Volume 10, Number 4, 2005 - American Biological Safety Association
Volume 10, Number 4, 2005 - American Biological Safety Association
Volume 10, Number 4, 2005 - American Biological Safety Association
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Volume</strong> <strong>10</strong>, <strong>Number</strong> 4, <strong>2005</strong>
213<br />
214<br />
216<br />
258<br />
Journal of the <strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong><br />
<strong>Volume</strong> <strong>10</strong>, <strong>Number</strong> 4, <strong>2005</strong><br />
Letter to the Editors<br />
President’s Page<br />
Articles<br />
Comparison of the Canadian Industrial Security Manual and the United States National<br />
Industrial Security Program Operating Manual<br />
Andrew Hammond .......................................................................................................................216<br />
The Infectious Dose of Francisella tularensis (Tularemia)<br />
Rachael M. Jones, Mark Nicas, Alan Hubbard, Matthew D. Sylvester, and Arthur Reingold .....227<br />
High-Dose Ultraviolet C Light Inactivates Spores of Bacillus Atrophaeus and Bacillus Anthracis<br />
Sterne on Nonreflective Surfaces<br />
Marie U. Owens, David R. Deal, Michael O. Shoemaker, Gregory B. Knudson,<br />
Janet E. Meszaros, and Jeffery L. Deal.....................................................................................240<br />
Autoclave Testing in a University Setting<br />
Richard N. Le, Amy L. Hicks, and Janice Dodge..........................................................................248<br />
Operating a BSL-4 Laboratory in a University Setting<br />
Tradeline Publications ..................................................................................................................253<br />
Special Features<br />
Use of Multiple SOP Styles to Increase Personnel Compliance and <strong>Safety</strong><br />
Within a BSL-2/BSL-3 Animal Facility<br />
Andrea Mitchell, Jeri Ellis, and Tim Ruddy..................................................................................258<br />
Book Review—Revenge of the Microbes by Abigail A. Salyers and Dixie D. Whitt<br />
Reviewed by George A. Pankey.....................................................................................................265<br />
Book Review—Biodefense: Principles and Pathogens Edited by Michael S. Bronze<br />
and Ronald A. Greenfield<br />
Reviewed by Michael P. Owen......................................................................................................266<br />
(continued on page 2<strong>10</strong>)
(continued from page 209)<br />
273<br />
2<strong>10</strong><br />
Ask the Experts—HEPA Filtered Supply Air for BSL-3 Laboratories?<br />
John H. Keene...............................................................................................................................268<br />
Biosafety Tips—Lymphocytic Choriomeningitis Virus—A Hazard in Rodent Animal Colonies<br />
Karen B. Byers ...............................................................................................................................270<br />
ABSA News<br />
<strong>2005</strong> ABSA Conference Photos.................................................................................................273<br />
<strong>2005</strong> ABSA Service Award Recipients......................................................................................274<br />
New ABSA Members for 2006 ...................................................................................................277<br />
<strong>2005</strong> ABSA Conference Sponsors.............................................................................................279<br />
Calendar of Events .......................................................................................................................280<br />
ABSA Journal Subscription Information ...................................................................................281<br />
ABSA Anthology Books Information and Order Form.............................................................282<br />
ABSA Chapters, Affiliates, and Affiliated Organizations........................................................283<br />
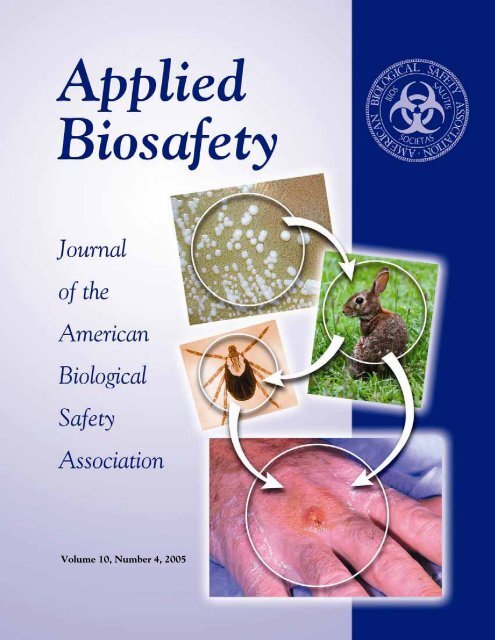
About the Cover<br />
Fransicella tularensis is the causative agent of tularemia. Exposure to F. tularensis has resulted in numerous<br />
laboratory acquired infections, some of which may have been due to aerosol exposures. Read more about<br />
infectious dose modeling on pages 227-239, “The Infectious Dose of Francisella tularensis (Tularemia)” by<br />
Rachael M. Jones, Mark Nicas, Alan Hubbard, Matthew D. Sylvester, and Arthur Reingold.<br />
One natural reservoir for this zoonotic disease is the rabbit. It can be transmitted to humans by handling<br />
infected blood or tissue, or consuming undercooked infected meat. The tick, an arthropod vector, can transmit<br />
the disease through its bite. The symptoms developed depend on the type of exposure route.<br />
Images from the CDC Public Health Image Library are: D. variabilis tick photo, taken by Andrew Brooks<br />
of CDC; Tularemia lesion on the dorsal skin of right hand photo, taken by Dr. Brachman of the CDC; and<br />
F. tularensis colony characteristics when grown on Chocolate, Martin Lewis or Thayer-Martin medium at<br />
48-72 hours, courtesy of Larry Stauffer, Oregon State Public Health Laboratory.
Applied Biosafety: Journal of the <strong>American</strong> <strong>Biological</strong> <strong>Safety</strong><br />
<strong>Association</strong> (ISSN 1535-6760) is published quarterly by the <strong>American</strong><br />
<strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (ABSA). ABSA members receive the<br />
journal as a benefit of membership. An additional annual subscription<br />
for members is $60. Nonmembers and institutions/libraries may<br />
subscribe at the annual rates of $92 and $122 respectively. Single issue<br />
rates are as follows: members $18; nonmembers $28; and institutions/<br />
libraries $35.<br />
Authorization to Copy: No part of this publication may be<br />
reproduced, stored in a retrieval system, or transmitted in any form or<br />
by any means, electronic, electrostatic, magnetic tape, photocopying,<br />
recording, or otherwise, without permission in writing from the<br />
copyright holder.<br />
Change of Address: A change of address notice should be sent at<br />
least 6 weeks in advance to the ABSA National Office to ensure that<br />
all mailings, including the journal and newsletter, will reach you.<br />
ABSA is not responsible for misrouted mail as a result of insufficient<br />
notification of an address change. Undelivered copies resulting from<br />
an insufficient address change notification will not be replaced, but<br />
issues may be purchased at the single issue price as detailed above.<br />
ABSA National Office<br />
<strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong><br />
1202 Allanson Road<br />
Mundelein, IL 60060-3808, USA<br />
847-949-1517 / Fax 847-566-4580<br />
E-mail: absa@absa.org<br />
Web Site: www.absa.org<br />
Advertising Rates<br />
Rates 1x 2x 4x<br />
Outside back cover $800 $720 $680<br />
Inside front cover $600 $540 $5<strong>10</strong><br />
Inside back cover $600 $540 $5<strong>10</strong><br />
Full page $500 $450 $425<br />
1/2 page $300 $270 $255<br />
1/4 page $200 $180 $170<br />
Color rates: $350 for first color (after black) and $300 each additional color.<br />
15% discount for agencies (orders must be supplied on agency letterhead).<br />
Mechanical Requirements Width Height<br />
Outside back cover (full bleed) 8-1/2” 11”<br />
Inside front cover (full bleed) 8-1/2” 11”<br />
Inside back cover (full bleed) 8-1/2” 11”<br />
Full page 7” <strong>10</strong>”<br />
1/2 page - horizontal 7” 4-7/8”<br />
1/2 page - vertical 3-3/8” <strong>10</strong>”<br />
1/4 page 3-7/8” 4-7/8”<br />
Trim size—8-1/2” x 11”<br />
Film—133 line screen, right reading, emulsion side down, color separated<br />
Submission Deadlines<br />
February 1 for Spring issue May 1 for Summer issue<br />
August 1 for Fall issue November 1 for Winter issue<br />
The publication of any advertisement by this journal is not an<br />
endorsement of the advertiser or of the products or services advertised.<br />
ABSA is not responsible for any claims made in any advertisement.<br />
ABSA Journal Editorial Board<br />
Co-Editors<br />
Barbara Johnson, Department of Defense, Arlington, VA<br />
Karen B. Byers, Dana Farber Cancer Institute, Boston, MA<br />
Associate Editor<br />
Elizabeth Gilman Duane, Wyeth, Cambridge, MA<br />
Lynn Harding, Biosafety Consultant, Chattanooga, TN<br />
Assistant Editors<br />
Richard Fink, Wyeth BioPharma, Andover, MA<br />
John H. Keene, Biohaztec Associates, Inc., Midlothian, VA<br />
Thomas A. Kost, GlaxoSmithKline, Research Triangle Park, NC<br />
Ed Krisiunas, WNWN International, Burlington, CT<br />
International Editors<br />
Allan Bennett, European <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (EBSA),<br />
United Kingdom<br />
Maureen Best, International Biosafety Working Group (IBWG),<br />
Canada<br />
Otto Doblhoff-Dier, European <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (EBSA),<br />
Austria<br />
Betty Kupskay, ABSA Canada, Canada<br />
Ai Ee Ling, Asia Pacific Biosafety <strong>Association</strong> (APBA), Singapore<br />
Leila Oda, Associação Nacional de Biossegurança (ANBio), Brazil<br />
Production Editor<br />
Karen D. Savage<br />
Editorial Board<br />
Matthew J. Bankowski, ViroMed (LabCorp), Minnetonka, MN<br />
Franklin R. Champlin, Mississippi State University, Mississippi<br />
State, MS<br />
Mary L. Cipriano, Abbott Laboratories, Abbott Park, IL<br />
Robert P. Ellis, Colorado State University, Fort Collins, CO<br />
Glenn A. Funk, Lawrence Livermore National Laboratory,<br />
Livermore, CA<br />
Raymond W. Hackney, Jr., University of North Carolina, Chapel<br />
Hill, NC<br />
Philip Hagan, Georgetown University, Washington, DC<br />
Robert J. Hawley, Midwest Research Institute, Frederick, MD<br />
Richard Henkel, Centers for Disease Control and Prevention,<br />
Atlanta, GA<br />
Debra L. Hunt, Duke University, Durham, NC<br />
Peter C. Iwen, University of Nebraska Medical Center, Omaha, NE<br />
John H. Keene, Biohaztec Associates, Inc., Midlothian, VA<br />
Paul Michael Kivistik, University of Nevada, Reno, NV<br />
Joseph P. Kozlovac, USDA-ARS, Beltsville, MD<br />
Jens H. Kuhn, Harvard Medical School, Southborough, MA<br />
Margy S. Lambert, University of Wisconsin, Madison, WI<br />
R. Thomas Leonard, University of Virginia, Charlottesville, VA<br />
Paul J. Meechan, Merck Research Laboratories, West Point, PA<br />
Mark Nicas, University of California, Berkeley, CA<br />
Beryl J. Packer, Iowa State University, Ames, IA<br />
Tim Ravita, Constella Health Sciences, Atlanta, GA<br />
Richard Rebar, GlaxoSmithKline R&D, King of Prussia, PA<br />
Jonathan Y. Richmond, Jonathan Richmond & Associates, Inc.,<br />
Southport, NC<br />
Deanna S. Robbins, Department of Veterans Affairs, Baltimore, MD<br />
Richard J. Shaughnessy, University of Tulsa, Tulsa, OK<br />
Allan Showler, USDA-ARS, Weslaco, TX<br />
Cecil R. Smith, Ohio State University, Columbus, OH<br />
Gerard J. Spahn, The Salk Institute, La Jolla, CA<br />
Donald Vesley, University of Minnesota, Minneapolis, MN<br />
Catherine L. Wilhelmsen, United States Army Medical Research<br />
Institute of Infectious Diseases (USAMRIID), Fort Detrick, MD<br />
Linda B. Wolfe, Whitehead Institute for Biomedical Research,<br />
Cambridge, MA<br />
Jeffrey D. Wolt, Iowa State University, Ames, IA<br />
Alan G. Woodard, International Environmental Health Alliance,<br />
Gansevoort, NY
Vision<br />
212<br />
ABSA, the leader in the profession of biological safety.<br />
Mission Statement<br />
The <strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> is dedicated to expanding biological safety awareness to<br />
prevent adverse occupational and environmental impact from biohazards.<br />
Goals<br />
• Expand professional and public awareness of biological safety through effective communication.<br />
• Participate in the development of biological safety and biosecurity standards, guidelines, and<br />
regulations.<br />
• Develop ABSA as the recognized resource for professional and scientific expertise in biological<br />
safety and biosecurity.<br />
• Advance biological safety as a scientific discipline through education, research, and professional<br />
development.<br />
ABSA Officers<br />
President<br />
Glenn A. Funk, Lawrence Livermore National Laboratory, Livermore, CA<br />
President-Elect<br />
Robert J. Hawley, Midwest Research Institute, Frederick, MD<br />
Secretary<br />
Rosamond Rutledge-Burns, National Institute Standards & Technology, Gaithersburg, MD<br />
Treasurer<br />
Leslie Delpin, University of Connecticut, Storrs, CT<br />
Past-President<br />
Elizabeth Gilman Duane, Wyeth, Cambridge, MA<br />
Council Members<br />
Robert P. Ellis, Colorado State University, Fort Collins, CO<br />
Joseph P. Kozlovac, USDA Agricultural Research Service, Beltsville, MD<br />
Patricia Olinger, Pharmacia Corporation, Kalamazoo, MI<br />
Chris Thompson, Greenfield, IN<br />
Executive Director<br />
Edward J. Stygar, Jr.
Letter to the Editors<br />
James J. Coogan<br />
Siemens Building Technologies, Buffalo Grove, Illinois<br />
Let me commend Allan Bennett et al. on valuable<br />
piece of research and an illuminating article<br />
entitled “Development of Particle Tracer Techniques<br />
to Measure the Effectiveness of High Containment<br />
Laboratories” in Applied Biosafety (<strong>Volume</strong> <strong>10</strong>, <strong>Number</strong><br />
3, <strong>2005</strong>). The facts and observations presented<br />
support some common engineering assumptions and<br />
challenge others. Both results are valuable.<br />
Definition of Laboratory Protection Factor and<br />
the test methods described advance our ability to<br />
discuss effective pressurization. The result that containment<br />
correlates more closely to infiltrating air<br />
flow than to pressure difference is intriguing. I expect<br />
it surprises many engineers as much as it does<br />
me.<br />
The explanation offered is that the air flowing<br />
inward through the door catches contaminants and<br />
prevents their escape while the door is open and a<br />
person walks through it. The authors themselves<br />
seem to find it unlikely that such low air velocity<br />
captures contaminants. (The air velocity reported<br />
through the open door is 0.14 m s-1 and lower:<br />
much less than the velocity of the swinging door or<br />
the walking person.)<br />
Perhaps it is appropriate to propose another explanation<br />
for the results. Consider the effect that the<br />
Editorial Note<br />
Letters to the Editors (approximately 400 words)<br />
discuss information published in Applied Biosafety in<br />
the past nine months or discuss topic areas of general<br />
interest in the biosafety profession. Letters can<br />
Applied Biosafety, <strong>10</strong>(4) p. 213 © ABSA <strong>2005</strong><br />
infiltrating air flow has on contaminant concentrations<br />
while the door is closed before and after entry<br />
or exit. Just inside the door, contaminated air is continuously<br />
replaced by the clean infiltrating air. This<br />
lowers the concentration near the door. When entry<br />
or exit occurs, certainly some air leaves the room,<br />
but this air is cleaner than it would be with a lower<br />
infiltrating air flow rate, so less contaminant leaves<br />
the room. After the entry or exit is complete and the<br />
door is closed, some quantity of contaminant lingers<br />
outside the room. A portion of it is picked up by the<br />
particle counters, but presumably, some of it is<br />
drawn back into the room by the on-going infiltration.<br />
In short, the supposition is that infiltrating air<br />
flow has a continuous cleaning effect near the door,<br />
and that this on-going effect (rather than several seconds<br />
of infiltration at very low velocity during entry<br />
or exit) increases the Laboratory Protection Factor.<br />
Do the authors have more information that will<br />
help us choose one mechanism or the other to explain<br />
the results? In some cases, the question is<br />
moot. Containment is the issue and the mechanism<br />
may be unimportant, but there are ventilation systems<br />
where the distinction is crucial.<br />
be submitted electronically to Karen D. Savage,<br />
Production Editor, at ksavage@covad.net or by mail<br />
to ABSA National Office, Applied Biosafety, 1202<br />
Allanson Road, Mundelein, IL 60060. Letters published<br />
in part or whole are subject to editing for clarity<br />
and special formatting.<br />
213
I suspect every new organization president wrestles<br />
with questions like “What do I want to achieve<br />
during my presidency?” and “Where do I want to<br />
lead the organization during the next year?” These<br />
are weighty issues that focus on the best interests of<br />
the membership in general and the institution in<br />
particular. They’re made especially challenging by<br />
the outstanding leadership and successes provided<br />
by recent past presidents. I have, appropriately, a<br />
very high standard to uphold.<br />
With 1,500 members representing 30 different<br />
countries and 16 Affiliates and affiliated organizations,<br />
ABSA is no longer a small club of friends. We<br />
are gaining the mass to be noticed, to be listened to,<br />
to be asked for advice and help, and to make a difference<br />
in the realms of science we impact. It would<br />
be easy for me to suggest that we grow the organization<br />
because as we grow larger, we grow stronger and<br />
we have a louder voice. There is truth in this, and<br />
growing ABSA is a worthy goal that we should pursue.<br />
However, at this point, I believe it is also important<br />
to “grow our profession”—to bring more highly<br />
qualified scientists into our ranks, to strengthen our<br />
knowledge base, and to provide additional ABSA<br />
members who will enrich our organization. I believe<br />
there are many scientists and health and safety professionals<br />
who are unaware of the challenges and<br />
rewards of biosafety as a career, or of the need for<br />
highly skilled biosafety professionals in the scientific<br />
community.<br />
To keep our profession attractive to others and<br />
respected within the scientific community, we must<br />
maintain, strengthen, and continue to demonstrate<br />
the high professional standards to which we adhere<br />
every day. Each of us must set the Gold Standard for<br />
professionalism, for technical competency, for cus-<br />
214<br />
President’s Page<br />
Glenn A. Funk<br />
Gualala, California<br />
Applied Biosafety, <strong>10</strong>(4) pp. 214-215 © ABSA <strong>2005</strong><br />
tomer service, and for flexibility and adaptability to<br />
meet the varied and often unanticipated needs of<br />
our customers. We must not simply continue to be<br />
the best of the best; we must continually get better at<br />
what we do. As “Neutron Jack” Welch, ex-CEO of<br />
General Electric, used to say, “You can’t just talk the<br />
talk; you’ve also got to walk the walk.”<br />
One of the things we do best in ABSA is share<br />
our knowledge through networking, seminars, training<br />
sessions, and professional courses. ABSA is your<br />
organization, and I urge you to use the opportunities<br />
it offers to improve your skills as a biosafety professional.<br />
Meanwhile, your ABSA Council and I will<br />
continue to make ABSA better for you. The management<br />
consultants who helped us restructure our<br />
business model also helped us identify important<br />
areas for Task Force study; we held off implementing<br />
these during the first year in order to focus on the<br />
business infrastructure. This year we’ll put Task<br />
Forces to work defining the parameters of the biosafety<br />
profession, enhancing the value and benefits<br />
of professional Registration and Certification, and<br />
determining the feasibility and usefulness of an<br />
ABSA Emergency Response capability to provide<br />
assistance during national and international emergencies<br />
that involve biosafety. If you have an interest<br />
in serving on one of these Task Forces, please let me<br />
know (gafunk@absa.org).<br />
One other effort soon to be underway is a renewed<br />
push to catalog the ABSA Historical Collection<br />
and transfer it to safe archival storage. Once<br />
that’s done, we can look at ways to make it accessible<br />
to members through, for example, displays at meetings<br />
and articles in this Journal. Ultimately, I’d like<br />
to see at least parts of the collection available online.<br />
In future columns I’ll discuss other ideas for
moving ABSA forward. As always, I greatly appreciate<br />
your volunteer efforts to help make ABSA what<br />
it is. We wouldn’t be here today if it weren’t for the<br />
active and positive participation of our many talented<br />
members. As President, my door is open to<br />
Corrections and Clarifications<br />
G. A. Funk<br />
you. Please send me e-mails with your ideas and suggestions.<br />
We’ll talk about them, I’ll take the great<br />
ideas to Council, and together we’ll continue to<br />
make ABSA better and stronger.<br />
Special Features, Ask the Experts: “USDA BSL-3 Facility Requirements: What’s the<br />
Concern?” authorship attribution in the Table of Contents is incorrect (<strong>Volume</strong> <strong>10</strong>, <strong>Number</strong><br />
3, page 133). It should be: John H. Keene.<br />
EPA Pesticide Program Update from EPA’s Office of Pesticide Programs<br />
<strong>10</strong>/11/05: EPA Approves New Non-Chemical Control for Corn Rootworm<br />
www.epa.gov/pesticides<br />
After an intensive, multi-year scientific analysis, EPA has approved applications submitted by Mycogen<br />
Seeds (c/o Dow AgroSciences, LLC) and Pioneer Hi-Bred International, Inc. for the use of a new corn<br />
plant-incorporated protectant (PIP) designed to control corn rootworm. Corn rootworm is a widespread<br />
and destructive insect pest responsible for the single largest use of conventional insecticides in the United<br />
States. The new product is the second PIP to offer protection against corn rootworm and is expected to<br />
result in a further reduction of chemical insecticide use by growers.<br />
The new corn plant-incorporated protectant, Event DAS-59122-7 Corn, produces its own insecticide<br />
within the corn plant derived from Bacillus thuringiensis (Bt), a naturally occurring soil bacterium. The Bt<br />
proteins used in this product, called Cry34Ab1 and Cry35Ab1 (Cry 34/35), control corn rootworm.<br />
To reduce the likelihood of corn rootworm developing resistance to Bt, EPA is requiring Mycogen and<br />
Pioneer to ensure that buffer zones within the planted acreage be planted with corn that is not protected<br />
from corn rootworm to serve as a “refuge.” The insect populations in the refuges will help prevent<br />
resistance development when they cross-breed with insects in the Bt fields. This resistance management<br />
strategy was developed as a condition of the registration, and EPA will require routine monitoring and<br />
documentation that these measures are followed.<br />
The reduction in chemical pesticide use will benefit the environment directly and can mean less<br />
chemical exposure to people who apply pesticides to corn. The availability of multiple corn rootwormprotected<br />
corn products will also increase grower choice and price competition, resulting in lower seed<br />
prices for consumers and higher adoption rates. The product provides yet another way to combat corn<br />
rootworm, as well as indirect benefits such as energy savings resulting from reduced chemical insecticide<br />
use. As with similar products, EPA has approved Cry 34/35 for time-limited use, which will be subject to<br />
reevaluation in five years. For more information on EPA’s regulation of biopesticide products, see<br />
www/epa.gov/pesticides/biopesticides/.<br />
215
Abstract<br />
Because of the potential for use as a bioterrorism<br />
agent or bioweapon, many governments have imposed<br />
strict regulations regarding the possession, use, and<br />
transfer of “select” biological agents. Consequently,<br />
much of the information surrounding the possession and<br />
use of these agents is potentially classified, and those<br />
contractors and their employees who require access to<br />
this information must receive Facility (contractor) and<br />
Personnel (employees) clearances. Both Canada and<br />
the United States (U.S.) have produced industrial security<br />
manuals—the Industrial Security Manual (ISM)<br />
(Canadian and International Industrial Security Directorate,<br />
2004) and the National Industrial Security<br />
Program Operating Manual (NISPOM) (Defense<br />
Technical Information Center, 1995)—for use by<br />
cleared government contractors. These documents set<br />
forth the requirements, restrictions, and other safeguards<br />
that are necessary to prevent unauthorized disclosure<br />
of classified information and assets provided to<br />
or produced by private government contractors. This<br />
article compares and contrasts the requirements set<br />
forth in the ISM and the NISPOM. The results of this<br />
comparison present a valuable security management<br />
tool for private organizations that wish to engage in<br />
classified work for the Canadian, U.S., or both governments.<br />
216<br />
Article<br />
Introduction<br />
Applied Biosafety, <strong>10</strong>(4) pp. 216-226 © ABSA <strong>2005</strong><br />
Comparison of the Canadian Industrial Security<br />
Manual and the United States National<br />
Industrial Security Program Operating Manual<br />
Andrew Hammond<br />
Constella Health Sciences, Atlanta, Georgia<br />
As a result of the October 2001 anthrax letter<br />
attacks, both the United States and Canada enacted<br />
new laws imposing additional restrictions on certain<br />
hazardous biological agents and toxins. The U.S.<br />
enacted the Public Health Security and Bioterrorism<br />
Preparedness and Response Act of 2002 (Public Law<br />
<strong>10</strong>7-188) (U.S. Government Printing Office, 2002)<br />
and Canada passed the Public <strong>Safety</strong> Act, 2002<br />
(Parliament of Canada, 2002). Because of the potential<br />
for “select” biological agents and toxins being<br />
used as bioterrorism agents or in a bioweapons program,<br />
both Acts impose strict regulations regarding<br />
their possession, use, and transfer. Consequently,<br />
much of the information surrounding the possession<br />
and use of these agents is potentially classified (or<br />
confidential), and those organizations and their employees<br />
who require access to this information must<br />
receive Facility (organization) and Personnel<br />
(employee) clearances. Both Canada and the U.S.<br />
have produced industrial security manuals—Industrial<br />
Security Manual (ISM) (Canadian and International<br />
Industrial Security Directorate, 2004) and the National<br />
Industrial Security Program Operating Manual<br />
(NISPOM) (Defense Technical Information Center,<br />
1995)—for use by cleared government contractors.<br />
These documents set forth the requirements, restrictions,<br />
and other safeguards that are necessary to prevent<br />
unauthorized disclosure of classified information<br />
(and assets) provided to or produced by private
government contractors and to control the authorized<br />
disclosure of classified information (and assets)<br />
released by the governments to their contractors.<br />
United States—National Industrial<br />
Security Program Operating Manual<br />
Security Classifications<br />
An original classification decision at any level<br />
can be made only by a U.S. Government official<br />
who has been delegated this authority in writing.<br />
Contractors may make derivative classification decisions<br />
based on the guidance provided by the Contract<br />
Security Classification Specification that is issued<br />
with each classified contract. Derivative classification<br />
is the act of classifying a specific item of information<br />
or material on the basis of an original classification<br />
decision already made by an authorized<br />
original classification authority. The source of authority<br />
for derivative classification ordinarily consists<br />
of a previously classified document or a classification<br />
guide issued by an original classification authority.<br />
Top Secret<br />
Top secret information or material is that information<br />
or material whose unauthorized disclosure<br />
could be reasonably expected to cause exceptionally<br />
grave damage to the national security that the original<br />
classification authority is able to identify or describe.<br />
Examples include armed hostilities against the<br />
United States or its allies, disruption of foreign relations<br />
vitally affecting the national security, and the<br />
disclosure of scientific or technological developments<br />
vital to national security.<br />
Secret<br />
Secret information or material is that information<br />
or material whose unauthorized disclosure<br />
could be reasonably expected to cause serious damage<br />
to the national security that the original classification<br />
authority is able to identify or describe. Examples<br />
of serious damage include significant impairment<br />
of a program or policy directly related to the<br />
national security and compromise of significant scientific<br />
or technological developments relating to national<br />
security.<br />
A. Hammond<br />
Confidential<br />
Confidential information or material is that information<br />
or material whose unauthorized disclosure<br />
could be reasonably expected to cause damage to<br />
the national security that the original classification<br />
authority is able to identify or describe. Examples<br />
include documents relating to clearance or assignment<br />
of personnel who will have knowledge of, or<br />
access to, classified information or materials or details<br />
pertaining to features of routes and schedules of<br />
shipments of confidential materials.<br />
Facility Security<br />
Facility Clearances<br />
A facility security clearance (FCL) is an administrative<br />
determination that a facility is eligible for access<br />
to classified information at the same or lower<br />
classification category as the clearance being granted.<br />
Contractors are eligible for custody of classified material,<br />
if they have an FCL and storage capability approved<br />
by the Cognizant Security Agency (CSA).<br />
A procuring activity of the Government or<br />
cleared contractor may request a facility clearance for<br />
a contractor or prospective contractor/<br />
subcontractor when a definite, classified procurement<br />
need has been established. Also, the contractor<br />
must be organized and existing under the laws of any<br />
of the 50 states, the District of Columbia, or Puerto<br />
Rico, and be located in the U.S. and its territorial<br />
areas or possessions.<br />
Meetings<br />
Classified disclosure at a meeting (e.g., conference,<br />
seminar, symposium, exhibit, convention,<br />
training course, or other such gathering) which<br />
serves a government purpose and at which adequate<br />
security measures have been provided in advance<br />
may be conducted by a cleared contractor provided<br />
the meeting is authorized by a Government Agency<br />
that has agreed to assume security jurisdiction. The<br />
Government Agency must approve security arrangements,<br />
announcements, attendees, and the location<br />
of the meeting. (Classified meetings shall be held<br />
only at a Federal Government installation or a<br />
cleared contractor facility where adequate physical<br />
security and procedural controls have been ap-<br />
217
proved.) Contractors wishing to conduct classified<br />
meetings shall submit their requests to the Government<br />
Agency having principal interest in the subject<br />
matter of each meeting.<br />
Personnel Security<br />
Security Officers<br />
The Facility Security Officer (FSO) shall be a<br />
U.S. citizen employee appointed by the contractor<br />
who is cleared as part of the facility clearance. The<br />
FSO will supervise and direct security measures necessary<br />
for implementing the NISPOM and related<br />
Federal requirements for classified information.<br />
The senior management official and the FSO<br />
must always be cleared to the level of the Facility<br />
Clearance (FCL). Other officials, as determined by<br />
the CSA, must be granted a Personnel Clearance<br />
(PCL) or be excluded from classified access.<br />
Personnel Clearances<br />
An industrial personnel security clearance is an<br />
administrative determination that an industrial employee<br />
is eligible for access to classified information.<br />
This determination is based on investigation and<br />
review of available personal data and a finding that<br />
access is clearly consistent with national interests.<br />
An individual may be processed for a personnel<br />
security clearance only when employed by a cleared<br />
contractor in a job requiring access to classified information.<br />
As an exception, a candidate for employment<br />
may be processed for a PCL provided a written<br />
commitment for employment that prescribes a fixed<br />
date for employment within the ensuing 180 days<br />
has been made by the contractor, and the candidate<br />
has accepted the employment offer in writing.<br />
Under rare circumstances, a non-U.S. citizen<br />
may be issued a Limited Access Authorization for<br />
access to classified information. Specific criteria and<br />
limitations are provided in the NISPOM.<br />
Contractors have no authority to grant, deny, or<br />
revoke personnel clearances for their employees.<br />
This authority is reserved by the U.S. Government.<br />
Subcontracting<br />
Before a prime contractor may release, disclose<br />
classified information to a subcontractor, or cause<br />
218<br />
Comparison of the Canadian Manual and the U.S. Manual<br />
classified information to be generated by a subcontractor,<br />
he or she must determine the security requirements<br />
of the subcontract and determine clearance<br />
status of prospective subcontractors. The prime<br />
contractor shall verify the clearance status and safeguarding<br />
capability of the subcontractor from the<br />
CSA. If a prospective subcontractor does not have<br />
the appropriate FCL or safeguarding capability, the<br />
prime contractor shall request the CSA of the subcontractor<br />
to initiate the necessary action.<br />
The prime contractor shall ensure that a Contract<br />
Security Classification Specification is incorporated<br />
in each classified subcontract. The contractor<br />
shall also review the security requirements during<br />
the different stages of the subcontract and provide<br />
the subcontractor with applicable changes in these<br />
security requirements. Upon completion of the subcontract,<br />
the subcontractor may retain classified material<br />
received or generated under the subcontract<br />
for a 2-year period, provided the prime contractor or<br />
GCA does not advise to the contrary.<br />
Education, Training, and Briefings<br />
Contractors shall provide all cleared employees<br />
with security training and briefings commensurate<br />
with their involvement with classified information.<br />
Contractors shall also be responsible for ensuring<br />
that the FSO, and others performing security duties,<br />
complete security training deemed appropriate by<br />
the CSA. (Training, if required, should be completed<br />
within 1 year of appointment to the position<br />
of FSO.) The contractor is responsible for providing<br />
all cleared employees with some form of security<br />
education and training at least annually.<br />
The SF 312 is an agreement between the United<br />
States and an individual who is cleared for access to<br />
classified information. An employee issued an initial<br />
PCL must execute an SF 312 prior to being granted<br />
access to classified information. The employee must<br />
also receive an initial security briefing that includes a<br />
Threat Awareness Briefing, a Defensive Security<br />
Briefing, an overview of the security classification<br />
system, employee reporting obligations and requirements,<br />
and security procedures and duties applicable<br />
to the employee’s job.<br />
Contractors shall debrief cleared employees at<br />
the time of termination (discharge, resignation, or
etirement); when an employee’s PCL is terminated,<br />
suspended, or revoked, and upon termination of the<br />
FCL.<br />
Visits<br />
The contractor must determine that the visit is<br />
necessary and that the purpose of the visit cannot be<br />
achieved without access to, or disclosure of, classified<br />
information. All classified visits require advance<br />
notification to, and approval of, the organization<br />
being visited. In urgent cases, visit information may<br />
be furnished by telephone provided that it is followed<br />
up in writing. The contractor shall issue a<br />
Visit Authorization Letter (VAL) to the organization<br />
being visited that shall include the following:<br />
• Contractor’s name, address, and telephone number,<br />
assigned CAGE Code, and certification of the<br />
level of the FCL<br />
• Name, date, place of birth, and citizenship of the<br />
employee intending to visit<br />
• Certification of the proposed visitor’s PCL and<br />
any special access authorizations required for the<br />
visit<br />
• Name of person(s) to be visited<br />
• Purpose and sufficient justification for the visit<br />
to allow for a determination of the necessity of the<br />
visit<br />
• Date or period during which the VAL is to be<br />
valid<br />
Contractors shall maintain a record of all visitors<br />
to their facility who have been approved for access<br />
to classified information.<br />
Document Security<br />
General Marketing<br />
All classified material shall be marked on the<br />
face of the document to show the name and address<br />
of the facility responsible for its preparation and the<br />
date of preparation. The highest level of classified<br />
information contained in a document is its overall<br />
marking. The overall marking shall be conspicuously<br />
marked or stamped at the top and bottom on the<br />
outside of the front cover, on the title page, on the<br />
first page, and on the outside of the back cover. Interior<br />
pages of classified documents shall be marked at<br />
A. Hammond<br />
the top and bottom with the highest classification of<br />
the information appearing thereon or marked UN-<br />
CLASSIFIED if all the information on the page is<br />
UNCLASSIFIED. The major components of complex<br />
documents are likely to be used separately.<br />
Therefore, each major component shall be marked<br />
as a separate document. Also, each section, part,<br />
paragraph, or similar portion of a classified document<br />
shall be marked to show the highest level of its<br />
classification, or that the portion is unclassified. Unclassified<br />
subjects and titles shall be selected for classified<br />
documents, if possible. If a classified subject or<br />
title must be used, it shall be marked with the appropriate<br />
symbol—(TS), (S), or (C)—placed immediately<br />
following and to the right of the item.<br />
All classified information shall be marked to<br />
reflect the source of the classification and declassification<br />
instructions. This required information shall<br />
be placed on the cover, first page, title page, or in<br />
another prominent position.<br />
General Storage<br />
Cognizant security officials shall work to meet<br />
appropriate security needs according to the intent of<br />
the NISPOM and at an acceptable cost.<br />
TOP SECRET material shall be stored in a<br />
GSA-approved security container, an approved vault,<br />
or an approved Closed Area. Supplemental protection<br />
is required.<br />
SECRET material shall be stored in the same<br />
manner as TOP SECRET material without supplemental<br />
protection.<br />
CONFIDENTIAL material shall be stored in the<br />
same manner as TOP SECRET or SECRET material<br />
except that no supplemental protection is required.<br />
Reproduction<br />
Contractors shall establish a reproduction control<br />
system to ensure that reproduction of classified<br />
material is held to the minimum consistent with<br />
contractual and operational requirements. Classified<br />
reproduction shall be accomplished by authorized<br />
employees knowledgeable about the procedures for<br />
classified reproduction. The use of technology that<br />
prevents, discourages, or detects the unauthorized<br />
reproduction of classified documents is encouraged.<br />
219
All reproductions of classified material shall be<br />
conspicuously marked with the same classification<br />
markings as the material being reproduced.<br />
Domestic Transmission Standards<br />
(Outside of Facility)<br />
Top Secret<br />
• Written authorization of the Government Contracting<br />
Activity (GCA)<br />
• Sealed, opaque inner and outer covers with the<br />
inner cover being a wrapper or envelope plainly<br />
marked with the assigned classification and addresses<br />
of both sender and addressee<br />
• A receipt that identifies the sender, the addressee,<br />
and the document shall be attached to or<br />
enclosed in the inner cover<br />
• Via:<br />
a. Defense Courier Service (DCS), if authorized<br />
by GCA<br />
b. A designated courier or escort cleared for<br />
access to TOP SECRET information<br />
c. By electrical means over CSA-approved secured<br />
communications security circuits provided<br />
such transmission conforms with the<br />
NISPOM, the telecommunications security<br />
provisions of the contract, or is authorized<br />
by the GCA<br />
Secret<br />
• Sealed, opaque inner and outer covers with the<br />
inner cover being a wrapper or envelope plainly<br />
marked with the assigned classification and addresses<br />
of both sender and addressee<br />
• A receipt that identifies the sender, the addressee,<br />
and the document shall be attached to or<br />
enclosed in the inner cover<br />
• Via:<br />
a. TOP SECRET methods<br />
b. USPS Express or Registered mail<br />
c. A cleared “Commercial Carrier”<br />
d. A cleared commercial messenger service engaged<br />
in the intracity/local area delivery<br />
(same day delivery only) of classified material<br />
e. A commercial delivery company approved by<br />
the CSA<br />
f. Other methods as directed, in writing, by<br />
the GCA<br />
220<br />
Comparison of the Canadian Manual and the U.S. Manual<br />
Confidential<br />
• Packaged by SECRECT material methods except<br />
that a receipt is required only if the sender deems it<br />
necessary<br />
• Via:<br />
a. SECRET methods<br />
b. USPS Certified mail<br />
International Transmission Standards<br />
Top Secret<br />
• Domestic requirements<br />
• Via:<br />
a. Defense Courier Service<br />
b. Department of State Courier System<br />
c. Courier service authorized by GCA<br />
Secret and Confidential<br />
• Domestic requirements<br />
• Via:<br />
a. Registered mail through U.S. Army, Navy,<br />
or Air Force postal facilities<br />
b. Appropriately cleared contractor employee<br />
c. U.S. civil service employee or military person<br />
designated by the GCA<br />
d. U.S. and Canadian registered mail with registered<br />
mail receipt to and from Canada and<br />
via a U.S. or Canadian government activity<br />
e. As authorized by the GCA<br />
Destruction<br />
Contractors shall destroy classified material in<br />
their possession as soon as possible after it has<br />
served the purpose for which it was intended.<br />
Classified material may be destroyed by burning,<br />
shredding, pulping, melting, mutilation, chemical<br />
decomposition, or pulverizing. Pulpers, pulverizers,<br />
or shedders may be used only for the destruction of<br />
paper products. Residue shall be inspected during<br />
each destruction to ensure that classified information<br />
cannot be reconstructed. Crosscut shredders<br />
shall be designed to produce residue particle size not<br />
exceeding 1/32 inch in width by 1/2 inch in length.<br />
Public destruction facilities may be used only<br />
with the approval of the CSA, and classified material<br />
removed from a cleared facility for destruction shall<br />
be destroyed on the same day it is removed.<br />
Destruction shall be performed only by appropri-
ately cleared employees of the contractor. For destruction<br />
of TOP SECRET material, two persons are<br />
required. For destruction of SECRET and CONFI-<br />
DENTIAL material, one person is required.<br />
Destruction records that indicate the date of<br />
destruction, identify the material destroyed, and are<br />
signed by the individuals designated to destroy and<br />
witness the destruction are required for TOP SE-<br />
CRET material.<br />
Information System Security<br />
Information systems (IS) that are used to capture,<br />
create, store, process, or distribute classified<br />
information must be properly managed to protect<br />
against unauthorized disclosure of classified information<br />
and loss of data integrity, and to ensure the<br />
availability of the data and system.<br />
Protection requires a balanced approach including<br />
IS security features to include. but not limited<br />
to, administrative, operational, physical, computer,<br />
communications, and personnel controls. Protective<br />
measures commensurate with the classification of<br />
the information, the threat, and the operational requirements<br />
associated with the environment of the<br />
IS are required.<br />
The requirements outlined in the NISPOM apply<br />
to all information systems processing classified<br />
information. Additional requirements for high-risk<br />
systems and data are covered in the NISPOM Supplement.<br />
The CSA is the Designated Accrediting/<br />
Approving Authority (DAA) responsible for accrediting<br />
information systems used to process classified<br />
information in industry. A formal certification and<br />
accreditation (C&A) occurs after the protection<br />
measures have been implemented and any required<br />
IS protection documentation has been approved.<br />
Certification validates that the protection measures<br />
described in the System Security Plan (SSP) have<br />
been implemented on the system and that the protection<br />
measures are functioning properly. Accreditation<br />
is the approval by the CSA for the system to<br />
process classified information.<br />
A. Hammond<br />
Canada—Industrial Security Manual<br />
Security Classifications<br />
The originator of the information and assets<br />
determines the classification level.<br />
Top Secret<br />
TOP SECRET refers to information and assets<br />
related to the national interest that may qualify for<br />
an exemption or exclusion under the Access to Information<br />
Act or Privacy Act and that the compromise<br />
of which would reasonably be expected to cause<br />
exceptionally grave injury to the national interest.<br />
Secret<br />
SECRET refers to information and assets related<br />
to the national interest that may qualify for an exemption<br />
or exclusion under the Access to Information<br />
Act or Privacy Act and that the compromise of<br />
which would reasonably be expected to cause serious<br />
injury to the national interest.<br />
Confidential<br />
CONFIDENTIAL refers to information and<br />
assets related to the national interest that may qualify<br />
for an exemption or exclusion under the Access<br />
to Information Act or Privacy Act and that the compromise<br />
of which would reasonably be expected to<br />
cause injury to the national interest.<br />
Protected “C”<br />
PROTECTED “C” refers to information and<br />
assets related to other than the national interest that<br />
may qualify for an exemption or exclusion under the<br />
Access to Information Act or Privacy Act that could<br />
reasonably be presumed to cause extremely serious injury,<br />
such as loss of life, if compromised.<br />
Protected “B”<br />
PROTECTED “B” refers to information and<br />
assets related to other than the national interest that<br />
may qualify for an exemption or exclusion under the<br />
Access to Information Act or Privacy Act that could<br />
reasonably be expected to cause serious injury if compromised.<br />
221
Protected “A”<br />
PROTECTED “A” refers to information and<br />
assets related to other than the national interest that<br />
may qualify for an exemption or exclusion under the<br />
Access to Information Act or Privacy Act that could<br />
reasonably be presumed to cause injury if compromised.<br />
Facility Security<br />
Facility Clearances<br />
A Facility Security Clearance is an administrative<br />
determination that an organization is eligible, from a<br />
security viewpoint, for access to CLASSIFIED and<br />
PROTECTED information and assets of the same<br />
or lower classification level as the clearance being<br />
granted.<br />
There are three types of Facility Security Clearances<br />
each of which may be authorized at the classification<br />
level of CONFIDENTIAL, SECRET, or TOP<br />
SECRET:<br />
1. Personnel Assigned (PA). This is the most basic<br />
type of Facility Security Clearance which involves<br />
security screening of the organization’s Key Senior<br />
Officials and employees. There is NO requirement<br />
to evaluate the physical security status of the organization’s<br />
facilities. The organization is not authorized<br />
to possess or store CLASSIFIED information and<br />
assets.<br />
2. Document Safeguarding Capability (D.Sc.). In addition<br />
to the security screening of the organization’s<br />
Key Senior Officials and employees, the physical security<br />
of the organization’s facilities is assessed to<br />
ensure safeguarding requirements are met. The organization<br />
is authorized to possess and store CLAS-<br />
SIFIED information and assets.<br />
3. Production (PROD). This includes all of the elements<br />
of a Document Safeguarding Facility Security<br />
Clearance. In addition, the security of the manufacturing,<br />
repairing, modifying, or otherwise working<br />
on CLASSIFIED components or items is assessed to<br />
ensure government security requirements are met.<br />
A Designated Organization Screening (at the PRO-<br />
TECTED level) is an administrative determination<br />
that an organization is eligible, from a security viewpoint,<br />
for access to PROTECTED information and<br />
assets of the same or lower level as the clearance be-<br />
222<br />
Comparison of the Canadian Manual and the U.S. Manual<br />
ing granted. The three types of Designated Organization<br />
Screening are equivalent to the three types of<br />
Facility Security Clearances except they pertain only<br />
to PROTECTED information and assets. Each of<br />
the three types may be authorized at one of the following<br />
levels: PROTECTED “A,” PROTECTED<br />
“B,” or PROTECTED “C.”<br />
An organization is eligible to obtain an organization<br />
security screening/clearance only if it is sponsored<br />
by an authorized sponsor in support of an existing<br />
or impending contract or bid solicitation<br />
which calls for access to CLASSI-<br />
FIED/PROTECTED information, assets, and/or<br />
certain restricted work sites.<br />
Meetings<br />
(No provisions are established within the Canadian<br />
Industrial Security Manual.)<br />
Personnel Security<br />
Security Officers<br />
All organizations that require a Designated Organization<br />
Screening or a Facility Security Clearance<br />
shall appoint a Company Security Officer. The Company<br />
Security Officer shall be appointed by the<br />
Chief Executive Officer (CEO) or the designated Key<br />
Senior Official (KSO) of the organization. The CSO<br />
must be a Canadian citizen employee, report to a<br />
designated KSO, and be security screened or cleared<br />
to the Reliability Status level or Facility Security<br />
Clearance level of the facility. The appointment of<br />
the Company Security Officer must be approved by<br />
the Canadian and International Industrial Security<br />
Directorate (CIISD).<br />
When a facility-cleared Canadian parent organization<br />
owns one or more cleared subsidiaries in Canada,<br />
a Corporate Company Security Officer (CCSO)<br />
should be appointed to oversee government industrial<br />
security matters for the entire corporation.<br />
Personnel Clearances<br />
Personnel Security Screening must be carried<br />
out according to the highest sensitivity level of information<br />
and assets that will be accessed during the
contracting process and/or required for access to<br />
restricted work sites. Access to PROTECTED information,<br />
assets, and restricted work sites requires that<br />
an individual has Reliability Status, and access to<br />
CLASSIFIED information, assets, and/or restricted<br />
work sites requires a Security Clearance at the appropriate<br />
level of sensitivity.<br />
Only individuals employed or under a contract<br />
to commence employment within 60 days by a private<br />
sector organization on a contract/subcontract<br />
requiring access to CLASSIFIED/PROTECTED<br />
information, assets, and/or certain restricted work<br />
sites may be security screened. Non-Canadian citizens<br />
may be security cleared with access limitations.<br />
The limitations include denying access to CLASSI-<br />
FIED/PROTECTED information and assets which<br />
are not of Canadian origin, do not come from the<br />
country of which the person is a citizen, or are not<br />
releasable to his/her nation of origin.<br />
Contractors have no authority to deny or revoke<br />
Personnel Security Clearances for employees. This<br />
authority is reserved by the Canadian Government.<br />
The contractor may suspend the access of an individual,<br />
while notifying CIISD of the circumstances.<br />
Subcontracting<br />
Contractors shall subcontract work only to companies<br />
holding a current Designated Organization<br />
Screening or a Facility Security Clearance of the type<br />
and at the level appropriate to the work to be performed<br />
under the subcontract. CIISD approval of<br />
the subcontractor must be obtained before award of<br />
the subcontract and the Designated Organization<br />
Screening or Facility Security Clearance for the proposed<br />
subcontractor(s) must be verified by CIISD<br />
before issue of bid solicitation documents. Contractors<br />
shall not assign a subcontract to organizations<br />
located outside of Canada without the prior written<br />
approval of CIISD and the Public Works and Government<br />
Services Canada (PWGSC) contracting authority.<br />
The prime contractor shall ensure the security<br />
safeguarding of work placed with subcontractors.<br />
Education, Training, and Briefings<br />
A major objective of the Company Security<br />
Officer in conducting a Security Education Program<br />
A. Hammond<br />
involves working closely with management, from the<br />
top down, to ensure proper company security. Managers<br />
and supervisors at all levels are responsible not<br />
only for their own personal security measures, but<br />
also for ensuring that proper security procedures are<br />
followed by all employees in the organization. An<br />
initial security briefing, reinforced by an ongoing Security<br />
Education and Awareness Program, is essential<br />
to the maintenance of an effective security program.<br />
Upon receiving a Personnel Security Clearance<br />
an employee acknowledges his or her responsibilities<br />
by reading and signing the Security Screening Certificate<br />
and Briefing Form, TBS/SCT 330-47 Rev.<br />
2002/06. A briefing from the Company Security<br />
Officer, which details the individual’s specific responsibilities<br />
and duties relative to security in the<br />
facility, must be presented. (New employees, even<br />
though not yet security-screened and therefore prohibited<br />
from access to CLASSIFIED information<br />
and assets, should be given a security briefing appropriate<br />
to their duties.)<br />
Visits<br />
A Visit Clearance Request (VCR) (submitted to<br />
CIISD via a Request for Visit form) is required<br />
when a security-cleared individual must visit a government/commercial<br />
organization in Canada or<br />
abroad, for the purpose of having access to CLASSI-<br />
FIED information and assets or where access to the<br />
installation is restricted in the interest of national<br />
security. Visitors must not proceed with CLASSI-<br />
FIED visits without prior visit clearance authorization<br />
from CIISD. The host organization shall deny<br />
access to CLASSIFIED information and assets or<br />
access to certain restricted work sites until the visitors’<br />
Personnel Security Clearance level and their<br />
need-to-know have been verified and confirmed by<br />
the CIISD through official visit protocol.<br />
Submission of a VCR initiates verification by<br />
CIISD that confirms:<br />
• The organization requesting the visit has an Facility<br />
Security Clearance to the required level<br />
• Each of the proposed visitors has a valid Personnel<br />
Security Clearance to the required level<br />
• Foreign disclosure limitations are identified and<br />
strictly observed<br />
Visit Clearance Request is approved when the<br />
223
equesting organization is notified by CIISD. Visitors<br />
must not proceed on CLASSIFIED visits without<br />
prior visit clearance authorization.<br />
Visit Clearance Request (VCR) requires strict<br />
lead-times imposed by the authorities of foreign nations.<br />
Every effort must be made to ensure that leadtimes<br />
are observed, as failure to do so will likely result<br />
in rejection of the RFV.<br />
Organizations shall maintain a record of all individuals<br />
who visit the facility for the purpose of having<br />
access to CLASSIFIED information. This record<br />
shall be separate from the record of unclassified visits.<br />
Document Security<br />
General Marketing<br />
All documents shall be marked on the outside of<br />
both the front and back covers with the highest level<br />
of classification and loose documents shall be<br />
marked on every sheet. Security markings should<br />
include the applicable classification/protection and<br />
the date or event at which declassification or downgrading<br />
is to occur. All covering or transmittal letters<br />
or forms or circulation slips must be marked to show<br />
the highest level of classification or protection of the<br />
attachments.<br />
For TOP SECRET information, mark the classification<br />
in the upper right corner of each document<br />
page and show the total number of pages on each<br />
page of the document.<br />
For SECRET information, mark the classification<br />
in the upper right corner of each document<br />
page.<br />
For CONFIDENTIAL information, mark the<br />
classification in the upper right corner of the face of<br />
the document.<br />
For PROTECTED information, mark the word<br />
“PROTECTED” in the upper right corner of the<br />
face of the document and, where required, with the<br />
letter “A,” “B,” or “C” to indicate the level of protection.<br />
General Storage<br />
PROTECTED B and PROTECTED C information<br />
and assets and all CLASSIFIED information<br />
must be stored in an approved security container.<br />
224<br />
Comparison of the Canadian Manual and the U.S. Manual<br />
PROTECTED A information and assets shall be<br />
stored in a locked container.<br />
CLASSIFIED or PROTECTED information<br />
and assets may be stored on open shelving in a secure<br />
room, only after inspection and approval by<br />
CIISD and only to the level approved by CIISD.<br />
Also, CLASSIFIED and PROTECTED information<br />
and assets shall not be stored in the same container<br />
as negotiable or attractive assets.<br />
Reproduction<br />
Reproduction of CLASSIFIED information<br />
shall be done only with the authorization of the<br />
Company Security Officer or an authorized Alternate<br />
Company Security Officer. Reproductions must<br />
be marked, registered, and accounted for in the<br />
same manner as for the originals. Reproductions of<br />
PROTECTED information must be marked in the<br />
same manner as the originals. TOP SECRET and<br />
PROTECTED C information shall NEVER be reproduced<br />
without written authorization from<br />
CIISD.<br />
Domestic Transmission Standards<br />
(Outside of Facility)<br />
Top Secret<br />
• Documents must be double enveloped (gum<br />
sealed, heavy duty) and sealed with government approved<br />
security tape.<br />
• A self-addressed receipt is enclosed in the inner<br />
envelope or wrapping and the inner envelope or<br />
wrapping is closed with an approved security tape.<br />
• Inner envelope or wrapping must bear the security<br />
marking and the recipient’s address.<br />
• Shipment must be recorded prior to leaving a<br />
Security Zone and the recipient must be notified in<br />
advance of shipment.<br />
• Documents are sent via a securitycleared/reliability-checked<br />
individual employed by<br />
the dispatching/receiving Facility Security Cleared<br />
Canadian organization.<br />
Secret, Confidential, and Protected “C”<br />
• Documents must be double enveloped (gum<br />
sealed, heavy duty) and sealed with government approved<br />
security tape.<br />
• A self-addressed receipt is enclosed in the inner
envelope or wrapping and the inner envelope or<br />
wrapping is closed with an approved security tape.<br />
• Inner envelope or wrapping must bear the security<br />
marking and the recipient’s address.<br />
• Via:<br />
a. Priority courier<br />
b. Registered mail<br />
c. A security-cleared/reliability-checked individual<br />
employed by the dispatching/receiving<br />
Facility Security Cleared Canadian organization<br />
Protected “A” and “B”<br />
• Single, gum-sealed, heavy duty envelope<br />
• Via:<br />
a. First class mail<br />
b. An individual employed with the organization<br />
c. Classified/Protected “C” methods<br />
International Transmission Standards<br />
Top Secret, Secret, Confidential, and Protected “C”<br />
• Double enveloped (gum sealed, heavy duty) and<br />
sealed with government approved security tape<br />
• Via CIISD<br />
Protected “B”<br />
• Single, gum sealed, heavy-duty envelope<br />
• Via CIISD<br />
Protected “A”<br />
• Single, gum sealed, heavy-duty envelope<br />
• Via first class mail, priority courier, or registered<br />
mail<br />
Destruction<br />
Unless otherwise specified, TOP SECRET, and<br />
PROTECTED “C” information and assets must be<br />
returned to CIISD for disposal.<br />
Unless otherwise specified, SECRET, CONFI-<br />
DENTIAL, and PROTECTED “A” and “B” information<br />
and assets of Canadian origin may be destroyed<br />
by the organization with the approval of<br />
CIISD.<br />
CLASSIFIED and PROTECTED information<br />
and assets which have been authorized for destruction<br />
must be disposed of in accordance with the<br />
following:<br />
A. Hammond<br />
• It must be destroyed only by approved destruction<br />
equipment, or at a facility authorized by CIISD.<br />
• Information awaiting destruction or in transit to<br />
destruction must be safeguarded in the manner prescribed<br />
for the most highly CLASSIFIED and PRO-<br />
TECTED information asset involved.<br />
• CLASSIFIED and PROTECTED information/assets<br />
awaiting destruction must be kept separate<br />
from other information/assets awaiting destruction.<br />
• An employee with a proper security clearance or<br />
with Reliability Status, as applicable, must be present<br />
to monitor the destruction of CLASSIFIED and<br />
PROTECTED information, respectively.<br />
• Surplus copies and waste that could reveal<br />
CLASSIFIED and PROTECTED information must<br />
be protected to the appropriate level and should be<br />
promptly destroyed.<br />
Information System Security<br />
The ISM establishes operational standards in<br />
Canadian industry for the safeguarding of Government<br />
information electronically processed, stored, or<br />
transmitted. This also applies to the safeguarding of<br />
technology assets. The administrative, organizational,<br />
physical, and personnel security standards as<br />
documented in the ISM also apply to the information<br />
technology environment.<br />
The Government Security Policy requires that<br />
the degree of safeguarding provided by industry be<br />
commensurate with the level of the information and<br />
assets and the associated threats and risks. The contracting<br />
authority is responsible for ensuring that the<br />
requirements of the Government Security Policy are<br />
met and that the security standards are applied by<br />
the private sector contractor. The security standards<br />
contained in the Government Security Policy, Information<br />
Technology Standards, are the minimum<br />
standards for security in the private sector. Assessments,<br />
advice, and guidance regarding these standards<br />
are available from the Canadian and International<br />
Industrial Services Directorate (CIISD) of<br />
Public Works and Government Services Canada<br />
(PWGSC).<br />
The prime contractor’s Information Technology<br />
Facility(s) must be approved by CIISD prior to processing<br />
government information.
Conclusions<br />
“It’s important to be responsible here and to be particularly<br />
careful after 9/11 that we’re not giving our<br />
enemies information or materials that would make<br />
their job easier.” (Chui, 2003)<br />
John H. Marburger III,<br />
Director, Office of Science & Technology Policy<br />
(and science adviser to President George W. Bush)<br />
To no surprise, the anthrax letter attacks of<br />
2001 led directly to national policy changes since<br />
they specifically targeted both lawmakers and media<br />
personnel at their workplaces. To better protect<br />
their citizens, the United States and Canadian governments<br />
established controls not only over the possession<br />
and use of hazardous biological agents, but<br />
also over the information pertaining to their possession<br />
and use. Legislation is now in place that forbids<br />
the disclosure of information that may identify<br />
which biological agents are possessed, who possesses<br />
that agent(s) and where, and any safeguard and security<br />
measures used to protect unauthorized access to<br />
the agent(s). Because of the genuine threat of bioterrorism,<br />
biodefense research has become a vital and<br />
necessary component of an overall national security<br />
program. The United States alone has committed<br />
billions of dollars towards biodefense research and<br />
development. To protect biodefense information<br />
and assets, organizations working on projects<br />
deemed to be “classified” (for the sake of national<br />
security) must follow precise requirements, restrictions,<br />
and safeguards established by their federal government.<br />
For Canada and the United States, these<br />
requirements are conveyed in the Canadian Industrial<br />
Security Manual (ISM) and the U.S. National Industrial<br />
Security Program Operating Manual (NISPOM). These<br />
manuals provide guidance in implementing a uni-<br />
226<br />
Comparison of the Canadian Manual and the U.S. Manual<br />
form and cost-effective security system, thus allowing<br />
an organization to focus mainly on research rather<br />
than the burden of developing and implementing<br />
security procedures. Without these standards and<br />
consistent security policies and practices the potential<br />
for compromise leading to a serious national<br />
security threat is enormous.<br />
References<br />
Canadian and International Industrial Security Directorate.<br />
(2004). Industrial security manual. Available<br />
at www.ciisd.gc.ca/ism/text/preface-e.asp. Accessed<br />
online 2004.<br />
Chui, G. (2003). Security concerns imperil research:<br />
Restrictions shackle scientists, some say. The Mercury<br />
News, March 3, 2003. Available at www.<br />
mercurynews.com/mld/mercurynews/news/<br />
5303757.htm?1c. Accessed online 2004.<br />
Defense Technical Information Center. (2004). National<br />
industrial security program operating manual<br />
(DoD 5220.22-M). Available at www.dtic.mil/whs/<br />
directives/corres/html/522022m.htm. Accessed<br />
online 2004.<br />
Parliament of Canada. (2004). Public <strong>Safety</strong> Act,<br />
2002. Available at www.parl.gc.ca/37/3/parlbus/<br />
chambus/house/bills/summaries/c7-e.pdf. Accessed<br />
online 2004.<br />
U.S. Government Printing Office. (2004). Public<br />
Health Security and Bioterrorism Preparedness and Response<br />
Act of 2002. Available at frwebgate.access.gpo.<br />
gov/cgi-bin/getdoc.cgi?dbname=<strong>10</strong>7_cong_public_<br />
laws&docid=f:publ188.<strong>10</strong>7.pdf. Accessed online<br />
2004.
Article<br />
The Infectious Dose of Francisella<br />
tularensis (Tularemia)<br />
Abstract<br />
Quantitatively estimating an individual’s risk of<br />
infection by an airborne pathogen requires knowledge<br />
of the expected dose and the pathogen’s infectious<br />
dose. Based on our review of the published literature on<br />
tularemia, we conclude that the infectious dose of Francisella<br />
tularensis varies among individuals, but that a<br />
substantial proportion of the population can be infected<br />
by a single bacillus. We also conclude that infection can<br />
be initiated by inhaling bacilli carried on respirable particles<br />
(diameters less than <strong>10</strong> µm) or nonrespirable particles<br />
(diameters between <strong>10</strong> µm and <strong>10</strong>0 µm). Regression<br />
analyses based on two-parameter Weibull and lognormal<br />
models of human inhalation dose-infection data<br />
aggregated across three studies indicate that approximately<br />
30% of individuals who inhale a single F. tularensis<br />
bacillus will develop tularemia. Further, when<br />
the organism is carried on particles with diameters on<br />
the order of 1 µm, it is estimated that the deposition of<br />
a single bacillus produces infection in 40% to 50% of<br />
individuals; thus, when F. tularensis is carried on respirable<br />
particles, the estimated ID50 via inhalation is close<br />
to one deposited bacillus. These results are consistent<br />
with separate analyses using nonparametric methods<br />
and with experimental animal models in which infection<br />
is observed after injection of a single bacillus. The risk<br />
of person-to-person transmission of tularemia is generally<br />
considered negligible, perhaps due to a low concentration<br />
of F. tularensis in respiratory fluids. However,<br />
viable F. tularensis bacilli are present in human respiratory<br />
fluids, and can be carried in inspirable particles<br />
(diameters less than <strong>10</strong>0 µm) which are emitted during<br />
coughs and sneezes.<br />
Introduction<br />
Applied Biosafety, <strong>10</strong>(4) pp. 227-239 © ABSA <strong>2005</strong><br />
Rachael M. Jones, Mark Nicas, Alan Hubbard, Matthew D. Sylvester, and Arthur Reingold<br />
University of California—Berkeley, Berkeley, California<br />
Francisella tularensis (formerly termed Pasteurella<br />
tularensis and Bacterium tularensis) is a bacterium that<br />
causes a spectrum of clinical illnesses termed<br />
“tularemia.” F. tularensis is a candidate agent for<br />
bioterrorism because it can be weaponized readily<br />
and is considered to have a low airborne infectious<br />
dose (Dennis et al., 2001; Franz et al., 1999). The<br />
World Health Organization (1970) has estimated<br />
that aerosol dispersal of 50 kg of F. tularensis over a<br />
metropolitan area with approximately 5 million inhabitants<br />
would result in 250,000 incapacitating<br />
casualties, including 19,000 deaths. Infection by the<br />
respiratory route has been demonstrated in Macaca<br />
mulatta using both respirable particles (diameters less<br />
than <strong>10</strong> m) and inspirable, but nonrespirable, particles<br />
(diameters between <strong>10</strong> m and <strong>10</strong>0 m) (Day &<br />
Berendt, 1972). Naturally occurring respiratory infection<br />
has been documented in Scandinavian farm<br />
workers exposed when handling hay contaminated<br />
by voles and their waste products (Dahlstrand,<br />
Ringertz & Zetterberg, 1971; Syjala, Kujala, Myllyla,<br />
& Sandstrom, 1996). Historically, laboratory personnel<br />
have become infected by bacterium-containing<br />
aerosols generated during normal laboratory procedures<br />
and accidents (Ledingham & Fraser,<br />
1923/1924; Overholt et al., 1961; Van Metre, Jr. &<br />
Kadull, 1959). Perhaps due to the low infectious<br />
dose by inhalation, implementation of careful handling<br />
procedures for F. tularensis in clinical laboratories<br />
has not entirely eliminated the potential for infection<br />
(Shapiro & Schwartz, 2002).<br />
Secondary (person-to-person) transmission of F.
tularensis is generally considered improbable. For<br />
example, the Centers for Disease Control and Prevention<br />
(2004) states: “Tularemia is not known to be<br />
spread from person-to-person.” Similarly, the Working<br />
Group on Civilian Biodefense (Dennis et al.,<br />
2001) concludes: “Isolation is not recommended for<br />
tularemia patients given the lack of human-tohuman<br />
transmission.” In 1951, however, Fillmore<br />
reported the case of a nurse’s aide who developed<br />
symptoms of tularemia 3 to 4 weeks after attending a<br />
patient with pleuropulmonary tularemia; the nurse’s<br />
aide had no contact with domestic or wild animals.<br />
In determining procedures to control airborne<br />
infection, it is useful to quantitatively estimate infection<br />
risk, which depends on the pathogen’s infectious<br />
dose, the concentration of the pathogen in air,<br />
and the duration of exposure. Variability in host<br />
susceptibility is captured, in part, by interindividual<br />
variability in a deterministic infectious dose. Given<br />
an appreciation of the potential intensity of airborne<br />
exposure to F. tularensis and of the pathogen’s infectious<br />
inhalation dose, one can evaluate existing biosafety<br />
protocols in laboratory and clinical settings. In<br />
this paper, we argue that the infectious dose of F.<br />
tularensis for a substantial portion of the population<br />
is on the order of one bacillus. We also argue that<br />
person-to-person transmission of tularemia is theoretically<br />
possible given low infectious dose values<br />
overall, and the presence of the bacillus in the sputum<br />
of some infected patients. However, the risk of<br />
secondary airborne infection may typically be low<br />
due to low pathogen concentrations in respiratory<br />
fluid and small aerosol volumes emitted in coughs<br />
commonly described as “nonproductive.”<br />
Background on Tularemia<br />
F. tularensis is a Gram-negative coccobacillus,<br />
with diameter ranging from 0.2 to 0.7 m (Evans,<br />
1985). The organism is rickettsial in that it cannot<br />
replicate outside a host cell, and it is pathogenic after<br />
being phagocytized by macrophages (Sjostedt,<br />
Tarnvik, & Sandstrom, 1996). Although originally<br />
described in ground squirrels in Tulare County,<br />
California, in 1911 by McCoy, the organism was<br />
renamed for Edward Francis who described the<br />
clinical and epidemiologic features of the disease<br />
228<br />
The Infectious Dose of Francisella tularensis (Tularemia)<br />
(Francis, 1927; Francis 1983). F. tularensis is found<br />
globally in mammals and arthropod vectors, and two<br />
strains produce infection in humans. Type A is associated<br />
with illness in North America; Type B is less<br />
virulent and is associated with illness in Europe<br />
(Reinjes et al., 2002). Type A has been traditionally<br />
considered for use as a biological weapon (Conlan et<br />
al., 2003), and the Schu strain of Type A, isolated<br />
from a finger ulcer (Bell, Owen, & Larson, 1955),<br />
was frequently used in experimental work until the<br />
late 1960s. At that time, investigators began using<br />
the live vaccine strain (LVS) of F. tularensis for experimental<br />
work because it is less virulent in humans yet<br />
is virulent in mice (Conlan et al., 2003).<br />
Note that the terms “infectivity” and “virulence”<br />
are distinct. Infectivity signifies the ability of a pathogen<br />
to penetrate into host tissue and multiply. Infectivity<br />
can be quantified by the metric of infectious<br />
dose, that is, the number of viable organisms<br />
(colony-forming units) that must penetrate into host<br />
tissue to initiate an infection, where infection is assessed<br />
by serology and clinical indicators. However,<br />
in nonhuman mammalian studies, the infectivity of<br />
F. tularensis is typically reported as the number of<br />
organisms that are lethal to 50% of exposed animals,<br />
termed the LD50. Virulence refers to the intensity of<br />
the disease produced by pathogen infection in a<br />
given host species (Black, 2002); the term is also<br />
used to compare the intensity of disease produced by<br />
a given pathogen in different host species. For F.<br />
tularensis, there is evidence that virulence is influenced<br />
by the dose of organisms received. For example,<br />
among Macaca mulatta receiving Schu S-4 strain<br />
organisms carried on 2.1 m diameter particles by<br />
inhalation, five inhaled bacilli infected 6/6 hosts but<br />
caused death in only 1/6 hosts, whereas higher inhaled<br />
doses caused death in a progressively greater<br />
proportion of animals (McCrumb, 1961).<br />
Infection with F. tularensis can occur through<br />
ingestion, dermal contact, and inhalation of the organism,<br />
and produces an array of clinical features<br />
(Centers for Disease Control and Prevention, 2003;<br />
Dennis et al., 2001). Ingestion of F. tularensis typically<br />
produces oropharnygeal tularemia (pharyngitis<br />
and cervical adenitis) (Reintjes et al., 2002). Dermal<br />
contact, arthropod bites, and intracutaneous inoculation<br />
often produce an ulcerated lesion at the site
of contact and/or swelling of the regional lymph<br />
nodes, although some individuals exposed through<br />
these routes can present with fever and other signs<br />
indicative of systemic infection (Dennis et al., 2001;<br />
Evans, 1985; Saslaw et al., 1961), including pulmonary<br />
involvement (bronchopneumonia and hilar<br />
adenopathy) (Miller & Bates, 1969). Inhalation of F.<br />
tularensis also produces systemic disease in humans<br />
and may produce pneumonia (McCrumb, 1961;<br />
Overholt et al., 1961), oval lesions in the lungs<br />
(Overholt & Tigertt, 1960), and/or bronchial<br />
changes (Syrjala et al., 1986). Although it has been<br />
demonstrated experimentally that humans can develop<br />
tularemia through inhalation of F. tularensis<br />
(McCrumb, 1961; Sawyer et al., 1966), rapid disease<br />
onset and delay in examination make it difficult to<br />
determine in some cases if pulmonary involvement<br />
precedes or follows systemic infection. Cough frequently<br />
occurs in patients with and without objective<br />
pulmonary involvement (Dennis et al., 2001;<br />
Saslaw et al., 1961). Although McCrumb (1961) reports<br />
that patients exhibited a lack of sputum production<br />
and nonproductive cough, case reports indicate<br />
that some patients exhibit increased mucous<br />
and sputum production, and productive cough<br />
(Cluxton, Jr., Cliffton & Worley, 1948; Syrjala et al.,<br />
1986).<br />
If untreated, pulmonary tularemia resulting from<br />
the type A strain has a case fatality proportion of<br />
40% to 60% (McCrumb, 1961). Mortality due<br />
to all clinical manifestations of tularemia has been<br />
approximately 5%, although in the United States,<br />
treatment with streptomycin and gentamicin has<br />
reduced the overall case fatality proportion to below<br />
2% (Dennis et al., 2001). The type B strain found in<br />
Europe is rarely fatal (Dennis et al., 2001).<br />
Experimental Airborne Infection<br />
Study Descriptions<br />
Airborne transmission of F. tularensis has been<br />
demonstrated using investigator-generated aerosol<br />
and respiratory aerosol emitted by infected animals.<br />
Work with investigator-generated aerosols commenced<br />
at Fort Detrick, Maryland in the mid-1940s,<br />
when infection of mice by “clouds” of F. tularensis<br />
was assessed (Rosebury, 1947). Animals were ex-<br />
R. M. Jones, et al.<br />
posed in a stainless steel chamber to aerosol generated<br />
by a Chicago atomizer from cultures suspended<br />
in water; the reported mass median diameter of the<br />
aerosol particles was less than 1 m. The inhalation<br />
dose was estimated based on the animal’s breathing<br />
rate (related to weight), duration of exposure, and<br />
the viable F. tularensis aerosol concentration as measured<br />
by impinger sampling of chamber air. The reported<br />
inhalation doses assumed that <strong>10</strong>0% of inhaled<br />
particles were retained in the respiratory tract.<br />
For mice, the doses ranged from 14 to 4,500 bacilli.<br />
Only one of thirty (1/30) mice receiving a dose of 14<br />
organisms died, while all 59 mice exposed to doses<br />
of 330 or more organisms died. All animals that did<br />
not die within 16 days subsequent to exposure were<br />
autopsied and found by gross evaluation and spleen<br />
culture to be negative for F. tularensis. It was estimated<br />
that 70 organisms would produce mortality in<br />
50% of exposed mice, with 95% confidence limits of<br />
2 to 2,063 organisms. The wide confidence interval<br />
was attributed to the large variability in recovery of<br />
aerosolized organisms. Rosebury (1947) also reports<br />
the results of Henderson, which were conveyed in a<br />
personal communication. Working at Porton Down<br />
in the United Kingdom, Henderson found that the<br />
50% lethal dose in mice exposed via inhalation was<br />
12 organisms.<br />
Hood (1961) exposed guinea pigs to aged F. tularensis<br />
(Schu D strain) aerosols generated with a<br />
Henderson apparatus and stored in a rotating<br />
stainless steel drum. Of the aerosols generated in the<br />
Henderson apparatus, approximately 98% of the<br />
dried particles had diameters less than 1 m, and<br />
90% of the droplets emerging from the spray apparatus<br />
had diameters less than <strong>10</strong> m (Henderson,<br />
1952). The inhaled dose was estimated based on the<br />
animal’s breathing rate (related to weight), exposure<br />
duration, the viable F. tularensis aerosol concentration<br />
as measured by impinger sampling near the<br />
guinea pigs, and an estimated inhaled particle retention<br />
factor of 0.55. When bacterial suspensions aged<br />
6 to 30 days were aerosolized and held in the drum<br />
for 3 seconds before the animals were exposed, the<br />
LD50 was 1 to 4 organisms. The investigators found<br />
that there was no significant loss of infectivity when<br />
aerosols were aged for 20 minutes in the drum, but<br />
significant infectivity was lost when aerosols were<br />
229
aged for 20 hours. It is unclear, however, what portion<br />
of the decreased infectivity was due to organism<br />
die-off versus deposition on the drum walls.<br />
A similar study was undertaken by Sawyer et al.<br />
(1966), who exposed Macaca mulatta and human<br />
volunteers to aerosols of the F. tularensis Schu-S4<br />
strain, generated with a two-fluid nozzle and stored<br />
in a spherical static chamber. The concentration of<br />
aerosol particles was measured by a total collector,<br />
and an impinger was used to determine the number<br />
of particles with diameters of 5 m or less; it was<br />
estimated that 65% of viable organisms were contained<br />
in particles with diameters of 5 m or less.<br />
Caged monkeys were placed in the test chamber for<br />
3 or <strong>10</strong> minutes; human subjects were exposed<br />
through a facemask for ten 1-liter breaths in 60 seconds.<br />
The inhaled dose was defined as the product<br />
of the duration of exposure, respiratory minute volume,<br />
and the concentration of viable organisms in<br />
particles with diameters 5 m or less; the fraction of<br />
organisms retained was not considered. It was found<br />
that an inhaled dose of 80 to 180 viable organisms<br />
from an aerosol aged for 60 minutes infected three<br />
of four (3/4) humans and seven of eight (7/8) monkeys.<br />
In another series of experiments, it was found<br />
that among human subjects who inhaled 150 viable<br />
organisms, two of four (2/4) became infected when<br />
the aerosol was aged 30 minutes, and three of four<br />
(3/4) became infected when the aerosol was aged 60<br />
minutes. Only results for aerosols aged 60 minutes<br />
or less are reported here because aerosols aged for<br />
120 and 180 minutes showed substantially decreased<br />
infectivity for humans and M. mulatta.<br />
One limitation of the Sawyer et al. study was<br />
that the dose estimate was based on particles with<br />
diameters less than 5 m. Day and Brendt (1972)<br />
noted that all particles with diameters greater than<br />
5 m contained F. tularensis bacilli, and that while<br />
these particles may not penetrate to the pulmonary<br />
region of M. mulatta, infection could result from<br />
deposition in the upper respiratory tract. This observation<br />
suggests that the inhaled doses were larger<br />
than reported by Sawyer et al. On the other hand,<br />
Sawyer et al. did not adjust the inhaled dose for the<br />
fraction of organisms that deposited in the respiratory<br />
tract, which signifies that the retained respirable<br />
dose was less than the dose reported.<br />
230<br />
The Infectious Dose of Francisella tularensis (Tularemia)<br />
Low dose infectivity of F. tularensis aerosols in<br />
vaccinated and nonvaccinated men has been reported<br />
by two investigators (Table 1). Saslaw et al.<br />
(1961) exposed men via a facemask to an aerosol<br />
with an average particle diameter of 0.7 m. The<br />
subjects were instructed to inhale through their nose<br />
and exhale through their mouths. Sixteen of the<br />
twenty (16/20) nonvaccinated men became infected<br />
after inhaling doses of <strong>10</strong> to 52 F. tularensis bacilli.<br />
The four men who did not develop infection had<br />
inhaled <strong>10</strong> to 45 organisms. The lowest doses producing<br />
infection among nonvaccinated and vaccinated<br />
men were <strong>10</strong> and 13 bacilli, respectively. We<br />
note that for particles with an aerodynamic diameter<br />
of 0.7 m, the approximate deposition fraction in<br />
the human pulmonary region is 0.2 (Hinds, 1999).<br />
Therefore, <strong>10</strong> to 52 inhaled F. tularensis bacilli represent<br />
approximately 2 to <strong>10</strong> deposited bacilli.<br />
McCrumb (1961) reported that among nonvaccinated<br />
individuals exposed to 20, 200, and 2,000 F.<br />
tularensis bacilli, all individuals (4/4, 4/4, and 2/2,<br />
in the respective dose groups) became infected;<br />
among 12 vaccinated individuals exposed to 20 organisms,<br />
four (33%) were infected. Unfortunately,<br />
McCrumb provided little information on the methodology<br />
used in these studies and did not account<br />
for the particle deposition fraction.<br />
Statistical Analysis of Aggregate Data<br />
To examine the infectious dose statistically, we<br />
began by pooling the inhalation dose-infection results<br />
obtained by McCrumb (1961) and Saslaw et al.<br />
(1961) for nonvaccinated individuals, and by Sawyer<br />
et al. (1966) for aerosols aged 60 minutes or less<br />
(Table 1). For this analysis, none of the inhaled<br />
doses were adjusted for the deposition fraction of<br />
the challenge particles in the respiratory tract, which<br />
is to say that the true deposited doses were less than<br />
the reported inhaled doses. We alternatively fit a<br />
discrete nonparametric maximum likelihood cumulative<br />
probability distribution and two continuous<br />
cumulative probability distributions (lognormal and<br />
Weibull) to the data to estimate the probability of<br />
remaining uninfected after being exposed to a fixed<br />
dose. These fitted probability distributions describe<br />
the survival distribution; the complement of the survival<br />
distribution is the cumulative infection distri-
ution (i.e., the proportion of individuals infected<br />
with increasing dose).<br />
The survival data structure can be considered<br />
“current status.” For each dose, one knows whether<br />
the dose given was either less than a subject’s minimum<br />
infectious dose (i.e., the subject was not infected)<br />
or greater than the minimum infectious dose<br />
(i.e., the subject was infected). The nonparametric<br />
maximum likelihood estimate of the survival function<br />
for current status data has been referred to as<br />
the pooled adjacent violator (PAV); the analysis involves<br />
a nonparametric, monotonically decreasing<br />
regression on the proportion of subjects left unin-<br />
R. M. Jones, et al.<br />
Table 1<br />
Infection dose-response data in human subjects used to determine low dose infectivity.<br />
Estimated Bacilli Dose<br />
Response<br />
#Infected/#Exposed<br />
Reference<br />
<strong>10</strong> 1/2 Saslaw, et al., 1961<br />
12 0/1 Saslaw, et al., 1961<br />
13 1/1 Saslaw, et al., 1961<br />
14 1/1 Saslaw, et al., 1961<br />
15 1/1 Saslaw, et al., 1961<br />
16 1/1 Saslaw, et al., 1961<br />
18 1/1 Saslaw, et al., 1961<br />
20 5/6<br />
Saslaw, et al., 1961;<br />
McCrumb, 1961<br />
23 2/2 Saslaw, et al., 1961<br />
25 1/1 Saslaw, et al., 1961<br />
30 1/1 Saslaw, et al., 1961<br />
45 0/1 Saslaw, et al., 1961<br />
46 2/2 Saslaw, et al., 1961<br />
48 1/1 Saslaw, et al., 1961<br />
50 1/1 Saslaw, et al., 1961<br />
52 1/1 Saslaw, et al., 1961<br />
150 5/8 Sawyer, et al., 1966<br />
200 4/4 McCrumb, 1961<br />
350 2/4 Sawyer, et al., 1966<br />
750 4/4 Sawyer, et al., 1966<br />
2,000 2/2 McCrumb, 1961<br />
fected at each dose (Kalbfleisch & Prentice, 2002).<br />
Inference can be derived from nonparametric bootstrapping.<br />
Because the data are sparse and thus the nonparametric<br />
estimates are highly variable, we also explored<br />
parametric regressions by fitting both a twoparameter<br />
Weibull model and a two-parameter lognormal<br />
model to the data. The Weibull survival<br />
function has the form:<br />
Eq. 1 S(d) = exp(— [d] )<br />
where S(d) is the probability of not being infected at<br />
dose d, and where > 0 and > 0 are scale and<br />
231
shape parameters, respectively. The lognormal survival<br />
function has the form:<br />
Eq. 2<br />
where GM and GSD denote the geometric mean<br />
(median value) and geometric standard deviation,<br />
respectively, and (z) denotes the cumulative standard<br />
normal distribution evaluated for the argument<br />
z. For improved readability, all fits are displayed<br />
graphically as the probability of infection, which is<br />
one minus the probability of survival.<br />
We note that the infectious dose models<br />
explored in this analysis are “deterministic” or<br />
232<br />
The Infectious Dose of Francisella tularensis (Tularemia)<br />
“threshold” models. It is assumed that if the host<br />
receives a threshold number of organisms or more,<br />
infection is certain to occur, whereas if the host receives<br />
fewer than the threshold number of organisms,<br />
infection is certain not to occur. Variability in<br />
host susceptibility is reflected by interindividual variability<br />
in the threshold dose value, and the ID50 is<br />
that deposited dose which will infect 50% of the<br />
population with certainty. In contrast, a purely<br />
“probabilistic” model assumes that a single organism<br />
can successfully infect the host with probability<br />
psuccess, such that the probability of infection is<br />
1 —(1 — psuccess) D , where D is the deposited number<br />
of organisms. If the value of psuccess is the same across<br />
individual hosts, the ID50 is that deposited dose<br />
which produces a 50% likelihood of infection in all<br />
Figure 1<br />
Estimated cumulative infection probability of humans experimentally exposed to increasing inhaled doses of<br />
F. tularensis based on the Table 1 data, via a nonparametric maximum likelihood analysis (black line with<br />
dashed lines representing the 95% CI), a lognormal parametric regression, and a Weibull parametric<br />
regression. The Table 1 data points are indicated by the diamonds.
hosts. A probabilistic model can also account for<br />
variability in the value of psuccess between individual<br />
hosts.<br />
Figure 1 displays the data listed in Table 1, the<br />
best fit curves for the lognormal and Weibull model,<br />
and the PAV fit along with the 95% pointwise confidence<br />
interval for the PAV fit. Over the range of<br />
data (inhaled doses of <strong>10</strong> and greater), the lognormal,<br />
Weibull, and PAV fits are consistent (the<br />
lognormal and Weibull fits are within the 95% confidence<br />
interval for the PAV fit). The lognormal and<br />
Weibull models allow extrapolation to inhaled doses<br />
below <strong>10</strong> bacilli. The lognormal model parameter<br />
estimates (GM = 3.71, GSD = 6.01) indicate that<br />
infection risk given inhalation of one bacillus is<br />
23%, while the Weibull model parameter estimates<br />
( = 0.191, = 0.412) indicate that infection risk<br />
given inhalation of one bacillus is 40%. Overall, the<br />
lognormal and Weibull models suggest that 20% to<br />
40% of the population would be infected due to inhaling<br />
a single F. tularensis bacillus.<br />
The PAV fit indicates that inhaling <strong>10</strong> bacilli<br />
would infect approximately 30% of the population;<br />
unfortunately, this nonparametric model does not<br />
permit estimating the percent infected below the<br />
inhaled doses for which data are available. However,<br />
it does not make sense that <strong>10</strong> bacilli is the minimum<br />
inhalation infectious dose. If inhaling <strong>10</strong> organisms<br />
produces infection with 30% probability, it<br />
is reasonable that inhaling 9 organisms should produce<br />
infection with some probability less than 30%<br />
but greater than zero, unless infection is a multihit<br />
process requiring a minimum of <strong>10</strong> organisms. In<br />
regard to the latter idea, we note that the infectivity<br />
of just one F. tularensis organism is supported by animal<br />
data. In mice, guinea pigs, and rabbits, the intracutaneous<br />
and intraperitoneal injection of a single<br />
F. tularensis bacterium is capable of producing<br />
lethal disease (Bell, Owen, & Larson, 1955; Downs<br />
et al., 1947; Emel’yanova, 1961; Rosebury, 1947).<br />
The distributions depicted in Figure 1 are somewhat<br />
confused by aggregating the results from aerosol<br />
exposure studies involving different or unknown<br />
particle size distributions. McCrumb (1961) did not<br />
specify the particle size distribution or describe the<br />
aerosol generating equipment, while Sawyer et al.<br />
(1966) considered the dose to be only those organ-<br />
R. M. Jones, et al.<br />
isms present in particles of diameter 5 m or less.<br />
Because particle size is inversely related to infectivity<br />
(Day & Berendt, 1972), we applied the same statistical<br />
analyses to the data of Saslaw et al. (1961) for<br />
which the aerosol size distribution was described as<br />
homogeneous with an average particle diameter of<br />
0.7 m. We also decreased Saslaw’s reported inhaled<br />
doses to account for a deposition fraction of 0.3 in<br />
the respiratory tract (Hinds, 1999). Figure 2 plots the<br />
Saslaw et al. (1961) data from Table 1, and the cumulative<br />
infection probability as a function of the<br />
deposited dose based on fitted lognormal and<br />
Weibull models; the 95% confidence intervals for<br />
the cumulative probability functions are also shown.<br />
The lognormal model parameter estimates are GM =<br />
1.48 and GSD = 5.75, and the Weibull model parameter<br />
estimates are = 0.427 and = 0.458.<br />
Given the deposition of one bacillus, the lognormal<br />
model parameter estimates indicate that infection<br />
risk is 41%, while the Weibull model parameter estimates<br />
indicate that infection risk is 49%. Overall,<br />
the parametric models suggest that 40% to 50% of<br />
the population would be infected by the deposition<br />
of a single F. tularensis bacillus. Figures 3 and 4 show<br />
that the 95% confidence intervals for the lognormal<br />
and Weibull cumulative probability functions, respectively,<br />
fall within the 95% confidence interval of<br />
the PAV cumulative probability function. Therefore,<br />
the lognormal and Weibull probability estimates are<br />
consistent with the PAV estimates in the dose range<br />
of three bacilli or more.<br />
Person-to-Person Transmission<br />
Based in part on the observation that surgeons<br />
did not become ill after incising or excising suppurating<br />
lymph nodes from tularemia patients, Francis<br />
concluded in 1927 that tularemia is not transmitted<br />
from person-to-person. This conclusion has been<br />
reiterated frequently in the tularemia literature.<br />
However, it is inconsistent with the report by Fillmore<br />
(1951) of tularemia in a health care worker<br />
who had treated a tularemia patient, and with<br />
reports of droplet spray transmission resulting<br />
from experimental animals “sneezing” at persons<br />
(Aagaard, 1944; Francis, 1983; Ledingham & Fraser,<br />
1923/1924). Further, airborne transmission between<br />
233
mice was demonstrated experimentally by Owen and<br />
Bucker (1956), who found that ten of twenty-eight<br />
(<strong>10</strong>/28) healthy mice strapped into tubes in near<br />
nose-to-nose contact with moribund mice succumbed<br />
to infection. For secondary airborne transmission<br />
to occur, viable organisms must be emitted<br />
from the infected animal and remain viable until<br />
reaching target tissues in the susceptible host. In this<br />
segment of the paper, we evaluate the feasibility that<br />
these events can occur and cause person-to-person<br />
transmission of tularemia.<br />
Viable F. tularensis bacilli are present in the human<br />
body, including respiratory fluids. Emel’yanova<br />
(1961) compared strains of F. tularensis isolated from<br />
234<br />
The Infectious Dose of Francisella tularensis (Tularemia)<br />
Figure 2<br />
Estimated cumulative infection probability of humans experimentally exposed to increasing inhaled doses of<br />
F. tularensis, based on the Saslaw et al. (1961) data adjusted for particle deposition, via a lognormal parametric<br />
regression and a Weibull parametric regression, including 95% confidence intervals. The Saslaw, et al. (1961)<br />
data points are indicated by the diamonds.<br />
the abscesses of two tularemia patients to strains isolated<br />
from well water which had caused a tularemia<br />
outbreak; all strains had the same biological properties<br />
and were lethal to mice, rats, guinea pigs, and<br />
rabbits in the same doses and at the same intervals.<br />
In addition, there are several reports that bacilli<br />
from throat swabs and/or sputum of tularemia patients<br />
with and without pulmonary involvement<br />
were fatal to experimental animals (Johnson, 1944;<br />
Larson, 1945). In a more extensive evaluation, gastric,<br />
pharyngeal, and sputum specimens were collected<br />
from patients with laboratory-acquired tularemia<br />
during the first 3 weeks of their illness; these<br />
specimens were inoculated into guinea pigs or cul-
tured on glucose-cysteine blood agar plates. A total<br />
of 14/16 sputum specimens, 18/32 pharyngeal<br />
specimens, and 22/31gastric specimens either killed<br />
the guinea pigs or produced cultures of F. tularensis<br />
(Overholt et al., 1961). Unfortunately, concentration<br />
data for viable F. tularensis bacilli in respiratory<br />
fluids have not been reported.<br />
The presence of F. tularensis in respiratory fluids<br />
implies that the organism will be present in the aerosol<br />
of respiratory fluids emitted during coughs and<br />
sneezes. The numbers and size distribution of respiratory<br />
aerosol particles have been summarized by<br />
Nicas, et al. (<strong>2005</strong>). Aerosolized F. tularensis remain<br />
viable in air for a sufficient time to be inhaled by<br />
health care workers or family members attending a<br />
R. M. Jones, et al.<br />
Figure 3<br />
Estimated cumulative infection probability of humans experimentally exposed to increasing inhaled doses of<br />
F. tularensis, based on the Saslaw et al. (1961) data adjusted for particle deposition, comparing the lognormal<br />
parametric regression to the nonparametric PAV regression, including 95% confidence intervals.<br />
tularemia patient. As described previously, Hood<br />
(1961) observed that F. tularensis aerosols retained a<br />
diminished, but still lethal, infectivity in guinea pigs<br />
when aged 20 hours. In humans, Sawyer et al. (1966)<br />
found that the inhaled dose of viable cells required<br />
to produce infection increased when the aerosol<br />
aged more than 120 minutes, but the severity of<br />
clinical illness and the incubation period did not<br />
vary with the age of the aerosol. Ambient temperature<br />
and relative humidity influence the viability of<br />
airborne F. tularensis, although the relationships are<br />
not linear. Peak recovery of viable airborne F. tularensis<br />
was observed between -7 o C and 3 o C (Ehrlich &<br />
Miller, 1973), and when disseminated from a wet<br />
state, survival of the organism in air was greatest at<br />
235
high relative humidity (Cox & Goldberg, 1972).<br />
Cough is frequently associated with tularemia,<br />
and increased sputum production has been observed<br />
in some patients. Coughing emits many particles<br />
that quickly attain diameters less than <strong>10</strong> m; these<br />
particles can penetrate to and deposit in the alveolar<br />
region. Coughing also emits many particles that<br />
quickly attain diameters in the <strong>10</strong> m to <strong>10</strong>0 m<br />
range; these particles can be inspired and deposit in<br />
the upper respiratory tract (Nicas, et al., 2004). Experimental<br />
evidence indicates that F. tularensis remains<br />
virulent in the human host and retains viability<br />
in air for prolonged periods of time. Coupled<br />
with an infectious dose of one bacillus, these conditions<br />
indicate that airborne person-to-person trans-<br />
236<br />
The Infectious Dose of Francisella tularensis (Tularemia)<br />
Figure 4<br />
Estimated cumulative infection probability of humans experimentally exposed to increasing inhaled doses of<br />
F. tularensis, based on the Saslaw et al. (1961) data adjusted for particle deposition, comparing the Weibull<br />
parametric regression to the nonparametric PAV regression, including 95% confidence intervals.<br />
mission of tularemia is possible. The overall lack of<br />
reported person-to-person transmission may be due<br />
to a low concentration of F. tularensis in respiratory<br />
fluids, such that the airborne concentration of the<br />
pathogen is usually low and the infection risk by inhalation<br />
is small.<br />
Conclusion<br />
Overall, we judge there is adequate evidence that<br />
infection can be produced by the respiratory tract<br />
deposition of a single F. tularensis bacillus. Human<br />
experimental work concerning inhalation infection<br />
by F. tularensis is limited to inhaled doses of <strong>10</strong> organisms<br />
or greater. However, regression parameter
estimates for the two-parameter lognormal and<br />
Weibull models indicate that the deposition of a<br />
single bacillus carried on a respirable particle will<br />
produce infection in 40% to 50% of individuals.<br />
This prediction is consistent with the observation<br />
that a single F. tularensis bacillus can initiate infection<br />
in experimental animals exposed via injection<br />
(Bell, Owen & Larson, 1955; Downs et al., 1947;<br />
Emel’yanova, 1961; Rosebury, 1947).<br />
Our review of the published literature indicates<br />
that airborne tularemia transmission in the laboratory<br />
has been frequent, and that person-to-person<br />
tularemia transmission is possible. In particular, Fillmore<br />
(1951) reported the case of a nurse’s aide who<br />
developed symptoms of tularemia 3 to 4 weeks after<br />
attending a case of pleuropulmonry tularemia, and<br />
virulent bacilli have been recovered from respiratory<br />
fluids of tularemia patients (Johnson, 1944; Larson,<br />
1945; Overholt et al., 1961). Coughing, which is<br />
associated with tularemia, emits many particles of<br />
respiratory fluid that quickly attain diameters less<br />
than <strong>10</strong>0 m; these particles can be inspired and<br />
deposit in the alveolar region or upper respiratory<br />
tract depending on particle diameter.<br />
The risk of person-to-person airborne infection<br />
is a multivariable function involving the pathogen<br />
concentration in respiratory fluid, the expiratory<br />
event rate, the size and volume distribution of particles<br />
emitted per respiratory event, the receptor’s<br />
breathing rate and exposure duration, and the receptor’s<br />
location in the room relative to the source case<br />
(Nicas, et al., <strong>2005</strong>). Given a specified infectious<br />
dose distribution for F. tularensis, and the concentration<br />
of bacilli in respiratory fluids, it is possible to<br />
estimate tularemia infection risk due to bacilli in<br />
emitted respiratory aerosol. Similarly, the risk of airborne<br />
infection in the laboratory involves the pathogen<br />
concentration in the materials being handled,<br />
the size and volume distribution of the aerosolized<br />
particles, the aforementioned receptor parameters,<br />
and the nature of the pathogen’s infectious dose. A<br />
quantitative estimate of infection risk, even if uncertain,<br />
serves to inform biosafety officers in their decision<br />
making about infection control procedures.<br />
R. M. Jones, et al.<br />
Acknowledgements<br />
This work was supported by a collaborative<br />
agreement with the <strong>Association</strong> of Schools of Public<br />
Health, S2148-22/23. The opinions expressed are<br />
solely those of the authors and do not necessarily<br />
reflect the views of the funding agency.<br />
References<br />
Aagaard, G. N. (1944). Involvement of the heart in<br />
tularemia. Minnesota Medicine, 27, 115-117.<br />
Bell, J. F., Owen, C. R., & Larson, C. L. (1955).<br />
Virulence of Bacterium tularense I: A study of the<br />
virulence of Bacterium tularense in mice, guinea pigs,<br />
and rabbits. Journal of Infectious Diseases, 97, 162-176.<br />
Black, J. (2002). Microbiology: Principles and explorations.<br />
New York: John Wiley and Sons, Inc.<br />
Centers for Disease Control and Prevention. (2003).<br />
Key facts about tularemia. Retrieved August 11,<br />
2004 from www.cdc.gov/agent/tularemia/facts.asp.<br />
Cluxton, Jr., H. E., Cliffton, E. E., & Worley, J. A.<br />
(1948). Primary tularemia of the lungs masquerading<br />
as other forms of lung pathology. The Journal of the<br />
Arkansas Medical Society, 44, 266-275.<br />
Conlan, J. W., Chen, W., Shen, H., Webb, A., &<br />
KuoLee, R. (2003). Experimental tularemia in mice<br />
challenged by aerosol or intradermally with virulent<br />
strains of Francisella tularensis: Bacteriologic and<br />
histopathologic studies. Microbial Pathogensis, 34,<br />
239-248.<br />
Cox, C. S., & Goldberg, L. J. (1972). Aerosol survival<br />
of Pasteruella tularensis and influence of relative<br />
humidity. Applied Microbiology, 23, 1-3.<br />
Dahlstrand, S., Ringertz, O., & Zetterberg, B.<br />
(1971). Airborne tularemia in Sweden. Scandinavian<br />
Journal of Infectious Diseases, 3, 7-16.<br />
237
Day, W. C., & Berendt, R. F. (1972). Experimental<br />
tularemia in Macaca mulatta: Relationship of aerosol<br />
particle size to infectivity of airborne Pasteurella tularensis.<br />
Infection and Immunity, 5, 77-82.<br />
Dennis, D. T., Inglesby, T. V., Henderson, D. A.,<br />
Bartlett, J. G., Ascher, M. S., Eitzen, E., Fine, A.D.,<br />
Friedlander, A. M., Hauer, J., Layton, M., Lillibridge,<br />
S. R., McDade, J. E., Osterholm, M. T.,<br />
O’Toole, T. O., Parker, G., Perl, T. M., Russell, P.<br />
K., & Tonat, K. (2001). Tularemia as a biological<br />
weapon: Medical and public health management.<br />
JAMA, 285, 2763-2773.<br />
Downs, C. M., Coriell, L. L., Pinchot, G. B., Maumenee,<br />
E., Klauber, A., Chapman, S. S., & Owen,<br />
B. (1947). Studies on tularemia I. The comparative<br />
susceptibility of various laboratory animals. Journal of<br />
Immunology, 56, 217-228.<br />
Ehrlich, R., & Miller, S. (1973). Survival of airborne<br />
Pasteurella tularensis at different atmospheric temperatures.<br />
Applied Microbiology, 25, 369-372.<br />
Emel’yanova, O. S. (1961). The virulence of strains<br />
of Pasteurella tularensis isolated from man. Journal of<br />
Microbiology, Epidemiology and Immunobiology, 32, 853-<br />
858.<br />
Evans, M. E. (1985). Francisella tularensis. Infection<br />
Control, 6, 381-383.<br />
Fillmore, A. J. (1951). Tularemia with report of six<br />
cases. Arizona Medicine, 8, 27-33.<br />
Francis, E. (1927). Tularemia. The Atlantic Medical<br />
Journal, 30, 337-344.<br />
Francis, E. (1983). Landmark article April 25, 1925:<br />
Tularemia by Edward Francis. JAMA, 250, 3216-<br />
3224.<br />
Franz, D. R., Jahrling, P. B., Friedlander, A. M.,<br />
McClain, D. J., Hoover, D. L., Byrne, W. R., Pavlin,<br />
J. A., Christopher, G. W., & Eitzen, E. M. (1999).<br />
Clinical recognition and management of patients<br />
238<br />
The Infectious Dose of Francisella tularensis (Tularemia)<br />
exposed to biological warfare agents. In J. Lederberg<br />
(Ed.), <strong>Biological</strong> weapons: Limiting the threat (pp. 38-<br />
80). Cambridge, MA: MIT Press.<br />
Henderson, D. W. (1952). An apparatus for the<br />
study of airborne infection. Journal of Hygiene, 50, 53-<br />
68.<br />
Hinds, W. C. (1999). Aerosol technology (2nd ed.).<br />
New York: John Wiley and Sons, Inc.<br />
Hood, A. M. (1961). Infectivity of Pasteurella tularensis<br />
clouds. Journal of Hygiene, 54, 497-504.<br />
Johnson, H. N. (1944). Isolation of Bacterium tularense<br />
from the sputum of an atypical case of human<br />
tularemia. Journal of Laboratory and Clinical Medicine,<br />
29, 903-905.<br />
Kalbfleisch, J. D., & Prentice, R. L. (2002). The statistical<br />
analysis of failure time data (2nd ed.). New Jersey:<br />
Wiley-Interscience.<br />
Larson, C. L. (1945). Isolation of Pasteurella tularensis<br />
from sputum: A report of successful isolations from<br />
3 cases without respiratory symptoms. Public Health<br />
Reports, 60, <strong>10</strong>49-<strong>10</strong>53.<br />
Ledingham, J. C. G., & Fraser, F. R. (1923/1924).<br />
Tularemia in man from laboratory infection. The<br />
Quarterly Journal of Medicine, 17, 365-382.<br />
McCrumb, F. R. (1961). Aerosol infection of man<br />
with Pasteurella tularensis. Bacteriological Reviews, 25,<br />
262-267.<br />
Miller, R. P., & Bates, J. H. (1969). Pleuropulmonary<br />
tularemia: A review of 29 patients. <strong>American</strong> Review<br />
of Respiratory Disease, 99, 31-41.<br />
Nicas, M., Nazaroff, W. W., & Hubbard, A. (<strong>2005</strong>).<br />
Toward understanding the risk of secondary airborne<br />
infection: Emission of respirable pathogens.<br />
Journal of Occupational and Environmental Hygiene,<br />
2,143-154.
Overholt, E. L., & Tigertt, W. D. (1960). Roentgenographic<br />
manifestations of pulmonary tularemia.<br />
Radiology, 74, 758-765.<br />
Overholt, E. L., Tigertt, W. D., Kadull, P. J., Ward,<br />
M. K., Charkes, N. D., Rene, R. M., Salzman, T. E.,<br />
& Stephens, M. (1961). An analysis of forty-two<br />
cases of laboratory acquired tularemia. <strong>American</strong> Journal<br />
of Medicine, 30, 785-806.<br />
Owen, C. R., & Buker, E. O. (1956). Factors involved<br />
in the transmission of Pasteurella tularensis<br />
from inoculated animals to healthy cage mates. Journal<br />
of Infectious Diseases, 99, 227-233.<br />
Reintjes, R., Dedushaj, I., Gjini, A., Jorgensen, T.<br />
R., Cotter, B., Lieftucht, A., D’Ancona, F., Dennis,<br />
D. T., Kosoy, M. A., Mulliqi-Osmani, G., Grunow,<br />
R., Kalaveshi, A., Gashi, L., & Humolli, I. (2002).<br />
Tularemia outbreak investigation in Kosovo: Case<br />
control and environmental studies. Emerging Infectious<br />
Diseases, 8, 69-73.<br />
Rosebury, T. (1947). Experimental airborne infection.<br />
Baltimore, MD: The Williams and Wilkins Company.<br />
Saslaw, S., Eigelsbach, H. T., Prior, J. A., Wilson, H.<br />
E., & Carhart, S. (1961). Tularemia vaccine study II.<br />
Respiratory challenge. Archives of Internal Medicine,<br />
<strong>10</strong>7, 702-714.<br />
<strong>Safety</strong> Library Reference<br />
R. M. Jones, et al.<br />
The National Academies Press provides, free of charge, Prudent<br />
Practices in the Laboratory: Handling and Disposal of Chemicals, 1995,<br />
in a searchable, printable format at:<br />
http://www.nap.edu/openbook/0309052297/html/index.html<br />
Sawyer, W. D., Jemski, J. V., Hogge, Jr., A. L., Eigelsbach,<br />
H. T., Wolfe, E. K., Dangerfield, H. G.,<br />
Gochenour, Jr., W. S., & Crozier, D. (1966). Effect<br />
of aerosol age on the infectivity of airborne Pasteurella<br />
tularensis for Macaca mulatta and man. Journal<br />
of Bacteriology, 91, 2180-2184.<br />
Shapiro, D. S., & Schwartz, D. R. (2002). Exposure<br />
of laboratory workers to Francisella tularensis despite a<br />
bioterrorism procedure. Journal of Clinical Microbiology,<br />
40, 2278-2281.<br />
Sjostedt, A., Tarnvik, A., & Sandstrom, G. (1996).<br />
Francisella tularensis: Host-parasite interaction. FEMS<br />
Immunology and Medical Microbiology, 13, 181-184.<br />
Syrjala, H., Kujala, P., Myllyla, V., & Salminen, A.<br />
(1985). Airborne transmission of tularemia in farmers.<br />
Scandinavian Journal of Infectious Diseases, 17, 371-<br />
375.<br />
Syrjala, H., Sutinen, S., Jokinen, K., Nieminen, P.,<br />
Touuponen, T., & Salminen, A. (1986). Bronchial<br />
changes in airborne tularemia. The Journal of Laryngology<br />
and Otology, <strong>10</strong>0, 1169-1176.<br />
Van Metre, Jr., T. E., & Kadull, P. J. (1959). Laboratory-acquired<br />
tularemia in vaccinated individuals: A<br />
report of 65 cases. Annals of Internal Medicine, 50,<br />
621-632.<br />
World Health Organization. (1970). Health aspects of<br />
chemical and biological weapons. Geneva: World<br />
Health Organization.<br />
239
240<br />
Article<br />
Introduction<br />
Ultraviolet light (UV) is frequently used in limited<br />
clinical settings to reduce the risk of nosocomial<br />
infections. The World Health Organization Global<br />
Solar UV Index (UVI) divides UV into A (315-400<br />
nm), B (280-315 nm), and C (<strong>10</strong>0-280 nm) bands.<br />
Light in the C band (UV-C) is listed in the UVI as<br />
the most harmful to living organisms because of its<br />
propensity to damage DNA and RNA. It is also the<br />
least relevant in the natural setting since it is completely<br />
filtered by the atmosphere and does not<br />
reach Earth’s surface in levels measurable with commercially<br />
available equipment.<br />
Often small surface areas or airflow in high-risk<br />
areas are treated with UV-C to decrease infectious<br />
microorganism populations. Other means of decontamination<br />
are sometimes employed when a large<br />
area has been contaminated. Gaseous disinfection<br />
with ethylene oxide, chlorine dioxide, or formaldehyde<br />
is costly, hazardous to workers and the environment,<br />
and requires prolonged evacuation of the<br />
treatment area (Rehork et al., 1990). Liquid disinfectants<br />
must be manually applied and removed and<br />
may damage exposed materials such as electrical devices.<br />
Ionizing radiation will kill in adequate doses<br />
but is hazardous to workers, difficult to contain, and<br />
not practical for general working space disinfection<br />
(Rehork et al., 1990).<br />
Applied Biosafety, <strong>10</strong>(4) pp. 240-247 © ABSA <strong>2005</strong><br />
High-Dose Ultraviolet C Light Inactivates<br />
Spores of Bacillus Atrophaeus and Bacillus<br />
Anthracis Sterne on Nonreflective Surfaces<br />
Marie U. Owens 1, David R. Deal 2, Michael O. Shoemaker 3, Gregory B. Knudson 3,<br />
Janet E. Meszaros 4, and Jeffery L. Deal 2<br />
1College of Charleston, Charleston, South Carolina; 2UVAS-LLC, Charleston, South Carolina; 3Armed Forces<br />
Radiobiology Research Institute, Bethesda, Maryland; and 4Steris Corporation, Mentor, Ohio<br />
The possibility of using UV-C (254 nanometer<br />
range) to decontaminate or sterilize work areas and<br />
to avoid the problems listed above led to the development<br />
by two of the authors (JLD, DRD) of the<br />
Ultraviolet Area Sterilizer (UVAS). The device is<br />
unique in that it generates intense levels of UV-C<br />
and then utilizes measured UV-C intensities reflected<br />
from the walls, ceilings, floors, or other<br />
treated areas to calculate the operation time to deliver<br />
the programmed lethal dose for infectious microorganisms.<br />
UV-C has been found to be highly<br />
effective against a wide spectrum of microorganisms<br />
(Banrud & Moan, 1999; Druce et al., 1995; Inamoto<br />
et al., 1979; Knudson, 1985). The development of a<br />
method to deliver a lethal and predictable UV-C<br />
dose can greatly increase the potential uses for UV-C<br />
in decontamination. Since the biological activity of<br />
UV-C is not limited to microorganisms, the UVAS<br />
has multiple safety features including remote controls,<br />
motion sensors, and audible voice warnings.<br />
These safety features were active during the course of<br />
this study.<br />
The ability of the UVAS device to deliver lethal<br />
doses of UV-C to bacterial spores on nonreflective<br />
surfaces was evaluated by comparing the susceptibilities<br />
of Bacillus atrophaeus (formerly named B. subtilis<br />
var. niger, and B. globigii) and Bacillus anthracis Sterne<br />
spores to incremental UV-C doses. Additionally, the<br />
susceptibility of Bacillus atrophaeus spores in the pres-
ence of silica-containing powder to simulate a bioterrorism<br />
attack weapon was tested to see if this modification<br />
altered the efficacy of UV-C deactivation.<br />
This investigation has shown that spore viability<br />
of both Bacillus atrophaeus as well as B. anthracis<br />
Sterne was significantly and reproducibly reduced by<br />
3-5 logs under extreme contamination levels following<br />
dosimetric UV-C exposure. Complete kill can be<br />
achieved when the spore contamination level is<br />
lower. These findings are consistent with those of<br />
Nicholson and Galeano (2003) and Knudson<br />
(1986). Spores of Bacillus atrophaeus in 1%-2% silica<br />
were likewise susceptible to killing by UV-C. However,<br />
the presence of gross particulate matter such as<br />
visible powder containing extremely high concentrations<br />
of spores significantly inhibits spore susceptibility<br />
to UV-C inactivation.<br />
Materials and Methods<br />
Bacterial Spore Suspensions/Preparations<br />
B. atrophaeus 93-PBA-1 spore mixture (provided<br />
by the Armed Forces Radiobiology Research Institute<br />
(AFRRI), Bethesda, MD) contained 1%-2% silica<br />
by weight and had an initial concentration of 2.5<br />
x <strong>10</strong> 11 Colony Forming Units (CFU)/g. This spore<br />
mix was diluted in 50% ethanol to achieve concentrations<br />
of <strong>10</strong> 9 , <strong>10</strong> 5 , <strong>10</strong> 4 , and <strong>10</strong> 3 CFU/ml. The dry,<br />
free-flowing silica spore mixture closely simulates a<br />
weapons-grade product used by bioterrorists. B. anthracis<br />
Sterne spores were produced at AFRRI using<br />
an inoculum from a live-spore veterinary vaccine<br />
(Colorado Serum Company, Denver, CO) as previously<br />
described (Elliott et al., 2002). The B. anthracis<br />
Sterne spores were washed twice in deionized sterile<br />
water and examined by phase-contrast microscopy to<br />
confirm that the refractile spore suspension was free<br />
of vegetative cells. The B. atrophaeus spores ATCC<br />
9372 (Steris Corp., Mentor, OH) were at initial concentrations<br />
of 3.0 x <strong>10</strong> 9 CFU/g and 2.5 x <strong>10</strong> <strong>10</strong><br />
CFU/ml, respectively. Both of these spore products<br />
were suspended in 50% ethanol and used at a concentration<br />
of <strong>10</strong> 9 , <strong>10</strong> 5 , and <strong>10</strong> 4 CFU/ml.<br />
Test Surfaces<br />
Aluminum plates, which measured 1276 cm 2 ,<br />
were painted with high heat-stable, flat-black enamel<br />
(7778-822, Rust-Oleum, Vernon Hills, IL). These<br />
M. U. Owens, et al.<br />
test surfaces were autoclaved prior to being evenly<br />
spread with suspensions of B. atrophaeus ATCC<br />
9372 and B. anthracis Sterne spores in ethanol. The<br />
dark surface was intended to minimize reflectance<br />
and, therefore, measured primarily the effect of direct<br />
UV-C exposure. For the test using the dry, freeflowing<br />
B. atrophaeus (93-PBA-1) spore powder, sterile<br />
90 mm Petri plates were used.<br />
Spore Distribution<br />
Two milliliters of the liquid spore suspensions in<br />
50% ethanol were uniformly distributed on the<br />
metal test and control surfaces using sterile, plastic,<br />
cell spreaders. An additional 5 ml of 50% ethanol<br />
was used to facilitate the even distribution over the<br />
entire surface area. Test surfaces were air dried for a<br />
minimum of 2 hours before UV-C exposure.<br />
Dry B. atrophaeus (93-PBA-1) spore powder was<br />
spread in the base of sterile 90 mm Petri plates by<br />
adding a uniform dry measure to 16 dishes. Each<br />
dish was gently rotated and tilted by hand to achieve<br />
a relatively uniform distribution of the powder. Excess<br />
spore powder was removed into a beaker by inverting<br />
and tapping the plates. To reduce shadowing<br />
effects during UV-C exposure, the powder was wiped<br />
from the sides and corners of the dishes with sterile<br />
cotton swabs. The mass of spores remaining in each<br />
plate was determined by weighing each plate before<br />
and after addition of spores. Each plate received 20<br />
to 50 mg of spore powder.<br />
Exposure<br />
The UVAS device employs 14 medium-pressure<br />
mercury bulbs (product #TUV 115W HHO, Philips<br />
Corporation, Sommerset, NJ) with a combined<br />
power output of approximately 3,000 microwatts/cm<br />
2 at 1 meter. The device was used to expose<br />
test surfaces in a room measuring 25 x 35 ft. For the<br />
flat-black metal surfaces, cumulative UV-C doses<br />
were measured using two National Institute of Standards<br />
and Technology-calibrated dosimeters<br />
(PMA2<strong>10</strong>0, Solar Light Company, Philadelphia, PA)<br />
placed on either side of the test surfaces and were<br />
reported as the average between both devices. For<br />
the Petri plates containing dry spore powder, a single<br />
PMA2<strong>10</strong>0 dosimeter was placed in the center of the<br />
plate array as shown in Figure 1.
Spore Recovery and Culture Media<br />
Two methods were used to recover spores from<br />
the metal test surfaces following each UV-C exposure.<br />
Rodac 45-mm contact culture plates containing<br />
trypticase soy agar with lecithin and polysorbate 80<br />
(TSALP, PML Microbiologicals, Mississauga, ON,<br />
Canada) were used to recover viable spores from<br />
28.3 cm 2 sample areas of the test surfaces by direct<br />
contact with the metal plates. Swab Dilution Samplers<br />
(MT00<strong>10</strong>025, Millipore Corp., Billerica, MA)<br />
were used for recovery of 16-cm 2 sample areas of the<br />
test surfaces. For each test surface, a minimum of<br />
three contact plates and one swab is used to obtain<br />
spore recovery at each targeted dose. The recovered<br />
spores adhering to the swabs were eluted in the Millipore<br />
buffer, subsequently diluted, and plated in<br />
triplicate as 150-l aliquots onto 90 mm trypticase<br />
242<br />
Recovered B. atrophaeus spores<br />
(CFU/ 1276 cm 2 )<br />
0<br />
250<br />
High-Dose Ultraviolet C Light Inactivates Spores<br />
Figure 1<br />
Recovery of B. atrophaeus spores containing ~1-2% silica after exposure to UV-C<br />
<strong>10</strong> <strong>10</strong><br />
<strong>10</strong> 9<br />
<strong>10</strong> 8<br />
<strong>10</strong> 7<br />
<strong>10</strong> 6<br />
<strong>10</strong> 5<br />
<strong>10</strong> 4<br />
<strong>10</strong> 3<br />
<strong>10</strong> 2<br />
<strong>10</strong> 1<br />
<strong>10</strong> 0<br />
500<br />
750<br />
<strong>10</strong>00<br />
1250<br />
1500<br />
UV-C Dose (milliJoules/cm 2 )<br />
Incremental doses of UV-C were administered to a total surface inoculum of 6.2 x <strong>10</strong> 8 CFU/1276 cm 2 .<br />
Following each dose, spores were recovered using Millipore swabs and Rodac contact plates. The average<br />
number of colonies were reported and used in calculations to determine the total viable spore count over the<br />
entire test surface. The curve represents the best-fit of a single exponential decay equation to the data.<br />
1750<br />
2000<br />
soy agar plates (TSA, BD Diagnostic Systems, Sparks,<br />
MD). Plates from both recovery methods were incubated<br />
at 35 o C for 15 hours before colonies were<br />
counted. Average plate counts were used to calculate<br />
the number of viable spores remaining on the metal<br />
plates and were plotted as a function of UV-C dose<br />
to generate inactivation curves (Figures 1-3).<br />
Spores in dry powder that were dispensed within<br />
the Petri plates were recovered by washing the Petri<br />
plates three times with sterile water (5 ml final volume)<br />
followed by recovering any material adhering<br />
to the bottom of the plate with a sterile rubber cell<br />
spreader. The suspensions were vortexed, diluted,<br />
inoculated as 150 l aliquots onto TSA plates in triplicate,<br />
and incubated at 35 o C for 15 hours before<br />
colonies were counted. Average plate counts were
used to calculate the number of viable spores remaining<br />
in each exposure plate and plotted as a<br />
function of UV-C dose (Figure 4).<br />
Calculations<br />
Total Population per Aluminum Plate Surface Area:<br />
Swab Dilution Samplers:<br />
= Mean Plate Count x Dilution<br />
Factor Vol. Plated (0.150 ml) x<br />
Swab Dilution Sampler Vol. (18<br />
ml) Aluminum Plate Surface Area<br />
Swabbed (16 cm 2 ) x Aluminum<br />
Plate Total Surface Area (1276 cm 2 )<br />
Rodac Contact Plates:<br />
= Mean Plate Count Aluminum<br />
Plate Surface Area Contacted (28.3<br />
cm 2 ) x Aluminum Plate Total Surface<br />
Area (1276 cm 2 )<br />
M. U. Owens, et al.<br />
Photo 1<br />
UVAS prototype in test room with sensor and test plates<br />
containing a thin layer of dry B. atrophaeus spore powder<br />
Results<br />
Inactivation of B. atrophaeus (93-PBA-1)<br />
Spores with Silica<br />
At extremely high spore-inoculum levels, contact<br />
plates could not provide population data from the<br />
control, unexposed plates due to the high number of<br />
colonies, but the swabbing method gave a viable<br />
spore count of 6.2 x<strong>10</strong> 8 CFU existed over the entire<br />
plate surface. The swab method was also the only<br />
procedure that could be used for recovery studies at<br />
lower UV-C doses of <strong>10</strong>0-600 milliJoules/cm 2 for<br />
the same reason. Results from the swab method indicated<br />
a 3-log reduction could be obtained at these<br />
UV-C exposure levels. At higher UV-C doses between<br />
600-1,800 milliJoules/cm 2 , a 3-4-log reduction<br />
was demonstrated with the swab recovery method<br />
and a 5-log reduction was obtained using the contact<br />
plates (Figure 1).<br />
For the test plates spread with less concentrated<br />
spore suspensions (theoretically <strong>10</strong> 5 , <strong>10</strong> 4 , and <strong>10</strong> 3<br />
243
CFU per test surface) recoveries were conducted using<br />
the contact plates alone after UV-C exposures of<br />
1,000 to 2,000 milliJoules/cm 2 . All plates indicated<br />
no survivors. Recoveries from unexposed control<br />
plates were 1 log lower than anticipated; therefore,<br />
at least a 4-log reduction can be ensured.<br />
Control surfaces, which were not exposed to<br />
UV-C, did not show any reduction in colony counts<br />
during the course of the experiment, eliminating the<br />
possibility that recoveries varied with time.<br />
Inactivation of B. atrophaeus<br />
(ATCC 9372) Spores<br />
Swab recoveries used for determining viable<br />
spore counts from the test plates spread with highly<br />
concentrated spore suspensions indicated a spore<br />
survival count of <strong>10</strong> 8 CFU per test surface. This recovery<br />
method demonstrated a 2-log reduction at 50<br />
244<br />
High-Dose Ultraviolet C Light Inactivates Spores<br />
Figure 2<br />
Recovery of B. atrophaeus (ATCC9372) spores from black-plate surfaces after exposure to UV-C.<br />
Recovered B. atrophaeus spores<br />
(CFU/ 1276 cm 2 )<br />
<strong>10</strong> <strong>10</strong><br />
<strong>10</strong> 9<br />
<strong>10</strong> 8<br />
<strong>10</strong> 7<br />
<strong>10</strong> 6<br />
<strong>10</strong> 5<br />
<strong>10</strong> 4<br />
<strong>10</strong> 3<br />
<strong>10</strong> 2<br />
<strong>10</strong> 1<br />
<strong>10</strong> 0<br />
0<br />
500<br />
<strong>10</strong>00<br />
1500<br />
2000<br />
2500<br />
3000<br />
3500<br />
UV-C Dose (milliJoules/cm 2 )<br />
Recovery of B. atrophaeus spores using the Millipore swab sampling recovery method. Curves represent best-fit<br />
of a single exponential decay equation to data.<br />
4000<br />
4500<br />
5000<br />
milliJoules/cm 2 and a 3–4-log reduction at <strong>10</strong>0 to<br />
4,647 milliJoules/cm 2 UV-C. The variability was attributed<br />
to the use of data from plates in which usable<br />
counts were less than 30 CFU per plate. Contact<br />
plates, which were used only at the doses from<br />
2,000 to 4,000 milliJoules/cm 2 UV-C, indicated that<br />
a 5-log reduction could be obtained in comparison<br />
to the unexposed spore population determined by<br />
swabbing (Figure 2).<br />
The control, contact plate viability counts from<br />
the less-concentrated test plates, theoretically <strong>10</strong> 4 and<br />
<strong>10</strong> 5 CFU, indicated a 2-log lower population than<br />
expected. The number of survivors was quite often<br />
zero for all the UV-C doses evaluated from 50 to<br />
2,000 milliJoules/cm 2 except in some instances low<br />
colony counts were obtained, which may have been<br />
environmental contamination.
B. anthracis Sterne Spores<br />
Millipore swab recoveries from nonirradiated<br />
test surfaces indicated 3.6 x <strong>10</strong> 8 CFU. Swab recoveries<br />
from UV-C doses of 150 and 1,000 milli-<br />
Joules/cm 2 resulted in a three and four log reduction<br />
respectively. Contact plates used for recoveries<br />
on the test surface exposed to UV-C doses of 2,000<br />
to 4,000 milliJoules/cm 2 demonstrated a 4 log reduction<br />
(Figure 3).<br />
Test surfaces spread with the diluted spore inoculum<br />
had <strong>10</strong> 4 CFU per test surface and showed<br />
total kill when exposed to 50 to 1,000 milli-<br />
Joules/cm 2 .<br />
Inactivation of Dry Spore Powder<br />
The last evaluation used dry, free-flowing B. atrophaeus<br />
spore powder in open Petri plates, with spore<br />
counts of <strong>10</strong> 8 to <strong>10</strong> 9 CFU per plates. A 1-log reduc-<br />
M. U. Owens, et al.<br />
Figure 3<br />
Recovery of B. anthracis Sterne spores from black plate surfaces after exposure to UV-C.<br />
Recovered B. anthracis spores<br />
(CFU/ 1276 cm 2 )<br />
<strong>10</strong> <strong>10</strong><br />
<strong>10</strong> 9<br />
<strong>10</strong> 8<br />
<strong>10</strong> 7<br />
<strong>10</strong> 6<br />
<strong>10</strong> 5<br />
<strong>10</strong> 4<br />
<strong>10</strong> 3<br />
<strong>10</strong> 2<br />
<strong>10</strong> 1<br />
<strong>10</strong> 0<br />
0<br />
500<br />
<strong>10</strong>00<br />
1500<br />
2000<br />
2500<br />
3000<br />
tion was obtained from duplicated plates after exposures<br />
of <strong>10</strong>,000 or 16,000 milliJoules/cm 2 (Figure 4).<br />
Discussion<br />
3500<br />
UV-C Dose (milliJoules/cm 2 )<br />
Recovery of B. anthracis Sterne spores using the Millipore swab sampling recovery method. Curves represent<br />
best-fit of a single exponential decay equation to data.<br />
4000<br />
4500<br />
5000<br />
This investigation has demonstrated that UV-C<br />
generated by the UVAS in the absence of visible particulate<br />
matter can be delivered at lethal doses on<br />
nonreflective, non-porous surfaces for partial spore<br />
reduction even when the contamination levels are<br />
extremely high and for total spore reduction in the<br />
presence of less-concentrated spore populations. A 3-<br />
5-log reduction can be assured following UV-C exposure<br />
to contamination levels simulating those used<br />
in bioterrorist weapons—<strong>10</strong> 8 to<strong>10</strong> 9 CFU/1276 cm 2 or<br />
<strong>10</strong> 5 to <strong>10</strong> 6 CFU/cm 2 —using doses of one hundred to<br />
several thousand milliJoules/cm 2 (Figures 1, 2, and<br />
3). In situations where the bioburden levels are more<br />
245
epresentative of the contamination in areas such as<br />
operating/emergency rooms (<strong>10</strong> 2 CFU/cm 2 ), UV-C<br />
is capable of completely deactivating the entire population<br />
at lower doses, most likely less than <strong>10</strong>0 milli-<br />
Joules/cm 2 . Test surfaces contaminated with high<br />
numbers of spores that are subsequently spread<br />
across the surface area as may occur during precleaning<br />
were readily decontaminated or sterilized with<br />
adequate doses of UV-C.<br />
Spores at contamination levels of <strong>10</strong> 5 to <strong>10</strong> 6<br />
CFU/cm 2 and applied in powder dense enough to<br />
be visible to the naked eye indicated a 1-log reduction<br />
after UV-C doses of 1,000 to 16,000 milli-<br />
Joules/cm 2 (Figure 4). These findings emphasize the<br />
need for precleaning contaminated surfaces soiled<br />
with gross material. Use of a precleaning step, such<br />
246<br />
Recovered B. atrophaeus spores<br />
(CFU/ 90 mm Petri plate)<br />
<strong>10</strong> <strong>10</strong><br />
<strong>10</strong> 9<br />
<strong>10</strong> 8<br />
<strong>10</strong> 7<br />
<strong>10</strong> 6<br />
<strong>10</strong> 5<br />
<strong>10</strong> 4<br />
<strong>10</strong> 3<br />
<strong>10</strong> 2<br />
<strong>10</strong> 1<br />
<strong>10</strong> 0<br />
0<br />
2000<br />
High-Dose Ultraviolet C Light Inactivates Spores<br />
Figure 4<br />
Recovery of a visible layer of dry B. atrophaeus spores containing<br />
~1% silica on Petri plates after exposure to UV-C.<br />
4000<br />
6000<br />
The curve represents the best-fit of a single exponential decay equation to the data.<br />
8000<br />
<strong>10</strong>000<br />
12000<br />
14000<br />
UV-C Dose (milliJoules/cm 2 )<br />
16000<br />
18000<br />
20000<br />
as HEPA-vacuuming or damp wiping, for heavily<br />
contaminated surfaces in the presence of visible soil,<br />
followed by UV-C exposure, should effectively decontaminate<br />
the area or surface. This is substantiated<br />
by the data in which total kill was demonstrated<br />
from surfaces contaminated with less-concentrated<br />
spore suspensions in the absence of visible powder.<br />
The presence of 1%-2% silica does not impede<br />
the germicidal effect of UV-C since the lethality was<br />
similar to that observed in the absence of silica. This<br />
finding demonstrates that the efficacy of UV-C is<br />
not altered in the presence of low concentrations of<br />
particulate matter or soil that could be present after<br />
precleaning.<br />
Prior studies in animal laboratory settings using<br />
UV light showed a significant reduction of bacterial
loads, and the addition of a chemical disinfectant<br />
followed by UV-C treatment was “particularly successful,<br />
reducing bacterial loads to extremely low levels”<br />
(Dix et al., 1992). In this study where the organisms<br />
were spread on the test surface without deactivation<br />
or removal by any cleaning agent, a significant<br />
spore reduction was observed after UV-C irradiation.<br />
A recent study by Nicholson and Galeano (2003)<br />
found “the data indicate that standard UV treatments<br />
that are effective against B. subtilis spores are<br />
likely also sufficient to inactivate B. anthracis spores,<br />
and spores of standard B. subtilis strains could reliably<br />
be used as a biodosimetry model for the UV inactivation<br />
of B. anthracis spores” Our investigations<br />
have confirmed this finding.<br />
Previous experience with the UVAS device suggested<br />
smooth materials that reflected UV-C may be<br />
more readily decontaminated than rough, nonreflective<br />
materials. Data obtained through this investigation<br />
will be useful in planning surface decontamination<br />
for many environmental applications, since determining<br />
the required decontamination doses<br />
should be based upon information obtained using<br />
the least reflective test surfaces, thus avoiding underexposure.<br />
From these experimental findings one may reasonably<br />
conclude that the UVAS device, or other<br />
UV-C generating devices, could decontaminate areas<br />
in which surface contamination was <strong>10</strong> 2 CFU/cm 2<br />
and could be used to decontaminate extremely concentrated<br />
surfaces as long as a precleaning step was<br />
instituted.<br />
Author’s Note<br />
The B. anthracis Sterne spores were washed twice<br />
in deionized sterile water and examined by phasecontrast<br />
microscopy to confirm that the refractile<br />
spore suspension was free of vegetative cells.<br />
References<br />
Banrud, H., & Moan, J. (1999). [Use of short wave<br />
ultraviolet radiation for disinfection in operating<br />
rooms]. Tidsskr Nor Laegeforen, 119, 2670-2673.<br />
M. U. Owens, et al.<br />
Dix, J., Nolan, G., Schlick, H., & Elliot, H. B.<br />
(1992). The efficiency of ultraviolet irradiation and<br />
chemical disinfection as a means of reducing bacterial<br />
contamination of animal rooms. Fifth FELASA<br />
Symposium: Welfare and Science.<br />
Druce, J. D., Jardine, D., Locarnini, S. A., & Birch,<br />
C. J. (1995). Susceptibility of HIV to inactivation by<br />
disinfectants and ultraviolet light. Journal of Hospital<br />
Infection, 30, 167-180.<br />
Elliott, T. B., Brook, I., Harding, R. A., Bouhaouala,<br />
S. S., Shoemaker, M. O., Knudson, G. B. (2002).<br />
Antimicrobial therapy for Bacillus anthracis-induced<br />
polymicrobial infection in 60 Co gamma-irradiated<br />
mice. Antimicrobial Agents and Chemotherapy, 46,<br />
3463-3471.<br />
Inamoto, H., Ino, Y., Jinnouchi, M., Sata, K., Wada,<br />
T., Inamoto, N., & Osawa, A. (1979). Dialyzing<br />
room disinfection with ultra-violet irradiation. Journal<br />
of Dialysis, 3, 191-205.<br />
Knudson, G. B. (1985). Photoreactivation of UVirradiated<br />
Legionella pneumophila and other Legionella<br />
species. Applied Environmental Microbiology, 49, 975-<br />
980.<br />
Knudson, G. B. (1986). Photoreactivation of ultraviolet-irradiated<br />
plasmid-bearing and plasmid-free<br />
strains of Bacillus anthracis. Applied. Environmental<br />
Microbiology, 52, 444-449.<br />
Nicholson, W. L., & Galeano, B. (2003). UV resistance<br />
of Bacillus anthracis spores revisited: Validation<br />
of Bacillus subtilis spores as UV surrogates for<br />
spores of B. anthracis Sterne. Appied Environmental<br />
Microbiology, 69, 1327-1330.<br />
Rehork, B., Martiny, H., Weist, K., & Ruden, H.<br />
(1990). [Performing surface and room disinfection in<br />
the hospital]. Offentl Gesundheitswes, 52, 36-45.<br />
247
Abstract<br />
248<br />
Article<br />
Potentially infectious wastes, if not properly<br />
treated, could expose both humans and the environment<br />
to untreated microbes and toxins, and create a potential<br />
for illness. Therefore, all pathogenic materials used in<br />
research must be destroyed by heat or chemical treatment<br />
prior to disposal as biomedical waste. Additionally,<br />
bacterial waste from nonpathogenic bacteria carrying<br />
antibiotic resistance must be treated before placement<br />
in the waste stream to avoid transmission of<br />
the antibiotic-resistant trait. In biomedical laboratories,<br />
glassware, beakers, test tubes, and other contaminated<br />
research material are usually treated by autoclaving before<br />
placing them into the waste stream or recycling for<br />
continued use in the laboratory.<br />
Introduction<br />
Florida Administrative Code (F.A.C.) Chapter<br />
64E-16, under the Biomedical Waste Code, requires<br />
an infectious waste treatment facility to maintain<br />
records of temperature and dwell time when wastes<br />
are rendered noninfectious by gas or steam<br />
sterilization. The F.A.C. further requires biological<br />
culture testing to assure proper sterilization of all<br />
autoclaved materials. Since this University is not a<br />
treatment facility but a generator facility, the<br />
University is not required to follow these records<br />
and testing requirements. However, in the best<br />
interest of the University’s environmental and<br />
research goals, the Department of Environmental<br />
Health & <strong>Safety</strong> (EH&S) is voluntarily complying<br />
with the sterilization aspect of the F.A.C.<br />
As a service, EH&S conducts annual sterilization<br />
testing for all departmental autoclave steam cycles<br />
Applied Biosafety, <strong>10</strong>(4) pp. 248-252 © ABSA <strong>2005</strong><br />
Autoclave Testing in a University Setting<br />
Richard N. Le, Amy L. Hicks, and Janice Dodge<br />
Florida State University, Tallahassee, Florida<br />
used for biological waste and materials decontamination.<br />
This testing is to ensure that the autoclave cycles<br />
used are sterilizing all microbial waste.<br />
Background on Steam<br />
Sterilization Testing<br />
Researchers who work with potentially infectious<br />
materials are at a higher risk of exposure, especially<br />
when exposed to untreated infectious waste.<br />
Infections may be transmitted through several different<br />
routes, including direct contact with untreated<br />
infectious waste, indirect contact with contaminated<br />
instruments or environmental surfaces, or inhalation<br />
of airborne contaminants. Infection via any of these<br />
routes requires that all five of the following conditions<br />
be present to form “the chain of infection”:<br />
1. A pathogen with sufficient infectivity and numbers<br />
to cause infection<br />
2. A reservoir or source that allows the pathogen to<br />
survive and multiply<br />
3. A mode of transmission from the source to the<br />
host<br />
4. A portal through which the pathogen may enter<br />
the host<br />
5. A susceptible host (CDC, 2003)<br />
Effective control measures are intended to break<br />
one or more of these “links” in the chain, thereby<br />
reducing the risk of, or completely preventing, exposure<br />
to potentially infectious materials. A key component<br />
in this link-breaking process is the proper use<br />
of steam sterilizers (autoclaves), which serve as an<br />
essential step toward eliminating the “pathogen<br />
links” in the chain of infection (DePaola, 2003;<br />
Quality America, Inc., 2001).<br />
The Occupational <strong>Safety</strong> and Health <strong>Association</strong>
(OSHA) relies on guidelines published by the Centers<br />
for Disease Control and Prevention (CDC) as a<br />
widely recognized and accepted standard to be followed<br />
by employers in carrying out their responsibilities<br />
under the Occupational <strong>Safety</strong> and Health Act.<br />
The CDC and OSHA recommend the use of <strong>Biological</strong><br />
Indicators (BI) for monitoring steam sterilization<br />
cycles in autoclaves. The CDC states [for medical<br />
autoclaves]...“proper functioning of sterilization<br />
cycles should be verified by the periodic use (at<br />
least weekly) of biological indicators (i.e., spore<br />
tests). Heat-sensitive chemical indicators (e.g., those<br />
that change color after exposure to heat) alone<br />
do not ensure the adequacy of sterilization cycle…”<br />
(CDC, 2004).<br />
In addition, F.A.C. 64E-16.007 states that a<br />
treatment facility that disposes of biomedical waste<br />
must utilize steam sterilization, incineration, or an<br />
alternative process approved by the Department of<br />
Health prior to disposal. Treatment shall occur<br />
within 30 days of collection from the generator. Additionally,<br />
steam treatment facility units should be<br />
evaluated for effectiveness with spores of Geobacillus<br />
stearothermophiluss at least once every 7 days for permitted<br />
treatment facilities, or once every 40 hours of operation<br />
for generators that treat their own biomedical<br />
waste.<br />
Sterilizer manufacturers also recognize the importance<br />
of routine testing of sterilizers and autoclaves.<br />
They recommend that a biological spore test<br />
indicator be used weekly in a representative load for<br />
sterilization assurance (Ritter; Tilton et al., 2004).<br />
Background on PROSPORE2<br />
<strong>Biological</strong> Indicators<br />
PROSPORE2 (HealthLink) is a self-contained<br />
biological indicator for validating and monitoring<br />
steam sterilization of solids. It consists of a paper<br />
disc carrier containing Geobacillus stearothermophilus<br />
(ATCC 7953) spores. The disc is enclosed in a plastic<br />
tube along with a glass vial containing growth media<br />
for the bacterial spores. Bromocresol purple has<br />
been added as a pH indicator to detect spore growth.<br />
The outgrowth of spores decreases pH, causing a<br />
color change from purple to yellow following a 24hour<br />
incubation period.<br />
R. N. Le, et al.<br />
A PROSPORE2 biological indicator is placed<br />
inside the autoclave and a specific cycle is selected.<br />
When the cycle is complete, the PROSPORE2 indicator<br />
is sealed by firmly depressing the cap. The glass<br />
ampoule of media is crushed inoculating the Geobacillus<br />
stearothermophilus disc. Then the indicator is<br />
incubated at 55 o -60 o C for a 24-hour time period<br />
along with an untreated PROSPORE2 indicator that<br />
serves as a control to ensure spore viability.<br />
Once the minimum incubation time of 24 hours<br />
has been achieved, both the control and autoclaved<br />
PROSPORE2 indicator are examined. If the autoclaved<br />
PROSPORE2 indicator retains its purple<br />
color, then the sterilization cycle is adequate and the<br />
result is recorded as passing. A failed sterilization<br />
cycle is indicated by turbidity or a change in color<br />
toward yellow, indicating spore growth due to a<br />
change in pH. The control indicator should exhibit<br />
turbidity and/or a color change to yellow after incubation<br />
to ensure the viability of the biological indicators.<br />
If the control indicator does not show signs of<br />
growth, the test is considered invalid and all the results<br />
are unacceptable and not considered.<br />
Evaluation of Autoclaves<br />
PROSPORE2 biological indicators were used to<br />
test the steam sterilization cycles of several departmental<br />
autoclaves. A total of three runs were conducted<br />
for each autoclave. For each autoclave, a test<br />
trial run using a PROSPORE2 biological indicator<br />
was run to see if the autoclaves were capable of sterilization<br />
without any load. The biological indicator<br />
in the test trial was placed in a horizontal position,<br />
as recommended by the manufacturer, in various<br />
locations within the autoclave chamber. This was<br />
done to verify the effectiveness of steam sterilization<br />
in different areas within the autoclave.<br />
Following the test trial run, two additional runs<br />
were performed in which PROSPORE2 biological<br />
indicators were placed in a representative load or<br />
challenge load to be autoclaved. The challenge load<br />
test consisted of placing a PROSPORE2 biological<br />
indicator in the center of an autoclave bag containing<br />
empty plastic pipette tip boxes. This bag was left<br />
partially open to allow for steam penetration and<br />
sterilization.
For the results, a “PASS” indicated that the<br />
PROSPORE2 biological indicator retained its purple<br />
color signifying an adequate sterilization cycle. A<br />
“FAIL” resulted in the PROSPORE2 biological indicator<br />
having turbidity or a color change toward<br />
yellow for that sterilization cycle. Untreated control<br />
PROSPORE2 biological indicators were incubated<br />
with each autoclaved ran PROSPORE2 biological<br />
indicator.<br />
The following results were compiled over a 3month<br />
testing period for several departmental autoclaves.<br />
These results are for the challenge load testing<br />
only. Challenges were performed using the temperatures<br />
preset by the research groups using the<br />
autoclaves.<br />
Test Findings<br />
Each test trial run resulted in a passing test for<br />
every autoclave. Based on this result, it was concluded<br />
that the autoclave was functioning properly.<br />
250<br />
Autoclave Testing in a University Setting<br />
An adequate amount of steam and heat were produced<br />
to sterilize any unobstructed contents such as<br />
glassware. However, problems occurred with the<br />
challenge load testing. Almost every challenge load<br />
test failed to sterilize the biological indicator. Therefore,<br />
the testing procedure was modified in an effort<br />
to sterilize the enclosed biological indicator. The<br />
challenge load volume was reduced by approximately<br />
half its original volume and the bag’s opening was<br />
increased. In addition, approximately 250 mL of<br />
water was added directly to the autoclave bag to generate<br />
additional steam within the bag to achieve sterilization.<br />
<strong>Biological</strong> indicators were also given to two separate<br />
departments to autoclave with their normal biohazardous<br />
waste load. One was autoclaved for 15<br />
minutes at 121°C gravity cycle and the other load<br />
was autoclaved at 121°C for 35 minutes on a liquid<br />
setting. Since the biological indicators were placed in<br />
actual bags of biohazardous waste, these tests were<br />
true representatives of what laboratories were gener-<br />
Autoclave<br />
Table 1<br />
Cycle Pass Fail<br />
Amsco 3021-S-A<br />
(Amsco)<br />
G15/D30<br />
L60 <br />
<br />
Amsco 3041<br />
All settings (Liquid and<br />
<br />
(Amsco)<br />
Gravity)<br />
Consolidated<br />
Addition of water to bag<br />
G60/D15<br />
<br />
<br />
(Consolidated) G30/D15 <br />
Primus Autoclaves-A<br />
(Primus)<br />
G20/D15 (Room 511)<br />
G15/D1 (Room 312)<br />
<br />
<br />
Amsco 3021-S-B All liquid cycles <br />
Amsco Scientific<br />
(Amsco)<br />
Amsco 3021-S-C<br />
(Amsco)<br />
G30/D30 (132°C) <br />
L30 <br />
L15 <br />
G15/D30 (132°C) <br />
L30 <br />
L15 <br />
Primus Autoclave(B) G15 <br />
Steris, Stage 1<br />
(Amsco)<br />
G30/D15 <br />
G30/D15 (addition of water) <br />
(“L”=liquid cycle, “G”=gravity cycle; and “D”=Dry time. Unless otherwise<br />
indicated, the standard 121°C and 15 psi were used at each autoclave)
ating. Unfortunately, both of these tests failed.<br />
Based on the information in the preceding table,<br />
it was evident that the results varied greatly with<br />
each autoclave due to the type of autoclave and differences<br />
in cycle times and temperatures. However,<br />
it can be shown that the shorter-timed cycles failed<br />
consistently for each challenge load tested. The exceptions<br />
to this were the results generated from the<br />
Amsco 3041 autoclave and the Amsco Scientific<br />
autoclave. For the Amsco 3041 autoclave, the 250<br />
mL of water added to the autoclave bag helped with<br />
the sterilization of the materials, resulting in a passing<br />
test for the challenge load. The Amsco Scientific<br />
autoclave was able to sterilize the PROSPORE2 biological<br />
indicator using a 30-minute cycle because of<br />
the higher temperature setting. However, the bags<br />
used for this autoclave were not compatible with the<br />
higher temperature, resulting in complete deterioration<br />
of the bags after autoclaving.<br />
Additional Findings<br />
It was observed that not all autoclaves had clear<br />
instructions available detailing proper usage and that<br />
no user log was present to record the users, cycle<br />
times, settings, and autoclave contents. In addition,<br />
it was unknown if the temperature sensors on each<br />
autoclave were properly calibrated due to inadequate<br />
record keeping concerning general maintenance on<br />
several autoclaves. However, each autoclave chamber<br />
temperature was verified during the runs using a<br />
high-low thermometer that was placed in the autoclave<br />
with each challenge load run. There was good<br />
consistency between the high-low thermometer temperature<br />
readings and the temperature indicated on<br />
the autoclaves.<br />
In addition, no records were kept to indicate<br />
when general or safety maintenance was last conducted<br />
on several autoclaves. Maintenance should be<br />
done yearly or as recommended by the autoclave<br />
manufacturer.<br />
Recommendations<br />
In keeping with the CDC and OSHA recommendations<br />
and using F.A.C. 64E-16.007 as a guide-<br />
R. N. Le, et al.<br />
line, EH&S will use biological indicators for validating<br />
the steam sterilization cycles on an annual basis.<br />
EH&S recommends that the following adjustments<br />
to policies and practices be implemented in order to<br />
better achieve sterilization and ensure proper maintenance<br />
for each autoclave:<br />
1. Readjustment of Cycle Times<br />
The standard 121°C, 15-psi, and 15-minute<br />
dwell time are adequate for sterilization of clean<br />
items or smaller loads, but were found to be inadequate<br />
for large bulky loads of biohazardous waste.<br />
For this type of waste, it is recommended that the<br />
sterilization time be increased to a minimum of 60<br />
minutes, while still maintaining the standard temperature<br />
and pressure. This setting has proven effective<br />
for sterilizing larger loads. The addition of water<br />
is not recommended because results were not consistent<br />
enough for this to be considered an effective<br />
option. It is also recommended not to leave the autoclave<br />
bag open for actual autoclaving of materials<br />
even though this procedure was used in the test procedure.<br />
The bag should be secured loosely with a<br />
rubberband or closed loosely with a small opening<br />
(at least 1 inch in diameter). This will minimize an<br />
individual’s risk of becoming exposed to hot materials<br />
within the bag. It is suggested that a “kill cycle”<br />
be set on each autoclave intended specifically for<br />
sterilization of contaminated dry waste loads.<br />
The Amsco Scientific autoclave did yield a passing<br />
result due to a higher temperature setting. However,<br />
the autoclave bags used could not withstand<br />
the higher temperature and the bags deteriorated<br />
during the procedure. This is a safety concern because<br />
the contents within the bag could spill onto<br />
the user exposing him or her to the extremely hot<br />
contents. To use this autoclave at the higher temperature<br />
settings, it is important to use an autoclave<br />
bag that is compatible with the 132°C temperature.<br />
In addition, the autoclaves should be retested using<br />
the new autoclave bags.<br />
2. Proper Autoclave Use<br />
The autoclave bag should never be over-packed<br />
or sealed too tightly. It is also important to make<br />
sure that the contents of the autoclave bag are kept<br />
at a minimum. An over-packed bag will insulate mi-<br />
251
crobes at the center of the bag compromising effective<br />
sterilization for the core contents (Churchill,<br />
2003).<br />
It is the responsibility of each department to ensure<br />
that all users understand and know how to use<br />
the autoclave correctly. EH&S recommends that<br />
proper personal protective equipment be worn when<br />
unloading materials from the autoclave. Any exposed<br />
skin should be covered when reaching into<br />
the autoclave after operation to prevent burns. Heatresistant,<br />
elbow-length gloves and other personal<br />
protective equipment are necessary to prevent burns<br />
from occurring when removing hot items. In addition,<br />
a shallow pan or container should be used<br />
when autoclaving bags of biohazardous waste to prevent<br />
potential spills of this material onto the user.<br />
3. Record Keeping<br />
The use of an autoclave logbook is recommended<br />
for each autoclave. Prior to autoclaving any<br />
items, users must fill in all information requested in<br />
the autoclave logbook. The logbook should be located<br />
adjacent to the autoclave and be maintained<br />
by the department. Information that should be part<br />
of the logbook includes: user’s name, cycle time, cycle<br />
setting, materials being autoclaved, contact number,<br />
time in, time out, and verification results.<br />
4. <strong>Safety</strong> Maintenance<br />
General maintenance should be conducted on<br />
an annual basis or as recommended by the manufacturer.<br />
Specifically, the safety valve should be checked<br />
and replaced as required. This information should<br />
be posted on the autoclave or maintained in a maintenance<br />
logbook for easy reference. In addition, a<br />
quick check of the autoclave should be conducted<br />
prior to each use to ensure that all parts are properly<br />
functioning (e.g., door closes and is sealed properly,<br />
the rack is in place, correct settings are being used,<br />
the interior is clean, etc.). Autoclaves should be<br />
cleaned after every use and the work area should be<br />
disinfected as needed. Appropriate cleaning protocols<br />
should be obtained from each manufacturer.<br />
252<br />
Autoclave Testing in a University Setting<br />
5. Training<br />
Each autoclave user should be trained on the<br />
proper use of the autoclave. The cycle settings<br />
should be posted next to the autoclave to inform<br />
each user of the types of settings available, such as<br />
gravity and liquid cycles, the temperatures for each<br />
cycle, and run times. A written sterilization procedure<br />
should be kept near each autoclave and a standard<br />
operating procedure should be developed. It<br />
should include the appropriate sterilization times for<br />
liquid and dry waste goods, identification of standard<br />
treatment containers and proper load placement<br />
procedures, personal protection equipment<br />
required for removing materials from the autoclave,<br />
instructions for loading and unloading the autoclave,<br />
and instructions on cleaning and maintaining<br />
the autoclave.<br />
References<br />
Centers for Disease Control and Prevention. (2003).<br />
Guidelines for infection control in dental healthcare<br />
settings-2003. MMWR, December 19/52(RR17), 1-<br />
98.<br />
DePaola, L. G. (2003). Infection control and the<br />
prevention of disease transmission in the dental office:<br />
Back to the basics. The Infection Control FO-<br />
RUM, 1(2).<br />
HealthLink. Prospore and Prosure Technical Bulletin 1.<br />
Frequency of Use for <strong>Biological</strong> Indicators.<br />
Quality America, Inc. (2001). Break the chain of infection.<br />
OSHA Watch, January/February, 3(1).<br />
Ritter©—Installation and Operation Manual M9/<br />
M11 UltraClave TM Steam Sterilizer. Sterilizer Manufacture<br />
Monitoring Recommendations.<br />
Tilton, G., & Kauffman, M. (2004). Sterilization: A<br />
review of the basics. STERIS Corporation white papers,<br />
document number M2712EN. www.steris.<br />
com/resources/resources_wp.cfm#. June.
Article<br />
The Viral Immunology Center at Georgia State<br />
University (GSU) is recognized as the national resource<br />
facility for research related to the early diagnosis<br />
and effective treatment of dangerous viral diseases,<br />
most notably B virus (Cercopithecine herpesvirus<br />
1), herpesviridae. Funded by the National Institutes<br />
of Health, the Center operates the National B<br />
Virus Resource Laboratory aimed at learning more<br />
about the deadly alpha herpes virus and preventing<br />
its transmission to laboratory workers.<br />
The GSU Center, located in downtown Atlanta,<br />
was the first BSL-4 facility in the country operating in<br />
a university setting. Under the direction of Julia Hilliard,<br />
the goal of the laboratory’s research is not only<br />
to diagnose viral diseases, but also to study the agents<br />
and use their infrastructure to design vaccines.<br />
The B Virus laboratory had been located at the<br />
Southwest Foundation for Biomedical Research in<br />
San Antonio, Texas, and operations were proceeding<br />
well in the BSL-4 environment. However, space constraints<br />
limited the size of the staff to <strong>10</strong> people and<br />
restricted the amount of work that could be done.<br />
Research officials at Georgia State University<br />
called upon Hilliard to move her facility to downtown<br />
Atlanta in 1997, noting the University’s proximity<br />
to Emory University, the Centers for Disease<br />
Control, and the Medical College of Georgia. The<br />
retrofitted lab at the University offers three times the<br />
amount of space that Hilliard was using at the Texas<br />
facility.<br />
“The thrill of working in a rich milieu and having<br />
a new facility was enough to engage my interest<br />
Applied Biosafety, <strong>10</strong>(4) pp. 253-257 © ABSA <strong>2005</strong><br />
Operating a BSL-4 Laboratory in a University<br />
Setting: Georgia State University Lab<br />
Studies Deadly Alpha Herpes Virus<br />
Tradeline Publications<br />
Orinda, California<br />
in moving the laboratory,” recalls Hilliard. “We now<br />
know what it’s like to build a BSL-4 laboratory in<br />
a highly concentrated downtown area. We were<br />
told this would not be a big problem because<br />
the residents were already aware that maximumcontainment<br />
laboratories were operating in the city.”<br />
Maximum-containment BSL-3 and -4 suites are<br />
necessary due to the nature of the alpha herpes virus,<br />
or B Virus, which is transmitted by the Macaca<br />
species of monkeys often used in biomedical research.<br />
Although there is a low frequency of infection<br />
among people, the virus is considered a severe<br />
occupational hazard for laboratory workers as a result<br />
of its lethal consequences if not diagnosed<br />
quickly after infection.<br />
“The virus causes death in 80 percent of the infected<br />
individuals (after it literally attacks the cervical<br />
spinal cord),” says Hilliard. “There have been five<br />
fatalities in the last 12 years at four different institutions<br />
in four states. The survivors are our first introduction<br />
to what happens when you put a pathogen<br />
like B virus into the human population. The reason<br />
we work with this agent is because we know that<br />
rapid identification means we can successfully treat<br />
the individuals.”<br />
The cost of moving to Atlanta was approximately<br />
$200,000, which included expenses for shipping the<br />
laboratory equipment, moving staff, and flying back<br />
and forth between the new lab and the Texas lab to<br />
verify that the performance standards of the new<br />
facility matched those of the well established lab.<br />
The cost to renovate the space to accommodate the<br />
253
Center was approximately $1 million, not including<br />
the daily maintenance costs of the hot lab. Both<br />
laboratories had to be operated concurrently in order<br />
to preserve the integrity of the testing until Hilliard’s<br />
team determined that the new Center could<br />
function efficiently on its own.<br />
The architectural firm of Lord, Aeck and Sargent<br />
designed the first phase of the Center, while<br />
construction of the BSL-4 lab was supervised by the<br />
architectural firm of HOK in cooperation with The<br />
Baker Co., which customized the 32-linear-foot<br />
glovebox cabinet.<br />
Designing a BSL-4 Laboratory<br />
The Viral Immunology Center, housed in the<br />
University’s six-floor, 500,000-sf natural sciences<br />
building, features a departmental animal facility in<br />
the basement and BSL-3 and -4 laboratories on the<br />
third floor, including a specialized BSL-4 for small<br />
animal models of disease. The Center, which occupies<br />
about 5,000 sf and employs 30 people, also includes<br />
two support BSL-2 laboratories, a biochemistry<br />
lab, robotics facility, offices, a fermentation lab,<br />
and shared departmental resources, including electron<br />
and confocal microscopy areas, a sequencing<br />
core, and a FACS-analysis core for cell sorting.<br />
The activities that take place in the Natural Science<br />
Center are of particular interest when designing<br />
a BSL-4 laboratory in a university setting. This<br />
building typically houses the departments of biology,<br />
chemistry, biochemistry, physics, and anatomy in<br />
addition to the BSL-4 lab. Research activities that<br />
are not part of the viral laboratories must also be<br />
taken into consideration when deciding where to<br />
locate the BSL-4 suites. Other activities to consider<br />
include teaching sessions and seminars.<br />
Providing access to the laboratories in a manner<br />
that protects visitors is critical to the efficient operation<br />
of the facility. Serious consideration is given to<br />
the type of barriers that are erected between common<br />
access hallways and restricted areas to ensure<br />
that lay visitors and research supporters can view the<br />
work taking place without being exposed to potential<br />
risks. Access is provided via keypad entry for students,<br />
faculty from other disciplines, visiting scientists,<br />
security and maintenance personnel, and inves-<br />
254<br />
Operating a BSL-4 Laboratory in a University Setting<br />
tigators. The BSL-3 and -4 laboratories have a magnetic<br />
card access so that entry and exit into the facilities<br />
can be tracked by a computer. With the additional<br />
restrictions imposed by the new Homeland<br />
Security Program, all individuals who work within<br />
the BSL-3 and -4 labs must first have federal security<br />
clearance after submission of extensive documentation<br />
to the FBI. The facilities must also meet Clinical<br />
Laboratory Improvement Amendments and Select<br />
Agent inspection requirements to carry out the<br />
research and diagnostic missions of the laboratory.<br />
Key Components of a Maximum-<br />
Containment Facility<br />
Each day Hilliard’s facility receives up to 20<br />
boxes from all over the world from individuals who<br />
may have been exposed to the secretions of a Macaca<br />
monkey. Minimizing the transport of materials going<br />
to high-containment areas is critical. When the samples<br />
arrive, they are triaged to determine what tests<br />
must be done so the results can be sent to the concerned<br />
individuals as quickly as possible.<br />
The packages, transported through an isolated<br />
hallway that is sectioned off from other areas of the<br />
facility, are opened in the Level 2 unpackaging<br />
room, attached to the BSL-3 and -4 suites. Each of<br />
these areas can be accessed only by computercontrolled<br />
keypad entry. Any materials that leave the<br />
BSL-4 facility undergo an intensive search for evidence<br />
of any live virus, using virus plaque assays to<br />
verify that all virus has been inactivated. If the assay<br />
is negative, the chain of custody for removal begins.<br />
Items that leave the BSL-4 laboratory must go<br />
through two sets of autoclaves or two sets of crosslinked<br />
glutaraldehyde dunk baths. Dunk baths enable<br />
chemical sterilization of the outside wall of submersed<br />
containers. This allows a live virus to be removed<br />
from the cabinet for ultra-low freezing and<br />
storage within the BSL-4 and passage of inactivated<br />
materials to the Level 2 labs. Live virus never leave<br />
the suite.<br />
The disposal system consists of two redundant<br />
150-gallon tanks that are released into a boilerdecontamination<br />
unit. A chilling mechanism cools<br />
the water, which is released into the public system
once it is steam disinfected and verified as inactivated.<br />
A drain is situated under the tanks to contain<br />
leakage, should that occur.<br />
The specialized HVAC unit dedicated to the<br />
independent air system of the BSL-3 and -4 suites is<br />
located on the roof of the Natural Sciences Center,<br />
while the decontamination facility is positioned under<br />
the BSL-4 laboratory. Computers are used to<br />
analyze temperatures, airflow, and the rooftop exhaust<br />
systems, which are actively engaged. In case of<br />
power failures, a natural gas backup system is in<br />
place to maintain air purification, negative pressure,<br />
and equipment power.<br />
It is critical to be able to monitor the temperature<br />
and air supply for each of the high-containment<br />
suites by computer on site or from remote locations<br />
by the extensively trained and certified engineer required<br />
to maintain the facility. The outer hallways<br />
are kept at negative pressure assessed by magnahelics,<br />
and with each step further into the biocontainment<br />
areas the negative pressure gradient increases<br />
according to the specifications outlined in the<br />
CDC’s Biosafety in Microbiological and Biomedical<br />
Laboratories.<br />
“The goal of the BSL-3 rooms is to isolate viruses<br />
from small samples. In order to process the samples,<br />
pull out the virus, and identify unusual agents, we<br />
have to have incubators that are fed five percent carbon<br />
dioxide and 95 percent air,” explains Hilliard.<br />
“We can’t bring tanks in and out of these rooms, so<br />
we have a separate alcove which houses the gas tanks<br />
feeding the incubators in the BSL-3 and BSL-4 labs.”<br />
It is challenging to keep the BSL-3 laboratories<br />
stocked and tidy at the same time, keeping in mind<br />
that many of the items that come into the labs are<br />
not going to leave until they are thoroughly melted<br />
down by repeated autoclaving. Disabled equipment<br />
cannot be removed from the laboratory for maintenance<br />
or repair. Tools for minor repairs are decontaminated<br />
with gas sterilization before they are removed<br />
from the maximum-containment suites.<br />
Keeping the Scientists Safe<br />
Necessary precautions are taken to protect the<br />
researchers while they are working in the laboratories.<br />
Scientists usually work in a cabinet or a suit lab,<br />
Tradeline Publications<br />
which relies on the standard biocontainment gear,<br />
in the BSL-4 facility. Working in a cabinet lab is extremely<br />
challenging, but considered safer than a suit<br />
lab because the individual uses large glove ports and<br />
is separated from the pathogen by thick stainless<br />
steel. The cabinet lab at the Center is 32-feet long<br />
and can accommodate three or four researchers at a<br />
time. A nearby animal section houses mice, rats, and<br />
rabbits, and a screen built into the cabinet allows<br />
investigators to visualize materials analyzed by an<br />
inverted, phase-contrast microscope.<br />
Working in the cabinet lab can sometimes lead<br />
to fatigue because scientists must do all of their work<br />
using arm-length gloves to maneuver materials<br />
within the stainless steel cabinet while working in a<br />
line with other researchers. Working in the suit lab<br />
allows scientists to use the traditional lab layout and<br />
to move around more freely. However, breathing the<br />
positive-pressure air in the suit can also cause fatigue.<br />
Barrier protection masks are worn at all times in<br />
the BSL-3 and -4 labs. Only <strong>10</strong> people on Hilliard’s<br />
staff are trained to work in the BSL-3 lab, while only<br />
five of these can enter the BSL-4 facility.<br />
“The masks are basically a reminder for us not to<br />
put our double-gloved hands up to our faces. If we<br />
relied on them as filtration or personal protection<br />
devices, we would go to something different,” says<br />
Hilliard. “All agents are handled in a Class 2 cabinet<br />
in the BSL-3, so there is no time at which an agent is<br />
uncapped in the room surrounding the cabinet.”<br />
Important Considerations<br />
Careful consideration must be given to the installation<br />
of all systems and how they will interact.<br />
The HVAC system at GSU had been repaired at an<br />
annual cost of $12,000 every year since Hilliard’s lab<br />
moved into the facility. A new HVAC system specifically<br />
engineered after analysis of previous failures<br />
was installed at a cost of $250,000 and 2003 marked<br />
its first year of operation.<br />
“This is an existing building that we modified. It<br />
wasn’t meant to be under constant negative pressure<br />
and that has caused substantial stress on the walls<br />
and ceiling,” says Hilliard. “Careful consideration of<br />
the systems that are linked is very important. We are<br />
255
ight in the middle of downtown on a rooftop so<br />
there are many issues to address.”<br />
Cabinet labs should be designed so they are ergonomically<br />
comfortable for researchers of varying<br />
physical stature. The cabinet labs at the Center were<br />
designed largely with the input of the former associate<br />
director, who is more than 6-feet tall, creating a<br />
challenge for other lab staff to do their work.<br />
Smaller gloves, extenders, and a few other modifications<br />
enable the other investigators to work relatively<br />
comfortably.<br />
It is also crucial to properly position the laboratories<br />
in a manner that is most conducive to the type<br />
of work being done. For example, a West Nile BSL-3<br />
is located adjacent to the robotics facilities that service<br />
the sera and viral culture laboratories.<br />
The BSL-2 labs have standard virology for lower<br />
containment agents like HSV-1 and HSV-2. The<br />
sum total of the work performed in these labs is to<br />
take core resources of the BSL-3 and -4 labs, combine<br />
them with the research missions, maintain a<br />
high-containment robotics lab for high-throughput<br />
virus identification, as well as serologic screening,<br />
perform microarray analysis, and be flexible enough<br />
to look at new agents as they come to the scientists’<br />
attention.<br />
“All of our work would be for naught if we<br />
didn’t have the supportive BSL-2 labs,” says Hilliard.<br />
The robotics unit can perform multiple tests and<br />
process thousands of sera daily. The viral culture<br />
robot can plate samples and screen them at multiple<br />
times during the day for the presence of a virus. This<br />
allows mass processing of thousands of diagnostic<br />
samples. If a disturbance in cell culture is noted, a<br />
pager is sounded and an investigator is called to the<br />
room for further analyses and to notify the institution<br />
submitting the sample for analysis.<br />
“In the BSL-4 laboratory, the goal of our work<br />
is the production of large amounts of virus and containing<br />
the supply very securely,” says Hilliard. “We<br />
can then look at drug sensitivities and how the virus<br />
256<br />
Operating a BSL-4 Laboratory in a University Setting<br />
behaves in cells in order to understand the pathogen<br />
and how to control it.”<br />
Biography<br />
Julia Hilliard is director of the Viral Immunology<br />
Center at Georgia State University in the Department<br />
of Biology. She is also the Georgia Research<br />
Alliance Eminent Scholar in Molecular Biotechnology<br />
and Director of the National B Virus<br />
Resource Center for global diagnostic resources. She<br />
has worked with the BSL-4, newly classified Select<br />
Agent, B Virus (Cercopithecine herpesvirus 1) for 23<br />
years, providing diagnostic resources to the biomedical<br />
community for the last 16 years.<br />
This report is based on a presentation given by<br />
Julia Hilliard at Tradeline’s International Conference<br />
on Biocontainment Facilities in May 2003.<br />
For more information, please contact: Julia Hilliard,<br />
Director, Viral Immunology Center, Georgia<br />
State University, Box 4118, Atlanta, GA 30302-<br />
4118, 404-651-0811, jhilliard@gsu.edu.<br />
Reprinted with Permission © December 2003 from<br />
TradelineInc.com, a registered product of Tradeline Inc.,<br />
a provider of leading-edge resources to facilities planning<br />
and management through conferences, publications, and<br />
the Internet community. Visit www.TradelineInc.com for<br />
more information.<br />
Resources<br />
Biosafety in Microbiological and Biomedical<br />
Laboratories:<br />
www.cdc.gov/od/ohs/biosfty/bmbl4/bmbl4toc.htm<br />
Clinical Laboratory Improvement Amendments:<br />
www.cms.hhs.gov/clia/<br />
Select Agents:<br />
www.cdc.gov/od/sap/docs/salist.pdf<br />
Viral Immunology Center:<br />
www.gsu.edu/~wwwvir/index.html
Figure 1<br />
The entry area for the maximum-containment<br />
labs includes a pass-through shower. Scientists<br />
prepare for their work by donning either a<br />
suit lab or working in the cabinet lab.<br />
(Photo courtesy of Julia Hilliard.)<br />
Tradeline Publications<br />
Figure 2<br />
Materials that leave the BSL-4 lab go through<br />
two sets of autoclaves or two sets of cross-linked<br />
glutaraldehyde dunk baths. A decontamination<br />
facility is situated under the lab. The disposal<br />
system consists of two redundant 150-gallon<br />
tanks released into a boiler-decontamination unit.<br />
(Photo courtesy of Julia Hilliard.)<br />
Figure 3<br />
When pathogen samples arrive, the packages are transported through an isolated hallway<br />
that is cordoned off from other areas of the facility. They are opened in a Level 2 unpackaging<br />
room, which is attached to the BSL-3 and -4 labs. (Photo courtesy of Julia Hilliard.)<br />
257
Abstract<br />
258<br />
Special Feature<br />
Use of Multiple SOP Styles to Increase<br />
Personnel Compliance and <strong>Safety</strong> Within<br />
a BSL-2/BSL-3 Animal Facility<br />
Andrea Mitchell, Jeri Ellis, and Tim Ruddy<br />
University of Arizona Animal Care, Tucson, Arizona<br />
Biohazard training and compliance of husbandry<br />
and research staff are often complicated at the University<br />
of Arizona by the sporadic nature of the work<br />
within the BSL-2/BSL-3 suite. Projects may last for a<br />
month and then not be repeated for a significant period<br />
of time. Failure to adhere to approved safety measures<br />
and techniques for specific rooms/projects over time<br />
increased the need for clear standard operating procedures<br />
(SOPs) that were easily accessed and utilized.<br />
SOPs available only in the employee lounge are of little<br />
use when a question arises while changing cages within<br />
a BSL-2 animal room. To this end, new SOP formats<br />
and display locations were developed and instituted to<br />
increase awareness and comprehension of techniques<br />
used within the BSL-2/BSL-3 suite. Changes included<br />
the placement of plain text as well as picture-enhanced<br />
SOPs in common areas such as the employee lounge<br />
and entrance to the biohazard suite, and within the animal<br />
rooms. The introduction of SOPs containing color<br />
photographs has been instrumental in increasing compliance<br />
of in-room procedures by both native English<br />
speakers and those who do not speak English as a first<br />
language. Overall, the use of multiple styles of SOPs<br />
has been a huge success. This process has helped to<br />
reduce confusion and increase compliance by both the<br />
husbandry and research staffs working within the University<br />
Animal Care facilities.<br />
Introduction<br />
In 2002, a review of University Animal Care<br />
(UAC) husbandry and research staff procedures<br />
within the biohazard suite at the Central Animal<br />
Facility identified several areas of concern. Even<br />
though SOPs formalized in the late 1990s were GLPcompliant,<br />
most husbandry technicians did not have<br />
a good understanding of the SOPs or biosafety basics<br />
and were using techniques and procedures that<br />
could potentially cause the spread of contamination<br />
to personnel and/or the environment. Less than<br />
optimal processes were immediately halted and all<br />
husbandry staff were retrained based on existing versions<br />
of SOPs. Fortunately, the agents in use were<br />
primarily ABSL-2, and appropriate personal protective<br />
equipment (PPE) was being worn when the animals<br />
were handled. Research staff used appropriate<br />
technique when working with their animals, but had<br />
difficulty packaging contaminated cages appropriately<br />
for autoclaving out of the suite, often necessitating<br />
the unpacking and repacking of cages.<br />
Data Gathering<br />
Staff Interviews<br />
UAC husbandry and research technicians were<br />
surveyed to establish the cause of the breakdown in<br />
technique and noncompliance with UAC SOPs.<br />
Numerous barriers were identified:
Complex or Unique Procedures. Husbandry<br />
technicians frequently used practices appropriate for<br />
sterile animal rooms instead of the required practices<br />
needed for biohazard rooms. As the bulk of<br />
their workload involved handling “clean” animals,<br />
they found it counter-intuitive to handle the “dirty”<br />
animals differently. The mindset that the animals<br />
must be protected from the technician and the environment<br />
was ingrained and using techniques to protect<br />
personnel, not animals, was reported as “feeling<br />
wrong.”<br />
Individual Variations Among Studies. Procedural<br />
differences based on the agent used confused<br />
the husbandry technicians. Often the techniques<br />
used with one study were applied to the next, without<br />
regard to the differences in agent or route of<br />
infection.<br />
Training. Husbandry technicians were often<br />
trained by the last person to work in the animal<br />
room, with minimal emphasis on SOPs. Incorrect<br />
techniques were passed from one technician to the<br />
next, creating the “we’ve always done it this way”<br />
mindset. A heavy reliance was placed on expecting<br />
the technician to memorize and retain verbal information<br />
rather than to consult written documentation.<br />
Sporadic Nature of the Studies. The sporadic<br />
nature of the biohazard studies hindered the process<br />
of knowledge “ownership” by the husbandry technicians.<br />
Often a study would last several weeks and not<br />
be repeated for 6 months to a year. It was found that<br />
husbandry technicians were trying to rely on memory<br />
rather than written documentation to refresh<br />
their memories about required processes.<br />
Imprecise and Tedious SOPs. A review of existing<br />
husbandry SOPs showed that there were process<br />
inaccuracies, as well as contradictory statements<br />
among SOPs. Husbandry technicians complained<br />
that reading SOPs was tedious and time-consuming.<br />
The inaccuracies caused confusion, often resulting<br />
in the technician abandoning the SOP and relying<br />
on memory to complete a task.<br />
Location of SOPs (distance to animal room).<br />
Husbandry technicians reported distance from the<br />
animal room to the employee lounge, where the<br />
GLP-compliant SOPs were kept, as an issue in the<br />
use of SOPs. They related that if a question arose<br />
A. Mitchell, et al.<br />
while in the animal room, they did not want to<br />
waste time by removing their PPE, leaving the room,<br />
and searching out the appropriate SOP. Instead,<br />
they would rely on memory and check the SOP after<br />
their animal room work had been completed.<br />
Language. Some husbandry and research staff<br />
identified difficulty comprehending written instructions<br />
as one barrier to bagging contaminated caging<br />
appropriately. The individuals experiencing the most<br />
difficulty were those for whom English was not their<br />
primary language.<br />
Communication. Instructions from research<br />
staff as to PPE and husbandry procedures used for<br />
their agent at times varied from the information included<br />
in the Institutional Animal Care and Use<br />
Committee (IACUC)-approved protocol.<br />
Institutional Input<br />
Next, the IACUC-approved protocols were reviewed<br />
for agents and species, PPE and equipment<br />
needed, and procedures involved in the study. This<br />
information was then compared to existing GLPcompliant<br />
UAC husbandry SOPs and the differences<br />
between the two were discussed with the University<br />
Biosafety Officer to facilitate changes needed<br />
in the SOPs to increase compliance with known industry<br />
standards for the agents used.<br />
Materials and Methods<br />
SOPs<br />
Based on the data gathered from the IACUC<br />
protocols and interviews with researchers, UAC husbandry<br />
staff, research staff, and the University Institutional<br />
Biosafety Officer, it was apparent that the<br />
UAC biohazard SOPs needed revamping. The information<br />
presented in the SOPs, as well as the location<br />
and format of the SOPs, needed to be addressed.<br />
It was found that new husbandry staff<br />
needed the in-depth presentation of the GLPcompliant<br />
SOPs during initial training and for occasional<br />
review, whereas experienced staff had no need<br />
to read hundreds of pages of SOPs every time they<br />
were assigned to a biohazard animal room for the<br />
week.<br />
To this end, all biohazard SOPs were reviewed<br />
and revised. Careful attention was paid to ensuring<br />
259
260<br />
Use of Multiple SOP Styles to Increase Personnel Compliance and <strong>Safety</strong><br />
that interconnecting SOPs “spoke” to each other<br />
with accuracy. Two non-GLP-compliant SOP formats<br />
were developed to distill the information presented<br />
in the GLP-compliant SOPs to an abbreviated<br />
format for use by experienced, trained husbandry<br />
staff members. SOP placement was also revised:<br />
Employee Lounge SOP Book. University Animal<br />
Care maintains master electronic copies of GLPcompliant<br />
standard operating procedures which are<br />
available for review on a computer located in the<br />
employee lounge. Pictures were added to those SOPs<br />
where a photo could illustrate a complex issue, increase<br />
comprehension, and reduce the wordiness<br />
inherent in complex SOPs. To increase accessibility<br />
specifically to the biohazard SOPs, photocopies were<br />
organized into a three-ring binder and placed in the<br />
employee lounge.<br />
Entrance to the Biohazard Suite SOP Binder.<br />
The biohazard suite is on a different floor from the<br />
employee lounge. Because of this, another three-ring<br />
binder containing photocopies of the GLPcompliant<br />
husbandry biohazard SOPs was placed in<br />
the entry airlock to the biohazard suite. SOPs were<br />
placed in plastic sleeves with closure flaps to keep<br />
the pages clean and facilitate updating the binder<br />
without spending excessive dollars to laminate the<br />
pages. This location allows the husbandry technicians<br />
to review procedures prior to entering the biohazard<br />
suite.<br />
Animal Room. Several changes were implemented<br />
at the animal room level:<br />
• A biohazard questionnaire was designed and<br />
implemented to address several of the issues identified<br />
during the data-gathering phase. The questionnaire<br />
(shown in abbreviated format in Figure 1) is<br />
completed by the PI before a new study begins (new<br />
agent or change in procedure). The Animal Facility<br />
Supervisor compares the information presented on<br />
the questionnaire with the listed IACUC protocol to<br />
determine if there are any differences in the PPE<br />
and procedures listed on the documents. Discrepancies<br />
are addressed prior to the start of the study. The<br />
Animal Facility Supervisor also searches the Web to<br />
gain third-party insight into the hazards associated<br />
with the agent. The multi-page questionnaire is converted<br />
into a single page SOP (Figure 2) for posting<br />
on the outside of the animal room door for the<br />
duration of the study. This SOP provides several<br />
key pieces of information that the husbandry technician<br />
needs prior to entering the animal room: agent<br />
used, species used, contaminated caging/dead animal/trash-processing<br />
procedures, contact name, and<br />
phone number. This SOP varies in format and<br />
length from the GLP-compliant SOPs in an attempt<br />
to increase comprehension and compliance by using<br />
a pared down, bullet-point presentation of information.<br />
The purpose of this SOP is to quickly answer<br />
the question “What do I need to do in this room?”<br />
leaving the “How do I do this task?” to the more extensive<br />
GLP-compliant SOP format. As an example,<br />
Figure 2 instructs the husbandry technician to autoclave<br />
the soiled cages. This translates roughly into 15<br />
individual GLP-compliant SOPs and 25+ pages of<br />
material for the naïve husbandry technician to read.<br />
The experienced husbandry technician needs to<br />
know only “Do I autoclave the dirty caging?” The<br />
naïve technician needs to know how to put on the<br />
PPE, change the cages, bag the cages, operate the<br />
autoclave, etc.<br />
• A photo-enhanced SOP (shown in abbreviated<br />
format in Figure 3) was designed to increase compliance<br />
by research and husbandry staff when bagging<br />
dirty caging for autoclaving. Including pictures with<br />
text has increased procedural compliance while decreasing<br />
the amount of caging that must be reprocessed.<br />
The laminated SOP is posted on each biosafety<br />
cabinet within the animal facility. This SOP<br />
also varies in format from the GLP-compliant SOPs<br />
in an attempt to increase comprehension and compliance<br />
by using bright, colorful, digital pictures to<br />
illuminate a process that is vital to ensure sterilization<br />
of contaminated caging. Autoclave package size<br />
limitations and autoclave operational idiosyncrasies<br />
increase the need for compliance to departmental<br />
SOPs.<br />
• Three-ring binders containing the GLPcompliant<br />
SOPs pertaining specifically to that room<br />
were placed in the BSL-3 anterooms. These rooms<br />
vary radically in equipment, procedures, and personnel<br />
risk from the BSL-2 rooms and each other. The<br />
additional reference material has been a key component<br />
in training new personnel. Once again, SOPs<br />
were placed in plastic sleeves with closure flaps to<br />
facilitate updating the information.
Training to the SOPs<br />
After the GLP-compliant SOPs were revised, the<br />
additional SOP designs formalized, and both styles<br />
put in place, departmental training packets were updated<br />
to reflect the changes in procedures and processes.<br />
Husbandry staff members were retrained and a<br />
“one size fits all” mindset was discouraged. Emphasis<br />
was placed on recognizing the differences in procedures<br />
in their daily routine. Husbandry staff members<br />
are now formally trained using all styles of biohazard<br />
SOPs and are fully aware of where to find the<br />
information they need to work safely in the animal<br />
rooms.<br />
Conclusion<br />
Compliance with standard operating procedures<br />
is a crucial step in ensuring the safety of husbandry<br />
A. Mitchell, et al.<br />
and research technicians working in areas housing<br />
animals exposed to biohazards. It is vital to identify<br />
barriers to comprehension of SOPs by the technicians.<br />
Physical location, language, and accuracy are<br />
all important factors to consider when reviewing<br />
SOPs. Is the SOP in an area where the technician<br />
can review it when actually performing the task? If<br />
not, is it possible to place the information where it<br />
will be readily accessible? Is it important that all of<br />
the information is presented in its entirety or can<br />
the SOP be abbreviated and the format changed to<br />
present a more readily comprehended and consumed<br />
product? Will using pictures reduce confusion<br />
and wordiness? Do all interrelated SOPs speak<br />
to one another accurately? By answering these questions,<br />
University Animal Care was able to produce<br />
stronger SOPs and a safer working environment for<br />
its technicians and research staff.<br />
IMPORTANT .................IMPORTANT......................IMPORTANT...............IMPORTANT<br />
Name<br />
A change of address notice should be sent at least 6 weeks in advance to the ABSA National Office to<br />
ensure that all mailings, including the journal, will reach you. ABSA is not responsible for misrouted mail as<br />
a result of insufficient notification of an address change. Undelivered copies resulting from an insufficient<br />
address change notification will not be replaced, but single issues may be purchased at the single issue price.<br />
Old Address<br />
Old Phone <strong>Number</strong><br />
NEW ADDRESS<br />
CHANGE OF ADDRESS FORM<br />
CITY STATE ZIP +4<br />
NEW PHONE NUMBER<br />
E-MAIL ADDRESS<br />
Effective Date<br />
261
FIGURE 1<br />
UAC Biohazard Information Questionnaire<br />
This worksheet has been prepared to aid in the establishment of investigator specific Standard Operating Procedures<br />
(SOPs) for biohazard studies. Completing this worksheet will better enable UAC to care for your biohazardous animals<br />
and assist you in meeting your research goals.<br />
This form must be filled out and submitted to the UAC Facility Supervisor prior to initiation of animal<br />
experiments.<br />
P.I. Office Phone # Research Tech:<br />
Lab Phone # Weekend/Holiday Contact Name and Phone #:<br />
Species used: Protocol #:<br />
Agent used: Please check all that apply and list agent (s). (Note: This form must be filled out in addition to the<br />
Authorization Form for Radioactive Material.)<br />
Carcinogenic agent(s):<br />
Radioactive agent(s):<br />
Human Infectious Agent(s):<br />
Animal Infectious Agent(s):<br />
Study size and duration:<br />
How many cages of animals do you expect to have in use at a time?<br />
How long will the animals be in the room?<br />
If using a radioactive compound, can the animals be housed in a general animal room?<br />
Husbandry Tasks. Please check one:<br />
UAC staff will do all husbandry tasks for the room. This includes changing the cages, removing dead animals,<br />
servicing the cages by adding food and water as needed and changing flooded cages.<br />
Investigator will perform all husbandry tasks. (Note-This includes packaging the used caging/bedding/trash for<br />
autoclaving.)<br />
Investigator and UAC staff will share husbandry tasks. Please explain:<br />
Diets: Please check one<br />
All mice will be fed Teklad NIH-31 diet<br />
All rats will be fed Teklad 4% Mouse/Rat diet<br />
Other, Please explain:<br />
Protective Equipment Needed:<br />
All personnel entering this room need to wear the following: Please check all that apply:<br />
Bonnet N95 Respirator Eye protection Yellow gown Jump suit Shoe covers Gloves<br />
Other:<br />
All personnel handling the animals in this room need to use the following when opening the cages:<br />
Biosafety Cabinet Glove Box Chemical Fume Hood Other:<br />
Check all that apply:<br />
All animal cages and bedding must be autoclaved after use in the animal room.<br />
All animal bedding must be disposed of in yellow radioactive bags and the label filled out.<br />
All trash must be autoclaved prior to disposal from the animal room.<br />
Trash may be disposed in the red barrels without autoclaving.<br />
All animal carcasses must be autoclaved prior to disposal.<br />
All animal carcasses must be disposed of in yellow radioactive bags and the label filled out.<br />
Animal carcasses may be disposed of in the red barrels without autoclaving.<br />
Other:
FIGURE 2<br />
UAC Biohazard SOP (Completed Sample)<br />
P.I. John Jones, DVM, PhD P.I. E-mail: jjones@u.arizona.edu Office Phone # 555-1234<br />
Research Technician: Jane Smith E-mail: jsmith@u.arizona.edu Fax # 555-2345<br />
Lab Phone # 555-3456 Weekend/Holiday Contact Name and Phone #: Jane 555-9023<br />
Species used: Mouse Protocol #: 04-555<br />
Agent used: Human and Animal Infectious Agent: Cryptosporidium parvum<br />
Study size and duration: Approximately <strong>10</strong>-12 cages will be in the room for 7-<strong>10</strong> days.<br />
Husbandry Tasks.<br />
UAC staff will do all husbandry tasks for the room. This includes changing the cages,<br />
removing dead animals, servicing the cages by adding food and water as needed and<br />
changing flooded cages.<br />
Diets: All mice will be fed Teklad NIH-31 non-irradiated mouse chow.<br />
Protective Equipment Needed:<br />
All personnel entering this room need to wear the following: Please check all that apply:<br />
Bonnet N95 Respirator Yellow gown Impervious shoe covers x 2 Gloves x 2<br />
All personnel handling the animals in this room need to use the following when opening the cages: Biosafety<br />
cabinet<br />
Check all that apply:<br />
All animal cages, bedding and trash must be autoclaved after use in the animal room.<br />
Animal carcasses may be disposed of in the red barrels without autoclaving.<br />
Personnel must ungown in the ante room.<br />
The PI will be responsible for terminating all moribund animals.<br />
Notification of Death: Death slips will be filled out and mailed as usual. Investigators will be notified<br />
immediately upon finding dead animals in order for them to harvest tissues or necropsy.<br />
P.I. UAC Supv.<br />
Signature Date Signature Date
264<br />
FIGURE 3<br />
Bagging animal caging using a biosaf ety cabinet with a dump station:<br />
1<br />
4<br />
5<br />
Join a Committee<br />
Use of Multiple SOP Styles to Increase Personnel Compliance and <strong>Safety</strong><br />
1. Gown up before entering the ani mal room.<br />
See door SOP for specific PPE worn.<br />
2. Line the dump station barrel with a red, or<br />
orange bi ohazard bag – see door SOP.<br />
3<br />
3. T urn the biosafety cabinet on.<br />
4. Clean cabinet with Clidox. Spray directl y on all surfaces except<br />
“ceiling” and wi pe down with paper towels. Follow the same<br />
process with alcohol.<br />
5. Place clean cages, water bottles, etc. i n the biosafety cabinet if<br />
changing cages.<br />
Have you ever considered joining a committee? When you choose to serve on a volunteer committee, you<br />
open up a world of possibilities for networking, professional growth, and career opportunities while serving<br />
your profession. Volunteer member groups are the backbone of the association because they:<br />
• Serve as a forum for exchange of information<br />
• Advance the science in all specialties of biosafety<br />
• Develop guidelines and standards<br />
• Provide education and training<br />
• Link ABSA to many other institutions<br />
You should explore committees in areas of the profession where you are active or have an interest. There<br />
is a great variety; you can be sure to find one of interest to you. Please review the list of committees and<br />
identify those areas in which you would like to participate or contact the chair of the committee (http://<br />
www.absa.org/abocommittees.html) that interests you to find out more information about the committee’s<br />
goals. You are also invited to attend the committee’s meeting during our national conference or at any other<br />
time (all committee meetings are open).<br />
2
Special Feature<br />
Book Review<br />
Reviewed by George A. Pankey<br />
Ochsner Clinic Foundation, New Orleans, Louisiana<br />
Revenge of the Microbes<br />
By Abigail A. Salyers and Dixie D. Whitt<br />
Washington, DC: ASM Press for Microbiology<br />
186 pp, $ 29.95<br />
ISBN: 1-55581-298-8<br />
This book, for “the general public about antibiotics<br />
and resistance to them,” is the authors’ first<br />
attempt at such a publication. They are both wellknown<br />
scientists and microbiology educators who<br />
have written textbooks on the subject.<br />
As would be expected, some of the material in<br />
Revenge of the Microbes is a little too advanced for the<br />
“general public”; however, for students of medicine,<br />
and members of ABSA, this is an excellent little<br />
book that makes a strong attempt to orient the<br />
reader to the problems of antimicrobial resistance<br />
and the potential etiologies. It is particularly refreshing<br />
that potential contributors to the problem are<br />
not lambasted. Discussions on the use and abuse of<br />
antibiotics by physicians, veterinarians, farmers, and<br />
industry are presented in a balanced fashion. The<br />
dentists somehow escaped discussion, although they<br />
are big antimicrobial users.<br />
I especially enjoyed the historical coverage and<br />
the issues to ponder that occur at the end of each of<br />
the 11 chapters. Following is my evaluation of each<br />
chapter, in parentheses, after each title:<br />
1. Magic Bullets, Miracle Drugs (Excellent)<br />
2. A Brief Look at the History of Antibiotics (Excellent)<br />
3. Bacteria Reveal Their Adaptability, Threatening the<br />
Brief Reign of Antibiotics (Simple and accurate)<br />
4. Antibiotic-Resistant Bacteria in the News (The re-<br />
porters get their due.)<br />
5. Antibiotics that Inhibit Bacterial Cell Wall Synthesis<br />
(Clearly detailed)<br />
6. Antibiotics that Inhibit the Synthesis of Bacterial Proteins<br />
(Good, but eperezolid has not “hit the market”<br />
yet)<br />
7. Fluoroquinolones, Sulfa Drugs, and Antituberculosis<br />
Drugs (Treatment specifics of antibiotic choices<br />
and side effects are not data-based and material<br />
ventures too far from the principles under discussion.)<br />
8. Bacterial Promiscuity: How Bacterial Sex Contributes<br />
to Development of Resistance (Beautifully written)<br />
9. The Looming Crisis in Antibiotic Availability (A<br />
must read)<br />
<strong>10</strong>. Antiseptics and Disinfectants (A practical and simple<br />
summary)<br />
11. Antiviral, Antifungal, and Antiprotozoal Compounds<br />
(Shows that bacteria are not the only antimicrobial-resistant<br />
microorganisms)<br />
The authors’ folksy writing style makes reading<br />
the book very pleasant. It reminded me of many of<br />
the authors in the United Kingdom whose writing<br />
style keeps one interested and awake.<br />
Revenge of the Microbes is appropriately illustrated<br />
and has an adequate suggested reading list. I<br />
did not find the “structures of antimicrobial agents<br />
mentioned in the text” in Appendix I or Appendix<br />
II regarding “how clinical laboratories measure resistance”<br />
to be necessary or appropriate for the intended<br />
audience. However, this book should be required<br />
reading for all medical, veterinary, nursing,<br />
and pharmacy students as well as those interested in<br />
biosafety.<br />
265
266<br />
Special Feature<br />
Book Review<br />
Reviewed by Michael P. Owen<br />
U.S. Food and Drug Administration Pacific Regional Laboratory Northwest, Bothell, Washington<br />
Biodefense: Principles and Pathogens<br />
Edited by Michael S. Bronze<br />
and Ronald A. Greenfield<br />
Wymondham, United Kingdom: Horizon Bioscience<br />
838 pp., $335, hardcover<br />
ISBN: 1-9094933-12-2<br />
Disclaimer: The opinions and conclusions expressed<br />
in this article are solely the views of the reviewer<br />
and do not necessarily reflect those of the<br />
U.S. Food and Drug Administration.<br />
The 2001 anthrax attacks on the East Coast of<br />
the United States, the 1984 release of Salmonella bacteria<br />
in Oregon, the multiple attempts by the Aum<br />
Shinrikyo cult in Japan to use biological weapons,<br />
and the regularly-reported threats of Al-Qa’ida and<br />
other terrorist movements attempting to use biological<br />
agents have demonstrated that the public health<br />
sector needs an increased sense of urgency to adequately<br />
prepare for bioterrorism events.<br />
One core component of biodefense is continuing<br />
education. Physicians, scientists, government<br />
officials, and other groups involved in public health<br />
need to be constantly aware of current developments<br />
in disease pathology, treatments, detection, biological<br />
safety, and biosecurity to provide an effective response<br />
to bioterrorism attacks. Michael S. Bronze<br />
and Ronald A. Greenfield, University of Oklahoma<br />
Health Sciences Center in Oklahoma City, Oklahoma,<br />
have edited a book about biodefense that assists<br />
with this challenge. One of the notable aspects<br />
of this text is that its information is current, including<br />
many references published in <strong>2005</strong>.<br />
Biodefense: Principles and Pathogens’ 23 chapters<br />
are detailed review articles and the book is actually<br />
two different texts in the same volume. The first<br />
seven chapters are a general discussion on biodefense,<br />
including a history of biological weapons, public<br />
health preparedness, public policy and legal issues<br />
surrounding terrorism in the U.S., hospital preparedness<br />
and infection control, surveillance and detection<br />
methods, and psychosocial issues.<br />
The remaining 16 chapters are detailed presentations<br />
about biological agents and biological toxins.<br />
Most of these chapters have sections on the agent’s<br />
history, microbiology, epidemiology, pathogenesis,<br />
veterinary manifestations, clinical manifestations in<br />
humans, diagnosis, treatment, prognosis, prevention,<br />
and research issues. Substances from all three<br />
CDC Bioterrorism Agent Categories A, B, C are<br />
presented. Chapters about food safety, water safety,<br />
agroterrorism, and emerging infectious diseases such<br />
as multi-drug resistant tuberculosis and severe acute<br />
respiratory syndrome are also included, along with a<br />
timely discussion on highly pathogenic avian influenza.<br />
Biodefense: Principles and Pathogens is almost entirely<br />
text. Although there are few images and tables,<br />
those that are included summarize many of the<br />
book’s important topics. The limited graphics is not<br />
necessarily a disadvantage because Biodefense: Principles<br />
and Pathogens is basically one large review article.<br />
As a result of this format, the book contains more<br />
information than tightly-packed chromatin in an<br />
eukaryotic cell. If the reader wants to see more<br />
graphics, the excellent citations and lists of references<br />
should minimize any effort to locate original<br />
publications containing the desired graphics.<br />
The first section presents many excellent points<br />
on preparedness. For example, the text compares<br />
nations such as the United Kingdom and Israel that
have national bioterrorism response plans in place to<br />
the United States which has 50 different plans, one<br />
for each state. Additionally, when discussing the<br />
Strategic National Stockpile of pharmaceuticals and<br />
vaccines, the text cautions that most communities<br />
will be on their own for at least 72 hours until these<br />
supplies can be distributed. It is a sad irony that a<br />
few months after this book was published, the U.S.<br />
was challenged by these issues during the strikes of<br />
Hurricane Katrina and Hurricane Rita. As a result of<br />
those two storms, adjusting the responsibilities of<br />
federal, state, and local agencies when responding to<br />
natural disasters and terrorist attacks and planning<br />
for the degree of self-sufficiency in disaster response<br />
each must assume will likely be often discussed topics<br />
over the next several years.<br />
The chapter on surveillance and detection is well<br />
written and lists methods that are both state-of-theart<br />
and in development. A longer discussion about<br />
the CDC Laboratory Response Network (LRN)<br />
would have been helpful; however, this subject is<br />
addressed in detail on the CDC web site<br />
and in <strong>Biological</strong> Weapons Defense:<br />
Principles and Mechanisms for Infectious Diseases<br />
Counter-Bioterrorism by Lindler et al (Humana Press,<br />
December 2004).<br />
The chapters on the agents are comprehensive.<br />
Because of their depth and detail, physicians and<br />
scientists will probably find them more useful than<br />
the general public. As in the first part of the book,<br />
the references continue to be very current and easily<br />
retrievable. The clinical information is written at a<br />
level of detail similar to the PDR Guide to <strong>Biological</strong><br />
and Chemical Warfare Response: Diagnosis, Treatment,<br />
Prevention by Sifton et al (Thomson PDR, February<br />
2002) and is oriented toward physicians and other<br />
healthcare personnel. The microbiology sections are<br />
in-depth summaries of current knowledge. The research<br />
issues presented at the end of each agent’s<br />
chapter list several new treatment strategies in development.<br />
The first half of the book could have been ex-<br />
M. P. Owen<br />
panded. These chapters offer only an overview of<br />
bioterrorism preparedness; however, they do provide<br />
a solid launching pad for further investigation into<br />
this topic, and the long lists of references make finding<br />
information on this subject easier.<br />
The food safety, water safety, and agroterrorism<br />
chapters would have been more useful if they were<br />
longer, too. However, this observation is not actually<br />
a weakness of the book. As mentioned above, the<br />
text is meant to be a review of biodefense. The relatively<br />
small size of these sections is most likely<br />
the result of most efforts in biodefense and infectious<br />
diseases being focused on higher-level threats.<br />
Longer reviews will likely appear when research efforts<br />
in these areas are increased.<br />
The main disadvantage of Biodefense: Principles<br />
and Pathogens is the cost, which is higher than many<br />
biodefense and biology books available today. Including<br />
an electronic version of the book on a CD-<br />
ROM, similar to <strong>Biological</strong> Weapons Defense: Principles<br />
and Mechanisms for Infectious Diseases Counter-<br />
Bioterrorism, would have been a helpful addition. Another<br />
option would have been access to a Web site<br />
that has book updates similar to Molecular Cloning: A<br />
Laboratory Manual by Sambrook and Russell (Cold<br />
Spring Harbor Laboratory Press, January 2001).<br />
Again, the lists of references at the end of each chapter<br />
are quite valuable, saving readers a great deal of<br />
time on literature searches.<br />
Biodefense: Principles and Pathogens is a good<br />
primer on current issues in biodefense. Although it<br />
will be most beneficial to physicians and researchers,<br />
the text will also be helpful to biological safety professionals,<br />
especially when performing risk assessments.<br />
It will be a nice addition to any biodefense,<br />
infectious disease, or biological safety library.<br />
Acknowledgement<br />
I would like to thank Karen B. Byers for providing<br />
the opportunity to review the text and submit a<br />
review for this journal.<br />
267
Do you have a biosafety question and you’re not<br />
sure who to ask? Send your questions to the “Ask<br />
the Experts” column and I’ll get them answered for<br />
you. Drawing from my own experience or that of<br />
other experts in the field, we’ll try to compile a thorough<br />
and comprehensive answer to your question.<br />
Please e-mail your questions to jkeene@biohaztec.<br />
com or to Co-Editor Barbara Johnson at barbara_johnson@verizon.net<br />
or Co-Editor Karen B.<br />
Byers at karen_byers@dfci.harvard.edu.<br />
HEPA-Filtered Supply Air for<br />
BSL-3 Laboratories?<br />
Question<br />
I have observed that NIH Design and Policy<br />
Guidelines (http://orf.od.nih.gov/policy/index.htm)<br />
do not appear to require HEPA filtration of air supply<br />
at the BSL-3 level. Isn’t there a possibility that<br />
microorganisms could be drawn into the intake air<br />
and potentially affect the outcome of the science<br />
being conducted in a BSL-3 lab (or any other lab)? If<br />
so, to satisfy the requirement for “flexibility,” wouldn’t<br />
it be more prudent to suggest that designers provide<br />
Air Handling Units (AHUs) with the capacity of<br />
adding HEPA filters?<br />
If I’m not mistaken, the source of the contamination<br />
in the air supply during the Legionnaire’s<br />
incident turned out to be carried on airborne dust<br />
from a construction site in close proximity to the air<br />
intakes of the hotel. Are the 30% prefilters and the<br />
95% filters that the guidelines require for supply air<br />
adequate to prevent a similar incident?<br />
268<br />
Special Feature<br />
Ask the Experts<br />
John H. Keene<br />
Biohaztec Associates, Midlothian, Virginia<br />
Response<br />
The question of HEPA filtration of supply air<br />
for containment laboratories is being asked more<br />
frequently as the construction of more containment<br />
laboratories is being considered. The intake air in<br />
most facilities is filtered by a prefilter and a 95% filter<br />
(not HEPA). This level of filtration is sufficient<br />
for both the general building and the containment<br />
laboratory. HEPA filtering of the air delivered to the<br />
BSL-3 laboratory is not necessary to protect the work<br />
since all open manipulations of infectious materials<br />
are performed in a biosafety cabinet or other physical<br />
containment devices. Moreover, these are leaky<br />
labs and air is drawn through the door from areas<br />
outside of the laboratory anyway.<br />
HEPA filtration of the air in these containment<br />
labs was considered because of concern about potential<br />
“backflow” of air from the lab to the supply system.<br />
This is not a valid concern for several reasons:<br />
1. The lab is not generally contaminated since the<br />
work is contained.<br />
2. In modern buildings control systems should ensure<br />
that the lab would not go positive in case of an<br />
exhaust fan failure.<br />
3. If for some reason the controls failed and the lab<br />
did go positive, the air would take the route of least<br />
resistance—the spaces around the doors and not the<br />
supply system which has a built-in resistance in the<br />
building filter system, and which, if it is still running,<br />
would be pushing air into the room so it<br />
would have to escape through another route.<br />
4. For any possible release, a highly unlikely sequence<br />
of events would have to occur, i.e., a spill in<br />
the laboratory at the same time that the exhaust
fans, primary and backup, failed as well as the supply<br />
fan failing at the same time.<br />
In addition, installing HEPA filters because of a<br />
concern about contamination of the supply duct<br />
work in a containment lab should be reviewed carefully.<br />
HEPA filtration of clean rooms is performed<br />
to reduce the particulate count in these rooms, not<br />
necessarily to remove infectious particles. The filters<br />
are placed so that the supply air blows against the<br />
filter and against the seal of the filter to the housing,<br />
thus ensuring, when properly installed, the continued<br />
seal of the filter. If one assumes that there is a<br />
possibility of contamination of the ducts (not a realistic<br />
assumption given the above discussion), one<br />
would want to install the HEPA filter so that it<br />
would seal in the direction of the potentially contaminated<br />
air flow, which would be toward the supply<br />
air duct. However, with the supply air blowing in<br />
the opposite direction the majority of the time, it<br />
would be difficult, if not impossible, to ensure that<br />
Fact Sheets on Terrorist Attacks<br />
J. H. Keene<br />
the filter seal was not disrupted by the push of air<br />
against it. Secondly, if it is assumed that the laboratory<br />
air is contaminated when it passes back through<br />
the filter, then the filter must be capable of being<br />
decontaminated and tested—a daunting task in itself.<br />
Consequently, the HEPA filtration of supply air in a<br />
BSL-3 laboratory is neither necessary nor desirable.<br />
Regarding the Legionella question: The outbreak<br />
resulted from outside air contamination, but not<br />
necessarily from construction dust. In fact, the outbreak<br />
resulted from Legionella contamination of the<br />
cooling tower water that was being aerosolized.<br />
While contamination of the intake air with Legionella<br />
or any other infectious agent might affect the<br />
personnel in a containment facility, as it has in many<br />
instances, it would not affect the work since good<br />
microbiological practice assumes that air in the laboratory<br />
is never sterile. In summary, the work in BSL-<br />
3 labs is not “clean room” work and does not have<br />
to be HEPA filtered to keep out potential pathogens.<br />
The National Academies is preparing, in cooperation with the Department of Homeland Security, fact<br />
sheets on four types of terrorist attacks. Drawing on our many reviewed publications, the expertise of our<br />
members, and the knowledge of other esteemed authorities, the fact sheets will provide reliable, objective<br />
information. Go to: www.nae.edu/nae/pubundcom.nsf/weblinks/CGOZ-642P3W?OpenDocument.<br />
They are being designed primarily for reporters as part of the project News and Terrorism:<br />
Communicating in a Crisis, though they will be helpful to anyone looking for a clear explanation of the<br />
fundamentals of science, engineering, and health related to such attacks.<br />
These fact sheets are a product of the National Research Council Division on Earth and Life Studies.<br />
<strong>Biological</strong> Attack (pdf file, 277 KB)—Where do biological agents originate? What’s the difference between<br />
“infectious” and “contagious”? How long after exposure will symptoms appear?<br />
Chemical Attack (pdf file, 72 KB)—What are the different origins of toxic chemicals that could be used? How<br />
do chemical toxicities vary? What are the practical steps to take if there’s a chemical release?<br />
Radiological Attack (pdf file, 68 KB)—What are radiological dispersal devices, a.k.a. “dirty bombs”? How are<br />
they different from nuclear bombs? What are their physical and psychological health effects?<br />
Nuclear Attack (pdf file, 192 KB) NEW!—What is radioactive fallout, and how is it dangerous? What are the<br />
short-term and long-term effects of radiation exposure? What is the likely size of a nuclear explosion from an<br />
attack by terrorists?<br />
269
Biosafety Tips brings you practical approaches to<br />
biosafety or “news you can use.” If you are looking<br />
for a useful and sensible solution to a biocontainment<br />
problem or perhaps a reference to help convince<br />
a skeptical researcher of the need for caution,<br />
this is the place to look. In this column I will share<br />
some biosafety insights for managing a variety of<br />
workplace situations. I welcome feedback or suggestions<br />
for future topics. Please e-mail any comments<br />
or suggestions to karen_byers@dfci.harvard.edu or<br />
to Co-Editor Barbara Johnson at barbara_johnson@<br />
verizon.net.<br />
Lymphocytic Choriomeningitis Virus—<br />
A Hazard in Rodent Animal Colonies<br />
In April <strong>2005</strong>, a woman died of a stroke and<br />
after a thorough work-up, her organs were donated<br />
to four recipients. In May, state authorities notified<br />
the CDC that three of the transplant recipients had<br />
died, and the fourth was ill. Extensive testing revealed<br />
that lymphocytic choriomeningitis virus<br />
(LCMV) was present in the transplanted organs. Review<br />
of the organ donor’s history indicated that she<br />
had a new pet hamster, and the hamster was positive<br />
for LCMV infection. Although the donor had a subclinical<br />
(asymptomatic) infection, the immunosuppressed<br />
organ recipients developed fatal or serious<br />
infections from the infected organs (CDC, <strong>2005</strong>).<br />
To prevent disease transmission from pet rodents,<br />
CDC has posted advice at: www.cdc.gov/ncidod/<br />
dvrd/spb/mnpages/dispages/lcmv/owners.htm.<br />
Wild, or house, mice are a far more common<br />
source of LCMV. LCMV is a rodent-borne Arenavirus,<br />
and about 5% of adults living in urban populations<br />
have antibodies indicating previous exposure<br />
270<br />
Special Feature<br />
Biosafety Tips<br />
Karen B. Byers<br />
Dana Farber Cancer Institute, Boston, Massachusetts<br />
to LCMV (CDC, <strong>2005</strong>). Subclinical LCMV infection<br />
in a healthy adult may go unnoticed, but the<br />
virus may also produce a flu-like illness, or aseptic<br />
meningitis. LCMV is not spread from person to person,<br />
except that it may spread vertically from a pregnant<br />
woman to a developing fetus. Exposures during<br />
the first or second trimester are a serious risk to the<br />
fetus (CDC, <strong>2005</strong>). To protect the general public<br />
from the risk of contracting LCMV from wild rodents,<br />
the CDC has posted practical guidelines on<br />
the Web and provided detailed information in the<br />
publication Interim Guidance for Minimizing Risk for<br />
Human Lymphocytic Choriomeningitis Virus Infection<br />
Associated with Rodents (CDC, <strong>2005</strong>).<br />
Case Study 1<br />
In the occupational setting, animal facilities are<br />
carefully designed to prevent entry by wild mice and<br />
colonies are routinely screened for LCMV. In addition<br />
to the zoonotic risk, infection with LCMV can<br />
affect a wide range of research results (National Research<br />
Council, 1991). The following case study describes<br />
the chain of events that lead to an LCMV<br />
outbreak at a research institute in 1989 (Dykewicz et<br />
al., 1992).<br />
• In 1964, a cancer research institute developed a<br />
proprietary cancer cell line. This institute routinely<br />
injected the cell line into rodents to induce tumors<br />
in order to study metastasis.<br />
• In 1988, the institute began replacing the hamster<br />
animal model with nude mice.<br />
• A lapse in the routine serological monitoring of<br />
rodent colony health occurred between August 1988<br />
and March 1989. When the monitoring resumed,<br />
the oldest sentinel hamsters were positive for LCMV.
• In May 1989, an animal care worker who had<br />
never worked with hamsters was hospitalized with<br />
aseptic meningitis. With the information that the<br />
sentinel animals had LCMV antibodies, the institute’s<br />
management requested testing to “rule out”<br />
LCMV. The hospitalized staff member was diagnosed<br />
with LCMV.<br />
• How could this infection have occurred? The<br />
proprietary cell line was tested, and it was positive<br />
for LCMV. Other staff members began reporting a<br />
range of complaints, so the CDC was alerted and an<br />
investigation followed.<br />
Results of CDC Investigation<br />
Eighty-two out of 90 staff members consented<br />
to serological monitoring for LCMV antibodies.<br />
Seven were positive, indicating previous exposure to<br />
LCMV, and one was a “probable” previous infection.<br />
The control group included 145 local blood<br />
donors with only one sample positive for LCMV<br />
(Dykewicz et al., 1992). Frozen aliquots of the proprietary<br />
cell line were thawed and it was discovered<br />
that aliquots as far back as 1975 were seropositive<br />
for LCMV. In addition, 13 out of 70 other cell lines<br />
passaged in animals were also positive.<br />
So why did the outbreak occur in 1988, if the<br />
cells had been infected for a long time? A review of<br />
all the factors the eight seropositive staff members<br />
had in common revealed no association with needlesticks<br />
or sharps injuries, bites or scratches, rural residence,<br />
pets, or noncompliance with the use of personal<br />
protective equipment. The facility had a policy<br />
of requiring gloves and a surgical mask. Only one<br />
fact stood out—the eight seropositive staff members<br />
had more contact with nude mice (median, <strong>10</strong> hours<br />
per week) compared to seronegative staff (median, 1<br />
hour per week) (Dykewicz et al.,1992).<br />
Nude mice are hairless, lack a thymus, and have<br />
an impaired immune system. They can become persistently<br />
infected with LCMV and excrete it in high<br />
titer; this characteristic is aptly called “viruria.”<br />
(Dykewicz et al., 1992). LCMV infection of nude<br />
mice does not produce symptoms in the mice and<br />
cannot be detected by direct serological monitoring<br />
since nude mice do not produce an antibody response.<br />
Apparently, the 80-fold increase in the use<br />
of nude mice resulted in a build-up of the viral reser-<br />
K. B. Byers<br />
voir in this facility and led to seven infections with<br />
two hospitalizations and one “probable” infection.<br />
The article goes on to describe the institute’s<br />
effort to contact former staff members and the many<br />
recipients of various cell lines to inform them of the<br />
LCMV infection. If the facility administration had<br />
not requested testing of the staff member hospitalized<br />
with aseptic meningitis, this outbreak might not<br />
have been recognized. Even if an animal colony is<br />
considered pathogen-free, the use of cell lines passaged<br />
in animals in another facility puts the colony,<br />
and the staff, at risk.<br />
Case Study 2<br />
An example similar to the one above was presented<br />
at the 2004 ABSA conference (Braun, 2004).<br />
In 1998, an animal technician developed a persistent<br />
high fever of unknown origin and “worrisome”<br />
symptoms. Several months later, three sentinel animals<br />
in the room where the technician worked were<br />
positive for LCMV infection. All of the other technicians,<br />
veterinarians, and investigators tested negative,<br />
but the animal technician who was ill tested<br />
positive. The source was a human cell line obtained<br />
from another institution that had been passaged in<br />
nude mice for <strong>10</strong> to 12 years without reports of contamination.<br />
Fortunately, that outbreak was limited<br />
to a single case.<br />
The research community must understand the<br />
importance of compliance with a cell line screening<br />
policy, since once a study has been approved, it is<br />
very difficult to monitor compliance. When incorporated<br />
into training programs, case studies such as the<br />
ones described above help researchers understand<br />
that noncompliance results in risks to themselves,<br />
the animal care staff, and their research results.<br />
Additional LCMV Resources<br />
Today, animal care staff and animal researchers<br />
receive training on zoonotic risks, including LCMV.<br />
For example, the University of California-Irvine<br />
web site has the following statement under<br />
“rodent health” at: www.rgs.uci.edu/ular/policies/<br />
rodentcolonyhealth.htm.<br />
271
The overwhelming significant feature of<br />
LCMV is its zoonotic potential. It can be<br />
predicted that T cell-deficient mice will amplify<br />
LCMV infection. The polytropic nature<br />
of LCMV and its wide host range allow<br />
this virus to readily infect transplantable<br />
tumors and cell lines, which can serve as a<br />
source of contamination for mouse colonies.<br />
• Organotropism—kidney, salivary gland,<br />
lymphohematopoietic cells<br />
• A zoonosis<br />
• Interference with research—immunology,<br />
oncology, physiology<br />
Well-established procedures for using immunocompetent<br />
sentinel animals are described at<br />
the University of Washington web site at:<br />
h tt p://depts.washington .edu/compmed/<br />
rodenthealth/#sentinels.<br />
Roughly analogous to the “canary in the<br />
coal mine,” sentinel rodents monitor the<br />
pathogen status of the investigator’s rodents.<br />
Every rack in a room is monitored. As you<br />
are facing a rack, the cage containing the<br />
two sentinels usually resides in the lower<br />
right-hand position. Every time an investigator’s<br />
rodent cage is changed (usually weekly),<br />
about a tablespoon of soiled bedding from<br />
that cage is transferred to the sentinel cage.<br />
In this way, sentinels are exposed to whatever<br />
pathogens may be present in the urine,<br />
feces, fur, saliva, dander, etc. from <strong>10</strong>0% of<br />
the cages on the rack. Because of this, investigators<br />
must not handle or move sentinels<br />
or sentinel cages.<br />
PCR testing for many zoonotic pathogens is also<br />
commercially available; this allows direct testing of<br />
immunocompromised strains. Charles River Laboratory<br />
has posted an explanation of test methods<br />
available at: www.criver.com/research_models_and_<br />
services/research_animal_diagnostics/LAD_DS_<br />
272<br />
Biosafety Tips<br />
MolecularW.pdf and www.criver.com/research_<br />
m o d e l s _ a n d _ s e r v i c e s / r e s e a r c h _ a n i m a l _<br />
diagnostics/LAD_DS_InVivoBiosafetyW.pdf.<br />
References<br />
Braun, A. (2004). Case report: Transmission of lymphocytic<br />
choriomeningitis virus from laboratory<br />
mice to an animal technician. 47th Annual <strong>Biological</strong><br />
<strong>Safety</strong> Conference, San Antonio, Texas.<br />
Centers for Disease Control Special and Prevention<br />
Pathogens Branch. (<strong>2005</strong>). Information for pet owners:<br />
Reducing the risk of becoming infected with LCMV from<br />
pet rodents. Available at: www.cdc.gov/ncidod/dvrd/<br />
spb/mnpages/dispages/lcmv/owners.htm. Accessed<br />
online <strong>2005</strong>.<br />
Centers for Disease Control and Prevention. (<strong>2005</strong>).<br />
Lymphocytic choriomeningitis virus infection in organ<br />
transplant recipients. Morbidity and Mortality<br />
Weekly Report, 54(21), 537-539.<br />
Centers for Disease Control and Prevention. (<strong>2005</strong>).<br />
Interim guidance for minimizing risk for human<br />
lymphocytic choriomeningitis virus infection associated<br />
with rodents. Morbidity and Mortality Weekly Report,<br />
54(30), 747-749.<br />
Dykewicz, C. A., Dato, V. M., Fisher-Hock, S. P.,<br />
Howarth, M. V., Perez-Oronoz, G. I., Ostroff, S. M.,<br />
Gary, H., Shonberger, L. B., & McCormick, J. B.<br />
(1992). Lymphocytic choriomeningitis outbreak associated<br />
with nude mice in a research institute. Journal<br />
of the <strong>American</strong> Medical <strong>Association</strong>, 267, 1349-1353.<br />
National Research Council. (1991). A companion<br />
guide to infectious diseases of mice and rats. Washington,<br />
DC: National Academy Press.
ABSA News<br />
<strong>2005</strong> ABSA Conference Photos<br />
Conference attendees visiting the Exhibit Hall<br />
Betsy Gilman Duane receives Past-<br />
President Award from Glenn Funk<br />
Affiliate Relations Exhibit Booth<br />
Conference attendees at the Scientific Program<br />
273
Award Presentations from the ABSA<br />
Conference, October <strong>2005</strong><br />
Arnold G. Wedum<br />
Distinguished Achievement Award<br />
David G. Stuart, PhD<br />
The Baker Company<br />
Sanford, Maine<br />
The award shall be given to an individual for<br />
outstanding contributions to biological safety through<br />
teaching, research, service or leadership.<br />
David Stuart has had a long and highly successful<br />
career at the Baker Company. He received his<br />
Doctorate in Microbiology, and is a Charter Member<br />
of ABSA. Through his distinguished career he<br />
has served on the original Steering Committee of<br />
ABSA, the Technical Review and Nominating Committees,<br />
and the Journal Editorial Board.<br />
He has mentored numerous colleagues in the<br />
certification profession regarding microbiology, de-<br />
274<br />
ABSA News<br />
<strong>2005</strong> ABSA Service Award Recipients<br />
David G. Stuart, PhD, accepting the Arnold G.<br />
Wedum Distinguished Achievement Award<br />
at the <strong>2005</strong> ABSA Conference in Vancouver.<br />
contamination and biocontainment and has been<br />
a constant source of reliable and timely information<br />
to the Controlled Environment Test <strong>Association</strong><br />
(CETA), ABSA, and the National Sanitation Foundation<br />
(NSF). He has had a profound influence in<br />
the area of standards writing as a participant in NSF<br />
committees. He is the voice on many panels that<br />
send the clear message that standards be developed<br />
based on scientific fact by ensuring participants provide<br />
research results to support their positions on<br />
standards development. He continues to make contributions<br />
to biosafety on international and national<br />
levels by teaching courses including “Advanced Certification”<br />
in the United States, Russia, and Hong<br />
Kong. He is noted by his colleagues and fellow biosafety<br />
professionals as an individual that leads by<br />
example. He is a dedicated researcher and teacher in<br />
the field of contamination control with an inspirational<br />
work ethic.<br />
Richard C. Knudsen<br />
Memorial Publication Award<br />
Janet E. Meszaros, MS<br />
Steris Corporation<br />
Mentor, Ohio<br />
The award shall be given, when merited, to the<br />
author(s) of an article that reports a significant contribution<br />
in scientific investigation and/or health and safety<br />
in areas of interest to Richard Knudsen during his career.<br />
The award recipient need not be a member of the<br />
<strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong>.<br />
Research Article: Meszaros, J. E., Antloga, K.,<br />
Justi, C., Plesnicher, C., & McDonnell, G. (<strong>2005</strong>).<br />
Area Fumigation with Hydrogen Peroxide Vapor.<br />
Applied Biosafety, <strong>10</strong>(2), 91-<strong>10</strong>0.<br />
Ms. Meszaros, the senior author of the article<br />
selected for the Richard Knudsen Memorial Publication<br />
Award, earned her BS and MS from Cleveland<br />
State University. She is a Senior Scientist at STERIS
Corp. where she has worked for over a decade, as<br />
well as serving the academic community as a Science<br />
Instructor at Cuyahoga Community College—also<br />
for over a decade.<br />
This original research article was selected for its<br />
contribution of knowledge to the field of biosafety.<br />
Results of this research quantitatively identified the<br />
sterilizing capabilities of hydrogen peroxide vapor<br />
across various classes of resilient organisms that were<br />
applied to numerous common laboratory surfaces<br />
over varied exposure times.<br />
Robert I. Gross Memorial Award<br />
Cassandra Kelly, BS<br />
New York State Department of Health<br />
Albany, New York<br />
Awarded to a student in recognition of academic<br />
achievement in biological safety.<br />
Cassandra Kelly is a Research Scientist and the<br />
Biosafety Level 3 Supervisor in the Biodefense Laboratory<br />
at the Wadsworth Center, New York State<br />
Department of Health (NYSDOH). Cassandra received<br />
a BS in 1997 from Carleton University and is<br />
currently pursuing a PhD in the Biomedical Sciences<br />
Department at the State University of New York,<br />
Albany. Prior to joining the NYSDOH Biodefense<br />
Laboratory in 2002, Ms. Kelly worked at the Canadian<br />
Science Center for Human and Animal Health<br />
conducting research in prion diseases, hepatitis viruses<br />
and emerging blood borne pathogens. Ms.<br />
Kelly is involved in the development of new diagnostics<br />
for select agents as well as training of laboratorians,<br />
first responders and members of the law enforcement<br />
communities in New York State.<br />
Abstract: Effects of bacillus spore decontamination<br />
methods on forensic evidence: an evaluation of<br />
decontamination methods: vaporized hydrogen peroxide,<br />
formaldehyde, and autoclaving.<br />
Many environmental samples submitted to the<br />
New York State Biodefense Laboratory for biothreat<br />
testing are often requested to be transferred, following<br />
select agent testing, to forensic laboratories in order<br />
to proceed with criminal prosecutions. Even after<br />
the presence of potential bioterrorism agents have<br />
been ruled-out, forensic laboratories may be unwilling<br />
to accept samples because they are restricted to working<br />
in biosafety level l or 2 facilities. In order for sam-<br />
<strong>2005</strong> ABSA Service Award Recipients<br />
ples to be analyzed safely and expeditiously to the forensic<br />
laboratories, all traces of infectious or toxic biological<br />
material must first be removed or inactivated.<br />
In collaboration with the New York State Police<br />
Forensics Investigation Center, a study has been<br />
conducted to determine which decontamination<br />
method(s) can render a letter/white powder sample<br />
free from infectious biological agents while at the<br />
same time preserving the integrity of forensic evidence.<br />
Several letters seeded with Bacillus spores, representative<br />
inks, drug surrogates, human hair or<br />
DNA, and fingerprints were exposed to three common<br />
decontamination methods: vaporized hydrogen<br />
peroxide, formaldehyde and steam autoclaving. Subsequent<br />
microbiological testing to insure spore inactivation<br />
and concomitant forensic analysis to evaluate the<br />
integrity of trace evidence has determined which decontamination<br />
method will be most useful to safely<br />
release and transfer suspect biothreat samples to forensic<br />
laboratories for additional testing.<br />
John H. Richardson<br />
Special Recognition Award<br />
J. Patrick Condreay, PhD<br />
GlaxoSmithKline<br />
Research Triangle Park, North Carolina<br />
The award shall be given to an individual in<br />
recognition of a specific contribution that has enhanced<br />
the <strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> and/or the<br />
profession of biological safety.<br />
Patrick Condreay received his undergraduate<br />
degree in biochemistry from Rice University and his<br />
PhD in microbiology from the University of Texas at<br />
Austin. For over 20 years he has pursued a career in<br />
research, studying the molecular biology of different<br />
microorganisms.<br />
Since first becoming an instructor at an ABSA-<br />
Eagleson Spring Seminar Series in 1998—where he<br />
helped teach the course “Viral Vectors and Biosafety<br />
Considerations”—he has helped develop and taught<br />
13 additional courses on similar topics. His ability to<br />
convey complex scientific topics that pose increasing<br />
challenges to biosafety professionals and his sustained<br />
commitment has made him one of the most<br />
prolific and sought-after teachers promoting biosafety<br />
for ABSA in the last decade. By the close of<br />
the Vancouver conference, he will have increased his<br />
275
number of ABSA or ABSA-related teaching assignments<br />
to 16 classes in 7 years, in topics of extreme<br />
relevance and importance to ABSA members and<br />
biosafety professionals around the globe.<br />
Everett Hanel, Jr. Presidential Award<br />
Robert J. Hawley, PhD<br />
Midwest Research Institute<br />
Frederick, Maryland<br />
The award shall be given to an individual for outstanding<br />
contributions to the <strong>American</strong> <strong>Biological</strong><br />
<strong>Safety</strong> <strong>Association</strong> by promoting the field of biological<br />
safety and by fostering the high professional standards<br />
of the <strong>Association</strong>’s membership.<br />
Bob Hawley is a Senior Advisor, for the Midwest<br />
Research Institute in Frederick, Maryland, and was<br />
previously employed at the U.S. Army Medical Research<br />
Institute of Infectious Diseases at Fort Detrick,<br />
Maryland, as Biosafety Officer, and later as Chief of<br />
the <strong>Safety</strong> and Radiation Protection Office. He holds<br />
276<br />
<strong>2005</strong> ABSA Service Award Recipients<br />
Thanks to the Elizabeth R. Griffin Research Foundation<br />
a PhD in Microbiology from the College of Medicine<br />
and Dentistry of New Jersey; an MS in Microbiology<br />
from the Catholic University of America, and a BS in<br />
Biology from Pennsylvania Military College.<br />
He has authored numerous journal articles and<br />
textbook chapters on biosafety and microbiology,<br />
and further promotes biosafety by teaching preconference<br />
courses, serving on ABSA committees<br />
and participating in IBCs and IACUCs. He is a Registered<br />
<strong>Biological</strong> <strong>Safety</strong> Professional serving as the<br />
Chair of the <strong>Biological</strong> <strong>Safety</strong> Examination Development<br />
Committee with the National Registry of Microbiology,<br />
and actively encourages biosafety practitioners<br />
to pursue registration and certification as<br />
Biosafety Professionals. He has expressed his commitment<br />
to the biosafety profession in many ways to<br />
include being elected President-Elect of ABSA, President<br />
of ChABSA, Editorial Review Board member<br />
for Applied Biosafety, and as an active promoter of<br />
biosafety in ASM.<br />
The ABSA Council would like to thank the Elizabeth R. Griffin Research Foundation for its continued<br />
support of ABSA activities and the field of biosafety. Through the generous support of the Foundation,<br />
ABSA was fortunate to have Benjamin J. Weigler, DVM, MPH, PhD, as the Elizabeth R. Griffin Research<br />
Foundation Lecturer at the <strong>2005</strong> Conference in Vancouver. Dr. Weigler is the Director of Animal Health<br />
Resources at the Fred Hutchinson Cancer Research Center. His<br />
presentation was titled “A National Survey of Occupationally<br />
Acquired Zoonotic Diseases in Laboratory Animal Workers.” He has<br />
published an article on this research. See Weigler, B. J., Di Giacomo,<br />
R. F., & Alexander, S. (<strong>2005</strong>, April). A national survey of laboratory<br />
animal workers concerning occupational risks for zoonotic diseases.<br />
[Journal Article]. Comparative Medicine, 55(2), 183-191.<br />
ABSA is also developing an animal biosafety training DVD with<br />
the support of the Foundation. We are grateful to have the<br />
opportunity to work with the Elizabeth R. Griffin Research<br />
Foundation in pursuit of safe science.
ABSA News<br />
New ABSA Members for 2006<br />
Natalie Barnett<br />
Sandia National Laboratories<br />
Albuquerque, NM<br />
Malcolm Barth<br />
Loyola University—Chicago<br />
Chicago, IL<br />
Shelley Belford<br />
Animal Resources Centre, Univ. Health Network<br />
Toronto, Ontario, Canada<br />
Arlisa Benford<br />
University of Houston<br />
Houston, TX<br />
Bill Biebesheimer<br />
Steris Corp.<br />
Rosemount, MN<br />
Asa Bjorndal<br />
Swedish Inst. for Infectious Disease Control<br />
Solna Sweden<br />
Sylvie Blondelle<br />
The Burnham Institute<br />
La Jolla, CA<br />
Mudu Ler Bok San<br />
Kowa Lab Engineering Pte. Ltd.<br />
Singapore, Singapore<br />
Jean-Luc Boudreau<br />
SFBC Anapharm<br />
Ste-Foy, Quebec, Canada<br />
Tiffany A. Brigner<br />
Colorado Department of Agriculture<br />
Denver, CO<br />
Neil Chin<br />
BC Centre for Disease Control<br />
Vancouver, British Columbia, Canada<br />
Benton Daw<br />
East Carolina University<br />
Greenville, NC<br />
Neville Debattista<br />
U of M<br />
Mosta, Malta<br />
Tina M. Ennis<br />
United States Army<br />
APO, AE<br />
Rowelle Enriquez<br />
UCLA Environment Health & <strong>Safety</strong><br />
Los Angeles, CA<br />
Jean Francois<br />
University of British Columbia<br />
Vancouver, British Columbia, Canada<br />
Sabrina Frank-DeBose<br />
Constella Group<br />
Snellville, GA<br />
Daniel Frasier<br />
Cornerstone Commissioning, Inc.<br />
Boxford, MA<br />
Claire Fritz<br />
Steris Corporation<br />
Lakewood, CO<br />
Joshua Jenkins<br />
Constella Health Sciences<br />
Stockbridge, GA<br />
277
Stephane Karlen<br />
Swiss Federal Institute of Technology<br />
Lausanne, VD, Switzerland<br />
William R. Lonergan<br />
SAIC-Frederick, Inc.<br />
Frederick, MD<br />
Bruce K. McDowell<br />
Lawrence Livermore National Laboratory<br />
Livermore, CA<br />
Paul Mehta, MD<br />
Constella Group, LLC<br />
Lawrenceville, GA<br />
Janet E. Meszaros<br />
Steris Corp.<br />
Mentor, OH<br />
Thomas Miller<br />
Constella Health Sciences<br />
Atlanta, GA<br />
Matt Mitchell<br />
Steris Corp.<br />
Mentor, OH<br />
Michael Penn<br />
Boston University<br />
Boston, MA<br />
Emily E. Pullins<br />
USDA APHIS BRS<br />
Riverdale, MD<br />
Emily Ranken<br />
MIT<br />
Cambridge, MA<br />
278<br />
New ABSA Members for 2006<br />
Jamie Stalker, MD<br />
Argonne National Laboratory<br />
Argonne, IL<br />
Clarence Stanley, Jr.<br />
Department of Army<br />
Ft. Gordon, GA<br />
Jan Vleck<br />
Western Institutional Review Board<br />
Olympia, WA<br />
Michael Wheatley<br />
City of Hope<br />
Duarte, CA<br />
New Student Members<br />
Donato Aceto<br />
Sandia National Laboratories<br />
Albuquerque, NM<br />
Changhua Chen<br />
University of Iowa Hospitals and Clinics<br />
Iowa City, IA<br />
New Corporate Memberships<br />
UAB-Comite de Bioseguretat<br />
Bellaterra, Barcelona<br />
Pere Ysern Comas<br />
Sebastian Calero Garnica<br />
Josep Santalo Pedro<br />
New Members of Existing Corporations<br />
Mike Brueggerhoff<br />
Siemens Building Technologies<br />
Norcross, GA
ABSA News<br />
<strong>2005</strong> ABSA Conference Sponsors<br />
We would like to thank the following sponsors of<br />
the <strong>2005</strong> ABSA Conference in Vancouver.<br />
Featured Sponsor<br />
Elizabeth R. Griffin Research Foundation—<br />
www.ergriffinresearch.org<br />
The Elizabeth R. Griffin Research Foundation is<br />
a 501(c)(3) non-profit foundation dedicated to the<br />
support of professional scientific and educational<br />
organizations that endeavor toward the common<br />
good of humankind. This includes, but is not limited<br />
to, supporting research that aims at the solution<br />
of human health and societal problems and supporting<br />
worker safety training in dealing with nonhuman<br />
primates and other animal subjects. The<br />
Foundation has an expressive interest in research of<br />
the macaque-borne B virus and the prevention of<br />
human exposure to B virus.<br />
Bronze Sponsors<br />
Germfree, Inc.—www.germfree.com<br />
Germfree Laboratories, Inc. was founded in<br />
1962. From its inception, Germfree’s primary objective<br />
has been to manufacture biological safety equipment<br />
for the scientific research and healthcare fields.<br />
Germfree systems have been purchased by more<br />
than 5,000 institutions and companies in the U.S.<br />
and 60 other countries worldwide. Our equipment<br />
has even gone in space.<br />
NuAire, Inc.—www.nuaire.com<br />
NuAire has been universally recognized as a<br />
leader for more than 30 years in providing laboratory<br />
professionals with reliable products such as biological<br />
safety cabinets, CO2 incubators, Laminar<br />
Airflow equipment, animal facility products, and<br />
ultra-low temperature freezers for the most demanding<br />
environments.<br />
The Baker Company—www.bakerco.com<br />
The Baker Company manufactures safety cabinets,<br />
clean benches, and fume hoods. Baker cabinets<br />
are designed for dependability, high performance<br />
and low life cycle costs.<br />
Certek, Inc.—www.certekinc.com<br />
Certek builds modular BL3 laboratories,<br />
safemod/safescan filters for hazardous exhausts, formaldehyde<br />
generators/neutralizers and other contaminations<br />
control equipment.<br />
National Select Agent Registry (NSAR) Sponsored<br />
by CDC and APHIS—www.cri-solutions.com<br />
The National Select Agent Registry (NSAR) is a<br />
system jointly developed by APHIS and CDC to allow<br />
Entities that possess or wish to possess Select<br />
Agents to register or amend their registration<br />
online—eliminating the need to use cumbersome<br />
paper forms. NSAR will be available for use in December<br />
<strong>2005</strong>.<br />
Siemens—www.sbt.siemens.com<br />
As a leading provider of building controls, fire<br />
safety and security system solutions, Siemens Building<br />
Technologies, Inc., makes buildings comfortable,<br />
safe, productive and less costly to operate. The company<br />
focuses on improving the performance of its<br />
customers’ buildings, so that its customers can focus<br />
on improving their business performance. With U.S.<br />
headquarters in Buffalo Grove, Illinois, Siemens<br />
Building Technologies employs 7,500 people and<br />
provides a full range of services and solutions from<br />
more than <strong>10</strong>0 locations coast-to-coast. Worldwide,<br />
the company has 29,000 employees and operates in<br />
more than 42 countries.<br />
H.E.P.A. Filter Services Inc./Design Filtration Inc.—<br />
www.hepafilterservices.com<br />
www.designfiltration.com
Calendar of Events<br />
280<br />
ABSA News<br />
October 15-18, 2006<br />
<strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (ABSA) 49th Annual Conference<br />
Marriott Copley Hotel, Boston, Massachusetts<br />
Contact: Phone: 847-949-1517, Fax: 847-566-4580, E-mail: absa@absa.org, Web Site: www.absa.org<br />
October 7-<strong>10</strong>, 2007<br />
<strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (ABSA) 50th Annual Conference<br />
Opryland Hotel, Nashville, Tennessee<br />
Contact: Phone: 847-949-1517, Fax: 847-566-4580, E-mail: absa@absa.org, Web Site: www.absa.org<br />
October 19-22, 2008<br />
<strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (ABSA) 51st Annual Conference<br />
John Ascuaga’s Nugget, Reno, Nevada<br />
Contact: Phone: 847-949-1517, Fax: 847-566-4580, E-mail: absa@absa.org, Web Site: www.absa.org<br />
ABSA ITEMS FOR SALE<br />
Pin $5.00<br />
Watch $30.00<br />
Men’s Women’s<br />
Total Enclosed: $ Charge my: VISA MasterCard <strong>American</strong> Express<br />
Card #:<br />
Exp. Date: Signature:<br />
Ship to Name:<br />
Address:<br />
City: State: Zip:<br />
Mail to: ABSA, 1202 Allanson Road, Mundelein, Illinois 60060-3808 or fax your credit card order to<br />
847-566-4580. Please allow two to three weeks for delivery.
Applied Biosafety is the Journal of the <strong>American</strong> <strong>Biological</strong><br />
<strong>Safety</strong> <strong>Association</strong> and publishes articles on the research, theory,<br />
and applied practice of biological safety. An expert panel of International<br />
Editors representing ABSA Canada, Associação Nacional de Biossegurança<br />
(ANBio), Asia Pacific Biosafety <strong>Association</strong> (APBA), European <strong>Biological</strong><br />
<strong>Safety</strong> <strong>Association</strong> (EBSA), and the International Biosafety Working Group<br />
(IBWG) contribute a global perspective on biosafety and biosecurity. As a<br />
service to the scientific community, online subscriptions are available at cost –<br />
$25/year.<br />
A free preview of Applied Biosafety, <strong>Volume</strong> <strong>10</strong>, <strong>Number</strong> 1, is at<br />
www.absa.org/resabj.html; for userID, type in “abj273” with password “8f9T74”
ABSA Announces Professional Publications for Purchase<br />
Anthology of Biosafety I:<br />
Perspectives on<br />
Laboratory Design<br />
❑ Member: $41.00<br />
❑ Nonmember: $55.00<br />
Anthology of Biosafety V:<br />
BSL-4 Laboratories<br />
❑ Member: $53.00<br />
❑ Nonmember: $67.00<br />
Anthology of Biosafety II:<br />
Facility Design<br />
Considerations<br />
❑ Member: $42.00<br />
❑ Nonmember: $57.00<br />
Anthology of Biosafety VI:<br />
Arthropod Borne Diseases<br />
❑ Member: $39.00<br />
❑ Nonmember: $52.00<br />
Anthology of Biosafety III:<br />
Application of Principles<br />
❑ Member: $49.00<br />
❑ Nonmember: $64.00<br />
Anthology of Biosafety VII:<br />
Biosafety Level 3<br />
❑ Member: $44.00<br />
❑ Nonmember: $57.00<br />
ADD POSTAGE/HANDLING: U.S. – $3.00 per book; Canada – $5.00 per book; Foreign – $15.00 per book<br />
Name __________________________________________ Member ID# ___________________________________________<br />
Address _____________________________________________________________________________________________________<br />
City/State/Zip ________________________________________________________________________________________________<br />
Total ___________________________ ❑ Check enclosed ❑ Please charge my: ❑ Visa ❑ MasterCard ❑ AmEx<br />
Card # ________________________ Exp. Date ________________________ Signature ____________________________<br />
Mail or fax this order form to:<br />
<strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (ABSA)<br />
1202 Allanson Road, Mundelein, IL 60060-3808<br />
Phone: 847-949-1517 • Fax: 847-566-4580<br />
Anthology of Biosafety IV:<br />
Issues in Public Health<br />
❑ Member: $42.00<br />
❑ Nonmember: $55.00<br />
Anthology of Biosafety VIII:<br />
Evolving Issues in<br />
Containment<br />
❑ Member: $36.00<br />
❑ Nonmember: $49.00<br />
NOTE: Please allow 2-3 weeks for delivery. If using a credit card, please mail or fax the form as we will need a signature on file.<br />
We do not accept purchase orders.
www.absa-canada.org<br />
Please visit our ABSA Chapters, Affiliates, and Affiliated<br />
Organizations for more biosafety information and news.<br />
www.anbio.org.br<br />
www.socalbionet.org<br />
biosafety@comcast.net www.duke.edu/~alder002 www.chabsa.org<br />
www.ebsa.be<br />
EGilman@absa.org<br />
www.mabsa.org www.sebsa.net<br />
Japanese <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong> (JBSA)<br />
(Note: JBSA affiliate status is in process.)<br />
ksugi@nih.go.jp
Guidelines for Submissions<br />
Authors will be acknowledged of submission receipt by the ABSA National Office. Final decisions regarding publication are<br />
made by the Editorial staff and reviewers. The following are the submission guidelines.<br />
Submission Categories<br />
Articles, Reviews, and Summary Articles—Reviews may focus on the theory, practice, and overarching areas relevant to<br />
biological safety, biosecurity or related areas. Articles must include an abstract not to exceed 250 words summarizing the<br />
main topic of the article. Typically articles do not exceed 20 pages in total length.<br />
Reports—Articles that focus on the results of research are appropriate for this section. Brief reports should include information<br />
on the research design, methods, and results. An abstract not to exceed 250 words must also be included. Articles vary in<br />
length.<br />
Viewpoints—Short articles focusing on personal experiences may be submitted to this section. Articles vary in length.<br />
Book and Video Reviews—Reviews of books and media (videos/CD/other) of interest to biological safety or biosecurity<br />
may be submitted at any time. Reviews typically do not exceed 1-2 pages in length. Books or media which authors wish to<br />
have considered for review may be sent directly to the ABSA National Office.<br />
Commentary/Editorial—Brief comments on submissions published in Applied Biosafety, issues critical to the profession and<br />
practice of biological safety, or letters to the Editor may be submitted to this section. Individuals may be invited by the Editors<br />
to submit a guest editorial article.<br />
Presentations—Articles that recount or summarize information relevant to the field of biological or biosecurity that has<br />
been presented at a conference. Presentation articles vary in length.<br />
Other Requirements<br />
1. Send an electronic submission or one (1) typeset copy with a disk of each submission to: Editor, Applied Biosafety:<br />
Journal of the <strong>American</strong> <strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong>, c/o ABSA, 1202 Allanson Road, Mundelein,<br />
IL 60060-3808, USA. Submissions that are under consideration by another periodical or publisher or submissions<br />
that have been previously published must be identified as such, and previous citing must be disclosed.<br />
2. Submission guidance:<br />
Format for 8-1/2” x 11” paper using 1” margins, double-spacing, and full-justification.<br />
References, footnotes, table captions, and quotations should be single-spaced, a guide to references can be found at<br />
www.absa.org.<br />
Use Times New Roman, Arial, AvantGarde, Helvetica, or Universal font in 12 point.<br />
Use high resolution laser printing if submission is made in hard copy media.<br />
Primary headings should be flush left, bolded, and have the first letter of all main words capitalized throughout the<br />
submission.<br />
Secondary headings should be flush left, italicized, and have the first letter of all main words capitalized.<br />
3. Submissions should follow ASM guidelines regarding fundamental style and ethics--refer to Applied and Environmental Microbiology<br />
at http://aem.asm.org.<br />
4. The Attention Authors Form may serve as a cover sheet with the full name(s) and degree(s) of the author(s), professional<br />
affiliations, and the return mailing address of the author to whom correspondence can be sent. Authors’ names, positions,<br />
titles, and places of employment should not appear in the body of the paper to facilitate the blind review process.<br />
5. Tables, charts, photographs (at least 3-1/2” x 5”) or diagrams must be computer-generated or professional quality and<br />
submitted as camera ready artwork. Tables, charts, or diagrams should be submitted on a separate page, referenced back<br />
to the text in a vertical (portrait) format including any legend, label, or number associated with them. Refer to each as<br />
Table 1, Table 2, etc., centered above the table. Captions should be single-spaced.<br />
6. It is the author’s responsibility to secure written permission from the original copyright holder to use quotations of over<br />
300 words from one source or use adaptation of tables or figures from copyrighted sources. A copy of the copyright<br />
holder’s written permission must be provided to the Editor immediately upon acceptance of the submission for publication.<br />
The author(s) bear full responsibility for the accuracy of all results, references, quotations, and materials accompanying<br />
their submissions.<br />
7. In the event a diskette it used, it should be prepared on either an IBM or IBM-compatible computer. All submissions<br />
should be formatted using either: Microsoft Word, Microsoft Publisher, or WordPerfect. ASC II files are also acceptable.
Attention Authors<br />
Please complete the following information and include with your submission.<br />
Name<br />
Degrees/Credentials<br />
Affiliation<br />
Address<br />
Phone <strong>Number</strong>s Work Home (opt.)<br />
E-mail Address<br />
Type of Submission (check one):<br />
Report Article, Review, Summary Article Viewpoint<br />
Book Review Video Review Presentation Commentary/Editorial<br />
Title of Submission<br />
Checklist<br />
Electronic submission or one (1) hard copy (typeset using 8-1/2” x 11” paper with 1” margins).<br />
Electronic submission or one (1) hard copy original of tables, figures, and/or illustrations.<br />
Submission follows ASM guidelines regarding fundamental style and ethics.<br />
Abstract of approximately 250 words (for Articles, Reviews, and Summary Articles only).<br />
This Attention Authors form.<br />
Author’s Signature Date<br />
Please send the completed form along with your submission to: Editor, Applied Biosafety: Journal of the <strong>American</strong><br />
<strong>Biological</strong> <strong>Safety</strong> <strong>Association</strong>, 1202 Allanson Road, Mundelein, IL 60060-3808, USA. Electronic submissions may be<br />
e-mailed to: Production Editor, Karen D. Savage, at ksavage@covad.net. If you have formatting, processing, or general<br />
questions, please contact Ms. Savage at the ABSA National Office Monday through Friday between 9:00 a.m. and<br />
5:00 p.m. Central Time at 847-949-1517.
Register through March 4th <strong>2005</strong><br />
and SAVE $150 US<br />
Learn more about Tradeline Inc<br />
and register today at:<br />
http://www.tradelineinc.com/bio2006<br />
Questions? Call 925.254.1744 x12<br />
Tradeline Inc.<br />
Biocontainment Facilities 2006<br />
Design • Construction • Operation<br />
Biocontainment Facilities 2006 Conference<br />
Design • Construction • Operation<br />
March 27-28, 2006<br />
Renaissance Vinoy Beach and Golf Resort<br />
St. Petersburg, Florida<br />
Here you’ll get the details on:<br />
• Developing efficient BSL-3 solutions for animal facilities<br />
• Sorting out certification, validation, commissioning and design guideline issues<br />
• Getting the design and construction details right<br />
• Benchmarking costs for new construction upgrades and conversions<br />
• Planning for BSL facilities operations and maintenance<br />
• New lab types - Bioaerosol, Bird Flu, Advanced Imaging in BSL environments<br />
Credit: CUH2A/George Ely<br />
Courtesy of Smith Carter Architects and Engineers Inc.