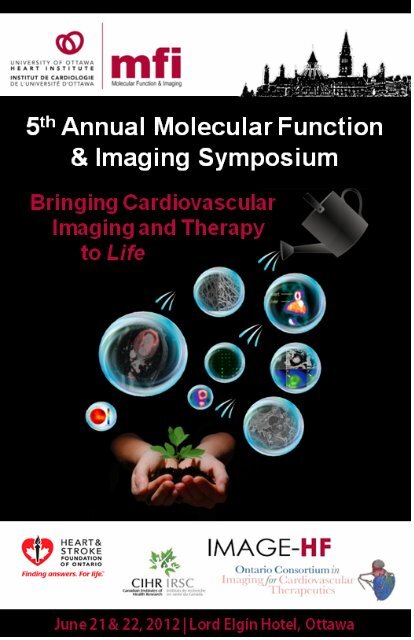
2012 MFI Symposium Program - University of Ottawa Heart Institute
2012 MFI Symposium Program - University of Ottawa Heart Institute
2012 MFI Symposium Program - University of Ottawa Heart Institute
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
INSIDE FRONT COVER
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
COVER PHOTO CREDITS:<br />
Joanne McBane<br />
Frank Prato<br />
Stephanie Thorn<br />
Elizabeth Orton<br />
Myra Cocker<br />
Concept: Kathie Drozd
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
WELCOME<br />
Dr. Rob Beanlands<br />
<strong>Program</strong> Director, <strong>MFI</strong> Director<br />
National Cardiac PET Centre and Chief<br />
Cardiac Imaging, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
This, the 5 th Annual Molecular Function and Imaging (<strong>MFI</strong>) <strong>Symposium</strong>,<br />
unique not only for its focus but also that it is <strong>of</strong> trainees, by trainees and for<br />
trainees - the backbone <strong>of</strong> the program itself. The <strong>MFI</strong> <strong>Program</strong> is supported<br />
by the <strong>Heart</strong> and Stroke Foundation as well as the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong><br />
<strong>Institute</strong>, the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>, Faculty <strong>of</strong> Medicine, and the Divisions <strong>of</strong><br />
Cardiology and Cardiac Surgery. This year the symposium highlights the<br />
translation <strong>of</strong> basic to clinical science through the application <strong>of</strong> imaging<br />
probes as tools for detection and prognostication or understanding disease and<br />
therapy. The vision <strong>of</strong> the <strong>MFI</strong> <strong>Program</strong> is to establish a focused research<br />
team through a unique integrated program with a primary emphasis on<br />
Molecular Function evaluation and translational research while also mentoring<br />
future scientific experts and leaders in the multiple disciplines <strong>of</strong> this field.<br />
We look forward to stimulating scientific interaction and the translation <strong>of</strong><br />
new knowledge forming the foundation for our future. Welcome to all<br />
participants and sponsors. Congratulations to the organizing committee <strong>of</strong><br />
trainees for this great achievement!<br />
i
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
WELCOME cont.<br />
Elizabeth Orton<br />
Chair, <strong>MFI</strong> <strong>Symposium</strong> Organizing Committee<br />
PhD. Candidate, Carleton <strong>University</strong><br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
The trainee organizing committee extends a great big welcome to all speakers<br />
and attendees for the 5 th Annual <strong>MFI</strong> <strong>Symposium</strong>! This year, the diversity and<br />
the collaboration underlying the <strong>MFI</strong> program are reflected in the use <strong>of</strong><br />
separate sessions for each scientific field, while emphasizing the cooperative<br />
translation <strong>of</strong> research both as it is necessarily integrated between fields and as<br />
it progresses from basic science to clinical application. In addition, we have<br />
aimed to incorporate as much informal social interaction between attendees as<br />
possible by including: a wine & cheese poster program, a career and<br />
networking lunch and, to encourage those with competitive nature, a<br />
cardiovascular-oriented Jeopardy match to help you digest after our awards<br />
dinner. Many thanks to our sponsors & we hope you enjoy this learning<br />
opportunity!<br />
Dr. Robert Roberts<br />
President and Chief Executive Officer<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Every year, the Molecular Function and Imaging <strong>Symposium</strong> brings together<br />
individuals in different fields to advance molecular imaging, and therapy,<br />
research as applied to the cardiovascular system. What makes this symposium<br />
unique is that it is organized by trainees for trainees. As a result, the event<br />
<strong>of</strong>fers a remarkable opportunity for young scientists to share their work,<br />
receive feedback and establish a network <strong>of</strong> potential collaborators. This year,<br />
the <strong>MFI</strong> <strong>Symposium</strong> will highlight the efficient, cooperative translation <strong>of</strong><br />
molecular methods for imaging and treating cardiovascular disease, from basic<br />
research to clinical application. As the field <strong>of</strong> molecular imaging evolves,<br />
increasing the exciting possibilities for medicine and research, participants in<br />
this symposium should take great pride as their contributions will, without a<br />
doubt, have a major impact on helping us better manage heart disease.<br />
ii
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
ORGANISING COMMITTEE & CONTRIBUTORS<br />
ORGANISING COMMITTEE<br />
Elizabeth Orton (chair)<br />
Joanne McBane<br />
James Haley<br />
Kathie Drozd<br />
Brian McArdle<br />
Lyne Sleiman<br />
Myra Cocker<br />
Jared Strydhorst<br />
Stephanie Chaisson<br />
ORGANIZING COMMITTEE ADVISORS<br />
Dr. Robert Beanlands<br />
Linda Garrard<br />
SYMPOSIUM ORGANISING ASSISTANCE<br />
Linda Garrard<br />
Carrie Barlow<br />
Matt McDonald<br />
Etienne Croteau<br />
Dr. Erik Suuronen<br />
Barbara IanniLucio<br />
Alex Norgaard<br />
<strong>MFI</strong> PROGRAM PRINCIPAL INVESTIGATORS<br />
Dr. Rob Beanlands<br />
Dr. Robert deKemp<br />
Dr. Mary-Ellen Harper<br />
Dr. Erik Suuronen<br />
Dr. Michael Gollob<br />
Dr. Jean DaSilva<br />
Dr. Marc Ruel<br />
iii
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
JUDGES & REVIEWERS<br />
ORAL PRESENTATION JUDGES<br />
Dr. Carolyn Anderson<br />
Dr. Jean DaSilva<br />
Dr. Richard Laforest<br />
Dr. Robert deKemp<br />
Dr. Markus Schwaiger<br />
Dr. Charles Cunningham<br />
Dr. Ren-Ke Li<br />
Dr. Ilona Skerjanc<br />
POSTER PRESENTATION JUDGES<br />
Dr. Carolyn Anderson<br />
Dr. Len Luyt<br />
Dr. Richard Laforest<br />
Dr. Rebecca Thornhill<br />
Dr. Aaron So<br />
Dr. Markus Schwaiger<br />
Dr. Ren-Ke Li<br />
Dr. Rob Beanlands<br />
ABSTRACT REVIEWERS<br />
Etienne Croteau<br />
Taylor Dowsley<br />
Brian McArdle<br />
Joanne McBane<br />
Jennifer Renaud<br />
Jared Strydhorst<br />
Branka Vulesevic<br />
iv
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
FINANCIAL SPONSORS<br />
FUNDING AGENCIES<br />
The <strong>MFI</strong> <strong>Program</strong> and <strong>Symposium</strong> Organizing Committee would like to thank the Ontario<br />
Consortium in Imaging for Cardiovascular Therapeutics and Image <strong>Heart</strong> Failure for their<br />
support and contributions to this event. The involvement <strong>of</strong> ICT has facilitated the assembly <strong>of</strong><br />
national and international experts in transitioning advances in basic cardiovascular research all<br />
the way to clinical imaging. Their contributions also encourage collaboration building between<br />
groups from key centers across Canada.<br />
INDUSTRY SPONSORS<br />
We are proud to have industry involvement in our symposium via financial support, attendance<br />
and participation in the program. Special thanks to our gold level sponsors (cumulative support<br />
2008 – <strong>2012</strong> > $5000): Jubilant DRAXIMAGE, Nordion, GE Healthcare, & Hermes Medical<br />
Imaging.<br />
v
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
TABLE OF CONTENTS<br />
WELCOME<br />
i<br />
ORGANIZING COMMITTEE & CONTRIBUTORS iii<br />
JUDGES & REVIEWERS<br />
iv<br />
FINANCIAL SPONSORS<br />
v<br />
TABLE OF CONTENTS<br />
vi<br />
DETAILED SCHEDULE 1<br />
ORAL ABSTRACTS 10<br />
SESSION I: Novel Probe Development 11<br />
SESSION II: Functional Imaging Technology 17<br />
SESSION III: Translational Imaging <strong>of</strong> Cardiovascular Disease 23<br />
SESSION IV: Application <strong>of</strong> Regenerative Research to Therapy 30<br />
POSTER ABSTRACTS 37<br />
Poster Index 38<br />
SESSION I: Novel Probe Development 41<br />
SESSION II: Functional Imaging Technology 43<br />
SESSION III: Translational Imaging <strong>of</strong> Cardiovascular Disease 46<br />
SESSION IV: Application <strong>of</strong> Regenerative Research to Therapy 52<br />
SPEAKER BIOGRAPHIES 64<br />
Keynote Speakers 65<br />
Workshop Speakers 70<br />
SOCIAL EVENTS INFORMATION 85<br />
SITE MAPS 88<br />
vi
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page<br />
DETAILED SCHEDULE<br />
1
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page back<br />
1
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
THURSDAY JUNE 21 ST , <strong>2012</strong><br />
WELCOME<br />
7:30 a.m. REGISTRATION, POSTER SET-UP & BREAKFAST<br />
8:00 a.m. OPENING REMARKS<br />
Dr. Rob<br />
Beanlands<br />
<strong>MFI</strong> <strong>Program</strong> Lead<br />
Investigator<br />
UOHI<br />
SESSION I: Novel probes<br />
<strong>MFI</strong> WORKSHOP I: NOVEL PROBE DEVELOPMENT AND APPLICATIONS<br />
8:20 a.m. The design <strong>of</strong> peptide-based<br />
molecular imaging agents<br />
Dr. Len Luyt<br />
London Health<br />
Sciences Centre<br />
Development <strong>of</strong> novel SPECT<br />
radiotracers for myocardial<br />
perfusion imaging<br />
Dr. Lihui Wei<br />
UOHI, Nordion<br />
The role <strong>of</strong> apoptosis in disease<br />
and the progress <strong>of</strong> apoptosis<br />
probes in molecular imaging<br />
applications<br />
Dr. Pasan<br />
Fernando<br />
UOHI, Nordion<br />
Moderator: Dr. Roberto Chica<br />
KEYNOTE LECTURE I<br />
9:30 a.m. Receptor-targeted imaging<br />
<strong>of</strong> cardiovascular disease<br />
Dr. Carolyn<br />
Anderson<br />
<strong>University</strong> <strong>of</strong><br />
Pittsburgh<br />
10:30 a.m. COFFEE BREAK<br />
2
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
THURSDAY JUNE 21 ST , <strong>2012</strong> cont.<br />
ORAL ABSTRACT SESSION I<br />
Moderators: Dr. Carolyn Anderson, Dr. Jean DaSilva<br />
Trainee Co-Moderator: Dr Ilias Mylonas<br />
10:45 a.m. Abstract#1: ‘Generation <strong>of</strong> a<br />
Longer Emission Wavelength Red<br />
Fluorescent Proteins Using<br />
Computationally Designed<br />
Libraries<br />
Roberto Chica<br />
Dept. <strong>of</strong> Chemistry,<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
10:57 a.m. Abstract#2: Characterizing Rho<br />
kinase activity using N-[ 11 C]-<br />
methyl-hydroxyfasudil in<br />
hypertrophied cardiomyocytes<br />
Pasan Fernando<br />
UOHI; Nordion<br />
11:09 a.m. Abstract#3: Decreased betaadrenoreceptor<br />
binding in highfat<br />
diet low dose streptozotocin<br />
rats is restored with similar<br />
efficacy by 2 or 7 weeks <strong>of</strong><br />
insulin-induced euglycemia<br />
James Haley<br />
UOHI,<br />
MSc candidate,<br />
Dr. JN DaSilva<br />
11:21 a.m. Abstract#4: [ 11 C] Methyl-<br />
EXP3174 as a potential<br />
radioligand for imaging<br />
AT1Receptor with PET<br />
Basma Ismail<br />
UOHI,<br />
PhD candidate,<br />
Dr. JN DaSilva<br />
11:33 a.m. Abstract#5: Imaging <strong>of</strong><br />
atherosclerotic vascular lesions in<br />
ApoE-/- mice using [ 18 F]-PyKYNEc(RGDyK)<br />
and PET<br />
Lyne Sleiman<br />
UOHI, R.A.,<br />
Dr. JN DaSilva<br />
11:45 a.m. LUNCH & POSTER BROWSING<br />
3
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
THURSDAY JUNE 21 ST , <strong>2012</strong> cont.<br />
SESSION II: Functional imaging technology<br />
<strong>MFI</strong> WORKSHOP II: PH-UNCTIONAL IMAGING PH-YSICS 101<br />
1:00 p.m. Magnetic resonance tools for<br />
the evaluation <strong>of</strong><br />
cardiovascular disease<br />
Dr. Rebecca<br />
Thornhill<br />
The <strong>Ottawa</strong> Hospital<br />
Fundamentals and advances<br />
<strong>of</strong> CT myocardial perfusion<br />
imaging<br />
Dr. Aaron So<br />
Robarts Research<br />
Centre<br />
Fundamentals <strong>of</strong> single photon<br />
emission tomography and<br />
technical advances<br />
Dr. R. Glenn Wells<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
<strong>Heart</strong> <strong>Institute</strong><br />
Fundamentals <strong>of</strong> positron<br />
emission tomography and<br />
advanced functional analysis<br />
Dr. Ran Klein<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
<strong>Heart</strong> <strong>Institute</strong><br />
Moderator: Dr. Robert<br />
deKemp<br />
2:15 p.m. AFTERNOON BREAK<br />
KEYNOTE LECTURE II<br />
2:30 p.m. Novel opportunities in<br />
imaging technology<br />
Dr. Richard<br />
Laforest<br />
<strong>University</strong> <strong>of</strong><br />
Washington in St.<br />
Louis<br />
4
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
THURSDAY JUNE 21 ST , <strong>2012</strong> cont.<br />
ORAL ABSTRACT SESSION II<br />
Moderators: Dr. Richard Laforest, Dr. Robert deKemp<br />
Trainee Co-Moderator: Dr Taylor Dowsley<br />
3:30 p.m. Abstract#6: Tc-99m/Tl-201<br />
crosstalk correction on a<br />
dedicated cardiac CZT<br />
SPECTcamera<br />
3:42 p.m. Abstract#7: Test-retest<br />
repeatability <strong>of</strong> myocardial<br />
blood flow measurements<br />
using rubidium-82 PET<br />
imaging<br />
Stephanie<br />
Chiasson<br />
UOHI,<br />
MSc candidate,<br />
Dr. G Wells<br />
Matthew Efseaff<br />
UOHI,<br />
MSc candidate,<br />
Dr. RA deKemp<br />
3:54 p.m. Abstract#8: Quantitative<br />
reconstruction <strong>of</strong> microSPECT<br />
data<br />
4:06 p.m. Abstract#9: A spline model<br />
for sampling <strong>of</strong> the right<br />
ventricle myocardium from<br />
cardiac PET images<br />
4:18 p.m. Abstract#10: Cross-talk<br />
correction in dual isotope In-<br />
Tc-99m small animal cardiac<br />
SPECT imaging<br />
Jared Strydhorst<br />
UOHI,<br />
PhD candidate,<br />
Dr. G Wells<br />
Simisani Takobana<br />
UOHI,<br />
MSc candidate,<br />
Dr. R Klein<br />
Rachel Timmins<br />
UOHI,<br />
MSc candidate,<br />
Dr. G Wells<br />
4:30 p.m. POSTER PRESENTATIONS & JUDGING WITH WINE &<br />
CHEESE<br />
6:00 p.m. END; POSTERS TAKEN DOWN<br />
5
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
FRIDAY JUNE 22 ND , <strong>2012</strong><br />
7:30 a.m. REGISTRATION & BREAKFAST<br />
SESSION III: Translational imaging <strong>of</strong> cardiovascular disease<br />
<strong>MFI</strong> WORKSHOP III: TRANSLATIONAL IMAGING OF CLINICAL<br />
CARDIOVASCULAR DISEASE<br />
SPONSORED BY IMAGING HEART FAILURE<br />
8:15 a.m. <strong>Heart</strong> failure and advances in<br />
PET for pre-clinical and clinical<br />
studies<br />
Ischemic heart disease and<br />
current CT approaches for preclinical<br />
and clinical studies<br />
Advancements in metabolic MRI<br />
and prospective detection <strong>of</strong><br />
clinical anomalies<br />
Dr. Lisa Mielniczuk<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
<strong>Heart</strong> <strong>Institute</strong><br />
Dr. Girish Dwivedi<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
<strong>Heart</strong> <strong>Institute</strong><br />
Dr. Charles<br />
Cunningham<br />
<strong>University</strong> <strong>of</strong> Toronto<br />
Molecular cardiac imaging with<br />
PET/MR<br />
Moderators: Dr. Mary-Ellen<br />
Harper; Dr. Rob Beanlands<br />
Dr. Kimberley<br />
Blackwood<br />
Lawson Health<br />
Research <strong>Institute</strong><br />
9:30 a.m. COFFEE BREAK<br />
KEYNOTE LECTURE III<br />
9:45 a.m. Translational imaging <strong>of</strong><br />
clinical cardiovascular<br />
disease<br />
Dr. Markus<br />
Schwaiger<br />
Technical <strong>University</strong><br />
<strong>of</strong> Munich<br />
6
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
FRIDAY JUNE 22 ND , <strong>2012</strong> cont.<br />
ORAL ABSTRACT SESSION III<br />
Moderators: Dr. Markus Schwaiger, Dr. Charles Cunningham<br />
Trainee Co-Moderator: Dr Mustafa Kazmi<br />
10:45 a.m. Abstract#11:<br />
Immunohistochemical Validation <strong>of</strong><br />
[18F]-fluorodeoxyglucose as a<br />
novel biomarker <strong>of</strong> inflamed<br />
vulnerable carotic plaque: A substudy<br />
<strong>of</strong> (CAIN)<br />
Myra Cocker<br />
UOHI, PDF,<br />
Dr. RS Beanlands<br />
10:57 a.m. Abstract#12: Sympathetic<br />
stimulation to evaluate coronary<br />
endothelial function in mice with<br />
11C-acetate positron emission<br />
tomography.<br />
11:09 a.m. Abstract#13: Integrin imaging <strong>of</strong><br />
hypertrophic cardiomyopathy<br />
identifies diffuse cardiac fibrosis:<br />
Direct comparison with<br />
cardiovascular magnetic resonance<br />
imaging-The SCAR Study<br />
11:21 a.m. Abstract#14: The prognostic<br />
value <strong>of</strong> change in RV function as<br />
measured on Radionuclide<br />
Ventriculography in patients with<br />
<strong>Heart</strong> Failure<br />
11:33 a.m. Abstract#15: Clinical trial<br />
standards and quality assurance<br />
for a low-dose 3D PET trial:<br />
Rubidium ARMI<br />
11:45 a.m. Abstract#16: Performance <strong>of</strong> CT<br />
coronary angiography in the<br />
elderly: does a life time <strong>of</strong><br />
exposure to cardiac risk factors<br />
preclude a diagnostic scan?<br />
Etienne Croteau<br />
UOHI, PDF,<br />
Dr. RA deKemp<br />
Myra Cocker<br />
UOHI, PDF,<br />
Dr. TD Ruddy<br />
Brian McArdle<br />
UOHI, Fellow,<br />
Dr. L Mielnizcuk<br />
Jennifer Renaud<br />
UOHI, RA,<br />
Dr. RA deKemp<br />
Gary Small<br />
UOHI, Fellow,<br />
Dr. B Chow<br />
12:00 p.m. SOCIAL LUNCH: CAREER DEVELOPMENT & NETWORKING<br />
Guest Speaker: Dr. R. Glenn Wells,<br />
Nuclear Cardiology, UOHI<br />
7
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
FRIDAY JUNE 22 ND , <strong>2012</strong> cont.<br />
SESSION IV: Application <strong>of</strong> regenerative research to therapy<br />
<strong>MFI</strong> WORKSHOP IV: REGENERATIVE THERAPY FROM TISSUE<br />
ENGINEERING TO IMAGING OUTCOMES<br />
SPONSORED BY IMAGING FOR CARDIOVASCULAR THERAPEUTICS<br />
1:15 p.m. Cardiomyogenesis in embryonic<br />
stem cells<br />
Dr. Ilona Skerjanc<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
Cardiac cell/biopolymer<br />
therapy: understanding effects<br />
and mechanisms<br />
Developments in clinical<br />
assessment, treatment<br />
planning, and therapeutic<br />
guidance for ischemic heart<br />
disease using MRI<br />
Dr. Marc Ruel<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
<strong>Heart</strong> <strong>Institute</strong><br />
Dr. Graham Wright<br />
<strong>University</strong> <strong>of</strong> Toronto<br />
Moderator: Dr. Darryl Davis<br />
2:15 p.m. AFTERNOON BREAK<br />
KEYNOTE LECTURE IV<br />
2:30 p.m. Cardiac rejuvenation to<br />
prevent heart failure after<br />
myocardial infarction<br />
Dr. Ren-Ke Li<br />
Toronto General<br />
Research <strong>Institute</strong><br />
8
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
FRIDAY JUNE 22 ND , <strong>2012</strong> cont.<br />
ORAL ABSTRACT SESSION IV<br />
Moderators: Dr. Ren-Ke Li, Dr. Ilona Skerjanc<br />
Trainee Co-Moderator: Dr. Brian McArdle<br />
3:30 p.m.<br />
Abstract#17: Enchanced matrix<br />
for cardiomyogenesis and<br />
regeneration <strong>of</strong> infarcted hearts<br />
3:42 p.m. Abstract#18: Human cardiac<br />
stem cells and circulating<br />
angiogenic cells possess equivalent<br />
capacity to regenerate damaged<br />
myocardium<br />
3:54 p.m. Abstract#19: Translationally<br />
controlled tumor protein (TCTP)<br />
revealed by proteomic analysis <strong>of</strong><br />
patient-specific blood outgrowth<br />
endothelial cells in heritable<br />
pulmonary arterial hypertension<br />
4:06 p.m. Abstract#20: Co-culture <strong>of</strong><br />
endothelial progenitor cells and<br />
monocytes for seeding the surface<br />
<strong>of</strong> a degradable polyurethane<br />
vascular graft material<br />
4:18 p.m. Abstract#21: Collagen matrices<br />
enhance CD34+ circulating<br />
angiogenic cell function through<br />
the integrin receptors<br />
4:30 p.m. CLOSING REMARKS<br />
Nick Blackburn<br />
UOHI,<br />
MSc candidate,<br />
Dr. EJ Suuronen<br />
Nick Latham<br />
UOHI,<br />
MSc candidate,<br />
Dr. D Davis<br />
Jessie Lavoie<br />
OHRI, PhD candidate,<br />
Dr. DJ Stewart<br />
Eva Mathieu<br />
UOHI, PDF,<br />
Dr. EJ Suuronen<br />
Brian McNeill<br />
UOHI, PDF,<br />
Dr. EJ Suuronen<br />
Dr. Robert Roberts<br />
President and CEO<br />
UOHI<br />
7:30 p.m. DINNER, AWARDS AND JEOPARDY!<br />
9
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page<br />
ORAL ABSTRACTS<br />
10
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page back<br />
10
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
ORAL ABSTRACTS<br />
SESSION I: Novel Probe Development<br />
11
Oral Abstract#1<br />
Generation <strong>of</strong> longer emission wavelength Red Fluorescent Proteins using<br />
Computationally Designed Libraries<br />
Roberto A. Chica 1,2 , Matthew M. Moore 3 , Benjamin D. Allen 3 , and Stephen L. Mayo 2,3 .<br />
1 Department <strong>of</strong> Chemistry, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 2 Division <strong>of</strong> Biology, California <strong>Institute</strong> <strong>of</strong><br />
Technology; 3 Division <strong>of</strong> Chemistry and Chemical Engineering, California <strong>Institute</strong> <strong>of</strong> Technology.<br />
Background: The longer emission wavelengths <strong>of</strong> red fluorescent proteins (RFPs) make them<br />
attractive for whole-body imaging because cells are more transparent to red light. Although several<br />
useful RFPs have been developed, the quest for further red-shifted and improved RFPs continues.<br />
Herein, we report a structure-based rational design approach to red shift the fluorescence emission <strong>of</strong><br />
RFPs.<br />
Methods/ Results: We applied a combined computational and experimental approach that uses<br />
computational protein design as an in silico pre-screen to generate focused combinatorial libraries <strong>of</strong><br />
mCherry mutants. The computational procedure helped us identify residues that could fulfill<br />
interactions hypothesized to cause red shifts without destabilizing the protein fold. These<br />
interactions include stabilization <strong>of</strong> the excited state through H-bonding to the acylimine oxygen<br />
atom, destabilization <strong>of</strong> the ground state by hydrophobic packing around the charged phenolate, and<br />
stabilization <strong>of</strong> the excited state by a p-stacking interaction. Our methodology allowed us to identify<br />
three mCherry mutants (mRojoA, mRojoB, and mRouge) that display emission wavelengths >630<br />
nm, representing red shifts <strong>of</strong> 20 to 26 nm. Moreover, our approach required the experimental<br />
screening <strong>of</strong> a total <strong>of</strong> 5000 clones, a number several orders <strong>of</strong> magnitude smaller than those<br />
previously used to achieve comparable red shifts. Additionally, crystal structures <strong>of</strong> mRojoA and<br />
mRouge allowed us to verify fulfillment <strong>of</strong> the interactions hypothesized to cause red shifts,<br />
supporting their contribution to the observed red shifts.<br />
Conclusion: These results suggest that this approach may be applicable to red-shift the emission<br />
wavelength <strong>of</strong> other RFPs. We expect that other useful properties, such as increased quantum yield<br />
and maturation rate, could also be improved using this method.<br />
I. Novel Probe Development – Oral Presentation<br />
12
Oral Abstract#2<br />
Characterizing Rho kinase activity using N-[ 11 C]-methyl-hydroxyfasudil in<br />
hypertrophied cardiomyocytes<br />
Steven Moreau 1,2,3 , A.C. Valdivia 2,3,5 , R.S.B. Beanlands 2,3,5 , T. Ruddy 3,5 , J.N. DaSilva 1,2,3,5 , Pasan<br />
Fernando 1,2,3,4<br />
1 Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 2 <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong><br />
<strong>Institute</strong> Molecular Function and Imaging Group; 3 <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>; 4 Nordion;<br />
5 <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong> Cardiac PET<br />
Background: Cardiac hypertrophy is a compensatory response to increased work load or stress on<br />
the heart, but over time can lead to heart failure and death. The molecular mechanisms underlying<br />
this disease are still not completely understood, however the Rho/Rho kinase pathway has been<br />
shown to play a role.<br />
Methods/ Results: The PET tracer N-[ 11 C]-methyl-hydroxyfasudil is an analog <strong>of</strong> the ROCK<br />
inhibitor hydroxyfasudil expected to bind to active Rho kinase. Hypertrophy was induced in vitro<br />
using the ß-adrenergic receptor agonist isoproterenol to evaluate optimal Rho kinase activity. Rho<br />
kinase activity data was correlated to N-[ 11 C]-methyl-hydroxyfasudil binding. Cardiac hypertrophy<br />
was verified with an increase in nuclear size (1.74 fold) and cell size (~2 fold), activation <strong>of</strong><br />
hypertrophic signalling pathways involving in particular ERK1/2 and mTOR phosphorylation, and<br />
increased Rho kinase activity (1.64 fold). This correlated to a 10.3% increase in N-[ 11 C]-methylhydroxyfasudil<br />
binding which was brought down to control levels by blocking with unlabeled<br />
hydroxyfasudil indicating the tracer’s specificity for its target, Rho kinase.<br />
Conclusion: This result suggests that N-[ 11 C]-methyl-hydroxyfasudil may be useful as a radiotracer<br />
for detecting cardiac hypertrophy in vivo and possibly to guide therapies.<br />
I. Novel Probe Development – Oral Presentation<br />
13
Oral Abstract#3<br />
Decreased ß-adrenoceptor binding in high-fat diet low dose streptozotocin<br />
rats is restored with similar efficacy by 2 or 7 weeks <strong>of</strong> insulin-induced<br />
euglycemia<br />
James Haley, J.T. Thackeray, S.L. Thorn, M. Kolajova, R.S.B. Beanlands, and J.N. DaSilva<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong> Cardiac PET Center; Dept. <strong>of</strong> Cellular and Molecular<br />
Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>.<br />
Background: Abnormal myocardial sympathetic nervous system and ß-adrenoceptor (ß-AR)<br />
signaling has been described in diabetes and may contribute to an increased risk <strong>of</strong> cardiovascular<br />
disease. While an early reduction <strong>of</strong> blood glucose by insulin treatment has been shown to prevent<br />
altered sympathetic and ß-AR signaling, the timeframe <strong>of</strong> this effect is not well established.<br />
[ 3 H]CGP12177 is a nonselective, hydrophilic ß-AR antagonist that has been used previously to<br />
assess ß-AR levels in high-fat diet fed, low-dose streptozotocin (STZ) rats. The aim <strong>of</strong> this study<br />
was to identify if a short timeframe <strong>of</strong> insulin treatment can restore myocardial ß-AR expression in<br />
high-fat-fed STZ hyperglycemic rats.<br />
Methods/ Results: Male Sprague-Dawley rats were fed a high-fat diet (32% kcal) to induce insulin<br />
resistance and given a single low-dose intraperitoneal injection <strong>of</strong> STZ (45mg/kg) (n=11) or vehicle<br />
(n=8) to evoke hyperglycemia (blood glucose >11mM). Additionally, two groups <strong>of</strong> the high-fat diet<br />
STZ hyperglycemics were stratified to receive insulin (4 U/day, continuous sc.) to normalize blood<br />
glucose at 1 week post-STZ for 7 weeks (n=3) or 6 weeks post-STZ for 2 weeks (n=4). Ex vivo<br />
[ 3 H]CGP12177 biodistribution was performed 8 weeks post-STZ to measure ß-AR binding 30 min<br />
following tracer injection. STZ-induced hyperglycemia was rapidly reversed by treatment with<br />
insulin at both 1 and 6 weeks post-STZ. Total myocardial [ 3 H]CGP12177 binding at 8 weeks was<br />
significantly (p
Oral Abstract#4<br />
[ 11 C]Methyl-EXP3174 as a Potential Radioligand For Imaging<br />
AT1Receptor With PET<br />
Basma Ismail, J. Fabre, T. Hadizad, J.T. Thackeray, S.L. Thorn, R.A. deKemp, R.S.B.Beanlands,<br />
J.N. DaSilva<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong> Cardiac PET Center; Dept. <strong>of</strong> Cellular and Molecular<br />
Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>.<br />
Background: AT1 receptor (AT1R) expression is altered in cardiac and renal disorders. EXP 3174,<br />
a major downstream metabolite <strong>of</strong> the clinically used drug Losartan, has 10 times the affinity for the<br />
AT1R as a reversible competitive antagonist than the parent compound. [11C]methyl-EXP3174 was<br />
evaluated as a potential radiotracer for quantifying AT1R.<br />
Methods/ Results: Male Sprague–Dawley rats (n=8) were administered i.v. [11C]methyl-EXP3174<br />
(0.5 – 1.5 mCi) and imaged for 60 min with the Siemens Inveon MicroPET camera to evaluate tracer<br />
pr<strong>of</strong>ile. Time activity curves were derived from the regions <strong>of</strong> interest (ROI) drawn from the<br />
reconstructed microPET images (Siemens IRW s<strong>of</strong>tware). Distribution volume (DV) was quantified<br />
using Logan slope graphical analysis with the left atrial cavity used to obtain the blood input<br />
function. Test-retest studies were conducted within 7 days to determine process reproducibility.<br />
Column switch HPLC with coincidence radioactivity detector was used to identify 11C- labeled<br />
metabolites in rat plasma and kidney at 10 minutes. Kidneys showed high tracer uptake with peak<br />
activity at 2 minutes and retained for 60 minutes. DV values were obtained from left kidney<br />
(2.5±0.64). Test-retest variability was found to be 21.7%. HPLC analysis revealed 13 - 25% <strong>of</strong> total<br />
radioactivity signal in plasma derived from hydrophilic labeled metabolites. Whereas these<br />
radiolabeled metabolites accounted for 52 - 86% <strong>of</strong> the total signal in kidney.<br />
Conclusion: In vivo studies support the use <strong>of</strong> [11C]methyl-EXP3174 as an imaging agent to assess<br />
AT1R in kidneys with good reproducibility. However, the presence <strong>of</strong> high proportion <strong>of</strong><br />
metabolites in the target tissue is a potential problem. Further studies to assess the specific binding<br />
<strong>of</strong> the tracer and labeled metabolites are warranted.<br />
I. Novel Probe Development – Oral Presentation<br />
15
Oral Abstract#5<br />
Imaging <strong>of</strong> atherosclerotic vascular lesions in ApoE-/- mice using [ 18 F]-<br />
PyKYNE-c(RGDyK) and PET<br />
A.C. Valdivia 1 , S.L. Thorn 1 , Lyne Sleiman 1 , R.S.B. Beanlands 1 and J.N. DaSilva 1<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Development <strong>of</strong> atherosclerosis occurs when fat, cholesterol, and other substances<br />
accumulate in the luminal walls <strong>of</strong> arteries. This results in a progressive inflammatory response<br />
deposit <strong>of</strong> macrophages and cholesterol filled foam cells to form the plaque core. Subsequent<br />
rupture <strong>of</strong> atherosclerotic plaques is one the leading causes <strong>of</strong> myocardial infarction and sudden<br />
cardiac death. Atherosclerotic plaques develop microvascular networks proposed to be important in<br />
sustaining plaque growth. Non-invasive imaging <strong>of</strong> atherosclerotic lesions is a promising approach<br />
for the early detection <strong>of</strong> vulnerable plaque and monitoring <strong>of</strong> anti-atherosclerotic therapies. The<br />
integrin a vß 3 receptor is a cell adhesion protein prominently expressed in the atherosclerotic plaque.<br />
18 F labeled RGD peptides have been investigated for imaging the a vß 3 integrin receptor expression in<br />
tumour neovascularization, but only 18 F-galacto-RGD has been evaluated for molecular imaging <strong>of</strong><br />
plaque-associated angiogenesis. In the present work, we developed [ 18 F]-PyKYNE-c(RGDyK), a<br />
new 18 F labeled RGD peptide, with the aim <strong>of</strong> investigating atherosclerotic plaques using PET.<br />
Methods/Results: [ 18 F]-PyKYNE-c(RGDyK) was synthesized via “click chemistry” by reacting the<br />
commercially available azido-c(RGDyK) with [ 18 F]PyKYNE in presence <strong>of</strong> Cu (I). 500 uCi <strong>of</strong> [ 18 F]-<br />
PyKYNE-c(RGDyK) was injected in ApoE-/- mice. 60-min whole body dynamic scans were<br />
acquired using the Inveon small animal PET camera. Mice were euthanized by cervical dislocation<br />
with the aorta dissected out and placed on a glass slide for a further 30 min static acquisition in the<br />
MicroPET camera. Additional tissues were collected and counted in a gamma counter to obtain ex<br />
vivo % injected dose (ID)/g <strong>of</strong> tissue measurements.<br />
[ 18 F]-PyKYNE-c(RGDyK) was produced in high purity (>95%) and in 10-20% radiochemical yield.<br />
High uptake is observed in the liver with low retention in the heart (13% ID/g <strong>of</strong> tissue) at 60 min<br />
post-injection. High uptake was found in the aorta, and confirmed by ex vivo imaging and<br />
biodistribution (35% ID/g <strong>of</strong> tissue).<br />
Conclusion: High uptake <strong>of</strong> [ 18 F]-PyKYNE-c(RGDyK) in the plaque-rich aorta <strong>of</strong> atherosclerotic<br />
prone ApoE -/- mice was observed and warrants further evaluation <strong>of</strong> this non-invasive approach.<br />
Future studies will be conducted with serial PET imaging <strong>of</strong> ApoE -/- mice using CT contrast for colocalization<br />
<strong>of</strong> plaques in vivo, ex vivo autoradiography and histological assessment.<br />
I. Novel Probe Development – Oral Presentation<br />
16
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
ORAL ABSTRACTS<br />
SESSION II: Functional Imaging Technology<br />
17
Oral Abstract#6<br />
Tc-99m/Tl-201 crosstalk correction on a dedicated cardiac CZT SPECT<br />
camera<br />
Stéphanie Chiasson, T.D. Ruddy, R.G. Wells<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Dual-isotope cardiac SPECT perfusion imaging <strong>of</strong>fers perfectly aligned rest/stress<br />
images and a greatly reduced imaging time. However, simultaneous imaging is hampered by high<br />
doses and crosstalk between the isotopes. Dedicated cardiac cameras based on solid-state (CZT)<br />
detectors have recently been introduced into the clinic, with improved energy resolution and greater<br />
sensitivity. Our study assesses the accuracy <strong>of</strong> using a modified Triple-Energy-Window (TEW)<br />
correction for Tl201/Tc99m-tetr<strong>of</strong>osmin dual-isotope imaging with a CZT-based dedicated cardiac<br />
SPECT camera. We are studying the correction accuracy using single-isotope clinical studies<br />
acquired on the camera at the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>.<br />
Methods/Results: The study includes 50 synthetic dual-isotope patients being corrected with a<br />
modified TEW correction with varying scatter window widths. Each patient consists <strong>of</strong> two singleisotope<br />
acquisitions, one <strong>of</strong> each Tc99m rest and Tl201 stress, matched by gender and BMI. For a<br />
first evaluation <strong>of</strong> the correction, it was originally done on the single isotope acquisitions to remove<br />
the residual scatter counts in the opposing primary energy window (i.e. remove Tc99m counts in the<br />
Tl201 window). The synthetic dual isotope patients were then created and the correction applied in<br />
each primary window. For the correction <strong>of</strong> the uncontaminated data, the TEW correction removes<br />
135% <strong>of</strong> the Tl201 scatter in the Tc99m window using the smallest scatter window width while it<br />
succeeds to remove 137% <strong>of</strong> the scatter using the largest. In the Tl201 window, the 3keV scatter<br />
window removed 101% <strong>of</strong> the Tc99m counts while the 10keV window removed 95%. Comparing<br />
the corrected synthetic images to the single isotope acquisition, we find 0.101%-0.38% <strong>of</strong> the Tc99m<br />
signal in the Tc99m window and 1.32%-2.39% <strong>of</strong> the Tl201 signal in the Tl201 window.<br />
Conclusion: a modified TEW correction provides a simple effective way <strong>of</strong> correcting for cross-talk<br />
in Tl201/Tc99m dual-isotope cardiac SPECT imaging.<br />
II. Functional Imaging Technology – Oral Presentation<br />
18
Oral Abstract#7<br />
Test-retest repeatability <strong>of</strong> myocardial blood flow measurements using<br />
rubidium-82 PET imaging<br />
Matthew Efseaff 1,2 , R. Klein 2 , M.C. Ziadi 2 , R.S.B. Beanlands 2 , R.A. deKemp. 1,2<br />
1 Carleton <strong>University</strong>, 2 <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: 82 Rb PET imaging has been proposed for routine myocardial blood flow (MBF)<br />
quantification. However, few studies have investigated the test-retest repeatability <strong>of</strong> this method.<br />
The goal <strong>of</strong> this study was to optimize same-day repeatability <strong>of</strong> MBF imaging with a highly<br />
automated analysis program using image-derived input functions and dual spillover corrections<br />
(SOC).<br />
Methods/Results: Test-retest repeatability <strong>of</strong> resting left-ventricle (LV) MBF was measured in<br />
patients (n = 27) with suspected coronary artery disease (CAD) and healthy volunteers (n = 9). The<br />
effects <strong>of</strong> scan-time, reconstruction and quantification methods were assessed with correlation and<br />
Bland-Altman repeatability coefficients. Factors affecting rest MBF included gender, suspected<br />
CAD, and SOC (p < 0.001). Significant test-retest correlations were found using all analysis<br />
methods tested (r > 0.79). The best repeatability coefficient for same-day MBF was 0.20 mL/min/g<br />
using a 6 min scan-time, iterative reconstruction, SOC, resting rate-pressure product adjustment<br />
(RPP), and left atrium input function. This protocol was significantly less variable than standard<br />
protocols using FBP reconstruction, longer scan-time, no SOC, or LV input function.<br />
Conclusion: 82 Rb PET MBF can be measured reproducibly using a 6 min scan length, iterative<br />
reconstruction, SOC, RPP, and an image-derived input function in the left atrium cavity.<br />
II. Functional Imaging Technology – Oral Presentation<br />
19
Oral Abstract#8<br />
Quantitative reconstruction <strong>of</strong> microSPECT data<br />
Jared Strydhorst, R.G. Wells<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Small animal microSPECT is an important pre-clinical imaging modality. However,<br />
quantitative accuracy is limited by photon attenuation in the subject and scatter in the subject and the<br />
collimator. In this study we investigate both scatter and attenuation correction in the reconstruction<br />
<strong>of</strong> a phantom.<br />
Method/ Results: Several phantoms consisting <strong>of</strong> a 9mm diameter cylinder <strong>of</strong> activity placed in the<br />
centre <strong>of</strong> progressively larger cylinders <strong>of</strong> water with (diameters: 23, 37, 49, and 52 mm), were<br />
scanned in a multiplexing multi-pinhole (MMP) SPECT scanner. Scan parameters were as follows: 9<br />
pinholes/detector, 2.5 mm diameter; 48 projections; helical scan; 3 minutes per projection.<br />
Projection data were recorded for two energy windows, one centered at the photopeak (140 keV) and<br />
a second window centered at 110 keV. The phantom was also scanned with a built-in CT scanner (45<br />
keV, cone beam). The SPECT data were reconstructed using an iterative ordered subsets expectation<br />
maximization algorithm with no correction, attenuation correction (AC) only, and AC and scatter<br />
correction (SC). Attenuation was estimated from the CT and incorporated into the system matrix as<br />
part <strong>of</strong> the reconstruction. Scatter was estimated using the dual energy window method to estimate<br />
the scattered photon distribution. The scatter projections were then smoothed and added to the<br />
forward projections during reconstruction. A point source with a known activity was used as a<br />
reference to convert the reconstructed data to absolute activity concentration.With neither<br />
attenuation nor scatter correction, the activity concentration measured using SPECT was 6 – 28%<br />
below the known activity. Attenuation correction alone resulted in measured activity concentrations<br />
4-8% above the true concentration. With both AC and SC, the measured activity concentration was<br />
within ±2% <strong>of</strong> the true value.<br />
Conclusion: With attenuation and scatter correction, tracer activity concentration can be<br />
quantitatively measured using multiplexed multi-pinhole microSPECT.<br />
II. Functional Imaging Technology – Oral Presentation<br />
20
Oral Abstract#9<br />
A Spline Model for Sampling <strong>of</strong> the Right Ventricle Myocardium from<br />
Cardiac PET Images<br />
Simisani Takobana 1,2 , A. Alder 1 , R.A. deKemp 2 , R. Klein 2<br />
1 Dept. <strong>of</strong> Systems and Computer Engineering, 2 Carleton <strong>University</strong>, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong><br />
<strong>Institute</strong><br />
Background: Conditions such as pulmonary hypertension usually alter right ventricular (RV)<br />
physiology and anatomy, in most cases making it hypertrophic and dysfunctional. Because <strong>of</strong> a wide<br />
range <strong>of</strong> RV anatomies among human and animals, with normal and hypertrophic hearts a spline<br />
model must be general. However, the model should minimize the number <strong>of</strong> control points as well as<br />
their degrees <strong>of</strong> freedom for computational efficiency and usability. The purpose <strong>of</strong> the study was to<br />
evaluate a proposed 12 spline points model with 13 degrees <strong>of</strong> freedom for sampling the RV in<br />
cardiac PET images.<br />
Methods/ Results: A sample set <strong>of</strong> 5 normal and 5 hypertrophic human, and 5 normal and 5<br />
hypertrophic rat hearts FDG PET images was used. The RV model was manually fit to each image,<br />
and the fit was evaluated. A pass was granted when the model was judged by the operator to<br />
sufficiently trace the RV mid-myocardium and appropriately intersect the LV. In normal rats, the<br />
RV was difficult to visualize due to its thinner wall, proximity to the thicker LV, and low image<br />
resolution. In all human and hypertrophic rat hearts the model was sufficient for tracing the RV.<br />
Conclusion: The proposed model is sufficiently flexible to describe normal and hypertrophic hearts<br />
in human and rat populations. It is possible that a simpler model, with fewer degrees <strong>of</strong> freedom may<br />
be sufficient, while further reducing the model complexity.<br />
II. Functional Imaging Technology – Oral Presentation<br />
21
Oral Abstract#10<br />
Cross-talk correction in dual isotope 111 In/ 99m Tc small animal cardiac<br />
SPECT imaging<br />
Rachel Timmins 1,2 , R.G. Wells 1,2<br />
1<br />
Dept. <strong>of</strong> Physics, Carleton <strong>University</strong>; 2 <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Dual-isotope imaging via energy discrimination is a major strength <strong>of</strong> SPECT<br />
imaging but image quality is degraded by cross-talk interference. Cross-talk correction techniques<br />
have been developed for clinical SPECT however application to small-animal imaging is not ideal.<br />
The reduced subject size & variability in small-animal imaging may allow simpler cross-talk<br />
correction methods to provide adequate quantification accuracy. The objective <strong>of</strong> this study is to<br />
evaluate the accuracy <strong>of</strong> three simple cross-talk correction methods for small-animal 111In/99mTc<br />
imaging.<br />
Methods/Results: We compared triple energy window (TEW), applied in both projection and image<br />
space, and convolution subtraction. Each was evaluated using a phantom consisting <strong>of</strong> 3 5ml<br />
syringes filled with Tc-99m, In-111 and a mixture <strong>of</strong> Tc-99m and In-111 respectively. Five ratios <strong>of</strong><br />
Tc-99m:In-111 activity concentrations were used in the mixture: 4.5:1, 3:1, 1:1,1:4, 1:8. Data were<br />
acquired on a 4-head NanoSPECT/CT small-animal camera (9x2mm pinholes/head) and<br />
reconstructed using OSEM with attenuation correction. Total counts in the uncorrected projection<br />
data were 61 and 96 M counts for the Tc99m (129-150keV) and In111 (158-185keV + 225-265keV)<br />
windows respectively. The corrected images were assessed visually and quantitatively as the percent<br />
reduction <strong>of</strong> the In-111 activity in the Tc-99m image and the accuracy <strong>of</strong> recovering the correct<br />
activity ratio in the mixed syringes. TEW applied in projection space gave the best reduction <strong>of</strong> In-<br />
111 cross-talk. It reduced the false Tc-99m image <strong>of</strong> the In-111 phantom by 96% and provided the<br />
best visual removal. TEW applied in image space and convolution subtraction reduced the In-111<br />
interference by 95% and 87% respectively and visual evaluation <strong>of</strong> the images showed greater<br />
residual signal. The concentration <strong>of</strong> Tc-99m in the mixed syringe was recovered to within 5% or<br />
less <strong>of</strong> the true value over the range evaluated.<br />
Conclusion: TEW applied in projection space was the most accurate cross-talk correction method in<br />
In-111/Tc-99m dual-isotope small-animal cardiac SPECT imaging and was able to achieve an<br />
accuracy <strong>of</strong> 4±1%.<br />
II. Functional Imaging Technology – Oral Presentation<br />
22
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
ORAL ABSTRACTS<br />
SESSION III: Translational Imaging <strong>of</strong> Cardiovascular<br />
Disease<br />
23
Oral Abstract#11<br />
Immunohistochemical Validation <strong>of</strong> [18F]-fluorodeoxyglucose as a Novel<br />
Biomarker <strong>of</strong> Inflamed Vulnerable Carotid Plaque: A Sub-study <strong>of</strong> the<br />
Canadian Atherosclerosis Imaging Network (CAIN)<br />
Myra Cocker, B. McArdle, R.A. deKemp, C. Lum, G. Youssef, R. Hammond, Y. Yer<strong>of</strong>eyeva, T.<br />
Karavardanyan, A. Adeeko, A. Hill, G. Stotts, M. Sharma, J.M. Renaud, J. Brennan, M. Alturkustani,<br />
L. Hammond, J.N. DaSilva, J.C. Tardif, J. David Spence, R.S.B. Beanlands<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Atherosclerosis is a leading cause <strong>of</strong> morbidity and mortality within Canada.<br />
‘Vulnerable’ rupture prone plaque is associated with pronounced inflammatory activity and<br />
increased density <strong>of</strong> macrophage cells. Macrophages have increased metabolic rates and require<br />
high-levels <strong>of</strong> energy for phagocytic activity. Therefore, the uptake <strong>of</strong> radiolabelled glucose or<br />
[18F]-fluorodeoxyglucose (18FDG) imaged with hybrid positron emission tomography (PET) and<br />
computed tomography (CT) may serve as a surrogate marker <strong>of</strong> inflammatory activity within plaque.<br />
We hypothesized that metabolic activity within carotid plaques, as determined by 18FDG studies<br />
with PET/CT, is associated with intraplaque inflammatory burden or macrophage expression using<br />
macrophage-specific CD68 staining immunohistology.<br />
Methods/Results: Twenty-two patients (mean age: 51±11 years, 18 male) scheduled for carotid<br />
endarterectomy within two weeks were prospectively recruited. Patients underwent PET-FDG and<br />
CT angiography <strong>of</strong> carotid vasculature but patients with baseline GFR 6 months or asymptomatic (n=16 plaques in 8 patients). Carotid<br />
18FDG uptake in recently symptomatic patients was greater (3.3±1.3 TBR n=28) than previously<br />
symptomatic or asymptomatic patients (2.6±1.0 TBR n=16) (p=0.044).<br />
Conclusion: The uptake <strong>of</strong> 18FDG in carotid vasculature is related to inflammatory burden within<br />
plaque, as evaluated by immunohistochemistry. 18FDG may serve as a non-invasive biomarker <strong>of</strong><br />
patients with plaque inflammation and macrophage activity, which may enable identification <strong>of</strong><br />
those at risk for events.<br />
III. Translational Imaging <strong>of</strong> Cardiovascular Disease –<br />
Oral Presentation<br />
24
Oral Abstract#12<br />
Sympathetic Stimulation to Evaluate Coronary Endothelial Function in<br />
Mice with 11 C-Acetate Positron Emission Tomography<br />
Etienne Croteau, M. Kordos, J.M. Renaud, R. Klein, J.N. DaSilva, R.S.B. Beanlands, R.A. deKemp.<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Endothelial dysfunction (ED) is a common early symptom <strong>of</strong> hypertension, diabetes<br />
and atherosclerosis. The main function <strong>of</strong> the endothelium is to regulate the microvascular blood<br />
supply according to local changes in demand. We propose a hyperemic stress protocol with<br />
norepinephrine (NE) to derive the endothelial-specific myocardial flow reserve (EFR).<br />
Methods/Results: N=5 mice were used to evaluate the stepwise response <strong>of</strong> norepinephrine (NE).<br />
Peripheral blood pressure (BP) was measured in the carotid artery using optical fiber sensor (SAII).<br />
The validity <strong>of</strong> using the image derive input function (IDIF) was experimentally confirmed by<br />
simultaneous blood sampling from the carotid during 11 C-acetate imaging. NE-Stress PET imaging<br />
(Siemens Inveon DPET) was conducted using an optimized radiotracer injection at 5 min post start<br />
<strong>of</strong> infusion. L-NAME (endothelial nitric oxide synthase inhibitor (eNOS)) pre-treated mice (drinking<br />
water 0.25mg/L for 1 week) and transgenic eNOS knockout mice were used to block the eNOSspecific<br />
vasodilatation <strong>of</strong> the coronary vessels. Rest/NE-stress protocol on C57BL mice (28 ± 1g)<br />
with I.V. injection <strong>of</strong> 34 ± 16 MBq 11 C-acetate was used to measure myocardial blood flow (MBF)<br />
at baseline and after NE-stress to evaluate EFR. IDIF is adequate in the kinetic analysis <strong>of</strong> 11 C-<br />
acetate. A steady state BP response was typically reached after 2 min <strong>of</strong> NE infusion, and was<br />
sustained in both healthy controls and pre-treated mice. Dosage in control groups has no significant<br />
effect on rate pressure product (RPP) [heart-rate × systolic blood pressure] ratio (NEstress:baseline).<br />
L-NAME pre-treatment showed a significant decrease <strong>of</strong> the RPP ratio to 1.07 ±<br />
0.03 (N=5) compared to the selected dose 3.2µg/Kg/min (Medium) with 1.23 ± 0.09 RPP (Unpaired<br />
t-test p
Oral Abstract#13<br />
Integrin Imaging <strong>of</strong> Hypertrophic Cardiomyopathy Identifies Diffuse<br />
Cardiac Fibrosis: Direct Comparison with Cardiovascular Magnetic<br />
Resonance Imaging<br />
The SCAR Study<br />
Myra Cocker*, G. Dwivedi*, B. Marvin, M. Poirier, C. Dennie, G. Wells, R. Roberts, A. Dick, K.<br />
Ascah, T.D. Ruddy (*Equal contributors.)<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> Instiute<br />
Background: Patients with hypertrophic cardiomyopathy (HCM) are at risk <strong>of</strong> developing heart<br />
failure secondary to the release <strong>of</strong> stress-responsive trophic factors. The disease process in HCM<br />
promotes diffuse myocardial collagen synthesis, disarray and hypertrophy. Cardiovascular magnetic<br />
resonance (CMR) imaging using T1-weighted late gadolinium enhancement (LGE) can be utilized to<br />
detect the extent <strong>of</strong> focal fibrosis in HCM. However, although the disease process in HCM is<br />
actually global, such diffuse injury cannot be visualized with LGE.<br />
avß3 is a unique vitronectin integrin receptor that is activated in infarcted tissue; is associated with<br />
fibroblasts as well as collagen synthesis. A novel 99 Technetium compound ( 99m Tc-NC100692, GE<br />
healthcare) that binds with high affinity to avß3 has been developed.<br />
99m Tc-NC100692 could be<br />
utilized to detect the extent <strong>of</strong> both focal and diffuse myocardial fibrosis in patients with HCM.<br />
Methods/Results:5 patients (mean age: 62±11 years, 1 female) with an established diagnosis <strong>of</strong><br />
HCM based upon findings from echocardiography were prospectively recruited. Patients underwent<br />
SPECT 99m Tc-NC100692 and CMR LGE imaging. Using the American <strong>Heart</strong> Association 17-<br />
segment model, 99m Tc-NC100692 images were visually assessed for the presence or absence <strong>of</strong><br />
myocardial uptake using a three-point scale. Similarly, LGE were also assessed for the presence or<br />
absence <strong>of</strong> enhancement using the 17-segment model. 85 left ventricular segments were assessed in<br />
5 patients. All 85 segments had some degree <strong>of</strong> evidence for 99m Tc-NC100692 uptake. 3 patients had<br />
CMR-based evidence for focal LGE present in 9 segments. Of these 9 segments, 5 had matched<br />
high-grade 99m Tc-NC100692 uptake. One patient had strong apical 99m Tc-NC100692 uptake without<br />
any evidence <strong>of</strong> hypertrophy nor LGE. The remaining 79 segments had low-grade 99m Tc-NC100692<br />
uptake with lack <strong>of</strong> evidence for LGE.<br />
Conclusion: There is evidence for diffuse low-grade left ventricular 99m Tc-NC100692 uptake,<br />
suggestive <strong>of</strong> fibrosis in patients with hypertrophic cardiomyopathy. In regions with CMR-based<br />
evidence for focal fibrosis, greater uptake <strong>of</strong> 99m Tc-NC100692 is noted. 99m Tc-NC10069 may be a<br />
marker <strong>of</strong> diffuse myocellular disarray and fibrosis that underlies the development <strong>of</strong> hypertrophic<br />
cardiomyopathy. Further studies are required in healthy subjects to determine the specificity <strong>of</strong><br />
99m Tc-NC100692.<br />
III. Translational Imaging <strong>of</strong> Cardiovascular Disease –<br />
Oral Presentation<br />
26
Oral Abstract#14<br />
The prognostic value <strong>of</strong> change in RV function as measured on<br />
Radionuclide Ventriculography in patients with <strong>Heart</strong> Failure<br />
Brian McArdle, M. Chiu, R. Ohle, H. Haddad, R.S.B. Beanlands, R. Davies,<br />
L. Mielniczuk<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Right Ventricular Function has been shown to have prognostic value in patients with<br />
heart failure but accurate estimation <strong>of</strong> RV Ejection Fraction (RVEF) with standard imaging<br />
techniques such as 2-D ECHO is difficult. RVEF as measured on Radionuclide Ventriculography<br />
(RNV) has recently been shown to have prognostic value independent <strong>of</strong> LV function. We aimed to<br />
evaluate the additional value <strong>of</strong> change in RV function over serial scans as measured on RNV in<br />
patients with heart failure.<br />
Methods/Results: We retrospectively analyzed the clinical records <strong>of</strong> patients with new- onset<br />
heart failure that attended our heart Function Clinic since January 2007 and included all patients who<br />
had undergone at least two RNV scans during the follow up period. Information on subsequent<br />
clinical events was obtained from patient records over the follow-up period. RV and LV EF were<br />
measured semi-quantitatively on planar gated equilibrium RNV and change in both RV (? RVEF)<br />
and LV (? LVEF) function was measured as: [R/LVEF1-R/LVEF2]/100. Using a Pearson’s test we<br />
correlated ? RVEF with ? LVEF and also evaluated the prognostic value <strong>of</strong> ? RVEF using a logistic<br />
regression model for the composite outcome <strong>of</strong> all cause mortality, heart transplant, or heart failure<br />
hospitalization. We included 118 patients for analysis (75% male, mean age 59 +/-27 years, 50%<br />
ischemic cardiomyopathy, mean follow-up 3.37 +/- 2.1 years, mean LVEF 31% +/-20, mean RVEF<br />
30%+/-22). During the follow up period there were 22 events (6 deaths, 3 transplants and 13 heart<br />
failure admissions). There was a statistically significant correlation between ? RVEF and ? LVEF (r=<br />
0.49 p
Oral Abstract#15<br />
Clinical trial standards and quality assurance for a low-dose 3D PET trial:<br />
Rubidium ARMI (Alternative Radiopharmaceutical for Myocardial<br />
Imaging)<br />
Jennifer M. Renaud 1 ; I. Mylonas 1 ; K. Yip 2 ; E. Turcotte 3 ; P. Pibarot 4 ; C. Maguire 5 ; K. Gulenchyn 6 ;<br />
G. Wisenberg 7 ; R.S.B. Beanlands 1 ; R.A. deKemp 1<br />
1 Cardiac PET Centre, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>, 2 KMH Cardiology & Diagnostic<br />
Centres, Mississauga ON, 3 Centre Hospitalier Universitaire de Sherbrooke, QC,, 4 Institut<br />
Universitaire de Cardiologie et de Pneumologie de Quebec, QC,, 5 <strong>University</strong> <strong>of</strong> Alberta Hospital,<br />
Edmonton, AB, 6 St Joseph’s Healthcare Hamilton,ON, 7 St Joseph’s Health Care, London ON.<br />
Background: The instability <strong>of</strong> Tc-99m supply requires alternative tracers for myocardial perfusion<br />
imaging (MPI). Rb-82 PET MPI has low radiation dose and may have superior accuracy, but<br />
requires further validation using 3D PET-CT. Rb-ARMI is a multicentre trial with an initial<br />
objective <strong>of</strong> standardizing Rb-82 PET MPI with highly repeatable interpretation in Canadian centers<br />
using 3D PET-CT technology.<br />
Methods/Results: Rest and stress phantom scans were conducted at all sites to standardize image<br />
reconstruction and quantitative scoring with 4DM-PET. Patients underwent low-dose (10 MBq/kg)<br />
rest and dipyridamole stress Rb-82 MPI. Sum stress, rest (SSS, SRS) and difference scores<br />
(SDS=SSS-SRS) were visually assessed using a 17-segment model. QA cases (n=25) from all sites<br />
were co-read to assess variability <strong>of</strong> scoring and overall interpretation. Cases with SDS differences =<br />
3 underwent a third review to reach consensus. Qualifying phantom scans resulted in the expected<br />
scores <strong>of</strong> SSS, SDS = 2 at all sites. Comparison <strong>of</strong> patient scores between core and recruiting sites<br />
showed very good agreement using the intraclass correlation coefficient (ICC): r = 0.91 for SSS and<br />
0.86 for SDS. 81% <strong>of</strong> SSS scores and 87% <strong>of</strong> SDS scores had differences (site-core) = 3. Most<br />
discrepancies occurred in large defects spanning multiple segments; however, these cases were all<br />
correctly interpreted as abnormal by recruiting and core sites. Following consensus review, overall<br />
agreement improved slightly to: r = 0.98 for SSS and 0.96 for SDS (p < 0.05 for both).<br />
Conclusion: With effective standardization and training, there was good agreement in scoring <strong>of</strong> Rb-<br />
82 MPI scans at the core and recruiting sites. Standardized and repeatable interpretation is<br />
achievable across imaging centers using different 3D PET-CT scanner.<br />
III. Translational Imaging <strong>of</strong> Cardiovascular Disease –<br />
Oral Presentation<br />
28
Oral Abstract#16<br />
Performance <strong>of</strong> CT coronary angiography in the elderly: does a life time <strong>of</strong><br />
exposure to cardiac risk factors preclude diagnostic scans?<br />
Gary R Small, Y. Yam, T.D. Ruddy, B.J.W. Chow.<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Coronary artery disease increases with age. Coronary artery calcification however<br />
accompanies atherosclerosis and can preclude the accurate assessment <strong>of</strong> luminal stenosis at CT<br />
coronary angiography (CTA). In elderly patients the presence <strong>of</strong> increased coronary atherosclerosis<br />
and accompanying coronary calcification may reduce the ability <strong>of</strong> CTA to perform diagnostic<br />
scans. We sought to determine whether advancing age would be associated with a reduced ability to<br />
perform diagnostic CT coronary angiograms.<br />
Methods/ Results: 2582 patients over the age <strong>of</strong> 60 years without a prior history <strong>of</strong> coronary<br />
revascularization and in sinus rhythm were identified from a registry <strong>of</strong> 9060 prospectively enrolled<br />
patients attending for a CT coronary angiogram at the <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>. Patients were divided<br />
into 5 age groups (60-64, 65-69, 70-74, 75-79 and >80 years old). Clinical data was recorded at the<br />
time <strong>of</strong> the CT scan. Coronary artery images were analysed according to a 17 segment model. Non<br />
evaluable scans were determined by the presence <strong>of</strong> >/=5 non evaluable segments. 45% <strong>of</strong> patients<br />
were male. The median age <strong>of</strong> patients was 66 years old. The number <strong>of</strong> non-evaluable studies was<br />
112. Univariable predictors <strong>of</strong> non diagnostic studies were age, diabetes, peripheral vascular disease,<br />
hypertension, serum creatinine, male gender, coronary calcium, the omission <strong>of</strong> nitro spray prior to<br />
imaging, baseline heart rate, metoprolol dose prior to imaging, imaging heart rate, retrospective<br />
image acquisition and the number <strong>of</strong> small coronary arteries (
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
ORAL ABSTRACTS<br />
SESSION IV: Application <strong>of</strong> Regenerative Research to<br />
Therapy<br />
30
Oral Abstract#17<br />
Enhanced Matrix for Cardiomyogenesis and Regeneration <strong>of</strong> Infarcted<br />
<strong>Heart</strong>s<br />
Nick Blackburn, 1,2 T. S<strong>of</strong>renovic, 1,2 A. Ahmadi, 1,2 D. Kuraitis, 1,2 K.A. McEwan, 1,3 D.T. Padavan, 1 M.<br />
Ruel, 1,2 and E.J. Suuronen 1,2<br />
1 Div. <strong>of</strong> Cardiac Surgery, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>; 2 Dept. <strong>of</strong> Cellular and Molecular<br />
Medicine, and 3 Dept. <strong>of</strong> Mechanical Engineering, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
Background: In CVD, the repair response is insufficient to restore blood flow, leading to the death<br />
<strong>of</strong> muscle and loss <strong>of</strong> tissue function. We have shown that a sialyl-lewis X (sLe X )-collagen matrix<br />
could enhance endogenous vascular and myogenic repair in a model <strong>of</strong> hindlimb ischemia. In this<br />
study, we explored the use <strong>of</strong> the sLe X -collagen matrix to augment regeneration after myocardial<br />
infarction (MI).<br />
Methods/Results: Seven-to-eight week old C57BL/6J mice underwent LAD ligation to induce MI.<br />
One week post-surgery the mice were treated via echo-guided injections with either: i) PBS, ii)<br />
collagen matrix or iii) sLe X -collagen matrix. <strong>Heart</strong> function was assessed by echocardiography at<br />
baseline (1-week post-MI) and 4 weeks post-treatment. Cardiac tissue was harvested for<br />
immunohistochemistry, cytokine arrays and western blots. Treatment with sLe X -collagen matrix<br />
reduced apoptosis in the heart by 33% compared to PBS (p=0.02), as measured by active caspase-3<br />
staining. The infarct area <strong>of</strong> the sLe X -collagen matrix-treated group had a 1.6-fold higher number <strong>of</strong><br />
proliferating cells, as measured by bromodeoxyuridine incorporation (p=0.008), and a higher number<br />
<strong>of</strong> cells per FOV that expressed the cardiac stem cell markers c-kit (2.0±0.2) and Nkx2.5 (5.2±0.4),<br />
compared to PBS (1.5±0.1 and 2.5±0.7, respectively; p=0.02). The expression <strong>of</strong> the cardiac gap<br />
junction protein connexin43 was 1.4-fold greater in sLe X -collagen matrix-treated mice compared to<br />
the other groups (p=0.0002). The increased expression <strong>of</strong> c-kit, Nkx2.5 and connexin43 suggests<br />
greater cardiomyogenesis in the sLe X -collagen matrix-treated hearts. Compared to baseline (1-wk<br />
post-MI), mice treated with the sLe X -collagen matrix had an improved ejection fraction (EF) <strong>of</strong><br />
+2.5%±2% compared to the PBS group (-4.1%±1.1%; p=0.008), while the collagen-treated group<br />
preserved EF at +0.6%±1.9% (p=0.05). Immunostaining for arterioles showed that the vascular<br />
network was greater in both matrix-treated groups (>8.0±0.5 per FOV) compared to PBS (5.5±0.5<br />
per FOV; p=0.004). The sLe X -collagen matrix also reduced inflammation, as indicated by fewer<br />
CD68 + macrophages (by 23%; p=0.03) and lower levels <strong>of</strong> inflammatory cytokines (e.g. IFN-?,<br />
TNF-a; by =22%; p
Oral Abstract#18<br />
Human cardiac stem cells and circulating angiogenic cells possess<br />
equivalent capacity to regenerate damaged myocardium<br />
Nicholas Latham 1 , B. Ye 1 , B. Lam 1 , D. Kuriatis 1 , M. Ruel 1 , E.J. Suuronen 1 , D.J. Stewart 2 , D.R.<br />
Davis 1<br />
1 <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>, 2 <strong>Ottawa</strong> Hospital Research <strong>Institute</strong><br />
Background: Stem cells hold the hope <strong>of</strong> mending the broken heart. Cell therapy with multiple cell<br />
types (including those that do not differentiate into new muscle) appears to be beneficial. Early<br />
attempts focused using blood derived endothelial progenitor cells (EPCs) has demonstrated these<br />
highly vascular cells restore perfusion and improve cardiac function after myocardial infarction<br />
through paracrine secretion and in the absence <strong>of</strong> significant engraftment, functional improvements<br />
are transient. Our lab has developed techniques to extract and grow cells directly from a patient’s<br />
own heart biopsy with a view towards transplanting these cells back into damaged myocardium. We<br />
have shown these cells have a complementary repertoire <strong>of</strong> sub-populations that are capable <strong>of</strong><br />
differentiating into cardiac lineage, secreting cardioprotective cytokines and improving postischemic<br />
cardiac function. Interestingly, the superiority <strong>of</strong> one cell type over the other has long been<br />
an area <strong>of</strong> speculation with no basic or clinical head to head trial ever being performed.<br />
Methods/Results: Human left atrial appendages and blood samples were obtained from patients<br />
undergoing clinically-indicated heart surgery after informed consent. In hypoxic culture designed to<br />
mirror infarcted myocardium, CSCs and EPCs provided a unique signature <strong>of</strong> pro-angiogenic and<br />
pro-cardiomyogenic growth factors. EPCs provided a more extensive paracrine pr<strong>of</strong>ile than CSCs (5<br />
vs. 14, respectively; p
Oral Abstract#19<br />
Translationally Controlled Tumor Protein (TCTP) Revealed by Proteomic<br />
Analysis <strong>of</strong> Patient-specific Blood Outgrowth Endothelial Cells in Heritable<br />
Pulmonary Arterial Hypertension<br />
Jessie R. Lavoie, 1, 2 , M. Ormiston 3 , C. Perez-Iratxeta 1 , B. Jiang 1 , D.W. Courtman 1,2 , N.W. Morrell 3 ,<br />
D.J. Stewart 1,2<br />
1 <strong>Ottawa</strong> Hospital Research <strong>Institute</strong>, Sprott Stem Cell Centre and Regenerative Medicine <strong>Program</strong>;<br />
2 Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 3 Dept. <strong>of</strong> Medicine, <strong>University</strong> <strong>of</strong><br />
Cambridge School <strong>of</strong> Clinical Medicine.<br />
Background: Pulmonary arterial hypertension (PAH) is a lethal disease, characterized by excessive<br />
proliferation <strong>of</strong> pulmonary vascular cells. Hereditary PAH is mainly caused by “loss-<strong>of</strong>-function”<br />
mutations in the bone morphogenetic protein type II receptor (Bmpr2). However, the mechanisms by<br />
which these mutations cause PAH remain unclear. The aim <strong>of</strong> this study was to identify dysregulated<br />
proteins in blood-derived endothelial cells <strong>of</strong> PAH patients with Bmpr2 mutations compared with<br />
healthy controls that may contribute to the pathogenesis <strong>of</strong> this disease.<br />
Methods/ Results: Blood-outgrowth endothelial cells (ECs) were expanded ex vivo from peripheral<br />
blood mononuclear cell samples <strong>of</strong> four patients with heritable PAH and four healthy subjects.<br />
Protein isolates were subjected to 2D gel electrophoresis and stained for total proteins with Sypro<br />
Ruby. Gels were scanned and subjected to quantitative computer-assisted analysis (PDQuest<br />
s<strong>of</strong>tware) and differentially regulated proteins determined by statistical tests (p-value
Oral Abstract#20<br />
Co-culture <strong>of</strong> endothelial progenitor cells and monocytes for seeding the<br />
surface <strong>of</strong> a degradable polyurethane vascular graft material<br />
Eva Mathieu 1 , J.E. McBane 1,2 , K.G. Battiston 3 , JP Santerre 3 , RS Labow 1 and EJ Suuronen 1,21 Div. <strong>of</strong><br />
Cardiac Surgery, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>; 2 Dept. <strong>of</strong> Cellular and Molecular Medicine,<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 3 <strong>Institute</strong>s <strong>of</strong> Biomaterials and Biomedical Engineering, <strong>University</strong> <strong>of</strong> Toronto<br />
Background: The interaction <strong>of</strong> endothelial progenitor cells (EPCs) and monocytes within the blood<br />
vessel endothelium is a process <strong>of</strong> wound repair. Therefore it was <strong>of</strong> interest to investigate their<br />
function when they were cultured on a degradable, polar, hydrophobic, and ionic polyurethane (D-<br />
PHI) material, prior to considering its use as a vascular graft. The present work investigated the<br />
cellular response <strong>of</strong> human EPCs when cultured on D-PHI films with and without monocytes.<br />
Methods/Results: Human EPCs isolated from human whole blood, were seeded onto fibronectincoated<br />
tissue culture polystyrene (TCPS), D-PHI films coated with fibronectin or D-PHI films with<br />
or without autologous monocytes for up to 7 days. EPCs were then analyzed for viability and<br />
attachment (WST assay and DNA), as well as nitric oxide (NO) and cytokine production. Lysates <strong>of</strong><br />
EPC cultures were analyzed by Western blot to assess EPC differentiation into an endothelial cell<br />
(EC) phenotype (CD31 expression). As indicated by a WST assay, EPCs alone remained viable over<br />
the 7-day culture period on D-PHI films (day 1 vs. day 7, 0.06±0.009 vs. 0.15±0.026 WST-1<br />
units/200,000 cells; p=NS) and in co-culture with monocytes (0.06±0.006 vs. 0.06±0.018 WST-1<br />
units/200,000 cells; p=NS). There was no significant difference in EPC attachment to D-PHI films or<br />
in NO production when EPCs were seeded on fibronectin-coated TCPS or with monocytes (p=NS).<br />
CD31 expression, linked to differentiation into ECs, was increased at the 7-day time point for each<br />
condition. EPCs cultured on fibronectin-coated TCPS or D-PHI films showed that EPCs were<br />
activated to a wound-healing phenotype, characterized by low TNF-a; and elevated IL-10 levels<br />
(10.62±4.01 vs. 106.22±40.10 pg/ g DNA for TNF-a; vs. IL-10, respectively, at day 7 for EPCs on<br />
D-PHI films); and in co-culture with monocytes, levels <strong>of</strong> the inflammatory cytokine TNF-a; were<br />
decreased (17.02±2.53 vs. 1.33±0.94; for day 1 vs. day 7, respectively).<br />
Conclusion: These results demonstrated that D-PHI films performed as well as fibronectin-coated<br />
TCPS in terms <strong>of</strong> the biological parameters assayed and that it was not necessary to coat the D-PHI<br />
films with fibronectin to promote EPC attachment or phenotype. Moreover, the data showed that<br />
EPC-monocyte co-culture might aid in promoting a wound-healing monocyte/macrophage<br />
phenotype. This suggests that co-culturing EPCs with autologous monocytes on D-PHI may be<br />
suitable for tissue engineering a vascular graft.<br />
IV. Application <strong>of</strong> Regenerative Research to Therapy – Oral Presentation<br />
34
Oral Abstract#21<br />
Collagen matrices enhance CD34+ circulating angiogenic cell function<br />
through the integrin receptors<br />
Brian McNeill, B. Vulesevic, M. Ruel, EJ Suuronen<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: We have previously demonstrated that culturing peripheral blood mononuclear cells<br />
(PBMCs) on a collagen-based matrix enhances the expansion and therapeutic potential <strong>of</strong> circulating<br />
angiogenic cells (CACs). The aim <strong>of</strong> this study was to investigate the involvement <strong>of</strong> integrin<br />
proteins in regulating the various collagen-mediated cellular processes that lead to the therapeutic<br />
enhancement.<br />
Methods/Results: The expression <strong>of</strong> several different integrin genes (18 a and 8 ß integrins) was<br />
evaluated in CD34+ CACs following 2, 4 and 7 day culture <strong>of</strong> human PBMCs on fibronectin or<br />
collagen matrix. CD34+ cells were collected by fluorescence-activated cell sorting and integrin<br />
expression was measured using quantitative RT-PCR. Positive findings were further investigated<br />
using specific integrin blocking antibodies and small molecule pathway inhibitors. The effects <strong>of</strong><br />
these blocking antibodies and inhibitors on collagen matrix-cultured CACs were evaluated by<br />
characterizing cell phenotype, adhesion, and angiogenic potential. Culturing PBMCs on the<br />
collagen-based matrix resulted in a 2.8-fold increase in the proportion <strong>of</strong> CD34+ cells compared to<br />
fibronectin (p=0.006). The integrin pr<strong>of</strong>ile between the fibronectin- and collagen-cultured cells was<br />
significantly different: integrins a5, a7, aV and ß3 were up-regulated 56 ±5.5, 60 ±6.4, 55 ±4 and 67<br />
±7.5 -fold respectively in collagen-cultured CD34+ cells, while integrin a3 and ß7 were downregulated<br />
by 30±4.5-fold and 58±6.8-fold, respectively (all p
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page<br />
POSTER ABSTRACTS<br />
37
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page back<br />
37
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
POSTER INDEX<br />
I: NOVEL PROBE DEVELOPMENT<br />
P1<br />
P2<br />
Besting Vitamin E: Sidechain Substitution<br />
Plays a Vital Role on the Activity <strong>of</strong><br />
Naphthyridinol Antioxidants in Lipid<br />
Bilayers<br />
In Vivo (R)-[ 11 C]Rolipram Positron<br />
Emission Tomography Imaging Detects<br />
Increased Phosphodiesterase-4 in<br />
Normally-perfused Rat Myocardial<br />
Regions 8-12 Weeks Following<br />
Myocardial Infarction<br />
Bo Li<br />
OHRI, PhD candidate<br />
Dr. D.A. Pratt<br />
Jonas Vaskas<br />
UOHI, M.Sc. candidate<br />
Dr. J.N. DaSilva<br />
II: FUNCTIONAL IMAGING TECHNOLOGY<br />
P3<br />
P4<br />
P5<br />
Dual Energy CT Myocardium Adenosine<br />
Stress Perfusion: Technique, Spectrum <strong>of</strong><br />
Imaging Findings and Clinical Applications<br />
Accuracy <strong>of</strong> Low-Dose Rubidium-82<br />
Myocardial Perfusion Imaging for<br />
Detection <strong>of</strong> CAD using 3D PET-CT<br />
Normal Database Limits: Initial Results<br />
from the ARMI Trial<br />
Comparison <strong>of</strong> SPECT RNA Phase<br />
Analysis Amplitude Values and Left<br />
Ventricular Lateral Wall Scar Size<br />
JR Inacio<br />
Medical Imaging,<br />
TOH, <strong>University</strong> <strong>of</strong><br />
<strong>Ottawa</strong>, PI<br />
Tyler Kaster<br />
UOHI,<br />
Medical Student<br />
Dr. R.A. deKemp<br />
Michel Lalonde<br />
UOHI,<br />
PhD Candidate<br />
Dr. R.G. Wells<br />
III: TRANSLATIONAL IMAGING OF CARDIOVASCULAR<br />
DISEASE<br />
P6<br />
P7<br />
Exercise Stress FDG Imaging as a More<br />
Sensitive Indicator <strong>of</strong> the Extent <strong>of</strong><br />
Myocardial Ischemia<br />
Transgenic Mice Overexpressing an<br />
Endothelial-Targeted Fas-inducing<br />
Apoptosis Construct Exhibit Pulmonary<br />
Hypertension Associated with Lung<br />
Vascular Lesions<br />
Taylor Dowlsey<br />
UOHI, Fellow<br />
Dr. TD Ruddy<br />
Heather Goldthorpe<br />
OHRI,<br />
M.Sc. Candidate<br />
Dr. DJ Stewart<br />
38
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
III: TRANSLATIONAL IMAGING OF CARDIOVASCULAR<br />
DISEASE cont.<br />
P8<br />
P9<br />
P10<br />
P11<br />
The Association between Pattern <strong>of</strong><br />
Myocardial Involvement and Clinical<br />
Presentation in Patients with Cardiac<br />
Sarcoidosis as Assessed by<br />
Fludeoxyglucose Positron Emission<br />
Tomography<br />
Incremental Value <strong>of</strong> Left Ventricular<br />
Function Assessment on Gated Rest /Stress<br />
Dipyridamole Technetium 99m SPECT<br />
Imaging in the Assessment <strong>of</strong> Myocardial<br />
Viability<br />
Transgenic Mice Lacking SIRT1 Catalytic<br />
Activity Exhibit Greater Susceptibility to<br />
Pulmonary Hypertension in Response to<br />
Chronic Hypoxia<br />
Right ventricular metabolic imaging in<br />
experimental pulmonary artery<br />
hypertension<br />
Brian McArdle<br />
UOHI, Fellow<br />
Dr. RSB Beanlands<br />
Gary Small<br />
UOHI, Fellow<br />
Dr. RSB Beanlands<br />
Mohamad Taha<br />
OHRI,<br />
M.Sc. Candidate<br />
Dr. DJ Stewart<br />
Kathie Drozd<br />
UOHI,<br />
M.Sc. Candidate<br />
Dr. L. Mielniczuk<br />
IV: APPLICATION OF REGENERATIVE RESEARCH TO<br />
THERAPY<br />
P12<br />
P13<br />
P14<br />
P15<br />
P16<br />
Characterization, Cytotoxicity, and<br />
Inflammatory Responses <strong>of</strong> Zinc Oxide<br />
Nanoparticles to Model Murine Cell Lines<br />
Altered Pattern <strong>of</strong> microRNA Expression in<br />
Blood Derived Mononuclear Cells During<br />
Maturation from Early to Late Outgrowth<br />
Endothelial Progenitor Cells.<br />
Physically Cross-Linked Chitosan Derived<br />
Hydrogels - An Alternative Approach for<br />
S<strong>of</strong>t Tissue Engineered Scaffolds for Cell<br />
Therapy<br />
CaMKinase II Anchoring Protein, aKAP, is<br />
a Novel Regulator <strong>of</strong> SERCA2a Activity in<br />
Cardiomyocytes.<br />
Inhibition <strong>of</strong> VEGFR2 is Sufficient to<br />
Produce Severe Plexogenic Pulmonary<br />
Arterial Hypertension in Rats without<br />
Exposure to Chronic Hypoxia<br />
Yan (Mary) Zhang<br />
Health Canada, PDF<br />
Dr. A Tayabali<br />
John Behbahani<br />
OHRI, PhD Candidate<br />
Dr. DJ Stewart<br />
Donna T. Padavan<br />
UOHI,<br />
Dr. E.J. Suuronen<br />
Omar Hawari<br />
Dept. <strong>of</strong> CMM,<br />
U <strong>of</strong> <strong>Ottawa</strong><br />
M.Sc. Candidate<br />
Dr. BS Tuana<br />
Baohua Jiang<br />
OHRI, R.A.<br />
Dr. DJ Stewart<br />
39
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
IV: APPLICATION OF REGENERATIVE RESEARCH TO<br />
THERAPY cont.<br />
P17<br />
P18<br />
P19<br />
P20<br />
P21<br />
P22<br />
Targeted Expression <strong>of</strong> the E2F6<br />
Transcriptional Repressor in Myocardium<br />
Collagen:Chitosan Hydrogels for<br />
Stimulation <strong>of</strong> Angiogenesis in a Type I<br />
Diabetic Mouse Model: Potential Use as a<br />
Pre-Vascularized Ectopic Site for Islet<br />
Transplantation<br />
Collagen-Laminin Hydrogels for Delivery<br />
<strong>of</strong> Insulin-Producing Tissue for the<br />
Treatment <strong>of</strong> Type 1 Diabetes<br />
Pharmacological Enhancement <strong>of</strong> Resident<br />
Cardiac Stem Cells via Activation <strong>of</strong> the<br />
Wnt Pathway<br />
Circulating Microrna Provice Potential<br />
Biomarkers <strong>of</strong> Pulmonary Arterial<br />
Hypertension.<br />
Development <strong>of</strong> PCSK9 Inhibitors for<br />
Regulating LDL-R and Cholesterol<br />
Jennifer Major<br />
OHRI, PhD Candidate<br />
Dr. BS Tuana<br />
Joanne E. McBane<br />
UOHI, PDF<br />
Dr. EJ Suuronen<br />
Kimberly McEwan<br />
UOHI,<br />
M.Sc. candidate<br />
Dr. EJ Suuronen<br />
Ola Qassim<br />
UOHI,<br />
Dr. D.R. Davis<br />
Kenny Schlosser<br />
OHRI, PDF<br />
Dr. DJ Stewart<br />
Priyambada Mishra<br />
OHRI, R.A.<br />
Dr. A Basak<br />
40
P1 – Poster Abstract #1<br />
Besting Vitamin E: Sidechain Substitution Plays a Vital Role on the<br />
Activity <strong>of</strong> Naphthyridinol Antioxidants in Lipid Bilayers<br />
Bo Li, D.A. Pratt<br />
Dept. <strong>of</strong> Chemistry, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
Background: A series <strong>of</strong> naphthyridinol analogs <strong>of</strong> α-tocopherol with varying sidechain substitution<br />
were synthesized in order to determine how changes in the lipophilicity <strong>of</strong> these potent antioxidants<br />
impact their radical-trapping reactivities in lipid bilayers and their binding to the human tocopherol<br />
transport protein (TTP), which determines the bioavailability <strong>of</strong> tocopherols.<br />
Methods/Results: The radical trapping activities <strong>of</strong> the compounds were assayed in egg<br />
phosphatidylcholine unilamellar lipsomes using a recently-developed assay which employs a<br />
BODIPY-conjugate <strong>of</strong> α-tocopherol (H 2B-PMHC) that undergoes a dramatic fluorescence<br />
enhancement upon oxidation. The assay was carried out in 96-well plate format such that the<br />
reactivity <strong>of</strong> the various compounds could be rapidly surveyed under several different reaction<br />
conditions. Liposomes supplemented with the different naphthyridinols were oxidized using either<br />
hydrophilic or lipophilic peroxyl radicals and consistently revealed a dose-dependent protection <strong>of</strong><br />
oxidation <strong>of</strong> the pro-fluorescent H 2B-PMHC. No detectable oxidation <strong>of</strong> H 2B-PMHC took place in<br />
the presence <strong>of</strong> any <strong>of</strong> the napthyridinols under conditions where α-tocopherol or its truncated<br />
analog, 2,2,5,7,8-pentamethyl-6-hydroxy-chroman (PMHC) were effective in only retarding the rate<br />
<strong>of</strong> oxidation. While sidechain length and/or branching did not have an effect on the apparent<br />
reactivity <strong>of</strong> the naphthyridinols to either hydrophilic or lipophilic peroxyl radicals, it had a dramatic<br />
effect on their stoichiometry – with more lipophilic compounds trapping 2 peroxyl radicals where<br />
more hydrophilic compounds trapped significantly less than 1.<br />
Conclusion: It is suggested that the more hydrophilic compounds autoxidize in the aqueous phase,<br />
and that the preferential partitioning <strong>of</strong> the more lipophilic compounds to the lipid phase protects<br />
them from this deleterious (and pro-oxidative) reaction. Studies on hydrophilic and hydrophobic<br />
pairs <strong>of</strong> less electron rich pyridinols (and related pyrimidinols) support this suggestion. The<br />
cooperativity <strong>of</strong> the most lipophilic naphthyridinol with the most physiologically important watersoluble<br />
reducing agents was also studied in liposomes using H 2B-PMHC. Binding assays with<br />
recombinant human TTP reveal that these compounds are strongly bound. In fact, naphthyridinols<br />
with sidechains <strong>of</strong> 8 or more carbons were comparable (and in some cases slightly better) ligands for<br />
the protein than α-tocopherol, suggesting they may have similar bioavailabilities in vivo.<br />
I. Novel Probe Development – Poster Presentation<br />
41
P2 - Poster Abstract #2<br />
In Vivo (R)-[ 11 C]Rolipram Positron Emission Tomography Imaging Detects<br />
Increased Phosphodiesterase-4 in Normally-perfused Rat Myocardial<br />
Regions 8-12 Weeks Following Myocardial Infarction<br />
Miran Kenk, S.L. Thorn, Jonas Vaskas, A.J. Thomas, J.M. Renaud, R. Klein, M. Lortie, R.A.<br />
deKemp, R.S.B. Beanlands, J.N. DaSilva.<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Sympathetic hyperactivity in heart failure is associated with changes in the<br />
noradrenergic signal transduction at the level <strong>of</strong> the beta adrenergic receptor (beta-AR) and<br />
intracellular second messenger cAMP. Cardiac cAMP-specific phosphodiesterase-4 (PDE4)<br />
enzymes are regulated by cAMP levels, with changes reported in cardiac diseases.<br />
Methods/Results: PDE4 enzymes are evaluated 8-12 weeks post-infarct in the current study using<br />
(R)-[ 11 C]rolipram and positron emission tomography. Sprague-Dawley rats underwent left anterior<br />
descending coronary artery ligations (n=8) or sham surgeries (n=4). Cardiac function was evaluated<br />
by echocardiography. Animals were injected with [13N]NH3 (2.9-4.6 mCi iv) at 8-12 weeks and<br />
scanned for 30 min, prior to a 60 min (R)-[11C]rolipram scan (0.5-1.2 mCi iv, cold mass
P3 - Poster Abstract #3<br />
Dual Energy CT Myocardium Adenosine Stress Perfusion: Technique,<br />
Spectrum <strong>of</strong> Imaging Findings and Clinical Applications<br />
JR Inacio 1 , S Nicolaou 2 , A Fong 3 , and JR Mayo 2<br />
1 Medical Imaging, TOH/ <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>, 2 Vancouver General Hospital, Radiology and<br />
3 Cardiology Depts., BC<br />
Background: The principles <strong>of</strong> Dual Energy Computed Tomography (DECT) applied in<br />
Myocardium Stress Perfusion in detecting reversible ischemia during first-pass contrast enhanced<br />
CT are reviewed.<br />
Methods/ Results: We explain the utility <strong>of</strong> this new emerging technique <strong>of</strong> combined evaluation <strong>of</strong><br />
coronary artery stenosis, cardiac morphology, function, perfusion and viability. The protocol <strong>of</strong><br />
DECT myocardium adenosine stress perfusion, radiation dose, post processing and interpretation <strong>of</strong><br />
DECT myocardium perfusion imaging is presented. This new technique has the potential <strong>of</strong><br />
evaluation coronary artery anatomy and stenosis, myocardium perfusion and function. With clinical<br />
examples we show how it compares to other modalities <strong>of</strong> Coronary Artery Disease assessment as<br />
Coronary Angiography, Myocardial Fractional Flow Reserve (FFR) and Cardiac MR.<br />
Conclusion: Comprehensive evaluation <strong>of</strong> anatomical and functional aspects <strong>of</strong> Coronary Artery<br />
Disease is feasible in a single low dose non invasive imaging study.<br />
II. Functional Imaging Technology – Poster Presentation<br />
43
P4 - Poster Abstract #4<br />
Accuracy <strong>of</strong> Low-Dose Rubidium-82 Myocardial Perfusion Imaging for<br />
Detection <strong>of</strong> CAD using 3D PET-CT Normal Database Limits: Initial<br />
Results from the ARMI Trial<br />
Tyler Kaster, I. Mylonas, J.M. Renaud, R.S.B. Beanlands and R.A. deKemp<br />
National Cardiac PET Centre, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>.<br />
Background: Rubidium (Rb-82) PET is a low-dose alternative to Tc-99m or Tl-201 SPECT for<br />
myocardial perfusion imaging (MPI). Previous studies using traditional 2D-mode imaging suggest<br />
that Rb-82 PET may be more accurate than SPECT; this study was performed to evaluate accuracy<br />
using current 3D PET-CT technology.<br />
Methods/Results: Low-dose (10 MBq/kg) Rb-82 3D PET-CT scans were performed in 1700<br />
patients with known or suspected CAD over a period <strong>of</strong> 18 months. N=40 patients (20 male) with<br />
low likelihood (LLK) <strong>of</strong> CAD were selected to construct normal database. Mean and SD polar maps<br />
<strong>of</strong> tracer uptake (0-100%) using 4DM-PET. LLK exclusion criteria included known CAD, diabetes,<br />
angina symptoms, abnormal rest or stress ECG. Uptake defects were scored using a 4-point scale<br />
(Mean = 1.5,3,4.5,6 SD) in 17 polar map segments. A sum stress score 4 was considered positive<br />
for detection <strong>of</strong> CAD. Sensitivity and specificity were evaluated in a group <strong>of</strong> 70 CAD patients using<br />
stenosis 50% by coronary angiography (ICA) as the gold-standard for presence <strong>of</strong> disease.<br />
Normalcy was evaluated in a separate validation group <strong>of</strong> 36 LLK normals to account for post-test<br />
referral bias in ICA results following PET. Sensitivity, specificity and overall accuracy were 100%,<br />
71% and 89% respectively in CAD patients without previous revascularization or LV dysfunction.<br />
When the validation group (94% normalcy) was combined with the CAD patients, specificity and<br />
accuracy increased to 87% and 92%. Positive and negative predictive values were 79% and 100%; a<br />
negative scans.<br />
Conclusion: These results using 3D PET-CT are similar to those obtained previously using 2D PET,<br />
suggesting that the proposed low-dose Rb-82 PET technique is accurate, and the normal database<br />
approach may be a useful adjunct for interpretation <strong>of</strong> these PET MPI studies.<br />
II. Functional Imaging Technology – Poster Presentation<br />
44
P5 - Poster Abstract #5<br />
Comparison <strong>of</strong> SPECT RNA Phase Analysis Amplitude Values and Left<br />
Ventricular Lateral Wall Scar Size<br />
Michel Lalonde 1 , D. Birnie 2 , T.D. Ruddy 2 , R. Wassenaar 1 , R.G. Wells 2<br />
1 Dept. <strong>of</strong> Physics, Carleton <strong>University</strong>, 2 Cardiology, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Phase analysis has previously been investigated for its potential at predicting the<br />
outcome <strong>of</strong> cardiac resynchronization therapy (CRT). Amplitude, defined as the extent <strong>of</strong><br />
contraction <strong>of</strong> a sector, is obtained from phase analysis but has not been investigated to the same<br />
extent as phase-based parameters. Furthermore, the extent <strong>of</strong> scar present in the lateral wall <strong>of</strong> the<br />
left ventricle (LV) has been shown in some studies to predict response to CRT. A scarred heart<br />
segment will not contract properly which may correspond to reduced amplitude values. Our<br />
objective is to determine the correlation between amplitude and scar size and to evaluate amplitude<br />
as a surrogate for scar in predicting response to CRT.<br />
Methods/Results: 46 LBBB patients (LVEF120 ms) underwent<br />
a baseline FDG PET scan and SPECT radionuclide angiography (RNA) scan prior to undergoing<br />
CRT. Scar size was obtained from the PET scan using a 5 segment model and phase analysis was<br />
performed on the SPECT RNA data. From the SPECT RNA data, 568 normalized LV amplitude<br />
values were acquired for each patient. Lateral wall scar size was then compared to average amplitude<br />
in that segment for both ischemic (N=26) and non-ischemic patients using a Pearson correlation<br />
coefficient (r). The ability <strong>of</strong> lateral amplitude to predict response was also investigated. Amplitude<br />
showed a strong correlation with scar size in all but non-ischemic responders, as shown below.<br />
Lateral amplitude did not present any significant differences between responders (N=30) and nonresponders<br />
(p>0.05). Though all patients with no lateral scar (N=9) were responders, these patients<br />
had variable lateral amplitude similar to non-responders.<br />
Conclusion: Amplitude obtained from SPECT phase analysis provides good correlation with scar<br />
size, but does not prove to be a suitable surrogate marker for response to CRT. This is likely due to<br />
differences in average amplitudes observed in patients with no lateral scar.<br />
II. Functional Imaging Technology – Poster Presentation<br />
45
P6 - Poster Abstract #6<br />
Exercise Stress FDG Imaging as a More Sensitive Indicator <strong>of</strong> the Extent <strong>of</strong><br />
Myocardial Ischemia<br />
Taylor Dowlsey, G. Dwivedi, M. Cocker, B.J.W. Chow, R.A. de Kemp, R.S.B. Beanlands, M. Poirier<br />
and T.D. Ruddy<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background:Single photon emission computed tomography myocardial perfusion imaging (SPECT-<br />
MPI) is established as a sensitive indicator for the detection <strong>of</strong> obstructive CAD. However in a<br />
substantial number <strong>of</strong> patients with an abnormal SPECT-MPI study, the extent <strong>of</strong> abnormal<br />
perfusion is underestimated. This relates to several factors including non-linear uptake <strong>of</strong> myocardial<br />
tracer and the fact that relative, not absolute perfusion is assessed such that <strong>of</strong>ten only the most<br />
severe areas <strong>of</strong> relative perfusion abnormality are discernable.The predominant energy substrate for<br />
the heart during normal metabolism is fatty acids. During an ischemic insult there is rapid and<br />
pr<strong>of</strong>ound upregulation <strong>of</strong> glucose extraction from the circulation via Glut 4-mediated transport. The<br />
purpose <strong>of</strong> the present study was to determine if PET imaging <strong>of</strong> FDG uptake during exercise stress<br />
will identify areas <strong>of</strong> stress-induced ischemia and be more accurate at defining the extent <strong>of</strong><br />
myocardium involved compared with stress MPI.<br />
Methods/Results:A total <strong>of</strong> 8 patients have been recruited to undergo FDG imaging including 4<br />
normals and 4 with CAD. The extent <strong>of</strong> ischemic myocardium was compared between FDG imaging<br />
and relative perfusion imaging with PET or SPECT MPI and correlated with areas <strong>of</strong> obstructive<br />
CAD on cardiac computed tomography angiography (CTA) or invasive coronary angiography. In<br />
normals, there was no focal myocardial uptake <strong>of</strong> FDG consistent with the absence <strong>of</strong> ischemic<br />
myocardium. Patients with stress-induced reversible perfusion defects on SPECT-MPI suggestive <strong>of</strong><br />
ischemia also showed corresponding focal uptake <strong>of</strong> FDG. However the extent <strong>of</strong> myocardium<br />
involved was greater for stress FDG PET than SPECT-MPI. In one representative example, SPECT-<br />
MPI showed evidence <strong>of</strong> ischemia in the RCA territory whereas there was focal FDG uptake in both<br />
the RCA and LCX territories. CTA showed significant obstructive disease in both the RCA and<br />
LCX territories indicating a more accurate representation from FDG PET than SPECT-MPI.<br />
Conclusion: These results suggest that exercise FDG PET imaging is feasible and shows potential to<br />
be a more sensitive indicator <strong>of</strong> the extent <strong>of</strong> myocardial ischemia than SPECT-MPI.<br />
III. Translational Imaging <strong>of</strong> Cardiovascular Disease –<br />
Poster Presentation<br />
46
P7 - Poster Abstract #7<br />
Transgenic Mice Overexpressing an Endothelial-Targeted Fas-inducing<br />
Apoptosis Construct Exhibit Pulmonary Hypertension Associated with<br />
Lung Vascular Lesions<br />
Heather A.M. Goldthorpe, J. Jiang, Y. Deng, S.H.J. Mei and D.J. Stewart<br />
Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; <strong>Ottawa</strong> Hospital Research<br />
<strong>Institute</strong><br />
Background: Pulmonary arterial hypertension (PAH) is a lethal disease, characterized by complex<br />
vascular lesions and increased pulmonary vascular resistance. Recent evidence points to endothelial<br />
cell (EC) apoptosis at the level <strong>of</strong> distal pulmonary arterioles as the underlying mechanism <strong>of</strong> this<br />
disease. Our objective is to establish a conditional transgenic system in mice, allowing us to test the<br />
hypothesis that lung EC apoptosis at the level <strong>of</strong> distal pulmonary arterioles is necessary and<br />
sufficient to cause a PAH phenotype.<br />
Methods and Results: In a pilot study, the Fas-Induced Apoptosis (FIA) construct was expressed<br />
under the control <strong>of</strong> an endothelial-specific, Tie2 promoter in transgenic mice (i.e. EFIA mice). Two<br />
lines <strong>of</strong> transgenic mice with differing levels <strong>of</strong> EFIA transgene expression were generated, termed<br />
low expressing (LE) and high expressing (HE) mice respectively, as well as a third hybrid (LE/HE)<br />
EFIA line. LE-EFIA exhibited normal pulmonary hemodynamics (RVSP; 24.8 ± 0.48 mmHg vs<br />
22.60 ± 0.48 WT control) and vascular structure at baseline; however, administration <strong>of</strong> a small<br />
molecule dimerizing agent, AP20187, for 1 week, resulted in lung microvascular apoptosis<br />
(TUNEL) and a modest dose-dependent (2 mg/kg or 10 mg/kg IP) increase in RVSP (29.0 ± 2.3 vs<br />
31.3 ± 1.9 mmHg, respectively) as well as evidence <strong>of</strong> inflammatory vascular lesions localized to the<br />
distal pulmonary arterioles (H&E). Interestingly, in the absence <strong>of</strong> the AP compound, a subset <strong>of</strong><br />
HE-EFIA transgenic mice at 8 weeks exhibited distal lung perivascular lesions, although there was<br />
no elevation in baseline RVSP compared to wild-type (WT) controls (24.9 ± 1.2 vs. 22.7 ± 0.99<br />
mmHg, respectively). Vascular lesions consisted mainly <strong>of</strong> inflammatory cells and were <strong>of</strong>ten<br />
obliterative, even occluding distal arterioles. Furthermore, in the absence <strong>of</strong> the dimerizing<br />
compound, the hybrid transgenic line exhibited a significant, although modest elevation in RVSP<br />
compared to WT controls (24.0 ± 0.44 vs. 21.6 ± 0.47 mmHg, respectively); however, pulmonary<br />
lesions were not observed in non-treated hybrid EFIA transgenic mice.<br />
Conclusion: Our current preliminary EFIA characterization suggests that EC apoptosis is sufficient<br />
to induce PAH, which is associated with marked inflammation and remodeling <strong>of</strong> pulmonary<br />
arterioles.<br />
III. Translational Imaging <strong>of</strong> Cardiovascular Disease –<br />
Poster Presentation<br />
47
P8 - Poster Abstract #8<br />
The Association between Pattern <strong>of</strong> Myocardial Involvement and Clinical<br />
Presentation in Patients with Cardiac Sarcoidosis as Assessed by<br />
Fludeoxyglucose Positron Emission Tomography<br />
Brian McArdle, D. Birnie, R.A. deKemp, R.S.B. Beanlands, E. Leung, P. Nery<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Evidence <strong>of</strong> Cardiac Sarcoidosis (CS) has been noted on advanced imaging in up to<br />
40% <strong>of</strong> patients with documented systemic Sarcoidosis but there is a broad spectrum <strong>of</strong> clinical<br />
manifestations, namely; conduction abnormalities, arrhythmia, heart failure and sudden death, with a<br />
significant proportion <strong>of</strong> patients remaining asymptomatic. Positron Emission Tomography (PET)<br />
using [18F]Fluorodeoxyglucose (FDG) has been shown to be an accurate modality for identification<br />
<strong>of</strong> active CS, but the association between the location and severity <strong>of</strong> FDG uptake within the<br />
myocardium and the clinical presentation has not been evaluated. In this study we quantitatively<br />
assessed the location and degree <strong>of</strong> FDG uptake in CS patients and correlated this with their clinical<br />
presentation.<br />
Methods/Results: We selected patients enrolled prospectively from our registry <strong>of</strong> patients<br />
undergoing PET for suspected CS. After an overnight fast each patient underwent rest perfusion<br />
scanning with either Rubidium-82 or N-13-Ammonia followed by FDG imaging. FDG activity was<br />
quantified as Standardized Uptake Values (SUV) using a 17-segment model <strong>of</strong> the LV myocardium.<br />
Summed Rest Score (SRS) was determined visually to quantify rest perfusion defects. A total <strong>of</strong> 24<br />
patients were included, <strong>of</strong> whom 19 (6 VT, 7 Complete <strong>Heart</strong> Block (CHB), 6 asymptomatic) had a<br />
diagnosis <strong>of</strong> CS based on Japanese criteria. Five patients with a negative FDG-PET and normal LV<br />
function were used as controls. LVEF in the VT group was normal in 4/6 patients with a mean <strong>of</strong><br />
51.6%. Mean overall LV SUV was higher in CS patients compared with controls (3.92 vs 0.91,<br />
P
P9 - Poster Abstract #9<br />
Incremental Value <strong>of</strong> Left Ventricular Function Assessment on Gated Rest<br />
/Stress Dipyridamole Technetium 99m SPECT Imaging in the Assessment <strong>of</strong><br />
Myocardial Viability<br />
Gary R. Small, T. Dowsley B.J.W. Chow, T.D. Ruddy, R.S.B. Beanlands<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Gated SPECT perfusion imaging is used in the evaluation <strong>of</strong> patients with ischemic<br />
cardiomyopathy to assess viability using resting perfusion and ischemia. The gated component <strong>of</strong> the<br />
scan assesses left ventricular function (LV) but is not used in the evaluation <strong>of</strong> viability. Changes in<br />
LV function on rest and stress imaging could indicate myocardial contractile reserve: measurement<br />
<strong>of</strong> which may contribute to viability assessment.The purpose <strong>of</strong> this study was to determine whether<br />
measurement <strong>of</strong> contractile reserve would have incremental utility in the assessment <strong>of</strong> myocardial<br />
viability using rest/stress SPECT imaging.<br />
Methods/ Results:: From a SPECT registry <strong>of</strong> 25,303 patients, 34 individuals were identified who<br />
had ischemic cardiomyopathy (LVEF/= 70% stenosis in >/=1 coronary artery) and had<br />
undergone an 18F- Fluorodeoxyglucose (FDG) /perfusion PET scan within 6 months <strong>of</strong> the<br />
dipyridamole/ technetium 99m tetrafosamin (Tc 99m ) SPECT study.<br />
Ischemic segments (/=10% improvement on rest) were declared<br />
viable and not used in wall motion analysis. Segments with persistent defects were analyzed for<br />
changes following stress in wall motion (using a 5 point scale) and wall thickness (>10% change).<br />
Segments with >/=50% FDG tracer uptake on FDG PET scanning were declared viable. 82% <strong>of</strong><br />
patients were male. The average age was 66. 578 segments were analyzed, 286 (49%) were ischemic<br />
and not used for contractile reserve assessment. Of the remaining 292 segments which had persistent<br />
perfusion defects, 57 demonstrated a change in wall motion, 141 showed a change in wall thickness.<br />
Segments with a change in wall motion correlated with viability at PET (45/57 (79%) r=0.88<br />
p
P10 - Poster Abstract #10<br />
Transgenic Mice Lacking SIRT1 Catalytic Activity Exhibit Greater<br />
Susceptibility to Pulmonary Hypertension in Response to Chronic Hypoxia<br />
Mohamad Taha, Y. Deng, M. McBurney and D.J. Stewart<br />
<strong>Ottawa</strong> Hospital Research <strong>Institute</strong><br />
Background: Pulmonary hypertension (PH) is a devastating disease characterized by increased<br />
pulmonary artery pressure, leading to right ventricle hypertrophy and ultimately heart failure and<br />
death. Pulmonary endothelial cell (EC) injury and apoptosis appear to be triggers for reactive<br />
vascular cell proliferation leading to narrowing and obliteration <strong>of</strong> distal lung arterioles. Sirt1 is a<br />
NAD+ dependent deacetylase that has been strongly implicated in maintaining EC homeostasis in<br />
systemic vessels, but little is known about its role in the lung vasculature. The purpose <strong>of</strong> this study<br />
was to investigate the role <strong>of</strong> Sirt1 catalytic activity in PH.<br />
Methods/Results: Sirt1Y/Y (H355Y point mutation) animals possess a Sirt1 protein lacking<br />
catalytic activity. Exposure <strong>of</strong> mutants (Sirt1Y/Y) to simulated normobaric hypoxia (9-10% O2) for<br />
3 weeks resulted in a significant increase in right ventricle systolic pressure (RVSP) compared to<br />
their WT littermates exposed to the same conditions (42.9±2.3 Sirt1Y/Y vs. 28.8±1.3 WT; n=9 and<br />
12 respectively, p< 0.001). Furthermore, mutant animals showed significantly greater RV<br />
remodeling, measured by the RV/LV+S weight ratio (0.55±0.03 Sirt1Y/Y vs. 0.40±0.01 WT, p<<br />
0.001) compared to the wild type littermates. In addition, hypoxia-induced pulmonary smooth<br />
muscle cell hyperplasia and perivascular cell infiltration seemed to be exacerbated in the mutant<br />
mice.<br />
Conclusion: Sirt1 protects against hypoxia-induced PH. This protection is most likely mediated<br />
through its well described role in maintenance <strong>of</strong> endothelial function and inhibition <strong>of</strong> apoptosis in<br />
response to stressors such as hypoxia.<br />
III. Translational Imaging <strong>of</strong> Cardiovascular Disease –<br />
Poster Presentation<br />
50
P11 - Poster Abstract #11<br />
Right ventricular metabolic imaging in experimental pulmonary artery<br />
hypertension<br />
S. Thorn, K. Drozd, J.N. DaSilva, J. Renaud, R.S.B. Beanlands, R.A. deKemp, D.J. Stewart, and<br />
L. Mielniczuk<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Pulmonary artery hypertension (PAH) is a disease <strong>of</strong> progressive vascular remodeling,<br />
vasoconstriction, and right heart failure (HF). There is heterogeneity in the development <strong>of</strong> right HF,<br />
and the mechanisms and predictors remain largely unknown. It has been suggested that alterations in<br />
cardiac metabolism may be related to progressive RV dysfunction. This study was designed to<br />
evaluate the changes in fatty acid and glucose metabolism with cardiac PET imaging in experimental<br />
PAH.<br />
Methods/Results: Monocrotaline (MCT) was given as a single injection (70 mg/kg) to adult<br />
Fischer rats to induce PAH. Glucose and fatty acid metabolism was assessed with FDG and FTHA<br />
PET imaging four weeks after injection and reported as Patlak Ki and as a standardized uptake value<br />
(SUV). Cardiac and pulmonary metabolism was correlated with RV size and pulmonary smooth<br />
muscle cell proliferation. PAH was associated with a significant increase in cardiac size (heart<br />
weight:body weight ratio 0.0026 vs. 0.0036 normals vs. PAH, p=
P12- Poster Abstract #12<br />
Characterization, Cytotoxicity, and Inflammatory Responses <strong>of</strong> Zinc Oxide<br />
Nanoparticles to Model Murine Cell Lines<br />
Yan (Mary) Zhang 1 , J. Tan 2 , P. Rippstein 2 , A. Tayabali 1<br />
1 Biotechnology Laboratory, EHSRB, HECSB, Health Canada, <strong>Ottawa</strong>, ON. 2 Histopathology<br />
Laboratory, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: Zinc oxide nanoparticles (nano-ZnO) have wide technological applications in<br />
industry, environment remediation, medical therapeutics, foods and cosmetics. However, the extent<br />
<strong>of</strong> hazards posed by nano-ZnO is not known. As a preliminary step towards understanding its<br />
toxicological effect on human health, two commercial nano-ZnO products (Z-COTE (uncoated) and<br />
Z-COTE HP1 (coated)) were characterized, and their toxicity and potential mechanisms were<br />
investigated.<br />
Methods/Results: Evaporated suspensions <strong>of</strong> Z-COTE, Z-COTE HP1 and fine ZnO (nonnanoparticle<br />
controls) were examined with transmission electron microscopy (TEM), scanning<br />
electron microscopy (SEM), and atomic force microscopy (AFM). All samples were highly<br />
agglomerated, and the individual particle appeared as crystalline rods or polygonal structures. There<br />
was no significant difference in size distribution or average size <strong>of</strong> Z-COTE (53.5±22.5 nm) and Z-<br />
COTE HP1 (60.1±26.4 nm), but the fine ZnO showed a larger average size (106.9±41.1 nm). Three<br />
types <strong>of</strong> mouse cell lines, lung epithelial cells (FE1-MML cells), monocytes (RAW 264.7), and<br />
lymphoblasts (LBRM33), were treated with 50, 25, 12.5, 6.25, and 3.125 g/mL <strong>of</strong> nano-ZnO for 24<br />
hours. Concentration dependent cytotoxicity (altered morphology, trypan blue viability, MTT<br />
bioreduction) was observed in all three cell lines, with the RAW 264.7 cells (LD50: 6.25-12.5<br />
g/mL) being more sensitive than FE1-MML cells (12.5-25 g/mL) and LBRM33 cells (12.5-25<br />
g/mL). The cell viability and metabolic activity were not significantly different between Z-COTE,<br />
Z-COTE HP1 and fine ZnO with any <strong>of</strong> cell lines. Exposure <strong>of</strong> the cells to a low concentration <strong>of</strong><br />
nano-ZnO (6.25 g/mL) did not significantly change the cell morphology, but increased the release<br />
<strong>of</strong> MCP-1, CD30L, MIP-1, KC, and TIMP-2.<br />
Conclusion: It is feasible to detect and characterize nano-ZnO using a combination <strong>of</strong> microscopybased<br />
imaging techniques. Nano-ZnO had toxic effects on mammalian cells, and this effect was<br />
dependent on the ZnO concentration and the cell type, rather than the size and surface coating <strong>of</strong><br />
particles. Nano-ZnO elevated levels <strong>of</strong> pro-inflammatory cytokine from cells, which might be a<br />
potential mechanism involved in the immunotoxicity induced by nano-ZnO. This study provided<br />
helpful information and direction for further in vitro and in vivo work to assess the toxicological<br />
effect <strong>of</strong> nano-ZnO.<br />
IV. Application <strong>of</strong> Regenerative Research to Therapy –<br />
Poster Presentation<br />
52
P13 - Poster Abstract #13<br />
Altered Pattern <strong>of</strong> microRNA Expression in Blood Derived Mononuclear<br />
Cells During Maturation from Early to Late Outgrowth Endothelial<br />
Progenitor Cells<br />
John Behbahani 1,2 , D.J. Stewart 1,2<br />
1 <strong>Ottawa</strong> Hospital Research <strong>Institute</strong>; 2 Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong><br />
<strong>Ottawa</strong><br />
Background: Endothelial Progenitor Cells (EPCs) circulate in the peripheral blood mononuclear<br />
cell (PBMC) fraction and can be selected under culture conditions which include appropriate matrix<br />
components and endothelial growth factors. Early outgrowth EPCs appear after the first 3 to 5 days<br />
<strong>of</strong> selective culture, and these non-proliferative cells still express MNC markers (i.e. CD14 and<br />
CD45), but also express some endothelial cell (EC) markers including CD31 and VEGFR2. Late<br />
outgrowth EPCs appear after 2 weeks, and exhibit a strong EC phenotype, and this highly<br />
proliferative population has lost all leukocyte markers. MicroRNAs (miRNAs) are small non-coding<br />
RNAs that have emerged as important regulators <strong>of</strong> gene expression. The aim <strong>of</strong> this study was to<br />
define the changes in miRNA expression pr<strong>of</strong>iles in MNC cultures during evolution from early to<br />
late outgrowth EPC.Changes in the expression <strong>of</strong> specific miRNAs contribute to the endothelial<br />
specification <strong>of</strong> cultured MNCs and the emergence <strong>of</strong> early or late outgrowth EPCs.<br />
Methods/Results: Mononuclear cells (MNCs) were isolated from healthy participants (n=4) by<br />
leukapheresis and cultured for 1, 3, 5, 7 and 9 days under conditions promoting endothelial<br />
differentiation. Late outgrowth EPCs were derived from the same cultures and appeared after 14-21<br />
days (n=3). MiRNA expression was assessed by (q)RT-PCR (Taqman), using a panel <strong>of</strong> 13<br />
miRNAs previously identified in PBMCs, EPCs or mature ECs. MiRNA expression pr<strong>of</strong>iles were<br />
very similar in cells between 1 and 3 days (cultured MNCs); and 5, 7 and 9 days (early outgrowth<br />
EPCs), and therefore these were grouped for further analysis. MiR-92a was highly dominant in day<br />
1-3 MNC cultures and remained relatively constant throughout the culture period. In early<br />
outgrowth EPCs (day 5-9), the expression <strong>of</strong> miR-146a increased 2.9±0.04 fold, (p
P14- Poster Abstract #14<br />
Physically Cross-Linked Chitosan Derived Hydrogels - An Alternative<br />
Approach for S<strong>of</strong>t Tissue Engineered Scaffolds for Cell Therapy<br />
Donna T. Padavan 1 , K.A. McEwan 1,2 , J.E. McBane 1,3 , A. Badner 1 , B. Vulesevic 1,3 , N. Nossova 1 , G.S.<br />
Korbutt 4 , and E.J. Suuronen 1,3<br />
1<br />
Div. <strong>of</strong> Cardiac Surgery, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>; 2 Dept. <strong>of</strong> Mechanical Engineering,<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 3 Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 4 Alberta Diabetes<br />
<strong>Institute</strong>, <strong>University</strong> <strong>of</strong> Alberta.<br />
Background: Ischemia is a central problem in cardiovascular disease and vascular complications<br />
associated with diabetes. Tissue engineered hydrogels have become popular scaffold platform<br />
materials for supporting cells and have demonstrated an ability to improve cell therapy in<br />
regenerative medicine. However, many hydrogels, although biocompatible, typically require<br />
chemical cross-linkers, limiting their therapeutic potential for transplanting cells, particularly as<br />
injectable materials. Thus, physically cross-linked hydrogels are attractive since they may improve<br />
the delivery <strong>of</strong> cells in a minimally invasive and non-toxic manner. This study aimed to develop<br />
chitosan-derived physically cross-linked hydrogels with tunable mechanical and cell responsive<br />
properties for supporting transplanted cells.<br />
Methods/ Results: Two injectable materials were developed via ionic cross-linking: a) chitosanderivative<br />
(HTCC) with sodium tripolyphosphate (TPP); and b) pure chitosan (PC) with betaglycerophosphate<br />
disodium salt (ßGP). Polymer hydrogels were characterized for the materials’<br />
chemical and physical properties, viscosity and mechanical properties. Cell-material interactions<br />
were evaluated using human blood-derived circulating progenitor cells (CPCs), human umbilical<br />
vein endothelial cells (HUVECs) and porcine islet cells, seeded onto the hydrogels and compared to<br />
their respective controls. Adhesion, viability and metabolic activity were evaluated on days 1, 2 and<br />
7 using standard adhesion, viability (live/dead) and WST-1 assays. PC-ßGP was less viscous<br />
(5.5±0.5Pa•s) at 37°C compared to HTCC-TPP (11±4Pa•s). The mean compressive stress and elastic<br />
modulus obtained from the regression analysis fit were calculated at 12% strain for PC-ßGP and<br />
HTCC-TPP hydrogels (n=7) and were found to be 0.45±0.16kPa and 6.33±0.87kPa, and<br />
0.06±0.007kPa and 0.05±0.01kPa, respectively. This indicated that PC-ßGP was significantly stiffer<br />
than HTCC-TPP. Morphology revealed uniform pore distribution for both hydrogels, with HTCC-<br />
TPP having higher (14%) porosity. Gels degraded 4× faster in alpha-amylase (pH 7, 37°C,<br />
250IU/ml) than in PBS over 7 days. Cell compatibility was assessed and the number <strong>of</strong> CPCs and<br />
HUVECs adherent on HTCC-TPP was less compared to PC-ßGP (p=0.001). Live/dead assays<br />
revealed comparable cell viability (>70%) between gels, and WST-1 showed greater cell metabolic<br />
activity on PC-ßGP (p=0.05). ELISA for insulin and flow cytometry labeling showed similar trends<br />
for both gels up to 7 days.<br />
Conclusion: Chitosan-derived hydrogels are promising as delivery vehicles and suitable for<br />
supporting multiple cell types for cardiovascular and islet transplantation tissue engineering<br />
therapies.<br />
IV. Application <strong>of</strong> Regenerative Research to Therapy –<br />
Poster Presentation<br />
54
P15 - Poster Abstract #15<br />
CaMKinase II Anchoring Protein, aKAP, is a Novel Regulator <strong>of</strong> SERCA2a<br />
Activity in Cardiomyocytes.<br />
Omar Hawari, P. Singh, M. Salih, B.S. Tuana<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>, Dept. <strong>of</strong> Cellular and Molecular Medicine<br />
Background: The Sarco-endoplasmic Ca2+ ATPase (SERCA2a) plays a crucial role in sequestering<br />
cytosolic calcium into the sarco-endplasmic reticulum (SR/ER) and is an important regulator <strong>of</strong><br />
muscle contraction and relaxation. Defective SERCA2a activity has been shown to result in heart<br />
failure. SERCA2a activity is triggered by cytosolic calcium with phospholamban (PLN) as a fine<br />
regulator <strong>of</strong> its affinity for calcium and uptake into the SR. Recent findings suggest that a novel<br />
CAMKIIa splice variant, aKAP, plays the role <strong>of</strong> a CAMKII anchoring protein in the myocardium,<br />
also directly interacts with SERCA2a.<br />
Methods/Results: We examined the effects <strong>of</strong> aKAP on SERCA2a activity using the NADH<br />
coupled enzymatic assay and thapsigargin as inhibitor <strong>of</strong> the Ca2+ ATPase. SERCA2a activity was<br />
assayed in microsomal fractions <strong>of</strong> HEK-293T co-expressing SERCA2a and aKAP. The rate <strong>of</strong><br />
NADH oxidation was correlated to the rate <strong>of</strong> ATP hydrolysis <strong>of</strong> SERCA2a. Our data showed that<br />
aKAP was without effect on the Ca2+ ATPase activity in microsomal fractions <strong>of</strong> SERCA2a<br />
transfected HEK-293T cells. Interestingly, neonatal mouse cardiomyocyte (NMCM) cultures<br />
infected with a lentivirus carrying the aKAP gene, demonstrated that aKAP actually inhibited the<br />
SERCA2a<br />
activity.<br />
Conclusion: The differences between the NMCM model and the HEK-293T cells indicate that the<br />
direct interaction <strong>of</strong> aKAP and SERCA2a alone is not sufficient and requires other factors not<br />
present in the HEK-293T cells. These data suggest that aKAP may be a unique regulator <strong>of</strong><br />
SERCA2a activity and may therefore serve as a novel target in the treatment <strong>of</strong> heart disease.<br />
IV. Application <strong>of</strong> Regenerative Research to Therapy –<br />
Poster Presentation<br />
55
P16 - Poster Abstract #16<br />
Inhibition <strong>of</strong> VEGFR2 is Sufficient to Produce Severe Plexogenic<br />
Pulmonary Arterial Hypertension in Rats without Exposure to Chronic<br />
Hypoxia<br />
Baohua Jiang 1,2 , Y. Deng 1 , M. Taha 1 , G. Li 1 , D.J. Stewart 1,2<br />
1 <strong>Ottawa</strong> Hospital Research <strong>Institute</strong>, Sprott Stem Cell Centre and Regenerative Medicine <strong>Program</strong>;<br />
2 Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>.<br />
Background: Pulmonary arterial hypertension (PAH) is characterized by elevated pulmonary<br />
vascular resistance due to obliteration <strong>of</strong> small arterioles. Sugen5416, a VEGFR2 inhibitor, has been<br />
reported to cause endothelial cell (EC) apoptosis resulting in severe PAH in chronically hypoxic<br />
(CH) rats, characterized by complex intimal and plexiform lesions. Recently, it was suggested that<br />
immune deficient, nude rats, were more susceptible to SU5416, demonstrating a severe PAH<br />
phenotype even without CH. The objective <strong>of</strong> this study was to establish whether chronic hypoxia is<br />
necessary for development <strong>of</strong> severe PAH after SU5416 injection.<br />
Methods/Results:Wild type (WT) Sprague Dawley or nude rats were divided into following groups:<br />
a single subcutaneous injection <strong>of</strong> vehicle (Control) or SU5416 (20mg/kg) (SU); 3 weeks <strong>of</strong> CH<br />
(10% oxygen) or SU5416 combined with 3 weeks <strong>of</strong> CH (SU+CH). After 3 weeks, the CH and<br />
SU+CH groups were returned to normoxia for an additional 5 weeks. SU+CH produced severe PAH<br />
in WT rats with increases in right ventricular systolic pressure (RVSP: 80±8 mmHg) compared to<br />
control rats (29±1 mmHg, p
P17 - Poster Abstract #17<br />
Targeted Expression <strong>of</strong> the E2F6 Transcriptional Repressor in<br />
Myocardium<br />
Jennifer Major, B. Westendorp, M. Nader, M. Salih, F. Leenen, B.S. Tuana<br />
Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; Dept. <strong>of</strong> Hypertension, <strong>University</strong><br />
<strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong><br />
Background: The E2F/Rb pathway is comprised <strong>of</strong> a dozen proteins which are expressed in a<br />
cell/tissue specific context to regulate genes involved in proliferation, differentiation, and death.<br />
Perturbation <strong>of</strong> the E2F/Rb pathway through modulation <strong>of</strong> its members induces changes in the cell<br />
cycle which could potentially be targeted in cell growth and death. However, the constellation <strong>of</strong><br />
E2F/Rb family members and their exact role in cardiac growth and development remains to be fully<br />
examined.<br />
Methods/ Results: In order to modulate the E2F pathway in vivo, we expressed E2F6 (a<br />
transcriptional repressor) in mice under the control <strong>of</strong> the a-myosin heavy chain promoter.<br />
Microarray, microRNA array, and protein expression pr<strong>of</strong>iling were utilized to identify targets which<br />
were sensitive to E2F6 in transgenic (Tg) myocardium. E2F6-Tg mice presented with symptoms <strong>of</strong><br />
Dilated Cardiomyopathy (DCM) leading to early mortality. Microarray analysis revealed that E2F<br />
responsive transcripts involved in cell cycle regulation including E2F1 and E2F3 were up regulated<br />
in Tg hearts (~19 and 3-fold respectively). Although thirty cell cycle genes were up-regulated they<br />
did not induce any changes in cardiomyocyte size or number. Western blot analysis indicated that<br />
E2F1 protein levels were unchanged and E2F3B was down-regulated ~60%, implying a posttranscriptional<br />
control mechanism for E2F6. We detected a 10-fold increase in the skeletal muscle<br />
enriched miR-206. Activation <strong>of</strong> miR-206 was linked to a post-transcriptional loss <strong>of</strong> the gap<br />
junction protein, connexin-43(~75% loss) and abnormal electrocardiogram in Tg mice. We also<br />
noted the activation <strong>of</strong> the Extracellular Receptor Kinase (ERK) which has been linked to the<br />
induction <strong>of</strong> miR-206 and a loss <strong>of</strong> connexin-43. The DCM noted in E2F6-Tg mice is similar to that<br />
initiated by mutations in nuclear proteins which are associated with the inappropriate docking <strong>of</strong> Rb<br />
and activation <strong>of</strong> E2F responsive transcripts as well as ERK activation and a loss <strong>of</strong> connexin-43.<br />
Conclusion: This study demonstrates a previously unrecognized role for E2F6 as a transcriptional<br />
activator and as a post-transcriptional regulator <strong>of</strong> gene expression in vivo. Further, the data suggest<br />
that a strict control <strong>of</strong> the E2F pathway by a subset <strong>of</strong> E2Fs is critical for normal cardiac<br />
development and function.<br />
IV. Application <strong>of</strong> Regenerative Research to Therapy –<br />
Poster Presentation<br />
57
P18 - Poster Abstract #18<br />
Collagen:Chitosan Hydrogels for Stimulation <strong>of</strong> Angiogenesis in a Type I<br />
Diabetic Mouse Model: Potential Use as a Pre-Vascularized Ectopic Site for<br />
Islet Transplantation<br />
Joanne E. McBane 1,2 , B. Vulesevic 1,2 , D.T. Padavan 1 , K.A. McEwan 1,3 , G.S. Korbutt 4 , E.J.<br />
Suuronen 1,2<br />
1 <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>; 2 Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong><br />
<strong>Ottawa</strong>; 3 Dept. <strong>of</strong> Mechanical Engineering,<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 4 Alberta Diabetes <strong>Institute</strong>, <strong>University</strong> <strong>of</strong> Alberta.<br />
Background: Islet transplantation to treat type 1 diabetes (T1D) has shown varied long term<br />
success, due in part to poor blood supply, suggesting that pre-vascularization <strong>of</strong> the transplant site is<br />
needed. In the current study, we compared preformed collagen (1C) and collagen:chitosan hydrogels<br />
(2C), +/-circulating progenitor cells (CPCs), as materials to promote angiogenesis in a T1D<br />
(streptozotocin (STZ)-induced) nude mouse model.<br />
Methods/Results: CPCs were isolated from human peripheral blood mononuclear cells cultured on<br />
fibronectin for 4d. 1C or 2C (10:1 collagen:chitosan) hydrogels +/- CPCs were crosslinked using<br />
EDC/NHS. Matrices were tested in vitro for: CPC viability (live-dead assay); mechanical strength<br />
(Instron), crosslinks and fiber diameter (scanning electron microscopy); and degradation rate<br />
(collagenase). Mice were injected via the tail vein with a single dose <strong>of</strong> STZ (220mg/kg). One week<br />
post-injection, blood glucose readings were taken and a level <strong>of</strong> >10mmol was taken as a positive<br />
reading for hyperglycemia. Matrices +/- CPCs were implanted subcutaneously for up to 6 weeks in<br />
the STZ mouse model and evaluated for cytokine production (cytokine array), cell infiltration<br />
(hematoxylin and eosin staining) and expression <strong>of</strong> vWF (immunohistochemistry). After gelation at<br />
37°C for 18h, live/dead staining showed greater CPC viability in the 2C gels compared to 1C gels<br />
(79% vs. 69%, p
P19 - Poster Abstract #19<br />
Collagen-Laminin Hydrogels for Delivery <strong>of</strong> Insulin-Producing Tissue for<br />
the Treatment <strong>of</strong> Type 1 Diabetes<br />
Kimberly A. McEwan 1,2 , DT.Padavan 2 , C. Ellis 4 , GS Korbutt 4 and EJ. Suuronen 1,2,3<br />
1 Dept. <strong>of</strong> Mechanical Engineering, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 2 Div. <strong>of</strong> Cardiac Surgery, <strong>University</strong> <strong>of</strong><br />
<strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>; 3 Dept. <strong>of</strong> Cellular and Molecular Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; Alberta<br />
Diabetes <strong>Institute</strong>, <strong>University</strong> <strong>of</strong> Alberta, Edmonton, AB<br />
Background: The lack <strong>of</strong> vasculature is a major limitation <strong>of</strong> islet transplantation therapy for the<br />
treatment <strong>of</strong> type 1 diabetes. Hydrogels are attractive bio-engineered materials for cell delivery, as<br />
they can provide an environment for cell survival and retention. The aim <strong>of</strong> this study was to develop<br />
and characterize a collagen-chitosan hydrogel to be used as an ectopic transplant site that will<br />
support vascularization and islet graft survival and function.<br />
Methods/Results:Type-I collagen, chitosan (10:1 and 20:1 collagen:chitosan) without or with<br />
laminin (40µg/mL) and chondroitin sulfate-C were cross-linked with EDC/NHS. Circulating<br />
progenitor cells (CPCs) in endothelial basal media (EBM) or islets in Ham’s media were added.<br />
Live/dead staining was used to assess CPC and islet viability. Scanning Electron Microscopy (SEM):<br />
surface morphology, porosity and pore diameter were evaluated. Mechanical Testing: compressive<br />
loading was applied to determine stiffness (modulus). Degradation: Degradation <strong>of</strong> hydrogels in<br />
water, PBS, collagenase (0.125U/mL) and amylase (220U/mL) was assessed. In 10:1 matrices, CPC<br />
viability was 1.4-fold greater with the addition <strong>of</strong> 40µg/mL <strong>of</strong> laminin, (p=0.01) at 24h. At 48h,<br />
20:1 matrices displayed 1.2-fold increase in viability with 40µg/mL laminin (p=0.0008). At 24h,<br />
islet survival was superior in the 20:1 matrix with 40µg/mL laminin (95.0±6.0%) compared to 10:1<br />
matrix without laminin (70.9±0.03%, p=0.02). At 48h, islet viability in 20:1 matrix with 40µg/mL<br />
laminin was 80.3±4.0% compared to 69.3±6.4% without laminin (p=0.03). SEM illustrated smoother<br />
surfaces with 40 g/mL laminin compared to matrices without laminin. The elastic moduli <strong>of</strong><br />
matrices synthesized with Ham’s media (7.8-13.9kPa) were all significantly higher than those with<br />
EBM (1.2-6.6kPa). Also, matrices with higher chitosan content were stiffer. After 72h in<br />
collagenase, degradation <strong>of</strong> matrices with EBM was greater than those with Ham’s (p
P20 - Poster Abstract #20<br />
Pharmacological Enhancement <strong>of</strong> Resident Cardiac Stem Cells via<br />
Activation <strong>of</strong> the Wnt Pathway<br />
Ola Qassim, M. Kamkar, B. Ye, N. Latham, and D.R. Davis<br />
Cardiac Translational Research Laboratory, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>.<br />
Background: Cardiac stem cell (CSC) therapy holds tremendous promise for patients suffering<br />
from chronic heart failure. We have developed techniques to extract and grow cells directly from a<br />
patient’s own heart biopsy with a view towards transplanting these cells back into damaged<br />
myocardium. Within the heterogeneous population <strong>of</strong> cells that spontaneous emigrates from plated<br />
tissue in culture, a modest subpopulation (
P21 - Poster Abstract #21<br />
Circulating Microrna Provice Potential Biomarkers <strong>of</strong> Pulmonary Arterial<br />
Hypertension<br />
Kenny Schlosser 1 , R.J. White 2 , D.J. Stewart 1<br />
1 <strong>Ottawa</strong> Hospital Research <strong>Institute</strong> & <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>; 2 <strong>University</strong> <strong>of</strong> Rochester Medical<br />
Center<br />
Background: Idiopathic pulmonary arterial hypertension (IPAH) is characterized by a progressive<br />
increase in lung vascular resistance, which leads to heart failure and premature death. The prognosis<br />
for IPAH is poor; however, early diagnosis and treatment can decrease morbidity and increase the<br />
patient's quality <strong>of</strong> life. Unfortunately, prompt diagnosis remains a challenge as the early stages <strong>of</strong><br />
PAH are asymptomatic, and there is no specific assay for this disease. Although the etiology <strong>of</strong> PAH<br />
remains unclear, there is increasing interest in microRNAs (miRNAs) as key regulators <strong>of</strong> cell<br />
differentiation, proliferation and survival in lung vascular disease. The objective <strong>of</strong> this study was to<br />
identify plasma miRNAs that could serve as novel diagnostic markers <strong>of</strong> IPAH.<br />
Methods/ Results: Blood samples were collected from the right ventricle <strong>of</strong> 9 patients with<br />
confirmed IPAH and 4 control participants with normal hemodynamics, as determined by right heart<br />
catheterization. Total RNA was extracted from EDTA-plasma and the levels <strong>of</strong> 85 different miRNAs<br />
were measured using reverse transcription and quantitative real-time PCR arrays. MicroRNA<br />
expression levels were normalized to the geomean <strong>of</strong> two novel internal miRNA reference genes that<br />
were identified specifically for this model system by systematically evaluating the expression<br />
stability <strong>of</strong> each miRNA using the NormFinder algorithm. Between 39-78 different miRNAs were<br />
detectable (PCR quantification cycle, Cq
P22 - Poster Abstract #22<br />
Development <strong>of</strong> PCSK9 Inhibitors for Regulating LDL-R and Cholesterol<br />
Alghamdi, R 1 , Mishra P 1 , Lagace T 2, 3 , and Basak A 1, 3<br />
1 Chronic Disease <strong>Program</strong>, <strong>Ottawa</strong> Hospital Research <strong>Institute</strong>, 2 Department <strong>of</strong> Pathology and<br />
Laboratory Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>, 3 Department <strong>of</strong> Biochemistry,<br />
Microbiology and Immunology, Faculty <strong>of</strong> Medicine, <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
Background: Since its discovery in 2003, PCSK9 (Proprotein Convertase Subtilisin/Kexin9) has<br />
drawn significant attention for its function in the degradation <strong>of</strong> Low Density Lipoprotein-Receptor<br />
(LDL-R). PCSK9-induced LDL-R degradation reduces LDL-cholesterol uptake by hepatocytes<br />
causing an accumulation <strong>of</strong> cholesterol in the blood - a condition known as Hypercholesterolemia.<br />
Owing to this biological property, confirmed by various studies including knock out mice, PCSK9<br />
became a major target for intervention <strong>of</strong> hypercholesterolemia. Crystal structure revealed that<br />
PCSK9’s catalytic domain binds with LDL-R’s EGF-A domain leading to re-routing <strong>of</strong> LDL-R<br />
towards lysosome for its degradation.<br />
Methods/Results: The precise location <strong>of</strong> catalytic domain(s) <strong>of</strong> PCSK9 involved in binding with<br />
LDL-R’s EGF-A domain has not yet been identified. This remains as the major focus <strong>of</strong> this study<br />
since peptides derived from such domains may likely interfere in the binding <strong>of</strong> PCSK9 with LDL-<br />
R, leading to possible reduction <strong>of</strong> LDL-R degradation. In addition, we are also interested in<br />
identifying non-peptide compounds from natural sources that may also block PCSK9’s ability to<br />
bind with LDL-R. For this we selected 5 natural products (berberine, allicin, forskolin, mimosine,<br />
swertiamarin) based on the known medicinal properties <strong>of</strong> the plants from which they were derived.<br />
The effects <strong>of</strong> all peptide and non-peptide compounds in human HepG2 cells following culture at<br />
various concentrations have been studied. The results suggested LDL-R promoting activity <strong>of</strong> 2<br />
PCSK9 catalytic loop peptides and. swertiamarin, while the rest <strong>of</strong> the compounds did not produce<br />
any significant effects. These effects may be mediated via inhibition <strong>of</strong> PCSK9 function. The results<br />
will be further confirmed using LDL-R uptake and other studies.<br />
Conclusion: Our study may lead to the development <strong>of</strong> new small molecule PCSK9 inhibitors as<br />
potential therapeutic agents for lowering cholesterol, as an alternative to the non-statin compounds.<br />
IV. Application <strong>of</strong> Regenerative Research to Therapy –<br />
Poster Presentation<br />
62
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
63
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page<br />
SPEAKER BIOGRAPHIES<br />
64
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page back
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE JUNE 21 ST & 22 ND , <strong>2012</strong>.<br />
LORD ELGIN HOTEL, OTTAWA<br />
SPEAKER BIOGRAPHIES<br />
KEYNOTES<br />
65
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
CAROLYN ANDERSON, PHD<br />
UNIVERSITY OF PITTSBURGH<br />
KEYNOTE LECTURE: NOVEL PROBES<br />
Receptor-targeted imaging <strong>of</strong> cardiovascular disease<br />
Dr. Anderson received her Ph.D. in Inorganic Chemistry in 1990 from Florida State <strong>University</strong>,<br />
where she carried out her dissertation research with Pr<strong>of</strong>. Gregory R. Choppin in the area <strong>of</strong> actinide<br />
chemistry. She is currently a Pr<strong>of</strong>essor <strong>of</strong> Radiology and Director <strong>of</strong> the Molecular Imaging<br />
Laboratory at the <strong>University</strong> <strong>of</strong> Pittsburgh. After obtaining her PhD, Dr. Anderson took a position as<br />
Research Associate in the Mallinckrodt <strong>Institute</strong> <strong>of</strong> Radiology at Washington <strong>University</strong> School <strong>of</strong><br />
Medicine in St. Louis, MO in Pr<strong>of</strong>. Michael J. Welch's group. In 1993 she was promoted to<br />
Assistant Pr<strong>of</strong>essor <strong>of</strong> Radiology, and held the position <strong>of</strong> Pr<strong>of</strong>essor in the departments <strong>of</strong><br />
Radiology, Biochemistry & Molecular Biophysics, and Chemistry from 2007-2011.<br />
Dr. Anderson’s research interests include the development and evaluation <strong>of</strong> novel radiometal-based<br />
radiopharmaceuticals for diagnostic imaging and targeted radiotherapy <strong>of</strong> cancer and cardiovascular<br />
disease. She pioneered the development <strong>of</strong> copper-64-based radiopharmaceuticals, and her research<br />
group carries out research on the interface <strong>of</strong> chemistry and biology. She has had NIH funding since<br />
1994 and has over 130 peer-reviewed and invited publications, mostly in the area <strong>of</strong> developing<br />
radiopharmaceuticals for oncological imaging and targeted radiotherapy. Dr. Anderson has also<br />
been actively involved in the education and training <strong>of</strong> graduate and undergraduate students in the<br />
areas <strong>of</strong> nuclear and radiochemistry, imaging sciences and nanotechnology.<br />
Dr. Anderson is currently the President <strong>of</strong> the Molecular Imaging Center <strong>of</strong> Excellence (MICoE;<br />
2010-<strong>2012</strong>). She is on the board <strong>of</strong> directors <strong>of</strong> the Society for Radiopharmaceutical Sciences (2007-<br />
present), and is a member <strong>of</strong> the American Chemical Society and the American Association for<br />
Cancer Research.<br />
In the leadership capacity <strong>of</strong> MICoE, she has lead the molecular imaging education task force, a<br />
dedicated group <strong>of</strong> scientists who have written a draft curriculum in Molecular Imaging for nuclear<br />
medicine residents.<br />
Source: http://www.snm.org/index.cfm?PageID=6886<br />
KEYNOTES<br />
66
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
RICHARD LAFOREST, PHD<br />
UNIVERSITY OF WASHINGTON IN ST. LOUIS<br />
KEYNOTE LECTURE: FUNCTIONAL IMAGING TECHNOLOGY<br />
Novel opportunities in imaging technology<br />
Dr. Laforest received his PhD in Experimental Nuclear Physics from Laval <strong>University</strong>. He is<br />
currently the Co-Director <strong>of</strong> the Washington <strong>University</strong> Small Animal Imaging Laboratory;<br />
composed <strong>of</strong> three small animal PET cameras and one small animal CT camera. This is the main<br />
laboratory in the Washington <strong>University</strong> Small Animal Imaging Resource (WUSAIR, PI.<br />
J.Ackerman, PhD) and the Siteman Cancer Center (SCC, PI: T.Eberlein MD). Dr. Laforest’s<br />
research involves the development <strong>of</strong> multi-modality small animal imaging instruments and<br />
techniques. Small animal imaging has become a main laboratory instrument around the world for the<br />
development <strong>of</strong> new agents for diagnostic and therapeutic use. The animal <strong>of</strong> choice for<br />
development is <strong>of</strong>ten the mouse, due to the wide availability <strong>of</strong> transgenic animal models exhibiting<br />
desired phenotypes <strong>of</strong> specific diseases. Novel tracers have been developed with positron emitting<br />
radionuclides having unfavorable decay characteristics for PET imaging. Dr. Laforest’s research<br />
focuses on suitable imaging techniques and adapted image reconstruction for these radionuclides, in<br />
order to provide high quality, optimized images.<br />
Source: http://chempet.wustl.edu/faculty/laforestr.htm<br />
KEYNOTES<br />
67
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
MARCUS SCHWAIGER, MD, PHD<br />
TECHNISCHE UNIVERSITÄT MÜNCHEN<br />
KEYNOTE LECTURE: TRANSLATIONAL IMAGING OF<br />
CARDIOVASCULAR DISEASE<br />
Translational imaging <strong>of</strong> clinical cardiovascular disease<br />
Dr. Schwaiger earned his MD from Kilinikum rechts der Isar, Technische Universitat Munchen,<br />
Germany. He then pursued a postdoctoral research fellowship in the departments <strong>of</strong> Physiology and<br />
Cardiology at the <strong>University</strong> <strong>of</strong> Cincinnati, USA. Dr. Schwaiger successfully completed his<br />
Cardiology and Nuclear Medicine fellowships at UCLA School <strong>of</strong> Medicine. Since then, he has had<br />
numerous pr<strong>of</strong>essional appointments, most recently as Dean <strong>of</strong> the School <strong>of</strong> Medicine and Director<br />
<strong>of</strong> the Department <strong>of</strong> Nuclear Medicine at the Technische Universitaet Muenchen, Germany.<br />
Dr. Schwaiger’s research expertise is the application <strong>of</strong> multimodal imaging, such as Magnetic<br />
Resonance Imaging (MRI), Positron Emission Tomography (PET), Computed Tomography (CT),<br />
and Single Photon Emission Tomography (SPECT), to visualize and quantify biological processes.<br />
His research also focuses on the use <strong>of</strong> PET in cardiology and oncology to monitor various therapies.<br />
Aside from Cardiology, Dr. Schwaiger has special interest in the diagnosis and treatment <strong>of</strong> thyroid<br />
endocrine and neuro-endocrine diseases in the Nuclear Medicine department.<br />
Dr. Schwaiger is very well published with more than 687 refereed publications; he is a Member and<br />
Chairman <strong>of</strong> DFG study section “Medizintechnik”, and is a Member <strong>of</strong> DFG study section “3.<br />
Sektion Herzkreislaufsystem”. In 2005, he was awarded an Unrestricted grant award for<br />
cardiovascular research from the BMS Foundation, Princeton, USA.<br />
KEYNOTES<br />
68
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
REN-KE LI, MD, PHD<br />
TORONTO GENERAL RESEARCH INSTITUTE<br />
KEYNOTE LECTURE: APPLICATION OF REGENERATIVE RESEARCH<br />
TO THERAPY<br />
Cardiac rejuvenation to prevent heart failure after myocardial<br />
infarction<br />
Dr. Li currently holds a Canada Research Chair in Cardiac Regeneration and his research focuses<br />
on cell transplantation for cardiovascular disease. Research projects include muscle cell<br />
transplantation to improve heart function after complete myocardial infarction; transplantation <strong>of</strong><br />
myogenic cells and angiogenic cells to improve heart function <strong>of</strong> the patients after incomplete<br />
myocardial infarction; cell transplantation to prevent ventricular dilation <strong>of</strong> hearts with dilated<br />
cardiomyopathy; and creation <strong>of</strong> autologous grafts using tissue engineering technique for congenital<br />
heart surgery.<br />
In 1996, Dr. Li’s group was the first to publish that transplanted muscle cells survived in myocardial<br />
scar tissue, stimulated angiogenesis and improved heart function in a small animal model and<br />
clinically relevant large animal models in 2000 and 2002.<br />
Dilated cardiomyopathy is one <strong>of</strong> the most prevalent etiologies <strong>of</strong> significant congestive heart failure<br />
and the most common indication for cardiac transplantation. However, the chronic shortage <strong>of</strong> donor<br />
organs and problems with immunosuppression and rejection limit the applicability and efficacy <strong>of</strong><br />
this therapy. Cell transplantation could be a new therapeutic means to prevent ventricular dilatation<br />
and improve heart function. Dr. Li’s group has implanted muscle cells into the genetic defect animal<br />
model with dilated cardiomyopathy, demonstrating that healthy transplanted cells survived in the<br />
diseased heart and prevented heart dilatation. Function <strong>of</strong> the heart with transplanted cells was much<br />
better than non-transplanted heart.<br />
Congenital heart defects <strong>of</strong>ten require surgical intervention, which may include graft materials. All<br />
currently available graft materials lack growth potential, are non-contractile and are thrombogenic. A<br />
viable, autologous, contractile, and less thrombogenic bio-engineered tissue graft would be ideal for<br />
the surgical repair <strong>of</strong> congenital cardiac defects. Dr. Li’s group has successfully grown fetal<br />
cardiomyocytes within a biodegradable gelatin mesh. The cells attached to the mesh, grew in 3<br />
dimensions, and formed a beating cardiac graft. The cells in the graft survived after implanted onto<br />
scar tissue <strong>of</strong> the hearts.<br />
KEYNOTES<br />
69
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
SPEAKER BIOGRAPHIES<br />
WORKSHOPS<br />
70
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
LEONARD LUYT, PHD<br />
LONDON HEALTH SCIENCES CENTRE<br />
UNIVERSITY OF WESTERN ONTARIO<br />
WORKSHOP SPEAKER: NOVEL PROBE DEVELOPMENT AND<br />
APPLICATIONS<br />
‘The design <strong>of</strong> peptide-based molecular imaging agents’<br />
Dr. Luyt received his Ph.D. from the <strong>University</strong> <strong>of</strong> Western Ontario in Organic Chemistry and<br />
subsequently undertook a post-doctoral fellowship with Swanlund Pr<strong>of</strong>essor John Katzenellenbogen<br />
at the <strong>University</strong> <strong>of</strong> Illinois, Urbana-Champaign. There he led a research team as a Senior Medicinal<br />
Chemist with the pharmaceutical company Bayer-Schering, where he authored two patents and<br />
received the CITE award for exemplary leadership. Dr. Luyt joined the <strong>University</strong> <strong>of</strong> Western<br />
Ontario in 2005 as a faculty member with a joint appointment between three departments: Oncology,<br />
Chemistry and Medical Imaging. He holds a position <strong>of</strong> Scientist at the London Regional Cancer<br />
<strong>Program</strong> and is also affiliated with the Lawson Health Research <strong>Institute</strong> within the Imaging<br />
<strong>Program</strong>. He is the Director <strong>of</strong> the SPECT Radiochemistry and Medicinal Chemistry facility for the<br />
Lawson. He was recently awarded the Early Researcher Award (ERA) from the Ministry <strong>of</strong><br />
Research and Innovation.<br />
The laboratory <strong>of</strong> Dr. Luyt is currently staffed with a total <strong>of</strong> 10 trainees and research associates.<br />
His research program spans from basic chemistry activities, looking at novel methods <strong>of</strong><br />
incorporating metal complexes into peptide structures, through to applied research, investigating<br />
new molecular imaging agents targeting cancer and diabetes. He collaborates closely with leading<br />
scientists in the areas <strong>of</strong> cancer biology and medical imaging. His lab also functions as a core<br />
facility at the Lawson Health Research <strong>Institute</strong> for peptide synthesis and for creating SPECT and<br />
PET molecular imaging agents.<br />
WORKSHOPS<br />
71
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
LIHUI WEI, PHD<br />
NORDION<br />
UNIVERSITY OF OTTAWA HEART INSTITUTE<br />
WORKSHOP SPEAKER: NOVEL PROBE DEVELOPMENT AND<br />
APPLICATIONS<br />
‘Development <strong>of</strong> novel SPECT radiotracers for myocardial<br />
perfusion imaging’<br />
Dr. Wei received her PhD degree in Inorganic Chemistry in 2005, with training in Bioinorganic and<br />
Radiopharmaceutical Chemistry at Syracuse <strong>University</strong> in Syracuse, New York. Her PhD research<br />
was design, synthesis and chemical and structural characterization <strong>of</strong> rhenium and technetium<br />
complexes for the development <strong>of</strong> diagnostic and therapeutic agents in nuclear medicine. She<br />
pursued her postdoctoral research at Mallinckrodt <strong>Institute</strong> <strong>of</strong> Radiology, Washington <strong>University</strong><br />
School <strong>of</strong> Medicine, in the laboratory <strong>of</strong> Michael Welch in St. Louis, Missouri. Her postdoctoral<br />
research focused on radiolabeling <strong>of</strong> peptides, proteins, antibodies and small molecules with Cu-64,<br />
Ga-68, Y-86, Zr-89, In-111 and Tc-94m and both in vivo and in vitro biology evaluation <strong>of</strong> the<br />
radiopharmaceuticals as PET/SPECT imaging agents and therapeutic agents.<br />
In 2007, Dr. Wei joined Nordion as a Research Chemist in the Global Research and Development<br />
department in Kanata, Ontario. In 2009, she transferred to Nordion’s lab at <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
<strong>Heart</strong> <strong>Institute</strong> and joined the Canadian Molecular Imaging Centre <strong>of</strong> Excellence (C-MICE) as a<br />
Research Scientist in Radiochemistry. She is an Adjunct Assistant Pr<strong>of</strong>essor at the Department <strong>of</strong><br />
Medicine, Division <strong>of</strong> Cardiology at <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>. Her current research interests are: a)<br />
SPECT myocardial perfusion imaging agents; b) Nanoparticle based therapeutic and multi-modality<br />
molecular imaging agents for the application in cancer and cardiovascular diseases; c) Development<br />
<strong>of</strong> novel radiotracers for imaging (SPECT and PET) <strong>of</strong> atherosclerosis and vascular inflammation.<br />
WORKSHOPS<br />
72
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
PASAN FERNANDO, PHD<br />
NORDION<br />
UNIVERSITY OF OTTAWA HEART INSTITUTE<br />
WORKSHOP SPEAKER: NOVEL PROBE DEVELOPMENT AND<br />
APPLICATIONS<br />
‘The role <strong>of</strong> apoptosis in disease and the progress <strong>of</strong> apoptosis<br />
probes in molecular imaging applications’<br />
Dr. Fernando is a Research Scientist in Biology and Imaging at Nordion, the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong><br />
<strong>Heart</strong> <strong>Institute</strong>’s partner in the Canadian Molecular Imaging Center <strong>of</strong> Excellence (CMICE).He<br />
received his PhD in Biology in 2002, with training in Developmental and Molecular Biology at the<br />
<strong>University</strong> <strong>of</strong> Waterloo in Waterloo, Ontario. He began his post-doctoral work at the <strong>Ottawa</strong> Health<br />
Research <strong>Institute</strong> in the laboratory <strong>of</strong> Lynn Megeney. With the support <strong>of</strong> a Post-doctoral<br />
Fellowship from the <strong>Heart</strong> and Stroke Foundation, Dr. Fernando researched bio-signalling<br />
mechanisms that govern skeletal muscle and cardiac cell transformation. His work with Lynn<br />
Megeney influenced a paradigm shift in the field <strong>of</strong> apoptosis by describing a non-death role <strong>of</strong><br />
caspase proteases in promoting cellular differentiation. Following his post-doctoral work, Dr.<br />
Fernando spent three years in the biotechnology sector leading a research team in developing protein<br />
therapeutics for cardiac regenerative medicine. He joined Nordion in 2008, is currently a member at<br />
the <strong>Heart</strong> and Stroke Foundation’s Center for Stroke Recovery and sits on the Board <strong>of</strong> Directors for<br />
the Multiple Sclerosis Society, <strong>Ottawa</strong> Chapter.<br />
Source: http://www.ottawaheart.ca/misc/pasan-fernando.htm<br />
WORKSHOPS<br />
73
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
REBECCA THORNHILL, PHD<br />
THE OTTAWA HOSPITAL<br />
WORKSHOP SPEAKER: PH-UNCTIONAL IMAGING PHYSICS 101<br />
‘Magnetic resonance tools for the evaluation <strong>of</strong><br />
cardiovascular disease’<br />
Dr. Thornhill obtained her M.Sc. and Ph.D. in Medical Biophysics from the <strong>University</strong> <strong>of</strong> Western<br />
Ontario under the supervision <strong>of</strong> Dr. Frank Prato, where she studied MRI methods for the<br />
assessment <strong>of</strong> myocardial viability. She then moved to Hamilton to do postdoctoral research in<br />
mitochondrial disorders using magnetic resonance and near-infrared spectroscopy with Dr. Gerald<br />
Moran (McMaster <strong>University</strong>). In 2008 Dr. Thornhill began a new postdoc at the <strong>University</strong> <strong>of</strong><br />
Toronto under the supervision <strong>of</strong> Dr. Andrea Kassner, applying MRI methods to assess blood-brain<br />
barrier disruption in acute ischemic stroke. She is currently a physicist in the Department <strong>of</strong> Medical<br />
Imaging (<strong>Ottawa</strong> Hospital), with particular research interests in cardiovascular MRI, perfusion<br />
analysis, image texture and pattern classification.<br />
WORKSHOPS<br />
74
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
AARON SO, PHD<br />
ROBARTS RESEARCH INSTITUTE<br />
ST. JOSEPH’S HEALTHCARE<br />
WORKSHOP SPEAKER: PH-UNCTIONAL IMAGING PHYSICS 101<br />
‘Fundamentals and advances <strong>of</strong> CT myocardial perfusion<br />
imaging’<br />
Dr. So is currently training as a clinical diagnostic imaging Medical Physicist at St. Joseph’s<br />
Healthcare, in London Ontario, while holding a research associate position at Robarts Research<br />
<strong>Institute</strong>. At Robarts, he works on cardiac CT perfusion imaging with Dr. Ting Lee, his former PhD<br />
supervisor. Dr. So’s research interest is in cardiac CT imaging, specifically quantitative CT<br />
myocardial perfusion imaging. Cardiovascular diseases are among the leading causes <strong>of</strong> mortality in<br />
the world and quantitative perfusion measurement allows a better understanding <strong>of</strong> the underlying<br />
hemodynamic causes and/or consequences <strong>of</strong> myocardial ischemia. During his PhD training, Dr. So<br />
received two Research Trainee Prizes from the Radiological Society <strong>of</strong> North America (RSNA) for<br />
the development <strong>of</strong> quantitative CT myocardial perfusion imaging for the assessment <strong>of</strong> coronary<br />
artery disease, and since then has received an RSNA Research Fellow Grant for the development <strong>of</strong><br />
a dynamic dual energy CT scanning technique which would improve the accuracy <strong>of</strong> quantitative CT<br />
myocardial perfusion measurement. Dr. So’s long term goal is to become a CT imaging scientist in a<br />
radiology department <strong>of</strong> an academic hospital with an equal division <strong>of</strong> time between clinical service<br />
and academic imaging research.<br />
Source: http://www.birc.ca/aaron-so-phd<br />
WORKSHOPS<br />
75
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
R. GLENN WELLS, PHD<br />
UNIVERSITY OF OTTAWA HEART INSTITUTE<br />
WORKSHOP SPEAKER: PH-UNCTIONAL IMAGING PHYSICS 101<br />
‘Fundamentals <strong>of</strong> single photon emission tomography and<br />
technical advances’<br />
CAREER DEVELOPMENT LUNCH: GUEST SPEAKER<br />
Dr. Wells received a PhD in Medical Physics (SPECT Imaging) in 1997 from the <strong>University</strong> <strong>of</strong><br />
British Columbia. He is a Medical Physicist in the Department <strong>of</strong> Nuclear Cardiology at the<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>, Assistant Pr<strong>of</strong>essor in the Division <strong>of</strong> Cardiology at the<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> and Adjunct Pr<strong>of</strong>essor in the Department <strong>of</strong> Physics at Carleton <strong>University</strong>.<br />
His research group has grown rapidly over the past few years and currently consists <strong>of</strong> five PhD and<br />
three MSc Medical Physics candidates. Dr. Wells’ research interests concentrate on the physics <strong>of</strong><br />
multi-modality cardiac imaging with nuclear medicine: the combination <strong>of</strong> multi-slice X-ray<br />
computed tomography (CT) with positron emission tomography (PET) and single-photon emission<br />
computed tomography (SPECT). Multi-modal cameras such as PET/CT and SPECT/CT are recent<br />
advances in medical imaging technology that combine two types <strong>of</strong> imaging in a single device.<br />
These cameras provide exquisite anatomical images from CT accurately aligned with nuclear<br />
medicine functional images from PET or SPECT. Beyond just providing pretty pictures, these<br />
cameras <strong>of</strong>fer new opportunities for using the CT information to improve the PET or SPECT images.<br />
A more complete integration <strong>of</strong> these two types <strong>of</strong> data sets will produce a “whole” that is “greater<br />
than the sum <strong>of</strong> its parts”.<br />
Source: http://www.ottawaheart.ca/misc/glenn-wells.htm<br />
WORKSHOPS<br />
76
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
RAN KLEIN, PHD<br />
UNIVERSITY OF OTTAWA HEART INSTITUTE<br />
WORKSHOP SPEAKER: PH-UNCTIONAL IMAGING PHYSICS 101<br />
‘Fundamentals <strong>of</strong> positron emission tomography and<br />
advanced functional analysis’<br />
Dr. Klein is manager <strong>of</strong> the Cardiac Imaging Core Lab at the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>,<br />
National Cardiac PET Centre. His research is focused on extracting quantitative physiologic<br />
information from cardiac images. In particular Ran has worked on quantification <strong>of</strong> cardiac blood<br />
flow using rubidium-82 positron emission tomography (PET). His research has resulted in<br />
commercially available s<strong>of</strong>tware for image analysis (FlowQuant). Ran’s work on an automated<br />
rubidium-82 infusion system is currently being commercialized by Jubilant DraxImage, Montreal.<br />
Ran obtained his PhD (2010) and MASc (2005) in Electrical Engineering from the <strong>University</strong> <strong>of</strong><br />
<strong>Ottawa</strong>, and has been conducting research at the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong> since 2001. He<br />
is an adjunct pr<strong>of</strong>essor at Carleton <strong>University</strong>.<br />
WORKSHOPS<br />
77
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
LISA MIELNICZUK, MD<br />
UNIVERSITY OF OTTAWA HEART INSTITUTE<br />
WORKSHOP SPEAKER: TRANSLATIONAL IMAGING OF<br />
CARDIOVASCULAR DISEASE<br />
‘<strong>Heart</strong> failure and advances in PET for pre-clinical and<br />
clinical studies’<br />
Dr. Mielniczuk is Staff Cardiologist in <strong>Heart</strong> Failure and Cardiac and Medical Director <strong>of</strong> both<br />
the Pulmonary Hypertension Clinic and the Telehealth Home Monitoring <strong>Program</strong> at the <strong>University</strong><br />
<strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>. She is also Assistant Pr<strong>of</strong>essor in the Department <strong>of</strong> Medicine at the<br />
<strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>. Dr. Mielniczuk obtained her BSc (Hons) in Biology and Psychology at<br />
McMaster <strong>University</strong> in Hamilton, Ontario, and her MSc in Clinical Epidemiology and Biostatistics<br />
at the Harvard School <strong>of</strong> Public Health in Boston, Massachusetts, before returning to McMaster<br />
<strong>University</strong> to obtain her MD. Dr. Mielniczuk was Chief Resident in the Internal Medicine <strong>Program</strong>,<br />
Department <strong>of</strong> Medicine, at Queen's <strong>University</strong> in Kingston, Ontario, and then Chief Resident in the<br />
Division <strong>of</strong> Cardiology at the <strong>Heart</strong> <strong>Institute</strong>.<br />
She became a Fellow <strong>of</strong> the Royal College <strong>of</strong> Physicians and Surgeons <strong>of</strong> Canada (FRCPC) in<br />
Internal Medicine in 2002 and in Cardiology in 2004. In 2003, she received the Resident Research<br />
Prize from the Canadian <strong>Institute</strong>s <strong>of</strong> Health Research. Both in 2004, Dr. Mielniczuk received a<br />
Certificate <strong>of</strong> Teaching Excellence Nomination from the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> and the <strong>Heart</strong><br />
<strong>Institute</strong>'s Wilbert J. Keon Award for Trainee Excellence and Clinical Research.<br />
Source: http://www.ottawaheart.ca/misc/lisa-marie-mielniczuk.htm<br />
WORKSHOPS<br />
78
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
GIRISH DWIVEDI, MRCP (UK), DM, PHD<br />
BANTING FELLOW<br />
UNIVERSITY OF OTTAWA HEART INSTITUTE<br />
WORKSHOP SPEAKER: TRANSLATIONAL IMAGING OF<br />
CARDIOVASCULAR DISEASE<br />
‘Ischemic heart disease and current CT approaches for preclinical<br />
and clinical studies’<br />
Dr. Dwivedi is a Banting Fellow in cardiac imaging at the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>. He<br />
has a particular research and clinical interest in cardiac imaging. His previous research was in<br />
developing myocardial perfusion methods with echocardiography (myocardial contrast tomography)<br />
using ultrasound contrast agents. He is a known expert in the field <strong>of</strong> echocardiography and cardiac<br />
magnetic resonance imaging with a number <strong>of</strong> peer reviewed publications and prestigious grants<br />
from his previous work in the United Kingdom. Presently, Dr Dwivedi is working on a CIHR funded<br />
project where he is evaluating the accuracy <strong>of</strong> myocardial perfusion assessed by cardiac computed<br />
tomography compared to that <strong>of</strong> positron emission tomography. Recently, Dr Dwivedi was awarded<br />
a Banting Fellowship, considered the most prestigious post doctoral fellowship award in Canada.<br />
WORKSHOPS<br />
79
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
CHARLES CUNNINGHAM, PHD<br />
SUNNYBROOK RESEARCH INSTITUTE,<br />
UNIVERSITY OF TORONTO<br />
WORKSHOP SPEAKER: TRANSLATIONAL IMAGING OF<br />
CARDIOVASCULAR DISEASE<br />
‘Advancements in metabolic MRI and prospective detection <strong>of</strong><br />
clinical anomalies’<br />
Dr. Cunningham received his PhD in Medical Biophysics from the <strong>University</strong> <strong>of</strong> Toronto in 2002.<br />
He is currently holds appointments as a scientist in the Physical Sciences division <strong>of</strong> the Schulich<br />
<strong>Heart</strong> Research <strong>Program</strong> at Sunnybrook Research <strong>Institute</strong>, assistant pr<strong>of</strong>essor, Medical Biophysics<br />
at the <strong>University</strong> <strong>of</strong> Toronto and as a McLaughlin Scholar from the McLaughlin Centre for<br />
Molecular Medicine. Molecular imaging is a new field that combines recent advances in noninvasive<br />
imaging modalities with molecular and cellular biology in order to improve our<br />
understanding <strong>of</strong> normal and disease processes. Although magnetic resonance imaging (MRI) has<br />
many characteristics that make it attractive as a molecular imaging platform, significant challenges<br />
remain.<br />
Dr. Cunningham’s research is focused on the fundamental physics underlying the MRI signal with<br />
the aim <strong>of</strong> advancing MRI methodology towards molecular imaging applications. Specific projects<br />
include development <strong>of</strong> novel methods for studying cell trafficking using magnetic nanoparticles,<br />
hyperpolarized carbon (13C) probes for metabolic characterization <strong>of</strong> diseased tissue, and<br />
radi<strong>of</strong>requency pulse design for high-field MRI applications.<br />
Source: http://sunnybrook.ca/research/team/member.asp?t=10&page=172&m=50<br />
WORKSHOPS<br />
80
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
KIMBERLEY BLACKWOOD, PHD<br />
LAWSON HEALTH RESEARCH INSTITUTE,<br />
WORKSHOP SPEAKER: TRANSLATIONAL IMAGING OF<br />
CARDIOVASCULAR DISEASE<br />
‘Molecular cardiac imaging with PET/MR’<br />
Dr. Blackwood received her PhD in Medical Biophysics from Western <strong>University</strong> studying the role<br />
<strong>of</strong> imaging in cardiac stem cell therapy, in large animals. While this initial work used clinical<br />
SPECT to assess transplanted cell viability, Dr. Blackwood currently studies the role <strong>of</strong> myocardial<br />
inflammation in transplanted cell viability as a post-doctoral associate at Western. Early work<br />
demonstrated that FDG-PET in infarcted myocardium, with suppressed glucose uptake, provided<br />
visualization <strong>of</strong> glucose dependent inflammatory cells within the infarct itself. This work is now<br />
being confirmed using tissue characterization with hybrid PET/MRI at Lawson Health Research<br />
<strong>Institute</strong>. The goal <strong>of</strong> this work is to understand the temporal changes in tissue remodelling in large<br />
animal models <strong>of</strong> acute heart disease in order to help optimize cell therapy, with the understanding<br />
that cell viability is important to long term improvements in heart function.<br />
WORKSHOPS<br />
81
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
ILONA SKERJANC, PHD<br />
UNIVERSITY OF OTTAWA<br />
WORKSHOP SPEAKER: REGENERATIVE THERAPY FROM TISSUE<br />
ENGINEERING TO IMAGING OUTCOMES<br />
‘Cardiomyogenesis in embryonic stem cells’<br />
Dr. Skerjanc received her PhD from McGill <strong>University</strong> in Biochemistry and is presently a Pr<strong>of</strong>essor<br />
in Biochemistry, Microbiology and Immunology at the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>. Her laboratory is<br />
interested in understanding the molecular mechanisms <strong>of</strong> muscle development with the long-term<br />
view <strong>of</strong> using stem cells to replace damaged muscle. Embryonic stem cells or embryonal carcinoma<br />
cells can be induced to differentiate into cardiac and skeletal muscle. However, this process is not<br />
very efficient and only a minority <strong>of</strong> the cells differentiates down a given developmental pathway.<br />
In order to enhance the extent <strong>of</strong> differentiation into muscle, it is essential to identify the network <strong>of</strong><br />
transcription factors that specify different types <strong>of</strong> muscle and to understand how signaling pathways<br />
control the expression and function <strong>of</strong> the individual transcription factors in the network. A solid<br />
grasp <strong>of</strong> the fundamental mechanisms involved in muscle development will be essential in designing<br />
future therapies based on adult or embryonic stem cells for restoring cardiac sufficiency or replacing<br />
muscle in patients with muscle atrophy.<br />
Source: http://www.medicine.uottawa.ca/bmi/eng/skerjanc.html<br />
WORKSHOPS<br />
82
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
MARC RUEL, MD<br />
UNIVERSITY OF OTTAWA HEART INSTITUTE<br />
WORKSHOP SPEAKER: REGENERATIVE THERAPY FROM TISSUE<br />
ENGINEERING TO IMAGING OUTCOMES<br />
‘Cardiac cell/biopolymer therapy: understanding effects and<br />
mechanisms’<br />
Dr. Ruel is a cardiac surgeon and endowed chair <strong>of</strong> cardiac surgery research at the <strong>University</strong> <strong>of</strong><br />
<strong>Ottawa</strong> <strong>Heart</strong> <strong>Institute</strong>. He holds the rank <strong>of</strong> Pr<strong>of</strong>essor <strong>of</strong> Surgery, with cross-appointments in<br />
Epidemiology and Community Medicine, and in Cellular and Molecular Medicine. He is the<br />
Assistant-Dean, Clinical and Translational Research, at the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>. After completion<br />
<strong>of</strong> his medical doctor degree and certification in cardiac surgery from the <strong>University</strong> <strong>of</strong> <strong>Ottawa</strong>, Dr.<br />
Ruel pursued minimally invasive surgery and translational research training at Harvard Medical<br />
School, where he also completed a Masters in Quantitative Methods at the Harvard School <strong>of</strong> Public<br />
Health.<br />
Dr. Ruel’s surgical areas <strong>of</strong> predilection include minimally invasive coronary and valve procedures,<br />
as well as complex and repeat cardiac operations. His research has been continuously funded by<br />
national granting agencies since his first faculty appointment. He introduced several novel cardiac<br />
surgical techniques in Canada and internationally, developed a successful translational regenerative<br />
medicine program in <strong>Ottawa</strong>, and continues to pursue clinical research on the long-term outcomes <strong>of</strong><br />
heart valve surgery and coronary bypass grafting. In 2007, he received the Gold Medal in Surgery<br />
from the Royal College <strong>of</strong> Physicians and Surgeons <strong>of</strong> Canada. He has published over 160 peerreviewed<br />
papers and book chapters, and was recently the editor <strong>of</strong> a cardiac surgery technique<br />
textbook published by Elsevier. He serves on the executive <strong>of</strong> the American <strong>Heart</strong> Association, the<br />
Society <strong>of</strong> Thoracic Surgeons, and the American Association for Thoracic Surgery.<br />
WORKSHOPS<br />
83
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
GRAHAM WRIGHT, PHD<br />
SUNNYBROOK RESEARCH INSTITUTE,<br />
UNIVERSITY OF TORONTO<br />
WORKSHOP SPEAKER: REGENERATIVE THERAPY FROM TISSUE<br />
ENGINEERING TO IMAGING OUTCOMES<br />
‘Developments in clinical assessment, treatment planning,<br />
and therapeutic guidance for ischemic heart disease using<br />
MRI’<br />
Dr. Wright received his PhD in Electrical Engineering from Stanford <strong>University</strong>. He is currently a<br />
Senior scientist in the Physical Sciences division <strong>of</strong> the Schulich <strong>Heart</strong> Research <strong>Program</strong> at<br />
Sunnybrook Research <strong>Institute</strong>, a Pr<strong>of</strong>essor <strong>of</strong> Medical Biophysics at the <strong>University</strong> <strong>of</strong> Toronto, and<br />
consultant to both the radiology department <strong>of</strong> The Hospital for Sick Children, Toronto, and the<br />
electrical engineering and radiology departments <strong>of</strong> Stanford <strong>University</strong>. His research focuses on<br />
cardiovascular imaging, particularly MRI, for disease assessment/intervention and guidance. Dr.<br />
Wright's research efforts include: basic biophysics to characterize the relationship between MR<br />
signals and underlying physiology in blood and tissue; engineering to develop more effective<br />
methods to acquire, analyze, and visualize medical images; and application <strong>of</strong> these tools to<br />
assessment, treatment planning, and therapy guidance in ischemic and congenital heart diseases and<br />
neurovascular and peripheral vascular diseases.<br />
Contributions from Dr. Wright's group include methods for characterizing the effects <strong>of</strong> oxygen in<br />
blood and tissue on MRI signal behaviour in vivo, development <strong>of</strong> a tool to automatically detect<br />
contrast agent arrival in a vessel (thus facilitating a rapid MR acquisition <strong>of</strong> 3-D vascular maps), and<br />
development <strong>of</strong> real-time adaptive MRI tools for improving the quality <strong>of</strong> coronary artery images.<br />
Through work with many clinical collaborators, these tools are being used in a wide range <strong>of</strong> patient<br />
studies.<br />
Current work builds on the group's central role in the Ontario Consortium for Cardiac Imaging<br />
where the focus is to develop and evaluate the role <strong>of</strong> multiple imaging modalities applied to cardiac<br />
diseases and in the Imaging Research Centre for Cardiac Intervention to design and test new imaging<br />
approaches to guide innovative minimally invasive cardiovascular therapies.<br />
Source: http://sunnybrook.ca/research/team/member.asp?t=13&page=172&m=184<br />
WORKSHOPS<br />
84
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page<br />
SOCIAL EVENTS INFORMATION<br />
85
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page back
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
SOCIAL EVENT 1:<br />
Poster Wine & Cheese<br />
Thursday, June 21<br />
4:30 – 6:00 p.m.<br />
While the <strong>MFI</strong> <strong>Symposium</strong> has always included poster presentations and the<br />
trainee “Best Poster Presentation” award, this year our organizing committee<br />
is testing the hypothesis that poster impact factors increase exponentially when<br />
presented along with drinks and appetizers! In addition, please note that, this<br />
year, posters will only be on display Thursday, June 21 during the first day <strong>of</strong><br />
the <strong>Symposium</strong>.<br />
SOCIAL EVENT 2:<br />
Career Development & Networking Lunch<br />
Friday, June 22<br />
12 :00p.m. – 1:15 p.m.<br />
The aim <strong>of</strong> this event is to give trainees the opportunity to learn about different<br />
career paths in cardiovascular research: from bench to bedside.<br />
At registration pick-up, students and fellows will sign up to share a lunch table<br />
with a specific group <strong>of</strong> PIs. Friday’s lunch will kick <strong>of</strong>f with a feature talk on<br />
career progression and networking by Dr. Glenn Wells. Following this,<br />
symposium PIs will, over lunch, discuss with their group <strong>of</strong> students and fellows<br />
how to network and progress within their field, en route to a final career<br />
destination.<br />
This event affords trainees the opportunity to listen, learn and ask questions<br />
about how to determine the most appropriate next steps in order to reach a<br />
particular career goal. As represented by our <strong>2012</strong> theme: translation in<br />
research, it’s easy to see that progression through collaboration is important.<br />
Our <strong>MFI</strong> PIs and invited speakers are a great resource for our talented trainees<br />
who will face decisions between many exciting career paths in the near future!<br />
Social Events Information<br />
86
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
SOCIAL EVENT 3:<br />
Awards Banquet & Social Evening<br />
Friday, June 22<br />
7:30 p.m. – 12:00 a.m.<br />
Awards granted for “Best Oral Presentation” and “Best Poster Presentation”<br />
will be presented and significant <strong>MFI</strong> program contributors and the symposium<br />
organizing committee members recognized. This will be followed by a banquet<br />
dinner, and Cardiovascular Jeopardy.<br />
***New*** in <strong>2012</strong>: Cardiovascular Jeopardy<br />
featuring <strong>MFI</strong> director Dr. Rob Beanlands as Alex Treeeeeeebek!<br />
Attendees will be divided into four teams and provided “signaling mechanisms”.<br />
Two rounds <strong>of</strong> hilarious cardiovascular and general skill-testing trivia will be<br />
presented… to be answered in the form <strong>of</strong> a question, <strong>of</strong> course! Come show <strong>of</strong>f<br />
your knowledge <strong>of</strong> random facts!<br />
Social Events Information<br />
87
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page<br />
SITE MAP<br />
88
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
Coloured cardstock page back
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
SITE MAP<br />
The 5 th Annual <strong>MFI</strong> <strong>Symposium</strong> is being held at the Lord<br />
Elgin Hotel, in downtown <strong>Ottawa</strong>. A parking is available at<br />
the National Arts Centre, the cost is $16/day for arrival<br />
before 4pm.<br />
100 Elgin Street, <strong>Ottawa</strong>, Canada, K1P 5K8<br />
P h o n e : ( 6 1 3 ) 2 3 5 . 3 3 3 3<br />
F a x : ( 6 1 3 ) 2 3 5 . 3 2 2 3<br />
To l l F r e e : 1 . 8 0 0 . 2 6 7 . 4 2 9 8<br />
Site Maps<br />
89
Poster<br />
session<br />
Site Maps<br />
90
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE JUNE 21 ST & 22 ND , <strong>2012</strong>.<br />
LORD ELGIN HOTEL, OTTAWA<br />
main<br />
sessions<br />
Site Maps<br />
91
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
NOTES
MOLECULAR FUNCTION & IMAGING SYMPOSIUM BRINGING<br />
CARDIOVASCULAR IMAGING & THERAPY TO LIFE<br />
JUNE 21 ST & 22 ND , <strong>2012</strong>. LORD ELGIN HOTEL, OTTAWA<br />
INSIDE BACK COVER
THANKS FOR COMING!