TXA - Casecag.com
TXA - Casecag.com
TXA - Casecag.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
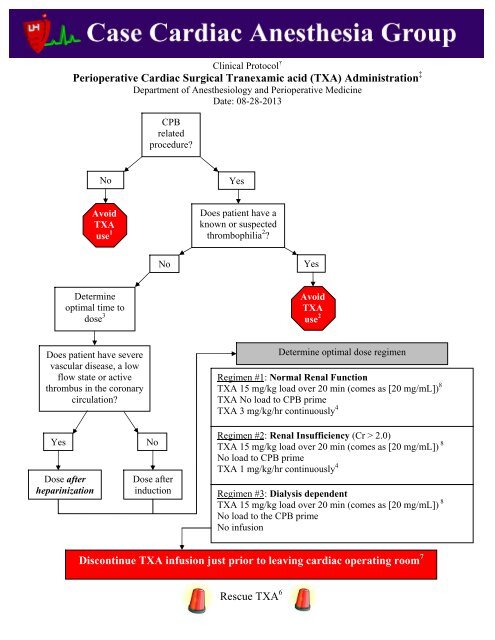
Clinical Protocol †Perioperative Cardiac Surgical Tranexamic acid (<strong>TXA</strong>) Administration ‡Department of Anesthesiology and Perioperative MedicineDate: 08-28-2013CPBrelatedprocedure?NoYesAvoid<strong>TXA</strong>use 1Does patient have aknown or suspectedthrombophilia 2 ?NoYesDetermineoptimal time todose 3Avoid<strong>TXA</strong>use 2Does patient have severevascular disease, a lowflow state or activethrombus in the coronarycirculation?Determine optimal dose regimenRegimen #1: Normal Renal Function<strong>TXA</strong> 15 mg/kg load over 20 min (<strong>com</strong>es as [20 mg/mL]) 8<strong>TXA</strong> No load to CPB prime<strong>TXA</strong> 3 mg/kg/hr continuously 4YesDose afterheparinizationNoDose afterinductionRegimen #2: Renal Insufficiency (Cr > 2.0)<strong>TXA</strong> 15 mg/kg load over 20 min (<strong>com</strong>es as [20 mg/mL]) 8No load to CPB prime<strong>TXA</strong> 1 mg/kg/hr continuously 4Regimen #3: Dialysis dependent<strong>TXA</strong> 15 mg/kg load over 20 min (<strong>com</strong>es as [20 mg/mL]) 8No load to the CPB primeNo infusionDiscontinue <strong>TXA</strong> infusion just prior to leaving cardiac operating room 7Rescue <strong>TXA</strong> 6
†Clinical protocols are based on the best and most recent available data and are expected to be followed by allCASECAG staff unless there is a <strong>com</strong>pelling clinical reason not to, or new data be<strong>com</strong>es available that suggestsan alternate treatment protocol. Standardizing our approach to some of our practices is expected to reduce drugerrors in the clinical environment and increase work flow for the trainees.‡Administration of <strong>TXA</strong> to cardiac surgical patients is considered a Class IA (I=Benefit>>>Risk, treatmentshould be performed, A=Strongest evidence supporting treatment based multiple prospective trials and/or metaanalyses)re<strong>com</strong>mendation to reduce the total number of patients who require blood transfusion and reduce theamount of blood loss after cardiac operations. (Ferraris et al.)1: The safety of <strong>TXA</strong> for OPCAB is not well established and therefore its use should be avoided in thiscircumstance. OPCAB surgery has been shown to be associated with a hypercoaguable state postoperativelyand without the anticoagulation effects of CPB its use may put the patient at risk for early graft closure or otherthromboembolic <strong>com</strong>plications. (Kon et al, Desai et al.) If <strong>TXA</strong> is being considered for a non-cardiac surgicalprocedure which is expected to involve heavy bleeding (e.g., trauma or redo orthopedic spine surgery) then itmay be permissible to electively and prophylactically administer <strong>TXA</strong> if the patient is known to not have severeperipheral vascular disease or a thrombophilia. (Verma et al., Berenholtz et al.)2: A screening for hypercoaguable states should be a regular part of each patient’s review of systems (e.g.,query whether the patient has ever had a DVT or pulmonary embolus). If the patient is known to possess any ofthe following conditions prophylactic administration of <strong>TXA</strong> may not be safe and it is not re<strong>com</strong>mended.Rescue administration of <strong>TXA</strong> to severely hemorrhaging patients with any of these diagnoses is left to thediscretion of the clinicians providing care.Heparin Induced Thrombocytopenia and Thrombotic Syndrome (HITTS)Factor V Leiden MutationProtein C Deficiency or ResistanceProtein S DeficiencyLupus AnticoagulantAnti-phospholipid antibody syndrome (APS)Prothrombin Gene 20210 MutationAntithrombin III DeficiencyAnticardiolipin antibody (IgG and IgM)Factor VIII Deficiency3: Pre-sternotomy administration of <strong>TXA</strong> is probably optimal to prevent the fibrinolysis that ac<strong>com</strong>paniessurgical trauma, inflammation and the institution of CPB. The efficacy of pre-sternotomy administration of<strong>TXA</strong> is supported by multiple prospective clinical trials. If the patient is known to possess severe occlusivecoronary disease, a low flow state (i.e. cardiogenic shock) or an active coronary thrombus the Amicar shouldnot be administered until the patient has been fully heparinzed for CPB (i.e., ACT > 400 seconds). In theabsence of severe vascular disease or an active coronary thrombus in an unheparinized patient it is optimal toadminister the <strong>TXA</strong> following induction but prior to sternotomy.4: Note 90% of IV administered <strong>TXA</strong> is excreted unchanged in the urine and higher levels of <strong>TXA</strong> areassociated with a greater incidence of seizures. The incidence of seizure may be higher in individuals with apre-existing seizure disorder.5: If deep hypothermic circulatory arrest (DHCA) is planned then the <strong>TXA</strong> infusion should be temporarilypaused while there is no systemic blood circulation (i.e. during DHCA). This will prevent a local accumulationof the <strong>TXA</strong> at the point where the drug is entering the vascular system. Failure to stop the <strong>TXA</strong> during DHCAcan result in a large thrombus formation local to the exit port on the catheter that the drug is infusing from.
6: Rescue <strong>TXA</strong> is a term that refers to the administration of <strong>TXA</strong> after the surgical procedure, or the majority ofit, has already been <strong>com</strong>pleted and no <strong>TXA</strong> was administered prophylactically at the start of the procedure. Inthis case if the patient is bleeding and other relevant clinical factors such as hypothermia, coagulopathy,thrombocytopenia and heparin rebound have been addressed then it may be helpful to administer <strong>TXA</strong> if thepatient is thought to be at risk for fibrinolysis and its associated increased hemorrhage. A Thromboelastograph(TEG) can establish the presence of fibrinolysis in approximately 30 minutes. If there is no detectablefibrinolysis by the TEG then administration of <strong>TXA</strong> would not be expected to help greatly with the bleeding.Conversely, not all patients with measurable fibrinolysis will demonstrate excessive hemorrhage.7: The <strong>TXA</strong> should be discontinued immediately before transport from the OR to the ICU. Stopping the drugwill allow the level to decrease and mitigate the chance of seizures postoperatively. It is strongly re<strong>com</strong>mendedto sedate patients treated with <strong>TXA</strong> postoperatively with propofol as it essentially eliminates the risk of seizurewhile it is running. Exceptions to continuing the <strong>TXA</strong> into the ICU course may include a patient who continuesto be significantly coagulopathic with active hemorrhage or a patient with TEG proven active fibrinolysis.8: Drug delivery: <strong>TXA</strong> is most safely administered using a volumetric pump. Outlined below is an example ofhow to deliver the <strong>TXA</strong> in Drug Delivery Mode.Step 1: Choose the appropriate channel on Alaris pumpand press the OPTIONS button and select AnesthesiaMode if the pump in not already in Anesthesia Mode.Step 2: Select Enable under Anesthesia Mode
Step 3: Select Tranexamic acidStep 4: Select Yes to confirm <strong>TXA</strong> concentration of5000 mg in 250 mL (20 mg/mL)Step 5: Confirm patient weight and drug concentration
References:Ferraris VA, Ferraris SP, Saha SP, et al. Perioperative Blood Transfusion and Blood Conservation in CardiacSurgery: The Society of Thoracic Surgeons and The Society of Cardiovascular Anesthesiologists ClinicalPractice Guideline. Ann Thorac Surg 2007;83:S27-86Kon ZN, Kwon MH, Kallam S, et al. Off-pump coronary artery bypass leads to a regional hypercoagulable statenot detectable using systemic markers. Innovations Phila Pa 2006;1:232–8Desai PH, Kurian D, Thirumavalavan N, et al. A Randomized Clinical Trial Investigating the RelationshipBetween Aprotinin and Hypercoagulability in Off-Pump Coronary Surgery. Anesth Analg 2009;109:1387-1394Verma K, Errico TJ, Vaz KM, Lonner BS. A prospective, randomized, double-blinded single-site control study<strong>com</strong>paring blood loss prevention of tranexamic acid (<strong>TXA</strong>) to epsilon aminocaproic acid (EACA) for correctivespinal surgery. BMC Surg 2010;10:13Berenholtz SM, Pham JC, Garrett-Mayer E, et al. Effect of epsilon aminocaproic acid on red-cell transfusionrequirements in major spinal surgery. Spine 2009, 34(19):2096-103.Koster A, Borgermann J, Zittermann A, Leuth J.U., Gillis-Januszewski T, Schirmer U. Moderate dosage oftranexamic acid during cardiac surgery with cardiopulmonary bypass and convulsive seizures: Incidence andClinical Out<strong>com</strong>e. Br J Anaesth 2012. http://bja.oxfordjournals.org/content/early/2012/09/16/bja.aes310.fullArmellin G, Vinciquerra A, Bonato R, Pittarello D, Giron GP. Tranexamic acid in primary CABG surgery:High verus Low dose. Minerva Anestesiol. 2004: 70(3):97-107