Georgia Nursing January 2022
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
“Nurses shaping<br />
the future of<br />
professional nursing<br />
for a healthier <strong>Georgia</strong>.”<br />
Since 1907<br />
The Official Publication of the <strong>Georgia</strong> Nurses Foundation (GNF).<br />
Quarterly publication distributed to approximately 58,000 RNs in <strong>Georgia</strong>.<br />
Brought to you by the <strong>Georgia</strong> Nurses Foundation<br />
(GNF) and the <strong>Georgia</strong> Nurses Association (GNA), whose<br />
dues-paying members make it possible to advocate for<br />
nurses and nursing at the state and federal level.<br />
Visit us online at www.georgianurses.org<br />
Volume 82 • Number 1 • <strong>January</strong>, February, March <strong>2022</strong><br />
<strong>Georgia</strong> <strong>Nursing</strong><br />
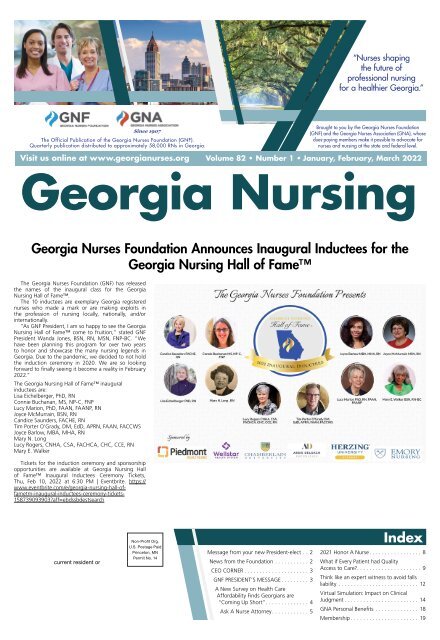
<strong>Georgia</strong> Nurses Foundation Announces Inaugural Inductees for the<br />
<strong>Georgia</strong> <strong>Nursing</strong> Hall of Fame<br />
The <strong>Georgia</strong> Nurses Foundation (GNF) has released<br />
the names of the inaugural class for the <strong>Georgia</strong><br />
<strong>Nursing</strong> Hall of Fame.<br />
The 10 inductees are exemplary <strong>Georgia</strong> registered<br />
nurses who made a mark or are making exploits in<br />
the profession of nursing locally, nationally, and/or<br />
internationally.<br />
“As GNF President, I am so happy to see the <strong>Georgia</strong><br />
<strong>Nursing</strong> Hall of Fame come to fruition,” stated GNF<br />
President Wanda Jones, BSN, RN, MSN, FNP-BC. “We<br />
have been planning this program for over two years<br />
to honor and showcase the many nursing legends in<br />
<strong>Georgia</strong>. Due to the pandemic, we decided to not hold<br />
the induction ceremony in 2020. We are so looking<br />
forward to finally seeing it become a reality in February<br />
<strong>2022</strong>.”<br />
The <strong>Georgia</strong> <strong>Nursing</strong> Hall of Fame inaugural<br />
inductees are:<br />
Lisa Eichelberger, PhD, RN<br />
Connie Buchanan, MS, NP-C, FNP<br />
Lucy Marion, PhD, FAAN, FAANP, RN<br />
Joyce McMurrain, BSN, RN<br />
Candice Saunders, FACHE, RN<br />
Tim Porter O’Grady, DM, EdD, APRN, FAAN, FACCWS<br />
Joyce Barlow, MBA, MHA, RN<br />
Mary N. Long<br />
Lucy Rogers, CNHA, CSA, FACHCA, CHC, CCE, RN<br />
Mary E. Walker<br />
Tickets for the induction ceremony and sponsorship<br />
opportunities are available at <strong>Georgia</strong> <strong>Nursing</strong> Hall<br />
of Fame Inaugural Inductees Ceremony Tickets,<br />
Thu, Feb 10, <strong>2022</strong> at 6:30 PM | Eventbrite. https://<br />
www.eventbrite.com/e/georgia-nursing-hall-of-<br />
fametm-inaugural-inductees-ceremony-tickets-<br />
158739093903?aff=ebdssbdestsearch<br />
current resident or<br />
Non-Profit Org.<br />
U.S. Postage Paid<br />
Princeton, MN<br />
Permit No. 14<br />
Message from your new President-elect. ..2<br />
News from the Foundation. ...........2<br />
CEO CORNER. .....................3<br />
GNF PRESIDENT’S MESSAGE. .........3<br />
A New Survey on Health Care<br />
Affordability Finds <strong>Georgia</strong>ns are<br />
“Coming Up Short”. ..............4<br />
Ask A Nurse Attorney. ............5<br />
Index<br />
2021 Honor A Nurse. .................8<br />
What if Every Patient had Quality<br />
Access to Care?. .....................9<br />
Think like an expert witness to avoid falls<br />
liability ........................... 12<br />
Virtual Simulation: Impact on Clinical<br />
Judgment. ........................ 14<br />
GNA Personal Benefits ............... 18<br />
Membership. ...................... 19
Page 2 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
GEORGIA<br />
NURSING<br />
Volume 82 • Number 1<br />
Message from your new President-elect<br />
Happy New Year!<br />
It is my hope that you and your family had a fun,<br />
safe and healthy holiday season. Many families<br />
returned to celebrating in person while many families<br />
continue to mourn lost loved ones. From the bottom<br />
of our hearts, the <strong>Georgia</strong> Nurses Association (GNA)<br />
is thinking of each person who has been affected<br />
by the pandemic over the past two years. The news<br />
reminds us of the need to continue to protect ourselves<br />
and those who we cherish. It is not unusual to hear<br />
the great debate going on amongst friends, family<br />
members, coworkers, and the like. The decision to be<br />
vaccinated versus the choice to remain unvaccinated<br />
has divided the nation and abroad. Boosters have<br />
sparked even more debate.<br />
As the conspiracies and mistrust rage on, remember<br />
whatever you decide, your immune system is your first<br />
line of defense, especially in the winter months. Here<br />
are some tips you can use to keep your immune system<br />
in good condition:<br />
1 Stop smoking if you are a smoker.<br />
2 Make sure your diet consists of plant-based<br />
items such as fruits and vegetables.<br />
3 Get moving! Stay active.<br />
4 Take time to rest. Sleep is important to<br />
immunity.<br />
5 Wash your hands or use hand sanitizer<br />
frequently.<br />
On another note, <strong>Georgia</strong>’s <strong>2022</strong> Legislative Session<br />
will commence on <strong>January</strong> 11th and conclude on day<br />
40. The GNA has an ambitious legislative platform that<br />
we believe will address some of the priority needs of<br />
our profession. We welcome your feedback, your input,<br />
and your participation. Do not hesitate to contact us<br />
at the GNA office or by email with your questions or<br />
concerns.<br />
The board of directors are poised and ready to<br />
represent the nurses of <strong>Georgia</strong> under the “Gold<br />
Dome.” We will periodically send out calls for your<br />
participation as we work to better working conditions<br />
for nurses in <strong>Georgia</strong>. Your stories, your experiences,<br />
and your insight are all invaluable.<br />
As your newly elected President-Elect, I would like to<br />
thank each of you for your vote for me, I am forever<br />
grateful for your trust and belief in my skills and ability<br />
to serve in this capacity.<br />
With gratitude,<br />
Erica Mills, PhD, RN, NPD-BC<br />
President-Elect, <strong>Georgia</strong> Nurses Association<br />
Board of Directors 2021-2023<br />
News from the<br />
Foundation<br />
The <strong>Georgia</strong> Nurses Foundation (GNF) awarded a<br />
Kathryn Chance Suggs Leonard Scholarship of $2,000<br />
this year to Morgan Clark-Youngblood.<br />
Congratulations Morgan!<br />
The <strong>Georgia</strong> Nurses Foundation and <strong>Georgia</strong><br />
Nurses Association <strong>Nursing</strong> Scholarship Awards<br />
provide financial assistance<br />
to qualified applicants who<br />
may be enrolled full- or parttime<br />
in an accredited nursing<br />
program. Interested students<br />
must have a GPA of at least<br />
a 2.5 (undergraduate) or 3.0<br />
(graduate) on a 4.0 scale<br />
in prior nursing education.<br />
For more information, visit<br />
<strong>Georgia</strong>Nurses.org.<br />
Communications Director: Charlotte Báez-Díaz<br />
GEORGIA NURSES FOUNDATION BOARD OF TRUSTEES<br />
Wanda Jones, BSN, RN, MSN, FNP-BC, President<br />
Orlin Marquez, DNP, MBA, APRN, FNP-BC, Vice President<br />
Vacant, Secretary<br />
Shawn Little, CNE, DNP, RN, Treasurer<br />
Catherine Futch, RN, MN, NEA-BC, CHC, FACHE,<br />
Immediate Past President<br />
Evelyn M. Olenick, DNP, RN, NEA-BC, Member<br />
Sherry Sims, RN, Member<br />
Mary Gullatte, PhD, RN, ANP-BC, AOCN, FAAN, Member<br />
Natalie Jones, MSN, RN, NPD-BC, Member<br />
Gerald Hobbs, RN, Member<br />
Brenda B. Rowe, RN, MN, JD, Member<br />
Katelyn Little, RN, BSN, Member<br />
Dina Hewett, PhD, RN, NEA-BC, Member<br />
Matt Caseman, Ex-Officio Member<br />
GEORGIA NURSES ASSOCIATION BOARD OF DIRECTORS<br />
President - Dina Hewett, PhD, RN, NEA-BC<br />
President-Elect & ANA Delegate-At-Large<br />
Erica Mills, PhD, RN, NPD-BC<br />
Secretary & ANA Delegate-At-Large<br />
Barbara Austin, MN, RN<br />
Treasurer & 1st Alternate ANA Delegate-At-Large<br />
Rachel E. Myers, PhD, RN, CDCES<br />
Director of Leadership Development & 2nd ANA<br />
Delegate-At-Large<br />
Linda Morrow, DPN, MSN, MBA, NE-BC, CPHQ<br />
Director Legislation/Public Policy<br />
Elizabeth K. Bolton-Harris, DNP, ACNP-BC, CHFN<br />
Director <strong>Nursing</strong> Practice & Advocacy<br />
Joy L. King-Mark, DNP, MBA, APRN, NP-C<br />
Director Advanced Practice Registered Nurse<br />
Victoria Gordon, MSN, RN, CNM<br />
Director Staff Nurse<br />
Natasha Laibhen-Parkes, PhD, RN, CPN<br />
Director Membership Development<br />
Bree Becker, MSN, FNP-C, RNC-MNN<br />
Director New Graduate<br />
Emily Kathryn Lewis, BSN, RN<br />
GNF President<br />
Wanda Jones, BSN, RN, MSN, FNP-BC<br />
For advertising rates and information, please contact Arthur L.<br />
Davis Publishing Agency, Inc., PO Box 216, Cedar Falls, Iowa<br />
50613, (800) 626-4081. GNF and the Arthur L. Davis Publishing<br />
Agency, Inc. reserve the right to reject any advertisement.<br />
Responsibility for errors in advertising is limited to corrections in<br />
the next issue or refund of price of advertisement.<br />
Acceptance of advertising does not imply endorsement or<br />
approval by the <strong>Georgia</strong> Nurses Foundation of products<br />
advertised, the advertisers, or the claims made. Rejection of an<br />
advertisement does not imply a product offered for advertising<br />
is without merit, or that the manufacturer lacks integrity, or<br />
that this association disapproves of the product or its use. GNF<br />
and the Arthur L. Davis Publishing Agency, Inc. shall not be held<br />
liable for any consequences resulting from purchase or use of<br />
an advertiser’s product. Articles appearing in this publication<br />
express the opinions of the authors; they do not necessarily<br />
reflect views of the staff, board, or membership of GNF or<br />
those of the national or local associations.<br />
<strong>Georgia</strong> <strong>Nursing</strong> is published quarterly every <strong>January</strong>, April,<br />
July and October for the <strong>Georgia</strong> Nurses Foundation, a<br />
constituent member of the American Nurses Association.<br />
GNA/GNF<br />
3032 Briarcliff Road, Atlanta, GA 30329<br />
www.georgianurses.org, gna@georgianurses.org<br />
(404) 325-5536<br />
FOLLOW GNA<br />
GNF President Wanda Jones and Morgan<br />
@georgianurses<br />
facebook.com/ganurses<br />
@<strong>Georgia</strong>Nurses<br />
<strong>Georgia</strong> Nurses Association
Calllliing<br />
A<br />
No Otheer.<br />
Liikee<br />
<strong>January</strong>, February, March <strong>2022</strong> <strong>Georgia</strong> <strong>Nursing</strong> • Page 3<br />
CEO CORNER<br />
GNF PRESIDENT’S MESSAGE<br />
Matt Caseman, GNA CEO<br />
As we head towards <strong>2022</strong>, GNA continues to<br />
progress and evolve because of our members’<br />
dedication and hard work. First and foremost, a<br />
new GNA Board of Directors was elected, and Dr.<br />
Dina Hewett took over as GNA President from<br />
Richard Lamphier. Dina has been a champion for the<br />
profession, and we are excited to have her leading<br />
<strong>Georgia</strong>’s oldest and largest professional nursing<br />
association.<br />
Richard, who fearlessly led GNA through the<br />
pandemic, a monumental task indeed, will not be<br />
going far from GNA. In fact, we are pleased to<br />
announce he will be the new Executive Director of<br />
our Peer Assistance Program (GNA-PAP) which received $150,000 in the state<br />
budget for a much-needed expansion. Established in the 1980s, GNA-PAP is<br />
nurses helping nurses with the disease of substance use disorder. Participants,<br />
who are drug tested weekly, meet in groups with a facilitator for many months<br />
until they get back on their feet. Thousands of <strong>Georgia</strong>’s nurses have been<br />
helped over the years through our PAP and I could not be prouder of its<br />
amazing success.<br />
Regarding legislative advocacy, lawmakers will be back in session in <strong>January</strong><br />
and GNA will be working the hallways and corridors under the Gold Dome in<br />
Atlanta to advance our priorities. SB 19, and companion legislation HB 371,<br />
would require hospitals and ambulatory surgical centers to utilize surgical<br />
smoke evacuation systems during surgical procedures. Smoke produced during<br />
surgery has been proven toxic and an extreme detriment to the health of our<br />
operating room nurses.<br />
Another focus during the <strong>2022</strong> legislative session is our APRNs. HB 340<br />
would create a separate APRN license, allow APRNs and PAs to do Home<br />
Health Service orders, and allow the Board of <strong>Nursing</strong> to collect nursing<br />
workforce data. HB 369 would allow APRNs and PAs to write prescriptions for<br />
Schedule II in an emergency for an amount not to exceed five days. HB 369<br />
also includes a section on allowing APRNs/PAs to authorize disability parking<br />
permits.<br />
Front and center is also the nursing shortage. GNA recently testified before<br />
the House Human Relations and Aging Committee on safe staffing and patient<br />
safety, and the need to recruit and retain bedside nurses. <strong>Georgia</strong> had the 5th<br />
worse nursing shortage in the country in 2019, and the pandemic has only<br />
exacerbated an already dire situation. GNA, along with other stakeholders, will<br />
be working to help ease the shortage during the <strong>2022</strong> General Assembly.<br />
Lastly, to honor our nurse legends from <strong>Georgia</strong>, the <strong>Georgia</strong> Nurses<br />
Foundation will be hosting the first annual <strong>Georgia</strong> <strong>Nursing</strong> Hall of Fame<br />
on February 10th in a ceremony at Piedmont Atlanta Hospital atrium and<br />
auditorium from 6 pm to 10 pm. The ten inaugural inductees have been<br />
announced and tickets for the ceremony are available for purchase on our<br />
website. Seating is limited. Please join us for what is sure to be a great night<br />
recognizing our state’s most accomplished nurses.<br />
We will also be holding an in-person annual conference in the Fall of <strong>2022</strong>.<br />
Location and date have yet to be determined. With Zoom fatigue at an all-time<br />
high, I think many agree that it is long overdue that we gather face to face.<br />
As always, thank you for your continued support of GNA/GNF and<br />
everything you do for our community.<br />
New Beginnings<br />
Wanda Jones, MSN, FNP-BC, RN<br />
As I begin my second term as your GNF President, I am<br />
looking forward to the great things we will accomplish in<br />
the next two years. Several projects were started in the past<br />
two years but had to be put on hold due to COVID-19.<br />
I am so honored and privileged to know that the<br />
<strong>Georgia</strong> <strong>Nursing</strong> Hall of Fame Inaugural Inductees<br />
Ceremony will finally take place on February 10, <strong>2022</strong>.<br />
Three judges outside of <strong>Georgia</strong> selected ten exemplary<br />
nurses who have met the required criteria for selection.<br />
These inductees will be the inaugural class for GNF’s Hall<br />
of Fame. It will be an exciting time to honor these nurses<br />
at Piedmont Hospital Marcus Heart Center. A limited<br />
number of tickets for this event, so please look on the<br />
GNA website for details to purchase your tickets. This will be a time we can honor<br />
these nurses who have made a difference for nurses and nursing in the state of<br />
<strong>Georgia</strong>, nationally and internationally.<br />
In addition, I am excited to report that the <strong>Georgia</strong> Center for <strong>Nursing</strong> Excellence<br />
(GCNE), led by Patricia Horton, RN, MN, MBA, CMC, CEEO, has acquired its<br />
articles of incorporation and is moving forward with various projects, starting with<br />
the hosting of the first <strong>Georgia</strong> <strong>Nursing</strong> Workforce Summit on <strong>January</strong> 20th and<br />
21st. Please go to GCNE’s website (www.gcnex.org) to learn more about the <strong>2022</strong><br />
Summit and other agenda items.<br />
Furthermore, GNF is planning on a golf tournament in the spring and Bobby<br />
Albert has committed to help us with this golf tournament. With our previous<br />
tournaments, before 2020, a fun time was had by all the participants.<br />
Lastly, we have a new diverse Board of Trustees that I am very honored to be<br />
able to work with. Their expertise and knowledge will only enhance the Foundation<br />
moving forward with new and innovative ideas.<br />
In closing, as I am writing this article, Thanksgiving is only a few days away. At<br />
this time of the year, we need to give thanks and blessings for our family, friends,<br />
work, health, and our freedom. I truly hope that everyone had a wonderful<br />
Thanksgiving with their family and friends, ate lots of healthy food, and finally<br />
talked with one another.
Page 4 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
A New Survey on Health Care Affordability Finds <strong>Georgia</strong>ns are<br />
“Coming Up Short”<br />
By Whitney Griggs, Policy Analyst<br />
The high cost of medical<br />
care has long been a concern<br />
for <strong>Georgia</strong>ns and a frequent<br />
topic of conversation among<br />
policymakers and industry<br />
leaders. Therefore, it’s no<br />
surprise to learn that many<br />
<strong>Georgia</strong>ns struggle to pay for<br />
health care or worry about<br />
their ability to pay for care<br />
in the future. A new survey<br />
conducted by Altarum’s<br />
Healthcare Value Hub, in<br />
consultation with <strong>Georgia</strong>ns for a Healthy Future, gives<br />
surprising new data on exactly how much <strong>Georgia</strong>ns<br />
struggle with the cost of healthcare.<br />
The purpose of Altarum’s Consumer Healthcare<br />
Experience State Survey (CHESS) is to provide<br />
advocates, policymakers, and industry leaders with<br />
a better understanding of consumers’ struggles with<br />
health care costs, reveal the cost-drivers that need to<br />
be addressed in <strong>Georgia</strong>, and provide support for<br />
system changes and policy solutions to improve health<br />
care affordability for consumers.<br />
The <strong>Georgia</strong> CHESS revealed that almost seven<br />
in ten (68%) respondents struggled with health<br />
care affordability burdens in the past 12 months.<br />
These burdens included being uninsured due to high<br />
premium costs (48%), delaying or forgoing care due<br />
to cost (58%), and struggling to pay medical bills<br />
(50%). The survey also found that four in five (80%)<br />
of respondents worried about affording care in the<br />
future, especially care related to aging or medical<br />
emergencies. Unsurprisingly, those with incomes<br />
below $50,000 struggled the most to afford care.<br />
However, health care cost challenges also affected<br />
families higher up the income ladder, with over half<br />
(56%) of residents with incomes of $100,000 or more<br />
struggling to afford care. When people are forced to<br />
delay or forgo health care due to cost, their conditions<br />
often become much more difficult and expensive to<br />
treat down the road. Additionally, taking on debt or<br />
choosing between necessities to pay for care affects<br />
individuals and family’s financial security and wellbeing<br />
for years to come. The survey found strong,<br />
bipartisan support for legislative action to address high<br />
medical costs. These actions include expanding health<br />
insurance options to make health insurance affordable<br />
and accessible for everyone, making it easier to switch<br />
plans if an insurer drops your provider, showing fair<br />
prices for procedures, and requiring insurers to provide<br />
up-front cost estimates to consumers. The results of the<br />
<strong>Georgia</strong> CHESS demonstrate the need for policymakers<br />
and stakeholders to address high costs across all areas<br />
of health care – from coverage to care to prescription<br />
drugs. Additionally, consumers need more protection<br />
from high health care costs and robust, easy-tounderstand<br />
tools to navigate the costs associated<br />
with care. Lawmakers can apply the CHESS results to<br />
their efforts in the <strong>2022</strong> legislative session, using the<br />
information to pass laws that eliminate cost as a barrier<br />
to care for <strong>Georgia</strong>ns, protect <strong>Georgia</strong>ns from rising<br />
health care costs, and require system-level changes so<br />
consumers can better tell what the actual cost of their<br />
care will be.<br />
wgriggs@healthyfuturega.org<br />
More information and evidence: https://<br />
healthyfuturega.org/2021/09/29/a-new-survey-onhealth-care-affordability-finds-georgians-are-comingup-short/<br />
Advocacy Update<br />
AMAZING<br />
REMARKABLE<br />
AWESOME<br />
American Renal Associates<br />
Our Staff Make the Difference!<br />
Opportunities for dialysis nurses in<br />
Augusta and Macon areas.<br />
Email resume to Brittany Winter<br />
at bwinter@americanrenal.com<br />
Tim Davis<br />
Sr. Director of Membership & Government Affairs<br />
On Wednesday, December 8, 2021, <strong>Georgia</strong> Nurses Foundation Treasurer Dr.<br />
Shawn Little spoke to the House Rural Development Council about the need for<br />
more support for schools of nursing in order to grow <strong>Georgia</strong>’s new nurse pipeline.<br />
In addition to some innovative ideas centered around how the state can invest in<br />
schools of nursing, she also offered feedback relating to the recently proposed<br />
Board of <strong>Nursing</strong> rule changes for schools of nursing and their potential impact.<br />
You can watch the Rural Development Council meeting at https://www.youtube.<br />
com/watch?v=InTG499rTOo<br />
Comments from Dr. Little begin at the 3hr and 10min mark.
<strong>January</strong>, February, March <strong>2022</strong> <strong>Georgia</strong> <strong>Nursing</strong> • Page 5<br />
Should nurse injectors<br />
carry liability insurance<br />
coverage and if yes<br />
what is best way to<br />
locate a reputable<br />
company?<br />
Hi HT,<br />
Thank you for your question. Any healthcare<br />
professional who provides patient care is susceptible<br />
to a medical malpractice lawsuit or professional license<br />
complaint. Therefore, all nurses who provide patient<br />
care should be covered by a professional liability<br />
insurance policy. If you are an employee of a healthcare<br />
facility, then you may be covered by your employer’s<br />
group professional liability insurance policy. However,<br />
you should always ask to make sure. Notably, you<br />
should also ensure that the employer’s policy includes<br />
license protection benefits, which covers the cost of<br />
your legal defense if a complaint is filed against your<br />
nursing license with the State Board of <strong>Nursing</strong>. If you<br />
are an independent contractor, then you should obtain<br />
your own individual professional liability insurance<br />
coverage. It is important to note that individual<br />
insurance policies typically provide license protection<br />
benefits. You can locate an individual insurance policy<br />
by using an online search engine and key search terms<br />
such as “individual liability insurance policy for nurses.”<br />
There are policies that cost as little as $250- $300<br />
per year! You can find these policies by doing a quick<br />
internet search.<br />
Best Wishes,<br />
Hahnah
Page 6 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
Report from the GNA <strong>Nursing</strong> Professional Development Units:<br />
New Scope and Standards of Practice<br />
Lynn Rhyne, MN, RNC-MNN<br />
I always struggle to develop an article for <strong>Georgia</strong><br />
<strong>Nursing</strong> that justly demonstrates the importance of nursing<br />
continuing professional development for nurses. As I have<br />
just received my 2021 update of the ANA <strong>Nursing</strong>: Scope<br />
and Standards of Practice, I thought this would be a timely<br />
update of nurses’ “Bible.”<br />
The <strong>Nursing</strong>: Scope and Standards of Practice are<br />
updated every six years. The definition of nursing has been<br />
reordered from 2015 and includes the art and science of<br />
caring, compassionate presence and recognition of the<br />
connection of all humanity.<br />
“<strong>Nursing</strong> integrates the art and science of caring and<br />
focuses on the protection, promotion, and optimization of health and human<br />
functioning of illness and injury; facilitation of healing; and alleviation of suffering<br />
through compassionate presence. <strong>Nursing</strong> is the diagnosis of human responses<br />
and advocacy in the care of individuals, families, groups, communities, and<br />
populations in recognition of the connection of all humanity (ANA, 2021, p. 1).<br />
The Scope of <strong>Nursing</strong> Practice describes the who, what, where, when, why, and<br />
how associated with nursing practice and roles (ANA, 2021, p. 3). The Standards are<br />
comprised of Professional <strong>Nursing</strong> Practice and Professional Performance.<br />
The Standards of Professional <strong>Nursing</strong> Practice provide nurses with insight into<br />
the actions and behaviors that nurses must demonstrate competently regardless of<br />
the practice setting. These are known as authoritative statements of nursing practice<br />
(ANA, 2021, p.4).<br />
A new standard was developed related to advocacy for the profession, healthcare<br />
consumer, and the communities we serve with an emphasis on a commitment for<br />
social justice in healthcare to address the social determinants of health and promote<br />
well-being.<br />
The Standards of Practice focus on a competent level of nursing practice<br />
demonstrated by the critical thinking model known as the nursing process. This<br />
model represents significant actions taken by nurses and forms the foundation<br />
of nurse’s decision-making, practice, and provision of care (ANA, 2015, p. 73).<br />
All nurses know the process of assessment, diagnosis, outcomes identification,<br />
planning, implementation, and evaluation. Within the fifteen standards are<br />
competencies the registered nurse must demonstrate.<br />
The Standards of Professional Performance provide an understanding of the<br />
competency of behavior in the professional role, including activities related to<br />
ethics, advocacy, respectful and equitable practice, communication, collaboration,<br />
leadership, education, scholarly inquiry, quality of practice, professional practice<br />
evaluation, resources stewardship, and environmental health (ANA, 2021, p. 74).<br />
Each of these performance standards are described in detail.<br />
An ANA Workgroup developed the ANA Professional <strong>Nursing</strong> Model that<br />
represents the “synergy of nurse’s caring, values, wisdom, and energy undergirded<br />
by ethical principles and situation ethics” (ANA, 2021, p. 9). The model is depicted<br />
by a flame with caring, values, wisdom, and energy within the flame with ethics<br />
providing the base of the flame upon which all the roles of nursing are grounded in.<br />
The model provides an in-depth analysis of ethics.<br />
The synopsis of the <strong>Nursing</strong>: Scope and Standards of Practice is my own<br />
interpretation of them. They must be read thoroughly by each person to develop<br />
an understanding and appreciation of them. They have been revised many times<br />
since I have been practicing as a professional registered nurse and each revision has<br />
provided more insight into professional practice and competent behaviors.<br />
References:<br />
American Nurses Association, <strong>Nursing</strong>: Scope and Standards of Practice, 4th ed., Silver Springs, MD,<br />
American Nurses Association, 2021.<br />
Visit nursingALD.com today!<br />
Search job listings<br />
in all 50 states, and filter by<br />
location and credentials.<br />
Browse our online database<br />
of articles and content.<br />
Find events<br />
for nursing professionals in your area.<br />
Your always-on resource for<br />
nursing jobs, research, and events.
Page 8 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
2021 Honor A Nurse<br />
Honoree<br />
Marilyn Williams<br />
Mitchell<br />
November 5, 2021<br />
In memory of nurse Marilyn Williams Mitchell.<br />
Ms. Williams Mitchell has been honored by her niece<br />
Lisa Oldham Sassaman through the <strong>Georgia</strong> Nurses<br />
Foundation Honor a Nurse Program. Mrs. and Mr. Betty<br />
and Don Parks also honored nurse Mitchell.<br />
The Foundation's Honor a Nurse Program provides<br />
a way to let individuals recognize nursing professionals<br />
who have made a difference in the lives of others as a<br />
friend, mentor, caregiver, or teacher. Proceeds from this<br />
program go to the Foundation's scholarship program<br />
and provide funding for nursing related activities.<br />
The <strong>Georgia</strong> Nurses Foundation salutes Ms. Williams<br />
Mitchell for her contribution to the nursing profession.<br />
Wanda Jones<br />
Wanda Jones, BSN, RN, MSN, FNP-BC<br />
GNF President<br />
Benton House and Benton Village, assisted living and<br />
memory care communities, are looking for qualified<br />
professionals for the following positions:<br />
LPN | Med Tech | CNA | CMA<br />
Locations in Augusta, Covington, Decatur, Douglasville,<br />
Grayson, Newnan, Stockbridge, Sugar Hill, and Woodstock.<br />
Applicants must be able to successfully pass a drug screening and background check.<br />
Ideal candidates will have Geriatric and Long Term Care experience. Three shift<br />
options are available at some locations.<br />
We offer a comprehensive benefits package including Health, Dental, Vision, Life<br />
Insurance, PTO and 401(k) plan.<br />
Only those truly committed to growth need apply. Apply online at<br />
www.bentonhouse.com/careers/
<strong>January</strong>, February, March <strong>2022</strong> <strong>Georgia</strong> <strong>Nursing</strong> • Page 9<br />
What if Every Patient had Quality Access to Care?<br />
By Monty Veazey, President/CEO <strong>Georgia</strong> Alliance<br />
of Community Hospitals<br />
In the spring of 2020, Laconyea Lynn of Albany went to<br />
Phoebe Putney Memorial Hospital with fatigue.<br />
Ms. Lynn woke up after six weeks on a ventilator and<br />
learned she’d had COVID-19, a disease she’d never heard<br />
of. She was among the first in the nation to catch the<br />
virus – and among the last to find out what it was. In total,<br />
she spent 72 days at Phoebe, walking out amid a tunnel<br />
of cheering nurses anxious to celebrate a survivor after<br />
witnessing so much heartache.<br />
In the first 100 days of the pandemic, Phoebe had<br />
2,728 positive COVID tests and 914 hospital admissions. Every bed was full. Offices<br />
were turned in to patient rooms. With PPE in short supply, staff sewed masks.<br />
Ms. Lynn was one of many struck by the virus. Albany became one of the first<br />
COVID hotspots, and its healthcare professionals at Phoebe found themselves on<br />
the front lines of a war with an unknown enemy. Survivors like Ms. Lynn were able<br />
to go back to their lives because they received compassionate, around-the-clock<br />
care from <strong>Georgia</strong>’s frontline healthcare workers.<br />
The COVID crisis shined a light on the heroic efforts of nurses, but it also exposed<br />
some of the significant challenges facing our industry and its workforce that require<br />
immediate action.<br />
Coming out of COVID, we must tell our stories of triumph. But we must also get<br />
help to solve the problems we face, or we run the serious risk of not having the<br />
healthcare infrastructure – both people and places – that we need to tackle the next<br />
healthcare crisis.<br />
First is the shortage of nurses and doctors that led to the state of <strong>Georgia</strong><br />
and our hospitals bidding for skilled nurses against other states and healthcare<br />
institutions. These shortages are long-standing, but COVID and its relentless<br />
consumption of healthcare resources brought the issue to a crisis point.<br />
This caused financial stress to institutions and personal stress to the professionals<br />
whose dedication to service pushed many beyond their personal limits.<br />
<strong>Georgia</strong> must redouble our efforts to address these shortages, and Community<br />
Hospitals are working to create new training programs to help. For example,<br />
Tift Regional Health System and Phoebe are partnering with Abraham Baldwin<br />
Agricultural College to create new nursing programs that identify expert<br />
practitioners and train them to become preceptors for nursing students.<br />
Efforts such as these are a great start, but there’s much more to do. <strong>Georgia</strong><br />
hospitals today face a nurse shortage of more than 25,000. To fill such a yawning<br />
gap will require a focused partnership from healthcare providers, state government<br />
and educational institutions. We must create incentives that inspire more bright<br />
young people to join this noble profession and encourage those who have left to<br />
consider returning.<br />
Part of creating a welcoming atmosphere is taking a stand for the safety and<br />
dignity of healthcare workers.<br />
That’s why <strong>Georgia</strong>’s hospitals are leading to stop the violence against healthcare<br />
workers that has spiked during the pandemic. We have worked with legislators<br />
to create the Senate Study Committee on Violence Against Health Care Workers<br />
and made the case for legislation to address the issue. We take seriously our<br />
responsibility to provide a safe workplace for all the professionals who work in our<br />
hospitals.<br />
And just as we must protect our healthcare workers so must we also protect their<br />
workplaces by fighting back efforts to repeal the CON laws that ensured <strong>Georgia</strong>ns<br />
maintain access to nearby hospitals.<br />
Together, we must stand strong and let our leaders know the importance to our<br />
communities of our hospitals and the “essential workers” who saved thousands of<br />
lives during the pandemic.<br />
That includes <strong>Georgia</strong>ns such as Laconyea Lynn of Albany.<br />
Veazey, of Tifton, is the president and CEO of the <strong>Georgia</strong> Alliance of Community<br />
Hospitals.<br />
HIRING<br />
RNs & LPNs<br />
Join the Crisp Regional Team!<br />
crispregional.org<br />
Contact: Ashley Purvis, Human Resource Recruiter at<br />
229-276-3113 • apurvis@crispregional.org<br />
Emergency<br />
Long-term Care<br />
Maternity<br />
Med/Surg<br />
Critical Care<br />
Telemetry<br />
Telemetry/Step Down<br />
Operating Room<br />
$5,000 SIGN ON BONUS for select RN positions!<br />
Competitive Salaries, Relocation Reimbursement & More!<br />
Apply Today!<br />
https://bit.ly/RNjobsSGHS<br />
Questions? Call 912-466-3146<br />
or email nurserecruiter@sghs.org
Page 10 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
<strong>Nursing</strong>ALD.com<br />
can point you right to that perfect<br />
NURSING JOB!<br />
<strong>Nursing</strong>ALD.com<br />
Free to Nurses<br />
Privacy Assured<br />
Easy to Use<br />
E-mailed Job Leads<br />
E-Store Now Open!<br />
Purchase GNA merchandise at GNA’s<br />
Café Press online store!<br />
Cups, bags, hats, t-shirts, hoodies,<br />
and more!<br />
www.cafepress.com/<br />
georgianursesassociation
Page 12 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
Think like an expert witness to avoid falls liability<br />
An 88-year-old patient slips on the floor, falling and<br />
breaking his hip. Your immediate concern is getting<br />
him the help he needs, but you also wonder if you<br />
could be legally liable for what happened. By thinking<br />
like an expert witness, you can help determine if this<br />
concern is valid and whether you could have taken<br />
steps to avoid the situation in the first place. But first,<br />
you need to understand some background information.<br />
Falls facts<br />
From 2007 to 2016, the fall death rate for older<br />
adults in the United States increased by 30%,<br />
according to data from the CDC. Each year, three<br />
million older adults are treated in emergency<br />
departments (EDs) for fall injuries, and more than<br />
800,000 people are hospitalized each year because<br />
of injuries related to a fall. These falls extract a high<br />
price—more than $50 billion for medical costs in a<br />
single year.<br />
Nurse professional liability claims involving falls are<br />
identified in the Nurse Professional Liability Exposure<br />
Claim Report: 4th Edition. The report notes that many<br />
of the closed claims analyzed in the report dataset<br />
which involved falls occurred because the nurse failed<br />
to follow fall-prevention policies and procedures.<br />
Further, the report states that falls most frequently<br />
occurred in inpatient hospital, surgical services, and<br />
aging services settings, as well as in patients’ homes.<br />
Given the statistics and the many places falls can<br />
occur, a fall is not an uncommon occurrence in a<br />
nurse’s career. A fall does not automatically mean the<br />
nurse is liable; for that to happen, key elements of<br />
malpractice need to be present.<br />
Elements of malpractice<br />
To be successful in a malpractice lawsuit, plaintiffs<br />
must prove four elements:<br />
1 Duty. A duty existed between the patient and<br />
the nurse: The nurse had a responsibility to care<br />
for the patient.<br />
2 Breach. The duty to care was breached; in other<br />
words, the nurse may have been negligent. To<br />
determine if negligence occurred, the expert<br />
witness would consider whether the nurse met<br />
the standard of care, which refers to what a<br />
reasonable clinician with similar training and<br />
experience would do in a particular situation.<br />
3 Injury. The patient suffered an injury. Even if<br />
a duty existed and it was breached, if no injury<br />
occurred, it’s unlikely the lawsuit would be<br />
successful. Keep in mind, however, that injury can<br />
be defined as not only physical injury, but also<br />
psychological injury or economic loss.<br />
4 Causation. The breach of duty caused the<br />
injury—the injury must be linked to what the<br />
nurse did or failed to do. This can be summed up<br />
in one question: Did the act or omission cause the<br />
negative outcome?<br />
Expert witnesses will consider these four elements as<br />
they review the case, and they’ll ask multiple questions<br />
(see Was there liability?). The questions primarily<br />
address prevention and what was done after the fall<br />
occurred.<br />
Prevention<br />
The following steps can help prevent falls and,<br />
if documented correctly, prove that the nurse took<br />
reasonable steps to protect the patient from injury:<br />
Take a team approach. Registered nurses, licensed<br />
practical/vocational nurses, and certified nursing<br />
assistants are ideal members for a team dedicated to<br />
creating a falls reduction plan for each patient.<br />
Assess the risk. Whether in the hospital,<br />
rehabilitation facility, clinic, or home, a comprehensive<br />
assessment is essential to identify—and then<br />
mitigate—falls hazards. This starts with assessing the<br />
patient for risk factors such as history of a previous fall;<br />
gait instability and lower-limb weakness; incontinence/<br />
urinary frequency; agitation, confusion, or impaired<br />
judgment; medications; and comorbid conditions such<br />
as postural hypotension and visual impairment. It’s also<br />
important to consider the environment, particularly<br />
in the home setting. For example, throw rugs are a<br />
known falls hazard.<br />
An excellent resource for assessing communitydwelling<br />
adults age 65 and older is the CDC’s STEADI<br />
(Stopping Elderly Accidents, Deaths & Injuries) initiative,<br />
which is an approach to implementing the American<br />
and British Geriatrics Societies’ clinical practice<br />
guideline for fall prevention. The initiative provides<br />
multiple resources for clinicians, such as a fall risk<br />
factors checklist with the categories of falls history;<br />
medical conditions; medications; gait, strength, and<br />
balance (including quick tests for assessing); vision; and<br />
postural hypotension. Keep in mind that assessment<br />
should be ongoing during the patient’s care because<br />
conditions may change.<br />
Develop a plan. Once the assessment is complete,<br />
the patient care team, including the patient and their<br />
family, can develop a falls-reduction plan based on the<br />
patient’s individual risk factors. The plan should address<br />
locations that are at greatest risk, such as bedside,<br />
bathrooms, and hallways, and detail action steps.<br />
Sample action steps include giving patients nonslip<br />
footwear, making sure call lights are within reach,<br />
removing throw rugs from the home, and providing<br />
exercises to improve balance.<br />
Communicate. It’s not enough to create a plan;<br />
communication is essential for optimal execution.<br />
All care team members, including patients and their<br />
families, need to be aware of the patient’s fall risk and<br />
the falls reduction plan.<br />
Communication also includes education. The STEADI<br />
initiative has falls prevention brochures for patients<br />
and family caregivers at www.cdc.gov/steadi/patient.<br />
html. Families often are underutilized as a resource for<br />
helping to prevent falls. They may know the best way<br />
to approach patients who are reluctant to follow fallsreduction<br />
recommendations and can take the lead to<br />
reduce home-related risks. The falls risk reduction plan,<br />
communication with others, and education provided<br />
should all be documented in the patient’s health<br />
record.<br />
Was there liability?<br />
If a patient falls, an expert witness will likely want<br />
to know the answers to the following questions
<strong>January</strong>, February, March <strong>2022</strong> <strong>Georgia</strong> <strong>Nursing</strong> • Page 13<br />
(developed by Patricia Iyers) when deciding if liability<br />
may exist:<br />
Before the fall:<br />
• Was the patient identified as being at risk for<br />
falls? How was that risk communicated to others?<br />
- What medications did the patient receive? Do<br />
they have side effects that may increase the<br />
risk of a fall?<br />
- Were there specific conditions present that<br />
could increase the risk of a fall?<br />
• Were measures implemented to prevent falls?<br />
- Was the patient capable of using the call light<br />
and was it used to call for assistance?<br />
- Was the bed in the lowest position?<br />
- Were the lights on in the room or under the<br />
bed to help light the area at night?<br />
- Was the patient given antiskid slippers?<br />
Immediately after the fall:<br />
• How soon was the individual found after he<br />
had sustained a fall (it’s not always possible to<br />
establish an exact time)?<br />
• What was done at the time of the fall?<br />
• Was the patient appropriately monitored after the<br />
fall to detect injuries?<br />
• What did the assessment (including vital signs)<br />
reveal?<br />
• Did the nurse communicate the findings to the<br />
patient’s provider?<br />
• Were X-rays ordered and performed?<br />
• Was there an injury? If so, how soon was it<br />
treated?<br />
• If the patient hit their head, was the chart<br />
reviewed to determine if mediations included<br />
an anticoagulant? If on anticoagulant, was this<br />
information communicated to the provider so<br />
head scans could be performed to check for<br />
cranial bleeding?<br />
Following up after a fall:<br />
• Was there a change in mental status after the<br />
fall?<br />
• Were additional assessments and monitoring<br />
done as follow up?<br />
• Was the patient’s risk for falls reassessed after the<br />
fall and the plan of care revised to minimize the<br />
risk of future falls?<br />
If a fall occurs<br />
Despite nurses’ best efforts, a patient may fall. An<br />
expert witness will scrutinize how the nurse responded<br />
to the event. The following steps will help to reduce<br />
the risk of a lawsuit or the chances that a lawsuit is<br />
successful:<br />
Assess the patient. Examine the patient for any<br />
obvious physical or mental injuries. For example,<br />
check vital signs; look for bleeding, scrapes, or signs of<br />
broken bones; ask the patient about pain; and check<br />
mental status. Do not move the patient if a spinal injury<br />
is suspected until a full evaluation can be made. Be<br />
particularly alert for possible bleeding if the patient is<br />
taking anticoagulants. When appropriate, ask patients<br />
why they think they fell and continue monitoring at<br />
regular intervals.<br />
Communicate assessment results. Notify<br />
the patient’s provider of the fall and results of the<br />
assessment. The provider may order X-rays for further<br />
evaluation. Remember to mention if the patient is<br />
taking anticoagulants, particularly in the case of a<br />
potential head injury, so the appropriate scans can be<br />
ordered.<br />
Revise the plan. As soon as possible after the fall,<br />
work with the team to reassess risk factors, revisit the<br />
falls reduction plan, and revise the plan as needed.<br />
For example, footwear may need to be changed, the<br />
amount of sedatives the patient is receiving may need<br />
to be reduced, or more lighting may need to be added<br />
to a hallway. It’s important that actions are taken to<br />
prevent future falls.<br />
Document. Each step should be documented in the<br />
patient’s health record, especially all assessment results<br />
and provider notifications. The expert witness can<br />
then see that the nurse followed a logical progression,<br />
with thorough evaluation and follow-up. Never alter<br />
a patient’s health record entry for any reason, or add<br />
anything to a record that could be seen as self-serving,<br />
after a fall or other patient incident. If the entry is<br />
necessary for the patient’s care, be sure to accurately<br />
label the late entry according to your employer’s<br />
policies and procedures.<br />
Reducing risk<br />
Unfortunately, patient falls are not completely<br />
avoidable. However, developing a well-conceived<br />
prevention plan can help reduce the risk, and taking<br />
appropriate actions after a fall can help mitigate further<br />
injury. Both prevention and post-fall follow up not only<br />
benefits patients, but also reduces the risk that the<br />
nurse will be on the losing side of a lawsuit.<br />
Article by: <strong>Georgia</strong> Reiner, MS, CPHRM, Senior Risk<br />
Specialist, Nurses Service Organization (NSO)<br />
RESOURCES<br />
Bono MJ, Wermuth HR, Hipskind JE. Medical malpractice. StatPearls.<br />
2020. www.ncbi.nlm.nih.gov/books/NBK470573.<br />
Centers for Disease Control and Prevention. Important facts about<br />
falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.<br />
html.<br />
Centers for Disease Control and Prevention. STEADI: Materials for<br />
healthcare providers. 2020. www.cdc.gov/steadi/materials.html.<br />
CNA, NSO. Nurse Professional Liability Exposure Claim Report: 4th<br />
Edition. 2020. www.nso.com/nurseclaimreport.<br />
Dykes PC, Adelman J, Adkison L, et al. Preventing falls in<br />
hospitalized patients. Am Nurs Today. 2018;13(9):8-13. https://<br />
www.myamericannurse.com/preventing-falls-hospitalizedpatients.<br />
Iyer P. Legal aspects of documentation. In: KG Ferrell, ed. Nurse’s<br />
Legal Handbook. 6th ed. Wolters Kluwer; 2015.<br />
Van Voast Moncada L, Mire GL. Preventing falls in older persons.<br />
Am Fam Physician. 2017;96(4):240-247. https://www.aafp.org/<br />
afp/2017/0815/p240.html.<br />
Disclaimer: The information offered within this article reflects<br />
general principles only and does not constitute legal advice by<br />
Nurses Service Organization (NSO) or establish appropriate or<br />
acceptable standards of professional conduct. Readers should<br />
consult with an attorney if they have specific concerns. Neither<br />
Affinity Insurance Services, Inc. nor NSO assumes any liability for<br />
how this information is applied in practice or for the accuracy of this<br />
information.<br />
This risk management information was provided by Nurses<br />
Service Organization (NSO), the nation's largest provider of nurses’<br />
professional liability insurance coverage for over 550,000 nurses<br />
since 1976. The individual professional liability insurance policy<br />
administered through NSO is underwritten by American Casualty<br />
Company of Reading, Pennsylvania, a CNA company. Reproduction<br />
without permission of the publisher is prohibited. For questions,<br />
send an e-mail to service@nso.com or call 1-800-247-1500. www.<br />
nso.com.
Page 14 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
Virtual Simulation: Impact on Clinical Judgment<br />
Amber Kool, MSN, RN<br />
Reprinted with permission<br />
Arizona Nurse April 2021 issue<br />
The need for newly licensed nurses to safely<br />
manage multiple complex patients requires strong<br />
clinical judgment skills to appropriately prioritize and<br />
delegate (Bittner & Gravlin, 2009). Direct patient care<br />
experiences in acute care settings are the typical way<br />
nursing students learn clinical judgment. However,<br />
these clinical experiences do not always provide an<br />
opportunity to collaborate, critical think, or make<br />
independent decisions that will improve patient<br />
outcomes (Lippincott <strong>Nursing</strong> Education, 2018). The<br />
most recent data from the American Association of<br />
Colleges of <strong>Nursing</strong> suggests that 80,407 qualified<br />
applicants were not admitted to baccalaureate and<br />
graduate nursing programs with insufficient clinical<br />
sites a contributing factor (2020). The COVID-19<br />
pandemic has significantly limited direct patient care<br />
clinical experiences for nursing students throughout<br />
the U.S. (Logue et al., 2021). There is an urgent need<br />
to develop teaching-learning practices that will<br />
support the development of clinical judgment as both<br />
NOW HIRING<br />
NURSING<br />
OPPORTUNITIES IN<br />
TALLAHASSEE, FL<br />
an augment and substitution for direct care clinicals<br />
(Thobaity & Alshammari, 2020).<br />
This study investigated the impact of a virtual<br />
simulation (VS) (Sentinel U’s Patient Management<br />
and Delegation and Prioritization of Care) on clinical<br />
judgment in a sample of pre-licensure BSN students.<br />
VS utilizes experiential learning as identified by Kolb’s<br />
Experiential Learning Theory (1984) to expose the<br />
learner to a new experience and requires the student<br />
to reflect, thereby integrating the learning into their<br />
knowledge bank (McLeod, 2017). As learners reflect<br />
on their decisions and reasoning, they integrate their<br />
previous experiences and the new knowledge gained<br />
through the VS.<br />
Design<br />
Using a one-group, repeated measures design,<br />
a paired-samples t-test was used to measure the<br />
change in perceived clinical judgment pre to post-<br />
VS intervention. The Skalsky Clinical Judgment Scale<br />
measures the construct using a four-point Likert<br />
Scale, with ten questions, which include assessing<br />
perceived abilities in prioritization, delegation, and<br />
communication.<br />
Psychiatric RNs & LPNs Full-Time<br />
Psychiatric APRN<br />
Medical Assisted Treatment (MAT) certified<br />
Inpatient & Residential Programs<br />
APRNs may qualify for the NHSC loan repayment. APRNs<br />
& RNs may qualify for the Nurse Corp loan repayment.<br />
Visit www.apalacheecenter.org or call Stephanie<br />
at 850-523-3212 for additional information.<br />
Apalachee Center, Inc participates in E-Verify. Federal law requires Apalachee Center, Inc to verify the identity and employment eligibility of all persons<br />
hired to work in the United States. Apalachee Center, Inc. is an at-will employer. An equal opportunity/affirmative action employer. Drug-free workplace.<br />
Looking for a<br />
rewarding new career?<br />
Make a difference in the lives<br />
of others. Come work by the<br />
sea and by our side!<br />
Sign-on bonus and relocation<br />
assistance for full-time RNs.<br />
Apply online at<br />
www.ssbythesea.com<br />
Equal Opportunity Employer M/F/D/V<br />
Major Findings<br />
There was a statistically significant increase<br />
in perceived clinical judgment scores from preintervention<br />
(VS) (M = 32.17, SD = 4.178) to postintervention<br />
(VS) (M = 34.10, SD = 4.992), t (41) =<br />
2.832, p < .007 (two-tailed). The mean increased in<br />
perceived clinical judgment scores was 1.929 with a<br />
95%.<br />
Discussion<br />
The positive results suggest that VS may be useful<br />
to support teaching-learning practices related to<br />
clinical judgment development. Perceived increases in<br />
clinical judgment may make students more confident<br />
and encourage them to practice skills further. Further<br />
research is needed to objectively measure clinical<br />
reasoning and resultant patient outcomes that result<br />
from the use of VS as a teaching-learning strategy.<br />
Implications for <strong>Nursing</strong> the <strong>Nursing</strong> Profession<br />
Recent evidence suggests that only 10% of newly<br />
licensed nurses score within an acceptable competency<br />
range using a performance-based (Kavanagh &<br />
Sharpnack, 2021). The most recent practice analyses<br />
by the National Council of States Boards of <strong>Nursing</strong><br />
suggest that newly licensed RNs are increasingly<br />
required to make more complex clinical decisions (2015,<br />
2018). COVID-19 exacerbated existing pre-licensure<br />
nursing education challenges by further limiting already<br />
scarce clinical practicum sites (Dewart et al., 2020). VS<br />
may be a useful addition to direct patient care and<br />
high fidelity human patient simulation to learn clinical<br />
reasoning skills. VS may be helpful as an additional<br />
strategy in addressing the critical nationwide shortage<br />
of clinical practicum sites. Also, VS may bridge the gap<br />
in clinical learning experiences during times when other<br />
opportunities may not exist, such as experienced during<br />
the COVID-19 pandemic and in times of emergencies<br />
and natural disasters.<br />
VS may likewise prove beneficial for skill<br />
development or assessment within clinical agency<br />
orientation and continuing competency efforts. Similar<br />
to its use in the academic environment, VS within<br />
practice and continuing education provides a safe<br />
environment to make decisions without potential harm<br />
to patients (Verkuyl et al., 2019). In conclusion, given<br />
the evolving technology that underpins VS and its<br />
increasing fidelity, the interest in and application of<br />
VS in academic and practice environments will likely<br />
increase. Nurse leaders will be challenged to implement<br />
VS in evidence-based ways and monitor and measure<br />
outcomes to assure its value.<br />
References<br />
American Association of Colleges of <strong>Nursing</strong>. (2019). <strong>Nursing</strong><br />
shortage. Retrieved from https://www.aacnnursing.org/newsinformation/fact-sheets/nursing-shortage<br />
Bittner, N. P., & Gravlin, G. (2009). Critical thinking, delegation,<br />
and missed care in nursing practice. JONA: The Journal<br />
of <strong>Nursing</strong> Administration, 39(3), 142-146. doi:10.1097/<br />
nna.0b013e31819894b7<br />
Dewart, G., Corcoran, L., Thirsk, L., & Petrovic, K. (2020). <strong>Nursing</strong><br />
education in a pandemic: Academic challenges in response to<br />
COVID-19. Nurse education today, 92, 104471. https://doi.<br />
org/10.1016/j.nedt.2020.104471<br />
Kavanagh, J.M., Sharpnack, P.A., (<strong>January</strong> 31, 2021) “Crisis in<br />
Competency: A Defining Moment in <strong>Nursing</strong> Education”<br />
OJIN: The Online Journal of Issues in <strong>Nursing</strong> Vol. 26, No. 1,<br />
Manuscript 2. DOI: 10.3912/OJIN.Vol26No01Man02<br />
Lippincott <strong>Nursing</strong> Education. (2018, June 7). Turning new<br />
nurses into critical thinkers. Combining Domain Expertise<br />
With Advanced Technology | Wolters Kluwer. https://www.<br />
wolterskluwer.com/en/expert-insights/turning-new-nurses-into<br />
critical-thinkers<br />
Logue, M., Olson, C., Mercado, M., McCormies, C.J., (<strong>January</strong><br />
31, 2021) “Innovative Solutions for Clinical Education during<br />
a Global Health Crisis” OJIN: The Online Journal of Issues<br />
in <strong>Nursing</strong> Vol. 26, No. 1, Manuscript 6. DOI: 10.3912/OJIN.<br />
Vol26No01Man06<br />
National Council of States Boards of <strong>Nursing</strong>. (2015). 2014 RN<br />
Practice Analysis: Linking the NCLEX-RN Examination to Practice<br />
- U.S. and Canada. 62. https://www.ncsbn.org/15_RN_Practice_<br />
Analysis_Vol62_web.pdf<br />
National Council of States Boards of <strong>Nursing</strong>. (2018). 2017 RN<br />
Practice Analysis: Linking the NCLEX-RN Examination to Practice<br />
- US & Canada 72. https://www.ncsbn.org/17_RN_US_Canada_<br />
Practice_Analysis.pdf<br />
McLeod, S. (2017, February 5). Kolb’s learning styles and experiential<br />
learning cycle. Retrieved from https://www.simplypsychology.<br />
org/learning-kolb.html<br />
Sentinel U. (2020, November 30). <strong>Nursing</strong> prioritization exercises.<br />
https://www.sentinelu.com/solutions/prioritization-anddelegation/<br />
Skalsky, K. (n.d.). Skalsky Clinical Judgment Scale validity. American<br />
Sentinel University<br />
Thobaity, A., & Alshammari, F. (2020). Nurses on the Frontline<br />
against the COVID-19 Pandemic: An Integrative Review. Dubai<br />
Medical, 1-6. https://doi.org/10.1159/000509361<br />
Verkuyl, M., Hughes, M., Tsui, J., Betts, L., St-Amant, O., & Lapum,<br />
J. L. (2017). Virtual gaming simulation in nursing education: A<br />
focus group study. Journal of <strong>Nursing</strong> Education, 56(5), 274-<br />
280. doi:10.3928/01484834-20170421-04
<strong>January</strong>, February, March <strong>2022</strong> <strong>Georgia</strong> <strong>Nursing</strong> • Page 15<br />
An Ethic of Justice Viewed through the Lens of an Ethic of Care: How<br />
Nurse Leaders May Combat Workplace Bullying<br />
Gloria Matthews, DNP, RN, CNL, CDE<br />
University of Oklahoma Medical Center<br />
Valerie Eschiti, PhD, RN, AHN-BC, CHTP, CTN-A<br />
University of Oklahoma Health Sciences Center<br />
Fran & Earl Ziegler College of <strong>Nursing</strong>,<br />
Lawton Campus<br />
Reprinted with permission from<br />
Oklahoma Nurse May 2021 issue<br />
The purpose of this paper is to present integration of<br />
two ethical approaches to combat workplace bullying<br />
within a clinical setting from an advance nursing<br />
practice leadership perspective. A description of ethic<br />
of care and ethic of justice is presented and critically<br />
appraised as it relates to managing workplace bullying.<br />
The importance of the application of the ethic of justice<br />
through the lens of the ethic of care will be elucidated.<br />
Description and Application to Workplace<br />
Bullying<br />
A failure of nursing leadership to address workplace<br />
bullying demonstrates a lack of compassion and<br />
organizational injustice. Bullying is the repeated and<br />
persistent, abusive mistreatment by one or more<br />
perpetrators towards one or more victims that is<br />
marked by threatening, humiliating or intimidating<br />
conduct, work interference, or verbal abuse (Fink-<br />
Samnick, 2018). Bullying is a systemic problem<br />
and reflects behavior patterns and surreptitious<br />
characteristics of a culture of violence that contributes<br />
to various expressions and manifestations of violence<br />
within an organization (Smit & Scherman, 2016). The<br />
Joint Commission (2008) notes that intimidating and<br />
disruptive behaviors contribute to medical errors, poor<br />
patient and staff satisfaction, staff turnover and poor<br />
collaborative work environments.<br />
Ethic of Care<br />
The ethic of care is a moral approach characterized<br />
by contextual, holistic empathy and is based on<br />
caring, strengthening and maintaining interpersonal<br />
relationships. It emphasizes the importance of insight<br />
gained from being open and receptive to the realities<br />
and needs of others (Simola, 2003). The ethic of care<br />
aligns with the authentic, servant and transformational<br />
leaders who put followers’ interests above their own<br />
and influence followers through building relationships,<br />
developing a collective vision, and attending to<br />
the needs and growth of their followers (Groves &<br />
LaRocca, 2011).<br />
Most occurrences of bullying are learned behaviors<br />
directed by reactions to stress and organizational<br />
norms and, therefore, can be unlearned (Berry et al,<br />
2016). Leaders guided by an ethic of care model take<br />
decisive action when confronted with behaviors that<br />
do not adhere to expected conduct. In combating<br />
workplace bullying, effective leaders are proficient<br />
in communication and competent in coaching,<br />
staff development, maintaining high standards of<br />
conduct, and fostering an environment of trust and<br />
mutual respect (Parker, Harrington, Smith, Sellers, and<br />
Millenbach, 2016).<br />
Bullying is an attempt to intimidate and gain<br />
power over someone else. Structural empowerment<br />
is an effective technique to mitigate the effects and<br />
incidents of bullying (Lachman, 2014). Effective nurse<br />
empowerment can be obtained through shared<br />
governance to minimize power imbalances and<br />
enhance shared responsibility and transparency in<br />
decision making (Berry et al, 2016; Parker et al, 2016).<br />
Skill development is an important weapon in the<br />
battle against bullying. Strategies such as cognitive<br />
rehearsal, skills-based training, and role-playing<br />
have been successful in raising staff awareness and<br />
combating bullying (Balevre, Balevre, & Chesire, 2018;<br />
Parker et al., 2016).<br />
Normative leadership models such as<br />
transformational, servant and authentic leadership<br />
constructively address the bullying by modeling an<br />
ethic of care perspective and seeking to facilitate<br />
followers’ self-actualization. The assumption is that<br />
ethical leadership styles promote social cohesion,<br />
professionalism, and empowerment (Webster, 2016).<br />
Ethic of Justice<br />
The ethic of justice is a moral approach that is<br />
characterized by justice, fairness, reciprocity and the<br />
protection of individual rights. Individuals demonstrate<br />
impartiality and the ability to reason abstractly through<br />
the application of formal, logical and impartial rules<br />
(Simola, 2003). The ethic of justice aligns with the<br />
transactional leader who influences followers by<br />
control, reward and corrective transactions (Groves &<br />
LaRocca, 2011).<br />
Structural empowerment is gained through<br />
establishment of an ethical infrastructure that<br />
reinforces ethical principles and behavioral expectations<br />
of members of the organization (Einarsen, Mykletun,<br />
Einarsen, Skogstad, & Salin, 2017). Aligned with the<br />
ethic of justice, organizations establish standardized<br />
policies, procedures and documents such as codes of<br />
ethics, procedures for handling complaints and zero<br />
tolerance policies (Einarsen et al., 2017).<br />
Hutchinson (2009) posits that rather than focusing<br />
on the individual, leaders should direct corrective<br />
measures towards the act of bullying itself and gain<br />
insight into work group and organizational factors that<br />
enable the behavior. The focus is on reintegration and<br />
restoration of social relationships within the context of<br />
a supportive group, such as a restorative circle, where<br />
the attention is placed on repairing harm rather than<br />
blame and punishment.<br />
Reflection on Integration of Ethical Approaches<br />
It is important for leaders to integrate the two<br />
ethical perspectives by distributing justice within a<br />
caring framework (Sorbello, 2008). Organizations and<br />
leaders must clarify and communicate that bullying is<br />
unacceptable. If corrective actions fail, termination is an<br />
acceptable consequence to continued behavior (Lee et<br />
al., 2014). At times, leaders must implement corrective<br />
actions and uphold values and policies set forth by the<br />
organization, but it is in the delivery and intent that<br />
determines a caring leader.<br />
Conclusion<br />
Combating bullying requires a multidimensional<br />
approach. By establishing a relationship-based ethics<br />
of care perspective, along with visible organizationalbased<br />
regulatory sanctions in communication and<br />
ethic of justice, organizations can create and sustain a<br />
respectful working environment for the prevention of<br />
workplace bullying. The integration of the divergent<br />
ethical perspectives of an ethic of care and an ethic<br />
of justice provides an environment of collegiality,<br />
transparency and support for improved patient-related<br />
and nurse-related outcomes.<br />
References<br />
Balevre, S. M., Balevre, P. S., & Chesire, D. J. (2018). <strong>Nursing</strong><br />
professional development anti-bullying project. Journal for<br />
Nurses in Professional Development, 34(5), 277-282. https://doi.<br />
org/10.1097/NND.0000000000000470<br />
Berry, P. A., Gillespie, G. L., Fisher, B. S., & Gormley, D. K. (2016).<br />
Recognizing, confronting, and eliminating workplace bullying.<br />
Workplace Health & Safety, 64(7), 337-341. https://doi.<br />
org/10.18291/njwls.v7i1.81398<br />
Einarsen, K., Mykletun, R. J., Einarsen, S. V., Skogstad, A., & Salin,<br />
D. (2017). Ethical infrastructure and successful handling of<br />
workplace bullying. Nordic Journal of Working Life Studies, 7(1),<br />
37–54. https://doi.org/10.18291/njwls.v7i1.81398<br />
Fink-Samnick, E. (2018). The new age of bullying and violence<br />
in health care: part 4: managing organizational cultures and<br />
beyond. Professional Case Management, 23(6), 294–306.<br />
https://doi.org/10.1097/NCM.0000000000000324<br />
Groves, K., & LaRocca, M. (2011). An empirical study of leader<br />
ethical values, transformational and transactional leadership, and<br />
follower attitudes toward corporate social responsibility. Journal<br />
of Business Ethics, 103(4), 511–528. https://doi.org/10.1007/<br />
s10551-011-0877-y<br />
Hutchinson, M. (2009). Restorative approaches to workplace<br />
bullying: Educating nurses towards shared responsibility.<br />
Contemporary Nurse, 32(1–2), 147–155. https://doi.org/10.5172/<br />
conu.32.1-2.147<br />
Lachman, V. D. (2014). Ethical issues in the disruptive behaviors<br />
of incivility, bullying, and horizontal/lateral violence. Medsurg<br />
<strong>Nursing</strong>, 23(1), 56-60.<br />
Parker, K. M., Harrington, A., Smith, C. M., Sellers, K. F., &<br />
Millenbach, L. (2016). Creating a nurse-led culture to minimize<br />
horizontal violence in the acute care setting: A multiinterventional<br />
approach. Journal for Nurses in Professional<br />
Development, 32(2), 56-63. https://doi.org/10.1097/<br />
NND.0000000000000224<br />
Simola, S. (2003). Ethics of justice and care in corporate crisis<br />
management. Journal of Business Ethics, 46(4), 351-361. https://<br />
doi.org/10.1023/A:1025607928196<br />
Smit, B., & Scherman, V. (2016). A case for relational leadership<br />
and an ethics of care for counteracting bullying at schools.<br />
South African Journal of Education, 36(4), 1-9. http://www.<br />
sajournalofeducation.co.za/index.php/saje/article/view/1312/668<br />
Sorbello, B. (2008). The nurse administrator as caring person: A<br />
synoptic analysis applying caring philosophy, Ray’s ethical theory<br />
of existential authenticity, the ethic of justice, and the ethic of<br />
care. International Journal of Human Caring, 12(1), 44-49.<br />
10.20467/1091-5710.12.1.44<br />
The Joint Commission. (2008). Behaviors that undermine a<br />
culture of safety. (Sentinel Event Alert, Issue 40). http://www.<br />
jointcommission.org/assets/1 /18/SEA_40.pdf<br />
Webster, M. (2016). Challenging workplace bullying: the role of<br />
social work leadership integrity. Ethics & Social Welfare, 10(4),<br />
316–332. https://doi.org/10.1080/17496535.2016.1155633
Page 16 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
Providing Competent, Supportive Care for People Who are Transgender<br />
F. Patrick Robinson, PhD, RN, ACRN, CNE, FAAN<br />
Sherry L Roper, PhD, RN<br />
Reprinted with permission from Illinois The <strong>Nursing</strong><br />
Voice, June 2021 issue<br />
The idea that gender is binary (male or female) and<br />
determined at birth predominates Western cultures.<br />
However, research evidence and lived experiences<br />
suggest that gender exists on a spectrum with many<br />
options. Some people identify as a gender different<br />
from their gender determined at birth (Deutsch, 2016).<br />
Our traditional understanding of gender, based on<br />
chromosomes and primary (genitalia) and secondary sex<br />
characteristics, is often called biological sex or gender<br />
(or sex) assigned at birth. Gender identity, on the other<br />
hand, is the innermost concept of self as male, female, a<br />
blend of both, or neither (Lambda Legal, 2016.).<br />
The majority of people are cisgender, which<br />
occurs when gender assigned at birth and gender<br />
identity are the same. However, the best available<br />
data suggest that approximately 1.4 million adults do<br />
not self-identify with their gender assignments (e.g.,<br />
someone assigned female at birth but identifies as<br />
male) (Flores et al., 2016). Transgender is an umbrella<br />
term for this population. A visibly growing segment of<br />
the U.S. population does not identify with the binary<br />
notion of gender. Nonbinary is a collective term for<br />
this population, but individuals may use terms such as<br />
genderqueer, gender fluid, or gender non-conforming.<br />
There is no standard or correct way to be (or<br />
be seen as) transgender. Some people who are<br />
transgender choose gender-affirming hormone therapy<br />
to achieve masculinizing or feminizing effects; others<br />
do not. Surgery that revises genitals to conform to<br />
gender identity is a critical part of the transition for<br />
many people who are transgender (Deutsch et al.,<br />
2019). Others do not feel that genital surgery is a<br />
necessary part of transition but may opt for non-genital<br />
surgeries to produce desired characteristics, including<br />
breast augmentation or removal and body contouring<br />
procedures. In other words, the importance of therapy<br />
related to the quality of life varies by individual. Also,<br />
some people who are transgender may want these<br />
services but do not have access to them because they<br />
are (a) unavailable in the community; (b) not covered<br />
by insurance (even if the individual has insurance, and<br />
many do not), and (c) too expensive.<br />
Remember: there is no one way to "be" transgender<br />
or cisgender. People choose to express their gender<br />
identities in personally satisfying ways, which may<br />
or may not match social expectations of what it<br />
means to look and behave as a male or female. Some<br />
transgender women choose not to wear makeup or<br />
dresses, and some cisgender men choose to wear their<br />
hair long and earrings.<br />
Health Disparities in People Who are Transgender<br />
Negative attitudes and discrimination toward the<br />
transgender community create inequalities that prevent<br />
the delivery of competent healthcare and elevate the<br />
risk for various health problems (Grant et al., 2011). In<br />
comparison to their cisgender counterparts, people<br />
who are transgender experience higher incidences<br />
of cancer, mental health challenges, and other health<br />
problems (Department of Health & Human Services,<br />
n.d.). For instance, transgender women, compared<br />
to all other populations, are at the highest risk of<br />
injury from violence and death by homicide. People<br />
who are transgender are also more likely to smoke,<br />
drink alcohol, use drugs, and engage in risk behaviors<br />
(Institute of Medicine, 2011).<br />
Furthermore, discrimination and social stigma<br />
increase poverty and homelessness in people who<br />
are transgender (Safer et al., 2017). The inability to<br />
afford basic living needs may lead to employment in<br />
underground economies, such as survival sex work or<br />
the illegal drug trade, which place the person who is<br />
transgender at an even higher risk for violence, drug use,<br />
and sexually transmitted infections (Deutsch, 2016).<br />
People who are transgender are more likely to rely<br />
on public health insurance or be uninsured than the<br />
general population. Even those insured report coverage<br />
gaps caused by low-cost coverage that does not<br />
include standard services for preventative, behavioral<br />
health, or gender-affirming therapies, including<br />
hormones (Deutsch et al., 2019). Lack of access to<br />
comprehensive health care leads some people who are<br />
transgender to seek hormones from the community<br />
and social networks without clinical support and<br />
monitoring, putting them at additional risk for adverse<br />
reactions and complications.<br />
Researchers suggest that healthcare providers'<br />
inability to deliver supportive and competent care serves<br />
as a powerful mechanism underlying health disparities<br />
(Fenway Institute, 2016). The experiences of people who<br />
are transgender are often not included in healthcare<br />
provider diversity and inclusiveness training. While<br />
transgender-related content in health professions basic<br />
education programs would effectively improve provider<br />
knowledge, skills, and attitudes, transgender health has<br />
not been prioritized in nursing education. The result is<br />
a nursing workforce inadequately prepared to care for<br />
people who are transgender (McDowell & Bower, 2016).<br />
<strong>Nursing</strong> Care of People Who Are Transgender<br />
Competent, supportive transgender care requires<br />
nurses to recognize potential biases and understand<br />
gender that may differ from their current beliefs and<br />
social norms. Honest reflection on these feelings is an<br />
essential step in providing competent transgender care.<br />
Using a lens of cultural humility, where cisgender nurses<br />
acknowledge that they do not adequately know about<br />
being transgender while also being open to learning,<br />
is helpful. In this spirit, open, transparent inquiry on<br />
the part of nurses when they do not know something<br />
(When I speak to your children, what name should I use<br />
to refer to you?) or how to proceed with care (I need to<br />
place a catheter into your bladder, and I know you have<br />
had gender-affirming surgery. Do you want to give me<br />
any special instructions?) can build trust.<br />
While gender-affirming care such as hormones,<br />
androgen-blocking agents, and surgeries require<br />
specialist care management, nurses will encounter<br />
transgender patients in all healthcare areas. Assessing<br />
the history and current status of gender-affirming<br />
therapies is critical to inform safe care. For example,<br />
hormone-induced changes in muscle and bone mass,<br />
along with menstruation or amenorrhea, can alter<br />
gender-defined reference ranges for laboratory tests<br />
such as hemoglobin/hematocrit, alkaline phosphatase,<br />
and creatinine (Deutsch, 2016). Nurses should consider<br />
the gender assigned at birth (especially if it is the<br />
only gender information to which the lab has access)<br />
and gender-affirming therapy-induced physiological<br />
changes to make valid inferences about lab values.<br />
Nurses should also ensure that a complete history of<br />
the use of hormones and androgen blockers (including<br />
those obtained from non-licensed providers) is taken.<br />
Nurses should work with other providers to ensure that<br />
hormone therapy does not stop with hospitalization<br />
unless contraindicated by current pathology or<br />
prescribed medications. Abrupt cessation of hormone<br />
therapy can have a significant and negative impact on<br />
emotional and physiological health.<br />
Systems-Level Policies, Processes, and Advocacy<br />
Professional nurses can play a crucial role by advocating<br />
for policies and processes that promote safe, effective,<br />
and supportive care for people who are transgender.<br />
Misgendering a patient (making an incorrect assumption<br />
about gender identity) can cause emotional distress and<br />
erode patient-provider trust. Unfortunately, electronic<br />
health records (EHR) often do not support competent care<br />
for people who are transgender. For instance, healthcare<br />
providers should use a 2-step gender identification<br />
process (Deutsch, 2016). However, many do not, and EHR<br />
systems rarely provide prompts for the processor space for<br />
easy documentation and access to information derived<br />
from the process. Asking about a patient's current gender<br />
identity can result in several responses. The EHR should<br />
make checkboxes for a reasonable number of those<br />
responses, including male, female, transgender male,<br />
transgender female, and nonbinary. A fill-in-the-blank is<br />
needed for other identifies. The gender assigned at birth<br />
also requires options beyond male or female; people<br />
born with external genitalia, gonads, or both that do not<br />
conform to what is typically male or female (intersex) may<br />
have been identified incorrectly at birth. The EHR should<br />
provide an intersex option to this question. Some people<br />
who are transgender are uncomfortable revealing gender<br />
assigned at birth, so decline-to-state should be another<br />
option. Note that this process should be the standard for<br />
all patients, not just those assumed to be transgender.<br />
People who are transgender may use names<br />
other than their legal names (Lambda Legal, 2016).<br />
Navigating a legal name change is complicated and<br />
costly. Some people who are transgender do not<br />
have the resources for a legal name change; for<br />
others, it may not be safe, given current social or<br />
legal circumstances. Using a patient's chosen name<br />
and pronouns is critical to patient-centered care.<br />
The EHR should prominently document the patient's<br />
chosen name and pronouns, which should also be<br />
used outside the EHR, including for appointments and<br />
prescriptions. Patients should only have to provide<br />
the information once, decreasing the need to correct<br />
providers and improving patient-provider relationships.<br />
EHRs should also contain an organ inventory, perhaps<br />
as part of surgical history, as providers will need to<br />
know about the presence or absence of reproductive<br />
and gonadal organs to inform clinical decision-making.<br />
This information must be clear, unambiguous, and<br />
easily accessible in the EHR to inform care and prevent<br />
medical and surgical errors.<br />
Nurses should work within governance processes to<br />
ensure that all institutional policies support transgender<br />
patients, staff, and visitors. Nondiscrimination<br />
statements should include gender identity. Policies<br />
about restrooms and staff changing rooms (usually<br />
labeled in gender-binary terms) should state that a<br />
person's gender identity rightly determines the room<br />
to be used and that that right should not require any<br />
proof (e.g., health provider confirmation) related to<br />
gender or gender identity. Finally, clear guidelines<br />
concerning non-private room assignments should<br />
include assigning roommates based on gender identity<br />
rather than gender assigned at birth.<br />
Power to Make a Difference<br />
The ANA Code of Ethics obligates nurses to practice<br />
"compassion and respect for the inherent dignity,<br />
worth, and unique attributes of every person" (ANA,<br />
2015, para 1). While some nurses may intentionally<br />
discriminate against people who are transgender, it is<br />
more likely that a lack of knowledge and experience<br />
leads to nursing actions that result in suboptimal care.<br />
Nurses play critical roles in transgender care by (a)<br />
providing supportive, affirming care, (b) creating an<br />
inclusive environment, and (c) leading interprofessional<br />
teams toward gender-affirming care. Education and a<br />
commitment to understanding the lived experiences of<br />
people who are transgender is, therefore, essential for<br />
all nurses.<br />
References<br />
American Nurses Association. (2015). What is the nursing code of<br />
ethics? https://nurse.org/education/nursing-code-of-ethics/<br />
Department of Health and Human Services, Office of Disease<br />
Prevention and Health Promotion. (n.d.). Healthy people.<br />
Lesbian, gay, bisexual, and transgender health. https://www.<br />
healthypeople.gov/2020/topics-objectives/topic/lesbian-gaybisexual-and-transgender-health<br />
Deutsch, M.B. (2016). Guidelines for the primary and genderaffirming<br />
care of transgender and gender nonbinary people<br />
(2nd ed.). Center of Excellence for Transgender Health, University<br />
of California at San Francisco. https://transcare.ucsf.edu/sites/<br />
transcare.ucsf.edu/files/Transgender-PGACG-6-17-16.pdf<br />
Deutsch, M.B, Bowers, M.L., Radix, A., & Carmel, T.C. (2019).<br />
Transgender medical care in the United States: A historical<br />
perspective. In J.S. Schneider, V.M.B. Silenzio, & Erikson-Schroth,<br />
L. (Eds.). The GLMA Handbook on LGBT Health (1, 83-131). Santa<br />
Barbara, CA: Praeger.<br />
Fenway Institute, National LGBT Health Education Center. (2016).<br />
Providing inclusive services and care for LGBT people. https://<br />
www.lgbtqiahealtheducation.org/publication/learning-guide/<br />
Flores, A.R., Herman, J.L., Gates, G.J., & Brown, T.N.T. (2016). How<br />
many adults identify as transgender in the United States? UCLA<br />
School of Law, William Institute. https://williamsinstitute.law.<br />
ucla.edu/publications/trans-adults-united-states/<br />
Grant, J. M., Mottet, L. A., Tanis, J., Harrison, J., Herman, J. L., &<br />
Keisling, M. (2011). Injustice at every turn: A report of the<br />
National Transgender Discrimination Survey. https://www.<br />
transequality.org/sites/default/files/docs/resources/NTDS_Report.<br />
pdf<br />
Institute of Medicine. (2011). The health of lesbian, gay, bisexual,<br />
and transgender people: Building a foundation for better<br />
understanding. http://www.nationalacademies.org/hmd/<br />
Reports/2011/The-Health-of-Lesbian-Gay-Bisexual-and-<br />
Lambda Legal. (2016). Transgender rights toolkit. https://www.<br />
lambdalegal.org/issues/transgender-rights<br />
McDowell, A. & Bower, K. (2016). Transgender health care for<br />
nurses: An innovative approach to diversifying nursing curricula<br />
to address health inequalities. Journal of <strong>Nursing</strong> Education,<br />
55(8), 476-479. DOI 10.3928/01484834-20160715-11<br />
Safer, J. D., Coleman, E., Feldman, J., Garofal, R., Hembree, W.,<br />
Radix, A., & Sevelius, S. (2017). Barriers to health care for<br />
transgender individuals. Current Opinion in Endocrinology,<br />
Diabetes, and Obesity, 23(2), 168-171. DOI: 10.1097/<br />
MED.0000000000000227<br />
Singh, S., & Durso, L. E. (2017). Widespread discrimination continues<br />
to shape LGBT people's lives in both subtle and significant ways.<br />
Center for American Progress. https://www.americanprogress.<br />
org/issues/lgbt/news/2017/05/02/429529/widespreaddiscrimination-continues-shape-lgbt-peoples-lives-subtlesignificant-ways/
<strong>January</strong>, February, March <strong>2022</strong> <strong>Georgia</strong> <strong>Nursing</strong> • Page 17
Page 18 • <strong>Georgia</strong> <strong>Nursing</strong> <strong>January</strong>, February, March <strong>2022</strong><br />
GNA Personal Benefits<br />
For ANA/GNA Members and GNA-Only Members!<br />
Everyone needs Auto and Home insurance – let<br />
ANA take the hassle out of finding the best provider<br />
and best rate. ANA is partnering with Liberty Mutual<br />
to offer auto and home insurance to members with<br />
a quick and convenient application process and<br />
great rates. Members can potentially save $947 with<br />
customized auto and home insurance.*<br />
Go to https://www.libertymutual.com/<br />
americannurses to apply now or find out more<br />
information on Auto and Home insurance or call 855-<br />
948-6267.<br />
*Savings validated by new customers who switched<br />
to Liberty Mutual between 1/2020-10/2020 and<br />
participated in a countrywide survey. Savings may<br />
vary. Comparison does not apply in MA. Coverage<br />
provided and underwritten by Liberty Mutual Insurance<br />
Company or its affiliates or subsidiaries, 175 Berkeley<br />
Street, Boston, MA 02116.<br />
Nurses need to protect themselves and their<br />
career by maintaining Professional Liability Insurance,<br />
a.k.a. Medical Malpractice Insurance. Do not assume<br />
your employer’s liability insurance will cover you<br />
when a lawsuit or complaint is filed. Nurses Service<br />
Organization (NSO) has a 45+ year history of<br />
defending nursing professionals from allegations of<br />
medical malpractice and licensing complaints. With<br />
over 500,000 nursing professionals insured and 60+<br />
professional nursing association partners, they are the<br />
premier administrator of nurses’ malpractice insurance<br />
in the U.S.<br />
We encourage you to explore NSO’s website, receive<br />
a quick rate quote, and browse the case studies and<br />
articles in NSO’s Learning Center. In the Learning<br />
Center, you will find NSO’s 4th Nurses Claim Report. It<br />
provides statistical data and an analysis of malpractice<br />
and licensing claims, as well as recommendations on<br />
how you can avoid potential problems in your practice.<br />
Learn more about NSO Professional Liability<br />
Insurance for ANA Members at https://www.nso.<br />
com/ana-csna-nurse-malpractice?refid=iiNW0T4i<br />
Watch the announcement video at https://<br />
vimeo.com/477619765/c825b287b3<br />
ANA’s collaboration with Prudential provides<br />
exclusive insurance plans for ANA Members. Term<br />
Life Insurance can help protect your loved ones in<br />
the event you pass away – and your coverage stays in<br />
place even if your health or employer changes. AD&D<br />
protects you from an accident that results in death or<br />
dismemberment. Both products offer competitive and<br />
affordable rates for ANA members with quick and<br />
simple access – applying takes about 10 minutes and<br />
you can get coverage in as little as 30 days! Products<br />
may not be available in all states.<br />
Go to https://ana.memberenroll.com/index.php to<br />
apply now or find out more information on Term Life<br />
and AD&D insurance.<br />
1044212-00001-00<br />
Prudential Financial, Inc. (NYSE: PRU), a financial<br />
services leader, has operations in the United States,<br />
Asia, Europe and Latin America. Prudential’s diverse<br />
and talented employees are committed to helping<br />
individual and institutional customers grow and protect<br />
their wealth through a variety of products and services.<br />
In the U.S., Prudential’s iconic Rock symbol has stood<br />
for strength, stability, expertise and innovation for<br />
more than a century. For more information, please visit<br />
news.prudential.com.<br />
Laurel Road specializes in helping nurses, with<br />
special interest rates available to nurses that allow<br />
them to save thousands of dollars. 1 Refinancing might<br />
help you consolidate your loans into one, manageable<br />
amount with one, potentially lower interest rate. ANA<br />
members also receive a special 0.25% rate discount or<br />
$300 cash bonus 1 when using this link https://www.<br />
laurelroad.com/partnerships/ana/ and below.<br />
Laurel Road’s quick and easy online application<br />
allows you to get preliminary rates in minutes –<br />
without impacting your credit and with no obligation<br />
to accept 2 . Laurel Road has no fees to apply. You'll<br />
also have the option to set up automatic payments to<br />
receive an additional 0.25% rate discount. 3<br />
Go to https://www.laurelroad.com/partnerships/ana/<br />
to learn more and check your rates now.<br />
To watch "Student Debt 101 and ANA<br />
Resources" webinar, visit https://www.<br />
nursingworld.org/membership/memberbenefits/personal-benefits/student-debt-videoregistration/<br />
All credit products are subject to credit approval.<br />
1) Savings vary based on rate and term of your<br />
existing and refinanced loan(s). Review your loan<br />
documentation for total cost of your refinanced loan<br />
2) Checking your rate with Laurel Road only requires<br />
a soft credit pull, which will not affect your credit<br />
score. To proceed with an application, a hard credit pull<br />
will be required, which may affect your credit score.<br />
Preliminary rates mean a delivery of personalized rates<br />
for those individuals who provide sufficient information<br />
to return a rate.<br />
3) The 0.25% American Nurses Association (ANA)<br />
member interest rate discount is offered for student<br />
loan applications from active ANA members. The rate<br />
discount will end if ANA notifies Laurel Road that<br />
borrower is no longer in good standing. An additional<br />
0.25% interest rate discount is available for making<br />
automatic payments from a bank account by electronic<br />
fund transfer (EFT) ( the AutoPay/EFT Discount). Neither<br />
discount reduces the monthly payment, instead the<br />
discounts are applied to the principal to help pay the<br />
loan down faster. The ANA member interest rate<br />
discount cannot be combined with other offers, except<br />
any discount for making automatic payments.<br />
Laurel Road is a brand of KeyBank National<br />
Association, Member FDIC.<br />
Travel discounts are the #1 requested benefit<br />
program from ANA members. ANA has partnered with<br />
Booking Community to offer members hotel room<br />
rates that are discounted up to 70% -- lower rates<br />
than you will find at any online travel or hotel website.<br />
ANA members get access to amazing deals that are not<br />
available to the public, at over 800,000 participating<br />
Hotels and Resorts Worldwide. Plan a trip and watch<br />
the savings grow – it pays to be an ANA member!<br />
Long Term Care Insurance is increasingly the choice<br />
of ANA Members seeking to protect their hard-earned<br />
assets from the high cost of long-term services along<br />
with the resulting financial spend-down and potential<br />
loss of self-reliance.<br />
Final Expense Insurance, also known as Burial or<br />
Funeral Insurance, is a type of whole life insurance<br />
designed for those over 40 years of age, to cover<br />
funeral expenses and existing bills when you pass.<br />
Through ANA’s partnership with Anchor Health<br />
Administrators (AHA), members receive specialized<br />
advocate services for these much-needed protections.<br />
AHA is a company that, for almost 30 years, has<br />
specialized in working with Nurses/Spouses to provide the<br />
best personal solutions for their planning needs. For more<br />
information on Long Term Care, or Final Expense coverage<br />
and to receive a free, no obligation consultation with a<br />
licensed advocate, visit https://www.anchorltc.com/<br />
http://careers.kindredathome.com
<strong>January</strong>, February, March <strong>2022</strong> <strong>Georgia</strong> <strong>Nursing</strong> • Page 19<br />
MEMBERSHIP<br />
As a GNA Member, you have …<br />
• The opportunity to serve as a GNA Board and/or Committee<br />
Member*<br />
• Access to shared interest and local chapters, and avenues to<br />
connect with leaders in the profession<br />
• Access to free and discounted educational opportunities<br />
• A free subscription to The American Nurse Today - the official<br />
journal of the American Nurses Association (ANA)<br />
• Member-only access to ANA’s Nurse Space<br />
• Free access to The Online Journal of Issues in <strong>Nursing</strong> (OJIN)<br />
• Access to free and discounted webinars at Navigate <strong>Nursing</strong><br />
Webinars<br />
• The LARGEST discount on initial ANCC certification ($120/full<br />
members only)<br />
• The LARGEST discount on ANCC re- certification ($150/full<br />
members only)<br />
• Discounts at NursesBook.Org<br />
* Serving as a GNA Board Member is subject to running in and winning the GNA<br />
Board of Directors’ Election for the position of interest.<br />
Become a GNA Member today! <strong>Georgia</strong>Nurses.org<br />
Member Lifestyle Benefits<br />
In addition, GNA Members<br />
receive special rates at:<br />
• Mutual of Omaha<br />
Insurance<br />
• Nurses Service<br />
Organization<br />
• Matchwell<br />
• Education Loan Finance<br />
• Commerce Bank<br />
• Grand Canyon University<br />
• Snazzy Traveler, and more!<br />
<strong>Georgia</strong> Nurses Association<br />
Political Action Committee<br />
(GN-PAC)<br />
About GN-PAC:<br />
The <strong>Georgia</strong> Nurses Association Political Action<br />
Committee (GN-PAC) actively and carefully reviews<br />
candidates for local, state and federal office. This<br />
consideration includes the candidate’s record on<br />
nursing issues and value as an advocate for the nursing<br />
profession. Your contribution to GN-PAC today will<br />
help GNA continue to protect your ability to practice<br />
and earn a living in <strong>Georgia</strong>. Your contribution will<br />
also support candidates for office who are strong<br />
advocates on behalf of nursing. By contributing $25<br />
or more, you’ll become a supporting member of GN-<br />
PAC. By contributing $100 or more, you’ll become a<br />
full member of GN-PAC! The purpose of the GN-PAC<br />
shall be to promote the improvement of the health<br />
care of the citizens of <strong>Georgia</strong> by raising funds from<br />
within the nursing community and friends of nursing<br />
and contributing to the support of worthy candidates<br />
for State office who believe, and have demonstrated<br />
their belief, in the legislative objectives of the <strong>Georgia</strong><br />
Nurses Association.<br />
TO DONATE VISIT:<br />
https://georgianurses.nursingnetwork.<br />
com/page/75371-gn-pac<br />
I Want to Get Involved:<br />
Joining and Creating a GNA Chapter<br />
Are you interested in Palliative Care? Nurse<br />
Navigation? Informatics?<br />
Whatever your nursing passion may be, <strong>Georgia</strong><br />
Nurses Association (GNA) can help you connect with<br />
your peers locally and across the state. Becoming<br />
involved in your professional association is the first step<br />
towards creating your personal career satisfaction and<br />
connecting with your peers. Now, GNA has made it<br />
easy for you to become involved according to your own<br />
preferences.<br />
Through GNA’s new member-driven chapter<br />
structure, you can join multiple chapters and also<br />
create your own chapter based on shared interests<br />
where you can reap the benefits of energizing<br />
experiences, empowering insight and essential<br />
resources.<br />
Visit http://www.georgianurses.org/?page=<br />
Chapter Chairs to view a list of current GNA Chapters<br />
and Chapters Chair contact information. Connect with<br />
Chapter Chairs to find out when they will hold their<br />
next Chapter meeting!<br />
The steps you should follow to create a NEW GNA<br />
chapter are below. If you have any questions, contact<br />
the membership development committee or GNA<br />
headquarters; specific contact information and more<br />
details may be found at www.georgianurses.org.<br />
1. Obtain a copy of GNA bylaws, policies and<br />
procedures from www.georgianurses.org.<br />
2. Gather together a minimum of 10 GNA<br />
members who share similar interests.<br />
3. Select a chapter chair.<br />
4. Chapter chair forms a roster to verify roster<br />
as current GNA members. This is done by<br />
contacting headquarters at (404) 325-5536.<br />
5. Identify and agree upon chapter purpose.<br />
6. Decide on chapter name.<br />
7. Submit information for application to become a<br />
chapter to GNA Headquarters. Information to be<br />
submitted includes the following:<br />
Chapter chair name and chapter contact<br />
information including an email,<br />
Chapter name, Chapter purpose, and Chapter<br />
roster.<br />
8. The application will then go to the Membership<br />
Development Committee who will forward it to<br />
the Board of Directors. The Board will approve or<br />
decline the application and notify the applicant<br />
of its decision.<br />
To become a member of GNA please review and<br />
submit our membership application located on the<br />
homepage of our website at www.georgianurses.org