MDCT in Acute Pancreatitis Nordic Forum ... - radiographia.ru
MDCT in Acute Pancreatitis Nordic Forum ... - radiographia.ru
MDCT in Acute Pancreatitis Nordic Forum ... - radiographia.ru
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
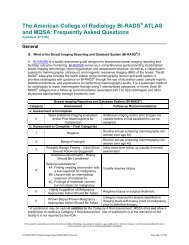
<strong>Nordic</strong> <strong>Fo<strong>ru</strong>m</strong> - Trauma & Emergency Radiology<strong>MDCT</strong> <strong>in</strong> <strong>Acute</strong> <strong>Pancreatitis</strong>Bo<strong>ru</strong>t Mar<strong>in</strong>cekInstitute of Diagnostic RadiologyUniversity Hospital Zurich, Switzerland<strong>Acute</strong> <strong>Pancreatitis</strong> (AP)EtiologiesMechanical (choledocho-/microlithiasis, ampullary/periampullary obst<strong>ru</strong>ction, anatomic variant, trauma),toxic-metabolic (alcohol, hyperlipidemia, hypercalcemia),vascular, <strong>in</strong>fectious (vi<strong>ru</strong>ses, bacteria, fungi, parasites),d<strong>ru</strong>g relatedMost common: gallstone disease & alcohol abuse (~70%)ClassificationThe 1992 Atlanta, Ga, International Symposium• based on cl<strong>in</strong>ical and morphological criteria• mild and severe AP (Bradley, Arch Surg 1993)
AP: Mild Form70-80% of all patientsMorphologyInterstitial edema, micronecrosisCl<strong>in</strong>ical courseResponds to supportive therapy, improve <strong>in</strong> 48-72 hrsNo organ failureImag<strong>in</strong>gNONEUS to evaluate gallstones & dilatation of CBDAP: Severe Form20-30% of all patientsMorphologyLarge confluent necrosis, hemorrhageCl<strong>in</strong>ical courseRequires <strong>in</strong>tensive monitor<strong>in</strong>g & specific therapiesAssociated with local (pseudocyst, abscess, <strong>in</strong>fectednecrosis) & extrapancreatic complicationsOrgan failure (renal and pulmonary most common)Pulmonary or pleural alterations: sens/spec60/88% for presence of necrosis73/75% for presence of <strong>in</strong>fected necrosis90/76% for mortality rate (Pezzilli, Hepatogastroenterology 1998)
AP: Imag<strong>in</strong>g EvaluationContrast-enhanced CT = imag<strong>in</strong>g modality of choiceMild AP:• Interstitial edema slight pancreas enlargement• Intrapancreatic fatty tissue necrosis heterogeneity of pancreatic parenchyma• Exudates, slight peripancreatic fatty tissuenecrosis or hemorrhage <strong>in</strong> various comb<strong>in</strong>ations blurred organ contours; peripancreatic fluidcollections, thickened fasciaMild AP• Peripancreatic fluid collection: enzyme rich pancreaticjuice• Lacks wall, occurs with<strong>in</strong> 48 hrs <strong>in</strong> 30-50%• Resolves spontaneously 50%
Mild APEtiology: hyperlipidemiaSlight pancreas enlargementPeripancreatic fluidcollection, thickened fasciaMild APCl<strong>in</strong>ical question: <strong>ru</strong>ptured AAA? History: 5 days afterlaparoscopic cholecystectomy ( gallstone caus<strong>in</strong>g APlikely)
Mild APERCP April 20, laparoscopic cholecystectomy April 26for gallstones and acute cholecyszitisApril 23 April 28AP: Indications for CTCT evaluation of patients with• Cl<strong>in</strong>ical diagnosis <strong>in</strong> doubt• Failure to improve with<strong>in</strong> 72 hrs of <strong>in</strong>itialconservative medical treatment• Cl<strong>in</strong>ical deterioration, early recognition of seriouscomplications• Guidel<strong>in</strong>es for assessment by CT:UK Work<strong>in</strong>g Party on AP (Gut 2005;54:1-9)JPN Guidel<strong>in</strong>es (J Hepatobiliary Pancreat Surg 2006;13:33-41)
AP: Imag<strong>in</strong>g EvaluationSevere AP:• Extensive peripancreatic fatty tissue necrosis,exudations, slight hemorrhage extensiveperipancreatic fluid collections• Parenchymal necrosis enhancement 30% of pancreas or >3 cm <strong>in</strong> diameter(Bradley, Arch Surg 1993)Severe APPotential pitfall oncontrast-enhanced CT:necrosis may not beapparent up to 48 hrsafter onset pancreatic necrosis more likely pancreaticduct dis<strong>ru</strong>pted8 dayslater
Severe APDec 3: endoscopy & biopsyof papilla Vateri ( biliaryobst<strong>ru</strong>ction?), no malignancyDec 4CT shortcom<strong>in</strong>g: <strong>in</strong>ability todifferentiate fluid collection -extrapancreatic fatty tissuenecrosisDec 17Severe APExtension of pancreatitisfluid collections:compression butpreservation of fat <strong>in</strong>posterior pararenal space
Severe APHistory of alcohol abuseSevere APDec 24Jan 1Heterogeneous enhancement& nonenhanc<strong>in</strong>gnecrotic areas of pancreas
Severe APStag<strong>in</strong>g AP: CT Severity Index (CTSI)• CTSI (10-po<strong>in</strong>t severity scale) based on degree ofpancreatic <strong>in</strong>flammation and necrosis (Balthazar, Radiology1990; Balthazar, Radiology 1994)• CTSI correlates with morbidity and mortality, but notwith development of organ failure or peripancreaticcomplications• Modified CTSI (by simplify<strong>in</strong>g scor<strong>in</strong>g for<strong>in</strong>flammation and necrosis, add<strong>in</strong>g weight factor forextrapancreatic complications, us<strong>in</strong>g <strong>MDCT</strong>)correlates more closely with patient outcomemeasures, with similar <strong>in</strong>terobserver variability(Mortele, AJR 2004)
Stag<strong>in</strong>g AP: Modified CTSI1. Image analysis:2. Outcome parameters: length of hospital stay, need forsurgical or percutaneous procedures, occurence of<strong>in</strong>fection, development of organ failure (Mortele, AJR 2004)CT Assessment of Severity of AP• Accuracy of CTSI for predict<strong>in</strong>g pancreatitis severitysignificantly higher than APACHE II (<strong>Acute</strong>Physiology and Chronic Health Evaluation,monitor<strong>in</strong>g system based on 12 physiologicmeasurements) and C-reactive prote<strong>in</strong> (Gurleyik, Pancreas2005)• Reliable method, widely available; patients with CTSI
MRI <strong>in</strong> APMRI as efficient as CT <strong>in</strong> recogniz<strong>in</strong>g necrosis andpredict<strong>in</strong>g severity (Arvanitakis, Gastroenterology 2004)Sensitivity of MRI may surpass CT (m<strong>in</strong>orperipancreatic <strong>in</strong>flammation) on T2w images(Pamuklar, Magn Reson Cl<strong>in</strong> NA 2005)Advantages MRI:- less nephrotoxicity of contrast medium (potentialfor extension of necrosis and exacerbation of renalimpairment after iv iod<strong>in</strong>e contrast media?)- allows evaluation of pancreatic duct & biliarysystem us<strong>in</strong>g MRCPMRI <strong>in</strong> APKnown biliary stonesM<strong>in</strong>or peripancreatic<strong>in</strong>flammation
AP: Complications1. Pseudocyst2. Abscess3. Infected necrosis4. Extrapancreatic: spontaneous fistulization, gastricoutlet obst<strong>ru</strong>ction, <strong>in</strong>test<strong>in</strong>al necrosis, bleed<strong>in</strong>gpseudoaneurysm, splenic ve<strong>in</strong> thrombosisPseudocyst• Collection of pancreatic fluid conta<strong>in</strong>ed by granulationtissue CT: well circumscribed, th<strong>in</strong> walled, lowattenuation collection• Develops as a consequence of AP <strong>in</strong> patients withperipancreatic fluid collections, pancreatic necrosis, orchronic pancreatitis• Requires usually >4 weeks from onset of acuteepisode(Baert, 1995)
Pseudocyst• Adjacent to, occasionally with<strong>in</strong> the pancreas• Resolves spontaneously with<strong>in</strong> 6 weeks 40%,80% if
Pseudocysts and MalignancyNon-Hodgk<strong>in</strong>-LymphomaAmylase and lipase AP secondary to tumorcompression of pancreatic ductor direct tumor <strong>in</strong>filtrationPancreatic Duct Injury: Posttraumatic Pseudocyst14 yo, f: epigastric pa<strong>in</strong>2 days after fall dur<strong>in</strong>g trampol<strong>in</strong>e jump<strong>in</strong>gJan 25Feb 13Feb 16
The cystic lesion shown is a .... (37 yo, f)Intermittent attacks of colicky epigastric pa<strong>in</strong>US diagnosis: large cystic lesion <strong>in</strong> the liver hilus Pancreatic Pseudocyst ?
Choledochal Cyst Type 1Choledochal Cysts: Todani-ClassificationType 1ACystic dilatation(80-90%)Type 1BFocal segmentaldilatationType 1CFusiform dilatationType 2DiverticulumType 3Choledochocele(rarest type)Type 4AIntra-and extrahepaticsegmentalcystic dilatationsType 4BExtrahepaticsegmental cysticdilatationsType 5Intrahepatic segmentalcystic dilatations(Caroli‘s disease)
Pancreatic Pseudocyst - Interventions• Criteria:- symptomatic cyst with pa<strong>in</strong>, <strong>in</strong>fection, or compressionof adjacent organs- diameter >6 cm• Techniques:- endoscopic (transgastric or transduodenal)- percutaneous- surgicalPseudocyst: Transgastric Dra<strong>in</strong>ageJan 18 Feb 9
AbscessEncapsulated collection of pus, usually <strong>in</strong> proximity to butoutside of pancreas; <strong>in</strong> 3% of patients with peripancreaticfluid collectionsCT: wall thicker ormore irregular thanwall of pseudocystAbscess: CT-guided Dra<strong>in</strong>ageMortality risk for <strong>in</strong>fected necrosis = double that forpancreatic abscess (Freeny, AJR 1998)
Infected Pancreatic Necrosis• Most serious local complication of AP• 30-70% of patients with pancreatic necrosis• 2nd – 3rd week follow<strong>in</strong>g onset of severe AP• Typically polymicrobial, E. coli <strong>in</strong> about 35% sourceof contam<strong>in</strong>ation = particularly colon translocationof bacteria directly through <strong>in</strong>test<strong>in</strong>al wall• Detection of gas bubbles <strong>in</strong> necrotic tissue <strong>in</strong>dicativeof <strong>in</strong>fective necrosis (extralum<strong>in</strong>al retroperitoneal gascaused by <strong>in</strong>test<strong>in</strong>al fistula very rare)• Surgical strategy: necrosectomyMore recently: percutaneous CT-guided catheterdra<strong>in</strong>age (Freeny, AJR 1998) or laparoscopic-assistedpercutaneous dra<strong>in</strong>age (Horvath, Surg Endosc 2001; Haan, Am Surg2006)Pseudocyst & Infected NecrosisCBD-obst<strong>ru</strong>ct<strong>in</strong>g pseudocyst pancreatic head stentInfected pancreatic & peripancreatic necrosisMay 7 May 31
Infected Necrosis Pancreatic HeadInfected Necrosis: CT-Guided Dra<strong>in</strong>ageJan 12 Jan 19
AP: Extrapancreatic ComplicationSpontaneous fistulization, oral contrast agentAP: Extrapancreatic ComplicationPseudoaneurysm of gastroduodenal/gastroepiploic artery(after <strong>ru</strong>pture <strong>in</strong>to preexist<strong>in</strong>g pseudocyst or digestion ofarterial wall by enzymes)
AP: Extrapancreatic ComplicationNon-occlusive mesenteric ischemia (NOMI) and associated<strong>in</strong>test<strong>in</strong>al gangrenePrevalence / mortality (N=120):NOMI 6.7% / 63%NOMI-associated<strong>in</strong>test<strong>in</strong>al gangrene 4.2% / 100%(Hirota, Pancreatology 2003)AP: Extrapancreatic ComplicationSplenic ve<strong>in</strong> thrombosis <strong>in</strong> 1-3% follow<strong>in</strong>g pancreatitisSVCVSVPseudocyst & stenosis splenic ve<strong>in</strong> (SV) collaterals via coronary ve<strong>in</strong> (CV, hepatopetal flow),gastric fundal varices left-sided portal hypertension
<strong>MDCT</strong> <strong>in</strong> AP: Conclusions• Contrast-enhanced CT: primary imag<strong>in</strong>g modalityfor assess<strong>in</strong>g the severity of AP and for follow-up• <strong>MDCT</strong> has changed the traditional Balthazar score<strong>in</strong> assess<strong>in</strong>g the severity of AP• MRI is the best alternative <strong>in</strong> patients withcontra<strong>in</strong>dications for CT• Optimal time for performance of a CT exam<strong>in</strong>ationto assess the early phase of AP is not yet def<strong>in</strong>ed