The Oklahoma Nurse - August 2022
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
THE<br />
OKLAHOMA<br />
NURSE<br />
<strong>The</strong> Official Publication of the <strong>Oklahoma</strong> <strong>Nurse</strong>s Association<br />
Quarterly publication delivered to approximately 64,000 Registered <strong>Nurse</strong>s and LPNs in <strong>Oklahoma</strong><br />
Volume 67 • Number 3<br />
<strong>August</strong> <strong>2022</strong><br />
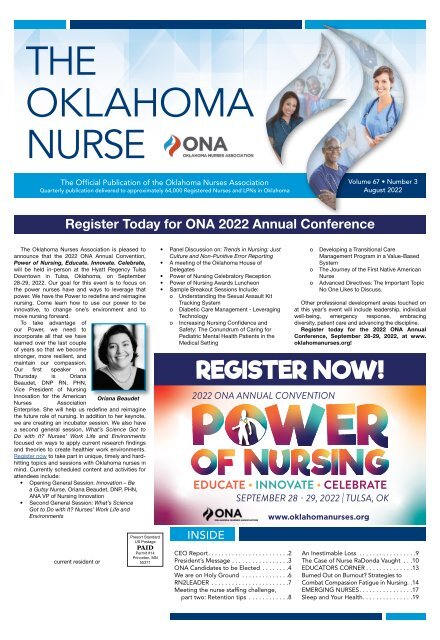
Register Today for ONA <strong>2022</strong> Annual Conference<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong>s Association is pleased to<br />
announce that the <strong>2022</strong> ONA Annual Convention,<br />
Power of Nursing, Educate. Innovate. Celebrate,<br />
will be held in-person at the Hyatt Regency Tulsa<br />
Downtown in Tulsa, <strong>Oklahoma</strong>, on September<br />
28-29, <strong>2022</strong>. Our goal for this event is to focus on<br />
the power nurses have and ways to leverage that<br />
power. We have the Power to redefine and reimagine<br />
nursing. Come learn how to use our power to be<br />
innovative, to change one’s environment and to<br />
move nursing forward.<br />
To take advantage of<br />
our Power, we need to<br />
incorporate all that we have<br />
learned over the last couple<br />
of years so that we become<br />
stronger, more resilient, and<br />
maintain our compassion.<br />
Our first speaker on<br />
Thursday is Oriana<br />
Beaudet, DNP RN, PHN,<br />
Vice President of Nursing<br />
Innovation for the American<br />
Oriana Beaudet<br />
<strong>Nurse</strong>s Association<br />
Enterprise. She will help us redefine and reimagine<br />
the future role of nursing. In addition to her keynote,<br />
we are creating an incubator session. We also have<br />
a second general session, What’s Science Got to<br />
Do with It? <strong>Nurse</strong>s’ Work Life and Environments<br />
focused on ways to apply current research findings<br />
and theories to create healthier work environments.<br />
Register now to take part in unique, timely and hardhitting<br />
topics and sessions with <strong>Oklahoma</strong> nurses in<br />
mind. Currently scheduled content and activities for<br />
attendees include:<br />
• Opening General Session: Innovation – Be<br />
a Gutsy <strong>Nurse</strong>, Oriana Beaudet, DNP, PHN,<br />
ANA VP of Nursing Innovation<br />
• Second General Session: What’s Science<br />
Got to Do with It? <strong>Nurse</strong>s’ Work Life and<br />
Environments<br />
• Panel Discussion on: Trends in Nursing: Just<br />
Culture and Non-Punitive Error Reporting<br />
• A meeting of the <strong>Oklahoma</strong> House of<br />
Delegates<br />
• Power of Nursing Celebratory Reception<br />
• Power of Nursing Awards Luncheon<br />
• Sample Breakout Sessions Include:<br />
o Understanding the Sexual Assault Kit<br />
Tracking System<br />
o Diabetic Care Management - Leveraging<br />
Technology<br />
o Increasing Nursing Confidence and<br />
Safety: <strong>The</strong> Conundrum of Caring for<br />
Pediatric Mental Health Patients in the<br />
Medical Setting<br />
REGISTER NOW!<br />
<strong>2022</strong> ONA ANNUAL CONVENTION<br />
EDUCATE • INNOVATE • CELEBRATE<br />
o<br />
o<br />
o<br />
Developing a Transitional Care<br />
Management Program in a Value-Based<br />
System<br />
<strong>The</strong> Journey of the First Native American<br />
<strong>Nurse</strong><br />
Advanced Directives: <strong>The</strong> Important Topic<br />
No One Likes to Discuss.<br />
Other professional development areas touched on<br />
at this year’s event will include leadership, individual<br />
well-being, emergency response, embracing<br />
diversity, patient care and advancing the discipline.<br />
Register today for the <strong>2022</strong> ONA Annual<br />
Conference, September 28-29, <strong>2022</strong>, at www.<br />
oklahomanurses.org!<br />
SEPTEMBER 28 - 29, <strong>2022</strong> | TULSA, OK<br />
www.oklahomanurses.org<br />
current resident or<br />
Presort Standard<br />
US Postage<br />
PAID<br />
Permit #14<br />
Princeton, MN<br />
55371<br />
INSIDE<br />
CEO Report. ....................... 2<br />
President’s Message. ................ 3<br />
ONA Candidates to be Elected ........ 4<br />
We are on Holy Ground .............. 6<br />
RN2LEADER ....................... 7<br />
Meeting the nurse staffing challenge,<br />
part two: Retention tips ............ 8<br />
An Inestimable Loss ................. 9<br />
<strong>The</strong> Case of <strong>Nurse</strong> RaDonda Vaught ... 10<br />
EDUCATORS CORNER. ............. 13<br />
Burned Out on Burnout? Strategies to<br />
Combat Compassion Fatigue in Nursing.. 14<br />
EMERGING NURSES. ............... 17<br />
Sleep and Your Health. .............. 19
2<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
<strong>Oklahoma</strong> <strong>Nurse</strong>s Association Regions and Regional Presidents<br />
Region 1:<br />
President: Lucas Richardson-<br />
Walker<br />
Region 2:<br />
President: Emma Kientz<br />
CEO REPORT<br />
Jane Nelson, CAE<br />
CEO, <strong>Oklahoma</strong> <strong>Nurse</strong>s<br />
Association<br />
Region 3:<br />
President: Mindy Thompson<br />
Region 4:<br />
Vacant<br />
Last year nurses<br />
were exhausted and<br />
overwhelmed. This year<br />
you are stressed and<br />
frustrated according to<br />
the ANF COVID-19 Two<br />
Year Impact Assessment.<br />
Add undervalued and Jane Nelson<br />
overworked to that list.<br />
However, in that impact assessment there are some<br />
positive answers too, such as 31% are grateful,<br />
23% hopeful, 21% supported and 9% empowered.<br />
Burnout is high as is bullying and incivility all of<br />
which provide challenges to our workplaces. Not<br />
only do each of us need to deal with these issues<br />
on an individual level, but employers are seeking<br />
solutions as well. <strong>The</strong> survey also indicates that only<br />
24% have sought mental health support and 36%<br />
feel that you should be able to manage your mental<br />
well-being yourself.<br />
Both ONA and ANA are working to provide<br />
resources to assist you as you continue to move<br />
forward on a daily basis. Time away from work, and<br />
spending time with family are all great solutions,<br />
but we need to figure out something on a day-today<br />
basis. On ONA’s website we have just posted a<br />
service called Emotional PPE that is free counseling,<br />
and we are getting ready to launch a stress-release<br />
course called Terra Firma. This Stress-Release<br />
course has a cost to it but it also has 15 hours of<br />
JOIN OUR TEAM AS A<br />
Clinical Health Facility Surveyor (ll, lll, lV)<br />
and make difference in the loves of <strong>Oklahoma</strong>ns.<br />
May be eligible for<br />
PAY INCENTIVES<br />
TRAVEL OPPORTUNITIES<br />
TUITION REIMBURSEMENTS<br />
Region 5:<br />
President: Nakeda Hall<br />
Region 6:<br />
President: Viki Saidleman<br />
Contact information available at www.oklahomanurses.org<br />
What is ONA Doing?<br />
Find out more:<br />
jobs.ok.gov<br />
Filter by keyword using<br />
“Surveyor”<br />
Competitive Salary and<br />
Benefits Package<br />
We Have More Information For You!<br />
Call: 405-426-8080<br />
Email: PHSWorkforce@health.ok.gov<br />
CE along with other resources. We hope that you<br />
will also take advantage of the other resources that<br />
ONA and ANA have to offer that can be found on<br />
the ONA website, www.oklahomanurses.org under<br />
<strong>Nurse</strong> Well-Being.<br />
Take a Breath...it changes your brain chemistry!<br />
Just about the time things feel like they are<br />
getting back to normal…we hit a spike. Breathe<br />
again. Hopefully with vaccines, boosters and<br />
treatments such as Paxlovid those affected with<br />
COVID will not have hospital stays, so, potentially<br />
focus can shift back to ways to build a positive work<br />
environment that includes tools such as shared<br />
governance and a just culture. ONA wants to get<br />
back to working on these issues so at the ONA<br />
Convention, we will have a session prior to the ONA<br />
House of Delegates on Trends in Nursing: Just<br />
Culture and Non-Punitive Error Reporting. This will<br />
include a panel of nurse leaders discussing how<br />
Just Culture, Culture of Safety, Shared Governance,<br />
and non-punitive error reporting are all part of where<br />
nursing is headed. During the House of Delegates,<br />
we will have a conversation around these same<br />
issues that will provide feedback to leaders on<br />
what is missing, what do we need to change to truly<br />
accomplish Just Culture and what does ONA need<br />
to do.<br />
For this to work, we need your engagement.<br />
Every ONA Member has an opportunity to<br />
participate in the House of Delegates. As you<br />
HIRING<br />
NURSES!<br />
APPLY HERE<br />
CEO Report continued on page 7<br />
10240 Broadway Ext.<br />
<strong>Oklahoma</strong> City, OK 73114<br />
or contact<br />
Nathan, CNO<br />
at<br />
405-900-8766<br />
today!<br />
<strong>Oklahoma</strong> <strong>Nurse</strong>s Association<br />
Editor: brendan@teamngage.com<br />
ONA 2021-<strong>2022</strong> BOARD OF DIRECTORS:<br />
President - Shelly Wells, PhD, MBA, APRN-CNS, ANEF<br />
Vice President - Angela Martindale, PhD, RN<br />
Secretary/Treasurer - Michele Bradshaw, MSN, RN<br />
President-Elect - Angie Kamermayer, DNP, APRN-CNS, NEA-BC<br />
Education Director - Vanessa Wright, PhD, MSN, RN<br />
Emerging <strong>Nurse</strong> Director - Rachael Bachhofer Kleckner,<br />
MSN, RN, CCRN-CMC-CSC<br />
Membership Development Director - Amy Hutchens, PhD, RN, CNE<br />
Political Activities Director - Cassy Abbott Eng, PhD, RN, LNC, CNE<br />
Practice Director - LaTonya Mason-Wilson, DNP, MS, RN, NE-BC<br />
Consultant to ONSA - Dean Prentice, Colonel, USAF (Ret),<br />
DHA, MA, BSN, NE-BC<br />
Region 1 President & Rep - Lucas Richardson-Walker, BSN, RN<br />
Region 2 President - Emma Kientz, DNP, RN<br />
Region 2 Rep & PE - April Loeffler, MSN, RN<br />
Region 3 President - Mindy Thompson, DNP, APRN, FNP-D, CNE<br />
Region 3 Representative - Julie Nevins, MS, RN<br />
Region 4 Representative - Leslie Collins, DNP, MS, RN<br />
Region 5 President & Rep - Nakeda Hall, DNP,APRN-CNP<br />
Region 6 President & Rep - Viki Saidleman, MSN, RN<br />
ONA STAFF:<br />
Jane Nelson, CAE — CEO<br />
Amber Feldpausch, CMP— Event Planner<br />
Katie Searl, Publications Editor<br />
Mariam Robinson, Membership Manager<br />
Tiffany Wilkinson, Member Services Specialist<br />
MAILING ADDRESS:<br />
<strong>Oklahoma</strong> <strong>Nurse</strong>s Association<br />
6608 N Western, #627, <strong>Oklahoma</strong> City, OK 73116<br />
405/840-3476<br />
Subscriptions:<br />
<strong>The</strong> subscription rate is $20 per year.<br />
THE OKLAHOMA NURSE (0030-1787), is published<br />
quarterly every February, May, <strong>August</strong> and November by<br />
the <strong>Oklahoma</strong> <strong>Nurse</strong>s Association (a constituent member<br />
of the American <strong>Nurse</strong>s Association) and Arthur L. Davis<br />
Publishing Agency, Inc. All rights reserved by copyright.<br />
Views expressed herein are not necessarily those of<br />
<strong>Oklahoma</strong> <strong>Nurse</strong>s Association.<br />
INDEXED BY<br />
International Nursing Index and Cumulative Index to Nursing<br />
and Allied Health Literature.<br />
Copies of articles from this publication are available from the UMI<br />
Article Clearinghouse. Mail requests to: University Microfilms<br />
International, 300 N. Zeeb Road, Ann Arbor, MI 48106.<br />
ADVERTISING<br />
For advertising rates and information, please contact Arthur<br />
L. Davis Publishing Agency, Inc., PO Box 216, Cedar Falls,<br />
Iowa 50613, (800) 626-4081, sales@aldpub.com. ONA and<br />
the Arthur L. Davis Publishing Agency, Inc. reserve the right<br />
to reject any advertisement. Responsibility for errors in<br />
advertising is limited to corrections in the next issue or refund<br />
of price of advertisement.<br />
Acceptance of advertising does not imply endorsement or<br />
approval by the <strong>Oklahoma</strong> <strong>Nurse</strong>s Association of products<br />
advertised, the advertisers, or the claims made. Rejection of an<br />
advertisement does not imply a product offered for advertising<br />
is without merit, or that the manufacturer lacks integrity, or that<br />
this association disapproves of the product or its use. ONA and<br />
the Arthur L. Davis Publishing Agency, Inc. shall not be held<br />
liable for any consequences resulting from purchase or use of<br />
an advertiser’s product. Articles appearing in this publication<br />
express the opinions of the authors; they do not necessarily<br />
reflect views of the staff, board, or membership of ONA or those<br />
of the national or local associations.<br />
CONTACT THE ONA<br />
Phone: 405.840.3476<br />
E-mail: ona@oklahomanurses.org<br />
Web site: www.oklahomanurses.org<br />
Mail: 6608 N Western, #627, <strong>Oklahoma</strong> City, OK 73116<br />
Questions about your nursing license?<br />
Contact the <strong>Oklahoma</strong> Board of Nursing at 405.962.1800.<br />
Want to advertise in <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong>?<br />
Contact Arthur L. Davis Publishing Agency, Inc.<br />
at 800.626.4081 or email at sales@aldpub.com.<br />
ONA CORE VALUES<br />
ONA believes that organizations are value driven<br />
and therefore has adopted the following core values:<br />
• Diversity<br />
• Safe Quality Care<br />
• Ethical Care<br />
• Health Parity<br />
• Integrity and Accountability<br />
• Practice Competence<br />
• Professional Development<br />
• Educational Advancement<br />
ONA MISSION STATEMENT<br />
<strong>The</strong> Mission of the <strong>Oklahoma</strong> <strong>Nurse</strong>s Association is to empower<br />
nurses to improve health care in all specialties and practice<br />
settings by working as a community of professional nurses.<br />
VISION<br />
Creating opportunities through advocacy, education and<br />
collaboration to become the leading voice for the nursing<br />
profession in the State of <strong>Oklahoma</strong>.<br />
BRAND PROMISE<br />
Engaging <strong>Nurse</strong>s to make a difference!
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 3<br />
PRESIDENT’S MESSAGE<br />
Shelly Wells, PhD, MBA,<br />
MS, APRN-CNS, ANEF<br />
As the hot summer starts<br />
to wind down, we start<br />
to think about Fall – my<br />
favorite season of the year!<br />
Fall is when the weather<br />
finally breaks, the leaves<br />
on the trees turn those<br />
gorgeous shades of yellow,<br />
red, orange, and purple, Shelly Wells<br />
the pumpkin spice aroma<br />
and flavor take their places on store shelves, and<br />
<strong>Oklahoma</strong> football season kicks into high gear. I<br />
am reminded that with the changing of seasons<br />
come new beginnings. Along with these seasonal<br />
changes, come changes within our nursing<br />
organization with the culmination of our officer<br />
elections and the naming of the new ONA Board<br />
Members at the Annual ONA Convention every<br />
fall.<br />
<strong>The</strong> past four years as your President<br />
-Elect and President of the <strong>Oklahoma</strong> <strong>Nurse</strong>s<br />
Association have been amazing, challenging, and<br />
frustrating all rolled into one! Who would have<br />
ever predicted the shifting of priorities we would<br />
see in nursing, health care, and policies because<br />
of a pandemic? Issues surrounding public health,<br />
safe staffing, workplace violence, and nurse wellbeing<br />
have been at the forefront of my term in<br />
office with the ONA Board.<br />
This has been such an important time for<br />
nurses to step forward to advocate for their<br />
profession, patients, and communities. As the<br />
most trusted profession in the United States,<br />
every individual nurse must be actively influencing<br />
health-related decisions and policies – not only<br />
for their patients and families, but also for their<br />
communities and our profession. As stated in<br />
the <strong>Nurse</strong>s’ Bill of Rights, we must continue<br />
to advocate for “safe work environments<br />
that prioritize and protect nurses’ well-being<br />
and provide support, resources, and tools to<br />
stay psychologically and physically whole”<br />
in order for us to provide for others (https://<br />
www.nursingworld.org/practice-policy/workenvironment/health-safety/bill-of-rights/).<br />
We<br />
accomplish this work through our effective<br />
leadership.<br />
Leadership does not require a title. In fact,<br />
every nurse is a leader. Leadership is a privilege<br />
that we must appreciate. Leadership can be<br />
challenging, but when you think about it, leading<br />
people can be one of the most fulfilling and<br />
rewarding experiences anyone can have since<br />
it affords the opportunity to change the lives of<br />
people every day. It is important that every nurse<br />
embraces their role as a leader to take the lead in<br />
activities and decisions in our work environments,<br />
communities, and policy making arenas. We must<br />
be heard in order to do the right thing to move<br />
forward. Attending the ONA convention: Power<br />
of Nursing: Educate, Innovate, Celebrate is a<br />
great way to recharge and learn about the many<br />
opportunities for nurses to engage in leadership<br />
activities. You can do this – lead by example and<br />
ask others to join in!<br />
I am optimistic about the future of nursing in<br />
<strong>Oklahoma</strong>. With over 52,000 registered nurses in<br />
the state, we collectively have the opportunity to<br />
lead <strong>Oklahoma</strong> and the profession of nursing to a<br />
place of excellence. We just have to “do it!” I look<br />
forward to your contributions!<br />
Thank you for placing your trust and confidence<br />
in me to serve as your President these past 2<br />
years. And thank you for your commitment to<br />
nursing and those we serve every day.<br />
JOIN OUR TEAM AS A<br />
Public Health <strong>Nurse</strong><br />
and make a difference in the lives of <strong>Oklahoma</strong>ns.<br />
May be eligible for the<br />
NURSE CORPS LOAN<br />
REPAYMENT PROGRAM<br />
Find out more:<br />
jobs.ok.gov<br />
Filter by Agency g State<br />
Department of Health<br />
Competitive Salary and Benefits Package<br />
Questions? Call: 405-426-8080<br />
HumanResources@health.ok.gov<br />
An opportunity<br />
you may not<br />
know exists!<br />
Join the FBI in <strong>Oklahoma</strong>. We’re hiring<br />
skilled nurses to become Special Agents.<br />
For more information, please contact<br />
cslandolt@fbi.gov.<br />
<strong>The</strong> best care starts with the best team.<br />
NOW HIRING FOR RN POSITIONS THROUGHOUT<br />
SAINT FRANCIS HEALTH SYSTEM!<br />
As a rapidly growing, locally owned, not-for-profit organization, Saint Francis<br />
is dedicated to the health and well-being of our patients and the entire<br />
community. We believe the best care starts with the best team, so we offer<br />
excellent benefits, competitive pay, career growth opportunities, a healthy<br />
work-life balance and an outstanding work environment.<br />
Learn more about available registered nurse positions and benefits,<br />
visit saintfrancis.com/nursing or call 918-502-8300 option 1.<br />
WHY NOW IS<br />
A GREAT TIME TO<br />
JOIN OUR TEAM:<br />
Generous<br />
sign-on bonus*<br />
Full comprehensive<br />
benefits package<br />
Generous relocation<br />
assistance*<br />
Clinical ladder<br />
program<br />
Tuition<br />
reimbursement<br />
CE opportunities<br />
On-site day care**<br />
EOE Protected Veterans/Disability<br />
*Some restrictions apply.<br />
See recruiter for details.<br />
**Only at select locations.
4<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
ONA Candidates to be Elected<br />
This year ONA members will elect the following<br />
positions, all for a two-year term:<br />
• Nominating Committee Members<br />
• Education Director<br />
• Membership Development Director<br />
• Secretary/Treasurer<br />
• President -Elect (serves 2 years as P-E and 2<br />
years as President)<br />
All candidates are listed below as well as on the<br />
ONA website. Voting will be conducted online and<br />
ballots will be available <strong>August</strong> 15 – September 9.<br />
ONA members will be emailed a username and<br />
password. If you prefer a paper ballot, one will be<br />
provided.<br />
Election results will be announced at the<br />
ONA House of Delegates, which will be held on<br />
September 28, <strong>2022</strong>.<br />
President-Elect (2 yrs as PE and 2 yrs as<br />
President) (Elect One)<br />
Cassy Abbott Eng, PhD,<br />
RN, CNE, LNC<br />
Educational Background:<br />
PhD Nursing Education<br />
<strong>The</strong> University of Northern<br />
CO Greeley, CO; MS<br />
Nursing UNC BS Nursing<br />
Marymount University; Legal<br />
<strong>Nurse</strong> Consultant Duke<br />
University; and Certified<br />
<strong>Nurse</strong> educator National<br />
League of Nursing<br />
Activities: ONA Political Activities Dir; Current<br />
Sigma <strong>The</strong>ta Tau President Zeta Delta at Large<br />
(July 2020-<strong>2022</strong>); National Charity League; Faculty<br />
Senate; and Strategic Planning Committee for<br />
Health Sciences<br />
Personal Statement: I firmly believe we, as<br />
nurses, have the ethical obligation and professional<br />
duty to advocate for the health and well-being<br />
of every individual. We are charged to protect<br />
human life and to ensure equality and justice for<br />
all. As nurses, we advocate for our patients and<br />
populations by becoming politically active and<br />
lobbying for policies that can be implemented.<br />
<strong>The</strong>se policies can potentially change the landscape<br />
of healthcare in our state. As nurses, we are charged<br />
to move beyond the point of recognizing current<br />
societal concerns and blaze the trail to promote<br />
change through active engagement and undeniable<br />
passion. We are the trusted voice for our patients<br />
and the vehicle for advancement. Now more<br />
than ever, we must advocate for all people while<br />
embracing and supporting their unique differences.<br />
Stagnation and complacency are not an option. We<br />
must embrace a plan of action that is patient driven<br />
not politically influenced. In addition, it is imperative<br />
nurses fight to increase resources in aiding optimal<br />
health and wellness of all citizens across our state.<br />
While the nation is burdened by a fog of chaos, as<br />
nurses we must cling to clarity and transparency.<br />
A rural hospital that is strong in its community.<br />
We are unique and one of a kind.<br />
We have a total of 26 beds with an occupancy rate of nearly 75%<br />
Once you join our team, you never want to leave!<br />
Opportunities for RNs and LPNs.<br />
New Graduates Welcome<br />
Full-Time, Flex & Double Time Available<br />
Competitive Pay with Benefits<br />
For more information and to apply contact Human Resources:<br />
Tammy White, HR Manager<br />
twhite@lindsaymunicipalhospital.com<br />
1305 W. Cherokee, Lindsay, <strong>Oklahoma</strong><br />
405-756-1404 phone • 405-756-1802 fax<br />
lindsayhospital.com<br />
EOE<br />
Optimal outcomes for the patient and honorable<br />
advancement of the profession must remain at<br />
the helm as our primary goal. Commitment to<br />
traveling the high road even if it's a lonely road at<br />
times. Acknowledging a challenge is the FIRST<br />
step. Fighting for the person and population that<br />
face that challenge ... is the RIGHT step. In doing<br />
so, we rightfully earn our title as the most trusted<br />
profession.<br />
Lucas Richardson-Walker,<br />
BSN, RN<br />
Educational Background:<br />
Rose State College ADN<br />
2002; and <strong>Oklahoma</strong> City<br />
University BSN 2017<br />
Activities: ONA, Region<br />
1 President ANA, Member<br />
Sigma <strong>The</strong>ta Tau, Member<br />
Founder of the Facebook<br />
Group "<strong>Nurse</strong>s Helping<br />
<strong>Nurse</strong>s" Reconciling Ministries Co-Chair St<br />
Stephens UMC Norman Youth Group Adult Sponsor<br />
St Stephens UMC Norman Administration Council St<br />
Stephens UMC<br />
Personal Statement: My name is Lucas<br />
Richardson-Walker BSN, RN. I am running for<br />
President-Elect. I have been a member of ONA<br />
for many years. I have served our profession on<br />
the ONA Board and represented our great state<br />
on the national stage as a Membership Assembly<br />
Representative at the ANA Membership Assembly<br />
in Washington D.C. I currently work as a Staff <strong>Nurse</strong><br />
in dialysis. As such, I have seen first-hand the<br />
pain and stress that our profession has struggled<br />
through during this trying pandemic. Too many<br />
have reached that breaking point. We have people<br />
leaving the profession at an alarming rate, in all<br />
areas of nursing! Seeing the struggle and knowing<br />
the power of the Professional <strong>Nurse</strong> is why I started<br />
the Facebook group “<strong>Nurse</strong>s Helping <strong>Nurse</strong>s”.<br />
As President-Elect, I will continue and expand on<br />
the current board’s focus of helping our essential<br />
profession through this hard time. I believe we<br />
will come out the other end of this pandemic a<br />
profession that is stronger and more resilient than<br />
ever! I am proud to be an <strong>Oklahoma</strong> nurse and<br />
member of ONA! I ask for your support to allow me<br />
to help lead our profession to the next level - coming<br />
out stronger and prepared for the challenging times<br />
ahead.<br />
Nathan Richmond, MSHA,<br />
BSN, RN<br />
Educational Background:<br />
OSU, Tulsa- MSHA, 2019<br />
OCU, OKC- BSN, 2016<br />
Activities: Member of<br />
ANA, ONA<br />
Member of ACHE<br />
Personal Statement:<br />
<strong>Nurse</strong>s represent the largest<br />
workforce in the healthcare<br />
sector to present date. <strong>Nurse</strong>s are also considered<br />
one of the most ethical professionals and most<br />
trusted not only in healthcare but out of all careers.<br />
<strong>Oklahoma</strong> also has some of the highest rates of<br />
health disparities and health outcomes in the nation.<br />
<strong>Oklahoma</strong> nurses are in a unique position to educate<br />
and help communicate healthy living strategies and<br />
the importance of over all health and well being to<br />
the communities we serve. I believe we need to<br />
increase the number of active members in ONA,<br />
so that the largest and most trusted workforce in<br />
healthcare is adequately represented and has a seat<br />
at the table in local and state policy making and<br />
reform.<br />
Secretary/Treasurer<br />
(2 yrs Term) (Elect One)<br />
Michele Bradshaw, MSN,<br />
RN<br />
Educational Background:<br />
<strong>Oklahoma</strong> City University,<br />
<strong>Oklahoma</strong> City, OK-<br />
Master’s in Nursing<br />
Administration (MSN)<br />
2019 <strong>Oklahoma</strong> Wesleyan<br />
University, Bartlesville, OK-<br />
Bachelors Nursing Science<br />
(BSN) 2005 Rose State<br />
College, Midwest City, OK- Associate Degree in<br />
Nursing Science (AAS) 1997 Metro Area Vocational<br />
School, <strong>Oklahoma</strong> City, OK- Practical Nursing<br />
Diploma- 1994<br />
Activities: ANA, ONA, OONE, AACN, Sigma-<br />
<strong>The</strong>ta Tau<br />
<strong>Oklahoma</strong> Christian <strong>Nurse</strong> Advisory Board<br />
Member Tri- City Youth and Family Services Board<br />
Member Nursing Education and Nursing Practice<br />
Advisory Committee<br />
Personal Statement: <strong>Nurse</strong>s have faced the<br />
greatest adversity of our careers in the last two<br />
years. We have shown innovation and resilience. I<br />
believe it is important for all nurses to be informed,<br />
and to have a strong voice on matters concerning<br />
nursing practice. With the predicted nursing<br />
shortage, I feel that we need to continue to seek<br />
innovative ways to recruit students to choose<br />
nursing as a career. We need to continue to<br />
advocate for safety for nurses with matters such as<br />
workplace violence and medical errors. It would be<br />
my honor to advocate for you and with you.<br />
Education Director<br />
(2 yr Term) (Elect One)<br />
Mindy Thompson, DNP,<br />
APRN, FNP-C, CNE<br />
Educational Background:<br />
Post-Masters Certificate,<br />
Family <strong>Nurse</strong> Practitioner:<br />
2019 Maryville University<br />
- St Louis, MO Doctor of<br />
Nursing Practice: Nursing<br />
Practice- Leadership and<br />
Innovation, Healthcare<br />
Nursing, 2017 University<br />
of Missouri - Columbia - Columbia, MO Master<br />
of Science: Nursing-Education Nursing, 2012<br />
Northeastern State University School of Nursing -<br />
Tahlequah, OK Bachelor of Science: Nursing, 2011<br />
Northeastern State University School of Nursing -<br />
Tahlequah, OK Associate: Applied Science Nursing,<br />
1998 Amarillo College School of Nursing - Amarillo,<br />
TX<br />
Activities: Dr. Thompson has been an active<br />
member of ONA for the past several years and over<br />
the past year has been the president of ONA Region<br />
3. She has served ONA Board of Directors by<br />
participating on ad-hoc committees. Dr. Thompson<br />
has served as an officer of other professional<br />
organizations such as two different chapters of<br />
Sigma <strong>The</strong>ta Tau-International.<br />
Dr. Thompson serves as a volunteer provider for<br />
Cura for the World providing primary care services<br />
for the uninsured of Creek County.<br />
Personal Statement: Advocacy is at the core of<br />
nursing and the values we embody. In recent events<br />
over the last couple of years from a global pandemic<br />
to changes impacting women's health and rights,<br />
advocacy is gaining even more importance. In<br />
order to be an effective advocate, we must take<br />
educated actions. Through maintaining current<br />
medical knowledge, we are better equipped to<br />
also protect the ethics we embody as a profession:<br />
nonmaleficence, beneficence, autonomy, justice,<br />
and privacy/confidentiality.
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 5<br />
Membership Development Director<br />
(Elect One)<br />
Amy Hutchens, Ph.D., RN<br />
Educational Background:<br />
Arizona State University,<br />
Ph.D., December, 2017<br />
Nursing and Health<br />
Innovation <strong>The</strong> University<br />
of <strong>Oklahoma</strong> M.S., May,<br />
2010 Nursing Education<br />
Health Sciences Center,<br />
<strong>The</strong> University of <strong>Oklahoma</strong>,<br />
B.S.N. May, 2003 Nursing<br />
Health Sciences Center <strong>Oklahoma</strong> City Community<br />
College A.D.N. December, 2001 Nursing<br />
Activities: From 2017-2018 Amy served as<br />
the director of education on the ONA Board of<br />
Directors. Dr. Hutchens developed educational<br />
initiatives put forth by the ONA. As an <strong>Oklahoma</strong><br />
<strong>Nurse</strong>s Association delegate representing Region 1,<br />
Amy supported the resolutions to define nurses as<br />
coordinators of care, and evaluated ONA bylaws.<br />
Dr. Hutchens also supported and advocated<br />
for full practice authority for APRNs through the<br />
<strong>Oklahoma</strong> Legislature. Amy served as Membership<br />
development director for the 2021-2021 term, and<br />
has presented multiple presentations across the<br />
state educating nurses and students on the benefits<br />
of ONA membership.<br />
Personal Statement: <strong>The</strong> nursing shortage has<br />
been and continues to be one of the most important<br />
issues facing ONA. Education, increasing availability,<br />
and resources for nursing students and faculty can<br />
contribute to alleviating this issue. I have and will<br />
continue to advocate for improved conditions at the<br />
bedside to recruit and retain nurses.<br />
Nominating Committee Representative<br />
(Elect Three)<br />
Monica Bowie, MSN, RN<br />
Educational Background:<br />
OSU-OKC, OKC, ADN,<br />
1997 Southern Nazarene<br />
University, Bethany, OK,<br />
BSN, 2001 <strong>Oklahoma</strong><br />
Wesleyan University (OKWU),<br />
Bartlesville, OK, MSN, 2020<br />
OKWU, Bartlesville, OK, DNP<br />
Student<br />
Activities: ANA, ONA<br />
Epidemiologist and Preventionists in Infection<br />
Control (EPIC) Oncology Nursing Society (ONS)<br />
Honor Society of Nursing, Sigma <strong>The</strong>ta Tau<br />
International (STTI), Beta Delta Chapter National<br />
League for Nursing (NLN) Association of Black<br />
Nursing Faculty, Inc (ABNF)<br />
Personal Statement: My views on nursing<br />
and issues facing ONA are to ensure nurses can<br />
practice their profession in a safe environment<br />
and to ensure nurses are compensated for their<br />
education and levels of expertise. I feel Advanced<br />
Practice Registered <strong>Nurse</strong>s (APRN) should be able<br />
to practice to the full extent of their education as<br />
independent practitioners. In addition, we should<br />
play a more active role in preventive healthcare.<br />
This includes patient education, increased access<br />
to healthcare, and elimination of food deserts and<br />
food insecurities. Finally, we should bring healthcare<br />
to the communities. This is where APRNs would be<br />
better utilized.<br />
Debra Johnston, RN, BSN,<br />
CEN, MBA<br />
Educational Background:<br />
ADN-Tarleton University<br />
Stephenville, TX 1994 BSN-<br />
OKWU 2012 MBA-OKWU<br />
2014<br />
Activities: ONA ANA ENA<br />
Personal Statement: <strong>The</strong><br />
field of nursing is harder than<br />
ever with COVID, resulting in many nurses moving to<br />
another career field and staffing issues. I have been<br />
in a leadership position for a few years and I want to<br />
make more of a positive impact on nursing.<br />
Nathan Richmond, MSHA, BSN, RN<br />
– See Bio Above<br />
Membership Assembly Representative<br />
(Elect Three)<br />
Cassy Abbott Eng, PhD,<br />
RN, CNE, LNC<br />
– See Bio Above<br />
Denise Barnett, MSN, RN<br />
Educational Background:<br />
OKCCC ADN 1989 OKWU<br />
MSN 2020<br />
Activities:<br />
ANA<br />
membership assembly rep<br />
ONA nominations committee<br />
Personal Statement: I have a MSN in nursing<br />
administration and am expected to graduate in Dec.<br />
<strong>2022</strong> with a MLS in Healthcare Law. My educational<br />
background combined with more than three<br />
decades of nursing experience puts me in a unique<br />
position for successfully expressing the concerns of<br />
our nurses to our legislators. It would be an honor to<br />
continue to serve <strong>Oklahoma</strong> nurses in this capacity.<br />
Thank you for supporting me as a representative for<br />
you at our next ANA membership assembly.<br />
Monica Bowie, MSN, RN<br />
– See Bio Above<br />
Debra Johnston, RN, BSN, CEN, MBA<br />
– See Bio Above<br />
Angie Kamermayer, DNP,<br />
APRN-CNS, NEA-BC<br />
Currently Serving as ONA<br />
President – Elect (ONA<br />
President <strong>2022</strong> – 2024)<br />
Rosalind Sims, RN BSN<br />
MBA PCCN<br />
Educational Background:<br />
Langston University -BSN<br />
2000 University of Phoenix<br />
MBA/HCM 2004<br />
Activities: ANA and ONA<br />
committees. Serving as<br />
nominee committee member<br />
Personal Statement:<br />
As we continue to advance<br />
into the 21st Century, the role of nurses continues<br />
to be a vital component of the success of our<br />
healthcare system. We are facing many challenges<br />
today in healthcare and our nursing profession.<br />
Some of the key challenges that we are facing are<br />
staff shortages, workplace hazards/violence, pay/<br />
salary compensation, working long hours and<br />
personal healthcare. To tackle these challenges,<br />
we need to have open dialogue discussions within<br />
our profession, focusing on a strategic plan with<br />
collaboration from our community leaders and<br />
healthcare professionals. I am committed to face<br />
these challenges as opportunities for our profession.<br />
Rachel Risner, Ph.D., DNP,<br />
APRN, C-FNP, CNE<br />
Educational Background:<br />
<strong>Oklahoma</strong> City University,<br />
<strong>Oklahoma</strong> City, OK, Ph.D.<br />
Nursing Education, 2016<br />
<strong>Oklahoma</strong> City University,<br />
<strong>Oklahoma</strong> City, OK, DNP,<br />
2013 Frontier Nursing<br />
University, Hyden, KY, MSN<br />
FNP, 2010 <strong>Oklahoma</strong> City<br />
University, <strong>Oklahoma</strong> City, OK, BSN 2007 <strong>Oklahoma</strong><br />
City Community College, <strong>Oklahoma</strong> City, OK, ASN,<br />
2005<br />
Activities: Nominating Committee<br />
Association of <strong>Oklahoma</strong> <strong>Nurse</strong> Practitioner<br />
Secretary National League for Nursing Nominations<br />
committee member (2) <strong>Oklahoma</strong> Indigenous<br />
<strong>Nurse</strong> Association President-elect <strong>Oklahoma</strong><br />
<strong>Nurse</strong>s Association Nominations Committee<br />
Chair NLN AARP representative for the American<br />
Indian/Alaska Native workgroup NLN AARP<br />
representative for the American Indian/Alaska<br />
Native Curriculum committee member NLN AARP<br />
representative for the American Indian/Alaska<br />
Native Webinar committee member and presenter<br />
NLN AARP representative for the American Indian/<br />
Alaska Native Workshop Development committee<br />
member presenter NLN AARP representative for<br />
the American Indian/Alaska Native Diversifying the<br />
Nursing Workforce: Mentoring for Student Retention<br />
and NCLEX Success at American Indian/Alaska<br />
Native-serving Institutions Toolkit contributor NLN<br />
Taking Aim Series committee member NLN Taking<br />
Aim Series Workshop Development Chair NLN<br />
Taking Aim Series Webinar committee member<br />
NLN Taking Aim Series Beyond Diversity and<br />
Between Equity and Inclusion webinar co-presenter<br />
NLN STEP into Leadership Coach NLN Strategic<br />
Action Group Accreditation Commission for<br />
Education in Nursing Peer Evaluator Accreditation<br />
Commission for Education in Nursing Evaluation<br />
Review Panel member American Academy of<br />
<strong>Nurse</strong> Practitioners Item Writer American Institute<br />
of Healthcare Quality teaching international nurses<br />
the Certified Professional in Infection Control<br />
course American Gulf International Consulting as an<br />
International Healthcare Consultant <strong>The</strong> American<br />
Association of Colleges of Nursing created the land<br />
acknowledgment Frontier Nursing University created<br />
the land acknowledgment American Leadership<br />
Academy participant <strong>Oklahoma</strong> State Plan to<br />
Decrease Prescription Drug Abuse committee<br />
member and contributor<br />
Personal Statement: My career has been<br />
guided by a mission to build an innovative, robust,<br />
and diverse nursing workforce that is responsive to<br />
stakeholders' needs. My educational background,<br />
leadership experience, and professional<br />
experiences have prepared me for the position of<br />
ANA Membership Assembly Representative. <strong>The</strong><br />
nursing profession is faced with a rapidly evolving<br />
healthcare landscape that must be addressed with<br />
innovation and bravery. Leaders in nursing must<br />
meet national and global healthcare needs while<br />
maintaining a commitment to the core nursing<br />
principles of compassionate care, honesty, and<br />
strong moral principles. It is our work as nurses to<br />
continue building a strong diverse, inclusive, and<br />
equitable nursing workforce.<br />
Lucas Richardson-Walker, BSN, RN<br />
– See Bio Above<br />
Nathan Richmond, MSHA, BSN, RN<br />
– See Bio Above
6<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
We are on Holy Ground<br />
Catherine White, MA, RN, FCN-BC Faith<br />
Community <strong>Nurse</strong> Coordinator Mental Health<br />
Coach, First Responder<br />
In the past several issues of THE OKLAHOMA<br />
NURSE there have been several articles about selfcare,<br />
wellness, holistic health care, faith-based<br />
care along with articles instructing nurses how to<br />
deal with stress – stress from academic pursuits,<br />
stress from pandemic situations of short staffing,<br />
insufficient or unavailable supplies, environmental<br />
hazards (e.g., incivility and conflict in the workplace)<br />
and the list goes on with topics about how to handle<br />
life’s difficulties. Authors did their best to write<br />
articles with optimism and actions to minimize if<br />
not eliminate the many problems nurses face in<br />
providing care while maintaining ethical standards.<br />
<strong>The</strong> articles were insightful but would lead the<br />
reader to wonder if there might be an option yet to<br />
be considered. <strong>The</strong> most recent article that made<br />
me want to answer the author's question "Where<br />
Do I Go From Here?" is in the May-July <strong>2022</strong> issue<br />
of THE OKLAHOMA NURSE publication by Sharon<br />
Broscious, page 22. <strong>The</strong>re is an answer.<br />
<strong>The</strong>re is indeed an option that needs to be<br />
shared. Traditional nursing care has been seen<br />
as meeting the patient's physical, mental and<br />
emotional, and to some extent spiritual needs. But<br />
over the years more attention has been given to the<br />
aspect of "spiritual care.” In the 1980s two efforts<br />
arose to address spiritual care from two different<br />
perspectives: holistic vs wholistic. It is interesting to<br />
note that these are different yet similar.<br />
<strong>The</strong> similarities are in the two organizations being<br />
founded. Holistic nursing as a clinical specialty<br />
came into being January 17, 1981, in Houston,<br />
Texas, when 33 nurses from eight states met to<br />
share their stories and implement a vision using<br />
a variety of healing and integrative therapies<br />
from a humanistic worldview such as imagery,<br />
visualization, relaxation, deep-breathing techniques,<br />
stress management, aromatherapy, subtle energy<br />
therapies (therapeutic touch) for patients in hospitals<br />
and in private practice. <strong>The</strong> faith-based or wholistic<br />
nursing, also an ANA clinical specialty, was<br />
founded in Chicago, Illinois, in the mid-1980s (1984)<br />
by a Lutheran Minister – Hospital Chaplain and<br />
medical doctor, Rev. Dr. Granger Westberg. Both<br />
organizations attempted to address the patient's<br />
needs for care of the body, soul and spirit but Dr.<br />
Westberg's efforts were to be based on the Judea-<br />
Christian worldview.<br />
Rev. Dr. Westberg made rounds daily at the<br />
hospital where he served and concluded that while<br />
the physical nursing care was excellent, there<br />
seemed to be a lack of attention to caring for the<br />
whole person spiritually. Intentionally using spiritual<br />
and religious practices such as prayer, anointing,<br />
religious and inspiring materials along with using<br />
one's presence helped the patient (and family) to<br />
know that healing as a desired healthcare outcome<br />
is from a right relationship with one's Creator, God.<br />
When people with diseases, disabilities, or mental<br />
illness manifestations approached Jesus, He, by<br />
word, touch, and presence, made them whole. He<br />
imparted the Shalom, or supernatural peace, healing<br />
and wholeness, that led to a healing only He could<br />
give them. <strong>The</strong> "Higher Power" Dr. Westberg saw as<br />
needed for health recovery was based on Biblical<br />
principles. As he taught these concepts to nursing<br />
staff at the hospital where he served, he helped<br />
them learn ways to provide self-care spiritually along<br />
with using skills to include in patient care providing<br />
a benefit to both giver and to receiver. <strong>The</strong> hospital<br />
administration was in full support of this education<br />
and, as word spread to other nursing staff at other<br />
hospitals in his community, he taught other medical<br />
staffs how to provide what he called "wholistic care"<br />
to enhance "traditional care.” He reminded the staff<br />
that one cannot give or use what one does not have<br />
or that one has not learned, so he taught the staff<br />
to use an in-filling of power to perform the tasks of<br />
caring – for self-first and then for others.<br />
Originally, the faith-based nursing organization<br />
was called Parish Nursing because denominations<br />
that are more formal in their ministries – Lutheran,<br />
Catholic, Episcopalian – have geographic<br />
boundaries called parishes for their congregations.<br />
As this type of faith-based nursing ministry<br />
expanded over the years, the name has been<br />
changed to Faith Community Nursing in order to<br />
include denominations of other groups. According<br />
to the Parliament of the World Religions, over 50<br />
world religions recognize the basic core values of<br />
faith nursing, which include respect for life and the<br />
promotion of charitable service to others (Kung &<br />
Kuschel, 1993).<br />
Originally, religious orders were known for caring<br />
for the sick, poor, widows, orphans, prisoners and<br />
other vulnerable populations as an expression<br />
of God's love and power toward mankind. While<br />
holistic principles and the inclusion of natural<br />
therapies (oils, liniments, salves, ointments, teas,<br />
plasters, poultices, compresses) were foundational<br />
in the early practice of nursing, they were largely<br />
abandoned by the mid to later part of the 1900s. In<br />
the later part of the 1900s technology superseded<br />
the human connection and the God-connection<br />
and healthcare began to change from a "service<br />
profession" to a "for-profit business.” <strong>The</strong> caring and<br />
healing connection that was fundamental to nursing<br />
was subdued by an emerging culture that valued<br />
efficiency and profit margins. Nursing early on had<br />
been seen as a calling of God and servanthood, but<br />
that view changed causing nurses to be frustrated<br />
by their inability to provide what they considered<br />
quality care and tend to the needs of the person as<br />
a whole entity. It was out of this milieu that these two<br />
organizations emerged, each with its own unique<br />
perspective on how to restore that care.<br />
<strong>The</strong>re is another organization that works<br />
collaboratively with the Faith Community <strong>Nurse</strong><br />
organization and that is <strong>Nurse</strong>s Christian<br />
Fellowship. This organization was founded in<br />
Chicago, Illinois, in early 1935 when three nurses<br />
met to pray at Children's Hospital about forming<br />
an organization intent on meeting the spiritual<br />
needs of nurses. Students in Chicago discovered<br />
this group and returned to their home school<br />
(diploma) and started a group like the one they had<br />
encountered. NCF reaches out to nurses needing<br />
their spiritual needs met while serving in various<br />
roles: faculty, administrators of nursing programs<br />
and departments of nursing in healthcare settings,<br />
staff nurses, nursing students, for example. Both<br />
organizations rely on the concept of wholeness that<br />
occurs when a person has a personal relationship<br />
with Jesus so that quality of nursing care is a reality<br />
even in the midst of indescribable and unbearable<br />
stress. Wholeness as a concept occurs in Matthew<br />
9: 1-13 with Jesus meeting a man with palsy, then<br />
in verse 22 with a woman who had a chronic<br />
hemorrhagic condition for 12 years to whom Jesus<br />
said, "Daughter, be of good comfort; your faith has<br />
made you whole. And the woman was made whole<br />
from that hour." (See also Mark 5:25-34). Other<br />
scenarios of supernatural healings – a 40-year-old<br />
crippled man – are recorded in the book of Acts 3:10<br />
and Acts 4: 5-10. People with seizures, self-cutting<br />
and mental illness, blind, deaf, dumb, dead, a<br />
withered hand and – the list goes on – all were made<br />
alive or well - whole - having had an encounter with<br />
Jesus.<br />
As a member of three organizations – Faith<br />
Community <strong>Nurse</strong> ministry, <strong>Nurse</strong>s Christian<br />
Fellowship and the Mental Health Coach First<br />
Responder ministry – I want to leave some passages<br />
of scripture that may lead a nurse colleague with the<br />
answer to Dr. Broscious question "Where Do I Go<br />
From Here?" <strong>The</strong> answer is found in the manual for<br />
life, i.e., the Holy Scriptures aka the Bible. Start your<br />
day with Psalm 5: 3, 8- "My voice shall You hear in<br />
the morning, O Lord; in the morning will I direct my<br />
prayer unto You and will look up...Lead me, O Lord...<br />
make Your way straight before my face." Add Psalm<br />
143:8- "Cause me to hear Your lovingkindness in the<br />
morning for in You do I trust; cause me to know the<br />
way wherein I should walk for I lift up my soul unto<br />
You."<br />
How about Psalm 37: 23 – ''<strong>The</strong> steps of a<br />
good man (person) are ordered of the Lord and<br />
He delights in his way." Isaiah 30: 21- "And your<br />
ears shall hear a word behind you saying, 'This is<br />
the way, walk you in it, when you turn to the right<br />
hand and when you turn to the left." Proverbs 3:<br />
S, 6 - "Trust in the Lord with all your heart and do<br />
not lean on your own under-standing. In all your<br />
ways acknowledge Him and He shall direct your<br />
paths." How about this one? 2 Chronicles 16:9a -<br />
"<strong>The</strong> eyes of the Lord run to and fro throughout the<br />
whole earth to show Himself mighty on behalf of<br />
those whose hearts are perfect (loyal) to Him." No<br />
one needs to be told that the times in which we live<br />
today are perilous and troublesome, so one needs<br />
Help From Above to live out one day. Our world is in<br />
chaos and spiritual warfare abounds. We need tools<br />
that are a match for such warfare and these tools<br />
(weapons) come from the Lord. See Isaiah 40:29 -<br />
"He gives power to the faint and to them that have<br />
no might He increases strength...they that wait upon<br />
the Lord shall renew their strength; they shall mount<br />
up with wings as eagles; they shall run and not be<br />
weary and they shall walk and not faint." Isaiah 41:<br />
10, 13a, 14a - "Fear not (DO NOT BE AFRAID) for I<br />
am with you; be not dismayed for I am your God. I<br />
will strengthen you; I will help you; yes, I will uphold<br />
you with the right hand of my righteousness...For I<br />
the Lord, your God will hold your right hand saying<br />
to you, 'Fear not; I will help you...Fear not...' ". See<br />
Micah 7:7 - "I will look unto the Lord and I will wait<br />
for the God of my salvation; my God will hear me...<br />
when I fall, I shall arise; when I sit in darkness, the<br />
Lord shall be a light unto me." Jeremiah 33:3 -" "Call<br />
unto Me and I will answer you and show you great<br />
and mighty things that you do not know."<br />
In answer to Dr. Broscious' question "Where Do I<br />
Go From Here?" - how about this answer: Matthew<br />
11:28-30 - "Come unto Me all you who are weary<br />
and heavy laden (burdened) and I will give you rest.<br />
Take My yoke upon you and learn of Me and you<br />
shall find rest unto your souls. For My yoke is easy<br />
and My burden is light." <strong>The</strong>n when the workday or<br />
shift is done, try this for encouragement. <strong>The</strong> 23rd<br />
Psalm which can be a form of prayer. "<strong>The</strong> Lord<br />
is my Shepherd. I shall not want (lack anything).<br />
He makes me to lie down in green pastures; He<br />
leads me beside still waters. He restores my soul;<br />
He leads me in the paths of righteousness for His<br />
name's sake. Yes, though I walk through the Valley<br />
of the Shadow of Death, I will fear no evil (harm) for<br />
You are with me and Your rod and Your staff they<br />
comfort me. You prepare a table in the presence of<br />
my enemies; You anoint my head with oil; my cup (of<br />
water) runs over. Surely goodness and mercy shall<br />
follow me all the days of my life and I shall dwell in<br />
the house of the Lord (heaven) forever (eternally)."<br />
Amen
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 7<br />
How Stress Affects the<br />
Physical Body<br />
Nicole Cerrini BSN, RN<br />
We are often consumed with how stress can cause us to experience mood<br />
changes, sleep pattern disruptions and overall anxiety. But what about the<br />
physical symptoms that appear and become chronic? Gastrointestinal (GI)<br />
distress, headaches, back pain, TMJ, hormonal imbalances and extreme<br />
fatigue, just to name a few, can all be the result of stress.<br />
So how do we know if our physical ailments are the result of stress, and how<br />
do we treat it? Learning to listen to your body is the first step in understanding<br />
if what you’re experiencing is directly related to stress. Do you find that your<br />
stomach gets upset when you have a lot going on, or you tend to lose your<br />
appetite (or eat more) when you feel overwhelmed? <strong>The</strong>se are both signs that<br />
your body is battling an internal imbalance, not a stomach bug. We’ve been<br />
conditioned to believe that all physical symptoms must be attributed to a true<br />
medical condition, instead of looking at it from a holistic perspective.<br />
<strong>The</strong>re are circumstances where you may in fact have a medical condition and<br />
may need specific treatment, but it should become a habit to analyze outside<br />
factors that may be contributing to your symptoms. <strong>The</strong> dreaded culprit of<br />
back pain is another good example. <strong>The</strong>re are millions of people suffering from<br />
back pain in our country, and a lot of times physicians are quick to recommend<br />
invasive procedures or prescription medication to help alleviate their symptoms.<br />
Chemical and physical reactions take place in your body when you are under<br />
stress, causing an involuntary tightening of your muscles due to an increase<br />
in cortisol and adrenaline levels. This can present as back pain in certain<br />
individuals and may branch out to include other physical symptoms.<br />
Becoming aware of physical symptoms that may be related to stress is the<br />
first step in treating these ailments. Once you're able to reflect and listen to<br />
your body, the next step is to make it a priority to listen to your needs! Holistic<br />
therapies are often ignored as a primary means of treatment. Analyzing the<br />
body through this perspective allows for a unique approach focusing on<br />
physical, emotional and spiritual health resulting in a plan to align and balance<br />
the body.<br />
Specific therapies for treating physical symptoms caused by stress include<br />
nutrition plans, mindset exercises, meditation, breathwork, hypnosis, reiki and<br />
many other modalities. Nutrition is one of the most important variables in your<br />
health, especially as it relates to stress and overall wellness. <strong>The</strong> term “food is<br />
medicine” was coined for a reason; how you fuel your body can have a direct<br />
impact on preventing and treating physical ailments.<br />
Try to keep an open mind when it comes to your health, and consider<br />
alternative therapies in your quest for relief of physical symptoms.<br />
CEO Report continued from page 2<br />
can see on the Call to the ONA House on the pages of this publication, every<br />
Region has representatives that are based on the number of members in each<br />
Region. We need nurses to volunteer and serve as Delegates to the House of<br />
Delegates.<br />
Breathe again…smile, another brain chemistry shift.<br />
RN2LEADER<br />
Joyful Noise<br />
Dr. Dean L. Prentice, Colonel (Ret), USAF, NC, DHA, MA, BSN, NE-BC<br />
Do you find joy in your job? I’m not asking if you like<br />
your job, but if you find joy in the basic heart of your job.<br />
When you started your professional life, I bet there was<br />
a part of you that really desired or even felt that being<br />
joyful, positive, or happy about going to work was what<br />
you wanted. You worked hard to earn that license, were<br />
proud of the accomplishment, and you were ready to<br />
take on the world.<br />
<strong>The</strong> positive outlook and desire to go to work is<br />
essential for ultimate job satisfaction. It increases your<br />
productivity, innovation, and performance at work.<br />
How you get to that joy at work can take many paths Dr. Dean Prentice<br />
which will require you to do some self-reflection on your<br />
current job. <strong>The</strong>n you will have to do some work if where you are currently is not<br />
where you want to be ultimately.<br />
People feel once they become successful, they will be happy. I am not sure<br />
that thought is entirely correct. Yes, becoming successful in your position does<br />
bring a sense of pride, of accomplishment, of fulfilling a need to be valued. That<br />
alone, I believe, is not going to guarantee joy at work.<br />
First you set out to create a work environment where you like going to work.<br />
This may include building a great team, defining the roles, looking for the right<br />
people for the team, and setting a vision all of which will encourage positive<br />
work environments. You also need to foster or create a work environment where<br />
you know you will enjoy working. Dreading coming to work, or facing daily<br />
challenges and not being able to improve them does not support your goal.<br />
Choosing to work for the right organization is another aspect of finding joy<br />
at work. <strong>The</strong> simple task of finding an organization whose mission, core values,<br />
and culture agree with yours can seem impossible at times. Networking with<br />
colleagues, talking with other professionals in the organization other than<br />
nurses, looking at the strategic plan of the organization, and observing where<br />
they invest their resources are great indicators of what the organization values.<br />
If what you see is not what you want, then look for another organization.<br />
Building strong interpersonal relationships helps build better feelings of joy at<br />
work. When you start to build stronger relationships with peers, both in and out<br />
of your profession, you have a sense of connectedness with the organization.<br />
Likewise these relationships help during times of crisis or disagreements.<br />
When challenges arise and you have an established positive relationship with<br />
another colleague, it is easier to walk through the resolution process to solve<br />
the problem. You are more confident in what you know and in the knowledge<br />
that you and your colleague are on the same team.<br />
Another great aspect about having a positive outlook on your job and finding<br />
joy at work is that your attitude spreads. A joyful attitude can positively affect<br />
your fellow workers and organization. You can be the change in your unit or<br />
organization that it needs to take it to the next level of excellence. Imagine if you<br />
and your fellow leaders looked forward to coming into work.<br />
So what is your next step to create joy at work? Don’t forget to take a<br />
colleague along for this journey. Working on this habit together can really pay<br />
dividends.<br />
FIVE-STAR RATED<br />
On another front, ONA has been advocating for nurses at the State Capitol.<br />
Our work has focused on solutions to our nursing shortage by supporting<br />
nursing education and other policy issues. Often Legislators have their own<br />
solutions, and we work to educate them on better solutions. One of the ways<br />
we are working to educate Legislators is to request an interim study focused<br />
on the nursing shortage. We want to highlight the current data, nursing’s<br />
educational needs, and the skills and education necessary for registered<br />
nurses as they deliver the highly skilled care required in todays’ patient care<br />
settings. This will take all of us to educate Legislators, both those running for<br />
election or reelection and those without elections this cycle. I encourage you to<br />
get involved…talk to those candidates knocking on your door, get involved in a<br />
campaign by volunteering or just voting. Voting is the most important thing you<br />
can do.<br />
Breathe again…smile you’re shifting your brain again<br />
I hope to see you at the ONA Annual Convention, <strong>The</strong> Power of Nursing, at<br />
the Hyatt Regency Tulsa Downtown in Tulsa, <strong>Oklahoma</strong> on September 28 - 29,<br />
<strong>2022</strong>. Look for more details on the ONA Convention in this newspaper and on<br />
the ONA website. ONA takes guidance from our members on where to focus<br />
our efforts. To ensure you have a voice in providing direction you need to be<br />
a member. We hope that you will become a member and get involved so that<br />
collectively we can make a difference in <strong>Oklahoma</strong>.<br />
Breathe again…you should be a different place then when you started!<br />
LEADERSHIP OPPORTUNITIES<br />
• RN, System Chief Nursing Officer<br />
• RN, Quality Director<br />
NURSING OPPORTUNITIES<br />
Community Hospital South:<br />
RN, FT*: ICU/Med Surg Days/Nights,<br />
Circulator, Med-Surg Days/Nights, ER Weekend<br />
PRIME Mid/Nights<br />
RN, PRN: ER Days/Nights, Med-Surg Nights,<br />
PACU, Pre-Admission Testing<br />
ADDITIONAL OPPORTUNITIES<br />
Paramedics, FT: Med-Surg<br />
*Sign On Bonus<br />
Community Hospital North:<br />
RN, FT*: Circulator, Pre-Admission<br />
Testing, PreOp/Phase II,<br />
Med-Surg Days/Nights<br />
RN, PRN: Med-Surg Days/Nights,<br />
PACU, Circulators<br />
$10,000 for FT Circulator • $10,000 for FT Med-Surg Nights<br />
$10,000 for FT Emergency • $7,500 for FT Med-Surg Days<br />
$5,000 for FT PACU • $3,000 for FT Pre-Admission Testing<br />
$3,000 for FT PreOp/PhaseII • $2,000 for FT Paramedics<br />
Learn about our benefits<br />
Northwest Surgical Hospital:<br />
RN, FT*: Med-Surg Days/Nights<br />
PACU<br />
RN, PRN: Med-Surg Days/Nights,<br />
PACU, PreOP/Phase II<br />
Come join our award winning team!<br />
3 LOCATIONS IN OKLAHOMA CITY!<br />
COMMUNITY HOSPITAL SOUTH<br />
COMMUNITY HOSPITAL NORTH<br />
NORTHWEST SURGICAL HOSPITAL<br />
Community Hospital/Northwest Surgical Hospital complies<br />
with Federal Civil Rights laws and doesn’t discriminate on the<br />
basis of race, color, age, disability or nationality. Community<br />
Hospital and Northwest Surgical Hospital are facilities in which<br />
physicians have an ownership or investment interest. <strong>The</strong> list<br />
of physician owners is available upon request.<br />
To apply, please visit www.communityhospitalokc.com or www.nwsurgicalokc.com.
8<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Meeting the nurse staffing challenge, part two: Retention tips<br />
By Georgia Reiner, MS, CPHRM,<br />
Risk Specialist, NSO<br />
As discussed in the first article in this two-part<br />
series on nursing recruitment and retention, ensuring<br />
appropriate nurse staffing levels is key to the financial<br />
health of healthcare organizations like hospitals and<br />
skilled nursing facilities. High-quality nursing care<br />
helps to reduce the likelihood of patient safety events<br />
and costly medical malpractice lawsuits related to<br />
missed errors. This means it is critical for leaders to<br />
engage in effective retention strategies.<br />
<strong>The</strong> second of a two-part series, this article<br />
addresses effective retention strategies that leaders<br />
can utilize to help reduce turnover of nursing staff.<br />
Retention<br />
<strong>The</strong> 2021 National Health Care Retention and<br />
RN Staffing Report notes that the average cost<br />
of turnover for a hospital-based RN was $44,400<br />
in 2020. This makes retention a key part of an<br />
organization’s staffing strategies. You need to<br />
work closely with human resources staff to ensure<br />
retention strategies are efficient, effective, and inline<br />
with organizational strategies.<br />
Conduct “stay” interviews. Stay interviews<br />
help you identify employees who might be thinking<br />
about leaving the organization and identify what<br />
factors are most important for staying. You can<br />
use the information to create an individual retention<br />
plan and to inform your larger retention efforts for<br />
the unit. Here are some examples of questions you<br />
can use to help elicit useful information during stay<br />
interviews:<br />
• What do you look forward to each day when<br />
you commute to work?<br />
• What are you learning here, and what do you<br />
want to learn?<br />
• Why do you stay here?<br />
• When is the last time you thought about<br />
leaving and what prompted it?<br />
• What can I do to make your job better for you?<br />
Promote a healthy work environment. For<br />
example, implement zero tolerance policies for<br />
patient or visitor violence against nurses and<br />
policies that discourage providers from bullying their<br />
colleagues. Beyond policies, it is also important to<br />
ensure lines of communication are open, so your<br />
staff feel comfortable speaking with you when they<br />
identify problem areas. Make rounds daily and listen<br />
to staff closely. Ask them questions such as, “What<br />
do you need to do your job more effectively?” If it’s<br />
something that you can take care of, do so and let<br />
them know it’s been done. If you can’t address the<br />
issue, explain why and, if appropriate, note that it<br />
may be able to be addressed in the future.<br />
Avoid sign-on bonuses. Sign-on bonuses<br />
may help to ease staffing woes short term, but<br />
don’t ensure commitment, and can even lead to<br />
resentment from current staff. Instead, focus on<br />
improving nurses’ pay scales or offering retention<br />
bonuses to show appreciation for your nursing<br />
staff’s commitment to the organization.<br />
Recognize employees. Recognition is an easy,<br />
but often underutilized, retention tactic. Take every<br />
opportunity to offer words of praise. To reinforce the<br />
behavior, specify what specifically was done to earn<br />
praise. Small rewards such as gift cards can also be<br />
effective, but try to match them to the individual’s<br />
interest. For example, a nurse who drinks coffee<br />
every day may enjoy a Starbucks card, but one who<br />
loves to read might prefer a card from Barnes &<br />
Noble.<br />
Support career development. Explore nurses’<br />
professional goals and how you can help meet<br />
them during stay interviews and other ongoing<br />
professional development conversations. It’s a good<br />
idea to keep a mental list of options such as serving<br />
on committees, acting as a preceptor, and leading<br />
project teams. Offer meaningful opportunities for<br />
professional growth based on performance, rather<br />
than solely based on tenure. Outline for your staff<br />
the types of experiences or skills that are most<br />
valuable for advancement and reinforce the value<br />
of bedside nursing experience for nurses’ long-term<br />
career growth.<br />
Consider a job embeddedness approach. Job<br />
embeddedness (JE) focuses on why people stay in<br />
their jobs as opposed to why they leave. A study<br />
by Reitz and colleagues found it’s a good predictor<br />
of nurses’ intent to stay. JE looks at ties related to<br />
organizations and the community where they exist.<br />
<strong>The</strong>se ties are considered in three dimensions:<br />
links (formal and informal connections people have<br />
with their organizations or communities), fit (how<br />
compatible people feel with their organizations<br />
or communities), and sacrifice (material and<br />
psychological losses people would experience by<br />
leaving their organizations or communities). You can<br />
leverage these dimensions to promote retention. For<br />
example, to help promote JE with the organization:<br />
• Links: Involve nurses in committees and<br />
shared governance.<br />
• Fit: Recruit nurses whose goals align with the<br />
organization’s goals.<br />
• Sacrifice: Align vacation time and retirement<br />
plans with the time of service.<br />
A multifaceted approach<br />
<strong>Nurse</strong> staffing challenges are unlikely to ease<br />
anytime soon. Leaders will need to be creative and<br />
take a multifaceted approach to recruitment and<br />
retention. <strong>The</strong>se efforts will help gain—and keep—<br />
staff. Doing so helps reduce the costs of lawsuits<br />
related to errors, but, most importantly, provides<br />
optimal patient outcomes.<br />
References<br />
Advisory Board. Struggling to keep entry-level staff<br />
engaged? Try a performance-based career<br />
ladder. 2017. https://www.advisory.com/<br />
blog/2017/02/pef-career-ladder<br />
CNA & NSO. <strong>Nurse</strong> Professional Liability Exposure Claim<br />
Report: 4th Edition: Minimizing Risk, Achieving<br />
Excellence. 2020. https://www.nso.com/<br />
Learning/Artifacts/Claim-Reports/Minimizing-<br />
Risk-Achieving-Excellence<br />
Malliaris AP, Phillips J, Bakerjian, D. Nursing and Patient<br />
Safety. Agency for Healthcare Research and<br />
Quality. 2021. https://psnet.ahrq.gov/primer/<br />
nursing-and-patient-safety<br />
NSI Nursing Solutions, Inc. 2021 National health care<br />
retention and RN staffing report. 2021. https://<br />
www.nsinursingsolutions.com/Documents/<br />
Library/NSI_National_Health_Care_Retention_<br />
Report.pdf<br />
Reitz O, Anderson M, Hill PD. Job embeddedness and<br />
nurse retention. Nurs Admin Q. 2010;34(3):190-<br />
200.<br />
Saver C. Retaining nurses in a post-pandemic era—Part 1.<br />
OR Manager. 2021;37(9):12-15.<br />
Sherman RO. <strong>The</strong> Nuts and Bolts of Nursing Leadership:<br />
Your Toolkit for Success. Rose. O. Sherman;<br />
2021.<br />
Disclaimer: <strong>The</strong> information offered within this article<br />
reflects general principles only and does not constitute<br />
legal advice by <strong>Nurse</strong>s Service Organization (NSO)<br />
or establish appropriate or acceptable standards of<br />
professional conduct. Readers should consult with an<br />
attorney if they have specific concerns. Neither Affinity<br />
Insurance Services, Inc. nor NSO assumes any liability<br />
for how this information is applied in practice or for the<br />
accuracy of this information.<br />
This risk management information was provided<br />
by <strong>Nurse</strong>s Service Organization (NSO), the nation's<br />
largest provider of nurses’ professional liability<br />
insurance coverage for over 550,000 nurses since<br />
1976. <strong>The</strong> individual professional liability insurance<br />
policy administered through NSO is underwritten by<br />
American Casualty Company of Reading, Pennsylvania,<br />
a CNA company. Reproduction without permission of the<br />
publisher is prohibited. For questions, send an e-mail to<br />
service@nso.com or call 1-800-247-1500. www.nso.com.
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 9<br />
An Inestimable Loss<br />
Nancy J Vitali, MS, DCSc, Caritas Coach<br />
Every arrival foretells a leave-taking: every birth a death. Yet each death and<br />
departure come to us as a surprise, a sorrow never anticipated. Life is a long<br />
series of farewells; only their circumstances should surprise us.<br />
Jessamyn West<br />
<strong>The</strong> Life I Really Lived<br />
<strong>The</strong> pandemic has proved to be an unprecedented challenge for nurses,<br />
with 52% of nurses considering a change in profession after two years of the<br />
pandemic (American <strong>Nurse</strong>s Foundation, <strong>2022</strong>) and a surprising 30% reporting<br />
poor emotional health across all age categories, with younger nurses having<br />
a much higher rate of 46%. <strong>The</strong> comprehensive impact of the past two-plus<br />
years on the profession of nursing is not measurable, with nurses reporting the<br />
overwhelming demoralization of witnessing deaths of patients in which families<br />
were not allowed to be present, doing their best to connect electronically and<br />
to act as proxy for their dying patients’ loved ones. This writer listened to the<br />
experiences of <strong>Oklahoma</strong> nurses who described the moral injury resulting from<br />
caring for several dying patients per shift on COVID units, day after day, during<br />
the worst of the pandemic. <strong>The</strong>se situations, combined with other stressors<br />
that were endemic in health care delivery, such as staffing shortages and<br />
inadequate equipment and supplies, multiply the distress to the level of trauma,<br />
whose effects will be a real presence in some nurses’ lives for years to come.<br />
Not mentioned yet are the pressures their families shouldered, such as home<br />
schooling and caring for their children, and the possibilities of contracting the<br />
illness themselves.<br />
Amid this climate of unprecedented distress, some of these nurses took their<br />
own lives. Early this year, Michael O’Dell of Muskogee was one of those nurses.<br />
He and several other nurses from <strong>Oklahoma</strong> had taken traveling contracts in<br />
different states over the previous several years, had coincidentally met in the<br />
workplace on the east coast, and had agreed to head to California. In California<br />
during the pandemic, they became each other’s support network, and even<br />
roommates, as Michael moved in with friend Joshua Paredes, a Tulsa nursing<br />
graduate. Friend Michael Walujo, also from Tulsa, worked in Southern California<br />
at Cedars-Sinai Medical Center. <strong>The</strong>y were in the habit of doing weekly mental<br />
health “check-ins” with one another and other friends. <strong>The</strong>y understood the<br />
combined vulnerabilities of being travelers and away from home, being part of a<br />
marginalized (LGBTQ+) community and working during the pandemic.<br />
Michael’s friends have shared that he was the life of their circle of friends,<br />
planning group trips to music festivals and abroad between contracts. He<br />
had been a precocious and inquisitive child, teaching himself the Swedish<br />
language at the age of 11. As an adult, he travelled to Spain, Italy, and Portugal<br />
to immerse himself in the languages and cultures of those countries. He also<br />
traveled to Iceland with a nurse friend between contracts. When he wasn’t at<br />
work in his travel positions, he hiked and attended electronic music festivals<br />
with friends, often as the orchestrator of the adventures for his companions. He<br />
was engaged in and in love with life and with the richness, diversity, and beauty<br />
of humanity. Michael was also recognized as an exceptionally caring nursing<br />
professional and patient advocate. Despite all of these attributes, the truth is<br />
that Michael also battled depression, and was experiencing the challenge<br />
of connecting with needed mental health services in the Bay Area when the<br />
tragedy of his death occurred.<br />
While working in an ICU at Stanford University Hospital on January 18<br />
of this year, Michael spoke to his supervisor, saying he needed to retrieve<br />
something from his car, and that he would return momentarily. Michael did not<br />
return. At their apartment in San Francisco, Joshua began to worry when he<br />
didn’t return from his shift at the expected time. A search began after his car<br />
was found on the Dumbarton Bridge (the southernmost bridge over the San<br />
Francisco Bay). Michael’s body was pulled from the bay several days later.<br />
Two months later, another nurse died by suicide/gunshot in the utility room of<br />
a Kaiser-Permanente facility in nearby Santa Clara. <strong>The</strong>se two deaths left Bay<br />
Area nurses and health care personnel in shock and disbelief, and galvanized<br />
Michael’s friends to reach out to other nurses to organize a peer-support<br />
organization for the purpose of preventing any further tragic events and loss of<br />
life. Not unrelated to this tragedy was the walkout of over 5,000 nurses from<br />
Stanford University Hospital and Lucille Packard Children’s Hospital on April<br />
25 over issues of better pay, more staffing, and more support for their mental<br />
health (NPR, April <strong>2022</strong>).<br />
<strong>The</strong> organization founded by Paredes, Walujo and others is currently<br />
seeking nurse volunteers. Its name is Don’t Clock Out.org and can be located<br />
at: www.dontclockout.org. <strong>The</strong>ir mission is “to provide a research-based peer<br />
support network for bedside nurses and nursing assistants; to share common<br />
experiences and emotional reactions with others who have had similar<br />
experiences, and to bridge the gap between bedside nursing caregivers and<br />
mental health treatment.” We who understand the nature of trauma and primary<br />
and secondary post-traumatic stress know that the pressure on health care<br />
workers has only begun. As the pandemic wanes, memories and experiential<br />
flashbacks are returning to plague our colleagues. Nightmares are undoubtedly<br />
a routine part of many nurses lives right now. <strong>Nurse</strong>s are generous with advice<br />
to those who are returning from war to avail themselves of mental health care<br />
services that specialize in trauma treatment, and may benefit from that same<br />
advice, for this pandemic is a war like no other that has been fought in health<br />
care organizations across the world. Ever.<br />
Peer support has been found to be advantageous as a community support<br />
net for the mental health of those affected by the COVID-19 pandemic,<br />
including health care workers. In a study by Suresh, Alam, and Karkossa (2021)<br />
it was found that peer support during the current pandemic can be a safe<br />
and beneficial resource, and that more research is needed. Individual peer<br />
support… “has been shown to provide beneficial practical, emotional, and<br />
social supports in a non-treatment based, normalizing relationship and lack<br />
evidence regarding the necessary duration, quality, or intensity to maximize<br />
its effectiveness.” (92). Individual peer support has also been electronically<br />
accessible during these times of isolation.<br />
As nurses from Stanford have said by their collective bargaining actions, the<br />
life of nursing depends on health care organizations investing in the profession’s<br />
well-being. This may include a well-researched approach that has had multiple<br />
successful applications in the past 50 years: mindfulness-based stressed<br />
reduction (Craigie, et al, 2016). In a recent address to the Fourth International<br />
Integrative Nursing Symposium, Billy Rosa, PhD, MBE, NP-BC, FAANP, FAAN<br />
stated that this responsibility is incumbent upon those organizations where<br />
work assignments place nurses’ health in dire risk. “Heroes work here!” signs<br />
and pizzas and gift bags and admonishments to self-care are not the answer<br />
to the problem of post-traumatic stress that in some health care workers is<br />
complicated by pre-existing human problems, membership in marginalized<br />
communities, and neurodiversity. <strong>The</strong>se realities of human existence deserve to<br />
be accepted and appropriately addressed in workers of all disciplines, without<br />
judgment or recrimination. As ANA’s Code of Ethics states in Provision 5: “<strong>The</strong><br />
nurse owes the same duties to self as to others; including the responsibility<br />
to promote health and safety, preserve wholeness of character and integrity,<br />
maintain competence, and continue personal and professional growth.” (ANA,<br />
2015). It follows that health care organizations ought not impede the nurses’<br />
progress to those ends but should provide protection during vulnerable times<br />
and encourage recovery, growth, and resiliency. Thoughtful and possibly costly<br />
investment that is informed by research is needed to preserve what we know<br />
that nursing is to humankind: a whole-human spiritual, emotional, and physical<br />
healing force and brilliant light in our clinics, hospitals, higher education, and<br />
communities. In the words of Dr. Jean Watson, American Academy of Nursing’s<br />
living legend, “We heal in community.” (Watson, <strong>2022</strong>).<br />
References<br />
American <strong>Nurse</strong>s Association. (2015). Code of ethics with interpretive statements. Silver<br />
Spring, MD.<br />
American <strong>Nurse</strong>s Foundation. (<strong>2022</strong>). Pulse on the nation’s nurses survey series:<br />
COVID-19 two-year impact assessment survey.<br />
Craigie, M., Slatyer, S., Hegney, D. et al. A pilot evaluation of a mindful self-care and<br />
resiliency (MCSR) intervention for nurses. Mindfulness 7, 764-774. (2016). DOI:<br />
https://doi.org/10.1007/s12671-016-0516-x<br />
Don’t Clock Out. www.dontclockout.org<br />
NPR. (March 31, <strong>2022</strong>). A nurse’s death raises the alarm about the profession’s<br />
mental health crisis. Retrieved from https://www.npr.org/sections/healthshots/<strong>2022</strong>/03/31/1088672446/a-nurses-death-raises-the-alarm-about-theprofessions-mental-health-crisis<br />
NPR. (April 25, <strong>2022</strong>). Thousands of nurses at Stanford Hospitals are striking<br />
over wages and mental health. Retrieved from https://www.npr.<br />
org/<strong>2022</strong>/04/25/1094689736/stanford-hospital-nurses-strike<br />
Rosa, Billy. (April 27, <strong>2022</strong>). <strong>Nurse</strong>s and health equity. 4th International integrative<br />
nursing symposium. Conference proceedings.<br />
Serrano, J., Hassamal, S., Hassamai, S., Dong, F., Neeki, M. (June, 2021). Depression<br />
and anxiety prevalence in nursing staff during the COVID-19 pandemic. Nursing<br />
Management. Volume52, issue 6. P 24-32.<br />
Suresh, R., Armaghan, A., and Karkossa, Z. (2021). Using peer support to strengthen<br />
mental health during the COVID-19 pandemic: A review. Frontiers in Psychiatry:<br />
Public mental health. July 12, 2021. https://doi.org/10.3389/fpsyt.2021.714181-<br />
Watson, J. (<strong>2022</strong>). Caring Community Conference. Boulder, CO. May 22, <strong>2022</strong>.
10<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
<strong>The</strong> Case of <strong>Nurse</strong> RaDonda Vaught – How Administering the<br />
Wrong Medication Resulted in a Criminal Conviction<br />
<strong>Nurse</strong>s across the country have followed and<br />
are now responding to the criminal prosecution and<br />
conviction of a Tennessee nurse who mistakenly<br />
injected a patient with a paralytic medication,<br />
resulting in her death. <strong>The</strong>re have been strong<br />
reactions to the guilty verdicts handed down against<br />
Ms. Vaught. Since not all material facts in this<br />
case were covered by the media, a more thorough<br />
discussion is provided below.<br />
Timeline of Events –<br />
12/26/2017 – <strong>Nurse</strong> Vaught mistakenly<br />
administered vecuronium (brand name Norcuron)<br />
instead of the prescribed Versed to a 75-year-old<br />
patient, Charlene Murphey, prior to a PET scan. In<br />
the PET scanning room, the patient arrested and<br />
was placed on a ventilator.<br />
12/27/2017 – <strong>The</strong> patient was declared brain<br />
dead and removed from the ventilator.<br />
12/27/2017 – Vanderbilt University Medical<br />
Center (“Vanderbilt”) reported the patient’s death to<br />
the county medical examiner. Vanderbilt’s report did<br />
not mention the medication error.<br />
12/27/2017 – <strong>The</strong> medical examiner determined<br />
the cause of death as “natural”.<br />
1/2018 – Vanderbilt did not report the patient’s<br />
death to state or federal officials, as required by<br />
law. Ms. Vaught’s employment at Vanderbilt was<br />
terminated.<br />
Early 2018 – Vanderbilt negotiated an out-ofcourt<br />
confidential settlement with the patient’s<br />
family.<br />
10/3/2018 – An anonymous tipster advised state<br />
and federal officials of the medication error which<br />
resulted in the patient’s death.<br />
10/23/2018 – <strong>The</strong> Tennessee Department of<br />
Health which oversees health professional licensing<br />
determined there was no violation by Ms. Vaught<br />
and issued her a letter indicating “this matter did not<br />
meet further action”.<br />
10/31/2018 – <strong>The</strong> Centers for Medicare<br />
and Medicaid Services (“CMS”) conducted an<br />
unannounced inspection of Vanderbilt.<br />
11/8/2018 – CMS confirmed the patient’s death<br />
was due to an accidental dose of vecuronium and<br />
that Vanderbilt did not report the medication error to<br />
the medical examiner and state officials.<br />
11/16/2018 – In response to CMS’s inspection<br />
Vanderbilt developed a plan of correction. No other<br />
action was taken against Vanderbilt or it’s Medicare<br />
provider status.<br />
2/4/2019 – Ms. Vaught is arrested and criminally<br />
charged with reckless homicide and impaired adult<br />
abuse.<br />
2/5/2019 – <strong>The</strong> CEO for Vanderbilt appeared<br />
before the Tennessee Board of Licensing for<br />
Health Care Facilities and admitted the death<br />
of Ms. Murphey was not reported and admitted<br />
the hospital’s response was “too limited”. <strong>The</strong><br />
Tennessee Board of Licensing for Health Care<br />
Facilities took no action against Vanderbilt.<br />
2/20/2019 – Ms. Vaught entered not guilty pleas<br />
to the criminal charges brought against her.<br />
8/20/2019 -- Law enforcement requested the<br />
medical examiner re-examine the circumstances of<br />
Ms. Murphey’s death. <strong>The</strong> medical examiner now<br />
with knowledge of the medication error, changed the<br />
official manner of death to “accidental”.<br />
9/27/2019 – <strong>The</strong> Tennessee Health Department<br />
overseeing the Board of Nursing re-opened <strong>Nurse</strong><br />
Vaught’s licensing case.<br />
3/22/<strong>2022</strong> – Criminal trial of Ms. Vaught began<br />
3/25/<strong>2022</strong> – After a three-day trial and 4 hours of<br />
deliberations the jury returns guilty verdicts against<br />
Ms. Vaught.<br />
5/13/<strong>2022</strong> – Sentencing of Ms. Vaught is<br />
scheduled to be held on May 13, <strong>2022</strong>.<br />
Facts – <strong>Nurse</strong> RaDonda Vaught became<br />
employed by Vanderbilt in October 2015. On<br />
December 26, 2017 she was working as a “help all<br />
nurse” for the Neuro ICU, step down and the 6th<br />
floor nursing units. 1 At that time Charlene Murphey,<br />
a 75 year woman with a subdural hematoma was a<br />
patient in the Neuro ICU. <strong>The</strong> patient was scheduled<br />
to undergo a full body PET scan at 2:00 pm. It is<br />
not clear when the patient arrived in radiology since<br />
there was no documentation of her arrival time. She<br />
was noted to be alert and oriented when she arrived<br />
in radiology. Prior to undergoing the PET scan the<br />
patient requested something to reduce her anxiety<br />
as she suffered from claustrophobia.<br />
<strong>The</strong> physician ordered 2 mg of Versed IV. 2 <strong>The</strong><br />
AcuDose report showed the order was entered<br />
at 2:47 pm and verified by pharmacy at 2:49<br />
pm. 3 <strong>The</strong> report also shows at 2:59 pm <strong>Nurse</strong><br />
Vaught removed 10 mg of vecuronium from the<br />
AcuDose cabinet, using an override. 4 <strong>The</strong>re was<br />
no order for vecuronium for this patient. <strong>The</strong>re<br />
was no override verified by pharmacy and there<br />
was no documentation by <strong>Nurse</strong> Vaught that she<br />
administered vecuronium. 5 At some time after the<br />
incident the family was told of a possible medication<br />
error. 6<br />
A physician’s note at 3:45 pm on 12/26/2017 7<br />
indicates a code was called in the PET scan area.<br />
Upon the physician’s arrival the patient was found<br />
to be pulseless and unresponsive. <strong>The</strong> patient<br />
was intubated and regained circulation after 2 – 3<br />
attempts at chest compressions. <strong>The</strong> patient was<br />
readmitted to the Neuro ICU.<br />
<strong>The</strong> next day, on December 27, 2017, a<br />
physician’s note 8 (time not specified) stated “I<br />
discussed the case with the neurology team and it<br />
is felt that these changes in exam likely represent<br />
progression towards but not complete brain<br />
death…very low likelihood of neurological recovery,<br />
we made the decision to pursue comfort care<br />
measures”.<br />
Hospital’s Actions after the Patient’s Death<br />
– <strong>The</strong> patient’s death was reported to the county<br />
medical examiner. <strong>The</strong> amended report from<br />
the county medical examiner’s office contains<br />
conflicting statements 9 as to the cause of death.<br />
<strong>The</strong> report indicates that the physician “will attest<br />
to the death as natural causes of complications<br />
of the intra-cerebral hemorrhage”. <strong>The</strong> cause of<br />
death is listed as “acute vecuronium intoxication”,<br />
contributing factors of death “intracerebral<br />
hemorrhage” and the manner of death as<br />
“accidental”. <strong>The</strong> medical examiner originally<br />
determined that the cause of death to be “natural”<br />
then after more information was made available,<br />
changed the cause of death to “acute vecuronium<br />
intoxication”.<br />
Vanderbilt did not report the medication error to<br />
either state or federal officials, as required by law.<br />
It appears that the only actions taken by Vanderbilt<br />
in January 2018 was to terminate <strong>Nurse</strong> Vaught’s<br />
employment and to negotiate an out-of-court<br />
settlement with Ms. Murphey’s family. <strong>The</strong> terms of<br />
the settlement are confidential.<br />
Anonymous Tip to State and Federal Health<br />
Officials – On October 3, 2018 an anonymous<br />
tipster advised state and federal health officials 10 of<br />
the unreported medication error that resulted in the<br />
patient’s death. <strong>The</strong> tipster reported <strong>Nurse</strong> Vaugh<br />
was orienting a new registered nurse when the<br />
patient’s nurse asked <strong>Nurse</strong> Vaught to give Versed<br />
to the patient. <strong>The</strong> report goes on to state that <strong>Nurse</strong><br />
Vaught removed the incorrect drug, did not read<br />
the label, and accidently administered vecuronium<br />
instead of Versed.<br />
Tennessee’s Board of Nursing Initial<br />
Determination -- <strong>The</strong> Tennessee Department<br />
of Health (“Department”) is responsible for the<br />
licensing of healthcare professionals. After receiving<br />
information from Vanderbilt the Department<br />
conducted an investigation which was reviewed<br />
by the Department’s nursing consultant and staff<br />
attorney. On October 23, 2018 the Department<br />
closed its files and issued letters to Vanderbilt and<br />
<strong>Nurse</strong> Vaught. 11<br />
A letter from the director of investigations to<br />
Vanderbilt stated in part, “the complaint received<br />
about <strong>Nurse</strong> Vaught has been reviewed by<br />
the nurse consultant and staff attorney for the<br />
Department and forwarded for investigation. As<br />
a result of the investigation and the review by<br />
the nursing consultant and staff attorney their<br />
determination was that the acts of the practitioner<br />
did not constitute a violation of statutes and/or<br />
rules governing the profession.” 12 On the same day<br />
<strong>Nurse</strong> Vaught was issued a similar letter indicating<br />
a “review of the complaint by the Board’s nursing<br />
consultant and staff attorney a decision was made<br />
that this matter did not merit further action”. 13<br />
Investigation by Centers for Medicare<br />
and Medicaid Services and State Officials –<br />
Interview of RaDonda Vaught -- Investigators<br />
conducted a surprise inspection at Vanderbilt. As<br />
part of this inspection investigators interviewed<br />
<strong>Nurse</strong> Vaught by telephone. According to the<br />
investigative report, <strong>Nurse</strong> Vaught stated, 14 “I was<br />
in a patient care role. I was the help-all nurse. As<br />
explained in the report a help-all nurse is a resource<br />
nurse. 15 <strong>Nurse</strong> Vaught was also orienting a new<br />
nurse.<br />
<strong>The</strong> patient’s primary care asked <strong>Nurse</strong> Vaught<br />
to go to the Radiology PET scanning room and<br />
administer Versed to the patient because she was<br />
not able to tolerate the PET scan procedure. <strong>Nurse</strong><br />
Vaught searched for the Versed under the patient’s<br />
AcuDose profile which she could not find. She then<br />
chose the override setting and searched for Versed.<br />
At the time she indicated she was talking to the<br />
orientee while she was searching for Versed and<br />
typed in the first two letters of Versed which are<br />
“VE” and chose the first medication on the list.<br />
According to the investigative report 16 , <strong>Nurse</strong><br />
Vaught could not remember the reason she gave<br />
for the override. <strong>The</strong> investigation also revealed<br />
there was no scanner in the radiology unit. 17 When<br />
<strong>Nurse</strong> Vaught discussed her medication error with<br />
the unit manager she was instructed not to scan the<br />
medication after the fact as the MAR would note it.<br />
<strong>Nurse</strong> Vaught also admitted that she was distracted<br />
by talking to the orientee about a swallow test they<br />
were going to do. She also admitted it struck her<br />
“as a little odd” that she had to reconstitute the<br />
medication and should have called the pharmacy.<br />
<strong>Nurse</strong> Vaught told the investigator 18 that she took<br />
out the medication vial and looked at the back of<br />
the vial for the directions on how to reconstitute it.<br />
She admitted she did not re-check the medication’s<br />
name on the vial. <strong>Nurse</strong> Vaught went on to say she<br />
grabbed a sticker from the patient’s file, a handful of<br />
flushes, alcohol swabs, and a blunt tip needle. She<br />
placed the medication vial in a baggie and wrote<br />
on the baggie, “PET scan, Versed 1-2 mg” and<br />
went to the radiology department to administer the<br />
medication to the patient. <strong>The</strong> medication was given<br />
but there is no documentation as to when it was<br />
administered.<br />
Once in the radiology department <strong>Nurse</strong> Vaught<br />
went to the patient, checked her identity and told<br />
her she was there to help her relax. She then<br />
proceeded to reconstitute the medication and<br />
measured what she needed. 19 When asked how<br />
much she gave the patient she indicated “I can’t<br />
remember. I am pretty sure I gave her 1 millimeter”. 20<br />
She put the left over medication in the baggie and<br />
gave it to another nurse [not identified]. 21 When<br />
asked her next actions <strong>Nurse</strong> Vaught indicated she<br />
left the radiology unit and did not monitor the patient<br />
after giving the medication. 22<br />
<strong>Nurse</strong> Vaught went on to tell the investigator that<br />
the family was standing outside in the hallway…”we<br />
heard a rapid response call for PET scan. That<br />
was a red flag since that patient was ours”. 23 <strong>The</strong><br />
investigative report indicates the rapid response<br />
team call occurred at 3:29 pm. <strong>Nurse</strong> Vaught went<br />
back into the PET scan area and saw that the<br />
patient was intubated and had regained a heartbeat.<br />
She told the physician, “I had given Versed a few
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 11<br />
minutes ago.” 24 <strong>The</strong> nurse who was present when<br />
<strong>Nurse</strong> Vaught administered the medication showed<br />
her the baggie and asked if this is what was given<br />
to the patient, <strong>Nurse</strong> Vaught responded “yes”. 25 <strong>The</strong><br />
other nurse in response said, “This isn’t Versed. Its<br />
vecuronium” 26 Other staff interviewed indicated the<br />
patient was estimated to be alone in the room for<br />
about 30 minutes once she was put in the scanning<br />
room. 27<br />
<strong>The</strong> investigation also revealed that in the days<br />
after the incident <strong>Nurse</strong> Vaught spoke with her nurse<br />
manager and risk management at Vanderbilt. 28<br />
<strong>Nurse</strong> Vaught indicated immediately after the events<br />
she spoke to several people in management and<br />
also completed a Veritas report around 4:00 pm on<br />
December 26th. 29<br />
Interview of the Vanderbilt Pharmacist – <strong>The</strong><br />
pharmacist reported the following events: 30 On<br />
December 26th a PET scan was ordered at 2:00<br />
pm, the Versed was ordered at 2:47 pm, and the<br />
vecuronium was removed from the AcuDose at 2:59<br />
pm. <strong>The</strong> pharmacist confirmed that the letters “VE”<br />
were entered in AcuDose which defaults to generic<br />
medications. That is why Versed did not show up.<br />
When vecuronium popped up a warning in the red<br />
box was visible for an override stating that is should<br />
be for STAT orders. <strong>The</strong> time of administration of the<br />
vecuronium was not documented.<br />
What the Baggie Contained – <strong>Nurse</strong> Vaught<br />
told the investigator that she labeled and placed the<br />
administration set up in a baggie bag before going<br />
to the Radiology department. <strong>The</strong> baggie contained<br />
the following: 31<br />
• Clear zip lock baggie with an orange<br />
biohazard label had “Versed 1 mg – 2 mg PET<br />
1251 handwritten in pink colored marker on it.<br />
• Inside the baggie was a vial with a few drops<br />
of clear liquid remaining in the vial. <strong>The</strong> vial<br />
was labeled as “Vecuronium Bromide 10<br />
mg. 1mg/ml when reconstituted to 10 ml.<br />
reconstitute with bacteriostatic water”.<br />
• <strong>The</strong> vial had a red top that said “WARNING:<br />
PARALYZING AGENT”.<br />
• <strong>The</strong>re was a 10 ml syringe labeled “Normal<br />
Saline” with a capped needle attached, with<br />
1.5 ml of a clear liquid remaining in it and<br />
caped with a white cap with no needle.<br />
• <strong>The</strong>re was also a 2-inch alcohol prep pad in<br />
the baggie.<br />
Vanderbilt Issues a Correct Action Plan -<br />
Following CMS’s investigation, Vanderbilt issued<br />
a corrective action plan in November 2018. <strong>The</strong><br />
corrective action plan included, among other<br />
actions: 32<br />
• Revising its medication administration policy;<br />
• Updating the transportation of critical<br />
care patient policy to require appropriate<br />
staff to accompany, monitor, and support<br />
patients’ needs, and document the<br />
handover of patients between nursing staff.<br />
If a no handover can be accomplished the<br />
transporting staff is to remain with the patient;<br />
• Revising high alert medication policy;<br />
• Establishing a work group to review paralyzing<br />
agents; and<br />
• Chief nursing officers conducting weekly<br />
chart reviews (5 patient/unit) for a total of 3<br />
months<br />
Criminal Charges Filed Against RaDonda<br />
Vaught -- On February 4, 2019 <strong>Nurse</strong> Vaught is<br />
arrested on a criminal indictment for her role in<br />
Ms. Murphey’s death, and charged with reckless<br />
homicide and abuse of an impaired adult. This is<br />
the first time Ms. Vaught is publicly identified. On<br />
February 20, 2019 Ms. Vaught enters not guilty pleas<br />
to both charges.<br />
Tennessee Board of Licensing Health Care<br />
Facilities – On February 5, 2019 the CEO of<br />
Vanderbilt appeared before the Tennessee Board<br />
of Licensing for Health Care Facilities. <strong>The</strong> CEO<br />
admitted the patient’s death was not reported<br />
to state regulators and admitted the hospital’s<br />
response was “too limited”. Officials also confirmed<br />
that they negotiated a confidential settlement<br />
with the family. <strong>The</strong> Board of Licensing for Health<br />
Care Facilities took no disciplinary action against<br />
Vanderbilt.<br />
<strong>The</strong> Licensing Board Reexamines Prior<br />
Licensing Decision Involving RaDonda Vaught –<br />
On September 27, 2019 the Tennessee Department<br />
of Health re-opened its prior decision not to pursue<br />
disciplinary action against Ms. Vaught’s license.<br />
She is charged with three violations, including<br />
unprofessional conduct, abandoning or neglecting a<br />
patient that required care, and failing to maintain an<br />
accurate patient record. 33<br />
<strong>The</strong> licensing violations brought against <strong>Nurse</strong><br />
Vaught included 34 :<br />
• Failure to follow the five rights of medication<br />
administration, right patient, right medication,<br />
right dose, right route, and right time;<br />
• After administrating the medication she failed<br />
to monitor the patient; and<br />
• Failed to document in the medical record that<br />
she administered vecuronium<br />
Licensing Hearing -- <strong>The</strong> licensing hearing<br />
began on July 22, 2021. At the hearing Ms. Vaught<br />
testified that the medication error was “completely<br />
my fault” because she did not double check<br />
the medicine she administered. 35 In addition to<br />
admitting to her error, Ms. Vaught argues, through<br />
her attorney, that there were flawed procedures at<br />
Vanderbilt. 36 <strong>The</strong>y argued that there was a problem<br />
that prevented communication between Vanderbilt’s<br />
electronic health records, medication cabinets and<br />
the hospital pharmacy. This flaw caused delays in<br />
accessing medications and the hospital’s short term<br />
workaround was to override the safeguards on the<br />
cabinets so they could remove drugs quickly.<br />
Ms. Vaught testified that “overriding was<br />
something we did as a part of our practice every<br />
day. 37 You couldn’t get a bag of fluids for a patient<br />
without using an override function”. <strong>Nurse</strong> Vaught<br />
testified that she allowed herself to become<br />
“complacent” and “distracted” while using the<br />
medication cabinet and did not double-check<br />
which drug she had withdrawn despite multiple<br />
opportunities. On July 23, 2021 the Tennessee<br />
Board of Nursing unanimously revokes Vaught’s<br />
nursing license.<br />
Ms. Vaught testified that overrides were common<br />
at Vanderbilt and that a 2017 upgrade to the<br />
hospital’s electronic health record system was<br />
causing rampant delays at medication cabinets.<br />
Because of that flaw Vanderbilt instructed nurses to<br />
use overrides to circumvent delays and get medicine<br />
as needed. A state investigator also told the board<br />
of nursing to her knowledge that computer issues<br />
caused problems with medication cabinets at<br />
Vanderbilt in 2017.<br />
Criminal Proceedings – As part of discovery<br />
process prosecutors reveal that Ms. Vaught<br />
made 10 separate errors when giving the wrong<br />
medication to the patient, including overlooking<br />
multiple warning signs. Court records state that<br />
Vaught would have had to look directly at a warning<br />
on the cap, saying “WARNING: PARALYZING<br />
AGENT” before injecting the drug.<br />
<strong>The</strong> State argued Ms. Vaught failed to scan<br />
the medication against the patient’s medical<br />
identification bracelet. 38 She also pointed out<br />
that vecuronium is a powder that needs to be<br />
reconstituted unlike Versed which is already in liquid<br />
form. 39<br />
<strong>The</strong> prosecution’s nursing expert testified that<br />
Ms. Vaught failed to meet the standard of care by: 40<br />
• Being distracted when administering the<br />
medication;<br />
• Not looking up the generic name for Versed;<br />
• Failing to read the name of the drug, not<br />
noticing a red warning on the top of the<br />
vial, and not staying with the patient after<br />
medication administration.<br />
• Administering the medication when a patient<br />
scanner was not available in the Radiology<br />
unit;<br />
• Not double checking the medication with a<br />
colleague; and<br />
• Not monitoring the patient even if she thought<br />
she was giving Versed.<br />
A lead investigator in the criminal trial<br />
testified that Vanderbilt had a “heavy burden<br />
of responsibility” for a grievous drug error…but<br />
pursued penalties and criminal charges only against<br />
the nurse and not the hospital itself. 41 Vanderbilt<br />
received no punishment for the fatal drug error.<br />
After three days of trial followed by four hours of<br />
deliberations the jury rendered its verdict. <strong>The</strong> jury<br />
was made up of six men and six women, with one<br />
juror being a practicing registered nurse and another<br />
a former respiratory therapist.<br />
<strong>The</strong> Verdict – <strong>The</strong> jury found Ms. Vaught guilty of<br />
criminal negligent homicide (a lesser charge under<br />
reckless homicide) and gross neglect of an impaired<br />
adult. She was acquitted of reckless homicide. <strong>The</strong><br />
neglect charge stemmed from the allegation that<br />
Ms. Vaught did not properly monitor Ms. Murphey<br />
after she was injected with the wrong drug.<br />
Stay Tuned -- RaDonda Vaught, a convicted<br />
felon, is scheduled to be sentenced on May 13,<br />
<strong>2022</strong>.<br />
Other Source Documents –<br />
• Kelman, Brett; <strong>The</strong> RaDonda Vaught case<br />
is confusing. This timeline will help. (msn.<br />
com); Nashville Tennessean; March 22, <strong>2022</strong>;<br />
https://www.msn.com/en-us/news/crime/<br />
the-radonda-vaught-case-is-confusing-thistimeline-will-help/ar-BB10EVFV<br />
• Kelman, Brett; Ex-Vanderbilt nurse RaDonda<br />
Vaught loses Nursing License for fatal<br />
drug error; Nashville Tennessean; July 23,<br />
2021; https://www.tennessean.com/story/<br />
news/health/2021/07/23/ex-vanderbiltnurse-radonda-vaught-loses-license-fatalerror/8069185002/<br />
• Timms, Mariah; Prosecutors, defense lay out<br />
framework in homicide trial of ex-Vanderbilt<br />
nurse RaDonda Vaught; March 22, <strong>2022</strong>;<br />
https://news.yahoo.com/prosecutorsdefense-lay-framework-homicide-193942097.<br />
html?fr=sycsrp_catchall<br />
• Kelman, Brett; In nurse’s trial, witness says<br />
hospital bears ‘heavy’ responsibility for<br />
patient death; Kaiser Health News; March<br />
24, <strong>2022</strong>; https://health.wusf.usf.edu/nprhealth/<strong>2022</strong>-03-24/in-nurses-trial-witnesssays-hospital-bears-heavy-responsibility-forpatient-death<br />
• Fruen, Lauren; Inside the trial of ex-nurse<br />
RaDonda Vaught who ‘killed a patient by<br />
giving her the wrong drug; March 24, <strong>2022</strong>;<br />
https://www.thesun.co.uk/news/18055626/<br />
nurse-radonda-vaught-trial-killed-patient/<br />
<strong>The</strong> Case of <strong>Nurse</strong> RaDonda...continued on page 12
12<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
<strong>The</strong> Case of <strong>Nurse</strong> RaDonda...continued from page 11<br />
• Sutton, Caroline, West, Emily, Davis, Chris;<br />
Trial of RaDonda Vaught: Jury to deliberate<br />
case starting Friday; March 25, <strong>2022</strong>; https://<br />
www.newschannel5.com/news/trial-ofradonda-vaught-former-vanderbilt-medicalcenter-nurse-continues-into-third-day<br />
• Kelman, Brett; <strong>Nurse</strong> Convicted of Neglect<br />
and Negligent Homicide for Fatal Drug Error;<br />
Nashville Tennessean; March 25, <strong>2022</strong>;<br />
https://khn.org/news/article/radonda-vaughtnurse-drug-error-vanderbilt-guilty-verdict/<br />
• Levine, Zachary, McClendon, Shannon;<br />
Statement in Response to the Conviction of<br />
<strong>Nurse</strong> RaDonda Vaught; American <strong>Nurse</strong>s<br />
Association, March 25, <strong>2022</strong>; https://www.<br />
nursingworld.org/news/news-releases/<strong>2022</strong>-<br />
news-releases/statement-in-response-to-theconviction-of-nurse-radonda-vaught/<br />
• Timms, Mariah; Former Vanderbilt nurse<br />
RaDonda Vaught found guilty on 2 charges in<br />
2017 death of patient; Nashville Tennessean;<br />
March 25, <strong>2022</strong>; https://www.yahoo.com/<br />
now/former-vanderbilt-nurse-radondavaught-184322536.html<br />
• Loller, Travis; Former nurse guilty of homicide<br />
in medication error death; Associated Press;<br />
March 25, <strong>2022</strong>; https://kstp.com/associatedpress/ap-us-international/former-nurse-guiltyof-homicide-in-medication-error-death/<br />
• Timms, Mariah; Ex-<strong>Nurse</strong> RaDonda Vaught<br />
found guilty on two charges in death of<br />
patient; Nashville Tennessean; March 29,<br />
<strong>2022</strong>; https://currently.att.yahoo.com/att/exnurse-radonda-vaught-found-175845609.html<br />
• Kelman, Brett, Norman, Hannah; Why<br />
<strong>Nurse</strong>s Are Raging and Quitting after the<br />
RaDonda Vaught Verdict; Kaiser Health; April<br />
5, <strong>2022</strong>; https://health.wusf.usf.edu/nprhealth/<strong>2022</strong>-04-05/why-nurses-are-ragingand-quitting-after-the-radonda-vaught-verdict<br />
Donna J. Craig, RN, JD is legal counsel to the<br />
ANA-Michigan Chapter and the Michigan Council<br />
of <strong>Nurse</strong> Practitioners. She practiced as a cardiac<br />
care nurse for several years before a chance<br />
opportunity to audit a graduate course in health<br />
care law and ethics changed her career path. That<br />
course propelled her to earn her law degree. After<br />
law school Ms. Craig joined a medical malpractice<br />
defense law firm before transitioning her focus<br />
to health care corporate and administrative law<br />
matters. For over 20 years she has maintained her<br />
private health law practice, representing health<br />
care providers and facilities in business, licensure<br />
and compliance matters. For her expertise and<br />
accomplishments, Detroit’s dbusiness Magazine<br />
awarded Ms. Craig its Top Lawyer in Health Care<br />
Law award on three occasions. Ms. Craig has the<br />
distinction and is proud of being a bar member of<br />
the Supreme Court of the United States of America.<br />
For more information about <strong>The</strong> Health Law Center,<br />
go to www.healthlawcenterplc.com.<br />
1 Anonymous Complaint, page 1 of 3 pages at: https://<br />
www.documentcloud.org/documents/6542003-<br />
CMS-Complaint-Intake.html<br />
2 Corrective Action Plan by Vanderbilt, page 7 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html.<br />
3 Id.<br />
4 Id.<br />
5 Id.<br />
6 Corrective Action Plan by Vanderbilt, page 33 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
7 Corrective Action Plan by Vanderbilt, page 8 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
8 Id.<br />
9 Amended County Medical Examiner Investigator’s<br />
Report, at: https://www.documentcloud.org/<br />
documents/6540657-Charlene-Murphey-ME-<br />
Investigation.html<br />
10 Report From the Anonymous Tipster at: https://www.<br />
documentcloud.org/documents/6542003-CMS-<br />
Complaint-Intake.html<br />
11 Closing Letters From Tennessee Department of<br />
Health at: https://www.documentcloud.org/<br />
documents/6785898-RaDonda-Vaught-Letters.<br />
html<br />
12 Id.<br />
13 Id.<br />
14 Corrective Action Plan by Vanderbilt, page 9 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
15 Id.<br />
16 Prosecutorial Discovery Documents, page 5 of 51<br />
pages at: https://www.documentcloud.org/<br />
documents/6785652-RaDonda-Vaught-DA-<br />
Discovery.html<br />
17 Prosecutorial Discovery Documents, page 6 of<br />
51 at: https://www.documentcloud.org/<br />
documents/6785652-RaDonda-Vaught-DA-<br />
Discovery.html<br />
18 Corrective Action Plan by Vanderbilt, page 9 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
19 Corrective Action Plan by Vanderbilt, page 10 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
20 Id.<br />
21 Id.<br />
22 Id.<br />
23 Id.<br />
24 Id.<br />
25 Corrective Action Plan by Vanderbilt, page 11 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
26 Id.<br />
27 Corrective Action Plan by Vanderbilt, page 12 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
28 Corrective Action Plan by Vanderbilt, page 11 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
29 Corrective Action Plan by Vanderbilt, page 25 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
30 Corrective Action Plan by Vanderbilt, page 33 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
31 Corrective Action Plan by Vanderbilt, page 35 of 105<br />
pages at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
32 Corrective Action Plan by Vanderbilt, pages 1 –<br />
105 at: https://www.documentcloud.org/<br />
documents/6535181-Vanderbilt-Corrective-Plan.<br />
html<br />
33 Licensing Charges Filed by the Board of Nursing<br />
at:<br />
https://www.documentcloud.org/<br />
documents/6483588 -Vaught-RaDonda-<br />
NOC-9-27-19.html<br />
34 xxxiv Id.<br />
35 Kelman, Brett; Ex-Vanderbilt nurse RaDonda<br />
Vaught loses Nursing License for fatal drug<br />
error; Nashville Tennessean; July 23, 2021;<br />
https://www.tennessean.com/story/news/<br />
health/2021/07/23/ex-vanderbilt-nurse-radondavaught-loses-license-fatal-error/8069185002/<br />
36 Id.<br />
37 Id.<br />
38 Fruen, Lauren; Inside the trial of ex-nurse RaDonda<br />
Vaught who ‘killed a patient by giving her the<br />
wrong drug; March 24, <strong>2022</strong>; https://www.<br />
thesun.co.uk/news/18055626/nurse-radondavaught-trial-killed-patient/<br />
39 Id.<br />
40 Sutton, Caroline, West, Emily, Davis, Chris; Trial<br />
of RaDonda Vaught: Jury to deliberate case<br />
starting Friday; March 25, <strong>2022</strong>; https://www.<br />
newschannel5.com/news/trial-of-radondavaught-former-vanderbilt-medical-center-nursecontinues-into-third-day<br />
41 Kelman, Brett; In nurse’s trial, witness says hospital<br />
bears ‘heavy’ responsibility for patient death;<br />
Kaiser Health News; March 24, <strong>2022</strong>; https://<br />
health.wusf.usf.edu/npr-health/<strong>2022</strong>-03-24/innurses-trial-witness-says-hospital-bears-heavyresponsibility-for-patient-death.
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 13<br />
Now for <strong>The</strong> Rest of the Story -<br />
<strong>The</strong> Sentencing of<br />
RaDonda Vaught<br />
On May 13th RaDonda Vaught, a former ICU nurse at Vanderbilt University<br />
Medical Center, was sentenced after being convicted of criminally negligent<br />
homicide and gross neglect of an impaired adult. Ms. Vaught lost her nursing<br />
license and was criminally prosecuted after she mistakenly administered the<br />
wrong medication to 75-year-old patient Charlene Murphey, resulting in her<br />
death. Ms. Vaught mistakenly gave Ms. Murphey vecuronium, a paralytic agent,<br />
instead of the ordered Versed, a sedative. Since the Vaught case has been the<br />
subject of discussion by nurses and nursing associations it is important that her<br />
sentencing be reported now.<br />
Hundreds of nurses from around the country were present in the courtroom,<br />
along with an overflow crowd outside the courthouse where they listened<br />
to the sentencing hearing over a public address system. <strong>Nurse</strong>s came to<br />
Tennessee and gathered in support of Ms. Vaught and wore “<strong>Nurse</strong> Strong”,<br />
#IAmRaDonda”, and “Seeking Justice for <strong>Nurse</strong>s and Patients in a BROKEN<br />
system” T-shirts to show their support.<br />
Before Judge Jennifer Smith handed down the sentence the prosecution and<br />
defense made sentencing arguments to the Judge. Ms. Vaught and the relatives<br />
of Charlene Murphey also addressed the court. <strong>The</strong> prosecution sought a<br />
prison term of 3 – 6 years, which was less than the 8 years Ms. Vaught was<br />
facing. Ms. Vaught’s attorney argued that probation, not jail time, was called for.<br />
Ms. Charlene Murphey’s son spoke of the toll his mother’s death has had on<br />
the family. He and his wife also said Charlene Murphey was a forgiving person<br />
and she wouldn’t have wanted jail time for Ms. Vaught. <strong>The</strong>y told the judge that<br />
they personally “didn’t want jail time, we just wanted to make sure she didn’t<br />
do this to anyone else”. It is reported that Ms. Murphey’s husband wanted the<br />
maximum sentence possible.<br />
When Ms. Vaught was given an opportunity to speak before being<br />
sentenced, she spoke directly to the family. She told them “Saying I'm sorry<br />
doesn’t seem like enough but you deserve to hear that and know that I am very<br />
sorry for what happened. When Ms. Murphey died, a part of me died with her.”<br />
Before announcing the sentence, Judge Smith addressed the family, telling<br />
them, “My hope that changes in the practices and protocols in the medical<br />
setting that have arisen since this event may at least be some positive aspect<br />
that has arisen. I recognize however, that will never be enough to heal your<br />
wounds.”<br />
In announcing the sentence Judge Smith acknowledged that the criminal<br />
charges warranted three years of prison, but then went on to say RaDonda<br />
Vaught wouldn’t face jail time. Judge Smith sentenced Vaught to three years<br />
supervised probation and then diverted that sentence which would allow her<br />
record to be expunged after successfully completing the terms of her probation.<br />
Prosecutors had argued against diversion, although they were not opposed to<br />
probation. In weighing whether to grant Vaught judicial diversion, Judge Smith<br />
cited Vaught's remorse, this being her first criminal offense, as well as her<br />
honesty about her medication error.<br />
Donna J. Craig, RN, JD is legal counsel to the ANA-Michigan Chapter and<br />
the Michigan Council of <strong>Nurse</strong> Practitioners. She practiced as a cardiac<br />
care nurse for several years before a chance opportunity to audit a graduate<br />
course in health care law and ethics changed her career path. That course<br />
propelled her to earn her law degree. After law school Ms. Craig joined a<br />
medical malpractice defense law firm before transitioning her focus to health<br />
care corporate and administrative law matters. For over 20 years she has<br />
maintained her private health law practice, representing health care providers<br />
and facilities in business, licensure and compliance matters. For her expertise<br />
and accomplishments, Detroit’s dbusiness Magazine awarded Ms. Craig its<br />
Top Lawyer in Health Care Law award on three occasions. Ms. Craig has the<br />
distinction and is proud of being a bar member of the Supreme Court of the<br />
United States of America. For more information about <strong>The</strong> Health Law Center,<br />
go to www.healthlawcenterplc.com.<br />
EDUCATORS<br />
CORNER<br />
Aligning Aristotle and Knowles<br />
Aristotle, known as a great public speaker and educator, once said (kind of)<br />
that educators should know their audience. https://www.cnbc.com/2021/01/12/<br />
aristotles-3-most-important-rules-for-being-more-persuasive-in-publicspeaking.html.<br />
What does our latest student nurse population look like?<br />
• 82% female and 18% male<br />
• 68.5% white, 10.7% black, 10.5% Asian, 8.2% Hispanic/Latino, 0.8%<br />
American Indian/Alaska Native<br />
• Average age 44<br />
• 67% stay less than one year at their first job<br />
https://www.zippia.com/student-nurse-jobs/demographics/<br />
Looking at the data, we realize that we have adult learners in a pedagogical<br />
setting. Malcolm Knowles is the Father of the Andragogical/Adult Learning<br />
<strong>The</strong>ory. Adapting what we teach could and frequently does look like:<br />
• Students need to know why specific areas are being taught – we need to<br />
emphasize the application.<br />
• Instruction should be application oriented instead of memorized — we<br />
need to provide learning activities that support areas studied.<br />
• Encourage adult learning and responsibility – identify an understood<br />
framework to demonstrate an area of learning when possible and allow<br />
students to fail and reflect when possible.<br />
• Understand the student population using a diverse architecture<br />
of experiences, learning materials, and activities to reinforce new<br />
information<br />
https://www.instructionaldesign.org/theories/andragogy/<br />
Other ideas? Send in your thoughts on how we can<br />
help our students prepare for the future.<br />
Marla Peixotto-Smith, MSN, PhD, RN, CNE, is an<br />
Associate Professor & Coordinator of the RN2BSN<br />
Program at Rogers State University. Marla invites<br />
you to contribute to the “Educators Corner.” Please<br />
send your thoughts, experiences, or strategies to<br />
marlasmith@rsu.edu.<br />
Marla Peixotto-<br />
Smith<br />
Timms, Mariah, et al; RaDonda Vaught Sentenced to Three Years’ Probation on a<br />
Diverted Sentence, Could See Record Wiped; Nashville Tennessean; May<br />
13, <strong>2022</strong>; https://finance.yahoo.com/news/radonda-vaught-sentenced-threeyears-194115731.html?fr=sycsrp_catchall<br />
Loller, Travis; Ex-<strong>Nurse</strong> Sentenced to Probation in Patient Medication Death; Associated<br />
Press; May 13, <strong>2022</strong>; https://apnews.com/article/health-homicide-tennesseenashville-1e196d4e4358a20141385494426cdbe7<br />
Timms, Mariah, et al; RaDonda Vaught Sentenced to Three Years’ Probation on a<br />
Diverted Sentence, Could See Record Wiped; Nashville Tennessean; May<br />
13, <strong>2022</strong>; https://finance.yahoo.com/news/radonda-vaught-sentenced-threeyears-194115731.html?fr=sycsrp_catchall<br />
RaDonda Vaught Receives Three Years’ Probation on Diverted Sentence; USA Today,<br />
May 13, <strong>2022</strong>; https://www.usatoday.com/story/news/crime/<strong>2022</strong>/05/13/<br />
radonda-vaught-vanderbilt-nurse-sentencing-live-updates/9717397002/<br />
Former <strong>Nurse</strong> RaDonda Vaught, Whose Medical Error Killed a Patient, Sentenced<br />
to Probation in Controversial Case; CBS News, May 13, <strong>2022</strong>; https://www.<br />
cbsnews.com/news/radonda-vaught-sentencing-nurse-whose-medical-errorkilled-a-patient-sentenced-to-probation-in-controversial-case/<br />
Id.<br />
PAM Health<br />
Specialty Hospital<br />
of <strong>Oklahoma</strong> City<br />
1407 North Robinson Ave<br />
<strong>Oklahoma</strong> City, OK 73103<br />
www.PAMHealth.com/jobs
14<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Burned Out on Burnout?<br />
Strategies to Combat Compassion Fatigue in Nursing.<br />
David Barron, DBA<br />
Saint Leo University<br />
For all the work and energy that nurses bring to<br />
their jobs, it is their compassion that is recognized<br />
internationally as one of the five professional values<br />
all nurses must demonstrate (Durkin et al., 2018).<br />
In healing professionals, compassion entails an<br />
aptitude to comprehend the distress of another,<br />
the familiarity of the sources and treatments of the<br />
distress, and the desire to help lessen the suffering<br />
(Godlaski, 2015). Researchers have described<br />
compassion as caring for someone suffering, the<br />
emotional feeling accompanying the care, and the<br />
desire to reduce and alleviate suffering (Greenberg<br />
& Turksma, 2015; Ledoux, 2015). However, there may<br />
be a ‘cost of caring’ which could unfortunately lead<br />
to compassion fatigue if not addressed early (Boyle,<br />
2015).<br />
In Stamm’s (2010) professional quality of<br />
life model compassion fatigue (Figure 1) stems<br />
from interactions with patients that leave the<br />
health professional preoccupied with the trauma<br />
experienced by the patient and enhanced emotional<br />
arousal or avoidance behaviors associated with<br />
the patient (Ray et al., 2013). Compassion fatigue<br />
has two parts. <strong>The</strong> first is burnout, which concerns<br />
issues such as exhaustion, hostility, frustration,<br />
anger, depression (Stamm, 2010), detachment,<br />
isolation, irritability, failure, despair, cynicism, and<br />
apathy (Circenis et al., 2013).<br />
Figure 1<br />
Diagram of Professional Quality of Life<br />
<strong>The</strong> second part is secondary traumatic stress,<br />
a negative feeling driven by fear and work-related<br />
trauma (Stamm, 2010). Some traumas at work<br />
can be direct (primary) trauma; therefore, workrelated<br />
trauma can be a combination of primary<br />
and secondary trauma (Stamm, 2010). Secondary<br />
traumatic stress can be viewed as an occupational<br />
hazard for persons who provide direct patient<br />
care to traumatized victims (Circenis et al., 2013).<br />
Witnessing traumatic experiences, such as providing<br />
end-of-life care, working with less experienced<br />
nursing staff, caring for young patients, and nursing<br />
insufficiency may all contribute to secondary<br />
traumatic stress (Partlak Gunusen et al., 2019).<br />
Together, burnout and secondary traumatic stress<br />
reflect the negative results of interactions with<br />
patients. <strong>The</strong>se aspects of the working life of nurses<br />
have been topics of great interest in academic<br />
bridget.bridger@rollinghillshospital.com<br />
Ada, <strong>Oklahoma</strong><br />
literature, linking several personal and work-relevant<br />
outcomes (Heritage et al., 2018).<br />
According to Lombardo and Eyre (2011; Table<br />
1), compassion fatigue symptoms can include<br />
work-related physical and emotional symptoms.<br />
However, it is important to note that generally<br />
more than one symptom is demonstrated before a<br />
nurse is identified as having compassion fatigue.<br />
With increasing numbers of nurses suffering from<br />
compassion fatigue, there is a negative impact<br />
on the quality of patient care, increased attrition<br />
of nurses, and enormous pressure placed on<br />
remaining health care providers (Figley, 2002;<br />
McMullen, 2007; Sprang et al., 2011). Compassion<br />
fatigue that is unrecognized and untreated may<br />
have serious detrimental effects on professional and<br />
personal functioning of nurses (Benoit et al., 2007);<br />
therefore, failure to provide support and assistance<br />
to those with symptoms of compassion fatigue<br />
can undermine an organization’s provision of care,<br />
especially if they lose talented nurses (Figley, 2002).<br />
Table 1<br />
Symptoms of Compassion Fatigue<br />
Work-Related Emotional Physical<br />
Avoidance<br />
or dread of<br />
working with<br />
certain patients<br />
Reduced ability<br />
to feel empathy<br />
toward patients<br />
or families<br />
Lack of<br />
joyfulness<br />
Frequent use of<br />
sick days<br />
Excessive use<br />
of substances:<br />
nicotine,<br />
alcohol, illicit<br />
drugs<br />
Restlessness<br />
Oversensitivity<br />
Irritability<br />
Anxiety<br />
Mood swings<br />
Depression<br />
Anger and<br />
resentment<br />
Loss of<br />
objectivity<br />
Memory issues<br />
Poor<br />
concentration,<br />
focus, and<br />
judgment<br />
Cardiac<br />
symptoms:<br />
chest pain/<br />
pressure,<br />
palpitations,<br />
tachycardia<br />
Sleep<br />
disturbances:<br />
inability<br />
to sleep,<br />
insomnia, too<br />
much sleep<br />
Digestive<br />
problems:<br />
diarrhea,<br />
constipation,<br />
upset stomach<br />
Fatigue<br />
Headaches<br />
Muscle tension<br />
On the positive side of the professional quality of<br />
life model is compassion satisfaction. Compassion<br />
satisfaction is about the pleasure you derive from<br />
being able to do your work well. You may feel like it<br />
is a pleasure to help others through your work. You<br />
may feel positively about your colleagues or your<br />
ability to contribute to the work setting or even the<br />
greater good of society (Stamm, 2010). Compassion<br />
satisfaction is considered a protective factor against<br />
compassion fatigue (Ruiz-Fernandez et al., 2020).<br />
It should come as no surprise that a balance<br />
between compassion satisfaction and compassion<br />
fatigue will ultimately determine the level of the<br />
professional’s quality of life. One such example<br />
was uncovered with my recent dissertation which<br />
included 202 registered nurses from seven South<br />
Florida counties during the height of the COVID-19<br />
pandemic, including the Delta virus outbreak in<br />
the summer of 2021. <strong>The</strong> research uncovered<br />
that one independent variable out of four showed<br />
statistical significance when determining nursing<br />
turnover intentions and this was burnout (p < .001),<br />
meaning that there is an imbalance in this cohort’s<br />
professional quality of life (Barron, <strong>2022</strong>). This is<br />
consistent withother research. For example, <strong>The</strong><br />
National Academy of Sciences, Engineering, and<br />
Medicine (2019) stated at least 50% of caretakers<br />
across medical fields reported symptoms of<br />
burnout, including emotional exhaustion, cynicism,<br />
and a low sense of professional accomplishment.<br />
Janeway (2020) stated that the prevalence of<br />
burnout among registered nurses in the United<br />
States ranged from 35-45%. Even in <strong>Oklahoma</strong>,<br />
nurses from across the state marched at the<br />
Capitol demanding better pay and a solution to<br />
staffing shortages leading to burnout (Arata, <strong>2022</strong>),<br />
highlighting the need for immediate attention by<br />
health care leaders.<br />
Consequently, due to existing nursing shortages,<br />
the aging of the nursing workforce, and the growing<br />
COVID-19 effect, the International Council of <strong>Nurse</strong>s<br />
(2021) estimate that up to 13 million nurses will be<br />
needed to fill the global nurse shortage gap in the<br />
future. Since nurses are considered the most trusted<br />
professionals among the general population, it is<br />
imperative health care organizations advocate for<br />
nurse well-being strategies to deliver optimal care<br />
for the patients.<br />
Strategies to Reduce Nursing Compassion<br />
Fatigue<br />
<strong>The</strong> Mayo Clinic (Shanafelt & Noseworthy, 2017)<br />
developed nine evidence-based organizational<br />
strategies that health system leaders could<br />
use to assess strengths and challenges in their<br />
organizations tohelp eliminate compassion fatigue,<br />
particularly burnout:<br />
• Acknowledge and assess the problem.<br />
Staff respond to sincere discussions with<br />
health system leaders and managers that<br />
reflect a genuine commitment to solving the<br />
problem of burnout and fostering well-being.<br />
• Harness the power of effective leadership.<br />
<strong>The</strong> impact of toxic leadership on worker<br />
burnout and well-being is proven. Effective<br />
leaders need to be developed and receive<br />
evaluative feedback about their leadership<br />
behaviors from those they lead. Health<br />
boards need to “have the courage” to make<br />
leadership changes when required.<br />
• Develop and implement targeted<br />
interventions. External compliance factors<br />
can increase pressure on health system<br />
leaders, managers, and practice leaders.<br />
Expectations of increased productivity,<br />
excessive documentation, and administrative<br />
burden are drivers of burnout. Factors<br />
requiring improvement must be identified<br />
in each department. Targeted interventions<br />
can then be developed and implemented<br />
to ensure maximum local impact and<br />
effectiveness.<br />
• Cultivate community at work. Formal<br />
and informal peer support is important to<br />
physicians and nurses. However, structural<br />
changes, such as loss of dedicated spaces<br />
to share ideas with colleagues, have resulted<br />
in the loss of relationships and connections<br />
as well as eroded peer support and sense<br />
of community. “<strong>The</strong> pause” is another<br />
strategy practiced in emergency and<br />
other clinical settings to honor the work of<br />
caring for patients who die. It is a minute of<br />
stillness when clinicians pause, listen to their<br />
breathing, focus, and prepare to care for the<br />
next patient with calmness and compassion<br />
(Bartels, 2014). This strategy could be a<br />
comforting balm for nurses caring for patients<br />
dying of COVID-19.<br />
• Greater work-life flexibility. Now more<br />
than ever during the COVID-19 crisis, leaders<br />
should collaborate with staff to identify ways<br />
to acknowledge and reward effort (Rosen,<br />
2015). Productivity-based compensation
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 15<br />
can encourage overwork, over-servicing<br />
and increasing burnout risk. Greater worklife<br />
flexibility (strategy seven) has been<br />
considered a valued reward. Today, flexibility<br />
is a necessity. Rewards and incentives convey<br />
respect, appreciation, and encourage work to<br />
fulfill organizational caring goals.<br />
• Align values and strengthen culture. <strong>The</strong><br />
triple bottom line model evaluates alignment<br />
between “what we say we do” (mission,<br />
values), “what we do” (actions and culture),<br />
and “what others say we do” (i.e., patients,<br />
families, community stakeholders). <strong>The</strong><br />
question is whether the values and actions<br />
are aligned to foster a healthy culture, staff<br />
well-being, optimal practice environments,<br />
and quality care delivery which requires<br />
collaborative dialogue and deliberate action to<br />
address any barriers undermining this goal.<br />
• Promote flexibility and work-life<br />
integration. <strong>The</strong> drivers of burnout can be<br />
embedded in rigid and out-of-date policies.<br />
It is wise to promote flexible, family-friendly<br />
work environments that meet the needs of a<br />
diverse workforce (Drury et al., 2014). Leaders<br />
need to be sincere about understanding<br />
what motivates their staff to do their best<br />
work and support work-life integration.<br />
Leaders need to promote flexibility so staff<br />
can adapt their work hours to accommodate<br />
personal obligations, and provide coverage for<br />
vacation, studying, and important life or family<br />
events.<br />
• Provide resources to promote resilience<br />
and self-care. Leaders can work with staff<br />
to co-create essential resources to cope with<br />
work-related stress, prevent burnout, and<br />
promote well-being and self-care. Meditation<br />
can improve emotion regulation and resilience<br />
(Singer & Klimecki, 2014). Staff members<br />
who are committed to self-care and worklife<br />
integration are better prepared to care for<br />
patients and fulfill the organization’s mission.<br />
• Facilitate and fund organizational science.<br />
Leading health care organizations (i.e.,<br />
Mayo Clinic) have the added responsibility<br />
to contribute to organizational science to<br />
generate robust scientific evidence to inform<br />
national benchmarks and evidence-based<br />
instruments that other organizations can<br />
implement to reduce burnout and promote<br />
staff well-being and engagement.<br />
References<br />
Arata, K. (<strong>2022</strong>, May 17). OKC medical facility battling<br />
health care worker burnout with a ‘culture of<br />
care’. https://ktul.com/local/okc-metro-medicalfacility-battling-healthcare-worker-burnout-valirnursing-shortage-covid-19-pandemic-culture-ofcare-hospital<br />
Barron, D. (<strong>2022</strong>). Professional Quality of Life and Fear of<br />
COVID-19 Moderated By Perceived Job Market<br />
Outlook: Predicting Registered <strong>Nurse</strong> Turnover<br />
Intentions In South Florida During the COVID-19<br />
Pandemic. [Doctoral dissertation, Saint Leo<br />
University]. https://www.proquest.com/openview<br />
/149726083d6a5f68f1a425627e5f2433/1<br />
Bartels, J. B. (2014). <strong>The</strong> pause. Critical Care <strong>Nurse</strong>, 34(1),<br />
74-75. doi:10.4037/ccn2014962<br />
Benoit, L. G., Veach, P. M., & LeRoy, B. S. (2007). When<br />
you care enough to do your very best: Genetic<br />
counselor experiences of compassion fatigue.<br />
Journal of Genetic Counseling, 6(3), 299-312.<br />
doi:10.1007/s10897-006-9072-1<br />
Boyle, D. (2015). Compassion fatigue: <strong>The</strong> cost of<br />
caring. Nursing, 45(7), 48-51. doi:10.1097/01.<br />
NURSE.0000461857.48809.a1<br />
Circenis, K., Millere, I., & Deklava, L. (2013). Measuring the<br />
professional quality of life among Latvian nurses.<br />
Procedia-Social and Behavioral Sciences, 84,<br />
1625-1629. doi:10.1016/j.sbspro.2013.07.003<br />
Drury, V., Craigie, M., Francis, K., Aoun, S., & Hegney, D.<br />
G. (2014). Compassion satisfaction, compassion<br />
fatigue, anxiety, depression, and stress in<br />
registered nurses in Australia: Phase 2 results.<br />
Journal of Nursing Management, 22(4), 519-531.<br />
doi:10.1111/jonm.12168<br />
Durkin, M., Gurbutt, R., & Carson, J. (2018). Qualities,<br />
teaching, and measurement of compassion in<br />
nursing: A systematic review. <strong>Nurse</strong> Education<br />
Today, 63, 50-58. doi:10.1016./j.nedt.2018.01.025<br />
Figley, C. R. (2002). Treating compassion fatigue.<br />
Routledge.<br />
Godlaski, T. M. (2015). On compassion. Substance Use<br />
and Misuse, 50, 942-947. doi:10.3109/10826084.<br />
2015.1007694<br />
Gonzalez, A. R. (2014). Approaches to approaching<br />
the neighbor. Lectora, 20, 11-14.<br />
doi:10.1344/105.000002148<br />
Greenberg, M. T., & Turksma, C. (2015). Understanding<br />
and watering the seeds of compassion.<br />
Research in Human Development, 12, 280-287.<br />
doi:10.1080/15427609.2015.1068060<br />
Heritage, B., Rees, C. S., & Hegney, D. G. (2018).<br />
<strong>The</strong> PROQOL-21: A revised version of the<br />
Professional Quality of Life (PROQOL) scale<br />
based on Rasch analysis. PLoS ONE, 13(2),<br />
e0193478. doi:10.1371/journal.pone.0193478<br />
International Council of <strong>Nurse</strong>s. (2021). <strong>The</strong> global nursing<br />
shortage and nurse retention. [Policy brief].<br />
https://www.icn.ch/sites/default/files/inline-files/<br />
ICN%20Policy%20Brief_<strong>Nurse</strong>%20Shortage%20<br />
and%20Retention_0.pdf<br />
Janeway, D. (2020). <strong>The</strong> role of psychiatry in treating<br />
burnout among nurses during the COVID-19<br />
pandemic. Journal of Radiology Nursing, 39(3),<br />
176-178. doi:10.1016/j.jradnu.2020.06.004<br />
Ledoux, D. G. (2015). Understanding compassion<br />
fatigue: Understanding compassion. Journal<br />
of Advanced Nursing, 71(9), 20141-2050.<br />
doi:10.1111/jan.12686<br />
Lombardo, B., & Eyre, C. (2011). Compassion fatigue: A<br />
nurses’ primer. Online of Issues in Nursing, 16(1),<br />
18. doi:10.3912/OJIN.Vol16No01Man03<br />
McMullen, L. (2007). Oncology nursing and compassion<br />
fatigue: Caring until it hurts. Who is caring for the<br />
caregiver? Oncology Nursing Forum, 34(2), 491-<br />
492. web.a.ebscohost.com/abstract?direct=true<br />
&profile=ehost&scope=site&authtype=crawler&jr<br />
nl=0190535X&AN=28835250&h=HPOSBZva3W7<br />
Jw<br />
National Academy of Sciences, Engineering, and<br />
Medicine. (2019). Taking actions against clinician<br />
burnout: A systems approach to professional<br />
well-being. <strong>The</strong> National Academies Press.<br />
doi:10.17226/25521<br />
Partlak Gunusen, N., Ustun, B., Sercekus, P., &<br />
Buyukkaya, D. (2019). Secondary traumatic<br />
stress experiences of nurses caring for cancer<br />
patients. International Journal of Nursing<br />
Practice, 25(e12717). doi:10.1111/ijn.12717<br />
Ray, S. L., Wong, C., White, D., & Heaslip, K. (2013).<br />
Compassion satisfaction, compassion fatigue,<br />
work-life conditions, and burnout among frontline<br />
mental health care professionals. Traumatology,<br />
19(4), 255-267. doi:10.1177/1534765612471144<br />
Rosen, J. (2015, May 30). Establishing a strong culture<br />
of compassion improves quality of care,<br />
bottom line. Modern Healthcare. https://www.<br />
modernhealthcare.com/article/20150530/<br />
magazine/305309976/establishing-a-strongculture-of-compassion-improves-quality-ofcare-bottom-line<br />
Ruiz-Fernandez, M. D., Perez-Garcia, E., & Ortega-<br />
Galan, A. M. (2020). Quality of life in nursing<br />
professionals: Burnout, fatigue, and compassion<br />
satisfaction. International Journal of<br />
Environmental Research and Public Health, 17(4),<br />
1253. doi:10.3390/ijerph17041253<br />
Shanafelt, T. D., & Noseworthy, J. H. (2017). Executive<br />
leadership and physician well-being: Nine<br />
organizational strategies to promote engagement<br />
and reduce burnout. Mayo Clinic Proceedings,<br />
92(1), 129-146. doi:10.1016/j.mayocp.2016.10.004<br />
Singer, T., & Klimecki, O. M. (2014). Empathy and<br />
compassion. Current Biology, 24(18), R875-R878.<br />
doi:10.1016/j.cub.2014.06.054<br />
Sprang, G., Craig, C., & Clark, J. J. (2011). Secondary<br />
traumatic stress and burnout in child welfare<br />
workers: A comparative analysis of occupational<br />
distress across professional groups. Child<br />
Welfare, 90(6), 149-168. doi:10.1037/a0021730<br />
Stamm, B. H. (2010). <strong>The</strong> Concise ProQOL Manual (2nd<br />
ed.) Pocatello, ID: https://www.proqol.org<br />
TAKE YOUR NURSING CAREER<br />
TO THE NEXT LEVEL!<br />
Find out how Kramer School of Nursing can<br />
prepare you for each step of your nursing career.<br />
LPN-BSN<br />
• In as little as 12 months!<br />
RN-BSN<br />
• In person or 100% online<br />
• No nursing exams, no prerequisites, competitive price<br />
• Complete in two semesters<br />
Master of Science in Nursing<br />
• MSN Available 100% online<br />
• Nursing Education and Nursing Leadership<br />
• Post Master’s Certificates: Education and Leadership<br />
• Post Master’s Certificates: FNP, AGACNP, and PMHNP<br />
Doctoral Programs<br />
• Doctor of Nursing Practice (BSN-DNP): FNP, AGACNP,<br />
and PMHNP<br />
• Doctor of Nursing Practice Completion (MSN-DNP):<br />
Executive Leadership, Clinical, and Community-Based<br />
Public Health<br />
• PhD and BSN-PhD<br />
Your Dream<br />
Find<br />
Job Now!<br />
Nursing<br />
okcu.edu/nursing<br />
UNDERGRAD 405-208-5000 • admissions@okcu.edu<br />
GRAD 405-208-5094 • gadmissions@okcu.edu
16<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Courage in Everyday Nursing Practice<br />
Carol Dobos PhD, RN-BC, NEA-BC<br />
Reprinted with permission from Arizona <strong>Nurse</strong>, July 2021 issue<br />
Courage is an important attribute in life and in your nursing practice. As Helen Keller<br />
said,<br />
“Security is mostly a superstition. It does not exist in nature nor do the children of<br />
men as a whole experience it. Avoiding danger is no safer in the long run than outright<br />
exposure. Life is either a daring adventure, or nothing.”<br />
Nursing is a noble profession that is not for the faint of heart. Opportunities to<br />
choose courageous acts present themselves on a regular basis because risk is<br />
everywhere. You can attempt to minimize the risks by playing it safe. However, there are<br />
risks to yourself, your colleagues, your profession, and those you serve when you don’t<br />
take risks in showing up, speaking up, or practicing according to the highest standards<br />
of evidence-based practice.<br />
Choosing to practice courageously, consistent with your personal and professional<br />
values, will cause some discomfort, bumps, and bruises to you and your career. It will<br />
also bring professional and personal fulfillment, strengthen the profession, and improve<br />
patient outcomes. You will know that you are making a difference in your daily practice<br />
and throughout your nursing career.<br />
One way to cultivate courageous behavior is through personal risk-taking (PRT),<br />
but first you need to understand the nature of risk and its related concept, positive<br />
deviance.<br />
What is Risk?<br />
Risk is defined as the possibility of losing something of value, which could be<br />
physical, psychological, or economic. Common risks include falling out of favor with<br />
others in authority, losing support, or damaging essential relationships. Any of these<br />
events could lead to losing status or influence at work, or even losing one’s position or<br />
employment.<br />
A related concept called “positive deviance” refers to an intentional act of breaking<br />
the rules to serve the greater good. Positive deviance is intentional and honorable<br />
behavior that departs or differs from an established norm. It contains elements of<br />
innovation, creativity, adaptability, or a combination thereof; and it involves risk for the<br />
nurse.<br />
For most nurses, whether a particular action is right or wrong will often be judged<br />
by others in charge of rules enforcement. <strong>The</strong> decision to engage in positive deviance,<br />
however, lies entirely with the nurse.<br />
Personal Risk-Taking<br />
PRT is behavior that is consciously and freely chosen among available alternatives,<br />
some of which are known to incur less risk than the chosen action. It is supported by<br />
the strength and belief of personal convictions. Courageous action upholds principles.<br />
Calculated inaction due to fear leaves one powerless, with values compromised.<br />
<strong>Nurse</strong>s promote courageous action by sharing courageous behavior, also called<br />
hero stories. This can be done formally and informally, verbally and in writing, one on<br />
one or in groups, during staff meetings, during change of shift report, or rounds. We<br />
create a culture based on what we talk about, what we value, and what we support and<br />
reward. Sometimes we stand alone, and sometimes we influence others to follow our<br />
lead and take their own personal risks. In one study, risk taking was found to be one<br />
of the key elements in attaining expert nursing practice, which supports effective and<br />
quality-based healthcare outcomes. Risk taking also was found to enhance clinical and<br />
professional development.<br />
Rather than sitting on the sidelines and hurling judgment or advice at others (for<br />
example, “Someone needs to do something about this.”), we must dare to show up<br />
and let ourselves be seen, which can result in change. (See Success story.)<br />
Success story<br />
When residents were not interacting appropriately with pediatric patients,<br />
risking psychological harm, I discussed this with the chief and arranged<br />
education. I advised our team that in identifying this issue, relationships<br />
might become strained, but we had an obligation to our patients to address<br />
this problem. I often used the mantra “I am doing the right thing for the right<br />
reason” stating it over and over in my head to help me stay the course and<br />
follow through with my convictions. As feared, the residents and even an<br />
attending physician demonstrated passive aggressive behavior towards us.<br />
<strong>The</strong> care of the children did improve, however, and we knew we had made the<br />
right call.<br />
We pay a price when we shut down and disengage, failing to take action. I have<br />
heard nurses talk about “staying under the radar.” In doing so they pay a dear price.<br />
<strong>The</strong>ir talents, wisdom, knowledge, and values are not being shared to positively<br />
influence care and support the development of new nurse graduates and other<br />
colleagues through courageous role modeling. Vulnerability occurs in sharing an<br />
unpopular opinion, standing up for oneself or others such as a colleague who is<br />
being bullied, being accountable, asking for help, trying something new, admitting<br />
uncertainty, and asking for forgiveness. When courage and fear meet, it often feels
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 17<br />
awkward and scary; however, “being all in” is to be alive. To act in alignment with your<br />
values is key to personal and professional happiness.<br />
PRT and Promoting Patient Safety<br />
Failing to take risks and practice courageously can lead to threats to patient safety.<br />
Focusing on my obligation to “First do no harm,” I made the decision not to deploy<br />
a transport team until all the team members demonstrated competency. I was<br />
transparent in discussing my concern and contingency plan to send another team with<br />
my medical and administrative colleagues. I was told that this was a “career-limiting<br />
move.” I simply stated, “I have to be able to sleep at night.”<br />
In another organization, I disagreed with a plan to move critically ill patients multiple<br />
times to accommodate unit renovation. I identified an alternative that required only one<br />
move. Although my plan was successfully implemented, my action caused me to fall<br />
out of favor with the administrator and eventually resulted in my having to move on<br />
to another position. In both instances, I had to put my patients first because when I<br />
became a member of the nursing profession, I made a promise to protect them.<br />
Why We May Not Take Personal Risks<br />
Understanding scarcity is key to understanding why nurses may not take justified<br />
risks. <strong>The</strong> three components of scarcity are shame, comparison, and disengagement.<br />
Shame is the fear of ridicule and belittling often used to control people and to keep<br />
them in line. Shame-based cultures are very unhealthy for nurses and patients. <strong>The</strong><br />
killer of innovation is shame. In these cultures, covert or sometimes overt messages<br />
are common, such as to dare not, you’re not good enough, who do you think you<br />
are, don’t you dare get too big for your britches.” Shame becomes fear, fear leads to<br />
risk aversion, and risk aversion kills innovation and can lead to unsafe patient care.<br />
Shame is the intensely painful feeling or experience of believing that we are flawed<br />
and therefore unworthy of belonging. Shame makes us feel unworthy of connection.<br />
Resilience to shame occurs when recognizing and speaking openly about shame,<br />
practicing critical awareness, and reaching out to others.<br />
Healthy competition can be beneficial, but constant overt or covert comparing and<br />
ranking suffocates creativity and risk taking. If nurses are held to one narrow standard,<br />
they may not question the relevance of a course of action to a specific situation and<br />
embrace evidence- based practice.<br />
Disengagement occurs when people are afraid to take risks and try new things.<br />
Too often it is easier to stay quiet than to share stories, experiences, and ideas. It is<br />
important to do what is right, not what is easy. <strong>The</strong> best way through a difficult situation<br />
is to address the situation directly with honesty and integrity, sharing your story and<br />
asking for what you need. An excellent resource for nurses is the book Crucial<br />
Conversations. Often what we fear does not happen, but even if it does, we have<br />
retained our self-respect and commitment to professional values.<br />
Courageous Practice<br />
I hope you choose to practice courageously, doing the right things for the right<br />
reasons. As <strong>The</strong>odore Roosevelt said,<br />
“Far better it is to dare mighty things, to win glorious triumphs, even though<br />
checkered by failure, than to take rank with those poor spirits who neither enjoy much<br />
nor suffer much, because they live in the gray twilight that knows not victory nor<br />
defeat.”<br />
Selected references<br />
Dobos C. Defining risk from the perspective of nurses in clinical roles. J Adv Nur.<br />
1992;17:1303-9.<br />
Dobos C. Understanding personal risk taking among staff nurses: critical information<br />
for nurse executives. J Nurs Adm. 1997;27(1):1-2.<br />
Gary JC, Exploring the concept and use of positive deviance in nursing. Am J Nurs.<br />
2013;113(8):26-34. Haag-Heitman B. <strong>The</strong> development of expert performance<br />
in nursing. J <strong>Nurse</strong>s Staff Dev. 2008;24(5):203-11.<br />
Brown B. Daring Greatly: How the Courage to be Vulnerable Transforms the Way We<br />
Live, Love, Parent, and Lead. Gotham Books; 2012.<br />
Patterson K, Grenny J, McMillan R, et al. Crucial Conversations: Tools for Talking When<br />
Stakes are High, 2nd ed. New York, NY: McGraw-Hill; 2011.<br />
Carol Dobos lives in Phoenix Arizona and is the past-president of the Arizona<br />
Association for Nursing Professional Development, a state affiliate of the<br />
Association for Nursing Professional Development.<br />
EMERGING<br />
NURSES<br />
Coming to a Coffee Shop<br />
Near You<br />
Rachael Kleckner, MSN, RN, CCRN-CNC-CSC<br />
With a dynamical healthcare climate, it’s no<br />
surprise that the typical new graduate is evolving<br />
alongside the profession. As your Emerging <strong>Nurse</strong><br />
Director, I have spent the past several months<br />
talking with you to identify what this looks like in<br />
order to best support you. One of the ways I chose<br />
to reach out is through the creation of the <strong>Oklahoma</strong><br />
Emerging <strong>Nurse</strong>s Facebook group, a page dedicated<br />
to students and those with less than five years of<br />
licensed experience.<br />
Rachael Bachhofer<br />
Through this page, many of you have identified Kleckner<br />
that you are already seeking advanced practice roles due to burnout,<br />
pay, scheduling, and lack of a work-life balance. With this in mind, I am<br />
now determining how to best represent you and ensure those new to the<br />
profession have a voice within our professional organization.<br />
<strong>The</strong>re will be networking events held later this year where you will have<br />
the opportunity to share your practice experience and learn how we plan to<br />
address your needs. Please request to join the above Facebook group so<br />
that you know when and where to join us — several group members have<br />
suggested that coffee may be the way to your heart and I couldn’t agree<br />
more!<br />
To access electronic copies of<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong>, please visit<br />
http://www.nursingALD.com/publications<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong>s Association has many members whose outstanding contributions should be<br />
recognized. We hope you will consider nominating a colleague, a coworker, or a friend for one of the<br />
ONA awards categories below:<br />
EXCELLENCE IN NURSING<br />
NURSING RESEARCH AWARD<br />
NURSING IMPACT ON PUBLIC POLICY AWARD<br />
NIGHTINGALE AWARD OF EXCELLENCE<br />
FRIEND OF NURSING AWARD<br />
EXCELLENCE IN THE WORKPLACE ENVIRONMENT<br />
<strong>The</strong> deadline for submission nominations is <strong>August</strong> 1, <strong>2022</strong>.<br />
NOMINATE SOMEONE TODAY AT:<br />
surveymonkey.com/r/ONAAWARDS22
18<br />
<strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Getting Clear on Bullying Versus Incivility<br />
Renee Thompson, DNP, RN, CSP<br />
Reprinted with permission<br />
from <strong>The</strong> Florida <strong>Nurse</strong>,<br />
February <strong>2022</strong> issue<br />
Numerous studies show the<br />
prevalence and devastating<br />
impact disruptive behaviors<br />
have on nurse retention and<br />
satisfaction, patient safety<br />
and the financial health of an<br />
organization. Today, more<br />
than ever, the unpredictable, Dr. Renee Thompson<br />
life-and-death nature of the<br />
pandemic has created an environment that is ripe for an<br />
increase in workplace bullying and incivility. Research at<br />
the Healthy Workforce Institute shows an uptick in bad<br />
behavior and nurses are experiencing greater workplace<br />
incivility now more than ever before. Additional studies<br />
show:<br />
• 45.7% of nurses said they witnessed more<br />
incivility than before the pandemic (El Ghaziri<br />
et al., 2021).<br />
• 14.3% of surgery patients had higher<br />
complications with surgeons who had one<br />
to three reports of unprofessional behaviors<br />
compared to those surgeons who had no<br />
reports of disruptive behaviors (Cooper et al.,<br />
2019).<br />
• 94% of individuals have worked with a toxic<br />
person in the last five years; 51% of the<br />
targets stated they are likely to quit as a result<br />
(Kusy, 2017).<br />
Developing successful, targeted interventions<br />
to reduce bullying and incivility among nurses<br />
will require that leaders develop awareness and<br />
understanding of nurses’ unique experiences with<br />
disruptive behavior. One of the biggest areas of<br />
confusion that makes it difficult to address and<br />
eliminate bad behavior is a misunderstanding about<br />
the differences between bullying and incivility.<br />
An important first step to educating yourself and<br />
your employees is to get clear on those differences.<br />
This will help you raise awareness, set expectations,<br />
and develop appropriate strategies to eliminate each<br />
type of disruptive behavior. Bullying should be a<br />
NEVER event, but not everything is bullying and when<br />
we call everything bullying, we lessen our chances of<br />
identifying and addressing true bullying behavior.<br />
BULLYING<br />
For a behavior to be considered bullying, it must<br />
include three things:<br />
A Target-This target can be a single person or<br />
group of people. Group targets can include the<br />
opposite shift, new nurses, or nurses who have a<br />
particular ethnic background.<br />
Harmful-<strong>The</strong> behavior must be harmful in some<br />
way. This harm can be to the target or harmful to a<br />
patient.<br />
Repeated-<strong>The</strong> most important element of<br />
bullying. <strong>The</strong> behavior can’t be just a one-time<br />
event, it must be repeated over time.<br />
INCIVILITY<br />
Incivility is different from bullying but tends to<br />
be much more pervasive. While the behaviors can<br />
be similar, they tend to be lower level. Incivility<br />
shows up as your typical rude, unprofessional,<br />
inconsiderate behaviors: eye-rolling, condescension,<br />
favoritism, alienation, gossiping, mocking, cursing.<br />
Make no mistake about it, incivility is a healthy<br />
and professional workplace killer, and needs to be<br />
addressed.<br />
<strong>The</strong> Bottom Line<br />
Bullying and incivility can destroy work<br />
environments and impact patients in a negative way.<br />
<strong>The</strong> key is to get very clear on the behavior – is it<br />
bullying (target, harmful, repeated) or incivility (low<br />
level, rude, and unprofessional). We are hemorrhaging<br />
nurses due to bad behavior and it’s time we get<br />
educated on how to recognize and address bullying<br />
and incivility so that we can cultivate a more<br />
respectful and professional work culture.<br />
References<br />
Cooper, W., Spain, D., Guillamondegui, O., et<br />
al. (2019, June). Association of Coworker Reports<br />
About Unprofessional Behavior by Surgeons<br />
with Surgical Complications in <strong>The</strong>ir Patients.<br />
JAMA Surgery, 154(9), 828–834. doi:10.1001/<br />
jamasurg.2019.1738<br />
El Ghaziri, M., Johnson, S., Purpora, C.,<br />
Simons, S. and Taylor, R. (2021, July). Registered<br />
<strong>Nurse</strong>s’ Experiences with Incivility During the<br />
Early Phase of COVID-19 Pandemic: Results of a<br />
Multi-State Survey. Workplace Health & Safety.<br />
doi:10.1177/21650799211024867<br />
Kusy, M. (2017). Why I don’t work here anymore:<br />
A leader’s guide to offset the financial and emotional<br />
cost of toxic employees. Boca Raton, FL: CRC Press<br />
Bio:<br />
As an international speaker and consultant, Dr.<br />
Renee Thompson tackles the challenges facing<br />
healthcare leaders today. With 30 years as a nurse,<br />
Renee is an expert on creating healthy workforces<br />
by eradicating bullying & incivility. She is in demand<br />
as a keynote speaker and has authored several<br />
books on bullying.<br />
HOUSE OF DELEGATES<br />
MEETING<br />
Official Call to the Delegates To Attend a Meeting of the ONA House of Delegates<br />
Hyatt Regency, Tulsa, <strong>Oklahoma</strong> | Wednesday, September 28, <strong>2022</strong>, 3:00 - 5:00 pm<br />
From— Michele Bradshaw, MSN, RN, ONA Secretary/Treasurer<br />
This notice constitutes the official call to meeting of the Meeting of the ONA House of<br />
Delegates. <strong>The</strong> House session will be held Wednesday, September 28, <strong>2022</strong>. <strong>The</strong> House of<br />
Delegates will convene at 3:00 p.m. adjourning at 5:00 p.m. Credentialing closes at 2:45<br />
p.m. so that we may start promptly at 3:00 p.m.<br />
Prior to the House we will have a session focused on issues facing nurses and nursing<br />
practice related to the work of the association. For more details regarding the agenda<br />
for the Annual Convention, please see the <strong>2022</strong> Convention schedule. <strong>The</strong> Agenda, 2021<br />
Minutes, and Registration for the ONA Convention are posted on the ONA website,<br />
oklahomanurses.org.<br />
Members of the ONA House of Delegates have a crucial role in providing direction and<br />
support for the work of the state organization. <strong>The</strong> House of Delegates also provides a<br />
courtesy seat to all Past ONA Presidents and one registered nurse participant from each<br />
organizational affiliate. <strong>The</strong>se delegates come to the House to work towards the growth<br />
and improvement of ONA and its constituencies. This requires a professional commitment<br />
to the preservation and creative growth of the professional society at all levels of the<br />
organization. Such a commitment will benefit the individual delegate, the Association<br />
and the nursing profession. <strong>The</strong> representation for each Regional <strong>Nurse</strong>s Association<br />
established for the <strong>2022</strong> House is below.<br />
Each delegate must study the issues thoroughly and is encouraged to participate in<br />
Region sponsored meetings prior to the ONA Annual Convention and the Issue Forum<br />
held prior to the House so that they may engage in open-minded debate, practice active<br />
listening and use the extensive resources and collective knowledge made available<br />
throughout these meetings to assist them in making informed decisions.<br />
If you are interested in having an issue considered by the ONA House, please submit a<br />
reference to be heard using the reference guidelines posted on the ONA website. Please<br />
refer to the Policies and Procedures posted on the website for guidance.<br />
Region #01....................................................43<br />
Region #02...................................................34<br />
Region #03...................................................35<br />
Region #04...................................................22<br />
Region #05...................................................20<br />
Region #06...................................................21<br />
ONA Board of Directors...........................16<br />
ONA Affiliates...............................................6<br />
Past ONA Presidents
<strong>August</strong>, September, October <strong>2022</strong> <strong>The</strong> <strong>Oklahoma</strong> <strong>Nurse</strong> 19<br />
Sleep and Your Health<br />
Cynthia Meyer, MSN, RN, CHSE<br />
Debra Rose Wilson,<br />
PhD, MSN, RN, IBCLC, AHN-BC, CHT<br />
Reprinted with permission from Tennessee <strong>Nurse</strong><br />
May <strong>2022</strong> issue<br />
To sleep, perchance to dream. – Shakespeare<br />
One in three adults do not get the uninterrupted<br />
sleep that is recommended, and inadequate<br />
sleep has a direct effect on the functioning of the<br />
immune system. <strong>Nurse</strong>s and other health care<br />
workers are part of the 18 to 20% of Americans<br />
who work alternating shift schedules. Sleep is<br />
essential, not only as restorative but because of its<br />
role in the regulation of immune response. <strong>The</strong>re<br />
has been some interesting research in the last<br />
20 years that explored the connections between<br />
sleep, inflammation, and immune function. With<br />
this information at hand, a nurse can improve selfcare<br />
and appreciate the importance of teaching<br />
sleep hygiene as part of holistic patient health care<br />
system.<br />
<strong>The</strong> sleep-wake cycle balances biological health,<br />
mental well-being, and helps the immune system<br />
adapt as needed. <strong>The</strong> sleep-wake is based on the<br />
24-hour circadian clock that regulates complex<br />
bodily functions, including the cardiovascular<br />
system, inflammation, and immune response.<br />
Cytokines are messenger proteins that can be<br />
pro-inflammatory or anti-inflammatory, triggering<br />
a response to infection or injury. People with<br />
chronic inflammatory disease, sleep problems, and<br />
depression have higher levels of circulating proinflammatory<br />
cytokines.<br />
While the body is awake, the immune system<br />
is protecting the body against foreign pathogens.<br />
Anti-inflammatory cytokines (IL-4, IL-10, IL-13,<br />
and TGF-β) are active. Natural killer (NK) cells act<br />
by stopping the growth of mutating cells such as<br />
cancer, and increase production during the wakeful<br />
state. <strong>The</strong>se immune cells are very responsive to<br />
stress and lower or discontinue production when<br />
the sympathetic nervous system spills the stress<br />
hormones. <strong>The</strong> longer you are stressed during<br />
wakeful periods, the less opportunity NK cells have<br />
to increase in numbers and the greater the chance<br />
that rogue cells will continue to mutate. <strong>The</strong> body<br />
can’t do maintenance work on immune function<br />
when the resources are being transferred to first aid<br />
and alarm response systems when stressed. For<br />
those who experience a great deal of stress, sleep<br />
is even more important. Once asleep, the body is<br />
put back into balance as CD4+ T cells and Th1 and<br />
Th2 respond, and production is higher. Natural killer<br />
cells, melatonin, and stress hormones can replenish<br />
themselves.<br />
Sleep Deprivation<br />
Both short-term and long-term sleep<br />
deprivation disrupts the 24-hour circadian clock<br />
and immunological functions. Sleep deprivation<br />
increases inflammation, so those with a pre-existing<br />
inflammatory disease (such as RA, depression,<br />
or bowel disease) need consistent sleep even<br />
more than others. With increased inflammation<br />
and decreased melatonin risk for CVD, breast<br />
cancer, and other inflammatory diseases rise.<br />
<strong>The</strong>rmoregulation, insulin levels, vaccine response,<br />
and cognitive flexibility are impaired with inadequate<br />
sleep. Those with sleep apnea are at higher risk for<br />
diabetes, hypertension, coronary issues related<br />
to the increased inflammation. For those who are<br />
significantly stressed, quality sleep is difficult to<br />
achieve. <strong>The</strong> sleep-wake cycle is disrupted when<br />
pro-inflammatory cytokines and stress hormones<br />
(e.g., cortisol, epinephrine, and norepinephrine) are<br />
released.<br />
Shift work<br />
Current estimates are that about 20% or one-fifth<br />
of the workforce currently participate in shift work.<br />
Of those working in the healthcare sector, 52%<br />
report short sleep duration. Studies also showed<br />
that those working the night shift reported poorer<br />
quality sleep and sleep deprivation. <strong>The</strong> general<br />
recommendation is for individuals to get between<br />
seven to nine hours of sleep, but shift workers get<br />
less than six hours daily or one to four hours less<br />
per week. Those working the night shift may not be<br />
able to make up for lost sleep which is needed for<br />
relaxation and physical restoration.<br />
Shift work is essential for healthcare. <strong>Nurse</strong>s<br />
must work hours that may not be conducive to sleep<br />
to provide round-the-clock care for patients. <strong>The</strong>se<br />
hours may cause a disruption in sleep. Circadian<br />
rhythms are what regulate the sleep-wake cycle, and<br />
these cycles rely on light to direct the cycle. Daylight<br />
causes us to become more alert and awake, while<br />
darkness leads to melatonin production, which<br />
prepares the body for sleep. Shift work disrupts the<br />
natural sleep-wake cycle, and research has shown<br />
that over time the physical and mental health of<br />
those who participate in shift work may be impacted<br />
by the disruption in sleep.<br />
Shift work has been shown to have a negative<br />
impact on the psychological and social health of<br />
the individuals working those hours. Shift work<br />
sleep disorder (SWSD) occurs when work schedules<br />
disrupt the natural circadian rhythms, and the<br />
disruptions cause excessive sleepiness, fatigue, or<br />
insomnia. Eventually, these symptoms may result<br />
in distress or impairment in mental, physical, and<br />
social functioning. Furthermore, sleep deprivation<br />
can lead to increased stress which in turn can lead<br />
to decreased job satisfaction for nurses. Studies<br />
showed that health professionals who worked night<br />
shifts had higher levels of psychological and mental<br />
health problems than their day shift counterparts.<br />
This included higher levels of depression, irritability,<br />
stress, OCD, and mood disorders. Shift workers<br />
also exhibited negative feelings, isolation, and<br />
difficulty in relationships.<br />
Sleep allows the body to heal itself, and it helps<br />
boost immune function. <strong>Nurse</strong>s who do shift<br />
work are not exempt from the negative effects of<br />
inadequate sleep. Obesity is more common in shift<br />
workers, and there is an increased risk of metabolic<br />
syndrome and diabetes. Shift work compromises<br />
immune function and places individuals at an<br />
increased risk for breast and colorectal cancer.<br />
When compared to day shift workers, those doing<br />
shift work have an increased risk of cardiovascular<br />
disease. Continued alterations in the circadian<br />
rhythms have also been linked to gastrointestinal<br />
issues such as gastritis, indigestion, appetite<br />
disorders, irregular bowel movements, constipation,<br />
heartburn, and pain. Since nursing is predominantly<br />
a female profession, it is worth noting the correlation<br />
between shift work and reproductive issues such<br />
as decreased fertility, altered menstrual cycles, and<br />
other reproductive issues.<br />
Tips<br />
Shift work can have negative effects on health;<br />
however, these crazy hours are necessary for the<br />
nursing profession. <strong>The</strong>re are things workers can do<br />
to improve sleep and maintain adequate rest. <strong>The</strong><br />
following tips are included for surviving shift work:<br />
• Maintain a consistent sleep schedule<br />
o Keep the same sleep-wake cycle on days<br />
off<br />
o Sleep directly after a shift or adopt a splitnap<br />
schedule<br />
o Take a short nap prior to shift on workdays<br />
but avoid naps longer than 30 minutes<br />
• Maintain an ideal sleep environment<br />
o Cool environment between 68-72 degrees<br />
Fahrenheit<br />
o Limit noise using white noise or earplugs<br />
o Limit light using an eye mask or blackout<br />
curtains<br />
o Stay away from electronic devices such<br />
as a computer screen or cell phone in the<br />
two hours prior to sleep.<br />
• Promote sleep<br />
o Take a hot shower, go for a walk, or use<br />
meditation for relaxation<br />
o Limit strenuous exercise<br />
o Limit caffeine, alcohol, nicotine three to<br />
four hours before bed<br />
o Maintain a healthy diet and avoid fatty,<br />
spicy foods before bed<br />
o If you tend to be cold, wear socks to bed<br />
• Things to do at work<br />
o Eat healthy<br />
o Use caffeine in moderation and avoid 4 to<br />
6 hours before sleep<br />
o Take short, frequent breaks<br />
o Keep the work environment well lit<br />
o Schedule wisely with no more than three<br />
consecutive 12-hour shifts and have 11<br />
hours off to ensure adequate rest time<br />
o Nap before driving home if needed<br />
o Get out into the sunshine on your breaks<br />
when possible<br />
o Give yourself stress management breaks<br />
where you rest, meditate, or practice<br />
breath work.<br />
Conclusion<br />
Shift work is part of our profession, but changes<br />
in sleep rhythms have a negative impact. Lack<br />
of sleep in nurses not only increases the chance<br />
of error but leads to health issues. This is a global<br />
issue for nurses. Assess your own sleep. <strong>The</strong><br />
National Sleep Foundation (NSF; sleepfoundation.<br />
org) has a Sleepiness Test that examines sleep<br />
patterns over the past 2 weeks. <strong>The</strong>re is the Epworth<br />
Sleepiness Scale that assesses daytime sleepiness<br />
and STOP BANG screening questions for sleep<br />
apnea. If you aren’t sure about your sleeping habits,<br />
try a sleep diary. <strong>The</strong> NSF can guide you through<br />
keeping a week of journaling with quality of sleep,<br />
caffeine intake, bedroom environment, and sleep<br />
hygiene. What are you going to do to improve your<br />
quality of sleep?<br />
References Available Upon Request<br />
Cynthia Meyer, MSN, RN, CHSE – Cindy is<br />
an Assistant Professor and the Simulation Lab<br />
Coordinator at Austin Peay State University,<br />
currently working on her PhD at East Tennessee<br />
State University.<br />
Debra Rose Wilson, PhD, MSN, RN, IBCLC,<br />
AHN-BC, CHT – Dr. Wilson is a Health Psychologist<br />
and a Professor of Nursing at Austin Peay State<br />
University and was the 2017-18 American Holistic<br />
<strong>Nurse</strong> of the year. She has been educating nurses<br />
in Tennessee for over 20 years, and has a private<br />
hypnosis practice in the Nashville area, and teaches<br />
hypnosis to nurses and psychologists.