Medical Technology: organ harvesting and Transplants
Medical Technology: organ harvesting and Transplants
Medical Technology: organ harvesting and Transplants
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
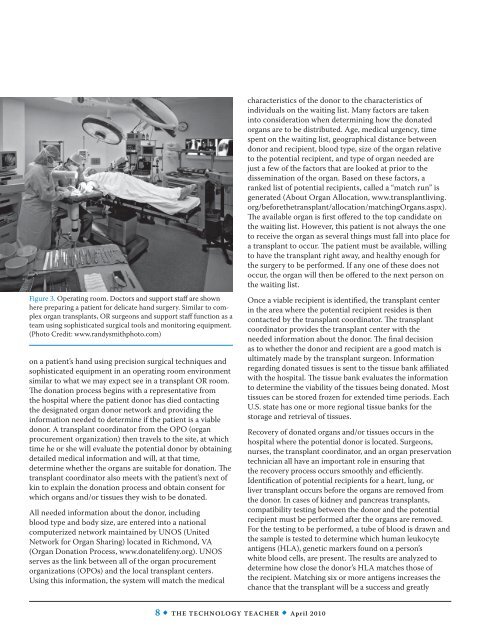
Figure 3. Operating room. Doctors <strong>and</strong> support staff are shown<br />
here preparing a patient for delicate h<strong>and</strong> surgery. Similar to complex<br />
<strong>organ</strong> transplants, OR surgeons <strong>and</strong> support staff function as a<br />
team using sophisticated surgical tools <strong>and</strong> monitoring equipment.<br />
(Photo Credit: www.r<strong>and</strong>ysmithphoto.com)<br />
on a patient’s h<strong>and</strong> using precision surgical techniques <strong>and</strong><br />
sophisticated equipment in an operating room environment<br />
similar to what we may expect see in a transplant OR room.<br />
The donation process begins with a representative from<br />
the hospital where the patient donor has died contacting<br />
the designated <strong>organ</strong> donor network <strong>and</strong> providing the<br />
information needed to determine if the patient is a viable<br />
donor. A transplant coordinator from the OPO (<strong>organ</strong><br />
procurement <strong>organ</strong>ization) then travels to the site, at which<br />
time he or she will evaluate the potential donor by obtaining<br />
detailed medical information <strong>and</strong> will, at that time,<br />
determine whether the <strong>organ</strong>s are suitable for donation. The<br />
transplant coordinator also meets with the patient’s next of<br />
kin to explain the donation process <strong>and</strong> obtain consent for<br />
which <strong>organ</strong>s <strong>and</strong>/or tissues they wish to be donated.<br />
All needed information about the donor, including<br />
blood type <strong>and</strong> body size, are entered into a national<br />
computerized network maintained by UNOS (United<br />
Network for Organ Sharing) located in Richmond, VA<br />
(Organ Donation Process, www.donatelifeny.org). UNOS<br />
serves as the link between all of the <strong>organ</strong> procurement<br />
<strong>organ</strong>izations (OPOs) <strong>and</strong> the local transplant centers.<br />
Using this information, the system will match the medical<br />
characteristics of the donor to the characteristics of<br />
individuals on the waiting list. Many factors are taken<br />
into consideration when determining how the donated<br />
<strong>organ</strong>s are to be distributed. Age, medical urgency, time<br />
spent on the waiting list, geographical distance between<br />
donor <strong>and</strong> recipient, blood type, size of the <strong>organ</strong> relative<br />
to the potential recipient, <strong>and</strong> type of <strong>organ</strong> needed are<br />
just a few of the factors that are looked at prior to the<br />
dissemination of the <strong>organ</strong>. Based on these factors, a<br />
ranked list of potential recipients, called a “match run” is<br />
generated (About Organ Allocation, www.transplantliving.<br />
org/beforethetransplant/allocation/matchingOrgans.aspx).<br />
The available <strong>organ</strong> is first offered to the top c<strong>and</strong>idate on<br />
the waiting list. However, this patient is not always the one<br />
to receive the <strong>organ</strong> as several things must fall into place for<br />
a transplant to occur. The patient must be available, willing<br />
to have the transplant right away, <strong>and</strong> healthy enough for<br />
the surgery to be performed. If any one of these does not<br />
occur, the <strong>organ</strong> will then be offered to the next person on<br />
the waiting list.<br />
Once a viable recipient is identified, the transplant center<br />
in the area where the potential recipient resides is then<br />
contacted by the transplant coordinator. The transplant<br />
coordinator provides the transplant center with the<br />
needed information about the donor. The final decision<br />
as to whether the donor <strong>and</strong> recipient are a good match is<br />
ultimately made by the transplant surgeon. Information<br />
regarding donated tissues is sent to the tissue bank affiliated<br />
with the hospital. The tissue bank evaluates the information<br />
to determine the viability of the tissues being donated. Most<br />
tissues can be stored frozen for extended time periods. Each<br />
U.S. state has one or more regional tissue banks for the<br />
storage <strong>and</strong> retrieval of tissues.<br />
Recovery of donated <strong>organ</strong>s <strong>and</strong>/or tissues occurs in the<br />
hospital where the potential donor is located. Surgeons,<br />
nurses, the transplant coordinator, <strong>and</strong> an <strong>organ</strong> preservation<br />
technician all have an important role in ensuring that<br />
the recovery process occurs smoothly <strong>and</strong> efficiently.<br />
Identification of potential recipients for a heart, lung, or<br />
liver transplant occurs before the <strong>organ</strong>s are removed from<br />
the donor. In cases of kidney <strong>and</strong> pancreas transplants,<br />
compatibility testing between the donor <strong>and</strong> the potential<br />
recipient must be performed after the <strong>organ</strong>s are removed.<br />
For the testing to be performed, a tube of blood is drawn <strong>and</strong><br />
the sample is tested to determine which human leukocyte<br />
antigens (HLA), genetic markers found on a person’s<br />
white blood cells, are present. The results are analyzed to<br />
determine how close the donor’s HLA matches those of<br />
the recipient. Matching six or more antigens increases the<br />
chance that the transplant will be a success <strong>and</strong> greatly<br />
8 • The <strong>Technology</strong> Teacher • April 2010