BlueCaid Coverage Chart - e-Referral - BCBSM.com
BlueCaid Coverage Chart - e-Referral - BCBSM.com
BlueCaid Coverage Chart - e-Referral - BCBSM.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
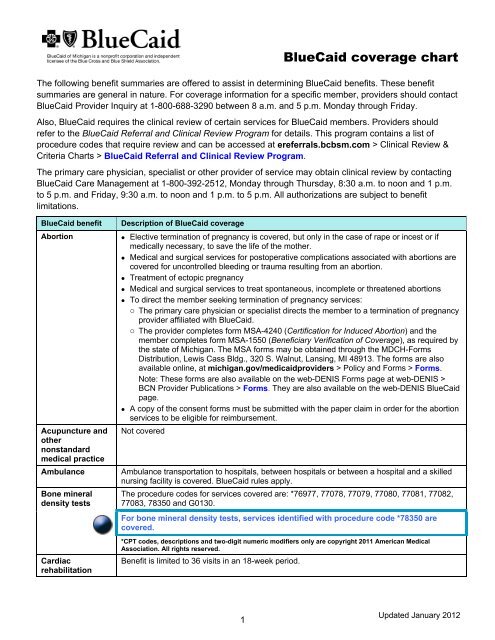
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefit(continued)EPSDT/Well ChildCare ProgramSee also: Leadtesting (blood)Description of <strong>BlueCaid</strong> coverage <strong>BlueCaid</strong> provides outreach and encourages participation based on notification from thestate of Michigan of members due or overdue for EPSDT/Well Child exams. Upon receipt ofthe names of those members eligible for the EPSDT/Well Child Care Program, <strong>BlueCaid</strong>sends each family a postcard advising the members to seek the appropriate services. Theprogram coverage specifics and reporting requirements include:o Vision: Diagnosis and treatment of refractive errors or abnormal visiono Oral health screening and flouride varnish: At age 1 (12 months), <strong>BlueCaid</strong> providers(pediatricians, family practitioners and nurse practitioners) will provide an oral healthscreen and flouride varnish treatment. <strong>Referral</strong> to a dentist will be made if dental care isneeded.Note: Medical providers must <strong>com</strong>plete online certification in order to provide flouridevarnish treatments. Providers can access infant oral health training and certificationmaterials at michigan.gov/medicaidproviders > Billing and Reimbursement > ProviderSpecific Information > Dental.o Hearing services must include at least the diagnosis of and treatment for hearing defects,including hearing aids, as appropriate. A conventional hearing aid, monaural or binaural,when medically necessary, is covered in full every third benefit year.o Providers may refer to a <strong>com</strong>munity mental health provider.o Hearing, vision and dental assessments: Medical record must show inspection of mouthand teeth.o Interpretative conference and appropriate counseling, for parents and guardians: Medicalrecord should show anticipatory guidance intended to help the parent or guardian andchild understand what to expect regarding growth and development. This includesinformation about healthy lifestyles and practices and the prevention of accidents anddiseases. Provider also provides the following services:o Objective testing for developmental behavior, hearing and vision must be performed inaccordance with the current American Academy of Pediatrics Re<strong>com</strong>mendations forPreventive Pediatric Health Care, which can be found at http://brightfutures.aap.org >Clinical Practice > Re<strong>com</strong>mendations for Preventive Pediatric Health Care.o State law requires that health professionals <strong>com</strong>ply with specified reporting requirementsfor <strong>com</strong>municable disease and other health indicators, as referenced atmichigan.gov/mdch/providers > Communicable and Chronic Diseases > InfectiousDiseases – Reporting and Tracking.o Providers must make appropriate referrals for a diagnostic or treatment servicedetermined to be necessary.o Oral screening should be part of a physical exam. Each child must have a direct referral toa dentist such that a dental exam can be <strong>com</strong>pleted by age 3. Note: <strong>Referral</strong> to a dentistat age 1 is re<strong>com</strong>mended but is not required.o Children should also be referred to a hearing and speech clinic, optometrist orophthalmologist or other appropriate provider for objective hearing and vision services, asnecessary.o <strong>Referral</strong> to <strong>com</strong>munity mental health services also may be appropriate.(continued on next page)4Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefit(continued)EPSDT/Well ChildCare ProgramSee also: Leadtesting (blood)Emergencyservices andpoststabilizationcareFamily planningservicesDescription of <strong>BlueCaid</strong> coverage Laboratory services for:o Tuberculin testing: Medical records should show evidence of a TB test performed. This isre<strong>com</strong>mended at 12 months, 4 to 6 years and 14 to 16 years.o Hematocrit and hemoglobin testing: Medical records should show evidence of ahemoglobin or hematocrit lab test being performed. This is re<strong>com</strong>mended between 6 and12 months, 15 months and 4 years, 5 and 12 years and 14 and 18 years.o Urinalysis: Medical records must show evidence of a urine test performed; this test isre<strong>com</strong>mended between 1 and 12 months, 15 months and 4 years, 5 and 12 years and 14and 18 years.o Other needed testing, as determined by the physician Vision services must include at least the diagnosis of and treatment for refractive errors orabnormal vision. This includes glasses, if appropriate. Dental services must include at least relief of pain and infections, restoration of teeth andmaintenance of dental health. (The <strong>BlueCaid</strong> provider is responsible for screening / referralonly. Other dental services are provided through the state, not through <strong>BlueCaid</strong>.) Also included are other health care, diagnostic services, treatment or services covered underthe state’s Medicaid Plan that are necessary to correct or ameliorate defects, physical ormental illnesses and conditions discovered during a screening. A medically necessaryservice may be available under the EPSDT/Well Child Care Program if listed in a federalstatute as a potentially covered service, even if Michigan’s Medicaid program does not coverthe service under its state’s Plan for Medical Assistance Program.Emergency services must be available 24 hours per day, seven days per week. <strong>BlueCaid</strong>covers emergency services and medical screening and stabilization exams without a referral orprior authorization. Members may go to any emergency facility.Emergency services are medically necessary services provided to a member to address thesudden onset of a medical condition that manifests itself in acute symptoms, including severepain, of sufficient severity that the absence of immediate medical attention could reasonably beexpected to result in: Serious jeopardy to the health of the member or, in the case of a pregnant woman, to thehealth of the woman or that of her unborn child Serious impairment of bodily functions Serious dysfunction of any body organ or partEmergency services also include covered inpatient and outpatient services that are furnishedby a provider that is qualified to furnish these services and needed to evaluate or stabilize anemergency medical condition.Poststabilization care includes services related to an emergency medical condition that areprovided after a member is stabilized, in order to maintain the member’s stabilized condition orto improve or resolve the member’s condition.Emergency services can be accessed anywhere in the world. <strong>BlueCaid</strong> members are asked tocontact their primary care physician within 24 hours of seeking emergency care to arrange forfollow-up. A <strong>BlueCaid</strong> member who receives emergency care from a non-<strong>BlueCaid</strong>-affiliatedhospital or facility may be transferred to a <strong>BlueCaid</strong> network hospital when it is safe to do so.<strong>BlueCaid</strong> is responsible for covering most family planning services through the member’sprimary care physician or obstetrician-gynecologist. The MDCH places special value on access to family planning services for <strong>BlueCaid</strong>members. <strong>BlueCaid</strong> members may obtain family planning services from any provider theywish (for example, in network or out of network, and without referral). <strong>BlueCaid</strong> membersmay self-refer to family planning providers for family planning services.(continued on next page)5Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefit(continued)Family planningservicesHearing examsand aidsDescription of <strong>BlueCaid</strong> coverage Family planning services include any medically approved diagnostic evaluation, drugs,supplies, devices and related counseling for the purpose of voluntarily preventing or delayingpregnancy or for the detection or treatment of sexually transmitted diseases. Services are tobe provided in a confidential manner to individuals of child-bearing age, including minorswho may be sexually active, who voluntarily choose not to risk initial pregnancy or who wishto limit the number and spacing of their children. Family planning services available to <strong>BlueCaid</strong> members are similar to benefits provided toBCN members, with the following considerations:o Over-the-counter family planning drugs and supplies are covered with a prescription.Members must go to a <strong>BlueCaid</strong>-affiliated pharmacy and present their <strong>BlueCaid</strong> ID card.o Infertility drugs are excluded.o Condoms are covered. These are distributed 12 at a time, up to a maximum of 36 permonth without prescription, from a family planning services provider Sterilization services are available within the following guidelines:o Sterilization must not be performed on males or females under 21.o When sterilization services are provided, providers are responsible for obtaining a signedconsent for sterilization 30 days prior to surgery, using either the MSA-1959 form from thestate of Michigan or the HHS-687 form from the U.S. Department of Health & HumanServices. These forms are available via links on the web-DENIS Forms page. Providerscan access that page at web-DENIS > BCN Provider Publications and Resources >Forms. These forms are also available on the web-DENIS <strong>BlueCaid</strong> page.In addition, the MSA-1959 form may be obtained through MDCH – Forms Distribution,Lewis Cass Bldg., 320 S. Walnut, Lansing, MI 48913. The form is also available online, atmichigan.gov/providers > Providers > Medicaid > Policy and Forms > Forms.o A copy of the consent form must be submitted with the paper claim in order for thesterilization services to be eligible for reimbursement.o Note: Federal regulations prohibit coverage for hysterectomies performed for familyplanning purposes. For additional information on hysterectomies, providers should referto “Hysterectomy claims submitted with consent form” in the “<strong>BlueCaid</strong> claimsprocessing” section of the <strong>BlueCaid</strong> chapter of the BCN Provider Manual. Hearing exams: For all <strong>BlueCaid</strong> members, hearing exams are provided if medicallynecessary when ordered by the primary care physician and provided by an audiologistaffiliated with <strong>BlueCaid</strong> and according to Medicaid guidelines. Hearing aids:o For <strong>BlueCaid</strong> members 21 years and older, hearing aids are not covered.o For <strong>BlueCaid</strong> members under 21 years, hearing aids are covered when re<strong>com</strong>mended asa result of a hearing exam. <strong>Coverage</strong> includes one hearing aid unit every five years, withone follow-up visit for fitting and evaluation of the unit’s conformance to the prescription. Batteries, maintenance and repair of hearing aids: For <strong>BlueCaid</strong> members under 21 years,these are covered and are provided by the hearing aid provider. For <strong>BlueCaid</strong> members 21years and older, these are covered only for hearing aids purchased prior to Feb. 1, 2010.When covered, batteries can be provided in a six-month supply and can be picked up at theMichigan Health System Department of Audiology or mailed to the member.Note: The names of providers affiliated with <strong>BlueCaid</strong> are available through <strong>BlueCaid</strong> ProviderInquiry at 1-800-688-3290 from 8 a.m. to 5 p.m. Monday through Friday.6Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefitHome health careservicesDescription of <strong>BlueCaid</strong> coverage Physical and occupational therapies are covered. Limited to 24 visits per episode in a 90-consecutive-day period. No clinical review is required for PT, OT or speech therapy. Skilled nursing visits are covered, with no limit. No clinical review is required. All services must be medically necessary, following or in lieu of a hospital stay.No clinical review is required for home health care services for <strong>BlueCaid</strong> members.Home infusionHospiceImmunizationsInpatient hospitalLaboratoryCovered services include total parenteral nutrition and enteral and formula feedings andantibiotic, hydration and other drug therapy. Clinical review is required when services involveTPN and enteral feedings. Hospice care services are a covered benefit for members not already receiving them at thetime of <strong>BlueCaid</strong> enrollment. Hospice services are covered when provided in the home, by anursing home or hospital affiliated with <strong>BlueCaid</strong>. Hospice services must be arranged andauthorized by <strong>BlueCaid</strong>, with a referral from the member’s primary care physician. Clinicalreview is required. Individuals enrolled in a hospice program on the effective date of <strong>BlueCaid</strong> enrollment areconsidered an enrollment error and should be disenrolled. Hospice must be requested by the member. There are no limit requirements on hospice services. For members under 21 years of age, <strong>BlueCaid</strong> covers hospice care concurrent withtreatment aimed at curing the member’s terminal illness. Providers may access additionaldetails from MDCH bulletin MSA 11-01 (Jan. 1, 2011).Clinical review is required for hospice services provided in the home. For all members, <strong>BlueCaid</strong> covers the administration fee for immunizations. The Vaccinesfor Children Program provides the serum for VFC-approved codes. For more detailed information on what the VFC Program involves, including a list of thevaccines that are covered, providers may access the MDCH VFC Resource Book online atmichigan.gov > Education & Children > Community Health > Pregnant Women, Children &Families > Children & Families > Immunization Info for Families & Providers > VFCResource Book > Vaccines for Children (VFC) Program Resource Book. UMHS providers can provide immunization services without obtaining an authorization. Vaccines are covered when given according to guidelines re<strong>com</strong>mended by the AdvisoryCommittee on Immunization Practices of the Centers for Disease Control and Prevention.Additional information is available at cdc.gov/HealthyLiving > Vaccines and Immunizations> Re<strong>com</strong>mendations > Advisory Committee on Immunization Practices (ACIP). Thiscoverage includes an increase in the maximum daily limit for vaccine administration effectiveOct. 1, 2010.Note: For additional information on the VFC Program, providers should refer to the “Vaccinesfor Children Program” subsection in the “<strong>BlueCaid</strong> primary care physician services” section ofthis chapter. <strong>BlueCaid</strong> <strong>Referral</strong> and Clinical Review Program rules apply. Members must go to a <strong>BlueCaid</strong> network hospital. (See the <strong>BlueCaid</strong> Provider Directory.) Includes semiprivate room, intensive care nursing, physician services, surgical services,anesthesia, X-rays and laboratory servicesCovered to the extent coverage is provided under <strong>BlueCaid</strong>; <strong>BlueCaid</strong> coverage rules apply.For information on <strong>BlueCaid</strong> laboratory providers, providers should refer to “Outpatientlaboratory services” elsewhere in this chapter.7Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefit(continued)Lead testing(blood)Maternal and childhealth: MichiganState UniversityExtension HealthPromotion ProgramMedical suppliesand disposableitemsMental healthservicesNutritionalcounselingObstetrics andgynecologyservicesOffice visitsDescription of <strong>BlueCaid</strong> coverageo Providers must also report blood lead test results to the MCIR.o Providers may call the BCN Quality Management department at 248-455-3471 withquestions.o Note: The provider guidelines for the statewide lead testing/lead screening program canbe accessed at web-DENIS > BCN Provider Publications and Resources > <strong>BlueCaid</strong> >MDCH Childhood Lead Poisoning Prevention Program or at web-DENIS > BCNProvider Publications and Resources > Clinical Practice Guidelines > Pediatric bloodlead testing: provider guidelines.o If a child is found to have elevated blood lead levels, in accordance with standardsdisseminated by the MDCH, a referral should be made to the local health department forfollow-up services that may include an epidemiological investigation to determine thesource of the blood lead poisoning.The MDCH offers online training in blood lead screening for primary care physicians and theirstaff members. Providers can access the online training modules at training.mihealth.org >Childhood Lead Poisoning Prevention for Primary Care Providers.A health promotion program for maternal and child health care education and support. Anumber of maternal and child health initiatives are coordinated throughout the state by theMDCH, Medicaid managed care plans and other entities. Medical supplies and disposable items deemed appropriate by the primary care physician orother <strong>BlueCaid</strong> provider are covered. Members must have an order to obtain supplies. All of the items must be provided by a<strong>BlueCaid</strong>-affiliated durable medical equipment-medical supply provider or pharmacy. Outpatient crisis intervention and short-term therapy are covered for up to 20 outpatientvisits per calendar year. Additional mental health services (for example, inpatient and outpatient partialhospitalization) are available through the Community Mental Health Service Programs. For mental health services, <strong>BlueCaid</strong> members should call the <strong>BlueCaid</strong> Mental Healthphone number on their member ID card or <strong>BlueCaid</strong> Customer Service at 1-800-228-8554(1-800-649-3777 for TTY users) between 8 a.m. and 5:30 p.m. Monday through Friday.Other mental health services for members are provided in conjunction with Community MentalHealth Service Programs, as follows: The Community Mental Health Service Programs coordinate all inpatient and partialhospitalization psychiatric care for <strong>BlueCaid</strong> members. For <strong>BlueCaid</strong> members determined by a Community Mental Health Service Program entity tobe severely and persistently mentally ill, the Community Mental Health Service Programprovides all the mental health care, including the outpatient visits. For severely and persistently mentally ill members who are receiving some services from aCommunity Mental Health Service Program, <strong>BlueCaid</strong> may also agree to authorize certainservices. These authorizations are handled on a case-by-case basis.Based on diagnosis, four to six visits per calendar year are covered.See Women’s health services.Physician office visits are covered.9Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefitOral surgicalservicesPediatric servicesDescription of <strong>BlueCaid</strong> coverageOral surgical services are limited to emergent and urgent services for the relief of pain orinfection and surgical services. <strong>BlueCaid</strong> members are covered for these oral surgical services: Emergency surgery of the jaw or maxillofacial area due to trauma, accident, or injury Diagnosis and treatment of cysts and of benign and malignant tumors of the maxilla andmandible and adjacent structures Hospital and medical expenses for extractions that must be performed in a hospital as theresult of an underlying critical medical condition Medically necessary medical or surgical, but not dental, management of internalderangements of the jaw, as determined by a <strong>BlueCaid</strong>-affiliated physician and authorizedby <strong>BlueCaid</strong><strong>BlueCaid</strong> covers routine preventive health care services rendered by a pediatrician or aninternist/pediatrician without a referral from the primary care physician.<strong>BlueCaid</strong> covers routine preventive health care services rendered by a pediatrician or aninternist/pediatrician without a referral from the primary care physician.PharmacyPhysical examsPodiatryPrenatal andpostpartumservicesProfessionalservices byphysiciansRadiologySkilled nursingfacilitiesSmokingcessation<strong>BlueCaid</strong> members have coverage for outpatient medications. Providers should refer to the“<strong>BlueCaid</strong> Pharmacy Services” section of this chapter for additional information.Physical exams with the member’s primary care physician are covered.For all <strong>BlueCaid</strong> members: Foot care services with the member’s physician or podiatrist are covered when the membermanifests signs and symptoms from a specific systemic disease of sufficient severity (suchas severe diabetes) that care by a nonprofessional would be hazardous. Treatment for subluxations, results of injury, mycotic infections, plantar warts and nailavulsions is also covered. Routine foot care, removal of corns and calluses and the trimming of nails are not covered.Prenatal and postpartum services are covered.Professional services rendered by primary care physicians are covered. Professional servicesrendered by specialists are covered but require a referral from the primary care physician.Radiology services are covered. Short-term, medically necessary restorative health services are covered for up to 45cumulative days of skilled care within a 12-month rolling period that starts with the initialadmission. Care must be provided in a SNF affiliated with <strong>BlueCaid</strong>. Long-term custodial care is not covered. After the 45-day limit is reached, the member will be disenrolled from the Medicaid plan.Individuals receiving long-term custodial care will also be disenrolled from <strong>BlueCaid</strong>. Members who use tobacco in any form may elect to enroll in the Quit the Nic program forsupport and phone counseling. For information, members can call 1-800-811-1764. <strong>Coverage</strong> is provided for prescription and over-the-counter smoking cessation aids with avalid prescription, subject to quantity limitations. <strong>Coverage</strong> for smoking cessation products is limited to a three-month supply every 12months.10Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefitSurgeryTelemedicine(telehealth)Termination ofpregnancyTherapy:outpatientphysical,occupational andspeechTransplants:human organ andtissueDescription of <strong>BlueCaid</strong> coverageOutpatient surgery coverage includes all related surgical services and anesthesia for coveredsurgical procedures.Note: <strong>BlueCaid</strong> covers services rendered in ambulatory surgical centers in the same way asthey are covered by the MDCH. Providers may access additional details from MDCH bulletinsMSA 10-63 (Dec. 2, 2010) and MSA 10-23 (June 15, 2010).Initial and follow-up consultations <strong>com</strong>pleted using telemedicine are covered by <strong>BlueCaid</strong> aslong as the services are rendered in line with the policies described in the MDCH Bulletin MSA06-22 (April 1, 2006).See: Abortion. Physical, occupational and speech therapy covered services include a maximum of 36 visitsin 90 consecutive days. Requests for visits beyond the initial 36 or the 90 consecutive daysrequire clinical review. Physical, occupational and speech therapy services are covered when medically necessary,when the condition is expected to improve in a relatively predictable time period. Physical, occupational and speech therapy services are available in a hospital outpatientfacility, freestanding facility or home health care. Names and addresses of providers for<strong>BlueCaid</strong> can be accessed through <strong>BlueCaid</strong> Provider Inquiry at 1-800-688-3290 between 8a.m. and 5 p.m. Monday through Friday. Physical and occupational therapy services provided in a physician’s office are eligible forcoverage, effective Feb. 1, 2010. Services must be performed by properly credentialedprofessionals under the supervision of the physician and billed with the physician’s NationalProvider Identifier. Physical, occupational and speech therapy for cognitive rehabilitation is excluded. Cornea and kidney transplants are covered. Extrarenal organ transplants (heart, lung, heart-lung, liver, pancreas, bone marrow includingallogenic, autologous and peripheral stem cell harvesting, and small bowel) are covered on apatient-specific basis when determined medically necessary according to current acceptablestandards of care. If a transplant is covered, additional benefits are provided to assure that the transplant will beprovided (including donor search fees). The Medical Services Administration mandates that transportation and lodging be provided, ifnecessary, so that transplant services can be accessed. <strong>BlueCaid</strong> has the right to direct themember to less costly services. <strong>BlueCaid</strong> covers small bowel transplants on a case-by-case basis following a review. Other transplants that <strong>BlueCaid</strong> considers to be investigational are reviewed on a case-by-casebasis. Transplants and evaluations are directed to Blue Distinction Centers for Transplants.11Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefitTransportation,non-ambulanceUrgent careDescription of <strong>BlueCaid</strong> coverageTransportation services may be available to members for medically necessary medical examsand treatment. This includes picking up prescriptions and durable medical equipment.The transportation provider provides non-emergency transportation to and from medicalappointments at facilities approved by <strong>BlueCaid</strong> for <strong>BlueCaid</strong> members, only if the member hasno other means of transportation available. This service is offered in line with MichiganDepartment of Human Services guidelines The <strong>BlueCaid</strong> member may contact the transportation provider, Access2Care, directly at1-888-803-4947 between 6 a.m. and 6 p.m. to schedule transportation. Arrangementsshould be made as soon as the member makes a medical appointment. Additional detailsrelated to the requirements for notifying the transportation provider are available in the<strong>BlueCaid</strong> Member Handbook.Note: Members who live in Wayne County and who need a ride for dental care, substanceabuse services, some types of mental health services or other services provided by the stateof Michigan should call LogistiCare ® at 1-866-569-1902 between 8 a.m. and 5 p.m. Mondaythrough Friday. The transportation provider determines the most appropriate mode of transportation (forexample, public transportation, taxi, minibus or van) for the member, based upon initialinterview information. The transportation provider informs <strong>BlueCaid</strong> members of the policies regardingtransportation benefits on initial contact. The transportation provider submits claims for reimbursement by <strong>BlueCaid</strong>. Claimssubmitted by other transportation providers will be denied. No referral or authorization is required. Urgent care services are those medically necessary services for a non-life-threateningcondition, injury or illness that should be treated within 24 hours. Urgent care services must be available 24 hours per day, seven days per week. <strong>BlueCaid</strong> members are asked to contact their primary care physician first, if they are unsurewhether their condition requires urgent care, to see whether the condition can be treated inthe primary care physician’s office. <strong>BlueCaid</strong> members who cannot reach their primary carephysician should contact <strong>BlueCaid</strong> Customer Service at 1-800-228-8554 (1-800-649-3777 forTTY users) anytime of the day or night. <strong>BlueCaid</strong> members who access urgent care are asked to contact their primary care physicianwithin 24 hours to arrange for follow-up care.12Updated January 2012
<strong>BlueCaid</strong> coverage chart<strong>BlueCaid</strong> benefitVisionVoluntarysterilizationWeightmanagementWomen’s healthservicesDescription of <strong>BlueCaid</strong> coverageFor <strong>BlueCaid</strong> members 21 years and older: Routine eye exams, eye glasses, contact lensesand other vision supplies and services are not covered. Services and supplies related to lowvision are covered, including low-vision eyeglasses, contact lenses, optical devices and otherlow-vision services and supplies. Services related to eye trauma and eye disease are covered.For <strong>BlueCaid</strong> members under 21 years: Vision exams, lenses and frames are covered. <strong>Referral</strong> is not required from the primary care physician. Routine eye exams are covered once every two years. (The member is eligible for an examtwo years from the date of the last exam.) The vision exam includes:o Obtaining a case history and binocular measureso Testing tonometry, visual acuity, performing refraction, external eye examination andrecord of findingso Prescribing lenses, if neededo Confirming the appropriateness of lenses under prescription, when indicated Corrective lens benefit: Providers are responsible for furnishing clear, non-oversizecorrective lenses of any focal length and conventional frames. Lens benefits are:o One pair of lenses and frames are covered every two years for members.o Orthoptics are covered.o Contact lenses are covered only if the member has a vision problem that cannot beadequately corrected by eyeglasses (monocular aphakia; keratoconus; anisometropia orantimetropia that results in aniseikonia; or other medical conditions that have noalternative treatment). Replacements for lost or damaged eyeglasses or contact lenses are covered up to twice peryear for members younger than 21 years and once per year for members 21 years or older.A year is 365 days from the initial dispensing.For <strong>BlueCaid</strong> members with a diagnosis of diabetes: <strong>BlueCaid</strong> members with diagnoseddiabetes (ICD-9-CM 250 through 250.99) may schedule an annual medical eye examinationwithout a written referral from their primary care physician. Providers should provide written<strong>com</strong>munication about the results of the dilated eye exam to the member’s primary carephysician.For all <strong>BlueCaid</strong> members: <strong>BlueCaid</strong> members must go to a <strong>BlueCaid</strong> vision provider. <strong>BlueCaid</strong> members should call <strong>BlueCaid</strong> Customer Service at 1-800-228-8554(1-800-649-3777 for TTY users) between 8 a.m. and 5:30 p.m. Monday through Friday forthe names of providers of vision services affiliated with <strong>BlueCaid</strong>.See: Family planning services <strong>BlueCaid</strong> coverage does not include treatment specifically for obesity or weight reductionand maintenance, except on a limited basis, for the purpose of controlling life-endangering<strong>com</strong>plications such as hypertension and diabetes. <strong>BlueCaid</strong> provides limited coverage for nutritional counseling.Under the Woman’s Choice program, <strong>BlueCaid</strong> covers all services rendered by a women’shealth specialist without a referral from the primary care physician. Additional information as towhich specialists are covered under this program is available in the Woman’s Choicespecialty and procedure/diagnosis code requirements document.<strong>BlueCaid</strong> covers all services rendered by a women’s health specialist without a referralfrom the primary care physician.13Updated January 2012