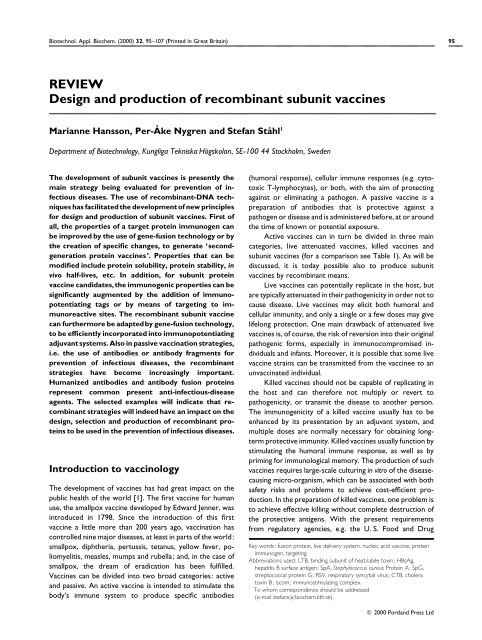
REVIEW Design and production of recombinant subunit vaccines
REVIEW Design and production of recombinant subunit vaccines
REVIEW Design and production of recombinant subunit vaccines
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Biotechnol. Appl. Biochem. (2000) 32, 95–107 (Printed in Great Britain) 95<br />
<strong>REVIEW</strong><br />
<strong>Design</strong> <strong>and</strong> <strong>production</strong> <strong>of</strong> <strong>recombinant</strong> <strong>subunit</strong> <strong>vaccines</strong><br />
Marianne Hansson, Per-A � ke Nygren <strong>and</strong> Stefan Sta� hl 1<br />
Department <strong>of</strong> Biotechnology, Kungliga Tekniska Ho� gskolan, SE-100 44 Stockholm, Sweden<br />
The development <strong>of</strong> <strong>subunit</strong> <strong>vaccines</strong> is presently the<br />
main strategy being evaluated for prevention <strong>of</strong> infectious<br />
diseases. The use <strong>of</strong> <strong>recombinant</strong>-DNA techniques<br />
has facilitated the development <strong>of</strong> new principles<br />
for design <strong>and</strong> <strong>production</strong> <strong>of</strong> <strong>subunit</strong> <strong>vaccines</strong>. First <strong>of</strong><br />
all, the properties <strong>of</strong> a target protein immunogen can<br />
be improved by the use <strong>of</strong> gene-fusion technology or by<br />
the creation <strong>of</strong> specific changes, to generate ‘secondgeneration<br />
protein <strong>vaccines</strong>’. Properties that can be<br />
modified include protein solubility, protein stability, in<br />
vivo half-lives, etc. In addition, for <strong>subunit</strong> protein<br />
vaccine c<strong>and</strong>idates,the immunogenic properties can be<br />
significantly augmented by the addition <strong>of</strong> immunopotentiating<br />
tags or by means <strong>of</strong> targeting to immunoreactive<br />
sites. The <strong>recombinant</strong> <strong>subunit</strong> vaccine<br />
can furthermore be adaptedby gene-fusion technology,<br />
to be efficiently incorporated into immunopotentiating<br />
adjuvant systems. Also in passive vaccination strategies,<br />
i.e. the use <strong>of</strong> antibodies or antibody fragments for<br />
prevention <strong>of</strong> infectious diseases, the <strong>recombinant</strong><br />
strategies have become increasingly important.<br />
Humanized antibodies <strong>and</strong> antibody fusion proteins<br />
represent common present anti-infectious-disease<br />
agents. The selected examples will indicate that <strong>recombinant</strong><br />
strategies will indeed have an impact on the<br />
design, selection <strong>and</strong> <strong>production</strong> <strong>of</strong> <strong>recombinant</strong> proteins<br />
to be used in the prevention <strong>of</strong> infectious diseases.<br />
Introduction to vaccinology<br />
The development <strong>of</strong> <strong>vaccines</strong> has had great impact on the<br />
public health <strong>of</strong> the world [1]. The first vaccine for human<br />
use, the smallpox vaccine developed by Edward Jenner, was<br />
introduced in 1798. Since the introduction <strong>of</strong> this first<br />
vaccine a little more than 200 years ago, vaccination has<br />
controlled nine major diseases, at least in parts <strong>of</strong> the world:<br />
smallpox, diphtheria, pertussis, tetanus, yellow fever, poliomyelitis,<br />
measles, mumps <strong>and</strong> rubella; <strong>and</strong>, in the case <strong>of</strong><br />
smallpox, the dream <strong>of</strong> eradication has been fulfilled.<br />
Vaccines can be divided into two broad categories: active<br />
<strong>and</strong> passive. An active vaccine is intended to stimulate the<br />
body’s immune system to produce specific antibodies<br />
(humoral response), cellular immune responses (e.g. cytotoxic<br />
T-lymphocytes), or both, with the aim <strong>of</strong> protecting<br />
against or eliminating a pathogen. A passive vaccine is a<br />
preparation <strong>of</strong> antibodies that is protective against a<br />
pathogen or disease <strong>and</strong> is administered before, at or around<br />
the time <strong>of</strong> known or potential exposure.<br />
Active <strong>vaccines</strong> can in turn be divided in three main<br />
categories, live attenuated <strong>vaccines</strong>, killed <strong>vaccines</strong> <strong>and</strong><br />
<strong>subunit</strong> <strong>vaccines</strong> (for a comparison see Table 1). As will be<br />
discussed, it is today possible also to produce <strong>subunit</strong><br />
<strong>vaccines</strong> by <strong>recombinant</strong> means.<br />
Live <strong>vaccines</strong> can potentially replicate in the host, but<br />
are typically attenuated in their pathogenicity in order not to<br />
cause disease. Live <strong>vaccines</strong> may elicit both humoral <strong>and</strong><br />
cellular immunity, <strong>and</strong> only a single or a few doses may give<br />
lifelong protection. One main drawback <strong>of</strong> attenuated live<br />
<strong>vaccines</strong> is, <strong>of</strong> course, the risk <strong>of</strong> reversion into their original<br />
pathogenic forms, especially in immunocompromised individuals<br />
<strong>and</strong> infants. Moreover, it is possible that some live<br />
vaccine strains can be transmitted from the vaccinee to an<br />
unvaccinated individual.<br />
Killed <strong>vaccines</strong> should not be capable <strong>of</strong> replicating in<br />
the host <strong>and</strong> can therefore not multiply or revert to<br />
pathogenicity, or transmit the disease to another person.<br />
The immunogenicity <strong>of</strong> a killed vaccine usually has to be<br />
enhanced by its presentation by an adjuvant system, <strong>and</strong><br />
multiple doses are normally necessary for obtaining longterm<br />
protective immunity. Killed <strong>vaccines</strong> usually function by<br />
stimulating the humoral immune response, as well as by<br />
priming for immunological memory. The <strong>production</strong> <strong>of</strong> such<br />
<strong>vaccines</strong> requires large-scale culturing in vitro <strong>of</strong> the diseasecausing<br />
micro-organism, which can be associated with both<br />
safety risks <strong>and</strong> problems to achieve cost-efficient <strong>production</strong>.<br />
In the preparation <strong>of</strong> killed <strong>vaccines</strong>, one problem is<br />
to achieve effective killing without complete destruction <strong>of</strong><br />
the protective antigens. With the present requirements<br />
from regulatory agencies, e.g. the U. S. Food <strong>and</strong> Drug<br />
Key words: fusion protein, live delivery system, nucleic acid vaccine, protein<br />
immunogen, targeting.<br />
Abbreviations used: LTB, binding <strong>subunit</strong> <strong>of</strong> heat-labile toxin; HBsAg,<br />
hepatitis B surface antigen; SpA, Staphylococcus aureus Protein A; SpG,<br />
streptococcal protein G; RSV, respiratory syncytial virus; CTB, cholera<br />
toxin B; iscom; immunostimulating complex.<br />
1 To whom correspondence should be addressed<br />
(e-mail stefans�biochem.kth.se).<br />
� 2000 Portl<strong>and</strong> Press Ltd
96 M. Hansson, P.-A� . Nygren <strong>and</strong> S. Sta� hl<br />
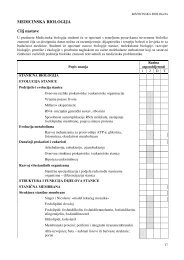
Table 1 A comparison <strong>of</strong> some properties <strong>of</strong> different vaccine types<br />
Vaccine type Advantages Drawbacks<br />
Live <strong>vaccines</strong> (attenuated) One or few doses normally required Controlled attenuation normally required<br />
Long-lasting protection Risk <strong>of</strong> reversion to pathogenicity<br />
Both humoral <strong>and</strong> cellular responses Certain risk <strong>of</strong> transmission<br />
Poorly defined composition<br />
Killed <strong>vaccines</strong> No risk <strong>of</strong> reversion to pathogenicity Multiple doses typically required<br />
No risk <strong>of</strong> transmission Poorly defined composition<br />
Antigen must be produced by cultivation <strong>of</strong> a pathogen<br />
Mainly humoral responses<br />
Adjuvants normally needed<br />
Subunit <strong>vaccines</strong> (non-<strong>recombinant</strong>) Defined composition<br />
Various delivery systems available<br />
Subunit <strong>vaccines</strong> (<strong>recombinant</strong>) No risk <strong>of</strong> pathogenicity since the pathogenic organism is<br />
not present<br />
Defined composition<br />
Various delivery systems available<br />
Simplified large-scale <strong>production</strong><br />
Further engineering possible<br />
Administration (FDA) <strong>and</strong> World Health Organization<br />
(WHO), for exact definitions <strong>of</strong> the vaccine preparations, it<br />
will probably become increasingly difficult to get new<br />
<strong>vaccines</strong> <strong>of</strong> this class accepted for human use.<br />
Subunit <strong>vaccines</strong> take advantage <strong>of</strong> the possibility <strong>of</strong><br />
using only part <strong>of</strong> the infectious micro-organism to raise a<br />
protective immune response, <strong>and</strong> since <strong>subunit</strong> <strong>vaccines</strong><br />
cannot replicate in the host, there is no risk <strong>of</strong> pathogenicity.<br />
The composition <strong>of</strong> a <strong>subunit</strong> vaccine can normally be clearly<br />
defined, which is a significant advantage in terms <strong>of</strong> safety<br />
considerations <strong>and</strong> minimization <strong>of</strong> side-effects. In order to<br />
elicit a vigorous immune response, <strong>subunit</strong> <strong>vaccines</strong> <strong>of</strong>ten<br />
require multiple doses, as well as the use <strong>of</strong> adjuvants.<br />
Subunit <strong>vaccines</strong> can be based on peptides, proteins or<br />
polysaccharides that have been shown to contain protective<br />
epitopes. Many <strong>of</strong> the cell-surface carbohydrates <strong>of</strong> pathogenic<br />
bacteria, e.g. capsular polysaccharides, are important<br />
antigenic determinants for vaccine development. Subunit<br />
conjugate <strong>vaccines</strong> [2,3] based on such polysaccharides, e.g.<br />
Haemophilus influenzae type b (Hib) <strong>vaccines</strong>, which are<br />
commonly delivered coupled to protein carriers such as the<br />
tetanus toxoid [4], will not be described further in this<br />
review.<br />
Immunogenic components can be isolated directly from<br />
pathogenic organisms, e.g. bacterial polysaccharides are<br />
<strong>of</strong>ten shed during growth <strong>and</strong> can be enriched from the<br />
culture medium. However, the <strong>production</strong> <strong>of</strong> <strong>subunit</strong><br />
<strong>vaccines</strong> <strong>of</strong>ten requires purification <strong>of</strong> the immunogens from<br />
large quantities <strong>of</strong> the pathogenic organism, which is not<br />
without risk <strong>and</strong> significant cost.<br />
Recombinant-DNA technology allows controlled <strong>production</strong><br />
<strong>of</strong> protein-<strong>subunit</strong> <strong>vaccines</strong> in heterologous hosts.<br />
Such strategies have several advantages, e.g. safe <strong>and</strong> cost-<br />
� 2000 Portl<strong>and</strong> Press Ltd<br />
Antigen must be produced <strong>and</strong> purified by cultivation <strong>of</strong><br />
a pathogen<br />
Multiple doses typically required<br />
Adjuvants needed<br />
Multiple doses typically required<br />
Adjuvants needed<br />
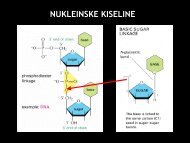
Table 2 Recombinant <strong>subunit</strong> <strong>vaccines</strong> <strong>and</strong> examples <strong>of</strong> their advantages<br />
(+) <strong>and</strong> drawbacks (�)<br />
Recombinant vaccine Advantages/drawbacks<br />
Protein immunogens + No risk <strong>of</strong> pathogenicity since the pathogenic<br />
organism is not present<br />
+ Efficient <strong>production</strong> systems available<br />
� Multiple doses required<br />
� Adjuvants needed<br />
Live delivery systems + May induce both humoral <strong>and</strong> cellular<br />
responses<br />
+ Adjuvants normally not needed<br />
� Risk <strong>of</strong> reversion when using attenuated<br />
pathogens as carriers<br />
Bacterial + Surface display <strong>of</strong> antigens possible<br />
+ Mucosal administration possible<br />
Viral + Efficient induction <strong>of</strong> cellular responses<br />
Nucleic acid <strong>vaccines</strong> + No risk <strong>of</strong> pathogenicity<br />
+ Simple <strong>production</strong><br />
+ May induce both humoral <strong>and</strong> cellular<br />
responses<br />
� Variable immune responses<br />
� Inefficient transfection<br />
DNA + Dedicated delivery systems exist<br />
� Inefficient delivery<br />
� Risk <strong>of</strong> integration into host chromosomes<br />
must be considered<br />
� Moderate <strong>and</strong> variable immune responses<br />
RNA + No risk <strong>of</strong> integration into host chromosomes<br />
+ No need to enter the nucleus for translation<br />
+ In vivo amplification systems available<br />
� Cumbersome large-scale <strong>production</strong><br />
� Unstable<br />
efficient <strong>production</strong> systems can be used. Recombinant<br />
strategies further <strong>of</strong>fer the possibility <strong>of</strong> delivering protein<br />
<strong>subunit</strong>s with the help <strong>of</strong> live delivery systems, bacterial or<br />
viral, or even as antigen-encoding genes, so-called nucleic<br />
acid <strong>vaccines</strong> (Table 2).
Recombinant <strong>subunit</strong> <strong>vaccines</strong><br />
Recent advances in immunology <strong>and</strong> protein engineering<br />
have allowed the design <strong>and</strong> <strong>production</strong> <strong>of</strong> <strong>recombinant</strong><br />
<strong>subunit</strong> <strong>vaccines</strong> [3,5–8]. The epitopes recognized by neutralizing<br />
antibodies are usually found in just one or a few<br />
proteins present on the surface <strong>of</strong> the pathogenic organism.<br />
Isolation <strong>of</strong> the genes encoding such epitope-carrying protein<br />
immunogens <strong>and</strong> their expression in heterologous hosts<br />
form the basis <strong>of</strong> <strong>recombinant</strong>-<strong>subunit</strong>-vaccine development.<br />
The main advantage <strong>of</strong> using single proteins displaying<br />
immunodominant epitopes as <strong>vaccines</strong> is the possibility <strong>of</strong><br />
inducing protective immunity without having side effects <strong>and</strong><br />
immune reactions caused by other parts <strong>of</strong> the pathogenic<br />
organism. Potential challenges in the development <strong>of</strong> <strong>subunit</strong><br />
<strong>vaccines</strong> are that they <strong>of</strong>ten are poorly immunogenic <strong>and</strong><br />
have short in vivo half-lifes. Another difficulty with <strong>subunit</strong><br />
<strong>vaccines</strong> is that they <strong>of</strong>ten elicit only strain-specific protection,<br />
so, to evoke full protection to a disease caused by<br />
several related strains, combinations <strong>of</strong> immunogens from<br />
the different strains might be needed.<br />
Protein immunogens<br />
Protein <strong>production</strong> in heterologous hosts is a wellestablished<br />
technique today, <strong>and</strong> <strong>recombinant</strong> strategies can<br />
thus combine the benefits <strong>of</strong> <strong>subunit</strong> <strong>vaccines</strong> with efficient<br />
<strong>production</strong> systems using non-pathogenic expression<br />
vehicles [8,9]. As will be discussed further, the use <strong>of</strong> fusion<br />
proteins can facilitate the downstream purification <strong>of</strong><br />
immunogens [8,10] <strong>and</strong>, in addition, fusion <strong>of</strong> the target<br />
immunogens to carrier proteins can increase both the halflife<br />
[11,12] <strong>and</strong> immunogenicity [13–15] <strong>of</strong> the immunogen.<br />
Live delivery systems<br />
Besides the possibility <strong>of</strong> producing <strong>recombinant</strong> protein<br />
immunogens in heterologous hosts, technologies to construct<br />
<strong>recombinant</strong> live viral <strong>and</strong> bacterial vaccine-delivery<br />
vectors carrying foreign immunogens have been developed.<br />
Several viruses have been investigated for their possible use<br />
as <strong>recombinant</strong> <strong>vaccines</strong> (for extensive reviews see [3,8,<br />
16,17]). The vaccinia vector is perhaps the most wellcharacterized<br />
viral vector, <strong>and</strong> a vaccinia vector encoding a<br />
rabies glycoprotein has been used for oral immunization <strong>of</strong><br />
wild animals [18,19]. Due to safety concerns, non-attenuated<br />
<strong>recombinant</strong> vaccinia virus is not likely to be used in humans.<br />
As alternatives, a highly attenuated <strong>recombinant</strong> vaccinia<br />
virus vector (NYVAC), which has been constructed through<br />
deletion <strong>of</strong> 18 open reading frames [20], as well as an avianpoxvirus<br />
vector (ALVAC) [21], have been developed. A<br />
NYVAC vector expressing seven different malarial antigens<br />
has been constructed <strong>and</strong> demonstrated to induce a<br />
Recombinant <strong>subunit</strong> <strong>vaccines</strong> 97<br />
Plasmodium-specific antibody response in rhesus macaques<br />
[22]. Adenoviruses have also been investigated as live vectors<br />
[17], <strong>and</strong> are especially interesting, since they are not<br />
particularly pathogenic in humans. The major disadvantage<br />
with adenoviruses is the limited cloning capacity compared<br />
with, for example, the vaccinia virus. Several other viruses<br />
have also been studied for the possible use as live vectors<br />
[17], but no virus-based vaccine, employed for live heterologous<br />
vaccine delivery, is yet accepted for human use.<br />
The use <strong>of</strong> live bacteria as mucosal <strong>vaccines</strong> has been<br />
studied extensively, both against the corresponding disease<br />
<strong>and</strong> also as delivery systems for heterologous diseases.<br />
Mucosal <strong>vaccines</strong> are easy to administer, e.g. by the oral or<br />
nasal route, <strong>and</strong> using bacteria as a delivery vehicle makes the<br />
vaccine comparatively inexpensive to produce [23]. The<br />
best-studied bacterial delivery systems are based on<br />
attenuated Salmonella spp. as live vectors expressing heterologous<br />
antigens <strong>and</strong> numerous studies have been performed<br />
for development <strong>of</strong> oral <strong>vaccines</strong> against bacterial,<br />
viral or parasitic diseases [24–26]. Live Salmonella, being an<br />
intracellular pathogen, is generally capable <strong>of</strong> eliciting cellular<br />
immune responses to the antigen delivered, a desired<br />
property <strong>of</strong> the immune responses protecting against viral or<br />
parasitic diseases.<br />
The possibility <strong>of</strong> expressing foreign proteins on the<br />
surface <strong>of</strong> bacteria makes live bacterial vectors highly<br />
interesting. Surface display <strong>of</strong> heterologous proteins for the<br />
construction <strong>of</strong> live vectors was first described for Gramnegative<br />
bacteria (for reviews see [26,27]) <strong>and</strong> more recently<br />
systems for surface display on Gram-positive bacteria have<br />
also been described [28,29]. Surface display for the development<br />
<strong>of</strong> live bacterial vectors is described in more<br />
detail below.<br />
Nucleic acid <strong>vaccines</strong><br />
Nucleic acid <strong>vaccines</strong> constitute a new class <strong>of</strong> <strong>recombinant</strong><br />
<strong>subunit</strong> vaccine, consisting <strong>of</strong>, for example, plasmid DNA<br />
containing the gene encoding the antigen <strong>of</strong> interest under<br />
the control <strong>of</strong> a strong mammalian viral promoter. The<br />
antigen-encoding gene will be expressed by the vaccinee<br />
upon delivery <strong>of</strong> the plasmid DNA. DNA <strong>vaccines</strong> have been<br />
shown to generate both humoral <strong>and</strong> cellular immune<br />
responses [30] <strong>and</strong> the first report <strong>of</strong> protective efficacy <strong>of</strong><br />
DNA immunization was against influenza [31]. Immunization<br />
<strong>of</strong> BALB�c mice with plasmid DNA encoding influenza A<br />
nucleoprotein resulted in the induction <strong>of</strong> nucleoproteinspecific<br />
antibodies, <strong>and</strong> protection from a subsequent<br />
challenge with a heterologous strain <strong>of</strong> influenza A virus [31].<br />
In addition to the advantage <strong>of</strong> a <strong>subunit</strong> vaccine<br />
including only the antigen (or antigens) required for protective<br />
immunization, nucleic acid <strong>vaccines</strong> present several<br />
other advantages. Nucleic acid <strong>vaccines</strong> are relatively easy to<br />
construct <strong>and</strong> produce, <strong>and</strong> considering the post-trans-<br />
� 2000 Portl<strong>and</strong> Press Ltd
98 M. Hansson, P.-A� . Nygren <strong>and</strong> S. Sta� hl<br />
lational modifications <strong>and</strong> the presentation <strong>of</strong> the antigen to<br />
the host’s immune system, they provide antigen synthesis in<br />
the host in a similar way to that which occurs during a natural<br />
infection.<br />
One drawback <strong>of</strong> DNA <strong>vaccines</strong> that has been extensively<br />
discussed is the potential risk for integration into<br />
the host’s genome. This risk could be minimized by using<br />
RNA instead <strong>of</strong> DNA for immunization. Due to the low<br />
stability <strong>of</strong> mRNA, preparation <strong>and</strong> administration <strong>of</strong> RNA<br />
<strong>vaccines</strong> are not entirely simple. These limitations could be<br />
circumvented by constructing RNA or DNA vectors based<br />
on parts <strong>of</strong> alphavirus genomes [32,33], carrying a gene<br />
encoding the foreign antigen <strong>and</strong> a gene encoding an<br />
alphaviral replicase. Upon transfection <strong>of</strong> such a construct,<br />
the replicase gene will be translated <strong>and</strong> the produced<br />
replicase will mass-replicate the antigen-encoding RNA. The<br />
transfected cell will express large amounts <strong>of</strong> the foreign<br />
protein for a short period <strong>of</strong> time, followed by cell death<br />
[32]. In a recent study, mice immunized with an alphaviral<br />
DNA vector encoding influenza antigens developed humoral<br />
<strong>and</strong> cellular responses at higher levels than mice that<br />
received a conventional DNA-vaccine vector [33]. In addition,<br />
protective immunity against influenza challenge was<br />
elicited in the immunized mice. Nucleic acid <strong>vaccines</strong>, based<br />
on either DNA or self-replicating RNA, will without doubt<br />
find a role in the future <strong>of</strong> vaccine development (for reviews<br />
see [30,34]).<br />
Recombinant <strong>production</strong> <strong>of</strong> protein<br />
immunogens<br />
Gene construction<br />
Recombinant-DNA techniques <strong>of</strong>fer several ways to construct<br />
genes coding for the immunogens to be produced.<br />
The use <strong>of</strong> the PCR enables direct isolation <strong>of</strong> the gene from<br />
its natural source, but requires knowledge <strong>of</strong> the target<br />
DNA sequence. In the PCR amplification, suitable restriction<br />
sites can be introduced for direct cloning into a desired<br />
expression vector. Building up genes de novo using synthetic<br />
oligonucleotides can sometimes be preferable [35–37], e.g. if<br />
only the protein sequence is known, or if the GC content <strong>of</strong><br />
the original gene would differ significantly from that <strong>of</strong> the<br />
host selected for expression. It may also be desirable to<br />
adapt the codons used to the chosen host [37], since<br />
heterologous genes rich in codons that are used rarely by,<br />
for example, Escherichia coli, may not be expressed efficiently<br />
in E. coli [38].<br />
Host vector systems<br />
The choice <strong>of</strong> expression system depends upon many<br />
factors, including (i) the requirements for post-translational<br />
� 2000 Portl<strong>and</strong> Press Ltd<br />
modification, (ii) the proteolytic stability <strong>of</strong> the target<br />
protein, (iii) whether the protein is secretable, (iv) the<br />
possibility <strong>of</strong> renaturation <strong>of</strong> a protein produced in a<br />
misfolded form <strong>and</strong> (v) the acceptable costs for the final<br />
product. There are four major expression hosts that are<br />
commonly used to produce vaccine antigens; bacterial,<br />
yeast, insect <strong>and</strong> mammalian expression systems. In addition,<br />
transgenic plant expression systems have started to emerge,<br />
with the aim <strong>of</strong> utilizing the plant both for <strong>production</strong> <strong>of</strong> the<br />
<strong>subunit</strong> vaccine <strong>and</strong> for vaccine delivery via the edible plant<br />
[39]. A plant-based <strong>subunit</strong> vaccine has indeed been tested in<br />
human volunteers. Transgenic potatoes expressing LTB, the<br />
binding <strong>subunit</strong> <strong>of</strong> the heat-labile toxin <strong>of</strong> enterotoxigenic E.<br />
coli, was consumed by volunteers who then developed<br />
significant LTB-specific antibody (IgG <strong>and</strong> IgA) responses<br />
[40]. Despite a costly development phase, transgenic plants<br />
might become interesting as future vaccine <strong>production</strong>�<br />
delivery vehicles, but their efficacy needs to be proven<br />
further.<br />
Bacterial systems can express antigens at very high<br />
levels <strong>and</strong> are suitable for expressing vaccine antigens that do<br />
not require significant post-translational modifications. E. coli<br />
is the most commonly used bacterium for <strong>production</strong> <strong>of</strong><br />
heterologous proteins, being easy to manipulate, genetically<br />
<strong>and</strong> physiologically well defined, <strong>and</strong> yielding high expression<br />
levels [41]. A multitude <strong>of</strong> vectors <strong>and</strong> strains are available,<br />
making it possible to design a suitable expression system.<br />
Expression <strong>of</strong> <strong>recombinant</strong> antigens in bacterial systems<br />
other than E. coli may sometimes be advantageous [42].<br />
Salmonella typhimurium [43,44], Vibrio cholerae [45] <strong>and</strong><br />
Bacillus brevis [46,47] are some examples <strong>of</strong> other bacteria<br />
that have been used for expression <strong>of</strong> antigens for vaccine<br />
<strong>production</strong> purposes. One particular feature in favour <strong>of</strong><br />
Gram-positive bacteria is that the risk <strong>of</strong> contaminating<br />
lipopolysaccharides is avoided.<br />
Among the eukaryotic expression systems, the baker’s<br />
yeast Saccharomyces cerevisiae is the most commonly used<br />
[48]. Yeast may not express proteins at the levels that can be<br />
obtained in E. coli, but Saccharomyces can easily be grown to<br />
high cell densities. The first human <strong>subunit</strong> vaccine produced<br />
by <strong>recombinant</strong> means was the hepatitis B vaccine, which<br />
consists <strong>of</strong> a major surface antigen (HBsAg) <strong>and</strong> which is<br />
produced in Sacc. cerevisiae [49]. In later years the yeast<br />
Pichia pastoris became a very promising <strong>production</strong> host due<br />
to high <strong>production</strong> levels [48]. Yeast cells possess some <strong>of</strong><br />
the eukaryotic possibilities for post-translationally modifying<br />
proteins, e.g. phosphorylation <strong>and</strong> glycosylation, but, since<br />
the glycosylations differ from the glycosylations in mammalian<br />
cells, it can potentially also be disadvantageous [50].<br />
Baculovirus-based expression systems take advantage<br />
<strong>of</strong> the ability <strong>of</strong> a virus to infect arthropod cells, <strong>and</strong><br />
heterologous proteins can be efficiently produced in both<br />
insect cells <strong>and</strong> larvae [51], but to a significantly higher cost
than in microbial expression systems. Advantages <strong>of</strong> baculovirus<br />
over other expression systems are that proteins are<br />
expressed at very high levels, <strong>and</strong> since these cells are<br />
eukaryotic, they are able to make many <strong>of</strong> the posttranslational<br />
modifications <strong>of</strong> mammalian cells, even though<br />
the glycosylations are not the same as in mammalian systems.<br />
Several mammalian expression systems for <strong>production</strong><br />
<strong>of</strong> <strong>recombinant</strong> proteins have been developed [51], but most<br />
<strong>vaccines</strong> requiring eukaryotic post-translational modifications<br />
are still being expressed in yeast. The main reasons<br />
are the higher product yield in yeast <strong>and</strong> the ease with which<br />
yeast can be manipulated <strong>and</strong> grown. The major advantage <strong>of</strong><br />
a mammalian expression system is that it will post-translationally<br />
modify the expressed product with the highest<br />
degree <strong>of</strong> fidelity compared with the other expression<br />
systems, <strong>and</strong> expressed viral proteins will thus be glycosylated<br />
in a human-like fashion. Drawbacks <strong>of</strong> mammalian<br />
expression systems are the laborious <strong>and</strong> time-consuming<br />
generation <strong>of</strong> stable cell lines, the high cultivation costs, <strong>and</strong><br />
the problems associated with viral <strong>and</strong> bacterial (e.g.<br />
Mycoplasma) infections.<br />
The choice <strong>of</strong> a suitable <strong>production</strong> system thus<br />
depends on several factors, e.g. the biochemical <strong>and</strong> biological<br />
properties <strong>of</strong> the protein <strong>of</strong> interest, the amount <strong>of</strong><br />
<strong>recombinant</strong> protein needed <strong>and</strong> the requirements for posttranslational<br />
modification. Concerning the latter point,<br />
bacterial antigens do not normally need such modifications<br />
<strong>and</strong> would thus be likely to be expressed successfully in<br />
bacteria. Parasitic antigens originating from eukaryotic<br />
organisms may have such requirements, <strong>and</strong> a eukaryotic<br />
expression system might be needed in cases where the posttranslational<br />
modifications are necessary for eliciting protective<br />
immune responses. Nevertheless, a normally highly<br />
glycosylated antigen can be found to be perfectly immunogenic<br />
when produced in bacteria [50]. Normally when<br />
setting up a <strong>production</strong> scheme for a target <strong>subunit</strong><br />
immunogen, the least-complicated bacterial expression<br />
systems are carefully investigated before more complicated<br />
<strong>and</strong> more costly host�vector systems are evaluated.<br />
Strategies for improved bioprocesses<br />
Recombinant-DNA techniques <strong>and</strong> the expression <strong>of</strong> heterologous<br />
proteins in E. coli <strong>and</strong> other hosts have provided a<br />
source <strong>of</strong> proteins <strong>of</strong> a quantity <strong>and</strong> quality that, previously,<br />
was difficult or impossible to achieve through their isolation<br />
from natural sources. In addition, gene technology can be<br />
used to engineer proteins to facilitate bioprocessing. Geneproduct<br />
design can influence the yield <strong>and</strong> the localization <strong>of</strong><br />
the product, as well as adapting the gene product by fusion<br />
technology to specific unit operations suitable for large-scale<br />
downstream processing. Since cost-efficient <strong>production</strong> <strong>of</strong><br />
<strong>subunit</strong> <strong>vaccines</strong> is <strong>of</strong> utmost importance, it is advisable to<br />
Recombinant <strong>subunit</strong> <strong>vaccines</strong> 99<br />
use careful genetic design, when possible, to simplify <strong>and</strong><br />
improve the overall <strong>production</strong> process.<br />
Secretion By taking advantage <strong>of</strong> a signal peptide (secretory<br />
leader), normally fused to the N-terminus <strong>of</strong> the target<br />
protein, efficient secretion <strong>of</strong> the protein can be achieved.<br />
For example, export <strong>of</strong> a protein from the cytoplasm into<br />
the periplasm <strong>of</strong> E. coli <strong>of</strong>fers several advantages [52,53].<br />
Secretion <strong>of</strong> the target protein to the periplasm functions as<br />
an initial purification step <strong>and</strong> simplifies the downstream<br />
purification considerably, since the periplasm contains<br />
approx. 100 host proteins [54] compared with more than<br />
4000 proteins in the cytoplasm [55]. The number <strong>of</strong><br />
proteases in the periplasm is also drastically fewer [56],<br />
which reduces the risk <strong>of</strong> degradation, <strong>and</strong> the oxidizing<br />
environment in the periplasm favours disulphide-bond<br />
formation, which thus stimulates a potentially correct folding<br />
<strong>of</strong> cysteine-containing target proteins. In addition to<br />
secretion into the periplasmic space <strong>of</strong> the E. coli cell, the<br />
protein can in some cases be recovered from the culture<br />
medium [57–59]. The mechanism for the release <strong>of</strong> proteins<br />
into culture medium by E. coli cells is not known in detail, but<br />
is probably due to non-specific leakage from the cells [60,61].<br />
Recovery <strong>of</strong> proteins from the culture medium has the<br />
advantages that cell disruption is not needed <strong>and</strong> that there<br />
is a low number <strong>of</strong> host proteins present [59]. A potential<br />
drawback may be the dilution <strong>of</strong> the protein, which could<br />
potentially complicate the purification in large-scale bioprocesses.<br />
Improved recovery by engineering <strong>of</strong> protein properties The<br />
addition <strong>of</strong> charged amino acid residues or mutation <strong>of</strong><br />
amino acids <strong>of</strong> a protein to alter the isolectric point (pI), can<br />
improve the purification by allowing ion-exchange chromatography<br />
[62]. Fusion <strong>of</strong> hydrophobic tails to the target<br />
protein has been shown to alter the partitioning <strong>of</strong> the fusion<br />
protein in aqueous two-phase systems, enabling the use <strong>of</strong><br />
such a system as a primary purification step for efficient<br />
recovery <strong>of</strong> the target protein [63,64]. Hydrophobic tagging<br />
<strong>of</strong> protein immunogens has the additional advantage, as will<br />
be discussed further below, that it could allow direct adjuvant<br />
incorporation <strong>of</strong> purified <strong>subunit</strong> <strong>vaccines</strong> through hydrophobic<br />
interaction [65,66].<br />
An illustrative example <strong>of</strong> how genetic design can be<br />
used to achieve integration <strong>of</strong> unit operations was presented<br />
in the process design for <strong>production</strong> <strong>of</strong> a malaria <strong>subunit</strong>vaccine<br />
c<strong>and</strong>idate [59,67]. The fusion protein ZZ-M5,<br />
constituting the malaria <strong>subunit</strong>-vaccine c<strong>and</strong>idate, was<br />
produced in E. coli using a secretion strategy. The M5<br />
polypeptide is derived from the central repeat region <strong>of</strong> the<br />
Plasmodium falciparum blood-stage antigen Pf155�RESA, <strong>and</strong><br />
the ZZ region represents an IgG-binding affinity tag derived<br />
from Staphylococcus aureus Protein A (SpA). More than 65%<br />
� 2000 Portl<strong>and</strong> Press Ltd
100 M. Hansson, P.-A� . Nygren <strong>and</strong> S. Sta� hl<br />
<strong>of</strong> the <strong>recombinant</strong> gene product was found to be excreted<br />
into the culture medium, from where it could be recovered<br />
in a single step directly from the crude fermentor broth<br />
without prior cell removal by exp<strong>and</strong>ed-bed anion-exchange<br />
adsorption. The fusion protein had a relatively low pI that<br />
allowed anionic-exchange adsorption at pH 5.5, at which<br />
most E. coli host proteins are not adsorbed. This strategy<br />
allowed an integration <strong>of</strong> the cell-separation step with the<br />
ion-exchange adsorption <strong>of</strong> the gene product with simultaneous<br />
volume reduction, which resulted in a highly<br />
condensed, but still efficient, recovery process [59]. Since<br />
the ZZ-M5 protein was to be used in a preclinical malaria<br />
vaccine trial in Aotes monkeys [67], a ‘polishing’ step was<br />
included in which the IgG-binding capacity <strong>of</strong> the fusion<br />
protein was employed. After affinity chromatography on<br />
IgG–Sepharose, contaminating DNA <strong>and</strong> endotoxin levels<br />
were well below the dem<strong>and</strong>s set by regulatory authorities.<br />
The overall yield <strong>of</strong> the process, performed in pilot scale,<br />
exceeded 90%, resulting in 550 mg <strong>of</strong> product�l <strong>of</strong> culture<br />
[59].<br />
Solubility <strong>and</strong> proteolytic stability Upon expression in bacterial<br />
expression systems, many proteins will precipitate <strong>and</strong><br />
form inclusion bodies [68]. If the target protein is sensitive to<br />
proteolytic degradation, this could be advantageous, since<br />
the formation <strong>of</strong> inclusion bodies normally protects unstable<br />
proteins from degradation. However, renaturation in vitro<br />
has to be employed to regain a native structure. This used to<br />
be a significant drawback in setting up a large-scale bioprocess,<br />
but today refolding can <strong>of</strong>ten be performed<br />
efficiently even on an industrial scale [68]. For many proteins<br />
that are not too proteolytically labile, improved solubility<br />
can be <strong>of</strong> significant importance, since higher in vivoexpression<br />
levels can be obtained without product precipitation<br />
<strong>and</strong> eventual in vitro refolding can be performed at<br />
significantly higher protein concentrations [69–72]. The<br />
solubility <strong>of</strong> a <strong>recombinant</strong> protein can be increased by fusing<br />
a target protein, at the level <strong>of</strong> the gene, to a highly soluble<br />
fusion partner, to thereby increase the overall solubility <strong>of</strong><br />
the fusion protein [37,68,70–72]. The SpA-derived ZZ, <strong>and</strong><br />
BB derived from streptococcal protein G (SpG), constitute<br />
relevant examples <strong>of</strong> fusion partners that have proven to be<br />
suitable in this context (for reviews see [73,74]). In addition,<br />
the proteolytic stability <strong>of</strong> a fusion protein can also be<br />
improved by single or double (N- <strong>and</strong> C-terminal) fusions to<br />
proteolytically stable fusion partners, such as the ZZ <strong>and</strong> BB<br />
tags [56,69,75].<br />
An illustrative example <strong>of</strong> how product engineering was<br />
employed to obtain increased product solubility <strong>and</strong> stability<br />
has been described in [37]. Site-directed mutagenesis was<br />
employed to engineer the hydrophobic properties <strong>of</strong> a 101amino-acid<br />
fragment from the human-respiratory-syncytial-<br />
� 2000 Portl<strong>and</strong> Press Ltd<br />
virus (RSV) major glycoprotein [37]. Hydrophobic engineering<br />
<strong>of</strong> four clustered phenylalanine residues, yielding<br />
mutant variants with the four phenylalanine residues either<br />
substituted for serine residues or deleted, increased the<br />
fraction <strong>of</strong> soluble protein in vivo from 27 to 75%. Interestingly,<br />
this effect was accompanied by a remarkable<br />
increase in product stability. Protein engineering <strong>of</strong> hydrophobic<br />
residues could obviously influence protein structure<br />
but, in the reported example, CD analysis <strong>and</strong> the antigenicity<br />
pattern suggested a retained structure [37]. These results<br />
indicate that, in certain cases, single amino acid substitutions<br />
<strong>and</strong> engineering <strong>of</strong> hydrophobic residues [76] (by substitution<br />
for more hydrophilic residues) might be used as<br />
tools to improve <strong>production</strong> processes for <strong>recombinant</strong><br />
<strong>subunit</strong> immunogens. Also other <strong>recombinant</strong> strategies can<br />
be utilized to improve proteolytic stability (for a review see<br />
[56]).<br />
Product yield The product yield is dependent on many<br />
factors, including mRNA <strong>and</strong> product stability, transcription<strong>and</strong><br />
translation-initiation efficiency, vector copy number <strong>and</strong><br />
stability [38,41]. In addition, a number <strong>of</strong> promoters <strong>of</strong><br />
different strengths <strong>and</strong> with different features are available<br />
for use in E. coli [38]. Large-scale <strong>production</strong> <strong>of</strong> <strong>recombinant</strong><br />
proteins preferably employs cell growth to high densities <strong>and</strong><br />
minimal expression <strong>of</strong> the target protein, followed by<br />
induction or de-repression <strong>of</strong> the promoter. Production <strong>of</strong><br />
heterologous proteins that might be toxic to the host<br />
require tight regulation <strong>of</strong> the promoter, e.g. the T7 system<br />
[77]. Constitutive promoters can preferably be used for<br />
non-regulated expression <strong>of</strong> secreted, non-toxic proteins<br />
[59]. Production <strong>of</strong> a target protein as a multicopy protein,<br />
followed by specific cleavage to release several copies <strong>of</strong> the<br />
native protein, is another way to increase product yield<br />
[78,79].<br />
Strategies to improve potency <strong>of</strong><br />
protein-<strong>subunit</strong> <strong>vaccines</strong><br />
The construction <strong>of</strong> gene fusions allows the generation <strong>of</strong><br />
fusion proteins potentially carrying the combined properties<br />
<strong>of</strong> each parental protein. The reasons for fusing a target<br />
protein to another protein by genetic means are several<br />
[74,80], e.g. to enable affinity purification, increase solubility,<br />
decrease proteolysis or to target the protein to a different<br />
compartment <strong>of</strong> the host cell. The fusion partner can also be<br />
used as a reporter molecule, to increase the half-life <strong>of</strong><br />
therapeutic proteins, provide carrier-related properties, or<br />
be used to enable display <strong>of</strong> the target protein on the<br />
surfaces <strong>of</strong> cells or phages. Gene-fusion strategies can also
e used to combine B- <strong>and</strong> T-cell epitopes in composite<br />
immunogens.<br />
Immunopotentiating fusion partners<br />
Gene-fusion strategies can be used as a powerful method to<br />
improve the immune response <strong>of</strong> an immunogen. For<br />
example, the fusion partner BB, derived from SpG [81],<br />
has been shown to possess immunopotentiating properties.<br />
Immunization <strong>of</strong> mice with a malarial antigen fused to the BB<br />
protein elicited an antibody response in mice strains that<br />
were non-responders to the malarial antigen alone [14].<br />
Furthermore, a c<strong>and</strong>idate RSV <strong>subunit</strong> vaccine, BB-G2N,<br />
comprising the BB protein fused to a 101-amino-acid<br />
sequence from the human RSV G protein, was shown to<br />
induce protective immunity in mice to RSV [15,50,82–85]. It<br />
was shown that, by inclusion <strong>of</strong> the BB part, a more potent<br />
G2N-specific B-cell memory response was evoked [15]. This<br />
indicates that the SpG-derived BB can function both as an<br />
affinity tag to facilitate purification <strong>and</strong> as a carrier protein<br />
with immunopotentiating properties. To date, it has not<br />
been fully elucidated whether this capacity is due to strong<br />
T-cell epitopes [14] or related to the serum-albumin-binding<br />
activity resulting in a prolonged exposure [11,12] <strong>of</strong> the<br />
immunogen to the immune system, or a combination <strong>of</strong><br />
both.<br />
Targeting <strong>of</strong> protein immunogens<br />
Targeting <strong>of</strong> chimaeric antigens to immunoreactive sites can<br />
be achieved, for example, by the use <strong>of</strong> adhesion factors,<br />
monoclonal antibodies or other molecules capable <strong>of</strong><br />
specifically binding to eukaryotic cell receptors or polysaccharides<br />
[8]. The cholera toxin B (CTB) <strong>subunit</strong> has been<br />
evaluated extensively as a fusion partner to various antigens<br />
for its immunopotentiating properties. Its capacity for<br />
binding to the ganglioside G M1 present on mucosal epithelial<br />
cells has been used for targeting <strong>of</strong> mucosal <strong>vaccines</strong> [13].<br />
Intracellular targeting <strong>of</strong> antigens is an elegant variation <strong>of</strong><br />
the theme. Fusions to the N-terminal catalytic domain <strong>of</strong><br />
adenylate cyclase toxin (CyaA) <strong>of</strong> Bordetella pertussis resulted<br />
in delivery <strong>of</strong> the foreign viral epitope to the cytosol <strong>of</strong> cells<br />
by the detoxified invasive toxin. Protective cytotoxic<br />
T-lymphocyte responses against challenge with intracerebral<br />
lymphocytic choriomeningitis virus (LCMV) challenge was<br />
obtained by this targeting strategy [86]. Chimaeric composite<br />
immunogens can also be created by fusion <strong>of</strong> different<br />
antigens, such as the hybrid CTB–LTB molecules, which are<br />
c<strong>and</strong>idate oral <strong>vaccines</strong> against both enterotoxic E. coli<br />
infections <strong>and</strong> cholera [87]. Such targeting strategies have<br />
also been utilized in efforts to improve live delivery vehicles<br />
(see below).<br />
Recombinant <strong>subunit</strong> <strong>vaccines</strong> 101<br />
Adjuvant incorporation<br />
Since single-protein antigens are normally rather weak<br />
immunogens, requiring co-administration <strong>of</strong> an adjuvant to<br />
increase the immune response, the development <strong>of</strong> novel<br />
adjuvants [88,89] <strong>and</strong> strategies for efficient antigen association<br />
are important topics in present vaccinology research.<br />
For several adjuvants, such as liposomes, cochleates,<br />
non-ionic block polymers <strong>and</strong> immunostimulating complexes<br />
(iscoms), the protein antigens are normally incorporated by<br />
means <strong>of</strong> hydrophobic interactions [88], <strong>and</strong> the physical<br />
association has been demonstrated to be essential for the<br />
adjuvant to exert its immunostimulating capacity. For iscoms,<br />
it has been shown that membrane antigens containing<br />
hydrophobic transmembrane sequences are efficiently incorporated.<br />
In contrast, hydrophilic antigens cannot be<br />
efficiently introduced into iscoms. Instead, such antigens<br />
could be incorporated by partial denaturation to expose<br />
hydrophobic sequences, or by chemical conjugation to<br />
preformed iscoms or iscom-matrix alone [88].<br />
In an attempt to simplify incorporation <strong>of</strong> hydrophilic<br />
protein immunogens into adjuvant systems, a <strong>recombinant</strong><br />
strategy was presented for <strong>production</strong> <strong>of</strong> immunogens<br />
furnished with a hydrophobic tag to improve incorporation<br />
into iscoms [65]. The benefits <strong>of</strong> two fusion partners were<br />
combined; an affinity tag, to enable efficient affinity purification<br />
<strong>of</strong> the target fusion protein, <strong>and</strong> a hydrophobic tag, to<br />
make direct incorporation into iscoms possible. Two <strong>of</strong> the<br />
evaluated hydrophobic tags were found to mediate efficient<br />
iscom association; a tryptophan�isoleucine-rich tag <strong>and</strong> a tag<br />
derived from the membrane-integration sequence from<br />
influenza haemagglutinin, <strong>and</strong> the formed iscoms were<br />
capable <strong>of</strong> efficiently eliciting antibody responses to the<br />
model antigen, a malaria peptide M5, derived from the<br />
central repeat region <strong>of</strong> the P. falciparum blood-stage antigen<br />
Pf155�RESA [65]. In a recent follow-up study, significant<br />
improvements in the <strong>production</strong> systems were presented<br />
[66], allowing high expression levels, efficient recovery <strong>and</strong><br />
adjuvant incorporation <strong>of</strong> hydrophobically tagged protein<br />
immunogens.<br />
Live bacterial <strong>and</strong> yeast vaccinedelivery<br />
systems<br />
Compared with proteinaceous <strong>subunit</strong> <strong>vaccines</strong>, <strong>recombinant</strong><br />
live <strong>vaccines</strong> would potentially be easier <strong>and</strong> less<br />
costly to produce, since they do not require extensive<br />
purification processes, <strong>and</strong> since they may be able to elicit<br />
long-lasting immunity without the need for adjuvants.<br />
Therefore, there is considerable interest in developing<br />
systems for heterologous protein expression in non-pathogenic<br />
micro-organisms to be used both as <strong>production</strong><br />
� 2000 Portl<strong>and</strong> Press Ltd
102 M. Hansson, P.-A� . Nygren <strong>and</strong> S. Sta� hl<br />
Table 3 Selected examples <strong>of</strong> immunization studies in which the antigens have been surface-displayed on heterologous bacteria or yeast<br />
i.p., intraperitoneally; i.v., intravenously.<br />
Micro-organism Display system Displayed antigen Animal model Result Reference<br />
Gram-negative<br />
E. coli E. coli LamB Hepatitis B virus fragment Rabbits/mice (i.v.) Antibodies recognizing viral fragments [93]<br />
S. typhimurium E. coli OmpA Malaria blood-stage antigen fragments Mice (orally) Antigen-specific antibody response [94]<br />
S. typhimurium<br />
Gram-positive<br />
E. coli/Shigella dysenteriae OmpA Malaria blood-stage antigen fragments Mice (i.p.) Antigen-specific antibody response [95]<br />
Streptococcus gordonii Strep. pyogenes M6 protein Hornet venom allergen Mice (orally, intranasally) Antigen-specific antibody response [96]<br />
Strep. gordonii Strep. pyogenes M6 protein Human papilloma virus protein Mice (orally, intranasally) Antigen-specific antibody response [97]<br />
Strep. gordonii Strep. pyogenes M6 protein Human papilloma virus protein Mice (vaginally) Antigen-specific antibody response [98]<br />
Strep. gordonii Strep. pyogenes M6 protein HIV-1 gp120 fragment human papilloma Cynomolgus monkeys Antigen-specific antibody response <strong>and</strong> [99]<br />
virus protein<br />
(vaginally)<br />
T-cell response<br />
Staphylococcus xylosus Staph. aureus protein A RSV protein fragment Mice (orally) Antigen-specific antibody response [100]<br />
Staph. carnosus Staph. aureus protein A Streptococcal model protein Mice (orally) Antigen-specific antibody response [101]<br />
Staph. carnosus Staph. aureus protein A RSV/CTB Mice (intranasally) Partial protection to RSV challenge [102]<br />
Bacillus subtilis spores<br />
Yeast<br />
B. subtilis cell wall (CwbA) protein Yersinia pseudotuberculosis invasin protein<br />
fragment<br />
Mice (orally) Antigen-specific antibody response [103]<br />
Sacc. cerevisiae Yeast α-agglutinin Hepatitis B virus protein fragments Mice (i.p.) Antigen-specific antibody response [104]<br />
systems <strong>and</strong> as vehicles for live delivery <strong>of</strong> <strong>subunit</strong> <strong>vaccines</strong>.<br />
For efficient presentation <strong>of</strong> the antigen to the immune<br />
system several techniques for displaying heterologous proteins<br />
on the surface <strong>of</strong> bacteria have been developed, since<br />
cell-surface display <strong>of</strong> antigens has been shown to be<br />
advantageous for the induction <strong>of</strong> an antigen-specific immune<br />
response when using live <strong>recombinant</strong> bacteria for immunization<br />
[76,90].<br />
Two basic strategies exist for the generation <strong>of</strong> bacterial<br />
live-delivery vehicles. One type <strong>of</strong> vehicle is based on<br />
colonizing normally pathogenic bacteria, <strong>and</strong> attenuated or<br />
non-pathogenic variants <strong>of</strong> that bacterium are employed in<br />
order to obtain suitable vehicles, e.g. Salmonella [26,29] <strong>and</strong><br />
mycobacterial strains [91]. A second type <strong>of</strong> vehicle is based<br />
on non-pathogenic commensal or food-grade bacteria, such<br />
as Streptococcus gordonii <strong>and</strong> certain staphylococcal or<br />
lactococcal strains. These approaches have been described<br />
in recent reviews [26,28,29,92].<br />
Gram-negative bacteria<br />
The first described examples <strong>of</strong> heterologous display on<br />
bacteria were with Gram-negative bacteria (Table 3), in<br />
which short peptides were displayed on the bacterial surface<br />
by genetic insertion into the exposed loops <strong>of</strong> E. coli outermembrane<br />
proteins LamB [105], OmpA [106] <strong>and</strong> PhoE<br />
[107]. The technique <strong>of</strong> inserting peptides into surfaceexposed<br />
loops <strong>of</strong> outer-membrane proteins has been used<br />
for other Gram-negative bacteria as well, e.g. S. typhimurium<br />
[108] <strong>and</strong> Pseudomonas aeruginosa [109]. The drawback <strong>of</strong><br />
using exposed loops <strong>of</strong> outer-membrane proteins is the<br />
limitation in the size <strong>of</strong> the peptide that can be inserted.<br />
Sequences <strong>of</strong> up to 70 amino acids have been reported as<br />
possible for insertion into the MalE protein [110]. Insertion<br />
<strong>of</strong> larger inserts (189 <strong>and</strong> 451 amino acids) <strong>of</strong> malarial<br />
antigens in E. coli OmpA <strong>and</strong> subsequent surface exposure<br />
on S. typhimurium has also been described [94]. Fusions to<br />
� 2000 Portl<strong>and</strong> Press Ltd<br />
fimbriae proteins [111–113] <strong>and</strong> flagellar proteins [114–116]<br />
have also been used to achieve surface display on Gramnegative<br />
bacteria. However, the use <strong>of</strong> cell appendages is<br />
limited by the size <strong>of</strong> the peptides that can be displayed.<br />
To allow display <strong>of</strong> larger protein fragments as well as<br />
entire proteins, different systems to anchor heterologous<br />
protein to lipoproteins have been used. Fused to a major<br />
outer-membrane protein, the TraT protein, a coat-protein<br />
fragment <strong>of</strong> type-1 poliovirus was demonstrated to be<br />
presented on the cell surface <strong>of</strong> E. coli [117]. Fusion <strong>of</strong> a<br />
lysozyme-binding single-chain fragment to E. coli peptidoglycan-associated<br />
lipoprotein (PAL) resulted in surface<br />
exposure <strong>of</strong> functional antibody fragments [118], <strong>and</strong> the<br />
entire Leishmania major glycoprotein gp63 has been displayed<br />
on the surface <strong>of</strong> E. coli by fusion to the P. aeruginosa major<br />
outer-membrane lipoprotein (opr1) [119]. Recently, a display<br />
system based on the ice-nucleation protein (Inp) from<br />
Pseudomonas syringae was described [120]. By fusion <strong>of</strong><br />
levansucrase to the C-terminus <strong>of</strong> Inp, an active enzyme<br />
could be displayed on the surface <strong>of</strong> E. coli.<br />
Taking advantage <strong>of</strong> the signal sequence <strong>and</strong> the first<br />
nine N-terminal amino acids <strong>of</strong> the E. coli major lipoprotein<br />
(Lpp) <strong>and</strong> a region <strong>of</strong> the E. coli OmpA, the entire βlactamase<br />
protein could be displayed in an active form on the<br />
surface <strong>of</strong> E. coli when fused C-terminally to the Lpp–OmpA<br />
complex [121]. This Lpp–OmpA display system has been<br />
shown to give efficient translocation <strong>and</strong> surface anchoring<br />
<strong>of</strong> fused gene products, resulting in a high number <strong>of</strong><br />
chimaeric surface proteins present in an accessible form on<br />
E. coli cells. Both <strong>recombinant</strong> enzymes <strong>and</strong> antibody<br />
fragments [122,123] have been surface-displayed on E. coli<br />
using this system. Reviews describing this system <strong>and</strong> other<br />
systems for surface display on Gram-negative bacteria have<br />
been published [26,27,124].<br />
Many <strong>of</strong> the E. coli surface-expression systems for the<br />
delivery <strong>of</strong> heterologous antigens to immunized animals have
een used for the surface-display <strong>of</strong> immunogens in Salmonella<br />
live-vaccine c<strong>and</strong>idates [26,29]. For example, malarial<br />
antigens have been surface exposed on S. typhimurium by<br />
genetic fusion to the ompA gene [94,95], <strong>and</strong> fusions to the E.<br />
coli LamB <strong>and</strong> MalE proteins have been used for the surface<br />
expression or periplasmic targeting, respectively, <strong>of</strong> viral<br />
antigens [125] <strong>and</strong> the Shiga toxin B <strong>subunit</strong> [126]. Shiga-like<br />
toxin IIe was exported by the use <strong>of</strong> an E. coli haemolysin<br />
transport system <strong>and</strong> fusion to the outer-membrane protein<br />
TolC [127]. Also, naturally existing Salmonella surface<br />
proteins or appendages (flagellae <strong>and</strong> fimbriae) have been<br />
used for surface display [128–130]. Despite extensive<br />
research efforts <strong>and</strong> the existence <strong>of</strong> numerous expression<br />
systems, the early optimism in using Salmonella spp. as<br />
delivery systems for foreign antigens has been hampered<br />
somewhat. The main reason is the risk <strong>of</strong> side effects due to<br />
potential reversion into virulence in immunocompromised<br />
humans, <strong>and</strong> lack <strong>of</strong> efficiency in human trials. Nevertheless,<br />
Salmonella provides an excellent tool for research into<br />
experimental <strong>vaccines</strong>, stimulating both the humoral <strong>and</strong><br />
cellular branches <strong>of</strong> the immune system.<br />
Gram-positive bacteria<br />
Several systems for heterologous surface display on Grampositive<br />
bacteria (Table 3) have also been described [28,29].<br />
The fibrillar surface M protein <strong>of</strong> Strep. pyogenes has been<br />
used to express a foreign antigen on the surface <strong>of</strong> the<br />
commensal bacterium Strep. gordonii [131]. The antigen was<br />
fused to the C-terminal attachment motif <strong>of</strong> the M protein<br />
<strong>and</strong> replaced nearly all <strong>of</strong> the surface-exposed region <strong>of</strong> the<br />
M protein. Using this system, a number <strong>of</strong> proteins have been<br />
displayed successfully on the surface <strong>of</strong> Strep. gordonii [92].<br />
The anchoring region <strong>of</strong> the surface-exposed SpA has<br />
also been used to display different heterologous immunogens<br />
on the non-pathogenic Staph. xylosus <strong>and</strong> Staph. carnosus<br />
[29,100,132–134]. An attempt to display tetanus toxin<br />
fragment C (TTFC) on the surface <strong>of</strong> Lactococcus lactis by<br />
fusion to the C-terminal anchoring domain <strong>of</strong> lactococcal<br />
cell-surface-associated proteinase (PrtP) did not result in a<br />
detectable surface exposure [135]. An interesting approach<br />
to making heat-resistant live bacterial vectors by employing<br />
sporulating Bacillus subtilis for surface display <strong>of</strong> an antigen,<br />
has been described by Acheson <strong>and</strong> co-workers [103].<br />
Antigenic domains <strong>of</strong> the Yersinia pseudotuberculosis invasin<br />
protein (Inv) were fused to B. subtilis cell wall (CwbA) protein<br />
<strong>and</strong> subsequently expressed on the surface. Mice<br />
immunized orally with spores from the <strong>recombinant</strong> B.<br />
subtilis developed an immune response to Inv [103].<br />
Yeast<br />
Surface display <strong>of</strong> an antigen on Sacc. cerevisiae has also been<br />
demonstrated [104]. The C-terminal cell-wall-anchoring<br />
Recombinant <strong>subunit</strong> <strong>vaccines</strong> 103<br />
sequence <strong>of</strong> the mannoprotein α-agglutinin was utilized to<br />
attach the antigen at the cell surface <strong>of</strong> yeast. Oral<br />
immunizations <strong>of</strong> mice with yeast cells expressing the HBsAg<br />
at their cell surface resulted in antigen-specific antibodies<br />
(IgG), <strong>and</strong> so baker’s yeast can thus be seen as a potential<br />
vaccine-delivery vehicle [104].<br />
Targeting <strong>of</strong> live bacterial vectors<br />
Although systemic antibody responses to surface-exposed<br />
antigens after oral delivery with the Staph. carnosus system<br />
have been reported [8,101], attempts have been made to<br />
improve the system in terms <strong>of</strong> antibody responses elicited<br />
to the surface-exposed antigenic determinants upon immunization<br />
via the mucosal routes [8,134,136,137]. The rationale<br />
has been to target the staphylococcal vaccine vehicles to the<br />
mucosa through the co-display <strong>of</strong> proteins that have binding<br />
partners present on the mucosal epithelium. The surface<br />
expression <strong>of</strong> a bacterial adhesion factor, a fibronectinbinding<br />
domain from Strep. dysgalactiae, on the surface <strong>of</strong><br />
Staph. carnosus, resulted in a 1.5 log 10 increase in the serum<br />
IgG responses to a co-displayed antigen upon intranasal<br />
immunization <strong>of</strong> mice [8,138]. In another approach, coexposure<br />
<strong>of</strong> a peptide (CTBp) comprising amino acids 50–75<br />
<strong>of</strong> the CTB <strong>subunit</strong> on the Staph. carnosus surface, was<br />
investigated. CTB is <strong>of</strong> significant interest for mucosal<br />
vaccine development, <strong>and</strong> its immunopotentiating capacity<br />
as a carrier molecule is considered to be related to its ability<br />
to bind to the monosialoganglioside G M1, present on mucosal<br />
epithelial cells [134,136,137]. The CTBp subfragment has<br />
been shown to have an immunopotentiating effect [139]. The<br />
introduction <strong>of</strong> CTBp into the chimaeric surface proteins,<br />
containing a model antigen, significantly increased (close to<br />
2 log 10) serum IgG responses upon intranasal immunization<br />
[137]. The same increase in immune responses was not<br />
observed upon oral delivery, <strong>and</strong> it was furthermore<br />
demonstrated that live delivery <strong>of</strong> the staphylococci was<br />
required to obtain this effect [137].<br />
In a subsequent vaccination study, the Staph. carnosus<br />
system, improved by co-display <strong>of</strong> CTBp, was used for<br />
delivery <strong>of</strong> peptides from the G glycoprotein <strong>of</strong> human RSV<br />
[102]. Three peptides, corresponding to the RSV G-protein<br />
amino acids 144–159 (denoted G5), 190–203 (G9) <strong>and</strong><br />
171–188 (G4S), were expressed separately by <strong>recombinant</strong><br />
means on the surfaces <strong>of</strong> three different cultures <strong>of</strong> Staph.<br />
carnosus, <strong>and</strong> their surface accessibility on the bacteria was<br />
verified by fluorescence-activated cell sorting (FACS). Intranasal<br />
immunization <strong>of</strong> mice with the live <strong>recombinant</strong><br />
staphylococci elicited significant anti-peptide as well as antivirus<br />
serum IgG responses, <strong>and</strong> upon viral challenge with 10 5<br />
tissue-culture infectious doses 50 (TCID 50, the virus dose<br />
infecting 50% <strong>of</strong> the cells), lung protection was demonstrated<br />
for approximately half <strong>of</strong> the mice in the G9 <strong>and</strong> G4S<br />
� 2000 Portl<strong>and</strong> Press Ltd
104 M. Hansson, P.-A� . Nygren <strong>and</strong> S. Sta� hl<br />
immunization groups. To our knowledge, this represents the<br />
first study in which protective immunity to a viral pathogen<br />
has been evoked using food-grade bacteria as vaccinedelivery<br />
vehicles [102].<br />
Concluding remarks<br />
Recombinant strategies are <strong>of</strong> great interest in the<br />
development <strong>of</strong> new <strong>vaccines</strong>, <strong>and</strong> in addition for the<br />
improvement <strong>of</strong> existing <strong>vaccines</strong>. New methods for<br />
construction, <strong>production</strong> <strong>and</strong> targeting <strong>of</strong> <strong>recombinant</strong><br />
immunogens have been presented. Several new <strong>and</strong> rational<br />
techniques have recently become available in the search for<br />
novel target antigens for use in new <strong>vaccines</strong>. The largescale<br />
genome-sequencing projects have provided enormous<br />
amounts <strong>of</strong> information to be deciphered. Vaccinology will<br />
most probably benefit through the identification <strong>of</strong> new<br />
target antigens <strong>and</strong> also from improved underst<strong>and</strong>ing <strong>of</strong><br />
the mechanisms <strong>of</strong> infection <strong>and</strong> immunity.<br />
New target antigens can also be identified for evaluation<br />
<strong>of</strong> immunogenicity using expression library immunization<br />
(ELI) [140]. To create an expression library, the genome <strong>of</strong><br />
a pathogen is digested into fragments, which are ligated into<br />
eukaryotic expression plasmids, forming the total library. By<br />
immunizing animals with sublibraries containing a large<br />
number <strong>of</strong> different plasmids, immune responses evoked in<br />
the animals are the basis for selection <strong>of</strong> a sublibrary to be<br />
studied further for the identification <strong>of</strong> the single protective<br />
plasmid. Another approach to the identification <strong>of</strong> target<br />
antigens have been envisioned by Jacobsson <strong>and</strong> co-workers<br />
[141], who used the method called ‘shotgun phage-display’<br />
for identifying genes encoding binding domains <strong>of</strong> bacterial<br />
adhesins [142,143]. Staph. aureus chromosomal DNA was<br />
fragmented by sonication <strong>and</strong> inserted into phagemid vectors<br />
for expression on phages. After affinity selection <strong>of</strong> the<br />
libraries against various human proteins, lig<strong>and</strong>-binding<br />
phages were identified that contained DNA encoding<br />
the bacterial binding protein fragment. Identified fragments<br />
<strong>of</strong> bacterial adhesins could be <strong>of</strong> interest in a future vaccine<br />
as c<strong>and</strong>idate antigens or as fusion partners for vaccine<br />
targeting.<br />
In the area <strong>of</strong> antigen targeting, proteins binding to a<br />
surface receptor or polysaccharide could potentially also be<br />
selected from protein libraries based on combinatorial<br />
r<strong>and</strong>omization <strong>of</strong> the surface <strong>of</strong> a suitable protein used as a<br />
scaffold [144,145]. After selection <strong>of</strong> a binder from the<br />
library, this protein can be used as a fusion partner for the<br />
antigen, for targeting <strong>of</strong> the antigen to certain tissues or cell<br />
types. Combinatorial protein libraries have also been described<br />
by others [146] as novel promising strategies in<br />
vaccine development.<br />
Taken together, it is evident that <strong>recombinant</strong>-DNA<br />
� 2000 Portl<strong>and</strong> Press Ltd<br />
technology will have a major impact on future strategies for<br />
the prevention <strong>of</strong> infectious diseases. The design, selection<br />
<strong>and</strong> <strong>production</strong> <strong>of</strong> <strong>recombinant</strong> <strong>subunit</strong> <strong>vaccines</strong> will be the<br />
basis <strong>of</strong> modern vaccinology. Various strategies to administer<br />
the <strong>subunit</strong> vaccine, as a protein immunogen, via a live<br />
delivery vehicle or as a nucleic acid construct, will be<br />
available.<br />
References<br />
1 Bloom, B. R. <strong>and</strong> Widdus, R. (1998) Nat. Med. 4, 480–484<br />
2 Hilleman, M. R. (1998) Nat. Med. 4, 507–514<br />
3 Ellis, R. W. (1999) Vaccine 17, 1596–1604<br />
4 Kristensen, K., Gyhrs, A., Lausen, B., Barington, T. <strong>and</strong> Heilmann,<br />
C. (1996) Pediatr. Infect. Dis. J. 15, 525–529<br />
5 Dertzbaugh, M. T. (1998) Plasmid 39, 100–113<br />
6 Liu, M. A. (1998) Nat. Med. 4, 515–519<br />
7 Babiuk, L. A. (1999) Vaccine 17, 1587–1595<br />
8 Liljeqvist, S. <strong>and</strong> Sta� hl, S. (1999) J. Biotechnol. 73, 1–33<br />
9 Plotkin, S. A. (1993) J. Infect. Dis. 168, 29–37<br />
10 Sjo� l<strong>and</strong>er, A., Sta� hl, S. <strong>and</strong> Nygren, P.-A� . (1993) Immunomethods<br />
2, 79–92<br />
11 Nygren, P.-A� ., Flodberg, P., Andersson, R., Wigzell, H. <strong>and</strong><br />
Uhle� n, M. (1991) in Vaccines 91 (Chanock, R. M., Ginsberg,<br />
H. S., Brown, F. <strong>and</strong> Lerner, R. A., eds.), pp. 363–368, Cold<br />
Spring Harbor Press, Cold Spring Harbor, NY<br />
12 Makrides, S. C., Nygren, P.-A� ., Andrews, B., Ford, P. J., Evans,<br />
K. S., Hayman, E. G., Adari, H., Uhle� n, M. <strong>and</strong> Toth, C. A. (1996)<br />
J. Pharmacol. Exp. Ther. 277, 534–542<br />
13 Hajishengallis, G., Hollingshead, S. K., Koga, T. <strong>and</strong> Russell,<br />
M. W. (1995) J. Immunol. 154, 4322–4332<br />
14 Sjo� l<strong>and</strong>er, A., Nygren, P.-A� ., Sta� hl, S., Berzins, K., Uhle� n, M.,<br />
Perlmann, P. <strong>and</strong> Andersson, R. (1997) J. Immunol. Methods<br />
201, 115–123<br />
15 Libon, C., Corvaı�a, N., Haeuw, J. F., Nguyen, T. N., Sta� hl, S.,<br />
Bonnefoy, J. Y. <strong>and</strong> Andreoni, C. (1999) Vaccine 17, 406–414<br />
16 Paoletti, E. (1996) Proc. Natl. Acad. Sci. U.S.A. 93,<br />
11349–11353<br />
17 Rolph, M. S. <strong>and</strong> Ramshaw, I. A. (1997) Curr. Opin. Immunol. 9,<br />
517–524<br />
18 Brochier, B., Kieny, M. P., Costy, F., Coppens, P., Bauduin, B.,<br />
Lecocq, J. P., Languet, B., Chappuis, G., Desmettre, P.,<br />
Afiademanyo, K. et al. (1991) Nature (London) 354, 520–522<br />
19 Pastoret, P. P. <strong>and</strong> Brochier, B. (1996) Epidemiol. Infect. 116,<br />
235–240<br />
20 Tartaglia, J., Perkus, M. E., Taylor, J., Norton, E. K., Audonnet,<br />
J. C., Cox, W. I., Davis, S. W., van der Hoeven, J., Meignier, B.,<br />
Rivie� re, M. et al. (1992) Virology 188, 217–232<br />
21 Taylor, J., Trimarchi, C., Weinberg, R., Languet, B., Guillemin, F.,<br />
Desmettre, P. <strong>and</strong> Paoletti, E. (1991) Vaccine 9, 190–193<br />
22 Tine, J. A., Lanar, D. E., Smith, D. M., Wellde, B. T., Schultheiss,
P., Ware, L. A., Kauffman, E. B., Wirtz, R. A., De Taisne, C., Hui,<br />
G. S. et al. (1996) Infect. Immunity 64, 3833–3844<br />
23 Staats, H. F., Jackson, R. J., Marinaro, M., Takahashi, I., Kiyono, H.<br />
<strong>and</strong> McGhee, J. R. (1994) Curr. Opin. Immunol. 6, 572–583<br />
24 Hackett, J. (1993) Curr. Opin. Biotechnol. 4, 611–615<br />
25 Chatfield, S. N., Roberts, M., Dougan, G., Hormaeche, C. <strong>and</strong><br />
Khan, C. M. (1995) Parasitology 110, S17–24<br />
26 Georgiou, G., Stathopoulos, C., Daugherty, P. S., Nayak, A. R.,<br />
Iverson, B. L. <strong>and</strong> Curtiss, R. I. (1997) Nat. Biotechnol. 15,<br />
29–34<br />
27 Georgiou, G., Poetschke, H. L., Stathopoulos, C. <strong>and</strong> Francisco,<br />
J. A. (1993) Trends Biotechnol. 11, 6–10<br />
28 Fischetti, V. A., Medaglini, D. <strong>and</strong> Pozzi, G. (1996) Curr. Opin.<br />
Biotechnol. 7, 659–666<br />
29 Sta� hl, S. <strong>and</strong> Uhle� n, M. (1997) Trends Biotechnol. 15, 185–192<br />
30 Donnelly, J. J., Ulmer, J. B., Shiver, J. W. <strong>and</strong> Liu, M. A. (1997)<br />
Annu. Rev. Immunol. 15, 617–648<br />
31 Ulmer, J. B., Donnelly, J. J., Parker, S. E., Rhodes, G. H., Felgner,<br />
P. L., Dwarki, V. J., Gromkowski, S. H., Deck, R. R., DeWitt,<br />
C. M., Friedman, A. et al. (1993) Science 259, 1745–1749<br />
32 Tubulekas, I., Berglund, P., Fleeton, M. <strong>and</strong> Liljestro� m, P. (1997)<br />
Gene 190, 191–195<br />
33 Berglund, P., Smerdou, C., Fleeton, M. N., Tubulekas, I. <strong>and</strong><br />
Liljestro� m, P. (1998) Nat. Biotechnol. 16, 562–565<br />
34 Kowalczyk, D. W. <strong>and</strong> Ertl, H. C. (1999) Cell. Mol. Life Sci. 55,<br />
751–770<br />
35 Sta� hl, S., Nygren, P.-A� ., Sjo� l<strong>and</strong>er, A. <strong>and</strong> Uhle� n, M. (1993) Curr.<br />
Opin. Immunol. 5, 272–277<br />
36 Nguyen, T. N., Uhle� n, M. <strong>and</strong> Sta� hl, S. (1994) in Advances in<br />
Biomagnetic Separation (Uhle� n, M., Hornes, E. <strong>and</strong> Olsvik, Ø.,<br />
eds.), pp. 73–78, Eaton Publishing Co., Natick, MA<br />
37 Murby, M., Samuelsson, E., Nguyen, T. N., Mignard, L., Power,<br />
U., Binz, H., Uhle� n, M. <strong>and</strong> Sta� hl, S. (1995) Eur. J. Biochem. 230,<br />
38–44<br />
38 Hannig, G. <strong>and</strong> Makrides, S. C. (1998) Trends Biotechnol. 16,<br />
54–60<br />
39 Arntzen, C. J. (1998) Nat. Med. 4, 502–503<br />
40 Tacket, C. O., Mason, H. S., Losonsky, G., Clements, J. D.,<br />
Levine, M. M. <strong>and</strong> Arntzen, C. J. (1998) Nat. Med. 4, 607–609<br />
41 Makrides, S. C. (1996) Microbiol. Rev. 60, 512–538<br />
42 Billman-Jacobe, H. (1996) Curr. Opin. Biotechnol. 7, 500–504<br />
43 Martin-Gallardo, A., Fleischer, E., Doyle, S. A., Arumugham, R.,<br />
Collins, P. L., Hildreth, S. W. <strong>and</strong> Paradiso, P. R. (1993) J. Gen.<br />
Virol. 74, 453–458<br />
44 Liljeqvist, S., Haddad, D., Berzins, K., Uhle� n, M. <strong>and</strong> Sta� hl, S.<br />
(1996) Biochem. Biophys. Res. Commun. 218, 356–359<br />
45 Viret, J. F., Cryz, Jr, S. J. <strong>and</strong> Favre, D. (1996) Mol. Microbiol. 19,<br />
949–963<br />
46 Ichikawa, Y., Yamagata, H., Tochikubo, K. <strong>and</strong> Udaka, S. (1993)<br />
FEMS Microbiol. Lett. 111, 219–224<br />
47 Nagahama, M., Michiue, K. <strong>and</strong> Sakurai, J. (1996) FEMS<br />
Microbiol. Lett. 145, 239–243<br />
Recombinant <strong>subunit</strong> <strong>vaccines</strong> 105<br />
48 Sudbery, P. E. (1996) Curr. Opin. Biotechnol. 7, 517–524<br />
49 Valenzuela, P., Medina, A., Rutter, W. J., Ammerer, G. <strong>and</strong> Hall,<br />
B. D. (1982) Nature (London) 298, 347–350<br />
50 Power, U. F., Plotnicky-Gilquin, H., Huss, T., Robert, A., Trudel,<br />
M., Sta� hl, S., Uhle� n, M., Nguyen, T. N. <strong>and</strong> Binz, H. (1997)<br />
Virology 230, 155–166<br />
51 Geisse, S., Gram, H., Kleuser, B. <strong>and</strong> Kocher, H. P. (1996)<br />
Protein Expr. Purif. 8, 271–282<br />
52 Sta� hl, S., Sjo� l<strong>and</strong>er, A., Nygren, P.-A� ., Berzins, K., Perlmann, P.<br />
<strong>and</strong> Uhle� n, M. (1989) J. Immunol. Methods 124, 43–52<br />
53 Fuh, G., Mulkerrin, M. G., Bass, S., McFarl<strong>and</strong>, N., Brochier, M.,<br />
Bourell, J. H., Light, D. R. <strong>and</strong> Wells, J. A. (1990) J. Biol. Chem.<br />
265, 3111–3115<br />
54 Pugsley, A. P. <strong>and</strong> Schwartz, M. (1985) FEMS Microbiol. Rev. 32,<br />
3–38<br />
55 Blattner, F. R., Plunkett, G. I., Bloch, C. A., Perna, N. T., Burl<strong>and</strong>,<br />
V., Riley, M., Collado-Vides, J., Glasner, J. D., Rode, C. K.,<br />
Mayhew, G. F. et al. (1997) Science 277, 1453–1474<br />
56 Murby, M., Uhle� n, M. <strong>and</strong> Sta� hl, S. (1996) Protein Expression<br />
Purif. 7, 129–136<br />
57 Abrahmse� n, L., Moks, T., Nilsson, B. <strong>and</strong> Uhle� n, M. (1986)<br />
Nucleic Acids Res. 14, 7487–7500<br />
58 Moks, T., Abrahmse� n, L., O� sterlo� f, B., Josephson, S., O� stling, M.,<br />
Enfors, S.-O., Persson, I., Nilsson, B. <strong>and</strong> Uhle� n, M. (1987)<br />
Bio/Technology 5, 379–382<br />
59 Hansson, M., Sta� hl, S., Hjorth, R., Uhle� n, M. <strong>and</strong> Moks, T. (1994)<br />
Bio/Technology 12, 285–288<br />
60 Alfthan, K., Takkinen, K., Sizmann, D., Seppala, I., Immonen, T.,<br />
Vanne, L., Keranen, S., Kaartinen, M., Knowles, J. K. <strong>and</strong> Teeri,<br />
T. T. (1993) Gene 128, 203–209<br />
61 Hewinson, R. G. <strong>and</strong> Russell, W. P. (1993) J. Gen. Microbiol.<br />
139, 1253–1259<br />
62 Dalbøge, H., Dahl, H.-H. M., Pedersen, J., Hansen, J. W. <strong>and</strong><br />
Christensen, T. (1987) Bio/Technology 5, 161–164<br />
63 Ko� hler, K., Ljungquist, C., Kondo, A., Veide, A. <strong>and</strong> Nilsson, B.<br />
(1991) Bio/Technology 9, 642–646<br />
64 Hassinen, C., Ko� hler, K. <strong>and</strong> Veide, A. (1994) J. Chromatogr. A<br />
668, 121–128<br />
65 Andersson, C., S<strong>and</strong>berg, L., Murby, M., Sjo� l<strong>and</strong>er, A., Lo� vgren-<br />
Bengtsson, K. <strong>and</strong> Sta� hl, S. (1999) J. Immunol. Methods 222,<br />
171–182<br />
66 Andersson, C., S<strong>and</strong>berg, L., Werne� rus, H., Johansson, M.,<br />
Lo� vgren-Bengtsson, K. <strong>and</strong> Sta� hl, S. (2000) J. Immunol. Methods<br />
238, 181–193.<br />
67 Berzins, K., Adams, S., Broderson, R., Chizzolini, C., Hansson, M.,<br />
Lo� vgren, K., Millet, P., Morris, C. L., Perlmann, H., Perlmann, P. et<br />
al. (1995) Vaccine Res. 4, 121–133<br />
68 Rudolph, R. (1996) in Protein Engineering: Principles <strong>and</strong><br />
Practice (Clel<strong>and</strong>, J. L. <strong>and</strong> Craik, C. S., eds.), pp. 283–298,<br />
Wiley–Liss, New York<br />
69 Murby, M., Cedergren, L., Nilsson, J., Nygren, P.-A� ., Hammarberg,<br />
B., Nilsson, B., Enfors, S. O. <strong>and</strong> Uhle� n, M. (1991)<br />
Biotechnol. Appl. Biochem. 14, 336–346<br />
� 2000 Portl<strong>and</strong> Press Ltd
106 M. Hansson, P.-A� . Nygren <strong>and</strong> S. Sta� hl<br />
70 Samuelsson, E., Wadensten, H., Hartmanis, M., Moks, T. <strong>and</strong><br />
Uhle� n, M. (1991) Bio/Technology 9, 363–366<br />
71 Murby, M., Nguyen, T. N., Binz, H., Uhle� n, M. <strong>and</strong> Sta� hl, S.<br />
(1994) in Separations <strong>of</strong> Biotechnology 3 (Pyle, D. L., ed.), pp.<br />
336–344, Bookcraft, Bath<br />
72 Samuelsson, E., Moks, T., Nilsson, B. <strong>and</strong> Uhle� n, M. (1994)<br />
Biochemistry 33, 4207–4211<br />
73 Sta� hl, S. <strong>and</strong> Nygren, P.-A� . (1997) Pathol. Biol. 45, 66–76<br />
74 Sta� hl, S., Nilsson, J., Hober, S., Uhle� n, M. <strong>and</strong> Nygren, P.-A� .<br />
(1999) in The Encyclopedia <strong>of</strong> Bioprocess Technology: Fermentation,<br />
Biocatalysis, & Bioseparation (Flickinger, M. C. <strong>and</strong><br />
Drew, S. W., eds.), pp. 8–22, John Wiley & Sons, New York<br />
75 Hammarberg, B., Nygren, P.-A� ., Holmgren, E., Elmblad, A., Tally,<br />
M., Hellman, U., Moks, T. <strong>and</strong> Uhle� n, M. (1989) Proc. Natl.<br />
Acad. Sci. U.S.A. 86, 4367–4371<br />
76 Nguyen, T. N., Gourdon, M. H., Hansson, M., Robert, A.,<br />
Samuelson, P., Libon, C., Andre� oni, C., Nygren, P.-A� ., Binz, H.,<br />
Uhle� n, M. <strong>and</strong> Sta� hl, S. (1995) J. Biotechnol. 42, 207–219<br />
77 Studier, F. W., Rosenberg, A. H., Dunn, J. J. <strong>and</strong> Dubendorff,<br />
J. W. (1990) Methods Enzymol. 185, 60–89<br />
78 Jonasson, P., Nygren, P.-A� ., Johansson, B. L., Wahren, J., Uhle� n,<br />
M. <strong>and</strong> Sta� hl, S. (1998) Gene 210, 203–210<br />
79 Jonasson, P., Nygren, P.-A� ., Jo� rnvall, H., Johansson, B. L., Wahren,<br />
J., Uhle� n, M. <strong>and</strong> Sta� hl, S. (2000) J. Biotechnol. 76, 215–226<br />
80 Sta� hl, S., Nygren, P.-A� . <strong>and</strong> Uhle� n, M. (1997) Methods Mol. Biol.<br />
62, 37–54<br />
81 Nygren, P.-A� ., Eliasson, M., Palmcrantz, E., Abrahmse� n, L. <strong>and</strong><br />
Uhle� n, M. (1988) J. Mol. Recognit. 1, 69–74<br />
82 Br<strong>and</strong>t, C., Power, U. F., Plotnicky-Gilquin, H., Huss, T., Nguyen,<br />
T., Lambert, P. H., Binz, H. <strong>and</strong> Siegrist, C. A. (1997) J. Infect.<br />
Dis. 176, 884–891<br />
83 Plotnicky-Gilquin, H., Goetsch, L., Huss, T., Champion, T., Beck,<br />
A., Haeuw, J. F., Nguyen, T. N., Bonnefoy, J. Y., Corvaı�a, N. <strong>and</strong><br />
Power, U. F. (1999) J. Virol. 73, 5637–5645<br />
84 Plotnicky-Gilquin, H., Huss, T., Aubry, J. P., Haeuw, J. F., Beck, A.,<br />
Bonnefoy, J. Y., Nguyen, T. N. <strong>and</strong> Power, U. F. (1999) Virology<br />
258, 128–140<br />
85 Siegrist, C. A., Plotnicky-Gilquin, H., Cordova, M., Berney, M.,<br />
Bonnefoy, J. Y., Nguyen, T. N., Lambert, P. H. <strong>and</strong> Power, U. F.<br />
(1999) J. Infect. Dis. 179, 1326–1333<br />
86 Saron, M. F., Fayolle, C., Sebo, P., Ladant, D., Ullmann, A. <strong>and</strong><br />
Leclerc, C. (1997) Proc. Natl. Acad. Sci. U.S.A. 94, 3314–3319<br />
87 Lebens, M., Shahabi, V., Ba� ckstro� m, M., Houze, T., Lindblad, N.<br />
<strong>and</strong> Holmgren, J. (1996) Infect. Immunity 64, 2144–2150<br />
88 Morein, B., Villacres-Eriksson, M., Sjo� l<strong>and</strong>er, A. <strong>and</strong> Bengtsson,<br />
K. L. (1996) Vet. Immunol. Immunopathol. 54, 373–384<br />
89 Cox, J. C. <strong>and</strong> Coulter, A. R. (1997) Vaccine 15, 248–256<br />
90 Leclerc, C., Charbit, A., Martineau, P., Deriaud, E. <strong>and</strong> H<strong>of</strong>nung,<br />
M. (1991) J. Immunol. 147, 3545–3552<br />
91 Stover, C. K., Bansal, G. P., Hanson, M. S., Burlein, J. E., Palaszynski,<br />
S. R., Young, J. F., Koenig, S., Young, D. B., Sadziene, A.<br />
<strong>and</strong> Barbour, A. G. (1993) J. Exp. Med. 178, 197–209<br />
� 2000 Portl<strong>and</strong> Press Ltd<br />
92 Pozzi, G. <strong>and</strong> Wells, J. M. (1997) Gram-Positive Bacteria:<br />
Vaccine Vehicles for Mucosal Immunization, L<strong>and</strong>es Bioscience,<br />
Georgetown, TX<br />
93 Charbit, A., Sobczak, E., Michel, M. L., Molla, A., Tiollais, P. <strong>and</strong><br />
H<strong>of</strong>nung, M. (1987) J. Immunol. 139, 1658–1664<br />
94 Schorr, J., Knapp, B., Hundt, E., Kupper, H. A. <strong>and</strong> Amann, E.<br />
(1991) Vaccine 9, 675–681<br />
95 Haddad, D., Liljeqvist, S., Kumar, S., Hansson, M., Sta� hl, S.,<br />
Perlmann, H., Perlmann, P. <strong>and</strong> Berzins, K. (1995) FEMS<br />
Immunol. Med. Microbiol. 12, 175–186<br />
96 Medaglini, D., Pozzi, G., King, T. P. <strong>and</strong> Fischetti, V. A. (1995)<br />
Proc. Natl. Acad. Sci. U.S.A. 92, 6868–6872<br />
97 Oggioni, M. R., Manganelli, R., Contorni, M., Tommasino, M.<br />
<strong>and</strong> Pozzi, G. (1995) Vaccine 13, 775–779<br />
98 Medaglini, D., Rush, C. M., Sestini, P. <strong>and</strong> Pozzi, G. (1997)<br />
Vaccine 15, 1330–1337<br />
99 Di Fabio, S., Medaglini, D., Rush, C. M., Corrias, F., Panzini,<br />
G. L., Pace, M., Verani, P., Pozzi, G. <strong>and</strong> Titti, F. (1998) Vaccine<br />
16, 485–492<br />
100 Nguyen, T. N., Hansson, M., Sta� hl, S., Bachi, T., Robert, A.,<br />
Domzig, W., Binz, H. <strong>and</strong> Uhle� n, M. (1993) Gene 128, 89–94<br />
101 Sta� hl, S., Samuelson, P., Hansson, M., Andre� oni, C., Goetsch, L.,<br />
Libon, C., Liljeqvist, S., Gunneriusson, E., Binz, H., Nguyen, T.<br />
N. <strong>and</strong> Uhle� n, M. (1997) in Gram-Positive Bacteria: Vaccine<br />
Vehicles for Mucosal Immunization (Pozzi, G. <strong>and</strong> Wells, J. M.,<br />
eds.), pp. 62–81, L<strong>and</strong>es Bioscience, Georgetown, TX<br />
102 Cano, F., Plotnicky-Gilquin, H., Nguyen, T. N., Liljeqvist, S.,<br />
Samuelson, P., Bonnefoy, J. Y., Sta� hl, S. <strong>and</strong> Robert, A. (2000)<br />
Vaccine 18, 2743–2752<br />
103 Acheson, D. W. K., Sonenshein, A. L., Leong, J. M. <strong>and</strong> Keusch,<br />
G. T. (1997) in Vaccines 97 (Brown, F., Burton, D., Doherty, P.,<br />
Mekalanos, J. <strong>and</strong> Norrby, E., eds.), pp. 179–184, Cold Spring<br />
Harbor Press, Cold Spring Harbor, NY<br />
104 Schreuder, M. P., Deen, C., Boersma, W. J., Pouwels, P. H. <strong>and</strong><br />
Klis, F. M. (1996) Vaccine 14, 383–388<br />
105 Charbit, A., Boulain, J. C., Ryter, A. <strong>and</strong> H<strong>of</strong>nung, M. (1986)<br />
EMBO J. 5, 3029–3037<br />
106 Freudl, R., MacIntyre, S., Degen, M. <strong>and</strong> Henning, U. (1986)<br />
J. Mol. Biol. 188, 491–494<br />
107 Agterberg, M., Adriaanse, H. <strong>and</strong> Tommassen, J. (1987) Gene<br />
59, 145–150<br />
108 Pistor, S. <strong>and</strong> Hobom, G. (1990) Res. Microbiol. 141, 879–881<br />
109 Wong, R. S., Wirtz, R. A. <strong>and</strong> Hancock, R. E. (1995) Gene 158,<br />
55–60<br />
110 Martineau, P., Guillet, J. G., Leclerc, C. <strong>and</strong> H<strong>of</strong>nung, M. (1992)<br />
Gene 113, 35–46<br />
111 Hedegaard, L. <strong>and</strong> Klemm, P. (1989) Gene 85, 115–124<br />
112 van Die, I., van Oosterhout, J., van Megen, I., Bergmans, H.,<br />
Hoekstra, W., Enger-Valk, B., Barteling, S. <strong>and</strong> Mooi, F. (1990)<br />
Mol. Gen. Genet. 222, 297–303<br />
113 Pallesen, L., Poulsen, L. K., Christiansen, G. <strong>and</strong> Klemm, P.<br />
(1995) Microbiology 141, 2839–2848
114 Kuwajima, G., Asaka, J.-I., Fujiwara, T., Fujiwara, T., Nakano, K.<br />
<strong>and</strong> Kondoh, E. (1988) Bio/Technology 6, 1080–1083<br />
115 Newton, S. M. C., Joys, T. M., Anderson, S. A., Kennedy, R. C.,<br />
Hovi, M. E. <strong>and</strong> Stocker, B. A. D. (1995) Res. Microbiol. 146,<br />
203–216<br />
116 Lu, Z., Murray, K. S., Cleave, V. V., LaVallie, E. R., Stahl, M. L.<br />
<strong>and</strong> McCoy, J. M. (1995) Bio/Technology 13, 366–372<br />
117 Harrison, J. L., Taylor, I. M. <strong>and</strong> O’Connor, C. D. (1990) Res.<br />
Microbiol. 141, 1009–1012<br />
118 Fuchs, P., Breitling, F., Dubel, S., Seehaus, T. <strong>and</strong> Little, M.<br />
(1991) Bio/Technology 9, 1369–1372<br />
119 Cornelis, P., Sierra, J. C., Lim, Jr, A., Malur, A., Tungpradabkul,<br />
S., Tazka, H., Leitao, A., Martins, C. V., di Perna, C., Brys, L. et<br />
al. (1996) Bio/Technology 14, 203–208<br />
120 Jung, H. C., Lebeault, J. M. <strong>and</strong> Pan, J. G. (1998) Nat. Biotechnol.<br />
16, 576–580<br />
121 Francisco, J. A., Earhart, C. F. <strong>and</strong> Georgiou, G. (1992) Proc.<br />
Natl. Acad. Sci. U.S.A. 89, 2713–2717<br />
122 Francisco, J. A., Stathopoulos, C., Warren, R. A., Kilburn, D. G.<br />
<strong>and</strong> Georgiou, G. (1993) Bio/Technology 11, 491–495<br />
123 Francisco, J. A., Campbell, R., Iverson, B. L. <strong>and</strong> Georgiou, G.<br />
(1993) Proc. Natl. Acad. Sci. U.S.A. 90, 10444–10448<br />
124 Francisco, J. A. <strong>and</strong> Georgiou, G. (1994) Ann. N.Y. Acad. Sci.<br />
745, 372–382<br />
125 Charbit, A., Martineau, P., Ronco, J., Leclerc, C., Lo-Man, R.,<br />
Michel, V., O’Callaghan, D. <strong>and</strong> H<strong>of</strong>nung, M. (1993) Vaccine<br />
11, 1221–1228<br />
126 Su, G. F., Brahmbhatt, H. N., Wehl<strong>and</strong>, J., Rohde, M. <strong>and</strong><br />
Timmis, K. N. (1992) Infect. Immun. 60, 3345–3359<br />
127 Tzschaschel, B. D., Guzman, C. A., Timmis, K. N. <strong>and</strong> de<br />
Lorenzo, V. (1996) Nat. Biotechnol. 14, 765–769<br />
128 Newton, S. M., Jacob, C. O. <strong>and</strong> Stocker, B. A. (1989) Science<br />
244, 70–72<br />
129 Wu, J. Y., Newton, S., Judd, A., Stocker, B. <strong>and</strong> Robinson,<br />
W. S. (1989) Proc. Natl. Acad. Sci. U.S.A. 86, 4726–4730<br />
130 McEwen, J., Levi, R., Horwitz, R. J. <strong>and</strong> Arnon, R. (1992)<br />
Vaccine 10, 405–411<br />
131 Pozzi, G., Contorni, M., Oggioni, M. R., Manganelli, R.,<br />
Recombinant <strong>subunit</strong> <strong>vaccines</strong> 107<br />
Tommasino, M., Cavalieri, F. <strong>and</strong> Fischetti, V. A. (1992) Infect.<br />
Immun. 60, 1902–1907<br />
132 Hansson, M., Sta� hl, S., Nguyen, T. N., Ba� chi, T., Robert, A., Binz,<br />
H., Sjo� l<strong>and</strong>er, A. <strong>and</strong> Uhle� n, M. (1992) J. Bacteriol. 174,<br />
4239–4245<br />
133 Samuelson, P., Hansson, M., Ahlborg, N., Andreoni, C., Go� tz,<br />
F., Bachi, T., Nguyen, T. N., Binz, H., Uhle� n, M. <strong>and</strong> Sta� hl, S.<br />
(1995) J. Bacteriol. 177, 1470–1476<br />
134 Liljeqvist, S., Samuelson, P., Hansson, M., Nguyen, T. N., Binz,<br />
H. <strong>and</strong> Sta� hl, S. (1997) Appl. Environ. Microbiol. 63,<br />
2481–2488<br />
135 Norton, P. M., Brown, H. W., Wells, J. M., Macpherson, A. M.,<br />
Wilson, P. W. <strong>and</strong> Le Page, R. W. (1996) FEMS Immunol.<br />
Med. Microbiol. 14, 167–177<br />
136 Liljeqvist, S., Sta� hl, S., Andreoni, C., Binz, H., Uhle� n, M. <strong>and</strong><br />
Murby, M. (1997) J. Immunol. Methods 210, 125–135<br />
137 Cano, F., Liljeqvist, S., Nguyen, T. N., Samuelson, P., Bonnefoy,<br />
J. Y., Sta� hl, S. <strong>and</strong> Robert, A. (1999) FEMS Immunol. Med.<br />
Microbiol. 25, 289–298<br />
138 Liljeqvist, S., Cano, F., Nguyen, T. N., Uhle� n, M., Robert, A. <strong>and</strong><br />
Sta� hl, S. (1999) FEBS Lett. 446, 299–304<br />
139 Delmas, A. <strong>and</strong> Partidos, C. D. (1996) Vaccine 14, 1077–1082<br />
140 Johnston, S. A. <strong>and</strong> Barry, M. A. (1997) Vaccine 15, 808–<br />
809<br />
141 Jacobsson, K., Jonsson, H., Lindmark, H., Guss, B., Lindberg, M.<br />
<strong>and</strong> Frykberg, L. (1997) Microbiol. Res. 152, 121–128<br />
142 Jacobsson, K. <strong>and</strong> Frykberg, L. (1995) Biotechniques 18,<br />
878–885<br />
143 Jacobsson, K. <strong>and</strong> Frykberg, L. (1998) Biotechniques 24,<br />
294–301<br />
144 Clackson, T. <strong>and</strong> Wells, J. A. (1994) Trends Biotechnol. 12,<br />
173–184<br />
145 Nygren, P.-A� . <strong>and</strong> Uhle� n, M. (1997) Curr. Opin. Struct. Biol. 7,<br />
463–469<br />
146 Arnold, G. F. <strong>and</strong> Arnold, E. (1999) Am. Soc. Microbiol. News<br />
65, 603–610<br />
Received 17 April 2000�2 June 2000; accepted 6 June 2000<br />
� 2000 Portl<strong>and</strong> Press Ltd