Spontaneous pneumomediastinum without pneumothorax in ...
Spontaneous pneumomediastinum without pneumothorax in ...
Spontaneous pneumomediastinum without pneumothorax in ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
THE NEW ZEALAND<br />
MEDICAL JOURNAL<br />
Journal of the New Zealand Medical Association<br />
<strong>Spontaneous</strong> <strong>pneumomediast<strong>in</strong>um</strong> <strong>without</strong> <strong>pneumothorax</strong> <strong>in</strong><br />
idiopathic pulmonary fibrosis<br />
Martyn P T Kennedy, Ahmed Fahim, Graham Smith<br />
A 58-year-old man with a background of idiopathic pulmonary fibrosis (IPF)<br />
presented with a sudden onset of breathlessness follow<strong>in</strong>g repeated cough<strong>in</strong>g. He was<br />
a life-long non-smoker. On exam<strong>in</strong>ation, there was evidence of extensive<br />
subcutaneous emphysema <strong>in</strong>volv<strong>in</strong>g his neck and chest. He was haemodynamically<br />
stable with oxygen saturations of 95% breath<strong>in</strong>g room air.<br />
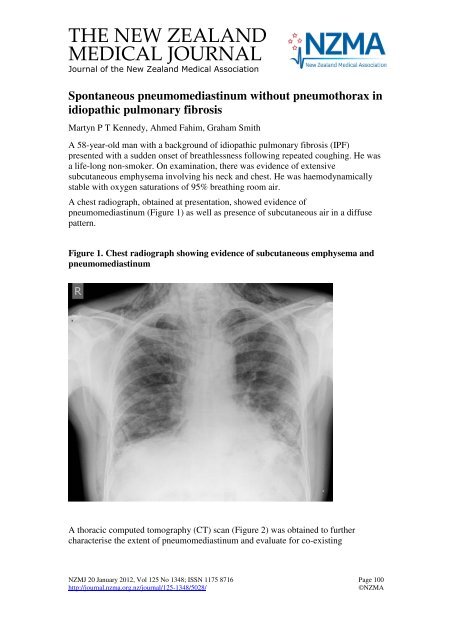
A chest radiograph, obta<strong>in</strong>ed at presentation, showed evidence of<br />
<strong>pneumomediast<strong>in</strong>um</strong> (Figure 1) as well as presence of subcutaneous air <strong>in</strong> a diffuse<br />
pattern.<br />
Figure 1. Chest radiograph show<strong>in</strong>g evidence of subcutaneous emphysema and<br />
<strong>pneumomediast<strong>in</strong>um</strong><br />
A thoracic computed tomography (CT) scan (Figure 2) was obta<strong>in</strong>ed to further<br />
characterise the extent of <strong>pneumomediast<strong>in</strong>um</strong> and evaluate for co-exist<strong>in</strong>g<br />
NZMJ 20 January 2012, Vol 125 No 1348; ISSN 1175 8716 Page 100<br />
http://journal.nzma.org.nz/journal/125-1348/5028/ ©NZMA
<strong>pneumothorax</strong>. The CT scan confirmed the radiographic f<strong>in</strong>d<strong>in</strong>gs of mediast<strong>in</strong>al air<br />
collection with no evidence of either a <strong>pneumothorax</strong> or oesophageal rupture.<br />
Figure 2. Images from a CT scan show<strong>in</strong>g subcutaneous emphysema and<br />
<strong>pneumomediast<strong>in</strong>um</strong> <strong>without</strong> any co-exist<strong>in</strong>g <strong>pneumothorax</strong><br />
NZMJ 20 January 2012, Vol 125 No 1348; ISSN 1175 8716 Page 101<br />
http://journal.nzma.org.nz/journal/125-1348/5028/ ©NZMA
The patient was treated conservatively with spontaneous improvement <strong>in</strong> symptoms<br />
and significant resolution of <strong>pneumomediast<strong>in</strong>um</strong> on follow-up chest radiographs.<br />
This case highlights the importance of consider<strong>in</strong>g spontaneous <strong>pneumomediast<strong>in</strong>um</strong><br />
(SPM) follow<strong>in</strong>g repeated attacks of cough <strong>in</strong> a patient with IPF. Although<br />
<strong>pneumothorax</strong> is commonly associated with SPM, this case suggests that this<br />
diagnosis should be considered even <strong>in</strong> the absence of a <strong>pneumothorax</strong>. The likely<br />
mechanism of the development of SPM is alveolar rupture secondary to <strong>in</strong>creased<br />
<strong>in</strong>trathoracic pressure. 1,2<br />
In this particular case, the <strong>in</strong>creased <strong>in</strong>trathoracic pressure is believed to be the result<br />
of extensive cough. CT scan is the diagnostic modality of choice <strong>in</strong> suspected SPM as<br />
it provides more precise <strong>in</strong>formation regard<strong>in</strong>g the presence, extent of extra-alveolar<br />
air and co-exist<strong>in</strong>g <strong>pneumothorax</strong>. 3<br />
Author <strong>in</strong>formation: Martyn PT Kennedy, SHO; Ahmed Fahim, SpR; Graham<br />
Smith, Consultant; Respiratory Medic<strong>in</strong>e, P<strong>in</strong>derfields Hospital, Mid Yorkshire NHS<br />
Trust, Wakefield, England<br />
Correspondence: Dr Martyn Kennedy, c/o Dr G Smith, P<strong>in</strong>derfields Hospital,<br />
Aberford Road, Wakefield WF1 4DG, UK. Email: martynkennedy@doctors.org.uk<br />
References:<br />
1. Mackl<strong>in</strong> CC. Transport of air along sheats of pulmonic blood vessels from alveoli to<br />
mediast<strong>in</strong>um. Arch Intern Med. 1939;64:913-926.<br />
2. Abolnik I, Lossos IS, Breuer R. <strong>Spontaneous</strong> <strong>pneumomediast<strong>in</strong>um</strong>. A report of 25 cases.<br />
Chest. 1991;100:93-95.<br />
3. Franquet T, Giménez A, Torrubia S, et al. <strong>Spontaneous</strong> <strong>pneumothorax</strong> and<br />
<strong>pneumomediast<strong>in</strong>um</strong> <strong>in</strong> IPF. Eur Radiol. 2000;10:108-13.<br />
NZMJ 20 January 2012, Vol 125 No 1348; ISSN 1175 8716 Page 102<br />
http://journal.nzma.org.nz/journal/125-1348/5028/ ©NZMA