Approach to Thrombocytopenia
Approach to Thrombocytopenia
Approach to Thrombocytopenia
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The McMasterat nightPediatricCurriculumConsolini, DM. “Thrombocy<strong>to</strong>penia in Infants &Children”. Pediatrics in Review 32 (4). 2011.
Objectives• Understand the evaluation of an infant or child presentingwith thrombocy<strong>to</strong>penia• Recognize signs and symp<strong>to</strong>ms that suggest lifethreateningdiagnoses• Triage patients for appropriate treatment based onunderlying etiology and risk of bleeding
Background• Platelets are irregular cell fragments derived from bonemarrow megakaryocytes• Platelets are responsible for primary hemostasis throughthe formation of platelet plugs• The coagulation cascade participates in secondaryhemostasis by creating a firm, stable fibrin clot• Thrombocy<strong>to</strong>penia is defined as a platelet count less than150 x 10 9 /L
Test Your Knowledge• At what level of platelets are children at risk forspontaneous hemorrhage?A. 10 x 10 9 /LB. 50 x 10 9 /LC. 100 x 10 9 /LD. 150 x 10 9 /L
The Answer• The normal platelet count is 150-450 x 10 9 /L• Patients with moderate thrombocy<strong>to</strong>penia (30-50 x 10 9 /L)are rarely symp<strong>to</strong>matic even with trauma• Spontaneous bleeding does not occur untilplatelets are < 10 x 10 9 /L, and may consis<strong>to</strong>f petichiae and bruising• Critical bleeding (ICH) occurs < 5 x 10 9 /L• Platelets should be > 50 x 10 9 /L for invasiveprocedures
The Case• A 3-year old boy presents <strong>to</strong> the emergency departmentwith a 24h his<strong>to</strong>ry of bruising, primarily over the lowerextremities, and a nosebleed for the past 15 minutes• His parents deny any trauma• The child has no significant medical his<strong>to</strong>ry and no familyhis<strong>to</strong>ry of bleeding or bruising
The Case
His<strong>to</strong>ryWhat would you ask?
His<strong>to</strong>ry• Past and current bleeding symp<strong>to</strong>ms, including bruisingwith little or no trauma, nosebleeds, hematuria,hema<strong>to</strong>chezia, melena, bleeding from the gums• Remember <strong>to</strong> ask about bleeding with dental and surgicalprocedures• Remember <strong>to</strong> ask post-menarchal females aboutexcessive menstrual bleeding• Family his<strong>to</strong>ry of all of the above
His<strong>to</strong>ry• Have symp<strong>to</strong>ms been present since birth?• Recent drug exposure, recent respira<strong>to</strong>ry or GI infection• Constitutional symp<strong>to</strong>ms (fever, night sweats, weight loss,fatigue) and bone pain• Always include non-accidental injury on the differential ofa child presenting with bruising without a his<strong>to</strong>ry of trauma
Physical ExamWhat would you look for?
Physical Exam• Ensure hemodynamic stability• Examine skin, gingivae, oral cavity for evidence ofbleeding, pallor; look for eczema in male patients• For infants, dysmorphyisms and malformations:(cataracts, hearing loss, limb defects, hemangiomas)• Palpate all accessible lymph nodes, liver, spleen• Check neurological status and focal deficits
WorkupWhat would you order?
Workup• CBC• Absolute platelet count• Assess severity of thrombocy<strong>to</strong>penia• Mean platelet volume• High suggests destructive process or congenitalmacrothrombocy<strong>to</strong>penia• Low suggests Wiskott-Aldrich syndrome• Hemoglobin• Concurrent anemia suggests au<strong>to</strong>immunehemolytic anemia, leukemia, or infiltration• Leukocyte counts and differential• Leukopenia suggests leukemia, infiltration
Workup• Peripheral Blood Smear• Confirm platelet count• Improper collection results in clumping andspurious thrombocy<strong>to</strong>penia• Red cell morphology• Spherocytes suggest au<strong>to</strong>immune hemolyticanemia (coupled with immune thrombocy<strong>to</strong>peniadefines Evans syndrome)• Schis<strong>to</strong>cytes suggest microangiopathic destruction(as in HUS, DIC, and TTP)
Workup• The remainder of the workup is guided by clinicalpresentation• A positive direct Coombs test suggests an immunemediatedprocess• Consider ANA and au<strong>to</strong>-antibodies in patients withpersistent thrombocy<strong>to</strong>penia• Fibrin degradation products are present in DIC; uremia ispresent in HUS
Workup• A bone marrow exam is not usually necessary, but isindicated if there is pancy<strong>to</strong>penia, peripheral blasts,constitutional symp<strong>to</strong>ms, or bone pain• For infants with multiple congenital anomalies, considerhead U/S, MRI, abdominal U/S, and echo• Consider genetic testing for patients with poor growth ordysmorphic features• HIV and Hepatitis C can be associated with chronicthrombocy<strong>to</strong>penia
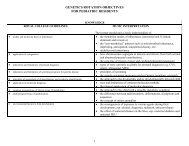
Differential DiagnosisIncreased DestructionImmune-mediatedImmune Thrombocy<strong>to</strong>penia PurpuraNeonatal Alloimmune Thrombocy<strong>to</strong>peniaNeonatal Au<strong>to</strong>immune Thrombocy<strong>to</strong>peniaSystemic Lupus Erythema<strong>to</strong>susDrug-induced thrombocy<strong>to</strong>peniaEvans SyndromeMechanical DestructionDialysisECMOPlatelet ConsumptionHemolytic-Uremic SyndromeThrombotic Thrombocy<strong>to</strong>penic PurpuraDisseminated Intravascular CoagulationKasabach-Merritt SyndromeSplenic sequestrationMalariaSickle-cell diseasePortal hypertensionVon-Willebrand Subtypes
Differential DiagnosisDecreased ProductionInfectionEBVHIVHCVParvovirusVaricellaCMV (congenital or acquired)Rubella (congenital)Nutritional DeficienciesFolateVitamin B12Bone Marrow Failure/InfiltrationLeukemiaMyelodysplastic syndromesOther malignanciesAcquired aplastic anemiaGenetic CausesFanconi anemiaWiscott-Aldrich SyndromeDyskera<strong>to</strong>sis congenitaThrombocy<strong>to</strong>penia Absent RadiiCongenital amegakaryoticthrombocy<strong>to</strong>penia
ITP• Acquired immune-mediated disorder characterized byisolated thrombocy<strong>to</strong>penia• Annual incidence of 3-8/100,000 children with peakincidence at 2-5 years• Sudden appearance of bruising or mucocutaneousbleeding in an otherwise healthy child (no constitutionalsymp<strong>to</strong>ms and no HSM); often preceded by viral infection• Over 2/3 will recover spontaneously within 6mo
ITP• Treatment is considered if platelets < 20 x 10 9 /L and iscontroversial unless there is active bleeding or significantrisk of bleeding• IVIG induces rise in 95% of patients within 48h; otheroptions include corticosteroids and anti-D for Rh+ patients(platelet transfusion is contraindicated unless there issignificant active hemorrhage)• < 1% will develop intracranial hemorrhage• 20% of children will develop chronic ITP and alternativeetiologies should be considered
Evans Syndrome• Immune thrombocy<strong>to</strong>penia with au<strong>to</strong>immune hemolyticanemia• Bruising and bleeding accompanied by pallor, fatigue,tachycardia +/- jaundice with positive Coombs test• Treatments include steroids, IVIG, immunosuppressantmedications• More likely <strong>to</strong> have a chronic relapsing course, oftenassociated with other au<strong>to</strong>immune disorders
Neonatal AlloimmuneThrombocy<strong>to</strong>penia (NAIT)• Isolated destruction of platelets by maternal antibodiesdirected against paternal antigens• Begins in utero and presents with petichiae, bruising andbleeding in an otherwise well neonate• Platelets recover over weeks, but ICH occurs in 10-20% ofinfants (50% in utero)• Treatment includes IVIG, steroids, maternal-matchedplatelet infusion
Neonatal Au<strong>to</strong>immuneThrombocy<strong>to</strong>penia (NAT)• Isolated destruction of platelets by maternal antibodiesdirected against maternal antigens, as in the case ofantepartum maternal ITP or SLE• Clinical presentation similar <strong>to</strong> NAIT, but higher plateletlevels and lower risk of serious hemorrhage• Treated with steroids or IVIG; maternal-matched plateletinfusion is ineffective
Kasabach-Merritt• Infant thrombocy<strong>to</strong>penia caused by a large or rapidlygrowinghemangioma that traps platelets• Aside from significant bleeding, complications include DICfrom consumption of coagulation fac<strong>to</strong>rs and high-outcardiac failure• If surgery is not an option, treatment includes steroids,vincristine, and embolization
Test Your Knowledge• An 8-month old boy presents <strong>to</strong> your office 1 week afterdischarge from the ICU for strep<strong>to</strong>coccal sepsis. You notescattered petichiae and eczema which his parents sayhave been present off-and-on since birth. What is themost likely diagnosis?A. Congenital HIV infectionB. LeukemiaC. Wiskott-Aldrich syndromeD. Congenital rubella syndrome
The Answer• Wiskott-Aldrich syndrome is a rare X-linked recessiveimmunodeficiency disorder characterized by the triad ofrecurrent bacterial infections, eczema, andthrombocy<strong>to</strong>penia with variable severity• WAS is caused by a mutation in the WASprotein which regulates platelet productionand antibody function• Treatment ranges from conservative, <strong>to</strong>symp<strong>to</strong>matic (platelet tranfusion, <strong>to</strong>picalsteroids, antibiotics), <strong>to</strong> hema<strong>to</strong>poietic stemcell transplant
Test Your Knowledge• You have been following a 14-year old girl with ITP for 10months, and her platelets have never recovered past 40 x10 9 /L. On review of her most recent labs you notice a Hbof 97. You request a urine dip that shows 3+ protein and2+ blood. What is the most likely diagnosis?A. Evans syndromeB. Chronic ITPC. Hemolytic uremic syndromeD. Lupus
The Answer• Persistent ITP can be the initial presentation ofau<strong>to</strong>immune disorders such as SLE, characterized byhema<strong>to</strong>logical manifestations, athralgias, skinmanifestations, serositis, nephritis, and other features• The older the ITP patient, the higher thelikelihood of chronicity and SLE• Chronic ITP is defined as >12 monthsduration• Evans syndrome alone does not featurenephritis, and HUS is not chronic
Summary• Thrombocy<strong>to</strong>penia is caused by increased destruction(immune, microangiopathic) or decreased production(congenital, infectious, marrow dysfunction) orsequestration of platelets• In a preschool child, ITP is the most common diagnosisbut thrombocy<strong>to</strong>penia must be isolated and a thoroughhis<strong>to</strong>ry and physical must rule out serious disorders suchas malignancy and NAI• Further investigation is required for chronicity, clinicalfeatures that suggest alternative diagnoses or treatmentfailure
Summary• There is no absolute threshold for treatment, which shouldbe administered based on underlying cause and anestimate of risk of significant hemorrhage• Platelet transfusions have limited utility in immunemediateddisorders