The FOSAMAX Induced Femur Fractures - HB Litigation Conferences
The FOSAMAX Induced Femur Fractures - HB Litigation Conferences
The FOSAMAX Induced Femur Fractures - HB Litigation Conferences
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
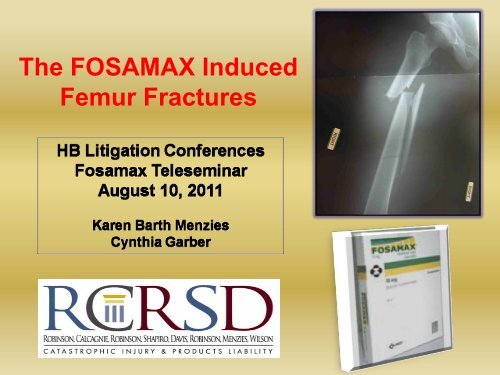
<strong>The</strong> <strong>FOSAMAX</strong> <strong>Induced</strong><br />
<strong>Femur</strong> <strong>Fractures</strong>
<strong>FOSAMAX</strong>®<br />
(ALENDRONATE SODIUM)<br />
• Manufactured by Merck<br />
• Belongs to class of drugs known<br />
as bisphosphonates, including:<br />
Actonel- Proctor & Gamble<br />
Aredia- Novartis<br />
Boniva- Roche<br />
Didronel- Proctor & Gamble<br />
Reclast - Novartis<br />
Skelid- Sanofi-Aventis<br />
Zometa- Novartis
Fosamax indications include:<br />
• Treatment of osteoporosis in<br />
postmenopausal women<br />
• Treatment to increase bone mass in<br />
men with osteoporosis<br />
• For prevention of osteoporosis, may be<br />
considered in postmenopausal who are<br />
risk of dev osteoporosis and for whom<br />
the desired clinical outcome is to<br />
maintain bone mass and to reduce risk<br />
of future fracture
What is Osteoporosis?:<br />
• A skeletal disorder characterized by<br />
compromised bone strength predisposing to an<br />
increased risk for fracture.<br />
• Bone strength reflects the integration of 2 main<br />
features: 1) bone mineral density (BMD); and 2)<br />
bone quality, (i.e., quantity<br />
and quality of bone)<br />
-- NIH Consensus Statement, 2000.
Normal Moderate Osteoporosis<br />
Severe Osteoporosis
WHO Criteria for Diagnosis of<br />
Osteoporosis: (Measurement of BMD)<br />
-- BMD is typically measured<br />
using a DEXA scanner<br />
-- Results are reported as a T score<br />
T Score Classifications<br />
>-1 Normal<br />
-2.5 to -1 Osteopenia<br />
Pathophysiology of the Injury<br />
<strong>The</strong> life of the skeleton is a highly active, living<br />
tissue<br />
Our bones are continually eaten<br />
away by osteoclasts…<br />
and rebuilt by osteoblasts…..<br />
and it’s this process of continuous<br />
remodeling that provides our bones with durability.
<strong>FOSAMAX</strong>:<br />
Mechanism of Injury<br />
• <strong>FOSAMAX</strong> inhibits osteoclastic mediated bone turnover (remodeling)<br />
which results in increased bone mineralization, which in turn increases<br />
brittleness of bone.<br />
•Microcracks tend to develop within highly mineralized bone.<br />
•Because remodeling is inhibited, microdamage accumulates, and in time,<br />
stress reactions arise which may develop into stress fractures and eventually<br />
complete fractures<br />
•Long term use of Fosamax is associated with reduced bone repair and<br />
accumulation of microdamage, leading to reduced bone toughness and<br />
adynamic fragile bones….and resulting in Atypical <strong>Femur</strong> <strong>Fractures</strong> (AFF)<br />
• <strong>FOSAMAX</strong> well bound in bone and so long lasting; <strong>FOSAMAX</strong> remains<br />
biologically active for over 10 years after final dose.
<strong>FOSAMAX</strong> Atypical <strong>Femur</strong><br />
<strong>Fractures</strong> (AFF): A Signature Injury<br />
• Subtrochanteric fracture:<br />
-Area between the lower border of the<br />
lesser trochanter to proximal third of<br />
femur (but can include to distal femur,<br />
less commonly.)<br />
-None to minimal trauma<br />
• Unique radiographic pattern:<br />
a) Cortical thickening of the subtrochanteric<br />
region;<br />
(b) A transverse or oblique fracture<br />
(c) Medial cortical spike<br />
(d) Some with bilateral stress fractures,<br />
(e) Often with associated prodromal pain.
Sample X-Rays of signature injury
Fracture Intervention Trial (FIT)<br />
• FIT consisted of 2 studies in postmenopausal women:<br />
the 3-year study (with vertebral fracture) and the 4-year<br />
study (with low BMD but no vertebral fracture.)<br />
• 3,236 women were treated with Fosamax 5mg for 2<br />
years, then the dose increased to 10mg for a total of 3-<br />
4.5 years.<br />
Results:<br />
• In women without osteoporosis, no clear reduction in<br />
fracture risk<br />
• 3 year: 47% reduction fx risk; 4 year: 44% reduction in<br />
fx risk<br />
Black DM et al. Fracture Risk Reduction vertebral fractures in women who had<br />
osteoporosis (femoral with Alendronate in Women with Osteoporosis: the Fracture<br />
Intervention Trial. J Clin Endoc Metab 2000 85:4118-4124.
Bisphosphonates Odvina et al, 2005<br />
9 patients sustained unusual spontaneous<br />
nonspinal fractures; on alendronate 3-8<br />
yr; bone biopsies showed markedly<br />
decreased matrix synthesis; 6 had delayed<br />
healing for 3 mo to 2 yr.<br />
J, Clin Endorinol Metab 90:1294-1301, 2005
Dr. Susan Ott M.D.<br />
“I believe the current evidence suggests that<br />
bisps should be stopped after 5 yr. Those<br />
patients who remain at high risk of fractures or<br />
who have had fractures despite BP therapy<br />
could be considered for treatment with<br />
intermittent PTH.”<br />
--Editorial, J Clin Endocrin Metab 2005.
S. Cummings, M.D.<br />
“It is reasonable to consider at least a 5-<br />
year holiday for patients who have been<br />
taking alendronate for at least 5 yrs but<br />
continue treatment in those with a high<br />
risk of vertebral fractures.<br />
-- JAMA 296:2601-2610, 2006.
T-1.8; 5 yrs on alendronate;<br />
FIT N = 6,459<br />
FLEX Trial<br />
Placebo N = 3,223 Alendronate N = 3,236<br />
Placebo N = 437<br />
Eligible for FLEX Screening<br />
N = 2,857<br />
Randomized in FLEX<br />
N = 1,099<br />
Alendronate, 5 mg<br />
N = 329<br />
Black D et al., 2006. J Clin Endocr Metab 85:4118-4124.<br />
FIT (3 to 4.5 yrs)<br />
Post-FIT Post FIT (1-2 (1 2 yrs)<br />
FLEX (5 yrs)<br />
Alendronate, 10 mg<br />
N = 333
Flex Fracture Outcome Years 1-3<br />
relative fracture rate<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
*<br />
VCFx<br />
Fosamax<br />
Placebo<br />
* statistically significant<br />
45% RRR
Flex Fracture Outcome Years 5-10<br />
% sustaining fracture<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
‡<br />
‡<br />
Hip Fx VCFx Any fx<br />
‡ not statistically significant<br />
‡<br />
Fosamax<br />
Placebo
Management recommendations:<br />
Dr. Joseph Lane<br />
“Lane advised physicians to check markers of bone<br />
metabolism in patients taking bisphosphonates and<br />
consider a drug holiday if bone metabolism appears<br />
to have stopped. He said he and his colleagues now<br />
discontinue bisphosphonate treatment in patients<br />
after 5 years; these patients are given calcium and<br />
vitamin D and are monitored for bone loss during that<br />
holiday. Bisphosphonate treatment is resumed in<br />
patients who experience bone loss, but at the lowest<br />
possible dose. ‘Until we get more data from industry<br />
and the FDA, we are stepping back,’ he said.”<br />
Source: Kuehn, B, 2009. Long-term risks of bisphosphonates probed.” JAMA 301:710-711.
Unusual Mid-shaft <strong>Fractures</strong> during Long-<br />
term Bisphosphonate <strong>The</strong>rapy - 2010<br />
13 women (from 2 hospitals) sustained atraumatic<br />
mid-shaft fractures – 11 femur, 1 humerus, and 1<br />
pelvis &right tibia. All had been only standing,<br />
walking, or turning around. 10 were on alendronate (3-<br />
11 yrs) and 3 on risedronate (Actonel) (2-5 yrs). 10<br />
were also on estrogen, tamoxifen, or prednisone. 3 of<br />
the 11 patients with a femur fracture had bilateral<br />
fractures. Of 11 patients with available information, 10<br />
had delayed fracture healing. Among 6 patients who<br />
had bone biopsies, all had severe depression of bone<br />
formation, with minimal or no osteoblasts.<br />
Note the high % who were also on other meds – a likely increased risk factor.<br />
Odvina CV, et al. 2010. Clinical Endocrinology 72:161-168.
Unusual Mid-shaft <strong>Fractures</strong> during Long-term<br />
Bisphosphonate <strong>The</strong>rapy - 2010<br />
Conclusion:<br />
“Long-term bisphosphonate therapy may increase the risk of<br />
unusual long bone mid-shaft fratures. This is probably due<br />
to prolonged suppression of bone turnover, which could<br />
lead to accumulation of microdamage and development of<br />
hypermineralized bone.”<br />
“Emerging data suggest that SSBT is a real clinical entity to<br />
be reckoned with. . . Coadministration of estrogens and<br />
SERMS, long-term steroid therapy, near-normal BMD<br />
before BP therapy and low initial bone turnover appear to<br />
be potential risk factors. Given the large number of patients<br />
exposed to bisphosphonates, even a small fraction of<br />
patients at risk of developing SSBT is not trivial and is<br />
clinically relevant.”<br />
Odvina CV, et al. 2010. Clinical Endocrinology 72:161-168.
Structural effects of long-term bisphosphonate<br />
treatment leading to atypical hip fractures<br />
• A DEXA- based study of the histology of bones of 111<br />
osteoporotic postmenopausal women compared 61<br />
treated with alendronate or risedronate for at least 4<br />
years with 50 controls not on BPs. (Pts on HRT,<br />
steroids, etc. were excluded) In the treated group, axial<br />
strength and structural integrity of the improved during<br />
the first 4 years of treatment, but later began to<br />
deteriorate back to baseline.<br />
• This BP effect can be explained by its inhibitory effect<br />
on bone remodeling, which may compromise the bone’s<br />
ability to bear loads and resist fractures. <strong>The</strong> results<br />
suggest that BP treatment beyond 4 years is<br />
counterproductive.<br />
Ding A et al. 2010. Presentation at the AAOS National Meeting.
Effects of long-term bisphosphonate<br />
use on bone quality.<br />
Bone samples were obtained from 21<br />
postmenopausal women hospitalized with femur<br />
fractures, 12 who’d been on BPs (mean 8.5 yrs)<br />
with 9 who had not. <strong>The</strong> treated group had<br />
reduced bone tissue heterogeneity of the<br />
mineral: matrix ration and significantly reduced<br />
crystallinity. “Our data suggest that suppression<br />
of bone turnover with long-term BPs results in a<br />
loss of heterogeneity of the tissue properties that<br />
may contribute to the risk of atypical fractures.”<br />
Gladnick B. Donnelly, Lorich, Lane et al, presentation at AAOS, 3/11/2010
Femoral insufficiency fractures associated<br />
with prolonged alendronate therapy -2010<br />
CONCLUSION<br />
“This is the largest study in the literature on<br />
femoral insufficiency fractures and alendronate<br />
therapy. Long-term alendronate use is<br />
associated with insufficiency fracture of the<br />
femoral shaft, which commonly presents with<br />
prodromal thigh pain and may be bilateral.<br />
Consideration should be given to ceasing<br />
alendronate therapy after 3 to 5 years of<br />
continuous use.”<br />
Isaacs JD et al. Presentation at AAOS 3/12/10
Black 2010: Risk of atypical femur fractures<br />
This study combined results of 3 large prior placebo-controlled studies of<br />
bisphosphonates: FIT (3-4.5 years on Fosamax, 5 mg for first 2 years, then 10 mg)<br />
and FLEX (additional up to 5 years on Fosamax) and HORIZON (up to 3 years on<br />
annual zolendronic acid). Among 14,195 women, 284 records showed hip or femur<br />
fractures, of which 12 were classified as subtrochanteric or diaphyseal, a combined<br />
rate of 2.3 per 10,000 patient-years.<br />
<strong>The</strong> authors calculated that treating 1,000 women with BPs for 3 years would prevent<br />
100 fractures, while the risk of atypical femur fractures would be about 0.3 cases.<br />
“<strong>The</strong> occurrence of [such] fractures of the femur was very rare, even among women<br />
who had been treated with bisphosphonates for as long as 10 years. <strong>The</strong>re was no<br />
significant increase associated with bisphosphonate use, but the study was<br />
underpowered for definitive conclusions.”<br />
-Black et al., 2010. Bisphosphonates and fracture of the subtrochanteric or<br />
diaphyseal femur. New England J Medicine 361:1761-71.
Management recommendations: Post-op<br />
1. Discontinue bisphosphonate; consider<br />
teriparatide (Forteo) post-op.<br />
2. Careful long-term follow-up for other fractures;<br />
imaging if pain in other leg. Bone scan if stress<br />
fracture is suspected.<br />
3. If stress fracture is found in other leg, do<br />
prophylactic rodding.<br />
DasDe S. et al, 2010. A rational approach to management of alendronate-related<br />
subtrochanteric fractures. J Bone Joint Surg 92:679-86.
Recent Studies:<br />
JAMA-Canadian Study<br />
NEJM-Swedish Study
JAMA, Park-Wyllie 2011:<br />
BP Use and the Risk of ST or Femoral Shaft<br />
<strong>Fractures</strong> in Older Woman (Canada)<br />
Adjusted OR 2.74<br />
With BP use > 5 years
NEJM: Schilcher, et al: BP Use and<br />
Atypical <strong>Fractures</strong> of the Femoral Shaft<br />
• 12,777 woman, age 55 sustaining femur fx in 2008<br />
• Reviewed 1234 x-rays reviewed of shaft fx<br />
• 59 patients with AFF indentified, 78% of these on BP (Longest<br />
duration of use 3 years)<br />
Results:<br />
Age adjusted RR 47.3<br />
Risk higher with longer use (OR 1.3). Risk was 10x as compared<br />
to normal risk within 2 years of use and 50X as high thereafter.<br />
Conclusion: “Absolute risk of atypical fractures associated with BP<br />
for patients with a high risk of osteoporotic fractures is small as<br />
compared with beneficial effects of the drug.”<br />
Schilcher, et al 2011, BP Use and Atypical <strong>Fractures</strong> of the Femoral Shaft
Fosamax Label:<br />
Timeline
March 10, 2010
Fosamax 2010 Task Force Report
ASBMR Symposium<br />
October 2010, Toronto<br />
• Task force of the American Society for Bone and<br />
Mineral Research (27 international experts)<br />
Results and Conclusions<br />
- Defined AFF<br />
- AFF associated with long-term BP use but no causal link<br />
- Data suggests that risk rises with increasing duration of<br />
exposure<br />
- Concern that lack of awareness and under-reporting may<br />
mask true incidence.
Information for FDA warning to doctors regarding<br />
BP-related femur fractures:<br />
• Fx are often bilateral. If one femur has a stress or completed<br />
fracture, assess the contralateral femur.<br />
• BP treatment should be stopped as soon as a stress or<br />
completed fracture is diagnosed.<br />
• Completed fractures are often preceded by stress fractures,<br />
which frequently cause thigh pain. Thigh pain in a patient<br />
on long-term BPs requires assessment with imaging studies.<br />
• BP-related stress fractures are at high risk of completion,<br />
and require early referral to an orthopedist for treatment<br />
(which often is prophylactic rodding).<br />
• BP-related fractures are at high risk of non-union or delayed<br />
union.<br />
• Despite stopping the BP, patients remain at risk for years of<br />
additional fractures and need to be followed up.
FDA Announces Label Change:<br />
October 13, 2010<br />
• FDA announced that it will be updating the public regarding<br />
information previously communicated regarding the risk of AFF<br />
in patients who take BP for osteoporosis (Class warning).<br />
• This information will be added to the Warnings and Precautions<br />
section of the label<br />
• “FDA will require a new Limitations of Use Statement in the<br />
Indications and Usage section of the label<br />
• “FDA will require that a Medication Guide be included with all<br />
BP medications approved for osteoporosis”<br />
-Based upon on-going FDA review and Task Force data of ASBMR
Fosamax Label<br />
Warnings/Precautions:<br />
Pre-January 2011<br />
• No Warnings or Precautions regarding AFF<br />
• No long term studies were performed according to label:<br />
– “<strong>The</strong> efficacy of <strong>FOSAMAX</strong> has been established in studies of two<br />
years’ duration. <strong>The</strong> greatest increase in bone mineral density<br />
occurred in the first year with maintenance or smaller gains during<br />
the second year. Efficacy of <strong>FOSAMAX</strong> beyond two years has not<br />
been studied.”
Jan. 2011: Update on <strong>Femur</strong> Fracture Risk with<br />
Bisphosphonates
Fosamax Label<br />
Warnings/Precautions:<br />
Precautions Section<br />
Issued January 2011<br />
“Atypical Subtrochanteric and Diaphyseal Femoral <strong>Fractures</strong>”<br />
• AFFs have been reported<br />
• Location of AFF<br />
• “Causality has not been established as these fractures also<br />
occur in osteoporotic patients who have not been treated<br />
with BP.”<br />
• Occur with minimal or no trauma, may be bilateral with<br />
prodromal pain<br />
• Number of reports note patients also txed with<br />
glucocorticoids
Fosamax Label<br />
Warnings/Precautions:<br />
Issued January 2011: (Continued)<br />
Precautions Section<br />
“Atypical Subtrochanteric and Diaphyseal Femoral <strong>Fractures</strong>”<br />
• Patients with hx of BP exposure with thigh/groin should be<br />
suspected for AFF and evaluated to rule out for incomplete<br />
femur fx.<br />
• Patients with AFF should be assessed for s/s of fx on<br />
contralateral limb<br />
• Interruption of BP should be considered, pending a<br />
risk/benefit assessment, on individual basis.
Jan. 2011: Update on <strong>Femur</strong> Fracture<br />
Risk with Bisphosphonates<br />
• FDA recommends that healthcare professionals:<br />
• be aware of the possibility of atypical femur fractures in patients taking bisphosphonates<br />
• rule out a femoral fracture if a patient presents with new thigh or groin pain, and discontinue<br />
potent anti-resorptive medications, including bisphosphonates, in patients who have evidence of a<br />
femoral fracture.<br />
• consider periodically re-evaluating whether continued bisphosphonate therapy is needed,<br />
especially in patients who have been treated for more than five years. Periodic reevaluation is<br />
recommended because the fracture reduction efficacy of these drugs has not been established, and<br />
the optimal duration of use is uncertain.<br />
• discuss the benefits and risks of these drugs with patients, and instruct them to seek medical<br />
attention if they experience new groin or thigh pain, which may be described as dull or aching. This<br />
pain can occur weeks or months before a complete fracture occurs.<br />
This safety information will appear in the drugs' labeling, as well as in a Medication Guide that will<br />
be distributed to patients with each prescription.
http://www.fda.gov/AdvisoryCommittees/Calendar/ucm262477.htm
FDA Bisphosphonate<br />
Advisory Committee Hearing<br />
Deadlines and Dates:<br />
Request to Speak August 17, 2011<br />
Written Submissions August 25, 2011<br />
Hearing September 9, 2011
AdComm Hearing Location<br />
Marriott Inn and Conference Center<br />
University of Maryland University<br />
College (UMUC)<br />
3501 University Blvd. East<br />
Adelphi, Maryland
FDA BP AdComm Speaker and Written<br />
Submission Contact Information<br />
Kalyani Bhatt<br />
Center for Drug Evaluation and<br />
Research<br />
Food and Drug Administration<br />
10903 New Hampshire Avenue<br />
WO31-2417<br />
Silver Spring, Maryland 20993-0002<br />
Phone: 301-796-9001<br />
Fax: 301-847-8533<br />
E-mail: ACRHD@fda.hhs.gov
FDA AdComm Info Line<br />
• FDA Advisory Committee Information<br />
Line<br />
1-800-741-8138<br />
(301-443-0572 in the Washington DC<br />
area) follow the prompts to the desired<br />
center or product area<br />
• Call the Information Line for up-to-date<br />
information on this meeting