Scheingraber S, Richter S, Igna D, Girndt M, Flesch S, Kleinschmidt ...
Scheingraber S, Richter S, Igna D, Girndt M, Flesch S, Kleinschmidt ...
Scheingraber S, Richter S, Igna D, Girndt M, Flesch S, Kleinschmidt ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
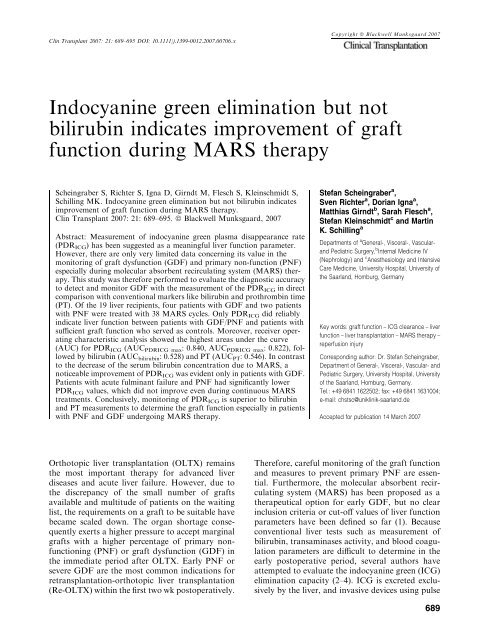
Clin Transplant 2007: 21: 689–695 DOI: 10.1111/j.1399-0012.2007.00706.x<br />
Copyright ª Blackwell Munksgaard 2007<br />
Indocyanine green elimination but not<br />
bilirubin indicates improvement of graft<br />
function during MARS therapy<br />
<strong>Scheingraber</strong> S, <strong>Richter</strong> S, <strong>Igna</strong> D, <strong>Girndt</strong> M, <strong>Flesch</strong> S, <strong>Kleinschmidt</strong> S,<br />
Schilling MK. Indocyanine green elimination but not bilirubin indicates<br />
improvement of graft function during MARS therapy.<br />
Clin Transplant 2007: 21: 689–695. ª Blackwell Munksgaard, 2007<br />
Abstract: Measurement of indocyanine green plasma disappearance rate<br />
(PDR ICG ) has been suggested as a meaningful liver function parameter.<br />
However, there are only very limited data concerning its value in the<br />
monitoring of graft dysfunction (GDF) and primary non-function (PNF)<br />
especially during molecular absorbent recirculating system (MARS) therapy.<br />
This study was therefore performed to evaluate the diagnostic accuracy<br />
to detect and monitor GDF with the measurement of the PDR ICG in direct<br />
comparison with conventional markers like bilirubin and prothrombin time<br />
(PT). Of the 19 liver recipients, four patients with GDF and two patients<br />
with PNF were treated with 38 MARS cycles. Only PDR ICG did reliably<br />
indicate liver function between patients with GDF/PNF and patients with<br />
sufficient graft function who served as controls. Moreover, receiver operating<br />
characteristic analysis showed the highest areas under the curve<br />
(AUC) for PDR ICG (AUC PDRICG max : 0.840, AUC PDRICG max : 0.822), followed<br />
by bilirubin (AUC bilirubin : 0.528) and PT (AUC PT : 0.546). In contrast<br />
to the decrease of the serum bilirubin concentration due to MARS, a<br />
noticeable improvement of PDR ICG was evident only in patients with GDF.<br />
Patients with acute fulminant failure and PNF had significantly lower<br />
PDR ICG values, which did not improve even during continuous MARS<br />
treatments. Conclusively, monitoring of PDR ICG is superior to bilirubin<br />
and PT measurements to determine the graft function especially in patients<br />
with PNF and GDF undergoing MARS therapy.<br />
Stefan <strong>Scheingraber</strong> a ,<br />
Sven <strong>Richter</strong> a , Dorian <strong>Igna</strong> a ,<br />
Matthias <strong>Girndt</strong> b , Sarah <strong>Flesch</strong> a ,<br />
Stefan <strong>Kleinschmidt</strong> c and Martin<br />
K. Schilling a<br />
Departments of a General-, Visceral-, Vascularand<br />
Pediatric Surgery, b Internal Medicine IV<br />
(Nephrology) and c Anesthesiology and Intensive<br />
Care Medicine, University Hospital, University of<br />
the Saarland, Homburg, Germany<br />
Key words: graft function – ICG clearance – liver<br />
function – liver transplantation – MARS therapy –<br />
reperfusion injury<br />
Corresponding author: Dr. Stefan <strong>Scheingraber</strong>,<br />
Department of General-, Visceral-, Vascular- and<br />
Pediatric Surgery, University Hospital, University<br />
of the Saarland, Homburg, Germany.<br />
Tel.: +49 6841 1622502; fax: +49 6841 1631004;<br />
e-mail: chstsc@uniklinik-saarland.de<br />
Accepted for publication 14 March 2007<br />
Orthotopic liver transplantation (OLTX) remains<br />
the most important therapy for advanced liver<br />
diseases and acute liver failure. However, due to<br />
the discrepancy of the small number of grafts<br />
available and multitude of patients on the waiting<br />
list, the requirements on a graft to be suitable have<br />
became scaled down. The organ shortage consequently<br />
exerts a higher pressure to accept marginal<br />
grafts with a higher percentage of primary nonfunctioning<br />
(PNF) or graft dysfunction (GDF) in<br />
the immediate period after OLTX. Early PNF or<br />
severe GDF are the most common indications for<br />
retransplantation-orthotopic liver transplantation<br />
(Re-OLTX) within the first two wk postoperatively.<br />
Therefore, careful monitoring of the graft function<br />
and measures to prevent primary PNF are essential.<br />
Furthermore, the molecular absorbent recirculating<br />
system (MARS) has been proposed as a<br />
therapeutical option for early GDF, but no clear<br />
inclusion criteria or cut-off values of liver function<br />
parameters have been defined so far (1). Because<br />
conventional liver tests such as measurement of<br />
bilirubin, transaminases activity, and blood coagulation<br />
parameters are difficult to determine in the<br />
early postoperative period, several authors have<br />
attempted to evaluate the indocyanine green (ICG)<br />
elimination capacity (2–4). ICG is excreted exclusively<br />
by the liver, and invasive devices using pulse<br />
689
<strong>Scheingraber</strong> et al.<br />
spectrophotometry became available for valid<br />
bedside calculation of ICG plasma disappearance<br />
rate (PDR ICG ) within 10 min (3, 5). It has been<br />
reported that the diminished ICG elimination<br />
reflects the degree of reperfusion injury and would<br />
be a good marker of primary graft function (6). In<br />
addition, ICG-clearance measurements showed a<br />
significant correlation with the severity of preservation<br />
injury, longer intensive care unit, and<br />
hospital stay, prolonged liver dysfunction, and<br />
septic complications (3). To further analyze the<br />
diagnostic accuracy of the ICG-clearance monitoring<br />
we (i) compared the PDR ICG with the<br />
conventional markers bilirubin and prothrombin<br />
time (PT) by calculation of receiver operating<br />
characteristic curves (ROC) and (ii) evaluated the<br />
possible superiority of PDR ICG measurements to<br />
indicate the improvement of liver function during<br />
MARS therapy in patients with PNF or GDF.<br />
Methods<br />
Patients and operative procedure<br />
A total of 19 patients undergoing orthotopic liver<br />
transplantation at the Department of General<br />
Surgery, University Hospital of the Saarland<br />
between June 2002 and April 2006 were entered<br />
in this study. Cadaveric liver grafts were harvested<br />
in cold UW-solution. After recipient hepatectomy,<br />
ABO-identical grafts matched for ratio of physiological<br />
body to liver weight were transplanted by<br />
the standard technique with venovenous bypass in<br />
16 and by the piggyback method in three cases. All<br />
OLTX operations were performed by two surgeons<br />
and the quality of reperfusion was estimated by the<br />
responsible surgeon. Impaired reperfusion was<br />
classified as prolonged discoloration of the grafts,<br />
patchy perfusion defects during reperfusion, and<br />
severe hepatic congestion. Reperfusion injury was<br />
confirmed by evidence of structural injury in the<br />
pre-and post-reperfusion liver biopsy.<br />
Postoperative management<br />
All patients received the same immunosuppressive<br />
regimen consisting of steroids, azathioprin, and<br />
continuous application of cyclosporin. Monitoring<br />
of postoperative infections was performed by daily<br />
determinations of procalcitonin, in addition to<br />
routine parameters such as white blood cell count<br />
and C-reactive protein as well as cultures of blood,<br />
sputum, urine, peritoneal fluid, and bile fluid. The<br />
diagnosis of rejection was made on the basis of<br />
clinical, laboratory and histology findings, and<br />
high-dose methylprednisone (1000 mg/d for three d)<br />
was given whenever acute rejection was suspected.<br />
Vascular complications were screened by frequent<br />
Doppler ultrasonography, followed by angiography<br />
whenever indicated. T-tube was placed routinely<br />
and the bile concentration was determined in<br />
the fluid sampled during 24 h. T-tube cholangiography<br />
was performed in cases with suspected<br />
biliary problems.<br />
ICG measurement and laboratory data<br />
Indocyaninine green plasma disappearance rate<br />
was measured immediately after admission on the<br />
surgical intensive care unit (SICU) and every<br />
morning at 7.00 am during stay on the SICU.<br />
Bilirubin and PT were determined on a daily<br />
clinical routine basis in the laboratory of the<br />
hospital using commercially available kits (Roche<br />
Diagnostics, Mannheim, Germany). PDR ICG was<br />
determined by means of a non-invasive monitor<br />
(LIMON Ò , Pulsion Medical Systems, Munich,<br />
Germany). A bolus of 0.25 mg/kg ICG was<br />
administered via the central venous catheter and<br />
the light absorption at two different wavelengths<br />
(805 and 905 nm) was measured non-invasively by<br />
a finger sensor for 10 min. After bolus administration,<br />
ICG binds to plasma proteins remains in<br />
the vascular compartment and is exclusively<br />
metabolized by the liver without undergoing<br />
enterohepatic circulation. Therefore, the PDR of<br />
ICG equals ICG clearance by the liver and<br />
depends on liver perfusion and hepatocellular<br />
function. Normal PDR ICG values of 18–25%/min<br />
with the Limon system were reported by the<br />
manufacturer.<br />
MARS treatment<br />
Between July 2003 and April 2006, 38 MARS<br />
cycles were performed in seven OLTX patients.<br />
One MARS cycle lasted eight h. One patient with<br />
fulminant liver failure (PT < 10%, encephalopathy<br />
grade 3) after acute hepatitis B infection<br />
received MARS for bridging to high urgent<br />
(HU)-OLTX. The remaining six patients were<br />
treated with MARS after OLTX, two patients<br />
with primary graft non-function [PT < 10% with<br />
continuous need for fresh frozen plasma (FFP),<br />
PDR ICG < 5%/min] as bridging therapy for<br />
HU-OLTX and four patients as support for<br />
GDF. GDF was defined by increased bilirubin<br />
serum concentrations >10 mg/dL or hepatic<br />
encephalopathy grade 2 or more. PNF was<br />
considered as a cause of graft failure only after<br />
excluding rejection and vascular problems.<br />
PDR ICG as well as bilirubin and PT were<br />
690
ICG clearance for graft function monitoring<br />
measured before and after each MARS cycle. All<br />
patients waiting for HU-OLTX required mechanical<br />
ventilation, whereas all other patients were<br />
breathing spontaneously. The decision to stop<br />
MARS therapy in patients with GDF was based<br />
on markers of liver function (hyperbilirubinemia<br />
5%/min). Plasma coagulation<br />
factors were not given when PT was below<br />
40% (normal range 75–140%) unless the patient<br />
was actively bleeding. During MARS dialysis<br />
unfractioned heparin was given continuously<br />
according to determinations of the activated<br />
clotting time in 30–60 min intervals.<br />
Statistics<br />
All variables are presented as mean ± SEM. For<br />
comparison of independent samples, ANOVA<br />
and the Mann–Whitney U-test were used. ROC<br />
curves and the respective AUC (7) were calculated<br />
for the maximum value of bilirubin and<br />
PDR ICG and the minimum value of PT and<br />
PDR ICG during the SICU-stay. The best cut-off<br />
was chosen as the value with optimal sensitivity,<br />
specificity and likelihood ratio. Statistical calculations<br />
were performed with the MedCalc Software<br />
package (MedCalc Ò ; Mariakerke, Belgium)<br />
(8). Values of p < 0.05 were considered significant.<br />
Results<br />
Patients’ characteristics<br />
In Table 1, patientsÕ sex and age, underlying<br />
etiology, hospital stay and graft, and overall<br />
outcome are demonstrated. All but two patients<br />
with multiple organ failure and sepsis survived.<br />
There were four patients with GDF and two<br />
patients with PNF in need for immediate<br />
Re-OLTX. One patient with fulminant liver failure<br />
caused by acute hepatitis B viral infection was<br />
admitted with encephalopathy and severe coagulation<br />
disorder and was listed for HU-OLTX. As<br />
shown in Table 1, seven patients with GDF and<br />
PNF received MARS-therapy. Mean SICU stay in<br />
patients with GDF and PNF was 32 ± 19 d<br />
(13–71 d) compared with 14 ± 8 d (4–34 d) in<br />
patients with a good functioning graft.<br />
Graft reperfusion<br />
Three grafts showed macroscopically insufficient<br />
reperfusion during OLTX with patchy ischemic<br />
zones, incomplete wash out, and a swollen graft<br />
after reperfusion. From these grafts, two (66%)<br />
developed PNF with need for Re-OLTX. Four<br />
other grafts showed moderate reperfusion in terms<br />
of prolonged time of wash out or patchy ischemic<br />
zones. From these, one (25%) graft was apparent<br />
Table 1. Patients’ characteristics<br />
Sex Age (yr) Etiology SICU-stay (d)<br />
MARS cycles<br />
(no. of cycles/days of treatment) Complication Outcome<br />
M 50 Hep. C 14 – Rebleeding Well<br />
F 56 Hep. B/D 13 – acRej, MOV Dead<br />
M 53 Hep. C 71 5/23 MOV, GDF Dead<br />
M 54 Hep. B/D, HCC 4 – None Well<br />
F 53 Hep. C 5 – None Well<br />
M 32 Hep. B, ALF 19 10/4 None (HU-OLTX) Well<br />
M 51 Hep. C, HCC 6 – None Well<br />
F 56 Hep. B/D 30 2/1 PNF [Re-OLTX] Well<br />
M 55 alc. LC 18 – cand. pneu. Well<br />
M 54 M. Wilson, HCC 11 – None Well<br />
F 56 Hep. B 12 – RF Well<br />
M 56 Hep. C, HCC 14 – None Well<br />
M 39 PSC 6 – None Well<br />
M 40 chron. GF 34 6/3 PNF [Re-OLTX] Well<br />
M 44 PSC 16 – PVT, anast. leak Well<br />
M 21 PBC 18 – PVT, acRej Well<br />
M 64 Hemochr., HCC 31 4/7 GDF, RF Well<br />
M 60 Hep. B 22 6/7 GDF, cholangitis Well<br />
M 50 Hep. B/D 23 5/3 GDF Well<br />
Hep., hepatitis; acRej, acute rejection; GDF, graft dysfunction; HCC, hepatocellular carcinoma; ALF, acute liver failure; PNF, primary non-function; HU-OLTX, high urgency<br />
listed orthotopic liver transplantation; Re-OLTX, recurrent orthotopic liver transplantation; alc. LC, alcoholic liver cirrhosis; cand. pneu., candida pneumonia; RF, renal<br />
failure (affording hemodialysis); PSC, primary sclerosing cholangitis; chron. GF, chronical graft failure; PVT, portal vein thrombosis; anast. leak., leakage of biliodigestive<br />
anastomosis; PBC, primary biliary cirrhosis; hemochr., hemochromatosis.<br />
691
<strong>Scheingraber</strong> et al.<br />
for GDF. Remaining 13 grafts showed homogeneous<br />
reperfusion. However, three of these 13 (23%)<br />
grafts developed GDF in the post-OLTX period.<br />
Graft dysfunction<br />
The differences in liver function markers between<br />
patients without GDF compared with patients with<br />
GDF were analyzed for the first seven d after<br />
OLTX (Table 2). During the first three d after<br />
OLTX, PDR ICG values were significantly higher in<br />
the group with sufficient graft function (controls)<br />
compared with graft, which presented with PNF or<br />
developed GDF. Seven d after OLTX the initially<br />
low-PDR ICG values increased markedly in the<br />
PNF/GDF group. In contrast, bilirubin levels were<br />
not significant between both study groups at the<br />
three examined time points nor did show any<br />
significant decrease in during the first week. Paradoxically,<br />
PT values remained significantly lower in<br />
the control group compared with the PNF/GDF<br />
group throughout all examined time points. Moreover,<br />
PT values did significantly increase in the<br />
PNF/GDF group. There were three patients in the<br />
control group with need of FFP (11 U for two<br />
patients, and 4 U for another patient) due to<br />
bleeding problems or marked consumption of<br />
coagulation factors. However, in all these patients<br />
with low PT values and need for FFP there were no<br />
indices for liver dysfunction and the patients course<br />
was well. Interestingly, despite low PT levels (44%,<br />
48%, 55%) the PDR ICG values were only slightly<br />
decreased (13.1%/min, 16.2%/min, 16.5%/min).<br />
As PNF and GDF developed at different time<br />
points, ROC analysis was calculated for the lowest<br />
as well the highest PDR ICG value, the highest<br />
bilirubin value and the lowest PT value during the<br />
first seven d after OLTX (Fig. 1A-D). The AUCs<br />
considering sensitivity as well as specifity showed<br />
significant differences between these three markers<br />
regarding the diagnosis of postoperative GDF. The<br />
highest AUC was found for the highest PDR ICG<br />
value (AUC PDRICG max : 0.840) followed by the<br />
lowest PDR ICG (AUC PDRICG min : 0.822), the AUC<br />
values for bilirubin (AUC bilirubin : 0.528) and for PT<br />
(AUC PT : 0.546). The differences between the AUC<br />
for the highest PDR ICG value and the AUC for<br />
bilirubin or PT were statistically significant (AUC bilirubin<br />
vs. AUCICGmax: p = 0.005; AUC PT vs. AUC<br />
ICGmax: p = 0.002). The optimal PDR ICG cut-off<br />
level with the highest sensitivity and specificity in<br />
the diagnosis of GDF was 10 mg/dL we did not observe a PDR ICG value<br />
>12%/min. On the other hand, at very high<br />
bilirubin levels >25 mg/dL, there were no very<br />
low-PDR ICG values (
A 100<br />
80<br />
Sensitivity<br />
60<br />
40<br />
20<br />
0<br />
B 100<br />
80<br />
Sensitivity<br />
60<br />
40<br />
20<br />
0<br />
C 100<br />
80<br />
Sensitivity<br />
60<br />
40<br />
20<br />
0 20 40 60 80 100<br />
100-Specificity<br />
0 20 40 60 80 100<br />
100-Specificity<br />
ICG clearance for graft function monitoring<br />
the dialysis filters. Patients with GDF received in<br />
median five cycles on 10 d, comprising 28% of the<br />
day, thus one cycle followed by a therapy break of<br />
16 h. MARS treatment caused a significant decrease<br />
of the serum bilirubin concentration from<br />
14.1 ± 1.3 mg/dL before to 10.7 ± 0.7 mg/dL<br />
(p < 0.05) after MARS therapy. The amount of<br />
the bilirubin decrease was correlated with the peak<br />
value of the serum bilirubin (r = 0.90, p < 0.05).<br />
In contrast to the decrease of the serum bilirubin<br />
concentration due to MARS, a noticeable improvement<br />
of PDR ICG was evident only in patients<br />
with GDF but not in patients with bridging<br />
therapy (Fig. 2). Patients with acute fulminant<br />
failure and PNF had significantly lower PDR ICG<br />
values, which did not improve even during continuous<br />
MARS treatments. Accordingly, there was<br />
no need for FFP in patients with GDF, whereas<br />
patients undergoing bridging therapy received<br />
3.6 ± 1.3 U (0–15 U) FFP. The PT values were<br />
significantly higher in the group with GDF<br />
(84.1 ± 2.4% vs. 37.2 ± 3.1%; p < 0.05). In<br />
patients with GDF there was no change in the<br />
PT values after MARS cycles compared to baseline<br />
levels before MARS (88.7 ± 2.6% vs. 84.4 ±<br />
2.5%; p = 0.10). In all patients after OLTX a<br />
T-tube was placed intraoperatively in the common<br />
hepatic bile duct. However, only in patients with<br />
GDF bile was produced and therefore only in this<br />
group the bilirubin concentrations could be analyzed<br />
before and after MARS treatment. We did<br />
not observe any change in the bilirubin concentration<br />
in the bile after any MARS cycles indicating<br />
0<br />
D 100<br />
80<br />
0 20 40 60 80 100<br />
100-Specificity<br />
20.0<br />
17.5<br />
15.0<br />
12.5<br />
10.0<br />
Bilirubin (mg/dL)<br />
PDR ICG (%/min)<br />
#<br />
#<br />
#<br />
Sensitivity<br />
60<br />
40<br />
20<br />
0<br />
0 20 40 60 80 100<br />
100-Specificity<br />
Fig. 1. Receiver operating characteristic curves of the most<br />
pathological post-orthotopic liver transplantation bilirubin<br />
(A), PT (B) the lowest (C) and the highest (D) plasma disappearance<br />
rate (PDR ICG ) values regarding the occurrence of<br />
graft dysfunction.<br />
7.5<br />
5.0<br />
2.5<br />
0.0<br />
Before MARS After MARS Before MARS After MARS<br />
Graft dysfunction<br />
20 cycles in four patients<br />
*<br />
Bridging in non-function<br />
18 cycles in three patients<br />
Fig. 2. Serum bilirubin concentrations and plasma disappearance<br />
rate (PDR ICG ) measured before and after molecular<br />
absorbent recirculating system (MARS) cycles in the group of<br />
patients with graft dysfunction (GDF) and the other group<br />
with graft non-function. Mean ± SEM; * p < 0.05 vs.<br />
patients with GDF, Mann–Whitney U-test;<br />
# p < 0.05 vs.<br />
baseline values, Mann–Whitney U-test.<br />
693
<strong>Scheingraber</strong> et al.<br />
that the hepatic bilirubin excretion did not<br />
improve.<br />
Discussion<br />
Indocyanine green is a synthetic dye that is<br />
eliminated by the liver without extrahepatic metabolism<br />
and excretion; therefore, its blood clearance<br />
depends on the plasma volume, hepatic perfusion,<br />
and the hepatocellular excretion rate. The PDR ICG<br />
has been applied to determine the liver donor<br />
function in liver transplantation. In an animal<br />
study, the PDR ICG decreased significantly after<br />
OLTX and correlated well with hypotensive episodes<br />
and ischemic time during the donor operation<br />
(2). In a clinical study, the PDR ICG measured<br />
just before procurement showed a good correlation<br />
with donor age and with the histologic score of<br />
liver damage (4). In addition, in this study, the<br />
PDR ICG had no relation to PT and transaminases.<br />
Comparing the PDR ICG measured just before<br />
procurement, the postoperative PDR ICG was significantly<br />
higher in accepted compared with discarded<br />
grafts (9). However, two grafts which were<br />
accepted had a PDR ICG < 15%/min and developed<br />
PNF.<br />
The PDR ICG and the clearance of ICG, which<br />
corresponds to the product of the PDR ICG and the<br />
volume of distribution of the dye, were measured<br />
in nine patients undergoing OLTX (10). The<br />
PDR ICG was at pathological low values before<br />
OLTX and diminished further during the anhepatic<br />
phase. Immediately after reperfusion the PDR ICG<br />
increased to almost normal values and showed a<br />
slight decrease 24 h after OLTX. However, the<br />
PDR ICG 24 h after OLTX was markedly higher<br />
than baseline levels before OLTX. As the plasma<br />
volume was increased at baseline and remained<br />
increased during surgery, the PDR ICG values tended<br />
to be relatively lower than the ICG-clearance values.<br />
However, the perioperative pattern and time course<br />
of the PDR ICG was very similar to that of the ICG<br />
clearance and thus the authors concluded that it<br />
seems justified to use the PDR ICG , which is<br />
independent of the amount of ICG administered.<br />
Another topic was the technique of how the PDR ICG<br />
should be measured, as a non-invasive finger probe<br />
has become available for routine clinical monitoring.<br />
It has been shown in several studies that the<br />
non-invasive transcutaneous pulse-densitometric<br />
method correlates well with the invasive aortic<br />
fiber-optic or with the conventional invasive ICG<br />
clearance test with the spectophotometric analyses<br />
of multiple blood samples (3, 11–13).<br />
In addition to the methodological considerations<br />
concerning the measurement of the PDR ICG , some<br />
studies focused on the role of PDR ICG as a test of<br />
graft function in the early post-OLTX period. In a<br />
multivariate analysis of the PDR ICG and other liver<br />
function tests with regard to the clinical outcome<br />
after 50 OLTX, a low-PDR ICG especially on POD 1<br />
after OLTX was closely correlated with the severity<br />
of preservation injury prolonged liver dysfunction,<br />
septic complications, a longer SICU and hospital<br />
stay (3). The finding that a low-PDR ICG reflects<br />
perfusion injury and that the PDR ICG measured<br />
24 h after OLTX is therefore an early predictor of<br />
graft function was also confirmed by another group<br />
(6). However, no study so far has reported a precise<br />
characterization of the diagnostic accuracy of<br />
PDR ICG as well as bilirubin and PT by calculating<br />
ROC curves. In this study, all three examined<br />
markers were significantly different between grafts<br />
with sufficient function and grafts with dysfunction.<br />
However, by calculating the AUC in ROC curves,<br />
we found the highest AUC for PDR ICG to detect<br />
GDF. Although levels >10 mg/dL of bilirubin<br />
were used to define GDF, and therefore bilirubin<br />
was part of the outcome criteria for the ROC<br />
analysis, the AUC for bilirubin was lower compared<br />
with the AUC of PDR ICG . The disadvantage<br />
of bilirubin might be its relatively long half-life. The<br />
relatively low AUC of PT can be explained by the<br />
fact that it is largely affected by bleeding episodes as<br />
well as the administration of FFPs. Especially in<br />
the initial phase, immediately after OLTX, we<br />
found in this study that interpretations of PT values<br />
can be very misleading and low-PT values can be<br />
associated with relatively normal PDR ICG values.<br />
Thus, the major advantage of PDR ICG compared<br />
with bilirubin and PT is that this marker shows<br />
marked differences even at the range of normal<br />
bilirubin and PT values.<br />
In this study, PNF and GDF were treated with<br />
MARS therapy. As there was no increase in the<br />
low-PDR ICG of the non-function group the efficacy<br />
of MARS in fulminant liver failure besides detoxification<br />
remains questionable. In contrast, the<br />
significant improvement in the PDR ICG of patients<br />
with GDF group favors our concept of MARS in<br />
post-OLTX GDF. Nevertheless, in this group,<br />
MARS could not improve bilirubin excretion as no<br />
significant changes of the bilirubin concentrations<br />
were detected in the collected bile. As the serum<br />
bilirubin concentration is lowered by the MARS<br />
treatment itself, the PDR ICG is obviously a better<br />
marker for monitoring of liver function during<br />
MARS therapy.<br />
As ICG is an organic anion like bilirubin, its<br />
hepatic uptake at the basolateral membrane of the<br />
hepatocyte is probably mediated by the same<br />
transport proteins (14). Therefore, lowering the<br />
694
ICG clearance for graft function monitoring<br />
serum bilirubin concentration due to MARS can<br />
increase the number of binding sites of the<br />
hepatocellular uptake. However, as this process is<br />
ATP-dependent (15), extensively damaged livers<br />
are unable for ICG-uptake resulting in a low<br />
PDR ICG . Conclusively, monitoring of PDR ICG is<br />
superior than bilirubin and PT measurements to<br />
determine the graft function especially in patients<br />
with PNF and GDF undergoing MARS therapy.<br />
Acknowledgement<br />
The authors wish to thank Bettina Rau, MD (Department<br />
General Surgery, University Hospital of the Saarland) for<br />
her assistance in calculation the ROC.<br />
References<br />
1. Hetz H, Faybik P, Berlakovich G et al. Molecular<br />
absorbent recirculating system in patients with early allograft<br />
dysfunction after liver transplantation: a pilot study.<br />
Liver Transpl 2006: 12: 1357.<br />
2. Jamanaka N, Okamoto E, Kato T et al. Usefulness of<br />
monitoring the ICG retention rate as an early indicator of<br />
allograft function in liver transplantation. Transpl Proc<br />
1992: 24: 1614.<br />
3. Tsubono T, Todo S, Jabbour N et al. Indocyanine green<br />
elimination test in orthotopic liver recipients. Hepatology<br />
1996: 24: 1165.<br />
4. Koneru B, Leevy C, Klein K, Zweil P, Wilson D. Indocyanine<br />
green clearance in the evaluation of donor livers.<br />
Transpl Proc 1993: 25: 1919.<br />
5. Faybik P, Krenn C, Baker A et al. Comparison of<br />
invasive and non-invasive measurement of plasma disappearance<br />
rate of indocyanine green in patients undergoing<br />
liver transplantation: a prospective investigator-blinded<br />
study. Liver Transpl 2004: 10: 1060.<br />
6. Pelvris J, Jalan R, Bzeizi K et al. Indocyanine green<br />
clearance reflects reperfusion injury following liver transplantation<br />
and is an early predictor of graft function.<br />
J Hepatol 1999: 30: 142.<br />
7. Beck J, Schultz E. The use of relative operating characteristic<br />
(ROC) curves in test performance evaluation.<br />
Arch Pathol Lab Med 1986: 110: 13.<br />
8. Schoonjans F, Zalata A, Depuydt C, Comhaire F.<br />
MedCalc: a new computer program for medical statistics.<br />
Comp Meth Prog Biomed 1995: 48: 257.<br />
9. Wesslau C, Krüger R, May G. Clinical investigations<br />
using indocyanine green clearance for evaluation of liver<br />
function in organ donors. Transplantology 1994: 5: 7.<br />
10. Von Spiegel T, Scholz M, Witasch G et al. Perioperative<br />
monitoring of indocyanine green clearance and plasma<br />
disappearance rat in patients undergoing liver transplantation.<br />
Anaesthesist 2002: 51: 359.<br />
11. Imai T, Takahashi K, Goto F, Morishita Y. Measurement<br />
of blood concentration of indocyanine green by pulse<br />
dye densitometry – comparison with the conventional<br />
spectrophotometric method. J Clin Monit Comput 1998:<br />
14: 477.<br />
12. Sakka SG, Reinhart K, Meier-Hellmann A. Comparison<br />
of invasive and non-invasive measurements of indocyanine<br />
green plasma disappearance rate in critically ill<br />
patients with mechanical ventilation and stable hemodynamics.<br />
Intensive Care Med 2000: 26: 1553.<br />
13. Hsieh C, Chen C, Chen T et al. Accuracy of indocyanine<br />
green pulse spectrophotometry clearance test for liver<br />
function prediction in transplanted patients. World J<br />
Gastroenterol 2004: 10: 2394.<br />
14. Keppler D, König J. Hepatic secretion of conjugated<br />
drugs and endogenous substances. Semin Liver Dis 2000:<br />
20: 265.<br />
15. Chijiiwa K, Mizuta A, Ueda J et al. Relation of biliary<br />
bile acid output to hepatic adenosine triphosphate level<br />
and biliary indocyanine green excretion in humans. World<br />
J Surg 2002: 26: 457.<br />
695