You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
the disease have been kept alive with steady<br />
and robust funding by international donors<br />
since 2010. With population growth and the<br />
emergence of resilient transmission patterns,<br />
existing levels of funding proved inadequate<br />
in recent years, especially in highest burden<br />
countries. Global funding for malaria control fell<br />
short of the estimated US$ 4.4 billion needed<br />
in 2017, with total funding estimated at US$<br />
3.1 billion, representing a yearly shortfall of<br />
US$ 1.3 billion. Investment in malaria R&D too<br />
fell in 2016. At a total of US$ 588 million, it<br />
represented about 85% of the US$ 693 million<br />
needed every year for malaria basic research<br />
and product development R&D, as estimated in<br />
the Global Technical Strategy (GTS) for malaria<br />
2016-2030.<br />
Investment in malaria vaccine development<br />
too is limited. Most financing into the<br />
development of vaccines to combat malaria<br />
comes from the public sector.<br />
The fact that malaria affects some of the<br />
world’s poorest means that there is a limited<br />
‘market’ for investment from the private sector.<br />
In the meantime, financing for vector<br />
control products and diagnostics have<br />
significantly increased.<br />
Among the systemic and technical<br />
measures identified by the WHO to accelerate<br />
malaria control are inadequate performance<br />
of health systems, weak management<br />
of supply chains, an unregulated private<br />
health sector in countries like India, a lack<br />
of surveillance systems, monitoring and<br />
evaluation, a dearth of adequate technical<br />
and human resource capacities to scale up<br />
efforts, and insufficient tools to diagnose and<br />
Malaria is caused<br />
by a different<br />
kind of pathogen<br />
– a parasite, as<br />
opposed to a virus<br />
or bacterium. You<br />
have to take into<br />
account a more<br />
complex lifecycle.<br />
We don’t have<br />
any vaccines in<br />
human use against<br />
parasites. They<br />
transit between two<br />
organisms—humans<br />
and mosquitoes.<br />
Dr Ashley Birkett<br />
Director of PATH’s<br />
Malaria Vaccine Initiative<br />
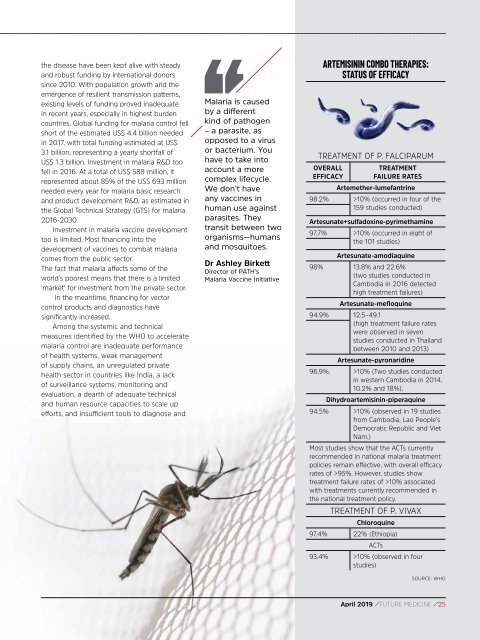
ARTEMISININ COMBO THERAPIES:<br />
STATUS OF EFFICACY<br />
TREATMENT OF P. FALCIPARUM<br />
OVERALL<br />
EFFICACY<br />
TREATMENT<br />
FAILURE RATES<br />
Artemether-lumefantrine<br />
98.2% >10% (occurred in four of the<br />
159 studies conducted)<br />
Artesunate+sulfadoxine-pyrimethamine<br />
97.7% >10% (occurred in eight of<br />
the 101 studies)<br />
Artesunate-amodiaquine<br />
98% 13.8% and 22.6%<br />
(two studies conducted in<br />
Cambodia in 2016 detected<br />
high treatment failures)<br />
Artesunate-mefloquine<br />
94.9% 12.5–49.1<br />
(high treatment failure rates<br />
were observed in seven<br />
studies conducted in Thailand<br />
between 2010 and 2013)<br />
Artesunate-pyronaridine<br />
96.9%. >10% (Two studies conducted<br />
in western Cambodia in 2014,<br />
10.2% and 18%),<br />
Dihydroartemisinin-piperaquine<br />
94.5% >10% (observed in 19 studies<br />
from Cambodia, Lao People’s<br />
Democratic Republic and Viet<br />
Nam.)<br />
Most studies show that the ACTs currently<br />
recommended in national malaria treatment<br />
policies remain effective, with overall efficacy<br />
rates of >95%. However, studies show<br />
treatment failure rates of >10% associated<br />
with treatments currently recommended in<br />
the national treatment policy.<br />
TREATMENT OF P. VIVAX<br />
Chloroquine<br />
97.4% 22% (Ethiopia)<br />
ACTs<br />
93.4% >10% (observed in four<br />
studies)<br />
SOURCE: WHO<br />
<strong>April</strong> <strong>2019</strong> / FUTURE MEDICINE / 25