APP1135277_Rice_Grant Proposal
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
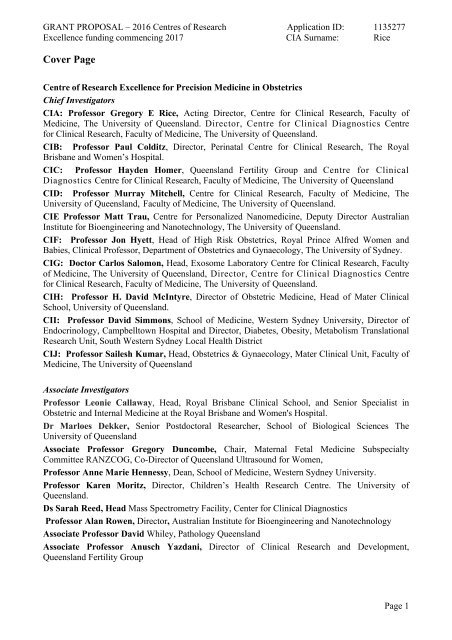
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Cover Page<br />
Centre of Research Excellence for Precision Medicine in Obstetrics<br />
Chief Investigators<br />
CIA: Professor Gregory E <strong>Rice</strong>, Acting Director, Centre for Clinical Research, Faculty of<br />
Medicine, The University of Queensland. Director, Centre for Clinical Diagnostics Centre<br />
for Clinical Research, Faculty of Medicine, The University of Queensland.<br />
CIB: Professor Paul Colditz, Director, Perinatal Centre for Clinical Research, The Royal<br />
Brisbane and Women’s Hospital.<br />
CIC: Professor Hayden Homer, Queensland Fertility Group and Centre for Clinical<br />
Diagnostics Centre for Clinical Research, Faculty of Medicine, The University of Queensland<br />
CID: Professor Murray Mitchell, Centre for Clinical Research, Faculty of Medicine, The<br />
University of Queensland, Faculty of Medicine, The University of Queensland.<br />
CIE Professor Matt Trau, Centre for Personalized Nanomedicine, Deputy Director Australian<br />
Institute for Bioengineering and Nanotechnology, The University of Queensland.<br />
CIF: Professor Jon Hyett, Head of High Risk Obstetrics, Royal Prince Alfred Women and<br />
Babies, Clinical Professor, Department of Obstetrics and Gynaecology, The University of Sydney.<br />
CIG: Doctor Carlos Salomon, Head, Exosome Laboratory Centre for Clinical Research, Faculty<br />
of Medicine, The University of Queensland, Director, Centre for Clinical Diagnostics Centre<br />
for Clinical Research, Faculty of Medicine, The University of Queensland.<br />
CIH: Professor H. David McIntyre, Director of Obstetric Medicine, Head of Mater Clinical<br />
School, University of Queensland.<br />
CII: Professor David Simmons, School of Medicine, Western Sydney University, Director of<br />
Endocrinology, Campbelltown Hospital and Director, Diabetes, Obesity, Metabolism Translational<br />
Research Unit, South Western Sydney Local Health District<br />
CIJ: Professor Sailesh Kumar, Head, Obstetrics & Gynaecology, Mater Clinical Unit, Faculty of<br />
Medicine, The University of Queensland<br />
Associate Investigators<br />
Professor Leonie Callaway, Head, Royal Brisbane Clinical School, and Senior Specialist in<br />
Obstetric and Internal Medicine at the Royal Brisbane and Women's Hospital.<br />
Dr Marloes Dekker, Senior Postdoctoral Researcher, School of Biological Sciences The<br />
University of Queensland<br />
Associate Professor Gregory Duncombe, Chair, Maternal Fetal Medicine Subspecialty<br />
Committee RANZCOG, Co-Director of Queensland Ultrasound for Women,<br />
Professor Anne Marie Hennessy, Dean, School of Medicine, Western Sydney University.<br />
Professor Karen Moritz, Director, Children’s Health Research Centre. The University of<br />
Queensland.<br />
Ds Sarah Reed, Head Mass Spectrometry Facility, Center for Clinical Diagnostics<br />
Professor Alan Rowen, Director, Australian Institute for Bioengineering and Nanotechnology<br />
Associate Professor David Whiley, Pathology Queensland<br />
Associate Professor Anusch Yazdani, Director of Clinical Research and Development,<br />
Queensland Fertility Group<br />
Page 1
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Response to Assessment Criteria<br />
1. Generate new knowledge that leads to improved health outcomes<br />
Pregnancy outcome in Australia<br />
The foundations of health throughout life are laid down during fetal development. Complications of<br />
pregnancy that compromise fetal development have profound effects not only on the immediate<br />
outcomes of pregnancy but also on the life-long disease risk susceptibility of the offspring.<br />
300,000 babies are born in Australia each year. The growth and development of more than 45,000<br />
of these babies is compromised by complications of pregnancy. Complications of pregnancy, such<br />
as: pregnancy-induced maternal high-blood pressure (preeclampsia, PE); pregnancy-induced<br />
diabetes (gestational diabetes mellitus, GDM); small for gestational age (intrauterine growth<br />
restriction, IUGR), stillbirth and preterm birth (delivery before 32 completed weeks of pregnancy,<br />
PTB), result in significant adverse health outcomes for the newborn; an increased short term risk of<br />
mortality and morbidity and an increased life time risk of metabolic and cardiovascular disease. 1-3<br />
Each year in Australia, 150,000 pregnancies are lost before 20 weeks of pregnancy (miscarriage),<br />
2000 are lost after 20 weeks (still birth), 2,500 babies die during the first 28 days of life and 800<br />
more before their first birth day. Poor pregnancy outcome (defined by these data) is a significant<br />
health and economic issue in Australia and, even more so, in developing nations.<br />
In most cases, poor pregnancy outcome is not anticipated or diagnosed early enough to significantly<br />
change health outcomes. Currently available tests are either not of sufficient accuracy for screening<br />
the general obstetric population or lack sufficient evidence-based data to define clinical utility and<br />
justify implementation into standard practice.<br />
Pregnancies resulting from Assisted Reproductive Technologies (ART) also suffer significantly<br />
higher rates of adverse outcomes such as preterm birth and low birthweight. Embryo screening for<br />
the steadily rising ART population offers an opportunity to identify and prevent at-risk pregnancies<br />
at the pre-implantation stage, but remains undeveloped.<br />
Most women who are triaged into high-risk obstetric units on the basis of poor previous obstetric<br />
history ultimately have uncomplicated pregnancies, whilst on the other hand it is those assumed to<br />
be low risk who comprise a large proportion of complicated pregnancies. Thus, critical health care<br />
resources are wasted and those who require high-risk care may not gain access to potential<br />
therapies. Early detection of risk is the first step in implementing efficacious treatment and<br />
improving pregnancy outcomes.<br />
One exception and a proof-of-concept establishing the feasibility of the approach to be used in this<br />
CRE is the work of CI Hyett. CI Hyett has implemented and evaluated first trimester screening for<br />
PE and reduced the prelevance of this complication of pregnancy at the Royal Prince Alfred<br />
Hospital in Sydney. 4 Based on the current performance of the screening test, however, only 1 in<br />
28 women triaged to treatment (i.e. low dose aspirin) would have developed PE. The current<br />
recommendations of the American College of Obstetricians and Gynecologists remain taking a<br />
detailed medical history to assess a patient's risks for developing PE but not using laboratory and<br />
imaging screening tests.<br />
There is a clear and well defined need to further improve screening test performance.<br />
Page 2
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Pregnancy is a stress test for life – a window into future health<br />
What happens during pregnancy informs us about the likelihood of developing adult disease, not<br />
only for the newborn 3 but also the mother. 5,6 Pregnancy, therefore, has been described as a<br />
stress test 7 and a window into future health. 8,9<br />
It is now well established that women who experience complications of pregnancy are at higher risk<br />
of developing obesity, diabetes and cardiovascular disorders in adult life. 10 In response, the<br />
American Heart Association acknowledged PE, GDM and IUGR as pregnancy-related risk factors<br />
for cardiovascular disease in the 2011 update of the Effectiveness-based Guidelines for the<br />
Prevention of Cardiovascular Disease in Women. 11<br />
Women who develop GDM, one of the most<br />
common maternal complications of pregnancy,<br />
have a 4- to 7-fold greater risk of developing type<br />
2 diabetes 12 ; an increased risk of developing<br />
metabolic syndrome 13 ; and a 66% to 85% higher<br />
risk of cardiovascular disease, including coronary<br />
artery disease, myocardial infarction, and/or<br />
stroke. 14 At present, there is a paucity of evidence<br />
with regard to the efficacy of a strategy of early<br />
identification and treatment of GDM prior to 24<br />
weeks of gestation.<br />
Women who develop PE during pregnancy are 4-fold more likely to develop hypertension later in<br />
15 16<br />
life and are twice as likely to develop heart disease, stroke and thrombosis in the future.<br />
Women with a previous history of preterm delivery, stillbirth or fetal growth restriction are<br />
similarly at increased risk of developing cardiovascular disease (~2-fold). 17<br />
Improving health outcomes for mothers and babies is a National priority, particularly for our<br />
indigenous populations (Closing the Gap, Department of Health, 11 October 2016) and remote<br />
communities.<br />
To achieve this objective requires:<br />
“Early detection and treatment may<br />
potentially improve outcomes.<br />
However, there is a dearth of<br />
evidence in this area.”<br />
ADIPS Consensus Guidelines for the<br />
Testing and Diagnosis of<br />
Hyperglycaemia in Pregnancy in<br />
Australia and New Zealand 2014<br />
Co-author CI McIntyre<br />
• more effective means to identify women who are at risk of developing complications of<br />
pregnancy; and<br />
• the implementation of effective prevention and/or intervention strategies.<br />
The earlier we can identify women who are at risk of developing complications of pregnancy, the<br />
greater the opportunity to improve the health outcomes for both mother and baby. This is the<br />
overall, ongoing objective of this CRE for Precision Medicine in Obstetrics.<br />
This CRE will build capacity by establishing a translational pipeline between innovation and<br />
technology intensive entities (AIBN, UQCCR) and clinical practice (including pathology service<br />
delivery, Pathology Queensland). This pipeline will promote clinical engagement, the opportunity<br />
to deliver end-user requirements. It will also provide unique training opportunities, new career<br />
pathways and development of future leadership in obstetric medicine and industry-standard<br />
translational research.<br />
Page 3
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
By investigating new classes of biomarker (exosomal) and implementing new genomic testing<br />
approaches (Single Drop DNA analysis); developing new multiple biomarker algorithms for risk<br />
assessment during pregnancy; and delivering clinical and health economic outcome data on their<br />
performance, this CRE will create tangible outcomes within five main aims:<br />
Generate new knowledge on the role of exosome signalling in embryo development by<br />
characterising developmental changes in the packaging and release of exosomes from blastocysts<br />
and the effects of blastocyst-derived exosome on decidua phenotype and implantation efficiency<br />
(CIs Homer, Salomon, Trau, Colditz, <strong>Rice</strong>; AIs Yazdani, Rowan). The data obtained from these<br />
studies will ultimately contribute to the development of new precision medicine management<br />
strategies for improving embryo quality, implantation efficiency and pregnancy and neonatal<br />
outcome.<br />
Identify and characterise biomarkers of complications of pregnancy that are present in biofluids of<br />
pre-symptomatic women that can be incorporated into existing or novel screening tests to improve<br />
risk assignment (positive predictive value) and patient triage to appropriate treatment (CIs Hyett,<br />
McIntyre, Kumar, Simmons, Salomon, Trau, Mitchell, <strong>Rice</strong>; AIs Moritz, Duncombe, Reed).<br />
Studies will be conducted within the Centre for Clinical Diagnostics (a NATA accredited<br />
ISO17025, medical device development environment) in accordance with ISO13485 guidelines.<br />
Develop and clinically evaluate a new generation of first trimester screening tests for GDM and PE<br />
by conducting prospective Phase 3 biomarker and clinical intervention trials translating research<br />
outcomes into clinical applications (CIs Hyett, McIntyre, Simmons, Kumar, Salomon, Trau,<br />
Mitchell, <strong>Rice</strong>; AIs Moritz, Duncombe, Reed).<br />
Facilitate collaboration across three national universities (The University of Queensland, University<br />
of Sydney, Western Sydney University), four hospitals (Royal Brisbane & Women’s Hospital,<br />
Mater Hospital, Royal Prince Alfred Hospital, Campbelltown Hospital) an international hospital<br />
network (Ochsner Health System, New Orleans. La, USA) and a State Pathology Department<br />
(Pathology Queensland). These collaborations will develop the health and medical research<br />
workforce in clinical obstetrics and neonatology, reproductive medicine and assisted reproductive<br />
technologies, in vitro diagnostics, nanotechnology and molecular biology.<br />
Inspire and train young clinicians and scientists to use the latest technological advances in<br />
reproductive medicine within an international industry standard environment (ISO17025,<br />
ISO13485) that focuses on end-user requirements and translational improvement in healthcare and<br />
commercial enterprise.<br />
The CRE team has the expertise, experience and capacity to deliver and implement new pregnancy<br />
screening tests that will improve the allocation of health care services and reduce the incidence and<br />
severity of complications of pregnancy and, thereby, improve outcomes for both mother and baby.<br />
Key Programs Conducted by the CRE<br />
This CRE for Precision Medicine in Obstetrics will geerate new knowledge, build translational<br />
capacity by creating a translational pipeline between T1 in-human medical device development, T2<br />
clinical evaluation of In Vitro Diagnostics, T3 clinical health outcomes and T4 health economic<br />
data to inform policy change. These objectives will be achieved within four CRE Core Programs.<br />
Page 4
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
PROGRAM 1: Exosomal Signalling In Pregnancy<br />
Program 1 is a discovery program that seeks to increase knowledge about the role of exosomal<br />
signalling in cell-to-cell communication during normal pregnancy and its complications. The<br />
program will be conducted in collaboration between AIBN and the UQ Centre for Clinical<br />
Diagnostics; the latter is one of only two such facilities in Australia that are NATA accredited for<br />
ISO17025 (General requirements for the competence of testing and calibration laboratories,<br />
codified for research).<br />
Research Questions<br />
• To characterize developmental changes (up to day 5) in the release and content of exosomes<br />
from human blastocysts, in vitro.<br />
• To establish the mechanism(s) by which blastocyst-derived exosomes interact with decidua<br />
cells; exosomes uptake and signal delivery.<br />
• To define the effects of blastocyst-derived exosomes on decidua cell phenotype and<br />
blastocyst attachment.<br />
Objectives: To define the role of exosomal signalling during embryo development. In partnership<br />
with the Queensland Fertility Group (AI Yazdani), Program 1 will deliver new knowledge that will<br />
allow the development of novel methods for non-invasive embryo testing (see Program 2) and<br />
ultimately the development of new treatments to improve implantation efficiency. The Program<br />
utilises established methodologies and expertise developed by the CIs and AIs in the study of<br />
human placental exosome biology (CIs: Salomon, <strong>Rice</strong>, Mitchell; AIs: Duncombe, Reed).<br />
Study Rationale: Exosomal signalling is a formative and burgeoning area of clinical research and<br />
one that offers great opportunity. Opportunity not only in terms of generating new knowledge<br />
about a novel cell communication system (i.e. exosomal signalling) but also in terms of identifying<br />
tissue- specific biomarkers and in developing naïve and engineered endogenous exosome-, and<br />
synthetic exosome-based therapeutics and drug delivery systems. These opportunities arise as a<br />
result of a paradigm shift in our understanding of how cells communicate and, in particular, the<br />
recognition of the role of exosomes in intercellular signalling. 18 Exosomes are small (40-100 nm),<br />
stable lipid bilayer nanovesicles that are formed by the inward budding of multivesicular bodies. 19<br />
Exosomes are package with tissue specific signalling molecules and once released are capable of<br />
regulating proximal and distal cell function. Exosomes are a unique source of biomarkers,<br />
therapeutics and theranostics as their content is stabilised and protected against enzymatic<br />
degradation; they are biocompatible, permeable to biological barriers; of low toxicity and low<br />
immunogenicity; able to be loaded with specific signalling molecules; and may be re-engineered or<br />
have molecules addressed to their surface, conveying exosome targeting capabilities to cells bearing<br />
cognate receptors. 20<br />
There is a paucity of data on exosomal signalling by the blastocyst and the functional role of<br />
exosomes in embryo development. The aim of this Core Program is to advance understanding of the<br />
role of exosomes in embryo development. This will result in the development of more informative<br />
diagnostics and opportunities for new therapeutic interventions.<br />
Proposed Research: In vitro discovery studies will be conducted to characterise: the release<br />
(number and size distribution) of exosomes from human blastocysts using nanoparticle tracking<br />
analysis (CI Salomon) 21 ; exosome protein (AI Reed, SWATH tandem mass spectrometry 22 and<br />
miRNA content 23 ; and the effect of blastocyst-derived exosomes on endometrial and endothelial<br />
cell phenotype using real-time cell imaging. 24 Exosome uptake by target cells will be assessed<br />
fluorescently-labelled exosomes (PKH67 green 25 ). Effects on cell phenotype will be defined using<br />
Page 5
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
real-time cell imaging 25 ; discovery-based proteomic analysis (Sequential Windowed Acquisition of<br />
All Theoretical Fragment Ion Mass Spectra, SWATH MS/MS; AI Reed 22 ) and targeted genomic<br />
methylation profiling (CI Trau) 26 , respectively. Studies will utilise human embryo-conditioned<br />
medium that we have obtained from our collaborative partner Queensland Fertility Group (AI<br />
Yazdani). The effects of blastocyst-derived exosomes on embryo attachment and invasion will be<br />
performed using in vitro pre-clinical models (CIs Mitchell and Homer). 27,28<br />
Significance: This T1 CRE Program will build capacity and generate knowledge that will inform<br />
clinical practice via the identification of potential biomarkers of embryo quality and consequently<br />
improving the rate of successful pregnancy. The Program is a direct collaborative engagement with<br />
healthcare service provider (Queensland Fertility Group), designed to meet a specific clinical need.<br />
PROGRAM 2: Non-invasive embryo testing<br />
Program 2 is a phase 2 biomarker trial; prospectively collected, retrospectively stratified cohort<br />
study) to clinically evaluate non-invasive embryo screening.<br />
Research Question: Are biomarkers (exosomal and genomic) present in day 3 and/or day 5 human<br />
embryo-conditioned media that correctly classify embryo quality based on pregnancy and neonatal<br />
outcome?<br />
Objectives: To establish the efficacy of exosomal and genomic biomarkers to correctly classify<br />
embryo quality on the basis of pregnancy and neonatal outcome.<br />
Rationale: Early prediction of the viability of in-vitro developed embryos before the transfer to a<br />
recipient still remains challenging. Presently, the predominant non-invasive technique for selecting<br />
viable embryos is based on morphology, where parameters such as rates of cleavage and blastocyst<br />
formation as well as developmental kinetics are evaluated, mostly subjectively. The per-oocyte<br />
pregnancy rate during IVF is surprisingly low with 7% or less of all oocytes producing a live-birth.<br />
Because of this low efficiency, multiple cycles of IVF are often required and in many areas of the<br />
world, multiple embryos are replaced leading to unacceptable rates of high-risk multiple<br />
pregnancies. Techniques capable of identifying the best quality blastocysts would greatly<br />
streamline and increase efficiency of IVF practice.<br />
Study Design: The clinical utility of biomarkers identified in Program 1 (including exosomal<br />
biomarker already identified in preliminary studies) will be determined in a phase 2 biomarker trial.<br />
Embryo-conditioned medium (n=2000) will be prospectively collected (QGF, AI Yazdani) and then<br />
retrospectively stratified on the basis of pregnancy and neonatal outcome. The efficiency of<br />
biomarkers to correctly classify cases will be established.<br />
Study endpoints: The primary endpoint (and stratification criterion of the study) will be live birth at<br />
term with a composite perinatal/health/neurodevelopment endpoint described in more detail below.<br />
Secondary endpoints are: the proportion of complicated vs uncomplicated pregnancies (i.e. GDM,<br />
PE, IUGR, spontaneous preterm birth and early pregnancy biomarkers).<br />
Newborn outcomes and screening: Each of the pregnancy cohort Programs in this CRE has<br />
newborn outcome as an additional final target for assessment of pregnancy outcome. Important<br />
Page 6
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
major newborn outcomes will be assessed in the following established ways which take into<br />
account a balance of data quality, cost, depth and availability of normative/comparative data:<br />
1. Birth data from the Perinatal Data Collection: livebirth/stillbirth, gestational age, growth<br />
parameters, need for resuscitation, Apgar scores, admission to neonatal nursery<br />
2. Routinely collected data to age 2 years: Medicare data (GP visits), Qld Hospital admitted<br />
patient data collection, QHAPDC (hospital admission diagnoses)<br />
3. Assessment at age 2 years: Bayley III assessment (neurodevelopment), medical assessment,<br />
health questionnaire, anthropometric measurements.<br />
These data sources will be used to define (i) a composite endpoint of low/high morbidity required in<br />
individual studies above, (ii) neurodevelopmental outcome, (iii) disease diagnostic categories, (iv)<br />
health service utilisation.<br />
Newborn screening is currently performed for a limited range (typically < 20) of genetic disorders<br />
with no two countries' screening programs the same. 29 Progress in technology has led to an increase<br />
in the number of conditions screened for, with tandem mass spectrometry which detects abnormal<br />
metabolites, now the dominant technology. Agreed criteria for screening include: a demonstrable<br />
benefit from early diagnosis; a suitable test with high specificity and sensitivity; a system of<br />
confirmation of results, counselling, treatment and follow-up; and the balance of harms and benefits<br />
is positive. Whole genomic testing is now available at a rapidly falling cost. However, its possible<br />
application to newborn screening poses a complex set of ethical, legal, and societal questions,<br />
particularly with the identification of mutations without knowledge of whether they represent<br />
pathological or benign polymorphisms.<br />
In this context to capture the best of new technology and to avoid the issues raised by whole<br />
genome screening, we propose a screening development and trial using a new relatively low cost<br />
technology developed by CI Trau to screen for 96 (as opposed to the current < 20) known genetic<br />
mutations that best meet agreed screening criteria. We will develop a 96-well plate using the<br />
multiplex PCR/SERS method 30 and evaluate it for its suitability to replace and enhance current<br />
newborn screening.<br />
Sample Size Determination: Sample sizes were established using Blume’s method 11 to allow 80%<br />
power to detect a 0.10 difference between an AUC of the new screening approach and current<br />
morphology-based embryo assessment.<br />
Analysis of Diagnostic Efficiency Outcomes: Statistical analyses have been developed to assess the<br />
hypothesis that a multimarker new screening test has greater discriminatory power to correctly<br />
classify embryos that result in normal pregnancy and neonatal outcome in comparison with current<br />
morphology based embryo assessment. Diagnostic performance will be summarized through the<br />
calculation of ROC curves, and by calculation of the area under the ROC curve (CI <strong>Rice</strong> 31,32 ). The<br />
difference in AUC between the diagnostics will be tested using a bootstrap procedure.<br />
Significance: The identification of biomarkers in embryo-conditioned media that are predictive of<br />
pregnancy outcomes will facilitate the development of non-invasive tests to aid in the assessment of<br />
embryo quality for assisted reproductive technologies.<br />
Page 7
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
PROGRAM 3 - First trimester Screening<br />
Program 3 will establish the classification efficiency of exosomal and genomic biomarkers present<br />
in maternal plasma at 12-14 week of pregnancy for complications of pregnancy. The data obtained<br />
will inform the composition of the screening algorithms used in Program 4.<br />
Research Question: To determine the performance of exosomal and genomic biomarkers present<br />
in maternal plasma, at 12 to 14 weeks of pregnancy and to classify women who have complicated<br />
and non-complicated pregnancy outcomes. Based on the outcome of these analyses, biomarkers<br />
will be selected for inclusion in multivariate screening assays to be used in Program 4.<br />
Study Rationale: Early identification of women at risk of developing complications of pregnancy<br />
is the first step in reducing the prevalence and severity of such complications. Currently available<br />
first trimester tests are either not of sufficient accuracy for first trimester of population-based<br />
screening or lack sufficient evidence-based data to define clinical utility and justify implementation<br />
into standard practice. 33 Our team has been developing multiple biomarker tests to identify women<br />
at 11-14 weeks of pregnancy who are at increased risk of subsequently developing complications of<br />
pregnancy. In order to introduce these tests into routine screening for the general obstetrics<br />
population, robust estimates of their classification efficiency and prognostic performance must be<br />
established. Thus, the primary objectives of Program 3 are to determine the classification<br />
performance of early-pregnancy screening tests to identify women at risk of developing<br />
complications of pregnancy and to identify and clinically evaluate additional exosome-associated<br />
and genomic biomarkers for inclusion in the screening test to improve test performance. The<br />
program is innovative in the development and application of placenta-specific exosomes for in vitro<br />
diagnostic screening tests and the application of high throughput and low cost genomic biomarker<br />
screening.<br />
Study Design: This is a multi-centre Phase 2 biomarker trial conducted at the RBWH, Mater<br />
Hospital, Campbelltown Hospital and the RPA Hospital. We are already screening 2000 women a<br />
year and store serum samples post first trimester analysis and collect pregnancy outcome data to<br />
describe five common adverse outcomes: spontaneous PE (early and late), GDM, PTB, IUGR. It is<br />
planned that 4758 women attending obstetric clinics will be recruited into this study. The<br />
involvement of four recruitment sites allows validation across different patient populations.<br />
Following recruitment and the recording of demography, past medical/surgical history and current<br />
medications, study participants will have a blood specimen collected and stored. Samples will be<br />
retrospectively stratified into two groups viz normal pregnancies and pregnancies complicated by<br />
GDM, PE or preterm birth. Plasma samples will be assayed for candidate biomarkers (i.e.<br />
biomarkers for which we have already completed proof-of-principle studies or are currently part of<br />
an existing algorithm (i.e. PE algorithm - CI Hyett). In a discovery component of this program,<br />
additional exosomal and genomic biomarkers present in first trimester plasma will be evaluated for<br />
inclusion in risk assessment algorithm. Classification performance will be summarized through<br />
ROC curve analysis and by calculation of the area under the ROC curve. 12<br />
Primary Endpoint: The primary study endpoint is the comparison of the area under the receiveroperator-characteristic<br />
curve for the new algorithms verse the standard risk assessment guidelines<br />
for identification of women at risk of developing complications of pregnancy.<br />
Sample Size Determination: Sample size was established using Blume’s method 11 to allow, at<br />
least, 80% power to detect a 15% difference between AUCs [based on a sample size calculation<br />
using P1 0.235 | P2 0.01475 | alpha=0.05 | 1-beta = 0.8 and assuming 20% women defined as high<br />
risk of early PE/late PE/IUGR or GDM through screening].<br />
Page 8
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Exosome Isolation and Processing: An exosome-enriched fraction will be prepared from clinical<br />
samples using ultra- and nano-filtration and disruption and solubilisation of exosomes. This<br />
extraction method allows direct translation of assays into routine clinical pathology platforms. The<br />
resultant soluble phase is available for direct assay on existing medical device approved, pathology<br />
platforms.<br />
Early pregnancy Screening Assay Exemplar: In proof-of-principle studies for GDM screening<br />
completed to date, we have identified a panel of 5 exosomal biomarkers (exosome-associated IL6,<br />
IL8, IL10, IFN γ, TNFα) that are strongly correlated with the subsequent development of<br />
gestational diabetes. First trimester HbA1c and Oral Glucose Tolerance Test will be determined on<br />
existing hospital pathology platforms. Furthermore, each assay will include defined positive and<br />
negative controls as well as internal standards.<br />
Receiver-operator-characteristic curve analysis: The ROC curve for the reference classification<br />
will be based simply on the RANZCOG and ACOG risk assignment guidelines. ROC curves for<br />
new classification algorithms will be based on the predicted probability of membership of the<br />
specific complication of pregnancy group. The area under the ROC curve (AUC) will be calculated<br />
using the Wilcoxon statistic. 34 The difference in AUC between methods will be tested using a<br />
bootstrap procedure. 35 Results from individual algorithms will be aligned with clinical data and<br />
pregnancy outcome and their performance compare to that of the current practice high assessment.<br />
That is, in the case of PE, the algorithm used by CI Hyett or previous obstetrics history and known<br />
risk factors for GDM and preterm birth. Tests will be developed in compliance with GLP<br />
principles as codified by ISO17025 and ISO13485, thus, enhancing translational and<br />
commercialisation opportunities. The final product will be a Class II medical device that will be<br />
commercialised with our industry partner; SeraCare LLC and Pathology Queensland (AI: Whiley).<br />
Significance: The outcome of this study will be the delivery of Level 2 clinical evidence on the<br />
performance; providing robust estimates of the classification performance (i.e. case-control cohort<br />
analysis) of multivariate models for the early pregnancy identification of women who subsequently<br />
develop PE, GDM or preterm labour. The outcome of this Program will inform Program 4 Triage to<br />
Treatment. The significance of this study resides in the delivery of a higher performance, single<br />
modality screening for early pregnancy risk assignment for complications of pregnancy that may be<br />
Page 9
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
implemented within routine pathology. The data obtained will inform and facilitate the development<br />
and clinical uptake early pregnancy screening and triage to treatment.<br />
Program 3 formalises an In Vitro Diagnostic medical device development core that is NATA<br />
accredited for ISO17025, complies with ISO13485. During the life of the CRE, application will<br />
also be made for accreditation for ISO15198 (Medical Testing). As such, this Program will be the<br />
only such accredited facility in Australia. It will provide a unique clinical research, development<br />
and training environment for scientific and clinical practitioners and an enabling capacity for<br />
leadership development.<br />
PROGRAM 4: Triage to High-risk Management<br />
First trimester screening algorithms for PE, IUGR and GDM have already been developed. There<br />
are a number of processes that need to be completed before these tools for individualised precision<br />
medicine can be robustly applied to population based screening. First, continued algorithmic<br />
development with inclusion of other biomarkers (Program 2) will improve screening efficacy<br />
(sensitivity, specificity and predictive values) and facilitate development of algorithms for preterm<br />
birth. Second, these algorithms need validation in separate populations to demonstrate applicability<br />
and consistency in performance. Third, the impact of preventative interventions applied based on<br />
the findings of first trimester screening (and therefore the value of prediction and prevention) needs<br />
to be demonstrated. These processes can potentially be completed simultaneously in multicentre<br />
randomised controlled trials that enrol patients prior to screening, randomising them to an<br />
intervention on the basis of the initial predictive test result.<br />
Research Questions:<br />
• Can the performance of current first trimester screening algorithms be reproduced in<br />
multiple centres with different population groups?<br />
• Can screening efficacy be improved by inclusion of other exosome or genome derived<br />
biomarkers?<br />
• Are preventative interventions (aspirin for PE and IUGR; metformin for late PE; diet and<br />
lifestyle advice / metformin / probiotics for GDM; progesterone / cerclage for preterm<br />
labour) effective in reducing disease prevalence for women defined as being at high risk of<br />
an adverse pregnancy outcome?<br />
Study Rationale: There is a clear need to collect more evidence-based data to define the clinical<br />
utility of first trimester risk assignment algorithms and to examine the impact of preventative<br />
therapeutic interventions. We have already developed multivariate algorithms to classify risk for<br />
subsequent development of PE, IUGR and GDM. The tests can variously be criticised for poor<br />
sensitivity (IUGR, late onset PE) and/or positive predictive value (early onset PE) and may be<br />
improved by including exosomal biomarkers or genomic markers. Novel algorithms, based on<br />
inclusion of these factors, can be compared to our current standards by comparing test performance<br />
through calculation of screening efficacy (sensitivity and specificity and positive and negative<br />
predictive values) and receiver operator characteristic curve analysis. Screening and identification<br />
of risk is only of value if preventative strategies are available that improve health outcomes. A<br />
number of interventions that prevent PE/ IUGR, GDM and spontaneous preterm birth have been<br />
proposed. Application is typically impacted by poor prediction of a high-risk group. The combined<br />
prediction and prevention strategy therefore needs assessing through a multicentre randomised<br />
controlled study.<br />
Page 10
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Study Design: This is a multi-centre clinical trial that is to be conducted at the Royal Brisbane and<br />
Women’s Hospital and Mater Hospital, Brisbane; Campbelltown Hospital; and the Royal Prince<br />
Alfred Hospital, Sydney. Women will be randomised to intervention or control arms. In the<br />
intervention arm biomarker-stratified analysis will be used to predict risk of PE, IUGR and GDM<br />
and high risk women will be treated with the intention of reducing the prevalence of disease. In the<br />
control arm, the data for biomarker –stratified analysis will be collected (and risks calculated after<br />
delivery) and pregnancies will be managed according to normal protocols. The primary outcome<br />
measure will be a composite of the prevalence of early and late onset PE, IUGR and GDM. The<br />
baseline prevalence of these disorders is 23.5% [0.5% early PE +3.0%late PE +5% IUGR + 15%<br />
GDM] and, based on available data of the effectiveness of first trimester screening and prevention<br />
strategies we anticipate a reduction to a prevalence of 14.75% [0.25% early PE +2.0% late PE +<br />
2.5% IUGR +10% GDM] (a 37% reduction in prevalence of disease). Demonstrating this<br />
difference requires randomisation of 732 women to intervention / control arms which, based on a<br />
20% screen positive rate and a 30% default rate in recruitment will require enrolment of 4758<br />
women in the screening program [based on a sample size calculation using P1 0.235 | P2 0.01475 |<br />
alpha=0.05 | 1-beta = 0.8 and assuming 20% women defined as high risk of early PE /late PE /<br />
IUGR or GDM through screening]. Analysis of data collected in women randomised to no<br />
intervention will allow validation and improvement of screening algorithms and the development of<br />
a validated algorithm for prediction of preterm birth that can be tested for preventative efficacy at a<br />
later date.<br />
Sample Size: Determination: Sample sizes were established using Blume’s method to allow, at<br />
least, 80% power to detect a 15% difference between AUCs.<br />
Significance: The successful completion of this study will provide Level III evidence for the<br />
implementation of early pregnancy screening for PE and permit the robust assessment of the<br />
efficacy of treatments for the prevention of PE, IUGR and GDM. Analysis of data collected in<br />
women randomised to no intervention will allow validation and improvement of screening<br />
algorithms for these complications of pregnancy as well as for preterm birth.<br />
Page 11
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
2. Promote effective transfer of research outcomes into health policy and/or practice<br />
This CRE increases capacity and research translation by bring together an exceptional<br />
multidisciplinary team who are nationally and internationally recognised healthcare professionals<br />
and researchers. The team is ideally placed to develop and implement new screening applications<br />
and medical devices into practice and to champion the update of practice and policy change.<br />
The governance structure of the CRE will include a Board of Management (CIs, + UQCCR Quality<br />
Assurance Office + Admin Officer), The Board will provide strategic planning and achievement of<br />
project KPIs. CRE Programs will be managed under an international quality management system<br />
and in compliance with FDA 21 CRF part 820. The ongoing review requirements of is code will be<br />
the responsibility of the Clinical Review Committee (McIntyre, Simmons, Colditz, Callaway,<br />
Hennessy + UQCCR QU officer + Health Economist).<br />
The Centre for Clinical diagnostics has already established an Industry Advisory Committee<br />
(Chaired by Prof Maree Smith, UQ). This committee will also facilitate and provide advice<br />
regarding industry engagement, CRE placement and career development. The currently community<br />
engagement activities of CRE members will be consolidated within the governance structure of the<br />
CRE to further enhance educational and awareness opportunities.<br />
The CRE will promote the transfer of research outcomes into health policy and practice as follows:<br />
2.1 The development and evaluation of new In Vitro Diagnostic screening tests for regulatory<br />
agency approval is requisite to implementation into practice. This will be achieved through the<br />
engagement of the CRE’s Biomarker Discovery and IVD Development capacity within the<br />
AIBN (Trau, Rowan), the Centre for Clinical Diagnostics (<strong>Rice</strong>, Salomon, Mitchell, Reed) and<br />
Pathology Queensland (Whiley) with Clinician Research teams directly engaged in high-risk<br />
patient management and the evaluation of new practice and policy - ART (Homer, Yazdani);<br />
complications of pregnancy (Hyett, McIntyre, Simmons, Kumar, Moritz, Duncombe); and<br />
pregnancy and neonatal outcome (Colditz, Moritz). As the IVDs are developed in compliance<br />
with ISO13485, they would be suitable for direct implementation within pathology services,<br />
such as Pathology Queensland or as niche diagnostics within the Centre for Clinical<br />
Diagnostics (once accredited for ISO15189) and be available for patient management. The<br />
intended label use of the tests (i.e. the uses submitted to TGA and/or FDA for approval as a<br />
Class II medical device, 510K submission) is as an IVD MIA to aid in the diagnosis of<br />
complications of pregnancies. Our team has a well-established track record in: the diagnosis<br />
and clinical management of complications of pregnancy, the discovery of biomarkers (using<br />
both protein display technologies and mass spectrometry-based approaches) 36-38 ; exosome<br />
biology 39,40 , in the development and evaluation of in vitro diagnostics 31 ; in the collection<br />
large pregnancy cohort 41 ; and in commercialisation and delivery of new diagnostics to market.<br />
2.2 Generation of technology advances, intellectual property and patents. It is anticipated the<br />
CRE will generate substantive advances in the development of devices and applications for<br />
rapid and or point-of-care use. Such devices would include, for example, hand-held devices for<br />
single drop DNA neonatal screening and/or embryo quality. New screening algorithms for<br />
assessing embryo quality and the risk of complications of pregnancy that have been<br />
appropriately evaluated and deliver increased sensitivity and specificity would represent<br />
significant intellectual property and the basis of patent applications. CRE members have a<br />
strong track record in patent development and commercialisation (e.g. Rowan, Trau, Homer,<br />
<strong>Rice</strong>). The development of new medical devices that more effectively informs the allocation<br />
of health care resources and patient management is a primary practice outcome of this CRE.<br />
Page 12
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
2.3 Best Practice Integrated Pregnancy Care Service. In addition, to the traditional modes of<br />
research outcome transfer, including: publication, profession and lay communications; patent<br />
submission; influence in peak professional bodies, this CRE will implement its research<br />
findings and education and training principles by establishing a best practice integrated<br />
pregnancy care service. Through its Clinical Practice Advisory Committee (Hyett, McIntyre,<br />
Simons, Colditz, Hennesey, Dumcombe, CEO, Health Economist, QA Officer, Project Officer)<br />
the CRE will deliver an iconic integrated pregnancy care service to deliver a best practice highrisk<br />
pregnancies care model. The healthcare model will dynamically and directly incorporate<br />
robustly validated clinical research advances into practice and provides a unique platform for<br />
workforce training and development. The Service will be coordinated by an independent web<br />
presence and serve not only as a referral portal for high-risk management but also as an enduser<br />
(community) education and awareness instrument.<br />
2.4 Health Economics and Policy Unit With the successful development of more effective<br />
screening test, the demonstration of clinical outcome benefit, the CRE’s Health Economics and<br />
Policy Unit (Health Economist, CEO, QA Officer, CRE Project Office) will generate health<br />
economic analyses for each of the practice changes supported by the work of the CRE<br />
enterprise and engage with the professional colleges and the TGA to provide an economic<br />
rationale for change. The Unit will facilitate and support T4, population-based activity that will<br />
bring the tests and the applied knowledge accrued under Programs 1, 2, 3 and 4 to<br />
implementation in the public health sphere. In addition, the Unit will conduct analyses of the<br />
economic impact of pre-clinical data failure in Australia and aid in generating a green paper on<br />
the Research Quality in Australia to enable an informed review of research quality management<br />
across the sector.<br />
2.5 Clinical and Research Champions Change in clinical practice and ultimately policy not only<br />
requires robust clinical evidence but “champions of change”; clinicians and scientists who are<br />
able to community the benefit of change in the health care system to their peers. Each CRE CI<br />
will be a change champion for the CRE research outcomes and leverage their professional<br />
networks as follows:<br />
2.5.1 Biomarker discovery and identification, development of in vitro diagnostics for clinical<br />
evaluation, validation and regulation will be championed by the AIBN- and UQCCR-based<br />
team of CIs <strong>Rice</strong>, Mitchell, Trau, Salomon, Rowan. The ISO17025 and ISO13485<br />
accredited environment enables the production of robust, reproducible industry-ready<br />
findings that will feed directly into a translational pathway. CI-<strong>Rice</strong> has served in leadership<br />
roles with the Australian Perinatal Society, the Perinatal Society of Australia & New<br />
Zealand the International Federation of Placenta Associations. CI-<strong>Rice</strong> is well placed to<br />
implement processes to ensure research integrity and alignment of academic research with<br />
industry standards to improved translational efficiency. CI-Mitchell is President Nominee<br />
of The Society for Reproductive Investigation in 2016 and will chair the Society’s annual<br />
meeting in Paris in 2019. He is Fellow ad eundem, Royal College of Obstetricians and<br />
Gynaecologists. CI-Mitchell has been at the forefront of organising global approaches to the<br />
issues of prematurity and stillbirth and has been invited speaker at the GAPPS International<br />
Conference on Prematurity and Stillbirth and March of Dimes/Burroughs Wellcome<br />
Meetings. CI-Salomon is a member of the Australian and New Zealand Placental Research<br />
Association, the International Society of Extracellular Vesicles, the Australasian Diabetes in<br />
Pregnancy Society and Society for Reproductive Investigation. CI-Salomon is a board<br />
member of the International Federation of Placenta Association and an editorial board<br />
member of The Journal of Reproductive Medicine, Gynaecology & Obstetrics. The<br />
UQCCR-based team will work closely with their UQ colleague, CI-Trau, Professor Matt<br />
Trau is currently a Professor of Chemistry at The University of Queensland (UQ) and<br />
Deputy Director and co-founder of the Australian Institute for Bioengineering and<br />
Page 13
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Nanotechnology. Prof Trau’s expertise are in nanobiotechnology, materials science,<br />
biomarkers, diagnostics, and personalised medicine. Matt’s involvement in the CRE is<br />
crucial to the development and application of new and innovative technologies in obstetrics<br />
medicine.<br />
2.5.2 Screening for early identification of PE will be championed by CI-Hyett. In addition to the<br />
largest public obstetric screening service in Australia that CI-Hyett runs, he will progress<br />
uptake through his professional network that includes his membership of the British Royal<br />
College of Obstetricians & Gynaecologists and NSW Commission Maternal and perinatal<br />
RCA Review Committee. CI-Hyett is Deputy Chair of Royal Australian and NZ college of<br />
Obstetricians & Gynaecologists, Education Subcommittee chair of the International Society<br />
in Obstetrics and Gynaecology, member of the Australian Pre-eclampsia Research Network<br />
and the Impact group that co-ordinates multi-centre RCTs in Australia and New Zealand<br />
Board member of Fetal Medicine Foundation, (UK) and member of the New Zealand<br />
Ministry of Health Down's syndrome screening technical support group. CI-Hyett is<br />
regularly invited to speak to international perinatal societies and has addressed International<br />
Federations of Placental Associations’ World congress in Fetal Medicine<br />
2.5.3 Screening for early identification of GDM will be championed by CIs-McIntyre and<br />
Simmons who have worked together for over 15 years. CI’s-McIntyre and Simmons hold<br />
honorary/ordinary membership of Diabetes in Pregnancy Study Group of the European<br />
Association for the study of Diabetes and are members of Australian Diabetes Society,<br />
Australasian Diabetes in Pregnancy Society, and American Diabetes Association, CI<br />
McIntyre is also a member of Society for Obstetric Medicine Australia and New Zealand<br />
and FIGO (International Federation of Gynaecology and Obstetrics), and CI Simmons is a<br />
member of the European Association for the study of Diabetes and Diabetes UK. Both of<br />
these CI’s have been president of the Australasian Diabetes in Pregnancy Society and Co-<br />
Chaired the [Australian] National Diabetes in Pregnancy Advisory Committee. CI McIntyre<br />
also maintains clinical involvement as Director of Obstetric Medicine at Mater Health<br />
Services and Head of the Mater Clinical School of the University of Queensland. Professor<br />
McIntyre is currently the Chair of the International Association of Diabetes in Pregnancy<br />
Study Groups (IADPSG). Through these networks CI-McIntyre has a track record of having<br />
contributed to the definition of priorities for the care of women with diabetes before, during<br />
and after pregnancy. CI-Simmons maintains clinical involvement as Head of the<br />
Campbelltown Hospital adult, paediatric and surgical endocrinology services, Chair of the<br />
Campbelltown Hospital Clinical Council and Chair of the Campbelltown Hospital Research<br />
Committee. CI-Simmons was also Co-Chair, NZ National GDM Working Group (2006);<br />
Diabetes UK Health Professional Education Chair (2010-2014); member, Mid Essex<br />
Clinical Commissioning Group (2013-2014); Deputy Divisional Director, Division of<br />
Medicine, CUH (2011-2014). While in Cambridge, besides being diabetes clinical lead, he<br />
was involved in the local diabetes network chairing the referral pathways and IT working<br />
groups. He has provided key data on the epidemiology of diabetes in the UK, Australia<br />
(including as a member of The Australian and NZ Diabetes and Cancer Collaboration) and<br />
New Zealand with studies of up to 100,000 participants, which continue to be used as source<br />
data in policy documents.<br />
2.5.4 Screening tests that contribute to the implementation of precision medicine in obstetrics to<br />
improve pregnancy and neonatal outcome will be championed by CIs-Colditz and Kumar.<br />
CI-Colditz is a practising neonatologist and his intellectual leadership is recognised at local,<br />
state and national levels: e.g. Chair QLD Clinician Scientists Assoc., senior roles in the<br />
Division of Paediatrics and Child Health within the Royal Australasian College of<br />
Physicians (President-elect, Chair of Research Committee, member of Council, member of<br />
Executive) as well as in the Royal Australasian College of Physicians (Chair, Research<br />
Page 14
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Committee, Director/board member RACP), member QLD Maternal and Perinatal Quality<br />
Council, Chair QLD Congenital Malformations Committee, and Leader State Clinical<br />
Guideline on Neonatal Seizures. CI-Kumar’s professional networks have already been<br />
identified as critical to his profile. In 2010/2011, the Times newspaper undertook an exercise<br />
to identify Britain's leading specialists based on information from professional bodies. Prof<br />
Kumar was one of only 2 fetal medicine specialists on this list.<br />
2.5.5 Embryo screening for the steadily rising Assisted Reproductive Technologies (ART) will be<br />
championed by CI-Homer. He is a practising fertility specialist and is the only such<br />
specialist in Australia who also conducts internationally-leading basic science research in<br />
reproductive biology thereby straddling key elements of the translational pipeline. He<br />
oversees a fully equipped laboratory for oocyte and embryo research at UQCCR, the first of<br />
its kind in Queensland. CI-Homer will be able to use his affiliations to the Royal Australian<br />
and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) and Fertility<br />
Society of Australia (FSA), their UK counterparts The Royal College of Obstetricians and<br />
Gynaecologists (RCOG) and British Fertility Service (BFS). At a more advanced stage of<br />
early screening implementation, CI-Homer will work networks within the European Society<br />
of Human Reproduction and Embryology (ESHRE) and the American Society of<br />
Reproductive Medicine (ASRM).<br />
3. Develop the health and medical research workforce by providing opportunity to advance<br />
the training of new researchers, particularly those with a capacity for independent<br />
research and future leadership roles<br />
Quality Research: A central and underpinning principle that distinguishes this CRE and delivers<br />
unique opportunities for advanced training is the implementation of an industry-standard quality<br />
management system (QMS) across the entire enterprise. Common to all QMS, is a process of<br />
continuing review and improvement. Quality Management Unit is an essential component of any<br />
successful QMS. As such, the CRE will establish a research Quality Management Unit to provide<br />
independent oversight of the operational and governance activities of the CRE. This will also<br />
provide a new career pathway for the research workforce in Australia, training and leadership<br />
development.<br />
Leadership Development: During the first five years, the CRE team will leverage its collaborative<br />
network to develop the future leaders in obstetric clinical practice and research in Australia. The<br />
CRE team includes expertise for investigating the basic biology of gametes and embryos thereby<br />
extending their reach to the prenatal stages, providing a unique opportunity for training in this niche<br />
area of rapidly growing significance due to the increasing uptake of ART. This will be achieved by<br />
mentoring trainees and providing unique opportunities for career development with the structure of<br />
the CRE. In particular, the CRE will actively promote the development and advancement of<br />
women to leadership positions within obstetric medicine and clinical research. To further reinforce<br />
the CRE’s commitment to leadership development of women in obstetrics, an award will be made at<br />
the CRE’s research workshop and community lecture series for Excellence in Obstetrics Research<br />
Translation. The CIs have an outstanding track record in mentoring and supervising research<br />
higher degree students, post-doctoral and clinical fellows.<br />
International industry standard training: The CRE provides a unique translational research<br />
training environment in Australia for clinicians and research scientists. Over the past four years CIs<br />
have established a clinical diagnostic facility within The University of Queensland Centre for<br />
Clinical Research that is NATA accredited. At the core of this facility is an industry standard<br />
research quality management system (ISO17025 and ISO13485). The significance of this<br />
accreditation is that clinical research conducted within this environment is regulator-ready. That is,<br />
Page 15
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
it complies with requirements of the FDA and TGA for regulatory approval. Thus, the time and<br />
cost from research to implementation is significantly reduced.<br />
Recent studies identify that one of the major barriers for the translation of academic research<br />
into clinical application is the inability of data to be replicated within industry standard<br />
environments. 42 The lack of research quality management systems and appropriate design control<br />
is a significant factor contributing to this failure. The research quality management systems<br />
developed over the past four years will encompass all activities conducted within the CRE. The<br />
CRE, thus, will function as an education and training platform in research quality management<br />
systems and the implementation of international industry standards in clinical research. Research<br />
conducted within its environment will align with industry and clinical practice and, therefore,<br />
facilitate its translation implementation. The CRE will be a national hub for training the next<br />
generation of industry-standard researchers and practitioners.<br />
To further promote the development of future clinical researchers and clinicians in obstetrics<br />
medicine the CRE will provide 5 PhD scholarship for exceptional PhD / MD PhD students (3<br />
national, 2 international). CRE team members will also develop and provide advanced training<br />
programs in research governance and compliance with industry standards and models of integrated<br />
pregnancy care. Annually, the CRE team will conduct a research workshop to review outcomes. In<br />
conjunction with the annual workshop, a public lecture series will be presented as a key community<br />
and end-user engagement activity. In addition, end-users will also engage via the CRE’s website<br />
and Facebook initiatives.<br />
Best Practice Integrated Pregnancy Care Service: In addition to the training and development<br />
opportunities identified above and to provide effective and immediate translation of the research<br />
outcomes of the CRE and a substantive platform for the development of the health and medical<br />
research workforce the CRE will establish an integrated pregnancy care service. BIPS will function<br />
as an iconic clinical unit for advanced training and practice for both clinical and scientific<br />
practitioners and students. BIPS will leverage the extensive expertise and experience of the CRE<br />
CIs and enhance transitional potential. It will deliver in-clinic outcome data necessary for uptake<br />
by end-users. Through the establishment of BIPS, a whole of pregnancy precision medicine-based<br />
management strategy will be implemented and will provide a unique clinical training environment.<br />
4. Facilitate collaboration<br />
CRE team members already have a strong existing collaboration and evidence of working together<br />
effectively (aspects of which have already been detailed in Section 2.5 of this application). Over<br />
the past 6 years, a strong, collaborative network can be evidenced between team members within<br />
the UQCCR viz Mitchell, <strong>Rice</strong>, Salomon, Colditz, Duncombe, Dekker, Callaway, Whiley and<br />
Homer. The QGF collaboration has been in place for 2 years; successfully providing clinical<br />
samples and resulting abstract and review publications. Colditz, Kumar and Callaway have a longstanding<br />
collaborative and professional engagement through the royal Brisbane and Women’s<br />
Hospital. McIntyre and Simmons have worked together for more than 15 years. A collaboration<br />
between AIBN and UQCCR has developed over the past 2 years and more recently between<br />
Rowan, Trau and <strong>Rice</strong>. While this later collaboration is still formative significant opportunity has<br />
been identified through this CRE, including the placement of AIBN research personnel within the<br />
NATA accredited facility within UQCCR to translate technological developments into clinical<br />
application; the conjoint appointment of a level B/C biomarker discovery and development research<br />
between the organisations; and the provision of PhD scholarship top-up to further promote<br />
collaborative engagement. These joint initiatives will generate new research capability, promote the<br />
Page 16
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
integration of preclinical and clinical research activities across the network; and enhance mentoring<br />
and career development opportunities.<br />
In the next five years, this CRE will be an international hub for: innovation in personalised<br />
reproductive medicine; the conduct of end-user oriented research and development activities to<br />
international industry standards; the delivery of Level 1 and 2 evidence that will inform clinical<br />
decision making through the implementation of precision medicine; excellence in clinical and<br />
research training; research quality management systems; biomarker discovery and the development,<br />
validation and implementation of In Vitro Diagnostics; translation of nanotechnology into<br />
personalised medicine (see Figure below). The CRE will enhance the capacity of its members,<br />
trainees and students to further develop collaborations; across the multiple disciplines within the<br />
CRE; within Australia and internationally.<br />
The CRE research will be conducted within three integrated capacities for which the CIs and AIs<br />
bring the necessary multidisciplinary expertise. Key elements of these capacities are already<br />
operational and support ongoing projects between the CIs and AIs.<br />
The core capacities of the CRE will provide advanced training, to international industry standard<br />
and within a research quality management system, for clinical trainees, post-doctoral fellows and<br />
research higher degree students as well as professional research and quality assurance staff. As the<br />
capacities are integrated in all projects they enhance collaborative engagement between CIs and AIs<br />
throughout the CRE. This collaboration is further facilitated by the current utilisation of 21 CFR<br />
part 11 compliant and NATA accredited cloud-based electronic notebooks and clinical sample<br />
tracking systems that are currently used by core members and that will be rolled out across the<br />
CRE. This system provides an instantaneous means of data sharing across the globe.<br />
The CRE will benefit from financial leveraging and industry engagement. The University of<br />
Queensland, and the Faculty of Medicine and the Faculty of Medicine will support the CRE with<br />
$50,000 annually. AIBN has committed to funding a PhD student in medical device development<br />
and precision medicine ($25,000 pa). Shimadzu Austrlaia has committed to funding a PhD student<br />
($27,000 pa) to work on MS-based biomarker discovery and to $30,000 in equipment upgrades to<br />
Page 17
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
enhance the capacity of the CRE. To further promote the development of future leaders, the CRE<br />
will provide five PhD top-up scholarships to exceptional RHD students with clear leadership<br />
potential.<br />
Building the Translational Pipeline: A strong, long-term multidisciplinary collaborative network<br />
has already been established between CRE CIs and AIs that spans multiple national and<br />
international organisation. This network provides opportunity for intellectual exchange and the<br />
enhancement of the interface between technological advances and patient care.<br />
For example, this CRE will establish a translational pipeline between technology and application<br />
intensive facilities (e.g. AIBN) and clinical practice. This will be achieved by the placement of<br />
research staff and students into clinical development environments (e.g. UQCCR) and their direct<br />
engagement with clinical practice in Australian and internationally. New technological<br />
achievement thus can be aligned with clinical and patient needs.<br />
Building National and International Collaborations: The CIs are well positioned to leverage their<br />
existing national and international collaboration to further advance the research and training<br />
objective of the CRE. In particular, UQ CIs have extremely productive collaborative clinical<br />
research and MD and PhD training programs with the Ochsner Health System in New Orleans (the<br />
largest provider of health care services in Louisiana). A similar partnership has been established<br />
with one of the largest private hospital networks in Chile through Clinica Davila, Santiago, Chile.<br />
Such partnerships provide opportunity to expand collaborative engagement between the members of<br />
the CRE and advancement of clinical and scientific enterprise.<br />
5. Record of research and translation achievement – relative to opportunity<br />
The CRE comes complete with a built-in capacity to translate its developments and these will<br />
represent the lasting legacy of the endeavour. The CI and AI team members each have outstanding<br />
records acquired on an international stage, of translating their research into practice within the very<br />
field addressed by the CRE. Past successes demonstrate a capacity to navigate and inject value to<br />
the service chain of delivery within healthcare systems.<br />
These are summarized in the attached table:<br />
CI<br />
<strong>Rice</strong><br />
Simmons<br />
RECORD OF TRANSLATION IN FIELD<br />
More than a decade of experience within the biotechnology sector (both private<br />
and public) in the development, evaluation and implementation of diagnostics<br />
tests.<br />
Conducted phase 2 and 3 biomarker trials to evaluate the clinical utility of an<br />
early detection, blood based diagnostic.<br />
Industry experience includes being co-founder of biotechnology company<br />
HealthLinx, (HTX, 2003), Executive Director (2006), General Manager Science<br />
and Operations (2007) and Chairman (2008-2013). This company listed on the<br />
ASX in 2006 as a diagnostic company that focuses on the development and<br />
delivery of in vitro diagnostics and multivariate index assays.<br />
Service as a member of Clinical and Scientific Advisory Committees of ASXlisted<br />
companies and as a member of the Technical and Regulatory Standing<br />
Committee of IVD Australia (2010-2012).<br />
Closely involved in the translation of clinical research findings into clinical<br />
practice, in particular through the redefinition of gestational diabetes (member of<br />
the WHO working group), establishment/redesign of pre-pregnancy and<br />
Page 18
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
McIntyre<br />
Kumar<br />
Trau<br />
Mitchell<br />
pregnancy services in Australia, New Zealand and UK.<br />
Established diabetes peer support across an English county, taken up by Diabetes<br />
UK across a further 5 counties (type 2 together)-training and other components<br />
now embedded in diabetes UK operations<br />
Developed and evaluated diabetes integrated care approach now in place in in<br />
parts of Cambridgeshire<br />
Part of team that developed/introduced RCT of school based intervention to<br />
reduce childhood obesity in the Waikato, NZ-now continued and extended<br />
beyond Waikato<br />
Study of random blood glucose screening for GDM at booking - now used by<br />
many services around the world<br />
Regional study of a systems approach to pre-pregnancy planning in T1/T2<br />
diabetes in a number of centres in East Anglia, now extended across more<br />
Hospitals<br />
Closely involved in the translation of clinical research findings into clinical<br />
practice, in particular through the redefinition of gestational diabetes and<br />
promotion of optimal diagnosis and treatment of this common pregnancy<br />
complication.<br />
Development of guidelines including most notably:<br />
Queensland Clinical Guidelines Translating evidence into best clinical practice<br />
GDM<br />
Local GDM implementation<br />
International (FIGO) guidelines<br />
Updating of guidelines in the light of new evidence<br />
Contributed to the most recent set of guidelines put out by the Fetal & Neonatal<br />
Transfusion sub-committee of the British Committee for Standards in<br />
Haematology (BCSH).<br />
Co-author of an RCOG guideline pertaining to the management of women with<br />
red cell antibodies in pregnancy. These guidelines influence and guide practice in<br />
many different countries.<br />
Specialist advice to the National Institute of Clinical Excellence for Fetal<br />
Medicine<br />
Interventional procedures and review of fetal medicine guidelines prior to<br />
publication<br />
Clinical advisor to the Healthcare Commission<br />
Developed nanoscale biosensors as a strategy for disease management<br />
Developed single drop DNA test with capacity to revolutionise the detection of<br />
diseases<br />
Initiated and led collaboration between leading nanotechnologists, molecular<br />
biologists, geneticists and commercial researchers with the goal of creating<br />
cutting edge diagnostics.<br />
Member Medicine and Public Health Panel (2012) for the Performance Based<br />
Research Fund that reviewed “quality” measures for all University Researchers<br />
in New Zealand (1,000).<br />
Reviewer for three Tommy’s research centres in the United Kingdom to<br />
determine their progress and whether the Campaign would continue funding<br />
them.<br />
Reviewer applications for the Preterm Labour Centre funded by Harris<br />
Wellbeing, UK<br />
Discovered true cause of Pre-term labour (Discovery in collaboration with Dr<br />
Roberto Romero)<br />
Page 19
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Advisor to Adeza Biomedical for Fetal Fibronectin Testing Development which<br />
remains the only FDA approved diagnostic for preterm labour.<br />
Hyett Internationally recognized for describing the underlying pathophysiology of<br />
increased nuchal translucency, a marker for aneuploidy and cardiac defects that<br />
forms a central part of the 12 week ultrasound scan. This scan is now a routine<br />
part of pregnancy care and the work underpins significant improvement in early<br />
diagnosis of fetuses affected by chromosomal or cardiac abnormalities.<br />
Member of the team that developed endoscopic laser ablation of the placental<br />
circulation that is now recognized as the key intervention for improving survival<br />
in affected twin pregnancies from 5% to 85%.<br />
Recognized internationally for his leadership in bringing cell free fetal DNA<br />
technologies to clinical practice in both RhD and aneuploidy screening.<br />
Homer Established an internationally recognised research programme focused on<br />
understanding mammalian oocyte maturation and oocyte quality and their impact<br />
on female reproductive health.<br />
Jointly set up and co-directed UNSW’s first Oocyte Biology Research<br />
Laboratory<br />
Established UQ’s first Oocyte Biology Lab located within UQ’s Centre for<br />
Clinical Research.<br />
Co-founder and director of Jumpstart Fertility Pty Ltd a company that is in the<br />
process of obtaining strategic investments from the NASDAQ listed company,<br />
Ovascience.<br />
Colditz Established a multidisciplinary, productive, collaborative, national and<br />
international network with paediatricians, neuroscientists, engineers,<br />
psychologists and obstetricians.<br />
Holds an Australian patent (2006 Approved 2006906381) for a method for<br />
detecting EEG seizures in a newborn.<br />
Possesses knowledge base relevant to commercialization and the application of<br />
research to clinical practice and health policy.<br />
Has undertaken key research that defines Clinical Practise in fetal monitoring and<br />
is author on several Cochrane reviews.<br />
Salomon Established and lead the UQCCR Exosome Biology Laboratory that conforms<br />
the ISO standards (ISO17025 and 13485)<br />
Established the mechanism of vascular dysfunction in the feto-placental<br />
circulation in GDM and the role of the insulin receptor isoform in this<br />
phenomenon. These results were the baseline to identify whether known<br />
vasoactive molecules whose plasma levels are elevated in the fetal blood in GDM<br />
pregnancies, play a functional role in the altered vascular reactivity and<br />
endothelial dysfunction in women who develop GDM.<br />
Several contributions to our understanding the role of placental exosomes during<br />
gestation, and my work demonstrated their nature as specific subcellular<br />
compartments and their ability to modify the biological function of target cells<br />
(maternal and/or fetal cells).<br />
Page 20
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI Track Record including top five publications in the last five years per CI)<br />
CI A TRACK RECORD: Prof Gregory <strong>Rice</strong>, PhD, Grad Dip MGT MAH, BSc (Hons)<br />
Career summary (selected qualifications, employment and appointment history)<br />
2010- NHMRC Principal Research Fellow, UQ Centre for Clinical Research<br />
2010-2015 Deputy Director (Translation), UQ Centre for Clinical Research<br />
2011-2015 Member, Centre Confirmation and Promotion Committee, UQ<br />
2011-2015 Member, Research Higher Degree Committee, Faculty of Health Science, UQ<br />
2010-2014 Director and Chairman, National Centre for Health Innovation Limited<br />
2010-2013 Member, Technical and Regulatory Standing Committee of IVD Australia.<br />
2008-2013 Chairman, HealthLinx Limited<br />
Honours and Awards<br />
2015 Senior Clinical Researcher, Ochsner Medical Foundation, New Orleans, LA, USA<br />
2012 Honorary Professor, University of the Andes, Santiago, Chile.<br />
2012 Honorary Member, Chilean Society of Ultrasound and Medical Biology<br />
Research Support (last 5 years (selected)<br />
2014-16 MECESUP Ministry of Education, Chile, $4,690,000<br />
2014-15 ARC Discovery $300,000<br />
2011-2014 SuperScience Translating Health Discovery, $6,700,00<br />
2014 CORFO Chilean Economic Development Agency, $335,953<br />
2010-2014 NHMRC Principal Research Fellowship $677,500<br />
2009-2011 NHMRC Project <strong>Grant</strong> #526686, $426,600,<br />
2009-2011 NHMRC Project <strong>Grant</strong> #546016 $528,750<br />
2008-2010 NHMRC Project <strong>Grant</strong> #509127 $461,625,<br />
Contribution to the field of research (selected)<br />
2014 Invited Speaker, “Preeclampsia: novel biomarkers and mediators” 46 th International<br />
Congress on Pathophysiology of Pregnancy, Tokyo, Sept 18-20.<br />
2013 Keynote Speaker “The Business of Biomarkers” AGM National Product Liability<br />
Association, Melbourne September 28 th .<br />
2013 Invited Speaker “Inflammation processes, oxidative stress and angiogenic factors in<br />
preeclampsia”. 45th International Meeting of Gestosis Organization, 6-8 December<br />
2013, Athens Greece.<br />
2013 Invited Speaker, “Exosomes - Nanomedicine Applications in Obstetrics and<br />
Gynaecology” Singapore International Congress of Obstetrics and Gynaecology,<br />
Singapore (22-24 August).<br />
2013 Invited Speaker, “The role of exosomes in the development of placental<br />
complications SLIMP (Latin American Symposium on Maternal Fetal Interaction<br />
& Placenta), Brazil (Feb 17 th , 2013).<br />
2012 Plenary Speaker “Molecular Biology in Routine Clinical Practice” IX Congress of<br />
the Sociedad Chilean de Ultrasonografia en Medicina Y Biologia, Vina del Mar,<br />
Chile June 7-9 th .<br />
Patents -<br />
WO2004019009 A1 currently licensed to Sigma Aldrich<br />
Collaborations - International - University of the Andes and Catholic University of Chile, Santiago<br />
(6 grants awarded > $5 million. 4 reviews, 4 papers); National: QUT two NHMRC<br />
Project grants submitted this round.<br />
Page 21
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Community engagement and participation - Chairman, National Centre for Health Innovation<br />
Professional Involvement (selected)<br />
2010-2012 Immediate Past President, International Federation of Placenta Associations<br />
2007-2009 President, International Federation of Placenta Associations<br />
2012-present Member, Editorial Board, Open Journal of Obstetrics and Gynecology<br />
2012- present Member, Editorial Board, Conference Papers in Biology<br />
2011-present Member, Editorial Board, Scientifica<br />
Supervision and Mentoring (last 5 year) Honours 8 (1 current); MSc 1(1); PhD 4 (3)<br />
Peer Recognition and Service last 5 year (selected):<br />
2013 NHMRC <strong>Grant</strong> Review Committee<br />
2012 NHMRC Research Translation Faculty<br />
2012 NHMRC <strong>Grant</strong> Review Committee<br />
2011 NHMRC Fellowship Review Committee<br />
Other contributions to NHMRC<br />
2014 NHMRC Assigner Academy<br />
Top 5 Publication in the last 5 years<br />
1. Sarker S, Scholz-Romero K, Perez ,. Illanes SE, Mitchell MD, <strong>Rice</strong> GE , Salomon C.<br />
Placenta-derived exosomes continuously increase in maternal circulation over the first<br />
trimester of pregnancy. Journal of Translational Medicine. (2014) 12:204<br />
doi:10.1186/1479-5876-12-204<br />
2. Salomon C, Torres MJ, Kobayashi M, Scholz K, Sobrevia L, Sobrevia L, Dobierzewska A,<br />
Illanes SE, Mitchell MD, <strong>Rice</strong> GE (2014) Pregnancy-Associated Changes in Placenta-<br />
Derived Exosome Concentration and Bioactivity in Maternal Plasma. PLoS One. DOI:<br />
10.1371/journal.pone.0098667<br />
3. Kobayashi M, Salomon C, Tapia J, Illanes, SE, Mitchell MD, <strong>Rice</strong> GE (2014) Ovarian<br />
cancer cell invasiveness is associated with discordant exosomal sequestration of Let-7<br />
miRNA and miR-200. Journal of Translational Medicine. 12:4. doi:10.1186/1479-5876-12-4<br />
These 3 papers establish leadership in exosome biology and analysis applied to placental<br />
development. In particular, through the work of Dr Salomon (a post-doctoral fellow in my<br />
group) and Ms Kobayashi (a PhD student in my group), we have improved the “bestpractice”<br />
protocol for isolating exosomes and begun to characterise the factors that regulate<br />
exosome protein and miRNA content, and their effects on target cells.<br />
4. Peiris HN, Ashman C, Vaswani K, Kvaskoff D, <strong>Rice</strong> GE, Mitchell MD (2014) Method<br />
Development for the Detection of Human Myostatin by High-Resolution and Targeted Mass<br />
Spectrometry. J Clin. Endocrinol Metab doi: 10.1210/jc.2014-2615 This paper establishes<br />
our expertise in developing and applying mass spectrometry approaches.<br />
5. <strong>Rice</strong> GE, Scholz-Romero K, Sweeney E, Peiris H, Kobayashi M, Duncombe G, Mitchell<br />
MD, Salomon C. (2015) The Effect of Glucose on the Release and Bioactivity of Exosome<br />
from First Trimester Trophoblast Cells. J Clin Endocrinol Metab. 2015 Aug 4:jc20152270.<br />
[Epub ahead of print] PMID:26241326 This paper delivers proof-of-concept of the<br />
involvement of exosomes in glucose homeostatis<br />
Page 22
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI B TRACK RECORD: Prof Paul Colditz<br />
Career summary Prof. Colditz is a practicing neonatologist with a DPhil in Medicine from the<br />
University of Oxford, UK. He is currently and for the past 20 years has been Director of the<br />
Perinatal Research Centre, one of the largest research centres in the School of Medicine and since<br />
2012 also Deputy Director University of Queensland Centre for Clinical Research (UQCCR). His<br />
research focuses on clinically important perinatal health problems and translation to clinical<br />
practice. It focuses on brain injury, neuroprotection and pathways to improving neurodevelopmental<br />
outcomes.<br />
Qualifications and dates of award/conferment<br />
Institution And Location Degree<br />
• Australian Institute Company Directors GAICD 2015 Business<br />
• Royal College of Paediatrics and Child Health FRCPCH 1997Medicine<br />
• University of Oxford DPhil 1988 Medicine<br />
• University of New South Wales, MBiomedE 1985 Engineering<br />
• Royal Australasian College of Physicians FRACP 1984 Medicine<br />
• University of New South Wales MBBS 1977 Medicine<br />
Contribution To The Field/Impact (include translation of research into health outcomes)<br />
Prof Colditz has been a lead CI on a number of perinatal randomized controlled trials where the<br />
measurement of infant outcomes has been a major component. He was responsible for the<br />
acquisition of the southern hemisphere’s first neonatal MRI compatible incubator as an indicator of<br />
his interests in accurate determination of outcomes. He has established a multidisciplinary,<br />
productive, collaborative, national and international network with paediatricians, neuroscientists,<br />
engineers, psychologists and obstetricians. CI Colditz has been granted over AUD$50m in project,<br />
equipment and fellowship funding for research, including being CI on 19 NHMRC grants, an<br />
NHMRC Practitioner Fellowship, 3 ARC grants and 6 International grants. Prof Colditz’s research<br />
group is recognized both nationally and internationally. He has received recognition in both a<br />
clinical context (Distinguished Research Medal for Research Excellence (2012) from the Royal<br />
Brisbane and Women’s Hospital) and academic context (recipient of University of Queensland of a<br />
‘Top 10’ Q Index Award).<br />
Patents<br />
He holds an Australian patent (2006 Approved 2006906381) for a method for detecting EEG<br />
seizures in a newborn.<br />
Collaborations<br />
Prof Colditz collaborates with the QLD Cerebral Palsy Research Centre; Children’s Nutrition<br />
Research Centre, UQ; the Uni. of Adelaide; Uni. of Sydney; Uni. of Melbourne; Uni. of Cork, and<br />
Uni. of Helsinki. He has an ongoing successful collaboration with the Uni. of Qatar, resulting grants<br />
>$9M in the last 5 years.<br />
Community Engagement & Participation<br />
Prof Colditz has a long standing involvement in supporting health consumer and advocacy<br />
organisations. He is currently a board member of the national SIDS & Kids Foundation. He has<br />
been awarded the Ray Phippard Award for services to medical research by the Lions Medical<br />
Research Foundation. In 2013 he was awarded life membership of SIDS & Kids (QLD).<br />
Professional Involvement (include committee membership, conference organisation and other<br />
service level participation)<br />
Page 23
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI Colditz’s intellectual leadership is recognised at local, state and national levels: e.g. Chair QLD<br />
Clinician Scientists Assoc., senior roles in the Division of Paediatrics and Child Health within the<br />
Royal Australasian College of Physicians (President-elect, Chair of Research Committee, member<br />
of Council, member of Executive) as well as in the Royal Australasian College of Physicians<br />
(Chair, Research Committee, Director/board member RACP), member QLD Maternal and Perinatal<br />
Quality Council, Chair QLD Congenital Malformations Committee, and Leader State Clinical<br />
Guideline on Neonatal Seizures. His experience in knowledge application includes<br />
commercialization and the application of research knowledge to clinical practice and health policy.<br />
CI Colditz is current lead on QLD Health Clinical Practice Guideline for neonatal seizures and<br />
member of perinatal Clinical Practice Guidelines (CPG).<br />
Supervision & Mentoring<br />
Professor Colditz has 14 current PhDs in the fields of basic science, engineering, medicine and<br />
allied health and has supervised 33 to completion. He has 6 current Postdoctoral fellows. CI Colditz<br />
supervises RHD students across medicine, nursing, allied health, engineering and maths/physics<br />
from Vietnam, China, Iran, Malaysia, Indonesia, Singapore, UK, US, Holland, Germany.<br />
Peer Review Involvement (include NHMRC, other granting organisations, manuscripts, editorial<br />
responsibilities)<br />
CI Colditz has been a member, including chair, of NHMRC project and program grant review<br />
panels regularly for more than a decade. He has been a member of NHMRC Australia Fellowship<br />
panel and for the past two years a member of a Career Development Fellowship Panel and for 2016<br />
a member of the Project <strong>Grant</strong> panel. In 2016 CI Colditz was on the scientific review team for the<br />
Cerebral Palsy Alliance Research Foundation <strong>Grant</strong>s Program and SIDS and Kids. He has been a<br />
peer reviewer for more than a dozen journals in recent years.<br />
Other Relevant Information<br />
Professor Colditz has published > 200 peer-reviewed publications (65 in the past 5 years), over 600<br />
conference abstract/proceedings, 3 books and 6 book chapters.<br />
TOP 5 PUBLICATIONS OVER THE LAST 5 YEARS (include reasons why these publications<br />
have been selected)<br />
1. Doyle L, Anderson P, Haslam R, Lee K, Crowther C, Australasian Collaborative Trial of<br />
Magnesium Sulphate (ACTOMgSO4). School age outcomes of very preterm infants after<br />
antenatal treatment with magnesium sulfate vs placebo. JAMA. 2014; 312(11):1105-1113.<br />
2. Pannek K, Guzzetta A, Colditz PB, Rose S. Diffusion MRI of the neonate brain: acquisition,<br />
processing and analysis techniques. Pediatric Radiology 2012 42;10: 1169-82.<br />
3. Pannek K, Hatzigeorgiou X, Colditz PB, Rose S. Assessment of structural connectivity in the<br />
preterm brain at term equivalent age using diffusion MRI and T2 relaxometry: a networkbased<br />
analysis. PLoS One 2013 8;8: e68593.<br />
4. Collins CT, Gibson RA, Anderson PJ, McPhee AJ, Sullivan TR, Gould JF, Ryan P, Doyle<br />
LW, Davis PG, McMichael JE, French NP, Colditz PB, Simmer K, Morris SA, Makrides M.<br />
Neurodevelopmental outcomes at 7 years’ corrected age in preterm infants who were fed<br />
high-dose docosahexaenoic acid to term equivalent: a follow-up of a randomised controlled<br />
trial. BMJ Open. 2015 Mar 18;5(3):e007314. doi: 10.1136/bmjopen-2014-007314.<br />
5. Jacobs SE, Morley CJ, Inder TE, Stewart MJ, Smith KR, McNamara PJ, Wright IM,<br />
Kirpalani HM, Darlow BA, Doyle LW, Colditz PB (Infant Cooling Collaboration). Wholebody<br />
hypothermia for term and near-term newborns with hypoxic-ischemic encephalopathy: a<br />
randomized controlled trial. Arch Pediatr Adolesc Med. 2011; 165: 692-700.<br />
Page 24
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CIC: Professor Hayden Homer (MBBS, PhD, MRCOG, CCSST [RCOG, UK], FRANZCOG)<br />
Career Summary: In January 2016, CIC Homer relocated to UQ to take up the fully endowed<br />
Christopher Chen Chair in Reproductive Medicine. Prior to that CIC Homer relocated from the UK<br />
to Australia in January 2014 after being recruited to UNSW through their Strategic Priority Funding<br />
route. Hayden has been dually accredited as a Specialist in Obstetrics & Gynaecology and a<br />
Subspecialist in Reproductive Medicine & Surgery through the British Royal College of<br />
Obstetricians & Gynaecologists (2012). CIA Homer was previously Clinical Senior Lecturer and<br />
Honorary Consultant in Reproductive Medicine at one of the world’s leading universities,<br />
University College London (UCL). Since moving to Australia he has also been elevated to Fellow<br />
of the Royal Australian and New Zealand College of Obstetricians & Gynaecologists (2014).<br />
Alongside clinical work, Hayden has established an internationally recognised research programme<br />
focused on understanding mammalian oocyte maturation and oocyte quality and their impact on<br />
female reproductive health. Hayden is 7 years post-PhD and is one of only a handful of basic<br />
science researchers in reproductive biology who is also clinically qualified and subspecialty trained<br />
in Reproductive Medicine. Since relocating from the UK, Hayden jointly set up and co-directed<br />
UNSW’s first Oocyte Biology Research Lab and more recently has established UQ’s first Oocyte<br />
Biology Lab located within UQ’s Centre for Clinical Research. In this time as well, CIA Homer<br />
completed equivalence requirements for Australian clinical registration and gained familiarity with<br />
clinical practice as a Staff Specialist in Gynaecology and Infertility. CIC Homer is 7 years post-PhD<br />
and although the last 3 years have been periods of major readjustment, he has successfully secured<br />
over $1.5 M dollars in NHMRC research funding and established highly productive research<br />
collaborations.<br />
Contribution to Field of Research, International and National Profile:<br />
Although only 7 years post-PhD, CIC Homer has placed leading papers in his field including 2<br />
high-impact senior author papers in the past 5 years (Developmental Cell and Development). In<br />
2013, he was invited editor for a prominent research protocols handbook on mammalian oocytes<br />
(Methods in Molecular Biology series) with 20 chapters from world-leading oocyte research labs.<br />
CIC Homer has also published landmark papers in the journals, Science (Homer et al. 2009) and<br />
Genes & Development (Homer et al. 2005) that were both cited by the Faculty of 1000 Biology for<br />
defining key regulatory facets in oocytes and are some of the most highly cited works in the field.<br />
In the last 5 years Hayden has had 12 invited contributions to various books and journals. He has<br />
been invited speaker at several international and national meetings including meetings of the<br />
Australian Society of Reproductive Biology (2014, 2016), the Fertility Society of Australia Annual<br />
Meeting (2013, 2015), Scientists in Reproductive Technology (2016) and Frontiers in Reproductive<br />
Medicine (2015) at Washington, USA.<br />
Research Funding:<br />
During his time in Australia (2014-2016), Hayden has received over $1.5 M funding as CIA<br />
including NHMRC Project (x2) and Development <strong>Grant</strong>s (x1) for oocyte- and fertility-related<br />
research (APP1078134, $515,615, APP1103689, $410,983 and APP1122484, $445,827) and a<br />
Ramaciotti Establishment <strong>Grant</strong> ($75,000). Hayden is also CIA on two Equipment <strong>Grant</strong>s, one from<br />
the NHMRC for a NanoString nCounter System (GNT9000249, $366,500) and the other from<br />
UNSW for an Oocyte Microinjection System ($56,000). He is Co-CI on two further Equipment<br />
<strong>Grant</strong>s at UNSW (see below). Hayden’s PhD student, Dave Listijono, recently secured an NHMRC<br />
Postgraduate Scholarship (APP1114631, 2016, $71,791.50) and won the Oozoa Award at the<br />
Society for Reproductive Biology Annual Meeting (2015). Another of his students, Nicholas Loh,<br />
was a finalist in this year’s Oozoa Awards (2016). Within the past 5 years, prior to moving to<br />
Australia, Hayden’s research at UCL was funded by a highly prestigious Wellcome Trust Clinician<br />
Scientist Fellowship ($1.26 million; 2007-2013), which was one of only two to have ever been<br />
awarded to Reproductive Medicine.<br />
Page 25
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Collaborations:<br />
Hayden was Principal Investigator in UCL’s world-leading Cross-Faculty Mammalian Oocyte &<br />
Embryo Research Laboratory (2007-2013). Since moving to Australia he has established productive<br />
collaborations with Professor David Sinclair, an international expert in sirtuin and NAD + regulation<br />
and aging with whom he has had success in NHMRC grant funding (APP1103689, APP1122484).<br />
CIC Homer’s NHMRC <strong>Grant</strong> APP1078134 involves collaborations with senior fertility clinicians<br />
(Prof William Ledger [Head of School, UNSW] and A/Prof Peter Illingworth [Director, IVF-<br />
Australia] and leading scientists (A/Prof Gilchrist [NHMRC Senior Research Fellow] and Prof John<br />
Carroll [Dean and Head of School, Monash University]). He led a successful bid for UNSW’s first<br />
NanoString nCounter System involving 17 co-CIs. Hayden is also co-CI on 2 further successful<br />
Equipment <strong>Grant</strong>s for a Zeiss Laser Micro-dissection System (2015, $392,000) and a Zeiss Light<br />
Sheet Microscope (2015, $565,000). Hayden previously co-directed UNSW’s oocyte research lab<br />
jointly with A/Prof Gilchrist.<br />
Supervision and mentoring:<br />
CIC Homer currently supervises 5 PhD students, one of whom is funded by an NHMRC<br />
Postgraduate Scholarships. Two further students will commence in 2016, one of whom is funded by<br />
an International Postgraduate Research Scholarship.<br />
Peer Review Involvement:<br />
CIC Homer has peer reviewed for high impact journals in the past 5 years including Nature Cell<br />
Biology, Nature Communications, Development, Journal of Cell Science and Journal of Molecular<br />
Cell Biology. In the past 5 years, he has been grant reviewer for NHMRC Project <strong>Grant</strong>s (2013 [x1];<br />
2014 [x3]; 2015 [x3]; 2016 [x3]), the UK’s MRC (Project and Program <strong>Grant</strong>s) and the French<br />
National Research Agency and has been a PhD examiner (x2, University of Newcastle, NSW).<br />
Top 5 publications in the last 5 years:<br />
CIC Homer is 7 years post-PhD. Alongside clinical practice and twice relocating his lab, he has 2<br />
high-impact papers as senior author both cited by the Faculty of 1000 Biology (asterisked below).<br />
1. Gui L and Homer H*. (2012) Spindle assembly checkpoint signalling is uncoupled from<br />
chromosomal position in mouse oocytes. Development 139(11):1941-1946.<br />
New insight into why chromosome segregation remains so error-prone in oocytes despite<br />
possessing a spindle assembly checkpoint surveillance mechanism.<br />
2. Gui L and Homer H*. (2013) Hec1-dependent cyclin B2 stabilization regulates the G2-M<br />
transition and early prometaphase in mouse oocytes. Developmental Cell 25(1):43-54<br />
Novel roles for kinetochores in regulating the G2-M transition in oocytes and new co-operative<br />
roles for cyclin B1 and cyclin B2 in promoting cyclin-dependent kinase 1 activation.<br />
3. Riris S, Webster P and Homer H. (2014) Digital multiplexed mRNA analysis of functionally<br />
important genes in single human oocytes and correlation of changes in transcript levels with<br />
oocyte protein expression. Fertility and Sterility 101(3):857-864.<br />
First paper to apply powerful NanoString technology to analyzing human oocytes and to report<br />
multi-gene profiling in any single cell without pre-amplification.<br />
4. Riepsamen A, Wu LE, Lau L, Listijono D, Ledger W, Sinclair DA, Homer HA. (2015)<br />
Nicotinamide Impairs Entry intro and Exit from Meiosis I in Mouse Oocytes. PLoS ONE<br />
10(5): e0126194. doi:10.1371/journal.pone.0126194.<br />
This paper showed that oocyte maturation is severely impaired by the pan-sirtuin inhibitor<br />
nicotinamide pointing to the importance of the sirtuin family of deacetylases in oocyte quality.<br />
5. Homer H. (2013) The APC/C in female mammalian meiosis I. Reproduction 146(2): R61-71.<br />
Invited review in one of the leading specialist journals in the field covering recent<br />
developments in oocyte cell-cycle regulation.<br />
Page 26
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI D TRACK RECORD Prof Murray Mitchell<br />
Career summary – (last 5 years)<br />
2015- Professorial Research Fellow, University of Queensland Centre for Clinical Research<br />
2010 - 2015 Director, University of Queensland Centre for Clinical Research<br />
2003-2009 Deputy Director ( Co-Director 2008-2009) National Research Centre for Growth and<br />
Development, N.Z.<br />
Research funding last 5 years (selected)<br />
I have received significant infrastructure funding through Therapeutic Innovation Australia (TIA),<br />
(8.9m-3.4m for UQCCR), A Clinical Academic Fellowship from The Queensland Government<br />
($375,000), NZ Government funding for Epigenetic Studies in Dairy Cows ($3m - $408,000) to<br />
Murray D Mitchell and an ARC Discovery <strong>Grant</strong> ($300,000). I have also received over $1m for UQ<br />
infrastructure mainly next generation sequencing items (Hi Seq and Mi Seq).<br />
Collaborations<br />
Our team has ongoing collaborations with investigators in Santiago, Chile, University of the Andes<br />
(Ilanes) and Catholic University of Chile (Sobrevia) (8 grants awarded >5m, 4 reviews, 4 papers –<br />
all jointly with Prof. G.E. <strong>Rice</strong>), Singapore (Choolani), Adelaide and several institutions in<br />
Brisbane.<br />
Committees – last 5 years<br />
I am a member on several hospital committees e.g. (Research Excellence and Academic Leadership,<br />
Royal Brisbane and Women’s Hospital) and Research Foundations (RBWH and Prince Charles<br />
Hospital). I have also served on many UQ committees through my position as Director,UQCCR<br />
Awards & commendations & leadership<br />
In 2012 I received an Award from the Society for Gynecologic Investigation (SGI) in recognition of<br />
outstanding organization for the 5th SGI International Summit “Prematurity and Stillbirth”:<br />
Antecedents, Mechanisms and Sequelae”. I developed the idea for this meeting, took it through the<br />
Society organization, my University organization and then presided over the meeting that attracted<br />
people from worldwide and opened the way for Perth to bid for a full meeting of the SGI in the near<br />
future. In 2009 I completed my second term on the SGI Council, having been their first<br />
International (non-North American) member.<br />
Presentations, plenary and invited lectures (selected)- last 5 years<br />
I have been invited to present regularly at International Meetings. In particular I have been invited<br />
to the GAPPS ‘International Conference on Prematurity and Stillbirth” in Seattle, 2009 and the<br />
March of Dimes/Burroughs Wellcome Meetings in 2010 and 2012 on Prematurity and Stillbirth.<br />
These meetings have been the major driving forces in organising global approaches to the issues of<br />
prematurity and stillbirth. I am invited to the next such meeting in Siena this year. I have also been<br />
invited to speak at the Perinatal Branch of NICHD in a special research lectureship.<br />
Supervision – last 5 years<br />
In the past 5 years I have supervised 5BSc (Hons), 1 MSc and 13 PhD students. Additionally I have<br />
mentored 3 postdoctoral Fellows, 3 MBBS Honours students and 1 Occupational Trainee from<br />
Universidad de Chile. My students have a 100% success rate in graduating with their degrees.<br />
Service – last 5 years<br />
I have received grants to review from the Wellcome Trust (UK) Programme, Canadian Institutes of<br />
Health Research, National Health and Medical Research Council (Australia) and Canadian<br />
Page 27
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Institutes of Health Research (China-Canada Joint Health Research Initiative). Separately, I was<br />
again asked to be a panel member of the Tertiary Education Commission (New Zealand). I was on<br />
the Medicine and Public Health Panel (2012) for the Performance Based Research Fund that<br />
reviewed “quality” measures for all University Researchers in New Zealand (1,000).<br />
PERTINENT – LAST 5 YEARS<br />
During the past five years I have moved from Auckland, New Zealand, to Brisbane, Australia (UQ).<br />
In my position as Director, UQCCR I have established a significant research infrastructure. The<br />
developments of a NATA accredited Centre for Clinical Diagnostics and a Centre for Clinical<br />
Genomics have been a major advance. My grants have excellent research infrastructure particularly<br />
with regards to mass spectrometry and next generation sequencing. Although this time commitment<br />
has reduced my outputs somewhat I believe that it is has been more beneficial to the overall<br />
research community.<br />
Top 5 Publications in the last 5 years<br />
1. Logan, P.C., Ponnampalam, A.P., Steiner, M. and Mitchell, M.D. Effect of cyclic AMP and<br />
estrogen/progesterone on the transcription of DNA methyltransferases during decidualization of<br />
human endometrial stromal cells Molecular Human Reproduction 19 (5): 302-312, 2013. This<br />
study was one of the first to describe the regulation by steroids of the transcription of DNA<br />
methyltransferases. This opened the way for developing novel therapeutic approaches to<br />
regulating pathways governed by epigenetic mechanisms.<br />
2. Sarker S, Scholz-Romero K, Perez ,. Illanes SE, Mitchell MD, <strong>Rice</strong> GE , Salomon C. Placentaderived<br />
exosomes continuously increase in maternal circulation over the first trimester of<br />
pregnancy. Journal of Translational Medicine. (2014) 12:204 doi:10.1186/1479-5876-12-204<br />
3. Salomon C, Torres MJ, Kobayashi M, Scholz K, Sobrevia L, Sobrevia L, Dobierzewska A,<br />
Illanes SE, Mitchell MD, <strong>Rice</strong> GE (2014) Pregnancy-Associated Changes in Placenta-Derived<br />
Exosome Concentration and Bioactivity in Maternal Plasma. PLoS One. DOI:<br />
10.1371/journal.pone.0098667<br />
4. Kobayashi M, Salomon C, Tapia J, Illanes, SE, Mitchell MD, <strong>Rice</strong> GE (2014) Ovarian cancer<br />
cell invasiveness is associated with discordant exosomal sequestration of Let-7 miRNA and<br />
miR-200. Journal of Translational Medicine. 12:4. doi:10.1186/1479-5876-12 These 3 papers<br />
establish leadership in exosome biology and analysis applied to placental development. In<br />
particular, through the work of Dr Salomon (a post-doctoral fellow in my group) and Ms<br />
Kobayashi (a PhD student in my group), we have improved the “best-practice” protocol for<br />
isolating exosomes and begun to characterise the factors<br />
5. Peiris, H.N, Ashman, C., Vaswani, K., Kvaskoff, D., <strong>Rice</strong>, G.E., Mitchell, M.D. (2014) Method<br />
development for the detection of human myostatin by high-resolution and targeted mass<br />
spectrometry. Journal of Proteome Research, 13 8: 3802-3809. doi:10.1021/pr5004642.<br />
Evidences expertise in proteomics and biomarker isolation.<br />
Additional pertinent publications include:<br />
Rahnama, F.,Thompson, B.,Steiner, M.,Shafiei, F., Lobie, P. and Mitchell, M.D., Epigenetic<br />
regulation of e cadherin controls endometrial receptivity. Endocrinology 150: 1466-1472, 2009.<br />
This study was among the first to describe epigenetic regulation of a key reproductive mechanism<br />
and demonstrate specific effects on functional as well as biochemical end points. As such it has<br />
been highly cited (40 citations); and<br />
Perry, J.K., Lins, R.J., Lobie, P. and Mitchell, M.D Regulation of invasive growth: similar<br />
epigenetic mechanisms underpin tumour progression and implantation in human pregnancy.<br />
Clinical Science 118: 451-457, 2010. This study described the not only the data supporting<br />
epigenetic regulation of critical pathways in human implantation but also drew parallels with<br />
similar regulation in pathways associated with tumour progression. Limits and opportunities that<br />
arise from this comparison were described.<br />
Page 28
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI E TRACK RECORD: Prof Matt Trau, PhD<br />
1992 The University of Melbourne, Melbourne, Australia<br />
PhD in Physical Chemistry<br />
1987 The University of Sydney, Sydney, Australia<br />
B.Sc. (Hons) 1 st Class (University Medal)<br />
Academic research, clinical, professional and industrial experience relevant to this<br />
application.<br />
Matt Trau is currently a Professor of Chemistry and Director of the Centre for Personalised<br />
Nanomedicine at the University of Queensland in Brisbane, Australia. His research is dedicated<br />
towards developing innovative nano-diagnostics to help transform the healthcare system towards<br />
early detection and personalized treatment of disease, and also to help enable the emerging<br />
“Wellness Industry” which aims to dramatically extend high quality human life through a<br />
combination of innovative diagnostic technology and preventative measures. Among Matt’s other<br />
roles, he is also deputy director and co-founder of the Australian Institute for Bioengineering and<br />
Nanotechnology (AIBN). Since graduating from the University of Sydney (BSc Hons I, University<br />
Medal) and the University of Melbourne (PhD in Physical Chemistry, 1993), he has held positions<br />
within industry and academia across the globe. These include a Fulbright Research Fellowship at<br />
Princeton University, USA, a research scientist at Dow Chemical and ICI Pty Ltd. Matt has also<br />
been a Visiting Professor at two of the largest Cancer Research Centres in the world: The Dana<br />
Farber Cancer Research Institute, Harvard Medical School, Boston (2000), and the Fred Hutchinson<br />
Cancer Research Centre, Seattle (2008). Matt is internationally recognised for his innovative and<br />
cross-disciplinary research at the interface between chemistry, nanotechnology, biology and<br />
medicine. He has co-authored more than 170 publications, many of which appear in the highest<br />
impact journals in his field, e.g., eight Science and Nature family journal publications overall to<br />
date – many of which have been highly cited. Over the past 10 years, he has raised greater than<br />
M$35 of competitive (category 1) research funding to support his work. His major awards and<br />
honours include an ARC Federation Fellowship (one of the most prestigious scientific fellowships<br />
in Australia), a Fulbright Research Fellowship to the US, a “Young Tall Poppy" Award for<br />
Queensland, a UQ Foundation/Vice Chancellor’s Research Excellence Award, a Paul Harris<br />
Fellowship, and a Pink Circle Award for breast cancer research excellence. Among other grants,<br />
Matt is currently the lead investigator on a 5-year M$5 national collaborative research grant from<br />
the National Breast Cancer Foundation (“Enabling Clinical Epigenetic Diagnostics: The Next<br />
Generation of Personalized Breast Cancer Care“).<br />
Matt has also initiated and led several large international multidisciplinary programs that involve<br />
close collaboration between leading nanotechnologists, molecular biologists, geneticists and<br />
commercial researchers. Significant examples include:<br />
1. A $4 million National and International Research Alliances Program (NIRAP) grant from<br />
the Queensland government, "International Partnership for Preventative and Personalised<br />
Medicine" (2009-11). An international collaborative grant between UQ, the Fred<br />
Hutchinson Cancer Research Centre (Seattle), the Seattle Biomedical Research Institute, and<br />
the University of Washington (Seattle). This consortium involved some of the highest<br />
calibre scientists in the world, e.g. Dr Lee Hartwell (2001 Nobel Laureate) from Seattle was<br />
a co-chief investigator on the grant.<br />
2. A $5 million National Institutes of Health (NIH) grant from the USA (co-lead with Prof<br />
Gerry Cangelosi, University of Washington, USA), “Accelerated Molecular Probe Pipeline”<br />
(2010-14). This consortium grant involves four partners across the US (University of<br />
Page 29
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Washington, PATH and University of Virginia), with my lab being the only non-US<br />
member. The success rate for NIH grants in this round was 6%.<br />
3. A $5 million multidisciplinary National Collaborative grant from the National Breast Cancer<br />
Foundation (NBCF), "Novel strategies for Prediction and Control of Advanced Breast<br />
Cancer via Nanoscaled Epigenetic-Based Biosensors" (2008-2013). This consortium grant is<br />
a national collaboration involving leading geneticists, pathologists and oncologists from<br />
across Australia. Participating organisations include: the Garvan Institute (Sydney), the<br />
Peter MacCallum Centre (Melbourne), and the University of Newcastle and Queensland<br />
Health. At the time of award, this was the largest competitively won grant ever awarded by<br />
the NBCF (the largest philanthropic organisation that funds Australian research). In 2014,<br />
this grant was ranked as one of the top-ten performing grants ever awarded by the NBCF<br />
(out of hundreds of grants previously awarded).<br />
4. A second $5 million multidisciplinary collaborative grant from the NBCF, "Enabling<br />
Clinical Epigenetic Diagnostics: The Next Generation of Personalized Breast Cancer Care",<br />
2013-2018. This collaborative grant greatly expands on the achievements from the first<br />
NBCF collaborative grant. As well as the original CIs and collaborative institutions, new<br />
partners now also include: the Olivia Newton-John Cancer Research Centre (Melbourne),<br />
the Ludwig Cancer Research Centre (Melbourne), and Hunter Area Pathology Services<br />
(Newcastle). This second consortium grant is the only time that a second (follow-on)<br />
National Collaborative grant has ever been awarded by the NBCF (success rates of the<br />
individual NBCF National Collaborative rounds are typically around 8%, and rounds are<br />
held every two or three years). At a cumulative total of M$10, these two grants in aggregate<br />
represent almost 10% of the total NBCF investment in Australian research since the NBCF<br />
was founded ten years ago.<br />
Top 5 publications in the last 5 years that reflects scholarly works in nanotechnology and<br />
nano-diagnostics (of 90 publications 2012-16)<br />
1. Clark, S.; Stone, A.; Zotenko, E.; Locke, W.; Korbie, D.; Millar, E.; Pidsley, R.; Stirzaker,<br />
C.; Graham, P.; Trau, M.; Musgrove, E.; Nicholson, R.; Gee' J. DNA methylation of<br />
estrogen regulated enhancers defines endocrine sensitivity in breast cancer. Nature<br />
Communications, 6, 7758, 2015.<br />
2. Stirzaker, C., Zotenko, E., Song, J., Qu, W., Nair, S., Locke, W., Stone, A., Armstong, N.,<br />
Robinson, M., Dobrovic, A., Avery-Kiejda, K., Peters, K., French, J., Stein, S., Korbie, D.,<br />
Trau, M., Forbes, J., Scott, R., Brown, M., Francis, G., Clark, S., Methylome sequencing in<br />
triple negative breast cancer reveals distinct methylation clusters with prognostic value,<br />
Nature Communications, 6, 5899,2015.<br />
3. Connolly, A. R.; Trau, M., Rapid DNA detection by beacon-assisted detection<br />
amplification, Nature Protocols, 6, 772-778, 2011.<br />
4. Vaidyanathan, R., Naghibosadat, M., Rauf, S., Korbie, D., Carrascosa, L.G., Shiddiky, M., Trau,<br />
M., Detecting Exosomes Specifically: A Multiplexed Device based on Alternating Current<br />
Electrohydrodynamic Induced Nanoshearing, Analytical Chemistry, 86, 11125-11132, 2014.<br />
5. Lane, R. E., Korbie, D., Anderson, W., Vaidyanathan, R., Trau, M., Analysis of exosome<br />
purification methods using a model liposome system and tunable-resistive pulse sensing.<br />
Scientific Reports, 5, 13, 7639, 2015 (Nature award for “Top 100” paper for Sci. Rep. in<br />
2015).<br />
Page 30
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI F TRACK RECORD Prof Jon Hyett<br />
Career summary<br />
2008 – Current Head of the High Risk Obstetric Service, Royal Prince Alfred (RPA) Hospital,<br />
Sydney<br />
2011 – Current Clinical Professor and Joint Head of Discipline, Obstetrics and Gynaecology,<br />
Faculty of Medicine, University of Sydney<br />
Research Support<br />
2015 – 2020 AI on NHMRC Project <strong>Grant</strong> APP1078142, $951,296 Reducing cardiovascular risk<br />
in children born with poor fetal growth: the Small baby Omega-3 (SO3) trial<br />
2015 - 2018 Project PhD Supervisor on McKern/University of Sydney <strong>Grant</strong> $135,000<br />
2012 – 2016 CIC on NHMRC Project <strong>Grant</strong> APP1029644, $516,175 The POP-OUT Trial:<br />
Persistent Occipto- Posterior Position: Outcomes following rotation<br />
Contributions to field of Research<br />
Jon has >100 publications in peer-reviewed journals and is internationally recognised for his<br />
research linking the 12-week ultrasound finding of increased fetal nuchal translucency with<br />
structural heart defects. Jon was part of the team that developed an effective intrauterine therapy for<br />
twin twin transfusion syndrome and has been a leader in the clinical application of cffDNA for<br />
RHD and fetal chromosomal abnormality.<br />
2014 Conference Convenor, International Society for Prenatal Diagnosis Scientific co-chair.<br />
Presented peer selected oral abstract on impact of aspirin on prevalence of early onset<br />
preeclampsia. Invited speaker on prediction of gestational diabetes for pre congress course.<br />
2014 Invited Speaker, Asia Pacific Congress in Maternal and Fetal Medicine, Singapore<br />
Presented data on NIPT, invasive prenatal diagnosis and on 'near miss' analysis of adverse<br />
metal outcomes. Chaired session on fetal surgery.<br />
2014 Invited Speaker, International Society Ultrasound in Obstetrics and Gynaecology (ISUOG):<br />
Annual Scientific Meeting, Spain. Convenor and speaker at pre-congress course on NIPT.<br />
2014 Speaker selected from abstract, World Congress in Fetal Medicine, France Prediction and<br />
prevention of early onset pre-eclampsia.<br />
Research translation<br />
cffDNA for non-invasive genotyping of RHD and for contingent aneuploidy screening.<br />
Validation and demonstration of prediction and prevention of early onset pre-eclampsia.<br />
Collaborations<br />
Charles Perkins Centre / University of Sydney<br />
Australasian Pre-eclampsia Research Network and the Australian Red Cross Blood Service<br />
Fetal Medicine Foundation (UK)<br />
Alberta Children’s Hospital Research Institute and the Danish Fetal Medicine Consortium<br />
Professional involvement<br />
2015 – Current Member Editorial Board, Associate Editor, Acta Obstet Gynecol Scand<br />
2010 – Current Member Editorial Board, Associate Editor, Prenatal Diagnosis<br />
2009 – Current Member Editorial Board, Associate Editor, Fetal Diagnosis and Therapy<br />
2014 Peer Reviewer, ANZJOG, BJOG, PLoS, Ultrasound Obstet and Gynecol<br />
2006 – Current NSW Medical Board<br />
2006 – Current Member RANZCOG 1st trimester screening committee<br />
1997 – Current Member RCOG, UK<br />
Supervision and mentoring<br />
Primary supervisor to five PhD students holders of University of Sydney scholarships.<br />
Five Masters’ students and one PhD student have completed in the last five years.<br />
Page 31
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Peer Recognition and Service<br />
2013 – 2015 Assessor for Singaporean grant funding scheme<br />
2014 – 2015 Assessor for Hong Kong grant funding scheme<br />
2013 UK national research grant funding schemes.<br />
Contributions to NHMRC<br />
2014 NHMRC Research Translation Faculty<br />
2013 - 2015 NHMRC External Assessor for project grants<br />
Top 5 publications in the last 5 years<br />
1: Park F, Russo K, Williams P, Pelosi M, Puddephatt R, Walter M, Leung C, Saaid R, Rawashdeh<br />
H, Ogle R, Hyett J. Prediction and prevention of early onset pre-eclampsia: The impact of aspirin<br />
after first trimester screening. Ultrasound Obstet Gynecol 2015; 46: 419-423.<br />
This prospective cohort study documents the value of prediction (with a 12 week algorithm defining<br />
risk for ePET) and prevention (with low dose Aspirin as a therapeutic intervention) of early onset<br />
pre-eclampsia.<br />
2: Park FJ, Leung CH, Poon LC, Williams PF, Rothwell SJ, Hyett JA. Clinical evaluation of a first<br />
trimester algorithm predicting the risk of hypertensive disease of pregnancy. Aust N Z J Obstet<br />
Gynaecol 2013; 53: 532-9.<br />
A validation study demonstrated the effectiveness of a first trimester algorithm for predicting risk of<br />
early onset pre-eclampsia; demonstrating 90% sensitivity at 90% specificity.<br />
3: Ridding G, Schluter PJ, Hyett JA, McLennan AC. Uterine artery pulsatility index assessment at<br />
11-13 weeks' gestation. Fetal Diagn Ther 2014; 36: 299-304.<br />
This paper defines normal ranges for uterine artery PI at 12 weeks’ gestation in an Australian<br />
population; used in the prediction of risk of early onset pre-eclampsia.<br />
4: Leung C, Saaid R, Pedersen L, Park F, Poon L, Hyett J. Demographic factors that can be used to<br />
predict early-onset pre-eclampsia. J Matern Fetal Neonatal Med. 2014 [Epub ahead of print].<br />
This paper describes demographic factors associated with the risk of developing early onset preeclampsia<br />
in an Australian population. It establishes the baseline for risk algorithms based on<br />
maternal demographic and investigational parameters.<br />
5: E Holanda Moura SB, Park F, Murthi P, Martins WP, Kane SC, Williams P, Hyett J, Silva Costa<br />
Fd. TNF-R1 as a first trimester marker for prediction of pre-eclampsia. J Matern Fetal Neonatal<br />
Med 2016; 29: 897-903.<br />
In collaboration with the group at The Royal Women’s Hospital in Melbourne, this paper explored<br />
the potential of other biomarkers for prediction of early onset pre-eclampsia.<br />
Research relevant to the proposed project<br />
Jon’s primary research interest is the prediction and prevention of adverse obstetric outcomes<br />
through population based screening. His research group has focused on developing predictive<br />
strategies for four major perinatal problems; screening for congenital abnormality, for preeclampsia<br />
and intrauterine growth restriction, for preterm birth and for gestational diabetes. All predictive<br />
testing occurs at 12 weeks’ gestation, the rationale being that this enables application of<br />
preventative interventions that will reduce the prevalence of disease. The group have had significant<br />
success in this area. Jon has lead the integration of some research findings into clinical practice.<br />
One example is the introduction of a pilot program demonstrating the effectiveness of prediction<br />
and prevention of pre-eclampsia; this program involves population-based assessment of maternal<br />
biophysical and biochemical parameters at the 12-week visit. High-risk women are treated with<br />
aspirin to prevent pre-eclampsia. This provides the platform on which women will be recruited to<br />
this study.<br />
Page 32
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI G TRACK RECORD: Dr. Carlos Salomon, PhD, MSc, BSc (Hons)<br />
Career summary<br />
2013-2016 University of Queensland Postdoctoral Fellowship, Brisbane Australia.<br />
2013- Staff, UQ Centre for Clinical Research (UQCCR), Brisbane, Australia.<br />
2013- Co-chair Early Career Researcher, International Federation of Placenta<br />
Association<br />
2009-2012 PhD program in Medical Science, School of Medicine, Pontificia<br />
Universidad Catolica de Chile<br />
Honours and Awards<br />
2013 Award excellence in doctoral thesis. Best PhD thesis, Pontificia Universidad Católica de<br />
Chile<br />
Best Basic Science Oral presentation. 22 nd annual Royal Brisbane and Women’s Hospital<br />
Healthcare Symposium<br />
2012 The University of Queensland Postdoctoral Research Fellowships 2013-2015<br />
University of Queensland Centre for Clinical Research (UQCCR), Brisbane, Australia.<br />
Sigma Aldrich Research Excellence Awards, Society for Gynecologic Investigation.<br />
International Federation of Placenta Associations (IFPA) Y.W. Charlie Locke Awards<br />
CONICYT (Comisión Nacional de Investigación Científica y Tecnológica)<br />
Internship Fellowship, UQCCR, Brisbane, Australia.<br />
UQCCR, Internship Fellowship<br />
CONICYT (Comisión Nacional de Investigación Científica y Tecnológica)<br />
Support fellowship for doctoral thesis, Chile.<br />
2011 International Federation of Placenta Associations (IFPA) Y.W. Charlie Locke Awards (<br />
VRAID (Vicerrectoría Adjunta de Investigación y Doctorado) Internship Fellowship,<br />
University Texas Health Science Center for Pregnancy and Newborn Research, USA.<br />
CONICYT (Comisión Nacional de Investigación Científica y Tecnológica)<br />
PhD Fellowship, Chile.<br />
CONICYT, Support to the participation in national meetings, Chile.<br />
2010 CONICYT, Support for participation in national meetings, Chile.<br />
VRAID , Fellowship Academic Instructor, Pontificia Universidad Católica de Chile.<br />
USPI (Universidade de São Paulo, Brazil), Support for participation in<br />
postgraduate workshop, Brazil<br />
Awards, Best Seminar, Workshop "Maternal Fetal", Universidade de São Paulo, Brazil.<br />
SCHRD (Sociedad Chilena de Reproducción y Desarrollo)<br />
Support for participation in anual meeting, Chile.<br />
Research Support<br />
2013-2016 University of Queensland Postdoctoral Fellowship AU$300,000<br />
2010-2012 Comision Nacional de Ciencia y Tecnologia de Chile (CONICYT), AU$6,000<br />
2009-2010 Vice-rectoría de investigación, Ponticifia Universidad Católica de Chile, AU$2,000<br />
Contribution to the field of research (selected)<br />
2013 Invited Speaker “Exosomes: surrogate biomarkers of placental function” UQCCR Seminars<br />
Series, The University of Queensland, Brisbane. Australia.<br />
Invited Speaker “The role of placental exosomes in intercellular communication in health<br />
and disease”. NUS-UQ Research Day @ The Changing Panorama of Women’s Health:<br />
Navigating New Frontiers 9 th Singapore International Congress of O&G 2013.<br />
Invited Speaker “Placento-Maternal Transfection: Exosomes as surrogate biomarkers of<br />
placental function”. Society for Reproductive Biology meeting, Australian & New Zealand<br />
Placental Research Association, Sydney Australia, 2013.<br />
Page 33
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Invited Speaker: Workshop “Stem cells: from biology to pathology”. International<br />
Federation of Placental Associations (IFPA) 2013, Whistler, CA.<br />
Invited Speaker: Workshop “Oxygen in placenta development and pathologies”.<br />
International Federation of Placental Associations (IFPA) 2013, Whistler, CA.<br />
Invited Speaker: Workshop “Use of ‘omics’ in understanding placental development and<br />
pathologies”. International Federation of Placental Associations (IFPA) 2013, Whistler, CA.<br />
Collaborations - International - University of the Andes and Catholic University of Chile, Santiago<br />
(4 reviews, 4 papers)<br />
Community engagement and participation<br />
Professional Involvement<br />
2012- Co-chair Early Carrier Researcher, International Federation of Placenta Associations.<br />
Supervision and Mentoring Honours 1 (1 current); MSc 0 (1 current); PhD 3 current<br />
Peer Recognition and Service<br />
2013 NHMRC <strong>Grant</strong> Reviewer<br />
Top 5 Publication in the last 5 years<br />
1. Salomon C, Kobayashi M, Ashman K, J, Sobrevia L, 2 Mitchell MD, <strong>Rice</strong> GE (2013)<br />
Hypoxia-induced changes in the bioactivity of cytotrophoblast-derived exosomes. PLoS<br />
ONE 8(11):e79636. doi: 10.1371/journal.pone.0079636.<br />
2. Salomon C, Ryan J, Sobrevia L, Kobayashi M, Ashman K, Mitchell M, <strong>Rice</strong> GE. Exosomal<br />
signalling during hypoxia mediates microvascular endothelial cell migration and<br />
vasculogenesis. (2013) PLoS One. Jul 8;8(7):e68451. doi: 10.1371/journal.pone.0068451.<br />
3. Kobayashi M, Salomon C, Tapia J, Illanes, SE, Mitchell MD, <strong>Rice</strong> GE (2014) Ovarian<br />
cancer cell invasiveness is associated with discordant exosomal sequestration of Let-7<br />
miRNA and miR-200. J. Translational Medicine 12:4. doi:10.1186/1479-5876-12-4<br />
The above 3 papers establish leadership in exosome biology and analysis applied to<br />
placental development and oncology.<br />
4. Westermeier F, Salomon C, González M, Puebla C, Guzmán-Gutiérrez E, Cifuentes F,<br />
Leiva A, Casanello P, Sobrevia L. (2011) Insulin restores gestational diabetes mellitusreduced<br />
adenosine transport involving differential expression of insulin receptor isoforms in<br />
human umbilical vein endothelium. Diabetes 60(6):1677-87. doi: 10.2337/db11-0155.<br />
5. Salomon C, Guzmán-Gutiérrez E, Westermeier F, Puebla C, Leiva A, Casanello P, Sobrevia<br />
L. (2012) Insulin Requires of Insulin Receptors A and B to Restore a Normal Phenotype in<br />
Human Placental Microvascular Endothelium from Patients with Gestational Diabetes<br />
Mellitus. PLoSONE; 7(7):e40578. doi: 10.1371/journal.pone.0040578.<br />
Paper 4 and 5 establish expertise in cell signalling and, in particular, in regulating placental<br />
vascular function.<br />
Page 34
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI H Professor David McIntyre<br />
Top 5 publications<br />
1) Mamun AA, Sutharsan R, O'Callaghan M, Williams G, Najman J, McIntyre HD, Callaway<br />
L. Cesarean Delivery and the Long-Term Risk of Offspring Obesity. Obstet Gynecol. 2013<br />
Nov 6. [Epub ahead of print] PubMed PMID: 24201680. This report addresses the putative<br />
influence of delivery by cesarean section and later obesity, refuting this association in a<br />
large Australian birth cohort with long term follow up.<br />
2) McIntyre HD, Gibbons KS, Flenady VJ, Callaway LK. Overweight and obesity in<br />
Australian mothers: epidemic or endemic? Med J Aust. 2012;196(3):184-8. This large<br />
epidemiologic study provides the most comprehensive long term data on the “obesity<br />
epidemic” and its relationship to a wide range of adverse pregnancy outcome in a birth<br />
cohort from the Mater Mothers’ Hospital in Brisbane.<br />
3) Catalano PM, McIntyre HD, Cruickshank JK, McCance DR, Dyer AR, Metzger BE, et al.<br />
The Hyperglycemia and Adverse Pregnancy Outcome Study: Associations of GDM and<br />
obesity with pregnancy outcomes. Diabetes Care. 2012;35(4):780-6. This study outlines the<br />
relative contributions of mildly elevated blood glucose levels and maternal obesity to<br />
adverse pregnancy outcomes.<br />
4) Flenady V, Koopmans L, Middleton P, Froen JF, Smith GC, Gibbons K, et al. Major risk<br />
factors for stillbirth in high-income countries: a systematic review and meta-analysis.<br />
Lancet. 2011;377(9774):1331-40. This systematic review outlines the major demographic<br />
and medical risk factors for still birth in the “developed world”, emphasising the<br />
importance of maternal obesity and diabetes.<br />
5) Barrett HL, Dekker Nitert M, McIntyre HD, Callaway LK. Normalizing metabolism in<br />
diabetic pregnancy: is it time to target lipids? Diabetes Care. 2014 May;37(5):1484-93. doi:<br />
0.2337/dc13-1934. PubMed PMID: 24757231. This major review in a highly cited journal<br />
considers the clinical relevance of treatments directed at modification of lipid parameters in<br />
pregnancies complicated by diabetes.<br />
OVERALL TRACK RECORD with an emphasis on the past 5 years<br />
Publications/Patents: I have published a total of 141 articles and 4 book chapters, with 57 articles<br />
in the last 5 years. The majority of these publications were achieved whilst working in a busy<br />
clinical role as I have had a part time research appointment (0.3 FTE) only since mid-2008, with no<br />
protected research time prior to this date. My recent publications are mostly in highly ranked<br />
specialist journals covering diabetes and obstetrics. My publications have received over 3400<br />
citations from other scientists and my “h” index via Google scholar is 29.<br />
Research Support: My research has attracted over $11.8M in funding as CI, including grants from<br />
NHMRC, National Institutes of Health (USA) and Canadian Institute for Health Research as well as<br />
smaller scale local grants (Diabetes Australia Research Trust, Queensland Health Strategic<br />
Partnerships, International Institute of Health (George Institute) and some pharmaceutical industry<br />
funding.<br />
Prizes (past 5y):<br />
INTERNATIONAL: Honorary membership of Diabetes in Pregnancy Study Group of the European<br />
Association for the Study of Diabetes, invited presentations to the Diabetes and Reproductive<br />
Health Interest Group of the American Diabetes Association (2011, 2013, 2015, 2016). Awarded<br />
Norbert Freinkel lecture (ADA) for 2016.<br />
NATIONAL: Invited presentations to the Developmental Origins of Health and Disease Society of<br />
Australia and New Zealand (2014) and Australasian Diabetes in Pregnancy Society (2014)<br />
International / National Reputation: I am a regular speaker at international and national meetings<br />
with over 40 presentations over the last 5 years, including invited presentations at peak gatherings<br />
such as the American Diabetes Association, International Federation of Gynecology and Obstetrics,<br />
Controversies in Gynecology, Obstetrics and Maternal Fetal Medicine and Diabetes in Pregnancy<br />
Page 35
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
meetings. I am frequently asked to serve as session chair at such meetings. I frequently undertake<br />
duties as a reviewer for high impact journals including Diabetes Care, Diabetologia, Clinical<br />
Endocrinology and the Journal of Clinical Endocrinology and Metabolism. I have recently been<br />
appointed as an Editorial Board Member for the premier clinical diabetes journal “Diabetes Care”.<br />
I currently serve as Chair of the International Association of Diabetes in Pregnancy Study Groups<br />
and I am an invited member of the FIGO Hyperglycemia in Pregnancy Workgroup<br />
Research Translation:<br />
Direct impact on clinical practice:<br />
• Testing for GDM. I have been centrally involved in the development and dissemination of<br />
the IADPSG recommendations for diagnosis of GDM. This has included membership of<br />
consensus conference which developed the consensus process and of the writing group<br />
which finalized the proposed criteria. On a national level, I have been involved in<br />
representations to the college of Obstetrics and Gynecology, ADIPS and the Australian<br />
Diabetes Society (ADS) as well as local within the Mater Mothers Hospital and on a<br />
Queensland level, where I have been Chair of the GDM workgroup for the Statewide<br />
Clinical Diabetes Network. Internationally, I have been closely involved in this process as<br />
Chair of IADPSG and a member of the FIGO GDM workgroup.<br />
• Intensive diabetes management. Since 2004, I have been a founding member of the<br />
OzDAFNE collaboration, which introduced the Dose Adjustment for Normal Eating<br />
(DAFNE) system of education in intensive insulin therapy for Type 1 diabetes patients into<br />
clinical practice in Australia. This has become the mainstay of such treatment in<br />
Queensland and is DAFNE courses are now offered in over 20 centres across Australia and<br />
New Zealand.<br />
• Type 2 diabetes management. As an investigator in the FIELD and ADVANCE studies, I<br />
have been an active participant in the integration of lipid lowering strategies and intensive<br />
blood pressure control strategies in the management of Type 2 diabetes.<br />
Clinical Practice Guidelines:<br />
I have participated in the development of clinical practice guidelines for Obesity in pregnancy via<br />
the Statewide Maternity and Neonatal Network and I served as Co-lead of the group which<br />
developed a guideline for GDM diagnosis and treatment published in 2015.<br />
Investigator-initiated Clinical Trials:<br />
• I have been involved in the MiG trial of metformin in the management of gestational<br />
diabetes and I have started the first Australian site for the “MiTY” (Metformin in Type 2<br />
diabetes) trial to further examine the use of this medication in pregnancy.<br />
• I am CI-B and lead at Mater Health Services for the “SPRING” (Supplementation with<br />
Probiotics in Gestation) trial which is examining the potential role for probiotics in GDM<br />
prevention.<br />
• I have initiated two RCTs dealing with lifestyle strategies in the prevention of progression to<br />
Type 2 diabetes following GDM.<br />
• I have been a CI on a further RCT “TRIM” (Trial of Weight Reduction in New Mums”<br />
dealing with optimal dietary follow up to reduce post-partum weight retention in obese<br />
pregnant women.<br />
Public Health: Through my role in the National Diabetes in Pregnancy Advisory Committee, I<br />
have contributed to definition of priorities for the care of women with diabetes before, during and<br />
after pregnancy. My contributions to GDM care also relate to Public Health as GDM is the<br />
commonest identifiable antecedent to overt Type 2 diabetes in parous women.<br />
Training: I have held advisory roles for 15 University of Queensland PhD candidates, of whom 8<br />
have successfully completed their degrees (7 ongoing). I am an associate advisor for one student<br />
based at the Menzies Institute in Darwin. In addition I developed and achieved accreditation for<br />
advanced physician training in Endocrinology and Obstetric Medicine at the Mater site and have<br />
supervised over 30 FRACP advanced trainees in these clinical areas.<br />
Page 36
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CI I: Professor David Simmons<br />
Professor David Simmons is Professor of Medicine at Western Sydney University, Head of the<br />
Department of Endocrinology and Chair of the Clinical Council at Campbelltown Hospital,<br />
Professorial Fellow at the University of Melbourne and Diabetes Physician at Cambridge University<br />
Hospitals. His interest is in the prevention of diabetes and its complications on a population basis<br />
and he brings expertise in the areas of health service redesign, the conduct of clinical trials and<br />
clinical epidemiology to the proposal. He has just completed 7 years (2007-2014) as diabetes<br />
clinical lead at Cambridge University Hospitals, England, having been the Foundation chair in<br />
Rural Health at the University of Melbourne 1998-2002, and the Foundation chair in Medicine at<br />
the Waikato Clinical School, University of Auckland, New Zealand 2003-2007. He was President<br />
of the Australasian Diabetes in Pregnancy Society (ADIPS) 1998-2002 and one of the two first cochairs<br />
of the Australian National Diabetes in Pregnancy Advisory Committee 2001-2002. He was<br />
chair of the Diabetes UK Diabetes Health Care Professional Education steering group 2009-2014,<br />
which generated a national position statement on competency in diabetes care. He has been awarded<br />
over $20 million in research funding previously including over $5 million (including 2 NHMRC<br />
grants) since starting back in Australia in January 2015. He has published (or in press) 254<br />
scientific articles (5,739 citations (GS)) and 8 book chapters.<br />
Research relevant to the proposed project<br />
Professor Simmons has been researching the interplay between diabetes, insulin resistance and<br />
adiposity for over 25 years in both epidemiological and prevention/treatment studies, commencing<br />
with South Asians in Coventry (Coventry Diabetes Study), Polynesians in South Auckland (South<br />
Auckland Diabetes Project), rural Victorians (Crossroads studies), Waikato (New Zealand: Te Wai<br />
o Rona: Diabetes Prevention Strategy), Cambridgeshire (England: DALI (RCT for preventing<br />
gestational weight gain/gestational diabetes), RAPSID (RCT of per support to assist selfmanagement<br />
in type 2 diabetes), East Cambs and Fenland Diabetes Integrated Care Initiative).<br />
Mental health issues have featured as barriers to care and self-care across many of these studies and<br />
he led the Cambridge diabetes service initiative to prevent ‘recurrent diabetic ketoacidosis’-a<br />
condition where 60% of patients have mental health issues: admissions were reduced by 60%.<br />
Top 5 publications in the last 5 years<br />
1. Meek CL, Murphy HR, Simmons D. Random plasma glucose in early pregnancy is a better<br />
predictor of gestational diabetes diagnosis than maternal obesity. Diabetologia, 2015.<br />
2. Simmons D, Jelsma JG, Galjaard S, Devlieger R, van Assche A, Jans G, et al. Results From a<br />
European Multicenter Randomized Trial of Physical Activity and/or Healthy Eating to Reduce<br />
the Risk of Gestational Diabetes Mellitus: The DALI Lifestyle Pilot. Diabetes Care,<br />
2015;38:1650-1656.<br />
3. Simmons D, Hartnell S, Watts J, Ward C, Davenport K, Gunn E, Jenaway A. Effectiveness of<br />
a multidisciplinary team approach to the prevention of readmission from acute glycaemic<br />
events. Diab Med. 2015: 1-7.<br />
4. Simmons D, Prevost AT, Bunn C, Holman D, Parker RA, Cohn S, Donald S, Paddison CAM,<br />
Ward C, Robins P, Graffy J. Impact of community based peer support in Type 2 diabetes: A<br />
cluster randomised controlled trial of individual and/or group approaches. PLOS One, 2015; 1-<br />
13.<br />
5. Yu D, Simmons D. Association between blood pressure and risk of cardiovascular hospital<br />
admissions among people with type 2 diabetes. Heart 2014;100:1444-1449.<br />
For papers 2-5, Professor Simmons role was as principal investigator (PI), leading in study design,<br />
and responsibility for the ethics submission, recruitment, implementation and publication. For<br />
paper 1, Professor Simmons was the senior author and supervised the analysis and publication.<br />
Page 37
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Overall track record in the last 5 years<br />
In spite of his heavy clinical and management responsibilities, over the last 5 years, Professor<br />
Simmons has generated 62 refereed publications, over 60 conference presentations and $11 million<br />
of research funding (mainly as PI or co-PI). He is currently the editor of a book on diabetes<br />
integrated care for Springer publications. His evaluated service designs won 3 of the 13 national<br />
QiC diabetes awards in 2013, his recurrent diabetic keto-acidosis prevention programme is reported<br />
as national best practice by the Joint British Diabetes Societies (December 2013). His research into<br />
diabetes in pregnancy has led to the Joseph Hoet award from the Diabetes in Pregnancy Study<br />
Group in 2009 with sentinel studies in the use of insulin pumps in GDM/Type 2 diabetes, random<br />
glucose screening at booking in pregnancy, the impact of the intrauterine milieu on Polynesian<br />
babies including their relative hyperleptinaemia at birth and the Australia/New Zealand pilot of<br />
diabetes in pregnancy structured audit and benchmarking. He was the only English/New Zealand<br />
member of the 2009 International Association Diabetes in Pregnancy Study Group consensus panel<br />
and one of 16 external experts for the 2013 World Health Organisation Diagnostic Criteria and<br />
Classification of Hyperglycaemia First Detected in Pregnancy.<br />
He has a proven track record in the conduct and coordination of clinical trials, epidemiological<br />
research and evaluated service development. Over the last 5 years, he has (i) successfully completed<br />
a National Institute for Health Research (NIHR) funded evaluation (as PI) of an integrated diabetes<br />
service in Cambridgeshire (n=8,000), leading to changes in the way that diabetes is delivered in the<br />
county (ii) successfully completed the largest global Randomised Controlled Trial of diabetes peer<br />
support (Peers for Progress/NIHR funded- RAPSID n=1,299-as PI) which has just had a £0.5<br />
million project funded to translate findings across 8 sites in the UK (iii) he has just finished as the<br />
trial coordinator, UK PI and overall deputy PI for DALI (Vitamin D and Lifestyle Intervention for<br />
the prevention of gestational diabetes), the EU FP7 funded RCT for the prevention of GDM across<br />
9 European countries. (iv) is a co-investigator for CONCEPTT, an international multicentre RCT<br />
of continuous glucose monitoring in pregnant and ‘pre-pregnant’ women with type 1 diabetes (v)<br />
He is one of the 17 PIs in The Australian and New Zealand Diabetes and Cancer Collaboration<br />
(ANZDCC), using data from the Crossroads Undiagnosed Disease Study 1999-2003.<br />
Professor Simmons is the clinical lead for the Cambridge Diabetes Education Programme, a Health<br />
Innovation and Education Cluster funded initiative, the first on line resource to comprehensively<br />
implement health care professional competency frameworks. In 2013, he was awarded the Diabetes<br />
UK Janet Kinson award for his achievements in educational research/development. He referees for<br />
multiple journals and has been an examiner for 4 PhD students (Denmark*2, Ireland, Australia) and<br />
international grants from Australia, Canada, New Zealand, Ireland and Wales. He still cosupervises<br />
one Doctor of Health Psychology (London) student in the UK. He has been a primary or<br />
co-supervisor for 4 PhD completions, 4 Masters students, 1 honours student in the past. He is an<br />
advisor to the Swedish National Diabetes in Pregnancy Register research in Orebro and Chief<br />
Technical Advisor to the Tongan GDM Taskforce.<br />
Page 38
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
CIJ: Professor Sailesh Kumar (MBBS MMed(O&G) FRCS FRCOG FRANZCOG DPhil(Oxon)<br />
CMFM)<br />
Top 5 publications in the last 5 years<br />
1. The relationship between maternal placental growth factor levels and intrapartum fetal<br />
compromise. L Bligh, R Greer, S Kumar. Placenta, Vol. 48, p63–67. Published online: October<br />
14, 2016 This paper details the association between low maternal PlGF levels and intrapartum<br />
complications and poor neonatal outcomes. It is the first report of this association in term<br />
pregnancies and provides evidence for the potential incorporation of this biomarker into a<br />
screening test for late pregnancy complications.<br />
2. Are babies that fail to reach their genetic growth potential at increased risk of intra-partum fetal<br />
compromise? Prior T, Paramasivam G, Bennett P, Kumar S. Ultrasound Obstet Gynecol. 2014 Dec<br />
9. doi: 10.1002/uog.14758. This paper demonstrated that term fetuses that developed intrapartum<br />
compromise had circulatory changes suggestive of suboptimal growth despite normal birthweights.<br />
The evidence presented in this paper is part of a small but growing body of evidence that challenges<br />
the conventionally held view that intrapartum fetal compromise is unpredictable.<br />
3. The magnitude of change in the fetal cerebro-placental ratio in the third trimester and the risk of<br />
adverse pregnancy outcome. C Flatley, R Greer, S Kumar. Ultrasound Obstet Gynecol. 2016 Nov<br />
22. doi: 10.1002/uog.17371.This paper demonstrated that the magnitude of change in the CPR<br />
influences the risk of intrapartum complications and adverse outcome providing evidence for the<br />
value of a late third trimester scan.<br />
4. Prediction of fetal compromise in labor. Prior T, Mullins E, Bennett P, Kumar S. Obstet<br />
Gynecol. 2014 Jun; 123(6):1263-71. This paper detailed a screening test for intrapartum<br />
compromise utilising the fetal cerebro-umbilical ratio and umbilical venous flow and demonstrated<br />
that it was capable of identifying the majority of fetuses at risk. It also showed that the test had a<br />
negative predictive value for intrapartum compromise of almost 100%.<br />
5. Prediction of intrapartum fetal compromise using the cerebroumbilical ratio: a prospective<br />
observational study. Prior T, Mullins E, Bennett P, Kumar S. Am J Obstet Gynecol. 2012 Nov 15.<br />
This was the first prospective study evaluating the utility of the fetal cerebro-umbilical ratio to<br />
predict intrapartum compromise. The results of this study demonstrated that identification of fetuses<br />
at risk was possible in an apparently low risk cohort.<br />
Overall Track Record in the last 5 years<br />
Career summary: Prof Kumar is a Maternal & Fetal Medicine Subspecialist at the Mater Mothers’<br />
Hospital in Brisbane and Head of the Academic Discipline of Obstetrics & Gynaecology at the<br />
University of Queensland. He leads an active research group collaborating across specialties both in<br />
basic science as well as clinical projects. He is also Visiting Professor at Imperial College London.<br />
He is actively involved in both clinical practice and research.<br />
Research Support: Prof Kumar has been a named investigator on grants worth >$2M both in the<br />
UK and in Australia including from the NHMRC.<br />
Contribution to the field of research: Prof Kumar’s current research programme has made<br />
significant contributions towards identifying at risk fetuses in late pregnancy. He has been invited to<br />
present his research findings at many national and international meetings and has given several key<br />
note lectures. His research contribution is evident in the research output of his group and the prizes<br />
won by some of his students. His area of research is particularly relevant in obstetrics given the<br />
appalling perinatal outcomes in low and middle income countries with high rates of stillbirth and<br />
other adverse pregnancy outcomes. He has authored/co-authored more than 80 peer reviewed<br />
papers, 18 book chapters and has written a textbook of fetal medicine. Over the last five years, Prof<br />
Kumar has authored over 40 publications. The majority of his publications is in the area of adverse<br />
pregnancy outcome, fetal growth restriction and fetal therapy. In recognition of Prof Kumar’s<br />
Page 39
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
professional achievements and contributions to the NHS in the UK, he was awarded a Bronze/Level<br />
9 Clinical Excellence Award in 2008 at the age of 42 years (The average age to attain this award<br />
nationally is 49 years). In 2010/2011, the Times newspaper undertook an exercise to identify<br />
Britain's leading specialists based on information from professional bodies. Prof Kumar was one of<br />
only 2 fetal medicine specialists on this list.<br />
Professional Involvement: In the UK he was a specialist advisor to the National Institute of<br />
Clinical Excellence for Fetal Medicine interventional procedures and reviewed some fetal medicine<br />
guidelines prior to publication. He was also a clinical advisor to the Healthcare Commission and<br />
gave advice on complex cases where local resolution had failed. He organised (since 2008) an<br />
annual Clinical Fetal Medicine Course at Imperial College, London which was aimed at advanced<br />
and subspecialty trainees in maternal and fetal medicine and specialists involved in perinatal care.<br />
This was an extremely popular course and attracted numerous local and international delegates. Prof<br />
Kumar has co-authored a RCOG guideline pertaining to the management of women with red cell<br />
antibodies in pregnancy. These guidelines influence and guide practice in many different countries.<br />
In addition, he was also a member of the Fetal & Neonatal Transfusion sub-committee of the British<br />
Committee for Standards in Haematology (BCSH) and contributed to the most recent set of<br />
guidelines. At the Mater Mothers’ Hospital/Mater Research Institute he is a member of the Human<br />
Research Ethics Committee.<br />
International standing: Prof Kumar is regularly invited to speak at international conferences<br />
including International Society for Prenatal Diagnosis, RANZCOG/RCOG, International Society of<br />
Obstetrics and Gynaecology Ultrasound, Singapore College of Obstetrics & Gynaecology and Hong<br />
Kong University.<br />
Supervision and/or mentoring: Prof Kumar is currently supervising 7 PhD and 3 Honours<br />
students and 8 medical student projects and is leading an RCT investigating the utility of Sildenafil<br />
to reduce the risk of intrapartum fetal compromise. In the UK, he has supervised to completion 5<br />
PhD students and 22 Masters students. In the UK, Prof Kumar was Clinical Programme Supervisor<br />
for the Maternal & Fetal Medicine Subspecialty training programme at Imperial College as well as<br />
preceptor for the Advanced Training Special Skills Module (ATSM) in Fetal Medicine for the<br />
Northwest Thames Perinatal Network<br />
Peer review involvement: Prof Kumar has reviewed for a number of international journals<br />
including Placenta, Prenatal Diagnosis, Journal of Maternal-Fetal Medicine and Neonatology,<br />
Journal of Perinatology, Australian & New Zealand Journal of Obstetrics & Gynaecology,<br />
Ultrasound in Obstetrics and Gynaecology and PLOSOne. In 2012 he was invited to be an<br />
associate editor of the journal Fetal and Maternal Medicine Review, Cambridge University Press.<br />
Contribution to the NHMRC and other funding agencies: Prof Kumar has reviewed funding<br />
proposals from the NHMRC and Wellcome Trust and other funding bodies.<br />
Page 40
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Associate Investigator (AI) Contribution,<br />
The AI team provides a pathway to end user organisations and will play a significant role within<br />
this CRE that will enable to CRE to influence policy and practice locally, nationally and<br />
internationally.<br />
AI – Professor Leonie Callaway holds a conjoint position as Head, Royal Brisbane Clinical<br />
School, and Senior Specialist in Obstetric and Internal Medicine at the Royal Brisbane and<br />
Women's Hospital. Prof Callaway is Deputy Chair of the Queensland Maternal and Perinatal<br />
Quality Council, and Co-Chair of the Queensland Clinician Scientists Association. Prof Callaway<br />
has an outstanding research track record in obesity and inflammation in pregnancy, the role of the<br />
maternal metabolism on fetal programming and neonatal body composition, lifestyle interventions<br />
in pregnancy, the role of pregnancy in unmasking the risks of future chronic disease and probiotics<br />
for the prevention of gestational diabetes mellitus. Prof Callaway is a member of the Council for the<br />
Australian Diabetes in Pregnancy Society, and is Deputy Chair of the Queensland Maternal and<br />
Perinatal Quality Council. Prof Callaway has an active interest in guideline development to support<br />
translation of research into clinical practice. Together with Dekker Nitert is a lead clinical<br />
researcher in the SPRING RTC study of probiotics in the prevention of gestational diabetes mellitus<br />
in overweight and obese women. Prof Callaway have a critical role in the translation of CRE<br />
research outcome into practice and policy change.<br />
AI- Professor Alan Rowan is Director of the Australian Institute for Bioengineering and<br />
Nanotechnology. He was awarded an ARC laureate in 2016 in the area of biomimetic materials and<br />
has active research in the fields of regenerative medicine, wound care, immunotherapy and<br />
nanomedicine. He co-director of the UQ StemCare center for stem cell ageing and a board member<br />
of the Dow Centre for Sustainable Engineering Innovation. Prof Rowan is co-founder of four spin<br />
companies Noviocell, Noviotech, Encapson and Wound-X in the field of biomaterials and their<br />
medical applications. Prof Rowan will play a crucial role in the transactional of new technological<br />
advances in bio engineering and nanotechnology into clinical practice. In particular, Prof Rowan<br />
will contribute to the development of exosome-based diagnostics and the development of new<br />
point- of-care medical devices. Prof Rowan will also leverage his extensive industry partnerships to<br />
provide in-house opportunities for career development and training for postdoctoral fellows and<br />
students involved in the CRE.<br />
AI-A/Prof Greg Duncombe is an active clinician scientist, with clinical involvement in many local<br />
institutions and access to Australia-wide clinical and basic science collaborations. He is the main<br />
clinical lead/connection between the exosome lab scientists at UQCCR and the local obstetric<br />
population in regards to fetal and maternal medicine research candidates (including GDM and<br />
others) and specimen availability. AI-Duncombe is the current Chair of the Maternal Fetal<br />
Medicine Subspecialty (MFM) in Australia and has unparalleled access to subspecialty trainees and<br />
colleagues and key responsibilities for development of guidelines. A/Prof Duncombe has played a<br />
crucial role in establishing clinical partnerships across the CRE collaborative network. In addition,<br />
he has an active collaborator in the exosomes signalling and biomarker aspects of the CRE.<br />
AI-A/Prof Anusch Yazdani is Director of Clinical Research and Development at Queensland<br />
Fertility Group Research Foundation. He is a distinguished subspecialist in reproductive<br />
endocrinology, infertility and minimally invasive pelvic surgery. He is the Program Director for<br />
Endoscopic Surgery and Reproductive Endocrinology at Eve Health and Director of Research at the<br />
Queensland Fertility Group. A/Prof Yazdani is a collaborator on ART research projects. Within the<br />
Queensland Fertility Group (QFG) he has facilitated access to human embryo-conditioned culture<br />
media for analysis. QFG staff collect and process these valuable clinical samples for the CRE team<br />
Page 41
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
and coordinate access to clinical records.<br />
contribution to the work of the CRE.<br />
As such they make extremely valuable in kind<br />
AI- A/Prof David Whiley is employed concurrently by The University of Queensland working at<br />
UQCCR and Pathology Queensland an organisation occupying the adjacent building. A/Prof<br />
Whiley has expertise in the successful development and implementation of in vitro diagnostics and<br />
their implementation to clinical practice. His working environment at Pathology Queensland<br />
contributes a clear pathway for translation. A/Prof Whiley conducts the development all phases of<br />
IVD development within the Centre of a Clinical Research and work closely with CRE members<br />
within the facility. He will play crucial role in is the translation of new screening tests into routine<br />
clinical pathology services.<br />
AI-Prof Karen Moritz is Director of the children’s health research Centre, University of<br />
Queensland and an NH&MRC Senior Research Fellow in the School of Biomedical Sciences at the<br />
University of Queensland. The aim of her work is to understand how prenatal perturbations<br />
contribute to an increased risk of developing cardiovascular, renal and metabolic disease in<br />
adulthood. Over the last 5-7 years, her research has focused on determining the pivotal role played<br />
by the kidney in the “developmental programming” of adult disease. Her research has shown a<br />
reduced nephron endowment is associated with hypertension and renal impairment in the adult<br />
following excess maternal glucocorticoid exposure, maternal low protein diet, placental<br />
insufficiency and most recently, prenatal alcohol exposure. Prof Moritz will play a substantive role<br />
in assessing the impact of complications of pregnancy on pregnancy and neonatal outcome and the<br />
development and evaluation of intervention strategies.<br />
AI – Dr Sarah Reed is the Head of the Mass Spectrometry Facility at the University of Queensland<br />
Centre for Clinical Research. She has over 12 years of experience in mass spectrometry across the<br />
research areas of proteomics, lipidomics, metabolomics, tissue imaging and small molecule<br />
analysis. Her background is from the industry where she was appointed as the senior application<br />
specialist for a global mass spectrometry company and was integral in the development,<br />
implementation and education of new technologies and workflows to researchers across Australia,<br />
New Zealand and the Rest of Asia regions. AI Reed is also involved in implementing and<br />
maintaining the international industry standard environment (ISO17025, ISO13485) within the<br />
facility. Dr Reid’s role in the CRC is one of a technical regulatory compliant expert.<br />
AI-Prof Annemarie Hennessy is the Dean of Medicine at the School of Medicine and currently<br />
holds the position of Foundation Professor of Medicine. Profe Hennessy is an active obstetric and<br />
renal physician based at the Campbelltown Hospital. Prof Hennessy has an extensive research track<br />
record in preeclampsia research and is actively involved in clinical and laboratory research into the<br />
causes of high blood pressure during pregnancy; collaborating with hospitals in Sydney, Canada<br />
and the USA. Her contribution to this CRE is indispensable for the successful completion of T3<br />
and T4 activities and for mentoring and training of clinical researcher and practitioners.<br />
AI – Dr Marloes Dekker Dr Dekker’s research focuses on the role of metabolism in<br />
complications of pregnancy. Dr Dekker is a Senior Lecturer in the School of Biomedical Sciences<br />
and heads a research group at the UQ Centre for Clinical Research studying the role of the gut<br />
microbiome in pregnancy, the role of food additives on placental function and placental gene<br />
expression and epigenetic markers in pregnancy complications. Dr Dekker works closely with<br />
clinician-scientists and clinicians at the Royal Brisbane and Women’s Hospital. She is part of the<br />
SPRING RCT team which assesses if probiotics can prevent gestational diabetes mellitus in<br />
overweight and obese women. Dr Dekker is a scientific representative on the SOMANZ council.<br />
Page 42
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
Consumer and Community Participation<br />
This work of this CRE is Precision Medicine that involves translation of research excellence and<br />
cutting edge technology through quality management systems into personalised medicine. The<br />
need for validation of personalised Medicine by end user populations is self-evident. While<br />
successful outcomes will be honed from presenting populations of mothers and babies, it is critical<br />
to the legacy of this CRE that those for whom successful pregnancy outcomes have not been<br />
possible will continue to have involvement. The CRE will endeavour to secure on going<br />
involvement of its end user populations and advocacy groups through the established health care<br />
provider organisations within its collaborative network but also directly through education<br />
programs offered to address lifestyle factors at preconception. Those who have experienced<br />
miscarriage and still birth are more likely to be engaged through the medium of support groups.<br />
The current engagement activities of the CRE CI and AI will be leveraged into CRE portfolio. The<br />
activities include their existing connections with stakeholder groups through which it is proposed<br />
the CRE will convene forums through which feedback and opinion may be elicited for new service<br />
models for improving pre-conception care and early pregnancy risk engagement. It is anticipated<br />
that the following engagements will be enhanced and strengthened by participation of other CIs;<br />
new engagements will be built:<br />
Professor Simmons is the clinical lead for the Cambridge Diabetes Education Programme, a Health<br />
Innovation and Education Cluster funded initiative, the first on line resource to comprehensively<br />
imple Professor Simmons presents to the local community (e.g. Rotary) on Diabetes. AHSP DOMS<br />
has set up an Aboriginal Reference group, a CALD reference group and a stakeholder group<br />
(including Diabetes Australia-NSW, Juvenile Diabetes Research Foundation, Pharma companies,<br />
Health Services). Prof Simmons engages with community group as President, Australasian<br />
Diabetes in Pregnancy Society (ADIPS 1998-2002); Co-Chair, National Diabetes in Pregnancy<br />
Advisory Committee, Australia (2001-2002); Co-Chair, NZ National GDM Working Group (2006);<br />
Diabetes UK Health Professional Education Chair (2010-2014); Mid Essex Clinical Commissioning<br />
Group (2013-2014); Deputy Divisional Director, Division of Medicine, CUH (2011-2014). He has<br />
also set up a Clinician Reference Group in Wollondilly for the Wollondilly Diabetes Programme<br />
(an integrated diabetes service).<br />
Professor Hyett contributes to ‘Miracle Babies’ as community advocates for a threatened preterm<br />
labor project being established across NSW and is involved in the James Lind style Charles Perkins<br />
Centre forum to identify research questions for the proposed Baby1000 (examining impacts of<br />
interventions through fetal life to two years of age) project. He has been involved in establishing the<br />
RPA/Sydney Local Health District iSAIL stillbirth clinic through community support (Canterbury<br />
NSW Leagues Club).<br />
Professor Colditz has a long standing involvement in supporting health consumer and advocacy<br />
organisations. He is currently a board member of the national SIDS & Kids Foundation. He has<br />
been awarded the Ray Phippard Award for services to medical research by the Lions Medical<br />
Research Foundation. In 2013 he was awarded life membership of SIDS & Kids (QLD).<br />
Page 43
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
References<br />
1. Barker DJ. The developmental origins of adult disease. Eur J Epidemiol 2003; 18(8): 733-6.<br />
2. Barker DJ. The developmental origins of chronic adult disease. Acta Paediatr Suppl 2004;<br />
93(446): 26-33.<br />
3. Ryckman KK, Borowski KS, Parikh NI, Saftlas AF. Pregnancy Complications and the Risk<br />
of Metabolic Syndrome for the Offspring. Curr Cardiovasc Risk Rep 2013; 7(3): 217-23.<br />
4. Park FJ, Leung CH, Poon LC, Williams PF, Rothwell SJ, Hyett JA. Clinical evaluation of a<br />
first trimester algorithm predicting the risk of hypertensive disease of pregnancy. Aust N Z J<br />
Obstet Gynaecol 2013; 53(6): 532-9.<br />
5. Manten GT, Sikkema MJ, Voorbij HA, Visser GH, Bruinse HW, Franx A. Risk factors for<br />
cardiovascular disease in women with a history of pregnancy complicated by preeclampsia<br />
or intrauterine growth restriction. Hypertens Pregnancy 2007; 26(1): 39-50.<br />
6. Christensen M, Kronborg CS, Eldrup N, Rossen NB, Knudsen UB. Preeclampsia and<br />
cardiovascular disease risk assessment - Do arterial stiffness and atherosclerosis uncover<br />
increased risk ten years after delivery? Pregnancy Hypertens 2016; 6(2): 110-4.<br />
7. Williams D. Pregnancy: a stress test for life. Curr Opin Obstet Gynecol 2003; 15(6): 465-71.<br />
8. Cain MA, Salemi JL, Tanner JP, Kirby RS, Salihu HM, Louis JM. Pregnancy as a window<br />
to future health: maternal placental syndromes and short-term cardiovascular outcomes. Am<br />
J Obstet Gynecol 2016; 215(4): 484 e1- e14.<br />
9. Chasan-Taber L. It Is Time to View Pregnancy as a Stress Test. J Womens Health (Larchmt)<br />
2016; 25(1): 2-3.<br />
10. Sattar N, Greer IA. Pregnancy complications and maternal cardiovascular risk: opportunities<br />
for intervention and screening? BMJ 2002; 325(7356): 157-60.<br />
11. Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of<br />
cardiovascular disease in women--2011 update: a guideline from the American Heart<br />
Association. J Am Coll Cardiol 2011; 57(12): 1404-23.<br />
12. Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational<br />
diabetes: a systematic review and meta-analysis. Lancet 2009; 373(9677): 1773-9.<br />
13. Noussitou P, Monbaron D, Vial Y, Gaillard RC, Ruiz J. Gestational diabetes mellitus and<br />
the risk of metabolic syndrome: a population-based study in Lausanne, Switzerland.<br />
Diabetes Metab 2005; 31(4 Pt 1): 361-9.<br />
14. Kim C, Cheng YJ, Beckles GL. Cardiovascular disease risk profiles in women with histories<br />
of gestational diabetes but without current diabetes. Obstet Gynecol 2008; 112(4): 875-83.<br />
15. Bellamy L, Casas JP, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular<br />
disease and cancer in later life: systematic review and meta-analysis. BMJ 2007; 335(7627):<br />
974.<br />
Page 44
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
16. Williams D. Long-term complications of preeclampsia. Semin Nephrol 2011; 31(1): 111-22.<br />
17. Robbins CL, Hutchings Y, Dietz PM, Kuklina EV, Callaghan WM. History of preterm birth<br />
and subsequent cardiovascular disease: a systematic review. Am J Obstet Gynecol 2014;<br />
210(4): 285-97.<br />
18. Simpson RJ, Jensen SS, Lim JW. Proteomic profiling of exosomes: current perspectives.<br />
Proteomics 2008; 8(19): 4083-99.<br />
19. Harding CV, Heuser JE, Stahl PD. Exosomes: looking back three decades and into the<br />
future. J Cell Biol 2013; 200(4): 367-71.<br />
20. Lener T, Gimona M, Aigner L, et al. Applying extracellular vesicles based therapeutics in<br />
clinical trials - an ISEV position paper. J Extracell Vesicles 2015; 4: 30087.<br />
21. Salomon C, Torres MJ, Kobayashi M, et al. A gestational profile of placental exosomes in<br />
maternal plasma and their effects on endothelial cell migration. PLoS One 2014; 9(6):<br />
e98667.<br />
22. Vaswani K, Ashman K, Reed S, et al. Applying SWATH Mass Spectrometry to Investigate<br />
Human Cervicovaginal Fluid During the Menstrual Cycle. Biol Reprod 2015; 93(2): 39.<br />
23. Escudero CA, Herlitz K, Troncoso F, et al. Role of Extracellular Vesicles and microRNAs<br />
on Dysfunctional Angiogenesis during Preeclamptic Pregnancies. Front Physiol 2016; 7: 98.<br />
24. Salomon C, Scholz-Romero K, Sarker S, et al. Gestational Diabetes Mellitus Is Associated<br />
With Changes in the Concentration and Bioactivity of Placenta-Derived Exosomes in<br />
Maternal Circulation Across Gestation. Diabetes 2016; 65(3): 598-609.<br />
25. Salomon C, Yee S, Scholz-Romero K, et al. Extravillous trophoblast cells-derived exosomes<br />
promote vascular smooth muscle cell migration. Front Pharmacol 2014; 5: 175.<br />
26. Wee EJ, Ngo TH, Trau M. Colorimetric detection of both total genomic and loci-specific<br />
DNA methylation from limited DNA inputs. Clin Epigenetics 2015; 7: 65.<br />
27. Rahnama F, Shafiei F, Gluckman PD, Mitchell MD, Lobie PE. Epigenetic regulation of<br />
human trophoblastic cell migration and invasion. Endocrinology 2006; 147(11): 5275-83.<br />
28. Rahnama F, Thompson B, Steiner M, Shafiei F, Lobie PE, Mitchell MD. Epigenetic<br />
regulation of E-cadherin controls endometrial receptivity. Endocrinology 2009; 150(3):<br />
1466-72.<br />
29. Jansen ME, Metternick-Jones SC, Lister KJ. International differences in the evaluation of<br />
conditions for newborn bloodspot screening: a review of scientific literature and policy<br />
documents. Eur J Hum Genet 2016.<br />
30. Wee EJ, Wang Y, Tsao SC, Trau M. Simple, Sensitive and Accurate Multiplex Detection of<br />
Clinically Important Melanoma DNA Mutations in Circulating Tumour DNA with SERS<br />
Nanotags. Theranostics 2016; 6(10): 1506-13.<br />
31. Edgell T, Martin-Roussety G, Barker G, et al. Phase II biomarker trial of a multimarker<br />
diagnostic for ovarian cancer. J Cancer Res Clin Oncol 2010; 136(7): 1079-88.<br />
32. <strong>Rice</strong> GE, Edgell TA, Autelitano DJ. Evaluation of midkine and anterior gradient 2 in a<br />
multimarker panel for the detection of ovarian cancer. J Exp Clin Cancer Res 2010; 29: 62.<br />
Page 45
GRANT PROPOSAL – 2016 Centres of Research Application ID: 1135277<br />
Excellence funding commencing 2017 CIA Surname: <strong>Rice</strong><br />
33. Brunelli VB, Prefumo F. Quality of first trimester risk prediction models for pre-eclampsia:<br />
a systematic review. BJOG 2015; 122(7): 904-14.<br />
34. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating<br />
characteristic (ROC) curve. Radiology 1982; 143(1): 29-36.<br />
35. Efron B. Bayesian inference and the parametric bootstrap. Ann Appl Stat 2012; 6(4): 1971-<br />
97.<br />
36. Di Quinzio MK, Oliva K, Holdsworth SJ, et al. Proteomic analysis and characterisation of<br />
human cervico-vaginal fluid proteins. Aust N Z J Obstet Gynaecol 2007; 47(1): 9-15.<br />
37. <strong>Rice</strong> GE, Georgiou HM, Ahmed N, Shi G, Kruppa G. Translational proteomics: developing<br />
a predictive capacity -- a review. Placenta 2006; 27 Suppl A: S76-86.<br />
38. Ahmed N, Barker G, Oliva KT, et al. Proteomic-based identification of haptoglobin-1<br />
precursor as a novel circulating biomarker of ovarian cancer. British Journal of Cancer<br />
2004; 91(1): 129-40.<br />
39. <strong>Rice</strong> GE, Illanes SE, Mitchell MD. Gestational diabetes mellitus: a positive predictor of type<br />
2 diabetes? Int J Endocrinol 2012; 2012: 721653.<br />
40. Salomon C, Ryan J, Sobrevia L, et al. Exosomal signaling during hypoxia mediates<br />
microvascular endothelial cell migration and vasculogenesis. PLoS One 2013; 8(7): e68451.<br />
41. Georgiou HM, Lappas M, Georgiou GM, et al. Screening for biomarkers predictive of<br />
gestational diabetes mellitus. Acta Diabetol 2008; 45(3): 157-65.<br />
42. Freedman LP, Cockburn IM, Simcoe TS. The Economics of Reproducibility in Preclinical<br />
Research. PLoS Biol 2015; 13(6): e1002165.<br />
Page 46