SCIENTIFIC REPORT 2010 - 2011 - IOV
SCIENTIFIC REPORT 2010 - 2011 - IOV
SCIENTIFIC REPORT 2010 - 2011 - IOV
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>SCIENTIFIC</strong><br />
<strong>REPORT</strong><br />
<strong>2010</strong> - <strong>2011</strong><br />
ISTITUTO ONCOLOGICO VENETO<br />
I.R.C.C.S.
FOREWORD 5<br />
THE INSTITUTE 9<br />
Chief Officer Address 13<br />
The <strong>IOV</strong> Governance 16<br />
CLINICAL ACTIVITY ORGANIZATION 19<br />
Chief Medical Officer Report 21<br />
Clinical Activity Data 24<br />
Multidisciplinary Groups 28<br />
THE DEPARTMENTS 31<br />
Department of Clinical Oncology 33<br />
Clinical Oncology 1 34<br />
Clinical Oncology 2 46<br />
Evaluation and Introduction of New Drugs<br />
in Cancer Therapy 54<br />
Department of Surgery 57<br />
Surgical Oncology 58<br />
Breast Surgery 64<br />
Melanoma and Soft Tissue Tumors 68<br />
Diagnostic and Operative Endoscopy 76<br />
Anesthesiology 82<br />
Department of Imaging, Radiology and Pathology 89<br />
Radiology 90<br />
Breast Imaging 96<br />
Pathology 104<br />
Department of Radiotherapy and Nuclear Medicine 107<br />
Radiotherapy and Nuclear Medicine 108<br />
Medical Physics 120<br />
Department of Experimental, Laboratory and<br />
Translational Oncology 127<br />
Immunology and Molecular Oncology 128<br />
Hereditary Endrocrine Cancer Unit 154<br />
CONTENTS<br />
CONTENTS<br />
3<br />
Department of Services 161<br />
Pharmacy 162<br />
Cardiology 168<br />
Psycho-Oncology 172<br />
Tumor Registry 178<br />
THE RESEARCH 185<br />
Scientific Director Address 187<br />
General Considerations 188<br />
Scientific Directorate Organization 191<br />
SWOT Analysis 195<br />
Research: Input and Output 197<br />
Clinical Trials and Biostatistics Unit 202<br />
Strategic Scientific Options 209<br />
Pharmacogenomics 212<br />
Cancer Stem Cells 214<br />
RESEARCH ACTIVITY <strong>REPORT</strong> 217<br />
Line 1 - Tumor Epidemiology and Prevention 218<br />
Introduction 218<br />
Workflow Project List 219<br />
Line 2 - Mechanisms of Cancerogenesis 220<br />
Introduction 220<br />
Workflow Project List<br />
Line 3 - Instrumental and Molecular Approaches<br />
221<br />
for Diagnosis, Staging and Follow-Up 222<br />
Introduction 222<br />
Workflow Project List<br />
Line 4 - Innovative Therapeutic Approaches:<br />
223<br />
Chemotherapy, Radiotherapy and Surgery 226<br />
Introduction 226<br />
Workflow Project List 227
Line 5 - Tumor Immunology and Innovative<br />
Therapeutic Approaches 230<br />
Introduction 230<br />
Workflow Project List 231<br />
Line 6 - Quality of Life in Cancer Patients<br />
and Geriatric Oncology 232<br />
Introduction 232<br />
Workflow Project List 233<br />
CLINICAL RESEARCH 235<br />
Ethics Committee 236<br />
Clinical Trials 237<br />
CONTENTS<br />
4<br />
VENETO ONCOLOGY NETWORK 245<br />
EDUCATION 249<br />
Internal Education & Training 250<br />
Post-graduate Schools 255<br />
Meetings and Seminars 257<br />
AWARDS 261<br />
PUBLICATIONS 265<br />
INDEx 305
FOREWORD<br />
FOREWORD<br />
5
This volume is the third edition of the Scientific<br />
Report of the IRCCS-Istituto Oncologico Veneto<br />
(<strong>IOV</strong>), and its format is very similar to that of the<br />
2008-2009 Report; since research programs which<br />
characterize the scientific profile of the Institute mostly<br />
have a wide breath, we felt that a biennial report of the<br />
results achieved and the developments foreseen could be<br />
appropriate. Again, we chose to publish this Report in<br />
English to stress the international dimension in which<br />
the Italian IRCCS must confront, and to underline the<br />
meaning of the report itself, as we intend it. Indeed, data<br />
reported in this kind of publications are also available<br />
in the yearly reports forwarded to the Italian Health<br />
Ministry; in any case, the array of research projects<br />
focused on specific aspects of oncologic research (the socalled<br />
Ricerca Corrente Programs) is summarized in a<br />
dedicated Section. We instead decided to privilege the<br />
presentation to colleagues involved in our field in Italy<br />
FOREWORD<br />
6<br />
and abroad a more faithful and comprehensive profile<br />
of the Institution we are working in. For this purpose,<br />
we gave more room to the analytical description of the<br />
Departments and of the clinical and research activities<br />
of the individual Units, who were asked to present<br />
in a more extended way a selection of their leading<br />
programs. The presence at the end of the book of an<br />
Analytical Index witnesses our hope to render this<br />
book a useful tool for researchers in Italy and abroad<br />
to establish new fruitful interactions on specific topics<br />
of interest.<br />
We did not feel it appropriate to distinguish our<br />
research activities into basic, translational and<br />
clinical investigation. Firstly, we are firmly convinced<br />
that only two types of research exist, good research<br />
and bad research. Secondly, progress is only achieved<br />
by the steady crosstalk of scientists belonging to very<br />
distant areas, and the interconnection of different
disciplines is terrific; it is impossible to foresee the<br />
future fallouts of an apparently “basic” research on the<br />
clinical management of patients in terms of diagnosis<br />
or therapy. In the light of the modern concepts in<br />
Oncology and more in general in Medicine, our work<br />
must go “from bed to bench and back from bench to the<br />
bed”, in search of innovative markers of disease and<br />
therapeutic targets. In this perspective, all the work at<br />
the Institute is carried out in a multidisciplinary way;<br />
this means that for every oncologic disease a group of<br />
concerned and dedicated workers (medical oncologists,<br />
radiologists, radiotherapists, surgeons, psychologists<br />
etcetera) strictly interact in the daily effort to provide<br />
patients with the best state-of-the-art standards of care.<br />
On the other hand, we are perfectly aware that<br />
clinicians and researchers also are only a part of the<br />
story. What we are daily carrying out in our labs,<br />
guards, and operating theaters would be vane, if our<br />
FOREWORD<br />
7<br />
activities were not complemented by the steady help<br />
of many people more or less directly involved in the<br />
management of the oncological disease. These include<br />
a wealth of persons, from the patients themselves to<br />
their relatives and caregivers, the nurses, the many<br />
volunteers belonging to the different Associations, and<br />
many others. This plethora of humble, often unknown,<br />
generous people do not have a place in this book, but<br />
without them our research would be a sterile, solipsistic<br />
exercise. To this silent multitude our grateful thinking;<br />
the struggle against cancer is a multifaceted task, and<br />
if we want to transform cancer into a curable disease,<br />
the efforts of everybody will be essential.<br />
Alberto Amadori, Scientific Director
THE INSTITUTE<br />
THE INSTITUTE<br />
9
The IRCCS Istituto Oncologico Veneto (Veneto Oncology<br />
Institute - <strong>IOV</strong>) was established in December 2005, after obtaining<br />
recognition of its scientific character from the Italian Health<br />
Ministry; following a site visit in 2008, this qualification was<br />
confirmed by the Ministry. The Institute has a juridical personality,<br />
and it is subordinate to both Veneto Regional Authorities and the<br />
Ministry of Health. The <strong>IOV</strong> is the only Cancer Center in the<br />
Veneto region; it participates in the Italian network of Cancer<br />
Institutes (Alliance Against Cancer), which includes the Italian<br />
Cancer Centers under the patronage of the Istituto Superiore di<br />
Sanità in Rome. Since January 2009, the <strong>IOV</strong> is a member of the<br />
Organization of European Cancer Centers (OECI), that includes<br />
over 70 Comprehensive Cancer Centers in Europe.<br />
The <strong>IOV</strong> stems from a long tradition of excellence<br />
in Oncology, which was first recognized in 1989 by the<br />
establishment of the Regional Oncology Center (COR) in Padova.<br />
The activity of COR was mainly devoted to fostering interactions<br />
among epidemiologists, clinicians and basic researchers in the<br />
field of Oncology, and to create a multidisciplinary approach<br />
to face the new frontiers of information on cancer genetics and<br />
biology. This strict collaboration among professionals involved<br />
in different areas of Oncology anticipated the modern concept<br />
of “translational medicine”, now considered as a strategic field<br />
within evidence-based medicine.<br />
The Institute<br />
THE INSTITUTE<br />
10<br />
Moreover, the <strong>IOV</strong> is a true Comprehensive Cancer Center,<br />
since it integrates in its mission clinical activity, research and<br />
education: the <strong>IOV</strong> offers, in fact, preventive, curative and palliative<br />
services to the population, and it combines this fundamental<br />
mission with a constant research activity on several different<br />
aspects of cancer, as well as maintaining a special commitment<br />
to educational issues, in strict collaboration with the Faculty of<br />
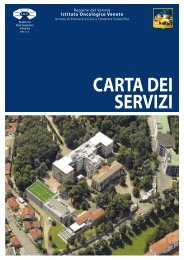
Medicine of the Padova University. The <strong>IOV</strong> is located in Padova in<br />
close proximity to the University Hospital, within an area known<br />
as “Ospedale Busonera”, a hospital that was established in 1932<br />
and was formerly dedicated to the care of tuberculosis patients.<br />
For this reason, the Ospedale Busonera is embedded in a park<br />
of about 40,000 square meters, populated by a collection of rare<br />
and magnificent trees, whose balsamic properties were thought<br />
to aid the recovery of tuberculosis patients; according to a recent<br />
agreement with the mayor of Padova, this park will soon be<br />
fully restored, and its beautiful environs shared by our patients<br />
and the general public. Because of its peculiar architectural<br />
characteristics, the major body of the hospital (recently flanked<br />
by a modern laboratory building) is under the patronage of the<br />
Artistic Superintendence of the Veneto Region; despite the great<br />
attention to our needs and the generous collaboration provided<br />
by this Authority, any refurbishment of the structures is complex<br />
and difficult.
Aerial view of the Busonera area<br />
THE INSTITUTE<br />
11
Map of Busonera Hospital area in the 30’s<br />
THE INSTITUTE<br />
12
Chief Officer<br />
Address<br />
THE INSTITUTE - CHIEF OFFICER ADDRESS<br />
13
Chief Officer Address<br />
When we started the project of the <strong>IOV</strong>, just five years ago,<br />
even with the most steady optimism we could not have thought<br />
that we would set up what has been created.<br />
The Veneto Region had believed in this project and the Italian<br />
Ministry of Health too, but we had an aura of skepticism and<br />
doubts around, that did not leave us completely calm.<br />
Today we can say we have worked hard and we have all worked<br />
well.<br />
Results are more than satisfying both in terms of clinical care<br />
and of research and innovation.<br />
<strong>IOV</strong> is recognized as a reality at a regional, national and<br />
international level.<br />
In this report, which sheds light<br />
on the improvements of the last two<br />
years and on the work in progress, the<br />
THE INSTITUTE - CHIEF OFFICER ADDRESS<br />
14<br />
achievements and the goal under implementation are described<br />
in detail.<br />
I would like to underline two important targets: the first is<br />
the extraordinary solidarity and generosity of our citizens already<br />
from the first year, the second is that the economic balance of the<br />
Institute has always been positive before tax, and today we have a<br />
significant income proving that also a public institution, even in its<br />
start-up, can be not a burden for the taxpayer, but an investment<br />
both at a scientific and a working level, as demonstrated by the<br />
patents taken out and now under development.<br />
We were few dozen of people at the beginning, today we are<br />
more than five hundred persons dedicated to research and medical<br />
care in the interests of the welfare of<br />
our patients.<br />
Thanks to each of you.<br />
Pier Carlo Muzzio
The <strong>IOV</strong> Governance<br />
The <strong>IOV</strong> is governed through the joint and coordinated effort of a Directive Board,<br />
which includes several persons each endowed with specific commitments and interacting<br />
within the Strategic Directorate.<br />
GENEral DirECTOraTE: legal representative of the Institution, responsible for legal and<br />
administrative affairs, through an Administrative Directorate.<br />
SCiENTifiC DirECTOraTE: responsible for scientific research and all activities connected<br />
to the scientific life of the Institute.<br />
The organization, monitoring and evaluation of clinical activities is the responsability<br />
of the Medical Directorate.<br />
According to the Italian law and regulations, the Institute functioning is superintended<br />
by a specific Committee (Comitato di Indirizzo e Verifica, CIV), whose duty is to supervise<br />
the strategic decisions of the General Directorate, to verify all the administrative aspects of<br />
the Institute, and to suggest lines of development to the Scientific Directorate, in order to<br />
guarantee a harmonic and fruitful development of the life and mission of the Institute.<br />
The CIV includes members endowed with scientific and administrative expertise, and<br />
it is presently composed by the following persons:<br />
Prof. Ermanno Ancona (President), Prof. Carlo Foresta, Dr. Eligio Grigoletto, Dr. Claudio<br />
Paccanaro and Dr. Adriano Paccagnella.<br />
The following diagram schematically illustrates the basic organization of the<br />
Institute.<br />
THE INSTITUTE - CHIEF OFFICER ADDRESS<br />
16
GENERAL DIRECTORATE<br />
ADMINISTRATIVE MARKETING &<br />
DIRECTORATE COMMUNICATION<br />
ECONOMICAL<br />
AFFAIRS<br />
IMAGING,<br />
RADIOLOGY<br />
& PATHOLOGY<br />
BREAST<br />
IMAGING<br />
RADIOLOGY<br />
MEDICAL<br />
PHYSICS<br />
LEGAL<br />
AFFAIRS<br />
PATHOLOGY<br />
RADIOTHERAPY<br />
& NUCLEAR<br />
MEDICINE<br />
RADIOTHERAPY<br />
& NUCLEAR<br />
MEDICINE<br />
CLINICAL<br />
ONCOLOGY 1<br />
MEDICAL<br />
DIRECTORATE<br />
CLINICAL<br />
ONCOLOGY<br />
SURGICAL<br />
ONCOLOGY<br />
CLINICAL<br />
ONCOLOGY 2<br />
EVALUATION & INTRODUCTION<br />
OF NEW DRUGS IN CANCER THERAPY<br />
DIAGNOSTIC<br />
& OPERATIVE<br />
ENDOSCOPY<br />
EDUCATION LIBRARY RESEARCH RESEARCH<br />
LABORATORIES ADMINISTRATION<br />
BREAST<br />
SURGERY<br />
THE INSTITUTE - CHIEF OFFICER ADDRESS<br />
17<br />
<strong>SCIENTIFIC</strong> DIRECTORATE<br />
SURGERY SERVICES<br />
CARDIOLOGY PSYCHO-<br />
ONCOLOGY<br />
ANESTHESIOLOGY<br />
PHARMACY<br />
MELANOMA<br />
& SOFT TISSUE<br />
TUMORS<br />
TUMOR<br />
REGISTRY<br />
IMMUNOLOGY<br />
& MOLECULAR<br />
ONCOLOGY<br />
CLINICAL<br />
TRIALS &<br />
BIOSTATISTICS<br />
UNIT<br />
EXPERIMENTAL<br />
LABORATORY<br />
& TRASLATIONAL<br />
ONCOLOGY<br />
HEREDITARY<br />
ENDOCRINE<br />
CANCER<br />
UNIT<br />
A S F A R A S S C I E N T I F I C A C T I V I T I E S A R E C O N C E R N E D
GENERAL DIRECTORATE<br />
Pier Carlo Muzzio (Director)<br />
Francesca Pagnin<br />
Bruno Bandoli (Marketing, Communication and Fund Raising)<br />
Flavia Dalla Rosa<br />
Daniela Chiusole (Certification and Quality Assurance)<br />
Marco Tria<br />
Maurizio Peci<br />
Andrea Azzalini<br />
Isabella Colpo<br />
Salvatore D’Amico<br />
Giuseppe Borella<br />
Ampelio Preo<br />
Marcello Valente<br />
<strong>SCIENTIFIC</strong> DIRECTORATE<br />
Alberto Amadori (Director)<br />
Daniela Battistuzzi<br />
Manuela Mtanis<br />
Mauro Apostolico<br />
Alessandro Andretto<br />
Gian Luca De Salvo<br />
Denise Marie Kilmartin<br />
Paola Del Bianco<br />
MEDICAL DIRECTORATE<br />
Maria Giacobbo (Director)<br />
Maria Pia Bellavere<br />
Antonella Frasson<br />
Maria Padovan (Nurses and Research Nurses, Coordinator)<br />
Massimo Cacco<br />
Martina Mattiazzi (Client Relation Office - URP)<br />
Paolo Turri (Medical Services)<br />
Alberto Bortolami<br />
Mauro Pegoraro<br />
Gianni Forzan<br />
Fortunata Marchese (Education)<br />
Stefania Facchin<br />
Luciana Nalin<br />
Roberta Candian<br />
Marta Amato<br />
Michelle Elisabeth Quinn<br />
THE INSTITUTE - CHIEF OFFICER ADDRESS<br />
18<br />
Nicoletta Zanotto<br />
Gloria Miarti<br />
Morena Piovan<br />
Donatella Pivetta<br />
Marica Pizzello<br />
Daniele Ciresola (Preventive Medicine)<br />
Cristina Maritan<br />
Michela Pinton<br />
Roberta Pozzani<br />
Lisa Rigato<br />
Silvia Volpi<br />
Marina Malipensa<br />
Sara Rossetti<br />
Federica Vascon<br />
Daniela Grosso<br />
ADMINISTRATIVE DIRECTORATE<br />
Pietro Girardi (Director)<br />
Marina Giusto (Deputy Director)<br />
Laura Scappin<br />
Giulia Di Chiara<br />
Simonetta Ive<br />
Cristina Ghirardello<br />
Roberta Signorini<br />
Paola Sorgato<br />
Emilio Pacchiega<br />
Isabella Calabrese<br />
Catia Farinea<br />
Franco Sterpi<br />
Margherita Casotto<br />
Manuela De Marchi<br />
Isabella Degli Agostini<br />
Lucia Lion<br />
Demis Sinigaglia<br />
Simone Polacco<br />
Filippo Paccanaro<br />
Michele Ferrin<br />
Federica Lea<br />
Margherita Merone Perone<br />
Emiliano Zabatta
CLINICAL ACTIVITY<br />
ORGANIZATION<br />
CLINICAL ACTIVITY ORGANIZATION<br />
19
Chief Medical Officer<br />
Report<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
21
Chief Medical Officer Report<br />
Graduated in Medicine in 1976, Maria Giacobbo was from<br />
the beginning involved in public health management. Since 1986<br />
she acted as Medical Director in several Hospitals and headed<br />
different Health Agencies of the Veneto Region; from 1993 to<br />
2000 she was also engaged as teacher at the Post-Graduate School<br />
of Hygiene and Preventive Medicine of the University of Verona.<br />
Since 2008 she acts as Medical Director of the <strong>IOV</strong>.<br />
The Medical Directorate is responsible for the management<br />
of all the clinical activities, and for the global governance and<br />
integration of the services provided by the individual Units of<br />
the Institute. In this setting, the Medical Directorate plays a key<br />
role in mediating among the requirements of the Clinics (efficacy<br />
of interventions and maintenance<br />
of high standards of care), of<br />
the Research activities (need of<br />
innovation and experimentation), and<br />
of the Administrative area (efficient<br />
resource employment). This function<br />
guarantees to both <strong>IOV</strong> workers and<br />
the public (patients and Institutions)<br />
elevated and consistent levels of care,<br />
also dedicating special attention to<br />
crucial aspects of modern Oncology<br />
and Medicine:<br />
safeness and risk prevention;<br />
treatment appropriateness;<br />
equal opportunity of access to care;<br />
care humanization and strict<br />
observation of deontological rules.<br />
In this frame, the Medical<br />
Directorate is strongly motivated<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
22<br />
to develop and optimize, in steady collaboration with the other<br />
Directorates, new models of organization and governance which<br />
could improve the quality of the services in terms of efficacy,<br />
efficiency, safety, and appropriateness.<br />
The Medical Directorate includes several Offices, which<br />
superintend specific aspects of the clinical governance of the<br />
Institute:<br />
Quality and accreditation<br />
Chief: Daniela Chiusole<br />
This Office is dedicated to the following activities:<br />
to guarantee, monitor and verify the maintenance and<br />
implementation of the quality of<br />
services, by providing appropriate<br />
indexes of control;<br />
to promote among the personnel of<br />
the Institute the culture and value<br />
of the quality, through dedicated<br />
tools such as educational courses on<br />
quality assurance and control;<br />
to plan and monitor all the activities<br />
needed to obtain and maintain<br />
the institutional accreditation,<br />
according to national and regional<br />
rules and requirements;<br />
to organize, monitor and maintain<br />
the ISO 9001 certification, now<br />
extended to all the clinical and<br />
administrative activities of the<br />
Institute;
to interact with other IRCCS to promote shared standards of<br />
the quality assurance system among Institutions with similar<br />
features and mission, and to favor the constant amelioration of<br />
governance tools also in view of international models of quality<br />
governance.<br />
Working risk prevention and radioprotection<br />
Chief: Daniele Ciresola<br />
This Office superintends to monitor the health of all the<br />
workers of the Institute, with particular attention to the evaluation,<br />
prevention and follow-up of the professional risks of individual<br />
categories and typologies of employment. This endeavor is carried<br />
out according to the regulations provided by both national and<br />
regional risk prevention agencies.<br />
Client satisfaction and claims<br />
Chief: Martina Mattiazzi<br />
This Office monitors the perception of the quality offered<br />
by the clients or patients, and his mission is to exploit all the<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
23<br />
claims and/or suggestions by the public to implement the quality<br />
of the medical assistance, in strict collaboration with the Quality<br />
and Accreditation office. To this end, a 24h phone line is active<br />
to facilitate the interactions with patients and their caregivers;<br />
more than 2,000 contacts are established yearly. Furthermore,<br />
in collaboration with volunteers operating within the Institute,<br />
a continuous analysis of client satisfaction is performed by<br />
appropriate forms exploring the opinion of the patients on<br />
waiting times, perceived quality of services, including information<br />
on health status, and availability of medical and non-medical<br />
personnel. The relevant information is periodically collected and<br />
analyzed within the Medical Directorate.<br />
The Medical Directorate also superintends to other Units, in<br />
collaboration with other structures of the Institute; in particular,<br />
the Education Office and the Clinical Trial Office will be<br />
mentioned within the appropriate section.
Hospitalisation<br />
9000<br />
8000<br />
7000<br />
6000<br />
5000<br />
4000<br />
3000<br />
2000<br />
1000<br />
6.100<br />
1.888<br />
5.157<br />
2.651<br />
2.304<br />
2.314<br />
0<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Clinical Activity Data<br />
2.343<br />
2.387<br />
Inpatients Day Hospital<br />
2.334<br />
2.516<br />
Inpatient admission by geographical areas<br />
Surgical index<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
24<br />
100<br />
80<br />
60<br />
40<br />
20<br />
57% 32%<br />
1%<br />
4%<br />
3%<br />
3%<br />
0<br />
94%<br />
6%<br />
85%<br />
15%<br />
67%<br />
33%<br />
66%<br />
34%<br />
60%<br />
40%<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Surgical Medical<br />
Padua<br />
Veneto except Padua<br />
Northen Italy except Veneto<br />
Central Italy<br />
Southern Italy and Islands<br />
Outside Italy
DRG average relative weight<br />
4,5<br />
4,0<br />
3,5<br />
3,0<br />
2,5<br />
2,0<br />
1,5<br />
1,0<br />
0,5<br />
0,0<br />
Pathological examinations<br />
3500<br />
3000<br />
2500<br />
2000<br />
1500<br />
1000<br />
500<br />
0<br />
Medical<br />
I n p a t i e n t s<br />
Surgical<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Cytological<br />
Istological<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Average length of stay<br />
Endoscopic procedures<br />
2500<br />
2000<br />
1500<br />
1000<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
25<br />
8<br />
7<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
500<br />
Medical<br />
Inpatients<br />
Surgical<br />
2006 2007 2008 2009 <strong>2010</strong><br />
0<br />
2006 2007 2008 2009 <strong>2010</strong>
Chemotherapy courses<br />
20000<br />
18000<br />
16000<br />
14000<br />
12000<br />
10000<br />
8000<br />
6000<br />
4000<br />
2000<br />
160000<br />
140000<br />
120000<br />
100000<br />
80000<br />
60000<br />
40000<br />
20000<br />
0<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Laboratory tests Outpatient visits<br />
0<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Radiodiagnostic and Nuclear Medicine examinations<br />
45000<br />
40000<br />
35000<br />
30000<br />
25000<br />
20000<br />
15000<br />
10000<br />
5000<br />
80000<br />
70000<br />
60000<br />
50000<br />
40000<br />
30000<br />
20000<br />
10000<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
26<br />
0<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Inpatients Outpatients Nuclear medicine<br />
Radiodiagnostic<br />
0<br />
2006 2007 2008 2009 <strong>2010</strong>
Radiation treatments<br />
1200<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
0<br />
2006 2007 2008 2009 <strong>2010</strong><br />
Inpatients Day Hospital<br />
Cardiologic examinations<br />
12000<br />
10000<br />
8000<br />
6000<br />
4000<br />
2000<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
27<br />
0<br />
2006 2007 2008 2009 <strong>2010</strong>
Multidisciplinary Groups<br />
The clinical and research activity of the Institute is carried out<br />
according to a model of multidisciplinarity. While this modality<br />
of approach to cancer patients fully fits the most accredited trends<br />
of modern Oncology, it also reflects the spirit of our Institute,<br />
where the presence of spikes of true excellence in some areas does<br />
not obscure the collegial work that permits the expression of this<br />
excellence. In other words, we are all convinced that the constant<br />
advancement of the clinical and research levels of our Institute,<br />
and the eventual steady improvement of the standards of care and<br />
the quality of life of our patients, only rely on the work of all of us.<br />
As in the functioning of a watch, the merit of indicating the real<br />
time is not attributable to one or the other piece composing the<br />
mechanism, but it is the result of the coordinated movement and<br />
function of all the parts of the watch. This spirit is reflected on the<br />
fact that most activities are carried out through organ-oriented<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
28<br />
multidisciplinary groups, which include all the experts needed to<br />
face a single pathology, from prevention to therapy to rehabilitation<br />
and palliation in terminal patients. This is possible because the<br />
<strong>IOV</strong> is embedded in a fertile milieu of different expertise, spread<br />
among the University of Padova and the other health structures<br />
operating in this area. Thus, some multidisciplinary groups also<br />
include researchers not formally belonging to <strong>IOV</strong>, and conversely<br />
many specialists belonging to <strong>IOV</strong> are asked to participate in<br />
clinical and research multidisciplinary groups based on other<br />
sanitary structures. This cross-fertilization makes it possible the<br />
constant rise to excellence of the Medicine and Oncology in<br />
Padova.<br />
The oncologic multidisciplinary groups operating since many<br />
years are listed in the Table with the indication of the contributing<br />
structures.
The experts of these groups meet at least at weekly intervals<br />
in fixed days, or if necessary in extemporary sessions. In these<br />
meetings, the clinical situation of every patient is collegially<br />
examined, and the most appropriate diagnostic/therapeutic plan<br />
is chosen. The patients are then also collegially re-evaluated during<br />
Field of interest Units<br />
Brain tumors Clinical Oncology 1, Radiotherapy and Nuclear Medicine, Immunology and Molecular Oncology - <strong>IOV</strong><br />
Pathology, Neurosurgery, Neuroradiology - University Hospital of Padua<br />
Breast tumors Breast surgery, Clinical Oncology 1 & 2, Radiotherapy and Nuclear Medicine, Breast Imaging, Radiology, Pathology,<br />
Immunology and Molecular Oncology, Hereditary Endrocrine Cancer Unit - <strong>IOV</strong><br />
Clinical Surgery II - University Hospital of Padua<br />
Esophageal tumors Clinical Oncology 2, Radiotherapy and Nuclear Medicine, Immunology and Molecular Oncology, Radiology,<br />
Surgical Oncology - <strong>IOV</strong><br />
Clinical Surgery I - University Hospital of Padua<br />
Lymphomas Clinical Oncology 2, Immunology and Molecular Oncology, Radiotherapy and Nuclear Medicine - <strong>IOV</strong><br />
Hematology Unit, Pediatric Hematology-Oncology Unit of Department of Pediatrics - University Hospital of Padua<br />
Gynecologic cancers Clinical Oncology 1, Radiotherapy and Nuclear Medicine, Radiology - <strong>IOV</strong><br />
Pathology, Clinical Surgery II, Gynecology - University Hospital of Padua<br />
Lung tumors Clinical Oncology 2, Radiotherapy and Nuclear Medicine, Radiology, Immunology and Molecular Oncology - <strong>IOV</strong><br />
Thoracic Surgery - University Hospital of Padua<br />
Head/neck tumors Clinical Oncology 2, Radiotherapy and Nuclear Medicine, Pathology - <strong>IOV</strong><br />
Otolaryngology Unit - University Hospital of Padua<br />
Thyroid tumors Clinical Oncology 1 & 2, Radiotherapy and Nuclear Medicine, Hereditary Endocrine Cancer Unit - <strong>IOV</strong><br />
Surgical Pathology Unit, Endocrinology Unit - University Hospital of Padua<br />
Gastro-Intestinal tumors Clinical Oncology 1, Radiotherapy and Nuclear Medicine, Pathology, Radiology, Immunology and Molecular<br />
Oncology, Family Cancer Clinics - <strong>IOV</strong><br />
Clinical Surgery II - University Hospital of Padua<br />
Surgery Branch - S. Antonio Hospital of Padua<br />
Melanoma Clinical Oncology 2, Melanoma and Soft Tissue Tumors Unit, Immunology and Molecular Oncology, Pathology,<br />
Radiotherapy and Nuclear Medicine - <strong>IOV</strong><br />
Clinical Surgery II, Dermatology - University Hospital of Padua<br />
Soft Tissue Sarcomas Melanoma and Soft Tissue Tumors Unit, Clinical Oncology 1, Radiotherapy and Nuclear Medicine, Radiology - <strong>IOV</strong><br />
Orthopedics, Radiology - University Hospital of Padua<br />
For Ewing sarcoma and rhabdomyosarcoma: periodical consultation with Pediatric Hematology-Oncology Unit -<br />
University Hospital of Padua<br />
Hepatic carcinoma<br />
and liver disease<br />
Clinical Oncology 1, Radiology - <strong>IOV</strong><br />
Hepatobiliary surgery, Pathology - University Hospital of Padua<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
29<br />
the treatment, and eventual decisions on the therapeutic layout<br />
stem from the discussion of the relevant experts. These meetings,<br />
beyond their importance for the management of the clinical<br />
situation of the patients, are also fundamental opportunities to<br />
generate new and foster existing scientific collaborations.
Peritoneal Carcinomatosis Melanoma and Soft Tissue Tumors Unit, Clinical Oncology1, Radiotherapy and Nuclear Medicine, Radiology - <strong>IOV</strong><br />
Clinical Surgery II - University Hospital of Padua<br />
Tumors of the Urinary<br />
System and Male genital<br />
organs<br />
Family Cancer Clinics<br />
Medical Oncology I, Radiotherapy and Nuclear Medicine, Radiology - <strong>IOV</strong><br />
Urology, Pathology, Cryopreservation of Male Gametes - Department of Medical and Surgical Sciences - University<br />
Hospital of Padua<br />
Pancreatic tumors Clinical Oncology 1, Radiology - <strong>IOV</strong><br />
Clinical Surgery I & II - University Hospital of Padua<br />
Pediatric Soft tissue<br />
sarcomas and Pediatric<br />
brain tumors<br />
Radiotherapy and Nuclear Medicine, Clinical Oncology 1, Anesthesiology - <strong>IOV</strong><br />
Pediatric Hematology-Oncology Unit - University Hospital of Padua<br />
The interest in heredo-familial tumors originated in the late<br />
’90s, much before the birth of <strong>IOV</strong>, thanks to the illuminated<br />
idea of a group of researchers of the Department of Oncology and<br />
Surgical Sciences of the University of Padua (Emma D’Andrea,<br />
Marco Montagna, Chiara Menin), who subsequently joined the<br />
<strong>IOV</strong>. At the beginning, the interest was centered on breast and<br />
ovary tumors, where inheritable alterations of the BRCA1-2<br />
genes had been first documented. Later on, the attention was<br />
extended to heredo-familial melanoma, and a further drive was<br />
given when an academic endocrinologist (Giuseppe Opocher)<br />
with a strong interest and expertise in inheritable neuroendocrine<br />
tumors joined the <strong>IOV</strong>. At that time (2009) an operative Unit<br />
was founded, denominated “Family Cancer Clinics”. This Unit,<br />
coordinated by Professor Opocher, collects the entire expertise on<br />
the field of heredo-familial tumors expressed within the Institute<br />
(and partly outside, as we shall see later). The Family Cancer<br />
Clinics structure has the responsibility for managing the afflux<br />
of patients to the structures where specific genetic testing and<br />
counseling is performed, organizing blood sampling for genetic<br />
CLINICAL ACTIVITY ORGANIZATION - CHIEF MEDICAL OFFICER <strong>REPORT</strong><br />
30<br />
tests, distributing these samples to the concerned laboratories,<br />
and collecting results for further contacts with the patients. Even<br />
though the interest in heredo-familial cancers is widespread<br />
among Italian IRCCS, the <strong>IOV</strong> Family Cancer Clinics is the sole<br />
structure collecting in a single operating unit the management of<br />
these conditions, thus contributing to increase the critical mass<br />
in the field. In addition, the Family Cancer Clinics works in<br />
strict contact and collaboration with a research group dedicated<br />
to the study of heredo-familial colorectal cancer. This surgical<br />
group, wich operates at the University of Padova-Padova General<br />
Hospital under the direction of Professor Donato Nitti, over<br />
the last 10 years has focused his interest on these neoplasms; its<br />
activity entails counseling, genetic testing, and most importantly a<br />
certified tissue bank which has collected over the years more than<br />
20,000 biological samples from about 2,000 patients. It is a firm<br />
auspice and hope of the Scientific Direction of the <strong>IOV</strong> that these<br />
structures could soon converge into a single inter-institutional<br />
Unit, where the critical mass, the mechanistic knowledge, and the<br />
quality of assistance could undergo a terrific growth.
THE DEPARTMENTS<br />
THE DEPARTMENTS<br />
31
CLINICAL<br />
ONCOLOGY<br />
THE<br />
DEPARTMENTS<br />
SURGERY IMAGING,<br />
RADIOLOGY<br />
& PATHOLOGY<br />
THE DEPARTMENTS<br />
32<br />
RADIOTHERAPY<br />
& NUCLEAR<br />
MEDICINE<br />
EXPERIMENTAL,<br />
LABORATORY<br />
& TRANSLATIONAL<br />
ONCOLOGY<br />
SERVICES
Department<br />
of<br />
Clinical Oncology<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
33
Main Pubblications<br />
Clinical Oncology 1<br />
Chief<br />
Vittorina Zagonel, MD<br />
Detecting functional impairment in older patients<br />
with cancer: is vulnerable elders survey-13 the right<br />
prescreening tool? An open question.<br />
Pegylated liposomal doxorubicin and gemcitabine in<br />
patients with advanced hepatocellular carcinoma: results<br />
of a phase 2 study.<br />
Primary tumor response to preoperative chemoradiation<br />
with or without oxaliplatin in locally advanced rectal<br />
cancer: pathologic results of the STAR-01 randomized<br />
phase III trial.<br />
Advanced gastric cancer (GC) and cancer of the gastrooesophageal<br />
junction (GEJ): focus on targeted therapies.<br />
Neoplastic meningitis from solid tumors: new diagnostic<br />
and therapeutic approaches.<br />
Vittorina Zagonel worked at the Clinical Oncology Division of the CRO Aviano Cancer Center<br />
(IRCCS) from 1983 to 1999. From 2000 to 2009, she served as Head of the Clinical Oncology<br />
Unit at the Fatebenefratelli Hospital, Rome, where she also acted as Director of the Department<br />
of Oncology for eight years. Since October 2009 she has been serving as Head of the Clinical<br />
Oncology 1 at Istituto Oncologico Veneto (Padua). She was a member of the National Oncologic<br />
Committee 2008-2009 and a member of the Ministry of Health board for palliative care in <strong>2010</strong>.<br />
She coordinates the AIOM task force on Continuous Care in Oncology since 2008. She is author<br />
and coauthor of more than 150 articles in indexed journals.<br />
Falci C, Brunello A, Monfardini S. J Clin Oncol. <strong>2010</strong>; 28:665-6<br />
Lombardi G, Zustovich F, Farinati F, Cillo U,<br />
Vitale A, Zanus G, Donach M, Farina M, Zovato<br />
S, Pastorelli D.<br />
Aschele C, Cionini L, Lonardi S, Pinto C, Cordio<br />
S, Rosati G, Artale S, Tagliagambe A, Ambrosini<br />
G, Rosetti P, Bonetti A, Negru ME, Tronconi MC,<br />
Luppi G, Silvano G, Corsi DC, Bochicchio AM,<br />
Chiaulon G, Gallo M, Boni L.<br />
Cappetta A, Lonardi S, Pastorelli D, Bergamo F,<br />
Lombardi G, Zagonel V.<br />
Lombardi G, Zustovich F, Farina P, Della Puppa<br />
A, Manara R, Cecchin D, Brunello A, Cappetta A,<br />
Zagonel V.<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
34<br />
Cancer. <strong>2011</strong>; 117:125-33<br />
J Clin Oncol. <strong>2011</strong>; 29:2773-80<br />
Crit Rev Oncol Hematol. <strong>2011</strong>; in<br />
press.<br />
Oncologist. <strong>2011</strong>; 16:1175-88
Clinical and Research<br />
Staff<br />
Vittorina Zagonel<br />
Umberto Basso<br />
Renato Ceravolo<br />
Sara Lonardi<br />
Ornella Nicoletto<br />
Fable Zustovich<br />
Antonella Brunello<br />
Elena Calore<br />
Alessandro Cappetta<br />
Maurizia Dalla Palma<br />
Miriam Farina<br />
Pasquale Fiduccia<br />
Giuseppe Lombardi<br />
Valeria Zafferri<br />
Administrative Staff<br />
Anna Schiavon<br />
Nursing Staff<br />
(Shared between Clinical<br />
Oncology 1 & 2)<br />
Barbara Giacomin (Coordinator)<br />
Samuela Aggio<br />
Monica Benetti<br />
Debora Bertin<br />
Flavio Berto<br />
Carmela Bisceglia<br />
Mariaelisa Bonaldo<br />
Elisabetta Bonfanti<br />
Silvia Bottazzo<br />
Chiara Canova<br />
Paola Canton<br />
Susanna Cedrone<br />
Cinzia Ciesa<br />
Maria Gliceria Collu<br />
Elisa Degortes<br />
Silvia Dell’Oste<br />
Sandra De Paoli<br />
Orejeta Diamanti<br />
Monica Patrizia Dori<br />
Eleonora Fontana<br />
Luisa Friso<br />
Debora Gabellotto<br />
Valeria Gallimberti<br />
Antonietta Gallocchio<br />
Nicola Galtarossa<br />
Monica Gechele<br />
Valentina Giurisato<br />
Maria Chiara Gobbo<br />
Evelina Lamberti<br />
Chiara Lando<br />
Patrizia Lazzaro<br />
Cristina Magro<br />
Elena Mancini<br />
Gabriella Maritan<br />
Jossie Veronica Mella<br />
Michela Michielotto<br />
Miriam Milanese<br />
Alessandra Modenese<br />
Cristina Naliato<br />
Ornella Nuccio<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
35<br />
Tatiana Peruffo<br />
Rossella Prando<br />
Caterina Pravato<br />
Antonella Prospero<br />
Cristina Raise<br />
Attilio Rambaldi<br />
Elena Rosa<br />
Laura Rossi<br />
Serena Ruzza<br />
Fabiola Sandonà<br />
Maria Cristina Saracini<br />
Paola Schiavon<br />
Veronica Schiavon<br />
Imelda Secondin<br />
Annalisa Spagolla<br />
Emanuela Tombolato<br />
Daniela Tonello<br />
Mbuyi Tshiala<br />
Elena Vittadello<br />
Anna Zambon<br />
Stefania Zanella<br />
Monica Zanocco
Mission<br />
The mission of the Unit of Clinical Oncology 1 is carrying<br />
out diagnosis and treatment of solid tumors in adult and<br />
senior patients, through multidisciplinary approaches involving<br />
surgeons, radiation oncologists, radiologists, pathologists,<br />
molecular biologists, geriatricians and different specialists. The<br />
principal aim is taking care of patients diagnosed with cancer,<br />
with special attention to all the needs of the person in order to<br />
have the best results for both cancer treatment and quality of life.<br />
Areas of Excellence<br />
Treatment of patients with gastrointestinal cancer (stomach,<br />
colon, rectum, anus, liver, pancreas and biliary tract);<br />
Treatment of patients with central nervous system tumors;<br />
Treatment of patients with gynecologic malignancies (ovary,<br />
uterus, vagina, vulva);<br />
Treatment of patients with breast cancer, in particular elderly<br />
patients and patients with heredo-familial cancers;<br />
Treatment of patients with genito-urinary tumors (kidney,<br />
bladder, prostate, testicle, penis);<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
36<br />
In this perspective, the effort of the Unit is to guarantee integration<br />
of the clinical interventions, together with implementation of<br />
clinical and translational research to allow patients to be treated<br />
with innovative antitumor therapies, as well as with supportive<br />
and palliative care. An important task of the Division of Clinical<br />
Oncology 1 is the theoretical and practical formation of Clinical<br />
Oncology fellows, in the fields of antitumor treatment, supportive<br />
and palliative care.<br />
Treatment of patients with soft tissue sarcomas;<br />
Diagnosis, assessment and therapeutic strategies for elderly<br />
patients with cancer;<br />
Phase I-II trials;<br />
Supportive and palliative care, with particular emphasis on<br />
continuity of care and socio-sanitary services;<br />
Treatment of patients with rare tumors (in particular GIST,<br />
neuroendocrine tumors).
Clinical Activity<br />
Distribution of patients by cancer site<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
271<br />
Colon<br />
96<br />
Rectum<br />
95<br />
Pancreas<br />
Clinical Activity <strong>2010</strong> No.<br />
Admissions 889<br />
Inpatients 486<br />
Outpatients 403<br />
Medical examinations 11.733<br />
First medical examinations 1.868<br />
Follow-up 4.432<br />
Medical examinations 5.433<br />
Hospital services 11.001<br />
67<br />
Stomach<br />
Chemotherapy 10.770<br />
Other treatments 231<br />
62<br />
Liver<br />
29<br />
Biliary tract<br />
18<br />
GIST<br />
174<br />
Urological cancer<br />
123<br />
Breast<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
37<br />
9<br />
Esophagus<br />
103<br />
Gynecologic cancer<br />
71<br />
Other types<br />
69<br />
Brain tumors<br />
64<br />
Sarcomas<br />
26<br />
Lung cancers
Major Collaborations<br />
Multidisciplinary Teams of Disease<br />
The Clinical Oncology 1 participates in multidisciplinary<br />
teams for studying cancers of the rectum, sarcomas, liver<br />
metastases, urologic tumors, brain tumors, breast cancer, liver<br />
tumors and peritoneal carcinomatosis.<br />
Within the <strong>IOV</strong>, steady interactions involve: Clinical<br />
Oncology 2, Molecular Immunology and Oncology, Surgery,<br />
Endocrinology, Radiotherapy and Nuclear Medicine, Psycho-<br />
Oncology, Cardiology, Radiology, Endoscopy, Pathology.<br />
National Collaborations<br />
Azienda Ospedaliera-Università, Padova<br />
Ulss 16, Padova<br />
CNR Aging Center, Padova<br />
Istituto Mario Negri (Milano)<br />
Istituto Nazionale Tumori (Milano)<br />
Istituto Humanitas (Milano)<br />
Istituto S. Raffaele (Milano)<br />
CRO (Aviano)<br />
Oncologia Medica (Pisa)<br />
Oncologia Medica (Ancona)<br />
Oncologia Medica Niguarda (Milano)<br />
IRST Meldola (Forlì)<br />
INRCA-Roma<br />
Neuro-oncologia, Università Torino<br />
Istituto Besta (Milano)<br />
Oncologia Medica (Verona)<br />
Oncologia Medica (Rovigo)<br />
Oncologia Medica (Vicenza)<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
38<br />
National Working Groups:<br />
GISCAD (Gruppo Italiano per lo Studio dei Carcinomi<br />
dell’Apparato Digerente)<br />
Mango (Mario Negri Gynecologic Oncology Group)<br />
ISG (Italian Sarcoma Group)<br />
GUONE (Gruppo Uro-oncologico del Nord Est)<br />
International Collaborations<br />
SENDO - Southern Europe New Drug Organization (Dott.<br />
Silvia Marsoni)<br />
New York University, Clinical Cancer Center, New York (Prof.<br />
F. Muggia)<br />
UCSF Medical Center, San Francisco (Prof. S. Chang)<br />
Memorial Sloan-Kettering Cancer Center, New York (Dr. A.<br />
Omuro)<br />
University of Losanne (Prof. R. Stupp)<br />
Division of Medical Genetics, Department of Medicine,<br />
Abramson Cancer Center, University of Pennsylvania (Prof.<br />
Katherine L. Nathanson)<br />
EORTC brain group<br />
EORTC elderly group<br />
EORTC sarcoma group
Major Ongoing Research Projects<br />
NEw ThErapEuTiC STraTEGiES iN ThE TrEaTmENT Of<br />
GaSTrO-iNTESTiNal (Gi) TumOrS<br />
Principal Investigators: Sara Lonardi, Davide Pastorelli, Vittorina<br />
Zagonel<br />
The management of GI tract cancers (both colorectal and<br />
non-colorectal) has widely changed over the last years, switching<br />
from a “tumor” perspective to a “patient’s tailored” approach.<br />
Identification of prognostic and predictive markers, optimization<br />
of multidisciplinary strategies, and new targeted drug development<br />
are some of the major points of interest for clinical and experimental<br />
research. Several trials are currently ongoing at our Institution in<br />
collaboration with multidisciplinary groups of Padua and others<br />
Oncology Units and national groups.<br />
A. prOGNOSTiC aND prEDiCTivE faCTOrS<br />
The identification of patients characterized by a worse<br />
prognosis or by a higher probability of response to certain<br />
treatments is crucial to select the “better population” for the<br />
“better therapeutic strategy”, and it is one of the main areas of<br />
research at our Institution.<br />
Molecular factors predictive of response to pre-operative<br />
chemo-radiation in locally advanced rectal cancer.<br />
Pre-operative chemo-radiotherapy (pCRT) approach for<br />
locally advanced rectal cancer is worldwide accepted as a standard<br />
treatment. The prediction of response to CRT has the potential<br />
to spare unnecessary toxic treatments for non-responders and,<br />
in selected cases, to allow a conservative surgery (local excision).<br />
Multiple patient- and tumor-related factors have been evaluated<br />
as potential predictors of response, but few studies take the tumor<br />
biology into account. Patients with rectal cancer, candidate to<br />
receive the same schedule of pCRT will be prospectively evaluated<br />
to assess the correlation of carcinoembryonic antigen (CEA),<br />
cell-free circulating DNA (cfDNA), levels of telomerase reverse<br />
transcriptase (h-TERT) and circulating tumor cells (CTC) with<br />
pathological response after pCRT and disease recurrence.<br />
Pharmacogenetic profiling and clinical outcome of patients<br />
with high-risk stage II and III colon cancer treated with adjuvant<br />
FOLFOX-4/XELOX chemotherapy and bevacizumab.<br />
Oxaliplatin plus a fluoropyrimidine (FOLFOX/XELOX) is<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
39<br />
the worldwide standard adjuvant therapy for high-risk stage II<br />
and III colorectal cancer, but the optimal duration of therapy and<br />
the management of toxicities remain to be resolved. Hopefully,<br />
it would be useful to find predictive/prognostic markers that<br />
could allow future adjuvant strategies to be optimized and<br />
individualized. Genomic polymorphisms in drug target genes,<br />
genes encoding DNA-repair enzymes and detoxification pathways<br />
may influence the activity of 5-Fluorouracil/capecitabine and<br />
Oxaliplatin, and their identification may improve the tailoring of<br />
chemotherapy and the choice of the optimal treatment strategy.<br />
In the present multicenter study, a panel of 17 polymorphisms<br />
within eleven genes in patients with radically resected high-risk<br />
stage II and III colon cancer undergoing adjuvant FOLFOX-4/<br />
XELOX chemotherapy and bevacizumab within a prospective<br />
phase III randomized clinical trial will be evaluated.<br />
Prospective evaluation of -1498 C/T VEGF polymorphism<br />
in the prediction of benefit from first-line FOLFIRI plus<br />
bevacizumab in metastatic colorectal cancer patients.<br />
Many studies have demonstrated that specific VEGF single<br />
nucleotide polymorphisms (SNPs) may affect gene transcription<br />
with a consequent variable production of VEGF and a probable<br />
indirect effect on pathogenesis and evolution of several disorders<br />
in which angiogenesis may be critical. Patients bearing -1498<br />
T/T genotype had significantly shorter progression-free survival<br />
(PFS) and worse, but not statistically significant, overall<br />
survival (OS) compared to patients carrying at least one C<br />
allele. On this basis we planned to prospectively evaluate the<br />
potential predictive role of -1498 C/T VEGF polymorphism in<br />
CRC patients treated with first-line FOLFIRI plus Bevacirumab.<br />
Primary objective is to evaluate the correlation between -1498<br />
C/T VEGF allelic variants and first-line PFS, while the secondary<br />
objectives is to evaluate the correlation with response rate, overall<br />
survival and toxicities attributable to Bevacizumab.<br />
B. OpTimizaTiON Of ThE TimiNG Of aDiuvaNT ChEmOThErapy<br />
Gastric and pancreatic cancers are a major cause of mortality<br />
worldwide. Prognosis is poor unless the cancer is diagnosed at<br />
a very early stage. Therapeutic options for patients with stage<br />
I-III gastric and pancreatic cancer include surgery plus adjuvant<br />
chemotherapy with or without radiotherapy, but the optimal
sequence of treatments and the role of radiotherapy in both<br />
diseases are still unclear.<br />
ITACA-S 2: comparison of the efficacy of pre-operative<br />
versus post-operative chemotherapy (CHT) in patients with<br />
resectable gastric cancer (GC).<br />
The role of adjuvant therapy in GC has been extensively<br />
studied during the past three decades in an attempt to improve<br />
the prognosis of patients who have undergone curative surgery.<br />
Metanalyses of some of these trials found that post-operative<br />
CHT led to marginal but statistically significant reductions in<br />
mortality compared to surgery alone. Neo-adjuvant CHT has<br />
recently received increasing attention in an attempt to improve<br />
the rate of complete tumor resection, to combat systemic<br />
metastases, and to prolong survival in patients with GC.<br />
Data from randomized, controlled, prospective trials comparing<br />
the two strategies are as yet not available. This Italian, multicentre,<br />
open-label, randomized, superiority, phase III trial enrolls patients<br />
with histologically confirmed, localized, resectable GC to compare<br />
the efficacy in terms of OS of a pre-operative vs. a post-operative<br />
CHT treatment.<br />
Randomized phase II-III study on pre-operative or<br />
post-operative chemotherapy in resectable pancreatic<br />
adenocarcinoma.<br />
Pancreatic tumor is the fourth leading cause of death in cancer<br />
patients. Only 10-20% of patients is amenable to surgery with<br />
a curative intent, and 5-yr survival is about 1-4%. Some phase<br />
III trials demonstrated a benefit of post-operative adjuvant<br />
chemotherapy vs. surgery alone in radically resected patients,<br />
but no data from randomized clinical trials on the role of neoadjuvant<br />
therapy are available. Some phase II studies suggest<br />
that a pre-operative treatment could increase the rate of patients<br />
operated with tumor-free margins and negative lymphnodes<br />
without affecting surgery morbidity and mortality.<br />
To evaluate the impact of a pre-operative CHT vs. a postoperative<br />
CHT, a multicentre national phase III trial has been<br />
recently launched. The primary objective is to compare the diseasefree<br />
survival in patients affected by resectable pancreatic cancer<br />
treated with pre-operative polychemotherapy (PEXG), postoperative<br />
PEXG or post-operative monotherapy (gemcitabine).<br />
C. NEw TarGETED DruG DEvElOpmENT<br />
Inhibition of angiogenesis is considered as a promising<br />
approach to the treatment of cancer. Disabling the function of<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
40<br />
the vascular endothelial growth factor receptor-2 (VEGFR-2)<br />
signaling pathway via a number of approaches, including anti-<br />
VEGF antibodies, anti-VEGFR-2 antibodies, and small molecule<br />
tyrosine kinase inhibitors (TKI), has been shown to inhibit new<br />
blood vessel formation and tumor growth in a variety of animal<br />
models. Ramucirumab is a recombinant human monoclonal<br />
antibody that specifically binds to the extracellular domain of<br />
VEGFR-2 with high affinity. Phase I studies and initial Phase II<br />
studies investigating Ramucirumab have provided information<br />
regarding safety and tolerability at clinically relevant doses, with<br />
preliminary evidence of clinical efficacy in a variety of human<br />
cancers. The drug is now undergoing Phase III studies in secondline<br />
treatment of multiple diseases.<br />
A randomized, double-blind, multicenter phase III study<br />
of irinotecan, folinic acid, and 5-fluorouracil (FOLFIRI)<br />
plus Ramucirumab or placebo in patients with metastatic<br />
colorectal carcinoma progressive during or following first-line<br />
combination therapy with bevacizumab, oxaliplatin, and a<br />
fluoropyrimidine<br />
This is a multicenter, randomized, double-blind, placebocontrolled<br />
phase III trial in which patients with metastatic<br />
colorectal cancer progressing to first-line combination therapy<br />
with bevacizumab, oxaliplatin, and a fluoropyrimidine will be<br />
randomized to receive either FOLFIRI plus placebo or FOLFIRI<br />
plus Ramucirumab. Approximately 1050 patients will be<br />
randomized to observe 756 events. The primary objective of this<br />
study is to compare overall survival; secondary objectives are to<br />
compare progression-free survival, objective response rate, patientreported<br />
outcome measures, safety profile, assessment of the<br />
association between biomarkers and clinical outcome, assessment<br />
of anti-Ramucirumab antibodies and assessment of serum levels<br />
of Ramucirumab.<br />
A randomized, multicenter, double-blind, placebo-controlled<br />
phase III study of weekly paclitaxel with or without<br />
Ramucirumab in patients with metastatic GC, refractory<br />
to or progressive after first-line therapy with platinum and<br />
fluoropyrimidine.<br />
To date, no randomized controlled trials have established a<br />
standard second-line treatment regimen for GC after failure of a<br />
cisplatin/fluoropyrimidine-containing regimen. At present, there<br />
is no evidence that any given single agent or combination therapy<br />
is clearly superior to other agents/regimens in terms of efficacy.<br />
This is a multicenter, randomized study evaluating the efficacy
of Ramucirumab using a double-blind, placebo-controlled<br />
design. The primary objective is to demonstrate efficacy in terms<br />
of OS in patients treated with paclitaxel plus Ramucirumab<br />
compared to patients treated with paclitaxel plus placebo as<br />
second-line treatment of metastatic gastric or gastro-esophageal<br />
adenocarcinoma after failure of any platin and fluoropyrimidine<br />
combination.<br />
Ramucirumab and best supportive care (BSC) versus<br />
placebo and BSC as second-line treatment in patients with<br />
hepatocellular carcinoma following first-line therapy with<br />
sorafenib.<br />
Hepatocellular carcinoma (HCC) confers a limited prognosis.<br />
Many patients present at a stage in which potentially curative<br />
surgery or orthotopic liver transplant is not feasible and, even<br />
when feasible, tumor recurrence is frequent. For patients with<br />
advanced disease, systemic chemotherapy is of marginal benefit<br />
and associated with significant toxicity. Sorafenib, a multitargeted<br />
TKI with activity against VEGFR-2, is now considered the<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
41<br />
standard first-line systemic treatment in this disease, based on<br />
favorable results of two phase III trials. No data from randomized<br />
trials on the role of a second-line treatment are available as yet.<br />
This is a Phase III multicenter, randomized study evaluating the<br />
safety and efficacy of Ramucirumab plus BSC as a double-blind,<br />
placebo-controlled (placebo plus BSC) comparison. The primary<br />
objective is to compare the overall survival in patients with HCC<br />
who had disease progression during or following sorafenib therapy,<br />
or were intolerant to this agent.<br />
TarGETiNG aNGiOGENESiS iN aDvaNCED rENal CEll<br />
CarCiNOma<br />
Principal Investigator: Umberto Basso<br />
The approval of six targeted therapies for advanced Renal Cell<br />
Carcinoma (RCC) has completely changed the management of<br />
this disease over the last 5 years, opening several fields of clinical
and experimental research. Several workers at <strong>IOV</strong> are now<br />
deeply involved in the treatment of this disease, aiming at buiding<br />
a multidisciplinary approach which has proven crucial for the<br />
progress of research in other more common cancers.<br />
a. CirCulaTiNG TumOr CEllS (CTC) iN paTiENTS TrEaTED wiTh<br />
firST-liNE SuNiTiNib<br />
CTC have a strong prognostic significange in breast,<br />
colorectal and prostate cancer, but their value in patients with<br />
advanced kidney cancer is sill poorly documented. A pilot study<br />
evaluating CTC counts in advanced RCC patients treated with<br />
first-line sunitinib has been carried out in cooperation with the<br />
Immunology and Molecular Oncology Unit of <strong>IOV</strong>, and other<br />
Oncological Units. More than 50 patients have been accrued so<br />
far, and about two thirds of them had one or more CTC in the<br />
blood. Total counts of CTC did not appear to correlate with the<br />
number of metastatic sites, and response or progression during<br />
sunitinib. However, when a count of apoptotic CTC was carried<br />
out, we found that an increase in these biologically inactive cells<br />
correlated with prolonged disease control. Based on these findings,<br />
we plan to extend the accrual to this study in order to prove the<br />
prognostic role of apoptotic CTC in advanced RCC.<br />
b. SuNiTiNib iN vON hippEl-liNDau SyNDrOmE<br />
Loss of function of the von Hippel-Lindau (VHL) gene located<br />
on chromosome 3 is the cause of this rare syndrome, but is also<br />
a key pathogenetic step in the development of sporadic clear cell<br />
RCC, with ensuing over-expression of VEGF-R, Platelet-Derived<br />
Growth Factor Receptor (PDGFR) and their ligands by the tumor<br />
and surrounding endothelial cells. In cooperation with the Unit<br />
for Hereditary Cancer of the <strong>IOV</strong> we started collecting data on<br />
VHL syndrome patients with advanced or recurrent RCC seen at<br />
our Institution. They were all treated with the TKI sunitinib as a<br />
first line regimen. Preliminary results have been presented at the<br />
ASCO Genitourinary Congress on February <strong>2011</strong>.<br />
C. SuNiTiNib iN ElDErly paTiENTS<br />
Since the activity and tolerability of sunitinib in unselected<br />
elderly patients ≥ 70 years are still poorly documented, we<br />
performed a retrospective analysis on feasibility and outcome<br />
of first or second-line sunitinib in 67 elderly patients with renal<br />
carcinoma followed in six oncological centers (<strong>IOV</strong>, Verona,<br />
Vicenza, Rovigo, Udine, Lucca). We found that dose reductions<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
42<br />
(up-front or after a few cycles) are frequently needed, but median<br />
PFS of about 13 months compares favourably with published data,<br />
with only three cases of cardiotoxicity. Results were presented at<br />
the ECCO Conference in October 2009. In cooperation with<br />
IRST-Meldola we are currently conducting a larger analysis in<br />
elderly patients receiving sunitinib as a first-line treatment for<br />
advanced cancer.<br />
D. pharmaCOkiNETiCS Of Oral DruGS aND COrrElaTiON wiTh<br />
rESpONSE aND TOxiCiTy<br />
Both sunitinib and everolimus (an inhibitor of m-TOR<br />
complex) are administered at fixed oral doses with no modifications<br />
according to age or body surface. Yet, recent data show that<br />
plasma drug levels may be different among patients due to dose<br />
reductions and heterogeneity in pharmacokinetics (mainly due<br />
to polymorphisms of Cytochrome P450 family proteins and/or<br />
concomitant medications). Different blood concentrations may<br />
translate into different toxicity rates as well as reduced tumor<br />
control. In cooperation with the Pharmacology Unit of CRO-<br />
Aviano and IRST-Meldola we plan to conduct a study evaluating<br />
the blood levels of sunitinib and everolimus administered to<br />
young and elderly RCC patients. Our aims are to assess agerelated<br />
differences, to clarify situations of unexpected toxicity and<br />
to elaborate predictive models in which daily dose modifications<br />
of sunitinib and everolimus might be driven by pharmacogenomic<br />
polymorphisms (Cytochrome 3A4 or other proteins), actual<br />
blood concentrations of native drug and its active metabolites as<br />
well as co-administration of other drugs interfering with hepatic<br />
drug metabolism.<br />
E. CarDiOTOxiCiTy Of Oral Tki<br />
Since hypertension, decrease in Left Ventricular Ejection<br />
Fraction (LVEF), clinically symptomatic congestive heart failure,<br />
myocardial hyschemia and rhythm alterations have been described<br />
in patients treated with sunitinib and sorafenib, all patients<br />
with RCC treated at <strong>IOV</strong> undergo cardiologic monitoring in<br />
cooperation with the Cardiology Unit. Over the years 2006-<strong>2010</strong>,<br />
around 70 patients were followed with clinical examination,<br />
electrocardiogram and echocardiography performed at 4 to 6<br />
months intervals. Several cardiac events were registered, mainly<br />
grade 1 or 2 according to CTCAE and reversible after appropriate<br />
treatments, allowing the majority of patients to resume treatment.<br />
A retrospective evaluation of type, treatment and outcome of these
events has been planned in order to establish the actual relevance<br />
and risk factors of cardiovascular events in unselected patients<br />
treated with sunitinib and sorafenib.<br />
GliOmaS Of ThE CENTral NErvOuS SySTEm: aNalyziNG<br />
iDh1, iDh2 aND mGmT GENES, prEDiCTivE faCTOrS,<br />
NEw DruGS aND rESpONSE TO TrEaTmENT iN ThE<br />
aNTiaNGiOGENiC Era<br />
Principal Investigators: Giuseppe Lombardi, Vittorina Zagonel,<br />
Fable Zustovich<br />
Gliomas are the most common form of primary brain tumors in<br />
adults. The majority of these are malignant, comprising glioblastomas<br />
and anaplastic astrocytomas, as well as other less common variants<br />
such as oligodendrogliomas and oligoastrocytomas. Low-grade<br />
gliomas also have the potential to became highly malignant neoplasms.<br />
Temozolomide, a DNA alkylating agent, is now the standard therapy<br />
against glioblastomas and anaplastic astrocytomas. In the recent<br />
period, new antiangiogenic drugs are emerging, such as bevacizumab,<br />
sorafenib and cilengitide; however, their effectiveness remains<br />
uncertain, and this is mainly due to the absence of randomized trials.<br />
Recent studies have shown the presence of IDH1 and IDH2 gene<br />
mutations in low-grade gliomas and secondary glioblastomas;<br />
this mutation leads to an increase of 2-HG levels in neoplastic<br />
cells and maybe in serum and urine. Elevated 2-HG levels could<br />
eventually lead to an increase in HIF-1 expression and VEGF levels.<br />
Furthermore, with the recent introduction of antiangiogenic drugs,<br />
which affect the permeability of tumor vasculature, there are significant<br />
limitations for evaluating the response by MRI, especially for the<br />
presence of pseudo-responses. Cerebral MIBI SPECT could help to<br />
define patients who really respond to therapy and patients who have a<br />
sole drop of the gadolinium uptake at MRI.<br />
Thus, for all these reasons, we have focused our attention on:<br />
Activity and efficacy of new antiangiogenic drugs<br />
Predictive and prognostic factors in patients treated with<br />
antiangiogenic drugs, with special attention to IDH1, IDH2 and<br />
MGMT mutations<br />
2-HG levels in serum and urine as a biomarker, in particular<br />
during follow-up<br />
Potential role of proton magnetic resonance spectroscopy in the<br />
evaluation of IDH mutation in neoplastic cells<br />
Potential role of cerebral MIBI SPECT in the evaluation of<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
43<br />
high grade glioma response to antiangiogenic treatments.<br />
Preliminary Results. We have interesting results in terms of<br />
activity and effectiveness reported from phase II and phase III<br />
clinical trials using new antiangiogenic drugs such as sorafenib,<br />
bevacizumab and cilengitide. Regarding predictive factors, in a<br />
recent work presented at the European Association of Neuro-<br />
Oncology Congress <strong>2011</strong>, we have shown that patients with a good<br />
ECOG-PS (0-1) have a better chance of prolonged survival when<br />
treated with antiangiogenic drugs, regardless of the type of agent.<br />
Furthermore, in another work submitted to the American Society<br />
of Clinical Oncology Congress <strong>2011</strong>, we have shown that patients<br />
with a good ECOG-PS and disease control on MRI according to<br />
Macdonald Criteria after two months of antiangiogenic treatment<br />
have a better chance of prolonged survival.<br />
Conclusions. Antiangiogenic drugs are emerging in the<br />
treatment of high-grade gliomas and recent evidence indicates<br />
that the molecular profile of gliomas may strongly influence the<br />
sensitivity of these tumors to both conventional treatments and<br />
targeted therapies. Thus, it is important to know new predictive<br />
factors for designing more personalized therapies and rapidly<br />
assess the real response to treatment by new radiologic methods<br />
and new possibly non-invasive biomarkers in urine and serum.<br />
CaNCEr iN ElDErly paTiENTS: COmprEhENSivE<br />
GEriaTriC aSSESSmENT aND TailOriNG TrEaTmENT<br />
OpTiONS<br />
Principal Investigators: Umberto Basso, Antonella Brunello,<br />
Vittorina Zagonel<br />
We are increasingly facing in the routine clinics cancer patients<br />
aged 70 years or more. Nevertheless, data show that elderly cancer<br />
patients (ECP) are less likely to be treated according to accepted<br />
treatment guidelines; the eventual undertreatment can have a<br />
detrimental effect on both relapse-free OS and quality of life.<br />
Understanding the physiologic and functional changes associated<br />
with aging can assist in developing useful strategies of treatment in<br />
elderly cancer patients. In our Unit we are currently studying the<br />
different aspects of ECP, especially in breast cancer, which is the<br />
most common neoplasm in the female population. In particular,<br />
we have focused our attention on:<br />
the impact of Comprehensive Geriatric Assessment on survival<br />
of ECP (“CGA” study);
the influence of the function of the immune system and<br />
thymic reserve on aging and tumor development, and the role<br />
of telomerase and telomere length in ECP vs. geriatric non-<br />
oncologic patients (“TELOTREC” study, in collaboration with<br />
Clinical Oncology 2, the Immunology and Molecular Oncology<br />
Unit and the Geriatric Unit, University of Padua);<br />
prevalence and assessment of pain in ECP (spontaneous study)<br />
and of depressive symptoms in ECP (“DAMA” study, in<br />
collaboration with INRCA, Rome);<br />
the polymorphisms of cytochrome CYP2D6 and activity and<br />
safety of Tamoxifen (“TAMOXIFENVENETO” study, in<br />
collaboration with other Clinical Oncology Units in Veneto);<br />
the polymorphism of aromatase gene and the activity of<br />
aromatase inhibitors in ECP with locally advanced/metastatic<br />
breast cancer;<br />
the impact of adjuvant treatment on cognitive functions in<br />
Conclusions and Future Perspectives<br />
Geriatric Oncology is a field of increasing interest, as<br />
demonstrated by the Italian National Oncologic Plan for the<br />
years <strong>2010</strong>-2012, and efforts are being put in developing models<br />
and strategies to optimize and tailor treatments. In the coming<br />
years we intend to continue our ongoing clinical and research<br />
activities, with the aim of optimizing care and facilitating clinical<br />
applications of the results obtained from translational studies.<br />
Several collaborations are underway to implement phase I-II<br />
studies with access to and availability of new antitumor drugs, as<br />
well as studies to recognize the factors that could predict response,<br />
and eventually be used in clinical practice.<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
45<br />
ECP with breast cancer (“ITACAm” study, in collaboration<br />
with INRCA, Rome.<br />
Preliminary results. So far, as to the above mentioned<br />
ongoing studies, we have been recruiting patients and enrolment<br />
is still ongoing. For the CGA study, data have been collected and<br />
analyzed and an abstract submitted to ASCO <strong>2011</strong>.<br />
The aim of the study was to compare a large cohort of ECP<br />
for all-cause survival according to their condition of fitness,<br />
vulnerability or frailty. All consecutive cancer pts ≥70 years<br />
admitted to our Geriatric Oncology Program underwent CGA and<br />
were prospectively followed. Kaplan-Meier survival method was<br />
used and univariate/multivariate (Cox) analyses were applied to<br />
different prognostic factors. In 880 patients enrolled from 9/2003<br />
to 10/<strong>2010</strong>, we observed that CGA correlates with mortality,<br />
independently from diagnosis of cancer stage and treatment.<br />
Moreover, multidisciplinary collaborations will be implemented<br />
to define an optimal diagnostic-therapeutic strategy for the main<br />
types of tumors (gastrointestinal, urologic, gynecologic, neurologic<br />
and breast cancer in the elderly), as it is already the case for other<br />
neoplasms.<br />
A further area of development is the activation of research<br />
programs in the field of support therapy and symptom control<br />
(pain, nutrition, comorbidities, etc.), with the intent of optimizing<br />
the quality of life and guaranteeing continuity of care for all cancer<br />
patients.
Main Pubblications<br />
Clinical Oncology 2<br />
Chief<br />
Vanna Chiarion-Sileni, MD<br />
Bleomycin-based electrochemotherapy: clinical outcome from a<br />
single institution’s experience with 52 patients.<br />
IL4Ralpha+myeloid-derived suppressor cell expansion in cancer<br />
patients.<br />
Multicentre, open, noncomparative phase II trial to evaluate<br />
the efficacy and tolerability of fotemustine, cisplatin, alpha<br />
interferon and interleukin-2 in advanced melanoma patients.<br />
Complete and lasting healing of bone melanoma metastasis after<br />
hypertermic limb perfusion.<br />
Role of the EGF +61A>G polymorphism in melanoma<br />
pathogenesis: an experience on a large series of Italian cases and<br />
controls.<br />
She earned her degree in Medicine from the University of Padova in 1980, subsequently specializing<br />
in Oncology (1983) and in Hematology (1988). Junior staff physician of Clinical Oncology at San<br />
Bortolo Hospital in Vicenza from 1987 to 1989, and then at the Padova Hospital from 1989 to 2007.<br />
Managing staff physician since 2007 at the Veneto Institute of Oncology; since 2008 head of the<br />
Melanoma and Skin Cancer Unit. Her experience abroad includes: observer at the Memorial Sloan<br />
Kettering Cancer Center (New York 1996); Yale University, Department of Medicine and Surgery<br />
(1997); Institute Gustave Roussy, Villejuif, Paris (1999). She received ESMO certification in Clinical<br />
Oncology in 1989. Since 1980, she is a member of AIOM and the Veneto Regional Secretary; since<br />
1987 member of ASCO; since 1989 member of ESMO, founder and elected member to the Italian<br />
Melanoma Intergroup from 1997. She was a professor for the post-graduate school in Oncology at<br />
the University of Padova. She published more than 150 papers in peer-reviewed journals.<br />
Campana LG, Mocellin S, Basso M, Puccetti<br />
O, De Salvo GL, Chiarion-Sileni V, Vecchiato<br />
A, Corti L, Rossi CR, Nitti D.<br />
Mandruzzato S, Solito S, Falisi E, Francescato<br />
S, Chiarion-Sileni V, Mocellin S, Zanon A,<br />
Rossi CR, Nitti D, Bronte V, Zanovello P.<br />
Ridolfi L, Fiorentini G, Guida M, Dichiara<br />
M, Bichisao E, Ridolfi R. Italian Melanoma<br />
Intergroup (IMI).<br />
Pigozzo J, De Rossi C, Rossi CR, Nitti D,<br />
Chiarion-Sileni V.<br />
Casula M, Alaibac M, Pizzichetta MA, Bono<br />
R, Ascierto PA, Stanganelli I, Canzanella S,<br />
Palomba G, Zattra E, Palmieri G. Italian<br />
Melanoma Intergroup (IMI).<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
46<br />
Ann Surg Oncol. 2009; 16: 191-9<br />
J Immunol. 2009; 182: 6562-8<br />
Melanoma Res. 2009; 19: 100-5<br />
Melanoma Res. 2009; 19: 193-4<br />
BMC Dermatol. 2009; 22: 9-7
Clinical and Research Staff<br />
Vanna Chiarion-Sileni<br />
Savina Aversa<br />
Cristina Falci<br />
Adolfo Favaretto<br />
Cristina Ghiotto<br />
Haralabos Koussis<br />
Davide Pastorelli<br />
Laura Bonanno<br />
Giovanni Faggioni<br />
Dario Marino<br />
Davide Maritan<br />
Giulia Pasello<br />
Jacopo Pigozzo<br />
Sara Polimini<br />
Giovanna Rossi<br />
Silvia Stragliotto<br />
Giulia Zago<br />
Nursing Staff<br />
(See Oncology 1)<br />
Administrative Staff<br />
Loredana Casagrande<br />
Silvia Salmaso<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
47
Mission<br />
The mission of this Unit is to provide patient access to new<br />
drugs and protocols through participation in major national and<br />
international studies. The whole staff is engaged in implementing<br />
the culture of quality and research as an added value that allows<br />
the activation of Phase I studies. Also, a major commitment is<br />
Areas of Excellence<br />
The Unit is especially dedicated to the following areas:<br />
study of new drugs and translational research in melanoma,<br />
lung neoplasms, and hepatocarcinoma;<br />
high-dose therapy and peripheral stem cell support in refractory<br />
lymphoma, myeloma and lymphomas of the elderly;<br />
development of protocols for patients with solid tumors or<br />
lymphoproliferative disease after organ transplantation or<br />
acquired immunodeficiency;<br />
assessment of the role of PET/CT in staging of breast cancer<br />
at high risk, in metastatic ocular melanoma, in the staging and<br />
restaging of esophageal cancer;<br />
Clinical Activity<br />
In <strong>2010</strong>, 1358 new patients were seen: the tumors most<br />
represented were, in the following order: breast cancer, lung cancer<br />
and melanoma, constituting 72% of the total. Two hundred-fifty<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
48<br />
to provide continuity and quality of care through a rigorous<br />
multidisciplinary approach and networking with both regional<br />
and extra-regional centers, in order to avoid the need for patients<br />
to migrate to gain access to study protocols.<br />
study and treatment of breast tumors in patients younger than<br />
35 years;<br />
definition of new criteria for evaluation of efficacy and<br />
immunomodulatory therapies;<br />
definition of new schemes in the combined treatment of head<br />
and neck and esophageal cancer;<br />
evaluation of risk factors in the development of brain metastases<br />
and their treatment;<br />
study of systemic and locoregional treatment combination in<br />
the treatment of metastatic melanoma.<br />
eight patients entered study protocols. Most services were provided<br />
in the outpatient setting with 11,626 accesses for treatment and<br />
9,821 for follow-up. The inpatient admissions were 389.
Distribution of patients by cancer site<br />
600<br />
500<br />
400<br />
300<br />
200<br />
100<br />
0<br />
540<br />
Breast<br />
299<br />
Lung<br />
212<br />
Melanoma<br />
Major Collaborations<br />
Esophagus<br />
Lymphoma<br />
Inside the <strong>IOV</strong><br />
For all the malignancies (lung, head-and-neck, esophagusstomach,<br />
liver, lymphoma, melanoma, breast, endocrine,<br />
hepatocellular carcinoma), multidisciplinary weekly meetings<br />
are active. Moreover, scientific investigations which involve<br />
the dedicated oncologist, the dedicated radiation oncologist,<br />
the appropriate surgeon, the radiologist, a nuclear physician, a<br />
gastroenterologist endoscopist are also ongoing. Multidisciplinary<br />
clinics and meetings are open to all specialists and trainees.<br />
National Collaborations<br />
Azienda ULSS “Veneziana” (Oncologia Medica)<br />
Dipartimento di Scienze Otorino-Odonto-Oftalmologiche-Cervico<br />
Facciali (Università degli Studi di Parma)<br />
IRCCS - HSR Ospedale San Raffaele (Milano)<br />
IRCCS - INT Istituto Nazionale dei Tumori (Milano)<br />
IRCCS - CRO Centro Riferimento Oncologico (Aviano)<br />
IRCCS - IEO Istituto Europeo di Oncologia (Milano)<br />
Azienda Ospedaliero Universitaria “Ospedali Riuniti”- Clinica<br />
di Endocrinologia (Ancona)<br />
Azienda Ospedaliera S. Croce e Carle - Oncologia Medica (Cuneo)<br />
89<br />
84<br />
Stomach<br />
Head & Neck<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
49<br />
44<br />
52<br />
37<br />
Endocrine<br />
12<br />
Mieloma<br />
7<br />
Post-transplant neoplasms<br />
Azienda Ospedaliera “Istituti Ospitalieri”- Chirurgia Generale<br />
(Cremona)<br />
Gruppo interdisciplinare per lo studio e trattamento dell’epatocarcinoma<br />
Gruppo interdisciplinare per lo studio e trattamento dei GIST<br />
(“G.I. - GIST”)<br />
Gruppo interdisciplinare per lo studio e trattamento dei tumori<br />
neuroendocrini (“G.I. - NET”)<br />
META (Melanoma Task Force)<br />
IMI (Italian Melanoma Intergroup)<br />
International Collaborations<br />
University Hospital, Zurich, Switzerland (Prof. R. Stahel)<br />
Istituto Oncologico Catalano, Barcelona, Spain (Prof. R. Rosell)<br />
Theaghenion Anticancer Hospital - Salonicco (Greece)<br />
EORTC Melanoma Group<br />
EORTC EBMT (European Bone Marrow Transplantation<br />
Group)<br />
ECOG (East Cooperative Oncology Group) Melanoma Group<br />
GMGT (Global Melanoma Task Force)
Major Ongoing Research Projects<br />
iDENTifiCaTiON Of NEw mOlECular TarGETS fOr<br />
biOlOGiCal aGENTS fOr ChEmOThErapy Of maliGNaNT<br />
plEural mESOThEliOma<br />
Principal Investigator: Giulia Pasello<br />
The objective of this study is to identify new biological<br />
agents to enhance the cytotoxic activity of chemotherapeutic<br />
regimens currently used to treat mesothelioma, forcing<br />
cancer cells to undergo apoptosis and to avoid cell cycle<br />
arrest in a metabolically active status (cellular senescence).<br />
In the first phase of the study, we plan to expose 3 mesothelioma<br />
cell lines to different treatments that can positively or negatively<br />
modulate the levels of ROS (reactive oxygen species) to induce<br />
apoptosis mediated by TRAIL (tumor necrosis factor-related<br />
apoptosis-inducing ligand). The analysis of the cell lines of<br />
malignant pleural mesothelioma ZL34, ZL55 and H28 is<br />
ongoing. The cell lines were kindly provided by the laboratories<br />
of Molecular Oncology, University Hospital of Zurich.<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
50<br />
We will evaluate the effect of these treatments associated<br />
with the inhibition of anti-apoptotic proteins of the<br />
IAP (inhibitors of apoptosis proteins) family and BCL2.<br />
At this stage, senescence and apoptosis will be evaluated using<br />
specific markers.<br />
In the second phase of the study, we will evaluate the<br />
potential therapeutic effect of biological agents identified<br />
in in vitro studies in a preclinical murine model. In the<br />
third year, the project will focus on the analysis of tumor<br />
samples from patients before and after chemotherapy.<br />
The expression of molecular markers of apoptosis and<br />
senescence will be correlated to the clinical and radiological<br />
response of patients to identify markers that can<br />
distinguish patients sensitive and refractory to treatment.<br />
Based on the results of this study, we will evaluate the possibility<br />
of developing a Phase I clinical trial in first-line treatment<br />
of pleural mesothelioma based on the association of selected<br />
biological agents with standard chemotherapy regimens.
aNalySiS Of ThE prOGNOSTiC aND prEDiCTivE impaCT Of<br />
EGfr aND kraS muTaTiONS, aND Of EGfr fiSh iN<br />
aDvaNCED luNG aDENOCarCiNOma<br />
Principal Investigator: Adolfo Favaretto<br />
The non-small cell lung cancer (NSCLC) has demonstrated<br />
considerable heterogeneity of biological and clinical behavior.<br />
Reversible inhibitors of EGFR have proven effective in a group of<br />
patients with specific clinical and molecular features. Mutations in<br />
the tyrosine domain of EGFR were found to be the best predictor<br />
in terms of objective response and PFS, while FISH for EGFR<br />
seems to identify a larger group of patients who might benefit<br />
from treatment. KRAS mutations are associated with failure to<br />
respond to such therapy. The three molecular markers will be<br />
analyzed retrospectively in patients with stage IIIB and IV NSCLC<br />
undergoing surgery for diagnostic or therapeutic purposes; the<br />
patients will be selected based on the presence of at least one of<br />
the clinical features which appear to be predictive of response to<br />
EGFR inhibitors (non-smoker status, female). The purpose of this<br />
study is to determine whether mutations in the tyrosine domain<br />
of EGFR or gene amplifications evaluated by FISH analysis can<br />
confirm their predictive value in a selected population of patients<br />
with clinical features indicative of response to inhibitors of EGFR<br />
tyrosine kinases, and to assess their prognostic value in a specific<br />
clinical context. Samples were collected from 67 patients with<br />
lung adenocarcinoma. Mutational analysis of EGFR (exons 18-<br />
21), KRAS (exon 2) and FISH analysis for EGFR are ongoing.<br />
The overall survival and disease-free survival will be analyzed in<br />
relation to the molecular findings to investigate their prognostic<br />
significance. The influence of treatment with inhibitors of EGFR<br />
on overall survival and disease-free survival in different patient<br />
groups will then be analyzed.<br />
EvaluaTiON Of CirCulaTiNG TumOr CEllS (CTC)<br />
aND ENDOThElial prOGENiTOr CEllS (EpC) aS a<br />
prOGNOSTiC faCTOr iN lOCally aDvaNCED luNG<br />
CaNCEr (NSClC)<br />
Principal Investigator: Adolfo Favaretto<br />
Patients with locally advanced NSCLC have a median survival<br />
of about 1 year, and at 3 years about 20% are still alive. Aim of this<br />
study is to assess whether two cell markers could partially explain<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
51<br />
this biological heterogeneity. CTC are present in many metastatic<br />
solid tumors. Their measurement in breast cancer has a prognostic<br />
and predictive value. EPC are cells derived from bone marrow and<br />
may play an important proangiogenetic role in the early growth<br />
of metastases. In 30 NSCLC patients we plan to count CTC<br />
and EPC at the beginning and at the end of concurrent chemoradiotherapy.<br />
In the case of sequential therapy, the count is also<br />
planned at the end of each treatment. The CTC will be evaluated<br />
with the CellSearch (Veridex, LLC, Warren, NJ) system.<br />
To this end, 15 ml of peripheral blood are incubated with<br />
magnetic nanoparticles conjugated with monoclonal antibody<br />
to the cell surface marker EpCAM, specific for epithelial cells.<br />
Through a magnetic field, EpCAM positive cells are selected<br />
and labeled with antibodies specific for white blood cells (anti-<br />
CD45) and epithelial cells (anti-cytokeratin 8, 18, 19) and a<br />
specific marker for cell nuclei (DAPI). A CTC, by definition,<br />
must express EpCAM, have a nucleus (DAPI positivity), and<br />
express markers for epithelial cells but not leukocytes. EPC are<br />
defined as endothelial cells in the peripheral blood expressing<br />
C-kit, VEGFR2, VE-cadherin but not expressing CD11b. Up to<br />
now, 6 patients with locally advanced NSCLC were enrolled and<br />
completed the counting of CTC and EPC.<br />
TumOr markErS fOr aDENOCarCiNOma Of ThE<br />
ESOphaGuS aND CarDiaS. a rETrOSpECTivE STuDy<br />
Principal Investigator: Vanna Chiarion-Sileni<br />
Tumor markers may correlate with the presence or progression<br />
of cancer. In cancers of the colon and pancreas, the predictive<br />
and prognostic value of CEA and Ca199 are defined, whereas<br />
for cancers of the esophagus and cardias only a few studies<br />
have evaluated the significance of their increase in the natural<br />
history of disease. The purpose of this study is to evaluate, both<br />
retrospectively and prospectively in patients treated from 1998<br />
with cardias gastric cancer, the significance and predictive value<br />
of CEA and Ca199 and their possible prognostic and predictive<br />
role.<br />
Data collection began in March <strong>2010</strong> and will continue until<br />
a suitable number of patients to obtain statistical significance will<br />
be reached. In case of evidence of a predictive and/or prognostic<br />
role, a prospective validation study will be proposed by the Italian<br />
Research Group on Biomarkers.
NEw ThErapEuTiC STraTEGiES iN ThE TrEaTmENT Of<br />
mElaNOma<br />
Principal Investigator: Vanna Chiarion-Sileni<br />
Within the clinical and translational research programs, many<br />
resources are devoted to melanoma. In addition to the design<br />
and coordination of non-profit, national clinical trials, the Unit<br />
has actively participated in and contributed to both academic<br />
(EORTC) and sponsored international studies, designed to test<br />
new molecules and identify new gene profiles and/or prognostic<br />
and predictive factors.<br />
Among the non-profit studies, the TRECEM trial (a phase<br />
III randomized, open-label study) prospectively evaluated the<br />
development of brain metastases in relation to the systemic use<br />
of Dacarbazine or Temozolomide, demonstrating that cerebral<br />
progression depends more on the effectiveness of the drug than its<br />
ability to cross the blood-brain barrier, and that the prognosis of<br />
patients who develop brain lesions is no worse than those who do<br />
not, thus supporting the issue that these patients are unjustifiably<br />
excluded from studies of new drugs. The Mel.A. trial (a phase III<br />
randomized, open-label study) has evaluated the effectiveness of<br />
intravenous intensified interferon alpha-2b compared to standard<br />
high-doses in patients after surgical excision of metastastatic<br />
lymph nodes, demonstrating that a shorter but more intensive<br />
treatment regimen is more feasible and not more toxic than a<br />
conventional one. In EORTC and sponsored trials, we have<br />
actively participated in the study of the anti-CTLA-4 antibodies<br />
(Ipilimumab) (BMS 008, BMS 024, BMS 025, BMS 029, BMS<br />
184 EAP studies). By treating more than 120 patients, we were<br />
able to identify new immune-related response patterns and<br />
implement the guidelines for the monitoring of immune-related<br />
adverse reactions for a more effective and safer drug use in the<br />
clinical practice. We are also studying possible surrogate markers<br />
of response that could be employed in the clinical evaluation of<br />
the patients during the phase of the immunological activaction<br />
when radiological imaging is not able to distinguish between true<br />
or false progression making the clinical decision difficult.<br />
Moreover, we contributed to the clinical evaluation of<br />
the MAGE 3 A recombinant protein by participating in the<br />
EORTC 16032-18031 study which allowed the identification<br />
of a predictive gene profile of efficacy, and we are now testing<br />
prospectively this profile in the metastatic (Predict study) and<br />
adjuvant setting (Derma study).<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
52<br />
Furthermore, we assessed and are currently evaluating the<br />
clinical activity and tolerance profile of several new molecules in<br />
the treatment of melanoma such as the antiCD137 (BMS006)<br />
monoclonal antibody, the intralesional allovectina-7 (VICAL),<br />
Vemurafenib and GSK 2118436 BRAF inhibitors.<br />
In testing the effect of Braf inhibitors we are particularly<br />
focused on defining the mechanism of resistance, the effect on<br />
brain metastases and the best combinations, schedules and timing<br />
in the treatment strategy and planning in order to improve the<br />
effect on survival.<br />
These studies will have important implications on the selection<br />
of the most appropriate drugs and combinations in the different<br />
context of the disease. In this regard, a strict collaboration with<br />
dermatologists is underway in order to better understand and<br />
manage the skin toxicities of these drugs.<br />
For mucosal and c-kit positive melanoma we are participating<br />
in the study of the evaluation of Nilotinib, and testing the<br />
effectiveness of Ipilimumab in the European access programme.<br />
Our Unit is a national reference center for choroid melanoma.<br />
For this very rare disease, we have developed a combined, systemic<br />
and local intrahepatic treatment method (TACE) with significant<br />
results, and we are currently testing the best integration of<br />
Ipilimumab in the treatment of the metastatic phase.<br />
We are also collaborating with colleagues at the Melanoma and<br />
Soft Tissue Tumor Unit regarding the combined use of systemic<br />
and electro-chemotherapy in order to define both prognostic and<br />
predictive factors related to the best local and systemic control<br />
and to an immunological response. In addition, a prospective<br />
assessment of the impact on the Quality of Life is underway.<br />
Clearly, training and educational activities are an important<br />
part of the Unit’s mission and specific programs on melanoma<br />
are provided also in collaboration with the Italian Melanoma<br />
Intergroup.<br />
Finally, the Unit was involved in the layout of regional<br />
guidelines for the diagnosis and treatment of melanoma and this<br />
task was a preparatory step in the implementation of the regional<br />
melanoma network now in progress. Currently we are involved<br />
with CNR in the set-up of the national melanoma guidelines.
Main Pubblications<br />
Evaluation and Introduction<br />
of New Drugs in Cancer Therapy<br />
Chief<br />
Antonio Jirillo, MD<br />
Mechanisms of acquired resistance to epidermal growth<br />
factor receptor tyrosine kinase inhibitors and new<br />
therapeutic perspectives in non small cell lung cancer.<br />
Platinum-based doublet chemotherapy in pre-treated<br />
malignant pleural mesothelioma (MPM) patients: a monoinstitutional<br />
experience.<br />
Sorafenib in hepatocellular carcinoma - a post marketing<br />
evaluation.<br />
Antonio Jirillo was born on 24 th September 1952. He graduated in Medicine at the University<br />
of Bari in 1977 cum Laude. He specialised in Oncology and Radiotherapy cum Laude. Then he<br />
attended the National Cancer Institute of Milan as a visiting fellow from 1977 to 1980. He worked<br />
as a Medical Doctor at the Division of Radiotherapy and Oncology at the Hospital of Legnago<br />
(Verona, Italy) from 1981 to 1987. He was Deputy Director at the same Division from 1988 to<br />
1996. Then he was the Director at the Division of Oncology of Legnago Hospital (Verona, Italy)<br />
from 1996 to 2000. From 2001 to June 2007 he was Deputy Director of Clinical Oncology of<br />
Azienda Ospedaliera di Padova and later Istituto Oncologico Veneto (<strong>IOV</strong>) (from 2005). During the<br />
period 2007-<strong>2010</strong> he was Director of the 2 nd Division of Clinical Oncology <strong>IOV</strong>. Since November<br />
<strong>2010</strong> he is Director of Unit of Evalutation and Introduction of New Cancer Therapies at <strong>IOV</strong>. He is<br />
author/coauthor of over 150 publications.<br />
Bonanno L, Jirillo A, Favaretto A. Curr Drug Targets. <strong>2011</strong>; 12:922-33<br />
Pasello G, Nicotra S, Marulli G, Rea F,<br />
Bonanno L, Carli P, Magro C, Jirillo A,<br />
Favaretto A.<br />
Trojniak MP, Palozzo AC, Mazurek M,<br />
Jirillo A.<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
54<br />
Lung Cancer. <strong>2011</strong>; 73:351-5<br />
Immunopharmacol Immunotoxicol. <strong>2011</strong>;<br />
in press.<br />
Evaluations of new drugs after they reach the market. Jirillo A, Trojniak MP. Health Aff (Millwood). <strong>2011</strong>; 30:2028
Clinical and Research Staff<br />
Antonio Jirillo Magdalena Mazurek Silvia Imbevaro<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
55
This Unit was founded in November <strong>2010</strong> and it is a part of the<br />
Department of Clinical Oncology.<br />
Objectives:<br />
critical evaluation of new cancer drugs when used in routine<br />
clinical practice;<br />
study of pharmacoeconomics;<br />
application of health technology assessment in Clinical<br />
Oncology;<br />
development of Phase I studies.<br />
Major Ongoing<br />
Research Projects<br />
Phase I study with agents dithiocarbamate gold (III) in cancer<br />
patients;<br />
Analysis of real clinical practice;<br />
Green Oncology: cultivating sustainability in Medical<br />
Oncology;<br />
Analysis of the first relapse in patients with operable breast<br />
cancer. A monoinstitutional experience.<br />
THE DEPARTMENTS - DEPARTMENT OF CLINICAL ONCOLOGY<br />
56
Department of Surgery<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
57
Main Pubblications<br />
Surgical Oncology<br />
Chief<br />
Carlo Castoro, MD<br />
Nodal Metastasis From Locally Advanced Esophageal Cancer:<br />
How Neoadjuvant Therapy Modifies Their Frequency and<br />
Distribution.<br />
Mucosal immune environment in colonic carcinogenesis:<br />
CD80 up-regulation in colonic dysplasia in ulcerative colitis.<br />
A systematic review of diagnostic procedures to detect midgut<br />
neuroendocrine tumors.<br />
Interval between neoadjuvant chemoradiotherapy and surgery<br />
for squamous cell carcinoma of the thoracic esophagus: does<br />
delayed surgery have an impact on outcome?<br />
Prophylactic thoracic duct mass ligation prevents chylothorax<br />
after transthoracic esophagectomy for cancer.<br />
Carlo Castoro obtained his degree in Medicine in 1983, his specialization in General Surgery in 1988<br />
and in Thoracic Surgery in 1993 at the University of Padua. He is an Assistant Professor of Surgery<br />
at the Postgraduate school of General Surgery at the University of Padua School of Medicine. His<br />
research interests and activities include thoracic and abdominal surgery, esophageal diseases, with<br />
special attention to multimodal treatments, Day Surgery and reorganization of surgical services,<br />
and Medical Education (new technologies and distance learning). He has published 45 indexed<br />
full papers; a book on Lichtenstein Hernia Repair, 1998; the Policy Brief “Day Surgery: Making it<br />
Happen” published in 2007 by the European Observatory on Health Systems and Policies, WHO<br />
Office for Europe; he is author of many videos and multimedia resources on surgical techniques. He<br />
is a member of the Executive Committee of the International Association for Ambulatory Surgery<br />
(IAAS), head of the sub-committee on Education and Training, and President elect of the IAAS for<br />
<strong>2011</strong>-2013.<br />
Castoro C, Scarpa M, Cagol M, Ruol A, Cavallin<br />
F, Alfieri R, Zanchettin G, Rugge M, Ancona E.<br />
Scarpa M, Bortolami M, Cecchetto A, Faggian D,<br />
Kotsafti A, Ruffolo C, Navaglia F, Pozza A, D’Incà<br />
R, Plebani M, Sturniolo GC, Angriman I.<br />
Scarpa M, Prando D, Pozza A, Esposti ED, Castoro<br />
C, Angriman I.<br />
Ruol A, Rizzetto C, Castoro C, Cagol M, Alfieri R,<br />
Zanchettin G, Cavallin F, Michieletto S, Da Dalt<br />
G, Sileni VC, Corti L, Mantoan S, Zaninotto G,<br />
Ancona E.<br />
Cagol M, Ruol A, Castoro C, Alfieri R, Michieletto<br />
S, Ancona E.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
58<br />
Ann Surg Oncol. <strong>2011</strong>; 18:3743-<br />
54<br />
Eur J Cancer. <strong>2011</strong>; 47:611-9<br />
J Surg Oncol. <strong>2010</strong>; 102:877-88<br />
Ann Surg. <strong>2010</strong>; 252:788-96<br />
World J Surg. 2009; 33:1684-6
Clinical and Research Staff<br />
Carlo Castoro<br />
Rita Alfieri<br />
Matteo Cagol<br />
Marco Scarpa<br />
Luigi Dall’Olmo<br />
Alessandra Fasolo<br />
Nursing staff<br />
Fabio Bassan<br />
Chiara Beghin<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
59<br />
Administrative Staff<br />
Christina Drace<br />
Enrica Malpeli<br />
Eleonora Pinto
Mission<br />
The Surgical Oncology Unit’s mission is to provide high<br />
standards of treatment, research and education on Gastro-<br />
Intestinal malignancies. It strives to deliver high quality care and<br />
appropriate follow-up for each patient. This is achieved through a<br />
multidisciplinary approach involving oncologists, radiotherapists,<br />
surgeons, pathologists and basic science researchers.<br />
Clinical Activity<br />
The unit performs surgery on abdominal and digestive tract<br />
tumors, especially esophagus, esophago-gastric junction, stomach<br />
and colon. Besides the inpatient ward, the Oncology Day<br />
Surgery Unit meets the clinical needs related to the placement of<br />
vascular access systems for chemotherapy, in collaboration with<br />
anesthesiologists, and interventional radiology procedures.<br />
In <strong>2010</strong> General surgery for cancer was performed on 339<br />
patients and procedures including:<br />
Major upper and lower Gastro-Intestinal surgery<br />
Laparoscopy, lymphnode radical dissection and biopsies<br />
Vascular access systems placement and other procedures<br />
The area of clinical excellence is the treatment of Upper G-I<br />
malignancies and the Surgical Oncology Unit is a high volume<br />
national referral center for esophageal cancer in collaboration with<br />
the Department of Surgery of the Padova University Hospital<br />
(Director Prof. E. Ancona).<br />
Admissions to the Surgical Oncology Unit are reported in<br />
the table, while the figure shows the relative caseload for major<br />
surgeries performed.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
60<br />
Clinical research involves the implementation of new<br />
protocols and new surgical techniques aimed at improving the<br />
surgical treatment of cancer. Research activities focus on clinical<br />
management, quality of life and cancerogenesis of digestive tract<br />
diseases.<br />
Clinical activity <strong>2010</strong><br />
Inpatient Admissions 207<br />
Day Surgery Admissions 320<br />
Admissions for tumors of the esophagus and cardias<br />
Admissions 147<br />
(61% from outside the Veneto Region)<br />
New Patients 112<br />
Admission by pathology<br />
Esophagus<br />
Stomach<br />
Colon - rectum<br />
Other
Major Research Collaborations<br />
Inside the <strong>IOV</strong><br />
Diagnostic and Operative Endoscopy Unit<br />
Clinical Oncology 1<br />
Clinical Oncology 2<br />
Radiotherapy and Nuclear Medicine<br />
Immunology and Molecular Oncology<br />
National Collaborations<br />
Dept. of Surgical and Gastroenterological Sciences, Università<br />
di Padova<br />
Major Ongoing Research Projects<br />
An integral part of the activity of the Unit of Surgical<br />
Oncology is research. The Unit collaborates with research groups<br />
from other departments of the <strong>IOV</strong> and University of Padua.<br />
Research activity focuses on clinical management, quality of life<br />
and cancerogenesis of digestive tract diseases. During the <strong>2010</strong>-<br />
<strong>2011</strong> period the research on clinical management of esophageal<br />
and esophago-gastric junction cancer has mainly been focused<br />
on quality of life after esophageal resection for cancer, and<br />
nodal metastasis distribution and prognostic role before and<br />
after neoadjuvant therapy for esophageal cancer. These studies<br />
were conducted in collaboration with the Dept. of Surgical and<br />
Gastroenterological Sciences, University of Padova (Prof. Ancona)<br />
and with the Endoscopy Unit, Veneto Institute of Oncology (Dr.<br />
Battaglia).<br />
Nodal metastasis from locally advanced<br />
esophageal cancer: how neoadjuvant therapy<br />
modifies their frequency and distribution<br />
Principal Investigator: Carlo Castoro<br />
Neoadjuvant chemoradiotherapy (CT-RT) before esophagectomy<br />
seems to affect the number of nodal metastases and to alter the<br />
distribution of those that remain. The aim of this study is to<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
61<br />
Dept. of Diagnostic Sciences and Special Therapy, Università di<br />
Padova (Pathology Unit)<br />
International Collaborations<br />
University of Sheffield – Sheffield (UK)<br />
Katholieke Universiteit te Leuven – Louvain, Belgium<br />
define how neoadjuvant CT-RT changes nodal metastasis patterns<br />
in locally advanced esophageal cancer. A total of 402 consecutive<br />
patients with cancer of the esophagus or esophagogastric junction<br />
(181 adenocarcinoma [AC] and 221 squamous cell carcinoma<br />
[SCC]) (evaluated at clinical stage T1N1, T2N1, T3N0, or<br />
T3N1 and pathological stage M0) presenting in our Department<br />
between 1992 and 2007 and who underwent complete resection<br />
(R0) were included in this retrospective study on a prospectively<br />
collected database. All dissected lymphnodes were retrieved and<br />
microscopically analyzed. Nodal metastasis patterns in patients<br />
who underwent chemotherapy (CT) or chemoradiotherapy (CT-<br />
RT) neoadjuvant therapy were compared with those in patients<br />
who underwent surgery alone. Almost 30% of the AC patients<br />
and approximately 40% of the SCC patients showed effective<br />
tumor downstaging after neoadjuvant therapy. There were fewer<br />
paracardial node metastases (P = .002) in the AC patients who<br />
underwent CT-RT neoadjuvant therapy. There were, likewise,<br />
significantly fewer paraesophageal, paracardial, and subcarinal<br />
node metastases in the SCC patients in whom the perigastric<br />
nodes became the second most frequent site of metastasis. In<br />
conclusion, not only was frequency of lymphnode metastases<br />
decreased after neoadjuvant therapy, but nodal localization and<br />
pattern were also significantly modified.
A systematic review on health-related quality<br />
of life after esophagectomy for esophageal<br />
cancer<br />
Principal Investigator: Marco Scarpa<br />
Recent studies concluded that esophageal resections are<br />
associated with significant deterioration of the health related<br />
quality of life (HRQL), which persists during the followup<br />
period. When esophageal resection is proposed, patients<br />
want to know, beside their prognosis, what their quality of life<br />
will be like. The aims of this study are to assess the long-term<br />
HRQL of these patients compared to the established norms and<br />
to evaluate HRQL evolution at the different step of follow-up<br />
after esophageal resection. A systematic review was performed by<br />
searching medical databases (Medline, EMBASE and Cochrane<br />
Library) for potentially relevant publications between January<br />
1975 and June 2009. Studies were included if dealing with HRQL<br />
after esophageal resection for esophageal cancer. Two researchers<br />
independently performed study selection, quality assessment, data<br />
extraction and analysis. Eleven observational, case series, studies<br />
were included with a total of 887 patients. Six studies analysed<br />
Other Programs and Future Perspectives<br />
Our research program in the future will be mainly focused on:<br />
perceived quality of care and quality of life in patients after<br />
radical and palliative treatment for gastrointestinal cancers;<br />
gut microbiota and innate immune environment in non<br />
inflammatory gastro-intestinal carcinogenesis;<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
62<br />
early generic HRQL of 651 patients with QLC-30 questionnaire<br />
and four studies analysed disease-specific HRQL of 521 patients<br />
with OES-18 questionnaire at different step of the early followup<br />
(3, 6, 9, 12 and 24 months, respectively). A trend to the<br />
improvement of the generic HRQL can be observed in the first<br />
24 months of follow-up after esophageal resection. This trend is<br />
confirmed by the progressive decrease of the symptoms burden in<br />
the first 12 months of the follow-up. Five studies analysed long<br />
term generic HRQL of 236 patients with SF-36 questionnaire.<br />
In these patients (median follow-up range: 24-63 months) the<br />
pooled physical function, role physical, social function, vitality,<br />
general health perception scores resulted lower than US and<br />
Canadian norms. On the contrary, the pooled bodily pain, mental<br />
health and emotional functional scores resulted comparable to US<br />
and Canadian norms. Although based on low-level evidence from<br />
uncontrolled studies, this systematic review showed a trend to the<br />
improvement of the generic and disease-specific HRQL in the first<br />
12 months of follow-up after esophageal resection. Nevertheless,<br />
in long term survivors the pooled physical function, role physical,<br />
social function, vitality, general health perception scores resulted<br />
lower than norms.<br />
molecular mechanisms at the basis of the association between<br />
obesity and esophageal carcinogenesis;<br />
immunosurveillance in the gastrointestinal carcinogenesis.
Main Pubblications<br />
Chief<br />
Breast Surgery<br />
Fernando Bozza, MD<br />
Phase II study of neoadjuvant gemcitabine, pegylated<br />
liposomal doxorubicin, and docetaxel in locally advanced<br />
breast cancer.<br />
Correlation between magnetic resonance imaging and<br />
histopathological tumor response after neoadjuvant<br />
chemotherapy in breast cancer.<br />
A Randomized clinical trial on sentinel lymph node biopsy<br />
versus axillary lymph node dissection in breast cancer:<br />
results of the Sentinella/GIVOM trial.<br />
Analysis of technical and clinical variables affecting sentinel<br />
node localization in patients with breast cancer after a single<br />
intradermal injection of 99mTc nanocolloidal albumin.<br />
Could the serial determination of Ca15.3 serum improve<br />
the diagnostic accuracy of PET/CT? Results from small<br />
population with previous breast cancer.<br />
Born in 1951, he graduated in Medicine in 1977 at the University of Padova. He then obtained<br />
a specialization in General Surgery and subsequently in Thoracic and Cardiovascular Surgery at<br />
the same University. Surgeon at the Padova General Hospital until 2009, when he moved to the<br />
<strong>IOV</strong> where acts as Head of the Breast Surgery Unit. He attended several national and international<br />
training courses at very qualified Institutions, such as Institute Gustave Roussy, Paris; Istituto Europeo<br />
di Oncologia, Milan; Istituto Nazionale Tumori, Milan; Memorial Sloan Kettering, New York;<br />
IRCARD, Strasbourg; Istituto Regina Elena, Rome. Member of the major surgical and oncologic<br />
Societies, he published several papers on general and breast surgery in national and international<br />
journals.<br />
Artioli G, Mocellin S, Borgato L, Cappetta<br />
A, Bozza F, Zavagno G, Zovato S, Marchet<br />
A, Pastorelli D.<br />
Nicoletto MO, Nitti D, Pescarini L, Corbetti<br />
F, Mencarelli R, Cappetta A, Galligioni A,<br />
Pogliani C, Marchet A, Bozza F, Ghiotto<br />
C, Griggio L, Zavagno G, Donach ME, Di<br />
Maggio C.<br />
Zavagno G, De Salvo GL, Scalco G, Bozza F,<br />
Barutta L, Del Bianco P, Renier M, Racano<br />
C, Carraro P, Nitti D, GIVOM Trialists.<br />
Rubello D, Zavagno G, Bozza F, Lise M, De<br />
Salvo GL, Saladini G, Mariani G, Casara D.<br />
Evangelista L, Baretta Z, Vinante L, Cervino<br />
AR, Gregianin M, Ghiotto C, Bozza F,<br />
Saladini G.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
64<br />
J Plast Reconstr Aesthet Surg. <strong>2011</strong>;<br />
64:1161-6<br />
Tumori. 2008; 94:481-8<br />
Ann Surg. 2008; 247:207-13<br />
Nucl Med Commun. 2004; 25:1119-24<br />
Ann Nucl Med. <strong>2011</strong>; 25:469-77
Clinical and Research Staff<br />
Fernando Bozza<br />
Raffaello Grigoletto<br />
Silvia Michieletto<br />
Tania Saibene<br />
Stefano Valente<br />
Nursing Staff<br />
Fabio Bassan<br />
Chiara Beghin<br />
Lisa Rigato<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
65
Mission<br />
The mission of the Breast Surgery Unit is to offer to patients<br />
with breast cancer a rapid and efficient diagnostic and therapeutic<br />
pathway, according to the most modern guidelines of management<br />
of mammary tumors. The Unit tackles the neoplastic disease in a<br />
multidisciplinary manner, and follows the patient from diagnosis to<br />
Clinical Activity<br />
Clinical activity (year <strong>2010</strong>) includes (see figure):<br />
187 mastectomies (21 bilateral with reconstruction, 143<br />
monolateral with reconstruction, 23 monolateral without<br />
reconstruction);<br />
290 conservative surgery interventions (233 with sentinel node<br />
technique, 82 with controlateral breast remodelling);<br />
246 mammary biopsies;<br />
13 prothesis application;<br />
151 day-hospital mammary surgery.<br />
Major Research Collaborations<br />
Inside the <strong>IOV</strong><br />
Clinical Oncology 1<br />
Clinical Oncology 2<br />
Breast Imaging Unit<br />
Familial Cancer Clinics<br />
Radiotherapy<br />
Nuclear Medicine<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
66<br />
the choice of the therapeutic program and reconstructive surgery/<br />
rehabilitation in strict collaboration with medical oncologists,<br />
radiotherapists, psycho-oncologists. One major interest is focused<br />
on new integrated therapeutic approaches, such as intra-operative<br />
radiation therapy.<br />
Number of surgical interventions<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
Mastectomy<br />
Conservative surgery<br />
National Collaborations<br />
IRCCS CRO, Aviano<br />
Breast Unit, Ospedale Morgagni (Forlì)<br />
Biopsies<br />
Day-hospital surgery<br />
International Collaborations<br />
Division of Surgery and Interventional Science, University<br />
College, London
Major Ongoing Research Projects<br />
Intra-operative Radiotherapy - The TARGIT<br />
Protocol<br />
Principal investigator: Fernando Bozza<br />
The combination of radiotherapy following surgery is now<br />
a gold standard in the management of breast cancer. While<br />
radiotherapy usually follows surgery and adjuvant chemotherapy,<br />
the recent introduction of intra-operative radiotherapy may<br />
present several advantages for the management of at least a part of<br />
breast malignancies. On the one hand, in fact, the simultaneous<br />
application of radiotherapy allows women to avoid the 5-7<br />
weeks of fractionated radiotherapy application; on the other, the<br />
local administration of radiation may allow a better focusing on<br />
affected tissues, while sparing surrounding non-target tissues and<br />
consenting a limitation of the cutaneous damage with eventual<br />
improvement of the esthetic results. The TARGIT protocol<br />
is an international multicenter study comparing the standard<br />
radiotherapy approach to intra-operative radiotherapy. The study<br />
entails the enrollment of patients >45 yr-old bearing non lobular<br />
infiltrating adenocarcinoma of the breast of
Main Pubblications<br />
Melanoma and Soft Tissue Tumors<br />
Chief<br />
Carlo Riccardo Rossi, MD<br />
Prognostic factors and oncologic outcome in 146 patients with<br />
colorectal peritoneal carcinomatosis treated with cytoreductive<br />
surgery combined with hyperthermic intraperitoneal<br />
chemotherapy: Italian multicenter study S.I.T.I.L.O.<br />
Long-term results of melphalan-based isolated limb perfusion<br />
with or without low-dose TNF for in-transit melanoma<br />
metastases.<br />
Targeted Therapy Database (TTD): a model to match patient’s<br />
molecular profile with current knowledge on cancer biology.<br />
A European project on incidence, treatment, and outcome of<br />
sarcoma.<br />
Interferon alpha adjuvant therapy in patients with high-risk<br />
melanoma: a systematic review and meta-analysis.<br />
Born in Rosolina (RO), Italy, on March 3 rd , 1950. He graduated in Medicine at the University of<br />
Padova in 1975, then specialized in General Surgery and Oncology. Full Professor of Surgery at<br />
the Department of Oncology and Surgical Sciences of the University of Padova, he has headed the<br />
Sarcoma and Melanoma Unit at <strong>IOV</strong> (Veneto Region Oncology Research Institute) since 2004.<br />
Member of several Italian and International surgical and oncological scientific societies. President of<br />
the Italian Melanoma Intergroup. He has published 131 scientific papers in international journals.<br />
Member of the Editorial Board of Melanoma Research and reviewer for many scientific journals.<br />
His research activity has been mainly focused on melanoma, sarcoma and loco-regional treatment<br />
of tumors. He has beeen financially supported by the University of Padova, the Veneto Region, the<br />
National Research Council and the European Commission.<br />
Cavaliere F, De Simone M, Virzì S, Deraco M, Rossi CR,<br />
Garofalo A, Di Filippo F, Giannarelli D, Vaira M, Valle M,<br />
Pilati P, Perri P, La Pinta M, Monsellato I, Guadagni F.<br />
Rossi CR, Pasquali S, Mocellin S, Vecchiato A, Campana<br />
LG, Pilati P, Zanon A, Nitti D.<br />
Mocellin S, Shrager J, Scolyer R, Pasquali S, Verdi D,<br />
Marincola FM, Briarava M, Gobbel R, Rossi C, Nitti D.<br />
Mastrangelo G, Fadda E, Cegolon L, Montesco MC, Ray-<br />
Coquard I, Buja A, Fedeli U, Frasson A, Spolaore P, Rossi<br />
CR.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
68<br />
Eur J Surg Oncol.<br />
<strong>2011</strong>; 37:148-54<br />
Ann Surg Oncol.<br />
<strong>2010</strong>; 17:3000-7<br />
PLoS One. <strong>2010</strong>;<br />
5:e11965<br />
BMC Public Health.<br />
<strong>2010</strong>; 10:188<br />
Mocellin S, Pasquali S, Rossi CR, Nitti D. J Natl Cancer Inst.<br />
<strong>2010</strong>; 102:493-501
Clinical and Research Staff Nursing Staff<br />
Carlo Riccardo Rossi<br />
Antonio Sommariva<br />
Antonella Vecchiato<br />
Luca Campana<br />
Sandro Pasquali<br />
Marco Rastrelli<br />
Francesco Russano<br />
Dermatology<br />
Mauro Alaibac<br />
Maria Paola Amici<br />
Cristina Bonacin<br />
Matteo Bordignon<br />
Paolo Del Fiore<br />
Elisabetta Oro<br />
Barbara Pigozzi<br />
Elena Tonin<br />
Plastic Surgery<br />
Leonardo Sartore<br />
Data Managers<br />
Cristina Bonacin<br />
Paolo Del Fiore<br />
Cinzia Bellesso<br />
Elisa Bonaldi<br />
Debora Borella<br />
Sabrina Carraro<br />
Concetta Collu<br />
Patrizia Gesuato<br />
Chiara Lando<br />
Michela Pinton<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
69<br />
Administrative<br />
Staff<br />
Marta Rotella<br />
Valeria Siscaro<br />
Elisa Tognana
Mission<br />
The Melanoma and Soft Tissue Tumors Unit main purpose is<br />
to be a leader in treatment, research and education on Melanoma,<br />
Sarcoma and Peritoneal Carcinomatosis. The Unit integrates<br />
different expertise in Surgery, Dermatology, Oncology, Pathology,<br />
Clinical Activity<br />
The out-patient clinical activity includes: first and followup<br />
visits for Melanoma, Sarcoma and Carcinomatosis patients;<br />
cutaneous biopsies for atypical nevi; and wide excisions for less<br />
advanced cutaneous malignancies. The Unit is also strongly<br />
involved in diagnosis of suspicious pigmented lesions and<br />
dermatologic follow-up of patients at risk.<br />
The caseload is constantly increasing and a report of our<br />
2009-<strong>2010</strong> ambulatory activities is shown in table 1.<br />
Table 1 2009 <strong>2010</strong><br />
Surgery<br />
Dermatology<br />
First visit 684 521<br />
Follow-up visit 1992 2315<br />
Biopsies/Wide excision 2569 3496<br />
First visit 2816 2679<br />
Follow-up visit 3350 4997<br />
Cutaneous Mapping 566 601<br />
Recently, a project for a Network in the Padova district for<br />
management of cutaneous pigmented lesions and melanoma<br />
(RETEMELA Project) has been promoted by our Unit.<br />
The main objective of this project is to improve early<br />
diagnosis (educating family physicians and favoring<br />
access to a dermatologist) and to define a more rational<br />
diagnostic and therapeutic course for these patients.<br />
RETEMELA should be effective in shortening the waiting<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
70<br />
Radiology and Molecular Biology in multidisciplinary groups<br />
specifically committed to patient care and clinical translational<br />
research.<br />
list and creating a dedicated database to provide an important<br />
amount of data for epidemiological studies.<br />
Before surgery, the clinical situation of almost all patients<br />
is discussed in weekly multidisciplinary meetings, in which the<br />
optimal diagnostic work-up and the most appropriate integrated<br />
treatments are planned. The in-patient surgical activity is<br />
performed weekly in three operating theaters, two for ordinary<br />
hospitalization and one for day or week surgery (figure 1).<br />
Figure 1.<br />
183 176<br />
Ordinary surgery<br />
Day surgery<br />
Surgery is mainly directed to melanoma and sarcoma patients<br />
and during <strong>2010</strong> more than 400 melanoma and sarcoma patients<br />
have been treated (table 2).<br />
Table 2 2009 <strong>2010</strong><br />
Melanoma 329 342<br />
Sarcoma 47 68
Clinical Areas of Excellence<br />
The Group has developed a specific competence on<br />
management of metastatic tumors confined in a unique organ<br />
and therefore amenable to the so-called “loco-regional therapy”.<br />
Under this definition we include different approaches: techniques<br />
developed to increase drug concentration in a specific area of the<br />
body (regional chemotherapy) or techniques that determine the<br />
immediate destruction of tumor nodules using physical or chemical<br />
approaches. Sometimes the loco-regional approach is proposed for<br />
improving radicality and functional outcome of surgery.<br />
The procedures set-up by the group in this field are: Isolated<br />
Limb Perfusion (ILP), Cytoreductive Surgery (CRS) associated<br />
with Hyperthermic Intra-Peritoneal Chemotherapy (HIPEC) and<br />
Electrochemotherapy (ECT).<br />
Isolated limb perfusion (ILP) consists of the injection under<br />
hyperthermic conditions of drugs (Melphalan and Tumor<br />
Necrosis Factor-alpha) into a limb-extracorporeal circuit. The<br />
therapeutic efficacy of ILP for the treatment of locally recurrent<br />
melanoma and in-transit metastases is well established as well<br />
for non resectable limb sarcoma. ILP has undoubtedly led to<br />
improvement in local results compared to those achieved with<br />
systemic drug administration, preventing the drawbacks of<br />
systemic toxicity.<br />
Education and Dissemination<br />
After a discussion forum among the most relevant specialists in<br />
the Veneto Region, the Unit coded and published the guidelines<br />
for Melanoma and Sarcoma patient treatment, which are freely<br />
accessible on the Unit’s Web Site. The Guidelines have also been<br />
divulgated in two different scientific sessions. With the same<br />
“educational” view, on the Website it is also possible, through a<br />
Major Research Collaborations<br />
Inside the <strong>IOV</strong><br />
Dermatopathology<br />
Immunology and Molecular Oncology<br />
Family Cancer Clinics<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
71<br />
Cyto-reductive Surgery (CS) combined with Hyperthermic<br />
Intra-Peritoneal Chemotherapy (HIPEC) has been developed as<br />
a loco-regional treatment for peritoneal carcinomatosis confined<br />
within the abdominal cavity. This multimodal approach is<br />
directed to surgically eliminate all the peritoneal visible nodules,<br />
followed by direct instillation of heated chemotherapy (Cisplatin,<br />
Doxorubicin and Mytomicin C at various combinations and<br />
doses) into the abdominal cavity, with the objective to eradicate<br />
the remaining microscopic tumoral foci and free cancer cells.<br />
Nowadays we have adopted this technique as a standard of care<br />
for pseudomixoma peritonei (PMP) and malignant peritoneal<br />
mesothelioma. In colon and ovary abdominal carcinomatosis,<br />
the role of CS+HIPEC is still under study and it is proposed only<br />
in selected cases. In gastric carcinomatosis and sarcomatosis the<br />
procedure must be considered still experimental and we do not<br />
recommend it outside clinical trials.<br />
Electrochemotherapy (ECT) is an effective method of drug delivery<br />
into cancer cells based on the mechanism of electroporation,<br />
consisting of the synergistic association of locally applied brief<br />
electrical voltages (reversible electroporation) and low permeant<br />
chemotherapeutic agents (bleomycin and cisplatin). At present,<br />
the technique is proposed as a palliative treatment for patients<br />
with melanoma and non-melanoma small cutaneous metastases.<br />
dedicated on-line form, to refer patients for clinical evaluation,<br />
multidisciplinary discussion and/or radiological/pathological<br />
second opinions. In the last few months, technical equipment has<br />
been put in place that will allow Oncology and Surgery Units of<br />
the Veneto region to attend our meetings and present and discuss<br />
complex cases in teleconference sessions.<br />
Clinical Oncology 1<br />
Clinical Oncology 2<br />
Radiotherapy and Nuclear Medicine<br />
Radiology
National Collaborations<br />
Italian Sarcoma Group<br />
Italian Melanoma Intergroup<br />
SITILO-Società Italiana di Terapie Integrate Locoregionali<br />
Major Ongoing Research Projects<br />
The research and clinical programs are focused on different<br />
research areas (figure 2):<br />
1. Describing disease distribution by characteristics relating to<br />
time, place, and person (descriptive epidemiology);<br />
2. Investigating and rating treatment options according to their<br />
benefits and side effects (patients selection);<br />
3. Testing further therapeutical procedures (innovative treatments);<br />
4. Defining the methods for monitoring the quality of therapies<br />
(quality control).<br />
Figure 2.<br />
QUALITY<br />
CONTROL<br />
DESCRIPTIVE<br />
EPIDEMIOLOGY<br />
MELANOMA<br />
CARCINOMATOSIS<br />
SARCOMAS<br />
PATIENT<br />
SELECTION<br />
INNOVATIVE<br />
TREATMENTS<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
72<br />
International Collaborations<br />
CONTICANET (CONnnective TIssue CAncer NETwork)<br />
Melanoma Institute of Australia, Sydney, Australia<br />
Rotterdam Cancer Center, The Netherlands<br />
Stanford University, California<br />
EORTC Sarcoma Group<br />
EORTC Melanoma Group<br />
Sentinel Lymphnode working group<br />
University of Leeds, United Kingdom<br />
The ongoing research activity is based on the following four<br />
main projects.<br />
The Molecular Melanoma Map Project<br />
(MMMP)<br />
Background and aim. MMMP is an open access, interactive<br />
web-based multidatabase dedicated to research on melanoma<br />
biology and therapy. MMMP has been built by six databases on<br />
molecular aspects of melanoma (Biomaps, Biocards, Melanoma<br />
Molecular Profile, Drug Development Database and Clinical<br />
Trial Database). The major aim of MMMP is to gather the huge<br />
amount of information scattered in thousand of papers about<br />
melanoma biology. Therefore, the investigators could formulate<br />
new mechanistic/therapeutic hypotheses and thus further<br />
stimulate basic, translational and clinical research. Considering<br />
the interests of our group in the research of new predictive and<br />
prognostic biomarkers for melanoma patients treated with surgical<br />
and medical therapies, we are implementing two new databases in<br />
the MMMP: the Individual Patients Database (IPD) and Targeted<br />
Therapy Database (TTD).<br />
The Individual Patients Database (IPD) is a collection of<br />
patient data about common clinico-pathologic features, such as<br />
those belonging to the 7 th edition of the AJCC TNM staging<br />
system and information regarding the availability of biological<br />
specimens, such as frozen tissues, serum samples, paraffin blocks.<br />
The Italian Melanoma Intergroup (IMI) has been involved in the<br />
IPD and several Italian melanoma centers have joined the project.<br />
Special interest has been raised by the recently implemented<br />
Targeted Therapy Database (TTD), a manually annotated
database where the relevant data on anti-melanoma therapies is<br />
gathered in a formal representation that can be computationally<br />
analysed. With the collaboration of Stanford University, dedicated<br />
algorithms have been set up and published for identification of the<br />
prevalent therapeutic hypotheses based on the available evidence<br />
from clinical and pre-clinical studies present in the literature.<br />
Achievements. Since its inception up to <strong>2010</strong>, the MMMP<br />
has gathered over 3,000 records, over 282,000 contacts and over<br />
1,200 registered users. It is also the #1 hit on Google when searching<br />
“melanoma database”, and it is increasingly quoted in articles.<br />
Future directions. The database needs constant updating<br />
(scientific information) and implementation of patients’ clinical<br />
and logistic data. This represents a remarkable opportunity to<br />
create a national/international network of Centers, collaborating<br />
in particular on quality control studies and search of molecular<br />
markers for patient selection. Moreover, the prediction performance<br />
of Targeted Therapy Database (TTD), in the light of its theoretical<br />
nature, must be validated before it could be implemented in a<br />
routine clinical setting.<br />
ONCOMIRS as new therapeutic targets for<br />
soft tissue sarcomas<br />
Background and aim. Soft tissue sarcomas<br />
(STS) are a group of solid tumors for which<br />
radical surgery remains the only therapeutic<br />
option with curative potential: conventional<br />
treatments (chemotherapy and radiotherapy)<br />
can only slightly change the dismal prognosis<br />
of patients affected by this type of cancer.<br />
Therefore, more effective therapeutic strategies<br />
are urgently needed and a new understanding of<br />
the cancerogenesis process could be of great help.<br />
A recently identified class of non-coding small<br />
RNAs, microRNAs (miRNAs), may provide<br />
new insights into cancer research. MicroRNAs<br />
are short single-stranded RNA molecules that<br />
control the expression of several genes involved<br />
in many cellular processes. They play important<br />
roles in almost all kinds of cancer, where they<br />
modulate key processes during tumorigenesis<br />
such as metastasis, apoptosis, proliferation, or<br />
angiogenesis (in which case they are defined<br />
total RNA<br />
GENE<br />
EXPRESSION<br />
PROFILING (mRNA)<br />
ANALYSIS OF<br />
EXPRESSION DATA<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
73<br />
“oncomiRs”). Some investigators have proposed to target these<br />
miRNA in view of a therapeutic perspective. Very little is known<br />
about the involvement of these short RNA sequences in the<br />
pathogenesis and aggressiveness of soft tissue sarcomas. The aim<br />
of the project is to obtain STS oncomiR expression patterns<br />
and thereafter to identify the deregulated oncomiRs as potential<br />
targets of new therapeutic strategies for the treatment of this class<br />
of tumors.<br />
Results. In these years we have obtained expression signatures<br />
of over 850 different miRNAs from several fibroblastic/<br />
myofibroblastic sarcomas and cell lines. From about 100<br />
differentially expressed miRNAs we focused our attention on the<br />
most deregulated oncomiRs that are involved in various phases<br />
of cancer progression (figure 3). We have also validated all the<br />
microarray data through the use of a more sensitive method than<br />
microarrays: the qRT-PCR with TaqMan® method.<br />
Future directions. At present we are studying the behavior of<br />
cell lines derived from STS in terms of proliferation, migration,<br />
apoptosis and invasiveness after overexpression or downregulation<br />
of oncomiRs identified in our previous studies. The therapeutic<br />
value of modulating oncomiR expression levels in STS biology<br />
will be also assessed in vivo in xenograft models of human soft<br />
tissue sarcomas. In particular, STS cell lines will be engineered to<br />
RNA ISOLATION<br />
Figure 3.<br />
Identification of target genes<br />
involved in the specific miRNA<br />
biological functions analyzing the<br />
functional correlation between miRNA<br />
and mRNA expression profiles.<br />
small RNA<br />
miRNA<br />
EXPRESSION<br />
PROFILING<br />
ANALYSIS OF<br />
EXPRESSION DATA<br />
FUNCTIONAL CORRELATION between miRNA<br />
and mRNA expression profiling of predicted targets<br />
IDENTIFICATION OF POTENTIAL<br />
TARGET GENES<br />
IN SILICO ANALYSIS OF<br />
PUTATIVE miRNA-mRNA TARGET<br />
INTERACTION<br />
miRanda PITA
express bioluminescent or fluorescent proteins, and the assessment<br />
of tumor cell growth and response to therapy will be carried out<br />
by an optical imaging approach. This project could also open the<br />
avenue to the development of new miRNA-based diagnostic/<br />
prognostic signatures and target therapies against this class of<br />
tumor, which is highly refractory to conventional anticancer<br />
agents.<br />
CONTICANET - CONnnective TIssue CAncer<br />
NETwork - the epidemiology project<br />
Background and aim. STS and GIST (Gastrointestinal<br />
Stromal Tumors) are rare tumors and their low incidence and<br />
the complex therapeutic approach to these tumors can justify, at<br />
least in part, the lack of an adequate initial treatment which can<br />
significantly worsen the clinical outcome. Moreover, data reporting<br />
from tumor registries is burdened by different and concurrent<br />
biases (i.e. wrong histological diagnosis, missing of visceral sarcoma<br />
registration) which bring to underestimate the actual incidence of<br />
these tumors. On the basis of these considerations, the European<br />
Commission has funded a Network of Excellence (CONnnective<br />
TIssue CAncer NETwork) with the following aims:<br />
to delineate the descriptive epidemiology and molecular<br />
epidemiology of STS & GIST in Europe;<br />
to evaluate quality control of diagnosis and the impact of<br />
molecular analysis on the final diagnosis;<br />
to evaluate conformity of medical practice to Standard Options<br />
Recommendations and its impact on patients prognosis.<br />
The project is structured according to three main tasks:<br />
descriptive epidemiology, molecular epidemiology and medical<br />
practice.<br />
Results. The project is ongoing in three European Regions:<br />
Rhone Alps, Aquitaine and Veneto, and some preliminary results<br />
have been reported. For the first task, the incidence of STS, after<br />
taking into account the distribution by age and sex, was not<br />
significantly different in the three European Regions. No major<br />
difference in incidence by histotype among the 3 Regions was<br />
observed except for Kaposi’s sarcoma, whose rate was higher in<br />
Veneto. Considering the second task (Molecular epidemiology),<br />
the histologic and molecular distribution of sarcomas and the<br />
impact of histologic review and molecular analysis on the final<br />
diagnosis have been defined. The reproducibility of molecular<br />
analysis has been tested, calculating difference between<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
74<br />
laboratories, techniques (RT-PCR versus FISH for traslocations)<br />
and tissue status (paraffin versus frozen). The third study area<br />
was focused on Medical practice. The ‘global’ conformity of<br />
management depends on eight categories; if one of them is not<br />
compliant, the ‘global’ patient management is considered not<br />
compliant. The ‘global’ conformity of this population is in most<br />
cases ‘not compliant’ (56%). Nevertheless, conformity is excellent<br />
for the following aspects: chemotherapy, radiotherapy and followup<br />
in more than 90% of patients; it is still good (80%) for initial<br />
examination, histology and secondary surgery revision. Surgery<br />
reaches conformity in only 46% of cases.<br />
Future directions. The following new projects are going to start:<br />
correlating geographical distribution of sarcomas and<br />
deprivation index in the three European countries;<br />
genotyping of NER and HR genes polymorphisms and<br />
evaluation of their potential use as predictive markers to the<br />
alkylating agent trabectedin in sarcoma subtypes from a<br />
representative population in the three European areas;<br />
cost-effectiveness profile evaluation for treatment of sarcomas<br />
in two European Regions (Veneto and Rhone-Alpes).<br />
Electrochemotherapy (ECT) as a new cancer<br />
treatment<br />
Background and aim. Electrochemotherapy (ECT) is<br />
based on the mechanism of electroporation, an effective way<br />
for drug delivery into cancer cells, on the basis of the synergistic<br />
association of locally applied brief electrical voltages (reversible<br />
electroporation) and low permeant chemotherapeutic agents<br />
(bleomycin and cisplatin). The aims of the project are: 1) to verify<br />
the palliative and possibly curative value of ECT at the present<br />
status of delivering; 2) to improve the methods of administration;<br />
3) to investigate the biological impact of ECT.<br />
Results and conclusions. In a previous paper we verified the<br />
validity of ECT in palliative treatment of small nodules in 52<br />
patients (34 with melanoma). In this setting, we demonstrated<br />
that ECT is highly active both in melanoma and non-melanoma<br />
tumors and that ECT proved to be safe and useful in preserving<br />
patients’ quality of life. Recently, we identified 85 patients with<br />
cutaneous metastases from melanoma who received repetitive<br />
bleomycin-based ECT. After the first ECT, an objective response<br />
was observed in 92% of patients, with a complete response up to<br />
78% after a second ECT. On multivariate analysis, the significant
positive predictive factors for response were the decreasing size<br />
and number of nodules; the number of electrode applications and<br />
ECT cycles were the only predictors for local control. On the other<br />
side, thickness of primary melanoma and anatomical location of<br />
cutaneous metastases were predictive factors for survival.<br />
Future directions. Once established that the procedure<br />
is effective, some limitations of ECT have emerged from its<br />
clinical application: 1) the lack of comparative studies with other<br />
therapies; 2) ECT can not be used for treating deep/large tumors<br />
because of the length of the currently available electrodes. Future<br />
investigations are focused in the clinical setting on testing ECT<br />
itself as a cure and on extending its indications, alone or in the<br />
context of new therapeutic associations. A planned phase II study<br />
will randomise patients with a limited number of limb metastases<br />
Other Programs and Future Perspectives<br />
Future research is mainly focused on developing new clinical<br />
projects, which could permit better patient selection and a more<br />
appropriate treatment.<br />
The following projects are underway or starting:<br />
RULL (Radioguided Ultrasound Lymphnode Localization in<br />
melanoma patients). The technique consists in detecting and<br />
removing non palpable lymphnodes suspicious for melanoma,<br />
after injection of radio-labelled albumin macro-aggregates<br />
under ultrasonography. The feasibility of the technique has been<br />
already confirmed and its diagnostic accuracy will be tested.<br />
ROLL (Radioguided Occult Lesion Localization). By using the<br />
same method of the RULL, the feasibility on suspected non<br />
palpable sarcoma lesions will be tested.<br />
Oncovision. Radioguided lymphnode localisation using an<br />
intra-operative portable gamma camera in conjunct with<br />
sentinel biopsy for melanoma.<br />
p53 status in Isolated Limb Perfusion (ILP). The aim of<br />
this study is to evaluate the role of p53 protein status and its<br />
correlation with histopathologic response after loco-regional<br />
delivering of TNF-alpha and melphalan in soft tissue sarcoma<br />
patients.<br />
PET volume leg/arm evaluation before ILP. The study will<br />
evaluate the efficacy of PET in defining leg/arm volume for drug<br />
dosing in patients candidates to ILP.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
75<br />
from melanoma between loco-regional chemotherapy and ECT.<br />
Moreover, the availability of new technical instrumentations<br />
(longer electrodes and hardware) could expand the indications<br />
for ECT allowing the treatment of bigger and deeper tumors.<br />
Up to now, ECT has been limited to the skin and subcutaneous<br />
tissue because of the current technology wich does not allow the<br />
treatment of deeply seeded or large tumors. A phase I/II study on<br />
ECT with longer needle electrodes for the treatment of deep and/<br />
or large soft tissue tumors (3-6 cm) is ongoing, mainly to assess<br />
the feasibility and safety of this new ECT modality. Beside testing<br />
ECT clinical activity/efficacy, a growing number of biological data<br />
on tumor response are going to be collected, which will permit<br />
to better understand the intrinsic mechanisms of action and the<br />
many factors that may influence it.<br />
Videoscopic groin dissection for melanoma. Feasibility study<br />
on a minimally invasive approach to lymphode groin dissection<br />
in melanoma patients.<br />
PET-CT and contrast-enhanced CT in carcinomatosis.<br />
Observational study on the diagnostic value of FDG-PET<br />
combined with a contrast-enhanced CT scan in selection of<br />
patients for cytoreductive surgery and HIPEC.<br />
Laparoscopy before CRS+HIPEC. The study is going to<br />
evaluate the potential diagnostic benefit of laparoscopic<br />
examination before cytoreductive surgery and HIPEC.<br />
MSLT II trial. Phase III multicenter randomised trial of<br />
sentinel node biopsy and complete lymphnode dissection versus<br />
sentinel node biopsy alone, in cutaneous melanoma patients<br />
with molecular or histopathologic evidence of metastases in the<br />
sentinel node.<br />
Stage IV. Randomised Multicenter Prospective Trial comparing<br />
metastasectomy versus best medical treatment in patients with<br />
resectable metastatic melanoma.<br />
Quality of life in melanoma. Multicenter Prospective Trial<br />
evaluating quality of life in early and advanced melanoma<br />
patients.<br />
Parameters for quality assurance in melanoma surgery.<br />
Retrospective study on the number of lymphnodes as a quality<br />
parameter after radical lymphnode dissection.
Diagnostic and Operative Endoscopy<br />
Main Pubblications<br />
Chief<br />
Giorgio Battaglia, MD<br />
High-frequency miniprobes and 3-dimensional EUS for<br />
preoperative evaluation of the etiology of congenital esophageal<br />
stenosis in children (with video).<br />
Quality of life in patients with esophageal stenting for the<br />
palliation of malignant dysphagia.<br />
Programmed cell death 4 (PDCD4) expression during multistep<br />
Barrett’s carcinogenesis.<br />
Giorgio Battaglia graduated in Medicine in 1974 at the University of Padova, and obtained the<br />
specialization in General Surgery and in Vascular Surgery in 1978 and 1981, respectively.<br />
Assistant Professor at the Padova University since 1980, he has been heading the Digestive Endoscopy<br />
Unit of the 1st Surgical Chair of the Faculty of Medicine of Padova from 1992 to 2007, when he<br />
moved to the <strong>IOV</strong> as Head of the Diagnostic and Operative Endoscopy Unit. He is member of several<br />
scientific Societies and Committees: Member of the Editorial Board of Acta Endoscopica; secretary<br />
of the Italian Society of Digestive Endoscopy from 2004 to 2007; Member of the Veneto Center<br />
for esophageal diseases and of the EBRA Registry for Barrett’s esophagus; Member of European<br />
RFA-Academia; Coordinator of the Italian Registry for radiofrequency in the therapy of Barrett’s<br />
esophagus. Throughout his career, his interest has been mainly focused on all the aspects related<br />
to digestive endoscopy, with special attention to the problems associated with gastro-intestinal<br />
bleeding. More recently, his attention is centered on pre-neoplastic and early neoplastic lesions of<br />
the gastro-intestinal tract, in particular of the upper portion, where innovative research approaches<br />
are allowed by the availability of unique technical devices such as confocal laser endoscopy and<br />
autofluorescence.<br />
Bocus P, Realdon S, Eloubeidi MA, Diamantis<br />
G, Betalli P, Gamba P, Zanon GF, Battaglia G.<br />
Diamantis G, Scarpa M, Bocus P, Realdon S,<br />
Castoro C, Ancona E, Battaglia G.<br />
Fassan M, Pizzi M, Battaglia G, Giacomelli L,<br />
Parente P, Bocus P, Ancona E, Rugge M. J.<br />
Aurora kinase A in Barrett’s carcinogenesis. Rugge M, Fassan M, Zaninotto G, Pizzi M,<br />
Giacomelli L, Battaglia G, Rizzetto C, Parente<br />
P, Ancona E.<br />
Caustic ingestion and esophageal cancer: intra- and peri-tumoral<br />
fibrosis is associated with a better prognosis.<br />
Ruol A, Rampado S, Parenti A, Portale G,<br />
Giacomelli L, Battaglia G, Cagol M, Ancona E.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
76<br />
Gastrointest Endosc. <strong>2011</strong>;<br />
74:204-7<br />
World J Gastroenterol. <strong>2011</strong>;<br />
17:144-50<br />
Clin Pathol. <strong>2010</strong>; 63:692-6<br />
Hum Pathol. <strong>2010</strong>; 41:1380-6<br />
Eur J Cardiothorac Surg. <strong>2010</strong>;<br />
38:659-64
Clinical and Research Staff<br />
Giorgio Battaglia<br />
Paolo Bocus<br />
Stefano Realdon<br />
Elisa Dassie<br />
Giorgio Diamantis<br />
Administrative Staff<br />
Martina Cesarotto<br />
Francesca Giacomini<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
77<br />
Nursing Staff<br />
Manuela Ruffato (Coordinator)<br />
Stella Bortolotto<br />
Loredana Celadin<br />
Cristina Gallo<br />
Andreina Schiavon<br />
Chiara Zampieri<br />
Emanuela Zoncapè
Mission<br />
The mission of the Unit is to provide patients the most advanced<br />
standard of care in gastrointestinal neoplasms, by implementing<br />
the quality of the offered services through careful monitoring<br />
of both medical results and patient satisfaction. Beside the<br />
state-of-the-art endoscopic and surgical procedures, in fact, one<br />
major commitment is to offer to patients a friendly, humanized<br />
surrounding, including a special attention to the communication<br />
Clinical Activity<br />
The Diagnostic and Operative Endoscopy Unit is located in a<br />
totally renovated area of the Institute, and it occupies 2 operating<br />
rooms plus one room with three beds for patient rest and awakening<br />
after the intervention. All these beds are under strict video and<br />
instrumental monitoring. Most procedures are performed in<br />
sedation, thanks to the collaboration of anesthesiologists. About<br />
2,700 endoscopic examinations are performed yearly; about 35%<br />
of these are operative endoscopies (it has to be stressed that the<br />
mean percentage in Italy is 6%). About 500 ecoendoscopies are<br />
performed yearly, 15% of whom are operative ecoendoscopies.<br />
Videoendoscopy. The Unit is equipped with the most upto-date<br />
instrumentation in the field. In particular, the personnel<br />
utilizes last generation Olympus Videoendoscopies equipped<br />
with Narrow Band Imaging (NBI) technology. Besides the highdefinition<br />
view normally allowed by the instrument, the selection<br />
of the NBI function exploits the green and blue light bands, thus<br />
permitting to highlight the mucosal vascularization and eventually<br />
evidence cancerous and pre-cancerous lesions, usually more<br />
vascularized: in addition, by activating a 150X lens, it is possible<br />
to reveal minimal lesions otherwise invisible at the standard vision.<br />
In addition, the Unit is the sole in Italy (and the second in Europe)<br />
equipped with a Fluorescence Videoendoscope; this technology<br />
exploits the autofluorescence generated by normal tissues and<br />
reveals as “black holes” areas of malignant transformation. Finally,<br />
the Unit recently acquired a new revolutionary technology,<br />
that thanks to a 1,000X magnification allows visualizing single<br />
mucosal cells in a sort of “in vivo histologic examination”. This<br />
technology is present in only 3 italian endoscopy Centers, and its<br />
use is limited to selected patients where a strong but otherwise non<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
78<br />
aspects with patients, families, and caregivers. This is obtained<br />
through a constant collaboration in a multidisciplinary team which<br />
includes several specialists, and in particular anesthesiologists and<br />
psycho-oncologists. Special attention is also dedicated to the<br />
educational aspects, in order to translate to peripheral Centers the<br />
critical mass acquired at the Unit.<br />
documented suspect of neoplastic transformation of the mucosa<br />
exists; this instrument allows very selective biopsies, and may also<br />
be useful in early monitoring of the effects of new anti-tumoral<br />
treatments, such as anti-angiogenic drugs.<br />
Ecoendoscopy. As far as ecoendoscopy is concerned, the<br />
Unit is fully equipped with standard ecoendoscopic probes as<br />
well as 3-D miniprobes; these latter allow accurate calculation of<br />
the tumor volume to better monitor the response to therapies.<br />
In addition, our Unit is the only Italian Center equipped with a<br />
“blind” probe which permits the study of stenotizing esophageal<br />
tumors. Finally, we can also utilize an operative probe, which<br />
permits to obtain biopsies from deeply located tissues (such as<br />
pancreas, lymphnodes etcetera), often avoiding the need for<br />
invasive surgical interventions.<br />
Operative endoscopy. The operative endoscopy activity<br />
is mostly focused on the therapy of Barrett’s esophagus, a precancerous<br />
lesion that affects over 500,000 patients in Italy.<br />
The mainstay of the surgical therapy of this condition is the<br />
removal of the metaplasic mucosa, which is obtained through<br />
radiofrequency or by a special hydro-dissector that very<br />
accurately detaches from the deeper layers the affected mucosa.<br />
All these invasive procedures are performed under deep sedation<br />
in collaboration with anesthesiologists; the level of sedation is<br />
monitored by a system (BIS) that records the cerebral waves of<br />
the patient, and automatically regulates the administration of the<br />
sedative according to a precise algorythm. Also, the recovery phase<br />
is strictly monitored by a computerized system.
<strong>2010</strong> Clinical Activity<br />
EGDS Esophageal-gastro-duodenoscopy 1318<br />
COLON Colonoscopy 295<br />
EUS Endoscopic ultrasononography 434<br />
EUS FNA<br />
Endoscopic ultrasononography Fine<br />
Needle Aspiration<br />
31<br />
RFA<br />
Radiofrequency ablation of Barrett’s<br />
esophagus<br />
22<br />
Areas of Excellence<br />
This Center stems from the very long experience and sound<br />
critical mass generated at the 1 st Surgical Clinic of the University<br />
of Padova (Director: Ermanno Ancona), and acts as the reference<br />
Center of this Clinic for all endoscopic approaches. The major<br />
fields of interest are: Early diagnosis and staging of neoplasms<br />
of the gastrointestinal tract; In vivo histologic diagnosis through<br />
confocal laser endomicroscopy; Early diagnosis of minimal<br />
disease by tissue autofluorescence; Endoscopic and ecoendoscopic<br />
therapy of early and advanced neoplastic lesions of the upper<br />
gastrointestinal tract.<br />
Major Collaborations<br />
National Collaborations<br />
Clinica Chirurgica I Università Policlinico (Padova)<br />
Radioterapia (Padova)<br />
Clinica Chirurgica Pediatrica (Padova)<br />
Banca Biologica, Università di Padova<br />
Gastroepatologia, Ospedale Molinette (Torino)<br />
Istituto Clinico Humanitas (Milano)<br />
Istituto Europeo di Oncologia – IEO (Milano)<br />
CRO (Aviano)<br />
Facoltà di design e arti – IUAV (Venezia)<br />
EMR-ESD<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
79<br />
Endoscopic Mucosectomy/Endoscopic<br />
submucosal dissection<br />
STENT Esophageal-gastric-colonic stent 40<br />
Diverticula Endoscopic esophageal diverticula section 19<br />
Dilation Gastrointestinal dilation 93<br />
Confocal<br />
endomicroscopy<br />
Confocal endomicroscopy 25<br />
AFI Auto-fluorescence endoscopy 40<br />
The Unit is involved in several management programs,<br />
including:<br />
coordination of the National Barrett’s esophagus Registry;<br />
coordination of the “Barrett’s Unit”, which collects in Padova<br />
in a multidisciplinary team personnel endowed with different<br />
expertise and specialization; the attractive potential of this Unit<br />
for patients from the rest of Italy is great;<br />
School of Ecoendoscopy on behalf of the Italian Ecoendoscopy<br />
Society (IEC);<br />
second level Masters in Diagnostic and Operative Endoscopy in<br />
Oncology;<br />
School of Esophageal Radiofrequency Ablation on behalf of<br />
International RFA – Academy.<br />
International Collaborations<br />
Division of Gastroenterology and Hepatology, American<br />
University of Beirut, Lebanon<br />
Department of Gastroenterology & Hepatology, Mayo Clinic,<br />
Jacksonville, Florida<br />
Metabolism Institute, Mount Sinai University, New York<br />
Laboratoire IMRCP (Interactions Moléculaires Réactivité<br />
Chimique et Photochimique, CNRS UMR 5623) Toulouse, France<br />
ITAV (Institut des Technologies Avancées pour le Vivant) UMS<br />
CNRS 3039 Université Paul Sabatier and Centre Hospitalier<br />
Universitaire (CHU) of Toulouse, France<br />
Faculty of Chemical and Process Engineering, Warsaw University<br />
of Technology, Poland<br />
31
Major Ongoing Research Projects<br />
frOm CONfOCal ENDOSCOpy TO TarGETED ENDOSCOpy:<br />
prECliNiCal aND CliNiCal STuDiES iN ESOphaGEal<br />
CaNCEr<br />
Principal Investigators: Giorgio Battaglia, Stefano Realdon<br />
This study aims at exploiting fluorochrome-labeled<br />
monoclonal antibodies and peptides to be used for the early<br />
diagnosis and eventually therapy of patients undergoing neoplastic<br />
transformation on a Barrett’s esophagus background. The study<br />
entails a pre-clinical approach, where a mouse/rat model of<br />
Barrett’s esophagus, already validated at our Institute, will be<br />
employed to explore the ability of transformed mucosal tissues<br />
to bind fluorescent monoclonal antibodies and peptides. In the<br />
clinical part of the project, these same fluoresceinated reagents<br />
will be administered to patients in a Phase I study, to assess their<br />
ability to detect early displastic/neoplastic lesions, compared to the<br />
results obtained by biopsy and canonical histologic examination.<br />
rOlE Of ObESiTy aND iNSuliN rESiSTaNCE iN ThE<br />
barrETT’S-DiSplaSia-aDENOCarCiNOma SEquENCE<br />
Principal Investigators: Giorgio Battaglia, Stefano Realdon<br />
The major risk factors recognized for Barrett’s esophagus and<br />
eventual malignant transformation are gastro-esophageal reflux and<br />
obesity. Even though these factors are at least in part independent, the<br />
possible interconnection of these elements is as yet unexplored. The<br />
mechanisms underlying the favoring effect of obesity on Barrett’s<br />
and adenocarcinoma development could be partly “mechanical”,<br />
but a role of obesity-associated metabolic alterations (such as high<br />
insulin and leptin levels) cannot be ruled out. In the pre-clinical<br />
part of this project we will study the effect of insulin resistance<br />
on the esophageal reflux carcinogenesis induced in rodents.<br />
To this end, we will take advantage of the mouse model of<br />
esophageal reflux set up at our Institute; in fact, following<br />
esophago-jejunal anastomosis, these animals undergo metaplastic<br />
transformation of the esophagus and carcinoma development.<br />
In collaboration with Mount Sinai Hospital, New York, we will<br />
compare the outcome of the anastomosis in a transgenic model of<br />
insulin resistance (MKR+/+ mice), in order to better understand<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
80<br />
the role of insulin resistance in esophageal carcinogenesis. From<br />
the clinical point of view, Barrett’s patients will be studied for<br />
a series of antropometric (body mass calculation, abdominal<br />
circumference) and serological parameters (serum levels of<br />
glucose, insulin, leptin, adiponectin, IRS-1, IGFBP-3, Homa-IR<br />
index). These insulin resistance indexes will be correlated to the<br />
extent of Barrett’s lesions, the levels of the eventual dysplasia, and<br />
the presence of frank adenocarcinoma.<br />
rESTaGiNG Of ESOphaGEal TumOrS ThrOuGh<br />
ECOENDOSCOpy (EuS)<br />
Principal Investigators: Giorgio Battaglia, Paolo Bocus<br />
The survival rate of esophageal cancer patients is strictly<br />
related to the clinico-pathologic staging at presentation. Recently,<br />
a neo-adjuvant chemotherapy has been proposed to reduce tumor<br />
mass, thus allowing more conservative interventions, with the<br />
aim of both preventing early recurrence and consenting a better<br />
quality of life to patients. In this setting, an accurate initial staging<br />
and a careful post-chemotherapy restaging are essential. Best<br />
results are obtained by ultrasound endoscopic ecography, which<br />
is able to provide precise information on the depth of tumor<br />
invasion of the surrounding tissues, on tumor dimensions, and<br />
on the possible lymphnode involvement. Restaging after radiochemotherapy<br />
also exploits TC-PET imaging, but reliability of<br />
this approach is uncertain. Aim of this project is to assess EUS<br />
accuracy in restaging of neo-adjuvant-treated esophageal masses,<br />
in comparison to the gold standard provided by macroscopic and<br />
microscopic examination following surgery.<br />
raDiOfrEquENCy TrEaTmENT Of DySplaSTiC barrETT’S<br />
ESOphaGuS<br />
Principal Investigators: Giorgio Battaglia, Giorgio Diamantis<br />
Intestinal metaplasia of the esophageal mucosa is the hallmark<br />
of Barrett’s esophagus. The eventual genomic instability leads over<br />
time to dysplasia, possibly followed by the appearance of localized<br />
foci of neoplastic transformation, which progressively evolve from
in situ neoplasia to diffuse, invasive adenocarcinoma. Aim of<br />
this study is to verify the feasibility of the eradication of the preneoplastic<br />
lesions through radiofrequency in patients with Barrett’s<br />
esophagus and low/high grade dysplasia. The major endpoints of<br />
this project are the evaluation of mucosal epithelium regeneration,<br />
Other Programs and Future Perspectives<br />
We have recently won two important GRANTS (AIRC<br />
investigation grant and Euronanomed 3 th Call) focused on the<br />
study of possible new applications of confocal endoscopy both<br />
in animal models and humans. It is intention of the Unit to<br />
implement an Internet network to foster discussion and sharing of<br />
projects among Clinical Oncology Units within the Veneto area.<br />
In addition, we plan to further expand our educational network<br />
for the diffusion of innovative techniques among colleagues<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
81<br />
and the evaluation of the recurrence of new dysplastic foci under<br />
the newly generated epithelium. The follow-up of these patients<br />
aims at establishing whether endoscopic surveillance could be<br />
reduced in these patients, thus minimizing both the patient<br />
distress and the eventual costs.<br />
strongly concerned with endoscopic approaches. As far as research<br />
is concerned, a special accent will be placed on developing all<br />
the possibilities offered by the most recent techniques, such as<br />
confocal endomicroscopy, in the firm convincement that these<br />
approaches will allow great advances in understanding the<br />
molecular mechanisms of esophageal carcinogenesis, in improving<br />
diagnosis, and in offering innovative therapeutic strategies.
Main Pubblications<br />
Chief<br />
Comparison of two methods for cardiac output<br />
measurement in critically ill patients.<br />
Protein C concentrate to restore physiological values<br />
in adult septic patients.<br />
Use of protein C concentrate in adult patients with<br />
severe sepsis and septic shock.<br />
Hepatocyte transplantation as a treatment for<br />
glycogen storage disease type 1a.<br />
Prognostic systems in intensive care: TRISS, SAPS<br />
II, APACHE III.<br />
Anesthesiology<br />
Muzio Meroni, MD<br />
Born in Induno Olona (Varese) on 22 nd May 1951. He graduated in medicine in 1979 and specialized<br />
in Anesthesiology in 1982 at the University of Padua. Head of Intensive Care Unit of the University<br />
Hospital of Padua since 2001 and Head of the Anesthesia Unit of Istituto Oncologico Veneto<br />
since <strong>2011</strong>.<br />
In 2005 he obtained the National Certification of Coordinators for Organ donation and<br />
transplantation activity.<br />
He has been a member of the Ethical Committee for clinical practice at the University hospital of<br />
Padua since December 2006. He is a Professor at the post-graduate school of Anesthesia, Nephrology,<br />
Dermatology and Venereology.<br />
Author of more than 20 papers published in International Journals and 27 abstracts presented at<br />
International meetings.<br />
Saraceni E, Rossi S, Persona P, Dan M, Rizzi S,<br />
Meroni M, Ori C.<br />
Baratto F, Michielan F, Meroni M, Dal Palù A,<br />
Boscolo A, Ori C.<br />
Baratto F, Michielan F, Gagliardi G, Di Gregorio G,<br />
Pasqualetto A, Meroni M, Giron GP.<br />
Muraca M, Gerunda G, Neri D, Vilei MT, Granato<br />
A, Feltracco P, Meroni M, Giron G, Burlina AB.<br />
Barbieri S, Michieletto E, Feltracco P, Meroni M,<br />
Salvaterra F, Scalone A, Gasparetto M, Pengo G,<br />
Cacciani N, Lodi G, Giron GP.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
82<br />
Br J Anaesth. <strong>2011</strong>;106:690-4<br />
Intensive Care Med. 2008;34:1707-12<br />
Minerva Anestesiol. 2004;70:351-6<br />
Lancet. 2002;359:317-8<br />
Minerva Anestesiol. 2001;67:519-38
Clinical and Research Staff<br />
Muzio Meroni<br />
Sandra Cappellato<br />
Connie Celentano<br />
Angelo Ciccarese<br />
Elisa Granziera<br />
Valentina Manfredi<br />
Donatella Soranzo<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
83<br />
Administrative Staff<br />
Matteo Vescuso
Mission<br />
The mission of the Unit of Anesthesiology is to provide the<br />
anesthesiologic help needed in most phases of the diagnostic/<br />
therapeutic/rehabilitative plan of patients with cancer, according<br />
to the international guidelines in this field. This fundamental role<br />
includes, only to make most obvious examples, deep sedation for<br />
Clinical Activity<br />
The clinical work burden of the Unit is very high, since<br />
the physicians must guarantee a non-interrupted, continuous<br />
availability for all the invasive procedure performed at the Institute.<br />
The paucity of the personnel in front of the commitments required<br />
to the Unit clearly impacts on the possibility of combining clinical<br />
activity with research; nevertheless, all the anesthesiologists<br />
are also engaged in research collaborations with the colleagues<br />
(mostly surgeons and radiotherapists, but also psycho-oncologists)<br />
to contribute to generating new models of intervention in both<br />
technical approaches and patient-physician interrelations.<br />
The major commitments of the Unit include:<br />
Anesthesiologic assistance to the Units of Surgical Oncology,<br />
Breast Surgery, Melanoma and Sarcoma Surgery, Diagnostic<br />
and Operative Endoscopy, Radiotherapy, Nuclear Medicine;<br />
Anesthesiologic assistance to all the <strong>IOV</strong> Units which require<br />
anesthesiologic help for the management of acute and/or<br />
chronic pain, or for emergency interventions in very critical<br />
patients;<br />
Intravascular device implant for chronic chemotherapies.<br />
The volume of activity is depicted in the accompanying Tables.<br />
Anesthesia for surgical interventions <strong>2010</strong><br />
1.1 – 31.12<br />
<strong>2011</strong><br />
1.1 – 30.4<br />
“Busonera” Theatres 1075 431<br />
“Giustinianeo” Theatres 918 286<br />
1993 717<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
85<br />
major invasive diagnostic techniques (such as endoscopy), full<br />
anesthesia in surgical interventions, acute post-surgical pain relief.<br />
Appropriateness, efficiency, steady attention to the patient anxiety<br />
and needs, and friendly approach to the patients and colleagues are<br />
the key words that inspire the work of this dedicated personnel.<br />
Deep Sedation for Digestive<br />
Endoscopy<br />
<strong>2010</strong><br />
1.1 – 31.12<br />
<strong>2011</strong><br />
1.1 – 30.4<br />
Operative 317 114<br />
EUS 438 179<br />
Diagnostic 343 132<br />
1098 425<br />
Deep Sedation for Radiotherapy <strong>2010</strong><br />
1.1 – 31.12<br />
Pediatric Patients<br />
<strong>2011</strong><br />
1.1 – 30.4<br />
Radiotherapy 353 233<br />
Nuclear Medicine 24 16<br />
Ce.Mu.RNI 395 110<br />
Central Vascular Access Positioning <strong>2010</strong><br />
1.1 – 31.12<br />
<strong>2011</strong><br />
1.1 – 30.4<br />
Port-a-Cath 301 124<br />
PiCC 86 36<br />
CVC 22 14<br />
409 174<br />
Anesthesiologic Consults <strong>2010</strong><br />
1.1 – 31.12<br />
<strong>2011</strong><br />
1.1 – 30.4<br />
3537 1281
Major Ongoing Research Project<br />
a raNDOmiSED STuDy ON ThE praCTiCE Of<br />
iNfOrmED CONSENT TO aNESThESia: COulD a SkillED<br />
COmmuNiCaTiON bE ThE kEy? COmpariSON bETwEEN<br />
a STruCTurED aNESThESiOlOGiC iNTErviEw aND aN<br />
iNTEGraTED pSyChO-ONCOlOGy apprOaCh<br />
Principal Investigators: Barbara Donà, Eleonora Capovilla<br />
Background. It has been suggested that emotional factors may<br />
contribute to alter the acquisition of information. The aim of this<br />
randomized study was to verify the hypothesis that an integrated<br />
psycho-oncology approach would reduce anxiety before the<br />
anesthesiologist visit and improve the comprehension of the<br />
information received.<br />
Methods. The study was designed as a single-center,<br />
randomized, controlled, open-label trial. Patients undergoing<br />
surgery for primary breast cancer were randomly assigned<br />
to the structured anesthesiologic interview group (SAI)<br />
or to the integrated psycho-oncological approach (IPA).<br />
In the IPA arm, before the pre-operative anesthesia evaluation,<br />
patients received the integrated psycho-oncology approach, that<br />
is patients underwent an interview with the psycho-oncologist<br />
and afterwards the anesthesiologist was instructed briefly on<br />
how to best communicate with the patient. To evaluate the<br />
efficacy of integrated psycho-oncology approach to reduce the<br />
anxiety of patients, the State-Trait Anxiety Inventory (STAI)<br />
questionnaire was used. In the SAI arm, patients received the<br />
anesthesiology interview only.<br />
Results. 251 patients were randomized: 130 in the IPA<br />
arm and 121 in the SAI arm. For both groups, mean anxiety<br />
scores were statistically lower after the anesthesiology visit<br />
than at baseline, with a reduction of 6.2 points for the IPA<br />
arm and of 4.5 points for the SAI arm [p
late (occurring after the first chemotherapy course administered<br />
through the device). Patients satisfaction or complaint about the<br />
device were also recorded.<br />
Results. 796 TIVAP implanted over a 4-year period were<br />
followed prospectively for overall complications. In 102 patients<br />
placement of TIVAP via the cephalic vein cutdown approach was<br />
initially attempted, 87 patients underwent successful insertion<br />
while 15 required conversion to a percutaneous approach, 11 using<br />
the blind technique, 3 using the ultrasound guided technique.<br />
In 1 patient it was impossible to access any central vessel for<br />
anatomical pitfalls and a peripheral inserted central venous access<br />
(PICC) was inserted under ultrasound guidance. Success rate was<br />
85.3%. The percutaneous blind technique was used initially in 48<br />
patients, and was successful in its first choice vessel in 45 patients.<br />
Three patients required conversion to a surgical approach.<br />
Success rate was 93.7%. The ultrasound guided approach was<br />
used as a primary technique in 646 patients and was successful<br />
in its first choice vessel in 644 patients. In 13 patients a second<br />
attempt changing vessel was necessary, while 2 patients required<br />
conversion to a surgical approach because of fibrotic or collapsed<br />
vein. Success rate was 99.7%. Mean operating time was 51<br />
minutes for cephalic vein cutdown approach, 49 minutes for blind<br />
percutaneous technique and 33 minutes for ultrasound guided<br />
technique. The only severe intraoperative complications requiring<br />
immediate treatment were three of the four pneumothoraces and<br />
one of the two arrythmias. All the other complications did not<br />
require any treatment except a longer monitoring before discharge.<br />
Late complications occurred in 49 of 796 pts (6.1%), requiring<br />
removal 42 (5.2%).<br />
Conclusions. The ultrasound guided technique using the low<br />
lateral approach with cannulation of the brachiocephalic vein has<br />
a lower rate of early and late complications and a higher success<br />
rate compared with the other implantation techniques.<br />
Future perspective. Statistical analysis to identify<br />
predictors of early and late complications is still ongoing. The<br />
identification of these factors may influence patient selection or<br />
timing of implantation, or suggest further clinical strategies of<br />
management.<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
87<br />
aNESThESiOlOGiCal maNaGEmENT fOr<br />
ElECTrOChEmOThErapy TrEaTmENTS DElivErED<br />
OuTSiDE OpEraTiNG rOOm: a prOpOSal fOr<br />
implEmENTaTiON Of STaNDarD OpEraNTiNG<br />
prOCEDurES<br />
Principal Investigator: Elisa Granziera<br />
Background. Electrochemotherapy (ECT) is a recent<br />
approach for treatment of superficial metastases, based on the<br />
synergistic association of locally applied brief electrical currents<br />
(reversible electroporation) and anticancer agents like bleomycin<br />
and cisplatin. The European Standard Operating Procedures of<br />
Electrochemotherapy (ESOPE) project has allowed to standardize<br />
treatments by developing guidelines to select properly drugs,<br />
delivery routes, type of electrodes and type of anesthesia.<br />
According to the Standard Operating Procedures (SOP)<br />
electrochemotherapy may be delivered under local anesthesia<br />
or analgosedation using reversible agents like propofol and<br />
remifentanil. Patients who complete treatment in our department<br />
have an advanced stage of disease, involving large anatomical<br />
regions. ECT is performed in a radiotherapy department requiring<br />
a non operating room anesthesia. Adequate strategies are required<br />
in order to avoid complications and improve the quality of life<br />
as far as possible. Pursuing a cost saving policy, early discharge<br />
is planned. Outpatients undergoing day-care procedures require<br />
a perioperative analgesic technique that is effective, has minimal<br />
side effects, is intrinsically safe, and can be easily managed away<br />
from the hospital or surgery center. Use of Monitored Anesthesia<br />
Care (MAC) techniques involving the use of local anesthesia<br />
via infiltration and sedative-analgesic drugs can facilitate a<br />
fast-track recovery after surgery and can be discharged home<br />
earlier due to the low incidence of post-operative side effects.<br />
However, careful intra-operative vigilance to avoid respiratory<br />
complications is mandatory to ensure patient safety. The<br />
combination of propofol and ketamine has the potential to provide<br />
better sedation with less toxicity than either drug alone or the<br />
propofol-opioid association. We therefore tested the hypothesis<br />
that the combination of local anesthesia, propofol and low-dose<br />
ketamine produces superior analgesia than propofol and opioids,<br />
minimizing the need for supplemental opioids, and that the<br />
combination is associated with improved spontaneous ventilation<br />
and faster recovery.
Methods. The main aim of this retrospective study was to<br />
evaluate the safety and efficacy of low doses of ketamine-based<br />
monitored anesthesia care to perform ECT procedures in an<br />
outpatient setting. The safety outcomes were the incidence<br />
of complications in terms of frequency and severity of<br />
cardiorespiratory events and adverse effects.<br />
Efficacy measures included procedural success (providing<br />
THE DEPARTMENTS - DEPARTMENT OF SURGERY<br />
88<br />
optimal surgical conditions in order to complete the<br />
planned procedure) as well as recovery and discharge times.<br />
Secondary aims of the study were the evaluations of patient’s<br />
satisfaction with the intraoperative and postoperative pain<br />
management.<br />
Results and conclusions. The study is still ongoing and the<br />
data underwent preliminary statistical analysis.
Department of Imaging,<br />
Radiology & Pathology<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
89
Main Pubblications<br />
Chief<br />
Prospective assessment of imaging after preoperative<br />
chemoradiotherapy for rectal cancer.<br />
Synovial sarcoma: CT imaging of a rare primary<br />
malignant tumor of the thorax.<br />
Digital breast tomosynthesis versus digital<br />
mammography: a clinical performance study.<br />
Positive experience of intraperitoneal chemotherapy<br />
followed by intravenous chemotherapy in heavily<br />
pretreated patients with suboptimal residual<br />
ovarian cancer and primary peritoneal cancer.<br />
Are Hodgkin and non-Hodgkin patients at a<br />
greater risk of atherosclerosis?<br />
Fabio Pomerri, MD<br />
Radiology<br />
Born on 22 nd September 1950. Degree in Medicine, University of Padua (1975). Post-Graduate<br />
specializations in: Radiology (1979), Gastroenterology (1983), and Nuclear Medicine (1990), University<br />
of Padua. Fellowship: Institute of Radiology, University of Padua (1975-1986). Assistant Professor of<br />
Radiology at the Department of Medical and Diagnostic Sciences and Special Therapies (Radiology<br />
Section), University of Padua (1987-2005). Associate Professor of Radiology at the Department of<br />
Medical and Diagnostic Sciences and Special Therapies (Radiology Section), University of Padua (since<br />
2005). Head of the <strong>IOV</strong> Oncological Radiology Unit (since <strong>2010</strong>). Member of the Italian Society of<br />
Medical Radiology (SIRM). Member of the European Society of Radiology (ESR). Member of the<br />
Gastrointestinal Radiology Advisory Board of SIRM (1986-1991). Member elected of the Abdominal<br />
and Gastrointestinal Radiology Advisory Board of the SIRM (since 2009). Member of the Editorial<br />
Board of “Pelviperineology” (since 1991). Publications: 230 papers, 56 of them in indexed journals,<br />
and three books. Main fields of radiologic experience and research: abdominal diseases, esophageal,<br />
colonic, rectal and thyroid cancer, pelvic floor diseases, obesity.<br />
Pomerri F, Pucciarelli S, Maretto I, Zandonà M, Del<br />
Bianco P, Amadio L, Rugge M, Nitti D, Muzzio PC.<br />
Polverosi R, Muzzio PC, Panunzio A, Pasquotti G,<br />
Schiavon M, Rea F.<br />
Gennaro G, Toledano A, Di Maggio C, Baldan E, Bezzon<br />
E, La Grassa M, Pescarini L, Polico I, Proietti A, Toffoli<br />
A, Muzzio PC.<br />
Nicoletto MO, Dalla Palma M, Donach ME, Gusella M,<br />
Cappetta A, Shams M, Marchet A, Nardin M, Pintacuda<br />
G, Di Maggio A, Marchesi M, Carli P, Fiduccia P, Artioli<br />
G, Nitti D.<br />
Bilora F, Pietrogrande F, Campagnolo E, Rossato A,<br />
Polato G, Pomerri F, Muzzio PC.<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
90<br />
Surgery. <strong>2011</strong>; 149:56-64<br />
Radiol Med. <strong>2011</strong>; 116:868-75<br />
Eur Radiol. <strong>2010</strong>;20:1545-53<br />
Tumori. <strong>2010</strong>; 96:918-25<br />
Eur J Cancer Care. <strong>2010</strong>; 19:417-9
Clinical and Research Staff<br />
Fabio Pomerri<br />
Elisabetta Bezzon<br />
Chiara Dal Bosco<br />
Davide Fiore<br />
Antonio Di Maggio<br />
Gisella Gennaro (Medical Physicist)<br />
Margherita Nardin<br />
Giovanna Pintacuda<br />
Roberta Polverosi<br />
Simone Corradin<br />
Manola Garato<br />
Technicians<br />
Elisa Baraldo<br />
Massimo Bedei<br />
Simonetta Cavinato<br />
Davide Discardi<br />
Federico Maggetto<br />
Roberta Sorgato<br />
Carla Versini (coordinator)<br />
Enrico Zennaro<br />
Nursing Staff<br />
Anna Bozzato<br />
Giorgia Ceccato<br />
Manuela Frasson<br />
Mauro Menon<br />
Linda Prunotto<br />
Patrizia Rossetti<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
91<br />
Administrative Staff<br />
Marina Bettin<br />
Antonella Ferrigno<br />
Maurizio Peci<br />
Maria Carmela Zorzato
Mission<br />
The mission of the Oncological Radiology Unit is to improve<br />
the length and quality of life of cancer patients through the<br />
conduct of clinical trials of diagnostic imaging and image-guided<br />
therapeutic technologies. The Oncological Radiology Unit intends<br />
to accomplish its mission by addressing a number of objectives, of<br />
which the following are among the most important:<br />
to evaluate innovative methods of diagnostic imaging and imageguided<br />
treatment that have the potential to improve survival and<br />
quality of life of cancer patients;<br />
to compare established patterns of imaging diagnosis, staging,<br />
and palliative or curative image-guided treatment to alternative<br />
Clinical Activity<br />
Major Collaborations<br />
Inside the <strong>IOV</strong><br />
All <strong>IOV</strong> Units<br />
Clinical Activity <strong>2010</strong> No.<br />
Diagnostic examinations performed: 24.858<br />
CT 9.366<br />
X-rays 8.273<br />
US 5.707<br />
approaches, in order to improve the effectiveness of care for<br />
patients with cancer and reduce the costs of this care;<br />
to examine diagnostic and therapeutic strategies that combine<br />
different imaging procedures with non-imaging technologies,<br />
in order to improve the efficiency of cancer detection and<br />
treatment;<br />
to assess the value of the use of imaging for detection of cancer in<br />
high-risk patient populations (ie, screening);<br />
to determine the value of imaging in reducing the anxiety of<br />
individuals who have symptoms suggestive of cancer but who are<br />
found to be free of malignancy.<br />
MRI 1.512<br />
National Collaborations<br />
University of Padua<br />
Azienda Ospedaliera di Padova<br />
ULSS 16 di Padova<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
92
Major Ongoing Research Projects<br />
DiffErENTiaTED ThyrOiD CarCiNOma (DTC) haS a<br />
GOOD prOGNOSiS wiTh a 10-yEar Survival raTE hiGhEr<br />
ThaN 90%, buT 5-24% Of paTiENTS ExpEriENCE<br />
pErSiSTENT Or rECurrENT DiSEaSE<br />
Principal Investigator: Fabio Pomerri<br />
DTC management guidelines recommend PET for imaging<br />
patients with 131 I-negative whole body scans and increasing serum<br />
thyroglobulin levels. The aim of this study is to assess the impact<br />
of PET/CT on the therapeutic management of patients with<br />
recurrent DTC.<br />
Materials and methods. DTC patients who have undergone<br />
surgery and post-operative thyroid remnant ablation with 131 I, and<br />
who develop rising basal or recombinant TSH-stimulated serum<br />
thyroglobulin levels will be studied using PET/CT.<br />
Preliminary results. Three clinical issues were identified:<br />
diagnostic indications for 131 I-negative scanning and increasing<br />
thyroglobulin levels; the planning of surgery for recurrent disease;<br />
and the effectiveness of systemic therapy.<br />
Conclusion. The emphasis will be placed on how imaging<br />
is changing from a purely diagnostic role in locating disease to<br />
supporting the design of appropriate therapeutic strategies.<br />
TO aSSESS ThE pOST-ChEmOraDiOThErapy pErfOrmaNCE<br />
Of DyNamiC CONTraST-ENhaNCED maGNETiC rESONaNCE<br />
imaGiNG iN DiSTiNGuiShiNG rESiDual CaNCEr frOm<br />
pOSTirraDiaTiON pEriTumOral vaSCulOpaThy aND<br />
DESmOplaSTiC rEaCTiONS<br />
Principal Investigator: Fabio Pomerri<br />
Materials and methods. Since 2009, 60 patients have been<br />
recruited. The patients considered to date had mid-low rectal<br />
tumors potentially amenable to neoadjuvant therapy. The sample<br />
mean age was 59.3 years (range, 21-78 years). Eleven patients did<br />
not meet the inclusion criteria. The outcome of dynamic magnetic<br />
resonance after radiochemotherapy has been evaluated for 49<br />
patients. The instrumental investigations were performed using<br />
a MRI equipment with a 1.5 T magnet, and local tumor stage<br />
was evaluated using the T parameter of the TNM staging system.<br />
Several pharmacokinetic parameters were also evaluated. Based on<br />
T status, patients were classified as either T0 or T1–4. Sensitivity,<br />
specificity, positive predictive value, negative predictive value, and<br />
accuracy were calculated for each staging modality used. Findings<br />
were compared with the pathological tumor stage.<br />
Preliminary results. On histopathological analysis, 9 patients<br />
had pT0 and 40 had pT1–4 lesions. The statistically significant<br />
parameter was the partition constant (the mean in the T0 group<br />
was 0.3 and in the T1-4 group 0.4) and the area below the curve<br />
up to 30 seconds (T0: 3.2; T1-4: 3.4). The sensitivity, specificity,<br />
positive predictive value, negative predictive value, and accuracy<br />
in predicting T status (T0 vs. T≥1) were 90%, 55.6%, 90%,<br />
55.6%, and 83.7%, respectively, for the partition constant and<br />
82.5%, 88.9%, 97.1%, 53.3%, and 83.7% for the area below the<br />
curve up to 30 seconds, with a cut-off of 2.65.<br />
Conclusions. The area below the curve up to 30 seconds<br />
and the partition constant showed a good accuracy, sensitivity<br />
and positive predictive value; these parameters can be applied in<br />
clinical practice to morphological MRI findings.<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
93
Other Programs and Future Perspectives<br />
Future prospects are mainly based on Interventional oncology.<br />
Areas of application are: intravascular and extravascular.<br />
Extravascular<br />
1) Percutaneous ablation of the lesions using radiofrequency,<br />
laser, cryoablation, or microwave to induce tissue necrosis. The<br />
procedure can be performed under ultrasound guidance (liver,<br />
thyroid and soft tissues in general) or CT guidance (lung, kidney<br />
and bone). The goals can be healing as in the case of primary<br />
and secondary liver lesions, lung, kidney and thyroid cancers.<br />
The thyroid lesions represent an area of clinical research. The<br />
treatment of liver lesions by combining radiofrequency and<br />
chemoembolization with drug eluting beads represents another<br />
area of clinical research. The percutaneous ablation using MRguided<br />
HIFU (High Intensity Focused Ultrasound) may be<br />
the main area of clinical research in oncology.<br />
2) Percutaneous biliary drainage. The procedure is performed<br />
under fluoroscopic guidance with the aim to treat obstructive<br />
jaundice before curative or palliative surgery. Pancreatic and<br />
biliary tract cancers, and in rare cases extrinsic compression<br />
of the biliary tract are possible clinical applications of this<br />
technique.<br />
3) Vertebroplasty is a palliative treatment to relieve pain in cases<br />
of spinal metastases and can be done by direct injection of<br />
cement into the spine or vertebral body following percutaneous<br />
ablation.<br />
4) Nephrostomy drainage may be performed under ultrasound<br />
guidance for puncturing the urinary tract or under fluoroscopy<br />
for placement of nephrostomy drainage.<br />
Intravascular<br />
1) Chemoembolization of primary and secondary liver cancers<br />
with drug eluting beads. Areas of clinical research are the<br />
treatment of hepatocellular carcinoma and liver metastases.<br />
The treatment may be employed in hepatocellular carcinoma<br />
patients out liver transplantation in order to re-include them in<br />
the MC (Milan Criteria) for liver transplantation. In the matter<br />
of metastases, the actual clinical utility of randomized studies<br />
using associated chemoembolization and systemic therapy<br />
(chemotherapy or biologic agents) is under investigation.<br />
2) Percutaneous isolated limb perfusion in the case of melanoma<br />
or sarcoma or percutaneous isolated liver perfusion.<br />
3) Embolization of hypervascular bone metastases.<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
94
Main Pubblications<br />
Chief<br />
Correlation between magnetic resonance<br />
imaging and histopathological tumor response<br />
after neoadjuvant chemotherapy in breast<br />
cancer.<br />
Automated analysis of phantom images for the<br />
evaluation of long-term reproducibility in digital<br />
mammography.<br />
Systematic approach to human error in<br />
radiology.<br />
Digital breast tomosynthesis versus digital<br />
mammography: a clinical performance study.<br />
Analysis of malpractice claims in mammography:a<br />
complex issue.<br />
Breast Imaging<br />
Luigi Pescarini, MD<br />
Born in Thiene (VI), on August 11, 1947, he earned his degree in Medicine at the University of<br />
Padova in 1972, subsequently specializing in Diagnostic Radiology (1975) and in Radiology (1977).<br />
Since 1973, his work has focused on breast imaging and is now acting as chief of the Breast Imaging<br />
Unit at the <strong>IOV</strong>. He is Associate Professor of Radiology at the Department of Oncology and Surgical<br />
Sciences of the University of Padova. His teaching activity includes the undergraduate schools of<br />
Medicine and Surgery, Dentistry and Dental Prosthetics, Radiology for technicians, and 5 postgraduate<br />
medical schools. As a member of the Italian Society for Medical Radiology (SIRM), he cofounded<br />
the Breast Imaging section of SIRM and has held positions in the directive council for the<br />
sections of Breast Imaging and Radiation Protection studies; he was president of the SIRM Regional<br />
Group for the Veneto Region (2001-2005) and President of the section of Ethics studies and forensic<br />
radiology (2006-2008). His scientific activity includes participation in numerous national and<br />
international congresses and publications predominant in breast imaging. He is part of the Editorial<br />
Board for the Ethics section of the journal “La Radiologia Medica”.<br />
Nicoletto MA, Nitti D, Pescarini L, Corbetti F, Mencarelli<br />
R, Cappetta A, Galligioni A, Pogliani C, Marchet A, Bozza<br />
F, Ghiotto C, Griggio L, Zavagno G, Donach M. E, Di<br />
Maggio C.<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
96<br />
Tumori. 2008; 94: 481-488<br />
Gennaro G, Ferro F, Contento G, Fornasin F, Di Maggio C. Phys Med Biol. 2007; 52:1387-1407<br />
Pescarini L., Inches I. Radiol Med. 2006; 111:252-267<br />
Gennaro G, Toledano A, Di Maggio C, Baldan E, Bezzon<br />
E, La Grassa M, Pescarini L, Polico I, Proietti A, Toffoli A,<br />
Muzzio PC.<br />
Eur Radiol. <strong>2010</strong>; 20:1545-53<br />
Fileni A, Magnavita N, Pescarini L. Radiol Med. 2009; 114:636-644
Clinical and Research Staff<br />
Luigi Pescarini<br />
Enrica Baldan<br />
Elisabetta Bezzon<br />
Chiara Dal Bosco<br />
Gisella Gennaro (Medical Physicist<br />
affiliated to the Radiology Unit)<br />
Ilaria Polico<br />
Alessandro Proietti<br />
Technicians<br />
Lorenzo Roverato (Head and Coordinator)<br />
Lina Ciampani<br />
Tiziana Masiero<br />
Maria Petrioli<br />
Tiziana Pisapia<br />
Administrative Staff<br />
Stefania Zaramella<br />
Nursing Staff<br />
Micaela Ceretta<br />
Eva Granziero<br />
Eliana Salviato<br />
Antonella Scelta<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
97
Mission<br />
The Breast Imaging Unit mission is manifested in the Diagnostic<br />
service for breast disease for the population of Padova, the Veneto<br />
Region and Italy, and in the specialist support given to the medical<br />
and surgical units of the <strong>IOV</strong>. The Breast Imaging Unit has been<br />
organized to provide tailored diagnostic paths, on the basis of<br />
individual patient needs, using multiple imaging techniques,<br />
and ensuring the integration of all diagnostic information, as well<br />
Clinical Activity<br />
The Breast Imaging Unit is equipped with all standard<br />
modalities used in breast imaging:<br />
Three direct digital mammography units, including review<br />
workstations;<br />
Four ultrasound scanners with suitable soft tissue probes;<br />
One dedicated prone table for vacuum-assisted breast biopsy,<br />
X-ray guided;<br />
One optical microscope for analysis of fine needle aspiration<br />
cytology specimens;<br />
One 1.5 magnetic resonance imaging (MRI) scanner, shared<br />
with the Radiology Unit, where the equipment is installed.<br />
This permits both diagnostic and interventional actions,<br />
according to clinical needs.<br />
Outpatient services<br />
The Breast Imaging Unit mission is diagnosis of breast diseases,<br />
in particular early cancer detection, using imaging techniques<br />
evidence-based. Each breast radiologist, after initial clinical<br />
assessment, is responsible, for the full patient management and<br />
workup, including integration of multiple imaging techniques<br />
and/or interventional procedures image-guided in sub-clinical<br />
lesions. Diagnostic actions include pretreatment cancer staging<br />
by MRI with contrast media.<br />
Inpatient services<br />
Priority is given to the needs of the Medical Oncology Units,<br />
with special care to consultations for surgical and/or pharmacological<br />
strategies. The Breast Imaging Unit works in close collaboration<br />
with all the other Units involved in breast cancer care, especially<br />
as humanization of doctor-patient relationship in all phases of<br />
workup, from communication of diagnosis to follow-up planning.<br />
Examinations are carried out under the direction of each radiologist<br />
who always works in team with a breast radiographer. The Breast<br />
Imaging Unit is ISO-certified since 2004 and its quality manual is<br />
continuously updated.<br />
for intervention planning of subclinical lesions which require<br />
ultrasound-or x-ray-guided localizations, as well as patient followup<br />
after treatment. Patient follow-up scheduled as planned by the<br />
medical oncology units. The “complex cases” are reviewed and<br />
discussed in consensus multidisciplinary meetings, involving<br />
radiologists, surgeons, oncologists, and any other specialist who<br />
is part of the Breast Unit. The Breast Imaging Unit represents<br />
an area of excellence for diagnosis of subclinical lesions, in both<br />
diagnostic and preoperative phases. The Breast Imaging Unit also<br />
represents a possible diagnostic reference during patient follow-up<br />
in detection of recurrences or in evaluation of breast reconstruction<br />
with implants and/or biological tissues.<br />
Types and amounts of examinations performed in <strong>2010</strong><br />
Clinical and instrumental breast examinations (breast<br />
examination, ultrasounds, and mammography)<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
98<br />
9.975<br />
MRI of the breast with and without contrast media 550<br />
Fine needle aspiration cytology 1.165<br />
Tru-cut needle aspiration biopsy (microbiopsy) 297<br />
External Consultation 474<br />
Preoperative localization ultrasound-guided 235<br />
Preoperative localization x-ray-guided 120<br />
Intraoperative mammographic evaluation 77
Major Research Collaborations<br />
Research activities are related to the Breast Imaging Unit field<br />
of interest and its mission. Therefore, the Unit is collaborating<br />
within the multidisciplinary Team of the Breast Unit with most<br />
<strong>IOV</strong> Units, and in particular with Breast Surgery, Medical<br />
Oncology, Molecular Oncology, Radiology.<br />
Research subjects include digital breast tomosynthesis, dose<br />
reduction in mammography, effects of neoadjuvant chemotherapy<br />
on circulating tumor cells in early stage breast cancer, surveillance<br />
Major Ongoing Research Projects<br />
SurvEillaNCE Of wOmEN aT hiGh GENETiC-familial<br />
riSk Of brEaST CaNCEr: iTaliaN NaTiONal iNSTiTuTE Of<br />
hEalTh NETwOrk “iSSiN hibCr-1 - hibrC2”<br />
Principal Investigator: Luigi Pescarini<br />
Background. Epidemiological knowledge on the incidence<br />
and onset of breast cancer at a young age in families leads to the<br />
control of high-risk groups of women, in order to assess the most<br />
of high risk women for familial-hereditary tumors, characterization<br />
of in situ tumors and so-called “border line” lesions.<br />
Moreover, clinical aspects related to breast imaging unit<br />
organization are specific interest of this Unit, within the frame<br />
of the workgroup “Breast Imaging” and “Ethics and Forensis<br />
Radiology” of the Italian Society of Medical Radiology.<br />
suitable techniques for detecting lesions starting at 25 years of age<br />
and, possibly, to demonstrate long-term reduction in mortality<br />
through screening strategies.<br />
Materials, methods and results. In 18 Italian centers<br />
participating in HIBCR-1, showed the superior sensitivity of<br />
magnetic resonance imaging (MRI) in detecting malignant<br />
lesions compared to other imaging techniques, as published by<br />
the National Institute of Health (ISS) (research leaders Podo F.<br />
and Sardanelli F).<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
99
Regarding the new HIBRC2 study, the Veneto Institute of<br />
Oncology focused its attention, unlike what was done in the<br />
previous study, to women “supposed to be healthy”, belonging<br />
to risk groups as identified by the national program. Main data<br />
from the Breast Imaging Unit collected during years 2009-<strong>2010</strong><br />
are reported: 79 healthy women with an alleged hereditary risk<br />
for breast cancer undergoing annual surveillance with integrated<br />
breast mammography and MRI, with and without contrast were<br />
enrolled in the study. Two breast cancers were identified, both<br />
with histologic findings of DCIS, one visible by mammography<br />
and MRI, the other by MRI only.<br />
qualiTy CONTrOlS iN DiGiTal brEaST SCrEENiNG<br />
Principal Investigator: Gisella Gennaro<br />
Background. High image quality is one of basic requirements<br />
within a breast screening program to ensure successful results.<br />
Some screening descriptors as Recall Rate (percentage of women<br />
recalled for further workup, caused by suspicious mammography<br />
images) and Detection Rate (cancers found in the screened<br />
population) are calculated assuming that mammography images<br />
evaluated by radiologist have high image quality. For this reason,<br />
in mammography, and even more in a screening program, quality<br />
controls (QC) of mammography equipment are considered<br />
important, and the definition of the QC protocol is one of the<br />
constraints in any accreditation process. Since 1 st Jan, 1996,<br />
quality controls are mandatory by law in Italy (DLg 195/230)<br />
for any radiology equipment; this duty was confirmed by the<br />
Decreto Legislativo n. 187 (May 26, 2000) “Attuazione della<br />
direttiva 97/43/EURATOM in materia di protezione sanitaria<br />
delle persone contro i pericoli delle radiazioni ionizzanti connessi<br />
ad esposizioni mediche”, better identifying responsibilities and<br />
roles of involved professions. In the last decade, transition from<br />
screen-film to digital mammography has required a review (still<br />
ongoing) of old QC protocols, to adapt them to needs of new and<br />
more complex technologies.<br />
In <strong>2010</strong>, the Veneto Region asked the Veneto Institute of<br />
Oncology to propose a Project to face the issue of quality controls<br />
for equipment used in mammography screening. After a quick<br />
preliminary survey, it was noticed that 80% of mammography<br />
systems used in screening were already digital (both direct digital,<br />
DR, and computed radiography, CR), while only 20% of systems<br />
still used films, and some of them were going to be replaced.<br />
This picture pushed us to propose a project addressed to digital<br />
screening only, on the basis of two simple considerations: (1) it is<br />
easy to guess that in a few years the last screen-film systems will be<br />
replaced by digital ones; (2) use of digital images support quality<br />
control automation and data sharing, simplifying the project<br />
management. Such Project, described in the following sections,<br />
was approved by the Veneto Region at the end of <strong>2010</strong>, and is<br />
now going to start.<br />
Methods. The Project proposes a unique Quality Assurance<br />
Program for all digital mammography systems involved in<br />
mammography screening of the Veneto Region. The Project is<br />
structured in two phases.<br />
Phase 1: regards Acceptance/Commissioning and Status tests,<br />
normally performed by a physicist (Medical Physics Expert,<br />
MPE) when the equipment is installed and subsequently with<br />
annual or semi-annual frequency. Goal of Phase 1 is to centralize<br />
collection of QC data resulting from physicists’ measurements,<br />
using a common protocol. This protocol, partially extracted from<br />
the “European Guidelines for Quality Assurance in Breast Cancer<br />
Screening and Diagnosis 4 th edition”, includes the following<br />
tests:<br />
1. Dosimetry (both measurements include the compression<br />
paddle in the beam):<br />
1.1 Tube output (all anode/filter combinations and<br />
kVp values used in the clinical practice)<br />
1.2 Half Value Layer, HVL (all anode/filter combinations<br />
and kVp values used in the clinical practice);<br />
2. Automatic Exposure Control (AEC):<br />
2.1. Contrast-to-Noise Ratio (CNR) versus object thickness;<br />
2.2. Average Glandular Dose (AGD) versus object<br />
thickness;<br />
2.3. Figure of merit (FOM): ;<br />
3. Detector:<br />
3.1. Response function;<br />
3.2. Noise evaluation;<br />
3.3. “Homogeneity”;<br />
3.4. Imaging plate variability (only for CR systems);<br />
4. Monitor:<br />
4.1. DICOM Grayscale Standard Display Function;<br />
4.2. Uniformity.<br />
Physicists of screening sites should perform tests according<br />
to procedures provided by the project manager, using their own<br />
calibrated instruments. Test results will be gathered from the<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
100
Veneto Institute of Oncology which will summarize them in a<br />
report and send to the Veneto Region.<br />
A web site will be developed to include all information related<br />
to the Project, the protocol, and possible analysis tools, which<br />
could simplify work of all people involved.<br />
Phase 2: it regards reproducibility tests, which should be<br />
performed by radiographers with weekly frequency. Purpose<br />
of Phase 2 is the application of an automatic procedure for<br />
reproducibility tests, using a software package for automatic<br />
analysis of images obtained by exposing an appropriate test-object<br />
(named “phantom” in the following) and an Expert System for<br />
diagnosis of malfunctions derived from the analysis of variations<br />
of image quality parameters compared to a baseline previously<br />
defined. Mammographic phantom used should have absorption<br />
characteristics equivalent to a “mean breast”, and include a proper<br />
number of “details” such as image analysis will allow to measure:<br />
Spatial resolution<br />
Contrast resolution<br />
Contrast<br />
Contrast-to-Noise Ratio (CNR)<br />
Structured noise.<br />
The Expert System should analyze variations of parameters<br />
listed above versus the baseline values and provide to the user realtime<br />
information regarding right operating of the system, or the<br />
existence of fluctuations which could be caused by a malfunction,<br />
suggesting possible causes and potential corrective actions.<br />
Results. At present, the project on quality controls has been<br />
presented to both reference radiologists for screening sites, and<br />
to physicists involved in Phase 1. In particular, the QC protocol<br />
has been shared with physicists, finding their agreement, and test<br />
procedures will be available by the end of <strong>2011</strong>. Phase 1 start and<br />
the first round of measurement collection should be closed within<br />
June 2012. The update of equipment used in mammography<br />
screening has shown that the number of digital systems is increased<br />
compared to the last year, up to 94% (figure 1).<br />
Conclusions. Application of the project described above<br />
will be an important step for harmonization of quality controls<br />
in digital mammography; this could have a significant impact in<br />
optimization of mammography screening program. Monitoring<br />
of image quality reproducibility using automatic procedures<br />
increases test efficacy and reliability, removing variability which<br />
would be unavoidable if image quality stability would be evaluated<br />
by human observers.<br />
Future perspectives. Automation of quality controls planned by<br />
the project will allow monitoring of an increasing number of systems.<br />
Proposed method could be extended to other imaging modalities.<br />
COmpariSON Of DiGiTal brEaST TOmOSyNThESiS aND<br />
STaNDarD mammOGraphy iN SympTOmaTiC wOmEN<br />
Principal Investigator: Gisella Gennaro<br />
Background. Mammography is an effective modality<br />
for the detection of early stage breast cancer. However it<br />
has significant limitations, due to masking of suspicious<br />
lesions by fibroglandular densities, reducing its diagnostic<br />
performance, particularly in denser breasts. Another limitation<br />
of mammography is that some features interpreted as lesions<br />
are merely summation densities. Digital breast tomosynthesis<br />
(DBT) is expected to overcome those inherent limitations of<br />
mammography by segmenting images of the breast into a number<br />
of planar images that can be individually reviewed by radiologists<br />
without the interference of superimposed fibroglandular tissues.<br />
A clinical study at the Veneto Institute of Oncology was designed<br />
in collaboration with GE Healthcare, aiming to compare clinical<br />
performance of DBT over full-field digital mammography (MX)<br />
in a diagnostic population, and is still ongoing. In the following,<br />
main summary results of Phase 2 are illustrated (Phase 1 study<br />
results already reported in the previous Annual Report).<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
101<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
digital analog<br />
Digital<br />
Analog<br />
Figure 1. Analog and digital equipment in mammography screening of the<br />
Veneto Region.
Methods. Patient accrual, following approval by competent<br />
authorities (Ethics Committee and Ministry of Health), started in<br />
April 2007 and finished in July 2008. Study population included<br />
250 women with a breast lesion found by mammography<br />
(two views: cranio-caudal, CC, and medio-lateral-oblique,<br />
MLO) or/and ultrasound, who consented undergoing also<br />
bilateral tomosynthesis (one view: MLO). The study (image<br />
interpretation) was conducted retrospectively in two phases,<br />
involving 6 readers per each: Phase 1, performed during patient<br />
accrual, aiming to compare clinical performance of tomosynthesis<br />
in one-view versus standard mammography in two-views; Phase<br />
2, performed after patient accrual, aiming to verify if the adjunct<br />
of the CC mammographic view could increase DBT performance<br />
compared to the reference standard (MX in two-views). Receiver<br />
Operating Characteristics (ROC) analysis of dataset from Phase<br />
1 demonstrated non-inferiority by 5% of DBT in one-view<br />
versus MX in two-views, at comparable dose level, while perlesion<br />
analysis of the same dataset showed that DBT significantly<br />
increased lesion detection compared to MX, especially for benign<br />
lesions. Figure 1 depicts the timeline of the DBT research at the<br />
Veneto Institute of Oncology. Results reported in the following<br />
section, regarding Phase 2, are still unpublished.<br />
Regulatory Approvals<br />
Patient Accrual<br />
START END<br />
Per-breast analysis<br />
(ROC)<br />
Per-lesion analysis<br />
(JAFROC)<br />
Per-breats analysis<br />
publication<br />
Results. Phase 2 dataset included image readings of<br />
469 breasts from 6 independent readers. The overall clinical<br />
performance analysis (ROC analysis) confirmed non-inferiority<br />
of DBT(MLO) versus MX(CC+MLO) already found in Phase 1,<br />
but showed a trend to superiority of DBT it was combined with<br />
the mammographic CC-view (DBT+MX CC ), as depicted in Figure<br />
2. The plot represents the space of difference between the mean<br />
areas under the ROC curves of DBT vs. MX and of (DBT+MX CC )<br />
vs. MX, respectively. Zero line represents the “equality” condition,<br />
and -0.05 line the “tolerance” accepted as possible difference<br />
between areas, set at 5%. The “tolerance” is named “noninferiority<br />
margin”. Confidence intervals (95%) together with<br />
the absolute differences between areas are represented, such as<br />
variability due to variance across multiple cases and readers is<br />
taken into account. If the difference and the related confidence<br />
interval are above the non-inferiority margin, non-inferiority of<br />
the investigational technique versus the reference standard can be<br />
concluded, otherwise, if the difference and the confidence interval<br />
are both above zero, superiority can be concluded.<br />
Thereby, adjunct of MX CC to tomosynthesis moved<br />
tomosynthesis alone towards superiority compared to<br />
mammography, even if it is not achieved. Moreover, in terms of<br />
Objective: compare clinical performance<br />
Phase 1: DBT(MLO) vs. MX(CC+MLO)<br />
Phase 2: DBT(MLO) + MX CC vs. MX (CC+MLO)<br />
2006 2007 2008 2009 <strong>2010</strong> <strong>2011</strong><br />
Readings: Phase 1<br />
Figure 1. Timeline of the DBT research at the Veneto Institute of Oncology.<br />
Readings: Phase 2<br />
Per-breast analysis<br />
(ROC)<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
102
mean AUC difference<br />
0.10<br />
0.08<br />
0.06<br />
0.04<br />
0.02<br />
0.00<br />
-0.02<br />
-0.04<br />
-0.06<br />
-0.08<br />
-0.10<br />
5% NI-margin<br />
sensitivity, it was found that DBT and MX detected comparable<br />
number of cancers, while the new protocol DBT+MX CC led to<br />
increase cancer detection: on average, DBT+MX CC detected<br />
2.3 extra-cancers compared to the reference standard. Finally,<br />
specificity was higher than MX with both DBT alone (significantly)<br />
and DBT+MX CC (not significantly).<br />
Conclusions. Results from Phase 2 showed the potential<br />
benefit of the new reading protocol, DBT+MX CC , combining<br />
tomosynthesis with one mammographic view. Furthermore,<br />
DBT - MX (DBT + MX CC ) - MX<br />
comparison of results obtained in the two phases of the clinical<br />
study suggested that further improvement in clinical performance<br />
of DBT alone could be expected, while the effect of radiologists’<br />
learning curve will get more evident.<br />
Future perspectives. Some manufacturers have already<br />
launched and others are going to launch tomosynthesis products<br />
onto the market. However, the clinical use of this new technology<br />
is still debated and it is easy to imagine it will be the subject of<br />
several papers in the next years.<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
103<br />
SUPERIORITY<br />
NON-INFERIORITY<br />
INFERIORITY<br />
Figure 2. ROC results from Phase 2: clinical performance of DBT(MLO) was confirmed to be non-inferior to MX(CC+MLO), while the combination of DBT(MLO)<br />
with one mammographic view (CC) showed an increase in clinical performance.
Mission and Clinical Activity<br />
The mission of the Patholgy Unit is the diagnosis of tumors.<br />
To this end, the Unit exploits histologic, histochemical, and<br />
immuno-histochemical techniques, as well as molecular biology<br />
approaches. In most instances, this activity is performed within<br />
the frame of a strict collaboration with Clinical Oncology and<br />
Surgical teams; for this reason the Pathology Unit participates in<br />
the activities of most Multidisciplinary Groups. Clinical activities<br />
range from secondary prevention screening activities to histologic<br />
and cytologic diagnosis of pre-neoplastic and neoplastic diseases,<br />
Pathology<br />
Research Collaborations and Projects<br />
The Unit maintains a strict collaboration with all the Clinical<br />
Units of the Institute and of the Azienda Università-Ospedale,<br />
with special attention to the Pathology Unit headed by Prof. M.<br />
Rugge, from which the Units depends for the administrative<br />
aspects. Translational research is a major commitment, with special<br />
including sentinel node examination, intra-operatory diagnosis,<br />
and pathologic staging of tumor. The Unit is also involved in<br />
organ transplant in tumor-bearing patients, as well as in the<br />
activities of Tumor Registry and Barrett’s Esophagus Registry.<br />
Most activities, coordinated by Dr. A. Galligioni, are performed<br />
under the supervision of and in collaboration with the Pathology<br />
Unit of the Azienda Università-Ospedale of Padova, headed by<br />
Professor Massimo Rugge. The <strong>IOV</strong> Institute is now re-organizing<br />
this area, in the frame of an autonomous Unit.<br />
attention to morphologic and molecular characterization of preneoplastic<br />
syndromes. Within the Veneto Oncology network,<br />
the Unit is involved in setting up guidelines and protocols for<br />
appropriate diagnostic and therapeutic approaches to several<br />
neoplastic diseases.<br />
THE DEPARTMENTS - DEPARTMENT OF IMAGING, RADIOLOGY AND PATHOLOGY<br />
104
foto
Department of Radiotherapy<br />
& Nuclear Medicine<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
107
Radiotherapy and Nuclear Medicine<br />
Main Pubblications<br />
Chief<br />
Patterns of care and survival in a retrospective<br />
analysis of 1059 patients with glioblastoma<br />
multiforme treated between 2002 and 2007: a<br />
multicenter study by the Central Nervous System.<br />
Infant ependymoma in a 10-year AIEOP<br />
(Associazione Italiana Ematologia Oncologia<br />
Pediatrica) experience with ometted or deferred<br />
radiotherapy.<br />
Sequential intensified chemotherapy with stem<br />
cell rescue for children and adolescents with<br />
desmoplastic small round-cell tumor.<br />
Clinical outcome of low risk differentiated<br />
thyroid cancer patients after radioiodine<br />
remnant ablation and recombinant human<br />
thyroid stimulating hormone preparation.<br />
Infant ependymoma in a 10-year AIEOP<br />
(Associazione Italiana Ematologia Oncologia<br />
Pediatrica) experience with omitted or<br />
deferred radiotherapy.<br />
Guido Sotti, MD<br />
University of Padova: MD (1973); University of Padova, specialisation in Radiology (1977), and<br />
Clinical Hematology (1980). Full time assistant at the U.O. of Radiotherapy and Nuc. Medicine,<br />
Padova Hospital (1974-1986); vice-Head Physician at the U.O. of Radiotherapy and Nuc.<br />
Medicine, Padova Hospital (1986-1997). Head Physician at the U.O. of Radiotherapy and Nuc.<br />
Medicine, Padova Hospital (1998 - 2006). Head Physician at the U.O. of Radiotherapy and Nuc.<br />
Medicine, <strong>IOV</strong> Padua (2006 - to date) 1983-<strong>2011</strong> University of Padova, teaching of the School of<br />
Specialisation in Oncology. 1989-<strong>2011</strong> University of Padova, teaching of the School of Specialisation<br />
in Radiology. 1997-1999 University of Padova, teaching of the School of Specialisation in Nuclear<br />
Medicine. Member of the Associazione Italiana di Oncologia Radioterapica (AIRO); Member of<br />
the International Society of Paediatric Oncology (SIOP); Member of the European Group for Bone<br />
Marrow Transplantation (EBMT). More than 100 publications and 10 books chapters cover many<br />
aspects of pediatric radiation oncology and adult cancer, including brain tumors, Hodgkin’s disease,<br />
malignant lymphomas, soft tissue sarcomas and the late effects of cancer treatment.<br />
Scoccianti S, Magrini SM, Ricardi U, Detti B, Buglione M, Sotti G, Krengli M, Maluta<br />
S, Parisi S, Bertoni F, Mantovani C, Tombolini V, De Renzis C, Lioce M, Fatigante L,<br />
Fusco V, Muto P, Berti F, Rubino G, Cipressi S, Fariselli L, Lupattelli M, Santoni R,<br />
Pirtoli L, Biti G. Study Group of Airo (italian Association of Radiation Oncology).<br />
Massimino M, Gandola L, Barra S, Giangaspero F, Casali C, Potepan P, Di Rocco C,<br />
Nozza P, Collini P, Viscardi E, Bertin D, Biassoni V, Cama A, Milanaccio C, Modena<br />
P, Balter R, Tamburrini G, Peretta P, Mascarin M, Scarzello G, Fidani P, Milano GM,<br />
Sardi I, Genitori L, Garrè ML.<br />
Bisogno G, Ferrari A, Rosolen A, Alaggio R, Scarzello G, Garaventa A, Arcamone<br />
G, Carli M.<br />
Vianello F, Mazzarotto R, Mian C, Lora O, Saladini G, Servodio O, Basso M,<br />
Pennelli G, Pelizzo MR, Sotti G.<br />
Massimino M, Gandola L, Barra S, Giangaspero F, Casali C, Potepan P, Di Rocco<br />
C, Nozza P, Collini P, Viscardi E, Bertin D, Biassoni V, Cama A, Milanaccio C,<br />
Modena P, Balter R, Tamburrini G, Peretta P, Mascarin M, Scarzello G, Fidani<br />
P, Milano GM, Sardi I, Genitori L, Garrè ML.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
108<br />
Neurosurgery <strong>2010</strong>; 67:<br />
446-58<br />
Int J Radiat Oncol Biol<br />
Phys <strong>2010</strong>; 18:1-8<br />
Bone Marrow Transplant.<br />
<strong>2010</strong>; 45:907-11<br />
Clin Oncol (R Coll<br />
Radiol). <strong>2011</strong>; in press.<br />
Int J Radiat Oncol Biol<br />
Phys. <strong>2011</strong>; 80:807-14
Clinical and Research Staff<br />
Guido Sotti<br />
Franco Berti<br />
Caterina Boso<br />
Maria Samaritana Buzzaccarini<br />
Anna Rita Cervino<br />
Luigi Corti<br />
Laura Evangelista<br />
Maria Luisa Friso<br />
Michele Gregianin<br />
Ornella Lora<br />
Lucio Loreggian<br />
Giorgio Saladini<br />
Giovanni Scarzello<br />
Federica Vianello<br />
Michela Basso<br />
Alessio Casetta<br />
Sara Galuppo<br />
Elena Groff (Psychologist)<br />
Federica Pellegrino (Speech therapist)<br />
Tiziana Proto<br />
Technical Staff<br />
Claudio Pagnin (Coordinator)<br />
Davide Bettin<br />
Francesca Bissacco<br />
Tommaso Brunoro<br />
Maria Colombis<br />
Michele Da Riva<br />
Doriana Di Tommaso<br />
Stefano Ferrioli<br />
Debora Gambetta<br />
Giorgio Lusiani<br />
Alessandro Novo<br />
Michela Raimondi<br />
Antonella Sanità<br />
Michael Sartori<br />
Giancarlo Zonzin (Coordinator)<br />
Marino Bortolami<br />
Giorgio Masiero<br />
Laura Memo<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
109
Riccardo Sanco<br />
Silvia Zampieri<br />
Manuela Anna Zappalà<br />
Elena Zaramella<br />
Nursing Staff<br />
Admission Department<br />
Cristina Tridello (Coordinator)<br />
Marina Bezzati<br />
Roberto Bilato<br />
Deborah Borella<br />
Giulia Carletti<br />
Fabiola Carrossa<br />
Franco Fiorotto<br />
Fabio Lincetto<br />
Roberta Luisetto<br />
Alessandro Paggiaro<br />
Monica Perotti<br />
Astrid Rossi<br />
Francesca Ruffo<br />
Graziella Sandon<br />
Elisa Zago<br />
Federico Zancato<br />
Carmela Zeoli<br />
Ambulatories<br />
Barbara Giacomin (Coordinator)<br />
Graziella Alfonsi<br />
Sandra Bonato<br />
Vania Boscolo<br />
Licia Canovese<br />
Daniela Filira<br />
Iolanda Fronzetti<br />
Carla Masiero<br />
Franca Smaniotto<br />
Liliana Spangaro<br />
Nuclear Medicine<br />
Morena Busatto<br />
Alessandra Biscotto<br />
Eva Carpin<br />
Michele Trevisan<br />
Socio-sanitary operators<br />
and Socio-sanitary auxiliaries (OSS – OT – OS)<br />
Fabrizio Boscolo<br />
Manola Colcera<br />
Miranda Longetti<br />
Pietro Marin<br />
Renza Meneghin<br />
Patrizia Quadrio<br />
Ivana Salvò<br />
Fabio Tamiazzo<br />
Renato Toffano<br />
Administrative Staff<br />
Daniele Bertin<br />
Marisole Celegato<br />
Sonia Celladin<br />
Simonetta Di Genni<br />
Graziella Formaggio<br />
Michele Pignataro<br />
Luigi Polanzan<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
110
Clinical Activity<br />
The acquisition of a helical tomotherapy system and a<br />
new accelerator is foreseen in the near future. Besides external<br />
radiotherapy, other treatments as high-dose rate brachytherapy<br />
for lung, esophageal, gynecologic cancer and choroidal melanoma<br />
are performed.<br />
A peri-intraoperative brachytherapy service is available for soft<br />
tissue sarcomas in adult and pediatric patients A photodynamic<br />
therapy (PDT) unit is also available, providing a photosensitizer<br />
chemical compound fixing on neoplasia, excited by light of<br />
a specific wavelength. Patients treated with this therapy are<br />
usually affected by Head&Neck, gynecological, esophageal and<br />
bronchial tumors no longer treatable with standard care. Other<br />
different lasers are used for endoscopic bronchial, esophageal and<br />
dermatologic surgery.<br />
Beds in admission department<br />
Ordinary 18<br />
Day Hospital 4<br />
Protected<br />
Patients in admission department<br />
8<br />
Ordinary 306<br />
DH 261<br />
Protected 481<br />
TOTAL 1.048<br />
Health services Ambulatories<br />
Examinations/visits 10.721<br />
First examinations/visits ambulatories and<br />
3500<br />
multidisciplinary examinations<br />
Patients 2600<br />
Treatments<br />
3583<br />
(performed 72.427 health services in the cure department)<br />
The Section of Nuclear Medicine, endowed with two 2-head<br />
gamma cameras, 1 hybrid PET-CT tomography and 1 gammacounter,<br />
offers traditional nuclear medicine tests to oncology<br />
patients such as bone scans, 131 I whole-body scans, sentinel node<br />
scintigraphy, somatostatin analogue scans etcetera, as well as<br />
functional examinations such as lung and myocardium perfusion<br />
scans, kidney, parathyroid and thyroid studies. FDG-PET scans<br />
are routinely performed in diagnosis, staging and clinical followup<br />
of patients. In <strong>2010</strong> over 15,000 nuclear medicine studies were<br />
performed, including about 1,000 sentinel node studies and more<br />
that 2,500 were PET-CT scans.<br />
Distribution by pathology (%)<br />
19,3<br />
Total activities in the cure department 72.427<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
111<br />
4,9<br />
1,4<br />
5,4 2,9<br />
10,8 20,7<br />
5,0<br />
3,8<br />
8,6<br />
6,7<br />
5,1<br />
5,4<br />
Breast tumors<br />
Head/neck tumors<br />
Lung tumors<br />
Esophagus<br />
Metastases<br />
Prostate cancer<br />
Gynecological<br />
tumors<br />
Brain tumors<br />
GI tumors<br />
(with ano-rectum)<br />
Lymphomas<br />
Thyroid tumors<br />
Germ cells tumors<br />
Other
Radiotherapy Equipment<br />
Radiotherapy systems:<br />
1 Accelerator PRIMUS Siemens – energy 6 MeV - El 5-14;<br />
1 Accelerator MX2 Siemens – energy 6 MeV;<br />
1 Accelerator ONCOR Siemens – energy 6-15 MeV - El 5-21;<br />
1 Accelerator MX2 Siemens – energy 6 MeV;<br />
1 Microseletron System HDR Nucletron (for therapy High Dose<br />
Rate);<br />
1 Simulator TAC PQ6000 – Picker;<br />
1 Radiology simulator Mevasin-Siemens;<br />
1 portable Radiology System (for simulations) Sirmobil-Siemens.<br />
Treatment planning system:<br />
1 Oncentra Masterplan;<br />
1 Oncologist Siemens;<br />
1 Plato Nucletron.<br />
Mission<br />
The mission of Radiotherapy and Nuclear Medicine Unit is<br />
the diagnosis and care of patients affected by malignant neoplasia.<br />
The Radiotherapy Unit provides multiple ways to deliver radiation<br />
therapy offered by modern oncology radiotherapy: conformal<br />
Lasers:<br />
1 Level M300 - bio-stimulant;<br />
1 Dornier MBB Nd Yag - endoscopy;<br />
1 Diomed D60 Diodo - surgery;<br />
1 Diomed PDT Diodo - photodynamic therapy;<br />
1 Deka laser CO2 - skin;<br />
1 Candela Dye-laser - skin.<br />
Nuclear medicine equipment<br />
1 γ Camera Siemens mod. Ecam;<br />
1 γ Camera Picker mod. Axis;<br />
1 TC-PET.<br />
radiation therapy, intraoperative radiation therapy, radiosurgery,<br />
fractionated stereotactic radiotherapy and total body irradiation<br />
for conditioning allogeneic bone marrow transplantation.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
112
Areas of Excellence<br />
Thyroid cancer<br />
The Unit is part of a multidisciplinary team involving experts<br />
from the Units of Surgery, Radiotherapy, Nuclear Medicine,<br />
Endocrinology, Clinical Oncology, Pathology, and Physics.<br />
Systemic isotope therapy is available in the form of:<br />
A) 131 I for remnant ablation or treatment of persistent or<br />
relapsed disease in patients with differentiated thyroid cancer.<br />
About 480 patients, both pediatric and adult, are treated each<br />
year. After treatment, all patients enter follow-up; more than<br />
2,500 patients are evaluated yearly in the follow-up program and<br />
the data from this large database permit evidence-based decisions<br />
for future patient management;<br />
B) Meta-I-benzyl-guanidine for metastatic medullary<br />
carcinoma or other neural crest tumors such as metastatic<br />
pheochromocytoma and paraganglioma, both in pediatric and<br />
adult patients.<br />
The major advance in thyroid cancer management over the last<br />
decades has been the ability to identify patients with or without<br />
disease after primary treatment by thyroglobulin measurement<br />
after recombinant human TSH stimulation (Tg test). Tg test<br />
also allows a more precise selection of patients who require<br />
further treatment or may enter follow-up. Another important<br />
advance in thyroid cancer management is the use of 18 FDG-<br />
PET for the prognostic evaluation of patients with differentiated<br />
thyroid cancer. All patients with advanced or metastatic disease<br />
undergo 18 FDG-PET, thus allowing to select patients who may<br />
benefit from 131 I treatment from those who need surgery or<br />
external beam radiotherapy. For anaplastic cancer, association of<br />
surgery (whenever possible), chemotherapy and external beam<br />
radiotherapy is performed with the aim of improving the poor<br />
control of loco-regional disease.<br />
Molecular tumor profiling is one of the most promising<br />
strategies for achieving an improvement of risk stratification<br />
and prognostic evaluation of differentiated thyroid carcinoma.<br />
Mutation analysis of the gene encoding B-type Raf kinase<br />
(BRAF) is performed in parallel to classic cytology before total<br />
thyroidectomy. It is a potential diagnostic and prognostic marker<br />
for papillary thyroid carcinoma (PTC) and is used 1) to increase<br />
diagnostic accuracy in fine-needle aspiration biopsies for PTC<br />
and for minimal disease metastatic to cervical lymphnodes, 2) in<br />
determining the aggressiveness of PTC because BRAF mutations<br />
could be associated to unfavorable patient outcome.<br />
Pediatric tumors<br />
Special attention is paid to pediatric patients, designing a<br />
section with a comfortable environment with toys and audiovisual<br />
systems and with the constant presence of an anesthesiologist for<br />
deep sedation treatment. The pediatric patients are about 150<br />
per year; sarcomas, brain tumors and hematologic malignancies<br />
predominate.<br />
Protocols within the International Society of Pediatric<br />
Oncology: EpSSG RMS & nRMS (Padova Center coordinator<br />
for radiotherapy); High-risk neuroblastoma; Hodgkin Euronet<br />
(Padova Center coordinator for radiotherapy); Wilms’ tumor;<br />
Low-grade glioma (Padova Center coordinator for radiotherapy);<br />
High-grade glioma (Padova Center coordinator for radiotherapy);<br />
Germ cell brain tumors; Craniopharyngioma; Ependymoma;<br />
Atipical theratoid rhabdoid tumors.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
113
125 Iodine episcleral plaque brachytherapy of<br />
choroidal melanoma<br />
The treatment of choroidal melanoma can be performed using<br />
several different therapeutic options, including surgery (partial<br />
resection or enucleation) and different modalities of radiotherapy.<br />
The application of episcleral plaques charged with 125 Iodine is<br />
an effective approach in the conservative treatment of choroidal<br />
melanoma. The Collaborative Ocular Melanoma Study (COMS),<br />
with over 20-year experience, has shown that the length of survival<br />
following radiation or enucleation is not different. Choroidal<br />
melanoma is a relatively radioresistant disease that grows in an<br />
organ very sensitive to radiation. Other tissues, such as optic<br />
nerve and chiasma, can be damaged by relatively low doses of<br />
radiation. A dose higher than 50 Gy can cause a permanent vision<br />
loss, and the therapeutic dose for treatment of the disease ranges<br />
between 50 and 100 Gy. For this reason, it is necessary to irradiate<br />
with a highly collimated technique that could preserve the more<br />
radiosensitive structures of the eye, with a significant decrease in<br />
dose outside the target. There are different isotopes that are used<br />
like Rutenium, but the 125 I energy can better cover the target up<br />
to the depth of 10 mm. The ophthalmic plaque is positioned by<br />
the ophtalmologist to direct contact of the sclera for a period<br />
determined by the Physicist. The dose administered is 85 Gy to<br />
the apex of the lesion, with a dose administration rate ranging<br />
between 50 and 105 cGy/h.<br />
From June 1994 to December <strong>2010</strong>, in collaboration with the<br />
Clinica Oculistica of the University of Padova, we have treated<br />
710 patients with choroidal melanoma and ciliary body with<br />
125 Iodine brachytherapy. Local control was obtained in more than<br />
90% of patients; useful visual acuity (>1/10) was maintained<br />
in 65% of treated eyes. The major complication was radiation<br />
chorioretinopathy (60% of treated eyes), in particular radiation<br />
maculopathy and optic neuropathy.<br />
The INFN Legnaro laboratories Boron<br />
Neutron Capture Therapy (BNCT) project<br />
The Legnaro BNCT project is a collaborative enterprise that<br />
involves the INFN Legnaro Laboratories, the Radiotherapy Dept.<br />
of the <strong>IOV</strong>, the Department of Physics of Padova University and<br />
the Department of Biology of Padova University. BNCT is a<br />
binary radiation therapy. First, a boronated substance is injected<br />
into patients, then the patient is irradiated with thermal or<br />
epithermal neutrons. The boron transport molecule is harmless<br />
and designed to be preferably captured by tumor cells. Because of<br />
the high 10 B thermal neutron capture cross section (3837 barn),<br />
the nuclear reaction 10 B(n, )7Li is likely to occur. The nuclear<br />
reaction fragments thus produced (4He of 1.47 MeV and 7Li of<br />
0.84 MeV) are densely ionizing charged particles, whose reach<br />
in soft tissues (~8 μm for the α particle, 5 μm for the lithium<br />
ion) is as short as cell diameter (~10 μm). Therefore, only cells<br />
Fig. 1a-b: a) left side. Complete RFQ structure installed at LNL. b) right side. First RFQ electromagnetic segment ready for the high power test in France.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
114
Fig. 2. The thick Beryllium target, with the inlet and outlet water pipes<br />
for cooling, has been designed at LNL and constructed at the Efremov<br />
Institute of St. Peterburg (Russia).<br />
containing 10 B are damaged, while the healthy surrounding cells<br />
are spared.<br />
The INFN Legnaro National Laboratory (LNL) has been<br />
constructing the high power proton accelerator that will be used<br />
to generate the intense neutron source for BNCT. The proton<br />
source (TRIPS) has been developed at the INFN South National<br />
Laboratory of Catania and optimized at LNL in 2007. Protons<br />
are transported into the accelerator through a beam line, which<br />
is ready to be assembled with magnets, pumping system, non<br />
interceptive profile and current diagnostics, interceptive profiler<br />
and current monitor. The proton accelerator, a radio frequency<br />
quadrupole (RFQ), has been completed in October 2009. The<br />
complete structure was installed at LNL in November 2009<br />
(Fig.1a) and was successfully tested at low power at the beginning<br />
of <strong>2010</strong>. The next step is the RFQ high power test. Such test will<br />
be performed at Saclay (France) in <strong>2011</strong>. Fig.1b shows the first<br />
RFQ electromagnetic section ready for the high power test.<br />
The 30 mA – 5 MeV proton beam will impinge the thick<br />
beryllium target (Fig.2), which will generate, because of a well<br />
known nuclear reaction, the intense neutron flux for BNCT<br />
clinical studies.<br />
Neutrons emerging from the Beryllium target have 1.35 MeV<br />
mean energy. They have to be slowed down to thermal energy to<br />
be used for BNCT on shallow tumors. Neutrons are slowed down<br />
with a multilayer, multi-material heavy structure (BSA), which<br />
has to be properly designed. The physical parameters for such a<br />
design have been measured with the Legnaro accelerator facility.<br />
The first BSA design points out that the Legnaro source will be the<br />
most intense and clean neutron source available in Italy. It will be<br />
ideal for shallow tumor BNCT treatment.<br />
Center for the study of Acute and Late<br />
Effects of Irradiation in Head-and-Neck Area<br />
We recently activated a center for the study, prevention and<br />
treatment of oropharyngeal toxicity. It is at the forefront in the<br />
provision of diagnostic and therapeutic services for patients<br />
suffering of dysphagia as an effect of either head-and-neck cancer<br />
or radiochemotherapy. Patients with suspected swallowing<br />
disorders should be carefully evaluated and appropriate treatment<br />
initiated in order to prevent complications such as dehydration,<br />
malnutrition, choking and pneumonia. The approach to dysphagia<br />
is interdisciplinary and performed by professionals skilled in the<br />
management of the disease. The interventions of the center are:<br />
Instrumental examination: fiberoptic examination of<br />
swallow (FEES).<br />
Speech and language therapy: evaluation and management of<br />
oropharyngeal diysphagia by means of clinical bedside assessment<br />
and swallowing therapy, such as diet modification, compensatory<br />
techniques and strategies designed to facilitate or stimulate the<br />
swallow.<br />
Psychological support: continuous evaluation of patients’<br />
quality of life, by offering help in disease control, renewed purpose<br />
in life, changes acceptance and late side effects adaptation.<br />
Nursing support: health education, weight control,<br />
management and monitoring of toxicity, such as oral mucositis,<br />
xerostomia, pain and dermatitis.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
115
Major Ongoing Research Projects<br />
Boron neutron capture therapy (bnct) in<br />
cutaneous recurrences of breast cancer: the<br />
utility of pet/ct<br />
Principal Investigator: Laura Evangelista<br />
The rational of our study is based on the execution of BNCT<br />
in cutaneous recurrences of breast cancer, mainly taking into<br />
account the knowledge about the selective adsorption of 10 B in<br />
tumor sites using molecular imaging. The 10 B is accumulated in<br />
cancer cells by a specific carrier: Boron Phenylalanine (BPA).<br />
Positron emission tomography/computed tomography (PET/<br />
CT) with 18 F-BPA is able to determine the in vivo concentration<br />
of BPA at the site of relapse, generating a clear map of 10 B-BPA<br />
distribution. The biodistribution of BPA is selective for the<br />
cells with high turnover; therefore 18 F-BPA PET/CT is able to<br />
characterize all sites of disease recurrence beyond those already<br />
known determining a change of the therapeutic management.<br />
The execution of 18 F-PBA PET/CT, as a valid alternative for<br />
the evaluation of 10 B-BPA concentration, could let us decide if the<br />
indication to the routine examination is correct and if the approach<br />
with BNCT can be considered as a valid choice.<br />
This is a prospective study recruiting patients with cutaneous<br />
recurrence of breast cancer. The selected patients will undergo 18 F-<br />
BPA PET/CT and subsequently surgery. Comparison between<br />
imaging and histologic examination will be made.<br />
Intrabeam project for intraoperative<br />
radiotherapy versus whole breast irradiation<br />
in breast cancer (TARGIT-A Trial)<br />
Principal Investigator: Guido Sotti<br />
Ninety percent of local breast cancer recurrences occur within<br />
the index quadrant despite the presence of multicentric cancers<br />
elsewhere in the breast. For selected patients with early breast<br />
cancer, a single dose of radiotherapy delivered at the time of surgery<br />
by use of intraoperative radiotherapy should be considered as an<br />
alternative to external beam radiotherapy delivered over several<br />
weeks. Women with early breast cancer are eligible for enrolment<br />
if aged 45 years or older and suitable for wide local excision for<br />
invasive ductal carcinoma, unifocal on conventional examination<br />
and imaging. Preoperative diagnosis of lobular carcinoma is an<br />
exclusion criterion. Patients’ assessments are scheduled at entry, 3<br />
months, and 6 months later; thereafter, they are scheduled every 6<br />
months up to 5 years, and then yearly for up to 10 years.<br />
The primary outcome of the trial is pathologically confirmed<br />
local recurrence in the conserved breast. The secondary outcome<br />
measure is local toxicity or morbidity.<br />
Intraoperative radiotherapy as a tumor bed<br />
boost (TARGIT−B)<br />
Principal investigator: Guido Sotti<br />
Patients with high risk of local recurrence are defined by either<br />
being 45 years or younger, or between 46 and 50 years but with any<br />
of the following risk factors: grade 3, ER negative, lymphovascular<br />
invasion, nodal involvement, positive margins. These patients will<br />
undergo a boost of intraoperative radiotherapy of the tumor bed<br />
followed by standard external beam irradiation. The control group<br />
will receive standard external beam radiotherapy only.<br />
Imaging Studies by Pet-Ct<br />
Principal investigators: Anna Rita Cervino, Laura Evangelista,<br />
Michele Gregianin, Giorgio Saladin<br />
PET-CT scans in Lymphoma<br />
Both Hodgkin’s lymphoma and non-Hodgkin’s lymphomas<br />
are potentially curable malignancies. A large part of patients<br />
with these diseases achieve complete clinical response, however<br />
disease relapse rate can be as high as 30-35%. Despite different<br />
efforts to define the impact of clinical and pathological factors on<br />
disease behavior, it is evident that risk stratifying systems are as<br />
yet inadequate to individualize or personalize therapy. The use of<br />
18 F-FDG and PET-CT integrated platforms has recently changed<br />
the definition of therapy response, but it has also imposed a<br />
significant change in disease management. Different national and<br />
international multicentric studies are in progress in this particular<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
116
field and the Nuclear Medicine Service of <strong>IOV</strong> is participating<br />
in two different studies, in particular in evaluating the rapidity<br />
of response to therapy (PET interim evaluation) that represents<br />
the main prognostic factor for these patients. The preliminary<br />
results demonstrate that an early poor response evaluated by<br />
means of FDG-PET may suggest a shift towards more intense<br />
chemotherapy regimens, and indicate that FDG-PET can be<br />
considered a very important diagnostic and prognostic tool in<br />
lymphoma management. FDG-PET is used with the same purpose<br />
also during clinical follow-up of patients with lymphoma at the<br />
end of therapy, because of its ability to detect an early relapse of<br />
the disease.<br />
PET-CT scans in Colorectal Carcinoma (CRC)<br />
CRC is the most frequent cancer in western countries and<br />
it is now considered as a social disease because of its impact on<br />
the health system. FDG-PET seems to be the most sensitive<br />
imaging approach for early detection of local recurrence and<br />
distant metastases. Recently our Nuclear Medicine Service in<br />
collaboration with Surgery and Oncology Departments undertook<br />
a prospective study aimed at comparing the diagnostic value of<br />
FDG-PET versus Multislice CT and MRI in distant metastasis<br />
detection, in particular for liver metastases. A second study is<br />
ongoing on FDG-PET scanning impact on CRC local recurrence<br />
detection after surgery and radiotherapy.<br />
PET-CT in Radiation Therapy Planning<br />
A recent report of IAEA agency stated that PET-CT is a<br />
significant advance in cancer imaging with great potential for<br />
optimizing radiation therapy planning, thus improving the patient<br />
outcome. Numerous studies support the routine use of FDG-<br />
PET for radiotherapy volume determination in lung cancer, headand-neck<br />
cancer, lymphomas and esophageal cancer. We began in<br />
patients affected by lymphoma a program of acquisition of PET-<br />
CT images in radiotherapy treatment position by means of the<br />
same carbon bed used during radiation treatment. Moreover, we<br />
are testing and validating a new technique to decide the volume<br />
to treat based on the contemporary acquisition of contrast CT<br />
images and PET images, and matching anatomical images of CT<br />
with functional PET images.<br />
PET-CT in Thyroid Cancer Management<br />
Thyroid cancer incidence is rising, even though mortality is<br />
today not significantly different from that recorded in the ’70s.<br />
The lack of increased mortality despite increasing incidence was<br />
interpreted as evidence of an early diagnosis and adequate therapy<br />
based on surgery and 131 I treatment. At <strong>IOV</strong> we follow a large series<br />
of differentiated thyroid carcinoma (DTC) patients undergoing<br />
different regimens of treatment based on the stage of disease. FDG-<br />
PET scanning is assuming a more central role in the follow-up of<br />
patients with DTC. It is well established that DTC lesions most<br />
visible by FDG-PET scans are those that are less able to capture<br />
iodine; in DTC management FDG-PET is used in our Department<br />
for many purposes: a) diagnosis of disease recurrence in patients with<br />
increased thyroglobulin and negative 131 I whole body scan; b) as a<br />
guidance for selective reintervention in patients with a local disease<br />
relapse; c) for patients with metastatic disease out of 131 I therapy<br />
to estimate the progression of disease and to enter the patient in a<br />
chemotherapy protocol; d) in selected cases, in combination with<br />
recombinant human TSH, with the aim of increasing diagnostic<br />
sensitivity of scanning in patients with increased thyroglobulin<br />
levels and negative 131 I whole body scan.<br />
PET-CT in Pediatric Oncology<br />
There is an increasing interest of PET-CT application in<br />
pediatric oncology, derived by an increasing number of papers<br />
indicating that lymphomas and other solid tumors in children<br />
accumulate FDG in the same manner as in adult patients. The<br />
European Nuclear Medicine Society recently published the<br />
Guidelines for FDG PET-CT imaging in pediatric oncology.<br />
In particular, in patients with soft-tissue sarcoma (STS), the<br />
early assessment of treatment response is important. We are<br />
determining in a group of patients with STS the usefulness of<br />
FDG-PET in evaluating treatment response after chemotherapy<br />
and chemoelectric therapy. FDG-PET is performed before therapy<br />
and after the first cycle of therapy to distinguish responder from<br />
non-responder STS patients.<br />
FCH PET-CT in Prostate Cancer<br />
Since <strong>2010</strong> we perform 18 F-choline PET-CT (FCH PET-<br />
CT) for evaluation of patients with prostate cancer after radical<br />
treatment. As reported in the literature, this survey is particularly<br />
indicated in patients with increased serum prostate-specific<br />
antigen (PSA) and negative conventional imaging. FCH PET-CT<br />
could become a crucial tool in radiotherapy target volumes and<br />
early therapy evaluation.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
117
Programs and Future Perspectives<br />
Set up of Intraoperative Radiotherapy (IORT) with<br />
INTRABEAM through participation in a clinical trial for the<br />
Prevention of recurrences in breast cancer. The study, called<br />
Targit A (Intraoperative Targeted Radiotherapy), is randomized and<br />
controlled, comparing conventional post-operative radiotherapy with<br />
intra-operative radiotherapy in patients over 45 years undergoing<br />
conservative surgery. There are more than 25 participating centers<br />
in the world and two in Italy. The study has already been approved<br />
by the Ethics Committee of the <strong>IOV</strong>. Another important study<br />
that will help to improve the knowledge and use of Intraoperative<br />
Radiation Therapy protocol will be the Targit B, in preparation,<br />
dedicated to breast cancer patients at high risk of relapse.<br />
The Boron Neutron Capture Therapy (BNCT) is a new<br />
technique of radiation therapy that uses the “Boron neutron<br />
Major Collaborations<br />
National Collaborations<br />
<strong>IOV</strong> (Breast Imaging, Clinical Oncology 1, Clinical Oncology<br />
2, Breast Surgery)<br />
University of Padova (Clin. Chir. II; Chir. Toracica; An.<br />
Patologica)<br />
Dip. of Pediatria (Oncoematologia, Chirurgia)<br />
CRO Aviano<br />
AIRO (Associazione Italiana Radioterapia Oncologica)<br />
INFN (Istituto Nazionale di Fisica Nucleare) Legnaro<br />
INFN (Istituto Nazionale di Fisica Nucleare) Pavia<br />
capture” by a substance injected into the patient carrying the 10 B<br />
isotope that binds selectively to cancer cells and is subsequently<br />
irradiated with an accelerator of protons. This allows a high<br />
selectivity of the target to be achieved with less damage to<br />
surrounding tissues. The project is advanced and two clinical<br />
trials, in collaboration with the Universities of Pavia, Catania<br />
and the laboratories of the Institute of Nuclear Physics (INFN),<br />
Legnaro are programmed.<br />
The acquisition of a tomotherapy is mandatory, due to the<br />
continuous search for improvement of therapy for patients with<br />
cancer who are referred to our Unit. The renewal of certain<br />
equipment as a new Rapid Arc accelerator, a simulator and a Spec-<br />
Tac CT dedicated to nuclear medicine is also foreseen.<br />
International Collaborations<br />
NYU Clinical Cancer Center – New York University School of<br />
Medicine<br />
University College, London<br />
International Society of Paediatric Oncology<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
118
Main Pubblications<br />
Chief<br />
Medical Physics<br />
Marta Paiusco, Physicist<br />
Commissioning Siemens Virtual Wedges in the Oncentra<br />
MasterPlan treatment planning system using Gafchromic EBT<br />
film.<br />
PET/CT and radiotherapy: data transfer, radiotherapy workflow<br />
and quality assurance.<br />
Physical radiotherapy treatment planning based on functional<br />
PET/CT data.<br />
Dosimetric verification of IMAT delivery with a conventional<br />
EPID system and a commercial portal dose image prediction tool.<br />
A two-variable linear model of parotid shrinkage during IMRT for<br />
head and neck cancer.<br />
Born in Mantova on June 6, 1962, she graduated in Physics at the University of Parma. Since 1996<br />
she has worked at the Department of Medical Physics of the “Arcispedale S.Maria Nuova” Hospital<br />
in Reggio Emilia. The principal field of interest is radiation dosimetry including: quality assurance,<br />
in vivo dosimetry and planning optimization, mainly dedicated to IMRT.<br />
Member of the ESTRO, AIFM and ISS groups, she is co-author of guidelines on IMRT dosimetry.<br />
She is co-investigator in a project on the use of functional images in Tomotherapy. Author of several<br />
articles she has been invited in many national and international congresses.<br />
Current research interests include image-guided radiotherapy, adaptive interventions for IMRT,<br />
radiation dose-response assessment and health technology assessment.<br />
Ferretti A, Simonato F, Zandonà R, Reccanello<br />
S, Fabbris R.<br />
Fioroni F, Iotti C, Paiusco M, Versari A, Grassi<br />
E, Salvo D, Iori M.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
120<br />
Med. Phys. <strong>2010</strong>; 37:6310-<br />
6316<br />
Q J Nucl Med Mol Imaging.<br />
<strong>2010</strong>; 54:476-89<br />
Thorwarth D, Geets X, Paiusco M. Radiother Oncol. <strong>2010</strong>; 96:317-<br />
24<br />
Iori M, Cagni E, Paiusco M, Munro P,<br />
Nahum AE.<br />
Broggi S, Fiorino C, Dell’Oca I, Dinapoli N,<br />
Paiusco M, Muraglia A, Maggiulli E, Ricchetti<br />
F, Valentini V, Sanguineti G, Cattaneo GM,<br />
Di Muzio N, Calandrino R.<br />
Med Phys. <strong>2010</strong>; 37:377-90<br />
Radiother Oncol. <strong>2010</strong>; 94:206-<br />
12
Clinical and Research Staff<br />
Marta Paiusco<br />
Davide Canonico<br />
Sonia Reccanello<br />
Lucia Riccardi<br />
Franca Simonato<br />
Roberto Zandonà<br />
Michele Bignotto<br />
Technical Staff<br />
Simonetta Bacco<br />
Carlo Merlo<br />
Nicola Pivato<br />
Marco Rossato<br />
Administrative Staff<br />
Grazia Rossetto<br />
Mariella Zuanon<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
121
Mission<br />
To assure safe, accurate and high-quality patient care in<br />
collaboration with Clinical Services in Diagnostic, Radiation<br />
Clinical Activity<br />
The Medical Physics Unit provides services for three Institution<br />
in Padua: Istituto Oncologico Veneto, Azienda Ospedaliera –<br />
Università di Padova, and ULSS16.<br />
In the field of radiation therapy the Unit provides quality<br />
assurance of imaging, treatment delivery equipment and<br />
treatment planning systems to ensure optimal, accurate and<br />
safe dose delivery. It is responsible for radiation dosimetry and<br />
QA of sophisticated radiotherapy treatments like Stereotactic<br />
Radiotherapy (SRT), Stereotactic Radiosurgery (SRS), Intensity<br />
Modulated Radiotherapy (IMRT), Image Guided Radiotherapy<br />
(IGRT), Total Body Irradiation (TBI), HDR Brachytherapy and<br />
COMS 125 I eye plaque Brachytherapy.<br />
In the area of Diagnostic and Nuclear Medicine, the Unit<br />
Major Research Collaborations<br />
National Collaborations<br />
Radiation Therapy and Nuclear Medicine Unit of the <strong>IOV</strong><br />
Breast Surgery of the <strong>IOV</strong><br />
Nuclear Medicine Department of Azienda Ospedaliera di<br />
Padova<br />
Radiology Department of Azienda Ospedaliera di Padova<br />
Neurological Surgery Department of Azienda Ospedaliera di<br />
Padova<br />
CRO Aviano<br />
Oncology, and Nuclear Medicine.<br />
supports clinical services in optimizing patient radiation exposure<br />
in diagnostic and interventional procedures, estimating fetal dose.<br />
It collaborates with clinical Units for Quality Assurance. In the<br />
field of Radiation Protection it covers all aspects dealing with<br />
radiation safety of the workers and the population, according to<br />
national regulations.<br />
The Medical Physics Unit evaluates and commissions<br />
equipment and systems appropriate for clinical practice and in<br />
any area takes an active role in research. The staff is involved in<br />
the teaching and training medical students of Padua University<br />
on Physics in Radiotherapy, Radiology and Nuclear Medicine and<br />
on Radiation Safety. Furthermore, the physicists are engaged in<br />
teaching courses and internships for the Post-Graduate School of<br />
Medical Physics.<br />
International Collaborations<br />
NYU Clinical Cancer Center -New York University School of<br />
Medicine<br />
University College, London<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
122
Major Ongoing Research Projects<br />
The Medical Physics Unit has been recently involved in two<br />
projects concerning the verification of the accuracy of the dose<br />
distribution calculated by a commercial treatment planning<br />
system.<br />
COmmiSSiONiNG SiEmENS virTual wEDGES iN ThE<br />
ONCENTra TrEaTmENT plaNNiNG SySTEm uSiNG<br />
GafChrOmiC EbT film<br />
Principal investigator: Franca Simonato<br />
Contributors: Roberto Fabbris, Alice Ferretti, Sonia Reccanello,<br />
Roberto Zandonà<br />
Purpose. Virtual Wedges were introduced in Siemens<br />
LINAC to improve the treatment workflow. The aim of the work<br />
was the validation of dose calculation by MasterPlan-Oncentra<br />
treatment planning system for virtual wedged beams.<br />
Methods. The Oncor Siemens accelerator installed in the<br />
Radiation Therapy Unit produces 6 and 15 MV photon beams.<br />
At first, the consistency of VW LINAC production was tested and<br />
the EBT film measuring method was verified. Then, the measured<br />
and calculated wedge factors and beam profiles were compared.<br />
For 15°, 30°, 45°, and 60° wedge angles, the wedge factors for<br />
different field sizes were measured by an ionization chamber and<br />
the dose profiles acquired by Gafchromic EBT film.<br />
Results. The comparison between measured and calculated VW<br />
factors shows discrepancies that increase with field size and angle.<br />
The OTP Enhanced algorithm fits better with measurements than<br />
the Classic one, with overall improvement visible for large angles.<br />
The agreement between measured and planned beam profiles is<br />
within the limits reported by the ESTRO Booklet No. 7 in terms<br />
of confidence limits.<br />
Conclusions. The MasterPlan-Oncentra treatment planning<br />
system determines wedge factors and VW profiles within the<br />
requested accuracy in the majority of treatment conditions. For<br />
big field dimensions and wedge angle, wedge factor accordance<br />
was worse, but it could be increased with an improvement of the<br />
LINAC dosimetric board calibration.<br />
COmmiSSiONiNG Of a COmmErCial TpS baSED ON ThE<br />
vmC++ mC CODE fOr ElECTrON bEamS: valiDaTiON<br />
aND COmpariSON wiTh EGSNrC<br />
Principal Investigator: Andrea Martignano<br />
Contributors: Alice Ferretti, Franca Simonato<br />
Purpose. Some commercial TPS already use MC engines<br />
for dose calculation. The aim of this work was to perform the<br />
commissioning of the VMC++ Monte Carlo (MC) engine<br />
implemented in the Oncentra Masterplan TPS for electron dose<br />
calculation, and to verify its accuracy comparing the results to the<br />
EGSnrc MC code.<br />
Methods. The commissioning procedure for the TPS consists<br />
of measurements of output factors and profiles in x,y and z<br />
direction, in both air and water. The BEAMnrc MC code was<br />
used as a benchmark: BEAMnrc required the geometries of the<br />
LINAC head, which were provided by Siemens; the optimisation<br />
was done considering PDD and profiles in water. Commissioning<br />
results were evaluated by means of 1D Gamma Analysis (2%,<br />
2mm), calculated with a home-made Matlab program.<br />
Masterplan dose distribution maps were compared to the<br />
results of BEAMnrc, in two virtual phantoms: one made of<br />
water with an air insert, and the second with a bone insert. The<br />
comparison was done by means of 2D Gamma Analysis (3%,<br />
3mm), and comparing significant profiles and PDD.<br />
Results and conclusions. The results of the commissioning<br />
of the TPS were good. The optimisation of the BEAMnrc model<br />
of the LINAC required the modification of some components to<br />
match the calculated and measured profiles: the final agreement<br />
was very good. The agreement of the dose distributions calculated<br />
with the TPS and with EGSnrc with the air-insert phantom was<br />
high; with the bone-insert phantom there were differences of<br />
about 10-15% in the bone region. This is due to the fact that<br />
the Masterplan implementation of VMC++ reports the dose as<br />
“dose to water”, instead of “dose to medium” (therefore it is not a<br />
dosimetric error).<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
123
Other Programs and Future Perspectives<br />
Three new treatment modalities are going to be implemented<br />
at the <strong>IOV</strong>: the Intra Operative RadioTherapy (IORT) for<br />
breast cancer, the Prone Breast radiotherapy and the IMRT for<br />
prostate and Head and Neck cancer. In close collaboration with<br />
the Radiotherapy Unit, the Medical Physics Staff will be involved<br />
in the technique development. The primary focus will be on the<br />
dosimetry aspects and three projects have been designed.<br />
Implementation and dosimetry optimization<br />
of IORT for breast cancer with IntraBeam<br />
System<br />
Principal investigator: Sonia Reccanello<br />
Contributors: Davide Canonico, Andrea Martignano, Marta<br />
Paiusco, Franca Simonato, Roberto Zandonà<br />
Purpose. Many studies demonstrate that after breastconserving<br />
surgery conventional post-operative whole breast<br />
radiotherapy might be unnecessary but could be suitable an<br />
intra-operative single fraction radiotherapy targeting only the<br />
peritumoral tissue. The Istituto Oncologico Veneto has recently<br />
bought the Intraoperative System IntraBeam and will participate<br />
in the breast protocol TargitA [1] by testing whether radiotherapy<br />
to the index quadrant alone can achieve as good a local control as<br />
radiotherapy to the whole breast.<br />
To determine the success of the radiotherapy treatment a key<br />
role is played by the dosimetric accuracy of the treatment. The<br />
project has therefore the aim to develop efficient and effective<br />
methods to verify the delivered dose.<br />
It will be divided in four phases:<br />
1. Equipment acceptance tests, dosimetric characterization and<br />
clinical implementation<br />
2. Dosimetric verification by Monte Carlo simulation<br />
3. Dosimetric characterization of a new specific dosimeter<br />
4. Research and development of a methods to optimize the dose<br />
distribution<br />
In addition, multicenter dosimetry will be programmed.<br />
[1] (Jayant S. Vaidya et al - Lancet Vol 376 - July 10, <strong>2010</strong>).<br />
Dosimetric verification and implementation<br />
of IMRT and IGRT for prostate and head-andneck<br />
cancer<br />
Principal investigator: Simonato Franca<br />
Contributors: Davide Canonico, Andrea Martignano, Marta<br />
Paiusco, Sonia Reccanello, Roberto Zandonà<br />
Purpose. Intensity-modulated radiation therapy (IMRT)<br />
is an advanced delivery technique that, thanks to the intensity<br />
modulation of the beams, allows doses highly conformed to the<br />
tumor. Moreover the possibility to create steep dose gradients<br />
makes it possible to escalate the dose inside the tumor while<br />
minimizing the dose to surrounding normal structures.<br />
On the other hand, because of the gradients, the IMRT can<br />
be safely implemented only with an Image Guided Radiotherapy<br />
system (IGRT). The IGRT has the aim to guarantee that the<br />
planning position is the same during the delivery time.<br />
IMRT- IGRT will be implemented for Head-and-Neck and<br />
prostate tumors according to several steps:<br />
Commissioning and clinical introduction of the IGRT system:<br />
BATCAM<br />
Margin definition for prostate<br />
Definition of a verification protocol for head-and-neck<br />
treatments<br />
Margin definition for Head-and-Neck<br />
Dosimetric verification with EPID<br />
Implementation and dosimetry optimization of<br />
prone breast radiotherapy<br />
Principal investigator: Sonia Reccanello<br />
Contributors: Davide Canonico, Andrea Martignano, Marta<br />
Paiusco, Franca Simonato, Roberto Zandonà<br />
Purpose. The radiotherapy goal is to increase the probability<br />
of locoregional tumor control without severe toxicity to the<br />
surrounding normal tissues. Highly conformed delivery techniques<br />
allow to escalate the dose to the tumor while sparing the organ<br />
at risk. Regarding breast cancer the “Prone Breast” technique,<br />
developed by Dr. Silvia Formenti, New York University School<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
124
of Medicine, seems to be a promising modality. The Medical<br />
Physics Department in collaboration with NYU will assess the<br />
actual feasibility of this new set-up. At first the technique will be<br />
clinically implemented as at the NYU. The reproducibility of the<br />
technique will then be evaluated. A dosimetric comparison, in<br />
term of tumor coverage and complication probability will be done<br />
between prone and supine position.<br />
THE DEPARTMENTS - DEPARTMENT OF RADIOTHERAPY AND NUCLEAR MEDICINE<br />
125
Department of Experimental,<br />
Laboratory & Translational<br />
Oncology<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
127
Main Pubblications<br />
Immunology and<br />
Molecular Oncology<br />
Chief<br />
Ligand-driven activation of the notch pathway in<br />
T-ALL and solid tumors: why Not(ch)?<br />
New Technologies for Cervical Cancer screening<br />
(NTCC) Working Group: Efficacy of human<br />
papillomavirus testing for the detection of invasive<br />
cervical cancers and cervical intraepithelial neoplasia:<br />
a randomised controlled trial.<br />
Relationship between telomere shortening, genetic<br />
instability, and site of tumor origin in colorectal<br />
cancers.<br />
Tumor-induced tolerance and immune suppression<br />
depend on the C/EBPbeta transcription factor.<br />
Annarosa Del Mistro, MD<br />
1976-1982: Medical School at the University of Padua. Degree of Doctor in Medicine (Honour)<br />
1982-1985: Postgraduate School in Oncology, University of Padua. 1987-1991: Postgraduate School<br />
in Pathology, University of Verona. 1982-1985: Scholarship from the Ministry of Education for the<br />
Postgraduate School in Oncology. 1985-1987: Research Associate at the Pathology Department,<br />
Montefiore Medical Center, New York, USA. 1987-2006: employment by Azienda Ospedaliera<br />
di Padova. 2006-ongoing: employment by Istituto Oncologico Veneto - Temporary Director since<br />
February 2008. Main research interests: Human Papilloma Viruses (HPV): prevalence, pathogenetic<br />
role and application of HPV tests in cervical screening and patient management (ano-genital and<br />
head-and-neck tumors); mechanisms of lymphomagenesis (studies on cases of human lymphomas<br />
and on the experimental SCID mouse model); HTLV-1/2 and HIV-1/2 infections and associated<br />
neoplastic diseases. Co-author of 70 papers on peer-reviewed journals.<br />
Indraccolo S, Minuzzo S, Masiero M, Amadori A. Cell Cycle <strong>2010</strong>; 9:80-85<br />
Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Dalla<br />
Palma P, Del Mistro A, Ghiringhello B, Girlando S, Gillio-<br />
Tos A, De Marco L, Naldoni C, Pierotti P, Rizzolo R,<br />
Schincaglia P, Zorzi M, Zappa M, Segnan N, Cuzick J.<br />
Rampazzo E, Bertorelle R, Serra L, Terrin L, Candiotto C,<br />
Pucciarelli S, Del Bianco P, Nitti D, De Rossi A.<br />
Marigo I, Bosio E, Solito S, Mesa C, Fernandez A, Dolcetti<br />
L, Ugel S, Sonda N, Bicciato S, Falisi E, Calabrese F, Basso<br />
G, Zanovello P, Cozzi E, Mandruzzato S, Bronte V.<br />
A MicroRNA targeting dicer for metastasis control. Martello G, Rosato A, Ferrari F, Manfrin A, Cordenonsi<br />
M, Dupont S, Enzo E, Guzzardo V, Rondina M, Spruce T,<br />
Parenti A R, Daidone M G, Bicciato S, Piccolo S.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
128<br />
Lancet Oncol <strong>2010</strong>; 11:249-257<br />
Brit J Cancer <strong>2010</strong>; 102: 1300-<br />
1305<br />
Immunity <strong>2010</strong>; 32:790-802<br />
Cell <strong>2010</strong>; 141:1195-1207
Clinical and Research Staff<br />
Annarosa Del Mistro<br />
Laura Bonaldi<br />
Roberta Bertorelle<br />
Vincenzo Bronte<br />
Maria Luisa Calabrò<br />
Vincenzo Ciminale<br />
Donna D’Agostino<br />
Emma D’Andrea<br />
Anita De Rossi<br />
Giovanni Esposito<br />
Antonella Facchinetti<br />
Stefano Indraccolo<br />
Susanna Mandruzzato<br />
Chiara Menin<br />
Marco Montagna<br />
Sonia Minuzzo<br />
Antonio Rosato<br />
Daniela Saggioro<br />
Rita Zamarchi<br />
Marisa Zanchetta<br />
Paola Zanovello<br />
Simona Agata<br />
Valentina Agnusdei<br />
Lorena Baboci<br />
Elisa Bergamo<br />
Lorena Biasini<br />
Cinzia Candiotto<br />
Francesco Carmona<br />
Silvia Dalla Santa<br />
Adamo Diamantini<br />
Helena Frayle Salamanca<br />
Riccardo Freguja<br />
Sonia Keppel<br />
Laura Lignitto<br />
Annalisa Martines<br />
Barbara Molon<br />
Giorgia Nardo<br />
Elena Negri<br />
Enrica Rampazzo<br />
Enrica Rumiato<br />
Mukherjee Subhamoy<br />
Elisabetta Tebaldi<br />
Silvia Tognazzo<br />
Administrative Staff<br />
and Technicians<br />
Vito Barbieri<br />
Emanuela Colucci<br />
Barbara Filippi<br />
Monica Gardin<br />
Antonella Ghinatti<br />
Margherita Marangoni<br />
Raffaella Marcato<br />
Monica Quaggio<br />
Elisabetta Rossi<br />
Cristina Sartorato<br />
Pietro Savelli<br />
Paola Sorgato<br />
Rossana Trevisan<br />
Salvatore Vettura<br />
Daniela Zullato<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
129
Mission<br />
The Unit includes personnel directly employed by the <strong>IOV</strong><br />
and academic personnel exploiting their institutional duties<br />
(research, assistance and teaching) in collaboration with <strong>IOV</strong>.<br />
Historically, two components constitute the nucleus of the Unit:<br />
Tumor Immunology and Viral and Molecular Oncology. These<br />
two components have been operating and creating a critical mass<br />
several decades before the <strong>IOV</strong> formation, and still continue to<br />
carry out their activities within the spirit of the new Institute.<br />
The mission of the Unit is to investigate the alterations which<br />
Clinical Activity<br />
Within the Unit molecular assays and innovative strategies for<br />
the characterization, the prognosis and the selection for the new<br />
targeted therapies of the main neoplastic diseases are implemented<br />
and performed. In particular:<br />
analyses for cytogenetic and molecular markers of oncohematologic<br />
diseases;<br />
analyses of the genes involved in the heredo-familiar forms of<br />
breast cancer and cutaneous melanoma;<br />
analyses for molecular markers of solid tumors;<br />
analyses for constitutive markers (farmacogenetics);<br />
search for circulating tumor cells in patients with metastatic<br />
breast carcinoma and other malignancies;<br />
viro-immunologic analyses of tumors and immunodeficiencies<br />
associated to infection with oncogenic viruses and retroviruses;<br />
virologic analyses of preneoplastic and neoplastic lesions of the<br />
ano-genital area.<br />
The Unit comprises 5 sub-units: Virologic Oncology<br />
(Responsible A. De Rossi); Cervical Cancer Screening<br />
(Responsible A. Del Mistro); Molecolar Biomarkers in Oncology<br />
(Responsible R. Bertorelle); Heredo-familiar Tumors of Breast<br />
and Ovary (Responsible M. Montagna); Tumor Immunotherapy<br />
(Responsible V. Bronte).<br />
characterize tumor development, on both the cancer cell site<br />
(intrinsic molecular alterations) and the host tissue in which the<br />
tumor grows (the tumor microenvironment). Along with research<br />
activity, a fundamental component of the mission of the Unit is the<br />
implementation, standardization and performance of molecular<br />
analyses and innovative strategies for up-to-date diagnostics, as<br />
well as effective follow-up and therapeutic regimens of patients<br />
affected by solid and hematologic neoplasms.<br />
Analyses for hematologic malignancies by year<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
130<br />
Number of analyses<br />
2500<br />
2000<br />
1500<br />
1000<br />
500<br />
0<br />
2008<br />
molecular analyses<br />
cytogenetic and FISH analyses<br />
2009 <strong>2010</strong> projection<br />
Year<br />
<strong>2011</strong>
Analyses for solid tumors by year Analyses for hereditary cancers by year<br />
Number of analyses<br />
500<br />
450<br />
400<br />
350<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
2008 2009 <strong>2010</strong><br />
Her2<br />
KRAS<br />
EGFR<br />
CTC<br />
Number of analyses<br />
Year<br />
Assays for oncogenic viruses<br />
2000<br />
1800<br />
1600<br />
1400<br />
1200<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
0<br />
projection<br />
<strong>2011</strong><br />
2008 2009 <strong>2010</strong><br />
Year<br />
projection<br />
<strong>2011</strong><br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
131<br />
Number of analyses<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
2008 2009 <strong>2010</strong><br />
HPV<br />
retroviruses<br />
EBV<br />
HHV8<br />
Year<br />
projection<br />
<strong>2011</strong><br />
number of new breast/ovarian cancer families (comprehensive test)<br />
number of family members tested for specific BRCA 1<br />
and BCRA 2 mutations<br />
number of new melanoma cases
Major Collaborations<br />
Inside the <strong>IOV</strong><br />
Clinical Oncology 1<br />
Clinical Oncology 2<br />
Familiar Cancer Clinics<br />
National Collaborations<br />
Azienda Ospedaliera di Padova (Clinica Pediatrica, Clinica<br />
Chirurgica 2, Ematologia, Clinica Oculistica)<br />
Registro Tumori del Veneto<br />
Azienda Ospedaliera di Verona<br />
Azienda Ospedaliera di Treviso<br />
CPO Piemonte<br />
ISPO Toscana<br />
CRO-IRCCS Aviano<br />
Università La Sapienza Roma<br />
CNR Milano<br />
Università di Modena<br />
Università di Trieste<br />
HSR Milano<br />
ISS Roma<br />
Areas of Excellence<br />
The long research activity of the components of the Unit of<br />
Immunology and Molecular Oncology translates into over 780<br />
publications in the last 20 years, with a total IF value of over 3,660.<br />
The major fields of interest, where the research groups are<br />
highly competitive on the national and international scenarios are<br />
the following:<br />
Study of heredo-familial tumors, with a particular accent<br />
on the genetic predisposition to breast and ovary tumors, and<br />
to melanoma. It is known that about 10% of the tumors are on a<br />
heredo-familial basis, due to inheritable alterations in some key genes<br />
controlling activation pathways or crucial DNA repair mechanisms<br />
within the cell. Two research groups within the Unit focus their<br />
interest on these aspects, and participate in several national and<br />
international networks aimed at characterizing all these alterations<br />
and unravelling the importance of accessory genes in determining<br />
the clinical manifestations of the genetic defects.<br />
Istituto Scientifico Romagnolo, Forlì<br />
Università di Genova<br />
ICGEB Trieste<br />
International Collaborations<br />
IARC Lyon, France<br />
Institute of Child Health, London, UK<br />
MRC, London, UK<br />
Imperial College, London, UK<br />
NCI, NIH, Bethesda<br />
Tokyo University, Japan<br />
University of Erlangen, Germany<br />
University of Miami, Miami<br />
University of Mainz, Germany<br />
IDIBELL, Barcelona, Spain<br />
Oncomed Pharm., USA<br />
Columbia University, New York<br />
Weatherall Institute of Molecular Medicine (WIMM), Oxford,<br />
UK<br />
Virologic oncology. It is known that about 20% of the<br />
tumors rely on the pathogenetic involvement of microrganisms,<br />
in particular viral agents. The interest for this aspect of oncology<br />
in humans has been steadily pursued for the last 30 years. Special<br />
attention is dedicated to: 1) the role of HPV in cancer of the<br />
uterine cervix and other sites (anus, esophagus); 2) the role of<br />
HHV-8 (also called KSV) in Kaposi’s sarcoma and Peritoneal<br />
Exudate Lymphomas; 3) the role of Retroviruses such as HTLV-I<br />
in adult leukemias; 4) the role of EBV in lymphomagenesis,<br />
especially in immunodeficient subjects (such as children and<br />
adults infected by HIV who eventually develop AIDS).<br />
Molecular oncology. The alterations arising in cells undergoing<br />
neoplastic transformation are a very hot issue in modern<br />
oncology, thanks to the availability of the most sophisticated<br />
techniques which allow an even deeper understanding of the<br />
molecular pathways governing cell cycle and the possibility of<br />
high-throughput genome and transcriptome analysis. In this<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
132
egard, the activity of some researchers of the Unit also entails<br />
a more applicative sense, since it allows dissecting the molecular<br />
alterations that confer a growing advantage to tumor cells by<br />
precluding apoptosis of the cells, and establishing whether some<br />
of these alterations could be exploited for therapeutic purposes<br />
with the so-called target molecules.<br />
Tumor-microenvironment relationship. It is becoming<br />
increasingly clear that tumor cells engage a strict interplay with the<br />
host cells that compose the bulk of tumor: fibroblasts, infiltrating<br />
inflammatory cells, endothelial cells. This relationship may be a<br />
double-edged sword; if it is undoubted that the host immune<br />
system can control tumor growth and keep neoplastic cells in check<br />
at least to a certain extent, it is also clear that some inflammatory<br />
cells of the host may play a favoring role for tumor expansion, by<br />
down-regulating the above immunological mechanisms of tumor<br />
growth control. The role of these cells, the so-called Myeloidderived<br />
Suppressor Cells, is at present a topic of great interest,<br />
because their elimination from the host could represent a smart<br />
strategy to potentiate the anti-tumor mechanisms of the host.<br />
Innovative approaches of immunotherapy. Immunotherapy<br />
of tumors is a constant dream of immunologists since the<br />
Major Ongoing Research Projects<br />
GENETiC prEDiSpOSiTiON TO brEaST aND OvariaN<br />
CaNCErS<br />
Principal Investigators: Marco Montagna, Emma D’Andrea<br />
Background. The hereditary breast and ovarian cancer Unit<br />
was established in 1995 as a multidisciplinary group interested<br />
in the identification, analysis and management of heredo-familial<br />
tumors. The Unit’s scientific projects represent one of the best<br />
examples of translational research as all research lines and clinical<br />
activities stem from the recruitment of families with breast and<br />
ovarian heredo-familial tumors. Most often research results are<br />
readily translated into the clinics with targeted medical interventions<br />
and/or preventive options and surveillance procedures for at risk<br />
healthy and affected subjects. Indeed, carriers of mutations in<br />
genes such as BRCA1 and BRCA2 face an exceedingly high risk of<br />
developing breast and ovarian cancer lifetime. Penetrance figures<br />
Burnett’s era, but the idea that vaccination against tumors<br />
could eradicate neoplasms has never maintained what it<br />
looked to promise. The reasons for this failure are numerous,<br />
and this report is not the right place to summarize them.<br />
In any case, the modern tendency of tumor immunology is to<br />
design innovative vaccination protocols by the use of more efficient<br />
adjuvants, and to combine immunotherapic approaches with the<br />
simultaneous administration of classical chemotherapeutic drugs.<br />
It is no longer time for standard interventions for everybody; a<br />
complex and well-balanced, personalized strategy that combines<br />
different therapeutic tools, including chemotherapy, will probably<br />
contribute to improve the success of these approaches in individual<br />
patients.<br />
Innovative therapeutic strategies. Several researchers at our<br />
Unit are attempting new strategies of tumor therapy, in particular<br />
anti-angiogenetic therapies aimed at deprivation of oxygen and<br />
nutrients in the tumor microenvironment. In this setting, the<br />
researchers are engaged in studying the factors that preclude<br />
a favorable response in a part of patients; this could be due to<br />
features inherent to the tumor cell itself, or rather depend on<br />
other factors linked to a particular microenvironment.<br />
range from 40 to 80% for breast cancer and from 18 and 40% for<br />
ovarian cancer.<br />
Research and clinical activities. The BRCA1 and BRCA2<br />
genetic tests are provided within the framework of a larger<br />
multidisciplinary clinical and diagnostic activity that includes<br />
pre- and post-test genetic counseling, psychological support to<br />
the patients and their relatives, as well as clinical indications for<br />
prevention and/or strict surveillance of the predisposed subjects.<br />
The Unit offers this Service to the <strong>IOV</strong> Clinical Oncology Units<br />
as well as to other oncology or medical genetics Units from<br />
the Veneto Region, by coordinating a network of Centers that<br />
extends to Trentino Alto Adige. Collaborating Centers include<br />
first level facilities where one or more clinicians keep in contact<br />
with the Unit by reporting new potential high-risk families,<br />
and second level facilities that perform the pre- and post-test<br />
counseling in-house and send directly patients’ samples to our<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
133
Unit. The Unit mission includes collaborative efforts with other<br />
regional hospitals to set up clinical genetic counseling facilities<br />
according to national and international guidelines for the genetic<br />
tests in hereditary breast and ovarian cancer patients. During the<br />
last three years, 577 new breast and ovarian cancer families were<br />
recruited and screened. A total of 760 BRCA1 and BRCA2 tests<br />
were performed using highly comprehensive mutation detection<br />
strategies that cover the entire BRCA1 and BRCA2 mutational<br />
spectra, including major genomic rearrangements. Mutationspecific<br />
tests were offered to eligible relatives of the positive cases,<br />
allowing for the identification of at risk family members who were<br />
counseled and clinically managed according to the result of the<br />
specific test. To date, the number of BRCA1/2 mutation positive<br />
families identified by the Unit from the start of its activity has<br />
raised to 253 for a total of more than 450 carriers of deleterious<br />
mutations.<br />
Results and conclusions. The understanding of the genetic<br />
determinants of the non-informative families is one of the key<br />
goals of our most recent studies. Evaluation of the clinical relevance<br />
of BRCA1 and BRCA2 sequence variants of unknown pathogenic<br />
significance, currently identified in 10-20% of individuals<br />
undergoing BRCA1/2 genetic testing, represents a valid possibility<br />
of increasing the number of informative tests. To address this<br />
problem we have used a combination of bioinformatic tools,<br />
based either on the predicted splicing effect, or the evolutionary<br />
conservation as well as the chemical/physical properties of<br />
aminoacid changes, and identified 12 unclassified variants with a<br />
high probability of being deleterious. Two of these variants have<br />
already reached classification: the BRCA c.301+6T>C classified<br />
as likely neutral or of low clinical significance and the BRCA1<br />
c.5074G>C p.Asp1692His which was previously mis-classified as<br />
a missense mutation. Using in vitro transcript assays we showed<br />
that this is a splicing mutation leading a cryptic splice site 153<br />
nucleotides in intron 17 of the BRCA1 gene that brings about<br />
a frame-shift in the protein and a premature termination codon.<br />
For the remaining ten variants we are currently collecting data and<br />
family members to be used in a multifactorial likelihood model,<br />
that integrates independent sources of evidence of disease causality<br />
derived from: co-segregation of the disease with the variant, LOH,<br />
and histopathology data on available tumor specimens, as well as<br />
evolutionary conservation and molecular epidemiology analyses.<br />
A second research line focuses on the identification of other<br />
susceptibility genes with moderate-low penetrance. While<br />
these genes are more likely to be critical in the development<br />
of the sporadic breast or ovarian cancer, at the same time they<br />
provide the tools for better defining the risk profile of BRCA1<br />
and BRCA2 carriers. To address these studies with a sufficiently<br />
powered approach, the Unit joined in 2007 the Consortium of<br />
Investigators of Modifiers of BRCA1/2 (CIMBA) that currently<br />
includes about 50 research groups located world-wide and with<br />
a sufficient sample size to allow large scale studies in order to<br />
evaluate reliably the effects of genetic modifiers. By the candidate<br />
gene approach, these studies have so far led to identification<br />
of five loci which modify the risk of breast cancer for BRCA1<br />
mutation carriers (CASP8, TOX3, 2q35, 19p13 and 6q25.1)<br />
and nine loci which modify the risk of breast cancer for BRCA2<br />
mutation carriers (FGFR2, TOX3, MAP3K1, LSP1, 2q35,<br />
SLC4A7, 5p12, ZNF365 and 1p11.2). For the ovarian cancer<br />
risk, one SNP rs3814113 at 9p22.2 was associated with a reduced<br />
risk of cancer among BRCA1 and BRCA2 mutation carriers (HR<br />
= 0.78). BRCA1 mutation carriers with the TT genotype were<br />
predicted to have an ovarian cancer risk to age 80 of 48%, and<br />
those with the CC genotype were predicted to have a risk of 33%.<br />
Two two-staged genome-wide association studies (GWAS) were<br />
also carried out within the Consortium as collaborative projects<br />
using the Affymetrix 6.0 SNP platform. The study of BRCA2<br />
mutation carriers identified several SNP previously associated with<br />
sporadic breast cancer risk and two novel loci on chromosome<br />
20 (rs311499) and chromosome 10 (rs16917302); FGFR2<br />
rs2981575 showed the strongest association with breast cancer<br />
risk (per allele HR = 1.28). Five SNP on 19p13 were associated<br />
with breast cancer risk from the GWAS in BRCA1 carriers. The<br />
five SNP were also associated with triple-negative breast cancers in<br />
a separate study of 2,301 triple-negative cases and 3,949 controls.<br />
Although altogether these variants account for a small proportion<br />
of the variability in the genetic risk of breast cancer (3-6%), it has<br />
been demonstrated that these SNP have implications for absolute<br />
risk prediction in mutation carriers.<br />
familial maliGNaNT mElaNOma<br />
Principal Investigator: Chiara Menin<br />
The studies on the genetics of familial melanoma are developing<br />
along two major lines: a) molecular analysis of constitutive genetic<br />
alterations in high/low penetrance genes which are considered<br />
predisposing to familial melanoma in probands/relatives belonging<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
134
to high-risk families; b) assessment of the bio-pathological role of<br />
CDKN2A unclassified variants (UV) in conferring predisposition<br />
to familial melanoma. The first line is part of a clinical/diagnostic<br />
service that is offered to patients for the diagnosis of hereditary<br />
melanoma and, when appropriate, for the implementation of<br />
specific protocols for primary and secondary prevention, while<br />
the second line represents a research project that should increase<br />
the number of families that could take advantage of the molecular<br />
assessment for their melanoma risk.<br />
a. GENETiC aNalySiS<br />
We have performed genetic testing and evaluation of the<br />
influence of the main genes with either high (CDKN2A and<br />
CDK4) or low (MC1R) penetrance for cutaneous melanoma<br />
in about 100 familial melanoma patients, recruited within the<br />
“Centro Regionale Specializzato per il Melanoma Cutaneo” of<br />
the <strong>IOV</strong>. The majority of the analysed families (72%) had only<br />
two cases of melanoma, and multiple primary melanoma (MPM)<br />
patients were present in 27% of them. No germline mutations were<br />
identified in the specific hot spot of CDK4 exon 2. Sequencing<br />
analysis of CDKN2A revealed 3 missense mutations: p.G23D,<br />
p.P48T, and p.G101. Altogether, only 6 families were found to<br />
be CDKN2A mutation positive, thus the mutation detection rate<br />
in melanoma-prone families from Veneto is approximately 8.5%,<br />
which is a much lower mutation rate compared to Italian figures.<br />
In fact, a recent Italian cooperative study on 204 families with<br />
two or more cases of melanoma reports a global 33% CDKN2A<br />
mutation rate, but single studies on families from different Italian<br />
regions report different mutation frequencies, and our data are<br />
more similar to those obtained in the Emilia Romagna region.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
135
The presence of at least one MPM case is a feature of all our<br />
mutated families. If we consider only the families with 2 or more<br />
melanoma cases and presence of at least one MPM, the CDKN2A<br />
mutation rate increases to 31.6%. In agreement with previous<br />
studies, our results support the presence of at least one MPM case<br />
in melanoma-prone families as the strictest criterion for identifying<br />
CDKN2A mutations. Additionally, we have investigated the<br />
influence of MC1R variants to melanoma susceptibility in these<br />
families, and we have found that MC1R variants are extremely<br />
common and they act as independent risk factor for melanoma as<br />
well as number of nevi or presence of atypical nevi.<br />
b. EvaluaTiON Of CDkN2a uv<br />
CDKN2A germline mutations have been associated with<br />
familial predisposition to melanoma and other tumor types.<br />
Besides bona-fide pathogenic mutations, many sequence variants<br />
have been identified, but their effect is not well known. We<br />
detected the p.Gly 23Asp missense mutation in one of two tested<br />
melanoma patients of a family with 3 melanoma cases. Even<br />
though the mutated amino acid is located in a conserved domain<br />
that specifically binds to and blocks the function of CDK4/6, its<br />
lack of segregation with disease suggested a series of functional<br />
assays to discriminate between a pathogenic variant and a neutral<br />
polymorphism.<br />
The effect of this mutation has been investigated exploiting<br />
four p16 INK4A properties: its ability (i) to bind CDK4, (ii) to<br />
inhibit pRb phosphorylation, (iii) to evenly localize in the cell,<br />
and (iv) to cause cell cycle arrest. The mutant protein properties<br />
were evaluated by transfecting three different cell lines (U2-OS<br />
and NM-39, both p16-null, and SaOS 2, p53 and pRb-null)<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
136
with plasmids expressing either p16 wt , p16 23Asp , or the p16 32Pro<br />
pathogenic variant. We found that p16 23Asp was less efficient than<br />
p16 wt in CDK4 binding, in inhibiting pRb phosphorylation and in<br />
inducing G1 cell cycle arrest; moreover, its pattern of distribution<br />
throughout the cell was suggestive of protein aggregation, thus<br />
assessing a pathogenic role for p16 23Asp in familial melanoma.<br />
Future prospects. Genetic counseling and testing will be<br />
extended to more melanoma-prone families from the Veneto<br />
region, through the recently developed regional network for<br />
hereditary cancers (Rete Veneta per i Tumori Eredo-Familiari).<br />
The functional analysis on the UV of the CDKN2A gene will<br />
be extended to the critical residues that are of vital importance for<br />
the specific folding and function of the p16INK4A protein.<br />
uSE Of hpv TEST iN ThE SCrEENiNG fOr CErviCal<br />
CaNCEr: mulTiCENTriC STuDy “NEw TEChNOlOGiES<br />
fOr CErviCal CaNCEr SCrEENiNG” (NTCC) aND ThE<br />
fEaSibiliTy prOjECT iN ThE paDOva arEa<br />
Principal Investigator: Annarosa Del Mistro<br />
Background. Cervical cancer screening by cytology (Pap<br />
test) is in use since many years and recognized as effective. In<br />
Italy organized programmes for women 25-64 year-old are<br />
recommended every three years. In recent years new technologies<br />
have become available for cervical cancer screening; the use of<br />
molecular search for HPV sequences is particularly promising<br />
since persistent infection with high risk human papillomavirus<br />
(hrHPV) types is a necessary cause for cervical cancer development.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
137
Cervical HPV infection is very common and its prevalence<br />
is higher among younger women; only a small percentage of<br />
women with persistent infection with high-risk types will develop<br />
the tumor, while the majority of infections clear spontaneously.<br />
Several randomized controlled studies investigating the use of<br />
HPV testing as primary screening test are ongoing. In 2001 the<br />
Italian multicentric NTCC trial started in 9 organized screening<br />
programs within 6 Italian Regions. Aim of the study is to evaluate<br />
the performance of HPV test in comparison to cervical cytology<br />
as primary test, by cross-sectional and longitudinal analyses. Since<br />
the results of NTCC and the other randomized studies ongoing in<br />
Europe indicate higher sensitivity but lower specificity of hrHPV<br />
test than cytology, in 2009 feasibility studies have been initiated<br />
in Italy to evaluate organizational impact, women’s compliance<br />
and costs derived from the routine introduction of hrHPV test as<br />
primary screening test, and to define the most effective protocols<br />
for triage and follow-up of hrHPV-positive cases.<br />
Methods. The NTCC trial is a randomized study with two<br />
arms (conventional: Pap test) and two phases for the experimental<br />
arm (phase 1: hrHPV test plus Pap test; phase 2: hrHPV test only).<br />
All women are followed-up by Pap test every six years. The hrHPV<br />
test used in both NTCC trial and feasibility project is Hybrid<br />
Capture 2 (HC2, Digene/Qiagen) with high-risk probes. In the<br />
feasibility project, triage of hrHPV-positive women is performed<br />
by cytology; women with atypical cells undergo colposcopy,<br />
women with negative cytology repeat hrHPV test one year later.<br />
Results and conclusions. In the NTCC trial some 95,000<br />
women (of whom 10,605 from the Veneto region, i.e. Padova and<br />
Verona) were enrolled during 2002-2005. During 2005-2008 rescreening<br />
by cytology at six years was performed in women of both<br />
arms; moreover, hrHPV test was repeated for a random group of<br />
hrHPV test negative patients at enrollement. During 2008-<strong>2010</strong><br />
re-screening by cytology at three years was performed in women<br />
of both arms; data analysis is ongoing.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
138
The results published so far indicate that hrHPV test is more<br />
sensitive than Pap test in the identification of women at risk of<br />
developing high-grade lesions and has higher efficacy in preventing<br />
invasive cervical cancer. Sensitivity and specificity of hrHPV test<br />
depend on women’s age; in particular, detection of transient<br />
infections and regressive lesions is most common among women<br />
younger than 35 years. Therefore means to increase specificity<br />
without affecting sensitivity are necessary; the triage strategies<br />
evaluated within the NTCC trial include cytology, higher cutoff<br />
of the HC2 test and p16INK4A immunocytochemistry. In<br />
2009 a feasibility project for the use of hrHPV test as a primary<br />
screening test has been started in the Veneto region; it includes all<br />
women of the 5 screening programs within Padova and Rovigo<br />
areas. The hrHPV test for the Padova area is performed at <strong>IOV</strong>;<br />
the target population for this area is about 80,000 women per<br />
year. Enrollement started April 2009 for the ULSS 17 program;<br />
July <strong>2010</strong> for the ULSS 15 program; June <strong>2011</strong> for the ULSS 16<br />
program. The results for the ULSS 17 and 15 programs indicate<br />
a 10% increase of the compliance as compared to the previous<br />
years, and good compliance to 1-year recall. Pap test was used as<br />
a triage test in both phase 1 of NTCC and feasibility project, and<br />
was performed blind and open to the hrHPV result, respectively;<br />
the results indicate the need to redefine the reading criteria of the<br />
triage Pap test, and to perform specific training for all operators<br />
involved in the screening.<br />
Future perspectives. For the NTCC trial, analyses for<br />
genotyping, viral load and viral variants of HC2-positive samples at<br />
enrollement and follow-up are ongoing. For the feasibility project,<br />
indicators of efficacy and quality control will be monitored and<br />
compared to those obtained with Pap test as primary screening<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
139
test within the same programs and those obtained in the other<br />
projects ongoing in other Italian regions.<br />
aSSESSmENT Of NEw NON-iNvaSivE STraTEGiES fOr<br />
DiaGNOSiS aND prOGNOSiS Of TumOrS: STuDy Of ThE<br />
TElOmErE/TElOmEraSE iNTErplay<br />
Principal Investigator: Anita De Rossi<br />
Brief description. Telomere/telomerase interplay is a key<br />
mechanism in controlling cellular replicative potential. While<br />
erosion of telomeres beyond a critical point may impair their<br />
function in protecting chromosome ends, resulting in genetic<br />
instability, a key event in the initiation of carcinogenesis, the<br />
maintenance of telomere length by telomerase is a critical step<br />
toward immortalization and tumorigenesis. Recent findings<br />
suggested that h-TERT, the rate limiting component of telomerase,<br />
may have prognostic value in several tumors and its detection in<br />
blood could constitute a marker for tumor diagnosis.<br />
We have developed PCR-based assays to quantify levels of<br />
h-TERT mRNA and to estimate the length of telomeres. We have<br />
set up methods to extract nucleic acids from blood and from cellfree<br />
biological fluids, and to quantify RNA and h-TERT mRNA<br />
from plasma.<br />
Our studies on hematological malignancies demonstrated that<br />
h-TERT mRNA is a useful prognostic marker in B-cell chronic<br />
lymphocytic leukemia (B-CLL). Studies aimed at evaluating the<br />
prognostic role of telomere/telomerase interplay and its relationship<br />
with chromosomal abnormalities are undergoing in a large series<br />
of B-CLL. Studies on colorectal cancers (CRC) demonstrated that<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
140
levels of h-TERT mRNA increased with tumor progression and<br />
that h-TERT mRNA in plasma significantly correlated with those<br />
in tumors. Furthermore, telomeres were significantly shorter<br />
in CRC than in adjacent tissues, thus suggesting that telomere<br />
shortening in CRC is a key initial event in colorectal carcinogenesis,<br />
before telomerase activation. Studies aimed at evaluating h-TERT<br />
mRNA as a predictive marker of tumor response to neoadjuvant<br />
chemoradiotherapy in rectal cancers are ongoing.<br />
rOlE Of miCrOENvirONmENT iN pEl paThOGENESiS<br />
Principal Investigator: Maria Luisa Calabrò<br />
Primary effusion lymphoma (PEL) is a HHV8-associated<br />
B-cell non-Hodgkin’s lymphoma growing as lymphomatous<br />
effusion within serous body cavities, which are lined by mesothelia.<br />
While the association between HHV8 and PEL development<br />
is widely accepted, the role of microenvironment remains to<br />
be fully elucidated. To analyze the specific role of the host<br />
microenvironment on tumor growth, we developed a xenograft<br />
SCID model of PEL that mimicks the liquid-phase growth and,<br />
most of all, the aggressive course of human PEL. We compared<br />
the activity of a murine (i.e. host-specific) interferon (IFN)-alphaexpressing<br />
lentiviral vector (mIFN-alpha-LV) to that of a human<br />
hIFN-alpha-LV. Treatment of PEL/SCID mice with hIFN-alpha-<br />
LV significantly prolonged mice survival and reduced ascites<br />
development. Interestingly, in vivo gene therapy experiments<br />
using the mIFN-alpha-LV showed an anti-neoplastic activity<br />
comparable to that observed with the hIFN-alpha-LV. As mIFNalpha<br />
did not exert any direct anti-proliferative, pro-apoptotic<br />
and antiviral effect on PEL cells in vitro, it likely acted in vivo on<br />
the intracavitary murine milieu, thus indicating that the specific<br />
targeting of microenvironment may impair PEL development.<br />
mIFN-alpha-treated murine mesothelial cells were found to<br />
express tumor necrosis factor-related apoptosis-inducing ligand<br />
(TRAIL) and to significantly induce apoptosis of co-cultured PEL<br />
cells in a TRAIL-dependent manner. These data suggest that the<br />
interaction between lymphomatous and mesothelial cells may be<br />
central to PEL pathogenesis, and also indicate that the specific<br />
targeting of microenvironment may impair PEL development.<br />
Ongoing studies are aimed at investigating the crosstalk between<br />
lymphomatous cells and mesothelial cells to dissect mechanisms<br />
involved in PEL cell survival and proliferation in body cavities. By<br />
co-culturing human primary mesothelial cells with PEL-derived<br />
cell lines, we reproduce in vitro the cellular interactions existing<br />
in body cavities to study: (i) the contribution of mesothelial cells<br />
to PEL cell turnover and cell-to-cell interactions; (ii) the role of<br />
IFN-induced genes expressed by mesothelial cells and involved in<br />
the in vivo anti-neoplastic activity of this cytokine, by analyzing<br />
the effects of TRAIL expression by human mesothelial cells on<br />
PEL cell apoptosis and by the identification of other IFN-induced<br />
genes expressed by mesothelial cells; (iii) the susceptibility to<br />
HHV8 infection of mesothelial cells and the effects of HHV8<br />
infection on mesothelial cell function.<br />
mOlECular markErS iN ESOphaGEal CaNCEr<br />
Principal Investigator: Daniela Saggiaro<br />
Esophageal cancer represents the eighth most common cancer<br />
in the world. Despite improvement in diagnosis and treatment,<br />
the overall survival remains lower compared to other solid tumors.<br />
Thus, understanding the molecular mechanisms underlying the<br />
onset and progression of esophageal cancer is mandatory to<br />
the development of better treatments. The two predominant<br />
histological subtypes of esophageal tumor are the squamous cell<br />
carcinoma (SCC) and the adenocarcinoma (ADC). The latter is<br />
thought to arise from an acquired precursor condition, known<br />
as Barrett’s esophagus (BE), in which the squamous epithelium<br />
of the lower esophagus is replaced by columnar epithelium. It is<br />
believed that BE is a premalignant condition caused by chronic<br />
gastro-esophageal reflux; other risk factors include smoking and<br />
obesity. SCC arise in the upper or middle esophagus and, although<br />
the etiology is unclear, factors such as smoking, alcohol, diet and<br />
chronic inflammation are considered as favoring elements. While<br />
the incidence of SCC has remained relatively stable over the last<br />
few decades, ADC incidence has steadily increased in the Western<br />
world and, though to lower extent, in Asia.<br />
It is generally accepted that initiation and progression of<br />
human cancer are associated with the accumulation of alterations<br />
in important regulatory genes. Indeed, DNA copy number<br />
abnormalities are a hallmark of nearly all advanced tumors and<br />
amplified genes represent attractive targets for the development of<br />
new diagnostic, prognostic and therapeutic approaches.<br />
In an attempt to define esophagus-specific biomarkers, we<br />
investigated DNA copy number changes of esophageal tumor<br />
samples, stratified into ADC and SCC. Analysis was carried<br />
out using the multiplex ligation-dependent probe amplification<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
141
(MLPA) technique. MLPA, contrary to chromosomal-CGH,<br />
allows detection of single gene alterations and represents an efficient<br />
method for simultaneous screening of copy number imbalance in<br />
multiple genomic regions while maintaining a single gene resolution;<br />
in terms of robustness MLPA has been compared to array-CGH.<br />
Our findings, in agreement with previous data, indicate that<br />
structural genetic changes involving several chromosomes are very<br />
frequent events in esophageal tumors. Nevertheless, by comparing<br />
the ADC and SCC samples we found that some chromosomal<br />
gains or losses were tumor subtype-specific. Looking for putative<br />
genes involved in DNA copy number alterations, we found that in<br />
ADC only a few genes were specifically altered at high frequency,<br />
and the same cytogenetic region often showed amplifications in<br />
one subset of patients and deletions in another, thus indicating<br />
that ADC are characterized by an elevated genetic instability.<br />
In contrast, in SCC the same probes exhibited either gains or<br />
losses at high level. The observed differences in DNA copy number<br />
patterns between ADC and SCC might suggest that genes within<br />
these regions are specific and could play a relevant role in the<br />
pathogenesis of the two esophageal cancer subtypes. On the other<br />
hand, the common alterations might indicate that shared genes<br />
are involved in tumor progression and growth.<br />
By analyzing the correlation between DNA copy number<br />
changes and overall survival (OS), we found that the total number<br />
of alterations in ADC correlated with OS and could be considered<br />
as an independent prognostic parameter. Thus, it seems that in<br />
ADC patients an increased genomic instability correlates with<br />
the aggressiveness of the tumor. On the contrary, no association<br />
between OS and total DNA alterations was found in SCC<br />
patients.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
142
More recently, given that the real benefit of a neoadjuvant<br />
therapy in esophageal cancer is still controversial, we undertook<br />
studies devoted to understanding the influence of patient genetic<br />
variants on response to neoadjuvant therapy. Indeed, there is a<br />
growing body of evidence suggesting that, beside variables such<br />
age, sex, diet and organ function, the drug therapeutic effects can<br />
be affected by genetic factors. Analyses devoted to the discovery<br />
of genetic variants involved in drug excretion and metabolism,<br />
as well as DNA repair, appear thus a promising tool to identify<br />
patients that will respond better to therapy.<br />
Cisplatin- and 5-fluorouracil (5-FU)-based chemotherapy<br />
in association with radiation still remains the cornerstone of<br />
treatment for esophageal cancer. Among polymorphic genes<br />
implicated in the response to cisplatin and 5-FU treatment,<br />
glutathione S-transferase family (GST), thymidylate synthase<br />
(TS), excision repair cross-complementation group 1 (ERCC1)<br />
and Xeroderma Pigmentosum group D (XPD/ERCC2) genes<br />
seem to play an important role due to their involvement in the<br />
drugs detoxification, inactivation or DNA adducts repair.<br />
The GST isoenzymes are divided into at least seven major classes;<br />
among these, the GST-P1, GST-M1 and GST-T1 polymorphic<br />
variants have been associated with changes in enzymatic activity.<br />
In GST-P1 gene, a change in exon 5 (A313G; rs1695) gives<br />
rise to Ile105Val amino acid substitution. This modification<br />
leads to an alteration in substrate affinity and consequently to a<br />
reduced detoxification activity. Activity of GST-T1 and GST-M1<br />
enzymes is modulated by inherited homozygous or heterozygous<br />
deletions that lead to a complete or partial absence of enzymatic<br />
activity, and their role in cisplatin detoxification is still debated.<br />
DNA adducts including those induced by cisplatin are removed<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
143
mainly by the nucleotide excision repair (NER) pathway, thus,<br />
suboptimal NER activity may render cancer cells more sensitive<br />
to cisplatin treatment. The ERCC1 and XPD gene products play<br />
a leading role in the NER pathway.<br />
It has been reported that variants rs11615 and rs3212986<br />
within ERCC1 and rs1799793 and rs13181 within XPD may<br />
alter their expression and subsequently their DNA repair capacity.<br />
As mentioned before, 5-FU remains an important drug in the<br />
chemotherapeutic treatment of esophageal cancer and high levels<br />
of its target, the thymidylate sinthase, have been correlated with<br />
drug resistance and a poor outcome. Several polymorphisms in<br />
the TS untranslated regions (UTR) which may influence TS<br />
mRNA transcription or protein expression, have been described<br />
recently. The prognostic significance of GST, ERCC1, XPD and<br />
TS polymorphisms have been studied in different solid cancer<br />
types treated with platinum compounds and 5-FU. Many of these<br />
studies have found an involvement of these genes in treatment<br />
response and in elevated risk of relapse.<br />
Although further analyses are required, preliminary results<br />
obtained in our cohort of esophageal cancer patients suggest a<br />
correlation between variants in NER genes and patient survival<br />
after neoadjuvant therapy.<br />
hTlv-1 TumOriGENESiS<br />
Principal Investigators: Vincenzo Ciminale, Donna M. D’Agostino<br />
HTLV-1 is the causative agent of adult T-cell leukemia/<br />
lymphoma (ATLL) and HTLV-1 associated myelopathy/tropical<br />
spastic paraparesis (HAM/TSP). Even though the mechanisms<br />
by which the virus engenders disease are not yet completely<br />
understood, numerous data indicate the multifunctional Tax<br />
protein as essential for malignant transformation. Indeed, Tax<br />
causes leukemia in transgenic mice, and immortalizes human<br />
lymphocytes when expressed in either a herpes- or retroviral<br />
vector. This oncogenic potential is accounted for by Tax ability<br />
to modulate the synthesis or the activity of many cellular proteins<br />
that control a variety of fundamental cellular processes.<br />
A key feature of malignant transformation is the induction of<br />
apoptotic resistance, and aberrant cell death is usually associated<br />
with uncontrolled cell growth. Tax contribution to apoptosis<br />
is still controversial since the protein was shown to possess<br />
both anti-apoptotic and pro-apoptotic activity. However, at<br />
present, it is generally accepted that the anti-apoptotic activity<br />
of Tax overrides its potential pro-apoptotic effects. In previous<br />
studies, using murine fibroblasts and human HeLa cells, we<br />
have shown that Tax expression induces resistance to apoptosis<br />
triggered by different stimuli. Analysis of potential mechanisms<br />
revealed that the observed resistance was linked to high levels of<br />
transcriptionally active CREB and to the presence of a functional<br />
Ras protein. Ras proteins are small GTPases that function as<br />
molecular switches, alternating between inactive (GDP-bound)<br />
and active (GTP-bound) states. Like many genes involved in<br />
the regulation of multiple cellular signaling pathways (i.e.,<br />
differentiation, proliferation and survival), Ras contributes to<br />
cancer development, when aberrantly expressed.<br />
While investigating the molecular mechanisms of Taxmediated<br />
resistance to apoptosis in T-cells, we found that cells<br />
expressing Tax either transiently or constitutively have higher<br />
levels of Ras-GTP (active form) than their control counterparts.<br />
Furthermore, by using FTS (S-farnesylthiosalicylic acid), a Ras<br />
farnesylcystein mimetic that selectively interacts with the activated<br />
form of Ras, we were able to increase the sensitivity of Tax-expressing<br />
cells to cisplatin treatment. These data strengthen previous<br />
findings indicating that Tax-mediated resistance to apoptosis is, at<br />
least in part, associated with Ras activity. Interestingly, increased<br />
apoptosis susceptibility of Tax-expressing cells to treatment with<br />
FTS was accompanied by a consistent reduction in phospho-<br />
ERK, suggesting a direct involvement of ERK activation in<br />
the apoptosis protection mediated by Tax. Moreover, although<br />
several reports stressed the potential relevance of Akt activation in<br />
survival of HTLV-1 infected or Tax-expressing cells, no reduction<br />
in phospho-Akt was observed after FTS treatment.<br />
The different behavior of ERK and Akt could be the result of<br />
the diverse activation pattern of the two proteins. Indeed, ERK<br />
activation is directly linked to Ras through the Raf-MEK pathway,<br />
whereas Akt is a downstream effector of PI3K, whose activation<br />
can be driven not only by Ras but also by diverse inducers. Thus,<br />
Ras inhibition has likely a more direct and rapid effect in ERK<br />
activation.<br />
Our data provide evidence of Ras signaling activation in Taxexpressing<br />
T-cells, and indicate this occurrence as a possible cause<br />
of ATLL cell resistance to death by chemotherapeutic agents.<br />
Although additional studies should evaluate whether the levels<br />
of Ras-GTP correlate with disease prognosis and the extent of<br />
apoptosis resistance, our data designate Ras as a possible target for<br />
ATLL therapy.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
144
aDvaNCED appliCaTiONS Of CirCulaTiNG TumOr CEllS<br />
iNvESTiGaTiON<br />
Principal Investigators: Rita Zamarchi, Elisabetta Rossi<br />
Background. Metastasis is the major cause of death from<br />
cancer. In the past decade the traditional model of metastasis<br />
has been challenged by direct and indirect evidence, contrasting<br />
the view that tumor cells spreading to secondary sites is a late<br />
event in the tumorigenesis. The implications for diagnosis and<br />
therapy are that it may not be sufficient to characterize the<br />
primary tumor to assess the risk for disease recurrence and to<br />
determine the appropriate therapeutic regimen. Investigation of<br />
tumor cells disseminated into bone marrow should be included in<br />
patient analysis. Nonetheless, bone marrow screening for occult<br />
metastatic tumor cells in patients with epithelial tumors has not<br />
been included as a standard clinical routine in the majority of the<br />
European Member States, remaining a research tool for clinical<br />
studies or in selected patients. Peripheral blood represents an<br />
alternative minimally invasive source of spreading tumor cells. In<br />
current practice, cancer tissue is usually taken at diagnosis and<br />
used to assess the presence of treatment targets. This however is<br />
a suboptimal approach, since tumor cells evolve due to genomic<br />
instability. Assessment of the phenotype and (hopefully) genotype<br />
of the tumor cells in peripheral blood will provide insights into<br />
treatments which could be most beneficial for the individual<br />
patient.<br />
Methods. Circulating tumor cells (CTC) refer to cells that<br />
detach from a primary tumor or metastatic site, and circulate<br />
in peripheral blood and may settle down at secondary sites<br />
forming metastasis. In the past decade, technology advances<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
145
enabled detection of these rare cancer cells, shedding some light<br />
on the disease natural history and showing promise to serve as a<br />
"liquid biopsy" used to tailor treatment for individual patients.<br />
At present, the only validated assay for CTC detection that has<br />
been cleared by the U.S. Food and Drug Administration is the<br />
CellSearch system. Prospective multicenter studies in metastatic<br />
breast cancer, prostate, and colon cancer, conducted with this<br />
system demonstrated that the presence of CTC was associated<br />
with poor survival; failure to eliminate the CTC after the first<br />
cycles of therapy strongly suggests futile therapy.<br />
Results. Addressing the role and mechanism of CTC in<br />
metastasis we started by quantifying apoptosis in these cells. Indeed,<br />
cell death is of fundamental importance for the development of<br />
multi-cellular organisms and homeostasis of their tissues; aberrant<br />
cell death can lead to many human diseases, including cancer.<br />
Furthermore, the induction of tumor cell death is a primary<br />
goal of many targeted therapies, directly or indirectly hinting to<br />
molecular components of apoptosis regulatory pathways. As a<br />
proof of concept that tumors respond to drug, we developed an<br />
M30-integrated CTC assay for quantifying apoptotic CTC, by<br />
using an anti-M30 mAb specific for epithelial cell apoptosis. To<br />
express the dynamic changes of live vs. apoptotic CTC during<br />
treatment, the difference (named Delta AUC) between live and<br />
apoptotic CTC concentration-time Area was calculated following<br />
a procedure which is commonly adopted for tumor markers. The<br />
integrated assay proved to disclose an active disease in metastatic<br />
breast cancer under chemotherapy. The new test and the<br />
companion algorithm are applied for the first time in metastatic<br />
renal cancer patients undergoing first-line Sunitinib, for which<br />
no predictive markers are currently available. We found that<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
146
the persistence of more aggressive (EpCam-positive, live) CTC<br />
predicts disease recurrence in these patients, and it is linked with<br />
distant relapses during first-line Sunitinib.<br />
Conclusions and Future perspectives. The renal cancer<br />
experience in CTC investigation is now applied to other<br />
malignancies. By exploiting the CellSearch platform we have<br />
developed integrated CTC assays for both phenotypic and<br />
molecular characterization, that is now included in multicenter<br />
clinical trials:<br />
To investigate the role of insulin/IGF pathway in metastatic<br />
breast cancer, we developed a new integrated assay for<br />
quantifying IGF1R-positive CTC as a proof of mechanism that<br />
drug hits target. The IGF1R-integrated assay is included in the<br />
multicenter Phase II comparative study of metformin plus firstline<br />
chemotherapy (CT) versus CT alone in HER2-negative,<br />
insulin-resistant (IR), no diabetic metastatic breast cancer, (PI:<br />
A. Gennari, D. Amadori) [<strong>2010</strong> ASCO Annual Meeting J Clin<br />
Oncol 28:7s, <strong>2010</strong> (suppl; abstr TPS134)]. The validation of<br />
the Insulin Sensitivity Score in these cells is ongoing.<br />
For monitoring tumor response to neoadjuvant treatments and<br />
tumor recurrence total and apoptotic CTC count is assessed in<br />
colorectal cancer patients, in collaboration with S. Pucciarelli<br />
(Dept. of Oncology and Surgical Sciences, University of<br />
Padova).<br />
Total and apoptotic CTC enumeration is assessed in prostate<br />
cancer patients during neoadiuvant treatment (Janus trial:<br />
A phase II study of Zoledronic Acid as Neoadjuvant therapy<br />
in invasive prostate cancer), in collaboration with D. Santini<br />
(Policlinico Universitario Campus Biomedico-Roma)<br />
For quantifying the dynamic changes of live vs. apoptotic<br />
Circulating Melanoma Cells (CMC) throughout anti-BRAF<br />
treatment [Pilot study “Predictive value of Circulating Melanoma<br />
Cells (CMC) in anti-BRAF treated Metastatic Melanoma” (PI<br />
P. Zanovello, University od Padova)] the CMC assay is used<br />
in conjunction with anti-DeltaH2AX mAb, specific for histone<br />
H2AX which undergoes phosphorylation in response to double<br />
strand DNA breaks, occurring during apoptosis. The study is<br />
conducted in collaboration with V. Chiarion-Sileni (Oncologia<br />
Medica 2, <strong>IOV</strong>) and C.R. Rossi (Melanoma e Sarcomi dei<br />
Tessuti Molli, <strong>IOV</strong>).<br />
iDENTifiCaTiON Of rEGulaTOry NETwOrk<br />
Of myElOiD-DErivED SupprESSOr CEllS by iNTEGraTiNG<br />
GENE ExprESSiON aND miCrOrNa ExprESSiON DaTa<br />
Principal Investigators: Susanna Mandruzzato, Paola Zanovello<br />
Background. Our research group is involved in studying<br />
myeloid-derived suppressor cells (MDSC), a cell population<br />
that comprise immature myeloid cells composed of monocytic,<br />
granulocytic and dendritic progenitor cells or myeloid cells at<br />
different stages of differentiation. Several groups have demonstrated<br />
that expansion of MDSC in tumor-bearing mice and in cancer<br />
patients is associated with an impairment of T cell responses.<br />
It is currently believed that the origin of MDSC is due to an<br />
arrest of myeloid development process caused by cytokines and<br />
growth factors released by the tumor microenvironment: the bone<br />
marrow immature myeloid cells fail to develop fully and do not<br />
acquire surface markers of mature monocytes and granulocytes.<br />
After being recruited into the peripheral lymphoid organs and in<br />
the tumor site, MDSC may undergo a process of activation and<br />
trigger mechanisms of suppression of T-cell function through cell<br />
surface receptors and the release of short-lived soluble mediators.<br />
Several works have demonstrated that different growth factors<br />
secreted by tumor cells are able to promote the development,<br />
the proliferation and the expansion of myeloid granulocytic and<br />
monocytic progenitors with inhibitory function. Therefore, by<br />
analyzing cytokines present in the microenvironment of tumors<br />
of different histologies, we found that GM-CSF, G-CSF, and IL-6<br />
allowed a rapid expansion of MDSC from progenitors present<br />
in mouse and human bone marrow (BM), that we termed BM-<br />
MDSC (Marigo et al., Immunity, <strong>2010</strong>).<br />
Aim of this project is the definition of the expression profile of<br />
BM-MDSC, that can rapidly be generated in vitro. Moreover, this<br />
information may guarantee a deeper comprehension of biological<br />
mechanisms if expression data can be integrated with other gene<br />
information; to this aim it is mandatory to use new platforms of<br />
expression profiling, and to study the regulation of gene expression<br />
at different levels.<br />
Main results. We have recently defined growth factors able to<br />
generate MDSC in vitro from human bone marrow precursors.<br />
We demonstrated that combinations of some cytokines, such<br />
as G-CSF, GM-CSF and IL-6 induce the expansion of BM<br />
immature myeloid populations (BM-MDSC), with phenotype<br />
and inhibitory activity comparable to patients’ MDSC. BM-<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
147
MDSC are able to suppress the activation of both alloactivated<br />
and mitogen activated T lymphocytes, while ex-vivo isolated BM<br />
cells and untreated BM cells do not interfere significantly with T<br />
lymphocyte proliferation. BM-MDSC consist of a heterogeneous<br />
cell population comprising myeloid cells at various stages of<br />
differentiation, ranging from more immature cells to mature<br />
granulocytes and monocytes. We investigated which myeloid<br />
subpopulation had the highest suppressive activity and our results<br />
clearly indicate that only one fraction of BM-MDSC, containing<br />
an immature myeloid population, has the suppressive activity.<br />
This immature cell population has morphology and phenotype<br />
resembling to promyelocytes, and it is able not only to block<br />
lymphocyte proliferation, but also to affect IFN-γ production and<br />
to induce T cell apoptosis.<br />
When we investigated the relationship between T cell<br />
activation and BM-MDSC-mediated suppression, we found that<br />
the promyelocytic-like population was able to proliferate and<br />
maintain its immature phenotype when co-cultured with activated<br />
T lymphocytes; conversely, the same myeloid subset showed a<br />
diminished proliferative index and differentiated to more mature<br />
myeloid cells when co-cultured with resting T lymphocytes.<br />
In the blood of breast and colorectal cancer patients we could<br />
clearly identify an immature myeloid population resembling in<br />
vitro generated BM-MDSC. Our data suggest that circulating<br />
MDSC levels, phenotypically similar to those described in<br />
human BM experiments, are clinically relevant and: (i) increase<br />
over time in patients with progressive disease; (ii) correlate with<br />
an established prognostic marker (i.e. circulating tumor cells)<br />
in advanced breast cancer; and (iii) their persistently high or<br />
increasing levels following chemotherapy are associated with poor<br />
survival.<br />
Conclusions and future perspectives. The identification of<br />
this population with inhibitory function, and the efficient and<br />
rapid in vitro generation gives us the opportunity to use this model<br />
of expansion of human MDSC to study its expression profile<br />
and to specifically define its regulatory network of expression.<br />
In fact, the integrative analysis of micro(mi)RNA/mRNA<br />
expression profiles allows to reconstruct a network of functional<br />
interactions occurring in cells by analyzing the panel of potential<br />
regulatory relationships predicted from sequence information.<br />
Our integrative approach assumes that the final effect of a truly<br />
functional interaction between miRNA and its predicted mRNA<br />
targets can be seen as a pair of anticorrelated expression profiles.<br />
According to the increasing experimental evidence supporting<br />
the miRNA mechanism of target degradation rather than<br />
translational repression, the integration of target predictions<br />
with miRNA and gene expression profiles has been proposed<br />
to improve the detection of functional miRNA-mRNA<br />
relationships. Since miRNA tend to down-regulate target mRNA,<br />
the expression profiles of genuinely interacting pairs are expected<br />
to be anti-correlated. Integrative analysis can be performed<br />
adopting a variational Bayesian model, or by using a non heuristic<br />
methodology based on the anti-correlation between miRNA and<br />
mRNA expression profiles.<br />
rEGulaTiON Of TumOr DOrmaNCy: DiSSECTiNG ThE<br />
mOlECular paThwayS DOwNSTrEam Of NOTCh fOr<br />
ThErapEuTiC purpOSES<br />
Principal Investigators: Stefano Indraccolo, Alberto Amadori<br />
Background. Angiogenesis contributes to regulate tumor<br />
dormancy, a condition defined by the presence in the host of<br />
fully transformed yet non-tumorigenic cells. Using a model of<br />
angiogenesis-dependent dormancy of T Acute Lymphoblastic<br />
Leukemia (T-ALL) cells, it was previously found that angiogenic<br />
factors induce expression of the Notch ligand Dll4 in the<br />
vasculature. Dll4 appears to activate Notch3 signalling in T-ALL<br />
cells, an event which protects them from apoptosis and initiates<br />
progressive tumor growth. These findings - reinforced by similar<br />
observations in colorectal cancer xenografts - suggest that<br />
endothelial cells embedded in tissues undergoing angiogenesis may<br />
communicate activation signals to tumor cells, which contribute<br />
to the switching towards an aggressive phenotype. Here we wish<br />
to investigate whether novel Notch-targeted drugs could maintain<br />
tumor dormancy in pre-clinical models of cancer.<br />
Methods. Studies on T-ALL make use of a clinically relevant<br />
model of engraftment of primary human leukemia samples in<br />
NOD/SCID mice recently set-up in the lab. Specifically, the<br />
hypothesis that blockade of the Notch3-Dll4 interaction by anti-<br />
Dll4 or anti-Notch1/3 antibodies could exert therapeutic effects<br />
in T-ALL as well as solid tumors is being tested. Tumor burden is<br />
quantified by measurement of blood parameters and live imaging<br />
of the tumors. Effects of anti-Notch drugs on gene expression will<br />
be analyzed by low density arrays on RNA extracted from FACSsorted<br />
T-ALL cells. The global effects of Notch inhibition on the<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
148
phosphokinome will be investigated by a microarray approach.<br />
Results. A correlation was seen between the Notch/Fbw7<br />
genetic status and expression levels of Notch-related transcripts in<br />
T-ALL xenografts. Preliminary results indicate that anti-Notch1<br />
treatment greatly delayed engraftment of T-ALL cells bearing<br />
an active Notch pathway, including samples derived from poor<br />
responders or relapsed patients. Anti-Notch1-treated mice had a<br />
significant reduction in the percentage of blasts in the blood, the<br />
spleen and the BM. Moreover, we observed an increase in the<br />
levels of T-ALL cell apoptosis and a strong inhibitory effect on<br />
Notch transcriptional profile following anti-Notch1 treatment.<br />
Conclusions. These results indicate that Notch1/Fbw7<br />
mutated T-ALL samples are suitable candidates for Notch targeted<br />
therapy and highlight the potential of measurements of Notch<br />
target genes as surrogate biomarkers of the therapeutic response.<br />
Perspectives. Upon completion, this pre-clinical study will<br />
enable us to plan a phase I clinical trial for Notch-targeted therapy<br />
of relapsed or chemotherapy-resistant T-ALL.<br />
mOlECular aNalySiS Of GaSTrOiNTESTiNal STrOmal<br />
TumOrS (GiSTS) iN CliNiCal praCTiCE<br />
Principal Investigator: Roberta Bertorelle<br />
Background. The discovery in 1998 of the pathogenic<br />
alteration of Gastrointestinal Stromal Tumor (GIST) has changed<br />
the natural history of this tumor highly resistant to conventional<br />
chemotherapy, providing a target for a molecular therapeutic<br />
approach.<br />
Mutations of KIT or PDGFRA gene, coding for class III<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
149
tyrosine kinase proteins, account for about 75-80% and 8-10%<br />
of the cases, respectively, and lead to a ligand-independent<br />
activation of the receptor. Most of the mutations involve exon<br />
11 of KIT gene (about 65%) being the spectrum of KIT exon<br />
11 mutations heterogeneous. Mutations in other exons of KIT<br />
gene include those in the regulatory extracellular domain (exon<br />
9) and mutations of kinase I domain (exon 13) and kinase II<br />
domain (exon 17), accounting for about 9%, 1% and 1% of cases,<br />
respectively.<br />
PDGFRA gene mutations involve much more frequently<br />
kinase domain II corresponding to exon 18 (6-8%). Rare (
algorithm that takes into account that mutations are mutually<br />
exclusive. Moreover clinico-pathological parameters like tumor<br />
size, mitotic index and tumor location were recorded for tumor<br />
risk assessment.<br />
Results. 157 GIST cases were collected so far. The frequency<br />
of mutated GIST in our Caucasian patients was 82% (65%<br />
KIT and 17% PDGFRA), while 18% were wild-type. The most<br />
frequent alterations involve KIT exon 11, followed by PDGFRA<br />
exon 18 and KIT exon 9 (65%, 16% and 10% of all mutated<br />
cases, respectively). KIT exon 13, exon 17 and PDGFRA exon 12<br />
were less frequently involved (3.9%, 0.8% and 3.9%).<br />
Although KIT and PDGFRA mutations have a controversial<br />
prognostic role, in our series KIT mutations, and in particular<br />
exon 11 deletion involving codon 557 or 558, associate to high<br />
risk of recurrence, to a worse prognosis compared to patients with<br />
other or no mutations, thus representing a strong independent<br />
negative prognostic factor.<br />
Molecular genetic status in GIST correlates with clinical<br />
behavior of the disease but it also predicts the response to treatment<br />
with tyrosine kinase inhibitors. Primary resistance is conferred<br />
by specific mutations, being exon 9 KIT and D842V PDGFRA<br />
mutations the most frequently involved, while a secondary<br />
resistance could occur during the course of therapy. These patients<br />
should therefore benefit from a higher dose of Imatinib or should<br />
be considered for a second-generation TKI treatment.<br />
Conclusions. Molecular analysis of GISTs plays an important<br />
role in the management of the disease. Mutational status could<br />
be considered as a prognostic and predictive factor both for<br />
metastatic and localized resected GISTs. Taking into account the<br />
genetic status of the tumor, the physician could select patients<br />
who benefit from Imatinib establishing the best dosage of the<br />
drug or choose a second-line therapy, also making a prediction<br />
of prognosis.<br />
aDOpTivE immuNOThErapy Of TumOrS aND prECliNiCal<br />
mOlECular imaGiNG<br />
Principal Investigator: Antonio Rosato<br />
Background. Adoptive T cell therapy (ACT) is a form of<br />
transfusion therapy involving the infusion of large numbers of<br />
T cells to treat malignancies or infectious diseases. Successful<br />
applications include the administration of virus-specific T<br />
lymphocytes to protect immunosuppressed patients from<br />
transplantation-associated viral diseases, donor lymphocyte<br />
infusions of ex vivo-expanded allogeneic T cells to treat relapsed<br />
hematological malignancies following allogeneic hematopoietic<br />
stem cell transplant, and melanoma by infusing patients with<br />
melanoma antigen-specific T cells. Nevertheless, a major obstacle<br />
to the clinical diffusion of ACT is represented by technical factors<br />
limiting the availability of adequate numbers of tumor-specific<br />
T cells to transfer. Viral vector-mediated genetic engineering<br />
of T lymphocytes may represent a valid tool to overcome such<br />
limitations, leading to the rapid generation of large amounts<br />
of tumor-specific T cells endowed with the desired specificity.<br />
This goal can be achieved by transferring a) the TCR derived<br />
from an antigen-specific T cell clone or b) a chimeric antigen<br />
receptor (CAR), an artificial T cell receptor that combines the<br />
extracellular single-chain variable fragment (scFv) of an antibody<br />
with intracellular signalling domains, such as CD3.<br />
Besides to chemical and biotechnological aspects, a powerful<br />
input towards analysis of in vivo behavior of new pharmaceuticals<br />
has come from development of detectors specifically dedicated<br />
to small animals. These innovative instruments, that permit to<br />
represent, characterize and quantify biological processes at cellular<br />
and subcellular levels within living organisms, constitute a real<br />
improvement for promotion and follow-up of new therapeutic<br />
approaches with a consequent acceleration in their transfer to<br />
clinical practice. In this regard, <strong>IOV</strong> has been equipped with an<br />
outstanding platform for in vivo imaging, comprising a MicroCT<br />
scanner, an apparatus for bioluminescence and a fluorescence<br />
optical imager; these instruments are currently used to analyse<br />
and monitor several experimental protocols.<br />
Methods. TCR cloning from tumor-specific cytotoxic T<br />
lymphocytes; development of CAR constructs; generation of<br />
retroviral and lentiviral vectors; transduction and expansion of<br />
antigen-specific mouse and human T cells; cytofluorimetric and<br />
functional assays (cytotoxic activity and cytokine release detection);<br />
in vivo monitoring of adoptively trasferred lymphocytes, and<br />
analysis of tumor growth and response to therapy by optical<br />
imaging.<br />
Main results. In collaboration with Verona University, we<br />
developed CAR directed to Prostate Specific Membrane Antigen<br />
(PSMA) and Prostate Stem Cell Antigen (PSCA). In particular, we<br />
could demonstrate that the anti-PSMA CAR construct inserted<br />
into an eukaryotic expression plasmid leads to the production of<br />
a membrane molecule on 293T cells, upon transient transfection,<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
151
which is identifiable by anti-c-myc tag cytometry analysis and<br />
has the correct molecular weight, as assessed by Western blotting.<br />
Moreover, a LV vector has been also developed that is capable<br />
of co-expressing both a CAR and a reporter gene (luciferase or<br />
fluorescence proteins) and is endowed with a high transduction<br />
efficiency in human T cells. These latter, upon repeated stimulations<br />
with PSMA+ tumor cells, undergo a rapid expansion and generate<br />
an effector population that exhibit strong and highly specific<br />
cytotoxic activity, and exert therapeutic activity in vivo upon<br />
adoptive transfer into mice bearing PSMA+ prostate tumors. On<br />
the imaging side, it was not only possible to follow the biological<br />
fate of transferred T cells, but several biodistribution studies<br />
have been also carried out involving monoclonal antibodies and<br />
the derived single chain fragments (scFv), and novel polymeric<br />
antitumor drugs (bioconjugates between cytotoxic drugs and<br />
hyaluronic acid).<br />
Conclusions and future perspectives. The development of a<br />
rapid and efficient protocol for the production of high amounts<br />
of antigen-specific effector T cells against prostate carcinoma,<br />
represents a fundamental prerequisite to translate this therapeutic<br />
approach to the clinical settings. Therefore, it will be interesting<br />
to verify the potentialities of the treatment with PSCA-redirected<br />
T lymphocytes and of the simultaneous combined redirectioning<br />
against both antigens to minimize the emergence of antigenic<br />
escape mutants. Finally, optical imaging studies of cell, antibody<br />
and drug biodistribution represent the basis for further in-depth<br />
examination and validation with the SPECT/PET/CT apparatus<br />
to be readily installed at our Institute.<br />
CONvENTiONal CyTOGENETiCS aND iNTErphaSE fiSh<br />
aNalySiS fOr a bETTEr prOGNOSTiC aSSESSmENT Of<br />
ChrONiC lymphOCyTiC lEukEmia<br />
Principal Investigator: Laura Bonaldi<br />
Background. The need for accurate prognostic markers<br />
in Chronic Lymphocytic Leukemia (CLL) is urgent. Major<br />
breakthroughs were achieved by identification of specific<br />
cytogenetic aberrations associated with clinical outcome by<br />
interphase Fluorescence in situ hybridization (FISH) analysis.<br />
FISH is able to identify genomic aberrations in approximately<br />
80% of CLL cases and the most frequent alterations are deletions<br />
in 11q, 13q, 17p, and trisomy 12. Deletions of 17p (17p-) or 11q<br />
(11q-) are highly predictive of decreased survival, whereas patients<br />
with del13q (13q-) as a single abnormality have an excellent<br />
prognosis with survival curves that are even better than those<br />
with normal karyotype. Trisomy 12 conveys high risk of disease<br />
progression, but in contrast to patients with deletions of 17p<br />
and 11q, patients with 12 trisomy respond to fludarabine-based<br />
therapy, and their survival is better. Due to the low proliferative<br />
activity of CLL lymphocytes and their weak responsiveness to<br />
classical B-cell mitogens, conventional cytogenetics does not<br />
yield satisfactory results. Recently, chromosome banding analysis<br />
has improved, thanks to the application of immunostimulatory<br />
oligonucleotides (CpG) in combination with IL-2 during culture.<br />
With this method the success rate reached almost 100% and<br />
chromosome abnormalities have been described in more than 80%<br />
of patients. Moreover, chromosome translocations, particularly<br />
those involving the IgH locus at 14q32, seem to identify a distinct<br />
subset of CLL with poor prognosis.<br />
Aim of the study:<br />
1) to evaluate the usefulness of conventional cytogenetics with<br />
CpG oligonucleotide for detecting chromosomal abnormalities<br />
in comparison to those described by interphase FISH<br />
2) to explore the possible prognostic role of cytogenetic<br />
aberrations, especially among the low-risk FISH group.<br />
Methods. Peripheral blood or bone marrow aspirates<br />
from patients with CLL at diagnosis are collected to perform<br />
conventional cytogenetics and FISH analysis. CpG oligonucleotide<br />
is added in association to the IL-2 to the medium for cytogenetic<br />
culture. Interphase FISH analysis is performed using commercially<br />
available probes for the loci of prognostic interest: 11q22.3<br />
(ATM), 13q14.3 (D13S319), 17p13.1 (TP53), and centromeric<br />
probe for chromosome 12. Preliminary data are available for 23<br />
patients.<br />
Results. In our case series, the success rate of cytogenetic<br />
analysis using CpG oligonucleotides was 96%, with 61% of<br />
samples showing clonal chromosomal aberrations. Among<br />
abnormal cases, 50% of samples showed a complex karyotype (≥<br />
3 chromosomal aberrations), and clonal evolution was described<br />
in 36%. Normal karyotype was established in 32% of cases.<br />
FISH analysis on interphase nuclei detected low-risk chromosomal<br />
abnormalities in 45% (13q- as a sole abnormality) and 23% (no<br />
cytogenetic aberrations) of the cases, and high-risk cytogenetic<br />
abnormalities in 9% (11q-), 4,5% (trisomy 12), and 14% (17p-) of<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
152
samples. Except for 13q deletions, that usually are cryptic changes,<br />
all the remaining abnormalities described by FISH were present<br />
at the banding analysis. Moreover, conventional cytogenetics<br />
was able to describe additional chromosome abnormalities in<br />
13 samples, and to better characterize 3 cases resulted normal as<br />
judged by FISH.<br />
Preliminary Conclusions. Mitogen stimulation with CpG<br />
oligonucleotides is particularly useful in uncovering additional<br />
chromosomal abnormalities compared to FISH. In particular,<br />
the identification of subgroups with complex aberrant karyotypes<br />
suggests that conventional cytogenetics might provide additional<br />
prognostic information. Moreover, cytogenetics may help to<br />
further understand the biology of CLL and its related lymphomas<br />
or to differentiate between atypical cases of CLL and other<br />
pathologic entities. We plan to provide a more exhaustive analysis<br />
after the collection of one hundred samples.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
153
Main Pubblications<br />
Hereditary Endocrine Cancer Unit<br />
Exome sequencing identifies MAX mutations<br />
as a cause of hereditary pheochromocytoma.<br />
Spectrum and prevalence of FP/TMEM127<br />
gene mutations in pheochromocytomas and<br />
paragangliomas.<br />
Peptide receptor radionuclide therapy in<br />
a case of multiple spinal canal and cranial<br />
paragangliomas.<br />
Research resource: Transcriptional<br />
profiling reveals different pseudohypoxic<br />
signatures in SDHB and VHL-related<br />
pheochromocytomas.<br />
Germline mutations in TMEM127 confer<br />
susceptibility to pheochromocytoma.<br />
Chief<br />
Giuseppe Opocher, MD<br />
Born in Treviso, November 5 th 1950. Graduated in Medicine; Specialist in Endocrinology and<br />
in Nuclear Medicine. Associate Professor of Endocrinology, Department of Medical and Surgical<br />
Sciences, University of Padua. Since 2009, Head of the Hereditary Endocrine Cancer Unit and<br />
Director of the Familial Cancer Clinic, Veneto Institute of Oncology.<br />
Research Experience: Adrenal gland and hypertension, Atrial Natriuretic Peptide, Angiotensin II<br />
receptors, NF1, VHL, SDHB and SDHC, SDHD, SDHAF2 and TMEN127 genes mutations<br />
in familial and sporadic pheochromocytoma and paraganglioma. Multiple endocrine neoplasias.<br />
Hereditary renal cancer. Author of 115 publications in peer-reviewed Journals (including top journals<br />
as JAMA and Nature Genetics), Chapters in National and International books.<br />
Comino-Méndez I, Gracia-Aznárez FJ, Schiavi F, Landa I, Leandro-García LJ,<br />
Letón R, Honrado E, Ramos-Medina R, Caronia D, Pita G, Gómez-Graña A,<br />
de Cubas AA, Inglada-Pérez L, Maliszewska A, Taschin E, Bobisse S, Pica G,<br />
Loli P, Hernández-Lavado R, Díaz JA, Gómez-Morales M, González-Neira A,<br />
Roncador G, Rodríguez-Antona C, Benítez J, Mannelli M, Opocher G, Robledo<br />
M, Cascón A.<br />
Yao L, Schiavi F, Cascon A, Qin Y, Inglada-Pérez L, King EE, Toledo RA,<br />
Ercolino T, Rapizzi E, Ricketts CJ, Mori L, Giacchè M, Mendola A, Taschin E,<br />
Boaretto F, Loli P, Iacobone M, Rossi GP, Biondi B, Lima-Junior JV, Kater CE,<br />
Bex M, Vikkula M, Grossman AB, Gruber SB, Barontini M, Persu A, Castellano<br />
M, Toledo SP, Maher ER, Mannelli M, Opocher G, Robledo M, Dahia PL.<br />
Cecchin D, Schiavi F, Fanti S, Favero M, Manara R, Fassina A, Briani C, Allegri<br />
V, Sansovini M, Bui F, Paganelli G, Opocher G.<br />
López-Jiménez E, Gómez-López G, Leandro-García LJ, Muñoz I, Schiavi F,<br />
Montero-Conde C, de Cubas AA, Ramires R, Landa I, Leskelä S, Maliszewska<br />
A, Inglada-Pérez L, de la Vega L, Rodríguez-Antona C, Letón R, Bernal C, de<br />
Campos JM, Diez-Tascón C, Fraga MF, Boullosa C, Pisano DG, Opocher G,<br />
Robledo M, Cascón A A.<br />
Qin Y, Yao L, King EE, Buddavarapu K, Lenci RE, Chocron ES, Lechleiter JD,<br />
Sass M, Aronin N, Schiavi F, Boaretto F, Opocher G, Toledo RA, Toledo SP,<br />
Stiles C, Aguiar RC, Dahia PL.<br />
Nat Genet. <strong>2011</strong>; 19:663-7<br />
JAMA. <strong>2010</strong>; 304:2611-9<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
154<br />
J Clin Oncol. <strong>2011</strong>; 29:e171-4<br />
Mol Endocrinol. <strong>2010</strong>; 24:2382-91<br />
Nat Genet. <strong>2010</strong>; 42:229-33
Clinical and Research Staff<br />
Giuseppe Opocher<br />
Stefania Zovato<br />
Francesca Schiavi (Head of the Laboratory)<br />
Francesca Boaretto<br />
Sara Bobisse<br />
Valentina Camozzi<br />
Marina Lorusso<br />
Beatrice Macino<br />
Isabella Mammi<br />
Paola Sartorato<br />
Eugenia Sharova<br />
Elisa Taschin<br />
Nursing Staff<br />
Roberta Pozzani<br />
Administrative Staff<br />
Christina Drace<br />
Marina Lorusso<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
155
Mission<br />
The mission of the Hereditary Endocrine Cancer Unit is<br />
to provide genetic counselling, genetic analysis and clinical<br />
surveillance to individuals with inherited endocrine tumors.<br />
The main interest is focused on neural crest-derived tumors, in<br />
particular pheochromocytoma and paraganglioma, von Hippel<br />
Lindau disease, MEN 1 and MEN 2 syndromes.<br />
Major Collaborations<br />
International Collaborations<br />
University of Freiburg, Germany (Hartmut Neumann);<br />
CNIO, Madrid, Spain (Mercedes Robledo);<br />
UT Health Science Center, San Antonio, Texas, (Patricia<br />
Dahia);<br />
Clinical Activity<br />
In <strong>2010</strong>, the Endocrine Hereditary Cancer Unit performed the followings activities:<br />
Significant activity was also performed in patients with<br />
inherited Cushing syndrome, Carney Complex, familial<br />
hyperparathyroidism and inherited renal cancer. Also, this unit<br />
performs clinical surveillance of individuals with genetic risk<br />
for breast and ovary tumor as well as endocrinological clinical<br />
activity.<br />
San Paulo Endocrine Genetics Unit, University of Sao Paulo<br />
School of Medicine, Brasil (Sergio Toledo);<br />
The Beaston Institute for Cancer Research, Glasgow, UK (Eyal<br />
Gottlieb).<br />
Counselling for inherited endocrine tumors 175<br />
Surveillance for inherited endocrine tumors 178<br />
Surveillance for individuals with genetic risk of breast cancer 283<br />
Clinical follow-up of individuals with oncological endocrine disease 692<br />
Analysis of fragments in inherited endocrine tumors 1.428<br />
Major Ongoing Research Projects<br />
paraGaNGliOma SyNDrOmE<br />
Principal Investigators: Giuseppe Opocher, Francesca Schiavi<br />
Paragangliomas are tumors of the paraganglia, a<br />
neuroendocrine organ which originates from the neural crest.<br />
The term paraganglioma includes two different tumors since<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
156<br />
No.<br />
paraganglia, after originating from the neural crest, differentiate<br />
into sympathetic and parasympathetic paraganglia. The<br />
main difference between the two types of paraganglia is the<br />
endocrine function, since sympathetic paraganglia secrete<br />
catecholamines while the parasympathetic paraganglia do not.<br />
The main sympathetic paraganglia is the adrenal medulla and
Figure 1.<br />
the tumor of the adrenal paraganglia is the pheochromocytoma.<br />
Retroperitoneal and thoracic paragangliomas are localized at the<br />
level of the organ of Zuckerkandl, prevertebral and paravertebral<br />
thoracoabdominal and pelvic paraganglia or ganglia in ovary,<br />
testis, vagina, urethra, prostate, bladder or liver. Adrenal and<br />
Campodenno<br />
extra-adrenal pheochromocytomas secrete catecholamines, which<br />
SP67<br />
are also responsible for the chromaffin reaction of these tumor<br />
Sporminore<br />
cells. Pheochromocytomas are usually benign tumors, and the rate<br />
SPORMINORE<br />
of malignant cases is about 10%. Parasympathetic paragangliomas<br />
are mainly localized in the head and neck (HNP), i.e. at the level<br />
of the carotid body and in the jugular tympanic region; most<br />
are benign with less than 10% malignant cases. Multiple lesions<br />
Cavedago<br />
occur in 20% of patients (50% in hereditary syndromes). The SP64<br />
incidence of all paragangliomas, HNP and PHEOS is estimated Andalo<br />
ANDALO<br />
to be less than 1/300,000 per year. They can occur as sporadic<br />
cases but up to 30% of the cases of paraganglioma may have a<br />
positive family history; in this case, paraganglioma may be part<br />
of the paraganglioma syndrome, a hereditary tumor syndrome<br />
in which parasympathetic- and sympathetic-derived tumors are % carrier<br />
associated. Less frequently, paraganglioma may be part of the von 11<br />
Hippel-Lindau syndrome, type 1 neurofibromatosis and, rarely,<br />
6<br />
type 2 multiple endocrine neoplasia.<br />
The loss of function of succinate dehydrogenase (SDH) gives 0<br />
origin to the tumors in paraganglioma syndromes. SDH is the<br />
eukaryotic complex II which directly connects the respiratory<br />
SP18<br />
SS45BIS<br />
chain of the inner mitochondrial membrane to the Krebs<br />
cycle enzymes in the mitochondrial matrix. SDH catalyses the<br />
oxidative dehydrogenation of succinate coupled to the reduction<br />
of ubiquinone and the formation of fumarate. SDHB, SDHC<br />
and SDHD genes encode three of the four subunits of the<br />
mitochondrial complex II (Fig. 1) and loss-of-function mutations<br />
of one of the three genes cause decrease of prolyl-hydroxylase and<br />
eventual hyperactivity of hypoxia inducible factor (HIF) 1 alpha,<br />
which delivers a potent angiogenic and anti-apoptotic signal.<br />
Loss-of-function mutations of SDHB, SDHC and SDHD genes<br />
have been found in the majority of familial paraganglioma as the<br />
cause of the paragangliomas syndrome type 4 (PGL 4), type 3<br />
(PGL 3) and type 1 (PGL 1), respectively. An additional locus has<br />
been identified (PGL 2), but the gene is still to be characterized.<br />
Approximately 20-30% of HNP that occur without a family<br />
history or syndromic stigmata may also have mutations in the<br />
SDHD or SDHB genes and, more rarely, in the SDHC gene.<br />
PGL1 can manifest as non-chromaffin head-and-neck tumors<br />
only, adrenal and/or extra-adrenal pheochromocytomas only, or<br />
a combination of the two types of tumors. In PGL1 a maternal<br />
genomic imprinting is associated with the dominant transmission,<br />
and the disease is only transmitted by the paternal branch. SDHD<br />
Denno<br />
MAGRÈ SULLA Bolzano<br />
STRADA DEL VINO<br />
SP10<br />
CAMPODENNO<br />
SP73<br />
SP124<br />
SP21<br />
A22 SALORNO<br />
SS90<br />
MEZZOCORONA<br />
Salorno<br />
Salurn<br />
Spormaggiore<br />
Mezzocorona<br />
Mezzolombardo<br />
SS43<br />
SPORMAGGIORE<br />
SS12<br />
MEZZOLOMBARDO<br />
SS612<br />
Grumes<br />
SS421<br />
CAVEDAGO FAI DELLA<br />
PAGANELLA<br />
Fai della<br />
SP90III<br />
San Michele<br />
SP71<br />
all’Adige<br />
SP58<br />
Paganella NAVE SAN<br />
ROCCO<br />
SP131I<br />
Cembra<br />
ZAMBANA<br />
Zambana<br />
SP131<br />
LAVIS<br />
SP76<br />
SP83<br />
SP224<br />
TERLAGO<br />
SP225<br />
EGNA<br />
TON<br />
ROVERE<br />
DELLA<br />
LUNA<br />
CAPRIANA<br />
Capriana<br />
ANTERIVO<br />
Rovere della Luna<br />
GRAUNO<br />
GRUMES<br />
FAEDO<br />
VALDA<br />
FAVER<br />
SOVER<br />
VALFLORIANA<br />
SEGONZANO<br />
CEMBRA<br />
T R E N T I N O A L T O A D I G E<br />
LONA-LASES<br />
G<strong>IOV</strong>O<br />
Bedollo<br />
LISIGNAGO<br />
Trento<br />
BEDOLLO<br />
Lavis<br />
Albiano<br />
ALBIANO<br />
BASELGA DI PINÈ<br />
PALÙ DEL<br />
FERSINA<br />
Baselga SANT’ORSOLA<br />
FORNACE di Pinè<br />
TERME<br />
SP85DIR<br />
SP85<br />
SS12 SP47<br />
Trento<br />
SP66<br />
PERGINE<br />
VALSUGANA<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
157<br />
TRENTO<br />
SS12<br />
SP17<br />
CIVEZZANO<br />
Civezzano<br />
SP8<br />
Pergine Valsugana<br />
Figure 2. PGL 1 syndrome risk map in Trentino.<br />
VIGNOLA-FALESINA<br />
SPI35<br />
FRASSILONGO<br />
FIEROZZO<br />
RONCEGNO<br />
TORCEGNO<br />
RONCHI<br />
VALSUGANA<br />
CAVALESE<br />
CASTELLO-MOLINA<br />
DI FIEMME<br />
TELVE<br />
TELVE<br />
DI SOPRA<br />
SP65<br />
Telve<br />
Borgo<br />
Valsugana
mutations confer 50% penetrance by 31 years and 86% by 50<br />
years. Despite the high risk of multiple paragangliomas, a strong<br />
variability in phenotype has been observed among SDHD<br />
mutation carriers and even among families segregating the same<br />
mutation; this can range from early-onset with multiple localization<br />
and malignancy, to late-onset with a single localization. We have<br />
identified and characterized the SDHD founder mutation,<br />
c.341 A>G p.Y114C. This founder effect occurs in a population<br />
established by a small number of people, living in a well-defined<br />
geographic area in Northern Italy (Fig. 2), comprising three<br />
alpine valleys (Val dei Mocheni, Altopiano di Pinè and Val di<br />
Cembra) and Alta Valsugana, being in the past a sort of a cultural<br />
and geographic enclave (SDHD Trentino population). Actually,<br />
for the SDHD c.341A>G founder mutation a large number<br />
of carriers are available; in three years we collected 75 families<br />
for a total of 233 mutation carriers. The penetrance and the<br />
expression of the disease in this founder population has been well<br />
characterized. Penetrance was about 80% and disease phenotype<br />
was variable with high prevalence of bilateral carotid glomus<br />
tumors, low prevalence of pheochromocytomas. The relative age<br />
of this founder mutation has been investigated by examining the<br />
distance over which haplotypes are conserved: it was estimated at<br />
1400 a.D. The age of the mutation together with the low rate of<br />
emigration/immigration have determined a high prevalence of the<br />
mutation in the population of this particular area of Trentino, so<br />
far estimated to be about 2%. In summary, we have detected and<br />
fully characterized the largest SDHD founder effect. Combining<br />
molecular medicine, history and molecular biology, now we know<br />
when, why and how PGL1 developed and spread in the Trentino.<br />
An example of how a rare disease may became endemic.<br />
Endemic type 1 paraganglioma syndrome:<br />
the search for new biomarkers and the<br />
identification of a possible drug treatment<br />
Principal Investigators: Giuseppe Opocher, Francesca Schiavi<br />
Trentino country harvests the largests (and probably the<br />
oldest) founder effect for PGL1 syndrome. Despite the success in<br />
the identification, description and characterisation of the endemic<br />
PGL1 syndrome in Trentino we think there are still several<br />
important questions to answer: 1) identification of a biomarker<br />
of the disease; 2) identification of a possible drug treatment of<br />
the paraganglioma; 3) set up of an in vitro models of the PGL1<br />
tumor where to test the biomarkers and the therapeutic effects of<br />
hypothetical new drugs. The major goal of this project is to use<br />
a combination of metabolomic and systems biology analyses to<br />
find biomarkers and synthetic lethal genes in SDH-mutant cells.<br />
Metabolomics has recently emerged as an invaluable analytical<br />
tool to investigate metabolic alterations in cancer cells; thanks<br />
to this approach, the metabolic profiles of prostate cancer,<br />
glioblastoma, and other tumors have been recently revealed.<br />
Metabolomics is not only crucial to uncover the determinants of<br />
the metabolic transformation of cancer cells but it can also be<br />
important to discover potential tumor biomarkers. In addition,<br />
metabolomic data can be used to improve in silico models of<br />
cellular metabolism, to better predict metabolic fluxes and also<br />
to discover potential synthetic lethal genes. Heterozygous germline<br />
mutations in SDHB, SDHC, and SDHD subunits have<br />
been found to predispose to a rare hereditary cancer syndrome,<br />
hereditary paragangliomas and pheochromocytomas (hPGL). This<br />
cancer syndrome is characterized by the development of tumors<br />
of the chromaffin tissue arising in the adrenal medulla, defined<br />
pheochromocytoma (PHEO), or derived from the parasympathetic<br />
tissue of the head and neck defined paraganglioma (PGL). In<br />
addition, SDHB mutation carriers have increased susceptibility<br />
to renal cell cancers (RCC). Generally, the germ-line mutations<br />
are followed by a somatic “second hit” of the normal allele in<br />
the tumor cells, causing a complete loss of SDH activity in these<br />
tissues. It is still unclear how SDH-deficient cells can survive and<br />
proliferate in the absence of a functional TCA cycle. In fact, the<br />
TCA cycle is in not only required to provide the mitochondrion<br />
with redox equivalents for oxidative phosphorylation but it also<br />
integrates several metabolic pathways that generate intermediate<br />
metabolites for cellular growth and proliferation.<br />
Therefore, it is reasonable to think that in the absence of an<br />
intact TCA cycle, SDH-deficient cells would require a metabolic<br />
adaptation, i.e. a rearrangement of the metabolic network of the<br />
cell, in order to proliferate and accomplish the metabolic request<br />
of a fast proliferating tumor tissue. Hence, SDH-deficient cells<br />
would become dependent on specific metabolic pathways to<br />
survive and proliferate but this will also represent their Achilles<br />
heel. In fact, the targeting of these alternative metabolic pathways<br />
should specifically affect the proliferation of mutant cells and will<br />
not have an effect on the normal cells. These metabolic pathways<br />
would be synthetic lethal (SL) with SDH. As we said, the major<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
158
goal of this project is to use a combination of metabolomic and<br />
systems biology analyses to find biomarkers and SL genes in<br />
SDH-mutant cells (see Table 1). First, we will perform a large scale<br />
unbiased metabolomic analysis of various body fluids and tumor<br />
tissues from SDH-mutant patients. This analysis will then lead to<br />
the characterization of the metabolic profiling of SDH mutant<br />
cells. Importantly, this analysis would reveal potential biomarkers<br />
to be used both for screening of the at-risk population and also to<br />
follow the success of chemotherapy. The parallel transcriptomic<br />
analysis will also be employed to establish the effects of different<br />
SDH mutations on metabolism. To further investigate the effect of<br />
SDH mutations on cellular metabolism, we will generate primary<br />
cell lines from tumor tissues and perform steady-state and flux<br />
endo- and exo-metabolomic analyses. With this metabolomic<br />
database, we will build a specific in silico model of SDH-mutant<br />
cells which will eventually allow us to predict SL metabolic<br />
pathways. The validation of these SL reactions will be initially<br />
performed on primary cell cultures.<br />
Table 1. Tasks of the project<br />
Enrolment of the cohort of SDH mutant patients and<br />
Task 1<br />
collection of body fluids<br />
Task 2 Metabolomic studies on human body fluids<br />
Task 3 In silico model of SDH-mutant cells<br />
Task 4 Establishment of human paraganglioma primary cell lines<br />
Task 5 Steady-state endo- and exo-metabolomic and flux analyses<br />
TmEm 127, ThE ElEvENTh GENE<br />
Principal Investigators: Giuseppe Opocher, Francesca Schiavi<br />
Characterization of the entire spectrum of disease-associated<br />
alleles is an overarching goal of contemporary and future medicine<br />
and can inform on patient diagnosis, treatment and surveillance.<br />
This may be particularly important in cancer genetics.<br />
We have many arguments to support the concept that genetics<br />
of pheochromocytoma and paraganglioma are really peculiar and<br />
that this scientific knowledge is rapidly expanding. In any other<br />
case of endocrine tumor a so strong relationship with genetics<br />
has been established: the overall prevalence of mutations is near<br />
to 40% of consecutive cases and more than 20% in apparently<br />
sporadic cases. Again, a very high number of different predisposing<br />
genes has been isolated, ten at the beginning of <strong>2010</strong>, but the<br />
number is increasing. Consequently, pheochromocytoma and<br />
paraganglioma can well be considered an extremely interesting<br />
model to study cancer genetics and to understand how multiple<br />
genes can affect cancer development.<br />
The eleventh gene, that we contribute to discover (Qin Y<br />
et al, Nature Genet <strong>2010</strong>), is the new tumor suppressor gene<br />
TMEM127. Mutations of this gene predispose to the development<br />
of pheochromocytoma: we have data supporting that TMEM127<br />
plays an important role in the regulation of the mTOR pathway.<br />
Genetic events leading to a deregulated mTOR signaling provide<br />
tumors with a selective growth advantage. Indeed, numerous<br />
oncogenes and tumor suppressors converge on the regulation<br />
of mTORC1, including those that most frequently underlie the<br />
development and progression of malignant tumors. Moreover,<br />
elevated mTORC1 signaling has been detected in a large<br />
percentage of the most common human cancers. These data could<br />
suggest a role for TMEM127 in other tumors with disruption of<br />
the mTOR pathway. In addition, they open the possibility that<br />
additional cancer-related genes remain to be identified.<br />
This project is aimed to the possibility to define the<br />
TMEM127 phenotype, to evaluate the pathogenetic role of<br />
sequence variant along the new gene, and to deeply investigate the<br />
role of TMEM127 in disregulation of mTOR pathway including<br />
the effect on new rapamycin inhibitors. The genetic analysis was<br />
extended to 200 new cases of pheochromocytoma referred to our<br />
clinic with apparently sporadic pheochromocytoma and wild type<br />
for RET, VHL, SDHB, SDHC, SDHD gene analysis. Based on<br />
preliminary data we have the possibility to clinically characterize<br />
7 families with different TMEM127 mutations. Our preliminary<br />
clinical data suggest an emerging pattern in association with<br />
TMEM127 mutations: while bilaterality combined with familial<br />
history accounts for almost half of the mutant cases, more than<br />
one-third of the mutation carriers presented with a sporadicappearing,<br />
benign pheochromocytoma after the age of 40.<br />
Although malignancy can also occur in association with these<br />
mutations, this was a very infrequent presentation.<br />
To address the problem of defining whether USV are<br />
pathogenetic or not, first we will perform experiments using<br />
in silico approaches in order to evaluate if they act as cis-acting<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
159
egulatory functional variants, disrupting or creating regulatory<br />
elements in DNA or RNA sequence.<br />
After evaluation of sequence conservation it is interesting to<br />
examine the different RNA stability when the variations are present<br />
in the 5’ or 3’UTR by using the RNAfold web server (http://rna.<br />
tbi.univie.ac.at/cgi-bin/RNAfold.cgi) that provides elements to<br />
perform RNA secondary structure analyses. Functional regulatory<br />
elements in TMEM127 will be identified by means of UTRScan<br />
(http://bighost.area.ba.cnr.it/BIG/UTRHome/).<br />
In addition, to better understand intronic mutations leading<br />
to splicing defects, further investigations will be performed using<br />
helpful tools like Human Splicing Finder website (http://www.<br />
umd.be/HSF/), the SpliceView (http://wwwspliceview.html),<br />
NNSPLICE0.9 (http://www.fruitfly.org/seq_tools/splice.html)<br />
and others.<br />
Secondly, by using in vitro analysis, in order to test whether<br />
the UTR variations could actually affect the expression levels of<br />
the TMEM127 gene we will prepare different plasmid constructs<br />
in which the luciferase reporter gene is under the control of either<br />
wild-type or mutant regions. We will use these plasmids to perform<br />
transient transfections of the HEK293 cell line. Instead we will<br />
investigate the effect of the intronic variations using minigene<br />
system in order to identify intronic elements that enhance or<br />
repress splicing.<br />
The study of the functionality of the wild type TMEM127<br />
protein as well as the effects of its newly described variants<br />
has just begun. The physiological and pathogenic roles of<br />
TMEM127 deserve further investigation. Wild type TMEM127<br />
protein encoded by exogenous vectors localizes to the plasma<br />
membrane and the cytoplasm, both in a punctuate pattern and<br />
as perinuclear clusters. Moreover, exogenous TMEM127 protein<br />
associates dynamically with endosomes. Transcription signature<br />
of TMEM127-mutant tumors revealed high statistical association<br />
with kinase receptor signals which had been previously linked to<br />
NF1 and RET mutants, inspiring further functional investigation.<br />
In particular, TMEM127 knockdown does not induce HIF1alpha<br />
and its targets in HEK293 or HeLa cells, nor increases RAS<br />
activity, nor enhances AKT phosphorylation. On the contrary,<br />
analogous tests demonstrated that TMEM127 knockdown leads<br />
to increased phosphorylation of 4EBP1 in various cell lines,<br />
establishing a relationship between TMEM127 and mTOR<br />
signalling. Based on these results, it is conceivable that the most<br />
important criterion for TMEM127 physiological and pathogenic<br />
role might be the evaluation of its effect on mTOR signalling.<br />
A reliable and clear functional assessment of the variants should<br />
explore TMEM127 properties, namely its ability to modulate<br />
mTORC1 pathway.<br />
To complement genetic studies, we will study whether<br />
TMEM127 mutations affect cellular sensitivity to pharmacological<br />
mTOR inhibition in vitro and in a preclinical setting. Transcription<br />
signature studies of TMEM127-mutant tumors revealed high<br />
statistical association with kinase receptor signals. In particular,<br />
the aberrant expression of TMEM127 results in an altered<br />
mTORC1, but not mTORC2 signalling, while co-localization<br />
studies denostrated that TMEM127 protein occupies the same<br />
intracellular domain as active mTOR. Overall, results suggest<br />
that TMEM127 contributes to controlling mTORC1 signals and<br />
support a role for TMEM127 as a tumor suppressor.<br />
THE DEPARTMENTS - DEPARTMENT OF EXPERIMENTAL, LABORATORY AND TRANSLATIONAL ONCOLOGY<br />
160
Department of Services<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
161
Main Pubblications<br />
Chief<br />
Photoreactivity of 5-fluorouracil under UVB light: photolysis<br />
and cytotoxicity studies.<br />
Short-term bisphosphonate therapy could ameliorate<br />
osteonecrosis: a complication in childhood hematologic<br />
malignancies.<br />
Italian Society for Parenteral and Enteral Nutrition Executive<br />
Committee. Prevalence of home artificial nutrition in Italy<br />
in 2005: a survey by the Italian Society for Parenteral and<br />
Enteral Nutrition (SINPE).<br />
Pharmacy<br />
Angelo Claudio Palozzo, Pharm D<br />
Graduated in Pharmacy in 1978 at the University of Padova, he specialized in Hospital Pharmacy<br />
in Milano 3 years later. From 1981 to 1991 he works as a Pharmacist in several Hospitals of the<br />
Veneto and Abruzzi regions. From 1991 he acts as Pharmacy Director in Veneto, and since 2007 he<br />
directs the <strong>IOV</strong> Pharmacy. Following some stages abroad (Providence, USA, 1985 and Barcelona,<br />
Spain, 1988), his interest has focused on pharmacokinetics, artificial nutrition, pharmacoeconomy,<br />
epidemiology, and health governance. He is the national referent for Oncology within the Pharmacist<br />
Italian Society SIFO, and he is member of several scientific societies (SINPE, ISOPP, ESOP).<br />
He teaches pharmacology in several post-graduate schools, and is very active in promoting educational<br />
issues. He is author of numerous scientific publications in the field of clinical pharmacology.<br />
Miolo G, Marzano C, Gandin V, Palozzo<br />
AC, Dalzoppo D, Salvador A, Caffieri S.<br />
Greggio NA, Pillon M, Varotto E, Zanin A,<br />
Talenti E, Palozzo AC, Calore E, Messina C.<br />
Pironi L, Candusso M, Biondo A, Bosco<br />
A, Castaldi P, Contaldo F, Finocchiaro E,<br />
Giannoni A, Mazzuoli S, Orlandoni P,<br />
Palozzo AC, Panella C, Pastò S, Ruggeri E,<br />
Sandri G, Stella E, Toigo G.<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
162<br />
Chem Res Toxicol. <strong>2011</strong>; 24:1319-26<br />
Case Report Med. <strong>2010</strong>; <strong>2010</strong>:206132<br />
Clin Nutr. 2007; 26:123-32
Clinical and Research Staff<br />
Angelo Claudio Palozzo<br />
Sonia Faoro<br />
Francesco Paganelli<br />
Maurizio Cavalli<br />
Lucia Esposito<br />
Enrico Gori<br />
Marta Paulina Trojniak<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
163<br />
Nursing and Technical Staff<br />
Fabiola Bellotti<br />
Silvia Bruno<br />
Giovanna Cazzadori<br />
Alessandra Misserianni<br />
Anita Moresco<br />
Francesca Pipitone<br />
Luisa Schivo<br />
Marinella Zanin
Mission<br />
The Pharmacy Unit of the <strong>IOV</strong> has the mission of performing<br />
and verifying all the activities involved in the preparation,<br />
Clinical Activity<br />
The clinical activities of the Unit include:<br />
the implementation of the quality system and the computerized<br />
management of all the prescriptions for individual patients;<br />
the manipulation of cytotoxic drugs, biotechnologic drugs, and<br />
antalgic recipes until the delivery of the ready-to-use product;<br />
the storing and conservation of all the pharmaceutical products<br />
in the appropriate quantities for satisfying the needs of the<br />
different Units and in the appropriate temperature and humidity<br />
conditions;<br />
Major Research Collaborations<br />
Inside the <strong>IOV</strong><br />
The Pharmacy Unit interacts with several structures, and in<br />
particular with the Clinical Oncology Units and the Unit for the<br />
Introduction of New Drugs.<br />
Major Ongoing Research Projects<br />
A retrospective observational study to<br />
evaluate effectiveness vs. efficacy and to<br />
determine the characteristics of patients with<br />
lung cancer responsive to Erlotinib treatment<br />
Principal Investigator: Angelo Claudio Palozzo<br />
This project intends to retrospectively analyze data obtained<br />
through the onco-AIFA register in lung cancer patients treated<br />
with the target drug Erlotinib. From this registry, in fact, it is<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
164<br />
distribution and administration of pharmacologic products.<br />
the management of the informative fluxes to central<br />
pharmaceutical authorities and agencies;<br />
the maintenance of the registries (Onco-AIFA for new oncologic<br />
drugs; NSIS; SIRFAC) and the computerized management of<br />
these databases;<br />
the vigilance on pharmaceuticals and medical devices;<br />
the appropriate periodical information to the personnel about<br />
AIFA regulations on single drugs.<br />
International Collaborations<br />
Christies NHS Trust, Pharmacy Unit, Manchester, UK<br />
Dept. of Public Health Science, School of Medicine, Kings<br />
College, London, UK.<br />
possible to obtain data on the efficacy of Erlotinib administered<br />
to NSCLC patients as a second line treatment following a<br />
therapeutic failure with conventional chemotherapy. The<br />
observation period goes from January 1, 2007 to January 31,<br />
<strong>2011</strong>, and comprehends 130 cases to be compared with data<br />
present in the registration study (RCT). The retrospective analysis<br />
will allow to identify critical points in the clinical practice, where<br />
conditions are less standardized than in RCT. The major clinical<br />
outcomes will be evaluated as Progression-Free Survival (PFS)
according to the onco-AIFA Registry, Overall Survival (OS) and<br />
Time to Progression (TTP), obtained from medical records. A<br />
detailed analysis of potential factors able to predict response (such<br />
as clinical features and genetic status) will also be performed, in<br />
order to better ascertain the prescriptive appropriateness of this<br />
drug.<br />
A retrospective study to evaluate<br />
effectiveness and prescriptive appropriateness<br />
of Pemetrexed in patients with lung cancer<br />
Principal Investigator: Francesco Paganelli<br />
The introduction of new anti-tumoral drugs often entails a<br />
conspicuous economic burden to the community. Thus, the use<br />
of these drugs is strictly regulated by a dedicated agency (AIFA),<br />
which emanates periodic guidelines on their use and continuously<br />
monitors the appropriateness of prescription. The extraction of<br />
data from the onco-AIFA Registry and the record-linkage with<br />
other administrative databases allows obtaining epidemiologic<br />
data (OS, PFS, TTP, toxicities) at different complexity levels (local,<br />
regional, national), thus contributing to delineate the effectiveness<br />
profile of single drugs. These data can be compared with those<br />
present in registration studies and for pharmacoeconomic analyses<br />
(LY, Budget Impact), and may help the decision-making of the<br />
health Authorities. Aim of this project is to compare therapeutic<br />
regimens containing pemetrexed vs. gemcytabine in the treatment<br />
of NSCLC. The project could also be a methodological example<br />
which could be extended to other settings and drugs. In fact,<br />
should the results be substantially different compared to those<br />
obtained in registrative studies, the data could be communicated<br />
to AIFA, with possible changes in the authorization to prescription<br />
of these drugs.<br />
Anti-emetic treatment in cancer patients<br />
Principal Investigator: Sonia Faoro<br />
It is known that a common side effect of most chemotherapic<br />
treatments is nausea and vomiting. The present project stems<br />
from the observation that in daily clinical practice, especially for<br />
non-hospitalized patients, anti-emetic treatment often differs<br />
from the guidelines of Scientific Societies, and it greatly varies<br />
among patients, with poor control of the efficacy of the different<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
165<br />
schedules. This study has two major objectives:<br />
1) to identify cost-effective anti-emetic treatments for every<br />
chemotherapic regimen associated with nausea and vomiting;<br />
2) to prepare appropriate anti-emetic kits to be distributed not<br />
only inside the Hospital, but also for at home use. This last<br />
approach could contribute to standardize the most appropriate<br />
anti-emetic intervention for every anti-tumoral medication, to<br />
obtain a better therapeutic compliance and hence quality of<br />
life of patients, and finally to potentially reduce the costs of the<br />
therapy of such adverse events.<br />
Retrospective analysis of the administration<br />
of Fulvestrant in patients with ER+ metastatic<br />
breast cancer: evaluation of appropriateness<br />
and effectiveness of the treatment<br />
Principal Investigator: Marta Paulina Trojniak<br />
The layout of this study is similar to that conducted on<br />
Erlotinib. The observation period goes from January 1, 2007<br />
to January 31, <strong>2011</strong>, and comprehends 100 cases of patients<br />
bearing metastatic hormone-sensitive breast cancer treated with<br />
Fulvestrant. Thanks to the data obtained from the onco-AIFA<br />
Registry and the medical records, this project will allow to<br />
calculate the effectiveness of the drugs in terms of TTP and OS.<br />
The data obtained will permit to identify the subset of patients in<br />
whom the therapy proved efficacious, and to define their clinical<br />
and biologic characteristics; at the same time, the results will allow<br />
to identify patients with clinical features which do not suggest the<br />
use of this treatment.
Other Programs and Future Perspectives<br />
Thanks to standardization, quality controls, and the availability<br />
of data from different sources and registries (AIFA, SIRFAC, SSI,<br />
SCI), the Unit has activated several lines of research in pharmacoepidemiology<br />
and pharmaco-economics. In this setting, Dr.<br />
Palozzo is the principal investigator of a regional <strong>2011</strong>-2012<br />
project on Health Technology Assessment, which involves most<br />
structures all over the region, and clearly delineates a leading role<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
166<br />
of this <strong>IOV</strong> Unit in the field of oncologic pharmaceutics within<br />
the Veneto region. A future challenge for the Pharmacy, which<br />
is going to move to a new and larger site within the Institute, is<br />
the distribution of cytotoxic drugs over the entire Padova health<br />
system; this implies an increment in work burden calculated in<br />
about 25,000 additional preparations per year.
Main Pubblications<br />
Chief<br />
Alberto Banzato, MD<br />
Low molecular weight heparin (parnaparin) for cardioembolic<br />
events prevention in patients with atrial fibrillation undergoing<br />
elective electrical cardioversion: a prospective cohort study.<br />
Large infero-posterior wall pseudoaneurysm of the left<br />
ventricle: an unusual presentation.<br />
Effectiveness of fixed minidose warfarin in the prevention of<br />
thromboembolism and vascular death in nonrheumatic atrial<br />
fibrillation.<br />
A comparison of a moderate with moderate-high intensity<br />
oral anticoagulant treatment in patients with mechanical heart<br />
valve prostheses.<br />
Revision and optimization of processes: a fundamental<br />
timing for adequate use of the resources and technological<br />
innovation. An example of intervention in the cardiology field<br />
and considerations on “total quality” in medicine.<br />
Cardiology<br />
Degree in Medicine and specialization in Cardiology at the University of Padua with full marks<br />
and honors. From 1994 to 2005 he participated in the opening and development of the Cardiology<br />
Department and Coronary Care Unit of Este General Hospital. Besides the clinical activity, he<br />
performs instrumental diagnostics and implants cardiac pacemakers and defibrillators. In 2006,<br />
he was responsible for the Electrophysiology Unit of Chioggia General Hospital. Since 2007 he<br />
has provided clinical and instrumental cardiology at the Veneto Oncology Institute with highly<br />
specialized tasks as “preoperative stratification of cardiovascular risk.” He was appointed chief of the<br />
Cardiology Unit in April <strong>2010</strong>. He is the author of more than 40 scientific publications.<br />
Angeloni G, Alberti S, Romagnoli E, Banzato<br />
A, Formichi M, Cucchini U, Pengo V.<br />
Targa L, Gaglione E, Scattolin G, Formichi<br />
M, Banzato A, Lucà MG, Corbara F.<br />
Pengo V, Zasso A, Barbero F, Banzato A,<br />
Nante G, Parissenti L, John N, Noventa F,<br />
Dalla Volta S.<br />
Pengo V, Barbero F, Banzato A, Garelli E,<br />
Noventa F, Biasiolo A, Zasso A, Dalla Volta S.<br />
Corbara F, Scattolin G, Gabellini A, Caneve<br />
F, Desideri A, Banzato A, Formichi M.<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
168<br />
Intern Emerg Med. <strong>2011</strong>; 6:117-23<br />
Ital Heart J. 2002; 3:758-61<br />
Am J Cardiol. 1998; 82:433-7<br />
Thromb Haemost. 1997; 77:839-44<br />
G Ital Cardiol. 1995; 25:859-75
Clinical and Research Staff<br />
Alberto Banzato<br />
Alessandra Bianchi<br />
Nursing Staff<br />
Caterina Fabris<br />
Maria Cristina Pancaro<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
169
Mission<br />
This Unit is mainly devoted to the cardiovascular surveillance<br />
of patients undergoing surgical and/or chemo-radiotherapy<br />
treatment, in order to determine individual cardio-vascular risk<br />
and to monitor the potential cardiotoxicity risks linked to these<br />
therapies. The activity is also addressed to the cardiovascular<br />
monitoring in patients treated with conventional chemotherapy or<br />
Clinical Activity<br />
The clinical and instrumental pathways are performed mostly<br />
on the same day in order to rapidly determine the cardiovascular<br />
status thus limiting further patient access to the Institute. To<br />
reduce the time between the diagnosis of cancer and its treatment,<br />
access to cardiologic assessment is divided into different priority<br />
levels that exclude the waiting lists for urgent situations (surgery,<br />
chemotherapy start), and provide separate lists for less urgent and<br />
follow-up patients. In the four years of activity, the Cardiology<br />
Unit has refined a work team that provides oncology and<br />
cardiology assessment, the definition of individual cardio-toxicity<br />
risk, the choice of treatment and subsequent oncologic and<br />
cardiologic follow-up. Early detection of cardiovascular damage<br />
through a careful clinical and instrumental monitoring helps<br />
to establish an early therapy in order to avoid worsening of the<br />
damage. The reporting activity is handled through the computer<br />
network in order to be able to ensure a real-time consultation.<br />
During <strong>2010</strong>, the Cardiology Unit carried out approximately<br />
10,000 procedures: cardiology consultation, electrocardiogram,<br />
transthoracic and transesophageal echocardiography at rest or with<br />
pharmacological stress, dynamic electrocardiogram, cycloergometer<br />
exercise test, carotid ultrasound, myocardioscintigraphy stress test<br />
(in collaboration with Nuclear Medicine).<br />
Major Collaborations<br />
In collaboration with other Units of the Institute, the Cardiology<br />
Unit participates in 19 clinical trials. It is currently involved in a<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
170<br />
more recent biological drugs for the potential risk of cardiotoxicity.<br />
The Unit also provides standard cardiologic support to other units<br />
at the Institute. The nursing staff has, by nature and training,<br />
human capacity and social skills appropriate to approach cancer<br />
patients.<br />
<strong>2010</strong> Cardiology Unit Activity<br />
Numbers<br />
4000<br />
3500<br />
3000<br />
2500<br />
2000<br />
1500<br />
1000<br />
500<br />
0<br />
3934<br />
ECG<br />
2801<br />
echocardiogram<br />
2491<br />
cardiology<br />
consultation<br />
dynamic ECG<br />
196 145 113<br />
carotid<br />
ultrasound<br />
project with the Italian Society of Echocardiography.<br />
exercise testing
Major Research in Progress<br />
Troponin dosage as an early marker of<br />
cardiotoxicity during chemotherapy.<br />
Principal Investigator: Alberto Banzato<br />
In view of the potential cardiotoxic effect of many chemotherapy<br />
regimens and radiotherapy, especially for left mammary gland<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
171<br />
irradiation, aim of this study is to identify early markers of<br />
cardiac damage. Troponin is a suitable candidate, but its use has<br />
not been as yet validated. The study enrolls patients undergoing<br />
standard chemotherapy and radiation therapy, patients treated<br />
with Trastuzumab monoclonal antibody, and patients undergoing<br />
IORT.
Main Pubblications<br />
Chief<br />
Positive experience of intraperitoneal<br />
chemotherapy followed by intravenous<br />
chemotherapy in heavily pretreated patients<br />
with suboptimal residual ovarian cancer and<br />
primary peritoneal cancer.<br />
La riabilitazione in psiconcologia: lo sviluppo<br />
dell’approccio psicosociale dall’adattamento<br />
alla spiritualità.<br />
Lo psicologo nell’accompagnamento al<br />
malato in fase terminale: l’esserci.<br />
Quality of life after radical cystectomy and<br />
orthotopic bladder substitution: a comparison<br />
between Italian and Swedish men.<br />
Psycho-Oncology<br />
Eleonora Capovilla, Psychologist<br />
Eleonora Capovilla, psychologist – psychotherapist, has developed and applies a psychological<br />
approach that is specific for the oncological field, called API (Integrated Psycho-oncological<br />
Approach). Formerly appointed to teach Psycho-oncology in the postgraduate course in Pain Therapy<br />
and Palliative Cares at the University of Verona, she is adjunct professor of the University of Padua.<br />
Besides teaching in various public training courses, she is author of a number of scientific works<br />
in the field of psycho-oncology. In 1997 she founded the Veneto Regional Section of the Italian<br />
Society for Psycho-oncology (SIPO) which she co-ordinated until 2002 and in that role she started<br />
the Project “Humanisation of Cares in Oncology”. From 2000 to 2007 she was Regional Board<br />
Member of the Italian Society of Palliative Care. From 2003 to 2007 she was vice-president of the<br />
SIPO. Since 2007 she is a member of the Regional Committee for Palliative Care and Cure of Pain<br />
in the Regional Observatory for Palliative Care and for Cure of Pain (Veneto Region). At present she<br />
coordinates the National SIPO Committee for Medical Humanities.<br />
Nicoletto MO, Dalla Palma M, Donach M.E,<br />
Gusella M, Cappetta A, Shams M, Marchet<br />
A, Nardin M, Pintacuda G, Di Maggio A,<br />
Marchesi M, Carli P, Fiduccia P, Artioli G,<br />
Nitti D.<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
172<br />
Tumori. <strong>2010</strong>; 96: 918-925<br />
Capovilla E, Serpentini S, Guglieri I, Cason E. Noos: aggiornamenti in psichiatria, Il Pensiero<br />
Scientifico Editore: Roma, in press.<br />
Capovilla E. I. Testoni, D. Di Lucia Sposito, F. Martini (a cura<br />
di) Atti del Convegno “Il morire tra ragione e fede.<br />
Universi che orientano le pratiche d’aiuto”. Padova 20-<br />
21 Marzo 2009. Monografia Endlife.it n°1. Capitolo<br />
Terzo. <strong>2010</strong><br />
Månsson A, Caruso A, Capovilla E, Colleen S,<br />
Bassi P, Pagano F, Månsson W.<br />
BJU Int. 2000; 85:26-31
Clinical and Research Staff<br />
Eleonora Capovilla<br />
Malihe Shams<br />
Lucia Bazzo<br />
Eleonora Cason<br />
Simona D’Ippolito<br />
Irene Guglieri<br />
Maria Rosa Mazzolini<br />
Eleonora Pinto<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
173<br />
Romina Spina<br />
Marco Zoncapè
Mission<br />
The Psycho-oncology Service offers to patients and families<br />
a welcoming setting to minimize the negative impact of cancer<br />
diagnosis and therapy. The main concern is to support the<br />
psychological needs of patients and family members in each<br />
Clinical Activity<br />
The service is addressed to patients in charge of the Operative<br />
Units of the Veneto Oncological Institute, from first entry into<br />
<strong>IOV</strong> up to the closure of follow-up, as well as to patients’ families.<br />
It is also open to patients from different Hospitals.<br />
The Psycho-oncological team supports patients according to<br />
the integrated model typical of the psycho-oncological discipline,<br />
which aims at the care of patients and families in collaboration<br />
with the other professional figures involved (medical oncologists,<br />
palliative care doctors, physicians, nursing and technical staff,<br />
social workers etc.) and in collaboration with volunteers who are<br />
active within the Operative Units of the Oncological Institute.<br />
Main psycho-oncological assistance available for patients:<br />
psycho-oncological entry structured interviews;<br />
counselling;<br />
psycho-educational interventions;<br />
individual and group therapies;<br />
Major Collaborations<br />
Inside the <strong>IOV</strong><br />
Anesthesia<br />
Clinical Oncology 1<br />
Clinical Oncology 2<br />
Oncological Surgery<br />
Radiotherapy<br />
Breast Unit<br />
Melanoma and soft tissue sarcomas<br />
Unit for hereditary cancers<br />
Nursing Service<br />
National Collaborations<br />
Orthopedic Clinic, Azienda<br />
Ospedaliera di Padova<br />
Unit of Physical Medicine and<br />
Rehabilitation<br />
Ospedale Sant’Antonio, ULSS 16,<br />
Padova<br />
Social Psychology - University of Padua<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
174<br />
phase of the illness, during both Day Hospital and ordinary<br />
hospitalisation, and during outpatient treatment, with individual<br />
as well as group treatments.<br />
mindfulness-based programs for stress reduction;<br />
relaxation groups.<br />
Assistance to family members. Psycho-oncological initial<br />
interviews, counselling and psychotherapy interventions.<br />
In addition the Unit guarantees:<br />
The presence of the psychologist in the ward team and the<br />
psycho-oncological interventions to accompany patients and<br />
families in advanced-terminal stages of illness.<br />
National point of reference for the promotion of “Medical<br />
Humanities” interventions, such as for example MBSR protocol<br />
(Mindfulness Based Stress Reduction), the only experience in<br />
progress at present for oncological patients in Italy.<br />
Continuing education and supervision of AVO and ANGOLO<br />
volunteers active in Clinical Oncology.<br />
International Collaborations<br />
Fabio Giommi, Radboud University,<br />
Nijmegen, (The Netherlands)<br />
Fawzy I. Fawzy, UCLA School of<br />
Medicine, Los Angeles, (California)<br />
Camilla Zimmermann, FRCPC Head<br />
Palliative Care program, University<br />
Health Network
Major Ongoing Research Projects<br />
Interventions for stress reduction and<br />
promotion of well-being based on the<br />
methodology of Mindfulness (MBSR)<br />
available to oncological patients in follow-up<br />
Principal Investigator: Eleonora Capovilla<br />
Background. MBSR is a program which has represented<br />
in the last twenty years a frontier in the area of medical and<br />
psychotherapeutic research called “integrative medicine” or<br />
“mind-body medicine”, which considers mind and body as a unit<br />
requiring to be understood beyond rigid divisions.<br />
The MBSR program is a scientific program developed in the<br />
field of behavioral medicine by Prof. Jon Kabat Zinn and his<br />
collaborators at University of Massachusetts.<br />
Aims: promoting in patients mindfulness-based strategies<br />
for fatigue and stress management.<br />
1) Promoting and implementing an approach of preventionrehabilitation<br />
which allows an improvement of the quality<br />
of life of cancer patients. The intervention is not limited to<br />
the acute therapeutic phase, it reduces hospitalisation and the<br />
pharmacologic load of assistance.<br />
2) Implementing a global approach to the patient according to<br />
the principle of “simultaneous care”.<br />
Methodology. Starting in January 2009, three interventions<br />
have been carried out, involving a total of 47 participants.<br />
Quantitative analysis. PRE-POST intervention administration<br />
of psychometric instruments : EORTC QLQ-30, Psychological<br />
Well being Index, Kentucky Inventory of Mindfulness Skills<br />
(KIMS), Mindful Attention Awareness Scale (MAAS), Hospital<br />
Anxiety and Depression Scale (HADS).<br />
Descriptive analysis. Main outcome variables, level of<br />
distress and specific abilities of Mindfulness: re-administration<br />
6-12 months.<br />
Qualitative analysis. Administration of a personal data form,<br />
assessment of motivation and expectations; content analysis;<br />
audio-recordings of sessions; administration of evaluation form<br />
12 months after the end of the course.<br />
Main results. The main results regard the first and second<br />
intervention and can be summarised as follows: an increase in<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
175<br />
the percentage of subjects without distress has been observed, a<br />
reduction of subjects with severe distress and an improvement<br />
of “state” aspects such as attention and awareness. As regards<br />
other variables, though not statistically significant, important<br />
improvements from the clinical point of view have been observed:<br />
an increase in the number of subjects with “Emotional level<br />
in the norm” and a decrease of the percentage of subjects with<br />
“adaptation disorder” or “major depression disorder”. The Quality<br />
of life appears tendentially increased.<br />
Re-administration of the instruments at 6 and 12 months<br />
confirms the results found in post-intervention as far as the<br />
principal outcome variables are concerned.<br />
The third intervention has just come to an end (January-<br />
March <strong>2011</strong>).<br />
In conclusion, the analysis of data, in line with the results of<br />
the literature, in the first evaluation post-intervention shows in<br />
the sample of participants to the Mindfulness course statistically<br />
significant improvements in the principal outcome variables, thus<br />
showing the efficacy of the intervention.<br />
Future prospects. Randomised study to evaluate the efficacy<br />
of an MBSR protocol modified for oncological patients under<br />
treatment.<br />
The practice of informed consent to<br />
anesthesia: a randomised study between<br />
conventional and integrated approaches<br />
Principal Investigator: Eleonora Capovilla<br />
Background. The project’s aim is to evaluate both the<br />
emotional state of patients in pre-surgery phase, considered as a<br />
particularly critical moment, when mood variations may condition<br />
also the ability of correctly receiving information and instructions<br />
from the curing staff, and – through such evaluation – to facilitate<br />
the communicative-relational process during the diagnosticinformative<br />
interview with the anesthesiologist. The present<br />
project, in collaboration with the Anesthesia Unit, originates<br />
from the perceived difficulties in clinical practice of managing the<br />
anxiety of patients during the anesthesiological pre-surgery visit<br />
and from the observation, on the day of surgery, that the patients<br />
have failed to understand some information.
An ad hoc intervention has therefore been devised, whose<br />
effectiveness will be tested. For the study, an experimental group<br />
of patients has been formed, to whom the anesthesiological presurgery<br />
visit has been preceded by a briefing with the psychooncologist<br />
and by a subsequent contact between the latter<br />
and the anesthesiologist, aimed at adopting the most efficient<br />
communicative strategies to be used with a patient. This group has<br />
been compared with a control group: traditional anesthesiological<br />
pre-surgery visit (with no intervention of the psycho-oncologist).<br />
Methodology. Randomised prospective monocentric study<br />
including a total of 240 patients (women with mammary<br />
carcinoma awaiting for surgery). The patients participating in the<br />
study are assigned to the two groups in a randomised way.<br />
In group P the integrated psycho-oncological approach<br />
is adopted: Group A (control group) simply undergoes the<br />
traditional anesthesiological visit.<br />
The following steps will be followed:<br />
1) Informative briefing and anesthesiological evaluation: the<br />
anesthesiologist after the clinical evaluation informs the patient,<br />
following a fixed protocol subject to periodic reassessment, in<br />
order to obtain the patient’s informed consent to anesthesia.<br />
2) Structured psycho-oncological interview: the psychooncologist<br />
gathers useful information for the subsequent<br />
anesthesiologist-patient communication and offers a setting for<br />
the aknowledgement and redefinition of the patient emotional<br />
experience.<br />
3) State Trait Anxiety Inventory (STAI) for the evaluation of<br />
the state of anxiety. This is administered in the two groups<br />
before randomisation and after the signature of the informed<br />
consent.<br />
4) Questionnaire for the patient to assess the subjective<br />
perception of the information received and the degree of its<br />
comprehension.<br />
5) Questionnaire for the anesthesiologist to assess the degree of<br />
difficulty perceived in managing the talk with the patient.<br />
Results. Data have not shown a significant decrease of anxiety<br />
in the experimental group. A significant difference between the two<br />
groups regarding anxiety is shown, instead, in the sub-population<br />
of patients with high anxiety (STAI>51). Both groups showed full<br />
comprehension and a high degree of perceived satisfaction for the<br />
information received.<br />
In conclusion, the results show that the basic factor for an<br />
adequate management of a pre-surgery anesthesiological interview<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
176<br />
is the relational quality. On the other hand, both the selection of<br />
the anesthesiologist for the study – highly motivated and sensitive<br />
to the emotional-relational issues – and the “learning factor”<br />
(training to relation and communication provided by the psychooncologist<br />
during the informative sessions between the latter and<br />
the surgeon in the two years of the study) could have reduced the<br />
difference in approaching the patient between the experimental<br />
and control group.<br />
Pilot project: emotions in music, “The sounds<br />
to tell it” Proposal for a social Music<br />
Therapy<br />
Principal Investigator: Maria Giacobbo<br />
This study aims to verify the influence of social Music Therapy<br />
on the oncological patient emotional and anxiety state and on<br />
his death representation. It also aims to evaluate the potential of<br />
music experience in conveying emotions and how music could be<br />
the starting point to revise the experience of illness and to give it a<br />
new meaning. The study takes place in Pollini’s academy of music,<br />
with the participation of the Oncological Institute of Veneto and<br />
the University of Padua, with the perspective of including and<br />
reinforcing a supportive social network.<br />
Subjects. 100 patients aged between 25 and 70, with first or<br />
second stage cancer diagnosis, on medication at the Oncological<br />
Institute of Veneto.<br />
Measures. After signing informed consent, research<br />
partecipants will fill in the following questionnaires, before and<br />
after the study:<br />
BDI-II (Beck Depression Inventory-II);<br />
POMS (Profile of Mood States);<br />
TDRS (Test Death Representation Scale).<br />
After each of the five meetings, partecipants will fill in a<br />
questionnaire to evaluate the emotional state related to listening<br />
to the music.
Programs and Perspectives for the Future<br />
The Unit intends to pursue and develop the field of researchintervention<br />
related to the Medical Humanities; to develop<br />
research projects regarding the advanced stage of illness, with<br />
particular regard to the areas of quality of life and doctor-patient<br />
communication, starting from the validation and creation of<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
177<br />
psychometric instruments of measure that may allow a rigorous<br />
approach (the Italian validation of the QUAL-EC test for the<br />
assessment of the Quality of Life in cancer patients in advancedterminal<br />
phase is already under way).
Main Pubblications<br />
Chief<br />
Cancer prevalence in Italy. Patients living<br />
with cancer, long-term survivors and cured<br />
patients.<br />
Cancer incidence in people with AIDS in<br />
Italy.<br />
Occupational exposure to pesticides and<br />
bile tract carcinoma in men: results from a<br />
European multicenter case-control study.<br />
Sarcoma risk and dioxin emissions from<br />
incinerators and industrial plants: a<br />
population-based case-control study (Italy).<br />
Efficacy of HPV 16/18 vaccines on sexually<br />
active young women and the impact on<br />
organized cervical cancer screening.<br />
Tumor Registry<br />
Paola Zambon, MD<br />
Born on 05.09.950, Researcher, Department of Oncology, University of Padua. Education: July 1976:<br />
Degree in Medicine, University of Padua (cum laude); 1979: OMS Epidemiology Course in Brussels;<br />
July 1979: Post graduate Specialization in Occupational Medicine, University of Padua (cum laude);<br />
December 1982: Post graduate Specialization in Allergology, University of Padua (cum laude); November<br />
1984: ISS Course for planning study on occupational epidemiology, Rome. Professional Activity: 1976 -<br />
1987: MD at the Institute of Occupational Medicine, University of Padua; 1979: Fellowship on primary<br />
aluminium production risk at the University of Padua; 1980-1986: Fellowship at the High Specialization<br />
Regional Centre on Environmental Cancerogenesis; 1988: Award for a study on cancer risk for silica<br />
exposure; 1988 - Researcher at the Faculty of Medicine - University of Padua. 2000-: coordinator of the<br />
Veneto Tumor Registry; From 2003-: she is in charge of the Regional Centre Veneto Tumor Registry.<br />
Guzzinati S, Dal Maso L, De Angelis R (Coordinators); Airtum<br />
Working Group.<br />
Polesel J, Franceschi S, Suligoi B, Crocetti E, Falcini F, Guzzinati S,<br />
Vercelli M, Zanetti R, Tagliabue G, Russo A, Luminari S, Stracci F,<br />
De Lisi V, Ferretti S, Mangone L, Budroni M, Limina Rm, Piffer S,<br />
Serraino D, Bellù F, Giacomin A, Donato A, Madeddu A, Vitarelli S,<br />
Fusco M, Tessandori R, Tumino R, Piselli P, Dal Maso L, Zambon P.<br />
Schmeisser N, Kaerlev L, Bourdon-Raverdy N, Ganry O, Llopis-González<br />
A, Guénel P, Hardell L, Merletti F, Zambon P, Morales-Suárez-Varela M,<br />
Olsen J, Olsson H, Vyberg M, Ahrens W.<br />
Zambon P, Ricci P, Bovo E, Casula A, Gattolin M, Fiore A R, Chiosi<br />
F, Guzzinati S.<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
178<br />
Epidemiologia e prevenzione<br />
<strong>2010</strong>; suppl2; 34: 1-188<br />
International journal of cancer<br />
<strong>2010</strong>; 127:1437-1445<br />
Cancer causes & control,<br />
<strong>2010</strong>; 21:1493-1502<br />
Environmental health: a global<br />
access science source 2007;<br />
6:1-10<br />
Giorgi Rossi P, Zorzi M. Acta Obstet Gynecol Scand.<br />
<strong>2010</strong>; 89:846-7
Clinical and Research Staff Administrative Staff<br />
Paola Zambon<br />
Maddalena Baracco<br />
Emanuela Bovo<br />
Antonella Dal Cin<br />
Anna Rita Fiore<br />
Stefano Guzzinati<br />
Daniele Monetti<br />
Alberto Rosano<br />
Carmen F. Stocco<br />
Sandro Tognazzo<br />
Manuel Zorzi<br />
Susanna Baracco<br />
Carla Cogo<br />
Chiara Fedato<br />
Melania Pendenza<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
179<br />
Alessandra Greco
Mission<br />
The main aims of the Veneto Tumor Registry are to define the<br />
incidence of neoplastic diseases; to conduct epidemiological studies<br />
and to evaluate the resources employed in the treatment of cancer;<br />
to coordinate the epidemiological aspects of the implementation,<br />
monitoring and evaluation of cancer screening, at a regional level.<br />
Research Activities<br />
Defining the incidence of neoplastic diseases in a population<br />
of 2,300,000 residents, the Registry develops indicators of risk<br />
(incidence), results (survival) and burden of care (prevalence)<br />
to provide health authorities with the necessary tools to control<br />
neoplastic diseases and plan health policy interventions.<br />
Analyses of the temporal and geographic variation in the<br />
incidence of cancer, at small area level (municipalities and Local<br />
Health Units), are periodically carried out.<br />
A study on the appropriateness of diagnostic and therapeutic<br />
procedures has been started. Evaluation of colorectal cancer is<br />
currently underway and we aim to expand this experience to breast<br />
cancer. Some analytical epidemiology studies have been activated.<br />
With regards to environmental risks, a study on the risk of<br />
leukemia and neuroblastoma in children in relation to exposure to<br />
electromagnetic fields and a case-control study on non-Hodgkin’s<br />
lymphomas and sarcomas in relation to environmental exposure<br />
to dioxins produced by incinerators are in progress.<br />
An update of the studies on occupational cancer and AIDS/<br />
cancer relationship are being carried out. A collaborative study<br />
aims to use population-based electronic health records to study<br />
the morbidity and mortality of cancer and non-cancer patients.<br />
Major Ongoing Research Projects<br />
Study on the Impact of Breast cancer<br />
screening<br />
As part of the multicenter study “Impact of mammographic<br />
screening”, the Veneto Tumor Registry participates in a cohort<br />
study whose objective is to estimate the reduction of breast cancer<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
180<br />
The Registry is part of the Italian Association of Cancer<br />
Registries network (AIRTUM), the European Network of Cancer<br />
Registries (ENCR) and the International Association of Cancer<br />
Registries (IACR).<br />
The Registry participates in the development and management<br />
of the Italian Network of Tumor Registries (AIRTum) database<br />
and in the preparation and publication at a national level of<br />
the incidence, survival and prevalence data. The Registry also<br />
participates in the same project at a European level involving<br />
the European Union and candidate states, in the automated<br />
information system of childhood cancer (ACCIS) and the<br />
European project to identify useful indicators for the organization<br />
of health care systems (CaMon ).<br />
Within the coordination of cancer screening, the Registry<br />
performs the following tasks: link between the National Screening<br />
Centres and Italian Regional Reference centres, coordination<br />
and epidemiological support for screening programs, design and<br />
maintenance of information systems, monitoring of process and<br />
quality indicators, organization of specific training programs,<br />
implementation and evaluation of the impact of screening,<br />
coordination of reporting.<br />
Furthermore, the Registry participates in the multicentre<br />
Italian IMPACT study, to assess the impact of mammographic<br />
screening and in the Italian multicenter NTCC study on the use<br />
of the HPV test in cervical cancer screening.<br />
mortality rates, of incidence rates of advanced lesions and of<br />
mastectomy rates in women who usually accept the mammographic<br />
screening invitation compared to those who usually do not.<br />
The study involves women aged 50-69 yrs invited to the first<br />
round of mammographic screening in selected areas, categorized
as “frequent”, “irregular” or “never” attenders in relation to<br />
adherence to subsequent screening invitations.<br />
Information on the possible diagnosis of breast cancer and life<br />
status is retrieved by means of linkage between different archives.<br />
The Registry is also involved in a sub-study involving the<br />
breast cancer screening program of the LHU of Rovigo, involving<br />
a cohort of 23,506 women aged 50-69 yrs, invited to the first<br />
round of screening in 1999-2001, in which a total of 509 were<br />
diagnosed with breast cancer. Data collection is in progress.<br />
Study on the Impact of Colorectal cancer<br />
screening<br />
The Registry coordinates the multicenter study entitled<br />
“Impact of screening”. This study aims to assess the impact of<br />
organized screening programs on colorectal cancer incidence and<br />
mortality in areas covered by cancer registries. More specifically,<br />
the study aims to describe temporal trends in incidence and<br />
mortality rates of colorectal cancer in the Italian areas covered<br />
by cancer registries during pre and post-screening periods, by<br />
age, geographic area, histology, stage at diagnosis and disease site,<br />
to compare the incidence rates during pre-and post-screening<br />
periods according to the different diagnostic modalities in relation<br />
to screening by record-linkage procedures, to evaluate the survival<br />
of populations in screening and non screening areas in relation to<br />
distributions of stage at diagnosis and to quantify other effects of<br />
screening programs such as the impact on invasive surgery rates as<br />
well as neo-adjuvant and adjuvant treatments.<br />
The study involves all cases of colorectal cancer diagnosed in<br />
areas covered by a Tumor Registry in subjects aged between 40-<br />
79yrs, before and after colorectal screening programs. For each<br />
case, specific data are collected regarding the screening history, the<br />
type of lesion and life status of the person.<br />
The Registry participates in the study with 2,086 colorectal<br />
cancer cases diagnosed between 2000 and 2005 in three LHUs<br />
(Feltre, Dolo Mirano and Rovigo). Data is currently being<br />
collected.<br />
Ulss 2 – Feltre 2000-05<br />
N°<br />
393<br />
Ulss 13 – Dolo Mirano 2000-05 935<br />
Ulss 18 – Rovigo 2000-05 758<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
181<br />
Study on the Impact of Cervical cancer<br />
screening<br />
The Registry is involved in the multicenter study entitled<br />
‘‘Impact of cervical screening”. This study aims to assess the<br />
impact of organized cervical screening programs on cervical cancer<br />
incidence and mortality in areas covered by cancer registries.<br />
More specifically, the study aims to describe the temporal trends of<br />
incidence and mortality rates of cervical cancer in the Italian areas<br />
covered by a Tumor Registry, by age, geographic area, histology<br />
and stage at diagnosis, to compare the incidence rates of cervical<br />
cancer before and after screening in the Italian areas covered by<br />
a Tumor Registry and to estimate the fraction of cervical cancers<br />
attributable to potential problems of the screening process.<br />
The study regards the cases of cervical cancer diagnosed<br />
in areas covered by a Tumor Registry, in women of all ages,<br />
before and after the activation of a cervical screening program.<br />
For each case, specific data on the screening history, the lesion and<br />
the life status of the person are collected.<br />
The Registry participates in the study with 342 cervical cancer<br />
cases diagnosed between 1997 and 2005 in eight LHUs (Belluno,<br />
Feltre, Bassano, Asolo, Dolo Mirano, Rovigo and Verona).<br />
Data collection ended in December <strong>2010</strong>. The central study<br />
coordinator is currently processing the data.<br />
Ulss 1 – Belluno 1997-2005<br />
N°<br />
56<br />
Ulss 2 – Feltre 1997-2005 44<br />
Ulss 3 – Bassano 1997-2005 38<br />
Ulss 8 – Asolo 1997-2005 68<br />
Ulss 13 – Dolo Mirano 1997-2005 31<br />
Ulss 18 – Rovigo 1997-2005 69<br />
Ulss 20 – Verona 1997-2005 36<br />
Evaluation of the costs of cancer care in Italy:<br />
an approach on colorectal cancer patients in<br />
the Veneto and Tuscany Regions<br />
The Veneto and Tuscany Cancer Registries are currently<br />
involved in a project on the estimated health care costs of cancer<br />
patients, initiated by the National Institute of Health, the<br />
University of Rome “Tor Vergata” and the Institute for Research on
Population and Social Policies. This is one of the first experiences<br />
on the “cost” evaluation of cancer patients in the Veneto and<br />
Tuscany Regions, using a record-linkage between the incidence<br />
data of “cancer registries” and the economic information obtained<br />
from the hospital discharge records by means of Drug Related<br />
Group (DRG).<br />
The preliminary results obtained by examining a limited<br />
cohort of incident cases were:<br />
a “U”-shaped trend of costs in the 3 stages of the disease (early<br />
stage - 12 months from diagnosis, intermediate and terminal -<br />
12 months from death);<br />
an increase in the cost for the more advanced stages of cancer;<br />
a decrease in the cost with increasing age.<br />
The final goal of this first study is to estimate the costs of cancer<br />
survivors, by combining the cost estimates with the estimates of<br />
prevalent cases. The possibility of using other administrative data,<br />
such as outpatient services and pharmaceutical expenditure files,<br />
could help to better determine the cost of cancer patients during<br />
different diagnostic and therapeutic phases, also taking into<br />
account the recent dynamics of moving some treatments from a<br />
day-hospital to an outpatient regimen, such as chemotherapy.<br />
Genetic-epidemiological study of BRCA1<br />
and BRCA2 founder mutations in sporadic<br />
and familial breast-ovarian cancer in the<br />
population of South Tyrol and the Alpine<br />
region.<br />
The aims of this study are to define:<br />
frequency of familial breast and ovarian cancer in the Alpine<br />
region;<br />
frequency of founder mutations in breast and ovarian cancer,<br />
both in familial and in sporadic cases;<br />
mutation spectrum in the Alpine region and the associated<br />
specific risks of cancer;<br />
variability of the clinical phenotype given specific mutations.<br />
The target is the patient population diagnosed with breast or<br />
ovarian cancer in the Alpine region of Northern Italy, in particular<br />
patients in the Provinces of Bolzano (commonly known as South<br />
Tyrol), Trentino, and Belluno. The annual incidence of breast<br />
THE DEPARTMENTS - DEPARTMENT OF SERVICES<br />
182<br />
cancer in these regions is approximately 300 cases in the Bolzano<br />
Province, 300 in Trento Province, and 200 in Belluno Province.<br />
Patients are identified through the records in the cancer registry.<br />
Study design/Analytical procedures<br />
The self-administered questionnaire that will be used in this<br />
study has been developed by the scientific coordinator of the<br />
study (FDV) and has been tested on a series of patients from the<br />
department.<br />
Participants indicate on the questionnaire, whether they are<br />
willing to provide a blood sample. Within three months after<br />
returning the questionnaire, patients are given a date for blood<br />
sampling. Blood sampling takes place in the hospital department,<br />
where the patient is usually followed-up.<br />
Sample elaboration is done in the molecular biology laboratory<br />
in Merano. DNA is extracted and stored; RNA is obtained from<br />
DNA. Direct sequencing will be used for mutation detection.<br />
Cases extracted from the Veneto Tumor Registry data base are:<br />
353 breast cancer and 89 ovary cancer.<br />
Statistical analysis<br />
Analysis will be done using standard descriptive and analytical<br />
statistical methods. Mutations will be described and compared<br />
to the database of the Breast Cancer Information Core (BIC)<br />
(Szabo, Hum Mutat 2000). The association between presence of<br />
a mutation and clinical-pathological factors will be assessed using<br />
the chi-squared test for categorical variables and the t-test test for<br />
continuous variables. To estimate the risk of carrying a mutation<br />
in relation to the degree of familiarity and other risk factors<br />
regression methods will be applied. Recurrent founder mutations<br />
will be validated by haplotyping.
THE RESEARCH<br />
THE RESEARCH<br />
185
Scientific Director Address<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
187
General Considerations<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
188<br />
The Scientific Directorate’s mission is to<br />
supervise basic, translational and clinical research<br />
at the <strong>IOV</strong>, as well as to implement strategies<br />
for pursuing cutting-edge areas in oncology.<br />
At the same time, a major endeavour is the<br />
constant scouting to offer all <strong>IOV</strong> researchers<br />
new opportunities to find the financial resources<br />
needed to face the challenges of modern<br />
biomedical research.<br />
In view of its nature as a true Comprehensive<br />
Cancer Centre, the <strong>IOV</strong> does not operate as<br />
an isolated entity in the medical and scientific<br />
milieu of the surrounding area, but more rather<br />
established strong links with all the subjects<br />
involved in biomedical sciences, allowing for a<br />
complete vision and integrated implementation<br />
of all clinical, management and research tasks<br />
undertaken. Indeed, many components of<br />
our staff are also Members of the Faculty of<br />
Medicine of Padua University, and as such are<br />
engaged in an articulated mission, which entails<br />
patient cure, research, and teaching.<br />
A leading, firm concept of the Scientific<br />
Directorate is that no excellence in clinical care<br />
can be reached in the absence of an outstanding<br />
level of research. Instead of detracting from the<br />
mission of improving prevention, diagnosis,<br />
treatment, and quality of life of cancer patients,<br />
the rapid application of knowledge emerging from<br />
research greatly helps in elevating the general<br />
levels of assistance. A virtuous circuit must be<br />
established between the ward and the laboratory;<br />
innovative results (such as the information<br />
acquired from pre-clinical models) must rapidly
e transferred from the bench to bedside, but also viceversa, in<br />
that samples from patients must come back to the laboratory to be<br />
examined and “teach” physicians and biologists newer and more<br />
refined information. In this frame, we do not feel it appropriate to<br />
distinguish research activities into basic, translational and clinical<br />
investigation.<br />
Although the Institute has undergone great cultural and<br />
scientific expansion since its establishment in 2006 and it is now<br />
fully mature as a true Comprehensive Cancer Center, the strategy<br />
underlying its foundation was complex, and it has required great<br />
prudence to succeed; much more attention will be needed to<br />
implement and foster this operation in the next few years. Indeed,<br />
the <strong>IOV</strong> was not created as a new entity in a cultural desert, but<br />
originated in a very fertile environment of public structures where<br />
oncology was already a piece of excellence within local medical<br />
culture. Thus, re-organizing the entire oncologic research and<br />
clinical assistance network was not a trivial task, but required<br />
great acquaintance with the pre-existing expertise and wise<br />
strategies, from both the political and scientific points of view.<br />
Due to its small dimension, the <strong>IOV</strong> does not aim (nor in fact<br />
could) at absorbing all the activities related to cancer research and<br />
care; instead, it is our purpose to select strategic areas where a critical<br />
mass has already been achieved or where high-quality expertise is<br />
scattered throughout different laboratories and/or clinical units,<br />
and to concentrate and implement this body of competence in<br />
order to get higher competitiveness levels.<br />
Near to the end of my commitment as Scientific Director,<br />
however, some general considerations on the role of the <strong>IOV</strong><br />
within the national IRCCS network are due. My Institution is<br />
part of the national health system and is not a private institution<br />
based on private funding, such as a sizable part of the IRCCS.<br />
It has always been unclear to me how different institutions with<br />
different status (public and private) could benefit from a common<br />
status (for instance the access to the Ricerca Corrente funding) but<br />
partly comply with different rules, nor did I understand how these<br />
different Institutions complying with partly different rules could<br />
by the end be melted in a single pot and evaluated all together<br />
according to identical parameters. I will briefly illustrate a few<br />
examples of this inconsistency.<br />
I. Public and private IRCCS benefit from, and in this regard<br />
they must comply with, rules shared among all the IRCCS; thus,<br />
it is unclear to me why the rules for hiring a Scientific Director<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
189<br />
are different among private and public IRCCS. In public IRCCS,<br />
the Scientific Director has an exclusive employment with the<br />
Ministry of Health, and no other activities are permitted (for<br />
absurd, a pedestrian interpretation of the law would also preclude<br />
scientific research!). Thus, to scientifically direct my Institute, I<br />
had to abandon my academic position, the teaching, the direction<br />
of a Department and of a Specialization School, the possibility of<br />
participating in the national academic life, and many other things.<br />
The same does not occur to colleagues scientifically directing<br />
private IRCCS, who maintain all these positions and prerogatives.<br />
This is not a trivial issue of syndical nature: the renounce to<br />
every commitment by the Scientific Director could preclude the<br />
engagement in public IRCCS of more young, active and motivated<br />
researchers, who would have trouble in abandoning their career<br />
track, and live room as Scientific Directors in public IRCCS to<br />
people at the end of their career, less creative and active.<br />
II. Public Institutions must comply with public Health System<br />
rules, which are much stricter compared to private institutions.<br />
This is true for hiring people, or for purchasing material from<br />
companies, even when the grant comes to the researcher from a<br />
private charity, and this may cause complications, delays and often<br />
the loss of convenient pricing of some material. As personnel who<br />
refer to both a University department and a public IRCCS, we<br />
several times experienced difficulties in spending money when<br />
the grant had to transit through the IRCCS administration. This<br />
is not attributable to a deficiency of our Administration (which<br />
instead always does its best, and more, to facilitate our problems)<br />
but to a viscous array of rules inherent to certain public entities.<br />
It is therefore easy to understand that the starting conditions for<br />
private and public IRCCS are not the same; yet, by the end of<br />
the year, all the IRCCS are classified in order of productivity (and<br />
eventual financing by the Ministry), irrespective of their public or<br />
private status. To me, this looks like a 100 yard contest in which<br />
males and females, adults and juniors participate all together, and<br />
the athletes are finally classified irrespective of their age or sex. Is<br />
this fully fair, when these classifications are publicized, and you can<br />
see them everywhere, in the specialized and non-specialized press,<br />
without any caveat, comment or explanation?<br />
III. A last observation to the IRCCS system, which is not<br />
dictated, as the former also are not, by a critical situation of my<br />
Institute, which instead has a very good positioning among the
IRCCS, in terms of both overall production and productivity. Can<br />
we compare the production of huge Institutes, having a long history<br />
and a great number of staff researchers, with the production of<br />
newly founded, small Institutes? Yet, as far as I know, the “Ricerca<br />
Corrente” funding is mostly based on total IF generated by the<br />
Institute, and the weight of other parameters (and in particular<br />
productivity, intended as the total research output divided by the<br />
number of staff members) is more limited. It is my firm hope that<br />
the recently established Research Direction of the Health Ministry<br />
could find more appropriate algorythms to evaluate private and<br />
public IRCCS; indeed, a series of very positive signals in terms<br />
of efficiency and transparency have already been sent by this<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
190<br />
Direction. Nevertheless, it would also be necessary to revise the<br />
legal frame regulating the IRCCS on the whole; the 288 law is not<br />
that recent, and it may be inadequate to face the changing world<br />
of the Italian sanitary research and of the Institutions that should<br />
lead this research.<br />
These things are very often said among Scientific Directors,<br />
but much more rarely publically discussed and even less written;<br />
it is probably time to tackle this matter in a transparent and<br />
appropriate manner, in the higher interest of the Institutions and<br />
the Health System which we have the honour and the burden to<br />
represent and serve.
Scientific Directorate Organization<br />
The Scientific Directorate is responsible for:<br />
Research Administration<br />
Responsible: Daniela Battistuzzi<br />
This Office is devoted to<br />
administrating research grants earned by<br />
<strong>IOV</strong> workers, as well as resources coming<br />
from the Health Ministry (Ricerca<br />
Corrente); the distribution of these latter<br />
resources is planned yearly partly on a<br />
merit basis, according to widely accepted<br />
scientific parameters, and partly on the<br />
basis of the needs of implementation and sustainment of the different<br />
areas. The management of the projects presented by the Researchers,<br />
as well as the monitoring of results, is facilitated by the availability at<br />
<strong>IOV</strong> of a managing software (SIFF-<strong>IOV</strong>, generated by CRBM, Pavia,<br />
Italy), as this system is fully compatible with the managing platform<br />
of the Italian Health Ministry (the so-called “Research Workflow”).<br />
At present, the burden of administrative duties, including the annual<br />
scientific and administrative reports to the Ministry of Health<br />
(“Ricerca Corrente”), and the maintenance of relationships with a<br />
wealth of players (Health Ministry, Alleanza Contro il Cancro, the<br />
Veneto Region, the other IRCCS, the national and international<br />
Agencies etcetera) only relies on the work of one administrative unit,<br />
Mrs. Daniela Battistuzzi, whose dedication is gratefully acknowledged<br />
here, with the precious help of Dr. Gian Luca De Salvo of the Clinical<br />
Epidemiogy and Biostatistics Unit, and of the Administrative Office<br />
(Dr. M. Giusto). The Scientific Directorate has recently potentiated<br />
his possibilities by recruiting on research grants a series of collaborators<br />
dedicated to maintain and foster interactions with European<br />
Community in view of FP7 Program, and to implement the librarian<br />
section and the Bibliosan platform.<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
191<br />
SIPS: a software tool for<br />
research administration<br />
Responsible: Alessandro Andretto<br />
The Italian Ministry of Health<br />
(MoH) allocates resources through a<br />
performance-based funding system to<br />
IRCCS. The total normalized impact<br />
factor of publications is the indicator<br />
of the scientific productivity of every<br />
IRCCS. Fifty percent of the total<br />
of MoH funds is allocated with regard to this indicator, while<br />
the capacity to attract resources for research and convert it into<br />
clinical practice accounts for another 15% of MoH funds. Thus,<br />
65% of the MoH funds are determined by scientific publications.<br />
The <strong>IOV</strong> Scientific Directorate recently put in place a new<br />
proprietary software for the management of the institutional<br />
scientific publication database. The new System was created on<br />
the basis of the afore-mentioned MoH criteria and is aimed at<br />
collecting quantitative (article, number of authors and researchers)<br />
and qualitative (bibliometric values and affiliation accuracy)<br />
data.<br />
The main purpose of this software to handle scientific<br />
productivity of <strong>IOV</strong>, called SIPS, (Information System of Scientific<br />
Publications), is to manage the publications and monitor the<br />
productivity of the <strong>IOV</strong>.<br />
The SIPS software is composed of three main modules:<br />
1. Publications management<br />
2. Research staff management<br />
3. Funds management.<br />
The “Publications management” is the core of the whole<br />
system: it allows the handling of bibliographic data of scientific
publications of <strong>IOV</strong> researchers while simplifying and automating<br />
the calculation of many important indexes, such as normalized<br />
impact factor, affiliation accuracy, author byline positions,<br />
citations, etc. The module of “Research staff management” is used<br />
to handle all data of researchers divided by operative units. “Funds<br />
management” allows the monitoring of funds.<br />
Through SIPS it is possible to cross-validate all data from<br />
different modules to create in-depth data analysis, by queries and<br />
significant indexes in order to evaluate publications, researchers<br />
and units together. SIPS is implemented through web-based<br />
technology and is only accessible within the Intranet network of<br />
the Scientific Directorate through members’ different accounts<br />
and distinct privileges, as required. The software also allows the<br />
import of bibliographic data from the citation manager RefWorks<br />
program (accessible to <strong>IOV</strong> through the BiblioSan consortium<br />
subscription) and it enables the export of data in many formats<br />
such as XML, CSV and Excel.<br />
The system simplifies the operations of data management<br />
as inserting, updating and searching records by automatic<br />
procedures and it also allows the creation of complex data queries<br />
in a few seconds. One of the main features of SIPS is the timely<br />
and labour-efficient creation of reports, formatted as requested<br />
by the user. In doing so, the original “administrative database” is<br />
currently developing into a fully implemented “Decision Support<br />
System” software, which will help to take decisions on the internal<br />
scientific priorities and funds management on the basis of the KPI<br />
(Key Performance Indicator).<br />
Laboratories<br />
An important part (about 1,500 square meters) of the<br />
Institute is occupied by research laboratories, fully equipped with<br />
state-of the-art instrumentation, including cytometry, confocal<br />
microscopy, Affimetrix and Agilent platforms, several real-time<br />
PCR platforms, sequencers, DHPLC etcetera. The acquisition of<br />
a last generation cytofluorimeter endowed with cell sorting is now<br />
underway, thanks to the funds deriving from the so-called “5 per<br />
mille” donations.<br />
The major labs, where research activities are strictly<br />
interconnected to the clinical management of patients in a<br />
translational research perspective, include the following Labs:<br />
Heredo-Familial Tumors; Molecular Immunology and Gene<br />
Therapy; Cellular and Molecular Immunology; Viral Oncology;<br />
Molecular Oncology and Cytogenetics; BL3 facility.<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
192<br />
Animal facility<br />
The activity performed in the Labs is complemented by the<br />
availability of a SPF animal facility (about 300 square meters),<br />
which hosts about 3,000 mice of wild-type/transgenic strains,<br />
and includes a BL3 room with isolated cages for containment of<br />
high-risk experimental procedures. Experimentation is carried<br />
out under strict control of the internal Ethical Committee<br />
and according to International Guidelines in the field; embryo<br />
transfer techniques are also available in the facility. A complete<br />
imaging platform, including computerized tomography,<br />
fluorescence and chemiluminescence, allows accurate followup<br />
of tumor progression in experimental tumor models, thus<br />
minimizing the number of animals needed for experimentation<br />
and the eventual invasive manipulations. Thanks to a “Conto<br />
Capitale <strong>2010</strong>” financing by the Health Ministry, the acquisition<br />
of a PET-TAC platform for small animals is now underway. This<br />
instrument will allow a fantastic advancement in the possibility<br />
of testing in a preclinical setting new drugs and biological agents,<br />
in view of their transfer into the clinical practice through phase I<br />
experimentation.<br />
Tissue banking<br />
In view of the growing importance of collecting tumor tissues<br />
according to standardized, reliable operating procedures, the<br />
<strong>IOV</strong> is implementing tumor tissue banking in collaboration with<br />
surgeons and pathologists. Presently, two bio-banks are established:<br />
a large collection of esophageal tissues, which forms the core of the<br />
Barrett’s Esophagus Italian Registry, including samples from more<br />
that 1,000 patients; a collection of more than 500 samples from<br />
patients with colo-rectal tumors. Work is in progress to extend<br />
biobanking to other pathologies, by also involving in this project<br />
surgeons, pathologists and clinicians all over the Veneto region,<br />
and participating in national and international networks. This<br />
will be made easier by the recent initiative of the Regional Health<br />
Authorities, who recently launched an initiative to count, catalogue,<br />
coordinate and regulate (by establishing minimal requirements<br />
and standard operating procedures to obtain accreditation) all<br />
the structures acting as biological sample repositories all over our<br />
Region. This aspect apart, it is an insofar unsuccessful dream of<br />
the Scientific Directorate to sample constitutive DNA from every<br />
cancer patient attending the Institute, in order to make available<br />
to the <strong>IOV</strong> researchers and to the oncologic network of the Veneto<br />
region a non-dispensable bank for pharmacogenetic studies.
library<br />
Responsible: Mauro Apostolico<br />
Library is seeking new ways<br />
to share <strong>IOV</strong> collection with its<br />
biomedical and academic audience in<br />
Padua. Being a member of Bibliosan,<br />
<strong>IOV</strong> Library is called to contribute to<br />
the health library network of Italian<br />
research centres.<br />
In recent years, the growth of<br />
technology and the widespread use of the net has stimulated<br />
rapid and huge strides to this regard. The Library is working<br />
with BiblioSan network partners to improve its digital resources<br />
program, paying a specific attention to user-oriented services and<br />
Institutional repositories in order to build a web-based digital<br />
library, constantly open to users, that can be consulted from<br />
everywhere and at anytime.<br />
The <strong>IOV</strong> Library is enhancing the Library services through the<br />
opportunities offered by new technologies: the development of a<br />
custom Key Performance Indicator (KPI) database or digitisation<br />
and web 2.0 applets, like NILDE 4.0 (“Network for Inter-Library<br />
Document Exchange”). Since September <strong>2010</strong>, <strong>IOV</strong> Library<br />
Website is a gateway to bibliographic and bibliometric sources,<br />
with fee-based and Open Access full text journals, links to health<br />
search engines, authoritative health websites and searchable<br />
catalogues and databases.<br />
<strong>IOV</strong> library website also include online access to librarian<br />
services such as document delivery and reference assistance.<br />
The regular addition of online periodicals to the BiblioSan<br />
catalogue, has enriched <strong>IOV</strong> collection in the field of oncology<br />
(125 periodicals) and allied sciences (700 periodicals).<br />
By the group agreements with BiblioSan, our Library has a<br />
collection of 3700 Medical and Health Sciences Journals and<br />
2000 Science Journals, a wide range of knowledge resources aimed<br />
at meeting the needs of oncologists, research scientists, nurses,<br />
healthcare professionals and postgraduates students from different<br />
disciplines. In the year <strong>2011</strong> NILDE, together with ACNP (the<br />
Italian “National Collective Catalogue of Periodicals”), connected<br />
<strong>IOV</strong> Library with the collections of 2,491 Libraries in Italy<br />
counting 922,922 journals. NILDE allows to borrow and lend<br />
a large number of articles and documents from Italian libraries,<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
193<br />
through a single platform, perfectly connected with a link resolver<br />
(called “Find Full Text by BiblioSan”) available on customized<br />
interfaces of most of the important and used scientific databases<br />
such as PubMed, ISI WoS, and new web-based tools such as<br />
Google Scholar. Strongly addressed to its audience, <strong>IOV</strong> Library<br />
serves institute staff, departments, internal and external operating<br />
units, recipients of <strong>IOV</strong> grants, postgraduates and PhD students<br />
training at <strong>IOV</strong>. Since the beginning of the digital library program<br />
in <strong>2010</strong>, <strong>IOV</strong> library services has increased by about 100 per cent<br />
and registered users have increased by 65 per cent.<br />
In the same year online BiblioSan - <strong>IOV</strong> catalogue’s page views<br />
were 64,879, an increase of 15% compared to the previous years,<br />
with an estimated growth of 25% in the current year.<br />
In <strong>2011</strong> the Library, with the <strong>IOV</strong> training office, has started<br />
staff training courses on BiblioSan resources. The courses aim to<br />
provide staff with the skills to use online bibliographic resources<br />
and to enhance research, clinical and health assistance activities.<br />
BiblioSan: Antonio Rosato<br />
Dr. Antonio Rosato is the <strong>IOV</strong><br />
delegate to interact with the BiblioSan<br />
librarian network and its Director<br />
(Prof. Moreno Curti) on behalf of the<br />
<strong>IOV</strong> Scientific Directorate.
<strong>IOV</strong> Library 2008-<strong>2011</strong> Nilde Exchange <strong>IOV</strong> Library 2007-<strong>2011</strong> Lending Time<br />
Articles<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
2007 2008 2009<br />
Order not filled<br />
Borrowing<br />
Lending<br />
Year<br />
<strong>IOV</strong> Library users<br />
Users<br />
350<br />
300<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
<strong>2010</strong><br />
35<br />
<strong>2011</strong><br />
96<br />
Time<br />
2009 <strong>2010</strong> <strong>2011</strong><br />
Year<br />
2.6<br />
2007<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
194<br />
7<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
Lending time<br />
(days) 250<br />
311<br />
Users<br />
200<br />
150<br />
100<br />
50<br />
2.8<br />
2008<br />
0<br />
6.5<br />
2009<br />
Year<br />
35<br />
0.7<br />
<strong>2010</strong><br />
96<br />
0.3<br />
<strong>2011</strong><br />
2009 <strong>2010</strong> <strong>2011</strong><br />
(30/06)<br />
Year<br />
Nilde users<br />
BiblioSan CLAS users<br />
RefWorks users<br />
<strong>IOV</strong> DD users<br />
Total users<br />
223
In the awareness of the difficult tasks that we are facing, and<br />
most of all our limits, we feel it appropriate to conclude this<br />
address by a SWOT analysis that may synthesize the Scientific<br />
Directorate spirit.<br />
Strength<br />
Four major points are to be considered.<br />
First, the <strong>IOV</strong> is greatly grown from its birth, in both<br />
dimensions and quality. The compilation of this Report offered<br />
to me the opportunity of summarizing my 4-year experience at<br />
the Scientific Direction of the Istitute, and to comprehensively<br />
address all the aspects of our life at <strong>IOV</strong>. All the aspects that<br />
I considered show a more than satisfactory improvement: the<br />
general organization of both research and clinical activity, the<br />
functioning of the Scientific Directorate, the number, and in<br />
particular the quality of the publications, the amount of grants<br />
earned by our Researchers, the growing success in funding by<br />
intenational agencies, in particular European Community.<br />
This progress is beyond any expectation, and it may represent<br />
the guarantee for a further, huge improvement.<br />
Second, the small dimension of the <strong>IOV</strong>, which only<br />
comprehends about 100 Researchers, greatly facilitates<br />
management, scientific coordination, and collaboration<br />
among groups. Due to the profound embedding in a preexisting<br />
excellent expertise in Oncology, we do not pursue a<br />
“generalistic” mission, aimed at tackling all oncological diseases;<br />
instead, we chose to select a few investigative fields and to<br />
implement these sectors by putting together all the experts into<br />
Multidisciplinary Units.<br />
Third, the great ability of our investigators to raise grants from<br />
both public and private agencies permits a high level of quality<br />
in both research and clinical applications.<br />
Finally, the <strong>IOV</strong> is a true Comprehensive Cancer Center,<br />
where basic and translational research, clinical activities, and<br />
educational programs are fully integrated.<br />
SWOT Analysis<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
195<br />
Weakness<br />
We are aware of several weakness points, whose removal<br />
would greatly potentiate our possibilities.<br />
A stronger support to the Scientific Directorate in terms of<br />
personnel resources would greatly help in improving the<br />
Institute’s presence within the national and international<br />
scenario; nowadays, steady scouting of financial resources,<br />
intelligent lobbying activities within the European Community,<br />
and careful maintenance of international relationship are<br />
mandatory activities for a Scientific Institute.<br />
Related to the former point, the lack of a structure responsible<br />
for scientific communication is a strong pitfall of the Institute;<br />
the importance of transmitting to the general public a correct<br />
information, with the right and professional modalities, is of<br />
paramount importance to acquire credit and sensitize people<br />
to understand and eventually support our work.<br />
Space constraints are also an important limit to <strong>IOV</strong> expansion;<br />
its location in an artistically protected and surveyed area renders<br />
any refurbishment intervention very long and difficult.<br />
The huge amount of money earned by <strong>IOV</strong> researchers to<br />
carry out their research is counterbalanced by the scarcity of<br />
personnel; the resources coming from the “Ricerca Corrente”<br />
are often employed not as a “plus” to implement research, but<br />
as a substitute to face routine clinical activities which would be<br />
difficult to perform due to the poor human resources.<br />
The University of Padova hosts a Specialization School in<br />
Clinical Oncology, which presently needs to be profoundly<br />
reorganized and implemented. Padova has never had in its<br />
Medical Faculty a Full Professor of Clinical Oncology; it is now<br />
time to tackle this problem as a vital priority of the School and<br />
of the <strong>IOV</strong> itself, where the post-graduate students carry out<br />
their formation in Oncology.<br />
Even though all the queries to the Research Direction of the<br />
Health Ministry are met whenever necessary, a more close and<br />
strict follow-up of the problems of the Scientific Directorate
would be auspicated, in the interest of a better and more<br />
harmonic governance of the <strong>IOV</strong>.<br />
Opportunities<br />
Several opportunities are at hand. The Institute has strict<br />
cultural and “physical” connections with the entire academic and<br />
non-academic medical milieu of Padova. Indeed, about one third<br />
of <strong>IOV</strong> researchers also hold a position at the Padova University;<br />
in addition, a full integration between the Azienda Ospedaliera<br />
and the Medical Faculty of Padova has been operating for more<br />
than 30 years. Also, the presence of a Doctorate School in<br />
Oncology and Surgical Oncology, presently directed by a Full<br />
Professor of the University of Padova working at <strong>IOV</strong>, guarantees<br />
the formation of new researchers, and for sure it represents a<br />
sort of cultural incubator and reservoir for the future. It is clear<br />
that the <strong>IOV</strong> may fully benefit from the contiguity with all<br />
these structures, in a common effort to mutually implement the<br />
individual expertise and vocation. Moreover, the greater critical<br />
mass generated by the convergence of different, complementary<br />
expertise will allow the entire Padua Medical School to become<br />
more competitive within the national and international research<br />
networks in Oncology.<br />
Threats<br />
Nowadays, also in view of the constraints due to the<br />
international economic crisis, the horizon may be more cloudy<br />
than in the past.<br />
One of the most relevant<br />
problems in doing research<br />
in Italy is the difficulty of<br />
recruiting into permanent<br />
or semi-permanent positions<br />
young post-PhDs who for<br />
many years have proven<br />
their research skills; in<br />
other words, in both the<br />
academic and non-academic<br />
settings the chance to<br />
offer career perspectives<br />
to most motivated young<br />
investigators is very poor.<br />
This problem is of<br />
paramount importance in<br />
the case of our Institute.<br />
As an infant, in fact, the<br />
Strength<br />
Novelty (no “original sin”)<br />
Small dimensions<br />
High ability to raise<br />
resources<br />
Comprehensive Cancer<br />
Center<br />
Opportunities<br />
Fertile scientific environment,<br />
with high opportunities for<br />
local collaborations<br />
Embedding in national/<br />
international research<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
196<br />
<strong>IOV</strong> would need special attention, care and feeding to foster<br />
its physiologic development. So, the first and more menacing<br />
danger is a lack of adequate support from the Regione Veneto,<br />
especially in terms of the possibility of attracting and hiring<br />
top-level investigators from Italy and abroad.<br />
A second worrying problem is that the ability to design ambitious<br />
research strategies could not be supported by the General<br />
Directorate through adequate platforms, both technologic<br />
(informatics, bio-informatics etcetera) and administrative<br />
(research administration, EC lobbying, international relations<br />
etcetera). We are perfectly aware that an “IRCCS mentality”<br />
has to be progressively acquired and built; however, the lack<br />
of these infrastructures would certainly hinder any effort to<br />
expand the <strong>IOV</strong> horizons from the relatively narrow visual<br />
angle of its birth.<br />
As far as spaces are concerned, the mid-to-long term possibility<br />
of moving into the future new Hospital of Padova may<br />
represent a menace, in virtue of the temptation of a long-term<br />
blocking of any enlargement/amelioration of the existing <strong>IOV</strong><br />
structures, in view of a future permanent location.<br />
The work in Oncology as well as in most medical branches<br />
greatly benefits of the possibility of network working. This<br />
need is particularly urgent for our Institutions, since Oncology<br />
in Veneto is distributed among more than 25 different<br />
Oncology Units scattered over the territory. If this on one<br />
hand represents an opportunity for a better, capillary survey of<br />
oncological diseases, on the other it may represent a difficulty<br />
for creating a network.<br />
Yet, to face the competition<br />
Weakness<br />
Novelty<br />
Space constraints/Uncertainties<br />
on future location<br />
Lack of adequate support<br />
to Scientific Direction (scouting,<br />
EC lobbying etc...)<br />
Threats<br />
Lack of far-reaching,<br />
ambitious strategies<br />
Lack of infrastructural support<br />
Constraints in researcher<br />
hiring<br />
from larger Institutions,<br />
from BigPharmas and<br />
from foreign countries, the<br />
Veneto Region must organize<br />
its oncological work as a<br />
network, sharing guidelines,<br />
case series, expertise, in the<br />
light of the key words “One<br />
for all, all for one”. Only by<br />
this spirit it will be possible<br />
to maintain the pace of<br />
innovation, progress, and<br />
improvement of research<br />
and care, the two nonseparable<br />
missions of an<br />
IRCCS.
Research: Input and Output<br />
The research activities of the <strong>IOV</strong> are supported by grants<br />
obtained from several national and international agencies, both<br />
public and private, as well as a few pharmaceutical industries and<br />
private charities. In addition, the <strong>IOV</strong> can count on a substantial<br />
support by the generous donations of patients, familiars, citizens,<br />
etcetera.<br />
The fund raising at <strong>IOV</strong> mainly relies on two structures, the<br />
one institutional, the other created by the Scientific Directorate to<br />
foster scouting of grants at the European level.<br />
fuND raiSiNG aND markETiNG<br />
OffiCE<br />
Head: Bruno Bandoli<br />
This institutional office, born<br />
since the foundation of the Institute<br />
in 2006, is responsible for the raising<br />
of grants from private citizens, local<br />
associations, private institutions<br />
within the basin of influence of the<br />
Institute. To this end, the Office must<br />
design communication and marketing strategies, which could<br />
render the Institute more visible to the general population. At<br />
the same time, a steady activity is dedicated to promoting and<br />
organizing special events where the income could be totally or<br />
mostly transferred to the <strong>IOV</strong>.<br />
Data on the events and the fund raising of the Office over the<br />
last 3 years are reported in the table (values in e):<br />
Source 2009 <strong>2010</strong> <strong>2011</strong><br />
5‰ 930,000 970,000 960,000<br />
Donations 270,000 300,000 550,000*<br />
* Data January-July<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
197<br />
iNTErNaTiONal rElaTiONS &<br />
EurOpEaN GraNTS OffiCE<br />
Responsible: Manuela Mtanis<br />
The International Relations and<br />
European Grants (IREG) Office<br />
is charged by the <strong>IOV</strong> Scientific<br />
Directorate to develop a strategy<br />
aimed at increasing the international<br />
presence of the Veneto Oncology<br />
Institute and obtaining new funds<br />
through highly competitive funding instruments set by the<br />
European Commission and other international agencies. These<br />
two major tasks are being carried out by expanding the scientific<br />
and institutional network base and by obtaining references in<br />
international project proposal participation.<br />
The progress in the implementation of the IREG Office<br />
activities, which started in June 2009, is in line with the slow<br />
but continuous EU funds awareness raising. This is accomplished<br />
after the staff attending courses on European project drafting and<br />
having been regularly notified of the funding opportunities in<br />
order to improve their drafting and networking skills. The <strong>IOV</strong><br />
participation in International funding programs has increased<br />
not only in the total number of project proposals but also in the<br />
quantity of researchers involved.<br />
The <strong>IOV</strong> expresses its needs and priorities while working<br />
towards the common good of the European Community: the<br />
lobbying activities and the strategic relations with international<br />
and national funding institutions that work in this field are carried<br />
out by the IREG Office with the scientific advice of the researcher<br />
involved in seeking for funding. This activity is monitored and<br />
coordinated by the Scientific Director.<br />
These ambitious aims are not pursued by the <strong>IOV</strong> alone.<br />
The <strong>IOV</strong> works within a variety of National, European and<br />
International Oncology Umbrella Organizations:
ACC (Alleanza Contro il Cancro);<br />
OECI (Organisation of European Cancer Institutes);<br />
UICC (Union International Contre le Cancer).<br />
To apply for funding from the European Commission Fund<br />
for Research and Development (the 7th Framework Programme),<br />
knowledge of the administrative and technical documentation is<br />
required. Information about this documentation is shared by the<br />
IREG Office with the following institutions:<br />
APRE (Agency for the European Promotion of Research);<br />
IRECOOP VENETO (Technical support service for the<br />
management of EU funds. 16 th Padova Company Health<br />
Authority);<br />
UNIVERSITY OF PADOVA, Service of International<br />
Research.<br />
European public relations have been a major consideration<br />
for the IREG Office. The <strong>IOV</strong> has been benefiting from the<br />
active presence of the Veneto Regional Representative office in<br />
Brussels. The <strong>IOV</strong> took part in information days for a variety of<br />
oncology-related funding opportunities in Brussels and in other<br />
FP7 countries such as those organised by:<br />
European Commission (Info days and Networking on 7PQ-<br />
Health Programme);<br />
Committee of the Regions (Regions and cities delivering<br />
growth);<br />
European Parliament (bilateral meetings with MEPs in charge<br />
of Research and Health policy);<br />
ECRIN (European Clinical Infrastructure Network: Pan-<br />
European, distributed infrastructure providing coordinated<br />
services to multinational clinical research in Europe);<br />
EATRIS (European Advanced Translational Research Infrastructure<br />
in Medicine: bridging basic research and medical innovation);<br />
EORTC (European Organization for Research and Treatment<br />
of Cancer);<br />
IMI JU (Innovative Medicine Initiative Joint Undertaking-Info<br />
days and Networking);<br />
EUREGHA (European Regional and Local Health Authorities);<br />
ERRIN (European Regions Research and Innovation<br />
Network);<br />
EPAAC (European Partnership for Action Against Cancer);<br />
ISRAEL BIOMED <strong>2011</strong> (Israeli SMEs looking for public<br />
partners in Biomedical Research).<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
198<br />
The <strong>IOV</strong>, through the scientific monitoring of Dr. Annarosa<br />
Del Mistro, was appointed for the EPAAC (European Partnership<br />
for Action Against Cancer – the EU platform on oncology<br />
policies) to conduct the activities of Work Package 6, objective<br />
3 on regional screening programs, concerning the Pan-European<br />
Regional implementation of guidelines on Cervical Cancer<br />
Screenings. In October 2012 the IREG staff will organize and<br />
host an International meeting on this specific issue, wich will<br />
be attended by local and Brussels based health and research<br />
stakeholders, European Commission officers and screening<br />
specialists, oncologists and policy markers form all over Europe.<br />
Dr. Indraccolo’s project proposal titled “Metabolic changes<br />
associated with ovarian cancer as possible new diagnostic tools to be<br />
transferred into clinical practice” was selected to be implemented<br />
by IATRIS (the Italian section of EATRIS).<br />
<strong>IOV</strong> participated in the The EuroNanoMed ERA-NET<br />
initiative. This initiative comprises 24 partners from 18 countries/<br />
regions. EuroNanoMed aims at fostering competitiveness of<br />
European nanomedicine players through the support of transnational<br />
collaborative and multidisciplinary Research and<br />
Technology Development (RTD) projects with participants from<br />
academia, clinical/public health communities and industry.<br />
Dr. Enzo Bronte project “Lymphotargh” was ranked as<br />
third in Europe for its scientific rigor. This study proposed to<br />
develop specifically targeted anticancer treatments, by associating<br />
anticancer drug to specific nanostructures composed of lipids and<br />
polymers, which have a specific affinity for the lymphnodes to<br />
prevent the process of metastatic spreading through lymphatic<br />
vessels. The project has as the final goal of achieving the preclinical<br />
evaluation stage with one of these novel nanocarrier systems.<br />
In October <strong>2011</strong> the Project FONDiag (Fluorescent Organic<br />
Nanocrystals for the Early Diagnosis of Esophageal and Colon<br />
Cancer) was ranked as first in Europe in the third call for proposal<br />
of the Euronanomed Programme. The three year European joint<br />
project wil be carried on by the <strong>IOV</strong> team leader Dr. Giorgio<br />
Battaglia from High Technogy Oncology Endoscopy Unit.<br />
In July <strong>2011</strong> <strong>IOV</strong> has been awarded with another FP7 grant<br />
in the field: “New Oral Nanomedicines: Transporting Therapeutic<br />
Macromolecules across the Intestinal Barrier”, a NMP Large scale<br />
project with a total cost of 9 million Euro. The consortium is<br />
composed by an international network of 17 partners from<br />
8 countries and among them 2 multinational industries and 3<br />
SMEs. There is an immense potential impact of Nanomedicine<br />
on public wellbeing and on economic growth for Europe. The<br />
field is of considerable importance for Europe and is a politically
strategic focus for the Government of Veneto Region too. Through<br />
the constant commitment of the office, we can now count on<br />
735Ke European funds dedicated to this field and with new<br />
renowned international partnerships.<br />
Bilateral cooperations:<br />
Christie Hospital, Manchester (UK)<br />
On March the 26th and 27th of <strong>2010</strong> a <strong>IOV</strong> delegation<br />
composed by the Scientific Director Prof. Alberto Amadori, Prof.<br />
Giuseppe Opocher, Dr. Carlo Castoro, Prof. Vincenzo Bronte, Dr.<br />
Angelo Palozzo and Ms. Manuela Mtanis has visited the Christies<br />
following the former visit made by the management of the English<br />
Comprehensive Cancer Centre to the <strong>IOV</strong> in 2008. The two-day<br />
visit layed the basis for mutual understanding agreements in the<br />
areas of basic and translational research, health and education.<br />
Bugando Medical Centre, Mwanza (Tanzania)<br />
In March <strong>2010</strong> the Scientific Director Prof. Alberto Amadori<br />
and Prof. Luigi Chieco Bianchi have visited the Bugando<br />
Medical Center (BMC) in order to identify priorities for the<br />
implementation of the collaborative program between <strong>IOV</strong> and<br />
the BMC, Mwanza. In particular, the collaboration between the<br />
<strong>IOV</strong> and the BMC could be achieved in the short / medium term<br />
according to the following guidelines:<br />
1) To start a pilot project for diagnostic and epidemiological<br />
monitoring of viral infections associated with cancer (HPV<br />
and uterine cervical cancer, HTLV-1 and adult T-cell leukemia;<br />
HHV-8 and Kaposi’s sarcoma and peritoneal effusion<br />
lymphonomas; EBV and Burkitt’s lymphoma).<br />
2) To provide accommodation for short periods of professional<br />
training to medical and paramedical staff, and reception of<br />
BMC staff for short stays in order to develop diagnostic tests.<br />
In particular, the <strong>IOV</strong> could accommodate at its facilities, for<br />
a period of 3-6 months, a general surgeon of the BMC, in<br />
order to gain initial experience, technical and theoretical, in<br />
oncological surgery.<br />
3) To investigate the prevalence of genetic alterations linked to<br />
cancer (BRCA1/2, Rb), transferring blood samples conveniently<br />
mounted on suitable supports, and therefore able to deal with<br />
transportation, to deepen the study of tumor pathology of<br />
hereditary basis.<br />
4) To activate a web-service to doctors within the BMC (possibly<br />
in cooperation with the Central Pathology Service in Venice<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
199<br />
and in coordination with the Foundation Tison), to give<br />
necessary advice in a pathologic cancer diagnosis.<br />
In the 2008-<strong>2010</strong> period, about 12 million euro were<br />
collected from funding agencies and charities, most of which on<br />
a competitive basis. This success in securing adequate grants to<br />
support research activities witnesses the high level of the research<br />
projects developed at the Institute.<br />
The major projects developed thanks to this support include:<br />
Ministry for University and Research<br />
Control of cell proliferation and death by HTLV-<br />
I-encoded proteins;<br />
EBV-associated lymphomagenesis: interactions<br />
between viral and cellular proteins;<br />
Functional interactions between mitochondria and<br />
proteins coded by human oncogenic viruses;<br />
Functional and pathological aspects of myelomonocytoid<br />
suppressor cells in cancer;<br />
Anti-angiogenic strategies in human tumors.<br />
Italian Ministry of Health/ISS<br />
Molecular bases of heredo-familial tumors;<br />
Genetic and functional analysis of regulatory<br />
proteins coded by oncogenic viruses;<br />
Virus-host interactions in a cohort of HIVinfected<br />
pediatric patients at risk of lymphoma;<br />
Immune response modulation as a novel<br />
therapeutic strategy in cancer patients;<br />
Idiotypic vaccination in patients with B cell<br />
lymphoproliferative diseases;<br />
Development of new drugs able to modify tumor<br />
microenvironment;<br />
Angiogenesis at the interface between tumor and<br />
microenvironment: therapeutic implications in<br />
hematologic malignancies;<br />
MicroRNA sequences in solid tumors and<br />
hematologic tumors;<br />
Tumor microenvironment: role in neoplastic<br />
progression;<br />
Biocompatible polymers as a carrier of antitumor<br />
agents.
Italian Association for Research on Cancer<br />
Innovative strategies for early diagnosis and<br />
treatment of esophageal cancer;<br />
Functional dissection of virus-host interactions in<br />
virus-associated lymphomagenesis;<br />
Blocking angiogenesis: a multifaceted approach to<br />
gene therapy in preclinical tumor models;<br />
Molecular and functional characterization of<br />
melanoma-associated myeloid suppressive cells;<br />
Virus-host interactions in EBV-associated<br />
lymphomagenesis;<br />
The role of telomerase in solid and hematologic<br />
malignancies;<br />
MicroRNA in human cancer: a high-throughput<br />
integrated approach based on tissue-specific<br />
microRNA libraries;<br />
Role of arginase in tumor development and in<br />
tumor-associated immune suppression;<br />
Implementation of an oncogenomic platform for<br />
the study of hemopoietic malignancies;<br />
Innovative diagnostic and therapeutic strategies for<br />
gastric and colo-rectal cancer.<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
200<br />
European Commission and Foreign Agencies<br />
Subset-specific immunotherapy of B cell<br />
lymphomas;<br />
Nanotechnologies in innovative approaches to<br />
cancer therapy;<br />
Role of chronic infections in the development of<br />
cancer;<br />
HIV infection-associated opportunistic tumors.<br />
Most of the above projects are conducted in collaboration with<br />
leading national and international Institutions; a non-exhaustive<br />
list includes: European Institute of Oncology, Milan (Italy);<br />
Istituto Clinico Humanitas, Milan; Istituto Superiore Sanità,<br />
Rome (Italy); Centro Riferimento Oncologico, Aviano (Italy);<br />
Universities of Padova, Rome, Milan, Verona (Italy); University<br />
of Santiago de Compostela (Spain), Universitè Catholique de<br />
Louvain (Belgium), University of Angers (France), University of<br />
London (United Kingdom), University College Dublin (Ireland),<br />
Uppsala University (Sweden), Warsaw University of Technology<br />
(Poland), Université Paul Sabatier de Toulouse (France), University<br />
of Twente (Netherlands), Ohio State University (USA); Columbia<br />
University, New York (USA); National Cancer Institute-NIH,<br />
Bethesda (USA); Sydney Melanoma Unit (Australia).
Impact Factor Trend<br />
1000<br />
800<br />
600<br />
400<br />
200<br />
0<br />
2007 2008 2009 <strong>2010</strong> <strong>2011</strong><br />
Total Impact Factor Articles Average IF<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
201<br />
6<br />
5<br />
4<br />
3<br />
2<br />
1<br />
0<br />
2007 2008 2009 <strong>2010</strong> <strong>2011</strong>
Clinical Trials and Biostatistics Unit<br />
Main Pubblications<br />
Chief<br />
Gian Luca De Salvo, MD<br />
Validity and reliability of the MSKCC Bowel Function<br />
instrument in a sample of Italian rectal cancer patients.<br />
Central nervous system failure in melanoma patients:<br />
results of a randomised, multicentre phase 3 study of<br />
temozolomide-and dacarbazine- based regimens.<br />
Patient-reported outcomes after neoadjuvant<br />
chemoradiotherapy for rectal cancer: a multicenter<br />
prospective observational study.<br />
Clinical considerations on sentinel node biopsy in<br />
melanoma from an Italian multicentric study on 1,313<br />
patients (SOLISM-IMI).<br />
A Randomized clinical trial on sentinel lymph node<br />
biopsy versus axillary lymph node dissection in breast<br />
cancer: results of the Sentinella/GIVOM trial.<br />
Born in Nuoro, Italy on 6 th March 1967. Graduated with honours in Medicine and surgery at the<br />
University of Padua in 1993 and specialized with honours in Internal Medicine at the University<br />
of Padua in 1998. Head of the Clinical Trials and Biostatistics Unit (previously named Clinical<br />
Epidemiology Unit) since its establishment in 1997. Research interests and activities include the<br />
methodology of clinical research with particular focus on phase II and III Randomised Clinical<br />
Trials; Quality of Life evaluation; innovative systems for data collection.<br />
Responsible for the organization and conduction of several National and International clinical<br />
trials in the field of oncology, particularly melanoma, breast cancer, colo-rectal cancer and pediatric<br />
tumors. Some of these trials are completely managed via a web-based system. Coordinator of the<br />
Statistical and Data Management panel of the European pediatric Sarcoma Study Group (EpSSG)<br />
and the SIOP-Low Grade Glioma study group. Published over 60 papers in peer-reviewed journals<br />
and presented over 40 abstracts at International scientific meetings (H-index 15).<br />
Zotti P, Del Bianco P, Serpentini S, Trevisanut P, Barba MC, Valentini<br />
V, De Paoli A, Pucciarelli S.<br />
Chiarion-Sileni V, Guida M, Ridolfi L, Romanini A, Del Bianco P,<br />
Pigozzo J, Brugnara S, Colucci G, Ridolfi R, De Salvo GL; Italian<br />
Melanoma Intergroup (IMI).<br />
Pucciarelli S, Del Bianco P, Efficace F, Serpentini S, Capirci C, De<br />
Paoli A, Amato A, Cuicchi D, Nitti D.<br />
Testori A, De Salvo GL, Montesco MC, Trifirò G, Mocellin S, Landi<br />
G, Macripò G, Carcoforo P, Ricotti G, Giudice G, Picciotto F,<br />
Donner D, Di Filippo F, Soteldo J, Casara D, Schiavon M, Vecchiato<br />
A, Pasquali S, Baldini F, Mazzarol G, Rossi CR; Italian Melanoma<br />
Intergroup.<br />
Zavagno G, De Salvo GL, Scalco G, Bozza F, Barutta L, Del Bianco P,<br />
Renier M, Racano C, Carraro P, Nitti D; GIVOM Trialists.<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
202<br />
Eur J Surg Oncol.<br />
<strong>2011</strong> 37:589-96<br />
Br J Cancer. <strong>2011</strong>;<br />
104:1816-21<br />
Ann Surg. <strong>2011</strong>;<br />
253:71-7<br />
Ann Surg Oncol.<br />
2009; 16:2018-27<br />
Ann Surg. 2008;<br />
247:207-13
Clinical and Research Staff<br />
Gian Luca De Salvo<br />
Paola Del Bianco<br />
Denise Kilmartin<br />
Angela De Paoli<br />
Paola Tellaroli<br />
Chiara Zaina<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
203
Mission<br />
The main aim of the Unit is to develop and coordinate clinical<br />
research program in oncology at national and international levels, in<br />
compliance with existing regulations and ethical requirements.<br />
Moreover, the Unit provides the institute’s researchers with<br />
biostatistical support in data analysis and interpretation of results<br />
Research Activities<br />
1) The Unit provides methodological, statistical and operative<br />
support for all phases (I, II, III, observational) of the development<br />
of research protocols and data management according to Good<br />
Clinical Practice (GCP) principles, in particular:<br />
Protocol development and preparation of case report forms;<br />
Statistical design and sample size;<br />
Data Base construction with the use of specific software<br />
programs;<br />
Data management;<br />
Development of methodologies for Data Quality Assurance<br />
according to GCP standards;<br />
Analysis of data and interpretation of results;<br />
Preparation of interim reports and manuscripts;<br />
Major Collaborations<br />
The Unit has general leadership responsibilities in developing<br />
and coordinating research programs with various departments<br />
and scientific institutions:<br />
Inside the <strong>IOV</strong><br />
Medical Oncology 1 and 2<br />
Radiotherapy and Nuclear Medicine<br />
Immunology and Molecular Oncology<br />
Radiology<br />
Anesthesia<br />
Melanoma and Sarcoma<br />
Psycho-oncology<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
204<br />
deriving from several types of oncological studies.<br />
Finally, the Unit supports the <strong>IOV</strong> Scientific Direction in<br />
retrieving, monitoring and evaluating the scientific activity of the<br />
Units at the <strong>IOV</strong>.<br />
2) The Unit supplies and manages operative tools for the<br />
monitoring and evaluation of the clinical and scientific activity<br />
of the Units at the Institute and assists in the collection and<br />
processing of the data by means of a dedicated web system (SIFF-<br />
<strong>IOV</strong>). The Unit collaborates in the collection and editing of data<br />
for the periodic publication of the Institute’s scientific report.<br />
The Unit deals with the collection, editing and input in the<br />
web data base of Ministry of Health (WorkFlow System) of all<br />
data concerning the clinical and scientific activities of the various<br />
departments at the Institute.<br />
National Collaborations<br />
Oncologic and Surgical Sciences Department, Padua<br />
University, Padova<br />
Pediatric Department, Padua University, Padova<br />
Medical Oncology, Giovanni Paolo II Cancer Institute, Bari<br />
Division of Melanoma and Soft Tissue Sarcoma, European<br />
Institute of Oncology, Milan<br />
Unit of Psychological-Oncology, National Cancer Institute<br />
CRO, Aviano
International Collaborations<br />
Emma Children’s Hospital, Academic Medical Center,<br />
Amsterdam, The Netherlands<br />
College of Public Health, University of Nebraska Medical<br />
Center, Omaha, USA<br />
Institut fur Biometrie und Klinische Forschung, Munster,<br />
Germany<br />
Major Ongoing Research Projects<br />
At present the Unit is involved in several multicentric clinical<br />
trials related to the diagnosis and treatment of melanoma, breast,<br />
head and neck cancer and pediatric tumors. In particular, two<br />
randomised phase III trials for the treatment of melanoma: one in<br />
the adjuvant setting for the treatment of patients at high risk of<br />
relapse and the other in advanced disease patients to evaluate the<br />
impact of temozolomide in preventing cerebral metastases.<br />
The unit carried out a randomized, multicenter study on the<br />
usefulness of the sentinel node biopsy as an indicator for axillary<br />
lymphadenectomy in patients with breast cancer less than 3cm.<br />
Since the sentinel node biopsy is becoming widely used in the<br />
current clinical practice, we believe it could be important to have<br />
solid evidence on its effectiveness. Therefore, we have recently<br />
started working on a meta-analysis regarding the sentinel node<br />
biopsy method vs axillary standard dissection in breast cancer.<br />
The unit has recently received approval from the Italian<br />
National Institute of Health (ISS) to commence a “first in man”<br />
Phase I study: adjuvant anti-ErbB-2 (RHuT-IDN 6439, plasmid<br />
for DNA vaccine) in patients treated for primary ErbB-2+<br />
stage III and IV carcinomas of the oral cavity, oropharynx and<br />
hypopharynx.<br />
In the pediatric setting, the unit manages several trials<br />
under the auspices of Italian or European co-operative groups:<br />
a comprehensive treatment strategy involving three clinical trials<br />
are offered to all children and adolescents up to an age of 18 years,<br />
with a low grade glioma arising in any part of the central nervous<br />
system; two clinical trials for the management and treatment<br />
of children and young people presenting with non-metastatic<br />
sarcoma. A particular characteristic of the above mentioned studies<br />
is that the management and data collection activities are carried<br />
out via web-based systems. In fact, the unit has a specific interest in<br />
the implementation of telematics for the management and remote<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
205<br />
The unit is also the coordinating centre for the activity of various<br />
collaborative clinical trial groups such as the Italian Melanoma<br />
Inter-group (IMI), the Italian Pediatric Haemato-Oncologic<br />
Association (AIEOP), the European Pediatric Sarcoma Study<br />
Group (EpSSG), the Society of Pediatric Oncology-Low Grade<br />
Glioma Consortium (LGG) and the Gruppo Interdisciplinare<br />
Veneto di Oncologia Mammaria (GIVOM).<br />
data collection as part of cooperative clinical trials. The Unit also<br />
supports an integrated project focused on pediatric patients with<br />
rare tumors. Specific aims are to collect epidemiological data,<br />
create a clinical and pathological database, develop diagnostic and<br />
therapeutic recommendations, create a cooperation network with<br />
expert specialists, and improve biological studies.<br />
The unit coordinated a randomized trial to evaluate whether<br />
an integrated psycho-oncologic compared to a conventional<br />
approach is more effective in reducing the anxiety of patients with<br />
breast cancer prior to surgery leading to a better understanding<br />
of informed consent to anesthesia and is now in the process of<br />
submitting a scientific paper to an international journal with the<br />
results of this study.<br />
Moreover, the unit is about to start up a study on “the<br />
early detection and prediction of cardiotoxicity in adjuvant<br />
Chemotherapy-Treated breast cancer patients”.<br />
Another area of interest includes the evaluation of Healthrelated<br />
quality of life (HRQOL), symptoms and other types of<br />
patient-reported outcomes that have become critical to fully<br />
evaluate overall treatment effectiveness. A number or research<br />
projects, aimed at evaluating how the HRQOL of patients with<br />
melanoma, breast and rectal cancer is affected by the disease,<br />
treatment and symptoms, within randomised clinical trials<br />
and observational studies, using a prospective and longitudinal<br />
approach, are being carried out. Moreover, activities related to<br />
the development of a new instrument to assess the HRQOL<br />
in melanoma patients undergoing electrochemotherapy, and in<br />
the validation of the Italian version of a questionnaire to assess<br />
the recovery and the normal bowel functions in patients after<br />
sphincter preserving surgery are being performed and another to<br />
assess quality of life in patients nearing the end of life.
Programs and Perspectives for the Future<br />
Performing no-profit clinical trials is a significant part of the<br />
Institute’s mission. Optimizing the management of these trials<br />
according to high quality standards respecting high ethical values<br />
are main objectives of the Institute. To better accomplish this issue,<br />
the Unit is in the process of applying for a quality certification<br />
according to international standards (ISO 9001).<br />
As far as clinical research is concerned, the Unit is currently<br />
involved in planning some trials in different contexts. Some details<br />
of these projects are reported below.<br />
Role of cytoreductive surgery plus hyperthermic<br />
intraperitoneal chemotherapy (HIPEC) in patients with<br />
colorectal cancer at high risk for peritoneal recurrence.<br />
This is a randomized phase II study to investigate the benefit<br />
of second look and hyperthermic intra peritoneal chemotherapy<br />
besides standard adjuvant chemotherapy in patients with colorectal<br />
cancer at high risk for peritoneal recurrence.<br />
Moreover, the Unit is planning a prospective sequential<br />
observational study to verify the additional role of the association<br />
of PET-TC with iodine contrast with respect to the traditional<br />
diagnostic work up in esophageal cancer potentially amenable to<br />
curative resection.<br />
Quality of life as a prognostic factor<br />
Health related quality of life (HRQOL) is recognized to<br />
complement biomedical measures in clinical decision making<br />
by providing relevant additional information for the assessment<br />
of overall burden and effectiveness of treatment. Additionally,<br />
recent research has shown that assessment of HRQOL scales<br />
in conjunction with clinical data might improve survival<br />
prediction.<br />
The aim of this research is to investigate the role of baseline<br />
HRQOL data and changes in HRQOL scores before and after<br />
treatment, combined with baseline clinical variables, as an<br />
independent prognostic factor for post-operative complications,<br />
progression-free and overall survival in patients with mid-low<br />
rectal cancer undergoing pCRT and surgery with curative intent.<br />
The analysis will be conducted on patients who had undergone<br />
THE RESEARCH - <strong>SCIENTIFIC</strong> DIRECTOR ADDRESS<br />
206<br />
surgery between February 2003 and June 2006. HRQOL baseline<br />
scores were assessed using the European Organisation for Research<br />
and Treatment of Cancer, Quality of Life Questionnaire-Core30<br />
(EORTC QLQ-C30), and the EORTC QLQ-CR38 colorectal<br />
module.<br />
Impact of treatment in advanced asymptomatic colorectal<br />
cancer and unresectable metastasis patients.<br />
The therapeutic strategy for stage IV colorectal cancer is driven<br />
by the resectability of the metastases. In the setting of asymptomatic<br />
primary tumor and unresectable metastases, although palliative<br />
systemic chemotherapy is clearly indicated, opinion is divided<br />
as to whether these patients should undergo primary tumor<br />
resection. Due to the complexity and cost of performing a<br />
randomized clinical trial, there is interest in using data from a<br />
multicentre observational study to evaluate the overall survival in<br />
patients undergoing asymptomatic primary tumor resection prior<br />
to chemotherapy and in patients receiving chemotherapy, with<br />
or without biological agents, followed by surgery if the primary<br />
becomes symptomatic or the metastases are resectable.<br />
Using observational data to compare outcomes associated<br />
with different treatments may result in biased estimates because of<br />
non-random treatment assignment. To correct for variables that<br />
may confound the association, a propensity score analysis and an<br />
instrumental variable analysis will be applied.
Strategic Scientific Options<br />
THE RESEARCH - STRATEGIC <strong>SCIENTIFIC</strong> OPTIONS<br />
209
Strategic Scientific Options<br />
In this frame, the major lines of research pursued at the <strong>IOV</strong><br />
can be summarized as follows:<br />
a. uNDErSTaNDiNG ThE COmplEx mOlECular mEChaNiSmS<br />
uNDErlyiNG maliGNaNT TraNSfOrmaTiON aND TumOr<br />
prOGrESSiON<br />
It is clear that cancer is a genetic disease, in which the stepby-step<br />
accumulation of genetic abnormalities leads the cell to<br />
eventually acquire a fully transformed, malignant phenotype.<br />
However, the molecular events which regulate cell proliferation<br />
and death are extremely complex, and high-throughput approaches<br />
at genomic, proteomic and metabolomic levels are needed to<br />
dissect this array of circuitries. At our Institute, special attention<br />
is devoted to the interaction between human genome and<br />
products of several human herpes-viruses and retroviruses, such<br />
as Epstein-Barr Virus (EBV), Human Herpes Virus-8 (HHV-8),<br />
Human Papilloma Virus (HPV) and Human T Lymphotropic<br />
Virus type I (HTLV-I), as well as to the alterations in signalling<br />
cascades that may preclude apoptotic pathways, thus leading to<br />
cell immortalization. Besides the use of gene expression analysis<br />
platforms, this work is also facilitated by the availability in our SPF<br />
animal facility of several animal tumor models, including models<br />
of EBV-associated human lymphomagenesis and transgenic/<br />
knockout models. A special focus is also dedicated to inheritable<br />
alterations of known genes, such as BRCA-1/2, CDKN2A and<br />
others, which are involved in the pathogenesis of heredo-familial<br />
cancers; through the collaboration with international leading<br />
groups, we are steadily searching for new, as yet unidentified genes<br />
responsible for some rare neuroendocrine tumors.<br />
In this setting, particular attention is paid to the search of<br />
modifier genes, which could affect the penetrance of the major<br />
genes, thus accounting for the different incidence of the disease<br />
in individuals sharing identical mutations. An operative unit,<br />
called “Family Cancer Clinics”, collects all the <strong>IOV</strong> expertise in<br />
THE RESEARCH - STRATEGIC <strong>SCIENTIFIC</strong> OPTIONS<br />
210<br />
this field, and stands as a reference point for all the people that in<br />
Padova and the surrounding region deal with hereditary cancer.<br />
b. SEarChiNG fOr NOvEl TOOlS fOr DiaGNOSiS, prOGNOSiS aND<br />
ThErapy Of TumOrS<br />
Over the last 30 years, early diagnosis has been a key element<br />
in contributing to improve the quality of life and survival of cancer<br />
patients. This issue is a central research interest at the <strong>IOV</strong>, and<br />
involves both basic/translational investigators (in search of new<br />
biomarkers through genomic, proteomic and phosphoproteomic<br />
approaches) and clinical researchers (through the identification of<br />
new imaging tools and non-invasive diagnostic procedures).<br />
As far as tumor prognosis is concerned, the most recent<br />
knowledge on tumor biology increasingly underscores how<br />
tumors of a same histotype, which are apparently identical<br />
based on histologic and phenotypic properties, may reflect<br />
totally different neoplastic diseases, destined to a completely<br />
different clinical course and also sensitive to different therapeutic<br />
approaches. Landscape examples of this are the case of lung<br />
tumors, where EGFR and K-ras status condition the response to<br />
Gefitinib, and the case of colon carcinoma, where the presence or<br />
absence of K-ras and B-RAF mutations is able to determine the<br />
efficacy of target therapies. A major goal of modern oncology is<br />
to molecularly characterize tumors, with the aim of designing a<br />
new classification of cancer, which could more closely correlate<br />
with patient prognosis and clinical course. In this setting, through<br />
the application of functional genomic platforms, tumor samples<br />
are studied for their gene expression profile in search of markers<br />
associated with a particular course of the disease or a given clinical<br />
response to therapy. By this means, the dream of a personalized,<br />
tailor-made treatment of cancer patients is becoming closer dayby-day.<br />
Finally, in reference to the search for innovative therapies,<br />
the most modern surgical, chemotherapic and radiotherapic
approaches are tested at the <strong>IOV</strong> within national or international<br />
multicentric studies. In this setting, special attention is paid to<br />
the so-called “target therapies” (such as Tyrosine Kinase Inhibitors<br />
-TKI- and monoclonal antibodies against molecule expressed at<br />
the cancer cell surface), which target particular signal transduction<br />
pathways that are key to cancer cell survival. One major issue that<br />
<strong>IOV</strong> researchers intend to address is why, despite similar molecular<br />
features in tumor cells, a part of the patients do not respond to<br />
these agents; also, a major focus of interest is the synergistic<br />
action of the combination of diverse therapeutic agents, targeting<br />
different steps of the complex cascade of alterations leading to<br />
malignant transformation.<br />
C. ExplOriNG ThE COmplEx iNTEraCTiONS bETwEEN TumOr CEllS<br />
aND hOST miCrOENvirONmENT aS a pOTENTial TarGET Of NEw<br />
ThErapEuTiC apprOaChES<br />
Even though cancer can be considered as a genetic disease, the<br />
interactions between tumor cells and cells of the host colonizing<br />
or infiltrating the tumor masses (fibroblasts, endothelial cells,<br />
inflammatory cells) may play a significant role in affecting tumor<br />
growth and progression. In some cases, factors released by neoplastic<br />
THE RESEARCH - STRATEGIC <strong>SCIENTIFIC</strong> OPTIONS<br />
211<br />
cells may recruit into tumors particular inflammatory cells able<br />
to down-regulate immune response to tumor antigens, thus<br />
preventing cancer rejection; attempts are underway to modulate<br />
the activity of these cells by appropriate drugs in experimental<br />
models as well as in man. On the other hand, some of these host<br />
components may represent a suitable therapeutic target; this is the<br />
case of endothelial cells, which may be targeted by appropriate<br />
reagents to induce a dramatic shortage of oxygen and nutrient<br />
support to tumor cells, thus inducing tumor regression.<br />
In this field, studies are currently underway in both experimental<br />
models and selected human tumors, often in combination<br />
with chemotherapic approaches. In addition, innovative active<br />
immunotherapy approaches with tumor antigens or adoptive<br />
immunotherapy strategies with tumor-specific lymphocytes<br />
are also being tested in several preclinical models as well as in a<br />
few phase I/II collaborative studies. In this regard, we are now<br />
launching the first phase I experimentation coordinated by our<br />
Institute, a first-in-man DNA vaccination trial with a Her-2coding<br />
plasmid, very recently authorized by the Health Ministry<br />
through the Istituto Superiore di Sanità.
Oncology has now entered an era in which the knowledge of<br />
genetic variability is helpful for optimal approach to patient care.<br />
Cancer is a complex disorder whose ultimate outcome is the result<br />
of numerous alterations affecting the regulation of genes, and it<br />
is well known that individuals with a same tumor type and stage<br />
do not necessarily carry the same cancer-driving mutations. This<br />
is a very important piece of information, as different molecular<br />
alterations or combinations of alterations may render the malignant<br />
cell sensitive or refractory to a drug targeting specific intracellular<br />
pathways. In this regard, the lesson learnt from non-small cell lung<br />
tumors (NSCLC), as an example of somatic mutations of key<br />
oncogenic pathways, in tumor DNA that are predictive of response<br />
to targeted therapy, is clear. The epidermal growth factor receptor<br />
(EGFR) has been found to be expressed or highly expressed in<br />
a variety of solid tumors, including NSCLC. Molecular studies<br />
revealed abnormal signal transduction in lung cancer cells, and high<br />
levels of EGFR expression have been associated with unfavorable<br />
clinical outcome, making the receptor a promising target for anticancer<br />
therapy. Somatic mutations in the kinase domain of EGFR<br />
have been linked to clinical response to Gefitinib, an orally active<br />
small molecule EGFR-associated tyrosine kinase inhibitor (TKI).<br />
These mutations are more common among women, never smokers<br />
and of Asian ethnicity, known clinical predictors of Gefitinib<br />
sensitivity. Recently, high EGFR copy number detected by FISH<br />
has been extensively studied and correlated with other prognostic<br />
factors. Moreover, increased EGFR copy number predicts Gefitinib<br />
sensitivity and has been proposed as an effective molecular predictor<br />
for Gefitinib efficacy in advanced NSCLC.<br />
Another example of the importance of specific genetic<br />
alterations in predicting the response to targeted therapies comes<br />
from colorectal cancer. In fact, patients with colorectal cancer<br />
benefit from the administration of TKI inhibitors only if the RAS<br />
gene is non-mutated; the additional role of the bRAF gene in this<br />
scenario is currently under investigation. Unfortunately, only a<br />
relatively small fraction of patients can benefit of these targeted<br />
Pharmacogenomics<br />
THE RESEARCH - STRATEGIC <strong>SCIENTIFIC</strong> OPTIONS<br />
212<br />
therapies while the majority is cured with classical non-targeted<br />
chemotherapeutic drugs. This standard anticancer therapy based<br />
on “one size fits all” modality often is ineffective or produces<br />
serious toxicities at doses retained optimal for anticancer effects<br />
(Figure 1). Inter-individual heterogeneity in drug response may<br />
be due to several factors including age, sex, race, organ function,<br />
and interactions among drugs. However, despite the potential<br />
importance of these clinical variables in determining drug effects, a<br />
growing body of evidence indicates that sequence variants (genetic<br />
polymorphisms) in genes encoding drug-metabolizing enzymes,<br />
drug transporter, drug targets or drug-induced DNA damage<br />
repair can have an even greater influence on the efficacy and<br />
toxicity of treatment. In many cases, the genetic polymorphism of<br />
drug metabolizing enzymes is associated with reduced activity of<br />
the encoded variant proteins, usually leading to a modulation of<br />
pharmacologic effects of therapy. Because anticancer drugs have a<br />
narrow therapeutic window, changes in their pharmacokinetics or<br />
pharmacodynamics may directly reduce efficacy or induce severe<br />
toxicity. In view of these premises, one strategy to increase the<br />
effectiveness of chemotherapy is to gain a better understanding<br />
of the influence exerted by the genetic background of patients<br />
in the response to treatment. Thus, development of genetic<br />
tests predicting which variant may influence the efficacy and/or<br />
toxicity of chemotherapy is one critical issue facing oncologists.<br />
The term pharmacogenetics usually refers to studies of genes that<br />
may influence response to drug and chemicals. However, recent<br />
advances in large genome scale sequencing and improvements<br />
in bioinformatics tools in processing large amounts of data led<br />
to the transition of pharmacogenetics (the analysis of one or a<br />
few candidate genes) to pharmacogenomics (study of the entire<br />
spectrum of genes in the human genome).<br />
Many genetic polymorphisms in some relevant drugmetabolizing<br />
enzymes are currently well-known, and data on<br />
new polymorphisms in the pathways involved in drug activation,<br />
detoxification and metabolisms are accumulating in the literature:
Thiopurine S-methyltransferase (TPMT). Thiopurine<br />
S-methyltransferase is relevant in the metabolism of<br />
6-mercaptopurine and 6-thioguanine; its activity shows<br />
population variability based on genetic polymorphism. Polymorph<br />
forms usually exhibit a reduced enzymatic activity, and reduced<br />
thiopurine S-methyltransferase activity is associated with severe<br />
toxicity and increased risk of secondary malignancies.<br />
Glutathione S-transferases. Glutathiones play a role in<br />
inactivation of many chemotherapeutics such as platinum agents<br />
and anthracyclines and in detoxification of exogenous products of<br />
reactive oxidation. Genotypes of glutathione S-transferases may<br />
predict not only treatment-related outcomes but will also predict<br />
the induction of severe cardiotoxicity induced by anthracycline,<br />
and severe myelosuppression induced by treatment with temerodal<br />
in glioblastoma and metastatic melanoma.<br />
Dihidropyrimidine dehydrogenase. Dihidropyrimidine<br />
dehydrogenase (DPD) represents the rate-limiting enzyme in<br />
the catabolism of pyrimidine antimetabolic drug 5-fluorouracil<br />
(5-FU); indeed the majority of 5-FU is degraded by DPD.<br />
Decreased activity of DPD accounts for approximately 43% of<br />
grade 3-4 toxicity in 5-FU-treated patients.<br />
Uridine diphosphate glucuronosyltransferase 1A1<br />
(UGT1A1). Uridine diphosphate glucuronosyltransferase 1A1<br />
plays a major role in detoxifying the active metabolite of irinotecan.<br />
Therefore, the analysis of UGT1A1 may be useful to predict<br />
patients at risk of irinotecan toxicity.<br />
Thymidylate syntase (TS). Thymidylate syntase, a<br />
critical enzyme in DNA synthesis, is also the target of 5-FU.<br />
The expression of TS is regulated by several polymorphic tandem<br />
All patients with<br />
the same diagnosis<br />
NO Benefit<br />
+ Toxicity<br />
NO Benefit<br />
NO Toxicity<br />
+ Benefit<br />
+ Toxicity<br />
+ Benefit<br />
NO Toxicity<br />
Figure 1. For an increasing number of situations, it is becoming clear that patients can be<br />
categorized into different classes, according to the benefit/toxicity they have following a<br />
given standard therapy (modified from Walgren RA et al., JCO 23:7342, 2005).<br />
Figure 2. Pharmacogenomics studies are<br />
not only beneficial to patients, but also help<br />
sparing money by preventing inappropriate<br />
expensive therapies.<br />
THE RESEARCH - STRATEGIC <strong>SCIENTIFIC</strong> OPTIONS<br />
213<br />
repeats in the TS promoter. Higher number of tandem repeat<br />
copies is related to increased TS activity and by consequence to<br />
a lower sensitivity to 5-FU treatment. By contrast, lower number<br />
of repeats is associated with a higher sensitivity, but also higher<br />
toxicity, to 5-FU treatment.<br />
Tamoxifen and CYP2D6. Tamoxifen is the most prominently<br />
prescribed drug for treating breast cancer; it is a prodrug, and its<br />
activation is mediated by cyrochrome P450 2D6. Polymorphisms<br />
in CYP2D6 are associated with a significantly higher risk of<br />
recurrent breast cancer. Furthermore, polymorphisms in the multi<br />
drug resistant gene-1 (MDR-1) and ATP-binding cassette (ABC)<br />
transporter genes can predict resistance to chemotherapeutic drugs,<br />
and patients with methylenetetrahydrofolate reductase (MTHFR)<br />
gene variants exhibit a higher response to 5-FU-based treatment.<br />
Thus, personalized medicine offers the opportunity to increase<br />
therapeutic efficacy by both targeting the cancer-driving genomic<br />
aberrations and, where the tumor biomarker is not known,<br />
identifying individuals who will benefit most from conventional<br />
“non-targeted” treatment, decreasing at the same time toxicity due<br />
to individually altered drug metabolism. All these tests are available<br />
to clinicians, and may greatly improve the management of most<br />
patients, in terms of both therapy effectiveness and safety. Of<br />
course, these tests may be expensive, but the costs of administering<br />
inappropriate, expensive therapies and of managing eventual<br />
untoward toxicities may largely compensate this effort (Figure 2).<br />
Indeed, pharmacogenomics can have a significant economic impact<br />
by driving therapeutic intervention and prospectively predicting<br />
patient’s drug activation and detoxification status.
Normal tissues are organized in a hierarchical fashion; rare<br />
somatic cells give origin to a population of differentiated cells<br />
forming the bulk of tissue. In this setting, the skin and the gastrointestinal<br />
tract undergo a tremendous turnover of the epithelial<br />
component, which entails the existence of a self-renewing<br />
population able to steadily face the continuous replacement of<br />
the dying epithelial cells. These self-maintaining cells, called stem<br />
cells, are able to divide symmetrically to perpetuate themselves<br />
(self-renewal) and asymmetrically to maintain the progeny<br />
(differentiation). Stem cell true nature can be entirely understood<br />
only within its natural microenvironment, the so-called “niche”,<br />
where the exposure to growth factors and extracellular matrix,<br />
secreted and organized by neighboring differentiated cells, allows<br />
stem cells to maintain their identity.<br />
A landscape example of stemness of solid tissues comes from<br />
the gastro-intestinal tract. The intestinal niche is organized into<br />
crypts and villi, populated by different types of cells that maintain<br />
their position along the intestinal architecture. All these cells<br />
originate from a small population of long-living cells located<br />
at the crypt base, as elegantly shown by clonal analysis. Thanks<br />
to a DNA-labeling method these cells have been recognized as<br />
intestinal stem cells. Exposure to niche signals may induce stem<br />
cells to divide asymmetrically and symmetrically, giving origin<br />
to transient amplifying progenitors (TA) that migrate along the<br />
crypt-villus axis. TA cells are faded to differentiate into three<br />
different mature cell types: enterocytes, entero-endocrine cells and<br />
goblet cells; in a few days these mature cells are entirely replaced.<br />
It has been recently shown that, akin normal tissues, malignant<br />
tissues as well present a hierarchical organization; only a few cells<br />
within the tumor are able to maintain indefinitely the bulk of<br />
cancer, and the term Cancer Stem Cells (CSC) was introduced<br />
for the first time in the ’80s. CSC origin is still a matter of debate;<br />
CSC could originate from genetic or epigenetic mutation(s) that<br />
occur in a normal stem or in a progenitor cell. In the former case,<br />
Cancer Stem Cells<br />
THE RESEARCH - STRATEGIC <strong>SCIENTIFIC</strong> OPTIONS<br />
214<br />
due to their unlimited replicative potential, normal stem cells<br />
accumulate oncogenic mutations over time, eventually acquiring<br />
specific malignant properties and at the same time retaining<br />
stemness properties. It is however also possible that differentiated<br />
cells could de-differentiate into stem cells upon genetic mutations,<br />
thus re-acquiring stemness properties.<br />
CSC share some features with normal stem cells, including<br />
long life-span, self-renewal and differentiation potential. CSC in<br />
fact are able to persist in vivo for long time perpetuating themselves<br />
thanks to the ability to divide asymmetrically generating a daughter<br />
differentiated cells and a daughter undifferentiated stem cell. Even<br />
in vitro, CSC can be maintained for long time in the absence of<br />
serum or other growth factors; under these culture conditions,<br />
one of the main characteristics of CSC is their ability to give rise<br />
to cellular structures named “spheroids”, which mimic tumor and<br />
micro-metastases organization in vivo and can be expanded in vitro<br />
for several months. In addition, CSC present high tumorigenic<br />
capability and metastatic phenotype; CSC disaggregated from<br />
spheroids are able to engraft and generate tumors at high efficiency<br />
when inoculated into immunodeficient mice, and also seem to be<br />
responsible for chemioresistance and tumor relapse. In fact, a large<br />
fraction of CSC is in a quiescent state, which prevents the response<br />
to conventional chemotherapeutics able to kill proliferating cells.<br />
CSC quiescence could be a reversible condition, and much work<br />
is focused on the possibility of uncovering the signals that drive<br />
CSC into proliferation or, conversely, induce their dormancy.<br />
Over the last 10 years researchers tried to isolate CSC<br />
thanks to the introduction of new technologies that allowed<br />
their characterization in several malignant tissues, including<br />
hematopoietic, breast, renal and colon cancer. Historically,<br />
two different approaches have led to their identification: (I)<br />
examination of the expression of tissue-specific surface markers<br />
(such as CD44, CD133, CD24) that are selectively expressed on<br />
CSC but not on the bulk of tumor cells, and (II) examination
of specific functional features of CSC. In some studies, CSC<br />
have been recognized by dual-wavelength flow cytometry as<br />
the so-called Side Population (SP) on the basis of their ability<br />
to efflux the fluorescent DNA-binding dye Hoechst 33342. In<br />
other studies, CSC have been identified on the basis of their<br />
replicative potential; under standard culture conditions CSC are<br />
poorly or non-proliferating cells compared to the bulk of tumor<br />
cells. By measuring fluorescence intensity following labelling with<br />
membrane-binding dyes such as PKH26, it is possible to identify<br />
cells that proliferate and eventually loose the dye from cells that<br />
remain in a quiescent state hence maintain high intensity of the<br />
dye. In other studies, CSC have been recognized by their ability<br />
to persist in vivo after chemotherapy treatment. It has been<br />
shown that the CD133- fraction of human colorectal cancer<br />
cells showed a dose-dependent sensitivity to oxaliplatin and/or<br />
5-Fluorouracil (5-FU), whereas the CD133+ fraction (recognized<br />
as the CSC subset) did not undergo drug-induced apoptosis, even<br />
by increasing drug concentration. Recent study has demonstrated<br />
that SP/CSC express multidrug resistance genes - including<br />
MDR-1, ABCG2, ABCA3 and BRC1 - that may contribute to<br />
the malignant phenotype and can explain the relative inefficiency<br />
of chemotherapeutic drugs.<br />
Based on the analogies between CSC and their normal<br />
counterpart, much interest has focused on the activation of<br />
certain signalling pathways involved in stem cell maintenance<br />
and proliferation, such as Notch-1, Wnt/β-catenin and Sonic<br />
Hedgehog pathways; it is reasonable that alterations in these<br />
pathways could contribute to neoplastic transformation of<br />
normal stem cells and permit to recognize CSC in different<br />
tissues. Aberrant Notch activation has been demonstrated in<br />
CSC from different tumors, including glioma, breast, colon and<br />
pancreatic cancer. Pancreatic CSC, identified by the expression of<br />
CD44, CD133, CD24, CD34 and ALDH, showed higher levels<br />
of Notch-1 and Notch-2 compared to pancreatic non-CSC. In<br />
colon cancer cells with CSC properties, inhibition of Notch-1<br />
induced a reduction in cell proliferation, a cell cycle arrest in G0-<br />
G1, and it increased the number of apoptotic cells. Moreover,<br />
Notch inhibition reduced both spheroid formation in vitro and<br />
tumorigenic capacity in mice, two established CSC features. In<br />
contrast, Notch-1 overexpression increased cell proliferation, cell<br />
cycle progression and it reduced apoptotic cells. Likewise, a recent<br />
study has demonstrated that some component of Sonic Hedgehog<br />
pathway are highly expressed in stem/progenitor mammary<br />
THE RESEARCH - STRATEGIC <strong>SCIENTIFIC</strong> OPTIONS<br />
215<br />
cells isolated from human normal breast tissue and cultured as<br />
mammospheres. Activation of Hedgehog signalling increased<br />
by 57% the mammosphere number and size; these effects<br />
were blocked by treatment with cyclopamine, which reduced<br />
mammospheres formation.<br />
Many of the markers used to identify CSC in different tissues<br />
(such as LGR5/GPR49, CD44, CD24 and Ep-cam) are part of<br />
the Wnt pathway. LGR5/GPR49, recognized as a putative colon<br />
stem cell marker, is overexpressed in the majority of colorectal<br />
cancer samples, compared to normal mucosal tissue; in addition,<br />
LGR5 expression was correlated to lymphatic and vascular<br />
invasion, lymph node metastasis and tumor stage, highlighting<br />
the involvement of aberrant Wnt signals in tumor progression<br />
driven by CSC.<br />
Despite all the work done, several key problems are still<br />
open:<br />
I) since CSC are usually obtained following long-term in vitro<br />
culture, the phenotypic and/or genotypic profile of spheroidderived<br />
CSC may not faithfully reflect their original in vivo<br />
properties;<br />
II) data on surface marker expression by CSC do not always<br />
coincide among the different workers, and different<br />
“cancer stemness” markers have been identified in different<br />
malignancies, or in a same malignant histotype by different<br />
Authors;<br />
III) assuming that a key property of CSC is their ability to<br />
form tumors when injected at very low cell number into<br />
immunodeficient animals, the estimated number of CSC in a<br />
tumor varies greatly among the Authors, depending on several<br />
factor such as tumor histotype, selection techniques, culture<br />
conditions, as well as the readout chosen for the assay of tumor<br />
generation, as recently elegantly shown in melanoma.<br />
Being conscious of all the difficulties to define a specific<br />
profile for CSC, a better understanding of their characteristics,<br />
the key signaling pathways in CSC and their role in the regulation<br />
of CSC quiescence could represent a fundamental point for a<br />
new therapeutic approach capable of improving the efficacy of<br />
established therapeutic approaches to cancer.
In the following Section we summarize<br />
the list of the Projects presented to the<br />
Health Ministry for the years <strong>2010</strong>-<strong>2011</strong><br />
“Ricerca Corrente”, grouped according<br />
to the appropriate Research Line.
RESEARCH ACTIVITY<br />
<strong>REPORT</strong><br />
RESEARCH ACTIVITY <strong>REPORT</strong><br />
217
LINE 1<br />
Tumor Epidemiology<br />
and Prevention<br />
Akin most (if not all) fields of medicine, progress in oncology firmly relies on the<br />
growing body of evidence about the mechanisms underlying neoplastic transformation<br />
and tumor progression. On the other hand, this wealth of knowledge cannot prescind<br />
from the careful consideration of the possible causes that promote cancer generation,<br />
including environmental factors, nor can the incidence of the different cancer forms be<br />
ignored, since its fluctuations over the years may reflect significant variations in the impact<br />
of these factors on the general population. Thus, in-depth knowledge of the prevalence<br />
and incidence of different cancer forms may greatly help in designing primary prevention<br />
strategies addressing exogenous factors or habits causally related to tumor generation.<br />
Secondary prevention as well may strongly impact on cancer morbidity and mortality,<br />
and the importance of appropriate screening strategies for early diagnosis of some tumors<br />
is largely proven. At the <strong>IOV</strong>, particular attention is paid to primary and secondary<br />
prevention of tumors, and the Institute has the mission of coordinating the three major<br />
cancer screening programs over the entire Veneto region, in strict collaboration with local<br />
health authorities.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 1<br />
218
N° Prog Titolo Responsabile<br />
L01P01 Registro Tumori del Veneto, studi di epidemiologia descrittiva ed analitica. Zambon Paola<br />
L01P02 Prevenzione secondaria dei tumori. Zambon Paola<br />
L01P03 Valutazioni epidemiologiche sui sarcomi delle parti molli. Rossi Carlo Riccardo<br />
L01P04 Epidemiologia delle patologie precancerose dell’esofago. Castoro Carlo<br />
L01P05<br />
L01P06<br />
Studio delle patologie neoplastiche e delle immunodeficienze associate ad infezione con retrovirus umani<br />
nel bambino.<br />
“Prevenire è meglio che curare”: Progetto educativo rivolto ai ragazzi delle scuole medie inferiori di<br />
Padova sui principali fattori di rischio associati al cancro e sull'importanza della prevenzione.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 1<br />
219<br />
De Rossi Anita<br />
Giacobbo Maria<br />
L01P07 Gravidanza dopo terapia per carcinoma della mammella. Ghiotto Cristina<br />
L01P08 Sorveglianza diagnostica di donne ad alto rischio genetico-familiare di tumore mammario. Pescarini Luigi<br />
L01P09 Familiarità e predisposizione genetica nel cancro esofageo e del cardias. Castoro Carlo<br />
L01P10<br />
L01P11<br />
Utilizzo del test Papillomavirus Umani (HPV) ad alto rischio nella prevenzione secondaria del carcinoma<br />
della cervice uterina.<br />
Analisi della prima recidiva in pazienti affetti da carcinoma mammario operato.<br />
Esperienza monoistituzionale.<br />
Del Mistro Annarosa<br />
Jirillo Antonio
LINE 2<br />
Mechanisms<br />
of Cancerogenesis<br />
Neoplastic transformation is a complex process that involves several initiating and/<br />
or promoting events, numerous as yet imperfectly understood molecular changes in<br />
the cell, and bidirectional interactions mediated by soluble or cell-associated molecules<br />
between tumor cells and the microenvironment (endothelial cells, stromal cells, infiltrating<br />
inflammatory cells). Among the causes underlying neoplastic transformation, infectious<br />
agents may play a relevant role, and it is estimated that >20% of human neoplasias are<br />
associated with viral infections. The immunocompromised status, due either to infection<br />
or iatrogenic immunosuppression in transplant recipients, also favors the development of<br />
virus-associated tumors. At the <strong>IOV</strong>, a great deal of expertise has accumulated over the past<br />
40 years on the pathogenic role of viruses, in particular the human T lymphotropic virus<br />
type 1 (HTLV-1), the Epstein-Barr virus (EBV), the human herpesvirus type 8 (HHV8 or<br />
Kaposi Sarcoma-associated HerpesVirus, KSHV), the human papilloma virus (HPV).<br />
These viruses play a direct role in oncogenesis and behave as causative agents of several<br />
tumors; instead, non-transforming retroviruses, such as the human immunodeficiency<br />
virus (HIV), are involved in the oncogenetic process through indirect mechanisms, by<br />
favoring reactivation of transforming viruses and/or interfering with the physiologic<br />
pathways that regulate cell proliferation and death. Analysis of the mechanisms by which<br />
viruses rearrange the cellular program of senescence/immortalization would shed new light<br />
into cell physiopathology and provide new tools for prevention/treatment strategies.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 2<br />
220
N° Prog Titolo Responsabile<br />
L02P01<br />
Analisi dei meccanismi coinvolti nella protezione dall’apoptosi mediata dalla proteina Tax del virus<br />
Tlinfotropico di tipo 1 (HTLV-1).<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 2<br />
221<br />
Saggioro Daniela<br />
L02P02 Melanoma maligno eredo-familiare: analisi funzionale di varianti geniche di CDKN2A. Menin Chiara<br />
L02P03<br />
Melanoma maligno: analisi genetica del gene CDKN2A e identificazione di modificatori genetici della<br />
penetranza in famiglie ad alto rischio.<br />
Menin Chiara<br />
L02P04 Analisi funzionali di proteine regolatorie codificate da retrovirus oncogeni umani. Ciminale Vincenzo<br />
L02P05 Identificazione delle famiglie ad alto rischio di cancro della mammella/ovaio. D’Andrea Emma<br />
L02P06<br />
Caratterizzazione del fenotipo e studio prospettico della sindrome paraganglioma in una popolazione ad<br />
alta prevalenza.<br />
Opocher Giuseppe<br />
L02P07 Ruolo dell’obesità e dell’insulino-resistenza nella sequenza esofago di Barrett-displasia-adenocarcinoma. Battaglia Giorgio<br />
L02P08 Role of cancer stem cells in gastrointestinal adenocarcinoma: potential targeted therapy. Scarpa Marco<br />
L02P09 Linfomagenesi EBV-associata. De Rossi Anita<br />
L02P10<br />
L02P11<br />
L02P12<br />
L02P13<br />
L02P14<br />
L02P15<br />
L02P16<br />
Modello chirurgico sperimentale di sviluppo di esofago di Barrett e adenocarcinoma indotto da reflusso<br />
biliare nel ratto e nel topo.<br />
Il nuovo gene oncosoppressore TMEM127: dalla caratterizzazione del fenotipo associato a mutazioni<br />
TMEM al meccanismo d’azione molecolare.<br />
Ricerca e tipizzazione HPV (papillomavirus umano) in tumori del capo-collo e dell’esofago, e relazione<br />
con la risposta alla terapia.<br />
Definizione della storia naturale della neoplasia endocrina multipla di tipo 1 (MEN1) e del ruolo di menina<br />
nella tumorigenesi a partire dalla caratterizzazione clinica-molecolare della più grande famiglia descritta per<br />
questa sindrome.<br />
Identificazione di nuovi alleli di predisposizione in famiglie con tumore della mammella/ovaio eredofamiliare<br />
non informative al test genetico BRCA.<br />
Carcinogenesi in esofago di Barrett: meccanismi di regressione della displasia di basso grado e costruzione<br />
di un vaccino contro l adenocarcinoma esofageo.<br />
Studio dei meccanismi patogenetici coinvolti nello sviluppo di tumori correlati all'herpesvirus oncogeno<br />
HHV8.<br />
Cagol Matteo<br />
Opocher Giuseppe<br />
Del Mistro Annarosa<br />
Opocher Giuseppe<br />
Montagna Marco<br />
Castoro Carlo<br />
Calabrò Maria Luisa<br />
L02P17 Imprinting materno nella Sindrome Paraganglioma di tipo 1: basi molecolari e tools diagnostici. Opocher Giuseppe<br />
L02P18 Tumorigenesi nella sindrome feocromocitoma/paraganglioma. Opocher Giuseppe<br />
L02P19 Ruolo dell’ipossia nella regolazione di SERPINB3 nell’epatocarcinoma. Amadori Alberto<br />
L02P20<br />
Studio sugli effetti della soppressione acida sulla carcinogenesi esofagea da reflusso nell’uomo e in un<br />
modello sperimentale di esofago di Barrett e adenocarcinoma indotto da reflusso biliare nel ratto.<br />
Castoro Carlo<br />
L02P21 Tumori ereditari del rene. Opocher Giuseppe
LINE 3<br />
Instrumental and Molecular<br />
Approaches for Diagnosis,<br />
Staging and Follow-Up<br />
A large body of evidence on accumulating genetic changes that underlie tumor<br />
development is providing more and more powerful tools for the clinical evaluation of<br />
the neoplastic disease. The characterization of new molecular features is significantly<br />
contributing to redefine both the criteria of tumor diagnosis and the formulation of<br />
prognosis. Indeed, if we only consider mammary tumors, what 20 or 30 years ago we<br />
called a “breast cancer” is now known to be an array of different transformation processes,<br />
each endowed with special phenotypic and genotypic properties, that differentiate this<br />
tumor from tumors apparently similar by conventional histology. As a matter of fact, a<br />
molecular classification of cancer is flanking the classical tumor taxonomy, and patients are<br />
increasingly classified based on the molecular profile of their tumor.<br />
Thus, the definition of new, non-invasive markers for tumor diagnosis, staging and<br />
prognosis is urgently needed. While the identification of new molecular markers (in tumor<br />
cells or in biological fluids) is clearly fundamental to the goal of improving the definition<br />
of prognosis of neoplastic diseases and to help in predicting the response of individual<br />
patients to targeted therapies, progress in tumor diagnosis and monitoring also firmly relies<br />
on the availability of new technological developments in several different fields. In this<br />
frame, the Institute has privileged the development of various instrument-based platforms,<br />
particularly those best suited to neoplastic conditions of major interest to the Institute.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 3<br />
222
N° Prog Titolo Responsabile<br />
L03P01<br />
L03P02<br />
Determinazione seriata delle cellule tumorali circolanti (CTCs) come indicatore di risposta alla terapia<br />
antiangiogenetica con Sunitinib (SUTENT®) nel carcinoma renale avanzato.<br />
Individuazione di nuove strategie non invasive per la diagnosi e monitoraggio dei tumori: studio della<br />
telomerasi come marcatore molecolare.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 3<br />
223<br />
Basso Umberto<br />
De Rossi Anita<br />
L03P03 Confronto tra Tomosintesi Digitale della Mammella e Mammografia Standard in donne sintomatiche. Gennaro Gisella Maria<br />
L03P04 Protocollo Italiano per i controlli di qualità in mammografia digitale. Gennaro Gisella Maria<br />
L03P05 Automazione controlli di qualità in mammografia digitale: sistemi DR e CR. Gennaro Gisella Maria<br />
L03P06<br />
Tecnica ROLL (Radioguided Occult Lesion Localization) nello studio di piccole lesioni in fase diagnostica<br />
o di ristadiazione in pazienti con sarcoma o altra patologia neoplastica.<br />
Gregianin Michele<br />
L03P07 Approfondimenti diagnostico-prognostici sulla biopsia del linfonodo sentinella del melanoma. Rossi Carlo Riccardo<br />
L03P08 Studio multicentrico AIMN. Stadiazione dei Linfomi mediante PET/CT. Gregianin Michele<br />
L03P09<br />
Accuratezza dell’endomicroscopia confocale nella diagnosi della displasia nell’Esofago di Barrett: studio<br />
prospettico in doppio cieco.<br />
Battaglia Giorgio<br />
L03P10 Valore prognostico incrementale della 18F-FDG-PET/CT nei pazienti con carcinoma della mammella. Evangelista Laura<br />
L03P11 Confronto tra tomosintesi digitale della mammella e mammografia standard in donne sintomatiche - Fase II. Gennaro Gisella Maria<br />
L03P12<br />
L03P13<br />
L03P14<br />
Fattori predittivi della risposta al trattamento e/o della prognosi nel melanoma o nei sarcomi delle parti<br />
molli.<br />
PET-CT diagnostica con m.d.c. vs. metodiche standard nella stadiazione del tumore esofageo: diagnosi e<br />
management.<br />
Determinazione delle Cellule Tumorali Circolanti prima e dopo chirurgia nelle pazienti con nuova diagnosi<br />
di carcinoma mammario in Stadio I-III.<br />
Rossi Carlo Riccardo<br />
Cervino Anna Rita<br />
Zamarchi Rita<br />
L03P15 Lesioni infracliniche mammarie e diagnosi precoce di neoplasia. Pescarini Luigi<br />
L03P16<br />
L03P17<br />
L03P18<br />
VEGF polymorphisms in the prediction of benefit from first-line FOLFIRI plus bevacizumab in metastatic<br />
colorectal cancer patients.<br />
Studio della distribuzione del drenaggio linfatico e guida alla biopsia del linfonodo sentinella nel melanoma<br />
del tronco. Studio linfoscintigrafico.<br />
Ruolo della PET-CT nella valutazione diagnostica precoce della cardiotossicità da chemioterapici in<br />
pazienti con Carcinoma della Mammella.<br />
Lonardi Sara<br />
Sotti Guido<br />
Evangelista Laura<br />
L03P19 Lo status di BRAF come marcatore prognostico nei pazienti con carcinoma papillare della tiroide (PTC). Vianello Federica<br />
L03P20<br />
L03P21<br />
Valore diagnostico della [18F]-Colina (FCH) PET/CT in pazienti con cancro della prostata al III stadio<br />
e a rischio di recidiva alto o intermedio.<br />
Il ruolo della 18F-DOPA PET-CT total body nella stadiazione e follow-up dei tumori neuroendocrini<br />
vs l imaging convenzionale morfologico (RMN, TC, US) o funzionale (111In-pentetreotide e 123/131I-<br />
MIBG).<br />
Saladini Giorgio<br />
Cervino Anna Rita
L03P22<br />
Ruolo della 18F-FDG PET/CT nel follow-up e nel sospetto di recidiva in pazienti con Cancro del<br />
colonretto operato.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 3<br />
224<br />
Gregianin Michele<br />
L03P23 Analisi prospettica con TC dei nodi/noduli polmonari nel cancro colon-rettale. Pomerri Fabio<br />
L03P24 Valutazione dell incidenza dell esofagite sovranastomotica nei pazienti operati di esofagectomia. Battaglia Giorgio<br />
L03P25<br />
Analisi delle mutazioni dei geni kit e PDGFRA in tumori stromali del tratto gastrointestinale (GIST):<br />
razionale per la terapia molecolare.<br />
Bertorelle Roberta<br />
L03P26 Espressione dei fattori di crescita endoteliali dopo chirurgia esofagea. Castoro Carlo<br />
L03P27 Personalizzazione dei trattamenti per i pazienti con tumori del tratto digestivo. Amadori Alberto<br />
L03P28<br />
L03P29<br />
Analisi dell’impatto prognostico delle mutazioni di EGFR e KRAS e della FISH per EGFR nei carcinomi<br />
polmonari non a piccole cellule trattati chirurgicamente.<br />
18F-FDG-PET/CT vs. CT nella stadiazione post-chirurgica nel carcinoma della mammella ad alto<br />
rischio.<br />
Favaretto Adolfo Gino<br />
Evangelista Laura<br />
L03P30 Fattori prognostici nel melanoma della coroide metastatico. Chiarion-Sileni Vanna<br />
L03P31 Marker tumorali nel carcinoma dell’esofago e del cardias. Studio retrospettivo. Chiarion-Sileni Vanna<br />
L03P32<br />
Studio delle caratteristiche cliniche e dei fattori prognostici delle pazienti con carcinoma della mammella<br />
diagnosticato
L03P44<br />
L03P45<br />
L03P46<br />
L03P47<br />
L03P48<br />
L03P49<br />
L03P50<br />
Utilizzo della SPECT con SestaMIBI nella valutazione della possibile istologia in pazienti con masse<br />
cerebrali di ndd.<br />
Utilizzo della SPECT con SestaMIBI nella valutazione della progressione vera in pazienti trattati<br />
radicalmente per glioblastoma multiforme.<br />
Mutazione dei geni IDH1 e IDH2 come fattore predittivo di risposta ai farmaci antiangiogenetici nei<br />
tumori cerebrali.<br />
18F-FDG-PET/CT vs. CT nella stadiazione post-chirurgica nei pazienti con carcinoma della mammella<br />
ad alto rischio.<br />
Effetto della ormonoterapia sulla accuratezza diagnostica della 18F-FDG PET/CT nei pazienti con<br />
carcinoma della mammella precedentemente trattate.<br />
Correlazione tra la presenza della mutazione dei geni IDH1 e IDH2 nei gliomi cerebrali e l’aumento della<br />
espressione del gene HIF-1 e del metabolita 2-HG nell’urina.<br />
Correlazione tra la presenza della mutazione dei geni IDH1 e IDH2 nei gliomi cerebrali, l’aumento del<br />
metabolita 2-HG nelle cellule tumorali e la sua rilevazione tramite RMN spettroscopica.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 3<br />
225<br />
Zustovich Fable<br />
Zustovich Fable<br />
Lombardi Giuseppe<br />
Bezzon Elisabetta<br />
Evangelista Laura<br />
Lombardi Giuseppe<br />
Lombardi Giuseppe<br />
L03P51 Dall’ Endoscopia Confocale all’Endoscopia Mirata: studi clinici e preclinici nel cancro dell’esofago. Battaglia Giorgio<br />
L03P52<br />
L03P53<br />
L03P54<br />
L03P55<br />
Metilazione MGMT come fattore predittivo di risposta al trattamento antiangiogenetico nei tumori<br />
cerebrali.<br />
Tumori del colon e della mammella: ottimizzazione della sorveglianza tramite analisi clinico-patologica e<br />
genetica della loro associazione.<br />
Indicazioni all’utilizzo di FDG-PET/CT nelle neoplasie ginecologiche: analisi di una casistica<br />
retrospettiva.<br />
Studio con endoscopia confocale della vascolarizzazione tumorale come “marcatore” di risposta alla terapia<br />
antiangiogenetica.<br />
Lombardi Giuseppe<br />
Cappetta Alessandro<br />
Dalla Palma Maurizia<br />
Battaglia Giorgio<br />
L03P56 L’ecografia endoscopica (EUS) nella ristadiazione dei pazienti chemio-radiotrattati per neoplasie esofagee. Battaglia Giorgio<br />
L03P57 Analisi delle mutazioni dei geni IDH1 e IDH2 nei gliomi. Bertorelle Roberta<br />
L03P58 Analisi FISH del riarrangiamento del gene ALK nei tumori non a piccole cellule del polmone. Bonaldi Laura<br />
L03P59<br />
Imaging con tc multidetettore e ricostruzioni 3d del mesotelioma pleurico: correlazioni con i riscontri<br />
operatori.<br />
Polverosi Roberta<br />
L03P60 Imaging delle Metastasi Pancreatiche da Carcinoma Renale. Polverosi Roberta
LINE 4<br />
Innovative Therapeutic<br />
Approaches: Chemotherapy,<br />
Radiotherapy and Surgery<br />
The wealth of knowledge accumulated on the molecular alterations that characterize<br />
tumors has profoundly changed pharmacological approaches to tumor therapy, with<br />
surgery, radiotherapy and chemotherapy now flanked by the so-called “target therapies”,<br />
which rely on the ability of small molecules to more or less specifically and selectively<br />
interfere with abnormal intracellular pathways responsible for the growth advantage of<br />
transformed tumor cells. Thus, several national and international clinical protocols are<br />
active at the Institute, with special attention placed on the possibility of combining small<br />
molecules such as kinase inhibitors with biologically active tools such as monoclonal<br />
antibodies. In any case, all cancer patients are offered an integrated approach to diagnosis<br />
and treatment that involves the expertise of medical oncologists, surgeons, radiotherapists,<br />
psycho-oncologists, and if needed specialists from many other fields, interacting in a<br />
multidisciplinary unit. Of course, the search for new, more active, selective and tolerated<br />
therapies cannot proceed in the absence of continuous exchange with the laboratory, and<br />
laboratory expertise is essential to this integrated approach. Many so-called “intelligent”<br />
drugs are now available, in fact; nothing, however, could be worse than using intelligent<br />
drugs in a stupid manner, that is, administering a drug to patients who cannot benefit from<br />
it due to their constitutional features or the molecular properties of their tumor.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 4<br />
226
N° Prog Titolo Responsabile<br />
L04P01<br />
Implementazione ed ottimizzazione dosimetrica della tecnica di irradiazione della mammella con<br />
posizionamento prono.<br />
Reccanello Sonia<br />
L04P02 Radioterapia Stereotassica Frazionata (RSF) nei gliomi a basso grado di malignità in età pediatrica. Scarzello Giovanni<br />
L04P03<br />
Studio randomizzato di fase III sull’efficacia dell’Interferone (IFN a2b) intensificato endovenoso vs IFN<br />
a2b secondo ECOG 1684 nel melanoma radicalmente operato.<br />
Chiarion-Sileni Vanna<br />
L04P04<br />
Studio di fase III di valutazione della sicurezza ed efficacia del trattamento con 2 mg di Allovectina-7<br />
intralesionale comparata con DTIC o Temozolomide nei soggetti con melanoma recidivato.<br />
Terapia neoadiuvante con Docetaxel,cisplatino e 5-fluorouracile(TPF) seguita da radioterapia e<br />
Chiarion-Sileni Vanna<br />
L04P05 chemioterapia concomitante o Cetuximab versus radioterapia più chemioterapia concomitante o<br />
Cetuximab in pazienti con carcinoma a cellule squamose della testa e del collo localmente avanzato.<br />
Koussis Haralabos<br />
L04P06 Trattamenti innovativi nel melanoma e nei sarcomi delle parti molli. Rossi Carlo Riccardo<br />
L04P07<br />
L04P08<br />
Chirurgia della malattia residua in pazienti con GIST metastatico responsivi ad imatinib (EORTC trial<br />
62032).<br />
ITACA-S 2: comparison of the efficacy ofa peri-operative versus a post-operative chemotherapy treatment<br />
in patients with operable gastric cancer and assessment of the benefit of a post-operative chemoradiotherapy.<br />
Studio multicentrico nazionale randomizzato.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 4<br />
227<br />
Basso Umberto<br />
Zagonel Vittorina<br />
L04P09 Screening for early predictors of Peripheral Neuropathy in Oxaliplatin-Treated patients. Lonardi Sara<br />
L04P10<br />
L04P11<br />
L04P12<br />
L04P13<br />
L04P14<br />
L04P15<br />
L04P16<br />
Studio multicentrico randomizzato di fase 3 di confronto tra dosaggio fisso e dosaggio modificato<br />
sulla base della tossicità della chemioterapia standard con cisplatino ed etoposide in pazienti affetti da<br />
microcitoma polmonare avanzato.<br />
Supporto metodologico ed informatico nella pianificazione, organizzazione e conduzione di<br />
sperimentazioni cliniche.<br />
Progetto “Ufficio di Coordinamento Trials Clinici”: gestione della ricerca clinica no-profit e profit<br />
all’interno dell’Istituto Oncologico Veneto.<br />
Attività anti-ossidante del cioccolato fondente in pazienti con carcinoma della mammella in terapia<br />
adiuvante.<br />
Analisi delle sequenze sorafenib/sunitinib versus sunitinib/sorafenib nel trattamento del tumore renale<br />
avanzato.<br />
ASL608LIOM02 (GLIMESOR): Sorafenib (nexavar) in associazione a terapia metronomica con<br />
temozolomide in pazienti con glioblastoma multiforme dopo fallimento di una chemioterapia di prima<br />
linea: studio clinico di fase II con valutazione farmacodinamica, farmacocinetica e farmacogenetica.<br />
Profilo farmacogenetico e risultati clinici di pazienti con cancro al colon in stadio II ad alto rischio e stadio<br />
III trattato con chemioterapia adiuvante Folfox-4 e bevacizumab.<br />
Favaretto Adolfo Gino<br />
De Salvo Gian Luca<br />
De Salvo Gian Luca<br />
Ghiotto Cristina<br />
Zustovich Fable<br />
Zustovich Fable<br />
Zagonel Vittorina<br />
L04P17 Radioterapia con modulazione della dose nel carcinoma dell’esofago cervicale. Corti Luigi<br />
L04P18 In-use stability dei farmaci oncologici. Palozzo Angelo Claudio<br />
L04P19<br />
Studio multicentrico nazionale randomizzato di fase II-III di chemioterapia peri o post chirurgica<br />
nell’adenocarcinoma pancreatico resecabile-PACT-15.<br />
Zagonel Vittorina
L04P20<br />
L04P21<br />
L04P22<br />
L04P23<br />
Studio randomizzato di fase II con taxotere, oxaliplatino, capecitabina (TOX) o epidoxorubicina,<br />
oxaliplatino e capecitabina (EOX) in pz con carcinoma gastrico loc avanzato o metastatico.<br />
Pemetrexed nel mesotelioma pleurico – un nuovo modello per valutare efficacia, efficienza e appropriatezza<br />
attraverso il registro AIFA.<br />
COMETS: Studio di fase III randomizzato controllato a gruppi paralleli che confronta due differenti<br />
sequenze di terapia (Irinotecan/Cetuximab seguito da FOLFOX-4 vs FOLFOX-4 seguito da Irinotecan/<br />
Cetuximab) in pazienti portatori di tumore del colon-retto metastatico trattati in prima linea di terapia<br />
con FOLFIRI/Bevacizumab.<br />
TRIBE: Studio randomizzato di fase III su Folfoxiri + Bevacizumab vs Folfiri + Bevacizumab come prima<br />
linea nel trattamento del tumore colon-retto metastatico.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 4<br />
228<br />
Zagonel Vittorina<br />
Jirillo Antonio<br />
Lonardi Sara<br />
Lonardi Sara<br />
L04P24 Barrx a completamento di mucosectomia eseguita per HGD e Ca in situ in esofago di Barrett. Battaglia Giorgio<br />
L04P25 Ablazione di esofago di Barrett mediante radiofrequenza. Battaglia Giorgio<br />
L04P26<br />
L04P27<br />
L04P28<br />
L04P29<br />
L04P30<br />
L04P31<br />
L04P32<br />
L04P33<br />
L04P34<br />
L04P35<br />
L04P36<br />
L04P37<br />
L04P38<br />
One-arm, multi-center, international prospective pivotal study to assess the safety and efficacy of<br />
BioProtect biodegradable implantable balloon in prostate cancer subjects undergoing radiotherapy.<br />
Studio retrospettivo sulla cardiotossicità in pazienti con carcinoma della mammella sottoposte a terapia<br />
adiuvante con trastuzumab.<br />
Studio randomizzato in doppio cieco di PF-804 in pazienti con tumore del polmone non a piccole cellule<br />
in stadio IIIb/IV dopo fallimento di una terapia standard per la malattia avanzata.<br />
Doxorubicina peghilata liposomiale (PLD) nella recidiva di carcinoma ovarico: migliore outcome nelle<br />
pazienti portatrici di mutazione BRCA?<br />
Studio di fase III randomizzato per la valutazione dell’efficacia di cisplatino e gemcitabina come prima<br />
linea di trattamento dei pazienti anziani con tumore del polmone non a piccole cellule (NSCLC) in stadio<br />
avanzato.<br />
Studio multicentrico randomizzato di fase II. Trattamento di pazienti anziani con carcinoma prostatico<br />
metastatico non suscettibili di trattamento standard.<br />
Valutazione retrospettiva multicentrica dell’attività di sunitinib nei pazienti anziani (70 anni o più) con<br />
carcinoma renale metastatico.<br />
Studio sull’impiego delle Gemcitabina come terapia di salvataggio nel carcinoma del colon-retto<br />
metastatico.<br />
Phase II Trial of Folfoxiri Plus Panitumumab as First-Line Treatment F for Kras and Braf Wild-Type<br />
Metastatic Colorectal Cancer.<br />
Boron Neutron Capture Therapy (Bnct) delle Recidive Cutanee da Cancro della Mammella: impiego<br />
della Pet/Ct.<br />
Verifica dosimetrica e implementazione della tecnica IMRT e IGRT per il trattamento di patologie del<br />
capo-collo e della prostata.<br />
Terapia settimanale con Carboplatino e Docetaxel in pazienti con tumore del capo-collo con importante<br />
comorbidità.<br />
Intrabeam project for intraoperative radiotherapy for breast cancer versus whole breast irradiation<br />
(TARGIT-A Trial): phase III trial.<br />
Scarzello Giovanni<br />
Ghiotto Cristina<br />
Favaretto Adolfo Gino<br />
Nicoletto Maria Ornella<br />
Favaretto Adolfo Gino<br />
Basso Umberto<br />
Basso Umberto<br />
Lonardi Sara<br />
Lonardi Sara<br />
Evangelista Laura<br />
Simonato Franca<br />
Koussis Haralabos<br />
Sotti Guido
L04P39 Chemioterapia adiuvante in pazienti Italiani ed Americani con tumore della mammella BRCA-associato. Cappetta Alessandro<br />
L04P40<br />
L04P41<br />
MITO 8\<strong>2011</strong>: Doxorubicina Liposomiale Stealth vs Carboplatino + Paclitaxel in pazienti con recidiva<br />
di carcinoma ovarico tra sei e dodici mesi dal precedente trattamento con platino: studio multicentrico<br />
randomizzato.<br />
Studio internazionale multicentrico, randomizzato, in doppio-cieco, di fase III, volto a valutare l’efficacia<br />
e la sicurezza di BIBF 1120 in combinazione con carboplatino e paclitaxel verso placebo più carboplatino<br />
e paclitaxel in pazienti con cancro ovarico avanzato.<br />
L04P42 Intraoperative radiotherapy as a tumor bed boost (TARGIT−B). Sotti Guido<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 4<br />
229<br />
Nicoletto Maria Ornella<br />
Nicoletto Maria Ornella<br />
L04P43 Studio di Fase I con agenti ditiocarbammici di oro(III) in pazienti oncologici. Jirillo Antonio<br />
L04P44 Implementazione e ottimizzazione dosimetrica della IORT con IntraBeam System. Reccanello Sonia<br />
L04P45<br />
L04P46<br />
Sorafenib nell’epatocarcinoma – un nuovo modello per valutare efficacia, efficienza e appropriatezza<br />
attraverso il registro AIFA.<br />
Pemetrexed nell’adenocarcinoma polmonare – un nuovo modello per valutare efficacia, efficienza e<br />
appropriatezza attraverso il registro AIFA.<br />
Jirillo Antonio<br />
Jirillo Antonio
LINE 5<br />
Tumor Immunology<br />
and Innovative Therapeutic<br />
Approaches<br />
It is now widely accepted that tumor growth is the result of the very complicated<br />
bidirectional interaction between cells that progressively acquire molecular alterations, a<br />
growth advantage and finally a fully transformed phenotype, and surrounding cells of<br />
the host that may contrast or in some instances also favor their autonomous growth and<br />
expansion. In addition, the interplay between tumor cells and host tissues may change<br />
during the course of tumor development. In a first phase a “sneaking through” situation<br />
may occur, where immune surveillance simply disregards cells on the way to premalignant<br />
or malignant transformation. Later on, an equilibrium may arise between tumor cell<br />
growth and death by apoptosis on the one hand, and active control by immune effectors<br />
on the other, with tumor expansion still in check. The final overt tumor expansion phase<br />
arises when this unstable equilibrium somehow breaks down, during which tumorderived<br />
factors often come into play to abate the residual contrasting potential of immune<br />
surveillance. For many years, one of the most popular dreams of tumor immunologists<br />
has been the so-called “magic bullet”; while this goal is close to becoming realized thanks<br />
to monoclonal antibodies and target molecules, the other great dream of potentiating<br />
the immune response against tumors has not lived up to its promise. Notwithstanding,<br />
tumor immunology is currently undergoing a new flare of development, thanks to the<br />
understanding that a combination of different strategies synergizing against all (or most)<br />
the different actors contributing to tumor growth could be a very effective, if not the<br />
ultimate, remedy. While several of these approaches are already in phase I/II clinical trials,<br />
frequently in combination with canonical chemotherapeutic tools, many others are still<br />
in a preclinical, translational research phase; hopefully, some of them will soon move<br />
to the human setting and become a part of the therapeutic armamentarium of clinical<br />
oncologists.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 5<br />
230
N° Prog Titolo Responsabile<br />
L05P01 Studio dei meccanismi molecolari che regolano la dormienza tumorale. Indraccolo Stefano<br />
L05P02<br />
Generazione di linfociti T citotossici survivina-specifici in topi HHD transgenici per HLA-A*0201, per<br />
l’isolamento di TCR utilizzabili nella ingegnerizzazione di cellule T umane per l’immunoterapia adottiva<br />
dei tumori.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 5<br />
231<br />
Rosato Antonio<br />
L05P03 Anticorpi terapeutici verso nuovi antigeni di EBV. Rosato Antonio<br />
L05P04<br />
Immunoterapia adottiva dei tumori mediante cellule T ingegnerizzate ad esprimere T Cell Receptor (TCR)<br />
transgenici o Recettori Chimerici per l'Antigene (CAR).<br />
Rosato Antonio<br />
L05P05 Ruolo dei microRNA nella maturazione e nel processo di trasformazione neoplastica dei linfociti T. Zanovello Paola<br />
L05P06<br />
L05P07<br />
L05P08<br />
L05P09<br />
L05P10<br />
Identificazione di reti regolatorie presenti nelle cellule soppressorie di derivazione mieloide mediante<br />
integrazione di dati di espressione genica e di microRNA.<br />
Analisi del profilo dei microRNA come strumento per studiare la biologia delle cellule mieloidi<br />
soppressorie.<br />
Identificazione di nuove molecole in grado di recuperare l’attività del sistema immunitario contro il tumore:<br />
basi molecolari e biologiche per nuove terapie.<br />
Chemo-immunoterapia: l’eliminazione selettiva delle cellule soppressorie di origine mieloide tramite<br />
somministrazione del chemioterapico 5-fluorouracile potenzia l’effetto terapeutico dell’immunoterapia<br />
anti-tumorale.<br />
Identificazione di reti regolatorie nelle cellule soppressorie di derivazione mieloide mediante integrazione<br />
di dati di espressione genica e di microRNA.<br />
Mandruzzato Susanna<br />
Bronte Vincenzo<br />
Bronte Vincenzo<br />
Bronte Vincenzo<br />
Mandruzzato Susanna<br />
L05P11 Effetti metabolici della terapia anti-angiogenica nei tumori sperimentali. Indraccolo Stefano
LINE 6<br />
Quality of Life in Cancer Patients<br />
and Geriatric Oncology<br />
Besides the effort spent in translational and clinical research, much attention is paid at<br />
the Institute to the issue of quality of life in cancer patients, with a special focus on geriatric<br />
oncology. Persons over the age of 65 years are the fastest growing segment of the population<br />
and will account for an estimated 20% of Americans and 25% of Europeans by the year<br />
2030. Cancer incidence is 11-fold higher in persons over the age of 65 years than in younger<br />
ones. Treatment of elderly patients with cancer is one of the key areas in which clinical<br />
and scientific activities of our Institute are focused. Close relationship with the Geriatric<br />
Clinics of the University of Padova is a peculiar feature of our Geriatric Oncology Program;<br />
a multidisciplinary team including oncologists, psychologists, geriatricians, cardiologists,<br />
dieticians, endocrinologists and other health professionals is currently involved in the<br />
evaluation and care of elderly patients. Multidimensional geriatric assessment (MGA) is<br />
regarded as an indispensable tool in the management of cancer patients. The Performance<br />
Status (PS) is one of the most useful instruments orienting the therapeutic decision in<br />
adult patients, but it is considered as a rather blunt tool when dealing with the elderly,<br />
for which MGA is much more appropriate, as it covers the multifaceted features of ageassociated<br />
conditions. Monthly case-oriented multidisciplinary meetings are organized<br />
in order to share clinical problems and to develop common algorithms of treatment<br />
according to tumor site, stage and MGA parameters. In this occasion a review of pertinent<br />
literature and results of our trials are presented to complete the discussion of clinical cases.<br />
A database containing demographic, clinical and follow-up data of more than 600 patients<br />
evaluated by MGA has been created and has provided data for several communications<br />
to international congresses and scientific articles. Particular attention has been devoted to<br />
proposing clinical trials to elderly patients whenever a national or international protocol is<br />
open at our Institution, because we believe that elderly patients must be enrolled in clinical<br />
trials, even though much more time and effort is needed.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 6<br />
232
Progr. Titolo Responsabile<br />
L06P01<br />
L06P02<br />
L06P03<br />
L06P04<br />
L06P05<br />
L06P06<br />
L06P07<br />
L06P08<br />
Valutazione dei disturbi cognitivi in pazienti con carcinoma mammario sottoposte a terapia con inibitori<br />
dell aromatasi.<br />
Confronto tra il questionario VES-13 (Saliba et al) e la Valutazione Geriatrica Multidimensionale (VGM)<br />
standard.<br />
Valutazione prospettica del significato prognostico della valutazione geriatrica multidimensionale in<br />
pazienti oncologici.<br />
L’esperienza terapeutica dello <strong>IOV</strong> nell utilizzo del Fulvestrant nel carcinoma mammario metastatico<br />
ormonosensibile:dati a confronto con gli studi registrativi.<br />
Studio prospettico sull’analisi dei costi economici reali dei pazienti inseriti all'interno di un trial<br />
sponsorizzato in rapporto al finanziamento erogato dallo Sponsor.<br />
Studio retrospettivo che valuta gli scostamenti dagli studi clinici, in termini di risposta e tossicità dei<br />
farmaci antitumorali nel registro Onco-AIFA.<br />
Studio prospettico sull’impatto prognostico della valutazione geriatrica multidimensionale alla prima visita<br />
del paziente oncologico anziano.<br />
Analisi retrospettiva dell’utilizzo di Fulvestrant (Faslodex) nel carcinoma mammario metastatico<br />
ormonosensibile per la valutazione dell’appropriatezza e dell’effectiveness del trattamento.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 6<br />
233<br />
Koussis Haralabos<br />
Falci Cristina<br />
Falci Cristina<br />
Jirillo Antonio<br />
Jirillo Antonio<br />
Jirillo Antonio<br />
Zagonel Vittorina<br />
Trojniak Marta Paulina<br />
L06P09 Appropriatezza e costi dei PDTA (Percorsi Diagnostico Terapeutici e Assistenziali). Giacobbo Maria<br />
L06P10 Consumi e costi dei farmaci presso l’Istituto Oncologico Veneto per il trattamento del dolore oncologico. Giacobbo Maria<br />
L06P11 Progetto Atmosfera Giacobbo Maria<br />
L06P12 Progetto Sole: Ansia, stress ed indagini diagnostiche in oncologia. Giacobbo Maria<br />
L06P13<br />
L06P14<br />
L06P15<br />
L06P16<br />
Studio retrospettivo di valutazione dell’effectiveness e dell’appropriatezza prescrittiva dei trattamenti<br />
contenenti il farmaco antitumorale pemetrexed (Alimta) sottoposto al monitoraggio Onco-AIFA nel<br />
trattamento delle neoplasie polmonari.<br />
Studio retrospettivo osservazionale di valutazione dell’effectiveness verso efficacy e determinazione delle<br />
caratteristiche di sottogruppi dei pazienti responders nel trattamento di neoplasie polmonari con erlotinib<br />
(Tarceva).<br />
Approccio psiconcologico integrato per la comunicazione di “cattive notizie” in pazienti oncologici<br />
ospedalizzati in fase avanzata di malattia: studio randomizzato per valutare l’efficacia nel migliorare la<br />
gestione del dolore e rispondere ai bisogni informativo-comunicativi.<br />
Proposta di un centro di prevenzione, cura e riabilitazione della disfagia grave nei pazienti sottoposti a<br />
trattamenti radiochemioterapici del capo-collo e dell esofago.<br />
Paganelli Francesco<br />
Palozzo Angelo Claudio<br />
Capovilla Eleonora<br />
Pellegrino Federica<br />
L06P17 Qualità di vita dopo esofagectomia per neoplasia. Castoro Carlo<br />
L06P18 Medicazioni avanzate e Qualità di Vita in Radioterapia. Corti Luigi<br />
L06P19 Valutazione della qualità della vita nell’ambito di trial clinici oncologici. Del Bianco Paola<br />
L06P20<br />
Studio retrospettivo di valutazione dell’effectiveness e dell'apropriatezza prescrittiva dei farmaci antitumorali<br />
sottoposti al monitoraggio Onco-AIFA.<br />
Palozzo Angelo Claudio
L06P21<br />
La dimensione religiosa e l’ansia di morte in pazienti oncologici. Analisi del fallimento della religione come<br />
fattore di protezione in base alle rappresentazioni della morte.<br />
RESEARCH ACTIVITY <strong>REPORT</strong> - LINE 6<br />
234<br />
Giacobbo Maria<br />
L06P22 Epidemiologia delle potenziali interazioni tra farmaci in pazienti oncologici ambulatoriali. Palozzo Angelo Claudio<br />
L06P23<br />
Programma multicentrico europeo per la valutazione del servizio di supporto della farmacia per i pazienti<br />
oncologici con rischio di nausea e vomito.<br />
Palozzo Angelo Claudio<br />
L06P24 Percorso di certificazione della galenica oncologica. Faoro Sonia<br />
L06P25<br />
Progetto collaborativo per il miglioramento del trattamento antiemetico nel paziente oncologico in<br />
ospedale e nel territorio, realizzando vantaggi farmacoeconomici.<br />
Faoro Sonia<br />
L06P26 Informatizzazione dei processi di farmacia oncologica Paganelli Francesco<br />
L06P27<br />
L06P28<br />
L06P29<br />
L06P30<br />
L06P31<br />
L06P32<br />
Quando la coppia incontra la malattia: ricerca-intervento sui ruoli tra i partner e sulla relazione che<br />
cambia.<br />
Prevalenza di neoplasie multiple sincrone o metacrone in pazienti oncologici anziani valutati secondo<br />
“valutazione geriatrica multidimensionale (VGM)”.<br />
Prevalenza del dolore, utilizzo degli oppioidi e modifiche del trattamento antalgico in pazienti ricoverati<br />
presso l’Oncologia 1.<br />
DAMA - Studio epidemiologico-osservazionale: prevalenza e decorso della Depressione in pazienti<br />
oncologici Adulti-anziani con Malattia in stadio Avanzato.<br />
ITACAm: Impatto del Trattamento Adiuvante sulle funzioni Cognitive nelle pazienti affette da Carcinoma<br />
mammario - Studio Pilota.<br />
Valutazione della sopravvivenza di pazienti affette da neoplasia ovarica seguite presso l’Istituto Oncologico<br />
Veneto (<strong>IOV</strong>-I.R.C.C.S)<br />
Giacobbo Maria<br />
Brunello Antonella<br />
Brunello Antonella<br />
Brunello Antonella<br />
Brunello Antonella<br />
Nicoletto Maria Ornella<br />
L06P33 Distiroidismo in pazienti affetti da CA rene e GIST sottoposti a target therapy Zovato Stefania<br />
L06P34<br />
Valutazione indici di metabolismo osseo nelle pazienti affette da CA della mammella trattate con<br />
ormonoterapia.<br />
Zovato Stefania<br />
L06P35 Progetto per la rilevazione e gestione della neurotossicita da chemioterapia. Padovan Maria<br />
L06P36<br />
L06P37<br />
L06P38<br />
L06P39<br />
Studio clinico randomizzato multicentrico aperto per la valutazione dell’efficacia del “lock” dei cateteri<br />
venosi centrali totalmente impiantabili con soluzione fisiologica verso soluzione eparinata.<br />
Medicina di genere e radioterapia: un’indagine retrospettiva in pazienti con tumore dell’orofaringe, della<br />
cavità orale e del colon-retto.<br />
Correlazione tra le alterazioni del metabolismo scheletrico, l’imaging medico nucleare e la comparsa di<br />
metastasi scheletriche.<br />
Validazione italiana del QUAL-EC per valutare la qualità di vita nei pazienti oncologici in fase avanzata<br />
di malattia.<br />
Padovan Maria<br />
Groff Elena<br />
Cervino Anna Rita<br />
Capovilla Eleonora<br />
L06P40 Progetto pilota: emozioni in musica - I suoni per dirlo - proposta per una musicoterapia sociale. Giacobbo Maria
CLINICAL RESEARCH<br />
CLINICAL RESEARCH<br />
235
Ethics Committee<br />
The <strong>IOV</strong> Ethics Committee (EC) is an independent body that has been formally<br />
designated to review biomedical research involving humans with the aim to protect the<br />
rights and welfare of the research subjects. Members are appointed for a period of three years<br />
and may serve two consecutive terms only. In force of its interdisciplinary composition,<br />
the <strong>IOV</strong> Ethics Committee also works as an advisory body whose purpose is to facilitate<br />
the discussion and resolution of ethical issues arising in patient care. Moreover, the Ethics<br />
Committee promotes training in Bioethics and working groups on medical ethics in the<br />
field of Oncology.<br />
The number of members is actually sixteen. The Ethics Committee comprises both<br />
healthcare professionals (doctors, nurses and pharmacists) and community representatives.<br />
More than half of the members are unaffiliated with the Institution. Five member are<br />
physicians with a thorough knowledge of the scientific aspects of clinical research. The<br />
Committee includes a biostatistician who is specifically expert of methods of research.<br />
The Ethics Committee’s President in office is a bioethics expert and the vice-President is a<br />
forensic scientist.<br />
CLINICAL RESEARCH<br />
236<br />
PRESIDENT<br />
Renzo Pegoraro<br />
VICE-PRESIDENT<br />
Daniele Rodriguez<br />
MEMBERS<br />
Alberto Amadori (ex-officio)<br />
Maria Giacobbo (ex-officio)<br />
Angelo Claudio Palozzo (ex-officio)<br />
Marilena Bertante<br />
Paolo Cadrobbi<br />
Patrizia Debetto<br />
Claudio Drago<br />
Fernando Gaion<br />
Giampiero Giron<br />
Francesco Grigoletto<br />
Daniela Grosso<br />
Roberto Labianca<br />
Carlo Moreschi<br />
Guido Sotti<br />
<strong>SCIENTIFIC</strong> SECRETARY<br />
Alessandra Bernardi
Numerous phase II and III, sponsored and spontaneous clinical<br />
trials are carried out at the <strong>IOV</strong>, mainly in breast, lung, gastrointestinal<br />
and cutaneous (melanoma) neoplasms. Unfortunately,<br />
phase I studies are not a major flag of the Institute, and only one<br />
phase I study addressing the effect of vaccination against Her-2/<br />
Clinical Trials<br />
Title Unit Type<br />
BRAIN<br />
Sorafenib in association with Metronomic Therapy with Temozolomide<br />
in Glioblastoma patients after first line chemotherapy failure: phase<br />
II clinical trial with pharmacodynamic, pharmacokinetic and<br />
pharmacogenetic evaluation.<br />
Cilengitide in patients diagnosed with glioblastoma multiform and<br />
methylated MGMT gene promotor plus standard TP (temozolomide<br />
with RT followed by maintenance temozolomide) vs standard<br />
treatment alone. A multicentre open label phase III trial.<br />
Cilengitide in patients diagnosed with glioblastoma multiforme and<br />
unmethylated MGMT gene promoter plus standard tp (temozolomide<br />
with radiotherapy followed by maintenance temozolomide). A<br />
multicenter, open-label phase II trial.<br />
BREAST<br />
Caelyx every 2 weeks in the treatment of metastatic breast carcinoma<br />
in elderly women.<br />
A phase III International Trial on the treatment with adjuvant<br />
Bevacizumab associated with standard CT in “triple negative” breast<br />
carcinoma patients.<br />
A two-arm randomised open label phase II study of CP-751,871 in<br />
combination with exemestane versus exemestane alone as first line<br />
treatment for postmenopausal patients with hormone receptor positive<br />
advanced breast cancer.<br />
CLINICAL RESEARCH<br />
237<br />
neu in patients with head-and-neck cancer, now in progress, is<br />
coordinated by our Institute. The fact that phase I studies are very<br />
scarce nationwide is not a sufficient justification; it is a strong<br />
priority of our Institute to implement these studies in a near<br />
future.<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Patients<br />
enrolled in<br />
2009<br />
Patients<br />
enrolled in<br />
<strong>2010</strong><br />
Total<br />
patients<br />
enrolled<br />
Phase II 9 18 28<br />
Phase III 0 0<br />
Phase II 1 1<br />
Observational 29 0 40<br />
Phase III 8 0 10<br />
Phase II 0 2 2
A phase III trial of Vinflunine + Capecitabine vs Capecitabine alone in<br />
previously treated or resistant to Anthracycline/Taxane advanced breast<br />
cancer patients.<br />
Pilot Study to evaluate the impact of adjuvant treatment on cognitive<br />
function in patients with metastatic breast. cancer. ITACam.<br />
A Phase III, randomized, open, two-arm trial with Neratinib in<br />
combination with paclitaxel vs Trastuzumab in Combination with<br />
Paclitaxel as first Line Treatment of Breast Cancer ErbB-2 Positive<br />
Locally Recurrent or Metastatic-3144A2-3005-WW patients.<br />
A randomized, double-blind, controlled trial versus placebo with<br />
Neratinib (HKI-272) after trastuzumab in women with early-stage<br />
Breast Cancer characterized by over-expression/amplification HER-2/<br />
neu- 3144A2-3004-WW.<br />
Adjuvant anti-estrogen therapy in women with breast cancer: possibility<br />
of a personalized approach. Multicenter study in the Veneto Region.<br />
HEAD AND NECK CANCERS<br />
A randomised phase III study of Pemetrexed in combination with<br />
Cisplatin versus Cisplatin monotherapy in Patients with recurrent or<br />
metastatic head and neck cancer.<br />
A Multicenter, Open-label, Randomised, Phase II/III Study to<br />
Evaluate the Safety and Efficacy of Combretastatin A-4 Phosphate in<br />
Combination with Paclitaxel and Carboplatin in Comparison with<br />
Paclitaxel and Carboplatin for Anaplastic Thyroid Cancer.<br />
Neo-adjuvant docetaxel plus cisplatin and 5-fluorouracil (TPF)<br />
followed by radiotherapy plus concomitant chemo or cetuximab versus<br />
radiotherapy plus concomitant chemo or cetuximab in patients with<br />
locally advanced squamous cell carcinoma of the head and neck.<br />
A randomised phase III factorial study (AVAPO).<br />
GASTROINTESTINAL CANCER<br />
A Phase III randomized controlled parallel group design comparing<br />
two different therapy sequences, (Irinotecan / Cetuximab followed by<br />
FOLFOX- 4 versus FOLFOX-4- followed by Irinotecan / Cetuximab)<br />
in patients with metastatic colorectal cancer treated in first-line therapy<br />
with FOLFIRI / Bevacizumab.<br />
A randomised trial investigating the role of FOLFOX 4 regimen<br />
duration (3 vs 6 months) and Bevacizumab as adjuvant therapy for<br />
patients with stage II/III colon cancer.<br />
Randomized study to evaluate the role of the duration of FOLFOX-4<br />
and XELOX (3 vs 6 Months) as adjuvant therapy for patients with<br />
stage II / III colon cancer.<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology<br />
1-2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
CLINICAL RESEARCH<br />
238<br />
Phase III 0 1 1<br />
Pilot Study 1 1<br />
Phase III 0 0<br />
Phase III 0 0<br />
Phase III 2 2<br />
Phase III 3 0 12<br />
Phase II-III 4 0 9<br />
Phase III 4 3 9<br />
Phase III 0 6 6<br />
Phase III 30 56 114<br />
Phase III 40 40
A Multicenter phase III trial to evaluate neo-adjuvant treatment<br />
with Epirubicine - Oxaliplatin - Xeloda and Oxaliplatin - Xeloda<br />
Radiotherapy in patients with operable gastric carcinoma.<br />
Randomised phase II study of maintenance therapy with Sunitinib in<br />
pancreatic adenocarcinoma.<br />
A phase III randomised study evaluating surgery of residual disease in<br />
patients with metastatic gastro-intestinal stromal tumor responding to<br />
mesylated Imatinib.<br />
A randomised phase II trial to evaluate FOLFOX or FOLFIRI<br />
treatment associated with AG-013736 or Bevacizumab in patients<br />
with metastatic colorectal carcinoma after failure with Irinotecan or<br />
Oxaliplatin as first line therapy.<br />
Comparison of the efficacy of peri-operative and postoperative<br />
chemotherapy in patients with operable gastric cancer and the<br />
evaluation of the benefit of chemotherapy combined with postoperative<br />
radiation therapy.<br />
Intensification Radiotherapy with Accelerated fractionation or<br />
ChemoTherapyAnd Local Excision after 3D External Radiochemotherapy<br />
INTE.R.A.CT-LEADER TRIAL.<br />
Prospective evaluation of 1498 C/T VEGF polimorphism in the<br />
prediction of benefit from first-line folfiri plus Bevacizumab in<br />
metastatic colorectal cancer patients. Pro.Ve.TT.A Study.<br />
A phase III randomized trial of Folfoxiri + Bevacizumab versus Folfiri +<br />
Bevacizumab as first-line treatment for metastatic colorectal cancer.<br />
Phase II study for first-line treatment of colorectal cancer in combination<br />
with FOLFOXIRI + Panitunumab in patients that express “wild type”<br />
KRAS and BRAF - TRIP.<br />
Phase I clinical study on intraperitoneal administration of ONCOFID<br />
in patients with peritoneal carcinomatosis from ovarian, stomach,<br />
breast, bladder and colon cancer.<br />
Open-label multicenter trial to evaluate the efficacy of nilotinib in adult<br />
patients with gastrointestinal stromal tumors resistant to imatinib and<br />
sunitinib.<br />
Prospective Evaluation of the quality of life (QoL) of patients with locally<br />
advanced rectal cancer after undergoing neoadjuvant radio-chemotherapy<br />
and surgery (performed as part of the INTERACT trial).<br />
An open-label trial on the efficacy and safety of Bevacizumab (Avastin®)<br />
combined with Xelox (Oxaliplatino + Xeloda®) as first line treatment<br />
of patients with locally advanced or metastatic colorectal cancer -<br />
OBELIX.<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
CLINICAL RESEARCH<br />
239<br />
Phase III 0 1 1<br />
Phase II 1 0 1<br />
Phase III 3 0 3<br />
Phase II 2 0 9<br />
Phase III 0 0<br />
Phase III 11 20 31<br />
Phase II 85<br />
Phase III 3 24 27<br />
Phase II 2 2<br />
Phase I 1 1<br />
Phase II 0 3 3<br />
Phase III 2 8 10<br />
Phase III 12 0 23
LYMPHOMAS<br />
A 3 arm multicenter phase III trial as first line treatment for patients<br />
with stage II-IV follicular lymphoma.<br />
Outcome of second-line treatment in patients with relapsed follicular<br />
lymphoma according to the type of first-line treatment received.<br />
Study to evaluate the prognosis of aggressive B-cell lymphoma treated<br />
with Anthracyclines + Rituximab. Combinations. ProDLBCL<br />
Phase II multicenter study of rituximab, cyclophosphamide,<br />
doxorubicin liposomal (Myocet®), vincristine, and prednisone<br />
(R-comp) in diffuse large B-cell non-Hodgkin’s disease of the cardiac<br />
patient. Italian Lymphoma Intergroup - Heart01.<br />
T-Cell Project: Collecting prospective data in patients with peripheral<br />
T lymphoma.<br />
MELANOMA<br />
Randomised adjuvant trial on patients with radically operated stage<br />
III malignant melanoma, comparison between different schedules of<br />
Interferon alfa 2B at high doses.<br />
Phase III clinical trial to evaluate the safety and efficacy of treatment<br />
with 2 mg of intralesional Allovectina-7® compared to Dacarbazine<br />
(DTIC) or Temozolomide (TMZ) in subjects with recurrent metastatic<br />
melanoma.<br />
A phase III double-blind placebo controlled randomised trial to<br />
evaluate the efficacy of recMAGE-A3 + AS15 as adjuvant therapy in<br />
patients with stage III Mage-A3 positive operable melanoma.<br />
Analysis of the expression of a specific series of tumor genes and antigens<br />
in patients with non small cell lung carcinoma and melanoma.<br />
Adjuvant immunotherapy with anti-CTLA-4 monoclonal antibody<br />
(Ipililumab) versus placebo after complete resection of high risk<br />
stage III melanoma: A randomised double blind phase III trial of the<br />
EORTC Melanoma Group.<br />
Treatment and outcome of patients with stage III or IV unresectable<br />
melanoma: a retrospective observational survey.<br />
Open-label multicenter phase III trial of ABI 007 versus dacarbazine in<br />
previously untreated metastatic malignant melanoma patients - CA33<br />
ABRAXIX.<br />
Open-label, single arm study to evaluate the clinical activity of<br />
recMAGE-A3 + AS15 in inoperable metastatic melanoma, MAGE-A3<br />
positive patients.<br />
Phase III randomized trial comparing TASISULAM vs. paclitaxel in<br />
previously treated metastatic melanoma patients. H8K-MC-JZAO.<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
CLINICAL RESEARCH<br />
240<br />
Phase III 3 0 7<br />
Phase II 13 13<br />
Phase II 11 0 11<br />
Phase II 2 2<br />
Observational 0 1 1<br />
Phase III 9 1 75<br />
Phase III 16 0 26<br />
Phase III 3 15 18<br />
Observational 13 2 18<br />
Phase III 13 16 36<br />
Observational 29 0 29<br />
Phase III 0 4 4<br />
Observational 0 0<br />
Phase III 0 6 6
LUNG<br />
An International multicenter randomised phase III study of first-line<br />
Erlotinib followed by second-line Cisplatin + Gemcitabine versus first<br />
line Cisplatin + Gemcitabine followed by second-line Erlotinib in<br />
advanced non small cell lung cancer - TORCH.<br />
Phase II, Randomised, double-blind, two-arm, parallel study of Vandetanib<br />
(ZACTIMA, ZD6474) plus Gemcitabine or Gemcitabine plus Placebo<br />
as first line treatment of advanced (stage IIIB or IV) Non Small Cell Lung<br />
Cancer (NSCLC) in Elderly patients.<br />
Phase II single arm trial of BIBW 2992 (Tovok) in patients with<br />
NSCLC and EGFR positive at FISH test.<br />
A single-arm, phase 2 trial of Pemetrexed,Cispatin and Bevacizumab as<br />
induction, followed by Pemetrexed and Bevacizumab as maintenance,in<br />
first-line treatment of Non Squamous Advanced NSCLC H3E-EW-S125.<br />
NGR015: Randomized double-blind phase III study of NGRhTNF<br />
plus best investigator s choice (BIC) versus placebo plus<br />
BIC in previously treated patients with advanced malignant pleural<br />
mesothelioma (MPM) (MOLMED).<br />
Open label study of bevacizumab maintenance therapy (AVASTINÒ)<br />
with or without pemetrexed after a first line treatment chemotherapy<br />
with bevacizumab-cisplatin-pemetrexed in patients with advanced,<br />
metastatic or recurrent non-squamous non-small cell lung cancer<br />
(NSCLC)- AVAPERL.<br />
A Phase III, open-label, randomized trial of CP-751, 871 in combination<br />
with paclitaxel and carboplatin versus paclitaxel and carboplatin in<br />
patients with non-small cell lung cancer. Protocol A4021016.<br />
Prospective randomised phase II trial of oral vinorelbine and cisplatin<br />
or pemetrexed and cisplatin in first-line metastatic or locally advanced<br />
non-small-cell lung cancer patients with non-squamous histological<br />
type PM 0259 CA227J1. NAVOTRIAL.<br />
International, randomized, double-blind trial evaluating Aflibercept vs<br />
placebo in patients treated with docetaxel in second-line after failure with<br />
a platinum-based therapy for locally advanced or metastatic non-small cell<br />
lung cancer (NSCLC). Protocol EFC10261 VITAL STUDY.<br />
Bevacizumab (Avastin) in combination with gemcitabine or<br />
attenuated doses of gemcitabine and cisplatin as a first line<br />
treatment of elderly patients with advanced or metastatic nonsquamous<br />
NSCLC.<br />
GENITO-URINARY CANCER<br />
HOPLITE Phase II clinical trial: evaluation of continuous or<br />
intermittent treatment with Docetaxel +/- Extramustine phosphate in<br />
androgen resistant prostate cancer.<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 1<br />
CLINICAL RESEARCH<br />
241<br />
Phase III 9 0 32<br />
Phase II 8 0 14<br />
Phase II 6 20 26<br />
Phase II 0 12 12<br />
Phase II 6 6<br />
Phase III 0 3 3<br />
Phase III 7 0 16<br />
Phase II 6 6<br />
Phase III<br />
Phase II 0 3 3<br />
Phase II 7 4 15
Randomised double blind clinical trial comparing Sunitib plus<br />
prednisone versus prednisone alone in patients with progressive<br />
hormone-refractory prostate cancer after failure with a docetaxel based<br />
regimen.<br />
Phase II open label randomised trial of Sorafenib alone or associated<br />
with Interleukin 2 as first line monotherapy in patients with advanced<br />
renal cancer.<br />
One-arm, multi-center, international prospective pivotal study to<br />
assess the safety and efficacy of Bio-Protect biodegradable implantable<br />
balloon in prostate cancer subjects undergoing radiotherapy.<br />
A phase II study of Sunitinib prior to and after or only after cytoreductive<br />
nephrectomy in patients with metastatic renal cell carcinoma.<br />
An International observational study on the quality of life of patients<br />
with testicular cancer with the aim of developing a questionnaire for<br />
future studies within the EORTC and other research groups.<br />
AXITINIB (AG-013736) as second line therapy for metastatic renal<br />
adenocarcinoma.<br />
SARCOMAS<br />
Prospective phase II trial with Sorafenib in patients with locally<br />
advanced or metastatic soft tissue sarcoma following chemotherapy<br />
with anthracycline.<br />
A study to establish the efficacy and safety of AP23573 administered as<br />
maintenance therapy in patients with soft tissue metastatic sarcoma or<br />
bone metastatic sarcoma.<br />
Therapeutic regimens for sarcomas and the impact of the disease in<br />
North America and Europe. SABINE.<br />
A Phase III, multicenter, randomized, double-blind trial on the<br />
efficacy of Ramucirumab (IMC-1121B) in combination with the best<br />
supportive care versus placebo plus best supportive care as second-line<br />
treatment in patients with hepatocellular carcinoma after first-line<br />
therapy with Sorafenib.<br />
GYNECOLOGIC CANCER<br />
A multicenter randomised trial on Caelix STEALTH versus Carboplatin<br />
+ Paclitaxel in patients with relapsed ovarian carcinoma 6-12 months<br />
after primary treatment with a platinum compound.<br />
Multicenter, randomized, double-blind, phase III trial designed to assess<br />
the efficacy and safety of BIBF 1120 in combination with carboplatin<br />
and paclitaxel versus placebo plus carboplatin and paclitaxel in patients<br />
with advanced ovarian cancer.<br />
Randomized phase II trial with carboplatin and paclitaxel + / -<br />
Cetuximab in advanced and / or recurrent cancer of the cervix.<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
CLINICAL RESEARCH<br />
242<br />
Phase III 3 1 4<br />
Phase II 0 1 1<br />
Observational 10 10<br />
Phase II 0 0 0<br />
Observational 20 0 20<br />
Phase II 2 0 2<br />
Phase II 1 0 9<br />
Phase II 4 0 7<br />
Observational 1 12 13<br />
Phase III 0 0<br />
Phase III 0 3 3<br />
Phase III 7 7<br />
Phase II 0 0
A randomized, double-blind, placebo-controlled, phase 3 study to<br />
assess the efficacy and safety of weekly Farletuzumab (morab-003) in<br />
combination with Carboplatin and Taxane in subjects with platinumsensitive<br />
ovarian cancer in first relapse.<br />
PEDIATRIC TUMORS<br />
Medical<br />
Oncology 2<br />
CLINICAL RESEARCH<br />
243<br />
Phase III 0 0 0<br />
A Prospective randomised controlled trial of hyperfractionated<br />
versus conventionally fractionated radiotherapy in standard risk<br />
medulloblastoma.(SIOP-PNET 4).<br />
Radiotherapy Phase III 3 3 15<br />
Nephroblastoma SIOP 2001. Radiotherapy Phase III 23<br />
International Randomised clinical trial for children and adolescents<br />
with low grade glioma (SIOP-LGG 2004).<br />
Radiotherapy Phase III 5 15 45<br />
Hodgkin’s Lymphoma - AIEOP - LH-2004.<br />
Phase III Randomized Study of Ifosfamide, Vincristine, and<br />
Radiotherapy Phase III 12 20 60<br />
Dactinomycin With or Without Doxorubicin in Pediatric Patients<br />
With Non-Metastatic Rhabdomyosarcoma (EpSSG RMS 2005 trial).<br />
Radiotherapy Phase III 16 19 65<br />
OTHER TOPICS<br />
A case control multicenter observational study on the epidemiology<br />
and risk factors for thromboembolic events in oncologic patients and<br />
the influence the venous thromboembolism has on the prognosis.<br />
Prospective observational study to evaluate the risk management of<br />
neutropenia and anaemia in subjects with solid tumors receiving<br />
mielotoxic chemotherapy.<br />
Open-label, randomized pilot study, to evaluate the change of wellbeing<br />
and quality of life induced by the use of a specific room equipped<br />
with complementary therapies, compared to no complementary<br />
therapies at all, in cancer patients facing chemotherapy for the first<br />
time. Atmosphere project.<br />
Screening For early predictors of peripheral neuropathy In oxaliplatintreated<br />
patients.<br />
Observational, prospective trial, to assess the intensity of nausea and<br />
vomiting in cancer patients receiving preventive therapy for nausea and<br />
vomiting caused by chemotherapy. Project N & V.<br />
Observational, multinational, multicenter, prospective study of adult<br />
patients receiving anti-emetic therapy in concomitance with the start<br />
of moderately or highly emetogenic chemotherapy drugs (HEC or<br />
MEC).<br />
Single-arm multicenter study of Denosumab in the treatment of<br />
hypercalcaemia in patients with high serum calcium levels after recent<br />
treatment with bisphosphonates.<br />
DAMA - Epidemiological - observational study: prevalence and course<br />
of depression elderly patients with advanced disease stage.<br />
Medical<br />
Oncology 1<br />
Medical<br />
Oncology 1<br />
Medical<br />
Office<br />
Medical<br />
Oncology 1<br />
Medical<br />
Office<br />
Medical<br />
Office<br />
Medical<br />
Oncology 2<br />
Medical<br />
Oncology 1<br />
Observational 12 0 12<br />
Observational 0 0 15<br />
Pilot Study 18 126 144<br />
Observational 24 24<br />
Observational 179 0 179<br />
Observational 13 43 56<br />
Observational 0 0<br />
Observational 2 2
VENETO ONCOLOGY<br />
NETWORK<br />
VENETO ONCOLOGY NETWORK<br />
245
Veneto Oncology Network<br />
The Istituto Oncologico Veneto has been established in<br />
Padova in view of the excellent background accumulated in this<br />
city over the decades in virtually all the aspects of Oncology.<br />
Notwithstanding, this expertise has slowly but steadily permeated<br />
the entire Veneto region, thanks to the presence in Padova of a<br />
post-graduate Specialty School in Oncology established in the late<br />
’70s and flanked a few years later by a Specialty School in Verona.<br />
A great number of clinical Oncologists now operating in the<br />
different Veneto provinces attended the post-graduate Specialty<br />
School in Padova.<br />
Thus, cancer patients can find elevated diagnosis and cure<br />
standards throughout our region, even though the most specialized<br />
approaches are performed at the major centres.<br />
At present, twenty seven Oncology Units are disseminated<br />
throughout the Veneto region. In most of them, Clinical Oncology<br />
is flanked by diagnostic (such as radiology, pathology and<br />
molecular biology) and therapeutic platforms (such as surgery and<br />
radiotherapy), whereas in some cases only day-hospital structures<br />
are present, offering patients only or mostly pharmacological<br />
treatments according to therapeutic programs discussed and<br />
planned in strict collaboration with major centres.<br />
A major aim of the <strong>IOV</strong> is to establish and foster an oncological<br />
network throughout our region, in order to improve and optimize<br />
all the aspects of the clinical management of cancer patients, as well<br />
as to implement research potential in an extremely competitive<br />
field.<br />
From an epidemiological point of view, the existence of an<br />
Oncologic Network will permit:<br />
to plan a capillary survey of the entire Veneto region, by<br />
collecting uniform data on the prevalence and incidence of<br />
different types of tumors through the extension of the activities<br />
of the Veneto Tumor Registry;<br />
to standardize primary prevention strategies throughout<br />
the region, in order to achieve the maximum efficacy of the<br />
interventions and avoid duplication of initiatives by the<br />
VENETO ONCOLOGY NETWORK<br />
246<br />
number of stakeholders possibly involved in tumor prevention<br />
campaigns;<br />
to define rational secondary prevention strategies, by designing<br />
screening plans for colon, mammary and uterine cervix cancer.<br />
A far as the clinical management of patients is concerned, a<br />
preliminary survey of all the Oncology Units will allow to have<br />
an outline of the situation within the Veneto region in order to<br />
better target specific interventions. In particular, the existence of<br />
an efficient network will permit:<br />
availability of a common informatics platform for the sharing of<br />
clinical data and other relevant material;<br />
definition of different levels of assistance, according to the<br />
diagnostic and therapeutic facilities present in different Units;<br />
development of shared guidelines for the different pathologies,<br />
and the identification of centers of excellence for particular<br />
tumors;<br />
careful planning of investments, to allow the access of oncologic<br />
patients to the state-of-the-art diagnostic and therapeutic<br />
facilities without duplication of expensive instrumentation and<br />
resource sparing.<br />
In reference to the research possibilities offered by an Oncologic<br />
Network spread throughout the entire region, it is evident that<br />
collaboration among centers may consent:<br />
promotion of coordinated initiatives in terms of education;<br />
delineation of research programs based on the strict<br />
interconnection of expertise in different fields (laboratory,<br />
medicine, surgery etc);<br />
better exploitation of top facilities, such as genomic and<br />
proteomic platforms;<br />
rapid collection of large case series of patients with a particular<br />
tumor, to allow the performing of in-depth research on their<br />
biological characteristics and adequate clinical trials.<br />
It is evident that careful scrutiny of all research and clinical<br />
resources presently available over the country is a preliminary<br />
step, mandatory for any future strategic planning.
Ospedale classificato<br />
ed equiparato Sacro Cuore,<br />
Don Calabria - Negrar (Verona)<br />
Head: Marco Venturini, MD<br />
UOC Oncologia,<br />
Ospedale di Bussolengo<br />
Az. ULSS 22<br />
Head: Tiziano Franceschi, MD<br />
UOC Oncologia, Ospedale di Thiene<br />
Az. ULSS 4 Alto Vicentino<br />
Head: Franco Bassan, MD<br />
UOC Oncologia, Ospedale di S. Bonifacio (VR)<br />
Az. ULSS 20 / UOC Oncologia<br />
Ospedale Civile Maggiore,<br />
Azienda Ospedaliero-Universitaria.<br />
Verona [Borgo Trento]<br />
Head: Anna Maria Molino, MD<br />
UOC Oncologia, Ospedale Civile Maggiore,<br />
Azienda Ospedaliero-Universitaria, Verona<br />
[Borgo Roma]<br />
Head: Giampaolo Tortora, MD<br />
UO Oncologia<br />
Casa di Cura Pederzoli,<br />
Peschiera del Garda<br />
Head: Annita Lusenti, MD<br />
UOC Oncologia,<br />
Ospedale di Montecchio Maggiore<br />
Az. ULSS 5<br />
Head: Cristina Oliani, MD<br />
UOC Oncologia,<br />
Ospedale di Legnago<br />
Az. ULSS 21<br />
Head: Andrea Bonetti, MD<br />
Peschiera<br />
Bussolengo<br />
Negrar<br />
Verona<br />
Legnago<br />
UOC Oncologia,<br />
Ospedale di Este<br />
Az. ULSS 17<br />
Head: Giorgio Bonciarelli, MD<br />
Thiene<br />
UOC Oncologia, Ospedale di Feltre<br />
Az. ULSS 2<br />
Head: Romana Segati, MD<br />
UO Oncologia,<br />
Bassano del Grappa (VI)<br />
Az. ULSS 3<br />
Head: Luigi Endrizzi, MD<br />
UOC Oncologia, Vicenza<br />
Az. ULSS 6<br />
Head: Paolo Morandi, MD<br />
Vicenza<br />
Montecchio<br />
Maggiore<br />
Medicina Oncologica,<br />
Ospedale Imm. Conc., Piove di Sacco<br />
Az. ULSS 16<br />
Head: Adriano Fornasiero, MD<br />
UOC Oncologia,<br />
Presidio Ospedaliero Piove di Sacco<br />
Az. ULSS 14<br />
Head: Carlo Gatti, MD<br />
Este<br />
Feltre<br />
Bassano<br />
del Grappa<br />
Camposampiero<br />
Rovigo<br />
Castelfranco<br />
Padova<br />
Piove<br />
di Sacco<br />
Adria<br />
Belluno<br />
Mirano<br />
SOC Oncologia,<br />
Ospedale di Rovigo<br />
Az. ULSS 18<br />
Head: Felice Pasini, MD<br />
VENETO ONCOLOGY NETWORK<br />
247<br />
UOC Oncologia, Ospedale di Belluno<br />
Az. ULSS 1<br />
Head: Mauro Giusto, MD<br />
Vittorio<br />
Veneto<br />
Mestre<br />
Treviso<br />
UOC Oncologia,<br />
Ospedale di Adria<br />
Az. ULSS 19<br />
Head: Silvia Toso, MD<br />
UOC Oncologia, Vittorio Veneto<br />
Az. ULSS 7<br />
Head: Luigi Salvagno, MD<br />
San Donà<br />
UOC Oncologia, Ospedale di Castelfranco<br />
Az. ULSS 8<br />
Head: Paolo Manente, MD<br />
SOC Oncologia, Ospedale di Treviso<br />
Az. ULSS 9<br />
Head: Giovanni Rosti, MD<br />
UOC Oncologia,<br />
Ospedale di San Donà<br />
Az. ULSS 10<br />
Head: Daniele Bernardi, MD<br />
UOC Oncologia,<br />
Ospedale di Camposampiero<br />
Az. ULSS 15<br />
Head: Fernando Gaion, MD<br />
UOC Oncologia ed Ematologia Oncologica (Mirano)<br />
Az. ULSS 13<br />
Head: Orazio Vinante, MD<br />
UOC Oncologia, Venezia Mestre<br />
Az. ULSS 12<br />
Head: Ottorino Nascimben, MD<br />
Istituto Oncologico Veneto (IRCCS),<br />
Oncologia 1, Padova<br />
Head: Vittorina Zagonel, MD<br />
Istituto Oncologico Veneto (IRCCS),<br />
Oncologia 2, Padova<br />
Head: Vanna Chiarion-Sileni, MD<br />
Istituto Oncologico Veneto (IRCCS),<br />
Valutazione e Introduzione Nuovi Farmaci<br />
nelle Terapie Oncologiche, Padova<br />
Head: Antonio Jirillo, MD
Building a network is not a trivial job, of course. Over the last<br />
35 years, the interactions among the different Veneto oncology<br />
centers were occasional, and in some instances troublesome, due<br />
to many complex reasons, including the lack of an academic<br />
Oncology chair in Padova. Since 2007, the Scientific Directorate<br />
tried hard to foster communication among all the Oncology<br />
Units, and to overcome the reciprocal difficulties in the interaction<br />
between major and peripheral centers. The Scientific Directorate<br />
is happy to see that these efforts met some significant success<br />
and were able to reconcile different feelings and behaviors; this<br />
allows to foresee even greater advancements in a near future.<br />
For sure, overcoming individualism is an essential ingredient for a<br />
successful recipe in the competition for excellence. In this regard,<br />
thanks to the joint efforts of Dr. Zagonel, Dr. Bonetti, Dr. Gaion,<br />
Dr. Pasini and a few other friends and colleagues, about a half<br />
VENETO ONCOLOGY NETWORK<br />
248<br />
of the Veneto Clinical Oncology Units will share an electronic<br />
clinical record platform, and other Units are expected to join<br />
this network. This choice will offer the opportunity to share data<br />
among Units, and to compare and study larger case series, thus<br />
rendering collaboration and scientific interactions much more<br />
easy and productive. In addition, two scientific projects have been<br />
recently launched. A first project is centered on the construction<br />
of a network on heredo-familial tumors, modelled according to<br />
a hub-and-spoke model; this network involves about two-thirds<br />
of the Veneto Clinical Oncology Units. A second project will be<br />
focused on the palliative care in non-small cell lung cancer; this<br />
project involves about ten Units of the nascent Veneto Oncology<br />
Network, and it is aimed at formulating shared guidelines on this<br />
important issue.
EDUCATION<br />
EDUCATION<br />
249
Internal Education & Training<br />
The <strong>IOV</strong> has an internal Continuous Education and Training<br />
Program, which in the period from 2005 to <strong>2010</strong> has involved over<br />
10,000 participants of the medical, nursing and administrative staff<br />
of both <strong>IOV</strong> and peripheral oncological Units. The courses, stages<br />
and seminars were centered on both basic/translational topics and<br />
issues of major clinical interest in Oncology; all the personnel<br />
2009<br />
Titolo<br />
EDUCATION<br />
250<br />
categories and specialties (technicians, nurses, clinical oncologists,<br />
radiotherapists, surgeons, pharmacists etc) were involved. Most<br />
of the formative events were organized according to the national<br />
program of Continuous Medical Education (ECM); overall, more<br />
than 1,000 ECM credits were administered. A list of the 2009-<br />
<strong>2011</strong> events is reported here.<br />
Responsabile<br />
Scientifico<br />
N.<br />
di partecipanti<br />
N.<br />
crediti ECM<br />
Lo Screening del Cervicocarcinoma con il Test HPV M. Vettorazzi 25 5<br />
Seminari “From Cloning To Clinic” G. Opocher 45 0<br />
Applicazioni cliniche e impatto farmacoeconomico dei nuovi farmaci biologici D. Pastorelli 75 3<br />
Convegno Nazionale Gisma 2009 M. Vettorazzi 200 7<br />
Evoluzione in mammografia digitale: la tomosintesi. Corso per fisici e tecnici<br />
di radiologia<br />
M. Vettorazzi 60 3<br />
Corso pratico di diagnostica mammografica integrata per radiologi M. Vettorazzi 60 3<br />
Corso teorico pratico di endoscopia operativa G. Battaglia 15 11<br />
Confronto interistituzionale in patologia mammaria da screening M. Vettorazzi 45 9<br />
Corso teorico-pratico: PET e linfomi M. Gregianin 10 21<br />
Psiconcologia: un ponte tra scienza e coscienza E. Capovilla 200 4<br />
Le terapie di supporto delle tossicità da antiblastici D. Pastorelli 20 8<br />
Il Carcinoma Ovarico: dalla ricerca di base alle novità terapeutiche<br />
S. Indraccolo<br />
P. Zanovello<br />
80 3<br />
I tumori ereditari del pancreas G. Opocher 100 4<br />
Sarcomi dei tessuti molli. Aggiornamento delle linee guida regionali e recenti<br />
innovazioni.<br />
C. R. Rossi 100 4
Integrative Oncology Care G. Opocher 60 8<br />
Riunione annuale Screening Colorettale M. Vettorazzi 90 4<br />
Riunione annuale Screening Citologico M. Vettorazzi 200 4<br />
Riunione annuale Screening Mammografico M. Vettorazzi 150 4<br />
Il Carcinoma del Colon: dalla ricerca di base alle novità terapeutiche<br />
EDUCATION<br />
251<br />
S. Indraccolo<br />
P. Zanovello<br />
90 2<br />
Le terapie di supporto nei pazienti oncologici D. Pastorelli 60 4<br />
La comunicazione tra infermiere e utente nel 2° livello dello screening<br />
colorettale<br />
M. Vettorazzi 25 26<br />
Il carcinoma della tiroide differenziato aspetti clinico assistenziali G. Sotti 50 15<br />
La sperimentazione clinica in oncologia e il nursing avanzato M. Padovan 25 28<br />
<strong>2010</strong><br />
Titolo<br />
Responsabile<br />
Scientifico<br />
N.<br />
di partecipanti<br />
N.<br />
crediti ECM<br />
La colonscopia di screening - Corso Regionale M.Vettorazzi 20 9<br />
Melanoma: novità nell’inquadramento diagnostico e modelli organizzativi C. R. Rossi 100 9<br />
Qualità della vita nei pazienti oncologici e update sulle terapie di supporto D. Pastorelli 70 4<br />
Cardioncologia <strong>2010</strong> A. Banzato 90 4<br />
Seminario “Predisposizione genetica al cancro: il problema delle varianti di<br />
incerto significato”<br />
G. Opocher 90 3<br />
Psiconcologia: interventi oncologici evidence-based e medical humanities E. Capovilla 150 4<br />
Re-ingegnerizzazione della prevenzione individuale e programmi di screening:<br />
efficacia, qualità e sostenibilità<br />
C. Cogo 100 6<br />
Convegno Nazionale Gisci <strong>2010</strong> C. Cogo 250 3<br />
Mindfulness: una pratica di self care E. Capovilla 50 7<br />
Carcinosi peritoneale: chirurgia citoriduttiva e chemioterapia ipertermica C. R. Rossi 90 11<br />
Agenti infettivi nella patogenesi dei tumori P. Zanovello 90 2<br />
Corso di aggiornamento in oncologia toracica A. Jirillo 20 3<br />
La comunicazione telefonica negli screening oncologici C. Cogo 25 25<br />
Corso di aggiornamento in oncologia mammaria F. Bozza 25 26<br />
Aggiornamento delle linee guida regionali e recenti innovazioni sul melanoma C. R. Rossi 100 13<br />
Il linfonodo sentinella nel carcinoma mammario: realtà e nuove prospettive F. Bozza 90 4
La comunicazione interpersonale negli screening oncologici C. Cogo 25 4<br />
Aggiornamenti in tema di carcinoma dello stomaco<br />
EDUCATION<br />
252<br />
V. Zagonel<br />
F. Adami<br />
50 26<br />
Aggiornamenti sulle neoplasie ginecologiche M. O. Nicoletto 90 5<br />
Riunione annuale screening colorettale C. Cogo 150 3<br />
Ruolo del TSRM nell’organizzazione e nella conduzione di uno screening<br />
mammografico di popolazione<br />
C. Cogo 100 4<br />
V Corso di Neuromodulazione: la terapia del dolore G. Pinato 80 5<br />
Riunione annuale screening citologico C. Cogo 200 4<br />
Riunione annuale screening mammografico C. Cogo 150 4<br />
Comunicare con tutti. 5° Seminario sulla comunicazione nei programmi di screening C. Cogo 240 4<br />
IX Convegno osservatorio nazionale screening C. Cogo 240 4<br />
La pratica del primary nursing: la sperimentazione del modello professionale<br />
in area oncologica<br />
Cartella oncologica informatizzata: sistema innovativo per la gestione dell’attività<br />
clinico assistenziale del malato oncologico, aspetti tecnici e gestionali<br />
Gli strumenti operativi delle sperimentazioni cliniche: il protocollo di ricerca<br />
e la scheda raccolta dati<br />
B. Burattin,<br />
M. Padovan<br />
50 25<br />
V. Zagonel 200 7<br />
V. Zagonel<br />
G. L. De Salvo<br />
25 36<br />
La gestione aziendale per la qualità D. Chiusole 25 20<br />
La sperimentazione clinica in oncologia e il nursing avanzato M. Padovan 50 33<br />
La sperimentazione clinica in oncologia e il nursing avanzato intensivo M. Padovan 25 33<br />
Strumenti diagnostici per la prevenzione e trattamento del tumore alla<br />
mammella<br />
M. Cacco 50 20<br />
<strong>2011</strong><br />
Titolo<br />
N.<br />
di partecipanti<br />
N.<br />
di partecipanti<br />
N.<br />
crediti ECM<br />
Percorsi integrati in oncologia. Il tumore del polmone G. Opocher 40 5<br />
Approccio multidisciplinare nel carcinoma della mammella F. Bozza 25 13<br />
Percorsi integrati in oncologia. Il tumore del colon retto G. Opocher 40 5<br />
Percorsi integrati in oncologia. Il tumore della mammella G. Opocher 40 5
Aggiornamento delle linee guida sulle terapie di supporto in chemioterapia V. Zagonel 35 2<br />
Corso itinerante in oncologia toracica R. Polverosi 60 6<br />
Approccio multidisciplinare sui gliomi V. Zagonel 90 3<br />
Percorsi integrati in oncologia. La collaborazione in una rete di relazioni<br />
integrate<br />
EDUCATION<br />
253<br />
G. Opocher 40 5<br />
Melanoma familiare: dal test genetico alla pratica clinica C. Menin 90 2<br />
Sarcomi delle parti molli e GIST: epidemiologia, clinica e “Network” C. R. Rossi 150 4<br />
La neoplasia mammaria nella donna giovane F. Bozza 200 5<br />
Systemic treatment selection and target therapies in NSCLC A. Favaretto 50 5<br />
1° Congresso Nazionale di Oncologia di genere V. Zagonel 250 4<br />
Aging and Cancer<br />
A. De Rossi<br />
V. Zagonel<br />
90 4<br />
La storia della nascita di un farmaco A. Jirillo 60 3<br />
Corso Teorico - Pratico. La diagnosi e il trattamento endoscopico delle lesioni<br />
“Early” del tratto digestivo<br />
G. Battaglia 12<br />
Nuovi approcci contro il cancro. Elettrochemioterapia: la rete del Nord-Est C. R. Rossi 100<br />
L’implementazione della qualità e sicurezza dell’assistenza chirurgica del paziente<br />
oncologico<br />
Corso di psicologia oncologica. Pazienti, famigliari, operatori: quali strumenti per<br />
una relazione efficace<br />
C. Castoro 25 30<br />
E. Capovilla 25 15<br />
La sperimentazione clinica in oncologia e il nursing avanzato intensivo M. Padovan 25 33<br />
Strumenti diagnostici per la prevenzione e trattamento del tumore alla mammella M. Cacco 50 20<br />
La gestione aziendale per la qualità D. Chiusole 25 20<br />
La gestione e verifica del workflow nella diagnostica per immagini con analisi degli<br />
errori comuni e delle possibili soluzioni<br />
M. Giacobbo 75 20<br />
Approccio ed assistenza al paziente disfagico G. Sotti 50 8<br />
Le patologie tiroidee: aspetti dosimetrici della terapia radiometabolica con iodio 131 F. Simonato 50 5<br />
Rilievo e trattamento del dolore cronico nel malato oncologico<br />
M. Giacobbo<br />
V. Zagonel<br />
M. Padovan<br />
G. Sotti<br />
25 20
Trattamento del dolore cronico nel malato oncologico<br />
EDUCATION<br />
254<br />
M.Giacobbo<br />
V. Zagonel<br />
M. Padovan<br />
G. Sotti<br />
25 20<br />
La scheda di dimissione ospedaliera: compilazione e codifica icd - 9 - cm 2007 M. Giacobbo 25 6<br />
Prevenzione e gestione delle infezioni ospedaliere nei pazienti oncologici ricoverati<br />
presso l’Istituto Oncologico Veneto<br />
Il Sistema BiblioSan: strumenti e metodi per l’implementazione del processo di<br />
ricerca scientifica e documentaristica<br />
Il Sistema BiblioSan: strumenti e metodi di ricerca finalizzato al miglioramento<br />
della pratica professionale<br />
P. Cadrobbi 50 17<br />
A. Rosato<br />
M. Apostolico<br />
M. Apostolico<br />
A. Rosato<br />
50 12<br />
50 12<br />
Sarcomi: valutazione e trattamento multidisciplinare. Studio e discussione di casi C. Rossi 25 15<br />
La gestione del rischio clinico: metodi di analisi M. Giacobbo 25 15<br />
Tutela della privacy e gestione dei dati sensibili in sanità M. Padovan 25 10
DOCTOraTE SChOOl iN ONCOlOGy<br />
aND SurGiCal ONCOlOGy<br />
Director: Paola Zanovello<br />
The Doctorate School in Oncology<br />
and Surgical Oncology is destined to<br />
physicians and biologists who want<br />
to acquire scientific methodology<br />
and appropriate expertise in basic,<br />
translational and clinical research in<br />
the field of Oncology and Clinical/<br />
Surgical Oncology. The School spans a 3-yr period, and about 10<br />
PhD students are admitted every year on a selective basis.<br />
pOST-GraDuaTE SpECializaTiON SChOOl iN CliNiCal ONCOlOGy<br />
Director: Fausto Adami<br />
The Specialization School in Clinical Oncology is dedicated to<br />
physicians who want to acquire special expertise in the different<br />
fields of Clinical Oncology. About 5 graduates are admitted to the<br />
School every year; during a 4-yr period, the educational program<br />
entails periods of internship in all the clinical Units of the Institute;<br />
the possibility of stages in outstanding Italian or foreign Cancer<br />
Institutes is also strongly encouraged.<br />
Post-graduate Schools<br />
EDUCATION<br />
255<br />
The major research themes implemented within the Doctorate<br />
School are:<br />
Molecular pathology of tumors;<br />
Virologic oncology;<br />
Tumor immunology and the role of tumor microenvironment;<br />
Animal models of human cancerogenesis;<br />
Genetic predisposition to cancer;<br />
Micro- and nano-biotechnologies in oncology;<br />
Novel therapeutic strategies (vaccination, gene therapy,<br />
immunoregulation);<br />
New molecular tools in onco-hematology.<br />
pOST-GraDuaTE SpECializaTiON SChOOl iN mEDiCal raDiOlOGy<br />
Director: Davide Fiore<br />
The Specialization School in Medical Radiology is dedicated<br />
to physicians who want to acquire special expertise in the different<br />
fields of imaging sciences and interventional radiology. A special<br />
attention is dedicated to the neuroradiology. About 10 graduates<br />
are admitted to the School every year.
EDUCATION<br />
256
2009<br />
Barbara Seliger How tumor cells fuel the immune system<br />
Peter Siesjö Immunotherapy of brain tumors: mission impossible?<br />
Graham Le Gros The differentiation in vitro and its relevance to allergy and parasitic diseases<br />
Maurizio Zanetti Immunologic aspects of ER stress<br />
Heiko Ihmels<br />
Varations on Annelated Quinzinium Derivatives: How the Shape of a Ligand Determines its Association<br />
with Duplex-, Triplex- and Quadruplex-DNA<br />
Stanley C. Froehner Nitric Oxide in Skeletal Muscle Function and Disease<br />
Napoleone Ferrara Regulation of tumor angiogenesis by VEGF- dependent and independent pathways<br />
Klemens Pichler<br />
Virus-mediated stimulation of anti-apoptotic genes as a survival strategy of HTLV-1-transformed<br />
lymphocytes<br />
Andrew Brack Self renewal of adult muscle stem cells during regeneration<br />
<strong>2010</strong><br />
Meetings and Seminars<br />
Scientific Conference “Highlights in Oncology: recent Advancements in Oncology”<br />
Veffa Franchini HTLV – the first human retrovirus to matter<br />
All you wanted to know about HIV but didn’t dare to ask<br />
Leonid Margolis<br />
HIV – A human virus that is much studied but not much understood<br />
War and peace between viruses<br />
Lionel Perrier Cost- Effectiveness Analysys: Methods and applications in oncology<br />
EDUCATION<br />
257
Charles R M Bangham How does HTLV-1 persist in vivo?<br />
Raymond White<br />
Genetics and Therapy Dopaminergic System and Addiction: Toward an individually-specific genetically<br />
based therapeutic approach<br />
Oriol Casanovas Evasive Resistance to Anti-angiogenic Therapies<br />
Joseph Schlessinger Cell signaling by receptor tyrosine kinases: from molecular mechanism to cancer therapy<br />
David Sassoon From cell stress responses to stem cells: a common link in muscle, skin and other adult stem cell niches?<br />
Pablo Menendez Hematopoietic and mesenchymal differentiation from hESC and iPS cells<br />
Luis A. Rokeach Aging effects of glucose in the model Schizosaccharomyces pombe<br />
Aichi Msaki Investigating the function of NF-kB subunit RelA<br />
David Y. Graham Barrett Esophagus: The Graham’s point of view<br />
Adolfo Ferrando The molecular pathogenesis of T-ALL<br />
Marina Cavazzana-Calvo Gene therapy: success and failure<br />
Martin Mueller Papillomavirus L2-based vaccination and high throughput pseudovirion neutralization assay<br />
<strong>2011</strong><br />
Rosa Maria Moresco<br />
Antonio Rosato<br />
International Workshop on VIRUSES, GENES AND CANCER – Venice <strong>2010</strong><br />
In Vivo Molecular Imaging in Translational Research<br />
Giovanni Cazzaniga Minimal residual disease monitoring in childhood ALL. Not only a diagnostic tool<br />
Esteban Czwan Classification of tumors based on the activity of oncogenic pathways<br />
Mauro Giacca<br />
“How can you mend a broken heart”: Searching for genes that induce myocardial protection, myocardial<br />
repair or neoangiogenesis by in vivo gene transfer using AAV vectors<br />
Marina Lusic Nuclear structures and chromatin determinants of HIV-1 infected cells<br />
Tim Hoey Development of new cancer therapeutics that reduce tumor initiating cell frequency<br />
Michael Stuerzl Molecular Dissection of the Pathogenicity of Kaposi‘s Sarcoma-associated Herpesvirus<br />
EDUCATION<br />
258
Genoveffa Franchini HTLV-1, the smooth operator of tumor transformation<br />
Ugo Cavallaro Neural adhesion molecules: old players with new functions in signaling and in cancer<br />
Rafael Rosell<br />
Adolfo Gino Favaretto<br />
Systemic treatment selection and targeted therapies in NSCLC<br />
Beghini Alessandro Leucemia acuta mieloide con riarrangiamenti del core binding factor: un paradigma senza fine<br />
Giorgio Stanta<br />
Ricerca traslazionale nei tessuti d’archivio: un’opportunità per accelerare l’applicazione della medicina<br />
personalizzata<br />
Francesco Dazzi The immunoregulatory activity of haemopoietic stem cell transplantation<br />
Giorgio Valle New generation sequencing:current limits and future perspectives<br />
Piero Dalerba Cancer Stem Cells: therapeutic implications<br />
Magnus Essand Viruses and T cells as cancer therapeutics<br />
Oliver Hohn The rise and fall of HMRV<br />
Vito Pistoia Nuovi meccanismi immunoregolatori mediati da HLA-G<br />
Marco Dotto Next Generation Sequencing: current applications for cancer care<br />
EDUCATION<br />
259
AWARDS<br />
VENETO ONCOLOGY AWARDS NETWORK<br />
261
Awards<br />
In November <strong>2010</strong> Dr. Giulia Pasello received<br />
the ESMO Fellowship Award<br />
for the IDENTIFICATION of NOVEL<br />
MOLECULAR TARGETS and BIOLOGICAL AGENTS<br />
for the CHEMOTHERAPY<br />
of MALIGNANT PLEURAL MESOTHELIOMA<br />
AWARDS<br />
263
PUBLICATIONS<br />
PUBLICATIONS<br />
265
2009 PUBLICATIONS / Journals indexed in ISI-JCR<br />
1 Aapro M, Monfardini S, Jirillo A, Basso U. Management of primary<br />
and advanced breast cancer in older unfit patients (medical treatment)<br />
Cancer treatment reviews; 35:6; 503-508; 2009<br />
2 Abbadessa G, Accolla R, Aiuti F, Albini A, Aldovini A, Alfano M,<br />
Antonelli G, Bartholomew C, Bentwich Z, Bertazzoni U, Berzofsky J A,<br />
Biberfeld P, Boeri E, Buonaguro L, Buonaguro F M, Bukrinsky M Burny<br />
A, Caruso A, Cassol S, Chandra P, Ceccherini-Nelli L, Chieco-Bianchi<br />
L, Clerici M, Colombini-Hatch S, Morghen C D G, De Maria A, De<br />
Rossi A, Dierich M, Della-Favera R, Dolei A, Douek D, Erfle V, Felber<br />
B, Fiorentini S, Franchini G, Gershoni J M, Gotch F, Green P, Greene<br />
W C, Hall W, Haseltine W, Jacobson S, Kallings L O, Kalyanaraman<br />
V S, Katinger H, Khalili K, Klein G, Klein E, Klotman M, Klotman<br />
P, Kotler M, Kurth R, Lafeuillade A, La PlacaM, Lewis J, Lillo F,<br />
Lisziewicz J, Lomonico A, Lopalco L, Lori F, Lusso P, Macchi B, Malim<br />
M, Margolis L, Markham P D, Mcclure M, Miller N, Mingari M C,<br />
Moretta L, Noonan D, O’Brien S, Okamoto T, Pal R, Palese P, Panet<br />
A, Pantaleo G, Pavlakis G, Pistello M, Plotkin S, Poli G, Pomerantz R,<br />
Radaelli A, Robert-Guroff M, Roederer M, Sarngadharan M G, Schols<br />
D, Secchiero P, Shearer G, Siccardi A, Stevenson M, Svoboda J, Tartaglia<br />
J, Torelli G, Tornesello M L, Tschachler E, Vaccarezza M, Vallbracht A,<br />
Van Lunzen J, Varnier O, Vicenzi E, Von Melchner H, Witz I, Zagury<br />
D, Zagury J F, Zauli G, Zipeto D. Unsung hero Robert C. Gallo.<br />
Science; 323:5911; 206- 207; 2009<br />
3 Adorno M, Cordenonsi M, Montagner M, Dupont S, Wong C, Hann<br />
B, Solari A, Bobisse S, Rondina M B, Guzzardo V, Parenti A R, Rosato<br />
A, Bicciato S, Balmain A, Piccolo S, A Mutant-p53/Smad Complex<br />
Opposes p63 to Empower TGFβ-Induced Metastasis. Cell; 137:1;<br />
87-98; 2009<br />
4 Agnelli G, Gussoni G, Bianchini C, Verso M, Mandalà M, Cavanna<br />
L, Barni S, Labianca R, Buzzi F, Scambia G, Passalacqua R, Ricci<br />
S, Gasparini G, Lorusso V, Bonizzoni E, Tonato M, PROTECHT<br />
Investigators [as collab. Falci C, Jirillo A]. Nadroparin for the<br />
prevention of thromboembolic events in ambulatory patients with<br />
metastatic or locally advanced solid cancer receiving chemotherapy:<br />
a randomised, placebo-controlled, double-blind study. Lancet<br />
Oncology; 10:10; 943-949; 2009<br />
5 Alaggio R, Bisogno G, Rosato A, Ninfo V, Coffin C M. Undifferentiated<br />
PUBLICATIONS<br />
266<br />
sarcoma: does it exist? A clinicopathologic study of 7 pediatric cases<br />
and review of literature. Human pathology; 40:11; 1600-1610;<br />
2009<br />
6 Amadori A, Rossi E, Zamarchi R, Carli P, Pastorelli D, Jirillo. A<br />
Circulating and disseminated tumor cells in the clinical management<br />
of breast cancer patients: unanswered questions. Oncology Basel;<br />
76:6; 375-386; 2009<br />
7 Antoniou A C, Sinilnikova O M, McGuffog L, Healey S, Nevanlinna<br />
H, Heikkinen T, Simard J, Spurdle A B, Beesley J, Chen X, Neuhausen<br />
S L, Ding Y C, Couch F J, Wang X, Fredericksen Z, Peterlongo P, Peissel<br />
B, Bonanni B, Viel A, Bernard L, Radice P, Szabo C I, Foretova L,<br />
Zikan M, Claes K, Greene M H, Mai P L, Rennert G, Lejbkowicz<br />
F, Andrulis I L, Ozcelik H, Glendon G, Gerdes A M, Thomassen M,<br />
Sunde L, Caligo M A, Laitman Y, Kontorovich T, Cohen S, Kaufman<br />
B, Dagan E, Baruch R G, Friedman E, Harbst K, Barbany-Bustinza<br />
G, Rantala J, Ehrencrona H, Karlsson P, Domchek S M, Nathanson<br />
K L, Osorio A, Blanco I, Lasa A, Benìtez J, Hamann U, Hogervorst<br />
F B L, Rookus M A, Collee J M, Devilee P, Ligtenberg M J, Van Der<br />
Luijt R. B, Aalfs C M, Waisfisz Q,Wijnen J, Van Roozendaal C E P,<br />
Peock S, Cook M, Frost D, Oliver C, Platte R, Evans D G, Lalloo<br />
F, Eeles R, Izatt L, Davidson R, Chu C, Eccles D, Cole T, Hodgson<br />
S, Godwin A K, Stoppa-Lyonnet D, Buecher B, Léoné M, Bressac-de<br />
Paillerets B, Remenieras A, Caron O, Lenoir G M, Sevenet N, Longy<br />
M, Ferrer S F, Prieur F, Goldgar D, Miron A, John E M, Buys S S,<br />
Daly M B, Hopper J L, Terry M B, Yassin Y, Singer C, Gschwantler-<br />
Kaulich D, Staudigl C, Hansen T V O, Barkardottir R B, Kirchhoff T,<br />
Pal P, Kosarin K, Offit K, Piedmonte M, Rodriguez G C, Wakeley K,<br />
Boggess J F, Basil J, Schwartz P E, Blank S V, Toland A E, Montagna<br />
M, Casella C, Imyanitov E N, Allavena A, Schmutzler R K, Versmold<br />
B, Engel C, Meindl A, Ditsch N, Arnold N, Niederacher D, Deissler<br />
H, Fiebig B, Suttner C, Schönbuchner I, Gadzicki D, Caldes T, De<br />
la Hoya M, Pooley K A, Easton D F, Chenevix-Trench G. Common<br />
variants in LSP1, 2q35 and 8q24 and breast cancer risk for BRCA1<br />
and BRCA2 mutation carriers. Human molecular genetics; 18:22;<br />
4442-4456; 2009<br />
8 Artioli G, Cassaro M, Pedrini L, Borgato L, Corti L, Cappetta A,<br />
Lombardi G, Nicoletto M O. Rare presentation of endometrial
carcinoma with singular bone metastasis. European Journal of Cancer<br />
Care; 19:5; 694-698; <strong>2010</strong> (E-pub 2009)<br />
9 Aschele C, Bergamo F, Lonardi S. Chemotherapy for operable and<br />
advanced colorectal cancer. Cancer treatment reviews; 35:6; 509-516;<br />
2009<br />
10 Atwal G S, Kirchhoff T, Bond E E, Montagna M, Menin C, Bertorelle<br />
R, Scaini M C, Bartel F, Böhnke A, Pempe C, Gradhand E, Hauptmann<br />
S, Offit K, Levine A, Bond G L. Altered tumor formation and<br />
evolutionary selection of genetic variants in the human MDM4<br />
oncogene. Proceedings of the National Academy of Sciences of the<br />
United States of America; 106:25; 10236-10241; 2009<br />
11 Aversa Savina M L, Trentin C, Sorarů M, Bona E D, Marino D,<br />
Canova F, Salvagno L, Adami F. Acute promyelocytic leukemia after<br />
Stanford V plus radiotherapy for advanced Hodgkin lymphoma.<br />
Leukemia & Lymphoma; 50:7; 1214-1216; 2009<br />
12 Baccarani U, Adani G L, Serraino D, Lorenzin D, Gambato M, Buda<br />
A, Zanus G, Vitale A, Piselli P, De Paoli A, Bresadola V, Risaliti A,<br />
Toniutto P, Cillo U, Bresadola F, Burra P. De Novo Tumors Are a Major<br />
Cause of Late Mortality After Orthotopic Liver Transplantation.<br />
Transplantation proceedings; 41:4; 1303-1305; 2009<br />
13 Banzato A, Rondina M, Meléndez-Alafort L, Zangoni E, Nadali A,<br />
Renier D, Moschini G, Mazzi U, Zanovello P, Rosato A. Biodistribution<br />
imaging of a paclitaxel-hyaluronan bioconjugate. Nuclear medicine<br />
and biology; 36:5; 525-533; 2009<br />
14 Baretta Z, Ghiotto C, Marino D, Jirillo A. Aloe-induced hypokalemia<br />
in a patient with breast cancer during chemotherapy. Annals of<br />
Oncology; 20:8; 1445-1446; 2009<br />
15 Baroncelli S, Ricci E, De Rossi A, Giuliano M. Response to Segat et al.<br />
Are DEFB1 gene polymorphisms associated with HIV-1 infection<br />
and virus replication? AIDS; 23:5; 649-650; 2009<br />
16 Basso U, Brunello A, Bertuzzi A, Santoro A. Sorafenib is active on<br />
lung metastases from synovial sarcoma. Annals of Oncology; 20:2;<br />
386-387; 2009<br />
17 Belloni-Fortina A, Piaserico S, Tonin Elena, Alaibac M. Melanoma<br />
and Immunosuppression. Dermatology; 218:1; 88; 2009 (E-pub<br />
2008)<br />
18 Berrino F, Verdecchia A, Lutz J M, Lombardo C, Micheli A, Capocaccia<br />
R, [as collab. Zambon P, Guzzinati S]. Comparative cancer survival<br />
information in Europe. European Journal of Cancer; 45:6; 901-908;<br />
2009<br />
19 Bertazza L, Mocellin S, Marchet A, Pilati P, Gabrieli J, Scalerta R,<br />
PUBLICATIONS<br />
267<br />
Nitti D. Survivin gene levels in the peripheral blood of patients with<br />
gastric cancer independently predict survival. Journal of Translational<br />
Medicine; 7; 111; 2009<br />
20 Biasco G, Velo D, Angriman I, Astorino M, Baldan A, Baseggio M<br />
Basso U, Battaglia G, Bertin M, Bertorelle R, Bocus P, Brosolo P,<br />
Bulzacchi A, Cannizzaro R, Da Dalt G F, Di Battista M, Errante D,<br />
Fedrigo M, Frustaci S, Lionetti I, Massani M, Mencarelli R, Montesco<br />
M C, Norberto L, Pantaleo M A, Pasquali C, Pastorelli D, Rossi C R,<br />
Ruffolo C, Salvagno L, Saponara M S, Vittadello F, Zaccaria F, Zovato<br />
S, Farinati F. Gastrointestinal stromal tumors: Report of an audit<br />
and review of the literature; European Journal of Cancer Prevention.<br />
18:2; 106-116; 2009<br />
21 Bilora F, Pietrogrande F, Campagnolo E, Rossato A, Polato G, Pomerri<br />
F, Muzzio P C. Are Hodgkin and non-Hodgkin patients at a greater<br />
risk of atherosclerosis? A follow-up of 3 years. European Journal of<br />
Cancer Care; 19:3; 417-419; <strong>2010</strong> (E-pub 2009)<br />
22 Bisogno G, Ferrari A, Prete A, Messina C, Basso E, Cecchetto G,<br />
Indolfi P, Scarzello G, D’Angelo P, Sio L D, Cataldo A D, Carli M.<br />
Sequential high-dose chemotherapy for children with metastatic<br />
rhabdomyosarcoma. European Journal of Cancer; 45:17; 3035-3041;<br />
2009<br />
23 Bisogno G, Ferrari A, Rosolen A, Alaggio R, Scarzello G, Garaventa<br />
A, Arcamone G, Carli M. Sequential intensified chemotherapy with<br />
stem cell rescue for children and adolescents with desmoplastic small<br />
round-cell tumor. Bone marrow transplantation; 45; 907-911; 2009<br />
24 Bobisse S, Rondina M, Merlo A, Tisato V, Mandruzzato S, Amendola<br />
M, Naldini L, Willemsen R. A, Debets R, Zanovello P, Rosato A.<br />
Reprogramming T lymphocytes for melanoma adoptive<br />
immunotherapy by T-cell receptor gene transfer with lentiviral<br />
vectors. Cancer research; 69:24; 9385-9394; 2009<br />
25 Bordignon M, Belloni-Fortina A, Pigozzi B, Tarantello M, Alaibac M.<br />
Bullous pemphigoid during long-term TNF1-α blocker therapy.<br />
Dermatology; 219:4; 357-358 2009<br />
26 Boscolo-Rizzo P, Da Mosto M C, Fuson R, Frayle-Salamanca H,<br />
Trevisan R, Del Mistro A. HPV-16 E6 L83V variant in squamous<br />
cell carcinomas of the upper aerodigestive tract. Journal of cancer<br />
research and clinical oncology; 135:4; 559-566 2009 (E-pub 2008)<br />
27 Brandes A A, Tosoni A, Franceschi E, Sotti G, Frezza G, Amistà P,<br />
Morandi L, Spagnolli F, Ermani M. Recurrence pattern after<br />
temozolomide concomitant with and adjuvant to radiotherapy<br />
in newly diagnosed patients with glioblastoma: Correlation with
MGMT promoter methylation status. Journal of Clinical Oncology;<br />
27:8; 1275-1279; 2009<br />
28 Brenner H, Francisci S, De Angelis R, Marcos-Gragera R, Verdecchia<br />
A, Gatta G, Allemani C, Ciccolallo L, Coleman M, Sant M,<br />
EUROCARE WG [as collab. Guzzinati S, Zambon P]. Long-term<br />
survival expectations of cancer patients in Europe in 2000-2002.<br />
European Journal of Cancer 45:6; 1028-1041; 2009<br />
29 Bronte V. Myeloid-derived suppressor cells in inflammation:<br />
Uncovering cell subsets with enhanced immunosuppressive<br />
functions. European Journal of Immunology; 39:10; 2670-2672;<br />
2009<br />
30 Bronte V, Mocellin S. Suppressive influences in the immune response<br />
to cancer. Journal of Immunotherapy; 32:1; 1-11 2009<br />
31 Brunello A, Loaldi E, Balducci L. Dose adjustment and supportive<br />
care before and during treatment. Cancer treatment reviews; 35:6;<br />
493-498; 2009<br />
32 Brunello A, Saia G, Bedogni A, Scaglione D, Basso U. Worsening of<br />
osteonecrosis of the jaw during treatment with sunitinib in a patient<br />
with metastatic renal cell carcinoma. Bone; 44:1; 173-175; 2009<br />
(E-pub 2008)<br />
33 Brunello A, Sandri R, Extermann M. Multidimensional geriatric<br />
evaluation for older cancer patients as a clinical and research tool.<br />
Cancer treatment reviews; 35:6; 487-492; 2009<br />
34 Bruno W, Ghiorzo P, Battistuzzi L, Ascierto P A, Barile M, Gargiulo<br />
S, Gensini F, Gliori S, Guida M, Lombardo M, Manoukian Menin C,<br />
Nasti S, Origone P, Pasini B, Pastorino L, Peissel B, Pizzichetta M A,<br />
Queirolo P, Rodolfo M, Romanini A, Scaini M C,Testori A,Tibiletti<br />
M G,Turchetti D, Leachman S A, Bianchi Scarrà G. Clinical genetic<br />
testing for familial melanoma in Italy: A cooperative study. Journal<br />
of the American Academy of Dermatology; 61:5; 775-782; 2009<br />
35 Burra P, Loreno M, Russo F P, Germani G, Galligioni A, Senzolo<br />
M, Cillo U, Zanus G, Fagluoli S, Ruggo M. Donor livers with<br />
steatosis are safe to use in hepatitis C virus-positive recipients. Liver<br />
Transplantation; 15:6; 619-628; 2009<br />
36 Cagol M, Ruol A, Castoro C, Alfieri R, Michieletto S, Ancona E.<br />
Prophylactic thoracic duct mass ligation prevents chylothorax after<br />
transthoracic esophagectomy for cancer. World journal of surgery;<br />
33:8; 1684-1686; 2009<br />
37 Calabrese F, Loy M, Lunardi F, Marino D, Aversa Savina M L, Rea<br />
F. Acute cellular rejection and Epstein-Barr virus-related posttransplant<br />
lymphoproliferative disorder in a pediatric lung transplant<br />
PUBLICATIONS<br />
268<br />
with low viral load. Transplant infectious disease; 12:4; 342-346;<br />
<strong>2010</strong> (E-pub 2009)<br />
38 Calabrò L, Gasperini P, Di Gangi I M, Indraccolo S, Barbierato M,<br />
Amadori A, Chieco-Bianchi L. Antineoplastic activity of lentiviral<br />
vectors expressing interferon-αlpha in a preclinical model of primary<br />
effusion lymphoma. Blood; 113:19; 4525-4533; 2009<br />
39 Campana L G, Mocellin S, Basso M, Puccetti O, De Salvo G L, Chiarion-<br />
Sileni V, Vecchiato A, Corti L, Rossi C R, Nitti D. Bleomycin-based<br />
electrochemotherapy: Clinical outcome from a single institution’s<br />
experience with 52 patients. Annals of Surgical Oncology; 16:1;<br />
191-199; 2009<br />
40 Capocaccia R, Martina L, Inghelmann R, Croeetti E, De Lisi V, Falcini<br />
F, Guzzinati S, Rosso S, Tagliabue G, Tumino R, Vercelli M, Zanetti<br />
R, De Angelis R. A method to estimate mortality trends when death<br />
certificates are Imprecisely coded: an application to cervical cancer<br />
in Italy. International Journal of Cancer; 124:5; 1200-1205; 2009<br />
41 Caumo F, Vecchiato F, Pellegrini M, Vettorazzi M, Ciatto S, Montemezzi<br />
S. Analysis of interval cancers observed in an Italian mammography<br />
screening programme (2000-2006). Radiologia Medica; 114:6;<br />
907-914; 2009<br />
42 Cavallari I, Micol S B, Rende F, Martines A, Fogar P, Basso D, Vella<br />
M D, Pedrazzoli S, Herman J G, Chieco Bianchi L, Esposito G,<br />
Ciminale V, D’Agostino D M. Decreased expression and promoter<br />
methylation of the menin tumor suppressor in pancreatic ductal<br />
Adenocarcinoma. Genes, Chromosomes and Cancer; 48:5; 383-396;<br />
2009<br />
43 Cecchin D, Chondrogiannis S, Puppa A D, Rotilio A, Zustovich<br />
F, Manara R, Gardiman M, Berti F, Zucchetta P, Carollo C, Bui F.<br />
Presurgical 99mTc-sestamibi brain SPET/CT versus SPET: A<br />
comparison with MRI and histological data in 33 patients with<br />
brain tumors. Nuclear medicine communications 30:9; 660-668;<br />
2009<br />
44 Chiarelli S, Padoan I, Parenti A, Ninfo V, D’Andrea E. Pathologic<br />
findings in 200 consecutive fallopian tube specimens. Human<br />
pathology; 40:4; 603-604; 2009<br />
45 Chiarion-Sileni V, Innocente R, Cavina R, Ruol A, Corti L, Pigozzo<br />
J, Del Bianco P, Fumagalli U, Santoro A, Ancona E. Multi-center<br />
phase II trial of chemo-radiotherapy with 5-fluorouracil, leucovorin<br />
and oxaliplatin in locally advanced esophageal cancer. Cancer<br />
chemotherapy and pharmacology; 63:6; 1111-1119; 2009 (E-pub<br />
2008)
46 Ciccolallo L, Licitra L, Cantù G, Gatta G, EUROCARE WG [as collab.<br />
Guzzinati S, Zambon P]. Survival from salivary glands adenoid cystic<br />
carcinoma in European populations. Oral oncology; 45:8; 669-674;<br />
2009<br />
47 Colavito D, Cartei G, Dal Bianco M, Stecca A, Zustovich F, Dalle<br />
Carbonare M, Ragazzi E, Farina M, Colombrino E, Leon A.<br />
Thymidylate synthetase allelic imbalance in clear cell renal carcinoma.<br />
Cancer chemotherapy and pharmacology; 64:6; 1195-1200; 2009<br />
48 Colombatti R, Calò A, Iacopetti T, Rosolen A, Lombardi G, Cesaro<br />
S. Successful treatment of severe iatrogenic calcinosis cutis with<br />
intravenous sodium thiosulfate in a child affected by T-acute<br />
lymphoblastic leukemia. Pediatric dermatology; 26:3; 311-315;<br />
2009<br />
49 Coltrini D, Ronca R, Belleri M, Zardi L, Indraccolo S, Scarlato V,<br />
Giavazzi R, Presta M. Impact of VEGF-dependent tumor microenvironment<br />
on EDB fibronectin expression by subcutaneous<br />
human tumor xenografts in nude mice. Journal of Pathology; 219:4;<br />
455-462; 2009<br />
50 Comper F, Antonello D, Beghelli S, Gobbo S, Montagna L, Pederzoli<br />
P, Chilosi M, Scarpa A. Expression pattern of claudins 5 and 7<br />
distinguishes solid-pseudopapillary from pancreatoblastoma, acinar<br />
cell and endocrine tumors of the pancreas. American Journal of<br />
Surgical Pathology; 33:5; 768-774; 2009<br />
51 Dal Maso L, Polesel J, Serraino D, Lise M, Piselli P, Falcini F, Russo<br />
A, Intrieri T, Vercelli M, Zambon P, Tagliabue G, Zanetti R, Federico<br />
M, Limina R M, Mangone L, De Lisi V, Stracci F, Ferretti S, Piffer S,<br />
Budroni M, Donato A, Giacomin A, Bellù F, Fusco M, Madeddu A,<br />
Vitarelli S, Tessandori R, Tumino R, Suligoi B, Franceschi S. Cancer<br />
and AIDS Registries Linkage, (CARL Study). Pattern of cancer risk<br />
in persons with AIDS in Italy in the HAART era. British journal of<br />
cancer; 100:5; 840-847; 2009<br />
52 Dall’Igna P, Cecchetto G, Bisogno G, Conte M, Chiesa P L, D’Angelo<br />
P, De Leonardis F, De Salvo G L, Favini F, Ferrari A. On Behalf of<br />
the TREP Group; Pancreatic tumors in children and adolescents:<br />
the Italian TREP project experience. Pediatric Blood & Cancer; 54:5;<br />
675-680; 2009<br />
53 D’Amico F, Schwartz M, Vitale A, Tabrizian P, Roayaie S, Thung S,<br />
Guido M, Martin J D R, Schiano T, Cillo U. Predicting recurrence<br />
after liver transplantation in patients with hepatocellular carcinoma<br />
exceeding the up-to-seven criteria. Liver Transplantation; 15:10;<br />
1278-1287; 2009<br />
PUBLICATIONS<br />
269<br />
54 De Angelis R, Francisci S, Baili P, Marchesi F, Roazzi P, Belot A,<br />
Crocetti E, Pury P, Knijn A, Coleman M, Capocaccia R, The<br />
EUROCARE-4,WG [as collab. Guzzinati S, Zambon P]. The<br />
EUROCARE-4 database on cancer survival in Europe: data<br />
standardisation, quality control and methods of statistical analysis.<br />
European Journal of Cancer; 45:6; 909-930; 2009<br />
55 De Corti F, Dall’Igna P, Bisogno G, Casara D, Rossi C R, Foletto M,<br />
Alaggio R, Carli M, Cecchetto G. Sentinel node biopsy in pediatric<br />
soft tissue sarcomas of extremities. Pediatric Blood & Cancer; 52:1;<br />
51-54; 2009<br />
56 De Rossi C, Brunello A, Jirillo G, Jirillo A. When an interim analysis<br />
of randomized trial changes the practice in oncology: the lesson of<br />
adjuvant trastuzumab and the HERA trial. Immunopharmacology &<br />
Immunotoxicology; 31:1; 1-4; 2009 (E-pub 2008)<br />
57 Della Puppa A, Dal Pos S, Zovato S, Orvieto E, Ciccarino P, Manara<br />
R, Zustovich F, Berti F, Gardiman M P, Scienza R. Solitary intraventricular<br />
brain metastasis from a breast carcinoma. Journal of<br />
Neuro - Oncology; 97:1; 123-126; 2009<br />
58 Di Filippo F, Giacomini P, Rossi C R, Santinami M, Anzà M,<br />
Garinei R, Perri P, Botti C, Di Angelo P, Sofra C, Pasqualoni R,<br />
Sperduti I, Cavaliere F, Di Filippo S, Corrias F, Armenti A, Ferraresi<br />
V, Ginebri A. Prognostic factors influencing tumor response,<br />
locoregional control and survival, in melanoma patients with<br />
multiple limb in-transit metastases treated with TNF1-α based<br />
isolated limb perfusion. In Vivo; 23:2; 347-352; 2009<br />
59 Erlic Z, Rybicki L, Peczkowska M, Golcher H, Kann P H, Brauckhoffm<br />
Müssig K, Muresan M, Schäffler A, Reisch N, Schott M, Fassnacht M,<br />
Opocher G, Klose S, Fottner C, Forrer F, Plöckinger U, Petersenn S,<br />
Zabolotny D, Kollukch O, Yaremchuk S, Januszewicz A, Walz M K,<br />
Eng C, Neumann H P H. Clinical predictors and algorithm for the<br />
genetic diagnosis of pheochromocytoma patients. Clinical Cancer<br />
Research; 15:20; 6378-6385; 2009<br />
60 Falci C, Morello E, Droz J P, Treatment of prostate cancer in unfit<br />
senior adult patients. Cancer treatment reviews; 35:6; 522-527;<br />
2009<br />
61 Fassan M, Castoro C, Saenz A J, Cagol M, Ninfo V, Rugge M.<br />
Inflammatory myofibroblastic tumor as adverse outcome of<br />
eosinophilic esophagitis. Endoscopy; 41: Suppl 2; e95-e96; 2009<br />
62 Favaretto A G, Pasello G, Loreggian L, Breda C, Braccioni F, Marulli<br />
G, Stragliotto S, Magro C, Sotti G, Rea F. Preoperative concomitant<br />
chemo-radiotherapy in superior sulcus tumor: a mono-institutional
experience. Lung Cancer; 68:2; 228-233; <strong>2010</strong> (E-pub 2009)<br />
63 Favaretto A G, Pasello G, Magro C, Schettino C, Gridelli C. Second<br />
and third line treatment in non-small cell lung cancer. Critical<br />
reviews in oncology/hematology; 71:2; 117-126; 2009<br />
64 Ficarra V, Novara G. Editorial Comment on: Cytological Punctures<br />
in the Diagnosis of Renal Tumors: A Study on Accuracy and<br />
Reproducibility. European urology; 55:1; 196; 2009<br />
65 Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M,<br />
Retropubic. Laparoscopic, and Robot-Assisted Radical Prostatectomy:<br />
A Systematic Review and Cumulative Analysis of Comparative<br />
Studies European urology; 55:5; 1037-1063; 2009<br />
66 Ficarra V, Novara G, Boscolo-Berto R, Artibani W, Kattan M W.<br />
How accurate are present risk group assignment tools in penile<br />
cancer? World journal of urology; 27:2; 155-160; 2009<br />
67 Ficarra V, Novara G, Fracalanza S, D’Elia C, Secco S, Iafrate<br />
M, Cavalleri S, Artibani W. A prospective, non-randomized<br />
trial comparing robot-assisted laparoscopic and retropubic radical<br />
prostatectomy in one european institution. BJU international; 104:4;<br />
534-539; 2009<br />
68 Ficarra V, Novara G, Galfano A, Brunelli M, Cavalleri S, Martignoni<br />
G, Artibani W. The ‘Stage, Size, Grade and Necrosis’ score is more<br />
accurate than the University of California Los Angeles Integrated<br />
Staging System for predicting cancer-specific survival in patients<br />
with clear cell renal cell carcinoma BJU international; 103:2;<br />
165-170; 2009<br />
69 Ficarra V, Novara G, Galfano A. Precursor Isoform of Prostate-<br />
Specific Antigen and Human Kallikrein 2: Two New Promising<br />
Biomarkers for the Unsolved Challenge of Early Prostate Cancer<br />
Detection. European urology; 55:3; 556-559; 2009<br />
70 Ficarra V, Novara G, Martignoni G. The Use of Simplified Versions of<br />
the Fuhrman Nuclear Grading System in Clinical Practice Requires<br />
the Agreement of a Multidisciplinary Panel of Experts. European<br />
urology; 56:5; 782-783; 2009<br />
71 Ficarra V, Novara Giacomo, Secco S, D’Elia C, Boscolo-Berto R,<br />
Gardiman M. Predictors of Positive Surgical Margins After<br />
Laparoscopic Robot Assisted Radical Prostatectomy. Journal of<br />
Urology; 182:6; 2682-2688; 2009<br />
72 Ficarra V, Novara G, Secco S, Macchi V, Porzionato A, De Caro R.<br />
Preoperative Aspects and Dimensions Used for an Anatomical<br />
(PADUA) Classification of Renal Tumors in Patients who are<br />
Candidates for Nephron-Sparing Surgery. European urology; 56:5;<br />
PUBLICATIONS<br />
270<br />
786-793; 2009<br />
73 Filen A, Magnavita N, Pescarini L. Analysis of malpractice claims<br />
in mammography: A complex issue. Radiologia Medica; 114:4;<br />
636-644; 2009<br />
74 Franceschi S, Dal Maso L, Zucchetto A, Talamini R, PACE SG [as<br />
collab. Stocco C F, Zambon P]. Alcohol consumption and survival<br />
after breast cancer. Cancer Epidemiology Biomarkers & Prevention;<br />
18:3; 1011-1012; 2009<br />
75 Francisci S, Capocaccia R, Grande E, Santaquilani M, Simonetti A,<br />
Allemani C, Gatta G, Sant M, Zigon G, Bray F, Janssen-Heijnen M,<br />
EUROCARE WG [as collab. Guzzinati S, Zambon P]. The cure of<br />
cancer: A European perspective. European Journal of Cancer; 45:6;<br />
1067-1079; 2009<br />
76 Frego M, Bridda A, Ruffolo C, Scarpa M, Polese L, Bianchera G. The<br />
hostile neck does not increase the risk of carotid endarterectomy.<br />
Journal of Vascular Surgery; 50:1; 40-47; 2009<br />
77 Garoli D, Pelizzo M G, Nicolosi P, Peserico A, Tonin E, Alaibac M.<br />
Effectiveness of different substrate materials for in vitro sunscreen<br />
tests. Journal of dermatological science; 56:2; 89-98; 2009<br />
78 Garolla A, Dinc R, Checchin D, Biagioli A, De Toni L, Nicoletti<br />
V, Scarpa M, Bolzonello E, Sturniolo G C, Foresta C. Reduced<br />
endothelial progenitor cell number and function in inflammatory<br />
bowel disease: A possible link to the pathogenesis. American Journal<br />
of Gastroenterology; 104:10; 2500-2507; 2009<br />
79 Gatta G, Zigon G, Capocaccia R, Coebergh J W, Desandes E, Kaatsch<br />
P, Pastore G, Peris-Bonet R, Stiller C A, EUROCARE WG [as collab.<br />
Guzzinati S, Zambon P]. Survival of European children and young<br />
adults with cancer diagnosed 1995-2002. European Journal of<br />
Cancer; 45:6; 992:1005; 2009<br />
80 Gennaro G, Toledano A, Di Maggio C, Baldan E, Bezzon E, La<br />
Grassa M, Pescarini L, Polico I, Proietti A, Toffoli A, Muzzio P C.<br />
Digital breast tomosynthesis versus digital mammography: a clinical<br />
performance study. European radiology; 20:7; 1545-1553; <strong>2010</strong><br />
(E-pub 2009)<br />
81 Gratwohl A, Baldomero H, Schwendener A, Rocha V, Apperley J,<br />
Frauendorfer K, Niederwieser D, EBMT WG [as collab. Aversa Savina<br />
M L]. The EBMT activity survey 2007 with focus on allogeneic<br />
HSCT for AML and novel cellular therapies. Bone marrow<br />
transplantation; 43:4; 275-291; 2009<br />
82 Grazzini G, Visioli C B, Zorzi M, Ciatto S, Banovich F, Bonanomi<br />
A G, Bortoli A, Castiglione G, Cazzola L, Confortini M, Mantellini
P, Rubeca T, Zappa M. Immunochemical faecal occult blood test:<br />
Number of samples and positivity cutoff. What is the best strategy<br />
for colorectal cancer screening? British journal of cancer; 100:2;<br />
259-265; 2009<br />
83 Gringeri E, Carraro A, Tibaldi E, D’Amico F E, Mancon M, Toninello<br />
A, Pagano M A, Vio C, Cillo U, Brunati A M. Lyn-mediated<br />
mitochondrial tyrosine phosphorylation is required to preserve<br />
mitochondrial integrity in early liver regeneration. Biochemical<br />
Journal; 425:2; 401-412; 2009<br />
84 Hersey P, Bastholt L, Chiarion-Sileni V, Cinat G, Dummer R,<br />
Eggermont A M, Espinosa E, Hauschild A, Quirt I, Robert C,<br />
Schadendorf D. Small molecules and targeted therapies in distant<br />
metastatic disease. Annals of Oncology; 20; Suppl 6; vi35-vi40; 2009<br />
85 Iacobone M, Barzon L, Porzionato A, Masi G, Macchi V, Viel G,<br />
Favia G. The extent of parathyroidectomy for HRPT2-related<br />
hyperparathyroidism. Surgery; 145:2; 250-251; 2009<br />
86 Indraccolo S, Minuzzo S, Masiero M, Pusceddu I, Persano L, Moserle<br />
L, Reboldi A, Favaro E, Mecarozzi M, Di Mario G, Screpanti I,<br />
Ponzoni M, Doglioni C, Amadori A. Cross-talk between tumor and<br />
endothelial cells involving the Notch3-DII4 interaction marks<br />
escape from tumor dormancy. Cancer research; 69:4; 1314-1323;<br />
2009<br />
87 Ingravallo G, Dall’Olmo L, Segat D, Fassan M, Mescoli C, Dazzo E,<br />
Castoro C, Polimeno L, Rizzetto C, Baroni M D, Zaninotto G, Ancona<br />
E, Rugge M. CDX2 hox gene product in a rat model of esophageal<br />
cancer. Journal of Experimental and Clinical Cancer Research; 28; 1;<br />
2009<br />
88 Jori G, Soncin M, Friso E, Vicente M G H, Hao E, Miotto G, Colautti<br />
P, Moro D, Esposito J, Rosi G, Nava E, Sotti G, Fabris C. A novel<br />
boronated-porphyrin as a radio-sensitizing agent for boron neutron<br />
capture therapy of tumors: In vitro and in vivo studies. Applied<br />
Radiation and Isotopes; 67:Suppl 7-8; 321-324; 2009<br />
89 Klug S J, Ressing M, Koenig J, Abba M C, Agorastos T, Brenna S M,<br />
Ciotti M, Das B R, Del Mistro A, Dybikowska A, Giuliano A R,<br />
Gudleviciene Z, Gyllensten U, Haws A L, Helland A, Herrington C S,<br />
Hildesheim A, Humbey O, Jee S H, Kim J W, Madeleine M M, Menczer<br />
J, Ngan H Y, Nishikawa A, Niwa Y, Pegoraro R, Pillai M R, Ranzani<br />
G, Rezza G, Rosenthal A N, Roychoudhury S, Saranath D, Schmitt<br />
V M, Sengupta S, Settheetham-Ishida W, Shirasawa H, Snijders P J,<br />
Stoler M H, Suàrez-Rincòn A E, Szarka K, Tachezy R, Ueda M, Van<br />
Der Zee A G, von Knebel Doeberitz M, Wu M. -T, Yamashita T, Zehbe<br />
PUBLICATIONS<br />
271<br />
I, Blettner M. TP53 codon 72 polymorphism and cervical cancer: a<br />
pooled analysis of individual data from 49 studies. Lancet Oncology;<br />
10:8; 772-784; 2009<br />
90 Landa I, Ruiz-Llorente S, Montero-Conde C, Inglada-Pérez L,<br />
Schiavi F, Leskelä S, Pita G, Milne R, Maravall J, Ramos I, Andìa V,<br />
Rodrìguez-Poyo P, Jara-Albarràn A, Meoro A, Del Peso C, Arribas L,<br />
Iglesias P, Caballero J, Serrano J, Picò A, Pomares F, Giménez G, Lòpez-<br />
Mondéjar P, Castello R, Merante-Boschin I, Pelizzo M-R, Mauricio D,<br />
Opocher G, Rodrìguez-Antona C, Gonzàlez-Neira A, Matìas-Guiu X,<br />
Santisteban P, Robledo M. The variant rs1867277 in FOXE1 gene<br />
confers thyroid cancer susceptibility through the recruitment of<br />
USF1/USF2 transcription factors. PLoS Genetics; 5:9; e1000637;<br />
2009<br />
91 Lombardi G, Zustovich F, Nicoletto M O, Donach M, Artioli G,<br />
Pastorelli D. Diagnosis and Treatment of Malignant Pleural Effusion:<br />
A Systematic Literature Review and New Approaches. American<br />
journal of clinical oncology; 33:4; 420-423; <strong>2010</strong> (E-pub 2009)<br />
92 Lumachi F, Borsato S, Tregnaghi A, Marino F, Polistina F, Basso S M<br />
M, Koussis H, Basso U, Fassina A. FNA cytology and frozen section<br />
examination in patients with follicular lesions of the thyroid gland.<br />
Anticancer Research; 29:12; 5255-5257; 2009<br />
93 Lumachi F, Brunello A, Roma A, Basso U. Cancer-induced<br />
hypercalcemia Anticancer Research; 29:5; 1551-1555; 2009<br />
94 Lumachi F, Marino F, Varotto S, Basso U. Oligonucleotide probe<br />
array for p53 gene alteration analysis in DNA from formalin-fixed<br />
paraffin-embedded breast cancer tissues. Annals of the New York<br />
Academy of Sciences; 1175; 89-92; 2009<br />
95 Luster M, Handkiewicz-Junak D, Grossi A, Zacharin M, Taïeb D, Cruz<br />
O, Hitzel A, Casas J A V, Mäder U, Dottorini M E, Pediatric rhTSH<br />
IG [as invest. Mazzarotto R, Vianello F]. Recombinant thyrotropin<br />
use in children and adolescents with differentiated thyroid cancer:<br />
A multicenter retrospective study. Journal of Clinical Endocrinology<br />
and Metabolism; 94:10; 3948-3953; 2009<br />
96 Mammano E, Belluco C, Bonafé M, Olivieri F, Mugianesi E, Barbi<br />
C, Mishto M, Cosci M, Franceschi C, Lise M, Nitti D. Association of<br />
p53 polymorphisms and colorectal cancer: Modulation of risk and<br />
progression. European Journal of Surgical Oncology; 35:4; 415-419;<br />
2009 (E-pub 2008)<br />
97 Mammano E, Cosci M, Zanon A, Picchi G, Tessari E, Pilati P, Nitti<br />
D. Celiomesenteric Trunk Aneurysm. Annals of Vascular Surgery;<br />
23(2):257; e9-e12; 2009
98 Mandruzzato S, Solito S, Falisi E, Francescato S, Chiarion-Sileni<br />
V, Mocellin S, Zanon A, Rossi C R, Nitti D, Bronte V, Zanovello P.<br />
IL4R-α+ myeloid-derived suppressor cell expansion in cancer<br />
patients. Journal of Immunology; 182:10; 6562-6568; 2009<br />
99 Mannelli M, Castellano M, Schiavi F, Filetti S, Giacchè M, Mori L,<br />
Pignataro V, Bernini G, Giachè V, Bacca A, Biondi B, Corona G, Di<br />
Trapani G, Grossrubatscher E, Reimondo G, Arnaldi G, Giacchetti G.,<br />
Veglio F, Loli P, Colao A, Ambrosio M R, Terzolo M, Letizia C, Ercolino<br />
T, Opocher G. Clinically guided genetic screening in a large cohort<br />
of Italian patients with pheochromocytomas and/or functional or<br />
nonfunctional paragangliomas. Journal of Clinical Endocrinology and<br />
Metabolism; 94:5; 1541-1547; 2009<br />
100 Marioni G, Koussis H, Gaio E, Giacomelli L, Bertolin A, D’Alessandro E,<br />
Scola A, Ottaviano G, De Filippis C, Jirillo A, Staffieri A, Blandamura<br />
S. MASPIN’s prognostic role in patients with advanced head and<br />
neck carcinoma treated with primary chemotherapy (carboplatin<br />
plus vinorelbine) and radiotherapy: Preliminary evidence. Acta Oto-<br />
Laryngologica; 129:7; 786-792; 2009<br />
101 Mazzaferro V, Llovet J M, Miceli R, Bhoori S, Schiavo M, Mariani L,<br />
Camerini T, Roayaie S, Schwartz M E, Grazi G L, Adam R, Neuhaus<br />
P, Salizzoni M, Bruix J, Forner A, De Carlis L, Cillo U, Burroughs<br />
A K, Troisi R, Rossi M, Gerunda G E, Lerut J, Belghiti J, Boin I,<br />
Gugenheim J, Rochling F, Van Hoek B, Majno P, Metroticket ISG [as<br />
collab. Vitale A]. Predicting survival after liver transplantation in<br />
patients with hepatocellular carcinoma beyond the Milan criteria:<br />
a retrospective, exploratory analysis Lancet Oncology; 10:1; 35-43;<br />
2009 (E-pub 2008)<br />
102 Melandez-Alafort L, Nadali A, Zangoni E, Banzato A, Rondina M,<br />
Rosato A, Mazzi U. Biokinetic and dosimetric studies of 188Rehyaluronic<br />
acid: a new radiopharmaceutical for treatment of<br />
hepatocellular carcinoma. Nuclear medicine and biology; 36:6;<br />
693-701; 2009<br />
103 Mian C, Barollo S, Zambonin L, Pennelli G, Bernante P, Pelizzo M R,<br />
Nacamulli D, Mantero F, Girelli M E, Opocher G. Characterization<br />
of the largest kindred with MEN2A due to a Cys609Ser RET<br />
mutation. Familial Cancer; 8:4; 379-382; 2009<br />
104 Micheli A, Ciampichini R, Oberaigner W, Ciccolallo L, De Vries E,<br />
Izarzugaza I, Zambon P, Gatta G, De Angelis R. The advantage of<br />
women in cancer survival: An analysis of EUROCARE-4 data.<br />
European Journal of Cancer; 45:6; 1017-1027; 2009<br />
105 Mocellin S, Thompson J F, Pasquali S, Montesco M C, Pilati P, Nitti<br />
PUBLICATIONS<br />
272<br />
D, Saw R P, Scolyer R A, Stretch J R, Rossi C R. Sentinel node status<br />
prediction by four statistical models: Results from a large biinstitutional<br />
series (n=1132). Annals of Surgery; 250:6; 964-969;<br />
2009<br />
106 Moserle L, Amadori A, Indraccolo S. The angiogenic switch:<br />
Implications in the regulation of tumor dormancy. Current Molecular<br />
Medicine; 9:8; 935-941; 2009<br />
107 Moserle L, Ghisi M, Amadori A, Indraccolo S. Side population and<br />
cancer stem cells: Therapeutic implications. Cancer letters; 288:1;<br />
1-9; 2009<br />
108 Mussolin L, Bonvini P, Ait-Tahar K, Pillon M, Tridello G, Buffardi S,<br />
Lombardi A, Pulford K, Rosolen A. Kinetics of humoral response to<br />
ALK and its relationship with minimal residual disease in pediatric<br />
ALCL. Leukemia; 23:2; 400-402; 2009 (E-pub 2008)<br />
109 Neumann H P H, Erlic Z, Boedeker C C, Rybicki L A, Robledo M,<br />
Hermsen M, Schiavi F, Falcioni M, Kwok P, Bauters C, Lampe K,<br />
Fischer M, Edelman E, Benn D E, Robinson B G, Wiegand S, Rasp<br />
G, Stuck B A, Hoffmann M M, Sullivan M, Sevilla M A, Weiss M M,<br />
Peczkowska M, Kubaszek A, Pigny P, Ward R L, Learoyd D, Croxson M,<br />
Zabolotny D, Yaremchuk S, Dra W, Muresan M, Lorenz R R, Knipping<br />
S, Strohm M, Dyckhoff G, Matthias C, Reisch N, Preuss S F, Esser D,<br />
Walter M A, Kaftan H, Stöver T, Fottner C, Gorgulla H, Malekpour M,<br />
Zarandy M M, Schipper J, Brase C, Glien A, Kühnemund M, Koseielny<br />
S, Schwerdtfeger P, Välimäki M, Szyfter W, Finckh U, Zerres K, Cascon<br />
A, Opocher G, Ridder G J, Januszewicz A, Suarez C, Eng C. Clinical<br />
predictors for germline mutations in Head and neck paraganglioma<br />
patients: cost reduction strategy in Genetic diagnostic process as failout.<br />
Cancer research; 69:8; 3650-3656; 2009<br />
110 Nicoletto M O, Bertorelle R, Borgato L, De Salvo G L, Artioli G,<br />
Lombardi G, Zustovich F, Marcato R, Parenti A, Montagna M, Donach<br />
M E. Family history of cancer rather than p53 status predicts efficacy<br />
of pegylated liposomal doxorubicin and oxaliplatin in relapsed<br />
ovarian cancer. International Journal of Gynecological Cancer; 19:6;<br />
1022-1028; 2009<br />
111 Nitti D, Marchet A, Mocellin S, Rossi G M, Ambrosi A, Mencarelli R.<br />
Prognostic value of subclassification of T2 tumors in patients with<br />
gastric cancer. British Journal of Surgery; 96:4; 398-404; 2009<br />
112 Novara G. Editorial Comment on: Mode-of-Action, Efficacy, and<br />
Safety of a Homologous Multi-Epitope Vaccine in a Murine Model<br />
for Adjuvant Treatment of Renal Cell Carcinoma. European urology;<br />
56:1; 131-132; 2009
113 Novara G, De Marco V, Aragona M, Boscolo-Berto R, Cavalleri S,<br />
Artibani W. Complications and Mortality After Radical Cystectomy<br />
for Bladder Transitional Cell Cancer. Journal of Urology; 182:3; 914-<br />
921; 2009<br />
114 Novara G, Ficarra V. Robotic-assisted laparoscopic radical cystectomy:<br />
Where do we stand? International journal of clinical practice; 63:2;<br />
185-188; 2009<br />
115 Novara G, Galfano A, Secco S, Ficarra V, Artibani W. Impact of surgical<br />
and medical castration on serum testosterone level in prostate cancer<br />
patients. Urologia internationalis; 82:3; 249-255; 2009<br />
116 Opocher G, Boaretto F, Pignataro V, Demattè S, Cecchini M E, Erlic<br />
Z, Schiavi F. The pheochromocytoma and paraganglioma syndrome:<br />
Founder effects and the PGL 1 syndrome. Annales d’Endocrinologie;<br />
70:3; 157-160; 2009<br />
117 Osorio A, Milne R L, Pita G, Peterlongo P, Heikkinen T, Simard<br />
J, Chenevix-Trench G, Spurdle A B, Beesley J, Chen X, Healey S,<br />
Neuhausen S L, Ding Y C, Couch F J, Wang X, Lindor N, Manoukian<br />
S, Barile M, Viel A, Tizzoni L, Szabo C I, Foretova L, Zikan M, Claes<br />
K, Greene M H, Mai P, Rennert G, Lejbkowicz F, Barnett-Griness O,<br />
Andrulis I L, Ozcelik H, Weerasooriya N, Gerdes A-M, Thomassen M,<br />
Cruger D G, Caligo M A, Friedman E, Kaufman B, Laitman Y, Cohen<br />
S, Kontorovich T, Gershoni-Baruch R, Dagan E, Jernstrom H, Askmalm<br />
M S, Arver B, Malmer B, Domchek S M, Nathanson K L, Brunet J,<br />
Ramon Y C, Yannoukakos D, Hamann U, Hogervorst F B L, Verhoef<br />
S, Garcia EB G, Wijnen J T, Van den Ouweland, Easton D F, Peock S,<br />
Cook M, Oliver C T, Frost D, Luccarini C, Evans D G, Lalloo F, Eeles<br />
R, Pichert G, Cook J, Hodgson S, Morrison P J, Douglas F, Godwin A<br />
K, Sinilnikova O M, Barjhoux L, Stoppa-Lyonnet D, Moncoutier V,<br />
Giraud S, Cassini C, Olivier-Faivre L, Revillion F, Peyrat J-P, Muller<br />
D, Fricker J-P, Lynch H T, John E M, Buys S, Daly M, Hopper J L,<br />
Terry M B, Miron A, Yassin Y, Goldgar D, Singer C F, Gschwantler-<br />
Kaulich D, Pfeiler G, Spiess A-C, Hansen Thomas v. O, Johannsson<br />
O T, Kirchhoff T, Offit K, Kosarin K, Piedmonte M, Rodriguez G C,<br />
Wakeley K, Boggess J F, Basil J, Schwartz P E, Blank S V, Toland A E,<br />
Montagna M, Casella C, Imyanitov E N, Allavena A, Schmutzler R<br />
K, Versmold B, Engel C, Meindl A, Ditsch N, Arnold N, Niederacher<br />
D, Deisler H, Fiebig B, Varon-Mateeva R, Schaefer D, Froster U G,<br />
Caldes T, De la Hoya, McGuffog L, Antoniou A C, Nevanlinna H,<br />
Radice P, Benitez J. Evaluation of a candidate breast cancer associated<br />
SNP in ERCC4 as a risk modifier in BRCA1 and BRCA2 mutation<br />
carriers. Results from the consortium of investigators of modifiers of<br />
PUBLICATIONS<br />
273<br />
BRCA1/BRCA2 (CIMBA). British journal of cancer; 101:12; 2048-<br />
2054; 2009<br />
118 Paccagnella A, Ghini M G, Loreggian L, Buffoli A, Koussis H, Mione<br />
C A, Bonetti A, Campostrini F, Gardani G, Ardizzoia A, Dondi D,<br />
Guaraldi M, Cavallo R, Tomio L, Gava A, Gruppo di Studio Tumori<br />
della Testa e del Collo. Concomitant chemoradiotherapy versus<br />
induction docetaxel, cisplatin and 5 fluorouracil (TPF) followed<br />
by concomitant chemoradiotherapy in locally advanced head and<br />
neck cancer: a phase II randomized study Annals of Oncology; 21:7;<br />
1115-1123; <strong>2010</strong> (E-pub 2009)<br />
119 Pasello G, Agata S, Bonaldi L, Corradin A, Montagna M, Zamarchi<br />
R, Parenti A, Cagol M, Zaninotto G, Ruol A, Ancona E, Amadori A,<br />
Saggioro D. DNA copy number alterations correlate with survival<br />
of esophageal adenocarcinoma patients. Modern Pathology; 22:1;<br />
58-65; 2009 (E-pub 2008)<br />
120 Pasello G, Favaretto A G. Molecular targets in malignant pleural<br />
mesothelioma treatment. Current Drug Targets; 10:12; 1235-1244;<br />
2009<br />
121 Pasini E, Caggiari L, Dal Maso L, Martorelli D, Guidoboni M, Vaccher<br />
E, Barzan L, Franchin G, Gloghini A, De Re V, Sacchi N, Serraino D,<br />
Carbone A, Rosato A, Dolcetti R. Undifferentiated nasopharyngeal<br />
carcinoma from a nonendemic area: Protective role of HLA allele<br />
products presenting conserved EBV epitopes. International Journal<br />
of Cancer; 125:6; 1358-1364; 2009<br />
122 Pastore G, De Salvo G L, Bisogno G, Dama E, Inserra A, Cecchetto<br />
G, Ferrari A. Evaluating access to pediatric cancer care centers<br />
of children and adolescents with rare tumors in Italy: The TREP<br />
project. Pediatric Blood & Cancer; 53:2; 152-155; 2009<br />
123 Pavesi G, Berlucchi S, Munari M, Manara R, Scienza R, Opocher G.<br />
Clinical and surgical features of lower brain stem hemangioblastomas<br />
in von Hippel-Lindau disease. Acta Neurochirurgica; 152:2;<br />
287-292; 2009<br />
124 Persano L, Moserle L, Esposito G, Bronte V, Barbieri V, Iafrate M,<br />
Gardiman M P, Larghero P, Pfeffer U, Naschberger E, Stürzl M,<br />
Indraccolo S, Amadori A. Interferon-α counteracts the angiogenic<br />
switch and reduces tumor cell proliferation in a spontaneous model<br />
of prostatic cancer. Carcinogenesis; 30; 5; 851; 860; 2009<br />
125 Pierobon M, Calvert V, Belluco C, Garaci E, Deng J, Lise M, Nitti D,<br />
Mammano E, Marchi F D, Liotta L, Petricoin E. Multiplexed cell<br />
signaling analysis of metastatic and nonmetastatic colorectal cancer<br />
reveals COX2-EGFR signaling activation as a potential prognostic
pathway biomarker. Clinical Colorectal Cancer; 8:2; 110-117; 2009<br />
126 Pigozzo J, De Rossi C, Rossi C R, Nitti D, Chiarion-Sileni V.<br />
Complete and lasting healing of bone melanoma metastasis after<br />
hyperthermic limb perfusion. Melanoma research; 19:3; 193-194;<br />
2009<br />
127 Pilati P, Mammano E, Mocellin S, Tessari E, Lise M, Nitti D.<br />
Hepatic arterial infusion for unresectable colorectal liver metastases<br />
combined or not with systemic chemotherapy. Anticancer Research;<br />
29:10; 4139-4144; 2009<br />
128 Pistollato F, Chen H -L, Rood B R, Zhang H-Z, D’Avella D, Denaro<br />
L, Gardiman M, Te Kronnie G, Schwartz P H, Favaro E, Indraccolo<br />
S, Basso G, Panchision D M. Hypoxia and HIF1-αlpha repress the<br />
differentiative effects of BMPs in high-grade glioma. Stem cells; 27:1;<br />
7-17; 2009<br />
129 Pomerri F, Dodi G, Nardin M, Muzzio P C. Colonic total and<br />
segmental transit times in healthy Italian adults. Radiologia Medica;<br />
114:6; 925-934; 2009<br />
130 Pomerri F, Maretto I, Pucciarelli S, Rugge M, Burzi S, Zandonà M,<br />
Ambrosi A, Urso E, Muzzio P C, Nitti D. Prediction of rectal lymph<br />
node metastasis by pelvic computed tomography measurement.<br />
European Journal of Surgical Oncology; 35:2; 168-173; 2009<br />
131 Pucciarelli S, Del Bianco P, Efficace F, Toppan P, Serpentini S, Friso M<br />
L, Lonardi S, De Salvo G L, Nitti D. Health-related quality of life,<br />
faecal continence and bowel function in rectal cancer patients after<br />
chemoradiotherapy followed by radical surgery. Supportive Care in<br />
Cancer; 18:5; 601-608; <strong>2010</strong> (E-pub 2009)<br />
132 Pucciarelli S, Gagliardi G, Maretto I, Lonardi S, Friso M L, Urso E,<br />
Toppan P, Nitti D. Long-term oncologic results and complications<br />
after preoperative chemoradiotherapy for rectal cancer: A singleinstitution<br />
experience after a median follow-up of 95 months.<br />
Annals of Surgical Oncology; 16:4; 893-899; 2009<br />
133 Quaglia A, Tavilla A, Shack L, Brenner H, Janssen-Heijnen M, Allemani<br />
C, Colonna M, Grande E, Grosclaude P, Vercelli M, EUROCARE WG<br />
[as collab. Guzzinati S, Zambon P]. The cancer survival gap between<br />
elderly and middle-aged patients in Europe is widening. European<br />
Journal of Cancer; 45; 6; 1006-1016; 2009<br />
134 Ridolfi L, Fiorentini G, Guida M, Michiara M, Freschi A, Aitini E,<br />
Ballardini M, Bichisao E, Ridolfi R, Italian Melanoma Intergroup<br />
[as collab. Chiarion-Sileni,V]. Multicentre, open, noncomparative<br />
Phase II trial to evaluate the efficacy and tolerability of fotemustine,<br />
cisplatin, α-interferon and interleukin-2 in advanced melanoma<br />
PUBLICATIONS<br />
274<br />
patients. Melanoma research; 19:2; 100-105; 2009<br />
135 Romanato G, Scarpa M, Angriman I, Faggian D, Ruffolo C, Marin R,<br />
Zambon S, Basato S, Zanoni S, Filosa T, Pilon F, Manzato E. Plasma<br />
lipids and inflammation in active inflammatory bowel diseases.<br />
Alimentary Pharmacology and Therapeutics; 29:3; 298-307; 2009<br />
136 Rossi P G, Zorzi M. Comment on: Efficacy of HPV 16/18 vaccines on<br />
sexually active young women and the impact on organized cervical<br />
cancer screening. Acta Obstetricia et Gynecologica Scandinavica; 89:6;<br />
846-847; 2009<br />
137 Rosso S, De Angelis R, Ciccolallo L, Carrani E, Soerjomataram I, Grande<br />
E, Zigon G, Brenner H, EUROCARE WG [as collab. Guzzinati S,<br />
Zambon P]. Multiple tumors in survival estimates. European Journal<br />
of Cancer; 45:6; 1080-1094; 2009<br />
138 Ruffolo C, Scarpa M, Bassi N, Angriman I. A systematic review<br />
on advancement flaps for rectovaginal fistula in Crohn’s disease:<br />
transrectal versus transvaginal approach. Colorectal disease; 12:12;<br />
1183-1191; <strong>2010</strong> (E-pub 2009)<br />
139 Ruffolo C, Scarpa M, Bassi D, Angriman I R C, Bassi D, Angriman I.<br />
Inflammatory fibroid polyp causing intestinal obstruction following<br />
restorative proctocolectomy for ulcerative colitis. Digestive surgery;<br />
26:4; 285-286; 2009<br />
140 Ruffolo C, Scarpa M, Faggian D, Basso D, D’Incà R, Plebani<br />
M, Sturniolo G C, Bassi N, Angriman I, Subclinical intestinal<br />
inflammation in patients with crohn’s disease following bowel<br />
resection: A smoldering fire. Journal of Gastrointestinal Surgery; 14:1;<br />
24-31; 2009<br />
141 Rugge M, Fassan M, Battaglia G, Parente P, Zaninotto G, Ancona E.<br />
Intestinal or gastric? The unsolved dilemma of Barrett’s metaplasia.<br />
Human pathology; 40:8; 1206-1207; 2009<br />
142 Ruol A, Castoro C, Portale G, Cavallin F, Chiarion-Sileni V, Cagol<br />
M, Alfieri R, Corti L, Boso C, Zaninotto G, Peracchia A, Ancona E.<br />
Trends in management and prognosis for esophageal cancer surgery:<br />
Twenty-five years of experience at a single institution. Archives of<br />
Surgery; 144:3; 247-254; 2009<br />
143 Rustighi A, Tiberi L, Soldano A, Napoli M, Nuciforo P, Rosato A,<br />
Kaplan F, Capobianco A, Pece S, Di Fiore P P, Del Sal G. The prolylisomerase<br />
Pin1 is a Notch1 target that enhances Notch1 activation<br />
in cancer. Nature cell biology; 11:2; 133-142; 2009<br />
144 Ruzza P, Rosato A, Nassi A, Rondina M, Zorzin M, Rossi C R, Floreani<br />
M, Quintieri L. Synthesis and preliminary in vitro biological<br />
evaluation of 4-[(4-hydroxyphenyl)sulfanyl]but-3-en-2-one, a
4-mercaptophenol derivative designed as a novel bifunctional<br />
antimelanoma agent. Journal of medicinal chemistry; 52:15;<br />
4973- 4976; 2009<br />
145 Saggioro D, Silic-Benussi M, Biasiotto R, D’Agostino D M, Ciminale<br />
V. Control of cell death pathways by HTLV-1 proteins. Frontiers in<br />
Bioscience-Landmark; 14; 3338-3351; 2009<br />
146 Sant M, Allemani C, Santaquilani M, Knijn A, Marchesi F,<br />
Capocaccia R, EUROCARE WG [as collab. Guzzinati S, Zambon<br />
P]. EUROCARE-4. Survival of cancer patients diagnosed in 1995-<br />
1999. Results and commentary. European Journal of Cancer; 45:6;<br />
931-991; 2009<br />
147 Sarzo G, Del Mistro A, Finco C, Frayle-Salamanca H, Marino F,<br />
Franzetti M, Ferrara R, Mistrangelo M, Savastano S, Vecchiato M,<br />
Merigliano S. Extensive anal condylomatosis: prognosis in relation<br />
to viral and host factors. Colorectal disease; 12: 7online; e128-e134;<br />
2009<br />
148 Scaini M C, Rossi E, De Siqueira Torres P L A, Zullato D, Callegaro<br />
M, Casella C, Quaggio M, Agata S, Malacrida S, Chiarion-Sileni V,<br />
Vecchiato A, Alaibac M, Montagna M, Mann G J, Menin C, D’Andrea,<br />
E. Functional impairment of p16INK4A due to CDKN2A<br />
p.Gly23Asp missense mutation. Mutation Research Fundamental and<br />
Molecular Mechanisms of Mutagenis; 671; 1-feb; 26-32; 2009<br />
149 Scarpa M, Bortolami M, Morgan S L, Kotsafti A, Ferraro S, Ruffolo C,<br />
D’Incà R, Polese L, Barollo M, D’Amico D F, Sturniolo G C, Angriman<br />
I. TGF-β1 and IGF-1 Production and Recurrence of Crohn’s<br />
Disease After Ileo-Colonic Resection. Journal of Surgical Research;<br />
152:1; 26-34; 2009<br />
150 Scarpa M, Erroi F, Ruffolo C, Mollica E, Polese L, Pozza G, Norberto L,<br />
D’Amico D F, Angriman I. Minimally invasive surgery for colorectal<br />
cancer: Quality of life, body image, cosmesis, and functional results.<br />
Surgical Endoscopy and Other Interventional Techniques; 23:3;<br />
577-582; 2009<br />
151 Scarpa M, Mescoli C, Rugge M, D’Incà R, Ruffolo C, Polese L, D’Amico<br />
D F, Sturniolo G C, Angriman I. Restorative proctocolectomy for<br />
inflammatory bowel disease: The Padova prognostic score for colitis<br />
in predicting long-term outcome and quality of life. International<br />
journal of colorectal disease; 24:9; 1049-1057; 2009<br />
152 Scarpa M, Pagano D, Ruffolo C, Pozza A, Polese L, Frego M, D’Amico<br />
D F, Angriman I. Health-related quality of life after colonic resection<br />
for diverticular disease: Long-term results. Journal of Gastrointestinal<br />
Surgery; 13:1; 105-112; 2009<br />
PUBLICATIONS<br />
275<br />
153 Scarpa M, Ruffolo C, Bassi D, Boetto R, D’Incà R, Buda A, Sturniolo<br />
G C, Angriman I. Intestinal surgery for Crohn’s disease: Predictors of<br />
recovery, quality of life, and costs. Journal of Gastrointestinal Surgery;<br />
13:12; 2128-2135; 2009<br />
154 Scarpa M, Victor C J, O’Connor B I, Cohen Z, McLeod R S. Validation<br />
of an English version of the Padova quality of life instrument to<br />
assess quality of life following ileal pouch anal anastomosis. Journal<br />
of Gastrointestinal Surgery; 13:3; 416-422; 2009<br />
155 Silic-Benussi M, Cannizzaro E, Venerando A, Cavallari I, Petronilli<br />
V, La Rocca N, Marin O, Chieco-Bianchi L, Di Lisa F, D’Agostino<br />
D M, Bernardi P, Ciminale V. Modulation of mitochondrial K+<br />
permeability and reactive oxygen species production by the p13<br />
protein of human T-cell leukemia virus type 1. Biochimica et<br />
Biophysica Acta - Bioenergetics; 1787:7; 947-954; 2009<br />
156 Sorgato N, Pennelli G, Boschin I M, Ide E C, Pagetta C, Piott A,<br />
Toniato A, De Salvo G L, Hindié E, Al-Nahhas A, Rubello D, Pelizzo<br />
M R. Can we avoid inadvertent parathyroidectomy during thyroid<br />
surgery? In Vivo; 23:3; 433-440; 2009<br />
157 Testori A, De Salvo G L, Montesco M C, Trifirò G, Mocellin S,<br />
Landi G, MacRipò G, Carcoforo P, Ricotti G, Giudice G, Picciotto<br />
F, Donner D, Di Filippo F, Soteldo J, Casara D, Schiavon M,<br />
Vecchiato A, Pasquali S, Baldini F, Mazzarol G, Rossi C R. Clinical<br />
considerations on sentinel node biopsy in melanoma from an<br />
Italian multicentric study on 1,313 patients (SOLISM-IMI).<br />
Annals of Surgical Oncology; 16:7; 2018-2027; 2009<br />
158 Testori A, Rutkowski P, Marsden J, Bastholt L, Chiarion-Sileni V,<br />
Hauschild A, Eggermont A M. Surgery and radiotherapy in the<br />
treatment of cutaneous melanoma. Annals of Oncology; 20:Suppl 6;<br />
22-29; 2009<br />
159 Toffoli G, Cecchin E, Gasparini G, D’Andrea M, Azzarello G, Basso<br />
U, Mini E, Pessa S, De Mattia E, Lo Re G, Buonadonna A, Nobili S,<br />
De Paoli A, Innocenti F. Genotype-driven phase I study of irinotecan<br />
administered in combination with fluorouracil/leucovorin in patients<br />
with metastatic colorectal cancer. Journal of Clinical Oncology; 28:5;<br />
866-871; <strong>2010</strong> (E-pub 2009)<br />
160 Tognazzo S, Bovo E, Fiore A R, Guzzinati S, Monetti D, Stocco C F,<br />
Zambon P. Probabilistic classifiers and automated cancer registration:<br />
An exploratory application. Journal of Biomedical Informatics; 42:1;<br />
1-10; 2009<br />
161 Toniato A, Boschin I, Bernante P, Foletto M, Guolo A M, Pelizzo M<br />
R, Opocher G, Ballotta E, Mantero F. Factors influencing the rising
ates of adrenal surgery: Analysis of a 25-year experience. Surgical<br />
Endoscopy and Other Interventional Techniques; 23:3; 503-507;<br />
2009<br />
162 Toniato A, Merante-Boschin I, Opocher G, Pelizzo M R, Schiavi F,<br />
Ballotta E. Surgical versus conservative management for subclinical<br />
cushing syndrome in adrenal incidentalomas: a prospective<br />
randomized study. Annals of Surgery; 249:3; 388-391; 2009<br />
163 Tosello V, Zamarchi R, Merlo A, Gorza M, Piovan E, Mandruzzato<br />
S, Bronte V, Wang X, Ferrone S, Amadori A, Zanovello P. Differential<br />
expression of constitutive and inducible proteasome subunits in<br />
human monocyte-derived DC differentiated in the presence of<br />
IFN-α or IL-4. European Journal of Immunology; 39:1; 56-66; 2009<br />
164 Turato C, Ruvoletto M G, Biasiolo A, Quarta S, Tono N, Bernardinello<br />
E, Beneduce L, Fassina G, Cavalletto L, Chemello L, Merkel C, Gatta<br />
A, Pontisso P. Squamous cell carcinoma antigen-1 (SERPINB3)<br />
polymorphism in chronic liver disease. Digestive and Liver Disease;<br />
41:3; 212-216; 2009 (E-pub 2008)<br />
165 Ugel S, Delpozzo F, Desantis G, Papalini F, Simonato F, Sonda N,<br />
Zilio S, Bronte V. Therapeutic targeting of myeloid-derived suppressor<br />
cells. Current Opinion in Pharmacology; 9:4; 470-481; 2009<br />
166 Ugel S, Scarselli E, Iezzi M, Mennuni C, Pannellini T, Calvaruso<br />
F, Cipriani B, De Palma R, Ricci-Vitiani L, Peranzoni E, Musiani<br />
P, Zanovello P, Bronte V. Autoimmune B-cell lymphopenia after<br />
successful adoptive therapy with telomerase-specific T lymphocytes.<br />
Blood; 115:7; 1374-1384; <strong>2010</strong> (E-pub 2009)<br />
167 Ugel S, Zoso A, De Santo C, Li Y, Marigo I, Zanovello P, Cipriani B,<br />
Oelke M, Schneck J P, Bronte V. In vivo administration of artificial<br />
antigen-presenting cells activates low-avidity T cells for treatment of<br />
cancer. Cancer research; 69:24; 9376-9384; 2009<br />
168 Vajente N, Trevisan R, Saggioro D. HTLV-1 Tax protein cooperates<br />
with Ras in protecting cells from apoptosis. Apoptosis; 14:2;<br />
153-163; 2009<br />
169 Verdecchia A, Guzzinati S, Francisci S, De Angelis R, Bray F, Allemani<br />
C, Tavilla A, Santaquilani M, Sant M. Survival trends in European<br />
cancer patients diagnosed from 1988 to 1999. European Journal of<br />
Cancer; 45:6; 1042-1066; 2009<br />
170 Vitale A, Boccagni P, Brolese A, Neri D, Srsen N, Zanus G, Pagano D,<br />
Pauletto A, Bonsignore P, Scopelliti M, D’Amico F E, Ometto G, Polacco<br />
M, Burra P, Gambato M, Feltracco P, Romano A, Cillo U. Progression<br />
of Hepatocellular Carcinoma Before Liver Transplantation: Dropout<br />
or Liver Transplantation? Transplantation proceedings; 41:4; 1264-<br />
PUBLICATIONS<br />
276<br />
1267; 2009<br />
171 Vitale A, D’Amico F, Gringeri E, Valmasoni M, Pauletto A, Bonsignore<br />
P, Bassi D, D’Amico F E, Polacco M, Burra P, Russo F, Angeli P, Poci<br />
C, Feltracco P, Romano A, Cillo U. Prognostic Evaluation of the<br />
Donor Risk Index Among a Prospective Cohort of Italian Patients<br />
Undergoing Liver Transplantation. Transplantation proceedings;<br />
41:4; 1096-1098; 2009<br />
172 Vitale A, Saracino E, Boccagni P, Brolese A, D’Amico F, Gringeri E,<br />
Neri D, Srsen N, Valmasoni M, Zanus G, Carraro A, Violi P, Pauletto<br />
A, Bassi D, Polacco M, Burra P, Farinati F, Feltracco P, Romano A,<br />
D’Amico D F, Cillo U. Validation of the BCLC Prognostic System in<br />
Surgical Hepatocellular Cancer Patients. Transplantation proceedings;<br />
41:4; 1260-1263; 2009<br />
173 Vitale A, Saracino E, D’Amico F E, Grigoletto F, Burra P, Angeli<br />
P, Boccagni P, Brolese A, Zanu G, Neri D, Gringeri E, D’Amico F,<br />
Valmasoni M, Carraro A, Gambato M, Feltracco P, Romano A, Buggio<br />
M, D’Amico D F, Cillo U. Prospective Validation of a New Priority<br />
Allocation Model for Liver Transplant Candidates: An Interim<br />
Analysis. Transplantation proceedings; 41:4; 1092-1095; 2009<br />
174 Vitaliani R, Spinazzi M, Del Mistro A, Manara R, Tavolato B,<br />
Bonifati D M. Subacute onset of deafness and vertigo in a patient<br />
with leptomeningeal metastasis from ovarian cancer. Neurological<br />
Sciences; 30:1; 65; 67; 2009<br />
175 Zancan M, Galdi F, Di Tonno F, Mazzariol C, Orlando C, Malentacchi<br />
F, Agostini M, Maran M, Del Bianco P, Fabricio A S C, Murer B,<br />
Pianon C, Gion M. Evaluation of cell-free DNA in urine as a marker<br />
for bladder cancer diagnosis. International Journal of Biological<br />
Markers; 24:3; 147-155; 2009<br />
176 Zanus G, Carraro A, Vitale A, Gringeri E, D’Amico F, Valmasoni M,<br />
D’Amico F E, Brolese A, Boccagni P, Neri D, Srsen N, Burra P, Feltracco<br />
P, Bonsignore P, Scopelliti M, Cillo U. Alcohol Abuse and De Novo<br />
Tumors in Liver Transplantation. Transplantation proceedings; 41:4;<br />
1310-1312; 2009<br />
177 Zattra E, Pigozzi B, Bordignon M, Marino F, Chiarion-Sileni V,<br />
Alaibac M. Anetoderma in cutaneous marginal-zone B-cell<br />
lymphoma. Clinical & Experimental dermatology; 34:8; e945-e948;<br />
2009<br />
178 Zattra E, Salmaso R, Montesco M C, Pigozzi B, Forchetti G, Alaibac<br />
M. Large plaque type blue nevus with subcutaneous cellular nodules.<br />
European Journal of Dermatology; 19:3; 287-288; 2009<br />
179 Zattra E, Tonin E Fortina A B, Pigozzi B, Alaibac M. Clinical tip:
Use of a manual dermatoscope with a compact digital camera in a<br />
pigmented lesion clinic. Skin Research and Technology; 15:4; 511-<br />
513; 2009<br />
180 Zustovich F, Lombardi G, Cartei G. Paraneoplastic diffuse cutaneous<br />
papillomatosis. Journal of the European Academy of Dermatology and<br />
Venereology : JEADV; 23:2; 220-221; 2009 (E-pub 2008)<br />
181 Zustovich F, Lombardi G, Della Puppa A, Rotilio A, Scienza R, Pastorelli<br />
D. A phase II study of cisplatin and temozolomide in heavily pre-treated<br />
patients with temozolomide-refractory high-grade malignant glioma.<br />
Anticancer Research; 29:10; 4275-4279; 2009<br />
182 Zustovich F, Lombardi G, Pastorelli D. Important role of gemcitabine in<br />
the treatment of classic Kaposi’s sarcoma. Tumori; 95:4; 562-563; 2009<br />
2009 PUBLICATIONS / Non indexed in ISI-JCR<br />
1 AIRTUM WG [as collab. Zambon P, Baracco M, Bovo E, Dal Cin A,<br />
Fiore A R, Greco A, Guzzinati S, Monetti D, Rosano A, Stocco C F,<br />
Tognazzo S], Crocetti E, Buzzoni C. New incidence and mortality<br />
data. 2003-2005 Epidemiologia e prevenzione 33:(1-2 Suppl 2); e1\3<br />
- e5\26; 2009<br />
2 Cillo U,Vitale A. Benefit and harm of deceased- or living-donor liver<br />
transplantation for hepatocellular carcinoma. Digestive and Liver<br />
Disease Supplements 3:4 88-92; 2009<br />
3 Diamantis G, Bocus P, Morbin T, Battaglia G. Endoscopic submucosal<br />
dissection of a non-polypoid gastric lesion. Giornale Italiano di<br />
Endoscopia Digestiva 32:3 228-229; 2009<br />
4 Fassan M, Rugge M, Parente P, Tieppo C, Battaglia G. The role of<br />
Helicobacter pylori in the spectrum of Barrett’s carcinogenesis.<br />
Cancer Prevention Research; 2:1; 94; 2009<br />
5 Favaretto A G, Pasello G, Magro C. Second and third line treatment<br />
in advanced non-small cell lung cancer. Discovery medicine; 8:43;<br />
204-209; 2009<br />
6 Ferretti S, Guzzinati S, Zambon P, Manneschi G, Crocetti E, Falcini F.<br />
Cancer incidence estimation by hospital discharge flow as compared<br />
with cancer registries data. Epidemiologia e prevenzione; 33; 4-5;<br />
147-153; 2009<br />
7 Gemelli A, Paciolla A, Oliosi F, Basso A, Moscardin R, Tineo M C,<br />
Romano P, Alaibac M, Aversa S M L, Furian L, D’Angelo A, Bonfante<br />
L. A case of Kaposi’s sarcoma in the rapamycin era. Giornale italiano<br />
di nefrologia; 26:1; 90-93; 2009<br />
8 Lombardi G, Zustovich F, Zovato S, Fiore D, Cappetta A, Pastorelli<br />
D. Characteristics and management of pancreatic lesions in von<br />
Hippel-Lindau disease: A systematic literature review. Oncology<br />
Reviews; 3:2; 103-106; 2009<br />
PUBLICATIONS<br />
277<br />
9 Mammano E, Pilati P, Tessari E, Cosci M, Mocellin S, Nitti D.<br />
Adjuvant chemotherapy after radical liver resection in the treatment<br />
of metastases from colorectal carcinoma. Minerva chirurgica; 64:5;<br />
457-463; 2009<br />
10 Merante-Boschin I, Fassan M, Pelizzo M R, Ide E C, Rugge M. Neck<br />
emergency due to parathyroid adenoma bleeding: a case report.<br />
Journal of Medical Case Reports; 3:1; 7404; 2009<br />
11 Montrone M, Martorelli D, Rosato A, Dolcetti R. Retinoids as critical<br />
modulators of immune functions: New therapeutic perspectives for<br />
old compounds. Endocrine, Metabolic and Immune Disorders - Drug<br />
Targets; 9:2; 113-131; 2009<br />
12 Morello E, Giordano G, Falci C, Monfardini S. Rehabilitation in older<br />
cancer patients. Aging Health; 5; 3; 369; 384; 2009<br />
13 Opocher G, Schiavi F, Cicala M V, Patalano A, Mariniello B,<br />
Boaretto F, Zovato S, Pignataro V, Macino B, Negro I, Mantero<br />
F. Genetics of adrenal tumors. Minerva endocrinologica; 34:2;<br />
107-121; 2009<br />
14 Palozzo A C, Paganelli F, Faoro S, Trojniak M P, Bertipaglia C.<br />
Registers as evaluation tool of clinical results of antiblastic therapy.<br />
Giornale Italiano di Farmacia Clinica; 23; 3; 128; 130; 2009<br />
15 Ronco G, Giubilato P, Naldoni C, Zorzi M, Anghinoni E, Scalisi A,<br />
Dalla Palma P, Zanier L, Barca A, Gaimo M D, Maglietta R, Mancini<br />
E, Pizzuti R, Iossa A, Segnan N, Zappa M. Extension of organised<br />
cervical cancer screening programmes in Italy and their process<br />
indicators: 2007 activity. Epidemiologia e prevenzione; 33:(3 Suppl 2);<br />
41-56; 2009<br />
16 Ruzza P, Rosato A, Rossi C R, Floreani M, Quintieri L. Glutathione<br />
transferases as targets for cancer therapy. Anti-Cancer Agents in<br />
Medicinal Chemistry; 9:7; 763-777; 2009
17 Savastano S, Vecchiato M, Sarzo G, Gruppo M, Cadrobbi R, Marcellan<br />
E, Mondi I, Cavallin F, Bazzolo G, Merigliano S. Surgery for<br />
obstructed defecation in over 65 year old patients. BMC Geriatrics;<br />
9:Suppl 1; A39; 2009<br />
18 Tomatis M, Mano M P, Baiocchi D, Barca A, Bordon R, Casella D,<br />
Donati G, Berti R, Filippini L, Frigerio A, Furini A, Mantellini P,<br />
Naldoni C, Pagano G, Ramera D, Ravaioli A, Sapino A, Taffurelli<br />
M, Vettorazzi M, Zorzi M, Cataliotti L, Rosselli Del Turco M, Segnan<br />
N, Ponti A. Audit system on Quality of breast cancer diagnosis<br />
and Treatment (QT): results of quality indicators on screendetected<br />
lesions in Italy for 2006 and preliminary results for 2007.<br />
Epidemiologia e prevenzione; 33:Suppl 2; 83-90; 2009<br />
<strong>2010</strong> PUBLICATIONS / Journals indexed in ISI-JCR<br />
1 Abbate I, Zanchetta M, Gatt M, Gabrielli L, Zanussi S, Milia M G,<br />
Lazzarotto T, Tedeschi R, Ghisetti V, Clementi M, De Rossi A, Baldanti<br />
F, Capobianchi M R. Multicenter comparative study of Epstein-Barr<br />
virus DNA quantification for virological monitoring in transplanted<br />
patients. Journal of clinical virology; 50:3; 224-229; <strong>2011</strong> (E-pub<br />
<strong>2010</strong>)<br />
2 Adami F, Scarin M, Pescarini L, Binotto G, Pavan L, Sgarabotto D,<br />
Semenzato G. Successful control of Blastoschizomyces capitatus<br />
infection in three consecutive acute leukaemia patients despite<br />
initial unresponsiveness to liposomal amphotericin B. Mycoses; 54:4;<br />
365-369; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
3 Adeegbe D, Serafini P, Bronte V, Zoso A, Ricordi C, Inverardi L. In vivo<br />
induction of myeloid suppressor cells and CD4Foxp3 T regulatory<br />
cells prolongs skin allograft survival in mice. Cell transplantation;<br />
E-pub <strong>2010</strong> E-pub<br />
4 Agostini M, Pucciarelli S, Calore F, Bedin C, Enzo MV, Nitti D.<br />
miRNAs in colon and rectal cancer: A consensus for their true<br />
clinical value. Clinica Chimica Acta; 411; 17-18; 1181-1186; <strong>2010</strong><br />
5 AIRTUM WG [as collab. Guzzinati S, Zambon P, Baracco M, Bovo E,<br />
Dal Cin A, Fiore A R, Greco A]. Italian cancer figures, report <strong>2010</strong>:<br />
Cancer prevalence in Italy. Patients living with cancer, long-term<br />
survivors and cured patients. Epidemiologia e prevenzione; 34:(5-6<br />
Suppl 2); 1-188; <strong>2010</strong><br />
PUBLICATIONS<br />
278<br />
19 Vecchiato M, Savastano S, Sarzo G, Cadrobbi R, Gruppo M, Mondi<br />
I, Cavallin F, Bazzolo G, Marcellan E, Merigliano S. Anterior<br />
laparoscopic rectal resection for cancer in the elderly: Long-term<br />
outcome, risk factors and health related quality of life. BMC<br />
Geriatrics; 9:Suppl 1; A43; 2009<br />
20 Zorzi M, Fedato C, Naldoni C, Sassatelli R, Sassoli De’Bianchi P, Senore<br />
C, Visioli C B, Cogo C. Screening for colorectal cancer in Italy: 2007<br />
survey. Epidemiologia e prevenzione; 33:Suppl 2; 57-74; 2009<br />
21 Zustovich F, Shams M, Anselmi P, Lombardi G, Pastorelli D, Cartei<br />
G. Cognitive and emotive state in elderly treatment-naive patients<br />
with advanced cancer compared with an elderly healthy control<br />
population. Cancer Therapy; 7; ISSUE A; 149-152; 2009<br />
6 Alaggio R, Cecchetto G, Bisogno G, Gambini C, Calabrò M L, Inserra A,<br />
Boldrini R, De Salvo G L, D’Amore E S G, Dall’Igna P. Inflammatory<br />
myofibroblastic tumors in childhood: A report from the italian<br />
cooperative group studies. Cancer; 116:1; 216-226; <strong>2010</strong><br />
7 Albini A, Indraccolo S, Noonan D M, Pfeffer U. Functional genomics<br />
of endothelial cells treated with anti-angiogenic or angiopreventive<br />
drugs Clinical & Experimental Metastasis; 27:6; 419-439; <strong>2010</strong><br />
8 Angeloni G, Alberti S, Romagnoli E, Banzato A, Formichi M,<br />
Cucchini U, Pengo V. Low molecular weight heparin (parnaparin) for<br />
cardioembolic events prevention in patients with atrial fibrillation<br />
undergoing elective electrical cardioversion: a prospective cohort<br />
study. Internal and emergency medicine; 6:2; 117-123; <strong>2011</strong> (E-pub<br />
<strong>2010</strong>)<br />
9 Angriman I, Scarpa M, Ruffolo C. Health related quality of life<br />
after surgery for colonic diverticular disease. World journal of<br />
gastroenterology : WJG; 16:32; 4013-4018; <strong>2010</strong><br />
10 Antoniou A C, Beesley J, McGuffog L, Sinilnikova O M, Healey S,<br />
Neuhausen S L, Ding Y C, Rebbeck T R, Weitzel J N, Lynch H T, Isaacs<br />
C, Ganz P A, Tomlinson G, Olopade O I, Couch F, J, Wang X, Lindor<br />
N M, Pankratz V S, Radice P, Manoukian S, Peissel B, Zaffaroni D,<br />
Barile M, Viel A, Allavena A, Dall’Olio V, Peterlongo P, Szabo C,<br />
I, Zikan M, Claes K, Poppe B, Foretova L, Mai P L, Greene M H,<br />
Rennert G, Lejbkowicz F, Glendon G, Ozcelik H, Andrulis I L, Ontario
Cancer Genetics Network, Thomassen M, Gerdes A M, Sunde L, Cruger<br />
D, Birk Jensen U, Caligo M, Friedman E, Kaufman B, Laitman Y,<br />
Milgrom R, Dubrovsky M, Cohen S, Borg A, Jernstrom H, Lindblom A,<br />
Rantala J, Stenmark-Askmalm M, Melin B, SWE-BRCA, Nathanson<br />
K, Domchek S, Jakubowska A, Lubinski J, Huzarski T, Osorio A, Lasa<br />
A, Duran M, Tejada M I, Godino J, Benitez J, Hamann U, Kriege<br />
M, Hoogerbrugge N, Van der Luijt R B, Van Asperen C J, Devilee<br />
P, Meijers-Heijboer E J, Blok M J, Aalfs C M, Hogervorst F, Rookus<br />
M, HEBON, Cook M, Oliver C, Frost D, Conroy D, Evans D G,<br />
Lalloo F, Picher G, Davidson R, Cole T, Cook J, Paterson J, Hodgson<br />
S, Morrison P J, Porteous M E, Walker L, Kennedy M J, Dorkins H,<br />
Peock S, EMBRACE, Godwin A K, Stoppa-Lyonnet D, Be Pauw A,<br />
Mazoyer S, Bonadona V, Lasset C, Dreyfus H, Leroux D, Hardouin A,<br />
Berthet P, Faivre L, GEMO, Loustalot C, Noguchi T, Sobol H, Rouleau<br />
E, Nogues C, Frenay M, Venat-Bouvet L, GEMO, Hopper J L, Daly<br />
M B, Terry M B, John E M, Buys S S, Yassin Y, Miron A, Goldgar D.<br />
Breast Cancer Family Registry, Singer C F, Dressler A C, Gschwantler-<br />
Kaulich D, Pfeiler G, Hansen T V, Jonson L, Agnarsson B, A, Kirchhoff<br />
T, Offit K, Devlin V, Dutra-Clarke A, Piedmonte M, Rodriguez G C,<br />
Wakeley K, Boggess J F, Basil J, Schwartz P E, Blank S V, Toland A<br />
E, Montagna M, Casella C, Imyanitov E, Tihomirova L, Blanco I,<br />
Lazaro C, Ramus S J, Sucheston L, Karlan B Y, Gross J, Schmutzler<br />
R, Wappenschmidt B, Engel C, Meindl A, Lochmann M, Arnold N,<br />
Heidemann S, Varon-Mateeva R, Niederacher D, Sutter C, Deissler<br />
H, Gadzicki D, Preisler-Adams S, Kast K, Schonbuchner I, Calde T,<br />
De la Hoya M, Aittomaki K, Nevanlinna H, Simard J, Spurdle A B,<br />
Holland H, Chen X, kConFab, Platte R, Chenevix-Trench G, Easton<br />
D. F, CIMBA. Common breast cancer susceptibility alleles and the<br />
risk of breast cancer for BRCA1 and BRCA2 mutation carriers:<br />
implications for risk prediction. Cancer research; 70:23; 9742-9754;<br />
<strong>2010</strong><br />
11 Antoniou A C, Wang X, Fredericksen Z, S, McGuffog L, Tarrell R,<br />
Sinilnikova O M, Healey S, Morrison J, Kartsonaki C, Lesnick T,<br />
Ghoussaini M, Barrowdale D, EMBRACE, Peock S, Cook M, Oliver<br />
C, Frost D, Eccles D, Evans D G, Eeles R, Izatt L, Chu C, Douglas<br />
F, Paterson J, Stoppa-Lyonnet D, Houdayer C, MazoyerS, Giraud S,<br />
Lasset C, Remenieras A, Caron O, Hardouin A, Berthet P, GEMO<br />
Study Collaborators, Hogervorst F B, Rookus M A, Jager A, Van den<br />
Ouweland A, Hoogerbrugge N, Van der Luijt R B, Meijers-Heijboer<br />
H, Gomez Garcia E B, HEBON, Devilee P, Vreeswijk M P, Lubinski J,<br />
Jakubowska A, Gronwald J, Huzarski T, Byrski T, Gorski B, Cybulski<br />
PUBLICATIONS<br />
279<br />
C, Spurdle A B, Holland H, kConFab Goldgar D E, John E M, Hopper<br />
J L, Southey M, Buys S S, Daly M B, Terry M B, Schmutzler R K,<br />
Wappenschmidt B, Engel C, Meindl A, Preisler-Adams S, Arnold N,<br />
Niederacher D, Sutter C, Domchek S M, Nathanson K L, Rebbeck<br />
T, Blum J L, Piedmonte M, Rodriguez G C, Wakeley K, Boggess J F,<br />
Basil J, Blank S V, Friedman E, Kaufman B, Laitman Y, Milgrom R,<br />
Andrulis I L, Glendon G, Ozcelik H, Kirchhoff T, Vijai J, Gaudet M M,<br />
Altshuler D, Guiducci C, SWE-BRCA, Loman N, Harbst K, Rantala<br />
J, Ehrencrona H, Gerdes A M, Thomassen M, Sunde L, Peterlongo P,<br />
Manoukian S, Bonanni B, Viel A, Radice P, Caldes T, De la Hoya M,<br />
Singer C F, Fink-Retter A, Greene M H, Mai P L, Loud J T, Guidugli<br />
L, Lindor N M, Hansen T V, Nielsen F C, Blanco I, Lazaro C, Garber<br />
J, Ramus S J, Gayther S A, Phelan C, Narod S, Szabo C I, MOD<br />
SQUAD, Benitez J, Osorio A, Nevanlinna H, Heikkinen T, Caligo M<br />
A, Beattie M S, Hamann U, Godwin A K, Montagna M, Casella C,<br />
Neuhausen S L, Karlan B Y, Tung N, Toland A E, Weitzel J, Olopade<br />
O, Simard J, Soucy P, Rubinstein W S, Arason A, Rennert G, Martin<br />
N G, Montgomery G W, Chang-Claude J, Flesch-Janys D, Brauch H,<br />
GENICA, Severi G, Baglietto L, Cox A, Cross S S, Miron P, Gerty S<br />
M, Tapper W, Yannoukakos D, Fountzilas G, Fasching P A, Beckmann<br />
M W, Dos Santos Silva I, Peto J, Lambrechts D, Paridaens R, Rudiger<br />
T, Forsti A, Winqvist R, Pylkas K, Diasio R B, Lee A M, Eckel-Passow<br />
J, Vachon C, Blows F, Driver K, Dunning A, Pharoah P P, Offit K,<br />
Pankratz V S, Hakonarson H, Chenevix-Trench G, Easton D F, Couch<br />
F J. A locus on 19p13 modifies risk of breast cancer in BRCA1<br />
mutation carriers and is associated with hormone receptor-negative<br />
breast cancer in the general population. Nature genetics; 42:10; 885-<br />
892; <strong>2010</strong><br />
12 Artioli G, Borgato L, Cappetta A, Wabersich J, Mocellin S, Dalla Palma<br />
M, Nicoletto M O. Overall survival in BRCA-associated ovarian<br />
cancer: case-control study of an Italian series. European journal of<br />
gynaecological oncology; 31:6; 658-661; <strong>2010</strong><br />
13 Artioli G, Mocellin S, Borgato L, Cappetta A, Bozza F, Zavagno G,<br />
Zovato S, Marchet A, Pastorelli D. Phase II Study of Neoadjuvant<br />
Gemcitabine, Pegylated Liposomal Doxorubicin, and Docetaxel<br />
in Locally Advanced Breast Cancer. Anticancer Research; 30:9;<br />
3817-3821; <strong>2010</strong><br />
14 Baccarani U, Piselli P, Serraino D, Adani G L, Lorenzin D, Gambato<br />
M, Buda A, Zanus G, Vitale A, De Paoli A, Cimaglia C, Bresadola<br />
V, Toniutto P, Risaliti A, Cillo U, Bresadola F, Burra P. Comparison<br />
of de novo tumors after liver transplantation with incidence rates
from Italian cancer registries. Digestive and Liver Disease; 42:1;<br />
55- 60; <strong>2010</strong><br />
15 Banna G L, Di Maio M, Follador A, Collova E, Menis J, Novello S,<br />
Bria E, ISA WG [as collab. Favaretto A G]. Italian Survey on Adjuvant<br />
treatment of non-small cell lung cancer (ISA). Lung cancer; 73:1;<br />
78-88; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
16 Barollo S, Pennelli G M, Vianello F, Watutantrige Fernando S, Negro<br />
I, Merante Boschin I, Pelizzo M, Rugge M, Mantero F, Nacamulli D,<br />
Girelli M E, Busnardo B, Mian C. BRAF in primary and recurrent<br />
papillary thyroid cancers: the relationship with 131-Iodine and<br />
2-[18F]-fluoro-2-deoxi-D-glucose uptake ability. European journal<br />
of endocrinology; 163:4; 659-663; <strong>2010</strong><br />
17 Bassi D, Ruffolo C, Scarpa M, Mescoli C, Bassi N, Angriman I. Ileal<br />
neuroendocrine carcinoma following restorative proctocolectomy<br />
for colonic adenocarcinoma in Crohn’s disease. International journal<br />
of colorectal disease; 26:2; 253-254; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
18 Bassi P F, Volpe A, D’Agostino D M, Palermo G, Renier D, Franchini<br />
S, Rosato A, Racioppi M. Paclitaxel-Hyaluronic Acid for Intravesical<br />
Therapy of Bacillus Calmette-Guérin Refractory Carcinoma In Situ<br />
of the Bladder: Results of a Phase I Study. Journal of Urology; 185:2;<br />
445-449; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
19 Bertazza L, Mocellin S. The Dual Role of Tumor Necrosis Factor<br />
(TNF) in Cancer Biology. Current medicinal chemistry; 17:29;<br />
3337-3352; <strong>2010</strong><br />
20 Bertolin C, Boaretto F, Barbon G, Salviati L, Lapi E, Divizia M T,<br />
Garavelli L, Occhi G, Vazza G I, Mostacciuolo M L. Novel mutations<br />
in the L1CAM gene support the complexity of L1 syndrome. Journal<br />
of the neurological sciences; 294; 1-2; 124-126; <strong>2010</strong><br />
21 Biasiotto R, Aguiari P, Rizzuto R, Pinton P, D’Agostino D M, Ciminale<br />
V. The p13 protein of human T cell leukemia virus type 1 (HTLV-1)<br />
modulates mitochondrial membrane potential and calcium uptake.<br />
Biochimica et Biophysica Acta - Bioenergetics; 1797; 6-7; 945-951;<br />
<strong>2010</strong><br />
22 Boaretto F, Vettori A, Casarin A, Vazza G, Muglia M, Rossetto M<br />
G, Cavallaro T, Rizzuto N, Carelli V, Salviati L, Mostacciuolo M<br />
L, Martinuzzi A. Severe CMT type 2 with fatal encephalopathy<br />
associated with a novel MFN2 splicing mutation. Neurology; 74:23;<br />
1919-1921; <strong>2010</strong><br />
23 Bonanno L, Schiavon M, Nardo G, Bertorelle R, Bonaldi L, Galligioni<br />
A, Indraccolo S, Pasello G, Rea F, Favaretto A G. Prognostic and<br />
Predictive Implications of EGFR Mutations, EGFR Copy Number<br />
PUBLICATIONS<br />
280<br />
and KRAS Mutations in Advanced Stage Lung Adenocarcinoma<br />
Anticancer Research; 30:12; 5121-5128; <strong>2010</strong><br />
24 Bordignon M, Belloni-Fortina A, Pigozzi B, Saponeri A, Alaibac<br />
M. The role of immunohistochemical analysis in the diagnosis of<br />
parapsoriasis. Acta Histochemica; 113:2; 92-95; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
25 Brunello A, Kapoor R, Extermann M. Hyperglycemia During<br />
Chemotherapy for Hematologic and Solid Tumors Is Correlated<br />
With Increased Toxicity American journal of clinical oncology; 34:3;<br />
292-296; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
26 Buja A, Perissinotto E, Compostella A, Tramarin A, Rebba V, Pastorelli<br />
D, Grigoletto F, Gallo C, Rausa G, Gregori D. Taking decisions on<br />
expenditure for high-cost drugs at the regional level: a model for<br />
evaluating the overall impact of Trastuzumab in the Veneto Region<br />
of Italy. Journal of evaluation in clinical practice; 17:2; 298-303; <strong>2011</strong><br />
(E-pub <strong>2010</strong>)<br />
27 Burra P, Germani G, Masier A, De Martin E, Gambato M, Salonia<br />
A, Bo P, Vitale A, Cillo U, Russo F P, Senzolo M. Sexual dysfunction<br />
in chronic liver disease: Is liver transplantation an effective cure?<br />
Transplantation; 89:12; 1425-1429; <strong>2010</strong><br />
28 Canova F, Marino D, Trentin C, Soldà C, Ghiotto C, Aversa Savina M<br />
L. Intrathecal chemotherapy in lymphomatous meningitis. Critical<br />
reviews in oncology/hematology; 79:2; 127-134; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
29 Cardin F, Minicuci N, Andreotti A, Pinetti E, Campigotto F, Donà<br />
B, Martella B, Terranova O. Maximizing the general success of<br />
cecal intubation during propofol sedation in a multi-endoscopist<br />
academic centre. BMC gastroenterology; 10:1; 123; <strong>2010</strong><br />
30 Carron M, Freo U, Zorzi M, Ori C. Predictors of failure of noninvasive<br />
ventilation in patients with severe community-acquired pneumonia<br />
Journal of critical care; 25:3; 540 e9-e14; <strong>2010</strong><br />
31 Caumo F, Vecchiato F, Strabbioli M, Zorzi M, Baracco S, Ciatto S.<br />
Interval cancers in breast cancer screening: Comparison of stage and<br />
biological characteristics with screen-detected cancers or incident<br />
cancers in the absence of screening. Tumori; 96:2; 198-201; <strong>2010</strong><br />
32 Cavaliere F, De Simone M, Virzì S, Deraco M, Rossi C R, Garofalo A,<br />
Di Filippo F, Giannarelli D, Vaira M, Valle M, Pilati P, Perri P, La<br />
Pinta M, Monsellato I, Guadagni F. Prognostic factors and oncologic<br />
outcome in 146 patients with colorectal peritoneal carcinomatosis<br />
treated with cytoreductive surgery combined with hyperthermic<br />
intraperitoneal chemotherapy: Italian multicenter study S.I.T.I.L.O.<br />
European Journal of Surgical Oncology (EJSO); 37:2; 148-154; <strong>2011</strong><br />
(E-pub <strong>2010</strong>)
33 Cecchin D, Schiavi F, Fanti S, Favero M, Manara R, Fassina A, Briani<br />
C, Allegri V, Sansovini M, Bui F, Paganelli G, Opocher G. Peptide<br />
Receptor Radionuclide Therapy in a Case of Multiple Spinal Canal<br />
and Cranial Paragangliomas. Journal of Clinical Oncology; 29:7;<br />
e171-e174; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
34 Cecchin E, Agostini M, Pucciarelli S, De Paoli A, Canzonieri V, Sigon<br />
R, De Mattia E, Friso M L, Biason P, Visentin M, Nitti D, Toffoli<br />
G. Tumor response is predicted by patient genetic profile in rectal<br />
cancer patients treated with neo-adjuvant chemo-radiotherapy. The<br />
pharmacogenomics journal; 11:3; 214-226; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
35 Centonze M, Visconti D, Doratiotto S, Silverio R, Fileni A, Pescarini L,<br />
Golfieri R. Clinical Risk Management in radiology. Part II: applied<br />
examples and concluding remarks. Radiologia medica; 115:7; 1147-<br />
1164; <strong>2010</strong><br />
36 Ceolotto G, Papparella I, Bortoluzzi A, Strapazzon G, Ragazzo F,<br />
Bratti P, Fabricio A S, Squarcina E, Gion M, Palatini P, Semplicini<br />
A. Interplay Between miR-155, AT1R A1166C Polymorphism,<br />
and AT1R Expression in Young Untreated Hypertensives. American<br />
journal of hypertension; 24:2; 241-246; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
37 Cillo U, Vitale A, Volk M L, Frigo A C, Grigoletto F, Brolese A, Zanus<br />
G, D’Amico F, Farinati F, Burra P, Russo F, Angeli P, D’Amico D F. The<br />
survival benefit of liver transplantation in hepatocellular carcinoma<br />
patients. Digestive and Liver Disease; 42:9; 642-649; <strong>2010</strong><br />
38 Corradin M T, Forcione M, Fiorentino R, Bordignon M, Alaibac M,<br />
Belloni-Fortina A. Verrucous cutaneous sarcoidosis in an adolescent<br />
with dark skin. European Journal of Dermatology; 20:5; 659-660;<br />
<strong>2010</strong><br />
39 Crescenzi M, Persano L, Esposito G, Zulato E, Borsi L, Balza,E.;Ruol<br />
A, Ancona E, Indraccolo S, Amadori A. Vandetanib improves antitumor<br />
effects of L19mTNFα in xenograft models of esophageal<br />
cancer. Clinical Cancer Research; 7:3; 447-458; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
40 Crocetti E, Buzzoni C, AIRTUM WG [as collab. Zambon P].<br />
Italy is one of the European countries with the greatest population<br />
observed by cancer registries. Epidemiologia e prevenzione; 34:5-6; 82<br />
<strong>2010</strong><br />
41 Crocetti E, Buzzoni C, AIRTUM WG [as collab. Zambon P].<br />
Childhood cancer: after the peak reached around 2000 the incidence<br />
seems to stabilize. Epidemiologia e prevenzione; 34:1; 2-4; <strong>2010</strong><br />
42 Crocetti E, Buzzoni C, AIRTUM WG [as collab. Zambon P]. Numbers:<br />
Colorectal cancer: if the actual trend persists, the gap between North<br />
and South will disappear in 2019 Acute effects of air pollution in<br />
PUBLICATIONS<br />
281<br />
Brindisi (Italy). Epidemiologia e prevenzione; 34:3; 69; <strong>2010</strong><br />
43 Cucchetti A, Vitale A, Gaudio M D, Ravaioli M, Ercolani G, Cescon<br />
M, Zanello M, Morelli M C, Cillo U, Grazi G L, Pinna A D. Harm<br />
and benefits of primary liver resection and salvage transplantation<br />
for hepatocellular carcinoma. American Journal of Transplantation;<br />
10:3; 619-627; <strong>2010</strong><br />
44 Dal Maso L, Lise M, Zambon P, Falcini F, Crocetti E, Serraino D,<br />
Cirilli C, Zanetti R, Vercelli M, Ferretti S, Stracci F, De Lisi V, Busco<br />
S, Tagliabue G, Budroni M, Tumino R, Giacomin A, Franceschi S,<br />
for AIRTUM WG. Incidence of thyroid cancer in Italy, 1991-2005:<br />
time trends and age-period-cohort effects. Annals of Oncology; 22:4;<br />
957-963; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
45 Dalla Palma M, Lombardi G, Donach M, Borgato Lucia, Zustovich F,<br />
Furini L, Nicoletto M O. Tolerability of PLD/Oxaliplatin Regimen<br />
in Recurrent Ovarian Cancer Patients With Previous Fragility<br />
to Carboplatin/Paclitaxel Treatment. American journal of clinical<br />
oncology; 34:3; 292-296; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
46 Dall’Olmo L, Moja L. Treatment for non-dysplastic Barrett’s<br />
oesophagus: a well-informed, demanding patient. Internal and<br />
emergency medicine; 5:5; 433-435; <strong>2010</strong><br />
47 De Leone A, Tonini M, Dominici P, Grossi E, Pace F, EMERGE<br />
SG [as collab. Battaglia G]. The proton pump inhibitor test for<br />
gastroesophageal reflux disease: optimal cut-off value and duration.<br />
Digestive and liver disease; 42:11; 785-790; <strong>2010</strong><br />
48 De Martin E, Senzolo M, Gambato M, Germani G, Vitale A,<br />
Russo F R, Burra P. Fibrosis Progression and the Pros and Cons<br />
of Antiviral Therapy for Hepatitis C Virus Recurrence After Liver<br />
Transplantation: A Review. Transplantation proceedings; 42:6;<br />
2223-2225; <strong>2010</strong><br />
49 De Palma A, Roveri A, Zaccarin M, Benazzi L, Daminelli S,<br />
Pantano G, Buttarello M, Ursini F, Gion M, Mauri P L. Extraction<br />
methods of red blood cell membrane proteins for Multidimensional<br />
Protein Identification Technology (MudPIT) analysis. Journal of<br />
chromatography. A; 1217:33; 5328-5336; <strong>2010</strong><br />
50 De Rossi A, Zanchetta M, Vitone F, Antonelli G, Bagnarelli P,<br />
Buonaguro L, Capobianchi M R, Clementi M, Abbate I, Canducci<br />
F, Monachetti A, Riva E, Rozera G, Scagnolari C, Tagliamonte M, Re<br />
M C, SIVIM WG. Quantitative HIV-1 proviral DNA detection: a<br />
multicentre analysis. The New Microbiologica; 33:4; 293-302; <strong>2010</strong><br />
51 Del Mistro A, Frayle-Salamanca H, Trevisan R, Matteucci M, Pinarello<br />
A, Zambenedetti P, Buoso R, Fantin G P, Zorzi M, Minucci D. Triage
of women with atypical squamous cells of undetermined significance<br />
(ASC-US): Results of an Italian multicentric study. Gynecologic<br />
Oncology; 117:1; 77-81; <strong>2010</strong><br />
52 Della Bella S, Taddeo A, Colombo E, Brambilla L, Bellinvia M,<br />
Pregliasco F, Cappelletti M, Calabro M L, Villa M L. Human<br />
herpesvirus-8 infection leads to expansion of the preimmune/natural<br />
effector B cell compartment. PloS one; 5:11; e15029; <strong>2010</strong><br />
53 Di Camillo B, Sanavia T, Iori E, Bronte V, Roncaglia E, Maran A,<br />
Avogaro A, Toffolo G, Cobelli C. The transcriptional response in<br />
human umbilical vein endothelial cells exposed to insulin: a dynamic<br />
gene expression approach. PloS one; 5:12; e14390; <strong>2010</strong><br />
54 Di Ieva A, Grizzi F, Tschabitscher M, Colombo P, Casali M, Simonelli<br />
M, Widhalm G, Muzzio P C, Matula C, Chiti A, Rodriguez y Baena<br />
R. Correlation of microvascular fractal dimension with positron<br />
emission tomography [11C]-methionine uptake in glioblastoma<br />
multiforme: Preliminary findings. Microvascular research; 80:2; 267-<br />
273; <strong>2010</strong><br />
55 D’Incà R, Barollo M, Scarpa M, Grillo A R, Brun P, Vettorato M G,<br />
Castagliuolo I, Sturniolo G C. Rectal Administration of Lactobacillus<br />
casei DG Modifies Flora Composition and Toll-Like Receptor<br />
Expression in Colonic Mucosa of Patients with Mild Ulcerative<br />
Colitis. Digestive diseases and sciences; 56:4; 1178-1187; <strong>2011</strong> (E-pub<br />
<strong>2010</strong>)<br />
56 Dolcetti L, Peranzoni E, Ugel S, Marigo I, Fernandez Gomez A, Mesa<br />
C, Geilich M, Winkels G, Traggiai E, Casati A, Grassi F, Bronte V.<br />
Hierarchy of immunosuppressive strength among myeloid-derived<br />
suppressor cell subsets is determined by GM-CSF. European Journal<br />
of Immunology; 40:1; 22-35; <strong>2010</strong><br />
57 Dolcetti R, De Rossi A.Telomere/telomerase interplay in virus-driven<br />
and virus-independent lymphomagenesis: Pathogenic and clinical<br />
implications. Medicinal research reviews; E-pub; <strong>2010</strong> E-pub<br />
58 European Collaborative Study, Boer K, England K, Godfried M H,<br />
Thorne C, [as collab. De Rossi A]. Mode of delivery in HIV-infected<br />
pregnant women and prevention of mother-to-child transmission:<br />
changing practices in Western Europe. HIV medicine; 11:6; 368-<br />
378; <strong>2010</strong><br />
59 Evangelista L, Baretta Z, Vinante L, Cervino A R, Gregianin M,<br />
Ghiotto C, Saladini G, Sotti G. Tumor markers and FDG PET/<br />
CT for prediction of disease relapse in patients with breast cancer.<br />
European journal of nuclear medicine and molecular imaging; 38:2;<br />
293-301; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
PUBLICATIONS<br />
282<br />
60 Falci C, Brunello A, Monfardini S. Detecting Functional Impairment<br />
in Older Patients With Cancer: Is Vulnerable Elders Survey-13 the<br />
Right Prescreening Tool? An Open Question. Journal of Clinical<br />
Oncology; 28:32; e665-e666; <strong>2010</strong><br />
61 Fassan M, Cagol M, Pennelli G, Rizzetto C, Giacomelli L, Battaglia<br />
G. Programmed cell death 4 protein in esophageal cancer. Oncology<br />
reports; 24:1; 135-139; <strong>2010</strong><br />
62 Fassan M, Pizzi M, Battaglia G, Giacomelli L, Parente P, Bocus P,<br />
Ancona E, Rugge M. Programmed cell death 4 (PDCD4) expression<br />
during multistep Barrett’s carcinogenesis. Journal of clinical pathology;<br />
63:8; 692-696; <strong>2010</strong><br />
63 Fassan M, Rea F, Clemente R, Rizzardi G, Pizzi M, Giacomelli L, Rugge<br />
M. Somatostatin Receptor Type 2 (SSTR2) in Bronchopulmonary<br />
Carcinoids. Endocrine Pathology; 21; 3; 204; 205; <strong>2010</strong><br />
64 Fassan M, Volinia S, Palatini J, Pizzi M, Baffa R, De Bernard M,<br />
Battaglia G, Parente P, Croce C M, Zaninotto G, Ancona E, Rugge M.<br />
MicroRNA expression profiling in human Barrett’s carcinogenesis;<br />
International journal of cancer. 129:7; 1661-1670; <strong>2011</strong> (E-pub<br />
<strong>2010</strong>)<br />
65 Fassina A, Cappellesso R, Schiavi F, Fassan M. Concurrent<br />
pheochromocytoma and cortical carcinoma of the adrenal<br />
gland. Journal of surgical oncology; 103:1; 103-104; <strong>2011</strong><br />
(E-pub <strong>2010</strong>)<br />
66 Fernandez A, Mesa C, Marigo I, Dolcetti L, Clavell M, Oliver L,<br />
Fernandez L E, Bronte V. Inhibition of tumor-induced myeloidderived<br />
suppressor cell function by a nanoparticulated adjuvant.<br />
Journal of immunology; 186:1; 264-274; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
67 Ferrari A, Miceli R, Rey A, Oberlin O, Orbach D, Brennan B, Mariani<br />
L, Carli M, Bisogno G, Cecchetto G, De Salvo G L, Casanova M,<br />
Vannoesel M M, Kelsey A, Stevens M C, Devidas M, Pappo A S, Spunt<br />
S L. Non-metastatic unresected paediatric non-rhabdomyosarcoma<br />
soft tissue sarcomas: Results of a pooled analysis from United States<br />
and European groups. European journal of cancer; 47:5; 724-731;<br />
<strong>2011</strong> (E-pub <strong>2010</strong>)<br />
68 Ferretti A, Simonato F, Zandonà R, Reccanello S, Fabbris R.<br />
Commissioning Siemens Virtual Wedges in the Oncentra<br />
MasterPlan treatment planning system using Gafchromic EBT film.<br />
Medical physics; 37:12; 6310-6316; <strong>2010</strong><br />
69 Fogar P, Navaglia F, Basso D, Zambon C-F, Moserle L, Indraccolo<br />
S,Stranges A, Greco E, Fadi E, Padoan A, Pantano G, Sanzari M C,<br />
Pedrazzoli S, Montecucco C, Plebani M. Heat-induced transcription
of diphtheria toxin A or its variants, CRM176 and CRM197:<br />
Implications for pancreatic cancer gene therapy. Cancer gene therapy;<br />
17:1; 58-68; <strong>2010</strong><br />
70 Frank-Raue K, Rybicki L A, Erlic Z, Schweizer H, Winter A, Milos I,<br />
Toledo S P, Toledo R A, Tavares M R, Alevizaki M, Mian C, Siggelkow<br />
H, Hufner M, Wohllk N, Opocher G, Dvorakova S, Bendlova B,<br />
Czetwertynska M, Skasko E, Barontini M, Sanso G, Vorlander C, Maia<br />
A L, Patocs A, Links T P, De Groot J W, Kerstens M N, Valk G D,<br />
Miehle K, Musholt T J, Biarnes J, Damjanovic S, Muresan M, Wuster<br />
C, Fassnacht M, Peczkowska M, Fauth C, Golcher H, Walter M A,<br />
Pichl J, Raue F, Eng C, Neumann H P, for the International RET Exon<br />
10 Consortium. Risk profiles and penetrance estimations in multiple<br />
endocrine neoplasia type 2A caused by germline RET mutations<br />
located in exon 10. Human mutation; 32:1; 51-58; <strong>2011</strong> (E-pub<br />
<strong>2010</strong>)<br />
71 Fritschi L, Guenel P, Ahrens W [as collab. Zambon P]. Breast cancer in<br />
priests: Follow-up of an observation made 167 years ago. European<br />
Journal of Epidemiology; 25:3; 219-221; <strong>2010</strong><br />
72 Gardiman M P, Fassan M, Orvieto E, D’Avella D, Denaro L,<br />
Calderone M, Severino M, Scarzello G, Viscardi E, Perilongo G.<br />
Diffuse leptomeningeal glioneuronal tumors: a new entity? Brain<br />
pathology; 20:2; 361-366; <strong>2010</strong><br />
73 Gatta G, Capocaccia R, Trama A, Martinez-Garcia C, RARECARE<br />
WG [as collab. Zambon P]. The burden of rare cancers in Europe.<br />
Advances in Experimental Medicine and Biology; 686:1; 285- 303;<br />
<strong>2010</strong><br />
74 Gaudet M M, Kirchhoff T, Green T, Vijai J, Korn J M, Guiducci C,<br />
Segre A V, McGee K, McGuffog L, Kartsonaki C, Morrison J, Healey<br />
S, Sinilnikova O M, Stoppa-Lyonnet D, Mazoyer S, Gauthier-Villars<br />
M, Sobol H, Longy M, Frenay M, GEMO Study Collaborators,<br />
Hogervorst F B, Rookus M A, Collee J M, Hoogerbrugge N, Van<br />
Roozendaal K E, HEBON Study Collaborators, Piedmonte M,<br />
Rubinstein W, Nerenstone S, Van Le L, Blank S V, Caldes T, De la<br />
Hoya M, Nevanlinna H, Aittomaki K, Lazaro C, Blanco I, Arason A,<br />
Johannsson O T, Barkardottir R B, Devilee P, Olopade O I, Neuhausen<br />
S L, Wang X, Fredericksen Z S, Peterlongo P, Manoukian S, Barile M,<br />
Viel A, Radice P, Phelan C M, Narod S, Rennert G, Lejbkowicz F,<br />
Flugelman A, Andrulis I L, Glendon G, Ozcelik H, OCGN, Toland A<br />
E, Montagna M, D’Andrea E, Friedman E, Laitman Y, Borg A, Beattie<br />
M, Ramus S J, Domchek S M, Nathanson K L, Rebbeck T, Spurdle A<br />
B, Chen X, Holland H, kConFab, John E M, Hopper J L, Buys S S,<br />
PUBLICATIONS<br />
283<br />
Daly M B, Southey M C, Terry M B, Tung N, Overeem Hansen T V,<br />
Nielsen F C, Greene M I, Mai P L, Osorio A, Duran M, Andres R,<br />
Benitez J, Weitzel J N, Garber J, Hamann U, Peock S, Cook M, Oliver<br />
C, Frost D, Platte R, Evans D G, Lalloo F, Eeles R, Izatt L, WalkerL,<br />
Eason J, Barwell J, Godwin A, K, Schmutzler R K, Wappenschmidt<br />
B, Engert S, Arnold N, Gadzicki D, Dean M, Gold B, Klein R J,<br />
Couch F J, Chenevix-Trench G, Easton D F, Daly M J, Antoniou A C,<br />
Altshuler D M, Offit K, Sinilnikova O M, Stoppa-Lyonnet D, Mazoyer<br />
S, Gauthier-Villars M, Sobol H, Longy M, Frenay M, Sinilnikova<br />
O, Barjhoux L, Giraud S, Leone M, Mazoyer S, Stoppa-Lyonnet D,<br />
Gauthier-Villars M, Houdayer C, Moncoutier V, Belotti M, De Pauw<br />
A, Bressac-de-Paillerets B, Remenieras A, Byrde V, Caron O, Lenoir<br />
G, Bignon Y, J, Uhrhammer N, Lasset C, Bonadona V, Hardouin A,<br />
Berthet P, Sobol H, Bourdon V, Noguchi T, Eisinger F, Coulet F, Colas<br />
C, Soubrier F, Coupier I, Peyrat J P, Fournier J, Revillion F, Vennin P,<br />
Adenis C, Rouleau E, Lidereau R, Demange L, Nogues C, Muller D,<br />
Fricker J P, Longy M, Sevenet N, Toulas C, Guimbaud R, Gladieff L,<br />
Feillel V, Leroux D, Dreyfus H, Rebischung C, Cassini C, Faivre L,<br />
Prieur F, Ferrer S F, Frenay M, Venat-Bouvet L, Lynch H T, Hogervorst<br />
F B, Rookus M A, Collee J M, Hoogerbrugge N, Van Roozendaal K E,<br />
Hogervorst F B, Verhoef S, Verheus M, Van’t Veer L J, Van Leeuwen F<br />
E, Rookus M A, Collee M, Van den Ouweland A M, Jager A, Hooning<br />
M J, Tilanus-Linthorst M M, Seynaeve C, Van Asperen C J, Wijnen J T,<br />
Vreeswijk M P, Tollenaar R A, Devilee P, Ligtenberg M J, Hoogerbrugge<br />
N, Ausems M G, Van der Luijt R B, Aalfs C M, Van Os T A, Gille J J,<br />
Waisfisz Q, Meijers-Heijboer H, Gomez-Garcia E B, Van Roozendaal<br />
C E, Blok M J, Oosterwijk J C, Van der Hout A H, Mourits M J, Vasen<br />
H F, Spurdle A B, Chenevix-Trench G. Common genetic variants<br />
and modification of penetrance of BRCA2-associated breast cancer.<br />
PLoS genetics; 6:10; e1001183; <strong>2010</strong><br />
75 Giaquinto C, Penazzato M, Rosso R, Bernardi S, Rampon O, Nasta<br />
P, Ammassari A, Antinori A, Badolato R, Castelli Gattinara G,<br />
D’Arminio Monforte A, De Martino M, De Rossi Anita, Di Gregorio P,<br />
Esposito S, Fatuzzo F, Fiore S, Franco A, Gabiano C, Galli L, Genovese<br />
O, Giacomet V, Giannattasio A, Gotta C, Guarino A, Martino A,<br />
Mazzotta F, Principi N, Regazzi M B, Rossi P, Russo R, Saitta M,<br />
Salvini F, Trotta S, Vigano A, Zuccotti G, Carosi G. Italian Paediatric<br />
HIV Infection Working Group. Italian consensus statement on<br />
paediatric HIV infection; Infection; 38:4; 301-319; <strong>2010</strong><br />
76 Goebell P J, Groshen S G, Schmitz-Dräger Bernd J. ISBC WG [as<br />
collab. Del Mistro A]. p53 immunohistochemistry in bladder cancer
a new approach to an old question. Urologic Oncology: Seminars and<br />
Original Investigations; 28:4; 377-388; <strong>2010</strong><br />
77 Golfieri R, Pescarini L, Fileni A, Silverio R, Saccavini C, Visconti D,<br />
Morana G, Centonze,M. Clinical Risk Management in radiology.<br />
Part I: general background and types of error and their prevention.<br />
Radiologia medica; 115:7; 1121-1146; <strong>2010</strong><br />
78 Gratwohl A, Baldomero H, Schwendener A, Gratwohl M, Apperley J,<br />
Frauendorfer K, Niederwieser D, EBMT WG [as collab. Aversa Savina<br />
M L, Marino D, Jirillo A, Canova F, Trentin C]. The EBMT activity<br />
survey 2008: impact of team size, team density and new trends. Bone<br />
marrow transplantation; 46; 2; 174-191; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
79 Greco M T, Corli O, Montanari M, Deandrea S, Zagonel V, Apolone<br />
G. On behalf of the Writing Protocol Committee and the Cancer<br />
Pain Outcome Research Study Group (CPOR SG) Investigators;<br />
Epidemiology and Pattern of Care of Breakthrough Cancer Pain in<br />
a Longitudinal Sample of Cancer Patients: Results From the Cancer<br />
Pain Outcome Research Study Group. The Clinical journal of pain;<br />
27-1; 9-18; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
80 Grohmann U, Bronte V. Control of immune response by amino acid<br />
metabolism. Immunological reviews; 236:1; 243-264; <strong>2010</strong><br />
81 Gusella M, Pasini F, Bolzonella C, Meneghetti S, Barile C, Bononi<br />
A, Toso C, Menon D, Crepaldi G, Modena Y, Stievano L, Padrini R.<br />
Equilibrative nucleoside transporter 1 genotype, cytidine deaminase<br />
activity and age predict gemcitabine plasma clearance in patients<br />
with solid tumors. British Journal of Clinical Pharmacology; 71:3;<br />
437-434; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
82 HAEMACARE W G [as collab. Zambon P]. Manual for coding and<br />
reporting haematological malignancies. Tumori; 96:4; i-A32; <strong>2010</strong><br />
83 Hsu W-M, Carraro A, Kulig K M, Miller M L, Kaazempur-Mofrad<br />
M, Weinberg E, Entabi F, Albadawi H, Watkins M T, Borenstein J T,<br />
Vacanti J P, Neville C. Liver-assist device with a microfluidics-based<br />
vascular bed in an animal model. Annals of Surgery; 252:2; 351-357;<br />
<strong>2010</strong><br />
84 Indraccolo S. Interferon-α as angiogenesis inhibitor: learning from<br />
tumor models. Autoimmunity; 43:3; 244-247; <strong>2010</strong><br />
85 Indraccolo S, Minuzzo S, Masiero M, Amadori A. Ligand-driven<br />
activation of the notch pathway in T-ALL and solid tumors: Why<br />
Not(ch)? Cell cycle; 9:1; 80-85; <strong>2010</strong><br />
86 International Prognostic Factors Study Group, Lorch A, Beyer J,<br />
Bascoul-Mollevi C, Kramar A, Einhorn L H, Necchi A, Massard C, De<br />
Giorgi U, Flechon A, Margolin K A, Lotz J P, Germa Lluch J R, Powles<br />
PUBLICATIONS<br />
284<br />
T, Kollmannsberger C K, [as collab. Basso U]. Prognostic factors in<br />
patients with metastatic germ cell tumors who experienced treatment<br />
failure with cisplatin-based first-line chemotherapy. Journal of<br />
Clinical Oncology; 28:33; 4906-4911; <strong>2010</strong><br />
87 Jirillo A, Vascon F. New rules on conflict of interest: what has to be<br />
done in Europe? Tumori; 96:1; 180-181; <strong>2010</strong><br />
88 Koussis H, Maruzzo M, Scola A, Ide Casal E, Fassina A, Marioni<br />
G, Lora O, Corti L, Karachontziti P, Jirillo A. A Case of Anaplastic<br />
Thyroid Cancer with Long-term Survival. Anticancer Research; 30:4;<br />
1273-1278; <strong>2010</strong><br />
89 Labianca R, Sobrero A, Isa L, Cortesi E, Barni S, Nicolella D, Aglietta<br />
M, Lonardi S, Corsi D, Turci D, Beretta G D, Fornarini G, Dapretto<br />
E, Floriani I, Zaniboni A, on behalf of Italian Group for the Study<br />
of Gastrointestinal Cancer-GISCAD. Intermittent versus continuous<br />
chemotherapy in advanced colorectal cancer: a randomised<br />
‘GISCAD’ trial. Annals of Oncology; 22:5; 1236-1242; <strong>2010</strong><br />
90 Lombardi G, Zustovich F, Della Puppa A, Borgato L, Orvieto E, Manara<br />
R, Cecchin D, Berti F, Farina P, Gardiman M P, Scienza R, Zagonel<br />
V. Cisplatin and temozolomide combination in the treatment of<br />
leptomeningeal carcinomatosis from ethmoid sinus intestinal-type<br />
adenocarcinoma. Journal of neuro-oncology; 104:1; 381-386; <strong>2010</strong><br />
91 Lombardi G, Zustovich F, Donach M, Dalla Palma M, Nicoletto M O,<br />
Pastorelli D. An update on targeted therapy in metastatic renal cell.<br />
carcinoma; Urologic Oncology; E-pub; <strong>2010</strong> E-pub<br />
92 Lombardi G, Zustovich F, Farinati F, Cillo U, Vitale A, Zanus<br />
G, Donach M, Farina M, Zovato S, Pastorelli D. Pegylated<br />
liposomal doxorubicin and gemcitabine in patients with advanced<br />
hepatocellular carcinoma: Results of a phase 2 study. Cancer; 117:1;<br />
125-133; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
93 Lopez-Jimenez E, Gomez-Lopez G, Leandro-Garcia L J, Munoz<br />
I, Schiavi F, Montero-Conde C, De Cubas Aguirre A, RamiresR,<br />
Landa I, Leskela S, Maliszewska A, Inglada-Perez L, De la Vega L,<br />
Rodriguez-Antona C, Leton R, Bernal C, De Campos J M, Diez-<br />
Tascon C, Fraga M F, Boullosa C, Pisano D G, Opocher G, Robledo<br />
M, Cascon A. Research Resource: Transcriptional Profiling Reveals<br />
Different Pseudohypoxic Signatures in SDHB and VHL-Related<br />
Pheochromocytomas. Molecular Endocrinology; 24:12; 2382-2391;<br />
<strong>2010</strong><br />
94 Lumachi F, Frigo A C, Basso U, Tombolan V, Ermani M. Estrogen<br />
therapy and risk of breast cancer in postmenopausal women: a<br />
case-control study and results of a multivariate analysis. Menopause;
17:3; 524-528; <strong>2010</strong><br />
95 Lumachi F, Luisetto G, Basso S M M, Basso U, Brunello A, Camozzi<br />
V. Endocrine therapy of breast cancer. Current medicinal chemistry;<br />
18:4; 513-522; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
96 Maio M, Nicolay H J, Ascierto P A, Belardelli F, Camerini R, Colombo<br />
M P, Queirolo P, Ridolfi R, Russo V, Fonsatti E, Parmiani G, NIBIT<br />
[as collab. Rosato A]. Sixth annual meeting of the Italian network<br />
for tumor biotherapy (NIBIT). Siena, 16-18 October 2008.; Cancer<br />
immunology, immunotherapy- CII; 59:6; 963-969; <strong>2010</strong><br />
97 Mano M P, Ponti A, Tomatis M, Baiocchi D, Barca A, Berti R, Bordon<br />
R, Casella D, Delrio D, Donati G, Falcini F, Frigerio A, Furini A,<br />
Mantellini P, Naldoni C, Pagano G, Piccini P, Ravaioli A, Rodella D,<br />
Sapino A, Sedda M L, Taffurelli M, Vettorazzi M, Zorzi M, Cataliotti<br />
L, Segnan N. Audit system on Quality of breast cancer diagnosis<br />
and Treatment (QT): results of quality indicators on screen-detected<br />
lesions in Italy, 2007. Epidemiologia e prevenzione; 34; 5-6 Suppl 4;<br />
81-88; <strong>2010</strong><br />
98 Marigo I, Bosio E, Solito S, Mesa C, Fernandez A, Dolcetti L, Ugel<br />
S, Sonda N, Bicciato S, Falisi E, Calabrese F, Basso G, Zanovello P,<br />
Cozzi E, Mandruzzato S, Bronte V. Tumor-induced tolerance and<br />
immune suppression depend on the C/EBPbeta transcription factor.<br />
Immunity; 32:6; 790-802; <strong>2010</strong><br />
99 Marino D, Burra P, Boccagni P, Calabrese F, Canova F, Trentin C, Boso C,<br />
Soldà C, Angeli P, Aversa Savina M L. Post-transplant Lymphoproliferative<br />
Disorders in Liver Transplanted Patients: A Single-centre Experience.<br />
Anticancer Research; 30:6; 2383-2391; <strong>2010</strong><br />
100 Marioni G, Koussis H, Scola A, Maruzzo M, Giacomelli L, Karahontziti<br />
P, Filippis C D, Staffieri A, Blandamura S. Expression of MASPIN<br />
and angiogenin in nasopharyngeal carcinoma: novel preliminary<br />
clinico-pathological evidence. Acta Oto-Laryngologica; 130:8; 952-<br />
958; <strong>2010</strong><br />
101 Martello G, Rosato A, Ferrari F, Manfrin A, Cordenonsi M, Dupont S,<br />
Enzo E, Guzzardo V, Rondina M, Spruce T, Parenti A R, Daidone M<br />
G, Bicciato S, Piccolo S. A microRNA targeting dicer for metastasis<br />
control. Cell; 141:7; 1195-1207; <strong>2010</strong><br />
102 Martini M, Testi MG, Pasetto M, Picchio MC, Innamorati G, Mazzocco<br />
M, Ugel S, Cingarlini S, Bronte V, Zanovello P, Krampera M, Mosna<br />
F, Cestari T, Riviera AP, Brutti N, Barbieri O, Matera L, Tridente G,<br />
Colombatti M, Sartoris S. IFN-gamma-mediated upmodulation of<br />
MHC class I expression activates tumor-specific immune response in a<br />
mouse model of prostate cancer. Vaccine; 28:20; 3548-3557; <strong>2010</strong><br />
PUBLICATIONS<br />
285<br />
103 Martorelli D, Muraro E, Merlo A, Turrini R, Rosato Antonio, Dolcetti<br />
R. Role of CD4+ cytotoxic T lymphocytes in the control of viral<br />
diseases and cancer. International reviews of immunology; 29:4;<br />
371-402; <strong>2010</strong><br />
104 Marulli G, Rea F, Nicotra S, Favaretto A G, Perissinotto E, Chizzolini<br />
M, Vianello A, Braccioni F. Effect of induction chemotherapy on<br />
lung function and exercise capacity in patients affected by malignant<br />
pleural mesothelioma. European journal of cardio-thoracic surgery;<br />
37:6; 1464-1469; <strong>2010</strong><br />
105 Massimino M, Gandola L, Barra S, Giangaspero F, Casali C, Potepan<br />
P, Di Rocco C, Nozza P, Collini P, Viscardi E, Bertin D, Biassoni V,<br />
Cama A, Milanaccio C, Modena P, Balter R, Tamburrini G, Peretta P,<br />
Mascarin M, Scarzello G, Fidani P, Milano G M, Sardi I, Genitori L,<br />
Garre M L. Infant Ependymoma in a 10-year AIEOP (Associazione<br />
Italiana Ematologia Oncologia Pediatrica) Experience with Omitted<br />
or Deferred Radiotherapy. International journal of radiation oncology,<br />
biology, physics; 80:3; 807-814; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
106 Mastrangelo G, Fadda E, Cegolon L, Montesco M, Ray-Coquard I, Buja<br />
A, Fedeli U, Frasson A, Spolaore P, Rossi C R. A European project on<br />
incidence, treatment, and outcome of sarcoma. BMC Public Health;<br />
10:1; 188; <strong>2010</strong><br />
107 Mastrangelo G, Lange J H, Fadda E, Agostini O, Agnesi R, Bardin A,<br />
Cegolon L. The evaluation of a health education campaign on use of<br />
leave from work during pregnancy. BMC public health; 10:1; 694;<br />
<strong>2010</strong><br />
108 Mercadante S, Zagonel V, Breda E, Arcara C, Gebbia V, Porzio G,<br />
Aielli F, David F, Gammucci T, Narducci F, Lanzetta G, Restuccia<br />
R, Lembo A, Passeri V, Virzi V, Casuccio A. Breakthrough pain in<br />
oncology: a longitudinal study. Journal of pain and symptom<br />
management; 40:2; 183-190; <strong>2010</strong><br />
109 Merlo A, Turrini R, Bobisse S, Zamarchi R, Alaggio R, Dolcetti R,<br />
Mautner J, Zanovello P, Amadori A, Rosato A. Virus-Specific Cytotoxic<br />
CD4+ T Cells for the Treatment of EBV-Related Tumors Journal of<br />
Immunology. 184:10; 5895-5902; <strong>2010</strong><br />
110 Merlo A, Turrini R, Dolcetti R, Martorelli D, Muraro E, Comoli P,<br />
Rosato A. The interplay between EBV and the immune system:<br />
a rationale for adoptive cell therapy of EBV-related disorders.<br />
Haematologica; 95:10; 1769-1777; <strong>2010</strong><br />
111 Merlo A, Turrini R, Trento C, Zanovello P, Dolcetti R, Rosato A. Impact<br />
of gamma-chain cytokines on EBV-specific T cell cultures. Journal of<br />
Translational Medicine; 8:1; 121; <strong>2010</strong>
112 Mescoli C, Castoro C, Sergio A, Ruol A, Farinati F, Rugge M. Hepatic<br />
spleen nodules (HSN). Scandinavian journal of gastroenterology;<br />
45:5; 628-632; <strong>2010</strong><br />
113 Mocellin S, Pasquali S, Rossi C R, Nitti D. Interferon alpha adjuvant<br />
therapy in patients with high-risk melanoma: a systematic review<br />
and meta-analysis. Journal of the National Cancer Institute; 102:7;<br />
493-501; <strong>2010</strong><br />
114 Montagnese S, Biancardi A, Schiff S, Carraro P, Carlà V, Mannaioni G,<br />
Moroni F, Tono N, Angeli P, Gatta A, Amodio P. Different biochemical<br />
correlates for different neuropsychiatric abnormalities in patients<br />
with cirrhosis. Hepatology; 53:2; 558-566; <strong>2010</strong><br />
115 Nacamulli D, Mian C, Petricca D, Lazzarotto F, Barollo S, Pozza D,<br />
Masiero S, Faggian D, Plebani M, Girelli ME, Mantero F, Betterle C.<br />
Influence of Physiological Dietary Selenium Supplementation on the<br />
Natural Course of Autoimmune Thyroiditis. Clinical endocrinology;<br />
73:4; 535-539; <strong>2010</strong> (E-pub 2009)<br />
116 Nicoletto M O, Dalla Palma M, Donach M E, Gusella M, Cappetta<br />
A, Shams M, Marchet A, Nardin M, Pintacuda G, Di Maggio<br />
A, Marchesi M, Carli P, Fiduccia P, Artioli G, Nitti D. Positive<br />
experience of intraperitoneal chemotherapy followed by intravenous<br />
chemotherapy in heavily pretreated patients with suboptimal<br />
residual ovarian cancer and primary peritoneal cancer. Tumori; 96:6;<br />
918-925; <strong>2010</strong> (E-pub 2009)<br />
117 Nicoletto M O, Parenti A, Del Bianco P, Lombardi G, Pedrini L, Pizzi<br />
S, Carli P, Della Palma M, Pastorelli D, Corti L, Becagli L. Vulvar<br />
cancer: prognostic factors. Anticancer Research; 30:6; 2311-2317;<br />
<strong>2010</strong><br />
118 Occhi G, Trivellin G, Ceccato F, De Lazzari P, Giorgi G, Dematté S,<br />
Grimaldi F, Castello R, Davì M V, Arnaldi G, Salviati L, Opocher G,<br />
Mantero F, Scaroni C. Prevalence of AIP mutations in a large series<br />
of sporadic Italian acromegalic patients and evaluation of CDKN1B<br />
status in acromegalic patients with multiple endocrine neoplasia.<br />
European Journal of Endocrinology; 163:3; 369-376; <strong>2010</strong><br />
119 O’Day S J, Maio M, Chiarion-Sileni V, Gajewski T F, Pehamberger<br />
H, Bondarenko I N, Queirolo P, Lundgren L, Mikhailov S, Roman L,<br />
Verschraegen C, Humphrey R, Ibrahim R, De Pril V, Hoos A, Wolchok J<br />
D. Efficacy and safety of ipilimumab monotherapy in patients with<br />
pretreated advanced melanoma: a multicenter single-arm phase II<br />
study; Annals of Oncology. 21:8; 1712-1717; <strong>2010</strong><br />
120 Opocher G, Schiavi F. Genetics of pheochromocytomas and<br />
paragangliomas. Best practice & research. Clinical endocrinology &<br />
PUBLICATIONS<br />
286<br />
metabolism; 24:6; 943-956; <strong>2010</strong><br />
121 Pace F, Riegler G, De Leone A, Pace M, Cestari R, Dominici P, Grossi<br />
E, EMERGE SG [as collab. Battaglia G]. Is it possible to clinically<br />
differentiate erosive from nonerosive reflux disease patients? A study<br />
using an artificial neural networks-assisted algorithm. European<br />
journal of gastroenterology & hepatology; 22:10; 1163-1168; <strong>2010</strong><br />
122 Paediatric European Network for Treatment of AIDS [as coord. De Rossi<br />
A]. Response to planned treatment interruptions in HIV infection<br />
varies across childhood. AIDS; 24:2; 231-241; <strong>2010</strong><br />
123 Palozzo A C. Structure and stabilty of G-CSF. Tumori; Suppl. 9:1;<br />
31-34; <strong>2010</strong><br />
124 Pasquali S, Mocellin S, Campana L G, Bonandini E Montesco MC,<br />
Tregnaghi A, Del Fiore P, Nitti D, Rossi C R. Early (sentinel lymph<br />
node biopsy-guided) versus delayed lymphadenectomy in melanoma<br />
patients with lymph node metastases: personal experience and<br />
literature meta-analysis. Cancer; 116:5; 1201-1209; <strong>2010</strong><br />
125 Pastorelli D, Zustovich F, Faggioni G, Zovato S, Donach M, Nicoletto<br />
M O, Farina M, Furini L, Ceravolo R, Carli P, Lombardi G. Good<br />
response to second-line bevacizumab and interferon-α in a sunitinibrefractory<br />
patient with metastatic renal cell carcinoma. Anti-Cancer<br />
Drugs; 21:2; 210-213; <strong>2010</strong><br />
126 Pastrello C, Pin E, Marroni F, Bedin C, Fornasarig M, Tibiletti M,<br />
Oliani C, De Leon M, Urso E, Della Puppa L, Agostini M, Viel A.<br />
Integrated analysis of unclassified variants in mismatch repair genes.<br />
Genetics in medicine; 13:2; 115-124; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
127 Pelizzo M R, Boschin I M, Barollo S, Pennelli G M, Toniato A,<br />
Zambonin L, Vianello F, Piotto A, Casal Ide E, Pagetta C, Sorgato<br />
N, Torresan F, Girelli M E, Nacamulli D, Mantero F, Mian C.<br />
BRAF analysis by fine needle aspiration biopsy of thyroid nodules<br />
improves preoperative identification of papillary thyroid carcinoma<br />
and represents a prognostic factor. A mono-institutional experience.<br />
Clinical chemistry and laboratory medicine; 42:2; 325-329; <strong>2011</strong><br />
(E-pub <strong>2010</strong>)<br />
128 Pelizzo M R, Losi A, Boschin I M, Toniato A, Pennelli G M, Sorgato N,<br />
Faggian D, Plebani M. Rapid intraoperative parathyroid hormone<br />
assay in fine needle aspiration for differential diagnosis in thyroid<br />
and parathyroid surgery. Clinical chemistry and laboratory medicine;<br />
48:9; 1313-1317; <strong>2010</strong><br />
129 Pengo V, Banzato A, Bison E, Denas G, Padayattil J S, Ruffatti A.<br />
Antiphospholipid syndrome: critical analysis of the diagnostic path.<br />
Lupus; 19:4; 428-431; <strong>2010</strong>
130 Peranzoni E, Zilio S, Marigo I, Dolcetti L, Zanovello P, Mandruzzato<br />
S, Bronte V. Myeloid-derived suppressor cell heterogeneity and subset<br />
definition. Current opinion in immunology; 22:2; 238-244; <strong>2010</strong><br />
131 Polacco M, Vitale A, Valmasoni M, D’Amico F, Gringeri E, Brolese A,<br />
Zanus G, Neri D, Carraro A, Pauletto A, Romanelli E, Lo Bello S,<br />
Cillo U. Liver Resection Associated With Mini Porto-Caval Shunt<br />
as Salvage Treatment in Patients With Progression of Hepatocellular<br />
Carcinoma Before Liver Transplantation: A Case Report.<br />
Transplantation proceedings; 42:4; 1378-1380; <strong>2010</strong><br />
132 Polese L, Angriman I, Scarpa M, Pagano D, Parente P, Erroi F, Frego<br />
M, D’Amico D F, Norberto L. Diode laser treatment of Barrett’s<br />
esophagus: Long-term results. Lasers in Medical Science; 26:2; 223-<br />
228; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
133 Polesel J, Franceschi S, Suligoi B, Crocetti E, Falcini F, Guzzinati S,<br />
Vercelli M, Zanetti R, Tagliabue G, Russo A, Luminari S, Stracci F,<br />
De Lisi V, Ferretti S, Mangone L, Budroni M, Limina R M, Piffer S,<br />
Serraino D, Bellu F, Giacomin A, Donato A, Madeddu A, Vitarelli<br />
S, Fusco M, Tessandori R, Tumino R, Piselli P, Dal Maso L, for the<br />
Cancer and AIDS Registries Linkage (CARL) Study Cancer and AIDS<br />
Registries Linkage Study. Cancer incidence in people with AIDS in<br />
Italy. International journal of cancer; 127:6; 1437-1445; <strong>2010</strong><br />
134 Pomerri F, Pucciarelli S, Maretto I, Zandon M, Del Bianco P, Amadio<br />
L, Rugge M, Nitti D, Muzzio P C. Prospective assessment of imaging<br />
after preoperative chemoradiotherapy for rectal cancer. Surgery; 149:<br />
1; 56-64; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
135 Pomerri F, Dodi G, Pintacuda G, Amadio L, Muzzio P C. Anal<br />
endosonography and fistulography for fistula-in-ano. Radiologia<br />
Medica; 115:5; 771-783; <strong>2010</strong><br />
136 Pomerri F, Foletto M, Allegro G, Bernante P, Prevedello L, Muzzio P C.<br />
Laparoscopic Sleeve Gastrectomy-Radiological Assessment of Fundus<br />
Size and Sleeve Voiding. Obesity Surgery; 21; 7; 858; 863; <strong>2010</strong><br />
137 Pucciarelli S, Del Bianco P, Efficace F, Serpentini S, Capirci C, De Paoli<br />
A, Amato A, Cuicchi D, Nitti D. Patient-reported Outcomes After<br />
Neoadjuvant Chemoradiotherapy for Rectal Cancer: A Multicenter<br />
Prospective Observational Study. Annals of Surgery; 253:1; 71-77;<br />
<strong>2011</strong> (E-pub <strong>2010</strong>)<br />
138 Qin Y, Yao L, King E E, Buddavarapu K, Lenci R E, Chocron E S,<br />
Lechleiter J D, Sass M, Aronin N, Schiavi F, Boaretto F, Opocher G, Toledo<br />
R A, Toledo S P, Stiles C, Aguiar R C, Dahia P L. Germline mutations<br />
in TMEM127 confer susceptibility to pheochromocytoma. Nature<br />
genetics; 42:3; 229-233; <strong>2010</strong><br />
PUBLICATIONS<br />
287<br />
139 Quarta S, Vidalino L, Turato C, Ruvoletto M, Calabrese F, Valente<br />
M, Cannito S, Fassina G, Parola M, Gatta A, Pontisso P. SERPINB3<br />
induces epithelial - Mesenchymal transition. Journal of Pathology;<br />
221:3; 343-356; <strong>2010</strong><br />
140 Ramonda R, Musacchio E, Campana C, Frigato M, Frallonardo P,<br />
Barbieri V, Piccoli A, Valvason C, Bronte V, Zanovello P, Punzi L.<br />
Immunogenetic aspects of erosive osteoarthritis of the hand in<br />
patients from northern Italy. Scandinavian journal of rheumatology;<br />
40:2; 139-144; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
141 Rampazzo E, Bertorelle R, Serra L, Terrin L, Candiotto C, Pucciarelli<br />
S, Del Bianco P, Nitti D, De Rossi A. Relationship between telomere<br />
shortening, genetic instability, and site of tumor origin in colorectal<br />
cancers. British journal of cancer; 102:8; 1300-1305; <strong>2010</strong><br />
142 Ramus S J, Kartsonaki C, Gayther S A, Pharoah P D, Sinilnikova<br />
O M, Beesley J, Chen X, McGuffog L, Healey S, Couch F J, Wang X,<br />
Fredericksen Z, Peterlongo P, Manoukian S, Peissel B, Zaffaroni D,<br />
Roversi G, Barile M, Viel A, Allavena A, Ottini L, Papi L, Gismondi<br />
V, Capra F, Radice P, Greene M H, Mai P L, Andrulis I L, Glendon<br />
G, Ozcelik H, OCGN, Thomassen M, Gerdes A M, Kruse T A, Cruger<br />
D, Jensen U B, Caligo M A, Olsson H, Kristoffersson U, Lindblom A,<br />
Arver B, Karlsson P, Stenmark Askmalm M, Borg A, Neuhausen S L,<br />
Ding Y C, Nathanson K L, Domchek S M, Jakubowska A, Lubinski J,<br />
Huzarski T, Byrski T, Gronwald J, Gorski B, Cybulski C, Debniak T,<br />
Osorio A, Duran M, Tejada M I, Benitez J, Hamann U, Rookus M A,<br />
Verhoef S, Tilanus-Linthorst M A, Vreeswijk M P, Bodmer D, Ausems<br />
M G, Van Os T A, Asperen C J, Blok M J, Meijers-Heijboer H E,<br />
HEBON, EMBRACE, Peock S, Cook M, Oliver C, Frost D, Dunning<br />
A M, Evans D G, Eeles R, Pichert G, Cole T, Hodgson S, Brewer<br />
C, Morrison P J, Porteous M, Kennedy M J, Rogers M T, Side L E,<br />
Donaldson A, Gregory H, Godwin A, Stoppa-Lyonnet D, Moncoutier<br />
V, Castera L, Mazoyer S, Barjhoux L, Bonadona V, Leroux D, Faivre<br />
L, Lidereau R, Nogues C, Bignon Y J, Prieur F, Collonge-Rame M A,<br />
Venat-Bouvet L, Fert-Ferrer S, GEMO Study Collaborators, Miron A,<br />
Buys S S, Hopper J L, Daly M B, John E M, Terry M B, Goldgar D,<br />
BCFR, Hansen T V, Jonson L, Ejlertsen B, Agnarsson B A, Offit K,<br />
Kirchhoff T, Vijai J, Dutra-Clarke A V, Przybylo J A, Montagna M,<br />
Casella C, Imyanitov E N, Janavicius R, Blanco I, Lazaro C, Moysich<br />
K B, Karlan B Y, Gross J, Beattie M S, Schmutzler R, Wappenschmidt<br />
B, Meindl A, Ruehl I, Fiebig B, Sutter C, Arnold N, Deissler H,<br />
Varon-Mateeva R, Kast K, Niederacher D, Gadzicki D, Caldes T, De<br />
la Hoya M, Nevanlinna H, Aittomaki K, Simard J, Soucy P, kConFab
Investigators, Spurdle A B, Holland H, Chenevix-Trench G, Easton D<br />
F, Antoniou A C, On behalf of Consortium of Investigators of Modifiers<br />
of BRCA1/2. Genetic Variation at 9p22.2 and Ovarian Cancer Risk<br />
for BRCA1 and BRCA2 Mutation Carriers. Journal of the National<br />
Cancer Institute; 103:2; 105-116; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
143 Rastrelli M, Soteldo J, Zonta M, Trifiro G, Mazzarol G, Vitali G C,<br />
Mosconi M, Testori A. Sentinel Node Biopsy for High-Risk Cutaneous<br />
Nonanogenital Squamous Cell Carcinoma: A Preliminary Result.<br />
European Surgical Research; 44:3-4; 204-208; <strong>2010</strong><br />
144 Rea F, Marulli G, Di Chiara F, Schiavon M, Perissinotto E, Breda C,<br />
Favaretto A G, Calabrese F. Multidisciplinary approach for advanced<br />
stage thymic tumors: Long-term outcome. Lung cancer; 72:1; 68-<br />
72; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
145 Reni M, Pasetto L M, Passardi A, Milella M, Mambrini A, Cereda<br />
S, Aprile G, Tronconi M C, Berardi R, Cordio S, Sartori N, Rognone<br />
A, Pederzoli P, Falconi M. Treatment trends in metastatic pancreatic<br />
cancer patients: Is it time to change? Digestive and liver disease; 43:3;<br />
225-230; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
146 Reni M, Sartori N, Mambrini A, Berardi R, Passardi A, Milella M,<br />
Cereda S, Tronconi M C, Aprile G, Cordio S, Pasetto L M, Rognone<br />
A, Pederzoli P, Falconi M. An Italian study on treatment trends and<br />
outcomes of patients with stage III pancreatic adenocarcinoma in<br />
the gemcitabine era: is it time to change? Anti-Cancer Drugs; 21:4;<br />
459-464; <strong>2010</strong><br />
147 Ricci E, Malacrida S, Zanchetta M, Mosconi I, Montagna M, Giaquinto<br />
C, De Rossi A. Toll-like receptor 9 polymorphisms influence motherto-child<br />
transmission of human immunodeficiency virus type 1.<br />
Journal of Translational Medicine; 8:1; 49-49; <strong>2010</strong><br />
148 Romei C, Mariotti S, Fugazzola L, Taccaliti A, Pacini F, Opocher G,<br />
Mian C, Castellano M, Degli Uberti E, Ceccherini I, Cremonini N,<br />
Seregni E, Orlandi F, Ferolla P, Puxeddu E, Giorgino F, Colao A, Loli<br />
P, Bondi F, Cosci B, Bottici V, Cappai A, Pinna G, Persani L, Uberta<br />
V, Boscaro M, Castagna M G, Cappelli C, Zatelli M C, Faggiano A,<br />
Francia G, Brandi M L, Falchetti A, Pinchera A, Elisei R, ItaMEN<br />
network. Multiple endocrine neoplasia type 2 syndromes (MEN<br />
2): results from the ItaMEN network analysis on the prevalence<br />
of different genotypes and phenotypes. European journal of<br />
endocrinology; 163:2; 301-308; <strong>2010</strong><br />
149 Ronco G, Giorgi-Rossi P, Carozzi F, Confortini M, Palma P D, Del<br />
Mistro A, Ghiringhello B, Girlando S, Gillio-Tos A, De Marco L,<br />
Naldoni C, Pierotti P, Rizzolo R, Schincaglia P, Zorzi M, Zappa M,<br />
PUBLICATIONS<br />
288<br />
Segnan N, Cuzick J. Efficacy of human papillomavirus testing for<br />
the detection of invasive cervical cancers and cervical intraepithelial<br />
neoplasia: a randomised controlled trial. Lancet Oncology; 11:3;<br />
249-257; <strong>2010</strong><br />
150 Ronco G, Giubilato P, Naldoni C, Zorzi M, Anghinoni E, Scalisi A,<br />
Dalla Palma P, Zanier L, Barca A, Angeloni C, Gaimo M D, Maglietta<br />
R, Mancini E, Pizzuti R, Iossa A, Segnan N, Zappa M. Extension of<br />
organised cervical cancer screening programmes in Italy and their<br />
process indicators: 2008 activity. Epidemiologia e prevenzione; 34:<br />
(5-6 Suppl 4); 35-51; <strong>2010</strong><br />
151 Rossi C R, Pasquali S, Mocellin S, Vecchiato A, Campana L G, Pilati<br />
P, Zanon A, Nitti D. Long-Term Results of Melphalan-Based<br />
Isolated Limb Perfusion With or Without Low-Dose TNF for In-<br />
Transit Melanoma Metastases. Annals of Surgical Oncology; 17:1;<br />
3000-3007; <strong>2010</strong><br />
152 Rossi E, Basso U, Celadin R, Zilio F, Pucciarelli S, Aieta M, Barile<br />
C, Sava T, Bonciarelli G, Tumolo S, Ghiotto C, Magro C, Jirillo A,<br />
Indraccolo S, Amadori A, Zamarchi R. M30 Neoepitope Expression<br />
in Epithelial Cancer: Quantification of Apoptosis in Circulating<br />
Tumor Cells by CellSearch Analysis. Clinical Cancer Research;<br />
16-21; 5233-5243; <strong>2010</strong><br />
153 Rossi G P, Seccia T M, Palumbo G, Belfiore A, Bernini G, Caridi G,<br />
Desideri G, Fabris B, Ferri C, Giacchetti G, Letizia C, Maccario M,<br />
Mallamaci F, Mannelli M, Patalano A, Rizzoni D, Rossi E, Pessina<br />
A C, Mantero F, PAPY Study Investigators [as collab. Opocher G].<br />
Within-patient reproducibility of the aldosterone: renin ratio in<br />
primary aldosteronism. Hypertension; 55:1; 83-89; <strong>2010</strong><br />
154 Rossi P, Baldazzi G, Battistella A, Bello M, Bollini D, Bonvicini V,<br />
Fontana C L, Gennaro G, Moschini G, Navarria F, Rashevsky A,<br />
Uzunov N, Zampa G, Zampa N, Vacchi A. Design and performance<br />
tests of the calorimetric tract of a Compton Camera for small-animals<br />
imaging. Nuclear Instruments and Methods in Physics Research Section<br />
A; 628:1; 430-433; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
155 Ruffolo C, Scarpa M, Bassi N. Infliximab, azathioprine, or<br />
combination therapy for Crohn’s disease. The New England journal<br />
of medicine; 363:11; 1086-1088; <strong>2010</strong><br />
156 Ruffolo C, Scarpa M, Polese L, D’Amico F E, Boetto R, Pozza A,<br />
D’Inca R, Checchin D, Sturniolo G. C, Bassi N, Angriman I. Clinical<br />
Presentation and Diagnosis of Intestinal Adenocarcinoma in Crohn’s<br />
Disease: Analysis of Clinical Predictors and of the Life-Time Risk.<br />
Journal of gastrointestinal surgery: official journal of the Society for
Surgery of the Alimentary Tract; 14:11; 1746-1751; <strong>2010</strong><br />
157 Rugge M, Fassan M, Zaninotto G, Pizzi M, Giacomelli L, Battaglia<br />
G, Rizzetto C, Parente P, Ancona E. Aurora kinase A in Barrett’s<br />
carcinogenesis. Human pathology 41:10; 1380-1386; <strong>2010</strong><br />
158 Ruggero K, Corradin A, Zanovello P, Amadori A, Bronte V, Ciminale<br />
V, D’Agostino D M. Role of microRNAs in HTLV-1 infection and<br />
transformation. Molecular aspects of medicine; 31:5; 367-382; <strong>2010</strong><br />
159 Ruol A, Rampado S, Parenti A, Portale G, Giacomelli L, Battaglia<br />
G, Cagol M, Ancona E. Caustic ingestion and esophageal cancer:<br />
intra- and peri-tumoral fibrosis is associated with a better prognosis.<br />
European Journal of Cardio-Thoracic Surgery; 38:6; 659-664; <strong>2010</strong><br />
160 Ruol A, Rizzetto C, Castoro C, Cagol M, Alfieri R, Zanchettin G,<br />
Cavallin F, Michieletto S, Da Dalt G, Chiarion-Sileni V, Corti L,<br />
Mantoan S, Zaninotto G, Ancona E. Interval between neoadjuvant<br />
chemoradiotherapy and surgery for squamous cell carcinoma of<br />
the thoracic esophagus: does delayed surgery have an impact on<br />
outcome? Annals of Surgery; 252:5; 788-796; <strong>2010</strong><br />
161 Safra T, Andreopoulou E, Levinson B, Borgato L, Pothuri B, Blank<br />
S, Tiersten A, Boyd L, Curtin J, Muggia F. Weekly paclitaxel with<br />
intermittent imatinib mesylate (Gleevec): tolerance and activity in<br />
recurrent epithelial ovarian cancer. Anticancer Research; 30:9; 3243-<br />
3247; <strong>2010</strong><br />
162 Salvador R, Costantini M, Zaninotto G, Morbin T, Rizzetto C, Zanatta<br />
L, Ceolin M, Finotti E, Nicoletti L, Da Dalt G, Cavallin F, Ancona<br />
E. The preoperative manometric pattern predicts the outcome of<br />
surgical treatment for esophageal achalasia. Journal of gastrointestinal<br />
surgery: official journal of the Society for Surgery of the Alimentary<br />
Tract; 14:11; 1635-1645; <strong>2010</strong><br />
163 Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser<br />
O, Marcos-Gragera R, Maynadie M, Simonetti A, Lutz J M, Berrino F,<br />
HAEMACARE WG [as part. Zambon P]. Incidence of hematologic<br />
malignancies in Europe by morphologic subtype: results of the<br />
HAEMACARE project. Blood; 116:19; 3724-3734; <strong>2010</strong><br />
164 Sartoris S, Mazzocco M, Tinelli M, Martini M, Mosna F, Lisi V, Indraccolo<br />
S, Moserle L, Cestari T, Riviera A P, Bifari F, Tridente G, Pizzolo G,<br />
Krampera M. Efficacy assessment of interferon-alpha-engineered<br />
mesenchymal stromal cells in a mouse plasmacytoma model. Stem Cells<br />
and Development; 20:4; 709-719; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
PUBLICATIONS<br />
289<br />
165 Scarpa M. Quality of life after surgery of the alimentary tract. World<br />
journal of gastroenterology WJG; 16:40; 5020-5023; <strong>2010</strong><br />
166 Scarpa M, Bortolami M, Cecchetto A, Faggian D, Kotsafti A, Ruffolo C,<br />
Navaglia F, Pozza A, D’Incà R, Plebani M, Sturniolo G C, Angriman<br />
I. Mucosal immune environment in colonic carcinogenesis: CD80<br />
up-regulation in colonic dysplasia in ulcerative colitis. European<br />
journal of cancer; 47:4; 611-619; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
167 Scarpa M, Pilon F, Pengo V, Romanato G, Ruffolo C, Erroi F, Elisa B,<br />
Frego M, Ossi E, Manzato E, Angriman I. Deep Venous Thrombosis<br />
After Surgery for Inflammatory Bowel Disease: Is Standard Dose<br />
Low Molecular Weight Heparin Prophylaxis Enough? World journal<br />
of surgery; 34:7; 1629-1636; <strong>2010</strong><br />
168 Scarpa M, Prando D, Pozza A, Esposti E D, Castoro C, Angriman<br />
I. A systematic review of diagnostic procedures to detect midgut<br />
neuroendocrine tumors. Journal of surgical oncology; 102:7; 877-<br />
888; <strong>2010</strong><br />
169 Scarpa M, Ruffolo C, Boetto R, Pozza A, Sadocchi L, Angriman I.<br />
Diverting loop ileostomy after restorative proctocolectomy:<br />
predictors of poor outcome and bad poor of life. Colorectal disease;<br />
12:9; 914-920; <strong>2010</strong><br />
170 Schiavi F, Milne R L, Anda E, Blay P, Castellano M, Opocher G,<br />
Robledo M, Cascon A. Are we overestimating the penetrance of<br />
mutations in SDHB? Human mutation; 31:6; 761-762; <strong>2010</strong><br />
171 Schmeisser N, Kaerlev L, Bourdon-Raverdy N, Ganry O, Llopis-Gonzalez<br />
A, Guenel P, Hardell L, Merletti F, Zambon P, Morales-Suarez-Varela<br />
M, Olsen J, Olsson H, Vyberg M, Ahrens W. Occupational exposure to<br />
pesticides and bile tract carcinoma in men: results from a European<br />
multicenter case-control study. Cancer causes & control: CCC; 21:9;<br />
1493-1502; <strong>2010</strong><br />
172 Scoccianti S, Magrini,S M, Ricardi U, Detti B, Buglione M, Sotti G,<br />
Krengli M, Maluta S, Parisi S, Bertoni F, Mantovani C, Tombolini V,<br />
De Renzis C, Lioce M, Fatigante L, Fusco V, Muto P, Berti F, Rubino<br />
G, Cipressi S, Fariselli L, Lupattelli M, Santoni R, Pirtoli L, Biti G.<br />
Patterns of care and survival in a retrospective analysis of 1059<br />
patients with glioblastoma multiforme treated between 2002 and<br />
2007: A multicenter study by the central nervous system study group<br />
of Airo (Italian association of radiation oncology). Neurosurgery;<br />
67:2; 446-458; <strong>2010</strong><br />
173 Serpentini S, Del Bianco P, Alducci E, Toppan P, Ferretti F, Folin M, De<br />
Salvo G L, Nitti D, Pucciarelli S. Psychological well-being outcomes<br />
in disease-free survivors of mid-low rectal cancer following curative
surgery. Psycho-oncology; 20:7; 706-714; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
174 Sidi R, Pasello G, Opitz I, Soltermann A, Tutic M, Rehrauer H Weder<br />
W, Stahel R A, Felley-Bosco E. Induction of senescence markers after<br />
neo-adjuvant chemotherapy of malignant pleural mesothelioma and<br />
association with clinical outcome: An exploratory analysis. European<br />
journal of cancer; 47:2; 326-332; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
175 Silic-Benussi M, Biasiotto R, Andresen V, Franchini G, D’Agostino D<br />
M, Ciminale V. HTLV-1 p13, a small protein with a busy agenda.<br />
Molecular aspects of medicine 31:5; 350-358; <strong>2010</strong><br />
176 Silic-Benussi M, Cavallari I, Vajente N, Vidali S, Chieco-Bianchi L,<br />
Di Lisa F, Saggioro D, D’Agostino D M, Ciminale V. Redox regulation<br />
of T-cell turnover by the p13 protein of human T-cell leukemia virus<br />
type 1: distinct effects in primary vs. transformed cells. Blood; 116-1;<br />
54-62; <strong>2010</strong><br />
177 Silic-Benussi M, Marin O, Biasiotto R, D’Agostino D M, Ciminale<br />
V. Effects of human T-cell leukemia virus type 1 (HTLV-1) p13 on<br />
mitochondrial K(+) permeability: A new member of the viroporin<br />
family? FEBS letters; 584:10; 2070-2075; <strong>2010</strong><br />
178 Sommariva A, Pasquali S, Rossi C R. Lymphadenectomy for<br />
melanoma: Toward a videoscopic approach. Annals of Surgical<br />
Oncology; 18:3; 898-899; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
179 Testori A, Rastrelli M, De Fiori E, Soteldo J, Della Vigna P, Trifiro<br />
G, Mazzarol G, Travaini L L, Verrecchia F, Ratto E L, Bellomi M,<br />
Radio-guided ultrasound lymph node localization: feasibility of a<br />
new technique for localizing and excising nonpalpable lymph nodes<br />
ultrasound suspicious for melanoma metastases. Melanoma research;<br />
20:3; 197-202; <strong>2010</strong><br />
180 Tramentozzi E, Zamarchi R, Pagetta A, Brunati A M, Rossi E, Tibaldi<br />
E, Finotti P. Effects of glucose-regulated protein94 (Grp94) on<br />
Ig secretion from human blood mononuclear cells. Cell stress &<br />
chaperones; 16:3; 329-338; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
181 Turato C, Calabrese F, Biasiolo A, Quarta S, Ruvoletto M, Tono N,<br />
Paccagnella D, Fassina G, Merkel C, Harrison T, Gatta A, Pontisso P.<br />
SERPINB3 modulates TGF-beta expression in chronic liver disease.<br />
Laboratory Investigation; 90:7; 1016-1023; <strong>2010</strong><br />
182 Ulisse S, Baldini E, Sorrenti S, Barollo S, Gnessi L, Catania A, Pellizzo<br />
M R, Nardi F, Mian C, De Antoni E, D’Armiento M, Frati L. High<br />
expression of the urokinase plasminogen activator and its cognate<br />
receptor associates with advanced stages and reduced diseasefree<br />
interval in papillary thyroid carcinoma. Journal of Clinical<br />
Endocrinology and Metabolism; 96:2; 504-508; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
PUBLICATIONS<br />
290<br />
1 83 Villano G, Quarta S, Ruvoletto M G, Turato C, Vidalino L, Biasiolo<br />
A, Tono N, Lunardi F, Calabrese F, Dall’Olmo L, Dedja A, Fassina G,<br />
Gatta A, Pontisso P. Role of squamous cell carcinoma antigen-1 on<br />
liver cells after partial hepatectomy in transgenic mice. International<br />
journal of molecular medicine; 25:1; 137-143; <strong>2010</strong><br />
1 84 Viola A, Contento R L, Molon B. Signaling amplification at<br />
the immunological synapse. Current topics in microbiology and<br />
immunology; 340:1; 109-122; <strong>2010</strong><br />
185 Vitale A, D’Amico F, Frigo A C, Grigoletto F, Brolese A, Zanus G,<br />
Neri D, Carraro A, D’Amico F E, Burra P, Russo F, Angeli P, Cillo U.<br />
Response to “Therapy as a Criterion for Awarding Priority to Patients<br />
With Hepatocellular Carcinoma Awaiting Liver Transplantation”.<br />
Annals of surgical oncology; 17:9; 2290-2302; <strong>2010</strong><br />
186 Vitale A, Volk M L, Gambato M, Zanus G, D’Amico F, Carraro A,<br />
Pauletto A, Bonsignore P, Scopelliti M, Polacco M, Russo F, Senzolo M,<br />
Burra P, Romano A, Angeli P, Cillo U. Estimation of the Harm to the<br />
Waiting List as a Crucial Factor in the Selection of Patients With<br />
Hepatocellular Carcinoma for Liver Transplantation. Transplantation<br />
proceedings; 42:4; 1194-1196; <strong>2010</strong><br />
187 Vitale A, Volk M L, Pastorelli D, Lonardi S, Farinati F, Burra P,<br />
Angeli P, Cillo U. Use of sorafenib in patients with hepatocellular<br />
carcinoma before liver transplantation: a cost-benefit analysis while<br />
awaiting data on sorafenib safety. Hepatology; 51:1; 165-173; <strong>2010</strong><br />
188 Yao L, Schiavi F, Cascon A, Qin Y, Inglada-Perez L, King E E, Toledo R<br />
A, Ercolino T, Rapizzi E, Ricketts C J, Mori L, Giacche M, Mendola A,<br />
Taschin E, Boaretto F, Loli P, Iacobone M, Rossi G P, Biondi B, Lima-<br />
Junior J V, Kater C E, Bex M, Vikkula M, Grossman A B, Gruber S B,<br />
Barontini M, Persu A, Castellano M, Toledo S P, Maher E R, Mannelli<br />
M, Opocher G, Robledo M, Dahia P L. Spectrum and prevalence<br />
of FP/TMEM127 gene mutations in pheochromocytomas and<br />
paragangliomas. JAMA: the journal of the American Medical<br />
Association; 304:23; 2611-2619; <strong>2010</strong><br />
189 Zigon G, Berrino F, Gatta G, Sanchez M J, Van Dijk B, Van Eycken<br />
E, Francisci S, EUROCARE WG [as collab. Guzzinati S, Zambon P].<br />
Prognoses for head and neck cancers in Europe diagnosed in 1995-<br />
1999: a population-based study. Annals of Oncology; 22:1; 165-174;<br />
<strong>2011</strong> (E-pub <strong>2010</strong>)<br />
190 Zorzi M, Baracco S, Fedato C, Grazzini G, Naldoni C, Sassoli de<br />
Bianchi P, Senore C, Visioli C B, Cogo C. Screening for colorectal<br />
cancer in Italy: 2008 survey. Epidemiologia e prevenzione; 34:(5-6<br />
Suppl 4); 53-72; <strong>2010</strong>
191 Zorzi M, Baracco S, Fedato C. Limited effect of summer warming on<br />
the sensitivity of colorectal cancer screening. Gut; E-pub; <strong>2010</strong><br />
192 Zorzi M, Fedato C, Grazzini G, Stocco C F, Banovich F, Bortoli A,<br />
Cazzola L, Montaguti A, Moretto T, Zappa M, Vettorazzi M. High<br />
sensitivity of five colorectal screening programmes with faecal<br />
immunochemical test in the Veneto Region, Italy. Gut; 60:7; 944-<br />
949; <strong>2011</strong> (E-pub <strong>2010</strong>)<br />
193 Zorzi M, Guzzinati S, Puliti D, Paci E. A simple method to estimate<br />
the episode and programme sensitivity of breast cancer screening<br />
programmes. Journal of medical screening; 17:3; 132-138; <strong>2010</strong><br />
194 Zuin J, Veggiani G, Pengo P, Gallotta A, Biasiolo A, Tono N, Gatta<br />
A, Pontisso P, Toth R, Cerin D, Frecer V, Meo S, Gion M, Fassina G,<br />
Beneduce L. Experimental validation of specificity of the squamous<br />
cell carcinoma antigen-immunoglobulin M (SCCA-IgM) assay in<br />
patients with cirrhosis. Clinical chemistry and laboratory medicine;<br />
48:2; 217-223; <strong>2010</strong><br />
195 Zustovich F, Lombardi G, Pastorelli D, Farina P, Furini L, Manara R,<br />
Dalla Palma M, Rotilio A, Nicoletto O, Zagonel V. Bevacizumab and<br />
glioblastomas, a single-centre experience: how disease history and<br />
characteristics may affect clinical outcome. Anticancer Research; 30:<br />
12; 5213-5216; <strong>2010</strong><br />
<strong>2010</strong> PUBLICATIONS / Non indexed in ISI-JCR<br />
1 Agostin M, Enzo M, Morandi L, Bedin C, Pizzini S, Mason S,<br />
Pizzini S, Mason S, Bertorelle R, Urso E, Mescoli C, Lise M,<br />
Pucciarelli S, Nitti D. A ten markers panel provides a more accurate<br />
and complete microsatellite instability analysis in mismatch repairdeficient<br />
colorectal tumors. Cancer biomarkers; 6:1; 49-61; <strong>2010</strong><br />
2 Colombini S, Cecchi M, Vaiani M, Palozzo A C, D’Arpino A. Survey<br />
and evaluation of the essential requirements of software used by a<br />
sample of italian cytotoxic drug units. Bollettino SIFO; 56; 6; <strong>2010</strong><br />
3 Corradin A, Di Camillo B, Rende F, Ciminale V, Toffolo G M, Cobelli<br />
C. Retrovirus HTLV-1 gene circuit: a potential oscillator for<br />
eukaryotes; Pacific Symposium on Biocomputing. Pacific Symposium<br />
on Biocomputing; 421:32; 421-432; <strong>2010</strong><br />
4 Della Puppa A, Rossetto M, Berti F, Zustovich F, Manara R,<br />
Gardiman M, P, Scienza R. Internal auditory canal metastasis<br />
Journal of neurosurgical sciences; 54:4; 159-162; <strong>2010</strong><br />
5 Dolcetti L, Peranzoni E, Bronte V. Measurement of myeloid cell<br />
immune suppressive activity. Current protocols in immunology;<br />
Chapter 14; Unit 14.17; <strong>2010</strong><br />
6 Donach M, Yu Y, Artioli G, Banna G, Feng W, Bast R C Jr, Zhang Z,<br />
Nicoletto M O. Combined use of biomarkers for detection of ovarian<br />
cancer in high-risk women. Tumor biology; 31:3; 209-215; <strong>2010</strong><br />
7 Endri M, Cartei G, Zustovich F, Serino F S, Fassina A. Differential<br />
diagnosis of lung nodules: breast cancer metastases and lung<br />
tuberculosis. Le infezioni in medicina; 18:1; 39-42; <strong>2010</strong><br />
8 Evangelista L, Cervino A R, Gregianin M, Saladini G, FDG-PET/<br />
CT visualises a case of primary hyperparathyroidism in patient<br />
with GIST. Minerva Endocrinologica; 35:3; 193-195<br />
PUBLICATIONS<br />
291<br />
9 Fadda V, Burchini G, Palozzo A C. La contrattazione del prezzo<br />
degli off- label in oncologia. Bollettino SIFO; 56; 1; <strong>2010</strong><br />
10 Fricia T, Sergi G, Lonardi S, Marin S, Falci C, Pintore G,<br />
Monfardini S, Coin A, Basso U, Perissinotto E, Enzi G, Manzato<br />
E. Adjuvant treatment with anastrazole in elderly women with<br />
early breast cancer: Risk of bone fractures and protective role of<br />
risedronic acid. Giornale di gerontologia; 58:1; 31-36; <strong>2010</strong><br />
11 Greggio N A, Pillon M, Varotto E, Zanin A, Talenti E, Palozzo A<br />
C, Calore E, Messina C Short-term bisphosphonate therapy could<br />
ameliorate osteonecrosis: a complication in childhood hematologic<br />
malignancies. Case reports in medicine; <strong>2010</strong>; 206132; 1; 6; <strong>2010</strong><br />
12 Lombardi G, Zustovich F, Nicoletto M O, Donach M, Pastorelli D.<br />
Important Role of Thiamine in Preventing Ifosfamide-Induced<br />
Encephalopathy. Journal of Oncology Pharmacy Practice; 16:2; 135-<br />
136; <strong>2010</strong><br />
13 Mastrangelo G, Fadda E, Rossi C R, Zamprogno E, Buja A, Cegolon<br />
L. Literature search on risk factors for sarcoma: PubMed and<br />
Google Scholar may be complementary sources. BMC Research<br />
Notes; 10:3; 131; <strong>2010</strong><br />
14 Palozzo A C. An Italian model to evaluate appropriateness and<br />
effectiveness of drugs. European Journal of Hospital Pharmacy<br />
Practice; 16:5; 54-55; <strong>2010</strong><br />
14 Pasello G, Altavilla G, Bonanno L, Rea,F., Favaretto A G. A<br />
pathological complete response after preoperative chemotherapy<br />
with carboplatin and pemetrexed in malignant pleural<br />
mesothelioma: A case report. Journal of Thoracic Disease; 2:4; 254;<br />
<strong>2010</strong>
<strong>2011</strong> PUBLICATIONS / Journals indexed in ISI-JCR<br />
1 Acampa W, Di Taranto M D, Morgante A, Salvatore B, Evangelista L,<br />
Ricci F, Costanzo P, De Sisto E, Filardi P P, Petretta M, Fortunato G,<br />
Cuocolo A. C-reactive protein levels are associated with paraoxonase<br />
polymorphism L55M in patients undergoing cardiac SPECT<br />
imaging. Scandinavian journal of clinical and laboratory investigation;<br />
71:3;179-84; <strong>2011</strong><br />
2 Agostini M, Pucciarelli S, Enzo M V, Del Bianco P, Briarava M, Bedin<br />
C, Maretto I, Friso M L, Lonardi S, Mescoli C, Toppan P, Urso E, Nitti<br />
D. Circulating cell-free DNA: A promising marker of pathologic<br />
tumor response in rectal cancer patients receiving preoperative<br />
chemoradiotherapy. Annals of Surgical Oncology; 18:9; 2461-2468;<br />
<strong>2011</strong><br />
3 AIRTUM Working Group, [as collab.] Zambon P, Baracco M, Bovo<br />
E, Dal Cin A, Fiore A R, Greco A, Monetti D, Rosano A, Stocco C F,<br />
Tognazzo S. Italian cancer figures, report <strong>2011</strong>: Survival of cancer<br />
patients in italy. Epidemiologia e prevenzione; 35:5-6 Suppl 3; 1-200;<br />
<strong>2011</strong><br />
4 Aliberti C, Fiorentini G, Muzzio P C, Pomerri F, Tilli M, Dallara S,<br />
Benea G. Trans-arterial chemoembolization of metastatic colorectal<br />
carcinoma to the liver adopting DC bead(R), drug-eluting bead<br />
loaded with irinotecan: Results of a phase II clinical study. Anticancer<br />
Research; 31:12; 4581-4587; <strong>2011</strong><br />
5 Ambrosini V, Campana D, Allegri V, Opocher G, Fanti S, 68Ga-<br />
DOTA-NOC PET/CT detects somatostatin receptors expression in<br />
von hippel-lindau cerebellar disease. Clinical nuclear medicine; 36:1;<br />
64-65; <strong>2011</strong><br />
6 Antoniou A C, Kartsonaki C, Sinilnikova O M, Soucy P, McGuffog L,<br />
Healey S, Lee A, Peterlongo P, Manoukian S, Peissel B, Zaffaroni D,<br />
Cattaneo E, Barile M, Pensotti V, Pasini B, Dolcetti R, Giannini G,<br />
Putignano A L V,L., Radice P, Mai P L, Greene M H, Andrulis I L,<br />
Glendon G, Ozcelik H, Thomassen M, Gerdes A M, Kruse T A, Birk<br />
Jensen U, Cruger D G, Caligo M A, Laitman Y, Milgrom R, Kaufman<br />
B, Paluch-Shimon S, Friedman E, Loman N, Harbst K, Lindblom<br />
A, Arver B, Ehrencrona H, Melin B, SWE-BRCA, Nathanson K L,<br />
Domchek S M, Rebbeck T, Jakubowska A, Lubinski J, Gronwald J,<br />
Huzarski T, Byrski T, Cybulski C, Gorski B, Osorio A, Ramon Y Cajal<br />
T, Fostira F, Andres R, Benitez J, Hamann U, Hogervorst F B, Rookus<br />
PUBLICATIONS<br />
292<br />
M A, Hooning M J, Nelen M R, van der Luijt R B, van Os T A, van<br />
Asperen C J, Devilee P, Meijers-Heijboer H E, Gomez Garcia E B,<br />
HEBON, Peock S, Cook M, Frost D, Platte R, Leyland J, Gareth Evans<br />
D, Lalloo F, Eeles R, Izatt L, Adlard J, Davidson R, Eccles D, Ong K<br />
R, Cook J, Douglas F, Paterson J, John Kennedy M, Miedzybrodzka<br />
Z, EMBRACE, Godwin A, Stoppa-Lyonnet D, Buecher B, Belotti<br />
M, Tirapo C, Mazoyer S, Barjhoux L, Lasset C, Leroux D, Faivre L,<br />
Bronner M, Prieur F, Nogues C, Rouleau E, Pujol P, Coupier I, Frenay<br />
M, CEMO Study Collaborators, Hopper J L, Daly M B, Terry M B,<br />
John E M, Buys S S, Yassin Y, Miron A, Goldgar D, Breast Cancer<br />
Family Registry, Singer C F, Tea M K, Pfeiler G, Catharina Dressler<br />
A, Hansen T V, Jonson L, Ejlertsen B, Bjork Barkardottir R, Kirchhoff<br />
T, Offit K, Piedmonte M, Rodriguez G, Small L, Boggess J, Blank S,<br />
Basil J, Azodi M, Ewart Toland A, Montagna M, Tognazzo S, Agata S,<br />
Imyanitov E, Janavicius R, Lazaro C, Blanco I, Pharoah P D, Sucheston<br />
L, Karlan B Y, Walsh C S, Olah E, Bozsik A, Teo S H, Seldon J L,<br />
Beattie M S, van Rensburg E J, Sluiter M D, Diez O, Schmutzler R K,<br />
Wappenschmidt B, Engel C, Meindl A, Ruehl I, Varon-Mateeva R, Kast<br />
K, Deissler H, Niederacher D, Arnold N, Gadzicki D, Schonbuchner<br />
I, Caldes T, de la Hoya M, Nevanlinna H, Aittomaki K, Dumont M,<br />
Chiquette J, Tischkowitz M, Chen X, Beesley J, Spurdle A B, kConFab<br />
investigators, Neuhausen S L, Chun Ding Y, Fredericksen Z, Wang X,<br />
Pankratz V S, Couch F, Simard J, Easton D F. Chenevix-Trench G,<br />
on behalf of CIMBA, Common alleles at 6q25.1 and 1p11.2 are<br />
associated with breast cancer risk for BRCA1 and BRCA2 mutation<br />
carriers. Human molecular genetics; 20:16; 3304-21; <strong>2011</strong><br />
7 Arlt W, Biehl M, Taylor A E, Hahner S, Libe R, Hughes B A, Schneider<br />
P, Smith D J, Stiekema H, Krone N, Porfiri E, Opocher G, Bertherat J,<br />
Mantero F, Allolio B, Terzolo M, Nightingale P, Shackleton C H, Bertagna<br />
X, Fassnacht M, Stewart P M. Urine steroid metabolomics as a biomarker<br />
tool for detecting malignancy in adrenal tumors. The Journal of clinical<br />
endocrinology and metabolism; 96:12; 3775-84; <strong>2011</strong><br />
8 Aschele C, Cionini L, Lonardi S, Pinto C, Cordio S, Rosati G, Artale S,<br />
Tagliagambe A, Ambrosini G, Rosetti P, Bonetti A, Negru M E, Tronconi<br />
M C, Luppi G, Silvano G, Corsi D C, Bochicchio A M, Chiaulon<br />
G, Gallo M, Boni L. Primary tumor response to preoperative<br />
chemoradiation with or without oxaliplatin in locally advanced
ectal cancer: Pathologic results of the STAR-01 randomized phase<br />
III trial. Journal of clinical oncology : official journal of the American<br />
Society of Clinical Oncology; 29:20; 2773-80; <strong>2011</strong><br />
9 Baldini E, Arlot-Bonnemains Y, Sorrenti S, Mian C, Pelizzo M R, De<br />
Antoni E, Palermo S, Morrone S, Barollo S, Nesca A, Moretti C G,<br />
D'Armiento M, Ulisse S. Aurora kinases are expressed in medullary<br />
thyroid carcinoma (MTC) and their inhibition suppresses in vitro<br />
growth and tumorigenicity of the MTC derived cell line TT. BMC<br />
cancer; 11:411; <strong>2011</strong><br />
10 Banzato A, Polverosi R, Polo V, Canal F, Bianchi A. An unusual<br />
mediastinal outline. Journal of cardiovascular medicine (Hagerstown,<br />
Md.); E-pub <strong>2011</strong><br />
11 Basso U, Maruzzo M, Roma A, Camozzi V, Luisetto G, Lumachi F.<br />
Malignant hypercalcemia. Current medicinal chemistry; 18:23; 3462-<br />
3467; <strong>2011</strong><br />
12 Biasi G, Facchinetti A, Cappellari R, Rossi E, Zanovello P. Immune<br />
response to moloney-murine leukemia virus-induced antigens in<br />
bone marrow. Immunology letters; 138:1; 79-85; <strong>2011</strong><br />
13 Bignotti E, Ravaggi A, Romani C, Falchetti M, Lonardi S, Facchetti F,<br />
Pecorelli S, Varughese J, Cocco E, Bellone S, Schwartz P E, Rutherford<br />
T J, Santin A D. Trop-2 overexpression in poorly differentiated<br />
endometrial endometrioid carcinoma: Implications for<br />
immunotherapy with hRS7, a humanized anti-trop-2 monoclonal<br />
antibody. International journal of gynecological cancer: official journal<br />
of the International Gynecological Cancer Society; 21:9; 1613-1621;<br />
<strong>2011</strong><br />
14 Bisogno G, Pastore G, Perilongo G, Sotti G, Cecchetto G, Dallorso S,<br />
Carli M. Long-term results in childhood rhabdomyosarcoma: A<br />
report from the italian cooperative study RMS 79. Pediatric blood &<br />
cancer; <strong>2011</strong><br />
15 Bocus P, Realdon S, Eloubeidi M A, Diamantis G, Betalli P, Gamba<br />
P, Zanon G F, Battaglia G. High-frequency miniprobes and<br />
3-dimensional EUS for preoperative evaluation of the etiology<br />
of congenital esophageal stenosis in children (with video).<br />
Gastrointestinal endoscopy; 74:204-207; <strong>2011</strong><br />
16 Bolognesi M, Zampieri F, Di Pascoli M, Verardo A, Turato C, Calabrese F,<br />
Lunardi F, Pontisso P, Angeli P, Merkel C, Gatta A, Sacerdoti D, Increased<br />
myoendothelial gap junctions mediate the enhanced response to<br />
epoxyeicosatrienoic acid and acetylcholine in mesenteric arterial vessels<br />
of cirrhotic rats. Liver International; 31:6; 881-890; <strong>2011</strong><br />
17 Bonanno L, Favaretto A G, Rugge M, Taron M, Rosell R. Role of<br />
PUBLICATIONS<br />
293<br />
genotyping in non-small cell lung cancer treatment: Current status.<br />
Drugs; 71:17; 2231-2246; <strong>2011</strong><br />
18 Bonanno L, Jirillo A, Favaretto A G. Mechanisms of acquired<br />
resistance to epidermal growth factor receptor tyrosine kinase<br />
inhibitors and new therapeutic perspectives in non small cell lung<br />
cancer. Current Drug Targets; 12:6; 922-933; <strong>2011</strong><br />
19 Bordignon M, Rottoli P, Agostini C, Alaibac M. Adaptive immune<br />
responses in primary cutaneous sarcoidosis. Clinical & developmental<br />
immunology; <strong>2011</strong>:235142; <strong>2011</strong><br />
20 Buzzoni C, AIRTUM Working Group [as member of AIRTUM WG:<br />
Zambon P.]. Population ageing effect on number of cancer cases:<br />
Italian cancer registries data. Epidemiologia e prevenzione; 35:3-4;<br />
216-221; <strong>2011</strong><br />
21 Caffo O, Sava T, Comploj E, Fariello A, Zustovich F, Segati R, Sacco<br />
C, Veccia A, Galligioni E. Impact of docetaxel-based chemotherapy<br />
on quality of life of patients with castration-resistant prostate<br />
cancer: Results from a prospective phase II randomized trial. BJU<br />
international; 108:11; 1825-1832; <strong>2011</strong><br />
22 Campiglio M, Bufalino R, Sandri M, Ferri E, Aiello R A, De Matteis<br />
A, Mottolese M, De Placido S, Querzoli P, Jirillo A, Bottini A, Fantini<br />
M, Bonetti A, Pedani F, Mauri M, Molino A, Ferro A, Pupa S M,<br />
Sasso M, Ménard S, Balsari A, Tagliabue E. Increased overall survival<br />
independent of RECIST response in metastatic breast cancer patients<br />
continuing trastuzumab treatment: Evidence from a retrospective<br />
study. Breast cancer research and treatment; 128:1; 147-154; <strong>2011</strong><br />
23 Cappetta A, Bergamo F, Mescoli C, Lonardi S, Rugge M, Zagonel V.<br />
Hepatoid adenocarcinoma of the colon: What should we target?<br />
Pathology oncology research: POR; E-pub <strong>2011</strong><br />
24 Cappetta A, Lonardi S, Pastorelli D, Bergamo F, Lombardi G, Zagonel<br />
V. Advanced Gastric Cancer (GC) and cancer of the Gastro-<br />
Oesophageal Junction (GEJ): Focus on targeted therapies. Critical<br />
reviews in oncology/hematology; E-pub <strong>2011</strong><br />
25 Carraro A, Mazloum D E, Bihl F. Health-related quality of life<br />
outcomes after cholecystectomy. World journal of gastroenterology:<br />
WJG; 17:45; 4945-4951; <strong>2011</strong><br />
26 Cartei G, Colombrino E, Sanzari M C, Plebani M, Micucci M, Fiorica<br />
F, Giraldi T, Zustovich F, Cartei F. Chronic anemia due to mitomycin<br />
C is drug dose-dependent, normocytic, progressive, related to<br />
erythropoietin levels and quantitatively predictable: Implications for<br />
radiochemotherapy. Journal of chemotherapy (Florence, Italy); 23:6;<br />
362-366; <strong>2011</strong>
27 Castelblanco E, Gallel P, Ros S, Gatius S, Valls J, De-Cubas A A,<br />
Maliszewska A, Yebra-Pimentel M T, Menarguez J, Gamallo C, Opocher<br />
G, Robledo M, Matias-Guiu X. Thyroid paraganglioma. Report of 3<br />
cases and description of an immunohistochemical profile useful in<br />
the differential diagnosis with medullary thyroid carcinoma, based<br />
on complementary DNA array results. Human pathology; E-pub<br />
<strong>2011</strong><br />
28 Castoro C, Scarpa M, Cagol M, Ruol A, Cavallin F, Alfieri R,<br />
Zanchettin G, Rugge M, Ancona E. Nodal metastasis from locally<br />
advanced esophageal cancer: How neoadjuvant therapy modifies<br />
their frequency and distribution. Annals of Surgical Oncology; 18:13;<br />
3743-3754; <strong>2011</strong><br />
29 Caumo F, Brunelli S, Zorzi M, Baglio I, Ciatto S, Montemezzi S.<br />
Benefits of double reading of screening mammograms: Retrospective<br />
study on a consecutive series. Radiologia Medica; 1-9; <strong>2011</strong><br />
30 Cavallari I, Rende F, D’Agostino D M, Ciminale V. Converging<br />
strategies in expression of human complex retroviruses. Viruses -<br />
Basel; 3:8; 1395-1414; <strong>2011</strong><br />
31 Chiarion-Sileni V, Guida M, Ridolfi L, Romanini A, Del Bianco P,<br />
Pigozzo J, Brugnara S, Colucci G, Ridolfi R, De Salvo G L. Central<br />
nervous system failure in melanoma patients: Results of a randomised,<br />
multicentre phase 3 study of temozolomide- and dacarbazine- based<br />
regimens. British journal of cancer; 104:12; 1816-1822; <strong>2011</strong><br />
32 Chioda M, Peranzoni E, Desantis G, Papalini F, Falisi E, Samantha<br />
S, Mandruzzato S, Bronte V. Myeloid cell diversification and<br />
complexity: An old concept with new turns in oncology. Cancer<br />
metastasis reviews; 30:1; 27-43; <strong>2011</strong><br />
33 Ciccarino P, Rotilio A, Rossetto M, Manara R, Orvieto E, Berti<br />
F, Lombardi G, d’Avella D, Scienza R, Della Puppa A. Multifocal<br />
presentation of medulloblastoma in adulthood. Journal of neurooncology;<br />
E-pub <strong>2011</strong><br />
34 Cipolletta S, Shams M, Tonello F, Pruneddu A. Caregivers of patients<br />
with cancer: Anxiety, depression and distribution of dependency.<br />
Psycho-oncology; n/a-n/a; <strong>2011</strong><br />
35 Colombo C, Verga U, Mian C, Ferrero S, Perrino M, Vicentini L, Dazzi<br />
D, Opocher G, Pelizzo M R, Beck-Peccoz P, Fugazzola L. Comparison<br />
of calcium and pentagastrin tests for the diagnosis and follow-up of<br />
medullary thyroid cancer. The Journal of clinical endocrinology and<br />
metabolism; E-pub <strong>2011</strong><br />
36 Comino-Mendez I, Gracia-Aznarez F J, Schiavi F, Landa I, Leandro-<br />
Garcia L J, Leton R, Honrado E, Ramos-Medina R, Caronia D, Pita<br />
PUBLICATIONS<br />
294<br />
G, Gomez-Grana A, de Cubas A A, Inglada-Perez L, Maliszewska A,<br />
Taschin E, Bobisse S, Pica G, Loli P, Hernandez-Lavado R, Diaz J A,<br />
Gomez-Morales M, Gonzalez-Neira A, Roncador G, Rodriguez-Antona<br />
C, Benitez J, Mannelli M, Opocher G, Robledo M, Cascon A. Exome<br />
sequencing identifies MAX mutations as a cause of hereditary<br />
pheochromocytoma. Nature genetics; 43:663-667; <strong>2011</strong><br />
37 Cordenonsi M, Zanconato F, Azzolin L, Forcato M, Rosato A, Frasson<br />
C, Inui M, Montagner M, Parenti A R, Poletti A, Daidone M G,<br />
Dupont S, Basso G, Bicciato S, Piccolo S. The hippo transducer TAZ<br />
confers cancer stem cell-related traits on breast cancer cells. Cell;<br />
147:4; 759-772; <strong>2011</strong><br />
38 Corradin A, Di Camillo B, Ciminale V, Toffolo G, Cobelli C.<br />
Sensitivity analysis of retrovirus HTLV-1 transactivation. Journal of<br />
Computational Biology; 18:2; 183-193; <strong>2011</strong><br />
39 Cox D G, Simard J, Sinnett D, Hamdi Y, Soucy P, Ouimet M, Barjhoux<br />
L, Verny-Pierre C, McGuffog L, Healey S, Szabo C, Greene M H, Mai<br />
P L, Andrulis I L, Ontario Cancer Genetics Network, Thomassen M,<br />
Gerdes A M, Caligo M A, Friedman E, Laitman Y, Kaufman B, Paluch<br />
S S, Borg A, Karlsson P, Stenmark Askmalm M, Barbany Bustinza G,<br />
SWE-BRCA Collaborators, Nathanson K L, Domchek S M, Rebbeck<br />
T R, Benitez J, Hamann U, Rookus M A, van den Ouweland A<br />
M, Ausems M G, Aalfs C M, van Asperen C J, Devilee P, Gille H J,<br />
HEBON, EMBRACE, Peock S, Frost D, Evans D G, Eeles R, Izatt L,<br />
Adlard J, Paterson J, Eason J, Godwin A K, Remon M A, Moncoutier<br />
V, Gauthier-Villars M, Lasset C, Giraud S, Hardouin A, Berthet P,<br />
Sobol H, Eisinger F, Bressac de Paillerets B, Caron O, Delnatte C,<br />
GEMO Study Collaborators, Goldgar D, Miron A, Ozcelik H, Buys S,<br />
Southey M C, Terry M B, The Breast Cancer Family Registry, Singer C<br />
F, Dressler A C, Tea M K, Hansen T V, Johannsson O, Piedmonte M,<br />
Rodriguez G C, Basil J B, Blank S, Toland A E, Montagna M, Isaacs C,<br />
Blanco I, Gayther S A, Moysich K B, Schmutzler R K, Wappenschmidt<br />
B, Engel C, Meindl A, Ditsch N, Arnold N, Niederacher D, Sutter<br />
C, Gadzicki D, Fiebig B, Caldes T, Laframboise R, Nevanlinna H,<br />
Chen X, Beesley J, Spurdle A B, Neuhausen S L, Ding Y C, Couch F J,<br />
Wang X, Peterlongo P, Manoukian S, Bernard L, Radice P, Easton D<br />
F, Chenevix-Trench G, Antoniou A C, Stoppa-Lyonnet D, Mazoyer S,<br />
Sinilnikova O M. On behalf of the Consortium of Investigators of<br />
Modifiers of BRCA1/2, common variants of the BRCA1 wild-type<br />
allele modify the risk of breast cancer in BRCA1 mutation carriers.<br />
Human molecular genetics; 20:23; 4732-4747; <strong>2011</strong><br />
40 Dal Maso L, De Angelis R, Guzzinati S, AIRTUM Working Group
[as member of AIRTUM WG: Zambon P, Baracco M, Bovo E,<br />
Dal Cin A, Fiore A R, Greco A, Tognazzo S. AIRTUM Numbers:<br />
200,000 young italians live with cancer. Epidemiologia e prevenzione;<br />
35:1; 59; <strong>2011</strong><br />
41 Danielli R, Ridolfi R, Chiarion-Sileni V, Queirolo P, Testori A, Plummer<br />
R, Boitano M, Calabro L, De Rossi C, Giacomo A M, Ferrucci P<br />
F, Ridolfi L, Altomonte M, Miracco C, Balestrazzi A, Maio M.<br />
Ipilimumab in pretreated patients with metastatic uveal melanoma:<br />
Safety and clinical efficacy. Cancer immunology, immunotherapy: CII;<br />
E-pub <strong>2011</strong><br />
42 De Corti F, Bisogno G, Dall’Igna P, Ferrari A, Buffa P, de Paoli A,<br />
Cecchetto G. Does surgery have a role in the treatment of local<br />
relapses of non-metastatic rhabdomyosarcoma? Pediatric Blood and<br />
Cancer; 57:7; 1261-1265; <strong>2011</strong><br />
43 De Vita F, Orditura M, Martinelli E, Vecchione L, Innocenti R, Chiarion-<br />
Sileni V, Di Maio M, Farella A, Troiani T, Morgillo F, Napolitano V,<br />
Ancona E, Di Martino N, Ruol A, Galizia G, Del Genio A, Ciardiello<br />
F. A multicenter phase II study of induction chemotherapy with<br />
FOLFOX-4 and cetuximab followed by radiation and cetuximab in<br />
locally advanced esophageal cancer. British journal of cancer; 104:3;<br />
427-432; <strong>2011</strong><br />
44 Della Puppa A, Denaro L, Rossetto M, Ciccarino P, Manara R, Lombardi<br />
G, Del Moro G, Rotilio A, d’Avella D, Scienza R. Postoperative seizure<br />
in high grade glioma patients treated with BCNU wafers. A monoinstitutional<br />
experience. Journal of neuro-oncology; 105:2; 275-280;<br />
<strong>2011</strong><br />
45 Della Puppa A, Persano L, Masi G, Rampazzo E, Sinigaglia A,<br />
Pistollato F, Denaro L, Barzon L, Palù G, Basso G, Scienza R, d’Avella<br />
D. MGMT expression and promoter methylation status may depend<br />
on the site of surgical sample collection within glioblastoma: A<br />
possible pitfall in stratification of patients? Journal of neuro-oncology;<br />
E-pub 1-9; <strong>2011</strong><br />
46 Diamantis G, Scarpa M, Bocus P, Realdon S, Castoro C, Ancona E,<br />
Battaglia G. Quality of life in patients with esophageal stenting for the<br />
palliation of malignant dysphagia. World Journal of Gastroenterology;<br />
17:2; 144-150; <strong>2011</strong><br />
47 Evangelista L, Rubello D, Saladini G. Can FDG PET/CT monitor<br />
the response to hormonal therapy in breast cancer patients? European<br />
journal of nuclear medicine and molecular imaging; E-pub <strong>2011</strong><br />
48 Evangelista L, Baretta Z, Vinante L, Cervino A R, Gregianin M,<br />
Ghiotto C, Bozza F, Saladini G. Could the serial determination of<br />
PUBLICATIONS<br />
295<br />
Ca15.3 serum improve the diagnostic accuracy of PET/CT? Results<br />
from small population with previous breast cancer. Annals of Nuclear<br />
Medicine; 25:7; 469-477; <strong>2011</strong><br />
49 Fabris L, Cadamuro M, Moserle L, Dziura J, Cong X, Sambado L,<br />
Nardo G, Sonzogni A, Colledan M, Furlanetto A, Bassi N, Massani M,<br />
Cillo U, Mescoli C, Indraccolo S, Rugge M, Okolicsanyi L, Strazzabosco<br />
M. Nuclear expression of S100A4 calcium binding protein increases<br />
cholangiocarcinoma invasiveness and metastasization. Hepatology<br />
(Baltimore, Md.); 54:3; 890-899; <strong>2011</strong><br />
50 Fadini G P, Albiero M, Menegazzo L, Boscaro E, Vigili De Kreutzenberg<br />
S, Agostini C, Cabrelle A, Binotto G, Rattazzi M, Bertacco E,<br />
Bertorelle R, Biasini L, Mion M, Plebani M, Ceolotto G, Angelini<br />
A, Castellani C, Menegolo M, Grego F, Dimmeler S, Seeger F, Zeiher<br />
A, Tiengo A, Avogaro A. Widespread increase in myeloid calcifying<br />
cells contributes to ectopic vascular calcification in type 2 diabetes.<br />
Circulation research; 108:9; 1112-1121; <strong>2011</strong><br />
51 Fassan M, Realdon S, Pizzi M, Balistreri M, Battaglia G, Zaninotto<br />
G, Ancona E, Rugge M. Programmed cell death 4 nuclear loss and<br />
miR-21 or activated akt overexpression in esophageal squamous<br />
cell carcinogenesis. Diseases of the esophagus: official journal of the<br />
International Society for Diseases of the Esophagus / I.S.D.E; E-pub<br />
<strong>2011</strong><br />
52 Fiocca R, Mastracci L, Milione M, Parente P, Savarino V. Microscopic<br />
esophagitis and Barrett’s esophagus: The histology report. Digestive<br />
and Liver Disease; 43:SUPPL. 4; S319-S330; <strong>2011</strong><br />
53 Fischer L, Trunečka P, Gridelli B, Roy A, Vitale A, Valdivieso A,<br />
Varo E, Seehofer D, Lynch S, Samuel D, Ericzon B, Boudjema K,<br />
Karpf C, Undre N. Pharmacokinetics for once-daily versus twicedaily<br />
tacrolimus formulations in de novo liver transplantation: A<br />
randomized, open-label trial. Liver Transplantation; 17:2; 167-177;<br />
<strong>2011</strong><br />
54 Franceschini L, Realdon S, Marcolongo M, Mirandola S, Bortoletto G,<br />
Alberti A. Reciprocal interference between insulin and interferonalpha<br />
signaling in hepatic cells: A vicious circle of clinical significance?<br />
Hepatology; 54:2; 484-94; <strong>2011</strong><br />
55 Frego M, Scarpa M, Lorenzo N, Iacobone M, Bianchera G. Dysplasia<br />
in ulcerative colitis: Still a challenge. Annali Italiani di Chirurgia;<br />
82:1; 5-10; <strong>2011</strong><br />
56 Freguja R, Gianesin K, Mosconi I, Zanchetta M, Carmona F, Rampon<br />
O, Giaquinto C, De Rossi A. Regulatory T cells and chronic immune<br />
activation in human immunodeficiency virus 1 (HIV-1)-infected
children. Clinical and experimental immunology; 164:3; 373-380; <strong>2011</strong><br />
57 Ghisi M, Corradin A, Basso K, Frasson C, Serafin V, Mukherjee S,<br />
Mussolin L, Ruggero K, Bonanno L, Guffanti A, De Bellis G, Gerosa G,<br />
Stellin G, D’Agostino D M, Basso G, Bronte V, Indraccolo S, Amadori<br />
A, Zanovello P. Modulation of microRNA expression in human<br />
T-cell development: Targeting of NOTCH3 by miR-150. Blood;<br />
117:26; 7053-7062; <strong>2011</strong><br />
58 Girardini J E, Napoli M, Piazza S, Rustighi A, Marotta C, Radaelli<br />
E, Capaci V, Jordan L, Quinlan P, Thompson A, Mano M, Rosato A,<br />
Crook T, Scanziani E, Means A R, Lozano G, Schneider C, Del Sal G.<br />
A Pin1/Mutant p53 axis promotes aggressiveness in breast cancer.<br />
Cancer cell; 20:1; 79-91; <strong>2011</strong><br />
59 Gori S, Greco M T, Catania C, Colombo C, Apolone G, Zagonel V,<br />
AIOM Group for the Informed Consent in Medical Oncology. A new<br />
informed consent form model for cancer patients: Preliminary<br />
results of a prospective study by the italian association of medical<br />
oncology (AIOM). Patient education and counseling; E-pub <strong>2011</strong><br />
60 Gridelli C, Gallo C, Morabito A, Iaffaioli R V, Favaretto A G, Isa L,<br />
Barbera S, Gamucci T, Ceribelli A, Filipazzi V, Maione P, Rossi A,<br />
Barletta E, Signoriello S, De Maio E, Piccirillo M C, Di Maio M,<br />
Rocco G, Vecchione A, Perrone F. G-STEP Investigators, Phase I-II<br />
trial of gemcitabine-based first-line chemotherapies for small cell<br />
lung cancer in elderly patients with performance status 0-2: The<br />
G-step trial. Journal of thoracic oncology: official publication of the<br />
International Association for the Study of Lung Cancer; E-pub <strong>2011</strong><br />
61 Gridelli C, Morgillo F, Favaretto A G, de Marinis F, Chella A, Cerea<br />
G, Mattioli R, Tortora G, Rossi A, Fasano M, Pasello G, Ricciardi S,<br />
Maione P, Di Maio M, Ciardiello F. Sorafenib in combination with<br />
erlotinib or with gemcitabine in elderly patients with advanced<br />
non-small-cell lung cancer: A randomized phase II study. Annals of<br />
Oncology: Official Journal of the European Society for Medical Oncology<br />
/ ESMO; 22:7; 1528-1534; <strong>2011</strong><br />
62 Gusella M, Pasini F, Bolzonella C, Meneghetti S, Barile C, Bononi<br />
A, Toso S, Menon D, Crepaldi G, Modena Y, Stievano L, Padrini R.<br />
Equilibrative nucleoside transporter 1 genotype, cytidine deaminase<br />
activity and age predict gemcitabine plasma clearance in patients<br />
with solid tumours. British journal of clinical pharmacology; 71:3;<br />
437-444; <strong>2011</strong><br />
63 Iacobone M, Schiavi F, Bottussi M, Taschin E, Bobisse S, Fassina A,<br />
Opocher G, Favia G. Is genetic screening indicated in apparently<br />
sporadic pheochromocytomas and paragangliomas? Surgery; 150:6;<br />
PUBLICATIONS<br />
296<br />
1194-1201; <strong>2011</strong><br />
64 Im K M, Kirchhoff T, Wang X, Green T, Chow C Y, Vijai J, Korn<br />
J, Gaudet M M, Fredericksen Z, Shane Pankratz V, Guiducci C,<br />
Crenshaw A, McGuffog L, Kartsonaki C, Morrison J, Healey S,<br />
Sinilnikova O M, Mai P L, Greene M H, Piedmonte M, Rubinstein<br />
W S, Hogervorst F B, Rookus M A, Collée J M, Hoogerbrugge N, van<br />
Asperen C J, Meijers-Heijboer H E J, Van Roozendaal C E, Caldes<br />
T, Perez-Segura P, Jakubowska A, Lubinski J, Huzarski T, Blecharz P,<br />
Nevanlinna H, Aittomäki K, Lazaro C, Blanco I, Barkardottir R B,<br />
Montagna M, D'Andrea E, Devilee P, Olopade O I, Neuhausen S L,<br />
Peissel B, Bonanni B, Peterlongo P, Singer C F, Rennert G, Lejbkowicz<br />
F, Andrulis I L, Glendon G, Ozcelik H, Toland A E, Caligo M A,<br />
Beattie M S, Chan S, Domchek S M, Nathanson K L, Rebbeck T R,<br />
Phelan C, Narod S, John E M, Hopper J L, Buys S S, Daly M B,<br />
Southey M C, Terry M -, Tung N, Hansen T v O, Osorio A, Benitez<br />
J, Durán M, Weitzel J N, Garber J, Hamann U, Peock S, Cook M,<br />
Oliver C T, Frost D, Platte R, Evans D G, Eeles R, Izatt L, Paterson J,<br />
Brewer C, Hodgson S, Morrison P J, Porteous M, Walker L, Rogers M<br />
T, Side L E, Godwin A K, Schmutzler R K, Wappenschmidt B, Laitman<br />
Y, Meindl A, Deissler H, Varon-Mateeva R, Preisler-Adams S, Kast K,<br />
Venat-Bouvet L, Stoppa-Lyonnet D, Chenevix-Trench G, Easton D F,<br />
Klein R J, Daly M J, Friedman E, Dean M, Clark A G, Altshuler D<br />
M, Antoniou A C, Couch F J, Offit K, Gold B. Haplotype structure<br />
in ashkenazi jewish BRCA1 and BRCA2 mutation carriers. Human<br />
genetics; 130:5; 685-699; <strong>2011</strong><br />
65 Jirillo A, Trojniak M P. Evaluations of new drugs after they reach the<br />
market. Health affairs (Project Hope); 30:10; 2028; <strong>2011</strong><br />
66 Jirillo A, Trentin C. Geriatric evaluation programs and elderly<br />
oncology patients. International Journal of Gerontology; 5:2; 129-<br />
130; <strong>2011</strong><br />
67 Kasic T, Colombo P, Soldani C, Wang C M, Miranda E, Roncalli M,<br />
Bronte V, Viola A. Modulation of human T-cell functions by reactive<br />
nitrogen species. European journal of immunology; 41:7; 1843-1849;<br />
<strong>2011</strong><br />
68 Leali D, Alessi P, Coltrini D, Ronca R, Corsini M, Nardo G, Indraccolo S,<br />
Presta M. Long pentraxin-3 inhibits FGF8b-dependent angiogenesis<br />
and growth of steroid hormone-regulated tumors. Molecular Cancer<br />
Therapeutics; 10:9; 1600-1610; <strong>2011</strong><br />
69 Lionello M, Blandamura S, Loreggian L, Ottaviano G, Giacomelli<br />
L, Marchese-Ragona R, Velardita C, Staffieri A, Marioni G. High<br />
mTOR expression is associated with a worse oncological outcome
in laryngeal carcinoma treated with postoperative radiotherapy:<br />
A pilot study. Journal of Oral Pathology and Medicine; E-pub <strong>2011</strong><br />
70 Lombardi G, Nicoletto M O, Gusella M, Fiduccia P, Dalla Palma M,<br />
Zuin A, Fiore D, Donach M, Zagonel V. Intrapleural paclitaxel for<br />
malignant pleural effusion from ovarian and breast cancer: A phase<br />
II study with pharmacokinetic analysis Cancer chemotherapy and<br />
pharmacology. E-pub <strong>2011</strong><br />
71 Lombardi G, Zustovich F, Farina P, Puppa A D, Manara R, Cecchin D,<br />
Brunello A, Cappetta A, Zagonel V. Neoplastic meningitis from solid<br />
tumors: New diagnostic and therapeutic approaches. The oncologist;<br />
16:8; 1175-1188; <strong>2011</strong><br />
72 Lorenzi L, Lonardi S, Petrilli G, Tanda F, Bella M, Laurino L, Rossi<br />
G, Facchetti F. Folliculocentric B-cell-rich follicular dendritic cells<br />
sarcoma: A hitherto unreported morphological variant mimicking<br />
lymphoproliferative disorders. Human pathology; E-pub <strong>2011</strong><br />
73 Loupakis F, Cremolini C, Salvatore L, Schirripa M, Lonardi S, Vaccaro<br />
V, Cuppone F, Giannarelli D, Zagonel V, Cognetti F, Tortora G, Falcone<br />
A, Bria E. Clinical impact of anti-epidermal growth factor receptor<br />
monoclonal antibodies in first-line treatment of metastatic colorectal<br />
cancer: Meta-analytical estimation and implications for therapeutic<br />
strategies. Cancer; E-pub <strong>2011</strong><br />
74 Lumachi F, Norberto L, Zanella S, Marino F, Basso S M M, Basso U,<br />
Brunello A, Fassina A. Axillary node sampling in conjunction with<br />
sentinel node biopsy in patients with breast cancer. A prospective<br />
preliminary study. Anticancer Research; 31:2; 693-697; <strong>2011</strong><br />
75 Lunardi F, Balestro E, Nordio B, Cozzi F, Polverosi R, Sfriso P, Braccioni<br />
F, Calabrese F. Undifferentiated connective tissue disease presenting<br />
with prevalent interstitial lung disease: Case report and review of<br />
literature. Diagnostic pathology; 6:50; <strong>2011</strong><br />
76 Magro G, Esposito G, Cecchetto G, Dall’Igna P, Marcato R, Gambini<br />
C, Boldrini R, Collini P, D’Onofrio V, Salfi N, d'Amore E, Ferrari A,<br />
Bisogno G, Alaggio R. Pediatric adrenocortical tumors: Morphological<br />
diagnostic criteria and immunohistochemical expression of matrix<br />
metalloproteinase type 2 and human leucocyte-associated antigen<br />
(HLA) class II antigens: Results from the italian pediatric rare tumor<br />
(TREP) study project. Human pathology; E-pub 1-9; <strong>2011</strong>.<br />
77 Marcos-Gragera R, Allemani C, Tereanu C, De Angelis R, Capocaccia<br />
R, Maynadie M, Luminari S, Ferretti S, Johannesen T B, Sankila R,<br />
Karjalainen-Lindsberg M L, Simonetti A, Martos M C, Raphael M,<br />
Giraldo P, Sant M, HAEMACARE Working Group [as a member<br />
Zambon P]. Survival of european patients diagnosed with lymphoid<br />
PUBLICATIONS<br />
297<br />
neoplasms in 2000-2002: Results of the HAEMACARE project.<br />
Haematologica; 96:5; 720-728; <strong>2011</strong><br />
78 Marino D, Farina P, Jirillo A, De Franchis G, Simonetto M, Aversa<br />
Savina M L. Neurological syndrome after R-CHOP chemotherapy<br />
for a non-hodgkin lymphoma: What is the diagnosis? International<br />
journal of hematology; 94:5; 461-462; <strong>2011</strong><br />
79 Marioni G, Blandamura S, Loreggian L, Koussis H, Lionello M,<br />
Giacomelli L, Fasanaro E, Lovato A, Staffieri A. Laryngeal carcinoma<br />
prognosis after postoperative radiotherapy correlates with CD105<br />
expression, but not with angiogenin or EGFR expression. European<br />
Archives of Oto-Rhino-Laryngology; 268:12; 1779-1787; <strong>2011</strong><br />
80 Martin F, Bangham C R, Ciminale V, Lairmore M D, Murphy E<br />
L, Switzer W M, Mahieux R. Conference highlights of the 15th<br />
international conference on human retrovirology: HTLV and<br />
related retroviruses. 4-8 june <strong>2011</strong>, Leuven, Gembloux, Belgium.<br />
Retrovirology; 8:86; <strong>2011</strong><br />
81 Marzocchi G, Castagnetti F, Luatti S, Baldazzi C, Stacchini M,<br />
Gugliotta G, Amabile M, Specchia G, Sessarego M, Giussani U,<br />
Valori L, Discepoli G, Montaldi A, Santoro A, Bonaldi L, Giudici G,<br />
Cianciulli A M, Giacobbi F, Palandri F, Pane F, Saglio G, Martinelli<br />
G, Baccarani M, Rosti G, Testoni N, (GIMEMA) Working Party on<br />
Chronic Myeloid Leukemia. Variant Philadelphia translocations:<br />
Molecular-cytogenetic characterization and prognostic influence<br />
on frontline imatinib therapy, a GIMEMA working party on CML<br />
analysis. Blood; 117:25; 6793-6800; <strong>2011</strong><br />
82 Masiero M, Minuzzo S, Pusceddu I, Moserle L, Persano L, Agnusdei<br />
V, Tosello V, Basso G, Amadori A, Indraccolo S. Notch3-mediated<br />
regulation of MKP-1 levels promotes survival of T acute<br />
lymphoblastic leukemia cells. Leukemia; 25:4; 588-598; <strong>2011</strong><br />
83 Massimino M, Solero C L, Garre M L, Biassoni V, Cama A, Genitori<br />
L, Di Rocco C, Sardi I, Viscardi E, Modena P, Potepan P, Barra S,<br />
Scarzello G, Galassi E, Giangaspero F, Antonelli M, Gandola L.<br />
Second-look surgery for ependymoma: The italian experience.<br />
Journal of neurosurgery. Pediatrics; 8:3; 246-250; <strong>2011</strong><br />
84 Mavaddat N, Barrowdale D, Andrulis I L, Domchek S M, Eccles D,<br />
Nevanlinna H, Ramus S J, Spurdle A, Robson M, Sherman M, Mulligan<br />
A M, Couch F J, Engel C, McGuffog L, Healey S, Sinilnikova O M,<br />
Southey M C, Terry M B, Goldgar D, O’Malley F, John E M, Janavicius<br />
R, Tihomirova L, Hansen T V, Nielsen F C, Osorio A, Stavropoulou<br />
A, Benitez J, Manoukian S, Peissel B, Barile M, Volorio S, Pasini B,<br />
Dolcetti R, Putignano A L, Ottini L, Radice P, Hamann U, Rashid M
U, Hogervorst F B, Kriege M, van der Luijt R B, for HEBON, Peock<br />
S, Frost D, Evans D G, Brewer C, Walker L, Rogers M T, Side L E,<br />
Houghton C, for EMBRACE, Weaver J, Godwin A K, Schmutzler R<br />
K, Wappenschmidt B, Meindl A, Kast K, Arnold N, Niederacher D,<br />
Sutter C, Deissler H, Gadzicki D, Preisler-Adams S, Varon-Mateeva<br />
R, Schonbuchner I, Gevensleben H, Stoppa-Lyonnet D, Belotti M,<br />
Barjhoux L, for GEMO Study Collaborators, Isaacs C, Peshkin B<br />
N, Caldes T, de la Hoya M, Canadas C, Heikkinen T, Heikkila P,<br />
Aittomaki K, Blanco I, Lazaro C, Brunet J, Agnarsson B A, Arason<br />
A, Barkardottir R B, Dumont M, Simard J, Montagna M, Agata S,<br />
D'Andrea E, Yan M, Fox S, for kConFab Investigators, Rebbeck T R,<br />
Rubinstein W, Tung N, Garber J E, Wang X, Fredericksen Z, Pankratz<br />
V S, Lindor N M, Szabo C, Offit K, Sakr R, Gaudet M M, Singer C F,<br />
Tea M K, Rappaport C, Mai P L, Greene M H, Sokolenko A, Imyanitov<br />
E, Toland A E, Senter L, Sweet K, Thomassen M, Gerdes A M, Kruse<br />
T, Caligo M, Aretini P, Rantala J, von Wachenfeld A, Henriksson K,<br />
for SWE-BRCA Collaborators, Steele L, Neuhausen S L, Nussbaum<br />
R, Beattie M, Odunsi K, Sucheston L, Gayther S A, Nathanson K,<br />
Gross J, Walsh C, Karlan B, Chenevix-Trench G, Easton D F, Antoniou<br />
A C, for the Consortium of Investigators of Modifiers of BRCA1/2.<br />
Pathology of breast and ovarian cancers among BRCA1 and BRCA2<br />
mutation carriers: Results from the consortium of investigators of<br />
modifiers of BRCA1/2 (CIMBA). Cancer epidemiology, biomarkers<br />
& prevention: a publication of the American Association for Cancer<br />
Research, cosponsored by the American Society of Preventive Oncology;<br />
E-pub 1-13; <strong>2011</strong>.<br />
85 Menin C, Vecchiato A, Scaini M C, Elefanti L, Funari G, De Salvo G<br />
L, Quaggio M, Tognazzo S, Agata S, Santa S D, Montagna M, Alaibac<br />
M, Chiarion-Sileni V, D’Andrea E. Contribution of susceptibility<br />
gene variants to melanoma risk in families from the veneto region of<br />
Italy. Pigment cell & melanoma research; 24:4; 728-730; <strong>2011</strong><br />
86 Merlo A, Turrini R, Dolcetti R, Zanovello P, Rosato A. Immunotherapy<br />
for EBV-associated malignancies. International journal of hematology;<br />
93:3; 281-293; <strong>2011</strong><br />
87 Mian C, Pennelli G, Barollo S, Cavedon E, Nacamulli D, Vianello<br />
F, Negro I, Pozza G, Boschin I M, Pelizzo M R, Rugge M, Mantero F,<br />
Girelli M E, Opocher G. Combined RET and ki-67 assessment in<br />
sporadic medullary thyroid carcinoma: A useful tool for patient risk<br />
stratification. European journal of endocrinology / European Federation<br />
of Endocrine Societies; 164:6; 971-976; <strong>2011</strong><br />
88 Miolo G, Marzano C, Gandin V, Palozzo A C, Dalzoppo D, Salvador<br />
PUBLICATIONS<br />
298<br />
A, Caffieri S. Photoreactivity of 5-fluorouracil under UVB light:<br />
Photolysis and cytotoxicity studies. Chemical research in toxicology;<br />
24:8; 1319-1326; <strong>2011</strong><br />
89 Mocellin S, Pasquali S, Rossi C R, Nitti D. Validation of the prognostic<br />
value of lymph node ratio in patients with cutaneous melanoma: A<br />
population-based study of 8,177 cases. Surgery; 150:1; 83-90; <strong>2011</strong><br />
90 Molon B, Ugel S, Del Pozzo F, Soldani C, Zilio S, Avella D, De Palma<br />
A, Mauri P, Monegal A, Rescigno M, Savino B, Colombo P, Jonjic<br />
N, Pecanic S, Lazzarato L, Fruttero R, Gasco A, Bronte V, Viola A.<br />
Chemokine nitration prevents intratumoral infiltration of antigenspecific<br />
T cells. The Journal of experimental medicine; 208:10; 1949-<br />
1962; <strong>2011</strong><br />
91 Monfardini S, Falci C, Brunello A, Lonardi S, Basso U. Cancer in the<br />
elderly. Internal and emergency medicine; 6 Suppl 1:115-118; <strong>2011</strong><br />
92 Mulligan A M, Couch F J, Barrowdale D, Domchek S M, Eccles D,<br />
Nevanlinna H, Ramus S J, Robson M, Sherman M, Spurdle A B,<br />
Wappenschmidt B, Lee A, McGuffog L, Healey S, Sinilnikova O M,<br />
Janavicius R, Hansen T V, Nielsen F C, Ejlertsen B, Osorio A, Munoz-<br />
Repeto I, Duran M, Godino J, Pertesi M, Benitez J, Peterlongo P,<br />
Manoukian S, Peissel B, Zaffaroni D, Cattaneo E, Bonanni B, Viel A,<br />
Pasini B, Papi L, Ottini L, Savarese A, Bernard L, Radice P, Hamann<br />
U, Verheus M, Meijers-Heijboer H E, Wijnen J, Gomez Garcia E<br />
B, Nelen M R, Kets C M, Seynaeve C, Tilanus-Linthorst M M, van<br />
der Luijt R B, van Os T, Rookus M, Frost D, Jones J L, Evans D G,<br />
Lalloo F, Eeles R, Izatt L, Adlard J, Davidson R, Cook J, Donaldson<br />
A, Dorkins H, Gregory H, Eason J, Houghton C, Barwell J, Side L E,<br />
McCann E, Murray A, Peock S, Godwin A, Schmutzler R K, Rhiem<br />
K, Engel C, Meindl A, Ruehl I, Arnold N, Niederacher D, Sutter C,<br />
Deissler H, Gadzicki D, Kast K, Preisler-Adams S, Varon-Mateeva<br />
R, Schoenbuchner I, Fiebig B, Heinritz W, Schafer D, Gevensleben<br />
H, Caux-Moncoutier V, Fassy-Colcombet M, Cornelis F, Mazoyer S,<br />
Leone M, Boutry-Kryza N, Hardouin A, Berthet P, Muller D, Fricker<br />
J P, Mortemousque I, Pujol P, Coupier I, Lebrun M, Kientz C, Longy<br />
M, Sevenet N, Stoppa-Lyonnet D, Isaacs C, Caldes T, de Al Hoya M,<br />
Heikkinen T, Aittomaki K, Blanco I, Lazaro C, Barkardottir R B,<br />
Soucy P, Dumont M, Simard J, Montagna M, Tognazzo S, D’Andrea<br />
E, Fox S, Yan M, Rebbeck T R, Olopade O I, Weitzel J N, Lynch H<br />
T, Ganz P A, Tomlinson G E, Wang X, Fredericksen Z, Pankratz V S,<br />
Lindor N M, Szabo C, Offit K, Sakr R, Gaudet M, Bhatia J, Kauff<br />
N, Singer C F, Tea M K, Gschwantler-Kaulich D, Fink-Retter A, Mai<br />
P L, Greene M H, Imyanitov E, O'Malley F P, Ozcelik H, Glendon
G, Toland A E, Gerdes A M, Thomassen M, Kruse T A, Birk Jensen<br />
U, Skytte A B, Caligo M A, Soller M, Henriksson K, von Wachenfeldt<br />
A, Arver B, Stenmark-Askmalm M, Karlsson P, Ding Y C, Neuhausen<br />
S L, Beattie M, Pharoah P D, Moysich K B, Nathanson K L, Karlan<br />
B Y, Gross J, John E M, Daly M B, Buys S M, Southey M C, Hopper<br />
J L, Terry M B, Chung W, Miron A F, Goldgar D, Chenevix-Trench<br />
G, Easton D F, Andrulis I L, Antoniou A C, Family Registry B C,<br />
Embrace, Collaborators G S, Hebon, Network O C, Swe-Brca, Cimba.<br />
Common breast cancer susceptibility alleles are associated with<br />
tumor subtypes in BRCA1 and BRCA2 mutation carriers: Results<br />
from the consortium of investigators of modifiers of BRCA1/2.<br />
Breast cancer research: BCR; 13:6; R110; <strong>2011</strong><br />
93 Nardo G, Favaro E, Curtarello M, Moserle L, Zulato E, Persano L, Rossi<br />
E, Esposito G, Crescenzi M, Casanovas O, Sattler U G, Mueller-Klieser<br />
W, Biesalski B, Thews O, Canese R, Iorio E, Zanovello P, Amadori<br />
A, Indraccolo S. Glycolytic phenotype and amp kinase modify the<br />
pathologic response of tumor xenografts to vegf neutralization.<br />
Cancer research; 71:12; 4214-4225; <strong>2011</strong><br />
94 Paraiso K H, Xiang Y, Rebecca V W, Abel E V, Chen Y A, Munko A C,<br />
Wood E, Fedorenko I V, Sondak V K, Anderson A R, Ribas A, Dalla<br />
Palma M, Nathanson K L, Koomen J M, Messina J L. Smalley K S,<br />
PTEN loss confers BRAF inhibitor resistance to melanoma cells<br />
through the suppression of BIM expression. Cancer research; 71:7;<br />
2750-2760; <strong>2011</strong><br />
95 Pasello G, Nicotra S, Marulli G, Rea F, Bonanno L, Carli P, Magro<br />
C, Jirillo A, Favaretto A G. Platinum-based doublet chemotherapy<br />
in pre-treated malignant pleural mesothelioma (MPM) patients:<br />
A mono-institutional experience. Lung cancer (Amsterdam,<br />
Netherlands); 73:3; 351-355; <strong>2011</strong><br />
96 Pasquali S, Mocellin S, Campana L G, Vecchiato A, Bonandini E,<br />
Montesco M C, Santarcangelo S, Zavagno G, Nitti D, Rossi C R.<br />
Maximizing the clinical usefulness of a nomogram to select patients<br />
candidate to sentinel node biopsy for cutaneous melanoma. European<br />
Journal of Surgical Oncology (EJSO); In Press, Corrected Proof:.<br />
97 Pennelli G, Vianello F, Barollo S, Pezzani R, Merante Boschin I, Pelizzo<br />
M R, Mantero F, Rugge M, Mian C. BRAF(K601E) mutation in a<br />
patient with a follicular thyroid carcinoma. Thyroid: official journal<br />
of the American Thyroid Association; 21:12; 1393-1396; <strong>2011</strong><br />
98 PENPACT-1 (PENTA 9/PACTG 390) Study Team [as part of<br />
study team De Rossi A, Zanchetta M, Babiker A, Castro nee Green<br />
H, Compagnucci A, Fiscus S, Giaquinto C, Gibb D M, Harper L,<br />
PUBLICATIONS<br />
299<br />
Harrison L, Hughes M, McKinney R, Melvin A, Mofenson L, Saidi Y,<br />
Smith M E, Tudor-Williams G, Walker A S. First-line antiretroviral<br />
therapy with a protease inhibitor versus non-nucleoside reverse<br />
transcriptase inhibitor and switch at higher versus low viral load in<br />
HIV-infected children: An open-label, randomised phase 2/3 trial.<br />
The Lancet infectious diseases; 11:4; 273-283; <strong>2011</strong><br />
99 Petrara M R, Cattelan A M, Zanchetta M, Sasset L, Freguja R, Gianesin<br />
K, Cecchetto M G, Carmona F, De Rossi A. Epstein-barr virus load<br />
and immune activation in human immunodeficiency virus type<br />
1-infected patients. Journal of clinical virology: the official publication<br />
of the Pan American Society for Clinical Virology; E-pub <strong>2011</strong><br />
100 Pharoah P D P, Palmieri R T, Ramus S J, Gayther S A, Andrulis I<br />
L, Anton-Culver H, Antonenkova N, Antoniou A C, Goldgar D,<br />
Beattie M S, Beckmann M W, Birrer M J, Bogdanova N, Bolton K L,<br />
Brewster W, Brooks-Wilson A, Brown R, Butzow R, Caldes T, Caligo<br />
M A, Campbell I, Chang-Claude J, Chen Y A, Cook L S, Couch F J,<br />
Cramer D W, Cunningham J M, Despierre E, Doherty J A, Doerk T,<br />
Duerst M, Eccles D M, Ekici A B, Easton D, Fasching P A, de Fazio A,<br />
Fenstermacher D A, Flanagan J M, Fridley B L, Friedman E, Gao B,<br />
Sinilnikova O, Gentry-Maharaj A, Godwin A K, Goode E L, Goodman<br />
M T, Gross J, Hansen T V O, Harnett P, Rookus M, Heikkinen T, Hein<br />
R, Hogdall C, Hogdall E, Iversen E S, Jakubowska A, Johnatty S E,<br />
Karlan B Y, Kauff N D, Kaye S B, Chenevix-Trench G, Kelemen L E,<br />
Kiemeney L A, Kjaer S K, Lambrechts D, LaPolla J P, Lazaro C, Le N<br />
D, Leminen A, Leunen K, Levine D A, Lu Y, Lundvall L, Macgregor<br />
S, Marees T, Massuger L F, McLaughlin J R, Menon U, Montagna<br />
M, Moysich K B, Narod S A, Nathanson K L, Nedergaard L, Ness R<br />
B, Nevanlinna H, Nickels S, Osorio A, Paul J, Pearce C L, Phelan C<br />
M, Pike M C, Radice P, Rossing M A, Schildkraut J M, Sellers T A,<br />
Singer C F, Song H, Stram D O, Sutphen R, Lindblom A, Terry K L,<br />
Tsai Y, van Altena A M, Vergote I, Vierkant R A, Vitonis A F, Walsh<br />
C, Wang-Gohrke S, Wappenschmidt B, Wu A H, Ziogas A, Berchuck<br />
A, Risch H A, BCFR Investigators, EMBRACE Investigators, GEMO<br />
Study Collaborators, HEBON Investigators, KConFab Investigators,<br />
Consortium Investigators, Modifiers, SWE-BRCA Investigators,<br />
Ovarian Canc Assoc Consortium. The role of KRAS rs61764370 in<br />
invasive epithelial ovarian cancer: Implications for clinical testing.<br />
Clinical Cancer Research; 17:11; 3742-3750; <strong>2011</strong><br />
101 Pisani P, Mosso M L, Buzzoni C, Crosignani P, Michiara M, Tumino<br />
R, AIRTUM Working Group [as member of AIRTUM WG:] Zambon<br />
P. Good news for italian children ince 2000 malignant CNS cancer
has stopped increasing. Epidemiologia e prevenzione; 35:3-4; 245; <strong>2011</strong><br />
102 Pizzi M, Fassan M, Balistreri M, Galligioni A, Rea F, Rugge M.<br />
Anterior gradient 2 overexpression in lung adenocarcinoma. Applied<br />
Immunohistochemistry & Molecular Morphology: AIMM/Official<br />
Publication of the Society for Applied Immunohistochemistry; E-pub <strong>2011</strong><br />
103 Polverosi R, Muzzio P C, Panunzio A, Pasquotti G, Schiavon M, Rea F.<br />
Synovial sarcoma: CT imaging of a rare primary malignant tumour<br />
of the thorax. La Radiologia medica; 116:6; 868-875; <strong>2011</strong><br />
104 Ponti A, Tomatis M, Baiocchi D, Barca A, Berti R, Bisanti L, Bordon<br />
R, Casella D, Cogo C, Deandrea S, Delrio D, Donati G, Falcini<br />
F, Frigerio A, Leonardo N, Mancini S, Mantellini P, Naldoni C,<br />
Pagano G, Ravaioli A, Pietribiasi F, Sedda M L, Taffurelli M, Zorzi<br />
M, Cataliotti L, Segnan N, Mano M P. Audit on quality of breast<br />
cancer diagnosis and treatment in Italy, 2008-2009. Epidemiologia e<br />
prevenzione; 35:5-6 Suppl 5; 87-95; <strong>2011</strong><br />
105 Porta C, Procopio G, Cartenì G, Sabbatini R, Bearz A, Chiappino<br />
I, Ruggeri E M, Re G L, Ricotta R, Zustovich F, Landi L, Calcagno<br />
A, Imarisio I, Verzoni E, Rizzo M, Paglino C, Guadalupi V, Bajetta<br />
E. Sequential use of sorafenib and sunitinib in advanced renal-cell<br />
carcinoma (RCC): An italian multicentre retrospective analysis of<br />
189 patient cases. BJU international; 108:8 Pt 2; E250-E257; <strong>2011</strong><br />
106 Pozza A, Scarpa M, Lacognata C, Corbetti F, Mescoli C, Ruffolo C,<br />
Frego M, D’Inca R, Bardini R, Rugge M, Sturniolo G C, Angriman<br />
I. Magnetic resonance enterography for Crohn’s disease: What the<br />
surgeon can take home. Journal of gastrointestinal surgery: official<br />
journal of the Society for Surgery of the Alimentary Tract; 15:10; 1689-<br />
1698; <strong>2011</strong><br />
107 Pozza A, Scarpa M, Ruffolo C, Polese L, Erroi F, Bridda A, Norberto L,<br />
Frego M. Colonic carcinogenesis in IBD: Molecular events. Annali<br />
Italiani di Chirurgia; 82:1; 19-28; <strong>2011</strong><br />
108 Pucciarelli S, Del Bianco P, Efficace F, Serpentini S, Capirci C, De Paoli<br />
A, Amato A, Cuicchi D, Nitti D. Patient-reported outcomes after<br />
neoadjuvant chemoradiotherapy for rectal cancer: A multicenter<br />
prospective observational study. Annals of Surgery; 253:1; 71-77; <strong>2011</strong><br />
109 Rampazzo E, Bonaldi L, Trentin L, Visco C, Keppel S, Giunco S,<br />
Frezzato F, Facco M, Novella E, Giaretta I, Del Bianco P, Semenzato<br />
G, De Rossi A. Telomere length and telomerase levels delineate<br />
subgroups of B-cell chronic lymphocytic leukemia with different<br />
biological characteristics and clinical outcomes. Haematologica;<br />
E-pub <strong>2011</strong><br />
110 Rastrelli M, Mosconi M, Tosti G. Epithelioid sarcoma of the thumb<br />
PUBLICATIONS<br />
300<br />
presenting as a periungual warty lesion: Case report and revision of<br />
the literature. Journal of Plastic, Reconstructive & Aesthetic Surgery;<br />
64:8; e221-e222; <strong>2011</strong><br />
111 Rende F, Cavallari I, Corradin A, Silic-Benussi M, Toulza F, Toffolo G<br />
M, Tanaka Y, Jacobson S, Taylor G P, D’Agostino D M, Bangham C<br />
R M, Ciminale V. Kinetics and intracellular compartmentalization<br />
of HTLV-1 gene expression: Nuclear retention of HBZ mRNAs.<br />
Blood; 117:18; 4855-4859; <strong>2011</strong><br />
112 Ronco G, Giubilato P, Naldoni C, Zorzi M, Anghinoni E, Scalisi A,<br />
Dalla Palma P, Zanier L, Barca A, Angeloni C, Gaimo M D, Maglietta<br />
R, Mancini E, Pizzuti R, Iossa A, Segnan N, Zappa M. Extension of<br />
organised cervical cancer screening programmes in italy and their<br />
process indicators, 2009 activity. Epidemiologia e prevenzione; 35:5-6<br />
Suppl 5; 39-54; <strong>2011</strong><br />
113 Rotondo R, Bertolotto M, Barisione G, Astigiano S, Mandruzzato S,<br />
Ottonello L, Dallegri F, Bronte V, Ferrini S, Barbieri O. Exocytosis<br />
of azurophil and arginase 1-containing granules by activated<br />
polymorphonuclear neutrophils is required to inhibit T lymphocyte<br />
proliferation. Journal of leukocyte biology; 89:5; 721-727; <strong>2011</strong><br />
114 Roxana Stan T, Piaserico S, Bordignon M, Salmaso R, Zattra E, Alaibac<br />
M. Bullous scabies simulating pemphigoid. Journal of cutaneous<br />
medicine and surgery; 15:1; 55-57; <strong>2011</strong><br />
115 Ruffolo C, Citton M, Scarpa M, Angriman I, Massani M, Caratozzolo<br />
E. Perianal Crohn’s disease: Is there something new? World Journal<br />
of Gastroenterology; 17:15; 1939-1946; <strong>2011</strong><br />
116 Rumiato E, Pasello G, Montagna M, Scaini M C, De Salvo G L, Parenti<br />
A, Cagol M, Ruol A, Ancona E, Amadori A, Saggioro D. DNA copy<br />
number profile discriminates between esophageal adenocarcinoma<br />
and squamous cell carcinoma and represents an independent<br />
prognostic parameter in esophageal adenocarcinoma. Cancer letters;<br />
310:1; 84-93; <strong>2011</strong><br />
117 Safra T, Borgato L, Nicoletto M O, Rolnitzky L, Pelles-Avraham<br />
S, Geva R, Donach M E, Curtin J, Novetsky A, Grenader T, Lai<br />
W - V, Gabizon A, Boyd L, Muggia F. BRCA mutation status and<br />
determinant of outcome in women with recurrent epithelial ovarian<br />
cancer treated with pegylated liposomal doxorubicin. Molecular<br />
Cancer Therapeutics; 10:10; 2000-2007; <strong>2011</strong><br />
118 Saggioro D. Anti-apoptotic effect of tax: An NF-kappaB path or a<br />
CREB way? Viruses; 3:7; 1001-1014; <strong>2011</strong><br />
119 Sant M, Minicozzi P, Lagorio S, Johannesen T B, Marcos-Gragera R, Francisci<br />
S, The EUROCARE,W.G. [as collab:] Guzzinati S, Zambon P. Survival of
european patients with central nervous system tumors. International journal<br />
of cancer.Journal international du cancer; E-pub <strong>2011</strong><br />
120 Sardanelli F, Podo F, Santoro F, Manoukian S, Bergonzi S, Trecate<br />
G, Vergnaghi D, Federico M, Cortesi L, Corcione S, Morassut S, Di<br />
Maggio C, Cilotti A, Martincich L, Calabrese M, Zuiani C, Preda L,<br />
Bonanni B, Carbonaro L A, Contegiacomo A, Panizza P, Di Cesare<br />
E, Savarese A, Crecco M, Turchetti D, Tonutti M, Belli P, Maschio<br />
A D, for the High Breast Cancer Risk Italian 1 (HIBCRIT-1) Study.<br />
Multicenter surveillance of women at high genetic breast cancer<br />
risk using mammography, ultrasonography, and contrast-enhanced<br />
magnetic resonance imaging (the high breast cancer risk italian 1<br />
study): Final results. Investigative radiology; 46:2; 94-105; <strong>2011</strong><br />
121 Scarpa M, Valente S, Alfieri R, Cagol M, Diamantis G, Ancona<br />
E, Castoro C. Systematic review of health-related quality of life<br />
after esophagectomy for esophageal cancer. World journal of<br />
gastroenterology: WJG; 17:42; 4660-4674; <strong>2011</strong><br />
122 Scarpa M, Angriman I, Prando D, Polese L, Ruffolo C, Pilon F, Erroi<br />
F, Mescoli C, Ninfo V, D’Amico D F, Norberto L. Helicobacter pylori<br />
and gastroesophageal reflux disease: A cross sectional study. Hepatogastroenterology;<br />
58:105; 69-75; <strong>2011</strong><br />
123 Scarpa M, Griggio L, Rampado S, Ruffolo C, Citton M, Pozza A,<br />
Borsetto L, Dall’Olmo L, Angriman I. Long-term health-related<br />
quality of life after minimally invasive surgery for diverticular<br />
disease. Langenbeck’s archives of surgery / Deutsche Gesellschaft fur<br />
Chirurgie; 396:6; 833-843; <strong>2011</strong><br />
124 Scarpa M, Grillo A, Faggian D, Ruffolo C, Bonello E, D’Inca R,<br />
Scarpa M, Castagliuolo I, Angriman I. Relationship between<br />
mucosa-associated microbiota and inflammatory parameters in the<br />
ileal pouch after restorative proctocolectomy for ulcerative colitis.<br />
Surgery; 150:1; 56-67; <strong>2011</strong><br />
125 Scarpa M, Grillo A, Pozza A, Faggian D, Ruffolo C, Scarpa M,<br />
D'Incà R, Plebani M, Sturniolo G C, Castagliuolo I, Angriman I.<br />
TLR2 and TLR4 up-regulation and colonization of the ileal mucosa<br />
by clostridiaceae spp. in Chronic/Relapsing Pouchitis1,2. Journal of<br />
Surgical Research; 169:2; e145-e154; <strong>2011</strong><br />
126 Scarpa M, Grillo A, Scarpa M, Brun P, Castoro C, Pozza A, Cavallo D,<br />
Faggian D, Ruffolo C, D’Incà R, Bardini R, Castagliuolo I, Angriman<br />
I. Innate immune environment in ileal pouch mucosa: Α5 defensin<br />
up-regulation as predictor of Chronic/Relapsing pouchitis. Journal<br />
of Gastrointestinal Surgery; E-pub <strong>2011</strong><br />
127 Serafin V, Persano L, Moserle L, Esposito G, Ghisi M, Curtarello M,<br />
PUBLICATIONS<br />
301<br />
Bonanno L, Masiero M, Ribatti D, Stürzl M, Naschberger E, Croner<br />
R S, Jubb A M, Harris A L, Koeppen H, Amadori A, Indraccolo S.<br />
Notch3 signalling promotes tumour growth in colorectal cancer.<br />
Journal of Pathology; 224:4; 448-460; <strong>2011</strong><br />
128 Sergi G, Pintore G, Falci C, Veronese N, Berton L, Perissinotto E, Basso<br />
U, Brunello A, Monfardini S, Manzato E, Coin A. Preventive effect<br />
of risedronate on bone loss and frailty fractures in elderly women<br />
treated with anastrozole for early breast cancer. Journal of bone and<br />
mineral metabolism; <strong>2011</strong><br />
129 Solito S, Bronte V, Mandruzzato S. Antigen specificity of immune<br />
suppression by myeloid-derived suppressor cells. Journal of leukocyte<br />
biology; 90:1; 31-36; <strong>2011</strong><br />
130 Solito S, Falisi E, Diaz-Montero C M, Doni A, Pinton L, Rosato A,<br />
Francescato S, Basso G, Zanovello P, Onicescu G, Garrett-Mayer E,<br />
Montero A J, Bronte V, Mandruzzato S. A human promyelocytic-like<br />
population is responsible for the immune suppression mediated by<br />
myeloid-derived suppressor cells. Blood; 118:8; 2254-65; <strong>2011</strong><br />
131 Sommariva A, Pilati P, Rossi C R. Cyto-reductive surgery combined<br />
with hyperthermic intra-peritoneal chemotherapy for peritoneal<br />
surface malignancies: Current treatment and results. Cancer<br />
treatment reviews; E-pub <strong>2011</strong><br />
132 Sonda N, Chioda M, Simonato F, Bronte V. Transcription factors in<br />
myeloid-derived suppressor cell recruitment and function. Current<br />
opinion in immunology; 23:2; 279-285; <strong>2011</strong><br />
133 Stoppa G, Rumiato E, Saggioro D. Ras signaling contributes to survival<br />
of human T-cell leukemia/lymphoma virus type 1 (HTLV-1) taxpositive<br />
T-cells. Apoptosis: An International Journal on Programmed<br />
Cell Death; E-pub <strong>2011</strong><br />
134 Thomassen M, Blanco A, Montagna M, Hansen T V O, Pedersen I<br />
S, Gutiérrez-Enríquez S, Menéndez M, Fachal L, Santamariña M,<br />
Steffensen A Y, Jønson L, Agata S, Whiley P, Tognazzo S, Tornero E,<br />
Jensen U B, Balmaña J, Kruse T A, Goldgar D E, Lázaro C, Diez<br />
O, Spurdle A B, Vega A. Characterization of BRCA1 and BRCA2<br />
splicing variants: A collaborative report by ENIGMA consortium<br />
members. Breast cancer research and treatment; E-pub 1-15; <strong>2011</strong><br />
135 Tieppo C, Betterle C, Basso D, Mescoli C, Rugge M, Martini C,<br />
Zorzetto V, Maddalo G, Cazzagon N, Nitti D, Farinati F. Gastric type<br />
I carcinoid: A pilot study with human G17DT immunogen vaccination.<br />
Cancer Immunology, Immunotherapy; 60:7; 1057-1060; <strong>2011</strong><br />
136 Trojniak M P, Jirillo A. Does chemotherapy have a role after erlotinib<br />
treatment in NSCLC? Lung Cancer; E-pub <strong>2011</strong>.
137 Trojniak M P, Palozzo A C, Mazurek M, Jirillo A. Sorafenib<br />
in hepatocellular carcinoma - a post marketing evaluation.<br />
Immunopharmacology and immunotoxicology; E-pub <strong>2011</strong><br />
138 Turato C, Biasiolo A, Pengo P, Frecer V, Quarta S, Fasolato S, Ruvoletto<br />
M, Beneduce L, Zuin J, Fassina G, Gatta A, Pontisso P. Increased<br />
antiprotease activity of the SERPINB3 polymorphic variant SCCA-<br />
PD. Experimental biology and medicine (Maywood, N.J.); 236:3;<br />
281-290; <strong>2011</strong><br />
139 Turato C, Buendia M A, Fabre M, Redon M J, Branchereau S, Quarta<br />
S, Ruvoletto M, Perilongo G, Grotzer M A, Gatta A, Pontisso P.<br />
Over-expression of SERPINB3 in hepatoblastoma: A possible<br />
insight into the genesis of this tumour? European journal of cancer;<br />
E-pub <strong>2011</strong><br />
140 Turrini R, Merlo A, Dolcetti R, Zanovello P, Rosato A. Differential<br />
down-modulation of HLA class I and II molecule expression on<br />
human tumor cell lines upon in vivo transfer. Cancer immunology,<br />
immunotherapy:CII; 60:11; 1639-1645; <strong>2011</strong><br />
141 Vianello F, Mazzarotto R, Mian C, Lora O, Saladini G, Servodio O,<br />
Basso M, Pennelli G, Pelizzo M R, Sotti G. Clinical outcome of lowrisk<br />
differentiated thyroid cancer patients after radioiodine remnant<br />
ablation and recombinant human thyroid-stimulating hormone<br />
preparation. Clinical oncology (RCR:UK); E-pub <strong>2011</strong><br />
142 Vianello F, Mazzarotto R, Taccaliti A, Lora O, Basso M, Servodio O,<br />
Mian C, Sotti G. Follicular thyroid carcinoma with metastases to the<br />
pituitary causing pituitary insufficiency. Thyroid: official journal of<br />
the American Thyroid Association; 21:8; 921-5; <strong>2011</strong><br />
143 Vitale A, Morales Ramirez R I, dalla Bona E, Scopelliti M, Zanus<br />
G, Neri D, d’Amico F, Gringeri E, Russo F, Burra P, Angeli P, Cillo<br />
U. Donor-model for end-stage liver disease and donor-recipient<br />
matching in liver transplantation. Transplantation proceedings; 43:4;<br />
974-976; <strong>2011</strong><br />
144 Vitale A, Navaglia F, Morales R R, Frigo A, Basso D, D’Amico F, Zanus<br />
G, Bonsignore P, Farinati F, Burra P, Senzolo M, Grigoletto F, Plebani<br />
M, Cillo U. Molecular refinement of clinical staging in hepatocellular<br />
carcinoma patients evaluated for potentially curative therapies. Plos<br />
One; 6:9; e23093; <strong>2011</strong><br />
145 Vitale A, Ramirez Morales R I, Zanus G, Farinati F, Burra P, Angeli P,<br />
Frigo A C, Del Poggio P, Rapaccini G, Di Nolfo M A, Benvegnu L, Zoli<br />
M, Borzio F, Giannini E G, Caturelli E, Chiaramonte M, Trevisani F,<br />
Cillo U, on behalf of the Italian Liver Cancer group. Barcelona clinic<br />
liver cancer staging and transplant survival benefit for patients with<br />
PUBLICATIONS<br />
302<br />
hepatocellular carcinoma: A multicentre, cohort study. The lancet<br />
oncology; 12:7; 654-662; <strong>2011</strong><br />
146 Zaninotto G, Parente P, Salvador R, Farinati F, Tieppo C, Passuello N,<br />
Zanatta L, Fassan M, Cavallin F, Costantini M, Mescoli C, Battaglia<br />
G, Ruol A, Ancona E, Rugge M. Long-term follow-up of Barrett’s<br />
epithelium: Medical versus antireflux surgical therapy. Journal of<br />
gastrointestinal surger: official journal of the Society for Surgery of the<br />
Alimentary Tract; Journal of gastrointestinal surgery; E-pub <strong>2011</strong><br />
147 Zappa M, Dardanoni G, Giorgi Rossi P, Grazzini G, Naldoni<br />
C, Paci E, Pirola M E, Pizzuti R, Segnan N, Zorzi M, Federici A.<br />
The diffusion of screening programmes in Italy, year 2009.<br />
Epidemiologia e prevenzione; 35:5-6 Suppl 5; 3-7; <strong>2011</strong><br />
148 Zattra E, Salmaso R, Tonin E, Alaibac M. Achromic superficial<br />
spreading melanoma accidentally treated with imiquimod. Acta<br />
Dermato-Venereologica; E-pub <strong>2011</strong><br />
149 Zattra E, Zambello R, Marino F, Bordignon M, Alaibac M. Primary<br />
cutaneous mantle cell lymphoma. Acta Dermato-Venereologica; 91:4;<br />
474-475; <strong>2011</strong><br />
150 Zorzi M, Baracco S, Fedato C, Grazzini G, Sassoli De’Bianchi P, Senore<br />
C, Visioli C B, Cogo C. Screening for colorectal cancer in Italy, 2009<br />
survey. Epidemiologia e prevenzione; 35:5-6 Suppl 5; 55-77; <strong>2011</strong><br />
151 Zotti P, Del Bianco P, Serpentini S, Trevisanut P, Barba M C, Valentini<br />
V, De Paoli A, Pucciarelli S. Validity and reliability of the MSKCC<br />
bowel function instrument in a sample of italian rectal cancer<br />
patients. European Journal of Surgical Oncology; 37:7; 589-596; <strong>2011</strong><br />
152 Zustovich F, Lombardi G, Nicoletto M O, Pastorelli D. Secondline<br />
therapy for refractory renal-cell carcinoma. Critical reviews in<br />
oncology/hematology; E-pub <strong>2011</strong>
<strong>2011</strong> PUBLICATIONS / Non indexed in ISI-JCR<br />
1 Boscolo-Berto R, Raduazzo D I, Vezzaro R, Marino D, Aversa Savina<br />
M L, Gardiman M. Aggressive non-Hodgkin’s lymphoma mimicking<br />
unilateral transitional cell carcinoma of renal pelvis. The risk of making<br />
a diagnostic mistake. Archivio Italiano di Urologia, Andrologia 83: 3;<br />
163-165; <strong>2011</strong><br />
2 Evangelista L, Baretta Z, Vinante L, Sotti G. What are the Best Ways to<br />
Reduce the False-positive Rate of 18F-FDG PET/CT in Patients with<br />
Breast Cancer? Nuclear Medicine and Molecular Imaging 45:1; 85-86; <strong>2011</strong><br />
3 Evangelista L, Sorgato N, Torresan F, Boschin I M, Pennelli G, Saladini<br />
G, Piotto A, Rubello D, Pelizzo M R. FDG-PET/CT and parathyroid<br />
carcinoma: Review of literature and illustrative case series.World journal<br />
of clinical oncology 2:10; 348-354; <strong>2011</strong><br />
4 Kaasa S, Apolone G, Klepstad P, Loge J H, Hjermstad M J, Corli O, Strasser<br />
F, Heiskanen T, Costantini M, Zagonel V, Groenvold M, Fainsinger R,<br />
Jensen M P, Farrar J T, McQuay H, Rothrock N E, Cleary J, Deguines<br />
C, Caraceni A. Expert conference on cancer pain assessment and<br />
classification: the need for international consensus: working proposals<br />
on international standards. BMJ Supportive & Palliative Care 1: 3; 281-<br />
287; <strong>2011</strong><br />
5 Opocher G, Schiavi F. Functional consequences of succinate<br />
dehydrogenase mutations. Endocrine Practice; 17 Suppl 3; 64-71; <strong>2011</strong><br />
6 Palozzo A C, Di Turi R. Pharmacoeconomic analysis of use of enteral<br />
nutrition in different clinical settings. Part 1: use of an antiinflammatory<br />
feeding formula in critically ill patients with acute lung injury/acute<br />
respiratory distress syndrome (ALI/ARDS). Nutritional Therapy &<br />
Metabolism; 29:2; 81-87; <strong>2011</strong><br />
7 Palozzo A C, Di Turi P. Pharmacoeconomic analysis of use of enteral<br />
nutrition in different clinical settings. Part 2: use of supplemental<br />
feeding in elderly long-term hospitalized patients. Nutritional Therapy<br />
& Metabolism; 29:3; 119-123; <strong>2011</strong><br />
8 Pegoraro R, Bernardi A, Turoldo F. Biobanks and Tissue Research<br />
the Public, the Patient and the Regulation: “Legal and Ethical Aspects of<br />
Biobanks for Research in the European-Mediterranean Area”. International<br />
Library of Ethics, Law and Technology; 8:3; 185-200; <strong>2011</strong><br />
9 Pellicano R, Bocus P, De Angelis C. Adolf Kussmaul, the sword eater and<br />
modern challenges of digestive endoscopy. Minerva gastroenterologica e<br />
dietologica; 57:2; 109-110; <strong>2011</strong><br />
10 Rastrelli M, Soteldo J, Vitali G C, Mazzarol G, Trifiro G, Tosti G, Testori A.<br />
PUBLICATIONS<br />
303<br />
Aggressive digital papillary adenocarcinoma. Indian Journal of Cancer;<br />
48:1; 126-127; <strong>2011</strong><br />
11 Spolverato G, Pucciarelli S, Bertorelle R, De Rossi A, Nitti D.<br />
Predictive Factors of the Response of Rectal Cancer to Neoadjuvant.<br />
Radiochemotherapy Cancers; 3:2; 2176-2194; <strong>2011</strong><br />
12 Stramare R, Scattolin G, Beltrame V, Gerardi M, Sommavilla M, Gatto C,<br />
Mosca P, Rubaltelli L, Rossi C R, Saccavini C. Structured reporting using<br />
a shared indexed multilingual radiology lexicon. International journal of<br />
computer assisted radiology and surgery. E-pub <strong>2011</strong><br />
13 Zustovich F, Lombardi G, Pastorelli D, Farina P, Dal Bianco M, De Zorzi<br />
L, Dalla Palma M, Nicoletto M O, Zagonel V. Clinical experience and<br />
critical evaluation of the role of sorafenib in renal cell carcinoma. Open<br />
Access Journal of Urology; 3:1; 69-82; <strong>2011</strong>
INDEX<br />
INDEX<br />
305
Index of Names<br />
A<br />
Alaibac Mauro 46, 69<br />
Alfieri Rita 58-59<br />
Aversa Savina M L 47<br />
B<br />
Baldan Enrica 90, 96-97<br />
Banzato Alberto 168-169, 171, 251<br />
Baracco Maddalena 179<br />
Basso Umberto 35, 41, 43, 223, 227-228<br />
Battaglia Giorgio 61, 76-77, 80, 198, 221,<br />
223-225, 228, 250, 253<br />
Berti Franco 108-109<br />
Bertorelle Roberta 128-130, 149, 224-225<br />
Bezzon Elisabetta 90-91, 96-97, 225<br />
Bianchi Alessandra 169<br />
Bocus Paolo 76-77, 80<br />
Bonaldi Laura 129, 152, 224-225<br />
Boso Caterina 109<br />
Bovo Emanuela 178-179<br />
Bozza Fernando 64-65, 67, 96, 202, 251, 253<br />
Bronte Vincenzo 46, 129-130, 199, 231<br />
Buzzaccarini Maria Samaritana 109<br />
C<br />
Cagol Matteo 58-59, 76, 221<br />
Calabrò Maria Luisa 129, 141, 221<br />
Canonico Davide 121, 124<br />
Capovilla Eleonora 86, 172-173, 175, 233-<br />
234, 250-251, 253<br />
Cappellato Sandra 83<br />
Castoro Carlo 58-59, 61, 76, 199, 219, 221,<br />
224, 233, 253<br />
Celentano Connie 83<br />
Ceravolo Renato 35<br />
Cervino Anna Rita 64, 109, 116, 223, 234<br />
Chiarion-Sileni Vanna 46-47, 51-52, 147, 202,<br />
INDEX<br />
306<br />
224, 227<br />
Ciccarese Angelo 83<br />
Ciminale Vincenzo 129, 144, 221<br />
Corti Luigi 46, 58, 109, 227, 233<br />
D<br />
Dal Bosco Chiara 91, 97<br />
Dal Cin Antonella 179<br />
D’Agostino Donna M. 129, 144<br />
D’Andrea Emma 30, 129, 133<br />
Del Bianco Paola 18, 64, 90, 128, 202-203,<br />
233<br />
Del Mistro Anna Rosa 128-130, 137, 198, 219,<br />
221<br />
De Rossi Anita 128-130, 140, 219, 221, 223,<br />
253<br />
De Salvo Gian Luca 18, 46, 64, 202-203, 227<br />
Di Maggio Antonio 90-91, 172<br />
E<br />
Esposito Giovanni 129<br />
Evangelista Laura 64, 109, 116, 223-225, 228<br />
F<br />
Facchinetti Antonella 129<br />
Falci Cristina 34, 47, 224, 233<br />
Faoro Sonia 163, 165, 234<br />
Favaretto Adolfo Gino 47, 51, 54, 224, 227-228,<br />
253, 259<br />
Fiore Anna Rita 178-179<br />
Fiore Davide 91, 256<br />
Friso Maria Luisa 109<br />
G<br />
Gennaro Gisella Maria 90-91, 96-97, 100-101,<br />
223-224<br />
Ghiotto Cristina 47, 64, 96, 219, 224, 227-228
Granziera Elisa 83, 86-87<br />
Gregianin Michele 64, 109, 116, 223-224,<br />
250<br />
Grigoletto Raffaello 64, 67<br />
Guzzinati Stefano 178-179<br />
I<br />
Indraccolo Stefano 128-129, 148, 198, 231,<br />
250-251<br />
J<br />
Jirillo Antonio 54-55, 219, 228-229, 233,<br />
251, 253<br />
K<br />
Koussis Haralabos 47, 227-228, 233<br />
L<br />
Lonardi Sara 34-35, 39, 223, 227-228<br />
Lora Ornella 108-109<br />
Loreggian Lucio 109<br />
M<br />
Mandruzzato Susanna 46, 128-129, 147, 231<br />
Manfredi Valentina 83<br />
Menin Chiara 30, 129, 134, 221, 253<br />
Meroni Muzio 82-83<br />
Minuzzo Sonia 128-129<br />
Monetti Daniele 179<br />
Montagna Marco 30, 129-130, 133, 221<br />
N<br />
Nardin Margherita 90-91, 172<br />
Nicoletto M. Ornella 35, 64, 90, 172,<br />
228-229, 234<br />
O<br />
Opocher Giuseppe 30, 154-156, 158-159,<br />
199, 221, 250-251, 253<br />
P<br />
Paganelli Francesco 163, 233-234<br />
Paiusco Marta 120-121, 124<br />
Palozzo Angelo Claudio 54, 162-166, 199,<br />
227, 233-234, 236<br />
Pastorelli Davide 34, 39, 47, 64, 250-251<br />
Pescarini Luigi 64, 90, 96-97, 99, 219,<br />
223-224<br />
Pintacuda Giovanna 90-91, 172<br />
Polico Ilaria 90, 96-97<br />
Polverosi Roberta 90-91, 225, 253<br />
Pomerri Fabio 90-91, 93, 224<br />
Proietti Alessandro 90, 96-97<br />
R<br />
Realdon Stefano 76-77, 80<br />
Reccanello Sonia 120-121, 123-124, 227, 229<br />
Riccardi Lucia 121<br />
Rosano Alberto 179<br />
Rosato Antonio 128-129, 151, 193, 231, 254,<br />
259<br />
Rossi Carlo Riccardo 46, 68-69, 147, 202,<br />
219, 223, 227, 250-251, 253<br />
S<br />
Saggioro Daniela 129, 221, 224, 224<br />
Saladini Giorgio 64, 108-109, 223<br />
Scarpa Marco 58-59, 62, 76, 221<br />
Scarzello Giovanni 108-109, 227-229<br />
Shams Malihe 90, 172-173<br />
Simonato Franca 120-121, 123-124, 228,<br />
254<br />
Sommariva Antonio 69<br />
Sotti Guido 108-109, 116, 223, 228-229,<br />
236, 251, 253-254<br />
Stocco Carmen Fiorella 179<br />
T<br />
Tognazzo Sandro 179<br />
V<br />
Vecchiato Antonella 46, 68-69, 202<br />
Vianello Federica 109, 223<br />
INDEX<br />
307<br />
Z<br />
Zagonel Vittorina 34-35, 39, 43, 227-228,<br />
233, 248, 252-254<br />
Zamarchi Rita 129, 145, 223-224<br />
Zambon Paola 178-179, 219<br />
Zandonà Roberto 120-121, 123-124<br />
Zanchetta Marisa 129<br />
Zanovello Paola 46, 128-129, 147, 231,<br />
250-251, 255<br />
Zorzi Manuel 128, 178-179<br />
Zovato Stefania 34, 64, 155, 234<br />
Zustovich Fable 34-35, 43, 227
Analytical Index<br />
A<br />
Acute Lymphoblastic Leukemia 148-149, 257,<br />
259<br />
ALL See Acute Lymphoblastic Leukemia<br />
Angiogenesis 39-41, 73, 148, 199-200, 257-<br />
258<br />
Apoptosis 50, 73, 141-, 144, 146-149<br />
B<br />
Barrett’s esophagus 76, 78, 79-81, 141<br />
Biostatistics 3, 191, 202<br />
Bone Marrow 49, 51, 108, 112, 145, 147, 152<br />
Boron Neutron Capture Therapy (BNCT) 114,<br />
116, 118, 228<br />
Brachytherapy 111, 114, 122<br />
BRCA 30, 131, 133-134, 199, 210, 221,<br />
228-229<br />
Breast Cancer 36, 38, 43, 45, 48, 51, 56, 64,<br />
66-67, 86, 96, 98-101, 116, 118, 130, 133-<br />
134, 146-148, 156, 165, 180-182, 202, 205,<br />
213, 222, 228, 237-238<br />
C<br />
Cancerogenesis 3, 60-61, 73, 178, 220, 255<br />
Chromosomes 142<br />
Chronic Lymphocytic Leukemia 140, 152, 153<br />
CLL. See Chronic Lymphocytic Leukemia<br />
Cytogenetics 152, 153, 192<br />
E<br />
EBV. See Epstein-Barr Virus<br />
EGFR 51, 131, 210, 212, 224, 241<br />
Elderly patients. See Geriatric Oncology<br />
Endoscopy 3, 38, 61, 76, 78, 79, 85, 198<br />
Epidemiology 3, 178, 202, 218<br />
Epstein-Barr Virus 131-132, 199-200, 210,<br />
220-221, 231<br />
INDEX<br />
308<br />
Erlotinib 164-165, 233, 241<br />
Esophageal Cancer 48, 58, 60-62, 76, 80, 117,<br />
142-144, 200, 206<br />
F<br />
FISH 51, 74, 130, 152-153, 212, 224-225,<br />
241<br />
G<br />
Gastro Intestinal Stromal Tumors 36, 49, 74,<br />
149-151, 224, 227, 234<br />
Gefitinib 210, 212<br />
Gene Therapy 141, 192, 200, 255, 259<br />
Geriatric Oncology 4, 45, 232<br />
GIST. See Gastro Intestinal Stromal Tumors<br />
H<br />
HHV-8 132, 199, 210<br />
HIV 128, 132, 199-200, 220, 258<br />
HPV 128, 131, 132, 137-138, 178, 180, 199,<br />
210, 219-221, 250<br />
h-TERT 39, 45, 140-141, 200<br />
HTLV-1 128, 144, 199, 220-221, 258<br />
Human Herpes Virus 8. See HHV-8<br />
Human Immunodeficiency Virus. See HIV<br />
Human Papilloma Virus. See HPV<br />
Human T-Lymphotropic Virus<br />
Type I. See HTLV-1<br />
I<br />
IL4R 46<br />
Imaging 3, 29, 52, 64, 66, 74, 78, 80, 89-90,<br />
92-93, 96, 98-101, 116-118, 120, 122, 148,<br />
151-152, 192, 221, 223, 225, 234, 256, 259<br />
Imatinib 151, 227, 239<br />
Immunology 3, 4, 29, 38, 42, 45, 61, 71, 128,<br />
130, 132-133, 192, 204, 230, 255
Immunotherapy 130, 133, 151, 200, 211, 240,<br />
258<br />
125 Iodine 114<br />
K<br />
KIT 149, 150-151, 224<br />
L<br />
Lung tumors 29, 51, 164-165, 210, 212, 224,<br />
228, 241, 253<br />
Lymphadenectomy 67, 205<br />
Lymphoma 48-49, 116-117, 141, 144, 199,<br />
240, 243<br />
M<br />
Mammography 90, 96, 98-102<br />
Melanoma 3, 29-30, 46, 48-49, 52, 68, 70-75,<br />
85, 94, 111, 114, 130-132, 134-137, 147, 151,<br />
174, 200, 202, 204-205, 213, 215, 205, 221,<br />
223-224, 240, 251, 253<br />
Monoclonal antibodies 80, 152, 211, 226, 230<br />
Mutation 43, 113, 134-136, 185-159, 182,<br />
214<br />
N<br />
Neo-adjuvant 40, 80, 181, 238-239<br />
NSCLC. See Lung tumors<br />
P<br />
Paraganglioma 113, 154, 156-159, 221<br />
PDGFRA 149-151, 224<br />
Pediatric tumors 113, 202, 205, 243<br />
Perfusion 46, 68, 71, 75, 94, 111<br />
PET 48, 64, 75, 93, 113, 116-117, 120, 152,<br />
223-225, 228, 250<br />
Prevention 3, 118, 218<br />
Q<br />
Quality of Life 4, 28, 36, 43,45, 52, 60-62, 74-<br />
75, 76, 80, 82, 87, 115, 165, 172, 175, 177,<br />
188, 202, 205-206, 210, 232, 239, 242-243<br />
R<br />
Registry 3, 76, 79, 104, 164-165, 178, 180-<br />
182, 192, 246<br />
RET 159, 160<br />
Retrovirus 130, 219, 221, 258<br />
S<br />
Sarcoma 29, 38, 68, 70-75, 85, 90, 94, 117,<br />
132, 178, 199, 202, 204-205, 220, 223, 242-<br />
243<br />
SCID mice 141, 148, 257<br />
Screening 92, 99-101, 104, 128, 130, 137-139,<br />
142, 145, 159, 178, 180, 198, 218, 227, 243,<br />
246, 250, 251, 250-252<br />
Sentinel Lymphnode 72<br />
Sunitinib 42-43, 146-147, 223, 227-228, 239,<br />
242<br />
T<br />
Telomerase. See h-TERT<br />
Thyroid tumors 29<br />
Tomosynthesis 90, 96, 99, 101-103<br />
Tumor antigens 211<br />
V<br />
VEGF 39, 40, 43, 223, 239, 258<br />
VHL. See Von Hippel Lindau Syndrome<br />
Von Hippel Lindau Syndrome 42, 154, 159,<br />
184<br />
Vulnerability. See Geriatric Oncology<br />
INDEX<br />
309
Colophon<br />
Title:<br />
Scientific Report <strong>2010</strong>-<strong>2011</strong><br />
Publisher:<br />
Istituto Oncologico Veneto<br />
I.R.C.C.S.<br />
Year / Month:<br />
2012, April<br />
Editorial committee:<br />
Alberto Amadori<br />
Elisabetta Mutto Accordi<br />
Gian Luca De Salvo<br />
Photographer:<br />
Maurizio Peci<br />
Graphic:<br />
Pallino & Co.<br />
Typographer:<br />
La Grafica Faggian<br />
Paper:<br />
Gardamat Art 135gr
April 2012