Defence Anaesthesia - Journal of the Royal Army Medical Corps
Defence Anaesthesia - Journal of the Royal Army Medical Corps
Defence Anaesthesia - Journal of the Royal Army Medical Corps
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
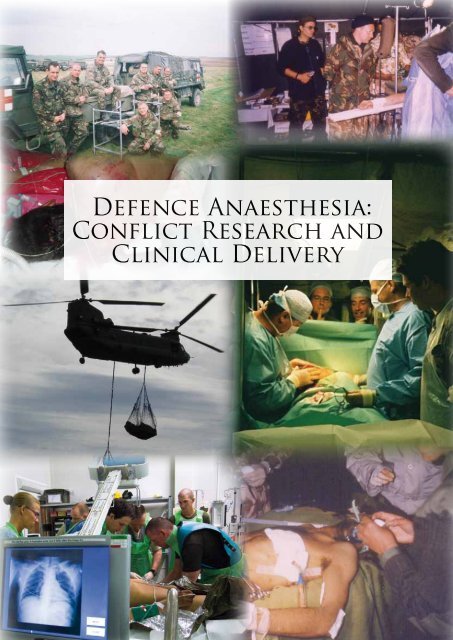
<strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong>:<br />
Conflict Research and<br />
Clinical Delivery
From The Editors<br />
Welcome to this <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> supplement to <strong>the</strong> <strong>Journal</strong> <strong>of</strong> <strong>the</strong> <strong>Royal</strong> <strong>Army</strong> <strong>Medical</strong> <strong>Corps</strong>. The supplement has a broad range<br />
<strong>of</strong> articles covering diverse aspects <strong>of</strong> our current practice and balances academic endeavour with pragmatic clinical advice. The guest<br />
editors are very grateful for <strong>the</strong> efforts <strong>of</strong> all <strong>the</strong> authors- both from DMS and our civilian colleagues in <strong>the</strong> NHS- and to <strong>the</strong> editor,<br />
Lt Col Jeff Garner for hosting us.<br />
Wg Cdr Simon Turner FRCA RAF<br />
Consultant in <strong>Anaes<strong>the</strong>sia</strong> and Intensive Care, Leeds General Infirmary; Research Lead, Department <strong>of</strong> Military <strong>Anaes<strong>the</strong>sia</strong>, Pain and<br />
Critical Care; Consultant, Critical Care Air Support Team, <strong>Royal</strong> Air Force<br />
Col Peter Mahoney OBE TD FRCA L/RAMC<br />
<strong>Defence</strong> Pr<strong>of</strong>essor <strong>Anaes<strong>the</strong>sia</strong> and Critical Care, <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine, Birmingham<br />
Front Cover Illustration: ‘Resuscitation on <strong>the</strong> MERT’ reproduced by kind permission <strong>of</strong> <strong>the</strong> artist, David Rowlands. David Rowlands is a<br />
pr<strong>of</strong>essional artist specialising in military paintings. He has worked with many Regiments and <strong>Corps</strong> <strong>of</strong> <strong>the</strong> British <strong>Army</strong> since his first military<br />
commission in 1983 and has deployed frequently to witness first hand soldiers in action in locations as diverse as South Armagh, Kuwait<br />
(Op GRANBY), Bosnia (Op GRAPPLE), Iraq (Op TELIC) and Afghanistan (Op HERRICK). In 2008, he flew with <strong>the</strong> <strong>Medical</strong> Emergency<br />
Response Team <strong>of</strong> Close Support <strong>Medical</strong> Regiment, 16 Air Assault Brigade in Helmand province which is when this sketch was made. Fur<strong>the</strong>r<br />
details are available at www.davidrowlands.co.uk<br />
282 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S282
Personal Views
<strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> - Look Back, Look Forward<br />
This supplement to <strong>the</strong> <strong>Journal</strong> <strong>of</strong> <strong>the</strong> <strong>Royal</strong> <strong>Army</strong> <strong>Medical</strong> <strong>Corps</strong><br />
examining <strong>the</strong> Challenges in <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> is <strong>the</strong> latest<br />
collection <strong>of</strong> articles that examine developments in <strong>the</strong> specialty<br />
<strong>of</strong> military anaes<strong>the</strong>sia in all its facets; previously <strong>the</strong> journal has<br />
Focused On… Pain Management (March 2009) and Intensive<br />
Care (June 2009). It is coincidentally being published close to <strong>the</strong><br />
20-year anniversary <strong>of</strong> <strong>the</strong> 1990-1991 Gulf War. Looking back to<br />
this conflict allows us to examine how much has changed in UK<br />
Military <strong>Anaes<strong>the</strong>sia</strong> in <strong>the</strong> intervening two decades.<br />
32 Field Hospital was one <strong>of</strong> four UK military hospitals<br />
deployed to <strong>the</strong> Arabian Gulf in 1991. It was located in <strong>the</strong><br />
desert in Nor<strong>the</strong>rn Saudi Arabia and housed 200 beds, eight<br />
operating tables, eight resuscitation bays and a treatment<br />
department. The resuscitation teams comprised three people (a<br />
doctor, nurse and medic) with responsibility for two resuscitation<br />
bays each. <strong>Anaes<strong>the</strong>sia</strong> duties were to be shared with Dental<br />
<strong>of</strong>ficers and <strong>the</strong> McVicar operating tables were arranged in zig-<br />
zag fashion in <strong>the</strong> open tented area with <strong>the</strong> two head ends close<br />
toge<strong>the</strong>r. This meant that, if required, one anaes<strong>the</strong>tist could<br />
look after two patients at once. <strong>Anaes<strong>the</strong>sia</strong> was given with<br />
<strong>the</strong> triservice kit using halothane and trilene. The ‘Cold War’<br />
template <strong>of</strong> <strong>the</strong> hospital meant that critical care as such did not<br />
exist. The long tented corridors <strong>of</strong> <strong>the</strong> hospital were dark and in<br />
January 1991 <strong>the</strong> complex was very cold at night. Fortunately <strong>the</strong><br />
anticipated casualty load did not arrive – and those patients who<br />
came through <strong>the</strong> hospital were given <strong>the</strong> best care <strong>the</strong> staff could<br />
<strong>of</strong>fer with <strong>the</strong> materials and equipment to hand. I am grateful to<br />
<strong>the</strong> mentors who gave a good grounding in <strong>the</strong> resuscitation and<br />
anaes<strong>the</strong>sia <strong>of</strong> <strong>the</strong> ballistic casualty.<br />
The Camp Bastion hospital in Afghanistan, 20 years later, is<br />
a very different place. The workload is intense. The equipment<br />
within <strong>the</strong> hospital is first class. CT scanners and digital X Ray<br />
have revolutionised our ability to image <strong>the</strong> severely injured and<br />
plan <strong>the</strong>ir care. Joint training on <strong>the</strong> MOST course and HOSPEX<br />
mean that <strong>the</strong> deployed teams have a shared understanding <strong>of</strong><br />
military damage control resuscitation concepts- and <strong>the</strong> role<br />
<strong>of</strong> anaes<strong>the</strong>sia within this. Our strong links with <strong>the</strong> Combat<br />
Casualty Care programme at DSTL Porton Down has meant that<br />
quality research is used to underpin our protocols- or where this<br />
is impractical give us a sound <strong>the</strong>oretical basis for what we want<br />
to achieve. The current state <strong>of</strong> development <strong>of</strong> <strong>the</strong> deployed<br />
hospital including intensive care and regional analgesia systems<br />
would not have been imagined by our teams in 1991.<br />
Getting to this point has not been straightforward. As a cadre<br />
we owe a great debt to a series <strong>of</strong> <strong>Defence</strong> Consultant Advisors<br />
and single service consultant advisers, supported by key members<br />
<strong>of</strong> <strong>the</strong> clinical cadres, who have pushed at <strong>the</strong> boundaries <strong>of</strong><br />
deployed anaes<strong>the</strong>sia and worked with <strong>the</strong> Surgeon General’s<br />
Department and PJHQ to get new equipment and materials into<br />
service.<br />
The collection <strong>of</strong> articles in this supplement gives a flavour <strong>of</strong><br />
<strong>the</strong> level <strong>of</strong> care that <strong>the</strong>se efforts have facilitated.<br />
Not all deployed operations are, or will be, like Bastion.<br />
Everyone who has been on short notice entry operations will<br />
know <strong>the</strong> compromises that have to be made when working<br />
within a strict air cargo constraint. <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> can be<br />
very proud <strong>of</strong> all <strong>the</strong> contributions made to <strong>the</strong> care <strong>of</strong> our combat<br />
casualties- but it is important as a cadre that we continually learn<br />
from our experiences, research emerging questions and contribute<br />
to ongoing operational training so <strong>the</strong> best <strong>of</strong> our practice can be<br />
adapted to whatever environments and situations we need to face<br />
in <strong>the</strong> future.<br />
This collection <strong>of</strong> articles is a very welcome contribution to<br />
this process and I am very grateful to <strong>the</strong> editor and <strong>the</strong> journal<br />
for supporting us.<br />
Col Peter F Mahoney<br />
<strong>Defence</strong> Pr<strong>of</strong>essor <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong><br />
The Future for Military <strong>Anaes<strong>the</strong>sia</strong> After<br />
Operations in Afghanistan<br />
Introduction<br />
The provision <strong>of</strong> military anaes<strong>the</strong>sia has evolved dramatically<br />
during <strong>the</strong> last few years and more specifically during Op<br />
HERRICK. The input from <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> into casualty<br />
care is greater now than at any previous time. <strong>Anaes<strong>the</strong>sia</strong> as a<br />
whole provides medical capability throughout <strong>the</strong> casualty<br />
pathway almost from point <strong>of</strong> wounding through all echelons<br />
<strong>of</strong> care including Aero <strong>Medical</strong> evacuation both tactically and<br />
strategically to Role 4 and beyond with input at <strong>the</strong> <strong>Defence</strong><br />
<strong>Medical</strong> Rehabilitation Centre at Headley Court and <strong>the</strong> Regional<br />
Rehabilitation Units.<br />
The foundation <strong>of</strong> deployed medical capability is rooted<br />
in three factors. Having <strong>the</strong> appropriately trained individual,<br />
equipped in <strong>the</strong> correct manner and commanded effectively<br />
to deliver <strong>the</strong> right care at <strong>the</strong> right time in <strong>the</strong> right place. The<br />
pace <strong>of</strong> change that has occurred during HERRICK has been<br />
frenetic. This has been in response to <strong>the</strong> demands placed upon<br />
us by <strong>the</strong> casualty load and complexity <strong>of</strong> injury. The fact that<br />
<strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> has been up to <strong>the</strong> challenge is in no small<br />
part due to <strong>the</strong> pr<strong>of</strong>essionalism and leadership <strong>of</strong> every single<br />
deployed anaes<strong>the</strong>tist as well as <strong>the</strong> guidance and tenacity <strong>of</strong><br />
various members <strong>of</strong> <strong>the</strong> cadre. As is inevitable at this time with<br />
<strong>the</strong> ramifications <strong>of</strong> <strong>the</strong> Strategic <strong>Defence</strong> and Security Review<br />
(SDSR) still to be fully absorbed, we must look to <strong>the</strong> future.<br />
What threats and challenges are likely to confront us in <strong>the</strong> future<br />
and how are we best to meet <strong>the</strong>se challenges?<br />
There are many lessons to learn from HERRICK, however we<br />
should not just try and duplicate <strong>the</strong> model that is so successful<br />
in Afghanistan in <strong>the</strong> next conflict. The pace <strong>of</strong> change that has<br />
occurred in Afghanistan was required to meet <strong>the</strong> challenges that<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S285–286 285
occurred in that particular <strong>the</strong>atre <strong>of</strong> operations and has produced<br />
an almalgamation <strong>of</strong> medical capabilities, a hybrid - a highly<br />
evolved military medical system that functions extremely well.<br />
However, removed from that environment with its established<br />
support mechanisms it will potentially fail like any o<strong>the</strong>r organism<br />
that has evolved in isolation. It becomes our responsibility to<br />
examine what lessons can be learnt from HERRICK that are<br />
transferable to future deployments.<br />
Command and Control & <strong>the</strong> <strong>Medical</strong> Plan.<br />
The first lesson must be that <strong>the</strong> severely injured soldier is a time<br />
sensitive casualty. Rapid medical intervention carried out at <strong>the</strong><br />
appropriate time saves life. This is reflected in <strong>the</strong> principle <strong>of</strong><br />
simultaneous initiation <strong>of</strong> treatment with casualty evacuation to<br />
<strong>the</strong> next level <strong>of</strong> care.<br />
The next conflict may not be as asymmetric as Afghanistan;<br />
ground forces may not have <strong>the</strong> ability to switch priority from<br />
aggressive patrolling to casualty extraction. During contingency<br />
operations <strong>the</strong> number <strong>of</strong> airframes will be severely limited and<br />
<strong>the</strong> area <strong>of</strong> operations will likely to be smaller in geographical area.<br />
The use <strong>of</strong> o<strong>the</strong>r casualty extraction vehicles o<strong>the</strong>r than airframes<br />
is potentially more likely. All <strong>the</strong>se factors are likely to delay<br />
casualty extraction to primary surgery or definitive care. How<br />
we as health care providers mitigate for this will be important<br />
if we intend to minimise mortality and morbidity. The concept<br />
<strong>of</strong> intelligent tasking will become more important to rationalise<br />
limited resources and requires flexible thinking and efficient<br />
decision making.<br />
Equipment<br />
The Role 3 facility at Camp Bastion operates above its designated<br />
deployed capability; <strong>the</strong> through put <strong>of</strong> casualties reflects <strong>the</strong> work<br />
load <strong>of</strong> a military Role 3 hospital with twice if not three times <strong>the</strong><br />
50 established beds. This is achievable because in certain areas<br />
<strong>the</strong> hospital is equipped and manned as if it was established for<br />
100 beds. It has eight resuscitation bays, four operating tables and<br />
10 intensive care beds which is soon to be expanded to 12. The<br />
Operational Establishment Table (OET) also reflects this uplift in<br />
capability. The o<strong>the</strong>r important force multiplier is <strong>the</strong> exceptional<br />
Aero <strong>Medical</strong> evacuation system that is working at full capacity<br />
nearly every day to keep <strong>the</strong> hospital functioning. The reason that<br />
<strong>the</strong> hospital in Bastion has been able to evolve in this way is that it<br />
is a fixed establishment with medical equipment and life support<br />
systems for <strong>the</strong> hospital such as power and environmental control<br />
being employed that would be impractical in all but <strong>the</strong> most<br />
enduring operation in <strong>the</strong> future.<br />
It is not only medical planners that need to be aware <strong>of</strong> this<br />
paradox. The expectation <strong>of</strong> those forces that rely on our care<br />
needs to be tempered. The next operational area by definition<br />
will be an entry operation <strong>of</strong> some nature. The logistical support<br />
including <strong>the</strong> air bridge will <strong>the</strong>refore be much more fragile and as<br />
a result <strong>the</strong> medical infrastructure will likely be different. This will<br />
impact on <strong>the</strong> way we deliver care and potentially <strong>the</strong> morbidity<br />
and mortality <strong>of</strong> <strong>the</strong> forces that we support.<br />
The Trained Individual<br />
Of <strong>the</strong> three factors or foundations that produce operational<br />
medical capability on operations outlined earlier (equipment,<br />
Command and Control and <strong>the</strong> trained individual), I believe <strong>the</strong><br />
most important is <strong>the</strong> appropriately trained individual. The most<br />
constant mitigating factor against <strong>the</strong> unpredictability <strong>of</strong> <strong>the</strong> future<br />
will be <strong>the</strong> clinician, be that <strong>the</strong> CMT, Nursing Officer, General<br />
Practioner or Secondary Health Care consultant. HERRICK has<br />
shown us that one way to increase capability, and thus success, is to<br />
increase <strong>the</strong> number <strong>of</strong> deployed consultants on <strong>the</strong> OET. When<br />
placed in multidisciplinary teams working toge<strong>the</strong>r to produce<br />
horizontal resuscitation great results can be achieved. However<br />
<strong>the</strong>se individuals must be trained for <strong>the</strong> environment that <strong>the</strong>y<br />
are deployed to. Pre-deployment training has become <strong>the</strong> main<br />
priority in <strong>the</strong> training arena. This emphasis must continue but<br />
change to encompass <strong>the</strong> generic entry operation. Old lessons<br />
need to be revisited. The deployed clinician <strong>of</strong> tomorrow should<br />
not only be trained to survive but to function in <strong>the</strong> austere<br />
environment. The next war will not be HERRICK and <strong>the</strong> next<br />
hospital will not be Bastion. The one known factor is that <strong>the</strong> team<br />
should aim to deliver consultant delivered care, and be trained to<br />
work in more austere environments. Instead <strong>of</strong> using <strong>the</strong> term<br />
Field Surgical Team (FST) to describe a deployed capability <strong>the</strong><br />
phrase Damage Control Resuscitation team (DCR) would be<br />
more appropriate. Such a phrase captures <strong>the</strong> multidisciplinary<br />
approach to <strong>the</strong> severely injured casualty including <strong>the</strong> specialities<br />
<strong>of</strong> Emergency and Intensive Care Medicine.<br />
Whatever challenges await, <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> will play<br />
a significant part and this will mean more anaes<strong>the</strong>tists being<br />
held at high readiness not only as part <strong>of</strong> <strong>the</strong> deployed surgical<br />
team but covering <strong>the</strong> o<strong>the</strong>r capabilities <strong>of</strong> Pre-Hospital care,<br />
Intensive Care and Aero <strong>Medical</strong> evacuation at both tactical and<br />
strategic level.<br />
The appropriately trained individual is <strong>the</strong> greatest assets <strong>the</strong><br />
DMS has and <strong>the</strong> training ethos <strong>of</strong> <strong>the</strong> future should be those that<br />
deploy toge<strong>the</strong>r need to train toge<strong>the</strong>r and this represents <strong>the</strong> true<br />
lesson from HERRICK that can be used in <strong>the</strong> future.<br />
Lt Col DA Parkhouse FRCA RAMC<br />
Consultant Anaes<strong>the</strong>tist 16 <strong>Medical</strong> Regiment; Consultant<br />
Adviser Anaes<strong>the</strong>tics (<strong>Army</strong>) to DGAMS;<br />
<strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> Operational Governance Lead and <strong>Defence</strong><br />
<strong>Anaes<strong>the</strong>sia</strong> Lessons Management Lead<br />
286 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S285–286
Clinical Practice
Pre-hospital <strong>Anaes<strong>the</strong>sia</strong><br />
RJ Dawes 1 , A Mellor 2<br />
1 Specialist Registrar in Anaes<strong>the</strong>tics and Intensive Care, Wessex Rotation. 2 Consultant Anaes<strong>the</strong>tist, Dept <strong>of</strong> Academic<br />
Emergency Medicine, James Cook University Hospital, Middlesbrough<br />
Abstract<br />
This review presents <strong>the</strong> history <strong>of</strong> Pre-hospital anaes<strong>the</strong>sia, it’s evidence base, required training and examines current<br />
arguments focusing on best practice such as who should undertake <strong>the</strong> procedure and how identifying appropriate patients,<br />
utilizing new techniques and drugs may benefit <strong>the</strong> Pre-hospital practitioner in optimum delivery <strong>of</strong> this important procedure.<br />
Introduction<br />
Pre-hospital anaes<strong>the</strong>sia is used to rapidly secure and protect <strong>the</strong><br />
airway, prevent secondary brain injury, for humanitarian reasons<br />
and to facilitate safe transfer when access to <strong>the</strong> patient may be<br />
less than ideal. Traditionally, <strong>the</strong> airway is secured by a technique<br />
known as Rapid Sequence Induction and Intubation (RSII).<br />
Securing <strong>the</strong> airway is second in importance only to <strong>the</strong> control<br />
<strong>of</strong> catastrophic haemorrhage, but pre-hospital anaes<strong>the</strong>sia is more<br />
than securing <strong>the</strong> airway, and intubation merely <strong>the</strong> first step .<br />
Once <strong>the</strong> airway is secured, supporting physiology, preventing<br />
secondary injury and safe transfer to an appropriate centre is <strong>the</strong><br />
goal in <strong>the</strong> pre-hospital phase.<br />
Definition and History <strong>of</strong> Rapid Sequence<br />
Induction/Intubation<br />
RSII is defined by Walls in <strong>the</strong> Manual <strong>of</strong> Emergency Airway<br />
Management 3rd Edition (Lippincott Williams & Wilkins) as<br />
“<strong>the</strong> administration, after preoxygenation, <strong>of</strong> a potent induction agent<br />
followed immediately by a rapidly acting neuromuscular blocking<br />
agent to induce unconsciousness and motor paralysis for tracheal<br />
intubation”<br />
The preoxygenation phase permits a period <strong>of</strong> apnoea to<br />
occur between administrating drugs and intubating <strong>the</strong> trachea.<br />
RSII is used on <strong>the</strong> predicated assumption that <strong>the</strong> patient has<br />
a full stomach and may be at risk <strong>of</strong> pulmonary aspiration <strong>of</strong><br />
gastric contents. This has long been recognized as a risk during<br />
anaes<strong>the</strong>sia. In 1950, <strong>the</strong> Association <strong>of</strong> Anaes<strong>the</strong>tists <strong>of</strong> Great<br />
Britain and Ireland (AAGBI) investigated deaths associated with<br />
anaes<strong>the</strong>sia and discovered 43 deaths caused by aspiration. Six<br />
years on, ano<strong>the</strong>r 110 deaths due to aspiration <strong>of</strong> gastric contents<br />
were reported.<br />
In 1961, Brian Sellick first described a manoeuvre attempting<br />
to control and minimize regurgitation <strong>of</strong> gastric contents before<br />
intubation by compressing <strong>the</strong> cricoid cartilage against <strong>the</strong> bodies<br />
<strong>of</strong> <strong>the</strong> cervical vertebrae. Prior to this, anaes<strong>the</strong>sia was induced in<br />
an upright position to provide airway protection, but debate still<br />
reigns regarding cricoid pressure [1].<br />
A ‘classical’ RSII incorporates Sodium Thiopentone (STP)<br />
as <strong>the</strong> induction agent and Suxamethonium for neuromuscular<br />
blockade (NMB) followed swiftly by tracheal intubation. Tracheal<br />
intubation was not routine until <strong>the</strong> 1940s when STP was used<br />
in WWII for military anaes<strong>the</strong>sia. Suxamethonium was first<br />
syn<strong>the</strong>sised in 1949, Ketamine in 1961, etomidate in 1964 and<br />
Corresponding Author: Surg Cdr Adrian Mellor , Consultant<br />
Anaes<strong>the</strong>tist, Dept <strong>of</strong> Academic Emergency Medicine, James<br />
Cook University Hospital, Middlesbrough, TS3 4BW<br />
Prop<strong>of</strong>ol in 1980. Despite <strong>the</strong>ir age, STP and Suxamethonium<br />
remain <strong>the</strong> most widely used agents. What is now apparent<br />
however, is that <strong>the</strong>re is no universal regime [2], and that RSII is<br />
evolving slowly as new drugs, equipment and knowledge emerge.<br />
Several induction agents as well as alternatives to Suxamethonium<br />
are used by both anaes<strong>the</strong>tists and non-anaes<strong>the</strong>tists. These<br />
include using <strong>the</strong> long acting non-depolarizing neuromuscular<br />
blocking agent Rocuronium, instead <strong>of</strong> Suxamethonium, as<br />
<strong>the</strong> ability now exists to rapidly reverse Rocuronium-induced<br />
paralysis with Sugammadex.<br />
Who should perform pre-hospital Rapid Sequence<br />
Induction/Intubation (PHRSII)?<br />
PHRSII brings with it its own unique challenges. It is an austere<br />
environment, <strong>of</strong>ten with little back up, with <strong>the</strong> capacity for failure<br />
higher than in hospital. These factors all undoubtedly contribute<br />
to why many studies looking for any benefit <strong>of</strong> pre-hospital<br />
intubation have been inconclusive. Note <strong>the</strong> deliberate use <strong>of</strong> <strong>the</strong><br />
term pre-hospital intubation. Many <strong>of</strong> <strong>the</strong> studies involved did not<br />
use NMB, used inadequate or no clinical monitoring, personnel<br />
<strong>of</strong>ten had short and poor training, had differing skill sets, and<br />
poor study design and methods [3]. The majority <strong>of</strong> pre-hospital<br />
intubations were not RSII’s. The Joint <strong>Royal</strong> Colleges Ambulance<br />
Liaison Committee have recently stated that UK paramedics<br />
should no longer be routinely trained in intubation [4], as evidence<br />
<strong>of</strong> benefit to patients intubated without drugs is lacking. London<br />
Ambulance Service have recently ceased training paramedics in<br />
endotracheal intubation (June 2010). A criticism <strong>of</strong>ten leveled<br />
by hospital practitioners regarding interventions undertaken<br />
on scene relates to <strong>the</strong> extra time taken to undertake those<br />
procedures, <strong>the</strong>reby prolonging <strong>the</strong> on scene time. Critical care<br />
is a process, not a place, and <strong>the</strong> patient requires an intervention<br />
when <strong>the</strong>y require it, not when <strong>the</strong>y have been transported to<br />
hospital. Interventions such as RSII, blood transfusion and large<br />
bore central access are undertaken routinely in <strong>the</strong> emergency<br />
department (ED) for conditions such as traumatic brain injury<br />
(TBI) and polytrauma, and are seen as minimum standards <strong>of</strong><br />
care. Hypoxia, hypotension and hypercapnia all increase mortality<br />
and morbidity in TBI. PHRSII allows control <strong>of</strong> oxygenation and<br />
ventilation early and safely in <strong>the</strong> pre-hospital phase.<br />
There is evidence that a well organised physician anaes<strong>the</strong>tist<br />
staffed pre-hospital organisation can deliver anaes<strong>the</strong>sia in <strong>the</strong><br />
pre-hospital phase as safely as in hospital [5-7]. The data on o<strong>the</strong>r<br />
groups is conflicting. This may be in part due to training and skill<br />
levels but also due to <strong>the</strong> drug combinations with midazolam and<br />
etomidate all reported as agents used to achieve a drug assisted<br />
intubation but without muscle relaxants [8-11].<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S289–294 289
Pre-hospital <strong>Anaes<strong>the</strong>sia</strong><br />
The two largest UK studies <strong>of</strong> ED RSII where ED staff were<br />
compared to anaes<strong>the</strong>tists showed that anaes<strong>the</strong>tists achieved<br />
significantly better views at laryngoscopy and more first time<br />
intubations [12-13]. A study <strong>of</strong> RSIIs performed by nonanaes<strong>the</strong>tists<br />
(critical care and ED staff) reported a significantly<br />
higher incidence <strong>of</strong> multiple attempts and unsuccessful<br />
intubation by <strong>the</strong> initial operator [14]. This finding is important<br />
as a large US study found that <strong>the</strong> incidence <strong>of</strong> complications<br />
increases significantly when more than one attempt at intubation<br />
is required [15]). Graham’s paper [13] reported almost three<br />
times as many oesophageal intubations (17 vs. 6), twice as many<br />
episodes <strong>of</strong> severe hypotension (17 vs. 8) and twice as many (6<br />
vs. 3) endobronchial intubations during RSII by ED staff. These<br />
numbers were not assessed for statistical significance and are small<br />
(in a series <strong>of</strong> 735 RSII) but may represent clinically significant<br />
harm. Reid’s study [14] showed a significantly higher incidence<br />
<strong>of</strong> multiple attempts and unsuccessful intubation when <strong>the</strong> initial<br />
intubator was not an anaes<strong>the</strong>tist; however overall (albeit selfreported)<br />
complications were similar. Similarly <strong>the</strong> Stevenson<br />
paper [12] reported overall comparable complication rates for ED<br />
vs. anaes<strong>the</strong>tic RSII. The choice <strong>of</strong> agent used is worthy <strong>of</strong> comment<br />
in that most anaes<strong>the</strong>tists choose to use prop<strong>of</strong>ol or thiopentone.<br />
One might speculate that <strong>the</strong> episodes <strong>of</strong> hypotension requiring<br />
treatment might have been significantly reduced for anaes<strong>the</strong>tists<br />
had <strong>the</strong>y used etomidate (ED 72% Etomidate vs. anaes 19%).<br />
This is possibly because <strong>the</strong> majority <strong>of</strong> anaes<strong>the</strong>tists were junior<br />
trainees with little or no experience <strong>of</strong> using etomidate, whereas<br />
<strong>the</strong> majority <strong>of</strong> ED physicians were consultants. Despite using<br />
drugs more likely to produce hypotension, <strong>the</strong> anaes<strong>the</strong>tists had<br />
no more episodes <strong>of</strong> hypotension than <strong>the</strong> ED staff. Familiarity<br />
with <strong>the</strong> side effects and appropriate doses <strong>of</strong> induction agents,<br />
and <strong>the</strong> ability to minimize and manage adverse effects is as<br />
important as <strong>the</strong> ability to get <strong>the</strong> tube in with <strong>the</strong> best view.<br />
The AAGBI produced a set <strong>of</strong> guidelines for PHRSII in<br />
2009 [16]. A panel concluded that practitioners “should have<br />
<strong>the</strong> same level <strong>of</strong> training and competence that would enable <strong>the</strong>m<br />
to perform RSII unsupervised in <strong>the</strong> emergency department”.<br />
This should include training through <strong>the</strong> acute care common<br />
stem (or equivalent). An expert panel in 2007 on behalf <strong>of</strong><br />
The National Confidential Enquiry into Patient Outcome and<br />
Death (NCEPOD) produced <strong>the</strong> report “Trauma who cares”<br />
[17] and concluded: “Airway management in trauma patients is<br />
<strong>of</strong>ten challenging. The pre-hospital response for <strong>the</strong>se patients should<br />
include someone with <strong>the</strong> skill to secure <strong>the</strong> airway, (including <strong>the</strong> use<br />
<strong>of</strong> rapid sequence intubation), and maintain adequate ventilation “<br />
and fur<strong>the</strong>rmore “If pre-hospital intubation is to be part <strong>of</strong> <strong>the</strong> prehospital<br />
trauma management plan , it needs to be in <strong>the</strong> context <strong>of</strong> a<br />
physician based pre-hospital care system”. Once a satisfactory level <strong>of</strong><br />
competency has been attained, this needs to be maintained, with<br />
at least one drug assisted intubation per month currently thought<br />
to be <strong>the</strong> absolute minimum required to maintain competency.<br />
These recent recommendations effectively limit <strong>the</strong> provision<br />
<strong>of</strong> PHRSII to those who regularly undertake RSII in <strong>the</strong> course<br />
<strong>of</strong> <strong>the</strong>ir job such as anaes<strong>the</strong>tists or occasionally emergency<br />
physicians and rarely to o<strong>the</strong>rs who have <strong>the</strong> flexibility to attain<br />
<strong>the</strong> competencies and maintain regular sessions undertaking RSII<br />
in a supervised environment.<br />
Indications for PHRSII<br />
After arrival in <strong>the</strong> ED, RSII will usually be carried out early<br />
to secure <strong>the</strong> airway, to improve physiological variables, for<br />
290<br />
RJ Dawes, A Mellor<br />
humanitarian reasons, and to facilitate safe fur<strong>the</strong>r investigation<br />
(e.g. CT). To carry this argument forward, should <strong>the</strong> patient<br />
require <strong>the</strong> intervention during <strong>the</strong> patient journey but in <strong>the</strong><br />
pre-hospital phase, <strong>the</strong>n <strong>the</strong>re is logic to carrying out RSII in <strong>the</strong><br />
pre-hospital environment if it can be done safely. The evidence<br />
above supports this, when undertaken by a well trained senior<br />
team under optimized conditions. However, <strong>the</strong> evidence to date<br />
does not support any survival benefit over non-RSII managed<br />
patients and if performed by those lacking experience or using<br />
sub-optimal techniques <strong>the</strong>n this may be harmful. It may be<br />
reasonable to be more conservative with pre-hospital RSII than in<br />
<strong>the</strong> Emergency department.<br />
Indications for PHRSII include:<br />
• Airway problems that cannot be reliably managed by simple<br />
manoeuvres e.g. severe facial injury<br />
• Respiratory insufficiency (SpO 2 < 92%) despite 15L/min<br />
O 2 or impending respiratory collapse due to exhaustion or<br />
pathology<br />
• GCS rapidly falling or < 9.<br />
• Patients at risk <strong>of</strong> deterioration when access is difficult<br />
during transfer to definitive care e.g. facial burns<br />
• Patients requiring analgesia and/or sedation prior to<br />
transfer to hospital because <strong>the</strong>y present a danger to <strong>the</strong>mselves<br />
or attending staff or for humanitarian reasons e.g. provide<br />
complete pain relief without respiratory depression.<br />
Using published and accepted guidelines, any patients in pain<br />
or at risk <strong>of</strong> deterioration should be considered for PHRSII.<br />
This effectively means any patient with major illness or injury.<br />
Clearly not all patients can or should receive anaes<strong>the</strong>sia and it is<br />
probably more helpful to think in terms <strong>of</strong> contraindications to<br />
<strong>the</strong> procedure;<br />
• Lack <strong>of</strong> a suitably trained team<br />
• Conditions likely to make intubation difficult or impossible<br />
where o<strong>the</strong>r techniques only available in hospital may be<br />
required e.g. facial deformity, epiglottitis, lack <strong>of</strong> difficulty<br />
airway equipment<br />
There is currently no randomized controlled data showing<br />
clear benefit in mortality or morbidity following pre-hospital<br />
intubation. The only randomized controlled trial <strong>of</strong> pre-hospital<br />
intubation performed so far involved paramedics intubating<br />
children without drugs [18] and in addition to <strong>the</strong> lack <strong>of</strong> doctors<br />
and drugs (i.e. not PHRSII), <strong>the</strong> study had major flaws. There<br />
have been several retrospective studies conducted in this area, and<br />
overall <strong>the</strong>se have not been conclusive. Some <strong>of</strong> <strong>the</strong> studies suggest<br />
survival advantage [19-20]. O<strong>the</strong>rs showed no improvement<br />
in neurological outcome or mortality [21] or even appeared to<br />
show an adverse outcome from pre-hospital intubation [22-<br />
23]. A recent review in <strong>the</strong> British <strong>Journal</strong> <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong> [24]<br />
reviewed <strong>the</strong> value <strong>of</strong> pre-hospital tracheal intubation in patients<br />
with traumatic brain injury and concluded <strong>the</strong>re was no evidence<br />
to support pre-hospital intubation. Unfortunately this detailed<br />
systematic review made no attempt to distinguish those patients<br />
given drugs (or not) to facilitate intubation nor operator skill<br />
level. In <strong>the</strong> majority <strong>of</strong> cases <strong>the</strong> drugs used were not stated and<br />
in o<strong>the</strong>r studies paramedics were taught to perform intubation<br />
with six or eight hours training. Comparing anaes<strong>the</strong>sia<br />
delivered by consultant anaes<strong>the</strong>tists (to standard guidelines) in<br />
<strong>the</strong> pre-hospital environment is very different to intubation by<br />
a paramedic with six hours training without <strong>the</strong> use <strong>of</strong> drugs.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S289–294
Pre-hospital <strong>Anaes<strong>the</strong>sia</strong> RJ Dawes, A Mellor<br />
Induction<br />
Agent<br />
Sodium<br />
Thiopentone<br />
(STP)<br />
General Info Dose Advantages for PHRSII<br />
Packaged as a yellow powder in<br />
a “multi-dose” glass bottle that<br />
requires reconstitution with 20mls<br />
<strong>of</strong> water to make up a 25mg/ml<br />
solution. Stable for days in this<br />
made up state.<br />
Induces sleep very quickly,<br />
but redistributed very quickly<br />
(5-10 mins)<br />
Is a dose dependant potent<br />
cardio-suppressant and venodilator<br />
Prop<strong>of</strong>ol Packaged as a ready made white<br />
emulsion in a break open glass<br />
bottle as 10mg/ml solution.<br />
Induces sleep quickly, redistributed<br />
quickly (5-10mins)<br />
Potent venodilator with no reflex<br />
tachycardia<br />
Ketamine Packaged in premixed multi-dose<br />
glass vial in three concentrations;<br />
10mg/ml (intravenous injection<br />
concentration), 50mg/ml and<br />
100mg/ml.<br />
Stable once drawn up for 24<br />
hours. There is a racaemic mixture<br />
(UK and USA) but <strong>the</strong> stereoselective<br />
S-isomer is available and<br />
is in widespread use in western<br />
Europe.<br />
Its pharmacodynamics are more<br />
favourable.<br />
Slower sleep onset time 30-60 secs.<br />
<strong>Anaes<strong>the</strong>sia</strong> for 10-20 mins<br />
Sympothomimetic: Excellent for<br />
hypotensive patients. Stabilises or<br />
increases MAP. Increase in MAP<br />
<strong>of</strong>fsets increase in intracranial<br />
pressure and sustains cerebral<br />
perfusion pressure in TBI<br />
Etomidate Packaged in break open glass vials<br />
as a premixed 2mg/ml solution<br />
Fast sleep onset time 15-45 secs.<br />
<strong>Anaes<strong>the</strong>sia</strong> for 3-12 mins<br />
Cardiovascularly stable for<br />
hypotensive patients<br />
Normotensive dose:<br />
3-7mg/kg.<br />
70kg patient<br />
= 8-20 mls <strong>of</strong><br />
standard solution<br />
Hypotensive dose:<br />
0.1-0.5 <strong>of</strong> normal dose.<br />
1.5-3.5mg/kg<br />
=4-10mls <strong>of</strong><br />
standard solution<br />
Normotensive dose:<br />
1-3mg/kg.<br />
70kg patient<br />
= 7-21mls <strong>of</strong><br />
standard solution<br />
Hypotensive dose:<br />
Not recommended<br />
for hypotensive<br />
patients unless very<br />
familiar with its use in<br />
hypotensive patients<br />
Dose is<br />
0.5-2mg/kg dependant<br />
on haemodynamic<br />
status.<br />
Always dilute to<br />
10mg/ml<br />
concentration<br />
for IV use.<br />
70kg patient<br />
3.5 – 14mls <strong>of</strong><br />
10mg/kg solution.<br />
Dose is 0.3mg/kg<br />
70 kg patient requires<br />
~10mls <strong>of</strong> premixed<br />
drug<br />
Table 1: The four main induction agents used for pre-hospital rapid sequence induction<br />
Cerebral protective<br />
(if CPP maintained)<br />
Reduces cerebral<br />
metabolic rate <strong>of</strong><br />
oxgygen (CMRO2)<br />
Will not mask<br />
hypovolaemia<br />
Raises seizure threshold<br />
Stable once drawn up<br />
Ready mixed<br />
Can be used to extend<br />
anaes<strong>the</strong>sia<br />
Useful as titrateable<br />
sedative<br />
Familiarity to many<br />
Ready mixed<br />
Maintains or increases<br />
MAP in hypotensive<br />
patients<br />
Bronchodilator, first<br />
choice for severely ill<br />
asthmatics<br />
Potent analgesic in subanaes<strong>the</strong>tic<br />
doses<br />
Avoids polypharmacy if<br />
also used as analgesic<br />
NMDA receptor<br />
antagonism in TBI<br />
<strong>the</strong>orectically useful<br />
Can be used IV, IN, IM<br />
and orally<br />
Premixed: 2 preparations<br />
– Clear (Hypnomidate)<br />
and Fat emulsion<br />
(Lipuro) both 2mg/ml<br />
Stable in hypotensive<br />
patients<br />
Disadvantages for<br />
PHRSII<br />
Needs mixing<br />
Will drop Mean<br />
Arterial Pressure<br />
(MAP) precipitously<br />
if not used cautiously<br />
Precipitous drop in<br />
MAP in hypotensive<br />
patients from whatever<br />
cause<br />
Cannot be pre<br />
drawn up<br />
Increases CMRO2<br />
Unfamiliarity<br />
Suppresses steroid axis<br />
(exact outcome from<br />
a single bolus dose<br />
unknown)<br />
Unfamiliarity<br />
Pain on injection<br />
particularly with<br />
clear solution<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S289–294 291
Pre-hospital <strong>Anaes<strong>the</strong>sia</strong><br />
Neuromuscular<br />
Blockers<br />
Suxamethonium<br />
(Short Acting)<br />
292<br />
General Information Dose Advantages Disadvantages<br />
Packaged as premixed solution<br />
in 2ml break open glass vials<br />
50mg/ml = 100mg per vial<br />
Induces paralysis very quickly,<br />
but redistributed very quickly<br />
dependant on metabolic rate<br />
and cardiac output. 3-7 mins<br />
Degrades once out <strong>of</strong><br />
temperature range (2-7 Deg<br />
C) but will retain up to 90%<br />
efficacy for up to 3 months<br />
out <strong>of</strong> fridge (dependant on<br />
ambient temperature)<br />
Rocuronium Packaged as premixed solution<br />
in 5ml multi dose glass vials<br />
10mg/ml = 50mg per vial<br />
Only long acting NMB<br />
that induces paralysis as<br />
quickly as Suxamethonium<br />
at high doses (1.2mg/kg) and<br />
<strong>the</strong>refore an alternative to<br />
Suxamethonium for PHRSII,<br />
and maintains paralysis for 20-<br />
40 mins dependant on patient<br />
pharmokinetics<br />
Specific reversal agent available<br />
(Sugammadex Schering-<br />
Plough, Schering-Plough<br />
House, Shire Park, Welwyn<br />
Garden City, Hertfordshire<br />
AL7 1TW)<br />
Pancuronium Packaged as premixed solution<br />
in 2ml break open glass vials<br />
2mg/ml = 4mg per vial<br />
Longest acting paralytic with<br />
vagolytic properties that can<br />
help maintain MAP.<br />
Vecuronium Packaged as two vials. 5mls <strong>of</strong><br />
sterile water in first break open<br />
glass vial and second glass vial<br />
containing vecuronium powder<br />
in glass vial. Vecuronium needs<br />
premixing before use. Once<br />
mixed solution is 2mg/ml =<br />
10mg per 5ml vial<br />
1.5-2mg/kg<br />
70kg patient<br />
= 105-140mg<br />
= 2-3 mls<br />
1.2mg/kg.<br />
70kg patient<br />
= 84mg<br />
= ~9mls<br />
0.1mg/kg.<br />
70kg patient<br />
= 7mg<br />
= 3.5mls<br />
0.1mg/kg.<br />
70kg patient<br />
= 7mg<br />
= ~4mls<br />
Quick onset<br />
Familiarity<br />
Can be used IV<br />
and IM<br />
Premixed<br />
Stable at ambient<br />
temperatures<br />
Reversible with<br />
Sugammadex<br />
Quick acting<br />
Long acting<br />
Negates need for<br />
second NMB post<br />
suxamethonium<br />
Premixed<br />
Helps maintain<br />
MAP<br />
Longest acting<br />
NMB >40 mins<br />
dependant<br />
on patient<br />
pharmokinetics<br />
Familiarity<br />
Predicticable<br />
phamodynamics<br />
Reversible with<br />
Sugammadex<br />
Table 2 The four Neuromuscular blocking agents used for pre-hospital rapid sequence induction<br />
RJ Dawes, A Mellor<br />
Difficult storage (needs to be<br />
exchanged frequently in hot<br />
climes if not refrigerated)<br />
Nearly always require two vials<br />
Short duration <strong>of</strong> action<br />
Second doses can precipitate<br />
pr<strong>of</strong>ound bradycardia<br />
especially in children<br />
Can cause cord spasm if not<br />
intubated before paralysis is<br />
extended leading to a<br />
“can’t intubate/can’t ventilate”<br />
scenario<br />
Some patients unable to<br />
metabolise drug leading to<br />
greatly leng<strong>the</strong>ned paralysis<br />
time (hrs)<br />
Not compatible (in same<br />
IV line) with STP without<br />
flushing first<br />
Need two vials in<br />
most patients<br />
Needs premixing from<br />
two vials<br />
Very stable<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S289–294
Pre-hospital <strong>Anaes<strong>the</strong>sia</strong> RJ Dawes, A Mellor<br />
Specific<br />
Reversal Agents<br />
General Information Dose Advantages Disadvantages<br />
Sugammadex First-in-class reversal agent<br />
that encapsulates and<br />
inactivates rocuronium or<br />
vecuronium<br />
Packaged as premixed<br />
multi dose glass vial<br />
in 1ml (100mg), 2ml<br />
(200mg) and 5ml<br />
(500mg) volumes.<br />
RSII reversal is 16mg/ml<br />
70kg patient dose is<br />
1120mg (11mls)<br />
Table 3 The properties <strong>of</strong> a specific neuromuscular blockade reversal agent<br />
Many <strong>of</strong> <strong>the</strong> studies in <strong>the</strong> literature focus on <strong>the</strong> process <strong>of</strong><br />
intubation, ra<strong>the</strong>r than <strong>the</strong> process <strong>of</strong> anaes<strong>the</strong>sia to facilitate<br />
intubation. Drug use is important as both failed intubations and<br />
complications are reduced by <strong>the</strong> use <strong>of</strong> NMB drugs [25]. For<br />
this reason one should be extremely cautious using <strong>the</strong>se studies<br />
to make conclusions about PHRSII.<br />
Importantly <strong>the</strong> published evidence does not show RSII to be<br />
detrimental and, when delivered as part <strong>of</strong> a well governed system,<br />
may be beneficial. Services such as <strong>the</strong> Whatcom Medic One<br />
(Washington state) have a relatively small number <strong>of</strong> well-trained<br />
paramedics using a recognized PHRSII technique and report very<br />
good results [26]. Improved outcome has been demonstrated for<br />
patients transferred by helicopter compared to land ambulance<br />
[27]. This may be due to speed <strong>of</strong> transfer to hospital, better<br />
trained staff or a combination <strong>of</strong> both. Toge<strong>the</strong>r this leads to<br />
<strong>the</strong> conclusion that small teams <strong>of</strong> well-trained staff on board<br />
helicopters are likely to improve outcomes if <strong>the</strong>y are able to<br />
perform PHRSII in certain patients.<br />
Attempting to tease out <strong>the</strong> exact benefits <strong>of</strong> PHRSII in <strong>the</strong> prehospital<br />
phase is difficult, but no more difficult than attempting<br />
to demonstrate <strong>the</strong> benefit <strong>of</strong> early intubation in <strong>the</strong> emergency<br />
department. Ano<strong>the</strong>r facet to pre-hospital care is appropriate<br />
triage. Good evidence exists indicating that direct triage bypassing<br />
district general hospitals with TBI conditions such as extradural<br />
and subdural haematomas to regional neurological centres<br />
significantly reduces morbidity and mortality [28,29]. PHRSII<br />
is merely one component <strong>of</strong> a package <strong>of</strong> care provided by a prehospital<br />
critical care team.<br />
Drugs<br />
There are four main induction agents (Table 1) and four NMB<br />
drugs (Table 2) used in PHRSII. Table 3 lists <strong>the</strong> properties <strong>of</strong> a<br />
specific reversal agent for some NMB agents.<br />
Training and standards<br />
There is an obvious dichotomy between <strong>the</strong> fact that in hospital<br />
anaes<strong>the</strong>sia for a polytrauma patient would usually be carried<br />
out by <strong>the</strong> most senior available anaes<strong>the</strong>tist, whereas historically<br />
pre-hospital anaes<strong>the</strong>sia and intubation has been carried out by<br />
enthusiastic amateurs with little or no governance. This situation<br />
has recently been reviewed and a set <strong>of</strong> guidelines published by<br />
<strong>the</strong> AAGBI [16] with <strong>the</strong> support <strong>of</strong> <strong>the</strong> British Association <strong>of</strong><br />
Immediate Care Schemes (BASICS), <strong>the</strong> Faculty <strong>of</strong> Pre-hospital<br />
Care at <strong>the</strong> <strong>Royal</strong> College <strong>of</strong> Surgeons <strong>of</strong> Edinburgh, <strong>the</strong> <strong>Royal</strong><br />
College <strong>of</strong> Anaes<strong>the</strong>tists and <strong>the</strong> Military.<br />
Complete and fast reversal<br />
<strong>of</strong> Rocuronium paralysis<br />
Shelf life 3 years<br />
Expensive – RSII reversal<br />
costs approximately £350<br />
(June 2010)<br />
These guidelines state <strong>the</strong> accepted level <strong>of</strong> monitoring, operator<br />
experience and team composition for delivering anaes<strong>the</strong>sia. Not<br />
surprisingly <strong>the</strong> monitoring standards remain <strong>the</strong> same as those<br />
for in hospital anaes<strong>the</strong>sia and minimal standards being noninvasive<br />
blood pressure, oxygen saturation, heart rate monitoring<br />
and end tidal carbon dioxide. The guidelines suggest that those<br />
undertaking PHRSII should perform at least one intubation per<br />
month. Whe<strong>the</strong>r this should be simulated or “live” is not stated.<br />
The process <strong>of</strong> pre-hospital anaes<strong>the</strong>sia is a complex process<br />
requiring over 100 individual tasks There is merit in practicing<br />
<strong>the</strong> process <strong>of</strong> intubation first in <strong>the</strong> elective surgical setting <strong>the</strong>n<br />
progressing to high fidelity simulation to practice crew resource<br />
management to successfully assess, anaes<strong>the</strong>tise, resuscitate and<br />
package a patient in this challenging environment.<br />
Courses do exist to train teams specifically to deliver PHRSII.<br />
These include <strong>the</strong> courses provided by <strong>the</strong> Great North Air<br />
Ambulance Service and <strong>the</strong> Mid Anglia General Practitioner<br />
Accident Service. They build team skills through realistic<br />
scenario training to familiarize providers with <strong>the</strong> procedures for<br />
anaes<strong>the</strong>sia, failed intubation drills, post intubation management<br />
and managing PHRSII as part <strong>of</strong> a complex pre-hospital scenario.<br />
Conclusions<br />
Taking anaes<strong>the</strong>sia to patients in <strong>the</strong> pre-hospital setting is<br />
a challenge in terms <strong>of</strong> individual skill and judgment and<br />
organization. The evidence base to support pre-hospital anaes<strong>the</strong>sia<br />
is by no means conclusive but what is clear is that outcomes are<br />
dependent upon <strong>the</strong> capabilities <strong>of</strong> <strong>the</strong> team delivering that care.<br />
PHRSII <strong>of</strong> anaes<strong>the</strong>sia should not just be seen as a treatment but<br />
merely one step in stabilizing a patient on a journey to definitive<br />
care.<br />
References<br />
1. Harris T, Ellis D, Foster L, Lockey D. Cricoid pressure and<br />
laryngeal manipulation in 402 pre-hospital emergency anaes<strong>the</strong>tics:<br />
Essential safety measure or a hindrance to rapid safe intubation?<br />
Resuscitation 81: 810–816.<br />
2. Morris J, Cook TM. Rapid sequence induction: a national survey<br />
<strong>of</strong> practice. <strong>Anaes<strong>the</strong>sia</strong> 2001; 56(11):1090-7.<br />
3. Davis DP, Fakhry SM, Wang HE et al. Paramedic rapid sequence<br />
intubation for severe traumatic brain injury: perspectives from an<br />
expert panel. Prehosp Emerg Care 2007; 11(1):1-8.<br />
4. Joint <strong>Royal</strong> Colleges Ambulance Liason Committee. A critical<br />
reassessment <strong>of</strong> ambulance service airway management in prehospital<br />
care. JRCALC Working Group.2008.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S289–294 293
Pre-hospital <strong>Anaes<strong>the</strong>sia</strong><br />
5. Fakhry SM, Scanlon JM, Robinson L et al. Pre-hospital rapid<br />
sequence intubation for head trauma: conditions for a successful<br />
program. J Trauma 2006; 60(5):997-1001.<br />
6. Gunning M, O’Loughlin E, Fletcher M, Crilly J, Hooper M, Ellis<br />
DY. Emergency intubation: a prospective multicentre descriptive<br />
audit in an Australian helicopter emergency medical service. Emerg<br />
Med J 2009; 26(1):65-9.<br />
7. Botker MT, Bakke SA, Christensen EF. A systematic review <strong>of</strong><br />
controlled studies: do physicians increase survival with pre-hospital<br />
treatment? Scand J Trauma Resusc Emerg Med 2009; 17(1):12.<br />
8. Dickinson ET, Cohen JE, Mechem CC. The effectiveness <strong>of</strong><br />
midazolam as a single pharmacologic agent to facilitate endotracheal<br />
intubation by paramedics. Prehosp Emerg Care 1999; 3(3):191-3.<br />
9. Bozeman WP, Young S. Etomidate as a sole agent for endotracheal<br />
intubation in <strong>the</strong> pre-hospital air medical setting. Air Med J 2002;<br />
21(4):32-5.<br />
10. Warner KJ, Cuschieri J, Jurkovich GJ, Bulger EM. Single-dose<br />
etomidate for rapid sequence intubation may impact outcome after<br />
severe injury. J Trauma 2009; 67(1):45-50.<br />
11. Swanson ER, Fosnocht DE, Jensen SC. Comparison <strong>of</strong> etomidate<br />
and midazolam for pre-hospital rapid-sequence intubation.<br />
Prehosp Emerg Care 2004; 8(3):273-9.<br />
12. Stevenson AG, Graham CA, Hall R, Korsah P, McGuffie AC.<br />
Tracheal intubation in <strong>the</strong> emergency department: <strong>the</strong> Scottish<br />
district hospital perspective. Emerg Med J 2007; 24(6):394-7.<br />
13. Graham CA, Beard D, Oglesby AJ et al. Rapid sequence intubation<br />
in Scottish urban emergency departments. Emerg Med J 2003;<br />
20(1):3-5.<br />
14. Reid C, Chan L, Tweeddale M. The who, where, and what <strong>of</strong> rapid<br />
sequence intubation: prospective observational study <strong>of</strong> emergency<br />
RSI outside <strong>the</strong> operating <strong>the</strong>atre. Emerg Med J 2004; 21(3):296-<br />
301.<br />
15. Mort TC. Emergency tracheal intubation: complications associated<br />
with repeated laryngoscopic attempts. Anesth Analg 2004;<br />
99(2):607-13.<br />
16. AAGBI. Pre-hospital <strong>Anaes<strong>the</strong>sia</strong>. 2009.<br />
17. NCEPOD. Trauma; who cares? 2007.<br />
294<br />
RJ Dawes, A Mellor<br />
18. Gausche M, Lewis RJ, Stratton SJ et al. Effect <strong>of</strong> out-<strong>of</strong>-hospital<br />
pediatric endotracheal intubation on survival and neurological<br />
outcome: a controlled clinical trial. JAMA 2000; 283(6):783-90.<br />
19. Winchell RJ, Hoyt DB. Endotracheal intubation in <strong>the</strong> field<br />
improves survival in patients with severe head injury. Trauma<br />
Research and Education Foundation <strong>of</strong> San Diego. Arch Surg 1997;<br />
132(6):592-7.<br />
20. Arbabi S, Jurkovich GJ, Wahl WL et al. A comparison <strong>of</strong> prehospital<br />
and hospital data in trauma patients. J Trauma 2004;<br />
56(5):1029-32.<br />
21. Stockinger ZT, McSwain NE, Jr. Pre-hospital endotracheal<br />
intubation for trauma does not improve survival over bag-valvemask<br />
ventilation. J Trauma 2004; 56(3):531-6.<br />
22. Murray JA, Demetriades D, Berne TV et al. Pre-hospital intubation<br />
in patients with severe head injury. J Trauma 2000; 49(6):1065-70.<br />
23. Eckstein M, Chan L, Schneir A, Palmer R. Effect <strong>of</strong> pre-hospital<br />
advanced life support on outcomes <strong>of</strong> major trauma patients. J<br />
Trauma 2000; 48(4):643-8.<br />
24. von Elm E, Schoettker P, Henzi I, Osterwalder J, Walder B. Prehospital<br />
tracheal intubation in patients with traumatic brain<br />
injury: systematic review <strong>of</strong> current evidence. Br J Anaesth 2009;<br />
103(3):371-86.<br />
25. Bulger EM, Copass MK, Sabath DR, Maier RV, Jurkovich GJ.<br />
The use <strong>of</strong> neuromuscular blocking agents to facilitate pre-hospital<br />
intubation does not impair outcome after traumatic brain injury. J<br />
Trauma 2005; 58(4):718-23<br />
26. Wang HE, Davis DP, Wayne MA, Delbridge T. Pre-hospital rapidsequence<br />
intubation--what does <strong>the</strong> evidence show? Proceedings<br />
from <strong>the</strong> 2004 National Association <strong>of</strong> EMS Physicians annual<br />
meeting. Prehosp Emerg Care 2004; 8(4):366-77.<br />
27. Davis DP, Peay J, Serrano JA et al. The impact <strong>of</strong> aeromedical<br />
response to patients with moderate to severe traumatic brain injury.<br />
Ann Emerg Med 2005; 46(2):115-22.<br />
28. Tasker RC, Morris KP, Forsyth RJ, Hawley CA, Parslow RC. Severe<br />
head injury in children: emergency access to neurosurgery in <strong>the</strong><br />
United Kingdom. Emerg Med J 2006; 23(7):519-22.<br />
29. London Severe Injuries Working Group. Modernising Major<br />
Trauma Centres in London. 2001.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S289–294
Prehospital Analgesia: Systematic Review <strong>of</strong><br />
Evidence<br />
CL Park 1 , DE Roberts 2 , DJ Aldington 3 , RA Moore 4<br />
1 Specialist Registrar in Anaes<strong>the</strong>tics, 2 ST4 in Anaes<strong>the</strong>tics & Intensive Care Medicine, St Georges Hospital, London and<br />
<strong>Royal</strong> Air Force; 3 Consultant in Pain Relief, John Radcliffe Hospital, Oxford; 4 Senior Research Fellow, Pain Research,<br />
Nuffield Department <strong>of</strong> Anaes<strong>the</strong>tics, John Radcliffe Hospital Oxford<br />
Abstract<br />
The purpose <strong>of</strong> this systematic review is to investigate current evidence for analgesic use in <strong>the</strong> prehospital environment using<br />
expert military and civilian opinion to determine <strong>the</strong> important clinical questions. There was a high degree <strong>of</strong> agreement<br />
that pain should be no worse than mild, that pain relief be rapid (within 10 minutes), that patients should respond to verbal<br />
stimuli and not require ventilatory support, and that major adverse events should be avoided. Twenty-one studies provided<br />
information about 6,212 patients; <strong>the</strong> majority reported most <strong>of</strong> <strong>the</strong> outcomes <strong>of</strong> interest. With opioids 60-70% <strong>of</strong> patients<br />
still had pain levels above 30/100 mm on a Visual Analogue Scale after 10 minutes, falling to about 30% by 30-40 minutes.<br />
Fascia iliaca blocks demonstrated some efficacy for femoral fractures. No patient on opioids required ventilatory support;<br />
two required naloxone; sedation was rare. Cardiovascular instability was uncommon. Main adverse events were dizziness or<br />
giddiness, and pruritus with opioids. There was little evidence regarding <strong>the</strong> prehospital use <strong>of</strong> ketamine.<br />
Introduction<br />
That analgesia should be provided in <strong>the</strong> pre-hospital<br />
environment has not always been as widely agreed at it is<br />
today. As late as 1981 thinking about pre-hospital analgesia<br />
was different: ‘Any agent that interferes with <strong>the</strong> patient’s normal<br />
pain response may frustrate <strong>the</strong> physician attempting to make<br />
a diagnosis’ and ‘A suitable agent for use by paramedics in prehospital<br />
treatment should be quick-acting and short-lived in<br />
order to preserve <strong>the</strong> pain response for diagnostic purposes in <strong>the</strong><br />
emergency department...‘ [1]. Many studies have shown inability<br />
to provide adequate pre-hospital analgesia [2-4]. Even as<br />
recently as 2000, only 1.8% <strong>of</strong> 1073 patients received any form<br />
<strong>of</strong> pre-hospital analgesia for extremity fractures [5].<br />
Morphine has been used in <strong>the</strong> pre-hospital environment<br />
for many years. There are descriptions <strong>of</strong> its use in <strong>the</strong> midnineteenth<br />
century during <strong>the</strong> Crimean War [6], but <strong>the</strong><br />
expansion in interest in pre-hospital analgesics came in <strong>the</strong> 1970s<br />
with <strong>the</strong> introduction <strong>of</strong> nitrous oxide and oxygen (Entonox),<br />
and <strong>the</strong>n with nalbuphine in <strong>the</strong> 1980s. More opioid drugs have<br />
subsequently become available by more routes <strong>of</strong> administration.<br />
In <strong>the</strong> non-opioid category, ketamine is <strong>of</strong>ten suggested for use<br />
in <strong>the</strong> pre-hospital environment.<br />
No systematic review <strong>of</strong> <strong>the</strong> available evidence has been<br />
published previously, although reviews have summarised<br />
options available for pre-hospital analgesia [7-9]. Most notable<br />
was a literature search for all available evidence using levels <strong>of</strong><br />
evidence [9]. Studies found at that time were limited and mainly<br />
descriptive, and <strong>the</strong> review described options available from <strong>the</strong><br />
various studies, ra<strong>the</strong>r than extracting data on efficacy and harm.<br />
Providing pre-hospital analgesia is not a simple matter; <strong>the</strong>re<br />
are a number <strong>of</strong> issues. These include <strong>the</strong> skills and knowledge <strong>of</strong><br />
<strong>the</strong> analgesic provider; if <strong>the</strong> provider is well versed in pre-hospital<br />
care (including appropriate intravenous access and ventilatory<br />
Corresponding Author: Dr RA Moore, Pain Research,<br />
Nuffield Department <strong>of</strong> Anaes<strong>the</strong>tics, University <strong>of</strong> Oxford,<br />
Level 6, West Wing, John Radcliffe Hospital OX3 9DU, UK<br />
Tel: 01865 231512 Fax: 01865 234539<br />
Email: andrew.moore@nda.ox.ac.uk<br />
support) <strong>the</strong> options are very different from those where <strong>the</strong><br />
provider has limited medical knowledge and skills. The location<br />
and type <strong>of</strong> o<strong>the</strong>r medical support may make a difference; if<br />
one is several days away from any medical help and specialised<br />
monitoring <strong>the</strong> options are different from those where <strong>the</strong>se may<br />
be less than an hour away. The type <strong>of</strong> injury is important; an<br />
isolated closed limb injury will <strong>of</strong>ten require a different approach<br />
from multiple injuries associated with massive tissue disruption,<br />
hypovolaemia and hypo<strong>the</strong>rmia.<br />
All <strong>of</strong> <strong>the</strong>se issues, and o<strong>the</strong>rs not detailed here, will affect<br />
choice <strong>of</strong> pre-hospital analgesic. Practical considerations are<br />
likely to outweigh academic ideals, but consideration <strong>of</strong> evidence<br />
<strong>of</strong> effectiveness or harm is important in ei<strong>the</strong>r case. One <strong>of</strong> <strong>the</strong><br />
drivers for this is <strong>the</strong> increasing number <strong>of</strong> buccal, sublingual and<br />
nasal opiates available, notably fentanyl, as well as increasing use<br />
<strong>of</strong> ketamine. While most <strong>of</strong> <strong>the</strong>se are usually licensed for cancer<br />
breakthrough pain <strong>the</strong>y may appear attractive to <strong>the</strong> pre-hospital<br />
care provider.<br />
The purpose <strong>of</strong> this systematic review is to investigate current<br />
evidence for analgesics in <strong>the</strong> pre-hospital environment.<br />
Methods<br />
We searched Medline (PubMed) and EMBASE using free<br />
text terms <strong>of</strong> pre-hospital pain relief, pre-hospital analgesia,<br />
and wilderness analgesia, alone and with individual drug names<br />
(morphine, fentanyl, etc) and routes (intravenous, intramuscular,<br />
intranasal, lollipop, oral, transmucosal, regional techniques<br />
etc). Reference lists from reviews and papers retrieved were also<br />
examined for possible inclusion. No language exclusion applied<br />
and <strong>the</strong> date <strong>of</strong> last search was November 2009.<br />
Any study, <strong>of</strong> any design, providing efficacy or adverse<br />
event results concerning pre-hospital analgesia was included<br />
if it reported results in adults. Studies were excluded if <strong>the</strong>y<br />
contained no numerical results, were not original studies, or<br />
were actually performed only in hospital. We also excluded<br />
studies involving nalbuphine [10 – 14] which is not now<br />
available in <strong>the</strong> UK, but did include a study on methoxyflurane<br />
[15] because it is used extensively by <strong>the</strong> Australasian military<br />
and civilian emergency services.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S295–300 295
Pre-hospital analgesia<br />
Data extraction was guided by a Delphi process, in which UK<br />
military emergency medicine and anaes<strong>the</strong>tic consultants were<br />
asked about criteria for an ideal pre-hospital analgesic, as well<br />
as civilian doctors involved with helicopter emergency services<br />
in sou<strong>the</strong>rn England. Their comments were used to determine<br />
which patient outcomes would be sought from included studies,<br />
for both efficacy and adverse events. They were asked whe<strong>the</strong>r<br />
<strong>the</strong>y agreed or disagreed with <strong>the</strong> following statements regarding<br />
adequacy <strong>of</strong> outcomes:<br />
1. Pain score <strong>of</strong>
Pre-hospital analgesia CL Park, DE Roberts, DJ Aldington et al<br />
Figure 1: Flow <strong>of</strong> references identified for <strong>the</strong> systematic review<br />
reviews (1,030 patients [36] and 2,129 patients [33]) both looking<br />
mainly at adverse events ra<strong>the</strong>r than pain scores and effectiveness.<br />
Delphi responses<br />
Forty <strong>of</strong> <strong>the</strong> military anaes<strong>the</strong>tic and emergency medicine<br />
consultants responded to <strong>the</strong> Delphi exercise, as well as 16<br />
civilian air ambulance doctors; <strong>the</strong>re was good agreement (Table<br />
2). There was a high degree <strong>of</strong> agreement that analgesia pain<br />
should be no worse than mild [16], that pain relief should be<br />
rapid (within 10 minutes), that patients should respond to<br />
verbal stimuli, not require ventilation, and that major adverse<br />
events should be avoided.<br />
They were also given an opportunity to make additional<br />
comments about what <strong>the</strong>y would find important in pre-hospital<br />
analgesia. These were concerned mainly with issues <strong>of</strong> adverse<br />
events, typically <strong>the</strong> severity <strong>of</strong> events like nausea and vomiting,<br />
and whe<strong>the</strong>r cardiovascular stability should also be a criterion<br />
for choosing pre-hospital analgesia. Civilian physicians were<br />
more accepting <strong>of</strong> possible adverse events in order to obtain high<br />
quality analgesia.<br />
Analgesic failure and timing<br />
The majority <strong>of</strong> included studies reported most <strong>of</strong> <strong>the</strong> outcomes<br />
<strong>of</strong> interest. Least <strong>of</strong>ten reported were <strong>the</strong> timing <strong>of</strong> analgesia<br />
(within 10-20 minutes; 10/21 studies) and <strong>the</strong> extent <strong>of</strong> analgesia<br />
(14/21). Need for ventilatory support, sedation, and adverse<br />
events were reported in 20/21 studies (Table 1).<br />
Many studies provided average pain scores, usually with a<br />
standard deviation. Initial average pain scores were above 60/100<br />
mm or equivalent, and typically 80/100 mm. After treatment,<br />
pain scores were usually lower, typically averaging 30-40/100<br />
mm, but with standard deviations almost as large as <strong>the</strong> average,<br />
indicating large disparity between individuals. These data were<br />
unhelpful in determining failure rate, but did indicate that<br />
analgesic failure was occurring.<br />
Some studies on opioids [17, 19 – 21, 23 – 27, 33 – 34] provided<br />
information on <strong>the</strong> proportion <strong>of</strong> patients achieving analgesic<br />
success and failure. Figure 2 shows <strong>the</strong> failure rates (pain ≥30/100<br />
mm) between 10 and 40 minutes after treatment with intravenous<br />
morphine, fentanyl, and tramadol, and transmucosal fentanyl.<br />
After 10 minutes, about 60-70% <strong>of</strong> patients still had pain levels<br />
above 30/100 mm, but by 30-40 minutes this had fallen to about<br />
30%. There was no obvious difference between opioid chosen in<br />
Military<br />
(n=40)<br />
Number Question Agree<br />
(%)<br />
1 Pain score <strong>of</strong> < 30/100 mm on<br />
VAS (or equivalent) achieved<br />
Civilian<br />
(n=16)<br />
this limited data set (Figure 2), and each study used different dose<br />
levels and dosing schedules. Failure rates on arrival at hospital were<br />
reported as 43% [17] and 17% [19], both involving battle injuries.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S295–300 297<br />
Agree<br />
(%)<br />
68 56<br />
2 Rapid onset <strong>of</strong> action. Pain<br />
relief achieved within:<br />
5 minutes 72 100<br />
10 minutes<br />
23<br />
15 minutes<br />
3<br />
20 minutes<br />
3<br />
3 Patients should remain<br />
responsive to verbal stimuli<br />
100 75<br />
4 Patient should not require<br />
any airway manoeuvres<br />
or ventilatory support to<br />
be performed following<br />
administration<br />
5 Absence <strong>of</strong> any harmful<br />
adverse events following<br />
administration<br />
97 88<br />
92 88<br />
Table 2: Results <strong>of</strong> <strong>the</strong> Delphi exercise – replies from 40 military<br />
anaes<strong>the</strong>tic and emergency medicine consultants and 16 civilian<br />
helicopter emergency service doctors<br />
Figure 2: Failure rates (pain greater than 30mm) between 10 and<br />
40 minutes after treatment with intravenous morphine (white),<br />
fentanyl (light gray), and tramadol (dark gray), and transmucosal<br />
fentanyl (black); <strong>the</strong> larger <strong>the</strong> circle’s diameter <strong>the</strong> larger <strong>the</strong><br />
number in <strong>the</strong> study.
Pre-hospital analgesia<br />
298<br />
Drug<br />
and route<br />
Number<br />
<strong>of</strong> patients<br />
IV morphine 815 Hypoventilation<br />
(3);only 1 treated<br />
with naloxone<br />
IV fentanyl 2224 Reduced respiratory<br />
rate or saturation<br />
(3), 1 given<br />
naloxone but no<br />
ventilatory support<br />
Transmucosal<br />
fentanyl<br />
Intranasal<br />
fentanyl<br />
Ventilatory support Sedation Nausea (N) &<br />
vomiting (V)<br />
22 Hypoventilation (1)<br />
given naloxone<br />
127 Reduced respiratory<br />
rate or saturations<br />
(7), none needed<br />
ventilatory support<br />
Fascia iliaca blocks demonstrated some efficacy for femoral<br />
fractures. Though some pain relief was noted after 10 minutes, low<br />
levels <strong>of</strong> analgesic failure were noted at later times, with 26/27 with<br />
mild pain on arrival at hospital [28], and 30-minute pain scores<br />
averaging below 30/100 mm [29]. For inhalational analgesia, three<br />
studies with 1550 patients using Entonox reported 30% marked<br />
or complete pain relief on arrival at emergency department, with<br />
53% partial, and 8% with mild or no relief [30-32]. Pain returned<br />
when gas was stopped. Inhalational methoxyflurane produced<br />
mean scores <strong>of</strong> 35/100 mm after 20 minutes in 83 patients [15].<br />
Table 3 shows <strong>the</strong> number <strong>of</strong> cases <strong>of</strong> need for ventilatory<br />
support, sedation, nausea and vomiting, and cardiovascular<br />
instability reported, as well as o<strong>the</strong>r adverse events recorded.<br />
Among opioids, <strong>the</strong> pattern <strong>of</strong> reporting was quite similar, though<br />
it was notable that no patient required ventilatory support and<br />
only two patients required naloxone. Sedation was rarely a problem<br />
3 Nausea (20),<br />
Vomiting (8),<br />
N & V (16)<br />
4 Nausea (6),<br />
vomiting (3)<br />
0 Nausea (3),<br />
vomiting (2)<br />
Cardiovascular<br />
instability<br />
↓ BP (9), no<br />
support given<br />
↓ BP (9), no<br />
support given<br />
0 Nausea (9) ↓ BP (8), no<br />
support given<br />
CL Park, DE Roberts, DJ Aldington et al<br />
O<strong>the</strong>r<br />
Pruritus (4), dizziness (5),<br />
dysphoria (1), fatigue (1),<br />
rash (1)<br />
Dysphoria (1)<br />
None Pruritus (5), light headed<br />
(2)<br />
IV alfentanil 16 0 0 Nausea (1) 0 Dizzy (4)<br />
IV tramadol 154 0 0 Nausea (40),<br />
vomiting (6)<br />
0 Dizzy (8)<br />
IV ketamine 870 0 0 0 0 Dizzy (3)<br />
IV pentazocine 9 0 9 0 0 0<br />
Sleepy/dizzy(5), bad taste<br />
(5), irritated throat (2),<br />
watery eyes (2), congestion<br />
(2), chest tightness (1),<br />
dysphoria (1)<br />
Fascia iliaca 79 0 0 0 0 Rapid absorption <strong>of</strong> local<br />
anaes<strong>the</strong>tic leading to<br />
headache, tachycardia, and<br />
increased BP (1)<br />
Inhalational<br />
Entonox<br />
Inhalational<br />
methoxyflurane<br />
1555 0 3 Nausea (15),<br />
N&V (69)<br />
83 0 Increased<br />
sedation<br />
score (29)<br />
0 Dizzy/light headed (177),<br />
drowsy (123), excitement<br />
(44), giddy (16), amnesia,<br />
numbness and headache<br />
(16)<br />
Nausea (7) 0 Euphoria (3), dizzy (2),<br />
headache (1), hallucinations<br />
(1), sore throat and lip<br />
paraes<strong>the</strong>sia (1)<br />
Table 3: Adverse events recorded according to treatment used. The numbers quoted are <strong>the</strong> number <strong>of</strong> patients with each adverse event.<br />
with any opioid treatment at <strong>the</strong> doses used. Nausea and vomiting<br />
were more frequent with intravenous tramadol and inhalational<br />
Entonox, but <strong>the</strong> severity was not mentioned. Cardiovascular<br />
instability again was uncommon, with a few instances <strong>of</strong> reduced<br />
blood pressure without necessity <strong>of</strong> intervention. O<strong>the</strong>r adverse<br />
events were mainly dizziness or giddiness, with <strong>the</strong> expected<br />
pruritus with opioids. Excitement experienced with Entonox was<br />
unexplained [30].<br />
Discussion<br />
The absence <strong>of</strong> evidence was <strong>the</strong> clearest outcome <strong>of</strong> this review,<br />
despite a broad search strategy and inclusion criteria, with 21<br />
studies and over 6,000 patients included. At least 11 different<br />
interventions were tested and outcomes used limited how much<br />
could usefully be adduced for any one <strong>of</strong> <strong>the</strong>m. There were no<br />
clear winners between <strong>the</strong> opioids, although fentanyl tended to<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S295–300
Pre-hospital analgesia CL Park, DE Roberts, DJ Aldington et al<br />
give <strong>the</strong> impression <strong>of</strong> being a good agent albeit with only a small<br />
sample, and a relatively large oral/transmucosal dose <strong>of</strong> 1,600 µg<br />
which is not without adverse effects [19].<br />
Despite early onset <strong>of</strong> analgesia being a desired outcome <strong>of</strong><br />
military and civilian physicians, <strong>the</strong> clear tendency was for up to<br />
30 minutes to be required for <strong>the</strong> proportion <strong>of</strong> patients with<br />
good analgesia to reach a maximum. It is also <strong>of</strong> interest to note<br />
<strong>the</strong> absence <strong>of</strong> efficacy data for <strong>the</strong> use <strong>of</strong> ketamine in <strong>the</strong> prehospital<br />
environment, despite its widely accepted use in this<br />
environment by both military and civilian practitioners. Fascia<br />
iliaca blocks showed great promise but are probably <strong>of</strong> limited use<br />
beyond analgesia for fractured femurs [28-29]. Finally, Entonox<br />
was characterised with a relatively high proportion <strong>of</strong> complete<br />
or partial failures while using <strong>the</strong> gas (53% partial, and 8% with<br />
mild or no relief) and with pain recurring within minutes <strong>of</strong><br />
stopping <strong>the</strong> gas [30-32].<br />
While <strong>the</strong> propensity <strong>of</strong> NSAIDs to increase bleeding and<br />
possible renal complications were an obvious reason why<br />
this class <strong>of</strong> drug has not been tested, it was less clear why<br />
cyclooxygenase-2-inhibitors have been omitted. These drugs<br />
can provide high levels <strong>of</strong> pain relief and long duration <strong>of</strong> action<br />
by virtue <strong>of</strong> a high acute pain dose without increasing bleeding<br />
[37-38]. There is also obvious scope for use <strong>of</strong> paracetamol<br />
and/or analgesic combinations, none <strong>of</strong> which was tested; only<br />
single analgesics were tested alone, and no test <strong>of</strong> multimodal<br />
analgesia was made.<br />
This review used several methodological techniques to<br />
maximise its relevance. These involved systematic searching<br />
and broad acceptance <strong>of</strong> study design, a consensus approach to<br />
desirable outcomes <strong>of</strong> efficacy and harm, and <strong>the</strong> definition <strong>of</strong><br />
analgesic failure as a universal outcome. Moreover, in addition<br />
to electronic searches, retrieved articles were read for any o<strong>the</strong>r<br />
sources <strong>of</strong> data, as were general review articles and book chapters,<br />
because observational studies can be poorly elicited by electronic<br />
searching [39,40].<br />
Although a number <strong>of</strong> reviews have been undertaken<br />
previously, this is, we believe, <strong>the</strong> first attempt at a systematic<br />
review <strong>of</strong> pre-hospital analgesia. As is so <strong>of</strong>ten <strong>the</strong> case, we<br />
found limited evidence without any clear-cut answer. It is likely<br />
that considerable valuable information exists as audits and<br />
surveys, but is not published because such methods are generally<br />
considered inferior to randomised trials. While that may be <strong>the</strong><br />
case for explanatory studies about whe<strong>the</strong>r an analgesic works,<br />
it may be less so for pragmatic issues <strong>of</strong> how to use analgesics<br />
<strong>of</strong> proven efficacy to obtain <strong>the</strong> best results in particular clinical<br />
circumstances [41].<br />
This reasoning underpinned <strong>the</strong> broad entry criteria used to<br />
maximise <strong>the</strong> amount <strong>of</strong> available data; restriction to randomised,<br />
double blind trials would have meant excluding 95% <strong>of</strong> <strong>the</strong><br />
patients. We balanced <strong>the</strong> broader inclusion criteria, with many<br />
more patients, against <strong>the</strong> increased possibility <strong>of</strong> bias.<br />
The Delphi study provided outcomes that experienced senior<br />
clinicians considered <strong>of</strong> pragmatic importance. Despite <strong>the</strong><br />
relatively small sample sizes it is still interesting to note that <strong>the</strong><br />
two populations <strong>of</strong> physicians rated analgesic onset and verbal<br />
response somewhat differently. The military tended to recognise<br />
that <strong>the</strong> onset could be slightly delayed if side effects were to<br />
be minimised; civilian physicians were less tolerant <strong>of</strong> delay in<br />
analgesic effect. This difference may be due to experiences <strong>of</strong><br />
treating multiple simultaneous casualties in a hostile environment<br />
ra<strong>the</strong>r than single casualties in a relatively benign environment.<br />
This dichotomy is important, since <strong>the</strong> only way <strong>of</strong> achieving<br />
rapid onset <strong>of</strong> analgesia, certainly with opiates, is by using<br />
relatively high doses with increased risks <strong>of</strong> adverse effects. Even<br />
<strong>the</strong> use <strong>of</strong> inhalational agents, which may provide a suitably rapid<br />
onset, may be expected to be associated with troublesome side<br />
effects such as <strong>the</strong> excitement <strong>of</strong> Entonox or <strong>the</strong> sedation with<br />
methoxyflurane.<br />
Most, but not all, physicians agreed that a pain score <strong>of</strong> below<br />
30/100 mm (mild pain, 1/3 numeric rating scale) was a desirable<br />
analgesic outcome. We chose this because it has been shown to be a<br />
consistent border between verbal and VAS scales [16], and because<br />
anything more than mild pain could reasonably be described as<br />
uncontrolled or unacceptable. Many studies reported average<br />
pain scores, but <strong>the</strong> wide standard deviations demonstrated how<br />
differently individuals had recorded <strong>the</strong>ir pain, indicating that <strong>the</strong><br />
average response was perhaps experienced only by a few. Future<br />
studies should consider reporting information on individuals,<br />
particularly after defining what constitutes analgesic or o<strong>the</strong>r<br />
failure. The failure rate <strong>the</strong>n becomes <strong>the</strong> primary outcome <strong>of</strong> any<br />
study <strong>of</strong> any design.<br />
The large number <strong>of</strong> options available for scoring pain, from<br />
100 mm visual analogue scale to 0-3 numerical rating scale, with<br />
<strong>the</strong>ir many variants, is a potential confusing factor. Teasing apart<br />
<strong>the</strong> effects <strong>of</strong> variation in dose levels and dosing schedules will<br />
always be difficult, but a simple scoring system may enable a<br />
clearer recognition <strong>of</strong> clinically significant differences between<br />
techniques. That should be <strong>the</strong> goal, ra<strong>the</strong>r than being lost in<br />
statistical differences <strong>of</strong> dubious clinical relevance. The military<br />
rule since 2008, has been to use <strong>the</strong> simpler 0-3 scale equating to<br />
no pain, mild, moderate, and severe pain [42].<br />
There is no obvious guidance from <strong>the</strong> evidence available.<br />
More, better, and better thought out research is needed, and<br />
this review suggests some ways in which that could be achieved;<br />
publication <strong>of</strong> surveys and audits <strong>of</strong> appropriate quality would<br />
help. Given <strong>the</strong> paucity <strong>of</strong> information and <strong>the</strong> extreme variation<br />
in patients, providers, and environments, <strong>the</strong> pragmatic advice<br />
would be to take heed <strong>of</strong> <strong>the</strong> title <strong>of</strong> Ella Fitzgerald’s 1939 song:<br />
“T’aint what you do (It’s <strong>the</strong> way that you do it)”, and <strong>the</strong>n find<br />
ways <strong>of</strong> doing it better.<br />
Disclaimer<br />
The views expressed in this work are those <strong>of</strong> <strong>the</strong> authors and<br />
are not necessarily those <strong>of</strong> <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services nor <strong>the</strong><br />
Ministry <strong>of</strong> <strong>Defence</strong>.<br />
Conflict <strong>of</strong> interest statement<br />
DJ Aldington and R A Moore have been consultants for various<br />
pharmaceutical companies and members <strong>of</strong> scientific and clinical<br />
advisory boards, <strong>the</strong>y have received speakers’ fees, participated in<br />
meetings supported by unrestricted grants from industry, and have<br />
received sponsored research funding from several companies. RAM<br />
is funded by NIHR Biomedical Research Centre Programme. All<br />
authors state that none <strong>of</strong> <strong>the</strong>se declarations presents a conflict <strong>of</strong><br />
interest in relation to <strong>the</strong> content <strong>of</strong> this review.<br />
References<br />
1. Amey BD, Ballinger JA, Harrison EE. Pre-hospital administration <strong>of</strong><br />
nitrous oxide for control <strong>of</strong> pain. Ann Emerg Med 1981; 10: 247-51.<br />
2. Hyland-McGuire P, Guly HR. Effects on patient care <strong>of</strong> introducing<br />
pre-hospital intravenous nalbuphine hydrochloride. J Acc Emerg<br />
Med 1998; 15: 99-101.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S295–300 299
Pre-hospital analgesia<br />
3. Hennes H, Kim MK, Pirrallo RG. Pre-hospital pain management:<br />
a comparison <strong>of</strong> providers’ perceptions and practices. Pre-hosp<br />
Emerg Care 2005; 9: 32<br />
4. McEachin CC, McDermott JT, Swor R. Few emergency medical<br />
services patients with lower-extremity fractures receive pre-hospital<br />
analgesia. Pre-hosp Emerg Care 2002; 6: 406-10.<br />
5. White LJ, Cooper JD, Chambers RM, Gradisek RE. Pre-hospital<br />
use <strong>of</strong> analgesia for suspected extremity fractures. Pre-hosp Emerg<br />
Care 2000; 4: 205-8.<br />
6. Gaunt C, Gill J, Aldington D. British military use <strong>of</strong> morphine: a<br />
historical review. JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155: 46-9.<br />
7. Thomas SH, Shewakramani S. Pre-hospital trauma analgesia. J<br />
Emerg Med 2008; 35: 47-57.<br />
8. Mackenzie R. Analgesia And Sedation. JR <strong>Army</strong> Med <strong>Corps</strong> 2004;<br />
150: 45-55.<br />
9. Borland ML, Jacobs I, Rogers IR. Options in pre-hospital analgesia.<br />
Emerg Med (Fremantle) 2002; 14: 77-84.<br />
10. Stene JK, St<strong>of</strong>berg L, MacDonald G, Myers RA, Ramzy A, Burns<br />
B. Nalbuphine analgesia in <strong>the</strong> pre-hospital setting. Am J Emerg<br />
Med 1988; 6: 634-9.<br />
11. Chambers JA, Guly HR. Pre-hospital intravenous nalbuphine<br />
administered by paramedics. Resuscitation 1994; 27: 153-8.<br />
12. Gray A, Johnson G, Goodacre S. Paramedic use <strong>of</strong> nalbuphine in<br />
major injury. Eur J Emerg Med 1997; 4: 136-9.<br />
13. Houlihan KP, Mitchell RG, Flapan AD, Steedman DJ. Excessive<br />
morphine requirements after pre-hospital nalbuphine analgesia. J<br />
Accid Emerg Med 1999; 16: 29-31.<br />
14. Robinson N, Burrows N. Excessive morphine requirements after<br />
pre-hospital nalbuphine analgesia. J Accid Emerg Med 1999; 16:<br />
392.<br />
15. Buntine P, Thom O, Babl F, Bailey M, Bernard S. Pre-hospital<br />
analgesia in adults using inhaled methoxyflurane. Emerg Med<br />
Austral 2007; 19: 509-14.<br />
16. Collins SL, Moore RA, McQuay HJ. The visual analogue pain<br />
intensity scale: what is moderate pain in millimetres? Pain 1997;<br />
72: 95-7.<br />
17. Beecher HK. Pain in men wounded in battle. Ann Surg 1946; 123:<br />
96-105.<br />
18. Bion JF. Infusion analgesia for acute war injuries. A comparison <strong>of</strong><br />
pentazocine and ketamine. <strong>Anaes<strong>the</strong>sia</strong> 1984; 39: 560-4.<br />
19. Kotwal RS, O’Connor KC, Johnson TR, Mosely DS, Meyer<br />
DE, Holcomb JB. A novel pain management strategy for combat<br />
casualty care. Ann Emerg Med 2004; 44: 121-7.<br />
20. Bounes V, Charpentier S, Houze-Cerfon CH, Bellard C, Ducassé<br />
JL. Is <strong>the</strong>re an ideal morphine dose for pre-hospital treatment <strong>of</strong><br />
severe acute pain? A randomized, double-blind comparison <strong>of</strong> 2<br />
doses. Am J Emerg Med 2008; 26: 148-54.<br />
21. Galinski M, Dolveck F, Borron SW et al. A randomized, doubleblind<br />
study comparing morphine with fentanyl in pre-hospital<br />
analgesia. Am J Emerg Med 2005; 23: 114-9.<br />
22. Silfvast T, Saarnivaara L. Comparison <strong>of</strong> alfentanil and morphine<br />
in <strong>the</strong> pre-hospital treatment <strong>of</strong> patients with acute ischaemic-type<br />
chest pain. Eur J Emerg Med 2001; 8: 275-8.<br />
23. Vergnion M, Degesves S, Garcet L, Magotteaux V. Tramadol, an<br />
alternative to morphine for treating posttraumatic pain in <strong>the</strong> prehospital<br />
situation. Anesth Analg 2001; 92: 1543-6.<br />
300<br />
CL Park, DE Roberts, DJ Aldington et al<br />
24. Rickard C, O’Meara P, McGrail M, Garner D, McLean A, Le<br />
Lievre P. A randomized controlled trial <strong>of</strong> intranasal fentanyl vs<br />
intravenous morphine for analgesia in <strong>the</strong> pre-hospital setting. Am<br />
J Emerg Med 2007; 25: 911-7.<br />
25. Bruns BM, Dieckmann R, Shagoury C, Dingerson A, Swartzell C.<br />
Safety <strong>of</strong> pre-hospital <strong>the</strong>rapy with morphine sulfate. Am J Emerg<br />
Med 1992; 10: 53-7.<br />
26. Ricard-Hibon A, Belpomme V, Chollet C et al. Compliance with<br />
a morphine protocol and effect on pain relief in out-<strong>of</strong>-hospital<br />
patients. J Emerg Med 2008; 34: 305-10.<br />
27. Ward ME, Radburn J, Morant S. Evaluation <strong>of</strong> intravenous<br />
tramadol for use in <strong>the</strong> pre-hospital situation by ambulance<br />
paramedics. Pre-hosp Disast Med 1997; 12: 158-62.<br />
28. Lopez S, Gros T, Bernard N, Plasse C, Capdevila X. Fascia iliaca<br />
compartment block for femoral bone fractures in pre-hospital care.<br />
Reg Anesth Pain Med 2003; 28: 203-7.<br />
29. Gozlan C, Minville V, Asehnoune K, Raynal P, Zetlaoui P,<br />
Benhamou D. Fascia iliaca block for femoral bone fractures in prehospital<br />
medicine. Ann Francaises d’Anes<strong>the</strong>sie et de Reanimation<br />
2005; 24: 617-20.<br />
30. McKinnon KD. Pre-hospital analgesia with nitrous oxide/oxygen.<br />
Can Med Assoc J 1981; 125: 836-40.<br />
31. Stewart RD, Paris PM, Stoy WA, Cannon G. Patient-controlled<br />
inhalational analgesia in pre-hospital care: a study <strong>of</strong> side-effects<br />
and feasibility. Crit Care Med 1983; 11: 851-5.<br />
32. Donen N, Tweed WA, White D, Guttormson B, Enns J. Prehospital<br />
analgesia with Entonox. Can Anaesth Soc J 1982; 29: 275-<br />
9.<br />
33. Kanowitz A, Dunn TM, Kanowitz EM, Dunn WW, Vanbuskirk K.<br />
Safety and effectiveness <strong>of</strong> fentanyl administration for pre-hospital<br />
pain management. Pre-hosp Emerg Care 2006; 10: 1-7.<br />
34. Thomas SH, Rago O, Harrison T, Biddinger PD, Wedel SK.<br />
Fentanyl trauma analgesia use in air medical scene transports. J<br />
Emerg Med 2005; 29: 179-87.<br />
35. Svenson JE, Abernathy MK. Ketamine for pre-hospital use: new<br />
look at an old drug. Am J Emerg Med 2007; 25: 977-80.<br />
36. Bredmose PP, Lockey DJ, Grier G, Watts B, Davies G. Pre-hospital<br />
use <strong>of</strong> ketamine for analgesia and procedural sedation. Emerg Med<br />
J 2009; 26: 62-4.<br />
37. Ouellet. Ibupr<strong>of</strong>en inhibits platelets more than etoricoxib (in<br />
vitro) Proc Nat Acad Sci 2001; 98: 14583-8<br />
38. Dallob A, Hawkey CJ, Greenberg H et al. Characterization <strong>of</strong><br />
etoricoxib, a novel, selective COX-2 inhibitor. J Clin Pharmacol<br />
2003; 43: 573-85.<br />
39. D Schwartz, J Lellouch. Explanatory and pragmatic attitudes in<br />
<strong>the</strong>rapeutical trials. J Chron Dis 1967; 20: 637–48.<br />
40. Lemeshow AR, Blum RE, Berlin JA, Stoto MA, Colditz GA.<br />
Searching one or two databases was insufficient for meta-analysis <strong>of</strong><br />
observational studies. J Clin Epidem 2005; 58: 867-873.<br />
41. Ruppen W, Derry S, McQuay H, Moore RA. Incidence <strong>of</strong> epidural<br />
hematoma, infection, and neurologic injury in obstetric patients<br />
with epidural analgesia/anes<strong>the</strong>sia. Anes<strong>the</strong>siology 2006; 105 :394-<br />
399.<br />
42. Looker J, Aldington D. Pain scores--as easy as counting to three. J<br />
R <strong>Army</strong> Med <strong>Corps</strong> 2009; 155: 42-3.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S295–300
Total Intravenous <strong>Anaes<strong>the</strong>sia</strong> for War Surgery<br />
S Lewis 1 , S Jagdish 2<br />
1 Specialist Registrar in <strong>Anaes<strong>the</strong>sia</strong> & Critical Care, St George’s Healthcare NHS Trust, London; 2 Associate Specialist in<br />
<strong>Anaes<strong>the</strong>sia</strong>, 33 Field Hospital, Gosport & Chief <strong>of</strong> Staff, Dept <strong>of</strong> Military <strong>Anaes<strong>the</strong>sia</strong>, Pain & Critical Care<br />
Abstract<br />
Total Intravenous <strong>Anaes<strong>the</strong>sia</strong> (TIVA) and Target-Controlled Infusion (TCI) <strong>of</strong> anaes<strong>the</strong>sia are techniques that have benefited<br />
from recent advances in microprocessor technology and drug design. Though dependant on technology, <strong>the</strong>y <strong>of</strong>fer significant<br />
clinical benefits and logistic advantages. Manipulation <strong>of</strong> complex data derived from population pharmacokinetics has enabled<br />
greater understanding <strong>of</strong> drug handling models, thus enabling individual patient titration <strong>of</strong> anaes<strong>the</strong>sia. This has also informed<br />
manual techniques <strong>of</strong> intravenous anaes<strong>the</strong>sia. These approaches constitute a useful and logical alternative in <strong>the</strong> field, both in<br />
austere circumstances as well as <strong>the</strong> more established deployed setting. The pharmacodynamics and pharmacokinetics <strong>of</strong> potent<br />
intravenous anaes<strong>the</strong>sia agents in <strong>the</strong> complex combat trauma patient require continued examination.<br />
Introduction<br />
Total Intravenous <strong>Anaes<strong>the</strong>sia</strong> (TIVA) describes <strong>the</strong> technique<br />
<strong>of</strong> inducing and maintaining anaes<strong>the</strong>sia purely by intravenous<br />
means. The use <strong>of</strong> Volatile Gas <strong>Anaes<strong>the</strong>sia</strong> (VGA) is consequently<br />
avoided. Agents are delivered ei<strong>the</strong>r by infusion or bolus to achieve<br />
<strong>the</strong> desired balance <strong>of</strong> hypnosis, analgesia and muscle relaxation.<br />
TIVA for war surgery can be traced back to <strong>the</strong> use <strong>of</strong><br />
barbiturates during <strong>the</strong> Spanish Civil War (1936-9). Despite<br />
being associated with an increased mortality rate in casualties<br />
<strong>of</strong> <strong>the</strong> attack at Pearl Harbour [1] (a proposition that has since<br />
been challenged [2]), British military anaes<strong>the</strong>tists successfully<br />
employed continuous thiopentone anaes<strong>the</strong>sia during World War<br />
II [3]. The use <strong>of</strong> ketamine during <strong>the</strong> Falklands conflict informed<br />
<strong>the</strong> development <strong>of</strong> TIVA regimes [4] and in <strong>the</strong> first Gulf War,<br />
fur<strong>the</strong>r examples <strong>of</strong> TIVA were described [5, 6]. Advances in<br />
pharmacology and technology continue to inform and help refine<br />
its use in current conflicts. Table 1 outlines <strong>the</strong> areas in which<br />
TIVA is employed by <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services (DMS).<br />
Pre-hospital care<br />
Role 2/Role 3<br />
surgical facilities<br />
Sedation<br />
During strategic<br />
transfer<br />
Role 4 hospitals<br />
During tactical transfer <strong>of</strong> intubated<br />
patients to <strong>the</strong> Field Hospital by <strong>the</strong><br />
<strong>Medical</strong> Emergency Response Team<br />
(MERT)<br />
As a substitute for <strong>the</strong> more traditional<br />
VGA<br />
For intubated patients on <strong>the</strong> Intensive<br />
Care Unit (ICU) and during transfers to<br />
CT scan<br />
For sedation <strong>of</strong> intubated patients to<br />
role 4 by RAF Critical Care Air Support<br />
Teams (CCAST)<br />
For fur<strong>the</strong>r surgical procedures (e.g.<br />
wound wash outs, second looks,<br />
reconstructive surgery)<br />
Table 1. Operational areas in which TIVA is employed<br />
Corresponding Author: Major S Lewis RAMC; C/O <strong>Army</strong><br />
<strong>Medical</strong> Directorate Support Unit, The Former <strong>Army</strong> Staff<br />
College, Slim Road, Camberley, Surrey GU15 4NP<br />
E-mail: drselewis@googlemail.com<br />
Comparison <strong>of</strong> TIVA against VGA for War Surgery<br />
TIVA possesses certain desirable features for war surgery when<br />
compared with VGA and <strong>the</strong>se are described below, followed by<br />
potential disadvantages.<br />
Advantages <strong>of</strong> TIVA<br />
Small Logistic Footprint<br />
Deployed surgical teams work in austere conditions at <strong>the</strong> end <strong>of</strong><br />
a long supply chain and must be prepared to move at short notice.<br />
Traditional anaes<strong>the</strong>tic machines are bulky, difficult to transport<br />
and require compressed oxygen and a power source to function.<br />
A method <strong>of</strong> waste gas disposal is also required. This is in contrast<br />
to a single programmable syringe driver, which can be carried in<br />
<strong>the</strong> pocket <strong>of</strong> a rucksack with space for additional batteries [7].<br />
Even <strong>the</strong> battle-proven lightweight Tri-Service Apparatus (TSA)<br />
cannot boast this simplicity and is known for its 20 separate tube<br />
connections [8].<br />
Recovery Characteristics<br />
Provision <strong>of</strong> post-operative recovery facilities is highly limited<br />
in a deployed field hospital, both in terms <strong>of</strong> space and trained<br />
personnel. A technique that reduces <strong>the</strong> burden on anaes<strong>the</strong>tic<br />
and recovery staff is beneficial for <strong>the</strong> facility as a whole. Whilst<br />
speed <strong>of</strong> recovery from prop<strong>of</strong>ol-based TIVA may not be<br />
significantly different to that from VGA with <strong>the</strong> newer volatile<br />
agents desflurane and sev<strong>of</strong>lurane, a recent systematic review [9]<br />
found that nausea, vomiting, antiemetic use and headache were<br />
all lowest in <strong>the</strong> prop<strong>of</strong>ol group.<br />
Modulation <strong>of</strong> <strong>the</strong> Stress Response<br />
The stress response to surgery is characterised by increased<br />
sympa<strong>the</strong>tic outflow, immunosuppression and a catabolic state.<br />
Attenuation <strong>of</strong> this response has become a treatment goal <strong>of</strong> perioperative<br />
medicine. Compared with VGA, prop<strong>of</strong>ol-based TIVA<br />
has been shown to delay and reduce <strong>the</strong> rise in IL-6 [10] (a proinflammatory<br />
cytokine) and stress hormone levels [11] in response<br />
to surgery. The clinical benefits <strong>of</strong> this effect, and whe<strong>the</strong>r it exists<br />
in <strong>the</strong> military trauma population, remain to be characterised.<br />
No potential for triggering Malignant Hyper<strong>the</strong>rmia (MH)<br />
MH is a rare but potentially fatal condition that is resource-heavy<br />
to treat. It may be triggered by halogenated volatile agents (or<br />
suxamethonium), but not by TIVA.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S301–307 301
TIVA for War surgery<br />
Continuity <strong>of</strong> anaes<strong>the</strong>sia<br />
The continuity <strong>of</strong> agent delivery with TIVA has benefits both during<br />
and after <strong>the</strong> operative phase. At intubation <strong>the</strong>re is no ‘twilight<br />
period’ as may occur in VGA between <strong>the</strong> <strong>of</strong>fset <strong>of</strong> intravenous<br />
induction agents and <strong>the</strong> onset <strong>of</strong> volatile agents, reducing <strong>the</strong> risk<br />
<strong>of</strong> awareness [12]. Also, intraoperative manipulation <strong>of</strong> <strong>the</strong> airway<br />
will not disrupt <strong>the</strong> delivery <strong>of</strong> anaes<strong>the</strong>tic.<br />
Severely injured patients who have undergone damage<br />
control surgery <strong>of</strong>ten remain intubated in <strong>the</strong> ICU and during<br />
CCAST transfer to Role 4. The sedation required to keep <strong>the</strong>se<br />
patients stable can be delivered by <strong>the</strong> same TIVA infusion<br />
as was used for <strong>the</strong> initial surgery (albeit at a reduced dose).<br />
It makes pharmacological sense to avoid <strong>the</strong> haemodynamic<br />
instability that may arise when one form <strong>of</strong> sedation is changed<br />
for ano<strong>the</strong>r [7].<br />
Disadvantages <strong>of</strong> TIVA<br />
Lack <strong>of</strong> familiarity<br />
All DMS anaes<strong>the</strong>tists are expected to be pr<strong>of</strong>icient in <strong>the</strong> use<br />
<strong>of</strong> TIVA, but are likely to be more familiar with VGA. Opinion<br />
remains divided whe<strong>the</strong>r TIVA is an appropriate technique for use<br />
in <strong>the</strong> cold, shocked, coagulopathic military trauma patient. Some<br />
consider it to be relatively contraindicated during <strong>the</strong> immediate<br />
resuscitation phase and prefer <strong>the</strong> security <strong>of</strong> an end-tidal volatile<br />
agent concentration to titrate delivery <strong>of</strong> a haemodynamically<br />
stable anaes<strong>the</strong>tic.<br />
Perceived risk <strong>of</strong> awareness<br />
With VGA <strong>the</strong> end-tidal volatile agent concentration is measured,<br />
providing an assurance that anaes<strong>the</strong>tic is actually reaching <strong>the</strong><br />
patient. By contrast, unrecognised disconnection and underdosing<br />
are major considerations when using TIVA as <strong>the</strong>re is<br />
no readily available clinical equivalent measure to <strong>the</strong> end-tidal<br />
volatile agent concentration. The closest would be <strong>the</strong> estimated<br />
blood (C p) or effect (C e) site concentration provided by a Target<br />
Controlled Infusion (TCI) pump.<br />
It is advisable to use a dedicated intravenous line for <strong>the</strong> TIVA<br />
infusion that is visible throughout <strong>the</strong> operation.<br />
Neuromuscular blockade increases <strong>the</strong> likelihood <strong>of</strong> awareness<br />
occurring since it prevents patient movement, a useful direct<br />
indication <strong>of</strong> nociception and indirectly one <strong>of</strong> inadequate<br />
anaes<strong>the</strong>sia. With TIVA, <strong>the</strong> use <strong>of</strong> muscle relaxants should be<br />
avoided or minimised where possible. Some advocate <strong>the</strong> use <strong>of</strong> a<br />
small dose <strong>of</strong> midazolam to reduce <strong>the</strong> risk <strong>of</strong> recall <strong>of</strong> awareness.<br />
Despite <strong>the</strong> above, <strong>the</strong> use <strong>of</strong> properly conducted TIVA/TCI is<br />
not associated with increased risk <strong>of</strong> awareness.<br />
Need to service and power infusion pumps<br />
Although TIVA represents a relatively small logistical requirement<br />
when compared with VGA, <strong>the</strong>re is still <strong>the</strong> need to service,<br />
maintain and power infusion pumps. In <strong>the</strong> event <strong>of</strong> pump<br />
failure, TIVA regimes that require only a standard intravenous<br />
giving set have been proposed.<br />
Dependant on intravenous access<br />
By definition, intravenous access is required for TIVA. This<br />
is likely to be difficult in <strong>the</strong> shocked, unresuscitated military<br />
trauma patient where intraosseous access is normally <strong>the</strong> first<br />
technique used. Any drug may be given by this route (e.g. a<br />
bolus <strong>of</strong> ketamine), but an ongoing infusion would require<br />
intravenous access.<br />
302<br />
S Lewis, S Jagdish<br />
Drugs used for TIVA<br />
Drugs available for use by DMS anaes<strong>the</strong>tists for TIVA consist<br />
<strong>of</strong> <strong>the</strong> anaes<strong>the</strong>tic agents prop<strong>of</strong>ol and ketamine. Thiopentone<br />
is available but is a poor choice for TIVA due to its tendency<br />
to accumulate within <strong>the</strong> body. Midazolam may be given by<br />
infusion to provide sedation in critical care patients but would<br />
rarely be used as a sole agent to maintain surgical anaes<strong>the</strong>sia.<br />
Some regimes include infusion <strong>of</strong> an opioid or muscle relaxant.<br />
Prop<strong>of</strong>ol<br />
Prop<strong>of</strong>ol is a phenol derivative that is thought to act by<br />
potentiating inhibitory gamma-aminobutyric acid (GABA)<br />
receptors. It is <strong>the</strong> most commonly used intravenous anaes<strong>the</strong>tic<br />
agent in Western medicine. Features that favour its use for TIVA<br />
in war surgery include:<br />
• Familiarity<br />
• Extensively characterised context-sensitive behaviour<br />
• Low incidence <strong>of</strong> allergy<br />
• Reduction in postoperative nausea and vomiting (consensus<br />
guidelines recommend its use in susceptible patients [13])<br />
Drawbacks to its use include:<br />
• Reduced cardiac output and systemic vascular resistance,<br />
which could be catastrophic in a shocked trauma patient.<br />
Dosage may need to be significantly reduced in such patients.<br />
A study <strong>of</strong> TIVA in a porcine model revealed that after<br />
haemorrhagic shock <strong>the</strong> blood prop<strong>of</strong>ol level increased by<br />
375% in unresuscitated animals [14].<br />
• Vulnerability to temperature damage. Prop<strong>of</strong>ol should<br />
be stored between 4°C and 22°C [15]. A study <strong>of</strong> a US<br />
helicopter drug box found that <strong>the</strong> temperature exceeded<br />
25°C for 37% <strong>of</strong> <strong>the</strong> time during <strong>the</strong> summer [16]. One<br />
author’s experience (SJ) during Operation TELIC was that a<br />
stock <strong>of</strong> prop<strong>of</strong>ol had almost solidified during its presumably<br />
unmonitored journey along <strong>the</strong> supply chain at <strong>the</strong> height <strong>of</strong><br />
an Iraqi summer.<br />
• Pain on injection<br />
Ketamine<br />
Ketamine is an intravenous anaes<strong>the</strong>tic agent derived from<br />
phencyclidine that acts via antagonism <strong>of</strong> N-methyl-D-aspartate<br />
(NMDA) receptors. It has many properties that favour its<br />
use within military and trauma anaes<strong>the</strong>sia, summarised by<br />
Grothwohl [17] as:<br />
• Haemodynamic stability with no evidence <strong>of</strong> human in vivo<br />
myocardial depression)<br />
• Reduced redistribution hypo<strong>the</strong>rmia [18]<br />
• Maintenance <strong>of</strong> protective airway reflexes and respiratory<br />
function<br />
• Bronchodilation<br />
• Maintenance <strong>of</strong> <strong>the</strong> hypoxic pulmonary vasoconstriction reflex<br />
• Analgesic effects (opioid synergy and reduced opioid tolerance)<br />
Concerns over certain side effects have prevented its use becoming<br />
widespread within <strong>the</strong> UK [17]. They include:<br />
• Increased ICP – which is now contested [19], ketamine may<br />
even be neuroprotective [20]<br />
• Psychotropic effects - <strong>the</strong>se may be reduced if benzodiazepines<br />
are used concurrently or as premedication. The S(+)-ketamine<br />
isomer may have reduced psychotropic effects whilst providing<br />
better analgesia than its R(-)-ketamine equivalent [21].<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S301–307
TIVA for War surgery S Lewis, S Jagdish<br />
• Increased salivation and tracheobronchial secretions – <strong>the</strong>se<br />
can be prevented or treated with an antisialogogue such as<br />
glycopyrrolate<br />
• Prolonged recovery time<br />
Recently <strong>the</strong> United States Tri-Services Anes<strong>the</strong>sia Research<br />
Group Initiative on TIVA (TARGIT) conducted a case-matched<br />
retrospective study <strong>of</strong> 214 cases <strong>of</strong> traumatic brain injury using<br />
data from <strong>the</strong>ir Joint Theatre Trauma Registry [22]. It compared<br />
those managed with ketamine-based TIVA against those who<br />
received VGA. They were unable to demonstrate a significant<br />
difference in neurological outcome.<br />
Midazolam<br />
Midazolam is a water-soluble imidazobenzodiazepine that acts<br />
at specific GABA-linked benzodiazepine receptors throughout<br />
<strong>the</strong> CNS. Its main actions are hypnosis, sedation, anxiolysis and<br />
anterograde amnesia. In bolus dose it has a short duration <strong>of</strong><br />
action due to its high lipophilicity (at body pH) and metabolic<br />
clearance. With infusion it may accumulate and elimination halflife<br />
is significantly increased in <strong>the</strong> critically ill patient. There is<br />
also <strong>the</strong> potential for withdrawal phenomena after prolonged<br />
infusion, particularly in children.<br />
In <strong>the</strong> context <strong>of</strong> TIVA for war surgery, midazolam is useful<br />
as an adjunct to a ketamine-based technique. Advantages<br />
include [23]:<br />
• Reduced potential for recall <strong>of</strong> awareness<br />
• Reduced psychotropic effects <strong>of</strong> ketamine<br />
• Reduced postoperative nausea and vomiting<br />
• Muscle relaxation<br />
• Modest cardiorespiratory depression<br />
• Reversibility with flumazenil<br />
Opioids<br />
Opioid infusions are <strong>of</strong>ten used as part <strong>of</strong> a TIVA technique.<br />
Studies examining <strong>the</strong> interaction <strong>of</strong> prop<strong>of</strong>ol and opioids<br />
have demonstrated a reduction in Cp50 [24, 25] (<strong>the</strong> plasma<br />
concentration <strong>of</strong> prop<strong>of</strong>ol required to prevent movement to a<br />
surgical stimulus in 50% <strong>of</strong> subjects – analogous to MAC). This<br />
prop<strong>of</strong>ol-sparing effect is useful as it allows a reduction in <strong>the</strong><br />
amount <strong>of</strong> prop<strong>of</strong>ol administered and thus greater haemodynamic<br />
stability.<br />
Remifentanil is now available to DMS anaes<strong>the</strong>tists and<br />
deserves special mention. It is a syn<strong>the</strong>tic anilidopiperidine that<br />
acts as a pure mu-opioid receptor agonist. It is notable for its<br />
short context-sensitive half time <strong>of</strong> 3-5 minutes, regardless <strong>of</strong> <strong>the</strong><br />
duration <strong>of</strong> infusion. Prop<strong>of</strong>ol TIVA with high-dose remifentanil<br />
provides a clean, rapid recovery that reduces <strong>the</strong> burden on<br />
recovery facilities. The obvious consequence <strong>of</strong> this property is<br />
that remifentanil will make no contribution to post-operative<br />
analgesia.<br />
Future Areas <strong>of</strong> Development<br />
Target Controlled Infusion (TCI) Pumps<br />
TCI pumps employ microprocessor technology to administer<br />
an infusion regimen at rates determined by models derived from<br />
population pharmacokinetics. Modern pharmacokinetic models<br />
are based around a ‘three-compartment model’, where <strong>the</strong> central<br />
compartment represents blood and <strong>the</strong> o<strong>the</strong>r compartments<br />
represent tissues into which <strong>the</strong> drug may distribute. The<br />
momentary drug concentration displayed on <strong>the</strong> device is a<br />
trended estimate, not <strong>the</strong> actual tissue concentration. The threecompartment<br />
model is <strong>the</strong> basis for <strong>the</strong> step changes performed by<br />
<strong>the</strong> TCI device in response to alterations in target concentration<br />
by <strong>the</strong> anaes<strong>the</strong>tist (Figure. 1).<br />
Figure 1: The traditional compartmental model <strong>of</strong> drug distribution<br />
with a continuous intravenous infusion. The effect site (represented by<br />
<strong>the</strong> blue compartment) is a recent addition that allows TCI systems to<br />
target brain concentration <strong>of</strong> drug. This compartment is considered<br />
volumeless for <strong>the</strong> purposes <strong>of</strong> ma<strong>the</strong>matical modelling [26]<br />
A detailed description <strong>of</strong> <strong>the</strong> practical aspects <strong>of</strong> using TCI<br />
techniques is beyond <strong>the</strong> scope <strong>of</strong> this article. However, two aspects<br />
<strong>of</strong> TCI that are central to safe practice are <strong>the</strong> pharmacokinetic<br />
models used and <strong>the</strong> site targeted. They are discussed below.<br />
Pharmacokinetic Models<br />
The two in widest use for prop<strong>of</strong>ol are <strong>the</strong> eponymously named<br />
Marsh and Schnider models. There are significant differences<br />
between <strong>the</strong>m. The volume <strong>of</strong> <strong>the</strong> central compartment (V c)<br />
used in <strong>the</strong> Marsh model is nearly four times greater than that <strong>of</strong><br />
<strong>the</strong> Schnider model. The Schnider model allows for <strong>the</strong> slowed<br />
rate <strong>of</strong> distribution between V c and V 1 (Figure 1). Though<br />
it has been suggested that <strong>the</strong> Marsh model correlates best for<br />
depth <strong>of</strong> anaes<strong>the</strong>sia [27], nei<strong>the</strong>r have been designed for use<br />
specifically in trauma patients. Failing to account for <strong>the</strong> altered<br />
pharmacokinetics <strong>of</strong> a patient with haemorrhagic shock could<br />
lead to dangerous overdosing and circulatory collapse. Reduced<br />
prop<strong>of</strong>ol and opioid requirements in haemorrhagic shock are<br />
thought to be partly due to decreases in central clearance and<br />
central and second compartment volumes <strong>of</strong> distribution [28].<br />
Additionally, <strong>the</strong>se models require patient parameters such as<br />
weight (and height in <strong>the</strong> case <strong>of</strong> <strong>the</strong> Schnider model), which can<br />
only be estimated in <strong>the</strong> immediate stages <strong>of</strong> treatment. This does<br />
not preclude <strong>the</strong> use <strong>of</strong> TCI in trauma patients, but constitutes an<br />
area <strong>of</strong> future research.<br />
Targeting<br />
Recognition <strong>of</strong> <strong>the</strong> need to titrate dosing strategies in order to<br />
influence <strong>the</strong> effect site (i.e. <strong>the</strong> brain) has driven <strong>the</strong> desire to<br />
target <strong>the</strong> effect site concentration. The newer generation <strong>of</strong> TCI<br />
pumps <strong>of</strong>fer <strong>the</strong> ability to target effect site for both prop<strong>of</strong>ol<br />
and remifentanil. The effect site is considered volumeless for <strong>the</strong><br />
purposes <strong>of</strong> ma<strong>the</strong>matical modelling (Figure 1). For prop<strong>of</strong>ol, it<br />
needs to be appreciated that effect site targeting is based on certain<br />
critical suppositions arising from population pharamacokinetics,<br />
thus underlining <strong>the</strong> importance <strong>of</strong> “calibrating” <strong>the</strong> patient<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S301–307 303
TIVA for War surgery<br />
during induction. The benefits <strong>of</strong> utilising effect site targeting<br />
for remifentanil are yet to be determined and given <strong>the</strong> rapid<br />
equilibration achieved by remifentanil, may even be irrelevant.<br />
The case for TCI pumps in <strong>the</strong> DMS<br />
TCI pumps are not yet available to DMS anaes<strong>the</strong>tists, although<br />
<strong>the</strong> provision <strong>of</strong> this capability in <strong>the</strong> operational setting is likely<br />
to add value and is being actively pursued. The advent <strong>of</strong> ‘open’<br />
TCI pumps has meant that generic prop<strong>of</strong>ol preparations can be<br />
used instead <strong>of</strong> expensive prefilled electronically-tagged syringes.<br />
Fur<strong>the</strong>rmore, <strong>the</strong> presence <strong>of</strong> a drugs library in <strong>the</strong>se devices<br />
means that <strong>the</strong>y are suitable for <strong>the</strong> safe infusion <strong>of</strong> o<strong>the</strong>r agents<br />
such as vasoactive drugs. The ability to deliver remifentanil and<br />
sufentanil as a TCI is an added feature <strong>of</strong> <strong>the</strong>se newer “open” TCI<br />
pumps.<br />
TCI pumps have been used successfully in <strong>the</strong> field by <strong>the</strong><br />
Austrailian <strong>Army</strong> <strong>Medical</strong> Services in East Timor, who concluded<br />
that TCI is a useful substitute for VGA [29].<br />
It is important that <strong>the</strong> user is aware <strong>of</strong> <strong>the</strong> ergonomics,<br />
capabilities and pharmacokinetic specifications <strong>of</strong> <strong>the</strong> chosen<br />
device, as <strong>the</strong>re are important aspects <strong>of</strong> drug handling to be<br />
considered. An understanding <strong>of</strong> <strong>the</strong> chosen pharmacokinetic<br />
model is essential to <strong>the</strong> rational administration <strong>of</strong> <strong>the</strong> relevant<br />
drug. Three commonly available commercial “open” TCI systems<br />
are shown in Figure 2:<br />
Figure 2: Commercially available open TCI systems<br />
A current area <strong>of</strong> research is closed-loop TCI technology, whereby<br />
depth <strong>of</strong> anaes<strong>the</strong>sia monitoring is employed to provide direct<br />
feedback to <strong>the</strong> microprocessor and facilitate automatic infusion<br />
rate adjustment.<br />
Depth <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong> Monitoring in <strong>the</strong> Field<br />
Systems available to monitor depth <strong>of</strong> anaes<strong>the</strong>sia may be divided<br />
into cortical activity-based and evoked potential systems. The<br />
system that enjoys widest support in <strong>the</strong> literature is <strong>the</strong> Bispectral<br />
Index (BIS) system. An electrode strip placed across <strong>the</strong> forehead<br />
measures potentials arising from <strong>the</strong> activity <strong>of</strong> <strong>the</strong> patient’s<br />
cerebral cortex. Data is integrated into an index between 0<br />
(cortical silence) and 100 (fully awake). Values below 60 indicate<br />
clinical anaes<strong>the</strong>sia and those below 40 indicate a deep hypnotic<br />
state. This single variable is meant to correlate with behavioural<br />
assessments <strong>of</strong> sedation and hypnosis.<br />
As a monitoring system, BIS possesses certain limitations. A<br />
study was published in 2003 in which <strong>the</strong> authors administered<br />
muscle relaxant to <strong>the</strong>mselves without anaes<strong>the</strong>tic agent,<br />
304<br />
S Lewis, S Jagdish<br />
Figure 3: The ASPECT BIS VISTA monitor in use toge<strong>the</strong>r with a<br />
TIVA system on Operation TELIC 12<br />
reporting that <strong>the</strong> BIS score was actually seen to fall [30]. Also BIS<br />
is incompatible with ketamine-based TIVA. BIS score is actually<br />
seen to increase following bolus injection <strong>of</strong> ketamine [31].<br />
The case for a Depth <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong> Monitoring System in<br />
<strong>the</strong> DMS<br />
Presently, clinical signs are <strong>the</strong> only guides that <strong>the</strong> DMS<br />
anaes<strong>the</strong>tist has to assess <strong>the</strong> adequacy <strong>of</strong> TIVA, though<br />
<strong>the</strong>se are known to lack sufficient specificity and sensitivity<br />
to confirm depth <strong>of</strong> anaes<strong>the</strong>sia. The quoted incidence <strong>of</strong><br />
awareness under anaes<strong>the</strong>sia ranges from 0.11% to 0.18%<br />
and haemodynamically compromised trauma patients are<br />
particularly at risk <strong>of</strong> under-dosage given <strong>the</strong> caution that is<br />
necessary when anaes<strong>the</strong>tising <strong>the</strong>m. Likewise, over-dosage can<br />
lead to cardiovascular compromise and prolonged recovery. The<br />
situation is also complicated by <strong>the</strong> use <strong>of</strong> remifentanil, which<br />
whilst possessing no hypnotic properties <strong>of</strong> its own, appears<br />
to allow downwards titration <strong>of</strong> co-administered prop<strong>of</strong>ol. An<br />
American Society <strong>of</strong> Anaes<strong>the</strong>siology (ASA) task force released<br />
a Practice Advisory in 2006 that recommended brain function<br />
monitoring should be considered in situations when <strong>the</strong>re was<br />
an increased risk <strong>of</strong> intraoperative awareness, including trauma<br />
surgery [32].<br />
The introduction <strong>of</strong> depth <strong>of</strong> anaes<strong>the</strong>sia monitoring may<br />
bring o<strong>the</strong>r benefits. A prospective observational study <strong>of</strong> over<br />
1000 high-risk patients undergoing major non-cardiac surgery<br />
identified three independent variables as significant predictors <strong>of</strong><br />
mortality [33]. These were patient co-morbidity, intra-operative<br />
systolic hypotension and cumulative deep hypnotic time (BIS <<br />
45). BIS scores in this range generated a 24.4% relative risk <strong>of</strong><br />
death per hour.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S301–307
TIVA for War surgery S Lewis, S Jagdish<br />
Technical<br />
Dependency<br />
‘Low Tech’<br />
TIVA Regimes<br />
(without<br />
electronic<br />
infusion<br />
pumps)<br />
‘Medium Tech’<br />
TIVA Regimes<br />
(electronic<br />
infusion pump<br />
required)<br />
‘High Tech’<br />
TIVA Regime<br />
(utilising TCI<br />
technology)<br />
Agents Indication Method Notes<br />
Ketamine<br />
Prop<strong>of</strong>ol,<br />
Fentanyl and<br />
Ketamine<br />
[17]<br />
Ketamine and<br />
Midazolam<br />
[35] (+/-<br />
Vecuronium)<br />
[4]<br />
Prop<strong>of</strong>ol and<br />
Alfentanil [5]<br />
‘Classical’<br />
Manual<br />
Prop<strong>of</strong>ol<br />
Infusion [37]<br />
Prop<strong>of</strong>ol and<br />
Remifentanil<br />
Prehospital<br />
care, austere<br />
environments<br />
Table 2. Suggested regimes for TIVA in <strong>the</strong> field<br />
Maintenance <strong>of</strong><br />
general anaes<strong>the</strong>sia<br />
with TIVA when<br />
electronic infusion<br />
pumps are<br />
unavailable<br />
Cardiac-stable<br />
regime in <strong>the</strong><br />
haemodynamically<br />
compromised<br />
casualty.<br />
Allows invasive<br />
ventilation.<br />
Invasive<br />
ventilation <strong>of</strong><br />
casualties without<br />
haemodynamic<br />
compromise<br />
<strong>Anaes<strong>the</strong>sia</strong> for<br />
casualties without<br />
haemodynamic<br />
compromise.<br />
Ventilated<br />
anaes<strong>the</strong>sia<br />
preferably<br />
without <strong>the</strong> use<br />
<strong>of</strong> neuromuscular<br />
blockade.<br />
0.5-2mg/kg iv for induction (use less<br />
than 1mg/kg if shocked). Maintain<br />
with 0.5mg/kg boluses or 20-<br />
100mcg/kg/min. 2mg midazolam<br />
reduces emergence delirium. 200mcg<br />
glycopyrrolate reduces salivation.<br />
40ml <strong>of</strong> 1% prop<strong>of</strong>ol, 5ml <strong>of</strong><br />
50mcg/ml fentanyl and 5ml <strong>of</strong><br />
50mcg/ml ketamine is mixed with<br />
50ml <strong>of</strong> NaCl 0.9% (solution<br />
will contain 4mg/ml prop<strong>of</strong>ol,<br />
2.5mcg/ml fentanyl and 2.5mcg/ml<br />
ketamine). Initially one drop every 3<br />
seconds through a standard 20 drop/<br />
ml giving set and titrate to effect.<br />
Induce anaes<strong>the</strong>sia with 1mg/<br />
kg ketamine plus 0.07mg/kg<br />
midazolam. Maintain by infusion<br />
<strong>of</strong> 200mg ketamine plus 5mg<br />
midazolam made up to 50ml and<br />
run at:<br />
(patient’s body weight in kg/2)ml/hr<br />
12mg vecuronium may be added for<br />
muscle relaxation.<br />
50ml <strong>of</strong> 1% prop<strong>of</strong>ol and 2.5mg<br />
(5ml) alfentanil. Infuse mixture at an<br />
initial rate <strong>of</strong> 1ml/kg/hr following a<br />
standard induction. Reduce rate by<br />
up to half according to clinical signs.<br />
Initial bolus <strong>of</strong> 1mg/kg for<br />
induction <strong>the</strong>n 10mg/kg/hour for<br />
10 minutes, 8mg/kg/hour for 10<br />
minutes followed by 6mg/kg/hour<br />
for subsequent maintenance <strong>of</strong><br />
anaes<strong>the</strong>sia.<br />
50ml 1% prop<strong>of</strong>ol infusion and<br />
a 40ml solution containing 2mg<br />
remifentanil.<br />
If TCI pump available for each drug:<br />
Initial blood prop<strong>of</strong>ol target<br />
4 to 6µg/ml<br />
Initial remifentanil target<br />
8 to 10ng/ml.<br />
If TCI is not available for<br />
remifentanil:<br />
Infuse remifentanil at 0.5µg/kg/<br />
min for 3 to 5 minutes followed by<br />
0.25µg/kg/min. Maintenance rates<br />
range from 0.12 to 0.5µg/kg/min.<br />
Commence prop<strong>of</strong>ol first as a rapid<br />
rise in effect site concentration <strong>of</strong><br />
remifentanil can induce apnoea<br />
before loss <strong>of</strong> consciousness.<br />
Full effect <strong>of</strong> bolus persists for<br />
about 10 minutes. In most<br />
cases airway reflexes and selfventilation<br />
should be preserved.<br />
Relatively high concentration<br />
<strong>of</strong> ketamine <strong>the</strong>refore good<br />
analgesic properties and slow<br />
return to full arousal after<br />
discontinuing. Omit ketamine<br />
for more rapid emergence.<br />
The mixture has a 72 hour<br />
shelf life.<br />
Facilitates rapid emergence<br />
compared with is<strong>of</strong>lurane-based<br />
VGA [36]. Low incidence <strong>of</strong><br />
nausea.<br />
Low incidence <strong>of</strong> nausea.<br />
It has been estimated that<br />
this schema delivers a steady<br />
state concentration <strong>of</strong> around<br />
3µg/ml.<br />
The initial Cp or Ce target<br />
for prop<strong>of</strong>ol is chosen to be<br />
just above <strong>the</strong> anticipated<br />
concentration required for<br />
loss <strong>of</strong> consciousness in that<br />
patient. The concept <strong>of</strong><br />
“patient calibration” is central<br />
to <strong>the</strong> success <strong>of</strong> this technique.<br />
Caution is required with <strong>the</strong>se<br />
targets especially where <strong>the</strong>re is<br />
cardiovascular instability.<br />
Estimated Ce should be noted<br />
at points during induction such<br />
as loss <strong>of</strong> response to command,<br />
instrumentation <strong>of</strong> <strong>the</strong> airway<br />
and incision. This will identify<br />
<strong>the</strong> Ce and Cp below which it<br />
would be inadvisable to drop<br />
and also helps identify <strong>the</strong> likely<br />
emergence point.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S301–307 305
TIVA for War surgery<br />
A field trial <strong>of</strong> <strong>the</strong> ASPECT BIS VISTA monitor was<br />
conducted by one <strong>of</strong> <strong>the</strong> authors (SJ) on OP TELIC 12 in 2008.<br />
A photograph <strong>of</strong> this monitor in use toge<strong>the</strong>r with a TIVA system<br />
is shown in Figure 3. Apart from one episode <strong>of</strong> dia<strong>the</strong>rmyrelated<br />
interference <strong>the</strong> system performed well across a spectrum<br />
<strong>of</strong> anaes<strong>the</strong>tic procedures.<br />
Figure 4: Depth <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong> monitoring employing auditoryevoked<br />
potentials during Operation TELIC 13<br />
Direct injection <strong>of</strong> volatile agents into <strong>the</strong> bloodstream<br />
This intriguing concept is still at <strong>the</strong> animal testing stage.<br />
Experiments using intravenous emulsified is<strong>of</strong>lurane have<br />
characterised potential advantages <strong>of</strong> this approach. Its use requires<br />
no specific ventilatory circuits or reliance on pulmonary function.<br />
There is evidence that onset and <strong>of</strong>fset is faster than prop<strong>of</strong>olbased<br />
TIVA whilst being very haemodynamically stable. A fur<strong>the</strong>r<br />
benefit is <strong>the</strong> preconditioning effect that is<strong>of</strong>lurane elicits against<br />
ischaemia-reperfusion injury [34].<br />
Suggested regimes for TIVA in <strong>the</strong> field<br />
The method <strong>of</strong> TIVA used will be dictated by anaes<strong>the</strong>tist<br />
preference, clinical presentation and <strong>the</strong> availability <strong>of</strong> drugs and<br />
equipment. The regimes outlined in Table 2 are all ‘battle-proven’<br />
techniques for use in adults that have been used by military<br />
anaes<strong>the</strong>tists. They also include approaches to TIVA for situations<br />
when electronic infusion pumps are unavailable.<br />
Conclusion<br />
There are some clear advantages <strong>of</strong> TIVA over VGA to <strong>the</strong><br />
deployed military anaes<strong>the</strong>tist. The drugs and technique used can<br />
be tailored to both <strong>the</strong> patient’s physiological status and <strong>the</strong> wider<br />
logistical situation in which <strong>the</strong> surgical team is working. Future<br />
developments may fur<strong>the</strong>r enhance <strong>the</strong> applicability <strong>of</strong> TIVA for<br />
war surgery.<br />
The purpose <strong>of</strong> this article is not to suggest that TIVA should<br />
replace VGA within <strong>the</strong> DMS, but to promote it as a valid<br />
alternative. It would certainly be wrong to assume that “…anyone<br />
who could depress <strong>the</strong> plunger <strong>of</strong> a syringe in response to movement in<br />
a patient could give an anaes<strong>the</strong>tic” [2]. There is great potential for<br />
harm with poorly administered TIVA, and advances in military<br />
pre-hospital care have meant that increasingly sick patients are<br />
now surviving to reach Role 2/3 facilities. When confronted with<br />
such patients, <strong>the</strong> best anaes<strong>the</strong>tic to give is probably <strong>the</strong> one<br />
with which <strong>the</strong> anaes<strong>the</strong>tist is most familiar, be that ei<strong>the</strong>r VGA<br />
or TIVA.<br />
306<br />
S Lewis, S Jagdish<br />
References<br />
1. Halford FJ. A Critique <strong>of</strong> intravenous anaes<strong>the</strong>sia in war surgery.<br />
Anes<strong>the</strong>siology 1943; 4: 67-9<br />
2. Bennetts FE. Thiopentone anaes<strong>the</strong>sia at Pearl Harbour. Br J<br />
Anaesth 1995; 75: 366-8<br />
3. Dunnil D. Continuous Pentothal anaes<strong>the</strong>sia. J R <strong>Army</strong> Med <strong>Corps</strong><br />
1943; 80: 217-20<br />
4. Restall J, Tully AM, Ward PJ, Kidd AG. Total intravenous<br />
anaes<strong>the</strong>sia for military surgery. A technique using ketamine,<br />
midazolam and vecuronium. <strong>Anaes<strong>the</strong>sia</strong> 1988; 43(1): 46-9<br />
5. Wilson RJ, Ridley SA. The use <strong>of</strong> prop<strong>of</strong>ol and alfentanil by<br />
infusion in military anaes<strong>the</strong>sia. <strong>Anaes<strong>the</strong>sia</strong> 1992; 47(3): 231-3<br />
6. Bacić A, Gluncić I, Buklijas J. Titrated total intravenous anaes<strong>the</strong>sia<br />
(TIVA) in war. J R <strong>Army</strong> Med <strong>Corps</strong> 1996; 142(3): 103-5<br />
7. Barras P, McMasters J, Grathwohl K, Blackbourne L. Total<br />
Intravenous Anes<strong>the</strong>sia on <strong>the</strong> Battlefield. U S <strong>Army</strong> Med Dept J<br />
2009 Jan-March: 68-72<br />
8. Beard D. Arguing against <strong>the</strong> TSA in modern conflict. Bull R Coll<br />
Anaesth 2010; 60: 19-20<br />
9. Gupta A, Stierer T, Zuckerman R, Sakima N, Parker S, Fleisher L.<br />
Comparison <strong>of</strong> Recovery Pr<strong>of</strong>ile After Ambulatory Anes<strong>the</strong>sia with<br />
Prop<strong>of</strong>ol, Is<strong>of</strong>lurane, Sev<strong>of</strong>lurane and Desflurane: A Systematic<br />
Review. Anesth Analg 2004; 98: 632-41<br />
10. Crozier TA, Muller JE, Quittkat D, Sydow M, Wuttke W, Kettler<br />
D. Effect <strong>of</strong> anaes<strong>the</strong>sia on <strong>the</strong> cytokine responses to abdominal<br />
surgery. Br J Anaesth 1994; 72: 280-5<br />
11. Ledowski T, Bein B, Hanss R et al. Neuroendocrine Stress Response<br />
and Heart Rate Variability: A Comparison <strong>of</strong> Total Intravenous<br />
Versus Balanced Anes<strong>the</strong>sia. Anesth Analg 2005; 101: 1700-5<br />
12. Peck TE, Hill SA, Williams M. Pharmacology for <strong>Anaes<strong>the</strong>sia</strong> and<br />
Intensive Care 2nd Edn. London: Greenwish <strong>Medical</strong> Media Ltd,<br />
2004<br />
13. Gan TJ, Meyer T, Apfel CC et al. Consensus guidelines for managing<br />
postoperative nausea and vomiting. Anesth Analg 2003; 97: 62-71<br />
14. Kazama T, Kurita T, Morita K, Nakata J, Sato S. Influence <strong>of</strong><br />
hemorrhage on prop<strong>of</strong>ol pseudo-steady state concentration.<br />
Anes<strong>the</strong>siology 2002; 97: 1156-61<br />
15. DIPRIVAN package insert. © AstraZeneca 2005<br />
16. Szucs P, Allegra J, Fields L et al. Storage temperatures <strong>of</strong> medications<br />
on an air medical helicopter Air Med J 2000; 19: 19-21<br />
17. Mahoney and McFarland. Field <strong>Anaes<strong>the</strong>sia</strong> and military injury. In:<br />
Smith CE (ed), Trauma Anes<strong>the</strong>sia 1st Edn. Cambridge University<br />
Press, 2008; Ch 31<br />
18. Ikeda T, Kazama T, Sessler DI, et al. Induction <strong>of</strong> anes<strong>the</strong>sia with<br />
ketamine reduces <strong>the</strong> magnitude <strong>of</strong> redistibution hypo<strong>the</strong>rma.<br />
Anesth Analg 2001: 93: 934-938<br />
19. Albanese J, Arnaud S, Rey M, Thomachot L, Alliez B,<br />
Martin C. Ketamine decreases intracranial pressure and<br />
electroencephalographic activity in traumatic brain injury patients<br />
during prop<strong>of</strong>ol sedation. Anes<strong>the</strong>siology 1997; 87: 1328-34<br />
20. Engelhard K, Werner C, Eberspächer E et al. The effect <strong>of</strong> <strong>the</strong> a2agonist<br />
dexmedetomidine and <strong>the</strong> N-methyl-d-aspartate antagonist<br />
S(+)-ketamine on <strong>the</strong> expression <strong>of</strong> apoptosis-regulating proteins<br />
after incomplete cerebral ischaemia and reperfusion in rats. Anesth<br />
Analg 2003; 96: 524-31<br />
21. White PF, Ham J, Way WL, Trevor AJ. Pharmacology <strong>of</strong> ketamine<br />
isomers in surgical patients. Anes<strong>the</strong>siology 1980; 52: 231-9<br />
22. Grathwohl KW, Black IH, Spinella PC et al. Total intravenous<br />
anes<strong>the</strong>sia including ketamine versus volatile gas anes<strong>the</strong>sia for<br />
combat-related operative traumatic brain injury. Anes<strong>the</strong>siology.<br />
2008; 109(1): 44-53<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S301–307
TIVA for War surgery S Lewis, S Jagdish<br />
23. Sasada M, Smith S. Drugs in <strong>Anaes<strong>the</strong>sia</strong> and Intensive Care 3rd<br />
Edn. Oxford University Press, 2005<br />
24. Smith C, McEwan AI, Jhaveri R, et al. The interaction <strong>of</strong> fentanyl<br />
on <strong>the</strong> Cp50 <strong>of</strong> prop<strong>of</strong>ol for loss <strong>of</strong> consciousness and skin incision.<br />
Anes<strong>the</strong>siology 1994: 81: 820-8<br />
25. Vuyk J, Lim T, Engbers FHM, Burm AGL, Vletter AA, Bovill<br />
JG. The pharmacodynamic interaction <strong>of</strong> prop<strong>of</strong>ol and alfentanil<br />
during lower abdominal surgery in female patients. Anes<strong>the</strong>siology<br />
1995; 83: 8-22<br />
26. Absalom AR, Struys MMRF. An Overview <strong>of</strong> TCI & TIVA. 2nd<br />
Edn. Academia Press, Ghent 2007<br />
27. Barakat R, Sutcliffe N and Schwab M. Effect site concentration<br />
during prop<strong>of</strong>ol TCI sedation: a comparison <strong>of</strong> sedation score with<br />
two pharmacokinetic models <strong>Anaes<strong>the</strong>sia</strong> 2007; 62(7): 661-6<br />
28. Egan TD, Kuramkote S, Gong G et al. Fentanyl pharmacokinetics<br />
in haemorrhagic shock: a porcine model. Anes<strong>the</strong>siology 1999;<br />
91(1): 156-66<br />
29. Harding J N, Wilson M. Use <strong>of</strong> target-controlled infusion <strong>of</strong><br />
prop<strong>of</strong>ol for military field anaes<strong>the</strong>sia. J Aust Def Health Service<br />
2003; 4(1): 23-6<br />
30. Messner M, Beese U, Romstöck J, Dinkel M, Tschaikowsky K. The<br />
Bispectral Index Declines During Neuromuscular Block in Fully<br />
Awake Persons. Anesth Analg 2003; 97: 488-91<br />
31. Hans P, Dewandre P-Y, Brichant J-F, Bonhomme V. Comparative<br />
effects <strong>of</strong> ketamine on bispectral index and spectral entropy <strong>of</strong> <strong>the</strong><br />
electroencephalogram under sev<strong>of</strong>lurane anaes<strong>the</strong>sia. Br J Anaesth<br />
2005; 94: 336-40<br />
32. American Society <strong>of</strong> Anes<strong>the</strong>siologists Task Force. Practice Advisory<br />
for Intraoperative Awareness and Brain Function Monitoring.<br />
Anes<strong>the</strong>siology 2006; 104: 847– 64<br />
33. Monk TG, Saini V, Weldon BC, Sigl JC. Anaes<strong>the</strong>tic management<br />
and one-year mortality after non-cardiac surgery. Anesth Analg<br />
2005; 100: 4-10<br />
34. Lucchinetti E, Schaub M, Zaugg M. Emulsified Intravenous Versus<br />
Evaporated Inhaled Is<strong>of</strong>lurane for Heart Protection: Old Wine in<br />
a New Bottle or True Innovation? Anes<strong>the</strong>sia and Analgesia. 2008<br />
106(5): 1346-9<br />
35. Roberts R. Military <strong>Anaes<strong>the</strong>sia</strong>. In Allman KG, Wilson I (eds)<br />
Oxford Handbook <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong>. Oxford University Press 2004; Ch<br />
32<br />
36. Saïssy JM. Simplified use <strong>of</strong> mixed prop<strong>of</strong>ol and alfentanil for<br />
anes<strong>the</strong>sia in remote locations. Mil Med. 2000; 165(3): 195-9<br />
37. Roberts FL, Dixon J, Lewis GT, Tackley RM, Prys-Roberts C:<br />
Induction and maintenance <strong>of</strong> prop<strong>of</strong>ol anaes<strong>the</strong>sia. A manual<br />
infusion scheme. <strong>Anaes<strong>the</strong>sia</strong> 1988; 43(S): 14-7<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S301–307 307
<strong>Anaes<strong>the</strong>sia</strong> at Role 4<br />
PR Wood 1 , AG Haldane 2 , SE Plimmer 2<br />
1 2 Consultant Anaes<strong>the</strong>tist; Speciality Registrars in <strong>Anaes<strong>the</strong>sia</strong> at University Hospital Birmingham NHS Foundation<br />
Trust<br />
Abstract<br />
The contribution <strong>of</strong> anaes<strong>the</strong>sia to <strong>the</strong> care <strong>of</strong> injured military personnel at Role 4 is described with particular emphasis on<br />
<strong>the</strong> working relationship between <strong>the</strong> <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine and <strong>the</strong> civilian department <strong>of</strong> anaes<strong>the</strong>sia. The<br />
implications for operating <strong>the</strong>atre activity are discussed.<br />
Philosophy and Infrastructure<br />
The aims <strong>of</strong> anaes<strong>the</strong>sia at Role 4 may be described as a horizontal<br />
integration with <strong>the</strong> care given in operational <strong>the</strong>atres, <strong>the</strong> current<br />
focus <strong>of</strong> which is Op HERRICK. While easily stated this is not<br />
without its challenges.<br />
The clinical care <strong>of</strong> military personnel was concentrated at Selly<br />
Oak Hospital (SOH) but in June 2010 this hospital relocated to<br />
<strong>the</strong> new Queen Elizabeth Hospital Birmingham (QEHB ).<br />
The Department <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong> <strong>of</strong> University Hospital<br />
Birmingham NHS Trust has 75 consultants, 30 <strong>of</strong> whom have<br />
intensivist duties distributed across four critical care units,<br />
containing a total <strong>of</strong> 100 beds. Military patients constitute just<br />
one per cent <strong>of</strong> <strong>the</strong> Trust’s population but are resource intensive<br />
- arrangements exist with <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services and local<br />
NHS Trusts to manage increased numbers <strong>of</strong> patients during<br />
periods <strong>of</strong> heightened activity in <strong>the</strong>atres <strong>of</strong> conflict.<br />
The new QEHB <strong>the</strong>atre complex has 23 in patient operating<br />
<strong>the</strong>atres and during busy periods up to four <strong>of</strong> <strong>the</strong>se may contain<br />
military casualties. Surgical care is dominated by ortho-plastics,<br />
hand and maxillo-facial surgeons with <strong>the</strong> input <strong>of</strong> general and<br />
urology surgery as necessary. The medical care <strong>of</strong> every military<br />
in-patient is reviewed at a weekly military ward round, which<br />
is a multi-disciplinary meeting starting at 0800hrs. Involving<br />
as many as 20 NHS and Tri-service clinicians with support staff<br />
every military casualty has all aspects <strong>of</strong> <strong>the</strong>ir present and future<br />
progress considered and plans made for ongoing surgery or key<br />
investigations.<br />
One <strong>of</strong> <strong>the</strong> authors (PW) participates in <strong>the</strong> first ‘sit down’<br />
part <strong>of</strong> <strong>the</strong> ward round. The presence <strong>of</strong> a civilian consultant<br />
anaes<strong>the</strong>tist allows observations or comment to be made in relation<br />
to current clinical issues and to take note <strong>of</strong> any preceding or<br />
forthcoming events that have particular relevance for anaes<strong>the</strong>sia.<br />
In particular his presence allows prompt and ongoing liaison with<br />
<strong>the</strong> <strong>Defence</strong> Pr<strong>of</strong>essor <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong>, <strong>the</strong> <strong>Army</strong> Subject Matter<br />
Expert (SME ) in pain and <strong>the</strong> consultant pain nurse responsible<br />
for <strong>the</strong> military ward.<br />
Patient admissions and <strong>the</strong>atre allocation<br />
Injured personnel arrive in Birmingham via <strong>the</strong> RAF Critical<br />
Care Air Support Team (CCAST ) or via routine aeromedical<br />
evacuation flights. By definition <strong>the</strong> first group require critical<br />
care and because <strong>of</strong> <strong>the</strong> rapid transit times from Afghanistan are<br />
still in <strong>the</strong> ‘damage control phase’ <strong>of</strong> <strong>the</strong>ir surgical journey.<br />
Corresponding Author: Dr Paul Wood, Dept <strong>of</strong> Anaes<strong>the</strong>tics,<br />
Queen Elizabeth Hospital Birmingham B15 2WB<br />
E-mail: paul.wood@uhb.nhs.uk<br />
For <strong>the</strong> anaes<strong>the</strong>tist back in <strong>the</strong> UK <strong>the</strong> process will <strong>of</strong>ten start<br />
with a phone call - a message that casualties are expected and will<br />
need fur<strong>the</strong>r care that day or night. The surgical teams and trauma<br />
co-ordinators meet up in <strong>the</strong> ‘bunker’- in reality a secure room in<br />
<strong>the</strong>atres - but with <strong>the</strong> addition <strong>of</strong> a series <strong>of</strong> white boards it has<br />
become a co-ordination centre (Figure 1). The new patients are<br />
on <strong>the</strong> boards with details summarised from <strong>the</strong> aeromed signals,<br />
injuries listed and teams allocated. On admission to QEHB<br />
CCAST patients enter <strong>the</strong> critical care unit ( CCU ) where an<br />
immediate assessment <strong>of</strong> <strong>the</strong>ir injuries and physiological status<br />
are made prior to continued stabilisation or immediate surgery<br />
- in most cases this is <strong>the</strong> ‘2nd look’ following <strong>the</strong>ir resuscitative<br />
surgery at Role 3.<br />
Figure 1. The ‘Bunker’<br />
Less severely injured aeromed admissions are admitted directly<br />
to <strong>the</strong> military ward , where an early review <strong>of</strong> <strong>the</strong>ir wounds is<br />
undertaken in <strong>the</strong> very likely event that within 2-8 hours <strong>the</strong>y will<br />
also be in an operating <strong>the</strong>atre having <strong>the</strong>ir wounds inspected, and<br />
initial surgical management carried out. The <strong>the</strong>atre bunker is not<br />
only essential in <strong>the</strong> planning <strong>of</strong> ‘casualty surges’ but is indispensable<br />
in <strong>the</strong> daily planning <strong>of</strong> <strong>the</strong>atre lists for both military and civilian<br />
trauma patients. Planning meetings held daily at 1230 and 1630<br />
help to ensure that <strong>the</strong> normal <strong>the</strong>atre activity is maintained.<br />
<strong>Anaes<strong>the</strong>sia</strong><br />
For those patients admitted to CCU <strong>the</strong>ir initial visits to <strong>the</strong>atre<br />
are characterised by rigorous attention in continuing to manage<br />
<strong>the</strong> lethal triad <strong>of</strong> coagulopathy, hypo<strong>the</strong>rmia and acidosis. Their<br />
surgery takes place in a designated emergency <strong>the</strong>atre under<br />
direct consultant surgical and anaes<strong>the</strong>tic supervision. The early<br />
care is an extension <strong>of</strong> <strong>the</strong> process carried out at Role 3 and initial<br />
<strong>the</strong>atre trips are <strong>of</strong>ten time critical if control <strong>of</strong> <strong>the</strong> lethal triad is<br />
to be maintained.<br />
308 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S308–310
Role 4 <strong>Anaes<strong>the</strong>sia</strong> PR Wood, AG Haldane, SE Plimmer<br />
There is significant use <strong>of</strong> blood and blood products – in<br />
particular fresh frozen plasma which is administered with packed<br />
red cells, most <strong>of</strong>ten in a 1:1 ratio, as practised during <strong>the</strong>ir<br />
haemostatic resuscitation in Role 3 [1]. When necessary platelet<br />
and cryoprecipitate preparations are also utilised.<br />
Critical care staff will undertake <strong>the</strong> changing <strong>of</strong> invasive<br />
monitoring and vascular access lines, however when <strong>the</strong> first<br />
surgical intervention is contemporaneous with <strong>the</strong> patients<br />
admission <strong>the</strong>se may be undertaken in <strong>the</strong> operating <strong>the</strong>atre. At<br />
this time fine bore nasogastric feeding tubes are inserted and a<br />
feeding regime established, which in intubated patients continues<br />
uninterrupted. As <strong>the</strong>ir wounds evolve <strong>the</strong> concept <strong>of</strong> damage<br />
control surgery continues until such time as <strong>the</strong>y are ready for<br />
transfer to <strong>the</strong> military ward and restorative surgery.<br />
For <strong>the</strong> less severely injured aeromed admissions <strong>the</strong>re is <strong>the</strong><br />
occasional unexpected ‘surprise’ when <strong>the</strong> dressings come down<br />
under anaes<strong>the</strong>sia.These patients are cross-matched prior to<br />
surgery and it is made clear to all - and <strong>the</strong> junior medical staff in<br />
particular - that <strong>the</strong>re is no such thing as ‘just a dressing change’.<br />
The complex nature <strong>of</strong> <strong>the</strong> ballistic wounds means that as<br />
<strong>the</strong> patients condition stabilises multiple surgical<br />
interventions are <strong>the</strong> norm. Particular challenges<br />
for anaes<strong>the</strong>sia include establishing and maintaining<br />
intravascular access, pain control and avoiding<br />
prolonged perioperative starvation. Trust policy<br />
limits preoperative omission <strong>of</strong> solids to 6 hours,<br />
while clear fluids are permitted up to 2 hours before<br />
surgery. Anaes<strong>the</strong>tic considerations are summarised<br />
in Box 1, while Figures 2 and 3 reveal aspects <strong>of</strong> <strong>the</strong><br />
surgical activity for all <strong>the</strong> military patients during<br />
February 2010, demonstrating some <strong>of</strong> <strong>the</strong> resource<br />
and clinical implications <strong>of</strong> managing <strong>the</strong>se patients.<br />
The six casualties whose <strong>the</strong>atre time exceeded 10<br />
hours are <strong>of</strong> particular note. One patient required<br />
45 hours <strong>of</strong> surgery - his operative interventions continued in <strong>the</strong><br />
following month. His situation is not unique – Table 1 details<br />
timings for three severely injured casualties treated in 2009.<br />
Critical Care<br />
• Damage control surgery - manage <strong>the</strong> lethal triad: acidosis,<br />
coagulopathy, hypo<strong>the</strong>rmia<br />
• Haemostatic resuscitation as per current CGO<br />
• Surgery is time critical<br />
• Sepsis – inotrope support<br />
• Renal function - K+ monitoring<br />
• Blast lung – complex ventilatory strategies may be required<br />
Military Ward<br />
• Recent transfer from intensive care – medically still<br />
challenging – high dependency<br />
• Reconstruction – prolonged procedures<br />
• Non opiate naive – high dose opiate background analgesia<br />
• Practical conduct <strong>of</strong> PNB regional anaes<strong>the</strong>sia made harder<br />
by stabilisation and negative pressure dressings<br />
• Epidural anaes<strong>the</strong>sia / analgesia not possible with unstable<br />
spinal fractures<br />
• Accentuation <strong>of</strong> tourniquet effect<br />
• Blood loss easily underestimated<br />
• Temperature control<br />
Box 1 Essential features <strong>of</strong> anaes<strong>the</strong>sia in Role 4 patients<br />
Figure. 2: Total time required in <strong>the</strong> operating <strong>the</strong>atre for patients<br />
undergoing surgery in February 2010<br />
Figure 3: Number <strong>of</strong> surgical operations performed on patients<br />
undergoing surgery in February 2010<br />
Number <strong>of</strong><br />
operations<br />
Total time<br />
in operating<br />
<strong>the</strong>atre (to<br />
nearest hour )<br />
Time required<br />
per operation<br />
A B C<br />
27 11 9<br />
75 hours 33 hours 17 hours<br />
shortest 1hr<br />
15 mins<br />
longest 6<br />
hours<br />
shortest 1hr<br />
longest 8hrs<br />
30 mins<br />
shortest 1 hr<br />
longest 3 hrs<br />
Table 1: Time utilised for three patients ( A ,B and C ). ( Data kindly<br />
supplied by Pr<strong>of</strong>essor K. Porter )<br />
Postoperative Care<br />
Critically injured patients are returned directly to <strong>the</strong> CCU. Noncritical<br />
patients are admitted to <strong>the</strong> recovery unit and returned<br />
to <strong>the</strong> ward when vital signs and analgesia are ensured. During<br />
awakening ‘flashbacks’ can be a problem requiring sensitive<br />
management from recovery staff.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S308–310 309<br />
Role 4 <strong>Anaes<strong>the</strong>sia</strong><br />
Despite <strong>the</strong>ir ‘non-critical’ status may <strong>of</strong> <strong>the</strong> patients on <strong>the</strong><br />
military ward can present challenging medical problems. In an<br />
effort to provide a standardisation <strong>of</strong> care <strong>the</strong>re are a number<br />
<strong>of</strong> protocols that are followed, in to which anaes<strong>the</strong>sia has had<br />
an input. Maintaining vascular access is a frequent issue and<br />
consequently peripherally inserted central ca<strong>the</strong>ter (PICC) lines<br />
(inserted under local anaes<strong>the</strong>sia by interventional radiologists)<br />
are used for maintenance fluids and repeat anaes<strong>the</strong>sia.<br />
Perioperative Analgesia<br />
This is managed by <strong>the</strong> acute pain team, lead by a consultant<br />
nurse, supported by a number <strong>of</strong> military and civilian consultant<br />
anaes<strong>the</strong>tic colleagues, including <strong>the</strong> <strong>Army</strong> SME in pain.<br />
Considerable attention has been given to <strong>the</strong> pain management<br />
<strong>of</strong> military patients. This has been well described elsewhere in<br />
this journal [2] but since that publication <strong>the</strong>re have been fur<strong>the</strong>r<br />
advances, particularly in respect <strong>of</strong> producing clinical guidelines<br />
and increased audit activity.<br />
A multimodal analgesic regime is prescribed for military<br />
patients and is described in detail in an analgesia document<br />
which is available on <strong>the</strong> Trust intra-net. Continued use is made<br />
<strong>of</strong> Peripheral Nerve Blockade (PNB) and epidural ca<strong>the</strong>ters sited<br />
in Role 3 [3] and where <strong>the</strong>ir removal is unavoidable replacement<br />
or substitution with a suitable alternative is <strong>of</strong>ten attempted. The<br />
department has two Sonosite (Sonosite Inc. Bo<strong>the</strong>ll, WA, USA)<br />
ultrasound machines available and a cadre <strong>of</strong> ultrasound trained<br />
anaes<strong>the</strong>tists who are available to assist in ca<strong>the</strong>ter placement. This<br />
has proved invaluable – particularly where complex reconstructive<br />
surgery to an upper limb has been undertaken.<br />
Epidural analgesia has despite some initial reticence concerning<br />
<strong>the</strong> risk <strong>of</strong> infection proved beneficial in patients with bilateral leg<br />
amputations. In <strong>the</strong>se injuries <strong>the</strong> use <strong>of</strong> femoral and or sciatic<br />
ca<strong>the</strong>ters can be limited by <strong>the</strong> high nature <strong>of</strong> <strong>the</strong> amputation<br />
sealed with bulky negative pressure dressings. In such a setting<br />
identification <strong>of</strong> complications associated with epidural regional<br />
analgesia can also be problematical – one practical development is<br />
<strong>the</strong> ‘four and no more’ rule, devised in an attempt to ensure that<br />
any patient suspected <strong>of</strong> having an epidural haematoma is MRI<br />
scanned within 4 hours <strong>of</strong> suspicion (Box 2).<br />
Research and development<br />
The contribution <strong>of</strong> anaes<strong>the</strong>sia to <strong>the</strong> patient’s onward progress<br />
does not stand still. A series <strong>of</strong> acute pain team initiatives<br />
have simplified <strong>the</strong> management <strong>of</strong> regional anaes<strong>the</strong>sia. The<br />
promotion <strong>of</strong> regional techniques will streng<strong>the</strong>n in <strong>the</strong> near<br />
future with <strong>the</strong> introduction <strong>of</strong> a military pain fellow who will be<br />
attached to <strong>the</strong> unit for nine months at a time. This is one marker<br />
<strong>of</strong> success to drive <strong>the</strong> developing policy <strong>of</strong> regional anaes<strong>the</strong>sia<br />
for limb trauma as <strong>the</strong> default analgesic method <strong>of</strong> choice [4].<br />
310<br />
PR Wood, AG Haldane, SE Plimmer<br />
We will consider an epidural infusion to be established in<br />
4 hours. The initial sensory level (if any) and motor function<br />
should be recorded in <strong>the</strong> patients notes (on an anaes<strong>the</strong>tic<br />
record). Thereafter:<br />
1. An awake patient should be assessed 4 hourly<br />
2. At each assessment <strong>the</strong> nurse should ask 4 questions:<br />
i. Is <strong>the</strong>re an increase in motor block?<br />
ii. Is <strong>the</strong>re back pain?<br />
iii. Is <strong>the</strong>re an increase in / development <strong>of</strong> a sensory level?<br />
iv. Are <strong>the</strong>re any o<strong>the</strong>r new abnormal/ unexpected<br />
symptoms i.e. bladder / bowel issues / increased pain in<br />
a previously comfortable limb.<br />
3. Positive answer to any one <strong>of</strong> <strong>the</strong> 4 questions - call <strong>the</strong><br />
anaes<strong>the</strong>tic SpR as per ‘S4 pain call’ agreement - while<br />
awaiting response - STOP THE INFUSION.<br />
4. Repeat examination by SpR 4 hours after infusion stopped.<br />
If no improvement or fur<strong>the</strong>r deterioration in neurology -<br />
patient needs EMERGENCY MRI.<br />
Box 2: Diagnosis <strong>of</strong> Epidural Haematoma – The ‘4 and no more’ Rule<br />
The management <strong>of</strong> patients in <strong>the</strong> operating <strong>the</strong>atre<br />
increasingly resembles <strong>the</strong> clinical guidelines for operations<br />
(CGO) employed in Role 3, an example <strong>of</strong> which is <strong>the</strong> near<br />
patient monitoring <strong>of</strong> coagulation with thromboelastography.<br />
This is available within CCU and <strong>the</strong> operating <strong>the</strong>atre suite. It<br />
is anticipated that this initiative will have <strong>the</strong> potential for more<br />
accurate administration <strong>of</strong> blood products, particularly in respect<br />
<strong>of</strong> <strong>the</strong> use <strong>of</strong> FFP [5].<br />
It is anticipated that <strong>the</strong> present system <strong>of</strong> care will continue<br />
to evolve as <strong>the</strong> QEHB matures with <strong>the</strong> constant aim <strong>of</strong> making<br />
<strong>the</strong> 8000 mile journey from Bastion to Birmingham as seamless<br />
as possible.<br />
References<br />
1. Hodgetts TJ, Mahoney PF, Kirkman E. Damage Control<br />
Resuscitation. JR <strong>Army</strong> Med <strong>Corps</strong> 2007; 153 (4): 299-300<br />
2. Edwards D, Bowden M, Aldington DJ. Pain management at role 4.<br />
JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155 (1): 61-64<br />
3. Hughes S, Birt D. Continuous Peripheral Nerve Blockade on OP<br />
Herrick 9. JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155 (1); 69-70<br />
4. Clasper J, Aldington D. Regional <strong>Anaes<strong>the</strong>sia</strong>, Ballistic Limb<br />
Trauma and Acute Compartment Syndrome. JR <strong>Army</strong> Med <strong>Corps</strong>.<br />
2010; 156 (2): 77-78<br />
5. Woolley T. Coagulation Study. Paper Presented at <strong>the</strong> Academia<br />
and Armed Conflict Conference. <strong>Royal</strong> College <strong>of</strong> Anaes<strong>the</strong>tists,<br />
London 21st September 2009.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S308–310
Field Intensive Care - Weaning and Extubation<br />
R Thornhill 1 , JL Tong 2 , K Birch 3 , R Chauhan 4<br />
1 Consultant in <strong>Anaes<strong>the</strong>sia</strong> and Intensive Care Medicine, Nottingham University Hospitals and RCDM 2 <strong>Royal</strong> Centre<br />
for <strong>Defence</strong> Medicine and Honorary Senior Lecturer at <strong>the</strong> University <strong>of</strong> Birmingham; 3 Consultant in <strong>Anaes<strong>the</strong>sia</strong> and<br />
Intensive Care, North Bristol NHS Trust; 4 StR in <strong>Anaes<strong>the</strong>sia</strong>, Queens Hospital, Burton-Upon-Trent.<br />
Abstract<br />
Injury following ballistic trauma is <strong>the</strong> most prevalent indication for providing organ system support within an ICU in <strong>the</strong><br />
field. Following damage control surgery, postoperative ventilatory support may be required, but multiple factors may influence<br />
<strong>the</strong> indications for and duration <strong>of</strong> invasive mechanical ventilation. Ballistic trauma and surgery may trigger <strong>the</strong> Systemic<br />
Inflammatory Response Syndrome (SIRS) and are important causative factors in <strong>the</strong> development <strong>of</strong> Acute Lung Injury<br />
(ALI) and Acute Respiratory Distress Syndrome (ARDS). However, <strong>the</strong>ir pathophysiological effect on <strong>the</strong> respiratory system<br />
is unpredictable and variable. Invasive mechanical ventilation is associated with numerous complications and <strong>the</strong> return to<br />
spontaneous ventilation has many physiological benefits. Following trauma, shorter periods <strong>of</strong> ICU sedation-amnesia and a<br />
protocol for early weaning and extubation, may minimize complications and have a beneficial effect on <strong>the</strong>ir psychological<br />
recovery. In <strong>the</strong> presence <strong>of</strong> stable respiratory function, appropriate analgesia and favourable operational and transfer criteria,<br />
we believe that <strong>the</strong> prompt restoration <strong>of</strong> spontaneous ventilation and early tracheal extubation should be a clinical objective<br />
for casualties within <strong>the</strong> field ICU.<br />
Introduction<br />
Injury following ballistic trauma is <strong>the</strong> most prevalent<br />
indication (50%) for providing organ system support to UK<br />
personnel within an intensive care unit (ICU) in <strong>the</strong> field [1].<br />
In general <strong>the</strong> role <strong>of</strong> <strong>the</strong> field ICU is to continue <strong>the</strong> postinjury<br />
resuscitation process and provide organ system support,<br />
until <strong>the</strong> casualty is discharged to <strong>the</strong> ward or evacuated to <strong>the</strong><br />
Role 4 facility.<br />
Trauma casualties may require admission to an ICU for<br />
mechanical ventilation, which may be indicated for a variety<br />
<strong>of</strong> reasons, which include: impaired ventilatory effort, impaired<br />
respiratory motor function, increased mechanical load and<br />
impaired alveolar gas exchange [2]. Postoperative respiratory<br />
support is also indicated in those casualties who require surgery<br />
for fur<strong>the</strong>r haemorrhage control or pack removal, bowel<br />
anastamosis and abdominal wall closure. Tracheal intubation is<br />
usually performed to facilitate invasive mechanical ventilation,<br />
but may also be instituted for endobronchial suctioning or<br />
maintenance <strong>of</strong> upper airway patency and protection.<br />
Mechanical ventilation is associated with multiple<br />
complications (Table 1) and prolonged periods <strong>of</strong> ventilation<br />
and intubation should <strong>the</strong>refore be avoided. In some studies,<br />
greater than 40% <strong>of</strong> <strong>the</strong> total duration <strong>of</strong> mechanical ventilation<br />
involves <strong>the</strong> weaning process [3, 4] and adopting an early weaning<br />
and extubation policy, may minimize <strong>the</strong> risk <strong>of</strong> complications<br />
associated with mechanical ventilation.<br />
Following mechanical ventilation, up to 20% <strong>of</strong> patients<br />
fail <strong>the</strong>ir first attempt at weaning [3, 4]. Whilst data on <strong>the</strong><br />
incidence <strong>of</strong> weaning failure in a military population remains<br />
unreported, premature extubation and re-intubation should<br />
be avoided, as this is associated with an increased morbidity<br />
and mortality [5]. The purpose <strong>of</strong> this manuscript is to review<br />
Corresponding Author: Lt Col R Thornhill, Department<br />
<strong>of</strong> Military <strong>Anaes<strong>the</strong>sia</strong> and Critical Care, <strong>Royal</strong> Centre<br />
for <strong>Defence</strong> Medicine, Raddlebarn Road, Selly Oak,<br />
Birmingham, B29 6JD<br />
Email: rjthorn@btinternet.com<br />
<strong>the</strong> evidence for a ‘prompt weaning protocol’ leading to <strong>the</strong><br />
restoration <strong>of</strong> spontaneous ventilation and tracheal extubation,<br />
within a field ICU.<br />
Causative Factor Complication<br />
Endo-tracheal intubation<br />
Mechanical ventilation<br />
Immobility<br />
Sinusitis<br />
Ventilator-associated pneumonia<br />
(VAP)<br />
Tracheal stenosis<br />
Vocal cord trauma<br />
Formation <strong>of</strong> fistulae (trachealoesophageal<br />
or tracheal-vascular)<br />
Pneumothorax<br />
Oxygen toxicity<br />
Hypotension<br />
Ventilator associated lung injury<br />
(VALI)<br />
Venous thrombo-embolism<br />
Loss <strong>of</strong> skin integrity and<br />
pressure necrosis<br />
Muscle wasting and weakness<br />
Atelectasis<br />
Table 1: Complications <strong>of</strong> mechanical ventilation.<br />
Effect <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong> & Sedation on normal<br />
respiratory function<br />
<strong>Anaes<strong>the</strong>sia</strong> causes an impairment <strong>of</strong> pulmonary function,<br />
irrespective <strong>of</strong> whe<strong>the</strong>r <strong>the</strong> patient is breathing spontaneously, or<br />
is being mechanically ventilated. Impaired oxygenation <strong>of</strong> blood<br />
occurs in most subjects who are anaes<strong>the</strong>tised [6]. Lung function<br />
remains impaired postoperatively, and clinically significant<br />
pulmonary complications can be seen in 1% to 2% after minor<br />
surgery, and in up to 20% after upper abdominal and thoracic<br />
surgery [7].<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S311–317 311
Early Extubation on ICU<br />
The effects <strong>of</strong> anaes<strong>the</strong>sia and mechanical ventilation on lung<br />
function are described below. These effects are causative - in that<br />
<strong>the</strong>y relate to a sequence <strong>of</strong> events <strong>the</strong> end result <strong>of</strong> which is a<br />
decrease in <strong>the</strong> lungs ability to oxygenate <strong>the</strong> blood and remove<br />
Carbon Dioxide. The first phenomenon that is seen following<br />
induction <strong>of</strong> anaes<strong>the</strong>sia is loss <strong>of</strong> muscle tone with a subsequent<br />
reduction in Functional Residual Capacity (FRC) due to a change<br />
in <strong>the</strong> balance between <strong>the</strong> outward forces (respiratory muscles)<br />
and inward forces (elastic tissue <strong>of</strong> <strong>the</strong> lung). This reduction in<br />
FRC is paralleled by an increase in <strong>the</strong> elastic behaviour <strong>of</strong> <strong>the</strong><br />
lung (reducing compliance) and an increased airways resistance.<br />
The decreased FRC also predisposes to airway closure and <strong>the</strong><br />
development <strong>of</strong> atelectasis - which is made worse by <strong>the</strong> application<br />
<strong>of</strong> high concentrations <strong>of</strong> inspired oxygen. These changes in lung<br />
patency alter <strong>the</strong> distribution <strong>of</strong> ventilation, and <strong>the</strong> matching<br />
<strong>of</strong> ventilation and perfusion, and impede efficient gas exchange.<br />
Lung Volume<br />
Resting lung volume (or FRC) is reduced by 0.8 to 1.0 L by<br />
changing body position from upright to supine, and <strong>the</strong>re<br />
is ano<strong>the</strong>r 0.4 to 0.5L decrease when anaes<strong>the</strong>sia has been<br />
induced [8]. End-expiratory lung volume is thus reduced from<br />
approximately 3.5 to 2L (this being close or equal to <strong>the</strong> Residual<br />
Volume <strong>of</strong> <strong>the</strong> lung (RV)). <strong>Anaes<strong>the</strong>sia</strong> itself causes a fall in FRC<br />
despite maintenance <strong>of</strong> spontaneous breathing [9, 10]; <strong>the</strong> average<br />
reduction corresponds to around 20% <strong>of</strong> awake FRC and may<br />
contribute to an altered distribution <strong>of</strong> ventilation. The decrease<br />
in FRC occurs regardless <strong>of</strong> whe<strong>the</strong>r <strong>the</strong> anaes<strong>the</strong>tic is inhaled or<br />
administered intravenously [11]. Muscle paralysis and mechanical<br />
ventilation cause no fur<strong>the</strong>r decrease in FRC.<br />
This decrease in FRC seems to be related to loss <strong>of</strong> respiratory<br />
muscle tone, which shifts <strong>the</strong> balance between <strong>the</strong> elastic recoil<br />
force <strong>of</strong> <strong>the</strong> lung and <strong>the</strong> outward force <strong>of</strong> <strong>the</strong> chest wall to a lower<br />
chest and lung volume.<br />
Compliance and Resistance<br />
Static compliance <strong>of</strong> <strong>the</strong> total respiratory system (lungs and chest<br />
wall) is reduced on average from 95 to 60 mL/cm H 2 O during<br />
anaes<strong>the</strong>sia [12]. Resistance <strong>of</strong> <strong>the</strong> total respiratory system and<br />
<strong>the</strong> lungs during anaes<strong>the</strong>sia increases during both spontaneous<br />
breathing and mechanical ventilation [12].<br />
Atelectasis<br />
Atelectasis (lung tissue collapse) appears in approximately 90%<br />
<strong>of</strong> all patients who are anaes<strong>the</strong>tised [13]. It is seen during<br />
spontaneous breathing and after muscle paralysis and whe<strong>the</strong>r<br />
intravenous or inhaled anaes<strong>the</strong>tics are used [11]. Up to 15%<br />
to 20% <strong>of</strong> <strong>the</strong> lung is regularly collapsed at <strong>the</strong> base <strong>of</strong> <strong>the</strong> lung<br />
during uneventful anaes<strong>the</strong>sia as a result <strong>of</strong> anaes<strong>the</strong>sia alone.<br />
Abdominal surgery does not add much to <strong>the</strong> atelectasis, but it<br />
can remain for several days in <strong>the</strong> postoperative period [14]. After<br />
thoracic surgery and cardiopulmonary bypass, more than 50%<br />
<strong>of</strong> <strong>the</strong> lung can be collapsed even several hours after surgery is<br />
complete [15]. It is likely that it is a focus <strong>of</strong> infection and can<br />
contribute to pulmonary complications [16].<br />
The amount <strong>of</strong> atelectasis decreases toward <strong>the</strong> apex, which is<br />
mostly spared and thus fully aerated. There is a weak correlation<br />
between <strong>the</strong> size <strong>of</strong> <strong>the</strong> atelectasis and body weight or body mass<br />
index (BMI), with obese patients showing larger atelectatic areas<br />
[11,17]. Atelectasis is independent <strong>of</strong> age, with children and<br />
young people showing as much atelectasis as elderly patients [18].<br />
312<br />
R Thornhill, JL Tong, K Birch et al<br />
There is a good correlation between <strong>the</strong> amount <strong>of</strong> atelectasis and<br />
<strong>the</strong> subsequent pulmonary shunt.<br />
Distribution <strong>of</strong> Ventilation and Perfusion<br />
Redistribution <strong>of</strong> inspired gas away from dependent to<br />
nondependent lung regions has been observed in anes<strong>the</strong>tized<br />
supine humans; ventilation was shown to be distributed mainly to<br />
<strong>the</strong> upper lung regions, and <strong>the</strong>re was a successive decrease down<br />
<strong>the</strong> lower half <strong>of</strong> <strong>the</strong> lung [19]. Positive end expiratory pressure<br />
(PEEP) increases dependent lung ventilation in anaes<strong>the</strong>tised<br />
subjects, so <strong>the</strong> distribution <strong>of</strong> ventilation is more similar to that<br />
in <strong>the</strong> awake state [20]. Thus, restoration <strong>of</strong> overall FRC toward<br />
or beyond <strong>the</strong> awake level returns gas distribution toward <strong>the</strong><br />
awake pattern. This is an effect <strong>of</strong> <strong>the</strong> recruitment <strong>of</strong> collapsed,<br />
dependent lung regions (atelectasis), <strong>of</strong> reopening <strong>of</strong> closed<br />
airways in <strong>the</strong> lower lung regions, and possibly <strong>of</strong> increased<br />
expansion <strong>of</strong> <strong>the</strong> upper lung regions so that <strong>the</strong>y become less<br />
compliant and less ventilated.<br />
PEEP will impede venous return to <strong>the</strong> right heart and<br />
<strong>the</strong>refore reduce cardiac output. It may also affect pulmonary<br />
vascular resistance, although this may have less <strong>of</strong> an effect on<br />
cardiac output. In addition, PEEP causes a redistribution <strong>of</strong> blood<br />
flow toward dependent lung regions [21]. By this means, upper<br />
lung regions may be poorly perfused, <strong>the</strong>reby causing a dead<br />
space–like effect.<br />
Respiratory Drive<br />
Spontaneous ventilation is frequently reduced during anaes<strong>the</strong>sia.<br />
Inhaled anaes<strong>the</strong>tics [22], as well as intravenous agents [23] reduce<br />
sensitivity to CO 2 . The response is dose dependent, with decreasing<br />
ventilation with deepening anaes<strong>the</strong>sia. <strong>Anaes<strong>the</strong>sia</strong> also reduces<br />
<strong>the</strong> response to hypoxia. Attenuation <strong>of</strong> <strong>the</strong> hypoxic response may<br />
be attributed to an effect on <strong>the</strong> carotid body chemoreceptors [24].<br />
Mechanical ventilation and acute lung injury<br />
Following major trauma, an acute lung injury (ALI) and <strong>the</strong> risk<br />
<strong>of</strong> Acute Respiratory Distress Syndrome (ARDS) is a significant<br />
clinical concern [25, 26]. The aetiology <strong>of</strong> ALI / ARDS following<br />
trauma is multifactorial and <strong>the</strong> risk factors are shown in (Table<br />
2). Recent studies have shown that inappropriate ventilator<br />
strategies can also induce ALI [27].<br />
Old age<br />
Preexisting physiological impairment (diabetes, etc)<br />
Direct pulmonary or chest wall injury<br />
Aspiration <strong>of</strong> blood or stomach contents<br />
Prolonged mechanical ventilation<br />
Severe traumatic brain injury<br />
Spinal cord injury with quadriplegia<br />
Massive transfusion<br />
Haemorrhagic shock<br />
Occult hypoperfusion<br />
Sepsis<br />
Table 2: Risk factors for development <strong>of</strong> ALI/ARDS after trauma.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S311–317
Early Extubation on ICU R Thornhill, JL Tong, K Birch et al<br />
Following injury, casualties are immobilized in <strong>the</strong> supine<br />
position. This posture is responsible for <strong>the</strong> development <strong>of</strong><br />
early dependent atelectasis, which may be fur<strong>the</strong>r exacerbated by<br />
opioid analgesia and sedation, due to cephalad movement <strong>of</strong> <strong>the</strong><br />
diaphragm into <strong>the</strong> thorax and compression <strong>of</strong> dependent lung<br />
parenchyma. General anaes<strong>the</strong>sia and <strong>the</strong> use <strong>of</strong> muscle relaxants<br />
may also exacerbate this problem [28]. Pulmonary contusions,<br />
if severe, can be life-threatening early in <strong>the</strong> hospital course and<br />
<strong>the</strong> disruption in pulmonary integrity due to “leaky” capillaries<br />
and lung parenchyma, may be fur<strong>the</strong>r exacerbated by volume<br />
resuscitation with blood and crystalloid solutions. Rib fractures<br />
can cause splinting <strong>of</strong> <strong>the</strong> diaphragm leading to atelectasis and<br />
hypoxaemia.<br />
Mechanical ventilation can initiate lung injury. High peak<br />
inspiratory pressure and low PEEP, may lead to inflammatory<br />
processes in <strong>the</strong> lung that can progress to multi-organ dysfunction.<br />
Animal studies that induce pulmonary damage to simulate<br />
ALI or ARDS cannot be distinguished from <strong>the</strong> lung damage<br />
occurring after studies that use mechanical ventilation strategies<br />
to induce injury [29]. ALI causes an alteration in lung mechanics<br />
that leads to an uneven distribution <strong>of</strong> ventilation, resulting in<br />
a disordered pattern <strong>of</strong> pressure / volume changes as <strong>the</strong> lung<br />
inflates and deflates [30]. This non-uniform ventilation results in<br />
alveolar stress which effects alveolar gas exchange. Alveolar shear<br />
forces may also develop in dependent regions. The early stages<br />
<strong>of</strong> ventilator-associated lung injury develop at commonly used<br />
airway pressures (transalveolar pressure >35 cmH 2 O) in animals<br />
with normal lungs, but <strong>the</strong> threshold for lung injury may occur at<br />
lower pressure in injured lungs.<br />
Several studies [31-33] have shown that modern ventilatory<br />
strategies using low tidal volumes (6 to 8 ml/kg), limiting alveolar<br />
distending pressures (plateau pressure 10<br />
PO 2 /FiO 2 ratio 14 days) mechanical<br />
ventilation. (PEEP = positive end expiratory pressure; PO 2 /FiO 2 =<br />
arterial partial pressure <strong>of</strong> oxygen divided by <strong>the</strong> fraction <strong>of</strong> inspired<br />
oxygen ratio; AIS score = abbreviated injury scale).<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S311–317 313
Early Extubation on ICU<br />
The weaning process – failure versus success<br />
Prior to discontinuing ventilatory support, <strong>the</strong> primary aim <strong>of</strong><br />
treatment is to correct <strong>the</strong> pathophysiological processes which<br />
created <strong>the</strong> need for mechanical ventilation. However, it is not<br />
essential to achieve complete resolution <strong>of</strong> <strong>the</strong> causative processes<br />
prior to attempting to wean and discontinue ventilation. Partial<br />
resolution <strong>of</strong> <strong>the</strong> underlying pathophysiology may be sufficient.<br />
Studies have shown that 40% <strong>of</strong> <strong>the</strong> period undergoing<br />
mechanical ventilation may be devoted to <strong>the</strong> weaning process<br />
[41]. Current evidence supports a protocol driven approach to<br />
weaning, as extubation performed over <strong>the</strong> shortest possible<br />
period is associated with improved patient outcomes [4, 42, 43].<br />
Extubation is 70 - 80% successful once <strong>the</strong> precipitating process<br />
has been corrected and <strong>the</strong> 20 - 30% who require re-intubation<br />
largely includes those who have been ventilated in excess <strong>of</strong> 48 hrs.<br />
Failure to wean can be viewed as an imbalance between <strong>the</strong><br />
capacity <strong>of</strong> <strong>the</strong> respiratory system and <strong>the</strong> load placed on that<br />
system. This imbalance may be due to: inadequate resolution<br />
<strong>of</strong> <strong>the</strong> primary problem, <strong>the</strong> occurrence <strong>of</strong> a new problem, a<br />
ventilator associated complication, or combinations <strong>of</strong> <strong>the</strong>se. The<br />
predominant pathophysiological characteristic <strong>of</strong> failure to wean<br />
is high levels <strong>of</strong> load relative to <strong>the</strong> strength <strong>of</strong> <strong>the</strong> respiratory<br />
muscles, which should be optimised to increase <strong>the</strong> success <strong>of</strong><br />
weaning (Table 4).<br />
Haemodynamic<br />
instability<br />
Acid-Base<br />
imbalance<br />
Electrolyte<br />
abnormalities<br />
Intravascular<br />
volume<br />
Mental status<br />
Nutrition<br />
314<br />
Avoiding myocardial ischaemia or new<br />
arrhythmias, which decrease cardiac<br />
function (or require high inotropic<br />
support).<br />
A normal pH is desirable but not essential.<br />
Avoid an acidaemia as this may increase<br />
<strong>the</strong> minute ventilation.<br />
Hypophosphataemia,hypocalcaemia,<br />
hypomagnesaemia and hypokalaemia<br />
reduce muscle contractility and adversely<br />
effect weaning [25].<br />
Avoid intravascular volume overloading,<br />
which increases <strong>the</strong> interstitial volume and<br />
decreases <strong>the</strong> functional residual capacity<br />
leading to alveolar collapse – leading to<br />
ventilation- perfusion mismatch and poor<br />
oxygenation.<br />
Mobilisation <strong>of</strong> <strong>the</strong> extra fluid usually<br />
occurs during resolution <strong>of</strong> <strong>the</strong><br />
inflammatory processes.<br />
The aetiology <strong>of</strong> mental status alteration<br />
is multifactorial, but over-sedation may<br />
prolong mechanical ventilation [26].<br />
Sedation holidays and a sedation scoring<br />
system is advised [27].<br />
Malnutrition decreases muscle mass,<br />
strength and reduces immunity.<br />
Nutritional supplementation improves<br />
respiratory capacity and weaning [5, 25].<br />
Table 4. Factors which effect weaning, by decreasing <strong>the</strong> capacity <strong>of</strong> or<br />
<strong>the</strong> demand on <strong>the</strong> respiratory system.<br />
R Thornhill, JL Tong, K Birch et al<br />
A protocol driven approach to weaning<br />
Physiological parameters have been evaluated, which allow<br />
casualties who may benefit from prompt weaning and extubation<br />
to be identified early [4, 42, 43]. Unfortunately specialised<br />
measuring equipment is required which is not available in a field<br />
ICU. However, <strong>the</strong> Rapid Shallow Breathing Index (RSBI) has<br />
been shown to accurately predict weaning outcome [48]. This is<br />
<strong>the</strong> ratio <strong>of</strong> frequency (f) to tidal volume (VT) measured after 1<br />
minute <strong>of</strong> spontaneous breathing. In general, casualties who fail<br />
to wean have low tidal volumes and a high respiratory rate. The<br />
advantage <strong>of</strong> f/VT is that it is easy to measure and is independent<br />
<strong>of</strong> patient cooperation and effort. The predictive value <strong>of</strong> RSBI is<br />
highest when measured during spontaneous ventilation through<br />
a tracheal tube.<br />
Casualties who pass <strong>the</strong> initial RSBI assessment should<br />
proceed to a formal Spontaneous Breathing Trial (SBT). The<br />
optimal mode <strong>of</strong> ventilation for this weaning trial has not been<br />
established, but it is generally accepted that SIMV weaning<br />
prolongs <strong>the</strong> duration <strong>of</strong> mechanical ventilation. Daily T-Piece<br />
trials have consistently been shown to be superior to SIMV, but<br />
<strong>the</strong>re is little evidence <strong>of</strong> an outcome difference between T-Piece<br />
based weaning and use <strong>of</strong> Pressure Support/Assist ventilation<br />
[44, 49]. An American task force has published evidence based<br />
guidelines [50] for discontinuing mechanical ventilation and <strong>the</strong><br />
first seven <strong>of</strong> <strong>the</strong>se guidelines which relate to weaning individual<br />
casualties are shown in Table 5.<br />
Evacuation to Role 4<br />
In a field hospital <strong>the</strong> general wards are usually staffed and equipped<br />
for basic care, observations and monitoring, which ensures that<br />
<strong>the</strong> ICU has a high bed occupancy rate. During a casualty surge,<br />
it is standard practice to review extubated casualties to determine<br />
<strong>the</strong>ir suitability for being moved to <strong>the</strong> ward, thus freeing beds<br />
and equipment for those who require ICU care. Adopting a<br />
prompt weaning and extubation protocol has obvious tactical and<br />
strategic implications for both current and future operations and<br />
may influence <strong>the</strong> decision process regarding whe<strong>the</strong>r to deploy<br />
<strong>the</strong> Critical Care Air Support Team (CCAST) or an aeromedical<br />
evacuation team.<br />
The CCAST provides an intercontinental critical care<br />
evacuation service. The well equipped team provides expert care<br />
in a flexible working environment aboard a fixed-wing airframe<br />
that can be adapted for transferring critically ill and ventilated<br />
casualties. Whilst vigilance should minimise many <strong>of</strong> <strong>the</strong> risks<br />
associated with transferring ventilated casualties, inadvertent<br />
extubation, disconnection and migration <strong>of</strong> tubes, may still<br />
occur. Some casualties require significant doses <strong>of</strong> sedation to<br />
allow optimal mechanical ventilation, which may mask <strong>the</strong> pain<br />
associated with a compartment syndrome. As a general rule if <strong>the</strong><br />
casualty is unstable or is at risk <strong>of</strong> requiring re-intubation during<br />
flight, extubation should not be attempted at <strong>the</strong> field ICU. As<br />
a CCAST consultant is collocated at <strong>the</strong> field hospital in Camp<br />
Bastion, <strong>the</strong> decision to extubate can be quickly confirmed. In<br />
flight, <strong>the</strong> cabin pressure is lower than at ground level; so oxygen<br />
requirements are increased and gas filled spaces expand. The cabin<br />
may be pressurized to ground or sea level, but this negatively<br />
impacts on aircraft range and flight duration.<br />
Whilst enteral feeding is important following trauma e.g.<br />
burns, at <strong>the</strong> time <strong>of</strong> writing, <strong>the</strong> current CCAST policy is that<br />
intubated casualties are not fed during <strong>the</strong>ir evacuation flight to<br />
<strong>the</strong> Role 4. Until <strong>the</strong>re is evidence to prove that in flight vibrations<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S311–317
Early Extubation on ICU R Thornhill, JL Tong, K Birch et al<br />
Recommendation 1<br />
Recommendation 2<br />
Recommendation 3<br />
Recommendation 4<br />
Recommendation 5<br />
Recommendation 6<br />
Recommendation 7<br />
A search for all contributing causes to ventilator dependence should be undertaken when mechanical<br />
ventilation is > 24 hours. All possible ventilatory and non-ventilatory issues should be corrected and are<br />
integral to <strong>the</strong> ventilator-discontinuation process.<br />
Casualties receiving mechanical ventilation for respiratory failure should undergo an individualised<br />
assessment <strong>of</strong> discontinuation potential if <strong>the</strong>re is:<br />
a. Evidence for some reversal <strong>of</strong> <strong>the</strong> underlying cause for respiratory failure.<br />
b. Adequate oxygenation (e.g. Pao 2 /Fio 2 ratio > 150 to 200, requiring positive end-expiratory<br />
pressure [PEEP] < 5 to 8 cmH 2 O and Fio 2 < 0.4 to 0.5) and pH (e.g., pH > 7.25)<br />
c. Haemodynamic stability, as defined by <strong>the</strong> absence <strong>of</strong> active myocardial ischemia and conditions<br />
requiring no vasopressor <strong>the</strong>rapy or <strong>the</strong>rapy with only low-dose vasopressors.<br />
d. The capability to initiate an inspiratory effort.<br />
Note: Those not satisfying <strong>the</strong>se criteria (e.g. casualties with chronic hypoxaemia values below <strong>the</strong><br />
thresholds cited) may still be ready to wean from mechanical ventilation.<br />
Formal discontinuation assessments for casualties receiving mechanical ventilation should be performed<br />
during spontaneous breathing ra<strong>the</strong>r than while <strong>the</strong> casualty is still receiving substantial ventilatory<br />
support. An initial brief period <strong>of</strong> spontaneous breathing can be used to assess <strong>the</strong> capability <strong>of</strong><br />
continuing onto a formal spontaneous breathing trial (SBT). The criteria with which to assess patient<br />
tolerance during SBTs are <strong>the</strong> respiratory pattern, <strong>the</strong> adequacy <strong>of</strong> gas exchange, haemodynamic<br />
stability, and subjective comfort. The tolerance <strong>of</strong> SBTs lasting 30 to 120 minutes should prompt<br />
consideration for permanent ventilator discontinuation.<br />
The removal <strong>of</strong> <strong>the</strong> artificial airway from a casualty who has successfully been discontinued from<br />
ventilatory support should be based on assessments <strong>of</strong> airway patency and <strong>the</strong> ability <strong>of</strong> <strong>the</strong> casualty to<br />
protect <strong>the</strong>ir airway.<br />
In casualties receiving mechanical ventilation for respiratory failure who fail an SBT, <strong>the</strong> cause <strong>of</strong><br />
<strong>the</strong> failure should be determined. After reversible causes are corrected subsequent SBTs should be<br />
performed every 24 hours.<br />
Casualties receiving mechanical ventilation for respiratory failure, who fail an SBT, require a stable and<br />
comfortable form <strong>of</strong> ventilatory support, to lower work <strong>of</strong> breathing and to allow for rest and recovery.<br />
<strong>Anaes<strong>the</strong>sia</strong> or sedation strategies and ventilator management aimed at early extubation should be used<br />
in postoperative patients.<br />
Table 5. Guidelines for discontinuing mechanical ventilation [50].<br />
do not exacerbate micro aspiration around <strong>the</strong> tracheal tube cuff,<br />
this policy is unlikely to change.<br />
Pain management<br />
In <strong>the</strong> polytrauma casualty, pain management issues may also<br />
influence <strong>the</strong> decision to prolong mechanical ventilation and<br />
sedation. Whilst regional anaes<strong>the</strong>sia and continuous peripheral<br />
nerve blockade has become an established method <strong>of</strong> providing<br />
analgesia for a large proportion <strong>of</strong> casualties with limb injuries<br />
[51], it may not be sufficient in every polytrauma casualty. Pain<br />
associated with thoraco-abdominal injuries can be difficult to<br />
manage and some casualties may require large supplementary<br />
doses <strong>of</strong> intravenous opioid. For this group, maintaining<br />
mechanical ventilation, analgesia and sedation until arrival at <strong>the</strong><br />
Role 4 would be more appropriate and is an exception to rapid<br />
weaning and extubation at <strong>the</strong> field ICU.<br />
Psychological Stress<br />
At present we are uncertain if prolonging <strong>the</strong> duration <strong>of</strong><br />
mechanical ventilation and sedation following traumatic injury<br />
and damage control surgery may affect <strong>the</strong> levels <strong>of</strong> postextubation<br />
psychological stress or post traumatic stress disorder<br />
(PTSD).<br />
In <strong>the</strong>ory, pharmacologically prolonging <strong>the</strong> period <strong>of</strong><br />
amnesia following injury, may potentially deny <strong>the</strong> casualty<br />
<strong>the</strong> opportunity to: begin to come to terms with <strong>the</strong> severity <strong>of</strong><br />
<strong>the</strong>ir injuries, to be debriefed by <strong>the</strong>ir own unit personnel and<br />
supported by <strong>the</strong>ir colleagues. Clearly this <strong>the</strong>ory requires fur<strong>the</strong>r<br />
clinical investigation using, e.g. <strong>the</strong> PTSD checklist (PCL-C),<br />
which is a self-report instrument designed to assess symptoms<br />
<strong>of</strong> post traumatic stress disorder [52, 53]. Until reliable evidence<br />
is available that supports early psychological debriefing and<br />
extubation following a traumatic injury, maintaining ventilation<br />
and sedation should be determined on an individual patient basis.<br />
Conclusion<br />
All injured or ill service personnel should, whenever possible<br />
be <strong>of</strong>fered medical care to a standard equal to that which <strong>the</strong>y<br />
receive in <strong>the</strong> UK. Therefore, applying an early weaning and<br />
extubation protocol to appropriate military casualties does<br />
reflect best practice in <strong>the</strong> UK. Restoring a patent airway and<br />
spontaneous ventilation early in <strong>the</strong> postoperative period has<br />
significant clinical and logistical advantages, but conversely also<br />
requires that adequate analgesia be provided.<br />
Maintaining mechanical ventilation and sedation during <strong>the</strong><br />
transfer to <strong>the</strong> Role 4 should be determined on an individual<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S311–317 315
Early Extubation on ICU<br />
basis. Ensuring early consultation with <strong>the</strong> deployed CCAST<br />
anaes<strong>the</strong>tist should significantly reduce <strong>the</strong> risk <strong>of</strong> both<br />
reintubation being performed prior to evacuation from <strong>the</strong><br />
field ICU, or conversely missing <strong>the</strong> opportunity to waken and<br />
extubate casualties early.<br />
References<br />
1. Roberts MJ, Fox MA, Hamilton-Davies C, et al. The experience<br />
<strong>of</strong> <strong>the</strong> Intensive Care Unit in a British <strong>Army</strong> Field Hospital during<br />
<strong>the</strong> 2003 Gulf Conflict. J R <strong>Army</strong> Med <strong>Corps</strong> 2003; 149: 284-90.<br />
2. Lavery GG, Lowry KG. Management <strong>of</strong> blast injuries and shock<br />
lung. Curr Opin Anes<strong>the</strong>siol. 2004; 17: 151-7.<br />
3. Chao DC, Scheinhorn DJ. Weaning from mechanical ventilation.<br />
Crit Care Clin 1998; 14: 799-817.<br />
4. Lellouche F, Mancebo J, Jolliet P, et al. A multicenter randomized<br />
trial <strong>of</strong> computer-driven protocolized weaning from mechanical<br />
ventilation. Am J Respir Crit Care Med 2006; 174: 894-900.<br />
5. Manthous CA, Schmidt GA, Hall JB. Liberation from mechanical<br />
ventilation. A decade <strong>of</strong> progress. Chest 1998; 114: 886-901.<br />
6. Hedenstierna G. Contribution <strong>of</strong> multiple inert gas elimination<br />
technique to pulmonary medicine: ventilation-perfusion<br />
relationships during anes<strong>the</strong>sia. Thorax 1995; 50: 85-91.<br />
7. Kroenke K, Lawrence VA, Theroux JF, et al. Postoperative<br />
complications after thoracic and major abdominal-surgery<br />
in patients with and without obstructive lung-disease.<br />
Chest 1993; 104: 1445-51.<br />
8. Wahba RWM. Perioperative functional residual capacity. Can J<br />
Anaesth 1991; 38: 384-400.<br />
9. Westbrook PR, Stubbs SE, Sessler AD, et al. Effects <strong>of</strong> anes<strong>the</strong>sia<br />
and muscle paralysis on respiratory mechanics in normal man. J<br />
Appl Physiol 1973; 34: 81-6.<br />
10. Ro<strong>the</strong>n HU, Sporre B, Engberg G, et al. Airway closure, atelectasis<br />
and gas exchange during general anaes<strong>the</strong>sia. Br J Anaes 1998; 81:<br />
681-6.<br />
11. Hedenstierna G, Edmark L. The effects <strong>of</strong> anes<strong>the</strong>sia and muscle<br />
paralysis on <strong>the</strong> respiratory system. Intensive Care Med 2005; 31:<br />
1327-35.<br />
12. Don H. The mechanical properties <strong>of</strong> <strong>the</strong> respiratory system during<br />
anes<strong>the</strong>sia. Int Anes<strong>the</strong>siol Clin 1977; 15: 113-126.<br />
13. Gunnarsson L, Tokics L, Gustavsson H, et al. Influence <strong>of</strong> age on<br />
atelectasis formation and gas-exchange impairment during generalanes<strong>the</strong>sia.<br />
Br J Anaesth 1991; 66: 423-432.<br />
14. Lindberg P, Gunnarsson L, Tokics L, et al. Atelectasis and<br />
lung-function in <strong>the</strong> postoperative period. Acta Anaes<strong>the</strong>siol<br />
Scand 1992; 36: 546-553.<br />
15. Tenling A, Hachenberg T, Tyden H, et al. Atelectasis and gas<br />
exchange after cardiac surgery. Anes<strong>the</strong>siology 1998; 89: 371-378.<br />
16. Van Kaam AH, Lachmann RA, Herting E, et al. Reducing atelectasis<br />
attenuates bacterial growth and translocation in experimental<br />
pneumonia. Am J Respir Crit Care Med 2004; 169: 1046-53.<br />
17. Ro<strong>the</strong>n HU, Sporre B, Engberg G, et al. Reexpansion <strong>of</strong> atelectasis<br />
during general anaes<strong>the</strong>sia: A computed tomography study. Br J<br />
Anaesth 1993; 71: 788-95.<br />
18. Gunnarsson L, Tokics L, Lundquist H, et al. Chronic obstructive<br />
pulmonary-disease and anes<strong>the</strong>sia-formation <strong>of</strong> atelectasis and gasexchange<br />
impairment. Eur Respiry J 1991; 4: 1106-16.<br />
19. Tokics L, Hedenstierna G, Svensson L, et al. V/Q distribution and<br />
correlation to atelectasis in anes<strong>the</strong>tized paralyzed humans. J Appl<br />
Physiol 1996; 81: 1822-33.<br />
316<br />
R Thornhill, JL Tong, K Birch et al<br />
20. Hedenstierna G, Baehrendtz S, Klingstedt C, et al. Ventilation and<br />
perfusion <strong>of</strong> each lung during differential ventilation with selective<br />
PEEP. Anes<strong>the</strong>siology 1984; 61: 369-76.<br />
21. West JB, Dollery CT, Naimark A. Distribution <strong>of</strong> blood flow in<br />
isolated lung—relation to vascular + alveolar pressures. J Appl<br />
Physiol 1964; 19: 713-24.<br />
22. Sakai EM, Connolly LA, Klauck JA. Inhalation anes<strong>the</strong>siology<br />
and volatile liquid anes<strong>the</strong>tics: Focus on is<strong>of</strong>lurane, desflurane, and<br />
sev<strong>of</strong>lurane. Pharmaco<strong>the</strong>rapy 2005; 25: 1773-88.<br />
23. Von Ungern-Sternberg BS, Frei FJ, Hammer J, et al. Impact <strong>of</strong><br />
depth <strong>of</strong> prop<strong>of</strong>ol anaes<strong>the</strong>sia on functional residual capacity<br />
and ventilation distribution in healthy preschool children. Br J<br />
Anaesth 2007; 98: 503-8.<br />
24. Ide T, Sakurai Y, Aono M, Nishino T. Contribution <strong>of</strong> peripheral<br />
chemoreception to <strong>the</strong> depression <strong>of</strong> <strong>the</strong> hypoxic ventilatory response<br />
during halothane anes<strong>the</strong>sia in cats. Anes<strong>the</strong>siology 1999; 90: 1084-<br />
91.<br />
25. Hoyt DB, Simons RK, Winchell RJ, et al. A risk analysis<br />
<strong>of</strong> pulmonary complications following major trauma. J<br />
Trauma 1993; 35: 524-31.<br />
26. Garber BG, Hevert PC, Yelle JD, et al. Adult respiratory distress<br />
syndrome: A systematic overview <strong>of</strong> incidence and risk factors. Crit<br />
Care Med 1996; 24: 687-95.<br />
27. McCunn M. Mechanical ventilation. Weapon <strong>of</strong> mass destruction<br />
or tool for liberation? Crit Care Med 2003; 31: 974-6.<br />
28. Brismar B, Hedenstierna G, Lundquuist H, et al. Pulmonary<br />
densities during anes<strong>the</strong>sia with muscular relaxation - a proposal <strong>of</strong><br />
atelectasis. Anes<strong>the</strong>siology 1985; 62: 422 -28.<br />
29. Dreyfuss D, Saumon G. Ventilator-induced lung injury: Lessons<br />
from experimental studies. Am J Respir Crit Care Med 1998; 157:<br />
294-323.<br />
30. Schiller HJ, McCann UG, Carney DE, et al. Altered alveolar<br />
mechanics in <strong>the</strong> acutely injured lung. Crit Care Med 2001; 29:<br />
1049-55.<br />
31. Amato MBP, Barbas CSV, Medeiros DM, et al. Effect <strong>of</strong> a protective<br />
ventilation strategy on mortality in <strong>the</strong> acute respiratory distress<br />
syndrome. N Engl J Med 1998; 338: 347-54.<br />
32. Hickling KG, Walsh J, Henderson SJ, et al. Low mortality rate<br />
in adult respiratory distress syndrome using low-volume, pressurelimited<br />
ventilation with permissive hypercapnia: A prospective<br />
study. Crit Care Med 1994; 22: 1568-78.<br />
33. The Acute Respiratory Distress Syndrome Network. Ventilation<br />
with lower tidal volumes as compared with traditional tidal volumes<br />
for acute lung injury and <strong>the</strong> acute respiratory distress syndrome. N<br />
Engl J Med 2000; 342: 1301-8.<br />
34. Putensen C, Rasanen J, Lopez FA. Ventilation-perfusion<br />
distributions during mechanical ventilation with superimposed<br />
spontaneous breathing in canine lung injury. Am J Respir Crit Care<br />
Med 1994; 150: 101-8.<br />
35. Davis K, Johnson DJ, Branson RD, et al. Airway pressure release<br />
ventilation. Arch Surg 1993; 128: 1348-52.<br />
36. Ritenour AE, Baskin TW. Primary Blast Injury: Update On<br />
Diagnosis And Treatment. Crit Care Med 2008; 36: S311-317.<br />
37. Sauaia A, Moore FA, Moore EE, et al. Pneumonia related multiple<br />
organ failure is not a primary cause <strong>of</strong> death in head trauma. Pan<br />
Am J Trauma 1992; 3: 90.<br />
38. Moore FA, Sauaia A, Moore EE, et al. Post-injury multiple organ<br />
failure: a bimodal phenomenon. J Trauma 1996; 40: 501-12.<br />
39. Agle SC, Kao LS, Moore FA, et al. Early predictors <strong>of</strong> prolonged<br />
mechanical ventilation in major torso trauma patients who require<br />
resuscitation. Am J Surg 2006; 192: 822-7.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S311–317
Early Extubation on ICU R Thornhill, JL Tong, K Birch et al<br />
40. Estenssoro E, Gonzalez F, Laffaire E, et al. Shock on admission day<br />
is <strong>the</strong> best predictor <strong>of</strong> prolonged mechanical ventilation in <strong>the</strong><br />
ICU. Chest 2005; 127: 598-603.<br />
41. Esteban A, Anzueto A, Alia I, et al. How is mechanical ventilation<br />
employed in <strong>the</strong> intensive care unit? An international utilization<br />
review. Am J Respir Crit Care Med 2000; 161: 1450-8.<br />
42. Esteban A, Alia I, Gordo F. Weaning: what <strong>the</strong> recent studies have<br />
shown us. Clin Pulm Med 1996; 3: 91-100.<br />
43. Horst HM, Mouro D, Hall-Jenssens RA, et al. Decrease in<br />
ventilation time with a standardized weaning process. Arch Surg<br />
1998; 133: 483-9.<br />
44. Esteban A, Alia I, Gordo F, et al. Extubation outcome after<br />
spontaneous breathing trials with T-tube or pressure support<br />
ventilation. Am J Respir Crit Care Med 1997; 156: 459-65.<br />
45. Aubier M, Murciano D, Lecocguic Y, et al. Effect <strong>of</strong><br />
hypophosphatemia on diaphragmatic contractility in patients with<br />
acute respiratory failure. N Engl J Med 1995; 313: 420-4.<br />
46. Brook A, Ahrens T, Schaiff R, et al. Effect <strong>of</strong> a nursing-implemented<br />
sedation protocol on <strong>the</strong> duration <strong>of</strong> mechanical ventilation. Crit<br />
Care Med 1999; 27: 2609-15.<br />
47. Kress JP, Dohlman AS, O’Connor MF, et al. Daily interruption <strong>of</strong><br />
sedative infusions in critically ill patients undergoing mechanical<br />
ventilation. N Engl J Med 2000; 342: 1471-7.<br />
48. Yang KL, Tobin MJ. A prospective study <strong>of</strong> indexes predicting <strong>the</strong><br />
outcome <strong>of</strong> trials <strong>of</strong> weaning from mechanical ventilation. N Engl J<br />
Med 1991; 324: 1445-50.<br />
49. Esteban A, Frutos F, Tobin MJ, et al. A comparison <strong>of</strong> four methods<br />
<strong>of</strong> weaning patients from mechanical ventilation. N Engl J Med<br />
1995; 332: 345-50.<br />
50. MacIntyre NR, Cook DJ, Ely Jr EW, et al: Evidence-based<br />
guidelines for weaning and discontinuing ventilatory support: A<br />
collective task force facilitated by <strong>the</strong> American College <strong>of</strong> Chest<br />
Physicians, <strong>the</strong> American Association for Respiratory Care, and<br />
<strong>the</strong> American College <strong>of</strong> Critical Care Medicine. Chest 2001; 120:<br />
375S.<br />
51. Buckenmaier CC 3rd, Rupprecht C, McKnight G, et al. Pain<br />
following battlefield injury and evacuation: a survey <strong>of</strong> 110<br />
casualties from <strong>the</strong> wars in Iraq and Afghanistan. Pain Med 2009;<br />
10: 1487-96.<br />
52. Adler AB, Castro CA, McGurk D. Time-driven battlemind<br />
psychological debriefing: a group-level early intervention in<br />
combat. Mil Med 2009; 174: 21-8.<br />
53. Ruggiero KJ, Del Ben K, Scotti JR, et al. Psychometric properties<br />
<strong>of</strong> <strong>the</strong> PTSD<br />
54. Checklist-Civilian Version. J Trauma Stress 2003; 16: 495-02.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S311–317 317
Traumatic Pneumorrhachis<br />
AG Haldane<br />
Specialty Registrar in <strong>Anaes<strong>the</strong>sia</strong>, Worcestershire <strong>Royal</strong> Hospital<br />
Abstract<br />
Pneumorrhachis or intraspinal air is an increasingly encountered phenomenon in <strong>the</strong> management <strong>of</strong> severe trauma. The case<br />
<strong>of</strong> a 23-year-old soldier, who sustained a gunshot wound to <strong>the</strong> chest, is presented and <strong>the</strong> subsequent discussion illustrates<br />
that while <strong>of</strong>ten benign this phenomenon may indicate serious occult injury.<br />
Introduction<br />
Pneumorrhachis is <strong>the</strong> presence <strong>of</strong> air in <strong>the</strong> spinal canal. This<br />
rare phenomenon has numerous aetiologies. It is a radiological<br />
diagnosis that, dependent on <strong>the</strong> location <strong>of</strong> <strong>the</strong> air, may be <strong>of</strong><br />
varying significance.<br />
Case History<br />
A 23-year-old United States Marine <strong>Corps</strong> soldier was admitted<br />
to <strong>the</strong> Joint Force <strong>Medical</strong> Group (R2E) facility at Camp<br />
Bastion in September 2009. He had sustained a gunshot wound<br />
to <strong>the</strong> left chest.<br />
Pre-hospital management had included high flow oxygen,<br />
a chest-seal dressing placed over <strong>the</strong> chest wound and vascular<br />
access with a 16G cannula in <strong>the</strong> left antecubital fossa. At <strong>the</strong><br />
primary survey on arrival in <strong>the</strong> emergency department he was<br />
alert and orientated and maintaining his own airway. Initial<br />
observations were: respiratory rate 16 breaths per minute, reduced<br />
air entry noted on <strong>the</strong> left, SpO 97%, pulse 78 beats per minute<br />
2<br />
and blood pressure 110/60 mmHg. No abdominal, pelvic or<br />
long bone injuries were<br />
identified. On examination<br />
<strong>of</strong> <strong>the</strong> back a single gunshot<br />
entry wound was identified<br />
in <strong>the</strong> left chest with an<br />
associated s<strong>of</strong>t tissue injury<br />
to <strong>the</strong> left triceps.<br />
Chest radiograph taken<br />
as part <strong>of</strong> <strong>the</strong> primary<br />
survey showed mediastinal<br />
shift and a large left sided<br />
haemo-pneumothorax.<br />
The penetrating round<br />
was seen clearly in <strong>the</strong><br />
left upper zone (Figure<br />
1). A thoracostomy tube<br />
was inserted and initially<br />
drained 300ml <strong>of</strong> fresh<br />
blood and a fur<strong>the</strong>r 100ml<br />
over <strong>the</strong> next 15 minutes.<br />
The patient remained haemodynamically stable throughout. No<br />
neurological deficit was detected.<br />
The patient was subsequently transferred for computerised<br />
tomography (CT) scanning and images <strong>of</strong> <strong>the</strong> thorax and<br />
Corresponding Author: Maj Andrew Haldane RAMC,<br />
Specialty Registrar in <strong>Anaes<strong>the</strong>sia</strong>, c/o AMDSU, FASC,<br />
Slim Road, Camberley, GU15 4NP<br />
Tel: 07958 739 437 E-mail: aghaldane1@doctors.org.uk<br />
Figure 2 – CT Scan <strong>of</strong> upper chest showing spinal air and retained round.<br />
Figure 1 – Chest radiograph showing injury to left chest and retained<br />
round.<br />
abdomen were obtained. The CT images confirmed <strong>the</strong><br />
haemo-pneumothorax, and also indicated large amounts <strong>of</strong><br />
subcutaneous emphysema with air extending into <strong>the</strong> spinal<br />
canal from above C5 to T7. The bullet was found to be lying<br />
between <strong>the</strong> left carotid and subclavian arteries (Figure 2). No<br />
bony injuries were identified.<br />
The patient remained stable and was admitted to <strong>the</strong> intensive<br />
care unit for observation. Initial debridement <strong>of</strong> his wounds was<br />
undertaken later that day. Post-operatively <strong>the</strong> patient underwent<br />
insertion <strong>of</strong> a thoracic epidural for analgesia at 24 hours post-<br />
318 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S318–320
1<br />
2<br />
3<br />
4<br />
5<br />
6<br />
7<br />
8<br />
9<br />
10<br />
11<br />
12<br />
13<br />
14<br />
15<br />
16<br />
17<br />
18<br />
19<br />
20<br />
21<br />
22<br />
23<br />
24<br />
25<br />
26<br />
27<br />
28<br />
29<br />
30<br />
31<br />
32<br />
33<br />
34<br />
35<br />
36<br />
37<br />
38<br />
39<br />
40<br />
41<br />
42<br />
43<br />
44<br />
45<br />
46<br />
47<br />
48<br />
49<br />
50<br />
51<br />
52<br />
53<br />
54<br />
55<br />
56<br />
57<br />
58<br />
59<br />
60<br />
61<br />
Traumatic Pneumorrhachis AG Haldane<br />
injury. Delayed primary closure <strong>of</strong> <strong>the</strong> extremity s<strong>of</strong>t tissue injury<br />
was undertaken at 48 hours.<br />
Discussion<br />
Air within <strong>the</strong> spinal canal is termed pneumorrhachis, first<br />
described by Newbold in 1971 [1]. O<strong>the</strong>r terms include: aerorachia,<br />
intraspinal pneumocele, epidural pneumatosis, pneumosaccus,<br />
and traumatic pneumomyelogram. It is a rare but increasingly<br />
recognised epiphenomenon [2]. The air can be within <strong>the</strong> epidural<br />
or subarachnoid spaces. While it can be difficult for clinicians<br />
to distinguish between <strong>the</strong>se two anatomical locations, varying<br />
distribution <strong>of</strong> air seen on CT may indicate its location. Air within<br />
<strong>the</strong> subarachnoid space may be located both anterior and posterior<br />
to <strong>the</strong> spinal cord. Air confined to <strong>the</strong> epidural space may be seen<br />
to have a predominantly posterior and/or lateral distribution [3,<br />
4]. This differentiation is important as <strong>the</strong> mechanism and causes<br />
<strong>of</strong> air entry are different and have different clinical implications<br />
[5]. Air in <strong>the</strong> epidural space is usually benign, while its presence<br />
in <strong>the</strong> subarachnoid space is commonly found in association with<br />
air within <strong>the</strong> cranial vault, basal skull fracture and dural tear, and<br />
is a marker <strong>of</strong> severe trauma.<br />
Epidural pneumorrhachis<br />
Epidural pneumorrhachis has numerous causes and <strong>the</strong>se can be<br />
broadly divided into iatrogenic, non-traumatic and traumatic.<br />
Iatrogenic causes include <strong>the</strong> administration <strong>of</strong> epidural analgesia.<br />
Non-traumatic cases have been reported in association with<br />
degenerative disc disease, epidural abscess, synovial cysts and<br />
following spontaneous pneumomediastinum and pneumothorax.<br />
In traumatic cases pneumorrhachis is most commonly seen in<br />
association with pneumomediastium and/or pneumothorax but<br />
has also been reported secondary to pelvic and vertebral fractures<br />
and dural-enteric fistulae [6].<br />
The mechanism whereby air enters <strong>the</strong> epidural space is a<br />
result <strong>of</strong> <strong>the</strong> fact that <strong>the</strong>re is no true fascial envelope protecting<br />
<strong>the</strong> space [7]. Air may dissect along fascial planes from ei<strong>the</strong>r <strong>the</strong><br />
posterior mediastinum or retropharyngeal space, through <strong>the</strong><br />
neural foramina and into <strong>the</strong> epidural space; this movement <strong>of</strong><br />
air occurs down <strong>the</strong> pressure gradient caused by a pneumothorax<br />
or pneumomediastinum. This continuous pathway between<br />
<strong>the</strong> intervertebral foramina and <strong>the</strong> epidural space was first<br />
demonstrated in 1973 [8]. It has also been established that air<br />
may track along fascial planes between <strong>the</strong> retroperitoneum and<br />
mediastinum and thus <strong>the</strong> epidural space [9]. Therefore injury to<br />
abdominal viscera may also result in pneumorrhachis [10].<br />
Epidural pneumorrhachis is usually benign. Identification<br />
<strong>of</strong> <strong>the</strong> underlying cause is important as its treatment will result<br />
in resolution <strong>of</strong> <strong>the</strong> intraspinal air. Criteria have been described<br />
that allow pneumorrhachis to be classified as benign, including:<br />
1) major thoracic trauma, 2) substantial pneumomediastinum<br />
with extensive subcutaneous emphysema, 3) a small amount <strong>of</strong><br />
epidural air, 4) air demonstrable only by CT scan, and 5) <strong>the</strong> air<br />
was an incidental finding on CT scan performed for an indication<br />
unrelated to <strong>the</strong> spine [11].<br />
It is rare for epidural pneumorrhachis to cause neurological<br />
symptoms; <strong>the</strong> few reported cases are most <strong>of</strong>ten in <strong>the</strong> context<br />
<strong>of</strong> <strong>the</strong> administration <strong>of</strong> epidural analgesia. The volumes <strong>of</strong> air<br />
injected during <strong>the</strong> “loss <strong>of</strong> resistance technique” are much larger<br />
than those likely to enter <strong>the</strong> spinal canal as a result <strong>of</strong> a traumatic<br />
injury [5]. Clinicians should rule out o<strong>the</strong>r possible causes <strong>of</strong><br />
neurological symptoms before attributing <strong>the</strong>m to intraspinal air.<br />
In cases <strong>of</strong> severe trauma consideration must be given that air<br />
may actually be present within <strong>the</strong> subarachnoid space.<br />
Subarachnoid pneumorrhachis<br />
Traumatic subarachnoid pneumorrhachis is a marker <strong>of</strong> severe<br />
injury. The most common reported causes are skull fractures and<br />
thoracic spine fractures and subarachnoid pneumorrhachis is<br />
almost always associated with pneumocephalus.<br />
In <strong>the</strong> case <strong>of</strong> skull fracture air enters <strong>the</strong> subarachnoid space<br />
ei<strong>the</strong>r directly from <strong>the</strong> atmosphere in <strong>the</strong> case <strong>of</strong> a fracture <strong>of</strong> <strong>the</strong><br />
cranial vault or from an air containing cavity or sinus. Once inside<br />
<strong>the</strong> intracranial subarachnoid space <strong>the</strong> air is free to migrate to <strong>the</strong><br />
spine through <strong>the</strong> foramen magnum, this usually occurs when <strong>the</strong><br />
patient has been in <strong>the</strong> head or face down position [5].<br />
Pneumocephalus may cause both general and focal neurological<br />
symptoms as a result <strong>of</strong> intracranial hypertension [12]. In addition<br />
<strong>the</strong>re is <strong>the</strong> risk <strong>of</strong> meningitis as a breach in <strong>the</strong> dura may act as a<br />
portal <strong>of</strong> entry for bacteria.<br />
Thoracic spine fractures may be associated with <strong>the</strong> formation<br />
<strong>of</strong> dural and pleural tears that may join to form a fistula. In<br />
penetrating trauma <strong>the</strong> missile may cause <strong>the</strong>se tears directly;<br />
fistula formation has been reported in a case <strong>of</strong> gunshot injury to<br />
<strong>the</strong> chest [13]. In blunt trauma extreme flexion and compression<br />
<strong>of</strong> <strong>the</strong> thoracic spinal nerve roots and thoracic cage is felt sufficient<br />
to allow <strong>the</strong> formation <strong>of</strong> a fistula [14].<br />
As with epidural air <strong>the</strong>re is no specific treatment for<br />
subarachnoid pneumorrhachis and <strong>the</strong>rapy is aimed at identifying<br />
and treating <strong>the</strong> underlying cause. Focussed investigation <strong>of</strong><br />
<strong>the</strong> spinal column and base <strong>of</strong> skull should be considered.<br />
Consideration should also be given to closure <strong>of</strong> defects in <strong>the</strong><br />
dura if such are present.<br />
Anaes<strong>the</strong>tic considerations<br />
Severely injured patients who are due to undergo surgery should<br />
not be exposed to anaes<strong>the</strong>tic techniques likely to increase <strong>the</strong><br />
pressure or volume <strong>of</strong> intraspinal gas collections. Therefore <strong>the</strong> use<br />
<strong>of</strong> nitrous oxide should be avoided [15]. A high inspired fraction<br />
<strong>of</strong> oxygen may help to speed resolution <strong>of</strong> air pockets.<br />
Air in <strong>the</strong> epidural space has been shown to cause <strong>the</strong> failure <strong>of</strong><br />
attempted epidural analgesia [16]. There are no reports <strong>of</strong> <strong>the</strong> use<br />
<strong>of</strong> epidural anaes<strong>the</strong>sia in <strong>the</strong> provision <strong>of</strong> analgesia for injuries<br />
associated with pneumorrhachis however we found that good<br />
analgesia was obtained from a thoracic epidural inserted 24 hours<br />
after injury despite <strong>the</strong> initial presence <strong>of</strong> intraspinal air. It would,<br />
however, seem prudent to use a “loss <strong>of</strong> resistance to saline” ra<strong>the</strong>r<br />
than a “loss <strong>of</strong> resistance to air” technique.<br />
Aeromedical evacuation considerations<br />
The aeromedical transfer <strong>of</strong> patients with pneumocephalus has<br />
always caused some concern. Pneumorrhachis may not always<br />
be associated with pneumocephalus. In <strong>the</strong> case <strong>of</strong> intracranial<br />
air a recent study concluded that <strong>the</strong> mechanism causing<br />
pneumocephalus, its time course, progression, and <strong>the</strong> rate <strong>of</strong><br />
altitude change are likely more important factors in determining<br />
its clinical significance [17], and this probably holds true for<br />
intraspinal air. Advice should be sought from those who will be<br />
responsible for <strong>the</strong> patient’s in-flight care.<br />
Conclusion<br />
Pneumorrhachis, or intraspinal air, is a rare phenomenon.<br />
However with <strong>the</strong> early use <strong>of</strong> CT in <strong>the</strong> assessment <strong>of</strong> <strong>the</strong><br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S318–320 319
Traumatic Pneumorrhachis<br />
severely injured patient it is likely to be increasingly encountered.<br />
The early management <strong>of</strong> <strong>the</strong> precipitating cause underpins <strong>the</strong><br />
management <strong>of</strong> pneumorrhachis. While in <strong>the</strong> majority <strong>of</strong> cases<br />
intraspinal air is benign and <strong>of</strong> little significance efforts must be<br />
made to identify those situations where <strong>the</strong> underlying cause may<br />
dictate that morbidity may be high.<br />
References<br />
1. Newbold RG, Wiener MD, Vogler III JB, Martinez Z. Traumatic<br />
pneumorrhachis. Am J Roentgenol 1987;148:615-6.<br />
2. Chaichana KL, Pradilla G, Witham TM, Gokaslan ZL, Bydon A.<br />
The clinical significance <strong>of</strong> pneumorachis: a case report and review<br />
<strong>of</strong> <strong>the</strong> literature. J Trauma 2010;68(3):736-44.<br />
3. Dwarakanath S, Banerji A, Chandramouli BA. Posttraumatic<br />
intradural pneumorrhachis: a rare entity. Ind J Neurotrauma<br />
2009;6(2):151-2.<br />
4. Oertel MF, Korinth MC, Reinges MHT, Krings T, Terbeck<br />
S, Gilsbach JM. Pathogenesis, diagnosis and management <strong>of</strong><br />
pneumorrhachis. Eur Spine J 2006;15(Suppl. 5):S636-S43.<br />
5. Goh BKP, Yeo AWY. Traumatic pneumorrhachis. J Trauma<br />
2005;58(4):875-9.<br />
6. Silver SF, Nadel HR, Flodmark O. Pneumorrhachis after jejunal<br />
entrapment caused by a fracture dislocation <strong>of</strong> <strong>the</strong> lumbar spine.<br />
Am J Roentgenol 1988;150:1129-30.<br />
7. Goh BK, Ng K-K, Hoe MNY. Traumatic epidural emphysems.<br />
Spine. 2004;29(22):E528-E30.<br />
320<br />
AG Haldane<br />
8. Burn JM, Guyer PB, Langdon L. The spread <strong>of</strong> solutions injected<br />
into <strong>the</strong> epidural space: a study using epidurograms in patients<br />
with lumbosciatic syndrome. Br J Anaesth 1973;45:334-8.<br />
9. Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and<br />
mediastinal empysema: pathophysiology, diagnosis and<br />
management. Arch Intern Med 1984;144:1447-53.<br />
10. Gautschi OP, Hermann C, Cadosch D. Spinal epidural air<br />
after severe pelvic and abdominal trauma. Am J Emerg Med<br />
2008;26:740.e3-.e5.<br />
11. Willing SJ. Epidural pneumatosis: a benign entity in trauma<br />
patients. Am J Neuroradiol 1991;12:345.<br />
12. Bilsky MH, Downey RJ, Kaplitt MG, Elowitz EH, Rusch VW.<br />
Tension pneumocephalus resulting from iatrogenic subarachnoid–<br />
pleural fistulae: report <strong>of</strong> three cases. Ann Thorac Surg 2001;71:455-7.<br />
13. Lloyd C, Saha SA. Subarachnoid pleural fistula due to penetrating<br />
trauma: a case report and review <strong>of</strong> <strong>the</strong> literature. Chest<br />
2002;122:2252-6.<br />
14. Rocha-Campos BA, Silva LB, Ballalai N, Negrao MM. Traumatic<br />
subarachnoid-pleural fistula. J Neurol Neurosurg Psychiatry<br />
1974;37:269-70.<br />
15. Day CJE, Nolan JP, Tarver D. Traumatic pneumomyelogram.<br />
Implications for <strong>the</strong> anaes<strong>the</strong>tist. <strong>Anaes<strong>the</strong>sia</strong> 1994;49:1061-3.<br />
16. Boezaart AP. Epidural air-filled bubbles and unblocked segments.<br />
Can J Anaesth 1989;36:603-4.<br />
17. Donovan DJ, Iskandar JI, Dunn CJ, King JA. Aeromedical<br />
evacuation <strong>of</strong> patients with pneumocephalus: outcomes in 21 cases.<br />
Aviat Space Environ Med 2008;79(1):30-5.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S318–320
Special Situations
Paediatric <strong>Anaes<strong>the</strong>sia</strong> in Afghanistan: a Review<br />
<strong>of</strong> <strong>the</strong> Current Experience<br />
GR Nordmann<br />
Consultant Paediatric Anaes<strong>the</strong>tist, MDHU Derriford; Consultant Anaes<strong>the</strong>tist, 16 <strong>Medical</strong> Regiment; Research Fellow,<br />
<strong>Defence</strong> Science and Technology Laboratory<br />
Abstract<br />
This paper describes <strong>the</strong> author’s experience <strong>of</strong> <strong>the</strong> paediatric patient load on <strong>the</strong> UK medical services in Afghanistan. Over a 3<br />
month period <strong>the</strong>re was a mean <strong>of</strong> 2.9 paediatric trauma admissions per week, mean age was 6.8 years with gunshot wound or<br />
explosive injury being <strong>the</strong> mechanisms <strong>of</strong> injury in 77% <strong>of</strong> <strong>the</strong> trauma admissions. Overall <strong>the</strong>se children represented 10.8%<br />
<strong>of</strong> <strong>the</strong> surgical workload. Some <strong>of</strong> <strong>the</strong> issues <strong>of</strong> paediatric anaes<strong>the</strong>sia in this environment are discussed including paediatric<br />
equipment, resuscitation for paediatric massive haemorrhage and regional anaes<strong>the</strong>sia. The need to formally recognise <strong>the</strong><br />
problem in training and equipping deployed medical personnel to deal with this challenge is examined.<br />
Introduction<br />
United Kingdom medical forces on operations are configured<br />
specifically to support <strong>the</strong> deployed military force in that<br />
area. In Afghanistan, as in most conflicts, civilians account<br />
for a significant number <strong>of</strong> <strong>the</strong> casualties. Present operations<br />
take place in close proximity to <strong>the</strong> local population and<br />
consequently UK forces in accordance with <strong>the</strong> Geneva<br />
Conventions will deliver medical support to non-combatants<br />
who are injured. Children are a prominent fraction <strong>of</strong> this<br />
group and are regularly placed in <strong>the</strong> UK medical treatment<br />
and evacuation chain where <strong>the</strong>y can impose a significant<br />
workload on <strong>the</strong> hospital in Camp Bastion.<br />
Historical Experience<br />
To appreciate <strong>the</strong> numbers <strong>of</strong> children involved it is appropriate<br />
to review what information has been published recently. This<br />
is predominantly from papers describing paediatric workload<br />
to UK and US hospitals in Iraq and Afghanistan over <strong>the</strong> past<br />
decade. Creamer’s [1] paper is <strong>the</strong> largest review and looked at<br />
US Combat Support Hospital (CSH) admissions in Iraq and<br />
Afghanistan. They reported that 10% <strong>of</strong> <strong>the</strong>ir overall workload<br />
was paediatric but <strong>the</strong>se children represented 50% <strong>of</strong> <strong>the</strong>ir civilian<br />
admissions. Of those admitted with trauma, penetrating injuries<br />
predominated (76.3%), <strong>the</strong> principal mechanisms <strong>of</strong> injury being<br />
gunshot wound (GSW, 39%) and explosive injury (32%). Just<br />
fewer than 6% required mechanical ventilation and mortality was<br />
6.9%, <strong>the</strong> primary causes <strong>of</strong> death being head injury and burns.<br />
Beitler [2] looked in more detail at <strong>the</strong>ir initial admissions in<br />
Afghanistan to <strong>the</strong> 48th Combat Support Hospital and found<br />
28.4% <strong>of</strong> all trauma victims were paediatric, paediatric admissions<br />
a week. Although <strong>the</strong>y didn’t look at mechanism <strong>of</strong> injury in<br />
<strong>the</strong> paediatric population specifically, <strong>the</strong>ir overall population<br />
had explosive injury (41%) and GSW (20%) as <strong>the</strong>ir highest<br />
mechanisms <strong>of</strong> injury. Mean age was 9 years (range 1-16 years)<br />
with <strong>the</strong> paediatric population having a longer length <strong>of</strong> stay (10<br />
days) compared to adults (8.5 days).<br />
Corresponding Author: Lt Col Giles R Nordmann BSc(Hons)<br />
MBChB FRCA RAMC, Consultant Paediatric Anaes<strong>the</strong>tist,<br />
MDHU Derriford, Plymouth<br />
Tel: 01822 853334 E-mail: nordmann@waitrose.com<br />
UK data from Iraq in <strong>the</strong> initial war fighting stage in 2003<br />
from two different hospitals illustrates <strong>the</strong> work load and differing<br />
mechanisms <strong>of</strong> injury at that time. Gurney’s [3] paper was an<br />
Emergency Department based review <strong>of</strong> 34 Field Hospital’s<br />
admissions over <strong>the</strong> first month when it was initially positioned<br />
in Shaibah, Iraq after <strong>the</strong> first few days <strong>of</strong> <strong>the</strong> conflict. He found<br />
paediatric patients comprised 2.9% <strong>of</strong> all recorded admissions,<br />
but accounted for nearly a third <strong>of</strong> civilian patients. The workload<br />
was 13 paediatric admissions per week with burns (77%) and<br />
explosive injury (12%) being <strong>the</strong> most common mechanisms <strong>of</strong><br />
injury in his trauma subset. Mean age was 7.9 years with a higher<br />
proportion being male (65.4%). Heller’s [4] review <strong>of</strong> paediatric<br />
patients followed <strong>the</strong>ir path through 22 Field Hospital based in<br />
Kuwait over <strong>the</strong> same initial war fighting stage. There were six<br />
paediatric admissions per week and again explosive (50%) and<br />
burns (42%) were <strong>the</strong> main mechanisms <strong>of</strong> injury. Mean age<br />
was 6.3 years in <strong>the</strong>ir trauma population (range 6 months to 15<br />
years). Their data is highly influenced by <strong>the</strong> number <strong>of</strong> transfers<br />
from <strong>the</strong> forward deployed 34 Field Hospital back to 202 Field<br />
Hospital in Kuwait.<br />
Local civilians without power were relying on Kerosene lamps<br />
for lighting and a high proportion <strong>of</strong> <strong>the</strong> injuries were burns<br />
secondary to accidents from this method <strong>of</strong> lighting ra<strong>the</strong>r than<br />
direct conflict casualties. None<strong>the</strong>less unexploded ordnance<br />
from this and previous conflicts were exposed in this phase <strong>of</strong><br />
<strong>the</strong> ground war and injuries secondary to <strong>the</strong>se accounted for a<br />
significant part <strong>of</strong> <strong>the</strong> remainder.<br />
Present military operations in Afghanistan are producing a<br />
greater proportion <strong>of</strong> explosive and GSW penetrating injuries in<br />
<strong>the</strong> paediatric population in UK facilities. Harris’ [5] paper in this<br />
journal reviewed <strong>the</strong> paediatric workload on Critical Care in 2008.<br />
In <strong>the</strong> two months <strong>the</strong>ir data was collected <strong>the</strong>y had 15 patients<br />
whose mechanism <strong>of</strong> injury was predominantly penetrating GSW<br />
or explosive. Mean age was 6 years (range 6 months to 17 years).<br />
This paediatric population was a significant workload for <strong>the</strong><br />
Critical Care unit leading to children accounting for 30% <strong>of</strong> all<br />
bed occupancy. They reported one death from multi organ failure<br />
subsequent a penetrating injury to <strong>the</strong> chest and abdomen.<br />
Methods<br />
In order to obtain a more accurate review <strong>of</strong> paediatric admissions<br />
to <strong>the</strong> Role 3 hospital at Camp Bastion, data was collected for<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S323–326 323
Paediatric <strong>Anaes<strong>the</strong>sia</strong> in Afghanistan<br />
a three month period over Op HERRICK 8b/9a looking at<br />
paediatric patients admitted with traumatic injuries. All paediatric<br />
surgical admissions medical records were examined retrospectively<br />
and <strong>the</strong> <strong>the</strong>atre operation log book was examined. Data collected<br />
included, age, sex, diagnosis, operations, number <strong>of</strong> operations,<br />
admission to ITU, length <strong>of</strong> admission.<br />
Results<br />
During <strong>the</strong> three months, 31 children were admitted for surgical<br />
intervention after trauma. There were 18 (58%) male and 13<br />
(42%) female patients with an average age <strong>of</strong> 6.8 years (range 6<br />
months to 14 years). This is similar to previous experience but <strong>of</strong><br />
more particular interest was that a quarter <strong>of</strong> <strong>the</strong>se were aged 2<br />
years or younger (Figure 1).<br />
Figure 1: Age distribution <strong>of</strong> paediatric trauma admissions as a<br />
percentage <strong>of</strong> total paediatric trauma admissions on Op HERRICK<br />
8b/9a.<br />
There were a mean <strong>of</strong> 2.9 paediatric admissions per week, a<br />
smaller number than in <strong>the</strong> previous papers, however this patient<br />
population still presented a significant workload for <strong>the</strong> surgical<br />
and anaes<strong>the</strong>tic teams. The quantity <strong>of</strong> surgical operations<br />
undertaken on this paediatric population was 10.8% <strong>of</strong> all<br />
operations carried out, with an operation on a child occurring<br />
every 1.9 days, each child needing a mean <strong>of</strong> 1.6 operations<br />
(range 1 to 5).<br />
The main mechanisms <strong>of</strong> injury were fragmentation (45.1%)<br />
and GSW (32.3%) and are shown in Figure 2 compared to <strong>the</strong><br />
previous UK and US experiences in Iraq.<br />
Figure 2: Paediatric patients; mechanism <strong>of</strong> injury as percentage <strong>of</strong><br />
total paediatric trauma admissions.<br />
324<br />
GR Nordmann<br />
Mean length <strong>of</strong> stay was 10.5 days (range 1 to 62 days) and<br />
35% <strong>of</strong> <strong>the</strong>se paediatric patients were admitted to critical care.<br />
This was 11.9% <strong>of</strong> its total admissions over <strong>the</strong> data collection<br />
period. In <strong>the</strong> critical care sub-group <strong>of</strong> <strong>the</strong> most gravely injured<br />
children penetrating wounds secondary to GSW or explosive<br />
injury accounted for 91% <strong>of</strong> <strong>the</strong> injuries. For those admitted<br />
to critical care a thoracotomy was needed in 27% <strong>of</strong> cases,<br />
laparotomy in 82% and injuries to <strong>the</strong> liver, spleen or pancreas<br />
were involved in 36%. There was one death from a penetrating<br />
explosive injury with multiple wounds to chest and abdomen.<br />
A summative review <strong>of</strong> <strong>the</strong> above data predicts that any<br />
anaes<strong>the</strong>tist deploying to Afghanistan would be expected to deal<br />
with two to four paediatric admissions per week. These patients<br />
will have an average age <strong>of</strong> seven and a quarter <strong>of</strong> <strong>the</strong>m may be less<br />
than two years <strong>of</strong> age. Each child will need around two operations<br />
and have an average length <strong>of</strong> stay <strong>of</strong> 10 days.<br />
Discussion<br />
This significant paediatric challenge means military anaes<strong>the</strong>tists<br />
need to be prepared to treat not just <strong>the</strong> injured paediatric patient<br />
but one that has had significant ballistic trauma and is suffering<br />
from <strong>the</strong> major haemorrhage and coagulopathy that can result<br />
from it, a rare occurrence in UK civilian practice. Military<br />
consultants and trainees need to be prepared to deal with this<br />
patient group by being adequately trained and equipped to<br />
provide <strong>the</strong> appropriate care.<br />
Critical Care<br />
Over a third <strong>of</strong> paediatric patients who had suffered trauma<br />
were admitted to critical care which seems a large proportion.<br />
It places a significant workload on <strong>the</strong> critical care staff who do<br />
not necessarily have <strong>the</strong> necessary paediatric experience. There is<br />
probably a combination <strong>of</strong> factors influencing this admission rate;<br />
significant penetrating injuries not normally seen in <strong>the</strong> UK, staff<br />
with little paediatric experience and <strong>the</strong> lack <strong>of</strong> local paediatric<br />
critical care provision are probably all <strong>of</strong> some significance. This is<br />
discussed in more detail in Harris’ paper [5].<br />
Equipment<br />
The design and choice <strong>of</strong> breathing systems is determined by <strong>the</strong><br />
child’s weight and age. The commonest being <strong>the</strong> Mapleson F and<br />
<strong>the</strong> circle system which comes in adult and paediatric sizes. The<br />
differences and advantages <strong>of</strong> <strong>the</strong>se systems can be found in any<br />
paediatric anaes<strong>the</strong>sia text [6]. In summary <strong>the</strong> Mapleson F is in<br />
most common use and its advantages are: no valves, low resistance,<br />
Continuous Positive Airway Pressure (CPAP) and Positive End<br />
Expiratory Pressure (PEEP) can be applied and it can be used for<br />
spontaneous and controlled ventilation. It is <strong>of</strong> particular use in<br />
smaller children but its disadvantage is <strong>the</strong> need for high fresh gas<br />
flows. The main disadvantages <strong>of</strong> circle systems are <strong>the</strong> resistance<br />
from unidirectional valves and <strong>the</strong>ir higher compliance reducing<br />
tactile feedback when hand ventilating. This reduces its ability to<br />
be used in smaller children (less than 10kg).<br />
Until recently in <strong>the</strong> military environment <strong>the</strong> Triservice<br />
anaes<strong>the</strong>tic apparatus (TSAA) has predominated. It has been<br />
studied in children in its original format previously by Bell [7].<br />
His team studied children weighing down to 10kg, comparing<br />
work <strong>of</strong> breathing between <strong>the</strong> Mapleson F breathing system<br />
and <strong>the</strong> TSAA. They found <strong>the</strong>re was no significant difference in<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S323–326
Paediatric <strong>Anaes<strong>the</strong>sia</strong> in Afghanistan GR Nordmann<br />
work <strong>of</strong> breathing between <strong>the</strong> two breathing systems proving <strong>the</strong><br />
TSAA is suitable to be used in children over that weight. Despite<br />
this endorsement <strong>the</strong> TSAA has a number <strong>of</strong> problems when<br />
being used to anaes<strong>the</strong>tise children. When manually ventilating<br />
children it also provides poor tactile feedback back from <strong>the</strong> bag<br />
and an inability to accurately measure and set <strong>the</strong> inspiratory<br />
pressure. In spontaneous ventilation it is difficult to visually<br />
monitor <strong>the</strong> tidal volume and respiratory rate in addition to being<br />
unable to easily provide PEEP or CPAP.<br />
This has prompted some users to use <strong>the</strong> TSAA in different<br />
formats when anaes<strong>the</strong>tising children. The Oxford Miniature<br />
Vaporisers (OMVs) can be added to <strong>the</strong> fresh gas flow arm <strong>of</strong><br />
<strong>the</strong> Mapleson F. This will require a high flow <strong>of</strong> gas through <strong>the</strong><br />
vaporisers (in excess <strong>of</strong> 6 litres per minute) to prevent rebreathing.<br />
Fur<strong>the</strong>r upstream from <strong>the</strong> OMVs is <strong>the</strong> oxygen inlet and <strong>the</strong> cage<br />
mount connector <strong>of</strong> <strong>the</strong> TSAA. This end has traditionally been<br />
occluded to minimise air entrainment and this occlusion is not an<br />
ideal solution for patient safety. Birt [8] describes <strong>the</strong> use <strong>of</strong> a short<br />
piece <strong>of</strong> extension tubing and a disposable Intavent adjustable<br />
pressure limiting (APL) valve at this end allowing pressure relief<br />
to occur when <strong>the</strong> circuit pressure exceeds a set level. This set up<br />
can be used for both spontaneous and manual ventilation in most<br />
paediatric weight groups.<br />
For children under 10kg, intubation and positive pressure<br />
ventilation is <strong>the</strong> norm. Manual ventilation compared to<br />
mechanical ventilation is useful as it provides constant feedback<br />
<strong>of</strong> airway resistance but it does not enable <strong>the</strong> anaes<strong>the</strong>tist to do<br />
concurrent tasks that are essential in resuscitation <strong>of</strong> <strong>the</strong> severely<br />
injured child. Ralph et al [9] addressed this issue recently and<br />
devised a method for ventilating children under 10kg using <strong>the</strong><br />
TSAA in conjunction with <strong>the</strong> Pneupac ComPAC 200 ventilator.<br />
The ComPAC 200 ventilator is a flow generator which is<br />
inadequate for paediatric use. Children have significantly smaller<br />
tidal volumes and are at higher risk <strong>of</strong> barotrauma so <strong>the</strong>y should<br />
be preferentially ventilated using a predetermined inspiratory<br />
pressure ra<strong>the</strong>r than volume. Ralph’s group described a series <strong>of</strong><br />
six children under 10kg who were successfully ventilated using<br />
<strong>the</strong> TSAA and ComPAC 200. In a similar move to <strong>the</strong> conversion<br />
<strong>of</strong> a Penlon Nuffield 200 ventilator from flow to a pressure<br />
generator by <strong>the</strong> addition <strong>of</strong> a Newton Paediatric valve <strong>the</strong>y added<br />
an Intavent APL valve between <strong>the</strong> ventilator and <strong>the</strong> OMVs thus<br />
converting <strong>the</strong> ComPAC 200 to a pressure generating ventilator.<br />
The changes described above give <strong>the</strong> military anaes<strong>the</strong>tist all<br />
options needed when anaes<strong>the</strong>tising a child using <strong>the</strong> TSAA. In<br />
recent months <strong>the</strong> new Dräger Fabius Tiro has been in place in<br />
Camp Bastion. This enables conventional methods <strong>of</strong> providing<br />
anaes<strong>the</strong>sia using <strong>the</strong> breathing systems discussed above that are<br />
well known in UK hospitals.<br />
Analgesia and Regional <strong>Anaes<strong>the</strong>sia</strong><br />
Adequate pain relief is an essential part <strong>of</strong> any anaes<strong>the</strong>tic<br />
technique and this is true for children <strong>of</strong> any age. Pain management<br />
in children presents additional challenges not seen in adults; in<br />
particular <strong>the</strong> difficulty <strong>of</strong> assessment <strong>of</strong> pain. Anticipation <strong>of</strong><br />
pain and pre-emptive treatment should be <strong>the</strong> norm. The use<br />
<strong>of</strong> regional anaes<strong>the</strong>sia is common in children and if given at<br />
induction has <strong>the</strong> advantage <strong>of</strong> providing good intra-operative<br />
analgesia where its effect can be assessed as to its subsequent postoperative<br />
effect. Blocks are virtually all performed under general<br />
anaes<strong>the</strong>sia. Virtually any block performed on adults can be used<br />
in children. The equipment does not have to be significantly<br />
different except for peripheral blocks in much smaller children<br />
and central blocks under a certain size. Paediatric regional<br />
anaes<strong>the</strong>sia though should only be carried out by an experienced<br />
practitioner who has <strong>the</strong> prior knowledge and skills to undertake<br />
<strong>the</strong>m. It is not in <strong>the</strong> scope <strong>of</strong> this article to discuss <strong>the</strong> equipment<br />
requirements in detail nor <strong>the</strong> different local anaes<strong>the</strong>tic doses,<br />
volumes or infusion rates.<br />
Massive Haemorrhage<br />
Adult management <strong>of</strong> massive haemorrhage has been well<br />
described and <strong>the</strong>re is formal guidance for all deployed physicians<br />
in its management [10]. The Paediatric <strong>Anaes<strong>the</strong>sia</strong> and Critical<br />
Care Specialist Interest Group (PACCSIG) has written a paediatric<br />
guide per weight that will enable anaes<strong>the</strong>tists to guide paediatric<br />
patient resuscitation and this is detailed fur<strong>the</strong>r in <strong>the</strong> article by<br />
Bree et al [11].<br />
Training<br />
It is imperative that military anaes<strong>the</strong>tists have adequate training<br />
to deal with this paediatric challenge. It is <strong>the</strong> author’s opinion<br />
that trainees should have at least 6 months paediatric training in<br />
<strong>the</strong>ir final 3 years <strong>of</strong> training, preferably at a tertiary paediatric<br />
hospital. Ideally this hospital should have a dedicated paediatric<br />
ED department and have a military anaes<strong>the</strong>tic consultant<br />
working <strong>the</strong>re. For consultants <strong>the</strong>re should be one consultant<br />
with a regular paediatric exposure in <strong>the</strong> UK deployed to Herrick<br />
at any one time. The o<strong>the</strong>r consultants should have refresher<br />
training in a tertiary paediatric centre before deploying.<br />
US experience<br />
The Americans have dealt with over 3,500 infants and children<br />
in Afghanistan and Iraq. Their combat support hospitals are<br />
‘doctrinally’ not staffed or equipped to provide care for this<br />
population. The US has recognised this and made changes to<br />
respond to this challenge [12]. Paediatric specific education<br />
including a web based education platform, modified paediatric<br />
equipment and a 24 hour paediatric critical care ‘teleconsultation’<br />
service have been designed to improve pre-deployment training<br />
and in <strong>the</strong>atre care <strong>of</strong> <strong>the</strong> injured child.<br />
Paediatric <strong>Anaes<strong>the</strong>sia</strong> and Critical Care Specialist<br />
Interest Group (PACCSIG).<br />
This group has been commissioned by <strong>the</strong> <strong>Defence</strong> Consultant<br />
Adviser in Anaes<strong>the</strong>tics and meets bi-annually to address some<br />
<strong>of</strong> <strong>the</strong> issues raised in this article. At present it is working on<br />
equipment concerns, massive haemorrhage, audit and training.<br />
As part <strong>of</strong> its work improved Role 1 Paediatric training has<br />
occurred for HERRICK 12 and 13. Consultant anaes<strong>the</strong>tists<br />
deploying to HERRICK 13 have had clinical refresher sessions<br />
at Birmingham Children’s Hospital and guidelines for paediatric<br />
massive haemorrhage are published in this journal.<br />
Conclusions<br />
The current spectrum <strong>of</strong> operations imposes a tough challenge<br />
on deployed <strong>Defence</strong> <strong>Medical</strong> Services (DMS) personnel to<br />
manage and treat civilian children. The data collected for this<br />
paper illustrates that children with considerable ballistic and<br />
penetrating injuries are a significant part <strong>of</strong> this challenge and<br />
military anaes<strong>the</strong>tists need to be prepared for this. As such, <strong>the</strong><br />
DMS has a duty to train and equip its personnel to <strong>the</strong> required<br />
standard in order to provide appropriate care to this population<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S323–326 325
Paediatric <strong>Anaes<strong>the</strong>sia</strong> in Afghanistan<br />
group. The PACCSIG is addressing some <strong>of</strong> <strong>the</strong> issues described<br />
in this article and is working towards a more formal recognition<br />
<strong>of</strong> <strong>the</strong> training and equipment needs in addition to guidelines<br />
for best practice in paediatric anaes<strong>the</strong>sia and resuscitation in <strong>the</strong><br />
deployed environment.<br />
Acknowldgements<br />
The author would like to thank Col P Mahoney OBE TD MSc<br />
FRCA L/RAMC for his advice on this article.<br />
References<br />
1. Creamer KM, Edwards MJ, Shields CH, Thompson MW, Yu CE,<br />
Adelman . Pediatric Wartime Admissions to US Military Combat<br />
Support Hospitals in Afghanistan and Iraq: Learning from <strong>the</strong> First<br />
2,000 Admissions. J Trauma 2009; 67 (4): 762-768.<br />
2. Beitler AL, Wortmann GW, H<strong>of</strong>mann LJ, G<strong>of</strong>f JM Jr. Operation<br />
Enduring Freedom: The 48th Combat Support Hospital in<br />
Afghanistan. Mil Med 2006; 171 (3): 189-193.<br />
3. Gurney, I. Paediatric Casualties During OP TELIC. J R <strong>Army</strong> Med<br />
<strong>Corps</strong> 2004; 150: 270-272.<br />
4. Heller D. Child Patients in a Field Hospital during <strong>the</strong> 2003 Gulf<br />
Conflict. J R <strong>Army</strong> Med <strong>Corps</strong> 2004; 151: 41-43.<br />
5. Harris CC, McNicholas JJK. Paediatric Intensive Care in <strong>the</strong> Field<br />
Hospital. J R <strong>Army</strong> Med <strong>Corps</strong> 2009; 155 (2): 157-159.<br />
326<br />
GR Nordmann<br />
6. Doyle E (Ed.). Paediatric <strong>Anaes<strong>the</strong>sia</strong>. 1st Edition. Oxford<br />
University Press.<br />
7. Bell GT, McEwen JP, Beaton SJ, Young D.. Comparison <strong>of</strong> work<br />
<strong>of</strong> breathing using drawover and continuous flow anaes<strong>the</strong>tic<br />
breathing systems in children. <strong>Anaes<strong>the</strong>sia</strong> 2007; 62: 359-363.<br />
8. Birt D. Modification <strong>of</strong> TSAA for Paediatric Use. Department<br />
<strong>of</strong> Military <strong>Anaes<strong>the</strong>sia</strong>, Pain and Critical Care website, Audit<br />
and Research, Clinical Answers. https://wss.armynet.mod.uk/<br />
anaes<strong>the</strong>sia/default.aspx<br />
9. Ralph JK, George R, Thompson J. Paediatric <strong>Anaes<strong>the</strong>sia</strong> Using<br />
<strong>the</strong> Triservice Anaes<strong>the</strong>tic Apparatus. J R <strong>Army</strong> Med <strong>Corps</strong> 2010;<br />
156 (2): 84-87.<br />
10. Surgeon General’s Operational Policy Letter, 2009. Management<br />
<strong>of</strong> Massive Haemorrhage on Operations.<br />
11. S Bree, K Wood, GR Nordmann, J McNicholas. The Paediatric<br />
Transfusion Challenge on Deployed Operations. J R <strong>Army</strong> Med<br />
<strong>Corps</strong> 2010; 156(4 Suppl 1): S361-364.<br />
12. Fuenfer MM, Spinella PC, Naclerio AL, Creamer KM. The US<br />
wartime pediatric trauma mission: how surgeons and paediatricians<br />
are adapting <strong>the</strong> system to address <strong>the</strong> need. Mil Med 2009; 174<br />
(9): 887-91.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S323–326
Toxicology and Military <strong>Anaes<strong>the</strong>sia</strong><br />
TC Nicholson-Roberts<br />
Specialist Registrar <strong>Anaes<strong>the</strong>sia</strong> and Intensive Care Medicine, MDHU Derriford<br />
Abstract<br />
The combination <strong>of</strong> trauma and poisoning is a situation likely to be faced by a deployed force at some point. This article provides<br />
practical advice on how to deal with poisoned patients without deviating from <strong>the</strong> concept <strong>of</strong> damage control resuscitation.<br />
The constraints <strong>of</strong> limited diagnostics, both at <strong>the</strong> scene and clinically, and lack <strong>of</strong> antidotal <strong>the</strong>rapy are fundamental to <strong>the</strong><br />
practice <strong>of</strong> clinical toxicology. Some <strong>of</strong> <strong>the</strong> specific <strong>the</strong>rapies such as atropine and oximes were not evaluated prior to <strong>the</strong>ir<br />
introduction and <strong>the</strong>re are few randomised controlled trials <strong>of</strong> poisoned patients. Most <strong>of</strong> <strong>the</strong> diagnoses will be made on<br />
clinical grounds and most <strong>of</strong> <strong>the</strong> <strong>the</strong>rapy will be supportive; this article aims to reassure military anaes<strong>the</strong>tists in <strong>the</strong> process<br />
<strong>of</strong> dealing with <strong>the</strong> poisoned trauma patient.<br />
Introduction<br />
The changing landscape <strong>of</strong> toxicological threats to deployed troops<br />
might now be inclined towards toxic industrial chemicals (TICs).<br />
Exposure to <strong>the</strong>se can be classified as an accidental or deliberate<br />
release and <strong>the</strong> casualties may or may not have associated trauma.<br />
For example, in <strong>the</strong> Bohpal disaster <strong>of</strong> 1984, an accidental release<br />
<strong>of</strong> methyl isocyanate, resulted in no direct trauma but thousands<br />
<strong>of</strong> poisoned patients. The Buncefield Oil Storage Depot fire in<br />
2005 had <strong>the</strong> potential to cause serious injury including blast and<br />
burns with <strong>the</strong> associated effects <strong>of</strong> inhaled combustion products<br />
and particles. Deliberate release would include <strong>the</strong> Iraq chlorine<br />
tanker incidents in 2007 [1]. Fortunately <strong>the</strong> temperature <strong>of</strong> <strong>the</strong><br />
blasts were such that a large proportion <strong>of</strong> <strong>the</strong> chlorine burnt and<br />
that which did not, was dissipated, however <strong>the</strong> accompanying<br />
blast would have resulted in much trauma. In <strong>the</strong> management <strong>of</strong><br />
a suspected chemical release, <strong>the</strong> identification <strong>of</strong> <strong>the</strong> compound,<br />
its combustion and reaction products are advantageous. Whilst<br />
this is relatively straightforward in <strong>the</strong> UK from registration <strong>of</strong><br />
COMAH (Control <strong>of</strong> Major Accident Hazards) sites, <strong>the</strong> use <strong>of</strong><br />
HazChem and a myriad <strong>of</strong> o<strong>the</strong>r data sources, it will be extremely<br />
difficult on operations. This knowledge is important, not only<br />
to determine scene management but also to establish levels <strong>of</strong><br />
exposure and <strong>the</strong> effects arising from that. The importance <strong>of</strong><br />
physicochemical properties such as solubility, volatility and<br />
reactivity are not confined to scene management. They are <strong>of</strong> equal<br />
importance in considering a compound’s journey through release,<br />
absorption, distribution to and metabolism by internal organs.<br />
These properties will not be known until much later during <strong>the</strong><br />
management <strong>of</strong> a release and toxicological data will follow from<br />
that. From <strong>the</strong> innumerable TICs only a small fraction have<br />
antidotes or specific <strong>the</strong>rapies that need instituting, most require<br />
supportive <strong>the</strong>rapy only, and will be considered later.<br />
Predicting likely chemical scenarios is always difficult and<br />
different agencies will come up with various solutions. In general<br />
terms threats were first described in quasi-ma<strong>the</strong>matical form by<br />
J David Singer over 50 years ago: Threat perception= Estimated<br />
Capability x Estimated Intent [2]. Whilst few traditional chemical<br />
warfare agents were discovered in Iraq, o<strong>the</strong>r threats such as<br />
Corresponding Author: Major TC Nicholson-Roberts BSc<br />
MRCP(UK) FRCA DipMedTox RAMC, Specialist Registrar<br />
<strong>Anaes<strong>the</strong>sia</strong> and Intensive Care Medicine, MDHU Derriford,<br />
Brest Road, Plymouth PL6 5YE<br />
Email: tcnr@doctors.org.uk<br />
chlorine abound. Rumours <strong>of</strong> chemical attacks on schools by<br />
Taliban indicate a degree <strong>of</strong> intent [3], however <strong>the</strong> exact nature<br />
<strong>of</strong> <strong>the</strong> agents used is not in <strong>the</strong> public domain. Locals likened <strong>the</strong><br />
odour to that <strong>of</strong> a compound used to poison foraging birds [4].<br />
Although <strong>the</strong> intent is high, <strong>the</strong> capability so far is limited to toxic<br />
substances readily available until superior agents become available<br />
to those hostile elements.<br />
The very nature <strong>of</strong> poisoning dictates that well performed<br />
studies are difficult, much data is derived from animal models,<br />
case reports and <strong>the</strong> experience <strong>of</strong> a few individuals. The poisoned<br />
patient presenting for surgery introduces an extra dimension<br />
to <strong>the</strong> care required. The immediate need for damage control<br />
resuscitation may result in continued treatment <strong>of</strong> poisoning in<br />
<strong>the</strong> operating <strong>the</strong>atre. Those patients who may be disadvantaged<br />
by general anaes<strong>the</strong>sia, for example in organophosphate poisoning,<br />
should have a regional anaes<strong>the</strong>tic technique where possible to<br />
avoid clouding <strong>of</strong> clinical assessment.<br />
Burns and Toxic Industrial Chemicals<br />
There are many thousands <strong>of</strong> chemicals in everyday use; some<br />
are inherently poisonous or react with o<strong>the</strong>rs to become so, or<br />
form toxic products <strong>of</strong> combustion. Trauma in <strong>the</strong> presence <strong>of</strong><br />
burns should be managed according to established guidelines<br />
with attention to management <strong>of</strong> airway burn, aggressive fluid<br />
resuscitation and prevention <strong>of</strong> sepsis. Early intubation is<br />
mandatory in <strong>the</strong> presence <strong>of</strong> an inhalation injury. After a burn<br />
extrajunctional expression <strong>of</strong> acetylcholine receptors is increased,<br />
<strong>the</strong>re is a general agreement that after a delay <strong>of</strong> 24h or more<br />
<strong>the</strong>n suxamethonium-induced hyperkalaemia becomes a real<br />
risk [5]. Potassium ions will leak out <strong>of</strong> myocytes in greater<br />
amounts, as a greater number <strong>of</strong> receptor ion channels are<br />
<strong>the</strong>n held open by suxamethonium. On <strong>the</strong> o<strong>the</strong>r hand, nondepolarising<br />
neuromuscular blocking agents (NMBAs) require<br />
a dose increase. Inhalation injuries represent a huge spectrum<br />
<strong>of</strong> illness dependent on duration <strong>of</strong> exposure, concentration,<br />
composition and temperature <strong>of</strong> smoke. A simple house fire will<br />
result in production <strong>of</strong> significant quantities <strong>of</strong> carbon monoxide<br />
(CO) and hydrogen cyanide (HCN). The abundance <strong>of</strong> syn<strong>the</strong>tic<br />
materials, some containing halogens and nitrogen, contribute to<br />
HCN formation and also to inorganic acids and nitrogen oxides<br />
with lung damaging properties [6]. Virtually all TICs have no<br />
specific treatment and supportive <strong>the</strong>rapy with appropriate organ<br />
support, good nursing care and attention to microbial sampling is<br />
all that can be <strong>of</strong>fered.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S327–334 327
Toxicology<br />
Smoke Inhalation<br />
Although rare, inhalation injury makes a considerable<br />
contribution to mortality and morbidity from burns. Efficient<br />
heat exchange in <strong>the</strong> upper airway reduces <strong>the</strong> risk <strong>of</strong> lower airway<br />
<strong>the</strong>rmal injury, but will not protect from soot, inorganic acids<br />
and o<strong>the</strong>r toxins. Hypoxaemia results from shunt; blockage <strong>of</strong><br />
bronchi by secretions, diffusion impairment; capillary leak and<br />
loss <strong>of</strong> hypoxic pulmonary vasoconstriction mediated by reactive<br />
oxygen and nitrogen species [7]. Cell necrosis will inevitably<br />
result in cytokine release and a generalised inflammatory response<br />
[8]. Lung compliance may be reduced by more than 50% in <strong>the</strong><br />
first 24h due to surfactant loss and increases in extravascular lung<br />
water and pulmonary lymph flow [9].<br />
The presence <strong>of</strong> hypoxia, pulmonary oedema or bronchospasm<br />
aside from anticipated or actual airway problems are indications<br />
for tracheal intubation and a period <strong>of</strong> postoperative ventilation<br />
and supportive care. This must include bronchial hygiene<br />
<strong>the</strong>rapy and physio<strong>the</strong>rapy to effect <strong>the</strong> removal <strong>of</strong> retained<br />
secretions and casts [9], as <strong>the</strong> mucociliary escalator will have<br />
been destroyed or disabled. Fraction <strong>of</strong> inspired oxygen (F I O 2 )<br />
and positive end expiratory pressure (PEEP) are titrated against<br />
arterial oxygen tension (P a O 2 ) and peripheral oxygen saturation<br />
(SpO 2 ); a protective ventilatory strategy is adopted for acute lung<br />
injury. There have been no well controlled studies comparing<br />
different modes <strong>of</strong> ventilation in inhalation injury [9]. O<strong>the</strong>r<br />
supportive measures are outside <strong>the</strong> scope <strong>of</strong> this article but must<br />
include adequate nutrition and attention to microbiological<br />
sampling and tissue viability. There is limited evidence to suggest<br />
that nebulised heparin and N- acetylcysteine can improve<br />
outcome in severe inhalation injury [9,10]. These measures are<br />
unlikely to cause harm in <strong>the</strong>mselves provided bronchodilators<br />
are used to counter <strong>the</strong> possibility <strong>of</strong> N- acetylcysteine mediated<br />
bronchospasm. O<strong>the</strong>r simple measures include bronchoscopy<br />
to confirm inhalation injury and bronchial lavage with 1.4%<br />
sodium bicarbonate [11].<br />
Carbon Monoxide<br />
Carbon monoxide poisoning (CMP) should be assumed, and if<br />
possible excluded, in any patient exposed to smoke, particularly<br />
in a confined space. It is a product <strong>of</strong> incomplete combustion <strong>of</strong><br />
hydrocarbons and o<strong>the</strong>r carbon containing substances - in isolation<br />
it is colourless and odourless. Features <strong>of</strong> CMP include headache,<br />
nausea and cerebral irritation (Table 1). Loss <strong>of</strong> consciousness<br />
from cerebral oedema, myocardial ischaemia and acidosis occur<br />
in severe poisoning. It is possible that personnel accommodated<br />
in an environment with significant carbon monoxide from<br />
incomplete combustion by a heater could all present with<br />
symptoms mimicking ‘flu or food poisoning. Thus CMP should<br />
be considered when faced with an outbreak <strong>of</strong> food poisoning or<br />
‘flu–like symptoms. It will not be filtered by conventional personal<br />
protective equipment (PPE). The pathophysiology <strong>of</strong> CMP is<br />
complex, based upon extreme left shift <strong>of</strong> <strong>the</strong> oxyhaemoglobin<br />
and myoglobin dissociation curves and interfering with <strong>the</strong><br />
mitochondrial respiratory chain and cellular oxygen utilisation.<br />
Common problems include cardiovascular injury, to heart and<br />
vascular endo<strong>the</strong>lium and neurological injury, particularly to<br />
‘watershed areas’ <strong>of</strong> <strong>the</strong> brain such as basal ganglia, with some<br />
long term sequelae [12,13]. Most blood gas analysers will measure<br />
carboxyhaemoglobin automatically, non-smokers will have a level<br />
Toxicology TC Nicholson-Roberts<br />
a relative deficiency <strong>of</strong> sulphur donors. Sodium thiosulphate<br />
(Na 2 S 2 O 3 ) given intravenously acts as a sulphur donor for <strong>the</strong><br />
enzyme rhodanase (thiosulphate: cyanide sulphurtransferase)<br />
located in mitochondria. This is a slower process than chelation<br />
by dicobalt edetate. First <strong>the</strong> rhodanase enzyme (E) forms a<br />
persulphide link with <strong>the</strong> thiosulphate ion [17]:<br />
E + S 2 O 3 2 - D ES + SO 3 2 -<br />
Rhodanase is <strong>the</strong>n cycled back to <strong>the</strong> sulphur free form [17]:<br />
ES + CN - D E + SCN -<br />
By doing so, cyanide (CN - ) is converted to relatively harmless<br />
thiocyanate (SCN - ) which is excreted by <strong>the</strong> kidney. In <strong>the</strong><br />
unlikely event that <strong>the</strong> diagnosis is confirmed <strong>the</strong>n dicobalt<br />
edetate 300mg in 50ml <strong>of</strong> 50% glucose can be given [13,18,19].<br />
Dicobalt edetate chelates cyanide in order that <strong>the</strong> kidneys can<br />
excrete it. There is a risk <strong>of</strong> hypotension, arrhythmias, laryngeal<br />
and facial oedema if dicobalt edetate is given in <strong>the</strong> absence <strong>of</strong><br />
cyanide poisoning [19]. In reality <strong>the</strong> diagnosis will not have been<br />
confirmed and a safer approach is to use sodium thiosulphate<br />
12.5g over 10min [19]. Formation <strong>of</strong> methaemoglobin using<br />
amyl nitrate or sodium nitrite is a strategy that has been used in<br />
severe cyanide poisoning. Cyanide avidly binds methaemoglobin<br />
reducing <strong>the</strong> amount binding to cytochromes, <strong>the</strong> bound<br />
cyanide is metabolised by <strong>the</strong> mechanisms outlined. Of course<br />
this will reduce <strong>the</strong> oxygen carrying capacity <strong>of</strong> blood which<br />
may be compromised already by a significant proportion <strong>of</strong><br />
carboxyhaemoglobin. Inducing methaemoglobinaemia in a<br />
patient with carboxyhaemoglobinaemia is not recommended<br />
unless <strong>the</strong>re has been a significant cyanide exposure with mild<br />
carboxyhaemoglobinaemia.<br />
Accordingly, trauma anaes<strong>the</strong>sia for <strong>the</strong> cyanide poisoned<br />
patient must involve an index <strong>of</strong> suspicion in cases <strong>of</strong> smoke<br />
inhalation where <strong>the</strong>re is hyperlactataemia contributing to a raised<br />
anion gap acidosis and a high central venous oxygen saturation.<br />
Sodium thiosulphate is likely to be <strong>the</strong> safest antidote unless<br />
cyanide poisoning is confirmed; o<strong>the</strong>r complications such as fits<br />
are managed in a conventional fashion.<br />
Chlorine<br />
Chlorine is in widespread use in industry and is familiar to all<br />
<strong>of</strong> us. Chlorine was used with devastating effect during <strong>the</strong> First<br />
World War [20], nowadays it is involved in both accidental<br />
(Figure 1) and deliberate releases.<br />
Chlorine is a largely predictable toxin. The effects <strong>of</strong> chlorine<br />
are predominantly in <strong>the</strong> eyes and respiratory tract and are worse<br />
with increasing dose, duration <strong>of</strong> exposure and in cases with<br />
underlying lung disease. Early features are, predictably, a sore<br />
throat, cough, chest tightness and dyspnoea [22]. Laryngeal<br />
oedema, bronchospasm and pulmonary oedema are seen with<br />
increasing doses (Table 2).<br />
Concentration Effect<br />
1-3ppm 3-10mgm-3 Mild mucous<br />
membrane irritation<br />
after 60min<br />
5-15ppm 15-45 mgm-3 Moderate irritation <strong>of</strong><br />
upper respiratory tract<br />
30ppm 90 mgm-3 Immediate chest pain,<br />
vomiting, coughing<br />
40-60ppm 115-175 mgm-3 Pneumonitis and<br />
pulmonary oedema<br />
430ppm 1250 mgm-3 Lethal after 30min<br />
1000ppm 2900 mgm-3 Fatal within a few<br />
minutes<br />
Table 2. Anticipated effects <strong>of</strong> increasing concentrations <strong>of</strong> chlorine<br />
[23].<br />
Cases <strong>of</strong> chlorine poisoning are managed in a supportive<br />
fashion as acute severe asthma with bronchodilator <strong>the</strong>rapy and<br />
nebulised steroids, however <strong>the</strong> role <strong>of</strong> corticosteroids is not<br />
completely established [21]. In more severe cases, pulmonary<br />
oedema is managed in conventional fashion with non-invasive<br />
continuous positive airway pressure (CPAP) and tracheal<br />
intubation if that fails. F I O 2 and PEEP are titrated against P a O 2<br />
and SpO 2 and a protective ventilatory strategy adopted for acute<br />
lung injury. Chlorine toxicity can be delayed such that a period<br />
<strong>of</strong> post operative observation should include <strong>the</strong> anticipation <strong>of</strong><br />
respiratory problems in patients with asymptomatic exposure.<br />
Phosgene<br />
Phosgene is widely used in <strong>the</strong> chemical manufacturing industry,<br />
however in UK most use is in factories that manufacture phosgene<br />
on site. This has virtually eliminated <strong>the</strong> transport <strong>of</strong> phosgene on<br />
<strong>the</strong> road and rail networks. It was first used as a War Gas during<br />
World War 1; initial exposure resulted in few symptoms and was<br />
succeeded by florid pulmonary oedema, sometimes up to a day<br />
later [20].<br />
Figure 1. Chlorine release from a tanker in <strong>the</strong> 2005 Graniteville,<br />
South Carolina rail crash. Approximately 54 tonnes (35 000 litres)<br />
<strong>of</strong> chlorine escaped from a ruptured tanker resulting in 8 deaths:<br />
according to <strong>the</strong> Coroner’s verdicts, seven were from asphyxia and<br />
one, <strong>the</strong> Train Engineer, who died several hours post-exposure from<br />
‘lactic acidosis’. 554 casualties attended local hospitals with breathing<br />
difficulties, 75 <strong>of</strong> those were admitted [21]. Note that Chlorine does<br />
not always take on <strong>the</strong> textbook yellow- green colour; it can also<br />
appear brown. It is denser than air and, in <strong>the</strong> absence <strong>of</strong> wind will<br />
settle in low areas.<br />
Photo: Environmental Protection Agency<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S327–334 329
Toxicology<br />
In common with o<strong>the</strong>r lung damaging chemicals <strong>the</strong>re is no<br />
specific <strong>the</strong>rapy for phosgene inhalation [24]. Lung damage occurs<br />
as a result <strong>of</strong> free radical generation leading to lipid peroxidation<br />
and associated glutathione depletion [24]. Supplementation or<br />
repletion <strong>of</strong> glutathione may be <strong>of</strong> value as demonstrated by a study<br />
in isolated rabbit lungs [25]. Postoperative patients exposed to<br />
phosgene require minimal exertion for 48h with close observations<br />
to identify <strong>the</strong> development <strong>of</strong> pulmonary oedema. The use <strong>of</strong><br />
steroids remain controversial and are probably not indicated. At<br />
present supportive <strong>the</strong>rapy using a protective ventilatory strategy<br />
with nebulised N-acetyl cysteine and bronchodilators is indicated;<br />
pulmonary oedema is managed with PEEP.<br />
Chemical Weapons<br />
The NATO definition <strong>of</strong> chemical weapons states that <strong>the</strong>y are<br />
substances intended for use on military operations to kill, injure or<br />
incapacitate as a result <strong>of</strong> <strong>the</strong>ir physiological effects. This does not<br />
confine <strong>the</strong>ir use to <strong>the</strong> battlefield as seen in Tokyo 1995 when sarin<br />
was released in <strong>the</strong> underground. Cyanides, chlorine and phosgene<br />
have all been weaponised and <strong>the</strong> management <strong>of</strong> <strong>the</strong> poisoned<br />
soldier during conflict does not differ in <strong>the</strong>se circumstances.<br />
Lung Damaging Agents<br />
Lung damaging agents, also known as choking agents include<br />
chlorine, phosgene and hydrochloric acid. These are non-persistent<br />
agents that do not require decontamination in current <strong>the</strong>atres <strong>of</strong><br />
operations. Treatment is supportive and if patients survive <strong>the</strong> first<br />
48 hours <strong>the</strong>y usually recover without sequelae [26].<br />
Blister Agents<br />
Vesicants or Blister Agents were first used during World War I to cause<br />
burning and blistering <strong>of</strong> exposed areas. They include <strong>the</strong> mustards<br />
and lewisite. They are persistent in temperate and colder climates.<br />
Unless <strong>the</strong>y have been ‘thickened’, decontamination should not be<br />
required in hotter climates, however vapour concentrations can be<br />
higher under <strong>the</strong>se circumstances. The effects <strong>of</strong> mustards are due<br />
to oxidation and alkylation <strong>of</strong> DNA, RNA and o<strong>the</strong>r important<br />
biological molecules. Crosslinking <strong>of</strong> DNA and RNA at guanine<br />
residues results in cytotoxicity, errors in DNA repair mechanisms<br />
can result in transformation and malignancy. Decontamination <strong>of</strong><br />
kit and equipment is beyond <strong>the</strong> scope <strong>of</strong> this article, however <strong>the</strong><br />
surgical patient with blister agent exposure may require ongoing<br />
decontamination in <strong>the</strong> operating <strong>the</strong>atre. Contaminated clothing<br />
fragments should be placed in a bleach solution to prevent<br />
fur<strong>the</strong>r vapour release, wounds are irrigated with 3000- 5000ppm<br />
chlorine (dilute Milton) solution before rinsing with crystalloid<br />
[27]. Mustards are degraded by water, forming hydrochloric<br />
acid. During its manufacture 0.9% Saline is rendered acidic with<br />
hydrochloric acid and <strong>the</strong>refore may not be <strong>the</strong> ideal solution to<br />
irrigate with. Decontamination <strong>of</strong> eyes and mucous membranes<br />
should not be attempted using skin decontamination preparations<br />
but 1.26% (isotonic) sodium bicarbonate should be used to irrigate<br />
if available, o<strong>the</strong>rwise saline or Hartmann’s solution will have to<br />
substitute. Mydriatics should be used in corneal damage to prevent<br />
adhesions with <strong>the</strong> iris and local anaes<strong>the</strong>tics should be avoided,<br />
permanent blindness is rare [27]. For intraperitoneal, intrathoracic<br />
and intracranial wounds crystalloid is used as irrigation fluid.<br />
Lung manifestations occur after a latent period up to six hours<br />
beginning with symptoms <strong>of</strong> a severe upper respiratory tract<br />
infection. Burning throat pain results in a reluctance to cough until<br />
copious secretions supervene. Epi<strong>the</strong>lial necrotic fragments and<br />
330<br />
TC Nicholson-Roberts<br />
pulmonary oedema will lead to hypoxaemia from shunt, diffusion<br />
impairment and a predisposition to pneumonia exacerbated by<br />
immune dysfunction [27]. There is a strong correlation between<br />
conjunctival damage and lung injury [27]. Lung support is<br />
achieved in a conventional fashion with escalation as necessary<br />
from non-invasive to invasive ventilation with titration <strong>of</strong> PEEP<br />
and F I O 2 against P a O 2 .<br />
Skin damage occurs within two minutes <strong>of</strong> exposure and<br />
progresses through ery<strong>the</strong>ma, blistering to full thickness burns.<br />
Skin damage is worst in warm wet skin [27]. The blister fluid is not<br />
vesicant and generally <strong>the</strong> blisters are not painful in postoperative<br />
patients with adequate systemic analgesia.<br />
Lewisite is an arsenical vesicant with a specific antidote,<br />
dimercaprol (British Anti Lewisite) which is used in metalloid and<br />
heavy metal poisoning. The onset <strong>of</strong> symptoms is faster than with<br />
mustard and although lung effects are less severe, blindness is more<br />
likely. Dimercaprol ointment can be applied to decontaminated<br />
skin and eyes or injected intramuscularly in severe exposure [27].<br />
Perioperative management is as for mustard.<br />
Organophosphorus compounds<br />
Organophosphorus (OP) compounds include <strong>the</strong> nerve agents and<br />
agricultural insecticides; o<strong>the</strong>r infrequent uses are as fire retardants<br />
and lubricants. The commonest cause <strong>of</strong> organophosphorus<br />
morbidity is from accidental or intentional ingestion from <strong>the</strong><br />
agricultural sector.<br />
OPs are irreversible inhibitors <strong>of</strong> plasma, red cell and tissue<br />
esterases, particularly butyrylcholinesterase (BChE) and<br />
acetylcholinesterase (AChE). It is inhibition <strong>of</strong> AChE that gives<br />
rise to <strong>the</strong> classic features <strong>of</strong> <strong>the</strong> cholinergic phase <strong>of</strong> nerve agent<br />
toxicity. This is brought about by overwhelming cholinergic<br />
stimulation by acetylcholine in <strong>the</strong> central nervous system,<br />
neuromuscular junction and autonomic nervous system. A<br />
summary <strong>of</strong> <strong>the</strong> effect sites <strong>of</strong> acetylcholine is shown in Figure 2.<br />
Figure 2. An outline <strong>of</strong> <strong>the</strong> utilisation <strong>of</strong> acetylcholine by <strong>the</strong> autonomic<br />
nervous system and neuromuscular junction. The parasympa<strong>the</strong>tic<br />
effects are demonstrated at <strong>the</strong> top where pre and post ganglionic<br />
fibres are stimulated by acetylcholine (ACh) at nicotinic (N) and<br />
muscarinic (M) receptors. Preganglionic sympa<strong>the</strong>tic fibres are<br />
generally shorter than those in <strong>the</strong> parasympa<strong>the</strong>tic nervous system,<br />
never<strong>the</strong>less <strong>the</strong>y utilise ACh to stimulate nicotinic receptors. The<br />
postganglionic sympa<strong>the</strong>tic fibres release catecholamines shown as<br />
red hexagons acting viscerally, and hormonally from <strong>the</strong> adrenal<br />
gland demonstrated by <strong>the</strong> brown triangle. Crucially <strong>the</strong> sympa<strong>the</strong>tic<br />
innervation <strong>of</strong> sweat glands is by ACh acting on muscarinic receptors.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S327–334
Toxicology TC Nicholson-Roberts<br />
The characteristics <strong>of</strong> OP toxicity are outlined in Table 3.<br />
Cholinergic crises are not only seen in indirectly acting toxins<br />
such as OPs and carbamates, such as pyridostigmine, but also<br />
with directly acting cholinomimetics, fungi and betel, sodium<br />
channel openers, some animal venoms and aconitine poisoning.<br />
Central Nervous<br />
System.<br />
Nicotinic and<br />
Muscarinic Effects<br />
Confusion<br />
Agitation<br />
Coma<br />
Respiratory Failure<br />
Autonomic Nervous System Neuromuscular<br />
Parasympa<strong>the</strong>tic<br />
Nervous System<br />
Muscarinic Effects<br />
Bradycardia,<br />
Hypotension<br />
Bronchospasm,<br />
Bronchorrhoea<br />
Salivation, Vomiting,<br />
Diarrhoea<br />
Miosis, Lacrymation,<br />
Urination<br />
Sympa<strong>the</strong>tic<br />
Nervous System<br />
Nicotinic Effects<br />
Tachycardia,<br />
Hypertension<br />
Sweating Paralysis<br />
Table 3. Summary <strong>of</strong> effects <strong>of</strong> OP poisoning. Generally <strong>the</strong><br />
parasympa<strong>the</strong>tic features prevail to <strong>the</strong> extent that mydriasis is not<br />
seen and hypovolaemia must be excluded as a cause <strong>of</strong> tachycardia<br />
should it occur. Note <strong>the</strong> multiple causes <strong>of</strong> respiratory failure and<br />
how all except <strong>the</strong> neuromuscular junction’s contribution can be<br />
reversed by atropine. After Eddleston et al [28].<br />
Low dose exposure to OPs may mimic an outbreak <strong>of</strong> influenza<br />
or gastroenteritis. On deployed operations <strong>the</strong> diagnosis is<br />
clinical. There may be no history (Figure 3); casualties presenting<br />
with pin point pupils, pr<strong>of</strong>ound salivation, respiratory distress<br />
and bradycardia should least arouse suspicion <strong>of</strong> OP poisoning<br />
and fasciculations are almost pathognomic. Assays for BChE and<br />
red cell AChE will not be available in <strong>the</strong> field. They are classed<br />
as specialist or infrequent assays ideally available within three<br />
hours including journey time in UK [29]. BChE activity more<br />
closely tracks <strong>the</strong> clinical picture [28, 29] except in patients with<br />
suxamethonium apnoea.<br />
Figure 3. Mo<strong>the</strong>r and child who have succumbed to nerve agent as<br />
a result <strong>of</strong> <strong>the</strong> attack on Halabja 16 March 1988. Observe <strong>the</strong> dried<br />
copious secretions from lacrimation and salivation. It is thought that<br />
mustard and cyanide were also used [30]<br />
Photo: Sipa Press/ Rex Features Ltd with permission<br />
OPs bound to AChE become less likely to dissociate through<br />
a process known as ageing. Ageing is thought to represent loss<br />
<strong>of</strong> an alkyl group which means that <strong>the</strong> complex is less likely to<br />
undergo spontaneous dephosphorylation. Of <strong>the</strong> nerve agents,<br />
ageing occurs most rapidly with soman with a t ½ (time required<br />
Junction.<br />
Nicotinic Effects<br />
Muscle weakness<br />
Mydriasis Respiratory failure<br />
Fasciculation<br />
for half <strong>the</strong> enzyme to become<br />
resistant to reactivation) <strong>of</strong> 1.3<br />
minutes, whereas <strong>the</strong> ageing t 1/2<br />
<strong>of</strong> sarin is five hours and that <strong>of</strong><br />
tabun, 46 hours [31]. Recovery<br />
is by syn<strong>the</strong>sis <strong>of</strong> new enzyme<br />
which occurs at a rate <strong>of</strong> about<br />
1% per day [32].<br />
Morbidity and mortality is<br />
primarily due to hypoxia from<br />
bronchospasm, bronchorrhoea<br />
and failure <strong>of</strong> ventilation<br />
by central and peripheral<br />
mechanisms. After <strong>the</strong> initial<br />
cholinergic phase follows a<br />
period <strong>of</strong> delayed neuromuscular<br />
weakness and respiratory failure first described as <strong>the</strong> Intermediate<br />
Syndrome [33], however fur<strong>the</strong>r observations have demonstrated<br />
less <strong>of</strong> a distinction and a variable constellation <strong>of</strong> signs [34]. The<br />
Intermediate Syndrome has not been observed in cases <strong>of</strong> nerve<br />
agent poisoning [35] and <strong>the</strong>re is no mention <strong>of</strong> it in <strong>the</strong> NATO<br />
Handbook on <strong>the</strong> <strong>Medical</strong> Aspects <strong>of</strong> NBC Defensive Operations<br />
AMedP-6(B) [36]. It is not clear why this is and clinicians should<br />
at least be alert to <strong>the</strong> possibility <strong>of</strong> it occurring.<br />
The principles <strong>of</strong> <strong>the</strong>rapy include pre-exposure prophylaxis,<br />
maintenance <strong>of</strong> oxygenation during acute exposure and<br />
maintaining a period <strong>of</strong> post exposure observation in cases <strong>of</strong><br />
agricultural OP poisoning. Pre-exposure prophylaxis is usually<br />
achieved using pyridostigmine 30mg eight hourly. Carbamates<br />
bind AChE less avidly, however <strong>the</strong>y disrupt <strong>the</strong> binding <strong>of</strong> OPs<br />
to <strong>the</strong> extent that reactivation <strong>of</strong> AChE is made easier. Unbound<br />
OPs undergo hydrolysis before spontaneous dissociation <strong>of</strong> <strong>the</strong><br />
carbamylated AChE produces active enzyme. Pyridostigmine<br />
should be discontinued once nerve agent poisoning has<br />
occurred as any unaffected AChE will be required to function.<br />
Unaffected patients who have been taking pyridostigmine may<br />
require antimuscarinic premedication and are likely to require<br />
increased doses <strong>of</strong> non-depolarizing neuromuscular blockers<br />
intraoperatively.<br />
The patient with OP poisoning presenting for surgery will need<br />
resuscitating first, and in patients who have been issued <strong>the</strong>m,<br />
combopens may have been used. They contain atropine 2mg,<br />
pralidoxime 500mg and avizafone which is a diazepam prodrug,<br />
equivalent to 5mg. The overarching principle is maintenance <strong>of</strong><br />
oxygenation and this is chiefly achieved by atropine in conjunction<br />
with standard resuscitative measures. In <strong>the</strong> presence <strong>of</strong> hypoxia<br />
or where oxygen supplementation is unavailable <strong>the</strong>re is always<br />
<strong>the</strong> concern <strong>of</strong> precipitating ventricular tachyarrhythmias,<br />
however this is not borne out by clinical practice in agricultural<br />
OP poisoning [28]. Atropine will rapidly decrease bronchospasm<br />
and dry secretions, thus alleviating hypoxia. A useful guide to<br />
atropine dosing is shown in Figure 4 which illustrates doubling<br />
<strong>of</strong> doses as recommended by Eddleston [28]; rapid atropinisation<br />
is crucial in severe OP poisoning and should take precedence<br />
over giving o<strong>the</strong>r drugs. One should give as much as it takes to<br />
reach a heart rate greater than 80 beats per minute and to break<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S327–334 331
Toxicology<br />
<strong>the</strong> bronchospasm, ei<strong>the</strong>r by assessing lung compliance through<br />
positive pressure ventilation, including bag valve mask, or by<br />
auscultation in <strong>the</strong> self ventilating patient. Assessment <strong>of</strong> pupils<br />
should not guide atropine dosing. An infusion <strong>of</strong> atropine after<br />
‘loading’ may result in a smoo<strong>the</strong>r recovery pr<strong>of</strong>ile [28,36].<br />
An oxime such as pralidoxime is given as soon as practicable in<br />
order to restore some AChE activity, however it is ineffective in<br />
<strong>the</strong> aged OP-AChE complex. There is evidence that it will bind<br />
unbound OPs, preventing <strong>the</strong>ir binding to AChE [32]. Oxime<br />
infusions have been used after <strong>the</strong> loading dose - pralidoxime<br />
should be started at 2.1 mgkg -1 h -1 [36].<br />
Fitting is commoner in nerve agent than agricultural OPs<br />
and should be treated in conventional fashion using diazepam.<br />
Agitated patients should also receive diazepam provided atropine<br />
is being given; paradoxically respiration under <strong>the</strong>se circumstances<br />
is enhanced [37].<br />
During <strong>the</strong> acute cholinergic phase, muscle relaxation will not<br />
be necessary as in moderate to severe poisoning <strong>the</strong> patient will<br />
already be paralysed and suxamethonium action will be greatly<br />
prolonged. Similarly, after carbamate pre-exposure prophylaxis<br />
<strong>the</strong> carbamylated BChE will not hydrolyse suxamethonium as<br />
readily resulting in prolonged action. It may be <strong>the</strong> case that non<br />
depolarising neuromuscular blockers will shield post synaptic<br />
nicotinic receptors from excess ACh stimulation during <strong>the</strong><br />
acute phase [35]. Whe<strong>the</strong>r this is beneficial is not known. A type<br />
II neuromuscular block is one that exhibits fade on repeated<br />
stimulation and potentiation after induced tetany. It is usually<br />
seen after <strong>the</strong> administration <strong>of</strong> non-depolarising neuromuscular<br />
blockers and in <strong>the</strong> Intermediate Syndrome. It can be assessed<br />
using a conventional <strong>the</strong>atre monitor; <strong>the</strong> ‘train <strong>of</strong> four’ [32].<br />
Consequently relaxants should be used with great care or avoided<br />
altoge<strong>the</strong>r in <strong>the</strong> Intermediate Syndrome. There is very little<br />
clinical experience in this regard.<br />
O<strong>the</strong>r measures can be employed to hasten recovery such as<br />
decreasing ACh at <strong>the</strong> synaptic cleft. Drugs such as magnesium<br />
and clonidine reduce ACh secretion in central and peripheral<br />
neurones. Magnesium will also be useful in averting torsade de<br />
pointes in <strong>the</strong> event <strong>of</strong> severe poisoning sufficient to prolong <strong>the</strong><br />
QT interval. Currently, <strong>the</strong>re is little evidence to support <strong>the</strong> use <strong>of</strong><br />
magnesium. A small study in Tehran <strong>of</strong> agricultural OP poisoning<br />
demonstrated a reduction in mortality and length <strong>of</strong> stay in an<br />
unrandomised and unblinded trial [38]. A larger Sri Lankan study<br />
is ongoing and will provide fur<strong>the</strong>r clarification [39].<br />
Surgery for <strong>the</strong> OP poisoned patient should be embarked upon<br />
following restoration <strong>of</strong> oxygenation and fur<strong>the</strong>r <strong>the</strong>rapy can be<br />
given intraoperatively. Consideration should be given to regional<br />
anaes<strong>the</strong>sia and interpretation <strong>of</strong> monitoring will be confused by<br />
a heart rate driven by atropine. It is likely, however in <strong>the</strong> event <strong>of</strong><br />
OP poisoned patient(s) arriving at a Field Hospital that <strong>the</strong>y will<br />
encounter anaes<strong>the</strong>tic expertise in managing a condition that is<br />
not too far removed from <strong>the</strong>ir own clinical experience.<br />
Future Developments<br />
OP poisoning represents a serious threat to health with<br />
approximately 200 000 deaths per year [28,32] mainly in<br />
developing countries. Advances in research by organisations such<br />
as <strong>the</strong> South Asian Clinical Toxicology Research Collaboration<br />
are limited by funding. Advances made in <strong>the</strong> military sector are<br />
<strong>of</strong>ten kept secret. Scavenging <strong>of</strong> OPs before <strong>the</strong>y have bound<br />
AChE is an area that is currently under investigation, this can only<br />
be accomplished with rapid intervention and may reduce length<br />
332<br />
<br />
<br />
<br />
15 min up<br />
to 3 doses<br />
Double <strong>the</strong><br />
previous<br />
atropine dose<br />
<br />
TC Nicholson-Roberts<br />
ORGANOPHOSPHORUS<br />
TREATMENT<br />
Buddy Aid/ Self Aid with<br />
Combopen (im)<br />
Atropine 2mg<br />
<br />
Pralidoxime 500mg<br />
Diazepam 5mg (equivalent)<br />
Atropine<br />
<br />
Begin with<br />
2-5 mg iv/ io<br />
Oxygen/<br />
Ventilation<br />
iv/ io access<br />
3-5min<br />
Reassess: Bronchospasm<br />
Bronchorrhea<br />
Bradycardia<br />
• Establish 2nd iv access and give Pralidoxime 2g over 5-10 min<br />
and infusion at 2.1 mgkg-1h-1 if dermal or gastric absorption<br />
continues<br />
• Diazemuls 5mg every 5min iv if fitting<br />
• Continue atropine until HR >80 and bronchospasm is broken<br />
• Consider fluid replacement <strong>of</strong> losses<br />
• Consider atropine infusion <strong>of</strong> 10-20% <strong>of</strong> “loading dose” per<br />
hour<br />
Figure 4. An algorithm for <strong>the</strong> treatment <strong>of</strong> OP poisoning, combopen<br />
use is currently unlikely. Atropine is given in doubling doses until<br />
atropinisation is achieved, an infusion <strong>of</strong> 10-20% <strong>of</strong> that total<br />
dose can <strong>the</strong>n be given per hour. Benzodiazepines should be given<br />
routinely in nerve agent poisoning but are less likely to be required in<br />
agricultural OP poisoning. Cutaneous VX absorption will continue<br />
after decontamination and will necessitate infusions <strong>of</strong> pralidoxime<br />
and atropine. After Bland [40] and Eddleston et al [28].<br />
<strong>of</strong> stay. Recombinant BChE has been trialled in vitro and binds<br />
OPs stoichiometrically [41]. Ano<strong>the</strong>r avenue that may be worth<br />
pursuing is <strong>the</strong> use <strong>of</strong> cyclodextrins. They have been in use for many<br />
years in pharmaceutical preparations but have only recently been<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S327–334
Toxicology TC Nicholson-Roberts<br />
used as drugs in <strong>the</strong> form <strong>of</strong> sugammadex that stoichiometrically<br />
binds <strong>the</strong> neuromuscular blocking agents rocuronium and<br />
vecuronium [42,43]. Sequestering <strong>of</strong> OPs by cyclodextrins is a<br />
possibility and candidates could rapidly be screened for activity<br />
as <strong>the</strong> act <strong>of</strong> sequestering represents a reduction in entropy. Any<br />
useful prototypes would <strong>the</strong>refore cool <strong>the</strong> reaction vessel. Whilst<br />
sequestering is useful, cyclodextrins can be modified to become<br />
catalysts [44] and this has been investigated with resulting<br />
hydrolysis <strong>of</strong> soman by b- cyclodextrins [45,46]. Unfortunately,<br />
due to rapid aging <strong>of</strong> soman this may not be clinically useful.<br />
Ano<strong>the</strong>r possible spin <strong>of</strong>f from <strong>the</strong> world <strong>of</strong> anaes<strong>the</strong>sia is <strong>the</strong><br />
use <strong>of</strong> intralipid for local anaes<strong>the</strong>tic toxicity. So far <strong>the</strong>re are two<br />
<strong>the</strong>ories as to its mechanism <strong>of</strong> action; <strong>the</strong> lipid sink hypo<strong>the</strong>sis<br />
and modulating carnitine acylcarnitine transferase activity in<br />
cardiac mitochondria [47,48]. A lipid sink hypo<strong>the</strong>sis may provide<br />
ano<strong>the</strong>r method <strong>of</strong> scavenging and <strong>the</strong>re is a current vogue for<br />
using intralipid successfully in various scenarios <strong>of</strong> massive drug<br />
overdose refractory to conventional resuscitative methods [49,50].<br />
Whe<strong>the</strong>r this might work in OP poisoning remains to be seen.<br />
Conclusions<br />
Military anaes<strong>the</strong>tists are familiar with <strong>the</strong> requirement for<br />
damage control resuscitation in military trauma [51]. Poisoned<br />
trauma patients will, at some point be delivered to a field hospital<br />
and undue delays in resuscitation will be detrimental. The<br />
additional complication <strong>of</strong> poisoning in trauma patients should<br />
not represent undue difficulty for <strong>the</strong> military anaes<strong>the</strong>tist in<br />
guiding <strong>the</strong> trauma patient through <strong>the</strong> perioperative period.<br />
There are few antidotes as compared to <strong>the</strong> number <strong>of</strong> potential<br />
toxins out <strong>the</strong>re; most treatment is supportive and reacting to<br />
changes in physiology.<br />
References<br />
1. Russell D. Personal communication. 13 March 2009<br />
2. Singer JD. Threat-Perception and <strong>the</strong> Armament-Tension<br />
Dilemma. J Confl Resolut 1958; 2: 90-105<br />
3. Stratfor Global Intelligence. Afghanistan: Schools Targeted by<br />
Chemical Weapons. May 12, 2009 http://www.stratfor.com/<br />
analysis/20090512_afghanistan_schools_targeted_chemical_<br />
weapons accessed 13 July 2009.<br />
4. The New Zealand Herald. Afghanistan: Young girls targeted in<br />
‘Taleban gas attack’. May 13 2009 http://www.nzherald.co.nz/<br />
world/news/article.cfm?c_id=2&objectid=10572008 accessed 13<br />
July 2009.<br />
5. MacLennan N, Heimbach D, Cullen B. Anes<strong>the</strong>sia for Major<br />
Thermal Injury. Anes<strong>the</strong>siology 1998; 89: 749-770<br />
6. Alarie Y. Toxicity <strong>of</strong> Fire Smoke. Crit Rev Tox 2002; 32: 259-289<br />
7. Traber DL, Hawkins HK, Enkhbaatar P et al. The role <strong>of</strong> <strong>the</strong><br />
bronchial circulation in <strong>the</strong> acute lung injury resulting from burn<br />
and smoke inhalation. Pulm Pharmacol Therapeut 2007; 20: 163-<br />
166<br />
8. Nguyen TT, Gilpin DA, Meyer NA, Herndon DN. Current<br />
Treatment <strong>of</strong> Severely Burned Patients. Ann Surg 1996; 223: 14-25<br />
9. Mlcak RP, Suman OE, Herndon DN. Respiratory management <strong>of</strong><br />
inhalation injury. Burns 2007; 33: 2-13<br />
10. Miller AC, Rivero A, Ziad S, Smith DJ, Elamin EM. Influence<br />
<strong>of</strong> nebulized unfractionated heparin and N-acetylcysteine in acute<br />
lung injury after smoke inhalation injury. J Burn Care Res 2009;<br />
30: 249-56<br />
11. Oxford Desk Reference: Critical Care. Waldman C, Soni N,<br />
Rhodes A. Oxford University Press. 2008. Chapter 28.7 Burns-<br />
general management<br />
12. Hardy KR, Thom SR. Pathophysiology and treatment <strong>of</strong> carbon<br />
monoxide poisoning. J Toxicol Clin Toxicol 1994; 32: 613-29<br />
13. Maynard R, Thompson J. Personal communication 13 February<br />
2008<br />
14. Calman K, Moores Y. Carbon Monoxide: The Forgotten Killer.<br />
Department <strong>of</strong> Health CMO Letter. 7 September 1998<br />
15. Henry JA. Carbon monoxide: not gone, not to be forgotten. J Accid<br />
Emerg Med 1999; 16: 91-103<br />
16. Breen PH, Isserles SA, Westley J, Roizen MF, Taitelman UZ.<br />
Combined carbon monoxide and cyanide poisoning: A place for<br />
treatment? Anesth Analg 1995; 80: 671-7<br />
17. Gliubich F, Gazerro M, Zanotti G, Delbonoi S, Bombieri G, Bernii<br />
R. Active Site Structural Features for Chemically Modified Forms<br />
<strong>of</strong> Rhodanese. J. Biol. Chem. 1996; 271: 21054–21061<br />
18. Bland SA. Personal communication. 12 July 2009<br />
19. British National Formulary Number 57. March 2009.<br />
20. Harris R, Paxman J. A Higher Form <strong>of</strong> Killing. Random House<br />
Publishing USA Inc 2002<br />
21. Collision <strong>of</strong> Norfolk Sou<strong>the</strong>rn Freight Train 192 With Standing<br />
Norfolk Sou<strong>the</strong>rn Local Train P22 With Subsequent Hazardous<br />
Materials Release at Graniteville, South Carolina January 6,<br />
2005. Railroad Accident Report. NTSB/RAR-05/04. PB2005-<br />
916304. Notation 7710A Adopted November 29, 2005. National<br />
Transportation Safety Board, 490 L’Enfant Plaza SW, Washington<br />
DC 20594<br />
22. Agabiti N, Ancona C, Forastiere F et al. Short term respiratory<br />
effects <strong>of</strong> acute exposure to chlorine due to a swimming pool<br />
accident. Occup Environ Med 2001; 58; 399-404<br />
23. International Programme on Chemical Safety (IPCS) (1996).<br />
Chlorine. Poisons Information Monograph. PIM 947<br />
24. Russell D, Blain PG, Rice P. Clinical management <strong>of</strong> casualties<br />
exposed to lung damaging agents: a critical review. Emerg Med J<br />
2006; 23: 421-424<br />
25. Sciuto AM, Holcombe HH. Therapeutic Treatments <strong>of</strong> Phosgene-<br />
Induced Lung Injury. Inhal Tox 2004; 16: 565-580<br />
26. NATO Handbook on <strong>the</strong> <strong>Medical</strong> Aspects <strong>of</strong> NBC Defensive<br />
Operations AMedP-6(B) Part III – Chemical. 1 February 1996.<br />
Chapter 4: Lung Damaging Agents (Choking Agents)<br />
27. NATO Handbook on <strong>the</strong> <strong>Medical</strong> Aspects <strong>of</strong> NBC Defensive<br />
Operations AMedP-6(B) Part III – Chemical. 1 February 1996.<br />
Chapter 3: Vesicants (Blister Agents)<br />
28. Eddleston M, Buckley NA, Eyer P, Dawson AH. Management <strong>of</strong><br />
acute organophosphorus pesticide poisoning. Lancet 2008; 371:<br />
597-607<br />
29. National Poisons Information Service and Association <strong>of</strong> Clinical<br />
Biochemists. Laboratory analyses for poisoned patients: joint<br />
position paper. Ann Clin Biochem 2002; 39: 328-339<br />
30. BBC: On This Day. 16 March 1988. Accessed 24 August 2009.<br />
http://news.bbc.co.uk/onthisday/hi/dates/stories/march/16/<br />
newsid_4304000/4304853.stm<br />
31. United States Environmental Protection Agency. Office <strong>of</strong><br />
Pollution Prevention and Toxics. NERVE AGENTS GA, GB, GD,<br />
GF (CAS Reg. Nos. 77-81-6, 107-44-8, 96-64-0, and 329-99-7)<br />
October 2000<br />
32. Karalliedde L. Organophosphorus poisoning and anaes<strong>the</strong>sia.<br />
<strong>Anaes<strong>the</strong>sia</strong> 1999; 54: 1073–1088<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S327–334 333
Toxicology<br />
33. Senanayake N, Karalliedde L. Neurotoxic effects <strong>of</strong><br />
organophosphorus insecticides. An intermediate syndrome. N Eng<br />
J Med 1987; 316: 761-763<br />
34. Eddleston M, Mohamed F, Davies J et al. Respiratory failure in<br />
acute organophosphorus pesticide self-poisoning. Q J Med 2006;<br />
99: 513–522<br />
35. Anes<strong>the</strong>sia and Perioperative Care <strong>of</strong> <strong>the</strong> Combat Casualty.<br />
Specialty Editors Brigadier General Russ Zajtchuk, Christopher M<br />
Grande. Published by <strong>the</strong> Office <strong>of</strong> The Surgeon General at TMM<br />
Publications 1995. Borden Institute, Walter Reed <strong>Army</strong> <strong>Medical</strong><br />
Center, Washington, DC 20307-5001. Chapter 30: Anes<strong>the</strong>sia for<br />
Casualties <strong>of</strong> Chemical Warfare Agents. Baker DJ, Rustick JM<br />
36. NATO Handbook on <strong>the</strong> <strong>Medical</strong> Aspects <strong>of</strong> NBC Defensive<br />
Operations AMedP-6(B) Part III – Chemical. 1 February 1996.<br />
Chapter 2: Nerve Agents<br />
37. Dickson E, Bird S, Gaspari R, Boyer E, Ferris C. Diazepam inhibits<br />
organophosphate-induced central respiratory depression. Acad<br />
Emerg Med 2003; 10: 1303–06<br />
38. Pajoumand A, Shadnia S, Rezaie A, Abdi M, Abdollahi M.<br />
Benefits <strong>of</strong> magnesium sulfate in <strong>the</strong> management <strong>of</strong> acute human<br />
poisoning by organophosphorus insecticides. Hum Exp Toxicol<br />
2004; 23: 565-569<br />
39. South Asian Clinical Toxicology Research Collaboration. http://<br />
www.sactrc.org/hospital_current_research_activities.html accessed<br />
1 September 2009<br />
40. Bland SA. Personal communication. 12 July 2009<br />
41. Huang Y-J, Huang Y, Baldassarre H et al. Recombinant human<br />
butyrylcholinesterase from milk <strong>of</strong> transgenic animals to protect<br />
against organophosphate poisoning. Proc Natl Acad Sci 2007; 104:<br />
13603–13608<br />
334<br />
TC Nicholson-Roberts<br />
42. British National Formulary 57 March 2009 15.1.6 Drugs for<br />
reversal <strong>of</strong> neuromuscular blockade > O<strong>the</strong>r drugs for reversal <strong>of</strong><br />
neuromuscular blockade<br />
43. Naguib M. Sugammadex: Ano<strong>the</strong>r Milestone in Clinical<br />
Neuromuscular Pharmacology. Anesth Analg 2007; 104: 575-581<br />
44. Easton C. Cyclodextrin-based catalysts and molecular reactors.<br />
Pure Appl Chem 2005; 77: 1865–1871<br />
45. Desire B, Saint-Andre S. Interaction <strong>of</strong> Soman with b-Cyclodextrin.<br />
Tox Sci 1986; 7: 646-657<br />
46. Seltzman H, Lonikar M. Catalytic beta-cyclodextrin enzyme<br />
mimics as soman hydrolases. Proceedings <strong>of</strong> <strong>the</strong> <strong>Medical</strong> Defense<br />
Bioscience Review 1993; 3: 1075-1083<br />
47. Weinberg G, Palmer J, VadeBoncouer T, Zuechner M, Edelman G,<br />
Hoppel C. Bupivacaine inhibits acylcarnitine exchange in cardiac<br />
mitochondria. Anes<strong>the</strong>siology 2000; 92: 523–8<br />
48. Picard J. Lipid emulsion to treat overdose <strong>of</strong> local anaes<strong>the</strong>tic: <strong>the</strong><br />
gift <strong>of</strong> <strong>the</strong> glob. <strong>Anaes<strong>the</strong>sia</strong> 2006; 61: 107–109<br />
49. Young A, Velez L, Kleinschmidt K. Intravenous fat emulsion<br />
<strong>the</strong>rapy for intentional sustained-release verapamil overdose.<br />
Resuscitation 2009; 80: 591-593<br />
50. Finn S, Uncles D, Willers J, Sable N. Early treatment <strong>of</strong> a quetiapine<br />
and sertraline overdose with Intralipid. <strong>Anaes<strong>the</strong>sia</strong> 2009; 64: 191-<br />
194<br />
51. Jansen J, Thomas R, Loudon M, Brooks A. Damage control<br />
resuscitation for patients with major trauma. Brit Med J 2009; 338:<br />
1436-1440<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S327–334
Operational <strong>Anaes<strong>the</strong>sia</strong> for <strong>the</strong> Management <strong>of</strong><br />
Traumatic Brain Injury<br />
CL Park 1 , P Moor 2 , K Birch 3 , PJ Shirley 4<br />
1 London HEMS Registrar; 2 Consultant in Neuroanaes<strong>the</strong>sia, MDHU Derriford; 3 Consultant, Intensive Care and<br />
<strong>Anaes<strong>the</strong>sia</strong>, Frenchay Hospital, Bristol; 4 Consultant, Intensive Care and <strong>Anaes<strong>the</strong>sia</strong>, <strong>Royal</strong> London Hospital,<br />
Whitechapel, London<br />
Abstract<br />
The primary brain insult that occurs at <strong>the</strong> time <strong>of</strong> head injury, is determined by <strong>the</strong> degree <strong>of</strong> neuronal damage or death<br />
and so cannot be influenced by fur<strong>the</strong>r treatment. The focus <strong>of</strong> immediate and ongoing care from <strong>the</strong> point <strong>of</strong> wounding<br />
to intensive care management at Role 4 should be to reduce or prevent any secondary brain injury. The interventions and<br />
triage decisions must be reassessed at every stage <strong>of</strong> <strong>the</strong> process, but should focus on appropriate airway management,<br />
maintenance <strong>of</strong> oxygenation and carbon dioxide levels and maintenance <strong>of</strong> adequate cerebral perfusion pressure. Early<br />
identification <strong>of</strong> raised intracranial pressure and appropriate surgical intervention are imperative. Concurrent injuries<br />
must also be managed appropriately. Attention to detail at every stage <strong>of</strong> <strong>the</strong> evacuation chain should allow <strong>the</strong> headinjured<br />
patient <strong>the</strong> best chance <strong>of</strong> recovery.<br />
Introduction<br />
Military patients sustaining severe traumatic brain injury (TBI)<br />
<strong>of</strong>ten pose particular challenges. The treatment <strong>of</strong> <strong>the</strong> injury can<br />
be highly complex, from <strong>the</strong> point <strong>of</strong> initial wounding, surgical<br />
intervention, intensive care and ultimately rehabilitation. It has<br />
been recognized that mild, moderate and severe brain injuries have<br />
become a major focus <strong>of</strong> military medical services during current<br />
operations due to <strong>the</strong> high levels <strong>of</strong> kinetic activity [1]. Changing<br />
patterns <strong>of</strong> head injury are being seen, with a penetrating injury<br />
now <strong>of</strong>ten also as a result <strong>of</strong> blast as well as direct ballistic injuries<br />
[1]. The management <strong>of</strong> traumatic brain injury raises many issues<br />
to be considered (Table 1). This article examines <strong>the</strong> management<br />
<strong>of</strong> brain injured patients through four phases <strong>of</strong> care from point<br />
<strong>of</strong> wounding through <strong>the</strong> deployed field medical facilities,<br />
aeromedical evacuation and UK based definitive care.<br />
• Consideration <strong>of</strong> <strong>the</strong> injury mechanisms and potential<br />
structures at risk in blunt and penetrating trauma.<br />
• Pre-hospital management and <strong>the</strong> time line to definitive care<br />
• Peri-operative management <strong>of</strong> <strong>the</strong> trauma patient<br />
including intubation and approaches to fluid<br />
management.<br />
• Clearance <strong>of</strong> <strong>the</strong> cervical spine in a sedated and ventilated<br />
trauma patient.<br />
• Timing <strong>of</strong> fracture fixation and o<strong>the</strong>r injury management.<br />
• Maintenance <strong>of</strong> blood pressure and cerebral perfusion<br />
pressure<br />
• Timing <strong>of</strong> aeromedical evacuation to role 4 care<br />
• Role 4 management and multi-modality monitoring<br />
• Timing <strong>of</strong> neurosurgical interventions such as<br />
decompressive craniectomy<br />
• Rehabilitation from injury<br />
Table 1: Issues raised in <strong>the</strong> treatment <strong>of</strong> brain-injured patients.<br />
Corresponding Author: Wg Cdr Peter Shirley, Consultant,<br />
Intensive Care and <strong>Anaes<strong>the</strong>sia</strong>, <strong>Royal</strong> London Hospital,<br />
Whitechapel, London E1 1BB<br />
Email: Peter.Shirley@bartsand<strong>the</strong>london.nhs.uk<br />
Pre-Hospital Management<br />
This encompasses care at all levels from Care Under Fire (CUF)<br />
and Tactical Field Care (TFC) [2], to <strong>the</strong> Combat <strong>Medical</strong><br />
Technician (CMT) or Regimental <strong>Medical</strong> Officer (RMO) at<br />
Role 1 and <strong>the</strong> <strong>Medical</strong> Emergency Response Team (MERT)<br />
retrieval. The level <strong>of</strong> intervention will depend on <strong>the</strong> stage <strong>of</strong><br />
evacuation and medical skills present, but <strong>the</strong> medical care at all<br />
stages should be based on similar underlying principles.<br />
The pre-hospital management <strong>of</strong> TBI aims to prevent secondary<br />
brain injury by provision <strong>of</strong> adequate oxygenation and cerebral<br />
perfusion and treatment <strong>of</strong> o<strong>the</strong>r significant injuries while ideally<br />
ensuring rapid transfer to a neurosurgical centre. It has been<br />
shown that even when surgical intervention is not required, all<br />
TBI patients do better when managed in a neurosurgical centre<br />
[3]. In <strong>the</strong> military setting, this may not be immediately possible,<br />
as current UK Role 2 or 3 facilities do not include a neurosurgical<br />
capability. However, all deployed general surgeons should be<br />
capable <strong>of</strong> performing a burr hole in order to decompress an<br />
extradural haematoma [2].<br />
MERT physicians in <strong>the</strong> operational setting should be aware<br />
<strong>of</strong> <strong>the</strong> location <strong>of</strong> neurosurgical facilities in <strong>the</strong>atre, and should<br />
make appropriate triage decisions immediately, and transfer<br />
directly to <strong>the</strong> available neurosurgical facility if <strong>the</strong> operational<br />
tempo will allow.<br />
Pre-hospital Resuscitation<br />
In accordance with Brain Trauma Foundation (BTF) guidelines<br />
[4], pre-hospital assessment <strong>of</strong> a head injured patient should<br />
include assessment and treatment priorities as listed in Table 2.<br />
Much <strong>of</strong> <strong>the</strong> civilian data for <strong>the</strong> pre-hospital management<br />
<strong>of</strong> TBI can be applied in <strong>the</strong> military setting. However, in some<br />
circumstances civilian guidelines will be impractical in <strong>the</strong> military<br />
setting, as discussed in <strong>the</strong> BTF Field management guidelines [5].<br />
CUF, TFC and Role One management should be performed as<br />
described by Battlefield Advanced Trauma Life Support (BATLS)<br />
2008 [2] and in <strong>the</strong> context <strong>of</strong> TBI <strong>the</strong> interventions in Table 3<br />
should be focused on.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S335–341 335
<strong>Anaes<strong>the</strong>sia</strong> for TBI<br />
Assessment <strong>of</strong>: Oxygenation<br />
Blood pressure<br />
Treatment: Maintenance <strong>of</strong> a patent airway<br />
Maintenance <strong>of</strong> adequate oxygenation and<br />
ventilation,<br />
Appropriate fluid resuscitation<br />
Treatment <strong>of</strong> cerebral herniation<br />
Appropriate triage and transport<br />
Table 2: Priorities in <strong>the</strong> Pre-hospital assessment <strong>of</strong> brain-injured<br />
patients<br />
336<br />
BATLS<br />
Stage<br />
Prevention <strong>of</strong> fur<strong>the</strong>r<br />
haemorrhage to<br />
maintain CPP.<br />
CUF / TFC Role 1<br />
A Maintenance <strong>of</strong> airway<br />
patency using adjuncts<br />
as necessary.<br />
B Optimisation <strong>of</strong><br />
chest injuries causing<br />
pathology by needle<br />
decompression, & / or<br />
Aschermann or Bolan<br />
chest seal.<br />
C 250ml fluid boluses to<br />
maintain a radial pulse.<br />
D Identification <strong>of</strong> head<br />
injury Assessment <strong>of</strong><br />
<strong>the</strong> Glasgow Coma<br />
Scale (GCS) score and<br />
pupil size.<br />
Alerting <strong>the</strong> casevac<br />
chain to <strong>the</strong> type <strong>of</strong><br />
injury and level <strong>of</strong><br />
consciousness will<br />
prompt accurate<br />
allocation <strong>of</strong> casevac<br />
assets.<br />
Continue to reassess<br />
adequate haemorrhage<br />
control.<br />
If <strong>the</strong> airway is not<br />
patent<br />
despite simple airway<br />
manoeuvres, a surgical<br />
airway should be<br />
performed as a definitive<br />
airway [2].<br />
If ventilation is<br />
inadequate, aid with a<br />
bag valve mask ei<strong>the</strong>r<br />
via face mask or surgical<br />
airway.<br />
250ml boluses <strong>of</strong> fluid<br />
should be given to<br />
maintain SBP <strong>of</strong> 90 if<br />
a BP cuff is available.<br />
O<strong>the</strong>rwise administer<br />
fluid boluses to maintain<br />
a good radial pulse, and<br />
verbal contact if <strong>the</strong><br />
casualty is able to speak.<br />
If <strong>the</strong> casualty is<br />
hypotensive with no<br />
palpable radial pulse,<br />
hypertonic saline would<br />
be an appropriate prehospital<br />
resuscitation<br />
fluid.<br />
A drop in GCS would<br />
require expedition<br />
<strong>of</strong> evacuation to a<br />
neurosurgical facility<br />
where possible.<br />
Table 3 Management during CUF / TFC and at Role One:<br />
CL Park, P Moor, K Birch et al<br />
MERT and initial hospital resuscitation<br />
These should be similar as MERT is a forward projection <strong>of</strong> <strong>the</strong><br />
resuscitation facilities available at Role 2 or 3.<br />
Airway<br />
A definitive airway should be obtained with a Rapid Sequence<br />
Induction (RSI) if <strong>the</strong> patient is unconscious, has airway<br />
compromise or ventilatory failure. A number <strong>of</strong> patients with<br />
head injury and a relatively high GCS (9 – 14) may also require<br />
intubation. Most <strong>of</strong> <strong>the</strong>se patients have cerebral agitation and<br />
it has been shown that patients with a significant mechanism<br />
<strong>of</strong> injury who have cerebral agitation have a high incidence<br />
<strong>of</strong> intracranial pathology. Patients with a skull fracture who<br />
are not orientated have a 1 in 4 risk <strong>of</strong> having an intracranial<br />
haematoma [6]. These patients require urgent management to<br />
prevent secondary brain damage, an expeditious CT scan and<br />
appropriate neurosurgical intervention.<br />
A well-trained pre-hospital team such as <strong>the</strong> MERT, should<br />
have low intubation failure rates and should practice more<br />
permissive use <strong>of</strong> intubation without causing an increase in<br />
mortality. However, if <strong>the</strong> RSI procedure and ensuing mechanical<br />
ventilation are performed poorly, <strong>the</strong> negative effects have been<br />
shown to outweigh potential benefits [7]. Agitated patients with<br />
head injuries and additional injuries <strong>of</strong>ten require sedation and<br />
/or analgesia in order to gain control <strong>of</strong> <strong>the</strong> patient, <strong>the</strong>refore<br />
preventing secondary brain injury by adequately pre-oxygenating<br />
and performing a controlled RSI.<br />
It is imperative that pre-hospital teams at Role 1 perform <strong>the</strong><br />
basics well, and do not attempt to perform an RSI when <strong>the</strong>y<br />
are not appropriately trained to do so. Basic airway management,<br />
appropriate administration <strong>of</strong> pre-hospital fluids to maintain<br />
a systolic <strong>of</strong> over 90mmHg (i.e. a good radial pulse) and rapid<br />
evacuation should be <strong>the</strong> focus <strong>of</strong> treatment. MERT personnel<br />
should be able to safely administer sedation and carry out an RSI<br />
when <strong>the</strong> patient’s condition requires it.<br />
Choice <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong>, Analgesia and Sedation by <strong>the</strong><br />
MERT or in <strong>the</strong> Emergency Department<br />
Current practice is commonly still to use etomidate as a prehospital<br />
induction agent for RSI in TBI, followed by morphine<br />
and midazolam to maintain analgesia and anaes<strong>the</strong>sia [8].<br />
Traditionally ketamine has rarely been used in patients with TBI<br />
because <strong>of</strong> concerns that it causes a rise in intracranial pressure<br />
(ICP). However, <strong>the</strong>re is emerging evidence that it in fact lowers<br />
ICP and maintains cerebral perfusion pressure (CPP) when used<br />
as an infusion on ITU [9-11] and <strong>the</strong>re is evidence that it decreases<br />
ICP spikes and prevents spikes in response to procedures[12].<br />
In hypotensive patients with TBI, ketamine is a more<br />
appropriate agent [13]. Especially in <strong>the</strong> presence <strong>of</strong> polytrauma,<br />
where brain injury and shock co-exist, and etomidate will<br />
reduce CBF as cerebral autoregulation is impaired and cerebral<br />
blood flow (CBF) is essentially CPP-related, <strong>the</strong> maintenance <strong>of</strong><br />
hemodynamic stability will maintain CBF. In addition ketamine<br />
reduces cerebral oxygen consumption (CMRO 2 ) and so <strong>the</strong><br />
overall balance <strong>of</strong> CBF and CMRO 2 in <strong>the</strong> presence <strong>of</strong> ketamine<br />
is favorable [13].<br />
RSI technique<br />
The RSI technique in head injury should minimise CO 2 increases<br />
and pharyngeal and laryngeal stimulation in an attempt to<br />
minimise ICP rises. Meticulous attention to oxygenation is also<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S335–341
<strong>Anaes<strong>the</strong>sia</strong> for TBI CL Park, P Moor, K Birch et al<br />
important as is <strong>the</strong> prevention <strong>of</strong> hyper and hypoventilation,<br />
which has been associated with poor outcomes [4,5,14].<br />
Ventilation Aims<br />
Ventilate to low normocapnia (end-tidal CO 2 <strong>of</strong> 30 mmHg,<br />
4.0KPa) [4, 5]. This equates to a PaCO 2 <strong>of</strong> approximately<br />
4.5KPa in normal individuals. This minimises <strong>the</strong> risk <strong>of</strong> cerebral<br />
vasodilation from high PaCO 2 and cerebral vasoconstriction<br />
from low PaCO 2 .<br />
Use <strong>of</strong> IV Fluids and CPP<br />
After significant head trauma, <strong>the</strong> brain may lose <strong>the</strong> ability<br />
to autoregulate cerebral blood flow. A fall in mean arterial<br />
pressure (MAP) may <strong>the</strong>refore result in a reduction in cerebral<br />
oxygen delivery even if <strong>the</strong> ICP is normal. When active external<br />
haemorrhage has been stopped and splintage <strong>of</strong> limbs / pelvis has<br />
been maximised, <strong>the</strong>n fluids should be administered to achieve<br />
a systolic blood pressure <strong>of</strong> 90mmHg. This can be increased to<br />
100 to 120mmHg in isolated head injury. On <strong>the</strong> MERT or<br />
during in-hospital resuscitation, if hypotension is secondary to<br />
traumatic injuries, damage control resuscitation (DCR) should be<br />
commenced. Fluid replacement should be with red blood cells and<br />
fresh frozen plasma in a 1:1 ratio, ra<strong>the</strong>r than crystalloid to replace<br />
blood loss. [15] Hypertonic saline may also be an appropriate<br />
fluid for use in multitrauma patients with head injuries – this is<br />
discussed below.<br />
Packaging<br />
Compression <strong>of</strong> <strong>the</strong> jugular veins will reduce venous return from <strong>the</strong><br />
head and neck which can increase ICP by an average <strong>of</strong> 4.5mmHg<br />
[16]; <strong>the</strong> cervical collar should be left slightly loose and cervical<br />
spine immobilisation maintained with head blocks and tape where<br />
possible. The neck veins can also be constricted by a tight tracheal<br />
tube tie, which should be checked and loosened if necessary.<br />
Ideally, <strong>the</strong> patient should be maintained and transported in a 20<br />
degrees head up position to maximise venous drainage.<br />
Control <strong>of</strong> ICP / impending herniation with hyperosmolar<br />
<strong>the</strong>rapies<br />
Mannitol<br />
The TBF guidelines [4, 5] support <strong>the</strong> use <strong>of</strong> mannitol in<br />
response to herniation at doses <strong>of</strong> 1.4–2.1 g/kg if supported by<br />
<strong>the</strong> capacity to provide high fluid volume compensation for any<br />
ensuing urine loss.<br />
In addition to <strong>the</strong> increased fluid requirement, however,<br />
mannitol is susceptible to cold and crystallizes in cold conditions,<br />
so is not practical in <strong>the</strong> military pre-hospital environment. A<br />
recent Cochrane review concluded that mannitol has a beneficial<br />
effect on ICP compared to pentobarbital, but may have a<br />
detrimental effect on mortality when compared to hypertonic<br />
saline. However, as that review highlights, <strong>the</strong>re is a lack <strong>of</strong> prehospital<br />
evidence on its effectiveness [17].<br />
Hypertonic Saline<br />
Hypertonic saline (HTS) has been shown to lower ICP in severe<br />
head injuries and in multiple studies has been shown to improve<br />
neurological outcome in TBI [18-21] especially in paediatric<br />
patients [22-26]. It may have o<strong>the</strong>r beneficial effects such as<br />
increasing circulating volume, minimal alteration to coagulation<br />
and anti-inflammatory properties [27].<br />
There are very few reports <strong>of</strong> any side effects due to its use.<br />
There are, however, some studies [28] showing no difference<br />
compared to isotonic solutions, although overall survival in <strong>the</strong>se<br />
studies has been shown to be better than predicted, which may be<br />
due to an adequate pre-hospital resuscitation protocol. HTS use<br />
with <strong>the</strong> goal <strong>of</strong> maintaining adequate haemodynamic parameters<br />
during resuscitation may <strong>the</strong>refore still be beneficial, especially<br />
in military pre-hospital care where transporting large volumes <strong>of</strong><br />
isotonic fluids is impractical[27].<br />
5% Sodium chloride is used by some pre-hospital services. It is<br />
available as a 250ml or 500ml infusion bag and is stable through<br />
a range <strong>of</strong> temperatures. A suggested policy for administration <strong>of</strong><br />
5% Hypertonic saline [8] is 6 ml / kg (to a maximum <strong>of</strong> 350ml)<br />
<strong>of</strong> 5% HTS delivered by a well secured large bore peripheral (><br />
18 gauge) cannula over 10 minutes in patients with signs <strong>of</strong> actual<br />
or impending herniation resultant from severe head injury with<br />
ei<strong>the</strong>r unilateral or bilateral pupil dilation and GCS < 8 (and<br />
usually 3) or progressive hypertension (systolic BP > 160mmHg)<br />
and bradycardia (pulse below 60).<br />
The dose is given only once and regardless <strong>of</strong> blood pressure.<br />
In patients with multiple traumatic injuries, hypotension and<br />
head injury a bolus <strong>of</strong> HTS as above will help restore circulating<br />
volume and may protect against cerebral hypoperfusion and<br />
reduce oedema. For this indication it is suggested by <strong>the</strong> BTF<br />
guidelines that one or two boluses <strong>of</strong> 250ml <strong>of</strong> 5% HTS would<br />
be appropriate. [5].<br />
Fur<strong>the</strong>r Management At Role 2+ / Role 3<br />
Initial management <strong>of</strong> ABCD should be as before for airway<br />
and ventilation. Rapid infusion <strong>of</strong> blood products in hypotensive<br />
multitrauma patients to maintain a systolic BP <strong>of</strong> over 100mmHg<br />
should be via a central, usually subclavian, trauma line, inserted<br />
on arrival in <strong>the</strong> Emergency Department (ED) and damage<br />
control resuscitation (DCR) should continue [15].<br />
There must be a rapid decision to proceed to CT scanning to<br />
look for intracranial haematoma and cervical spine clearance, or<br />
to go directly to <strong>the</strong>atre in <strong>the</strong> case <strong>of</strong> co-existing injuries requiring<br />
immediate surgical treatment.<br />
If <strong>the</strong> patient is haemodynamically stable, with no immediate<br />
need for surgical treatment, <strong>the</strong>n a CT scan to exclude intracranial<br />
pathology, most importantly an extradural haematoma, should<br />
be performed as a priority. If intracranial pathology is detected<br />
in a stable patient, including intracranial or intraocular foreign<br />
bodies, as is <strong>of</strong>ten seen from IED blasts, <strong>the</strong>n <strong>the</strong> images should<br />
be transmitted to <strong>the</strong> nearest neurosurgical facility. In Afghanistan<br />
at <strong>the</strong> time <strong>of</strong> writing, this is <strong>the</strong> US Role 3 facility at Kandahar<br />
Airfield. A neurosurgical opinion should be urgently sought,<br />
whilst <strong>the</strong> Tactical Critical care Air Support Team (CCAST)<br />
prepares to transport <strong>the</strong> patient.<br />
Intra- Operative Anaes<strong>the</strong>tic Management Of TBI<br />
Conduct <strong>of</strong> anaes<strong>the</strong>sia in <strong>the</strong> TBI patient should aim to preserve<br />
normal brain parenchymal homeostasis to reduce <strong>the</strong> risk <strong>of</strong><br />
secondary brain injury (Table 4) [14, 29].<br />
Any injury causing persistent hypotension should be<br />
addressed immediately and if intracranial space-occupying<br />
lesions are present, <strong>the</strong>se should be evacuated simultaneously.<br />
Limb-saving peripheral vascular surgery should be performed<br />
urgently. Subsequent, operative treatment <strong>of</strong> long bone and<br />
o<strong>the</strong>r fractures can be delayed until <strong>the</strong> head injury has been<br />
stabilized [30].<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S335–341 337
<strong>Anaes<strong>the</strong>sia</strong> for TBI<br />
GENERAL PRINCIPLES<br />
Maintenance <strong>of</strong> Mean Arterial Blood Pressure<br />
Control <strong>of</strong> Intracranial Pressure<br />
Maintenance <strong>of</strong> adequate Oxygenation<br />
Avoidance <strong>of</strong> hyper/hypocapnia<br />
Glycaemic Control<br />
Avoidance <strong>of</strong> Iatrogenic Injury<br />
Table 4: Physiological aims <strong>of</strong> anaes<strong>the</strong>sia for traumatic brain injury<br />
[4]<br />
Monitoring<br />
As with all military trauma patients, in addition to standard<br />
monitoring for anaes<strong>the</strong>sia, invasive arterial blood pressure,<br />
central venous pressure and core temperature monitoring should<br />
be initiated. Near-patient testing for blood gas analysis, blood<br />
glucose and coagulation is routinely available in <strong>the</strong> role 2E<br />
facility.<br />
Maintenance <strong>of</strong> anaes<strong>the</strong>sia<br />
After intubation, normoxia and low normal carbon dioxide<br />
should be <strong>the</strong> aim (ETCO 2 4.0-4.5 kPa). Hyperventilation<br />
should be preserved for herniation syndromes only. A systolic<br />
blood pressure <strong>of</strong>
<strong>Anaes<strong>the</strong>sia</strong> for TBI CL Park, P Moor, K Birch et al<br />
• Head Injury Traumatic brain injury<br />
guidelines followed?<br />
Tertiary survey completed?<br />
Cervical Spine cleared?<br />
Surgical plan robust?<br />
• Infection control Strict adherence to hand<br />
hygiene?<br />
Field-placed venous access lines<br />
changed?<br />
Assess need for current central<br />
venous access?<br />
Appropriate antibiotics?<br />
• Ventilated patients Head-<strong>of</strong>-bed elevation?<br />
EtCO 2 in 4.0-5.0 range?<br />
ICP/MAP/CPP all within<br />
agreed limits<br />
Oral care protocol?<br />
Is a weaning plan appropriate?<br />
Sedation and analgesia protocol?<br />
Cooling required?<br />
Is paralysis justified?<br />
Pressure area protection<br />
optimised?<br />
• Deep vein thrombosis prophylaxis optimised?<br />
• Stress ulcer prophylaxis required?<br />
• Glycaemic control best and safest for circumstance?<br />
• Nutrition optimal?<br />
• Candidate for evacuation? Safe for transport?<br />
CCAST arrangements?<br />
Records ready?<br />
• Rehabilitation plan commenced<br />
Table 5: Intensive Care Unit checklist for <strong>the</strong> brain-injured patient<br />
causes a reduction in PAO 2 and subsequently a reduction in<br />
PaO 2 . Any gas present in enclosed spaces with no ability to vent<br />
to <strong>the</strong> atmosphere will expand and cause compression <strong>of</strong> adjacent<br />
structures. If this gas lies within sensitive areas such as within <strong>the</strong><br />
cranium, <strong>the</strong> increase in pressure may have a deleterious effect.<br />
Noise prevents any effective auscultation and equipment alarms<br />
are unable to be heard and communication between crew members<br />
is degraded. Vibration can affect equipment and initial studies<br />
suggest that <strong>the</strong> risk <strong>of</strong> micro aspiration in intubated patients may<br />
beincreased (Unpublished data – K Birch). All <strong>the</strong>se factors must<br />
be considered and efforts made tominimize <strong>the</strong>ir impact.<br />
Haemodynamic Monitoring and Management<br />
Invasive monitoring <strong>of</strong> arterial blood pressure is important<br />
to ensure maintenance <strong>of</strong> adequate systemic blood pressure.<br />
Treatment should be titrated to aim for a CPP <strong>of</strong> 60-70mmHg.<br />
If <strong>the</strong> ICP is not known, as ICP monitors are not currently sited<br />
at UK Role 2 or 3 facilities, and <strong>the</strong>re are issues with accurately<br />
measuring ICP during flight, aiming for a MAP <strong>of</strong> 70-80mmHg<br />
would suffice. If augmentation <strong>of</strong> blood pressure is necessary,<br />
infusions <strong>of</strong> vasopressor agents or inotropes may be considered.<br />
Volume status <strong>of</strong> <strong>the</strong> patient should be assessed via a central<br />
venous ca<strong>the</strong>ter and/or by measuring hourly urine output. The<br />
aim is for a euvolaemic, normosmolar state with a haematocrit<br />
<strong>of</strong> around 0.3. If <strong>the</strong>re is evidence <strong>of</strong> active bleeding or risk <strong>of</strong> a<br />
fall <strong>of</strong> heamoglobin concentration in flight, blood for transfusion<br />
should be carried.<br />
Respiratory Monitoring and Management<br />
The majority <strong>of</strong> patients with traumatic brain injury require<br />
intubation and ventilation to ensure a secure airway (if GCS<br />
≤8/15), adequate oxygenation and control <strong>of</strong> PaCO 2 . Low levels<br />
<strong>of</strong> Positive End Expiratory Pressure (PEEP) should be employed<br />
during ventilation and PaCO 2 maintained within <strong>the</strong> normal<br />
range (4-0-5.0KPa). Equipment to be able to measure arterial<br />
blood gases during flight should be carried for transfer.<br />
Sedation and Muscle Relaxation<br />
The level <strong>of</strong> sedation required for head injured patients will<br />
depend on <strong>the</strong> injury and <strong>the</strong> systemic physiological condition<br />
<strong>of</strong> <strong>the</strong> patient. Increased doses <strong>of</strong> sedation, narcotics and/or<br />
benzodiazepines may be required during transfer due to increased<br />
stimulation due to noise and vibration on <strong>the</strong> aircraft. Routine<br />
use <strong>of</strong> muscle relaxants is not recommended, however if use is<br />
required, monitoring <strong>of</strong> <strong>the</strong> degree <strong>of</strong> neuromuscular blockade is<br />
mandatory.<br />
Patient Positioning<br />
Ideally a 30-45° head up attitude should be sustained as part <strong>of</strong><br />
<strong>the</strong> ventilatory care bundle and neurological management. The<br />
head should be maintained in a neutral position. The type and<br />
flying attitude <strong>of</strong> <strong>the</strong> aircraft will dictate if <strong>the</strong> patient is loaded<br />
head or feet first.<br />
Metabolic Treatment<br />
One should aim to maintain <strong>the</strong> patient’s biochemical parameters<br />
to as near normal as possible during transfer. If <strong>the</strong> ICP is known<br />
or believed to be significantly elevated, <strong>the</strong>rapy such as increasing<br />
serum sodium concentration and use <strong>of</strong> mannitol (used in<br />
conjunction with o<strong>the</strong>r <strong>the</strong>rapeutic measures) can be considered.<br />
The brain is an obligate glucose user so hypoglycaemia, as well as<br />
hyperglycemia must be avoided during transfer [37].<br />
Hyper<strong>the</strong>rmia is a recognized cause <strong>of</strong> secondary cerebral insult,<br />
<strong>the</strong>refore normo<strong>the</strong>rmia, or in certain circumstances <strong>the</strong>rapeutic<br />
hypo<strong>the</strong>rmia, should be maintained [38, 39]. This may require<br />
active or passive cooling methods.<br />
Nutrition<br />
Ideally early enteral feeding is initiated for patients suffering<br />
traumatic brain injury. However <strong>the</strong> potential risk <strong>of</strong> increased<br />
microaspiration in intubated patients during flight requires<br />
discontinuation <strong>of</strong> nasogastric or orogastric feeding during<br />
aeromedical transfer.<br />
Role 4 Treatment <strong>of</strong> TBI<br />
Intensive care treatment is aimed at lessening <strong>the</strong> impact <strong>of</strong><br />
secondary injury by controlling ICP. Maintenance <strong>of</strong> a CPP<br />
greater than 60 mm Hg is now widely recognized as a vital<br />
component <strong>of</strong> management <strong>of</strong> traumatic brain injury. A single<br />
recording <strong>of</strong> a hypotensive episode (SBP <strong>of</strong> < 90 ) is generally<br />
associated with a doubling <strong>of</strong> mortality and a marked increase in<br />
morbidity from a given head injury [40]. The highest blood sugar<br />
occurring in <strong>the</strong> first 24 hours <strong>of</strong> ICU care is linearly correlated<br />
with mortality [41]. Fever should be prevented in TBI patients,<br />
as it will merely increase <strong>the</strong> CMRO 2 . For <strong>the</strong> patient with TBI, a<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S335–341 339
<strong>Anaes<strong>the</strong>sia</strong> for TBI<br />
CPP <strong>of</strong> 60–70 mmHg is generally sufficient to maintain cerebral<br />
oxygenation. Excessive hyperventilation <strong>of</strong> patients with TBI will<br />
cause ischaemia if CO 2 reactivity is preserved. The interpretation<br />
<strong>of</strong> a given ICP measurement must be made in <strong>the</strong> light <strong>of</strong> <strong>the</strong><br />
underlying pathology and <strong>the</strong> speed <strong>of</strong> its evolution. Current<br />
evidence suggests that 20–25 mmHg is <strong>the</strong> upper threshold above<br />
which treatment to lower ICP should be started. The management<br />
<strong>of</strong> hypotension must include not only fluid replacement but also<br />
identification <strong>of</strong> <strong>the</strong> cause. There is minimal evidence for <strong>the</strong><br />
routine use <strong>of</strong> anticonvulsants to prevent seizures.<br />
Raised ICP after severe TBI is frequent in relation to altered<br />
cerebral compliance. Information obtained by ICP monitoring<br />
allows early detection <strong>of</strong> high ICP and goal directed <strong>the</strong>rapy. ICP<br />
monitoring allows informed <strong>the</strong>rapeutic decisions. Protocols need<br />
to be agreed jointly between <strong>the</strong> neurosurgical and intensive care<br />
medical team. There are a number <strong>of</strong> protocols for <strong>the</strong> prevention<br />
<strong>of</strong> secondary brain injury following major trauma. They are<br />
generally directed at <strong>the</strong> maintenance <strong>of</strong> CPP to ensure adequate<br />
cerebral blood flow. The Brain Trauma Foundation [42] found<br />
that mortality increased as <strong>the</strong> average CPP fell below 70 mm<br />
Hg, and that aggressive <strong>the</strong>rapy was required to control ICP<br />
and systemic arterial pressure. A number <strong>of</strong> historical trials have<br />
suggested that <strong>the</strong> mortality for patients with head injuries on a<br />
neurosurgical ICU is reduced by <strong>the</strong> implementation <strong>of</strong> a target<br />
CPP-guided protocol but <strong>the</strong>re are no pro spective randomised<br />
trials comparing goal-directed <strong>the</strong>rapy with previous conventional<br />
head injury management.<br />
The European Society <strong>of</strong> Intensive Care Medicine has published<br />
guidance on <strong>the</strong> use <strong>of</strong> monitoring in neurological injuries [43]:<br />
1. There are insufficient data to recommend ICP monitoring<br />
and management as standard care in all brain-injury patients.<br />
Never<strong>the</strong>less, <strong>the</strong> evidence is “good enough” to recommend<br />
ICP monitoring <strong>of</strong> patients with severe injuries who are at<br />
increased risk <strong>of</strong> intracranial hypertension.<br />
2. Which patients are at “high risk” <strong>of</strong> ICP elevation is a matter<br />
<strong>of</strong> controversy. We recommend ICP should be monitored in<br />
all salvageable patients with a severe TBI (i.e. Glasgow Coma<br />
Scale Score ≤ 8) and an abnormal CT scan.<br />
3. The management <strong>of</strong> raised ICP should follow BTF<br />
guidelines with care to exclude surgical lesions, including<br />
haematoma,contusion and hydrocephalus. Local protocols<br />
should be developed that conform to international guidelines<br />
and include neurosurgical consultation.<br />
Invasive ICP Monitors<br />
Invasive ICP monitors have been used on neuro-intensive<br />
care units in head injured patients for many years and <strong>the</strong>y<br />
have become a standard <strong>of</strong> care ei<strong>the</strong>r as external ventricular<br />
drains (EVD) or monitoring bolts. All evidence suggests that<br />
morbidity <strong>of</strong> head injured patients is improved if treated on a<br />
neuro-intensive care unit. Whilst not risk-free, <strong>the</strong> incidence<br />
<strong>of</strong> adverse events from inserting intra-cranial pressure<br />
monitoring equipment is small and it should be safe to use in<br />
<strong>the</strong> field. However it is clear that it is not <strong>the</strong> monitor itself<br />
which makes <strong>the</strong> difference, and it has been pointed out that<br />
all military intensivists and ITU nurses would need significant<br />
pre-deployment exposure to <strong>the</strong>se patients for all <strong>of</strong> <strong>the</strong> clinical<br />
governance issues to be covered [44].<br />
The use <strong>of</strong> brain tissue oxygenation (PO 2 ) monitors is gaining<br />
acceptance at established neuro-intensive care units. There is<br />
340<br />
CL Park, P Moor, K Birch et al<br />
now evidence that <strong>the</strong> combined use <strong>of</strong> ICP and brain tissue<br />
oxygenation monitoring can be associated with reduced mortality<br />
in TBI when compared with ICP monitoring alone [45].<br />
O<strong>the</strong>r considerations<br />
General supportive measures are as important as specialised<br />
neuro-intensive care or surgical interventions. Sepsis is a major<br />
threat in this group <strong>of</strong> patients and efforts should be made to<br />
prevent and treat infections. Infection control and hand-washing<br />
in particular have a major role to play, in this respect. Early feeding<br />
and thrombo-embolic prophylaxis are also important. Chest and<br />
limb physio<strong>the</strong>rapy should be performed at least daily on patients<br />
who are unconscious. Successful outcome is <strong>of</strong>ten measured in<br />
terms <strong>of</strong> mortality but from <strong>the</strong> patients perspective a return to a<br />
functionally useful life and full employment is usually what <strong>the</strong>y<br />
want. Intensive care only forms one link in <strong>the</strong> chain <strong>of</strong> survival<br />
and as such <strong>the</strong> goal should be viewed as enabling <strong>the</strong> patient to<br />
benefit from <strong>the</strong> rehabilitation phase, which commences in and<br />
follows discharge from ICU [46].<br />
Conclusion<br />
The principles <strong>of</strong> TBI management remain consistant<br />
throughout all levels <strong>of</strong> care. From <strong>the</strong> point <strong>of</strong> injury, <strong>the</strong> aim<br />
should be to prevent secondary brain damage by optimizing<br />
oxygenation, ventilation, cerebral perfusion pressure and<br />
adequate sedation and analgesia. Coexisting injuries must<br />
also be managed simultaneously in order to optimize cerebral<br />
perfusion and ventilation. The recognition <strong>of</strong> TBI must trigger<br />
appropriate triage decisions at all levels <strong>of</strong> <strong>the</strong> casevac chain.<br />
Timely CT scanning, neurosurgical intervention, appropriate<br />
critical care transfer and management including monitoring <strong>of</strong><br />
<strong>the</strong> intracranial pressure will allow optimization <strong>of</strong> <strong>the</strong> patient’s<br />
chances <strong>of</strong> recovery and rehabilitation.<br />
References<br />
1. Anakwe REB. The management <strong>of</strong> head injuries on military<br />
operations J R <strong>Army</strong> Med <strong>Corps</strong> 2005; 151: 87-92<br />
2. JSP 570 BATLS 2008 Ch 3,4,5,9, 21<br />
3. Poon WS, Li AK. Traumatic extradural hematoma <strong>of</strong> delayed onset<br />
is not a rarity. Neurosurgery 1992; 30(5): 681-6.<br />
4. Badjatia N, Carney N, Crocco T J et al. Guidelines for prehospital<br />
management <strong>of</strong> traumatic brain injury 2nd edition. Brain Trauma<br />
Foundation; BTF Center for Guidelines Management. Prehosp<br />
Emerg Care. 2008; 12 Suppl 1: S1-52<br />
5. Knuth T, Letarte PB, Ling G et al. Guidelines for <strong>the</strong> field<br />
management <strong>of</strong> combat-related head trauma. Brain Trauma<br />
Foundation New York: 2005<br />
6. Mendelow AD, Teasdale G, Jennett B, Bryden J, Hessett C, Murray<br />
G. Risks <strong>of</strong> intracranial haematoma in head injured adults. Br Med<br />
J (Clin Res Ed). 1983; 287: 1173-6<br />
7. Von Elm E, Schoettker P, Henzi I, Osterwalder J, Walder B. Br J<br />
Anaesth. 2009; 103(3): 371-86<br />
8. Head Injury Standard Operating Procedure. London HEMS. 2010<br />
9. Bourgoin A, Albanèse J, Wereszczynski N, Charbit M, Vialet R,<br />
Martin C. Safety <strong>of</strong> sedation with ketamine in severe head injury<br />
patients: comparison with sufentanil. Crit Care Med. 2003; 31(3):<br />
711-7<br />
10. Bourgoin A, Albanèse J, Léone M, Sampol-Manos E, Viviand X,<br />
Martin C. Effects <strong>of</strong> sufentanil or ketamine administered in targetcontrolled<br />
infusion on <strong>the</strong> cerebral hemodynamics <strong>of</strong> severely<br />
brain-injured patients. Crit Care Med. 2005; 33(5): 1109-13<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S335–341
<strong>Anaes<strong>the</strong>sia</strong> for TBI CL Park, P Moor, K Birch et al<br />
11. Schmittner MD, Vajkoczy SL, Horn P et al. Effects <strong>of</strong> fentanyl and<br />
S(+)-ketamine on cerebral hemodynamics, gastrointestinal motility,<br />
and need <strong>of</strong> vasopressors in patients with intracranial pathologies: a<br />
pilot study. J Neurosurg Anes<strong>the</strong>siol. 2007; 19(4): 257-62<br />
12. Bar-Joseph G, Guilburd Y, Tamir A, Guilburd JN. Effectiveness<br />
<strong>of</strong> ketamine in decreasing intracranial pressure in children with<br />
intracranial hypertension. J Neurosurg Pediatr 2009; 4(1): 40-6<br />
13. Morris C, Perris A, Klein J, Mahoney P. <strong>Anaes<strong>the</strong>sia</strong> in<br />
haemodynamically compromised emergency patients: does<br />
ketamine represent <strong>the</strong> best choice <strong>of</strong> induction agent? <strong>Anaes<strong>the</strong>sia</strong><br />
2009; 64(5): 532-9<br />
14. Guidelines for <strong>the</strong> management <strong>of</strong> severe traumatic brain injury. J<br />
Neurotrauma 2007; 24 Suppl 1: S1-106<br />
15. Dawes R, Thomas GO. Battlefield Resuscitation. Curr Opin Crit<br />
Care 2009; 15(6): 527-35<br />
16. Davies G, Deakin C, Wilson A. The effect <strong>of</strong> a rigid collar on<br />
intracranial pressure.Injury. 1996; 27(9): 647-9<br />
17. Wakai A, Roberts I, Schierhout G. Mannitol for acute traumatic<br />
brain injury. Cochrane Database Syst Rev 2007; 24(1): CD001049<br />
18. Vassar MJ, Perry CA, Holcr<strong>of</strong>t JW. Prehospital resuscitation <strong>of</strong><br />
hypotensive trauma patients with 7.5% NaCl versus 7.5% NaCl<br />
with added dextran: a controlled trial. J Trauma 1993; 34(5):<br />
622–32<br />
19. Wade CE et al Individual patient cohort analysis <strong>of</strong> <strong>the</strong> efficacy <strong>of</strong><br />
hypertonic saline/dextran in patients with traumatic brain injury<br />
and hypotension. J Trauma 1997; 42 (5 Suppl): S61–5<br />
20. Qureshi AI, Wilson DA, Traystman RJ Treatment <strong>of</strong> elevated<br />
intracranial pressure in experimental intracerebral hemorrhage:<br />
comparison between mannitol and hypertonic saline. Neurosurgery<br />
1999; 44(5): 1055–63<br />
21. Härtl R, Ghajar J, Hochleuthner H, Mauritz W. Hypertonic/<br />
hyperoncotic saline reliably reduces ICP in severely head-injured<br />
patients with intracranial hypertension. Acta Neurochir Suppl 1997;<br />
70: 126–9<br />
22. Berger S, Schwarz M, Huth R. Hypertonic saline solution<br />
and decompressive craniectomy for treatment <strong>of</strong> intracranial<br />
hypertension in pediatric severe traumatic brain injury. J Trauma<br />
2002; 53(3): 558–63<br />
23. Simma B, Burger R, Falk M, Sacher P, Fanconi S . A prospective,<br />
randomized, and controlled study <strong>of</strong> fluid management in children<br />
with severe head injury: lactated Ringer ’s solution versus hypertonic<br />
saline. Crit Care Med 1998; 26(7): 1265–70<br />
24. Pfenninger J, Wagner BP. Hypertonic saline in severe pediatric<br />
head injury. Crit Care Med 2001; 29(7): 1489<br />
25. Khanna S et al (2000) Use <strong>of</strong> hypertonic saline in <strong>the</strong> treatment<br />
<strong>of</strong> severe refractory post traumatic intracranial hypertension<br />
in pediatric traumatic brain injury. Crit Care Med 2000; 28(4):<br />
1144–51<br />
26. Peterson B et al (2000) Prolonged hypernatremia controls elevated<br />
intracranial pressure in head-injured pediatric patients. Crit Care<br />
Med 2000; 28(4): 1136–43<br />
27. Tyagi R, Donaldson K, L<strong>of</strong>tus CM, Jallo J. Hypertonic saline: a<br />
clinical review. Neurosurg Rev 2007; 30(4): 277-89<br />
28. Cooper DJ, Myles PS, McDermott FT et al. HTS Study<br />
Investigators. Prehospital hypertonic saline resuscitation <strong>of</strong> patients<br />
with hypotension and severe traumatic brain injury: a randomized<br />
controlled trial. JAMA 2004; 291(11): 1350-7<br />
29. Moppett IK. Traumatic brain injury: assessment, resuscitation and<br />
early management. Br J Anaesth 2007; 99(1): 18-31<br />
30. Wisner DH, Victor NS, Holcr<strong>of</strong>t JW. Priorities in <strong>the</strong> management<br />
<strong>of</strong> multiple trauma: intracranial versus intra-abdominal injury. J<br />
Trauma 1993; 35(2): 271-6<br />
31. Enderson BL, Reath DB, Meadors J, et al. The tertiary trauma<br />
survey: A prospective study <strong>of</strong> missed injury. J Trauma 1990; 30:<br />
666–9<br />
32. Morris CGT, McCoy E. Clearing <strong>the</strong> cervical spine in unconscious<br />
polytrauma victims. <strong>Anaes<strong>the</strong>sia</strong> 2004; 59: 464-82<br />
33. Sanchez B, Waxman K, Jones T, Conner S, Chung R, Becerra S.<br />
Cervical spine clearance in blunt trauma: evaluation <strong>of</strong> a computed<br />
tomography–based protocol J Trauma 2005; 59: 179–83<br />
34. Brohi K, Healy M, Fo<strong>the</strong>ringham T et al. Helical computed<br />
tomographic scanning for <strong>the</strong> evaluation <strong>of</strong> <strong>the</strong> cervical spine in<br />
<strong>the</strong> unconscious, intubated trauma patient. J Trauma 2005; 58:<br />
897–901<br />
35. Macnab AJ, Wensley DF, Sun C. Cost-benefit <strong>of</strong> trained transport<br />
teams: Estimates for head injured children. Prehospital Emergency<br />
Care 2001; 5: 3090-3127<br />
36. Helling E, McKinlay AJ. Considerations for <strong>the</strong> head injured airevacuated<br />
patient. A case report <strong>of</strong> frontal sinus fracture and review<br />
<strong>of</strong> <strong>the</strong> literature. Military Medicine 2005; 170: 577-9<br />
37. Bersten A, Soni N. Oh’s Intensive Care Manual. 5th Edition.<br />
Elsevier 2003.<br />
38. Treatment <strong>of</strong> traumatic brain injury with moderate hypo<strong>the</strong>rmia.<br />
NEJM 1997; 336: 540 – 6<br />
39. Zeiner A, Holzer M, Sterz F et al. Hyper<strong>the</strong>rmia after cardiac arrest<br />
is associated with an unfavourable outcome. Arch Intern Med 2001;<br />
161: 2007-12<br />
40. Chestnut RM, Marshall LF, Klauber MR, et al: The role <strong>of</strong><br />
secondary brain injury in determining outcome from severe head<br />
injury. J Trauma 1993; 34: 216-22<br />
41. Laird AM, Miller PR, Kilgo PD, Meredith JW, Chang MC.<br />
Relationship <strong>of</strong> early hyperglycaemia to mortality in trauma<br />
patients. J Trauma 2004; 56(5): 1058-62<br />
42. Guidelines for <strong>the</strong> management <strong>of</strong> severe traumatic brain injury. J<br />
Neurotrauma 2007; 24 Suppl 1: S1-106<br />
43. Andrews PJD, Citerio G, Longhi L, Polderman K, Sahuquillo<br />
J, Vajkoczy P. NICEM consensus on neurological monitoring in<br />
acute neurological disease. Intensive Care Med 2008; 34: 1362 – 70.<br />
44. Ralph JK, Lowes T. Neurointensive Care J R <strong>Army</strong> Med <strong>Corps</strong><br />
2009; 155: 147-51<br />
45. Stiefel MF, Spiotta A, Gracias VH et al. Reduced mortality rate in<br />
patients with severe traumatic brain injury treated with brain tissue<br />
oxygen monitoring J Neurosurg 2005; 103: 805–11<br />
46. Helmy A, Vizcaychipiand M, Gupta AK. Traumatic brain injury:<br />
intensive care management Br J Anaesth 2007; 99: 32-42<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S335–341 341
Critical Care at Role 4<br />
CPL Jones 1 , JP Chinery 2 , K England 3 , P Mahoney 4<br />
1 Core Trainee in <strong>Anaes<strong>the</strong>sia</strong>, University Hospitals Birmingham (UHB) NHS Foundation Trust; 2 Specialist Trainee in<br />
<strong>Anaes<strong>the</strong>sia</strong>, UHB NHS Foundation Trust; 3 Consultant in <strong>Anaes<strong>the</strong>sia</strong> and Intensive Care, UHB NHS Foundation<br />
Trust; 4 <strong>Defence</strong> Pr<strong>of</strong>essor <strong>Anaes<strong>the</strong>sia</strong>, <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine<br />
Abstract<br />
This descriptive paper focuses on <strong>the</strong> sequence <strong>of</strong> events that occur during <strong>the</strong> admission and ongoing management <strong>of</strong> <strong>the</strong><br />
Military Polytrauma patient to Critical Care, Area B, Queen Elizabeth Hospital Birmingham (QEHB). It is intended to<br />
inform new clinical staff, <strong>the</strong> wider DMS, and potentially o<strong>the</strong>r NHS intensive care units which may be called upon to manage<br />
such patients during a military surge or following a UK domestic major incident.<br />
Introduction<br />
Organisation <strong>of</strong> Critical Care at Role 4<br />
University Hospitals Birmingham NHS Foundation Trust (UHB)<br />
contains <strong>the</strong> combined clinical expertise to deliver optimum<br />
definitive care for injured personnel from military operations<br />
such as Operation HERRICK in Afghanistan. For this reason <strong>the</strong><br />
<strong>Defence</strong> <strong>Medical</strong> Services (DMS) uses UHB as its Role 4 facility.<br />
At Queen Elizabeth Hospital, Birmingham, <strong>the</strong>re are four critical<br />
care units, each <strong>of</strong>fering a specific clinical capability supported by<br />
on-site specialists.<br />
Area B, formerly based at Selly Oak Hospital (SOH), provides<br />
critical care to vascular, orthopaedic, maxill<strong>of</strong>acial, burns and<br />
plastic surgical patients, and is <strong>the</strong>refore well placed to <strong>of</strong>fer<br />
general critical care to <strong>the</strong> majority <strong>of</strong> severely injured military<br />
patients. QEHB’s o<strong>the</strong>r separate intensive care units, each has a<br />
particular sub-speciality interest:<br />
• Area A will soon house <strong>the</strong> Neurosciences Critical Care<br />
Unit (NCCU) providing tertiary level care for patients with<br />
neurosurgical and neurological problems - including head<br />
injuries.<br />
• Area C (formerly North 3 Critical Care) <strong>of</strong>fers general intensive<br />
care, with a special focus towards pre and post-operative care<br />
<strong>of</strong> patients undergoing liver surgery including transplantation,<br />
complex upper and lower GI surgery, and maxill<strong>of</strong>acial surgery.<br />
• Area D formerly <strong>the</strong> Welcome Building Critical Care (WBCC)<br />
is for patients with cardiothoracic pathology including those<br />
requiring heart and lung transplantation.<br />
All four units are supported by general and specialist surgeons<br />
and physicians, with full microbiology, radiology, pharmacy<br />
and laboratory services. Each has <strong>the</strong> clinical experience and<br />
infrastructure to deliver intensive care for all types <strong>of</strong> patients,<br />
regardless <strong>of</strong> underlying pathology.<br />
‘A new cohort <strong>of</strong> trauma patients’<br />
The predominant mechanism <strong>of</strong> injury for military patients<br />
received by Area B is <strong>the</strong> Improvised Explosive Device (IED).<br />
These devices can cause multiple patients from a single incident<br />
with extensive bone and s<strong>of</strong>t tissue defects, each potentially with<br />
Corresponding Author: Colonel PF Mahoney OBE FRCA<br />
L/RAMC, <strong>Defence</strong> Pr<strong>of</strong>essor <strong>Anaes<strong>the</strong>sia</strong>, <strong>Royal</strong> Centre for<br />
<strong>Defence</strong> Medicine, Birmingham Research Park, Vincent<br />
Drive, Birmingham B15 2SQ<br />
Tel: 0121 415 8858 Email: Peterfmahoney@aol.com<br />
multiple traumatic limb amputations, as well as facial, perineal,<br />
abdominal and ocular trauma. The cavitation effect <strong>of</strong> <strong>the</strong> IED<br />
blast sucks environmental contaminants high into wounds,<br />
beyond <strong>the</strong>ir obvious extent, sowing <strong>the</strong> seeds for subsequent<br />
infection and sepsis.<br />
This cohort <strong>of</strong> military patients, some who are surviving<br />
previously ‘non-survivable wounds’, are continually improving<br />
our understanding <strong>of</strong> <strong>the</strong> pathophysiology <strong>of</strong> major trauma.<br />
As such, many <strong>of</strong> <strong>the</strong> recommendations herein are based on<br />
consensus <strong>of</strong> expert pr<strong>of</strong>essional opinion, following evidence from<br />
civilian practice where applicable.<br />
The Initial Signal<br />
Shortly after military casualties are received at <strong>the</strong> deployed field<br />
hospital, Camp Bastion, Helmand Province, initial damage<br />
control surgery and resuscitation is completed. Following this,<br />
an initial secure signal is transmitted from <strong>the</strong> Aeromedical<br />
Communications Cell to <strong>the</strong> <strong>Royal</strong> Centre <strong>of</strong> <strong>Defence</strong> Medicine.<br />
On arrival, <strong>the</strong> message is presented to <strong>the</strong> Area B Consultant<br />
on-call. The signal contains a summary <strong>of</strong> a patient’s clinical<br />
condition in <strong>the</strong> form <strong>of</strong> a MIST (Mechanism <strong>of</strong> injury / Injuries<br />
identified / Vital Signs / Treatment given) report.<br />
This concise picture <strong>of</strong> <strong>the</strong> extent and severity <strong>of</strong> <strong>the</strong> injuries,<br />
prompts planning for optimal ongoing critical care. Unless <strong>the</strong><br />
patient has specific localised injuries indicating a need for ongoing<br />
neurosurgical or cardiothoracic surgery, <strong>the</strong> default plan is to<br />
admit to Area B. Repatriation to <strong>the</strong> UK is carried out by <strong>the</strong><br />
Critical Care Air Support Team (CCAST) normally within 24-48<br />
hours, via a seamless continuation <strong>of</strong> Role 3 critical care through<br />
to UHB. Fur<strong>the</strong>r description <strong>of</strong> this process is beyond <strong>the</strong> scope<br />
<strong>of</strong> this article [1, 2]<br />
Acute admission<br />
On arrival to Area B one <strong>of</strong> <strong>the</strong> CCAST anaes<strong>the</strong>tists provides a<br />
verbal handover to a receiving team <strong>of</strong> staff. During handover, <strong>the</strong><br />
patient remains monitored and supported by CCAST equipment.<br />
The receiving Area B team is composed <strong>of</strong> an ITU junior doctor,<br />
<strong>the</strong> allocated nurse, <strong>the</strong> On-call Consultant Intensivist and a<br />
variable number <strong>of</strong> o<strong>the</strong>r nurses. During times <strong>of</strong> heightened<br />
activity when several critically ill patients are admitted via <strong>the</strong><br />
same CCAST flight, a Second On-call Consultant Intensivist is<br />
also present to overlook o<strong>the</strong>r patients and guide ITU trainees.<br />
Once handover has taken place, patients are transferred to<br />
Area B monitoring and ventilators. The admitting ITU doctor<br />
performs a thorough top to toe clinical examination, assessing all<br />
342 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S342–348
Role 4 Critical Care CPL Jones, JP Chinery, K England et al<br />
systems and <strong>the</strong> extent <strong>of</strong> injuries sustained. This is a repeat <strong>of</strong><br />
<strong>the</strong> tertiary survey performed in Camp Bastion. Particular note<br />
is made to assess for unrecognised ocular and tympanic trauma.<br />
All patients injured by IEDs, regardless <strong>of</strong> <strong>the</strong> aero-med signal<br />
identifying ocular trauma, require a formal examination by a<br />
senior ophthalmologist.<br />
In addition to <strong>the</strong> above, more specific and focused clinical<br />
examinations quickly follow. The trauma co-ordinator from <strong>the</strong><br />
bunker [3] who also receives a copy <strong>of</strong> <strong>the</strong> initial signal pre-alerts<br />
<strong>the</strong> appropriate specialties so <strong>the</strong>y are ready to provide input. It<br />
is not uncommon to see a Senior Registrar or Consultant from<br />
<strong>the</strong> following specialties: Orthopaedic, Plastic, Vascular, ENT,<br />
Maxill<strong>of</strong>acial and Ophthalmological surgery, who attend to assess<br />
<strong>the</strong> patient’s immediate needs for <strong>the</strong>atre all within <strong>the</strong> damage<br />
control mindset (Box 1). Once a patient has been examined and<br />
clinical notes completed, <strong>the</strong> following points are addressed.<br />
• The Damage Control ‘mindset’ underpins clinical activity<br />
during <strong>the</strong> initial reception period as patients can rapidly<br />
become unstable, with unrecognised and/or evolving<br />
injuries.<br />
• It entails focussing activity towards providing life,<br />
limb and sight saving treatment in order to prevent<br />
<strong>the</strong> progression <strong>of</strong> <strong>the</strong> lethal physiological triad <strong>of</strong><br />
coagulopathy, hypo<strong>the</strong>rmia and acidosis.<br />
• Integrated Simulators including instructor<br />
and model driven mannequins.<br />
Box 1: Damage Control - <strong>the</strong> unifying principle directing initial<br />
clinical activity<br />
Vascular access<br />
Major polytrauma patients admitted to Camp Bastion commonly<br />
receive immediate placement <strong>of</strong> a subclavian 8.5 French Gauge<br />
pulmonary artery ca<strong>the</strong>ter introducer sheath to provide large<br />
bore central venous access for massive transfusion. All central<br />
and peripheral venous ca<strong>the</strong>ters are considered to have been<br />
inserted with potentially incomplete aseptic precautions in a less<br />
than ideal environment and are <strong>the</strong>refore subsequently removed<br />
on admission to Area B. The preferred site for replacement <strong>of</strong><br />
central venous ca<strong>the</strong>ters in Area B is <strong>the</strong> internal jugular vein,<br />
under ultrasound guidance. After placement, a portable chest<br />
radiograph is performed to confirm correct ca<strong>the</strong>ter position and<br />
exclude an iatrogenic pneumothorax.<br />
Arterial lines are also changed when possible. However<br />
alternative access can <strong>of</strong>ten be difficult with patients having<br />
multiple amputations, perineal and pelvic trauma. Placing a<br />
new arterial line into <strong>the</strong> brachial artery <strong>of</strong> an arm with a distal<br />
forearm amputation is considered inappropriate. Risk benefit<br />
analysis is required on an individual basis with consultant<br />
guidance. Routine blood investigations taken on admission are<br />
displayed in Table 1.<br />
Infection control<br />
Following an IED explosion, wounds become contaminated by<br />
endogenous host micro-flora and exogenous agents in <strong>the</strong> soldiers’<br />
environment such as soil, dust, stones, water, device fragments,<br />
uniform and equipment particles. Massive tissue devitalisation<br />
and haematoma compromise <strong>the</strong> microcirculation, producing<br />
tissue ischaemia. Such tissue <strong>of</strong>fers <strong>the</strong> ideal environment for<br />
microbial proliferation. On admission to Area B patients remain<br />
• Full blood count<br />
• Urea and electrolytes<br />
• Magnesium and Phosphate levels<br />
• Liver function test<br />
• Clotting screen<br />
• Fibrinogen level<br />
• Arterial blood gas measurement including lactate level<br />
• C-reactive protein<br />
• • Creatine Kinase level – assessed on admission and<br />
if high repeated daily to guide maintenance fluid<br />
prescription<br />
• Drug levels (as required)<br />
• ROTEM (thromboelastometry)<br />
Table 1: In order to guide fur<strong>the</strong>r clinical treatment <strong>the</strong> following tests<br />
are regularly repeated during a military patients admission to Area<br />
B. Once patients are clinically stable, requiring less frequent trips<br />
to <strong>the</strong>atre, daily blood requests reduce significantly. Fur<strong>the</strong>r daily<br />
blood tests help act as an early surveillance screen for infection, renal<br />
failure, adverse drug reactions etc.<br />
at high risk <strong>of</strong> wound infection and sepsis. Some patients present<br />
to Area B already in a “septic state” and commenced on inotropic<br />
support by CCAST in-flight.<br />
Nosocomially acquired MDR (multi-drug resistant) infections<br />
such as Acinetobacter baumanni and Pseudomonas aeruginosa,<br />
remain an extremely serious issue for injured military personnel<br />
[4,5] and concerns have previously been raised regards risk to<br />
civilian populations nursed in close proximity.<br />
Surprisingly, our experience with regards to MDR-Acinetobacter<br />
seems to be different to that published by allied forces, causing<br />
minimum serious infections in military personnel admitted<br />
to UHB since 2003. Transmission <strong>of</strong> MDR-Acinetobacter to<br />
civilians, especially those with chronic lung disease, remains<br />
a significant risk and is prevented on a daily basis by applying<br />
infection control measures.<br />
Standardization <strong>of</strong> infection control practice with emphasis on<br />
<strong>the</strong> basics <strong>of</strong> hand hygiene and isolation procedures remains key to<br />
prevent such organisms being a risk to o<strong>the</strong>rs. Table 2 summarises<br />
two key infection control measures that are addressed during <strong>the</strong><br />
admission <strong>of</strong> all military patients. Clinical audit can be used to<br />
assess if all <strong>the</strong>se measures are carried out correctly.<br />
Antimicrobial cover<br />
On admission to Area B all complex polytrauma patients are<br />
prescribed broader spectrum antimicrobials according to <strong>the</strong>ir<br />
injury pr<strong>of</strong>ile (Figure 1) and such treatment is guided by expert<br />
microbiological advice. A common question raised by new<br />
trainees on <strong>the</strong> unit is why patients’ are not commenced on such<br />
broader spectrums at Role 3?<br />
Routine Role 3 practice is to give early empirical antibiotic<br />
<strong>the</strong>rapy to help prevent severe infection caused by <strong>the</strong> well<br />
recognised and more aggressive pathogens in <strong>the</strong> period shortly<br />
after injury (Staphylococcus aureus, beta-haemolytic streptococci and<br />
clostridia causing gas gangrene and tetanus) [6]. Co-amoxiclav is<br />
used for non-penicillin allergic patients.<br />
The less pathogenic environmental organisms acquired as a<br />
result <strong>of</strong> an IED blast injury are unlikely to cause serious infection<br />
soon after injury, and are controlled in <strong>the</strong> early stages <strong>of</strong> treatment<br />
by surgical debridement. Debridement can be difficult and as a<br />
result some environmental organisms may remain in tissues for<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S342–348 343
Role 4 Critical Care<br />
Additional Barrier<br />
Protection<br />
Initial Septic<br />
Screen<br />
some time, hence <strong>the</strong> reason broad spectrum antibiotics, which<br />
cover such organisms, are started on Area B.<br />
An American study from Iraq assessed war wound bacteriology<br />
soon after initial injury and <strong>the</strong> results revealed a predominance<br />
<strong>of</strong> gram positive organisms <strong>of</strong> low virulence and pathogenicity,<br />
supporting <strong>the</strong> early use <strong>of</strong> narrow spectrum antibiotics, as first<br />
choice [7]. Our own experience in treating such patients from<br />
Iraq and Afghanistan supports this approach.<br />
After admission to Area B most patients are promptly taken to<br />
<strong>the</strong>atre for “a second look”, fur<strong>the</strong>r debridement and change <strong>of</strong><br />
dressing, or for more specific time critical surgical interventions.<br />
For such patients new antimicrobial treatment is delayed until<br />
tissue samples and wound swabs have been taken. Once all<br />
samples are collected <strong>the</strong> initial septic screen is complete and<br />
<strong>the</strong> anaes<strong>the</strong>tist commences appropriate broader spectrum cover<br />
(Figure 1). Once results return from microbiology, antimicrobials<br />
are changed according to sensitivities.<br />
During times <strong>of</strong> heightened activity when an initial trip to<br />
<strong>the</strong>atre may be delayed, or when patients are admitted in a septic<br />
state broader spectrum antimicrobials are given as soon as possible<br />
(Box 2).<br />
344<br />
Thumb looped gowns and gloves<br />
must be worn by all staff and family<br />
occupying patient bed spaces. This is<br />
practiced for <strong>the</strong> first seven days whilst<br />
an initial septic screen is completed<br />
and results confirmed. Once cleared<br />
normal infection control measures are<br />
taken; standard aprons worn within <strong>the</strong><br />
bed space, apron gown and gloves if<br />
clinically assessing <strong>the</strong> patient.<br />
Swab all wounds available to sample.<br />
Do not remove any dressings as fur<strong>the</strong>r<br />
samples are sent from <strong>the</strong>atre.<br />
Complete MRSA screen – axilla, groin<br />
and nasal swabs required.<br />
Send for microscopy, culture and<br />
sensitivity:<br />
Urine<br />
Sputum<br />
Pleural fluid (if intercostal chest drain<br />
in-situ)<br />
Abdominal drain fluid (if drains in-situ)<br />
Cerebral spinal fluid – consider lumbar<br />
puncture in all patients with penetrating<br />
head and spinal injuries (consultant<br />
request only)<br />
Blood cultures – required from all<br />
patients on admission regardless <strong>of</strong><br />
body temperature. Nursing staff to send<br />
cultures from new central and arterial<br />
lines. If insertion <strong>of</strong> new lines delayed<br />
perform a peripheral stab.<br />
Tips from all central lines removed.<br />
Tissue samples taken in <strong>the</strong>atre, include<br />
a samples for histology.<br />
Table 2 Infection Control measures implemented in Area B Critical<br />
Care.<br />
Box 2: Antimicrobial cover – an overview<br />
CPL Jones, JP Chinery, K England et al<br />
• Invasive fungal infections may present acutely or after<br />
several weeks <strong>of</strong> care [22].<br />
• All patients initially commenced on pre-emptive<br />
antifungal treatment need to continue this for fourteen<br />
days.<br />
• If an invasive fungal infection is diagnosed <strong>the</strong> treatment<br />
is much longer, stopping only when <strong>the</strong>re is no evidence<br />
<strong>of</strong> systemic spread or any surgical concern for wounds and<br />
graft healing.<br />
• When an initial septic screen is complete broad spectrum<br />
cover is started (Figure 1).<br />
• The default for any concerns regarding antimicrobial cover<br />
is to discuss with <strong>the</strong> consultant microbiologist on-call.<br />
• For all patients allergic to penicillin this discussion must<br />
occur as soon as possible.<br />
Malaria<br />
Afghanistan has a malarial season with <strong>the</strong> risk determined by<br />
military environmental health personnel, which generally runs<br />
from March to <strong>the</strong> end <strong>of</strong> October. Plasmodium Vivax malaria<br />
is <strong>the</strong> most prevalent; never<strong>the</strong>less up to 10% <strong>of</strong> infections<br />
can be due to <strong>the</strong> more pathogenic Falciparum malaria. Across<br />
Afghanistan <strong>the</strong>re have been about 400 malaria cases in NATO<br />
troops since 2001, all <strong>of</strong> which have been due to P. vivax to date<br />
(unpublished data confirmed by Military Infection Control)<br />
Malarial prophylaxis is prescribed to all military personnel<br />
deployed to at risk areas across <strong>the</strong> world and medication<br />
compliance is mandatory. Despite this soldiers on operational<br />
duties <strong>of</strong>ten fail to take prophylaxis treatment and should be<br />
considered high risk when <strong>the</strong>y develop persistent pyrexias.<br />
All military personnel admitted to Area B from Afghanistan<br />
during <strong>the</strong> “at risk” season are prescribed <strong>the</strong> standard regime <strong>of</strong><br />
Chloroquine 310mg once weekly and Proguanil 200mg once<br />
daily - both given via <strong>the</strong> nasogastric (ng) route. If <strong>the</strong>re are<br />
any contraindications, patients are prescribed Doxycycline or<br />
Malarone. All malaria prophylaxis is continued for <strong>the</strong> appropriate<br />
time, for example: four weeks on return to UK for those taking<br />
Chloroquine and Proguanil.<br />
Analgesia<br />
The timely aggressive provision <strong>of</strong> analgesia from time <strong>of</strong><br />
admission is <strong>of</strong> great importance, not only for humanitarian<br />
reasons. It has been widely recognised that adequate analgesia<br />
reduces sympa<strong>the</strong>tic nervous system activation, aids coagulation,<br />
and reduces <strong>the</strong> catabolic endocrine stress response to injury [8].<br />
Additionally, <strong>the</strong> nervous system retains <strong>the</strong> ability to remodel<br />
itself, particularly in response to excessive or untreated pain. This<br />
is thought to underpin <strong>the</strong> development <strong>of</strong> abnormal responses<br />
e.g. sensitisation to non-noxious stimuli, amplified responses<br />
to normally minimally noxious stimuli, and o<strong>the</strong>r chronic pain<br />
symptoms.<br />
Different types <strong>of</strong> analgesia impact on <strong>the</strong> nociceptive pathways<br />
at different points and/or at different sites, e.g. central/spinal/<br />
peripheral opioid receptors, so in combination complement each<br />
o<strong>the</strong>r’s activity [9].<br />
Critical Care Air Support Team (CCAST) patients arriving<br />
intubated and ventilated at Area B are commonly transferred with<br />
ongoing intravenous infusions <strong>of</strong> morphine and midazolam. This<br />
combination is usually effective at providing immediate strong<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S342–348
Role 4 Critical Care CPL Jones, JP Chinery, K England et al<br />
Figure 1 Antimicrobial cover according to injury pr<strong>of</strong>ile.<br />
opioid analgesia and sedation, facilitating mechanical ventilation.<br />
O<strong>the</strong>rs opioids such as Fentanyl and Alfentanil, as well as <strong>the</strong><br />
N-methyl-D-aspartic acid (NMDA) antagonist, Ketamine<br />
and <strong>the</strong> α2 receptor agonist Clonidine, although available, are<br />
infrequently utilised on Area B.<br />
Although designed for ward use, <strong>the</strong> Acute Pain Guidelines<br />
for Military Personnel [10] are a helpful benchmark for analgesic<br />
prescription on admission to Area B. They remind <strong>the</strong> clinician<br />
to prescribe regular and as required analgesia via both <strong>the</strong> oral/<br />
nasogastric and intravenous routes. If not already present, a<br />
nasogastric tube (NGT) is placed to allow early commencement<br />
<strong>of</strong> Amitriptyline 25mg at night and Pregabalin 75mg twice daily.<br />
This is <strong>of</strong>ten at <strong>the</strong> same time as placement <strong>of</strong> central venous lines<br />
to minimise radiation from check x-rays. This is appropriate for<br />
patients with amputations or extensive s<strong>of</strong>t tissue injuries who,<br />
having sustained direct neural damage, are likely to develop<br />
neuropathic and or phantom limb pain. Dose escalation <strong>of</strong> <strong>the</strong>se<br />
agents is carried out after three and seven days.<br />
NG tubes also facilitate feeding and delivery <strong>of</strong> Senna 10mls<br />
nocte and Docusate Sodium 100mg tds, <strong>the</strong> preferred stimulant<br />
and s<strong>of</strong>tening laxatives. These minimise constipation and aid<br />
onward intestinal motility and absorption <strong>of</strong> enteral nutrition<br />
and drugs. They are prescribed on admission and continue<br />
until patients develop persistent loose stools, diarrhoea or opiate<br />
medications are stopped.<br />
If <strong>the</strong> patient is not coagulopathic on admission, a NSAID,<br />
typically Dicl<strong>of</strong>enac is prescribed, along with a H2 receptor<br />
antagonist such as Ranitidine for gastric protection. It is likely<br />
that <strong>the</strong> increased use <strong>of</strong> thromboelastometry (ROTEM) [11]<br />
at Area B (to measure coagulation parameters) will enhance <strong>the</strong><br />
appropriate use/omission <strong>of</strong> NSAIDS. All patients should receive<br />
regular paracetamol, initially intravenously, as it enhances <strong>the</strong><br />
central effects <strong>of</strong> strong opioids<br />
and o<strong>the</strong>r NSAIDS [12].<br />
The <strong>Defence</strong> <strong>Medical</strong><br />
Services pain scoring system<br />
is used on <strong>the</strong> Area B charts.<br />
This is a verbal descriptive pain<br />
rating scale from 0-3[8]. When<br />
communication is impaired<br />
such as with a sedated intubated<br />
patient, o<strong>the</strong>r cues such as<br />
sedation score and autonomic<br />
reflexes, are used to provide an<br />
external indirect estimation <strong>of</strong><br />
<strong>the</strong> adequacy <strong>of</strong> analgesia.<br />
Patients with traumatic<br />
amputations <strong>of</strong>ten have<br />
adjuvant analgesia provided via<br />
low concentration Bupivicaine<br />
delivered by an epidural or<br />
continuous peripheral nerve<br />
block (CPNB) ca<strong>the</strong>ter. This<br />
modality <strong>of</strong> analgesia seems<br />
to reduce concomitant opioid<br />
use, resulting in less sedation,<br />
aiding weaning and earlier<br />
extubation. Although <strong>the</strong>re are<br />
a panoply <strong>of</strong> additional risks<br />
[13] associated with epidural<br />
and/or CPNB placement,<br />
<strong>the</strong>se have not occurred with great frequency at Area B. The<br />
Regional <strong>Anaes<strong>the</strong>sia</strong> Outcome Reporting system developed<br />
by Buckenmaiers’ <strong>Army</strong> Regional <strong>Anaes<strong>the</strong>sia</strong> and Pain<br />
Management Initiative (ARAPMI) group, indicate a very low<br />
rate <strong>of</strong> complications following CPNB [14].<br />
Nutrition<br />
High operational tempo on a day-to-day basis places <strong>the</strong> average<br />
infantry soldier working in <strong>the</strong> Green Zone at risk <strong>of</strong> malnutrition.<br />
Prevention strategies for this are currently being addressed and<br />
remain beyond <strong>the</strong> scope <strong>of</strong> this paper. Never<strong>the</strong>less, <strong>the</strong> premorbid<br />
state <strong>of</strong> malnutrition combined with a physiological<br />
catabolic response to major trauma places such patients at risk<br />
<strong>of</strong> severe nosocomial infections, delayed tissue healing, increased<br />
length <strong>of</strong> stay in critical care and increased muscle wasting,<br />
amongst o<strong>the</strong>r complications [15].<br />
Nutritional support with Nutrison HE (high energy)<br />
is commenced for all poly-trauma patients without<br />
contraindications, at an initial rate <strong>of</strong> 30ml/hr and increased<br />
according to <strong>the</strong> protocol to a final goal rate. Compensation<br />
for <strong>the</strong> catabolic response to trauma is paramount to improve<br />
long-term prognosis and is commenced as soon as possible<br />
on admission via NGT. Patients admitted with a NGT insitu,<br />
on free drainage are assessed for commencing immediate<br />
enteral feeding. Clinical Guidelines for Operations [16] dictate<br />
that enteral nutrition should be commenced at Role 2/3 when<br />
possible. However, enteral feed is paused during an aeromedical<br />
CCAST flights as it is thought patients may be at an increased<br />
risk <strong>of</strong> micro-aspiration and subsequent nosocomial pneumonia<br />
[17]. NGT sited in Afghanistan should not routinely be replaced,<br />
but prior to use for enteral feeding will require checking for<br />
correct placement.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S342–348 345
Role 4 Critical Care<br />
For patients failing to absorb enteral feed, with persistent large<br />
aspirates, prokinetics are prescribed early (Metoclopromide 10mg<br />
tds IV and Erythromycin 125mg qds ng).<br />
Patients with abdominal injuries, in particular bowel<br />
perforations require total parenteral nutrition (TPN). This is<br />
discussed with <strong>the</strong> critical care dietetics team and ordered by<br />
<strong>the</strong> unit pharmacist. Patients failing to absorb via <strong>the</strong> NG route<br />
are listed for endoscopic insertion <strong>of</strong> a nasojejunal tube (NJT).<br />
Unfortunately, this can take a number <strong>of</strong> days to organise and<br />
during this time TPN is given. Once <strong>the</strong> NJT is in-situ TPN<br />
continues concurrently until gut absorption is established.<br />
Blood products for <strong>the</strong>atre<br />
Massive blood transfusions provided during damage control<br />
resuscitation and surgery place patients at high risk <strong>of</strong> developing<br />
antibodies to subsequent blood products. As a result regular<br />
cross matches are required for this cohort increasing blood bank’s<br />
overall workload.<br />
During times <strong>of</strong> heightened tempo <strong>the</strong> total demand <strong>of</strong> blood<br />
products for military patients returning to and from <strong>the</strong>atre is<br />
significant. To preserve <strong>the</strong> pool <strong>of</strong> fresh frozen plasma and<br />
platelets particularly a general consensus now exists for blood<br />
product requests:<br />
• Initial <strong>the</strong>atre trip: Request a minimum <strong>of</strong> 4 x packed red blood<br />
cells (PBRC) and 4 x fresh frozen plasma (FFP). Total request<br />
is dictated by <strong>the</strong> extent <strong>of</strong> planned surgery and a patient’s<br />
pre-op condition – for example haemoglobin level, underlying<br />
state <strong>of</strong> coagulopathy or active bleeding.<br />
• Subsequent trips to <strong>the</strong>atre: Send a fresh group and save sample,<br />
and request only PRBC according to <strong>the</strong> extent <strong>of</strong> planned<br />
surgery and patient pre-op haemoglobin.<br />
Between <strong>the</strong>atre trips low platelet and haemoglobin counts are<br />
<strong>of</strong>ten tolerated on Area B, as long as patients are not coagulopathic<br />
or actively bleeding.<br />
Anticoagulation<br />
Initial damage control resuscitation with massive transfusions<br />
(delivery <strong>of</strong> blood products: PRBC and FFP at a ratio <strong>of</strong> 1:1<br />
with platelets when needed), use <strong>of</strong> recombinant factor VII,<br />
cryoprecipitate and antifibrinolytics controls coagulopathy in<br />
severe trauma [18-20]. Our understanding <strong>of</strong> <strong>the</strong> short and<br />
long term effects <strong>of</strong> such management never<strong>the</strong>less remains<br />
unclear.<br />
Lower limb and pelvic fractures place patients at a significant<br />
risk for developing venous thromboembolic disorders (VTED).<br />
For <strong>the</strong> military cohort <strong>of</strong> patients admitted to Area B, such<br />
injuries are common and generally form part <strong>of</strong> <strong>the</strong> long list <strong>of</strong><br />
o<strong>the</strong>r injuries sustained. Despite patients receiving prophylactic<br />
anticoagulation, Area B has diagnosed multiple deep vein<br />
thromboses and pulmonary emboli in <strong>the</strong> military cohort.<br />
Damage control resuscitation aims to return or maintain<br />
patients in a state <strong>of</strong> normal coagulation. In reality after such<br />
intensive treatment patients may move past “normality” and<br />
become pro-thrombotic, increasing <strong>the</strong> risk for VTED. Fur<strong>the</strong>r<br />
research relating to <strong>the</strong> following questions is required (Box 3)<br />
Currently anticoagulation prophylaxis is considered following<br />
a patient’s initial trip to <strong>the</strong>atre and after assessment <strong>of</strong><br />
coagulopathy (a full clotting screen completed, including<br />
fibrinogen and platelet levels).<br />
346<br />
CPL Jones, JP Chinery, K England et al<br />
• Does blast wave disruption caused by an IED explosion<br />
change <strong>the</strong> architecture <strong>of</strong> vessels on a micro and macro<br />
structural level, increasing overall risk <strong>of</strong> a VTED?<br />
• How does an IED blast wave affect <strong>the</strong> normal clotting<br />
cascade (e.g. clotting factor proliferation, platelet<br />
activation and function etcetera)?<br />
• Is <strong>the</strong>re a direct correlation between <strong>the</strong> amount <strong>of</strong> blood<br />
products, factor VII, cryoprecipitate etc used to control<br />
coagulopathy and risk for subsequent VTED?<br />
• Is <strong>the</strong>re a role for IVC filters to be used in such polytrauma<br />
patients? If so, when should <strong>the</strong>y be inserted? [21]<br />
• What is <strong>the</strong> optimum dose <strong>of</strong> anticoagulation for such<br />
patients, and when is it best to start treatment in order to<br />
minimise risk <strong>of</strong> VTED.<br />
• How do we best identify patients becoming prothrombotic?<br />
How effective is ROTEM for this?<br />
Box 3 – Current coagulation research questions<br />
A general consensus exists to prescribe Enoxaparin 40mg OD<br />
s/c when:<br />
• <strong>the</strong>re are no concerns regards active bleeding<br />
• fibrinogen level > 1.0<br />
• APTT Ratio and INR both < 1.5<br />
• Platelets are maintained at an adequate level (i.e. not being<br />
consumed requiring regular top up transfusions).<br />
A ROTEM has recently become available to assess, closer to real<br />
time, a patient’s coagulation status. Once in full practice, <strong>the</strong><br />
frequency <strong>of</strong> formal coagulation screens requested may be reduced.<br />
After initial damage control<br />
Once <strong>the</strong>se patients have been stabilized and have moved out <strong>of</strong><br />
<strong>the</strong> damage control phase, sometimes over several days, ongoing<br />
critical care management is as for any patient requiring multiple<br />
organ support.<br />
• Systems support is reduced as possible. For example, sedation<br />
will be reduced / stopped and ventilatory support gradually<br />
weaned. Similarly, if haem<strong>of</strong>iltration has been required for <strong>the</strong><br />
management <strong>of</strong> acute renal failure, this too will be paused to<br />
assess renal function etc.<br />
• Pre-operative optimisation and post-operative observations.<br />
Once a patient enters a period <strong>of</strong> relative stability, more<br />
definitive surgical interventions are planned and <strong>the</strong> frequency<br />
<strong>of</strong> <strong>the</strong>atre trips may increase once again.<br />
• Ongoing clinical surveillance. Early identification <strong>of</strong> sepsis,<br />
renal failure, disseminated invasive fungal infections, adverse<br />
reactions etc. remain key to patients overall prognosis.<br />
Sepsis<br />
When patients become septic, identifying <strong>the</strong> exact cause can be<br />
challenging. Deep-seated invasive infections and occult collections<br />
are commonly sought by performing CT scans and sometimes <strong>the</strong><br />
whole body is scanned in search <strong>of</strong> a source. Occasionally patients<br />
may be too unstable for transfer to a CT scanner, <strong>the</strong>atre or both<br />
and optimisation on Area B remains <strong>the</strong> only option.<br />
S<strong>of</strong>t tissue infection secondary to invasive fungi should be<br />
considered in all patients, even if previous microbiology results<br />
do not indicate a presence <strong>of</strong> fungi, and ‘pre-emptive’ antifungals<br />
have been commenced. Prompt review <strong>of</strong> wounds should be<br />
considered in <strong>the</strong>se patients as such infections can progress rapidly.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S342–348
Role 4 Critical Care CPL Jones, JP Chinery, K England et al<br />
Sepsis care bundles including fluid resuscitation (guided by<br />
oesophageal doppler studies), inotropic support, reinforced<br />
antimicrobial cover, and early input from appropriate specialties,<br />
including microbiology, are vital at such a time. During such<br />
periods <strong>of</strong> clinical deterioration, Area B consultants review all<br />
clinical steps regardless <strong>of</strong> <strong>the</strong> time <strong>of</strong> day.<br />
Hyperpyrexia<br />
Hyperpyrexia, with persistent temperatures above 39.5°C, is<br />
occasionally seen in Area B military patients (Box 4). The reason<br />
for this is not entirely understood. As expected when patients<br />
initially develop hyperpyrexia, <strong>the</strong> first thoughts are towards<br />
finding a possible septic source. All patients have a full septic screen<br />
completed, routine bloods sent for assessment, and surgeons<br />
are asked to review wounds etc. When all <strong>the</strong> results return as<br />
negative, <strong>the</strong> differential diagnosis for pyrexia <strong>of</strong> unknown origin<br />
(PUO) needs to be considered.<br />
Pre-deployment training for Op HERRICK may take soldiers<br />
to Kenya, Belize, Brunei and wider afield. Screening for tropical<br />
and communicable diseases appropriate to <strong>the</strong> areas <strong>the</strong>y have<br />
travelled must be included in <strong>the</strong> differential. Advice on such<br />
diseases is available from <strong>the</strong> Department <strong>of</strong> Infectious Diseases<br />
at Birmingham Heartlands Hospital. Malaria and “Helmand<br />
fever” (sand-fly fever, Q-fever and rickettsia spotted fever) are<br />
tropical diseases screened for during PUO. Malaria screens are<br />
sent to Haematology. Results from a Helmand fever screen (sent<br />
to HPA Porton Down) are usually not received in time to directly<br />
influence patient management. Hence if no o<strong>the</strong>r cause for fever<br />
is found, Doxycycline 200mg OD is prescribed on consultant<br />
microbiological advice.<br />
Following evidence that all wound samples are clear <strong>of</strong><br />
fungus and confirmation <strong>of</strong> a negative septic screen, discussion<br />
<strong>of</strong>ten takes place between consultant intensivists, surgeons and<br />
microbiologists to consider stopping antifungal treatment. After<br />
stopping treatment, hyperpyrexia has resolved in some patients,<br />
a phenomenon noted in haematology patients also taking<br />
antifungal treatment - cause and effect not yet understood.<br />
• It is advised all “unexplained fevers” be treated as<br />
objectively as possible. An initial logical approach is first<br />
explored to assess if <strong>the</strong> fever is related to:<br />
• Trauma and infection (which means occult collection(s) <strong>of</strong><br />
pus/blood, foreign bodies, necrotic tissue etc)<br />
• Health care associated infection and ICU stay (e.g: line<br />
infection, ventilator associated pneumonia, urinary tract<br />
infection)<br />
• Therapy (all antimicrobials can cause hyperpyrexia, not<br />
just antifungals)<br />
• Patient travel history (which means a work up for tropical<br />
diseases)<br />
Box 4 An overview <strong>of</strong> <strong>the</strong> diagnostic approach to hyperpyrexia,<br />
The Patient’s Family<br />
Following a patient’s admission and initial trip to <strong>the</strong>atre, one<br />
<strong>of</strong> <strong>the</strong> operating Consultant Surgeons and a Senior ITU doctor<br />
will explain <strong>the</strong> extent <strong>of</strong> <strong>the</strong> <strong>the</strong>ir injuries, <strong>the</strong> treatment given<br />
so far, and answer any questions <strong>the</strong> family raise. This discussion,<br />
although difficult, is <strong>of</strong> immense importance and <strong>the</strong> manner <strong>of</strong><br />
its delivery is not quickly forgotten.<br />
The military patient’s next <strong>of</strong> kin or immediate family have a<br />
vital role to play in <strong>the</strong> reassurance, reorientation, and recovery <strong>of</strong><br />
patients when sedation holds and extubation are on <strong>the</strong> clinical<br />
agenda. It is not uncommon for military patients to emerge from<br />
sedation agitated and showing signs <strong>of</strong> delirium. When extubated<br />
<strong>the</strong>y may believe <strong>the</strong> incident in which <strong>the</strong>y were injured is still<br />
ongoing, mistaken in <strong>the</strong> belief that <strong>the</strong>y are still in Afghanistan.<br />
Having family members present can <strong>of</strong>ten provide patients <strong>the</strong><br />
reassurance <strong>the</strong>y need to believe <strong>the</strong>y are safe and home in <strong>the</strong> UK.<br />
Occasionally agitation requires treatment with chlorpromazine or<br />
haloperidol in order to prevent invasive lines, epidural ca<strong>the</strong>ters,<br />
NGTs etc being pulled out.<br />
As well as explanation from medical and nursing staff,<br />
families at Area B may receive pastoral support from an<br />
experienced member <strong>of</strong> <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Welfare Services,<br />
Military Liaison Officers, <strong>the</strong> RCDM Padre and Hospital<br />
Chaplains. Coincidentally, many <strong>of</strong> <strong>the</strong>se support personnel<br />
at SOH come from a nursing background. This is in addition<br />
to <strong>the</strong> support provided by <strong>the</strong> individual patients’ Regimental<br />
Liaison Officer.<br />
Temporary residential accommodation onsite or at <strong>the</strong><br />
nearby SSAFA Norton House can be organised free <strong>of</strong> charge,<br />
to allow family who are not close residents, to remain in close<br />
proximity during this stressful period. They are also able to<br />
provide information about <strong>the</strong> relevant statutory and charitable<br />
organisations that can provide immediate and longer-term<br />
practical and financial assistance. Though adherence to set<br />
visiting times is encouraged – it is recognised that family<br />
members <strong>of</strong>ten desire to be with <strong>the</strong>ir relative outside <strong>the</strong>se<br />
periods, particularly shortly after admission and during times<br />
<strong>of</strong> clinical deterioration. Wherever possible a compassionate<br />
approach is adopted.<br />
Discharge from Area B<br />
Patients discharged from Area B are usually transferred to a military<br />
trauma ward with a six bed high dependency unit attached.<br />
Individuals with multiple amputations requiring ongoing<br />
intravenous medications, in particular antifungal treatment, need<br />
a more definitive, long-term solution for vascular access. For such<br />
patients Peripherally Inserted Central Ca<strong>the</strong>ters (PICC) lines are<br />
<strong>the</strong> ideal solution. These are placed under radiological guidance<br />
as early as possible when a discharge from Area B to <strong>the</strong> ward is<br />
planned. This process is coordinated by <strong>the</strong> hospital IV team who<br />
liaise with interventional radiology.<br />
Conclusion<br />
As with <strong>Anaes<strong>the</strong>sia</strong> at Role 4, Critical Care for complex<br />
polytrauma military patients is still evolving. Much has already<br />
been learned, but <strong>the</strong>re still remains many questions to be<br />
answered, some <strong>of</strong> which we have highlighted. To continually<br />
improve <strong>the</strong> level <strong>of</strong> care provided all possible avenues <strong>of</strong> research<br />
need to be fur<strong>the</strong>r explored.<br />
Acknowledgements<br />
The authors would like to acknowledge <strong>the</strong> extensive help and<br />
advice from Dr M Gill, Consultant Microbiologist UHB and Wg<br />
Cdr AD Green, Director <strong>of</strong> Infection Prevention and Control,<br />
DCA in Communicable Diseases in <strong>the</strong> writing <strong>of</strong> this article.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S342–348 347
Role 4 Critical Care<br />
References<br />
1. Turner S, Ruth M, Tipping R. Critical Care Air Support Teams and<br />
Deployed Intensive Care. JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155: 171-174<br />
2. Shirley P. Operational Critical Care. Intensive Care and Trauma. JR<br />
<strong>Army</strong> Med <strong>Corps</strong> 2009; 155:133-1140<br />
3. Wood PR, Haldane AG, Plimmer SE. <strong>Anaes<strong>the</strong>sia</strong> at Role 4. J R<br />
<strong>Army</strong> Med <strong>Corps</strong> 2010; 156(4 Suppl 1): S308-310<br />
4. Hospenthal DR, Crouch HK. Infection control challenges in<br />
deployed US military treatment facilities. J Trauma 2009; 66(4<br />
Suppl): S120-8<br />
5. Calhoun JH, Murray CK, Manring MM. Multidrug-resistant<br />
organisms in military wounds from Iraq and Afghanistan. Clin<br />
Orth Rel Res 2008; 466(6): 1356-62<br />
6. Green AD, Hutley EJ. Pre-hospital antibiotics administration: A<br />
response. JR <strong>Army</strong> Med <strong>Corps</strong> 2008; 154: 5-9<br />
7. Murray CK, Roop SA, Hospenthal DR et al. Bacteriology <strong>of</strong> war<br />
wounds at <strong>the</strong> time <strong>of</strong> injury. Military Medicine 2006; 171(9): 826-9<br />
8. Looker J, Aldington DJ. Pain Scores – As Easy As Counting To<br />
Three. JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155(1): 42-43<br />
9. Stannard C, Booth S. Pain 2nd Edn. London: Churchill<br />
Livingstone, 2004<br />
10. Edwards D, Bowden M, Aldington DJ. Pain Management at Role<br />
4. JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155: 58-6<br />
11. Brohi K. Trauma Induced Coagulopathy. JR <strong>Army</strong> Med <strong>Corps</strong> 2009;<br />
155: 320-322<br />
12. Oscier CD, Milner QJW. Peri-operative use <strong>of</strong> paracetamol.<br />
<strong>Anaes<strong>the</strong>sia</strong> 2009; 64: 65-72<br />
348<br />
CPL Jones, JP Chinery, K England et al<br />
13. DJ Conner, J Ralph, DJ Aldington. Field Hospital Analgesia. JR<br />
<strong>Army</strong> Med <strong>Corps</strong> 2009; 155: 49-55<br />
14. Buckenmaier CC 3rd, Croll SM, Shields CH et al. Advanced<br />
regional anaes<strong>the</strong>sia morbidity and mortality grading system:<br />
regional anaes<strong>the</strong>sia outcomes reporting (ROAR). Pain Med 2009;<br />
10(6): 1115-22<br />
15. Duff S, Price S, Gray J. The Role <strong>of</strong> nutrition in injured military<br />
personnel at Role 4: Current Practice. JR <strong>Army</strong> Med <strong>Corps</strong> 2008;<br />
154: 284 -291<br />
16. Clinical Guidelines for Operations. Joint Doctrine Publication<br />
4-03.1 Ministry <strong>of</strong> <strong>Defence</strong><br />
17. Turner S, Ruth MJ, Bruce DL. “In flight catering”: Feeding critical<br />
care patients during aeromedical evacuation. JR <strong>Army</strong> Med <strong>Corps</strong><br />
2008; 154: 282-283<br />
18. Hodgetts TJ, Mahoney PF, Kirkham E. Damage Control<br />
Resuscitation. JR <strong>Army</strong> Med <strong>Corps</strong> 2007; 153: 299-300<br />
19. Kirkman E, Watts S, Hodgetts T, Mahoney P, Rawlinson S,<br />
Midwinter M. A proactive approach to <strong>the</strong> coagulopathy <strong>of</strong><br />
trauma. The rationale and guidelines for treatment. JR <strong>Army</strong> Med<br />
<strong>Corps</strong> 2008; 153: 302-306<br />
20. Surgeon Generals Policy Letter: Management <strong>of</strong> Haemorrhage on<br />
Operations. 2009. <strong>Defence</strong> <strong>Medical</strong> Services Department.<br />
21. Parent P, Trottier VJF, Bennett DR, Charlebois PB, Schieff TD. Are<br />
IV filters required in combat support hospitals? JR <strong>Army</strong> Med <strong>Corps</strong><br />
2009; 155: 210-212<br />
22. Gill, M. Hospital Guideline: Invasive fungal infection &<br />
antifungals. UHB, Department <strong>of</strong> Microbiology.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S342–348
Maritime <strong>Anaes<strong>the</strong>sia</strong><br />
RM Heames 1 , JE Risdall 2<br />
1 Consultant Anaes<strong>the</strong>tist, Southampton University Hospitals NHS Trust and Role 2 Afloat, RFA Fort Victoria, BFPO<br />
442; 2 Consultant Anaes<strong>the</strong>tist, Honorary Visiting Specialist, Addenbrooke’s Hospital, Cambridge University Hospitals<br />
NHS Foundation Trust and Foundation Senior Lecturer, Department <strong>of</strong> Military <strong>Anaes<strong>the</strong>sia</strong> and Critical Care, <strong>Royal</strong><br />
Centre <strong>of</strong> <strong>Defence</strong> Medicine, Birmingham<br />
Introduction<br />
<strong>Anaes<strong>the</strong>sia</strong> (o<strong>the</strong>r than local infiltration) at sea, in <strong>the</strong> 21 st<br />
century, is a relatively unusual occurrence. It can only be provided<br />
in ships carrying a Role 2 (damage control resuscitation) or Role<br />
3 (hospital) medical capability. RFA ARGUS is <strong>the</strong> <strong>Royal</strong> Navy’s<br />
sole maritime Role 3 facility (Figure 1). She carries a bespoke<br />
hospital facility, <strong>of</strong> up to 100 beds, with a wide range <strong>of</strong> specialist<br />
capabilities and has <strong>the</strong> ability to hold patients at all levels <strong>of</strong><br />
dependency, until fur<strong>the</strong>r evacuation can be effected.<br />
Figure 1 Main <strong>the</strong>atre complex on board RFA Argus<br />
The maritime Role 2 capability is not linked to any specific<br />
platform. In <strong>the</strong> early 1990s, <strong>the</strong> aircraft carriers had a permanent<br />
complement <strong>of</strong> two medical <strong>of</strong>ficers as a Principal <strong>Medical</strong> Officer<br />
(PMO) and Deputy PMO. One <strong>of</strong> <strong>the</strong>se two medical <strong>of</strong>ficers was<br />
an anaes<strong>the</strong>tist and <strong>the</strong> o<strong>the</strong>r a surgeon and whilst one was usually<br />
an accredited consultant, <strong>the</strong> o<strong>the</strong>r was frequently a trainee. They<br />
provided an organic Role 2 capability for any task group with<br />
whom <strong>the</strong>y deployed (Figure 2). However, <strong>the</strong> limited numbers<br />
<strong>of</strong> <strong>the</strong>atre operations performed meant that core specialist medical<br />
skills were difficult to maintain. Following <strong>the</strong> Calman review and<br />
subsequent changes in training, and with <strong>the</strong> emergence <strong>of</strong> clinical<br />
governance, it was deemed inappropriate to have Secondary Care<br />
trainees working unsupervised. The surgical team was <strong>the</strong>refore<br />
removed from <strong>the</strong> permanent ship’s complement and replaced by<br />
an accredited General Practitioner.<br />
Corresponding Author: Surgeon Commander Richard M<br />
Heames FRCA <strong>Royal</strong> Navy, Role 2 Afloat, RFA Fort Victoria,<br />
BFPO 442<br />
Email: richard.heames@suht.swest.nhs.uk<br />
Figure 2 Administration <strong>of</strong> a general anaes<strong>the</strong>tic on board HMS Ark<br />
<strong>Royal</strong> in 2007<br />
When <strong>the</strong> ship deployed to an area <strong>of</strong> perceived risk (e.g.<br />
East <strong>of</strong> Suez), <strong>the</strong> medical department was augmented by a Role<br />
2 surgical team, consisting <strong>of</strong> a surgeon and anaes<strong>the</strong>tist (both<br />
consultants at OF4) and an Operating Department Practitioner.<br />
However, after several deployments in this configuration, it<br />
became apparent that resources for damage control surgery were<br />
still inadequate.<br />
From <strong>the</strong> early 2000’s, Fleet has scrutinised deployments<br />
requiring Role 2 support to ascertain which vessel is most suited<br />
to host this facility. Maritime Role 2 can <strong>the</strong>refore be expected<br />
to configure differently, due to differing platforms and medical<br />
schemes <strong>of</strong> complement, on each occasion it is utilised. At <strong>the</strong><br />
same time, advances in Role 2 care have developed based on <strong>the</strong><br />
experience gained in both Iraq and Afghanistan. This has also<br />
necessitated changes in <strong>the</strong> composition <strong>of</strong> <strong>the</strong> maritime Role 2<br />
team deployed. The current configuration encompasses casualty<br />
retrieval, emergency medicine, surgery and anaes<strong>the</strong>sia, critical<br />
care and onward transfer. The anaes<strong>the</strong>tist has <strong>the</strong> potential to<br />
play a part throughout this care pathway.<br />
In both <strong>the</strong> Role 3 platform and whichever vessel is selected for<br />
Role 2, certain constraints, unique to <strong>the</strong> maritime environment,<br />
influence <strong>the</strong> delivery <strong>of</strong> anaes<strong>the</strong>tic (and indeed all clinical) care.<br />
All ships are fighting platforms and although clinical care would be<br />
expected to continue during contact, no surgery and anaes<strong>the</strong>sia<br />
would be envisaged. The priority under <strong>the</strong>se circumstances is <strong>the</strong><br />
engagement and <strong>the</strong> survival <strong>of</strong> <strong>the</strong> ship. All embarked personnel,<br />
irrespective <strong>of</strong> speciality, are <strong>the</strong>refore required to support this aim<br />
and can be required to fight fires or undertake damage control as<br />
well as provide first aid medical care. These skills, plus sea survival<br />
in <strong>the</strong> event <strong>of</strong> ship loss, are a mandatory part <strong>of</strong> maritime predeployment<br />
training.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S349–352 349
Maritime <strong>Anaes<strong>the</strong>sia</strong><br />
Pre-Operative<br />
The anaes<strong>the</strong>tist is likely to be involved with any serious casualty,<br />
<strong>of</strong>ten at, or close to, <strong>the</strong> point <strong>of</strong> wounding or accident. The <strong>Royal</strong><br />
Navy has now formed and tested a Maritime <strong>Medical</strong> Emergency<br />
Response Team which variably includes an Emergency Nurse<br />
(Practitioner), a <strong>Medical</strong> Assistant and an anaes<strong>the</strong>tist (Figure 3).<br />
The process <strong>of</strong> reaching <strong>the</strong> casualty and <strong>the</strong>n extracting him to<br />
<strong>the</strong> medical facility can <strong>of</strong>ten be time-consuming and convoluted.<br />
This process may involve a helicopter or sea boat.<br />
Figure 3 Preparation for deployment as MERT from RFA Fort Victoria<br />
Utilising a helicopter for a patient transfer creates many<br />
difficulties. Of course, <strong>the</strong> issues with helicopters and casualties are<br />
applicable to any environment such as <strong>the</strong> limited space, vibration,<br />
poor lighting and noise. All <strong>of</strong> this would be complicated in a<br />
contact situation where <strong>the</strong> helicopter may have to perform evasive<br />
manoeuvres. A specific problem in <strong>the</strong> maritime environment is<br />
lifting <strong>the</strong> casualty from <strong>the</strong> deck <strong>of</strong> a vessel into <strong>the</strong> helicopter.<br />
The sea state could be such that it is taxing for <strong>the</strong> pilot to<br />
maintain a hover over <strong>the</strong> deck and <strong>the</strong> winch is only designed<br />
for <strong>the</strong> winchman, <strong>the</strong> casualty and <strong>the</strong> lightweight stretcher. It<br />
takes careful planning to manage an intubated casualty needing<br />
ventilation during winching. One potential solution is to have one<br />
medic in <strong>the</strong> helicopter ready to receive and take over ventilation<br />
and one medic with <strong>the</strong> lightweight stretcher on <strong>the</strong> deck. Once<br />
all parties are ready, ventilation is stopped and <strong>the</strong>re is a period <strong>of</strong><br />
apnoea whilst <strong>the</strong> winching occurs.<br />
Ships’ sea boats create <strong>the</strong>ir own difficulties when used<br />
for casualty transfer. Firstly, <strong>the</strong> sea state can result in extreme<br />
movements <strong>of</strong> <strong>the</strong> boat when ei<strong>the</strong>r stationary or under way.<br />
Attempting to treat or even handle a casualty in this situation is<br />
difficult. Many <strong>of</strong> <strong>the</strong> sea boats used are Rigid Inflatable Boats<br />
and have very limited space, especially if <strong>the</strong> patient is on a<br />
spinal board. Once <strong>the</strong> boat is back alongside <strong>the</strong> ship, it has to<br />
be winched up to deck level (providing <strong>the</strong> hoist is man-rated<br />
for lifting) with fur<strong>the</strong>r casualty handling required to bring <strong>the</strong><br />
casualty inboard.<br />
The transfer <strong>of</strong> casualties through <strong>the</strong> ship to <strong>the</strong> medical<br />
facility requires teams <strong>of</strong> personnel and frequent practice. <strong>Army</strong><br />
field pattern stretchers are not conducive to being carried up and<br />
down ladders and through narrow hatches. Certain platforms<br />
allow <strong>the</strong> use <strong>of</strong> lifts (e.g. aircraft lifts or bomb lifts) to facilitate<br />
movement between decks. The alternative is to use ei<strong>the</strong>r a spinal<br />
board, a Neil-Robertson stretcher or a hose lift technique to hoist<br />
<strong>the</strong> casualty between decks.<br />
350<br />
RM Heames, JE Risdall<br />
Per-Operative<br />
The layout <strong>of</strong> <strong>the</strong> hospital is very variable depending on <strong>the</strong><br />
platform. On <strong>the</strong> warships it is fixed, whereas <strong>the</strong> RFA platforms<br />
have a greater amount <strong>of</strong> space which can be utilised as a hospital.<br />
Modern anaes<strong>the</strong>sia providing damage control resuscitation<br />
requires laboratory support and preferably radiography, which in<br />
turn need fur<strong>the</strong>r dedicated space for equipment.<br />
An operating <strong>the</strong>atre, triage bay and critical care bed all require<br />
significant amounts <strong>of</strong> equipment to carry out <strong>the</strong>ir respective<br />
functions. Most ships have <strong>the</strong>ir core power supply running on<br />
115V although fur<strong>the</strong>r circuits <strong>of</strong> 230V have been overlaid for<br />
standard UK 3 pin plugs. There may be insufficient 230V plug<br />
sockets in <strong>the</strong> hospital area and even if extra sockets are added, <strong>the</strong><br />
system may not be rated to support <strong>the</strong> power required.<br />
The ship is a closed environment holding everything from fuel<br />
to armament in relative close proximity. Therefore, explosive gases<br />
such as oxygen and nitrous oxide, need to be carefully stored in a<br />
secure area that can be flooded to prevent explosions in <strong>the</strong> event<br />
<strong>of</strong> a ship fire.<br />
Overall, medical stores become an issue due to <strong>the</strong> limited<br />
storage space on board and <strong>the</strong> potential difficulty <strong>of</strong> resupply at<br />
sea. All stores whe<strong>the</strong>r in a hold or in <strong>the</strong> hospital need to be fully<br />
secured for sea when not in direct use, due to motion from sea<br />
states. It is very easy for an anaes<strong>the</strong>tic machine on wheels, stacked<br />
with kit and a monitor on top to roll and have equipment fall <strong>of</strong>f<br />
and break (Figure 4).<br />
Figure 4 The anaes<strong>the</strong>tic machine set up on board RFA Fort Victoria<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S349–352
Maritime <strong>Anaes<strong>the</strong>sia</strong> RM Heames, JE Risdall<br />
<strong>Anaes<strong>the</strong>sia</strong> at sea is similar to that on land in a Role 3 facility. It<br />
is based on an anaes<strong>the</strong>tic machine (currently <strong>the</strong> Smiths Lamtec<br />
330) which has pipeline input for oxygen, air and nitrous oxide<br />
and cylinder input for oxygen and nitrous oxide only. There is one<br />
vaporiser mount taking ei<strong>the</strong>r is<strong>of</strong>lurane or sev<strong>of</strong>lurane. A circle<br />
system is used with ventilator support from <strong>the</strong> field Compac 220.<br />
Monitors are <strong>the</strong> Datex S5 with full invasive capability. There is<br />
equipment to perform regional or neuraxial blocks, intravenous<br />
warming, rapid infusion and patient warming.<br />
The space <strong>of</strong> <strong>the</strong> operating <strong>the</strong>atres is minimal and usually <strong>the</strong><br />
size <strong>of</strong> a standard anaes<strong>the</strong>tic room in UK hospitals. This makes<br />
teamwork and communication absolutely essential between all<br />
members <strong>of</strong> <strong>the</strong> <strong>the</strong>atre team, as sterility and free movement<br />
become problematic (Figure 5).<br />
Figure 5 The narrow operating <strong>the</strong>atre on board RFA Fort Victoria<br />
Room ventilation in <strong>the</strong>atre is <strong>of</strong>ten on a shared, partially closed<br />
circuit with o<strong>the</strong>r compartments <strong>of</strong> <strong>the</strong> ship. It is unlikely to meet<br />
<strong>the</strong> standards <strong>of</strong> a modern orthopaedic <strong>the</strong>atre. Scavenging <strong>of</strong><br />
vapours can be done using a Cardiff Aldasorber, although with <strong>the</strong><br />
current scale <strong>of</strong> equipment it is impossible to scavenge and utilise<br />
PEEP at <strong>the</strong> same time. If nitrous oxide is used, <strong>the</strong> quantities<br />
which could build-up in <strong>the</strong>atre are unknown. Total intravenous<br />
anaes<strong>the</strong>sia could be used but <strong>the</strong> pumps on scale do not have<br />
target-controlled infusion capability.<br />
Re-sterilisation <strong>of</strong> anaes<strong>the</strong>tic and surgical instruments is<br />
an essential component <strong>of</strong> afloat anaes<strong>the</strong>sia and surgery. The<br />
steriliser used on board all ships is <strong>the</strong> Portoclave Field Steriliser<br />
which has now become obsolete. Future sterilisation should be<br />
delivered on board as a separate module covering all equipment<br />
needed for decontamination, disinfection and sterilisation.<br />
Post-Operative<br />
Post-operative care is delivered within <strong>the</strong> same constraints<br />
as pre- and peri-operative care. Low dependency patients are<br />
likely be nursed in <strong>the</strong> bottom bunks <strong>of</strong> standard mess deck<br />
accommodation, appropriated as a ward area. Such bunks are<br />
fixed and accessible from only one side. They have limited (or<br />
no 230V) power sockets and securing ancillary equipment<br />
(monitors, infusion pumps, oxygen cylinders or concentrators<br />
and even drips) is challenging. As standard sea-going berths<br />
<strong>the</strong>y do provide lee-cloths and straps to secure <strong>the</strong> occupant<br />
in <strong>the</strong> event <strong>of</strong> heavy wea<strong>the</strong>r. Access to toilet, sluice and<br />
washing facilities may also be less than optimal, raising issues<br />
<strong>of</strong> infection control.<br />
Higher dependency patients will require nursing in <strong>the</strong> critical<br />
care area. A limited number <strong>of</strong> standard hospital beds, with 360°<br />
access, are available as part <strong>of</strong> <strong>the</strong> Role 2 Afloat. These beds have<br />
to be secured to <strong>the</strong> deck and ideally secondary securing points<br />
should be available in <strong>the</strong> event that <strong>the</strong> bed has to be moved<br />
or re-angled (for example to facilitate access for re-intubation)<br />
(Figure 6). The scope and quality <strong>of</strong> <strong>the</strong> critical care capability in<br />
Role 2 Afloat is limited by <strong>the</strong> nature <strong>of</strong> <strong>the</strong> equipment and stores<br />
held and <strong>the</strong> fragility <strong>of</strong> <strong>the</strong> resupply chain.<br />
Figure 6 Critical care beds in RFA Fort Victoria<br />
The medical mission for any military operation is to<br />
contribute to <strong>the</strong> physical and moral wellbeing <strong>of</strong> <strong>the</strong> force<br />
deployed, in part through <strong>the</strong> timely treatment and evacuation<br />
<strong>of</strong> <strong>the</strong> sick and injured. Currently accepted clinical timelines for<br />
treatment are as follows [1]:<br />
1 hour from point <strong>of</strong> wounding to advanced resuscitation<br />
2 hours to damage control surgery<br />
4 hours to primary surgery<br />
Role 2 is configured to meet <strong>the</strong> requirement for damage control<br />
surgery. Primary surgery requires onward transfer to a Role 3<br />
facility at sea (RFA ARGUS) or ashore (foreign hospital) or to a<br />
Role 4 facility in <strong>the</strong> UK. These doctrinal timelines for casualty<br />
treatment may not be met at sea. An incident may occur remotely<br />
from <strong>the</strong> ship and <strong>the</strong> subsequent transit will delay receipt <strong>of</strong> Role<br />
2 care. Once on board, <strong>the</strong>re may be an extended timeline to<br />
reach <strong>the</strong> nearest Role 3 facility.<br />
There are many locations where <strong>the</strong> local hospital will not be<br />
able to provide <strong>the</strong> level <strong>of</strong> care that can be delivered by <strong>the</strong> Role 2<br />
Afloat team. Under <strong>the</strong>se circumstances it may be in <strong>the</strong> patient’s<br />
best interest to be held for longer at <strong>the</strong> Role 2 facility, whilst<br />
direct liaison takes place with <strong>the</strong> Critical Care Aeromedical<br />
Support Team (CCAST) to arrange transfer directly to UK Role<br />
4. However, <strong>the</strong> holding capacity and endurance <strong>of</strong> <strong>the</strong> Role 2<br />
Afloat is limited by <strong>the</strong> number <strong>of</strong> medical and nursing personnel<br />
embarked, <strong>the</strong> number <strong>of</strong> beds, <strong>the</strong> space available and <strong>the</strong><br />
quantity <strong>of</strong> stores held.<br />
Where an appropriate Role 3 facility has been identified, <strong>the</strong><br />
successful transfer <strong>of</strong> a patient can still be delayed due to <strong>the</strong><br />
sea state, an unserviceable helicopter or <strong>the</strong> distance <strong>of</strong> <strong>the</strong> ship<br />
from <strong>the</strong> facility.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S349–352 351
Maritime <strong>Anaes<strong>the</strong>sia</strong><br />
Patient Transfer<br />
<strong>Medical</strong> evacuation (medevac) is <strong>the</strong> process <strong>of</strong> moving patients<br />
between medical facilities. For maritime operations this transfer<br />
may be conducted by boat or helicopter. In <strong>the</strong> latter case it is<br />
more properly known as aeromedical evacuation (AE). Transfer<br />
to Role 3 or Role 4 facilities will usually be by AE. The <strong>Royal</strong> Air<br />
Force (RAF) is <strong>the</strong> UK lead service for AE. As a consequence,<br />
<strong>the</strong> <strong>Royal</strong> Navy has no bespoke maritime AE capability. However,<br />
since it is frequently inappropriate to fly <strong>the</strong> RAF transfer team<br />
out to maritime platforms on operations, it is accepted that <strong>the</strong><br />
Role 2 Afloat will generate its own transfer capability, including<br />
transfer ashore <strong>of</strong> critically ill patients, from within its own<br />
organic assets (Figure 7).<br />
Figure 7 Casualty being prepared for transfer on board RFA Fort<br />
Victoria<br />
352<br />
RM Heames, JE Risdall<br />
Although no RN personnel are currently trained to undertake<br />
CCAST, RN anaes<strong>the</strong>tists, intensivists and intensive care<br />
nurses are all experienced in patient transfer. In <strong>the</strong> absence <strong>of</strong><br />
a bespoke critical care transfer module, equipment for patient<br />
transfer has to be drawn from that available to <strong>the</strong> Role 2 Afloat<br />
which is unlikely to have been tested for aeromedical use in<br />
<strong>the</strong> airframe available. In removing equipment for transfer,<br />
<strong>the</strong> Role 2 capability is potentially reduced. The equipment<br />
available is not <strong>the</strong> most suitable for use in transfer, particularly<br />
with regard to portability (weight) and battery life (endurance).<br />
It is also unlikely to be directly compatible with that brought<br />
out by <strong>the</strong> CCAST team.<br />
Conclusion<br />
<strong>Anaes<strong>the</strong>sia</strong> in a maritime environment differs in many ways from<br />
that on land. The concept <strong>of</strong> operations has to remain totally<br />
flexible. Personnel and equipment may well change with <strong>the</strong><br />
differing platforms used, <strong>the</strong> operational area and <strong>the</strong> task group<br />
mission. At maritime Role 2, <strong>the</strong> anaes<strong>the</strong>tist will be involved<br />
in all aspects <strong>of</strong> patient care from retrieval and triage, through<br />
<strong>the</strong>atres and critical care to transfer to a Role 3 facility. Specialist<br />
knowledge <strong>of</strong> underwater medicine may also be required and <strong>the</strong><br />
anaes<strong>the</strong>tist has to be in date for fire fighting, damage control<br />
and sea survival. This makes <strong>the</strong> job <strong>of</strong> an anaes<strong>the</strong>tist at sea a<br />
challenging and rewarding one.<br />
Reference<br />
1. 1. JDP 4-30 2nd Ed <strong>Medical</strong> Support to Joint Operations<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S349–352
Challenges for <strong>the</strong> Future
Creating Airway Management Guidelines for<br />
Casualties with Penetrating Airway Injuries<br />
SJ Mercer 1 , SE Lewis 2 , SJ Wilson 3 , P Groom 4 , PF Mahoney 5 ,<br />
1 Specialist Registrar in <strong>Anaes<strong>the</strong>sia</strong> & Critical Care, University Hospital Aintree NHS Foundation Trust, Merseyside;<br />
2 Specialist Registrar in <strong>Anaes<strong>the</strong>sia</strong> & Critical Care, St George’s Healthcare NHS Trust, London; 3 Consultant<br />
Anaes<strong>the</strong>tist, James Paget University Hospital Foundation NHS Trust, Great Yarmouth; 4 Consultant Anaes<strong>the</strong>tist,<br />
University Hospital Aintree NHS Foundation Trust, Merseyside; 5 <strong>Defence</strong> Pr<strong>of</strong>essor <strong>Anaes<strong>the</strong>sia</strong> and Critical Care,<br />
<strong>Royal</strong> Centre for <strong>Defence</strong> Medicine Birmingham Research Park, Vincent Drive, Birmingham<br />
Abstract<br />
Anaes<strong>the</strong>tists in <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services (DMS) are currently dealing with casualties who have an increased prevalence<br />
<strong>of</strong> injuries due to blast, fragmentation and gunshot wounds. Despite guidelines already existing for unanticipated difficult<br />
tracheal intubation <strong>the</strong>se have been designed for a civilian population and might not be relevant for <strong>the</strong> anticipated difficult<br />
airway experienced in <strong>the</strong> deployed field hospital. In order to establish an overview <strong>of</strong> current practice, three methods <strong>of</strong><br />
investigation were undertaken; a literature review, a survey <strong>of</strong> DMS Anaes<strong>the</strong>tists and a search <strong>of</strong> <strong>the</strong> UK Joint Theatre Trauma<br />
Database. Results are discussed in terms <strong>of</strong> anatomical site, bleeding in <strong>the</strong> airway, facial distortion, patient positioning and an<br />
anaes<strong>the</strong>tic approach. There are certain key principles that should be considered in all cases and <strong>the</strong>se are considered. Potential<br />
pitfalls are discussed and our initial proposed guidelines for use in <strong>the</strong> deployed field hospital are presented.<br />
Introduction<br />
Combat trauma airway management is distinctive because <strong>of</strong><br />
<strong>the</strong> increased prevalence <strong>of</strong> penetrating airway injuries [1]. The<br />
majority <strong>of</strong> UK military deployed trauma consists <strong>of</strong> blast/<br />
fragmentation injuries (53.8%) and gunshot wounds (GSW)<br />
(29.9%), in contrast to National Health Service (NHS) trauma<br />
where <strong>the</strong> bulk is blunt airway injury due to motor vehicle<br />
collisions [2]. Penetrating injuries are <strong>of</strong>ten dramatic with severe<br />
disruption <strong>of</strong> both s<strong>of</strong>t tissue and bone [3], and airway injury is<br />
likely in ballistic and penetrating injury to <strong>the</strong> face and neck. The<br />
proximity <strong>of</strong> <strong>the</strong> carotid vessels means that penetrating carotid<br />
injury may impact airway patency. Consequently <strong>the</strong> team dealing<br />
with such injuries need to consider <strong>the</strong> likely fragment /projectile<br />
trajectory and potential airway effects.<br />
UK <strong>Defence</strong> <strong>Medical</strong> Services (DMS) anaes<strong>the</strong>tists spend<br />
<strong>the</strong> majority <strong>of</strong> <strong>the</strong>ir clinical practice working with civilian<br />
patients in <strong>the</strong> NHS and will generally deploy on military<br />
operations every six to 18 months. Not only does <strong>the</strong> deployed<br />
environment have a different case mix, but clinicians are also<br />
required to use what may be unfamiliar equipment and Standard<br />
Operating Procedures (SOPs). SOP’s have been developed for<br />
management <strong>of</strong> <strong>the</strong> difficult airway by <strong>the</strong> American Society <strong>of</strong><br />
Anes<strong>the</strong>siologists (ASA) [4], and for <strong>the</strong> unanticipated difficult<br />
airway by <strong>the</strong> Difficult Airway Society (DAS) [5]. Both protocols<br />
were designed to deal with a civilian patient population in <strong>the</strong><br />
setting <strong>of</strong> a general hospital and do not reflect <strong>the</strong> circumstances<br />
currently encountered in <strong>the</strong> deployed military environment.<br />
Although <strong>the</strong> management <strong>of</strong> anticipated difficult airway has<br />
recently been evaluated to some extent in a civilian setting [6], we<br />
felt <strong>the</strong> unusual nature <strong>of</strong> penetrating airway injury necessitated<br />
its own SOP for use in <strong>the</strong> deployed field hospital. It is hoped that<br />
this will allow anaes<strong>the</strong>tists to improve <strong>the</strong>ir non-technical skills<br />
Corresponding Author: Surgeon Lieutenant Commander<br />
Simon J Mercer <strong>Royal</strong> Navy, 22 The Knowles, Blundellsands<br />
Road West, Crosby, Liverpool, L23 6AB.<br />
Mobile number: 07970153168. Email: simonjmercer@hotmail.com<br />
or human factors [7] in a clinical environment that has recently<br />
be identified as exceptional by <strong>the</strong> Healthcare Commission [8].<br />
There is a lack <strong>of</strong> literature reporting <strong>the</strong> anaes<strong>the</strong>tic<br />
management <strong>of</strong> penetrating neck injuries [9,10] with manuscripts<br />
<strong>of</strong>ten concentrating on surgical management [11]. Currently,<br />
<strong>the</strong>re is no consensus amongst <strong>the</strong> anaes<strong>the</strong>tic community on<br />
<strong>the</strong> management <strong>of</strong> casualties with penetrating airway injuries<br />
[12] and much variability has been described [11]. We reviewed<br />
<strong>the</strong> current literature, <strong>the</strong> experience <strong>of</strong> previously deployed UK<br />
DMS anaes<strong>the</strong>tists as well as documented experience from <strong>the</strong><br />
UK Joint Theatre Trauma Registry (JTTR) [2] and present our<br />
initial guidelines.<br />
Methods<br />
In order to establish a complete overview <strong>of</strong> current practice, three<br />
separate methods <strong>of</strong> investigation were undertaken.<br />
Literature Review<br />
The databases and search terms used to identify papers published<br />
after 1995 are summarized in Table 1. Two <strong>of</strong> <strong>the</strong> authors (SEL/<br />
SJM) evaluated each paper for relevance to <strong>the</strong> anaes<strong>the</strong>tic<br />
management <strong>of</strong> penetrating head and neck injuries and<br />
summarized any case reports.<br />
Survey <strong>of</strong> DMS Anaes<strong>the</strong>tists<br />
All 185 DMS Anaes<strong>the</strong>tists whose details were held on <strong>the</strong><br />
<strong>Defence</strong> Consultant Advisor (DCA) database were contacted by<br />
e-mail on 23 November 2009. The details <strong>of</strong> any cases <strong>of</strong> blast or<br />
ballistic airway injury that <strong>the</strong>y had treated were requested. This<br />
email was repeated on 23 January 2010. All cases were collated in<br />
tabular form.<br />
Search <strong>of</strong> <strong>the</strong> UK Joint Theatre Trauma Registry (JTTR)<br />
The UK JTTR has already been described in this journal [13]<br />
and is maintained by <strong>the</strong> Academic Department <strong>of</strong> Military<br />
Emergency Medicine at <strong>the</strong> <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine.<br />
Essentially this registry contains continuous data from 2003 for<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S355–360 355
Guidelines for Penetrating Airway Injuries<br />
Database Search Terms<br />
Pubmed [14]<br />
Sciencedirect [15]<br />
Google Scholar[16]<br />
AMED<br />
BNI<br />
EMBASE<br />
HMIC<br />
MEDLINE<br />
PsycINFO<br />
CINAHL<br />
HEALTH BUSINESS ELITE<br />
Table 1. Literature Search Terms<br />
all casualties who trigger a trauma team activation in ei<strong>the</strong>r <strong>the</strong><br />
deployed field hospital or <strong>the</strong> Primary Casualty Receiving Facility<br />
afloat. Over 3000 records were interrogated for <strong>the</strong> search terms<br />
listed in Table 2. Cases identified by this search were analyzed by<br />
one <strong>of</strong> <strong>the</strong> authors (SJM) and those consisting <strong>of</strong> casualties with<br />
blast and ballistic head and neck trauma were recorded.<br />
Search Term<br />
Casualty Reference Numbers<br />
Gender<br />
Major Trauma<br />
UK Military<br />
Survivors<br />
Blast Injury or Ballistic Injury<br />
New Injury Severity Score (NISS) >16<br />
Airway Interventions<br />
Mechanism <strong>of</strong> Injury<br />
Brief Incident History<br />
Injuries<br />
Information from free text boxes.<br />
Table 2. Search terms used to identify cases in JTTR<br />
Results<br />
The literature review revealed 51 papers that were considered<br />
relevant to this study; 23 were civilian case reports and three<br />
contained military case reports. There were 17 case reports<br />
submitted by DMS Anaes<strong>the</strong>tists and <strong>the</strong> cause <strong>of</strong> injury in all<br />
cases was ei<strong>the</strong>r GSW or Improvised Explosive Device (IED).<br />
Over 3000 were searched on <strong>the</strong> JTTR and 19 were identified<br />
<strong>of</strong> soldiers with penetrating head and neck injury. These injuries<br />
were ei<strong>the</strong>r caused by blast (from IED, mine, mortar or rocket<br />
propelled grenade) or were due to GSW. Common <strong>the</strong>mes from<br />
all three areas <strong>of</strong> investigation are summarized in headings below.<br />
356<br />
Ballistic airway<br />
Blast airway<br />
Penetrating airway<br />
Laceration airway<br />
Fragmentation airway<br />
Gunshot airway<br />
Knife airway.<br />
Ballistic-airway<br />
Ballistic AND airway<br />
Blast-airway<br />
Blast AND airway<br />
Penetrating-airway<br />
Penetrating AND airway<br />
Laceration-airway<br />
Laceration AND airway<br />
Fragmentation-airway<br />
Fragmentation AND airway<br />
Gunshot AND airway<br />
Knife AND airway<br />
SJ Mercer, SE Lewis, SJ Wilson et al<br />
Penetrating injury though <strong>the</strong> mouth<br />
Case reports included projectiles or objects transfixing facial<br />
structures and interfering with mouth opening. Examples<br />
included transfixion through <strong>the</strong> floor <strong>of</strong> <strong>the</strong> mouth with a<br />
bamboo cane [17], penetration <strong>of</strong> <strong>the</strong> mouth floor with a nail<br />
[18], a spear gun shaft penetrating <strong>the</strong> floor <strong>of</strong> <strong>the</strong> mouth [19] and<br />
a crossbow arrow entering under <strong>the</strong> chin and passing through <strong>the</strong><br />
tongue, nasal cavity and between <strong>the</strong> frontal lobes [20]. Methods<br />
<strong>of</strong> management included awake fibreoptic intubation (AFOI)<br />
[17-20] rapid sequence induction <strong>of</strong> anaes<strong>the</strong>sia (RSI) [22,23]<br />
and surgical tracheostomy following failure <strong>of</strong> AFOI [19].<br />
Injuries to <strong>the</strong> Face<br />
Two articles summarized case series <strong>of</strong> GSW to <strong>the</strong> face from<br />
Level 1 Trauma Centres in <strong>the</strong> USA [23] and South Africa [24].<br />
Of 73 patients in <strong>the</strong> USA case series, 36 underwent AFOI, 30<br />
were conventionally intubated and seven had a cricothyroidotomy<br />
performed. In <strong>the</strong> South African case series <strong>the</strong>re were 28<br />
emergency orotracheal intubations (18 <strong>of</strong> which were performed<br />
in <strong>the</strong> prehospital phase), two cricothyroidotomies and six<br />
tracheostomies. The DMS survey revealed five case reports<br />
<strong>of</strong> soldiers with facial injuries as a result <strong>of</strong> IED blasts and<br />
four <strong>of</strong> <strong>the</strong>se underwent uneventful RSI (one had a surgical<br />
tracheostomy performed in <strong>the</strong> prehospital phase). There were<br />
4 case reports <strong>of</strong> GSW to <strong>the</strong> face <strong>of</strong> which two had RSI, one<br />
had a cricothyroidotomy and <strong>the</strong> o<strong>the</strong>r had an emergency surgical<br />
tracheostomy. The JTTR search contained three casualties who<br />
had undergone blast injuries to <strong>the</strong> face, two <strong>of</strong> which were<br />
managed by RSI and one who underwent cricothyroidotomy in<br />
<strong>the</strong> prehospital phase.<br />
Laceration to <strong>the</strong> neck<br />
There were several case reports <strong>of</strong> isolated neck laceration<br />
injuries [25,26] and an open laryngeal injury in a patient with<br />
multiple injuries [27]. Management included a pre-hospital<br />
cricothyroidotomy [27], surgical tracheostomy [25] and intubation<br />
directly though <strong>the</strong> defect [26,27]. There was a case report<br />
concerning a crush injury to <strong>the</strong> chest resulting in complete tracheal<br />
transection. This was managed with a surgical tracheostomy as<br />
<strong>the</strong> patient developed subcutaneous emphysema in <strong>the</strong> neck and<br />
anterior chest following orotracheal intubation [28].<br />
Penetrating Neck Injuries<br />
Case reports included a bullet fragment in <strong>the</strong> supraglottic region<br />
[29] and GSWs [30-32] to <strong>the</strong> neck. These were managed by<br />
orotracheal intubation [30], inhalational induction <strong>of</strong> anaes<strong>the</strong>sia<br />
[31], flexible bronchoscopy [32] and use <strong>of</strong> a light wand following<br />
failure <strong>of</strong> direct laryngoscopy [29]. Case series <strong>of</strong> penetrating neck<br />
injuries from US Trauma Centres [33,34] reported a combination<br />
<strong>of</strong> techniques including RSI, surgical tracheostomy, AFOI and<br />
orotracheal intubation without paralysis in comatose patients. A<br />
Canadian case series [11] also reported <strong>the</strong> use <strong>of</strong> AFOI and RSI.<br />
Ano<strong>the</strong>r case series from a Level 1 Trauma Centre in <strong>the</strong> USA [35]<br />
reviewed <strong>the</strong> airway management <strong>of</strong> 89 patients with penetrating<br />
neck injuries who had undergone blind nasal intubation. The<br />
authors concluded that this technique was a valuable tool for<br />
<strong>the</strong> management <strong>of</strong> patients with penetrating neck trauma.<br />
There were three case reports in <strong>the</strong> literature <strong>of</strong> soldiers who<br />
sustained penetrating neck injuries as a result <strong>of</strong> improvised<br />
explosive devices (IEDs). Management included emergency<br />
cricothyroidotomy following failed orotracheal intubation [36],<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S355–360
Guidelines for Penetrating Airway Injuries SJ Mercer, SE Lewis, SJ Wilson et al<br />
surgical tracheostomy in <strong>the</strong> operating <strong>the</strong>atre following failed<br />
orotracheal intubation [37] and orotracheal intubation followed<br />
by surgical tracheostomy [38].<br />
The DMS survey reported several cases <strong>of</strong> penetrating neck<br />
injury <strong>the</strong>se included:<br />
• A GSW causing damage to <strong>the</strong> posterior tracheal wall associated<br />
with bleeding into <strong>the</strong> airway, managed with a RSI.<br />
• An IED blast to <strong>the</strong> face and neck, managed by transferring<br />
<strong>the</strong> patient to <strong>the</strong>atre in <strong>the</strong> prone position to maintain <strong>the</strong>ir<br />
airway. RSI was performed as soon as <strong>the</strong> patient was turned<br />
supine. A trauma surgeon was ready to perform a surgical<br />
airway if needed.<br />
• A penetrating neck injury, managed by orotracheal intubation<br />
following gaseous induction using <strong>the</strong> Tri-service Anaes<strong>the</strong>tic<br />
Apparatus [39] with two Oxford Miniature Vaporizers filled<br />
with Sev<strong>of</strong>lurane.<br />
• A GSW through <strong>the</strong> larynx was managed by direct<br />
intubation through <strong>the</strong> defect and <strong>the</strong>n a subsequent surgical<br />
tracheostomy. A GSW injury disrupting <strong>the</strong> cricoid ring was<br />
managed with RSI.<br />
Results from <strong>the</strong> JTTR included four cases <strong>of</strong> penetrating neck<br />
injury <strong>of</strong> which one was managed by RSI. In addition to this<br />
<strong>the</strong>re were seven case reports <strong>of</strong> injury to <strong>the</strong> trachea and larynx.<br />
Of <strong>the</strong>se, four patients underwent RSI, (one <strong>of</strong> which failed and<br />
required cricothyroidotomy), one received a primary surgical<br />
tracheostomy and one had an endotracheal tube placed directly<br />
through <strong>the</strong> tracheal defect.<br />
Carotid Artery Injury<br />
One case reported <strong>the</strong> use <strong>of</strong> AFOI to manage a penetrating neck<br />
injury tearing <strong>the</strong> common carotid artery that was causing a rapidly<br />
expanding haematoma [40]. Ano<strong>the</strong>r case report describing a<br />
patient with neck compression due to strangulation with a chain<br />
and this was managed by conventional orotracheal intubation [41].<br />
There was also a case report <strong>of</strong> a patient who sustained internal<br />
and external common arteries injuries following a laceration from<br />
a flying metal sheet, this was managed by intubation into <strong>the</strong><br />
perforation <strong>of</strong> larynx [42]. A case report from <strong>the</strong> DMS survey<br />
described a casualty with a GSW to <strong>the</strong> neck associated with a<br />
laceration to <strong>the</strong> carotid artery resulting in respiratory distress and<br />
this was managed by inhalational induction <strong>of</strong> anaes<strong>the</strong>sia. There<br />
were an additional three cases <strong>of</strong> penetrating neck injury on <strong>the</strong><br />
JTTR database (all as a result <strong>of</strong> IED blast) resulting in laceration<br />
<strong>of</strong> <strong>the</strong> carotid artery. Anaes<strong>the</strong>tic details were entered for only one<br />
<strong>of</strong> <strong>the</strong>se cases, which was managed with an RSI.<br />
Discussion<br />
There are multiple potential approaches to <strong>the</strong> airway management<br />
<strong>of</strong> casualties penetrating injuries [43] and although <strong>the</strong> incidence<br />
is low, we felt that it was important to develop guidelines to allow<br />
planning and anticipation <strong>of</strong> <strong>the</strong>se cases prior to deployment as<br />
an aide memoire. The anaes<strong>the</strong>tist may wish to base <strong>the</strong>ir decision<br />
making process on <strong>the</strong> clinical scenario ra<strong>the</strong>r than a preset algorithm<br />
taking into account <strong>the</strong>ir own skills and equipment available [11].<br />
It has already been commented that most case series only contain<br />
small numbers <strong>of</strong> patients and that <strong>the</strong> injuries are diverse, meaning<br />
a didactic treatment algorithm would be unhelpful [12]. Our three<br />
different methods <strong>of</strong> investigating <strong>the</strong> anaes<strong>the</strong>tic management <strong>of</strong><br />
penetrating airway injury resulted in a wide variety <strong>of</strong> opinions and<br />
our conclusions are enumerated below.<br />
The anatomical site <strong>of</strong> <strong>the</strong> injury<br />
This is a crucial consideration as penetrating neck wounds are best<br />
approached on a zonal basis [44]<br />
Zone I - between <strong>the</strong> clavicles and <strong>the</strong> cricoid cartilage.<br />
Zone II - between <strong>the</strong> inferior margin <strong>of</strong> <strong>the</strong> cricoid cartilage and<br />
<strong>the</strong> angle <strong>of</strong> <strong>the</strong> mandible<br />
Zone III - between <strong>the</strong> angle <strong>of</strong> <strong>the</strong> mandible and <strong>the</strong> base <strong>of</strong> <strong>the</strong><br />
skull.<br />
Reference to a zone allows <strong>the</strong> prediction <strong>of</strong> potential injuries<br />
and so <strong>the</strong> potential for urgent airway management problems<br />
[12]. It should be noted that wounds in <strong>the</strong> anterior and lateral<br />
aspects <strong>of</strong> <strong>the</strong> neck compromise <strong>the</strong> airway more <strong>of</strong>ten than those<br />
in <strong>the</strong> posterior region [12]. Once <strong>the</strong> zone(s) involved have<br />
been identified <strong>the</strong> clinician should <strong>the</strong>n consider <strong>the</strong> presence <strong>of</strong><br />
injury to <strong>the</strong> airway’s lumen (with associated blood and debris),<br />
injury within <strong>the</strong> airways wall itself or injury outside <strong>the</strong> wall<br />
(e.g. expanding haematoma or surgical emphysema). Optimal<br />
intubation conditions may be difficult to achieve and injuries may<br />
compromise positive pressure ventilation with bag-valve-mask<br />
devices [11]. Not all patients will be in extremis however and <strong>the</strong>re<br />
may be time to consider additional investigations to characterise<br />
<strong>the</strong> injury. CT is considered <strong>the</strong> first-line investigation in stable<br />
patients with penetrating neck injuries [45] to identify <strong>the</strong><br />
location, nature and extent <strong>of</strong> any airway injury.<br />
Airway bleeding/facial distortion and patient positioning<br />
Blood and debris may be soiling <strong>the</strong> airway and if <strong>the</strong> casualty<br />
is maintaining <strong>the</strong>ir airway satisfactorily <strong>the</strong>y do not require<br />
immediate airway intervention apart from a jaw thrust. They<br />
should be allowed to adopt <strong>the</strong>ir most comfortable position.<br />
Lateral, sitting and prone positions have all be described in case<br />
reports and <strong>the</strong> importance <strong>of</strong> this must be reinforced during<br />
patient handover.<br />
Anaes<strong>the</strong>tic approaches to penetrating airway injury<br />
The principle clinical features mandating early tracheal<br />
intubation are acute or worsening respiratory distress, an airway<br />
that is compromised by blood and secretions, extensive surgical<br />
emphysema, tracheal deviation by haematoma and a decreasing<br />
level <strong>of</strong> consciousness [46]. Although anaes<strong>the</strong>tists perform<br />
endotracheal intubation routinely, it should be approached with<br />
great caution in a patient with a penetrating airway injury [47].<br />
Direct Laryngoscopy/ Rapid Sequence Induction (RSI)<br />
It is important that anaes<strong>the</strong>tists are aware that despite <strong>the</strong><br />
laryngeal inlet appearing intact, <strong>the</strong>re may be a tracheal tear<br />
present below this and placing an endotracheal tube under direct<br />
laryngoscopic vision could lead to <strong>the</strong> tip passing through <strong>the</strong><br />
defect. This may go unrecognized and risks airway obstruction,<br />
pneumomediastinum and <strong>the</strong> creation <strong>of</strong> a false passage [47] as<br />
this is in effect a ‘blind technique’, which may completely disrupt<br />
<strong>the</strong> larynx. The incidence <strong>of</strong> <strong>the</strong>se phenomena is unknown but is<br />
most likely lethal and difficult to reverse even with an emergency<br />
surgical airway (especially if gross surgical emphysema has been<br />
created) [12]. O<strong>the</strong>rs recommend an ‘awake look’ under topical<br />
anaes<strong>the</strong>sia but this will obviously not indicate if <strong>the</strong>re are any<br />
injuries distal to <strong>the</strong> vocal cords [11].<br />
Some authors hold that RSI should be <strong>the</strong> default method <strong>of</strong><br />
airway control [48]. Evidence is available to suggest that it is safe<br />
[49] and has a high success rate [33,34,50]. Despite this, <strong>the</strong>re are<br />
o<strong>the</strong>rs who argue against RSI in certain cases [36,37], where <strong>the</strong><br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S355–360 357
Guidelines for Penetrating Airway Injuries<br />
airway is penetrated below <strong>the</strong> vocal cords (risking unrecognized<br />
misplacement <strong>of</strong> <strong>the</strong> ETT). It is also not recommended in cases<br />
<strong>of</strong> near or total airway transection, where paralysis will abolish <strong>the</strong><br />
supportive muscle tone, which may be all that is holding <strong>the</strong> airway<br />
toge<strong>the</strong>r [11,51]. For <strong>the</strong>se reasons, some authors actively support<br />
<strong>the</strong> casualty maintaining spontaneous ventilation at all costs [47].<br />
Current UK anaes<strong>the</strong>tic practice includes <strong>the</strong> use <strong>of</strong> cricoid pressure<br />
[52] during an RSI but this may distort <strong>the</strong> airway, change <strong>the</strong><br />
anaes<strong>the</strong>tist’s view and result in a more difficult airway [47,53].<br />
Blind Nasal Intubation<br />
The consensus <strong>of</strong> opinion is that blind intubation methods<br />
including blind nasotracheal intubation should not be used in<br />
patients with penetrating neck injury because fur<strong>the</strong>r injury or<br />
complete airway obstruction may be induced [54]. A single paper<br />
reviewing a case series <strong>of</strong> patients successfully managed with blind<br />
nasotracheal intubation has challenged this advice [35]. As this<br />
technique is rarely taught in UK hospitals, we would discourage its<br />
use by clinicians for whom it is not part <strong>of</strong> <strong>the</strong>ir regular practice. It<br />
also requires extension at <strong>of</strong> <strong>the</strong> upper cervical spine while <strong>the</strong> lower<br />
cervical spine is extended, as part <strong>of</strong> <strong>the</strong> technique, which may risk<br />
neurological injury in <strong>the</strong> unstable cervical spine in trauma.<br />
Fiberoptic Intubation<br />
AFOI is <strong>the</strong> gold standard for safely securing <strong>the</strong> airway in a<br />
casualty with a traumatic airway injury. This technique allows <strong>the</strong><br />
lumen <strong>of</strong> <strong>the</strong> airway to be identified by direct vision throughout <strong>the</strong><br />
intubating process and allows <strong>the</strong> anaes<strong>the</strong>tist to be confident about<br />
siting <strong>the</strong> endotracheal tube (ETT) distal to any visualized tear.<br />
This technique depends on availability <strong>of</strong> a fiberscope, <strong>the</strong> cooperation<br />
<strong>of</strong> <strong>the</strong> patient [47,55] and <strong>the</strong> skills <strong>of</strong> <strong>the</strong> operator.<br />
Ano<strong>the</strong>r confounding factor to this method <strong>of</strong> securing <strong>the</strong><br />
airway is that any foreign bodies or blood will hinder <strong>the</strong> use<br />
<strong>of</strong> <strong>the</strong> fiberscope [47] although in skilled hands it has proved<br />
very effective [17-20, 23,24,40]. Difficulties regarding AFOI<br />
in <strong>the</strong> field hospital also arise from <strong>the</strong> sterilization aspect <strong>of</strong><br />
<strong>the</strong> fiberscope, however recently disposable versions have been<br />
developed, but are yet to be evaluated in this setting.<br />
Surgical Airway<br />
A case could be made to consider surgical airway as <strong>the</strong> first choice<br />
intervention for laryngeal injuries [47,56] as it is done under<br />
direct vision reducing <strong>the</strong> potential for worsening an injury by<br />
misplacement <strong>the</strong> endotracheal tube. Both cricothyroidotomy<br />
and tracheostomy have been described as safe techniques to<br />
perform in an awake, spontaneously ventilating patient with local<br />
anaes<strong>the</strong>tic infiltration [47]. Cricothyroidotomy itself has fur<strong>the</strong>r<br />
been described as a safe, rapid technique <strong>of</strong> obtaining an airway<br />
in an emergency setting [57]. Tracheostomy should be performed<br />
at least one tracheal ring below <strong>the</strong> injury to avoid complications<br />
[12]. Whenever a difficult intubation is suspected it is advisable to<br />
have <strong>the</strong> patient’s neck prepared and <strong>the</strong> surgeon ready to perform<br />
a surgical airway [47]. The anaes<strong>the</strong>tist should be mindful that<br />
<strong>the</strong> rapid creation <strong>of</strong> a surgical airway might be a difficult task for<br />
<strong>the</strong> surgeon, particularly if <strong>the</strong>re is overlying haematoma or o<strong>the</strong>r<br />
gross anatomical disruption.<br />
Recommendations<br />
Despite <strong>the</strong> variety <strong>of</strong> anaes<strong>the</strong>tic management strategies present<br />
in <strong>the</strong> literature, <strong>the</strong>re are certain key principles we believe should<br />
be considered in all cases. These are listed in Table 3. Human<br />
358<br />
SJ Mercer, SE Lewis, SJ Wilson et al<br />
factors play an important role in ensuring that individuals in a<br />
clinical team perform to <strong>the</strong> highest standard [58]. We believe<br />
that <strong>the</strong> principles <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong> Crisis Resource Management<br />
(ACRM) [59] are crucial to ensuring <strong>the</strong> best possible outcome<br />
when faced with a patient with severe blast or ballistic injuries.<br />
Monitor patient with full AAGBI standard monitoring<br />
[60] (especially ETCO 2 )<br />
Preoxygenation (even in patients with marginal functional<br />
reserve [43,47,54])<br />
Airway optimization<br />
• If conscious allow patient to adopt<br />
most comfortable position [46].<br />
• If unconscious use jaw thrust<br />
Consider <strong>the</strong> urgency with which a secure airway is<br />
required<br />
Consider <strong>the</strong> site <strong>of</strong> injury<br />
Availability <strong>of</strong> suction (preferably two devices)<br />
Table 3. Key principles to consider for all casualties with a penetrating<br />
airway injury<br />
Potential Pitfalls<br />
The literature review and DMS Anaes<strong>the</strong>tists experience and<br />
JTTR search have enabled us to suggest certain pitfalls when<br />
dealing with patients with penetrating airway injuries. These<br />
should be considered when constructing a plan <strong>of</strong> securing <strong>the</strong><br />
airway and are listed in Table 4.<br />
Ventilation: Positive pressure ventilation risks enlarging tears<br />
and causing surgical emphysema<br />
• Try to preserve spontaneous ventilation prior to<br />
intubation<br />
• Use bag-valve-mask ventilation is a last resort<br />
• Avoid LMA in injuries distal to cords<br />
• Avoid transtracheal jet ventilation<br />
Intubation: Blind placement <strong>of</strong> <strong>the</strong> tube risks <strong>the</strong> tip<br />
passing through <strong>the</strong> defect and lying outside <strong>the</strong> airway<br />
and is only avoided by fibreoptic intubation or a surgical<br />
airway.<br />
Intubation: Endotracheal intubation should be<br />
approached with caution<br />
• Avoid oral intubation when <strong>the</strong> injury is distal to <strong>the</strong><br />
vocal cords<br />
• Avoid blind nasal intubation<br />
• Fibreoptic intubation is likely to be difficult/<br />
impossible when <strong>the</strong>re is bleeding into <strong>the</strong> airway<br />
Surgical Airway<br />
• Is potentially extremely difficult in face <strong>of</strong> subcutaneous<br />
emphysema or an expanding haematoma (direct<br />
laryngoscopy is also likely to also be difficult).<br />
Drugs: Avoid muscle relaxants in near/complete airway<br />
transection<br />
• Muscle tone may be important for airway integrity<br />
Table 4 Potential Pitfalls to consider when drawing up plans to secure<br />
<strong>the</strong> airway.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S355–360
Guidelines for Penetrating Airway Injuries SJ Mercer, SE Lewis, SJ Wilson et al<br />
In proposing initial guidelines for DMS anaes<strong>the</strong>tists, we have<br />
been strongly influenced by <strong>the</strong> comments made in <strong>the</strong> review<br />
article by Abernathy [47] regarding <strong>the</strong> placing <strong>of</strong> an endotracheal<br />
tube when a distal airway injury has not been excluded. In such<br />
cases a primary surgical airway may be <strong>the</strong> most appropriate plan<br />
[43]. Whe<strong>the</strong>r it is <strong>the</strong> anaes<strong>the</strong>tist or <strong>the</strong> trauma surgeon who<br />
performs this will be decided by <strong>the</strong> skills and experience <strong>of</strong> <strong>the</strong><br />
individuals within <strong>the</strong> team.<br />
Our initial guidelines based on site <strong>of</strong> injury are summarized<br />
in Table 5. We anticipate that this preliminary work will now<br />
lead to fur<strong>the</strong>r studies to develop guidelines and training systems.<br />
We also hope to work with national bodies such as <strong>the</strong> Difficult<br />
Airway Society to fur<strong>the</strong>r develop our guidelines.<br />
Zone I injury<br />
• Consider direct intubation through a large defect<br />
• Consider tracheostomy<br />
• Consider a thoracotomy in complete tracheal<br />
transection [62]<br />
Zone II injury<br />
• Consider a CT scan to exclude distal airway injury<br />
• (Provided that <strong>the</strong>re is no immediate impending<br />
obstruction <strong>of</strong> <strong>the</strong> airway).<br />
• Consider oral intubation by RSI for injuries proximal<br />
to <strong>the</strong> larynx<br />
• Consider fibreoptic intubation for injuries distal to <strong>the</strong><br />
larynx<br />
• Consider a surgical airway for injuries distal to <strong>the</strong><br />
larynx<br />
Zone III injury<br />
• Consider oral intubation by RSI for small defects<br />
• Consider surgical airway for gross disruption.<br />
For any large airway defect<br />
• Consider direct intubation through <strong>the</strong> defect<br />
Table 5 Suggested Guidelines for <strong>the</strong> Airway Management <strong>of</strong><br />
Penetrating Airway Injury<br />
Acknowledgements<br />
The authors would like to thank Major Suzi Robinson QARANC<br />
and her team at <strong>the</strong> <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine for <strong>the</strong>ir<br />
help performing <strong>the</strong> search <strong>of</strong> <strong>the</strong> Joint Theatre Trauma Database<br />
and Mr. Michael Rowe, <strong>Defence</strong> Librarian for his help with <strong>the</strong><br />
Literature Search.<br />
References<br />
1. Adams BD, Cuniowski PA, Muck A, De Lorenzo RA. Registry <strong>of</strong><br />
Emergency Airways Arriving at Combat Hospitals. J Trauma 2008;<br />
64:1548–1554.<br />
2. Hodgetts TJ, Davies S, Russell R, McLeod J. Benchmarking <strong>the</strong><br />
UK Military Deployed Trauma System. JR <strong>Army</strong> Med <strong>Corps</strong> 2007;<br />
153: 237-238<br />
3. Pandit JJ, Popat M. Difficult Airway Management in Maxill<strong>of</strong>acial<br />
Trauma. Semin Anesth Perio M 2001; 20: 144-153<br />
4. An Updated Report by <strong>the</strong> American Society <strong>of</strong> Anes<strong>the</strong>siologists<br />
Task Force on Management <strong>of</strong> <strong>the</strong> Difficult Airway. Practice<br />
Guidelines for Management <strong>of</strong> <strong>the</strong> Difficult Airway. Anes<strong>the</strong>siology<br />
2003; 98:1269-77<br />
5. Henderson JJ, Popat MT, Latto PI, Pearce AC. Difficult Airway<br />
Society Guidelines for Management <strong>of</strong> <strong>the</strong> Unanticipated Difficult<br />
Intubation. <strong>Anaes<strong>the</strong>sia</strong> 2004; 59: 675–94.<br />
6. Aintree Difficult Airway Management. Available at: http://adam.<br />
liv.ac.uk [accessed 8 June 2010]<br />
7. Mercer SJ, Whittle CL, Mahoney PF. Human Factors in <strong>Defence</strong><br />
<strong>Anaes<strong>the</strong>sia</strong> – Lessons from <strong>the</strong> Battlefield. Br J Anaesth 2010 105:<br />
9-20<br />
8. Health Care Commission. <strong>Defence</strong> <strong>Medical</strong> Services : A Review <strong>of</strong><br />
<strong>the</strong> Clinical Governance <strong>of</strong> <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services in <strong>the</strong> UK<br />
and Overseas. Commission for Healthcare Audit and Inspection.<br />
March 2009. Available at: http://www.nhs.uk/<strong>Defence</strong>medicine/<br />
Documents/<strong>Defence</strong>_<strong>Medical</strong>_Services_review%5B1%5D.pdf.<br />
[accessed 26 February 2010]<br />
9. Kummer C, Netto FS, Rizoli S, Yee D. A review <strong>of</strong> traumatic<br />
airway injuries: Potential implications for airway assessment and<br />
management. Injury 2007: 38; 27-33<br />
10. Brywczynski JJ, Barrett TW, Lyon JA, Cotton BA. Management <strong>of</strong><br />
penetrating neck injury in <strong>the</strong> emergency department: a structured<br />
literature review. Emerg Med J 2008; 25: 711–715.<br />
11. Tallon JM, Ahmed JM, Sealy B. Airway management in penetrating<br />
neck trauma at a Canadian tertiary trauma centre. Can J Emerg<br />
Med Care 2007; 9:101-4<br />
12. Desjardins G, Varon AJ. Airway management for penetrating<br />
neck injuries: <strong>the</strong> Miami experience. Resuscitation 2001: 48;<br />
71–75<br />
13. Smith J, Hodgetts T, Mahoney PF, et al. Trauma Governance in<br />
<strong>the</strong> UK <strong>Defence</strong> <strong>Medical</strong> Services. JR <strong>Army</strong> Med <strong>Corps</strong> 2007; 153:<br />
239-242.<br />
14. PubMed. US National Library <strong>of</strong> Medicine. National Institutes<br />
<strong>of</strong> Health. Available at: http://www.ncbi.nlm.nih.gov/sites/<br />
entrez?db=pubmed [accessed 10 June 2010]<br />
15. ScienceDirect. Available at: http://www.sciencedirect.com<br />
[accessed 10 June 2010]<br />
16. GoogleScholar. Available at: http://scholar.google.co.uk [accessed<br />
10 June 2010]<br />
17. Ng KFJ, Lo CF. The bamboo skewer: Airway management in a<br />
patient with penetrating injury <strong>of</strong> <strong>the</strong> floor <strong>of</strong> mouth. Can J<br />
Anaesth 1996; 43: 1156-1160<br />
18. Dobson GT. Airway management in a patient with a nail-gun<br />
injury to <strong>the</strong> floor <strong>of</strong> <strong>the</strong> mouth. Ulster Med J 2000; 69: 148-51.<br />
19. Ban LH, Leone M, Visintini P, et al. Craniocerebral penetrating<br />
injury caused by a spear gun through <strong>the</strong> mouth: case report. J<br />
Neurosurg. 2008; 108: 1021-3.<br />
20. Joly LM, Oswald AM, Disdet M, Raggueneau JL. Difficult<br />
endotracheal intubation as a result <strong>of</strong> penetrating cranio-facial<br />
injury by an arrow. Anesth Analg 2002; 94: 231-2<br />
21. Incollingo F, Shevchenko Y. Airway management in a child with<br />
penetrating pharyngeal wall foreign body injury: a case report.<br />
AANA <strong>Journal</strong>. 2007; 75: 329-32.<br />
22. Rafique MB, Nesselrode R, de Armendi AJ. Difficult airway due<br />
to sprinkler spike in <strong>the</strong> head. Paediatr Anaesth 2008; 18: 903-4.<br />
23. Demetriades D, Chahwan S, Gomez H, Falabella A, Velmahos<br />
G, Yamashita D. Initial evaluation and management <strong>of</strong> gunshot<br />
wounds to <strong>the</strong> face. J Trauma 1998; 45: 39-41<br />
24. Glapa M, Kourie JF, Doll D, Degiannis E. Early management <strong>of</strong><br />
gunshot injuries to <strong>the</strong> face in civilian practice. World J Surg 2007;<br />
31: 2104-10.<br />
25. Ezeanolue BC. Management <strong>of</strong> <strong>the</strong> upper airway in severe cutthroat<br />
injuries. Afr J Med Med Sci 2001;30:233-5.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S355–360 359
Guidelines for Penetrating Airway Injuries<br />
26. Singh B., Kumar S., Kumar V. Management <strong>of</strong> complete<br />
cricotracheal separation following sharp edge injury. J Anaes<strong>the</strong>siol<br />
Clin Pharmacol 2004; 20: 79-82<br />
27. Steinig JP, DeLoach ED, Boyd CR. Transection <strong>of</strong> <strong>the</strong> base <strong>of</strong> <strong>the</strong><br />
tongue caused by penetrating injury. Am Surgeon 1999; 65: 133-4.<br />
28. Valerio P, Ivan M, Francisco R, et al. Survival after traumatic<br />
complete laryngotracheal transection. Am J <strong>of</strong> Emerg Med 2008;<br />
26: 837<br />
29. Sahu S, Agarwal A, Rana A, Lata I. Emergency intubation using a<br />
light wand in patients with facial trauma. J Emerg Trauma Shock.<br />
2009; 2: 51-3.<br />
30. Sari M., Baylancicek S., Inanli S. Atypical penetrating laryngeal<br />
trauma: A bullet in <strong>the</strong> larynx. Eur J Emerg Med 2007; 14: 230-<br />
232<br />
31. Young O, Watters K, Sheahan P, Hughes J. Penetrating air gun<br />
wound in <strong>the</strong> neck. Auris Nasus Larynx. 2008; 35: 426-8.<br />
32. O’Connor JV, Haan JM, Wright JL Spent bullet in <strong>the</strong> bronchus.<br />
Am Surgeon 2006; 72: 345-6.<br />
33. Mandavia DP, Qualls S, Rokos I. Emergency airway management<br />
in penetrating neck injury. Ann Emerg Medicine. 2000; 35: 221-5.<br />
34. Grewal H, Rao PM, Mukerji S, Ivatury RR. Management <strong>of</strong><br />
penetrating laryngotracheal injuries. Head Neck 1995;17 :494-502<br />
35. Weitzel N, Kendall J, Pons P. Blind nasotracheal intubation for<br />
patients with penetrating neck trauma. J Trauma 2004; 56: 1097-<br />
1101<br />
36. Gallo AC, Adams BD. Emergency battlefield cricothyrotomy<br />
complicated by tube occlusion. J Emerg Trauma Shock. 2009; 2:<br />
54-5.<br />
37. Sharma N, De M, Martin T, Pracy P. Laryngeal reconstruction<br />
following shrapnel injury in a British soldier: case report. J Laryngol<br />
Otol 2009; 123: 253-6.<br />
38. Banfield GK, Chowdhury CR, Brookstein R. Penetrating laryngeal<br />
injury: two case reports from Bosnia. J Laryngol Otol 1995; 109:<br />
144-6.<br />
39. Houghton I. The Triservice anaes<strong>the</strong>tic apparatus. <strong>Anaes<strong>the</strong>sia</strong><br />
1981; 36: 1094-1108<br />
40. Kotsev S. Airway management in a patient with a vascular injury<br />
and rapidly expanding neck haematoma. Eur J Anaes<strong>the</strong>siol 2005;<br />
22: 556-8.<br />
41. Venkatachalam S, Palaniswamy SD, Rangarajan M, Mani K,<br />
Palanivelu C. An unusual case <strong>of</strong> penetrating tracheal (“Cut throat”)<br />
injury due to chain snatching: The ideal airway management.<br />
Indian J Criti Care Med 2007: 11; 151-154<br />
42. Lin HL, Lin JN, Lin YK, Kuo LC, Lee WC, Chen CW. Damage<br />
control in <strong>the</strong> transection <strong>of</strong> carotid artery-a case report. Ann<br />
Emerg Medicine 2008; 26: 841<br />
43. Nelson LA. Airway trauma. Int Anes<strong>the</strong>siol Clin 2007; 45: 99–118.<br />
44. Baron BJ. Penetrating and blunt neck trauma. In: Tintinalli JE,<br />
Kelen GD, Stapczynski JS, (editors). Emergency Medicine: A<br />
Comprehensive Study Guide. 6th Ed, 1590-1595. New York:<br />
McGraw-Hill 2004.<br />
360<br />
SJ Mercer, SE Lewis, SJ Wilson et al<br />
45. Inaba K, Munera F, Mckenney M, et al. Prospective evaluation <strong>of</strong><br />
screening multislice helical computed tomographic angiography in<br />
<strong>the</strong> initial evaluation <strong>of</strong> penetrating neck injuries. J Trauma 2006;<br />
61: 144–9<br />
46. Bowley DM, Robertson SJ, B<strong>of</strong>fard KD Bhagwanjee S.<br />
Resuscitation and anaes<strong>the</strong>sia for penetrating trauma. Curr Opin<br />
Anes<strong>the</strong>sio 2003; 16: 165–171<br />
47. Abernathy JH III, Reeves ST Airway catastrophes. Curr Opin<br />
Anes<strong>the</strong>sio 2010; 23: 41-46<br />
48. Shearer VE, Giesecke AH. Airway management for patients with<br />
penetrating neck trauma: a retrospective study. Anesth Analg 1993;<br />
77: 1135–8.<br />
49. Brywczynski JJ, Barrett TW, Lyon JA, Cotton BA. Management <strong>of</strong><br />
penetrating neck injury in <strong>the</strong> emergency department: a structured<br />
literature review. Emerg Med J 2008; 25: 711–715.<br />
50. Eggen JT, Jorden RC. Airway management, penetrating neck<br />
trauma. J Emerg Med 1993; 11: 381–5.<br />
51. Chow JL, Coady MA, Varner J, et al. Management <strong>of</strong> acute<br />
complete tracheal transection caused by nonpenetrating trauma:<br />
report <strong>of</strong> a case and review <strong>of</strong> <strong>the</strong> literature. J Cardiothor Vasc An<br />
2004; 18: 475–478.<br />
52. Sellick BA. Cricoid pressure to control regurgitation <strong>of</strong> stomach<br />
contents during induction <strong>of</strong> anaes<strong>the</strong>sia. Lancet. 1961; 19: 404-6.<br />
53. Landsman I. Cricoid pressure: indications and complications.<br />
Paediatr Anaesth 2004; 14: 43–47<br />
54. Pandit JJ, Popat M. Difficult Airway Management in Maxill<strong>of</strong>acial<br />
Trauma. Semin Anesth 2001; 20: 144-153<br />
55. Prichayudh S, Pak-art R, Sriussadaporn S, et al. Airway<br />
management <strong>of</strong> penetrating neck injury by large foreign body<br />
impalement: Report <strong>of</strong> a case. Injury Extra 2009, doi:10.1016/j.<br />
injury.2009.10.025<br />
56. Schaefer SD. The acute management <strong>of</strong> external laryngeal trauma.<br />
A 27-year experience. Arch Otolaryngol 1992; 118: 598–604.<br />
57. Salvino CK, Dries D, Gamelli R, Murphy-Macabobby M, Marshall<br />
W. Emergency cricothyroidotomy in trauma victims. J Trauma<br />
1993; 34: 503–5<br />
58. Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis<br />
<strong>of</strong> errors reported by surgeons at three teaching hospitals. Surgery<br />
2003; 133: 614–21.<br />
59. Gaba DM, Fish KJ, Howard SK. Crisis management in<br />
anes<strong>the</strong>siology. New York: Churchill Livingstone, 1994<br />
60. Association <strong>of</strong> Anaes<strong>the</strong>tists <strong>of</strong> Great Britain and Ireland.<br />
Recommendations for Standards <strong>of</strong> Monitoring During <strong>Anaes<strong>the</strong>sia</strong><br />
and Recovery. 4th Edition March 2007. Available at: http://www.<br />
aagbi.org/publications/guidelines/docs/standards<strong>of</strong>monitoring07.<br />
pdf [accessed 01 May 2010]<br />
61. Kendall JL, Anglin D, Demetriades D. Penetrating neck trauma.<br />
Emerg Med Clin N Am 1998; 16: 85-105.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S355–360
The Paediatric Transfusion Challenge on<br />
Deployed Operations<br />
S Bree 1 , K Wood 2 , GR Nordmann 3 , J McNicholas 4<br />
1 Consultant Paediatric Anaes<strong>the</strong>tist, MDHU Derriford, Plymouth and Chair Paediatric <strong>Anaes<strong>the</strong>sia</strong> and Critical<br />
Care Special Interest Group (PACCSIG); 2 Specialist Registrar in <strong>Anaes<strong>the</strong>sia</strong>, James Cook University Hospital,<br />
Middlesborough; 3 Consultant Paediatric Anaes<strong>the</strong>tist, MDHU Derriford and 16 <strong>Medical</strong> Regiment, Colchester;<br />
4 Consultant in <strong>Anaes<strong>the</strong>sia</strong> and Intensive Care, MDHU Portsmouth, Department <strong>of</strong> Critical Care, Queen Alexandra<br />
Hospital, Portsmouth<br />
Abstract<br />
This paper briefly touches on <strong>the</strong> problem <strong>of</strong> dealing with <strong>the</strong> severely injured child requiring massive transfusion and produces<br />
a guide on <strong>the</strong> management <strong>of</strong> this based on <strong>the</strong> current Surgeon General’s Operational Policy Letter. There are no known<br />
UK guidelines on massive transfusion in trauma in <strong>the</strong> paediatric population although many specialist centres have guidance<br />
for dealing with cases in <strong>the</strong>atre during elective surgery. It is hoped that <strong>the</strong>se guidelines will be used by deployed military<br />
anaes<strong>the</strong>tists to aid in <strong>the</strong>ir management <strong>of</strong> <strong>the</strong>se difficult cases, not normally seen in <strong>the</strong> UK.<br />
Introduction<br />
The last few years have proved a busy time for <strong>the</strong> <strong>Defence</strong><br />
<strong>Medical</strong> Services (DMS) in terms <strong>of</strong> operational commitments<br />
and <strong>the</strong> development <strong>of</strong> military medical techniques. War fighting<br />
has historically provided a rich environment for <strong>the</strong> advance <strong>of</strong><br />
medical care including blood transfusion, antibiotics, wound<br />
care and casualty retrieval to name but a few. The recent conflicts<br />
have proved no exception with major advances in blood product<br />
<strong>the</strong>rapy, a refining <strong>of</strong> damage control resuscitation techniques,<br />
from <strong>the</strong> early extraction <strong>of</strong> casualties, through to rapid damage<br />
control time-limited surgery and <strong>the</strong> rapid evacuation back to UK<br />
Role 4 through our Critical Care Air Support Team (CCAST)<br />
capabilities.<br />
Much attention and energy has been directed towards improving<br />
<strong>the</strong> lot for our injured troops with a perceived improvement in<br />
outcome. An unfortunate but inevitable outcome <strong>of</strong> <strong>the</strong> current<br />
war fighting is <strong>the</strong> presence <strong>of</strong> casualties amongst <strong>the</strong> paediatric<br />
population. The causes for this are varied, but include legacy<br />
munitions, enemy and coalition activities, as well as ongoing<br />
domestic accidents. The UK military has traditionally treated all<br />
those appearing at our medical facilities according to an eligibility<br />
matrix whose interpretation can vary depending on tempo <strong>of</strong> ops<br />
and state <strong>of</strong> medical facilities. Irrespective <strong>of</strong> this, it is incumbent<br />
on UK medical personnel to provide <strong>the</strong> best quality care possible<br />
to those admitted to our Role 2 and 3 medical facilities. This is<br />
not always straightforward nor is it a purely medical decision.<br />
Very difficult ethical and logistic dilemmas can arise, which must<br />
be looked at on an individual basis.<br />
Paediatric <strong>Anaes<strong>the</strong>sia</strong> and Critical Care Special<br />
Interest Group<br />
The challenge <strong>of</strong> paediatric patients in <strong>the</strong> military environment is<br />
now accepted across <strong>the</strong> DMS and appropriate provision is being<br />
undertaken to provide <strong>the</strong> equipment to deal with this situation.<br />
As part <strong>of</strong> this process, <strong>the</strong> <strong>Defence</strong> Consultant Adviser (DCA)<br />
Corresponding Author: Surg Cdr Steve Bree RN,<br />
Consultant Paediatric Anaes<strong>the</strong>tist, MDHU Derriford,<br />
Plymouth PL6 8DH<br />
Tel 01752 439203/4/5 Email stephen.bree@phnt.swest.nhs.uk<br />
in Anaes<strong>the</strong>tics has commissioned <strong>the</strong> formation <strong>of</strong> <strong>the</strong> Paediatric<br />
<strong>Anaes<strong>the</strong>sia</strong> and Critical Care Special Interest Group (PACCSIG).<br />
The PACCSIG consists <strong>of</strong> four consultant anaes<strong>the</strong>tists (one an<br />
intensive care specialist), two trainees and a nurse with a sub<br />
speciality interest in paediatric issues across <strong>the</strong> board. It meets<br />
twice a year and has <strong>the</strong> following remit:<br />
1. Examine equipment issues, staff training and standards<br />
<strong>of</strong> care where anaes<strong>the</strong>tists may be involved in <strong>the</strong> care <strong>of</strong><br />
children including pre-hospital care, ED, <strong>the</strong>atres, ICU,<br />
wards and transfer.<br />
2. Outputs to include annual module review for <strong>the</strong> anaes<strong>the</strong>tic<br />
specialist interest group<br />
3. Production <strong>of</strong> an annual activity report to <strong>the</strong> DCA.<br />
Minutes <strong>of</strong> PACCSIG proceedings are sent to DCA’s in all<br />
relevant disciplines and it is hoped that it will act as a focus for<br />
paediatric issues throughout <strong>the</strong> DMS.<br />
Workload<br />
Current paediatric workload is still to be determined but some raw<br />
data has been retrieved. For <strong>the</strong> purpose <strong>of</strong> looking at paediatric<br />
casualties in both Iraq and Afghanistan a request was put in to <strong>the</strong><br />
Joint Theatre Trauma Registry (JTTR) at Birmingham to obtain<br />
data on all children treated under <strong>the</strong> age <strong>of</strong> 16 from March 2003<br />
to August 2009. On Op TELIC (Iraq) 29/271 (4%) <strong>of</strong> admissions<br />
were children compared to 147/1769 (8%) for Op HERRICK<br />
(Afghanistan). The age and gender <strong>of</strong> <strong>the</strong> children admitted are<br />
given in Figures 1 and 2.<br />
Figure 1. Age Breakdown <strong>of</strong> Paediatric admissions<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S361–364 361
Paediatric Transfusion<br />
Figure 2 Gender Breakdown<br />
A review <strong>of</strong> US data has recorded 10% <strong>of</strong> all admissions to<br />
<strong>the</strong>ir Combat Support Hospital (CASH) facilities in Iraq and<br />
Afghanistan as paediatric, with penetrating injuries accounting<br />
for three quarters <strong>of</strong> cases [1].<br />
This correlates well with data collected from Herrick 8B/9A [2]<br />
where 10.1% <strong>of</strong> all surgical operations within <strong>the</strong> UK Med facility<br />
were carried out in children and one third <strong>of</strong> all <strong>the</strong> paediatric<br />
surgical population were admitted to <strong>the</strong> ICU, which comprised<br />
11.9% <strong>of</strong> <strong>the</strong> total ICU admission load. These figures do not<br />
necessarily reflect <strong>the</strong> real contribution <strong>of</strong> paediatric casualties to<br />
ICU work. Coalition casualties are generally evacuated to <strong>the</strong> UK<br />
within 24 hours, whereas paediatric ICU admissions may spend a<br />
protracted period on <strong>the</strong> intensive care unit.<br />
A review by Gurney in 2004 [3] looked at activity in <strong>the</strong> UK<br />
surgical field hospital during <strong>the</strong> war fighting phase <strong>of</strong> <strong>the</strong> TELIC<br />
1 campaign and quoted paediatric patients as comprising 2.9%<br />
<strong>of</strong> all recorded admissions. This figure is lower than o<strong>the</strong>rs have<br />
experienced on previous campaigns and may be a reflection <strong>of</strong> <strong>the</strong><br />
relatively peaceful period which was in place prior to <strong>the</strong> sustained<br />
insurgency campaign when kinetic activity ie <strong>the</strong>- use <strong>of</strong> munitions<br />
and firearms, escalated considerably, <strong>of</strong>ten in an indiscriminate<br />
manner or directly targeting <strong>the</strong> civilian population This small<br />
figure <strong>of</strong> 2.9% has <strong>the</strong> potential to be slightly misleading as<br />
children accounted for nearly a third <strong>of</strong> all non-coalition patients,<br />
a figure which may need to be borne in mind when planning<br />
medical aspects <strong>of</strong> future operations.<br />
Present military operations in Afghanistan are generating a<br />
large number <strong>of</strong> fragmentation and gunshot wounds (GSW).<br />
Harris and McNicholas [4] in this journal reviewed <strong>the</strong> paediatric<br />
workload on Critical Care with 15 admissions over two months in<br />
mid-2008. Mechanism <strong>of</strong> injury was predominantly penetrating<br />
GSW or fragmentation (absolute numbers not given) and a mean<br />
age <strong>of</strong> six years (range 6 months to 17 years) was recorded. This<br />
population was a significant part <strong>of</strong> <strong>the</strong> Critical Care workload<br />
with a paediatric admission present for 66% <strong>of</strong> <strong>the</strong> time and<br />
accounting for 30% <strong>of</strong> all bed occupancy.<br />
PACCSIG continues to retrieve data, but it is clear that <strong>the</strong><br />
challenge <strong>of</strong> paediatric admissions is impacting significantly on<br />
field hospital resources and must be taken into account when<br />
planning personnel, equipment and patient disposal. The current<br />
matrix <strong>of</strong> <strong>Medical</strong> Rules for Eligibility (MRE) ensures that <strong>the</strong><br />
hospital front door is open for many <strong>of</strong> <strong>the</strong> civilian population<br />
at risk (PAR). Whilst considerable effort is being devoted to <strong>the</strong><br />
development <strong>of</strong> local medical facilities, <strong>the</strong> reality is that <strong>the</strong>y are<br />
a long way from providing critical care <strong>of</strong> a standard comparable<br />
to <strong>the</strong> joint UK/US hospital in Helmand.<br />
362<br />
S Bree, K Wood, GR Nordmann et al<br />
Massive Transfusion in Trauma<br />
The Surgeon Generals Operational Policy Letter (SGPL) on<br />
massive transfusion [5] updated <strong>the</strong> most recent advice on <strong>the</strong><br />
management <strong>of</strong> major haemorrhage on operations. This is an adult<br />
based guideline which has developed extensively over <strong>the</strong> past few<br />
years and is still part <strong>of</strong> <strong>the</strong> ongoing evolution <strong>of</strong> trauma transfusion<br />
medicine. The Association <strong>of</strong> Anaes<strong>the</strong>tists <strong>of</strong> Great Britain and<br />
Ireland (AAGBI) is in <strong>the</strong> process <strong>of</strong> generating a document on this<br />
subject and will include a section on <strong>the</strong> management <strong>of</strong> paediatric<br />
massive transfusion. As part <strong>of</strong> <strong>the</strong> process some <strong>of</strong> <strong>the</strong> authors <strong>of</strong><br />
this article in conjunction with <strong>the</strong> PACCSIG have developed a<br />
simple guideline based on reverse engineering <strong>of</strong> <strong>the</strong> adult SGPL.<br />
This has been carried out to provide a protocol on which to base<br />
a weight guided massive transfusion for situations where major<br />
haemorrhage is a problem in children. It enables physicians to<br />
guide paediatric patient resuscitation with greater confidence, and<br />
is intended to be used in conjunction with <strong>the</strong> clinical monitoring<br />
and near patient testing already available.<br />
The adult protocol dictates that on arrival in <strong>the</strong> ED, laboratory<br />
staff will provide 4 units <strong>of</strong> O negative packed red blood cells<br />
(PRBC) and 4 units <strong>of</strong> Fresh Frozen Plasma (FFP) for initial<br />
resuscitation in <strong>the</strong> massive transfusion case although a trend<br />
towards 2 unit packs <strong>of</strong> FFP and blood is now developing and<br />
may certainly be more appropriate for paediatric resuscuation.<br />
This constitutes <strong>the</strong> first phase. The second phase is entered when<br />
<strong>the</strong> lab issues <strong>the</strong> second major haemorrhage pack consisting <strong>of</strong> 6<br />
units <strong>of</strong> cross matched PRBC and 6 units <strong>of</strong> FFP.<br />
As a practical guide to <strong>the</strong> laboratory and <strong>the</strong> resuscitation<br />
teams we recommend <strong>the</strong> following guide (Figure 3) be used with<br />
reference to <strong>the</strong> key points in Table 1, to ensure appropriate fluid<br />
<strong>the</strong>rapy and efficient use <strong>of</strong> blood products.<br />
• In <strong>the</strong> first phase, order 1 unit (U) <strong>of</strong> PRBC and 1 U <strong>of</strong><br />
FFP for every 20kg weight <strong>of</strong> <strong>the</strong> child, e.g. a 23kg child<br />
will need 2 U blood and 2 U FFP initially. This will ensure<br />
a minimum <strong>of</strong> approximately 15 ml/kg, i.e. approx 300ml<br />
each <strong>of</strong> FFP and PRBC for a 20kg child.<br />
• A bag <strong>of</strong> PRBC or FFP for an adult is equivalent to<br />
approximately 4ml/kg for <strong>the</strong> child.<br />
• Alternate boluses <strong>of</strong> PRBC and FFP are given in a volume<br />
<strong>of</strong> 5ml/kg.<br />
• The first phase <strong>of</strong> transfusion for an adult, 4 U <strong>of</strong> PRBC<br />
and 4 U <strong>of</strong> FFP, is equivalent to approximately 15 ml/kg<br />
(3 boluses) <strong>of</strong> each product for <strong>the</strong> child.<br />
• Use all clinical signs to help guide resuscitation, including<br />
arterial wave form, central venous pressure, blood pressure<br />
and urine output, as well as laboratory results, particularly<br />
arterial blood gases and rotational thromboelastometry<br />
ROTEM® (TEM Innovations GmBH, Munich Germany).<br />
• Order more PRBC/FFP as required. (remember bool<br />
can be returned to labs within 30 minutes if cold box<br />
unopened)<br />
• Platelets should be given at 3ml/kg, however ROTEM®<br />
may indicate a requirement for more platelet transfusion.<br />
SGPL guideline aims for platelet count above 100 x 109/l.<br />
• The dose for Calcium Chloride is 0.2ml/kg.<br />
• The dose for Tranexamic Acid is 15mg/kg bolus, followed<br />
by an infusion <strong>of</strong> 1mg/kg/hr.<br />
Table 1 Paediatric Massive Haemorrhage Key Points<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S361–364
Paediatric Transfusion S Bree, K Wood, GR Nordmann et al<br />
Decision to enter massive<br />
transfusion protocol made<br />
early (first shock pack<br />
issued by labs containing<br />
non crossmatched blood)<br />
and FFP)<br />
Request clotting, full<br />
blood count, fibrinogen<br />
and ROTEM ® tests as<br />
soon as practical, as well<br />
as formal cross match<br />
Child arrives in ED<br />
Estimate weight (using<br />
Broselow tape or age<br />
formula [(age + 4) x 2]<br />
Blood 5ml/kg<br />
FFP 5ml/kg<br />
Alternating (ensuring<br />
warming <strong>of</strong> blood and<br />
FFP)<br />
End <strong>of</strong> 1 st phase, after a<br />
total <strong>of</strong> 15ml/kg blood<br />
and 15ml/kg FFP<br />
Consider<br />
Platelets 3ml/kg*<br />
Cryoprecipitate 3ml/kg**<br />
CaCl2 0.2ml/kg ***<br />
rFVIIa ****<br />
Transfusion end points<br />
Arresting <strong>of</strong> haemorrhage<br />
Heart rate, BP, CVP<br />
Cap refill<br />
Blood gases and lactate<br />
Hb<br />
Risks<br />
Hypo<strong>the</strong>rmia<br />
Hyperkalaemia<br />
Hypocalcaemia<br />
Hypomagnesaemia<br />
Give Tranexamic Acid<br />
bolus +/- infusion<br />
Start 2 nd phase <strong>of</strong> protocol<br />
again with aliquots <strong>of</strong><br />
blood and FFP in<br />
alternating 5ml/kg<br />
boluses<br />
Repeat <strong>the</strong> cycle using<br />
20ml/kg PRBC and<br />
20ml/kg FFP to indicate<br />
<strong>of</strong> <strong>the</strong> end <strong>of</strong> each “adult<br />
6 unit shock pack”<br />
*consider transfusing whole bag if platelets required and volume<br />
not an issue; ** aim for fibrinogen above 1g/l; *** Aim for ionised<br />
Ca above 1mmol/l; ****1 Dose <strong>of</strong> 100mcg/kg repeated after 20<br />
minutes if necessary. Aim for as near normal physiology as possible<br />
pre administration<br />
Fig 3. Framework for Paediatric Massive transfusion based on SGPL<br />
Paediatric Massive Haemorrhage: Practicalities <strong>of</strong><br />
Resuscitation<br />
The practicalities <strong>of</strong> this process are not as straightforward as<br />
for adult transfusion and a system for delivering <strong>the</strong> blood<br />
products must be assembled and rehearsed with all staff who<br />
may be involved in this process. There may be several “rigs”<br />
which staff may have used within different hospitals and but it<br />
is recommended one single assembly is agreed amongst deployed<br />
clinical staff to promote familiarity and minimise risk <strong>of</strong> mishaps.<br />
Practical points to be considered during major haemorrhage<br />
management in <strong>the</strong> paediatric population include <strong>the</strong> following:<br />
• Invasive pressure monitoring is essential.<br />
• Large bore central venous access is ideal. Multiple peripheral<br />
cannulae may not be possible and lead to <strong>the</strong> risk <strong>of</strong> multiple<br />
“ectopic” fluid transfusions.<br />
• A fluid warmer is essential.<br />
• The ability to deliver air free warmed boluses <strong>of</strong> blood products<br />
and fluids is an important practical issue. A set up such as <strong>the</strong><br />
one described below can be used successfully, but teams need<br />
to be briefed and trained in its safe use before <strong>the</strong> event.<br />
• At <strong>the</strong> proximal end <strong>of</strong> <strong>the</strong> fluid warmer 4 three way taps<br />
should be attached in series to 4 bags <strong>of</strong> fluid and <strong>the</strong>ir<br />
giving sets. The 4 bags may contain any <strong>of</strong> <strong>the</strong> following;<br />
crystalloid, colloid, blood and FFP. At <strong>the</strong> distal end <strong>of</strong><br />
<strong>the</strong> fluid warmer a fur<strong>the</strong>r 2 three way taps should be<br />
attached in series. One for a 50 ml syringe to use as <strong>the</strong><br />
main ‘pump’ to use for each fluid bolus and a fur<strong>the</strong>r tap<br />
for <strong>the</strong> addition <strong>of</strong> drugs. Distal to this should be a short<br />
connector to <strong>the</strong> central line. This connector should be<br />
secured in some manner to <strong>the</strong> bed so it takes <strong>the</strong> weight<br />
<strong>of</strong> <strong>the</strong> 50ml syringe and lines. This approach has been used<br />
to good effect in <strong>the</strong> ICU during <strong>the</strong> current phase <strong>of</strong> Op<br />
HERRICK. It shoud be borne in mind that with <strong>the</strong> Level<br />
1 Infusor (Smiths <strong>Medical</strong> Level 1® H-1200 Fast Flow<br />
Fluid Warmer) currently in use in rhe British military <strong>the</strong>re<br />
is a potentially significant dead space <strong>of</strong> up to 60 mls from<br />
<strong>the</strong> upstream to <strong>the</strong> down stream locations <strong>of</strong> <strong>the</strong> warming<br />
element. This will become increasingly important for <strong>the</strong><br />
smaller child and alternative arrangements should be<br />
explored in <strong>the</strong>se circumstances.<br />
• The physical arrangement described will provide an<br />
accurate method <strong>of</strong> administering specific volumes <strong>of</strong><br />
<strong>the</strong> required fluid. Fluid will be warmed and speed <strong>of</strong><br />
administration controlled by hand. Drugs can be given<br />
without interruption <strong>of</strong> transfusion.<br />
• It is vital to record <strong>the</strong> volumes given with accuracy. Ideally<br />
<strong>the</strong>se should be recorded concurrently and in a location which<br />
all can see (e.g. wipe board).<br />
• Platelets should be given through a different giving set to a<br />
different line and consideration should be given to transfusing<br />
<strong>the</strong> whole bag on <strong>the</strong> basis that our recommended 3ml/kg is<br />
reasonably conservative and once issued this scarce resource<br />
needs to be utilised efficiently.<br />
Management <strong>of</strong> major haemorrhage is <strong>of</strong>ten an obvious<br />
clinical picture in <strong>the</strong> emergency room and <strong>the</strong> operating <strong>the</strong>atre<br />
but it may also require recognition and initiation in o<strong>the</strong>r areas<br />
within <strong>the</strong> hospital and useful definition <strong>of</strong> massive transfusion in<br />
<strong>the</strong> paediatric population is given in Table 2 to aid in this aspect,<br />
particularly with respect to ongoing blood loss<br />
• Replacement <strong>of</strong> 1 blood volume in 24 hours<br />
• 10 units <strong>of</strong> Red Cells in 24 hours (40ml/kg)<br />
• 4 units in 1 hour (16ml/kg)<br />
• Replacement or loss <strong>of</strong>50% blood volume in 3 hours<br />
• Rate <strong>of</strong> blood loss >150ml/min (2ml/kg/min)<br />
Table 2: Definition <strong>of</strong> Massive Transfusion (proposed paediatric<br />
figures in brackets)<br />
Valuable lessons can be gained from observing treatment <strong>of</strong><br />
massive haemorrhage and coagulopathy in children undergoing<br />
elective surgery in UK specialist paediatric hospitals. Procedures<br />
such as hepatic transplantation, scoliosis surgery and crani<strong>of</strong>acial<br />
surgery are examples <strong>of</strong> practice in which important<br />
anaes<strong>the</strong>tic experience can be gained, not only in <strong>the</strong> practicalities<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S361–364 363
Paediatric Transfusion<br />
<strong>of</strong> resuscitation <strong>of</strong> massive haemorrhage and coagulopathy, but<br />
also in logistics <strong>of</strong> how <strong>the</strong> volumes can be transfused. It is <strong>the</strong><br />
opinion <strong>of</strong> <strong>the</strong> PACCSIG that military paediatric anaes<strong>the</strong>tists<br />
should have regular exposure to this experience or attend refresher<br />
training in a specialist paediatric unit prior to deploying.<br />
Conclusions<br />
This paper describes a guide for resuscitation in paediatric<br />
massive haemorrhage to be used by deployed anaes<strong>the</strong>tists in<br />
Afghanistan. It should be used in addition to conventional<br />
clinical signs and monitoring, including near patient laboratory<br />
investigations.<br />
Although not forming our core work on military operations<br />
<strong>the</strong> challenge <strong>of</strong> <strong>the</strong> injured and sick child is real and<br />
something that we face weekly on current deployed operations.<br />
It is important that we provide a well trained cadre with an<br />
appropriate skill mix, in order to deal with <strong>the</strong> full spectrum<br />
<strong>of</strong> clinical cases including children. Improved awareness and<br />
delivery <strong>of</strong> first class care to children will lead to both a better<br />
outcome for <strong>the</strong> injured child and a more efficient use <strong>of</strong> limited<br />
hospital resources.<br />
Fur<strong>the</strong>r work is being undertaken with <strong>the</strong> PACCSIG across<br />
a whole range <strong>of</strong> paediatric deployed issues and covering aspects<br />
<strong>of</strong> daily care, training and audit <strong>of</strong> outcome. It is hoped that <strong>the</strong><br />
authors can communicate developments through this journal as<br />
our work proceeds.<br />
364<br />
S Bree, K Wood, GR Nordmann et al<br />
Acknowledgments<br />
The authors would like to thank Dr Isabeau Walker, Consultant<br />
Anaes<strong>the</strong>tist, Great Ormond Street Hospital, London and Col T<br />
Hodgetts CBE QHP L/RAMC for <strong>the</strong>ir help and advice on <strong>the</strong><br />
massive haemorrhage protocol, <strong>the</strong> writing <strong>of</strong> this article and <strong>the</strong><br />
use <strong>of</strong> <strong>the</strong> JTTR data.<br />
References<br />
4. Creamer KM, Edwards MJ, et al. Pediatric Wartime Admissions to<br />
US Military Combat Support Hospitals in Afghanistan and Iraq:<br />
Learning from <strong>the</strong> First 2,000 Admissions. J Trauma 2009; 67 (4):<br />
762-8.<br />
5. Nordmann G. Paediatric anaes<strong>the</strong>sia in Afghanistan; a review <strong>of</strong><br />
current experience. J R <strong>Army</strong> Med <strong>Corps</strong> 2010; 156(4 Suppl 1):<br />
S323-326.<br />
6. Gurney I. Paediatric Casualties During OP TELIC. J R <strong>Army</strong> Med<br />
<strong>Corps</strong> 2004; 150: 270-272.<br />
7. Harris CC, McNicholas JJK. Paediatric Intensive Care in <strong>the</strong> Field<br />
Hospital. J R <strong>Army</strong> Med <strong>Corps</strong> 2009; 155 (2): 157-159.<br />
8. Surgeon General’s Operational Policy Letter Management <strong>of</strong><br />
massive haemorrhage on operations, June 2009, SGPL 08/09.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S361–364
Simulation, Human Factors and <strong>Defence</strong><br />
<strong>Anaes<strong>the</strong>sia</strong><br />
SJ Mercer 1 , C Whittle 2 , B Siggers 3 , RS Frazer 4<br />
1 Specialist Registrar in <strong>Anaes<strong>the</strong>sia</strong> & Critical Care, <strong>Royal</strong> Liverpool University Hospital, Prescot Street, Liverpool;<br />
2 Consultant in <strong>Anaes<strong>the</strong>sia</strong> & Critical Care, Frenchay Hospital, North Bristol NHS Trust, Bristol; 3 Consultant in<br />
<strong>Anaes<strong>the</strong>sia</strong>, Salisbury Hospital NHS Foundation Trust, Odstock Road, Salisbury, Wilts; 4 Consultant in <strong>Anaes<strong>the</strong>sia</strong>,<br />
SO1 Clinical, HQ 2 Med Bde, Strensall, York.<br />
Abstract<br />
Simulation in healthcare has come a long way since it’s beginnings in <strong>the</strong> 1960s. Not only has <strong>the</strong> sophistication <strong>of</strong> simulator<br />
design increased, but <strong>the</strong> educational concepts <strong>of</strong> simulation have become much clearer. One particularly important area is<br />
that <strong>of</strong> non-technical skills (NTS) which has been developed from similar concepts in <strong>the</strong> aviation and nuclear industries.<br />
NTS models have been developed for anaes<strong>the</strong>tists and more recently for surgeons too. This has clear value for surgical<br />
team working and <strong>the</strong> recently developed Military Operational Surgical Training (MOST) course uses simulation and NTS<br />
to improve such team working.The scope for simulation in <strong>Defence</strong> medicine and anaes<strong>the</strong>sia does not stop here. Uses <strong>of</strong><br />
simulation include pre-deployment training <strong>of</strong> hospital teams as well as <strong>Medical</strong> Emergency Response Team (MERT) and<br />
Critical Care Air Support Team (CCAST) staff. Future projects include developing Role 1 pre-deployment training. There is<br />
enormous scope for development in this important growth area <strong>of</strong> education and training.<br />
Introduction<br />
Simulation can be defined as <strong>the</strong> artificial representation <strong>of</strong><br />
<strong>the</strong> real-world to achieve an educational goal via experiential<br />
learning [1]. A number <strong>of</strong> different levels <strong>of</strong> simulation exist<br />
and in some areas <strong>Defence</strong> medicine is taking a leading role at<br />
national and international levels. This article will review current<br />
concepts <strong>of</strong> simulation and <strong>the</strong> increasingly important area <strong>of</strong><br />
non-technical skills (NTS) or human factors (HF). It will review<br />
current <strong>Defence</strong> <strong>Medical</strong> Services (DMS) simulation output and<br />
consider <strong>the</strong> future for simulation in <strong>the</strong> DMS and especially<br />
<strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong>, including <strong>the</strong> increasing opportunities for<br />
individuals to take part in this growth area.<br />
Simulation and Clinical Learning<br />
Simulation in medical education can be thought <strong>of</strong> as any<br />
educational activity involving <strong>the</strong> use <strong>of</strong> a simulated as opposed to<br />
live patient, thus in its broadest interpretation, a simple case-based<br />
discussion between consultant and trainee could be regarded as<br />
simulating <strong>the</strong> management <strong>of</strong> a “virtual” patient.<br />
Simulation can vary in complexity from <strong>the</strong> use <strong>of</strong> part-task<br />
trainers (<strong>of</strong>ten used in surgical training) through to <strong>the</strong> use <strong>of</strong><br />
mannequins for individual and small team training. Some<br />
common platforms are listed in Table 1. In addition to this a<br />
conceptual framework <strong>of</strong> three different levels <strong>of</strong> simulation has<br />
been proposed. Micro-simulation focuses on <strong>the</strong> needs <strong>of</strong> <strong>the</strong><br />
individual clinician and usually consists <strong>of</strong> basic motor skills (e.g.<br />
knot tying). The second level is Meso-simulation and this focuses<br />
on clinical teams looking at higher cognitive skills and behaviours<br />
(e.g. NTS). The highest level is Macro-simulation and this really<br />
focuses on an entire organisation [2].<br />
Corresponding author: Lt Col RS Frazer, SO1 Clinical, HQ 2<br />
Med Bde, Strensall, York. YO32 5SW.<br />
Tel: 01904 442611 Fax: 01904 442689<br />
Email: scottfrazer@doctors.net.uk<br />
• Part task trainers<br />
(e.g. for airway management or intravenous access)<br />
• Computer based systems<br />
• Virtual reality and haptic systems<br />
• Simulated patients<br />
• Simulated environments<br />
• Integrated Simulators including instructor<br />
and model driven mannequins.<br />
Table 1: Common simulation platforms<br />
<strong>Anaes<strong>the</strong>sia</strong> as a specialty has led <strong>the</strong> way in <strong>the</strong> development<br />
<strong>of</strong> simulation training in medicine. Following <strong>the</strong> creation <strong>of</strong><br />
<strong>the</strong> first mannequin in <strong>the</strong> late 1960s [3], <strong>the</strong>y have become<br />
increasingly sophisticated. Some are now completely wireless<br />
while o<strong>the</strong>rs possess an inherent s<strong>of</strong>tware-driven physiology. They<br />
have also become cheaper resulting in an increasing number <strong>of</strong><br />
centres delivering high-fidelity scenario-based training [4].<br />
In scenario-based training, learners are required to respond to<br />
simulated clinical situations as <strong>the</strong>y would to real situations and<br />
<strong>the</strong>n review and discuss <strong>the</strong>ir performance aided by <strong>the</strong>ir peers and<br />
a facilitator (debriefing). Clinicians can practice <strong>the</strong> management<br />
<strong>of</strong> uncommon emergencies to improve competence. An important<br />
element in this training, and its educational effectiveness, is<br />
<strong>the</strong> degree <strong>of</strong> realism, or ‘fidelity’ <strong>of</strong> <strong>the</strong> scenario. Physical (or<br />
Engineering fidelity) is <strong>the</strong> degree to which <strong>the</strong> training device or<br />
environment replicates <strong>the</strong> physical characteristics <strong>of</strong> <strong>the</strong> real task<br />
[5]. Functional or psychological fidelity is thought to be <strong>of</strong> greater<br />
importance and is <strong>the</strong> degree to which <strong>the</strong> skills in <strong>the</strong> real task are<br />
captured in <strong>the</strong> simulated task. The greater <strong>the</strong> reality, <strong>the</strong> more<br />
<strong>the</strong> learner will ‘buy into’ <strong>the</strong> process and <strong>the</strong> greater <strong>the</strong> learning.<br />
Numerous NHS anaes<strong>the</strong>tists have benefited from <strong>the</strong><br />
experience <strong>of</strong> mannequin based scenarios in a simulation centre<br />
and <strong>the</strong> majority <strong>of</strong> those surveyed have been positive about<br />
simulation as a means <strong>of</strong> delivering training [6]. A recent survey <strong>of</strong><br />
<strong>Defence</strong> Anaes<strong>the</strong>tists has shown similar enthusiasm, particularly<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S365–369 365
Simulation and <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong><br />
in pre-deployment training using operational clinical scenarios, for<br />
example massive transfusion and familiarisation with operational<br />
medical equipment [7].<br />
The increasing importance <strong>of</strong> simulation is such that <strong>the</strong> Chief<br />
<strong>Medical</strong> Officer <strong>of</strong> England & Wales has recently suggested that<br />
simulation-based training should be fully funded and integrated<br />
within training programmes for clinicians at all stages. He also<br />
states that simulation-based training needs to be valued and<br />
adequately resourced by NHS organisations, and that a faculty<br />
<strong>of</strong> expert clinical facilitators should be developed to deliver highquality<br />
simulation training [8].<br />
Non-technical Skills or Human Factors<br />
In <strong>the</strong> 1970s simulation in healthcare started to gain recognition<br />
as a means to limit human error and improve patient safety, taking<br />
a lead from <strong>the</strong> aviation and nuclear power industries as well as<br />
<strong>the</strong> National Aeronautics and Space Administration (NASA).<br />
NASA revealed that 70% <strong>of</strong> its errors were due to human factors<br />
such as failed interpersonal communication, decision-making<br />
and leadership [9]. Similar figures have been seen in an analysis<br />
<strong>of</strong> adverse events in anaes<strong>the</strong>sia [10]. Case reports and a report<br />
from <strong>the</strong> National Patient Safety Agency (NPSA) also suggest that<br />
human factors contribute to <strong>the</strong> majority <strong>of</strong> medical errors [11 -<br />
14]. The report “To err is human” confirmed <strong>the</strong> same situation in<br />
<strong>the</strong> USA [15].<br />
Much <strong>of</strong> <strong>the</strong> research from <strong>the</strong> airline and nuclear power<br />
industries into human factors is transferable to <strong>the</strong> clinical arena.<br />
Detailed analysis <strong>of</strong> critical events and in particular <strong>the</strong> human<br />
behaviours that contributed to <strong>the</strong>ir occurrence and management<br />
has led to <strong>the</strong> development <strong>of</strong> a set <strong>of</strong> behavioural principles.<br />
These behavioural `best practice` principles are known to aircrew<br />
as Crew Resource Management (CRM).<br />
Several groups have brought <strong>the</strong>se same principles into<br />
anaes<strong>the</strong>sia, notably a team led by David Gaba at Stanford,<br />
USA which developed <strong>Anaes<strong>the</strong>sia</strong> Crisis Resource Management<br />
(ACRM) [16] and ano<strong>the</strong>r led by Ronnie Glavin in Aberdeen,<br />
UK which developed <strong>Anaes<strong>the</strong>sia</strong> Non-Technical Skills (ANTS)<br />
[17]. These behavioural frameworks include elements such as<br />
‘knowing your environment’, ‘leadership’, ‘communication’,<br />
‘situational awareness’, ‘dynamic decision-making’, ‘prioritisation<br />
and delegation <strong>of</strong> tasks’. The key components <strong>of</strong> <strong>the</strong> two systems<br />
are shown in Table 2. It is easy for <strong>the</strong>se broad headings to sound<br />
trite and obvious. However, communication itself was found to<br />
be a causal factor in 43% <strong>of</strong> errors by surgeons in three American<br />
teaching hospitals [18].<br />
Clinical scenarios using a high-fidelity environment and<br />
mannequin, combined with carefully facilitated debriefing,<br />
are <strong>the</strong> ideal educational method for teaching <strong>the</strong>se principles<br />
[19]. However it must be stressed that training and experience<br />
in debriefing and NTS are key to <strong>the</strong> success <strong>of</strong> scenario based<br />
training. A poor debrief can adversely impact upon <strong>the</strong> educational<br />
aims <strong>of</strong> any scenario.<br />
<strong>Army</strong> <strong>Medical</strong> Training Centre (AMSTC)<br />
It is believed that <strong>the</strong> first <strong>Defence</strong> <strong>Medical</strong> establishment to<br />
develop simulation was <strong>the</strong> <strong>Army</strong> <strong>Medical</strong> Services Training<br />
Centre (AMSTC) at Strensall, York where <strong>the</strong> Hospital Exercise<br />
(HOSPEX) takes place. This is a macro simulation where layers<br />
<strong>of</strong> simulation exist, from <strong>the</strong> overall simulated hospital down to<br />
individual patient scenarios. This is in contrast to <strong>the</strong> majority<br />
<strong>of</strong> simulation centres which run single scenarios for individuals<br />
366<br />
ACRM [17] ANTS [19]<br />
Know <strong>the</strong> environment<br />
Anticipate and plan<br />
Call for help early<br />
Exercise leadership and<br />
followership<br />
Distribute <strong>the</strong> workload<br />
Mobilize all available<br />
resources<br />
Communicate effectively<br />
Use all available information<br />
Prevent and manage fixation<br />
errors<br />
Cross (double) check<br />
Use cognitive aids<br />
Re-evaluate repeatedly<br />
Use good teamwork<br />
Allocate attention wisely<br />
Set priorities dynamically<br />
Table 2: Two Non-Technical Skills Systems<br />
SJ Mercer, C Whittle , B Siggers et al<br />
Situational awareness:<br />
Ga<strong>the</strong>ring information<br />
Recognising & understanding<br />
Anticipating<br />
Decision Making:<br />
Identifying options<br />
Balancing risks and selecting<br />
options<br />
Re-evaluating<br />
Task management:<br />
Planning & preparation<br />
Prioritising<br />
Providing & maintaining<br />
standards<br />
Identifying & utilising<br />
resources<br />
Team working:<br />
co-ordinating team activities<br />
exchanging information<br />
using authority &<br />
assertiveness<br />
assessing capabilities<br />
supporting o<strong>the</strong>rs<br />
and small teams. At HOSPEX <strong>the</strong> staff <strong>of</strong> <strong>the</strong> entire hospital live<br />
out a simulated hospital day. One <strong>of</strong> <strong>the</strong> main aims is to allow<br />
multidisciplinary teams to rehearse toge<strong>the</strong>r in <strong>the</strong> safety <strong>of</strong> <strong>the</strong><br />
simulated environment. The team in question will be deploying<br />
toge<strong>the</strong>r and so can work, not only on <strong>the</strong>ir clinical skills, but also<br />
on <strong>the</strong>ir team dynamics.<br />
Figure 1: Mannequin based team scenario during HOSPEX<br />
AMSTC uses SimMan® and SimMan 3G® (Laerdal <strong>Medical</strong><br />
Ltd, Orpington, UK) but <strong>the</strong> use <strong>of</strong> simulators has been<br />
associated with a number <strong>of</strong> practical difficulties. The limitations<br />
that <strong>the</strong> original SimMan® imposed due to hard wiring are now<br />
being over come by <strong>the</strong> wireless version, however work-arounds<br />
are required for monitoring (<strong>the</strong> mannequin communicates to<br />
its own monitor and not to that used by <strong>the</strong> DMS) and <strong>the</strong><br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S365–369
Simulation and <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> SJ Mercer, C Whittle , B Siggers et al<br />
more dynamic or visual casualty simulation. The use <strong>of</strong> actors<br />
has developed enormously and a contract has been established<br />
with a civilian casualty make-up artist and “Amputees in Action”<br />
[20], <strong>the</strong> visual impact is now very striking. Although this has a<br />
number <strong>of</strong> advantages <strong>the</strong> Emergency Department team are still<br />
faced with a ‘casualty’ who is physiologically normal, however by<br />
using <strong>the</strong> SimMan® monitor and laptop to display <strong>the</strong> required<br />
physiology, elements <strong>of</strong> technology and live simulation are<br />
combined to create greater fidelity.<br />
Figure 2: View <strong>of</strong> 3 Resuscitation bays during HOSPEX<br />
Ano<strong>the</strong>r difference between <strong>the</strong> scenarios played out at<br />
HOSPEX and those at a high fidelity simulation centre is <strong>the</strong><br />
length <strong>of</strong> simulated case. At HOSPEX it is necessary for cases<br />
to run through <strong>the</strong> Hospital Trainer for 12 hours or more. Areas<br />
which are still being developed include <strong>the</strong> simulation <strong>of</strong> ITU<br />
cases to providing staff with changing physiology over long<br />
periods and, as for <strong>the</strong> Military Operational Surgical Training<br />
(MOST) course, <strong>the</strong> ability to provide simulation <strong>of</strong> surgery and<br />
anaes<strong>the</strong>sia concurrently.<br />
Triservice Anaes<strong>the</strong>tic Apparatus Simulation Course<br />
The tri-service anaes<strong>the</strong>tic apparatus (TSAA) was developed in<br />
<strong>the</strong> 1980s [21] for Air Assault Operations. It is a unique set <strong>of</strong><br />
equipment that is rarely used in <strong>the</strong> NHS and so <strong>the</strong> majority<br />
<strong>of</strong> trainees and new reserve consultants have had no experience<br />
<strong>of</strong> it. Although senior anaes<strong>the</strong>tists are familiar with it, many do<br />
not use it on a regular basis. A high fidelity simulation course<br />
has been developed to deliver training in this equipment. The<br />
course is delivered at <strong>the</strong> Cheshire and Merseyside simulation<br />
centre which uses <strong>the</strong> METI Human Patient Simulator® (<strong>Medical</strong><br />
Education Technologies, Inc., Sarasota, USA) as this can actually<br />
be given an anaes<strong>the</strong>tic. On <strong>the</strong> one-day course <strong>the</strong> anaes<strong>the</strong>tists<br />
and ODPs are introduced to <strong>the</strong> TSAA and to <strong>the</strong> capabilities<br />
<strong>of</strong> <strong>the</strong> simulator as familiarization is also important for effective<br />
non-technical skills [22]. Subsequently four scenarios are run<br />
with each scenario being designed by Military Subject Matter<br />
Experts (SMEs) and civilian simulation staff to combine realistic<br />
medical and equipment related problems and to explore <strong>the</strong> team<br />
dynamics in critical problem solving.<br />
Military Operational Surgery Training Course<br />
Although HOSPEX has an important role in delivering larger<br />
team training, developments in military anaes<strong>the</strong>sia, particularly<br />
<strong>the</strong> management <strong>of</strong> massive transfusion, have driven <strong>the</strong> need to<br />
provide specific clinical training for complex clinical scenarios<br />
not seen in <strong>the</strong> NHS. In 2008 <strong>the</strong> <strong>Defence</strong> Pr<strong>of</strong>essor <strong>of</strong> Surgery<br />
combined several pre-deployment surgical courses into one and at<br />
this stage <strong>the</strong> concept <strong>of</strong> a surgical team-training course emerged.<br />
The authors and colleagues have developed <strong>the</strong> anaes<strong>the</strong>tic<br />
component <strong>of</strong> <strong>the</strong> course and <strong>the</strong> team simulation element. The<br />
course is held at <strong>the</strong> <strong>Royal</strong> College <strong>of</strong> Surgeons (RCS) due to<br />
surgical training requirements and a dedicated simulated operating<br />
<strong>the</strong>atre with a Laerdal SimMan 3G® is used. The simulation based<br />
training is delivered to varying sized teams culminating in full<br />
team resuscitation scenarios. The clinical scenarios, developed<br />
from Operational cases use deployed equipment and are directed<br />
to specific learning objectives.<br />
Figure 3: Team scenario in RCS Team Skills Training Theatre during<br />
MOST course<br />
Although simulation and training in NTS has been undertaken<br />
before by anaes<strong>the</strong>tists and surgeons, MOST has been a clear step<br />
forward in bringing <strong>the</strong> entire surgical team toge<strong>the</strong>r. Future<br />
courses will bring ED staff into <strong>the</strong> team, adding complexity to<br />
<strong>the</strong> team dynamic as well as continuing <strong>the</strong> improvements in<br />
scenario design and fidelity. Ano<strong>the</strong>r aim is to develop an operative<br />
team simulator to improve surgical team training during Damage<br />
Control Resuscitation (DCR) and especially Damage Control<br />
Surgery which is part <strong>of</strong> DCR but although work on integrated<br />
procedure simulators has been described, <strong>the</strong> technology is at an<br />
early stage.<br />
MERT Course<br />
The <strong>Medical</strong> Emergency Response Team (MERT) course<br />
familiarises <strong>the</strong> paramedics, nurses and doctors with <strong>the</strong>ir<br />
operational team, environment and equipment. Clinical scenarios<br />
are exercised in a pre hospital setting, in <strong>the</strong> CH47 trainer and,<br />
airborne, in a C130. SimMan® and SimMan 3G® are used to<br />
rehearse clinical skills and drills such as rapid sequence induction<br />
(RSI). Actors are also used, as at HOSPEX. The final Exercise<br />
exposes <strong>the</strong> team to a mannequin based cardiac arrest scenario in<br />
<strong>the</strong> Hercules (C-130) during a live training flight.<br />
CCAST<br />
The development <strong>of</strong> affordable wireless simulators is changing<br />
<strong>the</strong> way Critical Care Air Support Teams (CCAST) are being<br />
trained. Using a SimMan 3G® <strong>the</strong> clinical instructors can deliver<br />
more realistic scenarios inside <strong>the</strong> C-130 and Chinook (CH-47)<br />
trainers at RAF Lyneham. Future training for both CCAST and<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S365–369 367
Simulation and <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong><br />
<strong>the</strong> Air Transportable Isolator (ATI) will benefit considerably<br />
by <strong>the</strong> improved fidelity and interaction <strong>of</strong> <strong>the</strong> mobile wireless<br />
mannequins. The use <strong>of</strong> simulators is also benefiting <strong>the</strong><br />
CCAST(E) equipment course held at John Radcliffe Hospital,<br />
Oxford, UK. Here candidates familiarise <strong>the</strong>mselves on <strong>the</strong><br />
Aeromedical transfer equipment and <strong>the</strong>n undertake transfer<br />
training initially using patient simulators and <strong>the</strong>n moving on to<br />
transfer patients within <strong>the</strong> hospital.<br />
Simulation for Role One Training<br />
Simulation is also being developed for <strong>the</strong> pre-deployment training<br />
<strong>of</strong> Role 1 clinical staff. A workshop has been held to examine<br />
<strong>the</strong> challenges facing Role 1 personnel [23]. Common <strong>the</strong>mes<br />
included team working, patient evaluation prior to transfer,<br />
equipment familiarisation and communication. Six scenarios<br />
have been developed which include technical and non-technical<br />
learning objectives. There are many aspects <strong>of</strong> NTS which can be<br />
transferred directly into a Role 1 healthcare setting. Simulation<br />
can deliver training in a safe, controlled environment and ensure<br />
that specific learning outcomes are achieved. A pilot course will<br />
take place in <strong>the</strong> near future.<br />
Clinical Fellowship in Simulation in Healthcare<br />
The need for competent instructors with training and experience<br />
<strong>of</strong> simulation and NTS has been recognised [8]. Faculty need to<br />
have a range <strong>of</strong> skills to design and run <strong>the</strong>se courses:<br />
• Generic course design<br />
• Scenario development in conjunction<br />
with subject matter experts<br />
• Control <strong>of</strong> <strong>the</strong> mannequin<br />
• Facilitating scenarios<br />
• Post Scenario debriefing in terms <strong>of</strong><br />
technical and non-technical skills<br />
Whilst <strong>the</strong> DMS has a number <strong>of</strong> anaes<strong>the</strong>tists who have<br />
been trained in recent years through fellowships at simulation<br />
centres <strong>of</strong> excellence, more are needed and <strong>the</strong> development <strong>of</strong><br />
a sizeable cohort will take time. Whilst overseas fellowships are<br />
attractive, internationally recognised simulation centres do exist<br />
in <strong>the</strong> UK, <strong>the</strong> most recent being undertaken at <strong>the</strong> Cheshire and<br />
Merseyside Simulation Centre [24]. Such fellowships combine<br />
<strong>the</strong> opportunity to maintain clinical skills whilst embarking on<br />
formal training in simulation and medical education. Interested<br />
DMS trainees are strongly encouraged to contact <strong>the</strong>ir <strong>Defence</strong><br />
Pr<strong>of</strong>essors for fur<strong>the</strong>r information.<br />
Conclusions<br />
<strong>Defence</strong> medicine is catching up rapidly with <strong>the</strong> growth in<br />
civilian simulation training and in some areas is taking a lead.<br />
The organisation is already a national leader in surgical trauma<br />
team training and an international exemplar in macro-simulation.<br />
Roles for simulation do not end with <strong>the</strong> areas described above. In<br />
<strong>the</strong> future, operational experience may not be so easily achieved as<br />
it is at present and simulation may be able to deliver elements <strong>of</strong><br />
<strong>the</strong> Military <strong>Anaes<strong>the</strong>sia</strong> Higher Training Module. Revalidation<br />
is also an area in which simulation may find a place in <strong>the</strong> future.<br />
The joint working with surgical colleagues to deliver MOST is<br />
developing important links with <strong>the</strong> <strong>Royal</strong> College <strong>of</strong> Anaes<strong>the</strong>tists<br />
(RCOA) and RCS. However, all those involved in <strong>Defence</strong><br />
Simulation must liaise closely with civilian simulation and<br />
educational bodies such as The Association for Simulated Practice<br />
368<br />
SJ Mercer, C Whittle , B Siggers et al<br />
in Healthcare and <strong>the</strong> Society for Education in <strong>Anaes<strong>the</strong>sia</strong> (UK)<br />
to ensure that valuable resources and expertise are used to best<br />
effect. The creation <strong>of</strong> a joint Senior Lecturer post in <strong>Anaes<strong>the</strong>sia</strong><br />
Education with <strong>the</strong> <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine and <strong>the</strong><br />
RCOA will assist here and also encourage research in this field.<br />
There is enormous scope for fur<strong>the</strong>r development in this area<br />
<strong>of</strong> clinical training, and for those with an interest in medical<br />
education, opportunities for involvement, including simulation<br />
fellowships, should be encouraged to ensure <strong>the</strong> future delivery <strong>of</strong><br />
<strong>Defence</strong> medical simulation.<br />
References<br />
1. Flanagan B, Nestel D, Joseph M. Making patient safety <strong>the</strong> focus:<br />
Crisis Resource Management in <strong>the</strong> undergraduate curriculum.<br />
Med Edu 2004; 38: 56–66.<br />
2. Arora S, Sevdalis N. Hospex and Concepts <strong>of</strong> Simulation. JR <strong>Army</strong><br />
Med <strong>Corps</strong> 2008; 154: 202-205.<br />
3. Carter DF. Man-made man: anes<strong>the</strong>siological medical human<br />
simulator. J Assoc Adv Med Instrum 1969; 3: 80–6.<br />
4. Glavin R. Simulation in Anes<strong>the</strong>sia and Acute Care Settings.<br />
EUROANAESTHESIA 2005: Annual Meeting <strong>of</strong> <strong>the</strong> European<br />
Society <strong>of</strong> Anaes<strong>the</strong>siology Vienna, Austria, May 28–31, 2005.<br />
European <strong>Journal</strong> <strong>of</strong> Anaes<strong>the</strong>siology. 2005; 22: 1-222.<br />
5. Miller RB. Psychological considerations in <strong>the</strong> design <strong>of</strong> training<br />
equipment. Report no. WADSC-TR-54-563, AD 71202. Wright<br />
Patterson Air Force Base, OH: Wright Air Development Center,<br />
1953.<br />
6. Weller J, Wilson L, Robinson B. Survey <strong>of</strong> change in practice<br />
following simulation-based training in crisis management.<br />
<strong>Anaes<strong>the</strong>sia</strong> 2003; 58: 471-479.<br />
7. Mercer SJ, Frazer RS. Simulation in <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong>. JR <strong>Army</strong><br />
Med <strong>Corps</strong> 2010; 156: 60.<br />
8. Department <strong>of</strong> Health. (2009). 150 years <strong>of</strong> <strong>the</strong> Annual Report<br />
<strong>of</strong> <strong>the</strong> Chief <strong>Medical</strong> Officer: On <strong>the</strong> state <strong>of</strong> public health 2008.<br />
Available at: http://www.dh.gov.uk/en/Publicationsandstatistics/<br />
Publications/AnnualReports/DH_096206 [accessed on 14 July<br />
2009].<br />
9. Helmreich RL. On error management: lessons from aviation. BMJ<br />
2000; 320; 781-785.<br />
10. Mallory S, Weller J, Bloch M, Maze M. The individual, <strong>the</strong> system,<br />
and medical error. BrJ Anaesth CEPD Reviews 2003; 6: 179-182.<br />
11. National Patient Safety Agency. Module 6. Why do errors occur?<br />
An introduction to human error. 2008. Available at: http://<br />
www.healthcareworkforce.nhs.uk/eventssuite/slideshow/booklet/<br />
Module%206%20-%20An%20Intro%20to%20Human%20<br />
Factors%20-%20Print%20double%20sided%20two%20<br />
slide%20to%20a%20page.pdf [accessed 20 May 2010].<br />
12. Bromiley M. Have you ever made a mistake? <strong>Royal</strong> College <strong>of</strong><br />
Anaes<strong>the</strong>tists Bulletin 2008; 48: 2442-5.<br />
13. Dyer O. Doctors suspended for removing wrong kidney.<br />
BMJ 2004; 328: 246.<br />
14. Holbrook J. The criminalisation <strong>of</strong> fatal medical mistakes. BMJ<br />
2003; 327: 1118-1119.<br />
15. Kohn LT, Corrigan JM, Donaldson MS. To Err is Human -<br />
Building a Safer Health System. Washington: National Academy<br />
Press 1999.<br />
16. Gaba DM, Fish KJ, Howard SK. Crisis management in<br />
anes<strong>the</strong>siology. New York: Churchill Livingstone 1994.<br />
17. Fletcher GC, McGeorge P, Flin RH, Glavin RJ, Maran NJ. The role<br />
<strong>of</strong> non-technical skills in anaes<strong>the</strong>sia: a review <strong>of</strong> current literature.<br />
BrJ Anaesth 2002; 88: 418-29.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S365–369
Simulation and <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> SJ Mercer, C Whittle , B Siggers et al<br />
18. Gawande AA, Zinner MJ, Studdert DM, Brennan TA. Analysis<br />
<strong>of</strong> errors reported by surgeons at three teaching hospitals. Surgery<br />
2003; 133: 614–21.<br />
19. Issenberg, SB, Mcgaghie WC Petrusa ER et al. Features and uses <strong>of</strong><br />
high-fidelity medical simulations that lead to effective learning: a<br />
BEME systematic review. Med Teach 2005; 27: 10-28.<br />
20. Amputees in Action. Available at: http://www.amputeesinaction.<br />
co.uk/ [accessed 20 May 2010].<br />
21. Houghton I. The Triservice anaes<strong>the</strong>tic apparatus. <strong>Anaes<strong>the</strong>sia</strong><br />
1981; 36: 1094-1108.<br />
22. Rall M, Gaba D. Human Performance and Patient Safety. In Miller<br />
R (editor). Miller´s Anes<strong>the</strong>sia, 3021-72. Philadelphia: Elsevier<br />
Churchill Livingstone, 2005.<br />
23. Mercer SJ, Howell M, Simpson R. Simulation training for <strong>the</strong><br />
Frontline- realistic preparation for Role 1 doctors. JR <strong>Army</strong> Med<br />
<strong>Corps</strong> 2010; 156: 87-89.<br />
24. Mercer SJ, Jones N, Guha A. A Clinical Fellowship in Simulation in<br />
Healthcare. BMJ Careers, 13 February 2010. Available from: http://<br />
careers.bmj.com/careers/advice/view-article.html?id=20000744.<br />
[accessed 10 February 2010].<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S365–369 369
Equipment
Use <strong>of</strong> Transoesophageal Echocardiography<br />
during <strong>the</strong> Peri-operative Period for Trauma<br />
Patients.<br />
K Smyth 1 , R Hebballi 2 , MK Peterson 3<br />
1 Specialist Registrar in Anaes<strong>the</strong>tics and Intensive Care Medicine, <strong>Royal</strong> Air Force, University Hospitals <strong>of</strong> Leicester<br />
NHS Trust, Glenfield Hospital, Groby Road, Leicester; 2 Consultant in Cardiothoracic <strong>Anaes<strong>the</strong>sia</strong>, University Hospitals<br />
<strong>of</strong> Leicester NHS Trust, Glenfield Hospital, Groby Road, Leicester; 3 Consultant in Anaes<strong>the</strong>tics and Intensive Care<br />
Medicine, <strong>Royal</strong> Air Force, Frimley Park NHS Foundation Trust, MDHU, Portsmouth Road, Frimley.<br />
Abstract<br />
The medical facility at Camp Bastion continues to evolve as a consequence <strong>of</strong> <strong>the</strong> increased throughput <strong>of</strong> battlefield trauma<br />
patients. There is a requirement for rapid and accurate diagnosis <strong>of</strong> haemodynamic instability and continued haemodynamic<br />
monitoring throughout <strong>the</strong> peri-operative period. Transoesophageal echocardiography (TOE) has been used for this purpose<br />
in <strong>the</strong> arena <strong>of</strong> cardiac anaes<strong>the</strong>sia since <strong>the</strong> mid 1980s. It is being introduced to o<strong>the</strong>r peri-operative settings where severe<br />
haemodynamic instability is expected. The old proverb: ‘There are none so blind as those who cannot see’ (Jeremiah 5:21)<br />
is applicable to this topic, in that TOE is proven to be a rapid, portable, safe and effective tool in <strong>the</strong> assessment <strong>of</strong> <strong>the</strong><br />
haemodynamically unstable patient. This paper explores <strong>the</strong> application <strong>of</strong> TOE for <strong>the</strong> assessment <strong>of</strong> <strong>the</strong> major causes <strong>of</strong><br />
haemodynamic instability in <strong>the</strong> trauma population.<br />
Introduction<br />
British military forces are currently committed to Operation<br />
HERRICK in Afghanistan. The medical support includes a<br />
Role IIE (enhanced) medical facility at Camp Bastion, Helmand<br />
Province, Afghanistan. The facility was initially designed as a<br />
surgical resuscitation node with limitation <strong>of</strong> clinical imaging,<br />
laboratory support and holding ability. As <strong>the</strong> operational<br />
workload has increased <strong>the</strong> facility has greatly expanded, but<br />
continues to be supported by a multi-national Role III facility<br />
at Kandahar. Records show that <strong>the</strong> majority <strong>of</strong> cases present as<br />
a consequence <strong>of</strong> traumatic injuries sustained in <strong>the</strong> battlefield<br />
[1,2]. The majority <strong>of</strong> <strong>the</strong> caseload presented for orthopaedic<br />
management <strong>of</strong> traumatic injury to <strong>the</strong> limbs. There was a wide<br />
variation in <strong>the</strong> severity <strong>of</strong> injuries, with 36% presenting with an<br />
injury severity score <strong>of</strong> greater than 16 during <strong>the</strong> period April 2006<br />
to July 2008 [2]. Battlefield injuries are incited by external forces<br />
produced by blast, deceleration and concussion, ei<strong>the</strong>r in isolation<br />
or in combination. It is well recognised that <strong>the</strong>se mechanisms<br />
can affect central structures in addition to <strong>the</strong> limbs [3-5]. Severe<br />
central vascular injury occurred in 27 UK military trauma patients<br />
during <strong>the</strong> period 2003-2007, with only 3 patients surviving [6].<br />
This is reported as <strong>the</strong> most common unsuspected visceral injury<br />
resulting in death in civilian accident victims [7]. In consideration<br />
<strong>of</strong> <strong>the</strong> potential compound pathology <strong>of</strong> <strong>the</strong> cases and <strong>of</strong> <strong>the</strong><br />
expansion <strong>of</strong> facilities at <strong>the</strong> Role IIE hospital, it seems reasonable<br />
to have access to accurate, rapid and portable imaging <strong>of</strong> <strong>the</strong> heart<br />
and great vessels. Transoesphageal Echocardiography (TOE) is<br />
becoming more established in <strong>the</strong> peri-operative period <strong>of</strong> civilian<br />
trauma patients [8-10]. The quality <strong>of</strong> images acquired with TOE<br />
is equivalent to that acquired by helical computed tomography<br />
Corresponding Author: Dr R Hebballi, Consultant in<br />
Cardiothoracic <strong>Anaes<strong>the</strong>sia</strong>, University Hospitals <strong>of</strong> Leicester<br />
NHS Trust, Glenfield Hospital, Groby Road,<br />
Leicester LE3 9QP<br />
Tel: 0300 303 1573 E-mail: hebballiravi@hotmail.com<br />
MINOR CAUSES MAJOR CAUSES<br />
Left ventricular systolic<br />
dysfunction<br />
Right ventricular systolic<br />
dysfunction<br />
Low systemic vascular<br />
resistance<br />
Dynamic left ventricular<br />
outflow obstruction<br />
Valvular pathology<br />
Massive pleural effusion<br />
Pericardial compression Ventricular septal rupture<br />
Hypovolaemia Pulmonary embolus<br />
Reduced left ventricular Traumatic myocardial<br />
compliance<br />
contusion<br />
Mitral regurgitation<br />
Abnormal heart rhythm<br />
Tension pneumothorax<br />
Table 1: Causes <strong>of</strong> haemodynamic disturbance that may be diagnosed<br />
by TOE.<br />
and magnetic resonance imaging for <strong>the</strong> assessment <strong>of</strong> aortic<br />
lesions [11-14]. The only exception being that <strong>the</strong> air space <strong>of</strong> <strong>the</strong><br />
trachea produces a blind spot in <strong>the</strong> distal ascending aorta and <strong>the</strong><br />
proximal aortic arch. The ability <strong>of</strong> TOE to predictably provide<br />
high quality images <strong>of</strong> <strong>the</strong> heart and guide surgical intervention<br />
has been well established in cardiac surgical patients [15-20].<br />
TOE has clear benefits over standard haemodynamic<br />
monitoring and <strong>the</strong> pulmonary artery ca<strong>the</strong>ter when assessing<br />
volume status and regional ventricular function [21-22].<br />
Diagnosis <strong>of</strong> some <strong>of</strong> <strong>the</strong> less common causes <strong>of</strong> haemodynamic<br />
instability (Table 1), are difficult to diagnose without some form<br />
<strong>of</strong> imaging. In 2003 <strong>the</strong> American College <strong>of</strong> Cardiology and<br />
American Heart Association Task Force on Practice Guidelines<br />
(ACC/AHA/ASE) published that <strong>the</strong>re was sufficient evidence<br />
<strong>of</strong> improved clinical outcome when TOE was utilised as a<br />
continuous haemodynamic monitor [23]. The mass <strong>of</strong> evidence<br />
supporting <strong>the</strong> utility <strong>of</strong> TOE since 1994 has led to a similar<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S373–379 373
Peri-operative Transoesophageal Echocardiography<br />
revision <strong>of</strong> <strong>the</strong> ‘Practice Guidelines for Peri-Operative TOE by<br />
<strong>the</strong> American Society <strong>of</strong> Anes<strong>the</strong>siologists (ASA) and <strong>the</strong> Society<br />
<strong>of</strong> Cardiovascular Anes<strong>the</strong>siologists’ in May 2010 [24]. They<br />
recommend <strong>the</strong> use <strong>of</strong> TOE when <strong>the</strong> nature <strong>of</strong> <strong>the</strong> planned<br />
surgery or <strong>the</strong> patient’s cardiovascular physiology may precipitate<br />
adverse haemodynamic, pulmonary or neurological sequelae.<br />
Fur<strong>the</strong>rmore, it is recommended for use when life-threatening<br />
circulatory instability persists despite corrective <strong>the</strong>rapy. It has<br />
been consistently demonstrated that examination with TOE can<br />
alter <strong>the</strong> management <strong>of</strong> <strong>the</strong> patient in <strong>the</strong> critical care and postoperative<br />
setting [25-30]. As a consequence, <strong>the</strong> ASA and <strong>the</strong><br />
Society <strong>of</strong> Cardiovascular Anes<strong>the</strong>siologists recommends its use if<br />
<strong>the</strong> clinician expects it will be beneficial and that o<strong>the</strong>r modalities<br />
can not be instituted in a timely manner [24].<br />
Equipment for Transoesophageal Echocardiography<br />
The equipment consists <strong>of</strong> an echocardiography machine toge<strong>the</strong>r<br />
with a TOE probe. Ultrasonic images are formed by <strong>the</strong> reflection<br />
<strong>of</strong> pulses <strong>of</strong> sound from tissues. The frequency <strong>of</strong> sound utilised<br />
in ultrasound is greater than 20 kHz, which is above <strong>the</strong> human<br />
audible frequency range (20 – 20 kHz). TOE probes are fitted<br />
with very high frequency transducers (3.5–7 MHz) to produce<br />
high resolution images. Low frequency transducers (2-4 MHz) are<br />
required in transthoracic echocardiography to penetrate through<br />
<strong>the</strong> chest wall, but <strong>the</strong> resolution is greatly attenuated.<br />
The multiplane angle TOE probe can be moved physically<br />
as well as steered electronically (‘phased array’ system) from 0 0 -<br />
180° to optimise <strong>the</strong> image. Fur<strong>the</strong>r optimisation is achieved<br />
by adjusting: image depth, focal zone, sector width, brightness,<br />
zoom and freeze. Two-dimensional images are supplemented<br />
with Doppler tracking <strong>of</strong> tissue motion. Colour Doppler, pulsed<br />
wave (PW) Doppler and continuous wave Doppler is applied<br />
depending on <strong>the</strong> tissue being analysed.<br />
Echocardiographic Evaluation for Trauma<br />
The American Society <strong>of</strong> Echocardiography (ASE) and <strong>the</strong><br />
Society <strong>of</strong> Cardiovascular Anes<strong>the</strong>siologists (SCA) have developed<br />
guidelines for comprehensive examination <strong>of</strong> <strong>the</strong> heart and great<br />
vessels, suggesting that between 12 and 20 standard views are<br />
required to avoid missing an unsuspected abnormality [31]. It<br />
has been demonstrated that this examination can be performed<br />
expeditiously [32, 33]. Brooks et al [34] reported a mean time<br />
<strong>of</strong> 27 minutes for complete examination in a series <strong>of</strong> patients<br />
presenting with trauma to <strong>the</strong> chest. This was in stark contrast to<br />
76 minutes required for arch aortography. Many algorithms have<br />
been postulated for rapid, focused, goal-directed and simplified<br />
transthoracic echocardiography in trauma and critically ill patients<br />
[35-38]. In a similar manner, <strong>the</strong> order <strong>of</strong> image acquisition for<br />
TOE could be tailored to clinical suspicion.<br />
Assessment <strong>of</strong> Hypovolaemia<br />
Hypovolaemia is <strong>of</strong>ten <strong>the</strong> main contributor to haemodynamic<br />
instability in multiple trauma patients. It appears as a small,<br />
vigorously contracting left ventricle with reduction <strong>of</strong> <strong>the</strong> end<br />
diastolic area (EDA) and end systolic area (ESA). Accurate<br />
measurement <strong>of</strong> <strong>the</strong> areas can be performed using <strong>the</strong> transgastric<br />
mid short axis view. These values have been shown to correlate<br />
well with pre-load [39, 40]. M-mode imaging at <strong>the</strong> level <strong>of</strong><br />
<strong>the</strong> papillary muscles will give <strong>the</strong> impression <strong>of</strong> obliteration<br />
<strong>of</strong> <strong>the</strong> cavity. This is termed ‘kissing’ <strong>of</strong> <strong>the</strong> papillary muscles.<br />
Hypovolaemia is associated with a reduction in <strong>the</strong> diastolic filling<br />
374<br />
K Smyth, R Hebball, MK Peterson<br />
velocity <strong>of</strong> <strong>the</strong> left ventricle (LV). This can be demonstrated by <strong>the</strong><br />
application <strong>of</strong> PW Doppler across <strong>the</strong> mitral valve. The tendency<br />
<strong>of</strong> <strong>the</strong> superior vena cava to collapse when it is under-filled<br />
provides a useful surrogate marker for hypovolaemia. The pressure<br />
across <strong>the</strong> wall <strong>of</strong> <strong>the</strong> vessel varies throughout <strong>the</strong> respiratory<br />
cycle, which is manifest by changes in its diameter. A variation in<br />
diameter <strong>of</strong> greater than 36% is indicative <strong>of</strong> hypovolaemia [41].<br />
Assessment <strong>of</strong> Left Ventricular Function<br />
It is vital to differentiate between hypovolaemia and pump failure.<br />
Injury to <strong>the</strong> myocardium can occur as a direct consequence <strong>of</strong><br />
<strong>the</strong> trauma or secondary to ischaemia. Cardiac contusion has<br />
been reported to occur in up to 70% <strong>of</strong> patients with blunt<br />
thoracic trauma [42, 43]. Changes in cardiac isoenzymes,<br />
electrocardiograph and increases in pulmonary artery wedge<br />
pressure may occur later and are insensitive [3, 44, 45].<br />
Global LV function is assessed by viewing <strong>the</strong> contractility and<br />
thickening <strong>of</strong> <strong>the</strong> myocardium. Quantification <strong>of</strong> contractility<br />
is achieved by measuring <strong>the</strong> EDA and ESA in <strong>the</strong> transgastric<br />
mid short axis view (Figure 1). The fractional area change can be<br />
calculated as (EDA-ESA)/EDA x 100. Derivation <strong>of</strong> <strong>the</strong> ejection<br />
fraction, stroke volume and cardiac output from a 2D image<br />
requires <strong>the</strong> application <strong>of</strong> formulae to calculate <strong>the</strong> end diastolic<br />
volume (EDV) and end systolic volume (ESV). The biplane and<br />
single plane ellipsoid methods have been recommended by <strong>the</strong> ASE<br />
[48]. The latter method requires acquisition <strong>of</strong> <strong>the</strong> end diastolic<br />
and end systolic frames from a single mid oesophageal four<br />
chamber loop. The endocardial borders are traced and volume is<br />
calculated (8A 2 /9L) using <strong>the</strong> assumption that <strong>the</strong> LV is ellipsoid.<br />
The volumes are applied to calculate <strong>the</strong> ejection fraction, defined<br />
as (EDV-ESV) / EDV x 100 and stroke volume, defined as EDV-<br />
ESV. Error can be incurred by foreshortening <strong>of</strong> <strong>the</strong> ventricle and<br />
by regional wall motion abnormalities (RWMA). RWMA are<br />
defined as areas <strong>of</strong> <strong>the</strong> myocardium that do not thicken during<br />
systole (Figure 2). The myocardium has been divided into 16<br />
anatomical segments to facilitate matching <strong>of</strong> <strong>the</strong> RWMA to its<br />
concomitant blood supply [31]. Five echocardiographic views are<br />
required to visualise all <strong>of</strong> <strong>the</strong>se segments.<br />
Figure 1. Assessment <strong>of</strong> left ventricular function (Transgastric mid<br />
short axis view). Doppler has been applied across <strong>the</strong> left ventricle.<br />
Movement <strong>of</strong> <strong>the</strong> inferior and anterior walls are plotted against time<br />
(M mode). EF, ejection fraction; FS, fractional shortening; LVIDs,<br />
left ventricular internal diameter in systole; LVIDd, left ventricular<br />
internal diameter in diastole.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S373–379
Peri-operative Transoesophageal Echocardiography K Smyth, R Hebball, MK Peterson<br />
Figure 2. Inferior wall akinesia (Transgastric mid short axis view).<br />
Doppler has been applied across <strong>the</strong> left ventricle. Normal thickening<br />
and movement <strong>of</strong> <strong>the</strong> anterior wall can be seen during systole. In<br />
contrast, <strong>the</strong> inferior wall is akinetic. EF, ejection fraction; FS,<br />
fractional shortening; LVIDs, left ventricular internal diameter in<br />
systole; LVIDd, left ventricular internal diameter in diastole.<br />
Assessment <strong>of</strong> Right Ventricular Function<br />
The right ventricular (RV) wall is most vulnerable to cardiac<br />
contusion by virtue <strong>of</strong> its proximity to <strong>the</strong> sternum. A multicentre<br />
trial demonstrated that 32% <strong>of</strong> 117 patients presenting<br />
with blunt chest trauma suffered damage to <strong>the</strong> right ventricle [3].<br />
The RV is best evaluated in <strong>the</strong> mid oesophageal four-chamber<br />
(Figure 3) and transgastric mid short axis views. Global function<br />
is assessed in a similar way to that discussed for <strong>the</strong> LV.<br />
Pulmonary embolism should always be considered in <strong>the</strong> context<br />
<strong>of</strong> cardiorespiratory deterioration in <strong>the</strong> trauma population. A<br />
large and sudden increase in RV afterload is manifest as: dilatation<br />
and hypokinesis <strong>of</strong> <strong>the</strong> RV, diastolic septal flattening, functional<br />
tricuspid regurgitation and pulmonary hypertension. In severe<br />
cases <strong>the</strong> thrombus can be visualised in <strong>the</strong> proximal pulmonary<br />
arteries or right heart chambers. Small emboli may not produce<br />
any echocardiographic abnormalities.<br />
Figure 3. Assessment <strong>of</strong> right ventricular function (Mid oesophageal<br />
four chamber view). The right sided heart structures are on <strong>the</strong> left<br />
and <strong>the</strong> atria are at <strong>the</strong> apex <strong>of</strong> <strong>the</strong> view. This view shows failure <strong>of</strong> <strong>the</strong><br />
right ventricle with concurrent dilatation <strong>of</strong> <strong>the</strong> right atrium.<br />
Assessment <strong>of</strong> Cardiac Tamponade<br />
Haemopericardium or pericardial effusion can present with<br />
or without frank tamponade. The classical clinical signs <strong>of</strong><br />
tamponade may not be present in <strong>the</strong> mechanically ventilated<br />
patient. Fur<strong>the</strong>r diagnostic difficulty may arise because<br />
<strong>the</strong> collection <strong>of</strong> blood can clot and become loculated in a<br />
specific area. Unclotted blood appears as an echolucent space<br />
encompassing under-filled or collapsed cardiac chambers. It is<br />
best evaluated in <strong>the</strong> four-chamber and transgastric mid short<br />
axis views (Figure 4). It is graded as small (2cm). As little as 1cm has been shown to<br />
cause tamponade [46].<br />
Figure 4. Pericardial effusion and tamponade <strong>of</strong> <strong>the</strong> heart (Transgastric<br />
mid short axis view)<br />
Assessment <strong>of</strong> Valvular Function<br />
The mitral valve (MV) and aortic valve (AV) are at a greater risk<br />
<strong>of</strong> traumatic injury than right-sided valves because <strong>of</strong> <strong>the</strong> higher<br />
pressures in <strong>the</strong> left side <strong>of</strong> <strong>the</strong> heart [42]. The aortic valve is <strong>the</strong><br />
most vulnerable to trauma, with laceration or detachment <strong>of</strong> <strong>the</strong><br />
cusps from <strong>the</strong> aortic annulus occurring [43]. The four standard<br />
views for systematic examination <strong>of</strong> <strong>the</strong> AV are: mid-oesophageal<br />
AV short axis and long axis views; deep transgastric long axis view;<br />
and transgastric long axis view. The most common traumatic<br />
injury to <strong>the</strong> mitral valve is rupture <strong>of</strong> <strong>the</strong> chordae tendinae and<br />
papillary muscles [47]. Examination <strong>of</strong> <strong>the</strong> MV and its apparatus<br />
requires four standard mid oesophageal views and two transgastric<br />
views. Each valve should be assessed using 2D imaging, colour<br />
flow Doppler and spectral Doppler. The normal area <strong>of</strong> <strong>the</strong> AV<br />
is 2.5 cm 2 and that <strong>of</strong> <strong>the</strong> MV is 4-6 cm 2 with pressure gradients<br />
across <strong>the</strong>m being
Peri-operative Transoesophageal Echocardiography<br />
attributed to <strong>the</strong> combination <strong>of</strong> hypovolaemia, increased LV<br />
contractility and reduced afterload. Clinically, it can result<br />
in collapse <strong>of</strong> <strong>the</strong> patient and requires urgent management<br />
with intravenous fluids, vasopressors and beta blockade. The<br />
latter treatment is quite distinct from routine management <strong>of</strong><br />
haemodynamic instability.<br />
Assessment <strong>of</strong> <strong>the</strong> Aorta<br />
TOE is becoming <strong>the</strong> tool <strong>of</strong> choice for <strong>the</strong> diagnosis <strong>of</strong> aortic<br />
dissection and <strong>the</strong> evaluation <strong>of</strong> its complications due to its<br />
high sensitivity and specificity [11-14]. Dissection involving<br />
<strong>the</strong> proximal aorta is best assessed in <strong>the</strong> mid oesophageal AV<br />
long axis view. An intimal flap may be seen to moving freely<br />
within <strong>the</strong> proximal aorta and can prolapse through <strong>the</strong> AV<br />
into <strong>the</strong> outflow tract. Entry and exit points may be identified<br />
using colour flow Doppler. The diagnosis is complicated<br />
when <strong>the</strong> false lumen contains haematoma, with <strong>the</strong> only<br />
echocardiographic finding being thickening <strong>of</strong> <strong>the</strong> wall <strong>of</strong> <strong>the</strong><br />
aorta. Various imaging artifacts can resemble dissection <strong>of</strong> <strong>the</strong><br />
aorta, including <strong>the</strong> presence <strong>of</strong> <strong>the</strong> innominate vein in <strong>the</strong><br />
upper oesophageal aortic arch view.<br />
Rupture <strong>of</strong> <strong>the</strong> aorta is associated with deceleration injury.<br />
The common site <strong>of</strong> injury is <strong>the</strong> isthmus, where <strong>the</strong> aorta is<br />
te<strong>the</strong>red by <strong>the</strong> ligamentum arteriosum just distal to <strong>the</strong> origin <strong>of</strong><br />
<strong>the</strong> subclavian artery. However, <strong>the</strong> site <strong>of</strong> rupture can vary and<br />
it is recommended that <strong>the</strong> whole <strong>of</strong> <strong>the</strong> aorta from <strong>the</strong> arch to<br />
<strong>the</strong> diaphragm is examined. The aorta is imaged in <strong>the</strong> short and<br />
long axis views, starting in <strong>the</strong> upper oesophagus and its course<br />
followed distally. The screen depth should be reduced to 6cm.<br />
The echocardiographic image <strong>of</strong> rupture is typically an intimal<br />
flap with a characteristic free edge (Figure 5). The aorta is usually<br />
surrounded with haematoma and a false aneurysm may be seen.<br />
The diameter <strong>of</strong> <strong>the</strong> aorta should decrease from <strong>the</strong> arch to <strong>the</strong><br />
proximal descending aorta, with even a small increase raising<br />
suspicion <strong>of</strong> rupture.<br />
Figure 5. Dissection <strong>of</strong> <strong>the</strong> descending thoracic aorta with intimal flap<br />
(Descending thoracic aorta short axis view)<br />
Assessment <strong>of</strong> Pleural Cavities<br />
Aerated lung tissue is poorly visualised with echocardiography,<br />
but pleural spaces and pleural fluid can be seen. The left pleural<br />
space is in <strong>the</strong> far field beyond <strong>the</strong> descending thoracic aorta in <strong>the</strong><br />
long and short axis views <strong>of</strong> <strong>the</strong> descending aorta. In <strong>the</strong> short axis<br />
view a pleural effusion is seen as an echo-free space in <strong>the</strong> shape <strong>of</strong><br />
a tigers claw (Figure 6). The right pleural space is in <strong>the</strong> right field<br />
376<br />
K Smyth, R Hebball, MK Peterson<br />
beyond <strong>the</strong> mid-oesophageal four chamber view. Pleural effusions<br />
can cause compression <strong>of</strong> <strong>the</strong> heart and haemodynamic instability<br />
if larger than 1.5 litres.<br />
Figure 6. Left pleural effusion (Descending thoracic aorta short axis<br />
view)<br />
Ventricular Septal Rupture<br />
Rupture <strong>of</strong> <strong>the</strong> ventricular septum can be a direct consequence <strong>of</strong><br />
<strong>the</strong> trauma or a late complication <strong>of</strong> infarction <strong>of</strong> <strong>the</strong> myocardium.<br />
The defect is best identified with <strong>the</strong> application <strong>of</strong> colour flow<br />
Doppler across <strong>the</strong> septum. A turbulent jet on <strong>the</strong> RV side <strong>of</strong> <strong>the</strong><br />
septum or a region <strong>of</strong> flow acceleration on <strong>the</strong> LV side is diagnostic.<br />
Associated findings may include: biventricular dysfunction;<br />
tricuspid regurgitation; and pulmonary hypertension. It should<br />
be remembered that a defect in <strong>the</strong> apex may be missed if <strong>the</strong> view<br />
<strong>of</strong> <strong>the</strong> ventricle is foreshortened.<br />
Safety <strong>of</strong> Transoesophageal Echocardiography<br />
This is an invasive form <strong>of</strong> imaging, but complications are<br />
infrequent provided <strong>the</strong> contra-indications are respected and<br />
care is exercised during manipulation <strong>of</strong> <strong>the</strong> probe. In three<br />
large surveys <strong>the</strong> incidence <strong>of</strong> complications associated with<br />
<strong>the</strong> procedure ranged from 0% to 0.5%, with only one death<br />
being reported. [20, 49, 50] This rate has been consistently<br />
quoted and is comparable to <strong>the</strong> complication rate <strong>of</strong><br />
0.08% to 0.13% associated with upper gastrointestinal tract<br />
endoscopy [51-53]. The most frequently reported symptom<br />
is odynophagia (Table 2). Haemorrhage and oesophageal<br />
perforation occur infrequently and are more likely to occur<br />
in patients with pre-existing upper gastrointestinal pathology.<br />
As a consequence, insertion <strong>of</strong> <strong>the</strong> probe is avoided in patients<br />
with proven or suspected upper gastrointestinal pathology. The<br />
management <strong>of</strong> patients presenting with mild dysphagia in <strong>the</strong><br />
absence <strong>of</strong> proven pathology is controversial. However, <strong>the</strong>re<br />
is evidence that <strong>the</strong>se patients tolerate <strong>the</strong> procedure; under<br />
<strong>the</strong> proviso insertion <strong>of</strong> <strong>the</strong> probe is performed cautiously and<br />
terminated if resistance is met [54]. Failure to insert or advance<br />
<strong>the</strong> probe has been reported to occur in 0.7% <strong>of</strong> sedated adult<br />
patients [49] and in 0.8% <strong>of</strong> anaes<strong>the</strong>tised patients [50]. This<br />
is associated with an increase in <strong>the</strong> incidence <strong>of</strong> injury to <strong>the</strong><br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S373–379
Peri-operative Transoesophageal Echocardiography K Smyth, R Hebball, MK Peterson<br />
COMPLICATION INCIDENCE (%)<br />
Odynophagia 0.1<br />
Swallowing abnormality 0.01<br />
Oesophageal abrasions 0.06<br />
No associated pathology 0.03<br />
Upper gastrointestinal<br />
haemorrhage<br />
0.03<br />
Oesophageal perforation 0.01<br />
Dental injury 0.03<br />
Endotracheal tube<br />
malposition<br />
0.03<br />
Table 2. Complications associated with TOE [50].<br />
oropharynx and odynophagia [55]. It is widely accepted that<br />
<strong>the</strong> procedure should be abandoned ra<strong>the</strong>r than risk injury to<br />
<strong>the</strong> patient.<br />
It has been suggested that prolonged contact <strong>of</strong> <strong>the</strong> probe with<br />
<strong>the</strong> oesophageal mucosa can result in pressure necrosis. It is fur<strong>the</strong>r<br />
proposed that <strong>the</strong>rmal injury from vibration <strong>of</strong> <strong>the</strong> piezoelectric<br />
crystals may be deleterious [55, 56]. Although <strong>the</strong>se hypo<strong>the</strong>ses<br />
have not been supported in animal studies [56], it may occur in<br />
patients suffering from circulatory compromise [57].<br />
Misinterpretation <strong>of</strong> <strong>the</strong> echocardiography data is an obvious<br />
risk, which is why <strong>the</strong> Association <strong>of</strong> Cardiothoracic Anaes<strong>the</strong>tists<br />
(ACTA) and <strong>the</strong> British Society <strong>of</strong> Echocardiography (BSE)<br />
have established a rigorous program for accreditation in<br />
echocardiography.<br />
Accreditation in Transoesophageal<br />
Echocardiography<br />
The Association <strong>of</strong> Cardiothoracic Anaes<strong>the</strong>tists (ACTA) and<br />
<strong>the</strong> British Society <strong>of</strong> Echocardiography (BSE) have jointly<br />
developed a process for training and accreditation in TOE in<br />
<strong>the</strong> UK [58]. It is not a compulsory or regulatory certificate<br />
<strong>of</strong> competence. The model is similar to that produced by <strong>the</strong><br />
BSE for accreditation in transthoracic echocardiography and<br />
is designed to include all specialities that utilise TOE. The<br />
accreditation process consists <strong>of</strong> <strong>the</strong> compilation <strong>of</strong> a logbook<br />
and a written examination [59]. A logbook <strong>of</strong> 125 TOE<br />
studies should be collected and reported on over a period <strong>of</strong> 24<br />
months. Ten <strong>of</strong> <strong>the</strong>se cases, with full reports, should be retained<br />
electronically. A supervisor is appointed by <strong>the</strong> BSE to oversee<br />
<strong>the</strong> compilation <strong>of</strong> <strong>the</strong> logbook and to certify <strong>the</strong> clinical<br />
practice <strong>of</strong> <strong>the</strong> candidate. The written examination consists<br />
<strong>of</strong> 125 single best answer questions covering <strong>the</strong> range <strong>of</strong> <strong>the</strong><br />
syllabus. The BSE states that <strong>the</strong> attainment <strong>of</strong> accreditation<br />
is a minimum standard and candidates will be expected to<br />
begin a process <strong>of</strong> continuing medical education towards reaccreditation.<br />
The re-accreditation process will include evidence<br />
<strong>of</strong> continuing clinical activity, distance learning and attendance<br />
at courses and conferences.<br />
Conclusion<br />
TOE equipment is evolving. Currently emphasis is being<br />
placed on <strong>the</strong> development <strong>of</strong> real time 3-dimensional imaging<br />
and miniaturisation <strong>of</strong> <strong>the</strong> probe. It is envisaged that this will<br />
improve portability and simplify <strong>the</strong> process for acquisition and<br />
interpretation <strong>of</strong> <strong>the</strong> images. The increasing availability <strong>of</strong> TOE<br />
equipment in <strong>the</strong> civilian sector combined with a structured<br />
training process means that it may become a routine tool in <strong>the</strong><br />
peri-operative management <strong>of</strong> unstable trauma patients.<br />
References<br />
1. Ramasamy A, Brooks A, Midwinter M, Stewart MPM, Hinsley D.<br />
Surgical workload during operation Herrick. JR <strong>Army</strong> Med <strong>Corps</strong><br />
2008; 154(3): 185-92<br />
2. Starkey KJ, Hodgetts TJ, Russell R, Mahoney PF. Combat trauma<br />
survival: where is <strong>the</strong> pro<strong>of</strong> <strong>of</strong> good outcomes? JR <strong>Army</strong> Med <strong>Corps</strong><br />
2008; 155(3): 230<br />
3. Garcia-Fernandez, Miguel A, Lopez-Perez, Jose M, et al. Role <strong>of</strong><br />
transoesophageal echocardiography in <strong>the</strong> assessment <strong>of</strong> patients<br />
with blunt chest trauma: Correlation <strong>of</strong> echocardiographic findings<br />
with <strong>the</strong> electrocardiogram and creatinine kinase monoclonal<br />
antibody measurements. Am Heart J 1998; 135(3): 476-81<br />
4. Tenzer ML. The spectrum <strong>of</strong> myocardial contusion: a review. J<br />
Trauma; 25: 620-7<br />
5. Sigler LH. Traumatic injury <strong>of</strong> <strong>the</strong> heart: incidence <strong>of</strong> its occurrence<br />
in forty-two cases <strong>of</strong> severe acidental bodily injury. Am Heart J<br />
1945; 30: 459-60<br />
6. Stannard A, Benson C, Bowley DM, Midwinter M, Tai N. Central<br />
vascular injuries in deployed military personnel. JR <strong>Army</strong> Med<br />
<strong>Corps</strong> 2008; 154(3): 188<br />
7. Leidtke AJ, DeMuth WE. Nonpenetrating cardiac injuries: a<br />
collective review. Am Heart J 1973; 86: 687-97<br />
8. Josephs SA. The use <strong>of</strong> current hemodynamic monitors and<br />
echocardiography in resuscitation <strong>of</strong> <strong>the</strong> critically ill or injured<br />
patient. Int Anes<strong>the</strong>siol Clin 2007; 45:31-59<br />
9. Hwang JJ, Shyu KG, Chen JJ, et al. Usefulness <strong>of</strong> transoesophageal<br />
echocardiography in <strong>the</strong> treatment <strong>of</strong> critically ill patients. Chest<br />
1993; 104: 861-6<br />
10. Colreavy FB, Donovan K, Lee KY, et al. Transoesophageal<br />
echocardiography in critically ill patients. Crit Care Med 2002; 30;<br />
989-96<br />
11. Shiga T, Wajima Z, Apfel C C, Inoue T, Ohe Y. Diagnostic<br />
accuracy <strong>of</strong> transoesophageal echocardiography, helical computed<br />
tomography and magnetic resonance imaging for suspected aortic<br />
dissection: systematic review and meta-analysis. Database <strong>of</strong><br />
Abstracts <strong>of</strong> Reviews <strong>of</strong> Effects 2006; No 12006008319<br />
12. Cinnella G, Dambrosio M, Brienza N, Tullo O, Fiore T.<br />
Transoesophageal echocardiography for diagnosis <strong>of</strong> traumatic<br />
aortic injury: an appraisal <strong>of</strong> <strong>the</strong> evidence. Database <strong>of</strong> Abstracts <strong>of</strong><br />
Reviews <strong>of</strong> Effects 2006; No 12005009446<br />
13. 13. Vignon P, Boncoeur M, Francois B, Rambaud G, Maubon<br />
A, Gastinne H. Comparison <strong>of</strong> multiplane transoesophageal<br />
echocardiography and contrast enhanced helical CT in <strong>the</strong><br />
diagnosis <strong>of</strong> blunt traumatic cardiovascular injuries. Anes<strong>the</strong>siol<br />
2001; 94: 615-22<br />
14. Smith M, Cassidy J, Sou<strong>the</strong>r S et al. Transoesophageal<br />
echocardiography in <strong>the</strong> diagnosis <strong>of</strong> traumatic rupture <strong>of</strong> <strong>the</strong><br />
aorta. N Engl J Med 1995; 332: 356-42<br />
15. Bergquist BD, Bellows WH, Leung JM. Transoesophageal<br />
echocardiography in myocardial revascularisation: influence on<br />
intraoperative decision making. Anesth Analg 1996; 82: 1139-45<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S373–379 377
Peri-operative Transoesophageal Echocardiography<br />
16. Kolev N, Brase R, Swanevelder J, et al. The influence <strong>of</strong><br />
transoesophageal echocardiography on intra-operative decision<br />
making. <strong>Anaes<strong>the</strong>sia</strong> 1998; 53: 767-73<br />
17. Click RL, Abel MD, Schaff HV. Intraoperative transoesphageal<br />
echocardiography: 5-year prospective review <strong>of</strong> impact on surgical<br />
management. Mayo Clin Proc 2000; 75: 241-7<br />
18. Michel-Cherqui M, Ceddaha A, Liu N, et al. Assessment <strong>of</strong><br />
systematic use <strong>of</strong> intraoperative transoesophageal echocardiography<br />
during cardiac surgery in adults: a prospective study <strong>of</strong> 203 patients.<br />
J Cardiothoracic Vasc Anesth 2000; 14: 45-50<br />
19. Couture P, Denault AY, McKenty S, et al. Impact <strong>of</strong> routine use <strong>of</strong><br />
intraoperative transoesophageal echocardiography during cardiac<br />
surgery. Can J Anaesth 2000; 47: 20-6<br />
20. Mishra M, Chauhan R, Sharma KK, et al. Real-time intraoperative<br />
transoesophageal echocardiography. How useful? Experience <strong>of</strong><br />
5016 cases. J Cardiothorac Vasc Anesth 1998; 12: 625-32<br />
21. Rose DD. Transoesophageal echocardiography as an alternative<br />
for <strong>the</strong> assessment <strong>of</strong> <strong>the</strong> trauma and critical care patient. AANA<br />
<strong>Journal</strong> 2003; 71(3): 223-8<br />
22. Schulmeyer MCC, Santelices E, Vega R, Schmied S. Impact<br />
<strong>of</strong> intraoperative transoesophageal echocardiography during<br />
noncardiac surgery. J Cardiothorac Vasc Anesth 2006; 20: 768-71<br />
23. Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/<br />
AHA/ASE 2003 Guideline update for <strong>the</strong> clinical application <strong>of</strong><br />
echocardiography: Summary article. Circ 2003; 108:1146-62<br />
24. Thys DM, Abel MD, Brooker RF, Cahalan MK, et al. Practice<br />
guidelines for perioperative transoesophageal echocardiography:<br />
An updated report by <strong>the</strong> American Society <strong>of</strong> Anes<strong>the</strong>siologists<br />
and <strong>the</strong> Society <strong>of</strong> Cardiovascular Anes<strong>the</strong>siologists task force on<br />
tranesophageal echocardiography. Anes<strong>the</strong>siol 2010; 112(5): 1-6<br />
25. Orme RMLE, Oram MP and McKinstry CE. Impact <strong>of</strong><br />
echocardiography on patient management in <strong>the</strong> intensive care<br />
unit: an audit <strong>of</strong> district general hospital practice. Brit J Anaes.<br />
2009; 102(3): 340-4<br />
26. Hwang J-J, Shyu K-G, Chin J-J, et al. Usefulness <strong>of</strong> transesophageal<br />
echocardiography in <strong>the</strong> treatment <strong>of</strong> critically ill patients. Chest<br />
1993; 104(3): 861-6<br />
27. Denault AY, Couture P, McKenty S, et al. Perioperative use <strong>of</strong><br />
tranesophageal echocardiography by anes<strong>the</strong>siologists: impact in<br />
noncardiac surgery and <strong>the</strong> intensive care unit. Can J Anesth 2002;<br />
49(3):287-93<br />
28. Suriani RJ, Neustein S, Shore-Lesserson, L, et al. Intraoperative<br />
transesophageal echocardiography during noncardiac surgery. J<br />
Cardiothorac and Vasc Anesth 1998; 12(3): 274-80<br />
29. Vignon P, Mentex H, Terre S, et al. Diagnostic accuracy<br />
and <strong>the</strong>rapeutic impact <strong>of</strong> transthoracic and transesophageal<br />
echocardiography in mechanically ventilated patients in <strong>the</strong> ICU.<br />
Chest 1994; 106: 1829-34<br />
30. Colreavy FB, Donovan K, Lee KY, et al. Transesophageal<br />
echocardiography in critically ill patients. Crit Care Med 2002;<br />
30(5): 989-96<br />
31. Shanewise JS, Cheung AT, Aronson S, et al. ASE/SCA<br />
guidelines for performing a comprehensive intraoperative<br />
multiplane transoesophageal echocardiographic examination:<br />
recommendations <strong>of</strong> <strong>the</strong> American Society <strong>of</strong> Echocardiography<br />
Council for Intraoperative Echocardiography and <strong>the</strong> Society <strong>of</strong><br />
Cardiovascular Anes<strong>the</strong>siologists Task Force for Certification in<br />
Perioperative Transesophageal Echocardiography. Anes<strong>the</strong>sia and<br />
Analgesia 1999; 89: 870-884<br />
378<br />
K Smyth, R Hebball, MK Peterson<br />
32. Mallod M and Felner J. Transesophageal echocardiography in <strong>the</strong><br />
evaluation <strong>of</strong> cardiothoracic trauma. Am Heart J 1996; 132(4):<br />
841-9<br />
33. Brooks SW, Cmolik BL, Young JC, Townsend RN, Diamond DL.<br />
Transesophageal echocardiographic examination <strong>of</strong> a patient with<br />
traumatic aortic transection from blunt chest trauma. J Trauma<br />
1991; 31: 841-5<br />
34. Brooks SW, Young JC, Cmolik B, et al. The use <strong>of</strong> transesophageal<br />
echocardiography in <strong>the</strong> evaluation <strong>of</strong> chest trauma. J Trauma<br />
1992; 32: 761-8<br />
35. Breitkreutz R, Walcher F, Seeger FH. Focused echocardiographic<br />
evaluation in resuscitation management: concept <strong>of</strong> an ALSconformed<br />
algorithm. Crit Care Med. 2007; 35: S150–S161<br />
36. Pershad J, Myers S, Plouman C, et al. Bedside limited<br />
echocardiography by <strong>the</strong> emergency physician is accurate during<br />
evaluation <strong>of</strong> <strong>the</strong> critically ill patient. Pediatrics 2004; 114: e667–<br />
e671<br />
37. Vignon P, Dugard A, Abraham J, et al. Focused training for goaloriented<br />
hand-held echocardiography performed by noncardiologist<br />
residents in <strong>the</strong> ICU. Intensive Care Med. 2007; 33: 1795–1799<br />
38. Beaulieu Y. Specific skill set and goals <strong>of</strong> focused echocardiography<br />
for critical care clinicians. Crit Care 2007; 35: S144–S149<br />
39. Scheuren K, Wente MN, Hainer C, et al. Left ventricular enddiastolic<br />
area is a measure <strong>of</strong> cardiac preload in patients with early<br />
septic shock. Eur J Anaes<strong>the</strong>siol 2009; 26: 759-65<br />
40. Thys DM, Hillel Z, Goldman ME et al. A comparison <strong>of</strong><br />
haemodynamic indices derived by invasive monitoring and twodimensional<br />
echocardiography. Anes<strong>the</strong>siol 1987; 67: 630-4<br />
41. Viellard-Baron A, Chergui K, Rabiller A, et al. Superior vena<br />
caval collapsibility as a gauge <strong>of</strong> volume status in ventilated septic<br />
patients. Intensive Care Med 2004; 30: 1734-9<br />
42. Tenzer ML. The spectrum <strong>of</strong> myocardial contusion: a review. J<br />
Trauma 1985; 25: 620-7<br />
43. Sigler, LH. Traumatic injury <strong>of</strong> <strong>the</strong> heart: incidence <strong>of</strong> its occurrence<br />
in forty-two cases <strong>of</strong> severe accidental bodily injury. Am Heart J<br />
1945; 30: 459-60<br />
44. Potkin RT, Werner JA, Trobaugh GB, et al. Evaluation <strong>of</strong><br />
noninvasive tests <strong>of</strong> cardiac damage in suspected cardiac contusion.<br />
Circ 1982; 66: 627-31<br />
45. Dolara A, Morando P, Pampaloni M. Echocardiographic findings<br />
in 98 consecutive nonpenetrating chest injuries. Dis Chest 1967;<br />
52: 50-6<br />
46. Bommer WJ, Follette D, Pollock M, et al. Tamponade in patients<br />
undergoing cardiac surgery: a clinical-echocardiographic diagnosis.<br />
Am Heart J 1995; 130: 1216-1223<br />
47. Perez de Prado A, Garcia-Fernandez MA, Barambio M, et al.<br />
Isolated mitral valve rupture caused by nonpenetrating trauma:<br />
recognition by transesophageal echocardiography. Am Heart J<br />
1995; 129: 1032-4<br />
48. Schiller NB, Shah PM, Crawford M, et al. Recommendations<br />
for quantification <strong>of</strong> <strong>the</strong> left ventricle by two-dimensional<br />
echocardiography. American Society <strong>of</strong> Echocardiography<br />
Committee on standards, subcommittee on quantification <strong>of</strong> two<br />
dimensional echocardiograms. J <strong>of</strong> Am Soc Echocardiography 1989;<br />
2: 358-367<br />
49. Daniel WG, Erbel R, Kasper W, et al. Safety <strong>of</strong> transesophageal<br />
echocardiography: a multi center survey <strong>of</strong> 10,419 examinations.<br />
Circ 1991; 83: 817-21<br />
50. Kallmeyer IJ, Collard CD, Fox JA, Body SC and Shernan SK. The<br />
safety <strong>of</strong> intraoperative transesophageal echocardiography: a case<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S373–379
Peri-operative Transoesophageal Echocardiography K Smyth, R Hebball, MK Peterson<br />
series <strong>of</strong> 7200 cardiac surgical patients. Anesth Analg 2001; 92:<br />
1126-30<br />
51. Steward JB, Khandheria BK, Oh JK, et al. Critical appraisal<br />
<strong>of</strong> transesophageal echocardiography: limitations, pitfalls and<br />
complications. J Am Soc Echocardioogr 1992; 5: 288-305<br />
52. Khandheria BK. The transesophageal echocardiographic<br />
examination: is it safe? Echocardiography 1994; 11: 55-63<br />
53. Silvis SE, Nebel O, Rogers G, et al. Endoscopic complications:<br />
results <strong>of</strong> <strong>the</strong> 1974 American Society for Gastrointestinal<br />
Endoscopy Survey. JAMA 1976; 235: 928-30<br />
54. Chan KL, Cohen GI, Sochowski RA, Baird MG. Complications<br />
<strong>of</strong> transesophageal echocardiography in ambulatory adult patients:<br />
analysis <strong>of</strong> 1500 consecutive examinations. J Am Soc Echocardiogr<br />
1991; 4: 577-82<br />
55. Savino JS, Hanson CW, Bigelow DC, et al. Oropharyngeal injury<br />
after transesophageal echocardiography. J Cardiothorac Vasc Anesth<br />
1994; 8: 76-8<br />
56. Urbanowicz JH, Kern<strong>of</strong>f RS, Oppenheim G, et al. Transesophageal<br />
echocardiography and its potential for esophageal damage.<br />
Anes<strong>the</strong>siol 1990; 72: 40-3<br />
57. Kharasch ED, Sivarajan M. Gastroesophageal perforation after<br />
intraoperative transesophageal echocardiography. Anes<strong>the</strong>siol 1996;<br />
85: 426-8<br />
58. Monaghan M, Chambers J, Leech G, et al. Training in<br />
echocardiography: British Society <strong>of</strong> Echocardiography Guidelines.<br />
Brit Heart J 1994; 71: S2-5<br />
59. British Society <strong>of</strong> Echocardiography. http://www.bsecho.org<br />
Accessed June 30, 2010<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S373–379 379
The Triservice Anaes<strong>the</strong>tic Apparatus: A Review<br />
RS Frazer 1 , DJ Birt 2<br />
1 Consultant in <strong>Anaes<strong>the</strong>sia</strong>, SO1 Clinical, HQ 2 Med Bde, Strensall, York; 2 Consultant in <strong>Anaes<strong>the</strong>sia</strong>, MDHU<br />
Derriford, Derriford Hospital, Plymouth.<br />
Abstract<br />
The Triservice Anaes<strong>the</strong>tic Apparatus was designed around 30 years ago as a robust and highly portable anaes<strong>the</strong>sia delivery<br />
system for medical support to airborne operations and it has been <strong>the</strong> core anaes<strong>the</strong>sia system for <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services<br />
since <strong>the</strong>n. Over this period <strong>the</strong>re have been a number <strong>of</strong> equipment changes but issues remain which are in part mitigated by<br />
recent training developments. This article reviews <strong>the</strong>se changes and developments and considers <strong>the</strong> future <strong>of</strong> this equipment.<br />
Introduction<br />
The Triservice Anaes<strong>the</strong>tic Apparatus (TSAA) was designed by<br />
Brigadier Ivan Houghton to improve <strong>the</strong> provision <strong>of</strong> surgical<br />
services to 23 Parachute Field Ambulance and was first described<br />
in <strong>Anaes<strong>the</strong>sia</strong> in 1981 [1]. It was designed to be robust, portable<br />
and minimally dependent on resources. Over <strong>the</strong> years it has been<br />
modified and although it has been replaced by a conventional<br />
anaes<strong>the</strong>tic machine at <strong>the</strong> UK deployed R3 facility in Camp<br />
Bastion, it remains in service as <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services<br />
(DMS) core anaes<strong>the</strong>tic equipment for contingent Operations.<br />
This article describes <strong>the</strong> history <strong>of</strong> <strong>the</strong> TSAA, its components<br />
and philosophy <strong>of</strong> use. We will highlight developments and issues<br />
over <strong>the</strong> years.<br />
Draw-over <strong>Anaes<strong>the</strong>sia</strong><br />
The delivery <strong>of</strong> anaes<strong>the</strong>sia in austere environments, including<br />
military operations depends on equipment with a minimal<br />
requirement for resources and infrastructure. For example,<br />
compressed gas cylinders are heavy, cumbersome and dangerous<br />
to move and, although a modern field surgical team would not<br />
have to exist without electricity, anaes<strong>the</strong>tic equipment that can<br />
continue to function during an interruption in supply is clearly<br />
an advantage. Table 1 lists suggested characteristics <strong>of</strong> anaes<strong>the</strong>tic<br />
equipment for use in austere environments. Regional and total<br />
intravenous anaes<strong>the</strong>sia also meet a number <strong>of</strong> <strong>the</strong>se requirements<br />
but draw-over techniques maintain <strong>the</strong>ir popularity amongst <strong>the</strong><br />
increasing competition.<br />
• Minimal reliance on compressed gases and electrical<br />
supplies<br />
• Robust<br />
• Compact and portable<br />
• Simple to operate<br />
• Able to withstand climatic extremes<br />
• Easily maintained and serviced<br />
• Economical in use<br />
• Versatile in <strong>the</strong> use <strong>of</strong> volatile agents<br />
• Versatile with regard to patient age/size<br />
Table 1. Anaes<strong>the</strong>tic system requirements for austere environments<br />
Corresponding author: Lt Col RS Frazer, SO1 Clinical,<br />
HQ 2 Med Bde, Strensall, York. YO32 5SW.<br />
Tel: 01904 442611 Fax: 01904 442689<br />
Email: scottfrazer@doctors.net.uk<br />
In its simplest form draw-over anaes<strong>the</strong>sia requires a suitable<br />
vaporiser and a one-way or non-return patient valve. In contrast to<br />
conventional anaes<strong>the</strong>tic machines which pass gases under pressure<br />
through flow meters and a vaporiser, draw-over systems rely on<br />
atmospheric air, usually enriched by oxygen, as <strong>the</strong> main carrier<br />
gas. During draw-over anaes<strong>the</strong>sia <strong>the</strong> patient’s respiratory effort<br />
moves air through <strong>the</strong> vaporiser in proportion to <strong>the</strong>ir minute<br />
ventilation. This requires a very low resistance system and <strong>the</strong><br />
ability to maintain vapour output despite wide variations in flow.<br />
The TSAA<br />
There are still a number <strong>of</strong> draw-over vaporisers available for<br />
use. Examples include <strong>the</strong> Epstein-Macintosh-Oxford (EMO),<br />
<strong>the</strong> Ohmeda Portable <strong>Anaes<strong>the</strong>sia</strong> Complete (PAC) and <strong>the</strong><br />
Oxford Miniature Vaporiser (OMV, Penlon, Oxford, UK).<br />
Despite <strong>the</strong> overwhelming numerical superiority <strong>of</strong> plenum<br />
vaporisers worldwide, developments in drawover vaporiser<br />
design continue [2].<br />
Figure 1: The OMV50<br />
The TSAA is designed around a modified OMV50. This has<br />
a capacity <strong>of</strong> 50mls <strong>of</strong> volatile agent, three fold-out “feet” and an<br />
interchangeable concentration indicator scale (Figure 1). Although<br />
some drawover vaporisers are temperature compensated, <strong>the</strong><br />
OMV50 is described as <strong>the</strong>rmally buffered. Changes in vapour<br />
output with temperature are smoo<strong>the</strong>d by <strong>the</strong> mass <strong>of</strong> metal in <strong>the</strong><br />
vaporiser and <strong>the</strong> presence <strong>of</strong> “Forlife” antifreeze in <strong>the</strong> base. As<br />
originally described two OMVs were used in series, one delivering<br />
halothane and <strong>the</strong> o<strong>the</strong>r trichloroethylene (TCE). This combined<br />
380 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S380–384
The Triservice Anaes<strong>the</strong>tic Apparatus RS Frazer, DJ Birt<br />
<strong>the</strong> analgesic properties <strong>of</strong> TCE with <strong>the</strong> anaes<strong>the</strong>tic properties<br />
<strong>of</strong> halothane. Reversible calibrated indicator scales were fitted for<br />
<strong>the</strong>se 2 agents. Subsequently scales became available for Is<strong>of</strong>lurane<br />
and this has been <strong>the</strong> agent <strong>of</strong> choice in later years.<br />
Circuit<br />
The o<strong>the</strong>r key component <strong>of</strong> any drawover anaes<strong>the</strong>sia circuit<br />
is <strong>the</strong> one-way patient valve. Although a number <strong>of</strong> options are<br />
available, Brig Houghton chose a Laerdal valve which was part<br />
<strong>of</strong> a set including a Self-inflating Bag (SIB), which provided <strong>the</strong><br />
means for manual ventilation. The system is still in existence<br />
today as <strong>the</strong> Resuscitator® (Laerdal <strong>Medical</strong> Ltd, Orpington,<br />
UK). In order to appropriately extend <strong>the</strong> circuit, corrugated<br />
silicone rubber tubing is used (Figure 2). Silicone rubber was<br />
originally specified because it was autoclavable, but it makes for<br />
a heavy system by modern standards. It should be noted at this<br />
stage that all <strong>of</strong> <strong>the</strong> connections in <strong>the</strong> circuit have cagemount<br />
(23.1mm) fittings (although <strong>the</strong> OMV50 can be supplied with<br />
22mm fittings if required).<br />
Figure 2: A common configuration for spontaneous respiration. For<br />
clarity <strong>the</strong> monitoring set-up is not shown.<br />
Although a number <strong>of</strong> variations are possible, <strong>the</strong> most common<br />
arrangement for spontaneous respiration is described here (Figure<br />
2). From <strong>the</strong> patient end, <strong>the</strong> one-way valve is connected to<br />
<strong>the</strong> SIB by a length <strong>of</strong> corrugated cage-mount tubing, <strong>the</strong> SIB<br />
is connected to <strong>the</strong> OMV50s by ano<strong>the</strong>r length <strong>of</strong> tubing and<br />
upstream <strong>of</strong> <strong>the</strong> OMVs is a T-piece to allow <strong>the</strong> connection <strong>of</strong><br />
supplementary oxygen followed by ano<strong>the</strong>r length <strong>of</strong> corrugated<br />
tubing to act as a reservoir.<br />
Additional Components<br />
The ventilator<br />
For mechanical ventilation, <strong>the</strong> original circuit simply replaced<br />
<strong>the</strong> SIB with an in-line ventilator such as <strong>the</strong> Penlon Oxford<br />
or <strong>the</strong> Cape TC 50. Following <strong>the</strong> Gulf war <strong>the</strong> Pneupac ®<br />
CompPACTM ventilator (Smiths <strong>Medical</strong>, Ashford, Kent, U.K.)<br />
was designed and replaced <strong>the</strong> TC50. It is a robust, relatively<br />
compact, time cycled, volume preset flow generator with an I:E<br />
ratio <strong>of</strong> 1:1.8 and can deliver minute volumes between 6 and 14<br />
litres per minute at rates <strong>of</strong> 10 to 30 breaths per minute. It can<br />
be powered by its internal air compressor using mains voltage,<br />
a vehicle supply or <strong>the</strong> internal battery. It is possible to deliver<br />
oxygen enrichment to a port at <strong>the</strong> rear <strong>of</strong> <strong>the</strong> machine when <strong>the</strong><br />
delivered FiO 2 can be calculated using a nomogram attached to<br />
<strong>the</strong> side <strong>of</strong> <strong>the</strong> ventilator. It can also be driven from an external<br />
compressed oxygen supply (e.g. in <strong>the</strong> Emergency Department)<br />
when it can provide an inspired oxygen fraction <strong>of</strong> 0.45, if<br />
switched to “airmix”, or 1.0 on “no airmix”. This is <strong>the</strong> only way<br />
to deliver 100% oxygen with <strong>the</strong> ComPACTM 200.<br />
Figure 3: A common configuration for mechanical ventilation<br />
When used with <strong>the</strong> TSAA <strong>the</strong> Sanders T-piece is kept in circuit<br />
to supply oxygen ra<strong>the</strong>r than <strong>the</strong> options above. The ventilator is<br />
used to provide a gas piston from <strong>the</strong> distal end <strong>of</strong> <strong>the</strong> circuit<br />
which is described colloquially as <strong>the</strong> “pushover” arrangement.<br />
The output from drawover vaporisers and for <strong>the</strong> OMV is similar<br />
in both arrangements [3]. As shown in Figure 3, <strong>the</strong> SIB must<br />
be removed from <strong>the</strong> circuit during mechanical ventilation due<br />
to its compliance and <strong>the</strong> tendency for <strong>the</strong> system to predispose<br />
to ”breath stacking”. This latter situation is due to a pressurised<br />
bolus <strong>of</strong> air being held between <strong>the</strong> one-way patient valve and<br />
<strong>the</strong> valve in <strong>the</strong> rear <strong>of</strong> <strong>the</strong> SIB: although ventilation occurs in<br />
inspiration, expiration is not possible. A detailed description <strong>of</strong><br />
<strong>the</strong> operation <strong>of</strong> <strong>the</strong> CompPACTM 200 is beyond <strong>the</strong> scope <strong>of</strong><br />
this article but may be found in <strong>the</strong> article by Roberts et al [4].<br />
DeVillbis Oxygen Concentrator<br />
Although <strong>the</strong> circuit can be supplied from an oxygen cylinder,<br />
in recent years it has been more usual to take this supply from<br />
an oxygen concentrator. Oxygen concentrators commonly use<br />
<strong>the</strong> properties <strong>of</strong> zeolite. The granules selectively absorb nitrogen<br />
from air under pressure, leaving a higher concentration <strong>of</strong> oxygen<br />
in <strong>the</strong> remaining gas, <strong>the</strong> zeolite is regenerated later in <strong>the</strong> process.<br />
The DeVillbis concentrator (DeVillbis, Somerset, Pennsylvania)<br />
has a maximum output <strong>of</strong> 5 litres/ minute producing an oxygen<br />
concentration <strong>of</strong> up to 95%. The device is simple to use <strong>the</strong> only<br />
controls being an on/<strong>of</strong>f switch and a flow knob for <strong>the</strong> rotameter.<br />
There are warning lights for oxygen concentration and an audible<br />
alarm if <strong>the</strong> oxygen output is less than 75%. At normal minute<br />
volumes, inspired oxygen concentrations <strong>of</strong> up to 80% are<br />
achievable with <strong>the</strong> concentrator at maximum flow.<br />
Monitoring<br />
Although a luxury in <strong>the</strong> developing world, modern monitoring<br />
is an absolute requirement for DMS anaes<strong>the</strong>tists. The current<br />
monitor is <strong>the</strong> Datex-GE S5 Compact (GE Healthcare, Chalfont<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S380–384 381
The Triservice Anaes<strong>the</strong>tic Apparatus<br />
St Giles, UK). It allows advanced monitoring <strong>of</strong> anaes<strong>the</strong>tic gas<br />
mixtures and has improved <strong>the</strong> safety <strong>of</strong> <strong>the</strong> TSAA more than any<br />
o<strong>the</strong>r recent development.<br />
Common Modifications and Clinical Strategies<br />
Alternative Reservoir<br />
Unlike a conventional anaes<strong>the</strong>tic circuit <strong>the</strong>re is little visible<br />
indication <strong>of</strong> respiration when using <strong>the</strong> TSAA. The final upstream<br />
piece <strong>of</strong> corrugated tubing acts purely as a reservoir but does<br />
not give any indication <strong>of</strong> spontaneous breathing. The Laerdal<br />
resuscitator 2.6L collapsible reservoir bag can be attached in its<br />
place to act as a crude respiratory monitor. It includes protective<br />
valves to allow entrainment and to protect against overpressure<br />
[5]. Figure 4 illustrates this setup.<br />
Figure 4: Use <strong>of</strong> <strong>the</strong> reservoir bag to indicate spontaneous respiration.<br />
Note also <strong>the</strong> alternative oxygen supply arrangement.<br />
The Revised Laerdal Resuscitator<br />
A recent change in <strong>the</strong> design <strong>of</strong> <strong>the</strong> Laerdal resuscitator has<br />
made <strong>the</strong> new model incompatible with <strong>the</strong> original TSAA<br />
configuration. Assembly with <strong>the</strong> new model requires <strong>the</strong><br />
“pushover” arrangement with <strong>the</strong> SIB and its reservoir bag<br />
connected to <strong>the</strong> distal (upstream) end <strong>of</strong> <strong>the</strong> OMVs (Figure 5)<br />
Figure 5: Laerdal Resuscitator®: <strong>the</strong> new version is on <strong>the</strong> right<br />
382<br />
RS Frazer, DJ Birt<br />
Paediatric Modification<br />
The non-return valve <strong>of</strong>fers little resistance and TSAA has been<br />
found to be safe in its original configuration for children <strong>of</strong> 10 kg<br />
and over [6]. For smaller children, <strong>the</strong> OMVs can be converted<br />
into a crude continuous flow anaes<strong>the</strong>tic machine for use with a<br />
Mapleson F system. To provide an overpressure blow-<strong>of</strong>f valve, an<br />
APL valve can be attached via a short length <strong>of</strong> corrugated tubing<br />
to <strong>the</strong> upstream end <strong>of</strong> <strong>the</strong> T-piece. Oxygen and o<strong>the</strong>r gases are<br />
introduced into <strong>the</strong> system via <strong>the</strong> T-piece to fill <strong>the</strong> Jackson-Rees<br />
bag and allow spontaneous breathing or hand ventilation. This is<br />
illustrated in Figure 6 and described in more detail in <strong>the</strong> recent<br />
article by Ralph et al [7].<br />
Figure 6: Setup for paediatric anaes<strong>the</strong>sia using an APL valve<br />
Preoxygenation<br />
Preoxygenation is normally undertaken with a supply from an<br />
oxygen cylinder in addition to <strong>the</strong> concentrator due to <strong>the</strong> limited<br />
flow from <strong>the</strong> latter device. This can be achieved by connecting<br />
<strong>the</strong> SIB to <strong>the</strong> cylinder and <strong>the</strong> T-piece to <strong>the</strong> concentrator. A<br />
disadvantage with this approach is that inadvertently leaving<br />
<strong>the</strong> cylinder supply on results in significant dilution <strong>of</strong> volatile<br />
agent and <strong>the</strong>refore awareness is likely. This is only <strong>the</strong> case where<br />
<strong>the</strong> SIB is in circuit so it should not be seen during established<br />
mechanical ventilation. A popular alternative is to connect both<br />
oxygen sources to a 3 way connector (typically a Luerlok 3-way<br />
tap) which is joined to <strong>the</strong> T-piece. As both supplies are upstream<br />
<strong>of</strong> <strong>the</strong> OMs, dilution <strong>of</strong> volatile agent is not seen.<br />
In preparation for induction, preoxygenation is achieved<br />
with both oxygen sources feeding into <strong>the</strong> circuit and <strong>the</strong> SIB<br />
connected. <strong>Anaes<strong>the</strong>sia</strong> is induced in <strong>the</strong> usual fashion and hand<br />
ventilation may be started using <strong>the</strong> SIB. For maintenance, <strong>the</strong><br />
SIB is removed, <strong>the</strong> cylinder supply switched <strong>of</strong>f, <strong>the</strong> ventilator<br />
tubing connected and mechanical ventilation begun. An<br />
alternative approach for RSI only is to preoxygenate and induce/<br />
intubate with <strong>the</strong> Bag-valve-mask separate from <strong>the</strong> rest <strong>of</strong> <strong>the</strong><br />
circuit which avoids <strong>the</strong> potential to leave <strong>the</strong> SIB in circuit<br />
during IPPV as well as <strong>the</strong> potential for dilution <strong>of</strong> volatile agent<br />
if <strong>the</strong> cylinder supply is left running.<br />
Volatile Agents and Gas Induction<br />
Although is<strong>of</strong>lurane is normally used in <strong>the</strong> OMV50, as it is a<br />
“universal” vaporiser a number <strong>of</strong> anaes<strong>the</strong>tists have looked<br />
at <strong>the</strong> possibility <strong>of</strong> using sev<strong>of</strong>lurane. Liu & Dhara tested <strong>the</strong><br />
vaporiser on a flow-bench and suggested that <strong>the</strong> output should<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S380–384
The Triservice Anaes<strong>the</strong>tic Apparatus RS Frazer, DJ Birt<br />
be suitable [8]. Brook and Perndt subsequently used sev<strong>of</strong>lurane<br />
clinically and stated that it was possible to perform an inhalation<br />
induction with two vaporisers [9] but <strong>the</strong> modern penchant for<br />
gas induction with sev<strong>of</strong>lurane has been difficult to satisfy with<br />
<strong>the</strong> TSAA. The OMV was designed when <strong>the</strong> relatively potent<br />
halothane was <strong>the</strong> volatile agent <strong>of</strong> choice and maximum outputs<br />
are limited when 4 MAC <strong>of</strong> sev<strong>of</strong>lurane is <strong>the</strong> target. Results are<br />
conflicting but <strong>the</strong> original TSAA does not appear to lend itself<br />
to this technique [10]. Sev<strong>of</strong>lurane has been used in <strong>the</strong> Universal<br />
PAC [11] and more recently Diamedica (Diamedica (UK) Ltd,<br />
Bratton Fleming, Devon, England) has developed a sev<strong>of</strong>lurane<br />
vaporiser which for <strong>the</strong> first time appears to produce a sufficient<br />
output for inhalational induction using a single vaporiser in a<br />
drawover system [2]<br />
Common Pitfalls<br />
The TSAA is not without its problems and has many critics. It is<br />
generally agreed that <strong>the</strong>re is still a need for a portable drawover<br />
anaes<strong>the</strong>tic system to be available to <strong>the</strong> UK military [12] but<br />
<strong>the</strong> original TSAA is overdue for replacement. It has a number <strong>of</strong><br />
particular problems:<br />
Disconnections and practical hazards<br />
Unfamiliarity, heavy tubing and complex procedures for changing<br />
configurations all contribute to <strong>the</strong> hazards <strong>of</strong> using <strong>the</strong> TSAA. It<br />
is a useful system for insertion and mobile operations but should<br />
not be <strong>the</strong> first choice equipment for an enduring mission. This<br />
was highlighted in January 2009 when a Patient Safety Incident<br />
report was submitted from Op HERRICK to PJHQ regarding<br />
<strong>the</strong> TSAA. The concerns identified included <strong>the</strong> potential for<br />
disconnection due to <strong>the</strong> number <strong>of</strong> connections in <strong>the</strong> circuit<br />
and <strong>the</strong> lack <strong>of</strong> familiarity amongst multi-national personnel.<br />
Scavenging<br />
Active scavenging is rarely available in <strong>the</strong> field so volatile agents<br />
are usually scavenged by activated charcoal in <strong>the</strong> form <strong>of</strong> a<br />
Cardiff Aldasorber (Shirley Aldred & Co Ltd, Derbyshire, U.K.).<br />
This adds to <strong>the</strong> hardware at <strong>the</strong> patient end as a scavenging<br />
connection must be made to <strong>the</strong> outlet <strong>of</strong> <strong>the</strong> non-return valve.<br />
Consumption <strong>of</strong> Volatile Agent<br />
Recycling <strong>of</strong> volatile agents cannot be achieved with <strong>the</strong> TSAA so<br />
consumption is high. Fur<strong>the</strong>rmore, as <strong>the</strong> capacity <strong>of</strong> <strong>the</strong> OMV is<br />
low refilling <strong>of</strong> vaporisers during anaes<strong>the</strong>sia is a common event.<br />
The presence <strong>of</strong> two vaporisers allows maintenance <strong>of</strong> anaes<strong>the</strong>sia<br />
but care must be taken to avoid disruption <strong>of</strong> <strong>the</strong> system, spillage<br />
and boluses <strong>of</strong> volatile to be delivered inadvertently.<br />
Dead Space<br />
Although it has improved safety, <strong>the</strong> addition <strong>of</strong> patient<br />
monitoring, spirometry, scavenging and heat and moisture<br />
exchange have increased <strong>the</strong> length <strong>of</strong> <strong>the</strong> TSAA beyond <strong>the</strong> nonreturn<br />
valve by an significant amount. This increases dead space<br />
and <strong>the</strong> potential for disconnections. That said, such additions<br />
would be needed on any modern anaes<strong>the</strong>tic system.<br />
Training<br />
Training on <strong>the</strong> TSAA has been difficult since <strong>the</strong> demise <strong>of</strong><br />
<strong>the</strong> military hospitals and <strong>the</strong> reluctance <strong>of</strong> NHS Trusts to use<br />
equipment which is unconventional. Although it is possible to<br />
view <strong>the</strong> equipment at <strong>the</strong> pre-deployment Hospital Exercise<br />
(HOSPEX), because <strong>of</strong> fidelity limitations it is not <strong>the</strong> ideal<br />
location to simulate an anaes<strong>the</strong>tic with <strong>the</strong> equipment. In view<br />
<strong>of</strong> <strong>the</strong>se short comings a high fidelity simulation course has<br />
been developed. The requirement to actually give an anaes<strong>the</strong>tic<br />
to a mannequin which would be monitored by <strong>the</strong> equipment<br />
that is deployed meant that only <strong>the</strong> physiologically modelled<br />
mannequin, METI HPS® was suitable and a contract has been<br />
established with <strong>the</strong> Cheshire and Merseyside Simulation Centre<br />
to deliver <strong>the</strong> training.<br />
On <strong>the</strong> one-day course <strong>the</strong> team is initially introduced to <strong>the</strong><br />
TSAA and to <strong>the</strong> capabilities <strong>of</strong> <strong>the</strong> simulator as familiarisation<br />
is also important for effective non-technical skills. Subsequently<br />
four scenarios are run with one or more anaes<strong>the</strong>tists and an ODP.<br />
Each scenario has been designed with input from military Subject<br />
Matter Experts and <strong>the</strong> civilian simulation staff to combine<br />
realistic medical and equipment related problems and to explore<br />
<strong>the</strong> team dynamics in critical problem solving.<br />
Allied Approaches to Drawover <strong>Anaes<strong>the</strong>sia</strong><br />
US forces have also used a draw-over apparatus for light scales <strong>of</strong><br />
effort. Their system has been based around <strong>the</strong> Ohmeda Universal<br />
PAC. This vaporiser has some differences from <strong>the</strong> OMV, <strong>the</strong><br />
main one being that it is temperature compensated. At present US<br />
forces still make use <strong>of</strong> it but are actively seeking a replacement<br />
because manufacture <strong>of</strong> <strong>the</strong> PAC has ceased.<br />
The Australian <strong>Defence</strong> Force use draw-over equipment<br />
also and <strong>the</strong> system <strong>the</strong>y have chosen is also based around <strong>the</strong><br />
OMV50. This has been developed into a set <strong>of</strong> equipment such<br />
that, although <strong>the</strong> OMV is not CE marked, <strong>the</strong> entire setup has<br />
been given type approval. It is <strong>the</strong> Field <strong>Anaes<strong>the</strong>sia</strong> Machine<br />
(FAM 100) manufactured by Ulco <strong>Medical</strong> (Marrickville, NSW,<br />
Australia) [11].<br />
Conclusion<br />
The TSA was first described in 1981 as <strong>the</strong> ideal anaes<strong>the</strong>tic<br />
apparatus for airborne and amphibious entry operations. Some<br />
equipment changes have been necessary over <strong>the</strong> years but <strong>the</strong><br />
original requirement for robust, portable equipment is unchanged.<br />
That said, anaes<strong>the</strong>sia no longer has to depend on volatile agents.<br />
Robust, lightweight and accurate intravenous pumps are available<br />
with long battery lives for TIVA and this also removes <strong>the</strong> need for<br />
scavenging. Although TIVA is increasing in popularity, especially<br />
for repeat procedures, <strong>the</strong> support for volatile agent based<br />
anaes<strong>the</strong>sia remains strong. Indeed <strong>the</strong> position <strong>of</strong> conventional<br />
anaes<strong>the</strong>sia worldwide, especially from drawover apparatus in<br />
austere environments is such that new equipment is still being<br />
developed.<br />
The DMS is likely to maintain a drawover volatile anaes<strong>the</strong>sia<br />
capability especially for entry operations and this is widely<br />
supported by <strong>Defence</strong> Anaes<strong>the</strong>tists. This article highlights a<br />
number <strong>of</strong> areas where <strong>the</strong> TSAA fails to satisfy <strong>the</strong> expectations <strong>of</strong><br />
DMS Anaes<strong>the</strong>tists and in a number <strong>of</strong> cases causes real concern.<br />
The disconnection risks, unfamiliarity and lack <strong>of</strong> CE marking<br />
<strong>of</strong> <strong>the</strong> OMV50 are examples. The issue <strong>of</strong> CE marking is an<br />
interesting one as <strong>the</strong>re is no CE standard for drawover vaporisers.<br />
It is, however, possible for a set <strong>of</strong> equipment (including a drawover<br />
vaporiser) to obtain CE certification (e.g. <strong>the</strong> FAM 100). The<br />
above concerns suggest that a replacement is required but many <strong>of</strong><br />
<strong>the</strong> original features <strong>of</strong> <strong>the</strong> TSAA are still relevant. Any replacement<br />
must be compact, lightweight and robust. It is difficult to envisage<br />
a modern field surgical unit without electricity, but an anaes<strong>the</strong>tic<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S380–384 383
The Triservice Anaes<strong>the</strong>tic Apparatus<br />
apparatus that is independent <strong>of</strong> compressed gas supplies would<br />
be preferable.<br />
Although <strong>the</strong> replacement for <strong>the</strong> TSAA is yet to be identified,<br />
options exist and are being examined. In <strong>the</strong> meantime potential<br />
users must be aware <strong>of</strong> <strong>the</strong> issues highlighted in this article<br />
and ensure that <strong>the</strong>y are appropriately trained in its use before<br />
deployment. Instruction from experienced users is available on<br />
pre-deployment training courses.<br />
References<br />
1. Houghton I. The Triservice anaes<strong>the</strong>tic apparatus. <strong>Anaes<strong>the</strong>sia</strong><br />
1981; 36: 1094-1108<br />
2. English WA, Tully R, Muller GD, Eltringham RJJ. The Diamedica<br />
Draw-Over Vaporizer: a comparison <strong>of</strong> a new vaporizer with <strong>the</strong><br />
Oxford Miniature Vaporizer. <strong>Anaes<strong>the</strong>sia</strong> 2009; 64: 84–92<br />
3. Taylor JC, Restall J. Can a drawover vaporiser be a pushover?<br />
<strong>Anaes<strong>the</strong>sia</strong> 1994; 49: 892-4<br />
4. Roberts MJ, Bell GT, Wong LS. The CompPAC and PortaPAC<br />
portable ventilators bench tests and field experience. J R <strong>Army</strong> Med<br />
<strong>Corps</strong> 1999; 145: 73-7<br />
384<br />
RS Frazer, DJ Birt<br />
5. Birt D. A reservoir bag for <strong>the</strong> Triservice Anaes<strong>the</strong>tic Apparatus.<br />
<strong>Anaes<strong>the</strong>sia</strong> 2006; 61, 510-511<br />
6. Bell GT, McEwen JPJ, Beaton SJ, Young D. Comparison <strong>of</strong> work<br />
<strong>of</strong> breathing using drawover and continuous flow breathing systems<br />
in children. <strong>Anaes<strong>the</strong>sia</strong> 2007; 62: 359-363<br />
7. Ralph JK, George R, Thompson J. Paediatric <strong>Anaes<strong>the</strong>sia</strong> using <strong>the</strong><br />
Triservice Anaes<strong>the</strong>tic Apparatus. J R <strong>Army</strong> Med <strong>Corps</strong> 2010; 156:<br />
84-86<br />
8. Lui EH, Dhara SS. Sev<strong>of</strong>lurane output from <strong>the</strong> Oxford Miniature<br />
Vaporizer in drawover mode. Anaesth Intensive Care 2000; 28: 532-<br />
6<br />
9. Brook PN, Perndt H. Sev<strong>of</strong>lurane drawover anaes<strong>the</strong>sia with two<br />
Oxford Miniature Vaporizers in series. Anaesth Intensive Care 2001;<br />
29: 616-8<br />
10. Mellor A, Hicks I. Sev<strong>of</strong>lurane delivery via <strong>the</strong> Triservice apparatus.<br />
<strong>Anaes<strong>the</strong>sia</strong> 2005; 60: 1151<br />
11. Pylman ML, Teiken PJ. Sev<strong>of</strong>lurane concentration available from<br />
<strong>the</strong> universal drawover vaporizer. Mil Med 1997; 162: 405-6<br />
12. Mercer SJ, Beard DJ. Does <strong>the</strong> Tri-Service anaes<strong>the</strong>tic apparatus<br />
still have a role in modern conflict? RCoA Bulletin 2010; 60: 18-20<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S380–384
Vascular Access on <strong>the</strong> 21 st Century Military<br />
Battlefield<br />
EJ Hulse 1 , GOR Thomas 2<br />
1 Specialty Registrar in Anaes<strong>the</strong>tics, <strong>Royal</strong> Cornwall Hospital, Truro, Cornwall; 2 Honorary Consultant Anaes<strong>the</strong>tist, The<br />
<strong>Royal</strong> London, and Queen Victoria’s Hospital, East Grinstead, London & 16 Air Assualt <strong>Medical</strong> Regiment.<br />
Abstract<br />
Timely and appropriate access to <strong>the</strong> vascular circulation is critical in <strong>the</strong> management <strong>of</strong> 21st century battlefield trauma. It<br />
allows <strong>the</strong> administration <strong>of</strong> emergency drugs, analgesics and rapid replacement <strong>of</strong> blood volume. Methods used to gain access<br />
can include; <strong>the</strong> cannulation <strong>of</strong> peripheral and central veins, venous cut-down and intraosseus devices. This article reviews <strong>the</strong><br />
current literature on <strong>the</strong> benefits and complications <strong>of</strong> each vascular access method. We conclude that intraosseus devices are<br />
best for quick access to <strong>the</strong> circulation, with central venous access via <strong>the</strong> subclavian route for large volume resuscitation and<br />
low complication rates. Military clinicians involved with <strong>the</strong> care <strong>of</strong> trauma patients ei<strong>the</strong>r in Role 2 and 3 or as part <strong>of</strong> <strong>the</strong><br />
<strong>Medical</strong> Emergency Response Team (MERT), must have <strong>the</strong> skill set to use <strong>the</strong>se vascular access techniques by incorporating<br />
<strong>the</strong>m into <strong>the</strong>ir core medical training.<br />
Introduction<br />
Timely and appropriate access to <strong>the</strong> vascular circulation is<br />
critical in <strong>the</strong> management <strong>of</strong> 21 st century battlefield trauma.<br />
This essential procedure allows <strong>the</strong> administration <strong>of</strong> emergency<br />
drugs, analgesics and rapid replacement <strong>of</strong> blood volume using<br />
crystalloid, colloid or blood products. It encompasses <strong>the</strong><br />
cannulation <strong>of</strong> peripheral and central veins, venous cut-down<br />
and intraosseus (IO) devices.<br />
The type <strong>of</strong> access employed in any given situation will be<br />
determined by <strong>the</strong> skill <strong>of</strong> <strong>the</strong> operator, <strong>the</strong> environment in which<br />
it is used, <strong>the</strong> degree <strong>of</strong> hypovolaemic shock and <strong>the</strong> extent and<br />
pattern <strong>of</strong> injury. Gaining access to <strong>the</strong> human vascular system<br />
has been practised for millennia, most notably for bloodletting<br />
procedures believed to improve health [1, 2]. IO access was first<br />
documented by Drinker in 1922 [3], but it was during <strong>the</strong> Second<br />
World War that IO infusions were more widely used to resuscitate<br />
patients in haemorrhagic shock [4]. After <strong>the</strong> war, it’s use largely<br />
died out in <strong>the</strong> adult population, but has seen resurgence during<br />
<strong>the</strong> Iraq and Afghanistan conflicts with <strong>the</strong> introduction <strong>of</strong><br />
modern needle and introducer systems [5].<br />
The Sapheno-femoral venous cut-down was popularised<br />
during <strong>the</strong> Vietnam conflict to manage casualties with severe<br />
haemorrhagic shock [6].<br />
During <strong>the</strong> recent conflict in Iraq and Afghanistan <strong>the</strong> use <strong>of</strong><br />
large bore central venous access (Figure 1) has been popularised<br />
by experienced military trauma clinicians. This has been driven<br />
by <strong>the</strong> severity <strong>of</strong> today’s battlefield casualties and <strong>the</strong> requirement<br />
for large volume fluid resuscitation. This is <strong>of</strong>ten used in<br />
conjunction with <strong>the</strong> transfusion protocol advocated by Borgman<br />
and colleagues [7] using <strong>the</strong> ratio <strong>of</strong> 1 bag <strong>of</strong> red cells: 1 bag <strong>of</strong><br />
plasma in <strong>the</strong> shocked trauma patient [8-11].<br />
Flow<br />
Flow through a vessel or tube is determined by Poiusselle’s<br />
equation describing laminar flow:<br />
Corresponding Author: Surg Lt Cdr Elspeth J Hulse MBChB<br />
FRCA, Specialty Registrar, Anaes<strong>the</strong>tics Department,<br />
Derriford Hospital, Plymouth PL6 8DH<br />
Tel: 0845 155 8155 Email: elspeth_uk@hotmail.com<br />
Figure 1: Size 9 French Cook Introducer central venous ca<strong>the</strong>ter which<br />
can be used for high volume fluid resuscitation<br />
With kind permission from Cook <strong>Medical</strong><br />
Q = ΔP π r 4<br />
8ηl<br />
Q = Flow rate ml/min, P = Pressure gradient between <strong>the</strong> proximal<br />
and distal ends <strong>of</strong> <strong>the</strong> tubing, r = radius <strong>of</strong> <strong>the</strong> tube, η = viscosity,<br />
l = length <strong>of</strong> <strong>the</strong> tube.<br />
Importantly, if you double <strong>the</strong> diameter <strong>of</strong> <strong>the</strong> cannulae, <strong>the</strong><br />
flow rate increases by a factor <strong>of</strong> 16. To aid flow, <strong>the</strong> venous<br />
cannulae and connecting tubing must be short and wide, <strong>the</strong><br />
fluid administered warm, pressurised and <strong>the</strong> viscosity <strong>of</strong> <strong>the</strong><br />
fluid reduced [12]. Although Poiseuille’s law demonstrates <strong>the</strong><br />
principles <strong>of</strong> flow, <strong>the</strong> actual flow rate <strong>of</strong> fluid under pressure is<br />
determined by a quadratic equation which takes into account<br />
<strong>the</strong> development <strong>of</strong> turbulence. Barcelona et al surmised that<br />
this partly explained why even large bore ca<strong>the</strong>ters are not<br />
capable <strong>of</strong> delivering <strong>the</strong> flows predicted using Poiseuille’s<br />
equation [13].<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S385–390 385
Vascular Access<br />
386<br />
Device Internal<br />
Radius (mm)<br />
Length<br />
(mm)<br />
Flow Rate<br />
Gravity<br />
ml/min<br />
(3.2mm<br />
tubing)<br />
Hartmann’s/<br />
H 2 O<br />
Intraosseous Access<br />
Many British casualties from <strong>the</strong> recent conflicts in Iraq and<br />
Afghanistan present with severe haemorrhagic shock associated<br />
with multiple traumatic limb amputations from improvised<br />
explosive devices. In <strong>the</strong>se situations IO can be utilised with<br />
substantial effect. The intravenous (IV) or IO route is now<br />
accepted as first line access in paediatric resuscitation by <strong>the</strong><br />
UK Resuscitation Council [18]. The <strong>Defence</strong> <strong>Medical</strong> Services<br />
(DMS) currently have two IO systems in place; The EZ-IO® and<br />
<strong>the</strong> FAST 1®.<br />
EZ-IO® System<br />
The EZ-IO® system (Vidacare, SanAntonio,USA) was introduced<br />
into UK DMS in December 2006. It consists <strong>of</strong> a battery<br />
powered disposable drill, a bevelled, hollow needle with a cutting<br />
needle central trocar and a short connection tube (with a one<br />
way valve) for fluid /drug administration. There are three needle<br />
sizes and <strong>the</strong> insertion point is just below and medial to <strong>the</strong> tibial<br />
tuberosity on <strong>the</strong> upper flat aspect <strong>of</strong> <strong>the</strong> tibia. EZ-IO can also be<br />
inserted into <strong>the</strong> lateral aspect <strong>of</strong> <strong>the</strong> humeral head or iliac crest.<br />
Contraindications are rare, but EZ-IO should not be inserted into<br />
a fractured bone to avoid extravasation into s<strong>of</strong>t tissues or through<br />
infected tissue.<br />
FAST 1 IO<br />
The FAST 1® sternal IO device (Pyng <strong>Medical</strong> Corporation,<br />
Richmond Canada) is designed exclusively for use in <strong>the</strong><br />
manubrium sternum (Figure 2) and has advantages <strong>of</strong> rapid,<br />
Flow Rate<br />
300mmHg<br />
ml/min<br />
(3.2mm<br />
tubing)<br />
Hartmann’s/<br />
H 2 O<br />
Flow rate<br />
300mg<br />
ml/min<br />
(5.0mm<br />
tubing with<br />
filter)<br />
Blood<br />
Level 1<br />
Infuser<br />
(300mm Hg)<br />
Ml/min<br />
Hartmann’s<br />
EJ Hulse, GOR Thomas<br />
Rapid<br />
Infusion<br />
System<br />
(approx<br />
285mm Hg)<br />
ml/min<br />
Hartmann’s<br />
20G venflon 0.423 32-33 40 - 67 n/a n/a 140 144<br />
18G Venflon 0.515 45-52 103 n/a n/a 209 205<br />
16G<br />
venflon<br />
14G<br />
venflon<br />
10G<br />
Angiocath<br />
0.705 45-55 151+/-3 - 236 448+/-19 444+/-25 368 412<br />
0.895 45-64 194+/-5 - 270 577+/-22 779+/-39 488 584<br />
2.25 76.2 162 496 1,248 n/a n/a<br />
8 French 2.2 160.02 162 492 1,200 n/a n/a<br />
8.5 French<br />
(Arrow)<br />
Sternal IO<br />
(FAST)<br />
Tibial IO<br />
EZIO<br />
Humeral IO<br />
EZIO<br />
1.43 112 245+/-4 645+/-20 1,622+/-120 596 857<br />
n/a 6 17.9+/-9.1<br />
(30-80)<br />
15G 25<br />
Paed 15<br />
15G 25<br />
Paed 15<br />
104.1+/-46.5<br />
- 125<br />
Table 1: Flow rates <strong>of</strong> vascular devices [12- 17] – The manufacturers’ details are marked in bold.<br />
n/a n/a n/a<br />
68-73 165-204 n/a n/a n/a<br />
81-84 148-153 n/a n/a n/a<br />
easy to locate placement, reasonable flow rates (Table 1), can<br />
be used during cardio-pulmonary resuscitation and has low<br />
risk <strong>of</strong> dislodgement. The device is not MRI compatible and is<br />
contraindicated in sternal fractures.<br />
Figure 2 : Photo <strong>of</strong> FAST 1® sternal insertion.<br />
With kind permission from Trauma.org<br />
Using <strong>the</strong> adhesive guide, <strong>the</strong> FAST is inserted perpendicular<br />
to <strong>the</strong> manubrium made possible by <strong>the</strong> 10 guide needles<br />
surrounding <strong>the</strong> I/O which will only release <strong>the</strong> cannulation<br />
mechanism when <strong>the</strong> pressure in all 10 needles is equal. The<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S385–390
Vascular Access EJ Hulse, GOR Thomas<br />
rationale for having 2 different IO systems is that multiple ballistic<br />
or fragmentation limb injuries are common and may preclude<br />
<strong>the</strong> use <strong>of</strong> EZ-IO. However, <strong>the</strong> large ballistic chest plate usually<br />
protects <strong>the</strong> sternum. Teaching is simplified by indicating that<br />
FAST1 is only for sternal placement and <strong>the</strong> EZ-IO for anywhere<br />
but <strong>the</strong> sternum. In <strong>the</strong> authors’ experience <strong>the</strong> preferred sites <strong>of</strong><br />
IO access are ideally tibial, <strong>the</strong>n humeral followed by sternal.<br />
Complications<br />
Operation <strong>of</strong> <strong>the</strong> EZ-IO device is intuitive and insertion times are<br />
fast with most operators being able to insert an IO in less than 10<br />
seconds. Published DMS experience involving EZ-IO for vascular<br />
access for 26 patients demonstrated 97% effective function. No<br />
complications <strong>of</strong> infection were noted, but pain was observed in<br />
responsive patients with <strong>the</strong> pain <strong>of</strong> infusion exceeding that <strong>of</strong><br />
<strong>the</strong>ir underlying injuries in three cases [5]. This was also reported<br />
by David<strong>of</strong>f et al who noted <strong>the</strong> average pain upon fluid infusion<br />
was rated as ‘5’ on a modified visual analogue scale (1-10) [19].<br />
From <strong>the</strong> authors experience this is indeed correct, however pain<br />
decreases markedly after completion <strong>of</strong> <strong>the</strong> first fluid flush.<br />
Frascone et al evaluated provider performance for obtaining<br />
IO access with <strong>the</strong> FAST1 and <strong>the</strong> EZ-IO and noted that 72%<br />
<strong>of</strong> FAST1 and 87% <strong>of</strong> EZ-IO were successful. EZ-IO (p=0.009)<br />
[20]. An interesting study was performed by Suyama et al<br />
comparing EZ-IO and peripheral intravenous cannulation in full<br />
personal protective equipment simulating a Chemical-Biological-<br />
Radionuclear (CBRN) environment. In all <strong>the</strong> scenarios <strong>the</strong> IO<br />
was found to be both faster and easier at gaining access [21].<br />
The most notable and recent complications with <strong>the</strong> FAST1<br />
have involved difficulty in removing <strong>the</strong> needle, some <strong>of</strong> which<br />
required surgery in order to extract. The device has apparently<br />
been modified so that no removal tool is required and <strong>the</strong> infusion<br />
tube can be pulled out by hand [22]. Although <strong>the</strong> observed risk<br />
<strong>of</strong> infection is low, this can take <strong>the</strong> form <strong>of</strong> cellulitis or in more<br />
severe forms osteomyelitis [23]. When <strong>the</strong> tibia is used as an IO<br />
site it has been reported that occasionally fluid resuscitation can<br />
lead to compartment syndrome in children [24].<br />
O<strong>the</strong>r potential but not as yet reported complication is<br />
<strong>the</strong> use <strong>of</strong> <strong>the</strong> IO in patients with an unstable pelvis. In <strong>the</strong><br />
authors opinion <strong>the</strong> practice <strong>of</strong> insertion <strong>of</strong> IO’s in patients at<br />
high risk <strong>of</strong> pelvic instability (Blast/Blunt trauma from victim<br />
operated explosive device) is potentially dangerous and should be<br />
discouraged. Misplacement <strong>of</strong> IO’s also seems to be increasingly<br />
common especially with <strong>the</strong> humeral approach. Common causes<br />
for this are: haste, patient movement on transfer, lack <strong>of</strong> training<br />
and not doing <strong>the</strong> ‘wiggle test’ (if <strong>the</strong> IO wiggles it’s not in).<br />
Peripheral venous access<br />
Combat medics, nurses, doctors and o<strong>the</strong>r health pr<strong>of</strong>essionals are<br />
trained to place intravenous peripheral cannulae. An experienced<br />
practitioner takes a mean <strong>of</strong> two minutes to cannulate a patient<br />
in <strong>the</strong> Emergency Department [25] , but in a case series over<br />
120, 000 procedures, gaining intravenous access (IVA) in <strong>the</strong><br />
pre hospital setting was associated with an increase in on-scene<br />
duration <strong>of</strong> between 3.17 - 5.4 minutes [26].<br />
Site<br />
Peripheral venous cannulae are usually sited in <strong>the</strong> dorsal<br />
metacarpal veins, tributaries <strong>of</strong> <strong>the</strong> basillic and cephalic veins in<br />
<strong>the</strong> forearm or ante-cubital fossa. The external jugular vein may<br />
also be utilised in arrest situations [27]. Battlefield advanced<br />
trauma life support (BATLS) recommends that two attempts<br />
should be made to secure two 14G cannulae [28]. In cases <strong>of</strong><br />
severe multi-trauma in which occult thoraco-abdominal damage<br />
is suspected, it is recommended to secure IV access both above<br />
and below <strong>the</strong> diaphragm and as close to <strong>the</strong> heart as possible.<br />
These measures attempt to secure a route to deliver fluid and<br />
medications to <strong>the</strong> central circulatory system with minimal risk<br />
<strong>of</strong> disruption [29]. IV access should ideally not be placed in limbs<br />
with massive oedema, burns, sclerosis, phlebitis, thrombosis or on<br />
<strong>the</strong> side <strong>of</strong> radical mastectomies. Cannulation at sites <strong>of</strong> cellulitis<br />
or extremities with shunts or fistulas should be avoided because it<br />
may cause bacteraemia or thrombosis [30].<br />
Complications<br />
Common complications include bruising, irritation, failure,<br />
haematoma, thrombophlebitis and extravasation <strong>of</strong> fluids or<br />
drugs causing pain and irritation to <strong>the</strong> surrounding tissue [29].<br />
Tricks<br />
Methods to increase peripheral venous distension include asking<br />
<strong>the</strong> patient to open and close <strong>the</strong>ir fist, light tapping <strong>of</strong> <strong>the</strong> vein,<br />
lowering <strong>the</strong> arm below <strong>the</strong> level <strong>of</strong> <strong>the</strong> heart and heat packs<br />
applied for 10 to 20 minutes [30]. A technique for up-gauging<br />
peripheral venous cannulae in volume resuscitation has been<br />
described whereby an initial small cannulae is inserted into a<br />
limb, and whilst <strong>the</strong> tourniquet remains up, 30-50mls <strong>of</strong> saline is<br />
injected into <strong>the</strong> veins via this cannulae. This <strong>the</strong>n allows a large<br />
bore cannulae >18G to be inserted into <strong>the</strong> same limb [31]. Small<br />
cannulae can also be up gauged using a Rapid Infusion Ca<strong>the</strong>ter<br />
which employs <strong>the</strong> Seldinger (guidewire) technique.<br />
The use <strong>of</strong> Ultrasound (US) guided peripheral IVA has shown<br />
to be <strong>of</strong> use and superior to external jugular IVA in <strong>the</strong> Emergency<br />
Department when IVA is difficult [32]. A review <strong>of</strong> <strong>the</strong> literature<br />
has shown that it requires less time, decreases <strong>the</strong> number <strong>of</strong> skin<br />
punctures and improves patient satisfaction [27].<br />
Venous Cut-down<br />
The practice <strong>of</strong> peripheral venous cut-down has declined due to<br />
<strong>the</strong> efficiency <strong>of</strong> <strong>the</strong> Seldinger technique for central venous access<br />
and limited clinician exposure [33].<br />
However, in <strong>the</strong> pr<strong>of</strong>oundly hypovolaemic trauma patient<br />
where <strong>the</strong>re may be distorted central anatomy, lack <strong>of</strong> femoral<br />
pulses and scarring <strong>of</strong> peripheral veins, it remains a useful tool. It<br />
enables reliable vascular access to be obtained with direct vision <strong>of</strong><br />
<strong>the</strong> vein and reduces cannulae misplacement.<br />
Westfall found that in shocked trauma patients, venous cutdown<br />
took longer to perform than inserting a femoral 8.5French<br />
Central Venous Ca<strong>the</strong>ter (CVC) with a mean <strong>of</strong> 5.6 and 3.2<br />
minutes respectively. The cut-down also had a decreased flow rate<br />
(150ml/min compared to 219ml/min for CVC) [34]. Venous<br />
cut-down sites include <strong>the</strong> proximal and distal greater saphenous<br />
vein, <strong>the</strong> cephalic and basillic veins.<br />
The most commonly used access is <strong>the</strong> greater saphenous<br />
vein proximally in <strong>the</strong> groin because <strong>of</strong> its large diameter and<br />
ease <strong>of</strong> dissection.<br />
This can be reliably located 5cm distal to <strong>the</strong> junction between<br />
<strong>the</strong> middle and medial one third <strong>of</strong> <strong>the</strong> imaginary line between<br />
<strong>the</strong> anterior superior iliac spine and <strong>the</strong> pubic tubercle or by <strong>the</strong><br />
“Rule <strong>of</strong> Two’s”; two fingerbreadths below and lateral to <strong>the</strong> pubic<br />
tubercle. These points form <strong>the</strong> midpoint <strong>of</strong> a 5cm horizontal<br />
incision which can also be approximated by a 5cm horizontal<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S385–390 387
Vascular Access<br />
incision starting just distal to where <strong>the</strong> labia/scrotal fold meet <strong>the</strong><br />
thigh [35]. A vertical venotomy in <strong>the</strong> vein can allow <strong>the</strong> passage<br />
<strong>of</strong> a straight wire (within <strong>the</strong> dilator) within <strong>the</strong> 8.5F CVC.<br />
Absolute contraindications are major blunt or penetrating<br />
trauma to <strong>the</strong> ipsilateral groin or limb. Complications occur in<br />
2-15% <strong>of</strong> cases and include haemorrhage, damage to <strong>the</strong> femoral<br />
artery and nerve, wound infection and dehiscence, thromboembolism<br />
and phlebitis [33].<br />
Central Venous Access<br />
The first central venous ca<strong>the</strong>ter was pioneered by a German<br />
surgeon in 1928 who described advancing a plastic tube near <strong>the</strong><br />
right atrium using his own left ante-cubital vein [36]. Aubaniac<br />
followed, when he described <strong>the</strong> insertion <strong>of</strong> a ca<strong>the</strong>ter using <strong>the</strong><br />
subclavian vein [37]. The technique was improved by <strong>the</strong> Swedish<br />
radiologist, Seldinger in 1953 with use <strong>of</strong> a guidewire whose<br />
technique we still use today [38].<br />
Obtaining central venous access is important to military<br />
clinicians as it is not only <strong>the</strong> most effective route for administering<br />
emergency drugs [39, 40], but is <strong>the</strong> quickest and most effective<br />
means to resuscitate haemorrhagic shock in trauma patients with<br />
a relatively low complication rate [41]. The 8.5F Swan introducer<br />
sheath for a pulmonary artery ca<strong>the</strong>ter (Figure 1 and 3) is<br />
commonly used for this purpose, delivering high volumes under<br />
pressure quickly (Table 1) [12, 41].<br />
Site<br />
In <strong>the</strong> trauma setting, cannulation <strong>of</strong> <strong>the</strong> internal jugular vein<br />
is <strong>of</strong>ten impractical due to neck collar and blocks for C-spine<br />
protection. Also, in severely hypovolaemic casualties <strong>the</strong> internal<br />
jugular vein (IJV) collapses and <strong>the</strong>refore increases <strong>the</strong> risk <strong>of</strong><br />
carotid puncture as 54% <strong>of</strong> people have <strong>the</strong>ir IJV overlying <strong>the</strong>ir<br />
carotid artery [42].<br />
Figure 3 : Photo showing <strong>the</strong> insertion <strong>of</strong> a left sided subclavian<br />
central venous trauma line (<strong>the</strong> light blue plastic tube placed on <strong>the</strong><br />
end <strong>of</strong> a blue syringe in <strong>the</strong> operators right hand).<br />
With kind permission <strong>of</strong> Major R Dawes.<br />
The subclavian vein is large and anatomically easy to locate<br />
in <strong>the</strong> face <strong>of</strong> hypovolaemia and so makes an ideal candidate for<br />
use in <strong>the</strong> trauma setting [11]. Subclavian lines should be placed<br />
on <strong>the</strong> ipsilateral side in <strong>the</strong> presence <strong>of</strong> penetrating trauma to<br />
chest wall, pneumothorax or haemothorax [8, 43]. Femoral vein<br />
cannulation may be complicated by arterial puncture if <strong>the</strong>re is<br />
388<br />
EJ Hulse, GOR Thomas<br />
no palpable femoral pulse [44]. It should be avoided in ipsilateral<br />
limb or presumed inferior vena caval injury to avoid extravasation<br />
[8, 44].<br />
Complications<br />
Controversy over <strong>the</strong> use <strong>of</strong> CVC’s in trauma casualties<br />
exists because <strong>of</strong> <strong>the</strong> perceived increase in complication rates.<br />
Complications include haematoma, arterial puncture, haemo/<br />
pneumothorax, malposition <strong>of</strong> <strong>the</strong> ca<strong>the</strong>ter, air embolism,<br />
line sepsis, thrombosis, embolism and thrombophlebitis. The<br />
most common complications in IJV ca<strong>the</strong>terisation are arterial<br />
puncture, and pneumothoraces with subclavian cathterisation<br />
[8, 41]. Abraham et al [45] and Ferguson et al [43] suggest that<br />
success rates are lower and complication rates higher (14% and<br />
15% respectively) in emergent CVC placement in trauma patients.<br />
The decrease in central blood volume following haemorrhage and<br />
potential venous anatomical changes in trauma patients may<br />
complicate <strong>the</strong> technique [9].<br />
However Pappas et al found no significant difference in<br />
complication rates (7.8%) between trauma patients irrespective<br />
<strong>of</strong> <strong>the</strong> degree <strong>of</strong> shock [10]. Scalea et al [9] noted that even in<br />
<strong>the</strong> presence <strong>of</strong> hypotension (
Vascular Access EJ Hulse, GOR Thomas<br />
Discussion<br />
In many patients IV <strong>the</strong>rapy cannot be initiated because <strong>of</strong><br />
inadequate access to peripheral veins. This lack <strong>of</strong> vascular access<br />
delays <strong>the</strong> resuscitation process and limits <strong>the</strong> benefit <strong>of</strong> medical<br />
intervention due to late administration <strong>of</strong> medications [51].<br />
Both speed and overall success <strong>of</strong> vascular access are important<br />
when evaluating potential methodologies for <strong>the</strong>ir use in <strong>the</strong> prehospital<br />
and hospital environment.<br />
In critically ill paediatric patients, vascular access may<br />
present substantial difficulties [52]. IO access will provide a<br />
significant time saving which will benefit critically ill trauma<br />
patients, both by decreasing <strong>the</strong> time to achieve access and<br />
time to drug administration. In 2005 <strong>the</strong> American Heart<br />
Associations’ resuscitation guidelines were updated to reflect<br />
this and now recommends <strong>the</strong> IO route be <strong>the</strong> first alternative<br />
to difficult or delayed intravenous access [53]. From Table 1 it<br />
is clear that if rapid fluid resuscitation is required, <strong>the</strong>n large<br />
bore IV access via <strong>the</strong> central route is preferable. However,<br />
<strong>the</strong>re is anecdotal use <strong>of</strong> multiple IO access ports to achieve<br />
increased fluid administration.<br />
Current medical training is heavily weighted towards<br />
<strong>the</strong>oretical ra<strong>the</strong>r than practical training. Placing IV cannulae<br />
in haemodynamically unstable casualties with multiple limb<br />
amputations is very challenging even for experienced clinicians<br />
in ideal situations. This should be balanced against IO insertion<br />
which is rapid, intuitive and requires minimal training and in less<br />
than ideal environments.<br />
The current Gold Standard for resuscitation is <strong>the</strong> subclavian<br />
large bore 8.5 French ‘Trauma Line’. It provides rapid access, fast<br />
flowing large volume fluid resuscitation. This technique however<br />
requires skill and training which currently only a limited number<br />
<strong>of</strong> specialities provide. The authors feel this should be updated<br />
and become a core competency for military clinicians involved in<br />
<strong>the</strong> management <strong>of</strong> severely injured trauma casualties providing<br />
advanced resuscitation on <strong>the</strong> <strong>Medical</strong> Emergency Response<br />
Team (MERT) Role 2 and 3 hospital setting.<br />
Conclusion<br />
Vascular access in <strong>the</strong> military polytrauma patient is difficult and<br />
can take up precious time that could be used for fluid resuscitation<br />
and drug administration.<br />
The authors propose that to avoid delay initiating resuscitation<br />
in pre-hospital or hospital setting, <strong>the</strong> IO approach should be<br />
<strong>the</strong> first line vascular access in casualties with severe trauma. This<br />
is <strong>the</strong>n to be augmented by two large bore peripheral cannulae<br />
or ideally an 8.5F central venous ca<strong>the</strong>ter in <strong>the</strong> subclavian vein<br />
depending on <strong>the</strong> experience <strong>of</strong> <strong>the</strong> practitioner and <strong>the</strong> severity<br />
<strong>of</strong> <strong>the</strong> injury.<br />
References<br />
1. Seigworth G. Bloodletting over <strong>the</strong> Centuries. NY State J Med<br />
1980;Dec:2022-2028<br />
2. www.braceface.com/medical/Civil_War_Articles/Bloodletting_<br />
during_Civil_War.htm<br />
3. Drinker CK, Drinker KR, Lund CC. The Circulation in <strong>the</strong><br />
mammalian bone marrow. Am J Physiology 1922;621-92<br />
4. Marvin AW. Adult Intraosseus access: An idea whose time has<br />
come. Israeli <strong>Journal</strong> <strong>of</strong> Emergency Medicine 2006;6;2:41-5<br />
5. Cooper BR, Mahoney PF, Hodgetts TJ, Mellor A. Intraosseus<br />
access (EZIO) for resuscitation: UK Military Combat Experience.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 2007;153(4):314-316<br />
6. Dronen SC, Yee AS, Tomlanough MC. Proximal saphenous vein<br />
cutdown. Ann Emerg Med 1981;10:328-30<br />
7. Borgman MA, Spinella PC, Perkins JG et al. The ratio <strong>of</strong> blood<br />
products transfused affects mortality in patients receiving massive<br />
transfusions at a combat support hospital. J Trauma 2007;63:805-<br />
813<br />
8. Sweeney MN. Vascular access in trauma. Anes<strong>the</strong>siol Clin N Am<br />
1999;17:97-106<br />
9. Scalea TM, Sinert R, Duncan AO et al. Percutaneous Central<br />
Venous Access for Resuscitation in Trauma. Acad Emerg Med<br />
1994;1:525-531<br />
10. Pappas P, Brathwaite CEM, Ross SE. Emergency Central Venous<br />
Ca<strong>the</strong>terization during Resuscitation <strong>of</strong> Trauma Patients. Am Surg<br />
1992;58(2):108-11<br />
11. Davis DP, Ramanujam R. Central Venous Access by Air <strong>Medical</strong><br />
Personnel. Prehosp Emerg Care 2007;11(2):204-206<br />
12. Miliken SJ, Cain TL, Hansbrough J. Rapid volume replacement for<br />
hypovolaemic shock: A comparison <strong>of</strong> techniques and equipment.<br />
J Trauma 1984;24:428-431<br />
13. Barcelona S, Vilich F, Cote C. A Comparison <strong>of</strong> Flow Rates and<br />
Warming Capabilities <strong>of</strong> <strong>the</strong> level 1 and Rapid Infuser System with<br />
Various Size Intravenous Ca<strong>the</strong>ters. Anaesth Analg 2003;97:358-63<br />
14. Su-Yin Ngo A, Oh JJ, Chen Y et al. Intraosseus Vascular Access in<br />
Adults using <strong>the</strong> EZIO in an Emergency Department. Int J Emerg<br />
Med 2009;2:155-160<br />
15. Ong ME, Chan YH, Oh JJ, Ngo AS. An observational, prospective<br />
study comparing tibial and humeral intraosseus access using <strong>the</strong><br />
EZIO. Am J Emerg Med 2009;27(1):8-15<br />
16. Mateer JR, Thompson BM, Tucker J et al. Effects <strong>of</strong> High Infusion<br />
Pressure and Large-bore Tubing on Intravenous Flow rates. Am J<br />
Emerg Med 1985;3:187-189<br />
17. Tiffany BR, Horwood BT, Pollack CV et al. Sternal Intraosseus<br />
Infusion: Flow Rates and Utility. Ann Emerg Med 1999;34(4):S15<br />
18. Paediatric Advanced Life Support (APLS). Resuscitation Council<br />
UK. 2005: 85-95<br />
19. David<strong>of</strong>f J, Fowler R, Miller L. Clinical evaluation <strong>of</strong> a novel<br />
intraosseus device for adults. J Em Med Serv 2005;30(10):20-23<br />
20. Frascone RJ, Jensen JP, Salzman JG. Consecutive field trials<br />
using two different intraosseus devices. Prehosp Emerg Care<br />
2007;11(2):164-171<br />
21. Suyama J, Knutsen C, Hostler D. IO Versus IV Access While<br />
Wearing Personal Protective Equipment In a HAZMAT Scenario.<br />
Prehosp Emerg Care 2007;11:467-472<br />
22. Fenton P, Bali N, Jeffrey SLA. A Complication <strong>of</strong> <strong>the</strong> use <strong>of</strong> an<br />
Intra-osseus needle. J R <strong>Army</strong> Med <strong>Corps</strong> 2009;155(2):110-111<br />
23. Rosovsky M, Fitzpatrick M, Goldfarb CR, Finestone H. Bilateral<br />
osteomyelitis due to intraosseus infusion: Case report and review<br />
<strong>of</strong> <strong>the</strong> English language literature. Pediatr Radiol 1994;24(1):72-3<br />
24. Galpin RD, Kronck JB, Willis RB, Frerwen TC. Bilateral lower<br />
extremity compartment syndrome secondary to intraosseus fluid<br />
resuscitation. J Pediatr Orthop 1991;11(6):773-6<br />
25. Lapostolle F, Catineau J, Garrigue B et al. Prospective evaluation <strong>of</strong><br />
peripheral venous access difficulty in emergency care. Intensive Care<br />
Med 2007;33:1452-1457<br />
26. Brendan G, Brachet T, David G et al. The Time Cost <strong>of</strong> Prehospital<br />
Intubation and Intravenous Access in Trauma Patients. Prehosp<br />
Emerg Care 2008;12(3):327-332<br />
27. Grevstad U, Gregersen P, Rasmussen LS. Intravenous access in <strong>the</strong><br />
emergency patient. Curr Anaes Crit Care2009;20:120-127<br />
28. Battlefield Advanced Trauma Life Support. 2010<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S385–390 389
Vascular Access<br />
29. Sweeney MN. Vascular access in trauma. Anes<strong>the</strong>siol Clin N Am<br />
1999;17(1):97-106<br />
30. Roberts JR, Hedges JR. Clinical Procedures in Emergency Medicine<br />
5th edition. Section IV. Saunders, 2009: Chap; 18-22<br />
31. Harvey M, Thumma V. Techniques for upguaging peripheral<br />
venous cannulae in volume resuscitation. Letter. Emerg Med J<br />
2007;24:371-373<br />
32. Constantino TG, Kirtz JF, Satz WA. Ultrasound guided peripheral<br />
venous access vs. <strong>the</strong> external jugular vein as <strong>the</strong> initial approach to<br />
<strong>the</strong> patient with difficult venous access. J Emerg Med 2009;Feb:1-6<br />
33. Chappell S, Vilke G, Chan TC et al. Peripheral Venous Cutdown:<br />
Technical tips. J Emerg Med 2006;31(4):411-416<br />
34. Westfall MD, Price KR, Lambert M et al. Intravenous access in<br />
<strong>the</strong> critically ill trauma patient: A multicentered, prospective,<br />
randomized trial <strong>of</strong> saphenous cutdown and percutaneous femoral<br />
access. Ann Emerg Med 1994;23:541-545<br />
35. Briers N, Morris I, Boon JM et al. Proximal Great Saphenous<br />
Vein Cut Down: An Evaluation <strong>of</strong> Techniques and Anatomical<br />
Considerations. Clin Anat 2008;21:453-460<br />
36. Forssmann WG, Hirsch JR. 50 years Nobel Prize: Werner<br />
Forssmann and <strong>the</strong> issue <strong>of</strong> commemorative stamps. Eur J Med Res<br />
2006;27;11(10):406-408<br />
37. Aubaniac R. L’injection intraveineuse sous-claviculaire: advantages<br />
et technique. Presse Med 1952;60:1456<br />
38. Seldinger SI. Ca<strong>the</strong>ter Replacement <strong>of</strong> <strong>the</strong> Needle in Percutaneous<br />
Arteriography: A new technique. Acta Radiologica 1953;39(5):368-<br />
376<br />
39. American Heart Association. Part 7.2: Management <strong>of</strong> Cardiac<br />
Arrest. Circulation 2005;112;IV-58-IV-66<br />
40. Fyntanidou B, Fortounis K, Amaniti K et al. The use <strong>of</strong> central<br />
venous ca<strong>the</strong>ters during emergency prehospital care: A 2 year<br />
experience. Eur J Emerg Med 2009;16:194-198<br />
41. Taylor R, Palagiri AV. Central venous ca<strong>the</strong>terisation. Crit Care<br />
Med 2007;35(5):1390-1396<br />
42. Troianos CA, Kuwik RJ, Pasqual JR et al. Internal Jugular<br />
Vein and Carotid Artery Anatomic Relation as Determined by<br />
Ultrasonography. Anes<strong>the</strong>siology 1996;85:43-48<br />
390<br />
EJ Hulse, GOR Thomas<br />
43. Ferguson M, Max MH, Marshall W. Emergency Department<br />
Infraclavicular Subclavian Vein Ca<strong>the</strong>terization in Patient with<br />
Multiple Injuries and Burns. South Med J 1988;81(4):433-5<br />
44. Mangiante EC, Hoots AV, Fabian TC. The Percutaneous Common<br />
Femoral Vein Ca<strong>the</strong>ter for Volume Replacement in Critically<br />
Injured Patients. J Trauma 1988;28(12):1644-1649<br />
45. Abraham E, Shapiro M, Podolsky S. Central venous ca<strong>the</strong>terization<br />
in <strong>the</strong> emergency setting. Crit Care Med 1983;11(7):515-517<br />
46. Schwab CW, Adcock OT. An eight French introducer as a primary<br />
resuscitation device. J Trauma 1983;23:660<br />
47. Sznajder JI, Zveibil FR, Bitterman H et al. Central Vein<br />
ca<strong>the</strong>terisation: Failure and Complication Rates by Three<br />
Percutaneous Approaches. Arch Intern Med 1986;146:259-261<br />
48. Mallory DL, McGee WT, Shawker TH et al. Ultrasound guidance<br />
improves <strong>the</strong> success rate <strong>of</strong> internal jugular vein cannulation. A<br />
prospective, randomized trial. Chest 1990;98(1):157-60<br />
49. Jones T, Barnhart GR, Gervin AS. Tandem 8.5 French Subclavian<br />
Ca<strong>the</strong>ters: A Technique for Rapid Volume Replacement. Ann<br />
Emerg Med 1987;16(12):1369-72<br />
50. National Institute for Clinical Excellence. Guidance on <strong>the</strong> use <strong>of</strong><br />
ultrasound locating devices for placing central venous ca<strong>the</strong>ters.<br />
Technology Appraisal Guidance No 49, http://www.nice.org.uk:<br />
September 2002<br />
51. Rittenberger JC, Bost J, Menegazzi JJ. Time to give <strong>the</strong> first<br />
medication during resuscitation in out-<strong>of</strong>-hospital cardiac arrest.<br />
Resuscitation 2006;70(2):201-6<br />
52. Rosetti VA, Thompson BM, Miller J, Mateer JR, Aprahamian C.<br />
Intraosseus infusion: an alternative route <strong>of</strong> pediatric intravascular<br />
access. Ann Emerg Med 1985;14(9):885-8<br />
53. American Heart Association. 2005 American Heart Association<br />
(AHA) guidelines for cardiopulmonary resuscitation (CPR) and<br />
emergency cardiovascular care <strong>of</strong> pediatric and neonatal patients:<br />
pediatric advanced life support. Pediatrics 2006;117(5):e1005-28<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S385–390
Research and Audit
Current Epidural Practice – Results <strong>of</strong> a Survey <strong>of</strong><br />
Military Anaes<strong>the</strong>tists<br />
KL Woods 1 , D Aldington 2 .<br />
1 Specialist Registrar Anaes<strong>the</strong>tics, James Cook University Hospital, Middlesbrough. 2 Consultant in Pain Medicine, Pain<br />
Relief Unit, Churchill Hospital. OXFORD.<br />
Abstract<br />
Objectives: As epidurals are now used for pain relief on deployment a survey was conducted to look at <strong>the</strong> current epidural<br />
practice <strong>of</strong> UK military anaes<strong>the</strong>tists. The aim was to identify any potential issues with regard to equipment and training to<br />
allow future development <strong>of</strong> pre-deployment training.<br />
Methods: An internet based survey was carried out. All military anaes<strong>the</strong>tists were sent an e-mail containing a link to <strong>the</strong><br />
survey and <strong>the</strong> results <strong>of</strong> those who responded were analysed.<br />
Results: A total <strong>of</strong> 49 surveys were completed. 78% <strong>of</strong> respondents carried out epidurals more than once a month, in a<br />
wide range <strong>of</strong> specialities. There was considerable variation in methods <strong>of</strong> securing epidurals and in drug choice amongst<br />
respondents.<br />
Conclusions: The results <strong>of</strong> this survey show that whilst epidurals are commonly carried out amongst military anaes<strong>the</strong>tists<br />
during <strong>the</strong>ir UK practice, <strong>the</strong>re is significant variation within <strong>the</strong> practice. Areas have been identified for development <strong>of</strong><br />
educational courses, for example methods <strong>of</strong> securing epidurals, and <strong>the</strong>se have already been acted upon.<br />
Introduction<br />
Epidurals are now carried out routinely whilst on deployment.<br />
However, on deployment <strong>the</strong> range and availability <strong>of</strong> equipment<br />
is limited when compared to <strong>the</strong> UK. As military anaes<strong>the</strong>tists<br />
deploy from a wide variety <strong>of</strong> hospitals within <strong>the</strong> UK and have a<br />
range <strong>of</strong> interests within <strong>the</strong>ir UK practice, it was felt that it would<br />
be useful to identify any potential problems that could arise from<br />
having to use unfamiliar equipment on deployment. Identification<br />
<strong>of</strong> any such problems allows training courses to be considered and<br />
allows deploying clinicians time to acquaint <strong>the</strong>mselves with issues<br />
and enhance <strong>the</strong>ir knowledge prior to deployment.<br />
The aim <strong>of</strong> this survey was to look at current UK epidural<br />
practice amongst military anaes<strong>the</strong>tists.<br />
Method<br />
We developed a series <strong>of</strong> questions for <strong>the</strong> survey and designed<br />
<strong>the</strong>se into an internet based survey using <strong>the</strong> Survey Monkey®<br />
tool [1]. Questions included frequency <strong>of</strong> insertion <strong>of</strong> epidurals,<br />
specialities in which <strong>the</strong>y were inserted, use and type <strong>of</strong> prepacked<br />
epidural sets and methods <strong>of</strong> securing epidurals. O<strong>the</strong>r questions<br />
involved drugs used within epidurals and choice <strong>of</strong> epidural<br />
pump. Anaes<strong>the</strong>tists were also asked <strong>the</strong> lowest age at which<br />
<strong>the</strong>y would be happy to insert an epidural. This questionnaire<br />
(See right) was distributed to all military anaes<strong>the</strong>tists on <strong>the</strong> Tri-<br />
Service Anaes<strong>the</strong>tic Society (TSAS) mailing list with a request<br />
asking <strong>the</strong>m to access <strong>the</strong> survey via a URL in <strong>the</strong> e-mail and<br />
complete <strong>the</strong> questionnaire. The results were analysed using <strong>the</strong><br />
built in analysis on Survey Monkey.<br />
Results<br />
The survey was started by a total <strong>of</strong> 58 people <strong>of</strong> whom 49<br />
completed <strong>the</strong> questionnaire. Sadly <strong>the</strong> “true” response rate is<br />
impossible to judge as <strong>the</strong> invitation to complete <strong>the</strong> questionnaire<br />
Corresponding Author: Lt Col Aldington, FFPMRCA<br />
RAMC, Consultant in Pain Medicine, Pain Relief Unit,<br />
Churchill Hospital. OXFORD.<br />
1: What grade are you?<br />
Consultant<br />
Staff and Associate Specialist<br />
ST 5,6,7 (SpR 3,4,5)<br />
ST 3,4<br />
ST 1,2<br />
O<strong>the</strong>r<br />
2: On average, how <strong>of</strong>ten do you carry out<br />
epidurals as part <strong>of</strong> your usual practice?<br />
More than once a week<br />
Once a week<br />
Once a fortnight<br />
Once a month<br />
Less than once a month<br />
Never<br />
3: Approximately how many epidurals do<br />
you carry out in a year?<br />
Please state<br />
4: What speciality do you carry out<br />
epidurals in routinely? Please tick all<br />
that apply<br />
General Surgery<br />
Orthopaedics<br />
Obstetrics<br />
Gynaecology<br />
Urology<br />
O<strong>the</strong>r (please specify)<br />
5: Do you use a pre-packed epidural set?<br />
Yes / No<br />
If yes please specify which set<br />
6: What do you use to secure your epidural<br />
ca<strong>the</strong>ters? Please tick all that apply<br />
Tegaderm<br />
Hypafix<br />
Epifix<br />
O<strong>the</strong>r (please specify)<br />
7: How <strong>of</strong>ten do you tunnel your routine<br />
epidurals?<br />
Always<br />
Occasionally<br />
Depends on <strong>the</strong> case<br />
Never<br />
8: Do you use glue to secure your epidural<br />
ca<strong>the</strong>ters?<br />
Always / Sometimes / Never<br />
9: What drug do you use for your test and<br />
loading doses? Please specify, including<br />
concentration and additives<br />
10: What drug mixture do you use for your<br />
standard epidural infusions?<br />
Please specify, including concentration<br />
and additives<br />
11: Do you use PCEA outside maternity?<br />
Yes / No<br />
12: What epidural pump do you use<br />
routinely? Please specify<br />
13: Is <strong>the</strong> epidural pump used exclusively<br />
for epidurals or does it have multiple<br />
uses?<br />
Epidural only / Multiple uses<br />
14: How comfortable would you be using<br />
<strong>the</strong> following drugs in epidurals on<br />
deployment?<br />
Very Comfortable/ Fairly Comfortable/<br />
Uncomfortable/ Never used<br />
Bupivacaine<br />
Levobupivacaine<br />
Lignocaine (Lidocaine)<br />
Ropivacaine<br />
15: In paediatric practice, what is <strong>the</strong><br />
youngest age you would be happy to<br />
insert an epidural in?<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S393–397 393
Epidural Practice Survey<br />
was sent by email with instructions to cascade which may or may<br />
not be accurate. The majority <strong>of</strong> respondents were consultants<br />
(Table 1).<br />
Grade Number (%)<br />
Consultant 35 (60.3)<br />
Staff and Associate Specialist<br />
(SAS)<br />
394<br />
1 (1.7)<br />
ST 5,6,7 (SpR 3,4,5) 11 (19.0)<br />
ST 3,4 7 (12.1)<br />
ST 1,2 4 (6.9)<br />
Table 1: The grade <strong>of</strong> respondents<br />
Of <strong>the</strong>se <strong>the</strong> majority carried out epidurals regularly as part <strong>of</strong><br />
<strong>the</strong>ir UK practice (Table 2) with <strong>the</strong> number <strong>of</strong> epidurals per year<br />
ranging from nil to approx 125. (Figure 1)<br />
Frequency Insertion Number (%)<br />
More than once a week 15 (26.3)<br />
Once a week 10 (17.5)<br />
Once a fortnight 9 (15.8)<br />
Once a month 7 (12.3)<br />
Less than once a month 14 (24.5)<br />
Never 2 (3.5)<br />
Table 2: Frequency with which respondents insert epidurals<br />
Figure 1: Frequency <strong>of</strong> epidural insertion<br />
KL Woods, D Aldington<br />
The majority <strong>of</strong> epidurals were carried out for General Surgery,<br />
Orthopaedics and Obstetrics (Figure 2)<br />
Figure 2: Specialty in which epidurals inserted<br />
48 <strong>of</strong> <strong>the</strong> responders used pre-packed epidural packs and <strong>of</strong> <strong>the</strong> 19<br />
who replied to <strong>the</strong> question regarding make <strong>of</strong> pre-packed set <strong>the</strong><br />
majority used Portex (9 respondents) with Braun being <strong>the</strong> next<br />
most commonly used (4 respondents). Hospital order and o<strong>the</strong>r<br />
brands each having 3 responses.<br />
The majority <strong>of</strong> people who responded used ei<strong>the</strong>r Tegaderm®<br />
or Epifix® to secure <strong>the</strong>ir epidural ca<strong>the</strong>ters (Figure 3). However<br />
most people do not routinely tunnel or use glue to secure <strong>the</strong><br />
ca<strong>the</strong>ter (Tables 3&4).<br />
Figure 3: Method <strong>of</strong> securing epidural ca<strong>the</strong>ter<br />
Frequency <strong>of</strong> tunnelling use Number (%)<br />
Always 1 (1.9)<br />
Occasionally 6 (11.3)<br />
Depends on <strong>the</strong> case 10 (18.9)<br />
Never 36 (67.9)<br />
<br />
Table 3: Frequency <strong>of</strong> epidural tunnelling<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S393–397
Epidural Practice Survey KL Woods, D Aldington<br />
Frequency <strong>of</strong> glue use Number (%)<br />
Always 9 (5.8)<br />
Sometimes 1 (1.9)<br />
Never 48 (92.3)<br />
Table 4: Frequency <strong>of</strong> glueing <strong>of</strong> epidurals<br />
There were a wide variety <strong>of</strong> drugs and concentrations used for a<br />
test dose but <strong>the</strong> commonest was 0.25% Bupivacaine followed by<br />
0.5% Bupivacaine (Figure 4).<br />
Figure 4: Choice <strong>of</strong> drug for epidural test dose<br />
There was a very wide range <strong>of</strong> drug combinations used for<br />
infusions. This was particularly noted with <strong>the</strong> added opiates<br />
and <strong>the</strong> concentration <strong>of</strong> opiate varied significantly. The most<br />
common drug combination for infusion was 0.1% Bupivacaine<br />
with 4mcg/ml fentanyl (Table 5).<br />
Patient controlled epidural anaes<strong>the</strong>sia (PCEA) is not used<br />
outside maternity in <strong>the</strong> majority <strong>of</strong> people’s current UK<br />
practice with only 36.7% <strong>of</strong> respondents using PCEA in nonobstetric<br />
settings<br />
The majority <strong>of</strong> responders to <strong>the</strong> questionnaire did not know<br />
<strong>the</strong> make <strong>of</strong> <strong>the</strong> epidural pump that was used in <strong>the</strong>ir hospital. Of<br />
those that did know, <strong>the</strong> most commonly used were <strong>the</strong> Gemstar<br />
and Graseby pumps. (Figure 5) In over 90% <strong>of</strong> those who replied<br />
<strong>the</strong>se pumps are used exclusively for epidural use.<br />
When asked how comfortable responders felt about using<br />
different drugs in epidurals on deployment, most people were<br />
happy using bupivacaine or levobupivacaine, but were less<br />
comfortable using lignocaine or ropivacaine (Figure 6).<br />
Drug Choice Number<br />
0.1% Bupivacaine + 4mcg/ml fentanyl 16<br />
0.125% Bupivacaine + 2mcg/ml fentanyl 8<br />
0.125% Bupivacaine + 4mcg/ml fentanyl 6<br />
0.1% Bupivacaine + opiate (range <strong>of</strong> doses) 5<br />
0.1% Bupivacaine (plain) 1<br />
0.125% Bupivacaine + opiate (range <strong>of</strong> doses) 1<br />
0.125% Bupivacaine (plain) 3<br />
0.15% Bupivacaine + opiate (range <strong>of</strong> doses ) 3<br />
0.2% Bupivacaine + 2 mcg/ml fentanyl 1<br />
0.075% Bupivacaine + 2 mcg fentanyl 1<br />
0.2% Ropivacaine 2<br />
0.125% Levobupivacaine + 2 mcg/ml fentanyl 1<br />
Depends 3<br />
Table 5: Combinations <strong>of</strong> drugs used for infusion<br />
Figure 5: Make <strong>of</strong> epidural pump used<br />
Figure 6: How comfortable responders would be to use different drugs<br />
on deployment<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S393–397 395<br />
<br />
Epidural Practice Survey<br />
When asked what <strong>the</strong> youngest age <strong>of</strong> child responders would<br />
be happy inserting epidurals in on deployment, <strong>the</strong> total number<br />
<strong>of</strong> people happy to insert an epidural decreased as <strong>the</strong> age <strong>of</strong> <strong>the</strong><br />
child decreased. (Figure 7)<br />
396<br />
Frequency<br />
Figure 7: Youngest age (vertical axis) responders were happy inserting<br />
epidurals into<br />
Discussion<br />
Although <strong>the</strong>re has been a recent national survey <strong>of</strong> central neuraxial<br />
block [2], <strong>the</strong>re are very few published audits or surveys <strong>of</strong> current<br />
practice with regards to personal epidural practice. It is only in<br />
recent years that epidurals have been carried out on established<br />
military deployments [3]. This change has been due to <strong>the</strong> move<br />
from tents to hard accommodation, which is significantly less dusty<br />
than a hospital under canvas and <strong>the</strong>refore allows epidural insertion<br />
in a clean environment. The move towards use <strong>of</strong> epidurals has also<br />
been facilitated by <strong>the</strong> ability <strong>of</strong> <strong>the</strong> Aeromedical Evacuation Teams<br />
to use <strong>the</strong>m during repatriation <strong>of</strong> patients. The military medical<br />
environment is, by necessity, relatively austere and <strong>the</strong> range <strong>of</strong><br />
equipment available to <strong>the</strong> deployed anaes<strong>the</strong>tist is reduced when<br />
compared to that <strong>of</strong> <strong>the</strong> NHS. Part <strong>of</strong> <strong>the</strong> reason for this is <strong>the</strong><br />
need to reduce <strong>the</strong> logistical requirement on operations. The intent<br />
behind our survey was to identify any issues with training and<br />
equipment in order to allow personnel to prepare and enhance<br />
<strong>the</strong>ir knowledge. This will <strong>the</strong>n help to allow for <strong>the</strong> provision <strong>of</strong><br />
an epidural service on deployment.<br />
The survey demonstrated that <strong>the</strong> vast majority <strong>of</strong> respondents<br />
do carry out epidurals regularly in <strong>the</strong>ir UK or NHS practice and<br />
in specialities that are comparable to those seen on deployment.<br />
Securing <strong>of</strong> epidurals was one area identified by <strong>the</strong> survey<br />
as having potential requirement for fur<strong>the</strong>r discussion and<br />
training. While <strong>the</strong> majority <strong>of</strong> people used Tegaderm, Epifix<br />
or Hypafix to secure <strong>the</strong>ir epidurals, only a minority tunnelled<br />
<strong>the</strong>ir epidurals. Tunnelling <strong>of</strong> epidurals reduces <strong>the</strong> incidence<br />
<strong>of</strong> movement <strong>of</strong> epidural ca<strong>the</strong>ters and so reduces <strong>the</strong> chance <strong>of</strong><br />
displacement [4-6] and in patients in whom an epidural may be<br />
<strong>of</strong> benefit for a prolonged time this is an advantage. This is also<br />
suggested in guidance on epidural management from <strong>the</strong> <strong>Royal</strong><br />
KL Woods, D Aldington<br />
College <strong>of</strong> Anaes<strong>the</strong>tists and The Association <strong>of</strong> Anaes<strong>the</strong>tists <strong>of</strong><br />
Great Britain and Ireland [7]. Although <strong>the</strong>re is some evidence<br />
suggesting that tunnelling <strong>of</strong> epidural ca<strong>the</strong>ters may reduce<br />
bacterial colonisation [8] <strong>the</strong>re is little to say that it reduces epidural<br />
infection rates. This is likely to be due to <strong>the</strong> fact<br />
that despite bacterial colonisation <strong>of</strong> ca<strong>the</strong>ters<br />
infection rates remain very low. However, <strong>the</strong>re is<br />
evidence that demonstrates tunnelling <strong>of</strong> caudal<br />
ca<strong>the</strong>ters in paediatric patients, where <strong>the</strong> site <strong>of</strong><br />
insertion is at higher risk <strong>of</strong> contamination than<br />
that <strong>of</strong> lumbar or thoracic epidurals, reduces<br />
colonisation <strong>of</strong> ca<strong>the</strong>ters to similar levels as that<br />
seen in lumbar epidurals [9]. This may be <strong>of</strong><br />
particular significance for <strong>the</strong> military patient<br />
population where patients may present having<br />
been contaminated by significant amounts <strong>of</strong><br />
dirt and dust.<br />
Glue can also be used to prevent accidental<br />
removal [10] and this survey has also highlighted<br />
<strong>the</strong> fact that very few responders use this as part<br />
<strong>of</strong> <strong>the</strong>ir routine UK practice. As with tunnelling<br />
<strong>the</strong> use <strong>of</strong> glue to reduce <strong>the</strong> chance <strong>of</strong> ca<strong>the</strong>ter<br />
displacement is <strong>of</strong> particular relevance on<br />
deployment where patients who have epidural<br />
ca<strong>the</strong>ters inserted in <strong>the</strong> Field Hospital may have <strong>the</strong>m running<br />
all through <strong>the</strong>ir repatriation (with all <strong>the</strong> moving and handling<br />
this entails) and on into <strong>the</strong>ir management in <strong>the</strong> UK. Securing<br />
epidural ca<strong>the</strong>ters as much as possible to minimise <strong>the</strong> chance<br />
<strong>of</strong> movement is <strong>the</strong>refore essential to help maintain epidural<br />
analgesia through this time.<br />
Drug choice for test and loading doses and also <strong>the</strong><br />
combinations used for infusions varied significantly amongst<br />
<strong>the</strong> responders to this survey. The guidelines on good practice<br />
in epidural management suggest that <strong>the</strong>re should be a strict<br />
limitation on <strong>the</strong> number <strong>of</strong> drugs and <strong>the</strong> concentration <strong>of</strong> <strong>the</strong>se<br />
drugs in each hospital [7]. On deployment plain local anaes<strong>the</strong>tic<br />
infusions are preferred ra<strong>the</strong>r than those containing opiates. This<br />
allows opiates to be used via PCA during repatriation, both<br />
for backup in case <strong>of</strong> problems with <strong>the</strong> epidural and also for<br />
analgesia for o<strong>the</strong>r wounds in areas not covered by <strong>the</strong> epidural.<br />
Education about which drugs are available in <strong>the</strong>atre will help<br />
prepare personnel prior to deployment.<br />
Ano<strong>the</strong>r area identified by <strong>the</strong> survey for fur<strong>the</strong>r training is that<br />
<strong>of</strong> paediatrics. As children form a proportion <strong>of</strong> those treated on<br />
deployment [11,12] it follows that some <strong>of</strong> <strong>the</strong>m will benefit from<br />
an epidural. The survey demonstrated that responders became less<br />
comfortable inserting epidurals as <strong>the</strong> age <strong>of</strong> <strong>the</strong> child reduced.<br />
How this can be improved for anaes<strong>the</strong>tists who do not routinely<br />
do any paediatric anaes<strong>the</strong>tics as part <strong>of</strong> <strong>the</strong>ir current UK practice<br />
is outside <strong>the</strong> remit <strong>of</strong> this survey.<br />
What next?<br />
The results <strong>of</strong> this survey have been fed back to both <strong>the</strong> <strong>Defence</strong><br />
Consultant Advisor (DCA) in Anaes<strong>the</strong>tics and Pr<strong>of</strong>essor <strong>of</strong><br />
Military <strong>Anaes<strong>the</strong>sia</strong>. The data has also been incorporated in<br />
some <strong>of</strong> <strong>the</strong> teaching on <strong>the</strong> Military Operational Surgical<br />
Training (MOST) course for personnel about to deploy and will<br />
also be used on <strong>the</strong> pre-deployment hospital validation exercise<br />
(HOSPEX).<br />
<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S393–397
Epidural Practice Survey KL Woods, D Aldington<br />
References<br />
1. URL: http://www.surveymonkey.com/s/HTGYLML<br />
2. Cook TM, Counsell D, Wildsmith JAW. Major Complications <strong>of</strong><br />
Central Neuraxial Block: report on <strong>the</strong> Third Audit Project <strong>of</strong> <strong>the</strong><br />
<strong>Royal</strong> College <strong>of</strong> Anaes<strong>the</strong>tists. Br J Anaesth 2009; 102: 179-90<br />
3. Connor DJ, Ralph JK, Aldington DJ. Field Hospital Analgesia. J R<br />
<strong>Army</strong> Med <strong>Corps</strong> 2009; 155: 49-56<br />
4. Bougher RJ, Corbett AR, Ramage DTO. The effect <strong>of</strong> tunnelling<br />
on epidural ca<strong>the</strong>ter migration. <strong>Anaes<strong>the</strong>sia</strong> 1996; 51: 191-194<br />
5. Kumar N, Chambers WA. Tunnelling epidural ca<strong>the</strong>ters: a<br />
worthwhile exercise? Editorial. <strong>Anaes<strong>the</strong>sia</strong> 2000; 55: 625-626<br />
6. Tripathi M, Pandey M. Epidural Ca<strong>the</strong>ter Displacement:<br />
Subcutaneous tunnelling with a loop to prevent displacement.<br />
<strong>Anaes<strong>the</strong>sia</strong> 2000; 55: 1113-1116<br />
7. Good practice in <strong>the</strong> management <strong>of</strong> continuous epidural analgesia<br />
in <strong>the</strong> hospital setting. The <strong>Royal</strong> College <strong>of</strong> Anaes<strong>the</strong>tists, The<br />
<strong>Royal</strong> College <strong>of</strong> Nursing, The Association <strong>of</strong> Anaes<strong>the</strong>tists <strong>of</strong> Great<br />
Britain and Ireland, The British Pain Society and The European<br />
Society <strong>of</strong> Regional <strong>Anaes<strong>the</strong>sia</strong> and Pain Therapy. November<br />
2004.<br />
8. Compere V, Legrand JF, Guitard PG et al. Bacterial Colonization<br />
After Tunneling in 402 Perineural Ca<strong>the</strong>ters: A Prospective Study.<br />
Anest Analg 2009; 108: 1326-1330<br />
9. Bebeck J, Books K, Krause H et al. Subcutaneous Tunneling <strong>of</strong><br />
Caudal Ca<strong>the</strong>ters Reduces <strong>the</strong> Rate <strong>of</strong> Bacterial Colonization to<br />
That <strong>of</strong> Lumbar Epidural. Anest Analg 2004; 99:689-93<br />
10. Wilkinson JN, Fitz-Henry J. Securing epidural ca<strong>the</strong>ters with<br />
Histoacryl glue. <strong>Anaes<strong>the</strong>sia</strong>. 2008; 63: 324<br />
11. Gurney I. Paediatric Casualties During OP TELIC. J R <strong>Army</strong> Med<br />
<strong>Corps</strong>. 2004; 150:270-272<br />
12. Creamer KM, Edwards MJ, Shields CH. Paediatric Wartime<br />
Admissions to US Military Combat Support Hospitals in<br />
Afghanistan and Iraq. Learning from <strong>the</strong> First 2,000 Admissions. J<br />
Trauma. 2009; 67: 762-768<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S393–397 397
Evolution <strong>of</strong> <strong>the</strong> Role 4 UK Military Pain Service<br />
L Devonport 1 , D Edwards 2 , C Edwards 3 , DJ Aldington 4 , PF Mahoney 5 , PR Wood 6<br />
1 <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine. 2 Consultant Nurse, Queen Elizabeth Hospital Birmingham, UHB NHS<br />
Foundation Trust. 3 Consultant Anaes<strong>the</strong>tist, <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine, 4 Consultant in Pain Medicine, DMRC<br />
Headley Court, 5 <strong>Defence</strong> Pr<strong>of</strong>essor <strong>Anaes<strong>the</strong>sia</strong>, Department <strong>of</strong> Military <strong>Anaes<strong>the</strong>sia</strong>, 6 Consultant Anaes<strong>the</strong>tist, Queen<br />
Elizabeth Hospital Birmingham, UHB NHS Foundation Trust.<br />
Abstract<br />
The early development <strong>of</strong> <strong>the</strong> UK Role 4 pain service has already been described. This article will describe developments up to<br />
October 2010, and present <strong>the</strong> results <strong>of</strong> projects used in assessing <strong>the</strong> effect <strong>of</strong> this service.<br />
Introduction<br />
The <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine (RCDM), based at<br />
University Hospital Birmingham NHS Foundation Trust (UHB)<br />
has been <strong>the</strong> primary Role 4 receiving unit for British military<br />
casualties since 2001 and <strong>the</strong> early development <strong>of</strong> <strong>the</strong> UK Role<br />
4 Pain service has already been described [1]. Although many <strong>of</strong><br />
<strong>the</strong> staff are military, <strong>the</strong>y are embedded in a new tertiary referral<br />
teaching hospital (Queen Elizabeth Hospital Birmingham,<br />
QEHB) that is currently undergoing accreditation as a Level 1<br />
Trauma centre. Prior to <strong>the</strong> opening <strong>of</strong> QEHB in June 2010 <strong>the</strong><br />
patients were treated by <strong>the</strong> same <strong>Defence</strong> <strong>Medical</strong> Services and<br />
civilian personnel at Selly Oak Hospital (SOH), which was also<br />
part <strong>of</strong> <strong>the</strong> UHB Trust.<br />
Patient Numbers<br />
The number <strong>of</strong> military casualties has varied over <strong>the</strong> past nine<br />
years, as have <strong>the</strong>ir injury patterns. Table 1 indicates admission<br />
rates for physical injury to both RCDM and <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong><br />
Rehabilitation Centre (DMRC) at Headley Court [2]. Table 2<br />
gives numbers <strong>of</strong> amputees that have been received [3]. Toge<strong>the</strong>r,<br />
<strong>the</strong>se tables reveal <strong>the</strong> work load has increased significantly in<br />
both <strong>the</strong> number <strong>of</strong> cases and complexity.<br />
Developments<br />
Personnel<br />
Key to improving <strong>the</strong> service was <strong>the</strong> development <strong>of</strong> a Military<br />
Pain Team (MPT) on <strong>the</strong> military ward. The core <strong>of</strong> this team<br />
has been 3 military nurses who spend at least 80% <strong>of</strong> <strong>the</strong>ir time<br />
with <strong>the</strong> Pain Team during <strong>the</strong>ir attachment. They are led by a<br />
civilian Consultant Nurse who also leads <strong>the</strong> hospital critical<br />
care outreach team and <strong>the</strong> team has daily consultant anaes<strong>the</strong>tic<br />
support. Each week <strong>the</strong>re is a multidisciplinary pain ward round.<br />
This multidisciplinary group is made up <strong>of</strong> <strong>the</strong> MPT, a senior<br />
physio<strong>the</strong>rapist and <strong>the</strong> ward pharmacist, <strong>of</strong>ten with <strong>the</strong> military’s<br />
Subject Matter Expert (SME) in Pain to help ensure integration<br />
with <strong>the</strong> o<strong>the</strong>r echelons.<br />
During <strong>the</strong> ward round every patient is asked about <strong>the</strong>ir pain,<br />
<strong>the</strong>ir sleep pattern and about side effects from pain medications.<br />
It must be stressed that every patient is interviewed and not only<br />
those requiring risk management because <strong>the</strong>y have epidurals<br />
Corresponding Author: Dr Paul Wood, Consultant<br />
Anaes<strong>the</strong>tist, Queen Elizabeth Hospital Birmingham,<br />
Mindelsohn Way, Edgbaston. Birmingham. B15 2WB<br />
Tel: 0121 627 2000 Email: paul.wood@uhb.nhs.uk<br />
2007 2008 2009 2010<br />
from 08<br />
Oct 07<br />
to 30<br />
June10<br />
or ca<strong>the</strong>ters in situ. Following <strong>the</strong> ward round <strong>the</strong> MPT have a<br />
group meeting to discuss clinical, audit, research and educational<br />
developments. At this point <strong>the</strong>y are joined by a Consultant<br />
Anaes<strong>the</strong>tist who attended <strong>the</strong> multidisciplinary military clinical<br />
care conference held on <strong>the</strong> same morning. This arrangement<br />
ensures that members <strong>of</strong> <strong>the</strong> MPT have an integrated role with<br />
<strong>the</strong> o<strong>the</strong>r specialties involved in <strong>the</strong> care <strong>of</strong> <strong>the</strong> patients. Finally,<br />
members <strong>of</strong> <strong>the</strong> MPT attend quarterly Military Pain Special<br />
Interest Group meetings that examine issues and developments<br />
in pain management from <strong>the</strong> point <strong>of</strong> wounding through to<br />
established rehabilitation.<br />
The relationship <strong>of</strong> <strong>the</strong> MPT to o<strong>the</strong>r essential clinical teams<br />
can be illustrated by a hub and spoke model (Figure 1).<br />
398 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S398–401<br />
Op<br />
Telic<br />
Op<br />
Herrick<br />
104 198 131 67<br />
148 432 736 643<br />
Table 1: Casualty admissions to RCDM and DMRC Headley Court [2]<br />
Op<br />
Telic<br />
Op<br />
Herrick<br />
2006 2007 2008 2009 2010<br />
from 01<br />
Apr 06<br />
to 30<br />
June10<br />
Amputees 6 10
UK Military Pain Service L Devonport, D Edwards, C Edwards et al<br />
Figure 1. Relationship <strong>of</strong> MPT to RCDM / UHB clinical teams<br />
Medication - <strong>the</strong> Military Standard Operating<br />
Procedure<br />
All patients admitted to <strong>the</strong> military ward are prescribed a<br />
standard analgesic regime with a minimum <strong>of</strong> regular paracetamol<br />
and a non-steroidal anti-inflammatory, toge<strong>the</strong>r with codeine<br />
or tramadol [1]. The details are described in a ward analgesic<br />
document which is made available to all <strong>the</strong> ward junior doctors<br />
and military and anaes<strong>the</strong>tic registrars. A paper copy is kept<br />
on <strong>the</strong> ward and an electronic version resides on <strong>the</strong> Trust’s<br />
intranet. Medication is prescribed electronically on <strong>the</strong> Patient<br />
Information and Communication System (PICS), which is a<br />
Trust development. This electronic tool is invaluable in tracking<br />
and auditing medication use. In tandem with <strong>the</strong> introduction<br />
<strong>of</strong> <strong>the</strong> PICS prescribing system <strong>the</strong> ability <strong>of</strong> nurses to prescribe<br />
regular oral morphine has been facilitated since March 2010 by<br />
<strong>the</strong> introduction <strong>of</strong> a Single Nurse Check Analgesia protocol.<br />
As a result <strong>of</strong> <strong>the</strong> mechanisms <strong>of</strong> injury, many <strong>of</strong> <strong>the</strong> patients<br />
are expected to have a neuropathic component to <strong>the</strong>ir pain,<br />
some, such as traumatic amputations, more than o<strong>the</strong>rs; thus<br />
<strong>the</strong>re is a low threshold for <strong>the</strong> early use <strong>of</strong> anti-neuropathic pain<br />
agents, particularly pregabalin and amitriptyline. A recent survey<br />
(Table 3 study V) showed 66% <strong>of</strong> <strong>the</strong> ward’s 25 patients were<br />
on a combination <strong>of</strong> <strong>the</strong>se, with half prescribed <strong>the</strong> maximum<br />
pregabalin dose.<br />
Regional <strong>Anaes<strong>the</strong>sia</strong><br />
Regional anaes<strong>the</strong>tic techniques are encouraged. Their use at<br />
<strong>the</strong> Role 3 Hospital has been described [4, 5]. In Birmingham<br />
it was noted that <strong>the</strong> number <strong>of</strong> patients returning with regional<br />
ca<strong>the</strong>ters in situ increased during Operation HERRICK 9B in<br />
early 2009. To date approximately 66% <strong>of</strong> <strong>the</strong> ca<strong>the</strong>ters have been<br />
initiated in <strong>the</strong> deployed field hospital (Table 3 Study VI) and<br />
will have been used to provide analgesia for <strong>the</strong> repatriation, a<br />
development anticipated in an earlier paper [6].<br />
There have been concerns about <strong>the</strong> use <strong>of</strong> regional ca<strong>the</strong>ters in<br />
limb injuries delaying diagnosis <strong>of</strong> compartment syndrome and<br />
its management [7]. A consensus meeting was undertaken at <strong>the</strong><br />
Birmingham Research Park to examine this issue in June 2009<br />
and a subsequent editorial <strong>of</strong>fered guidance on this issue [8].<br />
Managing Peripheral Nerve and Epidural Blocks<br />
When casualties arrive at RCDM, receiving clinicians know not<br />
to remove <strong>the</strong> ca<strong>the</strong>ters but to leave <strong>the</strong>m in place. If <strong>the</strong>re is any<br />
doubt about <strong>the</strong> neurological status <strong>of</strong> <strong>the</strong> limb <strong>the</strong> infusion is<br />
stopped. Once <strong>the</strong> degree <strong>of</strong> function has been confirmed, <strong>the</strong><br />
infusion can be restarted and analgesia restored. With <strong>the</strong> excellent<br />
support provided by <strong>the</strong> anaes<strong>the</strong>tic department at UHB, re-<br />
siting or de novo placement <strong>of</strong> both continuous peripheral nerve<br />
and epidural ca<strong>the</strong>ters can be facilitated with little delay.<br />
The duration that <strong>the</strong> peripheral nerve infusions are maintained<br />
is <strong>of</strong> interest. Our surveillance data <strong>of</strong> 133 cases show that our<br />
longest is 17 days, with approximately one quarter in place for<br />
a week or longer (Table 3, Study VI). It is also clear that <strong>the</strong><br />
geographical location <strong>of</strong> insertion does not influence duration<br />
<strong>of</strong> use. The most common technique (41%) in both Afghanistan<br />
and Iraq was a lumbar epidural, followed by femoral and <strong>the</strong>n<br />
sciatic nerve blocks (Table 3, Study VI).<br />
The concerns surrounding <strong>the</strong> use <strong>of</strong> epidurals in <strong>the</strong> current<br />
conflict are mentioned in a review <strong>of</strong> field hospital analgesia [4].<br />
It has been standard practice for all ca<strong>the</strong>ter tips to be sent for<br />
microscopy, culture and sensitivity testing after removal (Table<br />
3, Study VII). We have been supported in this venture by <strong>the</strong><br />
UHB microbiology department. While a number <strong>of</strong> <strong>the</strong> cultures<br />
have returned “positive” none have been <strong>of</strong> clinical significance;<br />
this data includes that for ca<strong>the</strong>ters for continuous peripheral<br />
nerve blockade (Table 3, Study VII). Ano<strong>the</strong>r concern is <strong>the</strong><br />
development <strong>of</strong> an epidural haematoma, particularly in patients<br />
who may be at greater risk following <strong>the</strong> coagulopathy associated<br />
with significant polytrauma [9]. Traditional signs <strong>of</strong> limb<br />
weakness rely on <strong>the</strong> existence <strong>of</strong> lower limbs; in <strong>the</strong> case <strong>of</strong> some<br />
<strong>of</strong> our patients this is not possible. O<strong>the</strong>r signs and symptoms<br />
that could be proxy measures are also difficult to use given <strong>the</strong><br />
frequency <strong>of</strong> perineal injury and urinary ca<strong>the</strong>terisation. Instead<br />
we have developed our “4 and No More Rule” supported by <strong>the</strong><br />
neuroradiologists as required [10].<br />
Practical procedures<br />
The ability to perform regional anaes<strong>the</strong>sia, changes <strong>of</strong> dressings<br />
and similar tasks <strong>of</strong>ten undertaken in <strong>the</strong>atre has been facilitated<br />
by equipping a room on <strong>the</strong> military ward exclusively for such<br />
tasks. This innovation has several advantages:<br />
• it allows <strong>the</strong> provision <strong>of</strong> appropriate sedation, analgesia (which<br />
may include <strong>the</strong> use <strong>of</strong> ketamine ), and monitoring;<br />
• it has a consequent reduction in demand on scarce operating<br />
<strong>the</strong>atre resources;<br />
• it provides rapid access with minimal transit time<br />
• it maintains continuity <strong>of</strong> nursing care<br />
• it enhances <strong>the</strong> education <strong>of</strong> both military medical and nursing<br />
staff in appropriate pain management<br />
Mental Health and psychosocial issues<br />
The importance <strong>of</strong> psychological support was emphasized in <strong>the</strong><br />
earlier article [1], and <strong>the</strong> broader issues and complexities <strong>of</strong> forces<br />
mental health have been <strong>the</strong> subject <strong>of</strong> a recent <strong>Journal</strong> <strong>of</strong> <strong>the</strong> <strong>Royal</strong><br />
<strong>Army</strong> <strong>Medical</strong> <strong>Corps</strong> Special edition [11]. The interface between<br />
pain, analgesia and mental health issues can be convoluted [12]<br />
and this fact is respected in liaison with <strong>the</strong> mental health team.<br />
After RCDM - Discharge Care<br />
Their stay at RCDM is just one phase <strong>of</strong> a patient’s rehabilitation<br />
and <strong>the</strong> importance <strong>of</strong> what will happen to <strong>the</strong> patients when <strong>the</strong>y<br />
leave RCDM is addressed. Most will go on a period <strong>of</strong> leave before<br />
posting to ei<strong>the</strong>r DMRC or one <strong>of</strong> <strong>the</strong> Regional Rehabilitation<br />
Units. Prior to leaving RCDM patients are provided with several<br />
leaflets about <strong>the</strong>ir analgesia toge<strong>the</strong>r with a telephone contact<br />
number should <strong>the</strong>y have any concerns about <strong>the</strong>ir medication.<br />
There are military consultants in pain medicine at DMRC some<br />
<strong>of</strong> whom also attend RCDM with <strong>the</strong> intention <strong>of</strong> ensuring this<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S398–401 399
UK Military Pain Service<br />
Serial Topic Dates Aim / Description<br />
400<br />
I Duration <strong>of</strong> Stay April – June<br />
2009<br />
II Surgical activity April 2008<br />
–January<br />
2009<br />
To record <strong>the</strong> mean duration<br />
<strong>of</strong> stay on <strong>the</strong> military ward<br />
To quantify <strong>the</strong> number<br />
<strong>of</strong> operations casualties<br />
undergo<br />
III Opioid use May 2010 To survey <strong>the</strong> use <strong>of</strong> opioids<br />
by interrogation <strong>of</strong> PICS<br />
IV Bowel Function February -<br />
April 2010<br />
V Anti -neuropathic<br />
Analgesic<br />
VI Regional analgesia<br />
techniques<br />
VII Surveillance<br />
<strong>of</strong> Regional<br />
Anaes<strong>the</strong>tic +<br />
Epidural Ca<strong>the</strong>ter<br />
Infections<br />
October<br />
2009<br />
January -<br />
April 2010<br />
January<br />
2008 -<br />
present<br />
VIII Ward Pain Scores February –<br />
March 2010<br />
IX S4 ( SOH )<br />
Military ward<br />
Take home<br />
medication<br />
X Trauma Pain<br />
Recollection<br />
Surveillance<br />
XI Patients<br />
experience <strong>of</strong> pain<br />
management<br />
XII Opiate Use in<br />
Amputees at<br />
DMRC<br />
April to<br />
June 2009<br />
February<br />
2010 - on<br />
going<br />
September<br />
2010<br />
Oct 2008<br />
and Feb<br />
2010<br />
To establish <strong>the</strong> prevalence<br />
<strong>of</strong> problems with bowel<br />
function given <strong>the</strong> opiate<br />
load some patients require<br />
To record how many <strong>of</strong> <strong>the</strong><br />
patients on <strong>the</strong> military ward<br />
were prescribed medication<br />
for neuropathic pain<br />
Where sited, geographically<br />
and anatomically, plus<br />
duration<br />
To establish whe<strong>the</strong>r or not<br />
infection <strong>of</strong> ca<strong>the</strong>ters is a<br />
clinical issue.<br />
A record <strong>of</strong> pain scores as<br />
measured twice daily over a<br />
5 week period<br />
Establish <strong>the</strong> discharge<br />
medication pr<strong>of</strong>ile at SOH<br />
To survey patient’s<br />
recollection <strong>of</strong> pain<br />
management from point <strong>of</strong><br />
wounding to discharge from<br />
UHB<br />
Examines patients concerns<br />
with pain and interaction<br />
with medical staff<br />
( interview questionnaire )<br />
Establish whe<strong>the</strong>r long term<br />
opiate use occurs in military<br />
amputees.<br />
Patient<br />
numbers<br />
L Devonport, D Edwards, C Edwards et al<br />
Outcome & Comment<br />
35 During <strong>the</strong> 3 month snap shot <strong>the</strong> mean<br />
duration reduced from 19 to 9 days. This study<br />
predated an increase in more seriously injured<br />
casualties during <strong>the</strong> second half <strong>of</strong> 2009<br />
144 Maximum 15. Averages 2.<br />
64% one operation only.<br />
8% experience more than 3.<br />
21 All taking opioids. 70% on more than one<br />
opioid. 30% are on 3 or more. 60% codeine,<br />
55% oramorph, 45% tramadol, 10% PCA<br />
(morphine),<br />
25% Morphine SR, 5% oxycontin<br />
Multiple concurrent opioid prescriptions are<br />
common (rare in NHS practice )<br />
All<br />
patients<br />
All inpatients assessed weekly<br />
Routine prescription <strong>of</strong> aperients maintains<br />
acceptable bowel function<br />
25 66% taking amitriptyline and pregabalin;<br />
33% on max. pregabalin dose. This is a very<br />
important departure from normal NHS practice.<br />
133 In both locations, epidurals were <strong>the</strong> most<br />
common technique used. Femoral and sciatic<br />
ca<strong>the</strong>ters were more common in Camp Bastion<br />
while axillary were sited in RCDM but not<br />
Camp Bastion<br />
153 This data is continually reviewed - no significant<br />
issues to date<br />
All<br />
patients<br />
Less than 10% experience moderate and severe<br />
pain -compared with 20-80% severe pain<br />
expected from o<strong>the</strong>r studies.<br />
35 75% on paracetamol became 86%.<br />
NSAID use increased from 60 - 76%, <strong>of</strong> <strong>the</strong>se<br />
dicl<strong>of</strong>enac accounted for 2/3.<br />
Codeine increased from 25 to 50%, while<br />
tramadol decreased from 55% to 39%.<br />
Amitriptyline, gabapentin and pregabalin all<br />
reduced: 30% to 8%, 35 to 11% and 30 to<br />
8%. MST reduced 25 to 3% The reduction<br />
in neuropathic medication reflected <strong>the</strong> injury<br />
patterns (see I above)<br />
All<br />
patients<br />
All<br />
patients<br />
Monthly review <strong>of</strong> all data.<br />
Excellent results to date.<br />
Overall satisfaction with pain management -<br />
69%<br />
49 + 50 Two iterations. No evidence <strong>of</strong> problem<br />
with opiate use.<br />
Table 3 List <strong>of</strong> audit and survey activity conducted by MPT from January 2008. Principle researchers for all studies were Cpl L G<strong>of</strong>ton RAF,<br />
Sgt L Devonport QARANC, Mrs D Edwards and Sqn Ldr C Flutter RAF except Study XII (Col S Jagdish L/RAMC ( October 2008 ) & Capt<br />
B.Coghill RAMC ( February 2010 ))<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S398–401
UK Military Pain Service L Devonport, D Edwards, C Edwards et al<br />
continuity <strong>of</strong> care. Steps are currently being taken to provide<br />
this military consultant support to <strong>the</strong> Regional Rehabilitation<br />
Units as well. The first joint clinics with consultants from DMRC<br />
were initiated in April 2010 and have already successfully been<br />
undertaken in Edinburgh, and Catterick. Going forward <strong>the</strong> plan<br />
is to also introduce <strong>the</strong>m in Tidworth and Plymouth, with <strong>the</strong><br />
intention <strong>of</strong> Colchester, Halton and Lichfield being supported in<br />
due course.<br />
Prior to leaving, Birmingham <strong>the</strong> casualties complete an<br />
audit questionnaire asking about <strong>the</strong>ir analgesia from point <strong>of</strong><br />
wounding to discharge from RCDM. Despite efforts to educate<br />
o<strong>the</strong>rwise <strong>the</strong> use <strong>of</strong> opioid analgesics, is still associated with a fear<br />
<strong>of</strong> “addiction”. Two completed surveys <strong>of</strong> amputees undertaken at<br />
DMRC have shown that <strong>the</strong>re is no evidence <strong>of</strong> this being an issue<br />
within our population (Table 3; Study XII).<br />
The Evidence<br />
It is suggested that 30-80% <strong>of</strong> post-operative patients experience<br />
moderate to severe pain [13, 14]. A collection <strong>of</strong> <strong>the</strong> twice daily<br />
ward pain scores was undertaken during a five week period (Table<br />
3, Study VIII). These scores are recorded routinely by <strong>the</strong> nursing<br />
staff but were later collected by <strong>the</strong> MPT for analysis. The results<br />
indicated that less than 10% <strong>of</strong> <strong>the</strong> casualties reported pain scores<br />
<strong>of</strong> 2 or 3 on our 4 point scale; this approximately equates to pain<br />
scores <strong>of</strong> 4/10 or more, or moderate and severe pain.<br />
Discussion<br />
The population we are treating <strong>of</strong>ten have complex pain issues.<br />
We are also dealing with mechanisms <strong>of</strong> injury that are not<br />
routinely seen except in a few centres around <strong>the</strong> world. To what<br />
extent <strong>the</strong>se various injuries create <strong>the</strong>ir own patterns <strong>of</strong> pain is<br />
impossible to quantify.<br />
In an attempt to support our approaches we have tried to<br />
look for evidence but have had to rely on fairly “weak” levels<br />
<strong>of</strong> evidence. This is because, fortunately, <strong>the</strong> actual numbers <strong>of</strong><br />
individuals coming thought our system are so small as to make<br />
high quality prospective double blind randomised control trials<br />
impossible. Instead we have relied on a number <strong>of</strong> surveillance<br />
projects, surveys and a few audit results and <strong>the</strong> more important<br />
<strong>of</strong> <strong>the</strong>se are mentioned in this text and are highlighted in Table 3.<br />
It is important to be clear that no one intervention is responsible<br />
for <strong>the</strong>se results. They derive from a combination <strong>of</strong> effects. Most<br />
importantly we would argue it is <strong>the</strong> change in attitude towards<br />
“pain”, and recognition by all healthcare workers, particularly <strong>the</strong><br />
ward nursing staff, that pain is not an acceptable experience. We<br />
also know to look at <strong>the</strong> wider aspects <strong>of</strong> a patient’s experience<br />
and not just focus on <strong>the</strong> medical aspects. We try to develop a<br />
patient’s sense <strong>of</strong> control as early as we can. It is <strong>the</strong>ir pain, <strong>the</strong>ir<br />
problem, and when <strong>the</strong>y are discharged <strong>the</strong>y will need to know<br />
how to manage it.<br />
Finally, we are clear that what occurs here must link with<br />
what has gone before and what will follow. The service’s name,<br />
<strong>the</strong> Military Pain Team, makes no reference to acute pain. This is<br />
because we see <strong>the</strong> service not as an isolated “acute” pain service<br />
but as one step in <strong>the</strong> continuum <strong>of</strong> care that may extend many<br />
miles and years from point <strong>of</strong> wounding to leaving <strong>the</strong> Service;<br />
<strong>the</strong> 30 year, 13,000 mile pain service.<br />
References<br />
1. Edwards D, Bowden M, Aldington DJ. Pain management at role 4.<br />
JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155:58-61.<br />
2. Monthly Op TELIC and Op HERRICK UK Patient Treatment<br />
Statistics- RCDM and DMRC Headley Court. Edition: 30 June<br />
2010 (Released 30 July 2010) http://www.dasa.mod.uk Accessed<br />
October 2010<br />
3. Quarterly Op HERRICK and Op TELIC amputation statistics.<br />
Edition: 1 April – 30 June 2010 (Released 30 July 2010) http://<br />
www.dasa.mod.uk Accessed October 2010<br />
4. Connor DJ, Ralph JK, Aldington DJ. Field hospital analgesia. JR<br />
<strong>Army</strong> Med <strong>Corps</strong> 2009; 155:49-56.<br />
5. Hughes S, Birt D. Continuous peripheral nerve blockade on OP<br />
HERRICK 9. JR <strong>Army</strong> Med <strong>Corps</strong> 2009; 155:57-58.<br />
6. Flutter C, Ruth M, Aldington D. Pain management during <strong>Royal</strong><br />
Air Force strategic aeromedical evacuations. JR <strong>Army</strong> Med <strong>Corps</strong><br />
2009; 155:61-63.<br />
7. Hayakawa H, Aldington DJ, Moore RA. Acute traumatic<br />
compartment syndrome: a systematic review <strong>of</strong> results <strong>of</strong><br />
fasciotomy. Trauma 2009; 11:5-35.<br />
8. Clasper JC, Aldington DJ. Regional anaes<strong>the</strong>sia, ballistic limb<br />
trauma and acute compartment syndrome. JR <strong>Army</strong> Med <strong>Corps</strong><br />
2010; 156:77-78.<br />
9. Walker C, Ingram M, Edwards D, Wood P. Use <strong>of</strong><br />
thromboelastometry in <strong>the</strong> assessment <strong>of</strong> coagulation prior to<br />
epidural insertion after massive transfusion. <strong>Anaes<strong>the</strong>sia</strong> 2010; In<br />
Press<br />
10. Wood PR, Haldane AG, Plimmer SE. Anes<strong>the</strong>sia at Role 4. JR<br />
<strong>Army</strong> Med <strong>Corps</strong> 2010; 156(4): 156(4 Suppl 1): S308-310<br />
11. Alexander DA, Klein S. Combat-related disorders: a persistent<br />
chimera. JR <strong>Army</strong> Med <strong>Corps</strong> 2008; 154:96-101.<br />
12. Holbrook TL, Galarneau MR, Dye JL, Quinn K, Dougherty AL.<br />
Morphine use after combat injury in Iraq and post-traumatic stress<br />
disorder. N Engl J Med 2010; 362:110-117.<br />
13. Dolin SJ, Cashman JN, Bland JM. Effectiveness <strong>of</strong> acute<br />
postoperative pain management: I. Evidence from published data.<br />
Br J Anaesth 2002; 89:409-423.<br />
14. Drew J, Aldington D. A Hospital Audit <strong>of</strong> Pain. IASP World<br />
Congress. 2005<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S398–401 401
Society <strong>of</strong> Triservice Anaes<strong>the</strong>tic Trainees<br />
Annual Scientific Meeting 2010<br />
This meeting was held at RAF Wyton, Cambridgeshire, on <strong>the</strong> 22-23 Jul 2010. Sq Ldr Elise Haites RAF won <strong>the</strong> Dave Hughes<br />
Memorial Prize for <strong>the</strong> best Trainees presentation. There were nine presentations in all and <strong>the</strong>ir abstracts are published here; three (*)<br />
have been written as full articles in this supplement <strong>of</strong> <strong>the</strong> <strong>Journal</strong> <strong>of</strong> <strong>Royal</strong> <strong>Army</strong> <strong>Medical</strong> <strong>Corps</strong>.<br />
Are CCAST patients developing a metabolic acidosis<br />
in-flight and if so is lactate monitoring necessary?<br />
EM Haites 1 , S Turner 2<br />
1 <strong>Royal</strong> Infirmary <strong>of</strong> Edinburgh; 2 Leeds General Infirmary<br />
Introduction: Critical care aeromedical transfer flights run by<br />
<strong>the</strong> <strong>Royal</strong> Air Force Critical Care Air Support Team (CCAST)<br />
serve to transfer severely ill trauma victims. At present on CCAST<br />
flights <strong>the</strong> base excess is used to assess acid-base balance. Lactate<br />
monitoring is not currently carried out although it is possible.<br />
Cardiac output monitoring is not available. The primary aim<br />
<strong>of</strong> this audit was to assess whe<strong>the</strong>r our patients are developing<br />
metabolic acidosis in flight as demonstrated by a change in base<br />
excess and to assess whe<strong>the</strong>r <strong>the</strong>re was a case for <strong>the</strong> introduction<br />
<strong>of</strong> routine lactate monitoring on CCAST flights. Secondary<br />
aims were to assess fluid balance in flight for CCAST patients<br />
and percentage <strong>of</strong> fluid delivered which is crystalloid. Methods:<br />
A retrospective audit was performed by analysis <strong>of</strong> aeromedical<br />
notes for all CCAST patients during <strong>the</strong> period <strong>of</strong> 12 July – 22<br />
December 2009 (n=70). Results: There was a mean change in<br />
base excess <strong>of</strong> -0.99 (95% CI -1.55 to -0.42) P
STAT 2010<br />
it useful. The majority <strong>of</strong> trainees (188/345) disputed <strong>the</strong> fairness<br />
<strong>of</strong> <strong>the</strong> Mini-CEX, found annual numbers difficult to achieve<br />
(173/340) and tended to conduct <strong>the</strong>m in a way to optimise<br />
results (173/340). The free text comment suggested <strong>the</strong> utility <strong>of</strong><br />
all <strong>the</strong> tools could be increased by improving assessor training.<br />
Conclusion: UK anaes<strong>the</strong>tic trainee attitudes do not mirror<br />
<strong>the</strong> New Zealand trainees’ positive acceptance <strong>of</strong> this style <strong>of</strong><br />
assessment tool and effort should be directed towards improving<br />
assessor training to help improve <strong>the</strong> perceived educational benefit.<br />
References:<br />
1. The <strong>Royal</strong> College <strong>of</strong> Anaes<strong>the</strong>tists. The CCT in Anaes<strong>the</strong>stics<br />
I: General Principles. A manual for trainees and trainers.<br />
Edition January 2007. Available at: http://www.rcoa.ac.uk/docs/<br />
CCTPartIJuly2010.pdf (accessed 11/10/10)<br />
2. Weller J, Jolly B, Merry A et al. Mini-clinical evaluation exercise in<br />
anaes<strong>the</strong>sia training. Br J Anaesth 2009;102: 633-41.<br />
Thin or Fat, Age or Beauty-The Red Cell in Critical<br />
Care<br />
MT Davies<br />
University <strong>of</strong> Leicester Hospitals NHS Trust<br />
Introduction: The transfusion <strong>of</strong> blood products has been<br />
occurring since <strong>the</strong> 17th century. The indication for treatment<br />
can be varied but <strong>the</strong> overriding indications are to increase <strong>the</strong><br />
circulating plasma volume and <strong>the</strong> concentration <strong>of</strong> <strong>the</strong> oxygencarrying<br />
molecule Haemoglobin. It is a <strong>the</strong>rapy that is not without<br />
side effects and annual Serious Hazards <strong>of</strong> Transfusion (SHOT)<br />
reports show an increasing number <strong>of</strong> incident reports though<br />
thankfully a reducing number <strong>of</strong> deaths as a result <strong>of</strong> transfusion.<br />
A paper from 2009 [1] suggested a link between <strong>the</strong> age <strong>of</strong> <strong>the</strong><br />
red blood cell transfused and mortality amongst trauma patients.<br />
A paper this year looked at transfusion in Paediatric patients and<br />
found a suggested increased risk when <strong>the</strong> blood transfused was<br />
over 15 days old. Methods: During a 6 month period I reviewed<br />
all transfusions given on 3 separate ITUs across Leicester and<br />
recorded <strong>the</strong> transfusion trigger level <strong>of</strong> Haemoglobin and <strong>the</strong> age<br />
<strong>of</strong> <strong>the</strong> packed red cell product given. 32 patients were given a<br />
total <strong>of</strong> 64 units <strong>of</strong> blood. All patients were from a general ITU<br />
and none were being actively resuscitated when <strong>the</strong> blood was<br />
administered. Results: 18 (56%) <strong>of</strong> patients were transfused when<br />
<strong>the</strong>ir haemoglobins were over 7 g d/l (our current transfusion<br />
trigger identified from <strong>the</strong> TRICC group). The graph below<br />
shows a plot <strong>of</strong> <strong>the</strong> age <strong>of</strong> each blood unit given. The red dotted<br />
line is 28 days, which was <strong>the</strong> age above that Spinella [1] group<br />
associated with increases risk. Karam group [2] identified a risk in<br />
blood aged 15 days and over.<br />
Conclusions: Red blood cells are administered on a regular basis<br />
in our military and civilian Critical Care patients. It is clearly a<br />
<strong>the</strong>rapy that provides enormous benefit but <strong>the</strong> question <strong>of</strong> when<br />
to transfuse and with what aged cell contains to be debated and on<br />
going research continues. I do not think <strong>the</strong>re is much doubt that<br />
<strong>the</strong> younger <strong>the</strong> red blood cell is <strong>the</strong> better it serves its purpose and<br />
we need to identify <strong>the</strong> patients in who that will make a difference.<br />
References:<br />
1. Spinella PC, Carroll CL, Staff I, et al. Duration <strong>of</strong> red blood<br />
cell storage is associated with increased incidence <strong>of</strong> deep vein<br />
thrombosis and in hospital mortality inpatients with traumatic<br />
injuries. Critical Care 2009, 13: R151<br />
2. Karam O, Tucci M, Bateman ST, et al. Association between length <strong>of</strong><br />
storage <strong>of</strong> red blood cell units and outcome <strong>of</strong> critically ill children: a<br />
prospective observational study. Critical Care 2010; 14: R57<br />
* Current Epidural Practice – Results <strong>of</strong> a Survey <strong>of</strong><br />
Military Anaes<strong>the</strong>tists<br />
KL Woods 1 , D Aldington 2 .<br />
1 James Cook University Hospital, Middlesbrough; 2 Pain Relief Unit,<br />
Churchill Hospital. Oxford.<br />
Introduction: Epidurals are now used for pain relief on<br />
deployment [1] and although a National Audit on complications<br />
<strong>of</strong> central neuraxial blocks [2] has been recently carried out <strong>the</strong>re<br />
are few published studies looking at personal epidural practice. A<br />
survey was conducted to look at <strong>the</strong> current epidural practice <strong>of</strong><br />
UK military anaes<strong>the</strong>tists. Due to <strong>the</strong> fact equipment available on<br />
deployment may vary from that in <strong>the</strong> UK, <strong>the</strong> aim <strong>of</strong> <strong>the</strong> survey<br />
was to identify any potential issues with regard to equipment and<br />
training to allow future development <strong>of</strong> pre-deployment training.<br />
Methods: An internet based survey was carried out. All military<br />
anaes<strong>the</strong>tists were sent an e-mail containing a link to <strong>the</strong> survey<br />
and <strong>the</strong> results <strong>of</strong> those who responded were analysed. Results:<br />
A total <strong>of</strong> 49 surveys were completed. Within <strong>the</strong>ir UK practice<br />
78% <strong>of</strong> respondents carried out epidurals more than once a<br />
month, in a wide range <strong>of</strong> specialities. There was considerable<br />
variation in methods <strong>of</strong> securing epidurals and in drug choice<br />
amongst respondents. Conclusions: The results <strong>of</strong> this survey<br />
show that whilst epidurals are commonly carried out amongst<br />
military anaes<strong>the</strong>tists during <strong>the</strong>ir UK practice, <strong>the</strong>re is significant<br />
variation within <strong>the</strong> practice. Areas have been identified for<br />
development <strong>of</strong> educational courses, for example methods <strong>of</strong><br />
securing epidurals, and <strong>the</strong>se have already been acted upon.<br />
References:<br />
1. Connor DJ, Ralph JK, Aldington DJ. Field Hospital Analgesia. J R<br />
<strong>Army</strong> Med <strong>Corps</strong> 2009; 155: 49-56<br />
2. Cook TM, Counsell D, Wildsmith JAW. Major Complications <strong>of</strong><br />
Central Neuraxial Block: report on <strong>the</strong> Third Audit Project <strong>of</strong> <strong>the</strong><br />
<strong>Royal</strong> College <strong>of</strong> Anaes<strong>the</strong>tists. Br J Anaesth 2009; 102: 179-90<br />
A Survey Of Ketamine Use Within The <strong>Defence</strong><br />
<strong>Medical</strong> Services<br />
J Warren 1 , DJ Aldington 2<br />
1 Frimley Park Hospital; 2 John Radcliffe Hospital, Oxford<br />
Introduction: Ketamine is a versatile drug that can be used for<br />
analgesia, sedation and anaes<strong>the</strong>sia. It is provided in military prehospital<br />
modules for use by General Duties <strong>Medical</strong> Officers.<br />
However, its use is not without side effects, some <strong>of</strong> which may<br />
be significant [1]. Unfortunately, while ketamine can be <strong>of</strong> great<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S402–404 403
STAT 2010<br />
use to <strong>the</strong> military healthcare provider [2], experience <strong>of</strong> its use<br />
in UK civilian practice is <strong>of</strong>ten very limited [3]. The aim <strong>of</strong><br />
this study was to establish how widely, within <strong>the</strong> UK <strong>Defence</strong><br />
<strong>Medical</strong> Services (DMS), ketamine is used, how <strong>of</strong>ten side effects<br />
occur, and how people are trained in its use. Method: An internet<br />
based questionnaire was designed (www.surveymonkey.com). It<br />
comprised 10 multiple-choice questions. Invitations to complete<br />
<strong>the</strong> questions were promulgated via <strong>the</strong> <strong>Defence</strong> Pr<strong>of</strong>essors <strong>of</strong><br />
<strong>Anaes<strong>the</strong>sia</strong>, General Practice and Emergency Medicine. Results:<br />
159 respondents completed <strong>the</strong> survey. Just under half (46%),<br />
73 respondents were trainees. <strong>Anaes<strong>the</strong>sia</strong> was <strong>the</strong> predominant<br />
speciality (63%), 19% from Emergency Medicine and 18%<br />
General Practice. 15% <strong>of</strong> respondents had never used ketamine<br />
citing lack <strong>of</strong> familiarity as <strong>the</strong> predominate reason. Of <strong>the</strong> 85%<br />
who had used it few reported having difficulties with side effects.<br />
Only 38% <strong>of</strong> those involved in military pre-hospital care reported<br />
receiving formal training. Discussion: A high proportion <strong>of</strong> <strong>the</strong><br />
respondents were anaes<strong>the</strong>tists so an inherently biased sample; but<br />
<strong>the</strong>y <strong>of</strong> all groups should have access to training and experience<br />
in its use in <strong>the</strong> UK, toge<strong>the</strong>r with experience <strong>of</strong> handling many<br />
<strong>of</strong> <strong>the</strong> side effects. This is <strong>the</strong> first survey <strong>of</strong> its kind to have<br />
been undertaken across such a broad-spectrum <strong>of</strong> physicians.<br />
This survey, despite its weaknesses, has been used to provide<br />
formal evidence <strong>of</strong> a training opportunity that has recently been<br />
recognised by <strong>the</strong> DMS.<br />
References:<br />
1. P P Bredmose, D J Lockey, G Grier, et al. Pre-hospital use <strong>of</strong><br />
ketamine for analgesia and procedural sedation. Emerg Med J 2009<br />
26: 62-64<br />
2. Mackenzie R. Analgesia and Sedation. J R <strong>Army</strong> Med <strong>Corps</strong> 2004;<br />
150: 45-55<br />
3. Green SM, Krauss B Ketamine is a safe, effective, and appropriate<br />
technique for emergency department paediatric procedural<br />
sedation. . Emerg Med J 2004; 21: 271–272.<br />
*Vascular Access on <strong>the</strong> 21st Century Military<br />
Battlefield<br />
EJ Hulse 1 , GOR Thomas 2<br />
1 <strong>Royal</strong> Cornwall Hospital, Truro, Cornwall; 2 The <strong>Royal</strong> London, and<br />
Queen Victoria’s Hospital, East Grinstead, London, 16 Air Assault<br />
<strong>Medical</strong> Regiment.<br />
404<br />
Introduction: Timely and appropriate access to <strong>the</strong> vascular<br />
circulation is critical in <strong>the</strong> management <strong>of</strong> 21st century battlefield<br />
trauma, allowing <strong>the</strong> administration <strong>of</strong> emergency drugs,<br />
analgesics and rapid replacement <strong>of</strong> blood volume. Methods<br />
used to gain access can include <strong>the</strong> cannulation <strong>of</strong> peripheral and<br />
central veins, venous cut-down and intraosseus devices. Method:<br />
We reviewed <strong>the</strong> current literature in both English speaking and<br />
non-English speaking countries on <strong>the</strong> benefits and complications<br />
<strong>of</strong> each vascular access method. Conclusion: Intraosseus devices<br />
are best for quick access to <strong>the</strong> circulation, with central venous<br />
access via <strong>the</strong> subclavian route for large volume resuscitation and<br />
low complication rates. Military clinicians involved with <strong>the</strong> care<br />
<strong>of</strong> trauma patients ei<strong>the</strong>r in Role 2 and 3 or as part <strong>of</strong> <strong>the</strong> <strong>Medical</strong><br />
Emergency Response Team (MERT), must have <strong>the</strong> skill set to<br />
use <strong>the</strong>se vascular access techniques by incorporating <strong>the</strong>m into<br />
<strong>the</strong>ir core medical training.<br />
*TIVA for War Surgery<br />
SE Lewis<br />
Total Intravenous <strong>Anaes<strong>the</strong>sia</strong> (TIVA) may be defined as <strong>the</strong><br />
delivery <strong>of</strong> agents into <strong>the</strong> bloodstream to achieve a balance <strong>of</strong><br />
hypnosis, analgesia and muscle relaxation. Military Anaes<strong>the</strong>tists<br />
have been using TIVA for war surgery since World War II and<br />
every conflict has produced advances in its practice. TIVA finds<br />
application at every echelon <strong>of</strong> care including <strong>the</strong> pre-hospital<br />
phase and during strategic transfer to <strong>the</strong> UK. Advantages that<br />
it possesses over Volatile Gas <strong>Anaes<strong>the</strong>sia</strong> (VGA) include a much<br />
smaller logistic footprint, favourable recovery characteristics, no<br />
potential for triggering malignant hyper<strong>the</strong>rmia and potentially<br />
beneficial modulation <strong>of</strong> <strong>the</strong> stress response. Disadvantages<br />
include a perceived increase in risk <strong>of</strong> awareness and reduced<br />
familiarity with its use amongst <strong>the</strong> anaes<strong>the</strong>tic cadre. A<br />
literature search and survey <strong>of</strong> subject matter experts within <strong>the</strong><br />
DMS anaes<strong>the</strong>tic cadre produced a selection <strong>of</strong> protocols for<br />
achieving TIVA appropriate to different patients and situations<br />
including one based on drip rate through a giving set with no<br />
infusion pump required. Future areas <strong>of</strong> development for TIVA<br />
within <strong>the</strong> DMS might include <strong>the</strong> introduction <strong>of</strong> Target<br />
Controlled Infusion (TCI) pumps and/or depth <strong>of</strong> anaes<strong>the</strong>sia<br />
monitoring. TIVA should be considered as a valid alternative to<br />
VGA for war surgery.<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S402–404
…And Finally
Images <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong><br />
Gulf War 1991- <strong>Anaes<strong>the</strong>sia</strong> at 32 Field Hospital (Photo: Col PF<br />
Mahoney L/RAMC)<br />
The Resus dept at 32 Field Hospital, Op Granby. Teams were <strong>of</strong> three<br />
people (a doctor, a nurse and a medic) to look after two trestles. At<br />
night teams slept in <strong>the</strong> department. (Photo: Col PF Mahoney L/<br />
RAMC)<br />
Receiving a casualty in Resus in Macedonia in 1999 prior to <strong>the</strong> move<br />
forward into Kosovo. (Photo: Col PF Mahoney L/RAMC)<br />
Retrieval <strong>of</strong> a casualty by <strong>the</strong> Immediate Response Team (IRT) from<br />
Macedonia, 1999. The IRT was <strong>the</strong> forerunner <strong>of</strong> <strong>the</strong> MERT. (Photo:<br />
Col PF Mahoney L/RAMC)<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S407–411 407
Images <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong><br />
Col Trip Buckenmaier undertaking<br />
regional anaes<strong>the</strong>sia with ultrasound<br />
guidance, Bastion 2009<br />
(Photo: Lt Col Simon Orr RAMC)<br />
Surgeon Commander Heames giving <strong>the</strong> first general anaes<strong>the</strong>tic<br />
(semi-elective) on RFA ARGUS in 2003 before <strong>the</strong> start <strong>of</strong><br />
operation TELIC. It is for a non-battle injury. Name <strong>of</strong> surgeon<br />
unknown. (Photo: Surg Cdr R Heames RN)<br />
408<br />
Emergency moulage on board RFA Fort Victoria (2010) where a<br />
patient is getting log-rolled. (Photo: Surg Cdr R Heames RN)<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S407–411
This was <strong>the</strong> portable operating <strong>the</strong>atre carried by <strong>the</strong> 22 Squadron<br />
FST <strong>of</strong> <strong>the</strong> <strong>Medical</strong> Support element <strong>of</strong> 16 Air Assault Brigade during<br />
<strong>the</strong> invasion phase <strong>of</strong> <strong>the</strong> Iraq campaign. Two MacVicar operating<br />
tables with supporting anaes<strong>the</strong>tic kit, based on <strong>the</strong> Tri-Service<br />
vapourizers and CompPac ventilators, and supplies were packed onto<br />
trailers towed by Pinz-Gaur non-armoured trucks. Two squadrons<br />
(22 and 19) leapfrogged, setting up and taking down every 48 hours,<br />
to keep abreast <strong>of</strong> <strong>the</strong> advancing Coalition forces. Op TELIC 1, 2003<br />
(Photo Lt Col NJ Jeffries RAMC)<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S407–411 409
Images <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong><br />
GIAT Industries (Groupement des Industries de l’Armée de Terre,<br />
a French government-owned weapons manufacturer) produced a<br />
modular, containerized operating <strong>the</strong>atre which was deployed in<br />
FRY to <strong>the</strong> SFOR UK Med Group hospital set up in a vacant shoe<br />
factory on <strong>the</strong> outskirts <strong>of</strong> Sipovo. It contained an operating table<br />
with associated lighting, a (barely...) overhead track to carry an<br />
X-ray, and a Kontron 5100 anaes<strong>the</strong>tic machine. There was a<br />
separate module for compressed gas supplies. The Kontron 5100<br />
was a sophisticated “civilian” apparatus in common use in French<br />
and o<strong>the</strong>r European hospitals. It featured several ventilation<br />
options including variable I:E ratios and SIMV, and two common<br />
gas outlets which was a little confusing. There was an option for<br />
a circle system but this had not been purchased. The instructions<br />
were only in French. Sipovo 1998.<br />
(Photo: Lt Col NJ Jeffries RAMC)<br />
ROTEM thromboelastometry analyser in use, revealing<br />
hyperfibrinolysis in a brain-injured patient, Camp Bastion Operating<br />
Room, Op HERRICK 11b (Photo: Maj N Tarmey RAMC)<br />
Vital signs displayed on an Operating Room monitor following<br />
successful resuscitation from hypovolaemic cardiac arrest. Camp<br />
Bastion, Op HERRICK 11b (Photo: Maj N Tarmey RAMC)<br />
410<br />
Air-freighted platelets for transfusion arrive at Camp Bastion Role 3<br />
Hospital Op HERRICK 11b (Photo: Maj N Tarmey RAMC)<br />
Incident involving multiple casualties in Iraq 2004. This was a<br />
fixed tented field hospital and highlight multiple resuscitation teams<br />
working simultaneously in a co-ordinated fashion. There is an<br />
anaes<strong>the</strong>tist in every resuscitation bay. (Photo: Lt Col DA Parkhouse<br />
RAMC)<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S407–411
Images <strong>of</strong> <strong>Anaes<strong>the</strong>sia</strong><br />
Preparation <strong>of</strong> equipment at <strong>the</strong> start <strong>of</strong> <strong>the</strong> day. Preanaes<strong>the</strong>tic<br />
equipment checks are similar to those carried<br />
out in hospitals in <strong>the</strong> UK everyday. Same skill set, different<br />
environment. (Photo: Lt Col DA Parkhouse RAMC)<br />
Transfer <strong>of</strong> casualty from CH47 to Battlefield<br />
Ambulance at Camp Bastion. Care is<br />
uninterrupted throughout.<br />
(Photo: Lt Col DA Parkhouse RAMC)<br />
Four man team carries out resuscitation on a<br />
MERT mission; <strong>the</strong> o<strong>the</strong>r troops look on calmly.<br />
(Photo: Lt Col DA Parkhouse RAMC)<br />
J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S407–411 411
The DMACC Coins<br />
PF Mahoney<br />
‘Challenge’ coins display <strong>the</strong> emblem or insignia <strong>of</strong> an organisation and are popular in <strong>the</strong> US military. Their origins and traditions<br />
are debated but probably originate in <strong>the</strong> United States <strong>Army</strong> Air Service in World War One. The coins have been used in a semi<br />
<strong>of</strong>ficial capacity to mark membership <strong>of</strong> a unit or as awards to denote special achievements. In some military units members can be<br />
‘challenged’ to produce <strong>the</strong>ir coin- and if <strong>the</strong>y fail to do so owe <strong>the</strong> challenger a drink. Members <strong>of</strong> <strong>the</strong> <strong>Royal</strong> Centre for <strong>Defence</strong><br />
Medicine (RCDM) academic units came across <strong>the</strong>se coins while working with US Forces in Iraq and Afghanistan- and thought <strong>the</strong><br />
tradition would translate well to <strong>the</strong> <strong>Defence</strong> <strong>Medical</strong> Services (DMS).<br />
The 2008 Coin has a Triservice <strong>the</strong>me. The three small pictures show a triservice anaes<strong>the</strong>sia<br />
apparatus, a CH47 and RFA Argus. The main picture is taken from a photograph <strong>of</strong> an<br />
anaes<strong>the</strong>tic being given for rapid sequence induction and endotracheal intubation on <strong>the</strong> MERT<br />
in Afghanistan in 2007.<br />
The 2010 Coin has a regional anaes<strong>the</strong>sia <strong>the</strong>me and shows a drawing <strong>of</strong> <strong>the</strong> brachial plexus above<br />
a picture <strong>of</strong> ultrasound being used to locate <strong>the</strong> brachial plexus. Col Trip Buckenmaier US <strong>Army</strong><br />
provided <strong>the</strong> original pictures from which <strong>the</strong>se images were created during his deployment to<br />
Bastion in 2009.<br />
The original coin was made by <strong>the</strong> Academic Department <strong>of</strong> Military<br />
Emergency Medicine (ADMEM) in 2006 and features <strong>the</strong> RCDM crest<br />
on one side and a medical team <strong>of</strong>f loading a patient from a CH47 on<br />
<strong>the</strong> o<strong>the</strong>r, based on images from <strong>the</strong> 2003 Gulf War. The Department<br />
<strong>of</strong> Military <strong>Anaes<strong>the</strong>sia</strong> and Critical Care (DMA&CC) coins have been<br />
designed to reflect <strong>the</strong> different elements <strong>of</strong> <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> and <strong>the</strong><br />
intention is to produce a different coin each year.<br />
The 2009 Coin was made jointly with ADMEM for OP HERRICK<br />
10 when <strong>the</strong> Role 3 hospital at Bastion became joint UK-US and also<br />
hosted <strong>the</strong> Danish Field Hospital. The coin includes UK, US, Danish<br />
and NATO flags surrounding a Red Cross on one side. One <strong>the</strong> o<strong>the</strong>r<br />
are <strong>the</strong> crests <strong>of</strong> <strong>Royal</strong> Centre for <strong>Defence</strong> Medicine, <strong>the</strong> <strong>Royal</strong> College<br />
<strong>of</strong> Anaes<strong>the</strong>tists and <strong>the</strong> College <strong>of</strong> Emergency Medicine.<br />
The 2011 Coin is <strong>the</strong>med around massive transfusion. The images used are <strong>of</strong> a surgical team working<br />
at Bastion, a pile <strong>of</strong> empty blood bags, and a member <strong>of</strong> <strong>the</strong> Field Hospital managing <strong>the</strong> infusions.<br />
These images were created from photographs taken by Lt Col Simon Orr RAMC during HERRICK<br />
10, 2009.<br />
To date <strong>the</strong> coins have been given out on operational deployments to mark special achievements, to mark presentations at military<br />
anaes<strong>the</strong>tic meetings, to thank people within <strong>the</strong> cadre for <strong>the</strong>ir efforts on behalf <strong>of</strong> <strong>Defence</strong> <strong>Anaes<strong>the</strong>sia</strong> and thank members <strong>of</strong> <strong>the</strong><br />
<strong>Royal</strong> College <strong>of</strong> Anaes<strong>the</strong>tists and <strong>the</strong> Association <strong>of</strong> Anaes<strong>the</strong>tists for support to DMA&CC.<br />
412 J R <strong>Army</strong> Med <strong>Corps</strong> 156 (4 Suppl 1): S412