You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
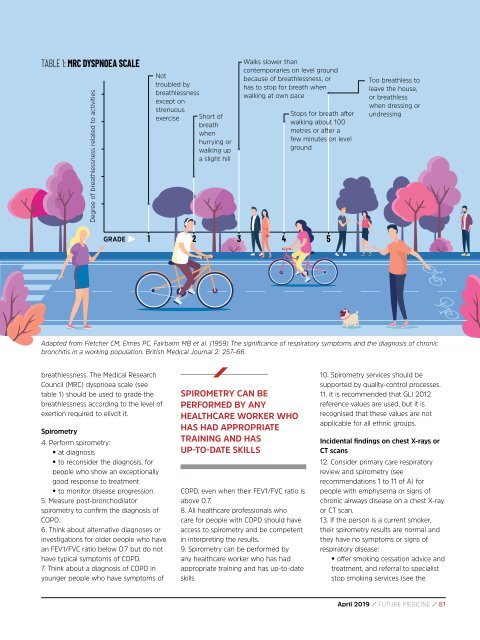
TABLE 1: MRC DYSPNOEA SCALE<br />
Degree of breathlessness related to activities<br />
Not<br />
troubled by<br />
breathlessness<br />
except on<br />
strenuous<br />
exercise<br />
Short of<br />
breath<br />
when<br />
hurrying or<br />
walking up<br />
a slight hill<br />
Walks slower than<br />
contemporaries on level ground<br />
because of breathlessness, or<br />
has to stop for breath when<br />
walking at own pace<br />
Stops for breath after<br />
walking about 100<br />
metres or after a<br />
few minutes on level<br />
ground<br />
Too breathless to<br />
leave the house,<br />
or breathless<br />
when dressing or<br />
undressing<br />
GRADE<br />
1 2 3 4 5<br />
Adapted from Fletcher CM, Elmes PC, Fairbairn MB et al. (1959) The significance of respiratory symptoms and the diagnosis of chronic<br />
bronchitis in a working population. British Medical Journal 2: 257–66.<br />
breathlessness. The Medical Research<br />
Council (MRC) dyspnoea scale (see<br />
table 1) should be used to grade the<br />
breathlessness according to the level of<br />
exertion required to elivcit it.<br />
Spirometry<br />
4. Perform spirometry:<br />
• at diagnosis<br />
• to reconsider the diagnosis, for<br />
people who show an exceptionally<br />
good response to treatment<br />
• to monitor disease progression.<br />
5. Measure post-bronchodilator<br />
spirometry to confirm the diagnosis of<br />
COPD.<br />
6. Think about alternative diagnoses or<br />
investigations for older people who have<br />
an FEV1/FVC ratio below 0.7 but do not<br />
have typical symptoms of COPD.<br />
7. Think about a diagnosis of COPD in<br />
younger people who have symptoms of<br />
SPIROMETRY CAN BE<br />
PERFORMED BY ANY<br />
HEALTHCARE WORKER WHO<br />
HAS HAD APPROPRIATE<br />
TRAINING AND HAS<br />
UP-TO-DATE SKILLS<br />
COPD, even when their FEV1/FVC ratio is<br />
above 0.7.<br />
8. All healthcare professionals who<br />
care for people with COPD should have<br />
access to spirometry and be competent<br />
in interpreting the results.<br />
9. Spirometry can be performed by<br />
any healthcare worker who has had<br />
appropriate training and has up-to-date<br />
skills.<br />
10. Spirometry services should be<br />
supported by quality-control processes.<br />
11. It is recommended that GLI 2012<br />
reference values are used, but it is<br />
recognised that these values are not<br />
applicable for all ethnic groups.<br />
Incidental findings on chest X‐rays or<br />
CT scans<br />
12. Consider primary care respiratory<br />
review and spirometry (see<br />
recommendations 1 to 11 of A) for<br />
people with emphysema or signs of<br />
chronic airways disease on a chest X‐ray<br />
or CT scan.<br />
13. If the person is a current smoker,<br />
their spirometry results are normal and<br />
they have no symptoms or signs of<br />
respiratory disease:<br />
• offer smoking cessation advice and<br />
treatment, and referral to specialist<br />
stop smoking services (see the<br />
<strong>April</strong> <strong>2019</strong> / FUTURE MEDICINE / 81