Managing Long-Term Issues – Post Lung Transplant
Managing Long-Term Issues – Post Lung Transplant
Managing Long-Term Issues – Post Lung Transplant
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
Jeff Golden, MD<br />
Professor of Medicine and Surgery<br />
University of California, San Francisco<br />
Medical Director, <strong>Lung</strong> <strong>Transplant</strong>ation<br />
Director of Clinical Research,<br />
Interstitial <strong>Lung</strong> Disease Program<br />
Email: jeffrey.golden@ucsf.edu<br />
ILD: SALLY MCLAUGHLIN 415 353-2577<br />
LUNG TRANSPLANTATION:<br />
KERRY KUMAR 415 353-9338<br />
What’s New, What Matters,<br />
What’s Next<br />
UCSF TRANSLANT 2010<br />
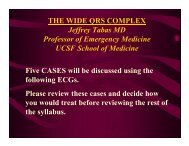
# of patients<br />
45<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
Number of <strong>Lung</strong> <strong>Transplant</strong>s Per<br />
Year at UCSF<br />
31<br />
32<br />
28<br />
29<br />
15<br />
13<br />
11<br />
12<br />
10 10 10<br />
8<br />
6<br />
6<br />
4<br />
1<br />
35<br />
41<br />
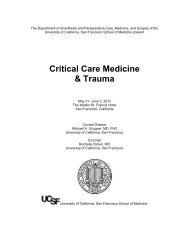
Heart and <strong>Lung</strong> <strong>Transplant</strong><br />
Quality Indicator<br />
Patient Survival<br />
UCSF Heart<br />
<strong>Transplant</strong><br />
Observed<br />
UCSF Heart<br />
<strong>Transplant</strong><br />
Expected<br />
UCSF <strong>Lung</strong><br />
<strong>Transplant</strong><br />
Observed<br />
UCSF <strong>Lung</strong><br />
<strong>Transplant</strong><br />
Expected<br />
1 Month 96.52% 94.97% 97.56% 95.85%<br />
1 Year 85.81% 81.14% 89.28% 83.18%<br />
3 Years 69.91% 60.44% 74.36%* 63.02%<br />
0<br />
1991<br />
1992<br />
1993<br />
1994<br />
1995<br />
1996<br />
1997<br />
1998<br />
1999<br />
2000<br />
2001<br />
2002<br />
2003<br />
2004<br />
2005<br />
2006<br />
2007<br />
2008<br />
SRTR- Scientific Registry <strong>Transplant</strong> Recipients<br />
•For Patients Receiving their First <strong>Transplant</strong> of this type between<br />
07/01/2006 and 12/31/2008 for the 1 Month and 1 Year Cohorts; between<br />
01/01/2004 and 06/30/2006 for the 3 Year Cohort<br />
• * Statistically Significant Updated 01/05/2010<br />
1
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
•50% Five Year Survival<br />
<strong>–</strong>15 - 20 years without improvement in five year survival<br />
<strong>–</strong>Risks to Improvement of <strong>Long</strong> <strong>Term</strong> Survival<br />
RISK TO LONG TERM OUTCOME<br />
Immunosuppression rather than understanding of mechanisms<br />
Bronchiolitis Obliterans - Chronic Rejection<br />
Challenges of newer categories of recipients<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
BRONCHIOLITIS OBLITERANS<br />
PROGRESSION OF SCAR<br />
Outline<br />
•Bronchiolitis Obliterans Syndrome (BOS)<br />
-Mortality & Morbidity<br />
- Mechanism - Immune and non-immune<br />
- Interventions<br />
<strong>–</strong>Complications <strong>Post</strong>-transplantation<br />
-Immunosuppression and morbidity<br />
i.e. Infection, cancer<br />
•New categories of recipients<br />
future management challenges<br />
What used to be the size of<br />
the dotted line has been<br />
scarred down to the central<br />
dark lumen<br />
2
Causes of Death Following<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
>3 years post transplant<br />
*Bronchiolitis Obliterans-80% of deaths<br />
Graft failure<br />
and/or<br />
Infection<br />
Bronchiolitis Obliterans<br />
Chronic Rejection<br />
“BOS” - Bonchiolitis Obliterans Syndrome<br />
FEV 1<br />
<strong>–</strong> BOS Major Barrier to <strong>Long</strong> <strong>Term</strong><br />
Success<br />
*BRONCHIOLITIS OBLITERANS SYNDROME<br />
“BOS”<br />
FEV 1 DECREASES >20%<br />
<strong>–</strong> Mechanism of BOS: Work in Progress<br />
• Immune Mechanism<br />
<strong>–</strong> Acute Vascular Rejection<br />
ACUTE VASCULAR REJECTION<br />
Transbronchial Biopsy (TBBx)<br />
Bronchiolitis Obliterans<br />
Chronic Rejection<br />
“BOS” - Bonchiolitis Obliterans Syndrome<br />
FEV 1<br />
<strong>–</strong> BOS Major Barrier to <strong>Long</strong> <strong>Term</strong> Success<br />
<strong>–</strong> Mechanism of BOS: Work in Progress<br />
• Immune Mechanism<br />
<strong>–</strong> Acute Vascular Rejection<br />
<strong>–</strong> Acute Airway Rejection<br />
» Lymphoycitic bronchitis/bronchiolitis<br />
3
Acute Airway Rejection<br />
Inhaled Cyclosporine<br />
Separate Interventions for Separate Processes<br />
Lymphocytic<br />
Bronchitis/Bronchiolitis(LBB):<br />
A Risk Factor for BO<br />
Youseem, 1993, Ross 1997, Hussain, 1999,<br />
Hays 2008 ATS<br />
Cyclosporine by inhalation<br />
Epithelial administration to<br />
avert airway rejection &<br />
ongoing injury, inflammation<br />
and fibrosis ending in<br />
bronchiolitis obliterans<br />
Systemic cyclosporine<br />
Systemic administration to<br />
avert vascular rejection,<br />
halting lymphocytic<br />
recruitment and activation<br />
Chronic rejection-free survival probability<br />
Inhaled Cyclosporine<br />
Kaplan-Meier Plot of Chronic<br />
Rejection-Free Survival<br />
1.0<br />
0.9<br />
0.8<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
0.0<br />
CyIS<br />
Placebo<br />
Relative risk = 0.279<br />
P = .001<br />
3.6-fold increase in median chronic<br />
rejection-free survival duration<br />
0 6 12 18 24 30 36 42 48 54 60<br />
N at risk<br />
Time, months<br />
Placebo 30 24 19 14 12 6 5 4 3 1 0<br />
CyIS 26 26 24 21 16 12 11 9 5 0 0<br />
Azithromycin: Prevention of BOS<br />
Randomized placebo-controlled trial to prevent<br />
BOS after lung transplantation<br />
2 year study, 83 patients<br />
Vos R. 2010<br />
Azithromycin reduced BOS v placebo<br />
12.5% vs 44.2% p= 0.0017<br />
4
Rejection:<br />
Newer Categories of Acute <strong>Lung</strong> Rejection<br />
Immune Mechanism of Bonchiolitis Obliterans Syndrome:<br />
• Acute Vascular Rejection<br />
• Lymphcytic bronchitis/bronchiolitis - Airway Rejection<br />
<strong>–</strong> Inhale Immunosuppression<br />
<strong>–</strong> azithromycin<br />
• Antibody Mediated Rejection-Donor Specific Antibody<br />
Humoral Mediated Rejection<br />
• Role in <strong>Lung</strong> <strong>Transplant</strong>ation?<br />
• How diagnose ?<br />
Donor Specific Antibodies (DSA)<br />
Measurement Technique (s)<br />
Pathology - C4D<br />
• Treatment?<br />
<strong>–</strong>Plasmapheresis, Rituxamab, IVIG<br />
Donor SpecificAntibody to Single HLA Antigen<br />
Humoral Mediated Rejection<br />
• Role in <strong>Lung</strong> <strong>Transplant</strong>ation?<br />
*<br />
• How diagnose ?<br />
Donor Specific Antibodies (DSA)<br />
Measurement Technique (s)<br />
Pathology - C4D<br />
• Treatment?<br />
<strong>–</strong>Plasmapheresis, Rituxamab, IVIG<br />
* PE - Phycoerthythrin<br />
5
Humoral Mediated Rejection<br />
• Role in <strong>Lung</strong> <strong>Transplant</strong>ation?<br />
• How diagnose ?<br />
Donor Specific Antibodies (DSA)<br />
Measurement Technique (s)<br />
Pathology - C4D<br />
• Treatment?<br />
<strong>–</strong>Plasmapheresis, Rituxamab, IVIG<br />
Donor Specific anti-HLA Antibodies<br />
and Antibody-Directed Therapy after<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
RR Hachem, MR Morrell, RD Yusen, AA<br />
Aloush, M Liu, BF Meyers, GA Patterson,<br />
T Mohanakumar, EP Trulock<br />
DSA clearance and survival<br />
DSA & BOS<br />
summary<br />
• DSA surprisingly<br />
common<br />
• Role of treatment?<br />
• DSA clearance<br />
favorable outcome<br />
Sensitization<br />
*PGD<br />
DSA<br />
BOS<br />
• NEED: Randomized<br />
Controlled Trial<br />
HLA mismatch<br />
*Primary Graft Dysfunction<br />
6
Chiron Briefing Document Figure 2.2-2<br />
Bronchiolitis Obliterans<br />
Syndrome (BOS)<br />
Immune Mechanisms<br />
• Acute Vascular Rejection<br />
• Acute Airway Rejection<br />
<strong>–</strong> Lymphocytic bronchitis/bronchiolitis<br />
• Antibody Mediated Rejection-Donor Specific Antibody<br />
The Path to Chronic Rejection<br />
Immune dependent factors<br />
• Acute rejection<br />
• Lymphocytic<br />
bronchitis/bronchiolitis<br />
• Humoral Mediated<br />
Rejection-<br />
<strong>–</strong> DSA- (donor specific<br />
antibody)<br />
Small airway epithelial injury<br />
Excessive fibroproliferation<br />
Aberrant tissue repair<br />
Immune independent factors<br />
• Primary Graft Dysfunction<br />
• GERD/microaspiration<br />
• CMV pneumonitis<br />
• Community Viral<br />
Bronchiolitis obliterans (OB)<br />
Gastroesophageal Reflux Disease<br />
Early Fundoplication Prevents Chronic Allograft<br />
Dysfunction in Patients with GERD<br />
Cantu 2004 Ann Thorac Surg<br />
•<strong>Post</strong>-<strong>Transplant</strong>ation<br />
14 <strong>Lung</strong> <strong>Transplant</strong> Recipients with GERD<br />
“immediate” fundoplication<br />
BOS free up to three years<br />
"…we suggest that GER should be considered as a<br />
potentially reversible cause of BOS among lung transplant<br />
recipients."<br />
7
Effect of GERD on Survival<br />
<strong>Lung</strong> <strong>Transplant</strong>ation:<br />
Bronchiolitis Obliterans Syndrome (BOS)<br />
&<br />
Gastroesophageal Reflux Disease<br />
•Increased GERD in Pre-<strong>Transplant</strong> Populations<br />
IPF, Cystic Fibrosis<br />
•GERD worse <strong>Post</strong>-<strong>Transplant</strong>ation<br />
•Esophageal Wrap Avoids BOS ?<br />
Davis RD Jr, et al. Improved lung allograft function after fundoplication in patients with<br />
gastroesophageal reflux disease undergoing lung transplantation. J Thorac Cardiovasc<br />
Surg. 2003 Mar;125(3):533-42.<br />
•Azithromycin reduces GE Reflux and aspiration<br />
»Mertins V<br />
<strong>–</strong>24 hour Impedance-pH<br />
<strong>–</strong>BAL bile acid level<br />
Chiron Briefing Document Figure 2.2-2<br />
The Path to Chronic Rejection<br />
Immune dependent factors<br />
• Acute rejection<br />
• Lymphocytic<br />
bronchitis/bronchiolitis<br />
• Humoral Mediated<br />
Rejection-<br />
<strong>–</strong> DSA- (donor specific<br />
antibody)<br />
Small airway epithelial injury<br />
Excessive fibroproliferation<br />
Aberrant tissue repair<br />
Immune independent factors<br />
• Primary Graft Dysfunction<br />
• GERD/microaspiration<br />
• CMV pneumonitis<br />
• Community Viral Infections<br />
Respiratory Syncytial Virus (RSV)<br />
in 75 year old <strong>Lung</strong> <strong>Transplant</strong> Recipient<br />
Bronchiolitis obliterans (OB)<br />
8
Viral Syndrome <strong>Post</strong>-Transpant<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
Community Acquired Respiratory Viruses<br />
• Novel Techniques of Detection<br />
• Pathogenesis - Bronchiolitis Obliterans Syndrome (BOS)<br />
• Clinical Management<br />
Eosinophils<br />
Bronchoscopy #2<br />
Clinical Presentation*<br />
Vessel<br />
• DFA neg<br />
• Viral PCR: metapneumovirus and rhinovirus<br />
• AFB and Fungal NGTD<br />
• Transbronchial <strong>Lung</strong> Biopsy: Rejection<br />
• Vascular Rejection A3*<br />
•<br />
_____________________________<br />
* Severity Scale A1 - A4<br />
9
Is community-acquired respiratory virus<br />
infection associated with Bronchiolitis<br />
Obliterans Syndroms<br />
• Gottlieb J 2009,<br />
Prospective Investigations<br />
of Community Acquired Virus in<br />
lung transplant recipients<br />
Community Acquired Respiratory Viruses (CARV)<br />
and Risk of BOS<br />
• Single center prospective cohort study, Hannover,<br />
Germany, Nov 2005- April 2006<br />
• 388 post lung transplant pts screened<br />
<strong>–</strong> viral sxs<br />
<strong>–</strong> URTI sxs: Nasopharyngeal swab for DFA, no PCR<br />
<strong>–</strong> LRTI sxs: Swab + BAL for DFA and PCR<br />
• 7.7% of patients enrolled had CARV<br />
<strong>–</strong> Parainfluenza, RSV, metapneumovirus, coronavirus,<br />
rhinovirus, influenza<br />
Gottlieb, <strong>Transplant</strong>ation 2009<br />
Kumar 2010<br />
Community Acquired Respiratory Viruses &<br />
Risk of Bronchiolitis Obliterans Syndrome<br />
Community Viruses Risk of BOS<br />
1year incidence of BOS<br />
25% in virus + pts<br />
9% in virus <strong>–</strong> pts<br />
P = 0.01<br />
Gottlieb, <strong>Transplant</strong>ation 2009<br />
Community Acquired<br />
Respiratory Viruses<br />
and <strong>Lung</strong> <strong>Transplant</strong>ation<br />
• Pathogenesis-Bronchiolitis Obliterans Syndrome (BOS)<br />
• Clinical Management Implications<br />
<strong>–</strong> Prevent Exposure<br />
<strong>–</strong> Call transplant center with “cold” symptoms<br />
<strong>–</strong> Vaccination -Danziger L, <strong>Transplant</strong>ation 2010<br />
10
Bronchiolitis Obliterans<br />
Challenge: Understanding Mechanism<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
Non-<br />
alloimmune<br />
factors: • Infection<br />
• GERD<br />
• Others<br />
Increase<br />
systemic<br />
immune<br />
suppression<br />
Immune<br />
activation<br />
Bronchiolitis<br />
obliterans<br />
Outline<br />
•Bronchiolitis Obliterans Syndrome (BOS)<br />
-Mortality & Morbidity<br />
- Mechanism - Immune and non-immune<br />
- Interventions<br />
<strong>–</strong>Complications <strong>Post</strong>-transplantation<br />
-Immunosuppression and morbidity<br />
i.e. Infection, cancer<br />
•New categories of recipients<br />
future management challenges<br />
Increased Potential for<br />
Infection<br />
Aspergillosis in <strong>Lung</strong><br />
<strong>Transplant</strong>ation<br />
• Immunosuppression<br />
• Donor lung infection<br />
• Acute epithelial injury<br />
• Ischemia<br />
• Rejection<br />
• Mucociliary clearance<br />
• No cough reflex<br />
• No Lymphatic defense<br />
• Airway function<br />
• Anastomosis<br />
• Obliterative bronchiolitis<br />
A Major Problem<br />
• Incidence (colonization or disease) 8 - 46%<br />
• Invasive Aspergillus mortality rate > 60%<br />
• Up to 13% of all post-lung transplant deaths<br />
Cahill. 1997 112(5):1160<br />
Nunley Chest. 2002 122(4):1185<br />
Westney. <strong>Transplant</strong>ation. 1996 61(6):915<br />
11
Aspergillosis in <strong>Lung</strong><br />
<strong>Transplant</strong>ation<br />
Management of <strong>Long</strong> <strong>Term</strong> Complications<br />
Voriconazole: Prophylaxis and Tx<br />
? Risk of skin cancer and Voriconazole<br />
Voriconazole and geographic location are<br />
independent risk factors for Squamous cell<br />
carcinoma<br />
SKIN CANCER INCIDENCE<br />
Kidney, Heart <strong>Transplant</strong><br />
Years post <strong>Transplant</strong>:<br />
10 years 10-30%<br />
20 years 40-60%<br />
<strong>Lung</strong> <strong>Transplant</strong><br />
7 years 12%<br />
Vadnerkar 2010<br />
Nguyen MH 2010<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
Outline<br />
•Bronchiolitis Obliterans Syndrome (BOS)<br />
-Mortality & Morbidity<br />
- Mechanism - Immune and non-immune<br />
- Interventions<br />
<strong>–</strong>Complications <strong>Post</strong>-transplantation<br />
-Immunosuppression and morbidity<br />
i.e. Infection, cancer<br />
•New categories of recipients<br />
future management challenges<br />
<strong>Lung</strong> <strong>Transplant</strong>ation & long term<br />
management:<br />
New recipient categories create future<br />
challenges<br />
•<strong>Lung</strong> Allocation Score: recipient risk<br />
»Russo MJ<br />
•<strong>Lung</strong> Fibrosis: DVT/emboli<br />
•Age<br />
•Coronary Artery Disease<br />
•Novel Patient Categories<br />
Bronchoalveolar cell carcinoma (BAC)<br />
Scleroderma<br />
Saggar R, UCLA<br />
12
<strong>Lung</strong> Allocation Score (LAS)<br />
Emergent <strong>Lung</strong> <strong>Transplant</strong>ation<br />
In Fibrotic <strong>Lung</strong> Disease<br />
• New transplant guidelines are based on a lung<br />
allocation score (LAS)<br />
• How sick is the patient?<br />
• LAS (0 - 100) prioritizes lung allocation<br />
• IPF & Cystic Fibrosis favored over Emphysema<br />
•<strong>Lung</strong> Allocation Score: Emergent Organ Availability:<br />
•ECMO extracorporeal membrane oxygenation<br />
RE-TRANSPLANTATION<br />
Yusen RD 2010<br />
<strong>Post</strong> LAS 5% of lung transplants<br />
May 2005<br />
Median waiting time<br />
Pre LAS 146 Days<br />
<strong>Post</strong> LAS 45 Days<br />
1-year survival<br />
Re-<strong>Transplant</strong>ation 70%<br />
Primary <strong>Transplant</strong> 83%<br />
<strong>Lung</strong> <strong>Transplant</strong>ation & long term<br />
management:<br />
New recipient categories create future<br />
challenges<br />
•<strong>Lung</strong> Allocation Score: recipient risk<br />
•<strong>Lung</strong> Fibrosis: DVT/emboli<br />
•Age<br />
•Coronary Artery Disease<br />
•Novel Patient Categories<br />
Bronchoalveolar cell carcinoma (BAC)<br />
Scleroderma<br />
Saggar R, UCLA<br />
13
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
Outline<br />
•Bronchiolitis Obliterans Syndrome (BOS)<br />
-Mortality & Morbidity<br />
- Mechanism - Immune and non-immune<br />
- Interventions<br />
<strong>–</strong>Complications <strong>Post</strong>-transplantation<br />
-Immunosuppression and morbidity<br />
i.e. Infection, cancer<br />
•New categories of recipients<br />
future management challenges<br />
<strong>Lung</strong> <strong>Transplant</strong>ation & long<br />
term management:<br />
future challenges<br />
•quality of life<br />
•<br />
<strong>–</strong>Assess more than survival<br />
<strong>–</strong>unique10 year survivors<br />
•Rutherford 2005<br />
<strong>–</strong>UCSF Jon Singer<br />
<strong>Lung</strong> <strong>Transplant</strong>ation<br />
“In it for the <strong>Long</strong> Haul:<br />
<strong>Long</strong>-<strong>Term</strong> Management”<br />
•50% Survival by 5 years post-transplant<br />
•Bronchiolitis Obliterans barrier to success<br />
Chronic Rejection<br />
•<strong>Lung</strong> transplant is a frontier<br />
•The standard of care is dynamic<br />
14