3B MEDIZIN | Biologie | Bachmann Lehrmittel
Sie wollen auch ein ePaper? Erhöhen Sie die Reichweite Ihrer Titel.
YUMPU macht aus Druck-PDFs automatisch weboptimierte ePaper, die Google liebt.
VR1528/4006700/1001566<br />
rectal ampulla<br />
Sagittal Section<br />
internal and external<br />
sphincter muscles of anus<br />
urogenital<br />
diaphragm<br />
Shape and Position<br />
In terms of size (3.5 – 5 cm x 3.2 - 4.2 cm) and shape the prostate gland<br />
somewhat resembles a chestnut and weights between 17 g and 28 g. Its<br />
compressive elasticity is similar to that of hard rubber. It surrounds the urethra<br />
between the base of the urinary bladder and the muscular plate spread<br />
between the lower rami of the pubic arch (urogenital diaphragm). The two<br />
common excretory ducts from the seminal vesicle and the ductus deferens,<br />
called the ejaculatory duct, rise posteriorly through the prostate and lead to<br />
the seminal colliculus of the prostate section of the urethra.<br />
seminal vesicle<br />
ejaculatory duct<br />
prostate<br />
diaphragmatic part<br />
of urethra<br />
ostium of<br />
ureter<br />
internal ostium of<br />
urethra<br />
prostate<br />
prostate part of<br />
urethra<br />
Function<br />
The prostate releases a thin, milky and turbid secretion containing various<br />
enzymes, prostaglandins, citric acid and richly acidic phosphatase. It is<br />
expelled into the urethra at the beginning of ejaculation during the male<br />
orgasmic phase due to contraction of the prostate.<br />
It accounts for 13 – 33 % of the entire sperm mass. The protein-cleaving<br />
enzymes contained in it liquefy the ejaculate after 15 – 30 minutes.<br />
Transurethral Resection (TUR)<br />
The glandular tissue surrounding the urethra is completely removed by means of<br />
an electroloop introduced via a resectioning instrument.<br />
Printed in Germany<br />
superior ramus<br />
of pubis<br />
body of urinary<br />
bladder<br />
mucosal folds<br />
ampulla of<br />
ductus deferens<br />
excretory<br />
duct<br />
ejaculatory duct<br />
prostate<br />
urethra<br />
urethral bulb<br />
urinary bladder<br />
rectovesticular pouch<br />
ostium of left ureter<br />
pubic symphysis<br />
internal ostium of urethra<br />
prostatic utricile<br />
prostate<br />
superficial dorsal<br />
vein of penis<br />
urethra<br />
corpus cavernosum<br />
penis<br />
corpus spongiosum<br />
penis<br />
testis<br />
epididymis<br />
apex of urinary<br />
bladder<br />
crus of the penis<br />
corpus cavernosum penis<br />
corpus spongiosum penis<br />
urinary bladder<br />
central zone<br />
ejaculatory duct<br />
peripheral zone<br />
prostatic part of<br />
the urethra<br />
Structure<br />
The prostate gland can be divided into the base situated at the<br />
top, the apex pointing downwards, a right and a left lobe, interconnected<br />
via the isthmus of the prostate, as well as a cone-shaped<br />
middle lobe, situated on the upper rear. The glandular tissue<br />
which is surrounded by a firm capsule is classified into four zones:<br />
the periurethral zone surrounding the urethra, the transitional zone, the central zone, correspondending<br />
to the middle lobe, as well as the peripheral zone, composed chiefly of the<br />
right and left lobes.<br />
Posterior Aspect of Male Pelvic Organs<br />
Ultrasound examination<br />
Adenoma<br />
60 % of all men over the age of 50<br />
years suffer from a begin, nodular<br />
enlargement of the central glandular<br />
part, producing concomitantly<br />
constriction of the urethra. This condition<br />
is called a prostate adenoma,<br />
benign prostate hyperplasia (BPH) or<br />
also prostate hypertrophy. With advancing<br />
age, production of the male sex hormones<br />
continually decrease, while the latter<br />
Symptoms<br />
Compression of the urethra leads to the<br />
are increasingly bound to plasma proteins, thus<br />
socalled „prostate patient sign“ (stage I):<br />
forfeiting their activity. A relative preponderance<br />
attenuated urinary stream, urge for frequent<br />
of female sex hormones begins to be manifest,<br />
micturition, increased urine production during<br />
the night and delayed or prolonged mic-<br />
generating an effect primarily on the glands of the central zone<br />
and producing the changes describbed. By means of an index<br />
turition. During stage II formation of residual<br />
finger introduced into the anus, the physician palpates through<br />
urine presents additionally, while stage III<br />
the wall of the rectum (rectal palpation) an enlarged, engorged,<br />
ranges from an „overflow bladder“ with<br />
smooth prostate.<br />
hydronephrotic kidney to renal failure.<br />
median + medial<br />
umbilical folds<br />
internal ostium<br />
of urethra<br />
prostatic ducts<br />
inferior ramus<br />
of pubis<br />
bulbo-urethral<br />
gland<br />
seminal vesicle<br />
Removal of a tissue sample<br />
isthmus of the prostate<br />
transitional zone<br />
periurethral zone<br />
base of the prostate<br />
median umbilical<br />
ligament<br />
apex of bladder<br />
vesical venous<br />
plexus<br />
vesical plexus<br />
pubic symphysis<br />
prostate plexus<br />
dorsal vein of<br />
penis<br />
inferior epigastric<br />
artery + vein<br />
ductus deferens<br />
inguinal<br />
ligament<br />
external iliac<br />
artery + vein<br />
ureter<br />
parietal<br />
peritoneum<br />
Effects of Hormones<br />
Male sex hormones (androgens) are produced by Leydig’s<br />
interstitial cells of the testes and by the adrenal cortex under the<br />
control of hypothalamic and anterior pituitary hormones. They<br />
provide for development and secretory functions of the prostate.<br />
Androgens generate an effect specifically on the peripheral zone.<br />
The female sex hormones also present in the male organism affect<br />
the central zone and the connective tissue of the prostate.<br />
Vascular and Nerve Supply of Urinary<br />
Bladder and Prostate<br />
Rectal Palpation<br />
left ureter<br />
ductus deferens<br />
superior vesicle<br />
vein<br />
superior vesicle<br />
artery<br />
autonomic<br />
nerve fibers<br />
inferior vesicle<br />
vein<br />
inferior vesicle<br />
artery<br />
Carcinoma<br />
Prostate carcinoma is one of the most common<br />
malignant tumors and one of the most common<br />
causes of death from cancer in men. Onset is<br />
between the age of 50 and 70 years. Unlike<br />
the adenoma, the tumor grows generally in the<br />
posterior or lateral parts of the prostate which<br />
are situated near the capsule and dependent on<br />
androgens. By means of an index finger introduced<br />
into the anus, the physician palpates through<br />
Metastasization<br />
the wall of the rectum a large, asymmetrical prostate,<br />
Distant seeding of cancer cells is effected via the lymph circulation<br />
featuring an irregular outline and with the hardness of wood.<br />
to lymph nodes in the vicinity of the aorta, iliac arteries and behind<br />
Treatment as well as prognosis are based on the clinical stage,<br />
the peritoneum as well as via the blood circulation to the bones,<br />
which is determined inter alia by the tumor size, invasion of lymph<br />
chiefly those of the pelvis and lumbar spine, into the liver and lungs.<br />
nodes, distatnt metastasization and the tumor markers (prostate-specific<br />
antigen=PSA, prostate-specific acidid phosphatase=PAP). To corroborate<br />
the diagnosis, a tissue sample is removed through the perineal region<br />
© <strong>3B</strong> Scientific GmbH<br />
(perineal fine-needle biopsy). In addition to localization of the smallest nonpalpable<br />
tumors, ultrasound examination (sonography) is used for determi-<br />
www.3bscientific.com<br />
Hamburg, Germany, 1997 - 2003<br />
nation of prostate size of residual urinary volume.<br />
Design and text: Wilfried Hennig, Antje Gottberg<br />
Illustrations: Holger Vaselow<br />
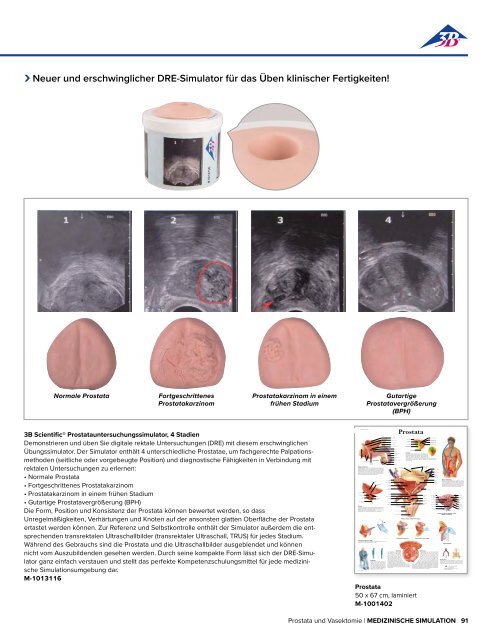
›<br />
Neuer und erschwinglicher DRE-Simulator für das Üben klinischer Fertigkeiten!<br />
Normale Prostata<br />
Fortgeschrittenes<br />
Prostatakarzinom<br />
Prostatakarzinom in einem<br />
frühen Stadium<br />
Gutartige<br />
Prostatavergrößerung<br />
(BPH)<br />
<strong>3B</strong> Scientific® Prostatauntersuchungssimulator, 4 Stadien<br />
Demonstrieren und üben Sie digitale rektale Untersuchungen (DRE) mit diesem erschwing li chen<br />
Übungssimulator. Der Simulator enthält 4 unterschiedliche Prostatae, um fachgerechte Palpationsmethoden<br />
(seitliche oder vorgebeugte Position) und diagnostische Fähigkeiten in Verbindung mit<br />
rektalen Untersuchungen zu erlernen:<br />
• Normale Prostata<br />
• Fortgeschrittenes Prostatakarzinom<br />
• Prostatakarzinom in einem frühen Stadium<br />
• Gutartige Prostatavergrößerung (BPH)<br />
Die Form, Position und Konsistenz der Prostata können bewertet werden, so dass<br />
Unregelmäßigkeiten, Verhärtungen und Knoten auf der ansonsten glatten Oberfläche der Prostata<br />
ertastet werden können. Zur Referenz und Selbstkontrolle enthält der Simulator außerdem die entsprechenden<br />
transrektalen Ultraschallbilder (transrektaler Ultra schall, TRUS) für jedes Stadium.<br />
Während des Gebrauchs sind die Prostata und die Ultraschallbilder ausgeblendet und können<br />
nicht vom Auszubildenden gesehen werden. Durch seine kompakte Form lässt sich der DRE-Simulator<br />
ganz einfach verstauen und stellt das perfekte Kompetenzschulungsmittel für jede medizinische<br />
Simulations umgebung dar.<br />
M-1013116<br />
Prostata<br />
Prostata<br />
50 x 67 cm, laminiert<br />
M-1001402<br />
Prostata und Vasektomie | <strong>MEDIZIN</strong>ISCHE SIMULATION 91