Why do we need to measure more than central ... - AtCor Medical
Why do we need to measure more than central ... - AtCor Medical
Why do we need to measure more than central ... - AtCor Medical
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Why</strong> <strong>do</strong> <strong>we</strong> <strong>need</strong> <strong>to</strong> <strong>measure</strong> <strong>more</strong> <strong>than</strong> <strong>central</strong> blood pressure alone<br />
While the prognostic value of brachial blood pressure is <strong>we</strong>ll established, there is now ample evidence of<br />
the pathophysiological importance of <strong>central</strong> haemodynamic <strong>measure</strong>ments. Central (aortic) sys<strong>to</strong>lic and<br />
dias<strong>to</strong>lic pressures are determinants of cardiac loading and coronary perfusion and are significant in<br />
identifying and understanding the development of cardiovascular disease.<br />
Central blood pressure and <strong>measure</strong>ments taken from the <strong>central</strong> arterial pulse wave have been shown <strong>to</strong><br />
be po<strong>we</strong>rful predic<strong>to</strong>rs of major cardiovascular events, independent of the traditional risk fac<strong>to</strong>rs, including<br />
brachial blood pressure. Further<strong>more</strong>, they are important markers for evaluating the effect of treatment.<br />
THE European Society of Hypertension 1 , as <strong>we</strong>ll as leading clinicians and researchers have recognized the<br />
importance of these values, specifically <strong>central</strong> SBP, PP and Aix. These <strong>measure</strong>s of arterial wave reflection<br />
indices and <strong>central</strong> pressure (along with aortic PWV) provide a comprehensive and integrated approach <strong>to</strong><br />
<strong>to</strong>tal cardiovascular assessment of a patient [1, 2, 3, 4, 5].<br />
PWA and <strong>central</strong> blood pressure<br />
In healthy and compliant arteries the pressure waves (generated by the left ventricle) travel through the<br />
arterial tree and are reflected at multiple peripheral sites. As a result, the arterial pressure waveform at any<br />
site is a combination of the forward travelling waveform and the backward (or reflection) waveform. The<br />
two waveforms merge during dias<strong>to</strong>le and augment coronary perfusion. With ageing, the arterial wall<br />
thickens and the arteries get stiffer resulting in the pressure waves travelling faster and the reflected<br />
pressure wave returning during the sys<strong>to</strong>lic phase. This increases aortic sys<strong>to</strong>lic pressure, widens pulse<br />
pressure and increases left ventricular load [6].<br />
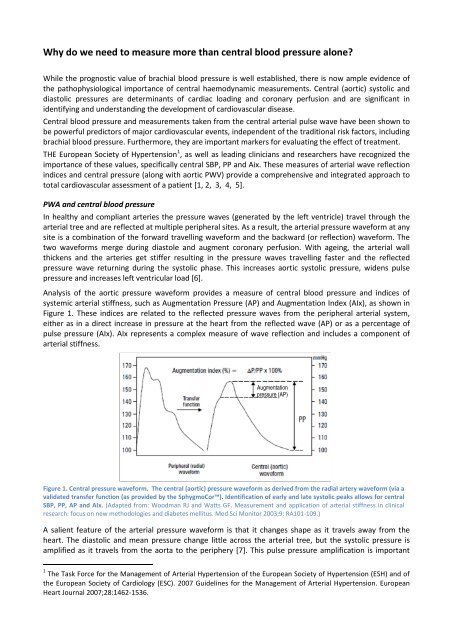
Analysis of the aortic pressure waveform provides a <strong>measure</strong> of <strong>central</strong> blood pressure and indices of<br />
systemic arterial stiffness, such as Augmentation Pressure (AP) and Augmentation Index (AIx), as shown in<br />
Figure 1. These indices are related <strong>to</strong> the reflected pressure waves from the peripheral arterial system,<br />
either as in a direct increase in pressure at the heart from the reflected wave (AP) or as a percentage of<br />
pulse pressure (AIx). AIx represents a complex <strong>measure</strong> of wave reflection and includes a component of<br />
arterial stiffness.<br />
Augmentation<br />
pressure (AP)<br />
Figure 1. Central pressure waveform. The <strong>central</strong> (aortic) pressure waveform as derived from the radial artery waveform (via a<br />
validated transfer function (as provided by the SphygmoCor). Identification of early and late sys<strong>to</strong>lic peaks allows for <strong>central</strong><br />
SBP, PP, AP and AIx. (Adapted from: Woodman RJ and Watts GF. Measurement and application of arterial stiffness in clinical<br />
research: focus on new metho<strong>do</strong>logies and diabetes mellitus. Med Sci Moni<strong>to</strong>r 2003;9: RA101-109.)<br />
A salient feature of the arterial pressure waveform is that it changes shape as it travels away from the<br />
heart. The dias<strong>to</strong>lic and mean pressure change little across the arterial tree, but the sys<strong>to</strong>lic pressure is<br />
amplified as it travels from the aorta <strong>to</strong> the periphery [7]. This pulse pressure amplification is important<br />
1 The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of<br />
the European Society of Cardiology (ESC). 2007 Guidelines for the Management of Arterial Hypertension. European<br />
Heart Journal 2007;28:1462-1536.
when considering the relationship bet<strong>we</strong>en brachial and <strong>central</strong> blood pressure as the pulsatile<br />
components may vary significantly. This was demonstrated in the Anglo-Cardiff Collaborative Trial II where<br />
data from 10,600 individuals sho<strong>we</strong>d that <strong>central</strong> pressure cannot be reliably inferred from peripheral<br />
pressure due <strong>to</strong> the variation in the gradient bet<strong>we</strong>en <strong>central</strong> and peripheral pressures [8].<br />
The most widely used device in clinical studies for PWA, the SphygmoCor, <strong>measure</strong>s the arterial pressure<br />
waveform at the radial artery and applies a validated generalised transfer function <strong>to</strong> provide the <strong>central</strong><br />
pressure waveform [2, 9, 10]. Along with <strong>central</strong> sys<strong>to</strong>lic blood pressure, a number of PWA indices provided<br />
have been shown <strong>to</strong> have clinical relevance.<br />
Predic<strong>to</strong>rs of disease and events<br />
Central blood pressure and AIx have been shown <strong>to</strong> be a significant predic<strong>to</strong>r of all-cause mortality and or<br />
major cardiovascular events in observational studies and over a range of diseases, such as coronary artery<br />
disease, end stage renal disease and diabetes as <strong>we</strong>ll as in the elderly [11, 12, 13, 14, 15, 16, 17, 18, 19, 20,<br />
21, 22]. Moreover, these <strong>measure</strong>ments have been shown <strong>to</strong> be independent of brachial blood pressure.<br />
Pulse pressure (PP), and in particular <strong>central</strong> PP have been shown <strong>to</strong> better predict cardiovascular events<br />
<strong>than</strong> brachial blood pressure [11]. Data from the Strong Heart Study 2 found that <strong>central</strong> pulse pressure<br />
predicted cardiovascular events <strong>more</strong> strongly <strong>than</strong> brachial pulse pressure, independently of traditional<br />
risk fac<strong>to</strong>rs, such as age, smoking, gender and cholesterol [11]. Further<strong>more</strong>, data from the same study<br />
sho<strong>we</strong>d in a 5-year follow-up that quartiles of <strong>central</strong> PP predicted cardiovascular outcomes <strong>more</strong> strongly<br />
<strong>than</strong> quartiles of brachial PP. Having a <strong>central</strong> PP, ≥ 50 mmHg, <strong>do</strong>ubled the risk of heart attack or stroke in<br />
both men and women, in the presence or absence of diabetes, and in people younger or older <strong>than</strong> 60<br />
years of age [12], as shown in Figure 2 .<br />
Figure 2 Quartiles of <strong>central</strong> pressure plotted against events rate for incident cardiovascular events in<br />
individuals from the STRONG heart study. The event rate in Q4 ≥ 50mmHg exceeded 20% compared <strong>to</strong> 10% in<br />
Q1 and Q2 * No significant difference bet<strong>we</strong>en Q1, Q2 and Q3 . ** Significant compared <strong>to</strong> Q1. (Data from:<br />
Roman MJ, Devereux RB, Kizer JR, et al. High <strong>central</strong> pulse pressure is independently associated with adverse<br />
cardiovascular outcome the strong heart study. J Am Coll Cardiol 27-10-2009,54:1730-1734.<br />
Central pressure has also been shown <strong>to</strong> be <strong>more</strong> closely related <strong>to</strong> other important cardiovascular<br />
intermediate endpoints such as left ventricular hypertrophy (LVH). LVH is commonly seen in hypertension<br />
and increases the risk for cardiac events, mostly as a result of increased left ventricular mass due <strong>to</strong> an<br />
increase in afterload of the left ventricle [23]. Recent work from the Strong Heart Study has shown that<br />
<strong>central</strong> sys<strong>to</strong>lic pressure has a has a stronger association with LVH <strong>than</strong> brachial or pulse pressure [24, 25].<br />
Central AIx has also been shown <strong>to</strong> have a significant correlation with LVH, as seen in end stage renal<br />
patients [26]. In a group of renal patients on haemodialysis, an increased AIx was associated with the<br />
development of LVH, independent of other fac<strong>to</strong>rs known <strong>to</strong> influence cardiac structure in ESRD patients,<br />
as shown in Figure 3. Further<strong>more</strong>, AIx is a strong independent predic<strong>to</strong>r of cardiovascular (and all-cause)<br />
mortality in end stage renal failure. For each 10% increase in AIx, the risk of cardiovascular events or allcause<br />
mortality increases by approximately 50% (RR of 1.51 and 1.48, respectively) [20].<br />
2 The Strong Heart Study is an observational study of prevalent and incident cardiovascular disease and their risk fac<strong>to</strong>rs in<br />
American Indians.
Figure 3 A scatterplot showing the correlation bet<strong>we</strong>en AIx and left ventricular mass index in end-stage renal disease<br />
patients. From: Marchais SJ, Guerin AP, Pannier BM, et al. Wave reflections and cardiac hypertrophy in chronic uremia.<br />
Influence of body size. Hypertension 1993,22:876-883.<br />
Similarly, <strong>central</strong> AIx has been shown <strong>to</strong> be an independent predic<strong>to</strong>r of severe cardiovascular events in<br />
patients with coronary artery disease [17, 18] and even in males in the general population without a his<strong>to</strong>ry<br />
of cardiovascular disease [13].<br />
A recent systematic review of pooled data of over 5500 patients confers that <strong>central</strong> AIx is predictive of<br />
cardiovascular events and all cause mortality in a range of populations [3]. For an absolute increase in AIx<br />
of 10% the risk for cardiovascular events increased by 31.8% and the risk for all cause mortality increased<br />
by 38.4%.<br />
The ability <strong>to</strong> <strong>measure</strong> <strong>central</strong> blood pressure and indices of wave reflection, such as AIx contributes<br />
valuable information on the cardiovascular risk of a patient.<br />
Precursor <strong>to</strong> hypertension<br />
Recent findings from a large a comprehensive longitudinal study have found that <strong>central</strong> AIx and forward<br />
wave amplitude are related <strong>to</strong> future sys<strong>to</strong>lic blood pressure, PP and incident hypertension. The<br />
community-based study of around 1700 normotensive participants (from the Framingham Offspring<br />
cohort 3 ) examined over a 7-year period sho<strong>we</strong>d that an increase in arterial stiffness was predictive of<br />
developing hypertension [27]. Treatments targeting arterial stiffness and function may play a significant<br />
role in prevention of incident hypertension. Arterial stiffness, as <strong>measure</strong>d by Aix, may become a treatment<br />
target in the future.<br />
Response <strong>to</strong> treatment<br />
Over the last decade there has been an increasing awareness that beneficial effect of pharmacological<br />
therapies beyond brachial blood pressure. As such, it is considered that the additional effects<br />
antihypertensive drugs have on <strong>central</strong> haemodynamics is associated with their ability <strong>to</strong> modify arterial<br />
properties, such as stiffness of large vessels (via pulse wave velocity) and pressure wave reflections via AIx.<br />
Although the current antihypertensive drugs have not been specifically designed <strong>to</strong> lo<strong>we</strong>r arterial stiffness,<br />
it is possible <strong>to</strong> assess the effect they have had either directly or indirectly on these arterial properties.<br />
In the largest prospective evaluation of cardiovascular drugs on <strong>central</strong> blood pressure and haemodynamics<br />
<strong>to</strong> date, the CAFÉ study 4 , differential effects of treatment can be seen in <strong>central</strong> blood pressure despite a<br />
3 The Framingham Heart study has follo<strong>we</strong>d three generation of participants since 1948 <strong>to</strong> identify common fac<strong>to</strong>rs or<br />
characteristics that contribute <strong>to</strong> cardiovascular disease. The Original Cohort consisted of 5209 participants aged 30-<br />
62 years. In 1971 the Offspring Cohort Study commenced and included 5124 men and women consisting of offspring<br />
from the Original Cohort and their spouses. Participants have undergone cardiovascular examinations every 4-6 years<br />
and PWA and PWV <strong>measure</strong>ments have been included since cycle 7 (1998-2001).<br />
4 CAFÉ study – Conduit Artery Function Evaluation study was a makor sub-study within the Anglo-Scandinavian Cardiac<br />
Outcome Trial (ASCOT) conducted across 5 centres in the UK and Ireland. Over 2000 patients with either untreated or
similar effect on brachial blood pressure. The improvement in <strong>central</strong> sys<strong>to</strong>lic and pulse pressures following<br />
amlodipine/perin<strong>do</strong>pril therapy are considered <strong>to</strong> have played a role in the superior cardiovascular<br />
outcomes observed in the larger ASCOT trial and would not have been detected if only brachial blood<br />
pressure was <strong>measure</strong>d [28].<br />
In a similar study of high risk patients with essential hypertension that extended over 12 months (REASON 5<br />
trial) brachial and <strong>central</strong> SBP, PP and AIx <strong>we</strong>re all significantly lo<strong>we</strong>r in patients on combination therapy<br />
(perin<strong>do</strong>pril/indapamide), with <strong>central</strong> changes being <strong>more</strong> pronounced <strong>than</strong> brachial changes [29]. These<br />
results are consistent with a number of smaller short term studies in hypertension [30, 31, 32, 33, 34, 35,<br />
36, 37].<br />
A recent study has also shown that an individual class of hypertensive drug should not be considered as a<br />
homogenous group and differences in hemo<strong>do</strong>dynamics can be observed. In this study, a relatively new<br />
beta blocker, Nebivolol, which is considered <strong>to</strong> have ancillary vasodila<strong>to</strong>ry properties, provided a<br />
significantly greater reduction in <strong>central</strong> PP, AIx and PP amplification compared with atenolol, a standard<br />
beta blocker, in patients with essential hypertension [32].<br />
Atenolol has also been shown <strong>to</strong> significantly increase <strong>central</strong> AIx, while still being able <strong>to</strong> reduce both<br />
brachial and <strong>central</strong> SBP.<br />
These studies highlight the importance of measuring <strong>central</strong> haemodynamic <strong>measure</strong>s including Aix and<br />
<strong>central</strong> pulse pressure in patient treatment. This may help <strong>to</strong> explain why some drugs with a similar effect<br />
on brachial pressure but a different affect on <strong>central</strong> blood pressure and significantly different<br />
cardiovascular outcomes.<br />
Perspective<br />
Central arterial blood pressure and <strong>measure</strong>s of arterial stiffness and wave reflection are important<br />
<strong>measure</strong>s for assessment of cardiovascular risk and evaluation of treatment. Central SBP, PP and AIx have<br />
all been shown <strong>to</strong> be po<strong>we</strong>rful predic<strong>to</strong>rs of major cardiovascular events across a range of diseases. Central<br />
SBP has consistently been shown <strong>to</strong> be better <strong>than</strong> brachial blood pressure in the determination of<br />
cardiovascular risk and the <strong>measure</strong>ment of <strong>central</strong> PP, AP and AIx provide additional information on the<br />
arterial stiffness of a patient, known <strong>to</strong> be a risk fac<strong>to</strong>r for the development of hypertension. As a result, all<br />
of these <strong>measure</strong>ments should be <strong>measure</strong>d and taken <strong>to</strong>gether <strong>to</strong> develop an accurate assessment of the<br />
patient’s cardiovascular risk. These <strong>measure</strong>ments have also become significant markers in the evaluation<br />
of, as <strong>we</strong>ll as potential targets for treatment.<br />
When selecting a device <strong>to</strong> <strong>measure</strong> arterial stiffness, it is imperative that the device <strong>measure</strong>s <strong>central</strong> SBP<br />
as <strong>we</strong>ll as <strong>central</strong> PP, AP and AIx using validated methods. The SphygmoCor device is the most widely used<br />
device in clinical trials and provides this information easily using gold standard techniques.<br />
References<br />
1. Mancia G, De BG, Dominiczak A, et al. 2007 Guidelines for the Management of Arterial Hypertension:<br />
The Task Force for the Management of Arterial Hypertension of the European Society of<br />
Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007,25:1105-1187.<br />
2. Agabiti-Rosei E, Mancia G, O'Rourke MF, et al. Central blood pressure <strong>measure</strong>ments and<br />
antihypertensive therapy: a consensus <strong>do</strong>cument. Hypertension 2007,50:154-160.<br />
treated hypertension participated in the study for up <strong>to</strong> 4 years, during which time multiple blood pressure<br />
<strong>measure</strong>ments <strong>we</strong>re made.<br />
5 REASON project – pREterax in regression of Arterial Stiffness in a controlled <strong>do</strong>uble blind study was a multicentre<br />
trial conducted across 13 countries.
3. Vlachopoulos C, Aznaouridis K, O'Rourke MF, et al. Prediction of cardiovascular events and all-cause<br />
mortality with <strong>central</strong> haemodynamics: a systematic review and meta-analysis. Eur Heart J<br />
2010,31:1865-1871.<br />
4. Lon<strong>do</strong>n GM and Pannier B. Arterial functions: how <strong>to</strong> interpret the complex physiology. Nephrol Dial<br />
Transplant 2010,25:3815-3823.<br />
5. Gurovich AN and Braith RW. Pulse wave analysis and pulse wave velocity techniques: are they ready<br />
for the clinic Hypertens Res 2011,34:166-169.<br />
6. McDonald's Blood Flow in Arteries. Theoretcial, experimental and clinical principles. 5th edition<br />
Hodder Arnold Lon<strong>do</strong>n 2005 370-373.<br />
7. Nichols WW and O'Rourke MF. McDonald's Blood Flow in Arteries. 5th Edition.2005,49-65.<br />
8. McEniery CM, Yasmin, McDonnell B, et al. Central pressure: variability and impact of cardiovascular<br />
risk fac<strong>to</strong>rs: the Anglo-Cardiff Collaborative Trial II. Hypertension 2008,51:1476-1482.<br />
9. Gurovich AN and Braith RW. Pulse wave analysis and pulse wave velocity techniques: are they ready<br />
for the clinic Hypertens Res 2011,34:166-169.<br />
10. Lon<strong>do</strong>n GM and Pannier B. Arterial functions: how <strong>to</strong> interpret the complex physiology. Nephrol Dial<br />
Transplant 2010,25:3815-3823.<br />
11. Roman MJ, Devereux RB, Kizer JR, et al. Central pressure <strong>more</strong> strongly relates <strong>to</strong> vascular disease<br />
and outcome <strong>than</strong> <strong>do</strong>es brachial pressure: the Strong Heart Study. Hypertension 2007,50:197-203.<br />
12. Roman MJ, Devereux RB, Kizer JR, et al. High <strong>central</strong> pulse pressure is independently associated with<br />
adverse cardiovascular outcome the strong heart study. J Am Coll Cardiol 27-10-2009,54:1730-1734.<br />
13. Janner JH, Godtfredsen NS, Ladelund S, et al. High aortic augmentation index predicts mortality and<br />
cardiovascular events in men from a general population, but not in women. Eur J Prev Cardiol 30-5-<br />
2012,Epub ahead of print:<br />
14. Jankowski P, Ka<strong>we</strong>cka-Jaszcz K, Czarnecka D, et al. Pulsatile but not steady component of blood<br />
pressure predicts cardiovascular events in coronary patients. Hypertension 2008,51:848-855.<br />
15. Danchin N, Bene<strong>to</strong>s A, Lopez-Sublet M, et al. Aortic pulse pressure is related <strong>to</strong> the presence and<br />
extent of coronary artery disease in men undergoing diagnostic coronary angiography: a multicenter<br />
study. Am J Hypertens 2004,17:129-133.<br />
16. Weber T, Auer J, O'Rourke MF, et al. Arterial stiffness, wave reflections, and the risk of coronary<br />
artery disease. Circulation 20-1-2004,109:184-189.<br />
17. Weber T, Auer J, O'Rourke MF, et al. Increased arterial wave reflections predict severe cardiovascular<br />
events in patients undergoing percutaneous coronary interventions. Eur Heart J 2005,26:2657-2663.<br />
18. Weber T, O'Rourke MF, Lassnig E, et al. Pulse waveform characteristics predict cardiovascular events<br />
and mortality in patients undergoing coronary angiography. J Hypertens 2010,28:797-805.
19. Cohen DL and Townsend RR. Central blood pressure and chronic kidney disease progression. Int J<br />
Nephrol 2011,2011:407801<br />
20. Lon<strong>do</strong>n GM, Blacher J, Pannier B, et al. Arterial wave reflections and survival in end-stage renal<br />
failure. Hypertension 2001,38:434-438.<br />
21. Schram MT, Kostense PJ, van Dijk RA, et al. Diabetes, pulse pressure and cardiovascular mortality: the<br />
Hoorn Study. J Hypertens 2002,20:1743-1751.<br />
22. Pini R, Cavallini MC, Palmieri V, et al. Central but not brachial blood pressure predicts cardiovascular<br />
events in an unselected geriatric population: the ICARe Dicomano Study. J Am Coll Cardiol 24-6-<br />
2008,51:2432-2439.<br />
23. Kaplan NM and Douglas PS. Clinical implications and treatment of left ventricular hypertrophy in<br />
hypertension.2011,<br />
24. Roman MJ, Okin PM, Kizer JR, et al. Relations of <strong>central</strong> and brachial blood pressure <strong>to</strong> left ventricular<br />
hypertrophy and geometry: the Strong Heart Study. J Hypertens 2010,28:384-388.<br />
25. Wohlfahrt P, Wichterle D, Seidlerova J, et al. Relation of <strong>central</strong> and brachial blood pressure <strong>to</strong> left<br />
ventricular hypertrophy. The Czech Post-MONICA Study. J Hum Hypertens 25-8-2011,<br />
26. Marchais SJ, Guerin AP, Pannier BM, et al. Wave reflections and cardiac hypertrophy in chronic<br />
uremia. Influence of body size. Hypertension 1993,22:876-883.<br />
27. Kaess BM, Rong J, Larson MG, et al. Aortic stiffness, blood pressure progression, and incident<br />
hypertension. JAMA 5-9-2012,308:875-881.<br />
28. Williams B, Lacy PS, Thom SM, et al. Differential impact of blood pressure-lo<strong>we</strong>ring drugs on <strong>central</strong><br />
aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation<br />
(CAFE) study. Circulation 7-3-2006,113:1213-1225.<br />
29. Asmar RG, Lon<strong>do</strong>n GM, O'Rourke ME and Safar ME. Improvement in blood pressure, arterial stiffness<br />
and wave reflections with a very-low-<strong>do</strong>se perin<strong>do</strong>pril/indapamide combination in hypertensive<br />
patient: a comparison with atenolol. Hypertension 2001,38:922-926.<br />
30. Mackenzie IS, McEniery CM, Dhakam Z, et al. Comparison of the effects of antihypertensive agents on<br />
<strong>central</strong> blood pressure and arterial stiffness in isolated sys<strong>to</strong>lic hypertension. Hypertension<br />
2009,54:409-413.<br />
31. Mackenzie IS, Wilkinson IB and Cockcroft JR. Assessment of arterial stiffness in clinical practice. QJM<br />
2002,95:67-74.<br />
32. Mahmud A and Feely J. Beta-blockers reduce aortic stiffness in hypertension but nebivolol, not<br />
atenolol, reduces wave reflection. Am J Hypertens 2008,21:663-667.<br />
33. Schneider MP, Delles C, Klingbeil AU, et al. Effect of angiotensin recep<strong>to</strong>r blockade on <strong>central</strong><br />
haemodynamics in essential hypertension: results of a ran<strong>do</strong>mised trial. J Renin Angiotensin<br />
Al<strong>do</strong>sterone Syst 2008,9:49-56.
34. Dhakam Z, McEniery CM, Yasmin, et al. Atenolol and eprosartan: differential effects on <strong>central</strong> blood<br />
pressure and aortic pulse wave velocity. Am J Hypertens 2006,19:214-219.<br />
35. Matsui Y, Eguchi K, O'Rourke MF, et al. Differential Effects Bet<strong>we</strong>en a Calcium Channel Blocker and a<br />
Diuretic When Used in Combination With Angiotensin II Recep<strong>to</strong>r Blocker on Central Aortic Pressure<br />
in Hypertensive Patients. Hypertension 10-8-2009,54:716-723.<br />
36. Jiang XJ, O'Rourke MF, Zhang YQ, et al. Superior effect of an angiotensin-converting enzyme inhibi<strong>to</strong>r<br />
over a diuretic for reducing aortic sys<strong>to</strong>lic pressure. J Hypertens 2007,25:1095-1099.<br />
37. Morgan T, Lauri J, Bertram D and Anderson A. Effect of different antihypertensive drug classes on<br />
<strong>central</strong> aortic pressure. Am J Hypertens 2004,17:118-123.<br />
Note alternative picture <strong>to</strong> Figure 1.<br />
From: Janner,J.H.; Godtfredsen,N.S.; Ladelund,S.; Vestbo,J.; Prescott,E. Aortic augmentation index:<br />
reference values in a large unselected population by means of the SphygmoCor device. Am.J Hypertens.<br />
2010;23:180-185