MOLECULAR ENGINEERS - Dana-Farber Cancer Institute
MOLECULAR ENGINEERS - Dana-Farber Cancer Institute
MOLECULAR ENGINEERS - Dana-Farber Cancer Institute
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
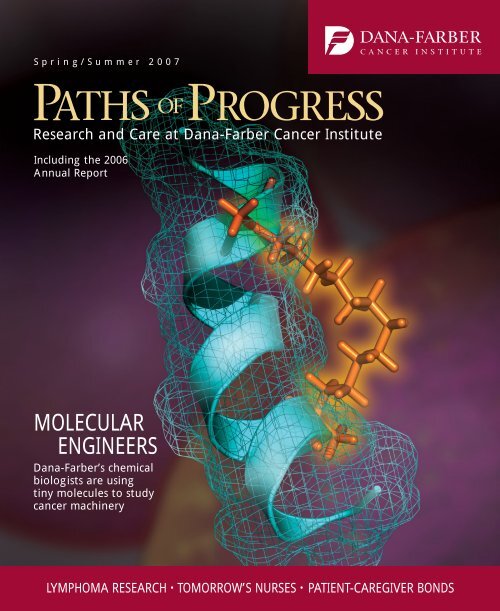
Spring/Summer 2007<br />
Research and Care at <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong><br />
Including the 2006<br />
Annual Report<br />
<strong>MOLECULAR</strong><br />
<strong>ENGINEERS</strong><br />
<strong>Dana</strong>-<strong>Farber</strong>’s chemical<br />
biologists are using<br />
tiny molecules to study<br />
cancer machinery<br />
LYMPHOMA RESEARCH • TOMORROW’S NURSES • PATIENT-CAREGIVER BONDS
From the President<br />
The more we learn about cancer’s complex and<br />
resilient nature, the more we are driven to strike it<br />
from all sides. Here at <strong>Dana</strong>-<strong>Farber</strong>, we are doing<br />
just that – through research in our laboratories, care in<br />
our clinics, and outreach in the community to spur prevention<br />
and early detection.<br />
The stories in this issue of Paths of Progress illustrate<br />
that multipronged approach. On the subcellular level,<br />
<strong>Dana</strong>-<strong>Farber</strong>’s chemical biologists are using tiny molecules<br />
to help block abnormal proteins implicated in<br />
various cancers. On the patient-care front, physicianscientists<br />
are seeking ways to stifle the growing number<br />
of lymphoma cases, both here and nationally. Beyond<br />
the <strong>Institute</strong>’s walls, we are helping train more minority<br />
nurse-leaders and researchers, in part through a new joint<br />
program with the University of Massachusetts Boston.<br />
Our successes over the years have paid off in<br />
enhanced survivorship, as evidenced by the feature on<br />
“special bonds” between caregivers and their now-grown<br />
patients, and Evie Goldfine’s powerful blog account of her<br />
multiple encounters with cancer.<br />
Our ability to continue our wide-ranging assault on this<br />
disease depends in large part on the generosity of <strong>Dana</strong>-<br />
<strong>Farber</strong>’s friends. With help from a $1 billion fundraising<br />
campaign – the largest in the <strong>Institute</strong>’s history – we look<br />
forward to achieving the next round of breakthroughs and<br />
watching the development of our planned Yawkey Center<br />
for <strong>Cancer</strong> Care.<br />
<strong>Dana</strong>-<strong>Farber</strong>’s Mission Possible campaign gives all of<br />
us hope, the same kind of hope we have been offering<br />
patients and their families for the past 60 years.<br />
Edward J. Benz Jr., MD<br />
President, <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong><br />
PATHS OF PROGRESS Spring/Summer 2007<br />
Volume 16, Number 1<br />
President, <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong> Edward J. Benz Jr., MD<br />
Chief of Staff Stephen E. Sallan, MD<br />
Chief Medical Officer Lawrence N. Shulman, MD<br />
Chief Scientific Officer Barrett J. Rollins, MD, PhD<br />
Chief Clinical Research Officer Philip W. Kantoff, MD<br />
Chair, Medical Oncology James D. Griffin, MD<br />
Chair, Pediatric Oncology Stuart H. Orkin, MD<br />
Chair, Radiation Oncology Jay R. Harris, MD<br />
Chair, Executive Committee for Research David M. Livingston, MD<br />
Senior VP for Experimental Medicine Lee M. Nadler, MD<br />
Senior VP for Patient Care Services, Chief Nurse Patricia Reid Ponte, RN, DNSc, FAAN<br />
Senior VP for Research, Beverly R. Ginsburg, MBA<br />
Senior VP for Communications Steven R. Singer<br />
Director of Publications Paul Hennessy<br />
Editor Debra Ruder<br />
Design John DiGianni<br />
Associate Editor Robert Levy<br />
Articles Editor Saul Wisnia<br />
Staff Writers Christine Cleary, Richard Saltus<br />
Production Assistance Nicole Bedard, Patricia Cleary, Kathleen Raven,<br />
Kim Regensburg, Irina Zlobina<br />
Photography Sam Ogden, Shawn Henry (pp. 29-30)<br />
Paths of Progress is published twice a year by <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong>’s<br />
Department of Communications. If you have any comments or would like to be<br />
removed from the mailing list, please contact:<br />
Debra Ruder, Editor, Paths of Progress<br />
<strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong>, Department of Communications<br />
44 Binney Street, Boston, MA 02115-6084<br />
(617) 632-4090<br />
debra_ruder@dfci.harvard.edu<br />
Copyright © 2007 <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong>. All rights reserved.<br />
On the cover: A hydrocarbon “staple”<br />
at right stabilizes a mini-protein,<br />
illustrated here as ribbon and mesh.<br />
(Courtesy of Peter Kutchukian and<br />
Eric Smith)<br />
Correction about breast cancer study<br />
A story in the last issue of Paths of<br />
Progress about the Study of Tamoxifen<br />
and Raloxifene (STAR) should have stated<br />
that the drug raloxifene reduces the<br />
chances of breast cancer occurrence<br />
(not recurrence) in postmenopausal<br />
women at increased risk for the disease.<br />
Please note that raloxifene is used to treat<br />
osteoporosis, not breast cancer. For more<br />
information about the STAR trial and<br />
other ongoing breast cancer risk-reduction<br />
studies at <strong>Dana</strong>-<strong>Farber</strong>, visit www.danafarber.org<br />
and go to “Patient Care” and<br />
“<strong>Cancer</strong> Risk and Prevention.”
Contents<br />
Spring/Summer 2007<br />
5 Divide and conquer<br />
By Richard Saltus<br />
Sorting lymphomas by their genetic signatures allows investigators<br />
to better target existing therapies or develop new ones<br />
needed to fight this varied group of cancers.<br />
11 The power of two<br />
By Robert Levy<br />
The <strong>Dana</strong>-<strong>Farber</strong>/Harvard <strong>Cancer</strong> Center and University<br />
of Massachusetts Boston are working to train minority nurses<br />
and reduce disparities in oncology awareness and treatment.<br />
16 Molecular engineers<br />
By Robert Levy<br />
Using advanced technology to build compounds from small<br />
molecules, chemical biologists are studying the genetic precursors<br />
for cancer and designing strategies to thwart them.<br />
24 Special bonds<br />
By Saul Wisnia<br />
As more children with cancer survive to adulthood, they are<br />
forging close ties with their caregivers while also educating<br />
them about aftereffects of pediatric treatment.<br />
29 First Person: Evie Goldfine<br />
Edited by Christine Cleary<br />
Through wise, witty, and poignant entries from her blog,<br />
lymphoma survivor Evie Goldfine discusses her encounters<br />
with cancer and reflects on loved ones lost.<br />
Departments<br />
2 Dateline DFCI<br />
20 Discoveries<br />
33 2006 Annual Report<br />
www.dana-farber.org
Dateline DFCI<br />
<strong>Dana</strong>-<strong>Farber</strong>’s $1 billion campaign to support top priorities<br />
To push cancer care and research to the next level,<br />
<strong>Dana</strong>-<strong>Farber</strong> this winter announced a $1 billion<br />
capital campaign. Mission Possible: The <strong>Dana</strong>-<br />
<strong>Farber</strong> Campaign to Conquer <strong>Cancer</strong> aims to help<br />
the <strong>Institute</strong> seize on a pivotal moment in cancer<br />
discovery and tap the latest knowledge and tools, as<br />
well as staff members’ talents and passion.<br />
“This year, physicians will diagnose another 1.5 million<br />
cancer cases in the United States,” notes <strong>Institute</strong><br />
President Edward J. Benz Jr., MD. “The numbers are<br />
daunting, and the stakes are high. But <strong>Dana</strong>-<strong>Farber</strong> is<br />
uniquely primed to alter these statistics and rewrite<br />
cancer’s prognosis once and for all.”<br />
Recent advances have made possible the use of precise,<br />
tailored therapies to attack a growing number of<br />
cancers at the molecular level, yet personalized cancer<br />
treatments remain the exception, not the rule. <strong>Dana</strong>-<br />
<strong>Farber</strong> is poised to change this, according to Benz.<br />
“Building on our time-tested, translational research<br />
model of moving promising findings from the laboratory<br />
quickly into the clinic for the benefit of patients,<br />
we have created a blueprint for definitive action.”<br />
Reflecting the priorities outlined in the <strong>Institute</strong>’s<br />
Strategic Plan, the Mission Possible campaign seeks<br />
investments in four areas: $450 million for research and<br />
care; $100 million for technology, especially in the areas<br />
of chemical biology, computational biology, genomics,<br />
imaging, and proteomics; $150 million for a planned<br />
13-story clinical building, recently named the Yawkey<br />
Center for <strong>Cancer</strong> Care, thanks to a $30 million gift<br />
from the Yawkey Foundation; and $300 million for the<br />
Jimmy Fund and unrestricted funds – which provide<br />
flexible dollars to help address the <strong>Institute</strong>’s most<br />
pressing needs.<br />
<strong>Dana</strong>-<strong>Farber</strong>’s largest-ever fund drive comes at a time<br />
of extraordinary growth here. Outpatient visits and infusions<br />
grew by more than 40 percent between 2001 and<br />
2005, and projections show continued demand for services<br />
as the population ages and people live longer with<br />
cancer. In addition to helping recruit and retain top physicians<br />
and scientists, the campaign will help <strong>Dana</strong>-<strong>Farber</strong><br />
provide a more welcoming, personalized experience for<br />
patients and their families.<br />
Mission Possible, which began its quiet phase in<br />
October 2003 and went public in January 2007, is<br />
already past the halfway mark in gifts and pledges<br />
from individuals, corporations, and foundations. As of<br />
February, it had raised more than $558 million. These<br />
contributions are essential for helping the <strong>Institute</strong><br />
continue pursuing its goals.<br />
“For the first time in human history, we know what<br />
causes cancer,” <strong>Dana</strong>-<strong>Farber</strong>’s Chief Scientific Officer,<br />
Barrett Rollins, MD, PhD, told The Boston Globe in<br />
January. “We know it’s a genetic disease. ... <strong>Cancer</strong> is<br />
hundreds and hundreds of diseases, each with its own<br />
genetic changes. We see the path before us pretty clearly.”<br />
The campaign supports <strong>Dana</strong>-<strong>Farber</strong>’s high-tech research, carried out here by Yi Zhang and Gordon Freeman.<br />
2 PATHS OF P ROGRESS Spring/Summer 2007
<strong>Institute</strong> expands beyond Longwood Medical Area<br />
As <strong>Dana</strong>-<strong>Farber</strong> aims to serve a growing number<br />
of cancer patients, it is building or planning<br />
several suburban clinics – and locating some<br />
employees off-site – to ease overcrowding at its main<br />
campus in the Longwood Medical Area and prepare for<br />
the planned Yawkey Center for <strong>Cancer</strong> Care there.<br />
In a partnership between <strong>Dana</strong>-<strong>Farber</strong>/Brigham and<br />
Women’s <strong>Cancer</strong> Center (DF/BWCC) and Milford<br />
Regional Medical Center, construction is well under<br />
way for a two-story, 54,000-square-foot building in<br />
Milford, Mass., 35 miles southwest of Boston. Slated<br />
to open early in 2008, the new facility will offer exam<br />
rooms, chemotherapy infusion, radiation therapy, and<br />
diagnostic imaging. Patients and families are helping<br />
plan the design for the building, which will include a<br />
healing garden to provide a peaceful environment for<br />
cancer patients.<br />
Milford is the second “satellite” DF/BWCC campus<br />
for adult clinical care, following a program at Faulkner<br />
Hospital in the Jamaica Plain neighborhood of Boston<br />
that opened last June. Plans are under way for additional<br />
satellite centers in Weymouth, Mass., through an affiliation<br />
with South Shore Hospital, and in Londonderry,<br />
N.H., in partnership with New Hampshire Oncology-<br />
Hematology and Elliot Hospital.<br />
In addition, several <strong>Dana</strong>-<strong>Farber</strong> departments have<br />
moved away from the main campus over the past several<br />
years, with the “Harbor Campus” as the latest venue.<br />
Staff members from the Health Information Services,<br />
Materials Management, and <strong>Cancer</strong> Registry units now<br />
work in this 49,000-square-foot waterfront building in<br />
Boston’s Marine Industrial Park. The “Drydock” site<br />
will also store dozens of freezers for patient tissue samples<br />
and other specimens, and will eventually house<br />
other research activities.<br />
“There is an urgent need to expand our capacity as<br />
a clinical center and extend our leadership in cancer<br />
research,” explains Richard Shea, <strong>Dana</strong>-<strong>Farber</strong>’s vice<br />
president for Facilities Management. “These moves support<br />
the <strong>Institute</strong>’s master plan to meet these challenges.”<br />
Kudos abound for <strong>Dana</strong>-<strong>Farber</strong> and its science, medical staff<br />
<strong>Dana</strong>-<strong>Farber</strong> received full accreditation for its<br />
hospital and clinical laboratory programs after<br />
a three-day survey in late January-early February.<br />
Surveyors from the Joint Commission (formerly the<br />
Joint Commission on Accreditation of Healthcare<br />
Organizations) praised the compassionate quality care<br />
they observed, the cleanliness and safety of the facility,<br />
and the knowledgeable staff. They also identified three<br />
non-care-related items needing improvement that the<br />
<strong>Institute</strong> began addressing immediately.<br />
“The surveyors’ parting comments were that this was<br />
one of the finest hospitals they have ever visited,” noted<br />
<strong>Dana</strong>-<strong>Farber</strong> President Edward J. Benz Jr., MD.<br />
In other news, <strong>Dana</strong>-<strong>Farber</strong> caregivers, scientists, and<br />
other staff members were recognized in recent months<br />
with awards, grants, and appointments for their outstanding<br />
and promising work. Here is a sampling of them:<br />
Several DFCI physicians were singled out at this<br />
year’s American Society of Hematology (ASH) conference,<br />
which drew thousands of hematologists from<br />
around the world. Among them was Kimberly<br />
Stegmaier, MD, an attending physician at <strong>Dana</strong>-<strong>Farber</strong><br />
and Children’s Hospital Boston who received the organization’s<br />
first Joanne Levy, MD, Memorial Award for<br />
Outstanding Achievement. This is bestowed on an ASH<br />
scholar with the highest-scoring research abstract at<br />
the annual meeting. Stegmaier’s paper was titled<br />
“Modulating AML1-ETO with Signature-Based Small<br />
Molecule Library Screening.”<br />
In addition, <strong>Dana</strong>-<strong>Farber</strong> research efforts were featured<br />
in more than 200 abstracts during the December<br />
conference, held to address issues involving disorders of<br />
the blood and bone marrow. Five <strong>Dana</strong>-<strong>Farber</strong> doctors<br />
also led educational sessions there.<br />
Brain researcher Rosalind Segal, MD, PhD, received<br />
a 2006 Director’s Pioneer Award from the National<br />
<strong>Institute</strong>s of Health, a five-year, $2.5 million grant<br />
designed to support biomedical scientists of “exceptional<br />
creativity” conducting innovative research.<br />
The grant will fund studies to determine how sugar<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 3
Dateline DFCI<br />
molecules provide information that spurs the production<br />
of stem cells in the brain, and whether targeting these<br />
specialized sugars can lead to new treatments for brain<br />
tumors and other cancers.<br />
Sarcoma expert George Demetri, MD, is now leading<br />
the Ludwig Center at <strong>Dana</strong>-<strong>Farber</strong> and Harvard Medical<br />
School, established with a $20 million gift last fall<br />
from the Virginia and D.K. Ludwig Fund for <strong>Cancer</strong><br />
Research. <strong>Dana</strong>-<strong>Farber</strong> is one of six leading U.S. academic<br />
institutions chosen to host a Ludwig Center; these<br />
now form a national network of collaborating institutes<br />
and investigators conducting cancer research.<br />
For her work on the fundamental biology of breast<br />
cancer, Kornelia Polyak, MD, PhD, recently earned the<br />
2006 Claire W. and Richard P. Morse Research Award.<br />
This <strong>Dana</strong>-<strong>Farber</strong> honor recognizes clinical or basic<br />
work “of the highest caliber.” Polyak leads a team investigating<br />
the biological mishaps that cause healthy breast<br />
cells to grow abnormally and evolve from a localized<br />
tumor into a cancer that spreads.<br />
Robert J. Mayer, MD, is the first holder of the<br />
Stephen B. Kay Family Professorship at <strong>Dana</strong>-<strong>Farber</strong><br />
and Harvard Medical School. Mayer directs the<br />
<strong>Institute</strong>’s Center for Gastrointestinal Oncology, which<br />
focuses on diseases of the digestive system, including<br />
esophageal, pancreatic, liver, stomach, and colorectal<br />
cancers. The professorship was created and endowed by<br />
<strong>Institute</strong> Trustee Stephen B. Kay.<br />
Nurse-scientist Susan Bauer-Wu, PhD, RN, is principal<br />
investigator of the first federally funded, nurse-led,<br />
randomized clinical trial at <strong>Dana</strong>-<strong>Farber</strong>. The five-year<br />
study is exploring the effects of mindfulness meditation<br />
for cancer patients undergoing autologous bone marrow<br />
transplantation. Bauer-Wu is outgoing director of the<br />
Phyllis F. Cantor Center for Research in Nursing and<br />
Patient Care Services, and she is collaborating on the<br />
study with Ann LaCasce, MD, Mary Cooley, PhD,<br />
RN, and other staff members.<br />
Clinical research by Marshall Posner, MD, director<br />
of Head and Neck Oncology at <strong>Dana</strong>-<strong>Farber</strong>, and his<br />
colleagues was listed as a “notable” advance in cancer<br />
treatment in a 2006 year-end review by the Journal of<br />
Clinical Oncology. The study involved adding the drug<br />
Taxotere to standard chemotherapy for patients with<br />
advanced head and neck cancer. It showed a significant<br />
increase in the number of patients cured with<br />
the three-drug treatment.<br />
William Kaelin,<br />
MD, earned a 2006<br />
Doris Duke Distinguished<br />
Clinical<br />
Scientist Award for<br />
his research on<br />
tumor suppressor<br />
proteins. He was<br />
one of seven investigators<br />
nationally<br />
to receive $1.5 million<br />
each to use<br />
over five to seven<br />
years on translational<br />
(bench-tobedside)<br />
research<br />
and mentoring of<br />
Rosalind Segal earns grant.<br />
junior colleagues.<br />
The awards are sponsored by the Doris Duke<br />
Charitable Foundation.<br />
<strong>Dana</strong>-<strong>Farber</strong> recently published a 100-page toolkit to<br />
help other healthcare organizations set up programs<br />
that involve patients and families in the quality and<br />
safety of their care. The patient safety rounds guide<br />
can be viewed at www.dana-farber.org/toolkit.<br />
In the comings and goings category, Janet Shaw<br />
retired in February after 38 years of working in<br />
<strong>Dana</strong>-<strong>Farber</strong>’s clinical laboratories, most recently as<br />
manager of the Core Laboratories. These units focus on<br />
analyzing blood, bone marrow, tissue, and other bodily<br />
specimens for patients undergoing care. Her calm<br />
demeanor, positive attitude, technical knowledge, and<br />
managerial skills helped Shaw guide staff through an<br />
extraordinary period of change at <strong>Dana</strong>-<strong>Farber</strong>.<br />
Beverly R. Ginsburg, MBA, joined the <strong>Institute</strong> as<br />
senior vice president for research in November after<br />
serving as executive director at the University of<br />
Pennsylvania’s comprehensive cancer center. Ginsburg,<br />
also associate director for administration of the<br />
<strong>Dana</strong>-<strong>Farber</strong>/Harvard <strong>Cancer</strong> Center, oversees a<br />
team providing the administrative infrastructure to<br />
support faculty members and facilitate the conduct<br />
of outstanding research. Ginsburg is dedicated to<br />
helping find better ways to prevent and treat cancer.<br />
“Part of the wonder of the scientific process,”<br />
she says, “is establishing the conditions in which<br />
scientists can best make use of their creativity.”<br />
4 PATHS OF P ROGRESS Spring/Summer 2007
Sorting<br />
lymphomas<br />
by gene<br />
signatures<br />
aids drug<br />
targeting<br />
Divide and conquer<br />
By Richard Saltus<br />
Scientists are dividing<br />
lymphomas into different<br />
genetic types based<br />
on the mutations that<br />
cause them. Above,<br />
Jennifer Brown uses a<br />
family tree to study<br />
rare cases of inherited<br />
lymphoma.<br />
In the winter of 2002, rapidly worsening leg pains and near-paralysis sent Carolyn Punzelt<br />
to an emergency room, where physicians discovered tumors encroaching on her spinal cord.<br />
Radiation treatment shrunk the cancer, forestalling immediate danger. After several biopsies,<br />
the Castine, Maine, woman was diagnosed with an aggressive form of non-Hodgkin’s lymphoma<br />
(NHL), a cancer of disease-fighting white blood cells.<br />
Despite their scary description, about 50 percent of fast-growing, aggressive non-Hodgkin’s<br />
cases can be cured with chemotherapy. Punzelt’s cancer, unfortunately, fell into the other half.<br />
Months of standard chemotherapy regimens failed to stop her disease and dangerously weakened<br />
her immune system.<br />
“At that point my oncologist said, ‘OK, you’re going to <strong>Dana</strong>-<strong>Farber</strong>,’” recalls Punzelt. “He<br />
said, ‘If you don’t do anything, I give you less than a year to live.’”<br />
That was in 2003. Today Punzelt is 75 and well, with no detectable cancer. A drug that was in<br />
clinical trials at <strong>Dana</strong>-<strong>Farber</strong>, enzastaurin, did what the toxic, cell-killing chemotherapy could<br />
not – put her in long-term remission. Taken as a pill, enzastaurin pinpointed a precise genetic<br />
defect within her cancer cells and shut down their growth. There were few side effects. Her hair,<br />
decimated by the chemotherapy, grew back.<br />
Continued on next page<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 5
“We’re very excited about these new, specific agents.<br />
They are going after what went wrong in the cancer<br />
cell to begin with.” — Ann LaCasce, MD<br />
At <strong>Dana</strong>-<strong>Farber</strong>’s pharmacy,<br />
Carolyn Punzelt picks up a supply<br />
of the experimental drug that has<br />
kept her lymphoma in remission<br />
for more than three years.<br />
“It’s really miraculous,” she says.<br />
“I’m active in a number of groups;<br />
I’m in the vestry of my church, and<br />
I live in a huge old house that needs<br />
a lot of work.” Oncologists in<br />
Maine monitor her remission, and<br />
she makes occasional 500-mile<br />
round trips to <strong>Dana</strong>-<strong>Farber</strong>/Brigham<br />
and Women’s <strong>Cancer</strong> Center to see<br />
her doctor, David C. Fisher, MD,<br />
and to pick up enzastaurin supplies.<br />
Punzelt’s story is more than a single<br />
patient’s reprieve; it represents a<br />
still-evolving, divide-and-conquer<br />
strategy using technology that takes<br />
“snapshots” of how all the genes in<br />
a cell are behaving. The approach is<br />
this: Separate tumors into subgroups<br />
by their distinctive genetic<br />
activity patterns. Using standard<br />
therapies, treat the cancers whose<br />
profiles suggest favorable outcomes.<br />
For those with poor-outcome<br />
gene profiles, develop and<br />
test new drugs to attack abnormal<br />
links in the cancer cell’s chain of<br />
molecular signals, or “pathways.”<br />
“We have a major commitment to<br />
understanding the genetic pathways<br />
that enable lymphoma cells to survive,<br />
and manipulating them with<br />
rational, targeted therapy,” says<br />
Margaret Shipp, MD, a <strong>Dana</strong>-<strong>Farber</strong><br />
oncologist and director of the <strong>Dana</strong>-<br />
<strong>Farber</strong>/Harvard <strong>Cancer</strong> Center<br />
Lymphoma Program.<br />
Different diseases<br />
Lymphoma originates in the network<br />
of lymph nodes, spleen, and<br />
bone marrow that forms part of the<br />
immune system (see box at right).<br />
The cancer may first be detected in<br />
lymph nodes in the chest, abdomen,<br />
or neck. As the malignant cells<br />
crowd out healthy white blood cells,<br />
patients typically experience pain,<br />
fatigue, night sweats, and swollen<br />
lymph nodes, and become susceptible<br />
to dangerous infections.<br />
Hodgkin’s lymphoma (also known<br />
as Hodgkin’s disease) is a special<br />
type that makes up about 12 percent<br />
of all lymphomas. The cancerous<br />
blood cells in Hodgkin’s lymphoma<br />
have a distinctive appearance, and<br />
incidence of the disease spikes in<br />
young adults, then rises again in<br />
later life. Non-Hodgkin’s lymphomas<br />
make up the remainder – a<br />
heterogeneous collection of lymphoma<br />
types. Unlike Hodgkin’s, the<br />
NHLs can occur at all ages, but<br />
they also increase in frequency as<br />
people age.<br />
Many of the 1,200 new lymphoma<br />
patients seen at <strong>Dana</strong>-<strong>Farber</strong><br />
every year participate in clinical<br />
trials testing combinations of drugs,<br />
both conventional and experimental,<br />
as well as radiation therapy, stem<br />
The<br />
lymphatic<br />
system<br />
Lymphomas are<br />
cancers of the<br />
lymphatic system,<br />
a network<br />
of nodes, vessels,<br />
ducts, tissues,<br />
and organs that<br />
distribute infection-fighting<br />
blood cells<br />
throughout the<br />
body. The lymphatic<br />
system<br />
plays a major<br />
role in the<br />
immune system.<br />
6 PATHS OF P ROGRESS Spring/Summer 2007
cell transplants, and cancer vaccines.<br />
“We’re very excited about these<br />
new, specific agents,” says Ann<br />
LaCasce, MD, a member of the<br />
lymphoma team who heads several<br />
clinical studies. “They are going<br />
after what went wrong in the cancer<br />
cell to begin with, and that’s very<br />
different from trying to kill dividing<br />
cells [with conventional treatments].”<br />
These newer “targeted” therapies<br />
are designed to attack the genetic<br />
pathways that cause cells to grow<br />
and divide in an unregulated way.<br />
Devices called microarrays, or<br />
“gene chips,” sift a cancer cell’s<br />
DNA and record genes that are<br />
unusually active or inactive compared<br />
to the same genes in normal<br />
cells. The resulting pattern is the<br />
cell’s genetic signature.<br />
Several years ago, Shipp and colleagues<br />
including Todd Golub, MD,<br />
analyzed genetic activity in tumors<br />
known as diffuse large B-cell lymphoma<br />
(DLBCL), the most common<br />
non-Hodgkin’s lymphoma in the<br />
Family ties: Searching for genetic clues in lymphoma<br />
What causes lymphoma to develop in one person<br />
but not another Aside from a few known or suspected<br />
risk factors such as aging, a compromised<br />
immune system, viruses, and environmental exposures,<br />
most forms of this blood cancer appear to result from random<br />
gene mutations – simply bad luck.<br />
A small number of cases, however, show evidence of a<br />
family connection. And therein may lie clues to the identification<br />
of lymphoma-causing genes.<br />
“There are reports of families in which several closely<br />
related individuals have lymphoma, and identical twins have<br />
a higher risk of both developing the disease than do fraternal<br />
twins,” says Jennifer Brown, MD, PhD, a physicianscientist<br />
in <strong>Dana</strong>-<strong>Farber</strong>’s Lymphoma Program. “These<br />
observations suggest that the development of lymphoma<br />
may have an inherited genetic component.”<br />
For the past two years, Brown and co-workers have asked<br />
all new lymphoma patients seen at <strong>Dana</strong>-<strong>Farber</strong> to complete<br />
detailed family history questionnaires. At last year’s<br />
American Society of Hematology meeting, they reported<br />
that 7.8 percent of new non-Hodgkin’s lymphoma patients<br />
had a first-degree relative (parent, sibling, or child) with a<br />
related lymphoma. For Hodgkin’s lymphoma, the figure was<br />
5.4 percent, and for chronic lymphocytic leukemia (CLL, a<br />
form of lymphoma) the number rose to 12.6 percent. Brown<br />
and co-workers have enrolled more than 125 families and<br />
200 individuals in a more detailed study of families with at<br />
least two individuals who have lymphoma.<br />
With blood and tumor samples from these participants<br />
in hand, Brown is comparing the DNA and gene activity<br />
in familial lymphoma tumors with DNA and gene<br />
activity in isolated, or “sporadic,” tumors. She hopes<br />
to identify genes that are abnormal<br />
in the familial cases, then<br />
determine whether they are also<br />
culprits in the more common<br />
sporadic lymphomas.<br />
“There are a lot of hypotheses<br />
about the types of genes that<br />
could lead to inherited lymphoma<br />
and how they might do<br />
so,” Brown explains. “We’re in<br />
the early stages of investigation.”<br />
Jennifer Brown<br />
A welcome boost to her research has come in the form of<br />
financial support from a familial lymphoma patient, Marilyn<br />
Lipton Okonow, her husband, Dale, and her brother, Roger<br />
Lipton. Marilyn came to <strong>Dana</strong>-<strong>Farber</strong> in 2005 for treatment of<br />
her diffuse large B-cell lymphoma, and in relating her family<br />
history, she told Brown that her father had survived CLL for<br />
20 years before dying at age 90 from other causes.<br />
“When Dr. Brown told me the two may be related, I didn’t<br />
waste a lot of time wondering where I got my lymphoma,” says<br />
Okonow, though it is impossible to know for certain whether<br />
the family link was involved. She says she is doing fine, and<br />
Brown welcomes the support as she searches for the factor, or<br />
factors, linking shared genes and the risk of lymphoma. – RS<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 7
United States and the type that<br />
affected Punzelt. About half of the<br />
patients with DLBCL and other<br />
aggressive lymphomas can be cured,<br />
while the remaining cases resist<br />
treatment. Physicians can’t yet accurately<br />
determine which group an<br />
individual patient belongs to.<br />
The Shipp team found a distinctive<br />
genetic profile in patients<br />
whose DLBCL recurred no matter<br />
what therapy they received. This<br />
gene profile pointed to overactivity<br />
in a signaling pathway called<br />
PKC-beta. It was this precise<br />
abnormality that enzastaurin,<br />
the drug that saved Punzelt, was<br />
supposed to block.<br />
Shipp reported in late 2006 that<br />
of the 55 patients with relapsed,<br />
poor-prognosis DLBCL who<br />
received enzastaurin, four of them<br />
– including Punzelt – had dramatic,<br />
long-term responses. Despite this<br />
small number, Shipp says, the fact<br />
that even four patients with<br />
advanced, previously treated disease<br />
had such outcomes “tells us<br />
that the cell signaling pathway<br />
blocked by enzastaurin may be<br />
particularly relevant to the survival<br />
of stubbornly resistant DLBCL<br />
tumors,” and that targeting this<br />
pathway is a promising line of<br />
attack. A larger clinical trial has<br />
been launched.<br />
Choosing therapies<br />
With the technology to sort<br />
patients into subgroups according<br />
to their tumors’ genetic profiles,<br />
clinical trials can be more tightly<br />
focused and powerful than studying<br />
drugs in clusters of patients with a<br />
variety of profiles. Genetic profiling,<br />
however, isn’t routinely used<br />
yet in lymphoma treatment. With<br />
aggressive lymphomas, physicians<br />
Arnie Freedman (front, center) with members of the <strong>Dana</strong>-<strong>Farber</strong>/<br />
Brigham and Women’s <strong>Cancer</strong> Center Lymphoma Program, including<br />
(first row, from left) Natalie Long, Elizabeth Ronan, Gabrielle Basile,<br />
Cynthia Vokey, Ann LaCasce, Barbara Virchick; second row: Michele<br />
Walsh, David C. Fisher, Virginia Dalton, Eric Jacobsen, Jennifer Brown,<br />
Andrea Ng, Hazel Reynolds.<br />
choose therapies based on standard<br />
tests and experience.<br />
At a routine checkup three years<br />
ago, Darren Baker, a drug company<br />
biochemist from Hingham, Mass.,<br />
mentioned he was having difficulty<br />
swallowing. An X-ray quickly<br />
revealed a fist-sized tumor in his<br />
chest that proved to be DLBCL.<br />
After eight cycles of chemotherapy<br />
plus rituximab (Rituxan), a form of<br />
immunotherapy, Baker was in complete<br />
remission; moreover, he has<br />
ridden in the Pan-Massachusetts<br />
Challenge bike-a-thon to benefit<br />
<strong>Dana</strong>-<strong>Farber</strong> the last three years.<br />
Unlike aggressive forms of the<br />
disease, slow-growing “indolent”<br />
8 PATHS OF P ROGRESS Spring/Summer 2007
lymphomas don’t pose an immediate<br />
threat to life, but they generally<br />
cannot be cured. Patients with these<br />
cancers, of which follicular lymphoma<br />
is the most common type, tend<br />
to have recurrences that become<br />
progressively more difficult to<br />
defeat. However, patients may live<br />
for years, and sometimes decades,<br />
with the disease.<br />
Retired civil engineer Gerald<br />
Rourke of Newburyport, Mass., for<br />
example, was diagnosed with follicular<br />
lymphoma after feeling swollen<br />
lymph nodes protruding from under<br />
his collarbone. The cancer responded<br />
well to treatment, but has returned<br />
three times – and been beaten back<br />
each time by therapies he received<br />
in clinical trials at <strong>Dana</strong>-<strong>Farber</strong>.<br />
His doctor, Arnie Freedman, MD,<br />
clinical director of the <strong>Dana</strong>-<strong>Farber</strong>/<br />
Brigham and Women’s <strong>Cancer</strong><br />
Center Lymphoma Program, says<br />
admiringly, “Like the Energizer<br />
Bunny, Gerry just keeps going and<br />
going and going.”<br />
NHL cases in 2007, compared with<br />
53,900 as recently as 2002. Deaths<br />
from NHL however, are estimated at<br />
18,660 in 2007, down from 24,400<br />
in 2002.<br />
The improvements can be credited<br />
to better and safer use of combination<br />
chemotherapy, stem cell transplants,<br />
radiation treatment, and the<br />
remarkable success of monoclonal<br />
antibody-based drugs such as rituximab.<br />
The latter are proteins made in<br />
the laboratory that mimic the body’s<br />
natural immune weapons for recognizing<br />
and disabling foreign intruders<br />
such as microbes.<br />
Rituximab is designed to latch onto<br />
an antigen, CD20, an identifying<br />
molecule on the surface of the malignant<br />
B-lymphocytes. These cancer<br />
cells exist in most lymphoma types,<br />
and rituximab kills them by activating<br />
certain parts of the patient’s<br />
immune system. The CD20 antigen<br />
was discovered more than 25 years<br />
ago by Lee Nadler, MD, now <strong>Dana</strong>-<br />
<strong>Farber</strong>’s senior vice president for<br />
Experimental Medicine, paving the<br />
way for monoclonal antibody treatment<br />
for lymphomas. Rituximab is<br />
routinely used with combination<br />
chemotherapy to treat both aggressive<br />
and indolent lymphomas.<br />
When given after chemotherapy as<br />
maintenance, it appears to prolong<br />
remissions in patients with the slowgrowing<br />
type.<br />
“Rituximab has substantially<br />
increased cure rates in diffuse large<br />
B-cell lymphoma,” says Freedman.<br />
“For indolent lymphomas, the addition<br />
of rituximab has improved<br />
remission rates, the length of<br />
remissions, and overall survival<br />
for these patients.”<br />
Another form of immunotherapy,<br />
cancer vaccines, are designed to<br />
stimulate the body’s natural defenses<br />
Survival on the rise<br />
The outlook for patients with<br />
lymphoma has brightened over the<br />
past few decades. Hodgkin’s lymphoma<br />
is considered one of the most<br />
curable kinds of cancer, with an<br />
86 percent five-year survival rate.<br />
For non-Hodgkin’s lymphomas,<br />
five-year survival has doubled, from<br />
31 percent in the early 1960s to<br />
62.9 percent in the period 1996-<br />
2002, according to the Leukemia<br />
and Lymphoma Society.<br />
In fact, NHL mortality continues<br />
to fall, even as the incidence has<br />
increased significantly for the past<br />
several decades. This trend has no<br />
single explanation and is not well<br />
understood. The American <strong>Cancer</strong><br />
Society projects almost 63,200 new<br />
Using microarray technology to capture a cell’s genetic signature,<br />
Margaret Shipp and her colleagues identify targets for precisely<br />
aimed “smart” drugs.<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 9
So much activity in basic and clinical research reflects the immense<br />
amount being learned about the molecular underpinnings of lymphoma.<br />
to recognize and attack tumors – but<br />
not prevent them. A clinical trial of<br />
a vaccine made from the cells of<br />
patients with relapsed follicular<br />
lymphoma is expected to open this<br />
year under the leadership of <strong>Dana</strong>-<br />
<strong>Farber</strong>’s Eric Jacobsen, MD, and<br />
Glenn Dranoff, MD.<br />
Molecular targets<br />
Among the newer compounds<br />
designed to hit molecular targets<br />
is one that blocks an overactive cell<br />
growth switch called spleen tyrosine<br />
kinase, or syk, that was first implicated<br />
by the genetic profiling of B-<br />
cell lymphomas. Another new agent<br />
inhibits an errant enzyme pathway<br />
known as PI3K. Still another target<br />
for new treatments is the protein<br />
Bcl-2, which in abnormal amounts<br />
turns cancer cells into renegade survivalists.<br />
Some compounds aimed at<br />
blocking Bcl-2 are being tested in<br />
early clinical trials, and more sophis-<br />
ticated versions are being developed<br />
in <strong>Dana</strong>-<strong>Farber</strong> laboratories.<br />
Targeting Bcl-2 is a strategy<br />
based on pioneering research by<br />
the late Stanley J. Korsmeyer, MD,<br />
who led <strong>Dana</strong>-<strong>Farber</strong>’s Program in<br />
Molecular Oncology. Korsmeyer<br />
studied programmed cell death, or<br />
apoptosis, a natural process intended<br />
to rid the body of damaged or<br />
otherwise abnormal cells. His key<br />
insight was that cancer can be<br />
caused not only by cells growing<br />
out of control, but also by cells failing<br />
to die – and that cancer cells<br />
use the Bcl-2 molecule to avoid<br />
dying as they should. Blocking<br />
Bcl-2 activity thus became a new<br />
approach to fighting the disease.<br />
One of the most promising<br />
anti-Bcl-2 candidates is Abbott<br />
Laboratories’ investigational compound<br />
ABT-737, expected to begin<br />
trials in patients with lymphoma<br />
and small-cell lung cancer at <strong>Dana</strong>-<br />
Darren Baker, left, survived aggressive lymphoma thanks to a combination<br />
of drugs and the care of oncologist Arnie Freedman.<br />
<strong>Farber</strong> and other centers this year.<br />
Anthony Letai, MD, PhD, formerly<br />
in Korsmeyer’s laboratory,<br />
says his group has tested ABT-737<br />
against lab-grown chronic lymphocytic<br />
leukemia (CLL) cells<br />
with striking results. “This drug is<br />
a member of a totally new class of<br />
agents with the potential to be a<br />
major addition to how we treat<br />
cancer,” Letai says.<br />
Loren Walensky, MD, PhD,<br />
another former Korsmeyer group<br />
colleague, is developing in his<br />
laboratory a “toolbox” of small<br />
peptides – fragments of proteins –<br />
that trigger programmed cell<br />
death. Walensky and chemical<br />
biologist Gregory Verdine, PhD,<br />
modified a key portion of a prodeath<br />
molecule and showed that<br />
when given to mice with lymphoma,<br />
it slowed the cancer’s<br />
advance. (See related story, p. 16.)<br />
So much activity in basic and<br />
clinical research reflects the<br />
immense amount being learned<br />
about the molecular underpinnings<br />
of lymphoma, and the creative<br />
energy directed to translating these<br />
findings into improved treatments.<br />
“The development of targeted<br />
therapies for lymphoma brings a<br />
lot of hope to patients,” says Hildy<br />
Dillon, a vice president at the<br />
Leukemia and Lymphoma Society,<br />
which supports research at <strong>Dana</strong>-<br />
<strong>Farber</strong> and other centers. “That’s<br />
why it’s important for patients<br />
to stay informed about clinical<br />
trials, discuss them with their<br />
oncologists, or have their cases<br />
reviewed in a center such as <strong>Dana</strong>-<br />
<strong>Farber</strong> that participates in lymphoma<br />
clinical research.”<br />
10 P ATHS OF P ROGRESS Spring/Summer 2007
Nursing leaders Greer Glazer (left) of<br />
UMass Boston and Patricia Reid Ponte<br />
of <strong>Dana</strong>-<strong>Farber</strong> and Brigham and<br />
Women’s Hospital chat at the UMass<br />
Boston campus.<br />
The power<br />
of two<br />
By Robert Levy<br />
The <strong>Dana</strong>-<strong>Farber</strong>/Harvard <strong>Cancer</strong> Center<br />
and University of Massachusetts Boston team up<br />
to train nurses, reduce health disparities<br />
When Paul Fonteyn<br />
became provost and vice<br />
president for academic<br />
affairs at the University of<br />
Massachusetts’ Boston campus in<br />
2002, he didn’t need a tutorial on<br />
health inequalities in the United<br />
States, or the nursing profession’s<br />
potential to reduce them.<br />
As an administrator at San<br />
Francisco State University, home<br />
to a large percentage of racial and<br />
ethnic minority students, Fonteyn<br />
was well aware that some groups<br />
have higher cancer rates, and less<br />
access to care, than others. He also<br />
knew that in many parts of the<br />
country the ranks of hospital nurses<br />
are not as ethnically diverse as the<br />
communities they serve – and that<br />
nursing schools and hospitals could<br />
work together to solve the problem.<br />
At a conference on partnerships<br />
between cancer centers and community<br />
organizations, Fonteyn met a<br />
particularly like-minded group:<br />
leaders of the <strong>Dana</strong>-<strong>Farber</strong>/Harvard<br />
<strong>Cancer</strong> Center (DF/HCC), a collection<br />
of more than 900 cancer<br />
scientists at seven Harvard-affiliated<br />
hospitals and schools. “My very<br />
first meeting as UMB [UMass<br />
Boston] provost was not even on my<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 11
own campus, but at <strong>Dana</strong>-<strong>Farber</strong>,<br />
with people who were interested in<br />
this project,” he recalls.<br />
That session planted the seed for<br />
further meetings between UMB and<br />
DF/HCC representatives. From initial<br />
gatherings of a half-dozen or<br />
so administrators and leaders, the<br />
meetings gradually began attracting<br />
faculty from both organizations,<br />
including biomedical researchers,<br />
nursing specialists, computing<br />
experts, and others.<br />
In 2005, after two years of planning<br />
and preparation, the group successfully<br />
competed for a five-year,<br />
$4.3 million U-56 grant from the<br />
National <strong>Cancer</strong> <strong>Institute</strong>, awarded to<br />
projects that link minority-serving<br />
institutions and NCI-designated<br />
Comprehensive <strong>Cancer</strong> Centers. The<br />
grant will fund a new graduate training<br />
program for nurses, as well as<br />
other initiatives (see box at right).<br />
The nursing program will commence<br />
this fall, with a new doctoral degree<br />
track, more research opportunities,<br />
and community outreach experiences<br />
becoming available to graduate students<br />
– particularly members of<br />
underrepresented minorities – at<br />
the UMB College of Nursing and<br />
Health Sciences.<br />
“The goal of the nursing training<br />
program is to reduce cancer disparities<br />
in Boston neighborhoods – to<br />
help people lower their risk of cancer<br />
and make sure they have the<br />
knowledge and resources to seek<br />
treatment,” says the project’s coleader,<br />
Patricia Reid Ponte, RN,<br />
DNSc, FAAN, senior vice president<br />
for Patient Care Services and chief<br />
nurse at <strong>Dana</strong>-<strong>Farber</strong>. “In line with<br />
that, we’re hoping to attract more<br />
minority students to careers in<br />
nursing, provide more training in<br />
community settings, and enable<br />
students to conduct research<br />
with DF/HCC nurse-scientists<br />
as their mentors.”<br />
UMass Boston and the <strong>Dana</strong>-<br />
<strong>Farber</strong>/Harvard <strong>Cancer</strong> Center are<br />
natural partners for this endeavor,<br />
Fonteyn adds: “UMB is an institution<br />
that has an urban mission, and<br />
reducing health disparities is a quintessentially<br />
urban issue. <strong>Dana</strong>-<strong>Farber</strong><br />
has been dedicated to overcoming<br />
cancer disparities in the community<br />
as part of its work in cancer prevention.<br />
From our very first meetings,<br />
there has been an enthusiasm and<br />
interest for this project that has been<br />
rewarding to be part of.”<br />
On the fast track<br />
The U-56 nursing training program<br />
has two major components:<br />
a “fast-track” Bachelor of Scienceto-PhD<br />
program that nursing students<br />
can complete in four years,<br />
and a new focus on cancer care and<br />
health disparities in graduate nursing<br />
training. Both will take students<br />
outside traditional hospital environments<br />
and help introduce them to<br />
the world of nursing research.<br />
The fast-track program addresses<br />
a problem that some are calling a<br />
public health crisis: a shortage of<br />
faculty at nursing schools across the<br />
country. The average age of doctorally<br />
trained nurse-educators in the<br />
United States is about 57 for full<br />
professors, according to the grant<br />
application. As more of these senior<br />
faculty retire, the pool of younger<br />
instructors is too small to replace<br />
them. Nationally, there has been an<br />
average increase of only 31 doctoral<br />
nursing students each year for the<br />
past half-decade.<br />
The shortfall is having ripple<br />
effects throughout the healthcare<br />
system. Fewer faculty translates into<br />
fewer openings for students. In a<br />
recent survey, two-thirds of U.S.<br />
nursing schools cited faculty shortages<br />
as a reason for not accepting<br />
all qualified applicants. At a time<br />
when many hospitals are struggling<br />
to hire enough registered nurses,<br />
nursing schools do not have enough<br />
graduates to fill the gap.<br />
The problem is compounded by<br />
an especially severe shortage of<br />
minorities in the profession. Only<br />
12 percent of registered nurses are<br />
members of minority groups, compared<br />
to one-third of the American<br />
Joint projects explore<br />
protocols and prayer<br />
Nursing training is the centerpiece<br />
of <strong>Dana</strong>-<strong>Farber</strong>’s alliance with<br />
UMass Boston, but the partnership<br />
is expanding into other areas as well.<br />
The federal U-56 grant supports a variety<br />
of pilot projects involving DFCI and<br />
UMB faculty, including:<br />
•<br />
Obesity/Weight Loss Intervention for<br />
African-American Women<br />
•<br />
Educating Underserved Communities<br />
About <strong>Cancer</strong> Clinical Trials<br />
•<br />
Training Minority Clinical Psychology<br />
Doctoral Students to be <strong>Cancer</strong><br />
Researchers<br />
•<br />
Understanding Prayer as a Coping<br />
Mechanism Among <strong>Cancer</strong> Patients<br />
• A Boston-Cambridge-Quincy<br />
Metropolitan Dominican Immigrant<br />
Household Survey<br />
12 P ATHS OF P ROGRESS Spring/Summer 2007
Nursing demands a combination of compassion and clinical<br />
expertise, as demonstrated by <strong>Dana</strong>-<strong>Farber</strong> nurses (left<br />
to right) Elizabeth Colon, Demetra McDonald, and Teresa<br />
Mazeika, pictured here with Len Bower.<br />
population. Among nurses holding<br />
doctorate degrees, the percentages<br />
are even smaller.<br />
The fast-track program tackles<br />
these issues and more as a group.<br />
The program is intended primarily<br />
for underrepresented minority<br />
students, and it focuses on health<br />
policy – long a hallmark of the<br />
UMass nursing curriculum.<br />
The emphasis on minority recruitment,<br />
cancer care, research, and<br />
community involvement taps the<br />
strengths of UMB and DF/HCC,<br />
says the Dean of UMass Boston’s<br />
College of Nursing and Health<br />
Sciences Greer Glazer, RN, CNP,<br />
PhD, FAAN, who helped lead the<br />
effort. “UMass Boston is the most<br />
diverse four-year institution of<br />
higher education in New England.<br />
About 40 percent of the university’s<br />
student population – and 30 percent<br />
of the college of nursing’s – consists<br />
of students of color,” she notes.<br />
For its part, the <strong>Dana</strong>-<strong>Farber</strong>/<br />
Harvard <strong>Cancer</strong> Center is not only<br />
a bastion of research, including<br />
nursing research, but also of neighborhood<br />
outreach projects that<br />
already involve UMB nursing students,<br />
says Reid Ponte, who is also<br />
the director of Oncology Nursing<br />
and Clinical Services at Brigham<br />
and Women’s Hospital. Oncology<br />
nurses at all DF/HCC hospitals –<br />
<strong>Dana</strong>-<strong>Farber</strong>, Brigham and Women’s,<br />
Massachusetts General Hospital,<br />
Beth Israel Deaconess Medical<br />
Center, and Children’s Hospital<br />
Boston – will provide research and<br />
clinical training to the students.<br />
“<strong>Dana</strong>-<strong>Farber</strong>’s Phyllis F. Cantor<br />
Center for Research in Nursing and<br />
Patient Care Services provides a<br />
base for research into the cancer<br />
patient experience, including life<br />
during and after cancer treatment<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 13
and the impact of the disease on<br />
families,” Reid Ponte remarks. The<br />
center’s nurse-scientists “are leading<br />
studies in areas ranging from<br />
smoking cessation to stress reduction<br />
for patients. They and their<br />
counterparts at other DF/HCC hospitals<br />
are an invaluable resource<br />
for students.”<br />
These specialists will serve as<br />
mentors in both the fast-track and<br />
regular-track PhD nursing programs.<br />
“Our aim is to help aspiring nurseresearchers<br />
acquire the skills to<br />
become independent investigators,”<br />
says the Cantor Center’s Susan<br />
Bauer-Wu, DNSc, RN.<br />
Approximately one-tenth of<br />
1 percent of U.S. nurses currently<br />
hold research doctorates. “Traditionally,<br />
nursing has been a<br />
practice-based discipline, and<br />
there hasn’t been a widespread<br />
awareness of the opportunities<br />
and need for nurse scientists,”<br />
Bauer-Wu continues. “That’s<br />
changing. The need for evidencebased<br />
research and the wider<br />
appreciation of the quality of<br />
life of cancer patients and their<br />
families underscores the value<br />
of nursing research.”<br />
Ending inequities<br />
The second part of the U-56 nurse<br />
training program – incorporating<br />
course work in cancer disparities into<br />
the nursing curriculum – will broaden<br />
students’ knowledge of the social,<br />
economic, and political aspects of<br />
healthcare. They’ll learn about the<br />
historical conditions that have caused<br />
some groups to be at increased risk<br />
of cancer, and about efforts to reduce<br />
such inequalities.<br />
This spring, eight UMB undergraduate<br />
nursing students assigned to<br />
<strong>Dana</strong>-<strong>Farber</strong> for their communityhealth<br />
rotation will help develop a<br />
Nursing students spread<br />
healthful messages<br />
Each semester since 2004, a group of eight UMass<br />
Boston nursing students has come to <strong>Dana</strong>-<strong>Farber</strong><br />
for their community-health rotations, working in<br />
patient-care areas under the direction of preceptors.<br />
Students also perform a “capstone” project – a final<br />
assignment to be completed before graduation – involving<br />
community outreach. They select a community to<br />
work in, assess the area’s health needs, choose a problem<br />
to focus on, and develop a program to address it,<br />
says <strong>Dana</strong>-<strong>Farber</strong>’s Lynn Thompson, RN, OCN, who<br />
directs the rotations.<br />
Projects developed and implemented by the<br />
students include:<br />
• A smoking and lung cancer prevention program<br />
delivered at the Roxbury Boys’ and Girls’ Club<br />
• A health fair at a Mattapan church focusing on<br />
diabetes, obesity, and colon cancer<br />
• A booth at a UMass Boston health fair offering<br />
information on human papillomavirus, which is<br />
linked to cervical cancer<br />
<strong>Dana</strong>-<strong>Farber</strong> nurse educator Lynn Thompson (second<br />
from right) and nursing students (left to right) Entela<br />
Topalli, Lisa Travers, and Kerry Rodden conducted<br />
blood pressure screenings and provided general<br />
health education at Hanscom Air Force Base last year.<br />
• A program on skin health offered at the UMB College<br />
of Nursing and Health Sciences<br />
•<br />
Participation in health fairs at Hanscom Air Force<br />
Base in Bedford, Mass., and at Rosie’s Place, a shelter<br />
for poor and homeless women in Boston<br />
14 P ATHS OF P ROGRESS Spring/Summer 2007
“We’re hoping to attract more minority students to careers in nursing,<br />
provide more training in community settings, and enable students to<br />
conduct research...” — Patricia Reid Ponte, RN, DNSc, FAAN<br />
smoking prevention program for elementary<br />
school children in South<br />
Boston, a section of the city with<br />
high rates of lung cancer mortality<br />
and cigarette smoking among adults.<br />
Marion Winfrey, MSN, EdD, associate<br />
dean of the College of Nursing<br />
and Health Sciences at UMB, and<br />
Lynn Thompson, RN, MPH, OCN, a<br />
nurse educator at <strong>Dana</strong>-<strong>Farber</strong>, have<br />
met with Boston Public School<br />
administrators to discuss how the<br />
program can be integrated into the<br />
existing school curriculum. “Our<br />
goal is for the nursing students,<br />
under faculty supervision, to work<br />
with school nurses, parents, students,<br />
teachers, and tobacco experts at<br />
DFCI,” says Winfrey. Plans call for<br />
the pilot program to be delivered in a<br />
South Boston elementary school this<br />
spring and expanded in the fall.<br />
“We hope there will be opportunities<br />
in the fall for students in the<br />
master’s nursing program and the<br />
new PhD fast-track program to<br />
become involved in research and policy<br />
development projects through<br />
this initiative,” says Thompson, who<br />
directs the UMB student nursing<br />
rotation at <strong>Dana</strong>-<strong>Farber</strong>. “It will teach<br />
children about smoking’s effect on<br />
their bodies and about the importance<br />
of good decision making.<br />
We hope the nursing students, who<br />
come from diverse backgrounds,<br />
can serve as role models for the<br />
children as well.”<br />
<strong>Dana</strong>-<strong>Farber</strong> and UMass Boston<br />
have been collaborating on community<br />
education projects for undergraduate<br />
nursing students since 2004.<br />
The new program is viewed as the<br />
beginning, rather than the fulfillment,<br />
of a partnership with Boston public<br />
schools. “We hope it will be the start<br />
of a relationship that lasts a long<br />
time,” Thompson asserts.<br />
Community learning experiences<br />
such as these can powerfully affect<br />
students’ perception of their future<br />
role as nurses, according to Reid<br />
Ponte. “For these young people to be<br />
successful, they need to understand<br />
how presence and professionalism<br />
play out in the community. Opportunities<br />
like this can assure that they’re<br />
aware of those responsibilities.”<br />
Setting the foundation<br />
The U-56 project is the result<br />
of work by dozens of people at<br />
DF/HCC and UMass Boston over the<br />
past five years, including nurse leaders<br />
at each DF/HCC hospital. Once<br />
the decision to apply for the grant<br />
was made, <strong>Dana</strong>-<strong>Farber</strong>’s Karen<br />
Emmons, PhD, associate director of<br />
DF/HCC’s Initiative to Eliminate<br />
<strong>Cancer</strong> Disparities, and Karen Burns<br />
White, its deputy director, led the<br />
effort to build an infrastructure of<br />
cooperation between the two institutions.<br />
Sarah Weiler, PhD, of Research<br />
Administration at <strong>Dana</strong>-<strong>Farber</strong> was<br />
instrumental as well, particularly<br />
in the basic science components of<br />
the partnership.<br />
“The NCI requires that institutions<br />
have a framework of collaborative<br />
efforts already in place, on which<br />
the U-56 grant can build,” Emmons<br />
explains. “We created an administrative<br />
structure with representatives<br />
from both organizations,<br />
including internal and external<br />
advisory committees. We also<br />
formed a core group to plan and<br />
evaluate the project, as well as a<br />
group to organize pilot studies<br />
involving faculty at DF/HCC<br />
and UMB.” The internal working<br />
groups included representatives<br />
of all DF/HCC hospitals.<br />
When the grant application<br />
was submitted, it carried a principal<br />
investigator at each organization:<br />
Emmons, who is also a<br />
professor at the Harvard School<br />
of Public Health, and Roderick<br />
Jensen, PhD, the Alton Brann<br />
Distinguished Professor of Physics,<br />
Biology, and Mathematics<br />
at UMass Boston.<br />
Ambitious as it is, the U-56<br />
effort is seen as a foundation for<br />
much more extensive collaborations<br />
in the future. Leaders hope<br />
to apply in a few years for another<br />
federal grant to fund a major<br />
expansion of the alliance.<br />
The partnership that has<br />
grown between UMB and<br />
DF/HCC is unique in Greer<br />
Glazer’s experience as a university<br />
administrator. “Usually such<br />
programs are designed by the<br />
academic institution, which then<br />
invites the hospital to join as a<br />
participant,” she says. “In this<br />
case, both organizations have<br />
been involved from the<br />
very beginning.”<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 15
Molecular<br />
engineers<br />
How chemical biologists<br />
explore the workings of cells<br />
By Robert Levy<br />
For every job, there is a tool – except, it might<br />
be said, in the field of cancer research. Despite<br />
galloping advances in biological knowledge,<br />
scientists have had no means of grappling with most<br />
of the malfunctioning machinery in cancer cells.<br />
An estimated 80 percent of the abnormal proteins<br />
involved in cancer are unreachable with existing classes<br />
of compounds, either because such compounds cannot<br />
get inside the cell or because “pits” on the surface of<br />
target proteins can’t accommodate them. As a result,<br />
researchers find themselves knowing very well which<br />
proteins they’d like to block with drug molecules, but<br />
lacking the means to do so.<br />
Enter the field of chemical biology, a relatively young<br />
discipline in which investigators use very small molecules<br />
to construct compounds of precise size and shape.<br />
The diminutive dimensions and key-like structure of<br />
such compounds give them an extraordinary versatility.<br />
They enable scientists to turn cell machinery on and off<br />
with almost pinpoint control. They provide a novel way<br />
of interrogating “suspect” genes to see if they’re<br />
involved in disease. And they vastly expand the pool<br />
of diseased genes and proteins – known as “druggable<br />
targets” in medical parlance – that can be attacked<br />
with therapies.<br />
Chemical biology has “cancer relevance” written all<br />
over it, which explains why it is part of <strong>Dana</strong>-<strong>Farber</strong>’s<br />
Strategic Plan. “The beauty of small molecules, from<br />
the standpoint of cancer, is that they allow us to alter<br />
the natural history of the disease process,” says Greg<br />
Verdine, PhD, who directs the Chemical Biology<br />
Initiative at <strong>Dana</strong>-<strong>Farber</strong> and is the Erving Professor of<br />
Chemistry in Harvard University’s Faculty of Arts and<br />
Sciences. Because cancer arises from a series of incorrect<br />
or incoherent messages between genes, the field<br />
A mini-protein locked into shape by a hydrocarbon<br />
“staple” represents a new approach to understanding<br />
and treating cancer. (Courtesy of Peter Kutchukian and<br />
Eric Smith)<br />
is uniquely capable of interrupting those messages,<br />
decoding them, and showing where they’ve gone astray.<br />
Chemical biology’s rise to prominence, Verdine notes,<br />
results from the growing “democratization” of biology<br />
and chemistry – the advent of technology that enables<br />
chemists to easily perform certain biological procedures,<br />
and biologists to do some chemistry.<br />
The partnership between <strong>Dana</strong>-<strong>Farber</strong> and Harvard’s<br />
Department of Chemistry and Chemical Biology grew<br />
out of that same sense of lowered barriers. “By associating<br />
with Harvard, <strong>Dana</strong>-<strong>Farber</strong> is connected to one of<br />
the foremost centers for synthetic chemistry [the construction<br />
of new chemical compounds] in the world,”<br />
says Verdine, who now splits his time between his<br />
Cambridge laboratory and the <strong>Institute</strong>. “When I get<br />
on the elevator in the Smith laboratories at <strong>Dana</strong>-<strong>Farber</strong>,<br />
I find myself riding with patients confronting their disease.<br />
That doesn’t happen at my lab in Cambridge. It<br />
makes the sense of urgency palpable.”<br />
The next pages offer a look at the work of the members<br />
of <strong>Dana</strong>-<strong>Farber</strong>’s Chemical Biology Initiative.<br />
16 P ATHS OF P ROGRESS Spring/Summer 2007
“The beauty of small molecules, from the standpoint of cancer, is that<br />
they allow us to alter the natural history of the disease process.”<br />
— Greg Verdine, PhD<br />
Biochemical braces<br />
Within every cell in<br />
the body, there is a<br />
contest for that cell’s<br />
future. Specialized<br />
proteins order it to<br />
die, while others<br />
instruct it to continue<br />
living. The cell’s<br />
course is dictated by<br />
the relative strength<br />
of these commands.<br />
Greg Verdine<br />
The vast majority of<br />
the time, there is a natural balance between the death of<br />
old cells and the creation of new ones. When the death<br />
mechanism fails because of a faulty gene, cells may<br />
persist long past the end of their natural lifespan. The<br />
resulting clump of cells can form a tumor.<br />
“In one of the classic models of cancer, cells produce<br />
an oversupply of survival proteins, which act as a shield<br />
against other proteins that signal the cell to die,” says<br />
Loren Walensky, MD, PhD, who joined <strong>Dana</strong>-<strong>Farber</strong> as<br />
its first chemical biologist in 2003. “The challenge is to<br />
find a way of restarting the death process.”<br />
Ideally, scientists could do that by disrupting the<br />
“blockade” that survival proteins exert on the cell’s<br />
death machinery. But the structural complexity of such<br />
proteins and their location deep within the cell nucleus<br />
have made it difficult to design drugs with that ability.<br />
Walensky and his colleagues knew that a protein<br />
called BID has a short, coiled segment – a helical peptide<br />
– that is capable of triggering the natural cell-death<br />
process, called apoptosis. When the peptide is produced<br />
in the laboratory, artificially disconnected from the<br />
entire protein, it loses its helical shape, which prevents<br />
it from entering cells to deliver its “die” message.<br />
With Verdine and Stanley J. Korsmeyer, MD, the<br />
late chairman of <strong>Dana</strong>-<strong>Farber</strong>’s Executive Committee<br />
for Research, Walensky constructed<br />
a tiny “staple”<br />
from synthetic amino<br />
acids (the building<br />
blocks of proteins) to<br />
Loren Walensky<br />
helped build a tiny<br />
“staple” to reinforce a<br />
compound involved in<br />
cancer cell death. The<br />
computerized image<br />
below shows the<br />
unstapled (left) and<br />
stapled compound.<br />
Illustration by Nicole Bedard<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 17
“It’s surprising how little we know about cell division, considering that<br />
it’s one of the most basic biological processes.” — Ulrike Eggert, PhD<br />
reinforce the natural peptide. In laboratory tests, the stapled<br />
peptides entered leukemia cells and activated their<br />
cell-death program. Even more intriguing, when the<br />
strengthened peptides were injected into mice with<br />
human-type leukemia, the disease was suppressed.<br />
The experiments demonstrated that stapled peptides<br />
can be used to study how proteins interact within cells,<br />
and to block interactions that lead to disease. “Stapling<br />
enables us to generate a brand-new ‘molecular toolbox’<br />
for probing and potentially treating the fundamental<br />
causes of cancer and other diseases,” Walensky remarks.<br />
Using the stapled peptide, Walensky recently proved<br />
that BID sets the cell’s death machinery in motion by<br />
binding to a protein called BAX, vindicating a theory<br />
first proposed by<br />
Stanley Korsmeyer.<br />
The<br />
finding has<br />
energized efforts to treat some cancers with molecules able<br />
to latch onto BAX.<br />
Stop-motion pictures<br />
Although it is described in every high school biology<br />
textbook, the process of cell division – cytokinesis –<br />
remains in many respects a mystery. In preparation for<br />
division, cells duplicate and divide their DNA, then form<br />
a ring at their center. The ring tightens until a new cell<br />
pinches off from the old one. Many of the details of the<br />
process, however, are unclear, because it is both very<br />
complicated and very fast – about 45 minutes from start<br />
to finish.<br />
Ulrike Eggert, PhD, who joined <strong>Dana</strong>-<strong>Farber</strong> last year<br />
at the same time as fellow chemical biologist Nathanael<br />
Gray, PhD, is using small molecules to halt cytokinesis<br />
at key points, creating freeze-frame pictures of dividing<br />
cells and revealing how their proteins change each step<br />
of the way.<br />
“It’s surprising how little we know about cell division,<br />
considering that it’s one of the most basic biological<br />
processes,” says Eggert, whose laboratory is alongside<br />
Gray’s at Harvard Medical School. “Small molecules can<br />
bring the process to a stop very quickly. Within a few<br />
seconds you can see them working.”<br />
As a postdoctoral fellow at Harvard Medical School<br />
and now as a <strong>Dana</strong>-<strong>Farber</strong> faculty member, Eggert has<br />
built a library of such cytokinesis-stoppers. She began by<br />
screening 50,000 candidate compounds, found 50 that<br />
had the desired effect, and chose the 25 most promising<br />
ones to study. The small molecules freeze the division<br />
Ulrike Eggert uses small molecules to trace<br />
the sequence of cell division, shown in the<br />
image below.<br />
18
process at different stages by binding to different<br />
cell proteins.<br />
The challenge now is to identify each of these target<br />
proteins within the cell. Eggert first used a technique<br />
called RNA interference, which stifles the production of<br />
specific proteins, to screen for proteins that play a role<br />
in cell division. She then treated cells with small molecules<br />
and compared the results of the two approaches.<br />
If small molecules and RNA interference produced a<br />
similar effect, it suggested that the same proteins were<br />
involved. Eggert is currently studying four small molecules<br />
known to inhibit cell division and plans to use<br />
them to understand how division takes place and how it<br />
goes out of control in many cancers.<br />
“If we can show that one of these molecules blocks a<br />
specific protein in the pathway,” Eggert explains, “that<br />
protein would be a natural target for drug therapy.”<br />
Wedge site story<br />
For Nathanael Gray, chemical biology offers a way<br />
to discover whether genes thought to be involved<br />
in cancer actually play that role and, if so, how they<br />
can be stopped. He focuses on a class of proteins known<br />
as kinases, which spark interactions between other<br />
proteins and are abnormally abundant in many types<br />
of cancer cells.<br />
Kinases work by allowing a chemical tag called a<br />
phosphate group to be transferred from one protein to<br />
another. Each type of kinase – there are more than 500<br />
in the human body – is responsible for transferring<br />
phosphates to a specific target protein. Many kinases<br />
work in a series and form a molecular signaling network<br />
that controls a cell’s fate.<br />
To restrain a kinase, scientists would like to use a biochemical<br />
“wedge,” a small molecule that attaches easily<br />
to the kinase’s binding site, a tiny pocket on its surface.<br />
That would bar the kinase from transferring phosphates<br />
to target proteins. Gray and his colleagues are working<br />
out the contours and dimensions of binding sites on a<br />
specific class of kinases and then testing small molecules<br />
whose size and shape is a close match. It’s as<br />
though the prince in the fairy tale “Cinderella” identified<br />
the owner of Cinderella’s glass slipper by measuring<br />
the slipper’s proportions and finding the<br />
maiden whose foot corresponded to them.<br />
“Chemical biology involves more than knowing<br />
that protein A interacts with protein B,” Gray says. “We<br />
want to know the exact positions of all the atoms in the<br />
protein interaction site. Armed with this knowledge, we<br />
can design and test compounds that have the potential to<br />
be specific inhibitors and that may become the starting<br />
point for future drugs.”<br />
Having a set of such molecules will enable researchers<br />
to selectively stifle whichever kinase, or group of kinases,<br />
they choose, to determine if they contribute to<br />
cancer. The “cancer kinases” could then be the target of<br />
small molecule-based therapies.<br />
“We’ve needed a way to dig deeper into the interactions<br />
between cell proteins,” Gray observes. “Chemical<br />
biology lets us explore them at the<br />
most basic level.”<br />
Nathanael Gray<br />
focuses on identifying<br />
and blocking genes<br />
involved in cancer.<br />
19
Discoveries<br />
Estrogen may offer key to new therapies for colon cancer<br />
News that estrogen supplements may raise the risk<br />
of heart disease and breast cancer has prompted<br />
many postmenopausal women to stop taking<br />
them. But the estrogen story is not entirely one-sided.<br />
Researchers at <strong>Dana</strong>-<strong>Farber</strong> have found that the hormone<br />
may hold important clues for the development of new<br />
therapies for colorectal cancer.<br />
Drawing on data from a long-running study of<br />
women’s health, the investigators found that postmenopausal<br />
women with colon cancer lived longer and<br />
were less likely to die of the disease if they had been<br />
taking estrogen supplements within five years of their<br />
diagnosis. The findings do not mean that estrogen<br />
should be viewed as a treatment or preventive therapy<br />
for colon cancer, but they do offer new insights into the<br />
cancer process, say the study authors, led by Jennifer<br />
Chan, MD, MPH, and Charles Fuchs, MD, MPH.<br />
“This work provides a rationale to further study the<br />
basic mechanism by which estrogen influences the<br />
development and progression of colon cancer,” says<br />
Chan. “By understanding how estrogen offers potentially<br />
beneficial effects in some types of cells, yet deleterious<br />
Research by Jennifer Chan and colleagues drew on<br />
data from more than 800 postmenopausal women.<br />
effects in others, it may be possible to design therapies<br />
that are effective against colon cancer without posing a<br />
significant risk of other health problems.”<br />
Study maps new route to making cells cancer-resistant<br />
Jean Zhao and Tom Roberts are probing the<br />
P13K cell-signaling pathway.<br />
It’s a cliché that a chain is no better than its weakest<br />
link, but in cancer biology, finding and removing that<br />
link can hinder a cell’s ability to become cancerous.<br />
Proof of that principle came from a recent study in<br />
which <strong>Dana</strong>-<strong>Farber</strong> investigators identified such a target<br />
in a cell-signaling pathway known as P13K, which often<br />
misfires in breast, colon, and other cancers. When the<br />
researchers disabled this target – a form of a protein called<br />
p110-alpha – in mouse cells, the cells became resistant to<br />
factors that normally would make them cancerous.<br />
“When you remove this subunit from the P13K pathway,<br />
genes associated with cancer quit working, key cell receptors<br />
shut down, and almost nothing can transform these<br />
cells into cancer cells,” says Tom Roberts, PhD, who led<br />
the study with colleague Jean Zhao, PhD. The findings<br />
have drawn new attention to p110-alpha, because they<br />
suggest that cancer therapies could be improved by<br />
blocking this molecule.<br />
20 P ATHS OF P ROGRESS Spring/Summer 2007
Discoveries<br />
Research reveals new breast cancer susceptibility gene<br />
Afew years ago, the existence of a gene now<br />
known as PALB2 was only hypothetical, not<br />
proven. Recently, <strong>Dana</strong>-<strong>Farber</strong> scientists and<br />
colleagues in Finland not only confirmed that PALB2 is<br />
real, but also found it heightens women’s risk of breast<br />
cancer when inherited in a mutated form. It may also<br />
raise the risk of prostate cancer in men.<br />
About 10 percent of all breast cancers result from<br />
inherited gene mutations, though the two best-known<br />
cancer-susceptibility genes, BRCA1 and BRCA2,<br />
account for only 20-30 percent of such inherited<br />
cancers, suggesting there are more such genes still<br />
to be discovered.<br />
Researchers led by <strong>Dana</strong>-<strong>Farber</strong>’s David Livingston,<br />
MD, and Bing Xia, PhD, determined that the PALB2<br />
protein enables the BRCA2 protein to repair damaged<br />
cell DNA. However, if PALB2 is defective, DNA repair<br />
can be hindered, increasing the chances that a cell will<br />
become cancerous.<br />
Finnish researchers working with the <strong>Dana</strong>-<strong>Farber</strong><br />
scientists screened tissues from breast cancer patients<br />
in Finland and found that about 1 percent had the same<br />
mutation in PALB2. A screening of other types of<br />
David Livingston (left) and Bing Xia collaborated<br />
with scientists in Boston, Finland, and Sweden.<br />
cancers indicated the mutation may play a role in some<br />
prostate cancers as well.<br />
“The screening suggests that carrying the mutation<br />
increases a woman’s risk of breast cancer approximately<br />
fourfold,” Xia said. “Our finding may improve the<br />
ability to identify some women at elevated risk for the<br />
disease and potentially lead to new prevention and<br />
treatment strategies.”<br />
Far-running mice may hold clues to human disease<br />
A magnified slice of mouse muscle showing fibers.<br />
The development of “marathon mice” by <strong>Dana</strong>-<br />
<strong>Farber</strong> researchers may one day benefit people<br />
with neuromuscular disorders and muscle wasting.<br />
Investigators led by the <strong>Institute</strong>’s Bruce Spiegelman,<br />
PhD, and Zoltan Arany, MD, PhD, used a genetic<br />
switch known as PGC-1 beta to change the type of skeletal<br />
muscle fibers in a group of laboratory mice. The<br />
altered mice had such muscular endurance that they ran<br />
on a treadmill 25 percent longer than normal mice before<br />
becoming exhausted. Had they been on a track, they<br />
would have covered nearly a half-mile before becoming<br />
fatigued, compared to less than one-third of a mile for<br />
normal mice.<br />
“We are working very hard on screening drugs that<br />
might benefit people with diseases like muscular dystrophy<br />
and amyotrophic lateral sclerosis (Lou Gehrig’s<br />
disease),” says Spiegelman.<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 21
Discoveries<br />
Study reveals need for more safety standards for prescribing<br />
chemotherapy drugs taken by pill<br />
Agrowing number of cancer medications are<br />
available in pill form, but the prescription<br />
safeguards so prevalent in infusion chemotherapy<br />
have yet to be implemented as thoroughly in oral<br />
chemo drugs, according to a recent study led by <strong>Dana</strong>-<br />
<strong>Farber</strong> researchers.<br />
A survey by the investigators found that few National<br />
<strong>Cancer</strong> <strong>Institute</strong>-designated comprehensive cancer centers<br />
had standardized prescribing practices for oral<br />
chemotherapy, that is, medications taken by pill rather<br />
than intravenously. The survey revealed significant differences<br />
among the centers in the way prescriptions<br />
were generated and in the amount of information needed<br />
to complete drug-order forms.<br />
Nearly 70 percent of the centers used handwritten<br />
orders for most oral chemotherapy; a minority used<br />
computer-based order entry systems or preprinted<br />
paper prescriptions.<br />
“Given how quickly oral chemotherapies have become<br />
standard care for a growing number of cancers, we were<br />
not surprised to find variations in how organizations<br />
prescribe and monitor their use,” says Saul N. Weingart,<br />
MD, PhD, vice president for patient safety at <strong>Dana</strong>-<br />
<strong>Farber</strong> and a leader of the study. “It was surprising,<br />
however, that few of the safeguards used with infusion<br />
chemotherapy are applied to oral chemotherapy.”<br />
Co-author Lawrence Shulman, MD, chief medical<br />
officer at <strong>Dana</strong>-<strong>Farber</strong>, added: “These findings underline<br />
the importance of forging a consensus in the oncology<br />
field on standardized safeguards and practices for prescribing<br />
and monitoring the use of these drugs.”<br />
Grief unfolds in stages for many, with yearning high<br />
Arecent study by <strong>Dana</strong>-<strong>Farber</strong> researchers and<br />
colleagues confirmed, in part, the commonly<br />
accepted stages of grief – disbelief, yearning,<br />
anger, depression, and acceptance – and the sequence in<br />
which these emotions normally occur.<br />
While describing how individuals, most of whom were<br />
widowed, mid-to-later-life adults, tend to adjust to a<br />
loved one’s death from “natural” causes such as cancer<br />
or heart disease, the study challenged existing clinical<br />
guidelines by showing that yearning – not depression –<br />
was the most common negative feeling among survivors.<br />
Acceptance was also high among them.<br />
“Up to now, people thought sadness was the most<br />
characteristic feature of bereavement, but these data<br />
show it is more about yearning and pining for and missing<br />
the person – a hunger for having him or her come<br />
back,” says senior author Holly Prigerson, PhD, director<br />
of <strong>Dana</strong>-<strong>Farber</strong>’s Center for Psycho-Oncology and<br />
Palliative Care Research.<br />
Forewarning about a pending death may help people<br />
cope emotionally, the investigators also found. “When<br />
patients and families knew about the terminal diagnosis<br />
ahead of time, specifically six months or longer,” Prigerson<br />
says, “they were better prepared for the death and had<br />
more acceptance and less disbelief afterwards.”<br />
The project involved interviews with 233 individuals in<br />
Connecticut who were mourning a loved one’s “natural”<br />
death; each participant was interviewed three times over<br />
two years. Study team members also included Susan<br />
Block, MD, of <strong>Dana</strong>-<strong>Farber</strong>/Brigham and Women’s<br />
<strong>Cancer</strong> Center; Baohui Zhang of <strong>Dana</strong>-<strong>Farber</strong>; and Paul<br />
Maciejewski, PhD, of Yale University School of Medicine.<br />
22 P ATHS OF P ROGRESS Spring/Summer 2007
Discoveries<br />
Patient stories in book reveal cancer treatment ‘revolution’<br />
Since the mid-1950s, when he witnessed some of<br />
the first patient experiments using combination<br />
chemotherapy, David G. Nathan, MD, has played<br />
a pivotal role in the dramatic history of cancer care<br />
and research.<br />
Now, Nathan – an acclaimed pediatric hematologist<br />
who served as <strong>Dana</strong>-<strong>Farber</strong>’s president from 1995 to 2000<br />
and has long been affiliated with Children’s Hospital<br />
Boston – recounts that history’s triumphs and struggles in<br />
a book called The <strong>Cancer</strong> Treatment Revolution: How<br />
Smart Drugs and Other New Therapies Are Renewing<br />
Our Hope and Changing the Face of Medicine.<br />
Published in March by John Wiley & Sons, the work<br />
recounts the stories of three patients with invasive cancers<br />
treated at <strong>Dana</strong>-<strong>Farber</strong> and its partners in care: Mario, a<br />
19-month-old boy diagnosed with leukemia; Joan, a 62-<br />
year-old woman facing metastatic breast cancer; and Ken,<br />
a 48-year-old who endured multiple clinical trials for<br />
gastrointestinal stromal tumor before his death in 2005.<br />
The pages are peppered with the insights of current and<br />
former <strong>Dana</strong>-<strong>Farber</strong> physicians, researchers, and other<br />
staff members.<br />
Nathan weaves the patients’ tales with the science<br />
behind them: how cancer behaves, how it is treated, and<br />
how the disease sometimes outsmarts the clinical investigators<br />
seeking to defeat it with “smart” drugs that attack<br />
specific proteins on which malignant cells thrive. His<br />
vivid prose brings the science to life: “Like the crab from<br />
which it gets its name, invasive cancer moves its claws in<br />
all directions, pushing abnormal cells into normal tissue<br />
and destroying normal organs in the process.”<br />
A longtime advocate for clinical research, Nathan spotlights<br />
the dedication of medical teams and the fortitude<br />
of patients and families – while calling for ongoing collaboration<br />
among oncologists, scientists, pharmaceutical<br />
companies, private foundations, and the government to<br />
continue the search for new and less toxic remedies.<br />
In one of the early chapters, Nathan depicts the first<br />
encounter between Mario, his mother, Flavia, and Scott<br />
Armstrong, MD, PhD, now a faculty member at <strong>Dana</strong>-<br />
<strong>Farber</strong> and Children’s Hospital. They were in the emergency<br />
room of Children’s, where Flavia and her husband,<br />
Walter, had rushed their toddler after a troubling blood<br />
test that indicated leukemia – though they didn’t yet know<br />
which type. The boy was being transferred to intensive<br />
care while Walter<br />
went home to learn<br />
whatever he could<br />
about his son’s<br />
dreaded disease:<br />
“Flavia stayed<br />
with Mario and the<br />
medical entourage.<br />
Out of the crowd<br />
of doctors stepped<br />
Scott Armstrong, a<br />
first-year fellow in<br />
oncology. She<br />
remembers their<br />
David G. Nathan<br />
first meeting in precise<br />
detail. Flavia felt as though she had been drifting in<br />
a turbulent sea, drowning in the unexpected wreck of her<br />
life. Suddenly a life ring was flung to her from the fog.<br />
Holding the rope was Scott. In his inexperience, Scott had<br />
no idea of the importance of that moment, but he saved<br />
Flavia from profound depression. ...<br />
“Scott knew he had to be careful in his initial conversations<br />
with Flavia. She was alone, exhausted, and<br />
extremely vulnerable. Whatever he told her would have<br />
to be backed with solid evidence and not conjecture. She<br />
immediately pressed him: ‘Is this the good leukemia’ His<br />
answer was that he could not be certain until other laboratory<br />
tests were concluded, but in any case, the immediate<br />
risk was not the type of leukemia but the very high<br />
white blood cell count. ...<br />
“Scott mobilized the specialized staff, and the exchange<br />
procedure [to replace the child’s diseased blood] started<br />
at once. Leaving Mario in the competent hands of the<br />
intensive care people, Scott called Lewis Silverman, a<br />
staff physician at Children’s Hospital and the <strong>Dana</strong>-<br />
<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong> and an assistant professor at<br />
Harvard Medical School, to go over the next steps in<br />
what would turn out to be a [successful] two-year effort<br />
to save Mario.”<br />
Excerpted from The <strong>Cancer</strong> Treatment Revolution:<br />
How Smart Drugs and Other New Therapies Are<br />
Renewing Our Hope and Changing the Face of Medicine<br />
(© 2007), by David G. Nathan, MD. Reprinted with permission<br />
from John Wiley & Sons.<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 23
SPECIAL BONDS<br />
PEDIATRIC PATIENTS, CAREGIVERS<br />
SHARE UNIQUE RELATIONSHIPS<br />
By Saul Wisnia<br />
The “no smoking” tie her doctor<br />
wore. The way he always<br />
made her feel safe in an<br />
environment filled with shots, blood<br />
tests, and other scary stuff. The college<br />
campuses her family drove by<br />
as they approached <strong>Dana</strong>-<strong>Farber</strong>,<br />
and her declaring, “I’m going to go<br />
there when I grow up,” at a time<br />
when her parents didn’t even know<br />
if she would grow up.<br />
These are the earliest memories<br />
Eileen Degregorio has of her cancer<br />
treatment. Just 2 years old when<br />
diagnosed with acute lymphocytic<br />
leukemia (ALL) in March 1989, she<br />
underwent aggressive chemotherapy,<br />
both then and after a relapse<br />
when she was 6. She had a bone<br />
marrow transplant and has since<br />
received follow-up care through<br />
annual visits to <strong>Dana</strong>-<strong>Farber</strong>’s<br />
Jimmy Fund Clinic.<br />
Eileen and her family’s challenges<br />
and concerns have changed over<br />
time, as has her role in monitoring<br />
her health as a young adult. But one<br />
thing has remained constant: her<br />
core caregivers. For nearly 20 years,<br />
David E. Fisher, MD, PhD, and<br />
Robin Griffey, RN, BSN, have been<br />
her primary oncologist and nurse<br />
at <strong>Dana</strong>-<strong>Farber</strong>.<br />
Theirs is a not an uncommon<br />
arrangement. With more pediatric<br />
cancer patients than ever recovering<br />
from their diseases, unique bonds<br />
are forming between these nowadult<br />
survivors and their caregivers.<br />
And as physicians and researchers<br />
here and at affiliated hospitals learn<br />
more about secondary cancers and<br />
other potential health problems<br />
resulting from childhood cancers<br />
and their treatment, they can both<br />
provide stronger follow-up care<br />
and see “their kids” reach milestones<br />
like graduations, marriages,<br />
and parenthood.<br />
“When I started here in 1981,<br />
many families still saw pediatric<br />
cancer as a death sentence,” says<br />
Holcombe Grier, MD, associate<br />
chief of Pediatric Clinical Oncology<br />
at <strong>Dana</strong>-<strong>Farber</strong> and its pediatric<br />
partner, Children’s Hospital Boston.<br />
“Now people are worrying not only<br />
about whether their sons and daughters<br />
will be cured, but also how they<br />
will continue to live as survivors.<br />
We’re able to change our mindset<br />
from talking about cures to talking<br />
about late effects like secondary<br />
cancers, and how to monitor them<br />
over time.”<br />
Photographs and memories<br />
Bulletin boards crammed with<br />
photos in many physician offices<br />
affirm the close ties that pediatric<br />
24 P ATHS OF P ROGRESS Spring/Summer 2007
As Eileen Degregorio has gone from<br />
preschool cancer patient to adult survivor,<br />
her oncologist David E. Fisher<br />
has “always been there for me.”<br />
doctors and their young patients<br />
build. Children of various ages grin<br />
in school pictures and action shots<br />
on ski slopes and Halloween routes,<br />
and caregivers often gain a sort of<br />
parental pride as youngsters continue<br />
growing. Although many children<br />
with ALL and other cancers<br />
are diagnosed as preschoolers or<br />
infants, the “well” visits continue<br />
long after their treatment ends –<br />
gradually moving from monthly<br />
to bi-monthly to twice and then<br />
once a year.<br />
“From the time I was about 10,<br />
every time I came in, Dr. Billett<br />
would introduce me to a new doctor<br />
and say, ‘This is the kid who was<br />
born with leukemia, and look how<br />
she’s doing,’” recalls Nakia Neff,<br />
now 19, of her visits with Amy<br />
Billett, MD, her primary caregiver<br />
for ALL since she was three weeks<br />
old. “They would all say how wonderful<br />
it was, and it made me feel<br />
great to be alive.”<br />
For Degregorio, time with Fisher<br />
was similarly reassuring. She<br />
remembers him asking her to draw<br />
a picture of her red and white blood<br />
cells – then praising her work as<br />
“just right.” When she was isolated<br />
in a sterilized hospital room after<br />
her transplant, she promised him<br />
she’d “set the record” for the quickest<br />
recovery. She did, getting out in<br />
just 13 days.<br />
“Usually when the doctor comes<br />
in a room, that’s when you panic,<br />
but I was always happy to see him,”<br />
she says. “Dr. Fisher took time to<br />
explain procedures to me before<br />
talking with my parents. He gave<br />
me strength.”<br />
Neither Neff nor Degregorio can<br />
remember her earliest visit to <strong>Dana</strong>-<br />
<strong>Farber</strong>, but Uri Berenguer-Ramos<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 25
will never forget his. When he was 3,<br />
the Panama native saw his first snow<br />
when he and his mother, Daisy, came<br />
to Boston and <strong>Dana</strong>-<strong>Farber</strong> in November<br />
1985. Uri had a rare blood<br />
disease known as histocytosis, and<br />
doctors back home had said he<br />
needed a right leg amputation due<br />
to a tumor. Daisy insisted on a second<br />
opinion, even if it meant flying<br />
to a city where she didn’t know any<br />
Uri Berenguer-Ramos (left) and Lindsay Frazier built a powerful connection<br />
during Uri’s long years of treatment; today they celebrate his good<br />
health and blossoming media career.<br />
people or the language.<br />
“That first day, after a Latino<br />
security guard helped us get settled<br />
in, I met Dr. Lindsay Frazier,”<br />
recalls Uri Berenguer-Ramos. “She<br />
was a warm, caring person, and<br />
helped me through those first terrifying<br />
days. She also helped save my<br />
leg, and over time, she became like<br />
my second mother.”<br />
Frazier, then a first-year hematology-oncology<br />
fellow at DFCI,<br />
recalls how Uri “appeared out of<br />
nowhere on our doorstep, radiating<br />
charisma even at age 3. He’s the<br />
kind of kid who, when he came into<br />
our world, it felt like somebody had<br />
turned on the lights – the Christmas<br />
lights.” Her young patient was also<br />
an excellent “bridge” to conversations<br />
with his mother, as he picked<br />
up English very quickly. Over the<br />
16 years of Uri’s treatment that followed,<br />
the three grew very close.<br />
Treating mom and dad<br />
In addition to forming strong<br />
bonds with young patients, caregivers<br />
develop distinctive ties with their<br />
parents. Joan Degregorio, Eileen’s<br />
mother, feels that Fisher, Griffey, and<br />
pediatric psychologist Nancy Frumer-<br />
Styron, PsyD, are a sort of “<strong>Dana</strong>-<br />
<strong>Farber</strong> trinity” that has watched over<br />
her family. “They didn’t just treat<br />
Eileen, they treated all of us,” Joan<br />
Degregorio says. “Dr. Fisher would<br />
tell you I’m the woman with a million<br />
questions, but they always<br />
answered every one.”<br />
Dad Anthony Degregorio agrees:<br />
“There is a comfort level you can’t<br />
describe – both for the continuity of<br />
services and the quality of care.<br />
When Eileen was first sick and we<br />
had to go back and forth to the emergency<br />
room, we had to memorize<br />
certain dates because we’d always<br />
be getting different doctors. At <strong>Dana</strong>-<br />
<strong>Farber</strong>, they knew everything; Dr.<br />
Fisher was reading his own notes,<br />
not dissecting someone else’s.”<br />
Eileen and John Sullivan’s son<br />
John Timothy was diagnosed with<br />
acute myelogenous leukemia (or<br />
AML) at age three weeks, forcing<br />
the family to begin a crazy schedule<br />
in which John would sleep nightly in<br />
26 P ATHS OF P ROGRESS Spring/Summer 2007
Uri Berenguer-Ramos was “the kind of kid who, when he came into<br />
our world, it felt like somebody had turned on the lights – the<br />
Christmas lights.” — Lindsay Frazier, MD<br />
their son’s room at Children’s<br />
Hospital Boston, while Eileen shuttled<br />
their two young daughters to<br />
relatives’ homes and spent her days<br />
by John Timothy’s bedside after<br />
dad went to work. There were many<br />
days the couple would literally pass<br />
each other in the hallway, and it was<br />
Billett who insisted they escape the<br />
hospital once a week for dinner.<br />
“Dr. Billett made us feel that she<br />
had our best interest at heart, and I<br />
came to count on her more and<br />
more,” says Eileen Sullivan. This<br />
closeness proved crucial when<br />
John Timothy needed a bone marrow<br />
transplant and his 4-year-old<br />
sister, Ciara, was a perfect match.<br />
“He had only a 40 percent chance<br />
for a successful transplant, and I<br />
don’t know what I would have<br />
done without Dr. Billett’s support.<br />
One by one, all of the other families<br />
we were friendly with at the<br />
hospital lost their kids, and sometimes<br />
it felt like we were in this<br />
alone with Dr. Billett. But she<br />
always gave us hope.”<br />
John Timothy recovered, and<br />
shortly thereafter Eileen became<br />
pregnant with her fourth child – just<br />
as Billett was conceiving her first.<br />
“We wound up having babies at the<br />
same time, and evolved into friends.<br />
After that, whenever I went in for<br />
appointments with John Timothy, he<br />
would have to sit there while Amy<br />
and I caught up. He’d stare at me<br />
with a look like, ‘Wrap it up, wrap<br />
it up,’ and I’d just laugh.”<br />
While invaluable to families,<br />
such closeness can make a physician’s<br />
job harder. “When you’re<br />
trying to make very difficult decisions<br />
about what to do next in<br />
treatment, especially if things are<br />
not going well, you need to make<br />
sure that you’re not so close with a<br />
family that your emotional involvement<br />
impedes your ability to make<br />
the best medical choices,” says<br />
Billett. “You need to weigh all the<br />
factors.” Even in those cases when<br />
a young patient does not survive,<br />
caregivers often continue their<br />
support by attending funerals and<br />
serving as a comforting presence<br />
to families.<br />
Growing up, staying close<br />
Vastly improving pediatric cancer<br />
outcomes have made bad outcomes<br />
far less common. The most common<br />
form of pediatric cancer, ALL,<br />
carried less than a 5 percent longterm<br />
survival rate in the 1960s<br />
and ’70s. Even into the mid-1980s,<br />
30-40 percent of children diagnosed<br />
with this leukemia didn’t make it<br />
far into adulthood, but today the<br />
Just three weeks old when Amy Billett (left) became her doctor, Nakia<br />
Neff can now talk with her “like she’s one of my girlfriends.”<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 27
“From the time I was about 10, every time I came in, Dr. Billett would<br />
introduce me to a new doctor and say, ‘This is the kid who was born<br />
with leukemia, and look how she’s doing.’” — Nakia Neff<br />
disease boasts an 80-90 percent cure<br />
rate. Other pediatric cancers such as<br />
Hodgkin’s lymphoma, Ewing’s sarcoma,<br />
and Burkitt’s lymphoma have<br />
also seen strong gains, thanks to<br />
improved regimens based partly on<br />
the experiences of children treated<br />
in the past.<br />
With extended survivorship, however,<br />
comes the potential for other<br />
health concerns down the road.<br />
Although <strong>Dana</strong>-<strong>Farber</strong>’s youngest<br />
patients maintain their primary<br />
oncologist after their treatment ends,<br />
this doctor can help lead them to<br />
other appropriate caregivers at DFCI<br />
and elsewhere.<br />
“It used to be that patients who<br />
came in after treatment were just<br />
screened to make sure the cancer was<br />
still gone, but now we approach survivorship<br />
differently,” says Lisa<br />
Diller, MD, clinical director of<br />
Pediatric Oncology at <strong>Dana</strong>-<strong>Farber</strong><br />
and Children’s Hospital Boston.<br />
Diller is founder and medical director<br />
of DFCI’s David B. Perini, Jr. Quality<br />
of Life Clinic, which focuses its<br />
research, patient care, and advocacy<br />
work on late effects such as secondary<br />
cancers, heart or fertility problems,<br />
and learning disabilities.<br />
“Today we can develop survivorship<br />
programs geared to each<br />
patient,” Diller explains. “Patients in<br />
the Perini Clinic can see a genetic<br />
counselor, a fertility expert, a mental<br />
health professional, and other specialists<br />
whose focus is the care of<br />
survivors. We can also link patients<br />
to the right adult caregivers at<br />
Brigham and Women’s Hospital or<br />
other institutions if they develop<br />
secondary conditions like hypertension<br />
or coronary heart disease.”<br />
Even patients who develop cancers<br />
at the cusp of adulthood can benefit<br />
from this arrangement. Michael<br />
Doto, now in his mid-40s, was diagnosed<br />
with Hodgkin’s disease at<br />
age 16 and began seeing Holcombe<br />
Grier a few years later. “Twelve years<br />
ago, I had bacterial meningitis and<br />
almost died, and Dr. Grier’s was the<br />
first face I saw when I woke. More<br />
recently, I developed a carcinoma in<br />
my ear and coronary artery disease<br />
as a result of my past radiation treatment,<br />
and in both cases he was great<br />
at helping me find the best specialists<br />
and make surgical decisions.”<br />
Getting on with life<br />
Another milestone occurs when<br />
patients grow old enough to check<br />
in with their doctors unaccompanied<br />
by a parent or adult. This rite of<br />
passage happens at different ages<br />
for each child, usually in the early<br />
teens, and can be exhilarating for all<br />
involved (although also tough for<br />
parents). Concerns can be discussed<br />
openly, like sex or fears about getting<br />
hurt playing sports.<br />
On one of his visits with Grier and<br />
his other longtime caregivers, Doto<br />
put together a collage of photos of<br />
his own two children and presented<br />
it to them with the comment, “You<br />
made this happen.” Doctors and<br />
nurses get their fair share of graduation<br />
and wedding invitations as well,<br />
and Degregorio asked Fisher to her<br />
high school graduation and five-year<br />
remission party.<br />
The best times, of course, are<br />
when patients get well and get on<br />
with their lives. Billett was attending<br />
a dance performance last December<br />
when she noticed a familiar face on<br />
stage. It was Neff, fully recovered and<br />
pursuing a performance career. John<br />
Timothy Sullivan also got better and<br />
is now in college at Massachusetts<br />
Maritime Academy; Doto is a<br />
senior vice president of operations<br />
at Citigroup.<br />
During baseball season, Frazier<br />
can turn on her radio and brush up<br />
on her Español by listening to Uri<br />
Berenguer-Ramos’ passionate broadcasts<br />
of the Boston Red Sox. Now<br />
cancer-free, Uri is the team’s leading<br />
Spanish radio broadcaster, and<br />
because of the close relationship<br />
between the Sox and <strong>Dana</strong>-<strong>Farber</strong>’s<br />
Jimmy Fund – one of the baseball<br />
club’s official charities – he has<br />
become a celebrity and inspiration<br />
to many other young patients. Like<br />
Doto, who volunteers at several DFCI<br />
events each year including the Jimmy<br />
Fund Clinic holiday party (where<br />
Grier plays Santa), Berenguer-Ramos<br />
also gives time to the <strong>Institute</strong> as a<br />
guest speaker.<br />
Then there is Eileen Degregorio,<br />
who is fulfilling her childhood promise<br />
by attending Wheelock College just<br />
down the road from <strong>Dana</strong>-<strong>Farber</strong>.<br />
Studying to be an elementary school<br />
teacher, she spent last summer as a<br />
counselor at Camp Sunshine, where<br />
children with cancer can get away<br />
from hospitals and checkups. A<br />
former camper there herself, she<br />
wants to help make kids feel happy<br />
and safe, just as Fisher and her other<br />
caregivers did for her.<br />
28 P ATHS OF P ROGRESS Spring/Summer 2007
First Person: Evie Goldfine<br />
A cancer survivor’s blog Edited by Christine Cleary<br />
Having a spouse die young from a brain tumor, raising two teenagers alone, enduring three bouts of lymphoma<br />
and a stem cell transplant, and losing a mother to lung cancer in just over 11 years would derail many<br />
people. Yet the spirited Evie Goldfine, 59, claims she has lived a charmed life, anchored by the love and<br />
support of family and friends.<br />
During her time as a <strong>Dana</strong>-<strong>Farber</strong> patient, Goldfine kept a lively Web log (blog) peppered with humor, pathos, and<br />
wisdom, and brimming with love for her family. In addition to allowing others to keep up with her progress, the site<br />
kept Evie from having to repeat her story to everyone who called. She was able to talk about, and think about, other<br />
things besides her cancer.<br />
A former technology executive and entrepreneur, Goldfine recalls, “When I got sick five years after my husband,<br />
Alan, died, I knew I could not leave my children. I’d say to my doctors, ‘Look, I can’t afford to die. My kids need me.’<br />
“I’m a pragmatic person,” she adds. “When I see a problem, I try to fix it. I’m not one to sit around saying,‘woe is<br />
me.’ I have always lived in the moment, so having cancer was no different.”<br />
In one entry, Evie’s daughter, Sarah, aptly compares this period of her family’s life with a track and field event<br />
called the steeplechase, a 3,000-meter race in which runners must jump over several barriers and a pit of water.<br />
Similarly, Evie had to clear several hurdles in addition to her cancer, such as life-threatening problems with the<br />
catheter implanted in her chest to administer drugs, a time when she thought Sarah also had lymphoma, and a<br />
near-death experience on the highway. Every time the reader breathes a sigh of relief, a new challenge appears.<br />
Her most recent obstacle was a stem cell transplant at <strong>Dana</strong>-<strong>Farber</strong>/Brigham and Women’s <strong>Cancer</strong> Center to<br />
replace her bone marrow with healthy new cells from a donor, driving her<br />
lymphoma into remission. With help from the Gift of Life, an organization that<br />
facilitates stem cell donations among the Jewish population (for whom matches<br />
are hard to find because of specific blood typing), Yisrael Meir Goldman, 23,<br />
was identified as a donor.<br />
When Goldfine met Goldman during a Gift of Life gathering a year later, she<br />
told the group, “It’s the ordinary things that are now extraordinary to me, and<br />
I owe this to my donor.” She gave the Israeli man her mother’s mezuzah, a<br />
symbol of Jewish faith, to thank him for saving her life.<br />
Here are some excerpts from Goldfine’s blog:<br />
8/1/00: Health update<br />
I don’t mean to be obnoxious by<br />
sending out a mass e-mail, but it<br />
seems easier. Then, when we speak I<br />
don’t have to go through the story.<br />
We can talk about the future – yours<br />
and mine.<br />
Today I met with the pathologist<br />
and he could not definitively say I<br />
have lymphoma, but he couldn’t say<br />
I don’t have it, either. So I took the<br />
slides and report to <strong>Dana</strong>-<strong>Farber</strong>.<br />
They will do their own pathology on<br />
the tissues, Thursday I will have CT<br />
scans, and Friday I will have blood<br />
tests and meet the oncologist.<br />
I really appreciate your support,<br />
love, words of encouragement,<br />
and extraordinary contacts. I was<br />
impressed with how quickly we could<br />
zero in on experts in the world of<br />
lymphoma. [Editor’s note: A definitive<br />
diagnosis could not be made yet.]<br />
12/25/00: Medical update<br />
The bottom line is, I have been diagnosed<br />
with aggressive lymphoma.<br />
Evie Goldfine’s optimism shines<br />
through the blog she kept during her<br />
six years as a lymphoma patient.<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 29
Already a devoted family, the Goldfines drew closer during Evie’s cancer experience. Pictured here (left to<br />
right) are Jason Rickles (Sarah’s fiancé), Sarah, Evie, Emma, Amy, Josh, and baby Jake.<br />
I have as much energy as ever – which<br />
means I can still run circles around<br />
20-year-olds.<br />
I have no time for second opinions<br />
on treatment. My oncologist [Arnie<br />
Freedman, MD] literally wrote the<br />
chapter on lymphoma in the textbooks,<br />
and I trust his judgment.<br />
The treatment consists of six 21-day<br />
cycles, where I get drugs intravenously<br />
on day one and then take drugs for the<br />
next four days. I will lose my hair, they<br />
should be able to control the nausea,<br />
I will feel tired (so now I’ll have the<br />
energy of a 40-year-old), I am susceptible<br />
to mouth sores and diarrhea, and<br />
I will have a much lower blood count –<br />
which means don’t visit me if you’ve<br />
been exposed to anyone who has<br />
been sick.<br />
The upside is, I pick up half an hour<br />
a day because I don’t have to wash and<br />
dry my hair, I save a ton of money on<br />
hair maintenance, I should lose some<br />
weight, I will get a lot of sympathy,<br />
AND I’ll find out a lot about myself<br />
and the people around me.<br />
The most difficult part is that [my<br />
kids] Josh and Sarah are terrified. This<br />
is my worst nightmare coming true.<br />
I am doing everything I can to help<br />
them with their fears, but I can’t promise<br />
that it will all turn out all right.<br />
12/30/00: Emergency update<br />
I am shaking. The doctor just called<br />
and said that I have an even more<br />
aggressive lymphoma than they originally<br />
thought. I will be hospitalized<br />
starting tomorrow. If this very aggressive<br />
treatment doesn’t work, my<br />
chances of survival are slim.<br />
How could this possibly be happening<br />
to me I still feel perfectly fine.<br />
Please surround my children with all<br />
the support and love they deserve.<br />
1/24/01: Update from Evie<br />
Everyone keeps asking me how<br />
Josh (and Amy) and Sarah are doing,<br />
so I thought I’d bring you up-to-date,<br />
trying not to embarrass them. Sarah<br />
went back to school, taking three<br />
courses, which gives her the ability to<br />
come home every other week. She<br />
is also training for a triathlon, May<br />
5th in California. I plan to be there,<br />
cheering her on.<br />
I don’t know what I would do<br />
without Josh and Amy. They visit<br />
me every day, and Josh has been<br />
sorting my mail and paying my<br />
bills. NO EASY FEAT, I can tell<br />
you. I probably get more mail than<br />
an average business.<br />
3/30/01: It just doesn’t get any<br />
better than today<br />
My bone marrow is cancer-free.<br />
My CT scan was clear and<br />
cancer-free.<br />
My gallium scan showed no signs<br />
of cancer, either.<br />
With me today at the hospital<br />
were Josh, Sarah, Amy, my nurse,<br />
and our family therapist (who has<br />
helped me and the children since<br />
Alan’s illness and death in 1994).<br />
My doctor told us about the test<br />
results, and I can’t describe the joy<br />
and elation in that room. Sarah<br />
30 P ATHS OF P ROGRESS Spring/Summer 2007
“I've been so consumed by world events this week that I almost forget<br />
how grave my own situation is.” — Sept. 16, 2001<br />
said, “It’s time to plan Josh and<br />
Amy’s wedding.”<br />
Life begins again for this family.<br />
I hate to be corny, but one of my<br />
favorite movie lines is, “Life is like<br />
a box of chocolates, you never<br />
know what you’re going to get.”<br />
I got the best chocolate in the<br />
box today.<br />
4/2/01: I have a blood clot<br />
In the main vein to my heart. I was<br />
in the hospital for seven hours and<br />
am completely wiped out. I get anticoagulation<br />
shots a couple of times a<br />
day and I will have surgery on<br />
Thursday or Friday to remove the<br />
port-a-cath [an implanted device for<br />
delivering medication]. Needless to<br />
say, a blood clot in the main vein to<br />
your heart is not exactly comforting.<br />
6/29/01: Sarah is ill<br />
Sarah has not been feeling well<br />
for the last six weeks. She has<br />
swollen lymph nodes and has been<br />
feeling run down and achy. She had<br />
a full round of blood tests and has<br />
an elevated LDH count [LDH is an<br />
enzyme associated with tissue damage].<br />
There are lots of viruses that<br />
could cause this, but it is also a<br />
symptom of lymphoma. The notion<br />
that she could be seriously sick<br />
is beyond my scope of thinking.<br />
We are all “maxed-out” on our<br />
coping skills.<br />
Editor’s note: July 2001, Sarah<br />
does not have lymphoma.<br />
8/17/01: Bad news<br />
I felt a lump in my neck<br />
Wednesday night. I am having a<br />
biopsy first thing in the morning.<br />
It will take until the middle of next<br />
week to get the results. Josh and<br />
Amy are getting married in two<br />
weeks, and I would not want to<br />
have any other procedures done<br />
until after the wedding. I think the<br />
cancer has returned.<br />
8/22/01: It could be worse<br />
My slides look exactly like the<br />
slides of the biopsy last July. The<br />
oncologist feels that my highly<br />
aggressive lymphoma has been<br />
cured, although there are no assur-<br />
ances. However, it appears that a<br />
low-grade lymphoma is still present.<br />
9/5/01: A few notes<br />
When I got the news last week<br />
that the cancer had returned, my<br />
first concern was that my health<br />
situation was going to put a huge<br />
damper on Josh and Amy’s wedding.<br />
Nothing could have been further<br />
from the truth. Everything went<br />
off perfectly. I don’t think anyone<br />
focused on my medical situation.<br />
Everyone was partying and celebrating<br />
with Josh and Amy, which<br />
is as it should be.<br />
9/16/01: More bad news<br />
I am going to be given a drug<br />
called Zevalin. The drug was<br />
approved Tuesday morning,<br />
“This is a celebration of the incredible, selfless deed of one young man<br />
who was willing to save a complete stranger’s life,” Evie said about her<br />
stem cell donor, Yisrael Meir Goldman.<br />
Spring/Summer 2007 P ATHS OF P ROGRESS 31
Sept. 11, moments before federal<br />
buildings were shut down in the<br />
wake of the terrorist attacks. I take<br />
this as a good sign. It’s the circle<br />
of life.<br />
This is the way cancer is. You feel<br />
fine and then you don’t. I’ve been so<br />
consumed by world events this week<br />
that I almost forget how grave my<br />
own situation is.<br />
11/18/01: A word about<br />
<strong>Dana</strong>-<strong>Farber</strong><br />
I vividly remember the time I<br />
was issued my <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong><br />
<strong>Institute</strong> plastic card. I couldn’t<br />
believe I had a card that labeled<br />
me as a cancer patient. Now<br />
when I walk into the hospital, I<br />
always have a smile on my face.<br />
Patients are treated with compassion<br />
beyond words.<br />
2/15/02: Great news!<br />
My CT scans were completely<br />
clean.<br />
My white blood count rebounded<br />
to normal.<br />
My red and platelet counts are<br />
normal, although my red count is<br />
down slightly.<br />
My LDH count increased and is<br />
definitely out of the range of normal.<br />
All in all this is terrific news. My<br />
doctor is not concerned about the<br />
LDH count.<br />
Editor’s note: From 2002 to 2005,<br />
son Josh Goldfine runs the Boston<br />
Marathon each April to raise money<br />
for <strong>Dana</strong>-<strong>Farber</strong>. Evie enjoys clean<br />
scans and good health while tending<br />
to her own mother, who has lung<br />
cancer and dies in Dec. 2004.<br />
4/21/05: I’ve had a recurrence<br />
Tuesday I went in for a routine<br />
exam and CT scan. Unfortunately the<br />
scan showed an enlarged lymph node<br />
in my abdomen. There is no question<br />
the cancer has returned; it’s<br />
only a matter of how aggressive it<br />
is. I am having surgery on Tuesday<br />
to remove the node. The results of<br />
the biopsy will take at least a<br />
week. If the cancer is aggressive I<br />
will need a stem cell transplant. I’ll<br />
be in the hospital for months, in<br />
isolation.<br />
5/17/05: Last night I got a call<br />
From the director of The Gift of<br />
Life Organization. These people<br />
are AMAZING. I asked him how<br />
people react when they are called<br />
and asked to be a donor. He said<br />
that they act like they’ve won the<br />
lottery. Imagine knowing that you<br />
are saving a life. “He who saves<br />
one life, it is as if he had saved the<br />
entire world.” – Talmud<br />
5/20/05: Except for the cancer,<br />
my life is charmed<br />
Going through a stem cell<br />
transplant is a huge juggling act.<br />
I have to admit, I’m highly qualified<br />
for the job. It’s all about dotting<br />
the “i”s and crossing the “t”s,<br />
and this is my forte. So, when I go<br />
through the transplant, I will know<br />
that I have done everything possible<br />
to give myself the best shot.<br />
7/26/05: First day<br />
This is the first day of the rest of<br />
my life. That’s the way the transplant<br />
team thinks of it.<br />
9/6/05: Truly remarkable test<br />
results today<br />
If I were to commit a crime<br />
and leave traces of blood at the<br />
scene, the police would never<br />
think it was me because my<br />
blood would show an XY chromosome.<br />
For those of you who<br />
remember your biology, my<br />
blood is now male. My blood type<br />
has changed from A+ to O+.<br />
However, the rest of my DNA is<br />
original. So, the DNA of my skin<br />
is different from my blood. If I<br />
had allergies, they would be gone<br />
because the donor doesn’t have<br />
allergies. Isn’t this all like science<br />
fiction And no, I’m not growing<br />
facial hair!<br />
7/19/06: This cat has a couple<br />
more lives left<br />
Restrictions are being lifted one<br />
by one. I can go to restaurants, shop<br />
in stores, and be in elevators without<br />
a mask and gloves. It takes discipline<br />
to let go of the barriers<br />
between me and the outside world.<br />
I’m not fully there yet. I still slip on<br />
a glove when opening doors, and<br />
put on a mask and gloves when<br />
using a public restroom.<br />
However, when I walked into<br />
<strong>Dana</strong>-<strong>Farber</strong> for my vaccinations,<br />
the nurse came over and said,<br />
“Look at you ... you look beautiful<br />
... no one would ever know what<br />
you’ve been through. I love your<br />
curls ... but then again, you handled<br />
bald very well.” She went on<br />
and on, reminiscing about how<br />
concerned I was for my children<br />
and the burden I placed on them.<br />
Here I was, with a clean scan, having<br />
sailed through the transplant,<br />
and I became very emotional.<br />
When she started checking the<br />
numbers on my bracelet to make<br />
sure the medication belonged to<br />
me, I broke down and cried. It just<br />
hit me that Josh, Sarah, and Amy<br />
were SOOOO sweet. They were<br />
always there to support me. It’s<br />
hard to believe that a year has<br />
gone by and it has been so effortless<br />
for me.<br />
It’s the story of my life. It has<br />
been charmed.<br />
32 P ATHS OF P ROGRESS Spring/Summer 2007
2006 ANNUAL R EPORT/TREASURER’ S R EPORT AND D ANA-FARBER G OVERNANCE<br />
A message from Chief Financial Officer Dorothy Puhy<br />
The past year was a strong one financially for <strong>Dana</strong>-<strong>Farber</strong>. The<br />
<strong>Institute</strong> reported an excess of revenues over expenses of approximately<br />
$21.5 million during 2006, an increase from the previous<br />
year’s excess of $13.3 million. The <strong>Institute</strong> ended the year with<br />
investment balances of $511.5 million, up from $462.5 million the<br />
previous year. Return on the investment portfolio was 9.9 percent,<br />
essentially the same as the market benchmark.<br />
The operating results improved from $4.5 million in 2005 to<br />
$17.7 million in 2006. Operating results benefited from strong revenue<br />
growth in all areas. Overall revenue grew 14.1 percent from<br />
2005 to 2006. Revenues from patient care services grew 24.9 percent,<br />
and research revenues were much better than expected, in<br />
light of a difficult environment in federal funding. I’m also pleased<br />
to report that donor funds used to support current activities grew<br />
substantially over the previous year. Unrestricted fundraising was<br />
up 18.6 percent, and programmatic support grew 23.3 percent.<br />
The results we achieved in 2006 were made possible by the work<br />
of staff throughout the <strong>Institute</strong>, as well as numerous friends of<br />
<strong>Dana</strong>-<strong>Farber</strong>. We are grateful for this strong and ongoing support.<br />
Annual Report 2006 / P ATHS OF P ROGRESS 33
D ANA-FARBER C ANCER I NSTITUTE, INC. AND S UBSIDIARIES*<br />
CONDENSED CONSOLIDATED BALANCE SHEETS<br />
For the Fiscal Year Ended Sept. 30 2006 2005<br />
(Dollars in thousands)<br />
Assets<br />
Current Assets 157,794 117,690<br />
Investments 511,450 462,493<br />
Property, Plant, and Equipment, net 247,079 235,893<br />
Contributions Receivable, less current portion 89,646 41,658<br />
Other Assets 14,041 16,829<br />
Total Assets $1,020,010 $874,563<br />
Liabilities and Net Assets<br />
Current Liabilities 118,584 103,821<br />
Long-Term Debt and Other Liabilities 144,062 147,209<br />
Net Assets<br />
Unrestricted 300,284 269,396<br />
Temporarily Restricted 341,311 244,478<br />
Permanently Restricted 115,769 109,659<br />
Subtotal Net Assets 757,364 623,533<br />
Total Liabilities and Net Assets $1,020,010 $874,563<br />
Summary Statistical Information<br />
(Unless otherwise noted, includes adult and pediatric patients)<br />
2006 2005<br />
Infusion Visits 87,784 84,458<br />
Outpatient MD Visits 106,994 100,342<br />
Number of Licensed Beds (as of year end) 27 27<br />
Adult Inpatient Discharges (from BWH) 1,036 949<br />
Clinical Trials (via <strong>Dana</strong>-<strong>Farber</strong>/Harvard <strong>Cancer</strong> Center) 629 589<br />
During FY’97, <strong>Dana</strong>-<strong>Farber</strong> moved its inpatient beds to partnering Brigham<br />
and Women’s Hospital as part of a longer-range strategy to emphasize the<br />
delivery of comprehensive outpatient care within DFCI facilities.<br />
* Subsidiaries include <strong>Dana</strong>-<strong>Farber</strong>, Inc., <strong>Dana</strong>-<strong>Farber</strong> Trust,<br />
and HealthCare Dimensions Hospice.<br />
34 P ATHS OF P ROGRESS / Annual Report 2006
D ANA-FARBER C ANCER I NSTITUTE, INC. AND S UBSIDIARIES<br />
CONDENSED CONSOLIDATED STATEMENTS OF OPERATIONS AND CHANGES IN NET ASSETS<br />
For the Fiscal Year Ended Sept. 30 2006 2005<br />
(Dollars in thousands)<br />
Revenues<br />
Research 235,912 228,289<br />
Patient Service, net 304,604 243,772<br />
Unrestricted Contributions and Bequests 49,980 42,147<br />
Other Operating 25,642 25,979<br />
Total Revenues $616,138 $540,187<br />
Expenses<br />
Fiscal Year 2006 Income<br />
Direct Research 203,931 190,937<br />
Direct Patient Care 192,392 160,309<br />
Indirect 202,149 184,464<br />
Total Operating Expenses $598,472 $535,710<br />
Operating Income 17,666 4,477<br />
Investment Return, net 3,848 8,871<br />
Excess of Revenues Over Expenses 21,514 13,348<br />
Net Unrealized Investment Gains 9,804 10,165<br />
Other (430) 264<br />
Increase in Temporarily Restricted Net Assets 96,833 58,272<br />
Increase in Permanently Restricted Net Assets 6,110 7,004<br />
Increase (Decrease) in Net Assets 133,831 89,053<br />
Net Assets at Beginning of Year 623,533 534,480<br />
Net Assets at End of Year $757,364 $623,533<br />
The preceding selected consolidated financial data as of Sept. 30, 2006, and 2005<br />
(except for the summary statistical data) have been derived from the consolidated<br />
financial statements of <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong>, Inc., <strong>Dana</strong>-<strong>Farber</strong>, Inc.,<br />
<strong>Dana</strong>-<strong>Farber</strong> Trust, and HealthCare Dimensions Hospice. These have been audited<br />
by Ernst & Young, LLP, independent auditors.<br />
Fiscal Year 2006 Expenses<br />
200<br />
150<br />
100<br />
50<br />
Comparison of<br />
Private Support<br />
($ i illi )<br />
In FY 2006, the <strong>Institute</strong> raised $203.4 million in new gifts, pledges,<br />
{<br />
and commitments through its Division of Development and the Jimmy<br />
Fund, representing an increase of 27 percent over FY 2005 results of<br />
$160.5 million. For accounting purposes, the financial charts above<br />
reflect new gifts and pledges calculated at present value and raised<br />
through the Division of Development and the Jimmy Fund, HealthCare<br />
Dimensions Hospice, and the Friends of DFCI, excluding commitments<br />
the <strong>Institute</strong> could not record due to conditionality.<br />
0<br />
Annual Report 2006 / P ATHS OF P ROGRESS 35
D ANA-FARBER C ANCER I NSTITUTE, INC.<br />
CORPORATE<br />
OFFICERS<br />
BOARD COMMITTEES<br />
AND CHAIRPERSONS<br />
BOARD DEVELOPMENT<br />
COMMITTEES AND CHAIRPERSONS<br />
Gary L. Countryman<br />
Chairman<br />
Edward J. Benz Jr., MD<br />
President and<br />
Chief Executive Officer<br />
Richard P. Morse<br />
Vice Chairman<br />
Vincent M. O’Reilly<br />
Vice Chairman<br />
Richard A. Smith<br />
Vice Chairman<br />
Richard K. Lubin<br />
Treasurer<br />
Dorothy E. Puhy<br />
Assistant Treasurer<br />
Neal J. Curtin, Esq.<br />
Secretary<br />
Richard S. Boskey, Esq.<br />
Assistant Secretary<br />
Kathleen Harkey<br />
Assistant Secretary<br />
Audit Committee<br />
Joseph E. Norberg<br />
Committee on Facility Planning<br />
and Construction<br />
John L. Marshall III<br />
Communications Committee<br />
Marjorie B. Salmon<br />
Community Programs Committee<br />
David Auerbach<br />
Amy Z. Reiner<br />
Compensation Committee<br />
Gary L. Countryman<br />
Executive Committee<br />
Gary L. Countryman<br />
Finance Committee<br />
Richard K. Lubin<br />
Governance Committee<br />
Neal J. Curtin, Esq.<br />
Investment Committee<br />
Stephen B. Kay<br />
Joint Committee on<br />
Quality Improvement<br />
and Risk Management<br />
Vincent M. O’Reilly<br />
Annual Giving<br />
Program Committee<br />
James W. Rappaport<br />
Jean S. Sharf<br />
Campaign Committee<br />
Josh Bekenstein<br />
Larry Lucchino<br />
Corporations and<br />
Foundations Committee<br />
Thomas J. May<br />
Development Committee<br />
Charles A. <strong>Dana</strong> III<br />
Richard P. Morse<br />
Gift Planning Committee<br />
M. Dozier Gardner<br />
Jimmy Fund Advisory Committee<br />
David Auerbach<br />
James P. Sadowsky<br />
Medical Staff Appointments Committee<br />
Gary L. Countryman<br />
Trustee Science Committee<br />
Michael R. Eisenson, Esq.<br />
Howard Cox<br />
The governance listings in this annual report are current as of January 1, 2007.<br />
36 P ATHS OF P ROGRESS / Annual Report 2006
D ANA-FARBER C ANCER I NSTITUTE, INC.<br />
TRUSTEES<br />
Andrea R. Abraham<br />
Gerhard R. Andlinger<br />
Mara G. Aspinall 3<br />
Arnold J. Auerbach 2+<br />
David Auerbach<br />
Joshua Bekenstein<br />
Baruj Benacerraf, MD 3<br />
Edward J. Benz Jr., MD 3<br />
Roger Berkowitz<br />
Alan J. Bernon<br />
Armin G. Biller<br />
John F. Blais<br />
Betty Ann Blum<br />
Justice Stephen G. Breyer 2<br />
Hon. Frederick L. Brown<br />
J. Gary Burkhead<br />
Kennett F. Burnes, Esq.<br />
Stephen J. Burton<br />
Richard A. Cantor<br />
Michael A. Champa<br />
George Cloutier<br />
Martha Coakley, Esq.<br />
Marc A. Cohen<br />
Joseph F. Cotter 2<br />
Gary L. Countryman 3<br />
Howard Cox<br />
Neal J. Curtin, Esq. 3<br />
Charles A. <strong>Dana</strong> III<br />
Lee S. Daniels<br />
Nader F. Darehshori<br />
Laura Weissman Davis<br />
David A. Dechman<br />
Daniel Dennis<br />
Peter I. deRoetth<br />
Emily F. DiMaggio<br />
Steven Dodge<br />
James H. Donovan<br />
James Dow<br />
John P. Dunfey<br />
Donald Dwares<br />
Michael R. Eisenson, Esq. 3<br />
Edward Eskandarian<br />
Darwin C. <strong>Farber</strong><br />
Stephen B. <strong>Farber</strong><br />
Thomas A. Farrington<br />
James L. Fine<br />
Stephen A. Fine<br />
Jane E. Fireman<br />
Robert C. First<br />
Stephen W. Foss<br />
Patricia L. Franchi<br />
Emil Frei III, MD<br />
Lauren Frei<br />
Orrie M. Friedman, PhD 2<br />
Michael Frieze<br />
M. Dozier Gardner<br />
Arthur Gelb, ScD 3<br />
Nancy Q. Gibson<br />
Charles K. Gifford<br />
William M. Gillen<br />
Michael S. Gordon<br />
Abraham D. Gosman<br />
James D. Griffin, MD 3<br />
David V. Harkins<br />
Marian L. Heard<br />
Alan J. Hirschfield<br />
Thomas F. Holt Jr., Esq.<br />
Barbara H. Hugus, PhD 2<br />
Jane P. Jamieson<br />
Glenn M. Johnson<br />
Hon. Scott L. Kafker<br />
William S. Karol<br />
Stephen B. Kay 3<br />
Phyllis Swerling Kellem 2<br />
Patricia D. Kelsey 2<br />
Robert P. Kelsey Jr. 2<br />
Michele Kessler<br />
Michael J. Kittredge<br />
Brian J. Knez<br />
Ruth Kopelman 2<br />
Paul B. Kopperl 3<br />
Stephen P. Koster, Esq.<br />
Robert K. Kraft 3<br />
Sandra G. Krakoff 3<br />
Phyllis Krock<br />
Judith Hurwitz Krupp<br />
Reuben Landau, Esq. 2<br />
Althea Lank<br />
Charles Larsen III<br />
Kenneth H. M. Leet<br />
Richard D. Leggat, Esq.<br />
Kenneth Levine<br />
Roger A. Lockwood<br />
Richard K. Lubin 3<br />
David G. Lubrano<br />
Bradley A. Lucas<br />
Lawrence Lucchino<br />
Hildegarde E. Mahoney<br />
Peter A. Maich<br />
Roger M. Marino<br />
John L. Marshall III<br />
Thomas J. May<br />
William F. McCall Jr.<br />
Joseph C. McNay<br />
William F. Meagher<br />
David S. Moross<br />
Richard P. Morse 3<br />
David G. Nathan, MD<br />
Charles Nirenberg<br />
Joseph E. Norberg<br />
Brian O’Connor<br />
John J. O’Connor<br />
Vincent M. O’Reilly 3<br />
Stuart H. Orkin, MD 3<br />
Edward O. Owens<br />
Peter Palandjian<br />
Arthur M. Pappas, MD 2<br />
Theodore Pasquarello<br />
Jean F. Pearlstein 3<br />
David B. Perini<br />
Eileen Perini<br />
Steven P. Perlmutter, Esq.<br />
Susan M. Poduska<br />
William J. Poutsiaka 3<br />
Irving W. Rabb 2<br />
John M. Randolph 2<br />
Kathleen M. Randolph, PhD 2<br />
James W. Rappaport<br />
John P. Reardon Jr.<br />
Shari E. Redstone<br />
Sumner M. Redstone 2<br />
Amy Z. Reiner<br />
Ann M. Rosenberg<br />
Harvey Rosenthal 3<br />
Edward F. Rover<br />
Robert J. Sachs, Esq.<br />
Barbara L. Sadowsky<br />
James P. Sadowsky<br />
Stephen E. Sallan, MD 3<br />
Marjorie B. Salmon<br />
Malcolm S. Salter<br />
H. Terrence Samway<br />
Judith P. Schlager<br />
Fredric E. Schluter 3<br />
Richard N. Seaman<br />
Paul Severino<br />
Jean S. Sharf<br />
Lawrence N. Shulman, MD 3<br />
Paula L. Sidman<br />
Laurence C. Siegel<br />
Marc E. Smith<br />
Richard A. Smith 3<br />
Susan F. Smith<br />
Ruth F. Snider<br />
Jerry M. Socol<br />
Nancy Socol<br />
Gloria H. Spivak<br />
Robert Stansky<br />
William Starr<br />
James M. Stoneman 2<br />
Patrick J. Sullivan<br />
Stephen B. Swensrud<br />
Delores Barr Weaver<br />
J. Wayne Weaver<br />
Karen L. Webster<br />
Thomas Werner<br />
T. Conrad Wetterau<br />
Donald W. White<br />
Gregory A. White<br />
Darnell L. Williams<br />
Frederica M. Williams<br />
Carl Yastrzemski 2<br />
George J. Yost III, Esq.<br />
Mortimer B. Zuckerman 2<br />
1 Trustee for Life<br />
2 Honorary Trustee<br />
3 Member, Executive Committee<br />
+ Deceased<br />
The governance listings in this annual report are current as of January 1, 2007.<br />
Annual Report 2006 / P ATHS OF P ROGRESS 37
D ANA-FARBER C ANCER I NSTITUTE, INC.<br />
EXECUTIVE MANAGEMENT<br />
Edward J. Benz Jr., MD<br />
President and Chief Executive Officer<br />
Richard S. Boskey, Esq.<br />
Senior Vice President and General Counsel<br />
Beverly R. Ginsburg, MBA<br />
Senior Vice President, Research, DFCI;<br />
Associate Director, Administration, DF/HCC<br />
James D. Griffin, MD<br />
Chair, Medical Oncology<br />
Jay R. Harris, MD<br />
Chair, Radiation Oncology<br />
Philip W. Kantoff, MD<br />
Chief Clinical Research Officer<br />
Lee M. Nadler, MD<br />
Senior Vice President,<br />
Experimental Medicine<br />
Stuart H. Orkin, MD<br />
Chair, Pediatric Oncology<br />
Susan S. Paresky, MBA<br />
Senior Vice President, Development and<br />
The Jimmy Fund<br />
Patricia Reid Ponte, RN, DNSc, FAAN<br />
Senior Vice President, Patient Care Services;<br />
Chief Nurse, <strong>Dana</strong>-<strong>Farber</strong><br />
Director, Oncology Nursing and Clinical<br />
Services, Brigham and Women’s Hospital<br />
Janet E. Porter, PhD<br />
Executive Vice President and<br />
Chief Operating Officer<br />
Dorothy E. Puhy<br />
Executive Vice President and<br />
Chief Financial Officer<br />
Barrett J. Rollins, MD, PhD<br />
Chief Scientific Officer<br />
Stephen E. Sallan, MD<br />
Chief of Staff;<br />
Chair, Medical Staff Executive<br />
Committee<br />
Lawrence N. Shulman, MD<br />
Chief Medical Officer;<br />
Senior Vice President, Medical Affairs;<br />
Chief, General Oncology, Medical<br />
Oncology<br />
Steven R. Singer<br />
Senior Vice President,<br />
Communications<br />
RESEARCH LEADERSHIP<br />
Professional Administration<br />
Edward J. Benz Jr., MD<br />
President; Director, DF/HCC<br />
Beverly R. Ginsburg, MBA<br />
Senior Vice President, Research, DFCI;<br />
Associate Director, Administration,<br />
DF/HCC<br />
Barrett J. Rollins, MD, PhD<br />
Chief Scientific Officer<br />
Executive Committee for Research<br />
David M. Livingston, MD<br />
Chair<br />
Harvey Cantor, MD<br />
Alan D. D’Andrea, MD<br />
Beverly R. Ginsburg, MBA *<br />
James D. Griffin, MD<br />
David P. Harrington, PhD<br />
J. Dirk Iglehart, MD<br />
Dennis C. Lynch, MD, PhD *<br />
Lee M. Nadler, MD<br />
Stuart H. Orkin, MD<br />
Thomas M. Roberts, PhD<br />
Barrett J. Rollins, MD, PhD *<br />
Jane C. Weeks, MD, MSc<br />
Department of Medical Oncology<br />
James D. Griffin, MD<br />
Chair<br />
Department of Biostatistics<br />
and Computational Biology<br />
David P. Harrington, PhD<br />
Chair<br />
Paul J. Catalano, ScD<br />
Associate Chair<br />
Department of <strong>Cancer</strong> Biology<br />
Thomas M. Roberts, PhD<br />
Charles D. Stiles, PhD<br />
Co-Chairs<br />
Department of <strong>Cancer</strong><br />
Immunology and AIDS<br />
Harvey Cantor, MD<br />
Chair<br />
Department of Pediatric Oncology<br />
Stuart H. Orkin, MD<br />
Chair<br />
Department of Radiation Oncology<br />
Jay R. Harris, MD<br />
Chair<br />
* ex-officio<br />
The governance listings in this annual report are current as of January 1, 2007.<br />
38 P ATHS OF P ROGRESS / Annual Report 2006
D ANA-FARBER, INC.<br />
CORPORATE OFFICERS<br />
Gary L. Countryman<br />
Chairman<br />
Edward J. Benz Jr., MD<br />
President and Chief Executive Officer<br />
TRUSTEES<br />
Edward J. Benz Jr., MD<br />
Gary L. Countryman<br />
Stephen B. Kay<br />
Richard K. Lubin<br />
Richard K. Lubin<br />
Treasurer and Vice Chairman<br />
Dorothy E. Puhy<br />
Assistant Treasurer<br />
Neal J. Curtin, Esq.<br />
Secretary<br />
Richard S. Boskey, Esq.<br />
Assistant Secretary<br />
Kathleen Harkey<br />
Assistant Secretary<br />
<strong>Dana</strong>-<strong>Farber</strong>, Inc. manages the investments of <strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong>, Inc.<br />
The governance listings in this annual report are current as of January 1, 2007.<br />
Annual Report 2006 / P ATHS OF P ROGRESS 39
D ANA-FARBER C ANCER I NSTITUTE, INC.<br />
FRIENDS OF DANA-FARBER CANCER INSTITUTE<br />
Co-Presidents<br />
Lauren Frei<br />
Nancy L. Socol<br />
Executive Vice President<br />
Diane Flynn<br />
Vice Presidents<br />
Cheryl Eckel<br />
Tobey Oresman<br />
Tina Peters<br />
Treasurer<br />
Loren Baum Edwards<br />
Assistant Treasurer<br />
Ed Perlmutter<br />
Recording Secretary<br />
Mary Ann Chase<br />
Members<br />
Andrea R. Abraham *<br />
Suzanne Fisher Bloomberg<br />
Maureen Champa<br />
Suzanne W. Conlin *<br />
Alice Cutler *<br />
Annette Feinstein<br />
Jean Feuer<br />
Jayne Bennett Friedberg *<br />
Nanci Gelb<br />
Christina Glen<br />
Elaine Goldenberg<br />
Micki Hirsch<br />
Jane M. Holt *<br />
Barbara Lapp<br />
Rebecca Latimore<br />
Elizabeth M. Loughlin<br />
JoAnne Marshall<br />
F. Jane May<br />
Jane B. Mayer<br />
Roberta McNulty<br />
Jane R. Moss<br />
Jean F. Pearlstein *<br />
Kelly Pesek<br />
Kristienne Perry Rassiger<br />
Kelly Sohn<br />
<strong>Dana</strong> Gerson Unger<br />
Members-at-Large<br />
Nikki Bialow<br />
Nancy Cutler<br />
Terri Hupalo<br />
Audra Lank<br />
Louise Nolan<br />
Robin Reibel<br />
Terri Tsagaris<br />
Honorary Directors<br />
Jean Speare Canellos *<br />
Louise S. Shivek<br />
Susan F. Smith<br />
Marilyn N. Wolman<br />
Founding President<br />
Sheila Driscoll Cunningham *+<br />
Program Coordinator<br />
Lindsay G. Fisch<br />
Administrative Assistants<br />
Linda R. Ciardi<br />
Elaine L. Tinetti<br />
TRUSTEE CHAIRS<br />
PRESIDENT’S VISITING<br />
COMMITTEES<br />
Gastrointestinal <strong>Cancer</strong> Center<br />
Michele Kessler<br />
Paula Sidman<br />
Hematologic Oncology<br />
Marc Cohen<br />
Alan Hirschfield<br />
Jimmy Fund<br />
Nancy Q. Gibson<br />
James P. Sadowsky<br />
The Lank Center for<br />
Genitourinary Oncology<br />
Bertram and Althea Lank<br />
(Honorary Co-Chairs)<br />
Arthur Gelb, ScD<br />
William Poutsiaka<br />
Women’s <strong>Cancer</strong>s Program<br />
Susan F. Smith<br />
HEALTHCARE DIMENSIONS<br />
HOSPICE<br />
Board of Directors prior to<br />
November 1, 2006<br />
President<br />
James B. Conway<br />
Treasurer<br />
Dorothy E. Puhy<br />
Assistant Treasurer<br />
Michael Desocio<br />
Clerk<br />
Patricia A. Evans, Esq.<br />
Assistant Clerk<br />
Nancy Ferrante<br />
Directors<br />
Janet Abrahm, MD<br />
Ndubuisi Azubuine<br />
Andrew Billings, MD<br />
Wayne F. Brasco Sr.<br />
Allen S. Danis<br />
Lachlan Forrow, MD<br />
Barbara Levine<br />
Craig M. Lilly, MD<br />
Debora Lingos<br />
Judith Miller<br />
Janet Porter<br />
Dorothy E. Puhy<br />
Evelyn Reading<br />
Celeste Robb-Nicholson, MD<br />
Suzanne Stoltmann-Dorsey<br />
Margaret Vettese, PhD, RN<br />
Jane Weingarten<br />
* Past President<br />
+ Deceased<br />
<strong>Dana</strong>-<strong>Farber</strong> transferred ownership of<br />
HealthCare Dimensions Hospice to Partners<br />
Home Care, a nonprofit provider of homebased<br />
medical care, as of Nov. 1, 2006. The<br />
now-named Partners Hospice provides comprehensive<br />
end-of-life services to adults and<br />
children with advanced terminal illnesses,<br />
including cancer.<br />
The governance listings in this annual report are current as of January 1, 2007.<br />
40 P ATHS OF P ROGRESS / Annual Report 2006
®<br />
DANA-FARBER CANCER INSTITUTE ...<br />
“Dedicated to discovery ... committed to care” is the mission of <strong>Dana</strong>-<strong>Farber</strong><br />
<strong>Cancer</strong> <strong>Institute</strong> (DFCI), described as “one of the world’s premier cancer centers”<br />
by the National <strong>Cancer</strong> <strong>Institute</strong>. Founded in 1947 by Sidney <strong>Farber</strong>, MD,<br />
<strong>Dana</strong>-<strong>Farber</strong> is renowned for its unique blend of basic and clinical research and<br />
for using its discoveries to improve the treatment of adults and children with<br />
cancer. It is a founding member of the <strong>Dana</strong>-<strong>Farber</strong>/Harvard <strong>Cancer</strong> Center –<br />
one of 39 nationally designated Comprehensive <strong>Cancer</strong> Centers. A teaching<br />
affiliate of Harvard Medical School, <strong>Dana</strong>-<strong>Farber</strong> is also one of 20 federal<br />
Centers for AIDS Research in the United States, and is consistently ranked one<br />
of the top cancer centers in the country by U.S.News & World Report. It has<br />
also earned “Magnet” status for excellence in nursing.<br />
<strong>Dana</strong>-<strong>Farber</strong> partners with Brigham and Women’s Hospital to deliver care for<br />
adults with cancer through <strong>Dana</strong>-<strong>Farber</strong>/Brigham and Women’s <strong>Cancer</strong> Center.<br />
It also has a longstanding alliance with Children’s Hospital Boston to care for<br />
pediatric cancer patients through <strong>Dana</strong>-<strong>Farber</strong>/Children’s Hospital <strong>Cancer</strong> Care.<br />
By bringing together the strengths of three world-class institutions, these partnerships<br />
provide an exceptional level of care for cancer patients and their families.<br />
... AND THE JIMMY FUND<br />
The Jimmy Fund supports the fight against cancer at <strong>Dana</strong>-<strong>Farber</strong>, helping to<br />
raise both funds and the chances of survival for children and adults around the<br />
world. Named to protect the anonymity of one of Dr. Sidney <strong>Farber</strong>’s young<br />
patients, the Jimmy Fund was established in 1948 by the Variety Club of New<br />
England in conjunction with the Boston Braves baseball team. Later adopted as<br />
the official cause of the Boston Red Sox, the Massachusetts Chiefs of Police<br />
Association, and the annual Pan-Massachusetts Challenge bike-a-thon, the Jimmy<br />
Fund is widely regarded as “New England’s favorite charity.” Individual and<br />
corporate gifts, many of them collected through hundreds of annual Jimmy Fund<br />
events, have helped the organization generate millions of dollars for cancer<br />
research and care at <strong>Dana</strong>-<strong>Farber</strong> over the decades.
A FATHER’S ILLNESS,<br />
ASON’S QUEST<br />
I first started thinking seriously about a career in<br />
cancer biology when my father was diagnosed with<br />
advanced prostate cancer while I was an MD-PhD<br />
student at Harvard Medical School. Although my<br />
graduate work was in a different field, I soon began<br />
to spend all of my spare time poring over the medical<br />
and scientific literature related to cancer. I<br />
became captivated by the scientific understanding<br />
of malignancy – but also somewhat distressed by the<br />
difficulties inherent in using this knowledge to help<br />
oncology patients such as my father. This goal of<br />
translating cancer science into medical advances has<br />
since become my passion and life’s work.<br />
I feel fortunate to be a physician-scientist at <strong>Dana</strong>-<br />
<strong>Farber</strong>. My research involves using genomics technologies<br />
to identify mutations in cancer cell DNA,<br />
and to understand how those mutations might make<br />
cancer cells vulnerable to new targeted therapies.<br />
I’m confident this type of work will help bring<br />
about a day when treatment for even the most deadly<br />
cancers can be tailored to the specific mutations in<br />
each patient’s tumor. <strong>Dana</strong>-<strong>Farber</strong> is a world leader<br />
in this effort to which I am honored to contribute.<br />
I know my father would be pleased.<br />
– Levi Garraway, MD, PhD<br />
Please visit us online at<br />
www.dana-farber.org<br />
<strong>Dana</strong>-<strong>Farber</strong> <strong>Cancer</strong> <strong>Institute</strong><br />
44 Binney Street<br />
Boston, MA 02115-6084<br />
(617) 632-4090<br />
www.dana-farber.org<br />
Non-profit Org.<br />
U.S. Postage<br />
P A I D<br />
<strong>Dana</strong>-<strong>Farber</strong><br />
A teaching affiliate of<br />
Harvard Medical School