DO - Ohio University College of Osteopathic Medicine
DO - Ohio University College of Osteopathic Medicine
DO - Ohio University College of Osteopathic Medicine
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
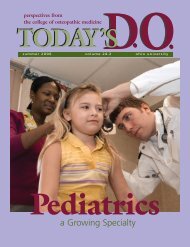
perspectives from<br />
<strong>DO</strong><br />
the college <strong>of</strong> osteopathic medicine<br />
TODAY’S<br />
summer/fall 2 0 0 7<br />
ohio university<br />
Our Alumni
Second-year student<br />
Kristen Conrad is the<br />
“Hamburgler” during<br />
the annual OU-COM<br />
Talent Follies.
<strong>DO</strong><br />
the college <strong>of</strong> osteopathic medicine<br />
TODAY’S<br />
perspectives from<br />
<strong>DO</strong><br />
TODAY’S<br />
F e a t u r e s<br />
12<br />
14<br />
18<br />
20<br />
A Family Physician takes an<br />
Alternative Path<br />
Out in “Custer Country,” Cmdr. George<br />
Ceremuga, D.O. (’93), provides health<br />
care to Native Americans on the Northern<br />
Cheyenne Reservation.<br />
Melting Pot <strong>Medicine</strong><br />
A new intercultural communications seminar<br />
at OU-COM fosters cultural competency in<br />
future physicians.<br />
Global Health<br />
By participating in international programs,<br />
students become aware <strong>of</strong> cultural differences<br />
and learn how to interact with patients from<br />
diverse backgrounds.<br />
The Long Road Back<br />
Injured when his humvee was hit by an<br />
improvised explosive device, Capt. Larry<br />
Robinson, D.O. (’02), describes his experience<br />
in Iraq.<br />
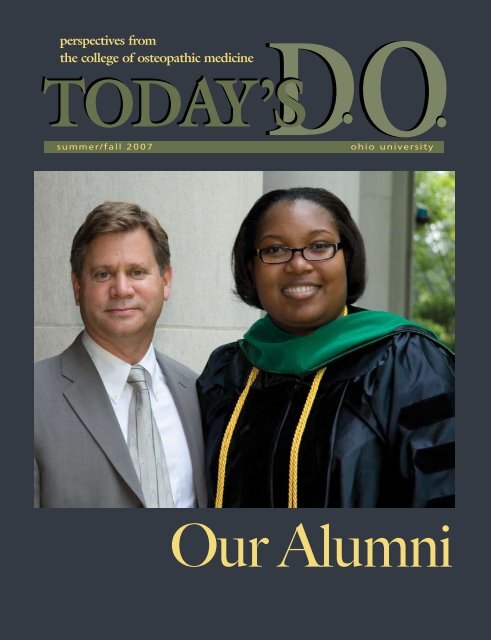
On the cover…<br />
Incoming Society <strong>of</strong> Alumni and<br />
Friends President Jeffrey A.<br />
Stanley, D.O. (’82), congratulates<br />
Kerwyn Flowers, D.O. (’07), after<br />
OU-COM’s 28th commencement<br />
exercises Saturday, June 2..pher:<br />
Christian Stork<br />
3 On Campus<br />
7 CORE News<br />
9 Commencement<br />
24 Research<br />
26 Alumni Note<br />
28 Alumni Board<br />
31 Alumni Events<br />
32 Class Notes<br />
36 Congratulations
<strong>DO</strong><br />
TODAY’S <strong>DO</strong><br />
volume 25.2<br />
Today’s D.O. is published two<br />
times a year by the Office <strong>of</strong><br />
Communication <strong>of</strong> the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Editorial <strong>of</strong>fices:<br />
Room 330, Grosvenor Hall,<br />
<strong>Ohio</strong> <strong>University</strong>, Athens, <strong>Ohio</strong>, 45701.<br />
Editorial Board<br />
George Dunigan II<br />
Director <strong>of</strong> Governmental Affairs<br />
Ryan Palmer<br />
Student Government President<br />
Edwin Rowland, Ph.D.<br />
Chair, Department<br />
<strong>of</strong> Biomedical Sciences<br />
John Schriner, Ph.D.<br />
Director <strong>of</strong> Admissions<br />
Sharon Zimmerman<br />
Director <strong>of</strong> Medical Development<br />
Executive Diretor Alumni Affairs<br />
Content Editor<br />
Susan Green<br />
Copy Editor<br />
Shelby Mullins<br />
Design<br />
Marie Graham<br />
Kari Gunter-Seymour<br />
Photography<br />
Leonardo Carrizo<br />
Tim Creamer<br />
John Sattler<br />
Writers and Contributors<br />
Anita Martin<br />
Mary Reed<br />
Jared Rutecki<br />
Carla Saavedra-Santiago<br />
Tracey Thomas<br />
Andrew Tillotson<br />
Administration<br />
Roderick McDavis, Ph.D<br />
President, <strong>Ohio</strong> <strong>University</strong><br />
A New <strong>Osteopathic</strong> Oath<br />
Recently, the <strong>Ohio</strong> Board <strong>of</strong> Regents commissioned the<br />
Robert Graham Center to perform a physician workload<br />
analysis for <strong>Ohio</strong>. The report showed that approximately 62<br />
percent <strong>of</strong> OU-COM graduates practice in <strong>Ohio</strong>—by far the<br />
most successful medical school in the state. This compares to<br />
42 percent <strong>of</strong> all the <strong>Ohio</strong> medical schools combined. It also<br />
showed that D.O.s are more likely to practice in underserved<br />
areas <strong>of</strong> the state.<br />
What explains these findings? While there are a number <strong>of</strong> factors,<br />
I believe the primary reason for our success is the CORE<br />
training hospital consortium. The seventeen institutions that<br />
make up the CORE provide exceptional training to students<br />
who enjoy a different atmosphere from most medical schools.<br />
Our clinical faculty teach because they enjoy it, and CORE<br />
staff develop personal relationships with our students. Our clinical faculty live the osteopathic<br />
physician’s oath they took when they graduated:<br />
“To my college I will be loyal and strive always for its best interests and for the interests<br />
<strong>of</strong> the students who will come after me.”<br />
Now the <strong>Ohio</strong> CORE is embarking on a new and broader mission. By 2020, it is estimated<br />
that there will be more than 95,000 active osteopathic physicians. That will be 79 percent<br />
higher than today. Recognizing the deficiency in postgraduate positions required to<br />
accommodate the large increase in graduates, the AOA has appealed to the pr<strong>of</strong>ession to<br />
establish new postgraduate training programs. A large part <strong>of</strong> this responsibility will<br />
rest on the shoulders <strong>of</strong> the osteopathic colleges, particularly those in states with high<br />
concentrations <strong>of</strong> D.O.s, such as <strong>Ohio</strong>. The <strong>Ohio</strong> CORE is rising to the task.<br />
Medical centers all over <strong>Ohio</strong> are interested in establishing new osteopathic GME<br />
programs. CORE hospitals have put aside their individual interests to support the<br />
pr<strong>of</strong>ession’s rapidly developing need for additional outstanding GME programs. It is<br />
exciting to watch the CORE grow in size, stature and quality. No wonder so many<br />
OU-COM students elect to stay in <strong>Ohio</strong>. As the premiere postgraduate training<br />
institution in the United States, the CORE provides osteopathic physicians an<br />
unparalleled environment in which to train and practice. The CORE hospitals have<br />
clearly adopted a variant to the osteopathic oath:<br />
“To our pr<strong>of</strong>ession we will be loyal and strive always for its best interests.”<br />
I couldn’t be prouder <strong>of</strong> them.<br />
Dean’s Message<br />
John Brose, D.O.<br />
Dean, <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Karoline Lane<br />
Director, Office <strong>of</strong> Communication<br />
Opinions expressed in Today’s D.O. are<br />
those <strong>of</strong> the authors and<br />
do not necessarily reflect<br />
viewpoints <strong>of</strong> the editors or <strong>of</strong>ficial<br />
policy <strong>of</strong> the <strong>Ohio</strong> <strong>University</strong><br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Jack Brose, D.O.<br />
Dean, <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong><br />
<strong>Osteopathic</strong> <strong>Medicine</strong><br />
© ’07 <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
Address updates for Today’s D.O.<br />
should be referred to Sheila Byc<strong>of</strong>ski<br />
OU-COM, 332 Grosvenor Hall<br />
Athens, OH 45701<br />
phone: (740) 593-2346<br />
e-mail: byc<strong>of</strong>ski@ohio.edu<br />
www.oucom.ohio.edu<br />
2<br />
oucom.ohio. www.<br />
edu
On Campus<br />
“…a gem in the neediest setting”<br />
This is how Joe Hallet, a senior editor at The Columbus Dispatch,<br />
described OU-COM in an editorial he wrote after a campus visit in<br />
February. In the photo below right, John Schriner, Ph.D., director<br />
<strong>of</strong> admissions, points out OU-COM’s Parks Hall clinic to Hallet during<br />
a campus tour. Hallet lived in Parks Hall as an <strong>Ohio</strong> <strong>University</strong> student<br />
more than 35 years ago<br />
In his editorial, Hallet wrote about the tough funding situation in<br />
<strong>Ohio</strong> for higher education and the reality that every college “soon may<br />
have to prove its worth to obtain state funding. That challenge is not<br />
feared by Dr. Jack Brose … His medical school is attracting the best<br />
and the brightest – 3,200 applicants for 100 first-year slots in 2006<br />
– in the state’s poorest and medically neediest region.”<br />
Thanks to Dean Jack Brose, D.O., and college advocacy efforts,<br />
government constituents are getting the same message that 54 percent<br />
<strong>of</strong> OU-COM alumni practice in primary care fields, and more than 60<br />
percent remain in <strong>Ohio</strong>, where they are more likely to practice in rural<br />
and other physician-shortage areas.<br />
<strong>Ohio</strong> Governor Ted Strickland, Representative Jimmy Stewart, OHIO<br />
President Roderick McDavis and Eric Fingerhut, chancellor <strong>of</strong> the <strong>Ohio</strong><br />
Board <strong>of</strong> Regents, toured campus in April, where they spoke to Dean<br />
Brose aboard OU-COM’s<br />
mobile health clinic, top and<br />
above right.<br />
State Senator Steve Stivers,<br />
and his brother Alan, also<br />
visited the college this spring.<br />
Here, left, they look at<br />
plasticized models with<br />
Dean Brose in the anatomy<br />
lab. Stivers is vice chair <strong>of</strong> the<br />
Senate’s Finance and Financial<br />
Institutions committee.<br />
-Karoline Lane<br />
summer/fall 2007 3
Rodeo roundup<br />
Karen Montgomery-Reagan, D.O.,<br />
assistant pr<strong>of</strong>essor <strong>of</strong> pediatrics,<br />
above, has fun with bubblemaking<br />
during the 5 th annual<br />
Bike Rodeo held at the Athens<br />
Community Center.<br />
James Schulz, an emergency<br />
nurse at O’Bleness Hospital,<br />
right, teaches Lander Zook, age<br />
9, left, how to handle his bike<br />
on rough terrain. Each year, the<br />
Bike Rodeo, which aims to teach<br />
young children about bicycle<br />
safety and helmet use, donates<br />
up to 200 helmets to local children<br />
and raffles <strong>of</strong>f one bicycle.<br />
About 20 OU-COM students and<br />
faculty volunteered alongside<br />
community members at this<br />
year’s event.<br />
-Carla Saavedra-Santiago<br />
4 www.oucom.ohio.edu
Go!<br />
Nearly 90 people participated in the annual 5k <strong>Medicine</strong> Run despite the cold, cloudy weather. A health fair,<br />
which provided free screenings for blood pressure, glucose and cholesterol, and a children’s obstacle course<br />
were part <strong>of</strong> the event as well. Booths were also available to educate people on a variety <strong>of</strong> health conditions.<br />
Close to 50 students volunteered their time throughout the year to make it all happen, noted second-year<br />
student Nicole Veitinger, who chaired the events. “Knowing we are giving so much back to the clinic as a<br />
result <strong>of</strong> our hard work is all the reward I need,” she said. The <strong>Medicine</strong> Run raised $2,000 for the Free Clinic,<br />
an amount that exceeds last year’s record donation <strong>of</strong> $1,350.<br />
-Andrew Tillotson<br />
OU-COM “Today”<br />
Jacqueline Wolf, Ph.D., associate<br />
pr<strong>of</strong>essor <strong>of</strong> social medicine, far left,<br />
appeared on NBC’s “Today,” April 26,<br />
to discuss pr<strong>of</strong>essional and informal<br />
wet nursing. Wolf, a nationally<br />
recognized expert in the history <strong>of</strong><br />
breastfeeding, is the author <strong>of</strong> Don’t<br />
Kill Your Baby: Public Health and the<br />
Decline <strong>of</strong> Breastfeeding in the 19 th<br />
and 20 th Centuries.<br />
Sinn to serve on national board<br />
Second-year student Clarice Sinn, right, was recently selected to serve on the<br />
national board <strong>of</strong> the Student <strong>Osteopathic</strong> Medical Association (SOMA) as the<br />
organization’s “preventative medicine” director. She was “preventative medicine”<br />
and public relations chair in SOMA’s OU-COM chapter last quarter.<br />
In her new position, Sinn will develop programs at osteopathic medical schools<br />
nationwide and collaborate with local coordinators to identify problems in<br />
specific regional populations. Her duties include developing relationships with<br />
national medical organizations like the American Lung Association and working<br />
with other members <strong>of</strong> the national board to develop the SOMA Fall<br />
Convention National Philanthropic Project in San Diego.<br />
This fall, Sinn begins her third year-clerkship at St. Vincent Mercy Medical<br />
Center in Toledo.<br />
-Jared Rutecki<br />
summer/fall 2007 5
Grant to benefit<br />
area children<br />
Young children and<br />
their families living in<br />
Appalachian <strong>Ohio</strong> will<br />
have greater access to<br />
health care thanks to<br />
a federal grant that<br />
will fund an innovative<br />
community-university<br />
partnership. The federal<br />
Health Resources and<br />
Services Administration<br />
has awarded a threeyear,<br />
$540,000 grant<br />
to <strong>Ohio</strong> <strong>University</strong> to<br />
support Interpr<strong>of</strong>essional Partners for Appalachian<br />
Children.<br />
“We are a community-university partnership with<br />
participants who are lay consumers trying to improve<br />
our community’s ability to identify, to refer and to<br />
provide comprehensive, coordinated care to young<br />
children with behavioral and developmental concerns,”<br />
says Jane Hamel-Lambert, Ph.D., director <strong>of</strong><br />
interdisciplinary mental health education in the<br />
Department <strong>of</strong> Family <strong>Medicine</strong> and principal<br />
investigator <strong>of</strong> the program.<br />
-Mary Reed<br />
Rewarding community service<br />
Sarah McGrew, B.S.N., received the Outstanding<br />
Arthritis Educator Award from the <strong>Ohio</strong> Rheumatic<br />
Diseases Coalition for her participation in arthritisrelated<br />
initiatives in the Appalachian region. For<br />
several years she has helped the <strong>Ohio</strong> Department<br />
<strong>of</strong> Health with teaching the Arthritis Foundation’s<br />
six-week, self-help program in several Southeastern<br />
<strong>Ohio</strong> communities. She is also a charter member <strong>of</strong><br />
the <strong>Ohio</strong> Rheumatic Diseases Coalition. McGrew,<br />
coordinator <strong>of</strong> clinical and community experiences at<br />
OU-COM, is the first person to receive the award.<br />
-Carla Saavedra-Santiago<br />
A winning proposal<br />
Earlier this year, the <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> received a Canon REALiS Sx6<br />
projector from Campus Technology magazine. The publication asked educators interested<br />
in bringing ultra-high-level projection capability into their classrooms to submit proposals<br />
to the magazine for an opportunity to win a projector.<br />
Out <strong>of</strong> 149 entries, OU-COM was among the four schools chosen to receive a top-<strong>of</strong>the-<br />
line video projector with a price tag <strong>of</strong> $5,999. Allen Reed’s winning proposal<br />
detailed how the projector would enable the college to deliver content in a new way<br />
in the Grosvenor 128 microbiology lab. The new equipment was installed at the end<br />
<strong>of</strong> January, replacing dated monitors, and has been in use since then.<br />
As part <strong>of</strong> an ongoing project, the magazine is studying the real-life usage <strong>of</strong> the<br />
projectors and will share with their readers the innovative ways educators and students<br />
are using the latest “smart classroom” equipment.<br />
This spring, Reed reported on the projector’s usage. Please visit campustechnology.<br />
com/articles/48230/ to read how the projector is making a difference in teaching and<br />
learning at OU-COM.<br />
6 www.oucom.ohio.edu
C O R E N e w s<br />
Whether working with students<br />
or members <strong>of</strong> the community,<br />
Nicholas Espinoza, D.O., is dedicated to<br />
making a difference By Anita Martin<br />
As a new assistant dean in the CORE, Nicholas Espinoza, D.O. (’90), coordinates third- and<br />
fourth-year clinical experiences for students at St. Vincent Mercy Medical Center in<br />
Toledo, <strong>Ohio</strong>.<br />
Espinoza’s got a knack for forging connections, whether between students and doctors,<br />
community members or among cultural groups. For years, he served Adelante, Inc.,<br />
a not-for pr<strong>of</strong>it resource center providing the Hispanic community in Northwest <strong>Ohio</strong><br />
with mental health services, support for victims <strong>of</strong> domestic violence and substance<br />
abuse prevention and intervention.<br />
“I served as a board member, assisting the development for programs to help people with<br />
substance abuse problems, which ranged from tobacco to crack cocaine,” he says.<br />
When he wasn’t practicing family, occupational or urgent medicine—or facilitating<br />
migrant health care—Espinoza has also moonlighted as a ringside physician for the<br />
Toledo Golden Gloves boxing club.<br />
These days, he’s focusing more on his private practice in Perrysburg, <strong>Ohio</strong>. But he<br />
still makes time to work around the greater Toledo area—Oakmont Medical Hospital,<br />
Bay Park Community Hospital, St. Charles Mercy Medical Hospital and St. Anne’s<br />
Hospital, where he has courtesy privileges.<br />
<strong>Ohio</strong> Occupational Health also employs Espinoza to help manage the return <strong>of</strong> plant<br />
workers who have sustained work-related injuries. And some weekends he provides<br />
urgent care at the Blanchart Valley Hospital.<br />
“I think that’s about enough,” he laughs.<br />
But even with all <strong>of</strong> his commitments, he still makes time to connect daily with third- and<br />
fourth-year medical students at the hospital. Espinoza began working with students<br />
as a CORE medical equity teacher with Harold C. Thompson III, D.O., to oversee<br />
and advise them, if necessary, on multicultural issues pertaining to their internships<br />
and residencies.<br />
And now as an assistant CORE dean, Espinoza supervises about 35 students, interns<br />
and residents from OU-COM and other participating colleges in <strong>Ohio</strong> and surrounding<br />
states.<br />
“I’ve always enjoyed working directly with students,” says Espinoza, who fondly remembers<br />
his own time spent as a student at <strong>Ohio</strong> <strong>University</strong>.<br />
Espinoza’s talent for making connections extends to his private practice, too. His group<br />
practice makes use <strong>of</strong> hospitalist internal medicine specialists (Intermed) to care for<br />
acutely ill patients who need in-hospital medical care.<br />
“Our Intermed colleagues, Drs. J. Retholz, Sheldon, Cifuentes, Orlo, Hooker, Blood<br />
and M. Retholz—all D.O.s—work great with us, our patient families and continually<br />
support the CORE teaching activities <strong>of</strong> the students, interns and residents,” Espinoza<br />
says. “Many <strong>of</strong> the Intermed physicians themselves trained right here at this CORE site<br />
and have chosen to stay here and practice. We are very fortunate for that.”<br />
Occasionally Espinoza returns to Athens to talk with students, and he fondly recalls the<br />
euphoria <strong>of</strong> spring. “I remember how nice it felt when the weather warmed up and the<br />
trees started to bloom,” he says.<br />
Espinoza interned at Parkview Hospital, and received board certification in family medicine<br />
in 1999. He and his wife, Carole, have two daughters, Valerie and Jacqueline.<br />
summer/fall 2007 7
Seven alumni named<br />
Master Faculty<br />
Honorees received a plaque and a gold lapel pin<br />
–lapel pin enlarged for detail<br />
Seven alumni are among the 28 physicians named a Master<br />
Faculty by <strong>Ohio</strong> Universty Co llege <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong>: Jeffrey Garman, D.O. (’84), Firlands<br />
Regional Medical Center; Joni Koren, D.O.<br />
(’84), Grandview Medical Center; Leonard<br />
Tamburro, D.O. (’85), Affinity Medical<br />
Center; Thomas Wehmann, D.O. (‘85),<br />
Cuyahoga Falls General Hospital;<br />
Roger Wohlwend, D.O. (’87), St.<br />
Vincent Mercy Medical Center;<br />
John Wolf III, D.O. (’88), St.<br />
John West Shore Hospital and<br />
John Yuhas, D.O. (’87), Firelands<br />
Regional Medical Center.<br />
The appointment <strong>of</strong> Master<br />
Faculty is the highest honor<br />
that the college gives to clinical<br />
faculty members at its Center<br />
for <strong>Osteopathic</strong> Research and<br />
Education (CORE), a statewide<br />
consortium <strong>of</strong> 15 hospitals<br />
across <strong>Ohio</strong>.<br />
“The award is truly an honor to<br />
receive,” Koren says. “Many times<br />
those <strong>of</strong> us who take students into our<br />
<strong>of</strong>fices wonder if we are appreciated, and it’s<br />
very encouraging to see that we are.<br />
“I’m thankful to be rewarded and recognized for<br />
teaching the students,” she adds. “It’s something I’ve<br />
always been passionate about and hope to continue<br />
doing for many years.”<br />
Master Faculty are chosen from hundreds <strong>of</strong> nominations and<br />
awarded once every four years. The college recognizes the doctors as innovators and leaders in clinical education<br />
and the osteopathic pr<strong>of</strong>ession. They have excelled as teachers and mentors. Medical students, interns and residents<br />
respect and esteem Master Faculty members for their contributions to undergraduate and graduate medical<br />
education, as well as for being outstanding role models.<br />
“One <strong>of</strong> the greatest parts <strong>of</strong> my job is recognizing my colleagues who have played such an important role in<br />
preparing our students, interns and residents to become caring, compassionate and competent physicians,” says<br />
Dean Jack Brose, D.O.<br />
For a complete list <strong>of</strong> Master Faculty, visit www.oucom.ohiou.edu/MasterFaculty.<br />
8 www.oucom.ohio.edu
Congratulations, you’re a D.O.<br />
Jubilation, hugs, pride and family were in abundance<br />
during the <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong>’s 28th commencement exercises Saturday<br />
morning, June 2, in Templeton-Blackburn Alumni<br />
Memorial Auditorium.<br />
President Roderick McDavis, Ph.D., hailed the college<br />
as “ … an outstanding example <strong>of</strong> our larger university<br />
mission … ” and congratulated the student doctors<br />
on the significant role they’ve played in the health <strong>of</strong><br />
<strong>Ohio</strong>’s citizens.<br />
In addressing the 102 graduates—59 women and<br />
43 men—Dean Jack Brose, D.O., said, “You have<br />
exceeded my expectations. … In a short while, you will<br />
understand why this ceremony is such an emotional<br />
event. There is no more pr<strong>of</strong>ound moment that<br />
watching you come to the stage as a lay person, and<br />
leave as a physician. As dean, congratulating each <strong>of</strong><br />
you is my favorite part <strong>of</strong> the job. I can’t imagine a<br />
greater honor.”<br />
Keynote speaker Alison Clarey, D.O. (Hon. ’98),<br />
president <strong>of</strong> the American <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
Surgeons, left the newly minted physicians with two<br />
thoughts: Know no limitations, and one person can<br />
make a difference.<br />
summer/fall 2007 9
Kerwyn Flowers<br />
the ministry <strong>of</strong> medicine<br />
By Mary Reed<br />
Ministering to people has been at the root <strong>of</strong> Kerwyn Flowers’<br />
lifework—from her stint as a 12-year-old Sunday school teacher<br />
to a medical school tutor to a doctor <strong>of</strong> osteopathic medicine.<br />
“God gives us gifts,” says Flowers, who received her medical<br />
degree from the <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong> June 2. “I think being a physician is a ministry<br />
within itself. Physicians are engaged in every aspect <strong>of</strong> their<br />
patients’ lives—they encourage, they counsel, they listen and<br />
so much more. In my opinion, physicians don’t heal, but rather,<br />
God gives us the opportunity and privilege to facilitate healing.”<br />
Even at a young age Flowers was resolved that her life’s work<br />
would focus on health and healing. The support <strong>of</strong> her<br />
mother, Sharon Smiley Gainous—the pastor <strong>of</strong> New Israel<br />
Church <strong>of</strong> Jesus Christ in Quincy, Florida—was a foundation for<br />
Flowers’ success in medical school. “My mother said you<br />
could be whatever you wanted to be. From the beginning she<br />
has always believed in me and supported me.” Flowers also<br />
observed her mother’s role as a teacher to the church<br />
congregation, and Flowers even dabbled in teaching Sunday<br />
school as a girl herself. It turns out that she was a natural<br />
teacher, a gift that would serve her well years later in<br />
medical school.<br />
After graduating with a degree in chemistry from Florida<br />
A&M <strong>University</strong>, Flowers worked as a chemist for<br />
GlaxoSmithKline and Lannett Pharmaceuticals. When she<br />
decided it was time to attend<br />
medical school, she needed more<br />
background in biological sciences.<br />
That’s when Flowers enrolled in<br />
the OU-COM Summer Scholars<br />
Program, a rigorous six-week<br />
medical school preparatory<br />
program for underrepresented<br />
minority students, and then the<br />
Post-Baccalaureate Program, a<br />
similar preparatory program that<br />
lasts one academic year.<br />
Flowers says she had never heard<br />
<strong>of</strong> osteopathic medicine prior to<br />
coming to OU-COM. But when<br />
a friend introduced her to the<br />
osteopathic principles <strong>of</strong> approaching<br />
the whole person, Flowers was<br />
sold. “The philosophy was so similar<br />
to what I had always believed<br />
about health and wellness.”<br />
After excelling in the Summer Scholars and Post-Baccalaureate<br />
programs, Flowers became a tutor and mentor for both.<br />
“Name it, I tutored it,” she says. She also became a mentor<br />
to first-year medical students as part <strong>of</strong> a program called<br />
COMrade. When she won COMrade <strong>of</strong> the Year in 2005,<br />
she was surprised—but she shouldn’t have been. “I tutored a<br />
lot <strong>of</strong> them,” she says, figuring that “all <strong>of</strong> the students who<br />
I tutored voted for me!” But in fact, she received even more<br />
votes than that.<br />
During that time, Flowers also served as president <strong>of</strong> the<br />
OU-COM Chapter <strong>of</strong> the Christian Medical and Dental<br />
Association. She organized a Bible study group every Wednesday<br />
night. “I tried to make sure the topics were relevant to people<br />
<strong>of</strong> our age group and (were) topics specific to physicians.”<br />
Now about to begin a residency in family medicine at Akron<br />
City Hospital, Flowers is embarking on yet a new ministry<br />
and believes that by becoming a physician, her destiny and<br />
purpose are fulfilled. She will bring her faith with her to every<br />
patient interaction. “I think faith gives us hope beyond<br />
our circumstances.”<br />
Flower‘s mother, left, and 25 members <strong>of</strong> her childhood church<br />
congregation from Quincy, Fla., were in Athens to see Flowers,<br />
center, receive her medical degree June 2.<br />
10 www.oucom.ohio.edu
Eric Greenfield<br />
all the right reasons<br />
By Mary Reed<br />
The ink is still drying on the <strong>Ohio</strong> <strong>University</strong> diploma that<br />
names Eric Greenfield a doctor <strong>of</strong> osteopathic medicine, but<br />
he has already made more house calls than most physicians will<br />
make in their entire careers. This is because prior to medical<br />
school, Greenfield was a paramedic for nine years – an experience<br />
that shaped his pr<strong>of</strong>essional trajectory as well as his philosophy<br />
as a practitioner and teacher <strong>of</strong> emergency medicine.<br />
“You get to make a big impact on people’s lives,” Greenfield<br />
says about his paramedic career. He remembers treating five<br />
cardiac arrest cases on five consecutive Christmas days.<br />
“When you’re in somebody’s house and you see somebody<br />
who’s collapsed literally in front <strong>of</strong> the Christmas tree, it<br />
gives you a perspective you can’t see anywhere else.”<br />
This in-home, pre-hospital assessment as a paramedic was<br />
the formative beginning to Greenfield’s medical career.<br />
He eventually earned a nursing degree through Regents<br />
<strong>College</strong>, and then went on to earn a bachelor’s degree in<br />
health sciences through Excelsior <strong>College</strong>. He was making<br />
a good living as a nurse when he became a part-time<br />
paramedic instructor at the <strong>University</strong> <strong>of</strong> Alabama, but he<br />
again changed careers to help establish a paramedic degree<br />
program at nearby Calhoun <strong>College</strong>. “It was the best job I<br />
ever had,” Greenfield recalls.<br />
Medical school had always been on his mind, however,<br />
and he eventually hit an educational ceiling as a nurse and<br />
a paramedic instructor. He knew it was time to pursue a<br />
medical degree, and he knew it would be at an osteopathic<br />
medical school.<br />
One <strong>of</strong> the things that drew Greenfield to OU-COM was<br />
the patient-centered continuum program, a student-directed<br />
curriculum where small groups <strong>of</strong> medical students are presented<br />
with patient cases, and they come up with their own learning<br />
objectives. “It was good for me because <strong>of</strong> my nontraditional<br />
background,” Greenfield says. Describing a typical PCC<br />
discussion, he says, “We might have a patient with a cough<br />
or pneumonia. We’d start talking about the differential<br />
diagnosis <strong>of</strong> a cough … a microbiologist in a previous life<br />
might say, ‘These are the typical bugs we see.’ My contribution<br />
is typically, ‘This is what you see in real patients, this is what<br />
you look for.’”<br />
Now Greenfield interacts with patients from the perspective<br />
<strong>of</strong> a resident physician—he’s starting an emergency medicine<br />
Eric Greenfield, left, and his mentor, Henry Gaillard, M.D.<br />
residency at the Medical <strong>College</strong> <strong>of</strong> Georgia. “I didn’t really<br />
want to do emergency medicine when I started medical school,”<br />
he says. “I wanted to do a little bit <strong>of</strong> everything—which left<br />
me with family medicine or emergency medicine. Then I realized<br />
it was emergency medicine that made me want to go to<br />
medical school to begin with.<br />
“From seeing people die to delivering babies—that experience<br />
at a formative age really changed me. I think life is precious<br />
and I think we have a duty to give back to people.”<br />
summer/fall 2007 11
A Family Physician Takes<br />
an Alternative Path<br />
By Tracey Thomas<br />
photo provided by Cmdr. George Ceremuga<br />
Out in “Custer Country,” Cmdr. George Ceremuga, D.O. ('93), plays an active<br />
role in the Indian Health Services’ commitment to promoting healthy American<br />
Indian communities.<br />
Every week, he makes a three-hour commute from his home in South Dakota to the<br />
pine-covered landscape <strong>of</strong> the Northern Cheyenne Indian Reservation in Lame Deer,<br />
Mont., where he provides medical care to Native Americans on the reservation.<br />
“One minute I could be delivering a baby and the next I could be dealing with an<br />
alcohol-related trauma patient,” he says. “I see much more than runny noses.”<br />
As clinical director <strong>of</strong> the Northern Cheyenne Indian Reservation Health Center, the<br />
ongoing struggle to stem the rampant spread <strong>of</strong> alcoholism, teen pregnancy, obesity,<br />
diabetes and drug addiction in native populations looms large in Ceremuga’s pr<strong>of</strong>essional<br />
life. And these are only a few <strong>of</strong> the pressing social issues on the reservation.<br />
12 www.oucom.ohio.edu<br />
He also works with tribal organizations to promote preventive<br />
health activities to improve the health and well-being <strong>of</strong> the<br />
reservation community.<br />
Facing serious health problems every day can take its toll,<br />
but Ceremuga has a prescription for that.<br />
“It’s important to separate yourself from your patients, which<br />
means not taking it personally when someone’s diabetes is<br />
getting worse because they won’t take their medicine,” he<br />
explains. “I see my role as a cheerleader for change, and if<br />
only one person makes a lifestyle change for the better, no<br />
matter how small, I’ve succeeded.<br />
“What I do is not glamorous, but it’s honorable,” he adds.<br />
“Sure we have problems and we’re understaffed, but we’re<br />
helping to make needed change.”<br />
He encourages medical students to do the same, taking what<br />
they’ve learned and using it to help people with the most<br />
need. And he’s quick to point out that helping others doesn’t<br />
mean living a diminished life.<br />
In fact, it’s quite the opposite.<br />
For Ceremuga, it meant exchanging an 80 – 100 hour work<br />
week in private practice, for a 40 – 50 hour work week on<br />
the reservation. Shorter weeks have allowed him to spend<br />
more time with his five children and to live the active and<br />
healthy lifestyle he advocates for his patients.<br />
“I’m constantly challenged in my work and really feel energized<br />
when I can provide patient care to those in need,” he says. “It’s<br />
the reason why I went into medicine.”<br />
TODAY’S<br />
<strong>DO</strong><br />
Don Shoulderblade, “sacred hat keeper” or holy man for the Northern Cheyenne Indian Reservation,<br />
prays daily for the safety and security <strong>of</strong> his people. Cmdr. Ceremuga and Shoulderblade are<br />
collaborating on a plan to integrate western medicine with traditional Northern Cheyenne medicine.
photo provided by Cmdr. George Ceremuga<br />
The Northern Cheyenne Indian Reservation Health Center is a modern, ambulatory<br />
care facility staffed with five family physicians, a pediatrician and two nurse<br />
practitioners who <strong>of</strong>fer outpatient care as well as 24-hour urgent care to nearly 5,000<br />
patients. Services <strong>of</strong>fered include optometry and dental care, physical and behavioral<br />
health therapy, and a full service lab and radiology unit. The clinic also includes<br />
a Healing Room for traditional ceremonies.<br />
In partnership with the Northern Cheyenne Community, the health center staff strives<br />
to raise the physical, mental, social and spiritual health <strong>of</strong> the population to the<br />
highest level in a culturally sensitive manner.<br />
Dr. Ceremuga is a Commander in the U.S. Public<br />
Health Service Commissioned Corps and is currently<br />
detailed to the Indian Health Service. The<br />
Commissioned Corps provides highly trained<br />
and mobile health pr<strong>of</strong>essionals who carry out<br />
programs to promote the health <strong>of</strong> the nation,<br />
understand and prevent disease and injury, assure<br />
safe and effective drugs and medical devices,<br />
deliver health services to federal beneficiaries,<br />
and furnish health expertise in time <strong>of</strong> war or<br />
other national or international emergencies.<br />
Cmdr. Ceremuga also participated in the<br />
Commissioned Corps relief effort immediately<br />
following Hurricane Katrina.<br />
For more information about the Commissioned<br />
Corps please visit www.usphs.gov.<br />
summer/fall 2007 13
Melting Pot<br />
By Anita Martin<br />
14 www.oucom.ohio.edu
<strong>Medicine</strong><br />
N e w i n t e r c u l t u r a l c o m m u n i c a t i o n<br />
t r a i n i n g s e r i e s f o s t e r s c u l t u r a l<br />
c o m p e t e n c y i n f u t u r e p h y s i c i a n s<br />
michaeldibari.com<br />
Medical school sharpens the senses. Eyes detect<br />
subtle imbalances, hands track changes, and ears<br />
listen with heightened diagnostic awareness. But<br />
anatomical savvy and keen diagnoses alone won’t<br />
cut it in today’s medical world. The various views<br />
and priorities <strong>of</strong> humanity’s diverse cultures<br />
rival—and perhaps surpass—the complexity <strong>of</strong> the<br />
human body itself. Culture informs a patient’s<br />
perception <strong>of</strong>, and decisions about, health care.<br />
From 1990 to 2000, the United States Census saw<br />
an increase in every minority population, including<br />
a 23 percent jump in the Hispanic population.<br />
Columbus, <strong>Ohio</strong>, is home to growing enclaves<br />
<strong>of</strong> East Asian Indian, African and other minority<br />
populations. “You don’t have to go very far to<br />
encounter enormous diversity,” says Pat Burnett,<br />
Ph.D., director <strong>of</strong> student affairs at the <strong>Ohio</strong><br />
<strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>.<br />
That’s why the staff <strong>of</strong> OU-COM’s Center <strong>of</strong><br />
Excellence (COE) is committed to sharpening<br />
the cultural acuity <strong>of</strong> the college’s diverse student<br />
body. Their latest project: a pr<strong>of</strong>essional development<br />
seminar conducted by Mark Orbe, Ph.D., an expert<br />
in cross-cultural medical communication.<br />
Cultural demand<br />
Orbe starts each session <strong>of</strong> his “Pr<strong>of</strong>essional<br />
Development in Cultural Competency” series for<br />
OU-COM by counting “1 – 2 – 3 … ”<br />
“Dumela!” his students shout on cue. The word<br />
dumela is a South African greeting that also<br />
means “I affirm you, I believe in you, and I see the<br />
great potential within you.” Orbe weaves this<br />
Mark Orbe, Ph.D., reviews material covered during the seminar—<br />
basic communication concepts, communication styles and<br />
explanatory models.<br />
michaeldibari.com<br />
summer/fall 2007 15
theme through the COE’s newly developed certificate<br />
program in intercultural communication at OU-COM.<br />
As warm and welcoming as this sounds, Orbe’s program is<br />
no feel-good affirmation fest. In fact, it can be downright<br />
uncomfortable. Participants must critically examine their<br />
own cultural identities, assumptions and biases; learn to<br />
implement communication principles and practice negotiating<br />
patients’ culturally based beliefs about medical care through<br />
simulated interviews.<br />
“This is not cultural sensitivity training. This is about developing<br />
strong communication skills so you get the most meaningful,<br />
productive exchange out <strong>of</strong> a 15-20 minute meeting with a<br />
patient,” Orbe says.<br />
Developing this dynamic series was a team effort. Burnett,<br />
Ann Brieck, associate director <strong>of</strong> student affairs, and Harold<br />
C. Thompson III, D.O., director <strong>of</strong> multicultural affairs, worked<br />
with Orbe to develop the OU-COM certificate program in<br />
intercultural communications, funded by a federal Health and<br />
Human Services Center <strong>of</strong> Excellence grant.<br />
“Cultural training is growing because <strong>of</strong> the demand <strong>of</strong> students,”<br />
Thompson says. “Our world is changing, and students<br />
understand the need to grasp it. We want to provide them<br />
with more practice inside and outside <strong>of</strong> the classroom.”<br />
Mindful approach<br />
As a biracial, first-generation college student, Orbe was drawn<br />
to the cultural aspects <strong>of</strong> communication. After earning his<br />
bachelor’s degree at <strong>Ohio</strong> <strong>University</strong>, he returned for a doctorate,<br />
also in communication studies, during which time his wife gave<br />
birth to their first child at O’Bleness Hospital. He now teaches<br />
intercultural communication at Western Michigan <strong>University</strong>.<br />
“There’s an inextricable relationship between culture and<br />
communication,” he says. “I explore ways in which that<br />
relationship manifests.”<br />
Orbe led his first OU-COM seminar, called “Physician-Patient<br />
Communication in a Multicultural Society,” during winter<br />
quarter 2006. Participants met twice, for a total <strong>of</strong> nine<br />
hours. They earned two academic credits and were given an<br />
overview <strong>of</strong> basic communication concepts and theories<br />
and how they relate to practical medical settings.<br />
“In terms <strong>of</strong> health-care communication, what you say and<br />
how you say it leads to different interpretations among<br />
different people,” says Becky Teagarden, a second-year<br />
medical student who attended this first seminar.<br />
In addition to differing disease propensities across cultural<br />
groups, there are differences in healing methods. Many<br />
groups trust traditional remedies—such as indigenous herbs<br />
and healing rituals—to Western medicine. Cultures can also<br />
express differences in their radius <strong>of</strong> personal space or level<br />
<strong>of</strong> family involvement in decision-making.<br />
Such cultural tips can be helpful, but it’s impossible to<br />
memorize the genetic predispositions, medical practices and<br />
social etiquette <strong>of</strong> every culture. The trick, according to<br />
Orbe, is to ask probing questions and cultivate mindfulness.<br />
michaeldibari.com<br />
From left, first-year students Nicholas Niemiec, Michael Finamore, Aaron Wolk<strong>of</strong>f, Ismail Oshogwemoh, Brett Buller, Jason<br />
Lane, and Baldassare Pipitone toss a ball <strong>of</strong> yarn to create a network <strong>of</strong> gratitude, admiration, appreciation and humanity as<br />
the seminar draws to a close.<br />
16 www.oucom.ohio.edu
Second-year students Rachel Polinski, left, and Antwon Morton, right, listen to second- year student Victoria Tong, center, as she<br />
relates one <strong>of</strong> her father’s experiences from World War II.<br />
“Most <strong>of</strong> us don’t communicate mindfully; we just say what<br />
we’re thinking and assume that there’s a shared meaning,”<br />
Orbe says. “I teach receiver orientation, a concept that says<br />
what’s more important is not what I’m saying, but how you<br />
receive it.”<br />
Investing in connecting<br />
Burnett, Brieck and Thompson knew, from the overwhelmingly<br />
positive response to the first seminar, that they needed to<br />
do more. Orbe returned to speak to OU-COM’s incoming<br />
first-year students in August 2006. They all participated in<br />
Orbe’s four-hour presentation on intercultural communication<br />
as it relates to medical practice.<br />
Meanwhile, second-year students who had attended Orbe’s<br />
winter quarter two-credit class and wanted more could<br />
attend a refresher course. Both groups had the option to<br />
attend three subsequent five-hour classes, but they earned<br />
the certificate in intercultural communication only if they<br />
attended all three.<br />
About 50 percent <strong>of</strong> this year’s first-year class completed this<br />
elective course. It’s no small feat considering the seminar’s<br />
extensive reading list and the fact that sessions are <strong>of</strong>ten on<br />
Friday evening or Saturday morning. This is in addition to<br />
the students’ already rigorous medical training schedule.<br />
“It’s a significant time commitment, but what you get out<br />
<strong>of</strong> it is well worth the hours you give up,” Teagarden says.<br />
“At medical school you’re so bombarded with the science<br />
that you don’t take the time to appreciate how intricately<br />
individual each situation is.”<br />
Through Orbe’s seminar, students gain new levels <strong>of</strong> cultural<br />
competency and mindful physician-patient communication,<br />
but they also deepen their bond with one another.<br />
Before bringing the final seminar class to a close, Orbe gathers<br />
his students into a circle and tosses a colorful ball <strong>of</strong> yarn to<br />
a young woman across the room. Still holding onto his end<br />
<strong>of</strong> the yarn, he affirms the humanity <strong>of</strong> that student, who<br />
tosses the yarn to another, and he to another. Soon multi-hued<br />
strands, each representing gratitude, admiration or appreciation,<br />
crisscross into an elaborate network <strong>of</strong> yarn.<br />
“It is through communication that we establish this web<br />
<strong>of</strong> dumela—<strong>of</strong> affirmation,” Orbe says. “Even though you<br />
didn’t speak to everyone in this room, and despite our<br />
many differences—look: we’re all connected.”<br />
TODAY’S<br />
<strong>DO</strong><br />
summer/fall 2007 17
Gl bal Hea<br />
International programs <strong>of</strong>fer research and clinical exp<br />
improve cultural sensitivity By Anita Martin<br />
A<br />
lthough Shawn Horwitz was born in South Africa, he<br />
grew up in the United States. Last year, as a second-year<br />
student at <strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong>,<br />
he made his first trip to Africa as an adult to conduct health<br />
care research through the Kenyan Grandparents Study.<br />
“I wanted to see the culture and the medical system <strong>of</strong> an<br />
African country,” says Horwitz, who also plans to explore the<br />
medical practices <strong>of</strong> South America and Asia. “I’m interested<br />
in going back to the third-world area. I’d like to have some<br />
kind <strong>of</strong> impact where it’s most needed.”<br />
Every year, Gillian Ice, Ph.D., founder <strong>of</strong> the Kenyan<br />
Grandparents Study and director <strong>of</strong> international programs<br />
at the college, facilitates training trips for students from<br />
the college and other participating medical schools across<br />
the country. Programming expanded last year to include El<br />
Salvador and the Dominican Republic, and participation in<br />
all programs—averaging about 30 students a year over the<br />
past few years—is growing.<br />
“Having experiences in international medicine helps students<br />
to think about the system in the U.S. with a different<br />
perspective—to not just assume that we provide the best<br />
system, but to really think about the decisions we make and<br />
why,” says Ice, also an associate pr<strong>of</strong>essor <strong>of</strong> social medicine.<br />
The college’s international programs feature tropical disease<br />
research in Ecuador, clinical and research rotations in Kenya,<br />
geriatric training in Scotland, new clinical rounds in El<br />
Salvador and the Dominican Republic, and, until recently,<br />
traditional medicine training in China.<br />
“If a third or fourth-year student wants to travel to a destination<br />
or participate in a program not <strong>of</strong>fered by OU-COM, they<br />
can set one up themselves with our approval,” Ice says. “But<br />
we still have a structure in place to ensure the student’s safety<br />
and a solid educational experience.”<br />
This past year students Andrea Molcutt and Zarinah Hudd,<br />
set up their own projects in Ghana and Ethiopia, respectively.<br />
Two more third-year students, Joseph Davis and Petter<br />
Vaagenes, traveled to Norway in 2005 to learn more about<br />
the practice <strong>of</strong> socialized medicine. All returning students<br />
Second-year student Shawn Horwitz, right, and Gillian Ice,<br />
Ph.D., distribute school uniforms to the local orphans.<br />
write and present papers comparing international medical systems<br />
based on their experiences.<br />
“Whether you practice right here, in Appalachia, or in some<br />
urban setting, it helps to be open to all cultures and be aware
lth<br />
eriences that<br />
<strong>of</strong> potential differences,” Horwitz says. “This is a good way<br />
to learn to interact with patients from different backgrounds<br />
within different health-care systems.”<br />
For example, students participating in the geriatric tutorial in<br />
Edinburgh <strong>of</strong>ten note how differently the United Kingdom<br />
rations care for its elderly. According to Ice, American doctors<br />
more <strong>of</strong>ten take extreme and intensive measures with elderly<br />
patients than do English doctors.<br />
Ice, herself, studied in the U.K. at the London <strong>University</strong><br />
while still a junior at Washington <strong>University</strong>. At the time, she<br />
majored in anthropology and worked in nursing homes on<br />
the side. Later, for her doctoral dissertation in gerontology at<br />
the <strong>University</strong> <strong>of</strong> Minnesota, Ice conducted research on the<br />
stress levels <strong>of</strong> U.S. nursing home populations.<br />
A few years after coming to OU-COM, Ice decided to diversify<br />
her research. “I was aware <strong>of</strong> the HIV epidemic in Africa<br />
and that many grandparents <strong>of</strong> orphans have unexpectedly<br />
become caregivers again,” she says. “I started thinking about<br />
the potential for stress there.”<br />
She headed to Kenya for the first time in 2002, to establish<br />
the Kenyan Grandparents Study, which examines how<br />
unanticipated childcare responsibilities affect the stress levels,<br />
nutrition and health <strong>of</strong> the elderly. What’s more, she fell in<br />
love with the place, and she’s returned every summer since<br />
with students in tow.<br />
“There are many situations in Kenya that will frustrate you or<br />
break your heart, but it’s amazing how much people appreciate<br />
the little things you do for them,” Ice says. “I always learn<br />
something new about myself and about Kenya. ... It’s neat<br />
to watch students go through the same process.”<br />
Even if students never return to the country where they studied<br />
or treat a tropical disease as physicians in the U.S., Ice believes<br />
international experience inspires better physicians.<br />
“Culture permeates everything,” she says. “We are an immigrant<br />
country, and immigrants arrive with their own attitudes, diseases<br />
and customs. It helps to be aware <strong>of</strong> all <strong>of</strong> those factors.”<br />
TODAY’S<br />
<strong>DO</strong><br />
Charles J. Cannon Edinburgh Geriatric Tutorial<br />
This clinical and educational program gives third-year medical<br />
students an opportunity to experience health care for the<br />
elderly in Scotland’s National Health Service.<br />
Deborah Meyer, Ph.D., director, 740.593.2266<br />
meyerd1@ohio.edu<br />
Community-Based Tropical Disease Research-Ecuador<br />
With a focus on Triatominae insects and mosquitoes in domestic,<br />
peridomestic and sylvatic habitats, this program seeks to<br />
reduce the spread <strong>of</strong> Chagas disease in Ecuador. Community<br />
education activities, including the production <strong>of</strong> educational<br />
tools to be used in the region, are also an important part <strong>of</strong><br />
this project.<br />
Mario Grijalva, Ph.D., director, 740.593.2192<br />
grijalva@ohio.edu<br />
Introduction to the Galapagos Islands Natural History<br />
This program provides an introduction to one <strong>of</strong> the most sensitive<br />
ecological habitats in the world. By visiting uninhabited<br />
and inhabited islands, students have a chance to compare and<br />
evaluate the impact <strong>of</strong> human activities on the island ecosystems<br />
and to discuss the struggle between economic development<br />
and conservation.<br />
Mario Grijalva, Ph.D., director, 740.593.2192<br />
grijalva@ohio.edu<br />
Tropical Disease Biology Workshop in Ecuador<br />
The objective <strong>of</strong> this multidisciplinary adventure is to gain a<br />
deeper understanding <strong>of</strong> the complex factors that play a role<br />
in the biology <strong>of</strong> tropical diseases.<br />
Mario Grijalva, Ph.D., director, 740.593.2192<br />
grijalva@ohio.edu<br />
Kenyan Grandparents Study<br />
This research project seeks to examine the effect that caregiving<br />
for orphaned children has on the health and wellbeing<br />
<strong>of</strong> Luo elders.<br />
Gillian Ice, Ph.D., M.P.H., director, 740.593.2128<br />
iceg@ohio.edu<br />
SHARE Kenya-<strong>Ohio</strong><br />
In this clinical program, students, faculty and clinicians deliver<br />
health care to residents in rural western Kenya.<br />
Christopher Simpson, D.O., M.A., director, 740.593.2257<br />
simpson@ohio.edu<br />
Village Mountain Mission<br />
This clinical program provides health care to the people <strong>of</strong><br />
Pueblo Nuevo, Dominican Republic. Identification <strong>of</strong> specific<br />
health conditions, for which there may be some immediate<br />
strategies, as well as those that require long-term strategies<br />
are an important part <strong>of</strong> this program.<br />
Roy Bontrager, M.D., director, 740.593.2207<br />
rbon@hocking.net<br />
<strong>Ohio</strong> <strong>University</strong> and CEDEINFA Partnership:<br />
Medical care for the “poorest <strong>of</strong> the poor” in San Salvador<br />
provides care for children and their families in collaboration<br />
with the Center for the Complete Development <strong>of</strong> Children and<br />
their Families.<br />
Eddith Dashiell, Ph.D., director, 740.593.2581<br />
dashiell@ohio.edu<br />
Clinical rotation in Ecuador<br />
This program provides students with an opportunity to rotate<br />
for four weeks in a variety <strong>of</strong> disciplines in select hospitals<br />
in Quito, Ecuador. Students will take orientation and training<br />
at Catholic <strong>University</strong> <strong>of</strong> Ecuador, receive classes in medical<br />
Spanish and conduct clinical rotations in the different services<br />
<strong>of</strong>fered by the participating hospitals.<br />
David Drozek, D.O., Ph.D., director, 740.593.2489<br />
drozek@oucom.ohiou.edu<br />
summer/fall 2007 19
Capt. Larry Robinson, D.O. (’02), was injured March 1, 2007, when an<br />
IED (improvised explosive device) hit his armored humvee. He required<br />
a craniotomy, cranioplasty and facial reconstruction surgery before<br />
returning to <strong>Ohio</strong>, where he’s recovering with the help <strong>of</strong> his wife,<br />
Emily, and his family.<br />
This is his story.<br />
This was my first deployment.<br />
I arrived in Iraq in August 2006 as part <strong>of</strong> the 5-73 Cavalry<br />
Squadron, which is part <strong>of</strong> the 3rd Brigade Combat Team,<br />
82nd Airborne Division out <strong>of</strong> Fort Bragg, N.C.<br />
As a family physician in the Army, it was my job to keep the<br />
nearly 600 people on my contingency operating base (COB)<br />
healthy with the help <strong>of</strong> one physician assistant and 24 medics<br />
in the squadron. We were based out <strong>of</strong> COB Caldwell in eastern<br />
Iraq, a short distance from the Iranian border. Medically, we<br />
were what the Army calls a level one aid station, which means<br />
personnel available to treat wounded soldiers. On these<br />
missions I felt well protected by the disciplined and<br />
pr<strong>of</strong>essional soldiers in the squadron.<br />
At the end <strong>of</strong> February, we left COB Caldwell to set up<br />
patrol bases in the Diyala River Valley, an area that had been<br />
infiltrated with terrorist and Al-Qaeda affiliated groups. It’s<br />
a dangerous place where many people, including U.S. soldiers,<br />
were killed. We used these bases to launch attacks and raids<br />
against terrorists.<br />
The long<br />
we had no radiology, laboratory, surgery, physical therapy or<br />
dentistry. But there was a small pharmacy along with supplies<br />
to stabilize trauma and to take care <strong>of</strong> sick call. The base<br />
was also home to around 3,000 Iraqi soldiers and to the 5th<br />
Division <strong>of</strong> the Iraqi Army.<br />
While accompanying the Iraqi Army and their medical<br />
team, we went out on several combined medical engagements<br />
where we provided free medical care to people in the<br />
village. These missions were generally well accepted by the<br />
Iraqi people and were an important way for them to see that<br />
their Army cared about them. The missions were fun for me<br />
because it gave me a chance to see Iraqi families with their<br />
children. It was also nice to help relieve a little <strong>of</strong> their suffering<br />
by treating some <strong>of</strong> their illnesses—even if it was just<br />
a temporary fix.<br />
I also went on many combat missions with my squadron.<br />
Treating trauma in the field is very different than treating<br />
trauma in an aid station or a hospital. Bombs and gunfire<br />
may be going <strong>of</strong>f, and there’s less equipment and fewer<br />
On what was to be my last mission, I went out with a<br />
platoon-sized element on a 24-hour mission to watch a<br />
dangerous stretch <strong>of</strong> road. The plan was to catch insurgents<br />
placing improvised explosive devices (IEDs) in the road.<br />
We were out all night watching and caught several insurgents.<br />
On the way back to the patrol base, we took a detour to observe<br />
a nearby town that was supposedly controlled by “The<br />
Islamic State <strong>of</strong> Iraq,” an Al-Qaeda-linked group.<br />
On the outskirts <strong>of</strong> town, our vehicle got stuck in a mud hole<br />
and began to sink. I was sitting in the back <strong>of</strong> the vehicle and<br />
could see angry villagers approaching us with Russian-made<br />
AK47 rifles and a few rocket-propelled grenades. Needless to<br />
say, I was concerned because our 50 caliber machine gun turret<br />
had malfunctioned and wouldn’t swivel. A vehicle behind us<br />
finally managed to pull us out <strong>of</strong> the mud hole. As we headed<br />
toward our patrol base, I praised God for getting me out <strong>of</strong><br />
that situation.<br />
Then my vehicle hit was hit by a large IED.<br />
20 18 www.oucom.ohio.edu
photo courtesy <strong>of</strong> Abigail Bobrow/Sandusky Register<br />
Road back<br />
A family physician recounts<br />
his experience in IraqBy Capt. Larry Robinson, D.O<br />
summer/fall 2007 21
When I woke up at Warhorse, I kept repeating “My head<br />
hurts!” I don’t remember any <strong>of</strong> this, but the doctors at<br />
Warhorse, good friends <strong>of</strong> mine, suspected I had an intracranial<br />
bleed and had me flown to LSA (logistical support area)<br />
Anaconda for treatment.<br />
Thankfully, my Kevlar helmet stopped the IED shrapnel<br />
from penetrating my skull. But the shrapnel did cause<br />
several comminuted fractures <strong>of</strong> my skull, along with facial<br />
bone fractures and epidural, subarachnoid and subdural<br />
hemorrahages. The increasing intracranial pressure from<br />
the bleeding inside my skull caused extreme nausea and<br />
unrelenting vomiting.<br />
My head hurt and I was confused.<br />
When my squadron commander, Lt. Col. Poppas, my<br />
physician’s assistant, Maj. Rather, and a few other friends<br />
from the squadron explained what happened to me and the<br />
extent <strong>of</strong> my injuries, I couldn’t believe it. I asked to see my<br />
CT scan right then and there.<br />
Lt. Col. Poppas pinned a Purple Heart on my shirt, and I<br />
remember thanking him and then jokingly told him it wasn’t<br />
the medal I wanted to receive in Iraq. Maj. Rather and<br />
I always referred to the Purple Heart as the “Iraqi Marksmanship<br />
Badge.”<br />
Capt. Larry Robinson on the Iranian border.<br />
Shrapnel struck me in the helmet and knocked me unconscious.<br />
Paratroopers in my squadron quickly pulled me from the<br />
burning wreckage before the ammunition exploded. I was<br />
taken to FOB (forward operating base) Warhorse and treated<br />
in the same trauma room that I’d worked in as a physician.<br />
Amazingly, I was the only one injured in the explosion!<br />
After that, I was evacuated to Landstuhl, Germany, and had<br />
surgery soon after landing. They performed a craniotomy<br />
with evacuation <strong>of</strong> the epidural hematoma and cranioplasty<br />
to stabilize my fractures. Four days later, I was able to fly<br />
back to the United States to the National Naval Medical<br />
Center (NNMC) in Bethesda, Md. I was very anxious to get<br />
back to the U.S. and to see my wife. I was told she had been<br />
flown to NNMC and was waiting for me.<br />
Capt. Larry Robinson,<br />
center, with Maj. Brad<br />
Rather, a physician<br />
assistant, left, and 1Lt.<br />
Braden Hestermann, a<br />
medical platoon leader,<br />
right, at LSA Anaconda<br />
before his evacuation<br />
to Germany.<br />
22 www.oucom.ohio.edu
Emily’s story<br />
I remember that morning very clearly.<br />
While chastising myself for sleeping in and leaving<br />
only 30 minutes to get ready for work, my cell phone<br />
rang. It was 7 a.m. A few days earlier, Larry told me<br />
that he was leaving for a month-long mission and<br />
would not be able to call me until the end <strong>of</strong> March.<br />
I answered. A male voice identified himself as the<br />
rear detachment <strong>of</strong>ficer for 5-73 CAV and he had news<br />
about Larry. I thought the call might be about some<br />
paperwork that Larry and I needed to fill out. It<br />
never occurred to me that he might have been hurt.<br />
Capt. Larry Robinson with an Iraqi child during a<br />
combined medical engagement mission.<br />
At NNMC I received first-rate medical care, for which I’m<br />
grateful. I wasn’t the most pleasant patient to care for—I<br />
would <strong>of</strong>ten awake from horrible nightmares where I thought<br />
the nurses were all trying to kill me. I was discharged from<br />
NNMC on March 13 to begin my three-month rehabilitation<br />
at Firelands Regional Medical Center.<br />
I did my internship and residency in family practice at Firelands.<br />
My father-in-law, Dr. James Preston, is the director <strong>of</strong> medical<br />
education there and was my first boss during my training.<br />
He’s become a great friend and an inspiration to me.<br />
The medical education I received at Firelands was great. It<br />
gave me everything I needed to be confident <strong>of</strong> my skills<br />
while in Iraq. My focus on hospital and in-patient training at<br />
Firelands—central lines, intubation, chest tubes, etc.—made<br />
procedures and trauma much easier for me in the field.<br />
Almost all soldiers in Iraq suffer from chronic thoracic and<br />
lumbar back pain. It’s one <strong>of</strong> the consequences <strong>of</strong> wearing 50<br />
pounds <strong>of</strong> body armor, spending hours sitting and sleeping in<br />
cramped humvees and sleeping outdoors on the ground while<br />
on missions. Because <strong>of</strong> my excellent OMM training, I was<br />
able to use manipulation to relieve their back pain.<br />
I still have some lingering problems, but I’m rapidly<br />
improving and expected to make a full recovery. After a few<br />
more months <strong>of</strong> rehabilitation, I’ll receive an extensive<br />
cognitive evaluation in the Traumatic Brain Injury Clinic at<br />
Walter Reed Army Hospital to see if I’m ready to return to<br />
active Army duty as a physician.<br />
My squadron has been hit really hard since my injury—I was<br />
the first—18 have been killed and over 40 have been injured<br />
during their long mission in the Diyala River Valley.<br />
I’m not sure if I’ll ever be asked to deploy to Iraq again.<br />
But this brush with death has made me realize that every<br />
day is a gift from God, and it’s important to make the<br />
most <strong>of</strong> every moment.<br />
TODAY’S<br />
<strong>DO</strong><br />
When he told me that Larry had a skull fracture, my<br />
mind went blank. He continued talking, but I couldn’t<br />
comprehend what this guy was saying. I gave the<br />
phone to my dad, hoping he could understand what<br />
was happening.<br />
The look on my father’s face told me the news wasn’t<br />
good—Larry had sustained a skull fracture and they’d<br />
call us when they had more information.<br />
I couldn’t stop crying. After praying and more crying,<br />
I called Larry’s brother, Mark, who is an OU-COM<br />
medical student at Firelands. He and his wife, Valerie,<br />
joined me and my parents for a prayerful wait at the<br />
kitchen table.<br />
We waited for what seemed like an intolerably long<br />
time, then, at 2 p.m., Larry called! His speech was<br />
slurred, but he assured me that his injuries weren’t<br />
“life-threatening,” he was going to be okay and that<br />
he loved me.<br />
I arrived in Bethesda, Md., at the National Naval Medical<br />
Center just a few hours after Larry checked into the<br />
ICU. When I saw him, he had 67 staples holding his<br />
scalp together, two black eyes from the broken bones<br />
in his face and the head trauma, and one blood-red<br />
eyeball. But I couldn’t take my eyes <strong>of</strong>f him—it was so<br />
good to see him.<br />
He’s had an amazing recovery. The doctors at Walter<br />
Reed Army Hospital are impressed with the care he’s<br />
receiving at Firelands and pleased with how well he’s<br />
healing. They expect a full recovery.<br />
We’re so blessed that we can resume our life together.<br />
What a gift.<br />
-Emily Robinson
quality<br />
Research<br />
<strong>of</strong> care<br />
Improving the<br />
By Susan Green<br />
It’s no secret that type 2 diabetes is on the rise.<br />
According to the Centers for Disease Control, 1 in 3<br />
people born in the United States in 2000 will develop<br />
diabetes in their lifetime. And over the next 50 years<br />
as those who develop diabetes continue to do so<br />
at a younger age, the number <strong>of</strong> people in nursing<br />
homes with diabetes will also increase due to the<br />
complexity <strong>of</strong> the disease in an aging population.<br />
“The fastest growing population <strong>of</strong> young people<br />
with diabetes is in this region,” says Rachel Holt, a<br />
second-year medical student at OU-COM. “Imagine<br />
the implications <strong>of</strong> this.”<br />
To examine the implications, Jay Shubrook, D.O.<br />
(’96), and Frank Schwartz, M.D., both affiliated<br />
with the Appalachian Rural Health Institute Diabetes<br />
Center at <strong>Ohio</strong> <strong>University</strong>, designed a research study<br />
to look at the quality <strong>of</strong> care diabetes patients receive<br />
in nursing homes. Holt joined the project in its early<br />
phase and was instrumental in its completion.<br />
The goal <strong>of</strong> the study was to examine physician<br />
management <strong>of</strong> patients with type 1 and type 2<br />
diabetes residing in extended care facilities and to<br />
compare this management to the American Diabetes<br />
Association Standards <strong>of</strong> Care for outpatients.<br />
After reviewing patient charts <strong>of</strong> more than 100<br />
elderly residents with diabetes in 11 nursing homes<br />
in <strong>Ohio</strong> and West Virginia, the researchers discovered<br />
that patients who had their diabetes under control<br />
either as outpatients or while hospitalized, had less<br />
success after entering a nursing home.<br />
Holt says an analysis <strong>of</strong> the data revealed the lack<br />
<strong>of</strong> a systematic approach to diabetes treatment in the<br />
facilities studied. The findings demonstrate that practice<br />
guidelines for this population are needed.<br />
Working closely with medical directors and directors<br />
<strong>of</strong> nursing, Schwartz and Shubrook are developing<br />
specific guidelines regarding the care <strong>of</strong> diabetes in<br />
the nursing home population. “The guidelines give<br />
physicians and nursing home staff a solid framework<br />
for developing treatment plans for this challenging<br />
population,” Shubrook says. “Phase 2 <strong>of</strong> the study,<br />
a second chart review <strong>of</strong> patients, will determine if<br />
following the treatment protocols results in quality<br />
<strong>of</strong> life changes for the residents.”<br />
This project is an excellent example <strong>of</strong> how the<br />
RSAF program gives medical students like Holt an<br />
opportunity to conduct valuable research. “I really<br />
enjoy research and had done basic science bench work,<br />
but I wanted to try clinical research,” she says. “And<br />
Dr. Shubrook’s project was a good fit. Next year I’ll<br />
be doing a family practice fellowship and will continue<br />
to work on phase 2 <strong>of</strong> the nursing home study.”<br />
As Holt’s research advisor, Shubrook gives her<br />
credit for the success <strong>of</strong> the project. He says she<br />
kept the project on track, analyzed the data and was<br />
the lead author on their research paper published in<br />
Diabetes Care.<br />
“The college is very supportive <strong>of</strong> research<br />
opportunities for students by helping us navigate<br />
our way through the process,” Holt adds. “Being<br />
here at OU-COM is advantageous. Through this<br />
experience and others, I’ll be better prepared to<br />
do my residency.”<br />
Holt RM, Schwartz FL, Shubrook JH. Diabetes Care<br />
in Extended Care Facilities: Appropriate Intensity <strong>of</strong><br />
Care? Diabetes Care. 2007 Jun;30(6):1454-1458;<br />
<strong>DO</strong>I: 10.2337/dc06-2311.<br />
From left, Jay Shubrook, D.O., Rachel Holt and Frank<br />
Schwartz, M.D.<br />
24 www.oucom.ohio.edu
“I really enjoy<br />
research and<br />
had done basic<br />
science bench<br />
work, but I<br />
wanted to try<br />
clinical research.”<br />
Curious Clinicians<br />
In an editorial in the New York Times, Susan Love, M.D., writes about the decline <strong>of</strong> “curious clinicians” in an age <strong>of</strong> increasingly<br />
complex medical and scientific research. What was common in the past—physicians who observed their patients and then went<br />
into the lab to test their hypothesis—is seldom practiced. Love advocates a return to medical research that begins with the<br />
patient and then leads to the lab.<br />
For nearly 30 years, the Research and Scholarly Advancement Fellowship (RSAF) has given selected OU-COM students an<br />
opportunity to conduct research. This ten-week summer program gives osteopathic medical students an introduction to<br />
scholarly work under the guidance <strong>of</strong> COM faculty members.<br />
And while not all research projects begin with the patient in mind, many do. Projects range from contributing to an ongoing<br />
faculty research project in the laboratory or clinic, to developing a review <strong>of</strong> a specific body <strong>of</strong> literature, or to an original<br />
research project designed by the student. In addition to conducting research, students are required to attend seminars on<br />
research-related topics, write a research paper and present a poster <strong>of</strong> their project during OU-COM’s annual Research Day<br />
held each fall quarter.<br />
This experience helps to set a strong foundation for future research they may pursue as clinicians.<br />
summer/fall 2007 25
A l u m n i a n d D e v e l o p m e n t<br />
Building our future together<br />
By Sharon Zimmerman<br />
This year has proven to be one <strong>of</strong> exciting changes.<br />
In January 2007, the <strong>of</strong>fices <strong>of</strong> alumni affairs and development merged in order to create a more<br />
unified outreach effort to our graduates and friends <strong>of</strong> the college. As a result <strong>of</strong> the reorganization,<br />
I’ve been named director <strong>of</strong> medical development and executive director <strong>of</strong> alumni affairs. While<br />
I’ll continue to oversee alumni programs at the college, most <strong>of</strong> my time will be dedicated to furthering<br />
the college’s fundraising efforts and working with you to enhance the alumni donor base.<br />
Our new director <strong>of</strong> alumni affairs, Jill Harman, who joined the <strong>of</strong>fice in May, is now responsible<br />
for planning alumni programs and events. Jill had been the associate director <strong>of</strong> admissions for the past<br />
five years, and she brings a wealth <strong>of</strong> knowledge about the college to her new position. Her energy and<br />
enthusiasm are unlike any I’ve seen, and if you haven’t already heard from Jill, you will. One <strong>of</strong> her first<br />
projects is to develop an easy way for you to stay in touch with us and for us to communicate with you.<br />
She has a lot <strong>of</strong> ideas and is interested in your input. Her e-mail address is: harmanj@ohio.edu.<br />
It is also my pleasure to welcome Jeffrey Stanley, D.O. (’82), as president <strong>of</strong> the Society <strong>of</strong> Alumni<br />
and Friends. Dr. Stanley joins the board after 20 years <strong>of</strong> practice as a vascular surgeon in Cleveland,<br />
<strong>Ohio</strong>. He was president <strong>of</strong> the <strong>Ohio</strong> <strong>Osteopathic</strong> Association in 2004, and in 2005 was recognized<br />
by OU-COM as Alumnus <strong>of</strong> the Year for his pr<strong>of</strong>essional achievements and for service to his alma<br />
mater. Also new to the board are Daryl Sybert, D.O. (’86), vice president, and Timothy Barreiro,<br />
D.O. (’97), secretary.<br />
Under Dr. Stanley’s leadership, the board has created several committees that will <strong>of</strong>fer suggestions<br />
concerning improved communication among alumni, and concerning alumni involvement in student<br />
recruiting, curricula and teaching, continuing medical education and development. It’s an exciting<br />
time to be an OU-COM graduate.<br />
I would like to thank Thomas Anderson, D.O. (’83), former president <strong>of</strong> the OU-COM Society<br />
<strong>of</strong> Alumni and Friends, for his three years <strong>of</strong> dedicated service to the board and to the Society.<br />
Dr. Anderson has just completed his first year <strong>of</strong> a three-year term on the <strong>Ohio</strong> <strong>University</strong> Alumni<br />
Association Board <strong>of</strong> Directors, where he’s representing 188,000 graduates. Congratulations Dr.<br />
Anderson!<br />
Congratulations also are in order for board member William ‘‘Rusty’’ Emlich, D.O. (’86), who<br />
was installed as president <strong>of</strong> the <strong>Ohio</strong> <strong>Osteopathic</strong> Association June 22, 2007.<br />
It remains our goal to engage each <strong>of</strong> you into the life <strong>of</strong> the college, whether through your time, talents<br />
or resources. Alumni are vital to the future <strong>of</strong> OU-COM’s continued success, and we look forward to a<br />
lasting relationship with you.<br />
To learn about supporting the<br />
integrated learning and research<br />
facility with a gift, contact Sharon<br />
Zimmerman, 740.593.2176.<br />
26 www.oucom.ohio.edu
C<br />
onstruction <strong>of</strong> the integrated learning and research<br />
facility—a special collaboration between the <strong>College</strong><br />
<strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong> and the Russ <strong>College</strong> <strong>of</strong><br />
Engineering—will mark the second time in <strong>Ohio</strong> <strong>University</strong><br />
history that a building has been constructed using funds<br />
primarily from private gifts.<br />
Members <strong>of</strong> the osteopathic medical community have<br />
demonstrated an unprecedented show <strong>of</strong> support for<br />
this project.<br />
For instance, Thomas Anderson, D.O. (’83), and<br />
his wife, Barbara, were the first to fund a named medical<br />
laboratory. Of his reason for giving, Dr. Anderson says,<br />
“ … Because it is our school, our osteopathic family and<br />
our future.”<br />
Richard A. Vincent, president <strong>of</strong> the <strong>Osteopathic</strong> Heritage<br />
Foundations, which made a considerable gift, says, “This<br />
facility provides a significant opportunity to advance the<br />
<strong>Osteopathic</strong> Heritage Foundations’ mission <strong>of</strong> improving<br />
health and quality <strong>of</strong> life while supporting the vision <strong>of</strong><br />
<strong>Ohio</strong> <strong>University</strong>.”<br />
Our own Society <strong>of</strong> Alumni and Friends made history at<br />
<strong>Ohio</strong> <strong>University</strong> with their gift <strong>of</strong> $50,000—the single<br />
largest gift ever made on behalf <strong>of</strong> an OHIO alumni society.<br />
These contributions are part <strong>of</strong> the remarkable $16.3<br />
million in private gifts garnered for the $30 million facility.<br />
Even with additional support from the State <strong>of</strong> <strong>Ohio</strong> and<br />
the <strong>University</strong>, we still need to raise $2.3 million to reach<br />
our goal.<br />
We will be asking for your support. So watch your mail for<br />
an important letter from Dean Jack Brose, D.O., and<br />
Jeffrey Stanley, D.O. (’82).<br />
As we continue fundraising efforts, I invite each <strong>of</strong> you to join<br />
fellow alumni and friends who have shown their support <strong>of</strong><br />
our commitment to excellence in learning and research.<br />
Just like Cutler Hall—built in 1819—this new facility<br />
symbolizes our pioneering spirit and sense <strong>of</strong> community.<br />
Sharon Zimmerman is the director <strong>of</strong> medical development<br />
and executive director <strong>of</strong> alumni affairs.<br />
www.oucom.ohio.edu/researchbuilding/<br />
An artist's rendering <strong>of</strong> the new the integrated learning and research facility.<br />
Research that will be<br />
enhanced by the new facility<br />
Diabetes<br />
Molecular biologist John Kopchick, Ph.D., is<br />
creating new therapies and diagnostics.<br />
Chemist Tadeusz Malinski, Ph.D., is developing<br />
therapies to accelerate wound healing.<br />
Scientist Leonard Kohn, M.D., and engineer<br />
Douglas Goetz, Ph.D., are developing new<br />
compounds to selectively target disease<br />
sites, and Kohn is studying how to detect<br />
early-stage diabetes.<br />
Heart Disease<br />
Goetz is combining engineering and biology<br />
to develop novel ways to treat heart disease.<br />
Technology<br />
The Center for Intelligent, Distributed and<br />
Dependable Systems is helping doctors diagnose<br />
patients, treat illnesses and plan for surgery.<br />
Engineer Robert Williams, Ph.D., in collaboration<br />
with John Howell, Ph.D., associate pr<strong>of</strong>essor <strong>of</strong><br />
biomedical sciences, is developing The Virtual<br />
Haptic Back to teach palpatory diagnosis.<br />
summer/fall 2007 27
Meet the<br />
Society <strong>of</strong> Alumni<br />
Jeffrey Stanley, D.O. (’82)<br />
president<br />
Vascular Surgery, Meridia South Pointe Hospital<br />
Words or phrases that<br />
describe you:<br />
Honest, fair, workaholic,<br />
generous, impatient<br />
Passion:<br />
My work as a vascular<br />
surgeon; this is what I was<br />
born to do<br />
Favorite movie:<br />
The Doctor<br />
Nicole Wadsworth, D.O. (’97)<br />
Emergency <strong>Medicine</strong>, OU-COM<br />
O’Bleness Memorial Hospital<br />
Words or phrases that<br />
describe you:<br />
Quiet, thoughtful, fair,<br />
driven, organized<br />
Wildest dream<br />
concerning health policy:<br />
Universal health care<br />
Peak patient<br />
experience:<br />
When patients ask me if<br />
I have an <strong>of</strong>fice practice<br />
because they would like<br />
me to be their physician.<br />
I’m deeply honored when<br />
this occurs<br />
Words or phrases that<br />
describe you:<br />
Out-<strong>of</strong>-the-box, inventive,<br />
integrative, humanistic,<br />
socially concerned<br />
Passion:<br />
Building systems that<br />
make life better for people<br />
Peak patient experience:<br />
Recognition for writing<br />
policy and developing<br />
a system that improved<br />
health care for the State<br />
<strong>of</strong> <strong>Ohio</strong><br />
Ronald Moomaw, D.O. (’80)<br />
Psychiatry,<br />
<strong>Ohio</strong> Department <strong>of</strong> Rehabilitation and<br />
Correction, Bureau <strong>of</strong> Mental Health Services<br />
28 www.oucom.ohio.edu
and Friends Board<br />
Daryl Sybert, D.O. (’86)<br />
vice president<br />
Orthopedics, New Albany Surgical Hospital<br />
Words or phrases<br />
that describe you:<br />
Optimistic, humorous,<br />
pr<strong>of</strong>essional, impatient,<br />
adventuresome<br />
Inspiration:<br />
My father, who was<br />
an osteopathic family<br />
physician<br />
Timothy Barreiro, D.O. (’97)<br />
secretary<br />
Internal <strong>Medicine</strong> – pulmonary, Pulmonary <strong>Medicine</strong> Consultants<br />
Words or phrases that<br />
describe you:<br />
Researcher, teacher,<br />
learner, overweight<br />
Perfect day:<br />
Save a life, cure a<br />
disease, learn something<br />
new, and go home to<br />
family<br />
Daily edification:<br />
Knowing I can make a<br />
difference in someone’s<br />
life by caring and listening<br />
Words or phrases<br />
that describe you:<br />
Patient, balanced, happy,<br />
motivated<br />
Biggest pr<strong>of</strong>essional<br />
challenge:<br />
Balancing practice and<br />
research<br />
Perfect day:<br />
All days are good<br />
Daily edification:<br />
I truly believe in the<br />
power <strong>of</strong> an optimistic<br />
attitude in life<br />
Mitchell Silver, D.O. (’89)<br />
Cardiology,<br />
Mid<strong>Ohio</strong> Cardiology Consultants<br />
summer/fall 2007 29
Sharon Van Nostran, D.O. (’98)<br />
Family <strong>Medicine</strong>,<br />
Primary Care Physicians<br />
Words or phrases that<br />
describe you:<br />
Dedicated educator,<br />
physician, bird watcher,<br />
ice cream eater<br />
Pr<strong>of</strong>essional bane:<br />
“What are you, some kind<br />
<strong>of</strong> chiropractor?”<br />
Peak patient experience:<br />
Hand-drawn cards from<br />
pediatric patients<br />
William Emlich, D.O. (’86)<br />
Internal <strong>Medicine</strong> - gastroentology, Consolidated<br />
Medical Specialists<br />
Tinisha Jordan, D.O. (’00)<br />
Family <strong>Medicine</strong>, Kaiser Permanente Marlow Heights<br />
Medical Center<br />
Paige Gutheil, D.O. (’02)<br />
Family <strong>Medicine</strong>,<br />
Family Practice West, Inc.<br />
Words or phrases that<br />
describe you:<br />
Honest, determined,<br />
reliable, open-minded,<br />
intelligent—with a touch<br />
<strong>of</strong> “blonde”<br />
First job:<br />
Filling out billing forms for<br />
my dad’s family practice<br />
<strong>of</strong>fice<br />
Pr<strong>of</strong>essional bane:<br />
Patients that come to the<br />
doctor expecting service<br />
equivalent to a fast-food<br />
drive-through: “I’m here<br />
for Nexium, Allegra, Viagra,<br />
and that medicine for<br />
your legs that I saw on TV.”<br />
Georgenna Riley, D.O. (’95)<br />
Radiology, Parma Medical Center<br />
Charles Mehlman, D.O. (’89)<br />
Orthopedics – pediatric, Cincinnati Children’s Hospital<br />
Medical Center<br />
Jay Shubrook, D.O. (’96)<br />
Family <strong>Medicine</strong>, OU-COM<br />
Cornwell Center for Cardiovascular Care<br />
Eric Beck, EMT-P, OMS IV<br />
30 www.oucom.ohio.edu
“Listening to doctors talk about the path they took in their career is a very educational experience<br />
because it helps students find their own paths,” says Tim Neely, a second-year medical student.<br />
Alumni on Campus<br />
This spring alumni talked about their work to OU-COM students during<br />
Career Medical Specialties Week and Minority Health Month.<br />
“There are many barriers to treating the under- and uninsured.<br />
Some <strong>of</strong> the barriers are cultural, but whatever they are, it<br />
prevents patients from seeing you, which means that they<br />
are less likely to receive appropriate care. To reach these<br />
people, you have to be a physician and a social worker.”<br />
–Tinisha Jordan, D.O. (’00), is a physician at Kaiser<br />
Permanente Marlow Heights Medical Center<br />
“I went to Honduras as an expert, and I returned to Athens a<br />
student looking to increase my knowledge.” Other advice:<br />
“Provide spiritual, medical and social help to people in need.”<br />
–David Drozek, D.O. (’83), is an assistant pr<strong>of</strong>essor<br />
<strong>of</strong> surgery at OU-COM<br />
“If you don’t respect their traditions or cultural differences,<br />
then you can’t expect elderly minorities to respect your<br />
advice.”<br />
–Michael Gerardo, D.O. (’01), was a fellow at<br />
Rhode Island Hospital, Brown <strong>University</strong>; beginning<br />
July 1, 2007, he will be an assistant pr<strong>of</strong>essor <strong>of</strong><br />
geriatric medicine at OU-COM<br />
“I want students to know that being an<br />
osteopathic doctor does not limit you to<br />
just primary care.”<br />
–Karen Thomas, D.O. (’96), treats<br />
patients with motor complications at<br />
the Movement District Center, <strong>Ohio</strong><br />
State <strong>University</strong><br />
“If you’re looking for a career with lots <strong>of</strong> hands-on<br />
with patients, radiology should probably not be your first<br />
choice. Patient interaction is very limited.” Other advice:<br />
“If you’re interested in becoming a radiologist, get as<br />
much exposure—no pun intended—as you can.”<br />
<br />
–Bradley Cole, D.O. (’99), ), is a cross imaging<br />
radiologist at the Cleveland Clinic<br />
summer/fall 2007 31
1980<br />
MacGregor E. Poll, D.O., is medical director <strong>of</strong> Northridge<br />
Surgery Center in Madison, Tenn.<br />
Gary W. Welch, D.O., was recently reappointed chairman<br />
<strong>of</strong> the board <strong>of</strong> directors at the Pennsylvania Trauma Systems<br />
Foundation, the agency which accredits all trauma centers in<br />
the state.<br />
1982<br />
Barbara A. Girz, D.O., was elected president <strong>of</strong> the New<br />
Jersey Maternal-Fetal <strong>Medicine</strong> Society for the 2006-2007<br />
term.<br />
David Lance, D.O., is senior medical director at Hospice<br />
and Palliative Care <strong>of</strong> Greater Wayne County in Wooster,<br />
<strong>Ohio</strong>.<br />
William Polinski, D.O.,<br />
gave an informative and entertaining<br />
presentation about<br />
cardiovascular medicine to<br />
OU-COM students in January<br />
2007. A practicing cardiologist<br />
for 18 years, Polinski talked about future testing<br />
and drug programs that could revolutionize cardiac<br />
care. He also <strong>of</strong>fered tips on vascular health, post-heart<br />
attack care utilizing aspirin and statin drugs, exercise,<br />
and metabolic syndrome to an audience that included<br />
his daughter, second-year student Rachel Polinski.<br />
His talk was sponsored by the OU-COM chapter <strong>of</strong><br />
the Student <strong>Osteopathic</strong> Medical Association, <strong>of</strong> which<br />
Rachel is vice president.<br />
OhiO <strong>University</strong> AlUmni AssOciAtiOn<br />
The Offical Ring <strong>of</strong><br />
<strong>Ohio</strong> <strong>University</strong><br />
Find information on<br />
the ring and how to order<br />
in our Bobcat Store.<br />
OHIO Alumna <strong>of</strong> the Year<br />
1984<br />
Roberta L. Kalafut, D.O., was appointed by Governor<br />
Rick Perry to the Texas Medical Board, as chairman <strong>of</strong><br />
licensure in 2002. She is currently serving as the board’s first<br />
female president.<br />
Louis B. Kasunic, D.O., is practicing at Castle Rock<br />
Family Physicians and is the director <strong>of</strong> the Colorado<br />
Cardiovascular Risk Reduction Center in Castle Rock,<br />
Colo.<br />
Anthony Montanaro, D.O., was named the Cleveland<br />
Clinic Foundation’s annual Educator <strong>of</strong> the Year for 2006.<br />
1986<br />
Kyle Allen, D.O., received a federal grant from the Agency<br />
for Healthcare Research and Quality to study a care management<br />
model for low-income elderly.<br />
E. Joseph Carter, D.O., was named a fellow <strong>of</strong> the<br />
American <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> Internists.<br />
Amelia Tunanidas, D.O. (’82), was<br />
named <strong>Ohio</strong> <strong>University</strong> Alumni Association<br />
2007 Alumna <strong>of</strong> the Year. She was recognized<br />
for her service to the osteopathic pr<strong>of</strong>ession<br />
and for her support <strong>of</strong> <strong>Ohio</strong> <strong>University</strong>.<br />
“I am most humbled and thrilled to have<br />
been selected for this recognition from<br />
my alma mater,” she says. “There are so<br />
many wonderful graduates <strong>of</strong> <strong>Ohio</strong><br />
<strong>University</strong> who are truly deserving <strong>of</strong><br />
this award, and I am spellbound to have been selected among such<br />
worthy honorees. It is quite an honor to join the ranks <strong>of</strong> OU’s<br />
finest, and I am grateful to the Lord to be blessed with this honor.”<br />
Tunanidas will be honored, along with other <strong>Ohio</strong> <strong>University</strong><br />
alumni at an awards ceremony during Homecoming Weekend,<br />
October 12-14, 2007.<br />
Gregory Hill, D.O., joined Spectrum Orthopedics in<br />
Canton, <strong>Ohio</strong>, after completing his second tour <strong>of</strong> duty in<br />
Iraq in December 2005.<br />
www.OhiOAlUmni.Org/stOre<br />
Robert Vaschak, D.O., recently gave a cardiovascular physical<br />
exam presentation to 3rd and 4th-year medical students<br />
in the OU-COM Internal <strong>Medicine</strong> Club.<br />
32 www.oucom.ohio.edu
1988<br />
Robert A. Cain, D.O., was named director <strong>of</strong> medical education<br />
at Grandview Hospital in Dayton, <strong>Ohio</strong>.<br />
Vicky Leo, D.O., is chair <strong>of</strong> the American <strong>Osteopathic</strong><br />
Board <strong>of</strong> Internal <strong>Medicine</strong> for the 2006-2007 term.<br />
Gwendolyn E. Niebler, D.O., accepted the position <strong>of</strong><br />
vice president <strong>of</strong> medical affairs at Shire Pharmaceuticals in<br />
Wayne, Pa.<br />
Michael Reeder, D.O., received the 2006 Teacher <strong>of</strong> the<br />
Year Award from St. Mary’s Family Practice Program in<br />
Grand Junction, Colo.<br />
Jill Vosler, D.O., published her first novel,<br />
Legal Larceny, a fictional depiction <strong>of</strong> the<br />
malpractice travails that shape the practice <strong>of</strong><br />
modern medicine. Inspired by a lawsuit leveled<br />
at a fellow physician, Vosler decided to take a<br />
closer look at “…our overly litigious climate”<br />
and the way it changes the practice <strong>of</strong> medicine.<br />
A family practitioner for over 17 years, Vosler practices<br />
in the same building where two <strong>of</strong> her three brothers also<br />
practice. Along with maintaining a busy practice, she serves as<br />
the Eaton High School team physician and also sits on the<br />
Preble county Mental Health and Recovery Board. And she<br />
recently became president <strong>of</strong> the Eaton Little League. How<br />
does she have time to write? “It’s tricky,” Vosler says. “But<br />
I’m quite good a making a few hours count.” Her next book<br />
will target the medical insurance industry.<br />
1990<br />
Franklin Demint, D.O., was certified by the AOA/<br />
AOBNMM in Neuromusculoskeletal <strong>Medicine</strong> and <strong>Osteopathic</strong><br />
Manipulative <strong>Medicine</strong>. He is also board certified in Family<br />
<strong>Medicine</strong> by the AOBFP and credentialed in pain management<br />
by the AAPM.<br />
1992<br />
Macy (Artis) Fox, D.O., started a solo ob/gyn practice<br />
in Snoqualmie, Wash., after relocating to the area with her<br />
husband and children.<br />
Roy Harris, D.O., received the Community Preceptor<br />
All-Star Award, selected by <strong>Ohio</strong> State <strong>University</strong> medical<br />
students. He is married to Mary “Beth” Harman, and they<br />
reside in Bucyrus, <strong>Ohio</strong>, with their two children.<br />
Tracy Marx, D.O., completed a Primary Care Faculty<br />
Development Fellowship with an emphasis on research<br />
methodology at Michigan State <strong>University</strong>.<br />
1994<br />
David D. Powell, D.O., has established a solo oncology<br />
practice, Cancer Care <strong>of</strong> West Central <strong>Ohio</strong>, in Lima, <strong>Ohio</strong>.<br />
John C. Sarantopoulos, D.O., and his wife Christina G.<br />
Sarantopoulos, D.P.M, announce the birth <strong>of</strong> a daughter, Kyra,<br />
born May 9, 2006.<br />
Charles E. Steiner, D.O., gave a lecture on somatic<br />
dysfunction and osteopathy at the Tennessee Academy <strong>of</strong><br />
Physicians Assistants CME conference Oct. 10, 2006.<br />
Timothy Wagner, D.O., and Joanne Nohra were married<br />
in July 2006. He was given command <strong>of</strong> Cc. 235 BSB (Med)<br />
in August, and was deployed to Iraq for the second time in<br />
December 2006.<br />
John J. Wilson, D.O., completed an Interventional<br />
Physiatry/Spine Fellowship at Orthopedic Specialists <strong>of</strong> the<br />
Carolinas in Winston-Salem, N.C. He opened a new practice,<br />
Piedmont Spine Specialists, PA, in Raleigh, N.C., with John G.<br />
Bentley, M.D. (B.S., ’93), and also serves as an instructor for<br />
the North American Spine Society spinal injection course.<br />
1996<br />
Susan Schrimpf Davis, D.O., completed a fellowship in<br />
geriatric medicine at the <strong>University</strong> <strong>of</strong> Cincinnati <strong>College</strong> <strong>of</strong><br />
<strong>Medicine</strong>. She is also an assistant pr<strong>of</strong>essor <strong>of</strong> family medicine<br />
at the college. She and husband, Craig M. Davis, Ph.D., have<br />
a 2-year-old son, Vincent.<br />
Deborah Gallo, D.O., and John Burlock Jr. were marred<br />
Aug. 5, 2006.<br />
Joseph M. Fabry, D.O., is practicing general and vascular<br />
surgery at the Santa Cruz Medical Clinic, a 150-physican,<br />
multi-specialty group in Santa Cruz, Calif.<br />
Michelle Kantor Herring, D.O., and husband, Jefferson<br />
Herring, M.D., have a son, Jacob, born Jan. 14, 2005.<br />
Miguel Krishnan, D.O., is an assistant pr<strong>of</strong>essor <strong>of</strong> pediatric<br />
otolaryngology at the <strong>University</strong> <strong>of</strong> Southern California, Keck<br />
School <strong>of</strong> <strong>Medicine</strong>. He and wife, Norma Marie Salmh<strong>of</strong>er,<br />
welcome their third daughter, Sara, to the family.<br />
Wayne J. Myles, D.O., is an assistant pr<strong>of</strong>essor <strong>of</strong> family<br />
medicine at OU-COM. He started a “practice within a<br />
practice” for people between 13 and 25 called TeenMed. He<br />
recently gave a presentation for the <strong>Ohio</strong> <strong>University</strong> Center for<br />
International Business Education and Development to business<br />
leaders and physicians from Brazil on how to start and run<br />
a successful family medicine practice in the U.S.<br />
Vernon Reynolds, D.O., and wife, Julie, announce the<br />
birth <strong>of</strong> a daughter, Lainey, Oct. 10, 2005.<br />
summer/fall 2007 33
William E. Saar, D.O., is the director <strong>of</strong> foot and ankle services<br />
at <strong>University</strong> Hospitals Health System-Primary and Specialty Care<br />
Practices.<br />
Mark J. Veronneau, D.O., opened an ear, nose and throat practice<br />
in Prestonsburg, Ky. He and wife, Lisa, announce the birth <strong>of</strong> a<br />
daughter, Adelle Grace, Feb. 4, 2006.<br />
1998<br />
Christopher Cirino, D.O., spent six weeks in the summer <strong>of</strong> 2006<br />
working as an HIV clinical mentor in Lesotho, Africa. He recently<br />
completed a Master <strong>of</strong> Public Health in Global Health at George<br />
Washington <strong>University</strong> School <strong>of</strong> Public Health and is currently<br />
working for St. Vincent’s Health System in Erie, Pa.<br />
Jessie Clairvil, D.O., announces the birth <strong>of</strong> a daughter, Justine,<br />
Sept. 14, 2005.<br />
Jason A. Fried, D.O., is in a vascular surgery fellowship at South Pointe<br />
Hospital in Cleveland, <strong>Ohio</strong>.<br />
Robert W. Garner, D.O., is the community physician liaison to the<br />
executive committee <strong>of</strong> Scott Air Force Base in Illinois, precepting for the<br />
St. Louis <strong>University</strong> Community and Family <strong>Medicine</strong> residency program<br />
as an individual mobilization augmentee.<br />
Vipin Koshal, D.O., is completing a Cardiology Fellowship at the<br />
<strong>University</strong> Hospital/<strong>University</strong> <strong>of</strong> Cincinnati <strong>College</strong> <strong>of</strong> <strong>Medicine</strong>.<br />
Cheryl Leuthaeuser, D.O., presented a lecture on integrated medicine<br />
and osteopathy for autism at the Autism and Asperger Association’s first<br />
international meeting last summer in Park City, Utah, August 2006. In July<br />
2006, the <strong>of</strong>fices <strong>of</strong> OsteoMed II in Middleburg Heights, <strong>Ohio</strong>, where Dr.<br />
Leuthaeuser’s practice resides, were destroyed by fire.<br />
Douglas Maurer, D.O., is completing a Madigan Faculty Development<br />
Fellowship at Madigan Army Medical Center, Fort Lewis, Wash., through<br />
which he’ll receive a Masters in Public Health from the <strong>University</strong> <strong>of</strong><br />
Washington this summer. He also is a recruiter for the Army Health<br />
Pr<strong>of</strong>essions Program.<br />
Leslie (Apacki) Nowell, D.O., and husband, Rob, announce the birth<br />
their second child, Ryan, Dec. 11, 2005.<br />
Ronald J. Russ, D.O., was named residency director <strong>of</strong> family medicine<br />
at Cuyahoga Falls General Hospital in January 2006.<br />
Jean (Weis) Schall, D.O., and husband, Steven, welcomed son, Jack,<br />
Nov. 30, 2005.<br />
Beth Schulz-Butulis, D.O., completed her Army duty last summer and<br />
entered private practice with Family Dermatology in Raleigh, N.C.<br />
Thomas Wagner, D.O., and wife, Lisa, announce the birth <strong>of</strong> a son,<br />
Jacob Thomas, born in April 2006.<br />
2000<br />
Lisa (Knight) Flarey, D.O., and her husband Anthony Flarey,<br />
D.O., (’97), finalized the adoption <strong>of</strong> a daughter, Noelle Christine,<br />
from China. Noelle was born April 3, 2005.<br />
James D. Heddleson, D.O., will complete a pulmonary/critical<br />
care fellowship at Doctors Hospital <strong>of</strong> Columbus in July 2007.<br />
Alexander Hewlett, D.O., received a Masters <strong>of</strong> Science in<br />
Clinical Investigation from the <strong>University</strong> <strong>of</strong> Texas Medical Branch in<br />
Galveston, Texas.<br />
Wendy (Morehead) Kissinger, D.O., and husband, Dan, welcomed<br />
their second son, Nicholas, to the family Dec. 16, 2005.<br />
Rebecca (Hauser) Tat, D.O., and David Tat, D.O. (’99)<br />
are the happy parents <strong>of</strong> twin girls, Madison and Kaitlyn, born June<br />
21, 2005.<br />
Marc Tressler, D.O., received the 2006-2007<br />
Orthopedic Trauma Association Kenneth Johnson<br />
Traveling Fellowship, which he is completing at the<br />
Harborview Medical Center in Seattle, Wash. He’s<br />
focusing on foot and ankle trauma and post-traumatic<br />
reconstruction. He also completed an orthopedic<br />
trauma fellowship at Vanderbilt <strong>University</strong> Medical<br />
Center, where he is now an assistant pr<strong>of</strong>essor.<br />
Kristin (Stenzel) Woodard, D.O., and husband, Todd, announce<br />
the birth <strong>of</strong> a daughter, Morgan Elizabeth, on Aug. 1, 2006.<br />
2002<br />
Gregory Applegate, D.O., completed an Anesthesiology Residency<br />
at Case Western Reserve <strong>University</strong>/<strong>University</strong> Hospital <strong>of</strong> Cleveland<br />
in June 2006 and accepted a position as an anesthesiologist at Walter<br />
Reed Army Medical Center.<br />
Dustin (Humienny) Blakeslee, D.O., is medical director <strong>of</strong><br />
consultation psychiatry at Akron General Medical Center and also<br />
maintains an outpatient private practice with the Center for Akron<br />
Psychiatry. She is involved in training NEOUCOM medical students<br />
and psychiatry residents.<br />
Patrick Blakeslee, D.O., is employed by Premier Medical Partners<br />
and is a hospitalist at Cuyahoga Falls General Hospital, Summa Health<br />
System, and Akron General Medical Center. He is a CORE assistant<br />
pr<strong>of</strong>essor <strong>of</strong> internal medicine.<br />
Catherine Kunzler Champagne, D.O., is an attending emergency<br />
medicine physician with Timberline Emergency Physicians in Saginaw,<br />
Mich.<br />
Marie Demosthenous, D.O., is in a child and adolescent psychiatry<br />
fellowship program. She and her husband, Greg Behbehani, M.D., Ph.D.,<br />
reside in Chicago.<br />
34 www.oucom.ohio.edu
James D. Heddleson, D.O., is currently the chief pulmonary/<br />
critical care fellow at Doctors Hospital in Columbus, <strong>Ohio</strong>.<br />
Brock Herring, D.O., will start an orthopedic foot and ankle fellowship<br />
at St. Joseph Mercy Hospital in Pontiac, Mich., in August.<br />
Anthony Karam, D.O., is a volunteer clinical faculty member<br />
for the <strong>University</strong> <strong>of</strong> California, Davis, and teaches family practice<br />
residents who rotate through emergency medicine at Mercy Medical<br />
Center in Redding, Calif.<br />
Sanjiv Lakhia, D.O., is working for Cincinnati Group Health<br />
Associates practicing PMR, OMT and acupuncture. He and wife,<br />
Teresa, announce the birth <strong>of</strong> a son, Kyran Sanjiv.<br />
Kari (Mann) Lucas, D.O., and husband, Jason, announce the birth<br />
<strong>of</strong> a son, Ethan, Nov. 23, 2006.<br />
Daniel Maurer, D.O., has accepted a shoulder and elbow surgery<br />
fellowship with Dr. Tom Norris in San Francisco, Calif. He announces<br />
the birth <strong>of</strong> a daughter, Mia, Aug. 9, 2006.<br />
Craig Peters, D.O., is completing a cardiology fellowship at the<br />
<strong>University</strong> <strong>of</strong> Arizona Medical Center in Tucson, Ariz.<br />
Larry Robinson, D.O., was deployed as a surgeon with the 5-73<br />
CAU (Recon), 82nd Airborne at FOB Caldwell in Iraq in August<br />
2006. He was wounded in February 2007 and flown to Germany,<br />
then on to Bethesda, where he underwent surgery at the National<br />
Naval Medical Center. The surgery went well.<br />
Tiffani Singleton, D.O., joined the family medicine faculty at the<br />
<strong>University</strong> <strong>of</strong> Alabama in Birmingham after completing an ob/gyn<br />
fellowship there.<br />
2004<br />
Andrew Guglielmi, D.O., and wife, Julie, announce the birth <strong>of</strong> a<br />
daughter, Alyssa. Andrew is a second-year radiology resident in the<br />
Aultman-NEOUCOM program in Canton, <strong>Ohio</strong>.<br />
Sarah Haley-Wien, D.O., received a Masters in Public Health from<br />
the <strong>University</strong> <strong>of</strong> Alabama at Birmingham.<br />
Alexis Johnston, D.O., received the Gold Foundation Humanism<br />
and Excellence in Teaching Award from the Northeastern <strong>Ohio</strong><br />
Universities <strong>College</strong> <strong>of</strong> <strong>Medicine</strong>.<br />
Deanna Ohms, D.O., and Joseph Anderson were<br />
married in November 2006 in Clearwater Beach, Fla.<br />
2006<br />
Jennifer (Paglia) Breedlove, D.O., and husband, Aaron, announce<br />
the birth <strong>of</strong> a son, Benjamin Aaron, Aug. 22, 2006.<br />
Jennifer A. Painter, D.O., will start aviation medicine training this<br />
summer with the U.S. Navy in Pensacola, Fla., for six months. She will<br />
then be stationed as a flight surgeon with a Navy Aviation Squadron.<br />
Keep us posted<br />
Please send us your news for the next issue.<br />
Fax: 740.593.0761<br />
E-mail: harmanj@ohio.edu<br />
Alumni Affairs, 203 Grosvenor Hall, Athens, <strong>Ohio</strong>, 45701<br />
Career_______________________________________<br />
____________________________________________<br />
__________________________________________________________________________________________<br />
_________________________________________________________________________________________<br />
_________________________________________________________________________________________<br />
Personal _____________________________________<br />
____________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
______________________________________________________________________________________<br />
Send us a photo!<br />
Name _____________________________________<br />
Home Address _______________________________<br />
____________________________________________<br />
___________________________________________<br />
Office Address _______________________________<br />
____________________________________________<br />
___________________________________________<br />
Address change ____yes_____no____<br />
Telephone - Home __________________________<br />
Office _____________________________________<br />
E-mail address _____________________________<br />
John J. Parente, D.O., will become an attending physician this summer<br />
at the Fisher-Titus Medical Center in Norwalk, <strong>Ohio</strong>. In addition,<br />
he will be teaching at the <strong>University</strong> <strong>of</strong> Toledo Medical School.<br />
Year <strong>of</strong> graduation __________________________<br />
I would like to read more about ________________<br />
____________________________________________<br />
___________________________________________<br />
____________________________________________<br />
____________________________________________<br />
____________________________________________<br />
summer/fall 2007 35
Peter Johnson, Ph.D.<br />
Three OU-COM<br />
pr<strong>of</strong>essors retire<br />
after 81 years <strong>of</strong> collective service<br />
David Stroh, D.O.<br />
William Duerfeldt, D.O.<br />
David Stroh, D.O.<br />
associate pr<strong>of</strong>essor <strong>of</strong> family medicine<br />
“The college has been a wonderful<br />
place to work, full <strong>of</strong> new adventures,<br />
great people and challenges. I’ve met<br />
lifelong friends here and had the<br />
opportunity to influence more than a<br />
few students.”<br />
Life after OU-COM “I’ll continue<br />
to teach one quarter each year and<br />
will continue my clinical practice in<br />
Coolville. I also plan to spend time<br />
reading, golfing, socializing and taking<br />
up new endeavors.”<br />
Peter Johnson, Ph.D.<br />
pr<strong>of</strong>essor <strong>of</strong> biomedical sciences<br />
“As a founding faculty member at<br />
OU-COM, I have been very pleased<br />
about the way our college has matured<br />
and strengthened over the years. Not<br />
only in terms <strong>of</strong> teaching, but also in<br />
that the college has developed a strong<br />
research focus. I have so much enjoyed<br />
working with the different units in the<br />
college, and I’m sure that I’ll undergo<br />
withdrawal symptoms in the early years<br />
<strong>of</strong> my retirement.”<br />
Life after OU-COM “I’ll be moving<br />
to the mountains <strong>of</strong> western North<br />
Carolina, but will be back in Athens<br />
for the next few summers to continue<br />
teaching in the Prematriculation and<br />
Summer Scholars programs. In North<br />
Carolina, I plan to continue some<br />
<strong>of</strong> my research, writing and editing.<br />
And, I also want to do some volunteer<br />
tutoring in middle and high schools.”<br />
William Duerfeldt, D.O.<br />
associate pr<strong>of</strong>essor <strong>of</strong> family medicine<br />
“I’ve been truly blessed to have had<br />
the opportunity to teach and practice<br />
medicine at OU-COM. It has been a<br />
privilege to share my experiences, and<br />
my patients, with the scores <strong>of</strong> medical<br />
students who rotated through my<br />
Nelsonville <strong>of</strong>fice these past 27 years.<br />
I think that is what I’m going to miss<br />
the most.”<br />
Life after OU-COM “My wife and<br />
I are moving to Asheville, N.C., and<br />
visiting family in Oregon this summer.<br />
We plan to spend 3-6 months each<br />
year—beginning in September—working<br />
in Jerusalem for the humanitarian aid<br />
organization “Vision for Israel.”<br />
36 www.oucom.ohio.edu
June 21 – 24, 2007<br />
<strong>Ohio</strong> <strong>Osteopathic</strong> Association Annual Convention<br />
The Lodge at Sawmill Creek Resort, Sandusky, <strong>Ohio</strong><br />
Alumni Reception: June 21, 2007<br />
5:00 – 7:30 pm, Wolf Room<br />
Recognizing William Emlich, D.O. (’86)President,<br />
<strong>Ohio</strong> <strong>Osteopathic</strong> Association<br />
OU-COM Alumni Board Breakfast Meeting: June 23, 2007<br />
8:00 – 9:30 am, Moose Room<br />
Save the Date<br />
alumni calendar<br />
June 27 – 30, 2007<br />
American Association <strong>of</strong> <strong>College</strong>s <strong>of</strong> <strong>Osteopathic</strong><br />
<strong>Medicine</strong> Annual Meeting<br />
Renaissance Harborplace Hotel, Baltimore, Md.<br />
August 1, 2007<br />
OU-COM 1st Year Classes Begin<br />
August 18, 2007<br />
OU-COM Convocation and White Coat Ceremony<br />
10:00 a.m., Templeton Blackburn Alumni Memorial Auditorium<br />
September 5, 2007<br />
OU-COM 2nd Year Classes Begin<br />
September 30 - October 4, 2007<br />
American <strong>Osteopathic</strong> Association Annual Convention<br />
San Diego Convention Center, San Diego, Calif.<br />
Alumni Lunch & Reception: October 1, 2007<br />
Marriott/Omni<br />
October 12 - 14, 2007<br />
<strong>Ohio</strong> <strong>University</strong> Homecoming & Alumni Awards Ceremony<br />
Recognizing Amelia G. Tunanidas Pantelis, D.O. (’82)<br />
Alumna <strong>of</strong> the Year<br />
October 18 - 21, 2007<br />
Annual OU-COM Reunion/CME and Alumni Awards Program<br />
Hilton Hotel at Easton, Columbus, <strong>Ohio</strong><br />
OU-COM Alumni Board Meeting: October 18, 2007<br />
Center <strong>of</strong> Excellence Reunion: October 19, 2007<br />
Class <strong>of</strong> 1982 25 Year Reunion: October 20, 2007<br />
Hotel Reservations 614.414.5000<br />
October 18 - 21, 2007<br />
2007 Annual Clinical Assembly <strong>of</strong> <strong>Osteopathic</strong> Specialists<br />
San Francisco Marriott, San Francisco, CA<br />
January 18 – 19, 2008<br />
Cleveland Academy <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Winter CME<br />
Embassy Suites, Independence, <strong>Ohio</strong><br />
Alumni Reception, January 18, 2008<br />
Co-sponsored by OU-COM Society <strong>of</strong> Alumni & Friends<br />
February 2008<br />
Cincinnati District Academy <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
Cincinnati, <strong>Ohio</strong><br />
Alumni Reception, Co-sponsored by<br />
OU-COM Society <strong>of</strong> Alumni & Friends<br />
February 2008<br />
Winter OU-COM Alumni Board Meeting<br />
Hilton Hotel, Easton, Columbus, <strong>Ohio</strong><br />
March 12 – 16, 2008<br />
ACOFP 45th Annual Convention<br />
Hyatt Regency, Denver, Colo.<br />
Alumni Recepton, Co-sponsored by<br />
OU-COM Society <strong>of</strong> Alumni & Friends<br />
cme<br />
All Class Reunion<br />
<strong>Ohio</strong> <strong>University</strong> <strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
& Society <strong>of</strong> Alumni and Friends<br />
&<br />
October 19–21, 2007<br />
Hilton at Easton<br />
Columbus, <strong>Ohio</strong><br />
Mark your calendar now for this this weekend <strong>of</strong> exciting medical education programs! You<br />
can earn up to 20 hours <strong>of</strong> CME credit and have the opportunity to meet with many <strong>of</strong> your<br />
colleagues and former classmates as well as members <strong>of</strong> the OU-COM faculty and staff.<br />
Special social events are planned, so call your classmates now and ask them to join<br />
you in Columbus.<br />
Make your reservation now for a special room rate. Call 614.414.5000 or go online at<br />
Hiltoncolumbus.com and enter Code OHU.<br />
Watch your mail for more information.<br />
For additional information, please call:<br />
740.593.4232<br />
Or e-mail:<br />
harmanj@ohio.edu<br />
To register online:<br />
http://www.oucom.ohiou.edu/Alumni/<br />
Sponsored by:<br />
OU-COM Society <strong>of</strong> Alumni & Friends<br />
OU-COM Area Health Education Center
what’s inside?<br />
a p r e v i e w o f t h e s u m m e r / f a l l i s s u e . . .<br />
Capt. Larry Robinson, D.O. (’02),<br />
recounts his experience in Iraq<br />
20<br />
Second-year<br />
24<br />
student Rachel Holt leads<br />
the way in a research paper published<br />
in Diabetes Care.<br />
<strong>College</strong> <strong>of</strong> <strong>Osteopathic</strong> <strong>Medicine</strong><br />
332 Grosvenor Hall<br />
Athens, OH 45701<br />
Non Pr<strong>of</strong>it Org.<br />
U.S. Postage<br />
PAID<br />
Permit No. 100<br />
Athens, OH<br />
ADDRESS SERVICE REQUESTED