Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
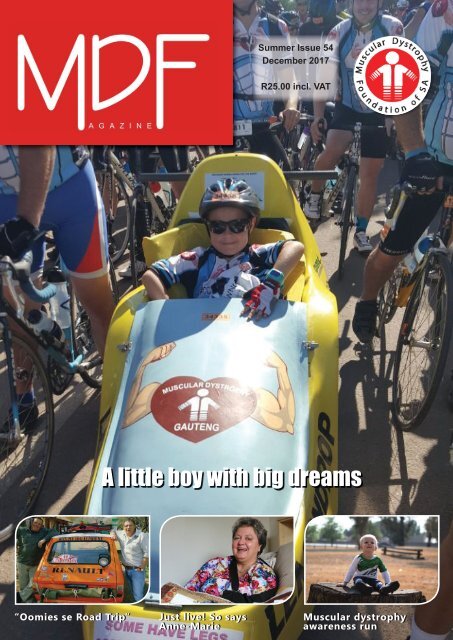
Summer <strong>Issue</strong> <strong>54</strong><br />
<strong>December</strong> <strong>2017</strong><br />
R25.00 incl. VAT<br />
A little boy with big dreams<br />
“Oomies se Road Trip”<br />
Just live! So says<br />
Anne-Marie<br />
Muscular dystrophy<br />
awareness run
Get 10% off any<br />
Power purchase<br />
Present this ad at any CE Mobility branch.<br />
The offer can not be used in conjunction with other discount offers.<br />
Valid until end <strong>2017</strong><br />
Roodepoort, Rivonia, Pretoria, Cape Town, Durban, Port Elizabeth, George & Bloemfontein . 0860 23 66 24 . www.cemobility.co.za
DF<br />
<strong>Magazine</strong><br />
05 <strong>MDF</strong> notice board<br />
06 National news<br />
07 MD information<br />
26 Health news<br />
MD INFORMATION<br />
07 Congenital muscular dystrophy<br />
10 Emergency alert cards<br />
Events<br />
14 Make Today Count Tandem Skydiving <strong>2017</strong><br />
15 Muscular dystrophy awareness run<br />
15 “Oomies se road trip”<br />
People<br />
16 Just live! So says Anne-Marie<br />
18 Iman Casoojee<br />
20 Tribute feature: Patrick John Artman<br />
21 Ride London: Barbara’s story<br />
22 Exondys 51: the Roe family’s story<br />
23 Ella and her ‘cheeky feet’<br />
Regular Features<br />
28 The View from Down Here<br />
29 Doctor’s corner<br />
30 Sandra’s thoughts on …<br />
Research<br />
24 Dystrophin mutation in Duchenne mouse model<br />
25 Myotubular myopathy gene therapy trial<br />
25 Bone health in people with FSHD<br />
C O N T E N T S<br />
Published by:<br />
Muscular Dystrophy Foundation of SA<br />
Tel: 011 472-9703<br />
Fax: 086 646 9117<br />
E-mail: national@mdsa.org.za<br />
Website: www.mdsa.org.za<br />
Publishing Team:<br />
Managing Editor: Pieter Joubert<br />
Copy Editor: Keith Richmond<br />
Publishing Manager: Gerda Brown<br />
Design and Layout: Divan Joubert<br />
Printer: Qualimark Printing<br />
Cover photo of Ludick Fouche courtesy<br />
of Angelos Frantzeskos.<br />
Future <strong>Issue</strong>s:<br />
April 2018<br />
(Deadline: 2 March 2018)<br />
The Muscular Dystrophy Foundation<br />
of South Africa<br />
We are a non-profi t organisation that supports<br />
people affected by muscular dystrophy and<br />
neuromuscular disorders and that endeavours to<br />
improve the quality of life of its members.
From The<br />
I was diagnosed with FSHD in my early twenties and have been using a wheelchair<br />
for 16 years. It was difficult to accept in the beginning but after a while you<br />
realise that you cannot change anything and a wheelchair makes a huge difference.<br />
It takes a lot of energy to shower, get dressed, eat, move around. I don’t<br />
complain, as there are many people in worse situations than I am. I try to do as<br />
much every day as I can. l try to stay positive and see the other blessings in my<br />
life, but it's hard not to wonder “what if...?” or “why did this happen to me?” It's<br />
a slowly progressing disease, but it's a very traumatising, suffocating disease<br />
at the same time.<br />
When I was diagnosed the only thing I thought of was the possibility that researchers<br />
would soon fi nd a cure. As time went by I realised this was not going<br />
to happen, but I still pray and believe that a cure will be found in the near<br />
future.<br />
I did not want to meet other people, but after I was invited to a meeting by Tina de Vente, who was<br />
working at the <strong>MDF</strong> offices at the time, I decided to meet with other affected members. After meeting parents<br />
of children diagnosed with Duchenne muscular dystrophy, my outlook changed. I realised it was selfi sh of me<br />
to think a cure should be found for my own condition and not to be as concerned about all the other conditions<br />
as well.<br />
I realised there were many people and families who needed help and the foundation should include and reach<br />
out to everybody affected by muscle diseases. Over the years I have met and become friends with many affected<br />
people and families. Families affected by muscle-wasting conditions are experts in what it means to live<br />
with these different conditions, and it is important that they share information and support each other.<br />
In this issue you will read of personal stories and awareness events. As usual you will also fi nd MD information<br />
and research articles.<br />
Thank you to everybody who has supported our foundation over the years. For those who are able to make<br />
donations, we thank you from the bottom of our hearts.<br />
Warmest greetings of the season, and best wishes for good health and happiness in 2018.<br />
Until next year!<br />
Regards<br />
Pieter Joubert<br />
4
Subscription and contributions to<br />
the magazine<br />
We publish three issues of <strong>MDF</strong> <strong>Magazine</strong><br />
a year and you can subscribe online<br />
to the magazine or by calling your nearest<br />
branch.<br />
If you have any feedback on our publications,<br />
please contact the National Office<br />
by email at national@mdsa.org.za<br />
or call 011 472-9703.<br />
Get all the latest news on the fight<br />
against muscle-wasting conditions and<br />
the latest research updates. It is our editorial<br />
policy to report on developments<br />
regarding the different types of dystrophy<br />
but we do not thereby endorse any<br />
of the drugs, procedures or treatments<br />
discussed. Please consult with your own<br />
physician about any medical interventions.<br />
If you are interested in sharing your inspirational<br />
stories, please let us know<br />
and we’ll be in touch to discuss this<br />
with you.The Foundation would love<br />
to hear from affected members, friends,<br />
family, doctors, researchers or anyone<br />
interested in contributing to the magazine.<br />
Articles may be edited for space<br />
and clarity.<br />
<strong>MDF</strong> SA database<br />
If you know people affected by muscular<br />
dystrophy or neuromuscular disorders<br />
who are not members, please<br />
ask them to contact us so that we can<br />
register them on our database. If we do<br />
not have your current e-mail and postal<br />
address, please contact your branch so<br />
that we can update your details on our<br />
database.<br />
How can you help?<br />
Branches are responsible for doing their<br />
own fundraising to assist members with<br />
specialised equipment. Contact your<br />
nearest branch of the Muscular Dystrophy<br />
Foundation of South Africa to find<br />
out how you can help with fundraising<br />
events for those affected with muscular<br />
dystrophy.<br />
Fundraising<br />
Crossbow Marketing Consultants (Pty)<br />
Ltd are doing invaluable work through<br />
the selling of annual forward planners.<br />
These products can be ordered from<br />
Crossbow on 021 700-6500. For enquiries<br />
contact National Office by email at<br />
national@mdsa.org.za or call 011 472-<br />
9703.<br />
<strong>MDF</strong> ::<br />
<strong>MDF</strong> support information<br />
For more information about the Muscular Dystrophy Foundation, the benefits of<br />
being a member and details on how to become a member, call your nearest branch.<br />
CAPE BRANCH (Western Cape,<br />
Northern Cape & part of Eastern<br />
Cape)<br />
E-mail: cape@mdsa.org.za<br />
Tel: 021 592-7306<br />
Fax: 086 535 1387<br />
Address: 3 Wiener Street, Goodwood,<br />
7460<br />
Banking details: Nedbank, current<br />
account no. 2011007631<br />
branch code 101109<br />
GAUTENG BRANCH (Gauteng,<br />
Free State, Mpumalanga, Limpopo<br />
& North West)<br />
E-mail: gauteng@mdsa.org.za<br />
Website: www.mdfgauteng.org<br />
Website: www.muscleriders.co.za<br />
Tel: 011 472-9824<br />
Fax: 086 646 9118<br />
Address: 12 Botes Street, Florida Park,<br />
1709<br />
Banking details: Nedbank, current<br />
account no. 1958323284<br />
branch code 192841<br />
Pretoria Office<br />
E-mail: swpta@mdsa.org.za<br />
Tel: 012 323-4462<br />
Address: 8 Dr Savage Road, Prinshof,<br />
Pretoria<br />
KZN BRANCH (KZN & part of<br />
Eastern Cape)<br />
E-mail: kzn@mdsa.org.za<br />
Tel: 031 332-0211<br />
Address: Office 7, 24 Somtseu Road,<br />
Durban, 4000<br />
Banking details: Nedbank, current<br />
account no. 1069431362<br />
branch code 198765<br />
General MD Information<br />
Cape Town<br />
Lee Leith<br />
Tel: 021 794-5737<br />
E-mail: leeleith@mweb.co.za<br />
Gauteng<br />
Pieter Joubert<br />
Tel: 011 472-9824<br />
E-mail: gauteng@mdsa.org.za<br />
General Support Group Gauteng<br />
East Rand<br />
Zigi Potgieter<br />
Cell: 082 499 9384<br />
E-mail: z.kerstholt@gmail.com<br />
Duchenne MD<br />
Cape<br />
Win van der Berg (Support Group)<br />
Tel: 021 557-1423<br />
Penny Cato<br />
Tel: 021 671-8702<br />
KZN<br />
Maxine Strydom (Support Group)<br />
Tel: 031 762-1592<br />
Cell: 083 290 6695<br />
Gauteng<br />
Jan Ferreira (Support Group – Pretoria)<br />
Tel: 012 998-0251<br />
Estelle Fichardt<br />
Tel: 012 667-6806<br />
Christine Winslow<br />
Cell: 082 608 4820<br />
Charcot Marie Tooth (CMT)<br />
Hettie Woehler<br />
Cell: 084 581 0566<br />
E-mail: hettie@leefvoluit.co.za<br />
Facioscapulohumeral (FSHD)<br />
Francois Honiball<br />
Tel: 012 664-3651<br />
Barry Snow<br />
Cell: 083 66 66 270<br />
E-mail: barry.snow@worleyparsons.<br />
com<br />
Friedreich Ataxia (FA)<br />
Linda Pryke<br />
Cell no: 084 405 1169<br />
Nemaline Myopathy<br />
Adri Haxton<br />
Tel: 011 802-7985<br />
Spinal Muscular Atrophy (SMA)<br />
Zeta Starograd<br />
Tel: 011 640-1531<br />
Lucie Swanepoel<br />
Tel: 017 683-0287<br />
Spinal Muscular Atrophy (Adult<br />
SMA)<br />
Justus Scheffer<br />
Tel: 012 331-3061<br />
E-mail: justusscheffer@gmail.com<br />
5
National<br />
What’s stopping you?<br />
By Gerda Brown<br />
Muscular dystrophy is physically destructive, but challenges can be greatly alleviated<br />
with assistive devices, support aids, surgery, physiotherapy, etc. It is the psychological<br />
and emotional issues related to physical disability that cause the main challenges. When<br />
people receive a diagnosis of muscular dystrophy, many adjust to it healthily and cope<br />
well but others do not. Feelings of hopelessness, social isolation, frustration and depression<br />
are all very common. The emotional wellbeing of a disabled person is incredibly<br />
important. Several types of interventions may be implemented to achieve wellness, such<br />
as therapy, counselling, support, etc.<br />
Many times, when we hear the word “support”, our minds go straight to formal programmes or services. This is, however,<br />
not always what support means. Support sources can provide assistance in day-to-day needs, provide much needed information,<br />
and provide comfort and assurance that you are not alone.<br />
It is with this in mind that <strong>MDF</strong>SA created a private social group for adults who share the bond of muscular dystrophy. The<br />
support group is based on Facebook and currently has 29 members. Facebook calls it a secret group, and only members will<br />
be able to view the content so as to ensure privacy and confidentiality.<br />
One of our members put it so eloquently: “It's amazing what beautiful difference little support can make, even just a few<br />
encouraging words from someone who cares. It makes your struggle less difficult but no support makes you feel like you<br />
left behind. So let's support each other, in deed, word and prayers.”<br />
If you would like to join us on the group, please leave a message on the Muscular Dystrophy Foundation of South Africa<br />
Facebook page. I will gladly add you as a member. I look forward to chatting to you soon.<br />
Did you know?<br />
Alfredo Ferrari (1932-1956) was an Italian automotive<br />
engineer and the first son of automaker<br />
Enzo Ferrari. Alfredo was nicknamed Dino. He had<br />
Duchenne muscular dystrophy and died at the age<br />
of 24. After his death the Ferrari ‘Dino’ was fitted<br />
with the engine that Alfredo was working on and<br />
Enzo Ferrari named the car in honour of his son.<br />
From an early age Enzo groomed Alfredo to be<br />
his successor. Alfredo studied economics in<br />
Bologna before moving to mechanical engineering<br />
in Switzerland. Over time, it became clear that<br />
something was wrong. Doctors had no idea what<br />
was afflicting him and he only managed to complete<br />
two years of his engineering education before<br />
returning to Modena.<br />
In his short career at Ferrari, Alfredo was credited<br />
for the 750 Monza racing car and to a limited<br />
extent a 1.5-litre V6 that would later see action in<br />
Ferrari’s early Formula racers. Alfredo suggested to<br />
his father the development of a 1.5 L DOHC V6 engine<br />
for F2 at the end of 1955. Twelve years later,<br />
to honour his son, Enzo named the Dino series of<br />
road and racing Ferraris using this V-6 engine after<br />
him.<br />
6<br />
Alfredo had Duchenne muscular dystrophy. In the<br />
final days of his life, while hospitalized, he discussed<br />
technical details of the 1.5-litre V6 with<br />
fellow engineer Vittorio Jano. Alfredo would never<br />
see the engine, he died in Modena on 30 June 1956<br />
at the age of 24. ...<br />
The Autodromo Dino Ferrari in Italy is also named<br />
in Alfredo’s honour, with his father’s name added<br />
after Enzo Ferrari’s death in 1988.<br />
Article from the website of Concours D’Élégance,<br />
Paleis Het Loo, at: http://www.concourselegance.<br />
com/alfredo-dino-ferrari-died-from-duchenne-muscular-dystrophy-60-years-ago-2/
Muscular Dystrophy Association, America<br />
https://www.mda.org/disease/congenital-muscular-dystrophy<br />
MD<br />
Congenital Muscular Dystrophy<br />
What is congenital muscular dystrophy<br />
(CMD)?<br />
Congenital muscular dystrophy (CMD) refers to a group of<br />
muscular dystrophies that become apparent at or near birth.<br />
Muscular dystrophies in general are genetic, degenerative<br />
diseases primarily affecting voluntary muscles. Babies with<br />
congenital muscular dystrophy are weak at birth and may<br />
have breathing or swallowing difficulties.<br />
Types of Congenital MD<br />
At least 30 different types of CMD are now recognized. At<br />
first glance, the various types of CMD seem to have little in<br />
common other than their early onset. But on the molecular<br />
level, the types can be grouped by how their faulty protein<br />
affects cells.<br />
A very small group of CMDs are linked to proteins that affect<br />
what happens inside muscle fibers, affecting how the fibers<br />
process signals from the nervous system, for example, or<br />
how they handle calcium.<br />
But the vast majority of CMD types are related to proteins<br />
that make up or interact with the extracellular matrix that surrounds<br />
muscle fibers.<br />
Several types of CMD that arise from gene mutations that<br />
initially seemed unrelated now appear to be related to defects<br />
in proteins that "sugar-coat" (glycosylate) a matrix protein,<br />
allowing it to connect with other proteins.<br />
The extracellular – outside the cell – matrix is the substance<br />
that surrounds the cells of a tissue, such as muscle, providing<br />
physical and biochemical support.<br />
An important role of the matrix around muscle fibers is force<br />
transmission. For a muscle to pull against bones, it needs to<br />
have contact with something that transmits force from the<br />
muscle fibers onto the tendons and bones. When all is going<br />
well, the matrix transmits that force, as well as chemical signals<br />
that muscles need to stay healthy.<br />
The matrix is a key supporting structure for the survival and<br />
regeneration of muscle. When cells lose touch with their surrounding<br />
matrix – as happens in most types of CMD – trouble<br />
follows.<br />
Signs and Symptoms<br />
CMD can cause contractures in the wrists, ankles and other<br />
joints.<br />
The term congenital muscular dystrophy (CMD) is actually<br />
the name for a group of muscular dystrophies united by the<br />
fact that muscle weakness begins in infancy or very early<br />
childhood (typically before age 2). Congenital diseases are<br />
those in which the symptoms are present at or soon after<br />
birth.<br />
Most children with CMD exhibit some progressive muscle<br />
weakness, although they can have different symptoms, degrees<br />
of severity and rates of progression.<br />
This weakness, usually first identified as hypotonia, or lack<br />
of muscle tone, can make an infant seem “floppy.” Later,<br />
infants and toddlers may be slow to meet motor milestones<br />
such as rolling over, sitting up or walking, or may not meet<br />
some milestones at all.<br />
Some of the rarer forms of CMD are also accompanied by<br />
significant learning disabilities, or mental retardation.<br />
What causes congenital muscular dystrophy<br />
(CMD)?<br />
It isn’t known why the CMDs cause muscle weakness earlier<br />
than other types of muscular dystrophy. One possibility is<br />
that the muscle proteins affected in CMD are required early<br />
in the development of an infant’s muscle, while muscle proteins<br />
linked to other muscular dystrophies don’t become important<br />
until the muscles begin to get a lot of use as a child<br />
grows.<br />
7
MD<br />
It’s important to note that just because the muscle weakness<br />
in CMD starts earlier, CMD isn’t automatically more severe<br />
than other forms of muscular dystrophy. The degree and<br />
rate of progression of muscle weakness varies with different<br />
forms of CMD and from one child to the next.<br />
In the mid-1990s, researchers found that a deficiency of a<br />
protein then called merosin and now more often called laminin<br />
211 was the underlying cause of at least some cases of<br />
CMD. Merosin normally anchors muscle cells to a structure<br />
that encases them (like the skin on a hot dog) called the basal<br />
lamina.<br />
Doctors began to classify CMD as either "merosin-deficient"<br />
or “merosin-positive.” The gene for merosin is on chromosome<br />
6.<br />
As the 20th century ended, researchers began to suspect that<br />
Ullrich’s disease, now known as Ullrich CMD, was caused<br />
by a lack of collagen 6, a ropelike protein located in the area<br />
where laminin 211 is found.<br />
Collagen 6, which helps support the muscle fiber, probably<br />
affects muscle cells via its connection to laminin 211. Laminin<br />
211, in turn, connects to muscle cells via either of two<br />
other proteins: integrin or dystroglycan.<br />
Dystroglycan links the outer surface of muscle cells with<br />
structures outside them via branches, made of sugar molecules,<br />
that protrude from its surface and stick to laminin.<br />
The branch structure helps explain why mutations in so many<br />
diverse genes all appear to cause CMD. Each of these proteins<br />
contributes in a different way to the process of “sugar-coating”<br />
(glycosylating) dystroglycan. Several forms of<br />
CMD — such as Fukuyama CMD, Santavuori muscle-eyebrain<br />
disease and Walker-Warburg syndrome — arise from<br />
defects in these glycosylation proteins.<br />
The illustration below shows the physical relationships<br />
among these proteins.<br />
What are the inheritance patterns in CMD?<br />
The CMDs are caused by genetic defects that affect important<br />
muscle proteins. Most forms of CMD are inherited in an autosomal<br />
recessive pattern.<br />
In brief, if a disease is recessive, two copies of the defective<br />
gene (one from each parent) are required to produce the<br />
disease. Each parent would be a carrier of the gene flaw but<br />
wouldn’t usually have the disease.<br />
If a disease is dominant, then only one copy of the genetic<br />
defect is needed to cause the disease. Anyone with the gene<br />
flaw will have disease symptoms and can pass the disorder<br />
to children.<br />
Many times, MD appears to have occurred “out of the blue,”<br />
but in reality, one or both parents may be carriers, unknowingly<br />
harboring the genetic mutation. Many parents have no<br />
idea they’re carriers of a disease until they have a child who<br />
has the disease.<br />
Medical Management<br />
General care<br />
The physician should meet with the family of a child with a<br />
clinical diagnosis of CMD as soon as possible, even before a<br />
specific genetic diagnosis is made. The first meeting with the<br />
family should include the following five components: diagnosis,<br />
prognosis, recurrence risk (if known), treatment plan,<br />
and family support and community resources.<br />
The treatment plan should introduce a multidisciplinary approach<br />
and include pulmonologists, cardiologists, ophthalmologists,<br />
physiotherapists, orthopedists, possibly others,<br />
and ideally, a palliative care specialist to optimize quality of<br />
life.<br />
A follow-up visit with a genetic counselor may be in order,<br />
but since 50 percent of children with CMD may not have a<br />
specific genetic diagnosis, supportive care should take place<br />
regardless of whether or not a specific genetic diagnosis is<br />
made.<br />
Cardiac (heart) care<br />
Some types of CMD, such as merosin-deficient CMD, are<br />
associated with severe cardiac complications. Cardiac investigations<br />
should be systematically performed during followup<br />
examinations, the frequency of which is dependent on the<br />
type of CMD and the level of cardiac involvement. Cardiac<br />
symptoms sometimes are atypical, especially in younger patients,<br />
and can start late in the course of the disease.<br />
Many forms of congenital muscular dystrophy stem from<br />
loss of firm connections between muscle fibers and their surroundings<br />
(extracellular matrix).<br />
8<br />
Since severe heart arrhythmia can lead to sudden death,<br />
implantation of a defibrillator should be considered.
MD<br />
Gastrointestinal, nutritional and oral care<br />
Feeding and swallowing difficulties are significant problems<br />
in some types of CMD. Individuals with this problem should<br />
be observed and evaluated by a qualified specialist, using a<br />
video-fluoroscopic swallow assessment, if possible.<br />
Recommendations for the treatment and management of<br />
feeding problems include adaptations to positioning and seating,<br />
supports for self-feeding, safe swallowing techniques<br />
and food texture modification.<br />
If these recommendations are insufficient, gastrostomy tube<br />
feeding should be considered.<br />
Muscle weakness and facial malformation can lead to speech<br />
problems in some people with CMD. There is no evidence<br />
that oral motor therapy and exercises help improve speech,<br />
but they may help resolve feeding problems.<br />
Neurological issues<br />
Specially adapted computers can help children with vision<br />
problems.<br />
Problems related to congenital brain malformation, which<br />
occurs in some forms of CMD, include intellectual disability,<br />
behavioral and learning problems, autistic features, emotional<br />
problems, seizures and vision problems.<br />
Orthopedics and rehabilitation<br />
Orthopedic symptoms, such as joint contractures, scoliosis,<br />
foot and spine deformities, rigid spine, hip dislocation and<br />
joint hypermobility are some of the most common aspects<br />
of CMD.<br />
A conservative and preventive approach to orthopedic symptoms<br />
is recommended. Regular stretching, maintaining proper<br />
positioning and environmental supports such as braces and<br />
orthotics are generally favored over surgical interventions.<br />
Although spinal surgery has been shown to improve the quality<br />
of life of older children with progressive spinal deformity,<br />
great care should be taken to minimize the risks of surgical<br />
intervention; postoperative, multidisciplinary care is essential.<br />
Palliative care<br />
Physical therapy is important in maintaining range of motion<br />
and reducing contractures. Palliative care seeks to incorporate<br />
the emotional, spiritual, developmental and physical aspects<br />
of caring for a person with a life-threatening disease. It<br />
is a comprehensive and multidisciplinary model that benefits<br />
patients, caregivers and practitioners as they seek to maximize<br />
the life span and well-being of the person with CMD.<br />
Problems that can be addressed through palliative care include<br />
fatigue, pain, depression, anger, anxiety, and other<br />
mental and emotional difficulties.<br />
Respiratory care<br />
All types of CMD can lead to the development of respiratory<br />
failure, and in some types, breathing problems may be severe<br />
from birth. A proactive approach is favoured because breathing<br />
problems can be present before they become noticeable.<br />
Weak crying, ineffective cough, choking on feedings, weight<br />
loss and repeated infections all can be signs of respiratory<br />
distress, even though, because of motor weakness, typical<br />
signs like breathlessness may not be present.<br />
Aggressive treatment of acute respiratory tract infections is<br />
particularly important, as these infections are the most common<br />
cause of hospital admissions and death in people with<br />
CMD.<br />
Research<br />
Research in the congenital muscular dystrophies centers<br />
around understanding the molecular processes that lead to<br />
muscle loss in these disorders and experimenting with methods<br />
to counteract these processes.<br />
Among the approaches being tried in laboratory rodents is<br />
gene addition (insertion of new genes, sometimes called gene<br />
therapy or gene transfer), either to directly supply the missing<br />
protein or to supply proteins that can help compensate for<br />
a missing or abnormal protein.<br />
A variant on this theme is blocking the activity of harmful<br />
genes, which is also being tried in lab models of CMD.<br />
An important component of MDA research in CMD is understanding<br />
early-stage muscle development in normal and<br />
abnormal situations, so that this knowledge can be applied to<br />
fixing what goes wrong with muscle development in CMD.<br />
This type of understanding could also lead to the use of stem<br />
cells as a treatment for CMD.<br />
Another theme in CMD research is the need to fully understand<br />
the process of glycosylation of proteins, such asalphadystroglycan,<br />
in the muscle-fiber membrane. Glycosylation<br />
of a protein means the addition of sugar molecules to the protein,<br />
which changes the way the protein interacts with other<br />
substances. Alpha-dystroglycan is not sufficiently glycosylated<br />
in several forms of CMD, so understanding and correcting<br />
this process is a promising avenue for treatment of these<br />
disorders.<br />
Article online at: https://www.mda.org/disease/congenitalmuscular-dystrophy<br />
9
EMERGENCY ALERT CARDS<br />
Muscular Dystrophy UK<br />
Muscular Dystrophy UK has created condition-specific alert cards for different muscle-wasting conditions.<br />
These new cards mean that people living with muscle-wasting conditions and their families will have the security of knowing<br />
they can easily inform emergency health care professionals of the vital and specific issues that affect children and adults<br />
with these conditions.<br />
Alert cards are conveniently shaped to fit inside a wallet and outline key recommendations and precautions that a nonspecialist<br />
clinician would need to know during a time of worsening health. To make sure the cards are effective, they cover a<br />
wide range of possible symptoms and situations. The card also includes important contact information on a person’s specialist<br />
neuromuscular and respiratory teams, which will ensure that expert advice will be much easier to access.<br />
Alert card information on the following four muscle-wasting conditions is reprinted with the permission of Muscular<br />
Dystrophy UK and appears on the website of the <strong>MDF</strong> Gauteng.<br />
LEG FRACTURE:<br />
► If ambulatory: Ask if internal fixation/surgery rather<br />
than casting may be possible. Surgery may help preserve<br />
walking.<br />
► If your child has had a fall or a leg injury and has rapid<br />
onset shortness of breath or difficulty breathing and<br />
changes in alertness (confusion, agitation, disorientation):<br />
This is an emergency. Go immediately to the ER<br />
and alert staff that symptoms could be due to Fat Embolism<br />
Syndrome (FES).<br />
RESPIRATORY CARE:<br />
► Risk: Respiratory failure. Please only give oxygen with<br />
close monitoring of CO2 levels; breathing may need to<br />
be supported (with BiPAP, for example).<br />
► If oxygen levels are low, assisted coughing (with cough<br />
assist machine or Amby bag) may help.<br />
► Take your equipment (cough assist, BiPAP, etc.) with<br />
you to the hospital/emergency room (ER); alert your<br />
neuromuscular team that you are going to ER/hospital.<br />
GENERAL RECOMMENDATIONS AND<br />
PRECAUTIONS:<br />
► Keep immunisations up to date and get influenza vaccine<br />
annually.<br />
► People taking daily, long-term steroids should avoid<br />
10<br />
Emergency information – for parents of boys with<br />
Duchenne MD (Parent Project Muscular Dystrophy)<br />
Becker muscular dystrophy is a progressive, inherited condition<br />
characterised by progressive muscle-wasting and weakness,<br />
affecting mostly the proximal lower and upper limb<br />
muscles. Symptoms and severity of the condition can vary<br />
from one person to another.<br />
Becker muscular dystrophy<br />
live vaccines when possible.<br />
► Always wear seat belts – in the car AND on the wheelchair/scooter.<br />
ANAESTHETIC PRECAUTIONS:<br />
► Avoid inhaled anaesthesia.<br />
► IV anaesthesia is considered to be safe (with close monitoring).<br />
► People with Duchenne should NOT receive succinylcholine.<br />
► Local anaesthetics and nitrous oxide are safe for minor<br />
dental procedures.<br />
IF VOMITING AND/OR UNABLE TO TAKE DAILY<br />
CORTICOSTEROIDS FOR 24 HOURS:<br />
► Go to a hospital emergency room; bring the PJ Nicholoff<br />
Steroid Protocol (ParentProjectMD.org/PJ).<br />
► Request substitute IV corticosteroid until oral medications<br />
are tolerated (6 mg of deflazacort equals 5 mg<br />
of prednisone).<br />
► Remind clinicals that high liver enzymes (AST/ALT)<br />
are normal for people with Duchenne MD.<br />
Patients usually have difficulties in walking and climbing<br />
stairs. They may present with frequent falls and may become<br />
non-ambulant as the condition progresses. Patients may also<br />
have difficulty raising their arms above their shoulders, as the<br />
condition progresses.
Fatigue and pain can occur after mild exercise and in walking.<br />
Paraspinal muscles are also affected and patients can develop<br />
scoliosis (curvature of the spine) and lower back pain.<br />
NOTE: Liver enzymes (AST/ALT) will be high on blood<br />
tests; this is normal in Becker muscular dystrophy and is attributed<br />
to muscle break-down. This should not prompt liver<br />
investigations unless otherwise indicated.<br />
Recommendations and precautions<br />
► Immunisations should be kept up-to-date. Do not use<br />
live vaccines if using corticosteroids.<br />
► Wear seat belt when using wheelchair to avoid dangerous<br />
falls.<br />
► Wear a medic alert bracelet.<br />
Anaesthetic precautions (continued)<br />
► Use intravenous general anaesthetics only (avoid suxamethonium).<br />
Inhaled anaesthetics should not be used.<br />
► Local anaesthetics and nitrous oxide are safe, e.g.<br />
for minor dental procedures.<br />
Cardiac<br />
► Patients with Becker muscular dystrophy can develop<br />
cardiomyopathy. Those with lesser muscle symptoms<br />
are at risk of severe heart involvement. All need regular<br />
heart checks.<br />
► Early ACE-inhibitor and beta-blocker usage slows the<br />
Congenital muscular dystrophy (CMD) is a neuromuscular<br />
condition caused by genetic mutations that lead to a lack of<br />
various proteins vital for healthy muscle structure or function.<br />
► Symptoms in small babies include hypotonia (floppiness)<br />
and low muscle tone. Contractures (tightness) in<br />
the hip, ankle, knee and elbow joints are common.<br />
► In children that do not have contractures, initial problems<br />
may be difficulties holding the head, and delays<br />
in sitting and walking.<br />
► Some forms of CMD can have associated brain changes<br />
on a magnetic resonance imaging (MRI) scan.<br />
► Some children with CMD and brain changes visible on<br />
an MRI scan may have learning difficulties with or without<br />
epileptic seizures.<br />
Respiratory<br />
► Respiratory failure in CMD may present without the<br />
usual signs of respiratory distress. Always consider<br />
underlying respiratory failure.<br />
► If presenting with respiratory symptoms or oxygen<br />
need, measure SpO2 in air and CO2 (transcutaneous,<br />
end-tidal or blood gas).<br />
► Titrate oxygen therapy to achieve SpO2 94-98% and<br />
monitor CO2.<br />
► If CO2 is raised, consider early initiation of mask ventilation.<br />
► Manage respiratory infections with chest physiotherapy,<br />
and consider use of nebulised saline and in-exsufflator<br />
(cough assist device).<br />
► For hypersecretion, consider use of glycopyrrolate<br />
40-100 micrograms/kg oral max 2mg six-hourly (use IV<br />
solution 200 mcg/ml) or oral atropine drops.<br />
MD<br />
progress of cardiomyopathy.<br />
► Heart failure symptoms will be subtle/absent in those<br />
with greater disability. If a patient has not been having<br />
regular heart checks, consider the possibility of a severe<br />
underlying cardiomyopathy.<br />
► Cardiac arrhythmias must be considered for patients<br />
with palpitations and/or dizziness/pre-syncope and investigated<br />
with ECG, 24-hour tapes or similar.<br />
Respiratory<br />
► Chronic respiratory failure in Becker muscular dystrophy<br />
may present without the usual signs of respiratory<br />
distress. Subtle signs include early morning headaches,<br />
fatigue, daytime sleepiness, reduced appetite and weight<br />
loss. Consider underlying respiratory failure in case of<br />
a chest infection.<br />
► If supplemental oxygen is required during a respiratory<br />
crisis, this must be carefully controlled. Healthcare professionals<br />
must be alert to the possibility of acute respiratory<br />
failure with an arterial blood gas assessment of<br />
oxygen, carbon dioxide and bicarbonate concentration.<br />
Non-invasive ventilation, with oxygen entrained, may<br />
be required.<br />
► Assisted coughing with chest physiotherapy and breathstacking<br />
techniques with an AMBU bag help to clear<br />
lower airways secretions. This can also be facilitated by<br />
a cough assist device.<br />
Congenital muscular dystrophy (CMD)<br />
► Collect cough swab or sputum for culture and use broadspectrum<br />
antibiotics.<br />
► Consult early with senior to discuss need for ITU care<br />
and escalation of respiratory support.<br />
Cardiac<br />
► The likelihood of heart involvement depends on the<br />
underlying CMD mutation and this guides the intensity<br />
of cardiac surveillance (i.e. Echo and ECG).<br />
► Cardiomyopathy occurs commonly in MDC1C (fukutin<br />
mutation) around age 10 years, progressing to heart failure.<br />
Periodic cardiac imaging is recommended from diagnosis.<br />
► LV-dysfunction may be mild or non-progressive<br />
(MDC1A; FKRP).<br />
► Even asymptomatic LV-dysfunction should be treated<br />
empirically with conventional regimes (e.g. ACE-inhibitors<br />
or angiotensin-receptor blockers; +/- beta-blockers;<br />
etc).<br />
► The possibility of severe LV-dysfunction should be<br />
considered when CMD patients present acutely or for<br />
other aspects of their condition.<br />
Speech and language therapy/swallowing<br />
► Swallowing difficulties can be common in CMD.<br />
► Symptoms such as recurrent chest infections, unintentional<br />
weight loss, the sensation of food and drink sticking,<br />
or feeling the need to clear the throat when eating<br />
or drinking, should be investigated more thoroughly.<br />
► Refer to a specialist speech and language therapist for<br />
an up-to-date swallowing assessment and/or the nutrition<br />
team for consideration of alternative means of hydration/<br />
nutrition, such as gastrostomy.<br />
11
MD<br />
Orthopaedics<br />
Low-energy fractures can occur in children with poor mobility<br />
and joint contractures.<br />
► In the limbs, these can appear as ‘greenstick’ or impacted<br />
fractures and can be difficult to see on X-ray.<br />
► A high level of suspicion is required if a child has minor<br />
trauma, pain, tenderness and limited, reduced mobility.<br />
► Refer to specialist paediatric orthopaedic services for<br />
fracture management.<br />
GI nutritional issues<br />
► Gastrostomy tube leakage can occur and may need<br />
replacement.<br />
► Infection should be treated with appropriate antibiotics<br />
or topical preparations.<br />
► If the site is very swollen, the tube may have to be<br />
removed to relieve pain.<br />
► If tube is removed/or falls out it is important to keep entry<br />
site open using XX and to contact the gastrointestinal<br />
specialist as soon as possible.<br />
12<br />
Facioscapulohumeral muscular dystrophy (FSHD)<br />
FSHD is a muscular dystrophy characterised by progressive<br />
muscle weakness affecting the facial, scapular, axial, upper<br />
arm and lower leg muscles. Wrist and hand muscles as well<br />
as those in the hips may be affected but usually later in the<br />
condition. Bulbar muscles can be affected in the more severe<br />
cases and at late stages of the condition. Extraocular and respiratory<br />
muscles tend to be spared. The severity of the condition<br />
varies from patient to patient even in the same family<br />
and is partly dependent on the severity of the mutation.<br />
Respiratory<br />
► Respiratory function is usually normal. In a minority of<br />
cases, however, type 2 respiratory failure may occur<br />
owing to weak breathing muscles, causing shortness<br />
of breath and nocturnal hypoventilation.<br />
► Patients can be prone to chest infections owing to respiratory<br />
failure. Patients reporting dysphagia might also<br />
be at risk of aspiration pneumonia.<br />
► Immunisations should be kept up to date, including the<br />
flu and pneumococcal vaccines.<br />
► If breathing function is impaired and if supplemental<br />
oxygen is required during a respiratory crisis it must<br />
be carefully controlled (aim for SpO2 target range of<br />
88-92%) and carbon dioxide levels monitored.<br />
Non-invasive ventilation (NIV) may be required.<br />
► Assisted coughing with chest physiotherapy and breathstacking<br />
techniques with an AMBU bag help to clear<br />
lower airways secretions during acute chest infections,<br />
or prophylactically when respiratory function is compromised.<br />
This can also be facilitated by a cough assist<br />
device.<br />
Cardiac<br />
Heart function is usually not affected. Potential cardiac<br />
symptoms (palpitation, fainting, dizziness and shortness of<br />
breath) require appropriate investigations. Coincidental cardiac<br />
problems, unrelated to FSHD, are more likely than causally<br />
related problems.<br />
Pain<br />
Chronic pain, probably secondary mechanical in origin rather<br />
than being directly related to the myopathy, is very frequent<br />
in FSHD patients. Mechanical cervical and lower back pain<br />
is common especially in patients who are developing an axial<br />
myopathy lumbar lordosis (often evident as a protuberant abdomen).<br />
Fractures and falls<br />
► Owing to weakness and poor balance, patients with<br />
FSHD are at high risk of frequent falls.<br />
► Consider checking vitamin D levels and bone mineral<br />
density, especially following a fall or fracture.<br />
► If ambulant, internal fixation is preferable to casting as it<br />
helps to preserve muscle by allowing earlier mobilisation.<br />
► Orthotics input is important, especially for ankle weakness.<br />
Orthotics can also be used to support the axial<br />
myopathy and periscapular weakness.<br />
Anaesthetics/sedation<br />
► Some patients can experience an increased sensitivity<br />
to sedatives, inhaled anaesthetics and neuromuscular<br />
blockade. It is essential that the anaesthetist is aware<br />
of the diagnosis of FSHD so that appropriate plans can<br />
be made for post-operative monitoring.<br />
► Patients with compromised respiratory function have<br />
a higher anaesthetic risk.<br />
► Local anaesthetics and nitrous oxide are safe, e.g. for<br />
minor dental procedures.<br />
Liver/GI<br />
Liver serum creatine kinase (CK) and ‘liver’ enzymes (AST/<br />
ALT, but not gamma GT) may be mildly raised owing to the<br />
muscle involvement. The clinical setting dictates whether<br />
further investigation of the apparent liver dysfunction is indicated.<br />
Gastrointestinal (GI)<br />
► Constipation is common in FSHD patients with substantially<br />
reduced mobility, but may need assessment to<br />
exclude other causes.<br />
► When dysphagia occurs in FSHD, patients are at risk<br />
of aspiration pneumonia.<br />
Other possible manifestations<br />
► Conjunctivitis and ulceration of the cornea can occur<br />
owing to limited blinking and inability to properly close<br />
the eyes, also when sleeping. The patients should consider<br />
using artificial tears and protect their eyes during<br />
sleep.<br />
► Retinal vasculopathy, usually asymptomatic, may affect<br />
FSHD patients.<br />
► High-frequency sensorineural hearing loss is common,<br />
not usually symptomatic.<br />
► Substantial facial muscle weakness may lead to misinterpretation<br />
of emotional expression, particularly in those<br />
with severe, childhood-onset FSHD.
QASA “EISH” CAMPAIGN <strong>2017</strong><br />
Taking Action when Disability Discrimination Occurs<br />
QASA launches a creative “EISH”* campaign by using the wheelchair Lego man in various environments identifying<br />
problems and issues experienced by persons with physical disabilities.<br />
*Term used in South African English and Afrikaans to express exasperation or disbelief. The word<br />
was first transliterated from the Xhosa language to Afrikaans, and then into South African English<br />
(Urban Dictionary). Also used to express surprise, annoyance, pain, etc (Oxford Living Dictionary).<br />
QASA manages a contact number for members to lodge a complaint, discuss an issue, seek advice and be heard.<br />
0860ROLLING (0860765<strong>54</strong>6) is manned by QASA staff from Monday to Friday 8am to 4pm.<br />
QASA will take note of each and every call which will allow the organisation to interrogate the issue, provide a<br />
solution, have a call to action and respond to the caller.<br />
Visit our website www.qasa.co.za if you want to become a member / learn more.<br />
JUSTICE TRANSPORT ACCESS PARKING EMPLOYMENT<br />
The National Road Traffic Act (1996), (Act 93 of 1996) in regulation 305 sub regulation (7) states the following:-“No<br />
person other than a disabled person or a driver of a vehicle conveying disabled persons which motor vehicle is<br />
issued with a sticker for conveying disabled persons shall park on a parking bay reserved for disabled persons”.<br />
QASA believes that wheelchair parking facilities, designed 3500mm wide, are for the use of wheelchair users only.<br />
This is to ensure that a wheelchair user has the required width in order to get in or out of a vehicle safely.<br />
QASA has a campaign whereby in the event of a non-wheelchair user misusing a wheelchair demarcated bay<br />
the public are encouraged to take a photo (ensuring the vehicle registration is clear & wheelchair parking sign is<br />
visible) and WhatsApp it to 0738539675 including the location, date and time and QASA will kindly sensitise the<br />
offender.<br />
If you have an EISH moment / experience with wheelchair parking not being provided, available<br />
or being abused, communicate this to QASA and QASA will investigate and follow up.<br />
QASA will strive to remove the EISH from your parking issues.
Events<br />
Make Today Count Tandem<br />
Skydiving <strong>2017</strong><br />
By Christo van den Berg<br />
Everyone in the cabin got ready and checked their<br />
seat belts, and as the plane approached the point<br />
from where we would jump, we slowed down and<br />
the door was opened. Corné Vorster, the instructor<br />
with whom I was doing the tandem jump, moved<br />
me to the point of exit from the plane and said,<br />
“Are you ready?” After a quick shuffle we jumped<br />
out. The feeling was overwhelming; it felt like I<br />
just dropped without any assistance, and so fast.<br />
It was hot on the ground, but up in the air it was<br />
very cold. You fall freely with your hands open and<br />
simply drift in the air.<br />
I looked around and everything looked different<br />
from up there, like you would see in the movies.<br />
After a few minutes, Corné held my head back,<br />
pulled my hands in and the parachute opened up.<br />
Corné gave me two handles, one right and one<br />
left, and said, “You're in control of parachute”. I<br />
turned left and then in a circle and then right into<br />
another circle.<br />
I am affected with Charcot-Marie-Tooth disease, and<br />
one of the things that I always wished to do was skydiving.<br />
When I read about the “Dare Me For Charity<br />
Skydiving” event, hosted by <strong>MDF</strong> Gauteng, which<br />
included the Make Today Count Tandem Skydiving<br />
event, I signed up for the challenge.<br />
We were ready to land, the plane having landed<br />
already, and softly we came back down to the<br />
ground. It was really nice and a great experience<br />
with such a professional team.<br />
On Saturday, 12 August <strong>2017</strong>, I had the opportunity<br />
to do a tandem jump at Leeukop Farm Airfield in<br />
Deneysville.<br />
When they lifted me up into the plane, my adrenaline<br />
began to pump and I began to get a hollow feeling in<br />
my stomach, the feeling that you get when you know<br />
what is coming next and you are full of excitement.<br />
They asked me if I was ready, and with great excitement<br />
I said “Yes!” The plane engines started and hot<br />
air from the exhaust pipe flowed into the cabin as the<br />
door was shut.<br />
The plane slowly began to move forward and the engine<br />
started to pick up and we were lifted up into the<br />
air. As the plane started to climb, my stomach felt<br />
awkward, that butterfly feeling. I looked out of the<br />
window to the ground below and realized how small<br />
everything looked from so high up.<br />
(Pictured: Christo van den Berg, from Bethlehem<br />
and Elvis Naya, from the Seychelles)<br />
14
Muscular Dystrophy<br />
Awareness Run<br />
By Doné and Hanti van Eyk<br />
Events<br />
The Little Hero Foundation held their inaugural muscular<br />
dystrophy awareness run on 30 September <strong>2017</strong> in conjunction<br />
with the Springs parkrun. More than 500 runners lined up<br />
to complete the five-kilometre course, most wearing green to<br />
show support and create awareness. The heart of the event<br />
was the intention to run for those who can’t. Before the start,<br />
an opportunity was provided to explain to the participants and<br />
the supporters what muscular dystrophy is and how it affects<br />
those who live with this condition.<br />
The Little Hero Foundation was established by<br />
Doné and Hanti van Eyk following the diagnosis in<br />
<strong>2017</strong> of their two-year old son, Lian, with LMNArelated<br />
congenital muscular dystrophy. The purpose<br />
of the foundation is to create awareness of all types<br />
of muscular dystrophy and actively participate in the<br />
“fight” to find a cure.<br />
“Oomies se<br />
Road Trip”<br />
By Pieter Joubert<br />
Earlier this year Bennie Hattingh, an <strong>MDF</strong> Gauteng<br />
member, and his friend Martin Kotze did an incredible<br />
road trip in a 1968 Renault 6 from Brits to Yzerfontein<br />
on the West Coast.<br />
They left on 22 August and travelled 300 km per day at<br />
60 km per hour, their car’s top speed. This unique journey<br />
was in honour of the life of André Hattingh, son of<br />
Bennie and Lynette Hattingh, and of others touched by<br />
Duchenne and various muscular dystrophies.<br />
The history of their Renault is also rather interesting. It<br />
was found in a scrapyard and cost a mere R3 000, but,<br />
to the surprise of everyone, purred to life after a few<br />
fluids were put in. After being fitted with new tyres and<br />
shocks and being freshly painted, the car was ready to<br />
hit the road once more.<br />
The Muscular Dystrophy Foundation Gauteng wishes to<br />
thank Bennie Hattingh, Martin Kotze and all who were<br />
involved for the awareness they have created. Following<br />
the trip every day on Facebook was an amazing<br />
experience.<br />
15
People<br />
Just live!<br />
So says Anne-Marie,<br />
diagnosed with FSHD<br />
at age 33<br />
[Extracts from the article “‘Lewe net!’, sê lyer”<br />
published in TygerBurger Goodwood, 5 September<br />
<strong>2017</strong> written by Carina Roux (translated and<br />
slightly adapted by Pieter Joubert)]<br />
TygerBurger spoke to Anne-Marie<br />
Stoman, 58, a resident of Panorama<br />
Palms Retirement Village.<br />
She was diagnosed with facioscapulohumeral<br />
muscular dystrophy<br />
(FSHD) at the age of 33.<br />
FSHD affects the muscles in the<br />
face, shoulders and upper arms.<br />
It goes even further to her waist<br />
and legs – even to her feet, Anne-<br />
Marie explains. “My whole body<br />
is affected. That's why I can tell<br />
a joke without emotion”, she<br />
laughs.<br />
The offbeat humour soon comes<br />
through in the conversation.<br />
She was very sporty and took<br />
part in hockey, squash, karate<br />
and modern dancing. It was in an<br />
aerobic exercise class that she<br />
"began to feel like an elephant –<br />
thud, thud, thud, I could not skip<br />
anymore”.<br />
She went home embarrassed,<br />
where she tried to stand on her<br />
heels. “I couldn’t. Even less on my<br />
toes. I thought I was going crazy.”<br />
She went from one doctor to the<br />
next. Eventually an intern friend<br />
referred her to a doctor at Mediclinic<br />
Constantiaberg. He made<br />
the diagnosis by sticking needles<br />
into her left leg, and was able to<br />
determine that the problem lay<br />
with her muscles.<br />
She continued with sport and with<br />
exercising at a women's gym until<br />
seven years ago, “until I really<br />
couldn’t do it any more”.<br />
About the diagnosis, she just<br />
thought “whatever” and did not<br />
even read up on FSHD. “I just<br />
went on with my life until I started<br />
falling – also at work.”<br />
She worked in the army's signal<br />
regiment, a fine-grained job<br />
where she sometimes had to install<br />
and carry equipment. She<br />
started falling and later could no<br />
longer work.<br />
She assists with administration<br />
functions at the Muscular Dystrophy<br />
Foundation Cape Branch and<br />
provides moral support for others<br />
– like the mother of a young man<br />
just diagnosed.<br />
“I give moral support and sometimes<br />
visit people when they are<br />
a bit depressed – I love helping<br />
people.”<br />
Many people struggle to accept<br />
the condition, she says, but she's<br />
very positive – “and I laugh at everything,<br />
maybe it's wrong! I know<br />
exactly how it feels for people who<br />
have just been diagnosed – you<br />
must try to get something positive<br />
out of your situation and it's difficult.<br />
Once you've done the mind<br />
switch, forget the rest, just live!”<br />
She emphasises that one must<br />
keep on going, but she admits<br />
you cannot force people, as they<br />
sometimes think it's a death sentence.<br />
Fit and active<br />
She was always fit and active and<br />
believes this definitely helped<br />
her body not to deteriorate too<br />
quickly. “I should have been in a<br />
wheelchair a long time ago – the<br />
longer you can keep your muscles<br />
supple, the longer you can keep<br />
their strength.”<br />
In the beginning, a person will<br />
feel the difference in their body,<br />
she says, and later you will find<br />
that you struggle with a drawer<br />
that you could still open the day<br />
before. Then you should be careful<br />
not to hurt yourself. “I give<br />
such advice on things that have<br />
happened to me.”<br />
It may sound strange, says Anne-<br />
Marie, but she has never been<br />
as happy as she is now. “In my<br />
work I was always on the ball<br />
and thought people should keep<br />
up with my fast pace. They were<br />
actually scared of me and didn’t<br />
want to talk to me.” Now she is<br />
much more relaxed.<br />
16
Recently a ballroom dance was<br />
held in the hall, and she told<br />
someone: “If the Lord asked me if<br />
he could give me my legs back so<br />
I could go dancing or if I'd rather<br />
have what I have now, I wouldn’t<br />
think twice. I'm incredibly happy<br />
here and in myself.” She still does<br />
things, says Anne-Marie. As long<br />
as she can, she will fold her walking<br />
frame and put it in her car,<br />
which she still drives. She is part<br />
of a support group where everyone<br />
can laugh and cry as they<br />
please and advise one another.<br />
She is also part of the Loslappie<br />
Quilting Group, although she initially<br />
doubted whether she’d be<br />
able to work with a needle because<br />
she couldn’t even pick up<br />
a glass with one hand. Where<br />
there’s a will, she finds a way.<br />
Now completely screwed<br />
After a fall, she recently underwent<br />
arm surgery. With three<br />
screws in her arm, she’s now<br />
completely screwed, she jokes.<br />
“I often tell people that I think I'm<br />
too stupid to realise what's happening<br />
to me, so I just carry on – I<br />
know, but just keep on going.”<br />
There have been many dark times<br />
in her life, but she has come<br />
through them. She realises that<br />
her children, aged 32 and 29,<br />
would have suffered. She has<br />
learnt to handle things with a<br />
sense of humour – that laughter<br />
can turn away wrath.<br />
You cannot walk around with the<br />
Bible under your arm, but you can<br />
display love and advise others.<br />
Original article online at: https://issuu.com/tygerburger/docs/tygerburger_de_grendel_<strong>2017</strong>0906<br />
KINGFISHER CORNER, SEDGEFIELD<br />
By Hilton Purvis<br />
For many years the little village of Sedgefield, on the<br />
Cape Garden Route, was a town that we always passed<br />
through on the way to somewhere else. Each time we<br />
would read signage indicating the "Wild Oats Farmers<br />
Market" which is held every Saturday morning. As we<br />
developed an interest in our local Cape Town farmers<br />
markets we started taking more notice of the Wild Oats<br />
market and decided to plan a holiday which would place<br />
us there on a Saturday morning.<br />
Finding accessible accommodation is always a challenge,<br />
and Sedgefield does not provide many choices,<br />
but we discovered "Kingfisher Corner" self-catering accommodation<br />
via the website of Disabled Travel (www.<br />
disabledtravel.co.za) and decided to give it a try.<br />
Built on a hillside overlooking the Sedgefield estuary,<br />
"Kingfisher Corner" consists of three separate houses.<br />
The lower house is the home of the owner, and the<br />
central unit has ramped access from the driveway and<br />
provides a fully accessible interior. The upper house is<br />
accessed from the road and provides a very spacious,<br />
accessible, home-like interior. All provide the necessary<br />
grab rails, roll-in showers, etc although the upper house<br />
is a little more difficult to access with a wheelchair from<br />
the road. The view from the veranda of the central unit<br />
is included for this article and provides a spectacular<br />
panorama of the estuary, which will have you spending<br />
a lot of time finding reasons to be sipping gins and tonic<br />
on lazy summer afternoons!<br />
"Kingfisher Corner"<br />
36 Kingfisher Drive, Sedgefield<br />
Tel/Fax: +27 (0)44 343 1715<br />
E-mail: lseals@arms.co.za<br />
See details online at: http://www.capestay.co.za/<br />
kingfishercorner/<br />
The Wild Oats Farmers Market is accessible with assistance<br />
(the car guards will direct you to parking places<br />
which are close to the action) provided you can manage<br />
undulating grass and hard ground under your wheels. It<br />
is one of the few genuine farmers markets servicing the<br />
residents of the town and not merely acting as a dining<br />
opportunity for visitors looking for entertainment as is<br />
so often the case in Cape Town. It is a large, busy and<br />
active market providing fresh produce, food, beverages<br />
and crafts over quite a large area and can keep you<br />
busy for a good couple of hours!<br />
Another Sedgefield institution worthy of a visit is the famous<br />
"Mr Kaai's" fish shop on the main road, just next<br />
to the one and only traffic robot in the town. We enjoyed,<br />
without doubt, the finest seafood platter we have<br />
ever eaten at Mr Kaai's, sitting outside the restaurant<br />
underneath the canvas awning. You really cannot drive<br />
through Sedgefield without stopping in at Mr Kaai's! It's<br />
as simple as that.<br />
17
People<br />
Iman Casoojee<br />
By Tasnim Jadwat Casoojee<br />
on my screen. After reading a few lines it was evident<br />
that Iman’s condition would ultimately result in her<br />
early demise, as Iman would be classified with type<br />
1, the most severe form of SMA.<br />
January 2010, a new year full of hope promise and<br />
prosperity for South Africa. But a time bomb had been<br />
placed on my child. “SMA type 1 Werdnigg Hoffmann<br />
disease” the doctor wrote, after a quick examination.<br />
Fasciculations? Tremor in her hand? I’m sorry.<br />
“Doctor, how much time do we have left with her?<br />
A month, plus another, and maybe another?”<br />
But it was just the beginning, a new outlook on life and<br />
the world around. Our little angel was special from<br />
the time she arrived in this world. Iman Casoojee was<br />
born 6 April 2009. “You have a girl” we were told, after<br />
a reasonably easy C-section. As I kissed her for<br />
the very first time, I thought, by God’s mercy she is<br />
healthy and beautiful, a child born with a single tooth.<br />
My husband and I couldn’t wait to take her home and<br />
start our new life together as a family. We named her<br />
Iman not knowing that it would be the most ironic<br />
name of all. Iman means faith.<br />
Even before Iman entered this world, I would follow<br />
her progress day by day on the internet. Once she was<br />
born, I wanted to learn everything about her and how<br />
to be the best mother possible. For a while everything<br />
seemed fine, and she reached all her milestones, but<br />
at six months Iman did not sit by herself and preferred<br />
lying down all the time. Being a first-time mother, I<br />
was not that concerned as I’d read that some kids just<br />
develop slowly. When Iman was nine months old, she<br />
still couldn’t sit. We noticed that she couldn’t even roll<br />
or lift her head when placed on her tummy. We knew<br />
something was wrong but never guessed it would be<br />
so devastating.<br />
When we returned to Johannesburg we took Iman to<br />
another neurologist. Although my heart told me it was<br />
serious, I prayed and cried, pleading to God to make<br />
things okay. This was before our world was turned<br />
upside down. The doctor examined Iman and said he<br />
had bad news for us. On a piece of paper he wrote<br />
down “SMA – Werdnigg Hoffman’s Disease”. I immediately<br />
started crying and asked the doctor how<br />
much time Iman had left with us. He responded that<br />
she could have a few months left, and that no cure or<br />
treatment was available.<br />
When someone tells you your child is going to die, you<br />
feel as though every bit of air in your body has been<br />
removed and your heart has been perforated. But the<br />
weirdest part of knowing is that you feel you already<br />
knew it, almost déjà vu. I immediately called my parents<br />
to inform them about Iman. We never thought<br />
that a condition like spinal muscular atrophy would<br />
ever manifest in our child; we did not even know it<br />
existed. For a parent, imagining that your child may<br />
never walk is hard enough, but being told your child’s<br />
time is limited is the worst feeling possible.<br />
In 2011 we attended the Cure SMA conference in<br />
Orlando, USA and decided to make a vacation of the<br />
trip. However, Iman contracted the RSV virus [respiratory<br />
syncytial virus] and spent 17 days in a Miami<br />
hospital. Her right upper lung collapsed and she was<br />
intubated. We were so close to losing her. Miraculously,<br />
she recovered. Fast forward to a few years<br />
later, and Iman is still alive and looking forward to<br />
starting a recently approved treatment for SMA, labelled<br />
Spinraza. This lifesaving treatment is making<br />
such a big difference to the lives of many affected<br />
with SMA.<br />
During a holiday to Durban, Iman was taken to my<br />
sister’s husband, Dr Ridwan Omar, a paediatrician,<br />
who disclosed that Iman was an extremely floppy<br />
baby and recommended we see a paediatric neurologist,<br />
who suggested that further testing would be<br />
required. While the doctor examined Iman, I made<br />
mental notes of all the symptoms she was pointing<br />
out. Although I did not understand any of the terms,<br />
I intended to find out what they meant. After returning<br />
home, I “googled” the symptoms, which included<br />
a tremor in Iman’s hand as well as “fasciculations”.<br />
The results were devastating: a degenerative muscle<br />
disease called “spinal muscular atrophy” popped up<br />
18
People<br />
Tribute feature for the<br />
late Patrick John Artman<br />
By Carol Artman<br />
vigour, but Pat struggled to climb the steps and get<br />
in and out of the swimming pool. With his “never say<br />
die” attitude, Pat started his own company manufacturing<br />
fibreglass basins for hairdressing salons. He<br />
was the sole worker and delivery man, doing everything<br />
on his own as he could not afford to hire help.<br />
He would sometimes fall, but pick himself up and<br />
carry on.<br />
My husband, Patrick, and I were married on 9 March<br />
1967. We lived in an old, run-down building in Crown<br />
Road, Fordsburg. After a few years we moved to a<br />
flat in Newclare, where I noticed that Pat couldn’t<br />
climb over the little embankment in front of the flat<br />
and had to walk a short way to where the surface<br />
was flat. It didn’t bother us much. We were in the<br />
prime of our lives and by this time had three children,<br />
the youngest being our son Sheldon (4). We<br />
had just purchased a piece of land in Fleurhof to<br />
start building our own home. Pat was so proud and<br />
happy, as he really wanted to have his own home.<br />
But that pride and joy turned to sadness when, at<br />
the age of 37, he was diagnosed with muscular dystrophy,<br />
which we had never heard of before.<br />
The news struck us like a death sentence. We cried,<br />
we prayed and cried again. Yes, we were also angry<br />
with God! But we decided to take one day at a time,<br />
and Pat soldiered on bravely. He was diagnosed<br />
with three types of dystrophy: limb girdle MD, spinal<br />
muscular atrophy, and Becker MD.<br />
During his long stay in Baragwanath Hospital undergoing<br />
countless tests, he was unexpectedly dismissed<br />
from his job for being absent for such a long<br />
period attending to his health. He had lined fibreglass<br />
pools, which required physical strength and<br />
During this time a very “special lady” by the name of<br />
Renske came into his life, having called him for an<br />
appointment to sell him life insurance. She played<br />
a very important role in our lives as she was instrumental<br />
in getting him a motorised wheelchair when<br />
he could no longer walk and his arms had become<br />
weaker. Before Pat passed away he referred to her<br />
as his “guardian angel”, which she indeed was.<br />
Before we fully understood muscular dystrophy, we<br />
were fortunate to meet another person with MD,<br />
Pieter Joubert, and his family, who shared the same<br />
challenges and made it easier for us to get through<br />
many of them. Through what has become the Muscular<br />
Dystrophy Foundation, Pieter introduced us<br />
to many other people with the condition, one of the<br />
most notable being Ilse Langenhoven, who was<br />
serving on the committee but has since also passed<br />
away.<br />
Pat tried for a long time not to become dependent<br />
on the wheelchair but as he became weaker it allowed<br />
us to continue enjoying holidays and outings,<br />
creating some beautiful memories. He worked tirelessly<br />
to give his family a good life despite his circumstances,<br />
but his long fight ended on 3 October<br />
<strong>2017</strong>.<br />
Thank you, Pat, for your brave fight and your love of<br />
me and the children. You indeed had a good name<br />
– “A good name is better than any fine perfume; and<br />
the day of death better than the day of birth” (Ecclesiastes<br />
7:1). We miss you, and you will forever be<br />
in our hearts.<br />
Rest in peace, Pa.<br />
<strong>MDF</strong> Gauteng and Cape wish to thank you for your continued support.<br />
20
People<br />
Ride London: Barbara’s story<br />
Just one year ago, Barbara was diagnosed with<br />
facioscapulohumeral muscular dystrophy (FSHD)<br />
which causes muscle wasting in the limbs, shoulders<br />
and face. A life-long cyclist, she was determined<br />
not to let her condition stop her love for the<br />
sport.<br />
“I’m doing Ride London because I want to prove<br />
to myself, and others, that my condition won’t stop<br />
me doing the sport I love. I have always cycled<br />
regularly, and I refuse to let my condition slow me<br />
down.”<br />
Barbara works in an office as a case consultant for<br />
a pensions company. She lives in Stockport, with<br />
her husband, their two sons and their daughter.<br />
She has big plans to compete in <strong>2017</strong>’s Ride London<br />
event – a 100 mile cycling challenge across<br />
London and Surrey.<br />
“Being diagnosed was devastating and a real<br />
shock to all the family. I had heard of muscular dystrophy<br />
before because my brother in law’s mother<br />
has limb girdle muscular dystrophy. But she had<br />
never really talked about it until I was diagnosed.<br />
Now, we openly share our experiences, which is<br />
really valuable.”<br />
Barbara’s road to diagnosis started at a sports<br />
massage clinic after cycling from Land’s End to<br />
John O’Groats.<br />
“My muscles felt stiff and tired, so I hoped a massage<br />
would ease the tension. I had also noticed<br />
physical differences, such as changes to my posture,<br />
and issues with my balance, but I didn’t think<br />
much of it. Then, at my appointment, my masseuse<br />
was shocked when she realised I had little<br />
muscle tissue around my neck. She was amazed<br />
and asked how I even held myself up on a bike.<br />
Worried, I booked an appointment with a physiotherapist,<br />
who referred me to hospital. Just before<br />
Christmas, in 2015, I was given the news I had<br />
FSHD.<br />
“It was such a tough period. I had no information<br />
about the condition and felt totally isolated. There<br />
is never a good time, but Christmas was a really<br />
tough time to get such life-changing news.<br />
Thankfully, not long after, I heard about Muscular<br />
Dystrophy UK. Through them, I was able to access<br />
information, specialist support, and heard about<br />
others with similar conditions.<br />
“After diagnosis, I was desperate to see someone<br />
with my condition living an active life. I needed to<br />
see someone else who was doing okay. As FSHD<br />
is so rare, I didn’t know anyone else with the condition.<br />
Then, a friend told me that I could be the<br />
person that others look to. She was right.<br />
“Since then, I’ve taken even more pride in maintaining<br />
as much cycling as possible, because I<br />
want to show others what’s possible. I have had<br />
to make adaptations, such as taking more breaks,<br />
but the enjoyment and drive is still there. Last summer<br />
I cycled the ‘Holy grail’ of cycling routes when<br />
I conquered the Madonna del Ghisallo, which is a<br />
10km climb from Lake Como and is a place of pilgrimage<br />
for Italian cyclists.<br />
“I am so fortunate to have already had cycling in<br />
my life, as it made me determined to just keep going.<br />
I’m not super fit, and you don’t have to be to<br />
get on a bike.<br />
“In <strong>2017</strong> I have two big bike rides planned – I will<br />
be cycling through Spain in February and France in<br />
July with some of the cyclists I met in in Italy. One<br />
day, I plan to cycle the length of the River Rhine<br />
through Switzerland and Germany to the Netherlands,<br />
which will be a real mental challenge.<br />
“I was really inspired to enter Ride London to raise<br />
funds and awareness of muscular dystrophy. It<br />
would be amazing to think I have contributed to a<br />
future cure. I’m also inspired to show others what<br />
can be done with a condition.<br />
“I always wanted to see someone with FSHD living<br />
an active life in the public. Now, I’m happy to be<br />
that person. So when the next person is diagnosed<br />
they can see that it’s not all doom and gloom – you<br />
can keep going.”<br />
Article online at: http://www.musculardystrophyuk.<br />
org/your-stories/ride-london-barbaras-story/<br />
21
People<br />
The Roe family’s<br />
story<br />
Mandy Roe’s son, five-year-old T-Jay, has Duchenne<br />
muscular dystrophy, and is eligible for new<br />
drug, Exondys 51.<br />
The drug – which was recently approved by<br />
the Food and Drug Administration in the United<br />
States – is currently being considered for a licence<br />
by the European Medicines Agency.<br />
Read the family’s story:<br />
“Exondys 51 is a piece of hope for T-Jay and us:<br />
a ray of light in a very dark tunnel”.<br />
T-Jay lives in Nottinghamshire with his parents<br />
and big sisters Cassidy (15) and Lexi (7). His<br />
mum, Mandy, sees the drug as potentially life<br />
changing for T-Jay, who has the devastating<br />
muscle-wasting condition, Duchenne muscular<br />
dystrophy.<br />
“T-Jay is a happy, fun loving young boy. He<br />
started school in September 2016 and is doing<br />
so well, with lots of friends who he enjoys running<br />
and playing with. He loves to read and is a<br />
real bookworm. He is brilliant at writing and very<br />
good with numbers.<br />
“When T-Jay grows up he wants to be a teenage<br />
mutant ninja turtle!”<br />
T-Jay was diagnosed with Duchenne on 1 July<br />
2015. He has a deletion amenable to the skipping<br />
of exon 51, meaning he is eligible for<br />
Exondys 51.<br />
Mandy says: “He had a fall off the sofa and after<br />
the blood test we got the devastating news.<br />
At that moment, our world fell apart. It really is<br />
heart-breaking to see your son get so upset because<br />
he falls or can’t keep up with his friends.<br />
It’s hard to see he can’t do things that other children<br />
would take for granted: walking, running or<br />
climbing the stairs.<br />
“If he were able to start treatment with Exondys<br />
51, he could carry on doing the things he loves<br />
for longer: playing with his friends, going to<br />
swimming lessons and dancing to his favourite<br />
songs.<br />
“If I could speak to the decision makers directly,<br />
I would ask them to please help my son, giving<br />
him the best chance possible to be a happy<br />
young boy.<br />
T-Jay isn’t a case note, or a name on a piece of<br />
paper: he is my universe.”<br />
Article online at: http://www.musculardystrophyuk.org/your-stories/exondys-51-the-roefamilys-story/<br />
The Muscular Dystrophy Foundation of SA would<br />
like to thank the National Lotteries Commission for<br />
their support.<br />
22
People<br />
Ella and her ‘cheeky feet’<br />
Lucy Brady lives in Huntingdon, Cambridgeshire,<br />
with her husband, Andrew, and their four-year-old<br />
daughter, Ella, who has Charcot-Marie-Tooth disease<br />
(CMT). Lucy talks about Ella’s diagnosis, and<br />
what life is like for her young daughter.<br />
“Ella started walking on her first birthday, but she<br />
never found her feet properly. We would always be<br />
following her around, waiting for her to fall.<br />
“By the time Ella was two, she was falling over<br />
all the time. We were getting quite worried by this<br />
point, and after numerous trips to see the GP, we<br />
were eventually referred to a physio. By this point,<br />
Ella’s feet were starting to turn under. She had an<br />
MRI, and from there, we were referred to a neurologist.<br />
In February 2015, a blood test confirmed<br />
Ella had CMT.<br />
“Ella’s diagnosis didn’t come as a massive shock<br />
to us, because I am a trained nurse, and had done<br />
lots of research when I was trying to find answers<br />
as to what was wrong with Ella. At first my husband<br />
and I were relieved that it wasn’t something worse,<br />
but then it hit us that there is no treatment, and this<br />
took a while to come to terms with.<br />
“Having ‘cheeky feet’ is how we describe Ella’s<br />
condition to her. We tell her that when she was<br />
made, CMT said they wanted to be part of her,<br />
they picked her. When we said this to Ella, she<br />
said “What if I don’t want CMT?” so I told her that<br />
CMT likes her, so it will always be with her, but the<br />
doctors will help her. To that, she said ‘OK, that’s<br />
fine.’<br />
“Ella loves school, she is really outgoing, bubbly<br />
and bright. She is learning phonics at the moment,<br />
which she is enjoying. Unfortunately she didn’t<br />
qualify for receiving any extra support at school,<br />
but she has physio at lunchtime. Ella’s classmates<br />
are very accepting of her condition – she wears<br />
splints to school, and the children will ask what<br />
they are and why she is wearing them. They hold<br />
her hand and help her where they can.<br />
“We recently got a dog, and as a family, we enjoy<br />
walking him, and Ella uses her wheelchair. We also<br />
like going on trips to London to visit the Natural<br />
History Museum – Ella loves dinosaurs.<br />
“Tiredness is becoming an issue for Ella. She is becoming<br />
dependent on her splints, and without them<br />
she really struggles to walk and wants to crawl, or<br />
be carried. She suffers with cramping at night, so<br />
we do massage to help with this, and watch cartoons<br />
to distract her from the pain.<br />
“My advice for parents who have recently had a<br />
child diagnosed with CMT would be to make sure<br />
you have a good support network around you. Let<br />
people who want to help, be there for you. There<br />
are lots of fantastic organisations out there who<br />
can offer advice and support, including Muscular<br />
Dystrophy UK. Don’t try and take everything on<br />
your shoulders. You have to get to the point where<br />
you accept your child’s condition is part of them.<br />
Take each day as it comes.<br />
“I think a support group for parents would be really<br />
helpful. It would give us a human link to people,<br />
and the chance to share experiences.<br />
“Ella’s neurologist told us about Muscular Dystrophy<br />
UK. We started looking on the website for information<br />
about Ella’s condition, we found this really<br />
helpful. It was at this point that we decided we<br />
wanted to start fundraising for the charity.<br />
“Last year, seven of us took part in the charity’s<br />
Town and Gown running event in Cambridge. We<br />
completed the 5km race, and thanks to the fantastic<br />
support from the local community, we raised<br />
more than £1,200 for the charity.<br />
“We are looking at what to do next. We might do a<br />
yearly challenge under the name ‘Ella’s team’.”<br />
Article online at: http://www.musculardystrophyuk.<br />
org/your-stories/ella4-has-charcot-marie-toothdisease-cmt-her-mum-lucy-shares-her-story/<br />
23
Research<br />
The following three articles, all by Jenny Sharpe, are from the Research section of the Muscular Dystrophy<br />
UK website (http://www.musculardystrophyuk.org/progress-in-research/news/).<br />
20/10/<strong>2017</strong><br />
Scientists at the University of California,<br />
Berkley, have developed a new<br />
way to deliver the genome-editing technology,<br />
CRISPR-Cas9 into cells. This<br />
new system, called CRISPR-Gold, corrected<br />
the mutated dystrophingene in<br />
a mouse model of Duchenne muscular<br />
dystrophy.<br />
CRISPR-Cas9 consists of a piece of<br />
RNA and the Cas9 enzyme that can cut<br />
DNA like a pair of ‘molecular scissors’.<br />
The RNA guides Cas9 to cut a specific<br />
region of DNA.<br />
In order to accurately correct a mutation,<br />
CRISPR-Cas9 must be delivered<br />
with the healthy DNA sequence (called<br />
the donor DNA). The cell uses the<br />
donor DNA to repair the cut made by<br />
Cas9, through a process called homology-directed<br />
repair. This has been difficult<br />
to achieve with adeno-associated<br />
virus (AAV) delivery systems, as they<br />
are too small to fit both the CRISPR-<br />
Cas9 and donor DNA.<br />
An advantage of CRISPR-Gold is that<br />
it can carry CRISPR-Cas9 and donor<br />
DNA simultaneously. It does this using<br />
tiny gold balls called gold nanoparticles.<br />
These are covered in a special<br />
coating that helps them to get inside<br />
24<br />
New CRISPR system corrects dystrophin mutation in<br />
Duchenne mouse model<br />
the cell. Once inside, the gold nanoparticles<br />
break apart and release the CRIS-<br />
PR-Cas9 and donor DNA. This triggers<br />
homology-directed repair, which corrects<br />
the mutation.<br />
In this study, the researchers designed<br />
CRISPR-Gold to target the mutated<br />
dystrophin gene in the mdx mouse<br />
model of Duchenne muscular dystrophy.<br />
It was injected directly into the<br />
muscles of the mice, as it cannot be delivered<br />
systemically.<br />
Two weeks later, the researchers found<br />
that about 5% of copies of the dystrophin<br />
gene were corrected. This significantly<br />
increased the amount of dystrophin<br />
protein in the muscle and reduced<br />
muscle scarring (fibrosis). The treated<br />
mice also performed better in muscle<br />
function tests compared to untreated<br />
mice. The researchers concluded that<br />
CRISPR-Gold was safe because it did<br />
not cause other mutations or an immune<br />
response.<br />
One of the leaders of the study, Professor<br />
Niren Murthy, told The Scientist:<br />
"In this paper, we were actually able<br />
to correct [the gene for] dystrophin<br />
back to the wild-type sequence. The<br />
other way of treating this is to do<br />
something called exon skipping,<br />
By Betty Kao<br />
which is where you delete some of<br />
the exons and you can get dystrophin<br />
to be produced, but it’s not [as functional<br />
as] the wild-type protein."<br />
CRISPR-Gold has not yet been tested<br />
in clinical trials, but some of the researchers<br />
have created a company<br />
called GenEdit to focus on translating<br />
the technology into humans. They are<br />
also developing a next generation of<br />
nanoparticles that can be injected into<br />
the bloodstream. This could potentially<br />
improve their clinical benefit, as<br />
they could get into every muscle of the<br />
body, including the heart and breathing<br />
muscles.<br />
Professor Vincent Rotello, a drug<br />
deli-very and nanotechnology expert at<br />
University of Massachusetts, who not<br />
involved in the study, told The Scientist:<br />
"There’s a lot of work to be done to<br />
move to the point where we’ll actually<br />
be able to cure diseases, but I think<br />
this [study] shows the way forward."<br />
The study was published in the scientific<br />
journal Nature Biomedical Engineering.<br />
Article online at: http://www.musculardystrophyuk.org/news/news/newcrispr-system-corrects-dystrophin-mutation-in-duchenne-mouse-model/
Research<br />
Myotubular myopathy gene therapy trial to start in the UK<br />
17/10/<strong>2017</strong><br />
Audentes Therapeutics is currently developing<br />
a gene therapy drug, named<br />
AT132, for the potential treatment<br />
of X-linked myotubular myopathy<br />
(XLMTM). AT132 uses a harmless<br />
adeno-associated virus to deliver a<br />
healthy copy of the MTM1 gene to the<br />
body. AT132 is currently being tested<br />
in the US, in a phase 1/2 trial named<br />
ASPIRO.<br />
Audentes Therapeutics recently announced<br />
that the Medicines and<br />
Healthcare Products Regulatory Agency<br />
(MHRA) has approved the Clinical<br />
Trial Authorisation (CTA) application<br />
for testing AT132 in the UK. This<br />
means Audentes Therapeutics can start<br />
working with UK based clinical study<br />
sites to start enrolling individuals with<br />
XLMTM into their ongoing ASPIRO<br />
trial.<br />
08/08/<strong>2017</strong><br />
Muscle strength tests could help to predict bone health<br />
in people with FSHD<br />
This article was kindly shared by June<br />
Kinoshita, FSH Society.<br />
Muscle plays an important role in bone<br />
health, and conditions such as Duchenne<br />
muscular dystrophy have been<br />
linked to low bone mineral density,<br />
abnormal bone turnover (the cycle of<br />
new bone formation and old bone removal),<br />
and increased risk of fractures.<br />
It was not known whether facioscapulohumeral<br />
muscular dystrophy (FSHD)<br />
also affects bone health, and a recent<br />
study published in Muscle & Nerve begins<br />
to address this question.<br />
Bone health is a concern for many people<br />
with muscular dystrophy, because<br />
weaker muscles increase the chance of<br />
falling and the risk of fracture. Fractured<br />
bones can take a long time to<br />
heal, and reduced mobility as a result<br />
of fractures can, in turn, further weaken<br />
muscles.<br />
Mr Matthew R Patterson, President and<br />
Chief Executive Officer at Audentes<br />
Therapeutics, said in a press release:<br />
"This CTA approval represents another<br />
important milestone for our<br />
AT132 program. We recently announced<br />
dosing of the first patient in<br />
ASPIRO at a U.S. clinical study site,<br />
and we are pleased to be working<br />
closely with the European XLMTM<br />
community as we continue to execute<br />
on our global plans to develop<br />
AT132 as a potentially transformative<br />
product to treat this devastating<br />
rare disease."<br />
ASPIRO is a multi-centre, open-label,<br />
dose-ascending study which will enrol<br />
12 children who are less than five<br />
years old with XLMTM. The study<br />
will compare the safety and efficacy<br />
of three different doses of AT312 in<br />
nine of the twelve participants. The remaining<br />
three participants will be part<br />
of a delayed-treatment control group,<br />
who will be treated once the optimal<br />
The study, led by Dr Kathryn Wagner<br />
of the Kennedy Krieger Institute in<br />
Maryland, USA, examined 94 people<br />
with FSHD, half in Australia and half<br />
in the U.S. The volunteers had genetically<br />
confirmed FSHD Type 1 and were<br />
examined for correlations among disease<br />
severity score, bone mineral density,<br />
blood biomarkers (molecules associated<br />
with bone turnover and health),<br />
strength tests and function.<br />
Overall, the study reported that a diagnosis<br />
of FSHD was not predictive<br />
of decreased bone mineral density or<br />
increased bone fractures. However,<br />
the researchers found that declines in<br />
whole-body and regional bone mineral<br />
density were moderately correlated<br />
with reduced muscle strength and function.<br />
These patients had a higher prevalence<br />
of traumatic fractures, as well as<br />
abnormally low levels of vitamin D3.<br />
By Sofia Nnorom<br />
dose of AT132 has been established.<br />
Primary efficacy analysis will be assessed<br />
twelve months after treatment,<br />
with participants being monitored for<br />
a further four years to assess long-term<br />
safety and developmental progression.<br />
Preliminary results from the ongoing<br />
ASPIRO study are expected by the end<br />
of the year.<br />
In September <strong>2017</strong> Audentes Therapeutics<br />
announced the US Food and<br />
Drug Administration (FDA) granted<br />
Rare Paediatric Disease and Fast Track<br />
status for AT132. In addition, AT132<br />
has also received Orphan Drug status<br />
from both the FDA and the European<br />
Medical Agency. These statuses will<br />
help speed-up the development and<br />
review process of AT132, which will<br />
help get the therapy to patients quicker.<br />
Article online at: http://www.musculardystrophyuk.org/news/news/myotubular-myopathy-gene-therapy-trial-tostart-in-the-uk/<br />
By Jenny Sharpe<br />
“Given the considerable variability<br />
of bone health in the FSHD population,<br />
strength and function can serve<br />
as predictors of bone mineral density,”<br />
the study concluded.<br />
The authors suggested that periodic<br />
bone-density scans should be done in<br />
people with FSHD whose strength and<br />
functional tests indicate a higher risk of<br />
lower bone mineral density. This will<br />
assist doctors in developing effective<br />
treatment plans tailored to individuals<br />
to help prevent fractures and promote<br />
bone health.<br />
The study was funded by a grant from<br />
FSHD Global Research Foundation and<br />
the U.S. National Institutes of Health.<br />
Article online at: http://www.musculardystrophyuk.org/news/news/musclestrength-tests-could-help-to-predictbone-health-in-people-with-fshd/<br />
25
Health<br />
Inspiratory muscle training in children and adolescents with<br />
neuromuscular disease: Never take breathing for granted<br />
By Anri Human<br />
“Life is not measured by the<br />
number of breaths we take,<br />
but by the moments that take<br />
our breath away.”<br />
– Maya Angelou<br />
People living with a neuromuscular<br />
disease (NMD) such as Duchenne<br />
muscular dystrophy (DMD) or spinal<br />
muscular atrophy (SMA) face<br />
the challenge of progressive muscle<br />
weakness caused by their condition.<br />
This weakness is clearly seen<br />
when there is difficulty with walking;<br />
getting in and out of the car; picking<br />
up objects and doing everyday<br />
life activities such as eating and<br />
dressing. In the same way as these<br />
large muscles progressively lose<br />
their bulk, strength and function as<br />
time passes, so breathing muscles<br />
also become progressively weaker.<br />
Breathing muscles include the diaphragm<br />
(the main muscle that assists<br />
in taking a deep breath), intercostal<br />
muscles (between the ribs)<br />
and abdominal muscles. Complications<br />
of breathing muscle weakness<br />
include not being able to expand the<br />
lungs enough to supply sufficient oxygen<br />
to the body; difficulty in clearing<br />
lung secretions because of a weak/<br />
ineffective cough; and frequent lung<br />
infections. The regression of breathing<br />
muscle strength, frequent infections,<br />
difficulty in breathing and decreased<br />
oxygen (hypoxia) lead to<br />
patients experiencing a poor quality<br />
of life. The effects of breathing muscle<br />
weakness become much more<br />
noticeable once a person loses the<br />
ability to walk. Therefore any treatment<br />
that slows down muscle weakness<br />
and keeps a person on their<br />
feet longer may also help maintain<br />
breathing function.<br />
26<br />
The solution might seem simple at<br />
first: if breathing muscles are weak,<br />
they should be strengthened in order<br />
to improve, slow down or maintain<br />
function in the same way as we<br />
try to maintain the function of our<br />
arms and legs. The principle is similar<br />
to strengthening your biceps by<br />
training with a weight or dumbbell.<br />
Devices used for inspiratory muscle<br />
training (IMT) provide resistance<br />
when the user takes a deep breath,<br />
leading to strengthening of the diaphragm.<br />
Although training has been<br />
shown to be effective in athletes and<br />
patients with asthma, IMT in people<br />
with NMD remains controversial.<br />
For this reason we did a study to<br />
find out if training the inspiratory<br />
breathing muscles (especially the<br />
diaphragm) can improve breathing<br />
muscle strength, lung function and<br />
quality of life of the patients using<br />
it. The main parts of the study and<br />
some of our early findings are outlined<br />
in this article.<br />
What did South African<br />
physiotherapists say?<br />
We conducted an electronic survey<br />
to find out how South African<br />
physiotherapists treat children and<br />
adolescents with NMD. Very few<br />
physiotherapists in our country have<br />
clinical experience and expertise in<br />
treating people with NMD, as this<br />
is a highly specialised field. However<br />
most of the physiotherapists<br />
who took part in this survey were<br />
aware of international clinical practice<br />
guidelines and recommended<br />
breathing exercises and strengthening<br />
of the breathing muscles in this<br />
patient group.<br />
An interesting case<br />
Previously published research studies<br />
have suggested that people with<br />
very poor lung function and severe<br />
breathing muscle weakness would<br />
not benefit from IMT and therefore<br />
should not undergo this treatment.<br />
However, we had a case of a<br />
10-year-old girl with advanced spinal<br />
muscular atrophy and severely<br />
affected breathing muscles which<br />
suggests that this might not necessarily<br />
be true in all cases. After only<br />
four weeks of training with a threshold<br />
IMT device (15 breaths, twice<br />
a day) we saw clear positive clinical<br />
effects. Her inspiratory muscle<br />
strength, her posture and her selfreported<br />
health-related quality of life<br />
improved. She rated her experience<br />
with the training regime as 9/10 and<br />
said that she would like to continue,<br />
as it made her “breathing better”.<br />
What did the observational<br />
study reveal?<br />
We then started a small-scale clinical<br />
study among eight children between<br />
the ages of 8 and 17 with a<br />
variety of neuromuscular diseases<br />
(including DMD and SMA). The children<br />
did 30 deep breaths against a<br />
resistance, twice a day, five days<br />
a week, for six weeks. We found<br />
significant improvements in their<br />
breathing muscle strength and the<br />
flow of air they could create with a
deep breath, and, excitingly, we also<br />
saw a marked improvement in the<br />
children’s upper limb function and<br />
coordination.<br />
What was even more encouraging<br />
was the feedback from patients<br />
themselves when asked what they<br />
thought of IMT:<br />
“It is fun and helps me to be able<br />
to run faster and for longer.”<br />
“I can breathe better during the<br />
course of the day.”<br />
“It helps me to improve and keeps<br />
me healthier.”<br />
“I can now come to the physiotherapy<br />
department, or go to<br />
the mall with my mother and do<br />
shopping without getting short of<br />
breath like I used to and have to<br />
take a break before going further<br />
[with her manual wheelchair].”<br />
Furthermore, we noticed other improvements<br />
that we did not expect:<br />
Some of the children had better posture,<br />
improved confidence, reported<br />
that they could sing better as their<br />
voice projection improved, used<br />
their asthma pumps less, were more<br />
motivated and concentrated better<br />
in class, and some even showed<br />
improved academic performance!<br />
Although probably not all of the outcomes<br />
can be directly attributed to<br />
IMT, and some children might benefit<br />
more than others depending on<br />
the disease progression and type of<br />
NMD, these early results are truly<br />
encouraging.<br />
Watch this space:<br />
what is currently being<br />
done?<br />
A randomised cross-over clinical<br />
study is currently being conducted<br />
in Cape Town and Gauteng (mainly<br />
Pretoria) in which approximately<br />
20 children and adolescents living<br />
with NMD are included. Children<br />
in the study train with a threshold<br />
IMT device for three months and<br />
are followed up on for another three<br />
months to see how long the effects<br />
of IMT last. We hope that by the<br />
end of 2018 our results will be able<br />
to guide clinical practice in order to<br />
Health<br />
implement effective and safe treatment<br />
strategies so that we can help<br />
to improve the quality of life for all<br />
people living with NMD.<br />
Acknowledgements:<br />
I would like to acknowledge the following<br />
very important role players:<br />
Profs Brenda Morrow and Jennifer<br />
Jelsma (supervisors); Dr Lieselotte<br />
Corten (research assistant in Cape<br />
Town), Sjaan Flanagan (Powerbreathe),<br />
my colleagues at Red<br />
Cross Children’s hospital (Cape<br />
Town), Dr George Mukhari Academic<br />
Hospital (Pretoria), Nuwe Hoop,<br />
Pretoria and Meerhof schools, and<br />
most importantly all the patients and<br />
their parents who have taken part in<br />
this study or are still part of it. I salute<br />
each and every one of you.<br />
Further information<br />
For further information or any queries,<br />
please contact us at:<br />
anrihuman@gmail.com (Gauteng),<br />
tel. 012 521-4047, or<br />
brenda.morrow@uct.ac.za (Cape<br />
Town)<br />
A little boy with big dreams<br />
Ludick Fouche is 8 years old and is affected with Duchenne<br />
muscular dystrophy. In June <strong>2017</strong>, Ludick was given the opportunity<br />
to go for a ride in a chariot pulled by one of our<br />
Muscle Riders cyclists, Angelos Frantzeskos. The ride then<br />
slowly became a more regular occurrence, and before we<br />
knew it Ludick and Angelos were teaming up to take on the<br />
Telkom 947 Cycle Challenge together. After many practice<br />
sessions in Muldersdrift and awesome adventures with the<br />
Muscle Riders team, Ludick and Angelos crossed the finish<br />
line on 19 November <strong>2017</strong> in 4 hours and 32 minutes flanked<br />
by a large group of Muscle Riders who helped. We could not<br />
be more proud, and together with Ludick’s family and everyone<br />
who attended, it was a day we will never forget.<br />
Look out for the April 2018 issue of <strong>MDF</strong> <strong>Magazine</strong>, in which<br />
we will revisit the Telkom 947 Cycle Challenge in a big way.<br />
Pictured: Front: Jan Ferreira, Ludick Fouche and<br />
Angelos Frantzeskos. Rear: Anzelle Fouche. ►<br />
27
This makes accessing the tremendous<br />
power of the smartphone so much easier<br />
and places the availability of all of<br />
the items mentioned earlier in this article<br />
right on the tip of my tongue!<br />
My smartphone died the other day,<br />
which led me to put together a list of<br />
items I needed to tote around all day in<br />
order to function normally. It amounted<br />
to quite a staggering collection of items<br />
which include a laptop/PC, diary, reference<br />
books, novels, multimedia discs,<br />
notebook and pen, calculator, GPS,<br />
stopwatch/timer/watch, torch, remote<br />
control for front gate, spirit level, alarm<br />
clock, telephone, video camera, stills<br />
camera, magnifying lens, USB memory<br />
stick, radio, music player, Scrabble,<br />
chess, photo album and sticky notes.<br />
It became clear to me only when I assembled<br />
all of these items just how<br />
much functionality I had placed on my<br />
smartphone. I would consider myself a<br />
relatively "lite" user and certainly not<br />
someone who has the phone permanently<br />
attached to the end of his arm!<br />
No doubt when I first obtained my<br />
smartphone it was intended to be used<br />
as a communication device, but as time<br />
passed and the technology developed,<br />
the phone took on additional work responsibilities<br />
and went from being a<br />
part-time assistant to a full-time employee!<br />
Some people might argue that<br />
the new phones are "employers" by the<br />
way they control our lives, but that is a<br />
debate for another time.<br />
The hopefully temporary hospitalisation<br />
of my smartphone led me to realise<br />
what a valuable contribution these devices<br />
make to the disabled community.<br />
I don't know about you, but I generally<br />
struggle to physically handle items such<br />
as computers, books, remote controls,<br />
etc. I battle to hold them, and my fingers<br />
struggle to operate them. Having<br />
to pick things up and put them down<br />
all the time is really a no-no, and even<br />
more so if they are bulky and heavy.<br />
When I have them all condensed into<br />
one small item, which is easily operated<br />
via a touch screen, then the advantages<br />
become immediately apparent.<br />
ALL-IN-ONE<br />
I shall focus on just one example for a<br />
moment. My Roberts Birds of Southern<br />
Africa guide, which for many years<br />
was a manageably sized printed book,<br />
has in its most recent incarnation become<br />
a monster coffee table book! This<br />
makes it essentially useless to me since<br />
it is impossible to hold the beast, never<br />
mind actually page through it. Even my<br />
able-bodied birdwatching friends have<br />
effectively shunned it. Along came the<br />
Roberts Birds of Southern Africa App<br />
for Android and iOS, which included<br />
all of the information from the book<br />
together with the functionality of being<br />
able to search, listen to bird calls, create<br />
lists, make notes and search maps.<br />
It provided all of the resources of the<br />
book, plus more, in an interactive package<br />
smaller than the size of my hand.<br />
Another feature I have enjoyed using<br />
on my smartphone is the ability to<br />
"ask" it to perform basic and simple<br />
tasks such as dialling a number, sending<br />
a message, opening a particular<br />
application and many more. The very<br />
enthusiastic voice activated Google Assistant<br />
(Android) and the equally helpful<br />
Siri (iOS) are always ready to do<br />
my bidding with suitably phrased voice<br />
commands. They don't always work so<br />
well in a noisy environment, but within<br />
the peace and quiet of your own home<br />
(where no one can see you talking to<br />
yourself on the phone!) it is remarkably<br />
useful.<br />
The opportunity to have my smartphone<br />
function as a remote control device has<br />
provided me with much satisfaction,<br />
and I am looking forward to seeing how<br />
this feature will develop in the coming<br />
years. My previous phone provided remote<br />
control via an infrared port, which<br />
worked very effectively on devices<br />
such as my television, video player, etc.<br />
It was however limited by this communication<br />
mechanism and by whether<br />
one had a phone with an infrared port.<br />
Now you can download applications<br />
which provide remote control for gates<br />
and doors (literally kilometres away<br />
from where you might be sitting) via<br />
the phone's communication mechanism<br />
without any need to have hardware features<br />
such as infrared ports or Bluetooth<br />
connectivity. Coupled to this, you can<br />
connect to video cameras which allow<br />
not only access control but also the<br />
ability to see activity and exactly who<br />
is coming or going.<br />
Somewhere along the line, after my<br />
smartphone died, I think I also missed<br />
the ability to make phone calls! I didn't<br />
notice it at first because all the added<br />
functionality provided for so many of<br />
my needs that the primary goal of the<br />
device was somehow lost in translation.<br />
Having to use a landline phone invokes<br />
a feeling of being in a museum, sampling<br />
a piece of technology from the<br />
past capable of performing only one<br />
task.<br />
I sure hope they can fix my smartphone<br />
soon – all this stuff I now have to carry<br />
around weighs a ton!<br />
28
Prof Amanda Krause, MBBCh, PhD MB BCh,<br />
Medical Geneticist/Associate. Professor.<br />
Head: Division of Human Genetics.<br />
National Health Laboratory Service (NHLS)<br />
& The University of the Witwatersrand.<br />
Please e-mail your questions about genetic counselling to national@mdsa.org.za.<br />
How to maintain muscle strength<br />
How do I maintain muscle strength if I have muscular dystrophy? Is there<br />
any medication, diet or exercise that is effective?<br />
Muscular dystrophies are a large group of conditions which vary significantly in age of onset, rate of sion and severity. It is thus very difficult to answer the question of how to maintain muscle strength apart from broad general<br />
progresprinciples.<br />
In almost all muscular dystrophies progressive weakness is a key part of the disease, as there is an inherent problem with the structure or function of the<br />
muscle. In addition, it is very hard for people to build new muscle cells after birth. People who do not have muscular dystrophy build muscle bulk by<br />
enlarging the muscle cells they have through exercising strenuously and pushing their limits. The approach as regards people with muscular dystrophy<br />
should be very different.<br />
It is good to work regularly with a biokineticist or physiotherapist who is aware of the specific areas of strength and weakness and can thus provide an<br />
individualised programme for each client. Biokineticists or physiotherapists may also be able to advise on how to use less affected muscles to overcome<br />
weaknesses of more affected muscles, so that function is maintained.<br />
People with muscular dystrophy should make every effort to improve muscle tone and fitness and maintain whatever strength they can. They should not<br />
try to build muscle or strength, as there is a significant risk of further damage to muscles that are already damaged and stressed. Thus, a person should<br />
exercise regularly and non-strenuously. Weights and resistance should generally not be used. Exercise should be aerobic. Individuals need to listen<br />
to their bodies and should stop exercising if they have any pain or fatigue. They should use stretching exercises to increase and maintain the range of<br />
motion and to avoid contractures developing or worsening. It is also important to strengthen stomach and back muscles (both being ‘core’ muscles) as<br />
this can improve posture and balance and enable you to breathe better.<br />
Cardiomyopathies and cardiac conduction defects are very common in several forms of muscular dystrophy. Individuals should be aware that if these<br />
are present they could also limit exercise capacity. Similar principles as those above apply, and exercise should be within the cardiac capacity of an<br />
individual. If there is any doubt about a person’s cardiac status, a cardiologist should be consulted before any exercise programme is initiated.<br />
As in healthy individuals, exercise used correctly can be beneficial in maintaining and improving strength and activities of daily living. Exercise also<br />
reduces fatigue, improves bone density, improves sleep and has positive psychological effects.<br />
Doctor’s<br />
In contrast to the benefits of exercise, there is little to suggest that diet or medication is beneficial in improving muscular dystrophy.<br />
A note on Guillain-Barré syndrome<br />
What is the relationship between Guillain-Barré syndrome and muscular dystrophy?<br />
Although Guillain-Barré syndrome and muscular dystrophy may appear to have overlapping<br />
symptoms of weakness, which can be progressive, they have completely different causes and<br />
disease courses. Guillain-Barré syndrome is a rare condition in which the body’s immune<br />
system attacks the nerves, leading to muscle weakness and even paralysis. Although the exact<br />
cause is unknown, it often occurs after a viral or bacterial infection. The onset may be<br />
rapid, but most people eventually make a full recovery, some more rapidly than others. This<br />
is in contrast to muscular dystrophies, which are due to genetic causes and do not generally<br />
improve after onset but continue to progress.<br />
29
Sandra’s thoughts on…<br />
Feeling lost in life’s maze<br />
Sandra Bredell (MSW)<br />
The feeling of being lost in life has been described in<br />
many ways – like being dropped in the centre of a maze<br />
with no map of how to get out, going around in circles,<br />
ending up in dead ends all the time, going backwards<br />
and forwards but not seeming to make any progress<br />
(Hounsell, 2016, <strong>2017</strong>). These experiences may sound<br />
familiar to you because they are real and we all experience<br />
some of them in our life from time to time.<br />
We feel that we are stuck in the middle, moving in circles<br />
and making no progress. We might be feeling walled in<br />
and with nowhere to turn. Maybe we have experienced<br />
a feeling of not having the capabilities for fi nding a way<br />
out of the situation. Why would this be? It might be that<br />
we think we should be able to control where we are going<br />
or where we want to go. Or we might be hoping for<br />
someone to rescue us from this route that is taking us in<br />
circles. Sometimes we do get a glimpse of the pathway<br />
but might think that we do not have the tools to conquer<br />
it. Maybe we accept that we are being guided by a higher<br />
power and that we should be calm and continue with<br />
what we need to deal with. On the other hand, it might<br />
also leave us angry and anxious, resulting in us blaming<br />
others for our situation, blaming people close to us, our<br />
parents, brothers and sisters and being disappointed in<br />
the higher power for not helping us out of this predicament.<br />
That is a lot to think about.<br />
So, how do we navigate our way out of this<br />
maze?<br />
When we fi nd ourselves tied up in the challenges of<br />
life’s maze, we have to keep our focus on the pathway<br />
and not get side-tracked by what people say or what<br />
we think they are going to say, by the economic situation<br />
in the country and the scarcity of water, et cetera.<br />
These are important aspects that can infl uence our life,<br />
but single-handed we cannot solve all of these situations.<br />
Regardless of how much we blame others, we<br />
can choose our emotions to restrict our moving forward<br />
or see this maze as an opportunity to develop life skills,<br />
believe in ourselves and trust the support that people<br />
are offering us in moving forward and making progress.<br />
We can take stock of our capabilities and our support<br />
systems and keep focused. That should build our confi -<br />
dence to conquer the maze.<br />
Remember, even if we fi nd ourselves at the same spot<br />
more than once, we are not falling behind. Life is not a<br />
race and defi nitely not linear. The goal of life is not to get<br />
things done but to allow ourselves to live. We so often<br />
want to be fi nished with pain, doubt, uncertainty and<br />
loss. We want to “solve the maze and get out” (Beck,<br />
2013). But in actual fact it gets us to move out of our<br />
comfort zones and gives us an opportunity to gain more<br />
skills and put them to work.<br />
Maybe we should also see the maze as a safe place<br />
where we can explore what feels dangerous. As <strong>2017</strong><br />
draws to an end, and I do not know where you are in the<br />
maze of life, my wishes are that you will fi nd the maze<br />
also to be a safe place where you can allow yourself<br />
to get to know yourself and trust your abilities to make<br />
a choice to move forward and make progress in 2018.<br />
For those who will be going on holiday, travel safely and<br />
enjoy the time with family and friends. Wishing you a<br />
wonderful and blessed 2018!<br />
Sources:<br />
Beck, M. 2013. The labyrinth of life. Martha Beck. Available<br />
at: marthabeck.com/2013/03/the-labyrinth-of-life<br />
Hounsell, S. 2016. Do you feel like you are lost in a<br />
maze? Sandy Hounsell. Available at: https://sandyhounsell.com/feel-like-i-am-lost-in-a-maze/<br />
Hounsell, S. <strong>2017</strong>. Do you feel like you are lost in a<br />
maze? LinkedIn. Available at: https://www.linkedin.com/<br />
pulse/do-you-feel-like-lost-maze-sandy-hounsell<br />
Marshall, J. <strong>2017</strong>. Feeling lost in life’s maze? Think<br />
again. LinkedIn. Available at: https://www.linkedin.com/<br />
pulse/feeling-lost-lifes-maze-change-think-again-joemarshall<br />
Pattakos, A. 2012. Life and the labyrinth of meaning.<br />
HuffPost. Available at: https://www.huffingtonpost.com/<br />
alex-pattakos/meaning-of-life_b_1584775.html<br />
30
Golf day<br />
Cape Branch<br />
Our sincere thanks to the Rotarian Club of Goodwood<br />
for the successful golf day on 6 October. A special<br />
thanks to Colin Jacobs and Judy Bird for the effort put<br />
into the arrangements for the day. Once again Anne-<br />
Marie Stoman and Sanjay Narshi were a huge help in<br />
promoting the muscular dystrophy cause.<br />
Wellness health fair<br />
at Bothasig Clinic<br />
On 9 September we joined other NPOs to raise awareness<br />
at the Bothasig Clinic. It was a great opportunity<br />
to promote awareness within our area.<br />
Family fun picnic<br />
World Duchenne Day on 2 September<br />
was celebrated at the beautiful Urban<br />
Park in Green Point. We enjoyed a funfilled<br />
day in the company of friends and<br />
members, with many fun activities for<br />
the children.<br />
31
Cape Branch<br />
Grand West outing<br />
On Thursday 21 September <strong>2017</strong> our <strong>MDF</strong> children<br />
enjoyed a fun day at our annual Grand West outing.<br />
The group got to do ten pin bowling and played<br />
arcade games to their heart’s content at the Magic<br />
Company. What a joy it was to watch the faces of<br />
our MD children enjoying the thrill and excitement<br />
of all the activities on the day. Everyone enjoyed a<br />
lovely lunch at Wimpy restaurant, and each child<br />
received a goodie bag to take home. Our sincere<br />
thanks to Reach for a Dream for their assistance on<br />
this special day. This was once again a wonderful<br />
fun-filled day for our MD children.<br />
Customized backs of<br />
wheelchairs<br />
Our sincere thanks to the Wetterhahn Foundation<br />
for their donation of R50 000, which<br />
was used to update five wheelchairs with<br />
new customised NXT backs. These NXT<br />
backs provide individual customised support<br />
for both back and head if or when necessary.<br />
This new back can be customised to<br />
recipients as they grow and as their posture<br />
changes. This donation has provided both<br />
comfort and safety for the recipients.<br />
32
Gauteng Branch<br />
Muscular dystrophy workshop<br />
By Robert Scott<br />
The morning of 2 September <strong>2017</strong> was a little on the chilly<br />
side, but that did not stop many <strong>MDF</strong> members from making<br />
their way to the muscular dystrophy workshop at Hope<br />
School in Westcliff.<br />
If you needed MD knowledge, some fun and some great<br />
tasting food, this was the best place to be!<br />
Talks were given by John Rodda (professor of<br />
paediatric neurology at Wits and head of department<br />
at Chris Hani Baragwanath Hospital),<br />
Suretha Erasmus (genetic counsellor), Kerrie<br />
Austin (physiotherapist) and Marinus Mans, who<br />
told his inspirational personal story as someone<br />
affected with MD. We would like to thank them all<br />
for spending the day with us.<br />
Furthermore we would like to thank all of our<br />
sponsors for assisting us with the amazing food!<br />
Thank you to:<br />
A group picture was taken of everyone in attendance with a red balloon to show their support for World<br />
Duchenne Awareness Day on 7 September.<br />
The workshop was informative and enjoyed by all. Lastly, thank you to Hope School, <strong>MDF</strong> staff and all the<br />
volunteers who helped make the day an amazing success!<br />
33
Gauteng Branch<br />
“Special guests from Prague” MDA Ride<br />
Muscular Dystrophy Foundation Gauteng recently had the<br />
pleasure of meeting some colleagues all the way from the<br />
Czech Republic!<br />
MDA Ride is a group of people who decided to band together<br />
to support those affected with muscular dystrophy<br />
in the Czech Republic, but with a twist. They do it with their<br />
motorcycles! They have been in operation for nine years<br />
and have managed to help many people in this time.<br />
It was an honour to have met these amazing individuals<br />
and wish them the best of luck with their work. We salute<br />
you and thank you for all that you do for those affected with<br />
muscular dystrophy!<br />
By Robert Scott<br />
A feel-good morning held in aid of muscular dystrophy<br />
Saturday 4 November witnessed the inaugural Redhill High School’s wellness<br />
Saturday – something for the body, mind and spirit. The morning was<br />
held primarily to help to raise money and awareness for muscular dystrophy<br />
and <strong>MDF</strong> Gauteng. The fine, hot day saw 22 enthusiastic, energetic people<br />
attend the 8:00 am to 9:00am boot camp session led by Sonio Fiandeiro,<br />
a Redhill teacher qualified in and passionate about fitness. This raised R1<br />
100. Approximately 100 yoga enthusiasts took part in the 1½-hour SUCO<br />
yoga session from 9:30 to 11:00am. This calmer yet invigorating session<br />
was led by members of the SUCO yoga company. The latter kindly donated<br />
20% of its takings to our cause.<br />
It was heartwarming to note how many participants revealed<br />
a keen interest in the charity and in informing<br />
themselves about muscular dystrophy. Hopefully this<br />
awareness will spread and many more people will support<br />
the 2018 event.<br />
We would like to thank Redhill School and<br />
The Sunshine Collective (SUCO) for their support.<br />
By Michelle Pretorius<br />
34
Gauteng Branch<br />
Thank you Old Mutual Foundation<br />
We are most grateful for your support and wish to express our<br />
deep gratitude to your company for the amount of R125 000<br />
received towards purchasing motorised wheelchairs for people<br />
in need. We appreciate your care and concern for the needs of<br />
people affected with muscular dystrophy.<br />
Thabo Maleho<br />
Thabo Maleho, aged 9, affected with Duchenne muscular dystrophy, has<br />
been assisted with a new motorised wheelchair. His father no longer has to<br />
carry him as he can move around independently. Thabo is very happy, and<br />
his father wishes to thank the <strong>MDF</strong> for assisting his son with a motorised<br />
wheelchair.<br />
Letsetsa Tobby Maphapo<br />
I am Toby Maphapo and I am from Limpopo. I would like to say thank<br />
you to the Muscular Dystrophy Foundation Gauteng for helping me to get<br />
a new motorised wheelchair. I am thrilled with it and cannot thank them<br />
enough. I am very happy.<br />
Yours sincerely,<br />
Toby Maphapo<br />
German Maleshane<br />
My name is German Maleshane, from Tlamelang Special School, and I would like to take this moment to<br />
thank the Muscular Dystrophy Foundation Gauteng for the new wheelchair.<br />
You guys gave me life, and life is good from now on. I will be able to go to places in my hometown, and I am<br />
also going to Grade 12, so thanks a lot!<br />
You gave me hope and changed my life, and I can also visit my friends and relatives now.<br />
Yours sincerely,<br />
German Maleshane<br />
Tshenolo Molapisi<br />
My name is Tshenolo Molapisi and I would like to take this opportunity to say thank you to the Muscular<br />
Dystrophy Foundation Gauteng for giving me the new wheelchair. I am so happy to have gotten the new<br />
wheelchair.<br />
Yours sincerely,<br />
Tshenolo Molapisi<br />
35
KZN Branch<br />
Casual Day <strong>2017</strong><br />
The Muscular Dystrophy Foundation KZN Branch participated with<br />
Casual Day sticker sales, and were delighted with the sale of 2 598 stickers.<br />
As in previous years, the branch could not have done this alone,<br />
and we wish to place on record our sincere thanks to the following volunteers,<br />
schools and companies that assisted us in our sticker sales:<br />
• Sister Namitha Chabilal from Inkosi Albert Luthuli Central Hospital<br />
• Cornel Smith, management and staff of Reutech Communication<br />
(New Germany, KZN) for their generous donation once again this<br />
year, matching the rand value of the stickers sold<br />
• U & G Fabrics<br />
• Staff, family and friends at Effingham Primary School<br />
• Staff and pupils of Effingham Secondary School<br />
• St Raphael’s School, Montclair<br />
• Volunteers – Cathy Khoon Khoon, Veronique Conner<br />
• Volunteers – Mercedes Benz, Riverhorse Valley<br />
• Bronz Salon<br />
• SA Homeloans, La Lucia<br />
• Parmalat, Riverhorse Valley<br />
• New Frontier Tours, Westville<br />
• Tetra Pak South Africa, Pinetown<br />
• Meltec Agencies, Pinetown<br />
Pictured: Maureen Malinga,<br />
Bronwen Goldstone, Chernice<br />
Singh, Alison Bruce and Adelle<br />
Hayes<br />
The KZN Branch also wishes to place on record our thanks and appreciation to the management and staff at the<br />
Westville Mall for allowing us the use of their premises over a few days. You assisted us greatly in promoting<br />
awareness of muscular dystrophy.<br />
A big thank you and appreciation also goes to Neil Goldstone and Duane Goldstone for generously providing<br />
time from their busy schedules in assisting with the selling of stickers.<br />
Thank you once again for your support and assistance in the sale of stickers. We look forward to your assistance<br />
and contribution again next year!<br />
KZN Branch AGM <strong>2017</strong><br />
The Muscular Dystrophy Foundation held its 43rd Annual General<br />
Meeting on 21 October <strong>2017</strong> at 24 Somtseu Road, Durban. It was<br />
a well-attended meeting, and it was great to see new as well as<br />
familiar faces. The <strong>MDF</strong> chairman of KZN, Mr Noel Pillay, reported<br />
that this year had been a rewarding year for the KZN Branch<br />
and was proud to say that the KZN office had progressed by leaps<br />
and bounds in pursuing and implementing some strategic goals.<br />
Our treasurer, Mr Raj Mahadaw, gave feedback indicating that,<br />
despite some challenges, all was not doom and gloom. He stated<br />
that we at <strong>MDF</strong> KZN were ever grateful to our companies and donors<br />
who had loyally supported us during the past financial year,<br />
and it was through their assistance that we could assist in providing<br />
motorised and manual wheelchairs and assistive devices for<br />
those who needed them. He also said that although we would<br />
have liked to assist more people, funding was a challenge.<br />
Pictured: Noel Pillay,<br />
Debbie Goldstone, Dr Pam Rapiti,<br />
Lovina Mahadaw, Namitha Chabilal,<br />
Raj Mahadaw<br />
We are proud to announce that we have a newly elected task force team that will assist the branch in marketing,<br />
the care of people with muscular dystrophy, and fundraising events. Dr Pam Rapiti stressed that the foundation<br />
is here to improve the lives of those with MD and their families.<br />
We would like to once again thank all staff, members, those with MD, and volunteers for attending our AGM, and<br />
everyone 36 for their assistance and support of the <strong>MDF</strong> KZN Branch!
KZN Branch<br />
Awareness at Genetic Congress<br />
Durban, <strong>2017</strong><br />
The 17th Biennial Genetic Congress was recently held at Elangeni Hotel,<br />
Durban. This was organised and facilitated by a group of enthusiastic and<br />
passionate people working in the field of human genetics in KZN, assisted<br />
by a conference convenor. The theme, ‘Ubuntu genetics: We are because<br />
you are’, focused on community genetics. It was well attended by national<br />
and international delegates including clinicians, geneticists, counsellors,<br />
nurses and allied health professionals. The academic programme highlighted<br />
various aspects of genetics including counselling, clinical cases,<br />
genetic testing available in SA and overseas, and research on various<br />
genetic topics. Learners from Westpark School for Learners with Special<br />
Educational Needs officially opened the congress with their electrifying<br />
rendition of the national anthem and showcased their talents with gumboot<br />
dancing and drums.<br />
An emotional and special tribute was delivered by Prof M Adhikari on the<br />
late Prof WS Winship, known as the father of genetics in KZN.<br />
Pictured: Namitha Chabilal<br />
and Debbie Goldstone<br />
As part of the social programmes, delegates had the opportunity to dress<br />
in colourful traditional wear, apply mehndi and eat traditional Indian<br />
meals at a colourful and entertaining Indian Evening at the Maharani Hotel.<br />
The gala dinner was held at the Ushaka Marine World, surrounded by hammerheads and sharks – it felt as<br />
though we were having dinner on the ocean bed – a breathtaking experience indeed!<br />
<strong>MDF</strong> KZN was invited to be part of this special meeting by Genetics Alliance SA – an umbrella body for support<br />
groups in SA. <strong>MDF</strong> KZN being a member of the alliance, we had the opportunity to be part of this prestigious<br />
gathering.<br />
An awareness table was set up and Casual Day stickers and licence disc holders were on sale. This was well<br />
supported by all. Members of the <strong>MDF</strong> also took the opportunity to market the foundation and its role in the community<br />
and networked with other societies and trade bodies.<br />
Amashova Cycle Challenge<br />
Amashova is a cycle race from Pietermaritzburg to<br />
Durban that took place on 22 October <strong>2017</strong>.<br />
In order to raise funds for the Muscular Dystrophy Foundation<br />
KZN, Dr Amith Keshave and his team formed<br />
The 100s Club – to get at least 100 people to support<br />
the team for cycling the Amashova by donating at least<br />
R100 each.<br />
By successfully completing the race, Dr Keshave’s team<br />
managed to raise R23 000 for the foundation. This initiative<br />
was inspired by one of Dr Keshave’s patients, Baby<br />
Arushi, diagnosed with spinal muscular atrophy type 1.<br />
Thank you for your donation and support!<br />
Pictured: Dr Amith Keshave, Namitha Chabilal,<br />
Sonam Nundkissoor (mom), Baby Arushi<br />
Nundkissoor, Akashen Nundkissoor (dad)<br />
37
KZN Branch<br />
KZN Branch Golf Day<br />
KZN Branch Golf Day<br />
By Debbie Goldstone<br />
On 17 September <strong>2017</strong>, Fairways Golf Club hosted a golf tournament<br />
in partnership with the Muscular Dystrophy Foundation<br />
KZN Branch at the picturesque Amanzimtoti Golf Course.<br />
Whilst the start of the day was preceded by ominous weather<br />
and light rain, the rest of the day was without rain and presented<br />
the golfers with perfect playing conditions. The club<br />
was gracious in welcoming representatives of the <strong>MDF</strong> and<br />
promised to consider an annual <strong>MDF</strong> golf day.<br />
Great prizes were presented to golfers bringing in the top<br />
scores at the end of the day, sponsored by Fairways Virtual<br />
Golf Club and the <strong>MDF</strong>.<br />
A big thank you goes out to Africa Training Centre for generously<br />
donating R8 000 and to Fairways Virtual Golf Club for<br />
also donating R4 000 to the Muscular Dystrophy Foundation<br />
KZN Branch. Thanks also goes to Indhu Meiser, Executive<br />
Manager of Dash Luxury Apartments, for generously sponsoring<br />
a one-night stay at their luxury apartments.<br />
A great thank you to all who assisted and for allowing us this<br />
opportunity to create awareness and bring in much needed<br />
funds. We raised a total of R13 020 (inclusive of donations<br />
and a lucky draw).<br />
<strong>MDF</strong> KZN awareness table at<br />
genetics congress<br />
An awareness table was set up at the 17th Biennial Congress<br />
of the Southern African Society for Human Genetics, which was<br />
held on 13 –16 August at the Elangeni Hotel, Durban. The sale of<br />
Casual Day stickers and licence disc holders was well supported<br />
by the delegates. Members of the <strong>MDF</strong> took the opportunity to<br />
market the foundation and its role in the community.<br />
Thank you for your support!<br />
38<br />
Pictured: Namitha Chabilal,<br />
Debbie Goldstone and<br />
Dr. Pam Rapiti
1 st<br />
WHEELCHAIR<br />
CUSHION<br />
For independent living<br />
sales@wheelchairs.co.za<br />
www.wheelchairs.co.za<br />
Tel (021) 592 3370
SOMEONE I LOVE<br />
Needs a Cure<br />
Please Support<br />
MUSCULAR DYSTROPHY<br />
AWARENESS & RESEARCH<br />
WE NEVER GIVE UP HOPE<br />
Contact us for further information:<br />
The term muscular dystrophy (MD) describes a disorder<br />
that affects the muscles, resulting in progressive<br />
wasting and weakness of the muscle. Symptoms may<br />
appear at birth, in early childhood, or later in life.<br />
Neuromuscular disorders affect not only the muscles<br />
but also the nervous system.<br />
Individuals of either sex and all ages<br />
and ethnic backgrounds can be<br />
affected by MD.<br />
NATIONAL OFFICE<br />
Tel: 011 472-9703<br />
E-mail: national@mdsa.org.za<br />
Website: www.mdsa.org.za<br />
CAPE BRANCH<br />
(Western Cape, Northern Cape & part of Eastern Cape)<br />
Tel: 021 592-7306<br />
E-mail: cape@mdsa.org.za<br />
GAUTENG BRANCH<br />
(Gauteng, Free State, Mpumalanga, Limpopo & North<br />
West)<br />
Tel: 011 472-9824<br />
E-mail: gauteng@mdsa.org.za<br />
KZN BRANCH<br />
(KZN & part of Eastern Cape)<br />
Tel: 031 332-0211<br />
E-mail: kzn@mdsa.org.za