Thirty years of CPAP - ResMed
Thirty years of CPAP - ResMed
Thirty years of CPAP - ResMed
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Snooze NewzA newsletter for people with sleep-disordered breathing (SDB) and their familiesISSUE 13Using <strong>CPAP</strong> for the long haul:an interview with Steve CreightonSteve Creighton didn’t realise hehad sleep apnea. It was only whenhe started using <strong>CPAP</strong> that he sawhow much <strong>of</strong> life he’d been missingout on.Steve Creighton is a pr<strong>of</strong>essionaldriver who lives in Western Sydneywith his wife Kate and their threeteenage children. Kate is a registerednurse, so she’s always on the alertfor health issues. When she waspregnant with their first child in 1994,she was worried about sudden infantdeath syndrome (SIDS) so she andSteve went to see a respiratoryspecialist. After speaking to thespecialist about SIDS, Kate added,“By the way, Steve’s got sleepapnea.”“This was news to me,” Steve says,recalling that day nearly 17 <strong>years</strong>ago. “I didn’t think that there wasa problem, but she said when Iwas sleeping I stopped breathingand she had to give me a nudge.“I felt, wow I’ve gotenergy now. I understoodwhy I needed treatment.Life was good again.”I had no idea. But I went to see asleep specialist and they said, ‘yes,you’ve got sleep apnea, you have20 episodes an hour.’ I rememberthinking, that’s every three minutes,which seemed like a lot. They putme on <strong>CPAP</strong> to see how it went. SoI got a Sullivan IV and the effectwas fairly dramatic. I felt, ‘Wow, I’vegot energy now’. It was really good. Iunderstood why I needed treatment.Life was good again.”They had no trouble with SIDS, norwith Steve’s treatment for OSA.“I’ve never had a problem using<strong>CPAP</strong>, ” Steve says. “Ok,” he adds,“the first time I tried it, it was a bitconfronting but I thought: yes—there’s a mask but let’s get over that,yes—there’s air flowing, but I couldput the machine on ramp so it wouldstart <strong>of</strong>f s<strong>of</strong>tly and gradually comeup to the required pressure. One <strong>of</strong>my sleep studies a few <strong>years</strong> agoshowed that I actually have borderlinenarcolepsy. I’ve always been ableto go to sleep very easily and nowI know why. So sleeping with themask has never been a problem.”Steve takes his <strong>CPAP</strong> with him whenhe travels, including an overseas tripin 2005. “No problems,” he says.When he was diagnosed withborderline narcolepsy Steve wasprescribed dexamphetamine.He notices that it adds anotherdimension to the treatment <strong>of</strong> hissleep apnea. “Before I started <strong>CPAP</strong>I’d be tired all the time,” he says. “OnceI started on <strong>CPAP</strong> I’d be fine, but if I hada big lunch I’d be falling asleep. Nowthat I’m having the dexamphetamine Ican take it after lunch and it takes thatedge <strong>of</strong>f the tiredness. So I needed thecombination—it’s not like one thing willfix you.” Another part <strong>of</strong> his treatmentwas a rhinoseptoplasty because hisseptum was crooked. His nose hadbeen broken when he was younger,blocking his left nostril. This meant hehad to work harder to breathe. Fixinghis septum didn’t affect his sleep apnea,but has let him breathe more easily ingeneral.Steve has noticed that a number <strong>of</strong>people he has worked with are also on<strong>CPAP</strong>, but he’s baffled by the peoplewho say they can’t stay on it. “Some> continued on page 2IN THIS ISSUE 30 Years Ago p5Both Sides <strong>of</strong> <strong>CPAP</strong> Therapy p8 Designing for Better Sleep p9
continued from page 1Using <strong>CPAP</strong> for the long haul: An interview with Steve CreightonRoad safety lawsand OSAAll drivers have a personal responsibility to ensure they are fit to drive.As road safety laws differ across countries, check with your country’sroad safety authority for respective laws related to driving with OSA.FROM THE EDITORCelebrating<strong>CPAP</strong> treatment“<strong>CPAP</strong> is somethingthat’s going to improveyour quality <strong>of</strong> lifeand it’s not just thetiredness, it’s the longtermeffects that sleepapnea has.”people say they have trouble stayingon the treatment. I can understand ifthey get claustrophobic, but if it’s justthat it feels uncomfortable then theyshould get through that. The first timeyou ever wore a hat it might have feltuncomfortable, but if you don’t weara hat and you go out in the sun youcould end up with skin cancer. <strong>CPAP</strong>is something that’s going to improveyour quality <strong>of</strong> life and it’s not just thetiredness, it’s the long-term effectsassociated with sleep apnea—thestress levels, the impact on the heartand the rest <strong>of</strong> the body. I’ve been onit now for 16–17 <strong>years</strong> and I’m glad. If Iwas just starting on it my health wouldhave been compromised by now.”Steve suggests a long-term approachto thinking about having OSA. “Thinkabout what sleep apnea can do to youif you’re not treated,” he says. “Youonly get one life so it’s up to you tosay, ‘Ok, if this is what I’ve got I’mgoing to look at all the options. Apartfrom <strong>CPAP</strong> what other options arethere? Is there a drug that’s an optionfor me? Surgery is invasive but isthere a possibility—removing adenoidsor tonsils, or fixing a broken nose?’Have a look at your diet and exercise.Obviously!”As Steve is a pr<strong>of</strong>essional driverhis use <strong>of</strong> <strong>CPAP</strong> is reportable—it’smarked on his drivers licence and hisgovernment authorization to drive abus. He has to see a specialist every12 months to check on his complianceand ensure treatment is working.Steve takes this responsibility veryseriously. “Even after a couple <strong>of</strong>days <strong>of</strong>f <strong>CPAP</strong> I feel the difference,”he explains. “If I’ve got a cold, I geta blocked nose, and I might pullthe mask <strong>of</strong>f during the night. But Iwouldn’t do that two nights in a row.I’ll go and get something for the coldso that when I get to bed I know I’llbe able to sleep.” He explains that hewouldn’t drive in those circumstances.“I’d know I wouldn’t be fit, wouldn’thave the judgment. Because <strong>of</strong> beinga pr<strong>of</strong>essional driver I’ve got to takeownership <strong>of</strong> it.”Recently Steve upgraded from theSullivan IV that he had been usingsince 1994. It was still workingeffectively, but Kate had heard abouta new generation <strong>of</strong> flow generators[<strong>ResMed</strong>’s new S9 <strong>CPAP</strong>]. AsSteve describes it, “Whereas the oldmachine was continuous air pressurethe newer one will start <strong>of</strong>f at a lowpressure, sense your breathing andthen only increase the pressure whenit registers that you’re having anapnea. It’s not continuous air pressure,it only gives you the pressure whenyou need it.” As a bonus, he’s als<strong>of</strong>inding that humidification with thenew machine is trouble-free.Kate is still helping Steve with hissleep apnea. She now works in a sleepunit and passes on the latest newson OSA and <strong>CPAP</strong>. Steve takes fulladvantage <strong>of</strong> this information. “If youdon’t keep up-to-date or have regularcheck-ups you don’t know what’shappening,” Steve says. “You mightfind out that what you’re doing is goodbut that something new is a lot better.That’s part <strong>of</strong> the treatment—makingsure you keep yourself informed.”AustraliaRoad safety laws in most parts <strong>of</strong>Australia require all drivers, whetherthey are driving a private car or acommercial vehicle, to report totheir Driver Licensing Authority anypermanent or long-term illness thatis likely to affect their ability to drivesafely. They may be required tohave their health assessed. Medicalconditions that affect a person’sdriving include sleep disorders,alcohol dependency, heart diseasesand respiratory disorders.See www.austroads.com.au formore information.EuropeA study <strong>of</strong> 25 European countriespublished in 2008 1 found that:“Excessive daytime sleepiness ismentioned in nine [driving licenceregulations], whereas sleep apnoeasyndrome is mentioned in 10countries. A patient with untreatedsleep apnoea is always consideredunfit to drive. To recover the drivingcapacity, seven countries rely ona physician’s medical certificatebased on symptom control andcompliance with therapy, whereas intwo countries it is up to the patientto decide (on their doctor’s advice) todrive again.”USARegulations about driving when youhave sleep apnea differ from stateto state in the USA. In some statesit is mandatory for doctors to reporta patient’s sleep apnea diagnosis.The Insurance Institute for HighwaySafety website states that if you have“a history <strong>of</strong> crashes or violations,or reports by physicians, police, orothers, state licensing agencies mayrequire renewal applicants to undergophysical or mental examinations orretake the standard licensing tests.” 2UKUK law requires drivers to tell theDriver and Vehicle Licensing Agency(DVLA) about any conditions suchas sleep apnea that may affect theirability to drive safely. Your ability todrive will be assessed. Generally, ifyou can prove that your treatmentfor your OSA is effective, you will beallowed to keep your licence.Beccy Mullins from <strong>ResMed</strong> UKrecently spoke on TalkSPORT Radioabout driving and sleep apnea.Go to www.realsleep.co.uk to hearher interview.CanadaThe Canadian Lung Associationreports that: “Doctors have a duty totell the motor vehicle board [<strong>of</strong> theirprovince or territory] about patientswho are not safe to drive. If youhave sleep apnea and you refusetreatment, your doctor is required toreport you. The motor vehicle boardcould suspend your license until youget your sleep apnea treated.” 3References:1. Alonderis A, Barbé F, Bonsignore M, Calverley P, DeBacker W, Diefenbach K, Donic V, Fanfulla F, Fietze I,Franklin K, Grote L, Hedner J, Jennum P, Krieger J, Levy P,McNicholas W, Montserrat J, Parati G, Pascu M, PenzelT, Riha R, Rodenstein D, Sanna A, Schulz R, Sforza E,Sliwinski P, Tomori Z, Tonnesen P, Varoneckas G, ZielinskiJ, Kostelidou K. Medico-legal implications <strong>of</strong> sleep apnoeasyndrome: driving license regulations in Europe. SleepMed. 2008;9(4):362-75.2. http://www.iihs.org/laws/olderdrivers.aspx3. http://www.lung.ca/diseases-maladies/apnea-apnee/drivers-camionneures/index_e.phpSteve Creightonhas been using<strong>CPAP</strong> (continuouspositive airwaypressure) fornearly 17 <strong>years</strong>.He is a veryexperienced andthoughtful <strong>CPAP</strong>user and he hassome advice forpeople who have just been diagnosedwith OSA (Obstructive Sleep Apnea):“Think about the long-term effects, whatsleep apnea can do to you if you’re nottreated. And realise that having OSAdoesn’t just affect you, it affects yourwhole family—your partner, your kids,how you react and interact with them,your whole quality <strong>of</strong> life. So, if you try<strong>CPAP</strong> and it’s a bit uncomfortable—yesit might be, but it’s going to be moreuncomfortable if you don’t persist andsee what sorts <strong>of</strong> benefits you might beable to get from it. I would say, hang inthere and even if you don’t like it, try it forat least a fortnight and within that timeyou should be able to see the benefits.”Steve is one <strong>of</strong> the thousands <strong>of</strong>people who have benefitted from <strong>CPAP</strong>treatment since it was invented in 1981.This edition <strong>of</strong> Snooze Newz celebrates30 <strong>years</strong> <strong>of</strong> <strong>CPAP</strong> with stories from theearliest days <strong>of</strong> its use through to howthe latest <strong>CPAP</strong> devices are designed.<strong>CPAP</strong> users and clinicians from all overthe world have shared their stories withus and we would like to thank all <strong>of</strong> themfor their generosity and good advice.If you’ve got a story to tell, let us know.Sleep well!Alison Hansford, Global Editor.2 Snooze Newz Snooze Newz 3
Nicholas Ward makes haywhile the sun shinesNicholas Ward is a company director in the UK. For many <strong>years</strong>before he was diagnosed, he suffered with what he now knows isobstructive sleep apnea (OSA).It was 30 <strong>years</strong> ago …This year, 2011, marks 30 <strong>years</strong> since the invention <strong>of</strong> continuous positive airway pressure(<strong>CPAP</strong>). Since then, <strong>CPAP</strong> devices have delivered a revolution in the treatment <strong>of</strong> sleep apnea.Research has kept pace and uncovered a raft <strong>of</strong> conditions associated with sleep apnea.Our understanding <strong>of</strong> sleep apnea, and how to treat it, has come a long way in 30 <strong>years</strong>.“It made a huge andrapid difference toboth our lives.”IF YOU’RE A <strong>CPAP</strong>USER IN THE UK, VISITwww.realsleep.co.ukTO SEE HOW THERESMED UK TEAMCAN HELP YOU WITHYOUR TREATMENT.It’s harvest time in England andNicholas Ward and his wife are helpingto make hay by hand while the haybaler lies quiet and motionless, inneed <strong>of</strong> repair. He’s just turned 70 andshe’s … younger. Twenty <strong>years</strong> ago, ifyou’d told Nicholas and his wife that hewould be baling hay in his 70th year,a successful, happy and healthy man,they would not have believed you.In the late 1980s, he wasn’t sleepingproperly and his wife was living anightmare. She’d lie awake in bedat night listening to him strugglingfor breath, then the silence as hisbreathing stopped, followed byexplosive gulps as he started breathingagain. It was a familiar and worryingcycle. At times, still asleep, Nicholaswould jump up to lean out thebedroom window gasping for air.In the early 1990s, she arrangedfor him to see a sleep consultant ina London hospital. The diagnosis?“You’re sleeping too much on yourback”! The consultant’s first step wasto recommend a tennis ball sewn intohis pyjamas, but this had no effect.“I was an irritable person,” admitsNicholas. “It affected my work, myrelationships with my colleagues,friends and family. I put on weight andit seemed to get worse.” Promptedby a newspaper article in 1994, hiswife organised an appointment withleading sleep specialist Pr<strong>of</strong>essor JohnStradling. By then, Nicholas says, “shewas absolutely desperate”.Nicholas still has the charts showing800 arousals on the night <strong>of</strong> the sleepstudy. He was given an “enormous andheavy crate” to trial, an early Sullivan<strong>CPAP</strong> machine. “It was noisy andleaked like mad,” he says, “but it madea huge and rapid difference to bothour lives.”He remembers ramp being a‘revolutionary’ new feature <strong>of</strong> theS6 he used in 2000. The S7 was amuch quieter machine, he recalls, buthis mask still leaked and rainout wasalways an issue.Nicholas has recently upgraded to anS9 Autoset and Mirage S<strong>of</strong>tGelmask and states that there is “nocomparison at all” with previousmodels. “They’re so improved, sodifferent,” he exclaims, “I get a muchbetter night’s sleep.” His wife’s life hasalso improved. “My wife finds it super,she’s very pleased with it. She can’tbelieve how quiet it is,” he says. “Shedoes notice the odd leak now,” heconfesses, “because they’reso unusual.”As a company chairman he travelsfrequently. The bulk and weight <strong>of</strong> early<strong>CPAP</strong> machines made flying difficultand everyone would ask what he wascarrying. “No one worries about my<strong>CPAP</strong> now. It’s so small and so manypeople carry laptops on planes.”Nicholas was once ashamed <strong>of</strong> talkingabout his sleep apnea. Now he speaks<strong>of</strong> it freely and shows his S9 to friends.He’s even recommended <strong>CPAP</strong> to afew people.So at the age <strong>of</strong> 70, fit and healthyNicholas and his slightly youngerwife enjoy <strong>ResMed</strong>’s evolutionary,intuitive and whisper quiet S9 Autoseteach night. Their happiness would becomplete if the hay baler wasn’t asquiet as the S9!The fat boy, Joe, in The PickwickPapers is Charles Dickens’ mostpopular creation among sleepresearchers. He falls asleep at everyopportunity. In this extract, Joe evensleeps through a battle that is beingre-enacted for the entertainment <strong>of</strong>the local gentry.Then there was such a rammingdown <strong>of</strong> the contents <strong>of</strong> enormousguns on the battery, with instrumentslike magnified mops; such apreparation before they were let <strong>of</strong>f,and such an awful noise when theydid go, that the air resounded withthe screams <strong>of</strong> ladies … Everybodywas excited, except the fat boy, andhe slept as soundly as if the roaring<strong>of</strong> cannon were his ordinary lullaby.‘Joe, Joe!’ said the stout gentleman,when the citadel was taken, and thebesiegers and besieged sat down fordinner. ‘Damn that boy, he’s gone tosleep again. Be good enough to pinchhim, sir—in the leg, if you please;nothing else wakes him—thank you.Undo the hamper, Joe.’ The fat boy,who had been effectually roused bythe compression <strong>of</strong> a portion <strong>of</strong> hisleg between the finger and thumb<strong>of</strong> Mr Winkle, rolled <strong>of</strong>f the box onceagain, and proceeded to unpack thehamper. [pages 101-102]In Joe, Dickens described thesymptoms <strong>of</strong> a person with possibleobstructive sleep apnea (OSA)decades before scientists did. ThePickwick Papers was written in1836–1837. A detailed scientificdescription <strong>of</strong> OSA came 40 <strong>years</strong>later from a London physician, WHBroadbent, in 1877.Snoring and other disturbances duringsleep have been with us forever, andthey have been noted since ancienttimes. The Ptolemy dynasty in Egyptis said to have had a genetic tendencyto obesity and sleep disorders. Ithas been suggested that NapoleonBonaparte, Queen Victoria and bothTheodore and Franklin D Roosevelt,U.S.A presidents, had OSA. But it wasnot until the 1950s that the cyclesand body movements <strong>of</strong> sleep couldeven be recorded, and 1981 beforecontinuous positive airway pressure(<strong>CPAP</strong>) treatment was developed.Sleep apneas and sleep clinicsIn 1965 the first polysomnographrecorded apneas during sleep. In 1970the first sleep clinic was establishedat Stanford University, California,U.S.A, by William Dement. In 1972Christian Guilleminault joined theclinic, concentrating on respiratorydisorders during sleep.The following five-year period,1975–80, was an intense time <strong>of</strong>research into sleep and apneas with319 articles appearing in the medicalliterature. In 1978 medical researcherslocated the source <strong>of</strong> the obstructionduring OSA, proving that the airwaywas closing at the oropharynx,not further down in the larynx aspreviously believed. 1Dogs with masksIn Toronto, Canada, Eliot Phillipsonhad started investigating respiratorycontrol in dogs in 1970. He was joinedin 1976 by Colin Sullivan on a postdoctoralresearch fellowship fromthe University <strong>of</strong> Sydney, Australia. In1979 Sullivan returned to Sydney anddevised a mask that would fit over adog’s snout to deliver air or a gas.> continued on page 64 Snooze NewzSnooze Newz 5
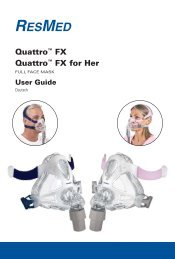
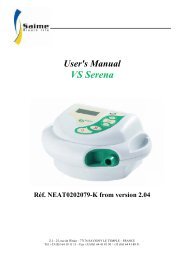
Designing for better sleep:an interview with Mark Bertinetti> continued from page 7My wonderful career: an interview with Bron LehrhaftEach <strong>CPAP</strong> therapy device that <strong>ResMed</strong> makes is a completely new design,from the motor to the latches. What goes into making a new device?Both sides <strong>of</strong><strong>CPAP</strong> therapyBron knows <strong>CPAP</strong> therapy from bothsides now. She started using it herself afew <strong>years</strong> ago and it has given her someunique insights into the treatment.“We see people at our clinic who arenot using their <strong>CPAP</strong> device properly sothey think it doesn’t work and it’s notimproving their condition. They mighthave a Ramp feature they can use toincrease the pressure until they drop<strong>of</strong>f to sleep, but they don’t know that.If the pressure starts <strong>of</strong>f too high you’llstruggle against it, and every time youswallow you take in a gulp <strong>of</strong> air, whichinflates your stomach, making you veryuncomfortable by the morning. So youwon’t keep the machine on all night. TheRamp feature lets you fall asleep beforethe pressure starts moving up.”“I still think that <strong>ResMed</strong> masks are, ifnot the best in the world, then they’reamong the best in the world. You haveto wear them firmly on your face, butif you do that they seem to suit thegreatest number <strong>of</strong> faces. I’m not paidto say this—it’s what I’ve experienced.I’ve tried every mask myself for at leasta week.”“<strong>ResMed</strong>’s latest, the S9, fulfils justabout every promise it makes. I use onemyself and it’s an outstanding device,a totally new concept. The ClimateControl on the tubing, the pressuredelivery, all the other features. Thiswinter was the first time since starting<strong>CPAP</strong> therapy that I haven’t had to putthe sheet over my face to keep thetubing and mask warm.”… and the patientsHer system was successful. In1986–88 she did a two-year study <strong>of</strong>the patients who had been throughthe sleep unit and found that 89%were still using <strong>CPAP</strong> therapy. “Therewere some people who’d fallen by thewayside and never returned, or wholived too far away and didn’t comeback, but the ones that came backwere still using <strong>CPAP</strong>” she says.“And it had made an enormousdifference in their lives. Absolutelyamazing differences.”“I still get excitedconducting a sleepstudy, watching theREM marching acrossthe page then watchingthe obstructions andknowing that I’mholding in my handssomething that willmake them better.”The improvements that she observedincluded: less depression and moremotivation; blood gas improvements;stabilization <strong>of</strong> pulmonary arterypressure; sleeping through the night;and reduction in skin problems. One <strong>of</strong>her observations about the diabetics inher care led to a study into the effect <strong>of</strong><strong>CPAP</strong> on diabetes. The outcome <strong>of</strong> thatstudy, Bron tells us, was that “<strong>CPAP</strong>will actually improve type 2 diabetesand improve the glucose levels in theblood, and obviously insulin levels aswell.”Bron Lehrhaft is still working inthe field <strong>of</strong> sleep, and is a NurseConsultant, Senior Technologist in aprivate clinic. Her face lights up asshe describes her work. “I still getexcited conducting a sleep study,watching the REM marching across thepage then watching the obstructionsand knowing that I’m holding in myhands something that will make thembetter. I’m the longest serving sleeptechnologist in Australia—I don’t knowif it’s in the world, but certainly inAustralia. Since 1984 to now. And it hasbeen just wonderful.”The first flow generators were bignoisy boxes with pool tubing attachedto handmade masks that were gluedon to each person’s face every night.They blew air at a constant pressure allnight, you needed a bank <strong>of</strong> monitors,and adjustments required an intimateunderstanding <strong>of</strong> the workings <strong>of</strong>a complex set <strong>of</strong> machines. <strong>Thirty</strong><strong>years</strong> <strong>of</strong> design work have reducedthese machines to tiny sleek devicesthat are almost silent and can delivercomfortable, individual treatment. Theycan tell you how many hours you werebeing treated, provide humidificationwithout condensation, and attach to arange <strong>of</strong> well-fitting masks.Each new <strong>CPAP</strong> therapy devicehas been designed by a team <strong>of</strong>engineers, <strong>of</strong>ten dedicated to solvinga particular problem. For <strong>ResMed</strong>’sS7, the challenge was to integratehumidification; for the S8 it was toreduce the size <strong>of</strong> the machine andmake it more portable. The aim forthe S9 was to make it easier to use,improve humidification and removerainout in the tube, and to be lessobtrusive in the bedroom.Translating the feedbackMark Bertinetti is the current SeniorIndustrial Designer for Sleep ProductDevelopment at <strong>ResMed</strong>. He hasworked at <strong>ResMed</strong> for almost 10 <strong>years</strong>on a range <strong>of</strong> <strong>CPAP</strong> therapy devicesand accessories. He describes his jobas being a ‘translator’.“I work with the marketing teamto gather information from <strong>CPAP</strong>users, sleep technicians, physicians,distributors and <strong>ResMed</strong> staff allaround the world,” Mark tells us. “It’sgreat to speak with patients directly.They tell me what would improvethe treatment for them, and whatfeedback they would like. I hear abouttheir basic daily routine—whetherthey wash their masks every day,whether they pull <strong>of</strong>f the tube, howthey store things, what settings theyuse. Then I feed this information backto the electrical, s<strong>of</strong>tware, mechanicaland system engineers. I have studieddesign, marketing, human factors,ergonomics, web design, materials anda range <strong>of</strong> manufacturing processes soI understand a little bit <strong>of</strong> everything.This lets me translate what I hear fromthe users into useful information for theengineers, and vice versa.”Mark studied industrial design atthe University <strong>of</strong> New South Wales,Sydney, and worked for a designcompany for a number <strong>of</strong> <strong>years</strong> beforemoving to <strong>ResMed</strong>. He says that twomain things attracted him to this job. “Ireally wanted to be part <strong>of</strong> a companywhere you get to interact with allthe major aspects <strong>of</strong> the design,” heexplains. “The other thing about thisjob is that it’s very fulfilling to knowthat your work is making a difference topeople’s lives.”Satisfying everyoneFor Mark, a <strong>CPAP</strong> therapy devicehas to satisfy a wide range <strong>of</strong> needs.He wants it to be a positive userexperience for all the different peoplethat touch it during its lifecycle. Thisincludes the people assembling it onthe assembly line, the physician orsleep technician using it to titrate in asleep lab, the dealer setting it up for apatient, and finally the patient and theirpartner’s experience with it in theirbedroom.As well as being easy to use,aesthetically pleasing and able to be> continued on page 10“It’s very fulfillingto know that yourwork is makinga difference topeople’s lives.”8 Snooze Newz Snooze Newz 9
Staying alive> continued from page 9Designing for better sleep: an interview with Mark BertinettiJody Chaitovitz is a retired judge, living in Columbia, Maryland(USA) with her husband Marty and their cat, Moee. It was a pleasureto interview Jody – a woman who is passionate, energetic andenthusiastic while coping with a very painful disability.“As technologychanges we’reconstantly able toinnovate and fixproblems that wecouldn’t fix before.”produced cost-effectively, each new<strong>CPAP</strong> therapy device has to meetstringent electrical, s<strong>of</strong>tware, andmechanical requirements. Mark thenhas to consider how it is manufactured,shipped, packaged, distributed andstored around the world. It has to meetbusiness needs, including environmentalresponsibilities. Mark describes the level<strong>of</strong> detail he went into with the latestmodel, the S9, to minimise its impactwherever possible. He thought aboutevery aspect, from the number <strong>of</strong> palletsthat are needed to carry it around theworld, to the number <strong>of</strong> wires going intothe motor.“We optimised the size <strong>of</strong> the S9 t<strong>of</strong>it more onto each pallet in a shippingcontainer, so we can ship 75% moreunits in a 40 foot container than with anS8. Now we’re not shipping air aroundthe world—we’re just shipping what weneed to ship. We use the bag to holdeverything in place during shipping, sothat minimises packaging.” Mark andhis team have thought about the wholelifecycle <strong>of</strong> the product. “Becausethe blower is so much quieter we canuse less foam than we used to. All <strong>of</strong>the materials that are used are ROHS(Removal <strong>of</strong> hazardous substances)compliant. This ensures that ourmaterials don’t have harmful substanceslike lead, so when you dispose <strong>of</strong> itand it breaks down it doesn’t releasehazardous substances. The s<strong>of</strong>tware andelectronics—everything is minimised.There’s less wiring—for example, weused to have seven or eight wiresgoing into the motor but now we onlyhave three because the sensing isdone externally.”Changes and challengesSome changes are made because peopleask for them, but others only becomepossible when the technology develops.Mark and his team are always lookinginto new technologies and this has ledto significant improvements in <strong>CPAP</strong>design and comfort. “For example,” Marksays, “the new ClimateLine heatedair tube delivers optimal temperatureand humidification all the way to themask while virtually eliminating rainout.This was only possible thanks to someincredible engineering and a new processthat enables us to wind wires into thetubing’s helix and capture tiny sensorsin the cuff. Prior to these technologies itwasn’t possible to cost-effectively makean automatically controlled heated tube.As technology changes we’re constantlyable to innovate and fix problems that wecouldn’t fix before.”Change has also occurred in the group <strong>of</strong>people who are treated by <strong>CPAP</strong> therapydevices. The wide range <strong>of</strong> devices cannow treat many more conditions, frombasic OSA through to Cheyne-StokesRespiration and respiratory failure.Added to this is a broad population <strong>of</strong>well-informed people seeking out <strong>CPAP</strong>treatment. “There’s been a definite shifttowards treating much younger users.Medical practitioners and the publichave become more aware <strong>of</strong> the effects<strong>of</strong> sleep-disordered breathing. Youthobesity is increasing, lifestyle stressesare increasing and diagnosis methods areimproving. The older, larger users haven’tgone away, but a lot more younger,socially active, working people are using<strong>CPAP</strong>. It’s been recognised that womenhave different symptoms <strong>of</strong> OSA, sothere’s a higher proportion <strong>of</strong> femalesthan ever before. As we treat people withdifferent needs, the design will evolveto accommodate a greater range <strong>of</strong>lifestyles, medical conditions, aspirations,gender differences and social pressures.”This is a challenge that Mark Bertinettiwelcomes.Jody has been married to Marty for two<strong>years</strong> now, but she insists that “withoutmy <strong>ResMed</strong> VPAP [variable positiveairway pressure device], the weddingwould never have happened.” Hercentral sleep apnea was so bad thatshe could not stay awake during theday. “I was afraid to drive because Iwould fall asleep at the wheel, and anytime we went to the movies, I wouldsleep through the film. The night thatDr. Schwartz and Chris Kane tested meon the VPAP, I slept through the nightlike a baby. When I woke up, I felt asif the world had been washed clean.I called Marty and told him that I wascoming over to pick him up. ‘Yeah,right,’ he said. And when I showed up,was he ever surprised! Things wentfrom good to better, and we married onDecember 27, 2009!”“Without my <strong>ResMed</strong>VPAP the weddingwould never havehappened.”“When I woke up, Ifelt as if the world hadbeen washed clean.”Her physician, Dr. Alan Schwartz,Director <strong>of</strong> the Sleep Center at JohnsHopkins, diagnosed her central sleepapnea (CSA) and Jody worked withhim to treat it. “CSA is a form <strong>of</strong> sleepapnea where”, as she cleverly puts it,“my brain sometimes forgets to tellmy lungs to breathe.” She became thefirst patient within the Johns Hopkinssystem <strong>of</strong> hospitals in Baltimore(USA) on Adaptive Servo Ventilation(ASV) therapy, using a VPAP device.ASV therapy continuously monitors andanalyzes a person’s breathing pattern,then provides the variable positiveairway pressure support that theyneed. It was created specifically for thetreatment <strong>of</strong> CSA in all its forms.Jody had some challenges adjustingto therapy and getting a proper seal onher mask, but worked with <strong>ResMed</strong>’sChris Kane to resolve the issues. Shehasn’t looked back since. Now, Jodysays she “owes her life back to her ASVand <strong>ResMed</strong>”. Since starting therapy,Jody has noticed a drastic improvementin her quality <strong>of</strong> life and has evenlost 120 pounds (54 kilograms). Shesays it’s not unusual for her to sleep9–10 hours each night, “with dreams inliving color” as she puts it.Jody’s perseverance was helped by hervery good understanding <strong>of</strong> medicalconditions. As an AdministrativeLaw Judge for the US Dept <strong>of</strong> Labor,rising to Deputy Chief AdministrativeLaw Judge for the New England area,she heard Black Lung, Long Shore,Whistleblower and Mine Safety cases,among others. Her career was cut shortonly when she became disabled bythe autoimmune disease, PolyarteritisNodosa. She describes this as “adisease which attacks the arteriesby shutting them down. Whicheverorgan system or nerves were servedby these arteries, including my lungs,were <strong>of</strong>ten disabled.” It also affectedthe nerves <strong>of</strong> her legs, which madewalking both difficult and painful.She tells how her rheumatologist,Dr. David Hellmann, Chairman <strong>of</strong> theDepartment <strong>of</strong> Medicine at HopkinsBayview, told her <strong>of</strong> his old mentor,“who described Polyarteritis Nodosa as‘a hurtin’ disease’, a description moreapt than I would care to take someone’sword for!”Jody is still using her original VPAPmachine.* “On the few occasions I fallasleep without it, I wake up with severeheadaches and nausea, and have terriblenightmares,” she says. “I still love it asmuch as ever, and to tell you the truth,I don’t know if I’d still be alive today if Ididn’t have it.”It’s not just the VPAP that keeps Jodyalive—her cat Moee has played a vitalrole as well. She describes Moee—aseven and a half year old, almost 20pound (over nine kilograms) Maine Cooncat—as her ‘assistance’, or ‘service’,cat. Jody had been worried about whatcould happen if she fell asleep whenshe wasn’t using her VPAP and theCSA caused a failure to breathe thatlasted too long. “But on two occasions,”Jody tells us, “when I fell asleep at thecomputer, I felt a tap, tap, tap on my leg,both times waking me up fairly quickly.Another two times, having fallen asleepreading, he jumped up on the table, andhead-butted me awake! This is not just‘cute’. This was brought home to mewhen I saw an obituary <strong>of</strong> a 37-year oldman who died <strong>of</strong> sleep apnea, leavinghis wife and four children. Dr. Schwartzshows that obituary to his patients asit’s not about someone ‘rich and famous’but an ordinary man who was everythingto his wife and children. He told me,‘Now maybe they will listen!’”* Jody is currently using <strong>ResMed</strong>’s VPAP Adapt SV TM ,available in the USA and Japan, and will be soonmoving to an S9 VPAP TM Adapt.10 Snooze NewzSnooze Newz 11
<strong>ResMed</strong> products receiveaward accolades<strong>ResMed</strong> staff members walked away happy fromthe 2011 Australian International Design Awards. Inthe Medical and Scientific category, the S9 Series<strong>of</strong> flow generators and the Mirage FX nasal maskboth won a Design Award, with the S9 Series named“Best in Category”. The Quattro FX Full Face Maskalso starred, being commended for “Good Design”.The Design Award recognises superior innovation,while the Good Design category signifies good levels<strong>of</strong> form, function, quality, safety and sustainability.<strong>ResMed</strong>’s Worldwide Offices:The right kind <strong>of</strong> support canmake all the difference to <strong>CPAP</strong>treatment. Whether you arenew to treatment or have beena user for many <strong>years</strong>, there aretimes when you need expertadvice and encouragement.Join <strong>ResMed</strong>’s freesleepVantage or Realsleep*programs to get the mostbenefit from your treatment atall times, with a free customersupport telephone line toanswer your questions about<strong>CPAP</strong>. As a sleepVantage orRealsleep member you won’tever have to feel alone withyour treatment.Go towww.sleepvantage.com.auor www.realsleep.co.uk andjoin today, or contact your local<strong>ResMed</strong> <strong>of</strong>fice.* Currently sleepVantage is only availablein Australia and Realsleep in the UK.Global OfficesUnited States<strong>ResMed</strong> Corp.San Diego CA USATel: +1 858 836 5000or 1800 424 0737Fax: +1 858 836 5001reception@resmed.comAustralia<strong>ResMed</strong> LtdBella Vista NSWTel: +61 2 8884 1000or 1800 658 189Fax: +61 2 8883 3114reception@resmed.com.auBelgiumTel: + 3215 305 673ChinaTel: +86-10-68492133EgyptTel: +20 3 546 8825FinlandTel: +358 0 9 8676 820FranceTel: +33 4 26 100 200GermanyTel: +49 0 89/99 01-00GreeceTel: + 30 210 876 4817AN IMPORTANT NOTE TO YOU, THE READERSnooze Newz publicationis the subject <strong>of</strong> copyrightowned by <strong>ResMed</strong> Ltd, allrights reserved.Requests for permission toreproduce contributions fromSnooze Newz should beaddressed in writing to theeditor:theeditor@resmed.com.auSnooze Newz is atrademark and servicemark<strong>of</strong> <strong>ResMed</strong> Ltd.Hong KongTel: +852 2366 0707IndiaTel: +91 11 2645 3592ItalyTel: +39 0331 931 707JapanTel: +81 3 5840 6781NetherlandsTel: +31 348 411 164New ZealandTel: +0800 737 633NorwayTel: +47 67 11 88 50PortugalTel: +351 210 865 760SingaporeTel: +65 6284 7177South AfricaTel: +2711 793 2356SpainTel: +34 916 393 579SwedenTel: +46 520 420 110SwitzerlandTel: +41 61 564 70 00United KingdomTel: +44 1235 862 997Snooze Newz is intended to serve as a forum for topics <strong>of</strong> interest to people with SDB andtheir families. Contributions by the editor and authors may contain information or opinionsthat have not been verified for accuracy or completeness by their authors or the editor.You should make your own independent inquiries before relying on Snooze Newzcontributions and accordingly neither the <strong>ResMed</strong> Group <strong>of</strong> companies nor the editor<strong>of</strong>fer to, nor will accept liability for, the consequences <strong>of</strong> any reliance you may placeon Snooze Newz contributions. Opinions by authors in Snooze Newz contributions arenot intended to be the opinions <strong>of</strong>, nor are they endorsed by, the <strong>ResMed</strong> Group <strong>of</strong>companies or the editor.While the editor has striven to make correct attributions <strong>of</strong> authorship and toacknowledge ownership <strong>of</strong> copyright any omission or error is unintentional and theeditor invites the notice <strong>of</strong> any suspected omission or error.Sullivan IV, S9, AutoSet, S7, S8, VPAP, Mirage FX, Mirage Quattro, Mirage S<strong>of</strong>tGel,VPAP Adapt SV are trademarks <strong>of</strong> <strong>ResMed</strong> Ltd © 2011 <strong>ResMed</strong> Ltd. 1015038 2011-1112 Snooze NewzGlobal leaders in sleep and respiratory medicine www.resmed.com