1) Basics on mechanical ventilation.pdf - Vula
1) Basics on mechanical ventilation.pdf - Vula
1) Basics on mechanical ventilation.pdf - Vula
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
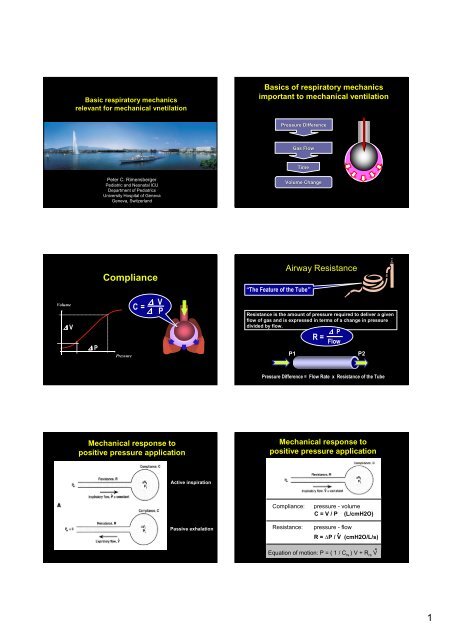
Basic respiratory mechanics<br />
relevant for <strong>mechanical</strong> vnetilati<strong>on</strong><br />
<str<strong>on</strong>g>Basics</str<strong>on</strong>g> of respiratory mechanics<br />
important to <strong>mechanical</strong> ventilati<strong>on</strong><br />
Pressure Difference<br />
Gas Gas Flow<br />
Time<br />
Peter C. Rimensberger<br />
Pediatric and Ne<strong>on</strong>atal ICU<br />
Department of Pediatrics<br />
University Hospital of Geneva<br />
Geneva, Switzerland<br />
Volume Change<br />
Volume<br />
∆ V<br />
∆ P<br />
Compliance<br />
Pressure<br />
C = ∆ V<br />
∆ P<br />
“The Feature of the Tube”<br />
Airway Resistance<br />
Resistance is the amount of pressure required to deliver a given<br />
flow of gas and is expressed in terms of a change in pressure<br />
divided by flow.<br />
R = ∆ P<br />
Flow<br />
P1<br />
P2<br />
Pressure Difference = Flow Rate x Resistance of the Tube<br />
Mechanical resp<strong>on</strong>se to<br />
positive pressure applicati<strong>on</strong><br />
Mechanical resp<strong>on</strong>se to<br />
positive pressure applicati<strong>on</strong><br />
Active inspirati<strong>on</strong><br />
Passive exhalati<strong>on</strong><br />
Compliance:<br />
Resistance:<br />
pressure - volume<br />
C = V / P (L/cmH2O)<br />
R = ∆P / V (cmH2O/L/s)<br />
Equati<strong>on</strong> of moti<strong>on</strong>: P = ( 1 / C rs ) V + R rs V .<br />
.<br />
pressure - flow<br />
1
Pressure – Flow – Time - Volume<br />
P = ( 1 / Crs ) x V + Rrs x V .<br />
Pressure – Flow – Time - Volume<br />
Time c<strong>on</strong>stant: T = Crs x Rrs<br />
Volume change requires time to take place.<br />
When a step change in pressure is applied, the instantaneous change in<br />
volume follows an exp<strong>on</strong>ential curve, which means that, formerly faster, it<br />
slows down progressively while it approaches the new equilibrium.<br />
Time c<strong>on</strong>stant: T = Crs x Rrs<br />
Will pressure equilibrium<br />
be reached in the lungs?<br />
Effect of varying time c<strong>on</strong>stants <strong>on</strong> the change<br />
in lung volume over time<br />
(with c<strong>on</strong>stant inflating pressure at the airway opening)<br />
A: Crs = 1, R = 1<br />
B: Crs = 2<br />
(T = R x 2C)<br />
C: Crs = 0.5<br />
(T = R x 1/2C)<br />
(reduced inspiratory<br />
capacity to 0.5)<br />
D: R = 0.5<br />
(T = 1/2R x C)<br />
E: R = 2<br />
(T = 2R x C)<br />
Pressure Difference<br />
Gas Gas Flow<br />
Time<br />
Volume Change<br />
Ventilators deliver gas to<br />
the lungs using positive<br />
pressure at a certain rate.<br />
The amount of gas<br />
delivered can be limited<br />
by time, pressure or<br />
volume.<br />
The durati<strong>on</strong> can be cycled<br />
by time, pressure or flow.<br />
Expiratory flow waveform:<br />
normal vs pathologic<br />
flow<br />
insufflati<strong>on</strong><br />
0<br />
time<br />
exhalati<strong>on</strong><br />
auto-PEEP<br />
Nunn JF Applied respiratory physiology 1987:397<br />
Premature flow terminati<strong>on</strong> during<br />
expirati<strong>on</strong> = “gas trapping” =<br />
deadspace (Vd/Vt) will increase<br />
2
Flow terminati<strong>on</strong> and<br />
auto-PEEP detecti<strong>on</strong><br />
Correcti<strong>on</strong> for Auto-PEEP<br />
- Br<strong>on</strong>chodilator<br />
PEEPi<br />
Trapped<br />
volume<br />
Dhand, Respir Care 2005; 50:246<br />
Analysing time settings of the respiratory cycle<br />
Appropriate inspiratory time<br />
1) Too short Te intrinsic PEEP 1) Correct Te<br />
2) Unnecessary l<strong>on</strong>g Ti 2) Too short Ti<br />
Optimizing tidal volume delivery at set ∆−pressure<br />
Vt 120 ml<br />
Lucangelo U, Bernabe F, and Blanch L Respir Care 2005;50(1):55– 65<br />
3
Vt 160 ml<br />
Vt 137 ml<br />
Progressive increase in inspiratory time<br />
Too short Ti will<br />
reduce delivered Vt<br />
unneccessary high<br />
PIP will be applied<br />
unnecessary high<br />
intrathoracic pressures<br />
Too short Te will not<br />
allow to deliver max.<br />
possible Vt at given P<br />
will induce PEEPi<br />
increases the risk for<br />
hemodynamic instability<br />
Lucangelo U, Bernabe F, and Blanch L Respir Care 2005;50(1):55– 65<br />
CAVE: you have to set Frequency and Ti (C<strong>on</strong>trol) or Ti and Te (TCPL)<br />
The patient respiratory mechanics dictate the maximal respiratory frequency<br />
4
Look at the flow – time curve !<br />
.<br />
V<br />
Leak<br />
Time<br />
Cave! Ti settings in presence of an<br />
endotracheal tube leak<br />
Flow<br />
Proximal Airway Pressure<br />
The <strong>on</strong>ly soluti<strong>on</strong> in presence<br />
P<br />
of an important leak:<br />
Alveolar Pressure<br />
Look how the thorax moves<br />
Volume<br />
Leak<br />
Vex < Vinsp<br />
Time<br />
Who’s Watching the Patient?<br />
Compliance ↓<br />
Compliance<br />
↓<br />
Pressure Ventilati<strong>on</strong><br />
Decreased Tidal Volume<br />
Increased Tidal Volume<br />
Volume Ventilati<strong>on</strong><br />
Increased Pressure<br />
Decreased Pressure<br />
Volume<br />
Volume<br />
Pressure<br />
Pressure<br />
Piers<strong>on</strong>, IN: Tobin, Principles and Practice of Critical Care M<strong>on</strong>itoring<br />
and do not forget, the time c<strong>on</strong>stant (T = Crs x Rrs) will change too!<br />
Compliance decrease<br />
Change in compliance after surfactant =<br />
change in time c<strong>on</strong>stant after surfactant<br />
pre<br />
post<br />
33 cmH2O<br />
52 cmH2O<br />
Volume<br />
0.4 (s) 0.65 (s) 0.35 (s) 0.5 (s)<br />
Lucangelo U, Bernabe F, and Blanch L Respir Care 2005;50(1):55– 65<br />
PEEP PIP PEEP PIP<br />
Pressure<br />
Kelly E Pediatr Pulm<strong>on</strong>ol 1993;15:225-30<br />
5
To measure compliance and<br />
resistance - is it in the clinical<br />
setting important ?<br />
Time c<strong>on</strong>stant: Τ = Crs x Rrs<br />
Use the flow curve for decisi<strong>on</strong> making<br />
about the settings for respiratory rate and<br />
duty cycle in the <strong>mechanical</strong> ventilator<br />
Volume Guarantee: New Approaches in Volume C<strong>on</strong>trolled Ventilati<strong>on</strong> for Ne<strong>on</strong>ates.<br />
Ahluwalia J, Morley C, Wahle G. Dräger Medizintechnik GmbH. ISBN 3-926762-42-X<br />
The saying “we ventilate at 40/min” or “with a Ti of 0.3”<br />
is a testim<strong>on</strong>y of no understanding !<br />
Pressure C<strong>on</strong>trol versus Pressure Support<br />
Pressure-Support and flow terminati<strong>on</strong> criteria<br />
Pressure Inspiratory Ventilati<strong>on</strong> time or cycle - Waveforms off criteria<br />
The n<strong>on</strong> synchr<strong>on</strong>ized patient during Pressure-Support<br />
(inappropriate end-inspiratory flow terminati<strong>on</strong> criteria)<br />
Peak<br />
Flow<br />
25%<br />
Flow<br />
PIP<br />
Ti Tinsp. set<br />
Ti given by the<br />
cycle off criteria<br />
Pressure<br />
Pressure C<strong>on</strong>trol<br />
Pressure Support<br />
Nilsestuen J Respir Care 2005;50:202–232.<br />
Pressure-Support and flow terminati<strong>on</strong> criteria<br />
Terminati<strong>on</strong> Sensitivity = Cycle-off Criteria<br />
Flow<br />
Peak Flow (100%)<br />
TS 30%<br />
TS 5%<br />
Leak<br />
Time<br />
Tinsp. (eff.)<br />
Set (max)<br />
Tinsp.<br />
Increase in RR, reducti<strong>on</strong> in VT, increase in WOB<br />
Nilsestuen J<br />
Respir Care 2005<br />
6
What do airway pressures mean?<br />
Palv = PPl + Ptp<br />
Etot = EL + Ecw<br />
when airway resistance is nil (static c<strong>on</strong>diti<strong>on</strong>)<br />
P airways (cmH2O)<br />
P pleural (cmH2O)<br />
Palv = Ppl + Ptp<br />
P transpulm<strong>on</strong>ary (cmH2O)<br />
Ptp = Palv - Ppl<br />
Where Ptp is transpulm<strong>on</strong>ary pressure, Palv is alveolar pressure, and Ppl is pleural pressure<br />
PPl = Paw x [E CW / (E L + E cw)]<br />
Ptp = Paw x [E L / (E L + E cw)]<br />
7
Paw = PPl + Ptp<br />
when airway resistance is nil (static c<strong>on</strong>diti<strong>on</strong>)<br />
soft<br />
stiff<br />
Ptp = Paw x [E L / (E L + E cw)]<br />
In normal c<strong>on</strong>diti<strong>on</strong>: EL = Ecw<br />
Ecw/ Etot = 0.5 and EL/ Etot = 0.5<br />
PTP ~ 50% of Paw applied<br />
Etot = EL + Ecw<br />
Ptp = Paw x [E L / (E L + E cw)]<br />
PPl = Paw x [E CW / (E L + E cw)]<br />
Gattin<strong>on</strong>i L<br />
Critical Care 2004,<br />
8:350-355<br />
In ARDS:<br />
PTP ~ 20 to 80% of Paw applied<br />
In primary ARDS: EL > Ecw (EL / Etot > 0.5)<br />
Stiff lung, soft thorax PTP > 50 % of Paw applied<br />
In sec<strong>on</strong>dary ARDS: EL < Ecw (EL / Etot < 0.5)<br />
Soft lung, stiff thorax PTP < 50 % of Paw applied<br />
Respiratory mechanics influence the efficiency of RM<br />
22 ARDS-patients: Vt 6 ml/kg, PEEP and FiO2 to obtain SO2 90–95%<br />
RM: CPAP to 40 cm H2O for 40 s<br />
Elastic properties, compliance and FRC in ne<strong>on</strong>ates<br />
Ne<strong>on</strong>ate chest wall compliance, C W = 3-6 x C L , lung compliance<br />
tending to decrease FRC, functi<strong>on</strong>al residual capacity<br />
By 9-12 m<strong>on</strong>ths C W = C L<br />
In infant RDS (HMD): EL >>> Ecw (EL / Etot >>> 0.5)<br />
Stiff lung, very soft thorax PTP >>> 50 % of Paw applied<br />
transpulm<strong>on</strong>ary pressure<br />
Grasso S Anesthesiology 2002; 96:795–802<br />
Elastic properties, compliance and FRC in ne<strong>on</strong>ates<br />
Ne<strong>on</strong>ate chest wall compliance, C W = 3-6 x C L , lung compliance<br />
tending to decrease FRC, functi<strong>on</strong>al residual capacity<br />
By 9-12 m<strong>on</strong>ths C W = C L<br />
Pplat = Palv;<br />
Pplat = Transpulm<strong>on</strong>ary Pressure ?<br />
transpulm<strong>on</strong>ary<br />
pressure = 15 cm H 2 O<br />
+15 cm H 2 O<br />
Dynamic FRC in awake, sp<strong>on</strong>taneously ventilating infants is maintained<br />
near values seen in older children and adults because of<br />
1. c<strong>on</strong>tinued diaphragmatic activity in early expiratory phase<br />
2. intrinsic PEEP (relative tachypnea with start of inspirati<strong>on</strong><br />
before end of preceding expirati<strong>on</strong>)<br />
3. sustained t<strong>on</strong>ic activity of inspiratory muscles (incl. diaphragma)<br />
(probably most important)<br />
By 1 year of age, relaxed end-expiratory volume predominates<br />
Pplat 30 cm H 2 O<br />
Stiff chest wall<br />
8
Pplat = Palv;<br />
Pplat = Transpulm<strong>on</strong>ary Pressure ?<br />
transpulm<strong>on</strong>ary<br />
pressure = 45 cm H 2 O<br />
PCV 20 cm H 2 O,<br />
PEEP 10 cm<br />
H 2 O; Pplat 30<br />
cm H 2 O<br />
-15 cm H 2 O<br />
Pplat 30 cm H 2 O,<br />
PCV<br />
Pplat = Palv;<br />
Pplat = Transpulm<strong>on</strong>ary Pressure?<br />
Pplat 30 cm H 2 O,<br />
PCV<br />
Pplat 30 cm H 2 O,<br />
PCV (PSV)<br />
Active inspiratory effort<br />
Active inspiratory effort<br />
Risk of VILI may be different with the same Pplat<br />
Pressure – Flow – Time - Volume<br />
Avoid ventilati<strong>on</strong> out of c<strong>on</strong>trol !<br />
V / P / V<br />
.<br />
t<br />
Curves<br />
.V or V<br />
P or V<br />
Loops<br />
Alveolar<br />
Pressure<br />
Airway<br />
Pressure<br />
The ventilator display can help us….<br />
but we still have to decide about respiratory rate, tidal<br />
volumes, pressure settings …<br />
Residual Flows<br />
… that have to be adapted to the patients respiratory<br />
mechanics<br />
9