Department of Surgical Education - Orlando Health
Department of Surgical Education - Orlando Health
Department of Surgical Education - Orlando Health
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
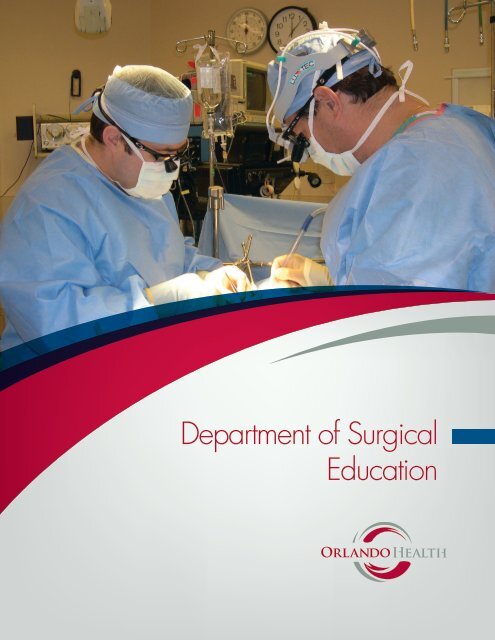
<strong>Department</strong> <strong>of</strong> <strong>Surgical</strong><br />
<strong>Education</strong>
Table <strong>of</strong> Contents<br />
<strong>Department</strong> <strong>of</strong> Surgery Faculty and Residents…….. ...........................................................................3<br />
<strong>Department</strong> <strong>of</strong> Surgery General Housestaff 2009 – 2010…….. ...........................................................4<br />
<strong>Department</strong> <strong>of</strong> Surgery Faculty…………….. .......................................................................................5<br />
Clerkships/Clinical Sites…………………….. ......................................................................................9<br />
Rotations Representative <strong>of</strong> a Typical Five-Year General Surgery Resident………… ......................10<br />
What We Offer ......................................................................................................................................11<br />
Conferences……………. .....................................................................................................................12<br />
ERAS Application…..............................................................................................................................13<br />
Publications…… ...................................................................................................................................14<br />
orlandohealth.com | pg 1
Welcome<br />
Thank you for your interest in our programs.<br />
The <strong>Department</strong> <strong>of</strong> <strong>Surgical</strong> <strong>Education</strong> at <strong>Orlando</strong><br />
<strong>Health</strong> is dedicated to graduate medical education,<br />
<strong>of</strong>fering a five-year, fully accredited general surgery<br />
residency program as well as accredited fellowships<br />
in surgical critical care and colon and rectal surgery.<br />
The department also <strong>of</strong>fers a one-year, non-<br />
accredited fellowship in trauma surgery.<br />
The residency structure includes four categorical<br />
and six non-designated preliminary first-year<br />
positions. There are four categorical residents at each<br />
subsequent year. Preliminary candidates are hired for<br />
a one-year period.<br />
<strong>Orlando</strong> <strong>Health</strong> has formal affiliations with several<br />
medical schools, including the University <strong>of</strong> Florida,<br />
Florida State University, University <strong>of</strong> Central Florida<br />
and the University <strong>of</strong> North Dakota.<br />
The program is based at <strong>Orlando</strong> Regional Medical<br />
Center (ORMC) which provides a total <strong>of</strong> 808 acute-<br />
care beds, performing more than 20,000 operative<br />
procedures and 80,000 emergency visits annually<br />
– an ideal environment for the education <strong>of</strong> our<br />
residents. The majority <strong>of</strong> surgical training occurs at<br />
ORMC, a designated Level One Trauma Center, and<br />
additional training is completed at Arnold Palmer<br />
Hospital for Children and Dr. P. Phillips Hospital.<br />
The campus serves as a major referral center for<br />
Central Florida.<br />
Mark L. Friedell, MD<br />
Program Director<br />
<strong>Department</strong> <strong>of</strong> Surgery 2009 – 2010<br />
Faculty and Residents<br />
Front row: First row: Drs. Karen Borman, Pat Quijada, David Graham, Bertrand Fonji, Chris Graham<br />
and Mark Friedell;<br />
Second row: Drs. Howard Smith, John Promes, Kyle Vincent, Jeremy Cravens, Joseph Bedway,<br />
Christopher DuCoin, Creighton Fiscina, Erin King and Sharon Noori;<br />
Third row: Drs. Guillermo Montes, Matt Lube, Ernest Block, Michael Kammerer, James Mayo, Kurt<br />
Gordon, Raj Nair, Lars Nelson and Christopher Schwan;<br />
Fourth row: Drs. Raj Patel, Raymond Green, Richard Sontchi, Marian Miller, Jason Clark, Jeremy<br />
Johnson, George Bishai, Hasan Kakli, Osmany Duany;<br />
Back row: Drs. Andre Teixeira, Mark Versnick and Aaron Seims<br />
pg 2 | orlandohealth.com<br />
orlandohealth.com | pg 3
General Surgery Housestaff 2009-2010<br />
PGY-5 Chief Residents Medical School<br />
Bertrand Fonji, MD SUNY Downstate Medical Center<br />
Chris Graham, MD Mercer University<br />
David Graham, MD West Virginia University<br />
PGY-4 Medical School<br />
Andre Teixeira, MD Morehouse School <strong>of</strong> Medicine<br />
Jason Clark, MD Medical University <strong>of</strong> South Carolina<br />
Mark Versnick, MD University <strong>of</strong> South Carolina<br />
Kyle Vincent, MD University <strong>of</strong> Oklahoma<br />
PGY-3 Medical School<br />
Jeremy Cravens, MD University <strong>of</strong> Missouri<br />
Michael Kammerer, MD Saint George’s University (Grenada)<br />
James Mayo, MD Medical University <strong>of</strong> South Carolina<br />
Aaron Seims, MD University <strong>of</strong> South Alabama<br />
PGY-2 Medical School<br />
Joseph Bedway, MD Jefferson Medical College <strong>of</strong> Thomas Jefferson University<br />
Erin King, MD Emory University<br />
Marian Miller, MD University <strong>of</strong> Toledo<br />
Sharon Van Duyne Noori, MD Morehouse School <strong>of</strong> Medicine<br />
PGY-1 Categorical Medical School<br />
Creighton Fiscina, MD Ross University (Dominica)<br />
Jeremy Johnson, MD University <strong>of</strong> South Alabama<br />
Lars Nelson, MD Saint George’s University<br />
Christopher DuCoin, MD Saint George’s University<br />
PGY-1 Preliminary Medical School<br />
George Bishai, MD University <strong>of</strong> North Carolina<br />
Osmany Duany, MD Institut Superior de Ciencias Medicas (Cuba)<br />
Kurt Gordon, MD University <strong>of</strong> Kentucky<br />
Hasan Kakli, MD Jefferson Medical College <strong>of</strong> Thomas Jefferson University<br />
Guillermo Montes, MD Baylor College<br />
Christopher Schwan, MD University <strong>of</strong> Texas Southwestern<br />
<strong>Department</strong> <strong>of</strong> Surgery Faculty<br />
Mark L. Friedell, MD, FACS<br />
Program Director, General Surgery<br />
Dr. Friedell completed his surgical residency at the University <strong>of</strong> Massachusetts and his<br />
vascular surgery fellowship at Newark Beth Israel Medical Center. He is board certified in<br />
general surgery with added qualifications in vascular surgery.<br />
His main research interest is carotid artery disease. He has published numerous articles<br />
on topics in general and vascular surgery in peer-reviewed journals. He is past-president<br />
<strong>of</strong> the Florida Vascular Society and this year was program chairman <strong>of</strong> the Association <strong>of</strong><br />
Program Directors in Surgery (APDS).<br />
Mark S. Roh, MD, FACS<br />
Academic Chairman, <strong>Department</strong> <strong>of</strong> Surgery<br />
Dr. Roh was recently named the academic chairman for the <strong>Department</strong> <strong>of</strong> Surgery. He<br />
completed his surgical residency at the University <strong>of</strong> Pittsburgh Medical Center. He also<br />
completed a clinical and research fellowship in surgical oncology at Memorial Sloan-<br />
Kettering Cancer Center in New York. He served for 10 years as chief <strong>of</strong> Liver Tumor<br />
Surgery at The University <strong>of</strong> Texas M. D. Anderson Cancer Center in Houston before<br />
becoming chairman <strong>of</strong> Surgery at Allegheny General Hospital. He received a master’s<br />
degree in Medical Management in 2007 from the University <strong>of</strong> Southern California<br />
Marshall School <strong>of</strong> Business.<br />
He has served in numerous leadership positions in international oncology organizations.<br />
Since 1994, Dr. Roh has been the executive editor <strong>of</strong> the Annals <strong>of</strong> <strong>Surgical</strong> Oncology. He is<br />
the associate director <strong>of</strong> Medical Affairs at the National <strong>Surgical</strong> Breast and Bowel Project<br />
(NSABP), an NIH supported clinical trials foundation. Dr. Roh is published widely in<br />
peer-reviewed journals and has lectured nationally and internationally.<br />
Pat B. Quijada, MD, FACS<br />
Associate Director, <strong>Surgical</strong> <strong>Education</strong><br />
Dr. Quijada completed his surgical residency at ORMC with additional postgraduate<br />
training at Memorial Sloan-Kettering Cancer Center in New York. He is board certified in<br />
general surgery.<br />
pg 4 | orlandohealth.com pg 5
<strong>Department</strong> <strong>of</strong> Surgery Faculty (CONTINUED)<br />
Michael Cheatham, MD, FACS, FCCM<br />
Director, <strong>Surgical</strong>/Trauma Intensive Care Unit<br />
Program Director, <strong>Surgical</strong> Critical Care Fellowship<br />
Dr. Cheatham completed both his general surgery residency and surgical critical care<br />
fellowship at Vanderbilt University. He is board certified in general surgery, with added<br />
qualifications in surgical critical care.<br />
Dr. Cheatham’s research interests include advanced hemodynamic monitoring, shock<br />
resuscitation, abdominal compartment syndrome, disaster preparedness, and third-world<br />
medicine. He is active in a number <strong>of</strong> national and international surgical, trauma, and<br />
critical care societies. He was recently elected as the president <strong>of</strong> the World Society for<br />
Abdominal Compartment Syndrome.<br />
Ernest Block, MD, MBA, FACS, FCCM<br />
Director, Trauma Services<br />
Dr. Block completed his general surgery residency at Albert Einstein Medical Center in<br />
Philadelphia and completed his surgical critical care fellowship and trauma fellowship<br />
at Jackson Memorial Hospital. He is board certified in general surgery with added<br />
qualifications in surgical critical care.<br />
Dr. Block is past-president <strong>of</strong> the Eastern Association for the Surgery <strong>of</strong> Trauma (EAST)<br />
and president-elect <strong>of</strong> the Florida Chapter <strong>of</strong> the American College <strong>of</strong> Surgeons. He<br />
recently received an MBA from University <strong>of</strong> Tennessee at Knoxville. His research interests<br />
include acute care surgery systems development, surgical infections and innovative<br />
technology for trauma.<br />
Matt W. Lube, MD, FACS<br />
Associate Director, <strong>Surgical</strong> <strong>Education</strong><br />
Dr. Lube completed his general surgery residency and surgical critical care fellowship<br />
at ORMC. He is board certified in general surgery with added qualifications in surgical<br />
critical care. He is currently the president <strong>of</strong> the Florida Society <strong>of</strong> Critical Care Medicine.<br />
Dr. Lube practices general and acute care surgery. He is actively involved in medical<br />
leadership at ORMC and is chairman <strong>of</strong> the <strong>Surgical</strong> Quality Committee. Dr. Lube serves<br />
as the director <strong>of</strong> the Basic Science Curriculum and will serve as the clerkship director for<br />
General Surgery for the University <strong>of</strong> Central Florida, College <strong>of</strong> Medicine.<br />
<strong>Department</strong> <strong>of</strong> Surgery Faculty (CONTINUED)<br />
Howard G. Smith, MD, FACS, FCCM<br />
Director, Burn Services<br />
Dr. Smith completed his general surgery residency at Indiana University and completed<br />
his surgical critical care fellowship at the University <strong>of</strong> Connecticut/Hartford Hospital. He<br />
is board certified in general surgery with added qualifications in surgical critical care.<br />
John T. Promes, MD, FACS, FCCM<br />
Director, Outpatient Center for Surgery<br />
Dr. Promes completed his general surgery residency at the Washington Hospital Center<br />
and completed his surgical critical care fellowship at Vanderbilt University Medical Center.<br />
He is board certified in general surgery with added qualifications in surgical critical care.<br />
Daryl Wier, MD, FACS<br />
Dr. Wier completed his general surgery residency at Louisiana State University (LSU)<br />
Medical Center in New Orleans and is board certified in general surgery. He is pastpresident<br />
<strong>of</strong> the Florida <strong>Surgical</strong> Society and a past-governor <strong>of</strong> the American College<br />
<strong>of</strong> Surgeons. An expert in the field <strong>of</strong> minimally invasive surgery, Dr. Wier specializes<br />
in advanced laparoscopic procedures for hiatal hernias, gastroesophageal reflux disease<br />
(GERD) and weight loss surgery.<br />
Marin Radulescu, MD, FACS<br />
Director, <strong>Surgical</strong> Skills Lab<br />
Dr. Radulescu completed his surgical residency at Nassau University Medical Center<br />
in Long Island New York and a fellowship in Minimally Invasive Surgery & Bariatrics<br />
at the Cleveland Clinic Florida. He is board certified in general surgery.<br />
Dr. Radulescu has published and presented at several pr<strong>of</strong>essional<br />
conferences on sleeve gastrectomy, gastric banding and gastroparesis.<br />
He is director <strong>of</strong> the <strong>Surgical</strong> Skills Lab.<br />
pg 6 orlandohealth.com | pg 7
<strong>Department</strong> <strong>of</strong> Surgery Faculty (CONTINUED)<br />
pg 8 | orlandohealth.com<br />
Raj Nair, MD<br />
Dr. Nair completed his surgical residency at ORMC. Upon graduation, he went to M<strong>of</strong>fitt<br />
Cancer Center in Tampa, Florida for a fellowship in surgical oncology. Dr. Nair oversees<br />
the general surgery tumor board grand rounds each month.<br />
Rajendra Patel, MD<br />
Vascular Surgery<br />
Dr. Patel completed his residency at University <strong>of</strong> Pittsburgh Medical Center and his<br />
vascular surgery fellowship at Massachusetts General Hospital. He is board certified<br />
in general surgery and board eligible in vascular surgery. His interests include aortic<br />
surgery, carotid surgery, venous disease and endovascular interventions for thoracic and<br />
abdominal aneurysms.<br />
Patrick Austin, MD<br />
Vascular Surgery<br />
Dr. Austin completed his general surgery residency at the University <strong>of</strong> Alabama at<br />
Birmingham. He completed his vascular surgery fellowship at the University <strong>of</strong> South<br />
Florida/Tampa General Hospital. He is board certified in general surgery and board<br />
eligible in vascular surgery. His interests include both open and endovascular approaches<br />
to aortic aneurysms, carotid disease, hemodialysis access, venous disease and lower<br />
extremity arterial occlusive disease.<br />
Clerkships<br />
Fourth-year electives in general<br />
surgery, surgical critical care, trauma<br />
surgery and vascular surgery are<br />
<strong>of</strong>fered throughout the academic<br />
year. Please visit orlandohealth.com<br />
for more information on how to<br />
apply for clerkships at ORMC.<br />
Clinical Sites<br />
Listed below are the clinical<br />
facilities for the teaching program<br />
in general surgery:<br />
• <strong>Orlando</strong> Regional Medical<br />
Center<br />
• Arnold Palmer Hospital for<br />
Children<br />
• Dr. P. Phillips Hospital<br />
• M. D. Anderson Cancer Center<br />
<strong>Orlando</strong><br />
pg 9
pg 10<br />
Rotations Representative <strong>of</strong> a Typical<br />
Five-Year General Surgery Resident<br />
PGY-I: General Surgery/Oncology, Acute Care Surgery,<br />
Vascular Surgery, Burn, Night Float, Pediatric Surgery,<br />
and a combined month <strong>of</strong> pathology/radiology.<br />
Designated preliminary residents will receive one<br />
elective month in their designated specialty.<br />
PGY-II: General Surgery/Oncology, SICU, Pediatric<br />
Surgery, Acute Care Surgery, Colorectal Surgery,<br />
Plastic Surgery and Night Float.<br />
PGY-III: General Surgery/Oncology, Vascular Surgery,<br />
Colorectal Surgery, Acute Care Surgery, SICU, Head<br />
and Neck and Night Float.<br />
PGY-IV: General Surgery/Oncology, Vascular Surgery,<br />
Acute Care Surgery, Thoracic Surgery, Transplantation<br />
and one month in either Colon and Rectal Surgery,<br />
SICU, Plastic Surgery or Pediatric Surgery.<br />
PGY-V: General Surgery/Oncology,<br />
Vascular Surgery, Acute Care<br />
Surgery, and in some cases,<br />
Thoracic Surgery.<br />
Acute Care Surgery<br />
Private General<br />
Surgery<br />
Our residents<br />
work closely<br />
with many busy<br />
private general<br />
surgeons who<br />
are committed to<br />
resident education.<br />
The experience in<br />
surgical oncology and<br />
advanced laparoscopic<br />
surgery is outstanding.<br />
ORMC is home to our Level One Trauma Center. As<br />
part <strong>of</strong> this, attending surgeons are in-house 24 hours<br />
a day and respond with the residents on the Acute<br />
Care Surgery team.<br />
Pediatric Surgery<br />
A very busy group provides a great experience in all<br />
aspects <strong>of</strong> pediatric surgery.<br />
<strong>Surgical</strong> Critical Care<br />
Our residents receive extensive experience in<br />
managing critically-ill patients. Numerous bedside<br />
diagnostic and therapeutic procedures are performed.<br />
For more information, please visit surgicalcriticalcare.net.<br />
Colon & Rectal Surgery<br />
This area <strong>of</strong>fers excellent experience in open and<br />
laparoscopic surgery as well as colonoscopy from a<br />
group that has developed a very busy practice and a<br />
Colorectal Fellowship Program.<br />
Vascular Surgery<br />
With the addition <strong>of</strong> two new surgeons, this<br />
has become an excellent rotation for open and<br />
endovascular cases.<br />
What We Offer<br />
• Excellent, well rounded clinical<br />
experience in all areas <strong>of</strong> general<br />
surgery<br />
• M. D. Anderson – <strong>Orlando</strong><br />
• Burn service<br />
• Physician extenders and ancillary<br />
services to help with the 80-hour<br />
resident work week<br />
• Sunrise XA computerized<br />
information system for easy<br />
tracking <strong>of</strong> patient charts<br />
• Animal lab<br />
• Computer lab<br />
• Skills lab<br />
• Book stipend<br />
• Free meals<br />
• Free parking<br />
• Notebook computers for access to<br />
clinical systems<br />
• Lab coats<br />
• Mock orals - years 2-5<br />
• ABS SCORE curriculum<br />
Total operative experience for the<br />
residents in our program can be as<br />
high as 1,100 cases – significantly<br />
higher than the national average.<br />
Each categorical resident is involved<br />
in at least one clinical research project<br />
which ultimately leads to presentation<br />
and publication.
Conferences<br />
The didactic experience includes weekly Grand<br />
Rounds, Mortality and Morbidity Conference and<br />
Basic Science Conference. Journal Club is held<br />
monthly.<br />
Fellowships Obtained<br />
Fifty percent <strong>of</strong> our chief residents choose to do a<br />
fellowship after graduation. Graduates have obtained<br />
fellowships in colorectal, cardiothoracic, plastic,<br />
vascular and pediatric surgery as well as surgical<br />
oncology and surgical critical care.<br />
Recent Fellowships<br />
• <strong>Surgical</strong> Critical Care Fellowship, University <strong>of</strong><br />
Oregon<br />
• <strong>Surgical</strong> Critical Care Fellowship, University <strong>of</strong><br />
Florida/Jacksonville<br />
• Breast Fellowship, Stanford University<br />
• Colon and Rectal Fellowship, Seattle, WA<br />
• MIS Fellowship, University <strong>of</strong> California, San Diego<br />
• Plastic Surgery Fellowship, LSU<br />
• <strong>Surgical</strong> Oncology Fellowship, M<strong>of</strong>fitt Cancer<br />
Center, Tampa, FL<br />
• Plastic Surgery Fellowship, University <strong>of</strong> South<br />
Florida, Tampa, FL<br />
• <strong>Surgical</strong> Critical Care Fellowship, ORMC<br />
• Plastic Surgery Fellowship, University <strong>of</strong> Akron, OH<br />
• Colon and Rectal Fellowship, ORMC<br />
Board Passage Rate<br />
We have a 92 percent first-time pass rate for the<br />
American Board <strong>of</strong> Surgery Qualifying and Certifying<br />
Exams ranking us in the top 10 percent <strong>of</strong> all<br />
programs nationally (absurgery.org).<br />
pg 12 | orlandohealth.com<br />
Intern Boot Camp<br />
Intern Boot Camp for PGY-1 residents is scheduled<br />
for two weeks in July. During this time, there will be<br />
courses to get you started with your technical training<br />
at <strong>Orlando</strong> <strong>Health</strong> including surgical instrument<br />
identification, knot tying, suture basics, stapling<br />
techniques and energy sources, basics <strong>of</strong> laparoscopy,<br />
Foley insertion and surgical biopsy.<br />
Skills Lab/Computer Lab<br />
The skills lab is located on the fourth floor near the<br />
operating rooms and the call rooms and is accessible<br />
24 hours a day. The computer lab is used for medical<br />
records completion, preparing presentations, literature<br />
searches, preparing abstracts and manuscripts,<br />
updating case logs, entering patients on your service<br />
lists and accessing all the surgical curricula that we use.<br />
ERAS Application<br />
ERAS application forms for the general surgery<br />
residency program are accepted September 1<br />
through October 31 each year.<br />
The ERAS application is considered complete when<br />
the personal statement, USMLE Steps one and two,<br />
three letters <strong>of</strong> recommendation, medical school<br />
transcripts and Dean’s Letter have been received.<br />
Interviews generally take place between November<br />
and January. The <strong>Department</strong> <strong>of</strong> <strong>Surgical</strong><br />
<strong>Education</strong> and <strong>Orlando</strong> <strong>Health</strong> participate<br />
and comply fully with the National Residency<br />
Matching Program (NRMP) rules and regulations.<br />
All available positions are for the standard July<br />
through June residency period.<br />
<strong>Orlando</strong> <strong>Health</strong><br />
<strong>Department</strong> <strong>of</strong> <strong>Surgical</strong> <strong>Education</strong><br />
86 W. Underwood St., Suite 201<br />
<strong>Orlando</strong>, FL 32806<br />
407.841.5142 • Fax: 407.648.3686<br />
For program or clerkship information, please<br />
visit our web site at orlandohealth.com.<br />
<strong>Orlando</strong> <strong>Health</strong> Highlights<br />
Facilities<br />
Hospitals 8<br />
Number <strong>of</strong> Beds 1,788<br />
People<br />
Team Members 14,310<br />
Physicians 2,206<br />
Medical <strong>Education</strong><br />
Faculty 88<br />
Residents 194<br />
Residency Programs 8<br />
Fellowship Programs 12<br />
Patients<br />
Total Admissions 107,405<br />
Total Births 14,705<br />
Total Surgeries 62,154<br />
Total Outpatient Visits 631,764<br />
Total Emergency Visits 290,275<br />
Total Trauma Admissions 4,786
Publications<br />
General Surgery<br />
1. Mesenteric venulitis in a 71-year-old man after acute<br />
appendicitis. Charron P, Smith JR. Am Surg 2005; 71:674-<br />
677.<br />
2. Free air induced secondary abdominal compartment<br />
syndrome following percutaneous endoscopic<br />
gastrostomy (PEG) Bhullar IS, Cheatham ML. Crit Care<br />
Med 2006; 34:A168.<br />
3. Pancreaticoduodenectomy in a community general<br />
surgery residency program. Smith CP, Lube MW,<br />
Cheatham ML, Safcsak K. Am Surg 2006; 72(8):750-753.<br />
4. A pitfall <strong>of</strong> protracted surgery in the lithotomy position:<br />
lower extremity compartment syndrome. Chow CE,<br />
Friedell ML, Freeland MB, DeJesus, S. Am Surg 2007;<br />
73(1)19-21.<br />
5. The death <strong>of</strong> George Washington: An end to the<br />
controversy. Cheatham ML. Am Surg 2008; 74:770-774.<br />
6. Guidelines for management <strong>of</strong> small bowel obstruction.<br />
Diaz JJ, Bokhari F, Block EFJ, et al. J Trauma 2008;<br />
64:1651-1664.<br />
7. Successful early fascial closure <strong>of</strong> an open abdomen<br />
during pregnancy. Pappas PA, Cheatham ML, Quijada P,<br />
O’Leary T, Carlan SJ. Am Surg (In press).<br />
8. Starting up a simulation and skills lab: What do I need<br />
and what do I want? Friedell, M, Smith CD, Seymour NE,<br />
Scott DJ, Dunnington GL. Journal <strong>of</strong> <strong>Surgical</strong> <strong>Education</strong><br />
2009 (In press).<br />
9. The general surgery residency at <strong>Orlando</strong> <strong>Health</strong>: Past,<br />
present and future. Friedell, M. Am Surg 2010 (In press).<br />
Vascular Surgery<br />
1. Carotid angioplasty and stenting is a safe and durable<br />
procedure in a community hospital. Friedell ML, Sandler<br />
BJ, Andriole JG, Cohen MJ, Martin SP, Howowitz JD. Am<br />
Surg 2007; 73(6) 543-47.<br />
2. Cerebral oximetry does not correlate with<br />
electroencephalography and somatosensory evoked<br />
potentials in determining the need for shunting during<br />
carotid endarterectomy. Friedell ML, Clark JM, Graham<br />
DA, Isley MR, Zhang XF. J Vasc Surg 2008; 48:601-6<br />
Trauma/<strong>Surgical</strong> Critical Care<br />
1. Abdominal and extremity compartment syndromes.<br />
Cheatham ML. In Ivy ME, Lipsett PA, eds. Adult<br />
Multipr<strong>of</strong>essional Critical Care Review Course. Society <strong>of</strong><br />
Critical Care Medicine, 2005, pp. 77-85.<br />
2. Ensuring adequate nutritional support: nitrogen balance,<br />
protein loss and the open abdomen. Cheatham ML,<br />
Safcsak K, Brezezinski SJ, Lube MW. ANZ J <strong>of</strong> Surgery<br />
75(4):a17-18, 2005.<br />
3. A liberal transfusion strategy does not improve survival<br />
in patients requiring open abdominal decompression.<br />
Cheatham ML, Safcsak K, Block EFJ, Lube MW. ANZ J <strong>of</strong><br />
Surgery 75(4):a14, 2005.<br />
4. Temporary abdominal closure should not be considered<br />
an age limited option. Al-Haddad A, Cheatham ML,<br />
Safcsak K. Crit Care Med 2005; 33:A42.<br />
5. Failure <strong>of</strong> observation <strong>of</strong> blunt splenic injury in adults:<br />
variability in practice and adverse consequences.<br />
Peitzman AB, Harbrecht BG, Rivera L, Block EFJ et al. J<br />
Am Coll Surg 2005; 201:179-187.<br />
6. Identifying undiagnosed diabetes in the trauma patient.<br />
Freeland M, Lube MW, Block EFJ, Cheatham ML, Safcsak<br />
K.Crit Care Med 2005; 33:A43.<br />
7. Does etomidate confound the diagnosis <strong>of</strong> adrenal<br />
insufficiency in the trauma patient? Turk BF, Cheatham<br />
ML, Safcsak K. Crit Care Med 2005; 33:A74.<br />
8. Higher hemoglobin levels during the first 48 hours<br />
<strong>of</strong> shock improve survival. Bhullar IS, Cheatham ML,<br />
Safcsak K, Block EF, Lube MW. Crit Care Med 2005;<br />
33:A23.<br />
9. The incidence <strong>of</strong> adrenal insufficiency in the critically ill<br />
trauma patient. Turk B, Cheatham ML, Safcsak K. Lube<br />
MW, Promes JT. J Trauma 2005; 59:1540<br />
10. Abdominal perfusion pressure. Cheatham ML, Malbrain<br />
MLNG. In: Ivatury RR, Cheatham ML, Malbrain MLNG,<br />
Sugrue M, editors. Abdominal Compartment Syndrome.<br />
Landes Biomedical, 2006.<br />
11. Cardiovascular implications <strong>of</strong> elevated intra-abdominal<br />
pressure. Cheatham ML, Malbrain MLNG. In: Ivatury<br />
RR, Cheatham ML, Malbrain MLNG, Sugrue M, editors.<br />
Abdominal Compartment Syndrome. Landes Biomedical,<br />
2006.<br />
12. Toward a consensus on intra-abdominal hypertension.<br />
Malbrain MLNG, Sugrue M, Cheatham ML, Ivatury R. In<br />
Ortiz-Ruiz G, Perafán MA, Faist E, and Castell CD, eds.<br />
Sepsis. Springer 2006; pp74-91.<br />
13. Results from the international consensus definitions<br />
conference on intra-abdominal hypertension (IAH)<br />
and abdominal compartment syndrome (ACS): Part I<br />
Definitions. Malbrain MLNG, Cheatham ML, Kirkpatrick<br />
A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi<br />
A, Olvera C, Ivatury R, D’Amours S, Wilmer A, Wendon J,<br />
Hillman K. Intensive Care Medicine 2006; 32: 1722-1732.<br />
14. Planned complex suicide: need for a high index <strong>of</strong><br />
suspicion. Parra MW, Al-Khayat H, Lube MW, Cheatham<br />
ML. Am Surg 2006; 72(5):454-455.<br />
15. Results from the international consensus definitions<br />
conference on intra-abdominal hypertension (IAH)<br />
and abdominal compartment syndrome (ACS): Part II<br />
recommendations. Malbrain MLNG, Cheatham ML,<br />
Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z,<br />
Leppäniemi A, Olvera C, Ivatury R, D’Amours S, Wilmer<br />
A, Wendon J, Hillman K. Intensive Care Medicine 2007;<br />
33(6):951-962.<br />
16. Consensus definitions for intra-abdominal hypertension<br />
and abdominal compartment syndrome. Cheatham ML.<br />
Critical Connections. 2006; 5(1):7.<br />
17. The use <strong>of</strong> diazepam for sedation <strong>of</strong> critically ill trauma<br />
patients. Gesin G, Dasta J, Birrer K, Cheatham ML, Kane-<br />
Gill S. Crit Care Med 2006; 34:A158.<br />
18. Decompressive laparotomy in the burn patient. Parra<br />
MW, Al-Khayat H, Smith HG, Cheatham ML. J Trauma<br />
2006; 60:1119-1121.<br />
19. Please pay attention to the abdominal compartment<br />
syndrome on your intensive care unit. Malbrain MLNG,<br />
Cheatham ML, Ivatury R, Sugrue M. Neth J Crit Care<br />
2006; 10: 422-430.<br />
20. Independent lung ventilation in the management <strong>of</strong><br />
traumatic bronchopleural fistula. Cheatham ML, Promes<br />
JT. Am Surg 2006; 72:530-533.<br />
21. Geriatric trauma. Block EFJ, Pearce J. In: Salomone JP,<br />
Pons PT et al, eds. Prehospital Trauma Life Support. Sixth<br />
Edition. St. Louis: Mosby 2006; 383-402.<br />
22. Abdominal compartment syndrome: It’s time to pay<br />
attention! Malbrain ML, Cheatham ML¸ Kirkpatrick A,<br />
Sugrue M, De Waele J, Ivatury R. Intensive Care Med<br />
2006; 32:1912-1914.<br />
23. Intravesicular pressure monitoring does not cause<br />
urinary tract infection. Cheatham ML, Sagraves SG,<br />
Johnson JL, White MW. Intensive Care Med 2006; 1640-<br />
1643.<br />
24. Admission serum glucose is a predictor <strong>of</strong> insulin therapy<br />
in trauma patients admitted to the intensive care unit.<br />
Pappas PA, Lube MW, Ibrahim JA. Crit Care Med 2006;<br />
23:A53.<br />
25. Shock: An overview. Cheatham ML, Block EFJ, Promes<br />
JT, Smith HG. In: Irwin RS, Cerra FB, Rippe JM,<br />
eds. Intensive Care Medicine. 6th Ed. Philadelphia:<br />
Lippincott-Raven, 2007, pp. 1831-1842.<br />
26. Consensus conference definitions and recommendations<br />
on intra-abdominal hypertension (IAH) and abdominal<br />
compartment syndrome (ACS) – The long road to<br />
the final publications, how did we get there? Malbrain<br />
MLNG, De laet I, Cheatham ML. Acta Clinica Belgica<br />
2007; 62(suppl); 44-59.<br />
27. Clinical awareness <strong>of</strong> intra-abdominal hypertension and<br />
abdominal compartment syndrome in 2007. Kimball EJ,<br />
Kim W, Cheatham ML, Malbrain MLNG. Acta Clinica<br />
Belgica 2007; 62(Supplement 1); 66-73.<br />
28. Cardiovascular implications <strong>of</strong> abdominal compartment<br />
syndrome. Cheatham ML, Malbrain MLNG. Acta Clinica<br />
Belgica 2007; 62(suppl); 98-112.<br />
29. Traumatic renal artery occlusion in a patient with<br />
a solitary kidney: case report <strong>of</strong> treatment with<br />
endovascular stent and review <strong>of</strong> the literature. Dowling<br />
JM. Lube MW. Smith CP. Adriole J. Am Surg 2007;<br />
73(4):351-3.<br />
30. Effect <strong>of</strong> patient positioning on intra-abdominal pressure<br />
monitoring. McBeth PB, Zygun DA, Widder S, Cheatham<br />
ML, Kirkpatrick AW. Am J Surgery 2007; 193: 644–647.<br />
31. Consensus conference definitions and recommendations<br />
on intra-abdominal hypertension (IAH) and abdominal<br />
compartment syndrome (ACS) – The long road to<br />
the final publications, how did we get there? Malbrain<br />
MLNG, De laet I, Cheatham ML. Acta Clinica Belgica<br />
2007; 62(suppl); 44-59.<br />
32. Clinical awareness <strong>of</strong> intra-abdominal hypertension and<br />
abdominal compartment syndrome in 2007. Kimball EJ,<br />
Kim W, Cheatham ML, Malbrain MLNG. Acta Clinica<br />
Belgica 2007; 62(suppl); 66-73.<br />
33. Cardiovascular implications <strong>of</strong> abdominal compartment<br />
syndrome. Cheatham ML, Malbrain MLNG. Acta Clinica<br />
Belgica 2007; 62(suppl); 98-112.<br />
34. Effect <strong>of</strong> patient positioning on intra-abdominal pressure<br />
monitoring. McBeth PB, Zygun DA, Widder S, Cheatham<br />
ML, Kirkpatrick AW. Am J Surgery 2007; 193: 644–647.<br />
35. Nitrogen balance, protein loss, and the open abdomen.<br />
Cheatham ML, Safcsak K, Brzezinski S, Lube MW. Crit<br />
Care Med 2007; 35(1):127-131.<br />
36. Biovailability <strong>of</strong> oral fluconazole in critically ill<br />
abdominal trauma patients with and without abdominal<br />
wall closure: A randomized crossover clinical trial.<br />
Barquist E, Gomez-Fein E, Block EFJ, et al. J Trauma<br />
2007; 63:159-163.<br />
37. Recombinant factor VIIa as an adjunct to control<br />
hemorrhage from chest trauma in a Jehovah’s Witness.<br />
Bhullar IS, Branman R, Block EFJ. Am Surg 2007; 73:818-<br />
819.<br />
38. The effect <strong>of</strong> body position on intra-abdominal pressure<br />
measurement: A multicenter analysis (WSACS Study<br />
001). Cheatham ML, DeWaele J, DeKeulenaer B, Widder<br />
S, Kirkpatrick A, Cresswell B, Malbrain M, Bodnar Z,<br />
Meija J, Reis R, Parr M, Schulze R. Acta Clinica Belgica<br />
2007; 62(suppl); 246.<br />
39. The optimal zero reference transducer position for intraabdominal<br />
pressure measurement: A multicenter analysis.<br />
DeWaele J, Cheatham ML, DeKeulenaer B, Widder S,<br />
Kirkpatrick A, Cresswell B, Malbrain M, Bodnar Z, Meija<br />
J, Reis R, Parr M, Schulze R. Acta Clinica Belgica 2007;<br />
62(suppl); 247.<br />
pg 14 orlandohealth.com | pg 15
Publications (CONTINUED)<br />
40. Long-term impact <strong>of</strong> the open abdomen: A prospective<br />
comparative analysis. Cheatham ML, Safcsak K. Acta<br />
Clinica Belgica 2007; 62(suppl); 246.<br />
41. Age should not limit the use <strong>of</strong> open abdominal<br />
decompression. Cheatham ML, Safcsak K. Acta Clinica<br />
Belgica 2007; 62(suppl); 261.<br />
42. Skin-only closure is superior to skin grafting in the open<br />
abdomen. Cheatham ML, Safcsak K. Acta Clinica Belgica<br />
2007; 62(suppl); 262.<br />
43. Is the evolving management <strong>of</strong> IAH/ACS improving<br />
survival? Cheatham ML, Safcsak K. Acta Clinica Belgica<br />
2007; 62(suppl); 268.<br />
44. Renal artery resistive index as the “canary” for critical<br />
intra-abdominal hypertension”. Ivatury RR, Kirkpatrick<br />
A, Cheatham ML. Acta Clinica Belgica 2007; 62(suppl);<br />
281.<br />
45. Results <strong>of</strong> the international survey on clinical awareness<br />
<strong>of</strong> intra-abdominal hypertension and abdominal<br />
compartment syndrome in critically ill patients (WSACS<br />
Study 003). Malbrain MLNG, Cheatham ML, for the<br />
WSACS Clinical Trials Working Group. Acta Clinica<br />
Belgica 2007; 62(suppl); 247.<br />
46. Fibrin glue improves skin graft adhesion to the open<br />
abdomen. Cheatham ML, Smith HK, Safcsak K. Acta<br />
Clinica Belgica 2007; 62(suppl); 301.<br />
47. Improved survival <strong>of</strong> critically ill trauma patients treated<br />
with recombinant human erythropoirtin. Napolitano<br />
LM, Fabian T, Bailey JA, Block EF, May AK, Corwin, HL. J<br />
Trauma 2007; 63:478.<br />
48. Natural course <strong>of</strong> citrulline during critical illness. Pappas<br />
PA, Cheatham ML, Safcsak, K. Crit Care Med 2007;<br />
35(suppl):A64.<br />
49. Citrulline versus arterial lactate during resuscitation <strong>of</strong><br />
the trauma patient. Pappas PA, Cheatham ML, Safcsak, K.<br />
Crit Care Med 2007; 35(suppl):A37.<br />
50. Resuscitation endpoints in severe sepsis: CVP, MAP,<br />
SvO2…and IAP. Cheatham ML. Crit Care Med 2008;<br />
36:1012-1014.<br />
51. Intra-abdominal pressure monitoring during fluid<br />
resuscitation. Cheatham ML. Curr Opin Crit Care 2008;<br />
14:327-333.<br />
52. The effect <strong>of</strong> different reference transducer positions on<br />
intra-abdominal pressure measurement: A multicenter<br />
analysis. De Waele JJ, Cheatham ML, De laet I, De<br />
Keulenaer BL, Widder S, Kirkpatrick AW, Cresswell AB,<br />
Malbrain M, Bodnar Z, Mejia-Mantilla JH, Reis Richard,<br />
Parr M, Schulze R, Puig S. Intensive Care Med 2008;<br />
34:1299-303.<br />
pg 16 | orlandohealth.com<br />
53. Serial hemoglobin levels play no significant role in the<br />
decision-making process <strong>of</strong> nonoperative management<br />
<strong>of</strong> blunt splenic trauma. Bhullar IS, Braman R, Block EFJ.<br />
Am Surg 2008; 9:876-878.<br />
54. Subcutaneous linea alba fasciotomy: A less morbid<br />
treatment for abdominal compartment syndrome.<br />
Cheatham ML, Fowler J. Am Surg 2008; 74:746-749.<br />
55. Traumatic perforation <strong>of</strong> a duodenal diverticulum.<br />
Fowler J, Cheatham ML, Sandler B, Padron A. Am Surg<br />
2008; 74:781-782.<br />
56. Are children really just small adults? Cheatham ML. Crit<br />
Care Med 2008; 36:2215-2216.<br />
57. Measuring intra-abdominal pressure outside the ICU:<br />
Validation <strong>of</strong> a simple bedside method. Cheatham ML,<br />
Fowler J. Am Surg 2008; 9:806-808.<br />
58. Long-Term Impact <strong>of</strong> Abdominal Decompression: A<br />
Prospective Comparative Analysis. Cheatham ML, Safcsak<br />
K. J American Coll Surg 2008; 207:573-579.<br />
59. Abdominal hypertension and abdominal compartment<br />
syndrome. Malbrain ML, Cheatham, ML. Core Topics<br />
in Cardiovascular Critical Care. Cambridge: Cambridge<br />
University Press, 2008 pp. 289-298.<br />
60. One hundred consecutive splenectomies for trauma: Is<br />
histologic evaluation really necessary? Fakhre GP, Berland<br />
T, Lube MW. J Trauma 2008; 64:1139-1141.<br />
61. Jugular venous air after basilar skull fracture. Anderson<br />
DR, Lube MW. J Trauma 2008; 64:847.<br />
62. Improved survival <strong>of</strong> critically ill trauma patients treated<br />
with recombinant human erythropoietin. Napolitano<br />
LM, Fabian TC,Block EFJ, et al. J Trauma 2008; 65:285-<br />
299.<br />
63. Nutritional support <strong>of</strong> the injured. Block EFJ, Lube MW.<br />
Trauma contemporary principles and therapy. Wolters<br />
Kluwer <strong>Health</strong>/Lippincott Williams & Williams. 2008;<br />
705-715.<br />
64. Dye pack injury causing third degree burns. Wroblewski<br />
RL, Smith HG. J Burn Care & Research. 2008, 29:406-407<br />
Colon and Rectal Surgery<br />
1. The gap in laparoscopic colorectal experience between<br />
U.S. general surgery and colon and rectal residency<br />
training programs. Charron P, Ferrara A, Campbell R,<br />
Gallagher JT, DeJesus S, Williamson PW. Dis Col Rectum,<br />
2007; 50:2023-2031.<br />
2. Novel murine model for colon cancer: Non-operative<br />
transanal rectal injection. Donigan M, Norcross LS,<br />
Aversa J, Colon J, Smith J, Ferrara A, Gallagher JT, Baker<br />
CH. J Surg Research, 2008; 5:1-5.
<strong>Department</strong> <strong>of</strong> <strong>Surgical</strong> <strong>Education</strong><br />
86 W. Underwood St., Suite 201<br />
<strong>Orlando</strong>, FL 32806<br />
407.841.5142 • Fax: 407.648.3686<br />
orlandohealth.com<br />
0359-111690 11/09