TheTayside Cardiology Unmet Needs Project (PDF Poster ...
TheTayside Cardiology Unmet Needs Project (PDF Poster ...
TheTayside Cardiology Unmet Needs Project (PDF Poster ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
HI 013<br />
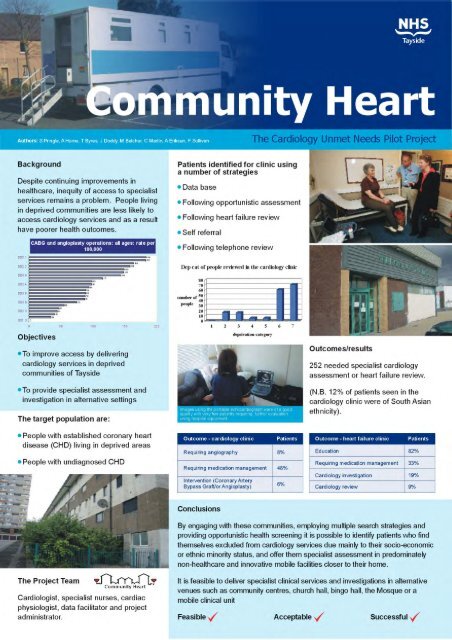
Community Heart:The Tayside <strong>Cardiology</strong> <strong>Unmet</strong> <strong>Needs</strong> <strong>Project</strong><br />
Authors: A Hume,T Byres, J Doddy, M Belcher, C Martin, A Eriksen, F Sullivan, S Pringle<br />
Lead Contact: Professor Stuart D Pringle, <strong>Cardiology</strong> Department, Ninewells Hospital, Dundee<br />
DD1 9SY,Tel: 01382 632263, E-mail: stuart.pringle@nhs.net<br />
Organisation: NHS Tayside<br />
Aim:<br />
Despite recent improvements in healthcare,<br />
inequity of access due to socio-economic and<br />
ethnic factors remains a problem. In cardiology,<br />
some patients with the highest clinical need<br />
have difficulty accessing specialist services.The<br />
aim of this project was to investigate different<br />
ways of engaging with patients and their<br />
communities to address this problem.<br />
Methodology:<br />
The clinical team, overseen by a multidisciplinary<br />
steering group, comprised two specialist nurses,<br />
a cardiac physiologist and a consultant<br />
cardiologist with additional support from a data<br />
facilitator and project administrator. Multiple<br />
methods of patient identification were<br />
employed. Hospital sector clinical IT systems<br />
were analysed for patients from post code areas<br />
with deprivation category 6 and 7 who had<br />
failed to attend outpatient appointments,<br />
defaulted from cardiac rehab or had known<br />
acute coronary events but no further<br />
investigation or hospital contact. In primary care,<br />
the practice-based disease registers were<br />
examined to find patients with a clinical<br />
diagnosis of heart failure or angina who had not<br />
had cardiac investigations or specialist referral.<br />
Communities were engaged with by attending<br />
organised social, educational and religious events<br />
in community centres, temples, church halls, and<br />
mosques including a feature on Ramadan Radio.<br />
Additional screening opportunities were<br />
provided at community gala days, shopping<br />
centres, the city square and a bingo hall. At<br />
clinics carried out in these non-healthcare<br />
facilities and in an adapted lorry, the patients<br />
had a clinical evaluation with a consultant<br />
cardiologist, 12 lead ECG, near patient blood<br />
testing and portable echocardiography. Patients<br />
requiring stress ECG or more specialised cardiac<br />
imaging had these tests arranged at the hospital.<br />
Outcomes/Results:<br />
Of the 1781 people seen so far 1632 had<br />
clinical evaluation and 252 needed specialist<br />
cardiology assessment or heart failure review.<br />
Very few required subsequent coronary<br />
angiography (n=8) with a view to coronary<br />
revascularisation but this was offset by a high<br />
proportion of the cardiology patients (48%)<br />
requiring a review of their diagnosis or change<br />
in medication.<br />
Conclusions:<br />
By engaging with these communities, employing<br />
multiple search strategies and providing<br />
opportunistic health screening it is possible to<br />
identify patients who find themselves excluded<br />
from cardiology services due mainly to their<br />
socio-economic or ethnic minority status, and<br />
offer them specialist assessment in<br />
predominately non-healthcare and innovative<br />
mobile facilities closer to their home.<br />
Health Improvement