Download - Macmillan Cancer Support
Download - Macmillan Cancer Support
Download - Macmillan Cancer Support
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
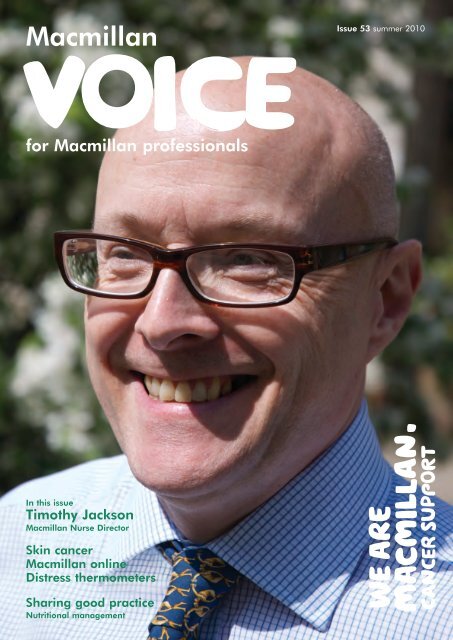
<strong>Macmillan</strong>voicefor <strong>Macmillan</strong> professionalsIssue 53 summer 2010In this issueTimothy Jackson<strong>Macmillan</strong> Nurse DirectorSkin cancer<strong>Macmillan</strong> onlineDistress thermometersSharing good practiceNutritional management
ContentsNews3 The latest news from across <strong>Macmillan</strong>, including our new partnershipswith Boots and TONI&GUY, the development of a strategy for the futureof cancer care, and more award-winning <strong>Macmillan</strong> professionalsFeatures10 ProfileTimothy Jackson, <strong>Macmillan</strong> Nurse Director, South East London<strong>Cancer</strong> Network11 Delivering cancer care in a rural setting<strong>Macmillan</strong> <strong>Cancer</strong> Information and <strong>Support</strong> Officer Moray Bradburyshares how cancer services are provided in a unique Welsh setting12 Improving supportive care for people in transitionOur third article in a series on the work of the <strong>Macmillan</strong> Palliativeand <strong>Cancer</strong> Care Research CollaborativePull out: Sharing good practiceStandardising nutritional management for people with cancer13 CARE – a unique rehabilitation serviceA proactive rehabilitation service for people with lung cancerand mesothelioma14 Distress thermometers – a holistic assessmentto help shape cancer servicesPiloting a screening tool for distress and anxiety in peopleaffected by cancer16 Taking healthy stepsA movement to music class for people with cancer17 Buddy <strong>Support</strong> – helping people newlydiagnosed with cancerA new buddy service delivered by people who have hada personal experience of cancer18 <strong>Macmillan</strong>’s online presence grows<strong>Macmillan</strong>’s Head of Digital Media Katie Smith provides anoverview of <strong>Macmillan</strong>’s online services and plans for 201019 Evaluating the safety of syringe driversin an acute hospital settingA project to evaluate the risks in delivering continuous medicationfor symptom control using a syringe driver20 Life as a lecturer practitioner<strong>Macmillan</strong> Palliative Care Lecturer Practitioner Pamela Wright sharessome education initiatives, and the challenges and variety of her work21 Travel and cancer – your patient’s questions answeredCommonly-asked questions about travel and cancer22 <strong>Support</strong>ing complex pathways of careNew nursing post helps create structured care for people with skin cancerDirectory23 Information for professionals – skin cancerUpcoming events<strong>Macmillan</strong> resources24 New and updated <strong>Macmillan</strong> resources available nowWe welcome feedback!Let us know your views on <strong>Macmillan</strong> Voice.Email macvoice@macmillan.org.ukWriters and news wanted<strong>Macmillan</strong> Voice is for you. It’s where<strong>Macmillan</strong> professionals can share newsabout their work, activities and successes,so please tell us what you’ve been doing.We’re also looking for new writers tocontribute articles. You can write aboutthe issues that matter to you and shareyour knowledge with other <strong>Macmillan</strong>professionals. You don’t need to be anexperienced writer to get involved in<strong>Macmillan</strong> Voice. We can help you turnyour idea into a news item or feature.All you have to do is get in touch withour Managing Editor Rosie Cotter atrcotter@macmillan.org.uk orcall her on 020 7091 2219.Maximum word counts: news storiesup to 300 words; features up to500 words. Please also send usphotographs if possible, using thehighest resolution on your camera.Contributors this issueCathy Alderson | Moray BradburyJean Campbell | Shoana ConnellGlenn Dawson | Sheila DifferAmanda Ford | Alison FreemantleCorrina Grimes | Timothy JacksonJanice Koistinen | Lisa Mann | Katie SmithAndrew Wilcock | Pamela WrightEditorial TeamRosie Cotter, Genevieve Osei-Kuffuor, Sajjad ShahEditorial BoardCharlotte Argyle, Carers <strong>Support</strong> ManagerKathy Blythe, <strong>Macmillan</strong> Development Manager, EMNEColin Cosgrove, Information Development ManagerHelen Foy, UK Postholder <strong>Support</strong> and Development Manager, EMNEAlison Hill, Nurse Director, South West London <strong>Cancer</strong> NetworkBeverly Hurst, <strong>Macmillan</strong> Gynaecology/Oncology CNSYvonne McKenna, <strong>Macmillan</strong> Lead <strong>Cancer</strong> NurseEileen Mullen, User representativeEsther Murray, <strong>Macmillan</strong> Consultant in Psychosocial OncologyHeather Nicklin, <strong>Macmillan</strong> Specialist Palliative Care Social WorkerTerry Priestman, Consultant Clinical OncologistChris Sansom, <strong>Macmillan</strong> Development Manager, LASERLouise Wem, <strong>Macmillan</strong> Specialist RadiographerTracy Williams, Senior Information Development NurseDesigned by Grade Design Consultants, Londonwww.gradedesign.comThis paper is 100% recycled.© <strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong> 2010. ISSN 1361-9020.No part of this publication may be reproduced without thepermission of <strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>. <strong>Macmillan</strong> <strong>Cancer</strong><strong>Support</strong>, registered charity in England and Wales (261017)and in Scotland (SC039907). Isle of Man charity number 604.MAC5772_06_10<strong>Macmillan</strong> Voice summer 2010
News 3Rewardingexcellencein palliative careDorothy Matthews (centre) with Liz Balance from Cephalon (left)and Jessica Corner, <strong>Macmillan</strong> Chief Clinician (right)<strong>Macmillan</strong> professionals were among those celebrated atthis year’s International Journal of Palliative Care Awards.Dorothy Matthews from Northumberland Tyne and WearNHS Trust won the Palliative Care Nurse of the Year Award,closely followed by Doreen Bulman from West CumberlandHospital in second place.Dorothy is a founding member of the National Networkfor Palliative Care for People with Learning Disabilities.Her insights have helped others better understand this areaof healthcare. Doreen is involved in mentoring, educatingand supporting other nurses. She regularly educates medicalstaff, creating a hospital-wide ‘palliative care ethos’ that isexceptional in an acute hospital setting.The <strong>Macmillan</strong> Palliative Care Team at Surrey and SussexHealthcare NHS Trust were awarded third prize in theDevelopment Award category for a collaborative venturewith a local hospice. This has helped bridge a gap in theservice for bereaved carers.The awards, which were held at the end of March,recognise and celebrate achievement and excellence in thework of nurses and their teams in palliative care. For moreinformation, go to ijpn.co.uk/awards<strong>Macmillan</strong> and Boots– an exciting new partnershipWe are delighted to tell you about our ambitious newpartnership with Boots. Much more than a normalfundraising partnership, we are working with Boots toreach everyone affected by cancer in the UK.‘<strong>Macmillan</strong> and Boots is not just an ordinary partnership.It is something that will give people access to informationand support from the high street that could change their lifeand the lives of their loved ones,’ says Ciarán Devane,<strong>Macmillan</strong> Chief Executive.This year, we are planning small pilots in some Bootsstores in Birmingham to help us understand how thepartnership can best reach people affected by cancer.We are testing ways we can provide cancer informationin-store and the potential for other activities, such asawareness or information events.This is also our biggest fundraising partnership – expectedto raise over £1.5 million a year for the next three years.Staff and customer fundraising started during April in storesthroughout the UK, and will officially launch at the end of June.A volunteering programme for Boots staff is also in development.By bringing together our expertise with that of the biggesthealth and beauty brand in the UK, we have the opportunityto reach and improve the lives of everyone living with cancer.For more information, please contact Steven Wibberley,Partnership Programme Lead, on 020 7840 4942 or atswibberley@macmillan.org.uk<strong>Macmillan</strong> Voice summer 2010
4NewsA body image tool kit tosupport self-managementA matterof detail<strong>Cancer</strong> and its treatment can havea dramatic effect on a person’sappearance, body function andsensation. Some people may be verydistressed due to changes to theirbody, which can result in low selfesteemand self-confidence, as wellas social anxiety and depression.<strong>Macmillan</strong> has funded an 18-monthproject in conjunction with NHSAyrshire and Arran to look at this issue.The project aims to improve the careof people with cancer who experiencechange(s) to their body.We ran focus groups and individualinterviews with 37 people who had arange of cancer diagnoses. We wantedto understand their experience of bodyimage issues and supportive care, andget their views on how to improveclinical care. In conjunction withresearch evidence, the themes andsub-themes identified from the focusgroup and interviews became thefoundation for a body image tool kit.The tool kit will be available in Julyand incorporates:• an e-learning programme forhealthcare professionals, whichcan be accessed throughmacmillan.org.uk/learnzone,cancernursing.org andtheknowledgenetwork.co.uk• a workbook to support individuals todevelop skills and strategies to adaptto change(s) to their body after cancer.This was developed together witheight people with cancer, and will beavailable through <strong>Macmillan</strong>.For more information please contactCaroline Hood, <strong>Macmillan</strong> ClinicalProject Lead – Body Image and <strong>Cancer</strong>,on 01563 527001, or atcaroline.hood@aaaht.scot.nhs.ukYou can also read about the projectand its developments in the March2010 issue of <strong>Cancer</strong> Nursing Practice.Dying Matters Week in Marchhighlighted that 65% of people in theUK have not written a Will, and onlya quarter of us have told anyoneabout our funeral arrangements.The second largest legacy everbestowed to <strong>Macmillan</strong> – £1.9 million– almost wasn’t awarded to us.Equivalent to funding nearly 13<strong>Macmillan</strong> professionals for threeyears, the incredible gift had beenleft in one generous person’s Will forthe benefit simply of ‘cancer relief’.Thanks to the support and backingof other UK cancer charities and aftera period of consultation, the gift wasawarded to us to support peopleaffected by cancer, as thought to havebeen intended by its benefactor.Carrying out people’s wishes isn’talways straightforward. If you or yourpatients have any questions aboutlegacies or Will writing, the <strong>Macmillan</strong>Legacy team is happy to help wherethey can. Call us on 0800 107 4448or visit macmillan.org.uk/legaciesStrength in StyleStrength in Style is a new programme<strong>Macmillan</strong> has developed inpartnership with hairdressing companyTONI&GUY to support and advise onhair care to people affected by cancer.Part of the new programme includesspecialist training for TONI&GUYstylists. A team from <strong>Macmillan</strong>’sLearning and Development department,led by Chele Lawrence, delivers the firstday of each training course, coveringhow to communicate effectively withpeople affected by cancer. This ensuresthe Strength in Style consultants arebetter equipped to deal with theemotional and practical issuessurrounding hair loss, and the effectsof treatment. Day two is run byTONI&GUY Academy staff and dealswith practical hair care before, duringand after treatment. The stylists arealso trained to style wigs.with TONI&GUYForty stylists have been trained to dateand we hope to train around 100stylists by the end of the year.The pilot programme, which isavailable in 40 salons across Englandand Scotland, will be reviewed andhopefully rolled out nationally by theend of the year. Initial Strength in Styleconsultations will be free and wig fittingand styling will cost the same as a blowdry (about half the cost of a standardhair cut).In addition to developing thisexciting new service, TONI&GUY staffhave pledged to raise £60,000 by theend of 2010.For a list of Strength in Style salons,please visit macmillan.org.uk/strengthinstyleuk If you have anyqueries about this partnership pleasecontact Sally Hill on 01904 756413or at shill@macmillan.org.uk<strong>Macmillan</strong> Voice summer 2010
News 5We evolve – buildingon our achievements<strong>Macmillan</strong>’s ambition is to reach and improve the livesof everyone living with cancer. Thanks to our work toimprove the data on cancer prevalence in the UK, andour efforts to measure the reach of our posts andservices, we know that we are reaching more than onein two of those living with cancer.In 2009 alone, we estimate that we increased our reach byaround 11%. Despite the challenging economic environment,we managed to raise £119 million last year. This enabled usto deliver some high-profile new services that increased thesupport we are able to provide. These included our newphone service and our redesigned website macmillan.org.ukThe phone service is now handling around 6,000 calls eachmonth, while over 450,000 people visit our website in thesame period. And you, our 5,000 professionals, helped usreach over 450,000 people in 2009.‘In 2009 alone, we estimate that weincreased our reach by around 11%.’As we look to the future, we will build on the good workalready achieved and evolve what we do. We will need tocontinue our success in innovation, as well as raising moremoney than ever before. We predict that the number ofpeople living with a cancer diagnosis will rise by around 3%each year. As more people survive a cancer diagnosis, therewill need to be a greater focus on recovery and support forpeople after treatment. We are committed to supportingcancer survivors to live a healthy and active life for as longas possible. We have worked in partnership with theDepartment of Health and NHS Improvement setting outthe vision and plan for the National <strong>Cancer</strong> SurvivorshipInitiative. Copies can be accessed at ncsi.org.uk‘As more people survive a cancerdiagnosis, there will need to bea greater focus on recovery andsupport for people after treatment.’Our new strategy, covering 2011–2015, will take account ofthis context. We have consulted with over 650 individuals inthe development of our strategy so far, including staff,professionals, volunteers, people affected by cancer, policymakers, commissioners and donors. We are very grateful forthe contribution you made at the <strong>Macmillan</strong> professionalsconference. We aim to publish our new strategy this summer.For more information, contact Gráinne Kavanagh, Head ofStrategy Implementation, on 020 7840 5081 or Hannah Marks,Planning and Performance Manager, on 020 7091 2126.ReferencesMaddams, J., Brewster, D., Gavin A., Steward, J., Elliot, J., Utley, M.and Moller, H. <strong>Cancer</strong> Prevalence in the UK: Estimates for 2008 <strong>Cancer</strong>Prevalence in the UK. British Journal of <strong>Cancer</strong>. 2009; 101, 541–547.<strong>Macmillan</strong>’s report, Two Million Reasons, can be accessed atbe.macmillan.org.ukTalking about sex– workshop for professionals<strong>Macmillan</strong>’s London, South East andAnglia office is hosting a workshop tohelp <strong>Macmillan</strong> professionals improvetheir understanding of the impact ofcancer on sexual relationships.People affected by cancer have toldus that it’s an area that they wouldlike more help in, and they foundthat professionals are not alwayscomfortable discussing the topic.This workshop is delivered by aRelate counsellor and nurse, who isalso a cancer and communicationexpert. The session starts with delegatesexploring their knowledge and feelingsabout sexuality by using fun, interactivetechniques. It then focuses on theproblems people with cancer experience,and how professionals can providesupport. Delegates complete a quizusing the sexual relationship resourceson Learn Zone and there is also a roleplayexercise so delegates can practicehaving difficult conversations. Delegatesare encouraged to use the sexualrelationship resources for their ongoingdevelopment and as teaching resources.Past delegates include occupationaltherapists, clinical nurse specialists andinformation professionals. Their feedbackhas been positive: ‘I’ll take back lots ofideas and information to disseminate‘It raised my confidenceand increased knowledgein different aspects.’among my colleagues,’ and, ‘It raisedmy confidence and increasedknowledge in different aspects.’The next sessions will be on19 October and 23 November.These are open to all <strong>Macmillan</strong>professionals, including those outsidethe region. Please contact ClaireBowen for details atcbowen@macmillan.org.uk<strong>Macmillan</strong> Voice summer 2010
6 NewsNew group focuses on improvinglife after treatmentTreatment for cancer can have a range of physical,psychological and social consequences. Too often, theseproblems are not recognised or addressed and they canhave a serious impact on people’s lives.‘A patient told me he had suffered from mild depressionand fatigue for several years after treatment for testicularcancer. He was finally able to get help only after hestumbled across hormone replacement therapy,’ says DianaGreenfield, a nurse consultant. ‘He said within two days hehad become “a different man”.’Diana belongs to a new group set up by <strong>Macmillan</strong>called the Consequences of <strong>Cancer</strong> Treatment Collaborative,which is part of the National <strong>Cancer</strong> Survivorship Initiative.The group aims to improve care for people living with the‘A patient told me how he had sufferedfrom mild depression and fatigue forseveral years after treatment for testicularcancer. He was finally able to get helponly after he stumbled across hormonereplacement therapy.’effects of treatment. The 12 members have expertise inresearch and clinical practice as nurses or allied healthprofessionals. As senior figures, they also have credibility ineducation and service development.Through their collective voice, the group aims to influenceservices, help bridge the gap between research and practice,and make consequences of treatment a far more visibleissue within the UK research and policy agendas. MembersSara Faithfull and Isabel White have already contributed to<strong>Macmillan</strong>’s booklets on the late effects of pelvicradiotherapy in men and women (free to order frombe.macmillan.org.uk).Other group members include: Karen Robb, ConsultantPhysiotherapist; Karen Roberts, <strong>Macmillan</strong> Reader and NurseConsultant in <strong>Cancer</strong> Care; Jo Armes, Research Fellow,Specialist Care; Natalie Doyle, Nurse Consultant; DeborahFenlon, Senior Research Fellow; Mary Wells, Senior Lecturerin <strong>Cancer</strong> Nursing; Gillian Knowles, Nurse Consultant;Claire Taylor, Lecturer in Gastrointestinal Nursing; TheresaWiseman, Lecturer and Nursing Research Fellow.For more information, contact Janice Koistinen,<strong>Macmillan</strong> Projects <strong>Support</strong> Manager, on 02476 575 509or j.koistinen@warwick.ac.ukA benchmark for good qualityStained glass window at the new breast centreThe Nightingale Centre Breast Unit atWythenshawe Hospital in Manchesterwas recently accredited during the<strong>Macmillan</strong> Quality Environment Mark(<strong>Macmillan</strong> QEM) pilot phase.The <strong>Macmillan</strong> QEM is a detailedframework for assessing whetherhealthcare facilities meet the standardsrequired by people living with cancer.Design began on the new centre in2005 because the original building wasunfit for purpose. A team of architects,estates department staff, clinical staff,the hospital arts team and patients wereactively involved in the design of thenew building.The centre diagnoses around 800people with breast cancer each year,as well as seeing women from the NHSbreast screening programme, womenwith a family history of breast cancer,and women on follow-up appointmentsafter surgery.The aim when designing the centrewas to maximise the number of servicesavailable to women. The new unitprovides sentinel node radio isotopeinjections (which used to be given inthe nuclear medicine department),bone density scanning, an extensiveprosthesis department with underwearand swimwear, and a gymnasium fordiet and exercise research programmes.The <strong>Macmillan</strong> QEM assessmentwas undertaken by Det Norske Veritas,the external assessment partner, and apatient representative.‘It was a very positive experience tohave a thorough external analysis of theprovision of care for our patients – andnot forgetting the staff facilities, whichI had not thought would be part of theassessment. I would encourage any unitor facility to participate in this veryworthwhile scheme,’ Barbara Eckersley,Superintendent Radiographer, said.For more information, pleasecontact Barbara on 0161 291 4466 orat barbara.eckersley@uhsm.nhs.uk.For more information about the <strong>Macmillan</strong>QEM, go to macmillan.org.uk/MQEM<strong>Macmillan</strong> Voice summer 2010
Expert benefits advice pays offAn everyday referral to <strong>Macmillan</strong> Benefits Adviser Glenn Dawsonleads to an unexpected reward for couple in needNews 7Mr James is 95 years old and has prostate cancer.His wife is 90 and has a disability. They both receiveAttendance Allowance for these disabilities, as well astheir State Pensions and Pension Credits.On checking their benefits I noticed that there was around£100 per week missing from their entitlement. I brought thisto the attention of Mrs James, who then discussed it with thePension Service.They wrote to her with a breakdown of her benefitentitlement and said that she and her husband werereceiving the correct amount of benefits. She was veryreluctant to take this further, as it was too much trouble andof course, the ‘Pension Service must be right’. However,Mrs James agreed to send me the letter so that I could followthis up on their behalf.‘The couple had been missing approx£100 per week since 2003.’When the letter arrived, I contacted the Pension Service andasked them to look again at the couple’s benefit entitlement.They still could not see the problem until I mentioned thatthe couple were both receiving Attendance Allowance, whichentitled them to the double severe disability premium of£105.70 per week, which was missing from their benefit.As a matter of interest I asked, ‘When was the last date thecouple claimed the premium?’ There was a bit of silenceand then the operator said 2003. The couple had beenmissing approx £100 per week since 2003.The Pension Service apologised for the mistake and arrangedfor a payment of £32,000 to be refunded to them. Thecouple also received the double carers premium back-dated12 weeks, totalling £708, and an extra £164.70 per weekin benefits.Mrs James was over the moon with the outcome. The firstthing they were going to buy was a new TV and the restwould go towards their funerals.‘Sometimes the rewards are small, butsometimes they can make a real difference.’A request has gone in to the Pension Service asking forcompensation for the couple on the grounds ofmaladministration as this mistake should have been rectifiedyears ago.This case is not unique. It is just one of many which allbenefits advisers come across at some point in their jobs.What it does show is how important it is to carry out basicbenefit checks for people with cancer. Sometimes the rewardsare small, but sometimes they can make a real difference.For more information on benefits and financial help forpeople affected by cancer, phone our cancer supportspecialists on 0808 808 00 00, visit macmillan.org.uk/financialissues or order Help with the cost of cancer atbe.macmillan.org.ukPutting pen to paper<strong>Macmillan</strong> Voice is for you. It’s yourforum to share news, innovative ideas,activities and successes.Have you written a thesis that you’dlike to share? Just finished work on anexciting project? Perhaps you havecreated an engaging poster presentationand would like to share your workwith even more professionals.Whatever your idea, we can helpyou turn it into a news item or feature.All you need to do is get in touch withRosie Cotter, Managing Editor, atrcotter@macmillan.org.uk oron 020 7091 2219.Group copiesIf your team would like to receiveone group copy of <strong>Macmillan</strong> Voiceinstead of individual copies,please emailmacvoice@macmillan.org.uk<strong>Macmillan</strong> Voice summer 2010
8NewsCapital’s cancer careprofessionals celebratedFive London healthcare professionalshave been presented with awards fortheir contribution to cancer care at theAction for London Conference 2010.Action for London is a partnershipbetween <strong>Macmillan</strong> and the five Londoncancer networks. It aims to set out anursing vision for cancer care in thecapital.The Action for London Awards2010 were presented to professionalswho have made a real contribution tothe cancer care experience throughinnovation and creative practice.Winners include a prostate cancernurse who took her work into thecommunity, running sessions at localbus garages and Post Office sortingoffices, and a clinical psychologist whohelped a breast cancer patient’sdaughter who was suffering fromobsessive compulsive disorder (OCD).This year’s winners are:Band 7/8 AwardMary Van Zyl, Clinical Nurse Specialistin prostate cancer care at St GeorgesHospital; Helen Keane, Day Care Sisterat University College HospitalBand 5/6 AwardRebecca Weeks, Staff Nurse at therehabilitation outreach team at TheRoyal Marsden NHS Foundation TrustPatient Choice AwardMary Burgess, Clinical Psychologist atThe Royal Marsden NHS Foundation Trustand University College London Hospital;Jane Coe, Clinical Nurse Specialist atUniversity College London Hospital.Carole Walford, <strong>Macmillan</strong> Actionfor London Programme Manager, said,‘We had some very strong applicationsthis year and it’s inspiring to see theexcellence in cancer care that ishappening in London.’Action for London Award winners 2010Each winner will receive an educationgrant, a small grant for their place ofwork, and an individual engravedglass award.For more information about Actionfor London and the award winners, pleasecontact Carole on 020 7380 9983 orat carole.walford@uclh.nhs.ukInaugural learn and share eventpopular with professionalsWe know how dedicated <strong>Macmillan</strong> professionals are toimproving the lives of people affected by cancer. But throughmy work as a <strong>Macmillan</strong> development manager, I noticedthat many teams were grappling with issues that otherteams had solved.‘Bringing together clinical staff withcommissioning teams was an excellentidea and removed barriers as theday progressed.’The East Midlands <strong>Cancer</strong> Network was keen to work withme to help remedy this. I met with Jo Kavanagh, NurseDirector, the lead nurses at the network and the learningdevelopment manager from <strong>Macmillan</strong>. Together we decidedto host a ‘learn and share’ day.As well as wanting to share good practice, many teamssaid they were struggling to understand the commissioningprocess and how this related to them in clinical practice –so we decided to invite a panel of commissioners to answertheir questions. We also asked teams from each of thenetwork areas to showcase their initiatives. These initiativesincluded e-learning, patient focus groups, therapy team work,first aid for family bereavement, outcome measures forpalliative care, and ‘learning to let go at the end of treatment’.The day was a great success and the delegates said theyhad gained a better understanding of the commissioningprocess.Maxine Astley-Pepper, <strong>Macmillan</strong> Development Manager,said, ‘The audience were hungry to learn aboutcommissioning and had (until that point) apparently notbeen included or not really fully engaged in the process.Bringing together clinical staff with commissioning teamswas an excellent idea and removed barriers as the dayprogressed, with the commissioners learning things too.’The workshops to share good practice were wellreceived,with over 80% of delegates asking for regularsharing days.For more information, please contact Kathy Blythe,<strong>Macmillan</strong> Development Manager, EMNE, on 01529307251 or at kblythe@macmillan.org.uk.<strong>Macmillan</strong> Voice summer 2010
News 9MPs vote ‘yes’ to cancer supportThe general election has been and gone, and after a lot ofexcitement and drama, we welcome the new government in placeThank you to all of you who took action in our ‘votecancer support’ campaign.Thousands of people wrote to their parliamentarycandidates asking them to support our calls. 163 new MPssupport our campaign, which is 25% of all MPs. This includesfour cabinet ministers and Deputy Prime Minister Nick Clegg.This is an amazing achievement. We think our three policycalls, detailed below, will dramatically improve the lives ofpeople affected by cancer and we will be asking the newgovernment to back our calls as quickly as possible.Living with cancerWe feel passionately that the new government shoulddemonstrate a clear commitment to the survivorship agendaand the two million people living with and after cancer. Thiscommitment should be based on the principles of a posttreatmentcare plan and appropriate support to help peopleget their lives back after treatment.Equal access to drugs for peoplewith rarer cancersWe want the new government to improve access to drugtreatments for people with rarer cancers by reforming theNational Institute for Health and Clinical Excellence (NICE)drug appraisal process.End-of-life care – access to 24/7community nursingWe want the new government to ensure people with cancernearing the end of their life have 24/7 access to communitynursing, allowing them to die at home if they wish.We will be asking every new MP who voted cancer support tobe a <strong>Macmillan</strong> champion in parliament. We will also beasking every parliamentary candidate who wasn’t elected tobe a <strong>Macmillan</strong> champion in their local area, too.We will continue to campaign on these issues and will letyou know ways to get involved over the coming months.<strong>Macmillan</strong> appointsnew ChairAfter nine years as Chairman of<strong>Macmillan</strong>, Jamie Dundas will bestepping down and handing over tohis successor after the charity’s AGMon 29 July.The Board of <strong>Macmillan</strong> is delightedto announce that the new Chair willbe Julia Palca. Julia has been a trusteeof <strong>Macmillan</strong> since 2001, and untilrecently, was a partner at law firmOlswang LLP.Jamie Dundas will be maintainingan association with <strong>Macmillan</strong> asDeputy President of the charity.‘It has been a great honour to serveas Chairman of <strong>Macmillan</strong> for the pastnine years. I’m very proud of what thecharity has achieved in the great causeof helping people with cancer,’ JamieDundas said.‘I’m delighted that Julia is steppinginto the role of Chair. As a cancersurvivor herself, Julia will continue toensure <strong>Macmillan</strong> keeps people withcancer at the heart of everything itdoes. She’s uniquely qualified andI wish her every success.’What do you really think?It’s our ambition that all <strong>Macmillan</strong>professionals feel valued, understoodand proud to be part of <strong>Macmillan</strong>.To help us make sure we are gettingit right, we need you to tell us what wecould be doing better. We havecommissioned research specialists GfKNOP to work with us on an in-depthstudy of your relationship with <strong>Macmillan</strong>so that we can continue to improve howwe work together. This research is ofgreater importance than anything wehave done with you in the past.Why participate?Wide-level participation is needed sothat we can ensure that all opinionsand voices are represented, and thatany changes we make work foreveryone. Knowing how busy you are,we have tried to make this processquick and easy so you all to take part.Remember, this is your opportunity tomake your opinion count.What do you have to do?Watch your inbox. Most professionalswill be contacted with two requestsaround this research – the first to ensurethat your contact details are up-to-date(you can expect this request in the nextfew weeks if you haven’t received italready) – the second asking you tocomplete our online survey (you canexpect this request in July).A small number of you will also becontacted by your regional team withan offer to take part in focus-groupsessions, which will explore commonthemes and issues.Then what?The results of the research will bepresented in early autumn. The findingswill be used to form recommendationsto develop and improve opportunitiesand ways of working: from inductionto learning and development, and alot in between.For more information please contactmarketing@macmillan.org.uk.We appreciate your participationand sharing.<strong>Macmillan</strong> Voice summer 2010
10ProfileTimothy Jackson<strong>Macmillan</strong> Nurse Director, South East London<strong>Cancer</strong> NetworkWhat does the role involve?The South East London <strong>Cancer</strong> Network (SELCN) covers a population of 1.5 millionpeople, and includes six primary care trusts (PCTs), a cancer centre, local hospitalsand hospices, and voluntary sector organisations. We work with acute teams in thehospitals and PCTs to modernise cancer and specialist palliative care.I lead on workforce development, user involvement, supportive and palliativecare, and specific tumour types, including brain, children, young people andsarcoma. I also manage a small team of programme managers.I work with other healthcare professionals, service users, managers, andcommissioners to ensure that patients receive national standards of treatmentand care, have a good patient experience, and receive high-quality information.What are the biggest challenges?I mostly work in a leadership role rather than as a direct line manager, so I have touse influence and credibility as a clinician and leader to get things done. Howeverstakeholders within SELCN have a ‘can do’ attitude and they want to help. It is achallenge sometimes but is also very liberating.The other challenge is trying to keep cancer on the agenda, alongside all of theother priorities in healthcare.What is your greatest success in the role?The ‘Cost of <strong>Cancer</strong>’ project with <strong>Macmillan</strong> and Southwark Citizens Advice Bureau.This put benefits advisers into a number of acute trusts to help people affected bycancer access grants. We have gained £1 million in benefits for our patients so far.How would you like the role and service to develop?We used to work with providers of cancer care, but we are now developing moreof a commissioning role, for example, developing a commissioning specificationfor systemic therapies like chemotherapy (biological and non-cytotoxic) andradiotherapy. The team are reviewing the current job roles and skills, and whatwe might need in the future given the changing work environment.What is the best thing about being a <strong>Macmillan</strong> professional?It is a privilege to be a <strong>Macmillan</strong> professional. You get a lot of support on apersonal level along with professional resources and expertise. The role supportsnetworking and you have access to people, experts, equipment grants, educationgrants and project money. <strong>Macmillan</strong> encourages innovative working and trustingyour instinct. It is a dynamic organisation that allows you to develop the evidencebase ahead of the rest. This helps you to deliver your agenda.Why did you choose to go into cancer care?I was watching the Horizon show one evening as a student nurse in York back in thelate 1970s. It featured the work of the Royal Marsden and a Professor McElwaintalking about this dynamic speciality called oncology. It showed cancer nurses anddoctors in very positive light and demonstrated good interdisciplinary working. Iapplied to do the oncology nursing course at the Marsden, which was the only oneavailable in the UK at the time. It was the best experience and anything was possible.Who has been your inspiration?My senior nurses from the Marsden – Robert Tiffany, Chief Nurse and RichardWells, Rehabilitation Nurse, both pushed the boundaries. They were human,approachable, and nothing was impossible. Marilyn Marks, Chemotherapy/Palliative Care Senior Nurse at the Marsden, and Professor Tony Goldstone,UCH Medical Director, also had a great impact.LocationSouth East London <strong>Cancer</strong> Networkmanagement offices, based in GuysHospital, LondonTimothy works as part of a coreteam that includes a networkdirector and medical directorIn postSince June 2004‘The challenge is tryingto keep cancer on theagenda, alongside allof the other prioritiesin healthcare.’Further informationTimothy JacksonNurse DirectorSouth East London <strong>Cancer</strong>Network12th Floor, Tower WingGuys Hospital, Great Maze PondLondon SE1 9RT020 7188 7121Timothy.Jackson@gstt.nhs.ukwww.patientinfo.selcn.nhs.uk<strong>Macmillan</strong> Voice summer 2010
Information and support 11Delivering cancer carein a rural setting<strong>Macmillan</strong> <strong>Cancer</strong> Information and <strong>Support</strong> Officer Moray Bradburyshares how cancer services are provided in a unique rural settingHealth and social care professionals will be aware of howdifficult it can be to deliver cancer services because ofpracticality versus reality, and the differing needs ofpeople with cancer.For the past five years I have worked within cancerservices, primary commissioning for the NHS, and deliveringservices in the community for people wishing to die at home.Within this time I have encountered a lack of provision forcancer services in particular.I joined <strong>Macmillan</strong> at the beginning of 2009 through ajoint initiative with The Bracken Trust, a Welsh cancer supportcentre supporting people with cancer within the Powys region.Both <strong>Macmillan</strong> and The Bracken Trust work well to supportpersonally-centred care.Wales is currently faced with supporting an aginggeneration and will be dependent on the voluntary sectorfor support. This increases the pressure of community care,which Powys has difficulties with because of its ruralgeography and social deprivation.‘Wales is currently faced withsupporting an aging generationand will be dependent on thevoluntary sector for support.’Powys is the largest county in Wales with an area of 2,006square miles, a quarter of the area of Wales. The countyhas borders with 11 other Welsh counties and two Englishcounties (Herefordshire and Shropshire). Powys is also theleast densely populated county in Wales. The estimatedpopulation in 2007 was 132,075 (4.4% of the Welshpopulation) and the Powys population is older than theaverage for Wales (19.9% of the population aged 65 orover compared to 17.4% for Wales and 15.9% for England).As a result, cancer diagnoses are now often found to besecondary rather than primary.Between 2003 and 2007 a total of 671 people living inPowys received chemotherapy treatment. The vast majority ofthose people (664) had to travel outside the county for theirtreatment and over half (52%) received their treatment inEngland during this period. Only people who take theirchemotherapy orally can have treatment in their own home.Almost every patient I meet in Powys is receiving treatment inone of the 18 different district general hospitals surroundingthe Powys borders. The average one-way distance thatpatients travel to receive their treatment is 37.4 miles, thehighest average for any county in Wales.‘Over half of Powys residents receivingchemotherapy in this period (52%)received their treatment in England.’This is very unique to Powys and it is not just cancer treatmentthat is affected. The average journey time for me to go to seea patient is a 40-mile return trip. A lot of my support isprovided over the phone, but this often turns into face-to-facesupport. My remit cannot be structured. My door is alwaysopen to new and old patients – I never close cases or files,not even if someone passes away, as family, friends andcarers need just as much information and support. Timing iskey when working in such a rural area, but sadly it doesn’talways happen.In England, people with cancer are allocated individualkey workers who are specialist, cancer-specific nurses. Thisis not the case in Powys – we do not have clinical nursespecialists. We have fantastic <strong>Macmillan</strong> nurses, but theirsupport limited as there are so few of them. This has a bigimpact on my role as the demand for services is huge.Since being in this post I have attempted to embracethese difficulties with the view that living in such a rural areain not always a disadvantage. I feel empowered by membersof the local community who I encounter on a regular basis.I support patients, carers, families and friends with allmanner of support from practical, emotional and welfareadvice, ensuring all their needs are provided for. We arealso very lucky to have such a fantastic charity in Powys –The Bracken Trust – which provides holistic support forpeople with cancer.Further informationMoray Bradbury<strong>Macmillan</strong> <strong>Cancer</strong> Informationand <strong>Support</strong> OfficerThe Bracken Trust, Cefnllys LaneLlandrindod Wells, Powys LD1 5LJ01597 823646 or 07817551142cic.bracken.trust@btopenworld.com<strong>Macmillan</strong> Voice summer 2010
12Research into cancer careImproving supportive carefor people in transitionA <strong>Macmillan</strong>-funded research project is investigating the supportneeds of people with progressive illness and their carersIn the last few editions of <strong>Macmillan</strong> Voice, we have beendescribing the work of the <strong>Macmillan</strong> Palliative and<strong>Cancer</strong> Care Research Collaborative (MacPaCC). Thegroup’s aim is to understand and improve cancer care.Earlier articles featured MacPaCC projects about:• how to care for people with cancer as early as possiblefollowing diagnosis (winter 2009)• how specialist and generalist nurses work with eachother and with other professionals, carers and patients inproviding supportive care to cancer survivors (spring 2010).In this edition, we profile a study about supportive care needsled by Dr Stephen Barclay. Stephen and his colleagues areespecially interested in exploring what patients and theircarers want as they approach the transition from supportivecare to palliative and end-of-life care.How to best support patients at a time of transitionStephen’s study involves two groups of people with contrastingprogressive illness: people recently diagnosed with incurablelung cancer and people with severe chronic obstructivepulmonary disease (COPD). The team want to find out whatStephen BarclayStephen is a practising clinician anda university researcher with a longstandingrelationship with <strong>Macmillan</strong>.Based part-time at the Universityof Cambridge, his main field ofacademic expertise is the GP’s rolein palliative care. He is also theSpecialty Director for Palliative Care in the medical schooland a practising GP in Cambridge and Honorary Consultantin Palliative Medicine at the Cambridge Hospice.Stephen’s work with <strong>Macmillan</strong> began in 1995 whenhe became a GP facilitator and continued with hisappointment as a <strong>Macmillan</strong> clinical fellow. He is currentlya <strong>Macmillan</strong> postdoctoral research fellow.‘Staying involved in clinical practice and academiahelps me do research that will be useful “on the ground”,’he says.Further informationDr Stephen BarclayCambridge Universitysigb2@medschl.cam.ac.uk01223 330300their care, support and information needs are at a time ofdeteriorating health and how these needs can best be addressed.For people with lung cancer, the prognosis is generallyvery poor. About half of people diagnosed with lung cancerwill die within four months according to a Scottish study.‘These people move from supportive care into thepalliative care stage very quickly,’ says Stephen. ‘We wouldlike to understand what they and their carers think are keymarkers of high-quality care during this very difficult time.’The challenges are different for people with COPD.Patients may have a transition from supportive to palliativecare, but this transition is not as clear cut or as easy toidentify as it is with cancer.Current services often do not meet these people’s needs,with lack of communication between doctors and patientshighlighted as a major barrier to better care.‘We need to understand much more about whatapproaches to care work best for this group of patients.There is a tendency to think that the cancer model of care isa “one size fits all”,’ Stephen says.‘I really want to get inside the mindsof my colleagues, to see how weapproach the care of these verydifferent illnesses.’Stephen’s team will explore priorities for care in interviewswith patients and carers. His team will also interview GPs andcommunity nurses who are looking after both a person withlung cancer and someone with severe COPD. The aim of theseinterviews is to see what these health professionals regard askey issues for patient care and service development. This willhelp the team compare approaches to these people’s care.‘As a GP myself,’ says Stephen, ‘I really want to get insidethe minds of my colleagues, to see how we approach thecare of these very different illnesses.’Through this study, <strong>Macmillan</strong> will gain a greaterunderstanding of caring for people in transition and providingservices that best meet the needs of patients and carers.Further informationJanice Koistinen<strong>Macmillan</strong> Projects <strong>Support</strong> ManagerWarwick Medical School02476 575 509j.koistinen@warwick.ac.uk<strong>Macmillan</strong> Voice summer 2010
Rehabilitation13CARE – a uniquerehabilitation serviceWho are we?The <strong>Macmillan</strong> Lung <strong>Cancer</strong> CAREService is a proactive rehabilitationservice for people with lung cancer andmesothelioma. Based at NottinghamUniversity Hospitals NHS Trust, theCARE service (cachexia, anorexia andrelated experiences), works closely withexisting cancer and specialist palliativecare services to provide holistic support.The multidisciplinary teamincludes Cheryl Percival, a dietitian;Rachel Hill, an occupational therapist;Helena Alvey, a physiotherapist; andVal Godfrey, a data manager.There is a particular focus on theeffects of the cachexia-anorexiasyndrome, where improvements aredesperately required. This syndromecauses a progressive wasting of skeletalmuscle which, together with symptomssuch as fatigue, impairs functionalability. Lung cancer has one of thehighest incidences of cachexia, withabout one-third of people alreadymalnourished at the time of diagnosis.What do we do?All people recently diagnosed with athoracic cancer are invited to completethe Sheffield Profile for Assessment andReferral to Care (SPARC) questionnaireto identify their supportive and palliativecare needs. This covers seven areas ofpotential need:• physical symptoms• psychological issues• personal issues• treatment issues• family and social issues• religious and spiritual issues• communication and information issues• independence and activity.The results are discussed at amultidisciplinary meeting, which includesthe lung cancer nurse specialists and aconsultant in palliative medicine. Basedon the needs uncovered, the appropriateteam members undertake a moredetailed assessment and provide therapy.All patients are assessed by the dietitian.The emphasis on rehabilitationhelps improve function, promoteindependence and helps people toadapt to their situation. This involvesproviding a routine nutritional assessmentand intervention, and for many, adviceon managing symptoms such as fatigueand breathlessness, the provision ofequipment and referral to other services.This proactive identification of needs, thetimely provision of appropriate supportand the continuity of care all contributeto a ‘crisis-prevention’ approach.Lynn Payne, one person to benefitfrom the service after having a lungremoved, said, ‘The new lung cancerteam has been brilliant, visiting me athome and providing the emotionalsupport I needed. I know they’re alwaysat the end of the phone if I need them.’What have we alreadyachieved?The team has already:• seen about 90 new patients andprovided 560 face-to-face episodesof care and 620 telephone reviews;about 60% of new and 30% of followupassessments take place in thepatient’s home• developed service documentationand some information leaflets to fillexisting gaps, for example, difficultysleeping at night• piloted the SPARC questionnaire in100 patients and found it to be wellreceived(this has also been acceptedfor publication and poster presentationat European Association for PalliativeCare Research Congress 2010)• summarised the supportive andpalliative care needs of 200 peoplewith thoracic cancer (accepted forposter presentation at EuropeanAssociation for Palliative CareResearch Congress 2010)• made links with national initiatives,such as the National <strong>Cancer</strong> TeamHolistic Needs Assessment and<strong>Cancer</strong> and Palliative CareRehabilitation Workforce projects• begun to evaluate the specificcontributions of the individualmembers of the team• made a successful bid to <strong>Macmillan</strong> fora therapy assistant to support the team• submitted a bid for a ‘Research forPatient Benefit’ grant for anindependent evaluation of the service.Dr Andrew Wilcock, <strong>Macmillan</strong>Reader/Honorary Consultant inPalliative Medicine and clinical lead forthe project says, ‘About 65,000 peoplein the UK are living with a diagnosisof thoracic cancer at any one time.Greater understanding of their needsand the provision of better support fromthe time of diagnosis has the potentialto optimise their independence andquality of life, and to help them toremain in their preferred place of care.This <strong>Macmillan</strong>-funded project will notonly influence local service provision,but will also feed into national palliativecare and rehabilitation initiatives. It willalso provide a model of care whichcould be rolled out to people with othercancers or conditions.’Related information<strong>Macmillan</strong> has a tool kit forprofessionals called the <strong>Macmillan</strong>Durham Cachexia Pack. It helps toguide professionals in the assessmentand management of common problemsseen in people with anorexia-cachexiasyndrome. It can be downloadedfrom the ‘health and social careprofessionals’ section of the Learn Zone.Go to macmillan.org.uk/learnzoneFurther informationDr Andrew Wilcock DM FRCP<strong>Macmillan</strong> Reader in PalliativeMedicine and Medical OncologyUniversity of NottinghamHayward House <strong>Macmillan</strong>Specialist Palliative Care <strong>Cancer</strong> UnitNottingham University HospitalsNHS Trust, Nottingham NG5 1PB0115 9627 7780115 9627 779andrew.wilcock@nottingham.ac.uk<strong>Macmillan</strong> Voice summer 2010
14SurvivorshipDistress thermometersA holistic assessment to help shape cancer servicesPsychological distress is commonamong people affected by cancer andis an understandable response to atraumatic and threatening experience.People draw on their inner resourcesto help cope and many seekemotional support from family andfriends. Some people however arelikely to benefit from additionalprofessional intervention because ofthe level and nature of their distress.In practice, psychological symptomsare often not identified and peoplewith cancer lack sufficient access topsychological support services.The <strong>Macmillan</strong> information andsupport radiographers at Ipswich HospitalNHS Trust provide accurate, evidencebasedinformation and support (psychosocial,psycho-sexual and emotional)to anyone affected by radiotherapytreatment. Relevant information andsupport is given sensitively and at anappropriate time for patients andcarers, and is available at any stageof the clinical care pathway.Patients and carers have differentneeds at different phases of their illnessand our service needs to be responsive tothis. It’s important that all patients haveequal and fair access to the <strong>Macmillan</strong>radiographer service. Due to resourcesand time constraints it’s impossible andnot always necessary to see and supporteveryone undergoing radiotherapy.‘Patients and carers havedifferent needs at differentphases of their illness.’Results from a recent audit of ourservice indicated that only 50% ofpeople having radiotherapy treatmenthad contact with our service and 35%were unaware that the service wasavailable to them. Therefore it was feltthat a tool would be useful forscreening everyone attending thedepartment to help identify those withinformation and support needs andto ensure all patients referred forradiotherapy are offered access to ourservice and followed up with extrainformation and support if required.The National Institute for ClinicalExcellence (NICE) clinical guidanceon supportive and palliative carerecommends that physical, psychological,social, spiritual and financial needs ofpeople with cancer should be assessed,and that this should be undertaken atkey points in their cancer experience.These should occur:• around the time of diagnosis• when treatment begins• when the primary treatment plan finishes• if the disease recurs• at the point when it is recognised thecancer cannot be cured• at the point at which dying is diagnosed• at any other time that the patientrequests.Professionals should also carry outthese assessments in partnership withpatients and carers.As a result, distress thermometershave been piloted in this departmentand we found them to be a useful toolfor two purposes:1. Screening and identifying patientswho need our service.2. Addressing the above keyrecommendations.What is distress?Distress is a feeling of unease stemmingfrom concerns or worries. Peopleundergoing cancer treatment and theircarers are subject to distress, depressionand anxiety. These can manifest inmany ways, such as:• panic attacks, irritability and poorsleeping• feelings of apprehension and worry• avoidance and poor concentration.Subsequently, distress can influencequality of life and participation inmedical treatment. Not everyone wantsto openly discuss their feelings andemotional distress, but research showsthat early advice, support, educationand intervention with small worries canstop the demand for intensiveintervention and clinically significantpsychological problems at a later stage.Why a distress thermometer?Quick screening tools involving fewer thanFigure 1.ExtremedistressNo distress109876543210five questions have been recommendedas a simple method of detecting distressanxiety or depression in several differenttypes of cancer settings.The distress thermometer wasdeveloped in 1998 by the NationalComprehensive <strong>Cancer</strong> Network(NCCN) in the United States, and it hasbeen widely used for people withcancer. Results of the research andevaluation show that:• People who score four or beloware considered to have ‘expecteddistress symptoms’ and need simpleintervention.• People who score above four areconsidered to have more seriousdistress symptoms and require morespecialist interventions.• People like it and it’s easy to use. Itgenerally takes about 20 seconds tocomplete and patients and carersreported that it helped them to focuson their true concerns and interactionswith their healthcare professionals.Our adaptation of the distressthermometer is an A5-sized sheet witha definition of distress, a thermometer(see figure 1), a list of causes of distressand areas of concern, and anexplanation of the role of the <strong>Macmillan</strong>information and support radiographers.Patients and carers are also invited towrite down anything they want to tellus that is not included on the form.<strong>Macmillan</strong> Voice summer 2010
Survivorship15Our contact details are given with theform along with instructions forreturning it.‘Patients and the <strong>Macmillan</strong>radiographers noticed thattheir interactions weremore focused, with amore efficient use of theconsultation time.’Patients are asked to consider theirlevels of distress over the last weekand score themselves between 0 (nodistress) and 10 (extreme distress).Pilot of distress thermometerThirty patients were given the tool tocomplete at their first appointment inthe radiotherapy department. All thedistress thermometers were returned tothe <strong>Macmillan</strong> information and supportradiographers for assessment.Patients scoring four or more onthe thermometer, or patients whohighlighted several concerns on theconcern list, were seen by the<strong>Macmillan</strong> information and supportradiographers. At this consultation theconcern list was looked at with thepatient to identify key areas of concern.Further questions were asked todetermine how the patient could be bestsupported to minimise their distress.This involved simple intervention forexpected distress symptoms. Symptomsmay include:• treatment concerns• concerns about the illness• sadness about the loss of good health• anger and the loss of control• poor sleep, concentration and appetite.Interventions include:• problem solving• listening and practical advice such asapplying for <strong>Macmillan</strong> Grants• explaining and managing side effects,fear, worry, and concerns aboutthe future• more complex intervention and referralon to other agencies such as supportgroups, social work, complementarytherapy and counselling.The distress thermometers wererepeated during treatment and alsoused to plan care and follow-up needsafter treatment.Results of pilotThe distress thermometer was easy andquick to fill in – only two were notreturned. It gave patients time toconsider their problems, talk aboutanxiety levels, explore issues openlyand allowed time for reflection.Patients and the <strong>Macmillan</strong>radiographers noticed that theirinteractions were more focused, with amore efficient use of the consultation time.Patients already known to the<strong>Macmillan</strong> service had less issues andscored lower than patients who hadnot met the <strong>Macmillan</strong> radiographersbefore attending the radiotherapydepartment. Levels of distress decreasedwhen the distress thermometer wasrepeated later in treatment.The distress thermometer was usefulin screening patients and identified thepatients who required help and accessto the service. In the free text areamany patients gave useful feedbackregarding the tool, which has beenused to make useful changes to theoriginal one. These have included athermometer that asks the patient howmuch help they would like, as somepeople who complete the forms havedistress and concerns, but do not wishto have any intervention.Guidelines for its use by theradiographers have been developedand it has been adopted within theradiotherapy department for all patients.However, if patients prefer not tocomplete one then this is respectedand annotated in their radiotherapytreatment sheet.Patients having more than 15treatments will be given another formto complete halfway or towards the endof their radiotherapy treatment in orderto plan care after their treatment.The distress thermometers can alsobe given to carers to help them withtheir concerns and emotional issues.We have found that carers’ levels ofdistress are often much higher thanpatients’. This is recognised by currentresearch and is an area that requiresmore recognition within informationand support roles.The distress thermometer has nowbeen adopted as the recommendedassessment tool by the oncologysite-specific clinical nurse specialistsat the Trust and we are in the processof rolling out the tool as pergovernment guidelines.This work has become part of thein-house ‘moving on’ programme to helppeople living with cancer, and a nationalsurvivorship project identifying peoplewith concerns for the future and to helpcare for them. We are hoping to providebetter signposting and a more effectiveservice for patients, as well as trainingfor treatment radiographers to helppatients requiring simpler interventions.Further informationAmanda Ford<strong>Macmillan</strong> Information and <strong>Support</strong> RadiographerAmanda.ford@ipswichhospital.nhs.ukorLisa Mann<strong>Macmillan</strong> Information and <strong>Support</strong> Radiographerlisa.mann@ipswichhospital.nhs.ukRadiotherapy No45Ipswich Hospital NHS TrustHeath Road, IpswichSuffolk IP4 5PD01473 704361<strong>Macmillan</strong> Voice summer 2010
TakinghealthystepsA movement to music class for people with cancerPeople who have been diagnosedwith cancer and undergone treatmentcan experience altered body image,lymphoedema, decreased range ofmovement and emotional distress.There is a growing recognition amonghealthcare professionals that exerciseplays a vital role in the physical,psychological and emotional aspects ofhealing. 1 Healthy Steps is a programmewhich uses slow, smooth-resisting,sequential exercises to open up thelymphatic system, promoting physical,emotional health and well-being.About Healthy StepsHealthy Steps is a therapeutic exercisewhich brings fun and laughter. Themovements are a mixture of jazz, balletand modern dance, set to a range ofmusic and incorporating a variety ofprops, such as top hats, canes andtutus. Hospitals, palliative care unitsand hospices are an ideal setting forHealthy Steps classes.BackgroundI work as a <strong>Macmillan</strong> lymphoedemaclinical nurse specialist at UniversityHospitals Coventry and WarwickshireNHS Trust. In May 2009, I attended athree-day Healthy Steps certificationand training programme. The courseteaches a programme which aims toreduce swelling, improve range ofmovement, posture and balance,increase upper and lower body mobility,and promote a positive body imageand quality of life.Literature reviewThere are many theories which suggestthat dancing can assist in the healingof illnesses, including cancer, byencompassing the individual’s physical,emotional, cognitive and socialintegration. 2 There are numerousstudies highlighting the benefits ofphysical activity and the effects on theincrease of endorphins within the brain,creating feelings of well-being. 3 Fedirkoet al 4 found that dance-orientedactivities have increased in popularityand provide an enjoyable, physicaland emotional outlet. This leads to amore positive self-image, as well asimproving daily functions anddeveloping a wider social network.Running the programmeAll participants have been diagnosedwith cancer – some recently andcurrently undergoing treatment, whileothers were diagnosed more than fiveyears ago. The class meet weekly andthere is a rolling programme of eightclasses, each lasting one hour. Memberscan attend further programmes if theywish. The first exercise involvesmovements used in lymphatic drainage.Further informationSheila Differ<strong>Macmillan</strong> Lymphoedema Clinical Nurse SpecialistRoom ABF00032, Arden CentreUHCW NHS Hospitals, Clifford Bridge RdCoventry CV2 2DX024 76965499sheila.differ@uhcw.nhs.ukThis stimulates the opening of the initiallymphatics, and can increase the optimumvolume of lymph flow. This exercise ismandatory and is crucial for thesuccessful outcome of the whole session.ResultsAll participants have reported increasein their range of movement, andelevation of confidence, mood and bodyimage. One participant said, ‘Before Istarted Healthy Steps my legs were soswollen that my ankles could not bend.After the first session I lost a lot of fluidand started to get moving.’The group network and supporteach other’s progress and friendshipshave formed which carry on outsidethe group.ConclusionHealthy Steps is an innovative system oftherapeutic movements and exercise tomusic. The exercises emulate manuallymphatic drainage, which helps topromote lymphatic flow, reducing therisk of developing lymphoedema andimproving existing lymphoedema. Itincreases range of movement, and canhelp to lighten mood and reduce anxiety.References[1] Susan L. Sandal, James O. Judge, NoraLandry, Lynn Faria, Robbie Ouellette, MartaMajczak. Dance and Movement Programimproves Quality-of-Life Measures in Breast<strong>Cancer</strong> Survivors. <strong>Cancer</strong> Nursing. 2005.Vol. 28, No. 4; 301–309.[2] Molinaro J, Kleinfeld M, Lebed S. PhysicalTherapy and Dance in the Surgical Managementof Breast <strong>Cancer</strong>. Physical Therapy. 1986.Vol 66, No. 6; 967–969.[3] Aktas G, Ogce F. Asian Pacific Journal of<strong>Cancer</strong> Prevention. 2005. Jul–Sept; 6(3): 408–11.[4] Fedirko et al. Dance as a PT modality:An experience in group treatment outside thehospital setting. Clinical Management inPhysical Therapy. 1985. 5(4):44–47.<strong>Macmillan</strong> Voice summer 2010
Buddy <strong>Support</strong><strong>Support</strong>17Helping people newly diagnosed with cancerJust being there for someone in their hour of need issometimes all that’s needed. Buddy <strong>Support</strong> – a supportedself-care in cancer project – aims to do just that.The service, which was piloted in conjunction with theScottish Government, provides people newly diagnosed withcancer with a buddy – someone who has had personalexperience of cancer and who can give them one-to-onesupport and advice.‘I wanted to show people that there islife after a cancer diagnosis and thatyou are still you, despite being on aslightly different journey than youhad anticipated.’Shoana Connell, <strong>Macmillan</strong> Patient and Public InvolvementOfficer, says, ‘People with cancer are given lots of informationthrough leaflets and verbal advice from staff on all aspectsof their disease and treatment. However, the softer, moresubtle information that can be shared through someonewho has had personal experience of cancer is sought afterby some patients.’The aim of this project is to create a group of individualsable to provide one-to-one information and support atthat level.For the pilot, potential buddies were recruited throughpromotional material, healthcare professionals, patientsand carer groups, and from talks to clinical nurse specialistgroups and other forums. Those who expressed interestattended a two-day ‘buddying and befriending’ course runby <strong>Macmillan</strong>. The course content includes:• What do you want to gain from this course?• What are the skills a buddy needs?• The purpose of buddying.• Exploring hopes and fears.• The difference between a ‘friend’ and a ‘buddy/befriender’.• Buddying by telephone, hospital/ward/clinic, face-to-face.Those who did the training were given a few weeks to considerif they wished to provide support to people with cancer. If theydid, interview and disclosure processes were undertaken.Guidelines and protocols for the service were developedwith the buddies. Psychological support for buddies and thepeople they support is available if required.One of our buddies Emma explains why she becamea buddy: ‘I wanted to show people that there is life aftera cancer diagnosis and that you are still you, despite beingon a slightly different journey than you had anticipated.After my cancer diagnosis, I was given great medical supportand advice but I also wanted to speak to someone who had“walked in my shoes”. <strong>Cancer</strong> can be very isolating.People around you don’t know what to say so you often findyourself reassuring them and ignoring the feelings youyourself are battling with.’John, also a buddy, said, ‘As a past patient with bowelcancer in 1999, who had “the operation” followed bychemotherapy, I now think of myself as one of the manyfortunate cancer survivors. When it was suggested that Iconsider becoming a cancer buddy I recalled that at the timeI was diagnosed I was not offered the opportunity to have aquiet chat with someone who’d been there and who facedthe future with confidence. On reflection I wished I had.‘My buddying experience to date is limited, but it hasconfirmed my belief that for anyone who wants to talk abouttheir situation and has concerns that can be discussed with aknowledgeable third party, the buddy system can offer thatindividual real help at a time when being isolated can suddenlybecome a very meaningful and at times frightening prospect.’Shoana adds, ‘Working with each and every personinvolved in the Buddy <strong>Support</strong> project has been aninspiration. It makes such a difference to someone who hasbeen given a diagnosis of cancer to speak to someone whounderstands how they feel.’‘The buddy system can offer thatindividual real help at a time whenbeing isolated can suddenlybecome a very meaningful andat times frightening prospect.’For more information about <strong>Macmillan</strong>’s buddying andbefriending course, visit the ‘members of the public’ sectionof the Learn Zone – macmillan.org.uk/learnzone For acopy of the literature review on the topic, please contactShoana Connell.Further informationShoana Connell, <strong>Macmillan</strong> PPIO(<strong>Cancer</strong>)0156 382 572607787 152206shoana.connell@aaaht.scot.nhs.uk<strong>Macmillan</strong> Voice summer 2010
18<strong>Macmillan</strong>’s online servicesMacmilLan’s oNlInEpresENCe gROwsLast year, more than three million people visitedmacmillan.org.uk Most of them came because they, orsomeone they know, has cancer and they are lookingfor information, support, or just someone to talk to.Increasing numbers of the UK population, young and old,are turning to the internet for health-related support andinformation. We provide them with high-quality content andservices from a trusted source, complementing what theyaccess offline.‘2010 will be an exciting year as wedevelop new online services and makethe most of the possibilities that newtechnologies can bring.’The merger with <strong>Cancer</strong>backup in 2008 meant that we wereable to create the biggest and most comprehensive cancerinformation and support website in the UK, bringing togetherthe very best of <strong>Cancer</strong>backup and <strong>Macmillan</strong> online. Withthousands of pages of quality-assured cancer content,information about services, financial advice, and a thrivingonline community with nearly 48,000 members, the websiteoffers an unparalleled source of support for anyone affectedby cancer. We’re always looking for ways to develop ourservices and help people make sense of their cancer experience,like our interactive guide to benefits entitlement – Benefitsmade clear at macmillan.org.uk/benefitsmadeclearAnd whether it is to make a donation, take part in anevent, volunteer your services or help us campaign for abetter deal for people living with cancer, there are plenty ofopportunities for anyone who wants to get involved. Sign upfor a coffee morning, email your MP about fuel poverty orfollow us on Facebook.We have plenty to offer for health and social careprofessionals too, including our online learning centre,the Learn Zone, at macmillan.org.uk/learnzone andbe.macmillan.org.uk where you can create <strong>Macmillan</strong>brandedmaterials, as well as order from our extensivecatalogue of information resources.2010 will be an exciting year as we develop new onlineservices and make the most of the possibilities that newtechnologies can bring. We will be joining all our onlineservices together so you only have to log in once. We areinvesting in more video content, a version of the websitefor mobile phones, and we are developing and expandingour online community so that there is more support forthe 1,000 new people who join every month.Visit our website at macmillan.org.uk and pass iton to anyone you know who might benefit from thiswonderful resource.‘Reasons why I love this site: I can rant andmoan and people understand; I can post aproblem and people come back with solutions;people know what I am going through.‘I have learnt that people are kind andthoughtful and care about me – a stranger.And tonight in the midst of all the sufferingand watching my lovely husband in pain withterminal cancer, another person, who hasvery recently been widowed herself throughthis cruel and nasty disease, took time outto post a response to my post and mademe laugh out loud.‘And I'm still laughing now. What a tonic.She has just made me feel so much better.’‘Claire58’, member of the <strong>Macmillan</strong> online communityFurther informationKatie SmithHead of Digital Media,<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>020 7840 7812katiesmith@macmillan.org.uk<strong>Macmillan</strong> Voice summer 2010
Evaluation 19Evaluating the safety of syringedrivers in an acute hospital settingGood symptom control for peoplein end-of-life care is an importantrecommendation of the End of LifeStrategy (2008). In response to this,our Trust ran a project to evaluatethe risks associated with our currentpractice of delivering continuousmedication subcutaneously (underthe skin) for symptom control usingthe MS16A syringe driver.Syringe driversThe MS16A syringe driver is a batteryoperatedpump that delivers continuousmedication for 12 or 24 hours. It issmall and lightweight, and can fit into alarge pocket. Continuous subcutaneousinfusion is an alternative to intravenousinfusion (into a vein) or intramuscular/subcutaneous injection. It is typicallyused when oral medication can nolonger be taken.The administration of medicationvia a syringe driver is an area of highrisk due to the type of drugsadministered. The MS16A wasdesigned over 30 years ago prior tothe introduction of internationalstandards to ensure the safety ofinfusion pumps. One example of thesestandards is that all modern infusiondevices are expected to have alarmsto alert users when therapy could becompromised, for example, theinfusion is tampering with, power isinterrupted, the syringe is displaced,or a line is blocked.Setting up the projectSyringe drivers are now manufacturedto meet new safety requirements, andin response to a number of clinicalincidents, a project team, which includedcommunity representation, was set upto identify a safer way forward.The project involved challengingestablished practice; interdisciplinaryworking; identifying and engaging keystakeholders from the acute Trust intothe community and other local hospitals;liaising with external agencies; settingup a trial to evaluate medical devices;designing new systems of work;communicating the vision for saferpractice across the region, anddevising new documentation toincorporate into the training andimplementation plan.Trialling different devicesA trial comparing the MS16A againsttwo new devices – the McKinley T34and the Alaris AD – both of whichcomplied with the new safetystandards, was conducted on fivewards. The results of this evaluationwere cross-referenced with discussionswith colleagues across the UK; onlineon the discussion forum ofpalliativedrugs.com and informationpublished by the NHS – Purchasingand Supply Agency for Evidence BasedPurchasing on Ambulatory SyringeDrivers (2008). Evaluation includedclinical, training and support, pricing,running costs and cleaning.OutcomesFrom this evaluation, we selected theMcKinley T34 for use in our Trust.Clinically, this device evaluated betterbecause it was robust and simple tooperate. We explored modifications toprotocols and practices before pilotingthe new syringe driver on threeoncology wards and the specialistpalliative care unit. We will evaluatethe training and new documentation,including new ways of prescribing andnew operating systems, beforeimplementing the device across bothhospitals in the Trust. We have alsoestablished a procurement contractinvolving 21 Trusts.‘The most challengingaspect of the project hasbeen to ensure systemsare in place across thehospital to make surepatients can be safelytransferred home or toa nursing home.’The project has not been withoutchallenges. Its scale was greater thanexpected, so developing resilience inthe face of conflicting priorities andsustaining energy and motivation wasa challenge. However, the vision for asafer system to deliver symptom controlto palliative and dying patients hasbeen fully embraced at all levels andacross disciplines throughout the Trust.In hindsight, a project managerwould have been helpful. We alsolacked political astuteness, includingthe ability to access the relevantstakeholders in other Trusts. It becameessential for us to ask senior managerswithin the Trust to identify and includecommunity colleagues with theappropriate level of authority toinfluence change and make decisions.The most challenging aspect of theproject has been to ensure systems arein place across the hospital to makesure patients can be safely transferredhome or to a nursing home.We found that developing a sharedvision and ensuring collaborativeworking with all stakeholders wasessential to make changes that wouldbenefit patients.Further informationAlison Freemantle<strong>Macmillan</strong> CNS, Hospital Palliative Care TeamNottingham University Hospitals NHS TrustCity Hospital campus, Hucknall RoadNottingham NG5 1PB0115 969 1169alison.freemantle@nuh.nhs.uk<strong>Macmillan</strong> Voice summer 2010
20Training and supportLife as a lecturer practitioner<strong>Macmillan</strong> Palliative Care Lecturer Practitioner Pamela Wright sharessome education initiatives, and the challenges and variety of her workI have seen many changes to the way palliative care isprovided since training in the 1980s. It is a privilege tonow have the ability to influence, even in small ways,how people in palliative care are looked after.I work alongside two other lecturer practitioners in theeducation team at Mount Vernon <strong>Cancer</strong> Centre – LizCarruthers, who specialises in communication andpsychological training, and Susan Alexander, OncologyLecturer Practitioner. We link in with the wider multidisciplinaryteam at the cancer centre to provide specialist education inoncology and palliative care. In 2009, we held 290 eventsfor over 3,000 participants from all healthcare disciplines.Clinical supervisionOver the last two years we have been developing the provisionof clinical supervision within the cancer centre. To date, allnurses from band 2 (healthcare assistants), to band 8 (leadnurses and modern matrons), have had access to it. Wechoose supervisors from within the centre, and we trainand support them throughout the year. Our next step in thisproject is to check whether or not staff are finding the clinicalsupervision beneficial.Peer group supportSusan also runs peer group support sessions for all newnursing staff at the centre. This helps them to settle into theirroles while learning about the speciality. These sessionsmainly comprise guided reflective practice where the newnurses meet and share their experiences of working in theclinical area, with Susan facilitating.Palliative care trainingAs a result of the End of Life Care Strategy (2008), we areinvolved in a project with the Hillingdon community<strong>Macmillan</strong> nurse specialists to provide palliative care trainingfor district nurses in Hillingdon. The strategy talks about theneed for specialist palliative care teams to be more involvedin providing education and support, for example, tocommunity staff and care homes. These training days lookat prognostic indicators of when it is appropriate for peopleto enter palliative care, and the difficult conversations thatcommunity staff have to undertake when people areapproaching end of life. We are also designing a similar dayfor nursing home staff which we will run later in the year.<strong>Support</strong>ing professionals: (from left) Susan Alexander, Pamela Wright and LizCarruthersKeeping it relevantOne of the most challenging aspects of the role is findingspeakers for our courses to keep them fresh, up-to-datewith current practice, and relevant to the speciality.Thankfully, working in a regional cancer centre providesus with a large pool of specialiststo approach as speakers, andwe rarely have to twist arms toachieve this.Being a lecturer practitioner hasmany components that would takemultiple pages to explain,but I hope that byhighlighting a few of ourcurrent projects andchallenges that it hasshown what aninteresting role it is.Further informationPamela Wright<strong>Macmillan</strong> Lecturer PractitionerMichael Sobell HouseMount Vernon Hospital01923 844567pamelawright@nhs.net<strong>Macmillan</strong> Voice summer 2010
Travel and cancer21Travel and cancer– your patient’s questions answeredWhat preparation can I dobefore going on holiday?It’s important to consult your doctor tocheck that you are medically fit totravel. Make sure you have insuranceto cover accidents or illness on holiday.Many insurers regard cancer as apre-existing condition, which can makeit difficult for people who have beendiagnosed to get affordable travelinsurance. For more information onpurchasing travel insurance, go tomacmillan.org.uk/travelinsuranceor call <strong>Macmillan</strong> on 0808 808 00 00.Be realistic. Places you have beenbefore may not be suitable now. Thinkabout what you need and make sureyour destination is suitable.What essential items shouldI take with me?Make sure you have a supply ofmedication and equipment to last for thewhole trip, plus a few extra days in caseof delays. It’s worth taking a prescriptionin case you lose your medicines.Any arrangements will depend onhow long you are going for, where youare going, and the type of medicinesyou are taking. Most people going ona two-week holiday won’t need to doanything special.If you have a stoma or any pumpson your body, a letter from yourdoctor is useful when going throughsecurity checks.Don’t forget your European HealthInsurance Card.How can treatment affect mysensitivity to the sun?Some cancer treatments can makeyour skin more sensitive to the sun.For example, radiotherapy will makethe treated area sensitive to the sun,often for years after treatment.You can protect your skin bywearing a wide-brimmed hat,sunglasses and a sunscreen that is atleast SPF 15. Sit in a shady place andalways cover areas that have beentreated with radiotherapy with loose,closely-woven clothing.Check with your cancer specialistbefore spending time in the sun.What other medical conditionsand side effects should I beaware of when travelling?Some types of cancer or cancertreatments may make you more proneto blood clots. Discuss this with yourcancer specialist.If you have anaemia, or sufferbreathlessness, you may be advised toavoid flying. This also applies to peoplewho have recently had surgery.People with stomas may find aproblem with wind in the stoma bagwhen flying. Your nurse will be able toadvise you about ways to avoid this.What do I need to considerwhen taking medicationabroad?Some countries have limits on the typeand amount of medicines you can takein. The restrictions vary a lot betweencountries and may include some drugsthat you can buy in the UK, for examplepainkillers containing codeine.The restrictions are likely to includecontrolled medicines, for examplemorphine, and drugs that you need tohave by injection. You will need tocheck with the country’s embassy orHigh Commission about any restrictionsthey have. You should take a letterwritten by your GP or specialist, listing:• your medicines• the type of cancer you have• the treatment you’ve had.It can help to list the chemical name ofthe drug and not just the brand name,because the brand name may bedifferent in the country you are visiting.Ask your doctor for the letter a coupleof weeks before you plan to go.Carry your letter in your handluggage so that you can show customsofficers if you need to, and carry all yourmedicines in the labelled containersthat your pharmacist gave you.What should I do when takingmedication in a different timezone?If the time difference is only one to twohours, take it at your usual time (UKtime), but if you are in a time zone thatmeans you would need to takemedication in the middle of the night,gradually change the time of day thatyou take it, until you reach ‘local time’.Ask your pharmacist for advice.Related informationOur booklet Travel and cancer and ourleaflet Getting travel insurance when youhave been affected by cancer can beordered through be.macmillan.org.ukor 0800 500 800.Further informationCathy Alderson<strong>Macmillan</strong> <strong>Cancer</strong> Information & <strong>Support</strong> ManagerThe Royal Liverpool and Broadgreen UniversityHospitals NHS Trust0151 706 3720 / 0151 600 1798catherine.alderson@rlbuht.nhs.uk<strong>Macmillan</strong> Voice summer 2010
22 Skin cancer<strong>Support</strong>ing complexpathways of careNew nursing post helps create structuredcare for people with skin cancerThe number of people diagnosed with skin cancer hasbeen increasing steadily over the past two decades.UK-wide non-melanoma skin cancer has trebled over thisperiod and incidence rates of malignant melanoma havemore than quadrupled in the UK since the 1970s. This hasled to a sharp rise in the number of lesion referrals to thedermatology services throughout Greater Glasgow andClyde. There have also been many changes in recentyears in the way dermatology services are delivered.Reduction in inpatient facilities, the introduction of waitingtime targets, and the reduction in junior doctor’s hourshave all had an impact.The <strong>Macmillan</strong> skin cancer nurse specialist (CNS) postwas introduced as a pilot project in October 2009, withfunding provided by <strong>Macmillan</strong> for two years. The post isbased at Southern General Hospital and covers thedermatology service throughout Greater Glasgow and Clyde.‘UK-wide non-melanoma skin cancerhas trebled and incidence rates ofmalignant melanoma have morethan quadrupled in the UK sincethe 1970s.’The main objective of introducing a CNS post for people withskin cancer is to develop a structured, supportive service forpeople and their families. The multi-site professionalsinvolved in the care of many of these people can make thisa complex and disjointed journey. For some, this will includeseeing the dermatologist, plastic surgeon and oncologist, aswell as support services such as counselling. Reinforcing andproviding relevant information and appropriate liaison withother professionals and agencies can help smooth thisprocess for the patient.Ongoing development of the service has been gradualand frustrating at times. Orientation to the various hospitalscovered by the dermatology service and developingrelationships with staff has taken time and perseverance.The number of consultants involved and differences in theirapproach has been an added consideration. Flexibility andadaptability have been essential elements of the role.The objectives of the post are quite varied and are likelyto change or expand over time as the post and postholderevolve. In addition to the main objective mentioned above,other aspects of the role include:• supporting healthcare professionals• developing needs-based education and training for staff• standardising and developing patient information• empowering patients to be proactive in their ownongoing care• delivering relevant health promotion messages to patientsand the public.This post puts me in an ideal position to manage thecomplexities and interdependencies of the various parts of thehealthcare journey. Organising and coordinating services andresources can help to control costs and prevent wasting timeand resources. Contact with a CNS can help smooth thepatient journey and I believe this is true for the patients andcarers I am involved with. Much of this work is not visible orquantifiable, but providing emotional support and signpostingto other agencies is an equally important aspect of the role,which is not always apparent to other staff and management.Providing telephone support also makes the service moreaccessible because of the wide geographic area covered.People with more advanced or metastatic disease arenormally referred on to the oncologist. Strong links have beendeveloped with the <strong>Macmillan</strong> melanoma CNS at theregional cancer centre to help ensure a smooth transition ofcare and to support these people and their families at allstages of their treatment and ongoing care.Because I am dealing directly with patients on an ongoingbasis, both face-to-face as well as telephone consultation,I feel I’m in an ideal position to identify areas where thepatient journey could be managed more efficiently andsympathetically. Ongoing assessment of the workload andplanning appropriate care delivery are now an integral partof any service provided. Appropriately trained and supportednursing staff can make a valuable contribution to the care ofpeople diagnosed with skin cancer.‘This post puts me in an ideal positionto manage the complexities andinterdependencies of the variousparts of the healthcare journey.’Further informationJean Campbell<strong>Macmillan</strong> Skin <strong>Cancer</strong> Nurse SpecialistThe Alan Lyell Centre for DermatologySouthern General HospitalGlasgow G51 5TF0141 201 2175jean.campbell4@nhs.net<strong>Macmillan</strong> Voice summer 2010
InformationSkin cancerWebsites for professionalsBMJ Evidence Updatesplus.mcmaster.ca/evidenceupdatesThe Evidence Updates service is unique.All citations (from over 120 premierclinical journals) are pre-rated for qualityby research staff, then rated for clinicalrelevance and interest by at least threemembers of a worldwide panel ofpracticing physicians. An email alertservice notifies you of important newresearch about the diagnosis, treatment,prognosis, aetiology and economics ofthe medical conditions of your choice.You can also register for free to receivetailored evidence updates.British Association ofDermatologistswww.bad.org.ukOn this website, health professionalscan access clinical guidelines on arange of skin conditions, includingmalignant melanoma, basal cellcarcinoma, squamous cell carcinoma,Bowen’s disease and topicalphotodynamic therapy.NHS Choices: Behind theHeadlines (<strong>Cancer</strong>)www.nhs.uk/newsBehind the Headlines provides anunbiased and evidence-based analysisof health stories that make the news.The service is intended for both thepublic and health professionals.NHS Evidence – <strong>Cancer</strong>Specialist Librarywww.library.nhs.uk/cancerThis is a comprehensive evidencebasedresource supporting busy healthprofessionals to find high-quality,up-to-date cancer information. The siteincludes evidence collections, annualevidence updates, and UK andinternational guidelines on all themajor cancers.NHS Evidence – Skin DisordersSpecialist Librarywww.library.nhs.uk/skinThis specialist online library aims tofor professionalsdevelop as a ‘one-stop’ resourcebringing together high-quality,evidence-based information on all ofaspects of skin disorders, includingtheir treatment and management, andthe impact they have on patients.Websites for the public<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong>www.macmillan.org.uk<strong>Macmillan</strong> provides high-quality,up-to-date cancer information. All ofthe information is written and reviewedby specialists. The website includesinformation on basal cell carcinoma,squamous cell carcinoma, malignantmelanoma and rarer types ofnon-melanoma skin cancer.<strong>Cancer</strong> Help UKwww.cancerhelp.org.uk<strong>Cancer</strong> Research UK’s website for thepublic containing a wealth of highqualityinformation on skin cancer,including basal cell and squamouscell skin cancers, and information onmelanoma skin cancers.NHS Choiceswww.nhs.ukThe NHS website for the publicproviding a variety of information onskin cancer and sun protection. Thewebsite has pages on non-melanomaskin cancers, such as basal cell andsquamous cell skin cancers. NHSChoices also has pages providinginformation on skin safety in the sun.SunSmartwww.sunsmart.org.ukSunSmart is the UK's national skincancer prevention campaign. TheSunSmart website contains a widerange of information for the generalpublic, including skin cancer facts, sunprotection advice, resources for schools,and personal stories from people whohave had skin cancer. You can alsoorder or download the whole rangeof SunSmart leaflets and publicitymaterials from the website.DirectoryUpcomingeventsJuly2 July 2010Action Mesothelioma Daywww.blf.org.uk236–12 July 2010Ethnic Minority <strong>Cancer</strong>Awareness Weekemcaw.co.ukSeptember13–19 September 2010Lymphatic <strong>Cancer</strong> Awareness Weekwww.lymphomas.org.uk25 September 2010World’s Biggest Coffee MorningHelp create a huge stir by havingcoffee and a slice of cake with yourfriends and colleagues.www.macmillan.org.uk/coffeeOctoberBreast <strong>Cancer</strong> Awareness Monthwww.breastcancercare.org.ukNovember4–5 November 2010<strong>Macmillan</strong> professionals eventPut this year’s event in your diaries.More information will be available atmacmillan.org.uk/learnzone andin Mac Mail in the near future.20117–16 May 2011Peru hiking challengeFrom high, remote mountain trails tothe first sight of the legendary LostCity of the Incas, Machu Picchu, thisis a truly memorable trek.www.macmillan.org/peruhiking@macmillan.org.uk020 7840 78876–16 October 2011Kilimanjaro hiking challengeKilimanjaro is the highest free-standingmountain in the world. <strong>Macmillan</strong> isoffering you the chance to reach newheights while raising money to helppeople living with cancer.www.macmillan.org/kilimanjarohiking@macmillan.org.uk020 7840 7887<strong>Macmillan</strong> Voice summer 2010
24<strong>Macmillan</strong> resourceswe sharE ReSourcEsNew and updated resources‘I think the bookletis great and Iwish I had hadsomething likethis when I wasdiagnosed.’<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong> reviewer talkingabout Self-employment and cancerHelp with the cost of cancer(updated)MAC4026_10 (Northern Irelandversion – MAC4026_10_NI)A comprehensive guide to benefits andfinancial help for people affected bycancer. Benefits rates apply from April2010 – April 2011. You can downloada Welsh version (PDF) frombe.macmillan.org.ukSelf-employment and cancer(new)MAC12818This booklet is designed to help peoplewho have a cancer diagnosis and areself-employed. It includes practicalinformation about cancer and treatments,balancing your health needs and yourwork, deciding who to tell and what tosay, keeping the business operating,and managing finances.Wide selection of skin cancer resources now available‘I found it informative,accessible and written in acalm, straightforward tone.’<strong>Macmillan</strong> <strong>Cancer</strong> <strong>Support</strong> reviewer talkingabout Understanding advanced melanomaA range of titles about skin cancer and the different stages of melanoma arenow available. The resources cover causes and symptoms, diagnosis, stagingand grading, treatments and clinical trials which may be offered for each typeof cancer. They also look at the emotional, practical and financial issues patientsmay face while living with cancer.Understanding skin cancerMAC11653For people who have, or are havingtests for skin cancer. The bookletfocuses on two common types of skincancer: basal cell and squamous cellcarcinoma. This title is also availableon CD and audiotape.Understanding advancedmelanomaMAC11918A new resource for people whosemelanoma has returned or has spreadto other areas of the body.Understanding thin melanoma(less than 1mm)MAC11633Also available in audio format, thisresource describes melanomas that areless than 1mm thick in depth and haveonly spread within the surface layersof the skin.Understanding melanoma(1mm and over)MAC11916Looks at melanoma that is 1mm thickand over in depth and has spread tothe deeper layers of skin.To view and order from our range of information resources,visit be.macmillan.org.uk or call 0800 500 800.