AMBULANCE VICTORIA STRATEGIC PLAN 2010 â 2012
AMBULANCE VICTORIA STRATEGIC PLAN 2010 â 2012
AMBULANCE VICTORIA STRATEGIC PLAN 2010 â 2012
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
PARTNERS FOR LIFE<br />
<strong>AMBULANCE</strong> <strong>VICTORIA</strong><br />
<strong>STRATEGIC</strong> <strong>PLAN</strong> <strong>2010</strong> – <strong>2012</strong><br />
DRAFT FOR CONSULTATION
1. Ambulance Victoria’s Role<br />
Ambulance Victoria is a critical link in Victoria’s Health Care<br />
System. AV provides pre-hospital care for patients experiencing<br />
medical emergencies, and medical transport by road and air to<br />
ensure both emergency and non-emergency patients access<br />
the appropriate level of health care. The overriding aim of the<br />
organisation is to improve the health outcomes of Victorians.<br />
In summary, Ambulance Victoria’s role is to:<br />
Improve the health of the Victorian community<br />
by providing high quality pre-hospital care and<br />
medical transport<br />
2. Overview of Services<br />
AV operates across the State, with major administrative centres in<br />
Melbourne and Ballarat. We have more than 3,000 career employees<br />
and almost 1,000 volunteers, with over 220 road ambulance response<br />
locations. Air ambulance services (fixed wing and helicopter) cover<br />
the entire State.<br />
AV’s primary focus is to deliver services that meet the needs of our<br />
patients, their families and carers, and a range of organisations using<br />
our services (including public and private hospitals, the Transport<br />
Accident Commission, WorkCover and other health bodies).<br />
AV’s Services include:<br />
• Emergency medical response and pre-hospital care<br />
• Emergency medical transport by road or air<br />
• Non-emergency patient transport (including road and<br />
air stretcher transport and clinic transport for walking<br />
and wheelchair patients)<br />
• Major incident management and response<br />
• Retrieval of critically ill adult patients (including advice<br />
and bed coordination)<br />
• Assistance for ambulance patients to access appropriate<br />
care when paramedic care or transport is not required<br />
• Support for other health services in communities where<br />
the full range of services are not easily accessible<br />
• Community education in pre-ambulance arrival<br />
emergency care<br />
• The Ambulance Membership Scheme (ambulance insurance)<br />
1
3. Principles<br />
AV is committed to a set of ten principles, which provide a guiding framework for<br />
our service delivery to the community and for our internal operations.<br />
AV is committed to:<br />
1. Providing an appropriate response to all requests for service<br />
2. Developing our services to improve patient outcomes, based on the best<br />
available evidence<br />
3. Delivering services efficiently and cost effectively<br />
4. Collaborating with other service providers and the community to improve<br />
health system performance<br />
5. Minimising risks to the safety of patients and staff<br />
6. Safeguarding patient confidentiality and privacy<br />
7. Identifying and addressing community concerns about our services<br />
8. Respecting the values of all members of the community<br />
9. Recognising and valuing our people and their contributions<br />
10. Encouraging and providing opportunities for our people to develop.<br />
4. Strategic Objectives<br />
2. Foster staff development and welfare<br />
Effective service delivery is critically dependent on the skills and<br />
well-being of AV’s staff and volunteers. Minimising the risks to staff health<br />
and safety and encouraging the professional development of all staff are key<br />
organisational commitments.<br />
3. Develop organisational systems and resources to support improved<br />
service delivery<br />
Service delivery is becoming increasingly complex and dependent on more<br />
sophisticated support systems. Ensuring information and business systems<br />
continue to evolve is an essential part of delivering better services to the community.<br />
4. Strengthen community relationships and promote community initiatives<br />
and policy to improve patient outcomes<br />
AV is committed to building on its relationships with all parts of the Victorian<br />
community, to ensure that it understands and responds appropriately to the full<br />
diversity of community needs. Initiatives to develop community capability and<br />
awareness can make an important contribution to improving health outcomes.<br />
AV’s overriding aim of improving health outcomes for Victorians is underpinned by<br />
four strategic objectives, relating to service delivery, staff welfare, organisational<br />
systems and community relationships.<br />
1. Improve service quality and efficiency to better meet patient needs<br />
Continuing development of service quality to ensure patient needs are being met<br />
is fundamental to delivering improved health outcomes. Improved efficiency and<br />
better health system integration can also play a significant role in enabling more<br />
effective service delivery.<br />
2
5. The Planning Environment<br />
Eleven key challenges have been identified, which AV will need to address<br />
during the planning period and beyond.<br />
Increasing demand for services<br />
Ambulance services in Victoria have been under stress as a result of continuing<br />
strong growth in demand for more than a decade. Since 1999-2000, ambulance<br />
caseload in Victoria has grown by an average of 5.7 per cent per annum, with<br />
both emergency and non-emergency incidents increasing by more than 50 per<br />
cent. Other ambulance services around the world are experiencing similar<br />
demand pressures.<br />
Demand management has been an important focus for more than five years.<br />
The referral system for lower priority 000 callers in Melbourne has played an<br />
important role in controlling demand, with more than 7 per cent of callers not<br />
receiving an emergency ambulance dispatch. There is scope for expansion<br />
of the service and exploration of new emergency demand management<br />
initiatives. Management of non-emergency demand, and ensuring<br />
appropriate allocation of resources to meet patient needs will also be a<br />
priority. These strategies will assist in moderating growth, but increasing<br />
demand is expected to remain a key challenge through the planning period.<br />
The drivers of ambulance demand are similar to those affecting demand for most<br />
other health services. These include demographic change (ageing and population<br />
growth), which accounts for about 25 per cent of the increase in emergency<br />
demand. Trends in the health of the community play a key role, notably the<br />
increasing burden of chronic disease. Other factors also include changes in<br />
medical practice and patient management (e.g. the trend to early discharge<br />
and treatment in the community), social changes (e.g. the increasing number of<br />
people living alone), reduced accessibility to other health services in some areas<br />
(especially general practitioners) and rising community expectations.<br />
Growth has slowed in the last eighteen months, but there is no reason to believe<br />
that the long-term trend has changed. Large numbers of seriously ill patients<br />
(about 40 per cent of triage category 1 to 3 patients in Melbourne) are not<br />
transported to hospital emergency departments by ambulance, indicating there<br />
is significant potential for further increases in demand.<br />
3
Health System development<br />
Ambulance service delivery in Victoria has become an increasingly<br />
well-integrated part of the wider health system in recent years. This process<br />
will continue during the planning period, placing new demands on AV as well as<br />
creating new opportunities to improve services.<br />
There is a clear trend of increasing specialisation of hospital facilities for high<br />
acuity patients, driven by infrastructure costs and the clinical benefits of high<br />
levels of exposure for practitioners. Timely access to these facilities can have<br />
a significant bearing on patient outcome. This may involve ambulances bypassing<br />
the closest hospital to transport a patient to the most appropriate level<br />
of care as quickly as possible. Victoria’s system for managing major trauma is<br />
a well established example of this approach.<br />
Transmission of clinical information from the scene can also assist in reducing<br />
the time to access definitive care by facilitating early activation of specialist<br />
hospital teams. A recent pilot of ECG transmission for Acute Coronary<br />
Syndrome patients in southeast Melbourne has yielded impressive reductions<br />
in the time to definitive treatment, and more widespread implementation is now<br />
occuring. Improved system approaches for stroke patients is another likely<br />
development during the planning period.<br />
There is a long-term trend for reduced length of stay in hospital and a wide<br />
range of demand management strategies designed to prevent or minimise<br />
hospitalisation have been implemented in recent years.<br />
At the same time, there is increasing pressure on primary care services.<br />
As noted above, access to a general practitioner is difficult in some areas,<br />
particularly in rural Victoria.<br />
These changes tend to increase ambulance demand, but there is potential<br />
for paramedics to play a part in managing this demand more effectively. A<br />
number of ambulance services have introduced paramedic or emergency care<br />
practitioner roles in recent years, generally on a trial basis. There is significant<br />
variation in how these roles have been defined, but most involve an extension<br />
of the paramedic scope of practice, with an emphasis on increased assessment,<br />
referral and primary care skills. In Victoria, new roles have been developed in<br />
two remote communities focused on increased support for the local community,<br />
but with no change in clinical practice.<br />
Further exploration of the relevance of these new models of care will be an<br />
important priority during the planning period, focusing on the potential to<br />
improve both ambulance service delivery and wider health system performance.<br />
Hospital specialisation also tends to increase the requirement for patient<br />
transfers between facilities. AV’s air ambulance and adult retrieval services<br />
play a critical role in high acuity transfers. Coordination of these patient<br />
movements can be complex and further development of systems to minimise<br />
delays will be a continuing focus for AV.<br />
A second important system trend affecting ambulance services is an increasing<br />
emphasis on care in the community as an alternative to hospital care.<br />
4
Equity in Service Delivery<br />
There are inherent difficulties in the provision of ambulance services in remote<br />
areas and areas with lower population densities. The Government’s response<br />
time targets reflect these difficulties, with one target for population centres of<br />
more than 7,500 people, and a somewhat lesser target for the State overall.<br />
Continuing improvements in air ambulance and retrieval systems, including<br />
the introduction of two new helicopters in 2009, will assist in providing better<br />
access to appropriate levels of care across the State.<br />
Nevertheless, a number of key areas have been identified where differentials<br />
in service standards are of particular concern. Cardiac arrest survival rates in<br />
rural areas are well below those achieved in the metropolitan area. This is not<br />
surprising given the importance of rapid response in cardiac arrest outcomes.<br />
However, a more complete understanding of the reasons for the difference is<br />
needed and new strategies to improve performance need to be developed.<br />
Call taking, dispatch and ambulance communications systems play a<br />
critical role in the quality of service delivery. There have been important<br />
improvements in these systems across the State in recent years, but rural<br />
call taking and dispatch systems remain well below best practice standards.<br />
The introduction of a new rural system managed by the Emergency Services<br />
Telecommunications Authority will be a key priority for the planning period.<br />
Another important focus will be further development of an integrated statewide<br />
major incident management system, ensuring there is appropriate capability in<br />
all parts of the State.<br />
Risk of major incidents<br />
AV’s major incident system has been tested by a number of recent events,<br />
including the 2009 bushfires, and has proved its effectiveness. However,<br />
learning from these experiences to strengthen systems is essential to ensure<br />
an appropriate level of preparedness for response to all types of incident<br />
(including pandemic) is maintained. Monitoring risk and close collaboration<br />
with the relevant planning and response agencies at all levels of government<br />
are cornerstones of the system. Further strengthening of national links is a<br />
particular priority for future development of the system. Another key aspect<br />
is the ability to maintain normal services while managing a major incident,<br />
especially if it is prolonged.<br />
Evidence Based Practice<br />
The introduction of the Victorian Ambulance Clinical Information System<br />
was one of the most significant ambulance initiatives in the State in the last<br />
five years. VACIS provides a rich source of clinical data which can assist<br />
in driving the development of clinical practice and education. A number of<br />
other Australian services are now using VACIS, creating the opportunity for<br />
national sharing of consistent data. Linkages with hospital data are also being<br />
established to provide a more complete picture of patient outcomes. Ensuring<br />
the full benefits of this data are realised is an on-going priority.<br />
More generally, quality systems and performance monitoring will continue<br />
to evolve, with particular focus on patient outcome measures. Further<br />
development of AV’s role in pre-hospital research, usually in partnership with<br />
universities or other health services, will also assist in strengthening the<br />
evidence base for service improvement.<br />
5
Advances in information and technology<br />
Recent developments in information management systems have created new<br />
opportunities to drive performance improvements, but significant challenges<br />
remain. Key priorities include the integration of a number of the systems<br />
inherited from AV’s predecessor organisations, increased real time performance<br />
reporting, wider dissemination of geographic information and improving access<br />
to information for in-field managers. Real time data linkages with hospitals and<br />
greater use of decision support technologies have the potential to significantly<br />
improve operational processes and system performance.<br />
Resource Constraints<br />
The Government provided a major injection of new funding for AV in 2008-2009,<br />
enabling significant recruitment for additional road response resources and<br />
the introduction of two new ambulance helicopters for the State. However, the<br />
demands on the organisation are continuing to grow and there is increasing<br />
competition for scarce resources within the health sector and beyond. In<br />
addition to the financial constraints, the recruitment of qualified paramedics may<br />
become more difficult as competition from other jurisdictions increases.<br />
Continuing improvement in the efficiency of operations is imperative in such a<br />
resource constrained environment. This will include maintaining the current<br />
focus on improving processes for patient handover at hospital emergency<br />
departments and further development of more dynamic deployment of response<br />
units. Complementing the focus on efficiency, strategies to protect and enhance<br />
revenue (especially from the Membership Scheme) will need to be pursued.<br />
Organisational Consolidation<br />
AV commenced operations on 1 July 2008, and integration of the key processes<br />
and systems of its predecessor organisations is now well advanced. However,<br />
a number of significant challenges remain to consolidate the transition process.<br />
These include further development of internal communications processes and<br />
completion of the transition to statewide information and business systems. An<br />
important benefit of the creation of the new organisation is the opportunity it<br />
provides for the refinement of existing processes and systems.<br />
6
Workforce demographics and expectations<br />
One of the most significant recent changes affecting ambulance services has<br />
been the move from training of paramedics following their employment to<br />
recruitment of graduate paramedics who have already completed a university<br />
degree. This change necessitates a new focus on workforce planning and<br />
liaison with the universities to ensure future staffing needs can be met. It<br />
has also required the development of programs to support the transition<br />
from university to the operational environment, and further evolution of these<br />
programs is expected.<br />
There has been a major emphasis on improving the health, safety and welfare of<br />
the workforce in recent years, and this will continue with further development of<br />
systems to facilitate early intervention and identification of the root causes<br />
of problems.<br />
The new recruitment and education model is also affecting workforce<br />
demographics, with increasing numbers of younger paramedics and women<br />
employed. At the same time, the number of paramedics in older age cohorts<br />
(greater than 50) is also increasing, especially in rural areas.<br />
These changes, as well as more general social trends, are affecting workforce<br />
attitudes and expectations. In particular, staff concerns about work/life balance<br />
will need to be addressed if AV is to remain an employer of choice. This is<br />
likely to involve increased access to part-time work and continuing development<br />
of alternative roster options. Promoting a constructive culture and further<br />
developing internal communications and consultation will also assist in meeting<br />
emerging staff expectations and improving organisational effectiveness.<br />
The availability of appropriate opportunities for professional development<br />
is another key aspect of meeting legitimate staff expectations, as well as<br />
strengthening organisational capability and facilitating succession planning.<br />
The focus on workforce development includes ensuring that opportunities are<br />
available for volunteers, especially those wishing to become career paramedics.<br />
7
Community expectations and capabilities<br />
There is a clear recognition in the Victorian community of the contribution<br />
paramedics make to its well-being. However, there are opportunities to<br />
improve services and increase access for specific communities through a<br />
better understanding of their needs.<br />
Environmental responsibilities<br />
Environmental change has the potential to impact on AV service delivery,<br />
most obviously by increasing the risk of major incidents such as bushfire or<br />
pandemic. More subtle impacts on the patterns of demand may also occur.<br />
These impacts clearly need to be factored into AV planning.<br />
There have been a number of recent initiatives to improve links with<br />
Culturally and Linguistically Diverse communities and the Aboriginal<br />
community and to improve staff awareness of community diversity.<br />
Work will continue with these groups to further strengthen relationships;<br />
collaborations with patient groups with special clinical needs will also be<br />
extended. Working with the Department of Health and local communities<br />
to identify opportunities to improve ambulance services and contribute to<br />
better health system performance in specific geographic locations will be<br />
another important priority.<br />
Engagement with the community has also been focused on improving<br />
community capability and preparedness to manage an emergency.<br />
Current programs include targeted promotion of CPR skills and a range of<br />
schools programs, and these will continue to develop.<br />
At the same time, AV has placed increasing emphasis on implementing more<br />
environmentally sustainable practices. However, there is significant scope for<br />
improvement to ensure the organisation meets appropriate environmental targets.<br />
.<br />
There are more than twenty five Community Emergency Response Teams<br />
across the State, providing invaluable access to early initial treatment and<br />
support for career paramedics. Ambulance Community Officers also play<br />
a critical role in AV’s emergency response in more remote areas. Further<br />
developing support systems to ensure the sustainability of AV’s volunteer<br />
response capability will be a high priority during the planning period.<br />
8
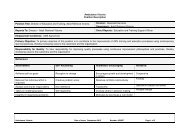
6. Strategic Framework<br />
A set of strategic themes, each linked to one of four strategic objectives set out in section 4, complete the framework for the Strategic Plan<br />
The strategic themes identify the primary aim of the specific initiatives within the plan. Each of the themes is related to one or more of the key<br />
issues outlined in the previous section, and the initiatives linked to the theme are designed to address these issues. A visual representation of<br />
this framework is included on page 26.<br />
Objectives Strategic themes Key issues<br />
1. Improve service quality and<br />
efficiency to better meet patient needs<br />
1.1 Demand management:<br />
Improve matching of patient needs & services<br />
1.2 Process efficiency:<br />
Increase the efficiency of resource use to deliver<br />
improved services<br />
1.3 Health System integration:<br />
Further develop collaboration with other health service<br />
providers to improve health system performance<br />
1.4 Emergency Services coordination:<br />
Further develop collaboration with emergency service<br />
organisations to improve effectiveness of ambulance<br />
service delivery<br />
• Increasing demand for service<br />
• Resource constraints<br />
• Community expectations<br />
• Health System developments<br />
• Resource constraints<br />
• Advances in technology<br />
• Equity in service delivery<br />
• Risk of major incidents<br />
• Environmental responsibilities<br />
• Health System developments<br />
• Evidence based practice<br />
• Community expectations<br />
• Advances in technology<br />
• Risk of major incidents<br />
• Equity in service delivery<br />
• Community expectations<br />
1.5 Standard and scope of care:<br />
Enhance clinical care to improve patient outcome<br />
• Evidence based practice<br />
• Equity in service delivery<br />
• Health System developments<br />
9
Objectives Strategic themes Key issues<br />
2. Foster workforce development<br />
and welfare<br />
3. Develop organisational systems<br />
and resources to support improved<br />
service delivery<br />
2.1 Workforce capability:<br />
Support workforce development to increase organisational<br />
effectiveness<br />
2.2 Workforce health and safety:<br />
Improve workforce health & safety<br />
2.3 Workforce wellbeing:<br />
Further develop working environment to promote<br />
workforce well-being<br />
3.1 Performance Monitoring<br />
Refine measurement of performance to drive improved<br />
service delivery<br />
3.2 Information Management<br />
Further develop information systems to support<br />
improvements in service delivery<br />
3.3 Financial Management<br />
Strengthen the organisation’s financial position to support<br />
service delivery development<br />
• Workforce expectations<br />
• Evidence based practice<br />
• Advances in technology<br />
• Community expectations<br />
• Workforce expectations<br />
• Community expectations<br />
• Workforce expectations<br />
• Community expectations<br />
• Community expectations<br />
• Resource constraints<br />
• Evidence based practice<br />
• Organisational consolidation<br />
• Advances in technology<br />
• Organisational consolidation<br />
• Resource constraints<br />
• Organisational consolidation<br />
3.4 Business Systems and processes:<br />
Further develop business systems to support consistency<br />
and quality of service<br />
• Resource constraints<br />
• Advances in technology<br />
• Organisational consolidation<br />
10
Objectives Strategic themes Key issues<br />
3. Develop organisational systems<br />
and resources to support improved<br />
service delivery (continued)<br />
3.5 Research:<br />
Increase research to support innovation in service delivery<br />
3.6 Environmental Sustainability:<br />
Reduce the environmental impact of AV activities<br />
• Evidence based practice<br />
• Health system developments<br />
• Community expectations<br />
• Environmental responsibilities<br />
4. Strengthen community<br />
relationships and promote community<br />
initiatives and policy to improve<br />
patient outcomes<br />
4.1 Community capability and awareness:<br />
Increase community awareness and skills to manage<br />
medical emergencies and collaborations with the community<br />
to improve patient outcomes<br />
4.2 Community relationships and accountability:<br />
Strengthen relationships with the community,<br />
improve understanding of the AV role and fulfil broader<br />
social responsibilities<br />
• Community expectations<br />
• Increasing demand for service<br />
• Workforce expectations<br />
• Resource constraints<br />
• Community expectations<br />
• Environmental responsibilities<br />
4.3 Policy and system development:<br />
Further develop the ambulance role in contributing to<br />
broader health policy and systems<br />
• Health system developments<br />
• Increasing demand for service<br />
• Resource constraints<br />
11
7. Strategic Initiatives <strong>2010</strong> to <strong>2012</strong><br />
Strategic initiatives have been developed to address the four organisational objectives and the aims expressed in the strategic themes. Target outcomes have<br />
been specified for each of the strategic initiatives. The initiatives and targets are described below, grouped according to the relevant AV service delivery area.<br />
1. Improve service quality and efficiency to better meet patient needs<br />
Emergency Response<br />
Strategic themes Strategies Outcomes<br />
Demand management:<br />
Improve matching of patient needs<br />
and services<br />
• Continue to refine 000 call prioritisation and ensure<br />
consistency of prioritisation statewide<br />
• Further develop the metropolitan Referral Service,<br />
increasing the referral options available and the scope of<br />
calls handled, and extend the Service statewide<br />
• Undertake further analysis of the drivers of demand<br />
and work with DH to identify new demand management<br />
strategies, including strategies to improve service delivery<br />
to specific patient categories and improved links to<br />
primary care services<br />
Improved identification of patient needs at the time of<br />
000 call for better targeted response<br />
Increased availability of appropriate alternatives to<br />
emergency ambulance response for lower priority<br />
000 callers<br />
Development of innovative strategies to address demand<br />
• Collaborate with nursing homes and other service<br />
providers to ensure a more appropriate ambulance response<br />
to nursing homes<br />
More appropriate matching of response to the needs<br />
of nursing home staff<br />
• Review planning criteria and methodology for<br />
emergency response resources in rural and remote areas<br />
Equitable basis for prioritising investment in response<br />
resources<br />
• Develop a long-term plan for statewide emergency<br />
response resources, taking into account demographic<br />
change and other drivers of demand<br />
Sufficient emergency response capacity to meet<br />
demand and achieve performance targets<br />
12
Strategic themes Strategies Outcomes<br />
Process efficiency:<br />
Increase the efficiency of resource<br />
use to deliver improved services<br />
• Improve the efficiency of the response process by:<br />
> Reducing case times<br />
> Improving the efficiency of logistic support processes<br />
> More dynamic deployment of resource units, building on<br />
current use of the Siren decision support system<br />
> Improving the management of urgent (Code 2) cases<br />
> Improving the efficiency of the interface with hospitals<br />
• Review dispatch rules (in conjunction with refinement<br />
of 000 call prioritisation), and ensure consistency of<br />
dispatch practice statewide<br />
• Complete implementation of a new operational<br />
front-line management model<br />
• Transfer rural call taking and dispatch to a single<br />
Communications Centre operated by ESTA, using a new<br />
Computer Aided Dispatch system<br />
• Continue to work with ESTA to improve call taking and<br />
dispatch processes<br />
• Develop and implement a statewide rostering system<br />
and paramedic placement model<br />
• Refine coordination processes for the management of<br />
time critical patient transfers<br />
Increased availability of response units and improved<br />
response times<br />
Better matching of dispatch with patient needs and<br />
more effective use of resources<br />
More effective management and improved<br />
operational performance<br />
More efficient and effective rural call taking and dispatch<br />
More efficient and effective call taking and dispatch<br />
More cost effective use of operational workforce and<br />
improved consistency of service delivery<br />
More efficient and timely transfer of time critical patients<br />
13
Strategic themes Strategies Outcomes<br />
Health system integration:<br />
Further develop collaboration with<br />
other health service providers to<br />
improve system performance<br />
• In conjunction with DH and the major health services,<br />
develop and implement improved processes for selection<br />
of hospital destinations<br />
• In conjunction with health services, further develop and<br />
implement systems for en route transmission of clinical<br />
information to receiving hospitals to enable early activation<br />
of the hospital response<br />
Better access for patients to definitive care<br />
Improved access for patients to definitive care<br />
• Continue development and implementation of an<br />
integrated strategy for acute coronary care patients,<br />
including early access to primary coronary angioplasty<br />
services and in-field thrombolysis where appropriate<br />
• Identify patient care pathways which provide a potential<br />
alternative to attendance at a hospital ED and explore<br />
options to improve their accessibility to paramedics<br />
Improved outcomes for acute coronary care patients<br />
Earlier access for patients to appropriate care<br />
• Work with DH and health services to evaluate and<br />
refine the current ambulance role in the response to<br />
mental health patients<br />
Improved service delivery for mental health patients<br />
• Work with DH regions to develop and implement strategies<br />
for improved integration and coordination of ambulance<br />
and health services<br />
Improved integration with regional health services<br />
14
Strategic themes Strategies Outcomes<br />
Emergency services coordination:<br />
Further develop collaboration with<br />
emergency service organisations to<br />
improve effectiveness of service delivery<br />
Standard and scope of care:<br />
Enhance clinical care to improve<br />
patient outcomes<br />
• Evaluate the pilot Country Fire Authority Emergency<br />
Medical Response program in outer Melbourne (involving<br />
simultaneous dispatch of AV and CFA resources to<br />
suspected cardiac arrest cases) and, subject to the outcome,<br />
implement the EMR program in appropriate areas statewide<br />
• Further develop the AV Clinical Risk Management System,<br />
including sentinel event and clinical incident systems<br />
• Strengthen systems for review of the Clinical Practice<br />
Guidelines by drawing on VACIS data, including<br />
establishment of links with hospital (and other) data to assist<br />
outcome analysis<br />
Improved cardiac arrest outcomes<br />
Identification of opportunities for system improvement<br />
Stronger evidence base for clinical practice<br />
• Improve systems to facilitate the clinical development of<br />
paramedics based on VACIS data<br />
• Review the current paramedic scope of practice and<br />
develop appropriate new model(s) of paramedic practice,<br />
taking into account the needs of the specific communities<br />
served by AV, health system developments and experience<br />
in other jurisdictions<br />
Improved clinical support and development<br />
for paramedics<br />
Evaluation of new models of paramedic practice to<br />
support improved health system performance and<br />
(if appropriate) initial implementation of new model(s)<br />
• Investigate statewide variation in cardiac arrest outcomes<br />
and develop strategies to reduce differences<br />
Improved cardiac arrest outcomes<br />
15
Non-Emergency Transport<br />
Strategic themes Strategies Outcomes<br />
Demand management:<br />
Improve matching of patient needs<br />
and services<br />
• In conjunction with DH, review and refine the current<br />
criteria for use of non-emergency transport<br />
Improved matching of resource type with patient need<br />
Process efficiency:<br />
Increase the efficiency of resource use<br />
to deliver improved services<br />
• Develop and implement a statewide non-emergency<br />
services strategy, with a particular focus on options for rural<br />
service delivery and appropriate use of non-emergency<br />
resources for high acuity transports<br />
• Complete statewide implementation of a non-emergency<br />
scheduling and vectoring system<br />
More efficient fleet management and improved<br />
service delivery<br />
Health system integration:<br />
Further develop collaboration with other<br />
health service providers to improve<br />
system performance<br />
• Explore options to assist hospital discharge processes in<br />
collaboration with DH and health services<br />
• Develop relationships with non-government agencies to<br />
assist with rural low acuity patient transport<br />
Improved patient flow in hospitals<br />
Improved allocation of resources and service delivery<br />
to rural and low acuity patients<br />
16
Air Ambulance<br />
Strategic themes Strategies Outcomes<br />
Demand management:<br />
Improve matching of patient needs<br />
and services<br />
• Continue to refine dispatch criteria to ensure appropriate<br />
use of aircraft<br />
Better matching of dispatch with patient needs and more<br />
effective use of resources<br />
Process efficiency:<br />
Increase the efficiency of resource use to<br />
delivery improved services<br />
• Prepare a strategy for the long term development of<br />
air ambulance operations and implement the strategy<br />
progressively<br />
More efficient and effective air ambulance operations<br />
Health system integration:<br />
Further develop collaboration with other<br />
health service providers to improve<br />
system performance<br />
• Work with rural and regional health services to improve the<br />
timeliness of aircraft activation<br />
Earlier access for patients to appropriate care<br />
Retrieval Services<br />
Strategic themes Strategies Outcomes<br />
Process efficiency:<br />
Increase the efficiency of resource use<br />
to deliver improved service<br />
• Implement the ARV service improvement plan and<br />
benchmark performance with other jurisdictions<br />
Improved service delivery for adult medical retrievals<br />
Health system integration:<br />
Further develop collaboration with other<br />
health service providers to improve<br />
system performance<br />
• Collaborate with DH and the non-adult retrieval services<br />
(peri-natal, neo-natal and paediatric) to improve the<br />
interface between the services and air ambulance<br />
Improved service delivery for non-adult medical<br />
retrievals<br />
• Continue to work with DH and health services to improve<br />
the management of access to critical care beds<br />
Improved accessibility of critical care beds<br />
17
Major Incident Preparedness<br />
Strategic themes Strategies Outcomes<br />
Demand management:<br />
Improve matching of patient needs<br />
and services<br />
Process efficiency:<br />
Increase the efficiency of resource use to<br />
deliver improved services<br />
• Continue close monitoring of the risks of all types of major<br />
incident, and ensure appropriate AV capability is developed<br />
and maintained<br />
• Continue development of major incident response<br />
processes to ensure statewide consistency of approach<br />
AV major incident capability meeting Government<br />
and community expectations<br />
Integrated and consistent statewide response to<br />
major incidents<br />
Health system integration:<br />
Further develop collaboration with other<br />
health service providers to improve<br />
system performance<br />
• Continue major incident planning, liaison and coordination<br />
with all relevant national and State response and planning<br />
bodies<br />
Improved coordination of major incident response<br />
agencies and strengthened system capability to<br />
respond to a major incident<br />
Emergency services coordination:<br />
Further develop collaboration with<br />
emergency service organisations to<br />
improve effectiveness of service delivery<br />
• Continue work with inter-state ambulance services (via the<br />
Council of Ambulance Authorities) and emergency services<br />
organisations to ensure appropriate ambulance involvement<br />
in national major incident planning<br />
Improved coordination of major incident response<br />
agencies and strengthened system capability to<br />
respond to a major incident<br />
18
2. Foster workforce development and welfare<br />
Strategic themes Strategies Outcomes<br />
Workforce capability:<br />
Support workforce development to<br />
increase organisational effectiveness<br />
• Develop a long-term workforce plan which identifies future<br />
organisational workforce needs and assists universities to<br />
plan student intakes<br />
• Support national initiatives on paramedic course<br />
accreditation through the Council of Ambulance Authorities,<br />
and continue AV liaison with universities regarding their<br />
selection procedures and curricula of paramedic courses<br />
Assured future supply of appropriately qualified<br />
paramedics<br />
Continuing development of paramedic education to meet<br />
service delivery needs<br />
• Review the current program for graduate paramedic<br />
recruits and explore options to improve their transition into<br />
the workforce<br />
Improved pathway for paramedic graduates to obtain<br />
the experience required to practice independently<br />
• Promote the career development of paramedics, including<br />
progression to specialist roles (MICA, Clinical Instructor,<br />
Clinical Specialist, Clinical Support Officer, Flight Paramedic<br />
etc)<br />
Improved AV clinical performance and workforce<br />
satisfaction<br />
• Further expand opportunities for all members of the<br />
workforce to develop their management and technical skills<br />
and strengthen the succession planning framework<br />
Improved management capability and succession<br />
planning<br />
• Develop and implement new strategies to attract and retain<br />
paramedics in regional and rural areas<br />
Improved retention of rural operational workforce<br />
19
Strategic themes Strategies Outcomes<br />
Workforce capability:<br />
Support workforce development to<br />
increase organisational effectiveness<br />
(continued)<br />
• Further develop strategies and support processes to ensure<br />
the engagement, sustainability, reward and recognition of the<br />
volunteer workforce<br />
• Further support the professional development of Ambulance<br />
Community Officers and Community Emergency Responders<br />
(including development of pathways to paramedic education)<br />
• Further develop and implement flexible learning options<br />
(e.g. on-line systems)<br />
• Further develop programs to promote workforce awareness<br />
of the needs of CALD and Aboriginal communities<br />
• Promote continuing development of a constructive and<br />
consistent organisational culture, including further<br />
development of mechanisms for workforce engagement,<br />
communication and consultation<br />
Improved integration of volunteers with AV operations<br />
and better patient outcomes in communities served by<br />
volunteers<br />
Improved level of service to rural communities and<br />
supply of paramedics in rural locations<br />
Improved workforce access to training and education<br />
programs<br />
Improved service delivery for CALD and Aboriginal<br />
communities<br />
Constructive attitudes and behaviours focused on<br />
common objectives<br />
Workforce health and safety:<br />
Improve workforce health and safety<br />
• Develop and implement an integrated AV Occupational<br />
Health and Safety Strategic Plan, with a focus on:<br />
> Health check and immunisation programs<br />
> Early intervention<br />
> Appropriateness of equipment<br />
> Manual handling injuries<br />
> Managing aggression/assault<br />
> Stress<br />
> Fatigue<br />
> Monitoring of trends and root cause analysis to identify<br />
underlying issues<br />
> Benchmarking with other jurisdictions<br />
Reduced workforce injuries and lost time<br />
20
Strategic themes Strategies Outcomes<br />
Workforce well-being:<br />
Further develop working environment to<br />
promote workforce well-being<br />
• Develop further initiatives to provide greater flexibility in<br />
working arrangements, including increased availability<br />
of part time options<br />
• Continue exploration of alternative rosters, taking into<br />
account workforce welfare impacts and service delivery<br />
requirements<br />
• Continue program of branch refurbishment to improve<br />
employees’ working environment<br />
Increased opportunities for a better work/life balance<br />
Identification of a suite of preferred future rosters<br />
Improved working environment for both operational<br />
and administrative workforce<br />
3. Develop organisational systems and resources to improve service delivery<br />
Strategic themes Strategies Outcomes<br />
Performance monitoring:<br />
Refine measurement of performance to<br />
drive improved service<br />
• Continue development of AV performance measures and<br />
targets (including operational, clinical and support services<br />
measures) and extend benchmarking with comparable<br />
services<br />
• In consultation with ESTA, further develop CAD<br />
performance measures for ambulance, reflecting both the<br />
speed and quality of call-taking and dispatch<br />
More complete view of AV performance and value<br />
Refined set of call-taking and dispatch performance<br />
measures, reflecting service delivery needs<br />
• Establish links with external data sources to facilitate<br />
further development of patient outcome measures<br />
• Work with DH and health services to develop measures of<br />
health system performance (including an AV component)<br />
Improved understanding of AV impact on<br />
patient outcomes<br />
More complete view of system performance and<br />
AV contribution<br />
21
Strategic themes Strategies Outcomes<br />
Information mangement:<br />
Further develop systems to support<br />
improvements in service delivery<br />
• Develop and implement a comprehensive Information<br />
Management Strategic Plan with a focus on:<br />
> Identification of future information requirements<br />
> Further integration of data from internal and external sources<br />
> Extending use of GIS data<br />
> Provision of real time management information<br />
> Real time transmission and receipt of clinical and management<br />
data with hospitals (e.g. pre-arrival ECG, projected arrivals,<br />
hospital status)<br />
> Infrastructure requirements to support systems development<br />
> Organisational consistency<br />
• Complete implementation of integrated statewide<br />
information systems for key processes, including<br />
financial, human resource, payroll, time and attendance,<br />
and clinical systems<br />
Increased accessibility, completeness, reliability and<br />
timeliness of management information to support<br />
improved decision-making<br />
Consistent management processes<br />
Financial mangement:<br />
Strengthen the organisation’s financial<br />
position to support service development<br />
• Explore opportunities to refine the current funding model and<br />
increase clarity about future funding<br />
• Continue development of strategies to improve the<br />
performance of the Membership Scheme (including the<br />
introduction of new products)<br />
• Develop and implement strategies to increase the capacity<br />
to fund new initiatives internally<br />
Increased certainty about future financial position<br />
to support longer term service planning<br />
Increased revenue from Membership Scheme<br />
Increased ability to implement service innovations<br />
22
Strategic themes Strategies Outcomes<br />
Business systems and processes:<br />
Further develop business systems to<br />
support consistency and quality of<br />
service delivery<br />
Research:<br />
Increase research to support innovation in<br />
service delivery<br />
• Further develop AV quality and risk management systems,<br />
including business continuity systems<br />
• Explore opportunities to establish further data links with<br />
business partners<br />
• Implement improved logistics management systems (for fleet,<br />
medical equipment, supplies etc)<br />
• Ensure AV clinical data is effectively used to support<br />
innovations in practice and promote the national roll-out<br />
of VACIS to facilitate national ambulance research and<br />
benchmarking<br />
• Continue to build research collaborations with universities,<br />
health services and other research bodies<br />
• Monitor international research and innovation in ambulance<br />
and the broader health sector to identify opportunities to<br />
improve service delivery<br />
Increased reliability and consistency of service delivery<br />
Increased efficiency of business processes<br />
Increased efficiency and effectiveness of operations<br />
support processes<br />
Further evidence-based development of practice<br />
Increased research to identify clinical and operational<br />
service improvement opportunities<br />
Early identification of options to improve services<br />
Environmental responsibilities:<br />
Reduce the environmental impact of<br />
AV activities<br />
• Implement an organisational plan to reduce the<br />
environmental impact of AV activities<br />
Reduced environmental impacts and improved<br />
environmental sustainability<br />
23
4. Strengthen community relationships and promote community initiatives and policy to improve patient outcomes<br />
Strategic themes Strategies Outcomes<br />
Community capability and awareness:<br />
Increase community awareness and skills<br />
to manage medical emergencies and<br />
collaborations with the community to<br />
improve patient outcomes<br />
• Continue to develop community CPR skills, with a focus<br />
on at risk groups, CALD communities and the Aboriginal<br />
community<br />
• Collaborate with partner organisations (including<br />
community safety organisations and first aid providers) to<br />
reduce preventable injuries and increase the community<br />
uptake of first aid training<br />
Increased community capability in CPR, contributing<br />
to improved cardiac arrest survival rates<br />
Increased community capability in injury prevention and<br />
first aid<br />
• Develop strategies for community engagement to improve<br />
the community/ambulance response for specific clinical<br />
conditions (e.g. asthma, stroke, diabetes, mental health<br />
and cardiovascular)<br />
Improved patient outcomes<br />
Community relationships and<br />
accountability:<br />
Strengthen relationships with the<br />
community, improve understanding of the<br />
AV role and fulfil broad social<br />
responsibilities<br />
• Further develop mechanisms for community engagement,<br />
including the Community Advisory Committee and auxiliaries<br />
• Continue to develop community relationships to improve<br />
access and equity, with a particular focus on CALD<br />
communities and the Aboriginal community, including the<br />
development of an AV Reconciliation Plan<br />
• Explore options to increase public awareness of appropriate<br />
ambulance use<br />
• Refine public reporting of AV performance, including<br />
additional reporting of clinical outcomes and clinical incidents<br />
Improved understanding of community needs<br />
Improved responsiveness to specific community needs<br />
More appropriate use of ambulance services<br />
Increased public accountability<br />
24
Strategic themes Strategies Outcomes<br />
Health policy and system<br />
development:<br />
Further develop the ambulance role in<br />
improving the health system performance<br />
• Provide policy input to DH to ensure unintended<br />
impacts of health system developments on ambulance<br />
service delivery are minimised<br />
• Collaborate with DH and health services to identify<br />
opportunities and develop strategies to improve the health<br />
system response for specific categories of high acuity patients<br />
• Strengthen links with the primary health care sector and<br />
explore options to improve service delivery via partnerships<br />
with other service providers, particularly general practitioners<br />
More effective and appropriate use of<br />
ambulance services<br />
Better coordination of ambulance and health<br />
services and improved outcomes for high<br />
acuity patients<br />
More appropriate use of ambulance services and<br />
improved patient outcomes<br />
• Work through the Council of Ambulance Authorities to<br />
improve the recognition of the ambulance role and issues<br />
at a national level<br />
Increased national recognition of the ambulance<br />
contribution to health system performance<br />
25
AV Strategic Framework<br />
AV role and principles<br />
Strategic objectives<br />
Improve Service<br />
Quality & Efficiency<br />
Foster Staff<br />
Development &<br />
Welfare<br />
Develop Systems &<br />
Resources<br />
Strengthen<br />
Community<br />
Relationships &<br />
Promote Initiatives<br />
Planning environment and issues<br />
Strategic themes<br />
• Demand Management<br />
• Process Efficiency<br />
• Health System Integration<br />
• Emergency Services Coordination<br />
• Standard & Scope of Care<br />
• Workforce Capability<br />
• Workforce Health & Safety<br />
• Workforce Well-being<br />
• Performance Monitoring<br />
• Information Management<br />
• Financial Management<br />
• Business Systems & Processes<br />
• Research<br />
• Environmental Sustainability<br />
• Community Capability & Awareness<br />
• Community Relationships & Accountability<br />
• Policy & System Development<br />
26
8. Performance measurement<br />
AV monitors its organisational performance using a suite of<br />
performance indicators grouped into four broad categories, which<br />
are closely aligned to the four strategic objectives outlined above:<br />
> Service delivery standards<br />
> Workforce development and welfare<br />
8.1 Service delivery standards<br />
These performance indicators measure the quality of AV service delivery<br />
Performance<br />
Indicator<br />
Measures<br />
> Resource management and cost effectiveness<br />
> Health system and community capability<br />
Further development of the indicator suite is proposed during the<br />
planning period, with particular focus on refinement and expansion<br />
of service delivery indicators including measures of response time,<br />
clinical outcome and non-emergency performance (see Section 7<br />
above). Where necessary, more specific measures will also be<br />
introduced to evaluate the effectiveness of each of the strategies<br />
outlined in Section 7.<br />
Existing performance indicators and related measurement<br />
definitions are detailed below. Specific targets are set for each<br />
measure every year in the AV Annual Plan.<br />
Call taking and<br />
dispatching times<br />
Emergency<br />
response times<br />
Standard of care<br />
Percentage of 000 calls answered within 5 seconds<br />
Percentage of Code 1 incidents with total time<br />
to dispatch within 150 seconds<br />
90th percentile response time to suspected<br />
cardiac arrests (Priority 0)<br />
Percentage of Code 1 incidents responded to<br />
within 15 minutes<br />
Percentage of Code 1 incidents responded<br />
to within 15 minutes in urban centres with<br />
population greater than 7,500<br />
Percentage of audited cases meeting standards<br />
(compliance with Clinical Practice guidelines)<br />
> emergency cases<br />
> non-emergency cases<br />
> CERT<br />
27
Performance<br />
Indicator<br />
Patient outcomes<br />
Measures<br />
1<br />
Percentage of adult cardiac arrest patients<br />
with vital signs at hospital<br />
Percentage of adult cardiac arrests patients<br />
surviving to hospital discharge<br />
Mean reduction in pain score for<br />
> ischaemic chest pain<br />
> traumatic pain<br />
Percentage of patients with initial severe cardiac<br />
relief or traumatic pain who receive significant<br />
pain relief<br />
Percentage of potential major trauma patients<br />
(non-trapped) with scene time less than or<br />
equal to 20 minutes<br />
1<br />
8.2 Workforce development and welfare<br />
These performance indicators measure the effectiveness<br />
of strategies to promote workforce development, health<br />
and safety<br />
Performance<br />
Indicator<br />
Workforce<br />
education and<br />
training<br />
Workforce health and<br />
safety<br />
Measures<br />
Average days of training per employee per year<br />
Sick leave rate<br />
> operational employees<br />
> non-operational employees<br />
Average annual days lost through work-related injury<br />
per operational employee<br />
Patient satisfaction<br />
Percentage of patients (or their carers)<br />
satisfied or very satisfied with service<br />
Number of complaints per thousand cases<br />
> total complaints<br />
> substantiated complaints<br />
Percentage of members satisfied or very<br />
satisfied with the Membership Scheme<br />
Workforce<br />
satisfaction<br />
Average full shift overtime per week (operational<br />
employees)<br />
Percentage of workforce satisfied (or better) working<br />
at AV<br />
> operational employees<br />
> non-operational employees<br />
1. Adult cardiac arrests not witnessed by a paramedic, presenting in VF/VT where resuscitation attempted<br />
28
8.3 Resource management and cost effectiveness<br />
These performance indicators measure the effectiveness of<br />
resource and cost management and of financial strategies to<br />
support service delivery<br />
8.4 Health system & community capability<br />
These performance indicators measure the effectiveness of<br />
other health care providers, partner organisations and the<br />
broader community in contributing to emergency outcomes<br />
Performance<br />
Indicator<br />
Measures<br />
Performance<br />
Indicator<br />
Measures<br />
Service delivery costs<br />
Overhead costs<br />
Cost per case for each service delivery category<br />
> emergency road<br />
> non-emergency road<br />
> air ambulance rotary wing<br />
> air ambulance fixed wing<br />
> adult retrieval<br />
Percentage of operating expenditure spent on<br />
administration<br />
Management of low<br />
priority 000 callers<br />
First responder<br />
programs<br />
Percentage of 000 callers receiving health<br />
advice or service from another health<br />
provider as an alternative to emergency<br />
ambulance response<br />
Percentage of suspected cardiac arrest cases<br />
(Priority 0) where (non-AV) first responder<br />
arrives first<br />
Generation of<br />
non-government<br />
revenue<br />
Financial liquidity<br />
Percentage of population (excluding pensioners<br />
and health care card owners), who are members<br />
of the Membership Scheme<br />
Administrative cost per member of the<br />
Membership Scheme<br />
• Quick asset ratio<br />
• Current asset ratio<br />
Community first aid<br />
skills<br />
Community<br />
satisfaction<br />
Health sector<br />
satisfaction<br />
Percentage of incidents where CERT is<br />
dispatched and arrives first<br />
Percentage of witnessed cardiac arrests where<br />
bystander CPR is undertaken<br />
Percentage of community satisfied or very<br />
satisfied with AV performance<br />
Percentage of health sector stakeholders<br />
satisfied with AV performance<br />
29
9. Ambulance Victoria in <strong>2012</strong><br />
AV’s strategies to <strong>2012</strong> build on the significant development of Victoria’s<br />
ambulance services which have occurred over the last ten years.<br />
The creation of a single statewide service in 2008 was a major step<br />
in a continuing process of transformation. On-going work to ensure<br />
consistency and integration of services and systems will be a continuing<br />
theme during the planning period.<br />
Major developments in service delivery by <strong>2012</strong> will include:<br />
• Rationalisation of rural communications centres, and statewide<br />
consistency in call taking and dispatching<br />
• Progress towards more consistent patient outcomes across the<br />
State (particularly cardiac arrest outcomes)<br />
• Continuing improvement in coordination and integration with the<br />
broader health sector, including improved performance at the hospital<br />
interface and extension of referral options<br />
• Evaluation of options for extending the scope of paramedic<br />
practice and (if appropriate) initial implementation of new model(s)<br />
• More efficient and dynamic management of emergency response<br />
resources<br />
• Strengthening of statewide major incident response systems and<br />
capability<br />
• More consistent statewide approach to the provision of nonemergency<br />
patient transport<br />
• More efficient and effective air ambulance services<br />
• Improved levels of service for adult retrievals statewide<br />
There will be a continuing focus on workforce development and welfare through<br />
the planning period. This will include promotion of a positive and consistent<br />
organisational culture and further development of mechanisms for workforce<br />
engagement and consultation.<br />
Strategies to minimise health and safety risks to the workforce will remain a key<br />
priority, and options to provide more flexible working arrangements will be developed.<br />
The program of facilities refurbishments will continue across the State.<br />
AV will work closely with the universities to ensure paramedic education meets<br />
organisational requirements and there is an appropriate future supply of qualified<br />
workforce.<br />
Organisational information systems will continue to evolve, with particular focus on<br />
integration of systems and data across the organisation, more real time reporting,<br />
more effective use of GIS data and better linkages with relevant external data.<br />
Use of VACIS data to support more evidence based approaches to clinical practice<br />
and training, and research to drive innovation will be significant priorities.<br />
Reducing AV’s environmental footprint will be an important objective for the planning<br />
period.<br />
AV is committed to further strengthening community relationships across the State,<br />
with a particular focus on improving its responsiveness to special needs and increasing<br />
the capability of communities to manage emergencies prior to ambulance arrival.<br />
30
Glossary & abbreviations<br />
ACO<br />
ARV<br />
AV<br />
CAA<br />
CAD<br />
CALD<br />
CERT<br />
CFA<br />
CPG<br />
DH<br />
Dispatch Code<br />
ECG<br />
ED<br />
EMA<br />
ESTA<br />
GIS<br />
MFB<br />
MICA<br />
MTS<br />
Single<br />
Responder<br />
Ambulance Community Officer<br />
Adult Retrieval Victoria<br />
Ambulance Victoria<br />
Council of Ambulance Authorities Australia<br />
Computer Aided Dispatch<br />
Culturally and Linguistically Diverse<br />
Community Emergency Response Team<br />
Country Fire Authority<br />
Clinical Practice Guidelines<br />
Department of Health<br />
Priority of ambulance dispatch (From 1 to 3; Code 1 means a<br />
time critical dispatch, with a response using lights and sirens)<br />
Electrocardiogram<br />
Hospital Emergency Department<br />
Emergency Management Australia<br />
Emergency Services Telecommunications Authority<br />
Geographic Information Systems<br />
Metropolitan Fire Brigade<br />
Mobile Intensive Care Ambulance<br />
Major Trauma Service (The Alfred Hospital, Royal Melbourne Hospital & Royal Children’s Hospital)<br />
MICA paramedic or Ambulance paramedic response unit<br />
without transport capability (usually a sedan)<br />
SHERP<br />
State Health Emergency Response Plan<br />
Triage Category Priority assigned to patients in hospital emergency departments (from 1 to 5)<br />
VACIS<br />
Victoria Ambulance Clinical Information System<br />
VACU<br />
Victorian Ambulance Counselling Unit<br />
31