136 - American Neurological Association
136 - American Neurological Association
136 - American Neurological Association
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>136</strong>th Annual Meeting of the<br />
<strong>American</strong> <strong>Neurological</strong> <strong>Association</strong><br />
September 25–27, 2011<br />
Manchester Grand Hyatt, San Diego, CA<br />
Poster Listings<br />
Derek Denny-Brown New Member<br />
Symposium Abstracts 1–3<br />
Poster Session Abstracts 4–18<br />
Works in Progress Abstracts 19–21<br />
Career Development Abstracts 22<br />
Author Index 112–123<br />
Subject Index 124–126
BLANK PAGE
J_ID: ANA Customer A_ID: SUPP11-2 Cadmus Art: 22574 Date: 31-August-11 Stage: Page: 1<br />
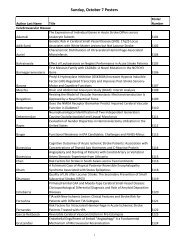
Poster Listings<br />
Sunday, September 25, 2011<br />
Topic Posters Poster Listing Pages Abstract Pages<br />
Cerebrovascular Disease 101–144 3–5; 19 23–32; 99–100<br />
Movement Disorders 201–240 5–7; 19 32–41; 100–101<br />
Sleep Disorders and Circadian Rhythm 301–303 7 42<br />
Education 401–408 7–8 42–44<br />
Career Development 515–531 22 111<br />
Monday, September 26, 2011<br />
Topic Posters Poster Listing Pages Abstract Pages<br />
Behavioral Neurology 601–622 8–9; 19 44–49; 102<br />
Epilepsy 701–732 9–10; 19–20 49–55; 102–104<br />
Neuromuscular Disease 801–841 10–11; 20 55–63; 104–105<br />
Neurogenetics 1001–1013 11–12; 20 63–65; 105–106<br />
Trauma/Injury 1101–1107 12 65–66<br />
Neurology Critical Care 1201–1206 12; 20 66–67; 106<br />
Pediatric Neurology 1301–1304 12–13 67–68<br />
Rehabilitation and Regeneration 1401–1403 13 68–69<br />
Tuesday, September 27, 2011<br />
Topic Posters Poster Listing Pages Abstract Pages<br />
Dementia and Aging 1501–1542 13–15; 20 69–79; 107–108<br />
Headache and Pain 1601–1623 15–16; 21 79–84; 108<br />
Neuroimmunology and Demyelinating Disease 1701–1747 16–28; 21 84–94; 108–110<br />
Neurooncology 1801–1809 18 94–96<br />
Neurovirology 1901–1908 18 96–98<br />
ID: senthilk I Black Lining: [ON] I Time: 07:59 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110240/APPFile/JW-ANA#110240<br />
Poster Listings
BLANK PAGE
J_ID: ZAY Customer A_ID: SUPP11-1 Cadmus Art: 22576 Date: 31-August-11 Stage: Page: 1<br />
<strong>136</strong> th Annual Meeting Tuesday,<br />
September 27, 2011 Derek<br />
Denny-Brown New Member<br />
Symposium Abstracts<br />
Derek Denny-Brown <strong>Neurological</strong> Scholar Award: Can<br />
We Detect Alzheimer’s Disease a Decade Before<br />
Dementia, and Why Would We Want To?<br />
Reisa Sperling, M.D. Center for Alzheimer Research and<br />
Treatment, Brigham and Women’s Hospital, Massachusetts<br />
General Hospital, Harvard Medical School<br />
The pathophysiological process of Alzheimer’s disease (AD)<br />
is thought to begin years, if not decades, prior to the onset<br />
of clinical dementia. Converging data from PET amyloid<br />
imaging, cerebrospinal fluid studies, and large autopsy series<br />
suggest that approximately one-third of clinically normal<br />
older individuals harbor a substantial burden of cerebral<br />
amyloid-b deposition. Recent multi-modality imaging studies,<br />
using PET amyloid imaging and functional MRI, have<br />
demonstrated that amyloid-b deposition in normal elderly is<br />
associated with aberrant fMRI activity in the default network,<br />
in a pattern strongly resembling that seen in AD dementia.<br />
AD-like patterns of atrophy have also been detected<br />
in amyloid-positive normal older individuals, and recent evidence<br />
suggests that specific patterns of cortical thinning are<br />
predictive of who will develop dementia a decade later. A<br />
small number of studies have reported an association<br />
between higher amyloid burden and lower memory performance<br />
even among the range of clinically normal older<br />
individuals, particularly those studies employing more challenging<br />
neuropsychological measures. These findings provide<br />
support for the hypothesis that amyloid-b accumulation is<br />
linked to synaptic dysfunction in the networks supporting<br />
memory processes, and that brain dysfunction is detectable<br />
prior to the emergence of significant cognitive impairment.<br />
It is likely, however, that many additional factors modulate<br />
the likelihood of subsequent clinical decline. Longitudinal<br />
studies are ongoing to determine if these amyloid-positive<br />
older individuals are indeed in the preclinical stages of AD,<br />
and to elucidate the endophenotype that best predicts those<br />
who will progress to AD dementia. In parallel with these<br />
natural history studies, we must begin secondary prevention<br />
trials to determine if altering amyloid burden can delay the<br />
emergence of clinical symptoms. It is likely that, similar to<br />
cancer, diabetes, cardiovascular and most other chronic diseases,<br />
many therapies for AD will be most efficacious in the<br />
early stages of the pathophysiological process.<br />
Derek Denny-Brown <strong>Neurological</strong> Scholar Award: The<br />
Human Sense of Smell at Millisecond Speed<br />
Jay A. Gottfried, MD, PhD, Northwestern University,<br />
Chicago, IL<br />
Very little is known about the basic anatomy, connectivity,<br />
and physiology of the human olfactory system. What we do<br />
know is largely inferential, derived from non-human animal<br />
studies that may hold scant relevance for the human sense<br />
of smell. Although functional imaging studies have<br />
expanded our general understanding of human olfactory<br />
neurobiology, these techniques have poor temporal resolution<br />
and provide only correlative information. Thus even<br />
the most basic assumptions about human olfaction have not<br />
been systematically tested. In this presentation I will discuss<br />
1<br />
new work using olfactory intracranial EEG techniques in<br />
patients with medically refractory epilepsy. By recording<br />
directly from olfactory limbic brain regions, we have begun to<br />
gain direct insights into the electrophysiological organization of<br />
the human olfactory system. Preliminary results suggest that<br />
the emotional content of a smell modulates piriform activity<br />
in the gamma-band range, and that cortical stimulation at piriform<br />
cortex elicits short-latency (
J_ID: ZAY Customer A_ID: SUPP11-1 Cadmus Art: 22576 Date: 31-August-11 Stage: Page: 2<br />
Results: Forty-three of 45 heterotopia (96%) showed<br />
functional correlation with discrete regions of overlying cortex<br />
(mean peak coefficient 0.61). Nodules also demonstrated<br />
correlation with contralateral cortex (62%), other nodules<br />
(51%), ipsilateral nonoverlying cortex (42%), and basal ganglia/cerebellum<br />
(13%). The peak degree of connectivity<br />
between heterotopia and other gray matter regions was significantly<br />
related to epilepsy duration.<br />
Interpretation: Nearly all heterotopia in PNH are functionally<br />
connected to overlying cortex, and the strength of<br />
aberrant connectivity increases with duration of epilepsy.<br />
Along with prior evidence that cortico-cortical tract defects<br />
underlie dyslexia in this disorder, these results suggest that<br />
altered connections are a critical substrate for neurological<br />
dysfunction in brain malformations.<br />
Study supported by: NIH/NINDS, Epilepsy Foundation,<br />
William F. Milton Fund<br />
M810. Evaluating Mechanoreceptors in Glabrous Skin<br />
in Diabetic Neuropathy<br />
Iliza Myers, Kay Artibee, Jun Li and Amanda C. Peltier;<br />
Nashville, TN<br />
Meissner corpuscles (MCs) and their myelinated afferents<br />
are found only in glabrous skin. We hypothesized that alterations<br />
in MCs occur in diabetic neuropathy and correlate<br />
with other measures of axonal loss. Immunohistochemistry<br />
was performed on 2 and 3 mm skin punches from the index<br />
finger and distal leg, respectively. Four diabetic patients<br />
(ages 45–75), with neuropathy confirmed by exam and<br />
nerve conduction studies and four control patients (aged<br />
35–50), were studied. Average Meissner corpuscle density<br />
(MCD) in control patients was 15.3 6 7.1 MCs/ mm 2 with<br />
significant reductions observed in two patients (3.3, 6.2 MCs/<br />
mm 2 ) with near normal or higher density in two other<br />
patients (11.1, 28.1 MCs/mm 2 ), suggestive of proliferation.<br />
MCs in diabetics often displayed abnormal morphology.<br />
Density of intrapapillary myelinated endings (IME) correlated<br />
with MCD in all patients (r ¼ 0.97). Diabetic<br />
patients’ intraepidermal nerve fiber density (IENFD) in the<br />
distal leg was 4.2 6 5.9 fibers/mm, compared to 13.7 6<br />
1.3 in controls. IME density did not correlate with IENFD,<br />
suggesting that these populations of fibers are independently<br />
affected by hyperglycemia. Glabrous skin biopsies afford<br />
evaluation of mechanoreceptors which are important in<br />
studying pathophysiology of diabetic neuropathy.<br />
Study supported by: Supported by NINDS K23<br />
NS056009 (A.C. P.), NINDS R01NS066927-01(J.L.), Vanderbilt<br />
CTSA grant 1 UL1 RR024975.<br />
T1501. Amyloid-Beta Dynamics and Prevention Trials<br />
in Dominantly Inherited Alzheimer’s Disease<br />
Randall J. Bateman and on behalf of the Dominantly<br />
Inherited Alzheimer Network; St. Louis, MO<br />
Amyloid-beta is a key pathologic protein in Alzheimer’s disease(AD)<br />
and extensive research has started an era of clinical<br />
trials targeting amyloid-beta. Understanding the dynamics<br />
of amyloid-beta formation and clearance in the human<br />
CNS and the processes that lead to clinical disease are essential<br />
to design better clinical trials. Developing efforts to prevent<br />
AD in autosomal dominant mutation carriers may test<br />
the amyloid hypothesis, determine the timing of treatment,<br />
and lead the way to AD prevention.<br />
Amyloid-beta production and clearance rates were measured<br />
with stable isotope labeling kinetics. The Dominantly<br />
Inherited Alzheimer’s Network interim findings of clinical,<br />
cognitive, MRI, PET, CSF, and blood biomarkers were analyzed<br />
with respect to the expected age of onset.<br />
2<br />
Amyloid-beta clearance rate is decreased by 30% in AD<br />
compared to controls. Changes in clinical, cognitive, MRI,<br />
PET, CSF, and blood biomarkers in autosomal dominant<br />
AD indicate the pathophysiologic cascade begins up to 20<br />
years before the expected age of onset.<br />
The pathophysiologic changes of AD can be specifically<br />
measured and targeted for clinical trials. Autosomal dominant<br />
AD prevention trials offer a unique opportunity to<br />
lead the way to effective treatments for all AD.<br />
Study supported by: NIH K-23-AG03094601, NIH R-01-<br />
NS065667, NIH 3P-01-AG02627603S1 (FACS), NIH 1U-<br />
01-AG03243801 (DIAN), ADRC (P50 AG05681-22),<br />
HASD (P01 AG03991-22), WU CTSA award (UL1<br />
RR024992), Mass Spectrometry Resource (NIH RR000954),<br />
Eli Lilly research collaboration<br />
R.J.B. is a co-founder of a company (C2N Diagnostics)<br />
that has licensed a Washington University patent on some<br />
of the technology described in this abstract.<br />
T1505. Components of Blood Pressure and Progression<br />
of Cerebral Leukoaraiosis: The ARIC Study<br />
Rebecca F. Gottesman, Diane J. Catellier, Laura H. Coker,<br />
Josef Coresh, Clifford R. Jack, Jr., David S. Knopman,<br />
Kathryn M. Rose, A. Richey Sharrett, Dean K. Shibata and<br />
Thomas H. Mosley; Baltimore, MD; Chapel Hill, NC;<br />
Winston-Salem, NC; Rochester, MN; Durham, NC; Seattle,<br />
WA and Jackson, MS<br />
Background The contribution of blood pressure (BP) components<br />
to the burden and progression of cerebral white<br />
matter hyperintensity (WMH) is poorly understood. We<br />
evaluated these associations in the population-based Atherosclerosis<br />
Risk in Communities (ARIC) cohort.<br />
Methods 983 participants each underwent 2 brain MRIs<br />
10 years apart. Systolic (SBP) and diastolic BP (DBP) were<br />
measured at 4 study visits. Four BP components were examined<br />
as predictors of WMH progression: 1) mean arterial<br />
pressure (MAP); 2) pulse pressure (PP); 3) orthostatic hypotension<br />
(OH); and 4) 10-year change in BP.<br />
Results Baseline (preceding MRI #1) MAP value predicted<br />
WMH progression (OR 1.39 (1.20–1.62), per 10<br />
mm Hg increase), but PP did not. Presence of OH did not<br />
predict WMH progression, but OH severity did (OR 1.21<br />
(1.02–1.42) per 10 mm Hg SBP decrease). Change in DBP<br />
over 10 years had a U-shaped relationship with WMH progression:<br />
extreme increases and decreases, independent of<br />
antihypertensive use, were both associated with greater<br />
WMH progression (p¼0.007).<br />
Discussion WMH progression is significantly predicted<br />
by MAP and extent of orthostatic SBP reduction. Significant<br />
changes over time in DBP, whether positive or negative, predict<br />
WMH progression, cautioning against simplified interpretations<br />
of blood pressure associations.<br />
Study supported by: The Atherosclerosis Risk in Communities<br />
Study is carried out as a collaborative study supported by National<br />
Heart, Lung, and Blood Institute contracts (HHSN26820<br />
1100005C, HHSN268201100006C, HHSN268201100007C,<br />
HHSN268201100008C, HHSN268201100009C, HHSN26820<br />
11000010C, HHSN2682011000011C, HHSN2682011000012C).<br />
Works in Progress Abstracts<br />
M839. Virtual Demyelination in pmp22 Deficiency<br />
Jiasong Guo, Qing Yan, Gina Sosinsky, Mark Elisman,<br />
Cameron McIntyre, Lily Wang, Ueli Suter and Jun Li;<br />
Nashville; San Diego; Cleveland; Zurich, Swaziland and<br />
Nashville, TN<br />
Safety factor for action potential propagation in pmp22þ/<br />
nerves appears impaired (Bai et al, J Neurosci 2010). The<br />
ID: senthilk I Black Lining: [ON] I Time: 08:03 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110239/APPFile/JW-ANA#110239
J_ID: ZAY Customer A_ID: SUPP11-1 Cadmus Art: 22576 Date: 31-August-11 Stage: Page: 3<br />
present study investigates mechanisms responsible for the<br />
impairment. Fluorescent dyes with different molecular sizes<br />
were injected into sciatic nerves. After 4-hour incubation,<br />
sciatic nerves were teased into individual nerve fibers, and<br />
examined under fluorescence microscopy. Fluorescence was<br />
of strong intensity in about a half of paranodal tomacula of<br />
pmp22þ/ nerves (15 mice), but absent or minimal in the<br />
paranodes of wild-type nerves (11 mice). This finding suggests<br />
that myelin is abnormaly leaky, and may result in excessive outward<br />
current. Application of potassium channel blocker, 4AP, to<br />
reduce outward current improved the amplitude of motor<br />
response during nerve stimulation. Western blot and immunohistochemistry<br />
revealed alterations of tight junction protein assembly,<br />
a potential molecular mechanism for the myelin leakage.<br />
Conclusions: Our results show excessive leakage in<br />
pmp22þ/ myelin in the absence of demyelination. This<br />
leakage is functionally similar to demyelination. These findings<br />
not only reveal novel mechanism for conduction block<br />
but also establish new therapeutic approach for this disease.<br />
Study supported by: NIH<br />
M1012. Exome Sequencing Identifies a Rare Variant in<br />
the CYP27B1 Gene Associated with Multiple Sclerosis<br />
George C. Ebers and Sreeram V. Ramagopalan; Oxford,<br />
Oxfordshire, United Kingdom<br />
Background: Multiple sclerosis (MS) is a complex neurological<br />
disease. We previously described the ascertainment of<br />
3<br />
43 Canadian families with 4 or more individuals with MS.<br />
Genetic linkage analysis and genotyping of candidate genes<br />
in these families has not fully explained familial disease<br />
clustering although alleles of GWAS genes are<br />
overrepresented.<br />
Methods: Whole exome sequencing was performed to<br />
further understand heightened prevalence of MS in these<br />
families.<br />
Findings: Forty-three individuals with MS (one/family)<br />
were sequenced. On average over 58000 variants were identified<br />
in each individual. Searching for rare variants in<br />
known or candidate MS susceptibility genes led to identification<br />
of a rare loss-of- function variant in the CYP27B1<br />
gene. This variant in 2716 parent-affected child trios<br />
showed significant association to MS P¼6 10 5 . Further<br />
genotyping of other variants in over 11,000 individuals<br />
showed that rare CYP27B1 variants conferred significant<br />
risk of MS, Peto odds ratio ¼ 4.1 (95% confidence interval<br />
1.5–11.1).<br />
Interpretation: Causative role for CYP27B1 in MS risk<br />
is supported. CYP27B1 encodes the vitamin D activating 1alpha<br />
hydroxylase enzyme. A role for vitamin D in MS<br />
pathogenesis is strongly implicated. We show the utility of<br />
using extreme multicase families to identify rare variants.<br />
Study supported by: This study was supported by grant<br />
funding from the MS Society of the United Kingdom and<br />
the Scientific Foundation of the Canadian MS Society.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:03 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110239/APPFile/JW-ANA#110239
<strong>136</strong> th Annual Meeting Sunday,<br />
September 25, 2011<br />
Poster Session<br />
Posters will be displayed in Elizabeth A-E of the Manchester<br />
Grand Hyatt from 10:00 am – 7:00 pm, with<br />
authors present from 6:00 pm – 7:00 pm.<br />
NOTE: An asterisk designates a resident/fellow travel award<br />
winner. Two asterisks represent a medical student travel award<br />
winner.<br />
Cerebrovascular Disease<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 4<br />
S101 Duration of Diabetes and Ischemic Stroke Risk:<br />
The Northern Manhattan Study<br />
Julio R. Vieira*, Chirantan Banerjee, Yeseon P. Moon,<br />
Myunghee C. Paik, Tatjana Rundek, Ralph L. Sacco and<br />
Mitchell S.V. Elkind; New York, NY and Miami, FL<br />
S102 Functional Outcomes in CREST among Patients<br />
with Periprocedural Stroke and Myocardial Infarction<br />
Bart M. Demaerschalk, Robert J. Hye, O.W. Brown, Donald<br />
V. Heck, Irfan Altafullah, Jenifer H. Voeks, George Howard,<br />
James F. Meschia and Thomas G. Brott; Phoenix, AZ; San<br />
Diego, CA; Royal Oak, MI; Winston Salem, NC; Robbinsdale,<br />
MN; Birmingham, AL and Jacksonville, FL<br />
S103 Inhibition and Scavenging of Complement as<br />
Therapeutic Targets in the Mouse Model of Acute<br />
Ischemic Stroke<br />
Xinzhi Chen, Mark P. Mattson and Milan Basta; Baltimore,<br />
MD and Potomac, MD<br />
S104 Does ACE (rs4646994) and a ADDUCIN (rs4961)<br />
Gene Polymorphisms Predicts the Recurrence of<br />
Hypertensive Intracerebral Hemorrhage<br />
Usha K. Misra, Jayantee Kalita, Bindu I. Somarajan,<br />
Bishwanath Kumar, Moromi Das and Balraj Mittal;<br />
Lucknow, Uttar Pradesh, India<br />
S105 Risk of Intracerebral Hemorrhage in t-PA Treated<br />
Patients with Elevated INR<br />
William P. Neil, Rema Raman, Ernstrom Karin and Thomas<br />
M. Hemmen; San Diego, CA<br />
S106 Toward a Further Clinical Physiological<br />
Elucidation: Immediate Regression of Leukoaraiosis after<br />
Carotid Artery Revascularization<br />
and Yu-Ming Chuang; New Taipei City, Taiwan<br />
S107 Ischemic Stroke Exome Pilot Study<br />
John W. Cole, Xinyeu Liu, Luke J. Tallon, Lisa K. Sadzewicz,<br />
Oscar C. Stine, Nicole Dueker, Yuching Cheng, Marcella A.<br />
Wozniak, Barney J. Stern, James F. Mitchell, Braxton D.<br />
Mitchell, Steven J. Kittner and Jeffrey R. O’Connell;<br />
Baltimore, MD and Jacksonville, FL<br />
S108 Phosphodiesterase Inhibitors Modulate Human<br />
Brain Microvascular Endothelial Cell Barrier Properties<br />
and Response to Injury<br />
Shuo Liu, Fan Yang, Chuanhui Yu, Annlia Paganini-Hill and<br />
Mark Fisher; Irvine, CA<br />
4<br />
S109 Incidence of Nocturnal Blood Pressure Dipping<br />
during Hospital Admission and Discharge among<br />
African <strong>American</strong> Stroke Patients<br />
Lien Diep, John Kwagyan, Joseph Kurantsin-Mills, Janaki<br />
Kalyanam, Amy Wong, Kermit Crowder, Bonnie Davis, Leia<br />
Harbour, Jean Edson and Annapurni Jayam-Trouth;<br />
Washington, DC and Baltimore, MD<br />
S110 Preoperative Factors Associated with In-Hospital<br />
Mortality Following Minimally Invasive Hematoma<br />
Aspiration and Thrombolysis for Intracerebral<br />
Hemorrhage<br />
Feng Xu, Zhouping Tang, Huicong Kang, Dengji Pan,<br />
Suiqiang Zhu and Wei Wang; Wuhan, China<br />
S111 Does Incidental Micro-Hemorrhage, Detected by<br />
Gradient Echo Sequence MRI, Predict Hemorrhagic<br />
Transformation of an Ischemic Stroke?<br />
Konark Malhotra and Yousef M. Mohammad; Chicago, IL<br />
S112 Younger Patients Have Lower Quality of Life after<br />
Intracranial Aneurysm Diagnosis<br />
Nerissa Ko, Richard Hornung, Charles Moomaw, Laura<br />
Sauerbeck and Joseph Broderick; San Francisco, CA and<br />
Cincinnati, OH<br />
S113 Aggressive Medical Management of Primary<br />
Intracerebral Hemorrhage: Cost/Benefit Analysis<br />
Luis Cava, Diane C. Andress-Rothrock and John F. Rothrock;<br />
Birmingham, AL<br />
S114 Withdrawn.<br />
S115 Genetic Analysis of Strain-Specific Stroke<br />
Sesceptibility in Mice: How To Classify C57BL/6?<br />
Amy K. Guzik, Sean S. Li, Ira M. Hall, Charles R. Farber,<br />
Brian H. Annex and Bradford B. Worrall; Charlottesville, VA<br />
S116 Risk Factor Control in a Phase 3 Carotid<br />
Revascularization Trial<br />
James F. Meschia, Pierre P. Leimgruber, Vito A. Mantese,<br />
Carlos H. Timaran, David Chiu, Bart M. Demaerschalk,<br />
Mary E. Longbottom, Jenifer H. Voeks, George Howard and<br />
Thomas G. Brott; Jacksonville, FL; Spokane, WA; St. Louis,<br />
MO; Dallas, TX; Houston, TX; Phoenix, AZ and<br />
Birmingham, AL<br />
S117 Radiologic Analysis of Thrombolysis-Induced<br />
Intracerebral Hemorrhage and the Role of Early Blood<br />
Pressure Management<br />
Maxim Mokin, Tareq Kass-Hout, Omar Kass-Hout, Robert<br />
Zivadinov and Bijal Mehta; Buffalo, NY<br />
S118 Anterior Circulation Stroke Causing Dizziness or<br />
Vertigo: A Systematic Review<br />
Yun Zhou, Seung-hun Lee, Ali S. Saber Tehrani, Karen A.<br />
Robinson and David E. Newman-Toker; Baltimore, MD and<br />
Gwangju, Korea<br />
S119 The Presence of Intracranial Vascular Calcification<br />
May Protect Against Vasospasm Following Subarachnoid<br />
Hemorrhage<br />
Joya Paul, Mohamed Zghouzi, Yousef Mohammad, Shyam<br />
Prabhakaran, Sudeep Bhabad and Bichun Ouyang; Chicago, IL<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 5<br />
S120 Stroke Knowledge: A Nation-Wide, Internet-Based<br />
Survey of 11,121 Inhabitants in Japan<br />
Hisanao Akiyama, Kanako Shimizu, Yoshiaki Tokuyama and<br />
Yasuhiro Hasegawa; Kawasaki, Kanagawa, Japan<br />
S121 Is Anti Epileptic Drug Necessary in Cortical<br />
Venous Thrombosis?<br />
Velmurugendran Cannigaiper Uthamaroyan, Kaushik Sundar,<br />
Meenakshisundaram Umaiorubahan and Shankar<br />
Venkatasubramaniam; Chennai, Tamilnadu, India<br />
S122 Race and Insurance Disparities in Cardiovascular<br />
Risk Factors Control in Patients with Acute Stroke<br />
Anna M. Cervantes, Jose R. Romero, Helena Lau, Feliks<br />
Koyfman, Aleksandra Pikula, Thanh N. Nguyen, Carlos S.<br />
Kase and Viken L. Babikian; Boston, MA<br />
S123 A Population-Based Verbal Autopsy Study of 1250<br />
Stroke Deaths in Bangladesh<br />
Farrah J. Mateen, Nurul Alam, Marco Carone and Robert E.<br />
Black; Baltimore, MD; Dhaka, Bangladesh and Berkeley, CA<br />
S124 Heparin-Induced Thrombocytopenia Associated<br />
with Cerebral Venous Sinus Thrombosis Following<br />
Postoperative Enoxaparin Administration in a 64 Year-<br />
Old Female<br />
Robert A. Fishman and Ashis Tayal; Pittsburgh, PA<br />
S125 Renal Failure Increases Risk for Intracranial<br />
Hemorrhage Following Stroke<br />
Elisabeth B. Marsh, Argye E. Hillis, Rafael H. Llinas and<br />
Rebecca F. Gottesman; Baltimore, MD<br />
S126 Dominant Vertebral Artery Occlusion during<br />
Ipsilateral Head Tilt<br />
In Soo Moon, Jae-Hwan Choi and Kwang-Dong Choi; Busan,<br />
Korea<br />
S127 A Novel Presentation of Mesodiencephalic<br />
Ischemic Stroke: Case Report and Literature Review<br />
Khalid S. Alqadi, Tariq Alfahad and Kathleen Burger;<br />
Washington, DC<br />
S128 Fatal Postpartum Cerebral Vasoconstriction<br />
Syndrome<br />
Jennifer E. Fugate, Eelco F.M. Wijdicks, Kelly D. Flemming<br />
and Alejandro A. Rabinstein; Rochester, MN<br />
S129 Racial Disparities in Secondary Stroke Prevention<br />
Practices<br />
Pratik Bhattacharya, Seemant Chaturvedi, Flicia Mada, Leeza<br />
Salowich-Palm, Sabrina Hinton, Scott Millis, Sam Watson<br />
and Kumar Rajamani; Detroit, MI and Lansing, MI<br />
S130 Predicting Ischemic Stroke Outcomes Based on<br />
Volume of Lesion<br />
Shazia Z. Choudhary, Jay-Ming Wang, Zahid Choudary,<br />
Michael Sloan, Harry R. Van Loveren, Karen R. Wilson,<br />
Morgan Wang and David A. Decker; Tampa, FL and<br />
Orlando, FL<br />
S131 Treatment Outside the NINDS Stroke Study<br />
Exclusion Criteria: A Case Report<br />
Nhu T. Bruce and Brett C. Meyer; San Diego, CA<br />
5<br />
S132 Size Matters: Predictors of Intracranial<br />
Hemorrhage in Stroke Patients on Anticoagulation<br />
Elisabeth B. Marsh, Argye E. Hillis, Rafael H. Llinas and<br />
Rebecca F. Gottesman; Baltimore, MD<br />
S133 A Rare Presentation of Anterior and Posterior<br />
Spinal Arteries Ischemia during Dilaysis<br />
Noor Yono, Adrian Marchidann and Rabih Kashouty;<br />
Manhasset, NY and New York, NY<br />
S134 Neurosarcoidosis: A Case Presentation<br />
Amtul Farheen, Nancy Gadallah, Rony Dekermenjian,<br />
Michael Rosenberg and Sushanth Bhat; Edison, NJ<br />
S135 Stroke Outcomes Based on MERCI/PENUMBRA<br />
Intervention and Hemodynamics<br />
Jay-Ming Wang**, Zahid I. Choudary, Shazia Z. Choudhary,<br />
Michael Sloan, Harry R. Van Loveren, Karen R. Wilson and<br />
David A. Decker; Tampa, FL<br />
S<strong>136</strong> Migraine-Related ICH – A Case Study and<br />
Review<br />
Shivani Ghoshal**, Sankalp Gokhale and Louis Caplan;<br />
Boston, MA<br />
S137 Stroke as a Complication of Tuberculous<br />
Meningitis<br />
Amtul Farheen, Sumaiya Salim, Zoha Fasih, Rony<br />
Dekermenjian and Sushanth Bhat; Edison, NJ<br />
S138 Patterns and Mechanisms of Head-Shaking<br />
Nystagmus in Anterior Inferior Cerebellar Artery<br />
Infarction<br />
Young Eun Huh and Ji Soo Kim; Seongnam-si,<br />
Gyeonggi-do, Korea<br />
S139 Co-Complaints Influence Odds of Stroke<br />
Diagnosis in ED Dizziness<br />
Ali S. Saber Tehrani, Yu-Hsiang Hsieh, Jonathan A. Edlow,<br />
Carlos A. Camargo and David E. Newman-Toker; Baltimore,<br />
MD and Boston, MA<br />
S140 Eclamptic Versus Non-Eclamptic PRES (Posterior<br />
Reversible Encephalopathy Syndrome): Comparison of<br />
Clinical Features and Response to Treatment<br />
Pavan Bhargava, Fazeel Siddiqui, Vivek Patel, Rodger J. Elble<br />
and Srikanth Vallurupalli; Springfield, IL<br />
Movement Disorders<br />
S201 Allele Specific RNAi Against Triplet Repeat<br />
Disease-Causing Alleles in Huntington Disease<br />
Hirokazu Furuya, Masaki Takahashi, Shoko Watanabe,<br />
Miho Murata, Ichiro Kanazawa, Keiji Wada and Hirohiko<br />
Hohjoh; Omuta, Fukuoka, Japan and Kodaira, Tokyo,<br />
Japan<br />
S202 Antigen-Sensitized Dendritic Cell Vaccine Against<br />
Human a-Synuclein: A Potential Cell-Based Therapy<br />
Against Parkinson’s Disease<br />
Chuanhai Cao, Xiaoyang Lin, Wang Li, Cai Jianfeng, Li<br />
Kunyu, Song Shijie and Juan Sanchez-Ramos; Tampa<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 6<br />
S203 Depressive Symptoms and Neurodegeneration in<br />
the Locus Coeruleus: The Honolulu-Asia Aging Study<br />
Ross Webster, Robert D. Abbott, Helen Petrovitch, Kamal H.<br />
Masaki, Caroline M. Tanner, Jane H. Uyehara-Lock and Lon<br />
R. White; Honolulu, HI; Hiroshima, Japan and Sunnyvale,<br />
CA<br />
S204 MRI in HDLS Shows a Unique Mechanism of<br />
Neuroaxonal Degeneration<br />
C. Sundal*, C. Wider, J.A. Van Gerpen, J. Lash, J.Y.<br />
Garbern, K.J. Schweitzer, J. Aasly, B. Goodman, B.K.<br />
Woodruff, C.W. Christine, M. Baker, J.E. Parisi, S. Roeber, S.<br />
DeArmond, R. Rademakers, D.W. Dickson, D.F. Broderick, O.<br />
Andersen and Z.K. Wszolek; Gothenburg, Sweden; Jacksonville,<br />
FL; Rochester, NY; Trondheim, Norway; Scottsdale, AZ; San<br />
Francisco, CA; Rochester, MN and Munchen, Germany<br />
S205 Appropriate Outcome Measures for Cognitive<br />
Trials in Huntington’s Disease<br />
Jody Corey-Bloom, Jody Goldstein, Shea Gluhm, Charles Van<br />
Liew, Stephanie Lessig, Jagan Pillai and Steven D. Edland; La<br />
Jolla, CA<br />
S206 Distinctive Neurocognitive Profiles Associated with<br />
Right and Left Motor Symptom Onset in Parkinson’s<br />
Disease<br />
Paul J. Eslinger, Daymond Wagner, Suman Sen, Mechelle M.<br />
Lewis, Guangwei Du, Michele L. Shaffer and Xuemei Huang;<br />
Hershey, PA<br />
S207 The Clinical and Pathological Features of Familial<br />
Parkinsonism with EIF4G1Gene Mutation<br />
Shinsuke Fujioka, Owen A. Ross, Rosa Rademakers, Matthew<br />
J. Farrer, Dennis W. Dickson and Zbigniew K. Wszolek;<br />
Jacksonville, FL and Vancouver, BC, Canada<br />
S208 Alcohol Consumption and Risk of Parkinson<br />
Disease<br />
Rui Liu, Yikyung Park, Xuemei Huang, Xuguang Guo, Albert<br />
Hollenbeck, Aaron Blair and Honglei Chen; Research Triangle<br />
Park, NC; Rockville, MD; Hershey, PA and Washington, DC<br />
S209 Hereditary Diffuse Leukoencephalopathy with<br />
Spheroids: An Under-Diagnosed Disease<br />
C. Sundal, C. Wider, J.A. Van Gerpen, J. Lash, J.Y. Garbern,<br />
E.A. Shuster, K.J. Schweitzer, J. Aasly, B. Goodman, B.K.<br />
Woodruff, W. Kupsky, A. Tselis, C.W. Christine, M. Baker,<br />
J.E. Parisi, S. Roeber, S. DeArmond, R. Rademakers, D.W.<br />
Dickson, O. Andersen and Z.K. Wszolek; Gothenburg, Sweden;<br />
Jacksonville, FL; Rochester, NY; Trondheim, Norway;<br />
Scottsdale, AZ; Detroit, MI; San Francisco, CA; Rochester,<br />
MN and Munchen, Germany<br />
S210 Co-Existing HTT and ATXN8OS Repeat<br />
Expansions and a ‘Face of the Giant Panda’ Sign on<br />
MRI in a Patient with a Complex Movement Disorder<br />
Shin C. Beh, Cherian A. Karunapuzha and Shilpa Chitnis;<br />
Dallas, TX<br />
S211 Clinical Differences among PD-MCI Subtypes<br />
Jennifer G. Goldman, Glenn T. Stebbins, Bryan Bernard and<br />
Christopher G. Goetz; Chicago, IL<br />
6<br />
S212 Loss of Cortical Gray Matter in Parkinson’s<br />
Disease<br />
Suman Sen, Paul J. Eslinger, Daymond Wagner, Guangwei<br />
Du, Mechelle M. Lewis, Michel L. Shaffer and Xuemei<br />
Huang; Hershey, PA<br />
S213 <strong>Association</strong> of PSP with Chemical Occupational<br />
Exposure Factors<br />
Irene Litvan, Christopher R. Cunningham, Peter Lees, Leila<br />
Jackson, Jorge Juncos, David Riley, Yvette Bordelon, David<br />
Standaert, Stephen Reich, Alex C. Cambon, Joseph Jankovic,<br />
Deborah A. Hall, Richard Dubinsky, Cassandra Shepherd,<br />
Claire Henchcliffe, Ryan Uitti, Benzi Kluger, David Shprecher,<br />
Connie Marras, Eliza Gallin, James Leverenz and Shesh N.<br />
Rai; Louisville, KY; Baltimore, MD; Cleveland, OH; Atlanta,<br />
GA; Los Angeles, CA; Birmingham, AL; Houston, TX; Chicago,<br />
IL; Kansas City, KS; New York, NY; Jacksonville, Fl; Boulder,<br />
CO; Salt Lake City, UT; Toronto, Canada and Seattle, WA<br />
S214 Psychiatric Co-Morbidities and Mortality among<br />
Hospitalized Parkinson Disease Patients<br />
Nicte Mejia and Zeina Chemali; Boston, MA<br />
S215 Comparison of Subthalamic (STN) and Pallidal<br />
(GPi) Deep Brain Stimulation (DBS) on Gait and<br />
Balance in Patients with Parkinson’s Disease (PD)<br />
Jyhgong Gabriel Hou, Minn Thant, Aliya Sarwar, Linda<br />
Fincher, Monthaporn S. Bryant, Farrah Atassi and Eugene C.<br />
Lai; Houston, TX and Galveston, TX<br />
S216 Reliability of Self-Reported Parkinson’s Disease<br />
(PD) Features<br />
Caroline M. Tanner, Cheryl Meng, Ira Shoulson, Anthony E.<br />
Lang, David Oakes, Roger Kurlan, Alberto Ascherio, Flint Beal,<br />
Emily Flagg, Jennifer Harman, Michael Schwarzchild, James<br />
Beck, Bernard Ravina, Kenneth Marek, Shirley Eberly, Karen<br />
Marder and Robin Elliott; Sunnyvale, CA; Washington, DC;<br />
Toronto, ON, Canada; Rochester, NJ; Summit, NJ; Boston,<br />
MA; New York, NY; Cambridge, MA and New Haven, CT<br />
S217 First <strong>Neurological</strong> Examination Can Predict<br />
Course of Parkinson’s Disease (PD)<br />
Ali H. Rajput, Michele L. Rajput and Alex H. Rajput;<br />
Saskatoon, SK, Canada<br />
S218 Difficulty with Balance Occurs Early in PD: It<br />
Isn’t Appreciated Because It’s Not Asked about Nor<br />
Tested For<br />
Abraham N. Lieberman, Samea Husain, Naomi Salins and<br />
Anthony Santiago; Phoenix, AZ<br />
S219 Poor Dementia Screening with Mattis Dementia<br />
Rating Scale Cutoffs in Highly Educated Parkinson’s<br />
Disease Patients<br />
Travis H. Turner and Vanessa Hinson; Charleston, SC<br />
S220 Impaired Social Problem-Solving in Huntington’s<br />
Disease<br />
Charles Van Liew, Jody Goldstein, Shea Gluhm, Jagan Pillai<br />
and Jody Corey-Bloom; San Diego, CA<br />
S221 <strong>Association</strong> of Psychological Symptoms with<br />
Impulse-Control Behaviors after Dopamine Agonist<br />
Therapy for Parkinson’s Disease: A Longitudinal Study<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 7<br />
Jennifer S. Hui, Steven Cen, Megan Gomez and Lauice Yang;<br />
Los Angeles, CA and Pasadena, CA<br />
S222 Balance Difficulty in PD Correlates with Step<br />
Length and Velocity<br />
Abraham Lieberman, Naomi Salins, Tiki Hussain, Di Pan<br />
and Anthony Santiago; Phoenix, AZ<br />
S223 Motor Asymmetry in SCAs<br />
Mitra Assadi, Bhavpreet Dham, Gazelle Zerafati, Jon Veloski<br />
and Paola Leone; Camden, NJ and Philadelphia, PA<br />
S224 Neurotoxin Injection for Treatment of Cervical<br />
Dystonia<br />
Chandler E. Gill, Anna L. Molinari, Neil D. Manus, Michael<br />
W. Pelster, Jason A. Cook, Wallace Title and David Charles;<br />
Maywood, IL; Nashville, TN; Minneapolis, MN and New<br />
Orleans, LA<br />
S225 The <strong>Association</strong> between Mediterranean-Type Diet<br />
Adherence and Parkinson’s Disease<br />
Roy N. Alcalay, Yian Gu, Helen Mehia-Santana, Lucien Cote,<br />
Karen S. Marder and Nicholas Scarmeas; New York, NY<br />
S226 Autonomic Dysfunction in Early Parkinson’s<br />
Disease<br />
Anna L. Molinari, Fenna T. Phibbs, Lily Wang, Yanna Song<br />
and P. David Charles; Nashville, TN<br />
S227 Balance Difficulty in PD Correlates with the BNI<br />
Balance Scale<br />
Abraham Lieberman, Naomi Salins, Tiki Hussain, Di Pan<br />
and Anthony Santiago; Phoenix, AZ<br />
S228 STEADY-PD. Safety and Tolerability of Isradipine<br />
CR in Early Parkinson’s Disease. Interim Tolerability<br />
Data Analysis<br />
Tanya Simuni, Kevin Biglan, David Oakes, Cheryl Deeley,<br />
Irenita Gardiner, Parkinson Study Group and STEADY PD<br />
Investigators; Chicago, IL and Rochester, NY<br />
S229 Nigella sativa Oil Controls Astrogliosis and<br />
Reduces Haloperidol-Induced Deficit in Rats<br />
Tafheem Malik**, Darakhshan Jabeen Haleem, Shema Husan,<br />
Shahid Pervez and Tasneem Fatima; Karachi, Sind, Pakistan<br />
and Karachi, Pakistan<br />
S230 Cost-Benefit Assessment of Two Forms of<br />
Botulinum Toxin Type-A in Different Pathologies<br />
Humberto Juarez, Santamaria Salvador, Leticia Hernandez<br />
and Enrique Molina; Mexico City, Mexico, Mexico<br />
S231 Weight and Height Distribution in Children with<br />
Tourette Syndrome<br />
Katie Kompoliti, Glenn T. Stebbins and Christopher G. Goetz;<br />
Chicago, IL<br />
S232 Motor Deterioration after Medication Withdrawal<br />
in Early Parkinson’s Disease<br />
Chandler E. Gill**, Anna L. Molinari, Thomas L. Davis,<br />
Mark Bliton, Stuart G. Finder, Michael G. Tramontana, Peter<br />
E. Konrad and David Charles; Maywood, IL; Nashville, TN<br />
and Los Angeles, CA<br />
7<br />
S233 Gender Differences in the Interleukin-6 G-174C<br />
Polymorphism and the Risk of Parkinson’s Disease<br />
Marta San Luciano, Laurie J. Ozelius, Richard B.. Lipton,<br />
Deborah Raymond, Kaili M. Stanley, Susan B. Bressman and<br />
Rachel Saunders-Pullman; New York, NY and Bronx, NY<br />
S234 Serum Cholesterol Is Linked with Nigrostriatal<br />
Iron Deposition in Parkinson’s Disease<br />
Guangwei Du, Mechelle M. Lewis, Michele L. Shaffer,<br />
Honglei Chen, Richard B. Mailman and Xuemei Huang;<br />
Hershey, PA and Research Triangle Park, NC<br />
S235 Balance Difficulty Differs from Gait Difficulty in PD<br />
Abraham Lieberman, Naomi Salins, Tiki Hussain, Di Pan<br />
and Anthony Santiago; Phoenix, AZ<br />
S236 Adult Onset Dopamine Responsive Dystonia<br />
(DRD): Is There a New Gene?<br />
Hossein Ansari, Ludwig Gutmann and Laurie Gutmann;<br />
Morgantown, WV<br />
S237 Dystonia Induced Mechanical Stress as a Cause of<br />
DBS Extension Fracture and Expulsion<br />
Massimo Mondani, Elisa Petacchi, Roberto Eleopra, Silvia<br />
Molteni, Sabrina Gualdi, Miran Skrap and Andrea<br />
Martinuzzi; Udine, UD, Italy; Conegliano, TV, Italy and<br />
Sesto San Giovanni, MI, Italy<br />
Sleep Disorders and Circadian Rhythm<br />
S301 Endogenous GABA A Receptor Enhancement<br />
Modulates Vigilance in the Primary Hypersomnias<br />
David B. Rye, Kathy Parker, Lynn Marie Trotti, Paul S.<br />
Garcia, James C. Ritchie, Michael J. Owens, Leslie Morrow,<br />
Donald L. Bliwise and Andrew Jenkins; Atlanta, GA;<br />
Rochester, NY and Chapel Hill, NC<br />
S302 Frequency of Parsaomnias in Patients with Non-<br />
Epileptic Seizures<br />
Mitchell G. Miglis, Michael Boffa, Sujata Thawani, Alcibiades<br />
Rodriguez and Anuradha Singh; New York, NY<br />
S303 Endothelial Function in Patients with Obstructive<br />
Sleep Apnea<br />
Kanika Bagai, James Muldowney, Yanna Song, Lily Wang,<br />
Douglas E. Vaughan and Beth A. Malow; Nashville, TN and<br />
Chicago, IL<br />
Education<br />
S401 The Effectiveness of Education Intervention on<br />
Health Knowledge among <strong>Neurological</strong> Patients<br />
Mercedes Jacobson and Polina Pomerants; Philadelphia, PA<br />
S402 Teleneurology in Leading U.S. Medical Institutions<br />
Benjamin P. George**, Nicholas J. Scoglio, Jason I. Reminick,<br />
Kevin M. Biglan and E. Ray Dorsey; Rochester, NY and<br />
Baltimore, MD<br />
S403 Standardized Sign-Out Improves Communication<br />
Skills<br />
Brian D. Moseley, Jonathan H. Smith, Gloria E. Diaz-<br />
Medina, Mateo Paz Soldan, Meredith Wicklund, Radhika<br />
Dhamija, Haatem Reda, Michael F. Presti and Jeffrey W.<br />
Britton; Rochester, MN<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
S404 Improved Scores on the AAN Resident Inservice<br />
Training Examination (RITE) after Lecture Curriculum<br />
Intervention<br />
L. John Greenfield, Vicki Ramsey-Williams, Theresa Marshall<br />
and Boyd Koffmann; Toledo, OH and Little Rock, AR<br />
S405 Evidence Based Medicine(EBM) in the 2 nd Year<br />
Neurosciences Curriculum<br />
Michael J. Schneck and Edward Neafsey; Maywood, IL<br />
S406 Adapting a Teaching Hospital Inpatient Neurology<br />
Service to New Duty Hour Requirements: The<br />
Washington University Adult Neurology Experience<br />
Robert Bucelli and Barbara J. Snider; Saint Louis, MO<br />
S407 Translational Research in Neuro-AIDS and Mental<br />
Health<br />
Amanda Brown, Valerie Wojna, Bruce Shiramizu, Avindra<br />
Nath and Justin C. McArthur; Baltimore, MD; San Juan, PR<br />
and Honolulu, HI<br />
S408 Relationship between Medical Student Feedback<br />
and Grading<br />
and James M. Stankiewicz; Boston, MA<br />
<strong>136</strong> th Annual Meeting Monday,<br />
September 26, 2011<br />
Poster Session<br />
Posters will be displayed in Elizabeth A-E of the Manchester<br />
Grand Hyatt from 10:00 am – 7:00 pm, with<br />
authors present from 6:00 pm – 7:00 pm.<br />
NOTE: An asterisk designates a resident/fellow travel award<br />
winner. Two asterisks represent a medical student travel award<br />
winner.<br />
Behavioral Neurology<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 8<br />
M601 Behaviorally-Driven Anatomical Mapping of<br />
Hemispatial Neglect<br />
Alex R. Carter, Mark P. Mcavoy, Serguei V. Astafiev, Jennifer<br />
Rengachary, Daniel L.W. Pope, Abraham Z. Snyder, Kristi<br />
Zinn, Nick Metcalf, Gordon L. Shulman and Maurizio<br />
Corbetta; Saint Louis, MO<br />
M602 Markers of Celiac Disease and Gluten Sensitivity<br />
in Patients with Cerebellar Ataxia<br />
Caroline Tan, Peter H. Green, Khalaf O. Bushara, Donald D.<br />
Kasarda, Ejaz Shamim, Norman Latov, Mark Hallett and<br />
Armin Alaedini; New York, NY; Minneapolis, MN; Albany,<br />
CA and Bethesda, MD<br />
M603 Early Signs of Cognitive Impairment among<br />
Multiple Sclerosis Patients with Clinically Isolated<br />
Syndrome<br />
Theodora Panou, Vasileios Mastorodemos, Efrosyni Papadaki,<br />
Panagiotis G. Simos and Andreas Plaitakis; Heraklion, Greece<br />
and Rethymnon, Greece<br />
M604 Motor Chunking Is Correlated with Sensorimotor<br />
Cortex and Striatum Activation<br />
Nicholas Wymbs and Scott T. Grafton; Santa Barbara, CA<br />
8<br />
M605 Areas of Ischemia Associated with ‘‘Frontal Lobe’’<br />
Task Failure<br />
Yessenia Gomez and Argye E. Hillis; Baltimore, MD<br />
M606 Thalamic Atrophy in Gastric Bypass Patients with<br />
Cognitive Complaints<br />
Jonathan Graff-Radford, Jennifer Whitwell, Max R. Trenerry,<br />
J.E. Ahlskog, Michael D. Jensen, Clifford R. Jack, Jr. and<br />
Keith A. Josephs; Rochester, MN<br />
M607 Parietal Lobe Lesions Affect the Generation of<br />
Antisaccades<br />
James A. Sharpe, Ping Cheng and Moshe Eizenamn; Toronto,<br />
ON, Canada<br />
M608 Cognitive Ability Correlates of Psychiatric and<br />
Social Behaviors in Williams Syndrome<br />
Rowena Ng, Anna Järvinen-Pasley and Ursula Bellugi;<br />
San Diego, CA<br />
M609 Human Brain Mapping at the Single Cellular<br />
Level: Neuronal and Area Specific Differences in Health<br />
and Diseases<br />
Ryan P. Moore, Irisa Mahaparn, Eliezer Masliah and<br />
Pavel V. Belichenko; La Jolla, CA<br />
M610 Cognitive and Behavioral Differences between<br />
ADHD Populations (Inattentive Type Versus ADHD<br />
Plus) Using Neuropsychological Testing and<br />
Self-Reported Symptoms in Diagnosed Population<br />
from Years 1991–2008<br />
Barbara C. Fisher, Danielle M. Garges and Stephany Fulda;<br />
Shelby Township, MI and Munich, Germany<br />
M611 The Use of Quetiapine in Agitated Patients<br />
with Acquired Brain Injury: A Case Control<br />
Study<br />
Sara Piccoli, Gabriella Paparella, Alec Vestri and Andrea<br />
Martinuzzi; Pieve di Soligo, TV, Italy<br />
M612 On-Line Lexical-Semantics in the Semantic<br />
Variant of Primary Progressive Aphasia<br />
David S. Race and Argye E. Hillis; Baltimore, MD<br />
M613 Differences in Time Interval Distributions<br />
Reveal Controlled and Automatic Contributions to<br />
Cued Word Retrieval<br />
Kyongje Sung, Erin J. Pickett, Kerry Ledoux, Tracy D.<br />
Vannorsdall, Mohammad Elsayed, Nia M. Billings,<br />
Jessica Silva, David J. Schretlen and Barry Gordon;<br />
Baltimore, MD<br />
M614 Gender Differences across the Lifespan in<br />
Neuropsychological Testing Performance in ADHD<br />
Population from the Years 1991–2008<br />
Barbara C. Fisher, Danielle M. Garges and Stephany Fulda;<br />
Shelby Township, MI and Munich, Germany<br />
M615 Hazard Perception in Cognitively Impaired Older<br />
Drivers<br />
Nazan Aksan, Monica Lees, John D. Lee, Shaun Vecera and<br />
Matthew Rizzo; Mountain View, CA; Madison, WI and Iowa<br />
City, IA<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
M616 Differentiation of Alzheimer’s Disease and<br />
Depression with Standard Cognitive Measures<br />
Meredith C. Frederick**, Stefan Sillau, David B. Arciniegas,<br />
C. Alan Anderson, Katherine L. Howard and Christopher M.<br />
Filley; Aurora, CO and Denver, CO<br />
M617 Attention Deficit Hyperactivity Disorder in<br />
Depressed Adults<br />
Ildefonso Rodríguez Leyva, Rubén Haro SIlva and Ana A.<br />
Rentería Palomo; San Luis Potosi, San Luis Potosi, Mexico<br />
M618 Cognition and EEG Abnormalities in Non-<br />
Epileptic AD(H)D/LD Patients with and without Anti-<br />
Epileptic Drug/Stimulant Therapy<br />
Brittany M. DiVito, Heather A. Koch, Spencer A. Leblang,<br />
Erik C. Bakken and Drake D. Duane; Scottsdale, AZ and<br />
Tempe, AZ<br />
M619 Evolution of EEG Abnormalities in Non-Epileptic<br />
AD(H)D/LD Patients with and without Anti-Epileptic<br />
Drug/Stimulant Therapy<br />
Heather A. Koch, Brittany M. DiVito, Spencer A. Leblang,<br />
Erik C Bakken and Drake D. Duane; Scottsdale, AZ and<br />
Tempe, AZ<br />
M620 Transection of CA3 Does Not Affect Memory in<br />
Rats<br />
Mohamad Z. Koubeissi, Saifur Rashid, Gemma Casadesus,<br />
Joseph LaManna, Kui Xu, Hans Luders and Dominique<br />
Durand; Cleveland, OH<br />
M621 Cruetzfeldt-Jakob Disease Presenting as a Rapidly<br />
Progressing Dementia with Non-Convulsive Status<br />
Epilepticus<br />
Natasha Tilluckdharry, Megan McGarry and Dipak P.<br />
Pandya; Paterson, NJ<br />
Epilepsy<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 9<br />
M701 Controlled Cortical Impact in Adult Rats and<br />
Posttraumatic Seizures and Epilepsy<br />
Kevin M. Kelly, Elena A. Kharlamov, Eric R. Miller, Bo Lu<br />
and Zakaria Mtchedlishvili; Pittsburgh, PA and<br />
Philadelphia, PA<br />
M702 Serotonin 1A Receptors and Memory in Temporal<br />
Lobe Epilepsy<br />
William H. Theodore, Edythe Wiggs, Ashley Martinez, Irene<br />
Dustin, Omar Khan, Shmuel Appel, Patricia Reeves-Tyer and<br />
Susumu Sato; Bethesda<br />
M703 Ictal Hypoxemia Is Associated with Cardiac<br />
Repolarization Abnormalities<br />
Lisa M. Bateman, Franchette Pascual, Michael Lee, Chin-<br />
Shang Li and Masud Seyal; Sacramento, CA and Los Angeles,<br />
CA<br />
M704 Gray Matter Heterotopia in an Epileptic Brain<br />
Malformation Are Functionally Connected to Overlying<br />
Cortex<br />
Joanna A. Christodoulou, Linsey M. Walker, Stephanie N. Del<br />
Tufo, Tami Katzir, Susan Whitfield-Gabrieli, John D.E.<br />
Gabrieli and Bernard S. Chang; Cambridge, MA; Boston, MA<br />
and Haifa, Israel<br />
9<br />
M705 JAK/STAT Inhibition Slows the Progression of<br />
Temporal Lobe Epilepsy in an Animal Model<br />
Heidi L. Grabenstatter, Yasmin Cruz Del Angel, Marco I.<br />
Gonzalez, Yogendra H. Raol, Shelley J. Russek and Amy R.<br />
Brooks-Kayal; Aurora, CO and Boston, MA<br />
M706 Long-Term Changes in mGluR-Mediated Long-<br />
Term Depression Following a Single Episode of Early<br />
Life Seizures in Rats<br />
Paul B. Bernard, Anna Castano and Tim A. Benke; Aurora,<br />
CO<br />
M707 Heterozygous Loss of the Epilepsy-Associated<br />
GABA A Receptor a1 Subunit Causes Spontaneous EEG<br />
Spike Discharges in Two Mouse Strains<br />
Fazal M. Arain and Martin J. Gallagher; Nashville, TN<br />
M708 Regional Network Disruption in Temporal Lobe<br />
Epilepsy<br />
Luigi Maccotta* and Edward Hogan; St. Louis, MO<br />
M709 Mice Deficient in SNAREs/SNARE Regulators<br />
Predict Kindling Phenotype<br />
John T. Slevin, Elena E. Matveeva, Sidney W. Whiteheart,<br />
Greg A. Gerhardt and Thomas C. Vanaman; Lexington, KY<br />
M710 Pharmacokinetic Equivalence between Immediate-<br />
Release and Extended-Release Topiramate<br />
Lawrence J. Lambrecht, Wesley M. Todd and Mark B.<br />
Halvorsen; Maple Grove, MN<br />
M711 Cingulate Epilepsy, Reporting 3 Clinical and<br />
Electrophysiologic Subtypes with Surgical Outcomes<br />
Mhd Rafeed Alkawadri, Norman K. So, Paul C. Van Ness<br />
and Andreas V. Alexopoulos; Cleveland, OH and Dallas, TX<br />
M712 GABAB Receptor Antagonists Reduce Pro-<br />
Epileptic Activity in Hippocampal Slices of Ts65Dn<br />
Mice, a Genetic Model of Down Syndrome<br />
Alexander M. Kleschevnikov, Brett Rasmuss, Pavel V.<br />
Belichenko and William Mobley; La Jolla, CA<br />
M713 Lacosamide: Long-Term Safety and Efficacy in<br />
Partial-Onset Seizures<br />
William Rosenfeld, Nathan B. Fountain, Gintaras Kaubrys,<br />
Elinor Ben-Menachem, Cindy McShea, Jouko Isojarvi and<br />
Pamela Doty; St. Louis; Charlottesville; Vilnius, Lithuania;<br />
Göteborg, Sweden and Raleigh<br />
M714 Lacosamide: Long-Term Safety in Partial-Onset<br />
Seizures<br />
Robert F. LeRoy, Gregory Krauss, Nathan B.. Fountain,<br />
Deanne Dilley, O’Neill D’Cruz and Pamela Doty; Dallas, TX;<br />
Baltimore, MD; Charlottesville, VA and Raleigh, NC<br />
M715 Withdrawn.<br />
M716 Computational Models of Ligand-Gated Receptor<br />
Function Characterize Anticonvulsant Drug Actions at<br />
GABAergic and Glutamatergic Synapses<br />
and David E. Naylor; Torrance, CA<br />
M717 Status Epilepticus: An Independent Predictor of<br />
Poor Survival after Anoxic Brain Injury<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
Jennie Luna, Nelly Awkar, Megan McGarry, Deepthi<br />
Karanam and Dipak P. Pandya; Paterson, NJ<br />
M718 Periodic Lateralized Epileptiform Discharges<br />
(PLEDs)-Rhythmic Discharges (RDs) in Anoxic<br />
Encephalopathy<br />
Sushanth Bhat, Sombabu Maganti, Eli S. Neiman, Divya<br />
Gupta and Sudhansu Chokroverty; Edison, NJ<br />
M719 Periodic Lateralizing Epileptiform Discharges<br />
(PLEDs) Causing Persistent Magnetic Resonance<br />
Imaging (MRI) Changes in Ipsilateral Thalamus<br />
Umang Shah, Umer Akber and Chunyang Wang; Camden, NJ<br />
M720 Ammoniacal Encephalopathy Presenting as<br />
Complex Partial Seizure-Like Episodes: A Case Series<br />
Darine Kassar and Stanley Iyadurai; Saint Louis, MO<br />
M721 Status Epilepticus as an Initial Manifestation of<br />
Sneddon’s Syndrome<br />
Anish Shah, Saurav Sen, Jennie Luna and Dipak P. Pandya;<br />
Paterson, NJ<br />
M722 Status Epilepticus Secondary to Milk Alkali<br />
Syndrome Induced by Hypercalcemia (Oral Antacids)<br />
Rabih Kashouty, Noor Yono and Mershed Al Samara;<br />
Manhattan, NY; Manhasset, NY and Southfield, MI<br />
M723 A Case of Magnesium-Responsive Paraneoplastic<br />
Non-Convulsive Status Epilepticus<br />
Robert K. Shin, Anna V. Rosenbaum and Nicholas Frost;<br />
Baltimore, MD<br />
M724 Withdrawn.<br />
Neuromuscular Disease<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 10<br />
M801 Nicotinamide Mononucleotide (NMN) Treatment<br />
of Diabetic Neuropathy<br />
Ankit Sura, Mitch Onken, Krish Chandrasekaran, Helen Chen<br />
and James W. Russell; Baltimore, MD<br />
M802 Defining Outcome Measures in Sporadic IBM for<br />
a Follistatin Gene Transfer Clinical Trial<br />
Linda P. Lowes, Lindsay N. Alfano, Laurence Viollet-<br />
Callendret, Xiomara Q. Rosales, Brian Kaspar, K. Reed Clark,<br />
Zarife Sahenk, Kevin M. Flanigan and Jerry R. Mendell;<br />
Columbus, OH<br />
M803 Tomaculous Formation in HNPP<br />
Jun Li, Zahara M. Jaffer, Xuebao Zhang, Qing Yan, Michael<br />
E. Shy, Ueli Suter, Jonathan Chernoff and Jiasong Guo;<br />
Nashville, TN; Philadelphia; Nashville; Detroit and Zurich,<br />
Swaziland<br />
M804 Zebrafish Models of Amyotrophic Lateral<br />
Sclerosis<br />
Stacey A. Sakowski, J. Simon Lunn, Angela S. Busta, Carey<br />
Backus, Sang Su Oh, James J. Dowling and Eva L. Feldman;<br />
Ann Arbor, MI<br />
M805 ALS-Like Spinal Cord Pathology in Transgenic Mice<br />
with a Mutation in the Valosin-Containing Protein Gene<br />
Hong Z. Yin, Tahseen Mozaffar, Virginia E. Kimonis and<br />
John H. Weiss; Irvine, CA<br />
10<br />
M806 Reevaluating Disease Progression in<br />
Facioscapulohumeral Dystrophy<br />
Jeffrey M. Statland*, William B. Martens, Kathryn R. Wagner,<br />
John Kissel, Shree Pandya, Michael P. McDermott and Rabi<br />
Tawil; Rochester, NY; Baltimore, MD and Columbus, OH<br />
M807 Dysferlin (DYSF) Is Absent from the Muscle-Fiber<br />
Sarcolemma in Various Neuromuscular Diseases, and in<br />
Sporadic Inclusion-Body Myositis (s-IBM) It Forms<br />
Cytoplasmic Inclusions Colocalizing with Amyloid-b42<br />
(Ab42)<br />
Mafalda Cacciottolo, Anna Nogalska, Carla D’Agostino, W<br />
King Engel and Valerie Askanas; Los Angeles, CA<br />
M808 Novel Demonstration of Conformationally-<br />
Modified Tau in Sporadic Inclusion-Body Myositis<br />
(s-IBM) Muscle Fibers. Possible Importance to s-IBM<br />
Pathogenesis<br />
Anna Nogalska, Carla D’Agostino, King W. Engel and Valerie<br />
Askanas; Los Angeles, CA<br />
M809 Anti-Ganglioside Antibodies Mimic CNS<br />
Inhibitors of Axon Regeneration<br />
Kazim Sheikh and Gang Zhang; Houston, TX<br />
M810 Evaluating Mechanoreceptors in Glabrous Skin in<br />
Diabetic Neuropathy<br />
Iliza Myers, Kay Artibee, Jun Li and Amanda C. Peltier;<br />
Nashville, TN<br />
M811 Amiodarone Associated Myopathy. A Report of 4<br />
Cases<br />
Eoin P. Flanagan, Charles M. Harper, Erik K. St. Louis,<br />
Michael H. Silber, Ronald C. Petersen and Keith A. Josephs;<br />
Rochester, MN<br />
M812 Cervical Cord 1 H-Magnetic Resonance Spectroscopy<br />
( 1 H-MRS) in Amyotrophic Lateral Sclerosis (ALS):<br />
Relationship to Clinoco- Electrophysiological Dysfunction<br />
Ken Ikeda, Yasuhiro Yoshii, Kiyoko Murata, Riya Nagata,<br />
Kiyokazu Kawabe, Osamu Kano and Yasuo Iwasaki; Tokyo, Japan<br />
M813 Localization of FIG4 in the Nervous System<br />
Jiasong Guo, Qing Yan and Jun Li; Nashville, TN<br />
M814 High Frequency Chest Wall Oscillation<br />
(HFCWO) in Amyotrophic Lateral Sclerosis (ALS)<br />
Patients Decreases Respiratory Infections Requiring<br />
Antibiotics and/or Hospitalization: A Pre-Post<br />
Observational Study<br />
Benjamin R. Brooks, Velma L. Langford, Amber L. Ward,<br />
Nicole M. Williams, Mindy S. Nichols, Elena Bravver and<br />
Scott C. Lindblom; Charlotte, NC<br />
M815 Dominant Cardiomyopathy and Very Distal<br />
Myopathy with Rod, Myofibrillar and AVSF<br />
Myopathology<br />
Stanley J. Iyadurai, Chris Weihl, Bob Baloh and Alan<br />
Pestronk; St. Louis, MO<br />
M816 Adult-Onset Rod Myopathy Syndrome (AORMS):<br />
Sustained Benefit from IVIG Plus Rituximab<br />
Shalini Mahajan, King W. Engel, Valerie Askanas,<br />
Indermohan Luthra and Varun Gupta; Los Angeles, CA and<br />
Rancho Mirage, CA<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 11<br />
M817 Geographic Trends of ALS in Minnesota<br />
Eric J. Sorenson and Lisa Kronk; Rochester, MN and<br />
Minneapolis, MN<br />
M818 Clinical Features Associated with Fine Specificity<br />
of IgG Anti-GQ1b Antibodies<br />
Susumu Kusunoki, Seiko Suzuki, Masami Ueda and Motoi<br />
Kuwahara; Osaka-Sayama, Osaka, Japan<br />
M819 Amyotrophic Lateral Sclerosis [ALS] Dashboard:<br />
Cognitive, Behavioral, Bulbar, Respiratory, Arm, Leg<br />
Domain-Specific Disease Staging – Statistically<br />
Significant Larger Proportion of Stage 3 Behavioral,<br />
Bulbar, Arm and Leg, but Not Cognitive or Re<br />
Benjamin R. Brooks, Mohammed S. Sanjak, Elena Bravver,<br />
William L. Bockenek, Urvi G. Desai, Scott C. Lindblom,<br />
Thomas J. Paccico, Nicole M. Williams, Mindy S. Nichols,<br />
Amber L. Ward, Kathryn A. Wright, Mifflin O’Neill, Velma<br />
L. Langford, Kristy Walgren, Priscilla Russo, Anne Blythe and<br />
Heather Oplinger; Charlotte, NC<br />
M820 A New Phenotype in Neurodegeneration:<br />
Trigeminal Sensory Deficits Preceding Rostro-Caudal<br />
Progressive Motor and Sensory Neuronopathy, Chorea<br />
and Dementia<br />
Camilo Toro, Justin Y. Kwan, Tanya J. Lehky, Bryan J.<br />
Traynor, Catherine A. Groden, Rena A. Godfrey, Michele E.<br />
Nehrebecky, Wiggs A. Edythe and Gahl William; Bethesda, MD<br />
M821 Update on a Phase 1 Study of ISIS 333611 in<br />
Familial ALS Due to SOD1 Mutations<br />
Timothy M. Miller, Richard Smith, Swati Aggarwal, Alan<br />
Pestronk, William David, Jeffrey Rothstein, Ericka Simpson,<br />
Benjamin Brooks, Isaac Bakst, Patricia Andres, Peggy Allred,<br />
Katie Alexander, Kathie Bishop, C.F. Bennett and Merit<br />
Cudkowicz; St. Louis, MO; La Jolla, CA; Boston, MA;<br />
Baltimore, MD; Houston, TX; Charlotte, NC and<br />
Carlsbad, CA<br />
M822 Retrospective Analysis of a Cohort of Non<br />
Systemic Vasculitic Neuropathy<br />
Raghav Govindarajan, Jagadish B. Agadi, Anita Mahadevan<br />
and S.K. Shankar; Weston, FL and Bangalore, India<br />
M823 Optimizing a Hospital Discharge Database for<br />
Passive Surveillance of Guillain-Barre Syndrome (GBS)<br />
Christopher D. Lee and Timothy F. Jones; Nashville, TN<br />
M824 Gene Expression Analysis in Patients with<br />
Amyotrophic Lateral Sclerosis and Multifocal Motor<br />
Neuropathy<br />
Alexander Shtilbans, Soon Gang Choi, Mary E. Fowkes, Greg<br />
Khitrov, Mona Shahbazi, Jess Ting, Stuart C. Sealfon and<br />
Dale J. Lange; New York, NY<br />
M825 Small-Fiber Polyneuropathy (SFPN) Can Cause<br />
Chronic Pain and Somatic Complaints in Youth<br />
and Anne Louise Oaklander; Boston, MA<br />
M826 Median Nerve Ultrasound in Diabetic PN with<br />
and without Carpal Tunnel Syndrome<br />
Anhar Hassan, Andrea Leep Hunderford, James Watson,<br />
Andrea Boon and Eric Sorenson; Rochester, MN<br />
11<br />
M827 Subacute Paraneoplastic Motor Neuronopathy<br />
with Ri Immunoeactivity and Breast Cancer: A<br />
Clinicopathologically Studied Patient<br />
and David S. Younger; New York, NY<br />
M828 Magnetic Resonance Neurography Versus<br />
Electromyography for the Diagnosis of<br />
Radigulopathy<br />
Youssef A. Dakka, Andrew Biondo, John Corrigan,<br />
Shehanaz Ellik and Ximena Arcilla-Londono;<br />
Detroit, MI<br />
M829 Denervation Causes Lower Expression of Heat<br />
Shock Protein 27 in Regenerating Skeletal Muscle<br />
Takahiro Jimi, Yoshihiro Wakayama and Hajime Hara;<br />
Yokohama, Japan<br />
M830 Rapid Magnetic Stimulation Versus Conventional<br />
Physiotherapy in Bell’s Palsy<br />
Devathasan Gobinathan and Lea Dosado; Singapore,<br />
Singapore<br />
M831 Establishing a Rare Disease Center in China: The<br />
Periodic Paralysis Program<br />
Qing Ke, Benyan Luo, Ming Ming, Michael Hanna, Jacob<br />
Levitt, Barbara Herr and Robert C. Griggs; Hang Zhou, Zhe<br />
Jiang, China; Rochester, NY; London, United Kingdom and<br />
New York, NY<br />
M832 Effect of Fatigue on Pulmonary Function Studies<br />
in ALS Patients<br />
Kathleen S. Alfuth, Ericka P. Simpson and Aparajitha K.<br />
Verma; Houston, TX<br />
M833 Monomelic Amyotrophy – A Rare Case<br />
Presentation<br />
Amtul Farheen, Manpreet Multani, Aiesha Ahmed, Raji<br />
Grewal and Raji Grewal; Edison, NJ<br />
M834 Botulism: A Case Report<br />
Peter Struck, Amtul Farheen and Sushanth Bhat; New<br />
Brunswick and Edison, NJ<br />
M835 A Novel Pentameric Thiophene Derivative<br />
(p-FTAA) Strongly Highlights Clusters of Paired Helical<br />
Filaments Containing Phosphorylated Tau in Sporadic<br />
Inclusion-Body Myositis (s-IBM) Muscle Fibers<br />
Therése Klingstedt, Anna Nogalska, Cristiane Blechschmidt,<br />
Stefan Prokop, Frank L. Heppner, King W. Engel, Valerie<br />
Askanas and Peter K.R. Nilsson; Linköping, Sweden; Los<br />
Angeles and Berlin, Germany<br />
Neurogenetics<br />
M1001 Withdrawn.<br />
M1002 Clinico-Genetic Characterization of a<br />
Large Italian Cohort with Primary Spastic<br />
Paraplegia<br />
Andrea Martinuzzi, Mariateresa Bassi, Grazia D’Angelo,<br />
Sara Bonato, Gabriella Paparella, Olimpia Musumeci,<br />
Mariagiovanna Rossetto, Marianna Fantin, Francesca Peruch,<br />
Alessia Arnoldi, Claudia Crimella, Erika Tenderini, Paolo<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
Bonanni, Vanessa Casanova, Giovanni Meola, Giacomo Comi,<br />
Antonio Toscano and Nereo Bresolin; Conegliano, TV,<br />
Italy; Bosisio Parini, LC, Italy; Messina, Italy and<br />
Milano, Italy<br />
M1003 A Study of ACE and ADD1 Gene Polymorphism<br />
in Extra and Intracranial Atherosclerosis in Patients with<br />
Ischemic Stroke<br />
Jayantee Kalita, Usha K. Misra, Sunil Kumar, Bishwanath<br />
Kumar, Bindu I. Somarajan and Balraj Mittal; Lucknow,<br />
Uttar Pradesh, India<br />
M1004 Generation and Characterization of MeCP2_270<br />
Mutant Mice<br />
Chiranjeevi Bodda, Karolina Can, Liakath Ali Kifayathulla,<br />
Hope Yao Agbemenyah and Ashraf U. Mannan; Goettingen,<br />
Germany<br />
M1005 Identification of Epigenomic Modifications as<br />
Biomarkers for Amyotrophic Lateral Sclerosis<br />
Claudia Figueroa-Romero, Junguk Hur, Yu Hong, John S.<br />
Lunn, Crystal Pacut, Colin E. Delaney, Raymond Yung,<br />
Brian Callaghan and Eva L. Feldman;<br />
Ann Arbor, MI<br />
M1006 A Drosophila Model of Williams Syndrome<br />
Ralph J. Greenspan and Jenee Wagner; La Jolla, CA<br />
M1007 Clinical and Pathological Features of Progressive<br />
Supranuclear Palsy with Family History<br />
Shinsuke Fujioka, Avi Algom, Audrey Strongosky, Dennis W.<br />
Dickson and Zbigniew K. Wszolek; Jacksonville, FL<br />
M1008 Aberrant Methylation by Mutations of DNA<br />
Methyltransferase 1 Cause Peripheral and Central<br />
Axonal Degeneration<br />
Christopher J. Klein, Maria V. Botuyan, Yanhong Wu,<br />
Christopher J. Ward, Garth A. Nicholson, Simon Hammans,<br />
Hiromitch Yamanishi, Adam R. Karpf, Douglas C. Wallace,<br />
Mariella Simon, Cecilie Lander, Julie M. Cunningham,<br />
Glenn E. Smith, William J. Litchy, Benjamin Boes,<br />
Elizabeth J. Atkinson, Sumit Middha, P. James Dyck,<br />
Joseph E. Parisi, Georges Mer, David I. Smith and Peter J.<br />
Dyck; Rochester, MN; Sydney, Australia; Southampton,<br />
United Kingdom; Hyogo, Japan; Buffalo, NY; Irvine, CA;<br />
Herston, Australia and Indianapolis, IN<br />
M1009 Common and Distinct <strong>Association</strong>s of<br />
HLA-DRB1 and -DPB1 Alleles with Neuromyelitis<br />
Optica and Multiple Sclerosis in Japanese<br />
Satoshi Yoshimura, Noriko Isobe, Takuya Matsushita,<br />
Tomomi Yonekawa, Katsuhisa Masaki and Jun-ichi Kira;<br />
Fukuoka, Japan<br />
M1010 Computer Simulations of Striatal Atrophy and<br />
Age at Onset of Huntington’s Disease<br />
Steven D. Edland and Jagan Pillai; La Jolla, CA<br />
Trauma/Injury<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 12<br />
M1101 A Human Natural IgM Drives Axon Outgrowth<br />
Xiaohua Xu, Arthur Warrington, Brent Wright, Allan Bieber,<br />
Virginia Van Keulen, Larry Pease and Moses Rodriguez;<br />
Rochester, MN<br />
12<br />
M1102 Computed Tomography Characteristics of<br />
Pediatric Traumatic Brain Injury<br />
Korak Sarkar and Kia Shahlaie; Sacramento<br />
M1103 <strong>Neurological</strong> Outcome Scale for Traumatic Brain<br />
Injury: Predictive Validity and Sensitivity to Change<br />
Paolo Moretti, Stephen R. McCauley, Elisabeth A. Wilde,<br />
James N. Scott and Guy L. Clifton; Houston, TX and Calgary,<br />
AB, Canada<br />
M1104 Determination of Awareness in Patients with<br />
Severe Brain Injury Using EEG Spectral Analysis<br />
Andrew M. Goldfine, Jonathan D. Victor, Mary M. Conte,<br />
Jonathan C. Bardin and Nicholas C. Schiff; New York, NY<br />
and White Plains, NY<br />
M1105 Orthopedic Injuries in Multiple Sclerosis<br />
Patients: Analysis of the Incidence of Injury in This<br />
Vulnerable Population<br />
Daniel Mandell** and William Tosches; Worcester, MA<br />
M1106 Raising the Dead: Barriers to Therapeutic<br />
Hypothermia Post Cardiac Arrest<br />
and Mark Andrews; Palo Alto, CA<br />
M1107 Abnormal Oculomotor Function among Blast-<br />
Injured Combat Veterans<br />
Bruce P. Capehart, Adam Mehlenbacher, Carol Smith-<br />
Hammond, Dale Bass and James Burke; Durham, NC<br />
Neurology Critical Care<br />
M1201 Withdrawn.<br />
M1202 Predictors of Outcome in Prolonged Refractory<br />
Status Epilepticus<br />
Sara Hocker, Jeffrey W. Britton, Jay Mandrekar, Eelco F.M.<br />
Wijdicks and Alejandro A. Rabinstein; Rochester, MN<br />
M1203 Refractory Status Epilepticus and Heart Damage<br />
– A Warning for Neurologists<br />
Sara Hocker, Jeffrey W. Britton, Jay Mandrekar, Eelco F.M.<br />
Wijdicks and Alejandro A. Rabinstein; Rochester, MN<br />
M1204 Safety and Feasibility of Intrathecal Nicardipine<br />
for Vasospasm after Subarachnoid Hemorrhage<br />
William D. Freeman, Sothear Luke, Christina Campbell, Dan<br />
Jackson and James F. Meschia; Jacksonville, FL<br />
M1205 Acute Bacterial Meningitis as a Possible Cause of<br />
Severe Dysautonomia Leading to Death<br />
Yadira Velazquez-Rodriguez, Umer Akbar and Evren<br />
Burakgazi-Dalkili; Camden, NJ<br />
Pediatric Neurology<br />
M1301 Diffusion Tensor MRI Tractography Reveals<br />
Altered Brainstem Fiber Connections Accompanying<br />
Agenesis of the Corpus Callosum<br />
Juebin Huang, Jian Chen, Haipeng Cai, Robert P. Friedland,<br />
Mohamad Z. Koubeissi, David H. Laidlaw and Alexander P.<br />
Auchus; Jackson, MS; Hattiesburg, MS; Louisville, KY;<br />
Cleveland, OH and Providence, RI<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
M1302 Neurofibromatosis 1 (NF1) Vasculopathy in<br />
Children – An Emerging Entity<br />
Partha S. Ghosh, A.D. Rothner and Manikum Moodley;<br />
Cleveland, OH<br />
M1303 Macro CK-1 a Cause of Spuriously<br />
Elevated CK Associated with Leukoencephalopathy<br />
in an Infant<br />
and John B. Bodensteiner; Phoenix, AZ<br />
M1304 Pharmaceuticals in the Environment: A<br />
Focus on <strong>Neurological</strong> Medications<br />
and Ilene Ruhoy; Seattle, WA<br />
Rehabilitation and Regeneration<br />
M1401 Human Induced Pluripotent Stem<br />
Cell-Derived Neural Progenitor Grafting into<br />
Rat Hippomcapus<br />
Alison L. Althaus, Yu Liu, Duriel Hardy and Jack M. Parent;<br />
Ann Arbor, MI<br />
M1402 Local Molecular Manipulation and Peripheral<br />
Nerve Regeneration<br />
Douglas W. Zochodne, Kimberly J. Christie, Christine A.<br />
Webber, Chu Cheng and Jose A. Martinez; Calgary, AB,<br />
Canada and Edmonton, AB, Canada<br />
M1403 Very Early Gait Training after Acute Stroke; a<br />
Dose-Escalation Study<br />
Randolph S. Marshall, Ying K. Cheung, Clare Bassile, Laura<br />
A. Evensen, Roujie Chen, Veronica Perez, Ronald M. Lazar<br />
and Bernadette Boden-Albala; New York<br />
<strong>136</strong> th Annual Meeting Tuesday,<br />
September 27, 2011<br />
Poster Session<br />
Posters will be displayed in Elizabeth A-E of the<br />
Manchester Grand Hyatt from 10:00 am – 7:00 pm,<br />
with authors present from 6:00 pm – 7:00 pm.<br />
NOTE: An asterisk designates a resident/fellow travel award<br />
winner. Two asterisks represent a medical student travel award<br />
winner.<br />
Dementia and Aging<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 13<br />
T1501 Amyloid-Beta Dynamics and Prevention Trials in<br />
Dominantly Inherited Alzheimer’s Disease<br />
Randall J. Bateman and on behalf of the Dominantly<br />
Inherited Alzheimer Network; St. Louis, MO<br />
T1502 Integrating Genome-Wide <strong>Association</strong> and<br />
Functional Validation To Understand Susceptibility for<br />
Alzheimer’s Pathology<br />
Joshua M. Shulman, Portia I. Chipendo, Lori B. Chibnik,<br />
Brendan T. Keenan, Dong Tran, Matthew A. Huentelman,<br />
Julie A. Schneider, Eric M. Reiman, Denis A. Evans, David<br />
A. Bennett, Mel B. Feany and Philip L. De Jager; Boston,<br />
MA; Chicago, IL and Phoenix, AZ<br />
T1503 Brain Expression Genome-Wide <strong>Association</strong><br />
Study (eGWAS) and Alzheimer’s Disease<br />
Nilufer Ertekin-Taner, Fanggeng Zou, High Seng Chai,<br />
Curtis S. Younkin, Julia Crook, V Shane Pankratz,<br />
13<br />
Mariet Allen, Minerva M. Carrasquillo, Christopher N.<br />
Rowley, Otto Pedraza, Morad Ansari, Caroline Hayward,<br />
Igor Rudan, Harry Campbell, Ozren Polasek, Nicholas D.<br />
Hastie, Asha A. Nair, Sumit Middha, Sooraj Maharjan,<br />
Thuy Nguyen, Li Ma, Kimberly G. Malphrus, Ryan Palusak,<br />
Sarah Lincoln, Gina Bisceglio, Constantin Georgescu,<br />
Christopher P. Kolbert, Jin Jen, Zbigniew Wszolek, Maria<br />
Barcikowska, Sigrid B. Sando, Jan Aasly, Kevin Morgan,<br />
Clifford Jack, Ronald C. Petersen, Neill R. Graff-Radford,<br />
Alan Wright, Dennis W. Dickson and Steven G. Younkin;<br />
Jacksonville, FL; Rochester, MN; Edinburgh, United<br />
Kingdom; Split, Croatia; Zagreb, Croatia; Warsaw,<br />
Poland; Trondheim, Norway and Nottingham,<br />
United Kingdom<br />
T1504 Insulin-Like Growth Factor 1 (IGF-1) and Risk<br />
of Alzheimer’s Disease: The Framingham Study<br />
Andrew J. Westwood*, Alexa S. Baiser, Ramachandran S.<br />
Vasan, Tamara B. Harris, Ronenn Roubenoff, Aleksandra<br />
Pikula, Rhoda Au, Charles DeCarli, Philip A. Wolf and<br />
Sudha Seshadri; Boston, MA; Framingham, MA; Bethesda,<br />
MD and Sacremento, CA<br />
T1505 Components of Blood Pressure and Progression<br />
of Cerebral Leukoaraiosis: The ARIC Study<br />
Rebecca F. Gottesman, Diane J. Catellier, Laura H. Coker,<br />
Josef Coresh, Clifford R. Jack, Jr., David S. Knopman,<br />
Kathryn M. Rose, A. Richey Sharrett, Dean K. Shibata and<br />
Thomas H. Mosley; Baltimore, MD; Chapel Hill, NC;<br />
Winston-Salem, NC; Rochester, MN; Durham, NC; Seattle,<br />
WA and Jackson, MS<br />
T1506 Therapeutic and Preventive Effects of a Novel<br />
AD Vaccine<br />
Carmen Vigo, Ivan Cuevas, Lucia Fernandez, Valter<br />
Lombardi, Richard Manivanh and Ramon Cacabelos;<br />
Sunnyvale, CA and Bergondo, La Coruna, Spain<br />
T1507 MoCA vs. MMSE: Patterns of Cognitive<br />
Performance across Adult Lifespan in a Non-Clinical<br />
Sample<br />
Shea Gluhm, Charles Van Liew, Jody Goldstein, Guerry Peavy,<br />
Mark Jacobson, Stephanie Lessig and Jody Corey-Bloom; La<br />
Jolla, CA and San Diego, CA<br />
T1508 Amyloid Imaging with Florbetapir-PET<br />
Correlates with Cognitive Performance in Non-<br />
Demented Oldest-Old<br />
Maria M. Corrada, Dana E. Greenia, Chris M. Clark, Carrie<br />
B. Peltz, Mark A. Mintun, Michael J. Pontecorvo, Abhinay D.<br />
Joshi and Claudia H. Kawas; Irvine, CA; Philadelphia, PA<br />
and St. Louis, MI<br />
T1509 FRET Measurements of Ab-Induced Glutamate<br />
Release from Astrocytes<br />
Sara Sanz-Blasco, Juan C. Piña-Crespo, Maria V. Talantova<br />
and Stuart A. Lipton; La Jolla, CA<br />
T1510 Is Poststroke Dementia Related to Amyloid<br />
Deposition and Microglia Activation?<br />
Wolf-Dieter Heiss, Basia Radlinska, Jean-Paul Soucy, Ralf<br />
Schirrmacher, Alexander Thiel and Vladimir Hachinski;<br />
Cologne, Germany; Montreal, QC, Canada and London, ON,<br />
Canada<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 14<br />
T1511 Cycad Methylazoxymethanol Linked to DNA<br />
Damage, Cancer and Neurodegeneration<br />
Glen E. Kisby, Rebecca C. Fry, Michael R. Lasarev, Theodor<br />
K. Bammler, Richard P. Beyer, Mona I. Churchwell, Daniel R.<br />
Doerge, Lisiane B. Meira, Valerie S. Palmer, Ana-Luisa<br />
Ramos-Crawford, Xuefeng Ren, Robert S. Sullivan, Terrance J.<br />
Kavanagh, Leona D. Samson, Helmut Zarbl and Peter S.<br />
Spencer; Portland, OR; Seattle, WA; Cambridge, MA;<br />
Jefferson, AR; Guildford, Kent, United Kingdom; Buffalo, NY;<br />
Piscataway, NJ and Chapel Hill, NC<br />
T1512 Genetic <strong>Association</strong>s between VPS10 Receptor<br />
Genes and Late-Onset Alzheimer’s Disease<br />
Christiane Reitz, Joseph Lee, Lindsay Farrer, Margaret Pericak-<br />
Vance, Jonathan Haines, Ekaterina Rogaeva, Peter St. George-<br />
Hyslop and Richard Mayeux; New York; Boston; Miami;<br />
Nashville and Toronto, Canada<br />
T1513 Cardiac Ejection Fraction, Cognitive Function<br />
and Leukoaraiosis in an Elderly Cohort: The<br />
Cardiovascular Health Study<br />
Rebecca F. Gottesman, Salvador Cruz-Flores, Annette<br />
Fitzpatrick, John Gottdiener, Traci Bartz, Richard Kronmal<br />
and W.T. Longstreth, Jr.; Baltimore, MD; St. Louis, MO and<br />
Seattle, WA<br />
T1514 Predicting MCI Outcome with Clinically<br />
Available MRI and CSF Biomarkers<br />
David S. Heister, James B. Brewer, Sebastian Magda, Kaj<br />
Blennow and Linda K. McEvoy; La Jolla, CA and Mölndal,<br />
Sweden<br />
T1515 Light and Electron Microscopic Analysis of FUS<br />
Immunoreactivity in 3 Variants of Tau and TDP-43<br />
Negative Frontotemporal Lobar Degeneration<br />
Keith A. Josephs, Wen-Lang Lin, Joseph E. Parisi, Neil Graff-<br />
Radford, Ronald C. Petersen and Dennis W. Dickson;<br />
Rochester, MN and Jacksonville, FL<br />
T1516 Effects of Once-Daily, Extended-Release<br />
Memantine (28 mg/day) on Cognitive Domains in<br />
Patients with Moderate to Severe Alzheimer’s Disease<br />
Michael Tocco, Suzanne Hendrix, Michael L. Miller, Vojislav<br />
Pejovic and Stephen M. Graham; Jersey City, NJ; Salt Lake<br />
City, UT and Chicago, IL<br />
T1517 Efficacy of Memantine by Baseline Disease<br />
Severity: A Pooled Post-Hoc Analysis of Trials in Mild to<br />
Moderate Alzheimer’s Disease<br />
Michael Tocco, Suzanne Hendrix, Michael L. Miller, Vojislav<br />
Pejovic and Stephen M. Graham; Jersey City, NJ; Salt Lake<br />
City, UT and Chicago, IL<br />
T1518 Clinical Gait Abnormalities and Hippocampal<br />
Morphometry in MCI: Preliminary Results from the<br />
ADNI Study<br />
Vincent S. DeOrchis and Joe Verghese; Bronx, NY<br />
T1519 Topography of Cortical Thinning in<br />
PIB-Negative Subcortical Vascular Dementia<br />
Versus Alzheimer’s Disease<br />
Chi Hun Kim, Sang Won Seo, Sung Tae Kim, Jae-Hong Lee,<br />
Jae Seung Kim, Seung Jun Oh, Suk-Hui Kim, Hae Kwan<br />
Cheong, Jong-Min Lee, Seun Jeon and Duk L. Na; Seoul,<br />
Korea and Suwon, Korea<br />
14<br />
T1520 The First Nationwide Survey of Bardet-Biedl<br />
Syndrome in Japan<br />
Makito Hirano, Toshihide Yamashita, Yasushi Ikuno, Hiromi<br />
Iwahashi, Mitsuru Ohishi, Toshiyuki Mano, Ryu Ishihara, Ichiro<br />
Tanaka, Keiko Yanagihara, Yusaku Nakamura and Susumu<br />
Kusunoki; Sakai, Osaka, Japan; Suita, Japan; Izumi, Japan;<br />
Osaka, Japan; Kashihara, Japan and Osaka Sayama, Japan<br />
T1521 P600 Word Repetition Effect Amplitude<br />
Correlates with Left Hippocampal Volume<br />
John M. Olichney, Rawi Nanakul, Alireza K. Javan, Patrick<br />
E. Adams, Andrea Schneider, Andreea Seritan, Randi J.<br />
Hagerman, Paul J. Hagerman and Susan M. Rivera; Davis,<br />
CA and Sacramento, CA<br />
T1522 Visuospatial Construction Measures and Their<br />
Utility in Identifying Dementia of the Alzheimer’s Type<br />
Bonnie M. Scott, G. Duncan, H. Carlson, Matthew Nance,<br />
Michele K. York, Angela Larery, Josephine Stouter and Adriana<br />
M. Strutt; Houston, TX<br />
T1523 Responder Analysis in a Trial of Once-Daily,<br />
Extended-Release Memantine (28 mg) in Patients with<br />
Moderate to Severe Alzheimer’s Disease<br />
Stephen M. Graham, Suzanne Hendrix, Michael L. Miller,<br />
Vojislav Pejovic and Michael Tocco; Jersey City, NJ; Salt Lake<br />
City, UT and Chicago, IL<br />
T1524 Rates of Cognitive Decline and Alzheimer’s<br />
Disease (AD) Neuropathology in Oldest-Old<br />
Archana B. Balasubramanian, Claudia H. Kawas, Daniel J.<br />
Berlau, Carrie B. Peltz and María M. Corrada; Irvine, CA<br />
T1525 Cortical Thickness on MR Imaging: Relation to<br />
Cognitive Reserve in Normal Aging and Mild Cognitive<br />
Impairment<br />
Jagan A. Pillai, Linda K. McEvoy, Donald J. Hagler, Jr,<br />
Dominic Holland, Anders M. Dale, David P. Salmon, Douglas<br />
Galasko and Christine Fennema-Notestine; San Diego, CA<br />
T1526 Effects of Once-Daily, Extended-Release<br />
Memantine on Individual Activities of Daily Living in<br />
Patients with Moderate to Severe Alzheimer’s Disease<br />
Michael Tocco, Suzanne Hendrix, Michael L. Miller, Vojislav<br />
Pejovic and Stephen M. Graham; Jersey City, NJ; Salt Lake<br />
City, UT and Chicago, IL<br />
T1527 Neurophysiologic Markers of Aging-Related<br />
Muscle Weakness<br />
Ela B. Plow, Dina Gohar, Mehmed B. Bayram, Jing Hou,<br />
Alexandria Wyant, Yin Fang, Vlodek Siemionow and Guang<br />
H. Yue; Cleveland, OH<br />
T1528 The Purkinje Cell of the Cerebellar Cortex in<br />
Alzheimer’s Disease<br />
and Stavros J. Baloyannis; Thessaloniki, Greece<br />
T1529 A Translational Program of BDNF Gene Delivery<br />
for Alzheimer’s Disease<br />
Mark H. Tuszynski, Alan Nagahara, Adrian P. Kells, J.<br />
Bringas, John Forsayeth and Krystopf S. Bankiewicz; La Jolla,<br />
CA and San Francisco, CA<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
T1530 Imaging Signatures of Pathology in Behavioral<br />
Variant Frontotemporal Dementia<br />
Jennifer L. Whitwell, Clifford R. Jack, David S. Knopman,<br />
Bradley F. Boeve, Ronald C. Petersen, Joseph E. Parisi, Dennis<br />
W. Dickson and Keith A. Josephs; Rochester, MN and<br />
Jacksonville, FL<br />
T1531 Improved Statistical Power To Detect Treatment<br />
Effects on Functional Outcomes in Alzheimer’s Disease<br />
(AD) Clinical Trials by Item-Response Theory (IRT)<br />
M. Colin Ard, Douglas R. Galasko and Steven D. Edland; La<br />
Jolla, CA<br />
T1532 Neuropathologic Basis of Age-Associated Brain<br />
Atrophy<br />
Deniz Erten-Lyons, Randy Woltjer, Hiroko Dodge, Lisa Silbert<br />
and Kaye Jeffrey; Portland, OR<br />
T1533 A Long-Term, Open-Label Extension Study<br />
Evaluating the Safety of Extended-Release Memantine<br />
(28 mg) in Patients with Moderate to Severe Alzheimer’s<br />
Disease<br />
Stephen M. Graham and James Perhach; Jersey City, NJ<br />
T1534 A Retrospective Analysis Using Data-Monitoring<br />
Algorithms: What Are the Logical Relationships between<br />
the ADAS-Cog and MMSE?<br />
Christian Yavorsky, Guillermo DiClemente, Mark Opler, Sofija<br />
Jovic, Brian Rothman and Ashleigh DeFries; New York, NY<br />
T1535 Withdrawn.<br />
T1536 Case of Bimodal Charles Bonnet Syndrome and<br />
Dementia<br />
Mirret El-Hagrassy and Gokhan Akfirat; New York, NY<br />
T1537 Lead Exposure Up-Regulated Autophagy<br />
Response in Neuroblastoma SH-SY5Y Cells Via mTOR<br />
Kinase Signaling Pathway<br />
Shun-Sheng Chen, Chueh-Tan Chen and Jiin-Tsuey Cheng;<br />
Kaohsiung, Taiwan<br />
Headache and Pain<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 15<br />
T1601 Withdrawn.<br />
T1602 OnbotulinumtoxinA for the Treatment of<br />
Chronic Migraine: Long-Term Outcome<br />
Hanlon T. Christopher, Silvia M. Weibelt,<br />
Diane C. Andress-Rothrock and John F. Rothrock;<br />
Birmingham, AL<br />
T1603 Utility of Orally-Inhaled Dihydroergotamine<br />
When Early Intervention Is Impractical<br />
Shashidhar Kori, Stewart Tepper, Peter J. Goadsby,<br />
Paul Winner, Min Wang and Stephen Silberstein;<br />
Mountain View; Cleveland; San Francisco;<br />
West Palm Beach and Philadelphia<br />
T1604 Characterization of Intraepidermal Nerve<br />
Fiber Morphology in Pain Associated with Diabetic<br />
Neuropathy and Impaired Glucose Tolerance<br />
Hsinlin T. Cheng, Jacqueline R. Dauch, Gordon A. Smith,<br />
Robinson J. Singleton, Brandon M. Yanik and Eva L.<br />
Feldman; Ann Arbor, MI and Salt Lake City, UT<br />
15<br />
T1605 Heavily T2-Weighted Magnetic Resonance<br />
Myelography for Post-Lumbar Puncture Headache:<br />
A Pilot Study<br />
Yen-Feng Wang, Jong-Ling Fuh, Jiing-Feng Lirng and<br />
Shuu-Jiun Wang; Taipei, Taiwan<br />
T1606 Angioplasty and Stenting for the Treatment of<br />
Idiopathic Intracranial Hypertension Associated with<br />
Dural Venous Sinus Stenosis<br />
Parisa P. Javedani**, Jeremy D. Fields, Kenneth C. Liu,<br />
Stanley L. Barnwell and Bryan Petersen; Portland, OR and<br />
Charlottesville, VA<br />
T1607 Adrenal Insufficiency Presenting as Postural<br />
Tachycardia Syndrome<br />
Darine Kassar and Stanley Iyadurai; Saint Louis, MO<br />
T1608 Prevalence of Chronic Migraine (CM), Headache-<br />
Related Disability and Sociodemographic Factors in the<br />
US Population: Results from the <strong>American</strong> Migraine<br />
Prevalence and Prevention (AMPP) Study<br />
Dawn C. Buse, Michael L. Reed, Kristina Fanning,<br />
Aubrey N. Manack, Catherine C. Turkel and<br />
Richard B. Lipton; Bronx, NY; Chapel Hill, NC and<br />
Irvine, CA<br />
T1609 Chronic Low Dose Methadone for the<br />
Suppression of Treatment-Refractory Chronic Migraine<br />
Keyvani Madjid and John F. Rothrock; San Diego, CA and<br />
Birmingham, AL<br />
T1610 Relationship between High Frequency Nausea<br />
and Treatment Satisfaction in Episodic Migraine (EM):<br />
Results of the <strong>American</strong> Migraine Prevalence and<br />
Prevention (AMPP) Study<br />
Richard B. Lipton, Michael L. Reed, Kristina M. Fanning and<br />
Dawn C. Buse; Bronx, NY and Chapel Hill, NC<br />
T1611 Frequent Nausea in Episodic Migraine (EM) Is<br />
Common and Associated with Increased Burden: Results<br />
from the <strong>American</strong> Migraine Prevalence and Prevention<br />
(AMPP) Study<br />
Dawn C. Buse, Michael L. Reed, Kristina M. Fanning and<br />
Richard B. Lipton; Bronx, NY and Chapel Hill, NC<br />
T1612 Medical Consultation and Headache-Impact<br />
among Persons with Chronic Migraine (CM) and<br />
Episodic Migraine (EM): Results from the <strong>American</strong><br />
Migraine Prevalence and Prevention (AMPP) Study<br />
Aubrey N. Manack, Dawn C. Buse, Daniel Serrano, Sepideh<br />
F. Varon, Catherine C. Turkel and Richard B. Lipton; Irvine,<br />
CA; Bronx, NY and Chapel Hill, NC<br />
T1613 Unmet Treatment Needs among Episodic<br />
Migraineurs (EM): Results of the <strong>American</strong> Migraine<br />
Prevalence and Prevention Study (AMPP)<br />
Richard B. Lipton, Dawn C. Buse, Daniel Serrano, Daisy S.<br />
Ng-Mak, Starr H. Pearlman and Michael Reed; Bronx, NY;<br />
Chapel Hill, NC; West Point, PA and Savannah, GA<br />
T1614 <strong>Association</strong> between Triptan Use and Cardiac<br />
Contraindications in Migraine<br />
Daisy S. Ng-Mak, Valerie P. Pracilio, Stephen Silberstein,<br />
Joseph Couto, Cary Sennett, Mary Hopkins, Jon Bumbaugh<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 16<br />
and Neil Goldfarb; West Point, PA; Philadelphia, PA and<br />
Bowie, MD<br />
T1615 ‘‘Let-Down Headache’’: Reductions in Stress and<br />
Improvement in Mood Predict Headaches in Persons<br />
with Migraine<br />
Dawn C. Buse, Sheryl R. Haut, Charles Hall, Howard<br />
Tennen, Tiffani DeFreitas, Thomas M. Borkowski and<br />
Richard B. Lipton; Bronx, NY and Storrs, CT<br />
T1616 Assessing the Consistency of LEVADEX TM<br />
(MAP0004, Orally Inhaled Dihydroergotamine)<br />
Pharmacokinetic Parameters in Healthy Volunteers:<br />
Results from 3 Clinical Studies<br />
Amy Forst, Julie Iwashita, Don Kellerman, Shashidhar Kori,<br />
Tracy Thomas and Glyn Taylor; Mountain View;<br />
Merthyr Tydfil, United Kingdom and Radyr,<br />
United Kingdom<br />
T1617 Migraine Recurrence Rates with Acute Treatment:<br />
Case for Standardizing the Definition<br />
Stewart Tepper, Shashidhar Kori, Peter J. Goadsby, Michel<br />
Ferrari, Richard Lipton, Scott Borland, Min Wang and David<br />
Dodick; Cleveland; Mountain View; San Francisco; Leiden,<br />
Netherlands; Bronx and Scottsdale<br />
T1618 Transdermal Sumatriptan for Acute Treatment of<br />
Migraine<br />
and Jerome Goldstein; San Francisco, CA<br />
T1619 Dejerine Roussy Syndrome in a Patient with<br />
Sneddon’s Syndrome as an Initial Manifestation<br />
Jennie Luna, Anish Shah, Sourav Sen and Dipak P. Pandya;<br />
Paterson, NJ<br />
T1620 Valproate-Responsive Subclinical Rhythmic<br />
Electrographic Disharges (SREDA) in a Migraineur<br />
Umer Akbar, Bhavpreet Dham, Evren Burakgazi and John<br />
Kelly; Camden, NJ and Washington<br />
T1621 Utriculo-Ocular Counterroll Reflex Disruption in<br />
Skew Deviation<br />
James A. Sharpe, Manokaraananthan Chandrakumar, Alan<br />
Blakeman, Herbert C. Goltz and Agnes M. Wong; Toronto,<br />
ON, Canada<br />
T1622 Superior Semicircular Canal Dehiscence (SSCD)<br />
and Osteoporosis in Elderly Asian Women<br />
Alexander Yu, Douglas L. Teich and Eric T. Wong; Boston,<br />
MA<br />
Neuroimmunology and Demyelinating Disease<br />
T1701 Antibodies to Metabotropic Glutamate Receptors<br />
in Ophelia Syndrome and Cerebellitis<br />
Eric Lancaster, Eugenia Martinez-Hernandez, Maarten J.<br />
Titulaer, Sarah Wong, Jian Xu, Anis Contractor, Rita Balice-<br />
Gordon and Josep Dalmau; Philadelphia, PA and Chicago, IL<br />
T1702 Mortality Outcomes for Interferon Beta-1b<br />
Versus Placebo 21 Years Following Randomization<br />
Douglas S. Goodin, Anthony T. Reder, George Ebers, Gary<br />
Cutter, Marcelo Kremenchutzky, Joel Oger, Mark Rametta,<br />
Karola Beckmann and Volker Knappertz; San Francisco, CA;<br />
16<br />
Chicago, IL; Oxford, United Kingdom; Birmingham, AL;<br />
London, ON, Canada; Vancouver, BC, Canada; Wayne, NJ;<br />
Berlin, Germany and Montville, NJ<br />
T1703 A Recombinant Human Neuron-Binding IgM<br />
Protects Spinal Cord Axons and Improves Motor<br />
Function in a Murine Model of Multiple Sclerosis<br />
Aleksandar Denic*, Slobodan Macura, Arthur E. Warrington,<br />
Istvan Pirko, Brandon R. Grossardt, Larry R. Pease and Moses<br />
Rodriguez; Rochester, MN<br />
T1704 Neuroprotection Mediated through Estrogen<br />
Receptor Alpha in Astrocytes<br />
Rory Spence, Mary Hamby, Elizabeth Umeda, Noriko Itoh,<br />
Sienmi Du, Galyna Bondar, Michael Sofroniew and Rhonda<br />
Voskuhl; Los Angeles, CA<br />
T1705 Genesis of Astrogliosis in an Autoimmune Model<br />
of Multiple Sclerosis<br />
Fuzheng Guo, Yoshiko Maeda, Joyce Ma, Monica Delgado and<br />
David Pleasure; Sacramento, CA<br />
T1706 Distinct Features of Neuromyelitis Optica<br />
According to Anti-Aquaporin-4 Antibody IgG Subclass<br />
Noriko Isobe, Tomomi Yonekawa, Takuya Matsushita, Yuji<br />
Kawano, Katsuhisa Masaki, Satoshi Yoshimura and Jun-ichi<br />
Kira; Fukuoka, Japan and Matsuyama, Japan<br />
T1707 Effect of Fingolimod on Relapse Rate by Prior<br />
Treatment Status and Reason for Discontinuation:<br />
FREEDOMS Subgroup Analyses<br />
Marcelo Kremenchutzky, Paul O’Connor, Reinhard Hohlfeld,<br />
Ernst-Wilhelm Radue, Ludwig Kappos, Lixin Zhang-Auberson,<br />
Dieter A. Häring, Philipp von Rosenstiel, Xiangyi Meng and<br />
Augusto Grinspan; London, ON, Canada; Toronto, ON,<br />
Canada; Munich, Germany; Basel, Switzerland and East<br />
Hanover, NJ<br />
T1708 Effect of Fingolimod on Relapse Rate by Prior<br />
Treatment Status and Reason for Discontinuation:<br />
TRANSFORMS Subgroup Analyses<br />
Bhupendra O. Khatri, Jean Pelletier, Ludwig Kappos, Hans-<br />
Peters Hartung, Giancarlo Comi, Frederik Barkhof, Jeffrey<br />
Cohen, Tracy Stites, Xiangyi Meng and Augusto Grinspan;<br />
Milwaukee, WI; Marseille, France; Basel, Switzerland;<br />
Dusseldorf, Germany; San Raffaele, Milan, Italy; Amsterdam,<br />
Netherlands; Cleveland, OH and East Hanover, NJ<br />
T1709 Safety Overview of Fingolimod in Relapsing<br />
Multiple Sclerosis: Phase 2 and 3 Studies<br />
Jeffrey A. Cohen, Ludwig Kappos, Gordon Francis, William<br />
Collins, Lixin Zhang-Auberson and Dejun Tang; Cleveland,<br />
OH; Basel, Switzerland and East Hanover, NJ<br />
T1710 Fingolimod Mechanism of Action (MOA) in<br />
Multiple Sclerosis (MS)<br />
Jerold Chun and Jeffery A. Cohen; La Jolla, CA and<br />
Cleveland, OH<br />
T1711 Antibodies to the VGKC-Complex Proteins LGI1<br />
and CASPR2 in Acquired Neuromyotonia<br />
Camilla Buckley, Philippa Pettingill, Rosie Pettingill, Matthew<br />
Kiernan, Osamu Watanabe, Sarosh Irani, Patrick Waters and<br />
Angela Vincent; Oxford, United Kingdom; Sydney, Australia<br />
and Kagoshima, Japan<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
T1712 Withdrawn.<br />
T1713 <strong>Association</strong> of MS Susceptibility Variants and<br />
Early Attack Location<br />
Ellen M. Mowry, Jean Pelletier, Maria R. Blasco, Pierre Duquette,<br />
Pablo Villoslada, Pierre-Antoine Gourraud, Irina Malikova,<br />
ChristophePicard,JamieMcDonald,ElaineRoger,StacyCaillier<br />
and Emmanuelle Waubant; San Francisco; Marseille, France;<br />
Madrid, Spain; Montreal, Canada and Pamplona, Spain<br />
T1714 Osmotic Demyelination Syndrome: Lack of<br />
<strong>Association</strong> between Outcome and Severity of<br />
Hyponatremia<br />
Jennifer E. Fugate*, Jonathan Graff-Radford and Alejandro A.<br />
Rabinstein; Rochester, MN<br />
T1715 Correlation of Brain Atrophy, Disability and<br />
Spinal Cord Atrophy in a Murine Model of MS<br />
M Mateo Paz Soldan, Jeffrey D. Gamez, Aaron J. Johnson,<br />
Anne K. Lohrey, Yi Chen and Istvan Pirko; Rochester, MN<br />
and Cincinnati, OH<br />
T1716 Anti-NMDA-Receptor Encephalitis: Clinical<br />
Analysis of 457 Patients<br />
Maarten J. Titulaer, Eugenia Martinez-Hernandez, Lindsey<br />
McCracken, Rita Balice-Gordon and Josep Dalmau;<br />
Philadelphia, PA and Barcelona, Spain<br />
T1717 Cigarette Smoke Induces Inflammation and<br />
Oxidative Stress in Brains of Lewis Rats<br />
Ashwani Khanna and Walter Royal, III; Baltimore, MD<br />
T1718 Withdrawn.<br />
T1719 Differential Sensitivity of Human PBMC Subsets<br />
to Alemtuzumab-Mediated Cytotoxicity<br />
William Siders, Sambasiva Rao, Juanita Campos-Rivera, Jose<br />
Sancho, Paula Boutin, Peter Severy, Johanne Kaplan, Bruce<br />
Roberts and Srinivas Shankara; Framingham, MA<br />
T1720 Transcriptional Profiles Uncover Population<br />
Structure among Multiple Sclerosis Patients<br />
Linda Ottoboni, David Hafler, Howard Weiner and<br />
Philip De Jager; Boston, MA and New Haven, CT<br />
T1721 Analysis of Immune Competence Following<br />
Alemtuzumab Treatment in huCD52transgenic Mice<br />
William Siders, Nathalie Chretien, Michael LaMorte, Bruce<br />
Roberts and Johanne Kaplan; Framingham, MA<br />
T1722 Withdrawn.<br />
T1723 Withdrawn.<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 17<br />
T1724 A Single Dose Escalation Study of the Safety,<br />
Pharmacokinetics, and Pharmacodynamics of<br />
Subcutaneous Pegylated Interferon-Beta in Healthy<br />
Volunteers<br />
Kenneth Grabstein, Aijun Wang, Natalie Winblade Nairn and<br />
Daniel J. Burge; Seattle, WA<br />
17<br />
T1725 Regulation of IL-12 by IL-23 in Bone Marrow<br />
Dendritic Cells<br />
Farinaz Safavi, Patricia Gonnella, Bogojub Ciric,<br />
Abdolmohamad Rostami and Farinaz Safavi; Philadelphia, PA<br />
T1726 Clinically Apparent MRI Activity Predicts 2-Year<br />
Outcomes in Patients with RRMS<br />
Thomas Scott, Xiaojun You and Pamela Foulds; Pittsburgh,<br />
PA and Weston, MA<br />
T1727 The Correlation of Brain MRI Lesion Load with<br />
Functional Outcome in Animal Models of MS<br />
Istvan Pirko, Jeffrey Gamez, Moses Rodriguez, Mihajlo<br />
Babovic and Slobodan I. Macura; Rochester, MN and<br />
Northfield, MN<br />
T1728 Comparison of CIDP Patients with Normal and<br />
Elevated CSF Protein<br />
YuanYuan Xue and Ericka P. Simpson; Houston, TX<br />
T1729 Are Anti-TAG-1 Autoantibodies Markers in<br />
Autoimmune Demyelinating Disorders of the PNS and<br />
CNS?<br />
Harry Alexopoulos, Pantelis P. Pavlakis, Domna Karagogeos,<br />
Clementine E. Karageorgiou and Marinos C. Dalakas; Athens,<br />
Greece and Heraklion, Greece<br />
T1730 Introduction and Diffusion of Multiple Sclerosis<br />
in the United States<br />
Mitchell T. Wallin and John F. Kurtzke; Washington, DC<br />
T1731 Withdrawn.<br />
T1732 Withdrawn.<br />
T1733 The Relationship between Conduction Block and<br />
Clinical Characteristics in Guillain-Barré Syndrome with<br />
Anti-GM1/GalNAc-GD1a Antibodies<br />
Go Ogawa, Ken-ichi Kaida, Susumu Kusunoki,<br />
Motoi Kuwabara, Fumihiko Kimura and Keiko Kamakura;<br />
Tokorozawa, Saitama, Japan and Osaka-Sayama,<br />
Osaka, Japan<br />
T1734 Withdrawn.<br />
T1735 Randomized, Open-Label Study To Evaluate<br />
Patient-Reported Outcomes (PRO) with Fingolimod<br />
after Changing from Prior Disease-Modifying Therapy<br />
(DMT) for Relapsing Multiple Sclerosis (MS): EPOC<br />
Study Rationale and Design<br />
Luigi M. Barbato, Lesley Schofield, Kevin McCague, Linda<br />
Pestreich, Kathy Tobias and Manoj Malhotra; East Hanover, NJ<br />
T1736 Novel Diagnostic Tool for MS<br />
Nancy L. Monson, Ann J. Ligocki, William H. Rounds,<br />
Diane Xiang, Lindsay G. Cowell, Doug Bigwood, Eric<br />
Eastman, Jeffrey L. Bennett, Scott D. Boyd, Andrew Z.<br />
Fire, Elliot M. Frohman and Benjamin M. Greenberg;<br />
Dallas, TX; Gaithersburg, MD; Denver, CO and<br />
Palo Alto, CA<br />
T1737 Efficacy of Combination Therapy in Marburg<br />
Variant Type of Multiple Sclerosis<br />
Jennifer Gabbard, Yasmin Bilal and Dipak Pandya; Paterson,<br />
NJ<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
T1738 Coma as an Inital Manifestation of Acute<br />
Disseminated Encephalomyelitis<br />
Megan McGarry, Natasha Tilluckdharry and Dipak P.<br />
Pandya; Paterson, NJ<br />
T1739 NMO-IgG in a Patient with Neurosarcoidosis<br />
Lena Derani** and Elham Bayat; Washington, DC<br />
T1740 Correlates of Dietary Intake in Individuals with<br />
Multiple Sclerosis<br />
Matthew A. Plow, Marcia Finlayson and Chi Cho; Cleveland,<br />
OH and Chicago, IL<br />
Neurooncology<br />
J_ID: ZAY Customer A_ID: SUPP11-3 Cadmus Art: 22575 Date: 31-August-11 Stage: Page: 18<br />
T1801 Comparative Uptake and Cytotoxicity of Anti-Hu<br />
and Anti-Ri Antibodies in Rat Cerebellar Slice Cultures<br />
John E. Greenlee, Susan A. Clawson, Blair Wood, Kenneth E.<br />
Hill and Noel G. Carlson; Salt Lake City, UT<br />
T1802 Cerebrospinal Fluid Chemokine/Cytokine<br />
Biomarkers for Melanoma Brain Metastasis<br />
Edwin Lok, Amy S. Chung, Szexian Lee, Tamar Melman,<br />
Kenneth D. Swanson and Eric T. Wong; Boston, MA<br />
T1803 Role of p75NTR and Its Signaling Pathways in<br />
Fenretinide (4-hydroxyphenyl Retinamide – 4HPR)<br />
Induced Apoptosis in Neuroblastoma Cells<br />
Veena R. Ganeshan and Nina F. Schor; Rochester, NY<br />
T1804 Relationship between Brain MRI Imaging<br />
Parameters and Molecular Biomarkers as Prognostic<br />
Indicators in Glioblastoma Multiforme<br />
Xiao-Tang Kong, Senxi Du, Beverly D. Fu, Mark E. Linskey<br />
and Daniela Bota; Orange, CA and Irvine, CA<br />
T1805 Secondary Intramedullary Spinal Cord Non-<br />
Hodgkin’s Lymphoma<br />
Eoin P. Flanagan, Brian P. O’Neill, Thomas M. Habermann<br />
and B. Mark Keegan; Rochester, MN<br />
T1806 Case Report: Optic Neuropathy in a Patient with<br />
Glioblastoma Receiving Bevacizumab<br />
Robert A. Fishman, Lara Kunschner and Erik Happ;<br />
Pittsburgh, PA<br />
T1807 Anti-Ri-Associated Paraneoplastic Brainstem<br />
Cerebellar Syndrome with Medically-Intractable Nausea<br />
in a Patient with Large Cell Neuroendocrine Lung<br />
Carcinoma: A Case Report<br />
Amber N. Mitchell, Jessica Levesque and Earl Zimmerman;<br />
Albany, NY<br />
T1808 Glioblastoma Multiforme: A Rare Presentation of<br />
Pineal Tumor with Leptomeningeal Seeding and Future<br />
Directions<br />
Noor Yono, Tulika Ranjan and Rabih Kashouty; Manhasset,<br />
NY, United States Minor Outlying Islands and New York, NY<br />
18<br />
T1809 Benign-Histology Meningioma with Extracranial<br />
Metastasis<br />
Umer Akbar, Bhavpreet Dham and Melissa Carran; Camden, NJ<br />
Neurovirology<br />
T1901 HIV Associated Neurocognitive Disorder<br />
(HAND) Is Not Associated with Increased Fibrillar<br />
Amyloid Deposits Using 11 C-PiB in Middle-Aged HIVþ<br />
Participants<br />
Beau Ances, Jewell Thomas, Tammie Benzinger, Jon Christensen,<br />
Mengesha Teshome, Patricia Aldea, Anne Fagan, David<br />
Holtzman, John Morris and David Clifford; Saint Louis, MO<br />
T1902 Modulation of HIV-Tat Neurotoxicity by<br />
Potassium Channel Blockers<br />
Srikant Rangaraju* and Jeffrey A. Rumbaugh; Atlanta, GA<br />
T1903 Varicella Zoster Encephalitis – Relationship<br />
between Viral Load, Time and Outcome<br />
Benedict D. Michael, Mike Griffiths, Anna Stewart, Charlotte<br />
Buckley, Mark Hopkins, Ian J. Hart, Alistair Miller, Sareen Galbraith<br />
and Tom Solomon; Liverpool, Merseyside, United Kingdom<br />
T1904 Acute Varicella Zoster Virus Encephalitis in<br />
Adults – Relationship between Viral Load, Time,<br />
Clinical Features and Outcome<br />
Benedict D. Michael, Michael Griffiths, Anna Stewart, Charlotte<br />
Buckley, Mark Hopkins, Ian J. Hart, Alistair Miller, Sareen E.<br />
Galbraith and Tom Solomon; Liverpool, United Kingdom<br />
T1905 TLR4 Expression Is Upregulated in<br />
HIV-Associated Neurocognitive Disorder (HAND)<br />
Amir H. Sabouri, Gursharan Chana, Amol Shah, Critian L.<br />
Achim, Ronald J. Ellis, Ian P. Everall and HNRC Group;<br />
La Jolla, CA; Melbourne, Australia and San Diego, CA<br />
T1906 Revisiting Reactivation of Calcified<br />
Neurocysticercosis: Report of Three Recent Cases<br />
Sanjna M. John** and Maria del Pilar Cortes Nino;<br />
Kingston, ON, Canada and Montreal, QC,<br />
Canada<br />
T1907 Clinical Features at Admission in Patients with<br />
Meningeal Cryptococcosis in a Third Level Hospital in<br />
Mexico<br />
Jesus F. Mendoza, Gilberto Vazquez, Jeronimo Rodriguez<br />
and Ildefonso Rodriguez; San Luis Potosí, San Luis Potosí,<br />
Mexico<br />
T1908 The Diagnosis of Tuberculous Meningitis:<br />
A Current Review of the Clinical and Laboratory<br />
Methods<br />
Brian Chisulo, Shan H. Jiang and Yue S. Pan; Guangzhou,<br />
GZ, China<br />
ID: srinivasanv I Black Lining: [ON] I Time: 21:55 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110241/APPFile/JW-ANA#110241
<strong>136</strong> th Annual Meeting Sunday,<br />
September 25, 2011 Works in<br />
Progress Poster Session<br />
WIP posters will be displayed in Elizabeth A-E of the<br />
Manchester Grand Hyatt from 10:00 am – 7:00 pm,<br />
with authors present from 6:00 pm – 7:00 pm.<br />
The Works in Progress category emphasizes ongoing<br />
clinical or basic research of an extraordinary nature, which<br />
warrants expediated presentation. These abstracts were<br />
selected based on scientific merit, timeliness, and anticipated<br />
interest to the membership. Key aspects of research<br />
must have been conducted after the regular abstract<br />
deadline.<br />
Cerebrovascular Disease<br />
S141 Polymorphism of Ninjurin2 in Korean<br />
Atherothrombotic Stroke Patients<br />
Dae-il Chang, Sung Hyuk Heo and Hye Ok Kim; Seoul,<br />
Korea<br />
S142 NMDA Receptor Biomarker for Acute Stroke<br />
Kerstin Bettermann and Svetlana Dambinova; Hershey, PA<br />
and Kennesaw, GA<br />
S143 Initial Transcranial Doppler Velocity Predicts<br />
Development of Symptomatic Vasospasm in Aneurysmal<br />
Subarachnoid Hemorrhage<br />
Shyam Prabhakaran, Konark Malhotra, Rajeev Garg, Sayona<br />
John, Richard Temes and Viven Lee; Chicago, IL<br />
S144 Relative Change in Transcranial Doppler Velocities<br />
Is Inferior to Absolute Thresholds in Prediction of<br />
Vasospasm after Subarachnoid Hemorrhage<br />
Konark Malhotra, James Connors, Viven Lee and Shyam<br />
Prabhakaran; Chicago, IL<br />
Movement Disorder<br />
J_ID: ZAY Customer A_ID: SUPP11-4 Cadmus Art: 22577 Date: 26-August-11 Stage: Page: 19<br />
S238 Dopamine Transporter Imaging Predicts Long<br />
Term Outcomes in Parkinson’s Disease<br />
Bernard M. Ravina, Kenneth Marek, Shirley Eberly, David<br />
Oakes and Ira Shoulson; Rochester and New Haven<br />
S239 Time to First Levodopa-Induced Motor<br />
Complication: Results from the STRIDE-PD Study<br />
C. Warren Olanow, Karl Kieburtz, Olivier Rascol,<br />
Werner Poewe, Anthony Schapira, Helena Nissinen,<br />
Mika Leinonen and Fabrizio Stocchi; New York, NY;<br />
Rochester, NY; Toulouse, France; Innsbruck, Austria;<br />
London, United Kingdom; Espoo, Finland; Kista,<br />
Sweden and Rome, Italy<br />
S240 Acute Effects of Preladenant, a Selective Adenosine<br />
A2A Antagonist, on Dyskinesia and Parkinsonism in<br />
Levodopa-Treated Subjects<br />
Penelope Hogarth, Matthew D. Troyer, Byung S. Park,<br />
Igor D. Grachev, Tatanisha Laguerre, Fengjuan Xuan, Amol<br />
Tendolkar and John G Nutt; Portland, OR and Whitehouse<br />
Station, NJ<br />
19<br />
<strong>136</strong> th Annual Meeting Monday,<br />
September 26, 2011 Works in<br />
Progress Poster Session<br />
WIP posters will be displayed in Elizabeth A-E of the<br />
Manchester Grand Hyatt from 10:00 am – 7:00 pm,<br />
with authors present from 6:00 pm – 7:00 pm.<br />
The Works in Progress category emphasizes ongoing clinical<br />
or basic research of an extraordinary nature, which warrants<br />
expediated presentation. These abstracts were selected<br />
based on scientific merit, timeliness, and anticipated interest<br />
to the membership. Key aspects of research must have been<br />
conducted after the regular abstract deadline.<br />
Behavioral Neurology<br />
M622 New Approaches to Unraveling the Multi-Scale<br />
Neuroanatomical Changes in Williams Syndrome<br />
Ann Lam and Elan L. Ohayon; La Jolla<br />
Epilepsy<br />
M725 HLA-B*1502 Genotyping in Carbamazepine and<br />
Phenytoin Induced Stevens-Johnson Syndrome<br />
Sivakumar M. Rajappa and Srinivasan A. Venkatesan;<br />
Chennai, Tamil Nadu, India<br />
M726 Filamin A Regulates Neural Progenitor<br />
Proliferation and Brain Size through wee1-Dependent<br />
cdk1 Phosphorylation<br />
Gewei Lian and Volney Sheen; Boston, MA<br />
M727 A Moderate-Throughput Screen for<br />
Antiepileptogenic Compounds<br />
Yevgeny Berdichevsky, Yero Saponjian, Michelle Mail and<br />
Kevin J. Staley; Boston, MA<br />
M728 Network Structure and Sensitivity to the<br />
Geometry of Stimuli in Epilepsy and Cognition<br />
Elan L. Ohayon, Ann Lam and Terrence J. Sejnowski; La<br />
Jolla, CA<br />
M729 Hypoglycemia Induced NMDA<br />
Receptor-Dependent Epileptiform Activity<br />
in the Hippocampal CA3 Area Causes Damage<br />
in CA1<br />
Carlos M. Florez, Jane Zhang, Peter Abdemalik,<br />
Liang Zhang and Peter L. Carlen; Toronto, ON, Canada<br />
M730 Alzheimer Disease in Lafora Epilepsy<br />
Jesus Machado-Salas, Maria Rosa Avila-Costa, Patricia<br />
Guevara, Jorge Guevara, Reyna M. Duron, Dongsheng Bai,<br />
Miyabi Tanaka and Antonio V. Delgado-Escueta; Los Angeles,<br />
CA and Mexico, Mexico<br />
M731 Antiepileptic Activity of Intrapulmonary<br />
Midazolam<br />
Ashish Dhir, Dorota Zolkowska and Michael A. Rogawski;<br />
Sacramento and Davis<br />
ID: kannanb I Black Lining: [ON] I Time: 16:18 I Path: N:/3b2/ANA#/Vol00000/110242/APPFile/JW-ANA#110242
M732 Do Brain Volumes in JME (juvenile myoclonic<br />
epilepsy) differ from normal controls?<br />
John T. Spitz, Long Vu, Lydia Su, Mark A. Mandelkern,<br />
Barbara E. Swartz; Berkely, CA, Irvine, CA, Los Angeles, CA,<br />
Irvine,CA and Newport Beach, CA<br />
Neuromuscular Disease<br />
M836 Disrupted Expression of Myogenin in Inclusion<br />
Body Myositis<br />
Akatsuki Kubota, Jun Shimizu, Atsushi Iwata and Shoji Tsuji;<br />
Tokyo, Japan<br />
M837 Abnormalities of a Novel Autophagy-Associated<br />
Protein, NBR1, in Muscle Fibers of Sporadic Inclusion-<br />
Body Myositis (s-IBM)<br />
Carla D’Agostino, Anna Nogalska, Mafalda Cacciottolo,<br />
W.King Engel and Valerie Askanas; Los Angeles, CA<br />
M838 Atrophy and Autophagy in Limb Girdle Muscular<br />
Dystrophy and Glycogen Storage Disease Type 2<br />
Corrado I. Angelini, Annachiara Nascimbeni, Marina Fanin<br />
and Marco Sandri; Padova, Italy<br />
M839 Virtual Demyelination in pmp22 Deficiency<br />
Jiasong Guo, Qing Yan, Gina Sosinsky, Mark Elisman,<br />
Cameron McIntyre, Lily Wang, Ueli Suter and Jun Li;<br />
Nashville; San Diego; Cleveland; Zurich, Swaziland and<br />
Nashville, TN<br />
M840 First in Human Phase 1 Trial of Neural<br />
Progenitor Cells in ALS: Results in the First 12 Patients<br />
Jonathan D. Glass, Nicholas Boulis, Meraida Polak, Crystal<br />
Kelly, Thais Federici, Jane Bordeau, Seward Rutkove, Karl<br />
Johe, Tom Hazel and Eva Feldman; Atlanta, GA; Boston,<br />
MA; Rockville, MD and Ann Arbor, MI<br />
M841 Clinical Development of an Antisense Therapy for<br />
the Treatment of Transthyretin Amyloidosis<br />
Shuling Guo, Elizabeth Ackermann, Sheri Booten, Luis<br />
Alvarado andrew Siwkowski, Merrill Benson, Steve Hughes<br />
and Brett Monia; Carlsbad, CA and Indianapolis, IN<br />
Neurogenetics<br />
J_ID: ZAY Customer A_ID: SUPP11-4 Cadmus Art: 22577 Date: 26-August-11 Stage: Page: 20<br />
M1011 EPI-A0001: New Potential Therapy for<br />
Friedreich Ataxia<br />
David R. Lynch, Steve M. Willi, Robert B. Wilson, Karlla W.<br />
Brigatti, Olena Kucheruck, Eric C. Deutsch, William D.<br />
Shrader, Patrice Rioux, Guy Miller, Amale Hawi and Thomas<br />
Sciascia; Philadelphia, PA; Patterson, NY and Mountain View,<br />
CA<br />
M1012 Exome Sequencing Identifies a Rare Variant in<br />
the CYP27B1 Gene Associated with Multiple Sclerosis<br />
George C. Ebers and Sreeram V. Ramagopalan; Oxford,<br />
Oxfordshire, United Kingdom<br />
M1013 Whole Genome Sequencing in Twins Discordant<br />
for 27 Diseases<br />
George C. Ebers and Sreeram V. Ramagopalan; Oxford,<br />
Oxfordshire, United Kingdom<br />
20<br />
Neurology Critical Care<br />
M1206 Imaging Biomarkers of Cerebral Edema in<br />
Malignant Infarction<br />
Kevin N. Sheth, Albert J. Yoo, R. G. Gonzalez, W. T.<br />
Kimberly, Zeshan A. Chaudhry, Jordan J. Elm, Sven Jacobson,<br />
Stephen M. Davis, Geoffrey A. Donnan, Gregory W. Albers<br />
and Barney J. Stern; Baltimore, MD; Boston, MA; Charleston,<br />
SC; New York, NY; Carlton South, Victoria, Australia and<br />
Stanford, CA<br />
<strong>136</strong> th Annual Meeting Tuesday,<br />
September 27, 2011 Works in<br />
Progress Poster Session<br />
WIP posters will be displayed in Elizabeth A-E of the<br />
Manchester Grand Hyatt from 10:00 am – 7:00 pm,<br />
with authors present from 6:00 pm – 7:00 pm.<br />
The Works in Progress category emphasizes ongoing clinical<br />
or basic research of an extraordinary nature, which warrants<br />
expediated presentation. These abstracts were selected<br />
based on scientific merit, timeliness, and anticipated interest<br />
to the membership. Key aspects of research must have been<br />
conducted after the regular abstract deadline.<br />
Dementia and Aging<br />
T1538 Proneurogenic Compound Reduces Synaptic<br />
Ab42 Oligomer Levels and Shows Cognitive Benefit in<br />
Alzheimer’s Mouse Model<br />
Sam Gandy, John W. Steele, Charles Glabe, Kai Treuner,<br />
Todd Albert, Carrolee Barlow, Michelle E. Ehrlich and<br />
Soong Ho Kim; New York, NY; Irvine, CA and<br />
San Diego, CA<br />
T1539 Alzheimer Risk Variant Clusterin (CLU) and<br />
Brain Function during Aging<br />
Madhav Thambisetty, Lori Beason-Held, Michael Kraut,<br />
Michael Nalls, Andrew Singleton, Luigi Ferrucci, Simon<br />
Lovestone and Susan Resnick; Baltimore and London, United<br />
Kingdom<br />
T1540 <strong>Association</strong> of High Density Lipoprotein to<br />
Alzheimer Disease<br />
Ramin Ebrahimi, Naser Ahmahi, Fereshteh Hajsadeghi and<br />
Hormoz Babaei; LA, CA<br />
T1541 Amyloid-b 42:40 Metabolism Is Altered in<br />
Autosomal Dominant Alzheimer’s Disease (ADAD)<br />
Rachel E. Potter, Vitaliy Ovid, Tom Kasten, Wendy Sigurdson,<br />
Kwasi Mawuenyega, Bruce Patterson, Don Elbert, Scot Fague,<br />
Sumi Chakraverty, Alison Goate, Kevin Yarasheski, John C.<br />
Morris, Tammie Benzinger and Randall J. Bateman; St. Louis,<br />
MO<br />
T1542 Acetylated Tau, a Novel Pathological Signature in<br />
Alzheimer’s Disease and Other Tauopathies<br />
David J. Irwin, Todd Cohen, Murray Grossman, Steven E.<br />
Arnold, Sharon X. Xie, Virginia M.Y. Lee and John Q.<br />
Trojanowski; Philadelphia, PA<br />
ID: kannanb I Black Lining: [ON] I Time: 16:18 I Path: N:/3b2/ANA#/Vol00000/110242/APPFile/JW-ANA#110242
Headache and Pain<br />
J_ID: ZAY Customer A_ID: SUPP11-4 Cadmus Art: 22577 Date: 26-August-11 Stage: Page: 21<br />
T1623 Retrospective Analysis of Major Congenital<br />
Malformations (MCMs) and Oral Clefts (OC) Associated<br />
with In-Utero Topiramate Exposure<br />
Mark W. Green and Arun Bhattachuria; New York, NY and<br />
Yardley, PA<br />
Neuroimmunology and Demyelinating Disease<br />
T1741 Comparison of MRI Techniques for Monitoring<br />
of Multiple Sclerosis<br />
Manuela Vaneckova, Jan Krasensky, Tomas Kalincik, Dana<br />
Horakova, Eva Havrdova and Zdenek Seidl; Prague, Czech<br />
Republic<br />
T1742 Effects of Rituximab on T-Cells in MS<br />
Uma Vinayagasundaram, Ellen M. Mowry, Ian R. Matthews,<br />
Julia Marino and Emmanuelle Waubant; San Francisco, CA<br />
T1743 Fast Macromolecular Proton Fraction (MPF)<br />
Mapping in Multiple Sclerosis (MS)<br />
Vasily L. Yarnykh, James D. Bowen, Bart P. Keogh, Pavle<br />
Repovic, Angeli Mayadev, Beena Gangadharan, Daniel S.<br />
21<br />
Rizzuto, Hunter R. Underhill, Kenneth R. Maravilla and Lily<br />
K. Jung-Henson; Seattle, WA<br />
T1744 Skull Is Skull and Not Simply Another Bony<br />
Structure<br />
Tsutomu Nakada, Yuji Suzuki, Yukihiro Nakayama, Vincent<br />
J. Huber and Ingrid L. Kwee; Niigata, Niigata, Japan and<br />
Martinez, CA<br />
T1745 Characteristics of the Long Latency Vestibular<br />
Electrical Evoked Potential in Control Human Subjects<br />
Benn E. Smith, Michael J. Cevette, Jan Stepanek, Daniela<br />
Cocco, Gaurav Pradhan, Kenneth H. Brookler, Lindsay<br />
Wagner, Sarah Oakley, David A. Zapala and Mark A. Ross;<br />
Scottsdale, AZ and Jacksoville, FL<br />
T1746 Regulatory T Cells Play Contrasting Roles in a<br />
Viral Model for Multiple Sclerosis<br />
Nicholas E. Martinez, Fridrik Karlsson, Fumitaka Sato,<br />
Seiichi Omura, Alireza Minagar, Mathew B. Grisham, and<br />
Ikuo Tsunoda; Shreveport, LA<br />
T1747 Idiopathic Relapsing Conus Myelitis<br />
Raghav Govindarajan and Efrain Salgado; Weston, FL<br />
ID: kannanb I Black Lining: [ON] I Time: 16:18 I Path: N:/3b2/ANA#/Vol00000/110242/APPFile/JW-ANA#110242
<strong>136</strong> th Annual Meeting Sunday,<br />
September 25, 2011 Career<br />
Development Poster Session<br />
Posters will be displayed in Elizabeth A-E of the Manchester<br />
Grand Hyatt from 10:00 am – 7:00 pm, with<br />
authors present from 6:00 pm – 7:00 pm.<br />
Epilepsy<br />
J_ID: ZAY Customer A_ID: SUPP11-5 Cadmus Art: 22578 Date: 26-August-11 Stage: Page: 22<br />
CD515 Non-Convulsive Status Epilepticus Is Associated<br />
with Mortality and Worse Short-Term Outcome in<br />
Critically Ill Children<br />
Nicholas S. Abend, Alexis A. Topjian, and Dennis J. Dlugos;<br />
Philadelphia, PA<br />
22<br />
Neuroimmunology and Demyelinating Disease<br />
CD531 TLR9 Processing in Multiple Sclerosis: A New<br />
Immunomodulatory Effect of Interferon-beta<br />
Konstantin E. Balashov, Suhayl Dhib-Jalbut, and Latt Aung;<br />
New Brunswick, NJ<br />
Neurogenetics<br />
CD522 Aberrant Channel Subunit Trafficking in the<br />
Neurodegenerative KCNC3R420H SCA13 Phenotype<br />
Michael F. Waters; Gainesville, FL<br />
ID: kannanb I Black Lining: [ON] I Time: 17:23 I Path: N:/3b2/ANA#/Vol00000/110243/APPFile/JW-ANA#110243
<strong>136</strong> th Annual Meeting Sunday,<br />
September 25, 2011<br />
Poster Session Abstracts<br />
Posters will be displayed in Elizabeth A-E of the Manchester<br />
Grand Hyatt from 10:00 am – 7:00 pm, with<br />
authors present from 6:00 pm – 7:00 pm.<br />
NOTE: An asterisk designates a resident/fellow travel award<br />
winner. Two asterisks represent a medical student travel award<br />
winner.<br />
Cerebrovascular Disease<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 23<br />
S101. Duration of Diabetes and Ischemic Stroke Risk:<br />
The Northern Manhattan Study<br />
Julio R. Vieira*, Chirantan Banerjee, Yeseon P. Moon,<br />
Myunghee C. Paik, Tatjana Rundek, Ralph L. Sacco and<br />
Mitchell S.V. Elkind; New York, NY and Miami, FL<br />
Background: Diabetes increases stroke risk, but whether<br />
time-dependent analyses improve estimates of effect, and<br />
whether duration is important, is less clear. We hypothesized<br />
that diabetes duration independently predicts ischemic<br />
stroke.<br />
Methods: Among 3,298 stroke-free participants, baseline<br />
diabetes and age at diagnosis were determined. Incident diabetes<br />
was assessed annually (median ¼ 9 years). We fit Cox<br />
proportional hazards models to examine associations<br />
between diabetes duration and ischemic stroke (IS) risk.<br />
Results: Mean age was 69 6 10 years (52% Hispanic,<br />
21% white, and 24% black); 22% were diabetic at baseline<br />
and 11% developed new diabetes. Diabetes at baseline was<br />
associated with IS (adjusted HR ¼ 2.5, 95% CI ¼ 1.9–<br />
3.3), and the magnitude was similar when analyzed as a<br />
time-varying covariate (adjusted HR ¼ 2.4, 95% CI ¼ 1.8–<br />
3.2). Duration of diabetes was associated with IS (adjusted<br />
HR ¼ 1.03 per year with diabetes, 95% CI ¼ 1.02–1.05).<br />
Compared to non-diabetics, those with diabetes for 0–5<br />
years (adjusted HR ¼ 1.7, 95% CI ¼ 1.1–2.7), 5–10 years<br />
(adjusted HR ¼ 1.8, 95% CI ¼ 1.1–3.0), and 10 years<br />
(adjusted HR ¼ 3.3, 95% CI ¼ 2.4–4.5) were at increased<br />
risk. There was a duration threshold effect at 10 years (p<br />
¼ 0.012).<br />
Conclusion: Duration of diabetes is independently associated<br />
with ischemic stroke. The risk triples in those with<br />
diabetes 10 years.<br />
Study supported by: This study was supported by NIH/<br />
NINDS (#R37 29993).<br />
Dr. Vieira reports no disclosures. Dr. Banerjee reports no<br />
disclosures. Ms. Moon reports no disclosures. Dr. Paik<br />
reports no disclosures. Dr. Rundek reports no disclosures.<br />
Dr. Sacco discloses receiving research support from the<br />
NIH/NINDS over the last 12 months. Dr. Elkind serves as<br />
a consultant to Bristol-Myers Squibb and Tethys Bioscience,<br />
Inc.; serves on an event adjudication committee for Jarvik<br />
Heart; and serves on speakers’ bureaus for Boehringer-Ingelheim,<br />
Inc., Bristol-Myers Squibb/Sanofi Pharmaceuticals<br />
Partnership, and Genentech; and receives research support<br />
from diaDexus, Inc., Bristol-Myers Squibb/Sanofi Pharmaceuticals<br />
Partnership, and the NIH/NINDS [# R01<br />
NS050724 (PI), #NS048134 (PI), # P50 NS049060 (Project<br />
PI), # R37 NS029993 (Co-PI), #R01 NS55809 (Co-I)<br />
and #R01 NS062820 (Co-I)]; and has given expert testimony<br />
on behalf of Novartis (Zelnorm VR<br />
and stroke litigation)<br />
and GlaxoSmithKline (Avandia VR<br />
and stroke litigation).<br />
23<br />
Dr. Elkind serves as Resident and Fellow Section Editor for<br />
Neurology, for which he receives compensation from the<br />
AAN.<br />
S102. Functional Outcomes in CREST among Patients<br />
with Periprocedural Stroke and Myocardial Infarction<br />
Bart M. Demaerschalk, Robert J. Hye, O.W. Brown, Donald<br />
V. Heck, Irfan Altafullah, Jenifer H. Voeks, George Howard,<br />
James F. Meschia and Thomas G. Brott; Phoenix, AZ; San<br />
Diego, CA; Royal Oak, MI; Winston Salem, NC; Robbinsdale,<br />
MN; Birmingham, AL and Jacksonville, FL<br />
Background: Stroke more frequently complicated stenting,<br />
and myocardial infarction (MI) more frequently complicated<br />
endarterectomy in the Carotid Revascularization Endarterectomy<br />
versus Stenting Trial (CREST).<br />
Purpose: To inform debate on importance of these components<br />
of the CREST primary endpoint.<br />
Methods: The modified Rankin Scale (mRS), a measure<br />
of function, was assessed at one year, and scales were available<br />
for 72 (89%) of the stroke patients and 34 (81%) of<br />
the MI patients.<br />
Results: There was no evidence of a difference in the distribution<br />
of mRS (pCMH ¼ 0.61). Complete or nearly complete<br />
recovery (mRS 0-1) was achieved for 43 (60%) of the<br />
stroke patients and 23 (68%) of the MI patients. Slight to<br />
severe disability (mRS 2–5) was achieved for 16 (22%) of<br />
the stroke patients and 5 (15%) of the MI patients. Death<br />
occurred in 13 (18%) of the stroke patients and in 6 (18%)<br />
of the MI patients. Disability and death were more frequent<br />
for both the stroke and MI patients compared to those with<br />
neither (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 24<br />
brain infarction volume and 35% vs. 22% inhibition of<br />
neurological deficit, respectively). Treatment with human serum<br />
albumin and vehicles (stabilizing solutions) for IVIG<br />
and C1-INH did not improve the magnitude of brain<br />
injury observed in non-treated controls. Our data suggest<br />
that complement attenuation could be considered as a novel<br />
interventional therapy for AIS.<br />
Study supported by: CSL Behring<br />
Salary and consulting fees.<br />
S104. Does ACE (rs4646994) and a ADDUCIN<br />
(rs4961) Gene Polymorphisms Predicts the Recurrence<br />
of Hypertensive Intracerebral Hemorrhage<br />
Usha K. Misra, Jayantee Kalita, Bindu I. Somarajan,<br />
Bishwanath Kumar, Moromi Das and Balraj Mittal;<br />
Lucknow, Uttar Pradesh, India<br />
Objectives: To evaluate ACE and aADDUCIN gene polymorphisms<br />
in patients with nonrecurrent and recurrent HICH.<br />
Methods: Out of 350 HICH, 33 (9.4%) patients had recurrence.<br />
ACE (rs4646994) and aADDUCIN (rs4961) gene<br />
polymorphisms was done in patients and 198 controls. Risk<br />
factors, clinical, CT, ACE (rs4646994) and aADDUCIN<br />
(rs4961) findings between recurrent and nonrecurrent<br />
HICH were compared.<br />
Results: The stroke risk factors and drug compliance were<br />
similar between the groups. Ganglionic-ganglionic recurrence<br />
was commonest(75.6%) and all had at least one ICH in hypertensive<br />
location. DD genotype (OR6.18,95%CI2.93-<br />
13.02) and D allele (OR2.43,95%CI1.70-3.47) of ACE was<br />
associated with nonrecurrent ICH compared to controls. In<br />
patients with recurrent ICH, DD genotype (OR7.46,95%<br />
CI2.8-19.4) and D allele (OR3.16, 95%CI1.83-5.46) of ACE<br />
and GW (OR3.49,95%CI 1.47-8.28) and WW (OR 2.9,<br />
95%CI 1.40-4.30) genotype and W allele<br />
(OR7.46,95%CI2.80-19.40) of aADDUCIN were more frequent<br />
compared to controls. Recurrent ICH also had higher<br />
frequency of WW genotype (OR9.43,95%CI1.49-59.50) and<br />
W allele (OR2.19,95%CI1.11-4.03) compared to nonrecurrent<br />
ICH. Higher frequency of DDþWW (P ¼ 0.008) and<br />
DD/WWþID/GW (P ¼ 0.0001) genotypes were found in<br />
recurrent compared to nonrecurrent ICH.<br />
Conclusion: Variant genotype combinations of ACE and<br />
aADDUCIN render the hypertensive patient vulnerable for<br />
recurrent ICH.<br />
Study supported by: Study is financially suppoerted by<br />
Indian Council of Medical Research, Government of India.<br />
S105. Risk of Intracerebral Hemorrhage in t-PA Treated<br />
Patients with Elevated INR<br />
William P. Neil, Rema Raman, Ernstrom Karin and Thomas<br />
M. Hemmen; San Diego, CA<br />
Use of Intravenous tissue Plasminogen Activator (IV t-PA)<br />
for stroke is limited to patients with an INR of less than<br />
1.7. Initial guidelines recommended against use of IV t-PA<br />
in patients with an INR >1.4. This was later revised<br />
to >1.7.<br />
We analyzed our database for safety and outcome in<br />
patients with acute ischemic stroke treated with IV t-PA<br />
from 2004–2010. We separated patients into two groups:<br />
those with INR 0.8–1.3, N ¼ 210 (group 1) and those<br />
with INR 1.4 - 1.7, N ¼ 12 (group 2).<br />
Intracerebral hemorrhage occurred in 19/210 (9.05%) in<br />
group 1 and 2/12 (16.67%) in group 2 (p ¼ 0.316). Symptomatic<br />
intracerebral hemorrhage (sICH) was found in 4/<br />
24<br />
210 (1.9%) in group 1, and 2/12 (16.67%) in group 2 (p<br />
¼ 0.036). At 90 days, 44/144 (30.56%) in group 1 had<br />
mRS 0-1, and in group 2, 1/8 (12.5%, p ¼ 0.437).<br />
We found no difference in sICH or clinical outcome in<br />
patients with high INR after IV t-PA. The data is limited<br />
to few patients. Larger prospective studies are needed to<br />
prove safety and efficacy of IV t-PA in those with higher<br />
INR.<br />
S106. Toward a Further Clinical Physiological<br />
Elucidation: Immediate Regression of Leukoaraiosis after<br />
Carotid Artery Revascularization<br />
and Yu-Ming Chuang; New Taipei City, Taiwan<br />
Background: To correlate leukoaraiosis, cerebral perfusion<br />
and circle of Willis (CoW) flow patterns after carotid artery<br />
revascularization.<br />
Methods: Leukoaraiosis (LA) on fluid attenuation<br />
inversion recovery (FLAIR) magnetic resonance (MR)<br />
images at the levels of the centrum semiovale and those<br />
of the frontal horns at both cerebral hemispheres were<br />
scored in 62 contiguous patients (men/women ¼ 38/24,<br />
mean age ¼ 63.2 þ- 8.4 years, range 44–82) before and<br />
after unilateral carotid artery revascularization (CAS). The<br />
pre-and post-stenting difference of LA scores, CoW flow<br />
pattern on MR angiography and MR perfusion parameters<br />
was analyzed.<br />
Results: Post-stenting sum of leukoaraiosis score on<br />
FLAIR imaging was regressed from 9.87þ 0.65 to<br />
8.33þ 0.72 (P ¼ 0.03). Subjects were assigned to the<br />
complete CoW group (N ¼ 21) vs. the incomplete CoW<br />
group (N ¼ 41). Incomplete CoW group had a higher preoperative<br />
LA load and higher interhemispheric asymmetry<br />
index of relative cerebral blood volume (rCBV) which could<br />
be significantly regressed post-operatively.<br />
Conclusions: A perfusion related remodeling of the leukoaraiosis,<br />
regarding the factor of CoW configuration was<br />
observed.<br />
Study supported by: CGMH<br />
S107. Ischemic Stroke Exome Pilot Study<br />
John W. Cole, Xinyeu Liu, Luke J. Tallon, Lisa K. Sadzewicz,<br />
Oscar C. Stine, Nicole Dueker, Yuching Cheng, Marcella A.<br />
Wozniak, Barney J. Stern, James F. Mitchell, Braxton D.<br />
Mitchell, Steven J. Kittner and Jeffrey R. O’Connell;<br />
Baltimore, MD and Jacksonville, FL<br />
Background: The genetic architecture of ischemic stroke is<br />
complex and likely to include rare or low frequency variants<br />
with high penetrance and large effect sizes. Because a<br />
significant portion of human functional variation may<br />
derive from the protein-coding portion of genes we undertook<br />
a pilot study to identify variation across the human<br />
exome.<br />
Methods: Tenischemicstrokecasesincluding8African-<br />
<strong>American</strong>s and 2 Caucasians, consisting of 2 dissections, 5<br />
lacunar, and 3 cryptogenic strokes underwent exome capture<br />
and sequencing implementing Illumina and Agilent<br />
technology. Whole-genome alignments of the sequence<br />
reads were performed using Burrows-Wheeler Aligner<br />
against NCBI build 36.1 with the resultant exome data<br />
evaluated for capture efficiency and rare variants as associated<br />
with stroke.<br />
Results: Sequencing generated an average of 25.5 million<br />
read pairs (75bp x 2) and 3.8Gbp per sample. After<br />
passing quality filters, screening the exomes against dbSNP<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 25<br />
demonstrated an average of 2839 novel SNPs among African-<strong>American</strong>s<br />
and 1105 among Caucasians. Nine gene<br />
isoforms demonstrated compound heterozygosity across all<br />
ten samples. Additional analyses are ongoing.<br />
Conclusions: We propose that rare coding variants predispose<br />
to the risk of ischemic stroke and that exomic-based<br />
analyses are a viable method to identify such variants.<br />
Study supported by: Department of Veterans Affairs<br />
S108. Phosphodiesterase Inhibitors Modulate Human<br />
Brain Microvascular Endothelial Cell Barrier Properties<br />
and Response to Injury<br />
Shuo Liu, Fan Yang, Chuanhui Yu, Annlia Paganini-Hill and<br />
Mark Fisher; Irvine, CA<br />
Brain microvascular disorders have high prevalence but few<br />
treatment options. To develop new strategies for these disorders,<br />
we analyzed effects of phosphodiesterase inhibitors<br />
on human brain microvascular endothelial cells (HBEC).<br />
We modified barrier properties and response to injury of<br />
HBEC with three phosphodiesterase (PDE) inhibitors: cilostazol<br />
(PDE-3 inhibitor), rolipram (PDE-4 inhibitor),<br />
and dipyridamole (non-specific PDE inhibitor). Cilostazol<br />
and dipyridamole altered distribution of endothelial Factin.<br />
Cilostazol increased expression of tight junction protein<br />
claudin-5 by 118 % compared to control (p
In this small sample size study, incidental MH as detected<br />
by Gradient Echo Sequence MRI was not associated with<br />
increased risk for HT of ischemic stroke. However, prior<br />
intake of anti-platelet agents was associated with decreased<br />
risk for HT of ischemic stroke.<br />
S112. Younger Patients Have Lower Quality of Life after<br />
Intracranial Aneurysm Diagnosis<br />
Nerissa Ko, Richard Hornung, Charles Moomaw, Laura<br />
Sauerbeck and Joseph Broderick; San Francisco, CA and<br />
Cincinnati, OH<br />
Objective: Quality of life (QOL) is an important outcome<br />
in patients with intracranial aneurysm (IA). EuroQol EQ-<br />
5D is a validated preference-based survey that incorporates<br />
functional, physical, and mental status into a single QOL<br />
value. We measured EQ-5D in subjects with and without<br />
IA in the Familial Intracranial Aneurysm (FIA) Study.<br />
Methods: Within FIA families, subjects with IA were<br />
identified after review of clinical and imaging data. Family<br />
members free of IA entered the study as non-cases. Subjects<br />
who completed the EQ-5D survey 365 6 60 days after diagnosis<br />
(75 cases) or study entry (885 non-cases) were<br />
included in the present analysis. Multivariable logistic<br />
regression was performed using the EQ-5D index adjusted<br />
for variables known to affect QOL.<br />
Results: EQ-5D index was significantly lower in subjects<br />
with IA than in those without IA (mean 6 SD 0.84 6<br />
0.19 vs. 0.90 6 0.15, p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 27<br />
Conclusion: Traditional stroke risk factors were comparably<br />
controlled for asymptomatic and symptomatic patients,<br />
with notable success only in smoking cessation. Protocoldriven<br />
approaches merit further study.<br />
Study supported by: This study was supported by the<br />
National Institute of <strong>Neurological</strong> Disorders and Stroke<br />
(NINDS) and the National Institutes of Health (NIH)<br />
(R01 NS 038384) and supplemental funding from Abbott<br />
Vascular Solutions (formerly Guidant).<br />
Dr. Carlos Timaran reports receiving Speakers’ fees and<br />
Honoraria from Abbott Vascular. Dr. George Howard<br />
reports receiving compensation for activities with Bayer<br />
Healthcare and research support from Amgen and Bayer<br />
Healthcare. He is also a consultant to Abbott for preparation<br />
of FDA materials.<br />
S117. Radiologic Analysis of Thrombolysis-Induced<br />
Intracerebral Hemorrhage and the Role of Early Blood<br />
Pressure Management<br />
Maxim Mokin, Tareq Kass-Hout, Omar Kass-Hout, Robert<br />
Zivadinov and Bijal Mehta; Buffalo, NY<br />
Introduction: The radiographic features of thrombolysisinduced<br />
intracerebral hemorrhages (ICH) and factors that<br />
influence early hematoma expansion are not well described.<br />
Methods: We performed volumetric analysis of hematoma<br />
volumes in patients who developed ICH from intravenous<br />
thrombolysis for acute ischemic stroke. Analysis of covariance<br />
was used to evaluate for the effect of baseline blood<br />
pressure (BP) on initial hematoma volume and further<br />
growth.<br />
Results: We found a positive correlation between systolic<br />
BP following thrombolysis and initial hematoma volume (r<br />
¼ 0.46, p ¼ 0.03) but not for the diastolic BP (r ¼ 0.07,<br />
p ¼ 0.40). There was a significant increase in mean hematoma<br />
volume expansion when comparing results between<br />
the first and second (median time 9 hours 22 min) CT<br />
study (14.9 6 19.6 cm 3 to 26.0 6 26.7 cm 3 ,p¼ 0.04).<br />
There was also a negative association between the reduction<br />
of systolic BP and hematoma growth (r ¼ 0.67, p ¼<br />
0.02), but no correlation with change in diastolic BP (r ¼ -<br />
0.22, p ¼ 0.28).<br />
Conclusion: Thrombolysis-induced ICH undergoes<br />
significant early expansion in size. Systolic BP plays a<br />
role in both initial hematoma development and early<br />
growth.<br />
Dr. Robert Zivadinov received personal compensation<br />
from Teva Neuroscience, Biogen Idec, EMD Serono and<br />
Questcor Pharmaceuticals for speaking and consultant<br />
fees, financial support for research activities from Biogen<br />
Idec, Teva Neuroscience, Genzyme, Questcor Pharmaceuticals,<br />
Greatbatch, EMD Serono and Bracco. Dr. Bijal<br />
Mehta received lecturing honoraria from Teva and Biogen<br />
Idec.<br />
S118. Anterior Circulation Stroke Causing Dizziness or<br />
Vertigo: A Systematic Review<br />
Yun Zhou, Seung-hun Lee, Ali S. Saber Tehrani, Karen A.<br />
Robinson and David E. Newman-Toker; Baltimore, MD and<br />
Gwangju, Korea<br />
Background: Determine frequency, localization of anterior<br />
circulation stroke causing dizziness/vertigo.<br />
Methods: Systematic review of observational studies.<br />
Search—electronic (MEDLINE) and manual search for English-language<br />
studies (1966–2011). Inclusions—dizziness/vertigo/syncope<br />
due to anterior circulation stroke or vascular<br />
27<br />
disease (e.g., carotid stenosis). Two independent reviewers<br />
selected studies, with differences adjudicated by a third.<br />
Study characteristics, patient symptoms, and lesion locations<br />
were abstracted.<br />
Results: We identified 414 unique citations, examined<br />
67 full manuscripts, and analyzed 39 studies describing<br />
1214 patients. Principal reasons for abstract exclusion<br />
were non-English language, no confirmed cerebrovascular<br />
diagnosis, and not anterior circulation (73%).<br />
Principal reasons for manuscript exclusion were no<br />
reported dizziness and no confirmed cerebrovascular diagnosis<br />
(53%). Unbiased studies of dizziness prevalence<br />
in anterior circulation stroke (i.e., dizziness not a mandatory<br />
symptom) reported a presenting symptom of<br />
dizziness in 12% (8.4% non-vertiginous, 3.2% vertiginous),<br />
syncope in 6.6% of n ¼ 683. Non-vertiginous<br />
symptoms were more commonly reported in right hemispheric<br />
lesions (73.9% vs. 26.1%, v 2 p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 28<br />
Method: The survey was conducted from November,<br />
2010 via internet using structured, self-applicable questionnaire<br />
addressed stroke knowledge.<br />
Results: We have valid responses from 11,121 people<br />
aged from 20 to 69 years old throughout all Japanese districts.<br />
66.2% of subjects were no source of informations<br />
about stroke. On the other hand, subjects of remaining<br />
33.8% can get the informations of stroke through mainly<br />
TV (85.2%). They understood the signs of stroke such as<br />
speech disturbance (95.5%). 67% of them request the ambulance<br />
and transport to the hospital promptly at the time<br />
of stroke onset but only 22.4% on the occasion of TIA.<br />
Importance of early diagnosis and treatment within 3<br />
hours of onset was well recognized among all age subjects<br />
(75.3%) and significantly associated with calling ambulance<br />
quickly when stroke (OR 4.458, 95%CI, 3.897–<br />
5.099, p ¼ 0.000) or TIA (OR 2.331, 95%CI, 1.923–<br />
2.825, p ¼ 0.000) occurred.<br />
Conclusions: Our survey demonstrates that it is important<br />
to educate stroke knowledges through TV such as judgment<br />
of stroke and calling ambulance when stroke or TIA<br />
occurred.<br />
S121. Is Anti Epileptic Drug Necessary in Cortical<br />
Venous Thrombosis?<br />
Velmurugendran Cannigaiper Uthamaroyan, Kaushik Sundar,<br />
Meenakshisundaram Umaiorubahan and Shankar<br />
Venkatasubramaniam; Chennai, Tamilnadu, India<br />
Introduction: Though CVT is associated with seizures,is it<br />
necessary to start AEDs in all patients with CVT?<br />
Aims To study the clinical profile of patients with CVT<br />
and to find out the incidence and etiology of seizures.<br />
Materials and methods: Patients who presented with<br />
signs and symptoms suggestive of CVT were admitted and<br />
brain imaging was done.If CVT was revealed,requisite investigations<br />
were done.Patients were then treated and followed<br />
up for a period of one year.<br />
Results: 50 (28 males/22 females) patients were diagnosed<br />
to have CVT.Of these 50 patients 25 of them presented with<br />
Seizures and all these 25 had an infarct/haemorrhage/ infarct<br />
with haemorrhagic transformation in their MRI.<br />
Discussion: We found that 50% of our study patients<br />
had seizures and all of them had an infarct/haemorrhage/or<br />
infarct with haemorrhagic transformation.The patients who<br />
did not have an infarct did not have a seizure and were not<br />
started on AEDs and remain seizure free till date.<br />
Conclusion: Patients with CVT who have no evidence of<br />
parenchymal lesion in the MRI need not be treated with<br />
AEDs as a prophylaxis and a wait and watch strategy can be<br />
followed.<br />
Study supported by: Self<br />
S122. Race and Insurance Disparities in Cardiovascular<br />
Risk Factors Control in Patients with Acute Stroke<br />
Anna M. Cervantes, Jose R. Romero, Helena Lau, Feliks<br />
Koyfman, Aleksandra Pikula, Thanh N. Nguyen, Carlos S.<br />
Kase and Viken L. Babikian; Boston, MA<br />
Objective: To investigate racial and socioeconomic disparities<br />
in cardiovascular risk factor control at the time of acute<br />
ischemic stroke at an urban hospital.<br />
Background: Racial and socioeconomic inequalities may<br />
play a role in the observed higher frequency and severity of<br />
stroke in minorities. Hypercholesterolemia, diabetes and<br />
28<br />
hypertension (HTN) are modifiable cardiovascular risk factors<br />
with higher prevalence in minorities.<br />
Design: We evaluated patients with acute ischemic<br />
stroke/TIA presenting to Boston Medical Center from 1/<br />
2009-12/2010. Patients were stratified by race (Whites,<br />
Blacks, Other) and insurance status (Medicaid/no insurance,<br />
Medicare, Private). Cardiovascular risk factor control<br />
(HTN, hyperlipidemia, diabetes) was evaluated on<br />
admission.<br />
Results: Among 833 patients (mean age 61yrs, 50.4%<br />
women), 34.8% were white, 45.5% black and 19.7% other<br />
races; 50.4% were insured and 49.6% uninsured. Compared<br />
to white, black and other races were more likely to be uninsured<br />
(p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 29<br />
arterial and venous thrombosis. The more common, and<br />
dangerous form of HIT, HIT II, is caused by prothrombotic<br />
anti-heparin/platelet factor PF4 complex antibodies, which<br />
activate platelets, induce their aggregation, and trigger coagulation<br />
(1). The consequences, especially if not diagnosed<br />
early, can be devastating, ranging from deep venous<br />
thromboses to myocardial infarctions and strokes. HIT is<br />
most commonly associated with the use of heparin after orthopedic<br />
procedures, as compared to cardiovascular surgeries<br />
and medical conditions requiring admission to an intensive<br />
care unit. HIT is much less frequently associated with the<br />
use of low molecular weight heparin, such as enoxaparin<br />
(3). Here, we present the case of a 64 year-old woman who<br />
developed both a lower extremity deep venous thrombosis<br />
and cerebral venous sinus thromboses from the administration<br />
of enoxaparin after an orthopedic surgery. Our patient<br />
is only the second reported case of HIT-induced CVST<br />
related to enoxaparin administration. Our poster will<br />
include brain imaging, graphs and tables regarding the clinical<br />
case.<br />
Study supported by: Residency Program<br />
S125. Renal Failure Increases Risk for Intracranial<br />
Hemorrhage Following Stroke<br />
Elisabeth B. Marsh, Argye E. Hillis, Rafael H. Llinas and<br />
Rebecca F. Gottesman; Baltimore, MD<br />
Background: Anticoagulation is associated with increased<br />
risk of intracranial hemorrhage. Renal failure can lead to<br />
platelet dysfunction, which may increase the risk further.<br />
We followed patients admitted with acute ischemic stroke<br />
who had an indication for anticoagulation, to determine if<br />
renal failure was associated with increased risk for intracranial<br />
hemorrhage.<br />
Methods: 63 patients admitted with acute ischemic<br />
stroke and with an indication for anticoagulation were<br />
included. Age-adjusted logistic regression was used to evaluate<br />
the association between history of renal failure and glomerular<br />
filtration rate (GFR) (>60 (normal), 30–60 (mildly<br />
reduced),
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 30<br />
rapid deterioration over hours to days with multi-territorial<br />
infarctions and global edema on imaging. All had angiographic<br />
findings of diffuse, severe, multifocal arterial narrowings.<br />
Aggressive treatment was attempted in most,<br />
including intravenous magnesium, corticosteroids, calcium<br />
channel blockers, balloon angioplasty, vasopressors, and osmotic<br />
agents. Despite aggressive measures, all patients suffered<br />
fulminant courses ending in death within 8–24 days<br />
after delivery.<br />
Conclusions: Postpartum vasoconstriction can be fatal<br />
with rapid progression of vasoconstriction, ischemia, and<br />
brain edema. Postpartum women with acute neurological<br />
symptoms deserve close monitoring with consideration of<br />
noninvasive cerebrovascular imaging.<br />
S129. Racial Disparities in Secondary Stroke Prevention<br />
Practices<br />
Pratik Bhattacharya, Seemant Chaturvedi, Flicia Mada, Leeza<br />
Salowich-Palm, Sabrina Hinton, Scott Millis, Sam Watson<br />
and Kumar Rajamani; Detroit, MI and Lansing, MI<br />
Racial differences in stroke risk, risk factor prevalence and<br />
outcomes are established. We explored racial differences in<br />
secondary stroke prevention practices among stroke patients.<br />
Methods: A retrospective review was conducted on ischemic<br />
stroke patients in 5 JC (Joint Commission) certified and 5<br />
noncertified hospitals. Secondary stroke prevention measures<br />
such as antiplatelet use, statin use, antihypertensives and<br />
smoking cessation steps were assessed. Results: 574 patients<br />
(430 white, 144 African <strong>American</strong>s(AA); 47.9% evaluated at<br />
JC certified centers) were included. AA were younger (mean<br />
age 64.4 vs 72.5; p 100 with one improved<br />
and 3 with worse outcome.<br />
Conclusion: High ischemic volume have higher NIHSS<br />
and worse outcome.<br />
Study supported by: USF College of Medicine<br />
S131. Treatment Outside the NINDS Stroke Study<br />
Exclusion Criteria: A Case Report<br />
Nhu T. Bruce and Brett C. Meyer; San Diego, CA<br />
Introduction: The original NINDS stroke trial established<br />
IV rt-PA as effective and defined treatment parameters.<br />
Some exclusions were well founded on data, others were<br />
chosen via consensus opinion. Successful use of rt-PA outside<br />
of some criteria raises concern over the continued utility<br />
of some exclusions. We report an intriguing case where a<br />
patient with prolonged PTT was successfully treated with IV<br />
rt-PA.<br />
Methods: Case report from the University of California,<br />
San Diego<br />
Results: An 86 year old woman with no hematologic history<br />
presented with acute ischemic stroke within the 3 hour<br />
window. Given her lack of being on anticoagulants or having<br />
hepatic dysfunction, her elevated PTT was felt to be<br />
spurious, and she was treated with rt-PA despite not meeting<br />
this inclusion criteria. Patient had significant improvement<br />
and work up was positive for a diagnosis of anti-phospholipid<br />
antibody syndrome.<br />
Conclusions: rt-PA treatment is effective, though only a<br />
minority of patients is treated. Multiple cohort studies have<br />
shown that deviations from the original exclusions may not<br />
result in worse outcomes for specific exclusion criteria.<br />
Reevaluating the significance and limiting the exclusion criteria<br />
may help to increase thrombolytic treatments.<br />
Study supported by: NIH SPOTRIAS<br />
S132. Size Matters: Predictors of Intracranial<br />
Hemorrhage in Stroke Patients on Anticoagulation<br />
Elisabeth B. Marsh, Argye E. Hillis, Rafael H. Llinas and<br />
Rebecca F. Gottesman; Baltimore, MD<br />
Background: Anticoagulation is associated with increased<br />
risk of intracranial hemorrhage. This may be higher in<br />
patients who have had a recent stroke. We followed patients<br />
with acute ischemic stroke who had an indication for anticoagulation,<br />
to determine what factors were associated with<br />
increased risk for hemorrhage.<br />
Methods: 63 patients admitted with acute ischemic<br />
stroke and with an indication for anticoagulation were<br />
included. We evaluated risk of hemorrhage associated with<br />
indicators of stroke severity; namely NIH Stroke Scale<br />
(NIHSS) score and infarct size (largest lesion and total<br />
lesion volume), using age-adjusted logistic regression.<br />
Results: Higher NIHSS scores predicted increased risk of<br />
hemorrhage. For every 3 point increase, risk for hemorrhage<br />
increased 51% (OR 1.51, 95% CI 1.01–2.25). Total volume<br />
of the infarct also approached statistical significance<br />
(OR 2.6 per larger quartile, 95% CI 0.86–7.56).<br />
Conclusions: In patients with acute ischemic stroke who<br />
also have an indication for anticoagulation, the severity of<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 31<br />
their stroke, indicated by their NIHSS score and volume of<br />
infarct, is a strong predictor of their risk for hemorrhage.<br />
Study supported by: The first author, EB Marsh, is supported<br />
in part by a NINDS R25 Research Grant- R25<br />
NS065729.<br />
EB Marsh is currently a resident, partially supported by<br />
funding from the R25 Research Grant.<br />
S133. A Rare Presentation of Anterior and Posterior<br />
Spinal Arteries Ischemia during Dilaysis<br />
Noor Yono, Adrian Marchidann and Rabih Kashouty;<br />
Manhasset, NY and New York, NY<br />
Spinal cord infarction is considered to be a rare event and<br />
usually presents with severe neurological deficits. Multiple<br />
etiologies have been described; however, this is the first case<br />
report of spinal cord infarction in the territory of the anterior<br />
and posterior spinal arteries secondary to hypotension<br />
during dialysis. We report a case of a 60 year-old man with<br />
past medical history of severe atherosclerosis, coronary artery<br />
disease and acute kidney failure, who presented with lower<br />
extremity paraplegia during hemodialysis secondary to hypotension.<br />
MRI of the spine demonstrated spinal cord infarction<br />
starting at the level of T8 and below. Clinical features<br />
suggested that the lesion was an ischemic infarct. In addition<br />
to paraplegia, he demonstrated absence of sensation to<br />
dull touch, pin prick, temperature, proprioception and<br />
vibration. Hypotension during dialysis could carry significant<br />
risk of spinal cord infarction. This unusual infarction<br />
demonstrates the importance of blood pressure control in<br />
susceptible patients with severe atherosclerotic disease. Physicians<br />
should be aware of such complications.<br />
S134. Neurosarcoidosis: A Case Presentation<br />
Amtul Farheen, Nancy Gadallah, Rony Dekermenjian,<br />
Michael Rosenberg and Sushanth Bhat; Edison, NJ<br />
27 y/o man with no significant medical history woke up<br />
with weakness and parasthesias of his right side. He smoked<br />
1ppd for more than 10yrs. <strong>Neurological</strong> examination was<br />
significant for decreased power on right side. Right upper<br />
extremity revealed power of 2/5 deltoid, 3/5 bicep/tricep/<br />
brachio, 1/5 intrinsic hand muscles, Right lower extremity<br />
revealed: 4/5 iliopsoas, hams, quads 0/5 dorsi and plantar<br />
flexion 0/5. Sensation was mildly decreased on right side.<br />
Reflexes were asymmetric and increased with upgoing toe<br />
on the right. MRI brain showed small left medullary hyperintensity.<br />
Csf had opening Pressure of 23, RBC 222, WBC<br />
7, Prot 57.8, Glucose 65. CSF was negative for gram stain,<br />
protein electrophoresis, oligoclonal bands, and infectious<br />
work up. Csf ACE 0.1. Serum ACE was 109. CT chest<br />
showed mediastinal and bilateral hilar lymphadenopathy.<br />
Mediastinal lymph node biopsy revealed noncaseating granulomas<br />
diagnostic of neurosarcoidosis. The patient was<br />
started on iv steroids and was discharged on oral prednisone.<br />
He improved clinically and was later almost back to<br />
his baseline.<br />
Although sarcoidosis is rarely confined to the nervous system,<br />
its neurological features frequently occur early in the<br />
course of the disease leading to diagnostic confusion.<br />
S135. Stroke Outcomes Based on MERCI/PENUMBRA<br />
Intervention and Hemodynamics<br />
Jay-Ming Wang**, Zahid I. Choudary, Shazia Z. Choudhary,<br />
Michael Sloan, Harry R. Van Loveren, Karen R. Wilson and<br />
David A. Decker; Tampa, FL<br />
Hypothesis: What are the effects of MERCI/PENUMBRA<br />
and blood pressure on stroke outcome?<br />
31<br />
Background: Not all guidelines for stroke are well supported<br />
by evidence. We seek to retrospectively study the<br />
effects of MERCI/PENUMBRA stroke interventions and<br />
hemodynamics to see ischemic stroke outcome.<br />
Methods: A retrospective chart review of 24 patients with<br />
hospitalization with ischemic stroke with age range 18 to<br />
90, mean age 70.6, 13 males, and 11 females. The blood<br />
pressure was correlated with ischemic stroke outcome. The<br />
patients undergoing MERCI/PENUMBRA intervention<br />
were analyzed.<br />
Results: We noted a significant positive correlation<br />
between higher blood pressures and worse outcomes in<br />
patients with large volume lesions.<br />
In the 8 patients with MERCI/PENUMBRA intervention,<br />
we had 3 with worse outcomes and 5 with improvement<br />
at discharge. Of the 3 with worse outcomes, 2 had<br />
large lesions and 1 had a small lesion. The 5 improved outcomes<br />
had 3 small lesions and 2 medium lesions. Three of<br />
the five had received IV tPA prior to interventional therapy.<br />
Two did not.<br />
Conclusion: MERCI/PENUMBRA intervention has an<br />
overall positive outcome on patients suffering from ischemic<br />
stroke.<br />
Higher blood pressures predict a worse outcome in<br />
patients with stroke lesions greater than 100 ml.<br />
Study supported by: USF College of Medicine<br />
S<strong>136</strong>. Migraine-Related ICH – A Case Study and Review<br />
Shivani Ghoshal**, Sankalp Gokhale and Louis Caplan;<br />
Boston, MA<br />
54 year-old right-handed male, with a 25-year history of<br />
frequent migraine headache, presented with an episode of<br />
severe migraine headache associated with visual changes;<br />
imaging revealed new left frontal intracranial hemorrhage.<br />
Since then, the patient had two different types of paroxysmal<br />
attacks. One consisted of prolonged severe headaches<br />
with multisystem sensory deficits, most consistent with migraine<br />
with aura. The second consisted of brief visual and<br />
auditory perseveration, likely representing focal seizures near<br />
the region of ICH. Excluding the initial presentation, the<br />
subsequent episodes left no discernible damage on clinical<br />
exam or imaging. Migraine is a form of vascular headache,<br />
postulated to cause direct vasoconstriction of cerebral vessels.<br />
This vasospasm may, in some cases, lead to reperfusion<br />
edema, with intracerebral bleeding to follow. Though migraine-related<br />
ischemia has been well-documented, there<br />
have been few noted cases of migraine-related ICH and<br />
none to date in male patients; the association of migraine<br />
and ICH is likely under-recognized and hence underreported.<br />
Given the dangers for cerebral hemorrhage, future<br />
migraine treatment may benefit from weighing the risk of<br />
vasoactive agents. We take this opportunity to review the<br />
current literature to provide guidance for improvement in<br />
care.<br />
S137. Stroke as a Complication of Tuberculous<br />
Meningitis<br />
Amtul Farheen, Sumaiya Salim, Zoha Fasih, Rony<br />
Dekermenjian and Sushanth Bhat; Edison, NJ<br />
A 28 y/o Hispanic man who moved to US from Guatemala<br />
four years before presentation, had no significant past medical<br />
history presented with 2 days of progressive confusion<br />
and headache. He reported weight loss, severe cough for few<br />
days with low grade temperatures and night sweats. He<br />
smoked occasionally. On examination he was lethargic and<br />
cachectic, neck stiffness noted, enlarged lymph nodes of the<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 32<br />
neck. He was tachycardic and had diminished breath sounds<br />
with bilateral crackles. <strong>Neurological</strong> examination revealed<br />
normal cranial nerve examination. He moved all extremities<br />
spontaneously. Initial CT head was normal. Lumbar puncture<br />
revealed WBC 53 (neutrophils predominantly), RBC 7,<br />
Protein 170, Glucose 7. Sputum was positive for AFB. HIV<br />
testing was negative. He was diagnosed with disseminated<br />
tuberculosis with tuberculous meningitis and started on<br />
antituberculous medications. On the third day of admission<br />
he had decreased movement of the left side of his body and<br />
a repeat CT of his head showed a new infarct in the right<br />
internal capsule.<br />
Vasculitis of the vessels of circle of Willis which may<br />
present as stroke is one of the most dreaded complications<br />
of Tuberculous meningitis.<br />
S138. Patterns and Mechanisms of Head-Shaking<br />
Nystagmus in Anterior Inferior Cerebellar Artery<br />
Infarction<br />
Young Eun Huh and Ji Soo Kim; Seongnam-si, Gyeonggi-do,<br />
Korea<br />
Infarctions involving the anterior inferior cerebellar artery<br />
(AICA) territory give rise to unique clinical features of combined<br />
peripheral and central vestibulopathies. Evaluation of<br />
head-shaking nystagmus (HSN) may provide information<br />
on central and peripheral vestibular dysfunction. We analyzed<br />
patterns of spontaneous nystagmus (SN) and HSN in<br />
18 patients with acute infarction involving the AICA territory<br />
which was confirmed on MRI. Patients also underwent<br />
head impulse and bithermal caloric tests, and pure tone<br />
audiogram. Twelve patients (12/18, 67%) showed unilateral<br />
caloric paresis (n ¼ 11) or abnormal head impulse test (n<br />
¼ 9) on the side of the infarction and most of them (10/<br />
12, 83%) also had acute hearing loss. Fifteen patients<br />
(83%) exhibited HSN, and the horizontal HSN was usually<br />
contralesional (10/14, 71%). However, 9 patients also<br />
showed patterns of central HSN which included perverted<br />
HSN (n ¼ 7), ipsilesional HSN (n ¼ 4), and HSN in the<br />
opposite direction of SN (n ¼ 4). Especially, perverted<br />
HSN was induced in half of the 6 patients without audiovestibular<br />
loss. In AICA infarction, HSN was common with<br />
both peripheral and central patterns. Careful evaluation of<br />
HSN may provide clues for AICA infarction in patients<br />
with acute unilateral audiovestibular loss.<br />
Study supported by: This study was supported by grant<br />
of the Korea Health 21 R&D Project, Ministry of Health<br />
& Welfare, Republic of Korea (A080750)<br />
S139. Co-Complaints Influence Odds of Stroke<br />
Diagnosis in ED Dizziness<br />
Ali S. Saber Tehrani, Yu-Hsiang Hsieh, Jonathan A. Edlow,<br />
Carlos A. Camargo and David E. Newman-Toker; Baltimore,<br />
MD and Boston, MA<br />
Background: Assess impact of co-complaints on stroke<br />
diagnosis in dizziness presentations to US emergency departments<br />
(EDs).<br />
Methods: Design—Cross-sectional study of ED visits<br />
from the National Hospital Ambulatory Medical Care Survey.<br />
Setting—Weighted sample of US ED visits (1993–<br />
2005). Participants— 16 years old; reason-for-visit code<br />
vertigo/dizziness (1225.0). Measures—co-complaints, ICD-9<br />
diagnoses. Co-complaints grouped as otologic (e.g., tinnitus);<br />
neurologic (e.g., weakness); medical (e.g., chest pain); or other<br />
(including multiple co-complaint groups). Diagnoses<br />
grouped using HCUP categories.<br />
32<br />
Results:7,925 dizzy patient complaints (3% of visits,<br />
weighted 28.3 million) sampled over 13 years. Dizziness<br />
was ‘‘isolated’’ (none, nausea/vomiting, or otologic co-complaints)<br />
in 21%; others with dizziness had only neurologic<br />
(10%), only medical (15%), or other (54%) co-complaints.<br />
Cerebrovascular causes were diagnosed in 4.1% (isolated),<br />
10% (neurologic), 0.9% (medical), 3.8% (other), 1.0%<br />
(non-dizzy controls). Neurologic co-symptoms increased<br />
odds (2.57, 95%CI 1.85 to 3.58) and medical co-symptoms<br />
decreased odds (0.21, 95%CI 0.10–0.41) of a cerebrovascular<br />
diagnosis relative to isolated dizziness.<br />
Conclusions: ED physicians use associated symptoms to<br />
diagnose dizzy patients. While this reflects an appropriate<br />
assessment of disease probability, it could increase the risk<br />
of stroke misdiagnosis in isolated dizziness or dizziness with<br />
medical symptoms.<br />
Study supported by: This study was supported principally<br />
by the National Institutes of Health, National Center for<br />
Research Resources (NCRR) grant K23 RR 17324-01.<br />
S140. Eclamptic Versus Non-Eclamptic PRES (Posterior<br />
Reversible Encephalopathy Syndrome): Comparison of<br />
Clinical Features and Response to Treatment<br />
Pavan Bhargava, Fazeel Siddiqui, Vivek Patel, Rodger J. Elble<br />
and Srikanth Vallurupalli; Springfield, IL<br />
Objective: To examine the hypothesis that eclamptic PRES<br />
responds more rapidly to treatment than non-eclamptic<br />
PRES.<br />
Background: PRES is characterized by reversible vasogenic<br />
edema, predominantly in the posterior circulation distribution,<br />
and can occur in various clinical settings such as<br />
eclampsia and malignant hypertension. It is unknown<br />
whether clinical, imaging and EEG features differ in<br />
eclamptic versus non-eclamptic PRES.<br />
Design/Methods: Retrospective data including clinical,<br />
EEG and MRI characteristics was collected on patients diagnosed<br />
with PRES between January 2003 and June 2010.<br />
Appropriate statistical methods were employed.<br />
Results: 45 episodes of PRES occurred in 43<br />
patients(69% women) with a mean age of 44.5 years(range<br />
9–82). The nine patients with eclampsia had significantly<br />
lower age(25 6 5 yrs vs. 50 6 20 yrs, p ¼ 0.002), shorter<br />
duration of stay following diagnosis(3.1 vs. 7.6 days, p ¼<br />
0.002), less incidence of renal impairment(0% vs. 39%, p<br />
¼ 0.04) and lower likelihood of abnormal EEG finding(33%<br />
vs. 85%, p ¼ 0.07) compared to non-eclamptic<br />
PRES. The etiologies of non-eclamptic PRES were hypertension(86%),<br />
sepsis(17%), transplant(11%) and connective<br />
tissue disorder(17%).<br />
Conclusions: Eclamptic PRES appears to respond more<br />
rapidly with treatment of the underlying condition than<br />
non-eclamptic PRES, which has a more varied etiology.<br />
Movement Disorders<br />
S201. Allele Specific RNAi Against Triplet Repeat<br />
Disease-Causing Alleles in Huntington Disease<br />
Hirokazu Furuya, Masaki Takahashi, Shoko Watanabe, Miho<br />
Murata, Ichiro Kanazawa, Keiji Wada and Hirohiko Hohjoh;<br />
Omuta, Fukuoka, Japan and Kodaira, Tokyo, Japan<br />
Suppression of disease-causing alleles is a potential approach<br />
to treatment of intractable diseases caused by dominate-negative<br />
alleles, such as triplet repeat diseases. RNAi may be an<br />
applicable tool in medical treatment; however, the identification<br />
of nucleotide variations and the design of siRNAs<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 33<br />
conferring disease allele-specific RNAi are quite difficult.<br />
Here we report an innovative procedure that facilitated allele-specific<br />
silencing of disease-causing alleles in Huntington<br />
disease (HD), a triplet repeat disease. We developed a<br />
pull-down method to rapidly identify coding SNP (cSNP)<br />
haplotypes of triple repeat, disease-causing alleles, and demonstrated<br />
disease allele-specific RNAi that targeted cSNP<br />
sites in mutant Huntingtin (HTT) alleles, each of which<br />
possessed a different cSNP haplotype. We examined 5<br />
patients with HD, found heterozygous cSNP sites in two<br />
patients, and successfully suppressed the disease-causing alleles<br />
in lymphoblastoid cells derived from the patients by<br />
means of RNAi. Therefore, the methods allow for diseasecausing<br />
allele specific silencing targeting disease-linked<br />
cSNP haplotypes of triplet repeat diseases.<br />
Study supported by: This work was supported by research<br />
grants from the Ministry of Health, Labour and Welfare of<br />
Japan<br />
S202. Antigen-Sensitized Dendritic Cell Vaccine Against<br />
Human a-Synuclein: A Potential Cell-Based Therapy<br />
Against Parkinson’s Disease<br />
Chuanhai Cao, Xiaoyang Lin, Wang Li, Cai Jianfeng, Li<br />
Kunyu, Song Shijie and Juan Sanchez-Ramos; Tampa<br />
The goal of this study was to develop a cell-based vaccine<br />
directed against human a-synuclein (hAS).<br />
Human recombinant a-synuclein (hrAS) was expressed in<br />
BL21 cells and AS peptides were synthesized based on antigen<br />
analysis. Mouse bone marrow-derived dendritic cells<br />
(DCs) were generated ex vivo, sensitized with hrAS or AS<br />
mixed peptides and then delivered i.v. to Tg hAS mice.<br />
Mice vaccinated with DCs sensitized with a peptide mixture<br />
(DC-ASpep) exhibited detectable anti-AS antibody earlier<br />
than mice vaccinated with DC-sensitized with human<br />
recombinant protein (DC-hrAS). With repeated treatments,<br />
antibody levels in the DC-hrAS was higher than in the DC-<br />
ASpep group. AS levels were significantly decreased at both<br />
3 rd and 5 th treatment compared to the control group. In behavioral<br />
tests, treatment groups performed better on the<br />
rotometer than control mice; the DC-ASpep group exhibited<br />
the best performance. Among all cytokines measured,<br />
only GM-CSF and IL1a were significantly changed after<br />
treatment, indicating that this treatment method has no<br />
potential to induce inflammation.<br />
Conclusions: AS-sensitized dendritic cell vaccination is<br />
effective, specific, long-lasting and unlike antigen-based vaccines,<br />
does not elicit non-specific activation of the immune<br />
system.<br />
Study supported by: Parkinson Study Group and Helen<br />
Ellis Endowed Chair Fund<br />
S203. Depressive Symptoms and Neurodegeneration in<br />
the Locus Coeruleus: The Honolulu-Asia Aging Study<br />
Ross Webster, Robert D. Abbott, Helen Petrovitch, Kamal H.<br />
Masaki, Caroline M. Tanner, Jane H. Uyehara-Lock and<br />
Lon R. White; Honolulu, HI; Hiroshima, Japan and<br />
Sunnyvale, CA<br />
Depression commonly occurs in Parkinson’s disease (PD),<br />
often pre-dating diagnosis. Lewy pathology in the locus<br />
coeruleus (LC) occurs early in PD and LC neurodegeneration<br />
occurs in depressed PD patients. Whether depressive<br />
symptoms (DS) are associated with LC neurodegeneration<br />
prior to onset of classic PD motor features remains unclear.<br />
Our objective is to examine the association of DS and LC<br />
neurodegeneration in decedents from the longitudinal Honolulu-Asia<br />
Aging Study. DS were assessed using the 11-item<br />
33<br />
modified Center for Epidemiologic Studies Depression Scale<br />
at examinations from 1991–1993 in 403 autopsied participants.<br />
A score >8 was defined as significant DS. LC neurodegeneration<br />
was based on semi-quantitative assessments by<br />
a neuropathologist shielded from clinical information. After<br />
age-adjustment, significant neurodegeneration was observed<br />
in 32.9% of 55 decedents with DS versus 17.8% in 348<br />
without DS (p ¼ 0.010). DS continued to be associated<br />
with LC neuron loss after removing 27 PD or dementia<br />
with Lewy bodies cases (p ¼ 0.044), and after removing 89<br />
cases with any Lewy pathology (p ¼ 0.010). Findings suggest<br />
that DS correlate with LC involvement in PD prior to<br />
development of classic motor symptoms as well as in some<br />
individuals without Lewy pathology.<br />
Study supported by: NIA, NIH; NINDS, NIH; Department<br />
of Defense; Office of Research and Developement,<br />
Veterans Affairs<br />
S204. MRI in HDLS Shows a Unique Mechanism of<br />
Neuroaxonal Degeneration<br />
C. Sundal*, C. Wider, J.A. Van Gerpen, J. Lash, J.Y.<br />
Garbern, K.J. Schweitzer, J. Aasly, B. Goodman, B.K.<br />
Woodruff, C.W. Christine, M. Baker, J.E. Parisi, S. Roeber, S.<br />
DeArmond, R. Rademakers, D.W. Dickson, D.F. Broderick, O.<br />
Andersen and Z.K. Wszolek; Gothenburg, Sweden; Jacksonville,<br />
FL; Rochester, NY; Trondheim, Norway; Scottsdale, AZ; San<br />
Francisco, CA; Rochester, MN and Munchen, Germany<br />
Background: Hereditary diffuse leukoencephalopathy with<br />
spheroids (HDLS) is an autosomal dominant neurodegenerative<br />
disorder with symptomatic disease onset usually in<br />
adult age and with relatively rapid course leading to death<br />
in less than a decade. It is clinically characterized by a constellation<br />
of symptoms including personality changes, cognitive<br />
dysfunction and motor impairments, often leading to a<br />
clinical misdiagnosis. Neuropathology is characterized by<br />
axonal spheroids. The disease-causing gene is unknown.<br />
Methods: Over the last 7 years, we have collected HDLS<br />
families both retrospectively and prospectively. We performed<br />
head magnetic resonance imaging (MRI) studies<br />
with only neuropathological proven HDLS cases/kindreds.<br />
Results: From all 13 families available to us, 14 cases<br />
were studied. 4 had repeated examinations. MRI demonstrated<br />
unique distribution of changes in the periventricular,<br />
deep and subcortical white matter of frontal/parietal lobes<br />
and in corpus callosum.<br />
Conclusions: MRI is helpful to substantiate the diagnosis<br />
of HDLS. It will be an important biomarker for HDLS<br />
progression after the gene is identified. It will also be very<br />
useful to follow the patients undergoing future experimental<br />
treatments if such are developed.<br />
Study supported by: C.Sundal supported by research<br />
grants through Gothenburg University, Sweden<br />
S205. Appropriate Outcome Measures for Cognitive<br />
Trials in Huntington’s Disease<br />
Jody Corey-Bloom, Jody Goldstein, Shea Gluhm, Charles Van<br />
Liew, Stephanie Lessig, Jagan Pillai and Steven D. Edland; La<br />
Jolla, CA<br />
Suitable measures are needed for clinical trials of therapeutic<br />
agents for cognition in Huntington’s disease (HD). The<br />
Montreal Cognitive Assessment (MoCA), Mini-Mental State<br />
Examination (MMSE), and Mattis Dementia Rating Scale<br />
(DRS) are commonly used cognitive instruments; however,<br />
little is known about longitudinal change on these measures<br />
in HD. We used mixed effects models to analyze MoCA,<br />
MMSE, and DRS scores obtained during 2.5–5 years of<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 34<br />
follow-up of up to 153 subjects with HD. Annual rates of<br />
decline on the MoCA and MMSE were 1.0 and 0.69<br />
points/year, respectively, over 2.5 years of follow-up. Rate of<br />
decline on the DRS was 3.04 points/year in the first 5 years<br />
of observation. For cognitive trials in HD, sample size<br />
requirements (90% power, critical alpha level 0.05) for a 3year<br />
trial to detect 50% reduction in mean rate of decline<br />
using the MoCA, MMSE, or DRS would be 106, 173, and<br />
165 subjects/ treatment arm, respectively. We conclude that,<br />
although all three measures decline significantly over time in<br />
an unselected HD population, the MoCA may be a more<br />
efficient instrument for assessing effects of a therapeutic<br />
agent for cognition in HD.<br />
Study supported by: Huntington’s Disease Society of<br />
America and Shiley-Marcos Alzheimer Disease Research<br />
Center NIH P50 AG005131.<br />
S206. Distinctive Neurocognitive Profiles Associated<br />
with Right and Left Motor Symptom Onset in<br />
Parkinson’s Disease<br />
Paul J. Eslinger, Daymond Wagner, Suman Sen, Mechelle M.<br />
Lewis, Guangwei Du, Michele L. Shaffer and Xuemei Huang;<br />
Hershey, PA<br />
Parkinson’s disease (PD) is commonly diagnosed in patients<br />
presenting with asymmetric motor impairments. However,<br />
the literature remains mixed with regard to the significance<br />
and prognostic value of identifying first-onset motor symptoms<br />
particularly for cognitive functioning and progression.<br />
We investigated the hypothesis that asymmetric motor<br />
impairment and attendant dopamine loss are associated with<br />
distinctive right- and left-onset profiles in 36 PD subjects<br />
(21 with right-sided,15 with left-sided motor symptom<br />
onset) and 44 matched healthy controls recruited for longitudinal<br />
cognitive and anatomical studies. Although samples<br />
did not differ on screening cognitive measures (Mini-Mental<br />
Status Examination, Montreal Cognitive Assessment), contrasting<br />
profiles of neurocognitive impairments were<br />
detected in PD. Specifically, left-sided motor symptoms<br />
were associated with prominent deficits in visuospatial learning<br />
and memory, visuospatial speed/accuracy in mirror tracing,<br />
and design fluency. In contrast, right-sided motor<br />
symptoms were associated with decline in cognitive flexibility<br />
and heightened symptoms of depression. Results support<br />
the hypothesis that asymmetric motor symptoms in PD are<br />
associated with distinctive patterns of early cognitive change<br />
that may require different management approaches. Analyses<br />
are underway to examine the relationship between such cognitive<br />
profiles and cortical changes in PD.<br />
Study supported by: National Institutes of Health<br />
S207. The Clinical and Pathological Features of Familial<br />
Parkinsonism with EIF4G1Gene Mutation<br />
Shinsuke Fujioka, Owen A. Ross, Rosa Rademakers, Matthew<br />
J. Farrer, Dennis W. Dickson and Zbigniew K. Wszolek;<br />
Jacksonville, FL and Vancouver, BC, Canada<br />
Recently, we have performed genome-wide linkage analysis<br />
of several families with autosomal-dominant late-onset parkinsonism<br />
and identified mutations in a novel susceptibility<br />
gene for Parkinson’s disease, eukaryotic translation initiation<br />
factor 4-gamma 1 isoform (EIF4G1) on chromosome 3q26-<br />
27. The missense mutations, EIF4G1 c.2057G>T<br />
(p.G686C) and c.3589C>T (p.R1197W) were identified<br />
together in two siblings of US 331-95 family. We reviewed<br />
available medical records and brain autopsy reports for both<br />
siblings. Mean age at symptomatic onset was 79 years and<br />
mean disease duration was 5.5 years. Both siblings presented<br />
34<br />
with hallucinations or depression followed by memory<br />
impairment. The younger brother developed levodopa responsive<br />
asymmetrical parkinsonism characterized by resting<br />
tremor, rigidity, and bradykinesia during the course of his<br />
illness. The autopsy showed transitional (limbic) type of<br />
Lewy body disease (LBD) in the brother and diffuse LBD<br />
in the older sister, with mild to moderate Alzheimer’s disease<br />
pathology (Braak stage II-IV) in both. We will present<br />
our clinicopathologic review with future genealogical and<br />
clinical research planned on this family.<br />
Study supported by: ZKW is partially supported by the<br />
NIH/NINDS 1RC2NS070276, NS057567, P50NS072187,<br />
Mayo Clinic Florida (MCF) Research Committee CR programs<br />
(MCF #90052018 and MCF #90052030), and gift<br />
from Carl Edw and Bolch, Jr., and Susan Boss Bolch (MCF<br />
#90052031/PAU #90052). FS is partially supported by<br />
Mayo Clinic Florida (MCF) Research Committee CR programs<br />
(MDF #90052018).<br />
S208. Alcohol Consumption and Risk of Parkinson<br />
Disease<br />
Rui Liu, Yikyung Park, Xuemei Huang, Xuguang Guo, Albert<br />
Hollenbeck, Aaron Blair and Honglei Chen; Research Triangle<br />
Park, NC; Rockville, MD; Hershey, PA and Washington, DC<br />
Objective: To prospectively examine the association between<br />
overall and individual types of alcohol consumption and<br />
risk of Parkinson disease (PD).<br />
Methods: Participants comprised 1,086 PD cases and<br />
299,684 individuals without PD from the NIH-AARP Diet<br />
and Health Study. Alcohol consumption was assessed in<br />
1995–1996 and PD was diagnosed in 2000–2006.<br />
Results: Total alcohol consumption was not associated<br />
with PD. However, moderate beer consumption was associated<br />
with lower risk of PD. After controlling for potential<br />
confounders and other types of alcohol consumption, the<br />
multivariate odds ratio (OR) for beer drinkers was 0.81<br />
(95% confidence interval [CI] 0.70–0.94) for
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 35<br />
kindred in 1984. An additional 11 kindreds and 8 sporadic<br />
cases have been reported over the years. Inheritance is autosomal<br />
dominant. HDLS presents with psychiatric, cognitive<br />
and motor symptoms. A definite diagnosis is made pathologically<br />
by demonstrating axonal spheroids. The causative<br />
gene is unknown.<br />
Method: Brains and brain biopsy specimens were collected<br />
through world wide collaborations and only those<br />
cases/families demonstrated pathological features of HDLS<br />
were included in our study.<br />
Results: 20 affected individuals were identified in 13 kindreds.<br />
During the course of the illness all patients developed<br />
parkinsonian signs along with other classic symptoms of<br />
HDLS. There was no response to levodopa. The mean age<br />
of onset was 45 years (range, 16–68), and mean disease duration<br />
was 4 years (range, 1–11).<br />
Discussion and Conclusions: HLDS is an under-diagnosed<br />
neurodegenerative condition. Cases are misdiagnosed<br />
as AD, PD, CBD, MS, FTD, FTDP, and others. Finding<br />
the gene for this condition will be of paramount importance<br />
in understanding the neurodegeneration associated with<br />
white matter abnormalities.<br />
Study supported by: C.Sundal supported by research<br />
grants through Gothenburg University, Sweden<br />
S210. Co-Existing HTT and ATXN8OS Repeat<br />
Expansions and a ‘Face of the Giant Panda’ Sign on<br />
MRI in a Patient with a Complex Movement Disorder<br />
Shin C. Beh, Cherian A. Karunapuzha and Shilpa Chitnis;<br />
Dallas, TX<br />
We present a 66 year old woman with a complex movement<br />
disorder syndrome. The disease began in her mid-fifties with<br />
fidgetiness. She later developed progressive gait ataxia and<br />
chorea. Unintended weight loss, mild dysphagia, depression<br />
and mild memory impairment were also present. Examination<br />
revealed square-wave jerks, grimacing, motor impersistence,<br />
generalized choreiform movements, hyperreflexia and<br />
an ataxic, choreic gait. Her mother had a similar movement<br />
disorder. In addition to cortical atrophy, T2-weighted brain<br />
MRI demonstrated mesencephalic white matter hyperintensity<br />
with areas of hypointensity in the red nuclei, substantia<br />
nigra and superior colliculi taking on the appearance of the<br />
‘‘face of the giant panda’’ sign. Genetic testing revealed coexisting<br />
huntingtin and ATXN8OS triplet repeat expansions.<br />
We discuss phenotype-genotype correlation and the unusually<br />
variable phenotypes of spinocerebellar ataxia 8.<br />
S211. Clinical Differences among PD-MCI Subtypes<br />
Jennifer G. Goldman, Glenn T. Stebbins, Bryan Bernard and<br />
Christopher G. Goetz; Chicago, IL<br />
Objective: To examine PD-MCI subtypes.<br />
Background: Mild cognitive impairment in PD (PD-<br />
MCI) may represent a pre-dementia state. MCI subtypes distinguish<br />
between amnestic (aMCI) and nonamnestic (naMCI)<br />
phenotypes and single (SD) or multiple-domain (MD)<br />
impairment. Whether PD-MCI subtypes differ in characteristics,<br />
progression or neuropathology remains unknown.<br />
Methods: 96 PD-MCI patients (not demented but with zscore<br />
of < 1.5 on at least 1 of 5 cognitive domains) were classified<br />
as: aMCI-SD, naMCI-SD, aMCI-MD, and naMCI-MD.<br />
Results: Group demographics included: age 71.8 (9.2),<br />
education 14.5 (2.9), PD duration 6.9 (5.2) years; MMSE<br />
26.9 (2.1); UPDRS motor score 31.6 (11.4). In our sample,<br />
25% had aMCI-SD, 44% naMCI-SD, 21% aMCI-MD,<br />
and 10% naMCI-MD. Subtypes differed significantly<br />
regarding age, PD onset age, MMSE, and H&Y stage. Post-<br />
35<br />
hoc analyses revealed older PD onset age in aMCI-SD,<br />
worse MMSE scores in naMCI-MD, and worse H&Y stage<br />
in naMCI-MD. Mean UPDRS motor scores were higher in<br />
both MD subtypes. Axial function differed among groups<br />
with worse scores in naMCI-MD.<br />
Conclusion: Nonamnestic and single domain impairment<br />
predominated. Multiple-domain PD-MCI had worse motor<br />
function. Increased burden of cognitive dysfunction (multiple-domain),<br />
rather than deficit type (amnestic/nonamnestic),<br />
may be associated with greater motor impairment and<br />
dementia risk.<br />
Study supported by: NIH K23060949, Parkinson’s<br />
Disease Foundation<br />
S212. Loss of Cortical Gray Matter in Parkinson’s<br />
Disease<br />
Suman Sen, Paul J. Eslinger, Daymond Wagner, Guangwei<br />
Du, Mechelle M. Lewis, Michel L. Shaffer and Xuemei<br />
Huang; Hershey, PA<br />
In addition to classic motor dysfunction, Parkinson’s disease<br />
(PD) patients exhibit cognitive deficits that are related to<br />
cortical network dysfunction. To investigate PD changes in<br />
cortical gray matter, high-resolution T1-weighted magnetic<br />
resonance images were acquired from 40 right-handed PD<br />
subjects and compared to 40 age-, gender-, education-, and<br />
handedness-matched healthy controls. Screening cognitive<br />
measures of Mini-Mental Status Examination (p ¼ 0.32) and<br />
Montreal Cognitive Assessment (p ¼ 0.81) were also comparable<br />
between groups. Imaging data were analyzed using<br />
voxel-based morphometry (VBM). Permutation-based, nonparametric<br />
testing (5000 permutations) was applied within<br />
the framework of a general linear model, adjusting for age<br />
and gender within groups. Group differences were considered<br />
significant at p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 36<br />
Methods: Analysis is based on 199 PSP cases and 129<br />
age-gender and geographically matched controls. Trained<br />
interviewers conducted standardized telephone surveys to<br />
collect information including demographics, residence history,<br />
lifetime occupational history and home pesticide use.<br />
An industrial hygienist and toxicologist blinded to whether<br />
data were from cases or controls assessed self-reported exposure<br />
to chemicals and determined if the subjects had direct,<br />
indirect or no exposure based on occupational histories.<br />
Odds ratios (OR) and 95% confidence intervals (CI) were<br />
estimated using univariable and multivariable logistic regression<br />
adjusting for significant covariates.<br />
Results: PSP cases were significantly more likely to report<br />
exposure to occupational pesticides (OR:2.22; CI:1.15-4.37,<br />
p ¼ 0.015) and organic solvents (OR:1.57; CI:1.05-2.34, p<br />
¼ 0.026) than controls. Using assigned exposures, cases<br />
were significantly more likely to have direct exposure to any<br />
chemical (OR:1.99; CI:1.26-3.16, p ¼ 0.003), and pesticides<br />
(OR:2.14; CI:1.06-4.61, p ¼ 0.034).<br />
Conclusions: This is the first epidemiological study to<br />
find a significant association between occupational chemical<br />
exposures and PSP. Future studies should determine which<br />
chemicals are associated with the development of this primary<br />
tauopathy and whether genetic and environmental risk<br />
factors interact.<br />
Study supported by: National Institutes of Aging,<br />
National Insitutes of Health<br />
S214. Psychiatric Co-Morbidities and Mortality among<br />
Hospitalized Parkinson Disease Patients<br />
Nicte Mejia and Zeina Chemali; Boston, MA<br />
Affective and anxiety disorders are determinants of poor<br />
quality of life and survival for Parkinson disease (PD)<br />
patients. Their impact on in-hospital PD mortality has not<br />
been examined.<br />
The study evaluates the effect of depression and anxiety<br />
on in-hospital PD mortality.<br />
PD patients with depression or anxiety would have higher<br />
in-hospital mortality compared to PD patients with no psychiatric<br />
co-morbidities. Alcohol or drug use would further<br />
increase mortality. We sampled 1998–2007 HCUP-NIS for<br />
PD, depression, anxiety, alcohol and drug use were identified<br />
through ICD-9 codes. All statistical models were<br />
adjusted for age, gender, and race/ethnicity.<br />
3,013,346 collected PD discharges-age 77.9 (SD 9.0<br />
years), 52.8% male, 84% white. Depression identified in<br />
10.6%; anxiety in 4.7%, an underestimate to population<br />
predicted prevalence for those disorders in same settings.<br />
Statistically significant lower mortality was found for PD<br />
patients with known depression (OR ¼ 0.64; p< 0.001) or<br />
anxiety (OR ¼ 0.50; p< 0.001). Substance and alcohol use<br />
were assessed as modifiers.<br />
Depression and anxiety are under-diagnosed in hospitalized<br />
PD patients. Contrarily when recognized and appropriately<br />
treated, depression and anxiety are associated with<br />
lower in-hospital PD mortality. Alcohol and illicit substances<br />
impact negatively on PD outcome.<br />
Study supported by: The authors have no disclosure. Dr.<br />
Nicte Mejia was awarded 2010 AAN Foundation Clinical<br />
Research Training Fellowships<br />
S215. Comparison of Subthalamic (STN) and Pallidal<br />
(GPi) Deep Brain Stimulation (DBS) on Gait and<br />
Balance in Patients with Parkinson’s Disease (PD)<br />
Jyhgong Gabriel Hou, Minn Thant, Aliya Sarwar, Linda<br />
Fincher, Monthaporn S. Bryant, Farrah Atassi and Eugene C.<br />
Lai; Houston, TX and Galveston, TX<br />
36<br />
Objective: To study if STN-DBS or GPi-DBS has different<br />
effects on gait and balance in individuals with PD.<br />
Background: Both STN- and GPi-DBS improve motor<br />
functions in PD. However, their differential benefits on gait<br />
and balance are unclear. Comparison of their effects may<br />
help clinical decisions in choosing the target.<br />
Method: Composite scores of 5-UPDRS items (arising, posture,<br />
gait, postural instability, bradykinesia) and 3-item standwalk-sit<br />
test of the STN-DBS (N ¼ 25) and GPi-DBS (N ¼<br />
23) groups were compared. Variables during ‘‘off-on’’ (medication-off,<br />
stimulation-on), ‘‘off-off’’ and ‘‘on-on’’ were measured.<br />
Result: During ‘‘off-on’’, the sum of 5-item UPDRS<br />
improved by 1.96(p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 37<br />
S217. First <strong>Neurological</strong> Examination Can Predict<br />
Course of Parkinson’s Disease (PD)<br />
Ali H. Rajput, Michele L. Rajput and Alex H. Rajput;<br />
Saskatoon, SK, Canada<br />
Our previous publications concluded that, when the entire<br />
clinical course is considered, the tremor dominant (TD),<br />
mixed (MX), and akinetic/rigid (AR) subtypes of PD have<br />
different pathology and different outcomes. There are no biological<br />
markers or early clinical manifestations to distinguish<br />
between those phenotypes.<br />
All patients were followed at Movement Disorders Clinic<br />
Saskatchewan and autopsied between 1972 and 2006. Those<br />
with Lewy body PD and no co-morbidity to modify the motor<br />
features were included. Excluded were cases that at baseline<br />
had 15 years or longer duration of PD motor symptoms. The<br />
patients were assessed in the state as they attended our clinic.<br />
We hypothesized that predominant tremor at baseline<br />
would evolve into lifelong TD, predominant akinesia/rigidity<br />
into AR and those with equal severity into MX subtypes.<br />
156 PD cases in the study, included 39 AR, 106 MX, and<br />
11 TD subtypes. Mean duration of symptoms at baseline was<br />
4.4 years. 133 (85%) of all – 90% of AR, 88% of MX, and<br />
55% of TD could be accurately identified at baseline.<br />
These observations are helpful for patient care, drug trials<br />
patient selection and for studies of pathophysiology of PD.<br />
Study supported by: Have received honorarium for lectures<br />
and meeting participation from Novartis. Have<br />
received travel support to meeting from Teva. Have been<br />
involved in Botulinum toxin study sponsored by Allergan.<br />
Research funding from Curling Classic, Parkinson Society<br />
Saskatchewan, and Greystone Golf Classic.<br />
S218. Difficulty with Balance Occurs Early in PD: It<br />
Isn’t Appreciated Because It’s Not Asked about Nor<br />
Tested For<br />
Abraham N. Lieberman, Samea Husain, Naomi Salins and<br />
Anthony Santiago; Phoenix, AZ<br />
Objective: Devise a question and tests to assess balance<br />
early, before patients fall.<br />
Background: Balance difficulty resulting in falls is a wellrecognized<br />
feature late in PD. Less well known is that balance<br />
difficulty occurs early in PD.<br />
Method: In addition to questions and testing of gait on<br />
the UPDRS we added a question about balance and 3 simple<br />
balance tests. We assessed balance and gait in 102 consecutive<br />
non-demented PD patients. The ANOVA analysis<br />
was used for continuous variables and a logistic regression<br />
analysis was used for categorical variables.<br />
Results: Duration of PD in patients who answered ‘‘yes’’<br />
on our balance question was 7.11 (6 4.5) versus 3.95 ( 6<br />
1.79) yrs in patients who answered ‘‘no.’’ This was significant:<br />
p< 0.0007. It’s noteworthy that 45% of 62 patients<br />
with PD for 1- 5 yrs had balance difficulty separate from<br />
gait difficulty. There were statistically significant differences<br />
on the tests between patients who complained of balance<br />
difficulty and those who did not.<br />
Conclusions: the balance question and tests provide a<br />
simple way of assessing balance early in PD.<br />
Study supported by: Self supported<br />
S219. Poor Dementia Screening with Mattis Dementia<br />
Rating Scale Cutoffs in Highly Educated Parkinson’s<br />
Disease Patients<br />
Travis H. Turner and Vanessa Hinson; Charleston, SC<br />
Introduction: The Mattis Dementia Rating Scale (DRS) is<br />
widely used to assess cognition and screen for dementia in<br />
37<br />
Parkinson’s disease (PD). In 2008, Llebaria and colleagues<br />
reported excellent sensitivity and specificity detecting dementia<br />
in PD using a DRS total score cutoff of 123. However,<br />
this study used a sample with rather low educational<br />
achievement.<br />
Methods: Linear discriminant function analysis was used<br />
cross-validate the 123 cutoff score in a sample of PD<br />
patients with rather high educational.<br />
Results: From a sample of 38 PD patients, 12 were diagnosed<br />
with dementia following comprehensive neuropsychological<br />
evaluation. A total score cutoff of 123 misidentified<br />
9 patients with dementia (25% sensitivity, 100% specificity).<br />
Age and education corrected scaled scores did not<br />
improve overall classification.<br />
Discussion: Results suggest caution in applying DRS-2<br />
total score cutoffs in highly educated patients, and highlight<br />
the importance of comprehensive neuropsychological evaluations<br />
for clinical diagnosis of dementia in PD.<br />
S220. Impaired Social Problem-Solving in Huntington’s<br />
Disease<br />
Charles Van Liew, Jody Goldstein, Shea Gluhm, Jagan Pillai<br />
and Jody Corey-Bloom; San Diego, CA<br />
Huntington’s disease (HD) is a genetic neurodegenerative<br />
disorder characterized by motor, cognitive, and psychiatric<br />
dysfunction. In HD, the inability to solve problems successfully<br />
affects not only disease coping, but also interpersonal<br />
relationships, judgment, and independent living. In the current<br />
study, we examined social problem-solving (SPS) in<br />
well-characterized HD and at-risk (AR) subjects using the<br />
Social Problem-Solving Inventory-Revised:Long (SPSI-<br />
R:L)—a 52-item, well-validated, standardized measure of<br />
SPS. Items are aggregated under five subscales (Positive,<br />
Negative, and Rational Problem-Solving; Impulsivity/ Carelessness;<br />
and Avoidance). Thirty-five subjects, including 12<br />
HD (mean age ¼ 53, mean CAG ¼ 44) and 23 gene-positive<br />
AR (mean age ¼ 41, mean CAG ¼ 42), were compared<br />
with two-tailed t-tests on SPSI-R:L scores. HD subjects<br />
scored significantly worse on Total SPS (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 38<br />
8/18 (44%) subjects developed ICBs. Subjects developing<br />
ICBs showed a significantly higher rate of progression on<br />
the Psychoticism (PSY) (p ¼ 0.004), Paranoid Ideation<br />
(PAR) (P ¼ 0.01), Global Severity Index (GSI)(p ¼ 0.03),<br />
and Positive Symptom Total (PST) (p ¼ 0.01) subscores.<br />
Subjects randomized to pramipexole had a significantly<br />
higher rate of progression on the PAR subscore (p ¼ 0.02).<br />
Careful monitoring of psychological symptoms after initiation<br />
of DA therapy may aid in identifying patients at risk<br />
for developing ICBs. Pramipexole may play a role in the<br />
manifestation of ICBs by augmenting certain psychological<br />
symptoms. Clinicians should consider medication effects<br />
when prescribing DA in patients with underlying or progressive<br />
psychological distress.<br />
S222. Balance Difficulty in PD Correlates with Step<br />
Length and Velocity<br />
Abraham Lieberman, Naomi Salins, Tiki Hussain, Di Pan<br />
and Anthony Santiago; Phoenix, AZ<br />
Objective: To determine step length and velocity in PD<br />
patients.<br />
Background: PD patients often report balance difficulty<br />
without falls.<br />
Method: In 102 consecutive non-demented PD patients,<br />
we compared patients with reported imbalance without falls<br />
to patients without imbalance as regards age, PD duration,<br />
UPDRS/Pull-Test, BNI Balance Scale, Stride Length and<br />
Velocity. There were no confounding causes of balance or<br />
gait difficulty upon historical review or physical exam.<br />
Results: Patients with balance difficulty had a shorter<br />
stride: 1.72 (60.47) vs 2.16 (60. 27) feet/ step, p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 39<br />
controls. Lower MeDi adherence was associated with higher<br />
odds for PD after adjustment for all covariates (OR per<br />
MeDi point ¼ 0.894, 95%CI ¼ 0.800–0.998, p ¼ 0.045).<br />
Mean age-at-PD-onset was 61.6yrs. Lower MeDi score was<br />
associated with earlier age-at-PD-onset (b ¼ 1.275, p ¼<br />
0.001).<br />
Conclusions: PD patients adhere less than controls to<br />
the MeDi. Dietary behavior may relate to PD risk.<br />
Study supported by: NIH (NS32527 and KL2<br />
RR024157) and the Parkinson’s Disease Foundation<br />
S226. Autonomic Dysfunction in Early Parkinson’s<br />
Disease<br />
Anna L. Molinari, Fenna T. Phibbs, Lily Wang, Yanna Song<br />
and P. David Charles; Nashville, TN<br />
Background: Orthostatic hypotension (OH) and suppressed<br />
heart rate (HR) response to standing are frequent symptoms<br />
of autonomic dysfunction (AD) in advanced Parkinson’s<br />
Disease (PD), but their incidence in early PD is unknown.<br />
Methods: 30 Hoehn & Yahr Stage II idiopathic PD subjects<br />
underwent a 7 day medication washout. Seated and<br />
standing blood pressure (BP) and HR measurements were<br />
recorded daily. Subjects were divided into 2 groups based<br />
on medication regimen: Group 1 levodopa only (n ¼ 9),<br />
Group 2 dopamine agonist monotherapy or in combination<br />
with levodopa (n ¼ 21).<br />
Results: HR response to standing improved in all 30 subjects<br />
during medication washout with an average increase of<br />
2.9 6 7.7 beats/minute (p ¼ 0.03). No subjects exhibited<br />
symptomatic OH. On average, systolic BP (SBP) decreased<br />
by 2.60 mmHg and diastolic BP (DBP) decreased by 3.13<br />
6 9.26 mmHg on Day 8, but these differences were not<br />
significant. Subjects in Group 1 experienced a smaller difference<br />
between seated and standing SBP and DBPs on Day 8,<br />
but these differences were also not significant.<br />
Conclusions: In early PD, the normal compensatory<br />
increase in HR upon standing is diminished while SBP and<br />
DBP are unaffected. HR response should be considered<br />
when evaluating AD in early PD.<br />
Study supported by: The clinical trial from which this case<br />
is reported is funded by Medtronic, Inc., by Vanderbilt CTSA<br />
grant 1 UL1 RR024975 from the NCRR-NIH, and by private<br />
donations. Medtronic representatives did not take part in<br />
data collection, management, analysis, or interpretation of the<br />
data or in preparation, review, or approval of the manuscript.<br />
Dr. Charles has received personal compensation and Vanderbilt<br />
University has received grants to support research<br />
from Medtronic in excess of $10,000. Dr. Charles has also<br />
received funding from Allergan for speaking and consulting<br />
services as well as research grants.<br />
S227. Balance Difficulty in PD Correlates with the BNI<br />
Balance Scale<br />
Abraham Lieberman, Naomi Salins, Tiki Hussain, Di Pan<br />
and Anthony Santiago; Phoenix, AZ<br />
Objective: To compare PD patients with and without<br />
reported balance difficulty by several variables to assess the<br />
validity of the BNI Balance Scale.<br />
Background: Balance difficulty is a late complication of<br />
PD. We devised a questionnaire and tested 3 tasks to calculate<br />
the BNI Balance Scale.<br />
Method: In 102 consecutive non-demented PD patients,<br />
we compared patients with reported balance difficulty without<br />
falls to patients without imbalance as regards age, PD<br />
duration,UPDRS/Pull-Test, BNI Balance Scale (one foot<br />
stance, turning 360 degrees, timed-gait). There were no<br />
39<br />
confounding causes of balance or gait difficulty upon historical<br />
review or physical exam.Results: Patients with reported<br />
balance difficulty had a longer duration of PD: 7.2 (6 4.6)<br />
vs 4.4 (6 2.4) yrs, p < 0.008; a worse BNI Balance Score:<br />
7.9 (6 3.8) vs 2.8 (6 2.3), p 30% difference relative to<br />
placebo. The interim tolerability analysis was preplanned after<br />
50 subjects (50%) completed 12 week dose titration phase.<br />
Results: The 20 mg dose was declared intolerable based<br />
on the interim tolerability data reviewed by the Data Safety<br />
Monitoring Board in July 2010. Investigators remained<br />
blinded to the dose assignment.<br />
Conclusion: These results support previously reported<br />
data on the dose dependent tolerability of isradipine in PD.<br />
Final data analysis and dose choice for the pivotal study will<br />
be available Fall 2011.<br />
Study supported by: Michael J. Fox Foundation and<br />
Northwestern Memorial Foundation Dixon Priority<br />
Research Initiative Award<br />
S229. Nigella sativa Oil Controls Astrogliosis and<br />
Reduces Haloperidol-Induced Deficit in Rats<br />
Tafheem Malik**, Darakhshan Jabeen Haleem, Shema Husan,<br />
Shahid Pervez and Tasneem Fatima; Karachi, Sind, Pakistan<br />
and Karachi, Pakistan<br />
The neuropathological status of Haloperidol (HP) induced<br />
Extrapyramidal symptoms (EPS) remains unclear.Evidence<br />
suggested persistent neuronal alterations in the basal ganglia<br />
cause EPS. This study evaluate the possible protective effects<br />
of the Nigella sativa (NS) oil on HP induced neuronal alterations<br />
and motor symptoms. EPS was monitored in HP<br />
treated groups and with NS oil alone and with placebo.HP<br />
treated group displayed (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 40<br />
astrogliosis with no indication of cell loss and 82% normal<br />
neuronal densities were observed. We conclude that NS may<br />
prevent HP induced neuronal degeneration.We believe that<br />
further preclinical research into the utility of NS may indicate<br />
its usefulness as a protective agent from irreversible EPS.<br />
Study supported by: The University of Karachi, Pakistan.<br />
S230. Cost-Benefit Assessment of Two Forms of<br />
Botulinum Toxin Type-A in Different Pathologies<br />
Humberto Juarez, Santamaria Salvador, Leticia Hernandez<br />
and Enrique Molina; Mexico City, Mexico, Mexico<br />
Botulinum Toxin Type-A has been successfully used since<br />
20 years in the treatment of different movement disorder<br />
pathologies.The comparison with Merz Pharma VR<br />
’s Botulinum<br />
Toxin Type A regarding its equivalency has not been<br />
trustfully demonstrated.The Social Security Hospitals have a<br />
high captive population for each disease group.In 2008, due<br />
to administrative restructure, a 150 kD assessment of Botulinum<br />
Toxin Type-A was initiated.To effectively compare the<br />
potency, efficacy and safety of the new biologic, the same<br />
dilution and application standards were maintained. Video<br />
and photography were taken for all patients with a standard<br />
procedure.From May 2008 to April 2009 the responses of 4<br />
types of 150 kD different batches of the toxin were employed.Comparatively,<br />
patients injected with onabotulinumtoxin<br />
A from May 2007 to April 2008 were selected.Our surveillance<br />
regarding potency, maximum time effect, and maximum<br />
duration was that in all parameters the Botulinum<br />
Toxin Type A at 150 kD was lower and oscillates at 6 weeks<br />
in average for all pathologies.<br />
S231. Weight and Height Distribution in Children with<br />
Tourette Syndrome<br />
Katie Kompoliti, Glenn T. Stebbins and Christopher G. Goetz;<br />
Chicago, IL<br />
Objective: To compare height and weight of untreated children<br />
with Tourette syndrome (TS) with age and gender<br />
matched controls.<br />
Background: TS children are reported to have lower<br />
height and weight, with normal body mass index (BMI),<br />
indicating a possible dopaminergic over-activity.<br />
Methods: Weight and height of consecutive TS patients<br />
under 20 years were recorded. Patients were considered<br />
untreated if they had never taken medications for tics or TS<br />
co-morbidities. Age and gender standardized weight z-score<br />
and BMI z-scores were compared between the TS group and<br />
the CDC normative data from 2000 using one-sample t-test.<br />
Results: A total of 195 patients (155 males, 40 females),<br />
mean 11.9years (SD 3.5), were included, with 95 never<br />
exposed to medications. Untreated patients had higher<br />
adjusted average weight compared to the CDC sample’s mean<br />
(p ¼ 0.0005), but no difference in height (p ¼ 0.08). Patients<br />
with medication exposure had a higher adjusted weight compared<br />
to those never treated but no difference in height.<br />
Conclusion: Un-medicated TS children are heavier than<br />
the general population, arguing against a generalized hyperdopaminergic<br />
state. Medication treatment increases weight<br />
further, alerting physicians to monitor weight when treating<br />
TS children.<br />
S232. Motor Deterioration after Medication Withdrawal<br />
in Early Parkinson’s Disease<br />
Chandler E. Gill**, Anna L. Molinari, Thomas L. Davis,<br />
Mark Bliton, Stuart G. Finder, Michael G. Tramontana, Peter<br />
E. Konrad and David Charles; Maywood, IL; Nashville, TN<br />
and Los Angeles, CA<br />
40<br />
Without a biomarker of Parkinson’s disease (PD) progression,<br />
we rely on clinical ratings to estimate disease progression.<br />
Medication washout may be useful in these ratings.<br />
We are conducting a prospective, blinded, pilot trial of deep<br />
brain stimulation (DBS) in early stage PD subjects aged 50<br />
to 75, Hoehn & Yahr II, without dyskinesias or motor fluctuations,<br />
and on PD medications < 4 years. Inpatient medication<br />
washout and motor rating is conducted at baseline<br />
and every six months for two years. On Day 1, subjects are<br />
rated ON medication and then medications are withheld<br />
and motor function is rated daily. Thirty subjects were<br />
randomized (15 MED; 15 DBSþMED). Participants are 27<br />
males and 3 females aged 60.3 6 6.6 years at study entry<br />
and taking medication an average of 2.1 6 1.5 years.<br />
UPDRS-III score at baseline Day 1 (ON medication) was<br />
14.9 6 7.9 which increased by 1.7 points per day to 27.0<br />
6 7.9 after one week withdrawal. Median ON Hoehn &<br />
Yahr Score was 2 (Range: 1-2) which remained at 2 after<br />
one week (Range: 2–2.5). Schwab & England ADL score<br />
also did not significantly change (Day 1: 92% 6 5%; Day<br />
8: 89% 6 4%).<br />
Study supported by: The clinical trial from which this<br />
case is presented is supported by Vanderbilt CTSA grant 1<br />
UL1 RR024975 from the National Center for Research<br />
Resources, National Institutes of Health, by a research<br />
grant from Medtronic, Inc., and by gifts from private<br />
donors.<br />
Vanderbilt University has received support from Allergan<br />
and Medtronic for research led by Drs. Charles and Medtronic<br />
for researcfh led by Dr. Konrad. Drs. Konrad and<br />
Davis have received personal compensation in the past from<br />
Medtronic for consulting fees or honoraria. Dr. Charles<br />
receives income from Allergan, Medtronic, and Pfizer for<br />
education and consulting services.<br />
S233. Gender Differences in the Interleukin-6 G-174C<br />
Polymorphism and the Risk of Parkinson’s Disease<br />
Marta San Luciano, Laurie J. Ozelius, Richard B.. Lipton,<br />
Deborah Raymond, Kaili M. Stanley, Susan B. Bressman and<br />
Rachel Saunders-Pullman; New York, NY and Bronx, NY<br />
Reports of associations between the -174G>C SNP in the<br />
promoter region of the interleukin-6 (IL6) gene and the<br />
1730G>A SNP in the estrogen receptor beta (ESR2) and<br />
PD are conflicting. We investigated the association of both<br />
SNPs in a sample of 121 unrelated Caucasian Parkinson’s<br />
disease (PD) cases and 329 control subjects. The G allele of<br />
the G-174C SNP was more common in the group of men<br />
with PD when compared to controls (p ¼ 0.022), but not<br />
among women with PD or in the overall group. In men,<br />
having the GG genotype increased the risk of PD by over<br />
two fold (OR ¼ 2.11, 95%CI: 1.14–3.89, p ¼ 0.017).<br />
Analysis restricted to young-onset PD cases showed no association.<br />
No differences in allele or genotype frequencies<br />
were observed between PD patients and controls for the<br />
ERBeta G-1730A SNP in the overall group or either gender<br />
separately, or between younger onset PD patients and controls.<br />
Our data supports a possible inflammatory role in PD<br />
for IL6, and concurs with a prior report linking the G allele<br />
with PD, although a gender effect was not found. These<br />
findings were not replicated in two other samples. The contradictory<br />
findings may be explained by ethnic differences<br />
in distribution of IL6 polymorphisms, the existence of other<br />
polymorphisms in tight linkage disequilibrium with the C/<br />
G SNP differentially influencing IL6 expression, methodological<br />
differences and sample size considerations, and<br />
inability to capture the complex functional network of<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 41<br />
cytokines and chemokines from single gene association studies.<br />
Analysis of IL6 SNPs in larger and more diverse populations<br />
and sequencing of surrounding regions is recommended<br />
to further assess a role for this cytokine in PD.<br />
Study supported by: Dr. San Luciano is supported by an<br />
<strong>American</strong> Academy of Neurology Foundation Clinical<br />
Research Training Fellowship. Dr. Saunders-Pullman is supported<br />
by the Pfizer Society for Women’s Health Research<br />
Scholar Grant for Faculty Development in Women’s Health.<br />
This study was supported by Grant Number K23NS047256<br />
from the National Institute of <strong>Neurological</strong> Disorders and<br />
Stroke (RSP), the Michael J. Fox Foundation (RSP, SBB),<br />
the Thomas Hartman Foundation (RSP), and The Einstein<br />
Aging Study is funded by the National Institute on Aging<br />
(AG03949, Principal Investigator: R.B. Lipton). This publication<br />
was made possible by the CTSA Grant UL1<br />
RR025750 and KL2 RR025749 and TL1 RR025748 from<br />
the National Center for Research Resources (NCRR), a<br />
component of the National Institutes of Health (NIH), and<br />
NIH Roadmap for Medical Research.<br />
S234. Serum Cholesterol Is Linked with Nigrostriatal<br />
Iron Deposition in Parkinson’s Disease<br />
Guangwei Du, Mechelle M. Lewis, Michele L. Shaffer,<br />
Honglei Chen, Richard B. Mailman and Xuemei Huang;<br />
Hershey, PA and Research Triangle Park, NC<br />
Higher nigrostriatal iron content has been related to Parkinson’s<br />
disease (PD). Higher serum cholesterol levels also have<br />
been suggested to be associated with lower occurrence of PD.<br />
To understand the relationship between serum cholesterol and<br />
nigrostriatal iron content, 3T MRI (T1-, T2-weighted, T2*)<br />
were obtained from 40 PD and 29 matched Controls. Fasting<br />
serum lipid profiles were measured in all subjects. The mean<br />
R2* values of bilateral substantia nigra (SN), caudate, putamen,<br />
globus pallidus (GP), and red nucleus (RN) were calculated,<br />
and correlated with serum cholesterol levels after controlling<br />
for age, gender, and statin usage. In PD, higher serum<br />
cholesterol levels were associated with lower iron content in<br />
SN (R ¼ 0.337, and p ¼ 0.048), striatum (R ¼ 0.403, p<br />
¼ 0.017 for caudate; R ¼ 0.366, p ¼ 0.031 for putamen),<br />
and RN (R ¼ 0.436, p ¼ 0.009), but not GP (R ¼<br />
0.250, p ¼ 0.147). In Controls, higher serum cholesterol<br />
levels were associated with lower iron content in striatum (R<br />
¼ 0.449, p ¼ 0.032 for caudate; R ¼ 0.451, p ¼ 0.027<br />
for putamen), but not associated with the SN (R ¼ 0.096, p<br />
¼ 0.654), RN (R ¼ 0.<strong>136</strong>, p ¼ 0.526), or GP (R ¼<br />
0.191, p ¼ 0.371) iron levels. Thus, higher serum cholesterol<br />
concentrations are associated with lower iron content in<br />
nigrostriatal structures, warranting further studies.<br />
Study supported by: NS060722, and the HMC GCRC<br />
(NIH M01RR10732) and GCRC Construction Grant<br />
(C06RR016499)<br />
S235. Balance Difficulty Differs from Gait Difficulty in<br />
PD<br />
Abraham Lieberman, Naomi Salins, Tiki Hussain, Di Pan<br />
and Anthony Santiago; Phoenix, AZ<br />
Objective: To compare reported balance difficulty from gait<br />
difficulty in PD.<br />
Background: Patients with PD often report imbalance<br />
without gait challenges.<br />
Method: In 102 consecutive non- demented PD patients,<br />
we compared 13 patients with reported imbalance without<br />
gait impairment with 22 patients with isolated gait difficulty<br />
as regards age, PD duration, UPDRS/Pull-Test, BNI Bal-<br />
41<br />
ance Scale. There were no confounding causes of balance or<br />
gait difficulty upon historical review or physical exam.<br />
Results: Patients with reported imbalance without gait<br />
challenges demonstrated postural instability to Pull-Test: odds<br />
ratio 6.00 (95% CL 1.331, 27.047), and one foot stance<br />
instability: odds ratio 5.440 (95% CL 1.217, 24, 321) compared<br />
with patients reporting isolated gait difficulty.<br />
Conclusions: Most patients with PD report a balance<br />
difficulty with a co-morbid gait challenge. We believe there<br />
is a subset of patients with subjectively perceived and objectively<br />
measurable impaired balance without noticeable gait<br />
challenges that may reflect a distinct circuitry aberration<br />
impacting balance separate from locomotion.<br />
S236. Adult Onset Dopamine Responsive Dystonia<br />
(DRD): Is There a New Gene?<br />
Hossein Ansari, Ludwig Gutmann and Laurie Gutmann;<br />
Morgantown, WV<br />
Background: DRD is a type of inherited dystonia typically<br />
presenting within the first decade of life. Various genes have<br />
been identified for this condition.<br />
Late-onset DRD is very rare and its gene has yet to be<br />
identified.<br />
Case Report: 29 y/o female with severe entire-body and<br />
facial dystonic movements. This was associated with occasional<br />
myoclonus. Mental status significantly decreased over<br />
the course of the patient’s nine-week hospitalization.Trials<br />
with different agents (including dopamine depletors) failed.<br />
Upon administration of Levopoda, however, the patient<br />
dramatically improved. After 2 doses, her mental status<br />
completely recovered and abnormal movements significantly<br />
decreased. With continued medication, patient normalized.<br />
Both the patient’s twin and one older sister have a history<br />
of similar movements.<br />
Conclusions: The rarity of late-onset DRD contributes<br />
to its misdiagnosis. Therefore, adult-onset DRD is probably<br />
an under-diagnosed condition with no known gene. We<br />
speculate this patient’s sisters also suffer from DRD.<br />
This family could be a prime case for genetic study used<br />
to identify the potential gene/mutation causing adult DRD.<br />
They are set to participate in a study by the NIH<br />
Undiagnosed Diseases Program.<br />
S237. Dystonia Induced Mechanical Stress as a Cause of<br />
DBS Extension Fracture and Expulsion<br />
Massimo Mondani, Elisa Petacchi, Roberto Eleopra, Silvia<br />
Molteni, Sabrina Gualdi, Miran Skrap and Andrea<br />
Martinuzzi; Udine, UD, Italy; Conegliano, TV, Italy and<br />
Sesto San Giovanni, MI, Italy<br />
The mechanical failure of the device, especially the most<br />
exposed and longest part connecting the electrode to the<br />
impulse generator (IPG) is a possible adverse eventa in DBS.<br />
We describe a 12 year old child in whom the successful<br />
treatment with GPi DBS for secondary generalized dystonia<br />
repeatedly failed for malfunction of the IPG-electrode connection<br />
including one internal fracture diagnosed by electrophysiology,<br />
and two aseptic scar breakage leading to expulsion<br />
of a 5 cm long stretch of the left extension and<br />
removal of the entire left implant.<br />
The study of the pattern of child’s movements and of the<br />
extension position along the left mastoid and neck revealed<br />
a region of mechanical stress on the left extension which<br />
was eluded by the right one thanks to its obliquity in<br />
respect to the axis of the prevalent neck movements.<br />
When implanting dystonia patients with DBS, especially<br />
when they are children and present neck dyskinesias, one<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 42<br />
should avoid positioning the IPG extension parallel to the<br />
major axis of the prevalent movement. A slight obliquity of<br />
the extension may suffice in preventing failures leading to<br />
suspension of an otherwise efficacious treatment.<br />
Sleep Disorders and Circadian Rhythm<br />
S301. Endogenous GABAA Receptor Enhancement<br />
Modulates Vigilance in the Primary Hypersomnias<br />
David B. Rye, Kathy Parker, Lynn Marie Trotti, Paul S.<br />
Garcia, James C. Ritchie, Michael J. Owens, Leslie Morrow,<br />
Donald L. Bliwise and Andrew Jenkins; Atlanta, GA;<br />
Rochester, NY and Chapel Hill, NC<br />
Primary hypersomnias lack an etiology or rational treatments.<br />
We investigated biological and neurobehavioral markers in 31<br />
such cases. Plasma and CSF assays ruled out sedative-hypnotic<br />
use, neurosteroid or gamma-aminobutryic acid (GABA)<br />
excess, pathological amino acid profiles, and hypocretin-1 deficiency.<br />
We tested for GABA-ergic activity employing ligand<br />
binding assays and electrophysiological recordings of cells<br />
expressing recombinant GABAA receptors. CSF from 31<br />
hypersomnolent and 16 control patients all enhanced a1b2c2s<br />
GABAA receptors. The magnitude of enhancement in hypersomnolent<br />
subjects exceeded that of controls (89% 6 46.5 vs<br />
41.4% 6 5.7, t ¼ 5.39, P < 0.001). Pharmacological profiling<br />
suggested that enhancement was due to an allosteric modulator<br />
unique to affected versus control CSF. Enhancement<br />
did not require a functional BZD binding site, was selective<br />
for a 2 > a1 receptors and negligible at a 4receptors,and<br />
was reversible with benzodiazepine antagonist flumazenil. Flumazenil<br />
normalized vigilance in seven index cases. Inhibitory<br />
GABAA receptor enhancement occurs by way of a positive allosteric<br />
modulator unique to patients with a primary hypersomnia.<br />
This altered biology is antagonized in vitro and in<br />
vivo by flumazenil and identifies a novel pathophysiology to<br />
primary hypersomnolence.<br />
Study supported by: Woodruff Health Sciences Center<br />
Fund and USPHS grants NS055015 and NS055015-03S1<br />
(D.B.R), NS-050595 (D.L.B), and GM073959 (A.J).<br />
S302. Frequency of Parsaomnias in Patients with<br />
Non-Epileptic Seizures<br />
Mitchell G. Miglis, Michael Boffa, Sujata Thawani, Alcibiades<br />
Rodriguez and Anuradha Singh; New York, NY<br />
Objective: To assess frequency of parasomnias in patients<br />
with Psychogenic Non-Epileptic Seizures (PNES)<br />
Background: PNES have been associated with a history<br />
of psychosocial stresssors, an association that has also been<br />
suggested for some parasomnias. There is little data on frequency<br />
of parasomnias in patients with PNES.<br />
Design/Methods: We selected a cohort of patients (n ¼<br />
9) with vEEG-confirmed PNES from our Epilepsy Unit<br />
and administered sleep questionnaires (Epworth, Munich<br />
Parasomnia Scale) on follow-up visits and phone interviews.<br />
An age-matched group of patients with vEEG-confirmed<br />
epilepsy (n ¼ 9) were interviewed for comparison. Participants<br />
were scored on responses relating to twenty-one parasomnias.<br />
Responses of PNES and epilepsy patient were<br />
compared (Chi square analysis, SPSS v16).<br />
Results: PNES patients reported a higher frequency of<br />
NREM parasomnias when compared to epilepsy patients,<br />
notably hypnic jerks (77.8% vs. 11.1%, p ¼ 0.004), rhythmic<br />
foot movements (55.6% vs. 0%, p ¼ 0.023), exploding<br />
head syndrome (44.4% vs. 0% p ¼ 0.023), and bruxism<br />
(66.7% vs. 0%, p ¼ 0.003).<br />
42<br />
Conclusions: Patients with PNES in our study population<br />
reported a higher frequency of NREM parasomnias<br />
compared to epilepsy patients, and a much higher frequency<br />
compared to general prevalence estimates. Parasomnias<br />
should always be considered in the differential of paroxysmal<br />
nocturnal events in these patients.<br />
Study supported by: Self Supported<br />
S303. Endothelial Function in Patients with Obstructive<br />
Sleep Apnea<br />
Kanika Bagai, James Muldowney, Yanna Song, Lily Wang,<br />
Douglas E. Vaughan and Beth A. Malow; Nashville, TN and<br />
Chicago, IL<br />
Background: Obstructive sleep apnea (OSA) is implicated in the<br />
pathogenesis of stroke, although mechanisms need clarification.<br />
Methods: Severity of OSA [apnea-hypopnea index (AHI)<br />
of 5 or greater] was defined by overnight polysomnography.<br />
Endothelial function testing was done using flow mediated<br />
dilatation and computerized arterial pulse waveform analysis<br />
in 17 patients with OSA and 17 normal controls.<br />
Results: The mean AHI (6 standard deviation) in the<br />
OSA group was 18.68(25.48) and in the non-OSA group was<br />
0.84 (0.80). Using a linear regression model, with AHI as the<br />
main effect, and age as covariates, there was a trend towards<br />
greater mean velocity change with higher AHIs (p ¼ 0.06).<br />
Conclusions: The severity of OSA selectively affects the<br />
percent velocity change after reactive hyperemia as measured<br />
by flow mediated dilation. Consistent with prior studies with<br />
altered endothelial function in OSA patients, our results show<br />
a trend towards significant difference in the markers of endothelial<br />
function as measured by brachial artery flow- mediated<br />
dilatation testing. One reason for the less dramatic difference<br />
noted in our study may be because we included patients with<br />
mild OSA, as compared with other studies which included<br />
patients with moderate to severe OSA.<br />
Study supported by: Supported in part by Vanderbilt<br />
CTSA grant 1 UL1 RR024975 from NCRR/NIH.<br />
Education<br />
S401. The Effectiveness of Education Intervention on<br />
Health Knowledge among <strong>Neurological</strong> Patients<br />
Mercedes Jacobson and Polina Pomerants; Philadelphia, PA<br />
Objective: To assess the impact of education intervention<br />
on patient’s health literacy in outpatient neurology<br />
setting.<br />
Background: Inadequate health knowledge is a strong indicator<br />
for higher risk of non-compliance, poor self-management,<br />
and negative health outcomes.<br />
Methods: A single-blind randomized study was conducted.<br />
Designed using Ask Me 3 principles, a questionnaire was<br />
administered to study group before and a week after onsite<br />
education intervention and to demographically matched control<br />
group a week after intervention. Performance was scored<br />
on consistency between subjects’ responses and congruence<br />
with information from subjects’ medical charts.<br />
Results: Control and study group population (N ¼ 118)<br />
consisted of unemployed (84%) middle-aged adults (44.2<br />
þ/ 12.4) who are legally disabled (66%) and lack postsecondary<br />
education (82%). Study subjects retained more<br />
health information (0.19þ/ 0.08, p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 43<br />
Conclusions: Statistically significant improvement in<br />
health knowledge resulted from education intervention using<br />
Ask Me 3 tool. Patient education with attention to health<br />
literacy should be employed in neurology teaching clinics to<br />
improve patients’ adherence to treatment and comprehension<br />
of health information.<br />
S402. Teleneurology in Leading U.S. Medical<br />
Institutions<br />
Benjamin P. George**, Nicholas J. Scoglio, Jason I. Reminick,<br />
Kevin M. Biglan and E. Ray Dorsey; Rochester, NY and<br />
Baltimore, MD<br />
Objective: Telemedicine is used for the care of neurological<br />
conditions yet little is known about the details of telemedicine<br />
use in neurology departments. The study purpose is to<br />
determine current teleneurology opinions and practices<br />
among neurologists at leading U.S. medical institutions.<br />
Methods: A survey on teleneurology was performed<br />
among neurologists at the top 50 hospitals in neurology<br />
based on U.S. News and World Report. The survey was<br />
sent to department chairs, faculty involved in teleneurology,<br />
or department administrators. Respondents indicated level<br />
of telemedicine use by department, current applications, and<br />
opinions of telemedicine.<br />
Results: The initial response rate was 32% (16 institutions,<br />
18 responses). 50% of respondents were neurology<br />
faculty, the remaining were department chairs (33%) and<br />
department administrators (17%). 69% of institutions provide<br />
telemedicine; of those, all use telemedicine for stroke,<br />
18% for movement disorders, and 9% for neuroimmunology.<br />
45% of institutions using telemedicine services initiated<br />
services within the last year, and 60% of institutions not<br />
providing telemedicine have plans to within a year. Additionally,<br />
61% of respondents find telemedicine to be equal<br />
to the in-person care model.<br />
Conclusions: There is increasing use and acceptance of<br />
teleneurology by neurologists at leading U.S. medical<br />
institutions.<br />
S403. Standardized Sign-Out Improves Communication<br />
Skills<br />
Brian D. Moseley, Jonathan H. Smith, Gloria E. Diaz-<br />
Medina, Mateo Paz Soldan, Meredith Wicklund, Radhika<br />
Dhamija, Haatem Reda, Michael F. Presti and Jeffrey W.<br />
Britton; Rochester, MN<br />
Objective: Unstructured handoffs are vulnerable to communication<br />
failures. We implemented standardized sign-out on<br />
our inpatient Neurology services and assessed its effect on<br />
communication skills.<br />
Methods: Residents spent the first half of their rotations<br />
utilizing unstructured sign-out. They switched to a structured<br />
sign-out system (using the Situation-Background-<br />
Assessment-Recommendation format) during the second<br />
half. We analyzed survey responses before and after implementation<br />
to evaluate for an effect.<br />
Results: We documented improvements in many variables,<br />
including being told: pertinent past medical history<br />
(14/33, 42% versus 14/20, 70%, p ¼ 0.088); pending laboratory<br />
studies/tests (26/33, 79% versus 19/20, 95%, p ¼<br />
0.234); recommendations for how to handle nursing/pharmacy<br />
calls (12/33, 36% versus 12/20, 60%, p ¼ 0.154);<br />
and up-to-date code status (14/33, 42% versus 14/20, 70%,<br />
p ¼ 0.088). Residents utilizing structured sign-out were significantly<br />
more likely to share test results with patients/family<br />
prior to shift changes (22/33, 67% versus 18/20, 90%, p<br />
¼ 0.037) and update our electronic service list (13/33, 39%<br />
43<br />
versus 15/20, 75%, p ¼ 0.045). The percentage who felt all<br />
important data were being transmitted increased from 49%<br />
(16/33) to 80% (16/20, p ¼ 0.041). Overall satisfaction<br />
(scale 1–10) increased from 6.2þ/ 1.6 to 7.4þ/ 1.3 (p ¼<br />
0.002).<br />
Interpretation: Structured sign-out results in improved<br />
communication skills, and may improve patient safety and<br />
quality of care.<br />
S404. Improved Scores on the AAN Resident Inservice<br />
Training Examination (RITE) after Lecture Curriculum<br />
Intervention<br />
L. John Greenfield, Vicki Ramsey-Williams, Theresa Marshall<br />
and Boyd Koffmann; Toledo, OH and Little Rock, AR<br />
Objective: Determine whether curriculum intervention has<br />
a positive impact on resident education as measured by<br />
RITE scores.<br />
Background: Performance on the RITE predicted scores<br />
on the ABPN Part I board examination, and has been used to<br />
assess readiness to take ABPN Part I (Goodman et al. 2002).<br />
Methods: Retrospective analysis of RITE and USMLE<br />
scores for 3 years preceding and following curriculum intervention,<br />
which consisted of realigning the didactic syllabus<br />
with the subject areas of the ABPN (Neurology) exam, and<br />
pre-and post-lecture quizzes.<br />
Results: All neurology residents at the Medical College of<br />
Ohio/University of Toledo between 2003 and 2010 were<br />
included. The mean percent of correct answers on the RITE<br />
significantly improved from prior to 2007 (55.561.4, n ¼<br />
30) to 2007 and after (61.361.6, n ¼ 27, p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 44<br />
S406. Adapting a Teaching Hospital Inpatient Neurology<br />
Service to New Duty Hour Requirements: The<br />
Washington University Adult Neurology Experience<br />
Robert Bucelli and Barbara J. Snider; Saint Louis, MO<br />
New duty hour regulations for ACGME accredited residency<br />
training programs will go into effect July 1, 2011.<br />
The complexity of neurological disorders makes balancing<br />
duty hours with educational and patient care goals particularly<br />
challenging for inpatient neurology services at teaching<br />
hospitals. The Washington University/Barnes Jewish Hospital<br />
(WU/BJH) Adult Neurology residency convened a workgroup<br />
of residents and faculty to create a rotation system<br />
designed to ease compliance with the proposed duty hour<br />
rules. This system was instituted July 1, 2010. We used a<br />
combination of local and national surveys of residents,<br />
patient satisfaction scores, and hospital quality data to assess<br />
whether this change altered duty hour compliance, resident<br />
satisfaction, patient satisfaction or patient outcomes. Our<br />
experience demonstrates the inherent difficulties in monitoring<br />
the effects of duty-hour driven changes in resident<br />
schedules and suggests that these changes may have unexpected<br />
negative effects on other aspects of residency education<br />
and patient care. Future adjustments will require resident<br />
feedback and patient care metrics to best balance<br />
resident education/quality of life and patient care responsibilities<br />
while maintaining compliance with program<br />
requirements.<br />
S407. Translational Research in Neuro-AIDS and Mental<br />
Health<br />
Amanda Brown, Valerie Wojna, Bruce Shiramizu, Avindra<br />
Nath and Justin C. McArthur; Baltimore, MD; San Juan, PR<br />
and Honolulu, HI<br />
HIV infection of the CNS frequently results in neuropsychiatric<br />
complications and is a major cause of disability. Despite<br />
effective antiretroviral treatment, nearly 80% of<br />
patients have asymptomatic cognitive impairment. HIV disproportionately<br />
affects racial/ethnic minorities and several<br />
barriers must be overcome for a significant impact on this<br />
illness to be realized. A better understanding of how social,<br />
cultural and genetics impact the pathophysiology of disease<br />
and the development of new therapies is needed. Another<br />
barrier is the dearth of scientists from racial/ethnic minority<br />
groups in the field of Neuro-AIDS research. The R25 program<br />
was designed to address these barriers by 1) supporting<br />
the education and training of minority graduate students,<br />
fellows and junior faculty and individuals who are<br />
not members of minority groups but are engaged in Neuro-<br />
AIDS disparity related research through a web-based didactic<br />
course; 2) to promote innovative Neuro-AIDS research,<br />
through pilot grants and 3) to provide long-term mentoring<br />
relationships to further career development. Since program<br />
inception 12 university partnerships have formed, 127 trainees<br />
have completed the course, 8 trainees were research<br />
scholars and/or received pilot grants, 11 independent grants<br />
were obtained by trainees, and more than 50 manuscripts<br />
have been published.<br />
Study supported by: 5R25MH080661, The National<br />
Institutes of Mental Health<br />
S408. Relationship between Medical Student Feedback<br />
and Grading<br />
and James M. Stankiewicz; Boston, MA<br />
It is common for students to be asked for feedback in order<br />
to foster clerkship improvement. It is less clear whether<br />
medical student feedback is ultimately related to perform-<br />
44<br />
ance on the clerkship and grade. Students were surveyed via<br />
zoomerang after completing their clerkship. Grades had not<br />
been assigned before evaluation, though students had<br />
received feedback from attendings and the clerkship director<br />
about floor performance. Attitudes towards night call, specific<br />
floor attendings, lecturers, and a clinical examination<br />
were numerically and qualitatively assessed. Histograms will<br />
be presented. Spearman rank correlations will be performed<br />
to relate student feedback ratings with their floor performance<br />
scores, clinical examination score, shelf performance,<br />
and overall grade. A Wilcoxon analysis will compare students<br />
assigning either extreme high/low feedback ratings and<br />
grades, shelf score, and clinical examination performance.<br />
Forty-six evaluations have to date been collected. Collection<br />
will continue until shortly before the meeting at which<br />
point the data will be analyzed.<br />
<strong>136</strong> th Annual Meeting Monday,<br />
September 26, 2011<br />
Poster Session<br />
Posters will be displayed in Elizabeth A-E of the Manchester<br />
Grand Hyatt from 10:00 am – 7:00 pm, with<br />
authors present from 6:00 pm – 7:00 pm.<br />
NOTE: An asterisk designates a resident/fellow travel award<br />
winner. Two asterisks represent a medical student travel award<br />
winner.<br />
Behavioral Neurology<br />
M601. Behaviorally-Driven Anatomical Mapping of<br />
Hemispatial Neglect<br />
Alex R. Carter, Mark P. Mcavoy, Serguei V. Astafiev, Jennifer<br />
Rengachary, Daniel L.W. Pope, Abraham Z. Snyder, Kristi<br />
Zinn, Nick Metcalf, Gordon L. Shulman and Maurizio<br />
Corbetta; Saint Louis, MO<br />
Objective: A wide range of lesions have been associated<br />
with hemispatial neglect. Some heterogeneity may be attributable<br />
to the use of varying tests. We used a single computerized<br />
test with high sensitivity for deficits in both topdown<br />
control of attention and reorientation to salient stimuli<br />
to predict which brain regions are more likely damaged<br />
in subjects with those deficits after right hemispheric stroke.<br />
Methods: Reaction times and accuracy were measured in<br />
61 right hemisphere stroke patients using a computerized<br />
Posner reaction time task. Stroke lesions were quantified by<br />
MRI. Behavioral scores and lesion data were entered into a<br />
novel voxel-wise logistic regression analysis.<br />
Results: Two distinct patterns were observed. Impaired<br />
target detection in the contralesional visual field predicted<br />
damage to the subcortical paraventricular white matter<br />
underlying the middle frontal and inferior frontal gyri.<br />
However, impaired shifting of attention predicted damage<br />
to more cortical regions between the inferior parietal lobule<br />
and the temporo-parietal junction complex.<br />
Interpretation: Lesions of long-range fronto-parietal<br />
white matter tracts may be associated with deficits in the<br />
maintenance of spatial representations; in contrast ventral<br />
parietal lesions may be associated with deficits in phasic<br />
reorientation of attention.<br />
Study supported by: This study was supported by the<br />
National Institute of Mental Health [R01 HD061117-05A2<br />
to M.C.; 1K08NS064365-01A1 to A.R.C.], the Robert<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 45<br />
Wood Johnson Foundation Amos Medical Faculty Development<br />
Program [65592 to A.R.C.].<br />
M602. Markers of Celiac Disease and Gluten Sensitivity<br />
in Patients with Cerebellar Ataxia<br />
Caroline Tan, Peter H. Green, Khalaf O. Bushara, Donald D.<br />
Kasarda, Ejaz Shamim, Norman Latov, Mark Hallett and<br />
Armin Alaedini; New York, NY; Minneapolis, MN; Albany,<br />
CA and Bethesda, MD<br />
Celiac disease is an autoimmune enteropathy resulting from<br />
sensitivity to wheat gliadin and related cereal proteins. A<br />
link between celiac disease and cerebellar ataxia has been<br />
postulated, based primarily on reports of increased anti-gliadin<br />
antibodies among patients with ataxia. Serum specimens<br />
from 21 patients with cerebellar ataxia and elevated antigliadin<br />
antibody titer, 20 celiac disease patients, and 20<br />
healthy subjects were assessed for antibodies to deamidated<br />
gliadin peptides and transglutaminase 2 (TG2) by ELISA.<br />
The anti-gluten antibody response was further characterized<br />
through examination of reactivity towards chromatographically<br />
separated gliadin and glutenin protein fractions by immunoblotting.<br />
In contrast to the celiac disease group, there<br />
was not a significant association between the anti-gliadin<br />
immune response and anti-TG2 or anti-deamidated gliadin<br />
antibodies in the ataxia group. Characterization of antibody<br />
specificity revealed differential reactivity towards specific<br />
gluten protein fractions between ataxia and celiac disease<br />
patients. The findings indicate that the mechanism and profile<br />
of the elevated antibody response to gluten in patients<br />
with cerebellar ataxia is significantly different from those in<br />
celiac disease patients.<br />
M603. Early Signs of Cognitive Impairment among<br />
Multiple Sclerosis Patients with Clinically Isolated<br />
Syndrome<br />
Theodora Panou, Vasileios Mastorodemos, Efrosyni Papadaki,<br />
Panagiotis G. Simos and Andreas Plaitakis; Heraklion, Greece<br />
and Rethymnon, Greece<br />
The study investigates primary and secondary verbal memory<br />
and motor/executive functions (response inhibition and<br />
strategy shifting ability) in multiple sclerosis (MS) patients<br />
with clinically isolated syndrome (CIS). We studied 44 CIS<br />
patients and compared them to 49 patients with relapsing<br />
remitting MS (RR-MS) displaying mild disability and to a<br />
large cohort of age- and education level-matched healthy<br />
volunteers. Results showed that both CIS and RR-MS<br />
patients evidenced a disproportionate impairment in the immediate<br />
and delayed recall of the second (as compared to<br />
the first) of two short narratives of the Logical Memory<br />
WMS-III subtest, and reduced performance on the Memory<br />
for Digits-Forward. Performance of either group on the executive<br />
tasks was not impaired, showing evidence of a<br />
reversed speed-accuracy trade-off. Illness duration emerged<br />
as a significant predictor of memory and executive task performance.<br />
Clinical, psychoemotional, and brain imaging<br />
findings were also examined as potential correlates of cognitive<br />
deficits and disease progression among CIS patients.<br />
These findings may signify early-onset decline of specific<br />
cognitive functions in CIS, which merits regular follow-up<br />
assessments and monitoring of psychoemotional adaptation<br />
and everyday functioning.<br />
Study supported by: This Research Project was partially<br />
supported by the <strong>Association</strong> for Research and Treatment of<br />
Neurologic Disorders of Crete (‘‘EY ZHN’’), which is philanthropic<br />
(non-profit) organization that supports the clini-<br />
45<br />
cal and research activities of the Neurology Department of<br />
the University Hospital of Crete.<br />
M604. Motor Chunking Is Correlated with<br />
Sensorimotor Cortex and Striatum Activation<br />
Nicholas Wymbs and Scott T. Grafton; Santa Barbara, CA<br />
Motor chunking facilitates the production of everyday<br />
movements by combining discrete motor elements into<br />
well-integrated units of behavior. We hypothesized that sensorimotor<br />
cortex and corresponding basal ganglia projection<br />
areas are essential for chunking. Healthy participants learned<br />
a motor sequencing task during fMRI scanning. Instructed<br />
to respond as quickly as possible, participants translated<br />
sequences from a pseudo-musical tablature displaying a series<br />
of twelve ‘notes’ on a four-lined staff to one of four<br />
response keys. Using multislice graph analysis, an unbiased<br />
estimator identified chunks on a trial-by-trial basis for a set<br />
of three extensively trained sequences (189 trials/sequence)<br />
performed over the course of three scanning sessions. A<br />
‘chunking score’ based on the element-to-element variance<br />
within each chunk was used to determine the strength of<br />
overall chunking for each trial and then entered as a covariate<br />
in the estimation of BOLD. Consistent with our predictions,<br />
we found activity in contralateral sensorimotor cortex<br />
and posterior putamen correlated with chunking strength,<br />
independent of movement speed or reaction time. Disruption<br />
of this circuit may result in deficits of concatenating<br />
complex serial actions into contiguous behavior and explain<br />
some symptoms of subcortical apraxia or Parkinson disease.<br />
Study supported by: Supported by PHS grant NS44393<br />
and contract no. W911NF-09-D-0001 from the U. S.<br />
Army Research Office.<br />
M605. Areas of Ischemia Associated with ‘‘Frontal Lobe’’<br />
Task Failure<br />
Yessenia Gomez and Argye E. Hillis; Baltimore, MD<br />
Hypothesis: Measures of ‘‘frontal lobe function’’ evaluate<br />
broad functional networks including left frontal, temporal,<br />
and parietal cortex.<br />
Methods: We identified acute areas of ischemia associated<br />
with impaired performance on Trail Making, Phonemic<br />
Word Fluency (word generation in 1 minute), and word<br />
span, in 95 patients with acute left hemisphere ischemic<br />
stroke within 48 hours of onset. DWI and PWI were evaluated<br />
for infarct or hypoperfusion in 14 Brodmann areas<br />
(4,6,10,11,44, 45,21,22,38,37,39,40,18,19). ANOVA was<br />
used to identify areas where ischemia was associated with<br />
mean decrement in performance.<br />
Results: Patients with ischemia (DWI or PWI abnormality)<br />
in BA 6, 44, 45 (posterior frontal), 21, 22, 37 (temporal),<br />
39 or 40 (inferior parietal) had significantly impaired<br />
performance on word span (p ¼ .03-.001). Patients with ischemia<br />
in BA 4, 6, 21, 22, 37 and 39 had impaired performance<br />
on word fluency. Only patients with ischemia in<br />
BA 37 had impaired Trail Making, but many could not complete<br />
the task. Lowest word span scores were associated with<br />
ischemia in BA 45 (mean 1.0 6 0); lowest word fluency<br />
were associated with ischemia in BA 21 (mean 4.7 6 3.9).<br />
Conclusion: Word fluency and span tasks are sensitive<br />
but not specific for frontal lesions.<br />
Study supported by: NIH R01 DC05375<br />
M606. Thalamic Atrophy in Gastric Bypass Patients<br />
with Cognitive Complaints<br />
Jonathan Graff-Radford, Jennifer Whitwell, Max R. Trenerry,<br />
J.E. Ahlskog, Michael D. Jensen, Clifford R. Jack, Jr. and<br />
Keith A. Josephs; Rochester, MN<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 46<br />
Background: Gastric bypass patients are at risk for developing<br />
neurological complications, often from nutritional deficiencies.<br />
We have noticed a series of patients presenting for<br />
cognitive complaints that developed after gastric bypass,<br />
without any identifiable etiology. We set out to determine<br />
whether such patients have any focal brain atrophy that<br />
could account for the complaints.<br />
Methods: Retrospective case series to identify patients (n<br />
¼ 10) with cognitive complaints following gastric bypass<br />
that had a volumetric MRI. Voxel-based morphometry and<br />
atlas-based parcellation were used to assess patterns of grey<br />
matter volume loss in all patients compared to a group of<br />
10 age and gender-matched controls, and a group of 10<br />
controls matched by body mass index before surgery.<br />
Results: Patients underwent gastric bypass at a median<br />
age of 54. Cognitive complaints began at a median age of<br />
57. All were taking multi-vitamins with nine receiving vitamin<br />
B12. Formal neuropsychometric testing revealed only<br />
minor impairments. No nutritional abnormalities were identified.<br />
Focal thalamic atrophy was identified in the gastric<br />
bypass patients when compared to controls.<br />
Conclusions: Patients with cognitive complaints after<br />
gastric bypass surgery have focal thalamic brain atrophy that<br />
could account for the cognitive impairment.<br />
Study supported by: KAJ is funded by the NIH grant<br />
R01 DC010367 (PI), the Dana Foundation (PI) and the<br />
Morris K. Udall PD Research Center of Excellence NIH/<br />
NINDS P50 NS40256 (Co-investigator).<br />
M607. Parietal Lobe Lesions Affect the Generation of<br />
Antisaccades<br />
James A. Sharpe, Ping Cheng and Moshe Eizenamn; Toronto,<br />
ON, Canada<br />
Antisaccades are directed away from visual targets, requiring<br />
suppression of reflexive saccades toward a target. Impaired<br />
antisaccade generation has been attributed to frontal lobe<br />
damage. The role of the parietal lobe is not established. We<br />
studied antisaccade generation by magnetic search coil technique<br />
in 13 patients (age 45 6 7 years) with unilateral focal<br />
parietal lobe lesions (9 tumors; 5 vascular lesions), and in<br />
10 age-matched controls.<br />
Patients were instructed to make horizontal antisaccades<br />
away from a 100ms target flashed randomly 10 degrees to<br />
the right or left of center. The task was to look 10 opposite<br />
to the target flash.<br />
The patient group made antisaccades in only 49.7 6<br />
32.7% of contraversive trials (visual target flash ipsilateral to<br />
lesions) and 49.6 6 38.4% of ipsiversive trials. In the other<br />
trials they made reflexive saccade errors toward the target<br />
flash. The control group made antisaccades in 82.8 6<br />
13.7% of trials. Eight patients showed subnormal antisaccade<br />
generation. Their imaged lesions overlapped in parietal<br />
lobe white matter.Generation of voluntary saccades is<br />
impaired by parietal lobe lesions. Antisaccades provide a<br />
means of measuring voluntary saccade function of the parietal<br />
lobes independent of visual guidance.<br />
Study supported by: Canadian Institutes of Health<br />
Research (CIHR)<br />
M608. Cognitive Ability Correlates of Psychiatric and<br />
Social Behaviors in Williams Syndrome<br />
Rowena Ng, Anna Järvinen-Pasley and Ursula Bellugi; San<br />
Diego, CA<br />
Williams syndrome (WS) is a genetic disorder characterized<br />
with cognitive impairment, a gregarious personality and significant<br />
anxiety. Research on WS indicates that individuals<br />
46<br />
with the disorder present a variety of psychiatric symptoms<br />
including obsessive compulsion, general anxiety, specific<br />
phobia, and depression. However, it is unknown the extent<br />
to which these behavioral problems are related to cognitive<br />
ability or hypersocial behaviors in WS. Thus, this study<br />
aimed to examine the relationships among cognitive ability<br />
(Verbal, Performance, Full IQ), psychiatric symptoms, and<br />
social behaviors (social-emotionality, social approach) in WS<br />
versus typical development (TD). A cognitive battery<br />
(WISC, WASI, WAIS), Brief Symptom Inventory and Salk<br />
Institute Sociability Questionnaire were administered to 41<br />
WS and 31 TD participants. Results suggest that verbal<br />
intelligence is predictive of greater psychiatric symptoms<br />
(e.g., somatization, interpersonal sensitivity, paranoid ideation,<br />
psychoticism) in WS but not in TD. Interestingly,<br />
greater reported psychiatric symptoms in WS were associated<br />
with poorer socio-emotionality (i.e., emotion recognition,<br />
desire to please) but not with approach behavior, while<br />
no significant correlations between social and psychiatric<br />
measures were observed in TD. Possible role of cognition in<br />
psychiatric ailments and social outcomes of WS will be<br />
discussed.<br />
Study supported by: Grant P01-HD033113-13<br />
M609. Human Brain Mapping at the Single Cellular<br />
Level: Neuronal and Area Specific Differences in Health<br />
and Diseases<br />
Ryan P. Moore, Irisa Mahaparn, Eliezer Masliah and Pavel V.<br />
Belichenko; La Jolla, CA<br />
The Human Brain Mapping Project is an ongoing effort to<br />
characterize neural circuitry at the level of single cells (Belichenko<br />
and Dahlstrom, 1994). Lucifer yellow microinjection<br />
and high resolution confocal microscopy imaging were<br />
employed to reveal disparities in dendritic geometry of von<br />
Economo neurons (VENs) vs. pyramidal neurons in the cingular<br />
cortex complemented with bilateral analysis of speech<br />
areas to find morphological substrates for the speech area<br />
asymmetry. For the VENs, significant differences were<br />
revealed in spine density (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 47<br />
(Inattentive Type) and 24% with ADHD plus additional<br />
disorder (i.e. sleep apnea; brain dysfunction excluded). Neuropsychological<br />
tests included Trail Making Tests (A and B)<br />
and SDMT-W. Self-report measures assessed hyperactivity<br />
and anxiety (PPCA, PHCA, PBC, PCC).<br />
Results: Hyperactivity (> 45%) and anxiety (> 50%)<br />
were frequent with no significant difference between<br />
ADHD and ADHD plus. We found a significant relationship<br />
between hyperactivity and anxiety. Individuals who<br />
reported yes to one or both anxiety items had higher hyperactivity<br />
scores than those who said no to both items.<br />
ADDþ performed worse on all neuropsychological tests (p<br />
< 0.001 for all comparisons).<br />
Conclusions: Findings indicate ADHD (Inattentive<br />
Type) and ADHDþ can be differentiated on cognitive<br />
measures, but not on self-reported symptoms of anxiety and<br />
hyperactivity as these co-morbid factors are highly prevalent<br />
in both populations.<br />
Study supported by: Personally funded and donated time<br />
M611. The Use of Quetiapine in Agitated Patients with<br />
Acquired Brain Injury: A Case Control Study<br />
Sara Piccoli, Gabriella Paparella, Alec Vestri and Andrea<br />
Martinuzzi; Pieve di Soligo, TV, Italy<br />
Background: Experimental studies on neurocognitive effects<br />
of quetiapine showed improvements of cognitive functions<br />
in psychiatric patients. Patients with Acquired Brain Injury<br />
(ABI) often present behavioral disturbances (BD) requiring<br />
drug treatment which might impair responsiveness and cognition.<br />
The use of quetiapine may provide in these patients<br />
adequate control of BD without cognitive side effects.<br />
Methods: 40 consecutive ABI patients (LCF 4–6) attending<br />
intensive neurorehabilitation were recruited, 20 of<br />
whom with BD scored by Aggressive Behaviour Scale (ABS)<br />
requiring medical treatment, and 20 with ABS score
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 48<br />
and females did not differ in performance on SDMT and<br />
Trail Making Tests.<br />
Conclusions: Gender differences are present across lifespan<br />
on tasks of information processing (PASAT). Depression<br />
moderates performance on tasks assessing distractibility<br />
(Stroop) to a greater degree for females than males. Significant<br />
gender differences did not occur systematically on<br />
SDMT and Trail Making Tests, which involve speeded performance<br />
and whole brain functioning.<br />
Study supported by: Personally funded<br />
M615. Hazard Perception in Cognitively Impaired Older<br />
Drivers<br />
Nazan Aksan, Monica Lees, John D. Lee, Shaun Vecera and<br />
Matthew Rizzo; Mountain View, CA; Madison, WI and Iowa<br />
City, IA<br />
Aging and neurological impairment reduce situation awareness<br />
and increase injury risk as in falls and car crashes. Hazard<br />
perception ability (HPA) is important to driver safety<br />
and can be indexed by reaction time (RT) to traffic scenarios<br />
(Horswill & McKenna, 2004; Horswill et al., 2008).<br />
Declines in HPA correlate with reductions in Useful Field<br />
of View (UFOV), a measure of spatial area within which<br />
individuals can detect visual stimuli (Ball & Rebok, 1994).<br />
We examined whether vehicular warning systems can<br />
improve RT in HPA paradigms in elderly drivers with and<br />
without UFOV deficits. 27 of 51 elderly (67-87yrs without<br />
neurodegenerative disease, min MMSE ¼ 25) were randomly<br />
assigned to receive auditory/visual warnings in a simulator<br />
while watching video scenarios and 10 of those had<br />
deficits in UFOV. Warnings improved RTs slightly<br />
(300msec) and a large difference of 1sec in RTs were noted<br />
between those with and without UFOV deficits. Warnings<br />
did not differentially improve RTs of those with deficits.<br />
However, they improved sensitivity, d’, of elderly without<br />
deficits more than those with deficits. Findings imply warning<br />
systems do not provide uniform benefits to elderly<br />
drivers.<br />
Study supported by: NIH R01 HL091917<br />
M616. Differentiation of Alzheimer’s Disease and<br />
Depression with Standard Cognitive Measures<br />
Meredith C. Frederick**, Stefan Sillau, David B. Arciniegas,<br />
C. Alan Anderson, Katherine L. Howard and Christopher M.<br />
Filley; Aurora, CO and Denver, CO<br />
Objective: Alzheimer’s disease (AD) and depression can<br />
both present with cognitive impairment. To compare the<br />
neurobiology of these disorders, we assessed patients with<br />
AD and depression using the Mini-Mental State Examination<br />
(MMSE) and Frontal Assessment Battery (FAB).<br />
Methods: Medical records were reviewed of 475 consecutive<br />
patients seen at a behavioral neurology clinic over 34<br />
months. From this group, patients with AD (n ¼ 59) and<br />
depression (n ¼ 44) were selected after receiving a consensus<br />
diagnosis by three physicians certified in Behavioral<br />
Neurology & Neuropsychiatry (DBA, CAA, CMF). MMSE<br />
and FAB data were analyzed using Z-score transformation.<br />
Results: AD patients performed significantly worse than<br />
those with depression on both the MMSE (z-scores 3.93<br />
vs. 0.05, p < 0.0001) and FAB ( 3.1 vs. 1.0, p ¼<br />
0.009). Patients with depression scored significantly worse<br />
on the FAB than the MMSE (p ¼ 0.0003). AD patients<br />
performed equally poorly on both tests.<br />
Conclusions: The MMSE and FAB may assist in the differentiation<br />
of AD and depression. Whereas both measures<br />
were abnormal in AD, depressed patients had poorer per-<br />
48<br />
formance on the FAB compared with the MMSE, consistent<br />
with frontal-subcortical dysfunction in depression.<br />
Study supported by: University of Colorado Denver<br />
School of Medicine.<br />
M617. Attention Deficit Hyperactivity Disorder in<br />
Depressed Adults<br />
Ildefonso Rodríguez Leyva, Rubén Haro SIlva and Ana A.<br />
Rentería Palomo; San Luis Potosi, San Luis Potosi, Mexico<br />
Objective: Attention deficit hyperactivity disorder (ADHD)<br />
is now recognized as a common disorder, as well as in<br />
children and adults. ADHD has an estimated prevalence of<br />
3–5% in adults. Evidence points to an increased rate of<br />
a co-morbidity in adult ADHD patients. The most common<br />
are disorders of the affective area, including depression.<br />
We investigated the comorbidity between these two<br />
conditions.<br />
Methods: Two questionnaires were applied, the first is<br />
the Hamilton Depression Scale D and the second is the<br />
Adult Self-Assessment Scale (EAVA), developed by the<br />
working group on adult ADHD, which includes the New<br />
York University Medical Center, Harvard Medical School<br />
and Massachusetts General Hospital.<br />
Results: 50 patients, 42 women and 8 men. 74% had<br />
some level of depression. 18% had criteria for ADHD<br />
(12% inattentive, 6% impulsive). By correlating the scale of<br />
Hamilton with the score of EAVA, results that in patients<br />
with ADHD and depression, impulsive symptom severity<br />
decreased in proportion to the degree of depression.<br />
Conclusions: In patients with ADHD and depression,<br />
the intensity of the symptoms of inattention and not those<br />
of impulsiveness, are related in proportion to the degree of<br />
comorbid depression measured by the Hamilton Scale.<br />
M618. Cognition and EEG Abnormalities in Non-<br />
Epileptic AD(H)D/LD Patients with and without Anti-<br />
Epileptic Drug/Stimulant Therapy<br />
Brittany M. DiVito, Heather A. Koch, Spencer A. Leblang,<br />
Erik C. Bakken and Drake D. Duane; Scottsdale, AZ and<br />
Tempe, AZ<br />
Background: Epileptiform EEG abnormalities of unknown<br />
but non-epileptic clinical significance are not rare in developmental<br />
disorders of attention and learning (ADD/LD).<br />
The fate of these EEG patterns, their correlation with behavioral<br />
manifestations and effects of AED therapy is<br />
unknown.<br />
Methods: Retrospective analysis of 56 non-epileptic<br />
ADD/LD with an initial Dysrhythmia Grade II or III EEG<br />
(Mayo Clinic classification) and subsequent EEG later for<br />
developmental dx, cognitive test profile, noting if stimulant,<br />
AED, both or none were employed.<br />
Results: Baseline Abnormal EEG-M38/F18, mean age 10<br />
5/12 years, Dx:AD(H)D-47, LD-40, both-32<br />
EEG and cognitive improvement in at least 1 of 5 cognitive<br />
tests: F/U EEG Nl-50%; F/U EEG Abn-52%<br />
In both, proof reading and verbal learning most apt to<br />
improve, rarely computerized attention<br />
Rx and cognitive improvement (cumulative score 5<br />
tests): No Rx-11, Stim-20, AED-12, Both-23<br />
Conclusions: In AD(H)D/LD with Abn EEG:<br />
-Normalization of EEG has no general correlation with<br />
improved cognition. When cognition is improved, it is most<br />
often in verbal learning/memory/proof reading not computerized<br />
attention tasks.<br />
-Irrespective of follow up EEG, cognition is most apt to<br />
improve when both an AED and stimulant are employed.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 49<br />
M619. Evolution of EEG Abnormalities in Non-Epileptic<br />
AD(H)D/LD Patients with and without Anti-Epileptic<br />
Drug/Stimulant Therapy<br />
Heather A. Koch, Brittany M. DiVito, Spencer A. Leblang,<br />
Erik C Bakken and Drake D. Duane; Scottsdale, AZ and<br />
Tempe, AZ<br />
Background: Epileptiform EEG abnormalities of non-epileptic<br />
clinical significance are not rare in developmental disorders<br />
of attention and learning (ADD/LD). The fate of<br />
these EEG patterns and their evolution over time with or<br />
without AED therapy is unknown.<br />
Methods: Retrospective analysis of 56 non-epileptic<br />
ADD/LD with initial Dysrhythmia Grade II or III EEG<br />
(Mayo Clinic classification) and subsequent EEG later for<br />
developmental dx, noting if stimulant, AED, both or none<br />
were employed. Population was contrasted with 56 control<br />
ADD/LD with normal EEG.<br />
Results: Baseline Nl EEG- M38/F18, mean age 10 9/12<br />
years, Dx: AD(H)D-49, LD-50, Both-43<br />
Baseline Abn EEG- M38/F18, mean age 10 5/12 years,<br />
Dx: AD(H)D-47, LD-40, Both-32<br />
Follow Up EEG: interval mean 3 9/12 years (range 8/12<br />
to 15 years)<br />
Nl- 25(45%) No Rx-3, Stim-5, AED-8, Both-9<br />
Abn- 31(55%) No Rx-9, Stim-11, AED-4, Both-7<br />
Conclusions: In AD(H)D/LD with abnormal EEG:<br />
-Diagnosis distribution is similar to normal EEG.<br />
-Whether on or off AED Rx, EEG abnormalities often<br />
persist, but less often if AED in use.<br />
M620. Transection of CA3 Does Not Affect Memory<br />
in Rats<br />
Mohamad Z. Koubeissi, Saifur Rashid, Gemma Casadesus,<br />
Joseph LaManna, Kui Xu, Hans Luders and Dominique<br />
Durand; Cleveland, OH<br />
Objective: To investigate the effect of CA3 transections on<br />
memory in rats.<br />
Rationale: Longitudinal hippocampal pathways are<br />
needed for seizure synchronization, and their transection<br />
may abolish seizures. However, the effect of such transection<br />
on memory is unknown.<br />
Methods: Sprague-Dawley Rats (247–285g) were used.<br />
A stereotactic knife was implanted 4mm ventrally, 3.3mm<br />
posterior and 4.0mm lateral to bregma, targeting CA3.<br />
The knife was protruded from its sheath to transect CA3.<br />
Sham surgery (n ¼ 4), unilateral (n ¼ 5), and bilateral (n<br />
¼ 5) CA3 transections were made. Novel object recognition<br />
(NOR) and Morris water maze (MWM) tests were<br />
started 18 days later. Cut locations were confirmed by cresyl-violet<br />
staining.<br />
Results: For MWM, the ratio of the amount of time<br />
spent in the target quadrant to that spent in the other three<br />
quadrants showed no difference between groups. For NOR,<br />
discrimination scores were also not different between controls<br />
and transected animals. Histology confirmed the locations<br />
of transections in the CA3 region.<br />
Conclusion: Normal performance in NOR and MWM<br />
does not appear to require intact transmission throughout<br />
the whole length of CA3.<br />
Significance: Since CA3 transections do not interfere<br />
with memory function, they may be tried for treatment of<br />
temporal lobe epilepsy.<br />
Study supported by: Dr. Durand is supported by the<br />
National Institute of Health (5R01NS032845-13,<br />
5R01NS060757-03, and 5R01NS064157-02) and the<br />
COULTER Foundation<br />
49<br />
M621. Cruetzfeldt-Jakob Disease Presenting as a Rapidly<br />
Progressing Dementia with Non-Convulsive Status<br />
Epilepticus<br />
Natasha Tilluckdharry, Megan McGarry and Dipak P.<br />
Pandya; Paterson, NJ<br />
Background Creutzfeldt-Jakob disease (CJD) is a fatal neurodegenerative<br />
disease caused by the accumulation of misfolded<br />
prion proteins in the brain. Although rare, it is the<br />
most common prion body disease. Clinical manifestations<br />
include rapidly progressive dementia, behavioral changes,<br />
extrapyramidal signs, akinetic mutism and myoclonus. We<br />
report a unique case of CJD with nonconvulsive status<br />
epilepticus.<br />
Case Report: 73 year old woman was admitted with a<br />
rapidly progressive dementia of one year. The patient was<br />
noted to have intermittent jerky movements, decreased<br />
responsiveness and mutism. Physical examination revealed<br />
vegetative mental state, whole body stiffness, myoclonic<br />
jerks and right sided rigidity. Electroenchephalogram (EEG)<br />
demonstrated generalized periodic,rhythmic and lateralized<br />
complexes. Magnetic Resonance Imaging (MRI) of the brain<br />
revealed global cerebral atrophy. CSF evaluation showed<br />
presence of 14-3-3 protein and extremely high levels of Tau<br />
protein. The brain biopsy was refused by family.<br />
Conclusion The clinical triad of rapid progressive dementia,<br />
myoclonus, akinetic mutism in conjunction with EEG<br />
and CSF findings are usually conclusive for CJD. Brain biopsy<br />
is the diagnostic choice with histopathologic findings<br />
of spongiform changes, cortical neuronal loss and abnormal<br />
deposition of prion protein. Nonconvulsive status epilepticus<br />
is usually a rare finding with CJD.<br />
Epilepsy<br />
M701. Controlled Cortical Impact in Adult Rats and<br />
Posttraumatic Seizures and Epilepsy<br />
Kevin M. Kelly, Elena A. Kharlamov, Eric R. Miller, Bo Lu<br />
and Zakaria Mtchedlishvili; Pittsburgh, PA and Philadelphia,<br />
PA<br />
The CCI model of TBI has been used in mice and immature<br />
rats to model posttraumatic epilepsy. We used young<br />
adult rats and long-term video and video-EEG with cortical<br />
and hippocampal electrodes to investigate posttraumatic epileptogenesis<br />
and associated neuropathological changes. A<br />
total of 28,956 hours of monitoring was obtained from 128<br />
CCI-injured and 15 sham-operated animals. Class 3–5 provoked<br />
seizures occurred in 7/72 (9.7%) animals video-monitored<br />
for 1 week immediately after CCI. Epileptic seizures<br />
occurred in 26/118 (22%) animals monitored beyond 1<br />
week post-CCI. Class 3–5 seizures occurred in 19 animals;<br />
ictal discharges appeared generalized at onset or from the<br />
contralateral frontal cortex. Nonconvulsive seizures occurred<br />
in 7 animals characterized by motor arrest or no behavioral<br />
change associated with continuous 1-2 Hz high amplitude<br />
spikes or spike-waves averaging 26.2 6 2.8 seconds. No<br />
control animal had seizures. CCI resulted in severe cortical<br />
and subcortical injury and alterations in NeuN and GFAP<br />
staining. Timm staining showed mossy fiber sprouting in<br />
the inner molecular layer of the dentate gyrus of epileptic<br />
and nonepileptic animals. These results indicate that the<br />
CCI model can be used in adult animals to investigate<br />
mechanisms underlying posttraumatic epileptogenesis.<br />
Study supported by: Pennsylvania Department of Health<br />
Research Formula Fund RFA 01-07-26 and Epilepsy Foundation<br />
Research Grant (ZM)<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 50<br />
M702. Serotonin 1A Receptors and Memory in<br />
Temporal Lobe Epilepsy<br />
William H. Theodore, Edythe Wiggs, Ashley Martinez, Irene<br />
Dustin, Omar Khan, Shmuel Appel, Patricia Reeves-Tyer and<br />
Susumu Sato; Bethesda<br />
Memory deficits are common in patients with temporal lobe<br />
epilepsy (TLE). Previous PET studies have shown reduced<br />
mesial temporal 5HT1A receptor binding. We studied 40<br />
patients (24 male; mean age 34.5). Seizure diagnosis and<br />
focus localization were based on ictal Video-Electoencephalographic<br />
recording. Patients had Weschler Adult Intelligence<br />
Score III, Weschler Memory Score III, Beck Depression inventory,<br />
and interictal PET with [18F]FCWAY, a highly specific<br />
5HT1A ligand. MRI partial volume correction for hippocampal<br />
atrophy and tracer plasma free fraction (f1)<br />
measurement were used to obtain [18F]FCWAY volume of<br />
distribution (V/f1). V/f1 was significantly lower ipsilateral<br />
than contralateral to the epileptic focus (73.7 þ/ 27.3 versus<br />
95.4 þ/ 28. We found a significant relation between<br />
left hippocampal FCWAY V/f1 and delayed auditory memory<br />
score (r ¼ 0.41; p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 51<br />
increased LTD (long term depression) and cognitive deficits<br />
at maturity (PND 60þ). These changes occur in the absence<br />
of pronounced hippocampal injury. We speculate that<br />
increased LTD expression may be responsible for the<br />
observed learning abnormalities. LTD induction can be<br />
mediated by two distinct mechanisms, NMDA receptor<br />
(NR) dependent and metabotropic glutamate receptor<br />
(mGluR) dependent. The NR-mediated and mGluR-mediated<br />
forms are differentiated by the effectiveness of different<br />
chemical and electrical LTD inducing stimulation paradigms.<br />
Using these paradigms, we found that alterations in<br />
LTD following ELS are the result of changes exclusively in<br />
mGluR-mediated LTD. Furthermore, we found that ELS<br />
results in abnormal signaling consistent with that mediated<br />
by the Fragile X Mental Retardation Protein (FMRP) to<br />
result in increased mGluR-mediated LTD, with similarities<br />
to that found in genetic disruption of FMRP. Expression of<br />
proteins associated with mGluR-mediated LTD and FMRP<br />
signaling were also altered in a consistent fashion, suggesting<br />
a mechanism for the observed changes in LTD and possible<br />
targets for therapeutic intervention.<br />
Study supported by: NIH-NINDS, Epilepsy Foundation,<br />
The Childrens Hospital Research Institute<br />
M707. Heterozygous Loss of the Epilepsy-Associated<br />
GABAA Receptor a1 Subunit Causes Spontaneous EEG<br />
Spike Discharges in Two Mouse Strains<br />
Fazal M. Arain and Martin J. Gallagher; Nashville, TN<br />
Autosomal dominant juvenile myoclonic epilepsy and absence<br />
epilepsy are associated with missense (A322D) and<br />
frameshift (S326fs328X) mutations in the GABAA receptor<br />
a1 subunit. Although both mutations substantially reduce<br />
a1 subunit protein expression in vitro, previous studies<br />
failed to detect seizures in heterozygous a1 subunit knockout<br />
(GABRA1 KO) mice. Here, we performed video-EEG<br />
studies in wild type and heterozygous GABRA1 KO mice in<br />
the seizure-resistant C57BL/6 and susceptible DBA/2J<br />
strains. Consistent with previous results, both strains of wild<br />
type mice had a low incidence of spike discharges (SD), and<br />
this baseline incidence was greater in DBA/2J (7 6 4SD/<br />
hr) than C57BL/6 (2 6 1 SD/hr) mice. Heterozygous<br />
GABRA1 KO caused an ethosuximide-sensitive increase in<br />
SD incidence to 14 6 3 SD/hr in DBA/2J mice and 12 6<br />
3 SD/hr in C57BL/6 mice. The typical SD duration was<br />
brief (1–3 seconds) and no definite associated behavior<br />
changes were observed. Therefore, heterozygous loss of a1<br />
subunit produces thalamocortical hypersynchrony in vivo<br />
and likely represents a principle mechanism by which the<br />
A322D and S326fs328X mutations cause seizures.<br />
Study supported by: National Institute Of <strong>Neurological</strong><br />
Disorders And Stroke R01NS064286<br />
M708. Regional Network Disruption in Temporal Lobe<br />
Epilepsy<br />
Luigi Maccotta* and Edward Hogan; St. Louis, MO<br />
Medial temporal cortex forms a network of connections<br />
with both the contralateral medial temporal lobe and with<br />
extratemporal brain regions. It is unclear how temporal lobe<br />
epilepsy (TLE) affects these connections, and whether the<br />
effect is pathologic/dysfunctional or compensatory. We<br />
investigated the functional connections of the medial temporal<br />
region with contralateral temporal and extratemporal<br />
brain regions in TLE patients using resting state fMRI.<br />
Twenty-three TLE patients underwent resting-state BOLD<br />
fMRI. Seizure localization was based on video-EEG.<br />
Healthy controls served as comparison. Regions of interest<br />
51<br />
were defined anatomically a priori and functioned as seeds<br />
in a functional connectivity analysis. Results indicate that<br />
TLE exerts a complex effect on the functional connections<br />
of the medial temporal region. Intrahemispheric coupling<br />
between the hippocampal head and entorhinal cortex was<br />
surprisingly stronger in TLE patients (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 52<br />
TPM exposure was equivalent between USL255 and<br />
TPM-IR; furthermore, USL255 displayed a lower C max and<br />
later T max than TPM-IR. While bioavailability of USL255<br />
was unaffected by food, T max was delayed by 4 hours with<br />
food as compared with the fasted condition.Single-dose<br />
USL255 demonstrated equivalent TPM exposure and a lack<br />
of food effect analogous to TPM-IR dosed twice-daily, suggesting<br />
that USL255 may provide a once-daily alternative to<br />
TPM-IR.<br />
Study supported by: Upsher-Smith Laboratories, Inc.<br />
All authors are employees of Upsher-Smith Laboratories,<br />
Inc. (study sponsor)<br />
M711. Cingulate Epilepsy, Reporting 3 Clinical and<br />
Electrophysiologic Subtypes with Surgical Outcomes<br />
Mhd Rafeed Alkawadri, Norman K. So, Paul C. Van Ness<br />
and Andreas V. Alexopoulos; Cleveland, OH and Dallas, TX<br />
Objective: To characterize epilepsy arising from the cingulate<br />
gyrus.<br />
Design/Methods: We describe 14 cases of lesional cingulate<br />
gyrus epilepsy treated surgically. The cases were identified<br />
from the Cleveland clinic and the UTSouthwestern epilepsy<br />
monitoring unit databases 1992–2009.<br />
Results: All 14 cases had cingulate epilepsy confirmed by<br />
MRI lesions and remarkable improvement after surgery.<br />
They were divided into 3 groups based on the anatomical<br />
location and the semiology. In the posterior cingulate group<br />
4 of 4 cases had clinical or electrophysiologic findings suggestive<br />
of temporal origin of the epilepsy. The anterior cingulate<br />
cases were divided into a ‘‘typical’’ (BANCAUD,<br />
1992) group: 6 cases with hypermotor seizures and infrequent<br />
generalization with the presence of fear, laughter, or<br />
interictal personality changes; and an ‘‘atypical’’ group: 4<br />
cases presenting with simple motor seizures and a tendency<br />
for more frequent generalization and less favorable surgical<br />
outcome. The pathology of the atypical cases was<br />
astrocytoma.<br />
Conclusions: Posterior cingulate gyrus epilepsy presents<br />
with electroclinical findings that are suggestive of temporal<br />
lobe epilepsy and can be considered an example of ‘‘pseudotemporal<br />
epilepsy’’. The electroclinical presentation and surgical<br />
outcome of lesional anterior cingulate epilepsy is possibly<br />
influenced by the underlying pathology.<br />
M712. GABAB Receptor Antagonists Reduce Pro-<br />
Epileptic Activity in Hippocampal Slices of Ts65Dn<br />
Mice, a Genetic Model of Down Syndrome<br />
Alexander M. Kleschevnikov, Brett Rasmuss, Pavel V.<br />
Belichenko and William Mobley; La Jolla, CA<br />
Epilepsy is a known co-morbidity of Down syndrome (DS).<br />
GABAB receptor antagonists have been proposed recently as<br />
medicines for improving memory in DS. We examined<br />
effects of GABAB antagonists on pro-epileptic properties in<br />
Ts65Dn mouse model of DS. In a high-potassium in vitro<br />
model of epilepsy, elevation of extracellular [Kþ] provoked<br />
seizures in the dentate gyrus in slices from both Ts65Dn<br />
and 2N (control) mice. The frequency of seizures was significantly<br />
greater in Ts65Dn (0.47 6 0.03 Hz vs. 0.33 6<br />
0.06 Hz, p ¼ 0.013), while the amplitude did not differ (p<br />
¼ 0.45). GABAB antagonist CGP52432 reduced the amplitude<br />
of seizures more considerably in Ts65Dn than in 2N<br />
slices (63.5 6 4.6% vs. 80.2 6 8.1%, p ¼ 0.033). The frequency<br />
of seizures was not affected (p > 0.4). GABAB<br />
antagonists reduced also ratio of amplitudes of population<br />
spikes (PSA2/PSA1) evoked by paired stimuli. This result<br />
suggests an increase in the feedback inhibitory efficiency fol-<br />
52<br />
lowing suppression of the GABAB receptors, an effect that<br />
may contribute to antiepileptic properties of the drug.<br />
Thus, GABAB receptor antagonists reduce pro-epileptic activity<br />
in DS model mice.<br />
Study supported by: Down syndrome research and treatment<br />
foundation (DSRTF); Larry L. Hillblom Foundation<br />
M713. Lacosamide: Long-Term Safety and Efficacy in<br />
Partial-Onset Seizures<br />
William Rosenfeld, Nathan B. Fountain, Gintaras Kaubrys,<br />
Elinor Ben-Menachem, Cindy McShea, Jouko Isojarvi and<br />
Pamela Doty; St. Louis; Charlottesville; Vilnius, Lithuania;<br />
Göteborg, Sweden and Raleigh<br />
Long-term ( 8 years exposure) safety and efficacy of the<br />
antiepileptic drug (AED) lacosamide were evaluated from a<br />
completed open-label extension (SP615; NCT00552305) in<br />
partial-onset seizures.<br />
Patients enrolled following double-blind or open-label<br />
lacosamide trials. Dosage adjustment of lacosamide (100-<br />
800mg/day) and/or concomitant AEDs occurred to optimize<br />
tolerability and seizure reduction. Treatment-emergent<br />
adverse events (TEAEs), vital signs, body weight, clinical<br />
laboratory data, electrocardiograms, and seizure frequency<br />
from subject diaries were evaluated.<br />
Of 370 enrolled patients, 77%, 51%, and 39% had >1,<br />
>3, or >5 years lacosamide exposure, respectively (median<br />
modal dose 400mg/day). Common TEAEs ( 15%) were<br />
dizziness, headache, nausea, diplopia, fatigue, upper respiratory<br />
tract infection, nasopharyngitis, contusion, and coordination<br />
abnormal. Discontinuations due to TEAEs were<br />
12.7%; only dizziness and convulsion led to discontinuation<br />
in 1% of patients. Median 28-day seizure frequency was<br />
12.0 at Baseline of previous trials; median percent reduction<br />
from Baseline was 50.8% across Treatment, and was 47.3%,<br />
56.8% and 65.2%, respectively, for 1-year, 3-year and 5year<br />
completers. The 50% responder rate was 51.2%<br />
across Treatment, and was 48.8%, 57.2% and 63.4% for 1year,<br />
3-year and 5-year completers, respectively.<br />
Long-term adjunctive lacosamide treatment was generally well<br />
tolerated, reduced seizure frequency and maintained efficacy.<br />
Study supported by: UCB Inc.<br />
Elinor Ben-Menachem, within the past year, has had contracted<br />
research, consulting, speaking, and teaching, relationship<br />
with UCB. Cindy McShea and Jouko Isojarvi are<br />
employed by UCB BioSciences Inc. Pamela Doty is<br />
employed by UCB BioSciences, Inc. as a Principal Clinical<br />
Program Director for Lacosamide Epilepsy. As Principal<br />
Clinical Program Director, she receives stock option grants.<br />
William Rosenfeld is a principal investigator and has<br />
received research support from UCB for participating in<br />
double-blind and open-label studies. William Rosenfeld is<br />
on the UCB speaker’s bureau.<br />
M714. Lacosamide: Long-Term Safety in Partial-Onset<br />
Seizures<br />
Robert F. LeRoy, Gregory Krauss, Nathan B.. Fountain,<br />
Deanne Dilley, O’Neill D’Cruz and Pamela Doty; Dallas, TX;<br />
Baltimore, MD; Charlottesville, VA and Raleigh, NC<br />
Long-term safety of the antiepileptic drug (AED) lacosamide<br />
was evaluated in an open-label extension trial SP926<br />
(NCT00655486).<br />
Eligible participants were enrolled from IV infusion trial<br />
SP925 (NCT00655551). Investigators could adjust lacosamide<br />
oral tablet (100–800mg/day) and/or concomitant AED<br />
dosage to optimize treatment. Safety assessments included<br />
adverse events (AEs), ECGs and clinical laboratory data.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
Of the 97 enrolled patients, 58.8% and 38.1% had<br />
>12- and >18-months of lacosamide exposure, respectively.<br />
The median modal lacosamide dose was 500mg/day.<br />
TEAEs (incidence 15%) included dizziness (44.3%), diplopia<br />
(17.5%), and vomiting (16.5%); most were mild/<br />
moderate in intensity. Only one serious AEs (SAEs)<br />
occurred in >1 patient(convulsion,n¼ 2). One patient<br />
discontinued due to SAEs (arrhythmia supraventricular<br />
and atrial fibrillation) and continued commercial lacosamide<br />
after treatment of the SAEs. One TEAE led to discontinuation<br />
in >1 patient (dizziness, n ¼ 3). Median<br />
clinical laboratory values remained within normal range;<br />
changes from Baseline were not of clinical relevance. Small<br />
increases in mean PR interval and QRS duration were consistent<br />
with the known lacosamide safety profile and did<br />
not vary with lacosamide exposure.<br />
Safety evaluations indicate long-term lacosamide administration<br />
(100–800mg/day) is generally well tolerated as adjunctive<br />
treatment for patients with partial-onset seizures.<br />
Study supported by: UCB Inc.<br />
Dr. RF LeRoy has a significant financial relationship with<br />
UCB, the sponsor of the study which generated this<br />
abstract. He participated in funded research as an investigator<br />
in study SP926 and other UCB funded studies as well<br />
as a speaker for the Vimpat Speaker ProgramHe has participated<br />
in UCB sponsored advisory boards for Vimpat. Dr. G<br />
Krauss has received research support from UCB S.A., Johnson<br />
& Johnson Inc., SK-Biosciences Corporation, Eisai Inc.,<br />
Sepracor Inc., and Icagen, Inc., and has served as a paid<br />
consultant for Eisai Inc. and UCB S.A. Deanne Dilley: Employee,<br />
UCB BioSciences, Inc. O’Neill D’Cruz: Employee,<br />
UCB BioSciences, Inc. Pamela Doty is employed by UCB<br />
BioSciences, Inc. as Principal Clinical Program Director for<br />
Lacosamide Epilepsy. As a Principal Clinical Program Director,<br />
she receives stock option grants<br />
M715. Withdrawn<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 53<br />
M716. Computational Models of Ligand-Gated Receptor<br />
Function Characterize Anticonvulsant Drug Actions at<br />
GABAergic and Glutamatergic Synapses<br />
and David E. Naylor; Torrance, CA<br />
Many neurological drugs act on inhibitory GABAergic or<br />
excitatory glutamatergic receptors. Little is known about the<br />
direct effects of endogenous ligand or drug exposure on<br />
receptors in situ, and even less about broader pharmacological<br />
effects on normal or pathological circuit activity. Here,<br />
computational models of receptors characterize drug actions<br />
on multiple scales from submillisecond transmitter release,<br />
diffusion and uptake at single synapses to near seconds of<br />
residual receptor desensitization after multisynaptic<br />
synchronized release. GABA-A and NMDA receptor-kinetic<br />
models at synaptic and extrasynaptic sites in dentate gyrus<br />
granule cells are optimized to fit inhibitory and excitatory<br />
postsynaptic currents (PSCs) as well as evoked paired-pulse<br />
and tonic current responses after ligand and drug exposure.<br />
Synaptic GABA-A receptors over-exposed to GABA paradoxically<br />
show rapid downregulation/amplitude reduction<br />
from receptor desensitization. Hi-frequency 200Hz pulsatile<br />
release of GABA for 400 ms (as with epileptic fast ripples)<br />
also degrades synaptic inhibition, and recovery from desensitization<br />
is prevented by 0.5 to 2 Hz interictal-like discharges.<br />
Subsequent model fits of IPSCs/EPSCs after exposure<br />
to anticonvulsant agents quantify and optimize the<br />
effects of single and combination agents on receptor<br />
properties.<br />
53<br />
M717. Status Epilepticus: An Independent Predictor of<br />
Poor Survival after Anoxic Brain Injury<br />
Jennie Luna, Nelly Awkar, Megan McGarry, Deepthi<br />
Karanam and Dipak P. Pandya; Paterson, NJ<br />
Introduction: Evaluation of prognosis in Anoxic brain<br />
injury is a very difficult task due to lack of clinical and biological<br />
markers. The delay in neurological recovery is a poor<br />
prognostic sign. Status epilepticus (SE) may present in up<br />
to one third of patients with cardiac arrest. We report the<br />
significance of SE and myoclonic status as an independent<br />
clinical marker in anoxic brain injury.<br />
Methods: After IRB approval, we studied adult patients<br />
with SE in anoxic brain injury. Status epilepticus was<br />
defined with clinical history and EEG findings. Patients<br />
without EEG findings were excluded. Total 48 patients were<br />
identified.<br />
Results: 20/48(41%) had SE. 16/20(80%) expired and 4/<br />
20(20%) survived. A 15% of the patients with SE had<br />
anoxic myoclonus with 100% mortality. All SE patients<br />
were comatose. Patients with SE, 60% reported duration of<br />
CPR 10 minutes. The other 40% had unknown duration.<br />
All our study patients were resistant to antiepileptic<br />
medications.<br />
Conclusion: Status epilepticus was present in 41% of<br />
patients and anoxic myoclonic status remains a grave prognostic<br />
sign for any survival. Overall, comatose mental status<br />
with SE or anoxic myoclonus remains an independent clinical<br />
marker for poor outcome.<br />
M718. Periodic Lateralized Epileptiform Discharges<br />
(PLEDs)-Rhythmic Discharges (RDs) in Anoxic<br />
Encephalopathy<br />
Sushanth Bhat, Sombabu Maganti, Eli S. Neiman, Divya<br />
Gupta and Sudhansu Chokroverty; Edison, NJ<br />
Objective: To describe an unusual EEG pattern of stereotypical<br />
PLEDs coupled with RDs in anoxic encephalopathy.<br />
Case Discussion: Following cardiac arrest, a comatose 79<br />
year-old woman had left facial twitching, sluggish pupils,<br />
absent corneal’s/Doll’s eyes reflexes and no withdrawal to<br />
stimuli. Facial twitching subsided with intravenous levetiracetam.<br />
CT scan of the head showed cerebral atrophy. An<br />
EEG showed right anterior/midtemporal PLEDs with slowsharp<br />
morphology recurring at 0.3–0.5 Hz, coupled with a<br />
9 Hz RD from the same area every 24–29 seconds and lasting<br />
5.5–7 seconds, not evolving into electrographic seizures<br />
and unchanged in morphology or frequency. There was no<br />
clinical/EEG background change to noxious stimulation.<br />
Discussion: PLEDs may be PLEDS-proper or PLEDSplus<br />
(associated with RDs). Both may occur with acute cerebral<br />
lesions, with PLEDs-plus more likely to be associated<br />
with seizures. However, focal and chronic lesions more often<br />
produce PLEDs-proper.<br />
The presented case is unusual, with no evolution of the<br />
PLEDs- RDs complex into electrographic seizures; such a<br />
pattern has not been described in acute, diffuse cortical injury<br />
such as anoxic encephalopathy, where BiPLEDs would be<br />
expected. Our EEG findings are reminiscent of those in isolated<br />
cortex in an animal model (Kristiansen, 1949).<br />
M719. Periodic Lateralizing Epileptiform Discharges<br />
(PLEDs) Causing Persistent Magnetic Resonance<br />
Imaging (MRI) Changes in Ipsilateral Thalamus<br />
Umang Shah, Umer Akber and Chunyang Wang; Camden, NJ<br />
Objective: To recognize PLEDs as potential cause of persistent<br />
MRI changes in ipsilateral thalamus.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 54<br />
Background: Transient diffusion weighted image (DWI)<br />
abnormalities in ipsilateral thalamus following status epilepticus<br />
are well-recognized, but persistent changes in fluidattenuated<br />
inversion recovery (FLAIR) and T2-weighted<br />
images (T2WI) are rare.<br />
Design/methods: We report a patient who had persistent<br />
ipsilateral signal change in thalamus after complex partial<br />
status epilepticus and PLEDs.<br />
Results: Case: A 56 year-old woman presented with<br />
recurrent partial seizures involving the right arm and change<br />
in mental status. Electroencephalography revealed PLEDs in<br />
the left temporal lobe causing partial status epilepticus. Immediate<br />
brain MRI was normal but repeat MRI ten days<br />
later showed a focus of increased signal on FLAIR and<br />
T2WI in the left posterolateral thalamus. No abnormal<br />
enhancement was seen. Follow-up MRI one-month later<br />
demonstrated a persistent area of signal abnormality in the<br />
left thalamus.<br />
Discussion: Thalamic role in ictal events is unclear, but<br />
afferent and efferent cortical-interconnections may explain<br />
thalamic involvement in epileptic activity, which is generally<br />
considered a cortical phenomenon. Although DWI thalamic<br />
abnormalities are reported after status epilepticus, persistent<br />
FLAIR and T2WI signal is rare.<br />
M720. Ammoniacal Encephalopathy Presenting as<br />
Complex Partial Seizure-Like Episodes: A Case Series<br />
Darine Kassar and Stanley Iyadurai; Saint Louis, MO<br />
Objective: To report a series of cases with hyperammonemia,<br />
presenting as seizure-like episodes.<br />
Background: Seizures are caused due to several causes.-<br />
While accumulation of ammonia is a common cause of<br />
encephalopathy, it is also known to cause a broad spectrum<br />
of neurological manifestations. Seizures have not been<br />
reported in association with chronic hyperammonemia.<br />
Methods: Case Series<br />
Case report: Index case: A 53-year old man with chronic<br />
hepatitis C presented with confusional episodes associated<br />
with stereo-typed movements. Physical examination revealed<br />
psychomotor slowing. Routine serological and CSF evaluations<br />
were normal, except elevated ammonia (177 mmol/l).<br />
A diagnosis of ammoniacal encephalopathy was made. The<br />
patient was started on lactulose therapy with improvement.<br />
Four other patients with similar history, presentation, and<br />
elevated ammonia levels were seen. Complete resolution of<br />
symptoms were observed with treatment of hyperammonemia<br />
with lactulose in these patients.<br />
Conclusion: Here we present a series of patients with<br />
episodes of various neurologic dysfunctions. The only metabolic<br />
abnormality that was identified was an elevated ammonia<br />
level. We believe that his seizure-like episodes are associated<br />
with hyperammonemia. To our knowledge, this is the<br />
first report that links complex partial seizure-like episodes to<br />
hyperammonemia.<br />
M721. Status Epilepticus as an Initial Manifestation of<br />
Sneddon’s Syndrome<br />
Anish Shah, Saurav Sen, Jennie Luna and Dipak P. Pandya;<br />
Paterson, NJ<br />
Background: Sneddon’s Syndrome is a rare progressive noninflammatory<br />
vasculopathic disease affecting small and medium<br />
size arteries in conjunction with ischemic cerebrovascular<br />
disease, possibly livedo reticularis in absence of well<br />
recognizable connective tissue disease stigmata. It may associate<br />
with hepatitis C, thrombocytopenia and positive antiphospholipid<br />
antibodies. Seizures are rare during the course<br />
54<br />
of the disease. Status epilepticus has not been reported as a<br />
clinical manifestation in Sneddon’s Syndrome.<br />
Results: A 68 year old man with history of hypertension<br />
admitted with confusion, decrease responsivessness and subtle<br />
left sided weakness. He had non-itchy skin rash and mild left<br />
sided paresis. His laboratory tests showed thrombocytopenia,<br />
Hepatitis C, positive antiphospholipid antibodies. MRI<br />
showed acute right middle cerebral artery distribution infarct.<br />
EEG showed Periodic Lateralized Epileptiform Discharges<br />
from right hemisphere with changing morphology and evolving<br />
in nature. Patient was treated with antiepileptic medications,<br />
intravenous immunoglobulins, antiplatelet agents, statin<br />
and ACE inhibitors. His acute condition was improved and<br />
he was discharged to rehabilitative facility.<br />
Conclusions: Most cases of Sneddon’s syndrome are sporadic.<br />
It is unclear whether the status epilepticus is due to<br />
acute brain injury, from antiphospholipid antibodies or<br />
from inflammatory mediators.<br />
M722. Status Epilepticus Secondary to Milk Alkali<br />
Syndrome Induced by Hypercalcemia (Oral Antacids)<br />
Rabih Kashouty, Noor Yono and Mershed Al Samara;<br />
Manhattan, NY; Manhasset, NY and Southfield, MI<br />
Milk-alkali syndrome is mainly caused by the ingestion of<br />
large amounts of calcium and absorbable alkali. This syndrome<br />
can lead to metastatic calcification, renal failure and<br />
metabolic alkalosis secondary to hypercalcemia. Hypercalcemia<br />
is rarely a cause of seizure activity. Very few case reports<br />
have been published linking seizure to hypercalcemia, but<br />
only one recent case report about mesial temporal sclerosis<br />
relates the seizure activity to Milk-alkali syndrome. This is<br />
the first report regarding seizures associated with excess calcium<br />
carbonate intake without evidence of mesial temporal<br />
sclerosis. The patient described in this article, suffered from<br />
status epilepticus most likely secondary to hypercalcemia.<br />
Evaluations for malignancy, thyroid, and parathyroid dysfunctions<br />
were non conclusive, therefore hypercalcemia in<br />
our patient was attributed to milk-alkali syndrome given the<br />
history of the prolonged calcium carbonate intake.<br />
M723. A Case of Magnesium-Responsive Paraneoplastic<br />
Non-Convulsive Status Epilepticus<br />
Robert K. Shin, Anna V. Rosenbaum and Nicholas Frost;<br />
Baltimore, MD<br />
Objective: We present a case of paraneoplastic non-convulsive<br />
status epilepticus resistant to multiple AEDs that<br />
resolved with magnesium.<br />
Background: Paraneoplastic syndromes affecting the<br />
nervous system have been described in association with<br />
numerous cancers, some presenting as limbic encephalites<br />
associated with seizures, including an encephalitis in young<br />
women with ovarian teratoma associated with anti-NMDA<br />
receptor antibodies.<br />
Results: A 57-year old female with clear cell ovarian cancer<br />
became unresponsive following a one week prodrome of<br />
increasing confusion and forgetfulness. EEG demonstrated<br />
non-convulsive status epilepticus. Imaging, serum and CSF<br />
studies were non-diagnostic. Over a course of two weeks, she<br />
did not respond to multiple anti-epileptic medications and<br />
continued to have up to 30 seizures daily. IV magnesium was<br />
administered, and the following morning she was alert, oriented<br />
and able to converse with her husband.<br />
Conclusions: While magnesium is routinely used to treat<br />
seizures in obstetrics, its use in neurology is uncommon.<br />
Given that it is a known NDMA inhibitor, it may represent<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
a useful treatment option, particularly in cases of paraneoplastic<br />
seizures.<br />
Study supported by: Study is a case report. There are no<br />
sponsors or affilitations associated with it. No individual<br />
associated with this case report (or their relatives) has a relevant<br />
financial interest relating to the support of the abstract.<br />
M724. Withdrawn<br />
Neuromuscular Disease<br />
M801. Nicotinamide Mononucleotide (NMN) Treatment<br />
of Diabetic Neuropathy<br />
Ankit Sura, Mitch Onken, Krish Chandrasekaran, Helen Chen<br />
and James W. Russell; Baltimore, MD<br />
Nicotinamide adenine dinucleotide (NAD) is a critical<br />
metabolite in energy metabolism and mitochondrial (Mt)<br />
electron transfer. Nicotinamide mononucleotide (NMN) is a<br />
direct substrate for generation of NAD. A decreased NAD<br />
level in diabetes may increase the severity of diabetic neuropathy.<br />
We determined if NMN prevented the development<br />
of diabetic neuropathy. Adult rats were made diabetic<br />
with streptozotocin. NMN was injected every second day.<br />
There were 4 treatment groups: (1) non-diabetic control<br />
with vehicle (2) diabetic (3) diabetic þ 50 mg/kg NMN (4)<br />
diabetic þ 100 mg/kg NMN. The Von Frey monofilament<br />
sensory withdrawal threshold was normalized in diabetic rats<br />
treated with 50 mg/kg or 100 mg/kg NMN for a period of<br />
2 months from the onset of diabetes (n ¼ 6 rats/group,<br />
P
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 56<br />
which reproduces key aspects of human disease, including<br />
the presence of MN cytosolic aaggregates, and pronounced<br />
astrocytic as well as MN pathology.<br />
Study supported by: NIH grant NS36548<br />
M806. Reevaluating Disease Progression in<br />
Facioscapulohumeral Dystrophy<br />
Jeffrey M. Statland*, William B. Martens, Kathryn R. Wagner,<br />
John Kissel, Shree Pandya, Michael P. McDermott and Rabi<br />
Tawil; Rochester, NY; Baltimore, MD and Columbus, OH<br />
Background: Recent breakthroughs in the molecular pathophysiology<br />
of Facioscapulohumeral dystrophy (FSHD) have<br />
identified potential therapeutic targets. Consequently, an<br />
accurate understanding of disease progression in FSHD is<br />
crucial for the design of future clinical trials.<br />
Methods: Data from 164 subjects in 2 negative clinical<br />
trials and 1 natural history study were combined to examine<br />
disease progression in FSHD. All studies utilized the same<br />
techniques for manual muscle testing (MMT) and quantitative<br />
myometry (QMT). Both techniques yield a total<br />
strength score that can be followed over time as an indicator<br />
of disease progression.<br />
Results: Whereas, natural history data showed a statistically<br />
significant decrease in strength by both QMT and<br />
MMT at 1 year, combined data from all 3 studies demonstrated<br />
a reduced estimate of loss of strength for both techniques<br />
at 1 year, which was no longer significant for QMT.<br />
Comparing natural history to combined clinical trial data<br />
suggested this reduced estimate of disease progression was<br />
due to a placebo effect, most noticeable at 6 months.<br />
Conclusions: Contrary to estimates based only on natural<br />
history data, treatment durations of longer than 1 year will<br />
be required to demonstrate arrest of disease progression in<br />
future FSHD therapeutic trials.<br />
M807. Dysferlin (DYSF) Is Absent from the<br />
Muscle-Fiber Sarcolemma in Various Neuromuscular<br />
Diseases, and in Sporadic Inclusion-Body Myositis<br />
(s-IBM) It Forms Cytoplasmic Inclusions Colocalizing<br />
with Amyloid-b42 (Ab42)<br />
Mafalda Cacciottolo, Anna Nogalska, Carla D’Agostino,<br />
W King Engel and Valerie Askanas; Los Angeles, CA<br />
DYSF is a transmembrane protein participating in muscle<br />
plasmalemma repair. In normal human biopsies, DYSF is<br />
present at the muscle-fiber sarcolemma. In dysferlinopathies<br />
– autosomal-recessive muscle diseases caused by mutations<br />
in the DYSF gene – DYSF is immunohistochemically absent<br />
from the sarcolemma, and is absent or prominently<br />
decreased by immunoblots. Immunohistochemically-absent<br />
DYSF at the sarcolemma is sometimes considered ‘‘diagnostic’’<br />
of dysferlinopathies. However, sarcolemmal absence of<br />
DYSF, and a cytoplasmic ‘‘neolocalization’’, was previously<br />
reported in some sarcoglyconopathies and DMD patients.<br />
We now report absence of DYSF at the sarcolemma of<br />
virtually all muscle fibers of 4 ALS, 4 peripheral neuropathy,<br />
5 s-IBM, and 1 polymyositis biopsies. In s-IBM, vacuolated,<br />
very abnormal muscle fibers often had DYSF-immunoreactive<br />
cytoplasmic inclusions that colocalized with Ab42. Four<br />
age-matched controls had normal sarcolemmal DYSF distribution.<br />
By immunoblots, DYSF levels were comparable in<br />
all biopsies. Thus: a) immunolocalization of DYSF cannot<br />
be a diagnostic criterion of dysferlinopathy; b) Ab42 might<br />
be a novel binding partner of DYSF, and in that complex<br />
DYSF might contribute to the s-IBM pathogenesis.<br />
Study supported by: MDA<br />
56<br />
M808. Novel Demonstration of Conformationally-<br />
Modified Tau in Sporadic Inclusion-Body Myositis (s-<br />
IBM) Muscle Fibers. Possible Importance to s-IBM<br />
Pathogenesis<br />
Anna Nogalska, Carla D’Agostino, King W. Engel and Valerie<br />
Askanas; Los Angeles, CA<br />
Molecular phenotype of s-IBM muscle fibers, the most<br />
common myopathy of older persons, has similarities to Alzheimer-disease<br />
(AD) brain, including intra-muscle-fiber<br />
accumulations of Ab42 and its oligomers, and large clusters<br />
of paired-helical filaments (PHFs) immunoreactive with various<br />
antibodies recognizing phosphorylated tau (p-tau).<br />
In AD brain, conformational changes of tau, including its<br />
modifications detectable with specific antibodies TG3,<br />
Alz50 and MC1, are early and important modifications<br />
leading to tau’s abnormal folding and assembly into PHFs.<br />
We have now identified conformationally modified tau (ctau)<br />
in 13 s-IBM muscle biopsies by a) light-and electronmicroscopic<br />
immunohistochemistry, b) immunoblots, and c)<br />
dot-immunoblots, using TG3, Alz50 and MC1 antibodies.<br />
Interestingly, in the very atrophic degenerating fibers, TG3<br />
co-localized with PHF-1 antibody recognizing p-tau, considered<br />
a later change in the PHFs formation; however, most<br />
of TG3-positive inclusions in non-atrophic fibers were<br />
PHF-1 immunonegative. None of the 12 disease- and normal-control<br />
muscle biopsies contained c-tau or PHF-1 immunoreactive<br />
tau. This first demonstration of c-tau in s-<br />
IBM suggests that, because of its abundance in non-atrophic<br />
muscle fibers, c-tau might play an early role in s-IBM PHF<br />
formation and thus be pathogenically important.<br />
Study supported by: MDA<br />
M809. Anti-Ganglioside Antibodies Mimic CNS<br />
Inhibitors of Axon Regeneration<br />
Kazim Sheikh and Gang Zhang; Houston, TX<br />
Anti-ganglioside antibodies (Abs) are strongly associated<br />
with axonal forms of Guillain Barré syndrome (GBS). Several<br />
studies indicate that GBS patients with anti-ganglioside<br />
Abs directed against GM1, GD1a, or ganglioside complexes<br />
have poor prognosis and/or incomplete recovery. We<br />
recently demonstrated that experimental monoclonal and<br />
GBS patient derived anti-ganglioside Abs can inhibit regeneration<br />
of injured axons in an animal model suggesting that<br />
Ab-mediated inhibition of nerve repair is one mechanism of<br />
delayed recovery. We have now established motor and sensory<br />
primary neuronal culture models to examine the cellular<br />
and molecular mechanisms of this Ab-mediated inhibition<br />
of axon regeneration. We found that GBS patient’s<br />
anti-ganglioside Abs can inhibit neurite outgrowth in primary<br />
neuronal cultures. This Ab-mediated inhibition of<br />
neurite outgrowth involves the activation of small GTPase<br />
RhoA and downstream effector ROCK pathway and this<br />
activation is through the engagement of specific cell surface<br />
gangliosides by Abs. In summary, these studies directly link<br />
patient autoantibodies to an intracellular inhibitory signaling<br />
pathway that is also central to inhibitory signaling induced<br />
by almost all CNS inhibitors of axon regeneration. Our<br />
results support the hypothesis that specific anti-ganglioside<br />
Abs mimic intracellular signaling induced CNS inhibitors of<br />
axon regeneration.<br />
Study supported by: NIH/NINDS<br />
M810. Evaluating Mechanoreceptors in Glabrous Skin in<br />
Diabetic Neuropathy<br />
Iliza Myers, Kay Artibee, Jun Li and Amanda C. Peltier;<br />
Nashville, TN<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 57<br />
Meissner corpuscles (MCs) and their myelinated afferents<br />
are found only in glabrous skin. We hypothesized that alterations<br />
in MCs occur in diabetic neuropathy and correlate<br />
with other measures of axonal loss. Immunohistochemistry<br />
was performed on 2 and 3 mm skin punches from the index<br />
finger and distal leg, respectively. Four diabetic patients<br />
(ages 45–75), with neuropathy confirmed by exam and<br />
nerve conduction studies and four control patients (aged<br />
35–50), were studied. Average Meissner corpuscle density<br />
(MCD) in control patients was 15.3 6 7.1 MCs/ mm 2<br />
with significant reductions observed in two patients (3.3,<br />
6.2 MCs/ mm 2 ) with near normal or higher density in two<br />
other patients (11.1, 28.1 MCs/mm 2 ), suggestive of proliferation.<br />
MCs in diabetics often displayed abnormal morphology.<br />
Density of intrapapillary myelinated endings (IME)<br />
correlated with MCD in all patients (r ¼ 0.97). Diabetic<br />
patients’ intraepidermal nerve fiber density (IENFD) in the<br />
distal leg was 4.2 6 5.9 fibers/mm, compared to 13.7 6<br />
1.3 in controls. IME density did not correlate with IENFD,<br />
suggesting that these populations of fibers are independently<br />
affected by hyperglycemia. Glabrous skin biopsies afford<br />
evaluation of mechanoreceptors which are important in<br />
studying pathophysiology of diabetic neuropathy.<br />
Study supported by: Supported by NINDS K23<br />
NS056009 (A.C. P.), NINDS R01NS066927-01(J.L.), Vanderbilt<br />
CTSA grant 1 UL1 RR024975.<br />
M811. Amiodarone Associated Myopathy. A Report<br />
of 4 Cases<br />
Eoin P. Flanagan, Charles M. Harper, Erik K. St. Louis,<br />
Michael H. Silber, Ronald C. Petersen and Keith A. Josephs;<br />
Rochester, MN<br />
Myopathy is a known side effect of amiodarone. However,<br />
the characteristic features and outcome are not widely<br />
known. We identified 4 patients from 1996 – 2010 at our<br />
institution with electrophysiologically confirmed myopathy<br />
and a final diagnosis of presumed amiodarone induced myopathy.<br />
The median age was 71 years (range, 67–75) and all<br />
had an insidious onset. Initial presenting symptoms<br />
included: lower extremity weakness, 3; and swallowing difficulty,<br />
1. Amiodarone was begun a median time of 20.5<br />
months (range, 1–36) before symptom onset. Laboratory<br />
features included elevations in: creatine kinase, 2; myoglobin,<br />
2; and aldolase, 1. EMG demonstrated short duration<br />
motor unit potentials in proximal muscles in all four<br />
patients and features of myonecrosis were seen in two. Muscle<br />
biopsies performed in two patients demonstrated severe<br />
necrotic myopathy with tubular aggregates in one and<br />
vacuolated atrophic fibers in the other. All 3 patients with<br />
follow up available improved after discontinuation of amiodarone,<br />
but in two the recovery was prolonged (>6 months)<br />
and incomplete. Amiodarone induced myopathy appears to<br />
affect mostly proximal muscles with variable electrophysiological<br />
and pathological findings. Discontinuation of amiodarone<br />
is associated with improvement, but recovery may be<br />
prolonged and incomplete.<br />
M812. Cervical Cord 1 H-Magnetic Resonance<br />
Spectroscopy ( 1 H-MRS) in Amyotrophic Lateral Sclerosis<br />
(ALS): Relationship to Clinoco- Electrophysiological<br />
Dysfunction<br />
Ken Ikeda, Yasuhiro Yoshii, Kiyoko Murata, Riya Nagata,<br />
Kiyokazu Kawabe, Osamu Kano and Yasuo Iwasaki; Tokyo,<br />
Japan<br />
Background: To examine whether clinico-electrophysiological<br />
aspects are related to spinal cord dysfunction on 1 H-MRS in<br />
57<br />
ALS patients. Methods: Fifteen patients with definite or<br />
probable ALS fulfilled the El Escorial revised criteria, and 15<br />
age- and sex-matched controls underwent cervical cord 1 H-<br />
MRS. A volume of interest with dimensions of approximately<br />
6.0 8.0 40.0 mm (19.2 mL) was located along the main<br />
axis of C1-C3 cord on T2-weighted images. N-acetyl-aspartate<br />
(NAA), choline-containing compounds (Cho), creatine<br />
plus phosphocreatine (Cr) and myo-Inositol (m-Ins) were<br />
determined. ALS functional rating scale (FRS) and forced<br />
vital capacity (FVC) were assessed monthly. Electromyography<br />
was performed. Results: NAA/Cr was decreased significantly<br />
(p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 58<br />
parameters. Mean infection rate 6 standard deviation(SD)before<br />
and after HFCWO was compared with paired, unpaired<br />
two-tailed t-tests and Wilcoxan rank tests.<br />
Results: ALS patients[36]patients pre-HFCWO had 0.07<br />
6 0.13(SD)infections/month which reduced to 0.02 6<br />
0.06 infections/[t test p ¼ 0.0638; Wilcoxon ranked test p<br />
¼ 0.0415]. Compliance in each patient compared well with<br />
the mean national compliance assessed by Hill-Rom in neuromuscular<br />
disease.<br />
Conclusion: HFCWO significantly reduces the perpatient<br />
infection rate in ALS patients. Observational studies<br />
employing pre-post-intervention design can provide important<br />
clinically meaningful information supporting certain respiratory<br />
interventions in ALS patients.<br />
Study supported by: Carolinas ALS Research Fund of the<br />
Carolinas Healthcare Foundation and Hill-Rom<br />
M815. Dominant Cardiomyopathy and Very Distal<br />
Myopathy with Rod, Myofibrillar and AVSF<br />
Myopathology<br />
Stanley J. Iyadurai, Chris Weihl, Bob Baloh and Alan<br />
Pestronk; St. Louis, MO<br />
We describe a multigenerational family with a distal myopathy<br />
with unusual features. The syndrome segregated by history<br />
as a dominantly-inherited disorder with affected family<br />
members of both sexes. Four affected patients without cardiac<br />
pacing died before age 40. Two affected patients with<br />
cardiac pacing were examined in their fifth decade. Symmetric<br />
weakness was most severe in intrinsic muscles of the<br />
hands and feet, averaging less than 10% of normal. Intrinsic<br />
muscles of the hands and feet were severely atrophic. Proximal<br />
muscle strength was normal. Tendon reflexes and sensation<br />
were normal. Serum CK was less than 250. EMG<br />
revealed a distal-predominant, irritable myopathy. Nerve<br />
conduction studies were normal. Muscle ultrasound showed<br />
a distal myopathy involving the hands and legs. Muscle biopsy<br />
showed varied fiber size, splitting, rods, desmin aggregates,<br />
and vacuoles containing granular debris with rims<br />
staining for sarcolemmal proteins, including dystrophin, sarcoglycans<br />
and caveolin. Distinctive features include very distal<br />
weakness and wasting, early sudden death, and myopathology<br />
with rods, myofibrillar changes in addition to<br />
AVSFs. Genotyping will be required to further define the<br />
identity of this distal myopathy syndrome.<br />
Study supported by: Department of Neurology and Psychiatry,<br />
Saint Louis University, St. Louis, MO.<br />
M816. Adult-Onset Rod Myopathy Syndrome<br />
(AORMS): Sustained Benefit from IVIG Plus Rituximab<br />
Shalini Mahajan, King W. Engel, Valerie Askanas,<br />
Indermohan Luthra and Varun Gupta; Los Angeles, CA and<br />
Rancho Mirage, CA<br />
AORMS (Engel WK,’66), is a rare, progressive, myopathy<br />
associated with intrafiber rods, often monoclonal gammopathy<br />
(MG), 6 dysschwannian neuropathy, and often fatal.<br />
Patients were unresponsive to anti-dysimmune therapies,<br />
including rituximab (Keller CE,’06). We report successful<br />
treatment of a 55yr old AORMS patient. Before treatment,<br />
he had for 1yr, sub-acute, progressively severe proximal limb<br />
and neck weakness, and dysphagia. Tendon reflexes were<br />
absent, vibratory and pinprick sensations decreased. Serum:<br />
IgG-kappa MG, normal CK. CSF: protein elevated, 59/45.<br />
NCVs: dyschwannian (demyelinating) neuropathy. EMG:<br />
fibrillations and brief small abundant motor-units. Muscle<br />
biopsy: groups of trichrome-red intrafiber rods, and a few<br />
small angular fibers. Rx: IVIG, 0.4 gm/kg infusions twice-<br />
58<br />
weekly, continuing for 6 yrs, arrested progression and sustained<br />
partially-improved strength, breathing and swallowing.<br />
In 3/10, added rituximab, 375mg/m2 q2wksx4 loading,<br />
plus q12-6wks maintenance, produced further increased<br />
strength, regained ability to walk independently 150ft, climb<br />
stairs, turn in bed, shower standing, and drive a car. This<br />
benefit from the continuing IVIG-plus-rituximab therapy<br />
emphasizes treatability of the AORMS and suggests a dysimmune<br />
pathogenesis. His concurrent CIDP-like aspect<br />
may be relevant to his beneficial response. (Interestingly,<br />
experimentally, tenotomy can produce rods (Engel et al,<br />
‘66).)<br />
M817. Geographic Trends of ALS in Minnesota<br />
Eric J. Sorenson and Lisa Kronk; Rochester, MN and<br />
Minneapolis, MN<br />
Background: This study examined geographic trends of<br />
ALS across Minnesota and assessed the completeness of ALS<br />
case ascertainment within the ALS association’s database<br />
(Minnesota/North Dakota chapter).<br />
Methods: The ALS association’s database was queried for<br />
deaths during 2009 in Minnesota with the county of residence<br />
recorded for each. 2009 census data was recorded for<br />
each Minnesota county with an incidence rate calculated for<br />
each county and for Minnesota overall. A chi-squared analysis<br />
compared incidence rates among the 88 counties.<br />
Results: 97 deaths occurred from a population of<br />
5,266,203, giving an incident rate of 1.8 cases per 100,000<br />
person-years (95% CI from 1.5 to 2.2). This agreed with<br />
incidence rates from Olmsted County of 1.7 per 100,000<br />
person-years suggesting that the ALS <strong>Association</strong>’s database<br />
has near complete case ascertainment throughout Minnesota.<br />
County incidence rates varied from 0 to 12.7 per<br />
100,000 person-years. However, comparison across counties<br />
failed to demonstrate any significant differences (p ¼ 0.42).<br />
Conclusions: No significant geographic trends were identified<br />
among the counties in Minnesota suggesting the clustering<br />
of cases in some counties is likely due to random case<br />
aggregation. The ALS association’s database proved effective<br />
at near complete case ascertainment in the state of<br />
Minnesota.<br />
Study supported by: ALS <strong>Association</strong><br />
M818. Clinical Features Associated with Fine Specificity<br />
of IgG Anti-GQ1b Antibodies<br />
Susumu Kusunoki, Seiko Suzuki, Masami Ueda and Motoi<br />
Kuwahara; Osaka-Sayama, Osaka, Japan<br />
Anti-GQ1b IgG antibodies are present in most cases of<br />
Fisher syndrome (FS), Bickerstaff brainstem encephalitis<br />
(BBE), and Guillain-Barré syndrome (GBS) with ophthalmoplegia.<br />
Anti-GQ1b antibodies frequently bind to GT1a,<br />
but the relative binding activities with the GQ1b and GT1a<br />
antigens vary. Some anti-GQ1b antibodies have higher activity<br />
against a mixture of GQ1b and phosphatidic acid<br />
(GQ1b/PA). We investigated anti-GQ1b IgG-positive cases<br />
including FS (n ¼ 197), BBE (n ¼ 20), GBS (n ¼ 78) and<br />
atypical FS (n ¼ 52) to see whether diversity in the fine<br />
specificity of IgG anti-GQ1b antibodies is related with variations<br />
in clinical features. Higher antibody activity with<br />
GQ1b compared to GT1a (GQ1b>GT1a) was significantly<br />
more frequent in BBE and FS than in GBS (pGQ1b/PA) was significantly more frequent in BBE<br />
than in FS (pGQ1b were found in patients<br />
with bulbar palsy (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 59<br />
titer was significantly higher in patients with ophthalmoplegia<br />
(pbulbar >depression<br />
>pseudobulbar affect.<br />
Study supported by: Carolinas ALS Research Fund of the<br />
Carolinas Healthcare Foundation<br />
M820. A New Phenotype in Neurodegeneration:<br />
Trigeminal Sensory Deficits Preceding Rostro-Caudal<br />
Progressive Motor and Sensory Neuronopathy, Chorea<br />
and Dementia<br />
Camilo Toro, Justin Y. Kwan, Tanya J. Lehky, Bryan J.<br />
Traynor, Catherine A. Groden, Rena A. Godfrey, Michele E.<br />
Nehrebecky, Wiggs A. Edythe and Gahl William; Bethesda,<br />
MD<br />
We describe five adults with a slowly progressive bulbaronset<br />
ALS like phenotype but preceded by trigeminal sensory<br />
symptoms, with or without late development of chorea<br />
and dementia. Age of onset was 53–69 years; disease duration<br />
was 5–12 years.<br />
Three women and two men experienced facial/oral sensory<br />
disturbance involving the unilateral infra-orbital area<br />
(3), tongue, or lips 6–18 months before bulbar motor deficits.<br />
At evaluation, all had impaired cornea reflexes, facial/<br />
oral hypoesthesia or anesthesia extending to posterior scalp<br />
plus truncal and shoulder weakness, while lower limb<br />
strength was relatively preserved. Three patients had frontotemporal<br />
dysfunction and two had chorea. Neuroimaging,<br />
CSF examinations, metabolic, toxic and immunological<br />
59<br />
screening (including Sjogren’s and anti-ganglioside antibodies)<br />
was uninformative. Electrophysiology revealed motor<br />
neuronopathy involving 3–4 body segments and sensory<br />
neuropathy. Blink reflexes in four and autonomic testing in<br />
two were abnormal. In 3 patients, nerve biopsies showed<br />
non-specific axonal degeneration/regeneration. Four patients<br />
failed immunotherapy. One autopsy examination revealed<br />
loss of spinal motor neurons.<br />
This disorder, distinct from sporadic bulbar-onset ALS<br />
resembles FOSMN, but with dementia and/or chorea. We<br />
are applying new genomics tools to study this unique<br />
patient group.<br />
Study supported by: National Institues of Health (NIH)-<br />
Intramural Program<br />
M821. Update on a Phase 1 Study of ISIS 333611 in<br />
Familial ALS Due to SOD1 Mutations<br />
Timothy M. Miller, Richard Smith, Swati Aggarwal, Alan<br />
Pestronk, William David, Jeffrey Rothstein, Ericka Simpson,<br />
Benjamin Brooks, Isaac Bakst, Patricia Andres, Peggy Allred,<br />
Katie Alexander, Kathie Bishop, C.F. Bennett and Merit<br />
Cudkowicz; St. Louis, MO; La Jolla, CA; Boston, MA;<br />
Baltimore, MD; Houston, TX; Charlotte, NC and<br />
Carlsbad, CA<br />
Objective: To evaluate the safety, tolerability, and pharmacokinetics<br />
of intrathecal infusion of ISIS 333611, an antisense<br />
oligonucleotide inhibitor of SOD1 mRNA.<br />
Background/Methods: Mutations in SOD1 cause 20%<br />
of familial ALS. In animal models, ISIS 333611 distributed<br />
widely in the brain and spinal cord, decreased<br />
SOD1 mRNA, and prolonged survival. A randomized,<br />
placebo controlled Phase 1 safety trial of ISIS 333611 is<br />
underway. In Cohort 1, ISIS 333611 (0.15 mg) was<br />
infused intrathecally over 12 hours in 6 SOD1-positive<br />
ALS patients (2 patients received vehicle control). Safety<br />
measures and neurological exams were assessed during the<br />
infusion and after 1, 8 and 29 days. CSF and plasma<br />
drug levels were measured. This completes 1 of 4<br />
cohorts, each with increasing dose and similar active:placebo<br />
ratio.<br />
Results: No serious adverse events occurred and common<br />
adverse events are consistent with procedure-related findings.<br />
Changes in neurological exams are consistent with ALS.<br />
CSF and plasma drug levels are consistent with levels predicted<br />
from preclinical studies. An update on the SOD1<br />
antisense program will be provided.<br />
Conclusion: In Cohort 1, ISIS 333611 was well tolerated<br />
and CSF drug levels are as predicted.<br />
Study supported by: ALS <strong>Association</strong>, Muscular Dystrophy<br />
<strong>Association</strong>, Isis Pharmaceuticals<br />
M822. Retrospective Analysis of a Cohort of Non<br />
Systemic Vasculitic Neuropathy<br />
Raghav Govindarajan, Jagadish B. Agadi, Anita Mahadevan<br />
and S.K. Shankar; Weston, FL and Bangalore, India<br />
Background: Nonsystemic vasculitic neuropathy (NSVN) is<br />
an infrequent neuropathy without systemic manifestations.<br />
Only few studies have reported the clinicopathologic spectrum.<br />
Fewer have looked into the treatment aspects.<br />
Methods: Nerve biopsies done over 10 years were<br />
reviewed. Patients who met criteria for NSVN at time of diagnosis<br />
and in whom 6 month follow-up was available were<br />
included. They were treated with steroid therapy (ST) or<br />
with steroids and azathioprine-combination therapy (CT).<br />
Independent T-tests were performed for age, duration of<br />
symptoms prior to therapy and improvement in Prineas<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 60<br />
disability score (PDS) between groups. Differences between<br />
pre and post-therapy PDS within groups were analyzed by<br />
paired T-tests and Chi-Square.<br />
Results: 21 cases were in the series with 12 males and 9<br />
females.Sensori-motor asymmetric axonopathy was seen in<br />
71%. Biopsy showed microvasculitis in 52%. 12 were<br />
treated with ST, 7 with CT,2 opted out. CT was superior in<br />
improving disability (1.57 vs. 1.08 p < 0.05). CT was 14<br />
times more likely to improve PDS by more >2 units (p ¼<br />
0.01). The percentage of improvement did not significantly<br />
differ between them (paired T-test 50% vs.42% p ¼ 0.37).<br />
Conclusion: NSVN is an asymmetric sensory predominant<br />
axonopathy. Combination therapy may be superior to<br />
steroids alone in improving disability.<br />
M823. Optimizing a Hospital Discharge Database for<br />
Passive Surveillance of Guillain-Barre Syndrome (GBS)<br />
Christopher D. Lee and Timothy F. Jones; Nashville, TN<br />
The 2009–2010 H1N1 pandemic influenza immunization<br />
program prompted a nationwide active surveillance effort to<br />
determine the risk of GBS following vaccination. Active surveillance<br />
is unsustainable in the long-term. Therefore, we<br />
sought to optimize a statewide hospital discharge database<br />
to evaluate its utility for GBS surveillance, compared to<br />
active surveillance data.<br />
We examined data from all patients discharged from Tennessee<br />
hospitals with an ICD-9 code for GBS, from 2000–<br />
2010. A total of 2659 cases with Tennessee residency were<br />
identified. Of these, 1098 (41%) were excluded due to a<br />
prior hospitalization with a GBS diagnosis in the database.<br />
Annual incident cases ranged from 143 to 161 (mean<br />
adjusted incidence calculated as 1.41 per 100,000 individuals).<br />
Variation in annual case tallies was significantly narrowed<br />
with this method, compared to aggregate ICD-9<br />
totals. We calculate capability of detecting an increase in<br />
GBS cases with an effect size of 1.20. Sensitivity compared<br />
to active surveillance was 0.81. Positive predictive value was<br />
0.45.<br />
Although incidence calculations are overestimated, an<br />
optimized hospital discharge database shows low variation<br />
and is capable of detecting small increases in GBS cases.<br />
Such a database can be useful for long-term surveillance.<br />
M824. Gene Expression Analysis in Patients with<br />
Amyotrophic Lateral Sclerosis and Multifocal Motor<br />
Neuropathy<br />
Alexander Shtilbans, Soon Gang Choi, Mary E. Fowkes, Greg<br />
Khitrov, Mona Shahbazi, Jess Ting, Stuart C. Sealfon and<br />
Dale J. Lange; New York, NY<br />
Objectives: To confirm the previously identified gene<br />
expression pattern in muscles from patients with Amyotrophic<br />
lateral sclerosis (ALS) and multifocal motor neuropathy<br />
(MMN) compared to controls.<br />
Methods: RNA extracted from skeletal muscles of 3-ALS,<br />
3-MMN and 3-control patients were subjected to RT-PCR<br />
confirmation analysis based on the previously published genome-wide<br />
microarray gene expression data (Shtilbans et al,<br />
Ann Neurol.,2009). Four additional ALS patients and four<br />
new controls were also used.<br />
Results: Validation analysis of the most significant expression<br />
pattern differences confirmed our previous microarray<br />
data for leucine-rich repeat kinase-2 (LRRK-2), follistatin,<br />
collagen type XIX alpha-1, ceramide kinase-like and sestrin-<br />
3 which were overexpressed only in the ALS group.<br />
CXorf64 was increased in ALS and decreased in MMN<br />
compared to controls. Western blot analysis of LRRK-2<br />
60<br />
gene protein level from ALS muscles showed no obvious<br />
difference compared to controls.<br />
Conclusions: The up-regulation of the above genes in<br />
the muscles of ALS patients relative to MMN and controls<br />
discovered previously by our microarray analysis is reproducible<br />
and statistically significant. Further studies are necessary<br />
to evaluate the identified genes in larger patient<br />
groups and different tissues.<br />
Study supported by: This work was supported by grants<br />
from the Muscular Dystrophy <strong>Association</strong> and the Horace<br />
Havemeyer Neuromuscular Research Fund.<br />
M825. Small-Fiber Polyneuropathy (SFPN) Can Cause<br />
Chronic Pain and Somatic Complaints in Youth<br />
and Anne Louise Oaklander; Boston, MA<br />
Patients with unexplained diffuse pain and multisomatic<br />
complaints are enigmatic and hard to treat, with pediatric<br />
cases especially concerning. An index youth with chronic<br />
pain from steroid-responsive SFPN prompted record analysis<br />
from 41 consecutive young patients with widespread<br />
pain and/or multisomatic complaints; age-matched volunteers<br />
provided controls. Age of onset averaged 13y; 73%<br />
were female. Most were seriously ill; 71% were hospitalized<br />
and 1 died. Half reported preceding injuries or infections.<br />
29% had other autoimmune illnesses. 98% had chronic<br />
pain and 98% had somatic symptoms, often cardiovascular<br />
and/or gastrointestinal. Abnormal fatigue, headaches, and<br />
sweating each affected more than half. Sensory abnormalities<br />
were present in 71% and erythromelalgia in 28%.<br />
94% of 33 autonomic-function tests were abnormal, 6%<br />
borderline, and most skin (25) and 2/2 nerve biopsies<br />
implicated SFPN. Etiologic testing spotlighted only<br />
immune markers (in 86%). Many symptoms became manageable<br />
once explained as neuropathic. Corticosteroids or<br />
IVIG helped 70% of 14 treated. This characterizes a disabling<br />
illness, juvenile-onset SFPN, sometimes caused by<br />
organ-specific autoimmunity. This verifiable and treatable<br />
diagnosis merits consideration in youngsters with syndromes<br />
of widespread pain and multisystem complaints, eg<br />
fibromyalgia, chronic fatigue, POTS, and seronegative<br />
Lyme.<br />
Study supported by: NINDS, Dept. of Defense, Bradley<br />
family foundation, Curvey family foundation<br />
M826. Median Nerve Ultrasound in Diabetic PN with<br />
and without Carpal Tunnel Syndrome<br />
Anhar Hassan, Andrea Leep Hunderford, James Watson,<br />
Andrea Boon and Eric Sorenson; Rochester, MN<br />
Background: Gold standard diagnosis for carpal tunnel syndrome<br />
(CTS) is nerve conduction study (NCS). However<br />
sensitivity decreases in peripheral neuropathy (PN). Ultrasound<br />
detects median nerve enlargement but its utility in<br />
coexistent PN is unknown.<br />
Methods: Case-control study enrolling diabetic PN<br />
patients (NCS-proven) referred to our EMG lab, with or<br />
without clinical symptoms of CTS. Demographics, CTS<br />
symptom score, median and ulnar NCS are recorded and<br />
correlated with blinded median and ulnar nerve ultrasound<br />
cross-sectional areas (CSA).<br />
Results: Full data to be presented. Six patients (100%<br />
male; 2 cases, 4 controls) are enrolled so far: age 50.5 years<br />
(range 35–68), with diabetes duration 106.5 months (10–<br />
300) and PN 13.5 months (0–93). Median nerve CSA was<br />
significantly larger (p ¼ 0.03) in CTS cases, and median<br />
antidromic sensory distal latency was significantly prolonged<br />
(p ¼ 0.04). There was no significant difference in diabetes<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 61<br />
(p ¼ 0.13) or PN duration (p ¼ 0.16); neurophysiologic<br />
PN severity (p ¼ 0.18); median motor (p ¼ 0.14) or sensory<br />
palmar NCS (p ¼ 0.05).<br />
Conclusions: In diabetic patients with peripheral neuropathy,<br />
median nerve CSA appears significantly enlarged with<br />
coexistent clinical CTS. If findings are confirmed, median<br />
nerve ultrasound may be a useful addition to NCS.<br />
M827. Subacute Paraneoplastic Motor Neuronopathy<br />
with Ri Immunoeactivity and Breast Cancer: A<br />
Clinicopathologically Studied Patient<br />
and David S. Younger; New York, NY<br />
A 49 year old woman had fatigue, cramps, and leg twitching<br />
in February 2010, four months before noting a breast<br />
mass. Lumpectomy in June 2010 showed stage II invasive<br />
ductal breast cancer, and estrogen and progesterone receptor<br />
positivity. Examination showed leg weakness, atrophy,<br />
and widespread twitching. Initial EMG/NCS showed<br />
motor predominant polyneuropathy of the legs with<br />
demyelinating features and persistent fasciculation. MRI of<br />
the brain, spinal cord, and cerebrospinal fluid showed no<br />
evidence of metastases. Blood studies showed positive<br />
ANNA-2 (Ri) titer 1:7680 from an extensive panel of paraneoplatic<br />
autoantibodies. Intravenous immunoglobulin<br />
(IVIg) was followed by combination chemotherapy. Followup<br />
EMG/NCS showed persistent motor polyneuropathy<br />
and fascicuation with resolution of demyelinating features.<br />
Prophylactic radiotherapy was well tolerated. She<br />
continued to decline whereupon followup EMG/NCS in<br />
February 2011showed motor neuropathy with active leg fibrillation<br />
and fasciculation. Sural nerve and soleus muscle<br />
biopsy were consistent with subacute motor neuronopathy.<br />
CSF evidenced Ri immunoreactivity using purified human<br />
recombinant antigen and Western blot analysis. Whole<br />
body PET/CT showed no evidence of malignancy. This is<br />
the first report of subacute motor neuronopathy in association<br />
with the Ri (ANNA-2) antibody.<br />
M828. Magnetic Resonance Neurography Versus<br />
Electromyography for the Diagnosis of Radigulopathy<br />
Youssef A. Dakka, Andrew Biondo, John Corrigan, Shehanaz<br />
Ellik and Ximena Arcilla-Londono; Detroit, MI<br />
Introduction: Evaluation of spinal nerve disorders relies on<br />
an accurate history, examination, MRI, MR Neurography<br />
and EMG/NCS. The purpose of our study was (a) to determine<br />
if MRN could detect radiculopathies earlier than<br />
EMG.<br />
Methods: Inclusion criteria included adults with cervical<br />
radiculopathy, MRN and EMG studies. Exclusion criteria<br />
included peripheral neuropathy, muscle disease, diabetes or<br />
tumor. Of the 438 patients reviewed, 64 patients were<br />
included. Symptoms, time course, MRN/EMG findings and<br />
consistency of MRN/EMG results with clinical findings<br />
were obtained retrospectively. The patient population was<br />
subdivided into males/females and symptom duration < or<br />
> 2 months. McNemars test and Generalized Estimating<br />
Equation Model were used. Interaction was evaluated at the<br />
significance level of 0.10.<br />
Results: Differences in agreement between MRN and<br />
EMG were 23.5% for females and 6.7% for males. For<br />
those with <br />
2 months duration, it was 20.9%. However, because of the<br />
small sample size, the power to detect these differences was<br />
reduced and they were not statistically significant.<br />
61<br />
Conclusion: In our study there were no significant benefits<br />
to MRN over EMG in radiculopathy diagnosis.<br />
M829. Denervation Causes Lower Expression of Heat<br />
Shock Protein 27 in Regenerating Skeletal Muscle<br />
Takahiro Jimi, Yoshihiro Wakayama and Hajime Hara;<br />
Yokohama, Japan<br />
We have studied changes of gene expression in denervated<br />
skeletal muscles and found a remarkably increased expression<br />
of genes relating to quality control. Denervation results<br />
in the incomplete regeneration of skeletal muscles. So we<br />
examined the mRNA expression of heat shock protein 27<br />
(HSP 27) in regenerating rat muscles in innervated and denervated<br />
conditions. We made rat regenerating muscles by<br />
injection of bupivacaine in both extensor digitorum longus<br />
(EDL) muscles. At the same time of injection, right sciatic<br />
nerve was removed. At 1, 2, 4, and 6 weeks after surgery,<br />
both EDL muscles were excised from five rats. The concentrations<br />
of HSP 27 mRNA were estimated by real-time<br />
PCR analysis. The mRNA level in the innervated condition<br />
was rapidly increased (ten times) at 1 week after surgery,<br />
and gradually decreased to the original level, whereas the<br />
increase in the denervated condition was mild (four times)<br />
and delayed (at two weeks). Thus, we speculated that denervation<br />
causes some effects on the regeneration of skeletal<br />
muscles, and the lower expression of proteins relating to<br />
quality control may be involved in the incomplete regeneration<br />
under denervation of skeletal muscle.<br />
M830. Rapid Magnetic Stimulation Versus Conventional<br />
Physiotherapy in Bell’s Palsy<br />
Devathasan Gobinathan and Lea Dosado; Singapore,<br />
Singapore<br />
We compared the use of rapid magnetic stimulation (RMS)<br />
therapy in 23 subjects with 22 others who elected conventional<br />
electrical, muscle stimulation (CS) treatment and acupuncture.<br />
All patients had acyclovir for 7 days with varying<br />
dose of steroids. After one year the parameters assessed were<br />
the strength of frontalis, orbicularis oculis, zygomaticus,<br />
orbicularis oris and for autonomic dysfunction–score 2<br />
being normal, 1 partial recovery and 0 no recovery or distressing.<br />
Patients did their own scoring.<br />
RMS was administered in 1 or 2 sessions ten times or<br />
days during the acute phase at 15Hz, 1500 pulses, 5 second<br />
pause, 50 in each of 30 trains at strength of 30 to 35A/us.<br />
Stimulation sites were at the mastoid and more distally at<br />
the facial area over the affected muscles away from the eye<br />
globe.<br />
Significant difference was noted in favor of RMS ( p <<br />
0.004, t ¼ 7.1, df ¼ 21 mean score RMS ¼ 9.9 and CS ¼<br />
6.0).<br />
High dose steroids may have introduced a bias element<br />
in favor of the RMS group as they received much less<br />
steroids.<br />
Study supported by: NIL<br />
M831. Establishing a Rare Disease Center in China: The<br />
Periodic Paralysis Program<br />
Qing Ke, Benyan Luo, Ming Ming, Michael Hanna, Jacob<br />
Levitt, Barbara Herr and Robert C. Griggs; Hang Zhou, Zhe<br />
Jiang, China; Rochester, NY; London, United Kingdom and<br />
New York, NY<br />
Objective: To establish a rare disease referral center in China.<br />
Methods: Analyze ways periodic paralysis (PP) patients<br />
reached Chinese centers and compare this process with US<br />
and UK approaches.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 62<br />
Results: 116 patients were evaluated with PP in two center<br />
(Beijing and Hangzhou) from 2003–2009. Only 20%<br />
patients were local, the remaining patients traveled distances<br />
without referrals from other areas. The deciding factor in<br />
seeking care largely depended on patients’ choice. In contrast,<br />
at University of Rochester Medical Center, over 90%<br />
of patients are referred from physicians throughout the<br />
country by virtue of published information concerning physician<br />
expertise or on the basis of referrals from a patient<br />
advocacy group. In UK, a single center, supported by the<br />
National Health Service, provides assessment and genetic<br />
testing for all patients in the country.<br />
Conclusions: Currently, PP patients in China are practising<br />
self-referral to a larger center for medical care. Most of<br />
them are evaluated in brief outpatient visits. With the rapid<br />
development of computer access and expertise coupled with<br />
a website locating one or more centers, patients in the country<br />
will be able to identify specific specialty centers.<br />
Study supported by: NIH F05NS065682<br />
M832. Effect of Fatigue on Pulmonary Function Studies<br />
in ALS Patients<br />
Kathleen S. Alfuth, Ericka P. Simpson and Aparajitha K.<br />
Verma; Houston, TX<br />
Objective: To measure change in pulmonary function tests<br />
(PFTs) as relates to time of day and fatigue in ALS patients.<br />
Methods: Cross-sectional cohort study evaluating %<br />
change in PFTs from early to late-day and correlation with<br />
fatigue severity scale (FSS), disability (ALSFRS-r), bulbar<br />
compromise (ALSFRS-r bulbar subscale). PFT measures<br />
include forced vital capacity (FVC), maximal inspiratory<br />
pressure (MIP), maximal expiratory pressure (MEP) at times<br />
T1 and T2 (5–9hrs after T1) in sitting and supine positions.<br />
Results: Eight patients were recruited [age 56.9 6 7.9<br />
yrs, 75% female, 25% bulbar onset, FSS 42.3 6 14.7,<br />
ALSFRS 35.5 6 8.1, ALSFRS-r bulbar 12.8 6 1.7]. Highest<br />
of three recorded attempts were used to calculate average<br />
change between T1 and T2. FVCsitting -13% 6 27%; FVCsu pine -13% 6 28%; MIPsitting þ7% 6 14%; MIPsupine -9%<br />
6 20%; MEPsitting -3 6 17%; MEPsupine þ7% 6 29%.<br />
Correlation analysis showed a trend association with increasing<br />
fatigue (FSS) and decrease in MIPsupine (p ¼ 0.13).<br />
Conclusion: Preliminary data suggests PFTs in ALS may<br />
significantly change from early to late-day and this may correlate<br />
with fatigue. This study is ongoing to determine significance<br />
of the results and possible impact upon<br />
management.<br />
Study supported by: Methodist <strong>Neurological</strong> Institute<br />
Employment<br />
M833. Monomelic Amyotrophy – A Rare Case<br />
Presentation<br />
Amtul Farheen, Manpreet Multani, Aiesha Ahmed, Raji<br />
Grewal and Raji Grewal; Edison, NJ<br />
A 26 year-old right handed Indian man presented with<br />
weakness and atrophy of the left upper extremity over seven<br />
years. He denied pain, numbness, diplopia, dysphagia, ptosis,<br />
muscle cramps, fasciculations and neck pain. There was<br />
no history of febrile illness, poliomyelitis, and exposure to<br />
toxins or heavy metals. On examination there was atrophy<br />
of entire left upper extremity and weakness (power of 4/5)<br />
of left deltoid, biceps, triceps, and wrist flexion and extension,<br />
and hand muscles. Motor exam was normal in other<br />
extremities. Sensation and cranialnerve examination were<br />
normal. Serum electrolytes, thyroid panel, ESR, CPK, HIV<br />
were normal. MRI of C-spine showed vertically oriented<br />
62<br />
signal alteration in left mid anterior spinal cord from C 3-<br />
C7. Electrodiagnostic testing revealed normal nerve conduction<br />
studies. EMG showed positive sharp waves, fibrillation<br />
potentials and motor unit action potentials of increased amplitude<br />
and duration with reduced recruitment in almost all<br />
of the muscles in left upper extremity.<br />
Monomelic amyotrophy is a rare disorder presenting with<br />
atrophy and weakness restricted to one limb. The benign<br />
nature of Monomelic amyotrophy helps distinguish it from<br />
other lower motor neuron disorders like ALS.<br />
M834. Botulism: A Case Report<br />
Peter Struck, Amtul Farheen and Sushanth Bhat; New<br />
Brunswick and Edison, NJ<br />
A 3 month old boy presented with 15 days of constipation<br />
and 5 days of progressive generalized weakness. Parents<br />
noted weak cry, poor appetite, lethargy, and generalized<br />
muscle weakness. No respiratory or ocular symptoms were<br />
reported. No history of sick contacts. The baby was full<br />
term, born by c-section but otherwise healthy. On examination<br />
facial weakness, weak gag,head lag and diffuse hypotonia<br />
were noted. There were no focal motor deficits. Deep<br />
tendon reflexes were 1 in bilateral upper extremities and 2þ<br />
in lower extremities. Babinski was positive bilaterally. Blood<br />
tests including CBC, CMP, UA, Newborn Screen were normal.<br />
Motor nerve conduction studies revealed normal conduction<br />
velocity, slightly decreased amplitudes. RNS of right<br />
median nerve at 3 Hz showed 9 % decrement and at 20 Hz<br />
showed 30 % increment. EMG showed fibrillations at rest,<br />
short duration low amplitude MUAPs. Stool revealed botulinum<br />
toxin. Baby was diagnosed to have botulism and was<br />
treated with Baby Botulism Immunoglobulin. After treatment<br />
patient was noted to have a stronger cry, improved<br />
appetite and improved weakness.<br />
The diagnosis of botulism should be considered in infants<br />
and children with hypotonia. The detection of toxin in the<br />
stool and EMG are diagnostic.<br />
M835. A Novel Pentameric Thiophene Derivative (p-<br />
FTAA) Strongly Highlights Clusters of Paired Helical<br />
Filaments Containing Phosphorylated Tau in Sporadic<br />
Inclusion-Body Myositis (s-IBM) Muscle Fibers<br />
Therése Klingstedt, Anna Nogalska, Cristiane Blechschmidt,<br />
Stefan Prokop, Frank L. Heppner, King W. Engel, Valerie<br />
Askanas and Peter K.R. Nilsson; Linköping, Sweden; Los<br />
Angeles and Berlin, Germany<br />
p-FTAA is a fluorescent amyloid-specific ligand that can be<br />
used for the detection of protein aggregates in vivo as well<br />
as pre-fibrillar and fibrillar species in vitro. The probe spectrally<br />
discriminate amyloid-beta (Ab) plaques and phosphorylated<br />
tau (p-tau)-containing neurofibrillary tangles in Alzheimer’s<br />
disease (AD) brain.<br />
Muscle biopsies of s-IBM, the most common muscle disease<br />
of older persons, have several pathologic similarities<br />
with the AD brain, including intra-muscle fiber accumulations<br />
of Ab and p-tau-containing clusters of paired helical<br />
filaments (PHFs). We now report that in all 6 s-IBM muscle<br />
biopsies studied, fluorescence evaluation of p-FTAA<br />
staining, using excitation 450–490 nm and emission 520<br />
nm, revealed a strong and specific signal from inclusions<br />
positive with AT100 antibody recognizing p-tau and p62<br />
antibody indicating clusters of PHFs. All 12 normal and<br />
disease-control muscle biopsies were negative.<br />
Our study demonstrates a novel staining method for<br />
detection of p-tau inclusions in s-IBM muscle fibers. The<br />
quick staining protocol together with the high signal-to-<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
noise ratio makes this probe an excellent tool for the diagnosis<br />
of s-IBM.<br />
Neurogenetics<br />
M1001. Withdrawn<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 63<br />
M1002. Clinico-Genetic Characterization of a Large<br />
Italian Cohort with Primary Spastic Paraplegia<br />
Andrea Martinuzzi, Mariateresa Bassi, Grazia D’Angelo, Sara<br />
Bonato, Gabriella Paparella, Olimpia Musumeci,<br />
Mariagiovanna Rossetto, Marianna Fantin, Francesca Peruch,<br />
Alessia Arnoldi, Claudia Crimella, Erika Tenderini, Paolo<br />
Bonanni, Vanessa Casanova, Giovanni Meola, Giacomo Comi,<br />
Antonio Toscano and Nereo Bresolin; Conegliano, TV, Italy;<br />
Bosisio Parini, LC, Italy; Messina, Italy and Milano, Italy<br />
Background: Diagnostic definition of hereditary spastic<br />
paraplegias (HSPs) is complicated by the wide genetic<br />
heterogeneity.<br />
Objectives: Establish in a large cohort of Italian HSP<br />
patients the relative frequency of the various forms, providing<br />
indications for an efficient diagnostic algorhythm.<br />
Methods: 478 index cases (72 familial, 98 pure, 380<br />
complicated) HSP were clinically and molecularly assessed.<br />
Results: 80 cases were molecularly defined. SPG4 was<br />
the most frequent form (55%), followed by SPG11 (16.6%)<br />
SPG7 (9%), SPG10 (8,8% ) and 5 (5.1%). SPG3a and<br />
SPG31 were rarer (2.5%). No mutations were identified in<br />
SPG6, 8, 13, 20, 21, 35, 48. There was wide inter and<br />
intrafamilial variation. Neurophysiology showed invariably<br />
increased central conduction time at lower limbs. Axonal<br />
polyneuropathy was detected in some SPG3a, 5, 10, 11, 17<br />
and SPG4 (15%). MRI showed abnormalities in SPG 5,<br />
10, 11 and 15.<br />
Conclusion: Frequency of SPG forms within this cohort<br />
of Italian HSPs confirms the prevalence of SPG4, reveals<br />
the recurrence of SPG11 and 7 and the low frequency of<br />
SPG3a and 31. Once SPG4 and SPG11 are excluded, family<br />
history, neurophysiology and neuroimaging may direct<br />
the choice of genetic testing.<br />
Study supported by: Italian Ministry of Health<br />
M1003. A Study of ACE and ADD1 Gene<br />
Polymorphism in Extra and Intracranial Atherosclerosis<br />
in Patients with Ischemic Stroke<br />
Jayantee Kalita, Usha K. Misra, Sunil Kumar, Bishwanath<br />
Kumar, Bindu I. Somarajan and Balraj Mittal; Lucknow,<br />
Uttar Pradesh, India<br />
Objective: To evaluate the hypertensive gene (ACE and<br />
aADDUCIN) and MR angiography (MRA) abnormality in<br />
patients with ischemic stroke (IS).<br />
Method: 151 patients with MRI proven IS were subjected<br />
to clinical and biochemical stroke risk factors evaluation.<br />
Both intra(IC) and extracranial(EC) MRA were done<br />
and more than 50% stenosis was considered significant.<br />
ACE and aADDUCIN gene polymorphism was done in<br />
patients and 188 controls.<br />
Results: The patients’ median was 60years and 26.5%<br />
were females. MRA was abnormal in 77.5%; ECMRA in<br />
58.3% and ICMRA in 66.7%. The conventional risk factors<br />
were not different between the patients with and without<br />
MRA abnormalities. Presence of DD genotype<br />
(OR3.86,95%CI0.78-2.28,P ¼ 0.0001) and aADDUCIN<br />
GW genotype (OR2.05, 95%CI1.28-3.27,P ¼ 0.003)<br />
increased the risk of IS significantly compared to controls.<br />
63<br />
Both genotype and allele frequency of ACE and<br />
aADDUCIN however were not different between patients<br />
with and without ECMRA or ICMRA abnormality after<br />
adjustment of putative stroke risk factors.<br />
Conclusions: ACE DD genotype and D allele and<br />
aADDUCIN GW genotype and W allele were associated<br />
with IS compared to controls but not related to IC or<br />
ECMRA abnormalities.<br />
Study supported by: Study financially supported by Indian<br />
council of medical research, Governmernt of India<br />
M1004. Generation and Characterization of MeCP2_270<br />
Mutant Mice<br />
Chiranjeevi Bodda, Karolina Can, Liakath Ali Kifayathulla,<br />
Hope Yao Agbemenyah and Ashraf U. Mannan; Goettingen,<br />
Germany<br />
MeCP2 is a transcription factor that binds to methylated<br />
target DNA sequence. Loss-of-function mutations in<br />
MECP2 gene is the main cause for Rett syndrome (RTT).<br />
The R270X is one of the most frequent recurrent MECP2<br />
mutations among RTT cohorts. The R270X mutation<br />
resides within the TRD-NLS region of MeCP2 and causes a<br />
severe clinical phenotype with increased mortality as compared<br />
to other mutations. To evaluate the functional role of<br />
R270X mutation, we first generated a transgenic mouse<br />
model expressing MeCP2_270 (human mutation equivalent)<br />
by BAC recombineering. The generated transgenic mice<br />
were crossed with Mecp2 knockout mice to produce<br />
Mecp2_R270X knockin mice. The expression pattern of<br />
MeCP2_270 was similar to that of endogenous MeCP2.<br />
Strikingly, MeCP2_270 localizes in the nucleus, contrary to<br />
the conjecture that the R270X could cause disruption of the<br />
NLS. Quantitative expression analysis of MeCP2 target<br />
genes revealed a similar trend in gene regulation pattern as<br />
observed in knock-out mice, however the level of differential<br />
regulation was variable. At the present, we are performing<br />
behavioral analysis to characterize the phenotype of the<br />
mice. Also, we are evaluating neuronal parameters to determine<br />
impairment in neuron development/differentiation<br />
and synaptic network dysfunction.<br />
Study supported by: DFG-Research Center Molecular<br />
Physiology of the Brain. Germany<br />
M1005. Identification of Epigenomic Modifications as<br />
Biomarkers for Amyotrophic Lateral Sclerosis<br />
Claudia Figueroa-Romero, Junguk Hur, Yu Hong, John S.<br />
Lunn, Crystal Pacut, Colin E. Delaney, Raymond Yung, Brian<br />
Callaghan and Eva L. Feldman; Ann Arbor, MI<br />
ALS is a progressive and terminal neurodegenerative disease<br />
leading to irreversible motor neuron degeneration. The high<br />
incidence of sporadic ALS (sALS) suggests that long-term<br />
influences of environmental factors on the genome may<br />
have a major impact in disease development. We hypothesize<br />
that epigenetic modifications play a key role in the<br />
pathogenesis of sALS. DNA from postmortem spinal cord<br />
(SC) tissue from sALS patients/controls was subjected to an<br />
epigene discovery phase. We identified 4,080 autosomal<br />
CpG sites with a significantly different methylation status in<br />
sALS compared to control (False Discovery Rate < 5%).<br />
The biological functions of ‘extracellular region’, ‘defense<br />
response’ and ‘immune response’ were highly associated<br />
with these differentially methylated sites. Furthermore, differential<br />
expression of six genes involved in human cytokine<br />
activity was observed in ALS/control human lymphocytes<br />
and/or SC. We have identified methylation profiles in diseased<br />
tissue, which might parallel those in blood as<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 64<br />
epigenetic biomarkers of sALS. This could enable early-stage<br />
diagnosis and therapeutic interventions to increase survival<br />
outcomes in sALS patients.<br />
Study supported by: The A. Alfred Taubman Medical<br />
Research Institute.<br />
M1006. A Drosophila Model of Williams Syndrome<br />
Ralph J. Greenspan and Jenee Wagner; La Jolla, CA<br />
Social cognition is a major frontier in neuroscience, and<br />
Williams Syndrome (WS) is a condition affecting social cognition<br />
associated with hemizygous deletions of 28 genes<br />
on human chromosome 7. The genetics of WS is apparently<br />
simple, consisting of a deletion of a defined chromosome<br />
segment, but complex because the deletions remove a block<br />
of genes, thus obscuring the contributions of interactions<br />
among subsets of the genes. These interactions are directly<br />
addressable in Drosophila, where ten of the genes in WS<br />
deletions have bona fide homologs in Drosophila, and one<br />
more has a more distant homolog, and all have extant mutant<br />
alleles.<br />
We are mapping the gene network interactions affected<br />
by different combinations of WS homologs in the fruit fly,<br />
capitalizing on the extensive conservation with humans of<br />
their genes and gene networks. Results from these experiments<br />
indicate that fly homologs of LIMK1 and CLIP190,<br />
among others, have substantial effects on behavior individually,<br />
but their contributions are not additive in combination<br />
with other WS genes. This non-linearity is reflected in the<br />
effects of these manipulations on gene network activities.<br />
Supported by NSF IOS-0840717 and NIH<br />
1R21EY020629-01 grants to R.J.G.<br />
Study supported by: NIH, NSF<br />
M1007. Clinical and Pathological Features of Progressive<br />
Supranuclear Palsy with Family History<br />
Shinsuke Fujioka, Avi Algom, Audrey Strongosky, Dennis W.<br />
Dickson and Zbigniew K. Wszolek; Jacksonville, FL<br />
Objective: To compare the clinical and pathological characteristics<br />
of progressive supranuclear palsy (PSP) patients<br />
with and without a family history of parkinsonism or PSP.<br />
Methods: We reviewed autopsy case records from Mayo<br />
Clinic Florida Brain Bank to retrieve PSP cases with positive<br />
family history of neurodegenerative disease, defined as PSP<br />
or parkinsonism, as well as PSP cases without a family history<br />
of neurologic disease.<br />
Results: This study was based on 375 pathologically confirmed<br />
PSP cases, of which 56 had a family history of PSP<br />
or parkinsonism. Among these, 19 patients had multiple<br />
affected family members with PSP, parkinsonism, or other<br />
neurodegenerative conditions, such as dementia or tremor.<br />
There was a trend (p ¼ 0.128) for PSP with a positive family<br />
history to have more atypical clinical features and diagnoses<br />
other than PSP, such as corticobasal syndrome or<br />
frontotemporal dementia. They also tended (p ¼ 0.131) to<br />
have more frequent atypical PSP pathology.<br />
Conclusion: PSP patients with a positive family history<br />
share many clinical and pathologic features with PSP<br />
patients without family history, but in general they tend to<br />
be atypical in clinical presentation and in final pathology.<br />
Study supported by: ZKW is partially supported by the<br />
NIH/NINDS 1RC2NS070276, NS057567, P50NS072187,<br />
Mayo Clinic Florida (MCF) Research Committee CR programs<br />
(MCF #90052018 and MCF #90052030), and gift<br />
from Carl Edw and Bolch, Jr., and Susan Boss Bolch (MCF<br />
#90052031/PAU #90052). FS is partially supported by<br />
64<br />
Mayo Clinic Florida (MCF) Research Committee CR programs<br />
(MDF #90052018).<br />
M1008. Aberrant Methylation by Mutations of DNA<br />
Methyltransferase 1 Cause Peripheral and Central<br />
Axonal Degeneration<br />
Christopher J. Klein, Maria V. Botuyan, Yanhong Wu,<br />
Christopher J. Ward, Garth A. Nicholson, Simon Hammans,<br />
Hiromitch Yamanishi, Adam R. Karpf, Douglas C. Wallace,<br />
Mariella Simon, Cecilie Lander, Julie M. Cunningham, Glenn<br />
E. Smith, William J. Litchy, Benjamin Boes, Elizabeth J.<br />
Atkinson, Sumit Middha, P. James Dyck, Joseph E. Parisi,<br />
Georges Mer, David I. Smith and Peter J. Dyck; Rochester,<br />
MN; Sydney, Australia; Southampton, United Kingdom;<br />
Hyogo, Japan; Buffalo, NY; Irvine, CA; Herston, Australia<br />
and Indianapolis, IN<br />
DNA methyltransferase 1 (DNMT1) is an essential component<br />
of genomic methylation. Neural gene expression, DNA<br />
mismatch repair and cell cycle regulation are all influenced<br />
by DNA methylation. Here we show mutations in DNMT1<br />
cause both central and peripheral axonal degeneration in<br />
one form of hereditary sensory and autonomic neuropathy<br />
with dementia and hearing loss. Two <strong>American</strong>, one European<br />
and one Japanese kindreds were studied. Next generation<br />
sequencing was utilized to identify two DNMT1 mutations,<br />
c.A1484G(p.Y495C) in <strong>American</strong> and Japanese<br />
kindreds and c.1470TCC-1472ATA(p.D490E-P491Y) in a<br />
European kindred. All mutations are within the DNA targeting<br />
sequence domain of DNMT1. Functional analysis<br />
shows premature degradation and reduced methyltransferase<br />
activity. Mutant proteins lost heterochromatin binding ability<br />
during the G2 cell cycle, leading to global hypomethylation<br />
measured by mass spectrometry analysis. Methylation<br />
of satellite 2 repetitive elements is preferentially decreased.<br />
Global hypomethylation and regional hypermethylation is<br />
shown in affected persons, a pattern commonly seen in<br />
unregulated cancer cells, suggesting post mitotic neural cells<br />
may undergo axonal degeneration by loss of cell cycle arrest.<br />
The discovered mutations in DNMT1 provide a new framework<br />
for the study of neurodegenerative diseases.<br />
Study supported by: NINDS K08 award<br />
M1009. Common and Distinct <strong>Association</strong>s of HLA-<br />
DRB1 and -DPB1 Alleles with Neuromyelitis Optica and<br />
Multiple Sclerosis in Japanese<br />
Satoshi Yoshimura, Noriko Isobe, Takuya Matsushita, Tomomi<br />
Yonekawa, Katsuhisa Masaki and Jun-ichi Kira; Fukuoka,<br />
Japan<br />
Background: A distinctive association between human leukocyte<br />
antigen (HLA) gene alleles and each clinical subtype,<br />
opticospinal multiple sclerosis (OSMS) and conventional<br />
MS (CMS), has been reported in Asians. However, patients’<br />
sample sizes were relatively small in the previous studies.<br />
OSMS is now suggested to be the same as a relapsing form<br />
of neuromyelitis optica (NMO) in Westerners.<br />
Objective: To clarify the association of HLA-DRB1 and -<br />
DPB1 alleles with NMO and non-NMO MS phenotypes in<br />
a large series of Japanese patients.<br />
Methods: Genotyping of HLA-DRB1 and -DPB1 alleles<br />
was performed in 288 MS patients including 83 who fulfilled<br />
the NMO criteria, and 367 healthy controls (HCs).<br />
Results: DRB1*0901 frequency was significantly lower in<br />
both NMO (p corr ¼ 0.0003, OR:0.133, 95%CI:0.048–<br />
0.374) and non-NMO MS patients (p corr
OR:0.301, 95%CI:0.181–0.499) as compared with HCs.<br />
Susceptibility alleles for non-NMO MS are DRB1*0405<br />
(p corr ¼ 0.0189, OR:1.867, 95%CI:1.300–2.683) and<br />
DPB1*0301 (p corr ¼ 0.0022, OR:3.328, 95%CI:1.747–<br />
6.337) while those for NMO are DRB1*1602 (p corr ¼<br />
0.0028, OR:12.942, 95%CI:3.355–49.923) and<br />
DPB1*0501 (p corr ¼ 0.0265, OR:2.608, 95%CI:1.412–<br />
4.816).<br />
Conclusion: There is a common resistant DRB1 allele<br />
between NMO and non-NMO MS while susceptibility alleles<br />
are distinct between the two conditions in Japanese.<br />
Study supported by: This work was supported in part by<br />
the Health and Labour Sciences Research Grant on Intractable<br />
Diseases (H20-Nanchi-Ippan-016) from the Ministry of<br />
Health, Labour and Welfare, Japan, and the grant-in-aid (B;<br />
no. 22390178) from the Ministry of Education, Culture,<br />
Sports, Science and Technology, Japan.<br />
M1010. Computer Simulations of Striatal Atrophy and<br />
Age at Onset of Huntington’s Disease<br />
Steven D. Edland and Jagan Pillai; La Jolla, CA<br />
Beyond polyglutamine repeat length on the huntingtin<br />
gene, little is known about predictors of age at onset of first<br />
symptoms of Huntington’s disease (HD). Cajevec et al.<br />
(Neurogenetics, 2006) proposed that variability in age at<br />
onset given repeat length could be explained by the random<br />
nature of striatal cell loss under the ‘‘one-hit’’ model of HD<br />
neurodegeneration proposed by Clarke et al. (Nature,<br />
2000). Alternatively, the rate of neuronal loss in HD could<br />
vary person to person due to environmental and background<br />
genetic influences affecting rate of neuronal loss or affecting<br />
susceptibility to the extent of cell loss. To investigate this,<br />
we simulated striatal neuron loss in HD as proposed by<br />
Cajevec et al. and under these alternative models. We found<br />
that stochastic cell death is unlikely to explain an appreciable<br />
fraction of variability in age at onset, while models<br />
with random rates of neuronal loss and susceptibility recapitulated<br />
empirical HD survival distributions perfectly. We<br />
conclude, contrary to Cajevec et al., that age at onset is a<br />
valuable phenotypic endpoint for investigations of environmental<br />
and background genetic factors affecting the expression<br />
of HD.<br />
Study supported by: NIH/NIA AG00513 and<br />
AG034439.<br />
Trauma/Injury<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 65<br />
M1101. A Human Natural IgM Drives Axon Outgrowth<br />
Xiaohua Xu, Arthur Warrington, Brent Wright, Allan Bieber,<br />
Virginia Van Keulen, Larry Pease and Moses Rodriguez;<br />
Rochester, MN<br />
We demonstrate that a human natural IgM, HIgM12 promotes<br />
axonal outgrowth by mechanisms coupling lipid raft<br />
to microtubule dynamics. Serum-derived human IgMs have<br />
been shown to support neurite extension of primary cerebellar<br />
granule neurons. In the current study with primary hippocampal<br />
neurons, we showed that a recombinant form of<br />
one of these IgMs, rHIgM12 regulated kinetics of membrane<br />
lipids. rHIgM12 bound to neuron surfaces and<br />
induced clustering of cholesterol and ganglioside, GM1.<br />
Following membrane association, rHIgM12 segregated into<br />
two pools, one associated with lipid raft fractions, and the<br />
other with detergent insoluble pellet composed of cytoskeletons.<br />
Moreover, rHIgM12 affected microtubule dynamics.<br />
65<br />
rHIgM12 co-localized with microtubules and was co-immunoprecipitated<br />
with b3-tubulin. rHIgM12 promoted tyrosination<br />
of a-tubulin. Finally, rHIgM12 enhanced polarized<br />
axon outgrowth when presented as substrate. Our results<br />
indicate that there exists a repertoire of natural IgMs with<br />
the potential to regulate membrane lipid and microtubule<br />
dynamics required for axonal outgrowth. These findings<br />
also identify a bioactive molecule that may be utilized to<br />
treat neurologic diseases.<br />
Study supported by: This work was supported by grants<br />
from the NIH (R01 GM092993, R01 NS024180, R01<br />
NS03219, R01 NS048357) and the National Multiple Sclerosis<br />
Society (CA 1011-A8). We also acknowledge with<br />
thanks support from the Applebaum and Hilton Foundations<br />
and the Minnesota Partnership Award for Biotechnology<br />
and Medical Genomics.<br />
M1102. Computed Tomography Characteristics of<br />
Pediatric Traumatic Brain Injury<br />
Korak Sarkar and Kia Shahlaie; Sacramento<br />
Little is known about the differences in CT findings<br />
between adult and pediatric TBI populations. A retrospective<br />
analysis of 1206 consecutive non-penetrating TBI<br />
patients treated at a Level 1 trauma center from August<br />
2008 to January 2011 was performed. Admission CT scan<br />
were evaluated for skull fractures, ICH, midline shift, and<br />
basal cistern compression. Of 1206 patients in our registry<br />
349(28.5%) were pediatric. Demographics and injury severity<br />
distribution were similar between the two populations<br />
(p> 0.05). The distribution of CT findings, however, was<br />
significantly different. Pediatric TBI patients were more<br />
likely to be associated with skull fractures (57.0% vs 23.4%)<br />
and EDH (17.2% vs 9.7%), and less likely to be associated<br />
with contusion, SDH, SAH, or basal cisterns compression<br />
(p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 66<br />
change in GOS or GOS-E between 3 and 6 months. The<br />
1- and 3-month NOS-TBI correlated with the 3- and 6month<br />
GOS, GOS-E and DRS (all p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 67<br />
Induction of anesthetic coma was necessary in 49/53 SE<br />
incidents. Patients required anesthetic agents for 9.6 (4, 0–<br />
60) days. Eighteen died, withdrawal of support preceded<br />
death in 13. Compared to a pre-morbid modified Rankin<br />
scale (MRS) of (2.09 6 1.6) 27 patients alive at 3–6<br />
months following hospital discharge had a MRS of (3.81 6<br />
1.52) (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 68<br />
Imaging Procedures: Whole brain DTT was performed<br />
using streamtube tracing and culling techniques. DTT of a<br />
normal subject was obtained as a control.<br />
Results: Conventional brain MRI displayed complete absence<br />
of the corpus callosum in both cases. Whole brain<br />
DTT showed no corpus callosum fibers crossing the midline<br />
in either ACC case. Instead, robust fiber bundles passing<br />
through middle cerebellum peduncles via transverse pontine<br />
fibers were seen.<br />
Conclusion: DTT was useful in visualizing expected and<br />
unexpected alterations of white matter fiber connections in ACC.<br />
Study supported by: National Science Foundation<br />
(1017921,1018769, 1016623)<br />
M1302. Neurofibromatosis 1 (NF1) Vasculopathy in<br />
Children – An Emerging Entity<br />
Partha S. Ghosh, A.D. Rothner and Manikum Moodley;<br />
Cleveland, OH<br />
Objective: Vasculopathy in children with NF1.<br />
Methods: Retrospective review of children with NF1<br />
from 2000- 2010 at Cleveland Clinic. NF1 associated vasculopathy<br />
divided into: (1) Cerebrovascular, (2) Cardiovascular<br />
(3) Other.<br />
Results: Of 398 patients, 26 (6.5%) had vasculopathy.<br />
Group1: Ten (2.5%) had cerebrovascular abnormalities<br />
(mean age 12.8 years; 5 males). Presentation- headache<br />
(4), seizures (1), asymptomatic (5): all had normal neurological<br />
examination. MRA brain: Moyamoya disease-4, stenosis/occlusion<br />
of Internal carotid artery-3, Middle cerebral<br />
artery stenosis-2, Posterior cerebral artery stenosis-1. Ischemic<br />
changes noted in 1. On follow-up (mean 5.2 years);<br />
1 died of brain tumor, others did not develop stroke. One<br />
had encephaloduromyosynangiosis for moyamoya.<br />
Group2: Fifteen (3.7%) had cardiovascular abnormalities<br />
(mean age 6.6 years; 8 males). Presentation: hypertension (2),<br />
shortness of breath (2), chest pain (1), syncope (1), murmur<br />
(6). Cardiac lesions: Pulmonary stenosis-5, Coarctation-4, mitral-valve<br />
prolapse-1, supra-valvular aortic stenosis-1, anomalous<br />
right coronary artery-1, pulmonary artery hypoplasia-1.<br />
On follow-up (mean 4.6 years), 3 had surgical procedures.<br />
Group3: Two girls had renal artery stenosis (RAS); 1 with<br />
coarctation. Both were hypertensive: 1 underwent RAS repair.<br />
Conclusion: Children with NF1 should be carefully<br />
screened for vasculopathy.<br />
M1303. Macro CK-1 a Cause of Spuriously Elevated CK<br />
Associated with Leukoencephalopathy in an Infant<br />
and John B. Bodensteiner; Phoenix, AZ<br />
Macro CK-1 is a complex formed by the Creatine Kinase isoenzyme<br />
BB and monoclonal IgG. The complex is not formed<br />
by abnormal CK enzyme but by an autoimmune reaction<br />
and occurs in about 1% of patients studied. First identified<br />
as a cause of spurious elevation of the total CK in patients<br />
suspected of myocardial infarction in the 1970s the test has<br />
been largely replaced by the measurement of Troponin levels.<br />
We present an infant with delayed milestones and persistently<br />
elevated CK measurements ( 1000–4000 IU) normal EMG<br />
and brisk DTRs. Suspicion that this was not a myopathy<br />
prompted the measurement of CK isoenzymes and brain<br />
imaging which showed the presence of Macro CK-1 and<br />
extensive signal abnormality of the cerebral white matter.<br />
Macro CK-1 has been associated with cancer, infection, myositis<br />
and heart disease, not described in association with leukoencephalopathy<br />
or in infants. Macro CK-1 may be a cause<br />
of elevated total CK in patients without primary muscle dis-<br />
68<br />
ease. The significance of the Macro-CK in relation to the<br />
Leukoencephalopathy in this patient or the frequency of this<br />
association is completely unknown.<br />
Study supported by: Supported by The William Pilcher<br />
Endowment for Pediatric Neurology<br />
M1304. Pharmaceuticals in the Environment: A Focus<br />
on <strong>Neurological</strong> Medications<br />
and Ilene Ruhoy; Seattle, WA<br />
Pharmaceutical residues in the environment have been an<br />
issue of increasing interest amongst environmental scientists,<br />
toxicologists, and policy makers. Physicians have recently<br />
expressed concern regarding the potential ill effects on<br />
humans from chronic exposures to these active pharmaceutical<br />
residues (APIs).<br />
Research has demonstrated the potential for neurological<br />
effects from exposure to the multitude of pharmaceutical<br />
residues identified in our environment, specifically in our<br />
water systems. Studies in aquatic organisms have revealed<br />
altered brain size, poor neuronal growth, and neuropathy. In<br />
addition, many of the pharmaceuticals that have been identified<br />
are centrally acting. Carbamazepine is one drug of significant<br />
concern in that it is largely refractory to most treatment<br />
technologies and indeed it has been identified in all<br />
water sampling studies. Benzodiazepines are another common<br />
culprit that are found with increasing frequency and<br />
are ubiquitous in its prescription patterns.<br />
This presentation will discuss the known and unknown<br />
with regards to medications commonly prescribed in the<br />
neurological setting and environmental presence. It will correlate<br />
research on aquatic wildlife with the potential for<br />
human health effects from exposures to these medications<br />
and will recommend actions to minimize human exposures.<br />
Rehabilitation and Regeneration<br />
M1401. Human Induced Pluripotent Stem Cell-Derived<br />
Neural Progenitor Grafting into Rat Hippomcapus<br />
Alison L. Althaus, Yu Liu, Duriel Hardy and Jack M. Parent;<br />
Ann Arbor, MI<br />
Induced pluripotent stem cells (iPSCs) offer potential<br />
advantages as a neural progenitor cell (NPC) source for regenerative<br />
therapy, including readily available supply, vast<br />
differentiation potential and autologous grafts that obviate<br />
the need for immunosuppression. To begin developing<br />
iPSC-based transplantation therapy, we injected human<br />
iPSC-derived NPCs into neonatal rat hippocampus to determine<br />
their differentiation potential. We also examined how<br />
the degree of in vitro differentiation influenced graft behavior.<br />
GFP- or mCherry-labeled human iPSCs were neurally<br />
differentiated and transplanted (10^5 cells) into postnatal<br />
day 4 rat hippocampus either at the primitive neural rosette<br />
stage or after 3-day neurosphere differentiation. Grafts were<br />
examined after 2, 4 or 8 weeks by immunostaining for<br />
human nuclear antigen or GFP/mCherry and neuronal or<br />
glial markers. Grafts generated GFAPþ glia and TuJ1þ<br />
neurons at all time points. Neural rosette grafts tended to<br />
form large neural tube-like structures that deformed host tissue.<br />
Neurosphere grafts dispersed more widely and gave rise<br />
to mature-appearing neurons, some of which expressed a pyramidal<br />
cell marker (Tbr1). These findings suggest that<br />
iPSCs autografts may be useful for treating brain disorders.<br />
Further work is needed to determine optimal NPC differentiation<br />
states for grafting.<br />
Study supported by: NIH NS065450<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 69<br />
M1402. Local Molecular Manipulation and Peripheral<br />
Nerve Regeneration<br />
Douglas W. Zochodne, Kimberly J. Christie,<br />
Christine A. Webber, Chu Cheng and Jose A.<br />
Martinez; Calgary, AB, Canada and Edmonton,<br />
AB, Canada<br />
Regeneration of peripheral neurons following injury or<br />
neuropathy is more challenging than usually assumed. We<br />
describe new molecular players that may offer insights into<br />
early axon outgrowth, the initiating step in regeneration.<br />
After complete nerve transection, axon outgrowth requires<br />
an intimate molecular exchange with partnering Schwann<br />
cells (SCs). Using an accessible conduit to connect the<br />
stumps of transected peripheral nerves in rats, we show<br />
that several forms of intervention, including local siRNA<br />
knock down, can alter regenerative outcome: (i) CGRP, an<br />
axonally synthesized peptide, signals local SCs to proliferate<br />
in order to support axon growth: knockdown interrupts<br />
regeneration. (ii) PTEN, a tumour suppressor molecule, is<br />
a regenerative roadblock that attenuates growth factor support<br />
of regeneration: knockdown dramatically enhances<br />
axon outgrowth. (iii) DCC and Unc5H are netrin facilitatory<br />
and inhibitory developmental pathfinding receptors<br />
respectively that are re-expressed in regenerating adult SCs:<br />
DCC knockdown attenuates adult regeneration whereas<br />
Unc5H knockdown enhances it. Local molecular manipulation<br />
can have significant impacts on the critical initiating<br />
step of peripheral nerve regeneration by eliminating roadblocks<br />
or upregulating growth signals. The approach may<br />
offer new forms of intervention for irreversible peripheral<br />
nerve lesions.<br />
Study supported by: Canadian Institutes of Health<br />
Research, Alberta Heritage Foundation for Medical<br />
Research<br />
M1403. Very Early Gait Training after Acute Stroke; a<br />
Dose-Escalation Study<br />
Randolph S. Marshall, Ying K. Cheung, Clare Bassile, Laura<br />
A. Evensen, Roujie Chen, Veronica Perez, Ronald M. Lazar<br />
and Bernadette Boden-Albala; New York<br />
Intensive rehabilitation within days of stroke may benefit<br />
from an altered inhibition/disinhibition environment which<br />
promotes neuroplasticity. Conversely, early rehab may be<br />
impeded by excitotoxicity, medical co-morbidities, logistics<br />
of diagnostic testing, and low motivation.<br />
We used a stepwise sequential probability ratio test<br />
(sSPRT) with 6 tiers to determine the maximal tolerated<br />
dose of standard gait training at 24–96 hours after ischemic<br />
or hemorrhagic stroke. A multidisciplinary acute stroke/<br />
rehab team assessed cardiac and neurological safety outcomes.<br />
Inclusion criteria: NIHSS leg motor or ataxia 1<br />
and prestroke Rankin 3.<br />
After 28 patients the study met the sSPRT algorithm<br />
requirements of dose-escalation to the highest tier, with 5 of<br />
6 patients completing 60 min/day at 24–96 hours. Safety<br />
outcomes included 3 cardiac withdrawals (2 patients at tier<br />
3, 1 at tier 6), and 3 fatigue withdrawals (1 at tier 4, 1 at<br />
tier 5, 1 at tier 6). One patient failed to complete his<br />
assigned dose because of sedation for diagnostic testing.<br />
These preliminary data suggest that very early rehabilitation<br />
with gait training is safe and feasible beginning<br />
24–48 hours after stroke. Further study is required to establish<br />
efficacy of early rehabilitation intervention in<br />
acute stroke.<br />
Study supported by: This work was supported by a Pilot<br />
Grant Award through Columbia University’s CTSA.<br />
69<br />
<strong>136</strong> th Annual Meeting Tuesday,<br />
September 27, 2011<br />
Poster Session<br />
Posters will be displayed in Elizabeth A-E of the Manchester<br />
Grand Hyatt from 10:00 am – 7:00 pm, with<br />
authors present from 6:00 pm – 7:00 pm.<br />
NOTE: An asterisk designates a resident/fellow travel award<br />
winner. Two asterisks represent a medical student travel award<br />
winner.<br />
Dementia and Aging<br />
T1501. Amyloid-Beta Dynamics and Prevention Trials in<br />
Dominantly Inherited Alzheimer’s Disease<br />
Randall J. Bateman and on behalf of the Dominantly<br />
Inherited Alzheimer Network; St. Louis, MO<br />
Amyloid-beta is a key pathologic protein in Alzheimer’s disease(AD)<br />
and extensive research has started an era of clinical<br />
trials targeting amyloid-beta. Understanding the dynamics<br />
of amyloid-beta formation and clearance in the human<br />
CNS and the processes that lead to clinical disease are essential<br />
to design better clinical trials. Developing efforts to prevent<br />
AD in autosomal dominant mutation carriers may test<br />
the amyloid hypothesis, determine the timing of treatment,<br />
and lead the way to AD prevention.<br />
Amyloid-beta production and clearance rates were measured<br />
with stable isotope labeling kinetics. The Dominantly<br />
Inherited Alzheimer’s Network interim findings of clinical,<br />
cognitive, MRI, PET, CSF, and blood biomarkers were analyzed<br />
with respect to the expected age of onset.<br />
Amyloid-beta clearance rate is decreased by 30% in AD<br />
compared to controls. Changes in clinical, cognitive, MRI,<br />
PET, CSF, and blood biomarkers in autosomal dominant<br />
AD indicate the pathophysiologic cascade begins up to 20<br />
years before the expected age of onset.<br />
The pathophysiologic changes of AD can be specifically<br />
measured and targeted for clinical trials. Autosomal dominant<br />
AD prevention trials offer a unique opportunity to<br />
lead the way to effective treatments for all AD.<br />
Study supported by: NIH K-23-AG03094601, NIH R-<br />
01-NS065667, NIH 3P-01-AG02627603S1 (FACS), NIH<br />
1U-01-AG03243801 (DIAN), ADRC (P50 AG05681-22),<br />
HASD (P01 AG03991-22), WU CTSA award (UL1<br />
RR024992), Mass Spectrometry Resource (NIH<br />
RR000954), Eli Lilly research collaboration<br />
R.J.B. is a co-founder of a company (C2N Diagnostics)<br />
that has licensed a Washington University patent on some<br />
of the technology described in this abstract.<br />
T1502. Integrating Genome-Wide <strong>Association</strong> and<br />
Functional Validation To Understand Susceptibility for<br />
Alzheimer’s Pathology<br />
Joshua M. Shulman, Portia I. Chipendo, Lori B. Chibnik,<br />
Brendan T. Keenan, Dong Tran, Matthew A. Huentelman,<br />
Julie A. Schneider, Eric M. Reiman, Denis A. Evans, David<br />
A. Bennett, Mel B. Feany and Philip L. De Jager; Boston,<br />
MA; Chicago, IL and Phoenix, AZ<br />
Gene discovery in Alzheimer’s disease (AD) is limited by etiologic<br />
heterogeneity of dementia in cases and subclinical<br />
disease in controls. We have implemented a novel strategy<br />
using quantitative AD pathology as an outcome for genome-wide<br />
association (GWA) analysis. Candidate susceptibility<br />
genes were subsequently tested for functional<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 70<br />
validation in a Drosophila model, based on transgenic<br />
expression of human Tau. In a pilot study of 227 subjects,<br />
6 out of 15 genomic regions associated with AD pathology<br />
contained genes showing interactions with Tau neurotoxicity<br />
in vivo. In the full cohort of 651 autopsies, GWA identified<br />
a variant in PFTK1 (rs11563839) associated with neurofibrillary<br />
tangle burden (p ¼ 6 10 6 ), and this polymorphism<br />
was also related to episodic memory decline (p ¼<br />
0.004) in 1600 prospectively-followed, elderly subjects. Significantly,<br />
in Drosophila, we find that both gain- and lossof-function<br />
of the PFTK1 ortholog, Eip63E, is associated<br />
with suppression and enhancement of Tau toxicity, respectively.<br />
Interestingly, PFTK1 encodes a cell cycle-related kinase<br />
strongly expressed in adult brain. Our strategy of integrating<br />
a GWA scan for pathologic phenotypes with<br />
functional validation in a model organism is likely to be a<br />
powerful approach for gene discovery in AD.<br />
Study supported by: National Institutes of Health/National<br />
Institute on Aging, Massachusetts Alzheimer’s Disease Research<br />
Center, the Harvard NeuroDiscovery Center, and the Clinical<br />
Investigator Training Program: Beth Israel Deaconess Medical<br />
Center–Harvard/MIT Health Sciences and Technology, in collaboration<br />
with Pfizer Inc. and Merck & Co.<br />
T1503. Brain Expression Genome-Wide <strong>Association</strong><br />
Study (eGWAS) and Alzheimer’s Disease<br />
Nilufer Ertekin-Taner, Fanggeng Zou, High Seng Chai, Curtis<br />
S. Younkin, Julia Crook, V Shane Pankratz, Mariet Allen,<br />
Minerva M. Carrasquillo, Christopher N. Rowley, Otto<br />
Pedraza, Morad Ansari, Caroline Hayward, Igor Rudan,<br />
Harry Campbell, Ozren Polasek, Nicholas D. Hastie, Asha A.<br />
Nair, Sumit Middha, Sooraj Maharjan, Thuy Nguyen, Li<br />
Ma, Kimberly G. Malphrus, Ryan Palusak, Sarah Lincoln,<br />
Gina Bisceglio, Constantin Georgescu, Christopher P. Kolbert,<br />
Jin Jen, Zbigniew Wszolek, Maria Barcikowska, Sigrid B.<br />
Sando, Jan Aasly, Kevin Morgan, Clifford Jack, Ronald C.<br />
Petersen, Neill R. Graff-Radford, Alan Wright, Dennis W.<br />
Dickson and Steven G. Younkin; Jacksonville, FL; Rochester,<br />
MN; Edinburgh, United Kingdom; Split, Croatia; Zagreb,<br />
Croatia; Warsaw, Poland; Trondheim, Norway and<br />
Nottingham, United Kingdom<br />
Genetic variants that modify brain gene expression may also<br />
influence risk for CNS diseases, including Alzheimer’s disease<br />
(AD). We performed an eGWAS of 24,526 transcript<br />
levels measured in the cerebella of 197 ADs and 177 non-<br />
ADs with 313,330 SNP genotypes. After elimination of<br />
probes with a known SNP within their sequence, cis-SNP/<br />
transcript level associations were sought. Corrections were<br />
made for technical and biological variables. Significant cerebellar<br />
associations were also tested in the temporal cortex of<br />
198 ADs and 193 non-ADs. Cerebellar expression was detectable<br />
for 69% of all transcripts. After accounting for<br />
technical variance, cis-SNPs explained 5–85% of the variance<br />
of >1,600 transcripts. There was an excess of significant<br />
associations. Substantial number of cis-SNP/transcript<br />
associations were significant in both ADs and non-ADs<br />
with similar direction and magnitude of effects. Many top<br />
cerebellar cis-SNPs were also detectable in the temporal cortex<br />
with similar effect sizes. We demonstrate that genetic<br />
factors influence brain expression for many genes, replicably<br />
across disease pathologies and tissue regions. eGWAS may<br />
be an excellent approach to identify candidate functional<br />
genetic variants implicated in AD. Top cis-SNPs are investigated<br />
for association with AD and its endophenotypes<br />
including plasma amyloid-b.<br />
Study supported by: R01 AG018023, P50 AG016574<br />
70<br />
T1504. Insulin-Like Growth Factor 1 (IGF-1) and Risk<br />
of Alzheimer’s Disease: The Framingham Study<br />
Andrew J. Westwood*, Alexa S. Baiser, Ramachandran S.<br />
Vasan, Tamara B. Harris, Ronenn Roubenoff, Aleksandra<br />
Pikula, Rhoda Au, Charles DeCarli, Philip A. Wolf and<br />
Sudha Seshadri; Boston, MA; Framingham, MA; Bethesda,<br />
MD and Sacremento, CA<br />
Objective: To relate serum IGF1 to risk of Alzheimer’s disease<br />
(AD) and to brain volumes in a dementia-free community<br />
sample.<br />
Background: IGF1 may be a biological link between lifestyle<br />
and risk of AD; exercise elevates and hyperinsulinemia<br />
depresses circulating IGF1. IGF1 levels correlate positively<br />
with cognition in older men and lower levels are reported in<br />
mouse models of AD.<br />
Method: Framingham participants (N ¼ 648, mean age<br />
79 6 4 yrs, 63% women) who had serum IGF1 measured<br />
(radioimmunoassay, coefficient of variation 4%) in 1990-94<br />
were followed prospectively for incident AD. Dementia-free<br />
survivors (N ¼ 161) underwent brain MRI in 1999–2005.<br />
Results: Mean IGF1 levels were 143 6 60lg/L. We<br />
observed 105 cases of incident AD over a mean follow-up<br />
of 9 6 4 years. In multivariable models adjusted for age-,<br />
sex-, APOE, plasma homocysteine and waist-hip ratio, each<br />
standard deviation increase in baseline IGF1 was associated<br />
with a 23% lower risk of AD (HR ¼ 0.77,95%CI:0.62-<br />
0.96;p ¼ 0.019). Persons with IGF1 levels in the lowest<br />
quartile had lower brain volumes (b 6 SD ¼ 0.6 6 0.28;<br />
p ¼ 0.033) cross-sectionally, and a 80% greater risk of<br />
developing AD (HR ¼ 1.80,95%CI:1.19–2.71;p ¼ 0.005)<br />
compared to others.<br />
Conclusions: Higher IGF1 levels may protect from clinical<br />
AD and subclinical brain atrophy.<br />
Study supported by: This work was supported by the Framingham<br />
Heart Study’s National Heart, Lung, and Blood<br />
Institute contract (N01-HC-25195) and by grants from the<br />
National Institute of <strong>Neurological</strong> Disorders and Stroke<br />
(R01 NS17950 to P.A.W.) and from the National Institute<br />
on Aging (R01 AG16495 to P.A.W., AG08122 to P.A.W.,<br />
AG033193 to S.S., AG031287 to S.S., AG033040 to<br />
P.A.W., P30AG013846 to S.S.). Dr. Roubenoff is an employee<br />
of Biogen Idec, Inc, but reports no conflict of interest<br />
with the subject of this paper<br />
T1505. Components of Blood Pressure and Progression<br />
of Cerebral Leukoaraiosis: The ARIC Study<br />
Rebecca F. Gottesman, Diane J. Catellier, Laura H. Coker,<br />
Josef Coresh, Clifford R. Jack, Jr., David S. Knopman,<br />
Kathryn M. Rose, A. Richey Sharrett, Dean K. Shibata and<br />
Thomas H. Mosley; Baltimore, MD; Chapel Hill, NC;<br />
Winston-Salem, NC; Rochester, MN; Durham, NC; Seattle,<br />
WA and Jackson, MS<br />
Background: The contribution of blood pressure (BP) components<br />
to the burden and progression of cerebral white<br />
matter hyperintensity (WMH) is poorly understood. We<br />
evaluated these associations in the population-based Atherosclerosis<br />
Risk in Communities (ARIC) cohort.<br />
Methods: 983 participants each underwent 2 brain MRIs<br />
10 years apart. Systolic (SBP) and diastolic BP (DBP) were<br />
measured at 4 study visits. Four BP components were examined<br />
as predictors of WMH progression: 1) mean arterial<br />
pressure (MAP); 2) pulse pressure (PP); 3) orthostatic hypotension<br />
(OH); and 4) 10-year change in BP.<br />
Results: Baseline (preceding MRI #1) MAP value predicted<br />
WMH progression (OR 1.39 (1.20–1.62), per 10<br />
mm Hg increase), but PP did not. Presence of OH did not<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 71<br />
predict WMH progression, but OH severity did (OR 1.21<br />
(1.02–1.42) per 10 mm Hg SBP decrease). Change in DBP<br />
over 10 years had a U-shaped relationship with WMH progression:<br />
extreme increases and decreases, independent of<br />
antihypertensive use, were both associated with greater<br />
WMH progression (p ¼ 0.007).<br />
Discussion: WMH progression is significantly predicted<br />
by MAP and extent of orthostatic SBP reduction. Significant<br />
changes over time in DBP, whether positive or negative, predict<br />
WMH progression, cautioning against simplified interpretations<br />
of blood pressure associations.<br />
Study supported by: The Atherosclerosis Risk in<br />
Communities Study is carried out as a collaborative study<br />
supported by National Heart, Lung, and Blood Institute<br />
contracts (HHSN268201100005C, HHSN268201100006C,<br />
HHSN268201100007C, HHSN268201100008C, HHSN2<br />
68201100009C, HHSN2682011000010C, HHSN2682011<br />
000011C, HHSN2682011000012C).<br />
T1506. Therapeutic and Preventive Effects of a Novel<br />
AD Vaccine<br />
Carmen Vigo, Ivan Cuevas, Lucia Fernandez, Valter<br />
Lombardi, Richard Manivanh and Ramon Cacabelos;<br />
Sunnyvale, CA and Bergondo, La Coruna, Spain<br />
A vaccine consisting of b-amyloid peptide (Ab) delivered in<br />
a liposomal matrix composed of phosphatidylcholine: phosphatidylglycerol:<br />
cholesterol: sphingosine-1-phosphate<br />
(EB101) was administered intraperitoneally for seven<br />
months to double transgenic mice (B6C3-Tg (APPswe,P-<br />
SEN1dE9)), before or after the AD pathology was developed.<br />
Ab plaques and neurofibrillary tangles were quantified<br />
by ELISAs and brain histology using specific antibodies. Basal<br />
immunological interaction between the T-cells in the<br />
affected hippocampal area and other immune activation<br />
markers, including glial fibrillary acidic protein (GFAP)<br />
(astroglia) and CD-45 (B-cells) were also studied. Both preventive<br />
and therapeutic vaccination with EB101 resulted in<br />
a marked inhibition of Ab deposits (from 60 to 90%), a<br />
reduction of neurofibrillary tangles (70 to 90%) and almost<br />
completely suppression of reactive gliosis as measured by<br />
GFAP immunoreactivity, consistent with a marked decrease<br />
in amyloidosis-induced inflammation. No external neurological<br />
deficits were observed as a result of EB101 immunization<br />
(limb paralysis or brain atrophy). Cognitive tests in<br />
these animals treated with EB101 also show a dramatic<br />
improvement in learning and psychomotor activity. The<br />
present results indicate that the immunization with EB101<br />
prevents and reverses AD neuropathology and underlined<br />
inflammation, thus warranting further studies.<br />
Study supported by: Euroespes Foundation<br />
T1507. MoCA vs. MMSE: Patterns of Cognitive<br />
Performance across Adult Lifespan in a Non-Clinical<br />
Sample<br />
Shea Gluhm, Charles Van Liew, Jody Goldstein, Guerry Peavy,<br />
Mark Jacobson, Stephanie Lessig and Jody Corey-Bloom; La<br />
Jolla, CA and San Diego, CA<br />
The Mini Mental State Examination (MMSE) is the most<br />
commonly used brief cognitive screening instrument; however,<br />
the Montreal Cognitive Assessment (MoCA) may be<br />
more sensitive to early cognitive dysfunction. The present<br />
study sought to compare age-related decline on these measures<br />
across the adult lifespan in a non-clinical sample. Performance<br />
on the MMSE and MoCA of 202, presumably<br />
normal, community-dwelling participants ranging in age<br />
from 20–89, divided by decade, were compared with<br />
71<br />
Wilcoxon Signed Ranks Tests. We found that, for the total<br />
sample, there were significant differences between MoCA<br />
and MMSE with regard to total score (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 72<br />
neuronal excitability and synaptic transmission. Here, we<br />
used the glutamate sensing fluorescent reporter (Super-<br />
GluSnFR) developed by Roger Tsien’s laboratory to perform<br />
sensitive optical measurements of glutamate release in<br />
response to Ab. This probe provides both a temporal and<br />
quantitative fluorescent readout of glutamate concentration<br />
by imaging FRET-dependent changes. We transfected HEK-<br />
293T cells with SuperGluSnFr, and then co-cultured these<br />
‘glutamate-sensing cells’ with astrocytes. Nanomolar concentrations<br />
of oligomerized (but not non-oligomerized) Ab<br />
induced release of several hundred-micromolar glutamate<br />
from astrocytes. These levels of glutamate can cause synaptic<br />
loss and excitotoxic damage to neurons. Taken together with<br />
prior studies, our work suggests that the neurotoxic effects<br />
of Ab may be mediated at least in part by local release of<br />
glutamate from astrocytes. Additionally, we found that<br />
newer congeners of memantine (called NitroMemantines)<br />
are able to prevent toxic glutamatergic effects of Ab to a<br />
greater degree than memantine itself.<br />
Study supported by: NIH and ADAMAS Pharmaceuticals,<br />
Inc.<br />
Stuart Lipton is the named inventor on patents for memantine<br />
and NitroMemantine for neurodegenerative disorders<br />
that are licensed to Forest Laboratories, Inc. and ADAMAS<br />
Pharmaceuticals, Inc., respectively. Concerning memantine,<br />
Dr. Lipton participates in a Royalty Sharing Agreement<br />
administered by his former institution, Harvard Medical<br />
School/Children’s Hospital, Boston.<br />
T1510. Is Poststroke Dementia Related to Amyloid<br />
Deposition and Microglia Activation?<br />
Wolf-Dieter Heiss, Basia Radlinska, Jean-Paul Soucy, Ralf<br />
Schirrmacher, Alexander Thiel and Vladimir Hachinski; Cologne,<br />
Germany; Montreal, QC, Canada and London, ON, Canada<br />
Amyloid deposition typical for Alzheimer’s Disease might be<br />
a predisposing factor for poststroke dementia and might be<br />
aggravated by inflammation accompanying ischemic changes.<br />
The relationship between amyloid deposition, inflammatory<br />
reaction and development of poststroke dementia is studied in<br />
5 patients with first supratentorial ischemic stroke by MRI (at<br />
2 weeks and 5 – 7 months) and PET with 11 C-PIB for amyloid<br />
imaging and with 11 C-PK 11195 for inflammation at 6<br />
months, the clinical course is followed for 12 months.<br />
Preliminary results indicate a significant increase in global<br />
PIB uptake (SUVR > 1.5) in the entire cortex compared to<br />
cerebellum. This amyloid deposition usually was asymmetric<br />
with peak values in prefrontal (SUVR ¼ 2.29 6 0.325) or<br />
parieto-temporal areas (SUVR ¼ 2.02 6 0.202). Increased<br />
PK-uptake as a marker of microglia activation was found in<br />
areas around the infarct, but also in connecting fiber tracts<br />
and distant from the ischemic lesion.<br />
These preliminary data demonstrate amyloid deposition<br />
and increased microglia activation in patients after stroke.<br />
The relationship between these two pathological processes<br />
and their impact on the development and progression of<br />
cognitive impairment will be further investigated.<br />
T1511. Cycad Methylazoxymethanol Linked to DNA<br />
Damage, Cancer and Neurodegeneration<br />
Glen E. Kisby, Rebecca C. Fry, Michael R. Lasarev, Theodor<br />
K. Bammler, Richard P. Beyer, Mona I. Churchwell, Daniel R.<br />
Doerge, Lisiane B. Meira, Valerie S. Palmer, Ana-Luisa<br />
Ramos-Crawford, Xuefeng Ren, Robert S. Sullivan, Terrance J.<br />
Kavanagh, Leona D. Samson, Helmut Zarbl and Peter S.<br />
Spencer; Portland, OR; Seattle, WA; Cambridge, MA;<br />
Jefferson, AR; Guildford, Kent, United Kingdom; Buffalo, NY;<br />
Piscataway, NJ and Chapel Hill, NC<br />
72<br />
Guam ALS-PD Complex (tauopathy) is linked epidemiologically<br />
to cycasin, methylazoxymethanol (MAM) glucoside, a<br />
neurotoxin, carcinogen and genotoxin. MAM produces O6methylguanine<br />
(O6-mG) DNA lesions that are repaired by<br />
O6-mG methyltransferase (MGMT). We asked whether<br />
MAM-induced DNA damage in MGMT-deficient<br />
(Mgmt / ) mouse brain (a model of the young adult<br />
human brain) activates signal transduction pathways perturbed<br />
in neurodegenerative disease. Brain transcriptional<br />
profiles of young adult Mgmt / and wild-type mice were<br />
determined at intervals after a single systemic dose of MAM<br />
or vehicle. Mgmt / mice treated with MAM vs. vehicle<br />
showed 362 differentially expressed genes, of which 57 were<br />
highly correlated with O6-mG levels. Sixty of 153 modulated<br />
genes correlated with O6-mG when the response of<br />
wild-type vs. Mgmt / mice to MAM vs. vehicle was<br />
determined. Top associations were with neurological disease,<br />
psychological disorders, cancer, and genetic disorders. Prominent<br />
MAM-modulated brain KEGG pathways included<br />
Wnt-beta-catenin, which is perturbed in Alzheimer Disease<br />
(AD) and in MAM-induced colorectal carcinoma. Thus,<br />
MAM modulates pathways common to cancer (in cycling<br />
cells) and cell degeneration (in non-cycling neurons). Exposure<br />
to environmental MAM-like genotoxins (e.g., nitrosamines)<br />
may have relevance to the etiology of other tauopathies,<br />
notably AD.<br />
Study supported by: National Institutes of Environmental<br />
Health Sciences: ES11384, ES11399, ES011387 and<br />
ES07033.<br />
T1512. Genetic <strong>Association</strong>s between VPS10 Receptor<br />
Genes and Late-Onset Alzheimer’s Disease<br />
Christiane Reitz, Joseph Lee, Lindsay Farrer, Margaret Pericak-<br />
Vance, Jonathan Haines, Ekaterina Rogaeva, Peter St. George-<br />
Hyslop and Richard Mayeux; New York; Boston; Miami;<br />
Nashville and Toronto, Canada<br />
Background: Genetic and functional studies showed that<br />
genetic variation in SORL1 and SORCS1 is associated with<br />
LOAD risk by modulating secretase processing of APP.<br />
Consequently, underexpression of SORL1 or SORCS1 leads<br />
to Ab overexpression and increased LOAD risk. We<br />
hypothesized that also genetic variation in the homologs<br />
SORCS2 and SORC3 is associated with LOAD.<br />
Methods: First, we analyzed associations between genetic<br />
variation in SORCS2 and SORCS3 and LOAD risk in several<br />
independent datasets. Then, we compared SORCS2<br />
and SORCS3 expression levels in brain regions from LOAD<br />
cases and controls, and performed cell biological experiments<br />
exploring the effect of both genes on APP processing.<br />
Results: Consistent with SORL1 and SORCS1, inherited<br />
variants in SORCS2 and SORCS3 were associated with<br />
LOAD risk. In addition, both genes were underexpressed in<br />
amygdala tissue from LOAD brains compared to control<br />
brains. Finally, we found evidence that - similar to SORL1<br />
and SORCS1- both SORCS2 and SORCS3 may influence<br />
APP processing by modulating gamma secretase processing<br />
of APP.<br />
Conclusions: In addition to SORL1 and SORCS1, also<br />
variants in SORCS2 and SORCS3 may play a role in the<br />
pathogenesis of LOAD through an effect on APP processing.<br />
Study supported by: R37-AG15473 (Mayeux), P01-<br />
AG07232 (Mayeux), R01-AG09029 (Farrer), R01-<br />
AG025259 (Farrer), P30-AG13846 (Boston University Alzheimer’s<br />
Disease Research Center grant), K23AG034550<br />
(Reitz). R01-AG027944 (Pericak-Vance), R01-AG019757<br />
(Pericak-Vance)<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 73<br />
T1513. Cardiac Ejection Fraction, Cognitive Function<br />
and Leukoaraiosis in an Elderly Cohort: The<br />
Cardiovascular Health Study<br />
Rebecca F. Gottesman, Salvador Cruz-Flores, Annette<br />
Fitzpatrick, John Gottdiener, Traci Bartz, Richard Kronmal<br />
and W.T. Longstreth, Jr.; Baltimore, MD; St. Louis, MO and<br />
Seattle, WA<br />
Background: Heart failure has been associated with cognitive<br />
dysfunction. To explore mechanism, we examined associations<br />
among ejection fraction (EF), cognition, and MRIdefined<br />
white matter hyperintensity (WMH) in the Cardiovascular<br />
Health Study (CHS), a longitudinal cohort study<br />
of participants 65 years old.<br />
Methods: We included 1972 CHS participants who underwent<br />
echocardiography, 2 brain MRIs 5 years apart, and cognitive<br />
assessments concurrent with the MRIs. Linear regression<br />
models including vascular risk factors, demographics, and EF<br />
(normal or impaired) were used to evaluate these outcomes:<br />
WMH grade on a 10-point scale, progression of WMH by<br />
1 grade, and change in cognitive performance on the 100point<br />
modified Mini-Mental State examination (3MS) and<br />
Digit Symbol Substitution test (DSST).<br />
Results: EF independently predicted WMH grade at the second<br />
MRI (p ¼ 0.05) and WMH progression (OR 1.61, 95%<br />
CI 1.07–2.43). Worse EF independently predicted more decline<br />
in 3MS (p ¼ 0.02) and DSST (p ¼ 0.02), but these relationships<br />
were partially attenuated with WMH grade as a covariate.<br />
Conclusions: In an elderly population, EF predicts volume<br />
and progression of WMH. EF also predicts cognitive<br />
performance, but this may be partially mediated through<br />
effects on the white matter.<br />
Study supported by: NIH/ NHLBI (not to the first / corresponding<br />
author directly)<br />
T1514. Predicting MCI Outcome with Clinically<br />
Available MRI and CSF Biomarkers<br />
David S. Heister, James B. Brewer, Sebastian Magda, Kaj<br />
Blennow and Linda K. McEvoy; La Jolla, CA and Mölndal,<br />
Sweden<br />
Cerebrospinal fluid (CSF) measures and medial temporal<br />
lobe atrophy (MTLA) on structural magnetic resonance<br />
images (MRIs) each predict decline to Alzheimer’s disease<br />
(AD), but how such measures can be used clinically to<br />
improve predictive prognosis is unclear.193 MCI participants<br />
were separated into risk groups (high/low) based on MTLA,<br />
quantified from FDA-approved software for volumetric imaging<br />
of MRIs, or based on cerebrospinal fluid (CSF) levels of<br />
total tau and Ab 1–42. Participants were also stratified into<br />
groups based on the combination of MTLA and CSF risk<br />
measures. Cox hazards models were used to assess group hazard<br />
ratios (HR) of converting to AD. MCI individuals with<br />
high atrophy or high CSF risk showed significantly greater<br />
hazard of AD conversion than those with low risk for each<br />
measure (HR: 3.52–4.20). Combining atrophy and CSF risk<br />
information substantially improved predictive ability. Individuals<br />
with both risk factors showed a significantly higher HR<br />
(13.68) than those with neither risk factor. Using both measures,<br />
80% of high-risk individuals developed AD in 3 years<br />
compared to 10% of low-risk individuals. Clinically available<br />
CSF and MRI measures can be combined to significantly<br />
improve predictive prognosis in MCI.<br />
Study supported by: L.K.M. is supported by NIA<br />
K01AG029218; J. B.B. is supported by NINDS<br />
K02NS067427. Data collection and sharing for this project<br />
was funded by the Alzheimer’s Disease Neuroimaging Initiative<br />
(ADNI) (National Institutes of Health Grant U01<br />
73<br />
AG024904). ADNI is funded by the National Institute on<br />
Aging, the National Institute of Biomedical Imaging and Bioengineering,<br />
and through generous contributions from the following:<br />
Abbott, AstraZeneca AB, Bayer Schering PharmaAG,-<br />
Bristol-Myers Squibb, Eisai Global Clinical Development,<br />
Elan Corporation, Genentech, GE Healthcare, GlaxoSmithKline,<br />
Innogenetics, Johnson and Johnson, Eli Lilly and Co.,<br />
Medpace, Inc., Merck and Co., Inc., Novartis AG, Pfizer Inc,<br />
F. Hoffman-La Roche, Schering-Plough, Synarc, Inc., and<br />
Wyeth, as well as non-profit partners the Alzheimer’s <strong>Association</strong><br />
and Alzheimer’s Drug Discovery Foundation, withparticipation<br />
from the U.S. Food and Drug Administration. Private<br />
sector contributions to ADNI are facilitated by the Foundation<br />
for the National Institutes of Health (www.fnih.org). The<br />
grantee organization is the Northern California Institute for<br />
Research and Education, and the study is coordinated by the<br />
Alzheimer’s Disease Cooperative Study at the University of<br />
California, San Diego. ADNI data are disseminated by the<br />
Laboratory for Neuro Imaging at the University of California,<br />
Los Angeles. This research was also supported by NIH grants<br />
P30 AG010129, K01 AG030514, and the Dana Foundation.<br />
None of the study sponsors had any role in the design and<br />
conduct of the current study, nor in data analysis, interpretation,<br />
preparation, review or approval of the manuscript.<br />
L. McEvoy’s spouse is President, CorTechs Labs, Inc. La Jolla,<br />
CA; Sebastian Magda is an employee of CorTechs Labs, Inc.<br />
T1515. Light and Electron Microscopic Analysis of FUS<br />
Immunoreactivity in 3 Variants of Tau and TDP-43<br />
Negative Frontotemporal Lobar Degeneration<br />
Keith A. Josephs, Wen-Lang Lin, Joseph E. Parisi, Neil Graff-<br />
Radford, Ronald C. Petersen and Dennis W. Dickson;<br />
Rochester, MN and Jacksonville, FL<br />
Background: The majority of frontotemporal lobar degenerations<br />
(FTLD) can be classified as tau or TDP-43 immunoreactive.<br />
Three rare variants were unclassified until recent<br />
evidence demonstrated FUS immunoreactivity: neuronal intermediate<br />
filament inclusion disease (NIFID), atypical<br />
FTLD with ubiquitin-immunoreactive inclusions (aFTLD-<br />
U) and basophilic inclusion body disease (BIBD).<br />
Aim: To assess the immunohistochemical profile of<br />
NIFID, aFTLD-U and BIBD.<br />
Methods: Light, electron and immunoelectron microscopic<br />
analysis of 15 cases of NIFID (n ¼ 5), aFTLD-U (n<br />
¼ 8) and BIBD (n ¼ 2).<br />
Results: All aFTLD-U and BIBD, and 3/5 NIFID cases<br />
were FUS immunoreactive. One FUS-negative NIFID case<br />
showed TDP-43 immunoreactivity. Electron microscopic<br />
examinations revealed FUS-immunoreactive granulofilament<br />
cytoplasmic inclusions in all aFTLD-U and BIBD cases,<br />
and in the FUS-positive NIFID cases. Granulofilament<br />
inclusions in the TDP-43 positive NIFID case were FUS<br />
negative, yet TDP-43-immunoreactive. Compact hyaline<br />
inclusions in all 5 NIFID cases were FUS-negative.<br />
Conclusions: Unlike in aFTLD-U and BIBD, FUS immunoreactivity<br />
in NIFID is variable and is limited to only certain<br />
types of inclusions, arguing against the notion that FUS is the<br />
primary pathological process in NIFID. Furthermore, TDP-<br />
43 immunoreactivity and NIFID are not mutually exclusive.<br />
Study supported by: NIH R01-AG037491<br />
T1516. Effects of Once-Daily, Extended-Release<br />
Memantine (28 mg/day) on Cognitive Domains in<br />
Patients with Moderate to Severe Alzheimer’s Disease<br />
Michael Tocco, Suzanne Hendrix, Michael L. Miller, Vojislav<br />
Pejovic and Stephen M. Graham; Jersey City, NJ; Salt Lake<br />
City, UT and Chicago, IL<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 74<br />
In this post hoc analysis of a 24-week, randomized, placebocontrolled<br />
trial (MEM-MD-50, NCT00322153) in ChEItreated<br />
patients with moderate to severe Alzheimer’s disease<br />
(AD), we examined the effects of a new, extended-release<br />
(ER) formulation of memantine (28 mg, once daily) on<br />
individual SIB domains, as well as on aggregated domains<br />
defined previously (Schmitt, 2006). Treatment groups were<br />
compared in terms of mean change from Baseline at Endpoint<br />
for nine SIB domains (Social Interaction, Memory,<br />
Orientation, Language, Attention, Praxis, Visuospatial Ability,<br />
Construction, and Orienting to Name) and combinations<br />
of domains aggregated using a face-valid approach<br />
into three higher-order subscales: MEMORY, LANGUAGE,<br />
and PRAXIS. Significant advantage of memantine ER over<br />
placebo was observed for the domains of Memory (OC, P<br />
¼ 0.021; LOCF, P ¼ 0.016), Language (OC, P ¼ 0.003;<br />
LOCF, P ¼ 0.004), Attention (OC, P ¼ 0.014; LOCF, P<br />
¼ 0.003), Praxis (OC, P ¼ 0.015; LOCF, P ¼ 0.002), Orientation<br />
(LOCF, P ¼ 0.043), and Construction (OC, P ¼<br />
0.042), and for all three higher-order subscales (MEMORY:<br />
OC, P ¼ 0.002; LOCF, P ¼ 0.003; LANGUAGE: OC,<br />
LOCF, P ¼ 0.003; PRAXIS: OC, P ¼ 0.012; LOCF, P ¼<br />
0.004). In conclusion, memantine ER treatment may be<br />
associated with significant improvements on several cognitive<br />
domains, including memory, language, praxis, and<br />
attention.<br />
Study supported by: Forest Research Institute<br />
Michael Tocco and Stephen M. Graham are employees of<br />
Forest Research Institute, Inc. Suzanne Hendrix is an employee<br />
of Pentara Corporation, an independent contractor<br />
to several pharmaceutical companies, including Forest<br />
Research Institute, Inc. Michael L. Miller and Vojislav<br />
Pejovic are employees of Prescott Medical Communications<br />
Group, an independent contractor to several pharmaceutical<br />
companies, including Forest Research Institute, Inc.<br />
T1517. Efficacy of Memantine by Baseline Disease<br />
Severity: A Pooled Post-Hoc Analysis of Trials in Mild to<br />
Moderate Alzheimer’s Disease<br />
Michael Tocco, Suzanne Hendrix, Michael L. Miller, Vojislav<br />
Pejovic and Stephen M. Graham; Jersey City, NJ; Salt Lake<br />
City, UT and Chicago, IL<br />
Several randomized, placebo-controlled trials have demonstrated<br />
benefits of memantine in patients with moderate to<br />
severe Alzheimer’s disease (AD); trials in mild to moderate<br />
AD have yielded less consistent results. The dementia severity<br />
range in which memantine may provide benefits should<br />
be determined with greater precision. In this post-hoc analysis,<br />
we pooled 713 memantine-treated (20 mg/day) and 559<br />
placebo-treated patients from three randomized trials in<br />
mild to moderate AD (MMSE range: 10–23). For each<br />
baseline MMSE value, mean change from baseline was estimated<br />
for measures of cognition (ADAS-cog), function<br />
(ADCS-ADL23), global status (CIBIC-Plus), and behavior<br />
(NPI). Furthermore, data (intent-to-treat population,<br />
observed cases) were analyzed by means of a mixed model<br />
with quadratic terms for time and baseline MMSE. Memantine<br />
treatment was associated with significant benefits versus<br />
placebo within the MMSE range of 12–20 for the ADAScog,<br />
15–18 for the ADCS-ADL, and 10–17 for the CIBIC-<br />
Plus; no significant differences between groups were<br />
observed for the NPI. In conclusion, memantine treatment<br />
may be associated with significant cognitive, functional, and<br />
global benefits in patients with MMSE scores corresponding<br />
to the early moderate stage of AD.<br />
Study supported by: Forest Research Institute<br />
74<br />
Drs. Stephen Graham and Michael Tocco are employed<br />
by Forest Research Institute. Dr. Suzanne Hendrix is an employee<br />
of Pentara Corporation, an independent contractor<br />
to several pharmaceutical companies, including Forest<br />
Research Institute, Inc. Drs. Michael L. Miller and Vojislav<br />
Pejovic are employees of Prescott Medical Communications<br />
Group, an independent contractor to several pharmaceutical<br />
companies, including Forest Research Institute, Inc.<br />
T1518. Clinical Gait Abnormalities and Hippocampal<br />
Morphometry in MCI: Preliminary Results from the<br />
ADNI Study<br />
Vincent S. DeOrchis and Joe Verghese; Bronx, NY<br />
Objective: To examine whether clinical gait abnormalities<br />
could identify aMCI subjects with reduced hippocampal<br />
volume and increased risk of cognitive decline.<br />
Methods: The population for this study included subjects<br />
with aMCI diagnosed using established criteria and with<br />
neuroimaging enrolled in the Alzheimer’s Disease Neuroimaging<br />
Initiative (ADNI) study. Hippocampal volume was<br />
assessed in 370 aMCI subjects using semiautomated voxel<br />
based morphometry available on the ADNI website. The<br />
association of gait abnormalities, as diagnosed by study<br />
clinicians, with hippocampal volume was assessed using linear<br />
regression adjusted for age, gender, education and total<br />
brain volume.<br />
Results: Subjects mean age was 72.8 years, average education<br />
was 15.4 years and 62.3% were women. The mean<br />
hippocampal volume was 3188.77 þ/ 562.27mm3 on the<br />
right and 3145.28 þ/ 549.78mm3 on the left. Clinical<br />
gait abnormalities were diagnosed in 35 (9.3%) subjects and<br />
were associated with right hippocampal volume (estimate<br />
264.646, 95% CI: 443.4 to 85.8, p ¼ 0.004), but<br />
not the left (p ¼ 0.053). Adding MMSE or memory test<br />
scores to the final model did not change the significance of<br />
association.<br />
Conclusions: Our preliminary study supports gait abnormalities<br />
as a clinical marker of worse hippocampal morphology<br />
in aMCI.<br />
T1519. Topography of Cortical Thinning in PIB-<br />
Negative Subcortical Vascular Dementia Versus<br />
Alzheimer’s Disease<br />
Chi Hun Kim, Sang Won Seo, Sung Tae Kim, Jae-Hong Lee,<br />
Jae Seung Kim, Seung Jun Oh, Suk-Hui Kim, Hae Kwan<br />
Cheong, Jong-Min Lee, Seun Jeon and Duk L. Na; Seoul,<br />
Korea and Suwon, Korea<br />
Objective: To determine the existence of cortical atrophy in<br />
Subcortical Vascular Dementia (SVaD) with negative 11 C-<br />
Pittsburgh compound B (PIB) PET scan and to compare<br />
the topography of cortical thinning between PIB (-) SVaD<br />
and Alzheimer’s disease (AD).<br />
Methods: Cortical thickness in 24 patients with PIB (-)<br />
SVaD, 81 clinically probable AD subjects with minimal ischemia,<br />
and 72 normal cognitive controls (NC) was measured<br />
using a surface-based morphometric method. The<br />
results were compared and mapped onto a 3D brain<br />
surface.<br />
Results: Compared with NC, significant cortical thinning<br />
of PIB (-) SVaD was noted in a widespread area including<br />
frontal, temporoparietal, medial frontal, posterior cingulate<br />
cortices, and ligual gyri. Compared with AD, PIB (-) SVaD<br />
demonstrated cortical thinning in bilateral perisylvian area,<br />
ligual gyri, and right medial frontal lobe. Compared with<br />
PIB (-) SVaD, AD showed significant cortical atrophy in<br />
bilateral medial temporal lobes and precuneus.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 75<br />
Interpretation: Small vessel disease without amyloid burden<br />
may lead to substantial cortical atrophy. PIB (-) SVaD<br />
demonstrated characteristic cortical thinning in bilateral<br />
perisylvian area, ligual gyri, and the right medial frontal<br />
lobe.<br />
Study supported by: The Korea Healthcare Technology<br />
R&D Project, Ministry for Health, Welfare & Family<br />
Affairs, Republic of Korea (A050079), grants from the Asan<br />
Institute for Life Sciences (2006-159), and the Conversing<br />
Research Center Program through the National Research<br />
Foundation of Korea (NRF) funded by the Ministry of<br />
Education, Science and Technology (2009-0081959)<br />
T1520. The First Nationwide Survey of Bardet-Biedl<br />
Syndrome in Japan<br />
Makito Hirano, Toshihide Yamashita, Yasushi Ikuno, Hiromi<br />
Iwahashi, Mitsuru Ohishi, Toshiyuki Mano, Ryu Ishihara,<br />
Ichiro Tanaka, Keiko Yanagihara, Yusaku Nakamura and<br />
Susumu Kusunoki; Sakai, Osaka, Japan; Suita, Japan; Izumi,<br />
Japan; Osaka, Japan; Kashihara, Japan and Osaka Sayama,<br />
Japan<br />
Bardet-Biedl syndrome (BBS) is an autosomal recessive disorder<br />
characterized by mental impairment, rod-cone dystrophy,<br />
polydactyly, central obesity, hypogonadism, and renal<br />
abnormalities. The causative genes have been identified as<br />
BBS1-14 genes encoding proteins that maintain cilia function,<br />
but more than 20% of patients have no mutations<br />
identified. This disease is extremely rare in Japan, where<br />
only a few patients have been reported. We conducted the<br />
first nationwide survey of this disease in 2010. We summarized<br />
clinical and genetic information of newly identified<br />
patients and previously reported patients. We found that<br />
rare liver fibrosis was detected in 20% of patients, while<br />
only 30% of patients had apparent renal abnormalities,<br />
thought to be a universal symptom. DNA array analysis<br />
(BBS1-10,12) was performed in 9 patients with clinically<br />
definite or possible BBS, but no known mutations were<br />
identified. However, cultured fibroblasts from two patients<br />
had reduced protein levels of BBS6 without any coding<br />
mutations, suggesting abnormalities in transcription/translation<br />
or protein instabilities affected by other regulatory proteins.<br />
In conclusion, we speculate that clinical symptoms<br />
and genetic background of BBS in Japan may differ from<br />
those in the Western countries.<br />
Study supported by: Health and Labour Science Research<br />
Grants in Japan (Research in intractable diseases)<br />
T1521. P600 Word Repetition Effect Amplitude<br />
Correlates with Left Hippocampal Volume<br />
John M. Olichney, Rawi Nanakul, Alireza K. Javan, Patrick<br />
E. Adams, Andrea Schneider, Andreea Seritan, Randi J.<br />
Hagerman, Paul J. Hagerman and Susan M. Rivera; Davis,<br />
CA and Sacramento, CA<br />
Background: Prior work has shown that hippocampal volume<br />
and certain ERP components (e.g. P600 repetition<br />
effect) can be predictors of memory ability. However, the<br />
relationship between hippocampal volume and electrophysiological<br />
measures of human memory remains unclear.<br />
Objective: To define the relationship between P600 word<br />
repetition effect amplitude and hippocampal volume. We<br />
hypothesized they would be moderately correlated, with<br />
each variable independently predicting verbal memory.<br />
Methods: 32 channel ERP data was recorded during a<br />
category decision task. Structural 3T MRI was acquired<br />
(Siemens Trio) and hippocampal volumes measured on 3D<br />
MPRAGE sequences.<br />
75<br />
Results: Across our mixed sample of subjects (n ¼ 33;<br />
21 with Fragile X-associated Tremor Ataxia Syndrome, 12<br />
normal controls, mean age ¼ 65, mean MMSE ¼ 27), a<br />
significant correlation (r ¼ 0.38, p ¼ 0.029) was present<br />
between P600 repetition effect amplitude and left, but not<br />
right, hippocampal volume. Linear regression models found<br />
that subsequent cued recall was predicted by left hippocampal<br />
volume and age. In contrast, free recall correlated with<br />
P600 repetition effect amplitude (rho ¼ .49, p ¼ 0.004)<br />
only.<br />
Conclusion: P600 word repetition effect correlates with<br />
left hippocampal volume. These two measures appear complementary<br />
and predict different aspects of memory<br />
performance.<br />
Study supported by: National Institutes of Health Roadmap<br />
Interdisciplinary Research Consortium Grant [Grant<br />
Numbers UL1DE019583 (NIDCR), RL1AG032115], NIH<br />
Grant R01-AG18442, California Alzheimer’s Disease<br />
Program<br />
Randi Hagerman receives research support from Neuropharm,<br />
Seaside therapeutics, Forest, Johnson and Johnson<br />
and Roche and consultation with Novartis for fragile X<br />
research studies.<br />
T1522. Visuospatial Construction Measures and Their<br />
Utility in Identifying Dementia of the Alzheimer’s Type<br />
Bonnie M. Scott, G. Duncan, H. Carlson, Matthew Nance,<br />
Michele K. York, Angela Larery, Josephine Stouter and Adriana<br />
M. Strutt; Houston, TX<br />
Objectives: To examine the psychometric properties and<br />
clinical utility of three visuospatial-construction (VC) measures<br />
in differentiating Mild Cognitive Impairment (MCI)<br />
and Alzheimer’s disease (AD).<br />
Background: Assessment of VC deficits aid clinicians in<br />
distinguishing AD from other forms of dementia and determining<br />
the patient’s functional status. However, there is currently<br />
no research comparing the psychometric properties of<br />
commonly employed VC measures with MCI subtypes and<br />
varying stages of AD.<br />
Methods: 37 MCI and 126 AD patients completed the<br />
Beery-Buktenica Developmental Test of Visual Motor Integration<br />
(Beery), Rey-Osterrieth Complex Figure Test (Rey-<br />
O), and the Block Design subtest of the WAIS-III.<br />
Results: Age and education significantly differed between<br />
groups, and were therefore utilized as covariates. ANCOVAs<br />
revealed significant between group differences (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 76<br />
measure (SIB, ADCS-ADL 19, NPI, CIBIC-Plus), 5 response<br />
levels were defined, based on change scores attained at Endpoint<br />
by the 10 th ,25 th ,50 th ,75 th , and 90 th percentile of<br />
placebo-treated patients. The proportions of memantineand<br />
placebo-treated patients attaining each response level<br />
(or better) were compared using Fisher’s exact test. For each<br />
outcome measure, the proportion of memantine-treated<br />
patients numerically exceeded that of placebo-treated<br />
patients at all response levels. On the SIB, the memantine<br />
group was significantly superior at the 90 th percentile level<br />
(improvement >11 points; P ¼ 0.003), on the NPI at the<br />
90 th percentile level (improvement 17 points; P ¼ 0.018)<br />
and the 75 th percentile level (improvement 8 points; P ¼<br />
0.016), and on the CIBIC-Plus at the 75 th percentile level<br />
(score 18 yrs) and<br />
low education (
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 77<br />
employee of Pentara Corporation, an independent contractor<br />
to several pharmaceutical companies, including Forest<br />
Research Institute, Inc. Michael L. Miller and Vojislav<br />
Pejovic are employees of Prescott Medical Communications<br />
Group, an independent contractor to several pharmaceutical<br />
companies, including Forest Research Institute, Inc.<br />
T1527. Neurophysiologic Markers of Aging-Related<br />
Muscle Weakness<br />
Ela B. Plow, Dina Gohar, Mehmed B. Bayram, Jing Hou,<br />
Alexandria Wyant, Yin Fang, Vlodek Siemionow and Guang<br />
H. Yue; Cleveland, OH<br />
Age-related muscle weakness is usually ascribed to peripheral<br />
factors, such as loss and change of muscle fibers. Recent evidence<br />
demonstrates that central neural drive diminishes<br />
with age, but its relation to strength remains unclear. We<br />
investigated the cortical neurophysiologic markers of agerelated<br />
muscle weakness using Transcranial Magnetic Stimulation<br />
(TMS). Ten healthy elderly (76.3 6 2.6yrs) and 15<br />
young individuals (22.3 6 0.9yrs) were enrolled. Measures<br />
included left elbow flexion strength, size of muscle evoked<br />
potential (MEP) following suprathreshold TMS delivered to<br />
Right Motor Cortex (RM1), size of RM1 map of left biceps<br />
brachii (BB) muscle, and inter-hemispheric inhibition (IHI)<br />
exerted upon RM1. Results demonstrate that elderly, compared<br />
to the young, were weaker (83.4 6 8.4N vs.105.9 6<br />
8.3N, p ¼ 0.04), possessed smaller RM1 map of BB (717.8<br />
6 150.8sq. mm vs.1034.4 6 116.1sq. mm, p ¼ 0.05) and<br />
showed stronger IHI (79.9 6 6.3% vs. 63.5 6 6.2%, p ¼<br />
0.04), although their size of MEP was larger (1.1 6 0.2mV<br />
vs. 0.4 6 0.1mV, p ¼ 0.02). Stronger IHI was associated<br />
with smaller RM1 map of BB (r ¼ 0.38, p ¼ 0.05) and<br />
poor strength (r ¼ 0.36, p ¼ 0.06). Thus, although compensatory<br />
processes ensue in the muscle, age-related weakness<br />
persists. Reduced motor cortical maps and stronger inhibition<br />
from ipsilateral motor areas may explain weakness<br />
in the elderly; interventions modulating these cortical factors<br />
may improve strength.<br />
Study supported by: National Institutes of Health R01<br />
NS035130<br />
T1528. The Purkinje Cell of the Cerebellar Cortex in<br />
Alzheimer’s Disease<br />
and Stavros J. Baloyannis; Thessaloniki, Greece<br />
Alzheimer’s disease is a heterogeneous neurodegenerative disorder,<br />
characterized by progressive memory loss, affective<br />
and behavioural changes.We studied the morphological findings<br />
of the cerebellar cortex, in twenty early cases of Alzheimer’s<br />
disease using electron microscopy and silver impregnation<br />
techniques. The Purkinje cells showed morphological<br />
alterations concerning dendritic profiles and axonic collaterals.<br />
Loss of dendritic branches was marked in Purkinje cells<br />
of the vermis. Large number of spines was lost in most of<br />
Purkinje cells. Axonic collaterals were also lost. The thick<br />
axonic network around the initial part of Purkinje cell<br />
axons, disappeard. The electron microscopy revealed morphological<br />
alterations of the mitochondria in the perikaryon,<br />
the dendritic processes and the axon of Purkinje cells. Fragmentation<br />
of the cisternae of Golgi apparatus was prominent.The<br />
loss of dendritic spines resulted in a dramatic<br />
decrease of the synapses in the molecular layer. However a<br />
tendency for regeneration of the spines was noticed, through<br />
a limited number of unattached spines. The synaptic alteration<br />
of the Purkinje cell emphasizes the importance of synaptic<br />
loss for the clinical and pathological profile of the<br />
disease,<br />
77<br />
T1529. A Translational Program of BDNF Gene<br />
Delivery for Alzheimer’s Disease<br />
Mark H. Tuszynski, Alan Nagahara, Adrian P. Kells, J.<br />
Bringas, John Forsayeth and Krystopf S. Bankiewicz; La Jolla,<br />
CA and San Francisco, CA<br />
Nervous system growth factors have extensive effects on neuronal<br />
function and survival. Nerve growth factor (NGF) prevents<br />
the death and stimulates the function of basal forebrain<br />
cholinergic neurons in correlational models of Alzheimer’s disease<br />
(AD), and is in a Phase 2 multi-center clinical trial using<br />
AAV2 gene delivery. Separately, Brain-Derived Neurotrophic<br />
Factor (BDNF) influences the survival and function of entorhinal<br />
cortical and hippocampal neurons in several animal<br />
models of AD, including transgenic mutant APP-expressing<br />
mice; aged rats and lesioned rats; and aged and lesioned primates.<br />
These effects occur independent of beta amyloid load.<br />
We are examining the safety and tolerability of BDNF gene<br />
delivery to the entorhinal cortex in rodent and primate dose<br />
escalation, safety and tolerability studies. Successful completion<br />
of these studies will lead to a Phase I trial of AAV2-<br />
BDNF gene delivery to target short term memory loss in Alzheimer’s<br />
disease. The translation of this clinical program will<br />
require development and utilization of real-time, MRI-guided<br />
AAV2 vector delivery with gadoteridol co-infusion to track<br />
and confirm vector distribution to the intended target.<br />
Study supported by: NIH, VA, Alz Assoc, Shiley Family<br />
Foundation<br />
T1530. Imaging Signatures of Pathology in Behavioral<br />
Variant Frontotemporal Dementia<br />
Jennifer L. Whitwell, Clifford R. Jack, David S. Knopman,<br />
Bradley F. Boeve, Ronald C. Petersen, Joseph E. Parisi, Dennis<br />
W. Dickson and Keith A. Josephs; Rochester, MN and<br />
Jacksonville, FL<br />
Background: Behavioral variant frontotemporal dementia<br />
(bvFTD) is pathologically heterogeneous. The most common<br />
pathologies underlying bvFTD are Pick’s disease (PiD),<br />
corticobasal degeneration (CBD), and FTLD-TDP type 1.<br />
We aimed to determine whether patterns of atrophy on<br />
imaging differed across these pathologies in bvFTD.<br />
Methods: We identified 15 bvFTD subjects that had a<br />
volumetric MRI and a pathological diagnosis of PiD (n ¼<br />
5), CBD (n ¼ 5) or FTLD-TDP type 1 (n ¼ 5). Voxelbased<br />
morphometry was used to assess patterns of atrophy<br />
in each group compared to 20 controls.<br />
Results: All groups showed frontal grey matter loss,<br />
although specific patterns of atrophy differed across groups.<br />
The PiD group showed widespread frontal loss with involvement<br />
of the anterior temporal lobes. The CBD group<br />
showed less severe loss predominantly involving posterior lateral<br />
and medial superior frontal lobe. The FTLD-TDP group<br />
showed widespread loss in frontal, temporal and parietal<br />
lobes. Greater parietal loss was observed in FTLD-TDP compared<br />
to both other groups, and greater anterior temporal<br />
loss was observed in PiD compared to CBD.<br />
Conclusions: Atrophy patterns in bvFTD vary according<br />
to pathology and may therefore be helpful in predicting<br />
these underlying pathologies.<br />
Study supported by: NIH grants R01 DC10367, R01<br />
AG037491, R21 AG38736, R01 AG11378 and P50 AG16574.<br />
T1531. Improved Statistical Power To Detect Treatment<br />
Effects on Functional Outcomes in Alzheimer’s Disease<br />
(AD) Clinical Trials by Item-Response Theory (IRT)<br />
M. Colin Ard, Douglas R. Galasko and Steven D. Edland; La<br />
Jolla, CA<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 78<br />
The Alzheimer’s Disease Cooperative Study-Activities of<br />
Daily Living (ADCS-ADL) scale assesses an individual’s<br />
ability to perform a range of everyday tasks and is frequently<br />
used as an endpoint in clinical trials for AD. While<br />
the ADCS-ADL has excellent face validity as a measure of<br />
the functional impact of AD, the manner in which it is constructed<br />
presents several challenges for longitudinal data<br />
analysis, including the use of different rating scales across<br />
items, item-specific gender and/or lifestyle biases, differences<br />
in the complexity or difficulty of indicated activities, and<br />
missing data at the item level. IRT constitutes a family of<br />
quantitative models that assume that responses on specific<br />
items are jointly probabilistically determined by item characteristics<br />
and underlying subject-level trait(s), and are well<br />
suited to handling item heterogeneity and missing data.<br />
Using data from an ADCS clinical trial of 409 mild to<br />
moderate AD patients we found that ADCS-ADL scores<br />
constructed from IRT-based re-weighted item scores displayed<br />
increased sensitivity to change and improved statistical<br />
power as an outcome measure in clinical trials.<br />
Study supported by: NIH/NIA AG010483 (SDE),<br />
AG005131 (SDE, DG), and AG034439 (MCA, SDE).<br />
T1532. Neuropathologic Basis of Age-Associated Brain<br />
Atrophy<br />
Deniz Erten-Lyons, Randy Woltjer, Hiroko Dodge, Lisa Silbert<br />
and Kaye Jeffrey; Portland, OR<br />
Objective: To examine the association between postmortem<br />
neuropathologic measures and antemortem brain atrophy in<br />
aging.<br />
Background: Better understanding of the neuropathologic<br />
basis of age-related brain atrophy is needed to differentiate<br />
disease processes from normal aging, and to optimize<br />
use of brain volume as an outcome in Alzheimer disease<br />
prevention studies.<br />
Methods: Seventy-three participants of a longitudinal aging<br />
study were followed until death. All subjects had 2MRI<br />
scans, with the last scan within 36 months of death, and cognitive<br />
evaluations within 24 months of death. The association<br />
between antemortem rate of ventricular volume expansion over<br />
time and three postmortem measures:neurofibrillary tangles<br />
(NFTs), neuritic plaques (NPs) and infarcts (large vessel and<br />
lacunar) was examined using a mixed-effects model adjusting<br />
for age at death, APOE e4 presence and cognitive status.<br />
Results: Presence of infarcts, high NFT and NP scores<br />
were significantly associated with higher rate of ventricular<br />
enlargement regardless of cognitive status. e4 carriers also<br />
had a significantly higher rate of ventricular enlargement.<br />
Conclusion: These results suggest that brain atrophy, as<br />
indexed by ventricular enlargement, is a marker of accruing<br />
age-associated neuropathology independent of presence of<br />
cognitive impairment.<br />
Study supported by: Merit Review Grant & Research Career<br />
Development Award, Office of Research and Development,<br />
Department of Veterans Affairs, National Institutes of<br />
Health (AG08017, MO1 RR000334)<br />
T1533. A Long-Term, Open-Label Extension Study<br />
Evaluating the Safety of Extended-Release Memantine<br />
(28 mg) in Patients with Moderate to Severe<br />
Alzheimer’s Disease<br />
Stephen M. Graham and James Perhach; Jersey City, NJ<br />
This study (MEM-MD-82) was a 52-week, multicenter,<br />
open-label extension (OLEX) of two previous trials of a 28mg,<br />
once-daily, memantine extended-release (ER) formulation:<br />
MEM-MD-51, a 52-week, open-label dosing trial in<br />
78<br />
patients with AD (MMSE 3–18; N ¼ 166) who were<br />
titrated or switched immediately to memantine ER, and<br />
MEM-MD-54, a 28-week OLEX of a pivotal, 24-week,<br />
randomized, placebo-controlled trial of memantine ER<br />
(MEM-MD-50; NCT00322153) in patients with AD<br />
(MMSE 3–14; N ¼ 677). All patients from Study MEM-<br />
MD-54 and most patients from MEM-MD-51 were taking<br />
a ChEI at Baseline, which continued throughout this study.<br />
Sixty-six patients received memantine during this trial; 44<br />
(66.7%) completed the study, and 8 (12.1%) discontinued<br />
due to an AE. A total of 50 (75.8%) patients experienced a<br />
treatment-emergent AE, including UTI (13.6%), agitation<br />
(12.1%), aggression (10.6%), exacerbation of AD (9.1%),<br />
and anemia, constipation, weight decrease, and back pain<br />
(7.6% each); 17 (25.8%) experienced a serious AE. In conclusion,<br />
treatment with once-daily, memantine ER (28 mg)<br />
for up to two years is well tolerated in patients with moderate<br />
to severe Alzheimer’s disease.<br />
Study supported by: Forest Laboratories, Inc.<br />
Drs. Stephen Graham and James Perhach are employed<br />
by Forest Research Institute.<br />
T1534. A Retrospective Analysis Using Data-Monitoring<br />
Algorithms: What Are the Logical Relationships between<br />
the ADAS-Cog and MMSE?<br />
Christian Yavorsky, Guillermo DiClemente, Mark Opler, Sofija<br />
Jovic, Brian Rothman and Ashleigh DeFries; New York, NY<br />
Background: The ADAS-Cog and MMSE are standard<br />
instruments in Alzheimer’s disease trials. The Critical Path<br />
Institute Online Data Repository (CODR) includes results<br />
of AD trials submitted by 11 sponsors. However, reliability<br />
and validity problems exist with clinician administered<br />
measures. Data-monitoring uses relationships between<br />
instruments to address this. We assessed the likelihood of<br />
error in assessments if they fell outside expected correlations<br />
between the ADAS-Cog and MMSE, and examined whether<br />
errors could have been detected by data-monitoring.<br />
Methods: Correlations of total ADAS-Cog and MMSE<br />
scores from AD patients in 11 trials were compared with<br />
known correlations. Assessments that fell out of previously<br />
reported ranges were evaluated using data-monitoring<br />
algorithms.<br />
Results: The correlation between MMSE and ADAS-Cog<br />
was .780 (p
dementia. Denied images, mentioned spirits, paranoid about<br />
witchcraft to make him look mad and get him locked up, implying<br />
pension would be stolen. He was hydrated, given Aricept,<br />
Seroquel, became calmer. He was discharged with diagnosis of<br />
Alzheimer’s dementia, bimodal CBS (Charles Bonnet Syndrome),<br />
possible resolved delirium and dehydration.<br />
Discussion: CBS involves complex visual hallucinations<br />
with partial or full insight; auditory variant rarely reported<br />
with visual, both associated with sensory deprivation.<br />
Patients often hide hallucinations, as our patient did. Management<br />
includes anticonvulsant, antipsychotic, and antidepressant<br />
trials, also reassurance, increasing sensory stimulation<br />
and socialization.<br />
CBS was suggested as early marker for dementia, particularly<br />
Alzheimer’s and Lewy Body dementias.<br />
Conclusion: Suggest screening blind or deaf patients for<br />
CBS; closely follow for signs of dementia if positive. Further<br />
studies to ascertain positive predictive value and if earlier diagnosis<br />
leads to improved outcomes.<br />
T1537. Lead Exposure Up-Regulated Autophagy<br />
Response in Neuroblastoma SH-SY5Y Cells Via mTOR<br />
Kinase Signaling Pathway<br />
Shun-Sheng Chen, Chueh-Tan Chen and Jiin-Tsuey Cheng;<br />
Kaohsiung, Taiwan<br />
Objective: To study the signal transduced interaction<br />
between b-amyloid accumulation and autophagy response of<br />
lead exposured neuroblastoma SH-SY5Y cells.<br />
Background: Cellular necrosis, apoptosis, and b-amyloid<br />
deposition frequently occur after chronic lead exposure, resulted<br />
in the amyloid-b formed during autophagic turnover of APPrich<br />
organelles supplied by both autophagy and endocytosis.<br />
Therefore, the new perspective wastriedtoprovetheroleof<br />
autophagy on amyloidogensis disorders of lead exposure.<br />
Methods: SH-SY5Y neurons were exposed with low concentration<br />
lead, and enhanced autophagy process was<br />
observed by western blot. The APP-mRNA levels, intracellular<br />
and secreted isoforms of APP, the mRNA levels, cell<br />
viability and b-amyloid production were also measured.<br />
Results: After lead exposure, SH-SY5Y cells were enhanced<br />
by their autophagy responses through increased LC3II from<br />
LC3I cleavage. Lead exposure also induced neuronal death by<br />
b-amyloid deposition. During autophagy process, neuronal<br />
death was accompanied with other autophagic characteristics<br />
as accumulation of the autophagosome and protein degradation<br />
regulated negatively by the mTOR kinase signaling.<br />
Conclusion: The autophagy processes have shown that<br />
enhancing chronic lead exposure in neurons is accompanied<br />
by accumulation of the autophagosome and protein degradation<br />
which regulated negatively via mTOR kinase signaling.<br />
Study supported by: National Science Council, Taiwan<br />
Headache and Pain<br />
T1601. Withdrawn<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 79<br />
T1602. OnbotulinumtoxinA for the Treatment of<br />
Chronic Migraine: Long-Term Outcome<br />
Hanlon T. Christopher, Silvia M. Weibelt, Diane C. Andress-<br />
Rothrock and John F. Rothrock; Birmingham, AL<br />
Background: The long-term clinical outcomederived from<br />
treatment of chronic migraine (CM) with onabotulinumtoxinA<br />
(onabotA) is unknown.<br />
Methods: From a series of CM patients treated twice<br />
with onabotA who experienced a 50% or greater reduction<br />
79<br />
in headache days/month, we continued to treat and follow<br />
123 consecutive patients for at least 2 years (mean 2.76<br />
years; range 24 months-61 months).<br />
Results: Ten subjects (8%) eventually worsened despite<br />
continued treatment and relapsed to CM. Thirty-one subjects<br />
(25%) were able to stop onabotA therapy and remain<br />
largely free of headache for >6 months (mean sets of injections<br />
required: 4.8; range 2–8). Eighty-two (67%) remained<br />
responders but required ongoing injection therapy throughout<br />
the study period (at intervals ranging from 3 months to<br />
6 months; mean 3.4 months). Out of 1,142 sets of injections,<br />
there was one serious adverse event (status migrainosus,<br />
requiring brief hospitalization).<br />
Conclusion: Most CM patients who initially respond to<br />
treatment with onabotA will maintain that response for at<br />
least 2 years, and a substantial minority will be able to discontinue<br />
treatment and do well without prophylactic therapy.<br />
Long-term therapy with onabotA for CM is associated<br />
with a very low incidence of SAEs.<br />
Member, Allergan Physician Advisory Board; Consultant,<br />
Allergan<br />
T1603. Utility of Orally-Inhaled Dihydroergotamine<br />
When Early Intervention Is Impractical<br />
Shashidhar Kori, Stewart Tepper, Peter J. Goadsby, Paul<br />
Winner, Min Wang and Stephen Silberstein; Mountain View;<br />
Cleveland; San Francisco; West Palm Beach and Philadelphia<br />
Background: Well-controlled studies have demonstrated<br />
substantial reductions in triptan efficacy with delayed migraine<br />
treatment, and surveys have revealed some patient reluctance<br />
to treat migraines early, leading to treatment failure<br />
and dissatisfaction.<br />
Methods: This post-hoc analysis of a randomized, double-blind,<br />
placebo-controlled phase 3 study of orally-inhaled<br />
DHE compared 2-hour pain-relief(PR) and pain-free(PF)<br />
rates among patients treating migraine within 1 hour, 1–4<br />
hours, 4–8 hours, or >8 hours of its start.<br />
Results: Of 903 patients randomized, 771 treating a single<br />
attack were included in the efficacy analysis. Two-hour PF<br />
and PF rates were: 66% and 38% (inhaled DHE) and 41%<br />
and 13% (placebo) when treated within 1 hour of migraine<br />
start; 60% and 28% (inhaled DHE) and 35% and 10% (placebo)<br />
when treated within 1–4 hours; 53% and 22% (inhaled<br />
DHE) and 30% and 8% (placebo) when treated within 4–8<br />
hours; and 49% and 19% (inhaled DHE) and 24% and 9%<br />
(placebo) when treated >8 hours after start.<br />
Conclusions: This analysis demonstrated the efficacy of<br />
orally inhaled DHE in moderate/severe acute migraine, even<br />
when administered >8 hours after migraine start. Inhaled<br />
DHE may help many migraineurs who are unable to treat<br />
migraine early.<br />
Study supported by: This study was sponsored by MAP<br />
Pharmaceuticals. Dr Kori is a full-time employee of MAP<br />
Pharmaceuticals. Dr Tepper, Dr Goadsby, Dr Winner and<br />
Dr Silberstein have consulted for MAP Pharmaceuticals.<br />
Shashi Kori, MD is a full-time employee of MAP<br />
Pharmaceuticals.<br />
T1604. Characterization of Intraepidermal Nerve Fiber<br />
Morphology in Pain Associated with Diabetic<br />
Neuropathy and Impaired Glucose Tolerance<br />
Hsinlin T. Cheng, Jacqueline R. Dauch, Gordon A. Smith,<br />
Robinson J. Singleton, Brandon M. Yanik and Eva L.<br />
Feldman; Ann Arbor, MI and Salt Lake City, UT<br />
Neuropathic pain is a common symptom associated with diabetes<br />
and. Measurement of intraepidermal nerve fiber<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 80<br />
density (IENFD) in distal skin samples is a standard<br />
method for the diagnosis of diabetic neuropathy (DN).<br />
IENFD, however, is not considered a good indicator for the<br />
diagnosis of painful diabetic neuropathy (PDN). To evaluate<br />
the use of skin biopsy to study neuropathic pain in PDN,<br />
we studied the IENFD and nerve morphology in skin samples<br />
from: normal control, diabetic control, PDN, and DN.<br />
Skin samples from both the distal leg and proximal thigh<br />
were examined. Quantification of IENFD demonstrated no<br />
significant difference between PDN and DN. Morphological<br />
studies on these skin samples demonstrated the presence of<br />
axonal swellings or microneuromas, round shape nerve segments<br />
in PDN. The microneuroma densities in the proximal<br />
thigh of PDN are significantly higher than that of the<br />
DN. In summary, IENFD does not have a diagnostic value<br />
for PDN. In contrast, the microneuroma densities in proximal<br />
skin samples could be used as an indicator for PDN.<br />
Study supported by: NIH<br />
T1605. Heavily T2-Weighted Magnetic Resonance<br />
Myelography for Post-Lumbar Puncture Headache:<br />
A Pilot Study<br />
Yen-Feng Wang, Jong-Ling Fuh, Jiing-Feng Lirng and<br />
Shuu-Jiun Wang; Taipei, Taiwan<br />
Objective: To investigate the utility of heavily T2-weighted<br />
magnetic resonance myelography (HT2W MRM) in postlumbar<br />
puncture (LP) headache (PLPH).<br />
Background: PLPH occurs in about one third of patients<br />
receiving diagnostic LPs. HT2W MRM was proved comparable<br />
to computed tomographic myelography in localizing<br />
CSF leaks in spontaneous intracranial hypotension.<br />
Methods: We prospectively enrolled inpatients with indications<br />
for diagnostic LPs. Whole-spine axial HT2W<br />
MRMs were carried out after LPs. PLPH was diagnosed<br />
according to the ICHD-2 criteria.<br />
Results: Sixteen patients (3M/13F, age 45.9 6 14.6<br />
years, range 24–82) were recruited. Five patients (31.3%)<br />
(1M/4F) developed PLPH. Twelve patients (75%) had post-<br />
LP CSF leakage, and all of them had CSF leaks along the<br />
nerve roots. Of these patients, four (33.3%) had epidural<br />
CSF collections, and five (41.7%) had lumbosacral retrospinal<br />
CSF collections. All of the patients with PLPH had<br />
CSF leaks along the nerve roots, but only 41.7% of the<br />
patients with CSF leakage developed PLPH.<br />
Conclusion: HT2W MRM was sensitive in detecting<br />
CSF leaks after LP. Although CSF leakage after LPs was<br />
common, it was not the only determinant in the development<br />
of PLPH.<br />
Study supported by: Taipei Veterans General Hospital<br />
The authors are employees of Taipei Veterans General<br />
Hospital.<br />
T1606. Angioplasty and Stenting for the Treatment of<br />
Idiopathic Intracranial Hypertension Associated with<br />
Dural Venous Sinus Stenosis<br />
Parisa P. Javedani**, Jeremy D. Fields, Kenneth C. Liu,<br />
Stanley L. Barnwell and Bryan Petersen; Portland, OR and<br />
Charlottesville, VA<br />
Introduction: Lumboperitoneal shunt, ventriculoperitoneal<br />
shunt, and optic nerve sheath fenestration are accepted surgical<br />
therapies for medically refractory idiopathic intracranial<br />
hypertension (IIH). Stenting of stenotic venous sinuses has<br />
emerged as a potential therapy.<br />
Methods: We retrospectively reviewed all cases of dural<br />
stents for IIH at our institution. Eligibility criteria included<br />
medically refractory IIH with documented papilledema and<br />
80<br />
dural venous sinus stenosis of the dominant venous outflow<br />
system (gradient 10 mmHg).<br />
Results: Thirteen cases were identified (all female; mean<br />
39 years); all failed medical therapy and 5/13 failed surgical<br />
intervention. Technical success was achieved in 13/13 without<br />
major peri-procedural complications. The mean pre-procedural<br />
gradient across the venous stenosis was reduced from<br />
23mmHg to 4mmHg post-procedure. Headache resolved or<br />
improved in 9/13. Papilledema resolved in 12/13 and<br />
improved in 1/13. Among the 9 patients with angiographic<br />
follow-up, there were no instances of restenosis.<br />
Conclusions: Venous sinus stenting can achieve a high<br />
degree of technical success and safety with excellent clinical<br />
outcomes. Our series suggests that angioplasty and stenting<br />
may be considered as an alternative to current surgical therapies<br />
in patients with IIH and dural venous sinus stenosis.<br />
Study supported by: This study was unfunded and no<br />
individuals other than the authors have contributed to the<br />
preparation of this manuscript.<br />
T1607. Adrenal Insufficiency Presenting as Postural<br />
Tachycardia Syndrome<br />
Darine Kassar and Stanley Iyadurai; Saint Louis, MO<br />
Objectives: To report a case of adrenal insufficiency presenting<br />
as Postural Tachycardia Syndrome (POTS).<br />
Background: POTS is a disorder of unknown etiology<br />
characterized by orthostatic intolerance and excessive<br />
tachycardia.<br />
POTS is believed to be caused by central hypovolemia.<br />
Adrenal insufficiency has not been described before as an<br />
etiology for POTS.<br />
Methods: Case report<br />
Case report: We report a case of a 20 year-old woman<br />
who presented for migraine headache. Headaches improved<br />
after hydration and treatment. She returned to emergency<br />
room 2 weeks after discharge, with dizziness and recurrent<br />
falls associated with loss of consciousness that occurred<br />
while she attempted to stand.<br />
Physical examination showed orthostatic tachycardia. Tilt<br />
table test was positive. A diagnosis of POTS was made.<br />
No major improvement was noticed with fluid hydration<br />
and treatment with fludrocortisone. Additional work up<br />
showed low morning cortisol level. A diagnosis of adrenal<br />
insufficiency was made and patient was placed on prednisone<br />
with relief of her symptoms.<br />
Conclusion: POTS remains a diagnosis of exclusion. Here<br />
we report the first case of POTS associated with adrenal insufficiency,<br />
which was successfully treated with prednisone.<br />
Given the right clinical setting, checking cortisol level should<br />
be a consideration in evaluation for an etiology for POTS.<br />
T1608. Prevalence of Chronic Migraine (CM),<br />
Headache-Related Disability and Sociodemographic<br />
Factors in the US Population: Results from the <strong>American</strong><br />
Migraine Prevalence and Prevention (AMPP) Study<br />
Dawn C. Buse, Michael L. Reed, Kristina Fanning, Aubrey N.<br />
Manack, Catherine C. Turkel and Richard B. Lipton; Bronx,<br />
NY; Chapel Hill, NC and Irvine, CA<br />
Objective: Estimate the prevalence of CM in the US population<br />
by sociodemographics and headache-related disability.<br />
Methods: In 2004 surveys were mailed to 120,000 US<br />
households; 162,756 individuals aged 12 returned surveys;<br />
28,621 reported severe headache. CM was defined as<br />
ICHD-2 migraine with headache frequency 15 headache<br />
days/month. Crude and sociodemographically adjusted prevalence<br />
ratios (PRs) were generated.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 81<br />
Results: 19,189 individuals (11.8%) met ICHD-2 criteria<br />
for migraine (17.3% of females; 5.3% of males); 0.9% met<br />
criteria for CM (1.3% of females; 0.5% of males). Prevalence<br />
was highest in males and females aged 40–49. When<br />
compared with persons aged 12–17, adjusted PRs in the<br />
40–49 age group were as follows: females 4.71 (95% CI<br />
3.24–6.83), males 3.31 (95% CI 1.99 ¼ 5.49.) Rates of<br />
CM were inversely correlated with annual household<br />
income. Severe-headache related disability was reported by<br />
38.0% of CM vs. 9.5% of EM respondents.<br />
Conclusions: Prevalence of CM in the US was 0.9%,<br />
and was highest in adjusted models among females, in midlife,<br />
and households with the lowest income. Severe headache-related<br />
disability was most common among persons<br />
with CM.<br />
Study supported by: The AMPP was funded through a<br />
grant to the National Headache Foundation by Ortho-<br />
McNeil Neurologics, Inc., Titusville, New Jersey with supplemental<br />
funding by Allergan Inc., Irvine, CA.<br />
Drs. Buse, Lipton, Serrano, and Reed have received consulting<br />
funds and/or research support from Allergan. Drs.<br />
Manack and Turkel are full time employees of Allergan.<br />
T1609. Chronic Low Dose Methadone for the<br />
Suppression of Treatment-Refractory Chronic Migraine<br />
Keyvani Madjid and John F. Rothrock; San Diego, CA and<br />
Birmingham, AL<br />
Objective: to determine the safety and effectiveness of<br />
methadone administered chronically to patients with treatment-refractory<br />
chronic migraine (TRCM).<br />
Methods: We administered low dose (range 2.5–10 mg<br />
TID) methadone to a series of patients with TRCM. A positive<br />
treatment response was defined as a 50% or greater<br />
reduction in headache days/month during the 3rd treatment<br />
month relative to the baseline pre-treatment month, with<br />
that response maintained for at least 6 months. At 6 months<br />
we attempted to taper all responders off methadone.<br />
Results: We treated 130 subjects, and 57 (44%) achieved<br />
a positive response. We followed all responders for a mean<br />
of 27 months (range 13–57 months). Only 5 patients (4%<br />
of the total and 7% of responders) eventually were able to<br />
discontinue methadone without relapsing to CM within 30<br />
days. There was one serious adverse event (death due to<br />
overdose of oxycodone and alprazolam).<br />
Conclusions: While chronic administration of low dose<br />
methadone may achieve remission of TRCM to episodic<br />
migraine in a significant minority of patients so treated, discontinuation<br />
of treatment typically is associated with rapid<br />
relapse to CM.<br />
T1610. Relationship between High Frequency Nausea<br />
and Treatment Satisfaction in Episodic Migraine (EM):<br />
Results of the <strong>American</strong> Migraine Prevalence and<br />
Prevention (AMPP) Study<br />
Richard B. Lipton, Michael L. Reed, Kristina M. Fanning and<br />
Dawn C. Buse; Bronx, NY and Chapel Hill, NC<br />
Objective: Report headache symptomology and satisfaction<br />
with medications among persons with EM by headacherelated<br />
nausea status.<br />
Methods: Respondents to the 2009 AMPP survey who<br />
met criteria for EM (ICHD-2 criteria and
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 82<br />
Objective: Compare patterns of medical consultation and<br />
headache-impact in persons with migraine in the general<br />
population.<br />
Methods: The AMPP study is a longitudinal, population<br />
study of persons with severe headache. 2009 survey respondents<br />
who met ICHD-2 criteria for migraine (CM [ 15<br />
headache days/month] or EM [
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 83<br />
Results: 17 patients entered 30 days of data (192 headache<br />
attacks [mean ¼ 5.5]). Lower PSS was associated with<br />
higher odds ratios (ORs) for headache within 12 hours (OR<br />
[95% CI] ¼ 1.81 [1.13, 2.91] per 4-unit difference on<br />
PSS). Improvement in mood was significantly associated<br />
with headache occurrence within 12, 18, and 24 hours for<br />
happy (ORs ¼ 1.20, 1.20, and 1.18, and relaxed ORs ¼<br />
1.26, 1.17, and 1.14. Increases of >10 points were associated<br />
with headache occurrence within 12 hours for happy<br />
OR ¼ 2.73 and relaxed OR ¼ 2.31.<br />
Conclusions: Reduced perceived stress and increased feelings<br />
of happiness and relaxation were associated with<br />
increased odds of headache.<br />
Study supported by: This study was supported by an investigator<br />
initiated grant from ENDO Pharmaceuticals,<br />
Chadds Ford, PA.<br />
Drs. Buse and Lipton have acted as consultants and/or<br />
received research support from Endo Pharmaceuticals.<br />
T1616. Assessing the Consistency of LEVADEX TM<br />
(MAP0004, Orally Inhaled Dihydroergotamine)<br />
Pharmacokinetic Parameters in Healthy Volunteers:<br />
Results from 3 Clinical Studies<br />
Amy Forst, Julie Iwashita, Don Kellerman, Shashidhar Kori,<br />
Tracy Thomas and Glyn Taylor; Mountain View; Merthyr<br />
Tydfil, United Kingdom and Radyr, United Kingdom<br />
Background: Rapid, consistent drug absorption is important<br />
for effectively treating migraine acutely. MAP0004, a<br />
novel, orally inhaled dihydroergotamine (DHE), has shown<br />
efficacy in treating migraine acutely. Data from pharmacokinetic<br />
studies were analyzed for consistency, adequacy, and<br />
speed of DHE absorption through inhalation.<br />
Methods: Three studies compared MAP0004 1.0mg<br />
nominal with 1.0mg of intravenous (IV) DHE, assessing<br />
pharmacokinetic differences between smokers and nonsmokers,<br />
effect of co-administration of ketoconazole on<br />
MAP0004, and acute effects of MAP0004 on pulmonary artery<br />
pressure.<br />
Results: MAP0004 delivered DHE rapidly in all studies<br />
(mean Tmax, 7–11 minutes). Peak plasma concentrations of<br />
DHE were consistent across studies in non-smokers (Cmax geometric mean, 2475–2551 pg/mL). MAP0004 Cmax values<br />
were substantially lower than IV values (average,<br />
45,000pg/mL) but higher than intranasal (1,004pg/mL).<br />
Cmax and clearance did not vary significantly based on lung<br />
function, age, or weight across studies. Co-administration of<br />
ketoconazole did not significantly impact DHE pharmacokinetics<br />
after MAP0004 administration. 80-hydroxy-dihydroer gotamine concentrations after MAP0004 administration<br />
were low (average Cmax,
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 84<br />
Introduction: Dejerine Roussy Syndrome(DRS) usually<br />
results from damage to sensory pathways from thalamus to<br />
spinal cord. It may occur after stroke, multiple sclerosis, after<br />
trauma or in brain tumor involving thalamus. Occurrence<br />
of DRS in a patient with Sneddon’s syndrome has not<br />
been reported. We report a patient diagnosed with Sneddon’s<br />
syndrome presenting with central pain syndrome.<br />
Case Report: 69 year-old man with hypertension, hepatitis<br />
C, right posterior cerebral artery stroke presented with<br />
left hemi body severe pain. He was diagnosed with Sneddon’s<br />
syndrome nine months ago. His pain was severe,<br />
burning in nature, tearing and excruciating deep pressure<br />
pain involving left face, and left hemibody. He had left<br />
sided spastic hemiparesis and hyperesthesia and tenderness<br />
to touch. He was treated with all neuropathic medications<br />
and narcotic medications without significant success.<br />
Conclusion: DRS can be long lasting or even life long<br />
occurs immediately or years after a stroke. The exact pathogenesis<br />
is unknown, it could be related with inflammatory<br />
mediators and pain peptides by denervated nerves. To the<br />
best of our knowledge, occurrence of DRS in Sneddon’s<br />
syndrome has not been reported in the literature.<br />
T1620. Valproate-Responsive Subclinical Rhythmic<br />
Electrographic Disharges (SREDA) in a Migraineur<br />
Umer Akbar, Bhavpreet Dham, Evren Burakgazi and John<br />
Kelly; Camden, NJ and Washington<br />
Objective: To report SREDA and its response to valproate<br />
in a patient with migraine headache.<br />
Background: The electroencephalogram (EEG) findings<br />
in migraine are typically non-specific, such as ictal and<br />
inter-ictal diffuse and focal slowing. More specific EEG<br />
findings in migraine are diffuse and focal slowing in theta<br />
and delta frequencies and decreased alpha activity with<br />
increased response to photic stimulation.<br />
Design: We report the case of SREDA during a migraine<br />
headache, improving after valproate administration.<br />
Case: A 45 year-old Caucasian female with catamenial<br />
migraines was admitted for dizziness, fogginess, and refractory<br />
migraines. Magnetic resonance imaging revealed deep white matter<br />
changes consistent with history of recurrent migraines. An<br />
otherwise unremarkable EEG showed intermittent episodes of<br />
SREDA in wakefulness and drowsiness. Valproate was initiated<br />
and repeat EEG two-weeks later showed no evidence of SREDA.<br />
Discussion: SREDA is an infrequent EEG pattern which<br />
occurs predominantly in adults after hyperventilation. It is<br />
generally thought to be benign with little clinical significance<br />
and has been noted in conditions as diverse as vascular<br />
events, syncope, transient global amnesia and epilepsy.<br />
Response to valproate confirms the electrical mechanism of<br />
migraines and suggests SREDA’s potential causal relationship<br />
with migraines.<br />
T1621. Utriculo-Ocular Counterroll Reflex Disruption<br />
in Skew Deviation<br />
James A. Sharpe, Manokaraananthan Chandrakumar, Alan<br />
Blakeman, Herbert C. Goltz and Agnes M. Wong; Toronto,<br />
ON, Canada<br />
Lateral head tilt activates the utricles to evoke a static ocular<br />
counterroll reflex (OCR) of torsional eye motion. Damage<br />
to utriculo-ocular reflex pathways with an abnormal static<br />
OCR might be the mechanism of skew deviation, a vertical<br />
strabismus caused by supranuclear lesions.<br />
OCR gains, the change in torsional eye position/change<br />
in head position after sustained passive lateral head tilt of<br />
20 , were recorded using search coils in 18 patients with<br />
84<br />
skew from brainstem or cerebellar lesions, and 18 controls.<br />
Patient group mean OCR gain was significantly reduced in<br />
both torsional directions. OCR gains were asymmetric<br />
between eyes and between directions in 16 patients. The<br />
hypotropic eye incyclotorting gain was lower than the<br />
hypertropic eye excyclotorting gain after head roll toward<br />
the hypotropic eye in 17 patients.<br />
The reduced static OCR gain and interocular and directional<br />
gain asymmetries provide evidence of disruption of<br />
utriculo-ocular pathways in the pathogenesis skew deviation.<br />
Study supported by: Canadian Institutes of Health<br />
Research (CIHR)<br />
T1622. Superior Semicircular Canal Dehiscence (SSCD)<br />
and Osteoporosis in Elderly Asian Women<br />
Alexander Yu, Douglas L. Teich and Eric T. Wong; Boston,<br />
MA<br />
SSCD is associated with vertigo caused by the absence of bone<br />
overlying the SSC. This opening acts as a third window for<br />
the vestibular system, resulting in vertigo that is triggered by<br />
sound (Tullio phenomenon) or external pressure exerted on<br />
the canal (Hennebert sign). Four elderly Asian women were<br />
evaluated for dizziness/vertigo in a community health clinic.<br />
Their age, 57–85, was significantly older than the median age<br />
of 40 originally reported for SSCD. They all complained of<br />
motion-induced vertigo without nausea or vomiting. Their<br />
cerebellar examinations were normal. Only one had inducible<br />
vertigo on Dix-Hallpike maneuver, and none had Tullio phenomenon<br />
or Hennebert sign. SSCD was confirmed in all cases<br />
by high-resolution CT, with longitudinal areas of dehiscence<br />
along the long axis of SSC, ranging from 0.4 to 3.0 mm, as<br />
seen on Poschl view. They also suffered from osteopenia or<br />
osteoporosis in the axial skeleton, as confirmed by bone density<br />
tests. SSCD may be associated with osteoporosis in elderly<br />
Asian woman without Tullio phenomenon or Hennebert sign.<br />
Further research is needed to determine the relationship of<br />
age, race, osteoporosis risk, and the development of SSCD.<br />
Study supported by: Chinese Center of Long Island<br />
Neuroimmunology and Demyelinating Disease<br />
T1701. Antibodies to Metabotropic Glutamate Receptors<br />
in Ophelia Syndrome and Cerebellitis<br />
Eric Lancaster, Eugenia Martinez-Hernandez, Maarten J.<br />
Titulaer, Sarah Wong, Jian Xu, Anis Contractor, Rita Balice-<br />
Gordon and Josep Dalmau; Philadelphia, PA and Chicago, IL<br />
Objective: The Ophelia syndrome is a presumed autoimmune<br />
disorder characterized by severe but treatment-responsive<br />
limbic encephalitis, in association with Hodgkin’s lymphoma.<br />
We aimed to determine the target autoantigen.<br />
Methods: Imunohistochemistry on brain tissue and cultures<br />
of rat hippocampal neurons was used to demonstrate<br />
antibodies. Immunoprecipitation, mass spectrometry, and<br />
mGluR5 knock outs served to identify the antigen.<br />
Results: Patient’s serum had antibodies that reacted with<br />
the hippocampus and cell surface of live, cultured neurons,<br />
immunoprecipitated mGluR5, and specifically labeled cells<br />
transfected with mGluR5. Reactivity of patient’s serum, but<br />
not control individuals, was abrogated in brain of mGluR5null<br />
mice, further confirming the specificity of the antibodies.<br />
Parallel studies with mGluR1, a receptor closely related<br />
to mGluR5, lead us to identify a case with cerebellar ataxia<br />
and mGluR1 antibodies. Despite the high homology of<br />
these receptors, each patient’s antibodies were specific for<br />
one type of receptor and a distinct syndrome, resembling<br />
the phenotype of genetic deletion of each receptor.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 85<br />
Conclusions: Antibodies to mGluR1 and mGluR5 should be<br />
considered in patients with cerebellitis and the Ophelia syndrome.<br />
Recognition is important because these disorders respond<br />
to immunotherapy. Our findings facilitate this diagnosis.<br />
Study supported by: Dr. Lancaster has a training grant<br />
from Talecris; his contribution to the current work was supported<br />
by a Dana Foundation Neuro-immunology Award.<br />
Dr. Martinez-Hernandez has a grant from the Fondo de<br />
Investigaciones Sanitarias, FIS, Spain (FI08/00285). Dr. Titulaer<br />
is supported by a KWF fellowship 2009–4451 of the<br />
Dutch Cancer Society. Dr. Dalmau receives royalties from<br />
the editorial board of Up-To-Date; from Athena Diagnostics<br />
for a patent for the use of Ma2 as autoantibody test. Dr.<br />
Dalmau has received a research grant from Euroimmun, and<br />
his contribution to the current work was supported in part<br />
by grants from the National Institutes of Health and<br />
National Cancer Institute (grant RO1CA89054). Drs. Dalmau<br />
and Balice-Gordon were supported by 1RC1NS068204-<br />
01, and a McKnight Neuroscience of Brain Disorders award.<br />
T1702. Mortality Outcomes for Interferon Beta-1b<br />
Versus Placebo 21 Years Following Randomization<br />
Douglas S. Goodin, Anthony T. Reder, George Ebers, Gary<br />
Cutter, Marcelo Kremenchutzky, Joel Oger, Mark Rametta,<br />
Karola Beckmann and Volker Knappertz; San Francisco, CA;<br />
Chicago, IL; Oxford, United Kingdom; Birmingham, AL;<br />
London, ON, Canada; Vancouver, BC, Canada; Wayne, NJ;<br />
Berlin, Germany and Montville, NJ<br />
Objective: To assess the effect of interferon beta-1b (IFNB-<br />
1b) 250 lg on mortality outcomes in multiple sclerosis<br />
(MS).<br />
Methods: Originally 372 patients were randomized to either<br />
IFNB-1b 50 lg (n ¼ 125), IFNB-1b 250 lg (n ¼<br />
124), or placebo (n ¼ 123), and remained on assigned<br />
treatment for a median 3.8 years (maximum 5.1 years),<br />
before licensed treatment became available. The primary<br />
outcome variable in this 21 year follow-up study was allcause<br />
mortality and the secondary cause-specific mortality.<br />
Results: At 21.1 years (median), vital status information<br />
was available for 366/372 (98.4%) of patients; of whom, 81<br />
(22.1%, 81/366) were deceased. Original randomization to<br />
IFNB-1b 250 lg showed a significant reduction in all-cause<br />
mortality versus placebo (log-rank test, P ¼ 0.0272) and<br />
risk of death was reduced by 39.3%. Cause of death data<br />
was assessed for 75% of deaths; of which, 50/61 (82%)<br />
were MS-related. Most of the excess mortality rate in placebo<br />
was MS-related.<br />
Conclusions: With near-complete ascertainment and over<br />
21 years of observation time, a substantial survival advantage<br />
was seen for patients receiving early IFNB-1b treatment<br />
versus placebo. Most of this striking difference appears to be<br />
due to MS-related deaths.<br />
Study supported by: Bayer HealthCare Pharmaceuticals,<br />
Montville, NJ, USA.<br />
Prof Douglas Goodin has received honoraria from Bayer<br />
HealthCare Pharmaceuticals for consulting fees and honoraria<br />
for speaking.<br />
T1703. A Recombinant Human Neuron-Binding IgM<br />
Protects Spinal Cord Axons and Improves Motor<br />
Function in a Murine Model of Multiple Sclerosis<br />
Aleksandar Denic*, Slobodan Macura, Arthur E. Warrington,<br />
Istvan Pirko, Brandon R. Grossardt, Larry R. Pease and Moses<br />
Rodriguez; Rochester, MN<br />
Our laboratory demonstrated that a natural human serum antibody,<br />
sHIgM12, binds to neurons in vitro and promotes neurite<br />
85<br />
outgrowth. We generated a recombinant form, rHIgM12, with<br />
identical properties. Intracerebral infection with Theiler’s Murine<br />
Encephalomyelitis Virus (TMEV) of susceptible mouse<br />
strains causes chronic demyelinating disease with progressive<br />
axonal loss and neurologic dysfunction similar to progressive<br />
forms of multiple sclerosis. We studied the effects of rHIgM12<br />
on motor function of TMEV-infected mice by recording spontaneous<br />
nocturnal activity continuously over several weeks using<br />
AccuScan activity boxes. Compared to control IgM- and salinetreated<br />
mice, rHIgM12-treated mice showed improved motor<br />
function which became statistically significant at 9 days post<br />
treatment (p ¼ 0.038 and p ¼ 0.043, respectively) until the<br />
end of experiment (56 days). To assess axonal integrity we performed<br />
retrograde-labeling, a technique that relies on anatomically<br />
continuous and functionally preserved axons. rHIgM12treated<br />
mice had more retrograde-labeled brainstem neurons, as<br />
compared to saline-treated controls. This study supports the hypothesis<br />
that peripheral treatment with a neuron-binding IgM<br />
not only protects spinal cord axons in vivo but also influences<br />
functional motor improvement.<br />
Study supported by: This work was supported by grants from<br />
the NIH (R01 GM092993, R01 NS024180, R01 NS03219,<br />
R01 NS048357) and the National Multiple Sclerosis Society<br />
(CA 1011-A8). We also acknowledge with thanks support from<br />
the Applebaum and Hilton Foundations and the Minnesota<br />
Partnership Award for Biotechnology and Medical Genomics.<br />
A patent for the use of rHIgM12 antibody has been issued<br />
to the Mayo Clinic and Foundation. Therefore some of the<br />
authors may receive financial compensation in the future.<br />
T1704. Neuroprotection Mediated through Estrogen<br />
Receptor Alpha in Astrocytes<br />
Rory Spence, Mary Hamby, Elizabeth Umeda, Noriko Itoh,<br />
Sienmi Du, Galyna Bondar, Michael Sofroniew and Rhonda<br />
Voskuhl; Los Angeles, CA<br />
Estrogen has well documented neuroprotective effects in<br />
central nervous system (CNS) disorders such autoimmune<br />
inflammation, traumatic injury, stroke, and neurodegenerative<br />
diseases, but the underlying mechanisms are uncertain,<br />
because diverse cell types express estrogen receptors in the<br />
immune system and CNS. We selectively deleted estrogen<br />
receptor alpha (ERa) from either astrocytes or neurons using<br />
well-characterized Cre-loxP systems for conditional gene<br />
knockout in mice. We found that signaling through ERa in<br />
astrocytes, but not in neurons, is essential for the neuroprotective<br />
effects of systemic treatment with ERa ligand on<br />
clinical function, CNS inflammation and axonal loss during<br />
experimental autoimmune encephalomyelitis. Our findings<br />
reveal a novel cellular mechanism for estrogen-mediated<br />
neuroprotective effects by signaling through astrocytes and<br />
have implications for understanding the pathophysiology of<br />
sex hormone effects in diverse CNS disorders.<br />
Study supported by: National Multiple Sclerosis Society<br />
(RRV), Adelson Medical Research Foundation (RRV and<br />
MVS), NIH NINDS grants NS 062117 (RRV) and<br />
NS057624 (MVS), Skirball Foundation, Hilton Foundation,<br />
and Sherak Family Foundation.<br />
T1705. Genesis of Astrogliosis in an Autoimmune Model<br />
of Multiple Sclerosis<br />
Fuzheng Guo, Yoshiko Maeda, Joyce Ma, Monica Delgado and<br />
David Pleasure; Sacramento, CA<br />
Astrogliosis is a prominent feature of multiple sclerosis<br />
(MS). We employed genetic fate-mapping and bromodeoxyuridine<br />
(BrdU) labeling to evaluate the cellular origins of reactive<br />
astroglia in spinal cords of mice with experimental<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 86<br />
autoimmune encephalomyelitis (EAE) induced by immunization<br />
with myelin oligodendrocyte glycoprotein peptide 35–55<br />
(MOG peptide). We found that oligodendroglial progenitor<br />
cells (OPCs) were stimulated to proliferate early in the course<br />
of MOG peptide EAE, and that many of these OPCs differentiated<br />
to oligodendroglia, but that OPC generation of<br />
astroglia was a rare event. Spinal cord ependymal cells, which<br />
have been reported to give rise to astroglia following spinal<br />
cord trauma, did not generate either OPCs or astroglia during<br />
MOG peptide EAE. Instead, virtually all reactive astroglia,<br />
identifiable by their expressions of nestin and vimentin<br />
in addition to glial fibrillary acidic protein, arose from resident<br />
spinal cord astroglia. In spinal cord white matter, astroglial<br />
proliferation increased overall astroglial numbers. In gray<br />
matter, in contrast, reactive astrogliosis was not accompanied<br />
by astroglial hyperplasia. Our study provides the first comprehensive<br />
view of the cellular origins of astrogliosis during<br />
an autoimmune demyelinative disorder.<br />
Study supported by: This work was supported by the<br />
Shriners Hospitals for Children, the California Institute for<br />
Regenerative Medicine (CIRM), NMSS and NINDS<br />
T1706. Distinct Features of Neuromyelitis Optica<br />
According to Anti-Aquaporin-4 Antibody IgG Subclass<br />
Noriko Isobe, Tomomi Yonekawa, Takuya Matsushita, Yuji<br />
Kawano, Katsuhisa Masaki, Satoshi Yoshimura and Jun-ichi<br />
Kira; Fukuoka, Japan and Matsuyama, Japan<br />
Objective: To clarify the clinical features of neuromyelitis<br />
optica (NMO) according to anti-aquaporin-4 (AQP4) antibody<br />
IgG subclass.<br />
Methods: We developed a quantitative flow cytometric<br />
assay for each anti-AQP4 antibody IgG subclass, and<br />
assessed 142 patients with multiple sclerosis (MS), 29 with<br />
neuromyelitis optica (NMO) fulfilling the 1999 criteria, 19<br />
with recurrent/longitudinally extensive myelitis, 86 with<br />
other inflammatory or non-inflammatory neurological diseases,<br />
and 28 healthy controls.<br />
Results: Anti-AQP4 antibody IgG was detected in 46<br />
patients, among whom 35 fulfilled either the 1999 or 2006<br />
NMO criteria, 9 had recurrent/longitudinally extensive spinal<br />
cord lesions, and two showed MS-like features. IgG1, 2,<br />
3 and 4 anti-AQP4 antibodies were detected in 97.8, 39.1,<br />
13.0 and 8.7% of patients, respectively. In patients not<br />
receiving corticosteroids, the levels of IgG1 anti-AQP4 antibody<br />
correlated positively with disease duration, while those<br />
of IgG2 antibodies correlated negatively with maximum spinal<br />
cord lesion length. IgG2 anti-AQP4 antibody carriers<br />
showed a younger age of onset, longer disease duration and<br />
lower Progression Index than those of other subclasses.<br />
Conclusion: IgG1 anti-AQP4 antibody levels increase<br />
with disease duration, while IgG2 antibodies are seen in relatively<br />
benign cases with a younger onset age.<br />
Study supported by: The Health and Labour Sciences<br />
Research Grant on Intractable Diseases (H20-Nanchi-Ippan-<br />
016) from the Ministry of Health, Labour and Welfare, Japan,<br />
and the grant-in-aid (B; no. 22390178) from the Ministry of<br />
Education, Culture, Sports, Science and Technology, Japan.<br />
T1707. Effect of Fingolimod on Relapse Rate by Prior<br />
Treatment Status and Reason for Discontinuation:<br />
FREEDOMS Subgroup Analyses<br />
Marcelo Kremenchutzky, Paul O’Connor, Reinhard Hohlfeld,<br />
Ernst-Wilhelm Radue, Ludwig Kappos, Lixin Zhang-Auberson,<br />
Dieter A. Häring, Philipp von Rosenstiel, Xiangyi Meng and<br />
Augusto Grinspan; London, ON, Canada; Toronto, ON,<br />
Canada; Munich, Germany; Basel, Switzerland and East<br />
Hanover, NJ<br />
86<br />
Fingolimod (FTY720) is a sphingosine-1-phosphate receptor<br />
modulator for the treatment of relapsing-remitting multiple<br />
sclerosis. In the phase 3 FREEDOMS study, fingolimod<br />
0.5-mg once daily reduced annualized relapse rate (ARR) by<br />
56% vs. placebo at 24 months (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 87<br />
companies and by grants from the Swiss MS Society, the<br />
Swiss National Research Foundation, the European Union,<br />
the Gianni Rubatto, Novartis and Roche Research Foundations.<br />
Dr. Zhang-Auberson, Dr. Häring, Dr. von Rosenstiel,<br />
Dr. Meng, and Dr. Grinspan are employees of Novartis.<br />
T1708. Effect of Fingolimod on Relapse Rate by Prior<br />
Treatment Status and Reason for Discontinuation:<br />
TRANSFORMS Subgroup Analyses<br />
Bhupendra O. Khatri, Jean Pelletier, Ludwig Kappos, Hans-<br />
Peters Hartung, Giancarlo Comi, Frederik Barkhof, Jeffrey<br />
Cohen, Tracy Stites, Xiangyi Meng and Augusto Grinspan;<br />
Milwaukee, WI; Marseille, France; Basel, Switzerland;<br />
Dusseldorf, Germany; San Raffaele, Milan, Italy; Amsterdam,<br />
Netherlands; Cleveland, OH and East Hanover, NJ<br />
In the phase 3 TRANSFORMS study of relapsing–remitting<br />
multiple sclerosis patients, fingolimod (FTY720) 0.5-mg<br />
once-daily significantly reduced annualized relapse rate<br />
(ARR) vs. once-weekly intramuscular interferon (IFN)b-1a<br />
30 lg by 52% at 1 year (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 88<br />
payments for all these activities have been exclusively used<br />
for funding of research of his department. Research and the<br />
clinical operations (nursing and patient care services) of the<br />
MS Center in Basel have been supported by non-restricted<br />
grants from one or more of these companies and by grants<br />
from the Swiss MS Society, the Swiss National Research<br />
Foundation, the European Union, the Gianni Rubatto,<br />
Novartis and Roche Research Foundations. Dr. Francis, Dr.<br />
Collins, Dr. Zhang-Auberson, and Dr. Tang are employees<br />
of Novartis.<br />
T1710. Fingolimod Mechanism of Action (MOA) in<br />
Multiple Sclerosis (MS)<br />
Jerold Chun and Jeffery A. Cohen; La Jolla, CA and<br />
Cleveland, OH<br />
Fingolimod, the first oral MS therapy, is thought to mediate<br />
its effects through actions of its metabolite, fingolimodphosphate,<br />
on sphingosine-1-phosphate (S1P) receptors on<br />
T-lymphocytes. This interaction produces ‘‘functional antagonism’’<br />
of the receptor subtype S1P1 on CCR7-positive Tcells<br />
(naïve, activated, central memory), whereby S1P1 is<br />
internalized and degraded, receptor signalling is lost, and<br />
egress from lymphoid organs is inhibited. Fingolimod exposure<br />
leaves CCR7-negative effector memory T-cells comparatively<br />
unaffected. In MS, the net effect is a relative preservation<br />
of immune surveillance, while proinflammatory<br />
subsets are prevented from reaching the CNS. Additionally,<br />
accumulating data support a distinct, nonmutually exclusive<br />
mechanism involving direct S1P-receptor modulation on<br />
CNS cells. To address this issue, studies in EAE-challenged<br />
mice have been pursued using a conditional-null mutation<br />
resulting in a lack of S1P1 in neurons and glia. This mutant<br />
demonstrated attenuated disease severity and loss of fingolimod<br />
efficacy despite maintaining immunologic effects on<br />
peripheral blood lymphocytes. Loss of fingolimod efficacy<br />
was apparent in astrocyte, but not neuronal, S1P1-null mutants. Additional data in this model will be discussed<br />
towards considering fingolimod as having a dual MOA<br />
involving S1P-receptor modulation in not only the immune<br />
system but also the CNS.<br />
Study supported by: NIH and Novartis Pharma AG,<br />
Basel, Switzerland<br />
Dr. Chun has received consulting fees from Novartis and<br />
Ono; lecture fees from Novartis; and research support from<br />
Novartis and Pfizer. Dr. Cohen has received consulting fees<br />
from Biogen Idec, Elan, Lilly, Novartis, and Teva.<br />
T1711. Antibodies to the VGKC-Complex Proteins LGI1<br />
and CASPR2 in Acquired Neuromyotonia<br />
Camilla Buckley, Philippa Pettingill, Rosie Pettingill, Matthew<br />
Kiernan, Osamu Watanabe, Sarosh Irani, Patrick Waters and<br />
Angela Vincent; Oxford, United Kingdom; Sydney, Australia<br />
and Kagoshima, Japan<br />
VGKC-complex-Abs are found in neuromyotonia, Morvan’s<br />
syndrome, or limbic encephalitis. It is now clear that<br />
VGKC-complex-Abs are mainly directed against proteins<br />
that are complexed with VGKCs in the brain, particularly<br />
LGI1 (mainly limbic encephalitis) and CASPR2 (mainly<br />
Morvans syndrome and neuromyotonia), but these antibodies<br />
have not been studied in detail in neuromyotonia<br />
patients. 68 sera from patients with neuromyotonia from<br />
centers in Kagoshima and Sydney (29 females, 39 males,12<br />
to 85 years) were assayed using cell-based assays for antibodies<br />
to LGI1 and CASPR2. 20/68 (30%) sera were positive<br />
for VGKC-complex-Abs (106–1560 pM) including three of<br />
the four with Morvans syndrome. 14 of these sera were pos-<br />
88<br />
itive with the cell based assays: eight for both CASPR2-Abs<br />
and LGI1-Abs, four only for CASPR2-Abs, two only for<br />
LGI1-Abs. In addition, ten of the 48 VGKC-complex-Ab<br />
negative sera had CASPR2-Abs. These results indicate that<br />
patients with neuromyotonia can have both CASPR2 and<br />
LGI1 antibodies. Moreover, the presence of CASPR2<br />
antibodies in 20% of the patients negative for VGKC-Abs<br />
by radioimmunoassay suggests that the cell-based assays<br />
may make a useful addition to the investigation of<br />
neuromyotonia.<br />
Study supported by: Medical Research Council of Great<br />
Britain and NIHR Oxford Biomedical Research Centre<br />
Angela Vincent, Sarosh Irani and Patrick Waters may in<br />
the future receive royalties from use of the LGI1 and<br />
CASPR2 antibodies for diagnosis of neuromyotonia and<br />
other diseases<br />
T1712. Withdrawn<br />
T1713. <strong>Association</strong> of MS Susceptibility Variants and<br />
Early Attack Location<br />
Ellen M. Mowry, Jean Pelletier, Maria R. Blasco, Pierre<br />
Duquette, Pablo Villoslada, Pierre-Antoine Gourraud, Irina<br />
Malikova, Christophe Picard, Jamie McDonald, Elaine Roger,<br />
Stacy Caillier and Emmanuelle Waubant; San Francisco;<br />
Marseille, France; Madrid, Spain; Montreal, Canada and<br />
Pamplona, Spain<br />
Background: The anatomic location of early MS relapses<br />
within the central nervous system is predicted by the first<br />
attack location. We sought to determine if genetic polymorphisms<br />
associated with multiple sclerosis (MS) susceptibility<br />
are associated with attack location.<br />
Methods: 17 well-documented MS susceptibility polymorphisms<br />
were genotyped in 354 white, non-Hispanic<br />
patients seen within a year of MS onset. Their association<br />
with the CNS location of the first two MS attacks was<br />
assessed.<br />
Results: The IL12A polymorphism was associated with<br />
increased odds of both attacks involving the spinal cord<br />
(OR ¼ 2.4, 95% CI 1.3, 4.3, p ¼ 0.003). The IL7R polymorphism<br />
was associated with reduced odds of both attacks<br />
involving the brainstem/cerebellum (OR ¼ 0.2, 95% CI<br />
0.0, 0.9, p ¼ 0.042). There was a strong trend for an association<br />
of EVI5 with reduced odds of both attacks featuring<br />
optic neuritis. Several other genes showed trends for association<br />
with attack locations.<br />
Conclusions: Some of the MS susceptibility genes predict<br />
MS attack location. This finding may lead to improved<br />
understanding of MS pathogenesis and treatment.<br />
Study supported by: National Multiple Sclerosis Society<br />
T1714. Osmotic Demyelination Syndrome: Lack of<br />
<strong>Association</strong> between Outcome and Severity of<br />
Hyponatremia<br />
Jennifer E. Fugate*, Jonathan Graff-Radford and Alejandro A.<br />
Rabinstein; Rochester, MN<br />
Objective: Little is known about outcome predictors in osmotic<br />
demyelination syndrome (ODS), though one study<br />
identified that severity of hyponatremia is an independent<br />
predictor. We aimed to characterize clinical and radiographic<br />
features of patients with ODS and identify variables that<br />
predict outcome.<br />
Methods: A retrospective study of patients with ODS<br />
identified by a search of Mayo Clinic medical records from<br />
1999–2010. Patients were diagnosed by clinical and<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 89<br />
radiographic features. Medical charts were reviewed. Favorable<br />
outcome was defined by Modified Rankin Scale (mRS)<br />
2.<br />
Results: Of 24 patients, 14 (48%) had central pontine<br />
myelinolysis and 10 (42%) extrapontine myelinolysis. Hyponatremia<br />
was documented in 18 (75%) with mean sodium<br />
nadir of 114 mmol/L. Favorable outcome was seen in<br />
15 (63%) at mean follow-up 3 years. Initial brain MRI was<br />
normal in 21%. The following variables were assessed: age<br />
(p ¼ 0.40), gender (0.68), sodium level (p ¼ 0.30), albumin<br />
(p ¼ 0.12), extrapontine involvement (p ¼ 1.00),<br />
GCS (p ¼ 0.33), alcoholism (p ¼ 1.00), and sepsis (p ¼<br />
0.17). None were predictive of outcome.<br />
Conclusions: Functional outcome in ODS is not associated<br />
with severity of hyponatremia. Serial brain imaging is<br />
of value as a substantial proportion of patients have normal<br />
initial MRIs.<br />
T1715. Correlation of Brain Atrophy, Disability and<br />
Spinal Cord Atrophy in a Murine Model of MS<br />
M Mateo Paz Soldan, Jeffrey D. Gamez, Aaron J. Johnson,<br />
Anne K. Lohrey, Yi Chen and Istvan Pirko; Rochester, MN<br />
and Cincinnati, OH<br />
Disability progression in MS remains incompletely understood.<br />
Unlike lesional measures, CNS atrophy has strong<br />
correlation with disability. TMEV infection in SJL mice is<br />
an established model of progressive MS. We utilized in vivo<br />
MRI to quantify brain and spinal cord atrophy in this<br />
model and analyzed the temporal relationship between atrophy<br />
and disability.<br />
Infected and control mice were followed for 12 months.<br />
Disability was assessed monthly using rotarod assay. Volumetric<br />
MRI datasets were acquired at 7 Tesla. Ventricular<br />
volume and C4-5 cord cross-sectional area measurements<br />
were performed using Analyze 10. At three months, brain<br />
atrophy reached statistical significance (p ¼ 0.009). In contrast,<br />
disability did not differ until four months post infection<br />
(p ¼ 0.0032). Cord atrophy reached significance by<br />
eight months (p ¼ 0.0088). By 12 months, brain atrophy<br />
resulted in 111.8% increased ventricular volume (p ¼<br />
0.000031), while spinal cord cross-sectional area was 25%<br />
reduced (p ¼ 0.0013) in cases.<br />
Our results suggest that significant brain atrophy precedes<br />
and predicts the development of disability, while spinal cord<br />
atrophy occurs late and correlates with severe disability. The<br />
observed temporal relationship establishes a framework for<br />
mechanisms of disability progression and enables further<br />
investigations of their underlying substrate.<br />
Study supported by: National MS Society Pilot Project<br />
Grant, NIH/NINDS R01 NS 058698<br />
T1716. Anti-NMDA-Receptor Encephalitis: Clinical<br />
Analysis of 457 Patients<br />
Maarten J. Titulaer, Eugenia Martinez-Hernandez, Lindsey<br />
McCracken, Rita Balice-Gordon and Josep Dalmau;<br />
Philadelphia, PA and Barcelona, Spain<br />
Introduction: Anti-NMDA-receptor encephalitis is the<br />
most common and best characterized antibody-mediated encephalitis.<br />
We provide the clinical features and follow-up of<br />
457 patients.<br />
Methods: Analysis of demographics, onset, syndrome,<br />
treatment, and outcome at 24 months.<br />
Results: 84% were female. Median age was 21 years<br />
(range 1–85; 39% 18 and 4.3% 45 years). 45% had a<br />
tumor (94% teratomas, 5.7% other). 62% of females >18<br />
years had ovarian teratoma(s), versus 35% 18 years. 84%<br />
89<br />
of patients had 3 of the following: psychiatric symptoms,<br />
speech disorder, seizures, dyskinesias, decreased consciousness,<br />
autonomic instability, or hypoventilation. Treatment<br />
included tumor removal when appropriate, and immunotherapy<br />
(91%). At the time of analysis, full recovery/minimal<br />
symptoms (back to all activities) have occurred in<br />
57.3% of the patients, mainly in those with teratoma<br />
(66.7% vs 48.8%); 6% died. The frequency of relapses varied<br />
according to the response to initial immunotherapy;<br />
87% of relapses occurred in patients without teratoma.<br />
Conclusions: Anti-NMDA-receptor encephalitis is a<br />
severe but treatable disorder of predominantly young individuals.<br />
Prompt diagnosis and treatment are important to<br />
improve outcome. In addition to the above, detailed analysis<br />
of the frequency of relapses, immunotherapy, timing of recovery,<br />
and prognostic factors will be provided.<br />
Study supported by: The current work is supported in<br />
part by grants from the National Institutes of Health and<br />
National Cancer Institute RO1CA89054 (Dalmau),<br />
1RC1NS068204-01 (Balice-Gordon and Dalmau), and a<br />
McKnight Neuroscience of Brain Disorders award (Balice-<br />
Gordon and Dalmau).<br />
Dr. Titulaer is supported by a KWF fellowship 2009–<br />
4451 of the Dutch Cancer Society; Dr. Martinez-Hernandez<br />
has a grant from the Fondo de Investigaciones Sanitarias,<br />
FIS, Spain (FI08/00285); Dr. Dalmau receives royalties<br />
from the editorial board of Up-To-Date; from Athena Diagnostics<br />
for a patent for the use of Ma2 as autoantibody test.<br />
Dr. Dalmau holds a patent application for the use of<br />
NMDA receptor as autoantibody test. Dr. Dalmau has<br />
received a research grant from Euroimmun.<br />
T1717. Cigarette Smoke Induces Inflammation and<br />
Oxidative Stress in Brains of Lewis Rats<br />
Ashwani Khanna and Walter Royal, III; Baltimore, MD<br />
Cigarette smoke (CS) exposure is a risk factor for developing<br />
multiple sclerosis. We examined this effect by analyzing<br />
brains from Lewis rats exposed to CS from 4 cigarettes /<br />
day for 30 days using a system developed to simulate<br />
human smoking behavior. Using quantitative PCR, we<br />
observed an increase in IFN-c, TNF-a, TGF-b, IL-10,IL-<br />
6, IL-17, IL-18 and IL-23 and in MCP-1/CCL2, MIP-1a/<br />
CXCR3 and SDF-1a/CXCL12 gene expression in the rat<br />
brains. Also gene expression for p22 phox , NOX-4, dual oxidase<br />
and Nfr2 was increased whereas thioredoxin gene<br />
expression was decreased. Immunocytochemical analysis of<br />
the brains from the rats showed, compared to rats not<br />
exposed to CS, increased staining for CD4, TNF-a, IFNc,<br />
class II MHC, ED1, Nrf2 and GFAP. Double immunofluorescence<br />
staining demonstrated cytoplasmic localization<br />
of Nrf2 in astrocytes from rats exposed to CS whereas nuclear<br />
localization was observed for non-exposed rats. These<br />
studies, therefore, demonstratethatCSexposurecanresult<br />
in increased brain immune cell trafficking, pro-inflammatory<br />
responses and oxidative stress. This model may be<br />
useful for elucidating mechanisms related to the link<br />
between CS and MS and for developing effective treatment<br />
strategies for the diseases.<br />
T1718. Withdrawn<br />
T1719. Differential Sensitivity of Human PBMC Subsets<br />
to Alemtuzumab-Mediated Cytotoxicity<br />
William Siders, Sambasiva Rao, Juanita Campos-Rivera, Jose<br />
Sancho, Paula Boutin, Peter Severy, Johanne Kaplan, Bruce<br />
Roberts and Srinivas Shankara; Framingham, MA<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 90<br />
Alemtuzumab(monoclonal antibody)currently in clinical<br />
trials for treatment of MS,recognizes CD52antigen<br />
expressed on lymphocytes&most myeloid cells. Its cytotoxic<br />
effects are reportedly influenced by density ofC-<br />
D52antigen on target cells. Using alemtuzumab in polychromatic<br />
flow cytometry assay,we examined levels<br />
ofCD52expression on 20distinct subsets of lymphoid<br />
&myeloid cells in peripheral blood mononuclear<br />
cells(PBMCs)from 11 healthy donors. Data demonstrated<br />
subsets of PBMCs express differing levels ofCD52. Quantitative<br />
analysis showed memory B-cells&myeloid dendritic<br />
cells(mDCs)display highest number while natural killer<br />
(NK) cells&plasmacytoid DCs have lowest number of CD52<br />
molecules per cell amongst lymphoid&myeloid cell populations,respectively.<br />
To test significance of differential CD52expression<br />
on sensitivity of PBMC subsets to alemtuzumabmediated<br />
cytotoxicity, we developed flow cytometry-based,<br />
complement-dependent cytotoxicity(CDC) assay allowing for<br />
simultaneous assessment of total number of dead cells&identification<br />
of phenotypes of surviving cells amongst PBMCs.<br />
Results from 4donors indicated, amongst lymphocytes, alemtuzumab-mediated<br />
profound cytotoxic effects on B-and Tcells<br />
with minimal effect on NKcells, correlating with density<br />
ofCD52 on these cells. Despite CD52 levels comparable to<br />
lymphocyte subsets, mDCs&monocytes were less susceptible<br />
to alemtuzumab-mediated CDC indicating antigen density<br />
alone doesn’t define susceptibility. Additionally, mDCs&monocytes<br />
expressed significantly higher levels of complement<br />
inhibitory proteins(CIPs) compared to lymphocyte subsets<br />
which may contribute to their resistance to alemtuzumabmediated<br />
CDC. Overall, results show while density of CD52<br />
antigen can influence cell susceptibility to alemtuzumabmediated<br />
CDC, factors such as, level of CIP expression, may<br />
also have an impact.<br />
Study supported by: Genzyme<br />
All authors received financial compensation (including<br />
stock) as employees of Genzyme.<br />
T1720. Transcriptional Profiles Uncover Population<br />
Structure among Multiple Sclerosis Patients<br />
Linda Ottoboni, David Hafler, Howard Weiner and Philip De<br />
Jager; Boston, MA and New Haven, CT<br />
There is extensive heterogeneity among subjects with multiple<br />
sclerosis (MS) in terms of their disease course and treatment<br />
response. Here, we explore the structure of the MS subject<br />
population using RNA expression profiles derived from peripheral<br />
blood mononuclear cells of 398 subjects. These subjects<br />
were untreated (n ¼ 148), treated with glatiramer acetate<br />
(GA) (n ¼ 101) or treated with interferon beta (IFNb) (n ¼<br />
143). We find the expected expression profile associated with<br />
IFNb treatment but find no significant difference in gene<br />
expression with GA treatment. Using unsupervised clustering,<br />
we define 2 subsets of untreated subjects, with enhanced type<br />
I interferon response gene expression in the smaller group and<br />
enhanced lymphocyte activation pathway gene expression in<br />
the larger group. This population structure is preserved in the<br />
GA subjects (Kappa coefficient ¼ 0.83) and IFNb subjects<br />
(Kappa ¼ 0.82). Retrospective data suggest that the smaller<br />
group is more likely to have an clinical or MRI event after<br />
sampling (p ¼ 0.02). We therefore report the identification of<br />
a gene expression profile discriminating 2 subsets of MS subjects<br />
and further report that this architecture captures a previously<br />
reported T cell gene expression signature associated with<br />
high-risk CIS subjects (Corvol et al. PNAS 2008).<br />
Study supported by: Affymetrix Inc. - donation of microarrays<br />
and processing<br />
90<br />
T1721. Analysis of Immune Competence Following<br />
Alemtuzumab Treatment in huCD52transgenic Mice<br />
William Siders, Nathalie Chretien, Michael LaMorte, Bruce<br />
Roberts and Johanne Kaplan; Framingham, MA<br />
Alemtuzumab (humanized monoclonal antibody) currently<br />
in clinical trials for treatment of MS, results in the overall<br />
depletion of lymphocyte subsets followed by extended period<br />
of repopulation. The goal, to evaluate functionality of<br />
lymphocytes following treatment, was accomplished by<br />
treating human CD52 (huCD52) transgenic mice w/alemtuzumab<br />
& evaluating ability of remaining T-lymphocytes<br />
to respond to polyclonal stimulation. While lymphocytes<br />
from animals treated with alemtuzumab are present in<br />
lower numbers, they retain ability to proliferate in response<br />
to T-cell receptor (TCR) ligation & produce similarTh1,<br />
Th2, & Th17 family cytokines compared to lymphocytes<br />
from untreated animals. Comparison of TCR Vbeta families<br />
represented in alemtuzumab-treated & untreated animals<br />
demonstrated no differences in diversity of T-cell repertoire.<br />
We next evaluated ability of alemtuzumab-treated<br />
animals to generate de novo & recall immune responses to<br />
adenovirus serotype2( Ad2). Animals were injected with<br />
Ad2 at various timepoints relative to treatment &evaluated<br />
for Ad2-specificT-cell frequency by IFNgamma ELIspot &<br />
development of antibodies to Ad2. This demonstrated animals<br />
immunized as early as 7 days developed detectable<br />
frequencies of antigen specific T-cells. Recall responses<br />
were unaffected in animals which memory responses were<br />
allowed to develop prior to treatment. These studies demonstrate<br />
alemtuzumab therapy doesn’t impact functional<br />
activity of remaining T-cells &doesn’t severely affect ability<br />
of host to generate functional T- and B-cell responses to<br />
foreign antigen.<br />
Study supported by: Genzyme<br />
All authors receive financial compensation from Genzyme<br />
(including stock) as employees.<br />
T1722. Withdrawn<br />
T1723. Withdrawn<br />
T1724. A Single Dose Escalation Study of the Safety,<br />
Pharmacokinetics, and Pharmacodynamics of<br />
Subcutaneous Pegylated Interferon-Beta in Healthy<br />
Volunteers<br />
Kenneth Grabstein, Aijun Wang, Natalie Winblade Nairn and<br />
Daniel J. Burge; Seattle, WA<br />
Purpose: A single-ascending dose study was conducted in<br />
healthy volunteers (HV) to establish the safety, tolerability,<br />
pharmacokinetic (PK) and pharmacodynamic (PD) profile<br />
of AZ01 (PEGylated interferon-beta). Methods: Eight HV<br />
in each of 5 escalation cohorts received one subcutaneous<br />
dose of AZ01 or placebo (6:2) at doses from 100mg to<br />
10mg. Safety, PK and PD parameters were evaluated.<br />
Results: The AE profile of AZ01 was consistent with that<br />
expected with IFN-beta therapy, especially in the 10mg<br />
group. Events included injection site reactions, headache,<br />
myalgia, chills, fatigue, nausea, and fever. No SAEs or AEs<br />
leading to discontinuation occurred. No laboratory parameter,<br />
vital sign measurement, or ECG was determined by the<br />
Investigator to be clinically significant. PK and PD analyses<br />
indicate a sustained exposure and response to single doses of<br />
AZ01, lasting about 14 days. Conclusion: Single subcutaneous<br />
AZ01 doses of up to 10mg were well tolerated by HV.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 91<br />
The prolonged PK and PD may allow dosing at greater<br />
intervals than with currently available interferon therapies.<br />
Less frequent injections are likely to decrease injection site<br />
reactions and flu-like symptoms and improve compliance.<br />
Study supported by: Allozyne Inc.<br />
Salaries, stock options, consulting fees<br />
T1725. Regulation of IL-12 by IL-23 in Bone Marrow<br />
Dendritic Cells<br />
Farinaz Safavi, Patricia Gonnella, Bogojub Ciric,<br />
Abdolmohamad Rostami and Farinaz Safavi; Philadelphia, PA<br />
Th1 and Th17 cells play important roles in the pathogenesis<br />
of Experimental Autoimmune Encephalomyelitis and other<br />
autoimmune models. IL-12 and IL-23 are heterodimeric<br />
cytokines produced mostly by dendritic cells (DCs) that<br />
promote development of Th1 and Th17 cells, respectively.<br />
Understanding the mechanisms that regulate production of<br />
these cytokines should advance our knowledge of the pathogenesis<br />
of Multiple Sclerosis (MS) and could lead to novel<br />
treatments for this disease. To test the effect of IL-23 on IL-<br />
12 production, Bone Marrow Dendritic cells(BMDCs) from<br />
IL-23p19 KO and WT mice were used. BMDCs were<br />
stimulated with LPS and mouse recombinant IL-23 (5 ng/<br />
ml) and IL-12p70 and IL-12p35 expression were measured<br />
after 6 and 24 hrs. WT DCs stimulated with both LPS and<br />
LPSþIL-23 secreted significantly larger quantities of IL-<br />
12p70 (p< 0.01) compared to IL-23p19 KO cells. RT-PCR<br />
analysis also showed significantly higher expression of IL-<br />
12p35 mRNA in WT DCs treated with either LPSþIL-23<br />
or LPS (p < 0.01 ). Our observations indicate that the<br />
expression of IL-12 is regulated by IL-23 in vitro.Finding<br />
similar regulatory mechanisms in vivo should increase our<br />
understanding of the role of these cytokines in the pathogenesis<br />
of autoimmunity.<br />
Study supported by: NIH grant number RO1NS046782<br />
T1726. Clinically Apparent MRI Activity Predicts 2-Year<br />
Outcomes in Patients with RRMS<br />
Thomas Scott, Xiaojun You and Pamela Foulds; Pittsburgh,<br />
PA and Weston, MA<br />
Background: Several studies report clinically apparent and<br />
clinically silent MRI lesions predict disease worsening in<br />
patients on IFNb-1a. The magnitude of risk, especially with<br />
clinically silent activity, remains uncertain.<br />
Methods: SENTINEL enrolled patients with > ¼ 12<br />
months of prior IFNb-1a treatment who continued with or<br />
without addition of natalizumab. MRI scans at baseline and<br />
year 1 were compared for new lesions. New lesions as a risk<br />
for clinical activity (relapses or progression) between years 1<br />
and 2 were examined.<br />
Results: New MRI and clinical activity in year 1 was<br />
associated with increased risk for relapse or progression in<br />
year 2 (P
T1729. Are Anti-TAG-1 Autoantibodies Markers in<br />
Autoimmune Demyelinating Disorders of the PNS and<br />
CNS?<br />
Harry Alexopoulos, Pantelis P. Pavlakis, Domna Karagogeos,<br />
Clementine E. Karageorgiou and Marinos C. Dalakas; Athens,<br />
Greece and Heraklion, Greece<br />
There is evidence of anti-TAG-1 autoantibodies (TAG-1<br />
is involved in the development of axonal connections),<br />
being associated with autoimmune syndromes of the<br />
CNS. Anti-TAG-1 antibodies have been found both in<br />
multiple sclerosis and in autoimmune limbic encephalitis.<br />
Also, polymorphisms in the TAG-1 gene influence<br />
treatment response in chronic inflammatory demyelinating<br />
polyradiculoneuropathy. We wanted to investigate<br />
whether anti-TAG-1 autoantibodies are present in<br />
CIDP.<br />
We tested serum samples from 12 patients with autoimmune<br />
demyelinating neuropathy (8 with CIDP, 2 with<br />
CIDP and CNS demyelination, 2 with MMN), 9 with<br />
Sjögren’s syndrome-associated axonal polyneuropathy and<br />
50 with relapsing–remitting MS. We established a cell-based<br />
assay previously used to detect anti-TAG-1 autoantibodies<br />
in LE. Briefly, either the FNIII or the IgC2 domains of<br />
TAG-1 were expressed in HEK cells and were incubated<br />
with patient sera. Antibody binding was visualized using a<br />
secondary anti-human fluorescent antibody.<br />
No positive staining was detected in any of the patients<br />
with autoimmune peripheral neuropathies or with RRMS.<br />
Our results suggest that neither anti-TAG-1 autoantibodies<br />
are a marker for demyelination in PNS or CNS nor TAG-1<br />
is a candidate autoantigen in CIDP or MS.<br />
Study supported by: Special Research Account, National<br />
and Kapodistrian University of Athens<br />
T1730. Introduction and Diffusion of Multiple Sclerosis<br />
in the United States<br />
Mitchell T. Wallin and John F. Kurtzke; Washington, DC<br />
Epidemiological evidence suggests that multiple sclerosis has<br />
spread from an origin in northwestern Europe. How and<br />
when it came to the US has not been well defined. Nationwide<br />
morbidity data here have arisen primarily from the<br />
military-veteran populations of our several wars. Prevalence<br />
rates for draftees rejected because of MS for military service<br />
in World War I provide its earliest distribution. Small numbers<br />
of cases required combination of states of residence<br />
into 23 areas. Prevalence rates for the 255 cases in these<br />
areas showing a strikingly high rate in area P, comprising<br />
Wisconsin and Minnesota. These states were settled in the<br />
mid-19 th century mainly by immigrants from south-central<br />
Norway and Sweden. Their original Scandinavian residences<br />
were principally in the high-risk areas for MS in both countries.<br />
When compared with two later military-veteran series,<br />
one from World War II and the Korean Conflict, the other<br />
from Vietnam and later service to 1994, a continuing spread<br />
from this north mid-western focus was seen. MS appears to<br />
have been introduced into the US in the mid-19 th by immigrants<br />
from Scandinavia to Wisconsin and Minnesota, with<br />
later diffusion throughout the land.<br />
Study supported by: VA Merit Review Grant Program &<br />
National MS Society<br />
T1731. Withdrawn<br />
T1732. Withdrawn<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 92<br />
92<br />
T1733. The Relationship between Conduction Block<br />
and Clinical Characteristics in Guillain-Barré Syndrome<br />
with Anti-GM1/GalNAc-GD1a Antibodies<br />
Go Ogawa, Ken-ichi Kaida, Susumu Kusunoki, Motoi<br />
Kuwabara, Fumihiko Kimura and Keiko Kamakura;<br />
Tokorozawa, Saitama, Japan and Osaka-Sayama, Osaka,<br />
Japan<br />
Patients with Guillain-Barré syndrome (GBS) with antibodies<br />
to a ganglioside complex GM1/GalNAc-GD1a frequently<br />
show motor conduction block (CB) at the intermediate<br />
portion of peripheral nerves. Clinical data of 57<br />
patients with anti-GM1/GalNAc-GD1a-IgG were studied to<br />
elucidate the association between CB and clinical and electrophysiological<br />
characteristics. Thirty patients (male/female,<br />
19/11) had CB, classified as CB(þ) (mean age, 43.1 6<br />
17.7 y/o), and 27 patients (male/female, 10/17) did not,<br />
classified as CB(-) (mean age, 46.8 6 16.5 y/o). Males are<br />
significantly more in the CB(þ). Both groups presented frequent<br />
preceding respiratory infection, infrequent cranial and<br />
sensory nerve disturbances, and were equal in the disability<br />
at the nadir. Twenty of 25 non-ambulatory patients could<br />
walk within three months, with no difference between both<br />
groups. The 17 CB(þ) patients were electrodiagnostically<br />
classified into acute inflammatory demyelinating polyneuropathy,<br />
one of whom changed to acute motor axonal neuropathy<br />
later. Serial electrophysiological results suggested<br />
Wallerian degeneration only in one and no evident remyelination.<br />
In view of the rapid recovery and lack of remyelination,<br />
axonal conduction failure with little pathological<br />
changes may be major mechanism in anti-GM1/GalNAc-<br />
GD1a antibody-associated nerve dysfunction.<br />
T1734. Withdrawn<br />
T1735. Randomized, Open-Label Study To Evaluate<br />
Patient-Reported Outcomes (PRO) with Fingolimod<br />
after Changing from Prior Disease-Modifying Therapy<br />
(DMT) for Relapsing Multiple Sclerosis (MS): EPOC<br />
Study Rationale and Design<br />
Luigi M. Barbato, Lesley Schofield, Kevin McCague, Linda<br />
Pestreich, Kathy Tobias and Manoj Malhotra; East Hanover,<br />
NJ<br />
The efficacy and safety profiles of fingolimod (FTY720)<br />
have been well characterized in phase 2 and 3 studies; however,<br />
limited data exist on PRO. The EPOC study is evaluating<br />
PRO and safety in relapsing–remitting MS patients<br />
who have received 6 months’ treatment with a single<br />
approved DMT and are randomized 3:1 to receive oncedaily<br />
fingolimod 0.5 mg with no washout or to continue<br />
standard DMT (interferon-b-1a, interferon-b-1b, or glatiramer<br />
acetate) for 6 months, followed by a 3-month openlabel<br />
extension, in which the DMT group can change to<br />
fingolimod with no washout. The primary endpoint is<br />
change in patient-reported treatment satisfaction using the<br />
global satisfaction subscale of the Treatment Satisfaction<br />
Questionnaire for Medication (TSQM). Secondary endpoints<br />
are safety/tolerability, changes in physician-reported<br />
Clinical Global Impression-Improvement, and changes in<br />
the following PRO: Fatigue Severity Scale; Beck Depression<br />
Inventory-II; activities of daily living using the Multiple<br />
Sclerosis Activities Scale (PRIMUS-Activities); effectiveness,<br />
side effects, and convenience subscales of the TSQM; and<br />
the Short-Form 36 Health Survey-v2-acute. The study is<br />
enrolling at approximately 175 US centers.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 93<br />
Study supported by: Novartis Pharma AG, Basel,<br />
Switzerland<br />
Dr. Barbato, Dr. Schofield, Dr. McCague, Dr. Pestreich,<br />
Dr. Tobias, and Dr. Malhotra are employees of Novartis.<br />
T1736. Novel Diagnostic Tool for MS<br />
Nancy L. Monson, Ann J. Ligocki, William H. Rounds, Diane<br />
Xiang, Lindsay G. Cowell, Doug Bigwood, Eric Eastman,<br />
Jeffrey L. Bennett, Scott D. Boyd, Andrew Z. Fire, Elliot M.<br />
Frohman and Benjamin M. Greenberg; Dallas, TX;<br />
Gaithersburg, MD; Denver, CO and Palo Alto, CA<br />
Multiple Sclerosis (MS) is the leading disease of the central<br />
nervous system and a significant, costly cause of disability in<br />
young adults. Patients at risk for MS often present with a<br />
single demyelinating event, typically called a ‘‘clinically isolated<br />
syndrome’’ (CIS) and present a challenging diagnostic<br />
and therapeutic dilemma. The community has an urgent<br />
need to develop tools that would assist in identifying<br />
patients who would develop MS in the future, since treatment<br />
with the appropriate immunomodulatory agents early<br />
in the disease course can delay long-term disability. Our laboratory<br />
has identified a completely novel type of biomarker,<br />
based on a pattern of antibody gene mutations (i.e. antibody<br />
gene signature or ‘‘AGS’’) that is exclusive to MS<br />
patients. In fact, the AGS demonstrated utility as a molecular<br />
diagnostic tool in a small cohort of patients who presented<br />
with optic neuritis (and were thus at risk to develop<br />
MS) with a sensitivity of 100%, specificity of 67%, positive<br />
predictive value of 89%, negative predictive value of 100%,<br />
and accuracy of 91%. Our current cohort, which includes<br />
both patients who presented with optic neuritis and patients<br />
that presented with transverse myelitis, has an increased accuracy<br />
of 94%.<br />
Study supported by: National MS Society<br />
T1737. Efficacy of Combination Therapy in Marburg<br />
Variant Type of Multiple Sclerosis<br />
Jennifer Gabbard, Yasmin Bilal and Dipak Pandya; Paterson,<br />
NJ<br />
Background: Marburg variant type of MS is a very rare<br />
form of disease which commonly consider fatal after weeks<br />
to months. The variant forms of multiple sclerosis are very<br />
rare and tend to have a rapid deteriorating course. We<br />
report an unusual case of Marburg variant MS, who<br />
responded to various combination therapy favourably.<br />
Results: 18-year-old male presented with imbalance,<br />
wide based gait and dizziness. His physical examination<br />
showed nystagmus, no signs of optic neuropathy, dysmetria,<br />
hyperreflexia and sustained clonus. The MRI brain<br />
showed extensive demyelinating plaques in periventricular<br />
white matter, brainstem and various areas of brain. The<br />
imaging findings were not consistent with Neuromyelitis<br />
optica. The patient was initally treated with pulse doses<br />
methylprednisone and plasmapheresis. Because of persisting<br />
clinical symptoms and imaging findings, patient was<br />
treated with induction doses of mitoxanthrone and interferone<br />
beta-1b. The patient had near complete resolution<br />
of his clinical symptoms and significant MRI<br />
improvement.<br />
Conclusions: Combination acute therapies like plasmapheresis<br />
and mitoxanthrone may reduce inflammatory cytokins<br />
in acute course of disease and may result in improvement.<br />
More multicenter clinical trial may help to<br />
understand nature of disease and management options.<br />
93<br />
T1738. Coma as an Inital Manifestation of Acute<br />
Disseminated Encephalomyelitis<br />
Megan McGarry, Natasha Tilluckdharry and Dipak P.<br />
Pandya; Paterson, NJ<br />
Background: Acute Disseminated Encephalomyelitis<br />
(ADEM) is a monophasic autoimmune demyelinating disease.<br />
Clinical manifestations include an altered behavior,<br />
headache, seizures and coma. We report a unique case which<br />
was presented as a coma an initial manifestation of ADEM.<br />
Case Report 21 year old woman was found unconscious<br />
with severe metabolic acidosis, renal failure requiring urgent<br />
dialysis and ventilatory support. Magnetic Resonance Imaging<br />
(MRI) of the brain showed extensive T2 signal in the<br />
periventricular area, deep white matter and bilaterally in the<br />
basal ganglia and hippocampus with enhancement. Her<br />
CSF studies were unremarkable. She was treated with pulse<br />
dose of solumedrol. Because of lack of initial response, she<br />
was treated with eight cycles of plasmapheresis. She recovered<br />
completely from illness. She had several follow up<br />
MRIs with significant improvement. Her neuropsychological<br />
evaluations showed significant improvement and currently<br />
she is pursuing higher studies without any difficulties.<br />
Conclusion: Based on our literature, this is the first case<br />
of coma patient as an initial manifestation of ADEM. Our<br />
patient has complete recovery of physical and neurcognitive<br />
symptoms which make onliest clinical features and outcome.<br />
We think that prompt and aggressive management may<br />
improve outcome from catastrophic neurological sequel.<br />
T1739. NMO-IgG in a Patient with Neurosarcoidosis<br />
Lena Derani** and Elham Bayat; Washington, DC<br />
Neurosarcoidosis is a rare manifestation of sarcoidosis in<br />
which inflammation and abnormal deposits occur in the<br />
nervous system. Neuromyelitis optica (NMO) is an inflammatory<br />
demyelinating disease that primarily targets the spinal<br />
cord and optic nerves. NMO-IgG (anti-aquaporin-4) is<br />
considered to be a sensitive and specific marker for NMO.<br />
However, NMO-IgG has also been found in patients with<br />
NMO spectrum disorders (NMOSD), paraneoplastic disease<br />
and systemic lupus erythematosus. We present the first<br />
reported case of NMO-IgG positivity in a patient with neurosarcoidosis<br />
but no evidence of NMO. We discuss autoimmunity<br />
in neurosarcoidosis, the specificity of NMO-IgG<br />
and its likelihood in autoimmune diseases, and the possibility<br />
of concomitant neurosarcoidosis and neuromyelitis<br />
optica. We suggest the possibility that NMO-IgG is a nonspecific<br />
indicator of autoimmunity present in patients with<br />
other autoimmune disorders, including neurosarcoidosis. We<br />
remind neurologists that patients who test positive for<br />
NMO-IgG do not necessarily carry the diagnosis of NMO<br />
or NMOSD, despite the documented specificity and sensitivity<br />
of NMO-IgG for these diseases. Further studies are<br />
needed to investigate the positive predictive value of NMO-<br />
IgG and the prevalence of positive NMO-IgG in the normal<br />
population and in patients with autoimmune diseases.<br />
T1740. Correlates of Dietary Intake in Individuals with<br />
Multiple Sclerosis<br />
Matthew A. Plow, Marcia Finlayson and Chi Cho; Cleveland,<br />
OH and Chicago, IL<br />
Since the multiple sclerosis (MS) population has a similar<br />
life expectancy as the general population and is characterized<br />
by impairments that can interfere with healthy eating habits,<br />
malnutrition, vitamin deficiencies, and obesity are prevalent<br />
problems among MS patients. However, few studies have<br />
been conducted to provide clinicians with evidence-based<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
approaches to support MS patients in developing healthy<br />
eating habits. Thus, the purpose of this study was to identify<br />
modifiable factors that predict dietary intake. Using<br />
data from an on-line validated survey of 271 MS patients, a<br />
stepwise multiple regression model was used to determine<br />
the relative importance of personal characteristics, symptoms,<br />
functional limitations, and coping skills in influencing<br />
dietary intake. Over 50% of the sample was overweight/<br />
obese. Four variables made the model: self-efficacy (b ¼<br />
0.51), physical activity (b ¼ 0.14), pessimism (b ¼ 0.13),<br />
age (b ¼ 0.12), and coping skills (b ¼ 0.10), which<br />
explained 40.5% of the variance in intake. Neither symptoms<br />
nor functional limitations significantly predicted<br />
intake. This is the first study to document a relationship<br />
between self-efficacy, coping skills, and nutritional habits in<br />
a large generalizable sample of MS patients. Future research<br />
should examine the effectiveness of efficacy-enhancing nutritional<br />
interventions that focus on improving coping skills.<br />
Study supported by: This work was supported through<br />
the National Multiple Sclerosis Society (NMSS) post-doctoral<br />
training grant. The information presented in this<br />
abstract does not necessarily reflect the position, ideas, or<br />
opinions of the NMSS<br />
Neurooncology<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 94<br />
T1801. Comparative Uptake and Cytotoxicity of Anti-<br />
Hu and Anti-Ri Antibodies in Rat Cerebellar Slice<br />
Cultures<br />
John E. Greenlee, Susan A. Clawson, Blair Wood, Kenneth E.<br />
Hill and Noel G. Carlson; Salt Lake City, UT<br />
Anti-Hu and anti-Ri antibodies label different neuronal antigens<br />
in western blots. However, both recognize intracellular<br />
antigens present in essentially all neurons. At autopsy, brains<br />
of patients with anti-Hu antibody show neuronal destruction.<br />
In contrast, anti-Ri antibody is less clearly associated with<br />
neuronal death, and patients with anti-Ri antibodies may<br />
respond to treatment. To study the effects of these two antibodies<br />
on living neurons, we incubated rat cerebellar slice<br />
cultures with either anti-Hu or anti-Ri antibodies and followed<br />
these cultures over time using TUNEL and FLICA<br />
methods to detect apoptosis, and uptake of SYTOX green to<br />
detect non-apoptotic cell death. Both anti-Hu and anti-Ri<br />
antibodies accumulated in essentially all neurons. Anti-Hu<br />
antibodies caused apoptosis within 72–96 hours in neurons<br />
throughout the cerebellum. In contrast, cells accumulating<br />
anti-Ri antibodies remained viable for over 200 hours, without<br />
evidence of apoptosis or necrotic cell death. Neurons in<br />
general may be able to internalize antibodies. Anti-Hu<br />
appears to be specifically cytotoxic, whereas anti-Ri appears<br />
less able to affect neuronal viability and may predominantly<br />
cause neuronal dysfunction rather than death.<br />
Study supported by: United States Department of Veterans<br />
Affairs<br />
T1802. Cerebrospinal Fluid Chemokine/Cytokine<br />
Biomarkers for Melanoma Brain Metastasis<br />
Edwin Lok, Amy S. Chung, Szexian Lee, Tamar Melman,<br />
Kenneth D. Swanson and Eric T. Wong; Boston, MA<br />
Because immunoregulatory chemokines and cytokines may<br />
modulate the biology of melanoma brain metastasis, we<br />
measured 26 of them in the CSF from 22 patients using<br />
multiplexed ELISA. Clustergram revealed segregation of<br />
non-disease controls from 5 identifiable clusters of patient<br />
94<br />
CSF with distinct chemokine/cytokine profiles. Cluster 1<br />
had the shortest time from initial melanoma diagnosis to<br />
brain metastasis (mean 7.5 months, P ¼ 0.0278). MIP-1b<br />
and IP-10 were elevated while GRO-a, IL-8, and Eotaxin<br />
were suppressed. Cluster 3 was associated with a shortened<br />
time from brain metastasis to death (mean 5.5 months, P ¼<br />
0.0714). Prior biologics treatment also correlated with the<br />
shortest time interval from brain metastasis to death (mean<br />
5.9 months, P ¼ 0.0396). In cluster 3, MIP-1a was elevated,<br />
while GRO-a, MPIF-1, MIG, and IL-1b were suppressed.<br />
Cluster 4 was associated with a trend for prolonged<br />
overall survival (mean 78.0 months, P ¼ 0.0847). This cluster<br />
also had the longest survival from date of biologics treatment<br />
to death (mean 58.5 months, P ¼ 0.0132). Cluster 4<br />
had elevated MPIF-1 while GRO-a, IL-8, IP-10, MDC, IL-<br />
5, MIG, and IL-1b were suppressed. Specific cytokine/chemokine<br />
profiles measured in the CSF of melanoma patients<br />
may have prognostic and predictive value for melanoma<br />
brain metastasis.<br />
Study supported by: A Reason To Ride research fund.<br />
T1803. Role of p75NTR and Its Signaling Pathways in<br />
Fenretinide (4-hydroxyphenyl Retinamide – 4HPR)<br />
Induced Apoptosis in Neuroblastoma Cells<br />
Veena R. Ganeshan and Nina F. Schor; Rochester, NY<br />
Objective: To understand the role of p75NTR and its signaling<br />
pathways in Fenretinide(4-hydroxyphenyl retinamide-<br />
4HPR)-induced apoptosis and determine if JNK phosphorylation<br />
mediates this effect in neuroblastoma cells.<br />
Background: 4HPR is well tolerated in clinical trials and<br />
causes apoptosis by increasing oxidative stress(OS) in cancer<br />
cells. p75NTR has pro and anti-apoptotic functions<br />
depending on the cell milieu and type.<br />
Methods: S-type neuroblastoma cells (SH-EP1) transfected<br />
with varying amounts of p75NTR are used in the<br />
4HPR-concentration experiments. 4HPR treatment results<br />
in changes in JNK phosphorylation and OS, which are<br />
recorded using western blotting and fluorescent microscopy.<br />
Results: 4HPR treatment reduces viability in SH-EP1<br />
and SK-N-SH cells within 24(15%)-72 hrs(40%) and causes<br />
an increase in mitochondrial O2- production. A sustained<br />
increase in Akt phosphorylation occurs in SH-EP1 cells<br />
with lower p75NTR levels. Within 1hr of 4HPR treatment,<br />
JNK phosphorylation increases by 100–150% in SH-EP1<br />
cells with lower levels of p75NTR.<br />
Conclusion: JNK phosphorylation appears to be protective<br />
against 4HPR-induced apoptosis. This will facilitate the<br />
development of combination chemotherapeutics for residual<br />
disease treatment and recurrence by increasing OS and<br />
enhancing response to conventional chemotherapeutics.<br />
Study supported by: Studies presented in this abstract<br />
were funded by grants to Nina F. Schor from the<br />
National Cancer Institute (CA07429), the National Institute<br />
of Neurologic Disorders and Stroke (NS038569),<br />
and the William H. Eilinger Endowment for Pediatric<br />
Research of the Golisano Children’s Hospital at the University<br />
of Rochester Medical Center. These organizations<br />
played no role in the interpretation of the data or the<br />
substance of the review presented herein. Veena R. Ganeshan<br />
is a doctoral student in the Integrated Graduate Program<br />
in Neuroscience of the University of Rochester<br />
School of Medicine and Dentistry. Neither of the authors<br />
have conflicts of interest of relevance for this abstract. No<br />
additional individuals played any role in the production<br />
of this abstract.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 95<br />
T1804. Relationship between Brain MRI Imaging<br />
Parameters and Molecular Biomarkers as Prognostic<br />
Indicators in Glioblastoma Multiforme<br />
Xiao-Tang Kong, Senxi Du, Beverly D. Fu, Mark E. Linskey<br />
and Daniela Bota; Orange, CA and Irvine, CA<br />
The purpose of this study is to explore the relationship<br />
between the potential MRI prognostic indicators and the<br />
molecular biomarkers in order to better evaluate the prognosis<br />
of the patients with GBM.<br />
Molecular biomarkers were determined using Immunohistochemistry.<br />
MIPAV software was used to quantify the volume<br />
of MRI parameters.<br />
Of the seventeen specimens that eventually included, 10<br />
had high and 6 low levels of MGMT expression; 5 were<br />
negative and 11 positive for EGFR wt amplification; 12<br />
negative and 5 positive for EGFRvIII expression; 14 had<br />
PTEN loss and 3 had intact PTEN. The vasogenic edema<br />
were more significant in the low MGMT expression group<br />
(P ¼ 0.04). The necrosis were larger in the group of non<br />
EGFR wt amplification (P ¼ 0.03) and the total volume of<br />
tumor involvement was significantly more in EGFRvIII variant<br />
expression group (P ¼ 0.0072). Our data suggest that<br />
the volume of vasogenic edema, necrosis and total tumor<br />
involvement are related to low MGMT level, lack of EGFR<br />
wt amplification, and increased EGFRvIII expression as<br />
prognostic indicators. Definitely, more cases will be added<br />
to the study to confirm the findings and to evalute the clinical<br />
prognosis.<br />
T1805. Secondary Intramedullary Spinal Cord Non-<br />
Hodgkin’s Lymphoma<br />
Eoin P. Flanagan, Brian P. O’Neill, Thomas M. Habermann<br />
and B. Mark Keegan; Rochester, MN<br />
Intramedullary spinal cord metastases are rare and associated<br />
with poor long-term survival. We present the clinical characteristics<br />
and outcome of secondary intramedullary spinal<br />
cord non-Hodgkin’s lymphoma (NHL) in 7 patients seen at<br />
Mayo Clinic from 1996–2010. All patients had myelopathy<br />
and imaging evidence of intramedullary spinal cord involvement<br />
of pathologically confirmed systemic NHL (B-cell, 6;<br />
T-cell, 1). Spinal cord NHL was diagnosed by: CSF cytology,<br />
4; PET hypermetabolism, 2; or MRI features alone, 1.<br />
In two, myelopathy was the initial presentation of systemic<br />
NHL and in the remainder the median time from NHL diagnosis<br />
to intramedullary involvement was 8 months (range,<br />
1–58). Median age was 60 years (range, 41–81) and 4 were<br />
wheelchair-dependent at diagnosis. MRI spine lesions (Thoracic,<br />
3; Cervical, 3; or both, 1) were typically gadolinium<br />
enhancing, expansile and associated with PET hypermetabolism.<br />
Two had leptomeningeal involvement and 4 had coexisting<br />
brain lesions. Six of the seven were treated: intravenous<br />
methotrexate, 3; radiation, 2; and R-CHOP, 1. Four<br />
improved (mild, 3; marked, 1) following treatment. The<br />
median survival was 11.5 months (range, 1–28). Secondary<br />
intramedullary spinal cord NHL appears to have longer survival<br />
than intramedullary metastases from most other<br />
cancers.<br />
T1806. Case Report: Optic Neuropathy in a Patient with<br />
Glioblastoma Receiving Bevacizumab<br />
Robert A. Fishman, Lara Kunschner and Erik Happ;<br />
Pittsburgh, PA<br />
Bevacizumab is a humanized monoclonal antibody developed<br />
to target and subsequently block vascular endothelial<br />
growth factor received FDA approval for single agent treatment<br />
of recurrent Glioblastoma multiforme in 2009. Estab-<br />
95<br />
lished Bevacizumab side effects include hypertension,<br />
delayed/impaired wound healing, gastrointestinal perforation<br />
and proteinuria. Recently a small number of case reports<br />
have reported six cases of optic neuropathy following Bevacizumab<br />
treatment for GBM.<br />
We report here a case of a 24 year old woman with Neurofibromatosis<br />
type I (NF-1) and right Thalamic GBM<br />
(WHO grade IV), who developed a severe, subacute optic<br />
neuropathy during treatment with Bevacizumab and Irinotecan<br />
for recurrent GBM following standard initial chemo<br />
radiotherapy with temozolamide. Following 4 cycles of salvage<br />
chemotherapy using Bevacizumab/Irinotecan, the<br />
patient developed diffuse blurring of vision, which progressed<br />
over 3-4 weeks-eventually resulting in total<br />
blindness.<br />
Six weeks following cessation of Bevacizumab the patient’s<br />
vision improved with return of light perception, and eventual<br />
return of baseline vision. Our completed poster will<br />
include a summary of our case, MRI images of the tumor,<br />
and results of ophthalmologic examination during and following<br />
Bevacizumab treatment.<br />
Study supported by: Residency program<br />
T1807. Anti-Ri-Associated Paraneoplastic Brainstem<br />
Cerebellar Syndrome with Medically-Intractable Nausea<br />
in a Patient with Large Cell Neuroendocrine Lung<br />
Carcinoma: A Case Report<br />
Amber N. Mitchell, Jessica Levesque and Earl Zimmerman;<br />
Albany, NY<br />
Paraneoplastic neurologic syndromes are rarely the first<br />
manifestations of occult malignancies, which if left<br />
untreated, often lead to significant morbidity and mortality.<br />
The presence of onconeural antibodies supports the paraneoplastic<br />
diagnosis, but is not absolutely essential. Anti-Ri<br />
autoantibodies are commonly associated with breast and<br />
small cell lung cancers. There are cases of anti-Ri paraneoplastic<br />
cerebellar degeneration reported, but none describe<br />
associated severe nausea and emesis as the major presenting<br />
and enduring symptoms. Here, we report a case of a 75year-old<br />
female with medically-intractable nausea, vomiting,<br />
diplopia, and vertigo for three months. Physical exam<br />
revealed rotary nystagmus, ocular skew deviation, limb dysmetria,<br />
and gait ataxia. After two courses of intravenous immunoglobulin,<br />
there was minimal improvement. Serum was<br />
Anti-Ri antibody positive. Computed tomography identified<br />
a 2.5 cm by 2.2 cm lung mass, and histopathology revealed<br />
large cell neuroendocrine carcinoma with smaller portions<br />
of adenocarcinoma. Post-lobectomy, the patient clinically<br />
improved. This is the first report of paraneoplastic brainstem<br />
cerebellar syndrome involving anti-Ri positivity from<br />
neuroendocrine tumor of the lung with nausea and vertigo<br />
as the major features and with improvement after tumor<br />
resection.<br />
T1808. Glioblastoma Multiforme: A Rare Presentation<br />
of Pineal Tumor with Leptomeningeal Seeding and<br />
Future Directions<br />
Noor Yono, Tulika Ranjan and Rabih Kashouty; Manhasset,<br />
NY, United States Minor Outlying Islands and New York, NY<br />
Glioblastoma Multiforme (GBM) is the most common primary<br />
malignancy of the Central Nervous System. Pineal<br />
GBM with leptomeningeal seeding is an exceedingly rare tumor.<br />
Only 18 cases have been reported in the literature. We<br />
present a case of pineal gland GBM with leptomeningeal<br />
disease treated with combination chemotherapy. A 55-yearold<br />
man presented with progressive headache, peduncular<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
hallucinations and perinaud syndrome. Brain MRI showed a<br />
heterogeneously enhancing pineal mass measuring 2.1 cm<br />
with hydrocephalus and infiltration into the midbrain and<br />
thalamus. The pathology was consistent with GBM with<br />
Ki-67 labeling index of 30–50%. Brain and total spine MRI<br />
showed diffuse linear leptomeningeal disease. Chemotherapy<br />
with Temozolomide was started on day 1st. Two high-volume<br />
lumbar punctures with intrathecal Methotrexate were<br />
performed. Within 24 hours following the first Methotrexate<br />
treatment, the patient showed significant improvement.<br />
Initial lumbar puncture showed markedly elevated protein<br />
count of 2856. He was further treated with Avastin every 2<br />
weeks and monthly Temozolomide. Recent CSF protein has<br />
improved to 315 and the pineal mass size has decreased to<br />
0.9mm after four months of starting treatment.<br />
T1809. Benign-Histology Meningioma with Extracranial<br />
Metastasis<br />
Umer Akbar, Bhavpreet Dham and Melissa Carran;<br />
Camden, NJ<br />
Objective: To recognize extracranial dissemination from a<br />
meningioma<br />
Background: Meningiomas are regarded as benign<br />
tumors, as malignant histology is uncommon and extracranial<br />
metastasis is an extremely rare occurrence.<br />
Design: We report a case of a histologically-benign meningioma<br />
with metastasis to the lungs.<br />
Case: A 36 year-old male with symptomatic epilepsy presented<br />
with a breakthrough seizure. Patient had a meningioma<br />
resection in 1998. Few months later, imaging revealed<br />
recurrent tumor which was treated with 48 Gy of radiation.<br />
Routine chest x-ray followed by computed tomography scan<br />
confirmed multiple scattered round nodules, averaging<br />
between 1 to 1.5 cm. Fine-needle aspiration showed clusters<br />
of meningothelial cells consistent with metastasis from the<br />
recurrent intracranial tumor.<br />
Discussion: Majority of meningiomas are benign (grade<br />
I), while few are atypical (grade II) and malignant (grade III)<br />
histology is rare. Aggressive behavior and metastatic potential<br />
is mainly seen in atypical and malignant histologic subtypes.<br />
With a metastasis rate of 0.1%, meningiomas are seldom<br />
seen extracranially. Very rarely, the metastasizing meningioma<br />
is of benign histology. Certain tumor tendencies for aggressive<br />
behavior have been observed and are discussed.<br />
Neurovirology<br />
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 96<br />
T1901. HIV Associated Neurocognitive Disorder<br />
(HAND) Is Not Associated with Increased Fibrillar<br />
Amyloid Deposits Using 11 C-PiB in Middle-Aged HIVþ<br />
Participants<br />
Beau Ances, Jewell Thomas, Tammie Benzinger, Jon<br />
Christensen, Mengesha Teshome, Patricia Aldea, Anne Fagan,<br />
David Holtzman, John Morris and David Clifford; Saint<br />
Louis, MO<br />
Objectives: Diagnostic challenges exist for differentiating<br />
HIV associated dementia (HAD) from Alzheimer disease<br />
(AD). Similar abnormalities in brain amyloid-b42 (Ab42)<br />
metabolism occur for both. We evaluated if 11 C-Pittsburgh<br />
compound B ( 11 C-PiB) discriminates AD from HAND.<br />
Methods: In this case-control study 16 HIVþ (11 cognitively<br />
normal, 5 HAND) and 19 HIV- (8 cognitively normal,<br />
11 symptomatic AD) participants were assessed using<br />
11<br />
C-PiB, clinical exam, and cerebrospinal fluid (CSF) testing.<br />
v 2 and t-tests investigated differences in clinical and de-<br />
96<br />
mographic variables amongst groups. An ANOVA assessed<br />
11 C-PiBregional differences.<br />
Results: Symptomatic AD were older (p < 0.001), had<br />
lower CSF Ab 42 (p < 0.001), and had higher CSF tau levels<br />
(p < 0.001). Regardless of degree of impairment, HIVþ<br />
participants had no increased 11 C-PiB. Mean and regional<br />
binding potentials were elevated for symptomatic AD participants<br />
(p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 97<br />
Study Design: The regional virology database was<br />
screened to identify VZV positive CSF over 5years. Viral<br />
load was determined by quantitative-polymerase chain reaction<br />
(qPCR).<br />
Results: 608 patients were screened, 36 had VZV qPCR<br />
performed, 12 were positive and had encephalitis. There was a<br />
strong negative correlation between time to LP and viral load<br />
(tau b ¼ 0.59, p ¼ 0.036). There was no significant difference<br />
in viral load between those with good and poor outcome.<br />
Conclusions: CSF viral load appears to more closely<br />
relate to time to LP than outcome. Timing of LP should be<br />
included in future studies to investigate the role of the viral<br />
load in the pathophysiology and prognosis of encephalitis.<br />
Study supported by: Study funded by the National Institute<br />
for Health Research (NIHR-UK) Biomedical Research<br />
Centre.<br />
T1904. Acute Varicella Zoster Virus Encephalitis in<br />
Adults – Relationship between Viral Load, Time,<br />
Clinical Features and Outcome<br />
Benedict D. Michael, Michael Griffiths, Anna Stewart,<br />
Charlotte Buckley, Mark Hopkins, Ian J. Hart, Alistair Miller,<br />
Sareen E. Galbraith and Tom Solomon; Liverpool, United<br />
Kingdom<br />
Background: Varicella zoster virus (VZV) is a common<br />
cause of viral encephalitis with a wide spectrum of outcomes.<br />
The pathophysiology remains poorly understood and<br />
few prognostic markers exist. A few studies have used viral<br />
load, determined by quantitative polymerase chain reaction<br />
(qPCR) of cerebrospinal fluid (CSF), to investigate this,<br />
with contradictory results. However, these have not assessed<br />
this in the context of time.<br />
Objectives: To determine the viral load in VZV encephalitis<br />
in relation to time and outcome.<br />
Study Design: The Liverpool Specialist Virology laboratory<br />
was screened to identify patients with VZV-positive<br />
CSF over 5years. Viral load was determined. Poor outcome<br />
was defined as moderate disability-death (Glasgow outcome<br />
score [GOS]2-5) and high viral load as (>5 10 4 GEq/ml).<br />
Results: Of 608 screened; 36 had VZV-PCR; 12 were<br />
positive. There was a strong negative correlation between<br />
time from symptoms to LP and viral load (tau b ¼ 0.59,<br />
p ¼ 0.036). There was no difference in viral load between<br />
those with good and poor outcome.<br />
Conclusions: In VZV encephalitis, viral load appears to<br />
better relate to time. Timing should be included in future<br />
studies aiming to relate viral load to outcome.<br />
Study supported by: This study recieved support from<br />
the National Institute for Health Research Biomedical<br />
Research Centre on Infectious Diseases. The authors have<br />
no other conflicts of interest to declare<br />
T1905. TLR4 Expression Is Upregulated in HIV-<br />
Associated Neurocognitive Disorder (HAND)<br />
Amir H. Sabouri, Gursharan Chana, Amol Shah, Critian L.<br />
Achim, Ronald J. Ellis, Ian P. Everall and HNRC Group; La<br />
Jolla, CA; Melbourne, Australia and San Diego, CA<br />
Despite the introduction of highly active antiretroviral therapy<br />
(HAART), HIV associated neurocognitive disorders<br />
(HAND) remain a significant cause of morbidity. In a previous<br />
investigation, we have demonstrated that the gene<br />
expression of a number of proteins related to the innate<br />
immune system toll-like receptor (TLR) signaling pathway<br />
correlate strongly with HIV associated neurodegeneration,<br />
most significantly TLR3 and 4. In this study, we examined<br />
gene expression of TLR4, the major signaling receptor<br />
97<br />
for lipopolysaccharide (LPS), within post-mortem brain tissue<br />
from HIV positive subjects (n ¼ 15) and HIV negative<br />
subjects (n ¼ 10) via quantitative real time PCR (qRT-<br />
PCR) and immunohistochemistry (IHC). We also assessed<br />
cognitive brain functions in 7 domains and their correlation<br />
with TLR4 mRNA expression. We found TLR4 expression<br />
was significantly higher in HIV positive subjects than HIV<br />
negative controls (p
J_ID: ZAY Customer A_ID: SUPP11-6 Cadmus Art: 22579 Date: 31-August-11 Stage: Page: 98<br />
All patients recieved treatment with Amphotericine B and<br />
fluconazole.Only half completed the induction phase as<br />
recommended.<br />
Discussion: Clinical presentation, CSF findings of<br />
patients presenting with MC in our hospital do not differ<br />
from what has been reported in the medical literature. This<br />
findings confirms the need to mantain a high suspicion<br />
index of CM in immunocompromised or immunocompetent<br />
patients with suggestive clinical picture.<br />
Special attention must be paid to appropiate treatment schemes<br />
in the future to achieve better outcomes in this population.<br />
Study supported by: The authors declare no conflict of<br />
interest. None of the authors recieved any financial benefits<br />
from the study.<br />
T1908. The Diagnosis of Tuberculous Meningitis: A<br />
Current Review of the Clinical and Laboratory Methods<br />
Brian Chisulo, Shan H. Jiang and Yue S. Pan; Guangzhou,<br />
GZ, China<br />
This review traces our understanding of the clinical<br />
manifestations and the laboratory methods commonly<br />
98<br />
considered in the diagnosis of tuberculous meningitis<br />
(TBM). In compiling this review, we searched electronic<br />
data bases in PubMed, Science Direct, Biomedical Central<br />
and Google Scholar. Firstly, we evaluate the more<br />
traditional diagnostic methods which have been commonly<br />
applied in the diagnostics of tuberculosis (TB).<br />
The role of direct cerebrospinal fluid (CSF) examination<br />
for acid-alcohol fast bacilli, CSF culture for Mycobacterium<br />
tuberculosis, and detection of mycobacterial nucleic<br />
acid in the CSF is evaluated. We also consider the role<br />
of brain imaging and chest X-ray. Secondly, the review<br />
evaluates the current evidence on the role of some newly<br />
prospective diagnostic techniques and the coverage is<br />
given to the role of CSF adenosine deaminase activity,<br />
Gen Probe amplified Mycobacterium tuberculosis direct<br />
test, microscopic observation drug susceptibility<br />
(MODS) culture technique, ex vivo Mycobacterium tuberculosis-specific<br />
enzyme-linked immunospot assay<br />
(ELISpot assay) and enzyme-linked immunosorbent assay<br />
(ELISA) in the diagnosis of TBM.<br />
Study supported by: This was a self-financed study.<br />
ID: senthilk I Black Lining: [ON] I Time: 08:46 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110244/APPFile/JW-ANA#110244
<strong>136</strong> th Annual Meeting Sunday,<br />
September 25, 2011 Works in<br />
Progress Poster Session Abstracts<br />
WIP posters will be displayed in Elizabeth A-E of the<br />
Manchester Grand Hyatt from 10:00 am – 7:00 pm,<br />
with authors present from 6:00 pm – 7:00 pm.<br />
The Works in Progress category emphasizes ongoing clinical<br />
or basic research of an extraordinary nature, which warrants<br />
expediated presentation. These abstracts were selected<br />
based on scientific merit, timeliness, and anticipated interest<br />
to the membership. Key aspects of research must have been<br />
conducted after the regular abstract deadline.<br />
Cerebrovascular Disease<br />
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 99<br />
S141. Polymorphism of Ninjurin2 in Korean<br />
Atherothrombotic Stroke Patients<br />
Dae-il Chang, Sung Hyuk Heo and Hye Ok Kim;<br />
Seoul, Korea<br />
Recently, in a genome-wide association study, the singlenucleotide<br />
polymorphisms (SNPs) rs12425791 and<br />
rs11833579 of ninjurin2 (NINJ2) were reported to be associated<br />
with atherothrombotic stroke. However, this finding<br />
has not been validated in Korean population yet. We therefore<br />
investigated an association between atherothrombotic<br />
stroke and SNPs of NINJ2 in 200 patients and 295 control<br />
subjects. Allelic discrimination assay was used. The A allele<br />
of rs11833579 increased stroke risk significantly (p ¼<br />
0.003, 1.50 (95% CI, 1.15 to 1.96), respectively). The A allele<br />
frequencies were higher in stroke patients with hypertension<br />
than in control subjects with hypertension (p ¼<br />
0.042 and p ¼ 0.001, respectively) in both SNPs of NINJ2<br />
(rs12425791 and rs11833579). Also, the A allele was more<br />
frequent in stroke patients with hyperlipidemia than in control<br />
subjects with hyperlipidemia (p ¼ 0.010 and p ¼<br />
0.005, respectively) in both. In addition, the A allele was<br />
more frequent in stroke patients with diabetes than in control<br />
subjects with diabetes (p ¼ 0.008, respectively) in SNPs<br />
rs11833579. In conclusion, SNPs of NINJ2 (rs12425791<br />
and rs11833579) confer a substantial genetic risk factor for<br />
atherothrombotic stroke in our population.<br />
S142. NMDA Receptor Biomarker for Acute Stroke<br />
Kerstin Bettermann and Svetlana Dambinova; Hershey, PA<br />
and Kennesaw, GA<br />
Background: The NR2 peptide, a breakdown product of<br />
brain specific NMDA receptors, is released into the bloodstream<br />
during cerebral ischemia and can be used as a marker<br />
for acute ischemic stroke (IS). Performance characteristics<br />
and critical values of the NR2 peptide in acute IS patients<br />
presenting within 24h of symptom onset are analyzed.<br />
Methods: NR2 peptide levels are correlated with neurological<br />
status and results of advanced neuroimaging studies.<br />
Plasma NR2 peptide concentrations are determined by plotting<br />
their absorbance values on a calibration curve constructed<br />
from the absorbance units of each calibrator and<br />
their known concentrations.<br />
Results: Controls and individuals with vascular risk factors<br />
have NR2 peptide concentrations below 0.25 and 0.3<br />
lg/l, respectively. Acute IS patients have significantly higher<br />
NR2 peptide levels (>0.5 lg/l) compared to all control<br />
groups (p75 cm/s was strongly predictive of symptomatic<br />
MCA vasospasm. The 3, 7, 10, and 14-day risks of symptomatic<br />
MCA vasospasm were 0.9%, 9.4%, 14.8%, and<br />
14.8% for those with initial MCA-MFV 75 cm/s (log-rank test: P ¼ 0.001).<br />
Elevated initial TCD velocity may provide a useful marker<br />
for those at high-risk for symptomatic vasospasm. The risk<br />
of vasospasm in those with elevated MCA velocity > 75<br />
cm/s was significantly higher, occurring earlier and for a<br />
longer period, than in those without.<br />
S144. Relative Change in Transcranial Doppler Velocities<br />
Is Inferior to Absolute Thresholds in Prediction of<br />
Vasospasm after Subarachnoid Hemorrhage<br />
Konark Malhotra, James Connors, Viven Lee and Shyam<br />
Prabhakaran; Chicago, IL<br />
We reviewed 350 consecutive SAH patients with aneurysmal<br />
source, who underwent serial TCD monitoring and survived<br />
at least 7 days. We recorded initial flow velocity(IFV) upto<br />
14 days, maximal flow velocity of middle cerebral artery<br />
(MCA), relative flow changes (MFV/IFV) >3, absolute<br />
maximal Lindegaard ratio (LR) >6, mean MCA maximum<br />
flow velocity (MFV) >175 cm/s, and MFV >200 cm/s.<br />
Among 211 patients selected, 48 (23%) developed symptomatic<br />
MCA vasospasm. Area under the ROC curve (AUC)<br />
was: MCA-MFV >175 ¼ 0.80, MFV >200 ¼ 0.73, LR<br />
>6 ¼ 0.71, and MFV/IFV >3 ¼ 0.60. The best characteristics<br />
were observed for MFV >175 cm/s or maximal LR<br />
>6 as: AUC ¼ 0.81; while sensitivity, specificity and negative<br />
predictive value were: 81%, 81% and 94%, respectively;<br />
the positive likelihood ratio was 4.1. MFV/IFV >3 performed<br />
the worst. MFV >175 cm/s and/or Lindegaard ratio<br />
>6 accurately predict symptomatic MCA vasospasm. Presence<br />
of either/both abnormalities in first 14 days after SAH<br />
increases the likelihood of symptomatic MCA vasospasm by<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
4 fold. Other thresholds including relative change from<br />
baseline appear inferior to these absolute thresholds.<br />
Movement Disorder<br />
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 100<br />
S238. Dopamine Transporter Imaging Predicts Long<br />
Term Outcomes in Parkinson’s Disease<br />
Bernard M. Ravina, Kenneth Marek, Shirley Eberly, David<br />
Oakes and Ira Shoulson; Rochester and New Haven<br />
Objective: Our objective is to measure the prognostic value<br />
of dopamine transporter (DAT) imaging for motor and<br />
non-motor outcomes in PD.<br />
Methods: We prospectively evaluated a PD cohort after<br />
enrollment in a de novo PD clinical trial with motor, cognitive,<br />
and behavioral measures. DAT imaging with [ 123 I][b]-<br />
CIT (b-CIT) and SPECT was performed at baseline and after<br />
22 months.<br />
Results: Four hundred and ninety-one (91%) of 537 subjects<br />
had evidence of dopamine deficiency consistent with<br />
PD. The cohort was followed for 5.5 (0.8) years and had a<br />
diagnosis of PD for 6.3 (1.2) years. Lower striatal binding<br />
of b-CIT at baseline was independently associated with significantly<br />
higher risk for important clinical milestones and<br />
measures of PD severity, including motor related disability,<br />
falling and postural instability, cognitive impairment, psychosis,<br />
and clinically important depressive symptoms. Subjects<br />
in the bottom quartile for DAT imaging compared to<br />
the top quartile had an odds ratio (95% CI) of 3.5 (1.7,<br />
6.9) for cognitive impairment and 12.8 (2.6, 61.8) for<br />
psychosis.<br />
Conclusions: Near the time of PD diagnosis, DAT imaging<br />
with b-CIT and SPECT is an independent predictor of<br />
clinically important motor and non-motor long term<br />
outcomes.<br />
Study supported by: This study was sponsored by the<br />
National Institute of <strong>Neurological</strong> Disorders and Stroke<br />
(NINDS) (5U01NS050095), Department of Defense<br />
(DOD) Neurotoxin Exposure Treatment Parkinson’s<br />
Research Program (W23RRYX7022N606), Michael J Fox<br />
Foundation (MJFF), Parkinson’s Disease Foundation (PDF),<br />
Cephalon Inc, and Lundbeck Inc.<br />
S239. Time to First Levodopa-Induced Motor<br />
Complication: Results from the STRIDE-PD Study<br />
C. Warren Olanow, Karl Kieburtz, Olivier Rascol, Werner<br />
Poewe, Anthony Schapira, Helena Nissinen, Mika Leinonen<br />
and Fabrizio Stocchi; New York, NY; Rochester, NY; Toulouse,<br />
France; Innsbruck, Austria; London, United Kingdom; Espoo,<br />
Finland; Kista, Sweden and Rome, Italy<br />
Introduction: The STRIDE-PD study compared initiation<br />
of levodopa/carbidopa (LC) to levodopa/carbidopa/entacapone<br />
(LCE) in PD patients.<br />
Objective: Determine the effect of levodopa dose on development<br />
of motor complications.<br />
Methods: A total of 745 patients participated in a 134–<br />
208-week, double-blind trial, with 3-monthly assessments of<br />
dyskinesia and wearing-off. Based on nominal levodopa<br />
dose per day, patients were divided into four groups: 400–600 mg (26.6%),<br />
and >600 mg (7.4%). Dose response was analyzed using<br />
log-rank test. Predictive factors for first motor complication<br />
were screened using multivariate analysis.<br />
Results: A dose response was observed between levodopa<br />
dose and first motor complication (p
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 101<br />
Outcome measures: Dyskinesia score(primary); fingertapping<br />
and walking speed, tremor score and blood<br />
pressure(secondary).<br />
Analysis: Area Under Curve statistical paradigm<br />
Results: Single doses of 100mg of preladenant increased<br />
levodopa-induced dyskinesia compared to placebo(p ¼<br />
0.003). Single doses of 10mg were not statistically significantly<br />
different from placebo(p ¼ 1.00). We found a trend<br />
suggesting a dose-response for dyskinesia, and observed dyskinesia<br />
in 4 of 12 subjects prior to levodopa infusion. Neither<br />
dose significantly improved any measure of parkinsonism.<br />
The drug was generally well-tolerated.<br />
101<br />
Conclusions: This proof of concept study does not support<br />
the hypothesis that A2A antagonists augment the<br />
effects of levodopa without increasing dyskinesia. Our<br />
results suggest that a supratherapeutic dose of preladenant<br />
may be pro-dyskinetic, perhaps independently of levodopa,<br />
in PD patients with pre-existing dyskinesias.<br />
Study supported by: Merck & Co, Inc<br />
Presenting author Hogarth and co-authors Nutt & Park<br />
received salary support from payments made by the sponsor<br />
to OHSU for contracted research design and execution services.<br />
Co-authors Troyer, Laguerre, Grachev, Xuan, and Tendolkar<br />
are/were employees of the sponsor.<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
<strong>136</strong> th Annual Meeting Monday,<br />
September 26, 2011 Works in<br />
Progress Poster Session<br />
WIP posters will be displayed in Elizabeth A-E of the<br />
Manchester Grand Hyatt from 10:00 am – 7:00 pm,<br />
with authors present from 6:00 pm – 7:00 pm.<br />
The Works in Progress category emphasizes ongoing clinical<br />
or basic research of an extraordinary nature, which warrants<br />
expediated presentation. These abstracts were selected<br />
based on scientific merit, timeliness, and anticipated interest<br />
to the membership. Key aspects of research must have been<br />
conducted after the regular abstract deadline.<br />
Behavioral Neurology<br />
M622. New Approaches to Unraveling the Multi-Scale<br />
Neuroanatomical Changes in Williams Syndrome<br />
Ann Lam and Elan L. Ohayon; La Jolla<br />
In this study we explore novel multi-scale approaches to<br />
investigate the role of neuroanatomy in cognitive phenotypes<br />
by imaging the distribution of metalloproteins across<br />
scales in Williams Syndrome tissue. Synchrotron-based rapid<br />
scanning imaging was used at whole hemisphere levels and<br />
resolutions of up to 10 microns to co-localize elements in<br />
postmortem samples of Williams Syndrome and typicaldeveloping<br />
individuals in prefrontal, temporal and occipital<br />
cortex. Comparisons between- and within-subjects revealed<br />
differences between brain areas in elemental distributions.<br />
For example, initial scans showed the expected high levels of<br />
iron in nuclei such as the substantia nigra and prominent<br />
zinc florescence along white matter tracts. To increase the<br />
resolution by a factor of 20, microprobe imaging was then<br />
used attaining resolutions as high as 0.5 microns. This<br />
microprobe analysis of 50–100 micron thick cortical sections<br />
showed the co-localization of iron, zinc and calcium<br />
in and around cell-like structures. The combination of these<br />
two synchrotron-based techniques thus enables the study of<br />
biologically relevant elements in postmortem brain tissue<br />
across large areas, while allowing for the co-registering of<br />
elements at high resolutions at the cellular level in regions<br />
of interest.<br />
Study supported by: NIH<br />
Epilepsy<br />
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 102<br />
M725. HLA-B*1502 Genotyping in Carbamazepine and<br />
Phenytoin Induced Stevens-Johnson Syndrome<br />
Sivakumar M. Rajappa and Srinivasan A. Venkatesan;<br />
Chennai, Tamil Nadu, India<br />
Objective: To study the association of HLA-B* 1502 allele<br />
in epileptic patients with carbamazepine and phenytoininduced<br />
Stevens Johnson Syndrome (SJS) in South Indian<br />
patients.<br />
Background: SJS and Toxic Epidermal Necrolysis (TEN)<br />
are severe cutaneous adverse drug reactions caused by carbamazepine<br />
(CBZ) and phenytoin. A strong association has<br />
been reported between human leucocyte antogen HLA-<br />
B*1502 and carbamazepine-induced SJS in Han Chinese<br />
patients.<br />
Design/Methods: Single center, prospective cross sectional<br />
study. After an informed consent, 7 ml of EDTA<br />
blood were collected from 100 patients on CBZ and 50 on<br />
102<br />
phenytoin therapy. Purified DNA were used for HLA-<br />
B*1502 typing by Sequence Specific Oligopeptide method<br />
using Polymerase Cahin Reaction.<br />
Results: Out of <strong>136</strong> patients on CBZ, HLA-B*1502<br />
were detected in 22 and 19 developed SJS/TEN. In 50<br />
patients on Phenytoin, HLA-B*1502 were detected in six<br />
patients and four had SJS. The mean duration from exposure<br />
to SJS was 14 days.<br />
Conclusion: There is a high prevalence of HLA-B*1502<br />
in South Indians on Carbamazepine and Phenytoin<br />
(18.66%). There was a strong association of HLA-B*1502<br />
allele and the developmment of SJS in South Indians, with<br />
the Positive Predictive Value for Carbamazepine and Phenytoin<br />
being 86% and 66.67% respectively.<br />
M726. Filamin A Regulates Neural Progenitor<br />
Proliferation and Brain Size through wee1-Dependent<br />
cdk1 Phosphorylation<br />
Gewei Lian and Volney Sheen; Boston, MA<br />
Mutations in the actin binding filamin A (FlnA) gene cause<br />
the human disorder periventricular heterotopia (PH). FlnAdependent<br />
regulation of cytoskeletal dynamics is thought to<br />
direct neural progenitor migration and proliferation. Here<br />
we show that late embryonic FlnA null mice exhibit a<br />
reduction in brain size, impairments in neural progenitor<br />
proliferation, and decline in neural progenitor numbers over<br />
time. The drop in the progenitor population is not attributable<br />
to changes in cell fate specification through altered<br />
asymmetric versus symmetric cell divisions, but to prolonged<br />
cell cycle duration. Suppression of FlnA leads to<br />
impaired degradation of cyclin b1-related proteins, thereby<br />
delaying the onset and progression through mitosis. We find<br />
that the cdk1 kinase wee1 binds FlnA, demonstrates<br />
increased expressions levels after loss of FlnA function, and<br />
is associated with increased phosphorylation of cdk1. Phosphorylation<br />
of cdk1 inhibits activation of anaphase promoting<br />
complex degradation system, which is responsible for<br />
cyclin b1 degradation and progression through mitosis. Collectively,<br />
our results demonstrate a molecular mechanism<br />
whereby FlnA impairs G2 to M phase entry, leading to cell<br />
cycle prolongation, impaired neural progenitor proliferation,<br />
and reduced brain size.<br />
Study supported by: This work was supported in part by<br />
the National Institutes of Health NS063997-01 to VLS.<br />
This work was also supported in part by the Empire State<br />
Stem Cell Fund through the New York State Department of<br />
Health Contract #C024324 to VLS. The opinions expressed<br />
here are solely those of the author and do not necessarily<br />
reflect those of the Empire State Stem Cell Board, the New<br />
York State Department of Health, or the State of New York.<br />
VLS is a Doris Duke Clinical Scientist Developmental<br />
Award Recipient.<br />
M727. A Moderate-Throughput Screen for<br />
Antiepileptogenic Compounds<br />
Yevgeny Berdichevsky, Yero Saponjian, Michelle Mail and<br />
Kevin J. Staley; Boston, MA<br />
Epilepsy is a frequent complication of traumatic, infectious<br />
and ischemic brain injury. The time interval between injury<br />
and epilepsy provides a tremendous opportunity for diseasemodifying<br />
therapies. Development of these therapies is limited<br />
by inadequate knowledge of the pathophysiology of epileptogenesis,<br />
the long time intervals required to observe<br />
changes in experimental epileptogenesis, and difficulties<br />
quantifying epileptogenesis.<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 103<br />
To address these difficulties we have developed a moderate-throughput<br />
drug screen for antiepileptogenic agents<br />
comprised of arrays of organotypic hippocampal brain slices<br />
that develop robust spontaneous electrographic seizure activity<br />
within two weeks in vitro. Seizure activity is quantified<br />
either electrographically or metabolically as cumulative lactate<br />
production over two weeks in vitro. Neuroprotection is<br />
quantified as cumulative lactate dehydrogenase release over<br />
two weeks in vitro.<br />
Using these techniques we have screened 50 compounds<br />
from the NINDS Custom Compounds Collection in less<br />
than 4 months. Most anticonvulsants demonstrated neither<br />
antiepileptogenic nor significant chronic anticonvulsant<br />
effects, although acute anticonvulsant effects were readily<br />
observable. With other compounds we have resolved chronic<br />
anticonvulsant or antiepileptogenic activities (which are<br />
indistinguishable in the first-level screen) evidenced by<br />
decreased lactate with no increase in LDH, as well as neuroprotective<br />
activity, evidence by reduction in LDH.<br />
Study supported by: NIH (NINDS)<br />
M728. Network Structure and Sensitivity to the<br />
Geometry of Stimuli in Epilepsy and Cognition<br />
Elan L. Ohayon, Ann Lam and Terrence J. Sejnowski; La<br />
Jolla, CA<br />
What modulates a brain’s sensitivity to stimuli? This question<br />
is central to the study of reflex epilepsies and cognition.<br />
Previously we have shown that network structure can affect<br />
the persistence of complex activity. Here we use computational<br />
models to demonstrate how anatomical changes can<br />
modulate sensitivity to initial conditions such as perceptual<br />
stimuli. Models consisted of large spatial networks with up<br />
to 20,000 spiking units with inhibitory and excitatory populations.<br />
Network structure was adjusted by randomly adding<br />
or removing cells at 5% increments. Simulations showed<br />
that homogeneous networks (density ¼ 1.0) were least likely<br />
to maintain activity with either single or distributed stimuli.<br />
In contrast, heterogeneous networks became more sensitive<br />
to a variety of stimuli (e.g., over 95% persistence at density<br />
¼ 0.6). Interestingly, the self-propagating responses generated<br />
in heterogeneous networks could be ‘‘grafted’’ back<br />
onto the homogenous networks and continue propagating.<br />
These experiments illustrate that changes in anatomy<br />
can modulate responses to stimulus geometry thereby helping<br />
explain how neurodegeneration and trauma might lead<br />
to changes in sensitivity and the lowering of seizure threshold.<br />
The findings also illustrate how network structure<br />
might modulate responses to stimuli in attention and<br />
cognition.<br />
Study supported by: NIH<br />
M729. Hypoglycemia Induced NMDA Receptor-<br />
Dependent Epileptiform Activity in the Hippocampal<br />
CA3 Area Causes Damage in CA1<br />
Carlos M. Florez, Jane Zhang, Peter Abdemalik, Liang Zhang<br />
and Peter L. Carlen; Toronto, ON, Canada<br />
Seizures are the most common clinical presentation of severe<br />
hypoglycemia in neonates. We characterized a new in vitro<br />
model for the study of hypoglycemia-induced seizures using<br />
mouse hippocampal thick slices. Changing the glucose concentration<br />
to 1mM produced seizures in 88% of the preparations.<br />
Isolation experiments revealed that CA3, less susceptible<br />
for hypoglycemia induced synaptic failure than CA1, is<br />
the epileptogenic area. The CA3 network showed decreased<br />
interneuronal activity and increased frequency and energy<br />
transfer of the pyramidal cell activity prior to the onset of<br />
103<br />
seizures. It was common to observe spreading depressionlike<br />
events (SD) and irreversible synaptic failure in the CA1<br />
region following the seizure activity originated in CA3 (8/<br />
12). SD also occasionally occurred in the CA3 area (3/12)<br />
following a SD event in the CA1 region. Hypoglycemic<br />
seizures required glutamatergic activity and NMDA receptor<br />
blockade prevented the hypoglycemia-induced seizures and<br />
SDs.<br />
Conclusions: Hypoglycemia-induced seizures in the hippocampus<br />
start in the CA3 region and cause SD and synaptic<br />
failure in the CA1 region. Activation of NMDA receptors<br />
is the key factor for the initiation of seizures and<br />
development of brain failure during severe hypoglycemia.<br />
Study supported by: JDRF<br />
M730. Alzheimer Disease in Lafora Epilepsy<br />
Jesus Machado-Salas, Maria Rosa Avila-Costa, Patricia<br />
Guevara, Jorge Guevara, Reyna M. Duron, Dongsheng Bai,<br />
Miyabi Tanaka and Antonio V. Delgado-Escueta; Los Angeles,<br />
CA and Mexico, Mexico<br />
Here we describe temporal progression of tau and amyloid<br />
pathology and subtypes of Lafora bodies (LB) in a Laforindeficient<br />
(epm2a / ) mice model. Wild type and<br />
epm2a / mice were sacrificed at different ages. Histological<br />
and immuonocytochemical techniques were used. We<br />
found in epm2a / mice that neurofibrilary tangles appear<br />
at 11 days-old while senile plaques are abundant at 6<br />
months. Type I LB are abundant inside neurons, type II LB<br />
are confined to neuron somata. Type I LB appear at 1<br />
month while type II LB with an external rim staining for<br />
Neurofilament L, appear at 3 to 5 months. Both types of<br />
LB increase in size and number with age but show regional<br />
differences. Diencephalon has meager or no LB, cell death<br />
and neurofibrillary tangles. All three features are abundant<br />
in hippocampus, amygdala, cerebellum, and in greatest<br />
amount in pons. Our results indicate that Lafora Disease is<br />
both a neurodegenerative disease and a glycogen metabolism<br />
disorder. We hypothesize that laforin deficiency upregulates<br />
tau protein kinase I/glycogen synthase kinase 3beta forming<br />
tau, amyloid and polyglucosan bodies. Our findings are critical<br />
for future experiments on disease mechanisms and<br />
therapies for both Lafora disease and Alzheimer disease.<br />
Study supported by: National Institutes of Health<br />
[1RO1NS055057], Chelsea’s Hope Foundation for Lafora<br />
Disease and Programa de Apoyo a Proyectos de Investigación<br />
e Innovación Tecnológica-DGAPA UNAM<br />
[IN214609, and PAPCA 2010-2011]<br />
M731. Antiepileptic Activity of Intrapulmonary<br />
Midazolam<br />
Ashish Dhir, Dorota Zolkowska and Michael A. Rogawski;<br />
Sacramento and Davis<br />
Midazolam is a short-acting central/peripheral benzodiazepine<br />
receptor modulator. It is widely used as an intravenous<br />
sedative and a fast-acting anticonvulsant to abort status epilepticus.<br />
In the present study, we sought to characterize<br />
intrapulmonary route to deliver midazolam for providing<br />
fast and potent antiepileptic action. Further, we explored<br />
the involvement of both central and peripheral benzodiazepine<br />
receptors in its mechanism of anticonvulsant action.<br />
Intraperitoneal administration of midazolam at 250–5000<br />
lg/kg protected mice against pentylenetetrazol, picrotoxin<br />
and kainic acid-induced convulsions. Similarly, the intratracheal<br />
route of midazolam administration demonstrated anticonvulsant<br />
activity but at much lower doses (25–100 lg/<br />
kg); the maximum anticonvulsant action was observed<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
etween 5–15 minutes. The anticonvulsant action of intratracheal<br />
midazolam (100 lg/kg) in PTZ i.v. seizure model<br />
was reversed by pre-administration of flumazenil (5 mg/kg.,<br />
i.p.), a centrally acting benzodiazepine receptor antagonist.<br />
Finasteride (100 mg/kg., i.p.), a 5-alpha reductase inhibitor<br />
and neurosteroid synthesis inhibitor partially blocked the<br />
anticonvulsant action of midazolam in PTZ seizure threshold<br />
model. Furthermore, the anticonvulsant action of intraperitoneal<br />
midazolam was reversed by PK-11195, a peripheral<br />
benzodiazepine receptor antagonist. In conclusion, the<br />
intrapulmonary midazolam provides fast and potent anticonvulsant<br />
action and involves both central and peripheral<br />
receptors in its mechanism of action.<br />
Study supported by: Epilepsy Laboratory<br />
M732. Do Brain Volumes in JME (juvenile myoclonic<br />
epilepsy) differ from normal controls?<br />
John T. Spitz, Long Vu, Lydia Su, Mark A. Mandelkern,<br />
Barbara E. Swartz; Berkely, CA, Irvine, CA, Los Angeles, CA,<br />
Irvine,CA and Newport Beach, CA<br />
Background: JME is a form of generalized epilepsy that<br />
accounts for 7% of all epilepsies. The natural history of<br />
JME and its brain morphology is explored in this study.<br />
Methods: We compared the volumes of 11 regions of interest<br />
(frontal and subcortical) and grey matter density<br />
between 17 JME subjects (33.8 þ/ 10.4 years) with sex<br />
and age-matched controls (35.4 þ/ 11.7) using automated<br />
and manual volumetric procedures and voxel based morphometry<br />
(VBM). Regional volumes were normalized to<br />
whole brain volumes prior to statistical analyses.<br />
Results: Initial analysis of the volumetric data using ttests<br />
with Bonferroni correction found no significant differences<br />
between the JME and controls. However, individual<br />
subjects with JME were more likely to have regions larger<br />
than control mean volumes than visa versa using VBM and<br />
volumetry (p ¼ .04, Binomial test, VBM). Additionally,<br />
both VBM and manual volumetric analysis found the left<br />
thalamus larger in JME subjects. These results will be<br />
expanded using ANCOVA and/or MANCOVA analyses to<br />
control for a number of covariates: duration of epilepsy, sex,<br />
seizure control and medications for final presentation. Discussion<br />
will emphasize the growing literature in this area.<br />
Study Supported By: Veteran’s Administration Merit<br />
Review Program 821/103.<br />
Neuromuscular Disease<br />
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 104<br />
M836. Disrupted Expression of Myogenin in Inclusion<br />
Body Myositis<br />
Akatsuki Kubota, Jun Shimizu, Atsushi Iwata and Shoji Tsuji;<br />
Tokyo, Japan<br />
Background: Inclusion body myositis (IBM) is a chronic<br />
progressive inflammatory myopathy, with degenerative pathology.<br />
Immunosuppressive therapies are ineffective to<br />
IBM, unlike other idiopathic inflammatory myositis (IIM).<br />
Muscle regeneration is also impaired in IBM, but the mechanism<br />
remains undetermined. Myogenin is one of the myogenic<br />
regulatory factors, and plays an essential role in maturation<br />
of myogenic cells.<br />
Purpose: We evaluated expression of myogenin in biopsied<br />
muscles from IBM and IIM patients.<br />
Materials and methods. We analyzed biopsied samples<br />
from 11 IBM and 19 IIM patients. We quantified myogenin-positive<br />
cells by immunohistochemistry, myogenin protein<br />
by Western blot, and myogenin mRNA by real-time<br />
reverse transcription PCR (RT-PCR).<br />
104<br />
Results: Biopsied samples from IBM patients showed<br />
lower expression of myogenin than those from IIM patients,<br />
in immunohistochemistry (IBM 4.761.4 cells/100myofibers,<br />
IIM 7.363.7, p ¼ 0.0352), Western blot (IBM<br />
0.04860.030 (relative amount to actin), IIM 0.09060.056,<br />
p ¼ 0.0297), and real-time RT-PCR (IBM 10.668.5 (relative<br />
amount to b-actin), IIM 19.6611.7, p ¼ 0.0344).<br />
Immunohistochemistry of biopsied samples from IBM<br />
patients also revealed that myogenin was aberrantly<br />
expressed within degenerative myofibers, and was aggregated<br />
in Ab-positive inclusion bodies.<br />
Conclusion: Disrupted expression of myogenin may<br />
reflect impaired regeneration in IBM.<br />
Study supported by: Grants-in Aid for Scientific Research<br />
and Health and Labour Sciences Research Grants for<br />
Research on Intractable Diseases from the Ministry of<br />
Health, Labour and Welfare of Japan, and Grants-in Aid for<br />
Scientific Research from the Ministry of Education, Culture,<br />
Sports, Science and Technology of Japan.<br />
M837. Abnormalities of a Novel Autophagy-Associated<br />
Protein, NBR1, in Muscle Fibers of Sporadic Inclusion-<br />
Body Myositis (s-IBM)<br />
Carla D’Agostino, Anna Nogalska, Mafalda Cacciottolo,<br />
W.King Engel and Valerie Askanas; Los Angeles, CA<br />
Intra-muscle fiber accumulation of ubiquitinated protein<br />
aggregates containing several conformationally modified proteins,<br />
including amyloid-b and phosphorylated tau, is characteristic<br />
of the pathologic phenotype of s-IBM, the most<br />
common degenerative myopathy of older persons. Impaired<br />
protein-degradation, involving both the 26S proteasome and<br />
autophagic-lysosomal pathways, we previously demonstrated<br />
in s-IBM muscle. NBR1 is a ubiquitin-binding scaffold-protein<br />
importantly participating in autophagic degradation of<br />
ubiquitinated proteins. Abnormalities of p62, another ubiquitin-binding<br />
protein, were previously described in s-IBM.<br />
Abnormalities of NBR1 have not been reported in s-IBM.<br />
We have now identified in 14 s-IBM muscle biopsies<br />
that NBR1, by: a) immunohistochemistry, was strongly<br />
accumulated within s-IBM muscle-fiber aggregates, where<br />
it closely co-localized with p62 and phosphorylated tau;<br />
b) immunoblots, was increased 3x, p< 0.01; and c) immunoprecipitation,<br />
was associated with p62. By real-time PCR,<br />
NBR1 mRNA was increased 2x, p< 0.01. None of the 15<br />
disease- and normal-control muscle biopsies had any NBR1<br />
abnormality.<br />
This first demonstration of NBR1 abnormalities in s-<br />
IBM: a) further suggests that abnormalities of the autophagic-lysosomal<br />
pathway may be critically involved in the s-<br />
IBM pathogenesis, and b) indicates a potential therapeutic<br />
focus.<br />
Study supported by: Muscular Dystrophy <strong>Association</strong><br />
M838. Atrophy and Autophagy in Limb Girdle Muscular<br />
Dystrophy and Glycogen Storage Disease Type 2<br />
Corrado I. Angelini, Annachiara Nascimbeni, Marina Fanin<br />
and Marco Sandri; Padova, Italy<br />
Few studies have investigated atrophy/autophagy gene<br />
expression in LGMDs and GSD type 2, to study the fate of<br />
misfolded proteins in ubiquitin-proteasome system and recovery<br />
in autophagy-lysosome pathway after Enzyme<br />
Repacement Therapy (ERT).<br />
We investigated gene expression from 40 muscle biopsies<br />
of LGMD 2A, 20 LGMD 2B and 12 GSD type 2, both infantile<br />
and late onset. We found evidence of activation of<br />
molecular pathways with upregulation of autophagy-related<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 105<br />
genes: BNIP3 and p62 in Pompe, of atrophy-related genes<br />
atrogin-1 and MuRF-1 in LGMD 2A (calpainopathy) and<br />
in LGMD 2B (dysferlinopathy). In one infantile, one juvenile<br />
and one adult GSD type 2 cases a second biopsy was<br />
done after ERT and analysed for morphology and gene<br />
markers: in the second biopsy we observed after ERT<br />
reduced vacuolated fibers and decreased autophagy related<br />
markers.<br />
Our study in GSD type 2 recognises an important contribution<br />
of autophagic process in the development of muscle<br />
pathology, after ERT autophagy markers are considerably<br />
decreased as well as vacuolisation of muscle fibers. Our<br />
observations in LGMDs are new and support future therapeutic<br />
interventions to rescue muscle atrophy.<br />
Study supported by: Telethon, Eurobobank.<br />
M839. Virtual Demyelination in pmp22 Deficiency<br />
Jiasong Guo, Qing Yan, Gina Sosinsky, Mark Elisman,<br />
Cameron McIntyre, Lily Wang, Ueli Suter and Jun Li;<br />
Nashville; San Diego; Cleveland; Zurich, Swaziland and<br />
Nashville, TN<br />
Safety factor for action potential propagation in pmp22þ/<br />
nerves appears impaired (Bai et al, J Neurosci 2010). The<br />
present study investigates mechanisms responsible for the<br />
impairment. Fluorescent dyes with different molecular sizes<br />
were injected into sciatic nerves. After 4-hour incubation,<br />
sciatic nerves were teased into individual nerve fibers, and<br />
examined under fluorescence microscopy. Fluorescence was<br />
of strong intensity in about a half of paranodal tomacula of<br />
pmp22þ/ nerves (15 mice), but absent or minimal in the<br />
paranodes of wild-type nerves (11 mice). This finding suggests<br />
that myelin is abnormaly leaky, and may result in excessive<br />
outward current. Application of potassium channel<br />
blocker, 4AP, to reduce outward current improved the amplitude<br />
of motor response during nerve stimulation. Western<br />
blot and immunohistochemistry revealed alterations of tight<br />
junction protein assembly, a potential molecular mechanism<br />
for the myelin leakage.<br />
Conclusions: Our results show excessive leakage in<br />
pmp22þ/ myelin in the absence of demyelination. This<br />
leakage is functionally similar to demyelination. These findings<br />
not only reveal novel mechanism for conduction block<br />
but also establish new therapeutic approach for this disease.<br />
Study supported by: NIH<br />
M840. First in Human Phase 1 Trial of Neural<br />
Progenitor Cells in ALS: Results in the First 12 Patients<br />
Jonathan D. Glass, Nicholas Boulis, Meraida Polak, Crystal<br />
Kelly, Thais Federici, Jane Bordeau, Seward Rutkove, Karl<br />
Johe, Tom Hazel and Eva Feldman; Atlanta, GA; Boston,<br />
MA; Rockville, MD and Ann Arbor, MI<br />
Twelve patients with ALS were injected into the lumbar<br />
spinal cord with fetal-derived neural stem cells. The design<br />
is one of ‘‘escalating risk’’, where each group of patients is<br />
progressively less impaired. The first 6 patients were nonambulatory,<br />
3 were supported by mechanical ventilation.<br />
The first 3 patients received 5 unilateral injections at L2-<br />
L4, and the next 3 received 5 injections bilaterally. Patients<br />
7–12 were ambulatory and had vital capacities > 60 %<br />
predicted. Patients 7–9 received 5 unilateral injections, and<br />
patients 10–12 received bilateral injections. Each injection<br />
was 10 ll of 10,000 cells/ll; patients received either<br />
500,000 or 1 million cells through 5 or 10 injections,<br />
respectively. There have been two deaths, one which was<br />
unrelated to either ALS or the clinical trial. The surgical<br />
procedure was well tolerated. There have been no adverse<br />
105<br />
events attributable to the cellular injections. We are using<br />
clinical evaluation, strength testing, and electrical impedence<br />
myography to monitor progression of disease. Following<br />
FDA review and approval of safety data from the<br />
first 12 patients we will move to injections into the cervical<br />
spinal cord.<br />
Study supported by: Neuralstem, Inc.<br />
M841. Clinical Development of an Antisense Therapy<br />
for the Treatment of Transthyretin Amyloidosis<br />
Shuling Guo, Elizabeth Ackermann, Sheri Booten, Luis<br />
Alvarado, Andrew Siwkowski, Merrill Benson, Steve Hughes<br />
and Brett Monia; Carlsbad, CA and Indianapolis, IN<br />
Transthyretin (TTR)-associated amyloidosis is a late-onset<br />
autosomal-dominant genetic disease. Mutations in TTR<br />
destabilize TTR tetramer thereby inducing the formation of<br />
amyloid fibrils. This disease mainly affects peripheral nerves<br />
as in familial amyloidotic polyneuropathy (FAP) or heart as<br />
in familial amyloid cardiomyopathy (FAC). Circulating<br />
TTR is predominantly produced by the liver, and the only<br />
available treatment as of June 2011 is orthotopic liver transplantation.<br />
Using antisense technology, we identified an<br />
antisense oligonucleotide, ISIS-TTRRx, for the treatment of<br />
TTR-associated amyloidosis. When tested in a human TTR<br />
transgenic mouse model, ISIS-TTRRx showed a dose-dependent<br />
reduction of human TTR at both the mRNA and protein<br />
levels. In cynomolgus monkeys, ISIS-TTRRx treatment produced<br />
a time-dependent reduction in plasma TTR levels. After<br />
12 weeks of treatment, liver TTR mRNA and plasma<br />
TTR protein levels were reduced by 80%. We also observed<br />
a significant decrease in plasma RBP4 levels correlating with<br />
TTR reduction. ISIS-TTRRx treatment was well tolerated in<br />
both rodents and monkeys and produced a PK/PD profile<br />
consistent with prior experience using this chemistry platform.<br />
ISIS-TTRRx is currently under evaluation in a Phase I<br />
clinical trial, with the first cohort dosed in May 2011.<br />
Study supported by: Isis Pharmaceuticals<br />
Shuling Guo, Elizabeth Ackermann, Sheri Booten, Luis<br />
Alvarado, Steve Hughes and Brett Monia are all employees<br />
at Isis Pharmaceuticals<br />
Neurogenetics<br />
M1011. EPI-A0001: New Potential Therapy for<br />
Friedreich Ataxia<br />
David R. Lynch, Steve M. Willi, Robert B. Wilson, Karlla W.<br />
Brigatti, Olena Kucheruck, Eric C. Deutsch, William D.<br />
Shrader, Patrice Rioux, Guy Miller, Amale Hawi and Thomas<br />
Sciascia; Philadelphia, PA; Patterson, NY and Mountain View,<br />
CA<br />
This study tested the ability of EPI-A0001(previously called<br />
A0001) (a-tocopherol quinone), to improve in vitro measures,<br />
glucose metabolism and neurological function in Friedreich<br />
ataxia. We used an in vitro assay of cell rescue followed<br />
by a double blind, placebo controlled trial of 2 doses<br />
of EPI-A0001 in 30 adults. The primary clinical trial outcome<br />
was disposition index, a measure of diabetic tendency,<br />
from an IVGTT, evaluated 4 weeks after treatment. Secondary<br />
neurologic measures included the Friedreich ataxia rating<br />
scale (FARS).<br />
EPI-A0001 inhibited cell death in FRDA models in vitro.<br />
For the clinical trial, mean GAA repeat length was 699, and<br />
mean age was 31. Four weeks after treatment initiation,<br />
changes in disposition index between subjects treated with<br />
EPI-A0001 and placebo were not statistically significant. In<br />
contrast, a dose dependent improvement in FARS score was<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 106<br />
found. Patients on placebo improved 2.0 FARS points while<br />
patients on low dose EPI-A0001 improved by 4.9 points (p<br />
¼ 0.04) and patients on high dose improved by 6.1 points<br />
(p
<strong>136</strong> th Annual Meeting Tuesday,<br />
September 27, 2011 Works in<br />
Progress Poster Session<br />
WIP posters will be displayed in Elizabeth A-E of the<br />
Manchester Grand Hyatt from 10:00 am – 7:00 pm,<br />
with authors present from 6:00 pm – 7:00 pm.<br />
The Works in Progress category emphasizes ongoing clinical<br />
or basic research of an extraordinary nature, which warrants<br />
expediated presentation. These abstracts were selected<br />
based on scientific merit, timeliness, and anticipated interest<br />
to the membership. Key aspects of research must have been<br />
conducted after the regular abstract deadline.<br />
Dementia and Aging<br />
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 107<br />
T1538. Proneurogenic Compound Reduces Synaptic<br />
Ab-42 Oligomer Levels and Shows Cognitive Benefit<br />
in Alzheimer’s Mouse Model<br />
Sam Gandy, John W. Steele, Charles Glabe, Kai Treuner, Todd<br />
Albert, Carrolee Barlow, Michelle E. Ehrlich and Soong Ho<br />
Kim; New York, NY; Irvine, CA and San Diego, CA<br />
Group II metabotropic glutamate receptors (Gp II mGluR)<br />
trigger production of Ab peptides from isolated synaptic terminals,<br />
and synaptic Ab42 generation is selectively suppressed<br />
by Gp II mGluR antagonists. Gp II mGluR antagonists<br />
also stimulate hippocampal neurogenesis and enhance<br />
cognition. Pilot studies were performed in old (18 mo) and<br />
young (6 mo) Dutch APP693Q x PS1D Exon 9 bigenic<br />
mice. After 3 wk oral BCI-838 treatment of 18 mo-old<br />
mice, levels of prefibrillar A11-immunoreactive Ab oligomers<br />
were decreased in hippocampi from treated mice (p<br />
0.01). In young Dutch APP693Q x PS1D Exon 9 mice,<br />
fibrillar OC-immunoreactive Ab oligomer levels were<br />
decreased in the treated young mice (p 0.01). Some<br />
Dutch APP693Q and wildtype littermates were given BCI-<br />
838 p.o. for 3 mo. BCI-838 treatment was associated with<br />
improved memory in cued fear conditioning (p ¼ 0.01<br />
TgþVeh vs TgþBCI-838). A trend toward reduced anxiety<br />
was also observed (p ¼ 0.086 for TgþVeh vs TgþBCI-<br />
838). GpII mGluR antagonists are promising compounds<br />
for prevention or treatment of AD because of their unique<br />
synaptic Ab42- and Ab-oligomer-lowering activity coexisting<br />
with pro-cognitive and pro-neurogenic activities.<br />
Study supported by: P01 AG10491<br />
Carrolee Barlow is CSO at BrainCells. Todd Albert and<br />
Kai Treuner are staff scientists at BrainCells.<br />
T1539. Alzheimer Risk Variant Clusterin (CLU) and<br />
Brain Function during Aging<br />
Madhav Thambisetty, Lori Beason-Held, Michael Kraut,<br />
Michael Nalls, Andrew Singleton, Luigi Ferrucci, Simon<br />
Lovestone and Susan Resnick; Baltimore and London, United<br />
Kingdom<br />
Recent genome wide association studies have identified common<br />
risk variants for Alzheimer’s disease (AD), although<br />
these exert small effects and are, by themselves, unlikely to be<br />
of clinical utility in risk prediction. However, these genetic<br />
risk variants may reveal mechanisms involved in the transition<br />
from normal aging to cognitive impairment. We examined<br />
the effect of the recently discovered AD risk variant<br />
rs11<strong>136</strong>000 single nucleotide polymorphism in the clusterin<br />
gene (CLU) on longitudinal changes in resting state regional<br />
cerebral blood flow (rCBF) during normal aging. 15O-water<br />
107<br />
positron emission tomography measurements of rCBF were<br />
available at baseline and up to 7 annual follow-up visits in 88<br />
cognitively normal older individuals in whom genome-wide<br />
genotyping data were collected. Cognitively normal carriers<br />
of the risk allele of the rs11<strong>136</strong>000 SNP in CLU show significant<br />
and dose-dependent longitudinal increases in resting<br />
state rCBF in brain regions intrinsic to memory processes.<br />
We propose that these increments in rCBF over time represent<br />
compensatory changes in neuronal activity required to<br />
maintain normal cognition during aging in at-risk individuals,<br />
and that their eventual failure in some may mark the<br />
transition from normal aging to Alzheimer’s disease.<br />
Study supported by: NIA Intramural Research Program<br />
T1540. <strong>Association</strong> of High Density Lipoprotein to<br />
Alzheimer Disease<br />
Ramin Ebrahimi, Naser Ahmahi, Fereshteh Hajsadeghi and<br />
Hormoz Babaei; LA, CA<br />
Background: Alzheimer’s disease (AD) is a devastating progressive<br />
neurologic disorder with increasing prevalence. Little<br />
data exists regarding association of HDL-c to AD. This<br />
study evaluates the association of different HDL-c levels<br />
with AD.<br />
Methods: This study consists of 2144 Veterans with AD<br />
and 16175 without AD. VA electronic medical records from<br />
veterans were used to evaluate the presence or absence of<br />
AD, HDL levels and risk factors. HDL-c was classified as<br />
HDL-c 50 mg/dl. Conditional<br />
logistic regression analysis was employed to assess the<br />
association of lower levels of HDL-c with AD.<br />
Results: The mean age was 7966 years. After adjustment<br />
for risk factors, odds ratio of AD was 2.20 (95% CI 2.09–<br />
2.31, p ¼ 0.0001) for those with HDL-c of 40–50 mg/dl and<br />
2.89 (95% CI 2.75–3.05, p ¼ 0.0001) for those with HDL-c<br />
50 mg/dL.<br />
Conclusion: There is a strong association between lower<br />
levels of HDL-c and AD. Furthermore, population attribution<br />
risk of lower levels of HDL-c for new AD is very high;<br />
warranting future studies evaluating the role of specific lipid<br />
therapy to improve HDL-c levels to potentially decreased<br />
future development of AD.<br />
Study supported by: Self<br />
T1541. Amyloid-b 42:40 Metabolism Is Altered in<br />
Autosomal Dominant Alzheimer’s Disease (ADAD)<br />
Rachel E. Potter, Vitaliy Ovid, Tom Kasten, Wendy Sigurdson,<br />
Kwasi Mawuenyega, Bruce Patterson, Don Elbert, Scot Fague,<br />
Sumi Chakraverty, Alison Goate, Kevin Yarasheski, John C.<br />
Morris, Tammie Benzinger and Randall J. Bateman; St. Louis,<br />
MO<br />
We hypothesized that ADAD is caused by mutations that<br />
lead to higher production rates for amyloid-beta (Ab) 42<br />
compared to Ab40. We measured Ab isoform production<br />
and clearance rates in ADAD participants to determine the<br />
effects of mutations which invariably lead to AD. Presenilin<br />
1 mutation carriers (46.2yrs 6 15.8 (N ¼ 7)), and related<br />
non-carriers (52.0yrs 6 20.5 (N ¼ 7)) completed Ab stable<br />
isotope labeling 13 C6-Leu kinetic studies of cerebrospinal<br />
fluid, and PET PIB imaging. Differences in the Ab42 relative<br />
to Ab40 labeling curves were specifically altered in<br />
mutation carriers versus non-carriers. Newly generated Ab42<br />
was detected before Ab40 or 38, and there were differences<br />
in area under the curve analyses. These findings support<br />
prior in vitro studies that Ab42 is overproduced relative to<br />
other Ab isoforms. Ab isoform production and clearance<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
may be used to define the therapeutic effectiveness of treatments<br />
which target abnormal Ab metabolism in AD.<br />
Study supported by: This work was supported by a grant<br />
from NIH (no. P01AG026276), an anonymous foundation,<br />
Eli Lilly research, the Knight Initiative for Alzheimer’s<br />
Research, and the James and Elizabeth McDonnell Fund for<br />
Alzheimer’s Research. R.J.B. is a cofounder of a company<br />
(C2N Diagnostics) that has licensed a pending Washington<br />
University patent on the technology described in this article.<br />
T1542. Acetylated Tau, a Novel Pathological Signature<br />
in Alzheimer’s Disease and Other Tauopathies<br />
David J. Irwin, Todd Cohen, Murray Grossman, Steven E.<br />
Arnold, Sharon X. Xie, Virginia M.Y. Lee and John Q.<br />
Trojanowski; Philadelphia, PA<br />
The microtubule-binding protein, tau, is the major component<br />
of neurofibrillary inclusions characteristic of Alzheimer’s<br />
disease (AD) and related tauopathies. Recently, we reported<br />
that the acetylation of tau at lysine residue 280 (ac-K280) is<br />
a novel, pathological post-translational modification. Here,<br />
we performed detailed immunohistochemistry (IHC) to further<br />
characterize tau ac-K280 expression in tauopathies.<br />
Ac-K280 tau IHC was conducted on 30 postmortem central<br />
nervous system (CNS) regions from AD (n ¼ 10), corticobasal<br />
degeneration (CBD; n ¼ 5), and progressive<br />
supranuclear palsy (PSP; n ¼ 5) patients. Ac-K280-immunoreactive<br />
(Ir) tau pathology was compared to multiple<br />
well-characterized tau epitopes.<br />
All cases showed significant CNS ac-K280-Ir tau pathology<br />
in a distribution pattern similar to hyperphosphorylated-tau.<br />
In AD cases, the majority of ac-K280-Ir tau pathology<br />
was in intracellular, thioflavin-S (ThS) positive tau<br />
inclusions, and also ThS negative tau pathology in CBD<br />
and PSP. Ac-K280-Ir was present throughout all stages of<br />
AD pathology, but more prominent in later stages.<br />
Ac-K280-Ir is a pathological modification of tau that<br />
may contribute to neurodegeneration by augmenting losses<br />
of normal tau properties, as well as toxic gains of function.<br />
Thus, inhibiting tau acetylation could be a disease modifying<br />
drug discovery target for tauopathies.<br />
Study supported by: NIH grants: T32-AG000255 Training<br />
in Age-Related Neurodegenerative Diseases and P30<br />
AG010124-20 Alzheimer’s Disease Core Center grant.<br />
Headache and Pain<br />
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 108<br />
T1623. Retrospective Analysis of Major Congenital<br />
Malformations (MCMs) and Oral Clefts (OC) Associated<br />
with In-Utero Topiramate Exposure<br />
Mark W. Green and Arun Bhattachuria; New York, NY and<br />
Yardley, PA<br />
Purpose: To analyze the prevalence of malformations<br />
among infants born to women exposed to topiramate.<br />
Methods: This study used retrospective data from Wolters-Kluwer<br />
Pharma Solutions that followed patients’ Pharmacy<br />
and Medical Claims (1/2003–12/2010) to identify<br />
infants exposed to topiramate during pregnancy (n ¼ 778).<br />
Probable exposure during pregnancy was refined using data<br />
on script fill date/supply, infant birth date, and ICD-9<br />
codes for birth term.<br />
Control cohorts included women with diagnosis of migraine<br />
without epilepsy (n ¼ 26,920) and a subset exposed<br />
to acute-preventive migraine drugs (APMD) during pregnancy<br />
(n ¼ 2,964). Topiramate was excluded from both<br />
groups. All cohorts excluded known or suspected teratogens.<br />
108<br />
Results: MCM rates were 4.11%, 4.02% and 4.15% for<br />
TPM, migraineurs, and APMD-treated migraineurs, respectively.<br />
Relative risks (95% CI) for TPM vs. migraineurs and<br />
APMD-treated migraineurs were 1.02 (0.73–1.45) and 0.99<br />
(0.68–1.45), respectively. OC rates were 0.26%, 0.17%, and<br />
0.37% for the TPM, migraineurs, and APMD-treated<br />
migraineurs, respectively. Relative risks (95% CI) for TPM<br />
vs. migraineurs and APMD-treated migraineurs were 1.50<br />
(0.37–6.19) and 0.69 (0.15–3.12), respectively.<br />
Conclusions: TPM exposure did not significantly<br />
increase the rates of OC or MCM.<br />
Study supported by: Vivus, Inc.<br />
Neuroimmunology and Demyelinating Disease<br />
T1741. Comparison of MRI Techniques for Monitoring<br />
of Multiple Sclerosis<br />
Manuela Vaneckova, Jan Krasensky, Tomas Kalincik, Dana<br />
Horakova, Eva Havrdova and Zdenek Seidl; Prague, Czech<br />
Republic<br />
Goal: To compare contemporary MRI measures for prediction<br />
of future clinical disability in multiple sclerosis patients<br />
by analysis of our MRI data (brain atrophy, T2 lesion volume,<br />
T1 lesion volume and corpus callosum atrophy).<br />
Methods: Long term (7-year) longitudinal MRI data of<br />
178 patients were analyzed Area of corpus callosum, T2<br />
lesion volume, T1 lesion volume, brain parenchymal fraction<br />
and brain atrophy were measured. Clinical disability<br />
was assessed with Expanded Disability Status Scale (EDSS).<br />
Patients were divided in two groups: clinically stable and<br />
those with sustained progression during seven years.<br />
Results: Statistically significant correlation of future clinical<br />
disability (as characterized by EDSS score) with brain atrophy<br />
and corpus callosum atrophy was found. In this retrospective<br />
study, clinically stable patients were distinguished from<br />
patients with sustained progression in less than 1 year using<br />
the corpus callosum atrophy (probability over 98%) and after<br />
3 years using the brain atrophy (with probability of 96%).<br />
Conclusions: We have shown that the corpus callosum<br />
atrophy is a superior marker of disease progression compared<br />
to the brain atrophy, which was considered to be its<br />
most significant marker.<br />
Supported by Biogen Idec Inc. and the grants<br />
MZOVFN2005, MSM 0021620849.<br />
Study supported by: Supported by Biogen Idec Inc. and<br />
the grants MZOVFN2005 and MSM 0021620849.<br />
T1742. Effects of Rituximab on T-Cells in MS<br />
Uma Vinayagasundaram, Ellen M. Mowry, Ian R. Matthews,<br />
Julia Marino and Emmanuelle Waubant; San Francisco, CA<br />
Objective: To examine rituximab effect on T-cell subsets.<br />
Background: Rituximab, an anti-CD20 antibody, profoundly<br />
depletes circulating B-cells. It is unclear how it<br />
impacts T-cells. Methods: In a retrospective study of<br />
patients who received >1 rituximab infusions at UCSF MS<br />
center, within-patient pre- and post-infusion (mean duration<br />
¼ 7 months) lymphocyte counts for the first rituximab<br />
course were compared. Results: Of 119 patients who<br />
received rituximab, 56 (45 MS, 10 NMO, 1 other indication)<br />
had both pre- and post-infusion labs. The mean (þ<br />
SD) absolute count of CD19þ B-cells dropped from 273<br />
(þ 25) pre- vs. 59 (þ17) post-rituximab (p
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 109<br />
count below 500, and 4 (6%) had a CD4 count below 200.<br />
NK cell number (CD56þ, CD16-) tended to increase postinfusion<br />
(182 þ 13 vs. 199 þ 14; p ¼ 0.2). Impact of retreatment<br />
is being analyzed. Conclusions: Rituximab induces<br />
long-term T-cell reduction, whose impact is unclear.<br />
Study supported by: Research grant from Roche<br />
T1743. Fast Macromolecular Proton Fraction (MPF)<br />
Mapping in Multiple Sclerosis (MS)<br />
Vasily L. Yarnykh, James D. Bowen, Bart P. Keogh, Pavle<br />
Repovic, Angeli Mayadev, Beena Gangadharan, Daniel S.<br />
Rizzuto, Hunter R. Underhill, Kenneth R. Maravilla and Lily<br />
K. Jung-Henson; Seattle, WA<br />
MPF mapping is a new quantitative imaging method, which<br />
determines relative concentration of macromolecular protons<br />
involved into the magnetization transfer effect. Literature suggests<br />
strong correlations between MPF and myelin content in<br />
neural tissues. We recently developed a fast 3D MPF mapping<br />
technique for clinical applications, which utilizes two images<br />
(with and without off-resonance saturation), and complimentary<br />
T1, B0, andB1maps, providing whole-brain coverage,<br />
1.5 1.5 4mm 3 resolution, and
J_ID: ZAY Customer A_ID: SUPP11-7 Cadmus Art: 22580 Date: 26-August-11 Stage: Page: 110<br />
immunopathology. Therefore, iTregs could play contrasting<br />
roles depending upon the stage of virus-mediated demyelinating<br />
diseases.<br />
Study supported by: National Center for Research<br />
Resources of the National Institutes of Health.<br />
T1747 Idiopathic Relapsing Conus Myelitis<br />
Raghav Govindarajan and Efrain Salgado; Weston, FL<br />
Background: Idiopathic acute transverse myelitis (TM)<br />
involves the thoracic cord. In rare cases conus might be the<br />
only site involved. Bladder symptoms can be a presenting<br />
feature without an obvious sensory level. Imaging studies<br />
might remain inconclusive thus posing a diagnostic challenge.<br />
Relapses in TM are rare and even more so restricted<br />
to the conus. We report a case of a 42 year-old female who<br />
presented with urinary retention (UR) that progressed to a<br />
flaccid paraplegia (FP). Imaging studies were negative ini-<br />
110<br />
tially with repeat imaging 5 days from symptom onset<br />
revealing a conus myelitis (CM).<br />
Case report: A 42-year-old female woke up with UR,<br />
which progressed to an ascending FP without a sensory<br />
level. MRI of spinal axis w/wo was normal. Lumbar<br />
puncture revealed 0 WBC, 1 RBC, normal protein,<br />
glucose and negative immune markers (IgG Index and<br />
oligoclonal bands). EMG was normal. MRI of the lumbar<br />
spine repeated 5 days later revealed CM. Extensive<br />
infectious, inflammatory and autoimmune work up<br />
including NMO was negative. Brain MRI w/wo was<br />
normal as were VEPs. She had a relapse 3 months after<br />
the initial bout.<br />
Conclusion: Idiopathic CM appears to be a rare clinical<br />
entity, which can have protean manifestations requiring a<br />
high index of clinical suspicion and a thorough systematic<br />
workup.<br />
Study supported by: None<br />
ID: kannanb I Black Lining: [ON] I Time: 17:25 I Path: N:/3b2/ANA#/Vol00000/110245/APPFile/JW-ANA#110245
J_ID: ZAY Customer A_ID: SUPP11-8 Cadmus Art: 22581 Date: 26-August-11 Stage: Page: 111<br />
<strong>136</strong> th Annual Meeting Sunday,<br />
September 25, 2011 Career<br />
Development Poster Session<br />
Abstracts<br />
Posters will be displayed in Elizabeth A-E of the Manchester<br />
Grand Hyatt from 10:00 am – 7:00 pm, with<br />
authors present from 6:00 pm – 7:00 pm.<br />
CD515. Non-Convulsive Status Epilepticus Is Associated<br />
with Mortality and Worse Short-Term Outcome in<br />
Critically Ill Children<br />
Nicholas S. Abend, Alexis A. Topjian and Dennis J. Dlugos;<br />
Philadelphia, PA<br />
Objective: Determine whether non-convulsive seizures<br />
(NCS) and non-convulsive status epilepticus (NCSE) were<br />
associated with higher mortality and worse short-term<br />
outcome.<br />
Methods: Critically ill children with acute encephalopathy<br />
underwent EEG monitoring. EEGs scored as no seizures,<br />
NCS, or NCSE. Co-variates included age, etiology of<br />
acute encephalopathy, and EEG background. Outcomes<br />
were mortality and change in Glasgow Outcome Scale<br />
(GOS) from admission to ICU discharge. Chi-squared analysis<br />
and multi-variable logistic regression were used to evaluate<br />
for associations.<br />
Results: 200 children underwent cEEG. NCS occurred<br />
in 84 (42%) of which 43 (22%) had NCSE. 83 (41%) had<br />
a decrease in GOS of which 36 (18%) died. In multi-variate<br />
analysis NCSE was associated with mortality (OR 3.05,<br />
p¼0.04) and change in GOS (OR 15.5, P
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 112<br />
Aasly, J. S204, S209<br />
Aasly, Jan T1503<br />
Abbott, Robert D. S203<br />
Abolfazlee, R. S114, T1732<br />
Achim, Critian L. T1905<br />
Adams, Patrick E. T1521<br />
Agadi, Jagadish B. M822<br />
Agbemenyah, Hope Yao M1004<br />
Aggarwal, Swati M821<br />
Ahlskog, J.E. M606<br />
Ahmed, Aiesha M833<br />
Akbar, Umer M1205, T1620,<br />
T1809<br />
Akber, Umer M719<br />
Akfirat, Gokhan T1536<br />
Akiyama, Hisanao S120<br />
Aksan, Nazan M615<br />
Al Samara, Mershed M722<br />
Alaedini, Armin M602<br />
Alam, Nurul S123<br />
Alcalay, Roy N. S225<br />
Aldea, Patricia T1901<br />
Alexander, Katie M821<br />
Alexopoulos, Andreas V. M711<br />
Alexopoulos, Harry T1729<br />
Alfahad, Tariq S127<br />
Alfano, Lindsay N. M802<br />
Alfuth, Kathleen S. M832<br />
Algom, Avi M1007<br />
Alkawadri, Mhd Rafeed M711<br />
Allen, Mariet T1503<br />
Allred, Peggy M821<br />
Alqadi, Khalid S. S127<br />
Altafullah, Irfan S102<br />
Althaus, Alison L. M1401<br />
Amini Harandi, Ali S114, T1712,<br />
T1718, T1722, T1723,<br />
T1731, T1732, T1734<br />
Ances, Beau T1901<br />
Andersen, O. S204, S209<br />
Anderson, C. Alan M616<br />
Andres, Patricia M821<br />
Andress-Rothrock, Diane C.<br />
S113, T1602<br />
Andrews, Mark M1106<br />
Annex, Brian H. S115<br />
Ansari, Hossein S236<br />
Ansari, Morad T1503<br />
Appel, Shmuel M702<br />
Arain, Fazal M. M707<br />
Arcilla-Londono, Ximena M828<br />
Arciniegas, David B. M616<br />
Ard, M. Colin T1531<br />
ABSTRACT AUTHOR INDEX<br />
Arnoldi, Alessia M1002<br />
Artibee, Kay M810<br />
Asadollahi, Marjan T1732<br />
Ascherio, Alberto S216<br />
Askanas, Valerie M807, M808,<br />
M816, M835<br />
Assadi, Mitra S223<br />
Astafiev, Serguei V. M601<br />
Atassi, Farrah S215<br />
Atkinson, Elizabeth J. M1008<br />
Au, Rhoda T1504<br />
Auchus, Alexander P. M1301<br />
Awkar, Nelly M717<br />
Azimi, Amirreza T1722<br />
Babikian, Viken L. S122<br />
Babovic, Mihajlo T1727<br />
Backus, Carey M804<br />
Bagai, Kanika S303<br />
Baiser, Alexa S. T1504<br />
Baker, M. S204, S209<br />
Bakken, Erik C. M618, M619<br />
Bakst, Isaac M821<br />
Balasubramanian, Archana B.<br />
T1524<br />
Balice-Gordon, Rita<br />
T1701, T1716<br />
Baloh, Bob M815<br />
Baloyannis, Stavros J. T1528<br />
Bammler, Theodor K. T1511<br />
Banerjee, Chirantan S101<br />
Bankiewicz, Krystopf S. T1529<br />
Barbato, Luigi M. T1735<br />
Barcikowska, Maria T1503<br />
Bardin, Jonathan C. M1104<br />
Barkhof, Frederik T1708<br />
Barnwell, Stanley L. T1606<br />
Bartz, Traci T1513<br />
Bass, Dale M1107<br />
Bassi, Mariateresa M1002<br />
Bassile, Clare M1403<br />
Basta, Milan S103<br />
Bateman, Lisa M. M703<br />
Bateman, Randall J. T1501<br />
Bayat, Elham T1739<br />
Bayram, Mehmed B. T1527<br />
Beal, Flint S216<br />
Beck, James S216<br />
Beckmann, Karola T1702<br />
Beh, Shin C. S210<br />
Belichenko, Pavel V. M609,<br />
M712<br />
Bellugi, Ursula M608<br />
Benke, Tim A. M706<br />
112<br />
Ben-Menachem, Elinor M713<br />
Bennett, C.F. M821<br />
Bennett, David A. T1502<br />
Bennett, Jeffrey L. T1736<br />
Benzinger, Tammie T1901<br />
Berlau, Daniel J. T1524<br />
Bernard, Bryan S211<br />
Bernard, Paul B. M706<br />
Beyer, Richard P. T1511<br />
Bhabad, Sudeep S119<br />
Bhargava, Pavan S140<br />
Bhat, Sushanth M718, M834,<br />
S134, S137<br />
Bhattacharya, Pratik S129<br />
Bieber, Allan M1101<br />
Biglan, Kevin S228<br />
Biglan, Kevin M. S402<br />
Bigwood, Doug T1736<br />
Bilal, Yasmin T1737<br />
Billings, Nia M. M613<br />
Biondo, Andrew M828<br />
Bisceglio, Gina T1503<br />
Bishop, Kathie M821<br />
Black, Robert E. S123<br />
Blair, Aaron S208<br />
Blakeman, Alan T1621<br />
Blasco, Maria R. T1713<br />
Blechschmidt, Cristiane M835<br />
Blennow, Kaj T1514<br />
Bliton, Mark S232<br />
Bliwise, Donald L. S301<br />
Blythe, Anne M819<br />
Bockenek, William L. M819<br />
Bodda, Chiranjeevi M1004<br />
Boden-Albala, Bernadette M1403<br />
Bodensteiner, John B. M1303<br />
Boes, Benjamin M1008<br />
Boeve, Bradley F. T1530<br />
Boffa, Michael S302<br />
Bonanni, Paolo M1002<br />
Bonato, Sara M1002<br />
Bondar, Galyna T1704<br />
Boon, Andrea M826<br />
Bordelon, Yvette S213<br />
Borkowski, Thomas M. T1615<br />
Borland, Scott T1617<br />
Bota, Daniela T1804<br />
Botuyan, Maria V. M1008<br />
Boutin, Paula T1719<br />
Boyd, Scott D. T1736<br />
Bravver, Elena M814, M819<br />
Brennan, K.C. T1601<br />
Bresolin, Nereo M1002<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 113<br />
Bressman, Susan B. S233<br />
Brewer, James B. T1514<br />
Bringas, J. T1529<br />
Britton, Jeffrey W. M1202,<br />
M1203, S403<br />
Broderick, D.F. S204<br />
Broderick, Joseph S112<br />
Brooks, Benjamin M821<br />
Brooks, Benjamin R. M814,<br />
M819<br />
Brooks-Kayal, Amy R. M705<br />
Brott, Thomas G. S102, S116<br />
Brown, Amanda S407<br />
Brown, O.W. S102<br />
Bruce, Nhu T. S131<br />
Bryant, Monthaporn S. S215<br />
Bucelli, Robert S406<br />
Buckley, Camilla T1711<br />
Buckley, Charlotte T1903, T1904<br />
Bumbaugh, Jon T1614<br />
Burakgazi, Evren T1620<br />
Burakgazi-Dalkili, Evren M1205<br />
Burge, Daniel J. T1724<br />
Burger, Kathleen S127<br />
Burke, James M1107<br />
Buse, Dawn C. T1608, T1610,<br />
T1611, T1612, T1613,<br />
T1615<br />
Bushara, Khalaf O. M602<br />
Busta, Angela S. M804<br />
Cacabelos, Ramon T1506<br />
Cacciottolo, Mafalda M807<br />
Cai, Haipeng M1301<br />
Caillier, Stacy T1713<br />
Callaghan, Brian M1005<br />
Camargo, Carlos A. S139<br />
Cambon, Alex C. S213<br />
Campbell, Christina M1204<br />
Campbell, Harry T1503<br />
Campos-Rivera, Juanita T1719<br />
Can, Karolina M1004<br />
Cannigaiper Uthamaroyan,<br />
Velmurugendran S121<br />
Cao, Chuanhai S202<br />
Capehart, Bruce P. M1107<br />
Caplan, Louis S<strong>136</strong><br />
Carlson, H. T1522<br />
Carlson, Noel G. T1801<br />
Carone, Marco S123<br />
Carran, Melissa T1809<br />
Carrasquillo, Minerva M. T1503<br />
Carter, Alex R. M601<br />
Casadesus, Gemma M620<br />
Casanova, Vanessa M1002<br />
Case, Amanda M1001<br />
Castano, Anna M706<br />
Catellier, Diane J. T1505<br />
Cava, Luis S113<br />
Cen, Steven S221<br />
Cervantes, Anna M. S122<br />
Chai, High Seng T1503<br />
Chana, Gursharan T1905<br />
Chandrakumar,<br />
Manokaraananthan T1621<br />
Chandrasekaran, Krish M801<br />
Chang, Bernard S. M704<br />
Charles, David S224, S232<br />
Charles, P. David S226<br />
Chaturvedi, Seemant S129<br />
Chemali, Zeina S214<br />
Chen, Chueh-Tan T1537<br />
Chen, Helen M801<br />
Chen, Honglei S208, S234<br />
Chen, Jian M1301<br />
Chen, Roujie M1403<br />
Chen, Shun-Sheng T1537<br />
Chen, Xinzhi S103<br />
Chen, Yi T1715<br />
Cheng, Chu M1402<br />
Cheng, Hsinlin T. T1604<br />
Cheng, Jiin-Tsuey T1537<br />
Cheng, Ping M607<br />
Cheng, Yuching S107<br />
Cheong, Hae Kwan T1519<br />
Chernoff, Jonathan M803<br />
Cheung, Ying K. M1403<br />
Chibnik, Lori B. T1502<br />
Chipendo, Portia I. T1502<br />
Chisulo, Brian T1908<br />
Chitnis, Shilpa S210<br />
Chiu, David S116<br />
Cho, Chi T1740<br />
Choi, Jae-Hwan S126<br />
Choi, Kwang-Dong S126<br />
Choi, Soon Gang M824<br />
Chokroverty, Sudhansu M718<br />
Choudary, Zahid S130<br />
Choudary, Zahid I. S135<br />
Choudhary, Shazia Z. S130,<br />
S135<br />
Chretien, Nathalie T1721<br />
Christensen, Jon T1901<br />
Christie, Kimberly J. M1402<br />
Christine, C.W. S204, S209<br />
Christodoulou, Joanna A.<br />
M704<br />
Christopher, Hanlon T. T1602<br />
Chuang, Yu-Ming S106<br />
Chun, Jerold T1710<br />
Chung, Amy S. T1802<br />
Churchwell, Mona I. T1511<br />
Ciric, Bogojub T1725<br />
113<br />
Clark, Chris M. T1508<br />
Clark, K. Reed M802<br />
Clawson, Susan A. T1801<br />
Clifford, David T1901<br />
Clifton, Guy L. M1103<br />
Cohen, Jeffery A. T1710<br />
Cohen, Jeffrey T1708<br />
Cohen, Jeffrey A. T1709<br />
Coker, Laura H. T1505<br />
Cole, John W. S107<br />
Collins, William T1709<br />
Comi, Giacomo M1002<br />
Comi, Giancarlo T1708<br />
Conte, Mary M. M1104<br />
Contractor, Anis T1701<br />
Cook, Jason A. S224<br />
Corbetta, Maurizio M601<br />
Coresh, Josef T1505<br />
Corey-Bloom, Jody S205, S220,<br />
T1507<br />
Corrada, Maria M. T1508,<br />
T1524<br />
Corrigan, John M828<br />
Cote, Lucien S225<br />
Couto, Joseph T1614<br />
Cowell, Lindsay G. T1736<br />
Crimella, Claudia M1002<br />
Crook, Julia T1503<br />
Crowder, Kermit S109<br />
Cruz Del Angel, Yasmin M705<br />
Cruz-Flores, Salvador T1513<br />
Cudkowicz, Merit M821<br />
Cuevas, Ivan T1506<br />
Cunningham,<br />
Christopher R. S213<br />
Cunningham, Julie M. M1008<br />
Cutter, Gary T1702<br />
D’Agostino, Carla M807, M808<br />
Dakka, Youssef A. M828<br />
Dalakas, Marinos C. T1729<br />
Dale, Anders M. T1525<br />
Dalmau, Josep T1701, T1716<br />
D’Angelo, Grazia M1002<br />
Das, Moromi S104<br />
Dauch, Jacqueline R. T1604<br />
David, William M821<br />
Davis, Bonnie S109<br />
Davis, Thomas L. S232<br />
D’Cruz, O’Neill M714<br />
De Jager, Philip T1720<br />
De Jager, Philip L. T1502<br />
DeArmond, S. S204, S209<br />
DeCarli, Charles T1504<br />
Decker, David A. S130, S135<br />
Deeley, Cheryl S228<br />
DeFreitas, Tiffani T1615<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 114<br />
DeFries, Ashleigh T1534<br />
Dekermenjian, Rony S134, S137<br />
del Pilar Cortes<br />
Nino, Maria T1906<br />
Del Tufo, Stephanie N. M704<br />
Delaney, Colin E. M1005<br />
Delgado, Monica T1705<br />
Demaerschalk,<br />
Bart M. S102, S116<br />
Denic, Aleksandar T1703<br />
DeOrchis, Vincent S. T1518<br />
Derani, Lena T1739<br />
Desai, Urvi G. M819<br />
Dham, Bhavpreet S223, T1620,<br />
T1809<br />
Dhamija, Radhika S403<br />
Diaz-Medina, Gloria E. S403<br />
Dickson, D.W. S204, S209<br />
Dickson, Dennis W. M1007,<br />
S207, T1503,<br />
T1515, T1530<br />
DiClemente, Guillermo T1534<br />
Diep, Lien S109<br />
Dilley, Deanne M714<br />
DiVito, Brittany M. M618, M619<br />
Dodge, Hiroko T1532<br />
Dodick, David T1617<br />
Doerge, Daniel R. T1511<br />
Dominantly Inherited<br />
Alzheimer Network T1501<br />
Dorsey, E. Ray S402<br />
Dosado, Lea M830<br />
Doty, Pamela M713, M714<br />
Dowling, James J. M804<br />
Du, Guangwei S206, S212, S234<br />
Du, Senxi T1804<br />
Du, Sienmi T1704<br />
Duane, Drake D. M618, M619<br />
Dubinsky, Richard S213<br />
Dueker, Nicole S107<br />
Duncan, G. T1522<br />
Duquette, Pierre T1713<br />
Durand, Dominique M620<br />
Dustin, Irene M702<br />
Dyck, P. James M1008<br />
Dyck, Peter J. M1008<br />
Eastman, Alison J. M1001<br />
Eastman, Eric T1736<br />
Eberly, Shirley S216<br />
Ebers, George T1702<br />
Edland, Steven D. M1010,<br />
S205, T1531<br />
Edlow, Jonathan A. S139<br />
Edson, Jean S109<br />
Edythe, Wiggs A. M820<br />
Eizenamn, Moshe M607<br />
Elble, Rodger J. S140<br />
Eleopra, Roberto S237<br />
El-Hagrassy, Mirret T1536<br />
Elkind, Mitchell S.V. S101<br />
Ellik, Shehanaz M828<br />
Elliott, Robin S216<br />
Ellis, Ronald J. T1905<br />
Elsayed, Mohammad M613<br />
Engel, King W. M808, M816,<br />
M835<br />
Engel, W. King M807<br />
Ertekin-Taner, Nilufer T1503<br />
Erten-Lyons, Deniz T1532<br />
Eslinger, Paul J. S206, S212<br />
Etemadifar, Masoud T1732<br />
Evans, Denis A. T1502<br />
Evensen, Laura A. M1403<br />
Everall, Ian P. T1905<br />
Faezi, Sholeh T1731<br />
Fagan, Anne T1901<br />
Fallah, A. T1712, T1723<br />
Fang, Yin T1527<br />
Fanning, Kristina T1608<br />
Fanning, Kristina M.<br />
T1610, T1611<br />
Fantin, Marianna M1002<br />
Farber, Charles R. S115<br />
Farheen, Amtul M833, M834,<br />
S134, S137<br />
Farrer, Lindsay T1512<br />
Farrer, Matthew J. S207<br />
Fasih, Zoha S137<br />
Fatima, Tasneem S229<br />
Feany, Mel B. T1502<br />
Feldman, Eva L. M804, M1005,<br />
T1604<br />
Fennema-Notestine,<br />
Christine T1525<br />
Fernandez, Lucia T1506<br />
Ferrari, Michel T1617<br />
Fields, Jeremy D. T1606<br />
Figueroa-Romero, Claudia M1005<br />
Filley, Christopher M. M616<br />
Fincher, Linda S215<br />
Finder, Stuart G. S232<br />
Finlayson, Marcia T1740<br />
Fire, Andrew Z. T1736<br />
Fisher, Barbara C. M610, M614<br />
Fisher, Mark S108<br />
Fishman, Robert A. S124, T1806<br />
Fitzpatrick, Annette T1513<br />
Flagg, Emily S216<br />
Flanagan, Eoin P. M811, T1805<br />
Flanigan, Kevin M. M802<br />
Flemming, Kelly D. S128<br />
Forsayeth, John T1529<br />
114<br />
Forst, Amy T1616<br />
Foulds, Pamela T1726<br />
Fountain, Nathan B. M713,<br />
M714<br />
Fowkes, Mary E. M824<br />
Francis, Gordon T1709<br />
Frederick, Meredith C. M616<br />
Freeman, William D. M1204<br />
Friedland, Robert P. M1301<br />
Frohman, Elliot M. T1736<br />
Frost, Nicholas M723<br />
Fry, Rebecca C. T1511<br />
Fu, Beverly D. T1804<br />
Fugate, Jennifer E. S128, T1714<br />
Fuh, Jong-Ling T1605<br />
Fujioka, Shinsuke M1007, S207<br />
Fulda, Stephany M610, M614<br />
Furuya, Hirokazu S201<br />
Gabbard, Jennifer T1737<br />
Gabrieli, John D.E. M704<br />
Gadallah, Nancy S134<br />
Galasko, Douglas T1525<br />
Galasko, Douglas R. T1531<br />
Galbraith, Sareen T1903<br />
Galbraith, Sareen E. T1904<br />
Gallagher, Martin J. M707<br />
Gallin, Eliza S213<br />
Gamez, Jeffrey T1727<br />
Gamez, Jeffrey D. T1715<br />
Ganeshan, Veena R. T1803<br />
Garbern, J.Y. S204, S209<br />
Garcia, Paul S. S301<br />
Garden, Gwenn A. M1001<br />
Gardiner, Irenita S228<br />
Garges, Danielle M. M610,<br />
M614<br />
George, Benjamin P. S402<br />
Georgescu, Constantin T1503<br />
Gerhardt, Greg A. M709<br />
Ghaffarpour, Majid T1732<br />
Ghaffar-Pour, Majid S114<br />
Gharagozli, Kourosh T1731<br />
Ghareghozli, Kourosh T1718<br />
Ghargozlee, Kourosh T1732<br />
Ghosh, Partha S. M1302<br />
Ghoshal, Shivani S<strong>136</strong><br />
Ghragozlee, Kourosh S114<br />
Gill, Chandler E. S224, S232<br />
Gluhm, Shea S205, S220,<br />
T1507<br />
Goadsby, Peter J. T1603, T1617<br />
Gobinathan, Devathasan M830<br />
Godfrey, Rena A. M820<br />
Goetz, Christopher G. S211, S231<br />
Gohar, Dina T1527<br />
Gokhale, Sankalp S<strong>136</strong><br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 115<br />
Goldfarb, Neil T1614<br />
Goldfine, Andrew M. M1104<br />
Goldman, Jennifer G. S211<br />
Goldstein, Jerome T1618<br />
Goldstein, Jody S205, S220,<br />
T1507<br />
Goltz, Herbert C. T1621<br />
Gomez, Megan S221<br />
Gomez, Yessenia M605<br />
Gonnella, Patricia T1725<br />
Gonzalez, Marco I. M705<br />
Goodin, Douglas S. T1702<br />
Goodman, B. S204, S209<br />
Gordon, Barry M613<br />
Gottdiener, John T1513<br />
Gottesman, Rebecca F. S125,<br />
S132, T1505,<br />
T1513<br />
Gourraud, Pierre-Antoine T1713<br />
Govindarajan, Raghav M822<br />
Grabenstatter, Heidi L. M705<br />
Grabstein, Kenneth T1724<br />
Graff-Radford, Jonathan M606,<br />
T1714<br />
Graff-Radford, Neil T1515<br />
Graff-Radford, Neill R. T1503<br />
Grafton, Scott T. M604<br />
Graham, Stephen M. T1516,<br />
T1517, T1523,<br />
T1526, T1533<br />
Green, Peter H. M602<br />
Greenberg, Benjamin M. T1736<br />
Greenfield, L. John S404<br />
Greenia, Dana E. T1508<br />
Greenlee, John E. T1801<br />
Greenspan, Ralph J. M1006<br />
Grewal, Raji M833<br />
Griffiths, Michael T1904<br />
Griffiths, Mike T1903<br />
Griggs, Robert C. M831<br />
Grinspan, Augusto T1707,<br />
T1708<br />
Groden, Catherine A. M820<br />
Grossardt, Brandon R. T1703<br />
Gu, Yian S225<br />
Gualdi, Sabrina S237<br />
Guo, Fuzheng T1705<br />
Guo, Jiasong M803, M813<br />
Guo, Xuguang S208<br />
Gupta, Divya M718<br />
Gupta, Varun M816<br />
Gutmann, Laurie S236<br />
Gutmann, Ludwig S236<br />
Guzik, Amy K. S115<br />
Habermann, Thomas M. T1805<br />
Hachinski, Vladimir T1510<br />
Hafler, David T1720<br />
Hagerman, Paul J. T1521<br />
Hagerman, Randi J. T1521<br />
Hagler, Jr, Donald J. T1525<br />
Haines, Jonathan T1512<br />
Haleem, Darakhshan Jabeen S229<br />
Hall, Charles T1615<br />
Hall, Deborah A. S213<br />
Hall, Ira M. S115<br />
Hallett, Mark M602<br />
Halvorsen, Mark B. M710<br />
Hamby, Mary T1704<br />
Hammans, Simon M1008<br />
Hanna, Michael M831<br />
Happ, Erik T1806<br />
Hara, Hajime M829<br />
Harbour, Leia S109<br />
Hardy, Duriel M1401<br />
Häring, Dieter A. T1707<br />
Harman, Jennifer S216<br />
Haro SIlva, Rubén M617<br />
Harper, Charles M. M811<br />
Harris, Tamara B. T1504<br />
Hart, Ian J. T1903, T1904<br />
Hartung, Hans-Peters T1708<br />
Hasegawa, Yasuhiro S120<br />
Hassan, Anhar M826<br />
Hastie, Nicholas D. T1503<br />
Hatemian, A. S114<br />
Haut, Sheryl R. T1615<br />
Hayward, Caroline T1503<br />
Heck, Donald V. S102<br />
Heiss, Wolf-Dieter T1510<br />
Heister, David S. T1514<br />
Hemmen, Thomas M. S105<br />
Henchcliffe, Claire S213<br />
Hendrix, Suzanne T1516,<br />
T1517, T1523,<br />
T1526<br />
Heppner, Frank L. M835<br />
Hernandez, Leticia S230<br />
Herr, Barbara M831<br />
Heshmat, Ramin T1722<br />
Hill, Kenneth E. T1801<br />
Hillis, Argye E. M605, M612,<br />
S125, S132<br />
Hinson, Vanessa S219<br />
Hinton, Sabrina S129<br />
Hirano, Makito T1520<br />
HNRC Group T1905<br />
Hocker, Sara M1202, M1203<br />
Hogan, Edward M708<br />
Hohjoh, Hirohiko S201<br />
Hohlfeld, Reinhard T1707<br />
Holland, Dominic T1525<br />
Hollenbeck, Albert S208<br />
115<br />
Holtzman, David T1901<br />
Hong, Yu M1005<br />
Hopkins, Mark T1903, T1904<br />
Hopkins, Mary T1614<br />
Hornung, Richard S112<br />
Hou, Jing T1527<br />
Hou, Jyhgong Gabriel S215<br />
Howard, George S102, S116<br />
Howard, Katherine L. M616<br />
Hsieh, Yu-Hsiang S139<br />
Huang, Juebin M1301<br />
Huang, Xuemei S206, S208,<br />
S212, S234<br />
Huentelman, Matthew A. T1502<br />
Huh, Young Eun S138<br />
Hui, Jennifer S. S221<br />
Hur, Junguk M1005<br />
Husain, Samea S218<br />
Husan, Shema S229<br />
Hussain, Tiki S222, S227, S235<br />
Hye, Robert J. S102<br />
Ikeda, Ken M812<br />
Ikuno, Yasushi T1520<br />
Irani, Sarosh T1711<br />
Ishihara, Ryu T1520<br />
Isobe, Noriko M1009, T1706<br />
Isojarvi, Jouko M713<br />
Itoh, Noriko T1704<br />
Iwahashi, Hiromi T1520<br />
Iwasaki, Yasuo M812<br />
Iwashita, Julie T1616<br />
Iyadurai, Stanley M720, T1607<br />
Iyadurai, Stanley J. M815<br />
Jack, Clifford T1503<br />
Jack, Clifford R. T1530<br />
Jack, Jr., Clifford R. M606,<br />
T1505<br />
Jackson, Dan M1204<br />
Jackson, Leila S213<br />
Jacobson, Mark T1507<br />
Jacobson, Mercedes S401<br />
Jaffer, Zahara M. M803<br />
Jankovic, Joseph S213<br />
Järvinen-Pasley, Anna M608<br />
Javan, Alireza K. T1521<br />
Javedani, Parisa P. T1606<br />
Jayadev, Suman M1001<br />
Jayam-Trouth, Annapurni S109<br />
Jeffrey, Kaye T1532<br />
Jen, Jin T1503<br />
Jenkins, Andrew S301<br />
Jensen, Michael D. M606<br />
Jeon, Seun T1519<br />
Jianfeng, Cai S202<br />
Jiang, Shan H. T1908<br />
Jimi, Takahiro M829<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 116<br />
John, Sanjna M. T1906<br />
Johnson, Aaron J. T1715<br />
Jones, Timothy F. M823<br />
Josephs, Keith A. M606, M811,<br />
T1515, T1530<br />
Joshi, Abhinay D. T1508<br />
Jovic, Sofija T1534<br />
Ju, Y. Sungtaek T1601<br />
Juarez, Humberto S230<br />
Juncos, Jorge S213<br />
Kaida, Ken-ichi T1733<br />
Kalita, Jayantee M1003, S104<br />
Kalyanam, Janaki S109<br />
Kamakura, Keiko T1733<br />
Kanazawa, Ichiro S201<br />
Kang, Huicong S110<br />
Kano, Osamu M812<br />
Kaplan, Johanne T1719, T1721<br />
Kappos, Ludwig T1707, T1708,<br />
T1709<br />
Karageorgiou, Clementine E.<br />
T1729<br />
Karagogeos, Domna T1729<br />
Karanam, Deepthi M717<br />
Karimi, Mehdi S114<br />
Karin, Ernstrom S105<br />
Karpf, Adam R. M1008<br />
Karunapuzha, Cherian A. S210<br />
Kasarda, Donald D. M602<br />
Kase, Carlos S. S122<br />
Kashouty, Rabih M722, S133,<br />
T1808<br />
Kaspar, Brian M802<br />
Kassar, Darine M720, T1607<br />
Kass-Hout, Omar S117<br />
Kass-Hout, Tareq S117<br />
Katzir, Tami M704<br />
Kaubrys, Gintaras M713<br />
Kavanagh, Terrance J. T1511<br />
Kawabe, Kiyokazu M812<br />
Kawano, Yuji T1706<br />
Kawas, Claudia H. T1508, T1524<br />
Ke, Qing M831<br />
Keegan, B. Mark T1805<br />
Keenan, Brendan T. T1502<br />
Kellerman, Don T1616<br />
Kells, Adrian P. T1529<br />
Kelly, John T1620<br />
Kelly, Kevin M. M701<br />
Khan, Omar M702<br />
Khanna, Ashwani T1717<br />
Kharlamov, Elena A. M701<br />
Khatri, Bhupendra O. T1708<br />
Khitrov, Greg M824<br />
Kiernan, Matthew T1711<br />
Kifayathulla, Liakath Ali M1004<br />
Kim, Chi Hun T1519<br />
Kim, Jae Seung T1519<br />
Kim, Ji Soo S138<br />
Kim, Suk-Hui T1519<br />
Kim, Sung Tae T1519<br />
Kimonis, Virginia E. M805<br />
Kimura, Fumihiko T1733<br />
Kira, Jun-ichi M1009, T1706<br />
Kisby, Glen E. T1511<br />
Kissel, John M806<br />
Kittner, Steven J. S107<br />
Klein, Christopher J. M1008<br />
Kleschevnikov, Alexander M.<br />
M712<br />
Klingstedt, Therése M835<br />
Kluger, Benzi S213<br />
Knappertz, Volker T1702<br />
Knopman, David S. T1505,<br />
T1530<br />
Ko, Nerissa S112<br />
Koch, Heather A. M618, M619<br />
Koffmann, Boyd S404<br />
Kolbert, Christopher P. T1503<br />
Kompoliti, Katie S231<br />
Kong, Xiao-Tang T1804<br />
Konrad, Peter E. S232<br />
Korczyn, Amos D. T1535<br />
Kori, Shashidhar T1603,<br />
T1616, T1617<br />
Koubeissi, Mohamad Z. M620,<br />
M1301<br />
Koyfman, Feliks S122<br />
Krauss, Gregory M714<br />
Kremenchutzky, Marcelo T1702,<br />
T1707<br />
Kronk, Lisa M817<br />
Kronmal, Richard T1513<br />
Kumar, Bishwanath M1003, S104<br />
Kumar, Sunil M1003<br />
Kunschner, Lara T1806<br />
Kunyu, Li S202<br />
Kupsky, W. S209<br />
Kurantsin-Mills, Joseph S109<br />
Kurlan, Roger S216<br />
Kurtzke, John F. T1730<br />
Kusunoki, Susumu M818,<br />
T1520, T1733<br />
Kuwabara, Motoi T1733<br />
Kuwahara, Motoi M818<br />
Kwagyan, John S109<br />
Kwan, Justin Y. M820<br />
Lai, Eugene C. S215<br />
Laidlaw, David H. M1301<br />
LaManna, Joseph M620<br />
Lambrecht, Lawrence J. M710<br />
LaMorte, Michael T1721<br />
116<br />
Lancaster, Eric T1701<br />
Lander, Cecilie M1008<br />
Lang, Anthony E. S216<br />
Lange, Dale J. M824<br />
Langford, Velma L. M814, M819<br />
Larery, Angela T1522<br />
Lasarev, Michael R. T1511<br />
Lash, J. S204, S209<br />
Latov, Norman M602<br />
Lau, Helena S122<br />
Lazar, Ronald M. M1403<br />
Leblang, Spencer A. M618, M619<br />
Ledoux, Kerry M613<br />
Lee, Christopher D. M823<br />
Lee, Jae-Hong T1519<br />
Lee, John D. M615<br />
Lee, Jong-Min T1519<br />
Lee, Joseph T1512<br />
Lee, Michael M703<br />
Lee, Seung-hun S118<br />
Lee, Szexian T1802<br />
Leep Hunderford, Andrea M826<br />
Lees, Monica M615<br />
Lees, Peter S213<br />
Lehky, Tanya J. M820<br />
Leimgruber, Pierre P. S116<br />
Leone, Paola S223<br />
LeRoy, Robert F. M714<br />
Lessig, Stephanie S205, T1507<br />
Leverenz, James S213<br />
Levesque, Jessica T1807<br />
Levitt, Jacob M831<br />
Lewis, Mechelle M. S206, S212,<br />
S234<br />
Li, Chin-Shang M703<br />
Li, Jun M803, M810, M813<br />
Li, Sean S. S115<br />
Li, Wang S202<br />
Lieberman, Abraham S222, S227,<br />
S235<br />
Lieberman, Abraham N. S218<br />
Ligocki, Ann J. T1736<br />
Lin, Wen-Lang T1515<br />
Lin, Xiaoyang S202<br />
Lincoln, Sarah T1503<br />
Lindblom, Scott C. M814, M819<br />
Linskey, Mark E. T1804<br />
Lipton, Richard T1617<br />
Lipton, Richard B. S233, T1608,<br />
T1610, T1611, T1612,<br />
T1613, T1615<br />
Lipton, Stuart A. T1509<br />
Lirng, Jiing-Feng T1605<br />
Litchy, William J. M1008<br />
Litvan, Irene S213<br />
Liu, Kenneth C. T1606<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 117<br />
Liu, Rui S208<br />
Liu, Shuo S108<br />
Liu, Xinyeu S107<br />
Liu, Yu M1401<br />
Llinas, Rafael H. S125, S132<br />
Lohrey, Anne K. T1715<br />
Lok, Edwin T1802<br />
Lombardi, Valter T1506<br />
Longbottom, Mary E. S116<br />
Longstreth, Jr., W.T. T1513<br />
Lowes, Linda P. M802<br />
Lu, Bo M701<br />
Luders, Hans M620<br />
Luke, Sothear M1204<br />
Luna, Jennie M717, M721,<br />
T1619<br />
Lunn, J. Simon M804<br />
Lunn, John S. M1005<br />
Luo, Benyan M831<br />
Luthra, Indermohan M816<br />
Ma, Joyce T1705<br />
Ma, Li T1503<br />
Maccotta, Luigi M708<br />
Macura, Slobodan T1703<br />
Macura, Slobodan I. T1727<br />
Mada, Flicia S129<br />
Madjid, Keyvani T1609<br />
Maeda, Yoshiko T1705<br />
Maganti, Sombabu M718<br />
Magda, Sebastian T1514<br />
Maghzi, Amir Hadi T1732<br />
Mahadevan, Anita M822<br />
Mahajan, Shalini M816<br />
Mahaparn, Irisa M609<br />
Maharjan, Sooraj T1503<br />
Mailman, Richard B. S234<br />
Malhotra, Konark S111<br />
Malhotra, Manoj T1735<br />
Malik, Tafheem S229<br />
Malikova, Irina T1713<br />
Malow, Beth A. S303<br />
Malphrus, Kimberly G. T1503<br />
Manack, Aubrey N. T1608,<br />
T1612<br />
Mandell, Daniel M1105<br />
Mandrekar, Jay M1202, M1203<br />
Manivanh, Richard T1506<br />
Mannan, Ashraf U. M1004<br />
Mano, Toshiyuki T1520<br />
Mantese, Vito A. S116<br />
Manus, Neil D. S224<br />
Marchidann, Adrian S133<br />
Marder, Karen S216<br />
Marder, Karen S. S225<br />
Marek, Kenneth S216<br />
Marras, Connie S213<br />
Marsh, Elisabeth B. S125, S132<br />
Marshall, Randolph S. M1403<br />
Marshall, Theresa S404<br />
Martens, William B. M806<br />
Martinez, Ashley M702<br />
Martinez, Jose A. M1402<br />
Martinez-Hernandez, Eugenia<br />
T1701, T1716<br />
Martinuzzi, Andrea M611,<br />
M1002, S237<br />
Masaki, Kamal H. S203<br />
Masaki, Katsuhisa M1009, T1706<br />
Masliah, Eliezer M609<br />
Mastorodemos, Vasileios M603<br />
Mateen, Farrah J. S123<br />
Matsushita, Takuya<br />
M1009, T1706<br />
Mattson, Mark P. S103<br />
Matveeva, Elena E. M709<br />
Matyushov, Alexei M1201<br />
Mayeux, Richard T1512<br />
McArthur, Justin C. S407<br />
Mcavoy, Mark P. M601<br />
McCague, Kevin T1735<br />
McCauley, Stephen R. M1103<br />
McCracken, Lindsey T1716<br />
McDermott, Michael P. M806<br />
McDonald, Jamie T1713<br />
McEvoy, Linda K. T1514,<br />
T1525<br />
McGarry, Megan M621, M717,<br />
T1738<br />
McShea, Cindy M713<br />
Mehia-Santana, Helen S225<br />
Mehlenbacher, Adam M1107<br />
Mehta, Bijal S117<br />
Meira, Lisiane B. T1511<br />
Mejia, Nicte S214<br />
Melman, Tamar T1802<br />
Mendell, Jerry R. M802<br />
Mendoza, Jesus F. T1907<br />
Meng, Cheryl S216<br />
Meng, Xiangyi T1707, T1708<br />
Meola, Giovanni M1002<br />
Mer, Georges M1008<br />
Meschia, James F. M1204, S102,<br />
S116<br />
Metcalf, Nick M601<br />
Meyer, Brett C. S131<br />
Meysamie, A. T1712<br />
Michael, Benedict D. T1903,<br />
T1904<br />
Middha, Sumit M1008, T1503<br />
Miglis, Mitchell G. S302<br />
Miller, Alistair T1903, T1904<br />
Miller, Eric R. M701<br />
117<br />
Miller, Michael L. T1516, T1517,<br />
T1523, T1526<br />
Miller, Timothy M. M821<br />
Millis, Scott S129<br />
Ming, Ming M831<br />
Mintun, Mark A. T1508<br />
Misra, Usha K. M1003, S104<br />
Mitchell, Amber N. T1807<br />
Mitchell, Braxton D. S107<br />
Mitchell, James F. S107<br />
Mittal, Balraj M1003, S104<br />
Mobley, William M712<br />
Moeller, Thomas M1001<br />
Mohammad, Yousef S119<br />
Mohammad, Yousef M. S111<br />
Mokin, Maxim S117<br />
Molina, Enrique S230<br />
Molinari, Anna L. S224, S226,<br />
S232<br />
Molteni, Silvia S237<br />
Mondani, Massimo S237<br />
Monson, Nancy L. T1736<br />
Moodley, Manikum M1302<br />
Moomaw, Charles S112<br />
Moon, In Soo S126<br />
Moon, Yeseon P. S101<br />
Moore, Ryan P. M609<br />
Moretti, Paolo M1103<br />
Morgan, Kevin T1503<br />
Morris, John T1901<br />
Morrison, Richard S. M1001<br />
Morrow, Leslie S301<br />
Moseley, Brian D. S403<br />
Moshirzadeh, Sasan T1718<br />
Mosley, Thomas H. T1505<br />
Mowry, Ellen M. T1713<br />
Mozaffar, Tahseen M805<br />
Mtchedlishvili, Zakaria M701<br />
Muldowney, James S303<br />
Multani, Manpreet M833<br />
Murata, Kiyoko M812<br />
Murata, Miho S201<br />
Musumeci, Olimpia M1002<br />
Myers, Iliza M810<br />
Na, Duk L. T1519<br />
Nafissi, Shahriar T1722<br />
Nagahara, Alan T1529<br />
Nagata, Riya M812<br />
Nair, Asha A. T1503<br />
Nakamura, Yusaku T1520<br />
Nanakul, Rawi T1521<br />
Nance, Matthew T1522<br />
Nath, Avindra S407<br />
Naylor, David E. M716<br />
Neafsey, Edward S405<br />
Nehrebecky, Michele E. M820<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 118<br />
Neil, William P. S105<br />
Neiman, Eli S. M718<br />
Newman-Toker, David E. S118,<br />
S139<br />
Ng, Rowena M608<br />
Ng-Mak, Daisy S. T1613, T1614<br />
Nguyen, Thanh N. S122<br />
Nguyen, Thuy T1503<br />
Nichols, Mindy S. M814, M819<br />
Nicholson, Garth A. M1008<br />
Nilsson, Peter K.R. M835<br />
Nogalska, Anna M807, M808,<br />
M835<br />
Nourian, A. S114, T1732<br />
Oakes, David S216, S228<br />
Oaklander, Anne Louise M825<br />
O’Connell, Jeffrey R. S107<br />
O’Connor, Paul T1707<br />
Ogawa, Go T1733<br />
Oger, Joel T1702<br />
Oh, Sang Su M804<br />
Oh, Seung Jun T1519<br />
Ohishi, Mitsuru T1520<br />
Olichney, John M. T1521<br />
O’Neill, Brian P. T1805<br />
O’Neill, Mifflin M819<br />
Onken, Mitch M801<br />
Opler, Mark T1534<br />
Oplinger, Heather M819<br />
Ottoboni, Linda T1720<br />
Ouyang, Bichun S119<br />
Owens, Michael J. S301<br />
Ozelius, Laurie J. S233<br />
Paccico, Thomas J. M819<br />
Pacut, Crystal M1005<br />
Paganini-Hill, Annlia S108<br />
Paik, Myunghee C. S101<br />
Pakdaman, Hosein T1734<br />
Pakdaman, Hossein S114, T1712,<br />
T1722, T1723, T1731, T1732<br />
Pakdaman, Hossien T1718<br />
Pakdaman, Reza T1712, T1723<br />
Palmer, Valerie S. T1511<br />
Palusak, Ryan T1503<br />
Pan, Dengji S110<br />
Pan, Di S222, S227, S235<br />
Pan, Yue S. T1908<br />
Pandya, Dipak T1737<br />
Pandya, Dipak P. M621, M717,<br />
M721, T1619, T1738<br />
Pandya, Shree M806<br />
Pankratz, V. Shane T1503<br />
Panou, Theodora M603<br />
Papadaki, Efrosyni M603<br />
Paparella, Gabriella M611,<br />
M1002<br />
Parent, Jack M. M1401<br />
Parisi, J.E. S204, S209<br />
Parisi, Joseph E. M1008, T1515,<br />
T1530<br />
Park, Yikyung S208<br />
Parker, Kathy S301<br />
Parkinson Study Group S228<br />
Pascual, Franchette M703<br />
Patel, Vivek S140<br />
Pati, Sandipan M715, M1201<br />
Paul, Joya S119<br />
Pavlakis, Pantelis P. T1729<br />
Paz Soldan, M Mateo T1715<br />
Paz Soldan, Mateo S403<br />
Pazdera, Ladislav M724<br />
Pearlman, Starr H. T1613<br />
Pease, Larry M1101<br />
Pease, Larry R. T1703<br />
Peavy, Guerry T1507<br />
Pedraza, Otto T1503<br />
Pejovic, Vojislav T1516, T1517,<br />
T1523, T1526<br />
Pelletier, Jean T1708, T1713<br />
Pelster, Michael W. S224<br />
Peltier, Amanda C. M810<br />
Peltz, Carrie B. T1508, T1524<br />
Perez, Veronica M1403<br />
Perhach, James T1533<br />
Pericak-Vance, Margaret T1512<br />
Peruch, Francesca M1002<br />
Pervez, Shahid S229<br />
Pestreich, Linda T1735<br />
Pestronk, Alan M815, M821<br />
Petacchi, Elisa S237<br />
Petersen, Bryan T1606<br />
Petersen, Ronald C. M811,<br />
T1503, T1515, T1530<br />
Petrovitch, Helen S203<br />
Pettingill, Philippa T1711<br />
Pettingill, Rosie T1711<br />
Phibbs, Fenna T. S226<br />
Picard, Christophe T1713<br />
Piccoli, Sara M611<br />
Pickett, Erin J. M613<br />
Pikula, Aleksandra S122, T1504<br />
Pillai, Jagan M1010, S205, S220<br />
Pillai, Jagan A. T1525<br />
Piña-Crespo, Juan C. T1509<br />
Pirko, Istvan T1703, T1715,<br />
T1727<br />
Plaitakis, Andreas M603<br />
Pleasure, David T1705<br />
Plow, Ela B. T1527<br />
Plow, Matthew A. T1740<br />
Polasek, Ozren T1503<br />
Pomerants, Polina S401<br />
118<br />
Pontecorvo, Michael J. T1508<br />
Pope, Daniel L.W. M601<br />
Prabhakaran, Shyam S119<br />
Pracilio, Valerie P. T1614<br />
Prakash, Neal T1601<br />
Presti, Michael F. S403<br />
Prokop, Stefan M835<br />
Rabinstein, Alejandro A. M1202,<br />
M1203, S128, T1714<br />
Race, David S. M612<br />
Rademakers, R. S204, S209<br />
Rademakers, Rosa S207<br />
Radlinska, Basia T1510<br />
Radue, Ernst-Wilhelm T1707<br />
Rahimian, E. T1723<br />
Rai, Shesh N. S213<br />
Rajamani, Kumar S129<br />
Rajput, Alex H. S217<br />
Rajput, Ali H. S217<br />
Rajput, Michele L. S217<br />
Raman, Rema S105<br />
Rametta, Mark T1702<br />
Ramos-Crawford, Ana-Luisa<br />
T1511<br />
Ramsey-Williams, Vicki S404<br />
Rangaraju, Srikant T1902<br />
Ranjan, Tulika T1808<br />
Rao, Sambasiva T1719<br />
Raol, Yogendra H. M705<br />
Rashid, Saifur M620<br />
Rasmuss, Brett M712<br />
Ravina, Bernard S216<br />
Raymond, Deborah S233<br />
Reda, Haatem S403<br />
Reder, Anthony T. T1702<br />
Reed, Michael T1613<br />
Reed, Michael L. T1608, T1610,<br />
T1611<br />
Reeves-Tyer, Patricia M702<br />
Reich, Stephen S213<br />
Reiman, Eric M. T1502<br />
Reitz, Christiane T1512<br />
Reminick, Jason I. S402<br />
Ren, Xuefeng T1511<br />
Rengachary, Jennifer M601<br />
Rentería Palomo, Ana A. M617<br />
Riley, David S213<br />
Ritchie, James C. S301<br />
Rivera, Susan M. T1521<br />
Rizzo, Matthew M615<br />
Roberts, Bruce T1719,<br />
T1721<br />
Robinson, Karen A. S118<br />
Rodriguez, Alcibiades S302<br />
Rodriguez, Ildefonso T1907<br />
Rodriguez, Jeronimo T1907<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 119<br />
Rodriguez, Moses M1101,<br />
T1703, T1727<br />
Rodríguez Leyva, Ildefonso M617<br />
Roeber, S. S204, S209<br />
Rogaeva, Ekaterina T1512<br />
Roger, Elaine T1713<br />
Romero, Jose R. S122<br />
Rosales, Xiomara Q. M802<br />
Rose, Kathryn M. T1505<br />
Rosenbaum, Anna V. M723<br />
Rosenberg, Michael S134<br />
Rosenfeld, William M713<br />
Ross, Owen A. S207<br />
Rossetto, Mariagiovanna M1002<br />
Rostami, Abdolmohamad T1725<br />
Rothman, Brian T1534<br />
Rothner, A.D. M1302<br />
Rothrock, John F.S113, T1602,<br />
T1609<br />
Rothstein, Jeffrey M821<br />
Roubenoff, Ronenn T1504<br />
Rounds, William H. T1736<br />
Rowley, Christopher N. T1503<br />
Royal, III, Walter T1717<br />
Rudan, Igor T1503<br />
Ruhoy, Ilene M1304<br />
Rumbaugh, Jeffrey A. T1902<br />
Rundek, Tatjana S101<br />
Russek, Shelley J. M705<br />
Russell, James W. M801<br />
Russo, Priscilla M819<br />
Rye, David B. S301<br />
Saber Tehrani, Ali S. S118, S139<br />
Sabouri, Amir H. T1905<br />
Sacco, Ralph L. S101<br />
Sadzewicz, Lisa K. S107<br />
Safavi, Farinaz T1725<br />
Sahenk, Zarife M802<br />
Sahraian, Mohammad T1732<br />
Sahraian, Mohammad Ali<br />
T1712, T1723<br />
Sakowski, Stacey A. M804<br />
Salami, Shiva T1722<br />
Salim, Sumaiya S137<br />
Salins, Naomi S218, S222,<br />
S227, S235<br />
Salmon, David P. T1525<br />
Salowich-Palm, Leeza S129<br />
Salvador, Santamaria S230<br />
Samadpour, Reza T1731<br />
Samson, Leona D. T1511<br />
San Luciano, Marta S233<br />
Sanchez-Ramos, Juan S202<br />
Sancho, Jose T1719<br />
Sando, Sigrid B. T1503<br />
Sanjak, Mohammed S. M819<br />
Santiago, Anthony S218, S222,<br />
S227, S235<br />
Sanz-Blasco, Sara T1509<br />
Sarkar, Korak M1102<br />
Sarwar, Aliya S215<br />
Sato, Susumu M702<br />
Sauerbeck, Laura S112<br />
Saunders-Pullman, Rachel S233<br />
Scarmeas, Nicholas S225<br />
Schiff, Nicholas C. M1104<br />
Schirrmacher, Ralf T1510<br />
Schneck, Michael J. S405<br />
Schneider, Andrea T1521<br />
Schneider, Julie A. T1502<br />
Schofield, Lesley T1735<br />
Schor, Nina F. T1803<br />
Schretlen, David J. M613<br />
Schwarzchild, Michael S216<br />
Schweitzer, K.J. S204, S209<br />
Scoglio, Nicholas J. S402<br />
Scott, Bonnie M. T1522<br />
Scott, James N. M1103<br />
Scott, Thomas T1726<br />
Sealfon, Stuart C. M824<br />
Sen, Saurav M721<br />
Sen, Sourav T1619<br />
Sen, Suman S206, S212<br />
Sennett, Cary T1614<br />
Seo, Sang Won T1519<br />
Seritan, Andreea T1521<br />
Serrano, Daniel T1612, T1613<br />
Seshadri, Sudha T1504<br />
Severy, Peter T1719<br />
Seyal, Masud M703<br />
Shaffer, Michel L. S212<br />
Shaffer, Michele L. S206, S234<br />
Shah, Amol T1905<br />
Shah, Anish M721, T1619<br />
Shah, Umang M719<br />
Shahbazi, Mona M824<br />
Shahbegi, Said S114<br />
Shahbeigi, Saeed T1734<br />
Shahkarami, Mohammad Amir<br />
T1722<br />
Shahlaie, Kia M1102<br />
Shamim, Ejaz M602<br />
Shankar, S.K. M822<br />
Shankara, Srinivas T1719<br />
Sharpe, James A. M607, T1621<br />
Sharrett, A. Richey T1505<br />
Sheikh, Kazim M809<br />
Shepherd, Cassandra S213<br />
Shibata, Dean K. T1505<br />
Shijie, Song S202<br />
Shimizu, Kanako S120<br />
Shin, Robert K. M723<br />
119<br />
Shiramizu, Bruce S407<br />
Shojaee, Maziar T1731<br />
Shojaei, Maziar T1718<br />
Shoulson, Ira S216<br />
Shprecher, David S213<br />
Shtilbans, Alexander M824<br />
Shulman, Gordon L. M601<br />
Shulman, Joshua M. T1502<br />
Shuster, E.A. S209<br />
Shy, Michael E. M803<br />
Siddiqui, Fazeel S140<br />
Siders, William T1719, T1721<br />
Siemionow, Vlodek T1527<br />
Silber, Michael H. M811<br />
Silberstein, Stephen T1603,<br />
T1614<br />
Silbert, Lisa T1532<br />
Sillau, Stefan M616<br />
Silva, Jessica M613<br />
Simon, Mariella M1008<br />
Simos, Panagiotis G. M603<br />
Simpson, Ericka M821<br />
Simpson, Ericka P. M832,<br />
T1728<br />
Simuni, Tanya S228<br />
Singh, Anuradha S302<br />
Singleton, Robinson J. T1604<br />
Skrap, Miran S237<br />
Slevin, John T. M709<br />
Sloan, Michael S130, S135<br />
Smith, David I. M1008<br />
Smith, Glenn E. M1008<br />
Smith, Gordon A. T1604<br />
Smith, Jonathan H. S403<br />
Smith, Richard M821<br />
Smith-Hammond, Carol M1107<br />
Snider, Barbara J. S406<br />
Snyder, Abraham Z. M601<br />
So, Norman K. M711<br />
Sofroniew, Michael T1704<br />
Solomon, Tom T1903, T1904<br />
Somarajan, Bindu I. M1003,<br />
S104<br />
Song, Yanna S226, S303<br />
Sorenson, Eric M826<br />
Sorenson, Eric J. M817<br />
Soucy, Jean-Paul T1510<br />
Spence, Rory T1704<br />
Spencer, Peter S. T1511<br />
St. George-Hyslop, Peter T1512<br />
St. Louis, Erik K. M811<br />
Standaert, David S213<br />
Stankiewicz, James M. S408<br />
Stanley, Kaili M. S233<br />
Statland, Jeffrey M. M806<br />
STEADY PD Investigators S228<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 120<br />
Stebbins, Glenn T. S211, S231<br />
Stern, Barney J. S107<br />
Stewart, Anna T1903, T1904<br />
Stine, Oscar C. S107<br />
Stites, Tracy T1708<br />
Stouter, Josephine T1522<br />
Strongosky, Audrey M1007<br />
Struck, Peter M834<br />
Strutt, Adriana M. T1522<br />
Sullivan, Robert S. T1511<br />
Sundal, C. S204, S209<br />
Sundar, Kaushik S121<br />
Sung, Kyongje M613<br />
Sura, Ankit M801<br />
Suter, Ueli M803<br />
Suzuki, Seiko M818<br />
Swanson, Kenneth D. T1802<br />
Tabasi, M. S114<br />
Tabatabae, Al S114<br />
Takahashi, Masaki S201<br />
Talantova, Maria V. T1509<br />
Tallon, Luke J. S107<br />
Tan, Caroline M602<br />
Tanaka, Ichiro T1520<br />
Tang, Dejun T1709<br />
Tang, Zhouping S110<br />
Tanner, Caroline M. S203, S216<br />
Tawil, Rabi M806<br />
Tayal, Ashis S124<br />
Taylor, Glyn T1616<br />
Teich, Douglas L. T1622<br />
Tenderini, Erika M1002<br />
Tennen, Howard T1615<br />
Tepper, Stewart T1603, T1617<br />
Teshome, Mengesha T1901<br />
Thant, Minn S215<br />
Thawani, Sujata S302<br />
Theodore, William H. M702<br />
Theriot, Jeremy J. T1601<br />
Thiel, Alexander T1510<br />
Thomas, Jewell T1901<br />
Thomas, Tracy T1616<br />
Tilluckdharry, Natasha<br />
M621, T1738<br />
Timaran, Carlos H. S116<br />
Ting, Jess M824<br />
Title, Wallace S224<br />
Titulaer, Maarten J. T1701,<br />
T1716<br />
Tobias, Kathy T1735<br />
Tocco, Michael T1516, T1517,<br />
T1523, T1526<br />
Todd, Wesley M. M710<br />
Toga, Arthur W. T1601<br />
Tokuyama, Yoshiaki S120<br />
Toro, Camilo M820<br />
Toscano, Antonio M1002<br />
Tosches, William M1105<br />
Tramontana, Michael G. S232<br />
Tran, Dong T1502<br />
Traynor, Bryan J. M820<br />
Trenerry, Max R. M606<br />
Trotti, Lynn Marie S301<br />
Tselis, A. S209<br />
Tufail, Yusuf M715, M1201<br />
Turkel, Catherine C. T1608,<br />
T1612<br />
Turner, Travis H. S219<br />
Tuszynski, Mark H. T1529<br />
Tyler, William J. M715, M1201<br />
Ueda, Masami M818<br />
Uitti, Ryan S213<br />
Umaiorubahan,<br />
Meenakshisundaram S121<br />
Umeda, Elizabeth T1704<br />
Uyehara-Lock, Jane H. S203<br />
Vallurupalli, Srikanth S140<br />
Van Gerpen, J.A. S204, S209<br />
Van Keulen, Virginia M1101<br />
Van Liew, Charles S205, S220,<br />
T1507<br />
Van Loveren, Harry R.<br />
S130, S135<br />
Van Ness, Paul C. M711<br />
Vanaman, Thomas C. M709<br />
Vannorsdall, Tracy D. M613<br />
Varon, Sepideh F. T1612<br />
Vasan, Ramachandran S. T1504<br />
Vaughan, Douglas E. S303<br />
Vazquez, Gilberto T1907<br />
Vecera, Shaun M615<br />
Velazquez-Rodriguez,<br />
Yadira M1205<br />
Veloski, Jon S223<br />
Venkatasubramaniam,<br />
Shankar S121<br />
Verghese, Joe T1518<br />
Verma, Aparajitha K. M832<br />
Vestri, Alec M611<br />
Victor, Jonathan D. M1104<br />
Vieira, Julio R. S101<br />
Vigo, Carmen T1506<br />
Villoslada, Pablo T1713<br />
Vincent, Angela T1711<br />
Viollet-Callendret, Laurence<br />
M802<br />
Voeks, Jenifer H. S102, S116<br />
von Rosenstiel, Philipp T1707<br />
Voskuhl, Rhonda T1704<br />
Vysata, Oldrich M724<br />
Wada, Keiji S201<br />
Wagner, Daymond S206, S212<br />
120<br />
Wagner, Jenee M1006<br />
Wagner, Kathryn R. M806<br />
Wakayama, Yoshihiro M829<br />
Walgren, Kristy M819<br />
Walker, Linsey M. M704<br />
Wallace, Douglas C. M1008<br />
Wallin, Mitchell T. T1730<br />
Wang, Aijun T1724<br />
Wang, Chunyang M719<br />
Wang, Jay-Ming S130, S135<br />
Wang, Lily S226, S303<br />
Wang, Min T1603, T1617<br />
Wang, Morgan S130<br />
Wang, Shuu-Jiun T1605<br />
Wang, Wei S110<br />
Wang, Yen-Feng T1605<br />
Ward, Amber L. M814, M819<br />
Ward, Christopher J. M1008<br />
Warrington, Arthur M1101<br />
Warrington, Arthur E. T1703<br />
Watanabe, Osamu T1711<br />
Watanabe, Shoko S201<br />
Waters, Patrick T1711<br />
Watson, James M826<br />
Watson, Sam S129<br />
Waubant, Emmanuelle T1713<br />
Webber, Christine A. M1402<br />
Webster, Ross S203<br />
Weibelt, Silvia M. T1602<br />
Weihl, Chris M815<br />
Weiner, Howard T1720<br />
Weiss, John H. M805<br />
Werner, Perla T1535<br />
Westwood, Andrew J. T1504<br />
White, Lon R. S203<br />
Whiteheart, Sidney W. M709<br />
Whitfield-Gabrieli, Susan M704<br />
Whitwell, Jennifer M606<br />
Whitwell, Jennifer L. T1530<br />
Wicklund, Meredith S403<br />
Wider, C. S204, S209<br />
Wiggs, Edythe M702<br />
Wijdicks, Eelco F.M. M1202,<br />
M1203, S128<br />
Wilde, Elisabeth A. M1103<br />
William, Gahl M820<br />
Williams, Nicole M. M814,<br />
M819<br />
Wilson, Karen R. S130, S135<br />
Winblade Nairn, Natalie T1724<br />
Winner, Paul T1603<br />
Wojna, Valerie S407<br />
Wolf, Philip A. T1504<br />
Woltjer, Randy T1532<br />
Wong, Agnes M. T1621<br />
Wong, Amy S109<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-9 Cadmus Art: 22582 Date: 26-August-11 Stage: Page: 121<br />
Wong, Eric T. T1622, T1802<br />
Wong, Sarah T1701<br />
Wood, Blair T1801<br />
Woodruff, B.K. S204, S209<br />
Worrall, Bradford B. S115<br />
Wozniak, Marcella A. S107<br />
Wright, Alan T1503<br />
Wright, Brent M1101<br />
Wright, Kathryn A. M819<br />
Wszolek, Z.K. S204, S209<br />
Wszolek, Zbigniew T1503<br />
Wszolek, Zbigniew K. M1007,<br />
S207<br />
Wu, Yanhong M1008<br />
Wyant, Alexandria T1527<br />
Wymbs, Nicholas M604<br />
Xiang, Diane T1736<br />
Xu, Feng S110<br />
Xu, Jian T1701<br />
Xu, Kui M620<br />
Xu, Xiaohua M1101<br />
Xue, YuanYuan T1728<br />
Yamanishi, Hiromitch M1008<br />
Yamashita, Toshihide T1520<br />
Yan, Qing M803, M813<br />
Yanagihara, Keiko T1520<br />
Yang, Fan S108<br />
Yang, Lauice S221<br />
Yanik, Brandon M. T1604<br />
Yavorsky, Christian T1534<br />
Yin, Hong Z. M805<br />
Yonekawa, Tomomi M1009,<br />
T1706<br />
Yono, Noor M722, S133, T1808<br />
York, Michele K. T1522<br />
Yoshihiro, Anna M715, M1201<br />
Yoshii, Yasuhiro M812<br />
Yoshimura, Satoshi M1009, T1706<br />
You, Xiaojun T1726<br />
Younger, David S. M827<br />
121<br />
Younkin, Curtis S. T1503<br />
Younkin, Steven G. T1503<br />
Yu, Alexander T1622<br />
Yu, Chuanhui S108<br />
Yue, Guang H. T1527<br />
Yung, Raymond M1005<br />
Zarbl, Helmut T1511<br />
Zerafati, Gazelle S223<br />
Zghouzi, Mohamed S119<br />
Zhang, Gang M809<br />
Zhang, Xuebao M803<br />
Zhang-Auberson, Lixin T1707,<br />
T1709<br />
Zhou, Yun S118<br />
Zhu, Suiqiang S110<br />
Zimmerman, Earl T1807<br />
Zinn, Kristi M601<br />
Zivadinov, Robert S117<br />
Zochodne, Douglas W. M1402<br />
Zou, Fanggeng T1503<br />
ID: kannanb I Black Lining: [ON] I Time: 17:26 I Path: N:/3b2/ANA#/Vol00000/110247/APPFile/JW-ANA#110247
J_ID: ZAY Customer A_ID: SUPP11-10 Cadmus Art: 22584 Date: 31-August-11 Stage: Page: 122<br />
Abdemalik, Peter M729<br />
Ackermann, Elizabeth M841<br />
Ahmahi, Naser T1540<br />
Albers, Gregory W. M1206<br />
Albert, Todd T1538<br />
Alvarado, Luis M841<br />
Angelini, Corrado I. M838<br />
Arnold, Steven E. T1542<br />
Askanas, Valerie M837<br />
Avila-Costa, Maria Rosa M730<br />
Babaei, Hormoz T1540<br />
Bai, Dongsheng M730<br />
Barlow, Carrolee T1538<br />
Bateman, Randall J. T1541<br />
Beason-Held, Lori T1539<br />
Benson, Merrill M841<br />
Benzinger, Tammie T1541<br />
Berdichevsky, Yevgeny M727<br />
Bettermann, Kerstin S142<br />
Bhattachuria, Arun T1623<br />
Booten, Sheri M841<br />
Bordeau, Jane M840<br />
Boulis, Nicholas M840<br />
Bowen, James D. T1743<br />
Brigatti, Karlla W. M1011<br />
Brookler, Kenneth H. T1745<br />
Cacciottolo, Mafalda M837<br />
Carlen, Peter L. M729<br />
Cevette, Michael J. T1745<br />
Chakraverty, Sumi T1541<br />
Chang, Dae-il S141<br />
Chaudhry, Zeshan A. M1206<br />
Cocco, Daniela T1745<br />
Cohen, Todd T1542<br />
Connors, James S144<br />
D’Agostino, Carla M837<br />
Dambinova, Svetlana S142<br />
Davis, Stephen M. M1206<br />
Delgado-Escueta, Antonio V.<br />
M730<br />
Deutsch, Eric C. M1011<br />
Dhir, Ashish M731<br />
Donnan, Geoffrey A. M1206<br />
Duron, Reyna M. M730<br />
Eberly, Shirley S238<br />
Ebers, George C. M1012, M1013<br />
Ebrahimi, Ramin T1540<br />
Ehrlich, Michelle E. T1538<br />
Elbert, Don T1541<br />
Elisman, Mark M839<br />
Elm, Jordan J. M1206<br />
Engel, W.King M837<br />
Fague, Scot T1541<br />
WIP AUTHOR INDEX<br />
Fanin, Marina M838<br />
Federici, Thais M840<br />
Feldman, Eva M840<br />
Ferrucci, Luigi T1539<br />
Florez, Carlos M. M729<br />
Gandy, Sam T1538<br />
Gangadharan, Beena T1743<br />
Garg, Rajeev S143<br />
Glabe, Charles T1538<br />
Glass, Jonathan D. M840<br />
Goate, Alison T1541<br />
Gonzalez, R. G. M1206<br />
Govindarajan, Raghav T1747<br />
Grachev, Igor D. S240<br />
Green, Mark W. T1623<br />
Grisham, Mathew B. T1746<br />
Grossman, Murray T1542<br />
Guevara, Jorge M730<br />
Guevara, Patricia M730<br />
Guo, Jiasong M839<br />
Guo, Shuling M841<br />
Hajsadeghi, Fereshteh T1540<br />
Havrdova, Eva T1741<br />
Hawi, Amale M1011<br />
Hazel, Tom M840<br />
Heo, Sung Hyuk S141<br />
Hogarth, Penelope S240<br />
Horakova, Dana T1741<br />
Huber, Vincent J. T1744<br />
Hughes, Steve M841<br />
Irwin, David J. T1542<br />
Iwata, Atsushi M836<br />
Jacobson, Sven M1206<br />
Johe, Karl M840<br />
John, Sayona S143<br />
Jung-Henson, Lily K. T1743<br />
Kalincik, Tomas T1741<br />
Karlsson, Fridrik T1746<br />
Kasten, Tom T1541<br />
Kelly, Crystal M840<br />
Keogh, Bart P. T1743<br />
Kieburtz, Karl S239<br />
Kim, Hye Ok S141<br />
Kim, Soong Ho T1538<br />
Kimberly, W. T. M1206<br />
Krasensky, Jan T1741<br />
Kraut, Michael T1539<br />
Kubota, Akatsuki M836<br />
Kucheruck, Olena M1011<br />
Kwee, Ingrid L. T1744<br />
Laguerre, Tatanisha S240<br />
Lam, Ann M622, M728<br />
Lee, Virginia M.Y. T1542<br />
122<br />
Lee, Viven S143, S144<br />
Leinonen, Mika S239<br />
Li, Jun M839<br />
Lian, Gewei M726<br />
Lovestone, Simon T1539<br />
Lynch, David R. M1011<br />
Machado-Salas, Jesus M730<br />
Mail, Michelle M727<br />
Malhotra, Konark S143, S144<br />
Maravilla, Kenneth R. T1743<br />
Marek, Kenneth S238<br />
Marino, Julia T1742<br />
Martinez, Nicholas E. T1746<br />
Matthews, Ian R. T1742<br />
Mawuenyega, Kwasi T1541<br />
Mayadev, Angeli T1743<br />
McIntyre, Cameron M839<br />
Miller, Guy M1011<br />
Minagar, Alireza T1746<br />
Monia, Brett M841<br />
Morris, John C. T1541<br />
Mowry, Ellen M. T1742<br />
Nakada, Tsutomu T1744<br />
Nakayama, Yukihiro T1744<br />
Nalls, Michael T1539<br />
Nascimbeni, Annachiara M838<br />
Nissinen, Helena S239<br />
Nogalska, Anna M837<br />
Nutt, John G S240<br />
Oakes, David S238<br />
Oakley, Sarah T1745<br />
Ohayon, Elan L. M622, M728<br />
Olanow, C. Warren S239<br />
Omura, Seiichi T1746<br />
Ovid, Vitaliy T1541<br />
Park, Byung S. S240<br />
Patterson, Bruce T1541<br />
Poewe, Werner S239<br />
Polak, Meraida M840<br />
Potter, Rachel E. T1541<br />
Prabhakaran, Shyam S143, S144<br />
Pradhan, Gaurav T1745<br />
Rajappa, Sivakumar M. M725<br />
Ramagopalan, Sreeram V.<br />
M1012, M1013<br />
Rascol, Olivier S239<br />
Ravina, Bernard M. S238<br />
Repovic, Pavle T1743<br />
Resnick, Susan T1539<br />
Rioux, Patrice M1011<br />
Rizzuto, Daniel S. T1743<br />
Rogawski, Michael A. M731<br />
Ross, Mark A. T1745<br />
ID: srinivasanv I Black Lining: [ON] I Time: 22:03 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110248/APPFile/JW-ANA#110248
J_ID: ZAY Customer A_ID: SUPP11-10 Cadmus Art: 22584 Date: 31-August-11 Stage: Page: 123<br />
Rutkove, Seward M840<br />
Salgado, Efrain T1747<br />
Sandri, Marco M838<br />
Saponjian, Yero M727<br />
Sato, Fumitaka T1746<br />
Schapira, Anthony S239<br />
Sciascia, Thomas M1011<br />
Seidl, Zdenek T1741<br />
Sejnowski, Terrence J. M728<br />
Sheen, Volney M726<br />
Sheth, Kevin N. M1206<br />
Shimizu, Jun M836<br />
Shoulson, Ira S238<br />
Shrader, William D. M1011<br />
Sigurdson, Wendy T1541<br />
Singleton, Andrew T1539<br />
Siwkowski, Andrew M841<br />
Smith, Benn E. T1745<br />
Sosinsky, Gina M839<br />
Spitz, John T. M732<br />
Staley, Kevin J. M727<br />
Steele, John W. T1538<br />
Stepanek, Jan T1745<br />
Stern, Barney J. M1206<br />
Stocchi, Fabrizio S239<br />
Suter, Ueli M839<br />
Suzuki, Yuji T1744<br />
Tanaka, Miyabi M730<br />
Temes, Richard S143<br />
Tendolkar, Amol S240<br />
Thambisetty, Madhav T1539<br />
Treuner, Kai T1538<br />
Trojanowski, John Q. T1542<br />
Troyer, Matthew D. S240<br />
Tsuji, Shoji M836<br />
Tsunoda, Ikuo T1746<br />
123<br />
Underhill, Hunter R. T1743<br />
Vaneckova, Manuela T1741<br />
Venkatesan, Srinivasan A. M725<br />
Vinayagasundaram, Uma T1742<br />
Wagner, Lindsay T1745<br />
Wang, Lily M839<br />
Waubant, Emmanuelle T1742<br />
Willi, Steve M. M1011<br />
Wilson, Robert B. M1011<br />
Xie, Sharon X. T1542<br />
Xuan, Fengjuan S240<br />
Yan, Qing M839<br />
Yarasheski, Kevin T1541<br />
Yarnykh, Vasily L. T1743<br />
Yoo, Albert J. M1206<br />
Zapala, David A. T1745<br />
Zhang, Jane M729<br />
Zhang, Liang M729<br />
ID: srinivasanv I Black Lining: [ON] I Time: 22:04 I Path: //xinchnasjn/01Journals/Wiley/3b2/ANA#/Vol00000/110248/APPFile/JW-ANA#110248
A<br />
Acute Cerebral Ischemia M721, S102, S105, S109, S116,<br />
S118, S120, S121, S128, S<strong>136</strong>, T1619<br />
Acute Ischemic Stroke S102, S103, S105, S109, S114,<br />
S116, S117, S120, S122, S124, S125, S127,<br />
S129, S130, S131, S132, S135<br />
Acute Neuropathies M818, M822, M823, M825, M827,<br />
M830, T1733<br />
Affective Functioning M608, M617, M819, S203<br />
Alzheimer’s Disease (AD) M616, M808, M1001, T1501,<br />
T1502, T1503, T1504, T1506, T1508, T1509,<br />
T1512, T1514, T1516, T1517, T1518, T1521,<br />
T1522, T1523, T1524, T1525, T1526, T1528,<br />
T1529, T1531, T1532, T1533, T1534, T1535, T1901<br />
Amyotrophic Lateral Sclerosis (ALS) M804, M805,<br />
M807, M813, M817, M821, M824,<br />
M829, M1005<br />
Antibodies M602, M809, M818, M822, M825, M1101,<br />
S202, T1506, T1701, T1703, T1706, T1711,<br />
T1716, T1719, T1721, T1729, T1733,<br />
T1736, T1739, T1801, T1908<br />
Apoptotic Cell Death T1537, T1801, T1803<br />
Astrocytes M1004, T1506, T1509, T1704,<br />
T1705, T1710<br />
Atherosclerosis M1003<br />
Attention-Deficit/Hyperactivity Disorder M610, M614,<br />
M617, M618, M619<br />
Autoimmune Demyelination M1105, M1303, T1704,<br />
T1713, T1729, T1731, T1732, T1734, T1738<br />
B<br />
Brain Imaging M601, M606, M704, M719, M1103,<br />
M1104, M1301, S117, S119, S125, S128,<br />
S132, S140, S204, S212, T1510, T1513, T1514,<br />
T1518, T1525, T1527, T1532, T1601, T1619,<br />
T1714, T1715, T1804, T1906, T1908<br />
Brain Ischemia M605, M1201, M1204, S103, S106,<br />
S114, S115, S126, T1519<br />
Brain Mapping M601, M604, M605, M609, M708,<br />
M724, S109, T1527, T1601<br />
C<br />
J_ID: ZAY Customer A_ID: SUPP11-12 Cadmus Art: 22585 Date: 26-August-11 Stage: Page: 124
I<br />
Interferon Treatments T1702, T1722, T1724<br />
Interferons M1001, T1722, T1726<br />
Intracerebral Haemorrhage (ICH) M1003, S104, S105,<br />
S110, S111, S113, S117, S124, S125,<br />
S128, S132, S<strong>136</strong><br />
Ischemia S124, S126, S133<br />
L<br />
L-Dopa Therapy S215<br />
Levodopa S232, S236<br />
Lewy Bodies (LB) S207<br />
Limbic Encephalitis T1701<br />
M<br />
Magnetic Resonance Imaging (MRI) M612, M719,<br />
M721, M828, M1301, S106, S204, S212, S234,<br />
T1504, T1505, T1514, T1519, T1521, T1525,<br />
T1530, T1532, T1605, T1726, T1727,<br />
T1737, T1738<br />
Magnetic Resonance Spectroscopy (H-MRS) M812<br />
Migraine S<strong>136</strong>, T1601, T1602, T1603, T1608, T1609,<br />
T1610, T1611, T1612, T1613, T1614,<br />
T1615, T1616, T1617, T1618, T1620<br />
Morvan Syndrome T1711<br />
Motoneuron Disease M804, M805, M812, M813,<br />
M814, M817, M819, M820, M832,<br />
M833, M1002, T1511<br />
Multiple Sclerosis (MS) M603, M1009, M1105, T1621,<br />
T1702, T1703, T1704, T1707, T1708,<br />
T1709, T1710, T1712, T1713, T1715, T1717,<br />
T1718, T1719, T1720, T1721, T1722, T1723,<br />
T1724, T1725, T1726, T1727, T1729, T1730,<br />
T1731, T1732, T1734, T1735, T1736,<br />
T1737, T1740<br />
Muscular Dystrophies M806, M807<br />
Myelin M803<br />
Myelin Oligodendrocyte Glycoprotein (MOG) T1737<br />
Myoclonus M621, M717<br />
Myopathic Syndrome M815, M816<br />
Myopathy M802, M806, M807, M808, M811,<br />
M815, M816, M829, M835<br />
N<br />
J_ID: ZAY Customer A_ID: SUPP11-12 Cadmus Art: 22585 Date: 26-August-11 Stage: Page: 125
A<br />
Acute Cerebral Ischemia S142<br />
Acute Ischemic Stroke M1206, S142<br />
Affective Functioning M622, T1745<br />
Alzheimer’s Disease (AD) M730, T1538, T1539,<br />
T1540, T1541, T1542<br />
Alzheimer’s Disease Mutants T1541<br />
Astrocytes T1744<br />
Atherosclerosis S141<br />
Autoimmune Demyelination T1742<br />
B<br />
Brain Imaging M622, M1206, S143, S144, S238,<br />
T1539, T1741, T1743, T1744<br />
Brain Ischemia M1206, S142<br />
Brain Mapping M622, T1745<br />
Brain Metabolism M727, M729, T1539, T1541<br />
C<br />
Cell Death M728, M1011<br />
Cerebrospinal Fluid (CSF) T1541<br />
Cognitive Outcomes M728, S238<br />
D<br />
Dementia T1538<br />
Demyelination M839, T1741, T1742, T1743<br />
E<br />
Epilepsy M726, M727, M731, M732<br />
Epilepsy Model M728, M729, M730, M731<br />
Epileptic Seizures M729<br />
Epileptogenesis M727, M728, M729<br />
F<br />
Frontotemporal Dementia (FTD) T1542<br />
G<br />
Gene Expression M838, S141<br />
Gene Regulation M726, M1013<br />
Genetic Mutations M726, M839, M841<br />
H<br />
J_ID: ZAY Customer A_ID: SUPP11-13 Cadmus Art: 22586 Date: 26-August-11 Stage: Page: 126<br />
Headache S143, S144, T1623<br />
WIP SUBJECT INDEX<br />
126<br />
L<br />
Lafora Disease M730<br />
L-Dopa Therapy S240<br />
M<br />
Magnetic Resonance Imaging (MRI) M1206, T1741,<br />
T1743<br />
Migraine T1623<br />
Multiple Sclerosis (MS) M1012, T1741, T1742, T1743<br />
Muscular Dystrophies M838<br />
Myelin M839, T1745<br />
Myoclonus M730<br />
Myopathy M836, M837, M838<br />
N<br />
Neurodegenerative Diseases M840, M841, T1538,<br />
T1542<br />
Neurogenesis M726, M839, T1538, T1744<br />
Neuromyelitis Optica (NMO) T1742<br />
Neuroprotection M727, M1011<br />
O<br />
Other M622, M725, M731, M836, M837, M840,<br />
M841, M1011, M1012, M1013, S141, S239,<br />
S240, T1540, T1623, T1745<br />
P<br />
Parkinson’s Disease (PD) S238, S239, S240<br />
PET T1539, T1744<br />
Pharmacokinetics M841, S240<br />
Pompe Disease M838<br />
R<br />
Reactive Oxygen Species (ROS) M1011<br />
S<br />
Single Photon Emission Computed Tomography S238<br />
Stroke S141, S142, S143, S144<br />
Subarachnoid Hemorrhage S143, S144<br />
T<br />
Tau M837, T1542<br />
ID: kannanb I Black Lining: [ON] I Time: 17:29 I Path: N:/3b2/ANA#/Vol00000/110251/APPFile/JW-ANA#110251
COVER 3 = BLANK PAGE
COVER 4 = BLANK PAGE