Inside Story - University College London Hospitals
Inside Story - University College London Hospitals
Inside Story - University College London Hospitals
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
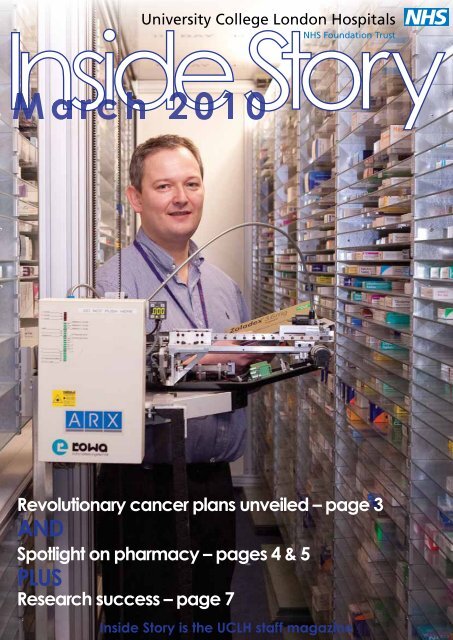
<strong>Inside</strong> <strong>Story</strong><br />
Revolutionary cancer plans unveiled – page 3<br />
AND<br />
Spotlight on pharmacy – pages 4 & 5<br />
PLUS<br />
Research success – page 7<br />
<strong>Inside</strong> <strong>Story</strong> is the UCLH staff magazine
news<br />
Honouring staff long service<br />
From researchers to registrars and<br />
nurses to managers, a whole host of<br />
UCLH staff have been honoured for<br />
their long service to UCLH.<br />
Some 35 members of staff who have<br />
achieved at least 25 years’ service<br />
were awarded with a crystal bowl<br />
during the ceremony organised by<br />
UCLH Charity and hosted by Peter<br />
Dixon, Trust chairman.<br />
Peter said: “You are the important<br />
people and what you do is fantastic.<br />
Yes, we have got the buildings and<br />
the technology but without the staff<br />
it’s nothing. It’s you people that make<br />
this the great place it is.”<br />
Pictured in the front row (l to r) are<br />
Kay Eaton, consultant nurse, cancer<br />
services who joined UCH as a<br />
student nurse in 1984 and<br />
Wihermina Rasay, deputy<br />
phlebotomy manager, who<br />
joined in 1972 as a<br />
phlebotomy nurse. In the<br />
back row (l to r) are Jim<br />
Waite, biomedical scientist,<br />
who has been with the<br />
Trust since 1978; David<br />
Starke, risk management<br />
and business continuity<br />
lead, who started at UCLH<br />
in 1972; and Howard<br />
Swanton, consultant<br />
cardiologist, who began<br />
work at the Middlesex<br />
Hospital in 1979.<br />
Louise wins top award<br />
Chief nurse Louise Boden has won a<br />
prestigious award in honour of her<br />
outstanding contribution to healthcare<br />
improvement and the nursing<br />
profession.<br />
She was presented with the Nursing<br />
Times lifetime achievement award<br />
after winning the public vote in an<br />
online poll.<br />
Louise was shortlisted by a<br />
distinguished panel who said she had<br />
won 'wide respect' for nurturing and<br />
developing talent both in promoting<br />
the careers of chief nurses at NHS<br />
trusts and in believing that every<br />
nurse, midwife and their support staff<br />
has the potential to develop.<br />
Louise said: "It is a great honour to be<br />
recognised by my peers but my<br />
achievement has only been possible<br />
because of the support I myself have<br />
received throughout my career and<br />
the remarkable nurses and midwives<br />
at UCLH."<br />
In memory<br />
Colleagues were<br />
saddened to hear of<br />
the unexpected<br />
death of John<br />
Golden (pictured<br />
left), Unison branch<br />
secretary and the<br />
senior database<br />
administrator in<br />
pharmacy.<br />
John had worked for the Trust for more<br />
than 20 years and was much valued<br />
for his long-standing trade union work.<br />
He stepped down as chair of staffside<br />
last year but continued to remain<br />
active in union matters.<br />
Colleagues remember John as<br />
someone who always thought of<br />
others rather than himself and would<br />
always make the time to try to resolve<br />
other people’s issues and problems.<br />
Bev Wallace, a local representative for<br />
another union, shared an office with<br />
John.<br />
She said: "If anyone had a problem he<br />
would always take the time to listen. I<br />
will really miss him and keep expecting<br />
him to walk back into the office at any<br />
moment. He wasn't just a colleague,he<br />
was a friend."<br />
Julia Whitehouse, interim workforce<br />
director, said: “On behalf of the Trust, I<br />
would like to take the opportunity to<br />
formally recognise all of John's hard<br />
work and achievements. Our thoughts<br />
are with John's family, friends and<br />
close colleagues at this difficult and<br />
tragic time."<br />
Pioneering<br />
bacteriologist Dr<br />
Joan Stokes<br />
(pictured), who<br />
died recently at<br />
the age of 97,<br />
was a trailblazing<br />
female in a<br />
predominantly<br />
male world.<br />
She was the first<br />
consultant clinical<br />
bacteriologist at UCH, developed<br />
ground-breaking work and was an<br />
inspiration to many. You can read<br />
more about this remarkable woman on<br />
the Insight news pages.<br />
Contact Us<br />
If you have any information you would like included in <strong>Inside</strong> <strong>Story</strong>, or on the Trust<br />
intranet site Insight, contact: Communications Unit, 2nd Floor Central, 250 Euston Road,<br />
<strong>London</strong> NW1 2PG. Email: communications@uclh.nhs.uk, Tel: ext 9897, Fax: ext 9401.<br />
Front cover: Simon Keady with robotic<br />
dispensing machines in UCH pharmacy which<br />
use barcode technology to store and later ‘pick’<br />
medicines with 100% accuracy. See pages 4 & 5.<br />
2
news<br />
(l-r) : Tahir Ahmed,<br />
deputy director capital<br />
investment; Ed Rose,<br />
strategic development<br />
manager: Daren Bubb,<br />
finance lead;Julia<br />
Solano, radiotherapy<br />
services manager; Dr<br />
Ivan Rosenberg,<br />
technical lead; Dr Yen-<br />
Ch’ing Chang, clinical<br />
lead and Matthew<br />
Metcalfe, deputy<br />
director of finance. The<br />
photo shows the PBT<br />
team on the former<br />
“Odeon” site near UCH<br />
which is owned by the<br />
Trust and is the<br />
proposed location for<br />
the new centre.<br />
UCL Partners bids for world-leading cancer treatment<br />
UCLH and five other <strong>London</strong><br />
<strong>Hospitals</strong> have announced plans to<br />
provide Proton Beam Therapy (PBT),<br />
one of the most advanced and<br />
effective forms of radiotherapy in the<br />
world. Proton Beam Therapy is far<br />
more precise than conventional<br />
radiotherapy, and is currently<br />
available in only a handful of locations<br />
worldwide – mostly in the US and<br />
Japan.<br />
More than a 1,000 patients a year –<br />
particularly children and teenagers –<br />
could benefit. It is also beneficial for<br />
adults with brain tumours, head and<br />
neck cancer, bone and soft tissue<br />
sarcomas.<br />
UCL Partners (UCLH, Great Ormond<br />
Street Hospital for Children, Barts and<br />
The <strong>London</strong>, The Royal Free<br />
Hampstead and Moorfields Eye<br />
Hospital) has now submitted a bid to<br />
the Department of Health to provide<br />
PBT. The service would be developed<br />
on land owned by UCLH which is<br />
large enough to house equipment<br />
weighing several hundred tonnes<br />
(see above).<br />
Dr Yen-Ch’ing Chang, a paediatric<br />
clinical oncologist working at UCLH<br />
and Great Ormond Street Hospital for<br />
Children, is leading the proposal. She<br />
said: “For a specific range of cancers,<br />
the advantages of PBT over<br />
conventional radiotherapy are now<br />
unquestionable. “For children in<br />
particular, we will be able to<br />
drastically reduce the chances of<br />
severe long-term side effects.”<br />
Ed Rose, who is project managing the<br />
development, said: "Developing PBT<br />
would allow UCLH to become one of<br />
the world’s leading radiotherapy<br />
centres – particularly for children, and<br />
for adults with complex cancers.<br />
Together with the opening of our new<br />
Cancer Centre in 2012, it would<br />
ensure UCLH continues to provide its<br />
patients with the best possible care.”<br />
If the Department of Health gives UCL<br />
Partners the go-ahead, it is hoped the<br />
new centre will be up and running<br />
within four years.<br />
New chairman to start work in the summer<br />
UCLH non-executive director Richard<br />
Murley (pictured) will take over as<br />
chairman of the Trust when Sir Peter<br />
Dixon steps down in June after nine<br />
years at the helm.<br />
Richard joined UCLH as a nonexecutive<br />
director in November<br />
2008. He is currently co-head of<br />
the UK advisory business at<br />
Rothschild in the City. He was<br />
previously the director general of<br />
the Takeover Panel, the City<br />
regulator. He chairs the<br />
UCLH Quality and Safety<br />
Committee and the<br />
Investment Committee.<br />
Richard has a real<br />
interest in the NHS,<br />
coming from a family of doctors. He is<br />
a Camden resident and his children<br />
were born in the old Elizabeth Garrett<br />
Anderson and Obstetric<br />
Hospital, part of UCLH.<br />
He said: “I am delighted<br />
to have been named<br />
chairman of UCLH. The<br />
Trust has a very high<br />
quality clinical and<br />
management team and I<br />
look forward to working with<br />
them as we strive for<br />
ever-higher<br />
standards of<br />
patient care.”<br />
Sir Peter has<br />
been chairman<br />
at UCLH since 2001.<br />
He said: “Richard is a splendid<br />
appointment for the Trust and will<br />
provide the leadership we need for<br />
turbulent times ahead in the NHS. I<br />
have been privileged to be part of an<br />
exciting time for this great institution<br />
and I am quite sure that Richard will<br />
take it on to even greater heights”.<br />
Sir Robert Naylor, UCLH chief<br />
executive, said: “I am delighted that<br />
one of our non-executive directors<br />
has been appointed as chairman – it<br />
gives continuity to the strategic<br />
direction of the organisation. I look<br />
forward to continuing to work closely<br />
with Richard in the future.”<br />
3
pharmacy special<br />
Change is sometimes the best medicine<br />
The Trust’s pharmacy team has cut<br />
waiting times by 50% over the last<br />
year: the majority of patients now<br />
wait just 15 minutes to pick up their<br />
medicines from the UCH outpatient<br />
dispensary.<br />
Not only that, complaints are<br />
down, staff and patient satisfaction<br />
is up.<br />
So how did they do it?<br />
Simon Keady, principal pharmacist,<br />
explained: “Every member of the<br />
team was empowered to make<br />
suggestions. We examined every<br />
step of the process to identify<br />
inefficiencies and bottlenecks that<br />
were acting as a barrier to<br />
providing a good service.<br />
Everyone rose to the challenge.<br />
“Some of the changes were<br />
relatively minor but together they<br />
had a huge impact: extended<br />
opening hours took the pressure<br />
off the busiest times and has given<br />
patients more choice; in-house<br />
customer care training has<br />
equipped our dispensary staff to<br />
provide a better patient experience<br />
and to deal more effectively with<br />
patient’s concerns and anxieties,<br />
especially those related around the<br />
use of their medicines.“<br />
Working with colleagues across<br />
the Trust continues to be a priority.<br />
For example, A&E and pharmacy<br />
have redesigned the A&E<br />
prescription to increase efficiency<br />
and reduce potential for errors. “It<br />
provides us with all the information<br />
we need – so reduces the need for<br />
phone calls.”<br />
To limit discharge delays, the Trust<br />
has agreed that 80% of discharge<br />
prescriptions should be prescribed<br />
on the day before a patient leaves<br />
the hospital and pharmacy are<br />
working with local clinical teams<br />
and the discharge nursing team to<br />
identify as early as possible those<br />
patients who are ready to go<br />
home.<br />
“We know that when discharge<br />
medicines are prescribed in<br />
advance, patients are not delayed.<br />
Unfortunately, many discharge<br />
prescriptions are written on the day<br />
and in some cases after patients<br />
have been told they can go. This<br />
inevitably causes delay and we are<br />
keen to work with colleagues to<br />
change this. Pharmacy is the last<br />
port of call for most patients, it’s<br />
important that their last memory of<br />
the Trust is a good one.”<br />
The lessons learnt at the UCH site<br />
are being used across all<br />
dispensaries at UCLH to improve<br />
the patient experience wherever<br />
they are being treated.<br />
The pharmacy team undertook a<br />
systematic review of their<br />
department using the Lean<br />
framework, looking closely at the<br />
time it was taking to complete each<br />
step of the process and targeting<br />
troublesome areas.<br />
Inge Edmondson, student pharmacy technician greets patients<br />
Fact file<br />
There are six dispensaries at UCLH<br />
Two are at UCH: over-the-counter for outpatients, A&E and clinical trials;<br />
another for inpatients and discharged patients<br />
390,000 medicines dispensed each year. That’s around one a minute<br />
Extended opening hours were introduced at UCH last year: now open until<br />
7pm three days a week, and weekend mornings<br />
Innovative IT tool designed by UCLH, gives visual “green amber red”<br />
warning about patient waiting times. To be introduced across all sites<br />
IT tool tracks medicine continuously: who has what, where?<br />
Two robotic dispensing machines at UCH automatically store and retrieve<br />
the correct medicines at lightning speed<br />
Future developments:<br />
A modern pharmacy is<br />
due to open at the NHNN<br />
next summer. It is<br />
currently located in a<br />
separate building<br />
Robotic dispensing is to<br />
be introduced at NHNN<br />
and the new cancer<br />
centre<br />
4
pharmacy special<br />
One of the five aspects of the UCLH approach to the recently<br />
launched Quality Efficiency and Productivity (QEP) programme is<br />
to ‘Make Life Simple’. This means getting all of our clinical<br />
services in place so that waste is minimised, duplication<br />
eliminated, flow is improved and unnecessary<br />
tasks reduced so we can all concentrate on<br />
our work for patients far more effectively.<br />
This pharmacy project is a shining<br />
example of how small changes can<br />
make a big difference.<br />
Read all about the five approaches to<br />
QEP, great examples of good practice<br />
and much more by visiting the newly<br />
updated QEP pages on Insight.<br />
UCLH has developed a<br />
new IT system which<br />
enables the pharmacy<br />
team to see at a<br />
glance how long a<br />
patient has been<br />
waiting and flags up<br />
delays. Simon<br />
Keady said: “It<br />
provides a minuteby-minute<br />
real time<br />
overview. We aim<br />
to expand it<br />
across all the sites with access<br />
for nursing staff – they could log on in their ward<br />
and see whether a patient’s discharge prescription is ready.”<br />
at the pharmacy counter<br />
L-r: Rakhee Mandalia, pharmacy technician, Bhavini Patel, Bola Oduwole, Panayiotis Sphikas, senior technicians behind the scenes at the UCH pharmacy<br />
5
interview<br />
Facing up to the biggest taboo<br />
Dr Chi-Chi Cheung talks to Elke Tullett<br />
6<br />
“Are you frightened of dying?”<br />
A bit of a conversation-stopper<br />
usually. But not for Dr Chi-Chi<br />
Cheung (pictured).<br />
“No, not frightened but I wouldn’t<br />
want it to happen yet,” she answered.<br />
“I don’t feel my time has come.”<br />
It’s the kind of talk that is a cultural<br />
taboo in England and one that Chi-<br />
Chi aims to challenge in her role as a<br />
palliative care consultant.<br />
“Culturally people don’t want to talk<br />
about it or even think about it, even<br />
though it is not a failure of care but a<br />
natural part of life. People who work<br />
in the health service are not any<br />
different. Many doctors are natural<br />
optimists whose aim is to make<br />
people well again. Death is not<br />
something we are necessarily keen<br />
to face.”<br />
Chi-Chi and her colleague, senior<br />
nurse Sue Hutton, co-chair the<br />
Trust’s End of Life Strategy Group<br />
which has developed a strategy to<br />
reflect the Department of Health’s<br />
mission to improve the quality of care<br />
for patients in the last year of life.<br />
The strategy advocates equipping<br />
clinical and non-clinical staff with the<br />
skills and confidence to support<br />
patients in their last months, weeks<br />
and days. All healthcare<br />
professionals should be able to deal<br />
with common end of life issues, be<br />
able to have conversations with<br />
patients and their families, and know<br />
Fact file<br />
70% of patients say they<br />
want to die at home<br />
60% die in hospital<br />
29% discuss their wishes<br />
about dying<br />
Only 4% have written<br />
advance care plans<br />
Over 50% of complaints<br />
to the former Health Care<br />
Commission related to<br />
end of life care<br />
when to seek specialist advice.<br />
The most difficult part is actually at<br />
the beginning – identifying when<br />
someone is reaching the end of their<br />
life. Once that has been<br />
acknowledged, the next part involves<br />
discussing with them their wants and<br />
need are (Where would they like to<br />
be cared for? Where would they<br />
prefer to die? Who would they like to<br />
be involved with decision making?<br />
What are their priorities?) and<br />
helping to co-ordinate care through<br />
the various stages. It also<br />
includes encouraging them to<br />
prepare for the inevitable so that<br />
family and friends are not left to<br />
'pick up the pieces', the wills left<br />
unmade, the things left unsaid,<br />
the loose ends of a life left<br />
untied.<br />
And whose role is it to have<br />
these conversations with<br />
patients?<br />
“It would be whoever the<br />
patient feels most<br />
comfortable with be they a<br />
GP, district nurse, specialist<br />
nurse, consultant or even a<br />
junior doctor or ward nurse.<br />
It is a sensitive process –<br />
trying to discover when<br />
someone is ready to talk<br />
about dying. Naturally, a<br />
person’s culture, religion or<br />
ethnicity is a major influence.<br />
Some people, of course, deny it<br />
to the end.”<br />
Chi-Chi splits her week between<br />
the UCLH and Islington<br />
community palliative care<br />
teams. It means that she has<br />
the opportunity to see people in<br />
their own home following<br />
discharge from hospital.<br />
“As a ward doctor I was firefighting<br />
and managing crises,<br />
always rushing from one patient<br />
to the next. I didn’t find that<br />
particularly fulfilling. Helping<br />
someone face the end of their life<br />
and allow them to die comfortably<br />
were aspects of medicine where I<br />
actually felt I was making a<br />
difference – we only get one<br />
chance to get it right, and when<br />
we do I find that very rewarding.”<br />
Dying Matters, a national coalition of<br />
more than 700 organisations, was set<br />
up by the National Council for Palliative<br />
Care to promote awareness and<br />
change attitudes and behaviour<br />
towards death and bereavement. The<br />
UCLH palliative care team held<br />
displays in the UCH atrium to mark an<br />
awareness week in March. Visit<br />
www.dyingmatters.org<br />
If staff need any advice they can<br />
contact the palliative care team on ext<br />
3672.
esearch<br />
Consultant wins £1 million funding to help stroke patients<br />
A stroke specialist has been awarded<br />
major research funding to prevent<br />
patients suffering life-threatening side<br />
effects following treatment.<br />
Dr David Werring, a consultant<br />
neurologist at the NHNN and leading<br />
member of the stroke research group<br />
at the UCL Institute of Neurology, aims<br />
to develop techniques to predict – and<br />
therefore protect – those patients at<br />
risk of suffering brain haemorrhage<br />
after being treated with blood thinning<br />
drugs.<br />
Anti-coagulants are often prescribed<br />
for long term use if blood clotting and<br />
stroke is due to an abnormal heart<br />
rhythm. This might follow the initial<br />
‘hyper acute’ treatment with clotbusting<br />
drugs given within the first few<br />
hours of stroke.<br />
The British Heart Foundation and The<br />
Stroke Association awarded his team<br />
nearly £1 million to help fund a fiveyear<br />
research programme into new<br />
types of MRI brain scans and genetic<br />
testing which could predetermine those<br />
most at risk.<br />
David said: “Blood thinning drugs are<br />
very effective for most patients who<br />
have suffered a stroke as a result of<br />
atrial<br />
fibrillation, an<br />
abnormal<br />
heart rhythm.<br />
However, in a<br />
small minority<br />
of patients it<br />
can put them<br />
at greater risk<br />
of devastating<br />
brain<br />
haemorrhage.<br />
“In some<br />
cases it is very<br />
hard to know<br />
the best thing<br />
to do. On the<br />
one hand<br />
there is a high risk of recurrent blood<br />
clots to the brain, on the other, a<br />
danger of bleeding in the brain. We<br />
want to identify those at highest risk of<br />
bleeding.”<br />
Sophisticated MRI scans can detect<br />
previous tiny bleeds (‘microbleeds’)<br />
that have occurred around fragile,<br />
leaky blood vessels.<br />
He added: “In patients with a lot of<br />
microbleeds, especially near the brain<br />
surface, anticoagulant drugs might<br />
L-r: Dr Rustam Al-Shahi Salman, MRC clinician scientist (<strong>University</strong> of<br />
Edinburgh), Dr David Werring clinical senior lecturer (stroke) and consultant<br />
neurologist UCLH, Dr Henry Houlden clinical senior lecturer (neurogenetics)<br />
and consultant neurologist UCLH.<br />
cause a life-threatening large<br />
haemorrhage. If this theory is correct,<br />
screening for microbleeds could help<br />
target the right anticoagulant treatment<br />
to the right patients, making them<br />
much safer to use."<br />
“This is a very exciting time for stroke<br />
research because the new hyper acute<br />
stroke unit at UCH will give many<br />
more patients the chance to take<br />
part in this and other important<br />
projects.”<br />
Pass me the painkillers – I’ve got an award to win<br />
Clinical research fellow Dr Andrew<br />
Flett used his initiative when<br />
emergency back surgery threatened to<br />
thwart his hopes of winning an<br />
international award.<br />
Undeterred, he recorded his<br />
presentation on webcam from his<br />
bedside and submitted it along with<br />
PowerPoint slides via a webcast to the<br />
panel of judges in Phoenix, Arizona.<br />
The next day The Society of<br />
Cardiovascular Magnetic Resonance<br />
declared him the winner of the Young<br />
Investigator Award at its annual<br />
scientific conference.<br />
Andrew, who underwent spinal surgery<br />
at the NHNN, said: “I knew I couldn’t<br />
travel to America as planned and<br />
thought ‘that’s the end of that award’.<br />
Then having recorded webcasts at<br />
conferences before, I realised this<br />
could be an option. I never really<br />
believed I could win it from the other<br />
side of the world though! “<br />
He was awarded the young<br />
investigator award for his work in<br />
developing a new technique to<br />
measure the amount of diffuse scar<br />
tissue in the heart using a cardiac MRI<br />
scanner. He found a strong correlation<br />
between the amount of scar tissue<br />
measured on the scan and that found<br />
on biopsy in two heart diseases, aortic<br />
stenosis and hypertrophic<br />
cardiomyopathy.<br />
He said:” Usually a biopsy is<br />
needed to measure scar tissue<br />
and is only undertaken as a last<br />
resort because it is very invasive<br />
and carries risk. Scanning is safe<br />
and will enable us to screen many<br />
more patients. This could play an<br />
important role in diagnosing<br />
patients, monitoring the rate of the<br />
disease and the effectiveness of<br />
treatments.”<br />
The research is being funded by<br />
The British Heart Foundation.<br />
7
the back page<br />
Secret lives<br />
If a silken voiced Italian promises you<br />
the moon and the stars you may feel<br />
a little taken aback. But in the case of<br />
Dr Giovanni Quarta (pictured left), a<br />
clinical researcher – and enthusiast<br />
astronomer – they may not be empty<br />
words. As his wife discovered.<br />
“On our honeymoon a couple of<br />
years ago we travelled to the Gobi<br />
desert to see the total eclipse of the<br />
Sun. It was amazing. As the moon<br />
passed over the sun, it got colder,<br />
darker, the wind dropped and shafts<br />
of light flared out. It is no wonder that<br />
ancient people were afraid. When<br />
you study the universe you start to<br />
appreciate how amazing it all is – to<br />
look at the very same sky that was<br />
present centuries ago, while almost<br />
everything else around us has<br />
changed.”<br />
Giovanni who works at The Heart<br />
Hospital alongside Professor William<br />
McKenna, Dr Perry Elliott<br />
(cardiomyopathy) and Dr James<br />
Moon (cardiovascular MRI) says he<br />
is fascinated in scientific subjects<br />
including mathematics and physics.<br />
He is currently attending an<br />
astronomy evening class at UCL and<br />
with fellow students makes regular<br />
trips to the Mill Hill Observatory to<br />
peer into infinity and beyond. Their<br />
lessons are filled with talk of<br />
galaxies, solar systems, dark matter:<br />
the stuff of unsettling dreams.<br />
“It’s true it makes most people feel<br />
very small and a little lonely. We think<br />
of distance as going from A to B but<br />
the scale of the universe is<br />
impossible to imagine and prompts<br />
so many philosophical questions.<br />
What are the chances of the right<br />
conditions all coming together at the<br />
same time, in the same place to<br />
support intelligent life? It certainly<br />
makes me appreciate being on<br />
Earth!”<br />
Our shooting stars<br />
Nurses,<br />
physiologists,<br />
administrative<br />
staff: it takes<br />
all sorts to<br />
make a<br />
winning team.<br />
They’ve<br />
formed the<br />
Trust’s first<br />
netball team<br />
‘All Blues’ and<br />
are ready to<br />
storm up the league tables!<br />
Tahlita Mabuza, a specialist in neurophysiology at UCH, said:<br />
“I posted a message on the intranet staff room last summer<br />
and we got an amazing response. We have a lot of fun – and<br />
yes, we are very competitive! The time invested in this team<br />
is worth every second and I hope I started something good<br />
that will last for many years to come. ”<br />
In the coming months, they’ll pitch their skills against rival<br />
teams such as MTV Skaters, Mediacoms Meertkats and<br />
Great Ormond Street Hospital.<br />
Logica has generously agreed to sponsor the team and<br />
funded their specially designed kit, equipment and hire<br />
charges.<br />
If you would like to join the team email Tahlita on<br />
Tahlita.Mabuza@uclh.nhs.uk<br />
Archives<br />
The dispensary in the outpatients department<br />
in the East Wing of the former Middlesex<br />
Hospital in 1924 before it was demolished and<br />
rebuilt. The pharmacist was Mr Sydney White<br />
and one of the dispensers seen here was Mr T<br />
C Willey. In 1924 there were nearly 190,000<br />
outpatient attendances.<br />
8