PARAphrase Fall 2012
PARAphrase Fall 2012
PARAphrase Fall 2012
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
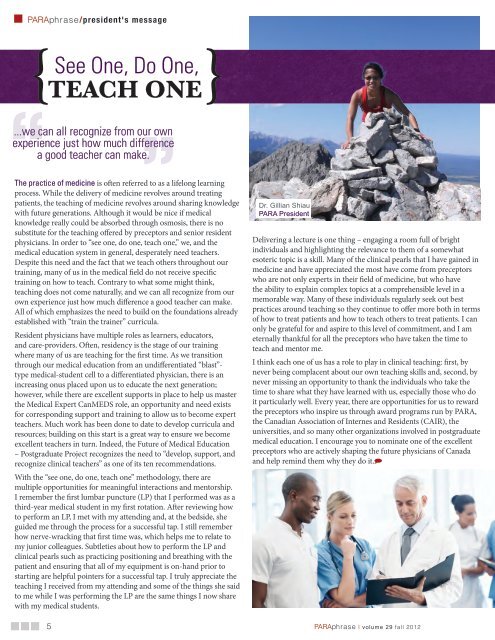
<strong>PARAphrase</strong>/president's message<br />
{<br />
See<br />
One, Do One,<br />
TEACH ONE}<br />
”<br />
The practice of medicine is often referred to as a lifelong learning<br />
process. While the delivery of medicine revolves around treating<br />
patients, the teaching of medicine revolves around sharing knowledge<br />
with future generations. Although it would be nice if medical<br />
knowledge really could be absorbed through osmosis, there is no<br />
substitute for the teaching offered by preceptors and senior resident<br />
physicians. In order to “see one, do one, teach one,” we, and the<br />
medical education system in general, desperately need teachers.<br />
Despite this need and the fact that we teach others throughout our<br />
training, many of us in the medical field do not receive specific<br />
training on how to teach. Contrary to what some might think,<br />
teaching does not come naturally, and we can all recognize from our<br />
own experience just how much difference a good teacher can make.<br />
All of which emphasizes the need to build on the foundations already<br />
established with “train the trainer” curricula.<br />
Resident physicians have multiple roles as learners, educators,<br />
and care-providers. Often, residency is the stage of our training<br />
where many of us are teaching for the first time. As we transition<br />
through our medical education from an undifferentiated “blast”-<br />
type medical-student cell to a differentiated physician, there is an<br />
increasing onus placed upon us to educate the next generation;<br />
however, while there are excellent supports in place to help us master<br />
the Medical Expert CanMEDS role, an opportunity and need exists<br />
for corresponding support and training to allow us to become expert<br />
teachers. Much work has been done to date to develop curricula and<br />
resources; building on this start is a great way to ensure we become<br />
excellent teachers in turn. Indeed, the Future of Medical Education<br />
– Postgraduate Project recognizes the need to “develop, support, and<br />
recognize clinical teachers” as one of its ten recommendations.<br />
With the “see one, do one, teach one” methodology, there are<br />
multiple opportunities for meaningful interactions and mentorship.<br />
I remember the first lumbar puncture (LP) that I performed was as a<br />
third-year medical student in my first rotation. After reviewing how<br />
to perform an LP, I met with my attending and, at the bedside, she<br />
guided me through the process for a successful tap. I still remember<br />
how nerve-wracking that first time was, which helps me to relate to<br />
my junior colleagues. Subtleties about how to perform the LP and<br />
clinical pearls such as practicing positioning and breathing with the<br />
patient and ensuring that all of my equipment is on-hand prior to<br />
starting are helpful pointers for a successful tap. I truly appreciate the<br />
teaching I received from my attending and some of the things she said<br />
to me while I was performing the LP are the same things I now share<br />
with my medical students.<br />
“...we can all recognize from our own<br />
experience just how much difference<br />
a good teacher can make.<br />
Dr. Gillian Shiau<br />
PARA President<br />
Delivering a lecture is one thing – engaging a room full of bright<br />
individuals and highlighting the relevance to them of a somewhat<br />
esoteric topic is a skill. Many of the clinical pearls that I have gained in<br />
medicine and have appreciated the most have come from preceptors<br />
who are not only experts in their field of medicine, but who have<br />
the ability to explain complex topics at a comprehensible level in a<br />
memorable way. Many of these individuals regularly seek out best<br />
practices around teaching so they continue to offer more both in terms<br />
of how to treat patients and how to teach others to treat patients. I can<br />
only be grateful for and aspire to this level of commitment, and I am<br />
eternally thankful for all the preceptors who have taken the time to<br />
teach and mentor me.<br />
I think each one of us has a role to play in clinical teaching: first, by<br />
never being complacent about our own teaching skills and, second, by<br />
never missing an opportunity to thank the individuals who take the<br />
time to share what they have learned with us, especially those who do<br />
it particularly well. Every year, there are opportunities for us to reward<br />
the preceptors who inspire us through award programs run by PARA,<br />
the Canadian Association of Internes and Residents (CAIR), the<br />
universities, and so many other organizations involved in postgraduate<br />
medical education. I encourage you to nominate one of the excellent<br />
preceptors who are actively shaping the future physicians of Canada<br />
and help remind them why they do it.<br />
5<br />
<strong>PARAphrase</strong> | volume 29 fall <strong>2012</strong>