HIV and AIDS response program, Mongolia - Australian Red Cross
HIV and AIDS response program, Mongolia - Australian Red Cross
HIV and AIDS response program, Mongolia - Australian Red Cross
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
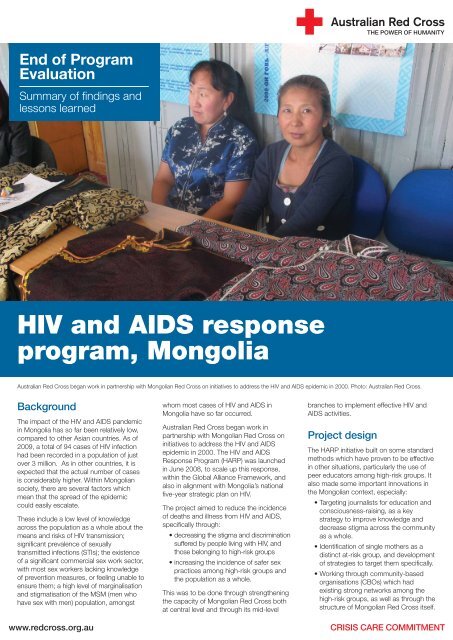
End of ProgramEvaluationSummary of findings <strong>and</strong>lessons learned<strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong> <strong>response</strong><strong>program</strong>, <strong>Mongolia</strong><strong>Australian</strong> <strong>Red</strong> <strong>Cross</strong> began work in partnership with <strong>Mongolia</strong>n <strong>Red</strong> <strong>Cross</strong> on initiatives to address the <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong> epidemic in 2000. Photo: <strong>Australian</strong> <strong>Red</strong> <strong>Cross</strong>.BackgroundThe impact of the <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong> p<strong>and</strong>emicin <strong>Mongolia</strong> has so far been relatively low,compared to other Asian countries. As of2009, a total of 94 cases of <strong>HIV</strong> infectionhad been recorded in a population of justover 3 million. As in other countries, it isexpected that the actual number of casesis considerably higher. Within <strong>Mongolia</strong>nsociety, there are several factors whichmean that the spread of the epidemiccould easily escalate.These include a low level of knowledgeacross the population as a whole about themeans <strong>and</strong> risks of <strong>HIV</strong> transmission;significant prevalence of sexuallytransmitted infections (STIs); the existenceof a significant commercial sex work sector,with most sex workers lacking knowledgeof prevention measures, or feeling unable toensure them; a high level of marginalisation<strong>and</strong> stigmatisation of the MSM (men whohave sex with men) population, amongstwww.redcross.org.auwhom most cases of <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong> in<strong>Mongolia</strong> have so far occurred.<strong>Australian</strong> <strong>Red</strong> <strong>Cross</strong> began work inpartnership with <strong>Mongolia</strong>n <strong>Red</strong> <strong>Cross</strong> oninitiatives to address the <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong>epidemic in 2000. The <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong>Response Program (HARP) was launchedin June 2008, to scale up this <strong>response</strong>,within the Global Alliance Framework, <strong>and</strong>also in alignment with <strong>Mongolia</strong>’s nationalfive-year strategic plan on <strong>HIV</strong>.The project aimed to reduce the incidenceof deaths <strong>and</strong> illness from <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong>,specifically through:• decreasing the stigma <strong>and</strong> discriminationsuffered by people living with <strong>HIV</strong>, <strong>and</strong>those belonging to high-risk groups• increasing the incidence of safer sexpractices among high-risk groups <strong>and</strong>the population as a whole.This was to be done through strengtheningthe capacity of <strong>Mongolia</strong>n <strong>Red</strong> <strong>Cross</strong> bothat central level <strong>and</strong> through its mid-levelbranches to implement effective <strong>HIV</strong> <strong>and</strong><strong>AIDS</strong> activities.Project designThe HARP initiative built on some st<strong>and</strong>ardmethods which have proven to be effectivein other situations, particularly the use ofpeer educators among high-risk groups. Italso made some important innovations inthe <strong>Mongolia</strong>n context, especially:• Targeting journalists for education <strong>and</strong>consciousness-raising, as a keystrategy to improve knowledge <strong>and</strong>decrease stigma across the communityas a whole.• Identification of single mothers as adistinct at-risk group, <strong>and</strong> developmentof strategies to target them specifically.• Working through community-basedorganisations (CBOs) which hadexisting strong networks among thehigh-risk groups, as well as through thestructure of <strong>Mongolia</strong>n <strong>Red</strong> <strong>Cross</strong> itself.CRISIS CARE COMMITMENT
Education around <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong> was complemented with livelihoods skills training. Photos: <strong>Australian</strong> <strong>Red</strong> <strong>Cross</strong>/ Tanya Cugura.Evaluation methodologyThe final evaluation of the project wasconducted over three months concluding inAugust 2011, with in-country work overtwo weeks from 20 June. The focus of theevaluation was on partner performance <strong>and</strong>project outcomes.MethodologyStages of the evaluation included:• Document review, encompassing allregular project reports; the report of theMay 2010 mid-term review; <strong>and</strong> thebaseline survey conducted in 2008.• Distribution of questionnaires tobeneficiaries, measuring knowledge<strong>and</strong> behaviour change against theresults of the original baseline survey.• Through this, all pertinent quantitativeinformation was readily available.• Direct interviews <strong>and</strong> focus groupdiscussions, including <strong>Mongolia</strong>n <strong>Red</strong><strong>Cross</strong> at national <strong>and</strong> branch level;other donor <strong>program</strong>mes in-country;beneficiaries; <strong>and</strong> local ‘opinionleaders’, including government figures<strong>and</strong> technical bureaus, <strong>and</strong> local police.Interviews were conducted in the capital,Ulaanbaatar, at both central <strong>and</strong> communitylevel; <strong>and</strong> in the two provinces (aimags) ofDornod <strong>and</strong> Arkhangai, respectively in thefar-east <strong>and</strong> the centre of the country.Only a small number of direct beneficiariescould be interviewed in the end, but as therewas extensive individual <strong>and</strong> FGDdiscussion with peer educators, all of whomwere drawn from the risk groups, <strong>and</strong> staffof the CBOs which have long <strong>and</strong> closeworking relationships with them, the reviewteam felt the qualitative information obtainedwas sufficiently reliable. Due to timeconstraints, it was only possible to have thesurvey questionnaires completed bybeneficiaries in Ulaanbaatar, so results havea possible bias towards urban respondents.Key findings of theevaluationResults of both document survey <strong>and</strong>interviews show real success inachievement of the project objectives; interms of changed behaviours <strong>and</strong> attitudesamong the primary target groups. In purelynumeric terms, of the 39 indicatorsincluded in the design, 32 were measurablein the evaluation, <strong>and</strong> of these, 22 wererated as fully achieved, <strong>and</strong> a further fivepartially achieved 1 . Quantifying the impacton the ultimate incidence of <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong>in the target groups <strong>and</strong> the broaderpopulation was beyond the scope of thisexercise; however, what is probably mostimportant <strong>and</strong> encouraging to note is thatthere appeared to be real qualitativechange in both behaviour <strong>and</strong> attitudeamong most of those who had beentargeted by the project, of a kind which islikely to substantially reduce risk of <strong>HIV</strong>transmission, <strong>and</strong> ensure better treatmentfor people living with <strong>HIV</strong> (PL<strong>HIV</strong>).Also important to note is that thesechanges were achieved in an unusuallydifficult operating environment, wherestrong stigma has been attached both to<strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong>, <strong>and</strong> to most of the high-riskgroups, particularly female sex workers(FSW) <strong>and</strong> MSM. Discussions with peereducators indicated notable shifts inawareness, but also in self-esteem, <strong>and</strong> theability of MSM, FSW <strong>and</strong> single mothers toprovide each other with support. This hasthe potential to serve as the foundation forlonger-term change <strong>and</strong> decreasedvulnerability to infection, as the capacitywithin target groups to share knowledge<strong>and</strong> reinforce safer sex practice increases.Results by groupMen who have sex with menMSM are currently the single most at-riskgroup in <strong>Mongolia</strong>. Of <strong>HIV</strong> infectionsrecorded in 2008, 68 percent had occurredthrough male-to-male sexual transmission.Both the group themselves, <strong>and</strong>government <strong>and</strong> other stakeholders statedthat the MSM population was highlyinvisible, <strong>and</strong> consistently subject todiscrimination <strong>and</strong> stigma; <strong>and</strong> that this iseven more so outside of the capital city.1. Noting that the indicators were a mixture of outcome <strong>and</strong> output <strong>and</strong> included qualitative measures around knowledge <strong>and</strong> behavior change.
The <strong>program</strong> focused on decreasing the stigma <strong>and</strong> discrimination suffered by people living with <strong>HIV</strong>, <strong>and</strong> those belonging to high-risk groups. Photo: <strong>Australian</strong> <strong>Red</strong> <strong>Cross</strong>.Outreach to the MSM community wasconducted mainly by Youth for Health, aCBO which also targeted female sexworkers. Peer educators were trained, <strong>and</strong> adrop-in centre established. 600 MSM madeuse of the centre over the project’s lifetime.Interestingly, reported rates of condom useamong MSM surveyed by questionnairehad not risen from the 2008 baseline of80 percent; though it should be noted thatthis is a higher rate than among MSMpopulations elsewhere in Asia. Respondentsalso expressed strong appreciation for thedrop-in centre as a safe space, whichfacilitated passing on of safer sex messages.Female sex workersThis group was also targeted through peereducation <strong>program</strong>s, with all educatorshaving themselves worked as sex workersin the past, <strong>and</strong> through drop-in centresrun directly by <strong>Mongolia</strong>n <strong>Red</strong> <strong>Cross</strong> <strong>and</strong>CBOs. The education model usedfocussed not only on safer sex practices,but also on how women could protectthemselves in violent or threateningsituations, <strong>and</strong> tactics to negotiate condomuse with clients.As well as reporting increased levels ofsafer sex practice, the peer educators saidthere was a change in women’s confidence<strong>and</strong> assertion, particularly in accessinghealth testing services, <strong>and</strong> in relations withtheir families. <strong>Red</strong>ucing alcoholconsumption was one strategy taught forreducing vulnerability; <strong>and</strong> positive changesin the behaviour of women attending thedrop-in centre were observed in this areaover the project’s lifetime.Single mothersInclusion of this population was because oftheir perceived higher vulnerability, as beingmore likely to have a number of differentsex partners, <strong>and</strong> particularly, undertakeeither occasional paid sex work, or othertransactional sex as a necessity for survival.They were more likely than average to beunemployed, <strong>and</strong> to have little or noknowledge about <strong>HIV</strong> transmission. Singlemothers were also targeted through a peereducator <strong>program</strong>, <strong>and</strong> peer supportgroups established. Education around <strong>HIV</strong><strong>and</strong> <strong>AIDS</strong> was complemented withlivelihoods skills training, <strong>and</strong> a key functionof the groups was to ensure better peersocial support than the women hadpreviously had access to.Women interviewed reported strongsatisfaction with the knowledge <strong>and</strong> skillsthey had acquired, <strong>and</strong> particularly that theyhad gained the confidence to talk openly totheir sex partners <strong>and</strong> to other women aboutsafer sex practices. Rates of increasedknowledge about <strong>HIV</strong> transmission <strong>and</strong> safersex practice varied according to location, butbetween 70 <strong>and</strong> 95 per cent of thosetargeted showing increased knowledge bythe end of the <strong>program</strong>.For example, one peer educator’s storyrecorded clearly demonstrates the effect ofthe <strong>program</strong> in breaking down isolation <strong>and</strong>raising confidence.Young peopleResults among young people were moredifficult to track, given the size <strong>and</strong> diversityof the target population, ranging from 17 to30 years of age. There were difficulties ofattribution, as it seemed young peoplewere exposed to a larger variety ofinformation sources on <strong>HIV</strong> <strong>and</strong> <strong>AIDS</strong>,including electronic media; information
Peer educator <strong>and</strong> peer support groups were central to the <strong>program</strong>. Photo: <strong>Australian</strong> <strong>Red</strong> <strong>Cross</strong>.through schools; educational institutions;<strong>and</strong> elsewhere. Peer educators alsoreported a greater degree of difficulty ingetting participation in <strong>HIV</strong> informationactivities.Peer educators’ experience with this groupalso showed up some of the deficiencies inmessage targeting. Counselling forabstinence was not considered useful;also, when talking about exercising greatercaution outside of ‘long term faithfulrelationships’, they found that youngpeople might well consider a six-monthrelationship as ‘long-term’. Centralmessages need to be fine-tuned todecrease risk.As with the three other target groups,young people who were recruited as peereducators reported high satisfaction withtheir work <strong>and</strong> its effectiveness, <strong>and</strong> theknowledge <strong>and</strong> skills they had gained.<strong>Red</strong>ucing stigma throughworking with journalistsA total of 246 journalists working in printmedia, television <strong>and</strong> internet weresuccessfully targeted by the <strong>program</strong>,specifically to improve media coverage byreducing sensationalist stories likely toincrease discrimination <strong>and</strong> maintainconfusion about the causes of <strong>AIDS</strong> <strong>and</strong>transmission of <strong>HIV</strong>. Final results in mediastories run during the project lifetime weremixed, partly due to one high-profile casein <strong>Mongolia</strong> of a blood donor being foundto be <strong>HIV</strong>-positive. However, focus groupdiscussions among journalists who hadparticipated showed significant change inknowledge <strong>and</strong> attitude for the better, <strong>and</strong>a greater preparedness to present storiesbased on fact, <strong>and</strong> to include the voices ofpeople living with <strong>HIV</strong>, <strong>and</strong> of those in highriskgroups.ConclusionHARP’s most important achievement hasbeen in laying a basic foundation for theon-going <strong>response</strong> to <strong>HIV</strong> in <strong>Mongolia</strong>. The<strong>program</strong> has broken important newground in not only demonstrably increasingthe capacity of <strong>Mongolia</strong>n <strong>Red</strong> <strong>Cross</strong> <strong>and</strong>its branches, but in establishing a peereducation model which can effectivelyreach high-risk groups <strong>and</strong> effect realknowledge <strong>and</strong> behaviour change there.<strong>Mongolia</strong>n <strong>Red</strong> <strong>Cross</strong>’ own knowledge<strong>and</strong> capacity to implement promotional<strong>and</strong> educational activities around <strong>HIV</strong> hasincreased, as has its ability to workthrough CBO partners <strong>and</strong> to use nontraditionalmodels of communityeducation. The community developmentwhich has taken place within high-riskgroups is a very distinctive <strong>and</strong> importantachievement, <strong>and</strong> it is hoped that this canbe built on further.- 2011