GP Pulse 03.2010 - The Royal New Zealand College of General ...
GP Pulse 03.2010 - The Royal New Zealand College of General ...
GP Pulse 03.2010 - The Royal New Zealand College of General ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
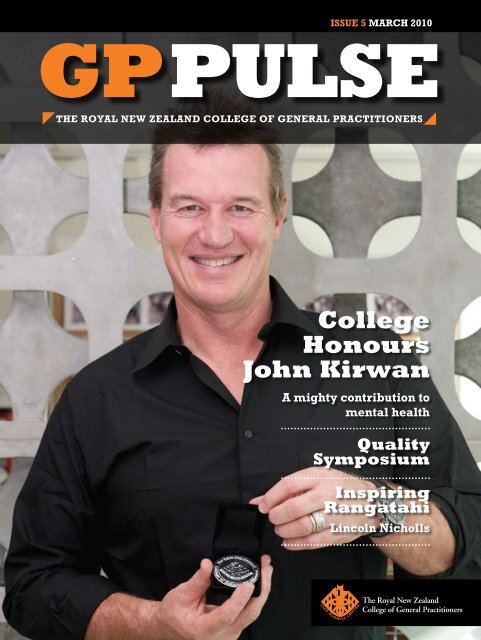
ISSUE 5 MARCH 2010<br />
<strong>GP</strong>PULSE<br />
THE ROYAL NEW ZEALAND COLLEGE OF GENERAL PRACTITIONERS<br />
<strong>College</strong><br />
Honours<br />
John Kirwan<br />
A mighty contribution to<br />
mental health<br />
Quality<br />
Symposium<br />
Inspiring<br />
Rangatahi<br />
Lincoln Nicholls
<strong>The</strong> Third Biennial<br />
<strong>GP</strong> Education Convention<br />
Supporting and Strengthening<br />
<strong>General</strong> Practice Education<br />
Friday 25–Saturday 26 June 2010,<br />
James Cook Hotel Grand Chancellor,<br />
Wellington<br />
Invitations will be sent to all current <strong>GP</strong> teachers in March<br />
For more information contact John Pearson: john.pearson@rnzcgp.org.nz
CONTENTS<br />
6<br />
Quality<br />
Symposium 2010<br />
20<br />
Inspiring rangatahi<br />
34<br />
<strong>The</strong> 2010 RNZC<strong>GP</strong> Annual<br />
Conference: Christchurch<br />
EDITORIAL<br />
4 Celebrating past successes, managing<br />
current challenges and looking to<br />
the future<br />
QUALITY<br />
6 <strong>The</strong> Annual Quality Symposium 2010<br />
8 <strong>The</strong> Quality agenda in your practice<br />
COLLEGE<br />
10 ‘More important than being<br />
an All Black’: John Kirwan and Mental<br />
Health<br />
CPD<br />
12 Prostate screening: defining the <strong>GP</strong>’s<br />
role<br />
14 Of pills and potions for coughs<br />
and colds<br />
RESEARCH<br />
16 Changes in community laboratory<br />
services in Auckland<br />
EDUCATION<br />
18 <strong>The</strong> (<strong>New</strong>) Educators<br />
19 Changes to your Maintenance <strong>of</strong><br />
Pr<strong>of</strong>essional Standards (MOPS)<br />
programme for 2011–2013<br />
20 Inspiring rangatahi<br />
PARTNERSHIP<br />
22 <strong>The</strong> evolving <strong>GP</strong>/physiotherapist<br />
partnership<br />
CORNERSTONE<br />
24 CORNERSTONE: the storage <strong>of</strong><br />
patient records<br />
25 CORNERSTONE notches up 500<br />
POLICY<br />
26 <strong>The</strong> role <strong>of</strong> the <strong>GP</strong><br />
28 Health insurance company requests<br />
for entire patient’s medical notes<br />
OBITUARIES<br />
29 William Grattan O’Connell QSM<br />
30 Brett Phillip Roche<br />
RURAL<br />
31 DHB Rural <strong>GP</strong> and Hospital Medicine<br />
Pilot Project<br />
LIFE & LEISURE<br />
33 Humour: Back to the Ark?<br />
Technophobia 101<br />
34 <strong>The</strong> 2010 RNZC<strong>GP</strong> Annual<br />
Conference: Christchurch<br />
36 Guide to <strong>New</strong> <strong>Zealand</strong> pinot noir<br />
regions<br />
MEMBER SUPPORT<br />
38 Becoming a member<br />
39 <strong>College</strong> services<br />
Cover picture—Photographer: Alistair Guthrie, <strong>The</strong> Collective Force<br />
<br />
<br />
Level 3, 88 <strong>The</strong> Terrace<br />
PO Box 10440<br />
Wellington 6143<br />
Phone: (04) 496 5999<br />
Fax: (04) 496 5997<br />
Email: rnzcgp@rnzcgp.org.nz<br />
Web: www.rnzcgp.org.nz<br />
© <strong>Royal</strong> <strong>New</strong> <strong>Zealand</strong> <strong>College</strong> <strong>of</strong> <strong>General</strong><br />
Practitioners. ISSN 1176–5445 (Print), ISSN<br />
1178–6795 (Online).<br />
All Rights Reserved. No part <strong>of</strong> this<br />
publication may be reproduced, stored in an<br />
electronic form or transmitted in any form or<br />
by any other means electronically, mechanical<br />
photocopying, recording or otherwise<br />
without express permission <strong>of</strong> the <strong>College</strong>.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 3
EDITORIAL<br />
<strong>GP</strong> <strong>Pulse</strong> is the <strong>of</strong>ficial magazine <strong>of</strong><br />
the <strong>Royal</strong> <strong>New</strong> <strong>Zealand</strong> <strong>College</strong><br />
<strong>of</strong> <strong>General</strong> Practitioners. It is<br />
published four times a year.<br />
Publisher<br />
Karen Thomas,<br />
Chief Executive;<br />
pam.berry@rnzcgp.org.nz<br />
Editor<br />
Heather Watt,<br />
Group Manager, Member Support;<br />
heather.watt@rnzcgp.org.nz<br />
Associate Editor<br />
Alexander Bisley,<br />
Communications Advisor;<br />
alexander.bisley@rnzcgp.org.nz<br />
Associate Editor<br />
John Pearson,<br />
Education Officer;<br />
john.pearson@rnzcgp.org.nz<br />
Subscription or<br />
advertising queries<br />
Cherylyn Borlase,<br />
Publications Coordinator;<br />
publications@rnzcgp.org.nz<br />
A subscription to <strong>GP</strong> <strong>Pulse</strong> is<br />
available at a cost <strong>of</strong> $60 for<br />
national subscriptions and $85 for<br />
international subscriptions.<br />
Joint subscriptions to <strong>GP</strong> <strong>Pulse</strong> and<br />
the Journal <strong>of</strong> Primary Health Care<br />
(JPHC) are available at a cost <strong>of</strong><br />
$150 for national subscriptions and<br />
$210 for international subscriptions.<br />
RNZC<strong>GP</strong>,<br />
PO Box 10440,<br />
Wellington 6143<br />
Phone: (04) 496 5999<br />
Fax: (04) 496 5997<br />
www.rnzcgp.org.nz/gp-pulse<br />
Celebrating past<br />
successes, managing<br />
current challenges and<br />
looking to the future<br />
Harry Pert<br />
President, RNZC<strong>GP</strong><br />
<strong>The</strong> <strong>College</strong>’s 2010 Annual Quality<br />
Symposium was an opportunity to think<br />
about what we would like for the future<br />
<strong>of</strong> <strong>New</strong> <strong>Zealand</strong> primary care; to consider<br />
some current and looming challenges, but<br />
also to do something we do all too rarely,<br />
celebrate. To quote visiting King’s Fund<br />
experts Dr Candace Imison and Dr Nick<br />
Goodwin from the UK: ‘<strong>New</strong> <strong>Zealand</strong><br />
already punches above its weight in delivering<br />
high quality primary care services<br />
with limited resources.’<br />
Some <strong>of</strong> those past successes include the<br />
Aiming for Excellence standards and the<br />
CORNERSTONE practice accreditation<br />
programme. As only the second country in<br />
the world to introduce such a scheme, the<br />
Symposium was a fitting opportunity to<br />
acknowledge the 398 practices nationwide<br />
who have now achieved accreditation<br />
(including 44 who have completed<br />
a second accreditation). Speaking at the<br />
Symposium, Health Minister Tony Ryall<br />
thanked the <strong>College</strong>, general practices and<br />
<strong>GP</strong>s for their leadership in improving public<br />
health care quality and safety through<br />
CORNERSTONE. Presently another 350<br />
practices are also working towards their<br />
accreditation.<br />
We continue to review and refine<br />
CORNERSTONE. Proposed future<br />
developments include delivery <strong>of</strong> the<br />
programme via four modules: practice<br />
organisation; clinical care; patient- and<br />
community-centred approach; and pr<strong>of</strong>essional<br />
development. Special modules could<br />
include teaching practices and environmental<br />
sustainability. We also need to<br />
review the business model that supports<br />
CORNERSTONE!<br />
This edition <strong>of</strong> <strong>GP</strong> <strong>Pulse</strong> includes some<br />
Quality Symposium highlights (pages six<br />
and seven), and an update on how the<br />
work being done for the <strong>College</strong> by the<br />
Wellington School <strong>of</strong> Medicine helps<br />
undertake and demonstrate Quality<br />
improvement activities within the context<br />
<strong>of</strong> your daily practice.<br />
One <strong>of</strong> the challenges in improving Quality<br />
has been that there are tremendous initiatives<br />
around the country which are not being<br />
shared and work is <strong>of</strong>ten unnecessarily<br />
replicated. <strong>The</strong> Quality Symposium was<br />
one opportunity to share and showcase<br />
quality work from around <strong>New</strong> <strong>Zealand</strong><br />
and to hear from international colleagues<br />
from around the world. <strong>The</strong>re are opportunities<br />
via networks and peer groups<br />
for us to share learning, so the really good<br />
initiative in Dunedin can be shared through<br />
the <strong>College</strong> and disseminated throughout<br />
the country. This would also allow the<br />
benchmarking and other Quality improvement<br />
activities to occur.<br />
If you are not already aware, I would also<br />
like to take this opportunity to inform you<br />
<strong>of</strong> changes to the governance arrangements<br />
<strong>of</strong> the <strong>College</strong> and to introduce<br />
members <strong>of</strong> our new Board.<br />
<strong>The</strong> <strong>College</strong> has been governed by a<br />
Council <strong>of</strong> 20, with additional observers<br />
also present at meetings. Fourteen<br />
members <strong>of</strong> Council were nominated by<br />
the <strong>College</strong> faculties and these nominees<br />
4 | <strong>GP</strong> PULSE | MARCH 2010
EDITORIAL<br />
changed quite frequently. Although this<br />
arrangement was good for debate and<br />
canvassing a range <strong>of</strong> opinions, it was too<br />
inefficient and time-consuming for fast<br />
decision-making. <strong>The</strong>re was also a lack<br />
<strong>of</strong> clarity within Standing Committees <strong>of</strong><br />
Council about governance versus operational<br />
matters and some confusion about<br />
lines <strong>of</strong> communication to both Council<br />
and the CEO.<br />
Council had recognised these problems<br />
and established the Constitution Steering<br />
Group in 2006: www.rnzcgp.org.nz/<br />
review-<strong>of</strong>-the-constitution. <strong>The</strong> proposals<br />
from this Committee, which have been<br />
modified following wide consultation<br />
with members, are due to be implemented<br />
at the 2010 <strong>College</strong> AGM.<br />
However in November last year, when<br />
the new <strong>College</strong> Executive met for two<br />
days to consider priorities for the coming<br />
year, it became clear that the <strong>College</strong><br />
urgently needed to rearrange its governance<br />
structures. we needed to accelerate<br />
the implementation <strong>of</strong> key recommendations<br />
from the Constitutional review<br />
and establish a small Board comprising<br />
the President and Deputy President, a<br />
nominee from Te Akoranga a Maui, two<br />
members appointed by Council and<br />
two independent members to establish<br />
the required skill-mix <strong>of</strong> the Board. <strong>The</strong><br />
CEO would be an ex <strong>of</strong>ficio member <strong>of</strong><br />
the Board. <strong>The</strong> changes could be made<br />
within the current rules and regulations<br />
<strong>of</strong> the <strong>College</strong>. In December at the<br />
<strong>College</strong> Council meeting this proposal<br />
was put to the meeting. Council decided<br />
that the President and the Deputy<br />
President should select the two Council<br />
members, ask the Chair <strong>of</strong> Te Akoranga<br />
a Maui to nominate their representative<br />
and seek suitable people to fill the other<br />
two places.<br />
<strong>The</strong> new Board members are: myself,<br />
Harry Pert, as President; Deputy<br />
President Tony Townsend; Te Akoranga<br />
Harry Pert: <strong>College</strong> President, Fellow since<br />
1995, practices at Ranolf Medical Centre<br />
in Rotorua.<br />
a Maui representative Peter Jansen; Tana<br />
Fishman to provide educational expertise;<br />
and Richard Tyler with his financial<br />
and governance experience. More<br />
information about each <strong>of</strong> us is provided<br />
below. As this edition <strong>of</strong> <strong>GP</strong> <strong>Pulse</strong> goes<br />
to print, the two others members are<br />
being sought (probably external appointments)<br />
to provide skills in governance,<br />
strategic thinking, marketing and business<br />
development. I look forward to working<br />
with them. I would like to emphasise<br />
these are interim arrangements, and will<br />
be reviewed at our September <strong>College</strong><br />
Conference in Christchurch.<br />
Tony Townsend: <strong>College</strong> Deputy President,<br />
Fellow since 1988, Distinguished Fellow<br />
since 2008, practices at Whangamata<br />
Medical Centre.<br />
Peter Jansen : Te Akoranga a Maui nominee,<br />
Fellow since 1998, Distinguished Fellow since<br />
2008, Mauri Ora Associates and Senior<br />
Medical Advisor for ACC.<br />
Tana Fishman: Representative with<br />
educational expertise, Fellow since 2004,<br />
practices at Manurewa’s Greenstone Family<br />
Clinic, Auckland.<br />
Richard Tyler: Representative with financial<br />
and governance expertise, Fellow since<br />
1991, practices at the Johnsonville Medical<br />
Centre, Wellington.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 5
QUALITY<br />
THE ANNUAL QUALITY SYMPOSIUM 2010<br />
Around the keynote table<br />
<strong>College</strong> staff, Maureen Gillon and Cathy Webber<br />
Dr Michael Lamont and <strong>College</strong> Board member<br />
Dr Richard Tyler<br />
RAC<strong>GP</strong> President Dr Chris Mitchell, Hon. Tony Ryall, Dr Peter Moodie <strong>of</strong> PHARMAC and Dr Jo Scott-Jones<br />
Group discussions<br />
Dr Candace Imison, Dr Nick Goodwin <strong>of</strong> the King’s Fund (UK)<br />
and <strong>College</strong> staff member Heather Watt<br />
Dr Jo Scott-Jones and <strong>College</strong> staff member<br />
Dr Frances Townsend<br />
6 | <strong>GP</strong> PULSE | MARCH 2010
IFHC Interactive Workshop<br />
QUALITY<br />
Dr Jim Vause, CORNERSTONE Assessor<br />
RNZC<strong>GP</strong> President Dr Harry Pert, Deputy President<br />
Dr Tony Townsend and keynote speaker Dr Nick Goodwin<br />
Highlights<br />
Keynote speaker Dr Candace Imison<br />
<strong>The</strong> 2010 Annual Quality Symposium in<br />
Wellington February 12–13 was attended<br />
by more than 220 key primary care<br />
stakeholders, with keynote presentations<br />
from <strong>Royal</strong> Australian <strong>College</strong> <strong>of</strong> <strong>GP</strong>s<br />
President Dr Chris Mitchell and British<br />
Kings’ Fund experts Dr Nick Goodwin<br />
and Dr Candace Imison. Goodwin and<br />
Imison pointed out that <strong>New</strong> <strong>Zealand</strong> can<br />
be very proud <strong>of</strong> its record: ‘<strong>New</strong> <strong>Zealand</strong><br />
already punches above its weight in delivering<br />
high quality primary care services<br />
with limited resources.’ Goodwin argued<br />
that reputation motivates initiatives like<br />
CORNERSTONE, and that there’s nothing<br />
more important to a <strong>GP</strong> than reputation.<br />
Health Minister Tony Ryall announced<br />
the establishment <strong>of</strong> the<br />
Quality and Safety Improvement<br />
Commission. Past RNZC<strong>GP</strong> president<br />
Jim Vause led a lively, wideranging<br />
workshop on the Ministerial<br />
proposal for Integrated Family Health<br />
Centres (IFHCs).<br />
Papatoetoe (and ProCare) <strong>GP</strong> Karl<br />
Cole also gave an excellent presentation<br />
on employing technology in general<br />
practice. <strong>GP</strong> Jo Scott-Jones delivered an<br />
inspirational presentation explaining<br />
how Opotoki wiped out terribly high<br />
rates <strong>of</strong> rheumatic fever.<br />
Pr<strong>of</strong>essor Peter Crampton, head <strong>of</strong> the<br />
Wellington School <strong>of</strong> Medicine, paid<br />
tribute to <strong>New</strong> <strong>Zealand</strong>’s world-leading<br />
public health system. According to the<br />
2009 Commonwealth Fund Survey, <strong>New</strong><br />
<strong>Zealand</strong> primary care physicians have the<br />
highest levels <strong>of</strong> satisfaction in the world.<br />
On the challenging side <strong>of</strong> the ledger,<br />
we have relatively low doctor numbers.<br />
Pr<strong>of</strong>essor Crampton illustrated how <strong>New</strong><br />
<strong>Zealand</strong> has, by international comparisons, a<br />
lean, effective system and lots <strong>of</strong> successes.<br />
For more, visit:<br />
www.rnzcgp.org.nz/quality-symposium<br />
Rowena Gotty and Maureen Gillon Vicky Noble and Debbie Gell Dr Tane Taylor, Chair <strong>of</strong> Te Akorangi a Maui<br />
<strong>GP</strong> PULSE | MARCH 2010 | 7
QUALITY<br />
<strong>The</strong> Quality agenda:<br />
How will it help your<br />
practice?<br />
<strong>The</strong> 2010 Annual Quality Symposium<br />
was an opportunity to hear about<br />
what the first year <strong>of</strong> work from<br />
the Wellington School <strong>of</strong> Medicine<br />
(WSM), on behalf <strong>of</strong> the <strong>College</strong>, has<br />
delivered. You’ll likely have heard<br />
about a Quality Framework and<br />
Quality Indicators, but how will they<br />
work in the real world <strong>of</strong> general<br />
practice?<br />
Paraparaumu <strong>GP</strong> Dr Chris Fawcett<br />
explains how the Quality Agenda will<br />
help him to ensure he delivers high<br />
quality care within his current day-today<br />
workload<br />
Like most <strong>GP</strong>s, Chris can identify some<br />
big health issues for his community.<br />
Many <strong>of</strong> them are common to communities<br />
across <strong>New</strong> <strong>Zealand</strong>, for example<br />
chronic diseases like CVD and diabetes.<br />
Others, like osteoporosis and mental<br />
health issues, are especially pertinent<br />
to the older Paraparaumu community<br />
where he practices. He does battle<br />
For Chris and his team, delivering quality<br />
care focuses on the patient in the consulting<br />
room with him, but he is aware<br />
there are many other concepts <strong>of</strong> quality<br />
which shape the health landscape.<br />
He is also aware that many factors affect<br />
patient care, both before the patient<br />
enters his/her room and after the<br />
patient leaves.<br />
But, how can he influence improved<br />
outcomes for his patients and his community<br />
across the board, and how can<br />
he demonstrate to the PHO and DHB<br />
that each successful intervention is<br />
one small battle won in the larger war<br />
on osteoporosis, CVD and diabetes?<br />
How can he be sure that he is doing<br />
the best and most effective things for<br />
his patients?<br />
<strong>The</strong> Quality Framework<br />
<strong>The</strong> framework is under development<br />
and is being built around existing <strong>GP</strong><br />
demands, e.g. workforce; capacity and<br />
<strong>The</strong> health landscape is complex and<br />
constantly changing. <strong>The</strong> quality<br />
framework will help identify those areas<br />
which are crucial to delivering quality care<br />
with these conditions (sometimes in<br />
combination) on any given day at the<br />
Paraparaumu Medical Centre. He follows<br />
guidelines, gives advice, prescribes<br />
drugs, and <strong>of</strong>ten good patient outcomes<br />
are achieved.<br />
resources and is based on knowledge<br />
gained <strong>of</strong> the structural interactions,<br />
and relationships and allegiances that<br />
already exist within the quality landscape.<br />
<strong>The</strong> health landscape is complex<br />
and constantly changing. <strong>The</strong> quality<br />
framework will help identify those<br />
areas which are crucial to delivering<br />
quality care, and how to have meaningful<br />
conversations with those with<br />
different <strong>of</strong> competing agendas. Chris,<br />
for example is aware that there are<br />
multiple concepts <strong>of</strong> quality and multiple<br />
agendas; the patient has a point<br />
<strong>of</strong> view, as does the <strong>GP</strong>, the nurse and<br />
all the clinical team. <strong>The</strong> funders, for<br />
example the PHO and DHB, also have<br />
a particular view <strong>of</strong> quality. In order to<br />
understand and have a conversation<br />
about these different views <strong>of</strong> quality<br />
Chris needs a framework and shared<br />
understanding within which a useful<br />
conversation can occur.<br />
What the survey data tells us<br />
A survey conducted in 2009 on behalf<br />
<strong>of</strong> the <strong>College</strong> by the WSM showed<br />
significant quality work is already being<br />
undertaken by practices and elsewhere<br />
within the primary care sector, but<br />
there are substantial time and workload<br />
pressures that provide barriers for<br />
practitioners:<br />
• Practices noted that it is vital that<br />
they be given mechanisms which<br />
allow them to rationalise and prioritise<br />
quality related activity within the<br />
context <strong>of</strong> clinical workloads.<br />
• <strong>The</strong> most immediate concern<br />
for practices is their day-to-day<br />
clinical work, and they believe some<br />
bureaucratically imposed activity is<br />
irrelevant.<br />
• Important tension points impacting<br />
on quality activity in primary<br />
care include a perceived disconnect<br />
8 | <strong>GP</strong> PULSE | MARCH 2010
etween a population and individual<br />
health focus, and managerial and<br />
clinical perspectives.<br />
Drawing on the survey results, the<br />
key aim <strong>of</strong> the Quality Agenda is to<br />
make it easier to fit quality activities<br />
into daily practice. It will support<br />
clinical leadership to determine how<br />
best to improve quality and will<br />
provide general practices with quality<br />
tools and processes to embed into<br />
practice systems.<br />
<strong>The</strong> key is to work smarter and not<br />
harder, to identify those activities<br />
which really do deliver a better quality<br />
<strong>of</strong> care, and which activities can be<br />
discarded.<br />
Some initial examples include:<br />
A how-to guide:<br />
A guide that can be used by staff working<br />
in primary care teams to determine<br />
what is feasible with respect to<br />
undertaking quality activity within their<br />
day-to-day work.<br />
An Indicator Development Tool<br />
To enable choice and prioritisation<br />
(which indicators are the best/most<br />
important for my practice?) for example<br />
through identifying gaps; and drawing<br />
on sentinel event reporting systems.<br />
<strong>GP</strong>s need confidence that the tools and<br />
processes they use are robust and appropriate<br />
for use in their own practice<br />
populations.<br />
How the Indicator<br />
Development Tool will work<br />
In the words <strong>of</strong> King’s Fund expert Dr<br />
Nick Goodwin, speaking at the <strong>College</strong>’s<br />
recent Quality Symposium: ‘You can’t<br />
improve what you can’t measure’. <strong>The</strong><br />
indicator development tool produced by<br />
the WSM will allow not just measurement,<br />
but will help ensure that we’re<br />
measuring the right things in our own<br />
communities, and identifying the best<br />
treatment and management options using<br />
robust, evidence based measures.<br />
<strong>The</strong>re are several options:<br />
• Use the online indicator development<br />
and implementation tool to<br />
develop a locally appropriate indicator<br />
that you own to help address<br />
a specific local or population-specific<br />
issue. One example might be<br />
skin infections in children. A child<br />
and siblings present on a regular<br />
basis with serious skin infections.<br />
<strong>The</strong>y are part <strong>of</strong> a large Pacific<br />
family that access the after hours<br />
service and general practice service<br />
on a regular basis for infections<br />
arising from skin conditions. <strong>The</strong><br />
practice team report that other<br />
members <strong>of</strong> the extended family<br />
have presented with the same<br />
problem and have been frequent<br />
attenders at the practice and after<br />
hours for the last six months. <strong>The</strong><br />
practice decides to investigate this<br />
issue. <strong>The</strong>y want to know if they<br />
are delivering quality care in this<br />
area for Pacific children and families<br />
in their practice so they use<br />
the indicator sieve to filter the data<br />
they have on skin conditions in this<br />
group <strong>of</strong> their practice population.<br />
<strong>The</strong>y want to isolate the causes<br />
to identify what clinical measures<br />
can be taken to prevent recurring<br />
infections. Using the sieve helps<br />
develop an appropriate indicator<br />
to measure improvement and to<br />
identify the best treatment and<br />
management options to achieve<br />
this. If the initiative is successful,<br />
the learning can be shared with<br />
other practices in the area via the<br />
common quality framework.<br />
• Use an indicator developed for <strong>New</strong><br />
<strong>Zealand</strong> primary care from the online<br />
library. One example might be<br />
an indicator for the assessment <strong>of</strong><br />
common mental health disorders.<br />
• Test an existing indicator being<br />
used in your practice/PHO/region<br />
against the ‘sieve tool’ on the website<br />
to ensure it is relevant for your<br />
patients and practice population.<br />
For example, the local community<br />
and funders consider that a <strong>GP</strong><br />
isn’t doing a good job in the area <strong>of</strong><br />
smoking cessation.. <strong>The</strong> <strong>GP</strong> is under<br />
pressure to measure and demonstrate<br />
improvement. <strong>The</strong> DHB<br />
wants him to measure number <strong>of</strong><br />
patients giving up smoking, number<br />
<strong>of</strong> patients having counselling for<br />
smoking cessation, number <strong>of</strong><br />
patients getting prescriptions for<br />
nicotine replacement therapy. <strong>The</strong><br />
<strong>GP</strong> can use the sieve to determine<br />
whether the measures are<br />
evidence based in order to respond<br />
to the DHB indicating which are<br />
invalid measures and which are<br />
useful. He will then be able to demonstrate<br />
that his practice provided<br />
advice, tools and interventions<br />
even if this has not produced the<br />
smoking cessation results sought<br />
by the funder. His practice’s results<br />
can also be shown against local<br />
population features, for example a<br />
high proportion <strong>of</strong> mental health<br />
consumers.<br />
All <strong>of</strong> this aims to support self-evaluation<br />
and learning and dissemination<br />
<strong>of</strong> knowledge gained. Would we do it<br />
again? What would we do next time?<br />
How can we showcase and share what<br />
we’ve learned? It can also be for quality<br />
assessment: how will we use it to<br />
demonstrate how well we are doing<br />
or to meet the expectations <strong>of</strong> PHOs,<br />
DHBs, or the PPP? How can we benchmark<br />
ourselves against other practices<br />
locally and nationally and demonstrate<br />
the success <strong>of</strong> or need for specific<br />
interventions?<br />
And, what happens next?<br />
We’ll be talking to you and your<br />
networks about ongoing development<br />
and usability and how a quality<br />
framework and the tools might be put<br />
into place.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 9
COLLEGE<br />
‘More important than being an All Black’<br />
John Kirwan and mental health<br />
Pr<strong>of</strong>essor Bruce Arroll<br />
<strong>General</strong> Practitioner, Auckland<br />
John Kirwan became famous through<br />
his sporting achievements. His work for<br />
mental health in <strong>New</strong> <strong>Zealand</strong> will leave<br />
a similar legacy to Sir Edmund Hillary.<br />
Political Plenary<br />
Early 2008 I was seeing a man in his forties<br />
with depression. I made the comment<br />
that the whole process <strong>of</strong> talking about<br />
and treating depression had been made<br />
much easier by the work <strong>of</strong> John Kirwan<br />
and the patient agreed. In a television<br />
campaign (which can be seen on the<br />
website www.depression.org.nz), John<br />
tells people about his experience with<br />
depression and <strong>of</strong>fers hope and advice<br />
on how to get help. I and many <strong>of</strong> my<br />
colleagues were hugely appreciative <strong>of</strong> his<br />
work and it occurred to me that John may<br />
not have been aware <strong>of</strong> this. Via email,<br />
it turned out that he was not aware <strong>of</strong><br />
<strong>GP</strong>s’ enthusiasm for his work and was<br />
pleased to get the message. <strong>The</strong> next<br />
step involved getting him the Meritorious<br />
Service Award from the <strong>College</strong> <strong>of</strong> <strong>GP</strong>s.<br />
Tim Kenealy was very pleased to be dual<br />
nominator. He has been photocopying<br />
pages from John Kirwan’s biography for<br />
his patients for many years. <strong>The</strong> application<br />
was supported by the awards<br />
committee for presentation at the annual<br />
<strong>College</strong> Conference in Wellington in<br />
September 2009.<br />
<strong>The</strong> <strong>of</strong>ficial citation read: ‘John Kirwan<br />
was born in <strong>New</strong> <strong>Zealand</strong> in 1964. He<br />
was an All Black from 1984 to 1994 and<br />
during his career he scored 67 tries<br />
in all matches for the <strong>New</strong> <strong>Zealand</strong><br />
All Blacks. This record stood for<br />
many years. In health his contribution<br />
Pr<strong>of</strong>essor Bruce Arroll pays tribute to John<br />
Kirwan’s achievements<br />
<strong>of</strong> depression. <strong>GP</strong>s in <strong>New</strong> <strong>Zealand</strong><br />
are grateful to him for making it easier<br />
for male patients to come forward and<br />
discuss depression.’ It’s interesting how<br />
far his work goes in the community.<br />
An old friend who is a barrister in the<br />
Family Court said that he frequently<br />
<strong>The</strong>re was a 19.1% decline from the Maori<br />
suicide rate in 1998 and a 46.6% reduction in<br />
the youth suicide rate since 1995<br />
John Kirwan with his <strong>College</strong> medal<br />
has been as the face <strong>of</strong> the National<br />
Depression Initiative. Market research<br />
has found a 96% recall <strong>of</strong> the ads, which<br />
is considered extremely high. Nationally<br />
there has been an increase in the<br />
public’s ability to recognise symptoms<br />
makes reference to John Kirwan when<br />
dealing with men who are depressed<br />
about marital separation. I spoke with a<br />
geriatric psychiatrist who says that she<br />
can now get elderly men in to groups to<br />
talk about depression.<br />
10 | <strong>GP</strong> PULSE | MARCH 2010
COLLEGE<br />
<strong>The</strong> Auckland award evening was attended<br />
by Auckland <strong>GP</strong>s, <strong>The</strong> <strong>Royal</strong><br />
<strong>New</strong> <strong>Zealand</strong> <strong>College</strong> <strong>of</strong> <strong>General</strong><br />
Practitioners, staff <strong>of</strong> advertising<br />
agency Draft FCB, National Depression<br />
Initiative leaders like Candace Bagnall,<br />
and John Kirwan’s family. William<br />
Ferguson was there, between patients,<br />
and said he could not miss such an occasion<br />
as JK’s award given the huge impact<br />
he has had on the issue <strong>of</strong> depression in<br />
<strong>New</strong> <strong>Zealand</strong>. I spoke about how much<br />
easier it was to work with men with<br />
depression as they were now willing to<br />
consider the diagnosis <strong>of</strong> depression.<br />
Twenty years ago patients were <strong>of</strong>ten<br />
convinced they had a physical condition.<br />
Kirwan’s work has contributed to the<br />
reduction <strong>of</strong> suicide rates. Latest figures<br />
(<strong>The</strong> Suicide Facts 2007 report) show<br />
there was a 19.1% decline from the<br />
Maori suicide rate in 1998 and a 46.6%<br />
reduction in the youth suicide rate<br />
since 1995. Market research says 96%<br />
<strong>of</strong> Maori men are aware <strong>of</strong> him and his<br />
message about depression. Such a high<br />
penetration rate among Maori men is<br />
unheard <strong>of</strong> in marketing terms.<br />
I spoke <strong>of</strong> John’s dedication. He has<br />
never been paid a penny, and when<br />
doing the filming he works tirelessly<br />
10 hours per day, five days per week.<br />
I have always been impressed with his<br />
work, but spending some time with<br />
John Kirwan and seeing him with the<br />
guests at the award ceremony I came<br />
to further realise how he is a special<br />
person. Speaking with everyone<br />
there, he showed himself to be a<br />
humble, sensitive and intelligent person.<br />
‘John, you’ve given <strong>New</strong> <strong>Zealand</strong><br />
hope,’ I concluded.<br />
John paid tribute to his family’s love<br />
helping him through his depression.<br />
He spoke about how he was initially<br />
reluctant to get involved as he was<br />
‘scared people would think I was a<br />
freak’, but the (continuing) campaign’s<br />
been ‘one <strong>of</strong> the greatest things I’ve<br />
ever done.’ He recalled Andy Hayden<br />
Former <strong>College</strong> President Jonathan Fox and John Kirwan<br />
MOH National Depression Initiative leader Candace Bagnall and Peter Huggard <strong>of</strong> the<br />
Goodfellow Unit<br />
telling him ‘Once an All Black, always<br />
an All Black’… ‘I wanted to keep giving<br />
back.’ Kirwan feels a pride in the<br />
campaign similar to the feeling when<br />
he first ran onto a rugby field wearing<br />
the All Black Jersey. ‘It’s a very <strong>New</strong><br />
<strong>Zealand</strong> thing, working together, helping<br />
each other out.’ He has had several<br />
people write letters to him and come<br />
up to him and thank him for saving<br />
their lives. ‘That’s more important<br />
than being an All Black.’<br />
<strong>The</strong> ceremony received extensive media<br />
coverage, such as this TV3 piece:<br />
www.3news.co.nz/Former-All-Blackhonoured-by-doctors-society/tabid/317/articleID/135268/Default.aspx.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 11
CONTINUING PROFESSIONAL DEVELOPMENT<br />
Prostate cancer screening:<br />
Defining the <strong>GP</strong>’s role<br />
Jim Vause<br />
Past RNZC<strong>GP</strong> President, Blenheim<br />
<strong>The</strong> world <strong>of</strong> prostate cancer screening is<br />
awash with rhetoric, opinion and conflicting<br />
research, a world in which a <strong>GP</strong> needs<br />
a clear understanding <strong>of</strong> his or her role.<br />
That role, as the first and most appropriate<br />
clinician <strong>of</strong> call for a man considering<br />
screening, is to facilitate their informed<br />
decision-making through provision <strong>of</strong><br />
unbiased, evidence-based information on<br />
the prostate gland, prostate cancer and<br />
the harms and benefit <strong>of</strong> screening.<br />
Central to defining this role is the<br />
Health and Disability Commission<br />
(HDC) code Clause 2, which covers<br />
both the content and the process with<br />
particular emphasis on Rule 6, the Right<br />
to be Fully Informed. 1 <strong>The</strong> process<br />
<strong>of</strong> patient communication should not<br />
need reiteration to vocationally trained<br />
<strong>GP</strong>s, except to emphasise that simply<br />
ordering a PSA test or doing a DRE test<br />
without first obtaining informed consent<br />
from the patient, could be regarded<br />
as an inappropriate standard <strong>of</strong> care.<br />
Note the importance <strong>of</strong> ‘informed’, for<br />
current media and interest group publicity<br />
is <strong>of</strong>ten poor in terms <strong>of</strong> quality and<br />
research base. Thus a man’s or, as <strong>of</strong>ten<br />
occurs, their spouse’s simple request<br />
for a PSA test flags the need to explore<br />
with the patient their knowledge and<br />
expectation <strong>of</strong> any such testing.<br />
Typically, the information provided to a<br />
man seeking screening should cover the<br />
anatomy, function and disease <strong>of</strong> the<br />
prostate, in particular the natural history<br />
<strong>of</strong> prostate cancer. This is the background<br />
information. More important is<br />
the foreground information, covering<br />
the harms and benefits <strong>of</strong> screening,<br />
including the full screening pathway<br />
within which lie the treatment options<br />
<strong>of</strong> prostate cancer, with all the regional<br />
practice variations which makes providing<br />
this information problematic to say<br />
the least. As for trying to meet the<br />
HDC standard <strong>of</strong> information on waiting<br />
times and service availability within a<br />
15-minute consult, after first prescribing<br />
a man’s blood pressure pills, dealing<br />
with his chest pain and checking his skin<br />
spots, the only answer that comes to<br />
mind is a Tui billboard.<br />
Fortunately, there are a few resources<br />
available to help, such as the <strong>New</strong><br />
<strong>Zealand</strong> Guidelines Group (NZGG)<br />
pamphlet which provides background<br />
and some foreground information. 2<br />
Harms and benefits is a different story,<br />
but a story that can be focused by the<br />
patient orientated question: ‘What<br />
chance is there that prostate screening<br />
will save my life?’ (benefit) and ‘What<br />
chance is there that prostate screening<br />
will cause me harm or even kill me?’<br />
(harm). Putting these questions to a man<br />
seeking screening helps focus thinking,<br />
for many men on first presentation<br />
presume benefit and ignore harm. That<br />
screening can kill you (through mortality<br />
from treatment <strong>of</strong> prostate cancer)<br />
seems to be a hidden fact.<br />
While we know a lot <strong>of</strong> the harms <strong>of</strong><br />
screening, it was not until March 2009<br />
that research answered the benefits<br />
question. Two key studies, both<br />
published in the 26 March NEJM gave<br />
answers, one being that there was no<br />
benefit, the other showing a small benefit.<br />
Both showed harm.<br />
<strong>The</strong> better quality study methodologically,<br />
the American PLCO trial, found that<br />
there was no benefit from prostate<br />
screening. 3 Screening did not reduce<br />
a man’s chance <strong>of</strong> dying from prostate<br />
cancer but did significantly increase his<br />
chance <strong>of</strong> being found to have prostate<br />
cancer. <strong>The</strong> researchers commented that<br />
there was a higher death rate from non<br />
prostate cancer causes in the screened<br />
group, probably due to over-diagnosis <strong>of</strong><br />
prostate cancer and treatment-related<br />
mortality. Commentators have pointed<br />
to the high number <strong>of</strong> patients in the<br />
non-screened (control) arm <strong>of</strong> this study<br />
who underwent screening; however the<br />
study design did allow for such contamination<br />
in calculating the power (number<br />
<strong>of</strong> men recruited) <strong>of</strong> the study.<br />
<strong>The</strong> other randomised controlled trial,<br />
the European ERSPC trial, did find a<br />
benefit, albeit small, from screening,<br />
with 1410 men having to be screened<br />
for nine years in order to prevent one<br />
man from dying from prostate cancer. 4<br />
This is the NNS (numbers needed to<br />
screen). Unfortunately, the study methodology<br />
was not as good as the PLCO<br />
study, there being variation in treatment,<br />
diagnosis and recruitment age between<br />
the many European study centres.<br />
So the benefit is most likely nil or possibly<br />
in the realm <strong>of</strong> one in 1410. <strong>The</strong> latter<br />
figure is comparable to other cancer<br />
screening such as breast and bowel (FOB<br />
test) cancer, but the difference is the<br />
high rate <strong>of</strong> harm from prostate cancer<br />
screening and the substantially older age<br />
<strong>of</strong> screening subjects (55–74) compared<br />
with breast cancer. For younger men, neither<br />
trial found benefit from screening.<br />
What <strong>of</strong> the magnitude <strong>of</strong> harm? In<br />
the ERSPC trial, one in three screening<br />
PSA tests were positive and one in six<br />
12 | <strong>GP</strong> PULSE | MARCH 2010
CONTINUING PROFESSIONAL DEVELOPMENT<br />
tested required a biopsy. One in 10 men<br />
screened were found to have prostate<br />
cancer and thus faced all the problems<br />
<strong>of</strong> deciding which therapy to have. This<br />
study also found that you have to detect<br />
by screening (and treat, including surveillance/watchful<br />
waiting) 48 prostate<br />
cancers in order to stop one man from<br />
dying from that cancer (numbers needed<br />
to detect) i.e. the other 47 did not benefit<br />
at nine years. <strong>The</strong>se rates seem high<br />
but remember this is a research trial with<br />
a good consistent screening protocol, not<br />
the real world <strong>of</strong> NZ with our difficulties<br />
with access to diagnostics.<br />
Back at the consultation, how do you<br />
get this data across to a man asking<br />
about prostate cancer screening, for the<br />
judgement <strong>of</strong> whether these numbers<br />
mean it is worthwhile to screen lies not<br />
with the <strong>GP</strong> or specialist, but the patient<br />
whose perception <strong>of</strong> benefit is substantially<br />
different from a <strong>GP</strong>s and more so<br />
compared with a specialist. 5 <strong>The</strong>re is<br />
extensive research on presenting statistics<br />
on harm and benefit to patients with the<br />
general consensus that graphic presentation<br />
appears better understood than<br />
numbers, as Goodyear-Smith et al. found<br />
in Auckland. 6 Whether you present (a)<br />
relative risk reduction, (b) absolute risk<br />
reduction, or (c) numbers needed to<br />
treat (NNT)/ screen favours (b) absolute<br />
risk reduction because <strong>of</strong> the difficulties<br />
<strong>of</strong> understanding NNTs/NNSs and<br />
the interpretation bias <strong>of</strong> relative risk<br />
reduction. However, there is significant<br />
work being done on what is the best way<br />
to present this type <strong>of</strong> data and how to<br />
achieve informed patient decision-making.<br />
Table 1<br />
Benefit<br />
Relative risk<br />
reduction death<br />
Harms <strong>of</strong> the magnitude in the above<br />
table, seems relatively easy to understand,<br />
qualified as always by the patient<br />
perspective, such as their feeling about<br />
being found to have a positive blood<br />
result for cancer (as might be influenced<br />
by their personality or mental<br />
conditions), their feeling about prostatic<br />
biopsy via biopsy needles inserted via<br />
the rectum or their understanding and<br />
feeling about the uncertainties around<br />
prostatic cancer treatment.<br />
Absolute risk<br />
reduction death<br />
Numbers needed to<br />
screen to prevent a death<br />
ERSPC 20% 0.71 in 1000 1 in 1410<br />
PLCO None None Infinite<br />
Harm, from the<br />
ERSPC trial<br />
a positive PSA<br />
needing a biopsy<br />
<strong>of</strong> a diagnosis <strong>of</strong><br />
prostate cancer<br />
Chance if screened <strong>of</strong> 1 in 3 1 in 4 1 in 10<br />
Out <strong>of</strong> 1000 341 292 100<br />
Presenting the benefits is a greater<br />
problem. Chance, such as one in 1410,<br />
is small and does not present well on<br />
the bar graphs that Goodyear-Smith<br />
et al. used in their research. A better<br />
method is to use pictograms showing<br />
the total number <strong>of</strong> men being recruited<br />
to screening (1410) and highlighting the<br />
one who gains benefit (Appendix 1) a<br />
technique developed by Dr John Paling. 7<br />
<strong>The</strong> same pictograms displaying 1410<br />
stock men can be used to show harm.<br />
Similar pictograms are used in the excellent<br />
online resource to be found at<br />
www.prosdex.com.<br />
Currently, medicine needs to have more<br />
information on the patient perception <strong>of</strong><br />
this magnitude <strong>of</strong> benefit versus harm on<br />
a screening issue and the impact <strong>of</strong> contextual<br />
factors, both individual and cultural,<br />
have on this perception. Until we have<br />
better information, the <strong>GP</strong>’s role will be to<br />
present statistical data to the patient in a<br />
manner which the patient—and family if<br />
necessary—can understand and interpret<br />
within their own context. It is also helpful<br />
if the <strong>GP</strong> understands the numbers.<br />
So, never simply just tick the lab box for<br />
a PSA test in response to an uninformed<br />
patient request. Make sure your patient<br />
understands the issues, has clarity<br />
around the outcome they are seeking,<br />
and make use <strong>of</strong> the written resources<br />
available, preferably the unbiased ones.<br />
Prostate screening charts available online<br />
at www.gponline.co.nz/Paling Charts.html<br />
References:<br />
1 <strong>The</strong> HDC Code <strong>of</strong> Health and Disability Services Consumers’ Rights Regulation 1996, 2. Rights <strong>of</strong> Consumers and Duties <strong>of</strong> Providers: Available online at http://<br />
www.hdc.org.nz/theact/theact-thecodeclause2<br />
2 Testing for Prostate Cancer. Published by the <strong>New</strong> <strong>Zealand</strong> Guidelines Group. ISBN (print): 978–1–877509–02–5 ISBN (electronic): 978–1–877509–03–2.<br />
Available online at http://www.nzgg.org.nz/guidelines/0153/Prostate_Cancer_Consumer_Resource.pdf<br />
3 Andriole GL, Grubb RL, Buys SS et al. Mortality results from a randomized prostate-cancer screening trial. N Engl J Med. 2009;360:1310–1319.<br />
4 Schröder FH, Hugosson J, Roobol MJ et al. Screening and prostate-cancer mortality in a randomized european study. N Engl J Med. 2009;360:1320–1328.<br />
5 Steel N. Thresholds for taking antihypertensive drugs in different pr<strong>of</strong>essional and lay groups: questionnaire survey. BMJ. 2000;320;1446–1447<br />
6 Goodyear-Smith F, Arroll B, Chan L et al. Patients prefer pictures to numbers to express cardiovascular benefit from treatment. Annals <strong>of</strong> Family Medicine.<br />
2008;6:213–217.<br />
7 <strong>The</strong> Risk Communication Institute. Available online at http://www.riskcomm.com<br />
<strong>GP</strong> PULSE | MARCH 2010 | 13
CONTINUING PROFESSIONAL DEVELOPMENT<br />
Primum non nocerE:<br />
Of pills and potions for<br />
coughs and colds<br />
Jim Vause<br />
Past RNZC<strong>GP</strong> President, Blenheim<br />
Once upon a time, boys and girls,<br />
when you went to your <strong>GP</strong> with a<br />
cold, he would have a special little<br />
mixture, a secret brew <strong>of</strong> magic<br />
potions, the formula handed down<br />
from generation to generation, to<br />
help quell your nasty hacking cough.<br />
Alas it is no more, gone forever into<br />
the mists <strong>of</strong> time, banished by the big<br />
bureaucrats in Medsafe. People who<br />
have decided the potions, concoctions<br />
and elixirs used in cough and cold<br />
remedies might cause a little harm,<br />
like poisoning, overdosing and death.<br />
A paradigm shift.<br />
Those <strong>College</strong> readers with more<br />
than a few decades <strong>of</strong> experience<br />
Such prescribing was mirrored by<br />
pharmacists, who <strong>of</strong>ten had equally<br />
heinous brews. But progress has seen<br />
them superseded by the pharmaceutical<br />
companies’ OTC preparations. Did<br />
you know you can buy one syrup for<br />
a wet cough and another for a dry<br />
cough? An elixir for blocked noses,<br />
another for running noses, dribbling<br />
noses and bent noses. And for the different<br />
types <strong>of</strong> phlegm.<br />
Fortunately Medsafe have made<br />
things a lot easier. DO NOT<br />
PRESCRIBE COUGH MIXTURES<br />
FOR CHILDREN UNDER THE AGE<br />
OF SIX YEARS as per their following<br />
statement.<br />
In this new order we are not alone.<br />
Authorities in the USA, UK and Canada have<br />
issued similar advice<br />
will recall pet formulations <strong>of</strong> opioids,<br />
alcohol, chlor<strong>of</strong>orm, ammonium chloride,<br />
ipecac and glycerine that were<br />
prescribed, <strong>of</strong>ten willy nilly, to URTI<br />
sufferers <strong>of</strong> all ages. More advanced<br />
prescribers added ephedrine to ‘dry<br />
things up’ and a little antihistamine<br />
to counteract the resultant insomnia,<br />
whilst the true ‘master class’ was a<br />
touch <strong>of</strong> extract <strong>of</strong> liquorice, to reach<br />
the prescribing climax <strong>of</strong> a ‘Linctus<br />
Forte’. Strong taste makes for a great<br />
cough mixture.<br />
‘Use <strong>of</strong> Cough and Cold Medicines in<br />
Children—<strong>New</strong> advice<br />
Medsafe has continued its review <strong>of</strong> the use <strong>of</strong><br />
cough and cold medicines in children with the<br />
assistance <strong>of</strong> the Cough and Cold Review Group.<br />
This Group assessed the available safety and efficacy<br />
data to support the use <strong>of</strong> cough and cold<br />
medicines in children.<br />
<strong>The</strong> Group have recommended to Medsafe that<br />
oral cough and cold medicines containing the following<br />
substances should not be used in children<br />
under six years <strong>of</strong> age:<br />
Guaifenesin, phenylephrine, doxylamine,<br />
ipecacuanha, brompheniramine, promethazine,<br />
dextromethorphan, chlorphenamine,<br />
triprolidine, pholcodine, diphenhydramine,<br />
pseudoephedrine 1 ’<br />
Accompanying this is a list <strong>of</strong> 162 OTC<br />
cough and cold preparations that contain<br />
these medicines.<br />
In this new order we are not alone.<br />
Authorities in the USA, UK and Canada<br />
have issued similar advice and every<br />
<strong>GP</strong> should be aware that the cut-<strong>of</strong>f <strong>of</strong><br />
six years is simply an extrapolation <strong>of</strong><br />
earlier Medsafe advice that set the cut<br />
<strong>of</strong>f at two years.<br />
So why now? After all we have known<br />
<strong>of</strong> the disutility <strong>of</strong> cough mixtures<br />
14 | <strong>GP</strong> PULSE | MARCH 2010
CONTINUING PROFESSIONAL DEVELOPMENT<br />
for a long time, so is this just another<br />
example <strong>of</strong> left-leaning do-gooders<br />
inflicting their world view on the<br />
populace? Or is it a backlash against<br />
inappropriate marketing <strong>of</strong> ineffectual<br />
pharmaceuticals?<br />
Harm versus benefit is the issue. <strong>The</strong><br />
benefit from cough mixtures is minimal,<br />
usually nil. Thus, it takes next to no harm<br />
to balance in the negative. We now have<br />
evidence on this harm!<br />
with these medications. 4 <strong>The</strong>re is little<br />
reason to believe NZ is any different<br />
either in magnitude or in social<br />
distribution <strong>of</strong> these remedies’ impact,<br />
but the small size <strong>of</strong> our population<br />
results in a very small number<br />
<strong>of</strong> adverse events. One example is a<br />
recent Coronial Court finding which<br />
questioned the role <strong>of</strong> antihistamines<br />
prescribed by a <strong>GP</strong>, against Medsafe<br />
advice, in a child’s death from infection.<br />
<strong>The</strong>re are issues around the<br />
How well informed are patients on the<br />
contents <strong>of</strong> cough mixtures when they<br />
receive advice from a health pr<strong>of</strong>essional,<br />
be it a doctor, a nurse or a pharmacist?<br />
Recent papers in paediatrics have<br />
shown a small but significant association<br />
<strong>of</strong> cough and cold remedies with<br />
increased death rates in children in the<br />
USA, an association due to a number<br />
<strong>of</strong> possible mechanisms ranging from<br />
accidental overdose to anaphylaxis<br />
to maliciousness. A higher incidence<br />
in more deprived communities has<br />
also been noted. 2,3 Data from the UK,<br />
Canada and Australia indicate a small<br />
number <strong>of</strong> adverse events associated<br />
quality <strong>of</strong> the evidence, but one child<br />
poisoning or one death requires significant<br />
provable benefit to justify using a<br />
cough mixture.<br />
<strong>The</strong>re are some other interesting<br />
issues to consider arising from the<br />
evidence, namely what <strong>of</strong> the safety<br />
<strong>of</strong> these medications in adults? Why<br />
are there such a large number <strong>of</strong><br />
OTC cough and cold mixtures on the<br />
market anyway? How well informed<br />
are patients on the contents <strong>of</strong> cough<br />
mixtures when they receive advice<br />
from a health pr<strong>of</strong>essional, be it a doctor,<br />
a nurse or a pharmacist?<br />
For many <strong>GP</strong>s, this restriction in<br />
prescribing will not be a problem.<br />
But for those used to reaching for a<br />
prescription pad when confronted<br />
by a toddler with rhinitis and cough,<br />
or a parent asking for a good syrup<br />
for wee Johnny’s hacking nocturnal<br />
cough, there will be a temptation to<br />
find an alternative not on the Medsafe<br />
list. But before you prescribe a little<br />
intranasal zinc, perhaps vitamin C,<br />
echinacea, Pelargonium sidoides or<br />
intranasal corticosteroids, check the<br />
evidence on the balance <strong>of</strong> their<br />
harms versus benefit.<br />
<strong>The</strong> best solution is not to prescribe,<br />
remembering that good advice and<br />
counselling <strong>of</strong>fers not only a better<br />
subsequent patient behaviour but also<br />
provides greater patient satisfaction. 5<br />
If you must have a fall back, try linctus<br />
simplex, a simple solution to a simple<br />
problem. It might not be effective, but at<br />
least causes no harm, we think.<br />
For the list <strong>of</strong> OTC medications containing<br />
the mentioned medicines go to:<br />
www.medsafe.govt.nz/hot/alerts/<br />
coughandcold/infooct2009.asp<br />
References<br />
1 Available online at http://www.medsafe.govt.nz/hot/alerts/coughandcold/infooct2009.asp<br />
2 Schaefer MK, Shehab N, Cohen AL, Budnitz DS. Adverse events from cough and cold medications in children. Pediatrics. April 2008;121(4):783–787. Available<br />
online at http://pediatrics.aappublications.org/cgi/reprint/121/4/783?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&fulltext=Melissa+K.+Schaefer&searchi<br />
d=1&FIRSTINDEX=0&sortspec=relevance&resourcetype=HWCIT<br />
3 Rimsza ME, <strong>New</strong>berry S. Pediatrics. Unexpected infant deaths associated with use <strong>of</strong> cough and cold medications. August 2008;122(2):e318–e322. (doi:10.1542/<br />
peds.2007–3813) Available online at http://pediatrics.aappublications.org/cgi/content/abstract/122/2/e318?maxtoshow=&HITS=10&hits=10&RESULTFORMAT=&<br />
fulltext=Mary+E.+Rimsza%2C+MDa+and+Susan+<strong>New</strong>berry%2C+MSW&searchid=1&FIRSTINDEX=0&sortspec=relevance&resourcetype=HWCIT<br />
4 Savage R. Review <strong>of</strong> OTC cough and cold medicines. Available online at http://www.medsafe.govt.nz/hot/alerts/coughandcold/Safety.pdf<br />
5 Welschen I, Kuyvenhoven M, Hoes A, Verheij T. Antibiotics for acute respiratory tract symptoms: patients’ expectations, <strong>GP</strong>s’ management and patient<br />
satisfaction. Family Practice. 2004;21(3):234–237. Available online at http://fampra.oxfordjournals.org/cgi/content/full/21/3/234<br />
<strong>GP</strong> PULSE | MARCH 2010 | 15
RESEARCH<br />
Changes in community<br />
laboratory services<br />
in Auckland<br />
Susan Dovey<br />
Associate Pr<strong>of</strong>essor, University <strong>of</strong> Otago, Dunedin School <strong>of</strong> Medicine<br />
<strong>The</strong> Labtests service in<br />
Auckland has improved a<br />
great deal since its start date<br />
in September 2009, but further<br />
improvements are needed.<br />
Making the right diagnosis, <strong>of</strong>ten assisted<br />
by timely laboratory results, is<br />
a major function <strong>of</strong> general practice.<br />
So when the established laboratory<br />
services were changed in the Auckland<br />
region in September last year, the<br />
<strong>College</strong> was concerned to ensure that<br />
the 40% <strong>of</strong> its members practising in<br />
the region could continue to provide<br />
the highest possible care. Three<br />
surveys were conducted between the<br />
start <strong>of</strong> the new Labtests services and<br />
the end <strong>of</strong> 2009. This is a report <strong>of</strong> the<br />
main results from these surveys.<br />
What <strong>College</strong> did<br />
<strong>The</strong> <strong>College</strong> invited all 1135 members<br />
practising in Auckland to complete a<br />
web-based survey about their experiences<br />
<strong>of</strong> the new laboratory service<br />
one, six and twelve weeks after the<br />
new service started. Retired <strong>GP</strong>s, affiliated<br />
members and <strong>GP</strong>s who may not<br />
have experienced the new laboratory<br />
services were included. <strong>The</strong>re were 442<br />
responses to the first survey, 196 to the<br />
second, and 166 to the third: 345 responses<br />
(43%) came from <strong>GP</strong>s practising<br />
in the Auckland DHB, 270 (34%) from<br />
Waitemata <strong>GP</strong>s, and (11%) from <strong>GP</strong>s in<br />
Counties Manukau DHB.<br />
What the <strong>College</strong> found<br />
Over 70% <strong>of</strong> <strong>GP</strong>s responding to the first<br />
and second surveys indicated they had<br />
experienced ‘significant’ or ‘major’ problems<br />
with the new laboratory service. In<br />
the third survey, this decreased to 55%.<br />
Figure 1 shows <strong>GP</strong>s’ overall experience<br />
with the new laboratory services in<br />
surveys 1, 2 and 3.<br />
In survey 2, 64% <strong>of</strong> <strong>GP</strong>s reported an<br />
improvement in services since the start<br />
<strong>of</strong> September and 68% reported an<br />
improvement in survey 3. <strong>The</strong> laboratory<br />
service had become ‘much better’ for<br />
14% in survey 2 and 23% in survey 3.<br />
Problem areas<br />
Given a choice <strong>of</strong> eight potential problems<br />
with the new laboratory service,<br />
the mean number <strong>of</strong> reported problems<br />
reduced from 3.2 at survey 1 to 3.0 in<br />
survey 2 and 2.0 in survey 3. Table 1<br />
shows changes in respondents’ experience<br />
in the three surveys <strong>of</strong> problems in<br />
the eight areas listed on the survey forms.<br />
Figure 1: Overall experience with the new laboratory services in surveys 1, 2 and 3<br />
Number <strong>of</strong> respondents<br />
250<br />
200<br />
150<br />
100<br />
50<br />
0<br />
no impact minor significant major<br />
problems problems problems<br />
Impact<br />
Survey<br />
1<br />
2<br />
3<br />
16 | <strong>GP</strong> PULSE | MARCH 2010
RESEARCH<br />
Table 1: Percent <strong>of</strong> respondents indicating experience with the eight problem areas listed on the three survey forms<br />
Percent reporting problems<br />
Survey 1 Survey 2 Survey 3<br />
p-value for change<br />
across surveys<br />
Delayed access to tests or results 75.4 61.4 33.1
EDUCATION<br />
<strong>The</strong> (new) educators<br />
Samantha Murton<br />
Clinical Leader <strong>GP</strong>EP1 & PG Rural<br />
Approachable and dedicated, Sam Murton enjoys time with her family:<br />
husband, three children, dog and cat. She likes fishing and cooking. She lives<br />
in Wellington for its beautiful weather and outdoor opportunities.<br />
Medical Council<br />
impressed with the RNZC<strong>GP</strong><br />
<strong>The</strong> Medical Council’s Education Committee<br />
has resolved that the RNZC<strong>GP</strong> be reaccredited<br />
as the standard-setter for <strong>GP</strong><br />
education for the maximum period. ‘We’re<br />
pleased the Council was impressed with our<br />
report. <strong>The</strong>y noted proposed “changes to<br />
the <strong>GP</strong>EP training programme are positive<br />
and will assist the <strong>College</strong> to develop a<br />
stronger training programme”,’ RNZC<strong>GP</strong><br />
Chief Executive Karen Thomas said. <strong>The</strong><br />
<strong>College</strong> is now accredited through to 2014.<br />
Anna Gilmour<br />
Co-Medical Educator, Otago/Southland<br />
Anna lives in Dunedin with her husband and two children.<br />
As a family they love living in Otago and having such easy<br />
access to some <strong>of</strong> their favourite pastimes such as skiing<br />
and mountain biking. She is a <strong>GP</strong> in urban Dunedin with a<br />
special interest in sexual health and is also a medical student<br />
tutor at the University <strong>of</strong> Otago. She has been involved<br />
with the <strong>GP</strong>EP1 programme for the last two years as a<br />
seminar facilitator and has been in the medical educator<br />
role since August 2009. Anna enjoys her involvement with<br />
the registrars, teachers and <strong>College</strong> staff and is looking<br />
forward to with enthusiasm.<br />
Craig Pelvin<br />
Co-Medical Educator, Otago/Southland<br />
Craig has returned to his home town <strong>of</strong> Dunedin again after<br />
living in various locations around the country. He works at the<br />
Gardens Medical Centre and maintains variety by doing fracture<br />
management at the local After Hours clinic and regular<br />
Emergency Department shifts. He has been involved in health<br />
politics over the last two years as a <strong>GP</strong> rep on a local PHO,<br />
and has some RNZC<strong>GP</strong> roles. What little time he has left, he<br />
spends with his wife and son, their cats and the veggie garden.<br />
His other interests include tramping, mountain biking and<br />
photography. He is a bit <strong>of</strong> a greenie and spends a lot <strong>of</strong> time<br />
trying to reduce his carbon footprint.<br />
18 | <strong>GP</strong> PULSE | MARCH 2010
EDUCATION<br />
Changes to your<br />
Maintenance <strong>of</strong> Pr<strong>of</strong>essional<br />
Standards (MOPS)<br />
programme for 2011–2013<br />
Rhett Emery<br />
Assessment Manager, RNZC<strong>GP</strong><br />
<strong>The</strong> MOPS programme is changing from<br />
June 2010 to reflect the direction <strong>of</strong> the<br />
Medical Council and the evidence base<br />
on the most effective methods <strong>of</strong> improving<br />
practice. From June, you will have<br />
the choice <strong>of</strong> two programmes for fulfilling<br />
the requirements for recertification.<br />
Option 1—Regular<br />
Practice Review (RPR)<br />
This option is based on a practice review<br />
visit undertaken by a trained vocationally<br />
registered peer. <strong>The</strong> completion <strong>of</strong> the<br />
practice review can occur at any time<br />
within the triennium and will satisfy the<br />
full MOPS credits for the triennium. <strong>The</strong><br />
reviewer can also gain full triennium credits<br />
for their involvement in the review.<br />
Doctors will register their intent to<br />
undertake the RPR with the RNZC<strong>GP</strong>.<br />
Prior to having a visit, the participant<br />
will supply a report based on feedback<br />
from colleagues and patients, and<br />
provide the reviewer with a personal<br />
reflection summary along with details <strong>of</strong><br />
their recent CPD portfolio and practice<br />
environment.<br />
<strong>The</strong> participant and the reviewer will arrange<br />
the practice visit for a time that is<br />
mutually acceptable. During the visit the<br />
reviewer will observe a series <strong>of</strong> patient<br />
consultations and review a selection <strong>of</strong><br />
patient records.<br />
Following the visit, the reviewer will<br />
meet with the participant at least once.<br />
This meeting will be used to provide<br />
verbal and written feedback to the<br />
participant—including specific information<br />
related to strengths and any<br />
identified areas for development—and<br />
formulate the participant’s personal<br />
development plan and future learning<br />
and CPD requirements.<br />
<strong>The</strong> costs associated with the RPR visit<br />
will be the responsibility <strong>of</strong> the participant<br />
and the reviewer.<br />
Option 2—Pr<strong>of</strong>essional<br />
Development Plan (PDP)<br />
This MOPS option is similar to the<br />
current programme, but is based on a<br />
Development Plan that identifies personal<br />
learning needs. This plan will be<br />
used to design the MOPS programme<br />
activities for the triennium. <strong>The</strong> MOPS<br />
credits are gained from the development<br />
plan and the activities that are<br />
undertaken as part <strong>of</strong> the plan.<br />
<strong>The</strong> annual submission <strong>of</strong> a completed<br />
Development Plan, reviewed by a peer,<br />
is required for the acceptance <strong>of</strong> all<br />
other credits.<br />
A minimum <strong>of</strong> 150 credits is required<br />
over the three years <strong>of</strong> the triennium.<br />
<strong>The</strong> credit requirement includes:<br />
• Development Plan (5 credits per<br />
annum)—compulsory<br />
• Clinical Audit (minimum 30 credits)<br />
• Peer Review (minimum 30 credits)<br />
• CME (minimum 30 credits).<br />
<strong>The</strong> <strong>College</strong> has designed the new MOPS<br />
triennium programme to give Fellows<br />
greater flexibility in creating personal programmes<br />
<strong>of</strong> relevance and meaning. <strong>The</strong>re<br />
is now evidence that traditional methods<br />
<strong>of</strong> maintaining pr<strong>of</strong>essional standards,<br />
such as lectures and conferences, aren’t<br />
always useful enough. <strong>The</strong> most effective<br />
methods <strong>of</strong> improving practice include<br />
educational initiatives that: are based on<br />
the real work <strong>of</strong> the practitioner; use<br />
individual practitioner data to compare<br />
with peers; take place in the working environment<br />
<strong>of</strong> the practitioner; and produce<br />
individualised education programmes<br />
based on identified learning needs.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 19
EDUCATION<br />
Inspiring rangatahi<br />
Alexander Bisley<br />
Communications Advisor, RNZC<strong>GP</strong><br />
Lincoln Nicholls (Ngati Raukawa), an<br />
acclaimed Maori medical student leader,<br />
is currently undertaking the <strong>GP</strong>EP<br />
training programme. <strong>GP</strong> <strong>Pulse</strong> caught up<br />
with Linc after he’d finished February’s<br />
Coast to Coast.<br />
Why do you want to be a <strong>GP</strong>?<br />
I like the continuity <strong>of</strong> care that a <strong>GP</strong> gets<br />
in their role. Serving the community has<br />
also always appealed to me and is something<br />
that I’ve always enjoyed since my<br />
days as a secondary school teacher. I like<br />
the pr<strong>of</strong>ile that a doctor can enjoy in the<br />
community and the role-modelling that<br />
comes with being a Maori doctor. I feel<br />
very passionate about being known as a<br />
Maori doctor so that our Maori rangatahi<br />
can be inspired and see that becoming a<br />
doctor is very achievable. We need more<br />
‘TKs from Shortland Street’ in Aotearoa<br />
and when this happens hey Maori health<br />
as a whole can only benefit.<br />
Anywhere in particular you’d<br />
like to practise once you finish?<br />
Currently I’m working as a <strong>GP</strong> Registrar<br />
in the NZ army and based at Linton<br />
Army Camp for two days a week,<br />
Consultation on a young Samoan girl with ‘Tsunami Lung’<br />
Feilding Medical Centre for two days,<br />
and one day <strong>of</strong> lectures in Wellington<br />
while on the first year <strong>GP</strong> training<br />
scheme. Following my three years with<br />
the <strong>College</strong> I will need to complete a<br />
further two years <strong>of</strong> return service with<br />
the army. Following this the options will<br />
be open which is a very exciting prospect<br />
for me. That’s the beauty <strong>of</strong> medicine:<br />
you can go anywhere and almost<br />
do anything. Something that has always<br />
sounded appealing to me is perhaps<br />
working for a Super 14 franchise.<br />
What’s your pitch to encourage<br />
Maori to become <strong>GP</strong>s?<br />
We need to break down the stereotypes<br />
and help our Maori rangatahi see the<br />
truth—becoming a doctor is extremely<br />
achievable and that there are Maori doctors<br />
out there ‘doing it!’ You know, if I go<br />
out on the town for a social night out with<br />
the mates and someone starts chatting<br />
to me, they inevitably ask me what I do<br />
for a job. When I disclose I’m a doctor,<br />
they <strong>of</strong>ten take one look at my moko on<br />
my arm and say ‘yeah right mate!’ <strong>The</strong>se<br />
are the stereotypes I’m talking about. We<br />
need to break them down.<br />
Lincoln and his 14-year-old daughter Awarangi<br />
Continuing with that topic, I’d like to say<br />
I’m disgusted with that <strong>New</strong> World ad<br />
that features a young ‘Maori Checkout<br />
Girl’. In the advertisement she goes on<br />
and on about how many <strong>of</strong> her whanau<br />
work at <strong>New</strong> World—this is feeding<br />
a stereotype that these are the jobs<br />
that Maori are good for and Maori do.<br />
It seems to me at times that in reality<br />
Aotearoa hasn’t come very far at<br />
all in closing disparity gaps. I quote a<br />
statement from the Director-<strong>General</strong><br />
<strong>of</strong> Education from back in 1931 which<br />
reflects the attitudes <strong>of</strong> that time. He<br />
declared that after noting the successes<br />
<strong>of</strong> Maori at Te Aute <strong>College</strong> <strong>of</strong> the time:<br />
‘Maori aptitude for maths was interesting,<br />
but not relevant to their present or<br />
future needs as agriculturalists.’<br />
Coming from a secondary school teaching<br />
background I see it as essential to<br />
expose Maori rangatahi to Maori doctors<br />
as role models and as real people in the<br />
community doing the business! This will<br />
help to break down those stereotypes.<br />
I take any opportunity I can to speak at<br />
colleges when invited, to promote medicine<br />
to Maori rangatahi. And when I can<br />
I send home the message to them about<br />
20 | <strong>GP</strong> PULSE | MARCH 2010
EDUCATION<br />
the importance <strong>of</strong> sciences as subjects<br />
at school. That’s what schools have to do<br />
for Maori rangatahi—they have to ‘G’<br />
up the sciences, make it interesting and<br />
appealing and inspire our kids to take<br />
science. It’s here where the seeds can be<br />
sown to grow our future Maori doctors.<br />
What are the crucial health<br />
issues for Maori at the moment?<br />
Understanding! I feel that the average<br />
<strong>New</strong> <strong>Zealand</strong>er doesn’t really know<br />
about the colonial history <strong>of</strong> Aotearoa<br />
and the impact <strong>of</strong> past unjust policies that<br />
have helped shape the current socioeconomical<br />
climate <strong>of</strong> Maori in Aotearoa.<br />
While at school as a student I remember<br />
learning about far away countries and<br />
their histories very <strong>of</strong>ten. I remain concerned<br />
however about the lack <strong>of</strong> NZ’s<br />
history that is taught in schools. Let’s face<br />
it; it’s our history that is so relevant to us<br />
as Kiwis. If we all know our past and the<br />
impact <strong>of</strong> the past and how it has shaped<br />
out today then we can understand why<br />
there are huge disparities in health between<br />
Maori and non-Maori. I believe that<br />
once there is understanding only then can<br />
we get together to reduce the gaps.<br />
How does being a father<br />
influence you?<br />
Being a role model to my daughter is<br />
tops for me. I’m stoked that one <strong>of</strong> her<br />
possible future pathways is to follow in my<br />
footsteps: becoming a doctor appeals to<br />
her, especially working in paediatrics. Every<br />
year I take her to the Te Ora hui (Maori<br />
Doctors Conference). <strong>The</strong>re she is always<br />
surrounded by Maori doctors and I have<br />
no doubt that this provides a significant<br />
source <strong>of</strong> inspiration. <strong>The</strong>y say that success<br />
breeds success and that’s what we should<br />
try to do for our kids.<br />
<strong>The</strong>re I gained huge experience in working<br />
in a mass casualty setting. I truly felt<br />
that I made a real difference in people’s<br />
lives there. I found it a huge privilege to<br />
treat desperate locals in their time <strong>of</strong> need<br />
and an honour to assist with the cause.<br />
Tell me about a particular<br />
medical mentor?<br />
Sir Mason Durie. Mason’s my best mate’s<br />
dad and I have been lucky enough to<br />
have known him now for 20 years. As a<br />
teacher his name kept popping up in education<br />
circles and education books. It was<br />
always cool to nudge the person next to<br />
me and say, ‘Hey I know him’.<br />
Since switching to medicine I have realised<br />
how much <strong>of</strong> a true legend Mason is.<br />
I have seen him deliver keynote speeches<br />
at conferences and have medical world<br />
VIPs eating out <strong>of</strong> the palm <strong>of</strong> his hand.<br />
Sir Mason is truly an inspiration and a<br />
fantastic Maori role model for all Maori.<br />
We’re very proud to say he is ours. Even<br />
cooler than that, he’s one <strong>of</strong> my referees.<br />
Who else has inspired you?<br />
Our Maori forefathers—Maui Pomare<br />
(1st Maori doctor), Te Rangihiroa (1st<br />
Maori doctor to graduate from NZ),<br />
Tutere Wirepa (3rd Maori doctor) and<br />
Pohau Ellison (4th Maori doctor).<br />
At the finish <strong>of</strong> the Coast to Coast with Robin Judkins<br />
(founder <strong>of</strong> the Coast to Coast)<br />
<strong>The</strong> late Dr Paratene Ngata, one <strong>of</strong> the<br />
founding members <strong>of</strong> Te Ora. Dr Ra<br />
Durie, Sport Med Physician in Palmerston<br />
North. Dr Don Stewart, my Yoda at the<br />
Linton Army Camp MTC.<br />
How do you wind down<br />
from medicine?<br />
Multisport! I’m loving doing multisport<br />
events at the moment as a form <strong>of</strong> maintaining<br />
sanity, health and fitness. In the<br />
last three years I have done two Ironman,<br />
five half Ironman, four marathons, three<br />
Lake Taupo Cycle Challenges and just<br />
completed the Speights Coast to Coast.<br />
When I’m not playing Dad, training or<br />
competing, you may just find me chucking<br />
down a few karaoke numbers at the<br />
China Inn in Palmy.<br />
How has working for the<br />
army influenced you?<br />
Last year I was fortunate enough to deploy<br />
to Samoa to provide medical aid and<br />
assistance following the Samoan tsunami.<br />
Samoa Tsunami medics<br />
<strong>GP</strong> PULSE | MARCH 2010 | 21
partnership<br />
<strong>The</strong> evolving <strong>GP</strong>/<br />
physiotherapist partnership<br />
Janet Copeland<br />
Research and Pr<strong>of</strong>essional Development, <strong>New</strong> <strong>Zealand</strong> Society <strong>of</strong> Physiotherapists<br />
What does partnership between <strong>GP</strong>s,<br />
physiotherapists and other health pr<strong>of</strong>essionals<br />
in primary care mean? What<br />
should it look like? How can it work?<br />
Up until 1982 the partnership between<br />
<strong>GP</strong>s and physiotherapists had to be strong<br />
because it was based on referrals. All<br />
physiotherapy patients were referred by a<br />
doctor. At least theoretically, physiotherapists<br />
acted ‘under the direction, supervision<br />
or approval <strong>of</strong> a registered medical<br />
practitioner’. This provision, quoted from<br />
the 1922 Rules <strong>of</strong> <strong>New</strong> <strong>Zealand</strong> Society<br />
<strong>of</strong> Physiotherapists’ (NZSP) Auckland<br />
Branch, remained in force until the NZSP<br />
Ethical Rules <strong>of</strong> 1982 allowed direct access.<br />
In 1999 an ACC regulation change removed<br />
the <strong>GP</strong> as gatekeeper for accidental injuries,<br />
meaning that physiotherapists and other<br />
treatment providers could claim ACC<br />
treatment subsidies for patients presenting<br />
directly to them. Only a medical practitioner,<br />
however, can sign a patient <strong>of</strong>f work.<br />
When patients began to access physiotherapists<br />
directly, the <strong>GP</strong>/physiotherapist partnership<br />
was challenged. Its nature changed.<br />
It had to evolve towards equality, which<br />
required a mind shift for both parties.<br />
• On the one hand, the <strong>GP</strong> needed to<br />
adjust to interacting with the physiotherapist<br />
as an autonomous health<br />
pr<strong>of</strong>essional and colleague whose independent<br />
judgement and skills contribute<br />
to the rehabilitation <strong>of</strong> their patient.<br />
• On the other hand, the physiotherapist<br />
had to realise that collaboration<br />
remains essential. Keeping the <strong>GP</strong><br />
informed regarding the progress <strong>of</strong><br />
their patient is just as important (or<br />
perhaps sometimes more important)<br />
when the patient is self-referred.<br />
Knowing when to refer a patient to<br />
the <strong>GP</strong> or other health pr<strong>of</strong>essional<br />
is a crucial element in the physiotherapist’s<br />
pr<strong>of</strong>essional expertise.<br />
A simple example <strong>of</strong> the requirement for<br />
good communication is when 18-year-old<br />
Amanda consults a physiotherapist the<br />
day after a fall while climbing on rocks.<br />
During the initial assessment, the physiotherapist<br />
discovers that in her fall Amanda<br />
also cut her foot. Taking a medical history<br />
establishes that Amanda has recently been<br />
diagnosed with Type 1 diabetes. Amanda<br />
has not yet absorbed all the information<br />
relating to her diabetes, such as warnings<br />
about care <strong>of</strong> the feet. <strong>The</strong> physiotherapist<br />
immediately informs her <strong>GP</strong>, who sees her<br />
to assess and treat the cut.<br />
Partnership in primary<br />
health care<br />
<strong>The</strong> growing emphasis on primary care<br />
reinforces the need for collaboration<br />
amongst health pr<strong>of</strong>essionals. <strong>The</strong> Primary<br />
Health Care Strategy stresses the importance<br />
<strong>of</strong> multidisciplinary involvement in<br />
<strong>of</strong>fering access to comprehensive services<br />
for local populations. A requirement for<br />
the recent expressions <strong>of</strong> interest from<br />
groups keen to develop ‘better, sooner,<br />
more convenient’ health care was pro<strong>of</strong><br />
<strong>of</strong> multidisciplinary involvement.<br />
Key principles for delivering primary<br />
health care are relevant to the <strong>GP</strong>/physiotherapist<br />
partnership.<br />
• Collaboration: <strong>The</strong> primary health<br />
system must evolve away from ‘the<br />
silo mentality’ to work as a team with<br />
strong lines <strong>of</strong> communication.<br />
• <strong>The</strong> patient at the centre: Working<br />
together in the best interests <strong>of</strong> the<br />
patient, from the patient’s point <strong>of</strong><br />
view. For instance, the decision on<br />
who should manage, say, a patient<br />
with COPD, is based on who is best<br />
for that patient.<br />
• Community base: Care is to devolve<br />
from the hospital to be delivered in<br />
patients’ own homes and in their own<br />
community. A patient needing chest<br />
physiotherapy, for example, is treated<br />
by the practitioner in a communitybased<br />
facility or their own home.<br />
• <strong>The</strong> need for clear pathways for the<br />
management <strong>of</strong> common conditions.<br />
22 | <strong>GP</strong> PULSE | MARCH 2010
partnership<br />
• Shared education for all practitioners<br />
involved. So each member <strong>of</strong> a<br />
multidisciplinary team implementing<br />
a particular pathway or programme<br />
understands their own role and how<br />
that fits with others. Understanding<br />
generates mutual respect as well as<br />
practical ways <strong>of</strong> working together.<br />
What can physiotherapists<br />
contribute to primary care?<br />
<strong>The</strong> traditional <strong>GP</strong> view <strong>of</strong> a private<br />
physiotherapist’s role is treatment <strong>of</strong> injuries.<br />
However, as <strong>New</strong> <strong>Zealand</strong> prepares<br />
to play its part in fighting the worldwide<br />
war against chronic non-communicable<br />
diseases, all health pr<strong>of</strong>essionals need to<br />
be fully engaged. Physiotherapists (and<br />
other allied health pr<strong>of</strong>essionals) are well<br />
placed to help the <strong>New</strong> <strong>Zealand</strong> public.<br />
Physiotherapists can add great value to<br />
the prevention and treatment <strong>of</strong> chronic<br />
diseases. <strong>The</strong>re is good evidence to support<br />
physiotherapy treatment for various conditions<br />
such as COPD, diabetes, cardiopulmonary<br />
rehabilitation, and chronic musculoskeletal<br />
conditions like osteoarthritis.<br />
Inactivity is an independent risk factor for<br />
development <strong>of</strong> chronic diseases and <strong>of</strong><br />
co-morbidities in those who already have a<br />
chronic condition. Overall, inactivity is estimated<br />
by the World Health Organization<br />
to cause 1.9 million deaths globally.<br />
‘Increasing physical activity is a societal, not<br />
just an individual problem. <strong>The</strong>refore it demands<br />
a population-based, multi-disciplinary,<br />
and culturally relevant approach,’ the World<br />
Health Organization stated in 2004.<br />
Physiotherapists can make a huge contribution<br />
by developing individual activity<br />
programmes for those with existing<br />
conditions who are afraid to become<br />
active or do not know how.<br />
An evolving example<br />
<strong>The</strong> Canterbury Clinical Network, a consortium<br />
<strong>of</strong> primary health care providers<br />
covering half a million people, was one <strong>of</strong><br />
the nine applicants (out <strong>of</strong> more than 70 expressions<br />
<strong>of</strong> interest) selected by the Minister<br />
<strong>of</strong> Health to develop a business case to<br />
deliver ‘better, sooner, more convenient care’.<br />
Canterbury practitioners were in a better<br />
position than most when the Minister <strong>of</strong><br />
Health made the call for expressions <strong>of</strong><br />
interest, because they had been reaching<br />
for years towards the above principles<br />
listed above. Through a project entitled<br />
Vision 20:20 they were already tackling the<br />
question, ‘If you redesigned primary health<br />
care in Canterbury, what would it look<br />
like?’ <strong>The</strong> Canterbury Initiative was working<br />
on clear pathways. Physiotherapists and<br />
a wide range <strong>of</strong> other health pr<strong>of</strong>essionals<br />
were already involved. Physiotherapy<br />
already had a lot <strong>of</strong> credibility in the region,<br />
for instance with a physiotherapist on the<br />
Canterbury DHB Clinical Board.<br />
<strong>The</strong> planning group includes physiotherapists,<br />
practice nurses, <strong>GP</strong>s, pharmacists,<br />
community nurses, rural care practitioners,<br />
PHO representatives, and other<br />
people with specialised expertise. ‘It’s a<br />
paradigm shift in attitudes,’ says physiotherapist<br />
Greg Knight. He gives credit<br />
to the visionary planners in Canterbury<br />
who have understood from the beginning<br />
the need to include everyone. Before<br />
finalising the business plan to be submitted<br />
mid-February, a two-day workshop<br />
brought together ideas from working<br />
groups which allowed each discipline to<br />
represent its own issues.<br />
Partnership models will vary<br />
How partnership amongst health<br />
pr<strong>of</strong>essionals will work may differ<br />
from one area to another, with varying<br />
models <strong>of</strong> primary health care provision.<br />
<strong>The</strong> Minister <strong>of</strong> Health is pushing for<br />
Integrated Family Health Centres, which<br />
may allow for flexible arrangements to<br />
meet local conditions.<br />
Different service models for Maori<br />
and Pasifika will no doubt continue to<br />
develop. Already physiotherapists form<br />
an integral part <strong>of</strong> some Maori PHOs.<br />
Co-location is one solution. <strong>The</strong>re are<br />
some very successful integrated health centres<br />
in smaller towns, for example. Shared<br />
facilities are a start—shared reception staff,<br />
shared medical records—but maybe the<br />
sharing can be virtual. A Wellington <strong>GP</strong> told<br />
me recently that he and a local physiotherapist<br />
are discussing how to share medical<br />
records. ‘We’ll probably just put in a router<br />
so the two computer systems can talk to<br />
each other,’ he said. Obviously in such a case<br />
issues <strong>of</strong> access and privacy will have to be<br />
carefully considered.<br />
Regular pr<strong>of</strong>essional networking for health<br />
providers in a local area also <strong>of</strong>fers one way<br />
to start developing partnership further.<br />
With plenty <strong>of</strong> good will and patience, and<br />
keeping the welfare <strong>of</strong> the patient as our<br />
focus, our future collaboration in primary<br />
health care will improve the health <strong>of</strong> <strong>New</strong><br />
<strong>Zealand</strong>ers.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 23
cornerstone<br />
CORNERSTONE: the<br />
storage <strong>of</strong> patient records<br />
Cathy Webber<br />
Principal Advisor, Medico-Legal<br />
How <strong>of</strong>ten have we all heard the mantra<br />
‘patient-centred care’? Quite <strong>of</strong>ten. But<br />
if patients’ needs are truly to be paramount,<br />
the information that <strong>GP</strong>s write<br />
down about those patients should surely<br />
be a key concern as well.<br />
Patients don’t tend to like the idea <strong>of</strong><br />
their medical records being accessible<br />
to all and sundry. Clearly security <strong>of</strong><br />
information ought to be a key priority<br />
for general practices, and the importance<br />
<strong>of</strong> security and privacy is reflected<br />
in the <strong>College</strong>’s policy on storing medical<br />
records. But after discussions between<br />
the <strong>College</strong> and the Office <strong>of</strong> the<br />
able in public,’ and that non-lockable files<br />
be used only in non-public working areas.<br />
In response to a member’s concern,<br />
the <strong>College</strong> attempted to clarify a 2007<br />
pamphlet from the Commissioner in<br />
regards to storage <strong>of</strong> paper files. <strong>The</strong><br />
pamphlet interprets Rule Five <strong>of</strong> the<br />
Health Information Privacy Code,<br />
which relates to storage and security <strong>of</strong><br />
health information; the core question<br />
was whether practices should have<br />
lockable cabinets for paper files.<br />
<strong>The</strong> Commissioner made it clear that<br />
she expects all practices to ensure<br />
they have lockable cabinets—having<br />
<strong>The</strong> Commissioner made it clear that she<br />
expects all practices to ensure they have<br />
lockable cabinets—having them unlocked,<br />
but behind reception, was not enough to<br />
meet this expectation<br />
Privacy Commissioner, in future, that<br />
definition <strong>of</strong> ‘secure’ needs to change.<br />
<strong>The</strong> <strong>College</strong>’s standards for storing medical<br />
records—developed with extensive consumer<br />
input, and in keeping with relevant<br />
legislation—are found in our publication<br />
Aiming for Excellence. This states that ‘the<br />
content <strong>of</strong> medical records and documents<br />
(paper or electronic) is not identifithem<br />
unlocked, but behind reception,<br />
was not enough to meet this expectation.<br />
<strong>The</strong> <strong>College</strong> agreed to inform<br />
RNZC<strong>GP</strong> members that they should<br />
plan to meet this expectation within<br />
the next five years. Discussions on the<br />
matter are continuing: in the meantime<br />
we refer you to the standards found in<br />
CORNERSTONE through the Aiming for<br />
Excellence document. <strong>The</strong>y can be found<br />
here: www.rnzcgp.org.nz/aiming-forexcellence.<br />
<strong>The</strong> Privacy Commissioner asked that<br />
the following note on storing paper<br />
records be passed on to <strong>GP</strong>s.<br />
Rule 5 <strong>of</strong> the Health Information Privacy<br />
Code requires that health agencies, such<br />
as <strong>GP</strong>s, take reasonable steps to keep the<br />
health information that they hold secure<br />
against loss, misuse and unauthorised access.<br />
It does not specify exactly how this<br />
should be achieved. What is ‘reasonable’<br />
depends on the circumstances, such as<br />
the nature <strong>of</strong> the information, the possible<br />
harm if it is lost or inappropriately<br />
accessed, and the practicality (including<br />
space and cost) <strong>of</strong> securing it. In the context<br />
<strong>of</strong> complaints that she has received,<br />
the Privacy Commissioner has been <strong>of</strong><br />
the view that having lockable cabinets in<br />
which to store sensitive personal information<br />
is an important component <strong>of</strong> secure<br />
information handling. Even where space<br />
is very limited, a range <strong>of</strong> lockable cabinets<br />
is now available to ensure information<br />
is secure.<br />
When deciding how to store your patients’<br />
paper records therefore remember<br />
that, while considerations <strong>of</strong> cost and<br />
practicality are relevant, you need to<br />
ensure that you are protecting your<br />
patients’ records in a way that recognises<br />
their sensitivity and confidentiality and<br />
your own legal obligations.<br />
24 | <strong>GP</strong> PULSE | MARCH 2010
cornerstone<br />
CORNERSTONE notches<br />
up 500<br />
When <strong>GP</strong> <strong>Pulse</strong> calls, Dunedin North<br />
Medical Centre project driver and practice<br />
manager Ali Barbara has just chaired an<br />
enthusiastic CORNERSTONE assessment<br />
debrief. ‘We’ve got strengthened policies<br />
and procedures now. We had an incident<br />
yesterday and everyone knew what to do.’<br />
<strong>The</strong> Centre is the 500th practice to have<br />
a CORNERSTONE assessment and,<br />
coincidently, the 100th practice funded<br />
under a Ministry <strong>of</strong> Health contract to<br />
be assessed. Staff, pictured below, found<br />
the process valuable. ‘CORNERSTONE<br />
drew the team together. It involved lots<br />
<strong>of</strong> teamwork, bringing all our information<br />
together. And the assessment visit<br />
highlighted the strength <strong>of</strong> our team.’<br />
Barbara says CORNERSTONE Assessors<br />
Judy Simpson and Diane Kelly put the<br />
team at ease with really useful, constructive<br />
and positive feedback through the<br />
day. Simpson, too, was pleased with<br />
Dunedin North Medical Centre. ‘It was<br />
a really nice, friendly practice. Everyone<br />
was very open. <strong>The</strong> whole team had got<br />
behind and understood the important<br />
CORNERSTONE journey.’<br />
In addition to ‘involving the whole team’,<br />
Barbara’s other key piece <strong>of</strong> advice to<br />
practices is having a CORNERSTONE<br />
project manager: ‘You’ve got to make<br />
sure your spokes and wheels are connected,<br />
driving the whole thing along.’<br />
Celebrating the 500th CORNERSTONE assessment at the Dunedin North Medical Centre<br />
<strong>GP</strong> PULSE | MARCH 2010 | 25
policy<br />
<strong>The</strong> Role <strong>of</strong> the <strong>GP</strong><br />
Jo Scott-Jones<br />
<strong>General</strong> Practitioner, Opotiki<br />
A perfect storm has gathered over<br />
primary medical care. Sweeping changes<br />
are afoot, but it’s not yet clear what role<br />
medically trained pr<strong>of</strong>essionals will have<br />
in primary care in 2020.<br />
<strong>GP</strong>s have evolved in a small business<br />
model <strong>of</strong> service provision. This model<br />
is becoming less attractive as the <strong>GP</strong><br />
workforce ages. Fewer young <strong>GP</strong>s are<br />
prepared to invest in the ‘corner dairy’<br />
business <strong>of</strong> family practice, and ongoing<br />
health disparities across our communities<br />
attest to the fact that the small<br />
business model did not always reach<br />
everyone equitably.<br />
Societal changes, including increasing<br />
democratisation, the breakdown <strong>of</strong> deferential<br />
attitudes, information technology<br />
creating a more knowledgeable population,<br />
workforce pressures, the recognition<br />
<strong>of</strong> the value <strong>of</strong> multidisciplinary<br />
All these factors have combined with the<br />
structural changes inherent in the ‘better,<br />
sooner, more convenient’ phase <strong>of</strong> the<br />
Primary Health Care Strategy to create<br />
a perfect storm requiring the role <strong>of</strong> the<br />
<strong>GP</strong> in primary care to be clearly defined.<br />
Without a clear definition <strong>of</strong> the role,<br />
there is a danger that the nature <strong>of</strong> the<br />
work <strong>GP</strong>s do will change in response to<br />
these pressures in ways which not only<br />
compromise the doctor–patient relationship,<br />
but also threaten the safety and<br />
quality <strong>of</strong> primary health care delivery in<br />
<strong>New</strong> <strong>Zealand</strong>.<br />
In a multidisciplinary team, who holds<br />
ultimate responsibility for patient care?<br />
What does it mean to work with a<br />
nurse who is autonomous? Should a<br />
<strong>GP</strong> be a part <strong>of</strong> every primary health<br />
care team? What is the value <strong>of</strong> medical<br />
training in primary care when so many<br />
<strong>The</strong> modern <strong>GP</strong> cannot function if<br />
isolated from the supportive network <strong>of</strong><br />
others working in primary health<br />
teams and the extension <strong>of</strong> the scope <strong>of</strong><br />
nursing practice put further pressure on<br />
primary medical care.<br />
Increasingly, whole-<strong>of</strong>-system approaches<br />
are being used in health policy development,<br />
and the language we use dividing<br />
care into primary, secondary and tertiary<br />
is coming into question, as it creates<br />
artificial barriers that keep funding and<br />
services in power vacuums.<br />
pr<strong>of</strong>essions have the training, ability and<br />
legislative support to diagnose, investigate<br />
and treat conditions?<br />
<strong>The</strong> modern <strong>GP</strong> cannot function if<br />
isolated from the supportive network<br />
<strong>of</strong> others working in primary health. In<br />
particular, the future role <strong>of</strong> the <strong>GP</strong> is<br />
tightly bound to the future role <strong>of</strong> the<br />
nurse, along with the practice manager,<br />
and the wider team <strong>of</strong> Hauora, NGO<br />
and other pr<strong>of</strong>essions working in the<br />
health sector.<br />
I sat on the Primary Health Care<br />
Advisory Council as RNZC<strong>GP</strong> representative<br />
until its demise in October<br />
2009, following the release <strong>of</strong> the<br />
Horn Report. Last year I also wrote<br />
a <strong>College</strong> occasional paper describing<br />
(appropriately in the year <strong>of</strong> the<br />
200th anniversary <strong>of</strong> Darwin’s birth)<br />
the ‘<strong>GP</strong> Genome’, and anticipating the<br />
‘<strong>GP</strong> Phenotype 2009–2020’ to help<br />
inform policy makers, planners and<br />
health pr<strong>of</strong>essionals in the formation <strong>of</strong><br />
new services as primary care continues<br />
to evolve. A copy can be found on the<br />
<strong>College</strong> website www.rnzcgp.org.nz/<br />
defining-the-role-<strong>of</strong>-the-gp.<br />
What is the <strong>GP</strong> genome? Is it possible<br />
to describe the total collection <strong>of</strong><br />
hereditary information held by a <strong>GP</strong>?<br />
What did the <strong>GP</strong> phenotype—the observable<br />
characteristics <strong>of</strong> a <strong>GP</strong>—look<br />
like in 2009?<br />
26 | <strong>GP</strong> PULSE | MARCH 2010
policy<br />
<strong>The</strong> International Labour Organisation<br />
(ILO) defines doctors as ‘clinical<br />
scientists who apply the principles and<br />
procedures <strong>of</strong> medicine to prevent,<br />
diagnose, care for and treat patients<br />
with illness, disease and injury and to<br />
maintain physical and mental health,’<br />
ILO says. ‘<strong>The</strong>y supervise the implementation<br />
<strong>of</strong> care and treatment plans<br />
by others in the health care team<br />
and conduct medical education and<br />
a vocationally registered <strong>GP</strong>; every<br />
person should be able to identify the<br />
<strong>GP</strong> with whom they have a relationship;<br />
every primary health care team should<br />
function well as a multidisciplinary<br />
team; every primary health care team<br />
should have a well functioning network<br />
<strong>of</strong> interdisciplinary connections; every<br />
primary health care team should be a<br />
learning environment; effective planning<br />
for change requires the engagement <strong>of</strong><br />
It is clear that within primary health<br />
every day, all pr<strong>of</strong>essionals are making<br />
difficult decisions in situations <strong>of</strong> clinical<br />
complexity and uncertainty. Is it the role <strong>of</strong><br />
the <strong>GP</strong> to take ‘ultimate responsibility’ for<br />
those decisions with the patient?<br />
research.’ A combined UK medical<br />
college consensus statement in 2009<br />
states: ‘Doctors alone amongst health<br />
pr<strong>of</strong>essionals must be capable <strong>of</strong> regularly<br />
taking ultimate responsibility for<br />
difficult decisions in situations <strong>of</strong> clinical<br />
complexity and uncertainty, drawing<br />
on their scientific knowledge and well<br />
developed clinical judgement and relationship<br />
with the patient.’ It is clear that<br />
within primary health every day, all pr<strong>of</strong>essionals<br />
are making difficult decisions<br />
in situations <strong>of</strong> clinical complexity and<br />
uncertainty. Is it the role <strong>of</strong> the <strong>GP</strong> to<br />
take ‘ultimate responsibility’ for those<br />
decisions with the patient?<br />
As we move forward into the future<br />
I would suggest that: every person<br />
should have an identifiable primary<br />
health care team; every primary health<br />
care team should include at least one<br />
<strong>GP</strong>; all medical pr<strong>of</strong>essionals working in<br />
primary health care should be working<br />
towards vocational registration or be<br />
those involved in change; primary care<br />
teams should continue to be actively<br />
engaged in the continuous development<br />
<strong>of</strong> quality services.<br />
Feedback on<br />
Dr Scott-Jones’s paper<br />
<strong>The</strong> RNZC<strong>GP</strong> invited comment on Dr<br />
Jo Scott-Jones’s paper Defining the role<br />
<strong>of</strong> the <strong>GP</strong> in a primary health care team:<br />
<strong>The</strong> <strong>GP</strong> genome and phenotype 2009–<br />
2020. Jo and the <strong>College</strong> have received<br />
responses to his paper reflecting<br />
a wide range <strong>of</strong> viewpoints. Most<br />
respondents agreed with the general<br />
direction <strong>of</strong> the paper. <strong>The</strong>re was some<br />
divergence <strong>of</strong> opinion both from the<br />
views put forward in the paper, and<br />
between respondents on several issues,<br />
including:<br />
1. Evidence-based practice. <strong>The</strong><br />
influences <strong>of</strong> large corporations on<br />
what research is undertaken and<br />
2.<br />
3.<br />
4.<br />
5.<br />
disseminated, the degree to which<br />
<strong>GP</strong>s follow scientific method, and<br />
the research base <strong>of</strong> nursing were all<br />
commented on.<br />
Practice size. <strong>The</strong> advantages<br />
<strong>of</strong> smaller or moderately sized<br />
practices in providing the ongoing<br />
one-to-one relationship at the core<br />
<strong>of</strong> patient care were noted. <strong>The</strong><br />
problem with the small business<br />
model was seen as its lack <strong>of</strong> attraction<br />
for investors.<br />
Multidisciplinary teams (MDT). This<br />
topic attracted a lot <strong>of</strong> comment.<br />
Some respondents considered<br />
these teams the obvious way <strong>of</strong><br />
the future, while others said that<br />
their practices already functioned as<br />
MDTs. Others referred to MDTs as<br />
‘management by committee’ and an<br />
institutionalised approach which was<br />
less conducive to patient-centred<br />
care. One respondent said ‘interdisciplinary<br />
environment yes, multidisciplinary<br />
teams—maybe, but very<br />
very carefully, and not merely to appease<br />
some group on a philosophical<br />
bandwagon.’ Others commented<br />
that a small team, such as already<br />
exists in many general practices, had<br />
advantages over a large team.<br />
Should <strong>GP</strong>s focus more on health<br />
and less on illness? Opinion was<br />
expressed that the focus should be<br />
more on areas such as nutrition and<br />
less on medication and the management<br />
<strong>of</strong> illness, accompanied by their<br />
expense and side effects.<br />
How much input should <strong>GP</strong>s seek<br />
into areas such as social work, housing,<br />
education etc? <strong>The</strong> view was<br />
expressed that although <strong>GP</strong>s need a<br />
good understanding <strong>of</strong> how health<br />
is affected by personal and social<br />
factors, it is more appropriate that<br />
there be good referral systems to<br />
appropriate agencies.<br />
<strong>The</strong> role <strong>of</strong> the <strong>GP</strong> continues to be a<br />
subject <strong>of</strong> much activity within the sector.<br />
<strong>The</strong> <strong>College</strong> welcomes further feedback<br />
via policy@rnzcgp.org.nz.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 27
policY<br />
Health insurance company<br />
requests for entire patient<br />
medical notes<br />
Cathy Webber<br />
Principal Advisor, Medico-Legal<br />
Over the past two years the RNZC<strong>GP</strong>,<br />
as part <strong>of</strong> the <strong>GP</strong>LF (<strong>General</strong> Practice<br />
Leaders Forum), worked with the<br />
Privacy Commissioner and the insurance<br />
industry in resolving the issue <strong>of</strong> health<br />
insurance companies’ requests for entire<br />
patient medical notes.<br />
In July 2009, the Privacy Commissioner<br />
published the results <strong>of</strong> her inquiry into<br />
this issue. * <strong>The</strong> (NZMA) also released a<br />
guidance note for its members. † Despite<br />
this information being available, a <strong>College</strong><br />
member raised her concerns with us<br />
that the average <strong>GP</strong> is probably still not<br />
aware <strong>of</strong> the outcome <strong>of</strong> the recent<br />
events and requested that the <strong>College</strong><br />
also bring it to your attention.<br />
information that is necessary to make<br />
insurance decisions.<br />
As the holder <strong>of</strong> the medical record, you<br />
need to be sure that the patient has properly<br />
authorised the insurer to collect the full<br />
medical record (for a specified period) and<br />
that the insurers that collect full medical<br />
notes (for a specified period) are collecting<br />
personal information that is necessary for<br />
the insurance decisions they have to make.<br />
<strong>The</strong> need to answer insurers’ questions<br />
will mean that in some cases<br />
considerable time may be required by<br />
your practice. <strong>The</strong> NZMA has provided<br />
clear advice on how to charge for this. ‡<br />
Essentially, ensure that the fee you charge<br />
<strong>The</strong> Privacy Commissioner has expressed<br />
her view that, in most cases, insurers<br />
that collect full medical notes—even for a<br />
specified period—are at risk <strong>of</strong> breaching<br />
the Health Information Privacy Code<br />
<strong>The</strong> nub <strong>of</strong> the issue is that the Privacy<br />
Commissioner has expressed her view<br />
that, in most cases, insurers that collect<br />
full medical notes—even for a specified<br />
period—are at risk <strong>of</strong> breaching the<br />
Health Information Privacy Code.<br />
Insurers can only collect personal health<br />
for the time spent meeting the request is<br />
reasonable and provide full details <strong>of</strong> this<br />
in your invoice.<br />
If you have a request for full medical<br />
notes, we recommend you respond with<br />
a brief letter along the lines <strong>of</strong>:<br />
Your request for full patient notes<br />
I am informed by the June 2009 Privacy<br />
Commissioner ruling on the collection <strong>of</strong> full<br />
medical notes by insurers that your request<br />
must be authorised by my patient and that it<br />
must be relevant to the decision you must make.<br />
I take my responsibilities under the Health<br />
Information Privacy Code seriously, but also<br />
do not want to jeopardise my patient’s insurance<br />
application. To this end I will provide the<br />
relevant medical information on receipt <strong>of</strong> a<br />
more specific request and with evidence <strong>of</strong><br />
my patient’s authorisation.<br />
<strong>The</strong> <strong>College</strong> appreciates members raising<br />
issues with us and encourages you to<br />
contact us with your queries. Email cathy.<br />
webber@rnzcgp.org.nz.<br />
Footnotes<br />
* <strong>The</strong> full report can be found at www.privacy.org.nz/collection-<strong>of</strong>-medical-notes-by-insurers-inquiry-by-the-privacy-commissioner/. If this link fails, go to the www.privacy.<br />
org.nz, go to the news and publications: commissioner inquiries section.<br />
† www.nzma.org.nz/membersonly/privacy-confidentiality/Patient%20notes%20and%20Insurers.pdf.<br />
‡ Ibid.<br />
28 | <strong>GP</strong> PULSE | MARCH 2010
OBITUARY<br />
William Grattan<br />
O’Connell QSM<br />
Ellis Greive<br />
Retired <strong>General</strong> Practitioner, Auckland<br />
William Grattan O’Connell FRNZC<strong>GP</strong><br />
died November 27 th 2009 aged 84<br />
years, thus ending a notable career<br />
in general practice and service to the<br />
community.<br />
Educated at Sacred Heart <strong>College</strong>,<br />
St Patrick’s Silverstream (where he was<br />
Head Boy) and Otago University, he<br />
began general practice at Glen Innes,<br />
Auckland in 1953 and never moved.<br />
With the initiation <strong>of</strong> a local work roster<br />
Grattan and I began playing golf on<br />
Thursday afternoons and continued to<br />
do so for more than 40 years. Sweet<br />
times indeed.<br />
He was devoted to his patients, devoted<br />
to medicine, devoted to excellence; an<br />
attribute shown by his three daughters.<br />
He was meticulous in everything. This did<br />
not compromise a wry sense <strong>of</strong> humour.<br />
His pastime was golf, his pr<strong>of</strong>ession was<br />
medicine, his passion was the Rotary<br />
movement, achieving high honours.<br />
International board member, a director <strong>of</strong><br />
the committee to eradicate polio, which<br />
was very successful. For these services he<br />
was awarded the Queen’s Service Medal.<br />
He is survived by his wife Verna whose<br />
unflagging support and care played a<br />
large part in Grattan’s success.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 29
OBITUARY<br />
Brett Phillip Roche<br />
Kate Braddock<br />
<strong>General</strong> Practitioner, North Shore<br />
Brett Roche MBChB, died tragically<br />
and unexpectedly at his home on 10th<br />
December 2009 aged 46.<br />
He will be missed by all who knew<br />
him—for his passion about general practice,<br />
for his caring, and for his challenging<br />
and penetrating wisdom regarding the<br />
future <strong>of</strong> primary care in <strong>New</strong> <strong>Zealand</strong>.<br />
Brett did a BSc, graduating in 1986, before<br />
going on to qualify from Auckland<br />
Medical School in 1992, and become<br />
one <strong>of</strong> the first registrars that I worked<br />
with at the Warkworth Medical Centre<br />
in 1996. Even then, he had an intense<br />
desire to better the care that was given<br />
in general practice and was full <strong>of</strong> ideas<br />
to help that happen.<br />
He went on to become a Member <strong>of</strong> the<br />
RNZC<strong>GP</strong>, and subsequently obtained a<br />
Diploma in Sports Medicine in 2005. He<br />
was involved in the medical care <strong>of</strong> the<br />
North Harbour Rugby Team and went<br />
on to be part <strong>of</strong> the Birkenhead Medical<br />
Centre, when he bought the practice<br />
from Peter Cunningham.<br />
During the last three years <strong>of</strong> his life<br />
he became very involved with the<br />
future <strong>of</strong> primary health care at a<br />
political level—sitting on the boards<br />
<strong>of</strong> the Independent Practitioners<br />
Association Council, Best Practice<br />
Advisory Council and Comprehensive<br />
Health Services (an Independent<br />
Practitioners Association based in<br />
North Harbour), and a member<br />
<strong>of</strong> the Performance Management<br />
Programme Governance Group<br />
representing the <strong>General</strong> Practice<br />
Leaders Forum.<br />
In all <strong>of</strong> these forums he presented<br />
thoughtful, penetrating and innovative<br />
ideas and was a well-respected and<br />
highly committed contributor.<br />
He was a reserved person in his public<br />
life but cared deeply and passionately<br />
for his patients and the care he could<br />
and did give them.<br />
He worked endlessly to extend his<br />
understanding and management <strong>of</strong> the<br />
problems he saw in primary care, and<br />
the work that he started will be continued<br />
by those who knew him and shared<br />
his passion.<br />
He will be sorely missed.<br />
<strong>The</strong> <strong>College</strong> publishes short obituaries in <strong>GP</strong> <strong>Pulse</strong>.<br />
Notifications can be submitted to the Editor via the <strong>College</strong><br />
address, RNZC<strong>GP</strong>, PO Box 10440, Wellington 6143, or email<br />
alexander.bisley@rnzcgp.org.nz. Pictures are encouraged.<br />
30 | <strong>GP</strong> PULSE | MARCH 2010
ural hospital medicine<br />
West Coast:<br />
DHB Rural <strong>GP</strong> and Hospital<br />
Medicine Pilot Project<br />
Anu Frances Shinnamon<br />
<strong>General</strong> Practitioner, RHM Registrar, West Coast<br />
Let’s be honest here, I am one <strong>of</strong> those<br />
new generation doctors, Generation Y<br />
according to Wikipedia. <strong>The</strong> ones they<br />
talk about at conferences when they<br />
labour over workforce planning and<br />
how the government can attract junior<br />
doctors to generalist roles in rural areas.<br />
During the past few years, the RNZC<strong>GP</strong><br />
has fostered two pilot programmes that<br />
have captured my attention.<br />
Luckily, I’ve been able to join a pioneering<br />
group <strong>of</strong> colleagues to test the waters as<br />
the <strong>College</strong> develops new ways <strong>of</strong> training<br />
and credentialling rural generalists. <strong>The</strong><br />
Type A in me was chomping at the bit to<br />
be one <strong>of</strong> the first on the block to undertake<br />
the Rural Hospital Medicine (RHM)<br />
pilot in 2009 and the <strong>GP</strong>/RHM Registrar<br />
Pilot at the West Coast DHB in 2010. <strong>The</strong><br />
Type B wanted to live rurally and indulge<br />
in the surrounding geography. <strong>GP</strong> <strong>Pulse</strong> has<br />
asked for some comment on my experience<br />
with the 2010 Pilot but I cannot<br />
restrain a bit <strong>of</strong> overlap with RHM.<br />
We are in the early days <strong>of</strong> 2010, but I<br />
dare say the <strong>College</strong> has hit the nail on<br />
the head in getting this training <strong>of</strong>f the<br />
ground. Greville Wood, the brainchild<br />
behind the West Coast DHB pilot,<br />
enticed me with an email that included<br />
this description: ‘<strong>The</strong> purpose <strong>of</strong> the<br />
programme’s to foster <strong>GP</strong> specialist skills<br />
whilst retaining the hospital skills that<br />
have been practised for years.’ To make<br />
the deal even sweeter, the year long<br />
Multi-Employer Collective Agreement<br />
(MECA) contracted post, meets the<br />
Primex requirements <strong>of</strong> <strong>GP</strong>EP1 and<br />
allows me to cross-credit the experience<br />
in the ever-flexible RHM programme. I<br />
love efficiency.<br />
<strong>The</strong> strengths <strong>of</strong> the WCDHB pilot are<br />
context and mentorship/collegiality. <strong>The</strong><br />
West Coast catchment <strong>of</strong> roughly 31000<br />
residents stretches between Haast and<br />
Karamea (which is in the midst <strong>of</strong> the<br />
best Rata bloom in 40 years). <strong>The</strong> pilot<br />
takes full advantage <strong>of</strong> the uniqueness<br />
<strong>of</strong> this geography and puts the trainee in<br />
the deep end <strong>of</strong> helping to oversee the<br />
community’s needs. For a relatively small<br />
head count, there is remarkable social<br />
diversity. <strong>The</strong>re is a blend <strong>of</strong> haves and<br />
have nots. Dairy, mining, fishing, conservation,<br />
education, tourism and health care<br />
dominate the workforce here. Grey and<br />
Westland High are decile four and six.<br />
<strong>The</strong> median individual income is $14,800.<br />
Many areas have no cell coverage.<br />
Seventy-five percent <strong>of</strong> households have<br />
no access to the Internet. <strong>The</strong>se social<br />
complexities combined with issues <strong>of</strong><br />
physical geography (which is very isolated<br />
at times) make for a satisfying and challenging<br />
training ground. I am honing my<br />
clinical acumen and my resourcefulness in<br />
the context <strong>of</strong> the available services. This<br />
is further enriched by the pairing <strong>of</strong> the<br />
in- and out-patient experience. <strong>The</strong> ability<br />
to follow patients between hospital<br />
and community is an invaluable educational<br />
modality. <strong>The</strong> continuity <strong>of</strong> looking<br />
after my chronic patients on the ward<br />
and following up the acute admissions in<br />
the community is the beauty <strong>of</strong> the training<br />
programme. It allows me to see the<br />
full cycle <strong>of</strong> the patient throughout their<br />
journey in the health care system.<br />
In a former career I evaluated health<br />
services education reform. A recurring<br />
theme in successful training programmes<br />
was good mentorship. Not the humiliating,<br />
bedside pimping style, but the dedicated,<br />
no question is too stupid, teaching is my<br />
modus operandi, type <strong>of</strong> mentorship. <strong>The</strong><br />
pilot has liberal amounts <strong>of</strong> protected<br />
mentorship and teaching time, alongside<br />
real-time advice and guidance during<br />
consults. <strong>The</strong> mentorship style brings<br />
together students, registrars and senior<br />
staff to challenge each other and learn<br />
together. It breaks the barrier <strong>of</strong> hiding<br />
weaknesses, which has dominated medical<br />
education through the years). Instead<br />
it fosters an open, case-based learning<br />
format which, put simply, suits me down<br />
<strong>GP</strong> PULSE | MARCH 2010 | 31
ural hospital medicine<br />
to the ground. Coming from the world <strong>of</strong><br />
public health and social services, I never<br />
quite adapted to the abrupt change in<br />
hierarchy that seems to dominate much<br />
<strong>of</strong> medicine. <strong>The</strong> smouldering adolescent<br />
certainly rejected the pecking order that<br />
put students at the bottom. I thought<br />
on graduation I might be embraced in a<br />
new-found collegiality with my peers and<br />
senior colleagues. I will forego the diatribe<br />
on that topic and acknowledge that I seem<br />
to have found my niche in rural medicine.<br />
<strong>The</strong> <strong>GP</strong>/RHM pilot is maximising the<br />
benefits <strong>of</strong> shared learning by fostering a<br />
refreshing collegiality.<br />
<strong>The</strong> two dominating highlights <strong>of</strong> the <strong>GP</strong>/<br />
RHM pilot are the lifestyle <strong>of</strong> the Coast<br />
and the unpredictability <strong>of</strong> the clinical<br />
presentation. At risk <strong>of</strong> sounding like a<br />
West Coast recruitment poster child, I’ve<br />
drunk the proverbial Kool Aid and can<br />
proselytise endlessly about the benefits <strong>of</strong><br />
training and living here. <strong>The</strong>re is the usual<br />
spiel about the coastline, forests, glaciers,<br />
tramping, climbing and paddling. It is all<br />
true. Even my husband, who has been at<br />
the mercy <strong>of</strong> the registrar life, can attest.<br />
You need to move on from your visions<br />
<strong>of</strong> endless rain and thoughts <strong>of</strong> parochialism.<br />
We have had dry skies for weeks and<br />
Tchaikovsky is being performed at the<br />
Cathedral this weekend. <strong>The</strong>re is a sense<br />
<strong>of</strong> community on the Coast, even if you<br />
are not born and bred. there It is an easy<br />
and fun place to live, without having to<br />
fight traffic to do the things I enjoy.<br />
For a person who likes order and<br />
predictability, I am always amazed at the<br />
rush I get from the unexpected. So far,<br />
there has been no predicting the variety<br />
<strong>of</strong> presenting complaints with which I’ve<br />
been faced. It is the essence <strong>of</strong> generalist<br />
medicine. It is the reason I’m doing this<br />
training. In the space <strong>of</strong> six weeks, I’ve<br />
been forced to resurrect medical school<br />
lectures I thought I’d never use and try<br />
to expand my RAM to keep pace with<br />
the patients that land in my care. Thank<br />
God for Google. Tempting as it may be to<br />
brag about what we treat on the Coast<br />
(in that macabre doctor way that we do),<br />
I’ll spare you the full list. Suffice it to say,<br />
however, I did not think I would come<br />
to manage cardiovascular risks, vaginal<br />
atrophy, career counselling, an ischemic<br />
bowel, a dislocated patella and a gaggle <strong>of</strong><br />
testosterone-poisoned, drunken teenagers<br />
with scalp lacerations all in one day.<br />
Unlike a big tertiary centre, there is no<br />
clamour to ‘get the interesting’ patients—<br />
when you are the only doctor in the<br />
hospital at night, all the patients are yours.<br />
Whether it is the injured farmer being<br />
flown in from up country or the octogenarian<br />
who needs advocacy and support<br />
for rest home placement, in this Registrar<br />
post I am seeing it all and learning how to<br />
manage it in the context <strong>of</strong> a rural setting.<br />
So, what more can I say? If you are one<br />
<strong>of</strong> those new generation (X, Y, or Z)<br />
doctors (Type A or B) consider a training<br />
opportunity that has come <strong>of</strong> age.<br />
Blending <strong>GP</strong> and rural hospital medicine<br />
opens up the best <strong>of</strong> both worlds and<br />
serves as meaty training grounds.<br />
32 | <strong>GP</strong> PULSE | MARCH 2010
wine • travel • books • humour and more<br />
Life&leisure<br />
Humour<br />
Back to the Ark? Technophobia 101<br />
Buzz Burrell<br />
<strong>General</strong> Practitioner, Blenheim<br />
She slowly moves her expressionless<br />
face towards the expectant questioner.<br />
With a detached, passive, defeated<br />
voice she announces the bad news:<br />
‘Computer says “No” ’.<br />
If only this were a real scene from Little<br />
Britain. Sadly it’s my receptionist imitating<br />
with scary accuracy the Little Britain character<br />
and she has two agendas. Firstly<br />
to raise a smile, since the TV sketches<br />
are funny to both <strong>of</strong> us. Secondly, to<br />
defuse the reality that for the third time<br />
this week the computer has completely<br />
locked up, and is as useful as a light bulb in<br />
an Auckland power cut.<br />
I feel old. I’m young enough to have<br />
attempted waterskiing over the summer<br />
holidays, and endure high-speed high<br />
colonic washouts trying to morph from<br />
anchor to floating towed vessel at 30<br />
miles an hour behind a speedboat. But<br />
I’m old enough to digress. Sorry.<br />
I’m also old enough to remember<br />
the days <strong>of</strong> my youthful entry into a<br />
small rural general practice where the<br />
only electronic gadget was a desk-top<br />
calculator. Computers were for playing<br />
space invaders, and a power cut was<br />
inconvenient only if it were dark and<br />
candles needed to be lit. Eventually<br />
we did invest in a fax machine, but this<br />
graduate from Technophobia 101 would<br />
usually phone immediately afterwards<br />
with the disbelieving ‘Did you really just<br />
get the fax?’<br />
I identify so well with the story <strong>of</strong> the<br />
young executive spotting the CEO<br />
standing in front <strong>of</strong> the shredder late<br />
one evening. ‘Listen lad,’ the CEO<br />
shouts: ‘This is a really important document,<br />
and I don’t know how this thing<br />
works?’ Eager to impress, the lad turns<br />
on the machine, inserts the paper, and<br />
presses the start button. Touched, the<br />
CEO exclaims: ‘That’s excellent, lad.<br />
Now where does the copy come out?’<br />
Sixteen years on, and I’m in a paperless<br />
environment. My notes, results, letters,<br />
recordings, referrals are all electronic,<br />
and for my peripheral clinic everything is<br />
also completely at the mercy <strong>of</strong> a fragile<br />
Internet connection between Havelock<br />
and Blenheim. When the connection<br />
is lost, the relationship between my<br />
terminal and the network collapses<br />
like a Hollywood marriage, and .... the<br />
computer says ‘No’.<br />
Perhaps it would help if I could type. In<br />
Australia, like an innocent schoolboy, I<br />
faithfully typed my referral letters before<br />
handing them into the cyber-teacher’s<br />
pigeon-hole for electronic spellchecking.<br />
I used to try to type ‘Thanks<br />
for your opinion’ etc. <strong>The</strong> ‘Thakns’<br />
would be cleverly corrected, but the<br />
veggie mistake which always followed<br />
would slip through, and for my first<br />
few months in Western Australia many<br />
Perth specialists must have wondered<br />
who this weird gardener was writing to<br />
them from the bush with the opening<br />
line ‘Thanks for your onion’.<br />
<strong>The</strong>re are times when I feel like I’ve just<br />
crawled <strong>of</strong>f the Ark.<br />
I think I’ve managed to trust the fax<br />
machine at last, largely because I don’t<br />
know how to use it, and my receptionist<br />
takes control. My trust <strong>of</strong> emailing new<br />
addresses remains unsure, cognisant <strong>of</strong><br />
vegetable typos, I frequently consider<br />
the case <strong>of</strong> the Illinois man who left<br />
the snow-filled streets <strong>of</strong> Chicago for<br />
a vacation in Florida. His wife was on<br />
a business trip and was planning to<br />
meet him there the next day. When he<br />
reached his hotel, he decided to send his<br />
wife a quick email. Unfortunately when<br />
typing her address, he missed one letter,<br />
and his note was directed instead to an<br />
elderly preacher’s wife whose husband<br />
had passed away only the day before.<br />
When the grieving widow checked her<br />
email, she took one look at the monitor,<br />
let out a piercing scream, and fell to the<br />
floor in a dead faint. At the sound, her<br />
family rushed into the room and saw<br />
this note on the screen: ‘Dearest Wife.<br />
Just got checked in. Everything prepared<br />
for your arrival tomorrow. P.S. Sure is<br />
hot down here.’<br />
Back to the Ark, I wonder how things<br />
would have worked with today’s technology<br />
assisting. <strong>The</strong> post-Ark days have<br />
special laws against relationships flourishing,<br />
I decide, after visiting www.datemypet.com.<br />
Little genetic thought has gone<br />
into the series <strong>of</strong> ‘this is sooooo cute’<br />
photos we receive in our email inbox,<br />
usually involving a big go<strong>of</strong>y dog sleeping<br />
with a duck. How did they manage to get<br />
all those animals on-board without an IT<br />
team, data entry clerks, spreadsheet and<br />
s<strong>of</strong>tware designer, and the constant virus<br />
protection upgrades?<br />
I can just imagine my receptionist being<br />
there. ‘And who is in charge here?’ ‘<strong>The</strong><br />
computer says Noah’.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 33
Life&leisure<br />
wine • travel • books • humour and more<br />
2–5 September—THE 2010 RNZC<strong>GP</strong> ANNUAL CONFERENCe<br />
Christchurch<br />
Attending the 2010 RNZC<strong>GP</strong> Conference<br />
in Christchurch in September will <strong>of</strong>fer<br />
the added benefit <strong>of</strong> some great nonconference<br />
enticements.<br />
Stroll leisurely around the beautiful, famous<br />
gardens; eat delicious Canterbury<br />
food and wine in the fine cafés and<br />
restaurants; or see the exhibitions at the<br />
excellent museums and galleries.<br />
For more on what’s on while you’re<br />
there: www.christchurchnz.com<br />
34 | <strong>GP</strong> PULSE | MARCH 2010
wine • travel • books • humour and more<br />
Life&leisure<br />
Top things to do in Christchurch<br />
Suggestions from RNZC<strong>GP</strong> staff and <strong>GP</strong>s with Garden<br />
City connections<br />
1. Take Christchurch Bike Tours’ two-hour excursion<br />
from Cathedral Square<br />
—Annie Fleetwood, Resources and Representation<br />
Coordinator<br />
2. Book ahead for <strong>The</strong> Bodhi Tree, great Burmese<br />
food on Colombo St near the conference centre<br />
—Margaret Metherell, <strong>GP</strong><br />
3. View the engaging exhibitions at Christchurch Art<br />
Gallery and eat at the enticing Arts Centre market<br />
—Alexander Bisley, Communications Advisor<br />
4. Go to the Antarctic Centre and the Crumpet Club<br />
(tapas bar)—Waveney Grennell, CORNERSTONE Manager<br />
5. Visit picturesque Akaroa or Canterbury vineyards<br />
—Karen Thomas, Chief Executive<br />
<strong>GP</strong> PULSE | MARCH 2010 | 35
Life&leisure<br />
wine • travel • books • humour and more<br />
Guide to <strong>New</strong> <strong>Zealand</strong><br />
pinot noir regions<br />
Jules van Cruysen<br />
<strong>New</strong> <strong>Zealand</strong> Pinot is gaining international momentum and reputation (and in my opinion rightly so), but while all<br />
good Kiwi Pinot share some characteristics, the differences between the regions are significant. Here I look at what<br />
to expect from the different regions in terms <strong>of</strong> style and look at the heavy hitters, the best value wines and what to<br />
avoid in Kiwi Pinot.<br />
WAIRARAPA<br />
<strong>The</strong> Wairarapa is the only significant Pinot region in the North Island and is centred on two sub-regions; Martinborough to the<br />
South and Gladstone in the North. Martinborough is surrounded by terraces <strong>of</strong> dried riverbeds and produces a number <strong>of</strong> the<br />
‘Grand Crus’ <strong>of</strong> Kiwi Pinot—notably Ata Rangi and Dry River, but for my money I would suggest Escarpment, Craggy Range<br />
Te Muna and Aroha and the wines <strong>of</strong> Kai Shubert. None <strong>of</strong> these are cheap. <strong>The</strong> wines are masculine with characteristic Black<br />
Dorris plum fruit, Earl Grey—like tannins (dry but floral) and a lot <strong>of</strong> oak—the best wines can be awkward in their youth but can<br />
last a long time. For something more accessible try Strugglers Flat. Avoid Martinborough Vineyards and Te Kairanga as these producers<br />
have both lost their edge in the last few years. Gladstone is based on old riverbeds but seems to produce s<strong>of</strong>ter, elegant,<br />
affordable wines that are less suited to ageing—as the vines age this will change. Johner Estate makes an excellent range <strong>of</strong> wines<br />
from this region at different price points.<br />
NELSON<br />
Nelson breaks down into two sub-regions: <strong>The</strong> Waimea Plains which centre around the towns <strong>of</strong> Hope and Brightwater on<br />
the flat gravel just to the south <strong>of</strong> Nelson, and the Moutere, to the west in the hills across the bay from Nelson where the soils<br />
are clay- based. From the Moutere go for Rimu Grove and Neudorf—from their entry level Tom’s Block to their Moutere and<br />
extremely rare Home Block the wines are stylish—full <strong>of</strong> ripe cherry, chocolate and spice! Greenhough and Brightwater make<br />
excellent wines on the flat.<br />
MARLBOROUGH<br />
Pinot has become the rising star <strong>of</strong> Marlborough—at their best they are light but intense, a balancing act between savoury and<br />
sweet, masculine game and feminine floral. Most <strong>of</strong> Marlborough is flat and is planted on old riverbed soils interspersed with other<br />
soil types, while the hills around the area are clay-based. <strong>The</strong>re are a handful <strong>of</strong> high performing affordable wines coming out<br />
<strong>of</strong> Marlborough like Spy Valley and Momo, but the top end really inspires. For supple, restrained, long-lived wines, producers like<br />
Dog Point, Seresin, Herzog and Fromm (and their second tier labels William Thomas and La Strada) cannot be beaten. <strong>The</strong> most<br />
complete Marlborough Pinot I have tried was the ‘07 Eaton Vineyards by Pyramid Valley. Intensely concentrated fruit balanced by<br />
acid and supple tannins with a beautiful floral lift—sadly it will be the last vintage <strong>of</strong> the wine that is produced. Like everything else<br />
in Marlborough there is a lot <strong>of</strong> commercial rubbish produced—avoid the mass-produced wines as, when it comes to Pinot they<br />
rarely <strong>of</strong>fer good value.<br />
36 | <strong>GP</strong> PULSE | MARCH 2010
wine • travel • books • humour and more<br />
Life&leisure<br />
NORTH CANTERBURY<br />
<strong>The</strong> wine growing region <strong>of</strong> North Canterbury (<strong>of</strong>ten referred to as the Waipara,<br />
but this also refers to a town and sub region as well) stretches about 50km along the<br />
inland <strong>of</strong> the east coast <strong>of</strong> the South Island from Amberley and Glasnevin in south<br />
moving up through Waipara and then Omihi and finishing at Waikari. Understandably<br />
it is a geographically diverse area which ranges from gravel plains in the south<br />
through to hillside sites heavy in clay and lime. <strong>The</strong> best wines are heavy, savoury,<br />
powerful beasts that only time will tame; the worst are foursquare, awkward and<br />
clumsy… and don’t get better. Pegasus Bay is the big name in the area and this reputation<br />
is well deserved as is that <strong>of</strong> Mountford. <strong>The</strong> new kids on the block are Crater<br />
Rim in the Waipara, Black Estate in Omihi. In Waikari Pyramid Valley and Bell Hill are<br />
commanding Grand Cru prices after only a couple <strong>of</strong> vintages. That’s if you can even<br />
get a hold <strong>of</strong> it.<br />
CENTRAL OTAGO<br />
<strong>The</strong> popularity <strong>of</strong> Central Otago Pinot has been driving the craze, both domestically<br />
and internationally, for NZ Pinot. <strong>The</strong>re are some stunning wines out there, but<br />
there is also a lot <strong>of</strong> dross, and expensive dross at that. It is a region that spans several<br />
geographically distinct sub-regions but the wines share some similarities—whether<br />
by style or soil (or more likely a combination <strong>of</strong> both). <strong>The</strong> wines are brightly fruited<br />
with ink black cherry fruit and many have a wild thyme herb and bramble component.<br />
<strong>The</strong>re are some big wines out there—14.5% ABV is pretty normal but with<br />
the best wines the fruit carry it well. <strong>The</strong> Grand Crus are Felton Road’s Block 3 and<br />
Block 5 wines from Bannockburn (their other wines are stunners as well) if you are<br />
prepared to wait five years before getting your money’s worth. Otherwise Grant<br />
Taylor’s Valli wines (he makes wines from the Bannockburn and Gibbston sub-regions)<br />
and Rippon based in Wanaka are very exciting. For something more affordable<br />
try Saddleback by Peregrine or Rabbit Ranch—both are a great introduction to the<br />
Central Otago style but are still pretty expensive for easy drinking reds.<br />
NORTH OTAGO<br />
I am particularly fond <strong>of</strong> the Waitaki as it is my home region and is one <strong>of</strong><br />
<strong>New</strong> <strong>Zealand</strong>’s most recently planted. <strong>The</strong> wines are very savoury and classically<br />
Burgundian in style—they vary depending on soil composition. <strong>The</strong> region has pockets<br />
<strong>of</strong> deep lime as well as schist and gravel and is already making serious, age-worthy<br />
wines that are getting better vintage after vintage. My picks are Ostler Caroline’s<br />
Pinot Noir as well as the Valli and Craggy Range wines. At five years’ old the Craggy<br />
Range Otago Station Vineyard is still a stunner—light and full <strong>of</strong> feral porcini, truffle<br />
and violets. And that was the first vintage. A region to watch!<br />
None <strong>of</strong> these wines are cheap. If you are going to invest in Kiwi Pinot I think it’s better<br />
to spend a few bucks and wait a few years and be rewarded rather than go for<br />
something cheaper and be let down.<br />
Jules van Cruysen is a wine critic and sommelier. He blogs at thewinewanker.blogspot.com<br />
Best Wine <strong>of</strong> 2009<br />
2009 being a year <strong>of</strong> recession<br />
it only fits that my favourite<br />
wine <strong>of</strong> the year is affordable<br />
and immediately drinkable:<br />
Forrest’s <strong>The</strong> Doctors’ Riesling<br />
2009, Marlborough. This wine<br />
is such a step up from previous<br />
vintages that it seriously blew<br />
me out <strong>of</strong> the water—and is<br />
textbook <strong>of</strong>f dry, low alcohol<br />
(that is Germanic) Riesling. Clean,<br />
fresh and pure. Green apple,<br />
pear, stony minerality and just a<br />
hint <strong>of</strong> floral meadow honey and<br />
honeysuckle. Just beautiful!<br />
forrestwines.co.nz/selectProduct.asp?RangeID=<strong>The</strong>%20<br />
Doctors&Product=Riesling<br />
Thanks to Forrest Wines<br />
we have six bottles <strong>of</strong><br />
the lovely 2009 Doctors’<br />
Riesling to give away.<br />
Give us feedback about<br />
what you like and don’t like<br />
about <strong>GP</strong> <strong>Pulse</strong> to get in the<br />
draw. Access the survey at<br />
the following link:<br />
www.surveymonkey.com/s/<br />
<strong>GP</strong><strong>Pulse</strong>Reader Survey<br />
<strong>GP</strong> PULSE | MARCH 2010 | 37
member support<br />
Becoming a member<br />
<strong>The</strong> <strong>College</strong> has over 4000 members,<br />
representing around 94 percent <strong>of</strong> all general<br />
practitioners in <strong>New</strong> <strong>Zealand</strong>.<br />
To Join<br />
Application forms may be obtained from the <strong>College</strong><br />
<strong>of</strong>fice, PO Box 10440, Wellington 6143. <strong>The</strong>y should be<br />
completed and sent to the Assessment Administrator<br />
Lynn Frew at the <strong>College</strong> <strong>of</strong>fice. Faculties are notified <strong>of</strong><br />
applications.<br />
Categories <strong>of</strong> Membership<br />
Full Membership and Fellowship is attainable only by<br />
examination and assessment. Associate membership<br />
therefore carries no implication <strong>of</strong> academic or pr<strong>of</strong>essional<br />
achievement or status.<br />
Fellow (FRNZC<strong>GP</strong>)<br />
Fellowship <strong>of</strong> the <strong>College</strong> is attained by completing the<br />
two-stage <strong>General</strong> Practice Education Programme, passing<br />
Primex (the primary membership exam) at the end<br />
<strong>of</strong> Stage 1, and the Fellowship Assessment in Stage 2.<br />
Fellows have full voting rights and have the privilege <strong>of</strong><br />
the floor at general meetings. <strong>The</strong>y may also hold any<br />
<strong>of</strong>fice within the <strong>College</strong>. Fellows are entitled to use the<br />
designation FRNZC<strong>GP</strong>.<br />
Member (MRNZC<strong>GP</strong>)<br />
<strong>The</strong> <strong>College</strong> awards Membership after successful completion<br />
<strong>of</strong> Primex at the end <strong>of</strong> <strong>GP</strong>EP1 or an equivalent<br />
programme. A Member who is <strong>of</strong> good standing is<br />
entitled to the privilege <strong>of</strong> the floor at general meetings,<br />
may vote and may hold <strong>of</strong>fice except where the <strong>of</strong>fice<br />
requires that it be filled by a Fellow. Members are entitled<br />
to use the designation MRNZC<strong>GP</strong>.<br />
Associate<br />
Most Associates <strong>of</strong> the <strong>College</strong> are engaged in general<br />
practice; however, doctors who are practising within<br />
a <strong>College</strong>-recognised special interest area <strong>of</strong> primary<br />
care are also entitled to Associate membership.<br />
Associates may take a full part in <strong>College</strong> affairs, except<br />
that they may not vote at the Annual <strong>General</strong> Meeting<br />
<strong>of</strong> the <strong>College</strong>.<br />
Affiliate<br />
Affiliate status may be granted to any individual who has<br />
special links with general practice and desires to become<br />
affiliated with the <strong>College</strong>. It may also be granted to<br />
organisations that have special links with general practice.<br />
Affiliates may not vote or hold <strong>of</strong>fice.<br />
All RNZC<strong>GP</strong> resources, including the <strong>GP</strong> <strong>Pulse</strong> and the Journal <strong>of</strong> Primary Health Care (JPHC), are produced using<br />
paper sourced only from sustainable and legally harvested forests (FSC Certified). <strong>GP</strong> <strong>Pulse</strong> and the JPHC are mailed<br />
in compostable film wrap.<br />
38 | <strong>GP</strong> PULSE | MARCH 2010
member support<br />
<strong>College</strong> services<br />
Everything we do is aimed at strengthening and supporting you in your practice.<br />
Advocacy<br />
You have tasked us with making your collective voice heard<br />
at the highest levels <strong>of</strong> Government about the issues facing<br />
general practice. Working as an integral part <strong>of</strong> the <strong>General</strong><br />
Practice Leaders Forum, we harness the power <strong>of</strong> a united <strong>GP</strong><br />
voice on major issues.<br />
<strong>College</strong> policy positions are developed using the expertise <strong>of</strong><br />
members. Once approved by the <strong>College</strong> Council they are<br />
posted on the <strong>College</strong> website: www.rnzcgp.org.nz/submissions<br />
If you would like to contribute your expertise to the development<br />
<strong>of</strong> <strong>College</strong> policy positions please contact policy@rnzcgp.<br />
org.nz or 04 496 5999.<br />
Education<br />
As a member <strong>of</strong> the <strong>College</strong> you can access our full range <strong>of</strong><br />
education programmes and resources that help you gain, then<br />
maintain, registration in the vocational scope <strong>of</strong> general practice,<br />
allowing you to practise independently. This includes online<br />
resources, particularly the highly-respected BMJ Learning that<br />
the <strong>College</strong> provides free to members.<br />
BMJ learning online<br />
Working in conjunction with the British Medical Journal, BMJ<br />
Learning <strong>of</strong>fers a range <strong>of</strong> learning resources which deal with<br />
everyday issues in primary care, general practice and hospital<br />
medicine. BMJ Learning currently <strong>of</strong>fers over 500 evidence-based<br />
learning modules, which are regularly updated. Plans are in development<br />
for specific <strong>New</strong> <strong>Zealand</strong> content. BMJ Learning forms<br />
part <strong>of</strong> the structured learning for the <strong>GP</strong>EP programme.<br />
Online resources<br />
MOPS Online allows you to enter and keep your Maintenance<br />
<strong>of</strong> Pr<strong>of</strong>essional Standards credits up to date. Already, our registered<br />
providers provide course attendances online and this year<br />
we have plans to make MOPS more interactive. It is all aimed at<br />
simplifying your compliance and reducing your paperwork.<br />
Quality<br />
Quality in everything we do is a focus <strong>of</strong> the <strong>College</strong>, with<br />
the member-developed Aiming for Excellence standard,<br />
together with CORNERSTONE practice accreditation.<br />
CORNERSTONE is gaining momentum as the vehicle to assure<br />
the delivery <strong>of</strong> a quality environment at your practice.<br />
Research<br />
<strong>The</strong> Journal <strong>of</strong> Primary Health Care (JPHC) is the <strong>College</strong>’s<br />
peer‐reviewed journal designed to meet the information needs<br />
<strong>of</strong> <strong>New</strong> <strong>Zealand</strong> general practitioners, practice nurses and community<br />
pharmacists plus other primary health care practitioners<br />
and the patients and communities we serve. It is also available<br />
on the <strong>College</strong> website, and we provide a local search engine<br />
for you to search the issues.<br />
Information<br />
At the core <strong>of</strong> the <strong>College</strong> is our website: www.rnzcgp.org.nz<br />
It’s there as your pathway to health information, and the services<br />
the <strong>College</strong> can provide.<br />
e<strong>Pulse</strong> is our electronic newsletter, bringing you the fastest and<br />
latest news in the health sector each week. We also publish ads<br />
for locums or <strong>GP</strong>s and, as a Fellow or Member, that service is<br />
FREE.<br />
<strong>GP</strong> <strong>Pulse</strong>, which you’re reading at the moment, covers every<br />
facet <strong>of</strong> the <strong>College</strong>’s work for you. It includes the latest news<br />
on <strong>College</strong> operations, the decisions <strong>of</strong> your representatives<br />
on the Executive and Council and the current issues facing the<br />
primary care sector.<br />
<strong>GP</strong> <strong>Pulse</strong> is the vehicle for you to have your say, either in response<br />
to something you’ve read, or as a request for a specific<br />
need you have identified. We welcome your comments on<br />
<strong>GP</strong> <strong>Pulse</strong> at gppulse@rnzcgp.org.nz or on 04 496 5999.<br />
We publish resources in response to the changing environment<br />
in general practice. All publications are free to members for the<br />
initial copy. <strong>The</strong>y are also available online at the <strong>College</strong> website:<br />
www.rnzcgp.org.nz/college-resources<br />
Articles from previous issues <strong>of</strong> <strong>GP</strong> <strong>Pulse</strong> and from the earlier<br />
<strong>College</strong> publication NZFP are available in the website archive.<br />
<strong>The</strong> Annual <strong>College</strong> Conference<br />
We rotate among our faculties with our annual conference,<br />
choosing a venue and theme that will stimulate and educate<br />
you. Registration is discounted for members.<br />
<strong>The</strong> 2010 Annual Conference will be held in Christchurch,<br />
2–5 September.<br />
Every year we also host a Quality Symposium noted for the<br />
input from national and international speakers and for the<br />
informed, erudite discussion generated by that input. Again,<br />
members get a substantial discount<br />
Every second year we host an Education Convention, bringing<br />
together <strong>GP</strong> teachers, educators and examiners and others<br />
interested in medical education.<br />
Advice for Members<br />
Sometimes it can all become too much for you. Where do you<br />
go, who can you speak to?<br />
Ring our HELPLINE: 0800 RNZC<strong>GP</strong> (769 247); we can pr<strong>of</strong>fer<br />
helpful suggestions. It is part <strong>of</strong> our mission to support you and<br />
in doing so to improve the health <strong>of</strong> all <strong>New</strong> <strong>Zealand</strong>ers.<br />
<strong>GP</strong> PULSE | MARCH 2010 | 39