Vermont Nurse Connection - August 2022
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Vermont</strong> <strong>Nurse</strong><br />
<strong>Connection</strong><br />
ANA-<strong>Vermont</strong><br />
Official Publication<br />
Quarterly Publication sent to 19,500 Registered <strong>Nurse</strong>s,<br />
Volume 25 • Number 4 LPNs, and LNAs in <strong>Vermont</strong><br />
<strong>August</strong>, September, October <strong>2022</strong><br />
Inside<br />
Change your<br />
thoughts. Change<br />
your life.<br />
Page 3<br />
Jessilyn Dolan<br />
What a beautiful summer it has been in <strong>Vermont</strong> so far!<br />
I hope this finds you and yours enjoying all that <strong>Vermont</strong><br />
has to offer.<br />
Whether you spend quiet time in nature or playing sports<br />
with teammates, we hope you are taking time for self-care, fun,<br />
and fresh air!<br />
We just returned from the ANA Annual Membership<br />
Assembly in Washington DC this June where we spent an<br />
amazing few days packed with education, excitement, and<br />
nurses from all over the country. ANA-VT is reinvigorated and<br />
ready to grow as a group and support you as an individual!<br />
ANA National is working hard to ensure that the mission<br />
and vision of nurses nationwide is being upheld, remaining<br />
vibrant, and surging ahead with positive and impactful<br />
progress on environmental stewardship, workplace violence,<br />
and our recently published Racial Reckoning statement.<br />
Your local ANA-VT team is excited to welcome Fritz<br />
Asuncion and Susan Shayne to the team and we are looking<br />
to you and our membership to see if you too would consider<br />
joining us. Together we can make our voices heard and make<br />
long lasting changes to better support our colleagues, patients,<br />
families, and communities.<br />
Thank you for being a member. We look forward to hearing<br />
from you, engaging with you, and working with you. With a<br />
warm heart, open mind, and the same excitement we all once<br />
had when we first passed our NCLEX – we are here for you!<br />
Wishing you sunshine, laughter, and light always.<br />
Warmly,<br />
Jessilyn<br />
Sigma Theta Tau International:<br />
Omega Mu At-Large Chapter Updates<br />
Page 4<br />
ANA VT Membership Assembly<br />
Jessilyn Dolan<br />
The <strong>2022</strong> Annual Meeting of the ANA Membership<br />
Assembly was Friday, June 10 and Saturday, June 11, <strong>2022</strong><br />
in Washington, DC at the Grand Hyatt Washington.<br />
Over 270 nurses gathered from 47 states, including (for<br />
the first time) Hawaii!<br />
The energy was contagious with excitement in the air.<br />
President Grant set the tone with his opening remarks,<br />
received more standing ovations than I could count, and<br />
beamed as he discussed ANA’s strong financial position<br />
and professed gratitude that ANA is investing thoughtfully<br />
and strategically in the future of nursing.<br />
You can view the <strong>2022</strong> ANA Membership Assembly<br />
Agenda here: https://www.nursingworld.org/~4962f7/<br />
globalassets/ana/leadership--governance/ma/<strong>2022</strong>/agenda-<br />
<strong>2022</strong>-ma-schedule-at-a-glance-external.pdf<br />
The first day started with a general networking<br />
breakfast and time to meet the candidates running for<br />
ANA’s board.<br />
There was an ANA-PAC meeting with ANA Rosa<br />
Potts who is on the National ANA Policy Committee and<br />
who has just moved to <strong>Vermont</strong>! The ANA-PAC has been<br />
meeting for nearly 50 years, and has been working to elect<br />
ANA VT Membership Assembly continued on page 6<br />
Benefit Bakes Fundraiser<br />
Page 7<br />
current resident or<br />
Presort Standard<br />
US Postage<br />
PAID<br />
Permit #14<br />
Princeton, MN<br />
55371<br />
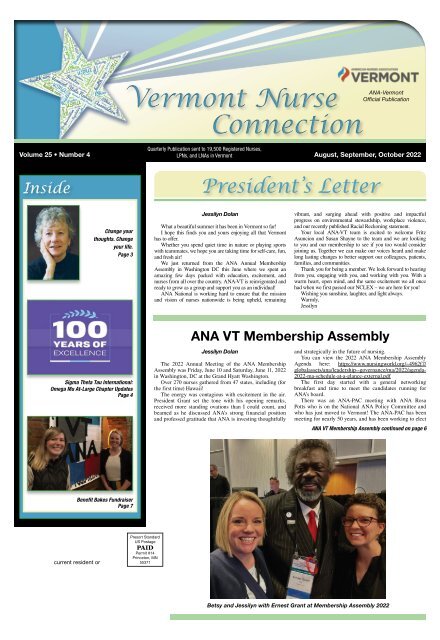
Betsy and Jessilyn with Ernest Grant at Membership Assembly <strong>2022</strong>
Page 2 • <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
A Message from the Executive Director<br />
Amy Martone, MBA, BSN, RN, NPD-BC<br />
It has been a very exciting three months for the<br />
ANA-<strong>Vermont</strong>! We welcomed two new Directors to<br />
our Board, participated in a fundraiser with Benefit<br />
Bakes, and sent two <strong>Vermont</strong> nurse representatives to<br />
the ANA Membership Assembly in Washington, D.C.!<br />
These successes have provided us with great energy and<br />
momentum forward. I am excited to see what we can<br />
achieve together in the next three months.<br />
The ANA-<strong>Vermont</strong> Board is working together to<br />
finalize a strategic plan that will be used to guide our<br />
initiatives in the coming year. Earlier this month, the<br />
Board met for an in-person strategic planning session in<br />
Burlington. It was a wonderful day filled with inspiration<br />
and collaboration! Our strategic plan will be finalized in<br />
the near future and shared with you.<br />
One item in our strategic plan is to engage with the<br />
members we represent by listening to their personal<br />
If you wish to submit a “Letter to the Editor,” please<br />
address it to:<br />
Cynthia Peterson<br />
<strong>Vermont</strong><strong>Nurse</strong><strong>Connection</strong>@gmail.com<br />
Please remember to include contact information,<br />
as letter authors may need to be contacted by the<br />
editors of the VNC for clarification. NOTE: Letters to<br />
the Editor reflect the opinions of the letter authors<br />
and should not be assumed to reflect the opinions<br />
of the ANA-<strong>Vermont</strong>.<br />
Cynthia Peterson, MSN, RN, Editor<br />
experiences, innovative ideas, and professional concerns.<br />
In doing this, the ANA-<strong>Vermont</strong> understands the<br />
prevalence of workplace violence in our practice settings,<br />
and the immediate need for action to advocate to protect<br />
nurses. The ANA-<strong>Vermont</strong> hosted a series of virtual<br />
Nursing Forums that connected <strong>Vermont</strong> nurses with<br />
States Attorneys from across the state for facilitated<br />
dialogue. Thank you to all that participated in this series<br />
as developing a relationship with key stakeholders was the<br />
first step in our advocacy and action.<br />
Lastly, we are excited for you to read this newsletter<br />
because we have been working to increase the content<br />
contributed by <strong>Vermont</strong> nurses. I hope that you will<br />
find the articles exciting and engaging as we focus on<br />
highlighting the achievements and accomplishments of<br />
nurses in our state and sharing a local nursing perspective<br />
on special interests. If you are interested in writing an<br />
article, I would encourage you to reach out to our editor<br />
Cynthia Peterson at <strong>Vermont</strong><strong>Nurse</strong><strong>Connection</strong>@gmail.<br />
com, or me at ExecutiveDirectorANAVT@gmail.com.<br />
Deadlines for the<br />
<strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong><br />
Are you interested in contributing an article to an<br />
upcoming issue of the <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong>? If so,<br />
here is a list of submission deadlines for the next 2 issues:<br />
Vol. 26 #1 – October 10, <strong>2022</strong><br />
Vol. 26 #2 – January 11, 2023<br />
Articles may be sent to the editor of the <strong>Vermont</strong><br />
<strong>Nurse</strong> <strong>Connection</strong> at:<br />
Cynthia Peterson<br />
<strong>Vermont</strong><strong>Nurse</strong><strong>Connection</strong>@gmail.com<br />
Official publication of ANA-<strong>Vermont</strong>, a constituent member<br />
of the American <strong>Nurse</strong>s Association. Published quarterly every<br />
January, April, July and October. Library subscription price is $20<br />
per year. ISSN# 1529-4609.<br />
Editorial Offices<br />
ANA-<strong>Vermont</strong>, 4 Carmichael Street, Suite 111, #215, Essex, VT<br />
05452, PH: (802) 651-8886, E-mail: <strong>Vermont</strong><strong>Nurse</strong><strong>Connection</strong>@<br />
gmail.com<br />
Editor: Cynthia Peterson<br />
Advertising<br />
For advertising rates and information, please contact Arthur<br />
L. Davis Publishing Agency, Inc., PO Box 216, Cedar Falls, Iowa<br />
50613, (800) 626-4081, sales@aldpub.com. ANA-<strong>Vermont</strong> and the<br />
Arthur L. Davis Publishing Agency, Inc. reserve the right to reject any<br />
advertisement. Responsibility for errors in advertising is limited to<br />
corrections in the next issue or refund of price of advertisement.<br />
Acceptance of advertising does not imply endorsement or<br />
approval by ANA-<strong>Vermont</strong> of products advertised, the advertisers,<br />
or the claims made. Rejection of an advertisement does not imply<br />
a product offered for advertising is without merit, or that the<br />
manufacturer lacks integrity, or that this association disapproves<br />
of the product or its use. ANA-<strong>Vermont</strong> and the Arthur L. Davis<br />
Publishing Agency, Inc. shall not be held liable for any consequences<br />
resulting from purchase or use of an advertiser’s product. Articles<br />
appearing in this publication express the opinions of the authors; they<br />
do not necessarily reflect views of the staff, board, or membership of<br />
ANA-<strong>Vermont</strong> or those of the national or local associations.<br />
Content<br />
ANA-<strong>Vermont</strong> welcomes unsolicited manuscripts and<br />
suggestions for articles. Manuscripts can be up to:<br />
• 750 words for a press release<br />
• 1500 words for a feature article<br />
Manuscripts should be typed double-spaced and spell-checked<br />
with only one space after a period and can be submitted:<br />
1) As paper hard copy<br />
2) As a Word Perfect or MS Word document file saved to a<br />
CD-Rom or zip disk<br />
3) Or e-mailed as a Word Perfect or MS Word document file to<br />
<strong>Vermont</strong><strong>Nurse</strong><strong>Connection</strong>@gmail.com.<br />
No faxes will be accepted. Authors’ names should be placed after<br />
title with credentials and affiliation. Please send a photograph of<br />
yourself if you are submitting a feature article.<br />
All articles submitted to and/or published in <strong>Vermont</strong> <strong>Nurse</strong><br />
<strong>Connection</strong> become the sole property of ANA-<strong>Vermont</strong> and may not<br />
be reprinted without permission.<br />
All accepted manuscripts may undergo editorial revision to conform<br />
to the standards of the newsletter or to improve clarity.<br />
The <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> is not a peer review publication.<br />
Articles appearing in this publication express the opinions of the<br />
authors; they do not necessarily reflect views of the staff, board,<br />
or membership of ANA-<strong>Vermont</strong> or those of the national or local<br />
association.<br />
Copyright Policy Criteria for Articles<br />
The policy of the ANA-<strong>Vermont</strong> Editorial Board is to retain<br />
copyright privileges and control of articles published in the <strong>Vermont</strong><br />
<strong>Nurse</strong> <strong>Connection</strong> unless the articles have been previously published<br />
or the author retains copyright.<br />
ANA-<strong>Vermont</strong> Officers and Board of Directors<br />
President ...................................Jessilyn Dolan<br />
Vice President ............................. Dionne Heyliger<br />
Secretary ...............................Samantha Gambero<br />
Treasurer ......................................Amy Swarr<br />
Director ....................................Michelle Wade<br />
Director .....................................Susan Shayne<br />
Director ....................................Fritz Asuncion<br />
Delegate Membership Assembly .................Betsy Hassan<br />
Alternative Delegate ........................Cynthia Peterson<br />
ANA-<strong>Vermont</strong> Foundation Board<br />
President ....................................Carol Hodges<br />
Vice President ..............................Christina Olcott<br />
Treasurer ......................................Amy Swarr<br />
Secretary ..................................Christina Olcott<br />
Trustee .....................................Jessilyn Dolan<br />
Trustee ...................................Meredith Roberts<br />
Trustee .....................................Michelle Wade<br />
Trustee ........................................... Vacant<br />
Trustee ........................................... Vacant<br />
VNC Editor<br />
Cynthia Peterson<br />
Committee Chairpersons<br />
Bylaws ........................................Amy Swarr<br />
Finance ........................................Amy Swarr<br />
Government Affairs ..........................Jessilyn Dolan<br />
Membership & Publicity ...................Amy Visser-Lynch<br />
Nominations & Elections ......................Michelle Wade<br />
Programs ......................................... Vacant<br />
Congressional Coordinator for Welch .........Meredith Roberts<br />
Senate Coordinator for Sanders ..............Meredith Roberts<br />
Senate Coordinator for Leahy ...............Meredith Roberts
<strong>August</strong>, September, October <strong>2022</strong> <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> • Page 3<br />
Change your thoughts. Change your life.<br />
“Every great dream begins<br />
with a dreamer. Always<br />
remember, you have within you<br />
the strength, the patience, and<br />
the passion to reach for the<br />
stars to change the world.”<br />
~ Harriet Tubman<br />
Early on in my career I was<br />
recruited into a position as the<br />
HIV Clinical <strong>Nurse</strong> Manager<br />
for an inner-city health center.<br />
One day the director of the<br />
center walked into my office,<br />
sat down and said, “Do you<br />
know some people are like<br />
Priscilla Smith-<br />
Trudeau<br />
trucks stuck in mud?” I sat there flummoxed and tonguetied<br />
waiting for her to continue so that I wouldn’t have<br />
to answer the question. She did continue to vent how the<br />
staff in general didn’t like change. After she left, I began<br />
to ponder if I was a person who didn’t like change. Could<br />
I be or become one of those people? Throughout my<br />
career I have encountered situations where I was asked to<br />
change something or adapt to the changes. When I felt like<br />
resisting the changes being made, I found myself asking<br />
“am I like a truck stuck in mud?”<br />
“Progress is impossible without change, and those who<br />
cannot change their minds cannot change anything.”<br />
~ George Bernard Shaw<br />
As nurses, we have come to understand that the concept<br />
of change is an inevitable part of life and that the way we<br />
practice today is increasingly dynamic. Realizing that<br />
nothing lasts forever is one of the keys to lasting happiness<br />
and peace. The other important factor is knowing what<br />
parts of our lives we can change and what parts we cannot.<br />
We discover in the course of our lives that reality refuses<br />
to bow to our commands. We are forced to let go when we<br />
want to hold on, and to hold on when we want so much to<br />
let go. There are unexpected twists, unwanted endings, and<br />
challenges of every puzzling kind. As nurses we know and<br />
understand that we must change our skills, behaviors, and<br />
ways of working with one another if we are to continue<br />
playing a valuable and meaningful role in our profession.<br />
As scary and difficult as it may be, change forces us to<br />
look at our lives and ourselves, with fresh eyes. Do I need<br />
to change? Do I need to change jobs? What am I looking<br />
for in a job? Am I searching for a job or the work I was<br />
born to do? What is my purpose in healthcare? Do I stay<br />
where I am or do I move on? Robert Quinn, a renowned<br />
expert on deep change suggests that deep change is the<br />
path to self-understanding and the key to revitalization<br />
of an individual. By finding our own moral core and<br />
beginning to see ourselves and our organizations in<br />
new and more productive ways, he explains, we can<br />
transform ourselves from victims to powerful agents of<br />
change. He goes on to say, “We need to look within for<br />
at least two reasons. The first has to do with purpose:<br />
Making fundamental choices about who we are. The<br />
second involves revisiting our fundamental choices and<br />
continuously realigning our behavior accordingly. By<br />
honoring and acting in alignment with our ideals, we grow<br />
within and increase what Gandhi called soul-force. The<br />
clearer we are about ourselves, the greater is our capacity<br />
for change.” i Dr. Mary-Frances Winters suggests in her<br />
book, Only Wet Babies Like Change, that we must first<br />
take a walk with ourselves. This journey of self-reflection<br />
and introspection involves asking the tough questions.<br />
Have I found my authentic self? How do I respond to<br />
change? What do I have to learn, unlearn, and relearn to<br />
find fulfillment in my job? ii Change is the operative word<br />
for successful and resilient nurses. If you can identify the<br />
sources of your resistance to this dynamic atmosphere, you<br />
can work to minimize the negative attitudes and results of<br />
changes you are going through. Equally important, you<br />
can make change your friend, not your enemy. Gandhi was<br />
correct when he said, “You must be the change you wish to<br />
see in the world.”<br />
“If you don’t like something change it. If you can’t change<br />
it, change your attitude.” ~ Maya Angelou<br />
Changes often hurt when they first emerge, but resisting<br />
them goes against the way the world works. Developing<br />
an appetite for the unknown might initially feel like a<br />
reckless act. But being with change is not haphazard. It’s<br />
an intentional practice that takes courage. It invites us to<br />
stand up and explore our lives with vigor, knowing we<br />
will never experience this moment again. As corny as<br />
it sounds, everything really is only here for now. It’s all<br />
ephemeral. When we realize this, we can open our eyes<br />
to what’s in front of us and be present to what is coming<br />
and going. You don’t have to want what’s coming. But<br />
you can always smile knowing that, whatever it is, it too<br />
shall pass. iii You’ll never change your life until you have<br />
stepped out of your comfort zone. It’s only after you’ve<br />
stepped out of your comfort zone that you begin to change,<br />
grow, and transform. Real change can be difficult at the<br />
beginning. Without the familiar to rely upon, you may not<br />
be in as much control as you had once been. When things<br />
are not going your way, you may start doubting yourself. iv<br />
Honoring the unease and discomfort that goes along with<br />
change is important, but taking the initiative to move past<br />
these emotions and master the art of change allows you to<br />
feel like you have agency and power in your life. You don’t<br />
need to be fearful or “just go along for the ride.” In fact,<br />
each and every change you encounter is a new opportunity<br />
for you to be a significant player in shaping the newfound<br />
world you now inhabit. v<br />
“The only way to make sense out of change is to plunge<br />
into it, move with it and join the dance.”<br />
~ Alan Watts English Writer<br />
It’s undeniable that change is integral to our personal<br />
development. You may think of yourself as someone who<br />
doesn’t like change, but it’s important to always remember<br />
that change is inevitable. Many huge career changes will<br />
not stop and ask your permission first. They will happen<br />
with or without your consent. However, there are still<br />
some changes that you can take control of, so it’s better to<br />
embrace the course of change and make it your own along<br />
the way. Choice, not chance, determines destiny. We have<br />
all said at one time or another, I need to change, but can<br />
I? Will I? Do I dare? What will become of my treasured<br />
past, the familiar sameness of my life? In the end as nurses<br />
we know that we will change because we want to achieve<br />
our maximal potential. We want to leave our signature,<br />
though invisible, on others’ lives so that when our career<br />
ends, others will begin. That is a nursing legacy of positive<br />
change.<br />
The ANA-<strong>Vermont</strong> website has been updated:<br />
ANA-<strong>Vermont</strong>.org. We will continue to update and<br />
expand the website.<br />
Do you want to stay updated on the latest ANA-<strong>Vermont</strong> has to offer?<br />
Learn of webinars offered by the ANA?<br />
How you can earn CEU hours?<br />
‘Like Us’ on Facebook. Find us at<br />
https://www.facebook.com/VT<strong>Nurse</strong>s<br />
REASONS WHY<br />
CHANGE IS GOOD<br />
1. IT ALLOWS US TO MOVE FORWARD.<br />
2. IT CAN MAKE US BREAK A<br />
ROUTINE.<br />
3. IT CAN ALLOW US TO THINK OUT OF<br />
THE BOX.<br />
4. IT CAN GIVE US HOPE FOR THE<br />
FUTURE.<br />
5. IT CAN HELP US TO BECOME MORE<br />
FLEXIBLE.<br />
6. IT CAN MAKE US STRONGER<br />
EMOTIONALLY.<br />
7. IT CAN BRING NEW INNOVATIONS<br />
TO LIFE.<br />
8. IT CAN REFRESH OUR ATTITUDE<br />
TOWARDS LIFE.<br />
ADAPTED FROM: HTTPS://WWW.<br />
MINIMALISMMADESIMPLE.COM/HOME/<br />
CHANGE-IS-GOOD/<br />
“The greatest discovery of all time is that a person can<br />
change his future by merely changing his attitude.”<br />
~ Oprah Winfrey<br />
Priscilla Smith-Trudeau, MSM, RN, BSN, CCM,<br />
CRRN, HNB-BC is board certified in holistic nursing<br />
and board certified in rehabilitation nursing. She has<br />
been a nurse for forty-five years and understands the<br />
interconnectedness of body, mind and spirit. She brings<br />
a comprehensive holistic and integrative approach to her<br />
practice for providing whole person care.<br />
i Quinn, R. E. (1996). Deep change: Discovering the leader<br />
within. Jossey-Bass, San Francisco, CA<br />
ii Winters, M.F., (2002). Only Wet Babies Like Change.<br />
Winters Group, Inc., St. Paul, MN<br />
iii Smookler, E., (2017). Why change is your greatest ally.<br />
Retrieved April 22, <strong>2022</strong> from: https://www.mindful.org/<br />
change-greatest-ally/<br />
iv Bennett, R., (2021). The Light in the Heart. Published by<br />
author<br />
v Koffler, T. (2017). The art of easing into change. Retrieved<br />
May 4, <strong>2022</strong> from: https://www.mindful.org/art-easingchange/<br />
South Burlington School District<br />
Seeking School <strong>Nurse</strong>s, <strong>Nurse</strong> Assistant, and<br />
Substitute <strong>Nurse</strong>s for the <strong>2022</strong>-2023 School Year<br />
RN: Full, part-time and on-call positions available. Provides health services and maintains<br />
records. A BSN from an accredited program, current RN license, and must hold/eligible for an<br />
Educator’s license in school nursing. Experience with school-aged population is preferred.<br />
LPN/Health Assistant: Under the direction of the School <strong>Nurse</strong>, provides health<br />
services and maintains records. Current Licensed Practical <strong>Nurse</strong> (LPN), Registered<br />
<strong>Nurse</strong> (RN), or EMT certified. Experience with adolescent aged students is preferred.<br />
Please apply through SchoolSpring.com, Keyword: South Burlington<br />
School District or contact Elissa Galvez, HR Employment Specialist<br />
at 802/652-7247 or egalvez@sbschools.net.<br />
Questions regarding our social media and website?<br />
E-Mail: vtnurse@ana-vermont.org<br />
SFC Theodore P. Provost<br />
AMEDD Specialty Branch Manager<br />
theodore.p.provost.mil@mail.mil<br />
802-338-3405
Page 4 • <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Sigma Theta Tau International:<br />
Omega Mu At-Large Chapter<br />
Updates<br />
By Susan Shayne, BSN, RN, CPPS<br />
Sigma Theta Tau International is celebrating 100 years of excellence on October<br />
5th this year. Chapters across the world will partner to showcase and celebrate the<br />
achievements of our organization. <strong>Vermont</strong>’s Omega Mu At-Large Chapter has many<br />
reasons to celebrate including successfully launching a chapter on Oct 6, 2019 and<br />
immediately being thrown into the pandemic. The lessons learned and challenges we<br />
faced have made us a stronger and more cohesive chapter with members from across the<br />
state and numerous practice settings. Stay tuned for more information on how we will be<br />
celebrating this year.<br />
<strong>Vermont</strong> Technical College and Norwich faculty banded together to bring Sigma and<br />
its membership benefits to their nursing students and nurse leaders. Starting out as the<br />
Greater <strong>Vermont</strong> Nursing Honor Society and working with Sigma leadership we were<br />
able to grow our honor society to 50 student and nurse leader members and worked<br />
to meet the rigorous standards to become our own STTI chapter. We were thrilled to<br />
become chartered in 2019 as the Omega Mu At-Large Chapter. Recently, we extended<br />
membership to Castleton University nursing students in order to support more nurses<br />
across the state in joining and benefitting from Sigma membership. Sigma Theta Tau<br />
International Nursing Honor society welcomes baccalaureate and graduate nursing<br />
students by invitation, or nurse leader members by application. You can apply online<br />
today at: https://join.sigmanursing.org or you can view our chapter website here: http://<br />
omegamu.sigmanursing.org/.<br />
One of our goals as a chapter is to increase the number of nurse leaders and this year<br />
have happily extended membership to six new nurse leaders. We are proud to announce<br />
that we currently have 147 members, 38 members living outside of <strong>Vermont</strong>, and one<br />
member is a Virginia Henderson Fellow. You can learn more about becoming a Virginia<br />
Henderson Fellow here: https://www.sigmanursing.org/docs/default-source/Foundation-/<br />
vhf-brochure---low-res-updated.pdf?sfvrsn=2.<br />
We encourage nurse leaders who promote healthy communities through education,<br />
research, and volunteer projects that transform healthcare locally and ultimately globally<br />
to apply online today to join us at https://join.sigmanursing.org by selecting “I am a nurse<br />
leader” on the webpage.<br />
Leaders increase diversity in an organization and can act as mentors assisting<br />
colleagues in promoting evidence-based practice and research and encouraging bravery<br />
to implement change (Wei & Horton-Deutch, <strong>2022</strong>). Leader mentoring is important<br />
work and supports new nurses as they embark on their journey in a very changeable<br />
environment. In mentoring, leaders are able to educate, model, and encourage nurses to<br />
collaborate, publish, engage in research, and develop relationships that support policy<br />
and practice. In doing this work and sharing information, news, and activities between<br />
Sigma chapters and our American <strong>Nurse</strong>s Association we strengthen all of our work.<br />
Sigma Theta Tau International provides a structured onboarding process that creates<br />
a succession plan to promote learning from each other; this includes an orientation to<br />
offices held and can encourage members to develop skills by participating in task forces<br />
and committees. Members also have access to many free or discounted continuing
<strong>August</strong>, September, October <strong>2022</strong> <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> • Page 5<br />
nursing education credits. Our new nurses have access to<br />
“Surviving Your First Years as a <strong>Nurse</strong>” and free online<br />
journal access that provides free contact hours.<br />
At the Spring Induction meeting, we hosted Dr. Sandra<br />
C. Garmon Bibb, DNSc, RN, FAAN Sigma Presidentelect,<br />
who passionately discussed this year’s Sigma’s<br />
missions and goals to twenty-four inductees. This set the<br />
stage for the installation of new board Omega Mu at-Large<br />
members <strong>2022</strong>-2023:<br />
• Paulette Thabault, President<br />
• Susan Shayne, Vice President<br />
• Karen McKenny, Treasurer<br />
• Mary Hill, Secretary<br />
• Carolyn Stannard-Carlo, Faculty Counselor -<br />
<strong>Vermont</strong> Technical College<br />
• Corey Bennett, Faculty Counselor - Norwich University<br />
• Virginia Kittell, Awards Committee, Char<br />
• Linda Havey, Governance Committee, Chair<br />
• Julie Jones, Membership Involvement Committee,<br />
Chair<br />
• Leadership Succession Committee Members: Jason<br />
Kirchick and Lisa Fox<br />
• Governance Committee Members: Jess Sherman and<br />
Ann Laramee<br />
The Strategic planning committee of the board also met<br />
to review specific goals to fulfill the mission and vision<br />
of Omega Mu at-Large for the next three, five, and ten<br />
years. Ideas included: community service, scholarship and<br />
research, programming, chapter benefits, communications,<br />
leadership development, financial, recruitment, and<br />
networking. The Omega Mu at-Large Membership will<br />
be surveyed soon to help direct the work they would like<br />
our chapter to undertake and how to get involved. We will<br />
narrow down our goals based on member feedback and<br />
how we can meet the needs as chapter leaders.<br />
In early <strong>2022</strong>, the board sent a survey to members to<br />
find out what our members were looking for in terms of<br />
programming. This review netted some of the following<br />
results: 54.5% of respondents attended an event last year,<br />
86.6 % wanted professional growth and development, and<br />
50% enjoyed the in-person networking we missed over the<br />
last few years. We will use this information and more as a<br />
planning guide moving forward.<br />
Decision Making Regarding Surgical Attire Guidance<br />
Adherence-Beyond New England” by Carole “Gert” Mayes,<br />
Ph.D., RN, NPD-BC, CNOR. Dates will be provided soon<br />
for their 2023 presentations to the membership.<br />
Sigma Theta Tau and the <strong>Vermont</strong> American <strong>Nurse</strong>s<br />
Association are hand in hand in supporting nurses across<br />
the state and having an impact on the health of all of our<br />
populations. <strong>Nurse</strong>s continue to be on the front line, in the<br />
board room, at the decision-making table, in the legislature, the<br />
classroom, hospital, public health department, senior housing,<br />
the list goes on and on. We are brave, bold, and know how to<br />
pull together to gather and share our expertise, our evidenced<br />
based practice, and to support each other as we move through<br />
these challenging times in healthcare and in our profession.<br />
Reference:<br />
Wei, H., & Horton-Deutsch, S. (<strong>2022</strong>). Visionary leadership in<br />
healthcare: Excellence in practice, policy and ethics. Sigma<br />
Theta Tau International.<br />
Susan Shayne, BSN, RN, CPPS has extensive experience<br />
in supporting nursing students and faculty in advocating<br />
for innovative clinical experiences and professional<br />
development. She holds a breadth of healthcare experience<br />
to include specialized pain management and regulatory<br />
compliance. Additionally, she hold specialty certification<br />
as a Certified Professional in Patient Safety. Susan is a<br />
Director on the ANA-<strong>Vermont</strong> Board of Directors and is the<br />
Sigma Theta Tau Omega Mu Chapter Vice President.<br />
The Medical Reserve<br />
Corps of SW <strong>Vermont</strong><br />
Thank you to all the volunteer nurses<br />
and clinicians who joined our Unit<br />
during COVID19 and helped <strong>Vermont</strong> be<br />
the national leader in State vaccinations.<br />
Come join our Unit and be ready for the next emergency or<br />
pandemic! Great training, teamwork and opportunities to<br />
help <strong>Vermont</strong>ers.<br />
Sign-up Today!<br />
VT Health RMS (vermont.gov) | 802-447-6401<br />
In the meantime, here are a few Omega Mu Save the<br />
Dates:<br />
• Walk to End Alzheimer’s at the Shelburne Museum<br />
September 18th: https://act.alz.org/site/TR/<br />
Walk<strong>2022</strong>/VT-<strong>Vermont</strong>?pg=entry&fr_id=15950<br />
• Breast Cancer Making Strides in South Burlington<br />
on October 9th: https://bit.ly/TeamJulieStrides<br />
• Breast Cancer Making Strides in Castleton on<br />
October 16th: https://secure.acsevents.org/site/<br />
STR?fr_id=102813&pg=personal&px=58057998<br />
We are also planning on our fall induction to name<br />
a few upcoming events. Please look for upcoming<br />
communications regarding these events on our Facebook<br />
page https://www.facebook.com/groups/2120701528180899/,<br />
newsletter, and email communication.<br />
The Omega Mu at-Large Chapter also awarded two<br />
research grants this year for research conducted by our<br />
members: “Changing Minds, Changing Lives for <strong>Vermont</strong><br />
<strong>Nurse</strong>s” by Cynthia Peterson, MSN, RN, and an honorable<br />
mention for “Exploring Intraoperative Team Members’<br />
• Inpatient Medical Surgical Unit<br />
• Charge RN- Emergency Room<br />
• Primary Care<br />
• Operating Room<br />
• Maternal/Child Health<br />
• PACU<br />
• ER RN<br />
Voices of <strong>Vermont</strong> <strong>Nurse</strong>s<br />
premiered at VSNA Convention 2000 and<br />
is available from the ANA-<strong>Vermont</strong> Office at:<br />
ANA - <strong>Vermont</strong><br />
4 Carmichael Street, Suite 111, #215<br />
Essex, VT 05452<br />
Price: $20 each book<br />
(plus $3.95 for postage and handling)<br />
Make check or money order payable to:<br />
VERMONT STATE NURSES FOUNDATION<br />
Name: _____________________________________<br />
Address: ___________________________________<br />
City: _______________________________________<br />
State: __________________ Zip: _______________
Page 6 • <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
ANA VT Membership Assembly continued from page 1<br />
and re-elect nurse champions to public office. It's critically<br />
important - now more than ever - to make sure nurses have<br />
a seat at the table.<br />
At one point during opening comments, immediately<br />
after a new nurse professed how nervous she was to speak<br />
out, I joyfully reminded the entire room to “Speak up,<br />
even if your voice shakes,” and thanked the new nurse,<br />
everyone in the room, and ANA for their service and<br />
advocacy.<br />
Together, we highlighted and celebrated the work<br />
that ANA has been doing with a hearing on our recently<br />
released ANA Racial Reckoning Statement which you can<br />
view here: https://www.nursingworld.org/practice-policy/<br />
workforce/racism-in-nursing/RacialReckoningStatement/<br />
After a report by the Nominations and Elections<br />
Committee, President Grant again entertained and<br />
educated us all with his elegant and elevating words.<br />
Detailed, concise reports by several ANA Subsidiaries<br />
and Constituent Associations helped us understand our<br />
partnerships and colleagues in the American Academy<br />
of Nursing, American Nursing Credentialing Center,<br />
American <strong>Nurse</strong>s Foundation, and National Student<br />
<strong>Nurse</strong>s Association.<br />
Reports from the ANA Chief Nursing Officer, ANA<br />
Treasurer, and ANA Vice President finished the morning<br />
leaving everyone ready for more, excited for the future of<br />
nursing, and reveling in all that ANA has accomplished.<br />
After lunch, we participated in several dialogue<br />
forums: Impact of Climate Change on Health, Advancing<br />
Solutions to Address Verbal Abuse and Workplace<br />
Violence Across the Continuum of Care, and <strong>Nurse</strong><br />
Staffing. These forums were ripe with discussion and<br />
debate as nurses from all across the country shared their<br />
thoughts, concerns, and aspirations.<br />
<strong>Vermont</strong>’s representatives urged the ANA to be<br />
mindful of “zero tolerance” language in Advancing<br />
Solutions to Address Verbal Abuse and Workplace<br />
Violence Across the Continuum of Care in regards to<br />
certain patient populations - such as children living with<br />
Autism, or adults living with Dementia.<br />
Voting delegates and board representatives of each<br />
state voted in support of all forums.<br />
That evening, we had another Candidate Forum<br />
to meet and greet those running for ANA, which was<br />
followed by Regional Meetings and an ANA-PAC<br />
Reception.<br />
Day two started off with your President and delegate<br />
proudly representing you and <strong>Vermont</strong> nurses, and voting<br />
to choose our new officials!<br />
The APRN Task Force met to work on “Enterprise:<br />
Tools to Dismantle APRN Practice Barriers.”<br />
It wouldn't be a nursing conference without discussing<br />
the impact and implications of COVID-19. We also heard<br />
a warm and heartfelt greeting from the International<br />
Council of Nursing (ICN) President with a message to all<br />
nurses about how important “influence” is and continues<br />
to be, as well as highlighting <strong>Nurse</strong>s For Peace and the<br />
efforts to support Ukraine.<br />
Our own ANA CEO spoke about ANA and nurses as<br />
having emerged from the COVID-19 pandemic stronger<br />
and more determined to achieve our vision and strategic<br />
plan, citing three E’s: Elevate, Engage, and Evolve.<br />
The second morning wrapped up with a Recognition<br />
of Outgoing Members on the ANA Board of Directors,<br />
a Nightingale Tribute, and announcements by ANA Vice<br />
President.<br />
At lunchtime, participants had the option to<br />
participate in one of several meetings: Amplifying the<br />
Voice of the <strong>Nurse</strong>, Addressing the US Opioid Crisis,<br />
The Role of State Nursing Leaders as Instrumental<br />
Stakeholders Feedback Opportunity, Revision of the<br />
Nursing Administration, or Scope and Standards of<br />
Practice<br />
The second day concluded with a Report of the ANA<br />
Professional Policy Committee and Head Teller. Newly<br />
elected officials were also recognized and honored.<br />
<strong>Nurse</strong>s were also given the opportunity to share both<br />
new business and issues they would like to engage in<br />
including reproductive freedom, gun rights, and inclusive<br />
language for LGBTQIA+ individuals.<br />
Closing remarks by the ANA President again left<br />
everyone teary-eyed, laughing, and enlightened. A roomshaking<br />
karaoke to “We Are Family” infused the room<br />
with energy and offered a powerful conclusion to an<br />
amazing and exciting two days!<br />
Join Our Team &<br />
Make a Difference!<br />
All people share a powerful need for the basic necessities of a<br />
good life and a place that understands that good health starts<br />
with a caring touch and a kind word. For over 50 years, the<br />
Community Health Centers of Burlington (CHCB) has provided<br />
access to high quality health care regardless of financial status or<br />
life circumstance. We strive to improve the health of all within the<br />
communities we serve in an environment that conveys respect,<br />
offers support, and encourages people to be actively involved in<br />
their own health care.<br />
<strong>Vermont</strong> <strong>Nurse</strong>s at Membership Assembly<br />
CHCB is an innovative Federally Qualified Health Center with<br />
sites throughout Chittenden County and southern Grand<br />
Isle County. We are an Equal Opportunity Employer and are<br />
especially interested in candidates who can contribute to the<br />
diversity and excellence of the organization.<br />
CHCB is growing and so is our<br />
nursing team!<br />
We have opportunities for<br />
Registered <strong>Nurse</strong>s, <strong>Nurse</strong> Educators,<br />
Clinical <strong>Nurse</strong> Supervisors,<br />
and more!<br />
Come join our mission-minded,<br />
collaborative, and creative team!<br />
Apply now on our Career Center at<br />
CHCB.ORG/CAREERS
<strong>August</strong>, September, October <strong>2022</strong> <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> • Page 7<br />
Celebrating <strong>Vermont</strong>’s <strong>Nurse</strong>s<br />
– Islane Louis, MSN, PMH-BC<br />
By Betsy Hassan, DNP, RN, NEA-BC, CPPS<br />
On May 13th, <strong>2022</strong> Islane Louis, MSN, PMH-BC was recognized by the <strong>Nurse</strong>s with<br />
Global Impact, Inc. at their 6th Annual <strong>Nurse</strong>s with Global Impact International <strong>Nurse</strong>s<br />
Day event for her work spanning 15 years of nursing.<br />
Islane began her international nursing work in 2007 while living in Haiti. She was<br />
practicing close to a nearby village that had no access to pediatric care. She became<br />
aware of Dr. Karen Schneider, Assistant Professor from Johns Hopkins University School<br />
of Medicine who participated in Mercy Medical Missions, Inc. in Haiti. This connection<br />
and mentorship with Dr. Schneider propelled Islane’s efforts in developing mobile<br />
pediatric clinics, implementing pediatric home visits, providing financial resources for<br />
medical interventions, and providing much needed care to the children of Haiti.<br />
Over her 15 years in this work Islane has had an incredible impact on patients,<br />
families and healthcare teams in Haiti. While she now lives in <strong>Vermont</strong>, she continues<br />
her connection to Haiti through supporting a nursing school there and hopes to plan to<br />
bring nursing students to Haiti as part of an international clinical experience as she is<br />
also Clinical Nursing Faculty for the University of <strong>Vermont</strong> College of Nursing.<br />
In asking Islane what she is most proud of she states, “Honestly, everything I do is<br />
what I am supposed to be doing. I never feel like I’m doing anything extraordinary. I am<br />
most proud of being able to make a difference, even it’s just providing hope to someone<br />
who is hopeless. I am privileged to be a part of their journey.” Islane’s humbleness is a<br />
testament to her benevolent character and aligns with nursing’s greatest work – caring for<br />
those most in need.<br />
<strong>Vermont</strong> is fortunate that Islane chose this as her home and her place of nursing<br />
practice. Our patients, families, nursing students, and communities benefit from her<br />
experience, expertise, and dedication to advancing nursing practice. Congratulations<br />
Islane – so well deserved!<br />
Benefit Bakes Fundraiser<br />
On Tuesday, May 17th the ANA-<strong>Vermont</strong> partnered with American Flatbread in<br />
Burlington for a Benefit Bake night! The Benefit Bake proceeds provide aid in funding<br />
the ANA-<strong>Vermont</strong> Annual Nursing Conference later this fall. Through the generosity of<br />
our community, the ANA-<strong>Vermont</strong> will continue to provide professional development<br />
and continuing education opportunities for <strong>Vermont</strong> <strong>Nurse</strong>s. Thank you for everyone that<br />
came out on May 17th and supported the ANA-<strong>Vermont</strong>!<br />
Pictured here Cynthia Peterson, MSN, RN, CCRN, ANA-<strong>Vermont</strong> <strong>Vermont</strong><br />
<strong>Nurse</strong> <strong>Connection</strong> Editor and Betsy Hassan, DNP, RN, NEA-BC, CPPS,<br />
ANA-<strong>Vermont</strong> Board of Directors<br />
Your next opportunity is at the <strong>Vermont</strong><br />
Veterans’ Home!<br />
We invite you to become part of our health-care<br />
team where we focus on resident-centered care<br />
fulfilling America’s promise to care for our country’s<br />
Veterans, their Spouses, and Gold Star Parents.<br />
Together we strive to create an environment that<br />
provides our residents with the dignity and respect<br />
that they so rightfully deserve.<br />
Pictured here is Islane Louis, MSN, RN, PMH-BC on May 13th, <strong>2022</strong> at the<br />
<strong>Nurse</strong>s with Global Impact, Inc. International <strong>Nurse</strong>s Day event in<br />
New Jersey!<br />
Nursing Employment Opportunities<br />
Licensed Nursing Assistant –<br />
Job Posting ID #32202<br />
Licensed Practical <strong>Nurse</strong> –<br />
Job Posting ID #32242<br />
Registered <strong>Nurse</strong> I – Job Posting ID #32264<br />
Registered <strong>Nurse</strong> II – Job Posting ID #32302<br />
<strong>Nurse</strong> Supervisor –<br />
Job Posting IDs #34301, 32262, 32263<br />
For more information on the above openings or other<br />
opportunities, contact Joyce.Santacross@vermont.gov.<br />
<strong>Vermont</strong> Veterans’ Home website:<br />
https://vvh.vermont.gov<br />
State of <strong>Vermont</strong> careers website:<br />
https://humanresources.vermont.gov/careers<br />
The State of <strong>Vermont</strong> offers an excellent total compensation package. To apply, you must use the online job application at https://careers.<br />
vermont.gov. For questions related to your application, please contact the Department of Human Resources Recruitment Services at<br />
(800) 640-1657 (voice) or (800) 253-0191 (TTY/Relay Service). The State of <strong>Vermont</strong> is an Equal Opportunity Employer.
Page 8 • <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
US Supreme Court’s Decision<br />
to Overturn Roe vs. Wade:<br />
Is a Serious Setback for<br />
Reproductive Health and<br />
Human Rights<br />
SILVER SPRING, MD – The American <strong>Nurse</strong>s Association (ANA) is dismayed by<br />
the 6-3 ruling of the U.S. Supreme Court in Dobbs v, Jackson Women’s Health which has<br />
overturned the longstanding and significant precedent of Roe v. Wade. The Dobbs ruling<br />
removes the right of all women to access high-quality health care and make personal<br />
decisions about their sexual and reproductive health care. In doing so, it potentially<br />
paves the way for laws that will fundamentally come between patients and health care<br />
professionals, including nurses, who must be guided by ethical obligations to their<br />
patients and the profession.<br />
“ANA is deeply disappointed in the decision to upend Roe v. Wade, which we view<br />
as a legal protection of basic reproductive health rights and human rights,” said ANA<br />
Enterprise CEO Loressa Cole, DNP, MBA, RN, FAAN, NEA-BC.<br />
<strong>Nurse</strong>s have an ethical obligation to safeguard the right to privacy for individuals,<br />
families, and communities, allowing for decision making that is based on full<br />
information without coercion. As the largest group of health care professionals, nurses<br />
have for decades assisted their patients with weighing the benefits, burdens, and available<br />
options, including the choice of no treatment, when discussing sexual health issues and<br />
pregnancy. ANA firmly believes that no nurse should be subject to punitive or judicial<br />
processes for upholding their ethical obligations to their patients and profession.<br />
In March <strong>2022</strong>, ANA affirmed that abortion is a reproductive health alternative<br />
that nurses can discuss when counseling patients. <strong>Nurse</strong>s have a duty to respect the<br />
decisions of their patients, including those decisions that are related to sexual health<br />
and pregnancy. Respect for patient decisions does not mean that the nurse must agree or<br />
support the decision. <strong>Nurse</strong>s can exercise their right to refuse to participate in sexual and<br />
reproductive health care based on ethical grounds, as long as patient safety is assured and<br />
care by others has been arranged.<br />
“No matter their philosophical differences or belief systems, all nurses must strive<br />
to remain consummate health care professionals and display empathy and respect<br />
to all,” said Cole. “This is a complicated issue and deeply personal for all, including<br />
nurses. <strong>Nurse</strong>s, leaders, all health care professionals, and the public must engage on this<br />
issue with empathy and respect.”<br />
ANA will continue to advocate for reproductive justice and sexual health that supports<br />
a patient’s decision and rights in a just society.<br />
###<br />
The American <strong>Nurse</strong>s Association (ANA) is the premier organization representing<br />
the interests of the nation's 4.3 million registered nurses. ANA advances the profession<br />
by fostering high standards of nursing practice, promoting a safe and ethical work<br />
environment, bolstering the health and wellness of nurses, and advocating on health care<br />
issues that affect nurses and the public. ANA is at the forefront of improving the quality<br />
of health care for all. For more information, visit www.nursingworld.org.<br />
have thousands<br />
We<br />
nursing jobs!<br />
of<br />
Find your dream job now.<br />
Springfield is nestled in the Connecticut River Valley, a short drive<br />
to lakes, mountains and the ocean. Whether your preference is<br />
hiking or skiing; biking or walking; sunbathing or sailing – or doing<br />
nothing at all – you don’t have far to go to find it in Springfield.<br />
Find Your New Career!<br />
Now hiring Registered <strong>Nurse</strong>s in the<br />
Emergency Department, Inpatient Care<br />
Unit, and Windham Center.<br />
If you are looking for new career<br />
opportunities, working with a team that is<br />
changing healthcare in new and exciting<br />
ways, visit springfieldhospital.org/careers<br />
or scan the QR code to apply today.
<strong>August</strong>, September, October <strong>2022</strong> <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> • Page 9<br />
Celebrating ONL’s <strong>2022</strong> Award<br />
Recipients<br />
The Organization of <strong>Nurse</strong> Leaders has been recognizing the many contributions<br />
and achievements of nurse leaders since 1982. This year, four <strong>Vermont</strong> nurses<br />
received awards. Please join us in congratulating the following nurse leaders on their<br />
achievements:<br />
ANA-<strong>Vermont</strong> - Representing<br />
<strong>Vermont</strong> <strong>Nurse</strong>s: <strong>Vermont</strong><br />
Commission on Women<br />
By Betsy Hassan, DNP, RN, NEA-BC, CPPS<br />
• Carol Conroy, DNP, RN, FAAN received the <strong>2022</strong> Mary B. Conceison Award<br />
which recognizes the outstanding contributions of a nursing service administrator.<br />
Dr. Conroy is a longtime ONL member and recently served as ONL President.<br />
Congratulations to Carol on this well-deserved award!<br />
• Susan Boyer, DNP, MEd, RN, NPD-BC, FAAN received the <strong>2022</strong> Pamela Leigh<br />
Vecchiarino award which recognizes nurse leaders who are patient-focused change<br />
agents committed to improving outcomes. Dr. Boyer was selected to receive this<br />
award based on her leadership, entrepreneurial approach, and scope of impact in<br />
her practice. Congratulations, Dr. Boyer!<br />
• Betsy Hassan, DNP, RN, NEA-BC, CPPS received one of the <strong>2022</strong> Sharon A.<br />
Smith Scholarship Awards this year. Betsy was selected as a recipient of this award<br />
that honors the legacy left by Sharon A. Smith to support nurse leader development<br />
and continued educational journeys. Betsy is currently pursuing a Master of Legal<br />
Studies at Seton Hall University School of Law. Congratulations, Betsy, on this<br />
scholarship award!<br />
• Cynthia Peterson, MSN, RN, CCRN received one of the <strong>2022</strong> Sharon A. Smith<br />
Scholarship Awards this year. Cynthia was selected as a recipient of this award<br />
that honors the legacy left by Sharon A. Smith to support nurse leader development<br />
and continued educational journeys. Cynthia is currently pursuing her PhD in<br />
nursing at the University of Massachusetts Amherst and a graduate certificate in<br />
Healthcare Administration from Champlain College. Congratulations, Cynthia, on<br />
this scholarship award!<br />
The <strong>Vermont</strong> Commission on Women (VCW) was founded in 1964 by Governor<br />
Philip Hoff. Nearly 60 years later, the <strong>Vermont</strong> Commission on Women is governed<br />
by 16 Commissioners appointed by the Governor, Speaker of the House, or the Senate<br />
Committee on Committees, and has an Advisory Council of 27 representatives of<br />
organizations serving women and girls in <strong>Vermont</strong>. 1 The <strong>Vermont</strong> Commission<br />
on Women purpose is “to advance rights and opportunities for women and girls in<br />
<strong>Vermont</strong>.” In supporting this purpose the VCW:<br />
• “conducts research and study of issues affecting the status of women in <strong>Vermont</strong>;<br />
• advises and consults with the executive and legislative branches of State<br />
government on policies affecting the status of women in <strong>Vermont</strong>;<br />
• educates and informs business, education, State and local governments, and the<br />
general public about the nature and scope of sex discrimination and other matters<br />
affecting the status of women in <strong>Vermont</strong>;<br />
• serves as a liaison and clearinghouse between government, private interest groups,<br />
and the general public concerned with services for women.” 1<br />
The ANA-<strong>Vermont</strong> serves as a member of the Advisory Council to the <strong>Vermont</strong><br />
Commission on Women. In this role the ANA-<strong>Vermont</strong> Advisor participates in<br />
meaningful dialogue on a monthly basis and adds the unique perspective of the nursing<br />
paradigm. Meetings occur monthly from September to June. If you’d like to learn more<br />
visit the website at https://women.vermont.gov/who_we_are.<br />
Betsy Hassan, DNP, RN, NEA-BC, CPPS is a board certified nurse leader and<br />
holds a doctorate of nursing practice from the MGH Institute of Health Professions.<br />
She represents <strong>Vermont</strong> <strong>Nurse</strong>s perspectives as an Advisory Council member to the<br />
<strong>Vermont</strong> Commission on Women. Her professional areas of expertise include workforce<br />
development, professional development, shared decision making, and leadership.<br />
1 About Us | Commission on Women (vermont.gov)
Page 10 • <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Marilyn Rinker Memorial<br />
Scholarship<br />
Marilyn Rinker Leadership Scholarship Application<br />
Application – 2023 deadline: March 25, 2023<br />
Name: ______________________________________________________________<br />
Address: _____________________________________________________________<br />
Telephone #: _____________________ Email Address: _______________________<br />
Vt RN Lic #______________________ VONL member since __________________<br />
School of Nursing: _____________________________________________________<br />
Currently in which year? 1 2 3 4 year of graduation (if applicable) ________________<br />
Graduate school ________________________ 1st yr __________ 2nd year__________<br />
expected date of graduation_______________<br />
If employed in nursing, current employer ___________________________________<br />
Currently receiving Financial Aid, Grants, Scholarships? Yes ________ No ________<br />
If yes please list the sources_______________________________________________<br />
Please attach to this form:<br />
1. Résumé<br />
2. Most recent transcript of grades demonstrating a cumulative average of 3.0 (B)<br />
3. A brief essay (500 words or less) describing nursing leadership experience and<br />
aspirations, community service experience, commitment to serve in <strong>Vermont</strong>,<br />
and financial need<br />
4. At least two (2) letters of recommendation (at least one academic and one work<br />
related)<br />
5. Evidence of acceptance in an accredited program leading to an advanced degree<br />
in nursing if not yet matriculated.<br />
I understand that if I receive an Advanced Degree <strong>Nurse</strong> Leaders<br />
Scholarship, I commit to practice nursing in <strong>Vermont</strong> for a minimum period<br />
of two years following graduation.<br />
Student signature: _______________________________ Date: __________________<br />
Return application (with attached materials) before March 25, 2023 to:<br />
Martha Buck, VAHHS/VONL<br />
148 Main Street, Montpelier, VT 05602<br />
(802)223-3461/ext. 111 Martha@vahhs.org<br />
The Marilyn Rinker Memorial Scholarship Award was established by the <strong>Vermont</strong><br />
Organization of <strong>Nurse</strong> Leaders in 2009 to honor Marilyn’s lifelong commitment and<br />
dedication to professional nursing practice, nursing education and leadership. Marilyn<br />
held many leadership positions during the course of her career such as Nursing<br />
Director for Medicine and Cardiology at Fletcher Allen Health Care (University of<br />
<strong>Vermont</strong> Medical Center); Oncology Clinical Coordinator at the <strong>Vermont</strong> Regional<br />
Cancer Center; Clinical Research <strong>Nurse</strong> and Educator in <strong>Vermont</strong> and Rhode Island;<br />
and, BSN Nursing Program Director at Norwich University. Marilyn also served as<br />
the Executive Director of the <strong>Vermont</strong> State <strong>Nurse</strong>s’ Association and President of the<br />
<strong>Vermont</strong> Organization of <strong>Nurse</strong> Leaders.<br />
This award provides scholarship support in the amount of $1000 for a qualified<br />
registered nurse to participate in an approved course of study leading to an advanced<br />
degree with an emphasis in nursing leadership.<br />
Application Criteria for the Marilyn Rinker Memorial Award<br />
1. Current member of ONL<br />
2. Registered nurse or advanced practice registered nurse currently licensed in the<br />
state of VT*<br />
3. Demonstrated commitment to nursing leadership as evidenced by participation<br />
in professional seminars, organizations, work accomplishments, project,<br />
recommendations of peers<br />
4. Currently enrolled or accepted in an accredited program that will lead to an<br />
advanced degree in nursing<br />
5. Willingness to commit to completing the program as indicated by realistic<br />
timeframe.<br />
6. GPA of 3.0 or the equivalent<br />
7. Two (2) supportive professional recommendations<br />
8. A double-spaced, short essay (500 words or less) of the reasons this nominee<br />
should receive the award according to the criteria listed above<br />
9. Nominee’s current Curriculum Vitae<br />
Nominations must be submitted by March 25, 2023. Annual scholarship award<br />
announcement will be made at the member reception and awards gala at the ONL<br />
Annual Meeting.<br />
*<strong>Vermont</strong> RNs will receive first priority. Applicants from other states will be<br />
considered if there are no applicants from <strong>Vermont</strong> or the scholarship criteria are not<br />
met by applicants from <strong>Vermont</strong>.<br />
https://survey.zohopublic.com/zs/6AbihO<br />
Do you consider yourself a patient champion?! Do you want to create a caring<br />
community, where patients seeking mental health find hope, compassion, and<br />
excellent clinical care? Collaborative Solutions Corporation/Second Spring<br />
Intensive Residential Programs is seeking energetic Registered <strong>Nurse</strong>s, like you,<br />
who are ready to be part of a holistic, collaborative, multidisciplinary team that<br />
is devoted to delivering high-quality residential care to <strong>Vermont</strong>ers with chronic<br />
and persistent mental health diagnoses.<br />
Apply directly to join our team:<br />
brattlebororetreat.org/careers<br />
Start on a Career Path with a Purpose<br />
Inspired by the courage of our patients, the Brattleboro Retreat is dedicated to children, adolescents<br />
and adults in their pursuit of recovery from mental illness, psychological trauma and addiction. We<br />
are committed to excellence in treatment, advocacy, education, research and community service.<br />
In addition to our beautiful campus, nurses enjoy:<br />
• 12 hour shifts<br />
• Competitive pay $34.51- $52.93/hr depending on experience<br />
• Peace of mind working in a safe, low-risk environment for COVID-19<br />
• Extensive clinical orientation<br />
• Collaborative work environment<br />
• Ongoing in-house clinical education<br />
• Training in Six Core Strategies, an evidenced-based framework to reduce<br />
conflict in the inpatient behavioral health setting<br />
• Robust benefits<br />
• Generous signing bonus<br />
Students encouraged to apply! Talk to our RN Recruiter:<br />
Grace Albert-Gardner, BSN, RN: galbertgardner@brattlebororetreat.org<br />
We are looking for <strong>Vermont</strong> RNs with great clinical skills and an even greater<br />
desire to provide compassion and hope to people who have frequently<br />
experienced many difficulties in their lives. We welcome applications from<br />
seasoned professionals and new graduates alike!<br />
A general description for this position is:<br />
• Provide primary and psychiatric nursing care to patients with both chronic<br />
and acute conditions; assess patients for signs and symptoms of mental<br />
illness and their response to treatment<br />
• Participate in daily primary-care in interdisciplinary treatment team<br />
population management planning; review and analyze clinical data to<br />
evaluate the effectiveness of the treatment plans<br />
• Perform disease prevention and infection prevention/control activities<br />
• Perform delegation to unlicensed staff<br />
This position is not for LPN’s, LNA’s, or Traveling <strong>Nurse</strong>s.<br />
Please check out our website to learn more:<br />
https://www.collaborativesolutionsvt.org/
<strong>August</strong>, September, October <strong>2022</strong> <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> • Page 11<br />
ANA-VT<br />
Membership Application<br />
Nursing continues to be the most trusted<br />
profession as indicated in annual surveys. This<br />
attests to the collective contributions nurses make<br />
as they care for patients, families and communities.<br />
Efforts of individual nurses however deserve special<br />
recognition by colleagues, employers, patients,<br />
families and friends. There are many reasons<br />
to Honor a <strong>Nurse</strong> such as: to thank a mentor, to<br />
acknowledge excellent care given by a nurse to a<br />
patient, to celebrate a milestone such as a birthday<br />
or retirement, or to recognize a promotion. Just<br />
think for a moment, you will know a nurse to honor.<br />
Celebration: The honored nurses and the persons<br />
nominating them will be recognized at the ANA-<br />
<strong>Vermont</strong> Convention in <strong>2022</strong>. The honored nurses<br />
each will receive a certificate identifying the person<br />
recognizing her/him as well as the reason for the<br />
honor. Submit nominations by: September 1, <strong>2022</strong>.<br />
All contributions are tax deductible to the full<br />
extent allowed by law. ANA-<strong>Vermont</strong> Foundation<br />
is a 501(c)3 organization. Nominations this year are<br />
online.<br />
Please go here to nominate someone:<br />
https://www.nursingworld.org/foundation/<br />
donate/honor-a-nurse/<br />
NOW ENROLLING FOR FALL 2023<br />
HELEN.PAPEIKA@CASTLETON.EDU<br />
IS YOUR NURSING<br />
ORGANIZATION PLANNING<br />
AN EDUCATION PROGRAM?<br />
CONSIDER APPLYING FOR<br />
CONTACT HOUR APPROVAL<br />
FOR MORE INFORMATION<br />
CALL THE ANA-<strong>Vermont</strong> OFFICE @<br />
(802) 651-8886<br />
The Northeast Multi-State Division, (NE-MSD) is accredited as an<br />
approver of continuing education in nursing by the American <strong>Nurse</strong>s’<br />
Credentialing Center’s Commission on Accreditation.
Page 12 • <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Where Do I Go From Here?<br />
Sharon Broscious, PhD, RN<br />
Program Director South University RN-BSN<br />
Online Program<br />
Reprinted with permission from Virginia <strong>Nurse</strong>s Today,<br />
<strong>August</strong> 2021 issue<br />
As the COVID-19 pandemic winds down, you may be<br />
asking yourself questions about your professional future.<br />
What’s my next career step? What does my professional<br />
future hold for me? The stress of the COVID-19 pandemic<br />
may have created these nagging questions for you, and<br />
you might be unsure what steps you should take to<br />
answer them. The physical, emotional, psychological, and<br />
financial impact of the pandemic on nurses has been well<br />
documented. A plethora of publications in professional<br />
journals and on websites as well as newspaper and television<br />
reports have discussed the impact of the COVID-19<br />
pandemic on nurses. Terms such as burnout, compassion<br />
fatigue, moral injury, PTSD, and healthcare worker<br />
exhaustion are used to describe the physical and mental<br />
effects of COVID-19 on healthcare providers (Chan, 2021;<br />
ICN, 2021). In an interview on NPR, the phrase “crushing<br />
stress” of the COVID-19 pandemic was used (Fortier, 2020).<br />
Not only did the nursing workload change – increased<br />
number of patients per assignment, increased number of<br />
shifts, increased length of workday due to insufficient<br />
staff – but also other factors compounded the stress on<br />
staff. Lack of equipment such as PPE, the unknowns about<br />
the disease itself with policies changing almost daily,<br />
and perceived lack of support from leadership have also<br />
contributed to the COVID effect (ICN, 2021) on nurses.<br />
Some facilities attempted to prepare and support staff for<br />
the pandemic surges, to varying levels of successful impact.<br />
While providing meals to nurses who could not take time<br />
for a meal break was helpful, as the pandemic persisted,<br />
nurses needed more support from their leadership teams.<br />
The recent COVID-19 report released by the<br />
International Council of <strong>Nurse</strong>s (ICN) (2021) describes the<br />
exacerbation of burnout and exhaustion of nurses during<br />
2020. National nursing associations reported approximately<br />
80% of their members identified as feeling stressed. In a<br />
survey of healthcare workers conducted by Mental Health<br />
America (Lagasse, 2020), 93% indicated feeling stressed,<br />
and 76% reported feeling burned out with 55% questioning<br />
their career focus. Similar results were found in a survey<br />
from Brexi (2020) with 84% of responding healthcare<br />
workers identifying some burnout and 18% reporting total<br />
burnout. In addition, almost half had considered quitting<br />
their job, retiring, or changing their career focus. The top<br />
five stressors that respondents identified, in order, were<br />
“fear of getting COVID-19, long hours/shifts, general state<br />
of the world, fear of spreading COVID-19, and family<br />
responsibilities/issues” (Berxi, 2020, para 2). Additional<br />
stressors identified by Shun (2021) include physical,<br />
emotional and moral distress related to ethical issues<br />
faced by nurses such as dealing with patient deaths, scarce<br />
resources, and forced changes in practice.<br />
The 2021 Frontline <strong>Nurse</strong> Mental Health and Well Being<br />
Survey (Trusted Health, 2021) revealed for nurses under<br />
age 40, 22% indicated they were less committed to nursing.<br />
Ninety-five percent of the nurses responding indicated<br />
their physical and mental health were not a priority in their<br />
workplace or the support received from leadership was<br />
inadequate. Finally, 66% of respondents indicated they<br />
were experiencing depression and a decline in their physical<br />
health. A poll by the Washington Post-Kaiser Family<br />
Foundation (2021) indicated 62% of healthcare workers felt<br />
mentally stressed from the pandemic with their greatest<br />
fears of them getting infected, infecting their families, or<br />
other patients. Another challenge identified was working<br />
while wearing PPE (Kirzinger et al., 2021).<br />
Prior to the pandemic, Shah, et al. (2021) reported<br />
burnout was the third leading cause of nurses leaving their<br />
jobs. However, the pandemic intensified levels of stress<br />
and burnout. From the perspective of Maslow’s hierarchy,<br />
Virkstis (2021) described the need for leadership to focus<br />
on basic needs of staff, not high level self-actualization.<br />
The basic needs were identified as: a safe working<br />
environment, clear mission, time to reflect on what was<br />
happening, and time to connect with peers.<br />
Considering the factors identified here, it is no surprise<br />
that you may be asking what is the next step for you in<br />
handling stress, burnout, and career questions.<br />
Step 1 – Do I stay where I am?<br />
You may be asking the following: Do I leave my job as<br />
other nurses have? Do I want to, or can I continue working<br />
where I am? Do I just need some time off?<br />
The first step to take is self-reflection or self-evaluation. If<br />
you are unsure about a change, pause and take some time to<br />
think about it. Consider staying where you are to determine<br />
how your workday has changed after COVID-19 and<br />
whether factors such as workload, staffing, and equipment,<br />
for example, have improved. Remember wherever you go,<br />
everyone will be rebuilding after the pandemic and trying to<br />
return to a previous level of normalcy, or an improved level<br />
based on lessons learned from the pandemic.<br />
Before making a decision, reflect on your job prior to<br />
the pandemic. Was this job a good fit for you? Were you<br />
happy with your job? Answers to these questions can<br />
guide you to remain in your current job to see if those<br />
same positive feelings come back after the pandemic. The<br />
area you work in may not be exactly the same as it was,<br />
but it could be even better. Other reasons leading you to<br />
consider a change may include the work environment,<br />
the leadership of your current unit, or lack of potential<br />
for growth in your current position. This introspective<br />
evaluation provides time to think about other opportunities<br />
or make plans for change if that is your final decision.<br />
Step 2 – Do I change my career path?<br />
There are numerous websites that provide steps to take<br />
when changing your specialty or your role, but the first<br />
step should be:<br />
1. Identify your passion. What makes you happy? Selfreflection<br />
and serious thought can help provide this<br />
answer.<br />
Additional steps to consider include:<br />
2. Complete a SWOT analysis. Guidelines for completing<br />
a SWOT analysis can be found on the internet.<br />
• Identify your strengths: skills, experiences,<br />
education, support from peers/family.<br />
• Identify weaknesses: communication skills,<br />
leadership skills, skills needed for a new path.<br />
• Identify opportunities: What specialty areas might<br />
be of interest? Do you want to be in a hospital
<strong>August</strong>, September, October <strong>2022</strong> <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> • Page 13<br />
or in the community? Do you want to move to<br />
administration or education and have less direct<br />
patient contact? What works for your family?<br />
The Johnson & Johnson Campaign for Nursing’s<br />
Future, provides information about 96 nursing<br />
specialties; this might be a good place to start<br />
looking for new opportunities as it may present some<br />
potential employment ideas you had not previously<br />
considered. A list of more than 100 nursing<br />
organizations is available at https://nurse.org/orgs.<br />
shtml In addition, the Illinois Nursing Workforce<br />
Center web page includes a list of professional<br />
nursing organizations (http://nursing.illinois.gov/<br />
nursingspeciality.asp).<br />
• Identify threats. What barriers exist that might<br />
keep you from making this change – family<br />
responsibilities, work hours desired, access to a<br />
new role in your geographic area, skills or specific<br />
educational background needed. A threat such as<br />
educational level may turn into an opportunity to<br />
return to school.<br />
3. What are your goals in five or ten years?<br />
4. When you have decided on a new role – develop an<br />
action plan or timeline to establish your transition<br />
to the new role. What steps do you need to take to<br />
make this change?<br />
5. Refresh your resume. While you may consider that a<br />
move from pediatrics to geriatrics would not provide<br />
you with appropriate skills, there are many skills<br />
you have that are transferable – your assessment<br />
skills for example, understanding lab results,<br />
providing care to someone who may be unable to<br />
describe how they feel, or organization skills.<br />
6. Network. Talk to someone who currently works in<br />
the specialty you are considering. If the specialty<br />
has a professional organization, peruse their website,<br />
attend a local meeting, or read their journals and<br />
social media networks to help you connect with<br />
nurses in the specialty you are considering.<br />
7. Draw on your support system and mentors to<br />
overcome any barriers/challenges that may be<br />
keeping you from making a change.<br />
8. Resources on the VNA/ANA websites provide<br />
information about available jobs, resume writing,<br />
and interviewing. Scheduling a live meeting with a<br />
career coach is also available.<br />
9. After you have made a specialty change, give<br />
yourself a chance to get acclimated to the new path<br />
you have chosen.<br />
10. Consider staying on good terms with your current<br />
employer. A reference will be needed when applying<br />
for a new position. Staying on good terms may also<br />
be beneficial if the new specialty or organization<br />
change does not work out.<br />
Step 3 – Do I leave nursing and change my profession?<br />
Your reflection may lead you to leaving the nursing<br />
profession. Many of the steps in this process are the same<br />
or similar to the steps above in changing your career path.<br />
1. Begin again with self-reflection/evaluation. What<br />
makes you feel fulfilled? What would you like to do?<br />
What are your interests?<br />
2. Identify areas of interest. There are a number of free<br />
aptitude tests available on the internet that can guide<br />
you in identifying a new career or attend a career<br />
fair. New careers could be with pharmaceutical<br />
companies, insurance companies, the government, or<br />
in education for example.<br />
3. Complete a SWOT analysis<br />
4. What are your goals?<br />
5. Identify the skills/education needed for the new career<br />
6. Develop action plan<br />
7. Network<br />
8. Career counseling – obtain a career coach, see the<br />
VNA/ANA websites<br />
9. Connect with your support system<br />
10. Keep your license current, you may decide at some<br />
point in time you want to return to nursing.<br />
The COVID-19 pandemic has likely changed you<br />
personally and professionally, has certainly changed<br />
healthcare, and has without a doubt changed the world.<br />
What you do to fulfill your life is a priority, so take time<br />
to carefully consider what you want to do and where you<br />
want to be.<br />
As Steve Jobs (2005) said, “Your work is going to<br />
fill a large part of your life, and the only way to be truly<br />
satisfied is to do what you believe is great work. And the<br />
only way to do great work is to love what you do. If you<br />
haven’t found it yet, keep looking. Don’t settle. As with all<br />
matters of the heart, you’ll know when you find it.”<br />
References<br />
Berxi. (December 8, 2020). State of healthcare workers in<br />
2020. Business Wire. https://www.businesswire.com/news/<br />
home/20201208005303/en/<br />
Chan, G.K., Bitton, J.R., Allgeyer, R.L., Elliott, D., Hudson,<br />
L.R., Moulton Burwell, P. (May 31, 2021) The impact of<br />
COVID-19 on the nursing workforce: A national overview<br />
OJIN: The Online Journal of Issues in Nursing 26 (2),<br />
Manuscript 2. DOI:10.3912/OJIN.Vol26No02Man02<br />
Fortier, J. (December 16, 2020). ICU Workers are quitting due<br />
to crushing stress from COVID-19 surge. (Radio broadcast)<br />
Morning Edition – NPR.<br />
International Council of <strong>Nurse</strong>s. (January 13, 2021). The<br />
COVID-19 Effect: World’s nurses facing mass trauma, an<br />
immediate danger to the profession and future of our health<br />
systems.<br />
ICN, https://www.icn.ch/news/covid-19-effect-worlds-nursesfacing-mass-trauma-immediate-danger-profession-andfuture-our<br />
Jobs, S. (June 12, 2005), Stanford Commencement Address.<br />
https://news.stanford.edu/2005/06/14/jobs-061505/<br />
Kirzinger, A, Kearney, A, Hamel, L., & Brodie M. (April 6,<br />
2021). KFF/The Washington Post Frontline Health Care<br />
Workers Survey. https://www.kff.org/report-section/<br />
kff-the-washington-post-frontline-health-care-workers-<br />
survey-toll-of-the-pandemic/?utm_campaign=KFF-2021-<br />
polling-surveys&utm_medium=email&_hsmi=2&_<br />
hsenc=p2ANqtz--iaCcoAuZ0CZUTZn7HHpdxV5L9Fup<br />
s2XQo2KMt8EYKKP_J3ppmXnSGWTPlbCKV22LE_<br />
QkSI0MO__BEFpHKrtaZ9CXF8w&utm_content=2&utm_<br />
source=hs_email<br />
Lagasse, J. ed (December 8, 2020) Healthcare workers<br />
experiencing burnout, stress due to COVID-19<br />
pandemic. Healthcare Finance News https://www.<br />
healthcarefinancenews.com/news/healthcare-workersexperiencing-burnout-stress-due-covid-19-pandemic<br />
Shun, S.C. (2021). COVID-19 Pandemic: The challenge to<br />
the professional identity or nurses and nursing education.<br />
The Journal of Nursing Research 29(2), e138. doi: 10.1097/<br />
JNR.0000000000000431<br />
Shah, M.K., Gandrakota, N., Cimiotti, J.P., Ghose, N., Moore,<br />
M., & Ali, M. (2021). Prevalence of and factors associated<br />
with nurse burnout in the US. JAMA Network Open 4(2),<br />
e2036469 doi:10.1001/jamanetworkopen.2020.36469<br />
Trusted Health. (2021). 2021 Frontline <strong>Nurse</strong> Mental Health &<br />
Well- Being Survey https://www.trustedhealth.com/notahero<br />
Virkstis, K. (March 11, 2021). <strong>Nurse</strong> burnout didn’t start with<br />
Covid-19. (And it won’t end with Covid-19, either.). Advisory<br />
Board https://www.advisory.com/daily-briefing/2021/03/11/<br />
nurse-burnout
Page 14 • <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> <strong>August</strong>, September, October <strong>2022</strong><br />
Challenges in the Nursing Workforce, Graduate Nursing<br />
Education, and Future of Nursing<br />
Georgianna Thomas, D.Ed., MSN, RN<br />
Somi Nagaraj, DNP, MSN, RN, CSSGB, CONTL<br />
Reprinted with permission from Illinois The Nursing Voice<br />
September 2021 issue<br />
The healthcare sector is an intricate, albeit<br />
fundamental, part of ancient and modern societies. It<br />
comprises a long list of agents, from the individual seeking<br />
healthcare services to the medical staff and nurses, all<br />
operating within a legal framework involving providers,<br />
consumers, insurance companies, government, medical<br />
schools, nursing schools, and regulatory institutions<br />
(Amorim Lopes et al., 2015).<br />
The healthcare market is always composed of both<br />
suppliers of health services and patients demanding their<br />
services. On the one side is the workforce of physicians,<br />
nurses, and remaining clinical staff educated according<br />
to standards and criteria, ready to assist those in need.<br />
On the other side stand the forces that drive the demand<br />
for medical services, strongly related to demographic,<br />
socioeconomic, and epidemiological factors. Analyzing<br />
these two market forces is a critical step in assessing<br />
whether the available health care human resources are<br />
enough in quantity and skills to meet the current and<br />
future demand in due time and may lay solid foundations<br />
for further research, considering perhaps changes to the<br />
existing health policy framework (Amorim Lopes et al.,<br />
2015).<br />
A high degree and extent of uncertainty affect supply<br />
and demand: asymmetric information between physicians,<br />
nurses, and patients, restrictions on competition, an aging<br />
workforce in all areas, strong government interference,<br />
and supply-induced demand are some of the most glaring<br />
differences that can be pinpointed. These may be relevant<br />
when assessing the impact of any policy involving<br />
Healthcare Human Resource [HHR] planning (Amorim<br />
Lopes et al., 2015).<br />
Supply<br />
Supplying human capital with the appropriate expertise<br />
to enable workers to perform and satisfy the demand for<br />
health care is no simple task. The time and effort required<br />
to equip HHR, especially physicians and advanced nurse<br />
practitioners, exceeds most other professions. In some<br />
particular healthcare professions, the set of necessary<br />
skills to qualify for medical practice is acquired through<br />
extensive academic learning, which involves enrollment in<br />
long courses that may take up decades to complete due to<br />
a strict licensing process. The analysis of the medical and<br />
nurse education process is relevant but may be insufficient,<br />
as several other factors may affect the efficiency and<br />
effectiveness of the care services delivered (Amorim<br />
Lopes et al., 2015).<br />
Despite the limitations, some measures to overcome<br />
imbalances in the quantity (number) of physicians and<br />
nurses have already been identified in the health policy<br />
literature (Chopra et al., 2008), namely the following:<br />
increasing the number of domestic- and foreign-trained<br />
medical graduates or increasing the number of medical<br />
and nursing schools and classroom sizes; increasing the<br />
enrollment limits; reducing the requirements for entry<br />
to medical and nursing schools; raising the wages of the<br />
medical and nursing staff, as well as the perspectives for<br />
their future career path; or reducing the costs of attending<br />
medical and nursing school, which may encourage<br />
potential students to enroll. These proposals are shortterm<br />
measures to alleviate the immediate stress put on<br />
the healthcare system triggered by an undersupply of<br />
personnel and may not be suitable for tackling long-term<br />
imbalances due to huge shortages or surpluses of medical<br />
and nursing staff (Amorim Lopes et al., 2015).<br />
Demand<br />
Demand for health care is a derived demand<br />
(Grossman, 1972), which means that people do not seek<br />
health care services as a final good for consumption but<br />
as an intermediate service allowing them to be healthy<br />
and to improve their stock of health capital (well-being).<br />
They want to improve their health, and to do so; they seek<br />
healthcare services (Amorim Lopes et al., 2015).<br />
The concept of needs in health care is not consensual<br />
in the health literature, with a semantic confusion arising<br />
from its use in health economics (Hall & Mejia, 2009).<br />
While the economic or effective demand translates the<br />
actual, observed demand, usually measured in terms<br />
of service utilization ratios such as bed occupancy<br />
rates, number of inpatients, the needs component tries<br />
to fully encompass the epidemiological conditions that<br />
characterize a given population, measured through<br />
morbidity and mortality rates or by the opinion of a<br />
panel of experts, and how that may translate into a given<br />
quantity of required healthcare services. Therefore, we see<br />
that the classical concept of economic demand may not<br />
reflect the biological needs of the population, as it may<br />
leave out the necessities of the population regardless of<br />
their ability to pay (Amorim Lopes et al., 2015).<br />
An integrated approach uses a dynamic, systemlevel<br />
perspective covering key drivers of supply and<br />
demand that includes manpower planning and workforce<br />
development is critical to overcoming such challenges<br />
(Stordeur et al., 2010). The importance of paying attention<br />
to needs is also continuously stressed, as changes<br />
in the health patterns of the populations take place<br />
(Tomblin et al., 2009). The impact of microeconomic<br />
and organizational changes in productivity and the<br />
skill mix, of the evolution of demand for healthcare<br />
services, and also of the evolution of health diseases<br />
and its potential impact on the health system. The given<br />
quantity of workers may provide more or less healthcare<br />
services depending on their productivity and skill mix,<br />
influencing the conversion from headcounts to full-time<br />
equivalents (FTEs). Such conversion is critical to properly<br />
assess the healthcare workforce, as a significant number<br />
of physicians and nurses work part-time only. For this<br />
reason, FTE is a more accurate measure as it normalizes<br />
headcounts. On the demand side, economic (effective)<br />
demand can be initially measured by analyzing utilization<br />
indicators. How this demand will evolve in the future<br />
will then be subject to typical economic factors such as<br />
demography and the growth of the income/GDP (Amorim<br />
Lopes et al., 2015).<br />
In parallel, potential needs can be assessed by<br />
incorporating the incidence and prevalence of diseases<br />
and then mapping a given disease to an estimate of FTE<br />
requirements. Whether future supply forecasts should<br />
tackle all of the estimated needs is a decision left to the<br />
consideration of the policymaker, as the analysis does not<br />
incorporate financial constraints. Despite the abundance<br />
of approaches and techniques to determine supply and<br />
need for professionals, none of the methodologies has<br />
ultimately proved to be superior (Ricketts, 2011).<br />
Recent studies testing current forecasting models show<br />
that there is still plenty of room for improvement given<br />
the gap between projected and actual results (Greuningen<br />
et al., 2013). It becomes even clearer that workforce<br />
planning should be accurate and performed in due time,<br />
given the attritions and the delays in enacting policies<br />
in the healthcare sector. Adapting medical and nursing<br />
schools, altering legislation, and changing roles is an effort<br />
that may take years to bring forth. Therefore, planning<br />
has to target a long enough time horizon to be useful and<br />
applicable and has to be done pre-emptively (Amorim<br />
Lopes et al., 2015).<br />
Accurate HHR planning requires an approach that is<br />
both integrated and flexible, featuring supply and demand<br />
(potential and effective) and incorporating less tangible<br />
factors, such as skill mix and productivity (Amorim Lopes<br />
et. al., 2015).<br />
Academia<br />
Looking at the area of academia, there are many issues<br />
at hand that present challenges for nursing education at the<br />
doctoral level. Having enough faculty to provide quality<br />
education to those interested in pursuing a doctoral degree<br />
in nursing relies on competent individuals. Presently there<br />
are two types of doctoral degrees one can earn, both are<br />
terminal degrees, and both allow nurses to continue<br />
to practice in the clinical field. The Doctor of Nursing<br />
Practice (DNP) has a clinical focus that allows the nurse<br />
to possess expert knowledge to influence healthcare<br />
outcomes across direct patient care, advocating for<br />
healthcare policy implementation, and collaborating with<br />
organizational leadership (Leveck, 2020, Chism 2010).<br />
The Doctor of Philosophy (PhD) focuses on research in<br />
advancing the nursing profession and change the quality<br />
of patient care and outcomes in the field. PhD nurses<br />
also teach and mentor nurses at the college and university<br />
level, growing the next cohorts of professional nurses.<br />
There is a difference between these two degrees in their<br />
primary foci and length of education (registerednursing.<br />
com). However, the DNP degree has become the more<br />
sought-after degree, and individuals who have earned it<br />
are considered equal at many institutions in academia in<br />
relation to tenure attainment and administrative positions.<br />
It was more common to see the individual with a PhD in<br />
the academic setting. However, individuals seeking this<br />
degree are decreasing in number, and some individuals are<br />
having difficulty completing their dissertation. This adds<br />
to the faculty shortage we continue to experience in the<br />
profession. There is a distinction between the two degrees<br />
and needs to be recognized and valued in advancing new<br />
nurses, however, the DNP graduate is more prepared for<br />
the clinical arena.<br />
According to Drs. Di Fang and Karen Kesten, one-third<br />
of the current nursing faculty workforce in all levels of<br />
education are expected to retire by 2025 (ANA Fact Sheet,<br />
2020). This will certainly have an effect on the numbers of<br />
students who will be accepted when they apply for nursing<br />
education overall.<br />
Continuous changes in the nursing and medical fields<br />
have been rapidly evolving because of technology and<br />
studies such as the genome project. Graduate student<br />
feedback to courses and discussions with clinical affiliates<br />
to the college/university are two ways that information can<br />
be ascertained in relation to curricular issues for content.<br />
Accreditation standard revisions and the recently adopted<br />
Essentials with emphasis on outcomes and competencies<br />
in learning have also added to many of the changes<br />
schools are making to revise overall curriculums (AACN,<br />
2021). Learning theories are used to expose students to<br />
various learning experiences. Online teaching, simulation,<br />
inter-professional learning, case studies, and other<br />
teaching formats take much time to prepare and grade and<br />
may not all be familiar for present faculty to fulfill.<br />
Interdisciplinary education (IPE) among the various<br />
healthcare providers is expected to be utilized in schools.<br />
This type of education provides shared experiences that<br />
allow for better understanding, improved engagement, and<br />
clearer insight into cooperation in the work environment<br />
and quality patient care. This activity in schools with<br />
major medical affiliations has an edge in providing<br />
this type of learning while many smaller colleges and<br />
universities struggle to gain this opportunity. Many IPE<br />
opportunities that do exist are noted through simulationenhanced<br />
activity (Fawaz, 2018). Although simulation<br />
is helpful, real-time situations may affect the learner<br />
differently when exposed.<br />
Technology has become more influential in our lives,<br />
especially after the past year and a half of pandemic<br />
experiences. However, online education is not a new<br />
concept in education. Use of learning platforms, Zoom<br />
meetings, Wiki’s, Google docs, social media, Electronic<br />
Health Records, and so on have not been mastered by<br />
all in education, faculty, or student. Many students like<br />
the idea behind online learning in that they can study at<br />
their own pace often or at a time that is most convenient<br />
for them. This strategy for education allows for flexibility<br />
to view course material in both an asynchronous and, at<br />
times, synchronous format. Faculty find this learning<br />
takes more time in their schedule for preparation and<br />
grading than when classes met traditionally. Class size<br />
is not always capped. Lack of support staff with course<br />
development and difficulty managing technological<br />
changes have been identified as barriers to distance<br />
education (Iwasiw et al., 2020). This becomes frustrating<br />
to both teacher and student in that the partnership that<br />
develops in learning is not fully developed.<br />
Future of Nursing<br />
The Future of Nursing 2020-2030: Charting a Path to<br />
Achieve Health Equity, study sponsored by Robert Wood<br />
Johnson Foundation identified, that a nation cannot thrive<br />
fully until everyone can live their healthiest possible life,<br />
and helping people live their healthiest life is and has<br />
always been the essential role of nurses. The ultimate<br />
goal is to achieve health equity in the United States built<br />
on strengthened nursing capacity and expertise (National<br />
Academies of Sciences, Engineering, and Medicine, 2021).<br />
The committee developed a framework identifying<br />
the key areas for strengthening the nursing profession<br />
to meet the challenges of the decade ahead. These areas<br />
include the nursing workforce, leadership, nursing<br />
education, nurse well-being, and emergency preparedness<br />
and response, as well as responsibilities of nursing with<br />
respect to structural and individual determinants of health<br />
(National Academies of Sciences, Engineering, and<br />
Medicine, 2021).<br />
In 1998 the Pew Health Professions Commission, a<br />
group of healthcare leaders charged with assisting health<br />
policymakers and educators teaching health professionals<br />
to meet the changing needs of healthcare systems,<br />
completed a report listing competencies healthcare<br />
providers of the future would need. The competencies are<br />
listed in the Fourth Report of the Pew Health Professions<br />
Commission (O’Neal & Pew Health Professions<br />
Commission, 1998).<br />
The book To Err Is Human: Building a Safer Health<br />
System (Kohn, Corrigan, & Donaldson, 1999) brought<br />
national attention to the issue of patient safety by
<strong>August</strong>, September, October <strong>2022</strong> <strong>Vermont</strong> <strong>Nurse</strong> <strong>Connection</strong> • Page 15<br />
discussing the number of people who die each year from<br />
medical errors. This, in turn, sharpened the focus of<br />
patient safety in nursing education (Scheckel, 2008).<br />
Despite the practice setting in which students learn<br />
nursing care, it will include using various technologies and<br />
knowledge of informatics to assist with patient care. These<br />
technologies can include but are not limited to medical<br />
devices patients will use to provide self-care, as well as<br />
information retrieval, clinical information management,<br />
and documentation technologies (Scheckel, 2008).<br />
Students’ use of these devices has important implications<br />
for improving their clinical judgment (Newman & Howse,<br />
2007). <strong>Nurse</strong>s are also being exposed to the use of variety<br />
of clinical management systems, like patient surveillance<br />
systems many of which have implications for ensuring<br />
quality and safety.<br />
A significant movement that accompanied the<br />
curriculum revolution involved using pedagogies to<br />
ensure students could think critically in clinical practice.<br />
Traditionally, students who learned the nursing process<br />
were thought to be learning critical thinking. During the<br />
past few decades, the nursing process has been challenged<br />
as the best approach to developing students’ critical<br />
thinking (Scheckel, 2008). However, current research<br />
in nursing education suggests that students also need<br />
to engage in thinking processes that promote reflective<br />
thinking, where they build practical knowledge, embodied<br />
thinking, where they learn the importance of intuition<br />
and pluralistic thinking, where they consider a clinical<br />
situation using many perspectives (Scheckel & Ironside,<br />
2006).<br />
Innovations<br />
As nurses assume increasing responsibility for<br />
patient care in primary care settings, the combination<br />
of increased clinical and systems knowledge, as well as<br />
the capability to apply and evaluate evidence to practice<br />
innovations, can only have a positive impact. The presence<br />
of DNP-prepared APRNs in primary care will expand<br />
educational opportunities. In the short term, the DNPprepared<br />
APRNs can mentor the MSN-prepared APRNs<br />
within the system. Equally important is the opportunity<br />
for enhanced preceptor education for nursing students in<br />
primary care (Dunbar-Jacob et al., 2013).<br />
Indeed, the preparation of the DNP will influence the<br />
perception of health care systems regarding the added<br />
value of DNP education. If graduates of such programs<br />
bring an increased depth of knowledge and skill to the<br />
clinical arena, the DNP will likely flourish. If graduates<br />
bring little more than what is offered by master’s-level<br />
education, the DNP will not be an attractive addition to<br />
the clinical arena. Thus, the quality of the preparation<br />
of the DNP will influence the adoption of the DNP<br />
practitioner and administrator by health care systems<br />
(Dunbar-Jacob et al., 2013).<br />
Conclusion<br />
Challenges in building DNP programs include the<br />
identification of qualified faculty for each specialty,<br />
qualified capstone advisors, and qualified clinical<br />
preceptors. A further challenge is the simultaneous<br />
education of master’s cohorts and DNP cohorts. The<br />
challenges by requiring faculty to obtain a doctoral degree,<br />
developing critical academic–service partnerships in<br />
mentoring students for practicum and capstone projects,<br />
and discontinuing MSN advanced practice specialty<br />
programs while focusing on the BSN-to-DNP and MSNto-DNP<br />
programs. High-quality DNP academics and<br />
DNP clinicians are crucial to help meet these challenges.<br />
Each educational program must assess its challenges<br />
and strategies for addressing those challenges. How we<br />
proceed will determine the impact of our programs on the<br />
future of the health care system (Dunbar-Jacob, Nativio, &<br />
Khalil, 2013).<br />
In academia, both the PhD and DNP prepared nurses<br />
can work together to ensure quality education for our<br />
nursing students. Both need an educational foundation to<br />
be learned to be successful educators. The distinction of<br />
the PhD concentrating on teaching theory and research<br />
to assist nursing to maintain its scientific foundation and<br />
the DNP concentrating on the clinical skills and acting as<br />
preceptor/clinical educator at any level of nursing appear<br />
to be the ideal partnership to develop. Both nurses can<br />
assist academia and the clinical arena in staying current<br />
and developing innovative care measures to provide<br />
quality care to clients. When looking at the definitions<br />
noted at the beginning of this work, this collaboration in<br />
teaching nurses fits what was noted.