Portosystemic Shunts - The University of Tennessee College of ...
Portosystemic Shunts - The University of Tennessee College of ...
Portosystemic Shunts - The University of Tennessee College of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Help!My dog wasdiagnosedwith a liverproblem!Understanding commonliver disorders inYorkshire Terriers& other toy breeds
Brief Overview <strong>of</strong><strong>Portosystemic</strong> <strong>Shunts</strong>What is a Liver Shunt?A liver shunt is a blood vessel that carries blood aroundthe liver instead <strong>of</strong> through it. In some animals a livershunt is a birth defect (“congenital portosystemicshunt”). In others, multiple small shunts (“acquiredportosystemic shunts”) form because <strong>of</strong> severe liverdisease such as cirrhosis.“Congenital PSS and MVDare related genetic disorders causingmalformation <strong>of</strong> the liver circulation.”—CenterWhy do animals with shunts have problems?In the normal animal, food and other ingestedmaterials are broken down or digested in the intestinesand absorbed into the portal blood stream, where theyare carried to the liver. <strong>The</strong> liver stores some <strong>of</strong> the foodfor energy, processes some <strong>of</strong> it into safe chemicals, anduses some <strong>of</strong> it to make proteins and other substances.Because the blood bypasses the liver in dogs withshunts, toxins may build up in the bloodstream orkidneys. Additionally, the animal lacks the necessarymaterials to give it a ready source <strong>of</strong> energy and to helpit grow.What are the most common types <strong>of</strong><strong>Portosystemic</strong> <strong>Shunts</strong> (PSS)?<strong>The</strong>re are a number <strong>of</strong> types <strong>of</strong> portosystemic shunts.Those present at birth are classified as “congenital.”1. Single extrahepatic shunt: a single shunting vesselthat is located outside the liver. This is the mostcommon type <strong>of</strong> congenital shunt.2. Single intrahepatic shunt: a single shuntingvessel within the liver. <strong>The</strong>se are congenital andmost commonly seen in large-breed dogs.3. Extrahepatic multiple acquired shunts: Whenblood pressure in the portal system becomes toohigh, multiple small blood vessels will open up toshunt blood around the liver. Multiple acquired shuntsoccur as a result <strong>of</strong> end stage liver disease (cirrhosis)and portal hypertension. <strong>The</strong>se are not congenital andthey are not surgically correctable.1
General Symptoms:GastrointestinalSymptoms:Urinary Symptoms:NeurobehavioralsymptomsHepaticEncephalopathy(HE):SymptomsandDiagnosissmaller body stature, pediatrichypoglycemia (especially toybreeds and this can causeneurologic signs), failure togrow, poor muscle development,poor haircoatfinicky eater, intermittentvomiting, diarrhea, episodicinappetence, anorexia, weightloss, gastrointestinal ulcerationurinary tract infections, cystitis/urinary obstruction, excessivethirst (polydipsia), excessiveurination (polyuria)behavior changes, lethargy,sudden aggressiveness,depression, may seem lessintelligent, dementia, stupor,pacing, circling, muscle tremors,head pressing, apparentblindness, seizures, comaClinical signs <strong>of</strong> dogs with congenitalportosystemic shunts(PSS)Animals with congenital PSS <strong>of</strong>ten present at a youngage, unless the flow through the shunt is small orintermittent. Dogs with congenital PSS are <strong>of</strong>tensmall in size and have and poor muscle mass andhair coat; breeders may note they are the “runts” <strong>of</strong>the litter. Most commonly these dogs have behaviorchanges such as weakness, a quiet demeanor, or dullattitude. Occasionally neurologic signs can be moresevere, particularly if blood sugar is low or if excessiveamounts <strong>of</strong> protein are consumed. In those instances,the dogs may pace, circle, act blind, press their headsagainst the wall, or even seizure. Because the liver is nolonger efficiently processing ammonia from proteins,large amounts <strong>of</strong> the toxin are excreted into the kidneysand bladder where the ammonia can concentrateinto spikey crystals (ammonium biurate crystals) orcondense into stones (urate stones). Both conditions willresult in urinary tract inflammation and infection. Dogswith congenital PSS may also urinate more frequently,and therefore drink more, because they lose the abilityto concentrate their urine. Occasionally dogs will benauseous, causing poor appetite, vomiting, or excessivesalivation. Some dogs may even develop stomach ulcers.Neurologic and gastrointestinal signs can vary from dayto day. (Figure 1)Other:Figure 1. Table <strong>of</strong> clinical signsjaundice (Acquired PSS), ascites(Acquired PSS), bleedingproblems (Acquired PSS)Clinical signs <strong>of</strong> dogs with multiple acquiredportosystemic shuntsDogs with multiple acquired PSS are <strong>of</strong>ten middle agedor older, although puppies can develop the condition.Sometimes the owners may have noted a previousepisode <strong>of</strong> severe illness or toxin ingestion associatedwith severe liver disease. If the bile system was affectedby the initial problem, the dog may have a yellow tintto its skin, gums, and the whites <strong>of</strong> its eyes and its urinemay be very dark. If the portal pressure is very high orthe dog is not making enough protein, fluid will collectin the belly cavity (“ascites”). In dogs with severe liverdisease, blood will not be able to clot effectively, andthe owner may notice tiny or even large patches <strong>of</strong>bruising.3
Clinical signs <strong>of</strong> dogs with PVH-MVDMany dogs with PVH-MVD are “asymptomatic”; in fact,most Yorkies and Maltese that have this condition haveno signs at all. However, some dogs do present withclinical signs that develop early or later in life. <strong>The</strong>sedogs may either have a very underdeveloped liver orthey may have another condition (e.g., epilepsy, toybreed hypoglycemia, hydrocephalus, inflammatorybowel disease, or behavioral issues) that is the actualcause <strong>of</strong> the signs. Unlike dogs with shunts, dogs withPVH-MVD rarely have neurologic signs from hepaticencephalopathy.How we can tell if clinical signs are caused by PVH-MVDWe can’t be sure that clinical signs in dogs with increasedbile acids and liver biopsy results consistent with PVH-MVD are actually caused by the liver abnormality. Ifthe biopsy changes are very severe, for instance, or theliver is inflamed or full <strong>of</strong> scar tissue, it is likely thatclinical signs are related to those changes. However, ifthe biopsy changes are mild, the dog may actually havesome other condition. We are especially suspicious thatanother condition is present if clinical signs do not goaway with appropriate medical management.What is hepatic encephalopathy?Hepatic encephalopathy is a group <strong>of</strong> neurologic signsor behavior changes caused by severe liver disease.It has been recognized in animals with congenital oracquired PSS, end-stage liver disease, and congenitalurea cycle enzyme deficiencies. Clinical signs includelethargy, dementia, stupor, and coma. Muscle tremors,motor abnormalities, and focal and generalizedseizures have also been reported. <strong>The</strong> etiology <strong>of</strong>hepatic encephalopathy is probably dependent onseveral factors, including circulating toxins, alterationsin amino acid concentrations, and increased cerebralsensitivity to drugs and toxins. A variety <strong>of</strong> toxins areimplicated in the condition, with the most notablebeing ammonia. It is important to realize that some <strong>of</strong>these signs are seen with other conditions; if a dog hasseizures but its liver function is normal or it does notrespond to medical management <strong>of</strong> liver dysfunction,it is quite likely that the seizures are not caused by ashunt or PVH-MVD.Conditions That Trigger HEHepatic Encephalopathy (HE) can be precipitatedby high protein meals, intestinal hemorrhage (such4as from parasites), transfusion with stored blood,infection, dehydration, constipation, and drugs such asanesthetics, analgesics, and tranquilizers.What are common laboratory changes foundwith congenital PSS?A basic work-up for a dog suspected to have congenitalPSS includes a complete blood count (CBC),chemistry analysis (biochemistry), urine analysis, andmeasurement <strong>of</strong> bile acids. Some veterinarians mayalso check protein C and ammonia concentrations;however, these tests require special processing to makesure they are accurate. Common laboratory changesinclude the following:• Small red cells (“microcytosis”) on CBC, andsometimes increases in white blood cells.• Decrease in total protein, albumin, BUN (bloodurea nitrogen) on chemistries. Animals may alsohave increased liver enzymes or low cholesterol.• Decreased urine specific gravity on urinalysis.Animals may also have ammonium biuratecrystals or evidence <strong>of</strong> urinary tract infection(white blood cells, red blood cells, protein, andbacteria) in their urine sediment.• Increases in fasting and fed serum bile acids. Bileacids are usually >70µmol/liter in dogs with PSS.• Increased blood ammonia, especially 6 hoursafter a meal.• Decreased protein C concentrations.On plain abdominal x-rays, the liver is usually smallerthan normal. Unfortunately, urate bladder stones maynot show up on an x-ray, but they can be seen withultrasound. Ultrasound can also be used to try and findthe shunt and to rule out cirrhosis <strong>of</strong> the liver.
What are common laboratory changes foundwith congenital PVH-MVD?Except for increases in bile acids, laboratory resultsfor dogs with PVH-MVD may be completely normal.In fact, dogs with PVH-MVD usually have normalfasting bile acids, red cell size, BUN, protein, albumin,cholesterol, and Protein C concentrations. <strong>The</strong>ir fedbile acids are <strong>of</strong>ten
What techniques or handling requirements areused for the bile acid test?How young can you test a patient for liverdysfunction by measuring bile acids?Unlike ammonia and protein C measurements, nospecial techniques are required for handling and storage<strong>of</strong> serum for bile acid samples. <strong>The</strong> most important stepis to separate the serum from the red cells. After that,the serum sample can be sent by regular mail or courierto a lab; it does not need to be refrigerated or frozen.Can bile acids be used to diagnose PSS orPVH-MVD?Most dogs with congenital PSS have high fasting andfed bile acids, while dogs with PVH-MVD usually havenormal fasting and increased fed bile acids. Bile acidscan increase with any liver disease, so high bile acidsare not specific to congenital portosystemic shuntsor PVH-MVD. To be certain a dog has a PSS orPVH-MVD, advanced imaging and liver biopsyare required. That being said, if a Yorkie puppypresents with signs <strong>of</strong> hepatic encephalopathy, hasammonium biurate crystals, and has chemistryand CBC changes consistent with a shunt and itsbile acids are over 100 micromoles/L, the mostlikely diagnosis is a congenital extrahepatic PSS.If a Yorkie has no clinical signs, normal urineand biochemistry results, and mildly increasedpostprandial bile acids, the most common causeis PVH-MVD.Can abnormalities other than liver diseasecause high bile acids?About 95% <strong>of</strong> bile acids are reabsorbed through theintestines and sent to the portal system. That meansthat anything that causes decreased absorption (e.g.,diarrhea or thickened intestines) can decrease bile acidconcentrations and anything that increases absorption(e.g., inflammation or constipation) can increase bileacids. However, because a normal liver is so effective atremoving bile acids from the bloodstream, we do NOTexpect normal dogs to have high bile acids. Owners maywant to blame diet changes, stress, or other conditionsfor their dog’s high bile acids, but high bile acids onlyoccur if there is liver disease.No one really knows how early we can detect increasedbile acids in dogs with congenital PSS or PVH-MVD.Liver function is considered to be normal by 8 weeks <strong>of</strong>age, and PSS have been diagnosed in dogs as early as 4weeks old. If bile acids are abnormal at 8 weeks <strong>of</strong> age,liver disease should be suspected, and the puppy’s bloodshould be retested at 12 weeks <strong>of</strong> age for abnormalitiesin bile acids and chemistries. Because congenital PSSand PVH-MVD are so common in certain breeds(e.g., Yorkies, Maltese, Cairn Terriers, Havanese, IrishWolfhounds), susceptible breeds should have their bileacids and chemistries evaluated at 4 to 6 months <strong>of</strong>age for evidence <strong>of</strong> liver dysfunction. This will help theveterinarian develop an individualized health care planfor each pet and will alert the owners <strong>of</strong> the potential forfuture illnesses.We do NOT expect normal dogs to have high bile“acids. Owners may want to blame diet changes, stress, orother conditions for their dog’s high bile acids, but highbile acids only occur if there is liver disease.—Tobias”Do all dogs with PVH-MVD have increasedbile acids?Most affected dogs will have at least a small increase inone <strong>of</strong> their bile acids samples; however, in rare cases wehave seen Yorkies with normal bile acids that have mildliver biopsy changes consistent with PVH-MVD.Do all dogs with congenital PSS haveincreased bile acids?Almost all dogs with PSS will have increased bile acids;however, congenital PSS have been reported in dogswith bile acids as low as 17 µmoles/L (normal,
Can bile acids be used to monitor thedog’s status?Bile acid concentrations have not been correlated tothe severity <strong>of</strong> liver disease (or shunting) and vary fromday to day within the normal or the abnormal range.Obviously, bile acids <strong>of</strong> 300 micromoles/L are muchworse than bile acids <strong>of</strong> 25 micromoles/L. However,many dogs may have bile acids <strong>of</strong> 40 one day and 80 thenext. Because <strong>of</strong> differences in how much bile is beingheld within the gallbladder at one time, how much thegallbladder contracts, how fast the bile is moving throughthe intestines, and how much <strong>of</strong> it is being reabsorbed,we cannot say that the dog is worse when the bile acidsare 80. We can only say that the bile acids are increasedon both days and the liver is still not working properly.“ Bile acid concentrations have not beencorrelated to the severity <strong>of</strong> liver disease(or shunting) and vary from day to day...”—TobiasWhy is this important?It means we need to use other methods to monitor howa dog with PVH-MVD or one that has undergone repairfor a congenital shunt is doing long term. If your doghas PVH-MVD, we do not expect the bile acids to everbe normal (unless they were high for another reason).So, instead <strong>of</strong> measuring bile acids, we will look at thedog’s chemistries to make sure it can still make protein,albumin, BUN, and glucose and that its liver enzymesremain normal. That will give us much more informationthan changes in bile acids.Can protein C be used to differentiate shuntsfrom PVH/MVD?Protein C is a measure <strong>of</strong> an animal’s ability to stop clotsfrom forming or to break them down. If you had a lowprotein C, you would be much more likely to developclots in your legs during long plane flights. Like manyclotting factors, protein C is made in the liver and isdecreased with severe liver disease and PSS. Most dogswith PVH-MVD do not have severe liver disease, so theywill have normal protein C concentrations. Unfortunately,however, a few dogs do not follow these rules. Currentlythere is no blood test that is 100% accurate fordifferentiating shunts from PVH-MVD or otherconditions.How do we differentiate congenital portal veinhypoplasia and congenital PSS?Many liver diseases can cause the same laboratory changesseen in dogs with congenital PSS or severe PVH-MVD.<strong>The</strong>refore, to confirm the diagnosis, advanced imagingand liver biopsy are required. <strong>Shunts</strong> can be detected withtrans-splenic scintigraphy, MRI, or a CT (“Cat” scan) orby an experienced ultrasonographer. If no shunting isfound on these tests, a liver biopsy is obtained to confirmthe diagnosis <strong>of</strong> PVH-MVD and rule out other liverdiseases caused by inflammation, infection, ortoxins. If no shunting is seen on CT or scintigraphyand the liver biopsy is positive for MVD, then thedog has PVH-MVD. Alternatively, an experiencedsurgeon may elect to explore the abdomen to lookfor a shunt and to obtain liver biopsies. If no shuntis found, a portogram (contrast x-ray study <strong>of</strong> theblood vessels) can be performed during surgery.<strong>The</strong> final x-ray, or “portogram”, highlights all thevessels to the liver and any shunting vessels carryingblood around it.Differential Diagnoses<strong>The</strong> term “differential diagnosis” refers to conditions thatcause similar signs or blood work changes. For instance,any liver disease could cause the blood work changesseen in dogs with congenital PSS, including increasesin ammonia and bile acids and decrease in Protein C.Besides liver disease, formation <strong>of</strong> ammonium biuratecrystals and urate stones can occur with certain metabolicconditions; these are particularly common in Dalmatians.Hepatic encephalopathy must be differentiated fromdistemper, hydrocephalus, hypoglycemia, toxicities, andepilepsy and even behavior changes....no special techniquesare required for handlingand storage <strong>of</strong> serum forbile acid samples.—Tobias7
If bile acids are abnormal at 8 weeks <strong>of</strong> age, liver disease should be suspected,and the puppy’s blood should be retested at 12 weeks <strong>of</strong> age for abnormalitiesin bile acids and chemistries. Because congenital PSS and PVH-MVD are socommon in Yorkies...bile acids and chemistries should be evaluated at 4 to 6months <strong>of</strong> age for evidence <strong>of</strong> liver dysfunction. This will help the veterinariandevelop an individualized health care plan for each pet and will alert theowners <strong>of</strong> the potential for future illnesses.—Tobias8
“If no shunting is seen on CT or scintigraphy and the liver biopsy ispositive for MVD, then the dog has PVH-MVD.”—TobiasWhat is Scintigraphy?What is a Portogram?What is a CT Scan?Scintigraphy is a nuclear scan that measures blood flow. To evaluate adog for a shunt, a radioactive material is inserted into the colon (by ahigh enema) or injected into the spleen (“trans-splenic” scintigraphy),and a special camera is used to measure the amount <strong>of</strong> radioactivity inthe dog’s heart and liver. Trans-splenic scintigraphy produces a betterimage and uses less radioactive material, so it is preferred over colonicscintigraphy. In a normal dog, over 95% <strong>of</strong> the radioactive materialinjected into the spleen will head to the liver; if more than 5% goes tothe heart, a shunt is diagnosed. Scintigraphy is safe and quick but doesrequire heavy sedation or anesthesia. Small dogs can <strong>of</strong>ten be releasedfrom the hospital on the same day <strong>of</strong> trans-splenic scintigraphy, butlarger dogs and those with multiple acquired shunts usually need to stayovernight until they have expelled the radioactive material by defecationand urination. Scintigraphy tells us that shunting is present and <strong>of</strong>tenlets us know if the shunts are congenital or acquired, but it does not tellus whether the shunt is inside or outside <strong>of</strong> the liver.A portogram is an X-ray <strong>of</strong> the blood vessels to the liver. Because bloodvessels are not easily seen on regular x-rays, a contrast material (a liquidthat looks white on X-rays) must be injected into a blood vessel in theabdomen. <strong>The</strong> injection can be performed through a surgical incisioninto the belly; by injecting the spleen directly through the skin; or bypassing a catheter down the jugular vein (in the neck), through theheart, and toward the abdomen. Portograms usually require anesthesiaand are more invasive than scintigraphy or CT scans. <strong>The</strong>y are usuallyquite safe, however, and are able to provide a picture <strong>of</strong> the PSS so thatthe veterinarian can see where it is located and whether there is morethan one. Many board certified surgeons have an X-ray machine, calleda C-arm, in their operating rooms, which allows them to quickly andsafely perform a portogram during surgery.Computed tomography, known as CT or “CaT” scan, is a techniquethat provides multiple cross-sectional X-rays <strong>of</strong> bones and organs.CT scans are usually performed under anesthesia. In a dog witha PSS, a CT can be used to make the diagnosis <strong>of</strong> a shunt and todetermine the specific location <strong>of</strong> the shunt. This makes surgicalintervention easier, particularly when the shunt is hidden insidethe liver. Preoperative CT scans are <strong>of</strong>ten performed on large breeddogs because they usually have intrahepatic shunts.9
“To be certain a dog has PVH-MVD, advanced imaging andliver biopsy are required.”—TobiasLiver BiopsyFigure 3. Photograph <strong>of</strong> the two small incisions made from alaparoscopic spay and biopsy.Liver biopsy can be obtained by open surgicaltechnique (“laparotomy”) or by laparoscopy (use <strong>of</strong> ascope). (Figure 3) Ultrasound-guided needle biopsiesare not recommended because small liver size in dogswith congenital PSS and PVH-MVD increases the risk<strong>of</strong> complications, and because the small sample sizeobtained by needle makes diagnosis <strong>of</strong> MVD difficult.Some clinicians recommend taking samples frommultiple liver lobes, since the amount <strong>of</strong> disease coulddiffer from lobe to lobe. (Figure 4)If a Yorkie has no clinical signs,normal urine and biochemistryresults, and mildly increasedpostprandial bile acids, the mostcommon cause is PVH-MVD.—TobiasFigure 4. Micrograph taken <strong>of</strong> a slide from a liver biopsy specimenrevealing the classical pathology <strong>of</strong> PVH-MVD.10
Medical and Nutritional ManagementWhat medical management is recommended fordogs with congenital PSS?DietMost <strong>of</strong> the toxins that cause problems in dogs withcongenital PSS come from proteins broken downby bacteria in the colon. <strong>The</strong>refore, the mostimportant treatment <strong>of</strong> dogs with congenital PSSis an appropriate diet. Commercial liver dietssuch as Hill’s Prescription Diet l/d Canine HepaticHealth and Royal Canin Veterinary Diet HepaticFormula provide quality proteins that are readilydigestible in the small intestine so that minimalamounts reach the colonic bacteria. <strong>The</strong>se dietshave protein concentrations that are higher thanthose in many <strong>of</strong> the kidney diets; in fact, they areconsidered “protein restricted” instead <strong>of</strong> “low protein”.This is important, because animals with liver diseasethat receive too little protein will break down their ownmuscle tissue to make more.ProbioticsSome dogs may benefit from the addition <strong>of</strong> yogurt withactive cultures to their diet. For example, 2.2 ounces <strong>of</strong>Activa vanilla yogurt can be added to each 1000 kcals<strong>of</strong> food. That is roughly 1-2 tsp <strong>of</strong> yogurt once or twicea day for a small Yorkie. This type <strong>of</strong> “probiotic” hasbeen shown to reduce signs <strong>of</strong> hepatic encephalopathyin people, and the yogurt also provides another source<strong>of</strong> high quality, readily digestible protein.LactuloseLactulose syrup is a double sugar that is brokendown by bacteria in the colon to two simple sugars.This reaction is beneficial in several ways. First, thereaction produces an acidic environment that may beunattractive to troublesome bacteria and that reducesammonia absorption. Second, the resulting sugarscause absorption <strong>of</strong> fluid into the feces, which makesthem move out faster. Because <strong>of</strong> this second effect,lactulose must be dosed carefully: too much could resultin diarrhea. In general, owners should give a dose thatresults in 2 to 3 s<strong>of</strong>t-but-formed stools per day. For mostYorkshire terriers, that means 2 mls by mouth 2 to 3times each day. <strong>The</strong> dose should be decreased if diarrheaor cow pie stools develop, and increased for constipateddogs.“...protein restricted instead <strong>of</strong> low protein...isimportant, because animals with liver disease thatreceive too little protein will break down their ownmuscle tissue to make more.”—TobiasAntibioticsAntibiotics are prescribed for animals with activeinfections (for instance, urinary tract infections) orthose with neurologic signs. Certain antibiotics will kill<strong>of</strong>f the bacteria in the colon that are causing ammoniaproduction. Antibiotics are not used routinely, however,because <strong>of</strong> potential side effects.SupplementsSome veterinarians will prescribe supplements that reduceinflammation <strong>of</strong> the liver, such as denosyl (“SAM-E”)and silymarin (milk thistle). While these supplementscan be purchased over the counter, their content andmanufacturing are not regulated by the FDA. <strong>The</strong>refore,use <strong>of</strong> veterinary products is recommended, since thesehave been appropriately tested for active ingredients.Denamarin (Nutramax Laboratories) is a common brand;the chewable form is preferred because it has greaterabsorption and causes less stomach upset. Use <strong>of</strong> thesenutriceuticals in dogs with congenital PSS or PVH-MVDhas not been studied, so no one knows whether they makeany difference in these dogs. Owners should never giveany supplements that could have negative effects on theirpet’s liver, nor should they use any chemical productsaround their house that have risks <strong>of</strong> toxicity.11
How is a dog diagnosed with PVH-MVD thathas clinical signs treated?Dogs with PVH/MVD that have clinical signs,ammonium biurate crystals, or abnormal bloodchemistries (for instance, high liver enzymes, lowprotein, low albumin) can be medically managedjust like dogs with congenital PSS. Most critical isthe use <strong>of</strong> a protein-restricted diet.“ Dogs with PVH-MVD that have clinical signs...can be medically managed just like dogs withcongenital PSS. Most critical is the use <strong>of</strong> aprotein-restricted diet.—Tobias”What about dogs with PVH-MVD that are“asymptomatic” and have normal chemistries?<strong>The</strong>re are no studies on medical management <strong>of</strong>dogs with PVH-MVD that only have increased bileacids. <strong>The</strong>refore, we have no idea whether affecteddogs have a shortened lifespan and whether medicalmanagement makes any difference.Don’t bother to ask whether lactulose, diet, yogurt,SAM-e, milk thistle, antibiotics, or anything elsewill be helpful to your ‘asymptomatic’ dog; the factis, nobody knows! All we can tell you is that many <strong>of</strong>our “normal” Yorkie patients have mildly increasedbile acids and live long lives, as long as they don’t getsick from something else.Response to therapy explainedOne option for owners <strong>of</strong> dogs with PVH-MVD is tobase the need for medical management on “responseto therapy”. In simple terms, “response to therapy”is what happens to the animals when a treatment isstarted or stopped. In other words, if dietary changeor administration <strong>of</strong> medications makes the animalfeel worse, the treatment should be discontinued; if itmakes the animal feel better, it should be continued.One problem with a positive response is a “placeboeffect”, which commonly happens when ownersgive their animals treatments. <strong>The</strong> owners believeit will work and therefore see positive changes intheir dogs, even if those changes are not reallycaused by the treatment. A more scientific methodfor monitoring response to therapy in dogs thathave abnormalities in their blood chemistries orammonia is to monitor these blood chemicals forchanges when treatment is started or stopped.For dogs with high blood ammonia, the ammoniaconcentration should drop to normal levelswhen appropriate treatment is given.Information on preparing homemade dietsHomemade diets formulated by veterinarynutritionists can be used for dogs that havecongenital PSS or PVH-MVD. An example canbe seen at: http://www.vet.utk.edu/clinical/sacs/shunt/pdf/GenericLiverShuntDiet.pdf. <strong>The</strong>re issome risk to use <strong>of</strong> a homemade diet because changesin the diet content can make it unbalanced. Thismost <strong>of</strong>ten occurs when an owner decides to changethe ingredients, but it can also occur if the quality <strong>of</strong>the dietary components change. For instance, dietsthat include chicken breast will have a different fatand calorie content than those made with the darker,thigh meat. Over several months, this could lead tonutritional deficits. If you are interested in feeding ahomemade diet, you will need to work closely withyour veterinarian or a veterinary nutritionist tomake a diet that is complete, balanced, and healthyfor your pet. Information about nutrition consultscan be found at: http://www.vet.utk.edu/clinical/sacs/nutrition.php.12
Routine Veterinary Care & PrognosisWhat type <strong>of</strong> rechecks are recommended fordogs with PVH-MVD?Blood chemistries and ammonia, if available, can berechecked every 6 to 12 months to make sure that thedog is producing a sufficient amount <strong>of</strong> proteins andno signs <strong>of</strong> inflammation or organ failure are present.Bile acids do not need to be rechecked—they do notcorrelate well with the amount <strong>of</strong> liver damage and willonly cause unnecessary worry for owners.“...because systemic illness may hitthem harder than dogs with normallivers, it’s important to continue anyrecommended preventatives.”—TobiasCan dogs with congenital PVH-MVD receivevaccinations and flea and tick preventatives?Because dogs with PVH-MVD are susceptible to allthe usual parasites and viruses, and because systemicillness may hit them harder than dogs with normallivers, it’s important to continue any recommendedpreventatives. Heartworm, flea, and tick preventativesand vaccines should be given as usual. If ownersare concerned about the stress vaccinations mayplace on their pet, they can ask their veterinarianto develop a schedule so that administration <strong>of</strong>individual vaccines is separated by at least a fewweeks. Preventative care is also safe and highlyrecommended for dogs with congenital PSS, whetheror not the shunts have been repaired.Can vaccinations cause PVH-MVD?PVH-MVD is not caused by vaccines because it is acongenital disease. It is important to continue routinevaccinations and preventatives in these dogs so they donot get other conditions that can make them ill.What is the prognosis for dogs diagnosed withcongenital PVH-MVD?We can comfortably say that dogs with mild increasesin bile acids and no other evidence <strong>of</strong> liver diseaseor clinical signs may live normal lifespans. In fact,most Yorkie owners never know their dogs havePVH-MVD because they never test for it. Basedon a routine survey <strong>of</strong> bile acids from 139 healthyYorkies, we suspect that over half <strong>of</strong> all Yorkies havethis condition. Perhaps we have even bred forit by selecting for smaller and smaller dogs. Sowhat about the dogs that have clinical signs?We know that dogs with PVH-MVD that arepresented because <strong>of</strong> illness can and do respondto medical management. We also know thatmany <strong>of</strong> these dogs will live for years when kepton an appropriate diet. In most cases, dogs withPVH-MVD succumb from other conditions,including old age. Rarely, the condition willprogress to liver failure. That is why yearly or twiceyearly check-ups are recommended.What is the prognosis for dogs diagnosed withcongenital PSS that are only treated medically?About 50% <strong>of</strong> dogs with congenital PSS will live longlives if they are medically managed appropriately andthey don’t get other illnesses. <strong>The</strong>se are usually the dogsthat are less severely affected based on their clinical signsand blood work. <strong>The</strong> outcome is much better for dogswith extrahepatic congenital PSS that undergo surgicalclosure with an ameroid constrictor or cellophaneband. In fact, 85% to 90% <strong>of</strong> these dogs do well longterm. Surgery does have risks, however, and about 5%<strong>of</strong> the dogs may die after the procedure because <strong>of</strong>seizures or pneumonia. Yorkiesthat undergo surgery will almostalways have mildly increasedbile acids the rest <strong>of</strong> their lives.This is because they usually alsohave PVH-MVD, which is notcured by surgery.13
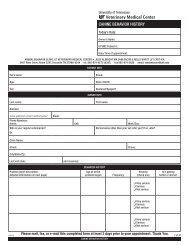
Helpful Links<strong>University</strong> <strong>of</strong> <strong>Tennessee</strong> Small Animal Clinical Scienceshttp://www.vet.utk.edu/clinical/sacs/index.phpDr. Karen M. Tobiashttp://www.vet.utk.edu/faculty/tobias.phpInformation relating to <strong>Portosystemic</strong> <strong>Shunts</strong>http://www.vet.utk.edu/clinical/sacs/shunt/index.phphttp://www.vet.utk.edu/clinical/sacs/shunt/pathophysiology.php#hepatichttp://www.vet.utk.edu/clinical/sacs/shunt/faq.phphttp://www.vet.utk.edu/clinical/sacs/shunt/diagnosis.phphttp://www.vet.utk.edu/clinical/sacs/shunt/management.phphttp://www.vet.utk.edu/clinical/sacs/shunt/surgery.phphttp://www.vet.utk.edu/clinical/sacs/shunt/postop.php#posthttp://www.vet.utk.edu/clinical/sacs/shunt/faq.pdfhttp://www.vet.utk.edu/clinical/sacs/nutrition.phphttp://www.vet.utk.edu/clinical/sacs/shunt/pdf/GenericLiverShuntDiet.pdfhttp://www.vet.utk.edu/giving/giving-makegiftnow.phpReferral Formhttp://www.vet.utk.edu/clinical/VMC-Referral_form_201210.pdf17