March 2013 - Institute of Physics and Engineering in Medicine
March 2013 - Institute of Physics and Engineering in Medicine
March 2013 - Institute of Physics and Engineering in Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
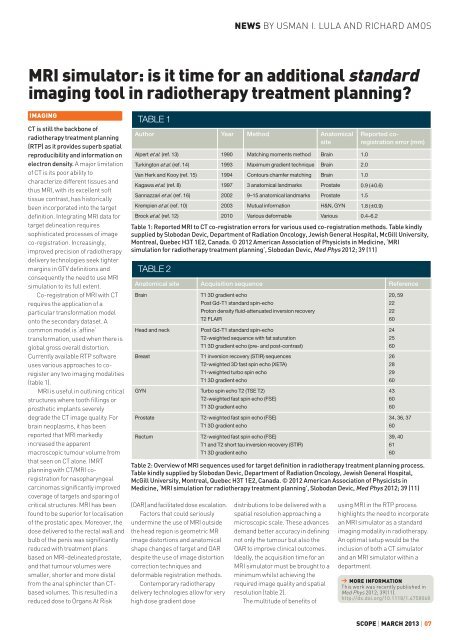
NEWS BY USMAN I. LULA AND RICHARD AMOSMRI simulator: is it time for an additional st<strong>and</strong>ardimag<strong>in</strong>g tool <strong>in</strong> radiotherapy treatment plann<strong>in</strong>g?IMAGINGCT is still the backbone <strong>of</strong>radiotherapy treatment plann<strong>in</strong>g(RTP) as it provides superb spatialreproducibility <strong>and</strong> <strong>in</strong>formation onelectron density. A major limitation<strong>of</strong> CT is its poor ability tocharacterize different tissues <strong>and</strong>thus MRI, with its excellent s<strong>of</strong>ttissue contrast, has historicallybeen <strong>in</strong>corporated <strong>in</strong>to the targetdef<strong>in</strong>ition. Integrat<strong>in</strong>g MRI data fortarget del<strong>in</strong>eation requiressophisticated processes <strong>of</strong> imageco-registration. Increas<strong>in</strong>gly,improved precision <strong>of</strong> radiotherapydelivery technologies seek tightermarg<strong>in</strong>s <strong>in</strong> GTV def<strong>in</strong>itions <strong>and</strong>consequently the need to use MRIsimulation to its full extent.Co-registration <strong>of</strong> MRI with CTrequires the application <strong>of</strong> aparticular transformation modelonto the secondary dataset. Acommon model is ‘aff<strong>in</strong>e’transformation, used when there isglobal gross overall distortion.Currently available RTP s<strong>of</strong>twareuses various approaches to coregisterany two imag<strong>in</strong>g modalities(table 1).MRI is useful <strong>in</strong> outl<strong>in</strong><strong>in</strong>g criticalstructures where tooth fill<strong>in</strong>gs orprosthetic implants severelydegrade the CT image quality. Forbra<strong>in</strong> neoplasms, it has beenreported that MRI markedly<strong>in</strong>creased the apparentmacroscopic tumour volume fromthat seen on CT alone. IMRTplann<strong>in</strong>g with CT/MRI coregistrationfor nasopharyngealcarc<strong>in</strong>omas significantly improvedcoverage <strong>of</strong> targets <strong>and</strong> spar<strong>in</strong>g <strong>of</strong>critical structures. MRI has beenfound to be superior for localisation<strong>of</strong> the prostatic apex. Moreover, thedose delivered to the rectal wall <strong>and</strong>bulb <strong>of</strong> the penis was significantlyreduced with treatment plansbased on MRI-del<strong>in</strong>eated prostate,<strong>and</strong> that tumour volumes weresmaller, shorter <strong>and</strong> more distalfrom the anal sph<strong>in</strong>cter than CTbasedvolumes. This resulted <strong>in</strong> areduced dose to Organs At RiskTABLE 1Author Year Method AnatomicalsiteAlpert et al. (ref. 13) 1990 Match<strong>in</strong>g moments method Bra<strong>in</strong> 1.0Turk<strong>in</strong>gton et al. (ref. 14) 1993 Maximum gradient technique Bra<strong>in</strong> 2.0Van Herk <strong>and</strong> Kooy (ref. 15) 1994 Contours chamfer match<strong>in</strong>g Bra<strong>in</strong> 1.0Kagawa et al. (ref. 8) 1997 3 anatomical l<strong>and</strong>marks Prostate 0.9 (±0.6)Sannazzari et al. (ref. 16) 2002 9–15 anatomical l<strong>and</strong>marks Prostate 1.5Krempien et al. (ref. 10) 2003 Mutual <strong>in</strong>formation H&N, GYN 1.8 (±0.9)Brock et al. (ref. 12) 2010 Various deformable Various 0.4–6.2Table 1: Reported MRI to CT co-registration errors for various used co-registration methods. Table k<strong>in</strong>dlysupplied by Slobodan Devic, Department <strong>of</strong> Radiation Oncology, Jewish General Hospital, McGill University,Montreal, Quebec H3T 1E2, Canada. © 2012 American Association <strong>of</strong> Physicists <strong>in</strong> Medic<strong>in</strong>e, ‘MRIsimulation for radiotherapy treatment plann<strong>in</strong>g’, Slobodan Devic, Med Phys 2012; 39 (11)TABLE 2(OAR) <strong>and</strong> facilitated dose escalation.Factors that could seriouslyunderm<strong>in</strong>e the use <strong>of</strong> MRI outsidethe head region is geometric MRimage distortions <strong>and</strong> anatomicalshape changes <strong>of</strong> target <strong>and</strong> OARdespite the use <strong>of</strong> image distortioncorrection techniques <strong>and</strong>deformable registration methods.Contemporary radiotherapydelivery technologies allow for veryhigh dose gradient dosedistributions to be delivered with aspatial resolution approach<strong>in</strong>g amicroscopic scale. These advancesdem<strong>and</strong> better accuracy <strong>in</strong> def<strong>in</strong><strong>in</strong>gnot only the tumour but also theOAR to improve cl<strong>in</strong>ical outcomes.Ideally, the acquisition time for anMRI simulator must be brought to am<strong>in</strong>imum whilst achiev<strong>in</strong>g therequired image quality <strong>and</strong> spatialresolution (table 2).The multitude <strong>of</strong> benefits <strong>of</strong>Reported coregistrationerror (mm)Anatomical site Acquisition sequence ReferenceBra<strong>in</strong>Head <strong>and</strong> neckBreastT1 3D gradient echoPost Gd-T1 st<strong>and</strong>ard sp<strong>in</strong>-echoProton density fluid-attenuated <strong>in</strong>version recoveryT2 FLAIRPost Gd-T1 st<strong>and</strong>ard sp<strong>in</strong>-echoT2-weighted sequence with fat saturationT1 3D gradient echo (pre- <strong>and</strong> post-contrast)T1 <strong>in</strong>version recovery (STIR) sequencesT2-weighted 3D fast sp<strong>in</strong> echo (XETA)T1-weighted turbo sp<strong>in</strong> echoT1 3D gradient echoGYN Turbo sp<strong>in</strong> echo T2 (TSE T2)T2-weighted fast sp<strong>in</strong> echo (FSE)T1 3D gradient echoProstateRectumT2-weighted fast sp<strong>in</strong> echo (FSE)T1 3D gradient echoT2-weighted fast sp<strong>in</strong> echo (FSE)T1 <strong>and</strong> T2 short tau <strong>in</strong>version recovery (STIR)T1 3D gradient echo20, 592222602425602628296043606034, 36, 376039, 406160Table 2: Overview <strong>of</strong> MRI sequences used for target def<strong>in</strong>ition <strong>in</strong> radiotherapy treatment plann<strong>in</strong>g process.Table k<strong>in</strong>dly supplied by Slobodan Devic, Department <strong>of</strong> Radiation Oncology, Jewish General Hospital,McGill University, Montreal, Quebec H3T 1E2, Canada. © 2012 American Association <strong>of</strong> Physicists <strong>in</strong>Medic<strong>in</strong>e, ‘MRI simulation for radiotherapy treatment plann<strong>in</strong>g’, Slobodan Devic, Med Phys 2012; 39 (11)us<strong>in</strong>g MRI <strong>in</strong> the RTP processhighlights the need to <strong>in</strong>corporatean MRI simulator as a st<strong>and</strong>ardimag<strong>in</strong>g modality <strong>in</strong> radiotherapy.An optimal setup would be the<strong>in</strong>clusion <strong>of</strong> both a CT simulator<strong>and</strong> an MRI simulator with<strong>in</strong> adepartment.‘ MORE INFORMATIONThis work was recently published <strong>in</strong>Med Phys 2012; 39(11).http://dx.doi.org/10.1118/1.4758068SCOPE | MARCH <strong>2013</strong> | 07