AvMed Physician
AvMed Physician
AvMed Physician
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>AvMed</strong> <strong>Physician</strong><br />
Orientation Manual
Dear <strong>Physician</strong>,<br />
Welcome to a 35-year-old tradition of medical excellence. We are<br />
pleased you’ve chosen the <strong>AvMed</strong> network as a partner in providing<br />
quality health care to Floridians of all ages and walks of life.<br />
The enclosed materials will help you work effortlessly with <strong>AvMed</strong> to<br />
ensure fast service and prompt payment. If you or your staff have any<br />
questions about our forms, policies or procedures, please call your<br />
<strong>Physician</strong> Service Representative or contact the Provider Service<br />
Center at 1-800-452-8633.<br />
Visit www.avmed.org to find several useful documents and tools.<br />
Accessing <strong>AvMed</strong> online can give you and your staff quick answers and<br />
easy access to important information. You are also invited to join our<br />
Quality Improvement Program and be part of our continuing efforts<br />
to provide you and your patients with the best service possible.<br />
On behalf of all of us at <strong>AvMed</strong>, we look forward to providing you with<br />
unparalleled service and peace of mind.<br />
Sincerely,<br />
Barry Wagner<br />
Vice President of Network<br />
<strong>AvMed</strong> Health Plans
<strong>Physician</strong><br />
Orientation<br />
Manual<br />
Table of Contents<br />
<strong>Physician</strong> Support /Responsibilities ............................................................................................................ 04<br />
Claims ................................................................................................................................................. 05<br />
Electronic Claims Submission<br />
Claims Entry Online<br />
Paper Claims Submission<br />
Benefit Coordination .............................................................................................................................. 06<br />
Benefit Coordination Team<br />
Authorizations<br />
Utilization Management .......................................................................................................................... 08<br />
Utilization Review<br />
Discharge Planning<br />
Clinical Pharmacy Management<br />
Care Management Programs<br />
Member Benefits & Eligibility .....................................................................................................................10<br />
Co-payments/Care Coordination<br />
Eligibility Listings<br />
Pharmacy Benefits/Drug Formulary<br />
Important Resources .............................................................................................................................. 12<br />
Credentialing ........................................................................................................................................ 13<br />
Quality Activity .......................................................................................................................................14<br />
<strong>AvMed</strong>’s Quality Improvement Program<br />
<strong>Physician</strong> Assessment Audits<br />
Clinical Guidelines ................................................................................................................................... 15
<strong>Physician</strong><br />
Support /<br />
Responsibilities<br />
<strong>AvMed</strong> makes sure that you receive all the support and information you need.<br />
You will be assigned a personal <strong>Physician</strong> Service<br />
Representative responsible for introducing you to<br />
<strong>AvMed</strong> Health Plans and to troubleshoot problems,<br />
explain responsibilities, offer assistance and to visit you<br />
and your staff. Our goal is to make your participation as<br />
rewarding as possible.<br />
The Provider Service Center is your chief link to <strong>AvMed</strong><br />
Health Plans. The staff at the Center can help you with<br />
any questions about policies and procedures, to report<br />
or request a change in your panel status, address/phone,<br />
covering physician, hospital privileges, Tax ID and<br />
Licensure or any other service issue. You may contact the<br />
Provider Service Center weekdays between 8:30 am and<br />
5:00 pm at 1-800-452-8633.<br />
<strong>Physician</strong> Services<br />
Important Contact Information<br />
Provider Service Center:<br />
PO Box 569004<br />
Miami, FL 33256-9004<br />
1-800-452-8633 (Option 3)<br />
Fax: 305-671-6149<br />
Toll Free: 1-877-231-7695<br />
E-mail: Providers@avmed.org<br />
In addition to your <strong>Physician</strong> Service Representative and<br />
the Provider Service Center, the <strong>Physician</strong> Reference<br />
Guide is an excellent support tool full of information.<br />
The <strong>Physician</strong> Reference Guide can be found on the<br />
<strong>AvMed</strong> Web Site at www.avmed.org.<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 1 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ <strong>Physician</strong> responsibilities<br />
■ In-office laboratory guidelines<br />
■ When to call the Provider<br />
Service Center<br />
■ Basic agreement highlights<br />
4 • <strong>AvMed</strong> <strong>Physician</strong> Orientation Manual
Claims<br />
Ninety-eight percent of <strong>AvMed</strong> claims are processed within 10 days.<br />
<strong>AvMed</strong> requires that all claims be submitted within 180<br />
days from the date of service. In addition, all requests<br />
for review or appeal have to be received within 150<br />
days from the date on which the explanation of<br />
payment was printed.<br />
Electronic Claims Submission<br />
<strong>AvMed</strong> receives claims electronically from the following<br />
clearinghouses: Emdeon, ProxyMed, ENS, ZirMed, Office<br />
Ally, Availity, SSI and eHDL.<br />
Claims Entry Online<br />
Please go to <strong>AvMed</strong>’s Web Site at www.avmed.org and<br />
click on <strong>Physician</strong>s & Care Providers. Then select the<br />
Provider Services Online section to learn more about<br />
submitting claims online.<br />
Paper Claims Submission<br />
<strong>Physician</strong>s should always bill their usual and customary<br />
fees. <strong>AvMed</strong> will pay the lesser of your contractual<br />
agreement or the Medicare allowance for Medicare<br />
members. When billing commercial member claims,<br />
<strong>AvMed</strong> will pay at your contractual agreement rates.<br />
Claims<br />
Important Contact Information<br />
To submit claims:<br />
PO Box 569000<br />
Miami, FL 33256-9000<br />
To query claims status:<br />
PO Box 569004<br />
Miami, FL 33256-9004<br />
1-800-452-8633 (Option 2)<br />
Fax: 1-800-452-5182<br />
To request claims<br />
review/appeal:<br />
PO Box 569004<br />
Miami, FL 33256-9004<br />
1-800-452-8633 (Option 2)<br />
Fax: 1-800-452-3847<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 2 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ Claims related information<br />
■ Adjustments<br />
■ Coordination of Benefits<br />
■ Reimbursements<br />
<strong>AvMed</strong> <strong>Physician</strong> Orientation Manual • 5
Benefit<br />
Coordination<br />
Ninety-eight percent of <strong>AvMed</strong> physicians find it easy to obtain referrals and authorizations.<br />
Benefit Coordination Team<br />
Each regional office is comprehensively supported by the Benefit<br />
Coordination Team, a highly trained clinical and administrative staff.<br />
When a request is submitted for authorization, an <strong>AvMed</strong> Medical<br />
Director and the Benefit Coordination Team will provide consistent<br />
application of internal procedures/guidelines, nationally recognized<br />
criteria and administration of benefit limitations. These initiatives<br />
can be best accomplished by coordinating your clinical expertise<br />
with the clinical and cost management know-how of the <strong>AvMed</strong><br />
Medical Directors and Benefit Coordination Team.<br />
<strong>AvMed</strong>’s authorization process has been designed to achieve and<br />
sustain coordinated and efficient service for <strong>AvMed</strong> members.<br />
This process also allows <strong>AvMed</strong> to identify and enroll members in<br />
pre-planned discharge planning (Speedy Recovery) and specialized<br />
programs, such as Disease and Case Management.<br />
The Benefit Coordination Team constantly strives to enhance<br />
the partnership with your office via a commitment to enhanced<br />
teamwork, effective communication and first-class customer<br />
service. Their goal is to provide you and <strong>AvMed</strong> Members — your<br />
patients — with high-quality and cost-effective care.<br />
Authorizations<br />
Authorizations for simple referrals/consultations to participating<br />
specialists, as well as for most services provided in a<br />
participating physician’s office, are not required; however, a<br />
referral is required by select plans. <strong>AvMed</strong> values the role of the<br />
Primary Care <strong>Physician</strong> (PCP) and requires that most members<br />
select a PCP. We expect that the PCP will continue to play the same<br />
integral role with our members by coordinating their medical care<br />
with specialists and other health care providers.<br />
6 • <strong>AvMed</strong> <strong>Physician</strong> Orientation Manual
For services requiring an authorization from <strong>AvMed</strong>, the<br />
prescribing physician should submit an Authorization<br />
Request Form via fax to 1-800-552-8633. If the service<br />
is deemed emergent or urgent, contact the Authorization<br />
Team directly by calling 1-800-816-5465.<br />
Primary Care <strong>Physician</strong>s and Specialists are encouraged<br />
to utilize the <strong>AvMed</strong> Link line and Web authorization<br />
modules to obtain select automated authorizations and to<br />
check member benefits and eligibility. <strong>AvMed</strong>’s automated<br />
authorization process is easy and fast. You and your staff can<br />
access <strong>AvMed</strong> Link by calling 1-800-816-LINK (5465). It’s<br />
as fast as the average credit card authorization. Additional<br />
information on authorizations can be found in the Quick Tips<br />
tab of this kit.<br />
The Service Plus department works closely with the Benefits<br />
Coordination Team and is responsible for admissions to an<br />
inpatient facility on an emergent/urgent basis either from the<br />
physician’s office or an emergency room.<br />
Benefits Coordination<br />
Important Contact Information<br />
Hours of Operation: 6:00 am – 10:00 pm<br />
Automated system is available seven days a<br />
week for simple referrals and authorization<br />
confirmation 8:30 am – 5:00 pm,<br />
Monday through Friday for<br />
coordinator-assisted authorizations<br />
Provider Authorizations<br />
Requests/confirmations:<br />
<strong>AvMed</strong> Link<br />
1-800-816-LINK<br />
(1-800-816-5465)<br />
Pre-Auth Fax: 1-800-55AVMED<br />
(1-800-552-8633)<br />
Service Plus: 7 days, 24 hours<br />
1-888-ER-AVMED (1-888-372-8633)<br />
Weekend Discharge Planner:<br />
1-888-372-8633 (Option 4)<br />
For Eye Care Referral:<br />
Primary Plus/CompBenefits, Inc.:<br />
1-800-393-2873<br />
For Mental Health Referral:<br />
Psychcare, LLC - North (Gainesville,<br />
Jacksonville, Orlando and Tampa):<br />
1-800-305-5886<br />
UMBH - South (Miami-Dade, Broward, Palm<br />
Beach and Southwest):<br />
1-800-294-8642<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 3 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ Authorization requirements<br />
■ Services requiring authorization<br />
■ Services not requiring authorization<br />
■ How to obtain an authorization<br />
<strong>AvMed</strong> <strong>Physician</strong> <strong>Physician</strong>s Orientation Manual • 00 • 7
Utilization<br />
Management<br />
<strong>AvMed</strong> provides the resources you need to give your patients the best care.<br />
Utilization Review<br />
In addition to daily authorizations by the Benefits Coordination<br />
Team, <strong>AvMed</strong>’s Utilization Management department examines the<br />
overall frequency of procedures by a doctor. Utilization Management<br />
(UM) approvals are handled by clinical personnel, all of whom<br />
have unrestricted licenses in the State of Florida, at the regional<br />
office level. Concurrent reviews are conducted both on site and by<br />
telephone. Doctors are invited to contact their regional office or<br />
Medical Director to discuss any UM denial decision.<br />
Discharge Planning<br />
Discharge planning is performed at each regional office. Discharge<br />
planners (RNs/LPNs) are licensed by the State of Florida and the<br />
Discharge Coordinators (non-clinical) work with the Utilization<br />
Management Coordinators in the facilitation of member’s access to<br />
benefits for discharge arrangements.<br />
<strong>AvMed</strong> recognizes that health care doesn’t stop after 5:00 pm.<br />
Service Plus performs Discharge Planning after normal business<br />
hours and weekends. The Service Plus program provides several<br />
24/7 services to help make things easier for you and your patients.<br />
Clinical Pharmacy Management<br />
The Clinical Pharmacy Management Department is located in<br />
Gainesville and administers the Prescription Drug Plan statewide.<br />
Pharmacists supervise clinical decision-making. Under the<br />
supervision of the Director of Clinical Pharmacy, non-clinical staff<br />
provides technical support.<br />
If you or your staff have any questions on dispensing limits and<br />
coverage guidelines you can access the latest information in the<br />
Coverage and Dispensing Limits Guide section at www.avmed.org,<br />
by clicking on the Useful Shortcuts and selecting Drug List.<br />
8 • <strong>AvMed</strong> <strong>Physician</strong> Orientation Manual
Care Management Programs<br />
<strong>AvMed</strong>’s Care Management and Disease Management<br />
programs are administered at both the regional offices<br />
and centralized locations. Interested <strong>AvMed</strong> members<br />
will discuss their eligibility and enrollment with you.<br />
Each eligible member is assigned a Registered Nurse,<br />
called a Care Coordinator, who works closely with you,<br />
medical directors and ancillary services to monitor and<br />
control their condition. If you are interested in enrolling<br />
a member, you should contact Disease Management at<br />
1-800-972-8633 and the Care Coordinator will contact<br />
you to discuss the referral. The programs are free and<br />
member participation is voluntary.<br />
Care Management Programs include:<br />
■ Complex Case<br />
■ Cancer Care<br />
■ Chronic Kidney Disease and Transplant<br />
Disease Management Programs include:<br />
■ Congestive Heart Failure<br />
■ Asthma/Chronic Obstructive Pulmonary Disease<br />
■ Wound Care<br />
■ Diabetes<br />
■ High Risk Pregnancy<br />
■ Coronary Artery Disease<br />
Utilization Management<br />
Important Contact Information<br />
Disease Management:<br />
1-800-972-8633<br />
Discharge Planning:<br />
1-888-372-8633<br />
Pharmacy:<br />
1-800-237-1255, ext. 40665<br />
Plan Medical Directors<br />
Broward: 954-462-2520<br />
Fax: 954-627-6280<br />
Miami-Dade: 305-671-0126<br />
Fax: 305-671-4770<br />
Gainesville: 352-337-8860<br />
Fax: 352-337-8870<br />
Jacksonville: 904 858-1311<br />
Fax: 904-858-1358<br />
Orlando: 1-800-227-4848<br />
Fax: 407-975-1634<br />
Tampa: 1-800-257-2273<br />
Fax: 1-800-572-6252<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 3 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ Utilization Management<br />
■ Access to Utilization Management staff<br />
■ <strong>AvMed</strong>’s Nurse On Call<br />
<strong>AvMed</strong> <strong>Physician</strong> <strong>Physician</strong>s Orientation Manual • 00 • 9
Member<br />
Benefits<br />
& Eligibility<br />
<strong>AvMed</strong> provides quick and easy access to eligibility listings at www.avmed.org.<br />
Co-payments/Care Coordination<br />
<strong>AvMed</strong> offers many benefit plans and riders. Most<br />
plans have varying co-payments, deductible and/or<br />
co-insurance, limitations and exclusions. Please be aware<br />
that the co-payment associated with various services may<br />
differ from plan to plan, and while not all plans require<br />
the member to select a Primary Care <strong>Physician</strong> (PCP),<br />
we emphasize the importance of coordination of care.<br />
Eligibility Listings<br />
Primary Care <strong>Physician</strong>s should receive a monthly<br />
“eligibility list” around the first day of each month for<br />
all members whose plan requires them to select a PCP.<br />
You can also view current eligibility listings via the web<br />
at www.avmed.org.<br />
Pharmacy Benefits/Drug Formulary<br />
Most members have a prescription rider for<br />
prescription medications coverage, which varies in terms<br />
of covered medications, co-payments and quarterly<br />
maximum benefit dollar amounts. All prescriptions must<br />
be filled at a participating pharmacy. In addition to the<br />
contracted independently owned pharmacies, <strong>AvMed</strong>’s<br />
pharmacy network includes: CVS, Winn Dixie, Long’s<br />
Drugs, Walgreens, Publix, Target, Navarro and Sedanos.<br />
We encourage the use of cost-effective prescribing<br />
habits. Use the <strong>AvMed</strong> Health Plans Two-Tier and Three-<br />
Tier Preferred Drug Lists, found on our Web site, for<br />
the most updated information available. If a physician<br />
or a member requests a brand name medication when a<br />
10 • <strong>AvMed</strong> <strong>Physician</strong> Orientation Manual
generic equivalent is available, most members will have<br />
to pay the cost difference between the brand and generic<br />
products plus their applicable co-payment, which is<br />
determined by the member’s prescription benefit.<br />
The Coverage and Dispensing Limit Guide is a reference<br />
that is used in addition to the Preferred Drug Lists.<br />
You can access the lists at www.avmed.org.<br />
This reference provides additional information about a<br />
member’s benefits including:<br />
■ Drugs requiring Prior Authorization<br />
■ Drug-Specific Quantity Limits<br />
■ Exclusion to the Prescription Drug Benefit<br />
This reference is provided as a tool for medication<br />
therapy selection. The final choice of medication selection<br />
for an <strong>AvMed</strong> member rests with the prescriber and<br />
the member. Situations may arise in which non-covered<br />
medications are medically warranted. If that occurs, you<br />
must complete and fax a Medication Exception Request<br />
Form to the Clinical Pharmacy Management Department,<br />
with supporting documentation to 1-800-552-8633.<br />
Member Benefit/Eligibility<br />
Important Contact Information<br />
Member Benefit/Eligibility:<br />
Member Services:<br />
1-800-882-8633<br />
Provider Service Center:<br />
1-800-452-8633 (Option 1)<br />
<strong>AvMed</strong> LINK Line:<br />
1-800-816-LINK<br />
North Fax: 352-337-8612<br />
South Fax: 305-671-4936<br />
<strong>AvMed</strong> Web Site: www.avmed.org<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 4 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ Member benefits<br />
■ Eligibility<br />
■ Product information<br />
<strong>AvMed</strong> <strong>Physician</strong> Orientation Manual • 11
Important<br />
Resources<br />
24/7 access to <strong>AvMed</strong> Service Plus for your administrative, home care and patient needs.<br />
For general questions and to<br />
request supplies:<br />
Provider Service Center<br />
P.O. Box 569004,<br />
Miami FL 33256-9004<br />
1-800-452-8633, Fax: 305-671-6149<br />
or Fax: 1-877-231-7695<br />
E-mail to: Providers@avmed.org<br />
To obtain authorizations, confirm<br />
authorizations and verify<br />
member eligibility:<br />
Pre-Authorization Call Center/(<strong>AvMed</strong> Link):<br />
1-800-452-8633, Fax: 1-800-552-8633<br />
(for all faxed requests)<br />
Confirm authorization online at our Web site,<br />
under <strong>Physician</strong>s & Care Providers<br />
To submit claims:<br />
Claims (Statewide)<br />
P.O. Box 569000<br />
Miami, FL 33256-9000<br />
To query claims status and request<br />
reviews/appeals:<br />
Claims & Reviews/Appeals Phone: 1-800-452-8633 (Option 2)<br />
Claims Status Fax: 1-800-452-5182<br />
Claims Review/Appeals Fax: 1-800-452-3847<br />
Review status claims online at our Web site, under<br />
<strong>Physician</strong>s & Care Providers<br />
For eye care referrals:<br />
Primary Plus/CompBenefits, Inc.<br />
(Jacksonville, Southwest, Orlando, Tampa,<br />
Miami-Dade, Broward & West Palm Beach):<br />
1-800-393-2873<br />
For questions regarding member benefits:<br />
Member Services – North<br />
(Gainesville, Jacksonville, Orlando,<br />
Tampa & Tallahassee):<br />
1-800-882-8633, Fax: 352-337-8612<br />
Member Services - South<br />
(Miami-Dade, Broward,<br />
West Palm Beach & Southwest):<br />
1-800-882-8633, Fax: 305-671-4736<br />
Verify member eligibility/benefits at our<br />
Web site, under <strong>Physician</strong>s & Care Providers<br />
For Mental Health/Behavioral Health:<br />
South - University of Miami<br />
Behavioral Health (UMBH)<br />
(Miami-Dade, Broward and West Palm Beach):<br />
1-800-294-8642<br />
North – Psychcare, LLC.<br />
(Gainesville, Jacksonville, Orlando,<br />
Tampa and SW Florida):<br />
1-800-305-5886<br />
To refer suspect issues, anonymously<br />
if preferred:<br />
Audit Services & Investigation Unit:<br />
1-877-286-3889<br />
For authorizations that originate in the ER<br />
or direct admits from the doctor’s office:<br />
Service Plus 24/7:<br />
1-888-372-8633<br />
For disease management:<br />
Disease Management:<br />
1-800-972-8633<br />
12 • <strong>AvMed</strong> <strong>Physician</strong> Orientation Manual
Credentialing<br />
<strong>AvMed</strong> wants you to become part of a 35-year tradition of quality health care.<br />
An important component of <strong>AvMed</strong> Health Plans’ Quality<br />
Improvement process is the Credentialing Program. The<br />
Credentialing Program is designed to ensure that participating<br />
practitioners possess the practice experience, licenses,<br />
certifications, privileges, professional liability coverage, education<br />
and other professional qualifications to provide a level of<br />
professionally recognized care. When selecting providers, <strong>AvMed</strong><br />
does not discriminate against sex, race, religion, creed, color, age<br />
and/or national origin.<br />
Composed of multi-disciplinary representation of participating<br />
community physicians, the Credentialing Committee reviews<br />
applications and credentials of each practitioner upon credentialing<br />
and re-credentialing. In the event that a practitioner is denied recredentialing,<br />
the practitioner will be given the right to a hearing.<br />
Credentialing<br />
Important Contact Information<br />
<strong>AvMed</strong>’s Credentialing<br />
Department:<br />
Contact your <strong>Physician</strong><br />
Service Representative<br />
Council for Affordable Quality Health<br />
care (CAQH):<br />
1-888-599-1771<br />
You will be notified of the Credentialing Committee’s decision within 30<br />
days following the monthly committee meeting. <strong>Physician</strong>s also have the<br />
right, upon request, to be informed of the status of their application.<br />
All practitioners may review information submitted in support of their<br />
credentialing applications. This information is limited to data that is<br />
not peer-review protected and can be obtained by the practitioner<br />
from the same primary sources utilized by <strong>AvMed</strong>.<br />
All practitioners have the right to correct erroneous information<br />
submitted to <strong>AvMed</strong> by another party. In the event that any<br />
information obtained during the credentialing process varies<br />
substantially from the information provided to <strong>AvMed</strong> by the<br />
practitioner, the practitioner will be notified in writing and asked<br />
to submit written clarification. All information obtained in the<br />
credentialing process is maintained in a confidential manner.<br />
There is no appeal mechanism available to a practitioner who is<br />
denied initial credentialing into <strong>AvMed</strong>’s Network.<br />
To start your credentialing process, please contact your<br />
<strong>Physician</strong> Service Representative.<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 6 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ Credentialing<br />
■ Re-credentialing<br />
■ Ambulatory Site Standards<br />
<strong>AvMed</strong> <strong>Physician</strong> Orientation Manual • 13
Quality Activity<br />
The Quality Improvement program lets you impact the future of <strong>AvMed</strong> health care.<br />
<strong>AvMed</strong>’s Quality Improvement Program<br />
The policies, procedure and activities of the <strong>AvMed</strong> Health Plans<br />
Quality Improvement (QI) Department are integrated into a<br />
single Quality Improvement Program. <strong>AvMed</strong>’s Board of Directors<br />
oversees the program to ensure that QI functions are timely,<br />
consistent and effective. The following are audits performed by<br />
<strong>AvMed</strong> as part of our QI initiatives.<br />
<strong>Physician</strong> Assessment Audits<br />
Medical Record Audits: Primary Care <strong>Physician</strong>s may receive an<br />
annual medical record review audit within their outpatient offices.<br />
A corrective action plan will be requested when your score is below<br />
<strong>AvMed</strong>’s minimum compliance level.<br />
Quality Activity<br />
Important Contact Information<br />
Quality Improvement:<br />
Contact your <strong>Physician</strong> Service<br />
Representative<br />
Risk Management:<br />
1-800-346-0231<br />
Fax: 352-337-8526<br />
Accessibility and Availability: Primary Care <strong>Physician</strong>s may<br />
be assessed annually to ensure their compliance with making<br />
appointments for members within the recommended <strong>AvMed</strong><br />
guidelines. A corrective action plan will be requested when your<br />
score is below <strong>AvMed</strong>’s minimum compliance level.<br />
After Hours Accessibility: Primary Care <strong>Physician</strong>s are assessed<br />
annually for member’s ability to reach their PCP after hours. According<br />
to the PCP contract, you or a designee must be available to members<br />
24 hours a day, 7 days a week.<br />
Member Satisfaction with their PCP: <strong>AvMed</strong> conducts surveys<br />
to determine member satisfaction with their PCP. These surveys<br />
are conducted and the results are tabulated for <strong>AvMed</strong> by an NCQA<br />
certified market research firm. When appropriate, results are<br />
calculated and forwarded to each PCP for review and action.<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 7 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ Quality Activities<br />
■ Advance Directives<br />
■ Disrobing Guidelines<br />
■ Risk Management<br />
■ A sample Membership<br />
Satisfaction Survey<br />
14 • <strong>AvMed</strong> <strong>Physician</strong> Orientation Manual
Clinical<br />
Guidelines<br />
The NCQA* rates <strong>AvMed</strong>’s clinical performance “Excellent.”<br />
<strong>AvMed</strong>’s comprehensive and informative Clinical Guidelines range<br />
from Asthma to Postpartum Care. These guidelines have been<br />
drawn from the National Institutes for Health and other leading<br />
health organizations such as the American Diabetes Association<br />
and the March of Dimes.<br />
It’s the physician’s responsibility to periodically check for<br />
updates to these guidelines, which can be found under Quality<br />
Improvements at www.avmed.org, or in the <strong>Physician</strong> Reference<br />
Guide set of PDFs.<br />
*The National Committee for Quality Assurance<br />
Additional Information<br />
found at www.avmed.org.<br />
Refer to Chapter 8 of the<br />
<strong>Physician</strong> Reference Guide for:<br />
■ Clinical Guidelines<br />
■ Behavioral Health<br />
Clinical Practice<br />
■ Pediatric Preventive Care<br />
■ Adult Preventive Care<br />
Recommendations<br />
<strong>AvMed</strong> <strong>Physician</strong> Orientation <strong>Physician</strong>s Manual • 00 15
www.avmed.org<br />
<strong>AvMed</strong> Health Plans<br />
Regional Offices<br />
Miami<br />
Ft. Lauderdale<br />
Tampa Bay<br />
Orlando<br />
Jacksonville<br />
Gainesville<br />
MP-0000 (00/06)<br />
AVM-EMKFR01ER<br />
<strong>AvMed</strong> Health Plans (health benefit plan) is the brand name used for products<br />
and services provided by <strong>AvMed</strong>, Inc. Plans contain limitations and exclusions.
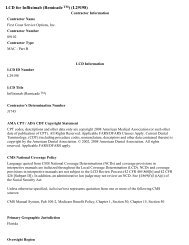
Authorization Request Form<br />
Link Line: 1-800-816-5465<br />
Fax: 1-800-552-8633<br />
For Urgent/Emergent requests, contact <strong>AvMed</strong>’s PreAuthorization Department at this number:<br />
1-800-816-5465<br />
NOTICE: Failure to complete this form in its entirety may result in delayed processing or an adverse determination due to<br />
insufficient information.<br />
Existing Authorization Number:<br />
Date(s) of Service:<br />
Member Information<br />
Name: (first and last)<br />
<strong>AvMed</strong> ID#:<br />
A ___ ___ ___ ___ ___ ___ ___ ___ - ___ ___<br />
Type of Request<br />
Outpatient Surgery<br />
Inpatient Admission<br />
Transplant<br />
Outpatient Drug / Chemotherapy<br />
Speedy Recovery<br />
Date Change only – DOS ______/ ______/ ______<br />
Wound Care<br />
Predetermination<br />
Non Par Request<br />
Home Health<br />
Date of Birth: ______/ ______/ ______<br />
Nuclear Cardiology (i.e. Thallium Scan)<br />
Complex Radiological Procedures<br />
i.e. CT/CT Angiogram, MRI, MRA, Pet Scans and<br />
includes in-office, DTF or outpatient settings<br />
Requesting <strong>Physician</strong> (PCP or Specialist) Referred to: Facility Hospital <strong>Physician</strong><br />
Name:<br />
Name:<br />
<strong>AvMed</strong> Provider#:<br />
Telephone #: (<br />
) _____________________________<br />
<strong>AvMed</strong> Provider#:<br />
Additional information as indicated:<br />
Fax#: ( ) _____________________________<br />
Contact Person:<br />
Diagnosis and Procedure Information<br />
ICD9 Diagnosis Code(s):<br />
Diagnosis Description:<br />
CPT4 Procédure / DME Code(s):<br />
Procedure Description:<br />
NOTE: This request cannot be processed without Supporting Clinical Documentation, e.g. office visit note(s); pertinent<br />
laboratory results; prior treatment(s) note(s).<br />
MP-1437 (7/2007)
Please fax completed form to <strong>AvMed</strong> Claims Department: FAX: 1-305-671-6121<br />
Dear Member:<br />
Your <strong>AvMed</strong> contract provides for benefits to be coordinated with other medical insurance by which you may<br />
be covered. The primary carrier pays first when there is more than one insurance company or health care<br />
provider. In order to expedite your claim(s) process, please complete the following information:<br />
NOTE: If the reason for your medical care was not due to an accident related injury, do not complete Section I<br />
of the questionnaire. You should complete Section I and III only when applicable.<br />
Patient Member ID Number _______________________<br />
Patient Name ______________________________<br />
Provider Name _________________________<br />
Date of Service ________________________<br />
SECTION I<br />
Is the reason for your visit to your doctor due to an injury caused by an accident?<br />
Yes _____ No _____<br />
If so, please indicate:<br />
Auto _______ Home _______ School _______ Other ___________________________________________<br />
Date of Accident ________________ How and where accident happened:<br />
__________________________________________________________________________________________<br />
__________________________________________________________________________________________<br />
Was a third party responsible for the injury? Yes ____ No ____<br />
If so, provide the following:<br />
Name of individual or company: _______________________________________________________________<br />
Name and address of attorney representing third party insurance company or party responsible:<br />
__________________________________________________________________________________________<br />
________________________________________________________________________________________<br />
SECTION II<br />
Full name of your spouse: _________________________________________________________________<br />
Spouse’s Birth date: ____________________ Social Security Number: ____________________________<br />
Spouse’s Employer: _______________________________________________________________________<br />
Employer’s Address: ______________________________________________________________________<br />
________________________________________________ Telephone Number: _____________________<br />
Is your spouse covered by any other Health Insurance Company: _____Yes ______No<br />
If YES, give name, address and telephone number of Health Insurance Company:<br />
_________________________________________________________________________________________<br />
________________________________________________ Telephone Number: _______________________<br />
Policy Number: ______________________________ Effective Date: _____________________________<br />
Type of Coverage: ______ Family ______Couple ______ Single<br />
Do you have Medicare coverage?<br />
Part A ____ Effective Date ______________<br />
Part B ____ Effective Date ______________<br />
SECTION III (Information to be filled out only if auto accident)<br />
Were you in your own or someone else’s vehicle? _____________________________________________<br />
Name of your insurance company: __________________________________________________________<br />
Amount of PIP coverage: _________________________ Amount of Deductible: ___________________<br />
If represented by an attorney, please provide the following: Attorney name, address and telephone #:<br />
__________________________________________________________________________________________<br />
________________________________________________________________________________________<br />
Subscriber/Member Signature______________________________________ Date _____________________<br />
MP-1488 Revised 5/17/06
<strong>AvMed</strong> Directory Information Change Form<br />
Please complete this form and return as soon as possible to have your directory changes<br />
reflected on the <strong>AvMed</strong> website and in the printed directories.<br />
Fax to 305-671-6149<br />
or email to: providers@avmed.org<br />
or mail to:<br />
<strong>AvMed</strong> Health Plans<br />
Provider Service Center<br />
9400 Dadeland Blvd, Ste 420<br />
Miami, FL 33156<br />
1. Please fill in ALL information in this section. Make Address corrections on next page.<br />
Provider Name<br />
(As it should appear in the directory. Use middle initial if desired)<br />
Provider <strong>AvMed</strong> # Provider Tax ID #<br />
Specialty<br />
(Heading in the directory under which your name should appear)<br />
Contact Name<br />
Phone#<br />
Person authorized to make these changes<br />
2. Fill in ONLY the information that should be changed.<br />
Fill in the parentheses as follows: (A) for Addition (D) for Deletion (C) for Change<br />
( ) Panel Comments<br />
(Age restrictions and/or other panel comments)<br />
( ) Board Certified (Year)<br />
(Attach a copy of certificate)<br />
( ) Group Practice Name<br />
(Please abbreviate. Field is limited to 24 characters)<br />
( ) Group Practice Name<br />
( ) Languages<br />
Your comments
<strong>AvMed</strong> Directory Information Change Form - continued<br />
Fill in ONLY the information that should be changed.<br />
Fill in the parentheses as follows: (A) for Addition (D) for Deletion (C) for Change<br />
First Location:<br />
County<br />
( ) Provider Address ( ) Suite<br />
( ) City ( ) State ( ) Zip<br />
( ) Phone ( ) Fax ( ) Email<br />
( ) Office Hours<br />
Second Location:<br />
County<br />
( ) Provider Address ( ) Suite<br />
( ) City ( ) State ( ) Zip<br />
( ) Phone ( ) Fax ( ) Email<br />
( ) Office Hours<br />
Third Location:<br />
County<br />
( ) Provider Address ( ) Suite<br />
( ) City ( ) State ( ) Zip<br />
( ) Phone ( ) Fax ( ) Email<br />
( ) Office Hours<br />
Fourth Location:<br />
County<br />
( ) Provider Address ( ) Suite<br />
( ) City ( ) State ( ) Zip<br />
( ) Phone ( ) Fax ( ) Email<br />
( ) Office Hours
AVMED VERIFICATION FORM<br />
Dear <strong>AvMed</strong> Patient:<br />
Our records show you are not on our AVMED eligibility list. You will receive services today with the understanding that<br />
you may be billed and held financially responsible in the unlikely event that your coverage is not effective for one of the<br />
following reasons:<br />
- Your membership has lapsed<br />
- The services are not a covered benefit<br />
- You have selected a different Primary Care <strong>Physician</strong> this month<br />
- Your enrollment application is still being processed, has not been received or cannot be verified by<br />
AVMED<br />
I HAVE READ THE ABOVE AND UNDERSTAND MY POSSIBLE FINANCIAL RESPONSIBILITY TO<br />
DOCTOR ___________________________________.<br />
I HEREBY AFFIX MY SIGNATURE AS AN ACKNOWLEDGEMENT OF THIS UNDERSTANDING. I<br />
AUTHORIZE AVMED TO DESIGNATE THIS PHYSICIAN AS MY PRIMARY CARE PHYSICIAN AS OF<br />
TODAY’S DATE.<br />
_____________________________<br />
Patient’s Signature/Date<br />
_____________________________<br />
Patient’s Name (Please Print)<br />
_____________________________<br />
AVMED/ID Number<br />
(If not sure, use *Subscriber’s SS#)<br />
_____________________________<br />
Office Staff Signature/Date<br />
_____________________________<br />
Employer/Group Name (If Applicable)<br />
_____________________________<br />
AVMED Provider Number<br />
*SUBSCRIBER IS THE PERSON WHO WORKS FOR THE EMPLOYER WHO OFFERS AVMED COVERAGE.<br />
TO PHYSICIAN’S OFFICE: AVMED members who are required to select a PCP and are not on your eligibility list should<br />
sign this form. Mail forms to AVMED so that your eligibility listing can be updated.<br />
Send to the following address:<br />
<strong>AvMed</strong> Health Plans<br />
P.O. Box 823<br />
Gainesville, FL 32602-0823<br />
Attn: Member Services<br />
Fax: (352) 337-8612
MP-3160 (10/07)<br />
Contact Numbers<br />
Phone: 800-452-8633<br />
Fax: 800-835-6132<br />
Medication Exception Request Form<br />
RETAIL PHARMACY AND IN OFFICE MEDICATIONS<br />
Please note, if your patient is on <strong>AvMed</strong> Medicare, this form cannot be used to request:<br />
• Medicare Part D excluded drugs, including but not limited to, barbiturates, benzodiazepines, fertility<br />
drugs, drugs prescribed for weight loss, weight gain or hair growth, over-the-counter drugs, or<br />
prescription vitamins (except prenatal vitamins and fluoride preparations).<br />
Please specify delivery requested:<br />
In Office (Supplied & Administered)<br />
Retail Pharmacy Pick-Up<br />
CuraScript Specialty Pharmacy<br />
Delivered to office<br />
Delivered to patient for self-injection<br />
Delivered to patient for Home Health to administer<br />
Facility (i.e. out-patient)<br />
Date of this request:<br />
Type of request:<br />
New<br />
Update<br />
Name:<br />
Member Information<br />
Name:<br />
Prescriber Information<br />
<strong>AvMed</strong> ID: Vendor #:<br />
DOB: Sex: M F Phone: Fax:<br />
Current Weight:<br />
Contact:<br />
Diagnosis:<br />
Diagnosis and Medication Information<br />
Diagnosis Code(s):<br />
Medication:<br />
Strength: Route: Frequency:<br />
Expected length of therapy:<br />
*Procedure Codes:<br />
This request cannot be processed without SUPPORTING DOCUMENTATION such as:<br />
• Office visit notes<br />
• Current lab results<br />
• Alternative therapies or treatments contraindicated/previously tried and failed<br />
(including dose, length of therapy, and adverse outcome)<br />
Please fax all URGENT/EMERGENT REQUESTS to <strong>AvMed</strong> Health Plans at 352-337-8737.<br />
(*ONLY REQUIRED FOR IN-OFFICE SUPPLY AND ADMINISTRATION.)
<strong>AvMed</strong> Health Plans<br />
Order Form<br />
Please complete this form and return as soon as possible.<br />
Fax: 305-671-6149<br />
Toll-free Fax: 1-877-231-7695<br />
or mail to: <strong>AvMed</strong> Health Plans<br />
Provider Service Center<br />
9400 Dadeland Blvd, Ste 420<br />
Miami, FL 33156<br />
1. Please fill in all information in this section.<br />
Person Requesting<br />
Phone Number<br />
Best time to call<br />
Provider <strong>AvMed</strong> # Provider Tax ID #<br />
Provider Name<br />
Mailing Address<br />
Suite<br />
City State Zip<br />
2. Please fill in quantities requested if applicable.<br />
Network Directory<br />
<strong>Physician</strong>s Reference Guide<br />
Office Orientation<br />
MP-1445 Advance Directives Member Pamphlet<br />
GP-1062 Allergy Stickers - For outside your Medical Record<br />
MP-1437 Authorization Request Form<br />
MP-1538 <strong>AvMed</strong> Link Referral Sheet (Pad)<br />
MP-1056 Envelopes - Attn: Claims Dept. (yellow)<br />
MP-1058 Envelopes - Attn: Claims Review & Appeal Dept. (pink)<br />
MP-1435 Lead Screening Labels - For Medical Records Documentation<br />
MP- 3160 Medication Exception Request Form<br />
MP- 2118 Prenatal Care Assessment Stickers<br />
MP-1843 Problems and Medication Summary (Pad) - For Medical Records Documentation<br />
MP- 2105 Request For Claims Review/Appeal<br />
MP- 2106 Request For Claims Status
Fax completed referral RX form to Priority Healthcare:<br />
PHONE# 877-634-8555 FAX# 866-877-1342<br />
<strong>Physician</strong> Name: ______________________________________ Office Contact/RN Name: ________________<br />
Phone Number: ________________________________ Fax Number: __________________________________<br />
Address: ___________________________________ City: ___________________ State: _____ Zip: _________<br />
DEA #: ______________________<br />
Patient Information<br />
Patient Name: _____________________________________ DOB: ___________ Member #: ________________<br />
Address: ___________________________________ City: ____________________ State: _____ Zip: _________<br />
Home Phone: ________________________________ Daytime Phone: __________________________________<br />
Allergies:__________________________________________________ Height: __________Weight: _________<br />
Primary Diagnosis: __________________________________________________Dx Code:__________________<br />
Insurance Information<br />
Primary Policy: Patient Spouse Parent<br />
Primary Insurance: <strong>AvMed</strong> Health Plans<br />
Insurance Phone: 1-800-816-5465<br />
Policy Holder's Name: _________________________<br />
Group Number: ______________________________<br />
Drug Delivery Information<br />
* If drug requires Prior Authorization send<br />
appropriate documents (i.e.: notes, test results, etc.).<br />
In-Office Delivery<br />
Just in Time Program*<br />
Drug Replacement Program*<br />
Home Delivery<br />
Other (ex: delivery to work): ________________<br />
*Program requires physician enrollment with <strong>AvMed</strong><br />
Prescription<br />
Prescription: (select, stamp or write below) New Patient Refill Request<br />
Medication Strength Directions Quantity<br />
Date: ______________________ <strong>Physician</strong>’s Signature: _________________________________<br />
Date Needed: ___________________________ (Please allow 48 hours for delivery)<br />
IMPORTANT NOTICE: This facsimile is intended to be delivered to the named addressee and may contain material that is confidential, privileged, proprietary or<br />
exempt from disclosure under applicable law. If it is received by anyone other than the named addressee, the recipient should immediately notify the sender at the address<br />
and telephone number set forth herein and obtain instructions as to disposal of the transmitted material. In no event should such material be read or retained by other than<br />
the named addressee, except by express authority of the sender to the named addressee.
REQUEST FOR CLAIM: REVIEW APPEAL<br />
INSTRUCTIONS FOR COMPLETING FORM<br />
1. Submit legible copies of CMS 1500 or UB92 form to process your request accordingly.<br />
2. Check the most appropriate box below for type of review requested.<br />
3. Use only one form per review type/per member. You may attach more than one claim per review type.<br />
PLEASE PRINT<br />
MEMBER IDENTIFICATION NUMBER<br />
MEMBER NAME<br />
Date of Request:<br />
-<br />
FIRST:<br />
_________________________________________________________________<br />
LAST:<br />
_________________________________________________________________<br />
DATE OF<br />
SERVICE:<br />
CLAIM #<br />
_________/_________/___________________<br />
_______________________________________<br />
Fax Your Request To:<br />
(800) 452-3847<br />
OR<br />
FROM: CONTACT PERSON PHONE FAX<br />
________________________________________________________________________________________________________________________________<br />
PROVIDER NAME<br />
PROVIDER NUMBER<br />
________________________________________________________________________________________________________________________________<br />
ADDRESS<br />
Mail To: (Statewide)<br />
<strong>AvMed</strong> Health Plans<br />
P O Box 569004<br />
Miami, FL 33256-9004<br />
________________________________________________________________________________________________________________________________<br />
CITY STATE ZIP<br />
________________________________________________________________________________________________________________________________<br />
TAX ID#<br />
Corrected Claim<br />
A corrected claim is enclosed for:<br />
Units<br />
Service Code (CPT / HCPCS / REVENUE CODE)<br />
Member ID Number<br />
Other Correction (please describe below)<br />
Implant / Prosthetic Device<br />
(Invoice or purchase order enclosed)<br />
Cost: $ + % = $ expected<br />
__________ _______ ____________ reimbursement<br />
Claim Paid Incorrectly<br />
Units Paid Incorrectly<br />
Payment Sent To Wrong Address<br />
Payment Made To Wrong Provider<br />
Payment Not Correct According To Contract<br />
DME: Purchase Authorized, Rental Paid<br />
Other: (Describe request in detail)<br />
Authorization Denial<br />
Claim denied for “no auth” but services do not<br />
require an authorization<br />
Services were authorized, please review<br />
Authorization # ________________________<br />
Specific services were not authorized, but were<br />
medically necessary<br />
(See enclosed appeal letter and supporting documentation<br />
describing the situation)<br />
Other Denial<br />
Consult Report Not Received<br />
(See enclosed consult report)<br />
Member Is Not Assigned To Your Panel<br />
(Proof of member assignment dates enclosed)<br />
Member Not Eligible At Time Of Service<br />
(See enclosed eligibility documentation)<br />
Untimely Filing<br />
(See enclosed appeal letter describing the situation)<br />
Lack Of COB Information<br />
(COB form signed by member is enclosed)<br />
Service Covered Under Capitation<br />
NOTE: Your contract allows a specified time period to request a review. This date is calculated from the date of the original notice of payment or denial<br />
on the explanation of payment report. Late claim reviews or appeals cannot be considered.<br />
TO REORDER ADDITIONAL FORMS CALL THE PROVIDER SERVICE CENTER AT 1-800-452-8633.<br />
MP-2105 (11/06)
REQUEST FOR CLAIM STATUS<br />
INSTRUCTIONS FOR COMPLETING FORM<br />
• Submit legible copies of CMS 1500 or UB92 form to process your request accordingly, or<br />
• Please enter the claims information on this form.<br />
Please Print<br />
FROM: CONTACT PERSON PHONE FAX<br />
Date of Request:<br />
______________________________________________________________________________________________________________________________________________<br />
PROVIDER NAME PROVIDER NUMBER<br />
______________________________________________________________________________________________________________________________________________<br />
ADDRESS<br />
_____________________________________________________________________________________________________________________________________________<br />
CITY STATE ZIP<br />
Fax Your Request To: Mail To:<br />
(800) 452-5182 OR P O Box 569004<br />
Miami, FL 33256-9004<br />
For <strong>AvMed</strong> Use Only<br />
Member<br />
ID #<br />
Member<br />
Name<br />
DOS<br />
Amount<br />
Billed<br />
Paid Amount or<br />
Denial Code Description<br />
Check<br />
Number<br />
Check<br />
Date<br />
Comments:<br />
_____________________________________________________________________________________________________________________<br />
_____________________________________________________________________________________________________________________<br />
REMINDER: Your contract allows a specified time period to request a review. This date is calculated from the date of the original notice of payment or denial on the<br />
explanation of payment report. Late claim reviews or appeals cannot be considered.<br />
Claims Service Rep: ________<br />
TO REORDER ADDITIONAL FORMS CALL THE PROVIDER SERVICE CENTER AT 1-800-452-8633.<br />
MP-2106 (12/04)
<strong>AvMed</strong> Risk Management<br />
Incident Report<br />
COVER SHEET<br />
Complete your identification in the “From” section.<br />
Transmit both sides of the completed Risk Management Incident Report within 24 hours<br />
of the occurrence and promptly mail original report to address at top of form.<br />
For assistance call <strong>AvMed</strong> Corporate Director of Risk Management at 1-800-346-0231<br />
Confidentiality: This transmission is a privileged communication and is<br />
protected by Florida Law.<br />
Date:<br />
To:<br />
<strong>AvMed</strong> Corporate Director, Risk Management<br />
Fax: 1-352-337-8526<br />
Phone: 1-800-346-0231<br />
From:<br />
(Provider)<br />
(Fax, Phone)<br />
(Address)<br />
(City, Sate, Zip)<br />
Number of Pages, Including Cover Sheet ______<br />
Confidentiality Note:<br />
The information contained in this facsimile message may be legally privileged and confidential<br />
information intended only for the use of the individual or entity named above. If the reader of this<br />
message is not the intended recipient, you are hereby notified that any dissemination, distribution, or<br />
copying of this telecopy is strictly prohibited. If you have received this telecopy in error, please<br />
immediately notify us by telephone and return the original message to us at the address above by the<br />
United States Postal Service. Thank you.<br />
HARD COPY WILL FOLLOW BY MAIL
Get a quick payment estimate!<br />
<strong>AvMed</strong>’s Cost Share Calculator allows<br />
you to quickly estimate the payment due<br />
from an <strong>AvMed</strong> member with a deductible<br />
or co-insurance benefit plan.* This Web<br />
tool is easy to access and can be used<br />
right at the time of service to determine<br />
the member’s responsibility. It can also<br />
be used to check deductible totals or<br />
co-insurance values.<br />
To access the Cost Share Calculator, log on to <strong>AvMed</strong>’s Web Site at www.avmed.org. Click on <strong>Physician</strong>s & Care<br />
Providers and then Provider Services Online. Once you enter your provider and PIN number, you will see the<br />
link to Cost Share Calculator under the left menu bar.<br />
To get an estimate of the member’s responsibility through the Cost Share Calculator, please follow these steps:<br />
1. Specify your county, the fee schedule your contract stipulates, along with the reimbursement percentage, then click Next.<br />
2. Enter member information including member number, deductible remaining and applicable co-insurance.<br />
Note: you can view deductible totals and co-insurance values from a link where the member information is entered.<br />
3. Enter CPT4 code information.<br />
4. Click Submit to display the estimated results for member responsibility.<br />
If you would like more information or if you need to confirm your provider or<br />
PIN number, please contact <strong>AvMed</strong>’s Provider Service Center at 1-800-452-8633.<br />
* Please note that this tool only supplies an estimate of the final costs for which the member is responsible. The actual value will not be determined until the claim<br />
is adjudicated.
<strong>AvMed</strong> ePay<br />
<strong>AvMed</strong> ePay<br />
<strong>AvMed</strong> ePay allows you to receive fast direct deposit payment,<br />
review patient eligibility and instantly check claim status, all<br />
through your e-mail. Your Explanation of Payment (EOP)<br />
can be delivered in the HIPAA 835 transaction format or as<br />
an interactive PDF attachment that has several convenient<br />
functions including downloading your claim to Excel,<br />
retrieving past EOPs and making a claim adjustment. You<br />
will need Adobe Acrobat Reader 6.0 or higher installed on your<br />
computer in order to enroll and use the EOP interactive PDF.<br />
<strong>AvMed</strong> ePay Advantages<br />
Using <strong>AvMed</strong> ePay gives you several advantages:<br />
■ Secure and private correspondence<br />
■ Simplified claims reconciliations for improved cash flow<br />
■ Payments electronically transferred into your bank<br />
account within minutes<br />
■ Access from your e-mail 24 hours a day, 7 days a week<br />
■ Reducing or eliminating costs and time associated with<br />
manual process<br />
Required Information<br />
Before enrolling in <strong>AvMed</strong> ePay, you will need to gather<br />
the following information:<br />
■ Provider Information<br />
• Provider Name<br />
• Provider Tax ID number<br />
■ Billing Information<br />
• E-mail address of recipient(s) to receive EOPs<br />
• Billing address<br />
• Contact name and telephone number<br />
■ Bank Account Information<br />
• Bank Routing Number<br />
• Bank Account Number<br />
• Bank Account Name<br />
• Type of account (savings, checking)<br />
• Bank’s name and address<br />
Enrollment<br />
If you belong to a group practice, only the group should<br />
enroll for <strong>AvMed</strong> ePay. Allow up to 10 days for <strong>AvMed</strong><br />
to process your enrollment after you have submitted the<br />
appropriate forms. You can easily enroll in <strong>AvMed</strong> ePay<br />
through these simple steps:<br />
1) Visit www.avmed.org and log on to Provider Services<br />
Online using your Provider ID and PIN.<br />
2) Click as directed to begin the enrollment process, fill out<br />
your Federal Tax ID number and click Next.<br />
3) On the next page enter your Provider or Group number<br />
and name, and a contact name and an email address<br />
to receive the enrollment invitation. You can specify a<br />
unique password to open the enrollment invitation or<br />
the password will default to your <strong>AvMed</strong> Payee number.<br />
Click the Enroll button in the “Action” section.<br />
4) <strong>AvMed</strong> will send you an invitation to the ePay program<br />
to authorize your Electronic Funds Transfer (EFT). You<br />
must open the secure PDF form attachment using the<br />
password you specified in Step 3 above. Fill out the<br />
required bank and billing information. Provide a password<br />
to protect and open your future EOPs, then click Submit<br />
to see a printable version. Print, sign and then fax or mail<br />
the document with a voided check to <strong>AvMed</strong>. Adobe<br />
Acrobat Reader is required for this step.<br />
Using the E-EOP<br />
Electronic funds transfers for approved claims are made once<br />
a week, and the e-mail containing your EOP attachment will<br />
be sent at that time. You will need your password to open the<br />
interactive PDF. The e-mail will include the hint that you chose<br />
during enrollment to help you remember your password. The<br />
functioning buttons of the EOP include:<br />
■ Overpayment Advice – Jumps to the page of the<br />
Overpayment Advice included with your EOP<br />
■ Request Previous EOP – Jumps to the page that allows<br />
you to obtain a copy of an earlier EOP for reference<br />
■ View FAQ – Opens a page of the <strong>AvMed</strong> Web Site<br />
containing ePay questions and answers<br />
■ Download Excel – Opens a new Excel document<br />
with the details of the claims<br />
■ Claim Adjustment – Allows you to submit an<br />
adjustment request and explanation online<br />
If you would like more information about <strong>AvMed</strong> ePay,<br />
please contact the <strong>AvMed</strong> Provider Service Center<br />
at 1-800-452-8633.<br />
MP-4088 (05/08)
Products<br />
<strong>AvMed</strong> Products at a Glance<br />
PRODUCT<br />
<strong>AvMed</strong><br />
Choice<br />
<strong>AvMed</strong><br />
Open<br />
Access<br />
<strong>AvMed</strong><br />
Consumer<br />
<strong>AvMed</strong><br />
HSA-Compatible<br />
HDHPs<br />
<strong>AvMed</strong><br />
Classic<br />
<strong>AvMed</strong><br />
Open<br />
Access POS<br />
<strong>AvMed</strong><br />
Classic POS<br />
Medicare<br />
Premier Care<br />
Medicare<br />
Preferred PPO<br />
DESCRIPTION<br />
Allows a member to use any doctor, any hospital, anywhere in the United States, all referral<br />
free. The member’s co-payments, deductible and co-insurance will vary depending on the<br />
network the member selects.<br />
A plan that allows members to freely see any <strong>AvMed</strong> physician without a referral. With <strong>AvMed</strong><br />
Open Access, members are not required to designate a Primary Care <strong>Physician</strong> (PCP) upon<br />
enrollment. However, <strong>AvMed</strong> encourages members to visit a PCP for routine and preventive<br />
care. Members agree to use an <strong>AvMed</strong> network doctor or hospital in order to have expenses<br />
covered, except for emergency care or in special situations when authorized by <strong>AvMed</strong>.<br />
<strong>AvMed</strong>’s consumer-directed (CDHP) product line allows employers to design plans for<br />
their employees by pairing the <strong>AvMed</strong> products with funding mechanisms such as Health<br />
Reimbursement Arrangements (HRAs and HSAs). The plans encourage preventive care and<br />
generally have higher deductibles and co-insurance. They are designed to lower premiums<br />
for employers while engaging consumers in all aspects of their health care.<br />
Specialized consumer-directed health plans (CDHPs) generally have lower premiums and can<br />
be paired with Health Savings Accounts (HSAs). The HSA-compatible High-Deductible Health<br />
Plans (HDHPs) are designed to actively engage consumers in using and choosing their health<br />
benefits, while providing them access to a tax-free account that can serve as a long-term<br />
savings mechanism for health care expenses.<br />
A plan that allows for fully coordinated health care within the <strong>AvMed</strong> network. With <strong>AvMed</strong><br />
Classic, members choose a Primary Care <strong>Physician</strong> (PCP) for routine and preventive care. A PCP<br />
coordinates visits to specialists. Members agree to use a network doctor or hospital to have<br />
expenses covered. Various co-payments, co-insurance and deductible options are available.<br />
A POS plan that allows members referral-free office visits for any <strong>AvMed</strong> physician and the<br />
freedom to go outside the <strong>AvMed</strong> network at any time for most services. With <strong>AvMed</strong> Open<br />
Access POS, members are not required to designate a Primary Care <strong>Physician</strong> (PCP) upon<br />
enrollment. However, <strong>AvMed</strong> encourages members to visit a PCP for routine and preventive care.<br />
A POS plan that allows for coordinated health care through a Primary Care <strong>Physician</strong> (PCP)<br />
within the <strong>AvMed</strong> network, and offers a member the freedom to seek care outside the<br />
network at any time for most services.<br />
A Medicare Advantage HMO plan that uses a full network of <strong>AvMed</strong> participating Primary Care<br />
<strong>Physician</strong>s, Specialists, Hospitals and other providers located in Miami-Dade and Broward<br />
counties. A member can use any provider who is part of the <strong>AvMed</strong> Premier Care Network.<br />
A Medicare Advantage PPO plan that uses a full network of <strong>AvMed</strong> participating Primary Care<br />
<strong>Physician</strong>s, Specialists, Hospitals and other providers located in Miami-Dade and Broward<br />
counties. A member can use any provider who is part of the <strong>AvMed</strong> Medicare Preferred<br />
PPO Network or providers who accept Medicare but do not participate in <strong>AvMed</strong>’s Medicare<br />
Preferred PPO Network at a nonparticipating provider rate.<br />
MP-4089 (05/08)
Authorizations<br />
Authorization Tips<br />
Services Requiring An Authorization<br />
■ Inpatient Hospitalizations (Acute, Observation, Skilled<br />
Nursing, Vent and Rehabilitation admissions Mental<br />
Health must be rendered through our capitated providers<br />
■ Outpatient Surgery in an Ambulatory Surgery Center<br />
or Hospital Setting* (Includes cardiac catherization and<br />
PTCA but excludes specific CPT4 codes that can be found<br />
on our Web Site at www.avmed.org)<br />
■ Complex Radiology Procedures performed In-Office,<br />
Outpatient Diagnostic Testing Facility, or Outpatient<br />
Hospital Setting* (Defined as CT, CT-Angiography, MRI,<br />
MRA, PET Scans, Myocardial Perfusion Imaging [MPI] and<br />
Cardiac Blood Pool Imaging Services)<br />
■ Hemodialysis<br />
■ Transplants<br />
■ Home Health Care* (Any service rendered by Home<br />
Health Care Agency, including therapy and drug<br />
administration/infusion services<br />
■ Outpatient Drug Infusion Services and Injection Therapy*<br />
(Defined as infusion/administration performed outside of<br />
a physician office not billed with a location 11)<br />
■ In-Office “Select” Drug Administration<br />
(Codes: See list of codes under Quick Tips)<br />
■ ALL Non-Participating Providers*<br />
* These services do not require authorization for Members who are covered<br />
by our Choice product, or our POS product while using the POS benefit for<br />
non-participating providers.<br />
Quick Tips<br />
■ Simple referrals no longer require authorization, however<br />
a referral from the PCP for select plans is required.<br />
■ WEB/VRU are available for quick entry authorizations,<br />
no faxing required. (excludes Complex Radiology, Home<br />
Health, Inpatient Admissions/Hemodialysis/Transplant<br />
Services/Outpatient Drug Therapy)<br />
■ Labs should still be sent to our contracted providers<br />
for processing unless they are listed on the In-Office<br />
Laboratory Guidelines and billed per guideline or member<br />
has out-of-network benefits. (Quest Diagnostics for<br />
Miami, Ft. Lauderdale, Southwest, Palm Beach, Tampa,<br />
Orlando and Gainesville Plan Areas and Consolidated<br />
Laboratory for Jacksonville Plan Area)<br />
■ Services rendered In-Office not outlined specifically under<br />
Services Requiring an Authorization will no longer require<br />
prior authorization. In-Office is defined as a physician<br />
office not contracted by <strong>AvMed</strong> as a facility and billed in<br />
a location 11.<br />
■ If you are unsure how your office is set up with <strong>AvMed</strong><br />
please contact your <strong>Physician</strong> Service Representative for<br />
further explanation.<br />
■ Services such as outpatient therapy in any setting,<br />
except therapy delivered in the Home setting, no longer<br />
requires authorization, as they are not noted in the above<br />
Authorization Requirements.<br />
■ No authorization is required for specific CPT4 Codes<br />
that are done in a participating providers office or<br />
outpatient surgical facility or hospital.<br />
■ The following codes require authorization in the<br />
physician office setting (location 11):<br />
Q0136 Procrit/Epogen J1440 Neupogen<br />
Q4055 Procrit/Epogen J1441 Neupogen<br />
J2505 Neulasta J2820 Leukine<br />
J0880 Aranesp J9999 Misc<br />
J1563 IVIG J3490 Misc<br />
J1745 Remicade C9003 Synagis<br />
J0215 Amevive<br />
■ Drug administration and infusion services delivered in any<br />
setting, excluding In-Office setting, require authorization<br />
(see specific drugs requiring authorization above)<br />
■ For more detailed information regarding Authorization<br />
Requirements, please refer to Chapter 3, Benefits<br />
Coordination/Utilization Management, of the <strong>Physician</strong><br />
Reference Guide.<br />
■ The following are not covered benefits<br />
when supplied In-Office:<br />
• Oral Medications<br />
• Inhaled Medications<br />
• Nebulized Medications<br />
(except Albuterol and Ipratroptium/Atrovent)<br />
• Self-injectables (some exceptions are made<br />
for Medicare Members)<br />
■ For the most current Authorization Request Fax Form,<br />
please refer to Forms on the Web.<br />
Continued on other side<br />
MP-4090 (05/08)
IN-OFFICE LABORATORY GUIDELINES<br />
The tests below are on the approved physician in-office lab list and will be considered routine.<br />
No chief complaint or sick diagnosis is required to receive payment.<br />
CODE<br />
DESCRIPTION<br />
82270 BLOOD, OCCULT, BY PEROXIDASE ACTIVITY (EG, GUAIAC), QUALITATIVE; FECES<br />
86580 SKIN TEST; TUBERCULOSIS, INTRADERMAL<br />
87210 SMEAR, PRIMARY SOURCE WITH INTERPRETATION; WET MOUNT FOR INFECTIOUS<br />
87220 TISSUE EXAMINATION BY KOH SLIDE OF SAMPLES FROM SKIN, HAIR, OR NAILS FOR<br />
The tests listed below are payable when services are rendered in the physician’s office and only<br />
when the member is treated for a chief complaint or sick diagnosis. If the visit is a well or preventive<br />
medicine visit, please send all specimens to your local <strong>AvMed</strong> contracted laboratory provider.<br />
CODE<br />
DESCRIPTION<br />
81000 URINALYSIS, BY DIP STICK OR TABLET REAGENT FOR BILIRUBIN, GLUCOSE<br />
81001 URINALYSIS, BY DIP STICK OR TABLET REAGENT FOR BILIRUBIN, GLUCOSE<br />
81002 URINALYSIS, BY DIP STICK OR TABLET REAGENT FOR BILIRUBIN, GLUCOSE<br />
81003 URINALYSIS, BY DIP STICK OR TABLET REAGENT FOR BILIRUBIN, GLUCOSE<br />
81015 URINALYSIS; MICROSCOPIC ONLY<br />
81025 URINE PREGNANCY TEST, BY VISUAL COLOR COMPARISON METHODS<br />
82247 BILIRUBIN, TOTAL<br />
82465 CHOLESTEROL, SERUM OR WHOLE BLOOD, TOTAL<br />
82803 GASES, BLOOD, ANY COMBINATION OF PH, PCO2, PO2, CO2, HCO3<br />
82947 GLUCOSE; QUANTITATIVE, BLOOD (EXCEPT REAGENT STRIP)<br />
82948 GLUCOSE; BLOOD, REAGENT STRIP<br />
82962 GLUCOSE, BLOOD BY GLUCOSE MONITORING DEVICE(S) CLEARED BY THE FDA<br />
83014 HELICOBACTER PYLORI; BREATH TEST ANALYSIS FOR UREASE ACTIVITY<br />
85004 BLOOD COUNT, AUTOMATED DIFFERENTIAL WBC COUNT<br />
85007 BLOOD COUNT; BLOOD SMEAR, MICROSCOPIC EXAMINATION WITH MANUAL<br />
85013 BLOOD COUNT; SPUN MICROHEMATOCRIT<br />
85014 BLOOD COUNT; HEMATOCRIT (HCT)<br />
85018 BLOOD COUNT; HEMOGLOBIN (HGB)<br />
85025 BLOOD COUNT; COMPLETE (CBC), AUTOMATED (HGB, HCT, RBC, WBC AND PLATELET<br />
85610 PROTHROMBIN TIME<br />
85651 SEDIMENTATION RATE, ERYTHROCYTE; NON-AUTOMATED<br />
86308 HETEROPHILE ANTIBODIES; SCREENING<br />
87081 CULTURE, PRESUMPTIVE, PATHOGENIC ORGANISMS, SCREENING<br />
87086 CULTURE, BACTERIAL; QUANTITATIVE COLONLY COUNTY, URINE<br />
87430 INFECTIOUS AGENT ANTIGEN DETECTION BY ENZYME IMMUNOASSAY TECHNIQUE<br />
87880 INFECTIOUS AGENT DETECTION BY IMMUNOASSAY WITH DIRECT OPTICAL<br />
If you have any<br />
questions regarding<br />
the information<br />
to the left,<br />
please contact<br />
the Provider<br />
Service Center at<br />
1-800-452-8633.<br />
All lab work<br />
should be sent<br />
to the following<br />
<strong>AvMed</strong> contracted<br />
Laboratories:<br />
Jacksonville<br />
Plan Area –<br />
Consolidated<br />
Laboratory<br />
Miami, Ft. Lauderdale,<br />
Southwest, Palm<br />
Beach, Tampa,<br />
Orlando, Gainesville<br />
Plan Areas –<br />
Quest Diagnostics
Web Site<br />
<strong>AvMed</strong> Web Site Guide<br />
www.avmed.org<br />
REQUIREMENTS<br />
<strong>AvMed</strong> Provider number and PIN. (Same numbers utilized<br />
when requesting authorization via the link)<br />
WELCOME PAGE<br />
Take an online tour and maximize the benefits of your<br />
online experience. Designed for use by all providers, the<br />
tour takes you through each of <strong>AvMed</strong>’s services for<br />
providers, explaining each page in detail. No Provider<br />
number or PIN required for tour.<br />
■ Click on <strong>Physician</strong>s & Care Providers<br />
(upper right hand circle)<br />
■ Click on Provider Services Online<br />
■ Insert <strong>AvMed</strong> Provider ID<br />
(<strong>AvMed</strong> six digit provider number)<br />
■ Insert PIN<br />
■ Click on Log In button<br />
PROVIDER SERVICES ONLINE<br />
Choose from the following menu options:<br />
■ Important Communications<br />
■ Authorization Requirements<br />
■ Claim Entry<br />
■ Claim Inquiries<br />
■ Clear Claim Connection<br />
■ Cost Share Calculator<br />
■ Medicare Benefits References<br />
■ Member Eligibility<br />
■ Mini Health Record (printable)<br />
■ Provider References<br />
■ Referral Entry<br />
■ Referral Inquiries<br />
■ Chan ge My PIN<br />
■ Update My E-mail Options<br />
Important Communications<br />
Recent important communications that have been mailed<br />
or faxed to providers can be found here.<br />
Authorization requirements<br />
A detailed description of services requiring authorization,<br />
quick tips and quick links to the following:<br />
■ In-Office Laboratory Guidelines<br />
■ Current list of Specific CPT4 Codes that do not require<br />
authorization<br />
■ Chapter 3 (Benefits Coordination/Utilization<br />
Management) of the <strong>Physician</strong> Reference Guide<br />
■ Current Authorization Request Fax Form<br />
Claim Entry<br />
This allows you to submit CMS1500 claims directly to <strong>AvMed</strong> via<br />
our Web Site. To enter a claim online, follow the steps below:<br />
1) Type the Patient/Insured’s last name and ID# and click<br />
on the Patient Lookup button. You will be taken to<br />
the CMS 1500 Form. The patient’s information will<br />
automatically be populated.<br />
2) Enter your Tax ID# and click the Lookup button. For<br />
multiple providers with the same Tax ID#, a drop<br />
down list will appear in order to select the treating<br />
physician. The provider information will automatically<br />
be populated.<br />
3) Enter all required claim information into the CMS 1500<br />
form and click the Submit button.<br />
4) Once you click Submit, you will receive a confirmation<br />
number. Please make a note of it for your records. Click<br />
New Claim to continue, or End Session to end your<br />
claims entry session.<br />
Helpful Tips:<br />
If a provider is not in our claim entry database, click on the<br />
link at the top of the CMS 1500 form: “click here to enter<br />
or modify provider data.”<br />
The member information can be changed once it is<br />
populated on the CMS 1500 form. If a patient is not found,<br />
click on the New Patient Click Below button. You will be<br />
able to status your claims within 24-48 hours.<br />
Reporting Options<br />
■ View Claims Log Sheet – This button will allow you to<br />
view a spreadsheet of all claims done for the date of<br />
entry you specify.<br />
■ View Claim – This button will allow you to view a<br />
spreadsheet of claims by one of the following options:<br />
• Member ID and Date of Service<br />
• Confirmation #<br />
• User Name and Date of Service<br />
Claim Inquiries – Search by:<br />
■ Authorization Number<br />
■ Claim Number<br />
■ Member ID<br />
■ Patient Account Number<br />
■ Rejected Claims (EDI claims only)<br />
■ Reports<br />
• Provider claims received report<br />
• Denied claims report<br />
For detailed claim information, click on the highlighted<br />
claim number.<br />
Continued on other side<br />
MP-4091 (05/08)
Web Site (continued)<br />
Clear Claim Connection<br />
You can view how <strong>AvMed</strong>’s code auditing software<br />
evaluates code combinations during the adjudication of a<br />
claim by entering certain claim data elements.<br />
To run a claim through Clear Claim Connection,<br />
follow these steps:<br />
1) Click one of the gender buttons<br />
2) Enter the member’s date of birth<br />
3) Enter the procedure codes and<br />
modifier (if applicable)<br />
4) Enter the date of service<br />
5) Enter the place of service<br />
6) Click Review Claim Audit Results<br />
The results will be shown with a recommended value of<br />
“Allow, Disallow or Review.” A Clinical Edit Clarification will<br />
be provided for claims with a recommendation value of<br />
“Disallowed or Review.” To view a Clinical Edit Clarification,<br />
double-click on the procedure line, and then click Review<br />
Clinical Edit Clarification.<br />
Cost Share Calculator<br />
This allows you to calculate an estimate of the patient’s<br />
responsibility at the time of service for <strong>AvMed</strong> members<br />
with a deductible and/or co-insurance benefit plan.<br />
Please note that this tool supplies an estimate of the final<br />
cost for which the member is responsible. The actual value<br />
will not be determined until the claim is adjudicated.<br />
To get an estimate of the member’s responsibility through<br />
the Cost Share Calculator, follow these steps:<br />
1) Specify your county, the fee schedule your<br />
contract stipulates, along with the reimbursement<br />
percentage, then click Next<br />
2) Enter member information including member<br />
number, deductible remaining and applicable<br />
co-insurance. Note: you can view deductible totals<br />
and co-insurance values from a link where the<br />
member information is entered<br />
3) Enter CPT4 code information<br />
4) Click Submit to display the estimated results for<br />
member responsibility<br />
MEdicare benefits references<br />
This provides you with the current years Medicare Benefits<br />
by Plan and County.<br />
Member Eligibility – Search by:<br />
■ Member ID<br />
■ Member’s Name<br />
■ Search your panel<br />
■ List Your Panel (Individual or Group)<br />
For detailed member information (including benefits),<br />
click on the highlighted member number.<br />
Mini Health record<br />
Allows you to print a Mini Health Record for <strong>AvMed</strong><br />
members/patients prior to a visit or whenever the<br />
information is required. The printable record shows the<br />
last 90 days of medical claims, pharmacy claims and<br />
authorizations.<br />
Provider References – To obtain:<br />
■ Medication List<br />
■ Decision Support Center<br />
■ Clinical Guidelines (Adobe Acrobat Required)<br />
■ Orientation Documents<br />
■ Provider Directory<br />
■ <strong>Physician</strong> Reference Guide (Adobe Acrobat Required)<br />
Referral Entry<br />
To obtain authorization for simple referrals:<br />
■ Enter Member ID number, referred to provider<br />
number, diagnosis code, CPT code<br />
■ Click the Request Authorization button on referral<br />
entry screen<br />
■ Authorization number with details will be displayed.<br />
This information can be printed.<br />
Note: At this time, referral entry is limited to those services<br />
that are currently authorized automatically via <strong>AvMed</strong> Link<br />
Referral Inquiries – Search by:<br />
■ Inpatient Admission<br />
■ Referred from provider<br />
■ Referred to Provider<br />
■ Inpatient by Tax ID Number<br />
■ Request by Tax ID Number<br />
For detailed authorization information, click on the<br />
highlighted Authorization Number. Authorization<br />
information can be printed.<br />
In addition, from the <strong>AvMed</strong> Homepage via Useful<br />
Shortcuts, the following can be accessed:<br />
Continued on next page
Web Site (continued)<br />
■ Urgent Care Centers<br />
■ Medication List (If no Internet access please contact Provider<br />
Services for a hard copy)<br />
■ Contact Provider Services (allows you to e-mail <strong>AvMed</strong>’s<br />
Provider Service Center)<br />
change my pin<br />
Allows you to change your current PIN. Please be aware that if<br />
you choose to change your PIN, it will be necessary for you to<br />
notify all internal and external users who will be conducting<br />
business utilizing your PIN.<br />
Update My E-mail Options<br />
You can provide an e-mail address for communications.<br />
Additional Web Site Resources<br />
■ Online Provider Directory<br />
■ Forms<br />
■ Emergency Preparedness Resources<br />
■ Electronic Data Interchange (EDI)<br />
■ Provider Publications<br />
■ Quality Improvement<br />
■ Fraud, Waste and Abuse<br />
■ Frequently Asked Questions<br />
If you do not have either a Provider ID Number<br />
or PIN Number, please contact the<br />
Provider Service Center at 1-800-452-8633
OB/GYN<br />
<strong>AvMed</strong> OB/GYN Guidelines<br />
These guidelines are for <strong>AvMed</strong>’s Obstetrician’s,<br />
Gynecologists, Midwives and their staff. They should answer<br />
most questions regarding procedures for <strong>AvMed</strong> members.<br />
OBSTETRICAL GUIDELINES<br />
As an obstetrician, you become the member’s primary<br />
care physician for the duration of the pregnancy. As such,<br />
members whose plan requires PCP assignment must be<br />
assigned to your panel of members. On or about the<br />
1 st of each month, you will receive a monthly eligibility<br />
listing. You can also obtain a current eligibility list on our<br />
Web site at www.avmed.org. Please check this listing<br />
when <strong>AvMed</strong> members present for services. If a member<br />
whose plan requires PCP assignment is not on your<br />
panel, please have the member contact Member Services<br />
for re-assignment to your panel for the duration of her<br />
pregnancy. Fetal non-stress tests performed in the office do<br />
not require authorization. OB ultrasounds do not require<br />
authorization. Please notify <strong>AvMed</strong> if the delivery does<br />
not occur in a hospital.<br />
<strong>AvMed</strong>’s global payment is inclusive of the delivery,<br />
antepartum and postpartum care, as well as all hospital<br />
and office services provided throughout the member’s<br />
pregnancy. When billing with the appropriate industry<br />
standard CPT code for the initial OB visit, the physician<br />
will be paid $100. This amount is prepaid and deducted<br />
from the global delivery fee and payment is contingent<br />
upon care being provided throughout the pregnancy<br />
(antepartum, delivery and postpartum). An additional<br />
amount of $100 will be withheld when billing for global<br />
OB care and will be reimbursed when postpartum care is<br />
provided 21-56 days following delivery and accompanied<br />
with CPT code 59430.<br />
Note: In order to receive your full contract rate for complete<br />
OB care, you must bill the initial OB visit and the postpartum<br />
visits as indicated above.<br />
Non-maternity related admissions are reimbursed on<br />
a fee for service basis with authorization from <strong>AvMed</strong>’s<br />
Pre-Authorization Department. Non-maternity office<br />
visits submitted with a non-maternity diagnosis code are<br />
also payable fee for service. The member’s co-payment/coinsurance<br />
for each maternity visit is deducted from the<br />
global maternity care payment. If <strong>AvMed</strong> does not receive<br />
an itemized claim, a standard of 10 visit co-payments will<br />
be deducted.<br />
NOTE: If additional day of confinement falls on a weekend<br />
or holiday, the physician may call for authorization on the<br />
next working day.<br />
Circumcisions performed in the hospital setting are<br />
reimbursable under the authorization number for the<br />
delivery. Circumcisions performed in office are covered up<br />
to 12 months after birth, and authorization is not required.<br />
In the event care is transferred or terminated during the<br />
maternity care period, <strong>AvMed</strong> will pay antepartum care<br />
using industry standard CPT codes. Billing guidelines for<br />
antepartum care are as follows:<br />
1-3 visits – bill appropriate Evaluation & Management CPT<br />
codes (1 co-payment per visit will be deducted)<br />
4-6 visits – bill using CPT code 59425 (6 co-payments will<br />
be deducted from this code)<br />
7 or more visits – bill using CPT code 59426<br />
(10 co-payments will be deducted from this code).<br />
HIGH-RISK GUIDELINES<br />
<strong>AvMed</strong> Health Plans will continue to reimburse<br />
additionally for pregnancies that are confirmed high risk<br />
by the <strong>AvMed</strong> Medical Department. It is no longer a<br />
requirement to bill the <strong>AvMed</strong> homegrown code for either<br />
moderate or extreme high-risk pregnancies in order to<br />
be reimbursed correctly. Once the provider has received<br />
authorization approval for the high-risk pregnancy, the<br />
provider will only bill for the appropriate global delivery<br />
code, vaginal or C-section.<br />
Continued on other side<br />
MP-4092 (2/07)
When the claim is submitted and processed, the system<br />
will reimburse based on the authorization in the system.<br />
If two OB/GYN physicians, from separate practices, are<br />
involved in the care of a member during an identified<br />
high-risk pregnancy, the additional payment will be<br />
divided between the two physicians.<br />
Midwives are not eligible for reimbursement<br />
of high-risk pregnancies.<br />
Requesting authorization for high-risk:<br />
When submitting an authorization request for a<br />
pregnancy that is considered high-risk, indicate in the<br />
Additional Information section of the authorization<br />
form “Requesting High Risk Payment”. This will flag the<br />
medical department to review for consideration. Be sure<br />
to enter the Diagnosis Code for High-risk OB and attach<br />
all necessary clinical documentation.<br />
General Medical Criteria for High Risk Pregnancy<br />
■ Multiple Gestation<br />
■ Gestational diabetes or pre-gestational IDDM<br />
■ Chronic hypertension on anti-hypertensive<br />
medication or PIH prior to 37 weeks<br />
■ Intrauterine growth retardation (IUGR) confirmed<br />
by ultrasound<br />
■ Preterm labor requiring tocolytic agents prior<br />
to 37 weeks<br />
■ Incompetent cervix<br />
■ Uterine Fibroids (symptomatic during pregnancy)<br />
■ Overweight when BMI equal to or > 30,<br />
Underweight when BMI is equal to or < 19<br />
■ Hemoglobinopathies including sickle cell disease,<br />
excludes sickle cell trait<br />
■ NYHA Class II, III and IV or cardiac history<br />
(excludes MVP)<br />
■ Chronic Renal Disease<br />
■ Lupus<br />
■ HIV Disease<br />
■ Miscellaneous high-risk patients (Refer to<br />
Medical Director)<br />
GYNECOLOGY GUIDELINES<br />
<strong>AvMed</strong> members may self refer for one annual<br />
gynecological (well woman) exam per calendar year. Use<br />
industry standard CPT codes with Dx. V72.31 when billing<br />
for this service. Reminder, all lab specimens must be sent<br />
to the <strong>AvMed</strong> contracted lab.<br />
Authorization is not required when medically necessary<br />
care is needed during the annual gynecological exam or<br />
follow-up care afterwards. All gynecological surgeries<br />
require authorization. Please do not schedule the surgery<br />
until you have received written confirmation that it has<br />
been authorized. This will avoid unnecessary delays in<br />
the event additional information is needed to process the<br />
authorization request.<br />
FAMILY PLANNING<br />
Family Planning is an <strong>AvMed</strong> covered benefit. Diaphragm<br />
fitting with instructions and insertion of an IUD are payable.<br />
Routinely, IUD supplies are not a covered benefit; please<br />
contact Member Services for benefit verification.<br />
Sterilization, both elective and for medical necessity,<br />
is a covered service with authorization. Elective sterilization<br />
may require a co-payment/co-insurance. Please contact<br />
Member Services to verify the benefit and co-payment/<br />
co-insurance amount. If sterilization is planned through<br />
tubal ligation, authorization is not required. If sterilization<br />
is planned through hysterectomy, authorization is required.<br />
Contraception for birth control is a covered benefit<br />
for members with a group RX benefit that includes<br />
contraceptives. Please contact Member Services to<br />
confirm whether a member has an RX plan that<br />
includes contraceptives.<br />
Depo Provera, when used as a contraceptive, is a covered<br />
service if the member has the contraceptive rider on their<br />
policy. No authorization is required for this service.<br />
When used as a contraceptive, the member will have a<br />
co-payment/co-insurance. Depo Provera, as a<br />
contraceptive, can be administered two ways:<br />
■ You may write a prescription for the drug. The pharmacy<br />
would collect the co-payment/co-insurance, when the<br />
member picks up the Depo. If the member returns to<br />
your office for the injection and you bill for an office visit,<br />
you may collect an office visit co-payment if applicable.<br />
■ The office can supply the drug and collect the<br />
co-payment/co-insurance. If you are billing an office<br />
visit in addition to the Depo injection, an office visit<br />
co-payment should be collected in addition to the<br />
drug co-payment.<br />
If Depo Provera is to be administered for medically<br />
necessary reasons other than birth control, no<br />
authorization is required. Co-payments are applicable<br />
for medically necessary injectable contraceptives.<br />
Termination of pregnancy procedures require<br />
authorization, for groups with said benefit. Please<br />
contact Member Services for benefit verification.
Q<br />
A<br />
Q<br />
A<br />
Q<br />
A<br />
Q<br />
A<br />
Q<br />
A<br />
Frequently Asked Questions<br />
Do I file with the Tax ID or provider number?<br />
You file with both your Federal Tax Number<br />
and your <strong>AvMed</strong> provider number.<br />
Why am I receiving rejects for member<br />
information?<br />
Verify that your Practice Management System<br />
is submitting the patient’s full 11-digit <strong>AvMed</strong><br />
Member ID number and that it is being<br />
submitted at the HIPAA patient level loop.<br />
Must I bill with a modifier on EDI Claims?<br />
The same rules apply as paper claims.<br />
What is a Pin Number?<br />
A Pin Number is an <strong>AvMed</strong> assigned and<br />
secured number that is used to grant access to<br />
our Web site and our Link Line. It is not part of<br />
the EDI Claims submission.<br />
How do I contact your EDI department?<br />
<strong>AvMed</strong> does not have a separate EDI<br />
department. Contact <strong>AvMed</strong>’s Provider Service<br />
Center at 800-452-8633 with your questions.<br />
Benefits of EDI<br />
✔ Increased billing and data<br />
entry accuracy<br />
✔ Reduced adjudication and<br />
payment cycle time<br />
✔ Reduced operating cost<br />
If you have questions, contact<br />
<strong>AvMed</strong>’s Provider Service Center<br />
at 800-452-8633 or write us an<br />
e-mail at providers@avmed.org.<br />
<strong>AvMed</strong>’s Provider Service Center<br />
Online Portal is an excellent tool<br />
for improving office efficiency.<br />
Visit us at<br />
www.avmed.org.<br />
Electronic Data Interchange<br />
for providers<br />
E-Z<br />
EDI<br />
Steps
Provider Select:MD<br />
A Comprehensive Cost Reduction Program for <strong>Physician</strong> Offices and Group Practices<br />
Provider Select, an operations-improvement company focused on<br />
the non-acute care market, is a unit of Premier, Inc., one of the<br />
nation’s largest healthcare alliances. Provider Select is setting a new<br />
standard in supply procurement, distribution and operating cost<br />
reduction through an outstanding portfolio of products and services.<br />
To remain competitive in an expanding and ever-changing marketplace,<br />
physician offices and group practices must identify and<br />
maximize cost-efficiencies while delivering quality patient care.<br />
Our programs and services have demonstrated success at helping<br />
physicians:<br />
• Reduce costs in many areas of their operations,<br />
• Better manage their purchasing, and<br />
• Improve administrative functions.<br />
• A comprehensive portfolio of high-quality products and services tailored<br />
for the physician market.<br />
• Savings on medical and non-medical products, equipment, and services.<br />
• Medical supply distribution and supply management through one source –<br />
McKesson Medical-Surgical – a proven leader in the physician market.<br />
PROVIDER SELECT: MD’S COMMITTED DISTRIBUTOR<br />
As a member of Provider Select: MD physicians and physician<br />
clinics can access favorable pricing from a broad range of leading<br />
healthcare manufacturers. Through our exclusive distribution<br />
agreement with McKesson Medical-Surgical, part of the nation’s<br />
largest multi-market distributor of pharmaceutical and medical<br />
supplies, Provider Select manages the entire supply chain function<br />
– from negotiating and contracting to inventory management and<br />
Streamlining practice operations can help physicians increase their<br />
competitiveness and create more time for quality assurance and<br />
delivering patient care. Through our exclusive physician program<br />
Provider Select: MD we offer measurable savings and unprecedented<br />
opportunity for the physician to control and reduce supplyprocurement<br />
costs and related operating expenses. Provider Select<br />
combines the national purchasing power of Premier’s group<br />
purchasing operations with a non-acute care-focused contracting<br />
approach to address the diverse and unique needs of the physician<br />
market. The comprehensive program encompasses medical supplies,<br />
services, office products, capital, equipment, pharmaceuticals and<br />
distribution.<br />
PROVIDER SELECT: MD BENEFITS<br />
Typical group purchasing organizations offer portfolios that do not<br />
adequately cover products used by physicians. The comprehensive<br />
Provider Select: MD portfolio includes medical and pharmaceutical<br />
products as well as an extensive range of service agreements.<br />
Provider Select: MD also offers:<br />
• Simple participation requirements.<br />
• Access to highly competitive pricing from market-leading manufacturers<br />
and service companies.
superior distribution services. By providing valuable cost<br />
reductions to physicians and group practices coupled with<br />
competitive pricing, McKesson Medical-Surgical has partnered<br />
with Provider Select to focus on lowering costs, improving<br />
productivity and enhancing the quality of patient care.<br />
The Primary Care Division of McKesson Medical-Surgical has a<br />
long history of servicing physician practices. Field-sales account<br />
managers respond to the specialized needs of the primary care<br />
market while collaborating with practices to achieve cost<br />
reductions and supply chain improvements. McKesson Medical-<br />
Surgical is committed to delivering superior healthcare supply<br />
chain management services by providing:<br />
• A nationwide network of over 45 state-of-the-art service centers offering<br />
the most flexible distribution programs to meet the individual needs of each<br />
customer<br />
• The most extensive product lines in the industry, including more than 3,000<br />
manufacturers and over 135,000 line items of product inventory<br />
• Experienced primary-care account managers to support inventory<br />
management using sophisticated information systems, customized order<br />
forms, and detailed product usage reports<br />
• Assistance with inventory levels, product standardization and Provider<br />
Select: MD contract utilization<br />
In addition, Provider Select: MD customers have access to<br />
educational programs to address industry issues and product<br />
information. These materials, including newsletters, videos and<br />
training manuals, inform customers on topics such as OSHA,<br />
CLIA, and Medicare reimbursement.<br />
PARTICIPATION REQUIREMENTS<br />
In return for these outstanding benefits, Provider Select: MD<br />
members agree to purchase at least 80 percent of their medical<br />
supplies through McKesson Medical-Surgical. Provider Select: MD<br />
is open to all physicians and group practices sponsored by a<br />
Premier acute care facility.<br />
For more information about the rewards and benefits of<br />
Provider Select: MD, call 877 777 1552.<br />
For more information on McKesson Medical-Surgical,<br />
call 888 234 7717, ext. 4456.<br />
ABOUT PREMIER<br />
Premier, Inc., is a strategic alliance in U.S. healthcare, entirely<br />
owned by nearly 200 of the nation’s leading hospital and healthcare<br />
systems. These systems operate or are affiliated with nearly 1,500<br />
hospital facilities in 50 states and hundreds of other care sites.<br />
Premier provides an array of resources supporting health services<br />
delivery, including group purchasing of $17 billion annually in<br />
supplies and equipment. Other resources offered by Premier are<br />
insurance programs and performance improvement services of<br />
many kinds. Premier is headquartered in San Diego, CA, with<br />
other major facilities in Chicago, IL, and Charlotte, NC. Advocacy<br />
and policy offices are located in Washington, DC. For more<br />
information, please visit www.premierinc.com.<br />
ABOUT MCKESSON CORPORATION<br />
McKesson has provided healthcare products for more than<br />
165 years. A publicly traded Fortune 40 company, McKesson has<br />
become the largest multi-market distributor of pharmaceutical<br />
and medical/surgical supplies while exceeding industry-leading<br />
standards for availability, accuracy, and efficiency. McKesson is<br />
committed to being the leader in healthcare supply management<br />
by providing tools, technologies and logistics programs such as<br />
Optima, SupplyNET, and ROBOT-Rx to help its customers exceed<br />
their goals for cost control and quality improvement.<br />
premierinc.com