Mayo Alumni Magazine 2011 Fall - MC4409-0811 - Mayo Clinic
Mayo Alumni Magazine 2011 Fall - MC4409-0811 - Mayo Clinic
Mayo Alumni Magazine 2011 Fall - MC4409-0811 - Mayo Clinic
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Mayo</strong> <strong>Alumni</strong><br />
mayo.edu/alumni | <strong>Fall</strong> <strong>2011</strong><br />
HAITI
<strong>Mayo</strong> <strong>Alumni</strong><br />
<strong>Fall</strong> <strong>2011</strong><br />
Features<br />
2 Helping Haiti<br />
<strong>Mayo</strong> <strong>Clinic</strong>, working with a proven partner, has provided additional resources<br />
to assist with ongoing recovery efforts at a medical center in Port-au-Prince,<br />
Haiti. <strong>Mayo</strong> physician team members share their experiences.<br />
8 An American doctor in Fukushima<br />
<strong>Mayo</strong> <strong>Clinic</strong> alumnus Kenneth Nollet, M.D., Ph.D., provides a bird’s-eye<br />
view of Japan in the aftermath of the March disaster.<br />
14 Government relations update<br />
Patricia Simmons, M.D., medical director of Government Relations,<br />
discusses her new role, and <strong>Mayo</strong> <strong>Clinic</strong> outlines this division’s priorities<br />
for relations with the federal government.<br />
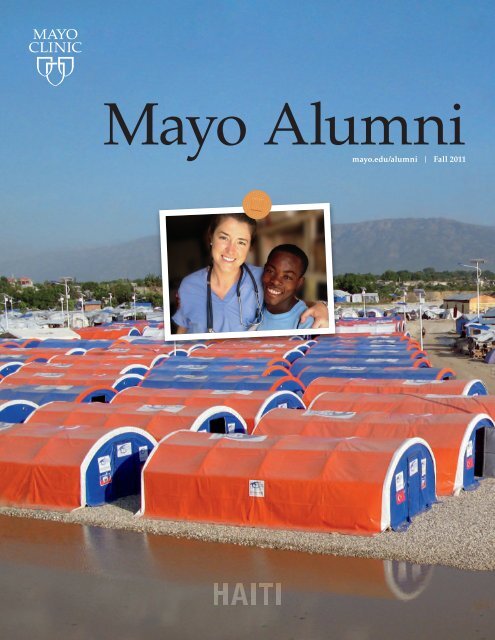
About the Cover<br />
Second-year <strong>Mayo</strong> <strong>Clinic</strong> resident<br />
Casandra Rosenberg, M.D. [inset photo,<br />
cover], who hails from St. Catharines,<br />
Ontario, Canada, was a first-time<br />
volunteer participating in <strong>Mayo</strong>’s efforts<br />
in Port-au-Prince, Haiti. She is pictured<br />
with an interpreter at St. Damien’s<br />
Hospital who hopes to continue his<br />
education and become a nurse.<br />
Dr. Rosenberg was humbled by the<br />
dedication of the Haitian staff and the<br />
conditions in which many staff and<br />
patients live. “We returned to a guesthouse<br />
each night after working, but some<br />
of the local hospital staff went home to<br />
tent cities,” she says. “Many patients<br />
also live in tent cities, without running<br />
water and electricity.” According to<br />
published reports, hundreds of thousands<br />
of Haitians live in thousands of tent<br />
cities near Port-au-Prince alone.<br />
Dr. Rosenberg kept a blog,<br />
www.handsoninhaiti<strong>2011</strong>.blogspot.com.<br />
“I want to share my story to help other<br />
first-time volunteers in underserved health<br />
care to feel more comfortable with the<br />
process,” she says.<br />
18 Learning from the ancient Greeks<br />
<strong>Mayo</strong> alumni and staff who attended the International CME Conference<br />
reflect on their visit to the ancient healing community of Epidaurus in Greece.<br />
<strong>Mayo</strong> Update<br />
20 New Arizona CEO, named professors, obituaries<br />
Recognize the exceptional<br />
It’s time to nominate fellow alumni with exceptional contributions<br />
to the field of medicine for the Distinguished <strong>Alumni</strong> Award.<br />
Information about the award is available at:<br />
http://www.mayo.edu/alumni/awards-distinguished.html<br />
An alumnus or alumna can nominate one candidate each year.<br />
Who do you think deserves this recognition?<br />
Nominations are due April 6, 2012.
A Letter from the Secretary-Treasurer<br />
I<br />
participated in the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association biennial international<br />
meeting in Greece in May. These meetings continue to surprise me in the<br />
high-quality presentations and enthusiastic, engaged attendees. The international<br />
meetings are among the few where a diverse group of <strong>Mayo</strong> staff provides a<br />
CME program in a setting with the opportunity to develop new relationships<br />
with colleagues and reconnect with alumni. Connecting and reconnecting in<br />
an unpressured environment is especially important to me, in the context of a<br />
fast-paced life in a busy academic medical center.<br />
As I connect with others who trained at <strong>Mayo</strong> or were or are on the <strong>Mayo</strong><br />
staff, I am continually reminded of the organization’s unique values — respect,<br />
compassion, integrity, healing, teamwork, excellence, innovation and stewardship.<br />
<strong>Alumni</strong> refer to these values in anecdotes about their past and in accounts about<br />
how they mirror these values in the institutions and practices they represent today.<br />
It’s heartwarming to learn how well regarded and enduring our founding values are.<br />
Two stories in this issue are representative of the <strong>Mayo</strong> <strong>Clinic</strong> values. <strong>Mayo</strong>’s<br />
recent efforts in Haiti (page 2) epitomize compassion, teamwork and healing.<br />
And Dr. Ken Nollet’s report of activities at Fukushima Medical University after<br />
the earthquake and tsunami (page 8 ) reflects the compassion, respect, integrity<br />
and healing honed, at least in part, during his 13 years at <strong>Mayo</strong> <strong>Clinic</strong>.<br />
As you read these stories, I hope you will take an opportunity to reflect on<br />
how these values may be applied in your work.<br />
Eric Edell, M.D.<br />
Secretary-Treasurer<br />
<strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association<br />
Be part of Innovation Into Action<br />
The <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association biennial meeting, Sept. 21–24 in Ponte Vedra Beach, Fla.,<br />
has a program packed with exciting and dynamic presentations on how innovation is<br />
changing the way we deliver health care. Speakers and panels will address issues such as<br />
research advances, health care delivery systems, accountable care organizations, knowledge<br />
management, social media and regenerative medicine.<br />
The <strong>Alumni</strong> Association will be reporting throughout the event on our interactive<br />
<strong>Alumni</strong> Blog: http://alumniblog.mayo.edu/.<br />
Visit the blog for overviews of the presentations, video interviews with speakers and<br />
participants, and a special sneak peek of the brand-new digital version of <strong>Mayo</strong> <strong>Alumni</strong>.<br />
Check out what’s happening at the meeting and join the conversation.
Helping after<br />
has faded from the headlines<br />
2 <strong>Mayo</strong> <strong>Alumni</strong>
The January 2010 earthquake in Haiti triggered a financial<br />
response from <strong>Mayo</strong> <strong>Clinic</strong> through its Disaster Relief<br />
Committee and an outpouring of support from physicians,<br />
faculty and staff members, including volunteerism and<br />
requests for leadership to do even more. When the disaster<br />
faded from the headlines, <strong>Mayo</strong> <strong>Clinic</strong> committed additional<br />
resources to assist with ongoing recovery.<br />
From February through May <strong>2011</strong>, almost 100 staff<br />
members representing all three <strong>Mayo</strong> <strong>Clinic</strong> sites and<br />
<strong>Mayo</strong> <strong>Clinic</strong> Health System provided patient care in Haiti.<br />
This project has been a combined effort by the <strong>Mayo</strong><br />
<strong>Clinic</strong> Disaster Relief Steering Committee, Emergency<br />
Preparedness Subcommittee, and Department of Medicine<br />
Program in Underserved Global Health (PUGH).<br />
“<strong>Mayo</strong> <strong>Clinic</strong>’s Disaster Relief Committee is focused on<br />
responding appropriately to disasters around the world and<br />
working with nongovernmental organizations to provide<br />
assistance for efforts that are sustainable,” says J. Christopher<br />
Farmer, M.D., chair of the <strong>Mayo</strong> <strong>Clinic</strong> Emergency Preparedness<br />
Subcommittee and a consultant in the Division of Pulmonary<br />
and Critical Care Medicine in Rochester. “We evaluate the<br />
nature of our response based on severity and location of the<br />
situation, fit with <strong>Mayo</strong>’s competencies and our ability to<br />
respond. Global health issues and disaster relief are a basic<br />
societal responsibility of health care organizations and,<br />
increasingly, we are engaged in these types of local, regional,<br />
national and international activities.”<br />
PUGH provides a coordinated and longitudinal program<br />
to address clinical and academic disparities in underserved<br />
health care — both when disasters have occurred and when<br />
they have not.<br />
“PUGH focuses on enhancing the quality and sustainability<br />
of health care delivery through on-site provider<br />
training, local community education and increasing health<br />
care availability in select locations lacking providers,” says<br />
John Wilson, M.D., PUGH chair and a consultant in the<br />
Division of Infectious Diseases at <strong>Mayo</strong> <strong>Clinic</strong> in Rochester.<br />
LEFT: Robin Georgeff, a registered nurse in <strong>Clinic</strong>al<br />
Informatics Support at <strong>Mayo</strong> <strong>Clinic</strong> in Arizona, bonded with<br />
Haitian youngsters while volunteering in Port-au-Prince.<br />
ABOVE RIGHT: Many patients and hospital employees live in<br />
tent cities, such as this one near Port-au-Prince. These areas<br />
lack running water and refrigeration.<br />
“<br />
In our response to Hurricane Katrina, <strong>Mayo</strong> learned<br />
the importance of partnering with other organizations<br />
in disaster relief. We’re using that lesson in our<br />
Haiti and future responses.”<br />
J. Christopher Farmer, M.D., chair, <strong>Mayo</strong> <strong>Clinic</strong><br />
Emergency Preparedness Subcommittee<br />
After making initial financial contributions, <strong>Mayo</strong> <strong>Clinic</strong><br />
took time to calculate planning, partnerships, logistics, team<br />
composition and specialty services for its Haiti involvement.<br />
“We very much believe that it’s critical to have relationships<br />
and to team with organizations in the areas affected by<br />
complex humanitarian emergencies,” says Robert Joyce,<br />
operations administrator and incident commander for the<br />
Haiti efforts. “We didn’t want to send in teams without being<br />
able to ensure their safety and efficacy. By choosing the right<br />
organization to partner with, we enabled our teams to focus<br />
on patient care and provider education, without having to<br />
worry about where to eat and sleep and other logistics.”<br />
In May and September 2010, individuals from <strong>Mayo</strong><br />
<strong>Clinic</strong> traveled to Haiti to assess the situation on the ground<br />
and advise about the organization’s response.<br />
The assessors recommended collaborating with Operation<br />
Blessing International, a nonprofit humanitarian organization,<br />
at St. Damien’s Hospital Center in Port-au-Prince. PUGH<br />
<strong>Fall</strong> <strong>2011</strong> 3
ABOVE: David Rushlow, M.D. (left), <strong>Mayo</strong> <strong>Clinic</strong> Health System,<br />
Franciscan Healthcare (La Crosse), treats a patient.<br />
AT LEFT: David Claypool, M.D. (right), Emergency Medicine,<br />
Rochester, treats a patient as Haitian providers assist.<br />
has worked with Operation Blessing on joint projects in<br />
El Salvador and Honduras.<br />
St. Damien’s leadership requested a rotation of small<br />
medical/surgical teams to assist with patient care. The<br />
St. Damien’s Hospital Center includes three hospitals —<br />
St. Damien’s Hospital, a 120-bed pediatric hospital providing<br />
care in pediatrics, maternal health and obstetrics; St. Luc’s<br />
Adult Field Hospital, a 40-bed facility providing medical<br />
care; and St. Philomena Rehydration Center, which provides<br />
“<br />
We would like to generate protocols and models of care<br />
appropriate to the resources, customs and diseases in<br />
Haiti, and to develop systems for virtual consultations,<br />
nursing training, skill set curricula development and<br />
health education material provision.”<br />
John Wilson, M.D., PUGH chair, Division of<br />
Infectious Diseases, <strong>Mayo</strong> <strong>Clinic</strong><br />
care for patients with cholera and has an emergency trauma<br />
and acute care center.<br />
Eight <strong>Mayo</strong> teams, comprised of 10 to 13 members, rotated<br />
for a week at a time, every other week, for four months. They<br />
provided general emergency medicine, acute medicine and<br />
trauma care, and bedside training and educational lectures<br />
for Haitian providers. The groups had a tag-team approach,<br />
in which each returning team shared its insights and experiences<br />
with the team on deck to go. This helped to ensure that<br />
teams were as prepared as possible for a dynamic situation.<br />
“The St. Luc’s facility was very busy and understaffed,”<br />
says Walter Franz III, M.D., a member of the <strong>Mayo</strong> <strong>Clinic</strong><br />
Disaster Relief Committee and PUGH, and a consultant in<br />
the Department of Family Medicine in Rochester. “I believe<br />
we helped to augment the level of care and the number of<br />
patients who could be seen. Our Haitian colleagues had been<br />
doing an outstanding job before we arrived and will continue<br />
to do so after our mission is complete. They were very<br />
appreciative of our assistance and information sharing, and<br />
we were eager to learn from them.”<br />
Dr. Franz and other team members were housed at a<br />
guesthouse run by Operation Blessing in Port-au-Prince.<br />
<strong>Mayo</strong> <strong>Clinic</strong> supported teams by paying for air and ground<br />
transportation, lodging and food. Team members donated<br />
their trip and vacation time.<br />
4 <strong>Mayo</strong> <strong>Alumni</strong>
Drs. Wilson and Franz hope the efforts in Haiti<br />
will continue with institutionally supported training<br />
and education. “We envision a continued close working<br />
relationship with St. Damien’s Hospital Center to enhance<br />
health care education and training, and provide a secure<br />
forum for ongoing staff volunteerism,” says Dr. Wilson.<br />
“The relationships we’ve developed with administrators,<br />
providers and nongovernmental organizations can<br />
facilitate ongoing efforts to most effectively use the vast<br />
clinical experiences and medical knowledge at <strong>Mayo</strong> <strong>Clinic</strong><br />
to continue to provide a supporting role for St. Damien’s,<br />
even from a long distance.”<br />
Dr. Farmer, an assessor in 2010 and a care provider team<br />
member in March <strong>2011</strong>, says the scope and magnitude of<br />
poverty and suffering in Haiti in particular and in underdeveloped<br />
countries in general means fixing the problems is an<br />
insurmountable endeavor. “Helping people is not the same as<br />
solving problems,” he says. “We can go and do our best to touch<br />
and help some people,” he says. “We do what we can. Mother<br />
Teresa said, ‘If you can’t feed 100 people, then just feed one.’”<br />
‘They’ve made remarkable progress’<br />
Like his physician colleagues, Walter Franz III, M.D., a member<br />
of the <strong>Mayo</strong> <strong>Clinic</strong> Disaster Relief Committee and PUGH,<br />
and a consultant in the Department of Family Medicine at<br />
<strong>Mayo</strong> <strong>Clinic</strong> in Rochester, brings much-needed clinical skills<br />
to less-developed parts of the world, including Haiti. He also<br />
brings significant organizational skills. He has 20 years of<br />
Army experience, including four overseas deployments<br />
— three to Iraq. He has served as commander of a forward<br />
trauma team; chief of staff of a field hospital; and civil affairs<br />
officer, going into Iraqi medical facilities to redevelop<br />
and reconstruct medical systems.<br />
“I use my military and civilian [nongovernmental organization]<br />
experiences and help to organize initiatives such as this<br />
one so they are as productive as possible, with systems and<br />
safety in order in a short period of time,” says Dr. Franz. “Haiti<br />
was in rough shape before the earthquake and is even more so<br />
now. The scope of needs is tremendous. There’s a unique oppor-<br />
tunity to reinitiate things for the betterment of the country, and<br />
to help with reconstruction and establishment of protocols to<br />
“<br />
help our Haitian colleagues improve their health care system<br />
using their tremendous clinical experience and energy.”<br />
Dr. Franz visited Haiti in early May. He’d been with the<br />
first <strong>Mayo</strong> team deployed in February, and had volunteered<br />
with <strong>Mayo</strong> colleagues three other times in the last 15 years.<br />
On his most recent trip, he reviewed progress at<br />
St. Damien’s Hospital. “They have hired additional physicians<br />
they astutely diagnose patients at the bedside.<br />
and developed a nursing cadre, and are expanding services<br />
These experiences are priceless.”<br />
to address changing patient care needs,” says Dr. Franz.<br />
“They’ve made remarkable progress since February.”<br />
Walter Franz III, M.D., <strong>Mayo</strong> <strong>Clinic</strong> Disaster Relief Committee and PUGH<br />
It strikes me how much clinicians in other parts of the<br />
world do without the resources we are accustomed to.<br />
In the absence of sophisticated equipment and testing,<br />
<strong>Fall</strong> <strong>2011</strong> 5
‘I’m optimistic it’s the start of something really good’<br />
Ritu Banerjee, M.D., Ph.D., was part of a team of 11 <strong>Mayo</strong><br />
physicians, physician assistants and nurses who served in<br />
Haiti for a week in late April <strong>2011</strong>. Dr. Banerjee, a consultant<br />
in the Division of Pediatric Infectious Diseases, joined the<br />
staff at <strong>Mayo</strong> <strong>Clinic</strong> in Rochester in 2009 and is interested in<br />
international health. “I’ve had a lot of privilege and education<br />
in the United States and wanted to take this opportunity to<br />
share my clinical skills to help people in need,” she says.<br />
Dr. Banerjee and her colleagues worked eight-hour shifts<br />
in the emergency room at St. Luc’s Hospital. Patients had<br />
conditions such as hypertension, stroke, trauma, diabetes,<br />
rheumatic heart disease, tuberculosis, HIV, cholera, malaria,<br />
asthma and sexually transmitted diseases.<br />
“It was sobering to see such severe manifestations<br />
of chronic disease — young people with terrible cerebral<br />
hemorrhages due to hypertension, very young women with<br />
advanced heart failure, diseases such as rheumatic fever<br />
that we no longer see in the United States, and a cholera<br />
epidemic,” says Dr. Banerjee. “The pathology and poverty<br />
is overwhelming.”<br />
The <strong>Mayo</strong> team treated patients and instructed Haitian<br />
providers at the bedside and in formal teaching sessions.<br />
“They seemed very receptive to our teaching and<br />
suggestions,” says Dr. Banerjee. “We talked to the physicians<br />
there about managing diabetes, managing pain and isolating<br />
patients with tuberculosis. In turn, they taught us about<br />
treating malaria.<br />
“The clinical needs in Haiti are huge. Little by little,<br />
we can make a difference. This partnership is in its<br />
infancy, but it has great potential to be a long-standing,<br />
sustainable relationship. I’m optimistic it’s the start of<br />
something really good.”<br />
ABOVE: Among the <strong>Mayo</strong> team members volunteering in Haiti in<br />
late April were (from left) Ritu Banerjee, M.D., Ph.D., Pediatric<br />
Infectious Diseases, Rochester; Lester Kiemele, certified physician<br />
assistant, Gonda Vascular Center, Rochester; and Robin Georgeff,<br />
registered nurse, <strong>Clinic</strong>al Informatics Support, Arizona.<br />
“<br />
On our last day, we attended a church service that<br />
honored two patients who had died. In broken English<br />
and despite his grief, a man spoke about his father and<br />
thanked us for coming to his country to provide care.<br />
It was a powerful moment and put the care we<br />
provided in a more personal context.”<br />
Ritu Banerjee, M.D., Ph.D., Division of Pediatric<br />
Infectious Diseases, <strong>Mayo</strong> <strong>Clinic</strong> Rochester<br />
6 <strong>Mayo</strong> <strong>Alumni</strong>
‘Winging it was challenging<br />
but exhilarating’<br />
While the conditions at St. Damien’s Hospital were far<br />
different from those at <strong>Mayo</strong> <strong>Clinic</strong>, second-year resident<br />
Casandra Rosenberg, M.D., found similarities among patients.<br />
“We saw all types of patient personalities and family dynamics<br />
just like we see at <strong>Mayo</strong>,” she says. “Because staff members’<br />
time is stretched so thin, involvement of family members in<br />
patients’ care is important. They provide food and water, do<br />
laundry and even alert staff about changes in a patient’s status.<br />
Everyone pitches in to help everyone else in the hospital.”<br />
Dr. Rosenberg, who is from St. Catharines, Ontario,<br />
Canada, speaks French, which assisted in communication<br />
with some patients. But many patients speak Creole, and<br />
many are illiterate. “Communication was a challenge in<br />
those cases,” she says. “I had a patient who we suspected<br />
had mitral stenosis. We treated her dyspnea and abdominal<br />
discomfort, and I wanted to explain to her what we’d<br />
done and how she should manage the condition at home.<br />
I drew a picture and described the path of blood past<br />
several ‘doors,’ or valves. If one door was hard to open, the<br />
rooms behind it would get full — like her lungs and belly.<br />
To describe stenosis, I grabbed two drinking straws and<br />
blew air through one to demonstrate the normal heart. To<br />
show stenosis, I squeezed the other in the middle, making<br />
it hard to puff air through. This experience reinforced<br />
how important communication with patients is, even if<br />
it is a hand gesture or a caring smile. This has definitely<br />
carried over into my practice back home.”<br />
Dr. Rosenberg is specializing in physical medicine and<br />
rehabilitation and was able to put her training to use. Patients<br />
use donated prosthetic limbs, which do not fit properly. “I<br />
worked with the Haitian nurses and the resources they had,<br />
such as wrap elastic bandages, to make the prostheses fit<br />
better,” says Dr. Rosenberg. “We brainstormed about how to<br />
prevent pressure sores in stroke patients. The hospital doesn’t<br />
have padding like we use. They fill hospital gloves with water<br />
and position them beneath patients to alleviate pressure. It<br />
was valuable to learn to think in different ways when we did<br />
not have every tool at our disposal.<br />
“It’s impressive how much Haitians are doing to improve<br />
their health care system. During the week I was there, a new<br />
building went up on the St. Damien’s campus. Vision translated<br />
to reality very quickly, with everything done by hand.<br />
“<br />
Nurses at the hospital worked 12-hour shifts, then<br />
some returned home to tents, without running water<br />
or electricity. Their strength and resourcefulness is<br />
truly courageous and humbling.”<br />
Casandra Rosenberg, M.D., resident, <strong>Mayo</strong> <strong>Clinic</strong> Rochester<br />
Patients’ family members brought buckets of water to the<br />
construction workers. The progress was amazing to see.”<br />
Initially, Dr. Rosenberg says she was nervous about<br />
having limited medical resources. “We had a patient with a<br />
rapid heart rate whose blood pressure was dropping, with<br />
signs of poor perfusion,” she says. “We needed to slow the<br />
heart rate, but we didn’t have an EKG or echocardiogram<br />
to diagnose the type of heart failure. We gave the patient a<br />
beta-blocker and observed with a pulse monitor and blood<br />
pressure cuff. The patient did well and the perfusion slowed.<br />
At <strong>Mayo</strong>, I’d have requested a cardiology consultation, the<br />
patient would have been monitored by nurses around the<br />
clock and we’d have had the luxury of various medications.<br />
Winging it was challenging, but it was exhilarating to learn<br />
to work with the available knowledge and resources.”<br />
<strong>Fall</strong> <strong>2011</strong> 7
8 <strong>Mayo</strong> <strong>Alumni</strong>
An American Doctor in Fukushima<br />
A bird’s-eye view of<br />
JApAn’s disAster AftermAth<br />
T<br />
he world rocked, tumbled and shook while<br />
Kenneth Nollet, M.D., Ph.D. (MMS ’93, BIOC<br />
’93, PATH ’97, TRMED ’98), and a colleague<br />
struggled to remain standing. The two moved from<br />
offices on the top floor of a research facility at<br />
Fukushima Medical University (FMU) in Fukushima<br />
City, Japan, to a hallway when the magnitude 9.0<br />
earthquake hit at 2:46 p.m. on March 11.<br />
FMU gave priority to severely injured patients<br />
and those directly affected by the earthquake<br />
and its aftermath. Patients arrived from inside<br />
and outside Fukushima Prefecture in buses,<br />
ambulances and medical evacuation helicopters.<br />
The medical center saw 28 life-threatening injuries,<br />
86 minor injuries and one fatality.<br />
Regularly scheduled bedside learning rotations<br />
and lectures for medical students were disbanded<br />
so that student volunteers and their faculty<br />
mentors could devote themselves to emergency<br />
care. Students not directly involved in FMU’s<br />
efforts attended to family and community needs.<br />
Within 48 hours of the disaster, Dr. Nollet<br />
started a blog, “An American Doctor in Fukushima”<br />
(http://cbbstoday.org/nollet_fukushima.php), to<br />
spur thinking about “this kind of event happening<br />
in your own backyard and redoubling institutional<br />
and personal preparedness initiatives.” The blog<br />
was published on the website of the California<br />
Blood Bank Society with which Dr. Nollet was<br />
involved as co-chair of its Emergency Planning<br />
Committee in 2003.<br />
“Helen Keller said, ‘Character cannot be developed<br />
in ease and quiet. Only through experience<br />
of trial and suffering can the soul be strengthened,<br />
ambition inspired and success achieved,’” says<br />
Dr. Nollet. “ We are all stronger as a result of this<br />
trial, but not as individuals. Strength in Japan is a<br />
collective attribute. The gossamer threads of interpersonal<br />
relationships, woven at FMU and in the<br />
community, held fast. Threads tested become<br />
threads trusted.”<br />
Dr. Nollet, a transfusion medicine specialist,<br />
is a specially appointed professor at FMU in the<br />
Division of Blood Transfusion and Transplantation<br />
Immunology. He joined Fukushima Medical<br />
University in 2008 and hopes to stay in Japan,<br />
noting that 13 years of practicing teamwork at<br />
<strong>Mayo</strong> <strong>Clinic</strong> helped to prepare him for life and<br />
work in Japan. “I would like to earn the right<br />
of permanent residency by mastering Japanese<br />
and making meaningful contributions to society,”<br />
he says. “Japan feels like home.”<br />
<strong>Fall</strong> <strong>2011</strong> 9
<strong>Mayo</strong> <strong>Alumni</strong> shares excerpts from Dr. Nollet’s blog throughout<br />
the days and weeks after the disaster.<br />
March 13<br />
Friday afternoon, March 11, buildings at Fukushima Medical<br />
University shook long and hard, and aftershocks continue.<br />
Fukushima City is not close to the eponymous nuclear plant,<br />
and we are inland from Sendai. No tsunami here, but no<br />
running water either. Electricity is OK, and I queued to fill<br />
some jugs from a water truck that came to the neighborhood.<br />
That took more than an hour, but this is Japan and people<br />
passed the time in friendly, quiet conversation. The medical<br />
center itself normally uses around 150 tons of water per day.<br />
Reserves fell below 500 tons over the weekend. A water<br />
rationing protocol started; laboratory procedures are being<br />
modified as much as possible, and employees have been<br />
asked to use chemical toilets in the parking lot instead of<br />
our usual indoor plumbing.<br />
People continue to exercise the good manners and<br />
cooperation that make living here worthwhile. As one person,<br />
I can’t do much, but as part of a team, I’m trying to be useful.<br />
March 14<br />
Being a specialist with an interest in disaster response is not<br />
quite the same as being a disaster specialist. Maybe my biggest<br />
contribution to the effort on Sunday was tracking down some<br />
bakery rolls, and then catching up with a surgeon who had<br />
been on overnight duty and still hadn’t eaten by mid-afternoon.<br />
Being human, he promptly inhaled two rolls. Being a surgeon,<br />
he washed them down with some strong coffee. Being Japanese,<br />
he put the rest in a freezer for others and went back to work.<br />
March 15<br />
We are still outside the radiation evacuation area, but some<br />
incoming patients are being wanded with a Geiger counter,<br />
in much the same way as some people are wanded with a<br />
Kenneth Nollet, M.D., Ph.D., has been at<br />
FMU since 2008 and hopes to stay in the<br />
country. “Japan feels like home,” he says.<br />
10 <strong>Mayo</strong> <strong>Alumni</strong>
Patients arrived at Fukushima Medical Center by helicopter,<br />
ambulance and bus.<br />
Fukushima Medical Center saw 28 life-threatening injuries,<br />
86 minor injuries and one fatality.<br />
magnatometer at airport security. Perhaps the most important<br />
place to measure radiation is the Neonatal Intensive Care Unit.<br />
March 26-27<br />
At a Japanese medical university, there is generally one full<br />
professor in each department, who serves as its chair, often<br />
until retirement. The system has been likened to a pyramid.<br />
But what is it like to be at the top?<br />
Professor Yasuhiro Hashimoto directs leading-edge<br />
glycomics research aimed at diagnosing serious neurological<br />
disorders. A weekend at the university would normally be<br />
for academic activities. But this Saturday and Sunday, he is<br />
also a radiation technologist [measuring radiation levels at<br />
the hospital with a portable gamma-ray detector].<br />
Scholars from around the world know Professor Hitoshi<br />
Ohto for research in transfusion-associated graft-versus host<br />
disease and other topics. To patients in Fukushima, however,<br />
he is a kindly physician who attends to therapeutic apheresis<br />
and personally draws blood from autologous donors.<br />
Power and service seem to be related here.<br />
April 2<br />
International media attention and domestic anxiety seem<br />
to focus on nuclear plant issues and possible long-term<br />
effects of stray radioactivity. Caregivers have to consider<br />
an even bigger picture. Our hospital is once again receiving<br />
non-urgent patients, but FMU teams continue to travel<br />
around the prefecture, attending to refugees.<br />
April 11<br />
Today marks one month since an earthquake changed<br />
everything. Or did it?<br />
Hourai East Primary School, a block from where I live,<br />
resumed classes today. Last night, there were students in the<br />
gymnasium, rather than refugees. Tens of thousands are still<br />
displaced and will be for some time. While new accommodations<br />
are being built, young doctors unaccustomed to making<br />
house calls are calling on the homeless. Earthquakes and<br />
tsunamis put every structure to the test, but social order has<br />
not collapsed.<br />
At 2:26 p.m. today, FMU observed a minute of silence for<br />
those removed from their homes, especially those removed<br />
from this world. I observed this silence from the vantage<br />
One month after the disaster, a decontamination tent remained<br />
outside of Fukushima Medical Center although Fukushima City has<br />
only slightly elevated radiation levels. “Worthy of surveillance but<br />
not worth worrying about, despite what people exposed only to mass<br />
media might believe,” says Kenneth Nollet, M.D., Ph.D.<br />
<strong>Fall</strong> <strong>2011</strong> 11
On March 24, a scaled back graduation ceremony was held for degree candidates from the School of Medicine, Graduate School of Medicine,<br />
School of Nursing and Graduate School of Nursing. In recent years, FMU introduced simulation technologies that allow students to learn medical<br />
procedures without putting themselves or patients in harm’s way. Students, in harm’s way themselves, learned from a disaster too big to simulate.<br />
point of a hallway window overlooking the courtyard. A small<br />
plaque in the courtyard commemorates the life and the oath<br />
of Hippocrates. It is a dull, overcast day and the courtyard<br />
trees are still bare. But this will change in the next week.<br />
Nature has the power to destroy; human artifice adds insult<br />
to injury, but nature also manifests creation and re-creation.<br />
May 8<br />
The entrance ceremony for new students was held May 6.<br />
Like other recent events, this one began with a minute of<br />
silence. Perhaps for anyone entering a caregiving profession,<br />
this ritual should be the norm rather than the exception. Near<br />
or far, there will always be people in need.<br />
Hana-mi-yama, or flower-viewing mountain, is a popular tourist<br />
destination in Fukushima City. Despite the disaster, residents and<br />
visitors made time to take in the cherry blossoms.<br />
12 <strong>Mayo</strong> <strong>Alumni</strong>
with Kenneth Nollet, M.D., Ph.D.,<br />
an American Doctor in Fukushima<br />
Why did you observe a moment of silence near a plaque<br />
commemorating the life and oath of Hippocrates?<br />
In the course of teaching medical English presentation<br />
skills, I convene students around this plaque. They compare<br />
and contrast the classic oath and modern variations. In common,<br />
every respectable oath is a promise of service to others.<br />
This comes naturally in times of disaster, but I also wanted to<br />
reflect on Hippocrates’ injunction to guide the next generation.<br />
Before the earthquake,<br />
we expected 100 medical<br />
students to matriculate<br />
in April. Circumstances<br />
forced Fukushima<br />
Medical University<br />
(FMU) to postpone the<br />
new academic year by one<br />
month, and for various<br />
reasons 11 students<br />
withdrew. The remaining<br />
students have made an<br />
extraordinary commitment.<br />
Those of us<br />
privileged to teach the art<br />
should do the same.<br />
Fukushima Medical<br />
University’s model<br />
of care translates to:<br />
“To show compassion, possess knowledge,<br />
apply skill, foster harmony, and build community.”<br />
How does it compare to the <strong>Mayo</strong> Model of Care?<br />
FMU’s model of patient care and education resembles<br />
what is practiced at <strong>Mayo</strong>. Of course, FMU cannot claim<br />
to be an international health care destination. On the other<br />
hand, I’ve never forgotten that farmers from southeastern<br />
Minnesota were as welcome at <strong>Mayo</strong> as princes and kings<br />
from around the world. Like southeastern Minnesota,<br />
much of Fukushima’s economy is agricultural, but not as<br />
mechanized. Farmers here work much harder for my meals<br />
than I do. Many of them come into old age and into hospital<br />
bent over from years of diligent crop tending. They deserve<br />
our best efforts.<br />
To what degree is daily life at FMU back to normal?<br />
FMU has resumed routine patient care. Radiation<br />
surveillance is a normal activity at any medical university<br />
but was scaled up when problems began at the nuclear plant.<br />
I walk past one radiation checkpoint every day, where log<br />
sheets are kept in plain view next to a Geiger counter. Between<br />
official measurements, I am at liberty to check myself or<br />
anything I might be wearing or carrying for radioactivity.<br />
My day-to-day<br />
life was never really<br />
disrupted. A doctor<br />
always has something<br />
to do. People in the<br />
community who<br />
wanted me to focus<br />
on my job made sure<br />
that other things<br />
were taken care of.<br />
Among those in the community who helped to take care of things so Kenneth Nollet,<br />
M.D., Ph.D., could focus on his job were the owners of a family-owned lunch<br />
counter. “The business could not operate when running water and gasoline were<br />
not available, but they kept their doors open for me,” says Dr. Nollet. At left, an<br />
FMU medical student joins Dr. Nollet (center) and members of the owner family.<br />
What would you<br />
like <strong>Mayo</strong> <strong>Clinic</strong><br />
alumni to know about<br />
disaster relief?<br />
<strong>Mayo</strong> alumni<br />
know firsthand<br />
what charitable giving<br />
can accomplish. Just<br />
as we are taught to practice evidence-based medicine, it<br />
behooves us to practice evidence-based benevolence.<br />
A compelling narrative suggests that Rochester’s<br />
F5 tornado in 1883 inspired an institution now known and<br />
respected around the world. We, as heirs to this legacy,<br />
should redouble our efforts to expect the unexpected and<br />
be of service in difficult times.<br />
visit dr. nollet’s ongoing blog<br />
for more information,<br />
http://cbbstoday.org/nollet_fukushima.php.<br />
<strong>Fall</strong> <strong>2011</strong> 13
... we face serious issues wiTh how healTh care<br />
is funded and insured, and how care<br />
is delivered To be high qualiTy, accessible and affordable.<br />
14 <strong>Mayo</strong> <strong>Alumni</strong>
pAtients Are<br />
‘GlAd mAyo is<br />
speAkinG up’<br />
Patricia simmons, M.d.<br />
new medical director of government relations<br />
patricia Simmons, M.D., is the medical director for <strong>Mayo</strong><br />
<strong>Clinic</strong>’s new Division of Government Relations. In this<br />
role, she is the physician leader for <strong>Mayo</strong> <strong>Clinic</strong>’s<br />
interactions with federal and state governments and other<br />
organizations. The new division encompasses the work of<br />
state legislative activity in Arizona, Florida, Minnesota and<br />
Wisconsin, and the work of the Health Policy Center and<br />
other federal government relations.<br />
Dr. Simmons came to <strong>Mayo</strong> <strong>Clinic</strong> in Rochester in 1977<br />
for her residency and fellowship and has remained ever since.<br />
She is chair of Pediatric and Adolescent Gynecology, a<br />
consultant in the Department of Pediatric and Adolescent<br />
Medicine and the Department of Obstetrics and Gynecology,<br />
and a professor of pediatric and adolescent medicine.<br />
<strong>Mayo</strong> <strong>Alumni</strong> interviewed Dr. Simmons about this new<br />
leadership position.<br />
why did you want to serve in this role?<br />
I’ve been privileged to be in leadership positions at <strong>Mayo</strong><br />
<strong>Clinic</strong> as well as on the “front lines,” and I have a passion for<br />
our values and model of care. <strong>Mayo</strong> is a wonderful place for<br />
people to receive health care, be educated and do research.<br />
I want to play a role in preserving the extraordinary thing<br />
that <strong>Mayo</strong> <strong>Clinic</strong> is. Serving at the decision-making table has<br />
given me insights and knowledge. I know to whom to go<br />
when I don’t have the answers I need. I want to use those<br />
resources and experiences in the broader environment.<br />
I also have had leadership positions outside of <strong>Mayo</strong>,<br />
such as serving on the Board of Regents of the University<br />
of Minnesota since 2003, including chair of the Board. The<br />
process involved in becoming a public servant and that<br />
engagement helped to stimulate my interest and provide<br />
experiences and relationships for my new role in <strong>Mayo</strong>’s<br />
government relations.<br />
Of course, I will protect my patient care responsibilities.<br />
One reason I took on this new role was because I care so<br />
much about patients. I don’t want to shortchange my primary<br />
reason for being at <strong>Mayo</strong> <strong>Clinic</strong>.<br />
Patricia Simmons, M.D., medical director of Government Relations,<br />
says she is grateful to Drs. Denis Cortese and John Noseworthy for<br />
making <strong>Mayo</strong> <strong>Clinic</strong> engagement in government relations a priority.<br />
<strong>Fall</strong> <strong>2011</strong> 15
kathleen harrington<br />
new division chair for<br />
Government relations<br />
Kathleen Harrington has<br />
joined <strong>Mayo</strong> <strong>Clinic</strong> as chair for<br />
the Division of Government<br />
Relations. She oversees a team<br />
that develops health policy<br />
recommendations, monitors<br />
congressional and legislative<br />
activity, and seeks to influence<br />
stakeholder groups at state and<br />
national levels.<br />
Prior to joining <strong>Mayo</strong> <strong>Clinic</strong>,<br />
Harrington spent 25 years in<br />
Washington, D.C., working on<br />
health policy issues in various<br />
roles, including serving as chief<br />
of staff for Congresswoman<br />
Nancy L. Johnson, vice president<br />
of federal government relations<br />
at Aetna, and director of the<br />
office of external affairs for<br />
the Centers for Medicare and<br />
Medicaid Services. Most recently,<br />
Harrington was director of<br />
government relations and public<br />
affairs for Carol Corp, a strategy<br />
and solutions company that<br />
empowers health systems to<br />
transition to accountable care.<br />
what challenges do health care organizations<br />
face in the government environment?<br />
At the state and federal levels, we face<br />
serious issues with how health care is<br />
funded and insured, and how care is<br />
delivered to be high quality, accessible<br />
and affordable.<br />
Now that the health reform law has<br />
passed, it’s time to work on the interpretation<br />
and what we know will be<br />
substantial revisions in the years ahead.<br />
We have to be prepared for change and<br />
to provide informed, valued input.<br />
who do you look to for support in this role?<br />
I’m helped by my colleagues throughout<br />
<strong>Mayo</strong>, including those who work in<br />
government relations. I still have a lot<br />
to learn, and I am grateful for their<br />
support. We’re doing this as a team in<br />
true <strong>Mayo</strong> style.<br />
I rely on fellow leaders at <strong>Mayo</strong><br />
<strong>Clinic</strong> for their ideas, skills and<br />
involvement. I admire <strong>Mayo</strong> leaders<br />
who have championed taking on a<br />
more public role with issues that are so<br />
important. Drs. [Denis] Cortese [former<br />
president and CEO] and [John]<br />
Noseworthy [president and CEO] have<br />
regarded this activity as important for<br />
<strong>Mayo</strong> to engage in. That says a lot<br />
about their sense of social responsibility<br />
and commitment to our patients<br />
and mission. Following their lead,<br />
<strong>Mayo</strong> has done this with dignity and<br />
style. Those of us who have trained<br />
here, work here and who are patients<br />
can be proud.<br />
Other organizations and individuals<br />
who share our values also are<br />
valuable resources. And the public is a<br />
tremendous ally for <strong>Mayo</strong> <strong>Clinic</strong>. In our<br />
engagement with national health<br />
policy, we’ve tried very hard to provide<br />
the public with a voice and a forum.<br />
I look forward to a new set of<br />
interactions with <strong>Mayo</strong> leadership and<br />
external leaders in federal and state<br />
government.<br />
has anything surprised you so far in this role?<br />
I was surprised at how engaged <strong>Mayo</strong><br />
<strong>Clinic</strong> is with government and active in<br />
health policy and how much my<br />
colleagues know. But I shouldn’t have<br />
been. <strong>Mayo</strong> <strong>Clinic</strong> has always been<br />
engaged, dating back to the <strong>Mayo</strong><br />
brothers. It’s part of our tradition to<br />
share what we know.<br />
It’s gratifying when a patient knows<br />
about <strong>Mayo</strong>’s or my activities in this area<br />
and expresses thanks. Patients have<br />
said, “I’m so glad you’re trying to do<br />
something — so glad <strong>Mayo</strong> is speaking<br />
up.” Patients, alumni and people around<br />
the state and country care deeply about<br />
health care in the United States and the<br />
future of <strong>Mayo</strong> <strong>Clinic</strong>.<br />
how will you measure success in this role?<br />
We’ll succeed when health care in the<br />
United States grows in value and <strong>Mayo</strong><br />
<strong>Clinic</strong> thrives.<br />
We would like everyone to advocate<br />
for continued federal funding for<br />
research, particularly for National<br />
Institutes of Health (NIH) funding.<br />
We believe that <strong>Mayo</strong> <strong>Clinic</strong> is<br />
the best health care model in the<br />
United States, and we have a moral<br />
obligation and responsibility to try to<br />
influence national and state policy.<br />
What’s good for <strong>Mayo</strong> <strong>Clinic</strong> is good<br />
for our patients and people everywhere.<br />
It’s wonderful to think you can<br />
improve health care for people and<br />
have the institution you love succeed.<br />
One goal serves the other.<br />
16 <strong>Mayo</strong> <strong>Alumni</strong>
division of governMenT relaTions<br />
federal PrioriTies<br />
through its new Division of Government Relations, <strong>Mayo</strong><br />
<strong>Clinic</strong> will work with groups who share similar points<br />
of view to advocate for extending high-value, efficient,<br />
affordable, accessible, patient-centered care for all. The goal<br />
of this activity is to ensure patients have access to <strong>Mayo</strong><br />
<strong>Clinic</strong> and that the <strong>Mayo</strong> <strong>Clinic</strong> Model of Care is used to<br />
help guide public policy decisions.<br />
<strong>Mayo</strong> <strong>Clinic</strong> is involved in state<br />
government relations activities in<br />
Arizona, Florida, Minnesota and<br />
Wisconsin. At the federal level, <strong>Mayo</strong><br />
<strong>Clinic</strong> has developed this message to<br />
guide its efforts:<br />
As the U.S. Courts examine<br />
the Patient Protection and Affordable<br />
Care Act, <strong>Mayo</strong> <strong>Clinic</strong> will continue<br />
to work toward the implementation<br />
of its provision and timelines until<br />
the court system’s judicial review<br />
reaches final resolution. <strong>Mayo</strong> <strong>Clinic</strong><br />
believes that the status quo in health<br />
care is not acceptable because too<br />
many patients lack access to patientcentered,<br />
high-value health care. <strong>Mayo</strong><br />
<strong>Clinic</strong> has consistently said that there must be two key<br />
principles in any successful reform effort:<br />
1 Incentives for physicians and hospitals to offer highquality<br />
care at a reasonable cost because this defines<br />
high-value health care<br />
2 A means to enable all Americans to purchase affordable<br />
health insurance<br />
The Affordable Care Act has begun to address the<br />
coverage aspect of health care, but much more needs to be<br />
done to advance the creation of a high-value health care<br />
system. Now is the time to focus on developing, testing and<br />
implementing concrete policies that will produce highquality,<br />
efficient, affordable, accessible, patient-centered care<br />
for all Americans.<br />
Priority areas for <strong>Mayo</strong> <strong>Clinic</strong> in <strong>2011</strong> within the framework<br />
of the Affordable Care Act are:<br />
• Guide the implementation of Accountable Care<br />
Organizations (ACO) that meet the needs of patients.<br />
• Contribute to the Institute of Medicine study on value<br />
so that new payment models effectively reward patientcentered,<br />
high-value health care.<br />
mAyo CliniC hAs AlwAys been enGAGed.<br />
it’s pArt of our trAdition<br />
to shAre whAt we know.<br />
• Work with the CMS Innovation Center on potential<br />
high-value health care projects.<br />
• Help develop workable guidelines for health insurance<br />
exchanges by working closely with states.<br />
• Provide input to CMS about the value modifier so that<br />
patient-centered, high-value health care is rewarded.<br />
• Guide the distribution of comparative effectiveness<br />
research funding through the Patient<br />
Centered Outcomes Research Institute.<br />
<strong>Mayo</strong> also is committed to advancing<br />
these initiatives, separate from the<br />
Affordable Care Act:<br />
• Advance health information technology<br />
standards and interoperability in health care<br />
systems by focusing on two priorities: unique<br />
patient identification and meaningful<br />
exchange of medication, allergy and<br />
problem lists between organizations.<br />
• Monitor unobligated funds from the<br />
2009 American Reinvestment and Recovery<br />
Act because these funds are at risk of<br />
being reclaimed. This may affect the health<br />
information technology efforts of the Office<br />
of the National Coordinator.<br />
• Determine and build support for a permanent solution<br />
to the sustainable growth rate formula issue within<br />
Medicare.<br />
• Monitor and protect National Institutes of Health and<br />
Graduate Medical Education funding.<br />
<strong>Mayo</strong> <strong>Clinic</strong> also is involved in state government relations<br />
activities in Arizona, Florida, Minnesota and Wisconsin.<br />
<strong>Mayo</strong> clinic’s government relations team<br />
Patricia Simmons, M.D. Medical Director, Government Relations<br />
Kathleen Harrington Division Chair, Government Relations<br />
Jennifer Mallard Director, Federal Government Relations<br />
Layne Smith<br />
Director, Florida Government Relations<br />
Erin Sexton<br />
Director, Minnesota Government Relations<br />
Michael Yardley Division Chair, Public Affairs, Arizona<br />
government relations operations Team<br />
Shelly Plutowski Judy Samson<br />
Nora O Sullivan Randy Schubring<br />
<strong>Fall</strong> <strong>2011</strong> 17
What can <strong>Mayo</strong> <strong>Clinic</strong> learn<br />
from the ancient Greeks?<br />
<strong>Alumni</strong>, <strong>Mayo</strong> staff reflect on visit to ancient healing community of Epidaurus<br />
Attendees of the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association International CME Conference,<br />
Living Long, Living Well, , visited the small community of Epidaurus, which dates<br />
back to the fourth century B.C.<br />
The asclepieion at Epidaurus was a healing center, where ill people went in<br />
the hope of being cured. The asclepieion featured a 160-person guest house,<br />
gymnasium, stadium, theatre and healing springs.<br />
<strong>Mayo</strong> <strong>Clinic</strong> staff and alumni marveled at the many parallels between Epidaurus<br />
and <strong>Mayo</strong> <strong>Clinic</strong>, and lessons we can learn from the ancient community. They<br />
share their reflections with <strong>Mayo</strong> <strong>Alumni</strong>, with photos by Eddie Greene, M.D.<br />
A museum on the Epidaurus grounds displays artifacts, including medical instruments<br />
that closely resemble those used today.<br />
Epidaurus at the time of its popularity<br />
embodied many of the concepts<br />
that we espouse as being important for<br />
health: Exercise, mind-body connection,<br />
and an environment that promoted<br />
health of the body and health of the<br />
spirit. However, even though this is<br />
regarded as important even in the age<br />
of more esoteric and scientifically based<br />
treatment of illness, this particular site<br />
is currently a ruin, and has been so<br />
for thousands of years. This begs the<br />
question: How did this site, which held<br />
the attention of healers and the sick for<br />
many years, with ideals and practices<br />
that we regard even today as being<br />
important to health and well-being, lose<br />
its connection for the community which<br />
18 <strong>Mayo</strong> <strong>Alumni</strong>
it served? What lessons can we as <strong>Mayo</strong><br />
<strong>Clinic</strong> learn and apply from this ancient<br />
“destination medical center?”<br />
The context of health, illness and<br />
healing is the context of the society<br />
in which the practices reside. Society<br />
and societies are not static organisms,<br />
but living organisms within which<br />
the accepted practices, ideals, mores<br />
and ethics may be in flux. The role of<br />
science and “best practices” may be<br />
more real or relevant to the practitioner<br />
than they are to the patient, and those<br />
practices and patient expectations can<br />
change over time. For example, within<br />
our own lifetimes the role of the physician<br />
and caregiver as an authoritarian<br />
and paternalistic figure has given<br />
way to a care partnership between<br />
the patient and the physician, with<br />
shared decision making on diagnostic<br />
testing and treatment the expectation.<br />
Providers that do not share and<br />
practice within the context of this new<br />
perception and expectation of medical<br />
care are likely to be marginalized and<br />
serve an increasingly small proportion<br />
of the population that continues to hold<br />
this view of the paternalistic provider<br />
and the compliant patient.<br />
It can be plausibly inferred from<br />
Epidaurus that the type of medicine and<br />
healing practiced at this site, though<br />
some of the practices performed there<br />
have withheld the test of time, somehow<br />
lost its relevance in Greek society.<br />
The basis for this loss of relevance is<br />
unknown. Could other cult followings<br />
of healing displaced it? Could political<br />
processes such as war, political fractionation<br />
of society or other rules imposed<br />
by society impeded its success through<br />
restricted access? Or did disease, famine<br />
or other natural disaster render its<br />
brand of healing as ineffective, unaffordable,<br />
or perhaps dangerous?<br />
The process that led to the demise<br />
of Epidaurus will likely never be<br />
known, yet the lessons from that early<br />
“destination medical center” should not<br />
be lost or discounted. The healing arts<br />
and sciences must remain relevant to<br />
the societies they serve. Practitioners<br />
must be vigilant and responsive to the<br />
societies they serve, holding the science<br />
and compassionate care as unyielding.<br />
They also must be nimble and flexible<br />
to meet patients on their terms and<br />
engage them in a partnership. As we<br />
strive to meet the guiding principle<br />
“The needs of the patient come first,”<br />
let’s make sure we are constantly and<br />
consistently asking our patients about<br />
their needs, listening carefully to their<br />
responses and crafting the delivery<br />
of our care to meet those needs. This<br />
process and practice will help us<br />
continue and improve our relevance to<br />
our patients, and prevent <strong>Mayo</strong> <strong>Clinic</strong><br />
from becoming the next Epidaurus.<br />
Terence Cascino, M.D. (’80 NEURo)<br />
James Garrity, M.D. (’85 oPh)<br />
Eddie Greene, M.D (NEPh)<br />
David herman, M.D. (’83 oPh)<br />
<strong>Fall</strong> <strong>2011</strong> 19
<strong>Mayo</strong> Update<br />
New Arizona CEO<br />
Board of Trustees honors new named professors<br />
The <strong>Mayo</strong> <strong>Clinic</strong> Board of Trustees has honored two new <strong>Mayo</strong> <strong>Clinic</strong> named professors.<br />
Wyatt Decker, M.D.<br />
Robert Spinner, M.D.<br />
Department of Neurologic Surgery<br />
Department of orthopedic Surgery<br />
<strong>Mayo</strong> <strong>Clinic</strong> Rochester<br />
Burton M. Onofrio, M.D.,<br />
Professor of Neurosurgery<br />
Michael Ackerman, M.D., Ph.D.<br />
Divisions of Cardiovascular Diseases<br />
and Pediatric Cardiology<br />
Department of Molecular Pharmacology<br />
and Experimental Therapeutics<br />
<strong>Mayo</strong> <strong>Clinic</strong> Rochester<br />
Windland Smith Rice Cardiovascular<br />
Genomics Research Professor<br />
At its quarterly meeting in May, the<br />
<strong>Mayo</strong> <strong>Clinic</strong> Board of Trustees appointed<br />
Wyatt Decker, M.D. (MMS ’90, I ’93,<br />
EM ’97) as the new vice president<br />
and chief executive officer in Arizona.<br />
Dr. Decker succeeds Victor Trastek, M.D.<br />
Dr. Decker has been with <strong>Mayo</strong><br />
<strong>Clinic</strong> for more than 16 years as a<br />
consultant and professor of emergency<br />
medicine. His leadership roles have<br />
included chair of Emergency Medicine,<br />
with responsibilities for the emergency<br />
departments at <strong>Mayo</strong> <strong>Clinic</strong> in<br />
Rochester and Jacksonville. Currently,<br />
he is chair of the <strong>Mayo</strong> <strong>Clinic</strong> Personnel<br />
Committee in Rochester and leads the<br />
Rochester Destination Medical<br />
Community initiative.<br />
Robert Spinner, M.D. (NS ’00) (left), and Michael Ackerman, M.D. (MMS ’95, PhAR ’95,<br />
PD ’98, PDC ’00) (right), are presented with named professorship certificates from Michael<br />
Camilleri, M.D. (center), a member of the <strong>Mayo</strong> <strong>Clinic</strong> Named Professorship Committee.<br />
For more information about these named professors, visit mayo.edu/alumni.<br />
Obituaries<br />
Hermance Legait, M.D. (N ’50),<br />
died May 15, <strong>2011</strong>.<br />
Alexander Lucas, M.D. (CAP ’71),<br />
died March 31, <strong>2011</strong>.<br />
James McPherson, M.D. (I ’59),<br />
died April 23, <strong>2011</strong>.<br />
20 <strong>Mayo</strong> <strong>Alumni</strong><br />
Douglas Pritchard, M.D. (OR ’72),<br />
died May 19, <strong>2011</strong>.<br />
Troy Rollins, M.D. (DERM ’58),<br />
died March 30, <strong>2011</strong>.<br />
Kevin Shaw, M.D. (CRANI ’87, PLS ’87),<br />
died Jan. 17, <strong>2011</strong>.<br />
Robert Sigler, M.D. (S ’66),<br />
died Jan. 27, <strong>2011</strong>.<br />
Gabriel Toro, M.D. (I ’48),<br />
died Jan. 2, <strong>2011</strong>.<br />
Complete obituaries and the Update section,<br />
with alumni and staff news, are available on<br />
the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Association website,<br />
mayo.edu/alumni.
<strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong><br />
Association Officers<br />
S. Mark Laney, M.D., St. Joseph, Mo.<br />
President<br />
Eric J. Grigsby, M.D., Napa, Calif.<br />
President-Elect<br />
Juan M. Sarmiento, M.D., Atlanta<br />
Vice President<br />
Eric S. Edell, M.D., Rochester, Minn.<br />
Secretary-Treasurer<br />
David K. Teegarden, M.D., Tyler, Texas<br />
Past President<br />
Karen D. Herman, Rochester, Minn.<br />
Director<br />
Executive Committee<br />
Peter C. Amadio, M.D., Rochester, Minn.<br />
Sarah Y. Boostrom, M.D., Rochester, Minn.<br />
(MSGME Representative)<br />
Terrence L. Cascino, M.D., Rochester, Minn.<br />
(Department of Education Representative)<br />
Maria L. Collazo-Clavell, M.D.,<br />
Rochester, Minn.<br />
Diane F. Jelinek, Ph.D., Rochester, Minn.<br />
Margaret M. Johnson, M.D.,<br />
Jacksonville, Fla.<br />
Clive P. Nyauncho, Rochester, Minn.<br />
(MMS Representative)<br />
Justin P. Peters, Rochester, Minn.<br />
(MGS Representative)<br />
Daniel L. Roberts, M.D., Scottsdale, Ariz.<br />
Carl W. Soderstrom, M.D., Peoria, Ill.<br />
Board of Directors 2009–<strong>2011</strong><br />
Carl L. Backer, M.D., Winnetka, Ill.<br />
Susheela Bala, M.D., San Bernardino, Calif.<br />
Wendelyn Bosch, M.D., Jacksonville, Fla.<br />
(MCF-MSGME Representative)<br />
Kenneth H. Brookler, M.D., New York<br />
Nancy L. Elwess, M.D., Plattsburg, N.Y.<br />
Juan Gallegos, M.D., Scottsdale, Ariz.<br />
(MCA-MSGME Representative)<br />
Robert P. Kazan, M.D., Chicago<br />
Peter H. Layer, M.D., Hamburg, Germany<br />
Kevin G. Madden, M.D., Scranton, Penn.<br />
Gregory K. Mayer, M.D., Phoenix<br />
M. Mark Melin, M.D., St. Louis Park, Minn.<br />
Nicole W. Pelly, M.D., Seattle<br />
David W. Romness, M.D., Arlington, Va.<br />
Scott R. Ross, D.O., Colorado Springs, Colo.<br />
Guillermo Ruiz-Arguelles, M.D.,<br />
Puebla, Mexico<br />
Marcia J. Sparling, M.D., Vancouver, Wash.<br />
Mack H. Sullivan, M.D.,<br />
West Bloomfield, Mich.<br />
Pamela B. Sylvestre, M.D., Memphis, Tenn.<br />
Karl F. Tamussino, M.D., Austria<br />
Robert L. Van Dervoort Jr., M.D.,<br />
Nashville, Tenn.<br />
Executive Editor — Karen Trewin<br />
Editorial Assistant — Emily DeBoom<br />
Advisory Board — Steven Altchuler, M.D., Ph.D., Brigitte Barrette, M.D., Matthew<br />
Bernard, M.D., Charles Burger, M.D., Eric Edell, M.D., chair, Michael Farnell, M.D.,<br />
Robert Giere, Colum Gorman, M.B.B.Ch., Ph.D., Nancy Henry, M.D., Ph.D., Karen<br />
Herman, Richard Hurt, M.D., Andrew Landstrom, Nicholas LaRusso, M.D., Paul<br />
Mueller, M.D., Lonzetta Neal, M.D., Robert Safford, M.D., Ph.D., Patricia Odean,<br />
Karen Trewin, Dietland Wahner-Roedler, M.D., Alexandra Wolanskyj, M.D.<br />
<strong>Alumni</strong> Center<br />
507-284-2317<br />
Karen Herman, director<br />
507-538-0162<br />
Email: mayoalumni@mayo.edu<br />
Website: http://www.mayo.edu<br />
Physician Referral<br />
Arizona 800-446-2279 (toll-free)<br />
Florida 800-634-1417 (toll-free)<br />
Rochester 800-533-1564 (toll-free)<br />
mayoclinic.org/medprofs<br />
Patient Transportation<br />
<strong>Mayo</strong> <strong>Clinic</strong> MedAir, <strong>Mayo</strong> One<br />
800-237-6822 (toll-free)<br />
mayomedicaltransport.com<br />
For information<br />
about alumni meetings<br />
and receptions,<br />
visit<br />
mayo.edu/alumni<br />
<strong>Alumni</strong> Philanthropy<br />
Contact: Robert W. Giere<br />
Director for <strong>Alumni</strong> Philanthropy<br />
800-297-1185<br />
tdms@mayo.edu<br />
<strong>Mayo</strong> <strong>Alumni</strong> magazine is published quarterly and mailed free of charge to<br />
physicians, scientists and medical educators who studied and/or trained at<br />
<strong>Mayo</strong> <strong>Clinic</strong>, and to <strong>Mayo</strong> consulting staff. The magazine reports on <strong>Mayo</strong> <strong>Clinic</strong><br />
alumni, staff and students, and informs readers about newsworthy activities<br />
throughout <strong>Mayo</strong> <strong>Clinic</strong>. Please send correspondence to: <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong><br />
Center, Siebens 5-33, <strong>Mayo</strong> <strong>Clinic</strong>, 200 First Street S.W., Rochester, MN 55905; or<br />
via e-mail to deboom.emily@mayo.edu; or telephone 507-284-4660; or fax<br />
507-284-8713. Send address changes to the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong> Center office<br />
at the preceding address or e-mail to mayoalumni@mayo.edu.<br />
<strong>Mayo</strong> <strong>Clinic</strong> is committed to creating and sustaining an environment that<br />
respects and supports diversity in staff and patient populations.<br />
<strong>MC4409</strong>rev<strong>0811</strong>
Division of Public Affairs<br />
<strong>Mayo</strong> <strong>Clinic</strong><br />
Rochester, Minnesota 55905<br />
ADDRESS SERVICE REquESTED<br />
Non-Profit Organization<br />
U.S. Postage<br />
PAID<br />
Rochester, MN 55905<br />
Permit No. 135<br />
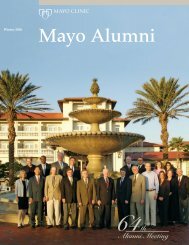
In May, the <strong>Mayo</strong> <strong>Clinic</strong> <strong>Alumni</strong><br />
Association hosted an International<br />
CME Conference in Greece. Many<br />
attendees visited Epidaurus, a former<br />
healing center dating back to the fourth<br />
century B.C. Numerous parallels exist<br />
between Epidaurus and <strong>Mayo</strong> <strong>Clinic</strong>,<br />
including an emphasis on health of body<br />
and spirit. One cannot help but wonder<br />
what led to the ruination of this ancient<br />
destination medical center. Did it cease<br />
to be relevant or ineffective?<br />
Several <strong>Mayo</strong> physicians provide their<br />
perspective about lessons <strong>Mayo</strong> <strong>Clinic</strong><br />
can learn from the ancient Greeks and<br />
Epidaurus in the story on page 18.<br />
Greece photos, Eddie Greene, M.D.