Fall 2009 - Mount Sinai Hospital
Fall 2009 - Mount Sinai Hospital
Fall 2009 - Mount Sinai Hospital
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
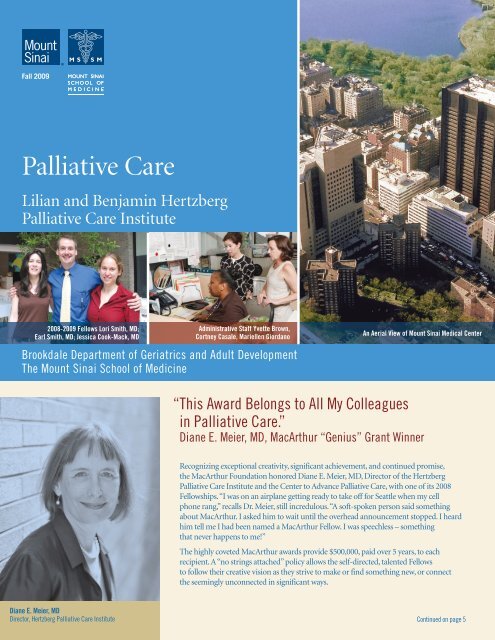
<strong>Fall</strong> <strong>2009</strong><br />
Palliative Care<br />
Lilian and Benjamin Hertzberg<br />
Palliative Care Institute<br />
2008-<strong>2009</strong> Fellows Lori Smith, MD;<br />
Earl Smith, MD; Jessica Cook-Mack, MD<br />
Administrative Staff Yvette Brown,<br />
Cortney Casale, Mariellen Giordano<br />
Brookdale Department of Geriatrics and Adult Development<br />
The <strong>Mount</strong> <strong>Sinai</strong> School of Medicine<br />
An Aerial View of <strong>Mount</strong> <strong>Sinai</strong> Medical Center<br />
“ This Award Belongs to All My Colleagues<br />
in Palliative Care.”<br />
Diane E. Meier, MD, MacArthur “Genius” Grant Winner<br />
Recognizing exceptional creativity, significant achievement, and continued promise,<br />
the MacArthur Foundation honored Diane E. Meier, MD, Director of the Hertzberg<br />
Palliative Care Institute and the Center to Advance Palliative Care, with one of its 2008<br />
Fellowships. “I was on an airplane getting ready to take off for Seattle when my cell<br />
phone rang,’’ recalls Dr. Meier, still incredulous. “A soft-spoken person said something<br />
about MacArthur. I asked him to wait until the overhead announcement stopped. I heard<br />
him tell me I had been named a MacArthur Fellow. I was speechless – something<br />
that never happens to me!”<br />
The highly coveted MacArthur awards provide $500,000, paid over 5 years, to each<br />
recipient. A “no strings attached” policy allows the self-directed, talented Fellows<br />
to follow their creative vision as they strive to make or find something new, or connect<br />
the seemingly unconnected in significant ways.<br />
Diane E. Meier, MD<br />
Director, Hertzberg Palliative Care Institute<br />
Continued on page 5
2<br />
Lilian and Benjamin Hertzberg<br />
Palliative Care Institute<br />
Brookdale Department of Geriatrics<br />
and Adult Development<br />
<strong>Mount</strong> <strong>Sinai</strong> School of Medicine<br />
One Gustave L. Levy Place, Box 1070, NY, NY 10029<br />
Tel. 212-241-1446<br />
www.mssm.edu/palliative<br />
Diane E. Meier, MD<br />
Director, Hertzberg Palliative Care Institute<br />
Director, Center to Advance Palliative Care<br />
Catherine Gaisman Professor of Medical Ethics<br />
Professor, Departments of Geriatrics and Medicine<br />
Albert L. Siu, MD, MSPH<br />
Ellen and Howard C. Katz Chairman’s Chair<br />
Brookdale Department of Geriatrics<br />
and Adult Development<br />
<strong>Mount</strong> <strong>Sinai</strong> School of Medicine<br />
Director of the GRECC at the James J. Peters<br />
VA Medical Center<br />
R. Sean Morrison, MD<br />
Vice-Chair for Research<br />
Director, National Palliative Care Research Center<br />
Director of Research, Hertzberg Palliative Care Institute<br />
Hermann Merkin Professor of Palliative Care<br />
Emily J. Chai, MD<br />
Medical Director<br />
Hertzberg Palliative Care Institute<br />
Assistant Professor, Brookdale Department<br />
of Geriatrics and Adult Development<br />
Gabrielle Goldberg, MD<br />
Education Director<br />
Hertzberg Palliative Care Institute<br />
Assistant Professor, Brookdale Department<br />
of Geriatrics and Adult Development<br />
Bette Kerr<br />
Writer and Editor<br />
Co-Editor: Susie West<br />
Photographer: Bruce Kushnick<br />
Art Director: E. Fitz Art, Inc.<br />
The Hertzberg Philanthropic<br />
Leadership Council<br />
Peggy Danziger<br />
Joseph Hertzberg<br />
Walter W. Hess, Jr.<br />
Diane E. Meier, MD<br />
Susan L. West<br />
Zena Wiener<br />
Doulas Volunteer as Patient Companions<br />
For Nurse Practitioner Marianne Gelber,<br />
the loneliness of hospitalized, critically<br />
ill patients was a major concern. Haunted<br />
by observations that Mr. A doesn’t have<br />
many visitors, or Ms. B’s family lives far<br />
away, she thought: “Wouldn’t it be great<br />
to have special volunteers, non-clinical<br />
companions, to visit, support, and sit with<br />
our patients I’d learned about Doulas to<br />
Accompany and Comfort, a non-sectarian<br />
program of the Shira Ruskay Center of<br />
the Jewish Board of Family and Children’s<br />
Services (JBFCS).”<br />
Nurse Practitioner Marianne Gelber<br />
with Doula Volunteer Marie Ginther.<br />
In a partnership embraced by Judith Kahn and Amy Levine, Director and Assistant<br />
Director of the Doula program at JBFCS, the first volunteers came to Hertzberg in April<br />
2008. In ancient Greece, “doulas” were companions for women in childbirth. Noting<br />
similarities between the sensitive care required at both the beginning and end of life,<br />
JBFCS chose this name for their program.<br />
Trained and supervised by Ms. Kahn and Ms. Levine, 5 Doulas now work in Palliative<br />
Care, under Ms. Gelber’s aegis. “I orient them, teach them about washing, gowning, and<br />
gloving, and assign them to patients weekly,” says Ms. Gelber. “I escort them to their first<br />
patient.” Depending upon the length of a hospital stay, Doulas may see a patient for 1 month,<br />
4 months, or longer. “They are beautiful people,” adds Ms. Gelber, “and have become an<br />
integral part of our Palliative Care team. We are grateful to them and to the JBFCS.”<br />
After 8 weeks of training at JBFCS, Doulas come to <strong>Sinai</strong> well-prepared. Ms. Levine<br />
describes their training as “a mixture of the didactic and experiential, stressing<br />
communication skills and introspection. We look at spirituality, at what we are like<br />
when we’re sick. How do our families handle critical illness” After the Doulas have<br />
been assigned, adds Ms. Levine, “We continue to support them via group meetings,<br />
monthly reports, and individual conferences. The in-hospital Palliative Care program<br />
is a new model for us and we are learning all the time how we can best support it.”<br />
Three Doulas comment on the impact of their work.<br />
“ I try to keep in mind that I am not there to do, but to make people feel<br />
less alone. It’s rewarding to realize I’ve added something to someone’s life,<br />
just by being there.” – Elaine Orr<br />
“ A recent experience with a patient and her family really struck me.<br />
She was nearing the end of life, and her son came in to play the violin for her.<br />
Everyone had tears. They were so loving, so strong.” – Marie Ginther<br />
“ I try to find common ground and start a conversation around it. I sense<br />
there’s a comfort for patients to have me with them at difficult times. At times<br />
I’ve experienced a depth of emotion that is hard to describe.” – Steve Polvent<br />
Strong testimony to the power of a Doula-patient relationship comes from patient<br />
Beth Stechman: “Steve and I often talk about music. When I’m upset, he is so patient.<br />
It can be easier to confide in a Doula than a staff or family member. Doctors and<br />
nurses can have a way of saying things that’s not always gentle. One day I got bad news<br />
and was crying. The Doula came in and I could unload. It was freeing.”
3<br />
The Inpatient Unit: A Vision Is Shaped<br />
Dreams for the future can materialize with the right combination<br />
of vision, leadership, planning, and support. With all these<br />
in place, the Hertzberg Palliative Care Institute, at press time,<br />
is two-thirds of the way toward a fundraising goal of $5 million<br />
for its new venture: a state of the art Inpatient Unit.<br />
“The new unit has the potential to transform completely the<br />
quality of care,” marvels Hertzberg Director Diane E. Meier, MD.<br />
She adds: “The <strong>Hospital</strong> has committed space on the 6th floor of<br />
Klingenstein Pavilion, overlooking Central Park. An aesthetically<br />
beautiful patient and family-centered unit will deliver efficient and<br />
effective care to the sickest, most complicated patients in a manner<br />
that is respectful, comforting and restorative. Attention to light,<br />
space, and design will be coupled with well-trained, expert, and<br />
adequate staffing.”<br />
“<strong>Mount</strong> <strong>Sinai</strong>’s commitment of space and support<br />
acknowledges the efficacy of palliative care.”<br />
– GABRIELLE GOLDBERG, MD<br />
While continuing to head Hertzberg’s educational programs,<br />
Gabrielle Goldberg, MD, will become Medical Director of the<br />
new unit. “<strong>Sinai</strong>’s commitment of space and support acknowledges<br />
the efficacy of palliative care,” says Dr. Goldberg. “Everyone<br />
who works on the unit – from physician to business associate –<br />
will be able to help us implement optimal symptom and pain<br />
management and increased patient and family satisfaction.”<br />
She sees “a wonderful opportunity for education for our medical<br />
students and all our house staff.”<br />
Nurse Practitioner Sue McHugh-Salera looks forward to seeing<br />
patients in “a place with a peaceful aura that will resemble a<br />
home-like situation for patient and family alike.” In her leadership<br />
role, Ms. McHugh-Salera is eager to educate and mentor nurses<br />
new to the unit. As the project moves toward fruition, she and<br />
Dr. Goldberg are working closely with: hospital, nursing, and<br />
Inpatient Unit Leadership: Sue McHugh-Salera, NP and Gabrielle Goldberg, MD<br />
facilities administrators; architects and design team; and everyone<br />
in Geriatrics and Palliative Care.<br />
<strong>Mount</strong> <strong>Sinai</strong> will provide the space, staffing, and overhead for<br />
the unit, but Hertzberg must raise funds to renovate and furnish<br />
the area. “As with all our projects,” says Development Director<br />
Jane MacDonald, “it’s a partnership between the hospital and<br />
philanthropic support from our community.”<br />
Dr. Meier emphasizes, “We could not do this without<br />
generous, consistent support from members of our community<br />
who believe in this kind of care.” Zena and Michael Wiener<br />
were among the unit’s first and major supporters. Mrs. Wiener<br />
comments: “We could have contributed to new drugs, new wings<br />
or medical centers. But to help provide a Palliative Care unit<br />
is the kindest contribution of all. This kind of care is as vital<br />
a part of medicine as the medicine itself.”<br />
Opportunities to name private rooms or public spaces in<br />
the Inpatient Unit are still available. For information, contact<br />
Jane MacDonald, Director of Development, at (212) 659-8517.<br />
What Is Palliative Care Anyway<br />
“Palliative care (pronounced pal-lee-uh-tiv) specializes in the relief of the pain,<br />
symptoms, and stress of serious illness. Palliative care is appropriate<br />
at any point in an illness, and it can be provided at the same time as treatment<br />
that is meant to cure you.”<br />
Information on free resources for<br />
help in situations that may require<br />
palliative care can be found at:<br />
www.getpalliativecare.org
Lilian and Benjamin Hertzberg Palliative Care Institute<br />
4<br />
Navigating the Labyrinth of Caregiving with Gail Sheehy<br />
After 14 tortuous years wending their way through the health<br />
care maze, prominent author Gail Sheehy and her husband,<br />
publisher Clay Felker, discovered palliative care. “Honest to God,<br />
a doctor insisted on making a house call,” recalls Ms. Sheehy.<br />
Sean Morrison, MD, took charge of Mr. Felker’s care and brought<br />
the resources of the Hertzberg Palliative Care Institute to the<br />
Felker-Sheehy home.<br />
Shortly before Dr. Morrison’s visit, Mr. Felker had developed<br />
pneumonia. His regular physician sent him to the emergency<br />
room, ordering yet another CAT scan. After a wait of 8 hours, the<br />
test was done only after Ms. Sheehy threw a small fit. By that time,<br />
“all the radiologists had left so no one could read it,” recounts Ms.<br />
Sheehy. “A sympathetic resident produced some results that<br />
sounded foreign. It was a scan taken 9 months before! I wheeled<br />
Clay out of the emergency room, and we congratulated ourselves<br />
on a jailbreak. We had spent several years frantically circling<br />
through the revolving doors of acute care.<br />
“After beating cancer 4 times, Clay wanted to spend the long<br />
afternoon of his life at home,” says Ms. Sheehy. “Treatment<br />
had left him with chronic conditions that made it difficult to<br />
talk or walk.” Yet, like many patients with long and serious illness,<br />
his vibrancy and zest for life prevailed. His mind and intellect<br />
remained sharp.<br />
“This is palliative care – a return of<br />
some control to people during a passage<br />
of life that is otherwise uncontrollable.”<br />
– GAIL SHEEHY<br />
Ms. Sheehy praises our health care system for excellent hospitals<br />
and professionals working toward one goal: cure. “But,” she warns,<br />
“chronic illnesses are impervious to cure; people often live with<br />
them for years, even decades, looked after at home by family<br />
members with no professional training, no financial support,<br />
and little respite. Properly funded home care could deliver huge<br />
savings to Medicare. But now it shifts the costs onto people’s<br />
personal bank accounts.”<br />
On the first of many home visits, Dr. Morrison sat at Mr. Felker’s<br />
bedside. According to Ms. Sheehy, “we had the first full and<br />
frank conversation about Clay’s wishes for this phase of his life.<br />
This is palliative care – a return of some control to people during<br />
a passage of life that is otherwise uncontrollable.”<br />
With assistance from Palliative Care and subsequent<br />
help from hospice, Ms. Sheehy cared for her husband at home<br />
for 7 months. Emboldened by Dr. Morrison’s ability to<br />
Susie West, Gail Sheehy, Diane Meier, MD and R. Sean Morrison, MD<br />
at the Douglas West Memorial Lecture in Geriatrics and Palliative Care<br />
keep Mr. Felker comfortable, she determined to take her eager<br />
husband on what would be his final excursion: hearing jazz<br />
at Dizzy’s Club Coca Cola, with its dazzling vistas across<br />
Central Park. Ms. Sheehy describes the evening: “Clay sat tall<br />
and straight in his wheelchair and drank in the music, tapping<br />
his fingers to the beat.” After returning home, “he gripped my<br />
hands,” remembers Ms. Sheehy, “and said clearly, with gusto,<br />
‘it was a magical evening.’”<br />
Gail Sheehy, author of 15 books, including the revolutionary<br />
“Passages,” shared her experiences as a caregiver at the<br />
June 3, <strong>2009</strong> Douglas West Endowed Memorial Visiting<br />
Lecture in Geriatrics and Palliative Care. She is the AARP<br />
Ambassador of Caregiving and offers weekly postings at<br />
AARP.org/Gail Sheehy. Her next book, “Labyrinth of Caregiving,”<br />
will be published in 2010.<br />
<strong>2009</strong>-2010 Palliative Care Fellows<br />
In July, the Hertzberg Palliative Care Institute welcomed 4 new fellows: Marcelo<br />
Bonomi, MD; Katharine Batt, MD, MSc; Aluko Hope, MD, MSCE; Mara Lugassy, MD
5<br />
Advancing the Science of Palliative Care Through Research<br />
While fully engaged in clinical work and teaching, Palliative<br />
Care faculty are also making major contributions to medical<br />
research. The following are a few of the many projects underway<br />
at Hertzberg.<br />
Diane E. Meier, MD, and R. Sean Morrison, MD, are Principal<br />
Investigators in a national study designed to improve the quality<br />
of palliative care for in-hospital cancer patients. With funding<br />
from the National Cancer Institute and National Institute for<br />
Nursing Research of the National Institutes of Health (NIH), this<br />
project has enrolled several thousand patients and their families.<br />
With awards from the Hartford Foundation and the National<br />
Institute of Aging of the NIH, Nathan Goldstein, MD, is<br />
pursuing questions about optimal care for patients with implanted<br />
defibrillators who are nearing the end of life. Defibrillators monitor<br />
the heart and, when necessary, deliver small electrical shocks to<br />
restore a normal pattern of beating. These shocks can impede the<br />
comfort of a patient who is seriously ill. Dr. Goldstein is working<br />
on a protocol that would help physicians communicate with<br />
patients in declining health about the possibility of deactivating<br />
their defibrillators.<br />
Investigating access to hospice care, Melissa Carlson, PhD,<br />
is conducting a 5-year study funded by the National Institute<br />
for Nursing Research of the NIH. Ultimately, she hopes to identify<br />
areas across the nation where there is no access to hospice and<br />
stimulate a quest to bring hospice to such regions.<br />
With support from the National Institute of Aging of the NIH,<br />
Dr. Morrison heads a project designed to improve pain<br />
management in older adults who experience hip fractures.<br />
Nathan Goldstein, MD and Melissa Carlson, PhD<br />
Immediately after a fracture, emergency room physicians are<br />
introducing regional nerve blocks, or injections of local anesthetic,<br />
in an attempt to minimize pain, avoid side effects of medications,<br />
and improve later functioning.<br />
Discussing the need for scientific evidence, Dr. Morrison,<br />
Director of the National Palliative Care Research Center (NPCRC;<br />
www.npcrc.org) cites the fact that more people are living longer<br />
with multiple chronic illnesses. Up to now, little research has<br />
focused on complicated patients. To provide the best quality of<br />
life to this growing patient population, palliative care professionals<br />
need to rely on a body of solid scientific evidence. “We aim to<br />
take our research findings and rapidly translate them into effective<br />
clinical practice,” says Dr. Morrison.<br />
“This Award Belongs to All My Colleagues in Palliative Care.” Continued from page 1<br />
Until all 25 awards were made public a week later, Dr. Meier<br />
was allowed to tell no one but her husband. Unable to call him or<br />
speak further with anyone at MacArthur until her flight landed<br />
hours later, she feared she was dreaming or hallucinating. She kept<br />
checking her cell phone to confirm that the incoming call had really<br />
taken place. By week’s end, when reporters were phoning, she broke<br />
the joyous news to her parents and to her chiefs at <strong>Sinai</strong>.<br />
MacArthur grants have often gone to people in the arts, but the<br />
2008 awardees included 4 groundbreaking physicians. “My award,”<br />
says Dr. Meier, “truly recognizes the importance of the whole field<br />
of palliative care, all that my colleagues from so many disciplines<br />
have contributed. Collectively, we have changed American medicine.<br />
It is gratifying, validating, and re-energizing.”<br />
A mere 15 years ago, palliative care’s original major funders, the<br />
Robert Wood Johnson Foundation and the George Soros Open<br />
Society Institute, demonstrated faith in a completely undeveloped<br />
field. Dr. Meier marvels: “Here we are, just 15 years later, with<br />
a new specialty. More than half the nation’s hospitals report<br />
a palliative care program. And we have a MacArthur award!”<br />
She credits <strong>Mount</strong> <strong>Sinai</strong> with being “100% supportive of our<br />
clinical and research endeavors and our efforts to train the next<br />
generation of physicians.” Grateful for support from the larger<br />
community as well, Dr. Meier adds: “Our donors’ farsighted and<br />
early investments have been validated by the judgment of the<br />
MacArthur Foundation.”<br />
Always planning for the future, Dr. Meier is grateful that the<br />
MacArthur award has raised the profile of palliative medicine<br />
with a number of audiences, including policy makers. “This will<br />
help me advocate for the pivotal role of palliative care as part<br />
of the solution to many aspects of our current health care crisis.”
6<br />
From Finance to Philanthropy<br />
Walter (Tommy) Hess, Jr. recalls his first meeting with Diane E.<br />
Meier, MD. “It was the weekend of the New York City Marathon.<br />
Central Park and all crossroads were closed to vehicles. My late wife<br />
Barbara, suffering from multiple myeloma, was in distress. We were<br />
fortunate to have made contact with Dr. Meier, who agreed to accept<br />
Barbara as a patient. Remarkably, this renowned physician would<br />
make a house call – and on a weekend. Answering my doorbell, I<br />
was astonished to see the doctor balancing her bicycle and carrying<br />
her helmet. ‘The only way to get across town,’ she casually said.”<br />
“I’m so impressed by the young doctors and health<br />
professionals being trained in palliative medicine.”<br />
– WALTER (TOMMY) HESS, JR.<br />
“When someone in your family is very sick, you’re nervous,” says<br />
Mr. Hess. “I’d call our prior physician, a very fine doctor at another<br />
hospital, to ask questions. When he didn’t return my call for two<br />
or three days, that drove me up the wall.” Contrasting this with the<br />
palliative care approach, Mr. Hess was incredulous that a member<br />
of the Hertzberg team would call Barbara several times a day when<br />
her symptoms were getting worse. “She was made as comfortable<br />
as possible at home, surrounded by family.”<br />
Soon to celebrate his 90th birthday, Mr. Hess<br />
decided it was time to retire from a long<br />
and distinguished career on Wall Street,<br />
including senior executive positions at two<br />
major firms. As a Board member of the<br />
Blythedale Children’s <strong>Hospital</strong> in Scarsdale, Walter (Tommy) Hess, Jr.<br />
a life Trustee of the Jewish Home and<br />
<strong>Hospital</strong> for the Aged, and head of the Wall Street Division of<br />
UJA/Federation of Jewish Philanthropies, he brought financial<br />
resources and expertise to many aspects of health care. Ever ready<br />
for new ways to contribute, Mr. Hess, who remarried several years<br />
after Barbara died, was delighted that his wife Peggy embraced<br />
and shared his commitment to furthering palliative medicine.<br />
“When Diane asked me to join the Hertzberg Philanthropic<br />
Leadership Council,” exclaims Tommy Hess, “I was thrilled!<br />
I’m so impressed by the young doctors and health professionals<br />
being trained in palliative medicine. They’re learning the<br />
clinical and communication skills needed to take care of seriously<br />
ill people. I get such pleasure from contributing and bringing<br />
others in to support Hertzberg.”<br />
Explaining how Walter Jr. became known as Tommy, Mr. Hess<br />
chuckles: “When I was a tot and my mother called ‘Walter,’ I would<br />
come running when it was my Dad she wanted. Mom decided:<br />
‘You look like a Tommy.’ The name stuck.” Mr. Hess laughs as<br />
he muses how young Tommy, always struggling to earn passing<br />
grades in mathematics classes, became a respected Wall Street<br />
executive, philanthropist, and forceful advocate for palliative care.<br />
Hertzberg Highlights<br />
In addition to the MacArthur Fellowship, Diane E. Meier, MD,<br />
has recently received awards from several other national<br />
organizations. At the Castle Connolly National Physician of<br />
the Year Awards Ceremony on March 23, <strong>2009</strong> in New York<br />
City, Dr. Meier was one of three physicians nationally honored<br />
by the Clinical Excellence Awards. Physicians listed in the<br />
Castle Connolly “Top Doctor” guides nominated Dr. Meier<br />
for this honor.<br />
The American Association of Retired Persons (AARP)<br />
selected Dr. Meier as a recipient of its 50th Anniversary Social<br />
Impact Award, bestowed upon “champions of social change”<br />
who “are enhancing the lives” of others.<br />
In February <strong>2009</strong>, the American Academy of Hospice and<br />
Palliative Medicine announced the election of R. Sean Morrison, MD,<br />
as its next President. On March 25, <strong>2009</strong>, at its annual conference<br />
in Austin, Texas, the Academy presented a Life Time Achievement<br />
Award to Dr. Diane E. Meier.<br />
Diane E. Meier, MD with Susie West and<br />
Bette Kerr at the Castle Connolly Awards<br />
John K. Castle, Diane E. Meier, MD,<br />
John J. Connolly, EdD<br />
On behalf of Hertzberg’s Nurse Practitioners, Marianne Gelber,<br />
Jay Horton, and Sue McHugh-Salera received this year’s Preceptor<br />
Award from The College of Nursing of New York University.<br />
The Award singled out the Palliative Care nursing practice for<br />
its outstanding contributions to the clinical education of NYU<br />
graduate nursing students.<br />
Gabrielle Goldberg, MD, received the <strong>2009</strong> <strong>Mount</strong> <strong>Sinai</strong> Teaching<br />
Excellence Incentive Plan Award, in recognition of her<br />
“valued contribution to educational efforts to create future<br />
leaders of academic medicine and clinical care.”


![December 2, 2012 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/51092274/1/190x245/december-2-2012-pdf-mount-sinai-hospital.jpg?quality=85)
![January 21, 2013 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/50916550/1/190x245/january-21-2013-pdf-mount-sinai-hospital.jpg?quality=85)
![February 3, 2013 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/50584982/1/190x245/february-3-2013-pdf-mount-sinai-hospital.jpg?quality=85)
![March 18, 2012 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/50462098/1/190x245/march-18-2012-pdf-mount-sinai-hospital.jpg?quality=85)


![Partners Program Guide [PDF] - Mount Sinai Hospital](https://img.yumpu.com/49411954/1/190x245/partners-program-guide-pdf-mount-sinai-hospital.jpg?quality=85)

![March 19 - April 1, 2012 [PDF] - Mount Sinai Hospital](https://img.yumpu.com/48990923/1/190x245/march-19-april-1-2012-pdf-mount-sinai-hospital.jpg?quality=85)
![PGY-1 Residency Application [PDF] - Mount Sinai Hospital](https://img.yumpu.com/48577701/1/190x245/pgy-1-residency-application-pdf-mount-sinai-hospital.jpg?quality=85)


