Pathology of the Head and Neck
Pathology of the Head and Neck
Pathology of the Head and Neck
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
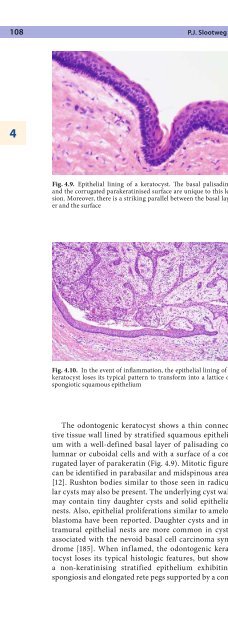
108 P.J. Slootweg4Fig. 4.9. Epi<strong>the</strong>lial lining <strong>of</strong> a keratocyst. The basal palisading<strong>and</strong> <strong>the</strong> corrugated parakeratinised surface are unique to this lesion.Moreover, <strong>the</strong>re is a striking parallel between <strong>the</strong> basal layer<strong>and</strong> <strong>the</strong> surfaceFig. 4.10. In <strong>the</strong> event <strong>of</strong> inflammation, <strong>the</strong> epi<strong>the</strong>lial lining <strong>of</strong> akeratocyst loses its typical pattern to transform into a lattice <strong>of</strong>spongiotic squamous epi<strong>the</strong>liumThe odontogenic keratocyst shows a thin connectivetissue wall lined by stratified squamous epi<strong>the</strong>liumwith a well-defined basal layer <strong>of</strong> palisading columnaror cuboidal cells <strong>and</strong> with a surface <strong>of</strong> a corrugatedlayer <strong>of</strong> parakeratin (Fig. 4.9). Mitotic figurescan be identified in parabasilar <strong>and</strong> midspinous areas[12]. Rushton bodies similar to those seen in radicularcysts may also be present. The underlying cyst wallmay contain tiny daughter cysts <strong>and</strong> solid epi<strong>the</strong>lialnests. Also, epi<strong>the</strong>lial proliferations similar to ameloblastomahave been reported. Daughter cysts <strong>and</strong> intramuralepi<strong>the</strong>lial nests are more common in cystsassociated with <strong>the</strong> nevoid basal cell carcinoma syndrome[185]. When inflamed, <strong>the</strong> odontogenic keratocystloses its typical histologic features, but showsa non-keratinising stratified epi<strong>the</strong>lium exhibitingspongiosis <strong>and</strong> elongated rete pegs supported by a connectivetissue containing a mixed inflammatory infiltrate(Fig. 4.10). Rarely, odontogenic keratocysts showdevelopment <strong>of</strong> epi<strong>the</strong>lial dysplasia <strong>and</strong> squamous cellcarcinoma [87].Immunohistochemical studies have not yielded data<strong>of</strong> diagnostic or prognostic significance [148, 149].Odontogenic keratocysts may also contain mucouscells, melanin-producing cells, dentinoid <strong>and</strong> intramuralcartilage [12, 74, 86, 105]. Ciliated cells may be seen,but in maxillary cases, <strong>the</strong>y could also be <strong>the</strong> result <strong>of</strong> acommunication with <strong>the</strong> maxillary sinus [122]. In addition,<strong>the</strong> cyst wall may contain intramural odontogenicepi<strong>the</strong>lial remnants. Occasionally, intraosseous cysts arelined by orthokeratinised epi<strong>the</strong>lium, thus having <strong>the</strong>appearance <strong>of</strong> an epidermoid cyst. Such cysts are knownas orthokeratinised odontogenic cysts. Their differentiationfrom <strong>the</strong> odontogenic keratocyst with parakeratinisationis clinically important as recurrence <strong>of</strong> orthokeratinisedcysts is rare [188]. Differential diagnosiswith unicystic ameloblastoma (see Sect. 4.4.1.1) maybe difficult. Odontogenic keratocyst exhibits a compactspinous layer <strong>and</strong> a corrugated superficial parakeratinlayer, <strong>and</strong> ameloblastoma a spinous layer with intercellularoedema.Keratocysts do not cause symptoms unless concomitantinflammation causes pain <strong>and</strong> swelling. Radiographsmay reveal extensive uni- or multilocular radiolucentlesions that occupy <strong>the</strong> major part <strong>of</strong> <strong>the</strong> jawwithout having caused any appreciable cortical expansion.When <strong>the</strong> odontogenic keratocyst forms part <strong>of</strong><strong>the</strong> nevoid basal cell carcinoma syndrome, patientsmay show any <strong>of</strong> <strong>the</strong> o<strong>the</strong>r features <strong>of</strong> this syndrome[72].Odontogenic keratocysts tend to recur after enucleation[147, 148, 149]. Sometimes, a partial jaw resectionis needed to a provide permanent cure [182]. If associatedwith <strong>the</strong> nevoid basal cell carcinoma syndrome, <strong>the</strong>chance <strong>of</strong> recurrence is even higher [18]. If located in <strong>the</strong>gingiva, <strong>the</strong> behaviour <strong>of</strong> <strong>the</strong> odontogenic keratocyst isless aggressive [65].As <strong>the</strong>re is sufficient evidence that this lesion actuallyrepresents a cystic neoplasm, <strong>the</strong> most recent WHOclassification proposes <strong>the</strong> diagnostic designation keratocysticodontogenic tumour [181].4.3.2.5 Gingival CystGingival cysts are divided in those occurring in adults<strong>and</strong> those in infants. They are located in <strong>the</strong> gingival tissues.Gingival cysts <strong>of</strong> adults are rarely larger than 1 cm<strong>and</strong> may be multiple. They are lined by ei<strong>the</strong>r thin epi<strong>the</strong>lium<strong>of</strong> one to three cell layers or thicker <strong>and</strong> exhibitkeratinisation. Plaques similar to those occurring in <strong>the</strong>lateral periodontal cyst (see Sect. 4.3.2.2) may be seen[107].