Anaplasmosis: The Unsung Tick Disease Pets a Go Go: Tips for ...
Anaplasmosis: The Unsung Tick Disease Pets a Go Go: Tips for ...
Anaplasmosis: The Unsung Tick Disease Pets a Go Go: Tips for ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
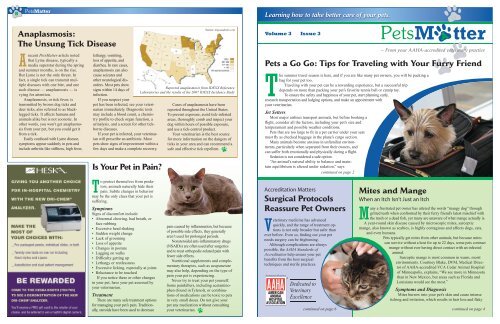
8<strong>Pets</strong>MatterLearning how to take better care of your pets.<strong>Anaplasmosis</strong>:<strong>The</strong> <strong>Unsung</strong> <strong>Tick</strong> <strong>Disease</strong>Arecent <strong>Pets</strong>Matter article notedthat Lyme disease, typically amedia superstar during the springand summer months, is on the rise.But Lyme is not the only threat. Infact, a single tick can transmit multiplediseases with one bite, and onesuch disease — anaplasmosis — isvying <strong>for</strong> attention.<strong>Anaplasmosis</strong>, or tick fever, istransmitted by brown dog ticks anddeer ticks, also referred to as blackleggedticks. It affects humans andanimals alike but is not zoonotic. Inother words, you won’t get anaplasmosisfrom your pet, but you could get itfrom a tick.Easily confused with Lyme disease,symptoms appear suddenly in pets andinclude arthritis-like stiffness, high fever,lethargy, vomiting,loss of appetite, anddiarrhea. In rare cases,anaplasmosis can alsocause seizures andother neurological disorders.Most pets showsigns within 14 days ofinfection.If you suspect yourpet has been infected, see your veterinarianimmediately. Diagnostic testsmay include a blood count, a chemistryprofile to check organ function, aurinalysis, and a screen <strong>for</strong> other tickbornediseases.If your pet is infected, your veterinarianwill prescribe an antibiotic. Mostpets show signs of improvement within afew days and make a complete recovery.Is Your Pet in Pain?Source: dogsandticks.comReported anaplasmosis from IDEXX ReferenceLaboratories and the results of the 2007 IDEXX Incidence StudyCases of anaplasmosis have beenreported throughout the United States.To prevent exposure, avoid tick-infestedareas, thoroughly comb and inspect yourdog within hours of possible exposure,and use a tick-control product.Your veterinarian is the best source<strong>for</strong> more in<strong>for</strong>mation on the dangers ofticks in your area and can recommend asafe and effective tick repellent.Volume 3 Issue 3— From your AAHA-accredited veterinary practice<strong>Pets</strong> a <strong>Go</strong> <strong>Go</strong>: <strong>Tips</strong> <strong>for</strong> Traveling with Your Furry Friend<strong>The</strong> summer travel season is here, and if you are like many pet owners, you will be packing abag <strong>for</strong> your pet too.Traveling with your pet can be a rewarding experience, but a successful tripdepends on more than packing your pet’s favorite tennis ball or catnip toy.To ensure the safety and happiness of your pet, start planning early,research transportation and lodging options, and make an appointment withyour veterinarian.Jet SettersMost major airlines transport animals, but be<strong>for</strong>e booking aflight, consider all the factors, including your pet’s size andtemperament and possible weather conditions.<strong>Pets</strong> that are too large to fit in a pet carrier under your seatmust fly as checked baggage in the plane’s cargo section.Many animals become anxious in unfamiliar environments,particularly when separated from their owners, andcan suffer both emotionally and physically during a flight.Sedation is not considered a safe option.“An animal’s natural ability to balance and maintainequilibrium is altered under sedation,” sayscontinued on page 2To protect themselves from predators,animals naturally hide theirpain. Subtle changes in behaviormay be the only clues that your pet issuffering.SymptomsSigns of discom<strong>for</strong>t include:• Abnormal chewing, bad breath, orface rubbing• Excessive head shaking• Sudden weight change• Lack of grooming• Loss of appetite• Changes in posture• Lagging on walks• Difficulty getting up• Lethargy or restlessness• Excessive licking, especially at joints• Reluctance to be touchedIf you notice these or other changesin your pet, have your pet assessed byyour veterinarian.Treatment<strong>The</strong>re are many safe treatment options<strong>for</strong> managing your pet’s pain. Traditionally,steroids have been used to decreasepain caused by inflammation, but becauseof possible side effects, they generallyaren’t used <strong>for</strong> prolonged periods.Nonsteroidal anti-inflammatory drugs(NSAIDs) are often used after surgeriesand to treat orthopedic-related pain withfewer side effects.Nutritional supplements and complementarytherapies, such as acupuncturemay also help, depending on the type ofpain your pet is experiencing.Never try to treat your pet yourself.Some painkillers, including acetaminophen(found in Tylenol), or combinationsof medications can be toxic to petsin very small doses. Do not give yourpet any medication without consultingyour veterinarian.Accreditation MattersSurgical ProtocolsReassure Pet OwnersVeterinary medicine has advancedquickly, and the range of treatment optionsis not only broader but safer thanever be<strong>for</strong>e. Even so, finding out your petneeds surgery can be frightening.Although complications are alwayspossible, the AAHA Standards ofAccreditation help ensure your petbenefits from the best surgicaltechniques and sterile practices.continued on page 6Mites and MangeWhen an Itch Isn’t Just an ItchMany a frustrated pet owner has uttered the words “mangy dog” throughgritted teeth when confronted by their furry friend’s latest mischief withthe trash or a dead fish, yet many are unaware of what mange actually is.A year-round skin disease caused by microscopic mites, sarcopticmange, also known as scabies, is highly contagious and affects dogs, cats,and even humans.<strong>Pets</strong> typically get mites from other animals, but because mitescan survive without a host <strong>for</strong> up to 22 days, some pets contractmange without ever having direct contact with an infectedanimal.Sarcoptic mange is most common in warm, moistenvironments. Courtney Blake, DVM, Medical Directorof AAHA-accredited VCA Cedar Animal Hospitalof Minneapolis, explains, “We see more in Minnesotathan in New Mexico, but areas such as Florida andLouisiana would see the most.”Symptoms and DiagnosisMites burrow into your pet’s skin and cause intenseitching and irritation, which results in hair loss and flakycontinued on page 4
2 <strong>Pets</strong>Matter7<strong>Tips</strong> <strong>for</strong> Traveling with Your Furry Friend Continued from page 1MRSA: Is It Time to Panic?Dr. Patricia Olson, DVM, PhD. “When thekennel is moved, a sedated animal may notbe able to brace and prevent injury.”Gary L. Rose, DVM, of AAHAaccreditedCabrillo Veterinary Hospitalin San Diego, Calif., adds “When heavilysedated, some short-nosed breedscan have trouble breathing.”Temperature extremes can also putyour pet at risk. Many airlines do nottransport pets during the hottest monthsof the year, or will not accept pets whenthe <strong>for</strong>ecasted temperature is above acertain point.Look <strong>for</strong> flights in the early morningor late evening, when temperatures areat their lowest.On the RoadOf course there are also safety concernswhen traveling by car. Pet cratesare strongly recommended.If an accident occurs, pet crates canprotect animals from impact injuriesand also prevent them from runningout into traffic.Marci Cook, DVM of AAHAaccreditedShiloh Veterinary Hospitalin Billings, Mt., says, “A crate offers asafe environment <strong>for</strong> your pet and helpsthem to feel com<strong>for</strong>table.”Rose recommends introducing yourpet to the crate over several weeks.“Get them used to it by feeding them init, and by taking short trips around theneighborhood to see how they do.”For pets prone to motion sickness,Rose advises, “Make sure there’s adequateventilation in the car. Keep [it] cooland com<strong>for</strong>table. If your pet still showssigns of motion sickness, medication isavailable through your veterinarian.”LodgingAlways research accommodationsbe<strong>for</strong>e leaving home, and make reservationswhenever possible.Many hotels and inns allow pets butmay have size and weight limits, breedrestrictions, or a limit on the numberof pets allowed per room.Campgrounds also have pet policiesand occasionally prohibit pets altogether.State and national parks that allowpets often restrict them from certainareas, such as hiking trails and beaches.Additional In<strong>for</strong>mationHealthyPet Hospital Locator:healthypet.aahanet.org/ewebBring Fido: www.bringfido.comTraveling with Your Cat: vet.osu.edu/2372.htmPet-Friendly Campgrounds in the U.S.:www.petfriendlytravel.com/?page=campgroundsTraveling with <strong>Pets</strong> to National Parks:usparks.about.com/library/weekly/aa042598.htmCrate Training (Dogs):www.hsus.org/pets/pet_care/our_pets_<strong>for</strong>_life_program/dog_behavior_tip_sheets/crate_training.htmlFree-Access Crate Training (FACT) <strong>for</strong> Cats:www.mmilani.com/feline-crate-training.htmlAmerican Animal Hospital Association: 800/252-2242Health CertificatesMost airlines require pets be examinedby a veterinarian no more than10 days prior to the date of travel. Beprepared to present health and rabiescertificates at the time of departure.If you are traveling by car, pack acopy of your pet’s prescriptions andvaccination records. Some states requireproof of rabies vaccination.Your veterinarian can also tell you ifyour pet needs additional vaccinationsor preventive medications <strong>for</strong> the areain which you will be traveling.If an accidentoccurs, petcrates canprotect animalsfrom impactinjuries and alsoprevent themfrom runningout into traffic.Methicillin-resistant Staphylococcusaureus (MRSA), anantibiotic-resistant “superbug”is receiving consistent media attention,with recent articles discussing whetherpets are transmitting the infectiousbacteria to people.Although some healthy people carryMRSA bacteria and never become ill,it can cause serious skin infections,which may develop into potentiallyfatal organ and bloodstream infectionsand pneumonia.Now considered an emergingzoonotic disease, meaning it may betransmitted between humans and animals,MRSA is of increasing concernto pet owners. However, the connectionbetween pets, people, and MRSA is notentirely clear.How Serious Is the Threat?<strong>The</strong>re is no doubt thatthe consequences ofMRSA infectionscan be dire, butare you andyour pet indanger oris the mediaattention generatingfear thatis unwarranted?Resources and Additional In<strong>for</strong>mationGregg Takashima,DVM, AAHA boardmember, and founder ofaccredited Parkway VeterinaryHospital in Lake Oswego, Ore.,says, “Animals are less of a risk <strong>for</strong>spread of the disease than humans.“This is an important disease, butto put it in perspective, in the UnitedStates, the common flu is responsible <strong>for</strong>approximately 200,000 hospitalizationsper year and 36,000 deaths. MRSA isestimated [by the Centers <strong>for</strong> <strong>Disease</strong>Control and Prevention] to be associatedwith approximately 94,000 hospitalizationsand 19,000 deaths per year.”“MRSA is a concern but…rates inpets are low,” says Scott Weese, DVM,of the Ontario Veterinary College.“People should remember thatother people are usually a greater risk ofMRSA than their pets,” contin-ues Weese, who is part ofa team of researchersstudying MRSAin humans andcompanionanimals.Colonization vs. Infection (Virginia Department of Health):www.vdh.virginia.gov/Epidemiology/Surveillance/MRSA/#ColonizationvsInfectionUnderstanding MRSA Symptoms:www.webmd.com/skin-problems-and-treatments/understanding-mrsa-symptomsCaring <strong>for</strong> an Infected Pet:tahilla.typepad.com/petsmrsa/files/annette_loeffler_advice_pets_at_home.pdfCenters <strong>for</strong> <strong>Disease</strong> Control and Prevention:www.cdc.gov/ncidod/dhqp/ar_mrsa_ca.htmlWorms and Germs Blog:www.wormsandgermsblog.com/articles/another-category/test-subcategoryJust the Facts• MRSA is spread by contact withpeople, animals, or objects with thebacteria on them.• <strong>Pets</strong> can become colonized by staffworking in veterinary clinics or humanhospitals.• Colonized pets and people areasymptomatic, but can becomeinfected if the bacteria enter the bodythrough a wound or an open sore.• Symptoms in humans begin with redbumps resembling pimples or spiderbites.• Symptoms in pets include fever, lossof appetite, and open sores.Weese explains, “MRSA infectionscan range from inapparent to rapidlyfatal,” but he goes on to say, “<strong>The</strong>majority of animals with MRSA willrecover with proper treatment.”Advice <strong>for</strong> pet ownersIf your pet shows signs of MRSA orhas been exposed to MRSA, call yourveterinarian immediately.“<strong>The</strong> single most effective preventionprotocol is appropriate hygiene— like washing your hands!” saysTakashima.Weese offers similar advice. “Routine,common sense practices such as handwashing,judicious antibiotic use, andgood veterinary care can reduce the riskof MRSA infection and transmission.”MRSA commonly lives in the nosein addition to the infection site, so Weesealso advises avoiding contact with yourpet’s face.MRSA is highly contagious.Takashima notes if you suspect yourpet is infected, alert staff and doctorsbe<strong>for</strong>e bringing your pet into a veterinaryclinic.
6<strong>Pets</strong>Matter3Travel <strong>Tips</strong> andCar SafetyBuckle Up Your Barker:Pet Seat Belts Save LivesDo you want your pet to befeatured in <strong>Pets</strong>Matter?Email a picture to <strong>Pets</strong>Matter@aahanet.org.Be sure to include your pet’s name, yourcity, state, a few lines about your pet,and the name of your veterinarian.Surgical Protocols Reassure Pet Ownerscontinued from page 1Surgical protocols at AAHAaccreditedclinics include:• Pre-surgical assessments. Prior tosurgery, the veterinary team verifiesthe specifics of the procedure;completes a physical exam of thepatient; and ensures blood tests havebeen completed, documented, andreviewed by the veterinarian. <strong>The</strong>seprecautions help determine if yourpet is at risk <strong>for</strong> complications whileunder general anesthesia.• Dedicated surgical suites. To preventpost-surgical infections andcross-contamination, surgeries areper<strong>for</strong>med in a room used only <strong>for</strong>sterile surgical procedures.• Surgical attire. Staff must weardisposable caps and masks whenentering the surgical suite. Anyoneinvolved in the procedure itselfmust also wear sterile gowns andsingle-use gloves.• Sterile packs and equipment.Surgical instruments are carefullycleaned, sterilized, and wrappedPhotos Courtesy of the Veterinary Referral Center of Coloradoprior to the procedure to help preventinfections.AAHA’s Standards of Accreditationdiminish the risks associated withsurgery and help ensure the highestlevel of care. <strong>The</strong> safety and com<strong>for</strong>tof your “best friend” are always of theutmost importance.• Be sure your pet is wearing a flatcollar with identification tags atall times.• If your pet doesn’t have amicrochip, consider having oneimplanted.• Know basic pet first aid, andcarry a first aid kit.• Never allow your pet to travelwith its head outside the carwindow.• Do not allow pets to ride in thefront seat. <strong>The</strong>y are at risk of beingthrown into the windshield,can interfere with your ability todrive, or could be injured by anairbag.• Disable electric window controls.Dogs have been known to gettheir heads stuck in windowsafter stepping on the buttons.• Stop <strong>for</strong> “potty breaks” every twohours.• Always leash your pet be<strong>for</strong>eopening the car door.For most of us, fastening ourseatbelts as soon as we get into acar is second nature. Now, a newconsumer group called Bark-BuckleUpis educating pet owners about the need<strong>for</strong> similar safety restraints <strong>for</strong> pets.<strong>The</strong> Travel Industry Association ofAmerica reports that 29 million U.S.dog owners travel with their caninecompanions, yet a 2007–2008 nationalsurvey of pet owners conducted by theAmerican Pet Products Manufacturer’sAssociation revealed that 80% of petowners who travel with their petsnever use a restraint.“In an accident, an unbuckledcat or dog can becomea projectile, risking seriousinjury to the pet, the driver,and passengers,” says Bark-BuckleUp’s cofounder ChristinaLynn.Some states have passedlaws restricting dogs from openvehicles, such as pick-up trucks,or require them to travel in crates, orwith cross-tie restraints. This followsin the wake of numerous accidents,including the widely publicized 1999incident in which author Stephen Kingwas struck by a car and gravely injuredafter the car’s driver became distractedwhile attempting to control an unrestraineddog.“My opinion is that requiring pets tobe appropriately restrained in pick-upsand cars is quite a positive and responsiblemove,” offers Alicia Faggella,DVM, and Critical Care Director atAAHA-accredited Dove Lewis EmergencyAnimal Hospital in Portland,Ore. “Too often, we see animals thathave been injured or killed secondaryto jumping or falling out of pick-uptrucks. Animals in closed vehicleshave also been injured or killed wheninvolved in car accidents where theanimal has not been restrained appropriately.”Faggella adds that restraints shouldbe applied appropriately, with the kindof restraint dependent upon vehicletype, size of pet being restrained, andthe animal’s temperament. She cautionsowners to buy restraints made expressly<strong>for</strong> that purpose, and not try to constructsomething on their own.For further in<strong>for</strong>mation on thistopic, visit these links:www.barkbuckleup.comwww.consumeraffairs.com/news04/2008/01/pet_seatbelts.html
4<strong>Pets</strong>Matter5Mites and Mangecontinued from page 1skin. Other symptoms are small redpustules and a yellow crust on theskin. If untreated, sores and infectionscan develop.According to Blake, “Some [infestations]look like a bad case of dandruff.”She adds, “Even mice, rats, and guineapigs can get mites. <strong>The</strong>ir flakes sometimeslook red instead of white.”Blake advises pet owners to havetheir animals evaluated as soon as theynotice symptoms. “Symptoms of mitesoften are mistaken <strong>for</strong> allergies or skininfections,” she says.To determine whether your pet isinfected, your veterinarian will analyzeskin scrapings. However, some infectedanimals don’t test positive <strong>for</strong> mites,so negative scrapings don’t always ruleout mange.<strong>The</strong> goodnews is that mangeis treatable. <strong>The</strong>re are topicalproducts on the market, aswell as a regimen of medicatedshampoo baths and body dipsthat may take care ofthe problem.Treatment<strong>The</strong> good news is that mange istreatable. <strong>The</strong>re are topical productson the market, as well as a regimen ofmedicated shampoo baths and bodydips that may take care of the problem.Getting rid of mites can be difficult,and the medication can have sideeffects. However, Blake states that nohome remedies effectively treat mites.She also reminds owners that treatmentvaries depending on the type of miteyour pet has.Lowell Ackerman, DVM, of theAAHA-accredited Harvard clinic,Foster Hospital <strong>for</strong> Small Animals,concurs. “Each condition is treatedseparately so there are no ‘general’treatment recommendations.”Ackerman also points out that thetreatments available from veterinariansare safer than home remedies. “Someof the products available over the counterare much more toxic than veterinarypreparations.”A Word of CautionSarcoptic mange can affect humans.Ackerman emphasizes following yourveterinarian’s instructions, saying, “Itis important to protect family membersfrom infection, so proper treatment iscritical.”If you have contact with a mangeinfectedanimal, you may develop anitchy rash of small raised bumps on yourchest and abdomen. Usually this conditionis temporary and will go away oncethe animal has been treated. Consult aphysician if the problem persists.Additional ResourcesCompanion AnimalParasite Council:www.petsandparasites.org/dog-owners/scabies.htmlDog Owner’s Guide:www.canismajor.com/dog/mange1.html<strong>The</strong> Pet Centerwww.thepetcenter.com/exa/mites.html<strong>The</strong> Pet Health Library:www.veterinarypartner.com/Content.plx?P=A&S=0&C=0&A=616Faces of the Veterinary ProfessionCancer Studies Put Khanna at Research Forefront“ Veterinarians don’t think or askquestions the same way as humandoctors,” says Chand Khanna,DVM, PhD, a senior scientist at theNational Cancer Institute (NCI), thefederal government’s principal agency<strong>for</strong> cancer research.“When I was pursuing my PhD atthe medical school of the University ofMinnesota, I learned that veterinariansthink differently from others in the biomedicalprofession,” Khanna explains.“Veterinarians are com<strong>for</strong>table movingbetween different systems and species…I realized this could be a competitiveadvantage <strong>for</strong> veterinarians who wanteda career in biomedical research.”Dr. Khanna applied this unique perspectivewhen he first joined the NCI.“My initial focus was on a diseasecalled osteosarcoma, a bone cancercommon in children. It’s very similarto a cancer that I see and treat in petanimals, mostly dogs.”Khanna is head of the NCI’s ComparativeOncology Program in Bethesda,Md. Working with 17 veterinaryschools across the country, his team ofphysicians, veterinarians, and biomedicalresearchers offer cutting-edgetherapeutics to treat pet cats and dogs“I truly think we’re on the cusp of where we imagine cancer ina different way.” — Dr. Chand Khanna, pictured below with Bogie,one of his patientssuffering from cancer.Historically, treating cancer in petsevolved from knowledge learned fromtreating humans. Dr. Khanna’s comparativeoncology program essentiallyreverses this process.“We help the pet animal who is beingtreated today and, hopefully, a child withthe same disease some time in the future.”Khanna emphasizes that his researchdoes not harm or infect any animals.“We’re managing cancers in petsthat have already developed the diseaseand aren’t responding to conventionaltreatments. <strong>The</strong>se pets don’t have otheroptions,” he says.Khanna also manages a laboratory atthe NCI focusing on metastasis, or howcancer spreads throughout the body.But he isn’t a stereotypic “ivory tower”researcher with his eye glued to a microscope.Khanna continues to be a practicingveterinarian, spending two days each weekat a clinic in Washington, D.C.“<strong>The</strong>re are no approved drugs totreat dogs with cancer,” he says. “<strong>The</strong>drugs we use in our clinic are all approved<strong>for</strong> human use.”But with 12 million pet dogs andcats being diagnosed with cancer everyyear, Khanna is seeing significant improvementin the standards of care andsays that more change is on the way.“This is an exciting time <strong>for</strong> us,” headds. “I truly think we’re on the cusp ofwhere we imagine cancer in a differentway. Until today, veterinarians have onlybeen able to control or manage cancer inpets. But I believe we’ll soon be able tostart using the term ‘cure.’”Additional ResourcesNational Cancer Institute:http://www.cancer.gov/Comparative Oncology Program:ccr.cancer.gov/resources/cop/public.aspCancer Clues from Pet Dogs:ccr.cancer.gov/resources/cop/8-ScientificAmerican.pdf