Expert Recommendations for Optimizing Outcomes ... - Wounds
Expert Recommendations for Optimizing Outcomes ... - Wounds
Expert Recommendations for Optimizing Outcomes ... - Wounds
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
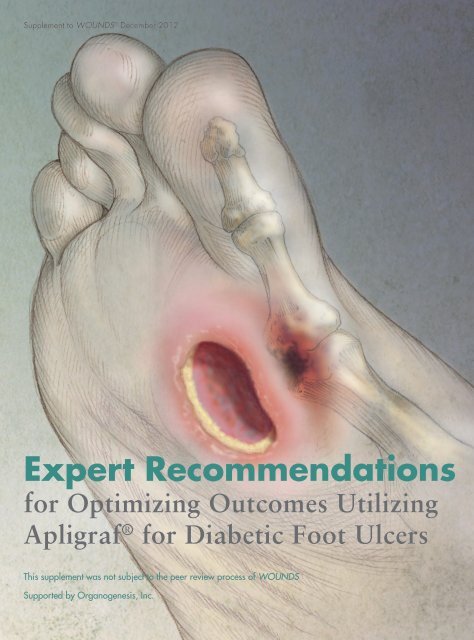
Supplement to WOUNDS ® December 2012<br />
<strong>Expert</strong> <strong>Recommendations</strong><br />
<strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing<br />
Apligraf ® <strong>for</strong> Diabetic Foot Ulcers<br />
This supplement was not subject to the peer review process of WOUNDS<br />
Supported by Organogenesis, Inc.
Table of Contents<br />
Purpose of this Supplement............................................................................................................4<br />
PART 1<br />
Patients with Diabetic Foot Ulcers<br />
1.1 The Challenge of Diabetic Foot Ulcers..................................................................................6<br />
1.2 Pathophysiology of Wound Healing in DFUs. .......................................................................7<br />
1.3 Initial Evaluation of Patients with a DFU... ............................................................................8<br />
1.4 Estimating the Likelihood of DFU Healing..........................................................................10<br />
1.5 Conventional Wound Therapies...........................................................................................11<br />
1.6 Evaluating Response to Conventional Therapy.....................................................................13<br />
Cover Photo Credit<br />
Photo Researchers Picture Number: BH3877<br />
Credit: Michele S. Graham / Photo Researchers, Inc<br />
License: Rights Managed<br />
Images and Text Copyright © 2012 Photo Researchers, Inc. All Rights Reserved.<br />
2 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
Table of Contents<br />
PART 2<br />
Advanced Therapy of DFUs with Apligraf ®<br />
2.1 Evidence-Based Selection of Advanced Therapy <strong>for</strong> DFUs.. ...................................................15<br />
2.2 Apligraf: Efficacy and Proposed Mechanism............................................................................17<br />
2.3 Initiating Apligraf Therapy.....................................................................................................18<br />
2.4 Evaluating Response to Apligraf & Reapplications.................................................................19<br />
2.5 Summary...............................................................................................................................20<br />
, LLC<br />
<br />
www.hmpcommunications.com. 130-218<br />
©2012 HMP Communications, LLC (HMP). All rights reserved. Reproduction in whole or in part prohibited. Opinions expressed by authors,<br />
contributors, and advertisers are their own and not necessarily those of HMP Communications, the editorial staff, or any member of the<br />
editorial advisory board. HMP Communications is not responsible <strong>for</strong> accuracy of dosages given in articles printed herein. The appearance<br />
of advertisements in this journal is not a warranty, endorsement, or approval of the products or services advertised or of their effectiveness,<br />
quality, or safety. HMP Communications disclaims responsibility <strong>for</strong> any injury to persons or property resulting from any ideas or products<br />
referred to in the articles or advertisements. Content may not be reproduced in any <strong>for</strong>m without written permission. Reprints of articles are<br />
available. Rights, permission, reprint, and translation in<strong>for</strong>mation is available at: www.hmpcommunications.com.<br />
HMP Communications, LLC (HMP) is the authoritative source <strong>for</strong> comprehensive in<strong>for</strong>mation and education servicing healthcare professionals.<br />
HMP’s products include peer-reviewed and non–peer-reviewed medical journals, national tradeshows and conferences, online programs,<br />
and customized clinical programs. HMP is a wholly owned subsidiary of HMP Communications Holdings LLC. Discover more about HMP’s<br />
products and services at www.hmpcommunications.com.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 3
Purpose of this Supplement<br />
Diabetic foot ulcers (DFUs) are one of the most common complications of diabetes mellitus (DM) and are associated<br />
with significant morbidity and mortality. Management of DFUs is complex and requires a systematic approach to<br />
achieve successful outcomes. The care of DFUs has evolved in recent years as new therapeutic options have become<br />
available with varying levels of evidence supporting their use. Education about the latest developments in the evaluation and<br />
treatment of DFUs has sometimes not kept up with the pace of this progress, especially with regards to advanced therapies,<br />
such as cell therapy, growth factors, negative-pressure therapy, and hyperbaric oxygen therapy.<br />
Six experienced wound care specialists reviewed the current status of evidence-based evaluation and therapy of DFUs with<br />
a focus on the optimal use of Apligraf ® , an allogeneic bilayered living-cell-based product that has FDA approval <strong>for</strong> treatment<br />
of DFUs.<br />
The objectives of this meeting were two-fold:<br />
(1) To highlight key aspects of the evaluation and evidence-based conventional therapy of DFUs<br />
(2) To make recommendations regarding the optimal use of Apligraf as evidence-based advanced therapy in the<br />
care of DFUs<br />
The overarching goal of both these objectives is to empower clinicians caring <strong>for</strong> patients with DFUs to optimize clinical<br />
outcomes by providing an educational resource that is concise and useful in their clinical practices.<br />
In this supplement, Part 1 | Initial Evaluation of Diabetic Foot Ulcers addresses the first objective and Part 2 | Advanced Therapy<br />
of DFUs with Apligraf addresses the second objective.<br />
Of note, this paper is not intended as an exhaustive review of DFU management. Rather, based on the group discussions<br />
during the meeting and the meeting participants’ extensive clinical experience with DFU management, the intention is to<br />
focus on a select number of issues that the group felt was most critical to achieving optimal clinical outcomes in DFU patients.<br />
The meeting participants provided a variety of perspectives including academic settings, teaching hospitals, and standalone<br />
wound care clinics. Robert Kirsner, MD, PhD, Professor and Vice Chairman of the Department of Dermatology<br />
and Cutaneous Surgery at the University of Miami Miller School of Medicine led the group discussions. Following the<br />
conference, a first draft summary of the group discussions was written and then extensively edited and finalized utilizing<br />
input from all meeting participants.<br />
Meeting Participants<br />
Dr. Robert S. Kirsner (Moderator)<br />
Dr. Kirsner is a tenured professor, Vice Chairman, and<br />
holds the endowed Stiefel Laboratories Chair in Dermatology<br />
in the Department of Dermatology and Cutaneous<br />
Surgery at the University of Miami Miller School of Medicine.<br />
He currently serves as director of the University of<br />
Miami Hospital Wound Center and chief of Dermatology<br />
at the University of Miami Hospital. Dr. Kirsner is also a<br />
recently retired board member of the Wound Healing Society<br />
and is past president of the Association <strong>for</strong> the Advancement<br />
of Wound Care. He co-directed the Symposium <strong>for</strong><br />
Advanced wound Care (SAWC) <strong>for</strong> the past 18 years. In<br />
addition to career development awards and industry sponsored<br />
funding, he is a recipient of NIH, ACS, CDC funding<br />
<strong>for</strong> his research. Independent of books, book chapters and<br />
abstracts, he has published over 350 articles.<br />
Dr. Desmond Bell<br />
Dr. Desmond Bell is the co-founder and executive<br />
director of the “Save A Leg, Save A Life” Foundation, a<br />
multidisciplinary non-profit organization dedicated to the<br />
reduction in lower extremity amputations and improving<br />
wound healing outcomes through evidence-based methodology<br />
and community outreach. He is a board certified<br />
wound specialist (CWS/American Board of Wound Management)<br />
and has served on their Board of Directors since<br />
2009. He serves on the Board of Directors of the Association<br />
<strong>for</strong> the Advancement of Wound Care, the Barbara<br />
Bates-Jensen Wound Reach Foundation, the Communications<br />
Committee of the Jacksonville Chapter of the American<br />
Diabetes Association and the Conference Planning<br />
Committee of the Symposium on Advanced Wound Care.<br />
He is also a member of the Wound Healing Society and<br />
the Vascular Disease Foundation/PAD Coalition. Dr. Bell<br />
has been in private practice in Jacksonville, Florida since<br />
1997 and is on staff at Memorial Hospital of Jacksonville, St.<br />
Vincent’s Medical Center Southside and Specialty Hospital<br />
of Jacksonville.<br />
4 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
Dr. Gary Gibbons<br />
Dr. Gibbons is medical director <strong>for</strong> South Shore Hospital<br />
Center <strong>for</strong> Wound Care and Hyperbaric Medicine and Professor<br />
of Surgery at the Boston University School of Medicine.<br />
Trained as a vascular surgeon, Dr. Gibbons was the first director<br />
of the Joslin-Beth Israel Deaconess Foot Center in Boston<br />
and his career has centered on diabetic patients with lower extremity<br />
wounds, especially those complicated by vascular disease.<br />
He has published and spoken extensively on the subject<br />
and has been honored with the Pecoraro (ADA), Olmos, and<br />
Georgetown Distinguished Achievement awards <strong>for</strong> his work.<br />
Dr. Bill Ennis<br />
Dr. Ennis is a professor of clinical surgery and chief of the<br />
section of wound healing and tissue repair at the University of<br />
Illinois Hospital and Health Sciences System. His active areas<br />
of research include healing outcomes measures, microcirculation,<br />
macrophage function and the impact of stem cells on<br />
wound healing.<br />
Dr. Arti Masturzo<br />
Dr. Masturzo is a published educator who has dedicated<br />
her career to the advancement of wound care best practices<br />
and the development of comprehensive wound care programs.<br />
She completed her internal medicine residency at the University<br />
of Cincinnati and went on to pursue a practice focusing<br />
entirely on the care of chronic wounds. She is currently the<br />
Medical Director of Comprehensive Wound Programs <strong>for</strong> Tri-<br />
Health Associates, overseeing inpatient and outpatient wound<br />
care, including hyperbarics, <strong>for</strong> multiple hospitals and clinics<br />
in greater Cincinnati. In addition, she is the Corporate Director<br />
of Medical Affairs of Accelecare Wound Centers. Dr.<br />
Masturzo is board-certified in internal medicine and undersea<br />
hyperbaric medicine.<br />
Dr. Gary Rothenberg<br />
Dr. Rothenberg is a board certified podiatrist, certified diabetes<br />
educator and certified wound specialist who currently<br />
serves as director of resident training and attending podiatrist<br />
at the Department of Veteran Affairs Medical Center in Miami,<br />
Florida. A graduate of the Ohio College of Podiatric<br />
Medicine, he completed 3 years of residency training at the<br />
University of Texas Health Science Center in San Antonio.<br />
His previous private practice experience and now academic<br />
practice have focused on conservative and surgical management<br />
of the diabetic foot.<br />
Conflicts of Interest<br />
Dr. Kirsner indicates advisory board participation with Organogenesis, Shire, Healthpoint, and KCI.<br />
Dr. Bell indicates he is a member of the Speaker’s Bureau of Organogenesis and Cordis and serves as a consultant<br />
with ev3, Cook, and Healiance.<br />
Dr. Gibbons indicates he is a consultant, speaker, and participates in a clinical experience program <strong>for</strong> Organogenesis, and<br />
that he is principal investigator <strong>for</strong> a venous leg ulcer study sponsored by Celleration.<br />
Dr. Ennis indicates he is a consultant to Organogenesis, KCI, and Accelecare wound centers.<br />
Dr. Masturzo indicates she is a member of the Speaker’s Bureau of Organogenesis and KCI. She has also served as a<br />
consultant to Shire.<br />
Dr. Rothenberg indicates he is a member of the Speaker’s Bureau <strong>for</strong> Organogenesis and Healthpoint.<br />
Acknowledgements<br />
This article is supported by a grant from Organogenesis. The authors would like to thank Ed Perper, MD, and James Radke,<br />
PhD, <strong>for</strong> editorial and manuscript assistance. This supplement is provided as a courtesy to the readers of WOUNDS. This<br />
supplement was not subject to the peer review process of WOUNDS.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 5
PART 1<br />
Patients with Diabetic Foot Ulcers<br />
1.1 The Challenge of Diabetic Foot Ulcers<br />
Review of Evidence<br />
DFUs are a common complication in patients with DM.<br />
The lifetime risk of developing a DFU is 15% to 25% and<br />
the prevalence of DFUs among diabetics is 4% to 10%. 1<br />
The morbidity and mortality associated with DFUs is<br />
very high. For example, 85% of leg amputations are preceded<br />
by DFUs 1 and more than 60% of nontraumatic lower<br />
extremity amputations per<strong>for</strong>med in the United States each<br />
year occur secondary to complications of DM. 2 Mortality<br />
rates following amputation are alarmingly high: up to 40%<br />
at 1 year and 80% at 5 years. 1<br />
Un<strong>for</strong>tunately, DFUs are notoriously difficult to heal.<br />
The healing rate even with good standard-of-care treatment<br />
is only 31% at 20 weeks 3 (Figure 1). Moreover, DFUs<br />
are frequently inadequately managed due to multiple factors<br />
including blunted signs of infection, limited understanding<br />
of current diagnostic and therapeutic approaches,<br />
and insufficient resources. 4<br />
Group Discussion<br />
The seriousness of DFUs is often underestimated by both<br />
clinicians and patients. A critical first step is <strong>for</strong> everyone involved<br />
to fully understand and explicitly acknowledge that<br />
achieving complete healing represents a significant challenge<br />
in a high-risk patient. This should motivate both the<br />
wound care practitioner and the patient to take all necessary<br />
steps to maximize the probability of success. It is important<br />
to not underestimate this disease as success is typically<br />
harder than many perceive. Educating patients about the<br />
challenge of healing their DFU will ideally motivate them<br />
to strictly comply with all therapeutic interventions; poor<br />
compliance is an important factor that often limits the success<br />
of therapy. Importantly, wound care clinicians should<br />
understand that even with well-delivered standard care of<br />
DFUs, the probability of complete healing is relatively low;<br />
there<strong>for</strong>e from the very start of treatment, clinicians should<br />
anticipate that advanced therapy will be required in many<br />
patients to achieve complete healing.<br />
%<br />
Weighted Mean Healing Rate<br />
100%<br />
75%<br />
25%<br />
0%<br />
24.2%<br />
30.9%<br />
12 Weeks 20 Weeks<br />
N = 4 trials<br />
N = 6 trials<br />
Time Elapsed<br />
Suggested Reading<br />
• Consensus Development Conference on Diabetic Foot Wound<br />
Care: 7-8 April 1999, Boston, Massachusetts. American Diabetes<br />
Association. Diabetes Care. 1999;22(8):1354-1360.<br />
• Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers<br />
in patients with diabetes. JAMA. 2005;293(2):217-228.<br />
• Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic<br />
foot ulcers receiving standard treatment. Diabetes Care.<br />
1999;22(5):692-695.<br />
Figure 1. Healing rates of control groups from<br />
meta-analysis of 10 randomized clinical trials of<br />
standard DFU care. 3 <br />
Margolis DJ, Kantor J, Berlin JA. Healing of diabetic neuropathic foot ulcers<br />
receiving standard treatment. Diabetes Care. 1999;22(5):692-695.<br />
• Maderal AD, Vivas AC, Zwick TG, Kirsner RS. Diabetic foot<br />
ulcers: evaluation and management. Hosp Pract (Minneap).<br />
2012;40(3):102-115.<br />
• Ramsey SD, Newton K, Blough D, et al. Incidence, outcomes,<br />
and cost of foot ulcers in patients with diabetes.<br />
Diabetes Care. 1999;22(3):382-387. n<br />
6 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
1.2 Pathophysiology of Wound Healing in DFUs<br />
Review of Evidence<br />
Acute wounds heal through a normal highly regulated<br />
process of cell replication, migration, protein synthesis,<br />
matrix deposition, and organization. In an acute wound,<br />
multiple growth factors, cytokines, and cells—including<br />
keratinocytes and fibroblasts—work in concert to heal the<br />
wound completely. 5-7 DFUs are chronic wounds that fail<br />
to heal in a regulated and systematic manner due to multiple<br />
abnormal physiologic, anatomic, and cellular factors:<br />
(1) decreased angiogenic response; (2) neuropathy; (3)<br />
ischemia; (4) endothelial dysfunction; and (5) increased<br />
susceptibility to wound infection 5 (Figure 2).<br />
In addition, in DFUs there is poor and disorganized regulation<br />
of the cytokines, growth factors, proteases, extracellular<br />
matrix components, and cells needed to achieve<br />
complete wound closure 8,9 : (1) keratinocyte migration and<br />
proliferation is impaired 10 ; (2) fibroblast response to growth<br />
factors 9 and the ability to synthesize collagen is impaired 11 ;<br />
and (3) there is a relative deficiency of tissue inhibitors<br />
of matrix metalloproteinases, which results in degradation<br />
of the extracellular matrix. 8,12,13 All these pathophysiologic<br />
factors contribute to the poor healing rates observed in<br />
patients with DFUs.<br />
Group Discussion<br />
All wound care practitioners should understand the<br />
multiple pathophysiologic defects that contribute to poor<br />
healing rates of DFUs. By therapeutically addressing as<br />
many of these factors as possible, the likelihood of wound<br />
healing can be increased. For example, clinicians must<br />
assess and reassess <strong>for</strong> ischemia, infection, and other factors<br />
throughout the course of management that may slow or<br />
prevent healing. If healing stalls, some advanced therapies<br />
may address the growth factor, cytokine, and cellular<br />
abnormalities that interfere with healing of DFUs.<br />
Suggested Readings<br />
• Brem H, Young J, Tomic-Canic M, et al. Clinical efficacy<br />
and mechanism of bilayered living human skin equivalent<br />
(HSE) in treatment of diabetic foot ulcers. Surg Technol Int.<br />
2003;11:23-31.<br />
Figure 2. Pathophysiologic factors contributing to<br />
poor healing rates of DFUs.<br />
• Werner S, Krieg T, Smola H. Keratinocyte–fibroblast<br />
interactions in wound healing. J Invest Dermatol.<br />
2007;127(5):998-1008.<br />
• Ghahary A, Ghaffari A. Role of keratinocyte–fibroblast<br />
cross-talk in development of hypertrophic scar. Wound Repair<br />
Regen. 2007;15(suppl 1):S45-S53. n<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 7
1.3 Initial Evaluation of Patients with a DFU<br />
Review of Evidence<br />
Several published clinical guidelines exist to assist wound<br />
care practitioners with proper evaluation and management of<br />
DFUs, including those from the Infectious Diseases Society<br />
of America, 14 the American College of Foot and Ankle Surgeons,<br />
15 the Wound Healing Society, 16 and the International<br />
Working Group on the Diabetic Foot Editorial Board. 17<br />
Common to these guidelines is the recommendation <strong>for</strong> a<br />
meticulous initial clinical evaluation of every patient with a<br />
DFU. Particular attention should be on the following issues:<br />
1) peripheral artery disease; 2) neuropathy; 3) nutritional status;<br />
4) wound infection, including osteomyelitis; and 5) hyperglycemia<br />
(Figure 3).<br />
In addition, a wound-specific history must be obtained,<br />
including location, duration, inciting event or trauma,<br />
previous ulcers and recurrences, hospitalization, previous<br />
wound care treatments, off-loading technique, wound response<br />
to treatment, patient compliance, family or social<br />
problems that are interfering with care, previous foot trauma<br />
or surgery, presence of edema, and history of Charcot<br />
foot and its treatment. 15<br />
Classification of DFUs is generally predictive of outcomes<br />
and may facilitate treatment (Figure 4). The most commonly<br />
used classification system is the Wagner system, which divides<br />
foot lesions into 6 grades based on the depth of the wound<br />
and extent of tissue infection and necrosis. However, the<br />
Wagner system does not consider the roles of infection, ischemia,<br />
and other factors. The University of Texas San Antonio<br />
(UTSA) system associates lesion depth with both ischemia<br />
and infection; this system has been validated and is generally<br />
predictive of outcome. 15<br />
If possible, the initial evaluation of the DFU should involve<br />
a multidisciplinary team that includes wound care professionals<br />
and, when indicated, diabetologists or endocrinologists,<br />
surgeons (vascular and podiatric), nurses, nutritionists,<br />
and pedorthotists. 4<br />
Assess Patient<br />
• H & P<br />
• Glycemic control<br />
• Nutritional evaluation<br />
• Immune status<br />
• Neurological evaluation<br />
• Vascular evaluation<br />
• Psychosocial evaluation<br />
Assess DFU<br />
• Duration<br />
• Size (~area in cm 2 Estimate Likelihood of<br />
)<br />
Succesful Closure &<br />
• Depth<br />
Discuss with Patient<br />
• Location<br />
• Charcot<br />
• Soft tissue infection & osteomyelitis<br />
• Consider advanced testing & imaging<br />
Appropriate<br />
Interventions<br />
Standard Therapy<br />
<strong>for</strong> all DFUs<br />
Debridement Infection Control Off-Loading Appropriate Dressing<br />
Figure 3. Clinical algorithm <strong>for</strong> initial assessment of patients with DFUs.<br />
Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious Diseases Society of America clinical practice guideline <strong>for</strong> the diagnosis and treatment of diabetic foot infections. Clin Infect Dis.<br />
2012;54(12):e132-173.<br />
Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot disorders. A clinical practice guideline (2006 revision). J Foot Ankle Surg. 2006;45(5 Suppl):S1-66.<br />
Steed DL, Attinger C, Colaizzi T, et al. Guidelines <strong>for</strong> the treatment of diabetic ulcers. Wound Repair Regen. 2006;14(6):680-692.<br />
Bakker K, Apelqvist J, Schaper NC; International Working Group on Diabetic Foot Editorial Board. Practical guidelines on the management and prevention of the diabetic foot 2011.<br />
Diabetes Metab Res Rev. 2012;28 Suppl 1:225-231.<br />
8 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
Wagner Classification System of DFUs<br />
Grade Lesion<br />
0 No open lesions: may have de<strong>for</strong>mity or cellulitis<br />
1 Superficial ulcer<br />
2 Deep ulcer to tendon or joint capsule<br />
3 Deep ulcer with abscess, osteomyelitis, or joint sepsis<br />
4 Local gangrene – <strong>for</strong>efoot or heel<br />
5 Gangrene of entire foot<br />
University of Texas Classification System of DFUs<br />
Stage<br />
A<br />
Pre- or post-ulcerative<br />
lesions, completely<br />
epithelized<br />
Grade<br />
0 I II III<br />
Superficial wound not<br />
involving tendon,<br />
capsule, or bone<br />
Wound penetrating in<br />
tendon or capsule<br />
Wound penetrating in bone<br />
or joint<br />
B Infected Infected Infected Infected<br />
C Ischemic Ischemic Ischemic Ischemic<br />
D Infected and ischemic Infected and ischemic Infected and ischemic Infected and ischemic<br />
Figure 4. Wagner and University of Texas Classification Systems <strong>for</strong> chronic wounds.<br />
Group Discussion<br />
Published evidenced-based guidelines should provide a<br />
roadmap <strong>for</strong> care <strong>for</strong> DFU. Clinicians should follow the<br />
recommendations of the published clinical guidelines <strong>for</strong><br />
initial evaluation of patients with a DFU. Too often inadequate<br />
evaluation or treatment of peripheral arterial disease<br />
(PAD), or in more severe instances, critical limb ischemia,<br />
is a major factor that slows or prevents complete DFU<br />
healing. Assessment of vascular status is critical prior to<br />
proceeding with other elements of care in patients with a<br />
DFU. Another important issue related to the initial evaluation<br />
of patients with a DFU is precise baseline measurement<br />
of wound size so that the response to treatment<br />
can be reassessed quantitatively and accurately (Section 1.6<br />
below: “Evaluating Response to Conventional Therapy”).<br />
Suggested Reading<br />
• Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious<br />
Diseases Society of America clinical practice guideline <strong>for</strong> the<br />
diagnosis and treatment of diabetic foot infections. Clin Infect<br />
Dis. 2012;54(12):e132-173.<br />
• Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot disorders.<br />
A clinical practice guideline (2006 revision). J Foot Ankle<br />
Surg. 2006;45(5 Suppl):S1-66.<br />
• Steed DL, Attinger C, Colaizzi T, et al. Guidelines <strong>for</strong> the treatment<br />
of diabetic ulcers. Wound Repair Regen. 2006;14(6):680-692.<br />
• Bakker K, Apelqvist J, Schaper NC; International Working<br />
Group on Diabetic Foot Editorial Board. Practical guidelines<br />
on the management and prevention of the diabetic foot 2011.<br />
Diabetes Metab Res Rev. 2012;28 Suppl 1:225-231.<br />
• Snyder RJ, Kirsner RS, Warriner RA, et al. Consensus recommendations<br />
<strong>for</strong> advancing the standard of care <strong>for</strong> treating<br />
neuropathic foot ulcers in patients with diabetes. Ostomy Wound<br />
Manage. 2010;56(suppl 4):S1-S24.<br />
• Gibbons GW, Shaw PM. Diabetic Vascular Disease: Characteristics<br />
of Vascular Disease Unique to the Diabetic Patient. Semin<br />
Vasc Surg. 2012;25:89-92. n<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 9
1.4 Estimating the Likelihood of DFU Healing<br />
Review of Evidence<br />
The likelihood of complete DFU healing is determined<br />
by multiple factors, both patient-related and wound-related.<br />
Important patient-related factors include vascular status,<br />
nutritional status, neurologic status, presence and severity of<br />
soft tissue infection, osteomyelitis, Charcot, and other factors,<br />
including glycemic control. Wound-related factors that have<br />
been demonstrated in prospective studies to have predictive<br />
value include the size, duration, depth, and grade of the<br />
DFU. Larger lesions (>2 cm 2 ), chronic lesions (>6 months<br />
- 12 months), deeper lesions, and higher grade lesions are<br />
associated with reduced likelihood of complete healing despite<br />
continued conventional therapy.<br />
Margolis et al 18 pooled data from the standard care arms<br />
of 5 clinical trials to determine the effect of wound size and<br />
duration on the probability of healing (Figure 5). Healing rates<br />
were lower in patients with larger wounds and longer duration<br />
wounds. For example, wounds 12 months, which had<br />
only a 26% probability of healing (n = 252 patients).<br />
Group Discussion<br />
Many DFUs heal slowly and many will not heal with<br />
standard treatment. Healthcare providers should be keenly<br />
aware of the serious challenges involved in treating any<br />
DFU successfully. Patients and families must be educated<br />
about the poor prognosis <strong>for</strong> healing in general and the<br />
critical importance of strict compliance in order to maximize<br />
the probability of success. The studies above clearly<br />
show that even in patients with DFUs that are small and<br />
of shorter duration, many lesions will not heal with conventional<br />
therapy, eg, in the Margolis trial described above,<br />
even among patients with small DFUs that were present<br />
<strong>for</strong> less than 6 months more than half (57%) did not heal at<br />
20 weeks. Of course, in larger wounds of greater duration<br />
the likelihood of healing is even lower. There<strong>for</strong>e, from the<br />
first day of treatment onwards, all patients need to understand<br />
that DFUs are very difficult to heal with conventional<br />
therapy and that most patients will ultimately need<br />
to receive evidence-based advanced therapy to maximize<br />
their odds of achieving complete healing.<br />
In addition, the group believed that in many cases the<br />
likelihood of successful healing is overestimated by both<br />
clinicians and patients and that greater awareness of the<br />
challenges DFUs present may lead to better clinical decisions<br />
and higher compliance.<br />
Suggested Readings<br />
• Margolis DJ, Kantor J, Santanna J, Strom BL, Berlin JA. Risk<br />
factors <strong>for</strong> delayed healing of neuropathic diabetic foot ulcers:<br />
a pooled analysis. Arch Dermatol. 2000;136:1531-1535. n<br />
100%<br />
% Healed Within 20 Weeks<br />
75%<br />
50%<br />
25%<br />
% Healed<br />
0 %<br />
4 12 12<br />
()*+,#-./0# ()*+,#1*234)+# ()*+,#-./0#3+,#<br />
Wound Size 1*234)+#<br />
& Duration<br />
Wound Size<br />
cm 2<br />
Wound Duration<br />
months<br />
cm 2 & months<br />
Sample Size: 347 123 116 202 88 189 120 252<br />
Figure 5. Cumulative healing rates within 20 weeks of care of DFUs.<br />
Adapted from Margolis DJ, et al. Risk factors <strong>for</strong> delayed healing of neuropathic diabetic foot ulcers: a pooled analysis. Arch Dermatol. 2000;136:1531-1535.<br />
10 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
1.5 Conventional Wound Therapies<br />
Review of Evidence<br />
Management of DFUs is complex and<br />
requires a systematic approach to achieve<br />
more consistent and successful outcomes. 4<br />
This includes addressing multiple issues: 1)<br />
peripheral artery disease; 2) neuropathy; 3)<br />
nutritional status; 4) ulcer and bone infection;<br />
and 5) glycemic control. Detailed discussion<br />
of these factors is beyond the scope of this<br />
paper. Addressing peripheral artery disease is<br />
particularly important. Depending on the<br />
population being treated, peripheral ischemia<br />
contributes to poor wound healing in 50% to<br />
60% of patients with DFUs.<br />
In addition, the wound itself must be treated<br />
directly. Below is a brief review of the<br />
clinical evidence supporting the administration<br />
of conventional wound therapies that are<br />
mandated in all patients with DFUs:<br />
Be<strong>for</strong>e debridement<br />
After debridement<br />
Offloading.<br />
The main mechanism by which DFUs<br />
develop is due to increased, sustained and/<br />
or repetitive trauma in the setting of peripheral<br />
neuropathy. Distributing and minimizing<br />
pressure in the affected area is crucial<br />
to achieve healing. Pressure offloading can<br />
be achieved with foot inserts, therapeutic<br />
shoes, casts, or by surgical procedures. The<br />
total-contact cast is considered the gold standard<br />
<strong>for</strong> the management of plantar DFUs as<br />
studies have shown the highest healing rates<br />
compared with other offloading devices. 19,20<br />
However, it is recognized that limitations to<br />
use of total-contact casting exist and alternatives<br />
are available which have been shown to<br />
be effective. 21,22 Poor patient compliance often<br />
limits success of offloading due in part to the fact that these<br />
devices limit per<strong>for</strong>mance of daily activities and the stability of<br />
patients’ gaits. 23 There<strong>for</strong>e, the best device is one with high adherence<br />
that best adapts to the patient, permitting continuous<br />
use and effective decrease in pressure.<br />
Figure 6. Examples of DFUs be<strong>for</strong>e and after surgical debridement.<br />
Photo credit: Arti B Masturzo MD ABPM/UHM<br />
Medical Director Advanced Wound Programs<br />
Bethesda North & Good Samaritan Hospitals<br />
Cincinnati, OH<br />
Debridement.<br />
Debridement is considered essential in DFU care although<br />
this is supported by data from secondary analyses of<br />
controlled trials per<strong>for</strong>med <strong>for</strong> reasons other than debridement.<br />
24 When undertaken, appropriate debridement includes<br />
removal of excess callus and necrotic tissue and likely results<br />
in reduction of unresponsive cells in the wound bed and<br />
edge, bacterial biofilms and excess matrix metalloproteinases.<br />
Among the different types of debridement (surgical, enzymatic,<br />
autolytic, mechanical, and biologic), surgical debridement<br />
is preferred. (See Figure 6 <strong>for</strong> examples of DFUs be<strong>for</strong>e<br />
and after surgical debridement.) Steed et al found topical<br />
application of a growth factor with frequent debridement<br />
increased the likelihood of healing as did debridement with-<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 11
out growth factor application, but to a lesser extent. 25 The<br />
“Debridement Per<strong>for</strong>mance Index,” which evaluates the<br />
adequacy of debridement of the wound and wound edges,<br />
was found to be an independent factor of wound closure. 26<br />
Finally, it has been suggested that frequent debridement<br />
of DFUs may increase wound healing and closure rates,<br />
which may be in part due to superior overall care provided<br />
to patients. 27<br />
Dressings.<br />
Important wound bed preparation principles are moisture<br />
balance, minimization of inflammation, infection control, and<br />
epithelial edge advancement. The goal is to promote healing<br />
via epidermal migration, angiogenesis, and connective tissue<br />
synthesis. The type of dressing will be dependent on the<br />
wound size, depth, location, the presence of eschar or slough,<br />
the amount of exudates, the wound margins, the need <strong>for</strong> adhesiveness,<br />
concern <strong>for</strong> infection, and con<strong>for</strong>mability. 5 However,<br />
there is not enough evidence to suggest that one dressing is<br />
more effective than another. Currently, no ideal dressing exists<br />
that possesses all properties ideal <strong>for</strong> all wound types. 4<br />
Group Discussion<br />
Standard wound management will succeed in healing<br />
only a percentage of DFUs. Un<strong>for</strong>tunately, optimal standard<br />
wound care is not always provided to all patients due<br />
to poor adherence to guidelines, diminished compliance,<br />
inadequate education of wound care practitioners, lack of<br />
close follow-up, insufficient resources, and other factors. Offloading<br />
is grossly underutilized, which is un<strong>for</strong>tunate given<br />
the strong evidence supporting its role in promoting wound<br />
healing. Practitioners are encouraged to remember that contact-casting<br />
is the most strongly supported by clinical evidence<br />
and is there<strong>for</strong>e considered the “gold standard.”<br />
Close follow-up with weekly reassessment is the standard<br />
of care; un<strong>for</strong>tunately, not all practitioners follow this guideline.<br />
Early, aggressive, and diligent management of DFUs is not<br />
only in the best interest of the patient but is also cost effective<br />
since it potentially prevents costly complications.<br />
Suggested Readings<br />
• Brem H, Sheehan P, Boulton AJM. Protocol <strong>for</strong> treatment of<br />
diabetic foot ulcers. Amer J Surg. 2004;187(suppl):1S-10S.<br />
• Lipsky BA, Berendt AR, Cornia PB, et al. 2012 Infectious<br />
Diseases Society of America clinical practice guideline <strong>for</strong> the<br />
diagnosis and treatment of diabetic foot infections. Clin Infect<br />
Dis. 2012;54(12):e132-173.<br />
• Frykberg RG, Zgonis T, Armstrong DG, et al. Diabetic foot<br />
disorders. A clinical practice guideline (2006 revision). J Foot<br />
Ankle Surg. 2006;45(5 Suppl):S1-66.<br />
• Steed DL, Attinger C, Colaizzi T, et al. Guidelines <strong>for</strong><br />
the treatment of diabetic ulcers. Wound Repair Regen.<br />
2006;14(6):680-692.<br />
• Bakker K, Apelqvist J, Schaper NC; International Working<br />
Group on Diabetic Foot Editorial Board. Practical guidelines<br />
on the management and prevention of the diabetic foot 2011.<br />
Diabetes Metab Res Rev. 2012;28 (suppl 1):225-231.<br />
• Snyder RJ, Kirsner RS, Warriner RA, et al. Consensus recommendations<br />
<strong>for</strong> advancing the standard of care <strong>for</strong> treating<br />
neuropathic foot ulcers in patients with diabetes. Ostomy Wound<br />
Manage. 2010;56(suppl 4):S1-S24.n<br />
12 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
1.6 Evaluating Response to Conventional Therapy<br />
Review of Evidence<br />
Patients with DFUs should be followed closely with weekly<br />
visits. A 2012 study comparing 206 patients with Wagner<br />
grade 1 or 2 DFUs who had weekly vs every-other-week<br />
visits found that weekly follow-up reduced the median time<br />
to wound closure by more than 50% (28 days vs 66 days). 43<br />
Several studies have shown that re-evaluation 4 weeks after<br />
initiation of standard wound healing therapy is clinically<br />
useful. These studies demonstrate that if wound size has not<br />
decreased by at least 50% by the 4th week of treatment, the<br />
likelihood of complete wound healing using the same treatment<br />
approach is very low. 28-30 For example, in a study of 704<br />
patients, only 18% of DFUs that were not healing adequately<br />
at 4 weeks healed at 12 weeks, whereas 58% of DFUs that<br />
were healing adequately at 4 weeks did so. 28 In another study,<br />
patients with DFUs receiving 4 weeks of conventional therapy<br />
whose wounds did not reduce in size by more than 53%<br />
had a decreased likelihood of healing at 12 weeks. 30 In addition<br />
to percent wound size reduction, Robson et al examined<br />
the data from 11 clinical trials and observed that by week<br />
4, the trajectories of the wounds that eventually would heal<br />
versus those that did not heal could be differentiated. 31 The<br />
Standard Therapy of DFU<br />
Reassess DFU within 4 Weeks<br />
• Wound healing trajectory<br />
• % area reduction<br />
Healing<br />
adequately<br />
Not healing<br />
adequately<br />
Follow-up<br />
Address factors<br />
interfering<br />
with healing<br />
• Ulcer infection<br />
• Osteomyelitis<br />
• Ischemia<br />
• Glycemic control<br />
• Inadequate offloading<br />
• Poor nutrition<br />
• Other factors<br />
Complete<br />
closure<br />
Evidence-based<br />
advanced<br />
therapy<br />
Figure 7. Clinical algorithm <strong>for</strong> initial assessment of patients with DFUs.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 13
Wound Healing Society’s guidelines recommend a change in<br />
treatment if wound size reduction is not observed at 4 weeks<br />
of conventional therapy. 16<br />
Group Discussion<br />
The evidence in favor of following DFU patients weekly<br />
is strong. Once the patient with a DFU is started on standard<br />
wound therapies, response to therapy should be re-evaluated<br />
at no later than 4 weeks. It is mandatory to per<strong>for</strong>m serial<br />
wound size measurements in all cases; but in real-world settings<br />
this is not always done. Although a ≥ 50% reduction<br />
in wound size is desirable and moderately predictive of the<br />
likelihood of healing, the overall trajectory of wound healing<br />
is most important. Other factors such as initial size, presence<br />
of infection, and quality of granulation tissue, in addition to<br />
percentage wound size reduction, should be considered in<br />
assessing the overall trajectory of wound healing. A suggested<br />
algorithm <strong>for</strong> follow-up evaluation is shown in Figure 7.<br />
If the clinician assesses that the wound healing trajectory<br />
is inadequate at 4 weeks, reassessment of the wound should<br />
be per<strong>for</strong>med and evidence-based advanced therapy should<br />
be considered. It is also important to note that the trials described<br />
above indicated that a sizeable proportion of patients<br />
(42% in one study 30 ) who are healing adequately at 4 weeks<br />
will ultimately fail to completely heal; these patients will also<br />
require advanced therapy.<br />
Suggested Readings<br />
• Coerper S, Beckert S, Küper MA, Jekov M, Königsrainer<br />
A. Fifty percent area reduction after 4 weeks of treatment<br />
is a reliable indicator <strong>for</strong> healing--analysis of a single-center<br />
cohort of 704 diabetic patients. J Diabetes Complications.<br />
2009;23:49-53.<br />
• Margolis DJ, Hoffstad O, Gelfand JM, Berlin JA. Surrogate<br />
end points <strong>for</strong> the treatment of diabetic neuropathic foot<br />
ulcers. Diabetes Care. 2003;26:1696-1700.<br />
• Sheehan P, Jones P, Casselli A, Giurini JM, Veves A. Percent<br />
change in wound area of diabetic foot ulcers over a 4-week<br />
period is a robust predictor of complete healing in a 12-week<br />
prospective trial. Diabetes Care. 2003;26:1879-1882.<br />
• Robson MC, Hill DP, Woodske ME, Steed DL. Wound healing<br />
trajectories as predictors of effectiveness of therapeutic<br />
agents. Arch Surg. 2000;135(7):773-777. n<br />
14 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
PART 2<br />
Advanced Therapy of DFUs with Apligraf<br />
2.1 Evidence-Based Selection of<br />
Advanced Therapy <strong>for</strong> DFUs<br />
Review of Evidence<br />
In many cases, standard DFU therapy is not sufficient to<br />
heal the wound. The appropriate use of advanced therapies<br />
in chronic, nonhealing wounds, can prevent limb loss,<br />
as well as improve quality of life <strong>for</strong> patients. 4 The use of<br />
advanced therapies is currently included in evidence-based<br />
treatment guidelines and algorithms <strong>for</strong> DFUs. 16<br />
At present there are only three products that are approved<br />
by the FDA <strong>for</strong> treatment of DFUs based on the<br />
results of rigorous clinical studies:<br />
1) Apligraf ® — bilayered (fibroblast/keratinocyte)<br />
cell-based product 32<br />
2) Dermagraft ® — human-fibroblast-derived<br />
dermal substitute 33<br />
3) Regranex ® — platelet-derived growth factor 34<br />
Level 1<br />
RCTs*<br />
Highest Level of Evidence<br />
Level 2<br />
COHORT<br />
StuDies<br />
Level 3<br />
Case-Controlled<br />
Studies<br />
Level 4<br />
Case Series<br />
Level 5<br />
Case Report or<br />
<strong>Expert</strong> Opinion<br />
Lowest Level of Evidence<br />
* RCT = randomized clinical trial<br />
Figure 8. The Centre <strong>for</strong> Evidence-Based Medicine: levels of clinical evidence.<br />
Adapted from Centre <strong>for</strong> Evidence-based Medicine. http://www.cebm.net/index.aspxo=1025. Accessed August 22, 2011.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 15
The FDA differentiates between wound dressings,<br />
which are intended to manage wounds and are classified<br />
as “non-interactive,” and cell-based wound care therapies,<br />
which are intended to heal wounds and are classified as<br />
“interactive.” To gain FDA approval <strong>for</strong> the treatment of<br />
DFUs, each of the above products was evaluated in large<br />
randomized multicenter clinical trials per<strong>for</strong>med in a DFU<br />
patient population.<br />
In contrast, many wound dressings and human tissue<br />
products receive a “510(K) Clearance,” which does not require<br />
clinical data and <strong>for</strong> which even preclinical efficacy<br />
studies are typically not per<strong>for</strong>med. 38<br />
The Centre <strong>for</strong> Evidence-Based Medicine published<br />
a “Levels of Evidence” document to help define a process<br />
<strong>for</strong> determining the value of clinical evidence-based on its<br />
source 35 (Figure 8). This pyramid ranks evidence from the<br />
highest (Level 1: randomized controlled trials) to the lowest<br />
(Level 5: expert opinion or case report). This process provides<br />
a guide to clinicians in their decision making to determine<br />
the merits of published clinical data.<br />
Group Discussion<br />
DFUs are a serious complication of DM associated with<br />
high morbidity, including limb loss and increased risk of mortality.<br />
Practitioners owe it to their patients to utilize the most<br />
proven therapies to maximize the likelihood of achieving successful<br />
healing, thereby potentially preventing additional complications.<br />
This commitment requires using evidence-based<br />
therapies that are supported by the highest level of scientific<br />
evidence, ie, randomized clinical trials. In real-world settings<br />
evidence-based medicine is sometimes delayed or not used as<br />
well as it should be. 39<br />
When a patient with a DFU fails to show wound progression<br />
with standard care (Section 1.6 above Evaluating Response<br />
to Therapy), transition to an evidence-based advanced therapy<br />
is appropriate. Three wound healing products have received<br />
FDA or postmarketing approval by the FDA <strong>for</strong> the treatment<br />
of DFUs: Apligraf, Dermagraft, and Regranex. Discussion of<br />
each of these products is beyond the scope of this paper. The<br />
main point here is that when new wound products become<br />
available, clinicians should inquire what level of clinical evidence<br />
supports their use. In the “hierarchy of scientific evidence,”<br />
randomized clinical trials represent the highest level of<br />
evidence while expert opinion and case reports represent the<br />
lowest level.<br />
Suggested Reading<br />
• Apligraf [prescribing in<strong>for</strong>mation].<br />
Canton MA: Organogenesis Inc; December 2010.<br />
• Dermagraft [prescribing in<strong>for</strong>mation]. Westpoint CT: Advanced<br />
Biohealing;2012.<br />
• Regranex (becaplermin) [prescribing in<strong>for</strong>mation].Fort<br />
Worth, TX: Healthpoint Biotherapeutics; 2012.<br />
• Veves A, Falanga V, Armstrong DG, Sabolinski ML, Apligraf<br />
Diabetic Foot Ulcer Study. Graftskin, a human skin equivalent,<br />
is effective in the management of noninfected neuropathic<br />
diabetic foot ulcers: a prospective randomized multicenter<br />
clinical trial. Diabetes Care. 2001;24(2):290–295.<br />
• Marston WA, Hanft J, Norwood P, Pollak R, Dermagraft<br />
Diabetic Foot Ulcer Study Group. The efficacy and safety<br />
of Dermagraft in improving the healing of chronic diabetic<br />
foot ulcers. Diabetes Care. 2003;26(6):1701–1705.<br />
• Wieman TJ, Smiell JM, Su Y. Efficacy and safety of a topical<br />
gel <strong>for</strong>mulation of recombinant human platelet-derived<br />
growth factor-BB (becaplermin) in patients with chronic<br />
neuropathic diabetic ulcers: a phase III randomized<br />
placebo-controlled double-blind study. Diabetes Care.<br />
1998;21(5):822–827.<br />
• Centre <strong>for</strong> Evidence-based Medicine. http://www.cebm.<br />
net/index.aspxo=1025. Accessed August 22, 2011.<br />
• Maderal AD, Vivas AC, Zwick TG, Kirsner RS. Diabetic foot<br />
ulcers: evaluation and management. Hosp Pract (Minneap).<br />
2012;40(3):102-115. n<br />
16 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
2.2 Apligraf: Efficacy and Proposed Mechanism<br />
Review of Evidence<br />
Apligraf is a bioengineered allogeneic bilayered living-cellbased<br />
product that is FDA-approved <strong>for</strong> treatment of DFUs of<br />
greater than 3 weeks duration. It consists of an epidermal layer<br />
of human keratinocytes overlying a dermal layer of human fibroblasts<br />
in a collagen matrix. Although the precise mechanism<br />
by which Apligraf promotes wound healing is not known, the<br />
mechanism of action is believed to be primarily related to its<br />
ability to modulate the healing response through the delivery of<br />
cytokines and growth factors (Figure 9).<br />
Apligraf was evaluated <strong>for</strong> treatment of DFUs in a randomized<br />
controlled trial by Veves et al 36 in which patients with chronic<br />
neuropathic DFUs (plantar, medial and lateral aspects of the foot)<br />
were randomized to receive up to 5 weekly applications of Apligraf<br />
(n=112) plus standard care or standard care alone (n=96).<br />
Standard care consisted of saline moistened gauze, wound debridement<br />
and offloading. Patients in the Apligraf group had<br />
higher rates of complete healing than those in the control group<br />
by 12 weeks (56% Apligraf, 38% control, P=0.0042). In addition,<br />
the median time to complete closure was reduced in the<br />
Apligraf group (65 days vs 90 days, P=0.0026).<br />
Similar results were observed in a second randomized controlled<br />
trial by Edmonds et al, 37 a multicenter randomized<br />
controlled trial in which patients with DFUs received Apligraf<br />
(n=33) or standard wound care (n=39). While this study was<br />
terminated prematurely <strong>for</strong> non-scientific reasons, at 12 weeks<br />
twice as many Apligraf subjects had achieved complete wound<br />
closure compared to conventional therapy subjects (52% vs 26%,<br />
P=0.049). Rates of adverse events were similar in the Apligraf<br />
and control groups in both of these trials.<br />
Group Discussion<br />
Use of Apligraf as an advanced treatment <strong>for</strong> DFUs is supported<br />
by two randomized clinical trials, which provides a high<br />
level of evidence <strong>for</strong> its use. Overall healing rates and the time<br />
to complete healing were substantially improved compared to<br />
standard wound therapy. From a pathophysiologic standpoint,<br />
this clinical response is understandable since Apligraf provides<br />
the cells (fibroblasts and keratinocytes), growth factors, and cytokines<br />
that are believed to play important roles in wound healing.<br />
Suggested Readings<br />
• Apligraf [prescription in<strong>for</strong>mation]. Canton MA: Organogenesis<br />
Inc; December 2010.<br />
• Veves A, Falanga V, Armstrong DG, Sabolinski ML, Apligraf<br />
Diabetic Foot Ulcer Study. Graftskin, a human skin equivalent, is<br />
effective in the management of noninfected neuropathic diabetic<br />
foot ulcers: a prospective randomized multicenter clinical trial.<br />
Diabetes Care. 2001;24(2):290–295.<br />
• Edmonds M; European and Australian Apligraf Diabetic Foot<br />
Ulcer Study Group. Apligraf in the treatment of neuropathic<br />
diabetic foot ulcers. Int J Low Extrem <strong>Wounds</strong>. 2009;8(1):11-18.<br />
• Kirsner RS. The science of bilayer cell therapy. <strong>Wounds</strong>. 2005<br />
(suppl):6-9. n<br />
Function 1<br />
Angiogenesis<br />
Growth, development,<br />
and differentiation<br />
Inflammation<br />
Proliferation<br />
Growth Factor or<br />
Cytokine*<br />
PDGF-A‡<br />
PDGF-B‡<br />
VEGF‡<br />
IGF-1<br />
IGF-2<br />
TGF-ß1<br />
TGF-ß3<br />
IL-1a‡<br />
IL-6‡<br />
IL-8‡<br />
IL-11‡<br />
FGF-1<br />
FGF-2<br />
FGF-7<br />
TGF-a‡<br />
Human 2<br />
Human 2<br />
Apligraf 2<br />
Keratinocytes † Fibroblasts †<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
3<br />
*As measured by mRNA levels † Cells were grown in monolayer cultures ‡ Cytokines and growth factors were also detected using enzyme-linked immunosorbent assay.<br />
1<br />
Barrientos S, et al. Wound Repair Regen. 2008;16:585-601 2<br />
Brem H, et al. Surg Technol Int. 2003;11:23-31<br />
Figure 9. Growth factors and cytokines identified in human keratinocytes, human fibroblasts, and Apligraf.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 17
2.3 Initiating Apligraf Therapy<br />
Review of Evidence<br />
The technique used to apply various wound therapies, including<br />
Apligraf, varies among different practitioners. However,<br />
since the goal of evidence-based therapy is to replicate<br />
the results of clinical studies in real-world clinical care, below<br />
is a summary of selected study entry criteria and application<br />
techniques employed in the 2 randomized controlled trials<br />
of Apligraf:<br />
Veves et al study (2001). 36 Study patients included patients<br />
with a full-thickness neuropathic DFU on the plantar, lateral<br />
or medial surface of the foot of ≥3 weeks duration and a<br />
post-debridement ulcer size between 1 and 16 cm 2 ; without<br />
signs of clinical infection at the ulcer site or active Charcot’s<br />
disease; and, with a good vascular supply as indicated by an<br />
audible dorsalis pedis and posterior tibialis pulses and ABI<br />
>0.65. The ulcer was debrided and irrigated with saline prior<br />
to initial application of Apligraf, which was placed directly<br />
over the ulcer site. Any excess edge was trimmed to fit the<br />
ulcer. The site was covered with a saline moistened non-adherent<br />
primary dressing (Tegapore) and secured with hypoallergenic<br />
tape. The wound was then covered with a layer of<br />
dry gauze, a layer of petrolatum gauze, and Kling ® .<br />
Edmonds et al study (2009). 37 Study patients had a full-thickness<br />
DFU of at least 4 weeks duration; with a surface area between<br />
1 and 16 cm 2 ; limited to the plantar <strong>for</strong>efoot region;<br />
with no signs of infection; and, with an adequate vascular<br />
supply to the target extremity. All patients received standard<br />
care therapies, including sharp debridement, saline-moistened<br />
dressings, and nonweight-bearing regimen. Apligraf<br />
was applied directly on the ulcer and Mepitel ® , a porous<br />
wound contact layer, was applied as a primary non-adherent<br />
dressing. Secondary dressings were also applied.<br />
Group Discussion<br />
What types of DFUs are appropriate <strong>for</strong> Apligraf Apligraf is<br />
appropriate <strong>for</strong> treatment of neuropathic DFUs, including<br />
large and deep ulcers (partial- and full-thickness ulcers). Ulcers<br />
at any location on the foot—including the plantar surface—are<br />
appropriate <strong>for</strong> Apligraf. Although Charcot disease<br />
was excluded in the clinical trials, with appropriate offloading<br />
this is not a contraindication to treatment with Apligraf.<br />
There is insufficient evidence to make recommendations<br />
regarding the use of Apligraf in patients with exposed bone<br />
or tendon, despite reports of clinical success. Frankly infected<br />
ulcers should not be treated and significant bioburden<br />
reduced, but optimization of granulation should not delay<br />
needed treatment.<br />
How should the wound be prepared Careful and complete<br />
sharp debridement followed by irrigation is essential. This<br />
may provide <strong>for</strong> a healing milieu and reduce bacterial load.<br />
How should Apligraf be applied to the ulcer Apligraf should<br />
be applied directly to the ulcer bed leaving a border (~5<br />
mm) beyond the edge of the ulcer. No evidence exists to<br />
suggest differences in outcomes between different types of<br />
dressings. Detailed directions regarding the application of<br />
Apligraf are beyond the scope of this paper.<br />
What post-Apligraf application measures are recommended<br />
Adhering Apligraf is critical, which is typically achieved<br />
with Steri-Strips TM , but other methods can be utilized. Negative<br />
pressure wound therapy may augment Apligraf wound<br />
bed interaction in highly exudative wounds. It is extremely<br />
important that offloading be continued.<br />
Suggested Readings<br />
•Apligraf [prescription in<strong>for</strong>mation]. Canton MA: Organogenesis<br />
Inc; December 2010.<br />
• Veves A, Falanga V, Armstrong DG, Sabolinski ML, Apligraf<br />
Diabetic Foot Ulcer Study. Graftskin, a human skin equivalent,<br />
is effective in the management of noninfected neuropathic diabetic<br />
foot ulcers: a prospective randomized multicenter clinical<br />
trial. Diabetes Care. 2001;24(2):290–295.<br />
• Zaulyanov L, Kirsner RS. A review of a bi-layered living cell<br />
treatment (Apligraf) in the treatment of venous leg ulcers and<br />
diabetic foot ulcers. Clin Interv Aging. 2007;2(1):93-98.<br />
• Graftskin (Apligraf) in neuropathic diabetic foot ulcers. <strong>Wounds</strong>.<br />
2000;12(5 suppl A):33A-36A.<br />
• Steinberg JS. Putting bilayered cell therapy to use. <strong>Wounds</strong>.<br />
2005 (Suppl):10-14. n<br />
18 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
2.4 Evaluating Response to Apligraf & Reapplications<br />
Review of Evidence<br />
In the randomized controlled trial of Apligraf by Veves et<br />
al, 36 DFU patients in the treatment group could have Apligraf<br />
reapplied at 4 weekly follow-up visits following the initial<br />
application, up to 5 applications. If Apligraf appeared to cover<br />
the wound at these follow-up visits, no reapplication was per<strong>for</strong>med.<br />
The average number of Apligraf applications was 3.9<br />
(range: 1 to 5); 9% of patients required one application, 10%<br />
two applications, 13% three applications, 15% four applications,<br />
and 53% five applications.<br />
In the randomized controlled trial of Apligraf by Edmonds<br />
et al, 37 all patients were followed weekly <strong>for</strong> clinical assessment<br />
of the target ulcer and, if necessary, debridement of the wound.<br />
The Apligraf group could have additional monthly applications<br />
of Apligraf at week 4 and week 8 if the wound was judged to<br />
not be healing, <strong>for</strong> a maximum of 3 applications. In the treatment<br />
group, 13 of the 33 subjects required only 1 application,<br />
15 received 2 applications, and 5 received 3 applications.<br />
There<strong>for</strong>e, in these controlled studies a majority of patients<br />
required multiple applications of Apligraf. This is<br />
consistent with findings from several small studies with different<br />
wound types that showed limited persistence. DNA<br />
evidence of Apligraf was short-lived, typically 3 weeks to 6<br />
weeks after application. 40-42<br />
Reassess<br />
Weekly<br />
Apligraf Application Healing #1<br />
adequately<br />
Application #2<br />
in 1 to 3 weeks<br />
H<br />
E<br />
Application #3<br />
in 1 to 3 weeks<br />
A<br />
Address factors<br />
interfering with healing<br />
No<br />
Wound<br />
healing<br />
progressing<br />
L<br />
• Ulcer infection<br />
• Osteomyelitis<br />
• Ischemia<br />
• Glycemic control<br />
• Inadequate offloading<br />
• Poor nutrition<br />
• Other factors<br />
Factors above<br />
addressed<br />
Yes<br />
Yes<br />
Application #4<br />
in 1 to 3 weeks<br />
Application #5<br />
in 1 to 3 weeks<br />
E<br />
D<br />
Figure 10. Clinical algorithm <strong>for</strong> Apligraf management of patients with DFUs.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 19
Group Discussion<br />
As with standard care of DFUs, patients treated with<br />
Apligraf should continue to be followed up on a weekly<br />
basis. Based on the available data and clinical experience,<br />
dosing of Apligraf should be undertaken as follows (Figure<br />
10): Initial Apligraf application (Apligraf #1) can be<br />
followed by reapplication (Apligraf #2) 1 to 3 weeks later.<br />
After an additional 1 to 3 weeks, Apligraf reapplication can<br />
be considered again (Apligraf #3). Apligrafs #2 and #3 can<br />
be applied even if healing is not progressing because the<br />
trajectory of healing may not become evident during the<br />
initial phase of therapy. However, if after 3 applications the<br />
wound is not progressing, reevaluate the patient <strong>for</strong> factors<br />
that may be interfering with healing, especially ischemia,<br />
ulcer infection, osteomyelitis, inadequate off-loading, poor<br />
nutritional status, and poor glycemic control. If these factors<br />
are under control, the patient should be considered <strong>for</strong><br />
2 additional applications (Apligraf #4 and Apligraf #5) to<br />
maintain the trajectory of healing. If these factors are not<br />
under control, they should be addressed be<strong>for</strong>e proceeding<br />
with additional applications. A maximum of 5 Apligraf applications<br />
is considered one course of therapy. The goal of<br />
treatment is complete closure of the DFU.<br />
Suggested Readings<br />
• Marston WA; Dermagraft Diabetic Foot Ulcer Study<br />
Group. Risk factors associated with healing chronic diabetic<br />
foot ulcers: the importance of hyperglycemia. Ostomy<br />
Wound Manage. 2006;52(3):26-32.<br />
• Apligraf [prescribing in<strong>for</strong>mation]. Canton MA:<br />
Organogenesis Inc; December 2010. n<br />
2.5 Summary<br />
The care of patients with a DFU requires careful attention to critical elements to optimize the potential <strong>for</strong> successful<br />
treatment. Thorough assessment of the patient, especially vascular status and the presence of soft tissue and bone infection,<br />
will lead to accurate staging of patients. Once peripheral arterial disease and infection have been either excluded or<br />
addressed, vigilance in offloading is the most important aspect of standard care. Coupled with debridement and appropriate<br />
dressing selection, conscientious weekly evaluation is recommended. Should a patient fail to improve by 4 weeks<br />
of care, reassessment is warranted as is consideration of advanced therapy.<br />
Three products have received FDA approval <strong>for</strong> the treatment of DFUs that have not responded to conventional therapy,<br />
Apligraf, Dermagraft and Regranex. Apligraf, a bilayered living-cell-based product, is supported by two randomized<br />
clinical trials showing benefit and effectiveness data demonstrating clinical utility. Optimally, wounds should be debrided<br />
and fastidious offloading continued as serial applications every 1 to 3 weeks of Apligraf are applied. If the wound has not<br />
responded after three applications, reassess factors that may be interfering with healing be<strong>for</strong>e proceeding with the two<br />
additional applications.<br />
Patients with DFUs are at risk <strong>for</strong> limb loss and death. The seriousness of this problem cannot be overstated and the<br />
best results are achieved with a thorough evidenced-based process of care. n<br />
20 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
References<br />
1. Singh N, Armstrong DG, Lipsky BA. Preventing<br />
foot ulcers in patients with diabetes. JAMA.<br />
2005;293(2):217-228.<br />
2. American Diabetes Association. Data from the<br />
2011 National Diabetes Fact Sheet (released Jan.<br />
26, 2011). http://www.diabetes.org/diabetes-basics/diabetes-statistics/.<br />
Accessed August 22, 2011.<br />
3. Margolis DJ, Kantor J, Berlin JA. Healing of diabetic<br />
neuropathic foot ulcers receiving standard<br />
treatment. Diabetes Care. 1999;22(5):692-695.<br />
4. Maderal AD, Vivas AC, Zwick TG, Kirsner RS.<br />
Diabetic foot ulcers: evaluation and management.<br />
Hosp Pract (Minneap). 2012;40(3):102-115.<br />
5. Brem H, Young J, Tomic-Canic M, et al. Clinical<br />
efficacy and mechanism of bilayered living human<br />
skin equivalent (HSE) in treatment of diabetic<br />
foot ulcers. Surg Technol Int. 2003;11:23-31.<br />
6. Werner S, Krieg T, Smola H. Keratinocyte–fibroblast<br />
interactions in wound healing. J Invest<br />
Dermatol. 2007;127(5):998-1008.<br />
7. Ghahary A, Ghaffari A. Role of keratinocyte–fibroblast<br />
cross-talk in development of hypertrophic<br />
scar. Wound Repair Regen. 2007;15(suppl<br />
1):S45-S53.<br />
8. Lobmann R, Schultz G, Lehnert H. Proteases<br />
and the diabetic foot syndrome: mechanisms<br />
and therapeutic implications. Diabetes<br />
Care.2005;28(2):461-471.<br />
9. Harding KG, Moore K, Phillips TJ. Wound chronicity<br />
and fibroblast senescence-implications <strong>for</strong><br />
treatment. lnt Wound J. 2005;2(4):364-368.<br />
10. Martin P. Wound healing--aiming <strong>for</strong> perfect skin<br />
regeneration. Science. 1997;276(5309):75-81.<br />
11. Herrick SE, Ireland GW, Simon D, McCollum<br />
CN, Ferguson MW. Venous ulcer fibroblasts compared<br />
with normal fibroblasts show differences<br />
in collagen but not fibronectin production under<br />
both normal and hypoxic conditions. J Invest Dermatol.<br />
1996;106(1):187-193.<br />
12. Vaalamo M, Leiva T, Saarialho-Kere U. Differential<br />
expression of tissue inhibitors of metalloproteinases<br />
(lIMP-I. -2, -l, and -4) in normal and aberrant<br />
wound healing. Hum Pathol. 1999;30(7):795-802.<br />
13. Muller M, Trocme C, Lardy B, et al. Matrix metalloproteinases<br />
and diabetic foot ulcers: the ratio<br />
of MMP-1 and TlMP-1 is a predictor of wound<br />
healing. Diabet Med. 2006;25(4):419-426.<br />
14. Lipsky BA, Berendt AR, Cornia PB, et al. 2012<br />
Infectious Diseases Society of America clinical<br />
practice guideline <strong>for</strong> the diagnosis and treatment<br />
of diabetic foot infections. Clin Infect Dis.<br />
2012;54(12):e132-173.<br />
15. Frykberg RG, Zgonis T, Armstrong DG, et al.<br />
Diabetic foot disorders. A clinical practice guideline<br />
(2006 revision). J Foot Ankle Surg. 2006;45(5<br />
Suppl):S1-66.<br />
16. Steed DL, Attinger C, Colaizzi T, et al. Guidelines<br />
<strong>for</strong> the treatment of diabetic ulcers. Wound Repair<br />
Regen. 2006;14(6):680-692.<br />
17. Bakker K, Apelqvist J, Schaper NC; International<br />
Working Group on Diabetic Foot Editorial Board.<br />
Practical guidelines on the management and prevention<br />
of the diabetic foot 2011. Diabetes Metab<br />
Res Rev. 2012;28 Suppl 1:225-231.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 21
18. Margolis DJ, et al. Risk factors <strong>for</strong> delayed healing<br />
of neuropathic diabetic foot ulcers: a pooled analysis.<br />
Arch Dermatol. 2000;136:1531-1535.<br />
19. Ali R, Qureshi A, Yagoob MY, Shakil M. Total contact<br />
cast <strong>for</strong> neuropathic diabetic foot ulcers. J Coll<br />
Physicians Surg Pak. 2008;18(11):695-698.<br />
20. Hanft JR, Surprenant MS. Is total contact casting<br />
the gold standard <strong>for</strong> the treatment of diabetic foot<br />
ulcerations Abstract presented at American College<br />
of Foot and Ankle Surgeons Joint Annual Meeting<br />
and Scientific Seminar; February 9, 2000; Miami, FL.<br />
21. Faglia E, Caravaggi C, Clerici G, et al. Effectiveness of<br />
removable walker cast versus nonremovable fiberglass<br />
off-bearing cast in the healing of diabetic plantar foot<br />
ulcer: a randomized controlled trial. Diabetes Care.<br />
2010;33(7):1419-1423.<br />
22. Armstrong DG, Short B, Espensen EH, Abu-Rumman<br />
PL, Nixon BP, Boulton AJ. Technique <strong>for</strong> fabrication<br />
of an “instant total-contact cast” <strong>for</strong> treatment<br />
of neuropathic diabetic foot ulcers. J Am Podiatr Med<br />
Assoc. 2002;92(7):405-408.<br />
23. van Deursen R. Footwear <strong>for</strong> the neuropathic patient:<br />
offloading and stability. Diabetes Metab Res Rev.<br />
2008;24(suppl 1):S96-100.<br />
24. The effect of intensive treatment of diabetes on the<br />
development and progression of long-term complications<br />
in insulin-dependent diabetes mellitus: the<br />
Diabetes Control and Complications Trial Research<br />
Group. N Engl J Med. 1993;329(14):977-986.<br />
25. Steed DL, Donohoe D, Webster MW, Lindsley L.<br />
Effect of extensive debridement and treatment on the<br />
healing of diabetic foot ulcers. Diabetic Ulcer Study<br />
Group. J Am Coll Surg. 1996;183(1):61-64.<br />
26. Saap LJ, Falanga V. Debridement per<strong>for</strong>mance<br />
index and its correlation with complete closure<br />
of diabetic foot ulcers. Wound Repair Regen.<br />
2002;10(6):354-359.<br />
27. Cardinal M, Eisenbud DE, Armstrong DG, et al.<br />
Serial surgical debridement: a retrospective study<br />
on clinical outcomes in chronic lower extremity<br />
wounds. Wound Repair Regen. 2009;17(3):306-311.<br />
28. Coerper S, Beckert S, Küper MA, Jekov M, Königsrainer<br />
A. Fifty percent area reduction after 4 weeks<br />
of treatment is a reliable indicator <strong>for</strong> healing--analysis<br />
of a single-center cohort of 704 diabetic patients.<br />
J Diabetes Complications. 2009;23:49-53.<br />
29. Margolis DJ, Hoffstad O, Gelfand JM, Berlin JA.<br />
Surrogate end points <strong>for</strong> the treatment of diabetic<br />
neuropathic foot ulcers. Diabetes Care.<br />
2003;26:1696-1700.<br />
30. Sheehan P, Jones P, Casselli A, Giurini JM, Veves<br />
A. Percent change in wound area of diabetic foot<br />
ulcers over a 4-week period is a robust predictor<br />
of complete healing in a 12-week prospective trial.<br />
Diabetes Care. 2003;26:1879-1882.<br />
31. Robson MC, Hill DP, Woodske ME, Steed DL.<br />
Wound healing trajectories as predictors of effectiveness<br />
of therapeutic agents. 2000;135(7):773-777.<br />
32. Apligraf [prescription in<strong>for</strong>mation]. Canton MA:<br />
Organogenesis Inc; December 2010.<br />
33. Dermagraft [prescription in<strong>for</strong>mation]. Westpoint<br />
CT: Advanced Biohealing; 2012.<br />
34. Regranex (becaplermin) [prescription in<strong>for</strong>mation].<br />
Fort Worth, TX: Healthpoint Biotherapeutics; 2012.<br />
35. Centre <strong>for</strong> Evidence-based Medicine. http://<br />
www.cebm.net/index.aspxo=1025. Accessed<br />
August 22, 2011.<br />
36. Veves A, Falanga V, Armstrong DG, Sabolinski ML,<br />
Apligraf Diabetic Foot Ulcer Study. Graftskin, a<br />
human skin equivalent, is effective in the management<br />
of noninfected neuropathic diabetic foot ulcers:<br />
a prospective randomized multicenter clinical<br />
trial. Diabetes Care. 2001;24(2):290-295.<br />
22 <strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers
37. Edmonds M; European and Australian Apligraf<br />
Diabetic Foot Ulcer Study Group. Apligraf in the<br />
treatment of neuropathic diabetic foot ulcers. Int J<br />
Low Extrem <strong>Wounds</strong>. 2009;8(1):11-18.<br />
38. Maderal AD, Vivas AC, Eaglstein WH, Kirsner RS.<br />
The FDA and designing clinical trials <strong>for</strong> chronic<br />
cutaneous ulcers. Semin Cell Dev Biol. 2012 Oct 9.<br />
doi:pii: S1084-9521(12)00179-6. 10.1016/j.semcdb.2012.09.014.<br />
[Epub ahead of print]<br />
39. Kirsner RS, Warriner R, Michela M, Stasik L, Freeman<br />
K. Advanced biological therapies <strong>for</strong> diabetic<br />
foot ulcers. Arch Dermatol. 2010 Aug;146(8):857-862.<br />
41. Griffiths M, Ojeh N, Livingstone R, Price R,<br />
Navsaria H. Survival of Apligraf in acute human<br />
wounds. Tissue Eng. 2004;10:1180-1195.<br />
42. Hu S, Kirsner RS, Falanga V, Phillips T, Eaglstein<br />
WH. Evaluation of Apligraf persistence and basement<br />
membrane restoration in donor site wounds: a pilot<br />
study. Wound Repair Regen. 2006;14:427-433.<br />
43. Warriner RA, Wilcox JR, Carter MJ, Stewart DG.<br />
More Frequent Visits to Wound Care Clinics Result<br />
in Faster Times to Close Diabetic Foot and Venous<br />
Leg Ulcers. Adv Skin Wound Care. 2012;25:494-501.<br />
40. Falabella AF, Valencia IC, Eaglstein WH, Schachner<br />
LA. Tissue-engineered skin (Apligraf) in the healing<br />
of patients with epidermolysis bullosa wounds. Arch<br />
Dermatol. 2000;136:1225-1230.<br />
<strong>Expert</strong> <strong>Recommendations</strong> <strong>for</strong> <strong>Optimizing</strong> <strong>Outcomes</strong> Utilizing Apligraf ® <strong>for</strong> Diabetic Foot Ulcers 23
TM<br />
, LLC<br />
©2012 HMP Communications, LLC (HMP). All rights reserved. Reproduction in whole or in part prohibited.<br />
www.hmpcommunications.com<br />
130-218