Heart rate response during exercise test and cardiovascular ...
Heart rate response during exercise test and cardiovascular ...
Heart rate response during exercise test and cardiovascular ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
584 K.P. Savonen et al.<br />
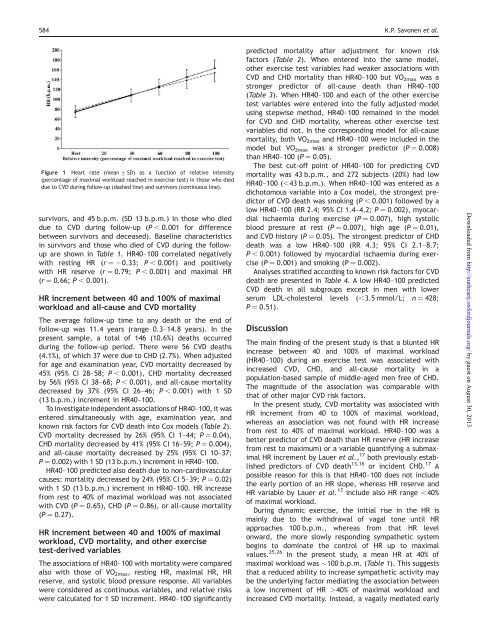
Figure 1 <strong>Heart</strong> <strong>rate</strong> (mean + SD) as a function of relative intensity<br />
(percentage of maximal workload reached in <strong>exercise</strong> <strong>test</strong>) in those who died<br />
due to CVD <strong>during</strong> follow-up (dashed line) <strong>and</strong> survivors (continuous line).<br />
survivors, <strong>and</strong> 45 b.p.m. (SD 13 b.p.m.) in those who died<br />
due to CVD <strong>during</strong> follow-up (P , 0.001 for difference<br />
between survivors <strong>and</strong> deceased). Baseline characteristics<br />
in survivors <strong>and</strong> those who died of CVD <strong>during</strong> the followup<br />
are shown in Table 1. HR40–100 correlated negatively<br />
with resting HR (r ¼ 20.33; P , 0.001) <strong>and</strong> positively<br />
with HR reserve (r ¼ 0.79; P , 0.001) <strong>and</strong> maximal HR<br />
(r ¼ 0.66; P , 0.001).<br />
HR increment between 40 <strong>and</strong> 100% of maximal<br />
workload <strong>and</strong> all-cause <strong>and</strong> CVD mortality<br />
The average follow-up time to any death or the end of<br />
follow-up was 11.4 years (range 0.3–14.8 years). In the<br />
present sample, a total of 146 (10.6%) deaths occurred<br />
<strong>during</strong> the follow-up period. There were 56 CVD deaths<br />
(4.1%), of which 37 were due to CHD (2.7%). When adjusted<br />
for age <strong>and</strong> examination year, CVD mortality decreased by<br />
45% (95% CI 28–58; P , 0.001), CHD mortality decreased<br />
by 56% (95% CI 38–68; P , 0.001), <strong>and</strong> all-cause mortality<br />
decreased by 37% (95% CI 26–46; P , 0.001) with 1 SD<br />
(13 b.p.m.) increment in HR40–100.<br />
To investigate independent associations of HR40–100, it was<br />
entered simultaneously with age, examination year, <strong>and</strong><br />
known risk factors for CVD death into Cox models (Table 2).<br />
CVD mortality decreased by 26% (95% CI 1–44; P ¼ 0.04),<br />
CHD mortality decreased by 41% (95% CI 16–59; P ¼ 0.004),<br />
<strong>and</strong> all-cause mortality decreased by 25% (95% CI 10–37;<br />
P ¼ 0.002) with 1 SD (13 b.p.m.) increment in HR40–100.<br />
HR40–100 predicted also death due to non-<strong>cardiovascular</strong><br />
causes: mortality decreased by 24% (95% CI 5–39; P ¼ 0.02)<br />
with 1 SD (13 b.p.m.) increment in HR40–100. HR increase<br />
from rest to 40% of maximal workload was not associated<br />
with CVD (P ¼ 0.65), CHD (P ¼ 0.86), or all-cause mortality<br />
(P ¼ 0.27).<br />
HR increment between 40 <strong>and</strong> 100% of maximal<br />
workload, CVD mortality, <strong>and</strong> other <strong>exercise</strong><br />
<strong>test</strong>-derived variables<br />
The associations of HR40–100 with mortality were compared<br />
also with those of VO 2max , resting HR, maximal HR, HR<br />
reserve, <strong>and</strong> systolic blood pressure <strong>response</strong>. All variables<br />
were considered as continuous variables, <strong>and</strong> relative risks<br />
were calculated for 1 SD increment. HR40–100 significantly<br />
predicted mortality after adjustment for known risk<br />
factors (Table 2). When entered into the same model,<br />
other <strong>exercise</strong> <strong>test</strong> variables had weaker associations with<br />
CVD <strong>and</strong> CHD mortality than HR40–100 but VO 2max was a<br />
stronger predictor of all-cause death than HR40–100<br />
(Table 3). When HR40–100 <strong>and</strong> each of the other <strong>exercise</strong><br />
<strong>test</strong> variables were entered into the fully adjusted model<br />
using stepwise method, HR40–100 remained in the model<br />
for CVD <strong>and</strong> CHD mortality, whereas other <strong>exercise</strong> <strong>test</strong><br />
variables did not. In the corresponding model for all-cause<br />
mortality, both VO 2max <strong>and</strong> HR40–100 were included in the<br />
model but VO 2max was a stronger predictor (P ¼ 0.008)<br />
than HR40–100 (P ¼ 0.05).<br />
The best cut-off point of HR40–100 for predicting CVD<br />
mortality was 43 b.p.m., <strong>and</strong> 272 subjects (20%) had low<br />
HR40–100 (,43 b.p.m.). When HR40–100 was entered as a<br />
dichotomous variable into a Cox model, the strongest predictor<br />
of CVD death was smoking (P , 0.001) followed by a<br />
low HR40–100 (RR 2.4; 95% CI 1.4–4.2; P ¼ 0.002), myocardial<br />
ischaemia <strong>during</strong> <strong>exercise</strong> (P ¼ 0.007), high systolic<br />
blood pressure at rest (P ¼ 0.007), high age (P ¼ 0.01),<br />
<strong>and</strong> CVD history (P ¼ 0.05). The strongest predictor of CHD<br />
death was a low HR40–100 (RR 4.3; 95% CI 2.1–8.7;<br />
P , 0.001) followed by myocardial ischaemia <strong>during</strong> <strong>exercise</strong><br />
(P ¼ 0.001) <strong>and</strong> smoking (P ¼ 0.002).<br />
Analyses stratified according to known risk factors for CVD<br />
death are presented in Table 4. A low HR40–100 predicted<br />
CVD death in all subgroups except in men with lower<br />
serum LDL-cholesterol levels (,3.5 mmol/L; n ¼ 428;<br />
P ¼ 0.51).<br />
Discussion<br />
The main finding of the present study is that a blunted HR<br />
increase between 40 <strong>and</strong> 100% of maximal workload<br />
(HR40–100) <strong>during</strong> an <strong>exercise</strong> <strong>test</strong> was associated with<br />
increased CVD, CHD, <strong>and</strong> all-cause mortality in a<br />
population-based sample of middle-aged men free of CHD.<br />
The magnitude of the association was comparable with<br />
that of other major CVD risk factors.<br />
In the present study, CVD mortality was associated with<br />
HR increment from 40 to 100% of maximal workload,<br />
whereas an association was not found with HR increase<br />
from rest to 40% of maximal workload. HR40–100 was a<br />
better predictor of CVD death than HR reserve (HR increase<br />
from rest to maximum) or a variable quantifying a submaximal<br />
HR increment by Lauer et al., 17 both previously established<br />
predictors of CVD death 13,16 or incident CHD. 17 A<br />
possible reason for this is that HR40–100 does not include<br />
the early portion of an HR slope, whereas HR reserve <strong>and</strong><br />
HR variable by Lauer et al. 17 include also HR range ,40%<br />
of maximal workload.<br />
During dynamic <strong>exercise</strong>, the initial rise in the HR is<br />
mainly due to the withdrawal of vagal tone until HR<br />
approaches 100 b.p.m., whereas from that HR level<br />
onward, the more slowly responding sympathetic system<br />
begins to dominate the control of HR up to maximal<br />
values. 25,26 In the present study, a mean HR at 40% of<br />
maximal workload was 100 b.p.m. (Table 1). This suggests<br />
that a reduced ability to increase sympathetic activity may<br />
be the underlying factor mediating the association between<br />
a low increment of HR .40% of maximal workload <strong>and</strong><br />
increased CVD mortality. Instead, a vagally mediated early<br />
Downloaded from http://eurheartj.oxfordjournals.org/ by guest on August 30, 2013