Name of Manual - Blue Cross and Blue Shield of Minnesota
Name of Manual - Blue Cross and Blue Shield of Minnesota
Name of Manual - Blue Cross and Blue Shield of Minnesota
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong><br />
<strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Provider Policy &<br />
Procedure <strong>Manual</strong><br />
2012
CPT codes copyright 2012 American Medical Association. All Rights Reserved. CPT is a trademark <strong>of</strong> the AMA.
Recent Chapter changes:<br />
Chapter 11<br />
Durable Medical Equipment<br />
Chapter 1 – At Your Service<br />
Date Topic Changes<br />
Chapter 2 – Provider Agreements<br />
Date Topic Changes<br />
Summary <strong>of</strong> Changes (2012)<br />
Chapter 3 – Health Care Improvement<br />
Date Topic Changes<br />
Chapter 4 – Care Management<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Date Topic Changes<br />
Content New Topic Deletions Topic Deleted<br />
1/31 Updated the language to this section in connection with annual<br />
review <strong>of</strong> policies <strong>and</strong> procedures.<br />
X<br />
06/20 Medical Policy <strong>and</strong> Behavioral Health Policy <strong>Manual</strong> X<br />
Chapter 5 – Health Care Options<br />
Date Topic Changes<br />
Chapter 6 – <strong>Blue</strong> Plus<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12) 1
Summary <strong>of</strong> Changes (2012)<br />
Date Topic Changes<br />
Chapter 7 – <strong>Blue</strong>Card<br />
Date Topic Changes<br />
Chapter 8 – Claims Filing<br />
Date Topic Changes<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
2/21 CMS 1500 Claim form information removed X<br />
2/21 Exceptions revised X<br />
05/10 Single facility claim submission X<br />
Chapter 9 – Reimbursement/Reconciliation<br />
Date Topic Changes<br />
Chapter 10 – Appeals<br />
Date Topic Changes<br />
06/20 Utilization Review Decision Appeal X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12) 2
Chapter 11 – Coding Policies <strong>and</strong> Guidelines<br />
Coding<br />
Date Topic Changes<br />
1/04 Reimbursement <strong>of</strong> HCPCS Codes, Page 11-2 x<br />
06/20 CPT / Level I<br />
Coding Immunizations <strong>and</strong> Injections<br />
07/12 Preventive Care Services X<br />
07/12 General Guides X<br />
08/15 Durable Medical Equipment X<br />
Copays<br />
Date Topic Changes<br />
Modifiers<br />
Date Topic Changes<br />
Anesthesia<br />
Date Topic Changes<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
2/21 HICF 1500 References Deleted, Page 2 X<br />
2/21 Qualifying Circumstances, Page 3 X<br />
2/21 Epidural Anesthesia, Page 5 X<br />
2/21 837P Added X<br />
3 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12)
Summary <strong>of</strong> Changes (2012)<br />
Behavioral Health<br />
Date Topic Changes<br />
06/20 Coding Restrictions X<br />
06/20 MHCP screening requirements X<br />
06/20 Intensive Residential Treatment Services (IRTS) changed to<br />
(Medicaid Government Programs Only)<br />
Chiropractic<br />
Date Topic Changes<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
3/6 Effective Date Removed from MHCP Requirements, Page 10 X<br />
Dental Services<br />
Date Topic Changes<br />
3/6 Electronic Claim Format, Page 3 X<br />
Durable Medical Equipment<br />
Date Topic Changes<br />
01/17 Medicare Advantage DME Rental Guidelines<br />
Waiver Claim Submission<br />
Coding Modifiers<br />
DME Repairs <strong>and</strong> Maintenance (Excluding Oxygen<br />
Equipment)<br />
Billing for Supplies<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12) 4<br />
X
Durable Medical Equipment<br />
Date Topic Changes<br />
03/23 New section/policy re: Enrollment Requirements when Providing<br />
Services to MHCP Members<br />
Prior authorization: delete "durable medical equipment"<br />
DME rental guidelines: large volume air compressors removed<br />
Sample waiver form: delete "durable medical equipment"<br />
Portable oxygen billing those added, these deleted<br />
Coding modifiers: revisions to the LL, RR, NR definitions<br />
DME repairs <strong>and</strong> maintenance (excluding oxygen equipment: add<br />
DME, delete "durable medical equipment"<br />
Billing for supplies: added "only" to first paragraph; corrected units<br />
reporting location; removed references (1500 hicf) claim form<br />
Pharmacies submitting DME Claims: delete "durable medical<br />
equipment" change to DME<br />
06/20 DME Rental Guidelines X<br />
Home Health, Home Infusion, Hospice<br />
Date Topic Changes<br />
3/6 PCA modifier information <strong>and</strong> requirements added, Page 8 X<br />
3/6 Corrected <strong>and</strong> added coding to grid, Page 10 X<br />
3/6 MHCP PA requirements added, Page 15 X<br />
4/6 Prior Authorization Verbiage updates, Pages 11-2 <strong>and</strong> 11-14 x<br />
06/20 Home Infusion X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
5 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12)<br />
X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic<br />
Deleted
Summary <strong>of</strong> Changes (2012)<br />
Hospital Care<br />
Date Topic Changes<br />
01/17 Critical Care<br />
Hospital Observation<br />
SNF Billing for <strong>Blue</strong> Plus Government Program<br />
Products<br />
03/12 critical care: added information/instructions re: time increments<br />
SNF billing for blue plus government program products (continued):<br />
add an "X" to the SNF type <strong>of</strong> bill - s/b 02XX<br />
added section/policy re: medical necessity vendor<br />
06/20 Leave <strong>of</strong> Absence (LOA) or furlough days X<br />
07/12 Home Health X<br />
Laboratory<br />
Date Topic Changes<br />
01/17 Introduction<br />
St<strong>and</strong>ing Orders<br />
Papanicolaou Smears<br />
Repeat Lab Services<br />
03/23 new section/policy for collection <strong>and</strong> h<strong>and</strong>ling <strong>of</strong> speciments for<br />
PMAP <strong>and</strong> <strong>Minnesota</strong>Care Members Only<br />
Maternity<br />
genetic testing modifiers: added "as appropriate"<br />
new section/policy for Lab billed through the <strong>Blue</strong>Card Program<br />
Date Topic Changes<br />
01/17 Newborn Care<br />
Reproduction Treatment<br />
06/20 Delivery X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
X<br />
X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
X<br />
X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12) 6<br />
X
Medical Emergency<br />
Date Topic Changes<br />
01/17 Emergency Department Services<br />
Extended/After-hours Clinics<br />
03/23 extended/after-hours clinics: deleted "1500 HICF" <strong>and</strong> "UB-04 X<br />
Medical Services<br />
Date Topic Changes<br />
06/20 Evaluation <strong>and</strong> Management (E/M)<br />
Office or Other Outpatient <strong>and</strong> Initial Inpatient Consultations<br />
Chemotherapy Administration<br />
Immunizations<br />
Infusion Therapy<br />
Coding<br />
Weight Management Care<br />
Assessment Management Program for Fully Insured<br />
Optometric Optical Services<br />
Date Topic Changes<br />
Pharmacy Services<br />
Date Topic Changes<br />
Public Services<br />
Date Topic Changes<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
7 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12)
Summary <strong>of</strong> Changes (2012)<br />
Public Programs<br />
Date Topic Changes<br />
Radiology Services<br />
Date Topic Changes<br />
01/17 Comparison X-ray X<br />
3/6 HTDI program information added, Pages 5-7 X<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12) 8
Rehabilitative Services<br />
Date Topic Changes<br />
01/17 Physical Therapy Procedures<br />
Physical Therapy Evaluation Codes<br />
Occupational Therapy Evaluation Codes<br />
Massage <strong>and</strong> <strong>Manual</strong> Therapy Exclusion<br />
Massage <strong>and</strong> <strong>Manual</strong> Therapy Exclusion<br />
Speech Therapy <strong>and</strong> Evaluation<br />
01/17 Hot <strong>and</strong> Cold Pack Exclusion<br />
MHCP PT, OT, ST Authorization Process<br />
03/23 physical therapy evaluation codes: revised guidelines re: submission<br />
<strong>of</strong> 97001-97002 with an E/M<br />
occupational therapy: deleted "4" - CPT is no longer referred to as<br />
CPT-4. It is only CPT<br />
occupational therapy continued: remove dash between codes 97750<br />
<strong>and</strong> 97755 <strong>and</strong> comma added. This is not a range <strong>of</strong> codes - there<br />
are only these two codes.<br />
occupational therapy evaluation codes: revised guidelines re:<br />
submission <strong>of</strong> 97003-97004 with an E/M<br />
mhcp pt, ot, st authorization process: deleted effective date<br />
reference; group numbers added to affected programs<br />
mhcp pt, ot, st authorization process continued: effective date <strong>and</strong><br />
information re; specialized maintenance therapy<br />
added section <strong>and</strong> policy for "medical necessity vendor"<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
9 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12)<br />
X<br />
X<br />
X
Summary <strong>of</strong> Changes (2012)<br />
Surgical Services<br />
Date Topic Changes<br />
02/22 General Guidelines X<br />
02/22 Global Surgical Package X<br />
02/22 Fractures X<br />
02/22 St<strong>and</strong>-by Services X<br />
03/23 Lesions: corrected code range<br />
Correct billing <strong>of</strong> Q1003 for Medicare advantage products: deleted<br />
section - code no longer valid<br />
Acne treatment/skin rejuvenation <strong>and</strong> rosacea treatment: deleted<br />
"<strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus"<br />
Intra-articular hyaluronan injections for osteoarthritis: deleted "<strong>and</strong><br />
<strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus"<br />
Assistant surgeons: added "or clinical nurse specialist"<br />
Multiple surgeries: corrected payment information - "billed" <strong>and</strong><br />
"charge" deleted; "highest allowed" <strong>and</strong> "allowed" added<br />
Type <strong>of</strong> Change(s)<br />
Content New Topic Deletions Topic Deleted<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/12) 10<br />
X
Table <strong>of</strong> Contents<br />
Chapter 1<br />
At Your Service<br />
Introduction................................................................................................................................ 1-3<br />
Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> ................................................................................. 1-3<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Plans..........................................................................................1-3<br />
<strong>Blue</strong> Plus ................................................................................................................................ 1-3<br />
CPT Copyright.....................................................................................................................1-4<br />
How to Contact Us ..................................................................................................................... 1-5<br />
Provider Services ...................................................................................................................1-5<br />
Federal Employee Program.................................................................................................... 1-5<br />
Calls Not H<strong>and</strong>led by Provider Services ............................................................................... 1-5<br />
Behavioral Health Service Numbers...................................................................................... 1-6<br />
<strong>Blue</strong>Card ® Benefits <strong>and</strong> Eligibility........................................................................................1-6<br />
Provider Claim Adjustment / Status Check ...........................................................................1-6<br />
General Address.....................................................................................................................1-6<br />
Claims Address ......................................................................................................................1-7<br />
Care Management Numbers <strong>and</strong> Addresses ..........................................................................1-7<br />
Other Numbers <strong>and</strong> Addresses............................................................................................. 1-12<br />
Address Changes <strong>and</strong> Other Demographic Information......................................................1-13<br />
BLUELINE............................................................................................................................... 1-14<br />
Introduction..........................................................................................................................1-14<br />
BLUELINE Availability...................................................................................................... 1-14<br />
Calling BLUELINE .............................................................................................................1-14<br />
System Assistance................................................................................................................ 1-14<br />
Provider Identification .........................................................................................................1-15<br />
Member Identification ......................................................................................................... 1-15<br />
Date...................................................................................................................................... 1-15<br />
Provider Web Self-Service ...................................................................................................... 1-16<br />
ID Cards.................................................................................................................................... 1-17<br />
Introduction..........................................................................................................................1-17<br />
ID Cards...............................................................................................................................1-17<br />
Helpful Tips .........................................................................................................................1-18<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-1
At Your Service<br />
Electronic Commerce .............................................................................................................. 1-19<br />
Overview..............................................................................................................................1-19<br />
Electronic Transactions........................................................................................................1-19<br />
Electronic Data Interchange (EDI) Guidelines.................................................................... 1-19<br />
Remote Access Services ...................................................................................................... 1-20<br />
Provider Communications ...................................................................................................... 1-23<br />
Member Rights <strong>and</strong> Responsibilities...................................................................................... 1-24<br />
Health Plan Members have the Following Rights ...............................................................1-24<br />
Health Plan Members have the Following Responsibilities ................................................1-25<br />
1-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Introduction<br />
Provider Policy <strong>and</strong><br />
Procedure <strong>Manual</strong><br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
<strong>Blue</strong> <strong>Shield</strong> Plans<br />
At Your Service<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> developed the Provider<br />
Policy <strong>and</strong> Procedure <strong>Manual</strong> for participating health care<br />
providers <strong>and</strong> your business <strong>of</strong>fice staff. This manual provides<br />
information about our claims filing procedures, payments, provider<br />
agreements, managed care requirements, communications <strong>and</strong><br />
other topics that affect patient accounts <strong>and</strong> patient relations. As<br />
policies <strong>and</strong> procedures change or clarification is needed, <strong>Blue</strong><br />
<strong>Cross</strong> will keep you updated through Provider Bulletins, Quick<br />
Points <strong>and</strong> the Provider Press, found at bluecrossmn.com.<br />
Information in this manual is a general outline <strong>and</strong> is part <strong>of</strong> your<br />
provider contract. Provider <strong>and</strong> member contracts determine<br />
benefits.<br />
<strong>Blue</strong> <strong>Shield</strong> plans for pr<strong>of</strong>essional services began to form across<br />
the nation in the 1940s, after the successful <strong>Blue</strong> <strong>Cross</strong> movement<br />
<strong>of</strong> the 1930s was well underway. Today, there are many <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Plans throughout the United States. <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Plans may be separate companies or<br />
combined as one company. Each plan is an independent business<br />
organization <strong>and</strong> a nonpr<strong>of</strong>it independent licensee <strong>of</strong> the <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Association.<br />
The <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Association, headquartered in<br />
Chicago, is an association <strong>of</strong> independent <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong><br />
<strong>Shield</strong> Plans. It sets performance st<strong>and</strong>ards <strong>and</strong> bids for national<br />
contracts <strong>and</strong> programs. It also organizes advertising campaigns,<br />
conducts research <strong>and</strong> coordinates legislative efforts on behalf <strong>of</strong><br />
the association’s members.<br />
<strong>Blue</strong> Plus <strong>Blue</strong> Plus, an affiliate <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong>, is a state-certified health<br />
maintenance organization (HMO). In most <strong>Blue</strong> Plus products,<br />
members select a participating primary care clinic that coordinates<br />
all <strong>of</strong> the patient’s medical care <strong>and</strong> authorizes treatment by<br />
specialists when necessary.<br />
Because <strong>Blue</strong> Plus is an affiliate <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong>, <strong>Blue</strong> Plus is<br />
subject to most <strong>of</strong> the same policies <strong>and</strong> procedures. For general<br />
information about <strong>Blue</strong> Plus, you may refer to Chapter 6 <strong>of</strong> this<br />
manual. <strong>Blue</strong> Plus primary care clinics should refer to the <strong>Blue</strong><br />
Plus Provider <strong>Manual</strong> for specific <strong>Blue</strong> Plus guidelines. <strong>Blue</strong> Plus<br />
is a nonpr<strong>of</strong>it independent licensee <strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong><br />
<strong>Shield</strong> Association.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-3
At Your Service<br />
CPT Copyright CPT codes copyright 2010 American Medical Association. All<br />
Rights Reserved. CPT is a trademark <strong>of</strong> the AMA. No fee<br />
schedules, basic units, relative values or related listings are<br />
included in CPT. The AMA assumes no liability for the data<br />
contained herein. Applicable FARS/DFARS restrictions apply to<br />
government use.<br />
1-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
How to Contact Us<br />
At Your Service<br />
Provider Services A conversation with one <strong>of</strong> our service representatives <strong>of</strong>ten can<br />
solve a problem immediately or give you an answer to a claims<br />
question. The representatives answering the provider services<br />
numbers are available to assist you:<br />
Federal Employee<br />
Program<br />
Calls Not H<strong>and</strong>led by<br />
Provider Services<br />
Monday – Thursday ..........8 a.m. – 5 p.m.<br />
Friday ................................9 a.m. – 5 p.m.<br />
In an industry that is constantly changing, ongoing education <strong>of</strong><br />
our provider services representatives is necessary. To meet this<br />
challenge, <strong>Blue</strong> <strong>Cross</strong> conducts staff training every Friday morning<br />
from 8 a.m. – 9 a.m.<br />
Please have your provider number or NPI <strong>and</strong> if applicable, the<br />
member’s identification number, account number <strong>and</strong> claim<br />
number ready when you call. The provider services telephone<br />
numbers listed are for the provider’s use only. Please refer<br />
members to the customer service telephone number on the back <strong>of</strong><br />
their member identification (ID) card.<br />
The general provider services phone numbers are (651) 662-5200<br />
(Twin Cities area) <strong>and</strong> 1-800-262-0820 (toll free). Listen for the<br />
current phone options when you call.<br />
The general provider services fax number is (651) 662-2745.<br />
Providers who are calling to check eligibility <strong>and</strong> benefits for<br />
Federal Employee Program members can utilize the voice response<br />
unit specific to FEP.<br />
Claim status is not available at this time. Providers will be<br />
prompted to speak to a service representative for all FEP claims<br />
questions. To access this service, call (651) 662-5044 or<br />
1-800-859-2128. FEP members are recognized by an “R” followed<br />
by eight numeric digits in their identification number.<br />
Calls for the accounts on the next page are not h<strong>and</strong>led by provider<br />
services. Please use the phone numbers listed. In addition, calls<br />
from independent social workers who are working as patient<br />
advocates should call the customer service phone number on the<br />
back <strong>of</strong> the member’s ID card.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-5
At Your Service<br />
Calls Not H<strong>and</strong>led by<br />
Provider Services<br />
(continued) Accounts <strong>and</strong> how to ID them Phone Numbers<br />
TRICARE/TRIWEST<br />
Behavioral Health<br />
Service Numbers<br />
<strong>Blue</strong>Card ® Benefits <strong>and</strong><br />
Eligibility<br />
Provider Claim<br />
Adjustment / Status<br />
Check<br />
Federal Employee Program<br />
ID number starts with an R<br />
General Address The general address is:<br />
(651) 662-5044<br />
1-800-859-2128<br />
Behavioral health customer service ................Call the number on<br />
the member’s card, or call 1-888-874-9378, local (651) 662-3484.<br />
Inpatient mental health fax..............................(651) 662-0856<br />
Outpatient mental health fax ...........................(651) 662-0854<br />
Inpatient chemical dependency fax.................(651) 662-0856<br />
Outpatient chemical dependency fax ..............(651) 662-0854<br />
Pre-certification: fax to the numbers listed above.<br />
To verify benefits or eligibility for <strong>Blue</strong>Card members, call<br />
1-800-676-BLUE (2583). Refer to Chapter 7 for additional<br />
information.<br />
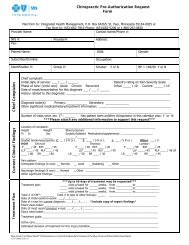
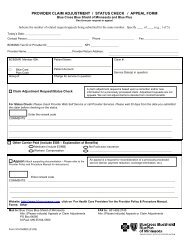
The Provider Claim Adjustment / Status Check Form is<br />
designed for providers to fax or mail their inquiries to <strong>Blue</strong> <strong>Cross</strong>.<br />
The applicable FAX number is listed on the form or mail it to the<br />
general <strong>Blue</strong> <strong>Cross</strong> address (see below).<br />
All the fields are required to be completed, if applicable. Make<br />
sure to clearly state the contact name, phone number <strong>and</strong> contact's<br />
FAX number.<br />
The inquiries can be an adjustment request or claim status request<br />
for regular or <strong>Blue</strong>Card business.<br />
The form will not be returned to you unless <strong>Blue</strong> <strong>Cross</strong> needs<br />
clarification on your request. All adjustments that are completed<br />
will be found on a future remittance advice.<br />
A sample <strong>of</strong> the Provider Claim Adjustment / Status Check<br />
Form can be found on our website, bluecrossmn.com.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
P.O. Box 64560<br />
St. Paul, MN 55164-0560<br />
(Claims adjustment requests inquires should be mailed to this<br />
address)<br />
1-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
At Your Service<br />
Claims Address Submit claims electronically whenever possible. All <strong>Minnesota</strong><br />
<strong>and</strong> out-<strong>of</strong>-state participating providers are required to<br />
electronically submit all claims according to <strong>Minnesota</strong> Statute<br />
62J.536 <strong>and</strong> the participating provider contracts. Paper claims<br />
submitted by <strong>Minnesota</strong> <strong>and</strong> out-<strong>of</strong>-state participating providers<br />
will be rejected to be resubmitted electronically. <strong>Blue</strong> <strong>Cross</strong> will<br />
not consider such paper claims to have been received until<br />
resubmitted electronically. Nonparticipating out-<strong>of</strong>-state providers<br />
may submit a scannable claim form to:<br />
Care Management<br />
Numbers <strong>and</strong><br />
Addresses<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Claims<br />
P.O. Box 64338<br />
St. Paul, MN 55164-0338<br />
The phone numbers, fax numbers <strong>and</strong> addresses for care<br />
management <strong>and</strong> utilization management are listed below.<br />
Area<br />
Phone/Fax Numbers<br />
<strong>and</strong> Addresses<br />
Case Management Non Government Programs<br />
(651) 662-5520<br />
FAX: (651) 662-1004<br />
Government Programs Case<br />
Management<br />
(PMAP, MNCARE, MN<br />
Senior Care Plus, MSHO –<br />
Secure<strong>Blue</strong> SM , Care<strong>Blue</strong> SM )<br />
(651) 662-5540 or<br />
1-800-711-9868<br />
FAX: (651) 662-6054 or<br />
1-866-800-1665<br />
Fraud Hot Line (651) 662-8363 or<br />
1-800-382-2000<br />
extension 28363<br />
Preadmission Notification<br />
(PAN)<br />
Medical <strong>and</strong> behavioral health<br />
inpatient admissions.<br />
Preadmission notifications are<br />
required to occur through<br />
provider web self-service.<br />
providerhub.com<br />
(651) 662-5270 or<br />
1-800-528-0934<br />
Medical FAX:<br />
(651) 662-6860<br />
Behavioral Health FAX:<br />
(651) 662-0856<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-7
At Your Service<br />
Care Management<br />
Numbers <strong>and</strong><br />
Addresses (continued)<br />
Area<br />
Utilization Management<br />
Prior authorization requests<br />
(may be called or Faxed)<br />
Home health services<br />
Home infusion services<br />
Hospice care<br />
Skilled nursing facility<br />
Admissions<br />
Phone/Fax Numbers<br />
<strong>and</strong> Addresses<br />
Commercial Intake<br />
(651) 662-5520 or<br />
1-888-878-0139, x25520<br />
FAX: (651) 662-1004<br />
Utilization Management For all other UM inquiries,<br />
contact provider services at<br />
1-800-262-0820 or<br />
(651) 662-5200 <strong>and</strong> they will<br />
triage your call appropriately.<br />
Government Programs<br />
Prior authorization requests or<br />
notifications<br />
(may be called or faxed)<br />
Home health care services<br />
Home infusion services<br />
PCA services<br />
Skilled nursing/nursing<br />
facility services (fax PMAP or<br />
Nursing Facility<br />
Communication Form)<br />
County waivered services<br />
Hospice services<br />
All services from<br />
nonparticipating providers<br />
Case Management,<br />
Government Programs<br />
(651) 662-5540 or<br />
1-800-711-9868<br />
FAX: (651) 662-6054 or<br />
1-866-800-1665<br />
1-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Care Management<br />
Numbers <strong>and</strong><br />
Addresses (continued)<br />
Area<br />
Medical Policy <strong>and</strong> Durable<br />
Medical Equipment (DME)<br />
Prior Authorization Requests<br />
(must be faxed or mailed)<br />
For commercial/nongovernment<br />
programs<br />
Cosmetic surgery<br />
Dental/oral surgery-inpatient<br />
Spinal cord stimulation<br />
DME<br />
Communication devices<br />
DME over $1,000 without<br />
an assigned HCPCS code<br />
Electrical bone growth<br />
stimulators<br />
Gravity lumbar reduction<br />
devices<br />
Specialty beds/overlays<br />
Vest percussor for cystic<br />
fibrosis<br />
Wheelchair (purchase<br />
only)<br />
Gastric bypass surgery<br />
Growth hormone<br />
Infertility service <strong>and</strong> drugs<br />
Investigative procedure (refer<br />
to Medical Policy Update on<br />
website)<br />
Weight-loss programs<br />
Services recommended by<br />
Medical Policy<br />
Phone/Fax Numbers<br />
<strong>and</strong> Addresses<br />
FAX: (651) 662-2810<br />
At Your Service<br />
Address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong><br />
Medical Review<br />
R4-72<br />
P.O. Box 64265<br />
St. Paul, MN 55164-0265<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-9
At Your Service<br />
Care Management<br />
Numbers <strong>and</strong><br />
Addresses (continued)<br />
Area<br />
Government Programs<br />
(PMAP, MNCare, MN Senior<br />
Care Plus, MSHO/Secure<strong>Blue</strong>,<br />
Care<strong>Blue</strong>)<br />
All <strong>of</strong> the above mentioned<br />
services, in addition to the<br />
following:<br />
DME over $500 (Secure<strong>Blue</strong>)<br />
Prosthetics over $1,000<br />
(MSHO)<br />
Wheelchair (rental <strong>and</strong><br />
purchase)<br />
Cesarean section<br />
Hysterectomy<br />
Tympanostomy tubes<br />
See website for complete list.<br />
Behavioral Health Outpatient<br />
Services<br />
Prior Authorization<br />
(must be mailed or faxed)<br />
For inpatient services, refer to the<br />
Preadmission Notification<br />
section.<br />
Chiropractic<br />
Prior Authorization Requests<br />
(must be faxed or mailed)<br />
Phone/Fax Numbers<br />
<strong>and</strong> Addresses<br />
FAX: (651) 662-6054 or<br />
1-888-800-1665<br />
Address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong><br />
Medical Review<br />
R244<br />
P.O. Box 64560<br />
St. Paul, MN 55164<br />
Outpatient Mental Health<br />
<strong>and</strong> Outpatient Chemical<br />
Dependency<br />
FAX: (651) 662-0854<br />
Address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong><br />
Behavioral Health<br />
P.O. Box 64265<br />
St. Paul, MN 55164-0265<br />
FAX: (651) 662-7816<br />
Address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong><br />
Allied Health Services<br />
R4-72<br />
P.O. Box 64265<br />
St. Paul, MN 55164-0265<br />
1-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Care Management<br />
Numbers <strong>and</strong><br />
Addresses (continued)<br />
Area<br />
Medical Dental<br />
Prior Authorization Requests<br />
(may be faxed or mailed)<br />
Surgical TMJ services<br />
Orthognathic/osteotomies<br />
Orthodontics for TMJ <strong>and</strong><br />
cleft lip/palate<br />
Bone grafts<br />
Bridges for accidental injuries<br />
Anesthesia <strong>and</strong><br />
inpatient/outpatient hospital<br />
charges for dental care<br />
provided to a covered person<br />
who is a child under age five<br />
(5); is severely disabled or has<br />
a medical condition that<br />
requires hospitalization or<br />
general anesthesia for dental<br />
treatment.<br />
PT/OT/ST<br />
Prior Authorization Requests<br />
(may be faxed or mailed)<br />
Participating providers<br />
(Refer to Chapter 4-Care<br />
Management for details)<br />
Transplants<br />
Prior Authorization Requests<br />
(may be mailed or phoned)<br />
Phone/Fax Numbers<br />
<strong>and</strong> Addresses<br />
FAX: (651) 662-7816<br />
At Your Service<br />
Address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong><br />
Medical-Dental Review<br />
R4-72<br />
P.O. Box 64265<br />
St. Paul, MN 55164-0265<br />
FAX: (651) 662-7816<br />
Address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong><br />
Allied Health Services<br />
R4-72<br />
P.O. Box 64265<br />
St. Paul, MN 55164-0265<br />
(651) 662-9936 or<br />
1-866-309-6564<br />
FAX: 651-662-1624<br />
Address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong><br />
P.O. Box 64179<br />
Route R4-72<br />
St. Paul, MN 55164-0265<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-11
At Your Service<br />
Care Management<br />
Numbers <strong>and</strong><br />
Addresses (continued)<br />
Other Numbers <strong>and</strong><br />
Addresses<br />
Area<br />
Phone/Fax Numbers<br />
<strong>and</strong> Addresses<br />
Referrals Provider web self-service:<br />
www.providerhub.com<br />
FAX: (651) 662-6860<br />
These phone numbers, fax numbers <strong>and</strong> addresses may be helpful<br />
to you.<br />
Company Phone Number Address<br />
Healthy Start ® Prenatal<br />
Support<br />
(651) 662-1818<br />
1-866-489-6948<br />
Healthy Start<br />
P.O. Box 64060<br />
St. Paul, MN 55164-0560<br />
<strong>Blue</strong>Link TPA Refer to Member’s ID card <strong>Blue</strong>Link TPA<br />
P.O. Box 64668<br />
St. Paul, MN 55164<br />
Delta Dental ® <strong>of</strong><br />
<strong>Minnesota</strong><br />
(651) 406-5900 or<br />
1-800-328-1188<br />
FAX: (651) 406-5934<br />
MII Life Inc. (651) 662-5065<br />
1-800-859-2144<br />
Prime Therapeutics LLC (612) 777 -4000<br />
or<br />
1-800-858-0723<br />
Pharmacy help desk:<br />
1-800-821-4795<br />
(for pharmacist or doctor use<br />
only)<br />
Customer Service Refer the member to their<br />
customer service number printed<br />
on the back <strong>of</strong> their member ID<br />
card. They may also call<br />
(651) 662-8000.<br />
Medicare & More<br />
Customer Service<br />
<strong>Minnesota</strong> Health Care<br />
Programs (through DHS)<br />
Eligibility Verification<br />
System (EVS)<br />
(651) 662-5020 or<br />
1-800-531-6686<br />
(612) 282-5354 or<br />
1-800-657-3613<br />
Delta Dental <strong>of</strong> <strong>Minnesota</strong><br />
3560 Delta Dental Drive<br />
Eagan, MN 55122<br />
MII Life Inc.<br />
3535 <strong>Blue</strong> <strong>Cross</strong> Road<br />
P.O. Box 64193<br />
St. Paul, MN 55164-9828<br />
Prime Therapeutics<br />
1305 Corporate Center Drive<br />
Eagan, MN 55121<br />
1-12 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Company Phone Number Address<br />
Public Programs Member<br />
Services (PMAP <strong>and</strong><br />
<strong>Minnesota</strong>Care)<br />
Address Changes <strong>and</strong><br />
Other Demographic<br />
Information<br />
(651) 662-5545 or<br />
1-800-711-9862<br />
At Your Service<br />
Promptly notify <strong>Blue</strong> <strong>Cross</strong> when any <strong>of</strong> your demographic<br />
information changes, including but not limited to your address,<br />
phone number, hospital affiliation or <strong>of</strong>fice hours. Use the<br />
Provider Demographic Change Form, available at<br />
providers.bluecrossmn.com. Enter “provider demographic<br />
change form” in the search window. <strong>Blue</strong> <strong>Cross</strong> uses your<br />
demographic information in provider directories, to help members<br />
find you easily, mail important information to you, etc. Call (651)<br />
662-5200 or 1-800-262-0820 for telephonic assistance. FAX<br />
completed forms to (651) 662-6684 or mail them to:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
PDO, S116<br />
P.O. Box 64560<br />
St. Paul, MN 55164-0560<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-13
At Your Service<br />
BLUELINE<br />
Introduction BLUELINE is a voice response system for our health care<br />
providers. It furnishes immediate information regarding covered<br />
<strong>Blue</strong> <strong>Cross</strong> members.<br />
BLUELINE <strong>of</strong>fers callers the following information:<br />
Prior authorization<br />
Member specific claim*<br />
Member specific eligibility*<br />
Member specific benefit*<br />
Member specific primary care clinic<br />
*A fax back <strong>of</strong> this information is available by following the menu<br />
options within BLUELINE.<br />
BLUELINE Availability BLUELINE is available 24 hours a day, seven days a week; except<br />
during scheduled maintenance.<br />
Calling BLUELINE You can access BLUELINE by calling (651) 662-5200 or<br />
1-800-262-0820.<br />
If the information you are requesting is not available within<br />
BLUELINE, you will be automatically routed to a service<br />
representative during normal service hours:<br />
Monday-Thursday....8 a.m. – 8 p.m.<br />
Friday 9 a.m. – 5 p.m.<br />
System Assistance If you require assistance in accessing BLUELINE or have not<br />
received your fax, call technical support at (651) 662-5555 or toll<br />
free at 1-800-711-9871 <strong>and</strong> select option three. <strong>Blue</strong> <strong>Cross</strong> will<br />
need the following information:<br />
Provider number <strong>and</strong> name<br />
Date <strong>and</strong> time <strong>of</strong> occurrence<br />
Caller’s name <strong>and</strong> telephone number<br />
Description <strong>of</strong> the problem<br />
FAX number, if applicable.<br />
1-14 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
At Your Service<br />
Provider Identification Provider identification is required for obtaining claim information<br />
or requesting a FAX back <strong>of</strong> claim information for a specific<br />
member.<br />
BLUELINE will prompt you when necessary for your provider ID.<br />
Your choices will be “<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Provider ID,” “NPI” or “TAX ID.”<br />
You may request any <strong>of</strong> these options just be speaking the words –<br />
such as saying, “NPI.” BLUELINE will then prompt you for the<br />
actual numbers for just that ID. Just speak naturally, one character<br />
or number at a time.<br />
Member Identification When BLUELINE prompts you for the member ID, just speak the<br />
numeric portion or enter it using your touch-tone keypad. For<br />
example, if the member ID is XZA XZ1234567, just speak or enter<br />
1234567, one digit at a time.<br />
Date When BLUELINE prompts you for the date <strong>of</strong> birth or date <strong>of</strong><br />
service, just say the date naturally, for example March 17, 1964 or<br />
3-17-1964. You may also enter the date using your touch-tone<br />
keypad. If using the keypad, enter all eight digits – i.e. 03171964.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-15
At Your Service<br />
Provider Web Self-Service<br />
Provider Web<br />
Self-Service<br />
Provider web self-service is a web-based service available to<br />
providers. This program allows you access to eligibility <strong>and</strong><br />
benefits, referrals, claim status <strong>and</strong> provider searches <strong>and</strong><br />
remittance advices.<br />
The system is available 24 hours a day, seven days a week except<br />
for scheduled maintenance times <strong>and</strong> the use <strong>of</strong> case functionality.<br />
For support in the Twin Cities call (651) 662-5743 or toll free at<br />
1-866-251-6743 or email support@providerhub.com.<br />
For additional information, including an application, visit the<br />
website at: providerhub.com.<br />
1-16 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
ID Cards<br />
At Your Service<br />
Introduction Your patient’s member ID card contains information that is<br />
essential for claims processing. <strong>Blue</strong> <strong>Cross</strong> recommends that you<br />
look at the patient’s ID card at every visit <strong>and</strong> have a current copy<br />
<strong>of</strong> the front <strong>and</strong> back <strong>of</strong> the card on file. There is a sample <strong>of</strong> some<br />
<strong>of</strong> the ID cards issued from <strong>Blue</strong> <strong>Cross</strong> on our website. Some <strong>of</strong><br />
the following information may be found on the ID card:<br />
<strong>Name</strong> <strong>of</strong> the plan<br />
Member’s ID number including alpha prefix<br />
Member’s name <strong>and</strong> group number<br />
Primary care clinic (PCC) name – for managed care plans only<br />
<strong>Blue</strong> <strong>Shield</strong> plan code<br />
<strong>Blue</strong> <strong>Cross</strong> plan code<br />
Prescription coverage<br />
Copay for prescription drugs<br />
Copay for <strong>of</strong>fice visits<br />
Dependent coverage indicator<br />
Claims submission information<br />
ID Cards <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> its affiliates do not use Social Security numbers for<br />
member identification numbers<br />
Members from the following <strong>Blue</strong> <strong>Cross</strong> line <strong>of</strong> business will<br />
retain their original identification number:<br />
<strong>Minnesota</strong> government programs<br />
Prepaid Medical Assistance Program<br />
<strong>Minnesota</strong>Care (identification numbers begin with an eight).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-17
At Your Service<br />
Helpful Tips <strong>Blue</strong> <strong>Cross</strong> plans have the option <strong>of</strong> creating identifiers with any<br />
combination <strong>of</strong> up to 14 letters or digits following the three-digit<br />
alpha prefix.<br />
Verify the identity <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus cardholders by<br />
asking for additional picture identification. If you suspect<br />
fraudulent use <strong>of</strong> a member ID card, please call our fraud hot<br />
line at (651) 662-8363. You may remain anonymous.<br />
Ask members for their current member ID card <strong>and</strong> regularly<br />
obtain new photocopies (front <strong>and</strong> back). Having the current<br />
card will enable you to submit claims with the appropriate<br />
member information <strong>and</strong> avoid unnecessary claims payment<br />
delays.<br />
Check eligibility <strong>and</strong> benefits by using provider web selfservice,<br />
BLUELINE, or call 1-800-676-BLUE (2583) <strong>and</strong><br />
provide the alpha prefix for <strong>Blue</strong>Card eligibility.<br />
If the member presents a debit card be sure to verify the<br />
copayment amount before processing payments.<br />
Do not use the card to process full payment up front. If you<br />
have questions about the debit card processing instructions or<br />
payment issues, please contact the toll-free debit card<br />
administrator’s number on the back <strong>of</strong> the card.<br />
1-18 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Electronic Commerce<br />
Overview An important part <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong>’ cost containment strategy is<br />
automating the electronic exchange <strong>of</strong> information.<br />
At Your Service<br />
Electronic Transactions <strong>Blue</strong> <strong>Cross</strong> accepts the submission <strong>and</strong>/or generates the following<br />
HIPAA compliant transactions:<br />
Electronic Data<br />
Interchange (EDI)<br />
Guidelines<br />
Health Care Claim (837 P <strong>and</strong> D)<br />
Health Care Claim Payment/Advice (835)<br />
Health Care Eligibility Benefit Inquiry <strong>and</strong> Response<br />
(270/271)<br />
Health Care Claim Status Request <strong>and</strong> Response (276/277)<br />
Health Care Services Review- Request for Review <strong>and</strong><br />
Response (278)<br />
<strong>Blue</strong> <strong>Cross</strong> uses Availity for exchanging HIPAA m<strong>and</strong>ated EDI<br />
transactions. You can get information on how to register <strong>and</strong><br />
conduct electronic transactions through Availity by going to<br />
Availity.com.<br />
<strong>Minnesota</strong> Statute 62J.536 requires all <strong>Minnesota</strong> providers<br />
<strong>and</strong> <strong>Minnesota</strong> group purchasers to exchange three transactions<br />
electronically: Health Care Claims, Health Care Claim<br />
Payment/Advice <strong>and</strong> Health Care Eligibility Benefit Inquiry<br />
<strong>and</strong> Response. In addition, participating out-<strong>of</strong>-state providers<br />
are required by contract to adhere to these electronic<br />
requirements.<br />
All nonparticipating, out-<strong>of</strong>-state providers who do not have<br />
electronic claim submission capabilities must submit their<br />
claims on an optical character recognition scannable claim<br />
form.<br />
All nonparticipating, out-<strong>of</strong>-state providers who are receiving<br />
direct payment must access their remittance advice via use <strong>of</strong><br />
the electronic transaction or provider web self-service.<br />
<strong>Blue</strong> <strong>Cross</strong> reserves the right to modify these guidelines with<br />
advance written notice.<br />
Providers are encouraged to obtain or develop EDI transaction<br />
s<strong>of</strong>tware from the many sources available.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-19
At Your Service<br />
Remote Access<br />
Services<br />
Providers may be permitted to use <strong>Blue</strong> <strong>Cross</strong>' remote access<br />
services, allowing them to obtain specific subscriber information<br />
<strong>and</strong> other information necessary for submitting claims <strong>and</strong> viewing<br />
claim status or payment information. Access may not be<br />
transferred to another entity by the provider <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong> retains<br />
all rights to the computer s<strong>of</strong>tware system. Providers may only use<br />
the system to:<br />
verify health plan coverage benefits <strong>of</strong> their patients<br />
verify claims status<br />
verify cases (such as referrals <strong>and</strong> admission notifications)<br />
create <strong>and</strong> update referrals (available only for primary care<br />
clinics)<br />
create <strong>and</strong> update admission notifications (available only to<br />
primary care clinics <strong>and</strong> inpatient facilities)<br />
for external security delegated administration<br />
view remittance advice information<br />
other purposes to be communicated by <strong>Blue</strong> <strong>Cross</strong><br />
Providers have certain responsibilities when using <strong>Blue</strong> <strong>Cross</strong>'<br />
remote access services. They include:<br />
Access is for the provider only, <strong>and</strong> third parties may not have<br />
access to the system without advance written approval <strong>of</strong> <strong>Blue</strong><br />
<strong>Cross</strong>.<br />
<strong>Blue</strong> <strong>Cross</strong> is the sole <strong>and</strong> exclusive owner <strong>of</strong> the system <strong>and</strong><br />
its components, <strong>and</strong> the provider does not have any rights to it,<br />
either intellectual property rights or other rights <strong>of</strong> any kind.<br />
The provider may not reverse assemble, decompile, duplicate<br />
or modify the system or any parts <strong>of</strong> it.<br />
At any time, <strong>Blue</strong> <strong>Cross</strong> may modify or enhance the system, or<br />
replace the system with an entirely new system.<br />
Provide all necessary components for using <strong>Blue</strong> <strong>Cross</strong>'<br />
system, such as compatible s<strong>of</strong>tware, hardware, access to the<br />
Internet <strong>and</strong> any other necessary technology to access the<br />
system.<br />
<strong>Blue</strong> <strong>Cross</strong> may discontinue the provider's access to the system<br />
or terminate use <strong>of</strong> the system upon thirty (30) days advance<br />
written notice to the provider.<br />
1-20 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Remote Access<br />
Services<br />
(continued)<br />
At Your Service<br />
Providers may access <strong>Blue</strong> <strong>Cross</strong>' system via the Internet (or other<br />
technology as approved by <strong>Blue</strong> <strong>Cross</strong>) at any time, except when<br />
the system is undergoing maintenance or repairs, or due to<br />
interruptions beyond the control <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong>. Providers are<br />
solely responsible for the necessary s<strong>of</strong>tware, hardware, access to<br />
the Internet, <strong>and</strong> other technology or services necessary for<br />
providers to use the system.<br />
Only authorized users may access the system <strong>and</strong> use its services.<br />
Authorized users are employees <strong>of</strong> the provider <strong>and</strong> others<br />
included in the provider's workforce (in accordance with 45<br />
C.F.R. 160.103).<br />
The provider must designate authorized users <strong>and</strong> obtain access<br />
through <strong>Blue</strong> <strong>Cross</strong> for them to use the system, either through a<br />
user request form or directly entering into the system the<br />
information required on the user request form.<br />
<strong>Blue</strong> <strong>Cross</strong> will assign a user name upon acceptance <strong>of</strong> the user<br />
request form.<br />
Each individual user name <strong>and</strong> password <strong>and</strong> each <strong>Blue</strong> <strong>Cross</strong><br />
assigned user identification number/code <strong>and</strong> password is used<br />
only by the respective authorized user <strong>and</strong> may not be shared<br />
with anyone.<br />
The provider must provide immediate written notification to<br />
<strong>Blue</strong> <strong>Cross</strong> whenever an authorized user terminates<br />
employment with the provider.<br />
The provider must also notify <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> any other changes,<br />
deletions <strong>and</strong>/or modifications to information originally<br />
submitted on the user request form.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-21
At Your Service<br />
Remote Access<br />
Services<br />
(continued)<br />
Disclaimer: provider’s use <strong>of</strong> the services <strong>and</strong> the system <strong>and</strong> any<br />
information obtained there from is subject at all times to<br />
instructions, notices <strong>and</strong>/or disclaimers appearing on-line on the<br />
system from time to time.<br />
The services <strong>and</strong> the system are provided “AS IS” <strong>and</strong> <strong>Blue</strong><br />
<strong>Cross</strong> makes no representation or warranty that the system will<br />
meet provider’s requirements or that the system will operate<br />
uninterrupted or error free, or that the information obtained is<br />
or will be accurate.<br />
<strong>Blue</strong> <strong>Cross</strong> makes no warranties <strong>of</strong> merchantability, fitness for<br />
a particular purpose, non-infringement or otherwise, all <strong>of</strong><br />
which are expressly disclaimed.<br />
Payment: <strong>Blue</strong> <strong>Cross</strong> reserves the right to require providers to pay<br />
remote access service fees. In such an event, <strong>Blue</strong> <strong>Cross</strong> will<br />
provide at least 90 days’ advance written notice to providers. Such<br />
fees will be due <strong>and</strong> payable within 30 days <strong>of</strong> any invoice <strong>and</strong> late<br />
payments will be subject to interest at a rate <strong>of</strong> the lesser <strong>of</strong> (a) one<br />
<strong>and</strong> one-half percent per month or (b) the highest rate allowed by<br />
law.<br />
Limitation <strong>of</strong> Liability: <strong>Blue</strong> <strong>Cross</strong>’ entire liability to provider for<br />
any <strong>and</strong> all damages incurred by provider for any <strong>and</strong> all claims<br />
arising out <strong>of</strong>, or otherwise relating to remote access services<br />
described above shall in the aggregate not exceed 100 percent <strong>of</strong><br />
the total remote access services fees received by <strong>Blue</strong> <strong>Cross</strong>. <strong>Blue</strong><br />
<strong>Cross</strong> will not be liable for any damages caused by provider’s<br />
failure to perform its responsibilities <strong>and</strong>/or for any indirect,<br />
special or punitive damages, even if <strong>Blue</strong> <strong>Cross</strong> has been advised<br />
<strong>of</strong> or is otherwise aware <strong>of</strong> the possibility <strong>of</strong> such damages.<br />
1-22 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Provider Communications<br />
Provider<br />
Communications<br />
At Your Service<br />
<strong>Blue</strong> <strong>Cross</strong> publishes the following communications for providers.<br />
They are available on our website at providers.bluecrossmn.com.<br />
Title Description<br />
Provider Bulletins <strong>Blue</strong> <strong>Cross</strong> communicates immediate policy<br />
<strong>and</strong> procedure changes through Provider<br />
Bulletins. The Provider Bulletins are<br />
contractually binding. Portions <strong>of</strong> this<br />
manual will also be updated periodically to<br />
reflect policy <strong>and</strong> procedure changes.<br />
Provider Press The goal <strong>of</strong> this publication is to make your<br />
job easier <strong>and</strong> to improve our service to you.<br />
The categories that are featured in the<br />
Provider Press include claims tips,<br />
PMAP/<strong>Minnesota</strong>Care, Coding Corner <strong>and</strong> a<br />
featured front page article.<br />
Provider<br />
Information<br />
Quick Points<br />
Medical Policy<br />
Update<br />
<strong>Blue</strong> Plus Referral<br />
Network for<br />
Primary Care<br />
Clinics<br />
This is a communication tool that <strong>Blue</strong> <strong>Cross</strong><br />
is using to get helpful information to you.<br />
Changes to Medical Policy impacting<br />
payment are communicated through Provider<br />
Bulletins. <strong>Blue</strong> <strong>Cross</strong> also includes updates in<br />
the Provider Press on a quarterly basis. The<br />
updates contain a summary <strong>of</strong> medical<br />
technologies that have been reviewed,<br />
revised, or are new to <strong>Blue</strong> <strong>Cross</strong>’<br />
investigative list. Prior authorization request<br />
requirements are also featured in this<br />
publication.<br />
This is a listing <strong>of</strong> specialty providers for<br />
referral purposes.<br />
<strong>Blue</strong> Plus <strong>Manual</strong> The <strong>Blue</strong> Plus <strong>Manual</strong> is published for our<br />
<strong>Blue</strong> Plus primary care providers. It includes<br />
information about the <strong>Blue</strong> Plus business,<br />
referrals, contacts, quality improvement, <strong>and</strong><br />
government programs.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-23
At Your Service<br />
Member Rights <strong>and</strong> Responsibilities<br />
Health Plan Members<br />
have the Following<br />
Rights<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Enrollee Rights <strong>and</strong> Responsibilities<br />
YOU HAVE THE RIGHT AS A HEALTH PLAN MEMBER:<br />
To be treated with respect, dignity <strong>and</strong> privacy.<br />
To receive quality health care that is friendly <strong>and</strong> timely.<br />
To have available <strong>and</strong> accessible medically necessary covered<br />
services, including emergency services, 24 hours a day, <strong>and</strong><br />
seven (7) days a week.<br />
To be informed <strong>of</strong> your health problems <strong>and</strong> to receive<br />
information regarding treatment alternatives <strong>and</strong> their risk in<br />
order to make an informed choice regardless, if the health plan<br />
pays for treatment.<br />
To participate with your health care providers in decisions<br />
about your treatment.<br />
To give your provider a health care directive or a living will (a<br />
list <strong>of</strong> instructions about health treatments to be carried out in<br />
event <strong>of</strong> incapacity).<br />
To refuse treatment.<br />
To have privacy <strong>of</strong> medical <strong>and</strong> financial records maintained<br />
by <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> its health care providers in accordance with<br />
existing law.<br />
To receive information about <strong>Blue</strong> <strong>Cross</strong>, its services, its<br />
providers <strong>and</strong> your rights <strong>and</strong> responsibilities.<br />
To make recommendations regarding these rights <strong>and</strong><br />
responsibilities policies.<br />
To have a resource at <strong>Blue</strong> <strong>Cross</strong> or at the clinic that you can<br />
contact with any concerns about services.<br />
To file a complaint with <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> the <strong>Minnesota</strong><br />
Commissioner <strong>of</strong> Commerce <strong>and</strong> receive a prompt <strong>and</strong> fair<br />
review.<br />
To initiate a legal proceeding when experiencing a problem<br />
with <strong>Blue</strong> <strong>Cross</strong> or its providers.<br />
1-24 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11)
Health Plan Members<br />
have the Following<br />
Responsibilities<br />
At Your Service<br />
YOU HAVE THE RESPONSIBILITY AS A HEALTH PLAN<br />
MEMBER:<br />
To know your health plan benefits <strong>and</strong> requirements.<br />
To provide, to the extent possible, information that <strong>Blue</strong> <strong>Cross</strong><br />
<strong>and</strong> its providers need in order to care for you.<br />
To underst<strong>and</strong> your health problems <strong>and</strong> work with your doctor<br />
to set mutually agreed-upon treatment goals.<br />
To follow the treatment plan prescribed by your provider or<br />
discuss with your provider why you are unable to follow the<br />
treatment plan.<br />
To provide pro<strong>of</strong> <strong>of</strong> coverage when you receive services <strong>and</strong> to<br />
update the clinic with any personal changes.<br />
To pay copays at the time <strong>of</strong> service <strong>and</strong> to promptly pay<br />
deductibles, coinsurance <strong>and</strong> if applicable, charges for services<br />
that are not covered.<br />
To keep appointments for care or to give early notice if you<br />
need to cancel a scheduled appointment.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/24/11) 1-25
Table <strong>of</strong> Contents<br />
Chapter 2<br />
Provider Agreements<br />
Participation <strong>and</strong> Responsibilities............................................................................................ 2-2<br />
Advantages <strong>of</strong> Participation................................................................................................... 2-2<br />
Responsibilities <strong>of</strong> Participating Providers............................................................................ 2-2<br />
Requirements <strong>of</strong> <strong>Minnesota</strong> Law...........................................................................................2-4<br />
<strong>Blue</strong> <strong>Cross</strong>' Responsibilities...................................................................................................2-5<br />
Written Notification <strong>and</strong> Provider Liability...........................................................................2-5<br />
Provider Numbers...................................................................................................................... 2-6<br />
Overview................................................................................................................................2-6<br />
National Provider Number (NPI)...........................................................................................2-6<br />
Credentialing.............................................................................................................................. 2-7<br />
Overview................................................................................................................................2-7<br />
Credentialing Requirements <strong>and</strong> Processes ...........................................................................2-7<br />
Questions about Credentialing............................................................................................... 2-7<br />
Accounting for Disclosure Request .......................................................................................... 2-8<br />
Guidelines for the Accounting Disclosure Request...............................................................2-8<br />
When to Use the Form ...........................................................................................................2-8<br />
Disclosures Related to Your Status as a Business Associate................................................. 2-9<br />
Carrier Replacement Law....................................................................................................... 2-10<br />
Carrier Replacement ............................................................................................................ 2-10<br />
How Carrier Replacement Works........................................................................................2-10<br />
Continuous Stay...................................................................................................................2-10<br />
Public Programs...................................................................................................................2-11<br />
Federal Employee Program..................................................................................................2-11<br />
InstaCare SM ..........................................................................................................................2-11<br />
Self-funded Groups <strong>and</strong> <strong>Minnesota</strong> Advantage Health Plan ............................................... 2-11<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10) 2-1
Provider Agreements<br />
Participation <strong>and</strong> Responsibilities<br />
Advantages <strong>of</strong><br />
Participation<br />
Responsibilities <strong>of</strong><br />
Participating Providers<br />
Advantages <strong>of</strong> being a participating provider include:<br />
• Direct payment from <strong>Blue</strong> <strong>Cross</strong> reduces administrative<br />
expense <strong>and</strong> improves cash flow<br />
• <strong>Blue</strong> <strong>Cross</strong> members have financial incentives to use<br />
participating providers<br />
• Participating providers’ names are included in directories that<br />
we publish for our members<br />
• <strong>Blue</strong> <strong>Cross</strong> contracts do not contain exclusivity clauses that<br />
prohibit you from participating with other health plans<br />
• Participating providers receive a Statement <strong>of</strong> Provider Claims<br />
Paid explaining how claims are processed<br />
• Opportunity to attend provider seminars <strong>of</strong>fered free <strong>of</strong> charge<br />
by <strong>Blue</strong> <strong>Cross</strong><br />
• Dedicated service staff available to assist participating<br />
providers<br />
• Electronic options such as provider web self-service to obtain<br />
information<br />
Responsibilities <strong>of</strong> being a participating provider include:<br />
• Participating providers are required to electronically submit all<br />
claims. Paper claims submitted by providers will be rejected<br />
<strong>and</strong> will need to be submitted electronically. <strong>Blue</strong> <strong>Cross</strong> will<br />
not consider such paper claims to have been received until<br />
resubmitted electronically.<br />
• Participating in the <strong>Blue</strong> <strong>Cross</strong> credentialing process.<br />
• Participating in <strong>Blue</strong> <strong>Cross</strong> managed care programs.<br />
2-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10)
Responsibilities <strong>of</strong><br />
Participating Providers<br />
(continued)<br />
Provider Agreements<br />
• Submitting preadmission notifications (PANs) or prior<br />
authorizations or pre-certifications when required. PANs must<br />
be submitted through provider web self-service.<br />
• Exceptions to this are:<br />
• non-rehab acute inpatient admissions to Bethesda<br />
Hospital<br />
• admissions for <strong>Blue</strong>Link TPA members<br />
• if your clinic/facility does not have web access<br />
• For these exceptions only, PANs may be faxed to<br />
(651) 662-6860.<br />
• Referring patients, whenever possible, to other participating<br />
providers including, but not limited to, anesthesiologists,<br />
radiologists, pathologists, surgical assistants <strong>and</strong>, where<br />
applicable, to Select network providers.<br />
• Accepting payment provisions outlined in the agreement. If<br />
<strong>Blue</strong> <strong>Cross</strong> determines that services are experimental,<br />
investigative, or not medically necessary, you may not bill the<br />
patient unless you give the patient written notification <strong>of</strong> noncoverage<br />
immediately before the services are performed <strong>and</strong><br />
the patient agrees in writing to be responsible for the services.<br />
• Notifying <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> new programs prior to implementation<br />
(i.e., technology, new procedures being performed).<br />
• Maintaining confidentiality <strong>of</strong> our contractual <strong>and</strong> financial<br />
arrangements.<br />
• Each provider’s services must be within the scope <strong>of</strong> the<br />
provider’s registration, license, <strong>and</strong> training <strong>and</strong> consistent<br />
with community st<strong>and</strong>ards for quality <strong>and</strong> utilization.<br />
• Not bill <strong>Blue</strong> <strong>Cross</strong> for any pr<strong>of</strong>essional services provided by<br />
physicians <strong>and</strong> health care pr<strong>of</strong>essionals to themselves, their<br />
immediate family members or those living in the same<br />
household. Immediate family members include the physician’s<br />
or health care pr<strong>of</strong>essional’s spouse, children, parents or<br />
siblings.<br />
• Not bill members for missed scheduled appointments except<br />
for a patient who misses a scheduled behavioral health<br />
appointment, provided you have notified the member in<br />
writing in advance that this is your policy. Please note that<br />
PMAP, <strong>Minnesota</strong>Care, <strong>and</strong> Medicare members may not be<br />
billed for missed appointments.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10) 2-3
Provider Agreements<br />
Responsibilities <strong>of</strong><br />
Participating Providers<br />
(continued)<br />
Requirements <strong>of</strong><br />
<strong>Minnesota</strong> Law<br />
• Promptly furnishing at the provider’s own expense any<br />
additional information that <strong>Blue</strong> <strong>Cross</strong> or the plan sponsor shall<br />
reasonably request as necessary to respond to claims,<br />
utilization review, coordination <strong>of</strong> benefits, quality<br />
improvement <strong>and</strong> care management reviews, pre-certification<br />
reviews, preadmission notification, prior authorization, medical<br />
necessity reviews, credentialing, <strong>and</strong> medical abstract reports.<br />
The provider shall be responsible for obtaining any<br />
authorization required to release such information to <strong>Blue</strong><br />
<strong>Cross</strong> or the plan sponsor.<br />
• Provider will collect appropriate copayment amounts <strong>and</strong> not<br />
waive these amounts.<br />
• Billing the patient for noncovered services listed as exclusions<br />
in the patient’s coverage certificate.<br />
• Participating providers may not collect any difference between<br />
the amount billed <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong>’ allowance for health<br />
services.<br />
• Charging members <strong>of</strong> the general public the same amounts as<br />
<strong>Blue</strong> <strong>Cross</strong> members (individual hardship cases are an<br />
exception).<br />
• Billing only for services personally performed by your medical<br />
staff or other pr<strong>of</strong>essionals employed by your facility that meet<br />
the eligibility criteria defined by <strong>Blue</strong> <strong>Cross</strong>.<br />
<strong>Minnesota</strong> law requires participating providers to look to <strong>Blue</strong><br />
<strong>Cross</strong> for payment <strong>of</strong> services covered by the member’s contract.<br />
Following are requirements:<br />
• Providers may not bill patients for services covered by their<br />
<strong>Blue</strong> <strong>Cross</strong> health plan only in accordance with <strong>Minnesota</strong> law<br />
for the applicable coinsurance, copayment or deductible <strong>and</strong><br />
providers may not withhold treatment in the event that a patient<br />
is unable to make payment in advance <strong>and</strong> prior to <strong>Blue</strong> <strong>Cross</strong><br />
completing processing <strong>of</strong> the claim or adjustment.<br />
• Providers may not refer a patient’s account to collection for<br />
nonpayment <strong>of</strong> services covered by the <strong>Blue</strong> <strong>Cross</strong> health plan.<br />
Copayments, coinsurance <strong>and</strong> deductibles can be coordinated<br />
through the clinic’s normal billing, <strong>and</strong> if applicable, their<br />
collections process.<br />
• Interest on services covered by <strong>Blue</strong> <strong>Cross</strong> may not be applied<br />
to a patient’s account.<br />
2-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10)
Requirements <strong>of</strong><br />
<strong>Minnesota</strong> Law<br />
(continued)<br />
<strong>Blue</strong> <strong>Cross</strong>'<br />
Responsibilities<br />
Written Notification<br />
<strong>and</strong> Provider Liability<br />
Provider Agreements<br />
• Effective August 1, 2010, <strong>Minnesota</strong> Statute [62Q.751] states:<br />
• Providers may collect deductibles <strong>and</strong> coinsurance from<br />
patients at or prior to the time <strong>of</strong> service.<br />
• Providers may not withhold a service to a health plan<br />
company enrollee based on a patient's failure to pay a<br />
deductible or coinsurance at or prior to the time <strong>of</strong> service.<br />
• Overpayments by patients to providers must be returned to<br />
the patient by the provider by check or electronic payment<br />
within 30 days <strong>of</strong> the date in which the claim adjudication<br />
is received by the provider.<br />
<strong>Blue</strong> <strong>Cross</strong>’ responsibilities include the following:<br />
• Make payment directly to the provider for covered services,<br />
respond to inquiries <strong>and</strong> resolve claims in a timely manner<br />
• Maintaining confidentiality <strong>of</strong> the provider’s charge data in<br />
accordance with the contract terms<br />
• Establishing a peer-review process to make decisions about<br />
medical necessity<br />
• Keeping members informed <strong>of</strong> participating providers through<br />
publication <strong>of</strong> directories<br />
• Keeping providers informed <strong>of</strong> changes which are<br />
contractually binding through Provider Bulletins or other<br />
communications (i.e. Provider <strong>Manual</strong>)<br />
If it is necessary to recommend that a patient see a<br />
nonparticipating provider, the participating physician must give the<br />
patient advance, written notification that the recommendation is to<br />
a nonparticipating physician. Once notice is given, the patient is<br />
responsible for any increased liability if he or she decides to<br />
schedule the service. If a patient is not properly informed, the<br />
provider making the recommendation to a nonparticipating<br />
provider will be liable for increased costs that a patient incurs.<br />
Please refer to Waivers in Chapter 4.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10) 2-5
Provider Agreements<br />
Provider Numbers<br />
Overview <strong>Blue</strong> <strong>Cross</strong> works with many different types <strong>of</strong> providers through<br />
contractual agreements. Agreements are in place with facilities <strong>and</strong><br />
physician clinics to establish networks <strong>of</strong> participating providers<br />
for our members.<br />
National Provider<br />
Number (NPI)<br />
The Health Insurance Portability <strong>and</strong> Accountability Act-<br />
Administrative Simplification (HIPAA-AS) is the result <strong>of</strong><br />
legislation passed by the U.S. Congress. The legislation m<strong>and</strong>ates<br />
st<strong>and</strong>ards for business to business electronic data interchange <strong>and</strong><br />
code sets, establishes uniform heath care identifiers <strong>and</strong> seeks<br />
protection for the privacy <strong>and</strong> security <strong>of</strong> patient data.<br />
The purpose <strong>of</strong> implementing the NPI is to improve the efficiency<br />
<strong>and</strong> effectiveness <strong>of</strong> the health care system by reducing the number<br />
<strong>of</strong> identifiers associated with any specific provider or provider<br />
facility. Implementation will simplify provider identification <strong>and</strong><br />
billing processes across multiple third party payers (including<br />
government programs) <strong>and</strong> prevent fraud <strong>and</strong> abuse.<br />
The NPI is a unique all numeric 10 digit number that is assigned<br />
by the Centers for Medicare & Medicaid Services (CMS). NPI<br />
eligible providers are to submit transactions with the NPI at the<br />
facility level as well as the practitioner level. Providers who are<br />
considered Atypical (not eligible for an NPI) are to submit<br />
transactions using their DHS assigned Unique <strong>Minnesota</strong> Provider<br />
Identifier (UMPI) or the <strong>Blue</strong> <strong>Cross</strong> proprietary identification<br />
number.<br />
To register online or to find the NPI paper application form, access<br />
the CMS website at http://nppes.cms.hhs.gov.<br />
It is your responsibility to report your NPI to payers. To access the<br />
NPI submission instructions, go to bluecrossmn.com for health<br />
care providers, HIPAA/NPI Compliance.<br />
2-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10)
Credentialing<br />
Provider Agreements<br />
Overview <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> uses a credentialing<br />
process to provide members with a selection <strong>of</strong> physicians <strong>and</strong><br />
other healthcare pr<strong>of</strong>essionals who have demonstrated<br />
backgrounds consistent with the delivery <strong>of</strong> high quality, costeffective<br />
health care. We have established credentialing criteria for<br />
network participation that is used to evaluate a provider’s<br />
credentials. The credentialing criteria serve as the foundation for<br />
determining a provider’s eligibility <strong>and</strong> continued eligibility in all<br />
<strong>Blue</strong> <strong>Cross</strong> networks. Providers are expected to remain in<br />
compliance with credentialing criteria at all times.<br />
Credentialing<br />
Requirements <strong>and</strong><br />
Processes<br />
Questions about<br />
Credentialing<br />
To learn more about credentialing requirements <strong>and</strong> processes,<br />
please reference the CREDENTIALING POLICY MANUAL<br />
found at providers.bluecrossmn.com.<br />
Call provider services at (651) 662-5200 or 1-800-262-0820.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10) 2-7
Provider Agreements<br />
Accounting for Disclosure Request<br />
Guidelines for the<br />
Accounting Disclosure<br />
Request<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> members have the right<br />
to an accounting <strong>of</strong> certain disclosures that are made <strong>of</strong> their<br />
protected health information (PHI) within six years prior to their<br />
request. <strong>Blue</strong> <strong>Cross</strong> will fulfill these requests with a member<br />
disclosure summary. Providers are requested to follow the<br />
guidelines listed below <strong>and</strong> forward required disclosures to:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus<br />
Attention: Compliance <strong>and</strong> Regulatory Affairs<br />
P.O. Box 64560<br />
St. Paul, MN 55164-0560<br />
When to Use the Form If a disclosure is subject to an accounting, providers must use the<br />
enclosed form to record the disclosure information. This form can<br />
be found on our website at bluecrossmn.com. Disclosures which<br />
require an accounting include disclosures which are made:<br />
1. pursuant to applicable law;<br />
2. for cadaveric organ donation purposes;<br />
3. to avert a serious threat to health or safety;<br />
4. for certain marketing or fundraising exceptions; <strong>and</strong><br />
5. to the Secretary <strong>of</strong> Health <strong>and</strong> Human Services.<br />
The attached form provides a more detailed list <strong>of</strong> those<br />
disclosures that must be accounted for. Not all disclosures <strong>of</strong> an<br />
individual’s PHI are subject to an accounting.<br />
Providers are not required to account for disclosures they make:<br />
• before the privacy rules compliance date (April 14, 2003)<br />
• to the individual<br />
• to or for notification <strong>of</strong> persons involved in an individual’s care<br />
• for treatment, payment, or health care operations<br />
• for national security or intelligence purposes<br />
• to correctional institutions or law enforcement <strong>of</strong>ficials<br />
regarding inmates<br />
• for research if it involves at least 50 records <strong>and</strong> we provide<br />
individuals with a list <strong>of</strong> all the research protocols <strong>and</strong> the<br />
researcher’s name <strong>and</strong> contact information<br />
• using de-identified health information<br />
2-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10)
Disclosures Related to<br />
Your Status as a<br />
Business Associate<br />
Provider Agreements<br />
Our agreement with you does not require that you account to us for<br />
any <strong>and</strong> all disclosures that do not fall within the exceptions listed<br />
above. We want to clarify how the disclosure requirements apply<br />
to you as our business associates. As you are aware, we have<br />
determined that you are our business associate because our<br />
provider agreement with you requires you perform certain<br />
activities on our behalf. We have identified these business<br />
associate activities as:<br />
• Compliance with <strong>and</strong> implementation <strong>of</strong> quality<br />
improvement/managed care requirements such as providing<br />
specific patient records for a quality study; <strong>and</strong><br />
• Receiving <strong>and</strong> resolving member complaints.<br />
You would only need to account for disclosures <strong>of</strong> records that you<br />
hold in your capacity as a business associate. For example, if you<br />
report a complaint to <strong>Blue</strong> <strong>Cross</strong> as required by your <strong>Blue</strong> <strong>Cross</strong><br />
Provider Agreement, you are gathering that information <strong>and</strong><br />
forwarding it to us as our business associate. You do not have to<br />
report the disclosure to us because it is part <strong>of</strong> health care<br />
operations. If, however, a regulator were to audit our compliance<br />
with h<strong>and</strong>ling member complaints <strong>and</strong> you had to release<br />
correspondence or records to the regulator, which is a disclosure<br />
you would have to account for. You created the record as our<br />
business associate <strong>and</strong> disclosed to a regulator, which is the type <strong>of</strong><br />
disclosure that must be accounted for.<br />
Another example would be records that you provided to us for<br />
Child <strong>and</strong> Teen Checkups. If the Department <strong>of</strong> Health were to<br />
decide to monitor managed care plans for child <strong>and</strong> teen checkups,<br />
they may ask you for all the information you provided to <strong>Blue</strong><br />
<strong>Cross</strong> as part <strong>of</strong> the on-site audits. The disclosure is permitted to<br />
the Department <strong>of</strong> Health without authorization as a public health<br />
activity, but it must be accounted for.<br />
You do not have to account for disclosure <strong>of</strong> records that you have<br />
in your capacity as a provider. For example, as discussed above,<br />
you might have medical records from providing a teen with a<br />
checkup. Subsequently, the teen is involved in a crime <strong>and</strong> the<br />
medical records are necessary for identification purposes. You<br />
may disclose the medical record to law enforcement authorities<br />
<strong>and</strong> must account to the teen for that disclosure. You do not,<br />
however, have to account to <strong>Blue</strong> <strong>Cross</strong> for that disclosure.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10) 2-9
Provider Agreements<br />
Carrier Replacement Law<br />
Carrier Replacement The Law<br />
How Carrier<br />
Replacement Works<br />
The <strong>Minnesota</strong> Carrier Replacement Law applies when a group<br />
terminates their fully insured coverage with one carrier <strong>and</strong><br />
replaces it with another fully insured group contract. This law<br />
dictates how <strong>Blue</strong> <strong>Cross</strong> determines liability for charges incurred<br />
by a member whose inpatient treatment occurred during this<br />
change in coverage.<br />
• The carrier whose coverage is in effect when a patient is<br />
admitted to a facility is liable for all institutional charges<br />
incurred by a member whose inpatient treatment spans the<br />
change in coverage.<br />
• The carrier in effect at the time <strong>of</strong> admission is liable for all<br />
pr<strong>of</strong>essional charges incurred up to the termination date <strong>of</strong> the<br />
coverage.<br />
• The new carrier is liable for all pr<strong>of</strong>essional charges incurred<br />
beginning on the effective date <strong>of</strong> the new coverage.<br />
• The definition <strong>of</strong> “discharge” is the date the patient is formally<br />
released from the inpatient facility with discharge papers<br />
completed.<br />
Continuous Stay Continuous stay occurs when the patient is sent to another facility<br />
for services unavailable at the current facility <strong>and</strong> no discharge or<br />
admission papers are processed upon transfer.<br />
• In the case <strong>of</strong> a patient who is discharged <strong>and</strong> transferred to<br />
another facility, both the transportation <strong>and</strong> charges incurred at<br />
the new facility will become the liability <strong>of</strong> the new carrier.<br />
When… Then…<br />
a new member was hospitalized<br />
prior to the effective date <strong>of</strong><br />
<strong>Blue</strong> <strong>Cross</strong> coverage<br />
a new member remains<br />
hospitalized on <strong>and</strong> after the<br />
first date <strong>of</strong> coverage<br />
the new member’s other carrier<br />
stops paying for the<br />
hospitalization or there is no<br />
other carrier<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong> pays the hospital<br />
claim on a pro rata basis<br />
beginning on the date coverage<br />
becomes effective.<br />
2-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10)
Provider Agreements<br />
Public Programs DHS requires the health plan active at the time <strong>of</strong> patient<br />
admission to be responsible for all services associated with an<br />
inpatient stay until the discharge date. This includes both facility<br />
<strong>and</strong> pr<strong>of</strong>essional charges.<br />
Federal Employee<br />
Program<br />
• All services occurring after the termination date <strong>of</strong> the contract<br />
for Individual contracts are denied as “No Coverage”.<br />
• Medicare supplement contracts will cover the Medicare<br />
inpatient deductible. However, Medicare Coinsurance Days are<br />
denied after the coverage termination.<br />
When Federal Employee Health Benefits coverage ends, the<br />
employee <strong>and</strong> eligible dependents may receive an additional 31<br />
days <strong>of</strong> coverage, for additional premium, when:<br />
• enrollment ends, unless the employee cancels their enrollment<br />
or<br />
• the employee family members are no longer eligible<br />
The employee may be eligible for spouse equity coverage or<br />
Temporary Continuation <strong>of</strong> Coverage (TCC), or a conversion<br />
policy.<br />
InstaCare SM This Contract terminates at the end <strong>of</strong> the contract term selected on<br />
the Contract Schedule <strong>and</strong> Application, except in instances where<br />
the member or their covered dependents are confined to a hospital<br />
on that date. For that person, we will extend the contract term only<br />
for the condition causing the hospital confinement. The extension<br />
will end when the person is no longer confined to the hospital or<br />
when the lifetime maximum has been paid, whichever occurs first.<br />
Self-funded Groups<br />
<strong>and</strong> <strong>Minnesota</strong><br />
Advantage Health Plan<br />
Carrier Replacement law does not apply to self-insured business.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (01/05/10) 2-11
Table <strong>of</strong> Contents<br />
Chapter 3<br />
Quality Improvement<br />
Introduction to Quality Improvement ..................................................................................... 3-2<br />
General Overview ..................................................................................................................3-2<br />
Basic Elements <strong>of</strong> a QI Program............................................................................................3-2<br />
Leadership..............................................................................................................................3-3<br />
Quality Improvement Projects ..............................................................................................3-3<br />
Cooperation with <strong>Blue</strong> <strong>Cross</strong> QI Program............................................................................. 3-4<br />
Telephone Care: During Office Hours...................................................................................3-4<br />
Telephone Care: In-coming Calls .......................................................................................... 3-4<br />
Telephone Care: After Hours.................................................................................................3-5<br />
Complaint Review System..................................................................................................... 3-6<br />
Quality <strong>of</strong> Care Complaints ...................................................................................................3-7<br />
Access & Availability............................................................................................................3-7<br />
Written Policies......................................................................................................................3-8<br />
Continuity <strong>and</strong> Coordination <strong>of</strong> Care................................................................................... 3-11<br />
Patient Safety .......................................................................................................................3-12<br />
Medical Record Keeping Practices...................................................................................... 3-13<br />
Medical Record Documentation .......................................................................................... 3-14<br />
Clinical Practice Guidelines.................................................................................................3-16<br />
Quality Improvement for Behavioral Health Providers ...................................................... 3-19<br />
General Overview ................................................................................................................3-19<br />
Cooperation with <strong>Blue</strong> <strong>Cross</strong> QI Program........................................................................... 3-19<br />
Complaint Review System................................................................................................... 3-20<br />
Additional requirements for Select Network Providers....................................................... 3-20<br />
Access <strong>and</strong> Availability .......................................................................................................3-20<br />
Physical Facility...................................................................................................................3-21<br />
Written Provider Policies..................................................................................................... 3-22<br />
Treatment Record Documentation.......................................................................................3-23<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-1
Quality Improvement<br />
Introduction to Quality Improvement<br />
General Overview This chapter contains detailed information about the <strong>Blue</strong> <strong>Cross</strong><br />
Quality Improvement (QI) program. The information provided in<br />
this chapter is intended for all Aware providers, however; some<br />
requirements may not apply in every facility. Additionally, some<br />
requirements for behavioral health providers are different than<br />
those described below. Requirements that are different or more<br />
stringent for behavioral health providers are detailed in the Quality<br />
Improvement for Behavioral Health Providers section. The<br />
material also explains what is expected from participating<br />
providers regarding their quality programs <strong>and</strong> defines provider<br />
requirements including medical record keeping practices.<br />
Basic Elements <strong>of</strong> a QI<br />
Program<br />
Rationale:<br />
<strong>Blue</strong> <strong>Cross</strong> subscribes to the philosophy <strong>of</strong> Quality Improvement<br />
(QI) <strong>and</strong> the multifaceted benefits it <strong>of</strong>fers. All providers<br />
associated with our <strong>Blue</strong> <strong>Cross</strong> networks must include quality<br />
improvement activities in their facilities. Striving to meet or<br />
exceed customer expectations should be a driver for a successful<br />
program. A well-established program enables you to discover root<br />
causes, use data to increase production, <strong>and</strong> maximize your<br />
available resources. A successful program has three basic<br />
elements: it must be customer-focused, data-driven, <strong>and</strong> processoriented.<br />
<strong>Blue</strong> <strong>Cross</strong> supports the six aims for improvement identified in the<br />
Institute <strong>of</strong> Medicine’s <strong>Cross</strong>ing the Quality Chasm. These six<br />
aims are that care should be safe, effective, patient-centered,<br />
timely, efficient, <strong>and</strong> equitable. All <strong>Blue</strong> <strong>Cross</strong> providers are<br />
expected to incorporate these aims into their Quality Improvement<br />
programs. Some models are available to guide <strong>and</strong> direct QI<br />
project efforts.<br />
Requirements:<br />
• Provide annual QI program report upon request to <strong>Blue</strong> <strong>Cross</strong>.<br />
3-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Leadership Rationale:<br />
Quality Improvement<br />
Projects<br />
Leadership within an organization must support <strong>and</strong> embrace the<br />
philosophy <strong>of</strong> Quality Improvement for it to succeed. Advising,<br />
supporting, <strong>and</strong> actively participating in the development <strong>and</strong><br />
implementation <strong>of</strong> process improvement is a vital function <strong>of</strong><br />
leadership.<br />
Improving processes within an organization promotes better care<br />
<strong>and</strong> services to customers, creating a marketplace advantage.<br />
Requirement:<br />
• Designated QI Medical Director, who is a practicing physician<br />
<strong>and</strong> is either a MD or DO.<br />
Rationale:<br />
Addressing problems or opportunities within your facility using<br />
the QI process <strong>of</strong>fers distinct advantages. Quality Improvement<br />
projects employ systematic analysis <strong>of</strong> current practices to reveal<br />
refined approaches to everyday operations. Using a defined model<br />
means that changes can be tested <strong>and</strong> adopted effectively.<br />
Requirements <strong>and</strong> changes regarding QI reporting are distributed<br />
annually in the first quarter to all main site primary care providers.<br />
Suggested project categories may include clinical guideline<br />
implementation or improvement, administrative or processoriented<br />
improvements, or improvements based on customer<br />
feedback. Often providers choose to do one project that is clinical<br />
<strong>and</strong> one that is service-related.<br />
We encourage you to conduct a survey or focus group <strong>of</strong><br />
customers as you develop system changes. <strong>Blue</strong> <strong>Cross</strong> does not<br />
routinely collect project information from providers however,<br />
requirements remain the same. The requirements listed below<br />
should be followed if your facility chooses to implement<br />
improvement activities.<br />
Requirements:<br />
• Provide QI program description, contact information, or<br />
project reports upon request.<br />
• Clinical projects must be based on approved <strong>and</strong> established<br />
guidelines [i.e., Institute for Clinical Systems Improvement<br />
(ICSI)].<br />
• Projects have completed a full PDCA Cycle or Seven-Step<br />
process. Refer to the PDCA or Seven-Step Process<br />
information.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-3
Quality Improvement<br />
Cooperation with <strong>Blue</strong><br />
<strong>Cross</strong> QI Program<br />
Telephone Care:<br />
During Office Hours<br />
Telephone Care:<br />
In-coming Calls<br />
Rationale:<br />
Collaborative efforts need to mutually service our<br />
members/patients with excellent care <strong>and</strong> services.<br />
Requirements:<br />
• Consultation <strong>and</strong> cooperation to resolve individual patient<br />
complaints.<br />
• Provide medical records for QI purposes upon request.<br />
• Collaborate on corrective action plan when <strong>Blue</strong> <strong>Cross</strong> quality<br />
thresholds are not met. The <strong>Blue</strong> <strong>Cross</strong> Quality Council<br />
determines thresholds.<br />
Rationale:<br />
Patients need telephone access to medical care with a response<br />
time based on the urgency <strong>of</strong> their symptoms.<br />
Requirements:<br />
During <strong>of</strong>fice hours, members calling a provider will be assessed<br />
according to patient care needs by a physician or designee:<br />
• Immediately for emergencies, 100% <strong>of</strong> the time<br />
• Within 30 minutes for urgent issues, 85% <strong>of</strong> the time<br />
• Within four hours for all other call types, 85% <strong>of</strong> the time<br />
Rationale:<br />
A timely response to incoming phone calls promotes patient<br />
satisfaction.<br />
Requirements:<br />
• Calls answered in six rings or fewer<br />
• On hold two minutes or less<br />
3-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Telephone Care:<br />
After Hours<br />
Rationale:<br />
Patients must have access to instructions for obtaining care 24<br />
hours a day, 7 days a week, <strong>and</strong> 365 days a year. When patients<br />
call your facility outside <strong>of</strong> routine business hours, it is important<br />
that they are able to receive directions on how to obtain care <strong>and</strong><br />
get answers to their questions. To achieve this, providers must<br />
have a telephone number that is answered 24 hours a day by either<br />
a live person, or an answering system that will provide patients<br />
information as outlined below.<br />
• The name <strong>of</strong> the clinic that the patient is calling is clearly<br />
stated.<br />
• Specific instructions on what the patient should do if they feel<br />
their situation is a medical emergency. This is <strong>of</strong>ten stated, “If<br />
you feel this is a medical emergency please hang up <strong>and</strong> dial<br />
911."<br />
• Information regarding who the patient should call if it is not a<br />
medical emergency, but feel they need medical advice. Be<br />
certain to include the name, area code <strong>and</strong> telephone number <strong>of</strong><br />
the individual or clinic to whom they are being directed.<br />
• If the patient is directed to leave a message, an acceptable call<br />
back time frame must be provided to the patient awaiting the<br />
return call.<br />
• All instructions should be articulated slowly <strong>and</strong> clearly in<br />
terms underst<strong>and</strong>able to non-health care pr<strong>of</strong>essionals.<br />
Additional tips:<br />
• If you are using an electronic answering system, minimize<br />
excess background noise when recording your message <strong>and</strong><br />
make sure the recording volume is set to an appropriate level.<br />
• If you are instructing the patient to call another location, that<br />
location must also have a detailed message or someone<br />
answering the phone that will provide the patient instruction on<br />
obtaining medical care or advice.<br />
• It is recommended that you audit your message according to<br />
these guidelines outside <strong>of</strong> normal business hours to make<br />
certain you are in compliance with the requirements.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-5
Quality Improvement<br />
Telephone Care:<br />
After Hours<br />
(continued)<br />
Complaint Review<br />
System<br />
Requirements:<br />
To provide all primary care patients access to a 24 hour telephonic<br />
resource that clearly articulates <strong>and</strong> identifies back-up coverage by<br />
another participating primary care physician; <strong>and</strong> referrals to<br />
urgent care centers, where available, <strong>and</strong>/or to hospital emergency<br />
care. Additionally, incorporating st<strong>and</strong>ards for call-back times<br />
based on what is medically appropriate to each situation when the<br />
patient must leave a message.<br />
Rationale:<br />
Patient complaints, concerns <strong>and</strong> grievances reflect their<br />
perceptions <strong>and</strong> expectations. Feedback, whether solicited or<br />
unsolicited, presents an opportunity to identify issues <strong>and</strong><br />
implement systematic processes to improve the quality <strong>of</strong> care or<br />
service. Aware providers <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong> share a joint commitment<br />
to patient satisfaction <strong>and</strong> to the improvement <strong>of</strong> care <strong>and</strong> services<br />
delivered to <strong>Blue</strong> <strong>Cross</strong> members.<br />
Requirements:<br />
All providers will have a policy <strong>and</strong> procedure in place detailing<br />
the following:<br />
• Process to receive written <strong>and</strong> verbal complaints for <strong>Blue</strong><br />
<strong>Cross</strong> members<br />
• Designate an individual to be the primary contact for complaint<br />
management, including the tracking <strong>of</strong> such complaints<br />
• Document the substance <strong>of</strong> the complaint, the investigation,<br />
<strong>and</strong> any actions taken<br />
• Notify members <strong>of</strong> the right to complain <strong>and</strong> appeal to their<br />
health plan<br />
• Track complaints by categories <strong>and</strong> report at least annually to<br />
an in-house committee<br />
3-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Quality <strong>of</strong> Care<br />
Complaints<br />
Access & Availability Rationale:<br />
A quality <strong>of</strong> care complaint is an additional right <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong><br />
members. Members may complain if they feel the quality <strong>of</strong> their<br />
care has been compromised.<br />
Some examples when members may file a complaint are:<br />
• They are not receiving an appointment in a reasonable amount<br />
<strong>of</strong> time.<br />
• The PCC is not referring them to a specialist when it is<br />
necessary.<br />
• The provider/provider <strong>of</strong>fice was rude or discourteous.<br />
• The provider is unable to diagnose or treat their condition.<br />
• There is a delay in communicating test results.<br />
• Confidentiality or privacy concern.<br />
• Incorrect test ordered or performed.<br />
• Infection control.<br />
• Equipment malfunction, cleanliness.<br />
We immediately supply the provider with a copy <strong>of</strong> the member’s<br />
complaint <strong>and</strong> involve the provider in the solution. We are<br />
required by the Department <strong>of</strong> Health to acknowledge these<br />
complaints within 30 days <strong>of</strong> receipt therefore we require your<br />
expedited attention to any request we may have.<br />
Members’ concept <strong>of</strong> the quality <strong>of</strong> care they receive <strong>of</strong>ten begins<br />
when they make an appointment. <strong>Blue</strong> <strong>Cross</strong> also wants to insure<br />
that members are able to schedule appointments within a timely<br />
manner, relative to the services they seek.<br />
Requirements:<br />
Satisfaction – Primary Care Providers Only<br />
• Routine Care: 85% <strong>of</strong> members will usually or always be<br />
satisfied with when they get a routine care appointment<br />
(routine care is that which the member does not need to see a<br />
practitioner right away.)<br />
• Urgent Care: 85% <strong>of</strong> members will usually or always be<br />
satisfied with when they get an urgent care appointment<br />
(urgent care is that which is needed right away for an illness,<br />
injury or condition).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-7
Quality Improvement<br />
Access &<br />
Availability<br />
(continued)<br />
Wait Times<br />
Written Policies Rationale:<br />
• Preventive Care – within 30 days 85% <strong>of</strong> the time for well<br />
child exam, annual physical exam, etc.<br />
• Routine Primary Care – within 7 days 85% <strong>of</strong> the time for<br />
non-urgent symptomatic conditions.<br />
• Urgent Care – Same day 85% <strong>of</strong> the time for medically<br />
necessary care which does not meet the definition <strong>of</strong><br />
emergency care.<br />
• Emergency Care – Immediate 100% <strong>of</strong> the time for<br />
immediately life threatening illnesses, injuries <strong>and</strong> conditions.<br />
To protect the safety <strong>and</strong> privacy <strong>of</strong> all patients, <strong>and</strong> for the<br />
protection <strong>of</strong> the provider, <strong>Blue</strong> <strong>Cross</strong> requires all providers to<br />
develop <strong>and</strong> implement written policies <strong>and</strong> procedures applicable<br />
to the services they provide. Providers are encouraged to have<br />
policies that are facility specific, signed, dated <strong>and</strong> reviewed<br />
annually.<br />
Requirement:<br />
Each provider will have policies <strong>and</strong> procedures in place for the<br />
following topics that apply to the services provided in the facility.<br />
Policy Required Recommended Risk Management Elements<br />
Advance<br />
Directives<br />
Child <strong>and</strong> Teen<br />
Check-ups<br />
• Information made available<br />
• Discussion is documented in medical record<br />
• Copies retained<br />
• Hospitals notified upon admission<br />
• Eligibility defined (birth through age 20,<br />
MA, PMAP, MNCare children)<br />
• Forms for documentation addressed<br />
• Age-appropriate services defined<br />
• Documentation in medical record<br />
• Correct coding<br />
3-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Written Policies<br />
(continued)<br />
Policy Required Recommended Risk Management Elements<br />
Communicable<br />
Disease<br />
Reporting<br />
Complaint<br />
Management<br />
• Requirement to report communicable<br />
diseases by State Health Department<br />
• Reporting timeframe (within one day)<br />
• Responsibility <strong>of</strong> reporting defined<br />
• Forms, completion <strong>and</strong> submittal addressed<br />
• See Complaint Review System Section<br />
Confidentiality • Training, including how soon initial training<br />
occurs, when or how <strong>of</strong>ten refresher training<br />
occurs, verified by signatures <strong>of</strong> trainer <strong>and</strong><br />
individual being trained, <strong>and</strong> on file for six<br />
years<br />
• Accountability, including how control is<br />
maintained (i.e., who has keys, who is<br />
allowed into the facility <strong>and</strong> when)<br />
• Protected health information (PHI) disposal<br />
• Security <strong>of</strong> both paper <strong>and</strong> electronic PHI,<br />
follow HIPAA guidelines<br />
• Reviewed annually<br />
Confidentiality<br />
<strong>and</strong> Security <strong>of</strong><br />
Medical<br />
Records<br />
Foreign<br />
Language<br />
Translation <strong>and</strong><br />
Hearing<br />
Impaired<br />
Services<br />
• Refer to the Medical Records section<br />
• Assistance provided for both situations<br />
• Interpreter available for phone calls <strong>and</strong><br />
face-to-face interactions<br />
• Patients/family are notified that interpreter<br />
is provided<br />
• Resources are identified<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-9
Quality Improvement<br />
Written Policies<br />
(continued)<br />
Policy Required Recommended Risk Management Elements<br />
Hazardous<br />
Materials <strong>and</strong><br />
Waste<br />
Management<br />
Infection<br />
Control<br />
Medical<br />
Emergency<br />
• Written plan in place <strong>and</strong> maintained<br />
• Hazardous material <strong>and</strong> waste defined<br />
• Mechanism in place for responding to a spill<br />
• MSDS (material safety data sheets)<br />
available<br />
• Hazardous materials <strong>and</strong> waste are<br />
identified <strong>and</strong> inventoried<br />
• Mechanism defined for responding to a<br />
spill/breach <strong>of</strong> containment<br />
• Chemical <strong>and</strong> regulated medical waste<br />
addressed<br />
• Hazardous gas <strong>and</strong> vapors addressed<br />
• Orientation <strong>and</strong> education <strong>of</strong> staff outlined<br />
• Basic overview <strong>of</strong> infection control <strong>and</strong> how<br />
it relates to controlling disease<br />
• H<strong>and</strong> washing outlined, when <strong>and</strong> how<br />
• Universal precautions addressed, including<br />
glove use<br />
• Personal protection equipment addressed<br />
• Screening employees for TB<br />
• Vaccinating employees for Hepatitis B<br />
• Steps taken when employee is exposed to<br />
breach <strong>of</strong> infection control or exposure, how<br />
to report to OSHA<br />
• Mechanism in place for responding<br />
• Medical emergency code is identified<br />
• Identify who directs activities<br />
• Identify who determines if 911 is called<br />
3-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Written Policies<br />
(continued)<br />
Continuity <strong>and</strong><br />
Coordination <strong>of</strong> Care<br />
Policy Required Recommended Risk Management Elements<br />
Medication<br />
Management<br />
Non-Medical<br />
Emergency<br />
Policy<br />
Treating<br />
Unaccompanied<br />
Minors Policy<br />
Rationale:<br />
• Mechanism in place for procuring, storing,<br />
controlling <strong>and</strong> distributing medications<br />
• Narcotics addressed, even if to say they are<br />
not kept at the facility<br />
• Recalls addressed<br />
• Emergency <strong>and</strong> sample drugs addressed<br />
• Sign-out log covered<br />
• Prescription pad accessibility addressed<br />
• Mechanism in place for responding<br />
• Include power outages, weather<br />
emergencies, bomb threats, <strong>and</strong> both fire<br />
<strong>and</strong> fire drills<br />
• Minor defined, exceptions covered<br />
• Scheduling appointments addressed<br />
• Mechanism in place to respond when an<br />
unaccompanied minor calls/arrives asking to<br />
be seen<br />
• Sample <strong>of</strong> authorization to consent to<br />
treatment <strong>of</strong> a minor is provided<br />
Patient continuity <strong>and</strong> coordination <strong>of</strong> care (COC) across settings<br />
such as inpatient <strong>and</strong> ambulatory care <strong>and</strong> transition from specialty<br />
to primary care, is critical in ensuring the best care for our<br />
members <strong>and</strong> your patients. All providers share a joint<br />
responsibility to ensure continuity <strong>and</strong> coordination <strong>of</strong> care.<br />
Guidelines:<br />
Health Records:<br />
• Establish a consistent location(s) for external communications<br />
from facilities <strong>and</strong>/or consultants including but not limited to<br />
discharge summaries or notes, consult letters, progress notes,<br />
<strong>and</strong> test or lab results.<br />
• Communication is maintained in a chronological order.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-11
Quality Improvement<br />
Continuity <strong>and</strong><br />
Coordination <strong>of</strong> Care<br />
(continued)<br />
Referrals:<br />
• Communicate with specialists/consultants the rationale for the<br />
referral (is the patient being referred for a consultation or<br />
ongoing care) <strong>and</strong> set expectations for future communications.<br />
• Information, radiology, lab/test results, etc. are made available<br />
to the specialist/consultant in time for the patient’s visit.<br />
Specialty Care <strong>and</strong> Consultants:<br />
• Provider written communication to the patients’ primary care<br />
provider including, but not limited to progress notes,<br />
consultation letters, <strong>and</strong> test or lab results.<br />
Inpatient:<br />
• The attending physician copies all discharge summaries <strong>and</strong><br />
discharge notes to the primary care provider.<br />
Emergency <strong>and</strong> Urgent Care:<br />
• Correspondence regarding all emergency room <strong>and</strong> urgent care<br />
visits are copied to the primary care provider.<br />
Patient Safety <strong>Blue</strong> <strong>Cross</strong> is committed to establishing high st<strong>and</strong>ards <strong>of</strong> care for<br />
our members. In order to assure these high st<strong>and</strong>ards, we expect<br />
all participating practitioners <strong>and</strong> providers to be familiar with <strong>and</strong><br />
actively involved in patient safety practices. We support the work<br />
<strong>of</strong> the Leapfrog Group, a national coalition <strong>of</strong> major employer<br />
groups, which has established patient safety st<strong>and</strong>ards. <strong>Blue</strong> <strong>Cross</strong><br />
also supports national health improvement initiatives, such as the<br />
recent “5 Million Lives Campaign” sponsored by the Institute for<br />
Health Improvement.<br />
<strong>Blue</strong> <strong>Cross</strong> also works to ensure patient safety by monitoring <strong>and</strong><br />
addressing quality-<strong>of</strong>-care issues identified through pharmacy<br />
utilization data, continuity <strong>and</strong> coordination <strong>of</strong> care st<strong>and</strong>ards,<br />
disease management program follow-up, <strong>and</strong> member complaints.<br />
3-12 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Patient Safety<br />
(continued)<br />
Medical Record<br />
Keeping Practices<br />
Resources<br />
Resources are available to you for information <strong>and</strong> to assist in the<br />
continuation <strong>of</strong> safe practices.<br />
The following websites have patient safety programs <strong>and</strong> materials<br />
that you may find useful:<br />
Website Website Address<br />
Agency for Healthcare Research <strong>and</strong><br />
Quality (Dept <strong>of</strong> HHS)<br />
www.ahrq.gov<br />
Institute for Healthcare Improvement www.ihi.org<br />
The Joint Commission International<br />
Center for Patient Safety<br />
www.jcipatientsafety.org<br />
Leapfrog Group for Patient Safety www.leapfroggroup.org<br />
<strong>Minnesota</strong> Alliance for Patient Safety www.maps.org<br />
National Quality Forum www.qualityforum.org<br />
Rationale:<br />
<strong>Blue</strong> <strong>Cross</strong> requires its providers to have a policy <strong>and</strong> procedure<br />
for confidentiality <strong>of</strong> health information <strong>and</strong> medical records that<br />
meet state <strong>and</strong> federal requirements.<br />
<strong>Blue</strong> <strong>Cross</strong> expects strict adherence to state <strong>and</strong> federal laws with<br />
regards to maintaining members’ medical information <strong>and</strong> records<br />
in a confidential manner. <strong>Blue</strong> <strong>Cross</strong> requires medical records to<br />
be maintained in a manner that is current, detailed <strong>and</strong> organized.<br />
Providers must have a tracking process in place for ease <strong>of</strong><br />
retrieval.<br />
Requirements:<br />
• A written policy <strong>and</strong> procedure <strong>of</strong> medical record keeping<br />
practices, which includes the confidentiality <strong>and</strong> security <strong>of</strong><br />
medical records, <strong>and</strong> release <strong>of</strong> information, is available.<br />
• Medical records are kept in a secure or electronically secure<br />
location.<br />
• Review <strong>of</strong> the confidentiality policy <strong>and</strong> procedure is<br />
performed at least annually with staff.<br />
• A tracking system for medical records is in place.<br />
• The medical record forms are available for release.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-13
Quality Improvement<br />
Medical Record<br />
Documentation<br />
Rationale:<br />
The patient medical record is a vehicle for documenting services<br />
provided <strong>and</strong> evaluating continuity <strong>and</strong> coordination <strong>of</strong> care. It also<br />
serves as legal protection for the patient <strong>and</strong> practitioner. <strong>Blue</strong><br />
<strong>Cross</strong>, per contractual agreement with both the subscriber <strong>and</strong><br />
provider, has access to the member’s medical record for<br />
examination <strong>and</strong> evaluation. <strong>Blue</strong> <strong>Cross</strong>’ corporate confidentiality<br />
policy requires that the personal <strong>and</strong> health information <strong>of</strong> its<br />
members be maintained as confidential information. All employees<br />
are required to attest to their knowledge <strong>of</strong> this policy <strong>and</strong> their<br />
intent to comply with it.<br />
Medical record review is an essential component <strong>of</strong> a<br />
comprehensive Quality Improvement program. The <strong>Blue</strong> <strong>Cross</strong><br />
Quality Council, which includes practicing physicians, establishes<br />
minimum patient medical record documentation st<strong>and</strong>ards.<br />
Requirements:<br />
All providers will have a policy <strong>and</strong> procedure in place to address<br />
the following:<br />
Format<br />
• The content <strong>and</strong> format <strong>of</strong> the medical record is organized <strong>and</strong><br />
includes patient’s address <strong>and</strong> home <strong>and</strong> work phone numbers.<br />
• Each page in the medical record contains the patient’s name or<br />
identification number.<br />
• All entries in the medical records contain the author’s<br />
identification. Author identification may be a h<strong>and</strong>written<br />
signature, a unique electronic identifier, or a stamped signature<br />
verified with initials.<br />
• Medical records are legible to someone unfamiliar with the<br />
author’s h<strong>and</strong>writing.<br />
• All encounters/entries are dated.<br />
• Immunization status information for all ages is recorded on a<br />
single page location.<br />
• A summary <strong>of</strong> preventive services screening is documented in<br />
a consistent place.<br />
3-14 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Medical Record<br />
Documentation<br />
(continued)<br />
Content<br />
• Medication allergies <strong>and</strong> adverse reactions are prominently<br />
noted in the record. If the patient has no known allergies or<br />
history <strong>of</strong> adverse reactions, this is appropriately noted in the<br />
record.<br />
• Significant illnesses <strong>and</strong> medical conditions are indicated on a<br />
problem list.<br />
• Past medical history (for patients seen three or more times) is<br />
easily identified <strong>and</strong> includes, as appropriate, significant family<br />
history, serious accidents, operations <strong>and</strong> illnesses. For<br />
children <strong>and</strong> adolescents (18 years <strong>and</strong> younger), past medical<br />
history relates to prenatal care, birth, operations <strong>and</strong> childhood<br />
illnesses.<br />
• For patients 10 years <strong>and</strong> older, there is an appropriate notation<br />
concerning the use <strong>of</strong> tobacco, alcohol <strong>and</strong> substances.<br />
• The history <strong>and</strong> physical exam identifies appropriate subjective<br />
<strong>and</strong> objective information pertinent to the patient’s presenting<br />
complaints <strong>and</strong> includes medications.<br />
Assessment <strong>and</strong> Plan<br />
• Laboratory <strong>and</strong> other studies are ordered, as appropriate<br />
• Assessment <strong>of</strong> each encounter reflects patient’s chief<br />
complaint<br />
• Treatment plans are consistent with diagnoses<br />
Follow-up<br />
• Encounter forms or notes have a notation, when indicated,<br />
regarding follow-up care calls or visits. The specific time <strong>of</strong><br />
return is noted in weeks, months or as needed.<br />
• Unresolved problems from previous <strong>of</strong>fice visits are addressed<br />
in subsequent visits.<br />
• If a consultation is requested, there is a note concerning this<br />
visit in the record.<br />
• Consultation, lab <strong>and</strong> imaging reports filed in the chart are<br />
reviewed by the primary care physician.<br />
• Clinically significant abnormal consultation results, lab or<br />
imaging study results have an explicit notation in the follow-up<br />
plans.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-15
Quality Improvement<br />
Clinical Practice<br />
Guidelines<br />
Institute for Clinical Systems Improvement (ICSI)<br />
Website Website Address<br />
ACS: Diagnosis <strong>and</strong> Treatment<br />
<strong>of</strong> Chest Pain <strong>and</strong> Acute<br />
Coronary Syndrome<br />
Diagnosis <strong>and</strong> Management <strong>of</strong><br />
Asthma<br />
ADHD, Attention Deficit<br />
Hyperactivity Disorder in<br />
Primary Care for Children <strong>and</strong><br />
Adolescents<br />
At <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus, we<br />
believe that the use <strong>of</strong> clinical practice guidelines is a key<br />
component <strong>of</strong> Quality Improvement. Each year our Quality<br />
Council approves the adoption <strong>of</strong> select guidelines that are used to<br />
support various programs <strong>and</strong> initiatives. The guidelines do not<br />
substitute for sound clinical judgment; however, they are intended<br />
to assist clinicians in underst<strong>and</strong>ing key processes for<br />
improvement efforts.<br />
Please note that some treatment <strong>and</strong> management options<br />
recommended in clinical practice guidelines may not be covered<br />
benefits under a <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong><br />
<strong>Blue</strong> Plus member’s health plan.<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/cardi<br />
ovascular/acs_acute_coronary_syndrome/acs__acute_coro<br />
nary_syndrome_<strong>and</strong>_chest_pain__diagnosis_<strong>and</strong>_treatme<br />
nt_<strong>of</strong>__full_version_.html<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/respi<br />
ratory/asthma__outpatient/asthma__diagnosis_<strong>and</strong>_outpa<br />
tient_management_<strong>of</strong>_12572.html<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/beha<br />
vioral_health/adhd/adhd_in_primary_care_for_children_<br />
__adolescents__diagnosis_<strong>and</strong>_management_<strong>of</strong>_.html<br />
Colorectal Cancer Screening http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/preve<br />
ntive_health_maintenance/colorectal_cancer_screening/col<br />
orectal_cancer_screening_6.html<br />
Diagnosis <strong>and</strong> Management <strong>of</strong><br />
Chronic Obstructive<br />
Pulmonary Disease (COPD) by<br />
ICSI<br />
Major Depression in Adults in<br />
Primary Care<br />
Diagnosis <strong>and</strong> Management <strong>of</strong><br />
Diabetes in Adults, type 2<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/respi<br />
ratory/chronic_obstructive_pulmonary_disease/chronic_o<br />
bstructive_pulmonary_disease__guideline_.html<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/beha<br />
vioral_health/depression_5/depression__major__in_adults<br />
_in_primary_care_4.html<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/other<br />
_health_care_conditions/diabetes_mellitus__type_2/diabet<br />
es_mellitus__type_2__management_<strong>of</strong>___6.html<br />
3-16 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Institute for Clinical Systems Improvement (ICSI)<br />
Website Website Address<br />
Healthy Lifestyle http://www.icsi.org/chronic_disease_risk_factors__primar<br />
y_prevention_<strong>of</strong>__guideline__23506/chronic_disease_risk_<br />
factors__primary_prevention_<strong>of</strong>__guideline__23508.html<br />
Heart Failure in Adults http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/cardi<br />
ovascular/hypertension_4/hypertension_diagnosis_<strong>and</strong>_tre<br />
atment__11.html<br />
Immunizations http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/preve<br />
ntive_health_maintenance/immunizations___guideline_/i<br />
mmunizations__guideline__38399.html<br />
Lipid Management in Adults http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/cardi<br />
ovascular/lipid_management_3/lipid_management_in_adu<br />
lts__4.html<br />
Low Back Pain, Adult by ICSI http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/musc<br />
ulo-skeletal/low_back_pain/low_back_pain__adult_5.html<br />
Prevention <strong>and</strong> Management <strong>of</strong><br />
Obesity<br />
http://www.icsi.org/for_patients/for_patients_families/obes<br />
ity__mature_adolescents_<strong>and</strong>_adults___prevention___ma<br />
nagement_<strong>of</strong>__for_patients___families_.html<br />
Preventive Services for Adults http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/preve<br />
ntive_health_maintenance/preventive_services_for_adults/<br />
preventive_services_for_adults__11.html<br />
Preventive Services for<br />
Children <strong>and</strong> Adolescents<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/preve<br />
ntive_health_maintenance/preventive_services_for_childr<br />
en__guideline_/preventive_services_for_children_<strong>and</strong>_ado<br />
lescents_762.html<br />
Routine Prenatal Care http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/wom<br />
ens_health/prenatal_care_4/prenatal_care__routine__3.ht<br />
ml<br />
Stable Coronary Artery<br />
Disease (CAD)<br />
http://www.icsi.org/guidelines_<strong>and</strong>_more/gl_os_prot/cardi<br />
ovascular/coronary_artery_disease/coronary_artery_disea<br />
se__stable__3.html<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-17
Quality Improvement<br />
Other<br />
Website Website Address<br />
KDOQI Clinical Practice<br />
Guidelines for Chronic Kidney<br />
Disease from NKF<br />
NCCN Clinical Practice<br />
Guidelines in Oncology<br />
(copyrighted material; need<br />
registration)<br />
NIAAA Helping Patients Who<br />
Drink Too Much<br />
SAMHSA Substance Abuse<br />
Treatment for Persons with Co-<br />
Occurring Disorders<br />
http://www.kidney.org/pr<strong>of</strong>essionals/kdoqi/guidelines_ckd<br />
/toc.htm<br />
http://www.nccn.org/pr<strong>of</strong>essionals/physician_gls/f_guideli<br />
nes.asp<br />
http://pubs.niaaa.nih.gov/publications/Practitioner/Clinici<br />
ansGuide2005/clinicians_guide.htm<br />
https://ncadistore.samhsa.gov/catalog/productDetails.aspx<br />
?ProductID=16979<br />
3-18 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Quality Improvement for Behavioral Health<br />
Providers<br />
General Overview This section contains detailed information about the <strong>Blue</strong> <strong>Cross</strong><br />
Quality Improvement (QI) program that is specific to behavioral<br />
health providers. The information in this section is in addition to or<br />
more specific than the requirements in the greater chapter. The<br />
material explains what is expected from participating providers<br />
regarding their quality programs <strong>and</strong> defines provider<br />
requirements.<br />
Cooperation with <strong>Blue</strong><br />
<strong>Cross</strong> QI Program<br />
Rationale:<br />
Collaborative efforts need to mutually serve our members/patients<br />
with excellent care <strong>and</strong> services.<br />
Requirements:<br />
Actively participate in the following <strong>Blue</strong> <strong>Cross</strong> QI activities.<br />
St<strong>and</strong>ardized substance abuse screening in mental health<br />
assessment.<br />
• Routinely incorporate a substance abuse screening<br />
questionnaire, e.g., CAGEAID, AUDIT, during mental health<br />
assessment <strong>of</strong> new patients age 12 <strong>and</strong> under.<br />
• Recommend or complete diagnostic assessment for a substance<br />
use disorder based on positive screening results <strong>and</strong><br />
corroborating clinical information.<br />
Exchange <strong>of</strong> information with primary care physicians<br />
• Routinely ask new patients to authorize communication with<br />
their physician <strong>and</strong> document authorization or refusal.<br />
• When authorized, document communication with the<br />
physician, e.g., report, letter, telephone or email.<br />
• Authorized communication should include diagnosis, general<br />
treatment plan, <strong>and</strong> if treated by a psychiatric practitioner,<br />
initial medication management information.<br />
St<strong>and</strong>ardized treatment response monitoring for depression<br />
• Routinely administer the Patient Health Questionnaire-9 for<br />
adults with Major Depressive or Dysthymic Disorder to<br />
monitor treatment response.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-19
Quality Improvement<br />
Complaint Review<br />
System<br />
Additional<br />
requirements for<br />
Select Network<br />
Providers<br />
Rationale:<br />
The practice <strong>of</strong> managing patient complaints in behavioral health<br />
clinics is consistent with practices in primary care clinics. Please<br />
review the Complaint Review System section found under<br />
Introduction to Quality Improvement for additional information on<br />
maintaining a complaint review system.<br />
Requirements:<br />
Access <strong>and</strong> Availability Rationale:<br />
All providers will have a policy <strong>and</strong> procedure in place detailing<br />
the following:<br />
• Process to receive written <strong>and</strong> verbal complaints for <strong>Blue</strong><br />
<strong>Cross</strong> members<br />
• Designate an individual to be the primary contact for complaint<br />
management, including the tracking <strong>of</strong> such complaints<br />
• Document the substance <strong>of</strong> the complaint, the investigation,<br />
<strong>and</strong> any actions taken<br />
• Notify members <strong>of</strong> the right to complain <strong>and</strong> appeal to their<br />
health plan<br />
• Track complaints by categories <strong>and</strong> report at least annually to<br />
an in-house committee<br />
Members’ concept <strong>of</strong> the quality <strong>of</strong> care they receive <strong>of</strong>ten begins<br />
when they make an appointment. <strong>Blue</strong> <strong>Cross</strong> wants to ensure that<br />
members are able to schedule appointments in a timely manner;<br />
commensurate with the level <strong>of</strong> care they need.<br />
Requirements:<br />
Routine initial appointments: 90% <strong>of</strong> requests within 10 business<br />
days. Routine care is defined as a circumstance in which the<br />
individual does not present either emergent or urgent conditions<br />
<strong>and</strong> requests clinical services.<br />
Follow-up appointment: 90% <strong>of</strong> requests within 10 business days<br />
<strong>of</strong> the initial appointment.<br />
3-20 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Physical Facility Rationale:<br />
Urgent appointment: 100% <strong>of</strong> requests within 24 hours. Urgent<br />
care is defined as a circumstance in which the individual presents<br />
no emergency or immediate danger to self or others; however, the<br />
individual, clinician, or concerned party believes that the<br />
individual’s level <strong>of</strong> distress <strong>and</strong>/or functioning warrants<br />
assessment as soon as possible. An urgent condition is a situation<br />
that has the potential to become an emergency in the absence <strong>of</strong><br />
prompt treatment.<br />
Non-life-threatening emergency appointment: 100% <strong>of</strong> requests<br />
within 6 hours. A non-life-threatening emergency is defined as a<br />
circumstance in which the individual is experiencing a severe<br />
disturbance in mood, behavior, thought, or judgment. There may<br />
be evidence <strong>of</strong> uncontrolled behavior <strong>and</strong>/or deterioration in ability<br />
to function independently that could potentially require intense<br />
observation, restraint, or isolation.<br />
Emergency care: 100% <strong>of</strong> member requests immediately. An<br />
emergency is defined as a circumstance in which there is imminent<br />
risk <strong>of</strong> danger to the physical integrity <strong>of</strong> the individual; the<br />
individual cannot be maintained safely in his or her typical daily<br />
environment.<br />
<strong>Blue</strong> <strong>Cross</strong> requires behavioral health clinics to provide a safe<br />
environment, which protects patient privacy <strong>and</strong> ensures h<strong>and</strong>icap<br />
accessibility for disabled patients. <strong>Blue</strong> <strong>Cross</strong> will monitor <strong>and</strong><br />
review physical environment to evaluate conformity with<br />
regulatory, plan, <strong>and</strong> accreditation st<strong>and</strong>ards.<br />
Requirements:<br />
• Provider is open reasonable working hours<br />
• Provide 24 hour/7 day on-call coverage<br />
• Accessibility for h<strong>and</strong>icapped members as defined by the<br />
Americans with Disabilities Act, 1990<br />
• Controlled substances are secure in a locked cabinet or space<br />
<strong>and</strong> dispensation is logged<br />
• A system is in place to ensure that all medications are within<br />
the expiration date<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-21
Quality Improvement<br />
Written Provider<br />
Policies<br />
Rationale:<br />
To protect the safety <strong>and</strong> privacy <strong>of</strong> all patients, <strong>and</strong> for the<br />
protection <strong>of</strong> the clinic, <strong>Blue</strong> <strong>Cross</strong> requires all behavioral health<br />
clinics to develop <strong>and</strong> implement written policies <strong>and</strong> procedures.<br />
Providers are encouraged to have policies that are specific to the<br />
clinic <strong>and</strong> are signed, dated <strong>and</strong> reviewed annually.<br />
Requirement:<br />
Each clinic will have policies <strong>and</strong> procedures in place for the<br />
following topics in addition to policies listed previously in this<br />
chapter including Complaint Management, Confidentiality,<br />
Confidentiality <strong>and</strong> Security <strong>of</strong> Medical Records, Foreign<br />
Language Translation <strong>and</strong> Hearing Impaired Services, Medical<br />
Emergency, Medication Management (if applicable), Non-Medical<br />
Emergency Policy <strong>and</strong> Treating Unaccompanied Minors.<br />
• Behavioral Health Accessibility St<strong>and</strong>ards<br />
Policy Required<br />
Behavioral Health<br />
Accessibility<br />
St<strong>and</strong>ards<br />
Recommended Risk Management<br />
Elements<br />
• Access to behavioral health<br />
appointments commensurate with<br />
clinical need<br />
• Access to follow-up appointments<br />
commensurate with clinical need<br />
• Crisis access to clinician 24 hours a<br />
day/7 days a week<br />
3-22 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Treatment Record<br />
Documentation<br />
Rationale:<br />
The patient behavioral health treatment record is a vehicle for<br />
documenting services <strong>and</strong> evaluating continuity <strong>and</strong> coordination<br />
<strong>of</strong> care. It also serves as legal protection for the patient <strong>and</strong><br />
practitioner. <strong>Blue</strong> <strong>Cross</strong>, per contractual agreement with both the<br />
subscriber <strong>and</strong> provider, has access to the member’s record for<br />
examination <strong>and</strong> evaluation. <strong>Blue</strong> <strong>Cross</strong>’ corporate confidentiality<br />
policy requires that the personal <strong>and</strong> health information <strong>of</strong> its<br />
members be maintained as confidential information. All employees<br />
are required to attest to their knowledge <strong>of</strong> this policy <strong>and</strong> their<br />
intent to comply with it.<br />
Treatment record review is an essential component <strong>of</strong> a<br />
comprehensive Quality Improvement program. The <strong>Blue</strong> <strong>Cross</strong><br />
Quality Council establishes minimum record documentation<br />
st<strong>and</strong>ards.<br />
Annually, <strong>Blue</strong> <strong>Cross</strong> audits a r<strong>and</strong>om sample <strong>of</strong> patient records<br />
from the <strong>Blue</strong> <strong>Cross</strong> population. The records are reviewed in<br />
accordance with the required documentation elements. If potential<br />
deficiencies are identified at a given site, a more intensive review<br />
may occur.<br />
Requirements for Treatment Record Format <strong>and</strong> Content<br />
Record Organization<br />
• The format <strong>of</strong> the treatment record must be logical <strong>and</strong><br />
organized.<br />
• All forms used in the treatment process must be st<strong>and</strong>ardized<br />
<strong>and</strong> consistent for all records.<br />
• The treatment record must contain the patient’s current<br />
address, employer or school, home <strong>and</strong> work phone numbers,<br />
marital or legal status, appropriate consent forms, <strong>and</strong><br />
guardianship status information.<br />
• Special status situations, such as imminent risk <strong>of</strong> harm,<br />
suicidal or homicidal ideation, or elopement potential, must<br />
be prominently documented <strong>and</strong> updated.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-23
Quality Improvement<br />
Treatment Record<br />
Documentation<br />
(continued)<br />
• There must be a signed patient authorization for all external<br />
persons with whom treatment information is exchanged. No<br />
treatment information can be exchanged without patient<br />
authorization or court order.<br />
• Each page in the record must contain the patient’s name or<br />
identifying number.<br />
• All entries must be dated <strong>and</strong> contain the author’s name,<br />
pr<strong>of</strong>essional degree/designation, <strong>and</strong> relevant identification<br />
number if applicable. If a non-degreed pr<strong>of</strong>essional completes<br />
the entry, the title <strong>of</strong> the author must accompany the signature,<br />
e.g., Family Skills Worker. Author identification may be a<br />
h<strong>and</strong>written signature or unique electronic identifier. Initials<br />
alone are not an acceptable form <strong>of</strong> identification. Initials may<br />
be used in conjunction with a typed signature block that clearly<br />
identifies the author.<br />
• Errors in documentation must be corrected with a single line<br />
drawn through the error with the author’s initials.<br />
Initial Assessment<br />
• Presenting problem(s), as well as relevant psychological or<br />
social conditions affecting the patient's medical or psychiatric<br />
status, must be documented.<br />
• Presenting symptoms that are consistent with DSM-IV-TR<br />
criteria must be clearly identified <strong>and</strong> documented, including<br />
the onset, duration, <strong>and</strong> intensity <strong>of</strong> symptoms as well as<br />
functional impairment.<br />
• A psychiatric history must be documented. The psychiatric<br />
history should include, if applicable, previous treatment dates,<br />
identification <strong>of</strong> former treating practitioner(s), therapeutic<br />
interventions <strong>and</strong> responses, relevant family psychiatric<br />
history, lab test results, <strong>and</strong> consultation reports.<br />
• A medical history must be documented which includes current<br />
<strong>and</strong>/or past major or chronic medical conditions <strong>and</strong> a current<br />
list <strong>of</strong> medications. Medication allergies <strong>and</strong> adverse reactions<br />
must be prominently noted. If the patient has no known<br />
allergies or history <strong>of</strong> adverse reactions, this must be noted.<br />
• For children <strong>and</strong> adolescents through age 17, a comprehensive<br />
developmental history must be documented that includes<br />
prenatal <strong>and</strong> perinatal events, achievement <strong>of</strong> developmental<br />
milestones, <strong>and</strong> psychological, social, intellectual, <strong>and</strong><br />
academic history.<br />
3-24 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Treatment Record<br />
Documentation<br />
(continued)<br />
• For individuals 10 years <strong>and</strong> older, a substance use history<br />
must be documented. The history must include past <strong>and</strong> present<br />
use <strong>of</strong> tobacco, alcohol, illicit drugs <strong>and</strong> any misuse <strong>of</strong><br />
prescription or over-the-counter drugs. Additionally, negative<br />
consequences <strong>of</strong> use <strong>and</strong> history <strong>of</strong> assessment <strong>and</strong>/or<br />
treatment should be documented.<br />
• St<strong>and</strong>ardized substance abuse screening questionnaire results<br />
should be incorporated into the assessment <strong>of</strong> all new patients<br />
12 years <strong>and</strong> older.<br />
• A social history that includes family history, current family<br />
status, history <strong>of</strong> physical, sexual or mental abuse or trauma,<br />
current social network, <strong>and</strong> academic or vocational status must<br />
be documented.<br />
• A mental status examination which includes, at minimum,<br />
information about appearance, speech, affect, mood, thought<br />
content, judgment, insight, attention, concentration, memory,<br />
<strong>and</strong> impulse control must be documented.<br />
• A risk assessment that identifies level <strong>of</strong> risk for harm,<br />
including suicidal, homicidal or elopement risk, must be<br />
predominantly documented.<br />
• Patient strengths <strong>and</strong> weaknesses that enable or inhibit the<br />
individual’s ability to achieve treatment goals must be<br />
documented.<br />
• An initial treatment plan must be documented.<br />
• All behavioral health practitioners must attempt consultation<br />
<strong>and</strong> coordination <strong>of</strong> treatment with the patient’s primary care<br />
or treating physician. Patient authorization must be obtained<br />
prior to the release <strong>of</strong> any information. If the patient does not<br />
wish to have treatment information exchanged, patient refusal<br />
must be documented.<br />
Diagnosis<br />
• A DSM-IV-TR diagnosis must be documented. The diagnosis<br />
must be consistent with presenting problems, symptoms,<br />
clinical history, mental status exam, <strong>and</strong> other clinical data.<br />
• All fives axes must be documented according to the DSM-IV-<br />
TR multi-axial diagnostic system. The fifth digit <strong>of</strong> Axes I <strong>and</strong><br />
II diagnoses must be listed when applicable.<br />
• ICD-9-CM codes must be used when submitting claims for<br />
payment.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-25
Quality Improvement<br />
Treatment Record<br />
Documentation<br />
(continued)<br />
Treatment Plan<br />
• The treatment plan must be comprehensive, current, <strong>and</strong><br />
consistent with the diagnosis. The formal treatment plan must<br />
be completed within the first three visits.<br />
• The treatment plan must contain clear, objective, <strong>and</strong><br />
measurable goals as well as the estimated timeframes for goal<br />
attainment or problem resolution. Interventions must be<br />
appropriate for the diagnosis <strong>and</strong>/or presenting problem(s).<br />
• The patient must participate in the development <strong>of</strong> the<br />
treatment plan <strong>and</strong> should sign the initial plan <strong>and</strong> sign or<br />
initial all updates or revisions.<br />
Progress Notes<br />
• All entries must contain the date, actual face-to-face contact<br />
time, <strong>and</strong> current diagnosis.<br />
• All entries must document the persons present during the visit<br />
without using the names <strong>of</strong> persons other than the identified<br />
patient.<br />
• The interventions must be consistent with the diagnosis <strong>and</strong><br />
correspond with current treatment goals.<br />
• Recommendations or referrals for preventive or other external<br />
services, e.g., stress management, relapse prevention, or<br />
community services, must be documented.<br />
• The documentation <strong>of</strong> each entry must clearly state the chief<br />
complaint <strong>and</strong> current status <strong>of</strong> symptoms as well as patient<br />
strengths <strong>and</strong> limitations in reaching treatment goals.<br />
• There must be a notation in each entry about need for followup<br />
care, plans for a return visit, or termination <strong>of</strong> treatment.<br />
The specific date or timeframe <strong>of</strong> a return visit must be noted.<br />
• There must be documentation <strong>of</strong> patient cancellation or failure<br />
to show for a visit.<br />
• Evidence <strong>of</strong> coordination <strong>of</strong> care with other relevant behavioral<br />
health providers <strong>and</strong>/or medical pr<strong>of</strong>essionals must be<br />
documented.<br />
• Unresolved problems from previous visits must be addressed<br />
<strong>and</strong> the outcomes documented.<br />
• If safety or risk characteristics are identified, they must be<br />
prominently documented <strong>and</strong> addressed during each visit.<br />
• Phone conversations with persons relevant to treatment, e.g.,<br />
referral sources, physicians, or parents, must be documented.<br />
3-26 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11)
Quality Improvement<br />
Treatment Record<br />
Documentation<br />
(continued)<br />
Medication Management<br />
• Significant illnesses, clinical risks, <strong>and</strong> medical conditions are<br />
to be clearly noted <strong>and</strong> revised periodically.<br />
• Current medications prescribed by all prescribing physicians<br />
must be listed. Dosages <strong>and</strong> dates <strong>of</strong> initial prescription <strong>and</strong>/or<br />
refills must be documented.<br />
• Evidence <strong>of</strong> informed patient consent for the receipt <strong>of</strong><br />
medication must be documented.<br />
• Laboratory orders <strong>and</strong> results must be documented as well as<br />
review <strong>of</strong> the results by the ordering physician. If abnormalities<br />
are found, follow-up plans must be documented.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/11/11) 3-27
Chapter 4<br />
Integrated Health Management<br />
Table <strong>of</strong> Contents<br />
Integrated Health Management................................................................................................ 4-3<br />
Introduction............................................................................................................................4-3<br />
Objectives ..............................................................................................................................4-3<br />
Provider Contractual Obligations – Important Program Points............................................. 4-4<br />
Integrated Health Management Decision Making .................................................................4-5<br />
Utilization Management ............................................................................................................ 4-6<br />
Purpose................................................................................................................................... 4-6<br />
Goals ...................................................................................................................................... 4-6<br />
Integrated Health Management Medical <strong>and</strong> Behavioral Health Clinical Staff ....................4-7<br />
Medical Policy ............................................................................................................................ 4-8<br />
Medical <strong>and</strong> Behavioral Health Policy Development............................................................4-8<br />
Medical Policy <strong>and</strong> Behavioral Health Policy <strong>Manual</strong>.......................................................... 4-9<br />
Prior Service Request Form................................................................................................. 4-10<br />
High Technology Diagnostic Imaging Decision Support...................................................... 4-11<br />
Overview..............................................................................................................................4-11<br />
Pre-Certification/Authorization ............................................................................................. 4-14<br />
Overview..............................................................................................................................4-14<br />
Scope <strong>and</strong> Purpose ...............................................................................................................4-15<br />
Decision Making <strong>and</strong> Notification Time frames ................................................................. 4-16<br />
Definition <strong>of</strong> Urgent Request...............................................................................................4-17<br />
Services Requiring Pre-Certification Utilization Management Pre-<br />
Certification/Authorization Requirements............................................................................ 4-19<br />
Overview..............................................................................................................................4-19<br />
Inpatient & Residential Pre-Service Admission Requirements........................................... 4-19<br />
Out-<strong>of</strong>-area <strong>Blue</strong> Plan Patients............................................................................................. 4-19<br />
For Local <strong>Blue</strong> <strong>Cross</strong> Plan Patients ..................................................................................... 4-19<br />
Where to Send Requests..........................................................................................................4-21<br />
Inpatient Admissions ........................................................................................................... 4-21<br />
Inpatient Pre-Certification/Authorization Requests.............................................................4-21<br />
Appeals ................................................................................................................................4-22<br />
On-site Concurrent Review..................................................................................................4-22<br />
Compliance Audit .................................................................................................................... 4-23<br />
Overview..............................................................................................................................4-23<br />
Case & Disease Management.................................................................................................. 4-24<br />
Overview..............................................................................................................................4-24<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-1
Integrated Health Management<br />
Program Goals ..................................................................................................................... 4-24<br />
Referrals to Case <strong>and</strong> Disease Management ......................................................................... 4-25<br />
Case Management................................................................................................................ 4-25<br />
Referrals to Commercial Case Management .......................................................................4-25<br />
Referrals to Government Programs Case Management....................................................... 4-25<br />
Disease Management ...........................................................................................................4-25<br />
Disease States.......................................................................................................................4-26<br />
Access Management Programs............................................................................................ 4-26<br />
Focused Utilization Review ..................................................................................................... 4-28<br />
Overview..............................................................................................................................4-28<br />
Messages You May Receive................................................................................................ 4-29<br />
Special Investigations ..........................................................................................................4-30<br />
Documentation in the Medical Record .................................................................................. 4-31<br />
Documentation Requirements.............................................................................................. 4-31<br />
Overview..............................................................................................................................4-32<br />
GA Modifier.........................................................................................................................4-33<br />
Medical Referrals To Nonparticipating Providers............................................................... 4-34<br />
Sample Waivers ................................................................................................................... 4-34<br />
Upgraded/Deluxe Durable Medical Equipment (DME)......................................................4-35<br />
DME Waiver Requirement .................................................................................................. 4-35<br />
DME Claims Submissions ................................................................................................... 4-35<br />
Sample DME Waiver...........................................................................................................4-36<br />
4-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Integrated Health Management<br />
Integrated Health Management<br />
Introduction As part <strong>of</strong> your participation agreement with <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong><br />
<strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>), you have agreed to comply with<br />
Integrated Health Management programs administered by <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus. These Integrated Health Management<br />
programs are designed to ensure that the treatment members<br />
receive is reimbursable according to the medical necessity<br />
guidelines in their contracts. In addition, we review investigative<br />
<strong>and</strong> new procedures/services for coverage determinations.<br />
Integrated Health Management programs also ensure the most<br />
cost-effective <strong>and</strong> appropriate use <strong>of</strong> the health care delivery<br />
system.<br />
These programs include:<br />
Pre-Certification/Authorization <strong>of</strong> selected procedures,<br />
services, supplies, <strong>and</strong> drugs<br />
Preadmission Notification (PAN), Pre-Certification <strong>and</strong><br />
concurrent reviews for selected inpatient admissions<br />
Case <strong>and</strong> Disease Management<br />
Retrospective review <strong>of</strong> claims <strong>and</strong> medical records<br />
To make utilization decisions, <strong>Blue</strong> <strong>Cross</strong> uses written utilization<br />
review decision criteria based on sound clinical evidence. The<br />
criteria used to evaluate an individual case is available, free <strong>of</strong><br />
charge, upon request for your review.<br />
Objectives Integrated Health Management Programs are designed to:<br />
Maximize the coordination <strong>of</strong> care <strong>and</strong> health outcomes.<br />
Ensure appropriate <strong>and</strong> efficient utilization <strong>of</strong> health care<br />
resources.<br />
Promote efficient use <strong>of</strong> health care resources.<br />
Define <strong>and</strong> agree upon appropriate st<strong>and</strong>ards <strong>of</strong> care.<br />
Manage service for members with complex care coordination<br />
needs.<br />
Identify gaps in our members’ care <strong>and</strong> navigation <strong>of</strong><br />
resources.<br />
Identification <strong>of</strong> members with conditions that will benefit<br />
from self-care efforts, care intervention <strong>and</strong> communication.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-3
Integrated Health Management<br />
Provider Contractual<br />
Obligations –<br />
Important Program<br />
Points<br />
The following points pertain to all <strong>of</strong> the Integrated Health<br />
Management programs. Any medical necessity denial<br />
determination may be discussed with a physician reviewer by<br />
telephone.<br />
Any services denied using <strong>Blue</strong> <strong>Cross</strong>’ medical necessity<br />
guidelines cannot be billed to the member/patient unless you<br />
have specifically notified the member/patient prior to the<br />
service being rendered that the service is medically<br />
unnecessary <strong>and</strong> will not be covered, <strong>and</strong> the member/patient<br />
has agreed in writing to pay for the service. This applies to<br />
investigative services as well as some non-covered services for<br />
mental health. (Refer to Waiver Section.)<br />
The Integrated Health Management process is a review for<br />
medical necessity only. Payment for services is still subject to<br />
all other terms <strong>of</strong> the member contract. Therefore, denials may<br />
occur for preexisting conditions, benefit maximums,<br />
coordination <strong>of</strong> benefits or riders in the member’s contract, that<br />
supersede medical necessity.<br />
We recommend that you utilize provider web self-service,<br />
BLUELINE or contact provider services to verify coverage,<br />
benefits, contract eligibility <strong>and</strong> limitations for all patients.<br />
Service representatives will also verify which Integrated<br />
Health Management procedures apply to a patient’s contract.<br />
Providers will be held financially liable for services that are<br />
determined to be not medically necessary during a review or an<br />
audit process, even though pre-certification/pre-authorization<br />
<strong>and</strong>/or admission review has been requested or is not<br />
recommended.<br />
4-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Integrated Health<br />
Management Decision<br />
Making<br />
Integrated Health Management<br />
Integrated Health Management including utilization management<br />
(UM) decision-making is based only on appropriateness <strong>of</strong> care,<br />
service <strong>and</strong> existence <strong>of</strong> coverage. <strong>Blue</strong> <strong>Cross</strong> does not compensate<br />
practitioners or other individuals conducting utilization review<br />
decision-making activities for denials <strong>of</strong> coverage or service. <strong>Blue</strong><br />
<strong>Cross</strong> does not <strong>of</strong>fer incentives to decision-makers to encourage<br />
denials <strong>of</strong> coverage or service that would result in less than<br />
appropriate care or underutilization <strong>of</strong> appropriate care <strong>and</strong><br />
services.<br />
<strong>Blue</strong> <strong>Cross</strong> UM decision-making processes ensure that members<br />
are not discriminated against in the delivery <strong>of</strong> health care services<br />
consistent with the benefits covered in their health coverage plan<br />
based on race, ethnicity, national origin, religion, sex, age, mental<br />
or physical disability, sexual orientation, genetic information or<br />
source <strong>of</strong> payment through the use <strong>of</strong> specific clinical criteria <strong>and</strong><br />
consideration <strong>of</strong> the individual needs <strong>of</strong> each case.<br />
This statement exists to inform <strong>and</strong> remind providers, their<br />
employees, their supervisors, upper management, medical<br />
directors, UM directors or managers, licensed UM staff, <strong>and</strong> other<br />
personnel <strong>and</strong> UM staff employed by participating providers, who<br />
make utilization management decisions <strong>of</strong> this philosophy <strong>and</strong><br />
practice. This includes delegates conducting utilization<br />
management services on behalf <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong>.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-5
Integrated Health Management<br />
Utilization Management<br />
Purpose The purpose <strong>of</strong> the UM Program is to promote effective,<br />
appropriate <strong>and</strong> efficient use <strong>of</strong> medical <strong>and</strong> behavioral health care<br />
resources for our members.<br />
UM is defined by the Utilization Review Accreditation Committee<br />
(URAC) as “the evaluation <strong>of</strong> the necessity, appropriateness, <strong>and</strong><br />
efficiency <strong>of</strong> the use <strong>of</strong> health care services, procedures, <strong>and</strong><br />
facilities under the auspices <strong>of</strong> the applicable health benefit plan.”<br />
IHM uses the UM program processes, procedures <strong>and</strong> criteria to<br />
review <strong>and</strong> coordinate members’ benefits to enhance the<br />
efficiency, affordability <strong>and</strong> quality <strong>of</strong> care.<br />
The UM program is a set <strong>of</strong> continuously improving processes,<br />
designed to both meet our member’s needs, as well as regulatory<br />
<strong>and</strong> accreditation requirements. The UM program includes<br />
processes for:<br />
Identifying over <strong>and</strong> under utilization<br />
Identifying members with complex health issues that may<br />
benefit from case management<br />
The collection <strong>and</strong> distribution <strong>of</strong> UM data<br />
Goals The UM program purpose <strong>of</strong> promoting effective, appropriate, <strong>and</strong><br />
efficient use <strong>of</strong> health care resources is accomplished by adhering<br />
to the UM processes described in this program. The program goals<br />
are to:<br />
Ensure objective <strong>and</strong> consistent utilization management<br />
decision-making<br />
Ensure that members have access to appropriate <strong>and</strong> timely<br />
medical <strong>and</strong> behavioral health care across the provider network<br />
Improve service <strong>and</strong> claims processes to provide optimal<br />
h<strong>and</strong>ling <strong>of</strong> pre-service authorization <strong>and</strong> post-service payment<br />
Ensure timely resolution <strong>of</strong> identified problems<br />
Continually build <strong>and</strong> maintain collaborative relationships with<br />
medical <strong>and</strong> behavioral health care providers<br />
4-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Integrated Health<br />
Management Medical<br />
<strong>and</strong> Behavioral Health<br />
Clinical Staff<br />
Integrated Health Management<br />
IHM medical <strong>and</strong> behavioral health clinical staff is responsible for<br />
the coordination <strong>of</strong> utilization management functions for eligible<br />
members. Clinical staff is required to maintain an active<br />
unrestricted health license in <strong>Minnesota</strong>. The IHM medical <strong>and</strong><br />
behavioral health clinical staff is permitted to approve requested<br />
authorizations based on plan documents, policies, procedures, <strong>and</strong><br />
established medical <strong>and</strong> behavioral health clinical criteria.<br />
Physicians or appropriately licensed peer reviewers make<br />
necessary medical necessity denials.<br />
Contractual benefits, medical necessity, appropriateness, <strong>and</strong><br />
individual needs are evaluated during the review process to<br />
determine coverage <strong>of</strong> services. All requests for services that do<br />
not meet medical necessity criteria are reviewed through the<br />
physician peer review process.<br />
UM decision-making is based only on appropriateness <strong>of</strong> care <strong>and</strong><br />
service, <strong>and</strong> existence <strong>of</strong> coverage. No financial incentive is<br />
awarded to clinical staff for denying requests for service or based<br />
on coverage decisions.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-7
Integrated Health Management<br />
Medical Policy<br />
Medical <strong>and</strong> Behavioral<br />
Health Policy<br />
Development<br />
Medical <strong>and</strong> behavioral health policies are developed by the <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) Medical <strong>and</strong><br />
Behavioral Health Policy Committee, which is comprised <strong>of</strong><br />
practicing physicians <strong>and</strong> providers representing a variety <strong>of</strong><br />
specialties in the local community <strong>and</strong> one <strong>Blue</strong> <strong>Cross</strong><br />
representative.<br />
<strong>Blue</strong> <strong>Cross</strong> makes its determination <strong>of</strong> experimental, investigative<br />
or unproven based upon a preponderance <strong>of</strong> evidence after the<br />
examination <strong>of</strong> the following reliable evidence, none <strong>of</strong> which<br />
shall be determinative in <strong>and</strong> <strong>of</strong> itself:<br />
1. Whether there is final approval from the appropriate<br />
government regulatory agency, if approval is required;<br />
2. Whether there are consensus opinions <strong>and</strong> recommendations<br />
reported in relevant scientific <strong>and</strong> medical literature, peerreviewed<br />
journals, or the reports <strong>of</strong> clinical trial committees<br />
<strong>and</strong> other assessment bodies; <strong>and</strong><br />
3. Whether there are consensus opinions <strong>of</strong> national <strong>and</strong> local<br />
health care providers in the applicable specialty or subspecialty<br />
that typically manages the condition as determined by a survey<br />
or poll <strong>of</strong> a representative sampling <strong>of</strong> these providers.<br />
The committee considers a number <strong>of</strong> additional factors when<br />
evaluating each <strong>of</strong> the criteria. These factors include, but are not<br />
limited to: quality <strong>of</strong> the available peer-reviewed medical<br />
literature; safety, effectiveness, appropriateness <strong>of</strong> technology;<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Association requirements <strong>and</strong> Medical<br />
Policies; <strong>and</strong> the relevant impact <strong>and</strong> consequences <strong>of</strong> coverage for<br />
the technology (for example, patient, <strong>Blue</strong> <strong>Cross</strong>, ethical, societal,<br />
legal).<br />
A drug, device, medical treatment, diagnostic procedure,<br />
technology or procedure for which reliable evidence does not<br />
permit conclusions concerning its safety, effectiveness, or effect on<br />
health outcomes. <strong>Blue</strong> <strong>Cross</strong> bases its decision upon an<br />
examination <strong>of</strong> the following reliable evidence, none <strong>of</strong> which is<br />
determinative in <strong>and</strong> <strong>of</strong> itself.<br />
Drugs <strong>and</strong> devices cannot be lawfully marketed without the<br />
approval <strong>of</strong> the U.S. Food <strong>and</strong> Drug Administration <strong>and</strong> approval<br />
for marketing has not been given at the time the drug or device is<br />
furnished.<br />
4-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Medical <strong>and</strong> Behavioral<br />
Health Policy<br />
Development<br />
(continued)<br />
Medical Policy <strong>and</strong><br />
Behavioral Health<br />
Policy <strong>Manual</strong><br />
Integrated Health Management<br />
The drug, device, diagnostic procedure, technology, or medical<br />
treatment or procedure is the subject <strong>of</strong> ongoing Phase I, II, or III<br />
clinical trials:<br />
Phase I clinical trials determine the safe dosages <strong>of</strong> medication<br />
for Phase II trials <strong>and</strong> define acute effects on normal tissue.<br />
Phase II clinical trials determine clinical response in a defined<br />
patient setting. If significant activity is observed in any disease<br />
during Phase II, further clinical trials usually study a<br />
comparison <strong>of</strong> the experimental treatment with the st<strong>and</strong>ard<br />
treatment in Phase III trials. Phase III trials are typically quite<br />
large <strong>and</strong> require many patients to determine if a treatment<br />
improves outcomes in a large population <strong>of</strong> patients); or<br />
Medically reasonable conclusions establishing its safety,<br />
effectiveness or effect on health outcomes have not been<br />
established. For purposes <strong>of</strong> this subparagraph, a drug, device,<br />
diagnostic procedure, technology, or medical treatment or<br />
procedure shall not be considered investigative if reliable<br />
evidence shows that it is safe <strong>and</strong> effective for the treatment <strong>of</strong><br />
a particular patient.<br />
Medical <strong>and</strong> behavioral health policies are available for your use<br />
<strong>and</strong> review on the <strong>Blue</strong> <strong>Cross</strong> website at<br />
providers.bluecrossmn.com. From this site, there are two ways to<br />
access medical policy information depending on the patient’s <strong>Blue</strong><br />
Plan membership.<br />
For Out-<strong>of</strong>-area <strong>Blue</strong> Plan Patients<br />
1. Select Medical Policy Pre-Cert/Auth Router<br />
2. Click Go.<br />
You will be taken to the page where you select either medical<br />
policy or pre-certification/prior authorization<br />
3. Enter the patient’s three-letter alpha prefix (as found on their<br />
member ID card)<br />
4. Click Go.<br />
Once you accept the requirements, you will be routed to the<br />
patient’s home plan where you can access medical policy or precertification/pre-authorization<br />
information.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-9
Integrated Health Management<br />
Medical Policy <strong>and</strong><br />
Behavioral Health<br />
Policy <strong>Manual</strong><br />
(continued)<br />
Prior Service Request<br />
Form<br />
For local <strong>Blue</strong> <strong>Cross</strong> Plan Patients<br />
1. Under the Tools <strong>and</strong> Resources, select “Medical Policy”<br />
2. Read <strong>and</strong> accept the <strong>Blue</strong> <strong>Cross</strong> Medical Policy Statement<br />
3. Select “View All Active Policies.” You have now navigated to<br />
the <strong>Blue</strong> <strong>Cross</strong> Medical <strong>and</strong> Behavioral Health Policy <strong>Manual</strong>,<br />
where there are several selections to assist with your inquiry.<br />
The “What’s New” section identifies our latest new or<br />
revised policies approved by <strong>Blue</strong> <strong>Cross</strong>’ Medical <strong>and</strong><br />
Behavioral Health Policy Committee at least 45 days ago.<br />
These policies are now effective <strong>and</strong> providers should<br />
begin following these policies immediately.<br />
These policies also appear in the “Active Policy” section <strong>of</strong><br />
the Medical <strong>and</strong> Behavioral Health Policy <strong>Manual</strong>.<br />
The “Upcoming Policies” section lists new or revised<br />
policies approved by the <strong>Blue</strong> <strong>Cross</strong> Medical <strong>and</strong><br />
Behavioral Health Policy Committee. They are effective 45<br />
days from the date they were posted to the “Upcoming<br />
Policies” section <strong>of</strong> the Medical <strong>and</strong> Behavioral Health<br />
Policy <strong>Manual</strong>.<br />
The “Active Policy” section contains the entire list <strong>of</strong><br />
policies effective at the time <strong>of</strong> your inquiry.<br />
Note: DHS programs have a separate section titled<br />
“Coverage Guidelines for DHS Programs (MHCP<br />
<strong>Manual</strong>).”<br />
A sample <strong>of</strong> the Prior Authorization Request, form number F1676<br />
is available on our website. The Transplant Prior Authorization<br />
Request form number X16519 is available on our website.<br />
For behavioral health, please refer to Prior Authorization-<br />
Outpatient Mental Health <strong>and</strong> Prior Authorization-Chemical<br />
Dependency.<br />
4-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Integrated Health Management<br />
High Technology Diagnostic Imaging Decision<br />
Support<br />
Overview <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus (<strong>Blue</strong><br />
<strong>Cross</strong>) have entered a relationship with Nuance for the Institute <strong>of</strong><br />
Clinical Systems Improvement (ICSI) sponsored HTDI automated<br />
decision support program. This change could impact the processes you<br />
currently follow today regarding data submission <strong>and</strong> precertification/pre-authorization<br />
decision support services for HTDI.<br />
Key process changes<br />
Effective November 1, 2011, ordering providers are required to<br />
use a decision support system as part <strong>of</strong> their process for<br />
elective, outpatient HTDI procedures. This can be performed<br />
either by Electronic Medical Record (EMR) integrated RadPort<br />
s<strong>of</strong>tware or the web-based version. Providers who choose to<br />
use other programs should contact <strong>Blue</strong> <strong>Cross</strong>.<br />
All providers must continue to follow Medical <strong>and</strong> Behavioral<br />
Health Policies for selected HDTI procedures as summarized<br />
in the section below both before <strong>and</strong> after November 1,<br />
2011.<br />
For specific questions about Nuance's RadPort tool, or to<br />
schedule training <strong>and</strong> implementation <strong>of</strong> the tool, contact ICSI<br />
at (952) 814-7067 or htdi@icsi.org<br />
Imaging procedures included in the automated decision support<br />
HTDI program<br />
The new program covers the following elective, outpatient HTDI<br />
procedures:<br />
Computed tomography <strong>and</strong> angiography (CT/CTA) scans<br />
Positron emission tomography (PET scans)<br />
Magnetic resonance imaging <strong>and</strong> magnetic resonance<br />
angiography (MRI/MRA) scans<br />
Nuclear cardiology scans<br />
Combinations <strong>of</strong> PET, CT, MRI, etc.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-11
Integrated Health Management<br />
Overview (continued) Medical <strong>and</strong> Behavioral Health Policies relating to HTDI<br />
Commercial Products<br />
All providers must continue to follow current pre-certification/preauthorization<br />
<strong>and</strong> investigative policies in the Medical <strong>and</strong><br />
Behavioral Health Policy <strong>Manual</strong> for commercial products. The<br />
following procedures have coverage criteria, are subject to medical<br />
review <strong>and</strong> continue to require the st<strong>and</strong>ard pre-certification/preauthorization<br />
process as noted:<br />
Computed tomography angiography (CTA) for evaluation <strong>of</strong><br />
coronary arteries<br />
CT colonography (virtual colonoscopy) as a screening test for<br />
colorectal cancer (pre-certification/pre-authorization required)<br />
MRI <strong>of</strong> the breast (pre-certification/authorization required<br />
EXCEPT in individuals with biopsy proven breast cancer).<br />
Positron emission tomography (PET)<br />
<strong>Minnesota</strong> Health Care Programs (MHCP)<br />
All providers must continue to follow current pre-certification/preauthorization<br />
<strong>and</strong> investigative policies in the Medical <strong>and</strong><br />
Behavioral Health Policy <strong>Manual</strong> for <strong>Minnesota</strong> Health Care<br />
Programs (MHCP) as defined in your Provider Service Agreement.<br />
The following procedures continue to require the st<strong>and</strong>ard precertification/pre-authorization<br />
process:<br />
MRI <strong>of</strong> the breast<br />
CT colonography (virtual colonoscopy)<br />
Computed tomography angiography (CTA) for evaluation <strong>of</strong><br />
coronary arteries, including coronary CT <strong>and</strong> EBCT for<br />
calcium Scoring<br />
PET scans<br />
SPECT scans<br />
Capsule endoscopy<br />
4-12 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Overview (continued) Non-Covered Procedures<br />
Integrated Health Management<br />
These procedures are not covered for either commercial or<br />
<strong>Minnesota</strong> Health Care Programs (MHCP) members:<br />
Computed tomography (CT) screening for coronary artery<br />
disease<br />
Full body CT scanning<br />
Spiral CT screening for lung cancer<br />
Members covered by the program<br />
To date, this program includes the following <strong>Blue</strong> <strong>Cross</strong> lines <strong>of</strong><br />
business in the <strong>Minnesota</strong> service area <strong>and</strong> surrounding counties in<br />
Wisconsin, South Dakota, North Dakota <strong>and</strong> Iowa (surrounding<br />
counties are relevant only to contracting with providers, not with<br />
location <strong>of</strong> members):<br />
<strong>Blue</strong> <strong>Cross</strong> fully insured members<br />
A limited number <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> self-insured <strong>Minnesota</strong><br />
members<br />
<strong>Blue</strong> Plus subscribers enrolled in <strong>Minnesota</strong> Health Care<br />
Programs(MHCP)<br />
The HTDI program does not apply to any Medicare products,<br />
<strong>Blue</strong>Link TPA, or FEP ®<br />
The EMR integrated RadPort s<strong>of</strong>tware or the web-based version<br />
will display the member's name if they are included under the<br />
HTDI program. (<strong>Blue</strong> <strong>Cross</strong> membership feeds to RadPort contain<br />
only members who are part <strong>of</strong> HTDI program, so if the member is<br />
not displayed in RadPort that member is not included.)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-13
Integrated Health Management<br />
Pre-Certification/Authorization<br />
Overview The purpose <strong>of</strong> pre-certification/authorization is to review services<br />
prior to being rendered to determine if the services are<br />
contractually eligible <strong>and</strong> medically necessary. Medical policy<br />
criteria <strong>and</strong> member contract language is used to assist in<br />
determining if benefits are available for the requested service.<br />
Certification/Authorization for a service, device or drug does<br />
not in itself guarantee coverage, but notifies you that as<br />
described, the service, device or drug meets the criteria for medical<br />
necessity <strong>and</strong> appropriateness. Payment for services <strong>and</strong>/or<br />
supplies <strong>Blue</strong> <strong>Cross</strong> approves in advance is based on the following<br />
requirements: if the policy is in force the date the member receives<br />
care, premiums have been paid, lifetime or benefit maximums<br />
have not been exceeded, the condition is not subject to a<br />
preexisting condition limitation period, <strong>and</strong> the procedure that is<br />
authorized is the service <strong>and</strong>/or supply that is billed by the<br />
provider. Deductibles, coinsurance, allowed amount <strong>and</strong> copayments<br />
will apply.<br />
The “pre-certification/authorization” section identifies various<br />
services, procedures, prescription drugs, <strong>and</strong> medical devices that<br />
require pre-certification/pre-authorization. Please note, commercial<br />
(including <strong>Blue</strong>Link TPA) <strong>and</strong> MN Government Programs have<br />
different pre-certification/authorization lists <strong>and</strong> requirements.<br />
These lists are not exclusive to medical policy services only; they<br />
encompass other services that are subject to precertification/authorization<br />
requirements. For your convenience,<br />
links to the “Commercial Forms,” “<strong>Blue</strong>Link TPA Forms,” CMS<br />
<strong>and</strong> DHS criteria websites have also been provided.<br />
The <strong>Blue</strong> <strong>Cross</strong> clinical reviewer uses local <strong>and</strong> national medical<br />
policy, Medicare guidelines, MHCP Guidelines, behavioral health<br />
criteria <strong>and</strong> member contract language to assist in determining if<br />
benefits are available for the request. Criteria are determined by<br />
the type <strong>of</strong> plan in which the member is enrolled. Authorization for<br />
a service, device, or drug does not in itself guarantee coverage but<br />
notifies you if the request meets the criteria for medical necessity<br />
<strong>and</strong> appropriateness. The provider should always check with<br />
customer service to make sure the member, or patient has contract<br />
benefits <strong>and</strong> that the coverage is up to date.<br />
We will evaluate your request for pre-certification <strong>and</strong> will make a<br />
determination once all the necessary medical information is<br />
received. Review decisions will be made <strong>and</strong> communicated<br />
within required time frames as defined by state <strong>and</strong> federal law.<br />
4-14 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Integrated Health Management<br />
Scope <strong>and</strong> Purpose These policies are applicable to all commercial <strong>and</strong> government<br />
program products; medical, surgical, <strong>and</strong> behavioral health<br />
services are included.<br />
Benefit plans vary in coverage <strong>and</strong> some plans may not provide<br />
coverage for certain services discussed in the medical policies.<br />
Medicaid products may have additional policies <strong>and</strong> prior<br />
authorization requirements, as well as some self <strong>and</strong> fully insured<br />
plans. Coverage decisions are subject to all terms <strong>and</strong> conditions <strong>of</strong><br />
the applicable benefit plan, including specific exclusions <strong>and</strong><br />
limitations, <strong>and</strong> to applicable state <strong>and</strong>/or federal law.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-15
Integrated Health Management<br />
Decision Making <strong>and</strong><br />
Notification Time<br />
frames<br />
(Electronic or written)<br />
To ensure timely processing <strong>and</strong> assist us in meeting compliance<br />
with state <strong>and</strong> federal guidelines, please submit precertification/authorization<br />
requests at least 15 business days prior<br />
to any elective services being rendered.<br />
File Type Decision-Making Time frame Initial Notification Time frame<br />
(Telephone Practitioner only) Follow-up Notification Time frame<br />
(Members <strong>and</strong> Practitioners)<br />
Pre-certification Request – Nonurgent:<br />
Initial <strong>and</strong> Concurrent: Commercial: Within 10 business days* <strong>of</strong> receiving request, not to exceed 15<br />
calendar days**.<br />
Government Programs: Within 10 business days/14 calendar days, whichever is sooner. Within 1<br />
business day* <strong>of</strong> making decision <strong>and</strong> within time frame. Commercial: Within 10 business days* <strong>of</strong><br />
receiving request, not to exceed 15 calendar days**.<br />
Government Programs: Within 10 business days/14 calendar days, whichever is sooner<br />
Pre-certification Request – Urgent Commercial: Within 72 hours <strong>of</strong> receiving request or as<br />
expeditiously as the member's health condition warrants Government: Within 72 hours <strong>of</strong> receiving<br />
request or as expeditiously as the member's health condition warrants. Same day as decision.<br />
Commercial: Within 72 hours <strong>of</strong> receiving request or as expeditiously as the member's health condition<br />
warrants. Government: Within 72 hours <strong>of</strong> receiving request or as expeditiously as the member's health<br />
condition warrants.<br />
Concurrent Review:<br />
Urgent Within 24 hours <strong>of</strong> receiving request. Applicable to Commercial & Government Programs<br />
business. Within 24 hours <strong>of</strong> receiving request. Within 24 hours <strong>of</strong> receiving request. Applicable to<br />
Commercial & Government Programs business.<br />
Post-service Request (Retrospective) Within 30 calendar days** <strong>of</strong> receiving the request.<br />
Applicable to Commercial & Government Programs business. Within 30 calendar days** <strong>of</strong> receiving the<br />
request. Within 30 calendar days** <strong>of</strong> receiving the request. Applicable to Commercial & Government<br />
Programs business.<br />
*Business day: Day in which <strong>Blue</strong> <strong>Cross</strong> is open for business, does not include weekends or holidays.<br />
** Calendar day: Days in sequence on calendar, including weekends <strong>and</strong> holidays<br />
4-16 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Definition <strong>of</strong> Urgent<br />
Request<br />
The federal regulations define an urgent request as:<br />
Integrated Health Management<br />
Requires immediate action to prevent a serious deterioration <strong>of</strong><br />
a member’s health that results from an unforeseen illness or an<br />
injury, or<br />
Could jeopardize the ability <strong>of</strong> the individual to regain<br />
maximum function based upon a prudent layperson’s<br />
judgment, or<br />
In the opinion <strong>of</strong> the treating physician, would subject the<br />
individual to severe pain that cannot be adequately managed<br />
without the treatment being requested. An urgent condition is a<br />
situation that has the potential to become an emergency in the<br />
absence <strong>of</strong> treatment.<br />
Requests not meeting the conditions for an urgent request will be<br />
considered nonurgent. Both urgent <strong>and</strong> nonurgent requests will be<br />
reviewed <strong>and</strong> completed within current state <strong>and</strong> federal timelines.<br />
For expedited requests, <strong>Blue</strong> <strong>Cross</strong> adheres to federal <strong>and</strong> state<br />
requirements for decision-making time frames. <strong>Blue</strong> <strong>Cross</strong> uses the<br />
following definitions to determine if a request is expedited:<br />
For Commercial Plans<br />
Requires immediate action to prevent a serious deterioration <strong>of</strong> a<br />
member’s health that results from an unforeseen illness or an<br />
injury, or<br />
Could jeopardize the ability <strong>of</strong> the individual to regain maximum<br />
function based upon a prudent layperson’s judgment, or<br />
In the opinion <strong>of</strong> the treating physician, would subject the<br />
individual to severe pain that cannot be adequately managed<br />
without the treatment being requested. An urgent condition is a<br />
situation that has the potential to become an emergency in the<br />
absence <strong>of</strong> treatment.<br />
Requests not meeting the criteria for the urgent definition for an<br />
urgent request will be considered nonurgent. Providers submitting<br />
the request will be notified by <strong>Blue</strong> <strong>Cross</strong> that the request does not<br />
meet urgent criteria <strong>and</strong> will be managed according to nonurgent<br />
criteria. Both urgent <strong>and</strong> nonurgent requests will be reviewed.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-17
Integrated Health Management<br />
Definition <strong>of</strong> Urgent<br />
Request (continued)<br />
For <strong>Minnesota</strong> Government Programs<br />
The attending health care pr<strong>of</strong>essional believes that an expedited<br />
determination is warranted when the st<strong>and</strong>ard decision time frame<br />
may jeopardize the member’s health or ability to regain maximum<br />
functioning.<br />
An expedited determination is completed as the enrollee's medical<br />
condition requires, but no later than 72 hours from the initial<br />
request.<br />
Requests not meeting the criteria for the urgent definition for an<br />
urgent request will be considered nonurgent. Providers submitting<br />
the request will be notified by <strong>Blue</strong> <strong>Cross</strong> that the request does not<br />
meet urgent criteria <strong>and</strong> will be managed according to nonurgent<br />
criteria. Both urgent <strong>and</strong> nonurgent requests will be reviewed <strong>and</strong><br />
completed within current state <strong>and</strong> federal timelines.<br />
4-18 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Integrated Health Management<br />
Services Requiring Pre-Certification Utilization<br />
Management Pre-Certification/Authorization<br />
Requirements<br />
Overview Medical <strong>and</strong> behavioral health policies are available for your use<br />
<strong>and</strong> review on the <strong>Blue</strong> <strong>Cross</strong> website at<br />
providers.bluecrossmn.com. From this site, there are two ways to<br />
access medical policy information depending on the patient’s <strong>Blue</strong><br />
Plan membership.<br />
Inpatient & Residential<br />
Pre-Service Admission<br />
Requirements<br />
Out-<strong>of</strong>-area <strong>Blue</strong> Plan<br />
Patients<br />
For Local <strong>Blue</strong> <strong>Cross</strong><br />
Plan Patients<br />
Note: Providers are required to report all inpatient admissions <strong>and</strong><br />
discharges to <strong>Blue</strong> <strong>Cross</strong>. Refer to “Where to Send<br />
Requests” section.<br />
Providers are required to report all inpatient admissions <strong>and</strong><br />
discharges to <strong>Blue</strong> <strong>Cross</strong>.<br />
The member’s ID card has a number to call for precertification/pre-authorization<br />
for inpatient admissions.<br />
1. Under the Tools <strong>and</strong> Resources, select “Medical Policy”<br />
2. Read <strong>and</strong> accept the <strong>Blue</strong> <strong>Cross</strong> Medical Policy Statement<br />
3. Select “View All Active Policies.”<br />
You have now navigated to the <strong>Blue</strong> <strong>Cross</strong> Medical <strong>and</strong><br />
Behavioral Health Policy <strong>Manual</strong>. Within in the manual, there are<br />
several selections to assist with your inquiry.<br />
1. Under the Tools <strong>and</strong> Resources, select “Medical Policy”<br />
2. Read <strong>and</strong> accept the <strong>Blue</strong> <strong>Cross</strong> Medical Policy Statement<br />
3. Select “View All Active Policies.”<br />
You have now navigated to the <strong>Blue</strong> <strong>Cross</strong> Medical <strong>and</strong><br />
Behavioral Health Policy <strong>Manual</strong>. Within in the manual, there are<br />
several selections to assist with your inquiry.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-19
Integrated Health Management<br />
For Local <strong>Blue</strong> <strong>Cross</strong><br />
Plan Patients<br />
(continued)<br />
The “What’s New” section identifies our latest new or revised<br />
policies approved by <strong>Blue</strong> <strong>Cross</strong> Medical <strong>and</strong> Behavioral<br />
Health Policy Committee at least 45 days ago. These policies<br />
are now effective <strong>and</strong> providers should begin following these<br />
policies immediately. These policies also appear in the “Active<br />
Policy” section <strong>of</strong> the Medical <strong>and</strong> Behavioral Health Policy<br />
<strong>Manual</strong>.<br />
The “Upcoming Policies” section lists new or revised policies<br />
approved by the <strong>Blue</strong> <strong>Cross</strong> Medical <strong>and</strong> Behavioral Health<br />
Policy Committee <strong>and</strong> are effective 45 days from the date they<br />
were posted to the “Upcoming Policies” section <strong>of</strong> the Medical<br />
<strong>and</strong> Behavioral Health Policy <strong>Manual</strong>.<br />
The “Active Policy” section contains the entire list <strong>of</strong> policies<br />
effective at the time <strong>of</strong> your inquiry.<br />
Note: DHS programs have a separate section titled “Coverage<br />
Guidelines for DHS Programs (MHCP <strong>Manual</strong>).”<br />
The “Pre-Certification/Authorization” section identifies<br />
various services, procedures, prescription drugs, <strong>and</strong> medical<br />
devices that require pre-certification/authorization. Please note,<br />
Commercial (including <strong>Blue</strong>Link TPA) <strong>and</strong> MN Government<br />
Programs have different pre-certification/authorization lists<br />
<strong>and</strong> requirements. These lists are not exclusive to medical<br />
policy services only; they encompass other services that are<br />
subject to pre-certification/authorization requirements. These<br />
lists are maintained on the provider website.<br />
4-20 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Where to Send Requests<br />
Integrated Health Management<br />
Inpatient Admissions Providers are required to report all inpatient admissions <strong>and</strong><br />
discharges to <strong>Blue</strong> <strong>Cross</strong>.<br />
Inpatient Pre-<br />
Certification/Authoriza<br />
tion Requests<br />
Commercial<br />
Enter admissions through our PWSS portal <strong>and</strong> for *Services<br />
requiring pre-certification providers should call our provider<br />
services center at 1-800-262-0820 or (651) 662-5200.<br />
(* Services that require pre-certification are: FEP, newborn,<br />
Mental Health <strong>and</strong> Chemical Dependency/Detox, Inpatient Acute<br />
Rehab <strong>and</strong> Long Term Acute Care admissions)<br />
Government Programs<br />
Enter admissions through our PWSS portal <strong>and</strong> for *Services<br />
requiring pre-certification providers should call our provider<br />
services center at 1-800-262-0820 or (651) 662-5200.<br />
(* Services that require pre-certification are: Newborn, Mental<br />
Health <strong>and</strong> Chemical Dependency/Detox, Inpatient Acute Rehab<br />
<strong>and</strong> Long Term Acute Care admissions)<br />
Commercial<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
P.O. Box 64265 Attn: Pre-certification<br />
St. Paul, MN 55164-0265<br />
Fax: (651) 662-2810<br />
Government Programs<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Attn: Pre-certification<br />
P.O Box 64255<br />
St. Paul, MN 55164-0255<br />
1-866-800-1665<br />
Fax: (651) 662-4022<br />
Transplants (Commercial <strong>and</strong> Government Program requests):<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Attn: Transplant Coordinator<br />
Route R472<br />
PO Box 64179<br />
St. Paul, MN 55164-0179<br />
Fax: (651) 662-1624<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-21
Integrated Health Management<br />
Appeals Information regarding appeals for denied pre-certification requests<br />
can be found in the Appeals section (Chapter 10) <strong>of</strong> this manual.<br />
On-site Concurrent<br />
Review<br />
<strong>Blue</strong> <strong>Cross</strong> conducts on-site inpatient concurrent review at select<br />
MN hospitals. The goal <strong>of</strong> the on-site clinical program is to:<br />
Identify members who have been admitted, discharged to home<br />
or to another level <strong>of</strong> care.<br />
Underst<strong>and</strong> length <strong>of</strong> stay <strong>of</strong> member who may be at risk <strong>of</strong><br />
hitting outlier status.<br />
Assist members with transition <strong>of</strong> care needs <strong>and</strong> bridge the<br />
gap between facility <strong>and</strong> community.<br />
Engage members in our plan-based case/disease management<br />
activities sooner <strong>and</strong> more reliably.<br />
Inpatient concurrent review will continue to exp<strong>and</strong>. Although we<br />
will not be on-site at each hospital or inpatient facility, we may be<br />
in contact with you telephonically.<br />
Note: Preadmission notification or certification is required by <strong>Blue</strong><br />
<strong>Cross</strong>. Refer to “Where to Send Requests” for details on<br />
how <strong>and</strong> where to submit a hospital/inpatient admission.<br />
4-22 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Compliance Audit<br />
Integrated Health Management<br />
Overview Your provider services agreement includes certain quality<br />
assurance requirements. Pursuant to this agreement, <strong>Blue</strong> <strong>Cross</strong><br />
may conduct audits to evaluate a provider’s compliance with<br />
medical necessity guidelines <strong>and</strong> st<strong>and</strong>ards <strong>of</strong> practice in the<br />
community. Such an audit could include post-service claims<br />
review, which may result in provider liability if the care is<br />
determined to be not medically necessary or medically<br />
inappropriate.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-23
Integrated Health Management<br />
Case & Disease Management<br />
Overview Mission Statement<br />
Integrated Health Management (IHM) combines historically<br />
fragmented Disease <strong>and</strong> Case Management services to provide a<br />
whole person approach to improving member health, working with<br />
members who are facing chronic, complex, catastrophic injuries,<br />
illness or diseases.<br />
IHM clinicians work collaboratively with members, providers, <strong>and</strong><br />
the community to promote optimal health, <strong>and</strong> coordinate access to<br />
services across the continuum <strong>of</strong> care that is holistic, seamless <strong>and</strong><br />
easily accessible.<br />
Clinicians<br />
Licensed Dedicated Nurses/Clinicians, using a collaborative<br />
process, advocate, assess, plan, implement, coordinate, monitor<br />
<strong>and</strong> evaluate options <strong>and</strong> services to meet an individual’s specific<br />
health care needs through education <strong>and</strong> communication <strong>of</strong><br />
available resources to promote high quality, cost effective<br />
outcomes for members with medical <strong>and</strong> behavioral conditions that<br />
require ongoing or intermittent care. Clinicians are required to<br />
maintain an active unrestricted health license in <strong>Minnesota</strong>.<br />
Program Goals Maximize optimal health <strong>and</strong> functional outcomes.<br />
Identify gaps in care.<br />
Reach out to the members with the greatest need <strong>and</strong> educate<br />
them about their condition.<br />
Support <strong>and</strong> encourage individual accountability for health <strong>and</strong><br />
wellness (self-care management).<br />
Help members coordinate their needs <strong>and</strong> navigate services in<br />
the health care system.<br />
Tailor interventions <strong>and</strong> outreach to promote the appropriate<br />
use <strong>of</strong> health care services.<br />
Improve member satisfaction with the health plan <strong>and</strong> health<br />
care system.<br />
4-24 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Referrals to Case <strong>and</strong> Disease Management<br />
Case Management Maximize optimal health <strong>and</strong> functional outcomes<br />
Referrals to<br />
Commercial Case<br />
Management<br />
Referrals to<br />
Government Programs<br />
Case Management<br />
Identify gaps in care<br />
Integrated Health Management<br />
Reach out to the members with the greatest need <strong>and</strong> educate<br />
them about their condition<br />
Support <strong>and</strong> encourage individual accountability for health <strong>and</strong><br />
wellness (self-care management)<br />
Help members coordinate their needs <strong>and</strong> navigate services in<br />
the health care system<br />
Tailor interventions <strong>and</strong> outreach to promote the appropriate<br />
use <strong>of</strong> health care services<br />
Improve member satisfaction with the health plan <strong>and</strong> health<br />
care system<br />
A referral can be made by contacting the case management support<br />
staff at (651) 662-5520 <strong>and</strong> toll free at 1-888-878-0139 extension<br />
25520.<br />
A referral to case management can be made by calling<br />
(651) 662-5540, or toll free at 1-800-711-9868.<br />
Please contact Government Programs Case Management when you<br />
have a patient who may need additional supportive services, such<br />
as a Restricted Recipient referral.<br />
Disease Management Disease management is a multidisciplinary, continuum-based<br />
approach to health care delivery that proactively identifies<br />
populations who have or are at risk for, chronic medical <strong>and</strong><br />
behavioral health conditions. Disease management supports the<br />
practitioner-patient relationship <strong>and</strong> plan <strong>of</strong> care, emphasizes the<br />
prevention <strong>of</strong> exacerbation <strong>and</strong> complications using cost-effective,<br />
evidence-based practice guidelines <strong>and</strong> patient empowerment<br />
strategies such as education <strong>and</strong> self-management. The process <strong>of</strong><br />
disease management evaluates clinical, social/humanistic <strong>and</strong><br />
economic outcomes with the goal <strong>of</strong> improving overall health <strong>of</strong><br />
the whole person.<br />
Members who receive disease management services receive<br />
support from a dedicated clinician, who assists in facilitating the<br />
health <strong>of</strong> the whole person, not just their individual condition.<br />
*Services are <strong>of</strong>fered to members, participation is optional.<br />
* Member eligibility for disease management is determined by the<br />
member/subscriber contract.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-25
Integrated Health Management<br />
Disease States Commercial Government Programs<br />
Access Management<br />
Programs<br />
Asthma<br />
Coronary Artery Diseases (CAD)<br />
Chronic Kidney Disease (CKD)<br />
Chronic Obstructive Pulmonary Disease (COPD)<br />
Depression<br />
Diabetes<br />
Heart Failure<br />
Low Back Pain<br />
Oncology<br />
In addition to the above conditions, <strong>Blue</strong> <strong>Cross</strong> also <strong>of</strong>fers a<br />
prenatal support program (Healthy Start ® Prenatal Support) to<br />
eligible members. Please contact customer service to determine if a<br />
member is eligible.<br />
A dedicated nurse or clinician may contact your <strong>of</strong>fice for<br />
assistance with a <strong>Blue</strong> <strong>Cross</strong> member’s needs. They may also send<br />
you a letter including member goals <strong>and</strong>/or gaps in care to inform<br />
you on what we are working with the member to advance their<br />
health care needs. We look forward to working with our member’s<br />
practitioners to make a healthy difference in our member’s health.<br />
Access management is a specialized program for fully insured<br />
commercial <strong>and</strong> <strong>Minnesota</strong> Health Care Program members.<br />
<strong>Blue</strong> Plus members include members with coverage through:<br />
Prepaid Medical Assistance Program Services for Persons<br />
Under Age 65 (PMAP <strong>and</strong> <strong>Minnesota</strong>Care Program Services<br />
(MNCare). MHCP also refers to this program as the Restricted<br />
Recipient Program.<br />
Restrictions <strong>of</strong> Medicare services are not allowable per DHS<br />
contract 2.119. For members who are on Medicare integrated<br />
product (Secure<strong>Blue</strong> SM [HMO SNP]), it is permissible to restrict<br />
Medicaid-only services. <strong>Blue</strong> Plus is not able to restrict Part D<br />
drug coverage <strong>and</strong> implement physician sole prescribers for public<br />
program members with Medicare (MSC+). If a MSC+ member is<br />
not Medicare eligible, restriction is permissible.<br />
4-26 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Access Management<br />
Programs (continued)<br />
Integrated Health Management<br />
Access management members/restricted recipients are members<br />
who have used services at a frequency or amount that is not<br />
medically necessary <strong>and</strong>/or who have obtained services in an<br />
inappropriate manner.<br />
Access management specialists in Integrated Health Management<br />
review members’ medical <strong>and</strong> pharmacy claims for potential<br />
restriction. Members who meet the access management program<br />
criteria are assigned to a specific physician for the primary care<br />
needs who, in turn, will coordinate all their care <strong>and</strong> medication<br />
needs. The member will also be assigned to a single pharmacy <strong>and</strong><br />
a single hospital. Access to specialty care may be discussed with<br />
the access manager assigned to the member. Access management<br />
program restriction is for 24 months.<br />
As a provider, you need to verify if a member has a restriction<br />
before providing services.<br />
If you provide services to a member enrolled in this program <strong>and</strong><br />
you are not the assigned physician, pharmacy or hospital claims<br />
payment may be impacted.<br />
Eligible services provided to a member in the access management<br />
program will be reimbursed only when one <strong>of</strong> the following<br />
criteria is met:<br />
The service is provided by the member’s assigned provider.<br />
The service is <strong>of</strong> a provider type or type <strong>of</strong> service that is not<br />
listed as needing access management.<br />
This includes durable medical equipment (DME), home care,<br />
ambulance services, mental health or chemical health services.<br />
Access management specialists will refer suspect cases to the<br />
special investigation unit (SIU) as needed.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-27
Integrated Health Management<br />
Focused Utilization Review<br />
Overview Focused utilization review programs contribute to our goals <strong>of</strong><br />
containing health care costs by assuring that services are contract<br />
benefits <strong>and</strong> appropriate. <strong>Blue</strong> <strong>Cross</strong> systematically monitors<br />
services <strong>of</strong> providers for patterns <strong>of</strong> overuse, underuse, misuse <strong>and</strong><br />
abuse in addition for obsolete or questionable practices.<br />
<strong>Blue</strong> <strong>Cross</strong> has data warehousing <strong>and</strong> s<strong>of</strong>tware programs that look<br />
for patterns outside established norms. The analysts review<br />
medical records <strong>and</strong> work with providers to resolve questions on<br />
coding, benefits <strong>and</strong> medical necessity. On-site audits, using a<br />
sample <strong>of</strong> up to the last three years <strong>of</strong> claims history may be<br />
performed. Prompt response to medical records requests will speed<br />
up processing <strong>of</strong> claims under review. Claims are denied as<br />
provider liability if the necessary information is not received<br />
within 14 calendar days.<br />
4-28 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Messages You May<br />
Receive<br />
Integrated Health Management<br />
The following message appears on the Statement <strong>of</strong> Provider<br />
Claims Paid to tell you that we did not receive the information<br />
needed to review the claim:<br />
We cannot continue processing <strong>of</strong> this claim because the<br />
medical information we requested has not been received. We<br />
will reprocess your claim upon receipt <strong>of</strong> the requested<br />
information.<br />
During utilization review, claims are screened for medical<br />
necessity. Peer review agents or consultants deny claims only after<br />
careful evaluation. Slightly longer processing time is required for<br />
claims that must go through the utilization review process. The<br />
following messages appear on the Statement <strong>of</strong> Provider Claims<br />
Paid for utilization review denials:<br />
This contract does not cover charges for treatment, services, or<br />
supplies which do not meet our criteria for medical necessity or<br />
are not normally provided for the treatment <strong>of</strong> this condition as<br />
determined by our medical staff <strong>and</strong>/or an independent health<br />
care pr<strong>of</strong>essional reviewer.<br />
These charges are not covered because this contract does not<br />
allow services from a provider performing this type <strong>of</strong> health<br />
care.<br />
This service <strong>and</strong> related charges are considered investigative<br />
<strong>and</strong> are not covered according to this contract. Our Medical<br />
Policy Committee continually reviews medical procedures in<br />
order to determine the investigative status <strong>of</strong> this <strong>and</strong> other<br />
services.<br />
These charges are not allowed because there was no<br />
documentation in the medical records to support this level <strong>of</strong><br />
care.<br />
Participating providers agree not to bill the member for any<br />
services <strong>Blue</strong> <strong>Cross</strong> determines to be not medically necessary or<br />
investigative. Medical necessity denials can be appealed within 30<br />
days from the date you are notified. We request that you submit<br />
written appeals outlining the issues <strong>and</strong> ATTACH supporting<br />
documentation such as medical records, operative reports, <strong>and</strong> any<br />
medical information documenting unusual circumstances at the<br />
time <strong>of</strong> the request.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-29
Integrated Health Management<br />
Special Investigations <strong>Blue</strong> <strong>Cross</strong> actively investigates possible fraudulent claims<br />
submissions from both members <strong>and</strong> providers. Fraud <strong>and</strong> abuse<br />
investigations conducted by our special investigations department<br />
are among the most thorough in the industry. Inconsistent charges,<br />
forged or altered charges, or services billed but never rendered are<br />
just a few examples <strong>of</strong> inappropriate practices that we may verify<br />
when conducting our investigation. Our investigation process may<br />
include, but is not limited to, record requests, audits, <strong>and</strong> survey<br />
letters.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>of</strong>ten conducts our investigations <strong>and</strong> criminal<br />
proceedings in collaboration with outside agencies such as the<br />
state attorney general’s <strong>of</strong>fice, the FBI, postal inspectors, or local<br />
authorities. Our goal is to protect <strong>Blue</strong> <strong>Cross</strong> members <strong>and</strong><br />
providers from losses due to fraudulent acts.<br />
Information about any person’s inappropriate use <strong>of</strong> a <strong>Blue</strong> <strong>Cross</strong><br />
policy, member ID card, or questionable billing practices should<br />
be reported by calling our fraud hot line. The phone number is<br />
listed in Chapter 1 — At Your Service. You may remain<br />
anonymous if you wish.<br />
4-30 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Documentation in the Medical Record<br />
Documentation<br />
Requirements<br />
Integrated Health Management<br />
To avoid denials for medical necessity, the patient’s medical<br />
record must contain certain pertinent information that may be<br />
subject to our review. The Centers for Medicare <strong>and</strong> Medicaid<br />
Services (CMS) in conjunction with the American Medical<br />
Association (AMA) has developed guidelines for the medical<br />
documentation necessary to support a given level <strong>of</strong> evaluation <strong>and</strong><br />
management service. <strong>Blue</strong> <strong>Cross</strong> adopted these guidelines to<br />
ensure that our members receive quality care <strong>and</strong> that the services<br />
are consistent with the health plan coverage provided.<br />
The general guidelines are listed below:<br />
The medical record should be complete <strong>and</strong> legible.<br />
The documentation <strong>of</strong> each patient encounter should include:<br />
reason for the encounter <strong>and</strong> relevant history, physical<br />
examination findings <strong>and</strong> prior diagnostic test results;<br />
plan <strong>of</strong> care; <strong>and</strong><br />
date <strong>and</strong> legible signature <strong>of</strong> the practitioner.<br />
If not documented, the rationale for ordering diagnostic <strong>and</strong><br />
other ancillary services should be easily inferred.<br />
Past <strong>and</strong> present diagnoses should be accessible to the treating<br />
<strong>and</strong>/or consulting physician.<br />
Appropriate health risk factors should be identified.<br />
The patient’s progress, response <strong>and</strong> changes in treatment, <strong>and</strong><br />
revision <strong>of</strong> diagnosis should be documented.<br />
The CPT/HCPCS <strong>and</strong> ICD-9-CM codes reported on the health<br />
insurance claim form or billing statement should be supported<br />
by the documentation in the medical record.<br />
Charge slips, super bills, travel cards, or <strong>of</strong>fice ledgers are not<br />
considered supporting documentation for services provided to a<br />
patient.<br />
Use <strong>of</strong> the term IBID (same as above) <strong>and</strong>/or the use <strong>of</strong> quotation<br />
marks to replace or repeat previously documented information is<br />
not acceptable. All information must be in date-sequence order.<br />
Services not documented as indicated above are not covered by<br />
<strong>Blue</strong> <strong>Cross</strong>. Patients are not financially liable for services that are<br />
denied for inadequate documentation.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-31
Integrated Health Management<br />
Overview Per your provider service agreement, you may not bill:<br />
Any member for medically unnecessary or investigative<br />
services.<br />
Prepaid Medical Assistance Program (PMAP) <strong>and</strong><br />
<strong>Minnesota</strong>Care members for services that are not covered at<br />
your <strong>of</strong>fice, but may be covered if the member went to another<br />
provider.<br />
You may bill the patient only if the following conditions are met:<br />
The patient is notified prior to the service being rendered that<br />
the service is not covered, etc.<br />
The member agrees, by signing a waiver, to pay for the service.<br />
In addition, you should not direct your fee-for-service members to<br />
nonparticipating providers (Refer to Referrals to Nonparticipating<br />
Providers).<br />
One <strong>of</strong> the DHS regulations includes enrollee rights to notification<br />
<strong>of</strong> non-covered services. General signed statement information is<br />
included in the <strong>Blue</strong> <strong>Cross</strong> Provider Policy <strong>and</strong> Procedure<br />
<strong>Manual</strong>, Chapter 6.<br />
The signed statement is allowed only when the service provided is<br />
a non-covered service, <strong>and</strong> must be:<br />
Specific to the procedure/service (including the cost)<br />
Specific to a date <strong>of</strong> service<br />
Signed <strong>and</strong> dated by the enrollee for each date <strong>of</strong> service<br />
If the signed statement is not signed by the Public Programs<br />
enrollee prior to the service, then according to DHS rules, the<br />
enrollee cannot be billed for the service. This includes services that<br />
are investigative, not medically necessary, or excluded from<br />
coverage under the contract. You may bill an enrollee for noncovered<br />
services only when <strong>Minnesota</strong> Health Care Programs<br />
(MHCP) never covers the services <strong>and</strong> only if you inform the<br />
enrollee before you deliver the services that he/she would be<br />
responsible for payment. If MHCP normally covers a service but<br />
the enrollee does not meet coverage criteria at the time <strong>of</strong> the<br />
service, the provider cannot charge the enrollee <strong>and</strong> cannot accept<br />
payment from the enrollee.<br />
For example, if an enrollee did not receive a referral for a service<br />
that required one, the service is not eligible for a signed statement;<br />
<strong>and</strong>, the provider cannot bill the member for the service.<br />
4-32 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Integrated Health Management<br />
Overview (continued) When submitting claims, indicate with a –GA in box 24D modifier<br />
those services that have a valid signed statement on file.<br />
We do not consider blanket (nonspecific) waivers sufficient<br />
notice to meet the patient notification requirements in your<br />
provider services agreement. The waiver must be dated <strong>and</strong><br />
must specifically identify the procedure or service. The waiver<br />
must also advise the patient that he or she would not be liable<br />
for these charges unless the waiver is signed.<br />
GA Modifier Use the -GA modifier in field 24D <strong>of</strong> the CMS-1500 form to<br />
indicate:<br />
you have notified a patient that a specific service has been<br />
determined by <strong>Blue</strong> <strong>Cross</strong> to be investigative or not medically<br />
necessary, <strong>and</strong><br />
those services will most likely not be covered under the<br />
member’s contract.<br />
After this notice, <strong>and</strong> prior to receiving the services, the patient<br />
must have agreed in writing that charges incurred will be the<br />
patient’s liability.<br />
The use <strong>of</strong> this modifier will result in allowed amounts related to<br />
these services being reported in the patient responsibility column<br />
<strong>of</strong> your provider remittance.<br />
Note: The -GA modifier should not be used routinely on all <strong>of</strong><br />
your claims submittals. Inappropriate use <strong>of</strong> the -GA<br />
modifier may result in an audit <strong>of</strong> your files <strong>and</strong> possible<br />
payment adjustments.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-33
Integrated Health Management<br />
Medical Referrals To<br />
Nonparticipating<br />
Providers<br />
<strong>Blue</strong> <strong>Cross</strong> participating providers are required to direct their feefor-service<br />
patients to other participating providers, including<br />
anesthesiologists, radiologists, pathologists <strong>and</strong> surgical assistants.<br />
Directories <strong>of</strong> participating providers are available upon request by<br />
contacting provider services. Many times the member will have<br />
reduced benefits <strong>and</strong> higher patient responsibility when using<br />
nonparticipating providers.<br />
Directing patients to nonparticipating providers may be necessary<br />
in the following situations:<br />
medical emergency<br />
participating providers are not available within certain<br />
geographic areas<br />
quality <strong>of</strong> care or specialty care requires use <strong>of</strong> a<br />
nonparticipating provider<br />
Note: This is for <strong>Blue</strong> <strong>Cross</strong> fee-for-service contracts. Use the<br />
Referral Network directory available on our website for<br />
<strong>Blue</strong> Plus managed care referrals. Typically, the member<br />
will receive the highest level <strong>of</strong> their benefits when<br />
receiving a referral for those services that require a referral.<br />
For complete information on Government Programs<br />
requirements, please refer to Chapter 3 in the <strong>Blue</strong> Plus<br />
Provider <strong>Manual</strong>.<br />
If it is necessary to refer to a nonparticipating provider, the<br />
participating physician must give the patient advance,<br />
written notification that the referral is to a nonparticipating<br />
physician. Once notice is given, the patient is responsible for<br />
any increased liability if he or she decides to schedule the<br />
service. If the patient is not properly informed, the provider<br />
making the referral to a nonparticipating provider will be<br />
liable for increased costs incurred by a patient.<br />
Sample Waivers A sample waiver for use in your <strong>of</strong>fice is available on our website.<br />
The waivers include the information required in order for you to<br />
hold the member financially liable for services. The waiver should<br />
be incorporated into your usual business forms <strong>and</strong> should be<br />
customized to include your business letterhead.<br />
4-34 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Upgraded/Deluxe<br />
Durable Medical<br />
Equipment (DME)<br />
DME Waiver<br />
Requirement<br />
DME Claims<br />
Submissions<br />
Commercial Business<br />
Integrated Health Management<br />
Participating durable medical equipment (DME) suppliers may bill<br />
members for an equipment upgrade or deluxe charge if a waiver is<br />
on file <strong>and</strong> the DME charges are billed correctly to <strong>Blue</strong> <strong>Cross</strong>. We<br />
continue to reimburse for medically necessary st<strong>and</strong>ard DME.<br />
Government Business<br />
Participating durable medical equipment (DME) suppliers may bill<br />
members for an equipment upgrade or deluxe charge if a waiver is<br />
on file <strong>and</strong> the DME charges are billed correctly to <strong>Blue</strong> <strong>Cross</strong>.<br />
Participating DME suppliers must obtain a signed, written waiver<br />
from the member that includes the cost for the deluxe features or<br />
upgrade. The waiver must also state the following:<br />
the st<strong>and</strong>ard piece <strong>of</strong> equipment or least costly alternative<br />
<strong>of</strong>fered to the member,<br />
the member is aware <strong>and</strong> agrees that <strong>Blue</strong> <strong>Cross</strong> will only pay<br />
the st<strong>and</strong>ard allowance, <strong>and</strong><br />
the member will be responsible for the deluxe or upgrade<br />
charge in addition to his or her contractual obligation.<br />
This waiver must be kept on file at your <strong>of</strong>fice. If a precertification/authorization<br />
are required for the item being provided,<br />
please send the waiver form along with your request. For all<br />
services that do not require a pre-certification/authorization, do<br />
not send it to <strong>Blue</strong> <strong>Cross</strong>. We do, however, reserve the right to<br />
see it.<br />
Two lines <strong>of</strong> service must be billed. The first line will include the<br />
DME HCPCS code <strong>and</strong> the st<strong>and</strong>ard charge for the equipment. The<br />
second line must include the same DME HCPCS code with the -<br />
GA modifier (waiver <strong>of</strong> liability statement on file) <strong>and</strong> the upgrade<br />
or deluxe charge. For example:<br />
E0202 -- $550.00 (st<strong>and</strong>ard charge that will be subject to<br />
st<strong>and</strong>ard allowance <strong>and</strong> reductions)<br />
E0202 GA -- $150.00 (deluxe/upgrade charge that will be<br />
denied as member liability)<br />
The -GA modifier must be submitted as the first modifier on the<br />
second service line. Other applicable modifiers, such as -NU<br />
(Purchase), should be submitted on the first service line.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 4-35
Integrated Health Management<br />
Sample DME Waiver A sample waiver for use in your <strong>of</strong>fice is available on our website.<br />
The waiver includes the information required in order to hold the<br />
member financially liable for deluxe features or upgrades to a<br />
durable medical equipment purchase. The waiver should be<br />
incorporated into your usual business forms <strong>and</strong> customized to<br />
include your business letterhead.<br />
4-36 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Table <strong>of</strong> Contents<br />
Chapter 5<br />
Health Care Options<br />
Member ID Cards/Health Coverage Options.......................................................................... 5-3<br />
Fully Insured Groups .............................................................................................................5-3<br />
Self-Insured Groups...............................................................................................................5-3<br />
Member ID Cards ..................................................................................................................5-4<br />
Member ID Card Conversion.................................................................................................5-4<br />
Helpful Tips ...........................................................................................................................5-5<br />
Verify Identity <strong>of</strong> Cardholder ................................................................................................5-5<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Coverage Options................................................ 5-6<br />
Overview................................................................................................................................5-6<br />
Aware Gold ® ..........................................................................................................................5-6<br />
Aware Gold Limited ..............................................................................................................5-6<br />
Aware PPO.............................................................................................................................5-6<br />
<strong>Blue</strong> Selections....................................................................................................................... 5-7<br />
Options <strong>Blue</strong> HRA/HSA........................................................................................................5-7<br />
Comprehensive Major Medical..............................................................................................5-7<br />
Double Gold...........................................................................................................................5-8<br />
Freedom 1-2-3........................................................................................................................5-8<br />
Simply <strong>Blue</strong> SM ........................................................................................................................5-8<br />
Personal <strong>Blue</strong> SM .....................................................................................................................5-8<br />
Go<strong>Blue</strong> ...................................................................................................................................5-8<br />
InstaCare ................................................................................................................................5-8<br />
Medicare Supplemental Plans................................................................................................5-9<br />
Medicare Basic <strong>Blue</strong> ® ..........................................................................................................5-10<br />
Extended Basic <strong>Blue</strong> ® ..........................................................................................................5-10<br />
Senior Gold SM ......................................................................................................................5-11<br />
Platinum <strong>Blue</strong> SM (Cost)........................................................................................................ 5-12<br />
Medicare<strong>Blue</strong> PPO (Regional PPO) ....................................................................................5-13<br />
Medicare<strong>Blue</strong> Rx (PDP) ......................................................................................................5-14<br />
Guidelines for Determining Submissions to Medicare or <strong>Blue</strong> <strong>Cross</strong>.................................5-15<br />
Inquiries <strong>and</strong> Claims Platinum <strong>Blue</strong> (Cost) .........................................................................5-15<br />
<strong>Blue</strong> Plus Coverage Options.................................................................................................... 5-19<br />
Comprehensive Plan ............................................................................................................ 5-19<br />
Preferred Gold SM ..................................................................................................................5-19<br />
Triple Gold...........................................................................................................................5-19<br />
Medicare Select Product ......................................................................................................5-19<br />
<strong>Minnesota</strong> Senior Health Options (MSHO) / Secure <strong>Blue</strong> (HMO) .....................................5-20<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-1
Health Care Options<br />
Prepaid Medical Assistance Program (PMAP), <strong>and</strong> <strong>Minnesota</strong> Senior Care Plus (MSC+) /<br />
<strong>Blue</strong> Advantage....................................................................................................................5-21<br />
<strong>Minnesota</strong>Care Program ...................................................................................................... 5-22<br />
Federal Employee Program .................................................................................................... 5-23<br />
Federal Employee Program (FEP).......................................................................................5-23<br />
Provider Statements .............................................................................................................5-23<br />
Benefit Changes...................................................................................................................5-23<br />
<strong>Blue</strong>LinkTPA .............................................................................................................................. 5-24<br />
Healthy Start ® Prenatal Support............................................................................................ 5-25<br />
Healthy Start ® Prenatal Support........................................................................................... 5-25<br />
Delta Dental .............................................................................................................................. 5-26<br />
History.................................................................................................................................. 5-26<br />
Inquiries ...............................................................................................................................5-26<br />
MII Life, Incorporated ............................................................................................................ 5-27<br />
History..................................................................................................................................5-27<br />
Products <strong>and</strong> Services ..........................................................................................................5-27<br />
Prime Therapeutics LLC......................................................................................................... 5-28<br />
History..................................................................................................................................5-28<br />
Formularies ..........................................................................................................................5-28<br />
Workers’ Compensation, No-Fault Auto & Subrogation .................................................... 5-29<br />
Overview..............................................................................................................................5-29<br />
Workers' Compensation, No-Fault Auto & Subrogation.....................................................5-29<br />
Networks ................................................................................................................................... 5-34<br />
<strong>Blue</strong> <strong>Cross</strong> (Aware)..............................................................................................................5-34<br />
Select Networks ...................................................................................................................5-34<br />
<strong>Blue</strong> Plus ® ............................................................................................................................5-34<br />
<strong>Blue</strong>Card ® ............................................................................................................................5-34<br />
<strong>Blue</strong> Distinction Centers ® ....................................................................................................5-34<br />
<strong>Blue</strong> Precision ® ....................................................................................................................5-34<br />
Accord Network...................................................................................................................5-34<br />
Value Network.....................................................................................................................5-34<br />
5-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Member ID Cards/Health Coverage Options<br />
Health Care Options<br />
Fully Insured Groups <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus (<strong>Blue</strong><br />
<strong>Cross</strong>) fully-insured contracts are available for employers that<br />
select our st<strong>and</strong>ard benefits. The employer can choose the<br />
deductible/coinsurance <strong>and</strong> copay amounts.<br />
Fully insured contracts generally:<br />
• <strong>of</strong>fer consistent benefit options<br />
• follow state m<strong>and</strong>ates<br />
• follow federal m<strong>and</strong>ates<br />
• have st<strong>and</strong>ard member identification (ID) cards<br />
• are regulated by the Department <strong>of</strong> Commerce (fee-for-service)<br />
or the Department <strong>of</strong> Health (managed care)<br />
Self-Insured Groups We also administer self-insured contracts in which the employer<br />
selects the benefits <strong>and</strong> assumes all or part <strong>of</strong> the financial risk.<br />
These may also be referred to as ASOs (Administrative Services<br />
Only). Self-insured contracts generally:<br />
• <strong>of</strong>fer many contract benefit options<br />
• are not required to follow state m<strong>and</strong>ates<br />
• follow federal m<strong>and</strong>ates<br />
• have member ID cards that may not be st<strong>and</strong>ard <strong>and</strong> may<br />
include the employer name <strong>and</strong>/or logo<br />
Patients who belong to self-insured groups administered by <strong>Blue</strong><br />
<strong>Cross</strong> are to be treated as any other member for purposes <strong>of</strong> the<br />
provider contract. Because your <strong>of</strong>fice must bill us directly for<br />
these patients, it is important to check the back <strong>of</strong> the member ID<br />
card to see if we are listed as the administrator <strong>of</strong> the health plan.<br />
The front <strong>of</strong> the card may have the company’s plan name.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-3
Health Care Options<br />
Member ID Cards Your patient’s member ID card contains information that is<br />
essential for claims processing. We recommend that you look at<br />
the member’s ID card at every visit <strong>and</strong> have a current copy <strong>of</strong> the<br />
front <strong>and</strong> back <strong>of</strong> the card on file. There is a sample <strong>of</strong> some <strong>of</strong> the<br />
member ID cards issued at <strong>Blue</strong> <strong>Cross</strong> on our website. Not all <strong>of</strong><br />
the following information is found on each member ID card:<br />
Member ID Card<br />
Conversion<br />
• name <strong>of</strong> the plan<br />
• member’s ID number including alpha prefix<br />
• member’s name <strong>and</strong> group number<br />
• primary care clinic (PCC) name – for managed care plans only<br />
• <strong>Blue</strong> <strong>Shield</strong> plan code<br />
• <strong>Blue</strong> <strong>Cross</strong> plan code<br />
• prescription coverage<br />
• copay for prescription drugs<br />
• copay for <strong>of</strong>fice visits<br />
• dependent-coverage indicator<br />
• claims submission information<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> its affiliates converted member identification<br />
numbers from Social Security numbers as <strong>of</strong> December 31, 2004.<br />
Members from the following <strong>Blue</strong> <strong>Cross</strong> lines <strong>of</strong> business will<br />
retain their original identification number:<br />
• Federal Employee Program - Identification numbers are not<br />
the member’s social security number <strong>and</strong> are assigned by the<br />
federal government.<br />
• <strong>Minnesota</strong> government programs, including Prepaid<br />
Medical Assistance Program <strong>and</strong> <strong>Minnesota</strong> Care -<br />
Identification numbers are not the member’s social security<br />
number, they being with an “8”.<br />
• Workers’ Compensation - The <strong>Minnesota</strong> Department <strong>of</strong><br />
Labor <strong>and</strong> Industry requires the use <strong>of</strong> social security numbers<br />
for anyone who has ever filed a work compensation claim.<br />
5-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Health Care Options<br />
Helpful Tips • Ask members for their current member ID card <strong>and</strong> regularly<br />
obtain new photocopies (front <strong>and</strong> back) <strong>of</strong> the member ID<br />
card. Having the current card will enable you to submit claims<br />
with the appropriate member information (including alpha<br />
prefix) <strong>and</strong> avoid unnecessary claims payment delays.<br />
• Check eligibility <strong>and</strong> benefits by using provider web selfservice,<br />
BLUELINE or call 1-800-676-BLUE (2583) <strong>and</strong><br />
provide the alpha prefix.<br />
• If the member presents a debit card (st<strong>and</strong>-alone or combined),<br />
be sure to verify the copayment amounts before processing<br />
payment.<br />
• Please do not use the debit card to process full payment<br />
upfront. If you have questions about the debit card processing<br />
instructions or payment issues, please contact the debit card<br />
administrator’s toll-free number on the back <strong>of</strong> the card.<br />
Verify Identity <strong>of</strong><br />
Cardholder<br />
We recommend that you verify the identity <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong><br />
cardholders by asking for additional picture identification.<br />
Identification numbers <strong>and</strong> group numbers must be submitted<br />
correctly on electronic or paper claims in order for us to identify<br />
the patient.<br />
If you suspect fraudulent use <strong>of</strong> a member ID card, please call our<br />
fraud hot line at (651) 662-8363. You may remain anonymous.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-5
Health Care Options<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Coverage<br />
Options<br />
Overview <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong>fer a wide variety <strong>of</strong> health coverage options. A<br />
summary <strong>of</strong> those benefit options available to individuals <strong>and</strong><br />
groups follows in this chapter. All benefits are subject to the terms<br />
<strong>of</strong> the member’s contract <strong>and</strong> certificate.<br />
Please use provider web self-service, BLUELINE or provider<br />
services to identify your patient’s eligibility <strong>and</strong> benefits.<br />
Aware Gold ® Aware Gold is <strong>Blue</strong> <strong>Cross</strong>’ premier health plan. When using<br />
participating providers, Aware Gold members usually receive 100<br />
percent coverage for everything from preventive care, such as<br />
annual physical examinations <strong>and</strong> lab <strong>and</strong> x-ray services, to<br />
hospital inpatient services. Office visit copays may apply.<br />
Members may choose to see specialists without referrals. If<br />
members select out-<strong>of</strong>-network providers for non-emergency care,<br />
deductibles <strong>and</strong> coinsurance may apply.<br />
Aware Gold Limited Aware Gold Limited, a companion plan to Aware Gold, covers a<br />
wide range <strong>of</strong> medical services from routine <strong>of</strong>fice visits to major<br />
surgery, including chiropractic, mental health, <strong>and</strong> substance abuse<br />
treatment. Aware Gold Limited members receive the highest level<br />
<strong>of</strong> benefits when they see a network provider, do little or no<br />
paperwork, <strong>and</strong> have coverage outside the network, anywhere in<br />
the world. Under this plan, members pay a modest portion <strong>of</strong> their<br />
health care costs in the form <strong>of</strong> a copay or coinsurance for many<br />
services. An annual deductible applies only to certain services<br />
from out-<strong>of</strong>-network providers.<br />
Aware PPO Aware PPO is a fully insured open access product. Attractive to<br />
groups that have members headquartered in <strong>Minnesota</strong> with a<br />
concentrated population <strong>of</strong> employees also living in other<br />
geographical areas. This plan covers eligible medial services, such<br />
as inpatient <strong>and</strong> outpatient hospital services <strong>and</strong> doctor visits, at a<br />
percentage after the deductible. Preventive care <strong>and</strong> well child<br />
visits are covered at 100 percent under this plan.<br />
Several calendar-year deductibles <strong>and</strong> out-<strong>of</strong>-pocket maximum<br />
options are available.<br />
Once the deductible has been met, Aware PPO pays a percentage<br />
<strong>of</strong> the allowed amount for all eligible expenses, up to an<br />
established out-<strong>of</strong>-pocket maximum. If eligible expenses during a<br />
calendar year exceed the out-<strong>of</strong>-pocket maximum, Aware PPO<br />
pays 100 percent <strong>of</strong> the allowed amount through the end <strong>of</strong> that<br />
calendar year.<br />
5-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Health Care Options<br />
<strong>Blue</strong> Selections Benefit plans that use the <strong>Blue</strong> Precision network <strong>of</strong> tiered<br />
providers based upon quality <strong>of</strong> care <strong>and</strong> cost effective care.<br />
Members receive the highest level <strong>of</strong> benefits by utilizing<br />
providers in Tier 1.<br />
Options <strong>Blue</strong> HRA/HSA Options <strong>Blue</strong> is the suite <strong>of</strong> consumer-directed health care<br />
solutions. The components <strong>of</strong> Options <strong>Blue</strong> are a high-deductible<br />
open access health plan (CMM or PPO), alongside an account that<br />
is funded by the employer or employee, or both, that helps pay for<br />
eligible out-<strong>of</strong>-pocket expenses (please note that HRAs can only<br />
be funded by the employer). In most cases, any dollars that are<br />
unused in the account at the end <strong>of</strong> the benefit year will roll over<br />
<strong>and</strong> be added to new dollars in the next benefit year. The dollars<br />
can be used to help pay for future out-<strong>of</strong>-pocket health care<br />
expenses. Additionally, the <strong>Blue</strong> <strong>Cross</strong> Health Support member<br />
health improvement tools (including Dedicated Nurse support,<br />
Healthy Start <strong>and</strong> 24-Hour Nurse Advice Line) add to the overall<br />
value <strong>of</strong> the product.<br />
Comprehensive Major<br />
Medical<br />
From a health plan perspective, this plan works like any other<br />
high-deductible health plan. Members are responsible for paying<br />
providers for services that are not paid by the health plan.<br />
Available account funds can be used by members to pay their<br />
provider(s) for eligible care not reimbursed by the health plan.<br />
Employers have an option to allow employees to have account<br />
funds go directly to the provider. Providers will receive a check<br />
directly from SelectAccount ® , the account administrator.<br />
The Comprehensive Major Medical (CMM) plan is designed for<br />
employer groups <strong>and</strong> individuals who are willing to pay a small<br />
portion <strong>of</strong> their medical bills <strong>and</strong> still receive protection against the<br />
costs <strong>of</strong> major illness or injury. This plan covers eligible medical<br />
services, such as inpatient <strong>and</strong> outpatient hospital services, at a<br />
percentage after a deductible. Preventive Care <strong>and</strong> well-child care<br />
is covered at 100 percent under this plan.<br />
Several calendar-year deductible <strong>and</strong> out-<strong>of</strong>-pocket maximum<br />
options are available. Generally, the higher the deductible, the<br />
lower the cost for comprehensive coverage.<br />
Once the deductible has been met, CMM pays a percentage <strong>of</strong> the<br />
allowed amount for all eligible expenses, up to an established out<strong>of</strong>-pocket<br />
maximum. If eligible expenses during a calendar year<br />
exceed the out-<strong>of</strong>-pocket maximum, CMM pays 100 percent <strong>of</strong> the<br />
allowed amount through the end <strong>of</strong> that calendar year.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-7
Health Care Options<br />
Double Gold Double Gold is a self-insured fee-for-service plan administered by<br />
<strong>Blue</strong> <strong>Cross</strong>. Members have the freedom to see participating doctors<br />
<strong>of</strong> their choice, however, the provider network for chiropractic <strong>and</strong><br />
behavioral health care may be limited depending on the employer<br />
group. Office visit copays may apply.<br />
Freedom 1-2-3 Is a new low-cost plan designed especially for employer groups<br />
with 2-50 members? There is no coverage for certain m<strong>and</strong>ated<br />
benefits like chiropractic, mental health care, infertility <strong>and</strong><br />
bariatric surgery. This plan has a low deductible, with no <strong>of</strong>fice<br />
visit copays. It includes generous upfront benefits for:<br />
• One preventive care visit <strong>and</strong> one eye exam each year<br />
• Two doctor’s <strong>of</strong>fice or urgent care visits each year<br />
• Three retail health clinic visits each year<br />
The group has the option to choose one <strong>of</strong> two networks. The<br />
statewide Accord network or, in the 11-county metro area, our new<br />
Value network.<br />
Simply <strong>Blue</strong> SM Simply <strong>Blue</strong> <strong>of</strong>fers essential health care coverage. The plan is<br />
single coverage only ages 19-64. This plan <strong>of</strong>fers three deductible<br />
options, two drug options, <strong>and</strong> <strong>of</strong>fice visit copays. Substance abuse<br />
coverage is optional. This plan <strong>of</strong>fers the statewide Accord<br />
network.<br />
Personal <strong>Blue</strong> SM Personal <strong>Blue</strong> is a comprehensive major medical Individual plan<br />
with some upfront coverage for <strong>of</strong>fice <strong>and</strong> retail health clinic <strong>of</strong>fice<br />
visits <strong>and</strong> generic drug copay. There are a variety <strong>of</strong> deductible<br />
options for members to choose from. This plan has family<br />
coverage. Substance abuse coverage is optional. This plan <strong>of</strong>fers<br />
the statewide Accord network.<br />
Go<strong>Blue</strong> Go<strong>Blue</strong> is our lowest cost plan that takes care <strong>of</strong> major expenses.<br />
There are four deductible options <strong>and</strong> <strong>of</strong>fers an urgent care <strong>and</strong><br />
generic drug copay. This plan is single coverage only for ages 19<br />
through 64. This plan <strong>of</strong>fers the statewide Accord network.<br />
InstaCare InstaCare is our short-term coverage plan that <strong>of</strong>fers immediate<br />
protection. This plan does not cover preexisting conditions. There<br />
are three deductible options to choose from <strong>and</strong> three contract term<br />
durations – 30 day, 60 day, or 90 day.<br />
5-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Medicare<br />
Supplemental Plans<br />
Health Care Options<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>of</strong>fers <strong>and</strong> has a variety <strong>of</strong> Medicare supplement plans.<br />
Medicare supplement plans are designed to help fill the gaps in<br />
Medicare coverage. <strong>Blue</strong> <strong>Cross</strong> has several Medicare supplement<br />
plans that are no longer open for enrollment, however, members<br />
who had signed up previous to plan closure are eligible to keep<br />
their plan.<br />
As <strong>of</strong> June 2006, <strong>Blue</strong> <strong>Cross</strong> currently has two Medicare<br />
Supplement plans open for enrollment by individuals (as opposed<br />
to employer groups), Basic Medicare<strong>Blue</strong> <strong>and</strong> Extended Basic<br />
<strong>Blue</strong> <strong>and</strong> one Medicare Select plan, Senior Gold.<br />
Under these plans, Medicare is the primary payer. Claims must be<br />
submitted to <strong>Blue</strong> <strong>Cross</strong> with a copy <strong>of</strong> the Medicare Remittance<br />
Advice (RA) form.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-9
Health Care Options<br />
Medicare Basic <strong>Blue</strong> ® Medicare Basic <strong>Blue</strong> is our low-cost Medicare Supplement plan.<br />
Members can enroll in the base plan <strong>and</strong> then select from a number<br />
<strong>of</strong> additional coverage options to suit their needs.<br />
The base plan for Medicare Basic <strong>Blue</strong> covers the Medicare<br />
coinsurance for Part A <strong>and</strong> B, but does not cover the annual<br />
deductibles. When the deductible has been met, coverage is<br />
provided for the Medicare Part B coinsurance amount up to<br />
Medicare’s approved charge <strong>and</strong> for the cost <strong>of</strong> the first three pints<br />
<strong>of</strong> blood per calendar year. Additional coverage is furnished for<br />
residential <strong>and</strong> nonresidential treatment programs, cancer<br />
screening <strong>and</strong> temporom<strong>and</strong>ibular joint syndrome (TMJ). It also<br />
covers 80 percent <strong>of</strong> emergency care received in a foreign country.<br />
The plan also <strong>of</strong>fers four separate additional coverage options,<br />
which include: Preventative care coverage, coverage <strong>of</strong> Medicare<br />
Part A inpatient hospital deductible, coverage <strong>of</strong> Medicare Part B<br />
annual deductible, <strong>and</strong> coverage <strong>of</strong> 100 percent <strong>of</strong> eligible medical<br />
expenses <strong>and</strong> supplies not covered by Medicare Part B that exceed<br />
Medicare approved charges. These options can be purchased to<br />
supplement coverage available through the base plan according to<br />
the needs <strong>of</strong> the member.<br />
Under this plan, Medicare is the primary payer. Claims must be<br />
submitted to <strong>Blue</strong> <strong>Cross</strong> with a copy <strong>of</strong> the Medicare Remittance<br />
Advice (RA) form.<br />
Extended Basic <strong>Blue</strong> ® The Extended Basic Medicare supplement plan is the most<br />
comprehensive plan that <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong>fers. Coverage is furnished<br />
Medicare coinsurance, deductibles, preventive care up to $120 <strong>of</strong><br />
eligible charges annually, 20 extra days in a skilled nursing facility<br />
<strong>and</strong> extra home health care expenses. Member out <strong>of</strong> pocket is<br />
limited to $1,000 <strong>of</strong> eligible charges each year.<br />
Members who were enrolled in this plan with optional drug prior<br />
to January 1, 2006 are able to retain their 80 percent prescription<br />
drug coverage. That prescription coverage plan is creditable<br />
according to CMS guidelines.<br />
Under this plan, Medicare is the primary payer. Claims must be<br />
submitted to <strong>Blue</strong> <strong>Cross</strong> with a copy <strong>of</strong> the Medicare RA form.<br />
5-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Health Care Options<br />
Senior Gold SM Senior Gold, also referred to as the Medicare Select plan, <strong>of</strong>fers<br />
seniors comprehensive coverage within the <strong>Blue</strong> <strong>Cross</strong><br />
participating provider network <strong>and</strong> the freedom <strong>of</strong> choice<br />
associated with fee-for-service plans. Senior Gold has been, <strong>and</strong><br />
continues to be, our most popular Medicare supplemental product.<br />
Members receive the highest level <strong>of</strong> benefits for services in the<br />
participating provider network <strong>and</strong> also have excellent coverage<br />
when traveling. There are no copays or deductibles for services<br />
received from <strong>Blue</strong> <strong>Cross</strong> participating providers. Senior Gold also<br />
<strong>of</strong>fers optional preventive screenings <strong>and</strong> services not covered by<br />
Medicare. Senior Gold members enrolled in the optional<br />
prescription drug coverage prior to January 1, 2006 may retain that<br />
coverage, however; that coverage is not creditable according to<br />
Medicare guidelines. The optional prescription drug coverage is<br />
not available to new Senior Gold enrollees (those enrolling after<br />
December 31, 2005).<br />
On claims where assignment is taken, <strong>Blue</strong> <strong>Cross</strong> pays Medicare<br />
coinsurance <strong>and</strong> deductible only. Under this plan, Medicare is the<br />
primary payer. Claims must be submitted to <strong>Blue</strong> <strong>Cross</strong> with a<br />
copy <strong>of</strong> the Medicare RA form.<br />
This product is also available for fully insured employer groups to<br />
purchase for their Medicare eligible members. The logo on the<br />
member ID card for any such group members will be prefaced<br />
with “Group”. Benefits may vary by group.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-11
Health Care Options<br />
Platinum <strong>Blue</strong> SM (Cost) <strong>Blue</strong> <strong>Cross</strong> has made a commitment to <strong>of</strong>fer a broader variety <strong>of</strong><br />
Medicare products to eligible <strong>Minnesota</strong> Medicare beneficiaries. In<br />
mid-2005, <strong>Blue</strong> <strong>Cross</strong> introduced its Medicare Cost product,<br />
Vantage<strong>Blue</strong>, statewide. Effective January 1, 2010, Vantage<strong>Blue</strong><br />
was renamed Platinum <strong>Blue</strong> <strong>and</strong> <strong>of</strong>fered three plan options.<br />
Platinum <strong>Blue</strong> is an open access product for Medicare<br />
beneficiaries who are residents <strong>of</strong> <strong>Minnesota</strong>, <strong>of</strong>fered through a<br />
contract with the Centers for Medicare <strong>and</strong> Medicaid Services<br />
(CMS).<br />
Members can chose from three different medical benefits plan<br />
options:<br />
• Core<br />
• Choice<br />
• Complete<br />
Platinum <strong>Blue</strong> is also <strong>of</strong>fered to employer groups. There are three<br />
options for employer groups: Plan A, Plan B, <strong>and</strong> Plan C. All<br />
individual <strong>and</strong> employer group options provide coverage for<br />
Medicare eligible services with exp<strong>and</strong>ed coverage levels <strong>and</strong><br />
additional benefits. Members who have only Medicare Part B<br />
coverage will not receive any plan coverage for Medicare Part A<br />
services.<br />
The Core option requires copays for inpatient hospital, inpatient<br />
mental health care, urgently needed care <strong>and</strong> emergency room<br />
visits, but requires 20 percent coinsurance for many other services<br />
covered.<br />
The Choice option also requires $50 to $100 copays for inpatient<br />
hospital care, inpatient mental health care, urgently needed care<br />
<strong>and</strong> emergency room visits, as well as $10 copays for many other<br />
services. Some benefits require coinsurance.<br />
The Complete option <strong>of</strong>fers the most comprehensive coverage,<br />
having all the benefits <strong>of</strong> the Core <strong>and</strong> Choice options but<br />
generally at $0 copay. A few benefits require 20 percent<br />
coinsurance.<br />
All individual <strong>and</strong> group plan options include travel coverage (innetwork<br />
benefit levels when traveling in the United States, but<br />
outside <strong>of</strong> <strong>Minnesota</strong>), health <strong>and</strong> wellness education, <strong>and</strong> a fitness<br />
program. The Choice <strong>and</strong> Complete individual <strong>and</strong> Plan A, Plan B<br />
<strong>and</strong> Plan C group plan options also include benefits for hearing<br />
aids <strong>and</strong> fittings <strong>and</strong> vision exams <strong>and</strong> eyewear.<br />
5-12 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Platinum <strong>Blue</strong> SM (Cost)<br />
(continued)<br />
Medicare<strong>Blue</strong> PPO<br />
(Regional PPO)<br />
Health Care Options<br />
The Plan C employer group option requires copays for most<br />
services, including inpatient hospital, mental health services <strong>and</strong><br />
emergency room visits. The Plan B option requires similar copays,<br />
but does not require a copay for inpatient hospital care <strong>and</strong><br />
inpatient mental health.<br />
No referrals are needed for in-network doctors, specialists or<br />
hospitals. It is important to note that both individual <strong>and</strong> group<br />
Platinum <strong>Blue</strong> members can receive plan benefits for services<br />
received outside <strong>of</strong> <strong>Minnesota</strong> when traveling for up to nine<br />
months per year. This differs from out <strong>of</strong> network coverage while<br />
in <strong>Minnesota</strong>. If, while in <strong>Minnesota</strong>, members go to a provider<br />
outside <strong>of</strong> the Platinum <strong>Blue</strong> (Cost) network who accepts Medicare<br />
patients, members are covered under Original Medicare <strong>and</strong> would<br />
pay the Part A <strong>and</strong> Part B deductibles <strong>and</strong> coinsurance.<br />
Claims administration for Platinum <strong>Blue</strong> is shared by <strong>Blue</strong> <strong>Cross</strong><br />
<strong>and</strong> Medicare. Medicare is the primary claim processing entity for<br />
most Medicare Part A eligible services, with some exceptions.<br />
Claims for services eligible under Medicare Part B will generally<br />
be administered by <strong>Blue</strong> <strong>Cross</strong>, again, with some exceptions.<br />
This product is also available for fully insured employer groups to<br />
purchase for their Medicare eligible members. The logo on the<br />
member ID card for any such group members will be prefaced<br />
with “Group”. Benefits may vary by group.<br />
A more recent introduction in the <strong>Blue</strong> <strong>Cross</strong> Medicare product<br />
expansion is Medicare<strong>Blue</strong> PPO. This is a regional Medicare<br />
Advantage product <strong>of</strong>fered through the coordination <strong>of</strong> six <strong>Blue</strong><br />
<strong>Cross</strong> plans covering seven states.<br />
The service area for this plan encompasses Iowa, <strong>Minnesota</strong>,<br />
Montana, Nebraska, North Dakota, South Dakota <strong>and</strong> Wyoming.<br />
The plan was introduced across the region with a first effective<br />
date <strong>of</strong> January 1, 2006.<br />
This product <strong>of</strong>fers one medical benefit level option with Medicare<br />
Part D (prescription drug) coverage included. The plan covers the<br />
full range <strong>of</strong> basic Medicare covered services, with exp<strong>and</strong>ed<br />
coverage levels <strong>and</strong> additional benefits. Additional benefits<br />
include: hearing services, vision services, physical exams,<br />
health/wellness education (newsletter, nurse hotline, <strong>and</strong> disease<br />
management).<br />
Medicare<strong>Blue</strong> PPO members are free to receive care either in or<br />
out <strong>of</strong> network, however; while in-network care is generally<br />
subject to a copay, out-<strong>of</strong>-network care is generally subject to<br />
coinsurance.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-13
Health Care Options<br />
Medicare<strong>Blue</strong> PPO<br />
(Regional PPO)<br />
(continued)<br />
PLEASE NOTE: The <strong>Blue</strong> <strong>Cross</strong> provider manual is not<br />
applicable to this product, nor is the <strong>Blue</strong> <strong>Cross</strong> provider<br />
services number. Provider information for Medicare<strong>Blue</strong> PPO<br />
can be found at:<br />
http://www.yourmedicaresolutions.com/for_providers/<br />
This product is also available for fully insured employer groups to<br />
purchase for their Medicare eligible members. Benefits may vary<br />
by group.<br />
Medicare<strong>Blue</strong> Rx (PDP) Another recent introduction in the <strong>Blue</strong> <strong>Cross</strong> Medicare product<br />
portfolio is Medicare<strong>Blue</strong> Rx. This is a regional Medicare Part D<br />
Program product <strong>of</strong>fered through the coordination <strong>of</strong> six <strong>Blue</strong><br />
<strong>Cross</strong> plans covering seven states. The service area for this plan<br />
encompasses Iowa, <strong>Minnesota</strong>, Montana, Nebraska, North Dakota,<br />
South Dakota <strong>and</strong> Wyoming. The plan was introduced across the<br />
region with a first effective date <strong>of</strong> January 1, 2006.<br />
This product, as <strong>of</strong> January 1, 2011, <strong>of</strong>fers two different benefit<br />
level options: St<strong>and</strong>ard <strong>and</strong> Premier. The design <strong>of</strong> St<strong>and</strong>ard<br />
includes a $310 annual deductible, 25 percent coinsurance <strong>and</strong> a 4<br />
tier formulary. Premier has no annual deductible <strong>and</strong> has copays or<br />
coinsurance depending on the drug’s formulary placement, which<br />
is 4 tiers, <strong>and</strong> has some benefits in the coverage gap. Both plan<br />
options include catastrophic coverage after $4,550 annual out <strong>of</strong><br />
pocket <strong>and</strong> formulary exceptions processes. Drugs in the<br />
formularies may be subject to step therapy, quantity limits, or prior<br />
authorization.<br />
PLEASE NOTE: Forms, formularies <strong>and</strong> provider<br />
information for Medicare<strong>Blue</strong> Rx can be found at:<br />
http://www.yourmedicaresolutions.com/for_providers/<br />
This product is also available for fully insured employer groups to<br />
purchase for their Medicare eligible members. The logo on the<br />
member ID card for any such group members will be prefaced<br />
with “Group”. Benefits may vary by group.<br />
5-14 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Guidelines for<br />
Determining<br />
Submissions to<br />
Medicare or <strong>Blue</strong> <strong>Cross</strong><br />
Inquiries <strong>and</strong> Claims<br />
Platinum <strong>Blue</strong> (Cost)<br />
Health Care Options<br />
For services provided to Medicare members enrolled in our<br />
Medicare supplement or Platinum <strong>Blue</strong> plan that are eligible under<br />
Medicare Part A, Medicare is primary. CMS will continue to be<br />
the primary payor for these services with electronic claims<br />
crossing over from Medicare intermediaries. <strong>Blue</strong> <strong>Cross</strong> will serve<br />
as secondary payor for these services with members being subject<br />
to Medicare coinsurance <strong>and</strong> deductibles.<br />
<strong>Blue</strong> <strong>Cross</strong> is the administrator for Medicare Part B nonfacilitybased<br />
services <strong>and</strong> any additional Platinum <strong>Blue</strong> benefits.<br />
Reimbursement for pr<strong>of</strong>essional providers utilize <strong>Blue</strong> <strong>Cross</strong>’<br />
contracted fee schedule methodology. Current reimbursement uses<br />
2005 RVUs with Medicare conversion factors <strong>and</strong> is GPCI<br />
adjusted (geographical adjustment). For the initial product launch,<br />
Medicare part B services will apply CCI edits at the claim level; as<br />
<strong>Blue</strong> <strong>Cross</strong>’ functionality evolves; auto adjudication will occur. To<br />
ensure CMS compliance, follow the guidelines outlined in<br />
st<strong>and</strong>ard Medicare bulletins <strong>and</strong> the Provider Policy <strong>and</strong> Procedure<br />
manual.<br />
For Medicare members enrolled in our Medicare Advantage plans,<br />
including Medicare<strong>Blue</strong> PPO, <strong>Blue</strong> <strong>Cross</strong> replaces Medicare as<br />
primary payor. Please see the information available on medical<br />
policy, claims submission <strong>and</strong> payment, etc at:<br />
http://www.yourmedicaresolutions.com/for_providers/<br />
Provider claim <strong>and</strong> benefit inquiries for Platinum <strong>Blue</strong> can be<br />
directed to provider web self-service, BLUELINE or provider<br />
services at (651) 662-6500 or 1-800-262-0820.<br />
Care management inquires should be directed to (651) 662-5520 or<br />
1-800-528-0934.<br />
Services eligible under Medicare part B <strong>and</strong> that would otherwise<br />
be billed to the Medicare carrier on a pr<strong>of</strong>essional claims<br />
form/format, should be submitted directly to <strong>Blue</strong> <strong>Cross</strong><br />
electronically, whenever possible.<br />
Group number for Platinum <strong>Blue</strong> individual members are:<br />
• Y0704 - C0 - Platinum <strong>Blue</strong> Core Option<br />
• Y0704 - C4 - Platinum <strong>Blue</strong> Core Option-Medicare B only<br />
members<br />
• Y0704 - H1 - Platinum <strong>Blue</strong> Core Option - Medicare Hospice<br />
enrolled members<br />
• Y0705 - C0 - Platinum <strong>Blue</strong> Choice Option<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-15
Health Care Options<br />
Inquiries <strong>and</strong> Claims<br />
Platinum <strong>Blue</strong> (Cost)<br />
(continued)<br />
• Y0705 - C4 - Platinum <strong>Blue</strong> Choice Option-Medicare B only<br />
members<br />
• Y0705 - H1 - Platinum <strong>Blue</strong> Choice Option - Medicare hospice<br />
enrolled members<br />
• Y0706 - C0 - Platinum <strong>Blue</strong> Complete Option<br />
• Y0706 - C4 - Platinum <strong>Blue</strong> Complete Option-Medicare B<br />
only members<br />
• Y0706 - H0 - Platinum <strong>Blue</strong> Complete Option - Medicare<br />
hospice enrolled members<br />
Please see the grid that follows for an overview <strong>of</strong> services, CMS<br />
billing format, <strong>and</strong> Medicare Part A or Part B eligibility.<br />
5-16 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Health Care Options<br />
The following grid provides an overview <strong>of</strong> Platinum <strong>Blue</strong> services, CMS billing format, <strong>and</strong> Medicare Part A or Part B eligibility.<br />
Institutional = electronic format or paper (UB) form pr<strong>of</strong>essional = electronic format or paper (1500) form<br />
Billable to Medicare<br />
Inpatient <strong>and</strong> outpatient hospital including Acute<br />
Care Hospital, Indian Health Service Facility<br />
(IHS), Critical Access Hospital, Sole Community<br />
Hospital, Rehabilitation Hospital, etc.<br />
Medicare<br />
submission<br />
form/format Billable to <strong>Blue</strong> <strong>Cross</strong><br />
institutional<br />
Physician services rendered in the inpatient<br />
hospital setting <strong>and</strong> separately billed<br />
Hospital-based surgical center institutional Free-st<strong>and</strong>ing ambulatory surgical center (ASC)<br />
Inpatient <strong>and</strong> outpatient blood transfusions<br />
Outpatient hospital radiology <strong>and</strong> laboratory<br />
services<br />
Hospital based therapy including physical,<br />
occupational, <strong>and</strong> speech<br />
Individual private practice physical therapy <strong>of</strong>fice<br />
meeting CMS variance qualifications<br />
institutional<br />
<strong>and</strong>/or<br />
pr<strong>of</strong>essional<br />
institutional<br />
institutional<br />
Skilled Nursing Facility (SNF) institutional<br />
Hospice except for services not related to<br />
treatment <strong>of</strong> terminal condition<br />
ESRD facility (CMS approved dialysis facility) Bills<br />
for support services <strong>and</strong> back up dialysis <strong>and</strong><br />
emergency services only. (global fee<br />
includes some physician services)<br />
<strong>Blue</strong> <strong>Cross</strong><br />
submission<br />
form/format<br />
pr<strong>of</strong>essional<br />
institutional<br />
(deviates<br />
from CMS)<br />
Physician <strong>of</strong>fice visits pr<strong>of</strong>essional<br />
Pr<strong>of</strong>essional behavioral health services including<br />
Community Mental Health Centers<br />
Freest<strong>and</strong>ing clinic/physician group physical,<br />
occupational or speech therapy<br />
pr<strong>of</strong>essional<br />
pr<strong>of</strong>essional<br />
pr<strong>of</strong>essional Chiropractic services pr<strong>of</strong>essional<br />
institutional<br />
institutional<br />
<strong>and</strong>/or<br />
pr<strong>of</strong>essional<br />
Home health agencies institutional<br />
Federally Qualified Health Centers (FQHC) [both<br />
Independent <strong>and</strong> Provider based]<br />
Rural Health Clinic (RHC)<br />
[both Independent <strong>and</strong> Provider Based]<br />
institutional<br />
institutional<br />
SNF provision <strong>of</strong> certain prosthetics (PEN<br />
therapy) billed to DMERC<br />
Hospice services unrelated to treatment <strong>of</strong><br />
terminal condition <strong>and</strong> Medicare eligible<br />
Laboratory <strong>and</strong> X-rays including hospital<br />
reference labs<br />
Home health agencies (also approved as DME<br />
suppliers) billing for DMEPOS services<br />
Durable Medical Equipment (DME), prosthetics,<br />
orthotics, <strong>and</strong> medical supplies<br />
pr<strong>of</strong>essional<br />
pr<strong>of</strong>essional<br />
pr<strong>of</strong>essional<br />
pr<strong>of</strong>essional<br />
pr<strong>of</strong>essional<br />
Hospital-based ambulance institutional Ambulance pr<strong>of</strong>essional<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-17
Health Care Options<br />
Additional information available from CMS at:<br />
http://www.cms.hhs.gov/healthplans/rates/out-<strong>of</strong>-network/default.asp#_Toc77576994<br />
Sample Member ID card<br />
Front <strong>of</strong> member ID card Back <strong>of</strong> member ID card<br />
<strong>Name</strong><br />
ELIZABETH SAMPLENAME<br />
ID Member #<br />
XZVXZ0000000 00<br />
Svc Types<br />
Office Copay 20.00<br />
ER Copay 60.00<br />
RxNetwork SELECT<br />
GRP<br />
Care<br />
Type<br />
RxBIN<br />
RxPCN<br />
Platinum<br />
<strong>Blue</strong><br />
(Cost) H2461<br />
Y0704-C0<br />
MEDICARE COST<br />
CNTRCT<br />
610455<br />
PGIGN<br />
Members: See your Evidence <strong>of</strong> Coverage for<br />
covered services or other important<br />
information. Possession <strong>of</strong> this card does not<br />
guarantee eligibility <strong>of</strong> benefits.<br />
Providers: If you are a Platinum <strong>Blue</strong> (Cost)<br />
provider, submit Medicare part A claims to<br />
Medicare, <strong>and</strong> Medicare part B claims to<br />
BCBSM. For all providers, submit both<br />
Medicare part A & B to Medicare.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> is an<br />
independent licensee <strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
<strong>Blue</strong> <strong>Shield</strong> Association<br />
www.bluecrossmn.com<br />
Customer Service or Complaints<br />
(651) 662-5654<br />
1-866-340-8654<br />
Provider Service: 1-800-<br />
262-0820<br />
24-Hour Nurse Advice: 1-800-<br />
622-9524<br />
Medical TTY: 1-888-<br />
878-0137<br />
Find a Pharmacy: 1-800-<br />
509-0545<br />
Pharmacist Only: 1-800-<br />
821-4795<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong><br />
<strong>of</strong> <strong>Minnesota</strong><br />
P.O. Box 64338<br />
St. Paul, MN 55164-0338<br />
5-18 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
<strong>Blue</strong> Plus Coverage Options<br />
Health Care Options<br />
Comprehensive Plan This <strong>Blue</strong> Plus plan places a major emphasis on staying well,<br />
maintaining fitness, <strong>and</strong> preventing potential health problems by<br />
providing full coverage for basic care, such as annual physical<br />
examinations, PAP tests, immunizations, <strong>and</strong> vaccinations, when<br />
members use their predesignated clinic. Basic to this<br />
comprehensive plan is coverage for lab work, X-rays, hospital care<br />
<strong>and</strong> specialists’ consultations when provided or authorized by the<br />
predesignated clinic. The plan also covers emergency treatment<br />
anywhere in the world.<br />
Preferred Gold SM Preferred Gold, a ‘‘triple option’’ plan, <strong>of</strong>fers its members three<br />
levels <strong>of</strong> benefits, depending on which provider network they elect<br />
to use. Preferred Gold members select a primary care clinic <strong>and</strong><br />
receive the highest level <strong>of</strong> coverage for medical care provided or<br />
authorized by that clinic. Access to ob/gyn care <strong>and</strong> other open<br />
access benefits is available without a referral. Office visit copays<br />
may apply. Specialist care, when referred by the primary care<br />
clinic, is also covered.<br />
Preferred Gold also <strong>of</strong>fers its members the opportunity to self refer<br />
to any provider or hospital <strong>and</strong> still receive coverage at a reduced<br />
level. Under this second benefit level, Preferred Gold members<br />
may use providers from <strong>Blue</strong> <strong>Cross</strong>’ extended network <strong>and</strong> receive<br />
80 percent coverage after an annual deductible for most services.<br />
Under the third level, out-<strong>of</strong>-network providers may be used, but<br />
benefits are reduced or unavailable.<br />
Triple Gold Triple Gold is a ‘‘triple option’’ plan for self-insured groups. It is<br />
structured very much like Preferred Gold, but benefits may vary.<br />
Medicare Select<br />
Product<br />
Medicare is primary for all services. For the highest level <strong>of</strong><br />
benefits, all care must be provided or referred by the member’s<br />
primary care clinic. There are no benefits under the Medicare<br />
Select contract for services outside the network, although coverage<br />
through Medicare for eligible services is still available to the<br />
member. Medical emergencies, however, are covered whether a<br />
member is at home or traveling. The applicable Medicare<br />
deductible <strong>and</strong> coinsurance amounts are the member’s<br />
responsibility. Enrollment in Medicare Select is closed.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-19
Health Care Options<br />
<strong>Minnesota</strong> Senior<br />
Health Options (MSHO)<br />
/ Secure <strong>Blue</strong> (HMO)<br />
<strong>Blue</strong> Plus <strong>of</strong>fers a <strong>Minnesota</strong> Senior Health Options (MSHO)<br />
product called Secure<strong>Blue</strong> for dual eligible seniors. Secure<strong>Blue</strong> is<br />
a Special Needs Plan (SNP) <strong>of</strong>fered under Medicare Advantage by<br />
<strong>Blue</strong> Plus. <strong>Blue</strong> Plus has a contract with both the Centers for<br />
Medicare <strong>and</strong> Medicaid Services (CMS) <strong>and</strong> the <strong>Minnesota</strong><br />
Department <strong>of</strong> Human Services (DHS) for Secure<strong>Blue</strong> that creates<br />
an alternative delivery system for acute <strong>and</strong> long-term care<br />
services <strong>and</strong> integrates Medicare <strong>and</strong> Medicaid funding.<br />
Secure<strong>Blue</strong> combines the services <strong>and</strong> benefits <strong>of</strong> Medicare Parts<br />
A <strong>and</strong> B, including Part D prescription drug coverage, <strong>and</strong><br />
Medicaid benefits.<br />
A personal care coordinator will work closely with individual<br />
Secure<strong>Blue</strong> members to assist them in achieving optimal medical<br />
<strong>and</strong> social stability.<br />
For Secure<strong>Blue</strong> members, <strong>Blue</strong> Plus is billed as primary not<br />
Medicare. Secure<strong>Blue</strong> members can be identified by ID numbers<br />
beginning with an “XZS8” + the member’s PMI# <strong>and</strong> group<br />
numbers that begin with “PP2”. Enrollment eligibility may change<br />
monthly. Providers must verify eligibility through any electronic<br />
data system currently being used to access Medical Assistance<br />
eligibility such as Medifax, BLUELINE, the Department <strong>of</strong><br />
Human Services Eligibility Verification System (EVS), provider<br />
web self-service, or <strong>Blue</strong> <strong>Cross</strong> provider services.<br />
Secure<strong>Blue</strong> includes 180 days <strong>of</strong> nursing home coverage <strong>and</strong><br />
Elderly Waiver services. The only copays for Secure<strong>Blue</strong> members<br />
are for prescriptions. Members must designate a primary care<br />
clinic, however, referrals are not required for services at<br />
participating providers. Services are coordinated through a<br />
personal care coordinator. All <strong>Blue</strong> Plus referral providers are<br />
included in the specialty network. Providers should file their<br />
claims with <strong>Blue</strong> <strong>Cross</strong>.<br />
5-20 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Prepaid Medical<br />
Assistance Program<br />
(PMAP), <strong>and</strong> <strong>Minnesota</strong><br />
Senior Care Plus<br />
(MSC+) / <strong>Blue</strong><br />
Advantage<br />
Health Care Options<br />
The <strong>Blue</strong> Advantage Prepaid Medical Assistance Program<br />
(PMAP) <strong>and</strong> <strong>Minnesota</strong> Senior Care Plus (MSC+) are <strong>Minnesota</strong><br />
health care programs funded jointly by the state <strong>and</strong> federal<br />
governments. <strong>Blue</strong> Plus has a contract with <strong>Minnesota</strong> Department<br />
<strong>of</strong> Human Services (DHS) to provide services for specific county<br />
Medicaid enrollees (MSC+ is for seniors 65+).<br />
<strong>Blue</strong> Plus <strong>Blue</strong> Advantage members can be identified by ID<br />
numbers beginning with “XZG8” <strong>and</strong> group numbers that start<br />
with “PP0”. Enrollment eligibility may change monthly. Providers<br />
must verify eligibility through any electronic data system currently<br />
being used to access Medical Assistance eligibility such as<br />
Medifax, BLUELINE, the Department <strong>of</strong> Human Services MN-<br />
ITS, provider web self-service, or <strong>Blue</strong> <strong>Cross</strong> provider services.<br />
Members designate a primary care clinic to provide or coordinate<br />
their care. No referrals are required for access to services from<br />
providers who participate in the <strong>Blue</strong> Plus or Aware networks,<br />
except for chiropractic services. Members must obtain<br />
chiropractic services from providers in the Select Chiropractic<br />
network. There are some providers in the Public Programs referral<br />
network that are not listed in the provider directory (i.e., nonambulatory<br />
transportation, hearing aids, <strong>and</strong> public health). For<br />
behavioral health, members have direct access to in-network<br />
providers. In rare instances, out-<strong>of</strong>-network exceptions may be<br />
considered. Call the number on the back <strong>of</strong> the member’s ID card,<br />
or call 1-800-262-0820 (local 651-662-5200). Providers should<br />
file their claims with <strong>Blue</strong> <strong>Cross</strong>. Please refer to Chapter 3 <strong>of</strong> the<br />
Blus Plus <strong>Manual</strong> for more detailed information on Government<br />
Programs.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-21
Health Care Options<br />
<strong>Minnesota</strong>Care<br />
Program<br />
<strong>Minnesota</strong>Care is a state-subsidized health program. It is funded<br />
by member premiums, the state <strong>of</strong> <strong>Minnesota</strong>, a tax on health care<br />
providers <strong>and</strong> some federal matching dollars. It is open to all<br />
<strong>Minnesota</strong>ns who meet program <strong>and</strong> income guidelines <strong>and</strong> do not<br />
have access to health insurance.<br />
<strong>Minnesota</strong>Care members can be identified by ID numbers<br />
beginning with an “XZG8” <strong>and</strong> group numbers that begin with<br />
“PP1”. Enrollment eligibility may change monthly. Providers must<br />
verify eligibility through any electronic data system being used to<br />
access Medical Assistance eligibility such as Medifax,<br />
BLUELINE, the Department <strong>of</strong> Human Services MN-ITS,<br />
provider web self-service, or <strong>Blue</strong> <strong>Cross</strong> provider services.<br />
Member ID cards look similar to cards for PMAP.<br />
Benefits for children under 21 <strong>and</strong> pregnant women are the same<br />
as the PMAP benefits except for common carrier transportation.<br />
Adults have a reduced benefit set <strong>and</strong> have some copays. Members<br />
must designate a primary care clinic <strong>and</strong> referrals are not required<br />
if within the participating provider network. All <strong>Blue</strong> Plus Referral<br />
providers are included in the specialty network. Providers should<br />
file their claims with <strong>Blue</strong> <strong>Cross</strong>.<br />
See Chapter 3 <strong>of</strong> the <strong>Blue</strong> Plus Provider <strong>Manual</strong> for more complete<br />
information.<br />
5-22 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Federal Employee Program<br />
Federal Employee<br />
Program (FEP)<br />
Health Care Options<br />
The Federal Employee Program (FEP), one <strong>of</strong> the health benefit<br />
plans available to federal government employees <strong>and</strong> their<br />
dependents, is administered by <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> plans<br />
throughout the country. Enrollment, eligibility, <strong>and</strong> claims records<br />
for all FEP members are maintained in Washington, D.C. We have<br />
access to the records through a national telecommunications<br />
system.<br />
The unique federal ID number, which always begins with an “R”<br />
<strong>and</strong> is followed by eight digits, identifies FEP members.<br />
Federal employees may choose Basic Option or St<strong>and</strong>ard Option<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> coverage. Providers should file all<br />
claims for FEP benefits within the local plan, (i.e., <strong>Minnesota</strong><br />
providers submit to <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> North Dakota providers submit<br />
to <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> North Dakota). All claims must<br />
be submitted no later than December 31 <strong>of</strong> the calendar year after<br />
the one in which the covered care or service was provided, unless<br />
timely filing was prevented by administrative operations <strong>of</strong><br />
government or legal incapacity, provided the claim was submitted<br />
as soon as reasonably possible. Once benefits have been paid, there<br />
is a three-year limitation on the reissuance <strong>of</strong> uncashed checks.<br />
Providers can call a new automated voice response unit (VRU) to<br />
check eligibility <strong>and</strong> benefits for FEP members. To access this<br />
service, call (651) 662-5044 or 1-800-859-2128. Claim status is<br />
currently not available through the VRU.<br />
Provider Statements Your Statement <strong>of</strong> Provider Claims Paid <strong>and</strong> Statement <strong>of</strong><br />
Institutional Claims Paid for FEP members will be posted on a<br />
separate remit. You will also receive a separate check titled<br />
“Federal Employee Program” with the <strong>Blue</strong> <strong>Cross</strong> logo for your<br />
FEP members. Recoupments <strong>and</strong> credit claim activities for FEP<br />
members will be reflected on a separate Accounts Receivable<br />
Recoupment Report which will be titled “Federal Employee<br />
Program.”<br />
Benefit Changes Visit www.fepblue.org for current benefit information.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-23
Health Care Options<br />
<strong>Blue</strong>LinkTPA<br />
<strong>Blue</strong>Link TPA<br />
<strong>Blue</strong>Link is an affiliate <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> an independent licensee<br />
<strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Association serving residents<br />
<strong>and</strong> businesses <strong>of</strong> <strong>Minnesota</strong>. <strong>Blue</strong>Link utilizes the <strong>Blue</strong> <strong>Cross</strong><br />
network <strong>of</strong> participating providers, provider contract pricing, <strong>Blue</strong><br />
Distinctions Centers <strong>of</strong> excellence <strong>and</strong> the Care Comparison online<br />
tool.. Plan benefits vary by employer, all which are self-insured.<br />
Some <strong>Blue</strong>Link employer customers use remote processing,<br />
meaning that claims come to <strong>Blue</strong> <strong>Cross</strong>, they are priced, <strong>and</strong> then<br />
sent to the employer to complete the claims processing. There are<br />
also employers who utilize our <strong>Blue</strong> <strong>Cross</strong> networks but process<br />
their claims through a third-party administrator.<br />
Providers have access to benefits information for <strong>Blue</strong>Link<br />
members through PWSS.<br />
The <strong>Blue</strong>Card program enables a <strong>Blue</strong>Link member obtaining<br />
health care services while traveling or living in another plan’s<br />
service area to receive the benefits <strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> plan listed on<br />
their member ID card <strong>and</strong> to access the local plan’s provider<br />
networks <strong>and</strong> savings.<br />
For inquiries, adjustments or appeals contact the employer or the<br />
third-party administrator directly. File electronic claims to <strong>Blue</strong><br />
<strong>Cross</strong>. Mail scannable paper claims to:<br />
<strong>Blue</strong>Link TPA<br />
P.O. Box 64668<br />
St. Paul, MN 55164<br />
5-24 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Healthy Start ® Prenatal Support<br />
Healthy Start ® Prenatal<br />
Support<br />
Healthy Start ®<br />
Prenatal Support<br />
(continued)<br />
Health Care Options<br />
Healthy Start is a personalized program designed to assess, educate<br />
<strong>and</strong> support pregnant women <strong>and</strong> their health care providers to<br />
achieve optimal childbirth outcomes. Registered nurses who are<br />
experienced in obstetrics work with the expectant mother to help<br />
her achieve a normal full-term delivery. With a quick phone call, a<br />
Healthy Start nurse is there to give answers <strong>and</strong> support.<br />
Healthy Start <strong>of</strong>fers these features:<br />
• An experienced obstetrics registered nurse who educates the<br />
mother-to-be on having a healthy pregnancy <strong>and</strong> answers her<br />
questions.<br />
• Comprehensive educational material that is tailored to the<br />
specific needs <strong>of</strong> the mother-to-be.<br />
• Guidance on nutrition, exercise, birth planning, stress<br />
management, relieving discomfort, explanation <strong>of</strong> procedures<br />
<strong>and</strong> much more.<br />
• A reward card to the participant’s choice <strong>of</strong> major retail stores.<br />
There is no cost for participation in the Healthy Start program.<br />
Healthy Start is available to all <strong>Blue</strong> <strong>Cross</strong> fully insured members,<br />
<strong>Blue</strong> Plus members <strong>and</strong> members <strong>of</strong> self-insured groups that have<br />
purchased this program. It is not available to members with<br />
individual policies.<br />
To enroll, please instruct members who are expecting a baby to the<br />
back <strong>of</strong> their member ID card for the appropriate contact number.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-25
Health Care Options<br />
Delta Dental<br />
History Delta Dental <strong>of</strong> <strong>Minnesota</strong> <strong>of</strong>fers dental coverage to individuals<br />
<strong>and</strong> small <strong>and</strong> large groups in <strong>Minnesota</strong>. Delta Dental operates<br />
pursuant to an administrative service agreement with <strong>Blue</strong> <strong>Cross</strong>.<br />
Delta Dental <strong>of</strong> <strong>Minnesota</strong> is independent from <strong>Blue</strong> <strong>Cross</strong>. Delta<br />
Dental provides administrative services for dental benefits.<br />
Inquiries Delta Dental inquiries may be directed to:<br />
Delta Dental<br />
3560 Delta Dental Drive<br />
Eagan, MN 55112<br />
Phone: (651) 406-5900 or 1-800-328-1188<br />
Fax: (651) 994-5035<br />
Website: www.deltadentalmn.org<br />
5-26 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
MII Life, Incorporated<br />
Health Care Options<br />
History MII Life, Incorporated administers reimbursement account<br />
products (flexible spending accounts, health reimbursement<br />
arrangements, health savings accounts) under the name<br />
SelectAccount ® .<br />
MII Life, Inc., d.b.a. SelectAccount, is an independent company<br />
providing account administration services.<br />
Products <strong>and</strong> Services SelectAccount’s product line includes:<br />
• Flexible spending accounts (FSAs)<br />
• Medical savings accounts (MSAs)<br />
• Health reimbursement arrangements (HRAs)<br />
• Health savings accounts (HSAs)<br />
• VEBA accounts<br />
• Transportation reimbursement accounts<br />
These products are <strong>of</strong>fered as st<strong>and</strong>-alone products or in<br />
conjunction with <strong>Blue</strong> <strong>Cross</strong> plans.<br />
• SelectAccount customer service ............1-800-859-2144<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-27
Health Care Options<br />
Prime Therapeutics LLC<br />
History Prime Therapeutics, LLC is <strong>Blue</strong> <strong>Cross</strong>’ pharmacy benefits<br />
manager (PBM).<br />
Prime Therapeutics, LLC is an independent company providing<br />
pharmacy benefit management services.<br />
Formularies <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong>fers two formulary options to meet customer <strong>and</strong><br />
member needs.<br />
GenRx is the formulary option designed for maximum value in<br />
pharmacy spending for clients <strong>and</strong> members while maintaining the<br />
highest st<strong>and</strong>ards in therapeutic safety <strong>and</strong> effectiveness. Its focus<br />
is to provide the same high therapeutic st<strong>and</strong>ard as FlexRx by<br />
having both br<strong>and</strong>-name <strong>and</strong> specialty drugs on this formulary<br />
while placing greater emphasis on lower-cost generic equivalents.<br />
GenRx addresses a rapidly growing need in a marketplace looking<br />
for high-quality, cost-conscious benefit solutions.<br />
FlexRx is the broadest formulary option providing the highest<br />
st<strong>and</strong>ard <strong>of</strong> therapeutic safety <strong>and</strong> effectiveness through a<br />
combination <strong>of</strong> br<strong>and</strong>-name <strong>and</strong> generic drugs, including specialty<br />
drugs.<br />
5-28 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Workers’ Compensation, No-Fault Auto &<br />
Subrogation<br />
Health Care Options<br />
Overview Following is a Question <strong>and</strong> Answer guide to assist you in<br />
reimbursement <strong>of</strong> Workers Compensation, No-Fault Auto <strong>and</strong><br />
Subrogation claims.<br />
Workers'<br />
Compensation, No-<br />
Fault Auto &<br />
Subrogation<br />
1. What does <strong>Blue</strong> <strong>Cross</strong> need if the workers’ compensation<br />
carrier, or the automobile carrier/third party liability<br />
carrier denies?<br />
We need a letter from the other carrier, stating the specific date<br />
<strong>of</strong> service on the claim they are wanting paid <strong>and</strong> the reason<br />
the other carrier is not paying claims.<br />
2. Why do claims deny when they are not marked<br />
work/auto/subro related?<br />
Once we have identified a workers’ compensation or<br />
automobile or subrogation claim, an indicator is placed on the<br />
patient’s file. All claims that are possibly related to the<br />
indicated injury are denied.<br />
3. Why do claims continue to deny when a denial has been<br />
sent in?<br />
The denial must be valid in order for <strong>Blue</strong> <strong>Cross</strong> to pay the<br />
claims under the health benefits. The denial is not valid unless<br />
it specifies why the other insurance carrier is denying <strong>and</strong> they<br />
provide a specific reason behind the denial such as doctor’s<br />
opinion, IME, etc. If the denial is date specific, only the dates<br />
listed on the denial are adjusted.<br />
4. Why does <strong>Blue</strong> <strong>Cross</strong> need a denial from the workers’<br />
compensation carrier if the doctor states it is not work<br />
related?<br />
A notification from the workers’ compensation carrier is<br />
needed if the treatment is similar to the work injury. The<br />
workers’ compensation carrier must make the final<br />
determination.<br />
5. Why do some claims pay <strong>and</strong> some deny?<br />
If the diagnosis is non-specific (like pain in a limb) <strong>and</strong> we are<br />
unable to determine what is being treated the claim may deny.<br />
If we have limited information on what the injury is, some<br />
claims may pay while others may deny.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-29
Health Care Options<br />
Workers'<br />
Compensation, No-<br />
Fault Auto &<br />
Subrogation<br />
(continued)<br />
6. When does <strong>Blue</strong> <strong>Cross</strong> need chart notes to adjust claims?<br />
The chart notes should indicate what the patient was treated<br />
for. If the chart notes indicate the treatment was not related to<br />
the work injury, the motor vehicle accident or the third party<br />
accident, then claims can be adjusted. If chart notes are nonspecific<br />
or treatment is similar to the accepted injury, a valid<br />
denial is needed from the other insurance carrier.<br />
7. If there is an intervention case does <strong>Blue</strong> <strong>Cross</strong> pay claims?<br />
Depending on the circumstances surrounding the litigation,<br />
<strong>Blue</strong> <strong>Cross</strong> may or may not pay claims. If you have case<br />
specific questions you should contact the Special Services Unit<br />
directly at 1-866-251-6691.<br />
8. If the member has a pre-paid medical or MNCare group<br />
can we bill them?<br />
No. As a provider you need to bill the other insurance carrier.<br />
If you do not know who the other insurance carrier is, then you<br />
must try to contact the member three times for this<br />
information. If you are unable to get a response from the<br />
member, then <strong>Blue</strong> <strong>Cross</strong> will adjust claims to pay, under the<br />
health benefit, once the documentation is received showing the<br />
three attempts to contact the member.<br />
9. What are the no-fault laws for <strong>Minnesota</strong> <strong>and</strong> surrounding<br />
states?<br />
<strong>Minnesota</strong> <strong>and</strong> North Dakota have m<strong>and</strong>atory medical pay<br />
laws. This means all drivers insured in <strong>Minnesota</strong> or North<br />
Dakota have medical pay on their auto insurance. <strong>Minnesota</strong><br />
has a $20,000 medical pay limit. North Dakota has a<br />
$30,000.00 medical pay limit. South Dakota, Iowa <strong>and</strong><br />
Wisconsin are optional states which mean the member can<br />
chose to either have or not to have medical pay on their auto<br />
policy.<br />
10. What are some uncommon injuries that may be covered by<br />
the workers’ compensation carrier?<br />
The workers’ compensation carrier may cover injuries that<br />
occur when an employee trips or falls at work, is injured in the<br />
parking lot, is hurt volunteering or is hurt when traveling for<br />
work. If you have specific questions regarding a potential work<br />
related injury contact the Special Services Unit.<br />
5-30 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Workers'<br />
Compensation, No-<br />
Fault Auto &<br />
Subrogation<br />
(continued)<br />
HICF 1500 Form Locator 837P<br />
Health Care Options<br />
11. What are some uncommon injuries that maybe covered by<br />
the automobile or third party insurance?<br />
The automobile or third party insurance may cover injuries that<br />
occur while the individual is at someone else’s home, on<br />
someone else’s private property, at a place <strong>of</strong> business, due to a<br />
dog bite, or when they are a pedestrian or bicyclist injured by a<br />
motor vehicle.<br />
12. Does health insurance coordinate with auto/third party or<br />
workers’ compensation insurance?<br />
No. In most circumstance the other insurance is primary. Once<br />
the other insurance carrier has exhausted their payments,<br />
claims may be payable under the health insurance policy.<br />
13. Who should claims be filed to if the patient is working <strong>and</strong><br />
has an auto accident?<br />
The claims should first be filed to the workers’ compensation<br />
carrier. If they deny stating the employee was not in the scope<br />
<strong>of</strong> their employment, then the claim should be filed to the auto<br />
insurance carrier. If the auto insurance carrier denies or<br />
benefits are exhausted, the claim should be billed to <strong>Blue</strong> <strong>Cross</strong><br />
with a copy <strong>of</strong> both the workers’ compensation denial <strong>and</strong> the<br />
auto carriers exhaust letter, EOB, or payment log.<br />
14. What should be done if a claim was paid by both <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> another insurance company?<br />
Option 1: Request a void/replacement claim. Refer to Chapter<br />
10 for information regarding submission <strong>of</strong> void/replacement<br />
claims. Note that effective July 15, 2009, only out <strong>of</strong> state,<br />
nonparticipating providers are allowed to submit paper claim<br />
forms per <strong>Minnesota</strong> Statute 62J.536 <strong>and</strong> the <strong>Blue</strong> <strong>Cross</strong><br />
provider contracts.<br />
Information indicating if the patient’s condition is related to<br />
employment, auto or other accident, or workers‘ compensation<br />
should be indicated on the replacement claim.<br />
For pr<strong>of</strong>essional claims (HICF-1500 or 837P) complete the<br />
items indicated below.<br />
Item # Title Loop ID Segment Notes<br />
10a Is Patient’s<br />
Condition<br />
Related to:<br />
Employment<br />
2300 CLM11 Titled Related Causes Code in<br />
the 837P<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-31
Health Care Options<br />
HICF 1500 Form Locator 837P<br />
Item # Title Loop ID Segment Notes<br />
10b Is Patient’s<br />
Condition<br />
Related to: Auto<br />
Accident<br />
10c Is Patient’s<br />
Condition<br />
Related to: Other<br />
Accident<br />
10d Reserved for<br />
local use<br />
14 Date <strong>of</strong> Current<br />
Illness, Injury,<br />
Pregnancy<br />
2300 CLM11 Titled Related Causes Code in<br />
the 837P<br />
2300 CLM11 Titled Related Causes Code in<br />
the 837P<br />
2300 K3 This is specific for reporting<br />
Workers’ Compensation<br />
Condition Codes.<br />
2300 DTP03 Titled in the 837P:<br />
a. Onset <strong>of</strong> current illness or<br />
injury date.<br />
b. Acute manifestation date.<br />
c. Accident date.<br />
d. Last menstrual period<br />
date.<br />
For institutional claims (UB-04 or 837I) report the appropriate<br />
occurrence code. Occurrence codes <strong>and</strong> dates are entered in<br />
Form Locator(s) 31-34, 35-36 on the UB-04 or in Loop 2300<br />
<strong>of</strong> the 4010A1 837I transaction. The following occurrence<br />
codes may be submitted as appropriate.<br />
01:Accident / Medical Coverage<br />
Code indicating accident-related injury for which there is<br />
medical payment coverage. Provide the date <strong>of</strong> accident /<br />
injury.<br />
02: No Fault Insurance Involved - Including Auto<br />
Accident/ Other<br />
Code indicating the date <strong>of</strong> an accident, including auto or other<br />
where state has applicable no-fault liability laws (i.e., legal<br />
basis for settlement without admission or pro<strong>of</strong> <strong>of</strong> guilt).<br />
5-32 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Workers'<br />
Compensation, No-<br />
Fault Auto &<br />
Subrogation<br />
(continued)<br />
03: Accident/Tort Liability<br />
Health Care Options<br />
Code indicating the date <strong>of</strong> an accident resulting from a third<br />
party’s action that may involve a civil court process in an<br />
attempt to require payment by the third party, other than n<strong>of</strong>ault<br />
liability.<br />
04: Accident/ Employment-Related<br />
Code indicating the date <strong>of</strong> an accident allegedly relating to the<br />
patient’s employment.<br />
OPTION 2: Contact the Special Services Unit at<br />
1-866-251-6691 <strong>and</strong> request the claim is adjusted.<br />
15. Should claims that are related to a work/auto/third party<br />
injury be billed to <strong>Blue</strong> <strong>Cross</strong>?<br />
Claims that are related to a work/auto/third party injury should<br />
be billed to the liable insurance carrier <strong>and</strong> not to <strong>Blue</strong> <strong>Cross</strong>.<br />
If the other insurance carrier denies, then the claim should be<br />
billed to <strong>Blue</strong> <strong>Cross</strong> with a copy <strong>of</strong> the other insurance carrier’s<br />
denial <strong>and</strong>/or EOB attached.<br />
On occasion the other insurance carrier may not process the<br />
claim in a timely manner <strong>and</strong> due to <strong>Blue</strong> <strong>Cross</strong> timely filing<br />
guidelines, you may need to bill to <strong>Blue</strong> <strong>Cross</strong> prior to getting<br />
an EOB or denial from the other carrier. If this occurs, you<br />
should submit the claim to <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> note in the HICF<br />
1500, form locator 10 or the 837P for pr<strong>of</strong>essional claims (as<br />
noted under 14. above) or the appropriate occurrence code for<br />
institutional claims. Occurrence codes <strong>and</strong> dates are entered in<br />
Form Locator(s) 31-34, 35-36 on the UB-04 or in Loop 2300<br />
<strong>of</strong> the 4010A1 837I transaction.<br />
16. How can I reach the Special Services Unit if I have other<br />
questions or concerns related to a work/auto/third party<br />
injury?<br />
The Special Services Unit can be reached by direct dial at<br />
1-866-251-6691. Monday through Thursday 8:00 am -<br />
4:30 pm, Friday 9:00 am - 4:30 pm, CT<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 5-33
Health Care Options<br />
Networks<br />
<strong>Blue</strong> <strong>Cross</strong> (Aware) An extensive open access network which includes nearly every<br />
physician <strong>and</strong> hospital in <strong>Minnesota</strong>. This network is used with<br />
major medical plans <strong>and</strong> open access/preferred provider-type<br />
products.<br />
Select Networks Available for substance abuse, behavioral health <strong>and</strong> chiropractic<br />
care services. They are st<strong>and</strong>ard for small <strong>and</strong> large insured groups<br />
<strong>and</strong> <strong>of</strong>fer a savings advantage.<br />
<strong>Blue</strong> Plus ® Our most exclusive primary network that includes more than 7,500<br />
physicians. Members enrolled in managed care products choose a<br />
primary care clinic from the <strong>Blue</strong> Plus network to coordinate their<br />
care <strong>and</strong> make referrals to network specialists.<br />
<strong>Blue</strong>Card ® A national network managed by the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong><br />
Association. Local <strong>Blue</strong> plans can sell national account business<br />
by leveraging the 50-state <strong>Blue</strong>s provider network.<br />
<strong>Blue</strong> Distinction<br />
Centers ®<br />
A national centers <strong>of</strong> excellence program that enables members to<br />
make more informed health care decisions to improve outcomes.<br />
Facilities must meet strict clinical criteria to earn the <strong>Blue</strong><br />
Distinction Centers designation for transplants, transplants <strong>and</strong><br />
cardiac care.<br />
Note: Designation as <strong>Blue</strong> Distinction Centers means these<br />
facilities’ overall experience <strong>and</strong> aggregate data met<br />
objective criteria established in collaboration with expert<br />
clinicians’ <strong>and</strong> leading pr<strong>of</strong>essional organizations’<br />
recommendations. Individual outcomes may vary. To find<br />
out which services are covered, please call <strong>Blue</strong> <strong>Cross</strong>.<br />
<strong>Blue</strong> Precision ® A high performance, tiered network. In it, all providers within the<br />
<strong>Blue</strong> <strong>Cross</strong> (Aware) network are tiered into one <strong>of</strong> two levels, <strong>and</strong><br />
members make value-based decisions at the point <strong>of</strong> care. There<br />
are two <strong>Blue</strong> Precision networks available in <strong>Minnesota</strong>, one with<br />
greater access to Level 1 providers (Perform) <strong>and</strong> one with greater<br />
savings (Achieve).<br />
Accord Network Our st<strong>and</strong>ard network that includes 97 percent <strong>of</strong> <strong>Minnesota</strong><br />
doctors <strong>and</strong> hospitals.<br />
Value Network Value is our Minneapolis/St. Paul metro area PPO network that<br />
<strong>of</strong>fers access to the most affordable physicians <strong>and</strong> hospitals<br />
available to provide a lower cost health plan.<br />
5-34 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Table <strong>of</strong> Contents<br />
Chapter 6<br />
<strong>Blue</strong> Plus<br />
Member Information................................................................................................................. 6-2<br />
Introduction to <strong>Blue</strong> Plus ® .....................................................................................................6-2<br />
<strong>Blue</strong> Plus Network Participation............................................................................................ 6-2<br />
Department <strong>of</strong> Health.............................................................................................................6-2<br />
Member Rights <strong>and</strong> Responsibilities .....................................................................................6-3<br />
Member Benefits....................................................................................................................6-8<br />
Member PCC Selection..........................................................................................................6-9<br />
Claim Processing ...................................................................................................................6-9<br />
Statement <strong>of</strong> Provider Claims Paid Form ..............................................................................6-9<br />
Quality <strong>of</strong> Care Complaint...................................................................................................6-10<br />
Referrals.................................................................................................................................... 6-11<br />
Overview..............................................................................................................................6-11<br />
Referral Policy .....................................................................................................................6-11<br />
Referral Points .....................................................................................................................6-12<br />
Referral Required.................................................................................................................6-13<br />
Referral Not Required.......................................................................................................... 6-14<br />
St<strong>and</strong>ing Referral .................................................................................................................6-16<br />
Clarifications <strong>of</strong> Terms ........................................................................................................6-17<br />
Referral Letter......................................................................................................................6-18<br />
Sample Patient Referral Authorization Letter ..................................................................... 6-19<br />
Special Member Benefits......................................................................................................... 6-22<br />
Overview..............................................................................................................................6-22<br />
Chiropractic Benefits ...........................................................................................................6-22<br />
Continuity <strong>of</strong> Care After Facility Discharge........................................................................6-22<br />
Durable Medical Equipment................................................................................................6-22<br />
Mental Health <strong>and</strong> Chemical Dependency Services............................................................6-23<br />
OB/GYN Services................................................................................................................ 6-23<br />
OB/GYN Open Access Additional Services........................................................................6-23<br />
OB/GYN Open Access Diagnosis .......................................................................................6-24<br />
Vision Care ..........................................................................................................................6-26<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-1
<strong>Blue</strong> Plus<br />
Member Information<br />
Introduction to<br />
<strong>Blue</strong> Plus ®<br />
<strong>Blue</strong> Plus Network<br />
Participation<br />
We developed this chapter for all <strong>Blue</strong> Plus providers <strong>and</strong> their<br />
business staff. The information contained in this chapter will give<br />
the referral (specialty care) providers access to <strong>Blue</strong> Plus<br />
information. The <strong>Blue</strong> Plus Provider <strong>Manual</strong> for participating<br />
primary care clinics (PCCs) details the information necessary for<br />
the PCC to conduct business with <strong>Blue</strong> Plus <strong>and</strong> is intended as a<br />
complement to this manual.<br />
<strong>Blue</strong> Plus, an affiliate <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong>,<br />
is a state-certified health maintenance organization (HMO). In<br />
most <strong>Blue</strong> Plus plans, Members select a participating PCC that<br />
coordinates the patient’s medical care <strong>and</strong> authorizes treatment by<br />
specialists when necessary.<br />
Because <strong>Blue</strong> Plus is an affiliate <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong>, <strong>Blue</strong> Plus is subject to most <strong>of</strong> the same policies <strong>and</strong><br />
procedures as <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong>.<br />
To be listed as a participating <strong>Blue</strong> Plus provider, you need to have<br />
a signed <strong>Blue</strong> Plus agreement. After participation is established in<br />
the Aware ® network, you can make a written request for a <strong>Blue</strong><br />
Plus agreement. Send this request to:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
<strong>Blue</strong> Plus Contracting<br />
P.O. Box 64560<br />
St. Paul, MN 55164-0560<br />
<strong>Blue</strong> Plus will review the request <strong>and</strong> make a written response.<br />
Note: <strong>Blue</strong> Plus will not <strong>of</strong>fer <strong>Blue</strong> Plus agreements to all<br />
requesting health care providers.<br />
Department <strong>of</strong> Health The <strong>Minnesota</strong> Department <strong>of</strong> Health (MDH) regulates HMOs<br />
licensed in <strong>Minnesota</strong>. It governs the fully insured HMO products,<br />
which includes <strong>Blue</strong> Plus. The MDH is involved in approving <strong>and</strong><br />
monitoring contract changes, provider network access <strong>and</strong><br />
changes, appeals, identification cards, quality improvement, <strong>and</strong><br />
much more.<br />
6-2 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Member Rights <strong>and</strong><br />
Responsibilities<br />
<strong>Blue</strong> Plus Member Rights <strong>and</strong> Responsibilities. <strong>Blue</strong> Plus<br />
Members receive the following statement <strong>of</strong> rights:<br />
Your rights as a health plan member:<br />
<strong>Blue</strong> Plus<br />
• To be treated with respect, dignity <strong>and</strong> privacy.<br />
• To receive quality health care that is friendly <strong>and</strong> timely.<br />
• To have available <strong>and</strong> accessible medically necessary covered<br />
services, including emergency services, 24 hours a day, seven<br />
(7) days a week.<br />
• To be informed <strong>of</strong> your health problems <strong>and</strong> to receive<br />
information regarding treatment alternatives <strong>and</strong> their risk in<br />
order to make an informed choice regardless if the health plan<br />
pays for treatment<br />
• To participate with your health care providers in decisions<br />
about your treatment.<br />
• To give your provider a health care directive or a living will (a<br />
list <strong>of</strong> instructions about health treatments to be carried out in<br />
the event <strong>of</strong> incapacity).<br />
• To name the person who can make health care decisions for<br />
you in the event <strong>of</strong> your incapacity.<br />
• To refuse treatment.<br />
• To have privacy <strong>of</strong> medical <strong>and</strong> financial records maintained<br />
by <strong>Blue</strong> Plus <strong>and</strong> its health care providers in accordance with<br />
existing law.<br />
• To receive information about <strong>Blue</strong> Plus, its services, its<br />
providers, <strong>and</strong> your rights <strong>and</strong> responsibilities.<br />
• To make recommendations regarding <strong>Blue</strong> Plus’ rights <strong>and</strong><br />
responsibilities policies.<br />
• To have a resource at <strong>Blue</strong> Plus or at the clinic that you can<br />
contact with any concerns about services.<br />
• To file a complaint with <strong>Blue</strong> Plus <strong>and</strong> the Commissioner <strong>of</strong><br />
Health <strong>and</strong> receive a prompt <strong>and</strong> fair review.<br />
• To initiate a legal proceeding when experiencing a problem<br />
with <strong>Blue</strong> Plus or its providers.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-3
<strong>Blue</strong> Plus<br />
Member Rights <strong>and</strong><br />
Responsibilities<br />
(continued)<br />
• Medicare enrollees have the right to voluntarily disenroll from<br />
<strong>Blue</strong> Plus. <strong>Blue</strong> Plus may not encourage or request you to<br />
disenroll except in circumstances specified in federal law.<br />
• Medicare enrollees have the right to a clear description <strong>of</strong><br />
nursing home <strong>and</strong> home health care benefits covered by <strong>Blue</strong><br />
Plus.<br />
You have the responsibility as a health plan member:<br />
• To know your health plan benefits <strong>and</strong> requirements.<br />
• To provide, to the extent possible, information that <strong>Blue</strong> Plus<br />
<strong>and</strong> its providers need in order to care for you.<br />
• To participate in underst<strong>and</strong>ing your health problems <strong>and</strong><br />
developing mutually agreed-upon treatment goals.<br />
• To follow the treatment plan prescribed by your provider or to<br />
discuss with your provider why you are unable to follow the<br />
treatment plan.<br />
• To provide pro<strong>of</strong> <strong>of</strong> coverage when you receive services <strong>and</strong> to<br />
update the clinic with any personal changes, such as name <strong>and</strong><br />
address.<br />
• To pay copays at the time <strong>of</strong> service <strong>and</strong> to promptly pay<br />
deductibles, coinsurance <strong>and</strong>, if applicable, charges for services<br />
that are not covered.<br />
• To keep appointments for care or to give early notice if you<br />
need to cancel a scheduled appointment.<br />
6-4 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Member Rights <strong>and</strong><br />
Responsibilities<br />
(continued)<br />
<strong>Minnesota</strong> Health Care Programs Member Rights <strong>and</strong><br />
Responsibilities:<br />
<strong>Blue</strong> Plus<br />
You have the right to know about your rights <strong>and</strong> responsibilities.<br />
If you have any questions, please call member services at<br />
(651) 662-5545 or toll free at 1-800-711-9862.<br />
Your rights as a health plan member:<br />
• To get quality health care that’s timely, accessible, <strong>and</strong><br />
friendly.<br />
• To be treated with respect, dignity <strong>and</strong> consideration for<br />
privacy.<br />
• To get medically necessary covered services, including<br />
emergency services 24 hours a day, seven (7) days a week.<br />
• To be told about your health problems.<br />
• To get information about treatment, your treatment choices <strong>and</strong><br />
how they may help or harm you – whether or not the health<br />
plan would pay for these treatments.<br />
• To participate with your providers in the decisions about your<br />
health care.<br />
• To participate in underst<strong>and</strong>ing your health problems <strong>and</strong><br />
developing your treatment goals.<br />
• To refuse treatment. To get information about what might<br />
happen if you refuse treatment.<br />
• To refuse care from specific providers.<br />
• To expect that we will keep your medical <strong>and</strong> financial records<br />
private.<br />
• To request <strong>and</strong> receive a copy <strong>of</strong> your medical records. You<br />
also have the right to ask to correct the records.<br />
• Get notice <strong>of</strong> our decisions if we deny, reduce, or stop a<br />
service, or deny a payment for a service.<br />
• To file a grievance or appeal with <strong>Blue</strong> Plus. You can also file<br />
a complaint with the <strong>Minnesota</strong> Department <strong>of</strong> Health.<br />
• To request a State Fair Hearing with the <strong>Minnesota</strong><br />
Department <strong>of</strong> Human Services (also referred to as “the<br />
State”). You may request a State Fair Hearing before or at any<br />
time during the <strong>Blue</strong> Plus appeal process. You do not have to<br />
file an appeal with <strong>Blue</strong> Plus before you request a State Fair<br />
Hearing.<br />
• To get a clear explanation <strong>of</strong> covered nursing home <strong>and</strong> home<br />
care service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-5
<strong>Blue</strong> Plus<br />
Member Rights <strong>and</strong><br />
Responsibilities<br />
(continued)<br />
• Give written instructions that inform other <strong>of</strong> your wishes<br />
about your health care. This is called a “health care directive.”<br />
It allows you to name a person (agent) to decide for you if you<br />
are unable to decide, or if you want someone else to decide for<br />
you.<br />
• To choose where you will get family planning services.<br />
• To get a second opinion for medical, mental health <strong>and</strong><br />
chemical dependency services.<br />
• To be free <strong>of</strong> constraints or seclusion used as a means <strong>of</strong><br />
coercion, discipline, convenience or retaliation.<br />
• To request a copy <strong>of</strong> the Certificate <strong>of</strong> Coverage at least once a<br />
year.<br />
• To recommend changes regarding <strong>Blue</strong> Plus’ rights <strong>and</strong><br />
responsibilities policies.<br />
• To freely exercise your rights. The exercise <strong>of</strong> your rights will<br />
not badly affect the way you are treated.<br />
• Get the following information from us, if you ask for it:<br />
• Whether we use a physician incentive plan that affects the<br />
use <strong>of</strong> referral services;<br />
• The type(s) <strong>of</strong> incentive arrangement used;<br />
• Whether stop-loss protection is provided; <strong>and</strong><br />
• Results <strong>of</strong> member survey if one is required because <strong>of</strong> our<br />
physician incentive plan.<br />
• Get the results <strong>of</strong> an external quality review study from the<br />
State, if you ask for them.<br />
• To be told when a health care provider cancels their contract<br />
with <strong>Blue</strong> Plus. You may choose from the rest <strong>of</strong> the <strong>Blue</strong> Plus<br />
providers.<br />
• To have a person at <strong>Blue</strong> Plus or at the clinic to contact with<br />
any concerns about services.<br />
• To get information about <strong>Blue</strong> Plus, our services, network <strong>of</strong><br />
providers <strong>and</strong> your rights <strong>and</strong> responsibilities.<br />
6-6 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Member Rights <strong>and</strong><br />
Responsibilities<br />
(continued)<br />
<strong>Blue</strong> Plus<br />
• To start a legal proceeding when having a problem with <strong>Blue</strong><br />
Plus or our providers.<br />
• To file a grievance or appeal with <strong>Blue</strong> Plus <strong>and</strong> receive a<br />
prompt <strong>and</strong> fair review.<br />
• To contact the State ombudsman for help in filing a grievance<br />
or appeal.<br />
• To ask for a speedy hearing.<br />
Your responsibilities as a health plan member:<br />
• Read your Certificate <strong>of</strong> Coverage <strong>and</strong> know which services<br />
are covered under the Plan <strong>and</strong> how to get them.<br />
• To show your <strong>Blue</strong> Plus member ID card <strong>and</strong> your <strong>Minnesota</strong><br />
Health Care Programs card every time you go for health care.<br />
Also show the cards <strong>of</strong> any other health coverage you have,<br />
such as Medicare or private insurance.<br />
• To establish a relationship with a <strong>Blue</strong> Plus primary care<br />
doctor before you become ill. This helps you <strong>and</strong> your primary<br />
care doctor underst<strong>and</strong> your total health condition.<br />
• To give information that <strong>Blue</strong> Plus <strong>and</strong> our providers need to<br />
give care to you. Share information about your health history.<br />
• To follow all your doctor’s instructions. If you have questions<br />
about your care, you should ask your doctor.<br />
• Work with your doctor to underst<strong>and</strong> your total health<br />
condition. It is important to know what to do when a health<br />
problem occurs, when <strong>and</strong> where to seek help, <strong>and</strong> how to<br />
prevent health problems.<br />
• To practice preventive health care. To have tests, exams <strong>and</strong><br />
shots recommended for you based on your age <strong>and</strong> gender.<br />
• To tell the clinic about changes in your name or address.<br />
• To keep appointments for care or to give early notice if you<br />
need to cancel.<br />
This information is available in other forms to people with<br />
disabilities by calling <strong>Blue</strong> Plus customer service at<br />
(651) 662-5545, toll free at 1-800-711-9862 (voice), or<br />
(651) 662-8700 or 1-888-878-0137 (TDD), or 711, or through<br />
the <strong>Minnesota</strong> Relay Service at 1-877-627-3848 (speech-tospeech<br />
relay service).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-7
<strong>Blue</strong> Plus<br />
Member Benefits Members’ benefits depend upon their type <strong>of</strong> contract. Benefits for<br />
our st<strong>and</strong>ard fully insured contracts may vary from our self-insured<br />
contracts. Because members’ benefits will vary, please use<br />
BLUELINE, provider web self-service, or contact provider service<br />
for specific member benefits.<br />
• Highest level <strong>of</strong> benefits – Members generally receive the<br />
highest level <strong>of</strong> benefits when they receive their services from<br />
their PCC or when the PCC authorizes a referral to a specialist.<br />
A list <strong>of</strong> participating referral providers which is online at<br />
www.providerhub.com is available in the Referral Network<br />
for PCCs directory or at bluecrossmn.com.<br />
• Self-referral – Members may decide to manage their own<br />
health care without involving their PCC. We consider this a<br />
self-referral. In doing so, members usually take on additional<br />
financial responsibilities. A claim may be paid at a lesser<br />
benefit or completely denied, depending on if the member has<br />
a self-referral option.<br />
• Referral bypass – There are some services that will be paid at<br />
the highest level <strong>of</strong> the member’s benefits without a referral<br />
from the PCC. This is known as a referral bypass or referral<br />
exception. For a listing <strong>of</strong> referral bypasses, please refer to the<br />
Referral Not Required section <strong>of</strong> this chapter.<br />
• PCC/Care System - Referral bypass- There may be situations<br />
where a particular PCC or care system has communicated their<br />
wish to have a referral bypass implemented for a particular<br />
situation. This allows the specified service to be paid at the<br />
highest level <strong>of</strong> benefits without you communicating a referral<br />
to us. If you have questions regarding a PCC specific referral<br />
bypass, please contact provider service. These requests are<br />
h<strong>and</strong>led on an individual basis <strong>and</strong> must be implemented by<br />
<strong>Blue</strong> Plus <strong>and</strong> an authorized person at your clinic.<br />
• Open access – Some contracts have open access for specified<br />
services. The member usually uses a designated participating<br />
network provider <strong>and</strong> will receive the highest level <strong>of</strong> benefits<br />
without a referral from the PCC. Some examples include<br />
vision, chiropractic, obstetrics/gynecology (ob/gyn), or<br />
behavioral health care.<br />
6-8 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
<strong>Blue</strong> Plus<br />
Member PCC Selection Members are responsible for selecting their primary care clinic<br />
(PCC). Every member in the family may select their own PCC;<br />
they are not required to select the same PCC. Members may also<br />
change their designated PCC. To do so they must contact <strong>Blue</strong><br />
Plus customer service. The phone number is on the back <strong>of</strong> the<br />
member’s ID card.<br />
The effective date assigned to all PCC changes will be generally<br />
the first day <strong>of</strong> the month following <strong>Blue</strong> Plus’s receipt <strong>of</strong> the<br />
request. This provision may be waived under certain situations.<br />
The effective date <strong>of</strong> the change will be communicated on the<br />
instructions mailed with the member’s ID card.<br />
Claim Processing When a claim is received for specialty care (not by the PCC), we<br />
will review our records for a referral. If a referral has not been<br />
received or does not match an open referral in our records, we will<br />
process the claim as a self-referral if the member has a self-referral<br />
option. If the member does not have a self-referral option, we may<br />
contact the PCC to inquire if a referral is desired. If no referral is<br />
authorized, then the claim will be denied or processed at the lower<br />
level <strong>of</strong> benefits.<br />
Statement <strong>of</strong> Provider<br />
Claims Paid Form<br />
Providers will be notified <strong>of</strong> claims processing details as outlined<br />
in Chapter 10-Reimbursement/ Reconciliation Programs <strong>of</strong> this<br />
manual for more details regarding the <strong>Blue</strong> Plus Statement <strong>of</strong><br />
Provider Claims Paid <strong>and</strong> reimbursement.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-9
<strong>Blue</strong> Plus<br />
Quality <strong>of</strong> Care<br />
Complaint<br />
A quality <strong>of</strong> care complaint is an additional right <strong>of</strong> <strong>Blue</strong> Plus<br />
members. Members may complain if they feel the quality <strong>of</strong> their<br />
care has been reduced. Some examples <strong>of</strong> quality <strong>of</strong> care<br />
complaints are listed below. Members may file a complaint if they<br />
believe:<br />
• They are not receiving an appointment in a reasonable amount<br />
<strong>of</strong> time<br />
• The PCC is not referring them to a specialist when it is<br />
necessary<br />
• The provider/provider <strong>of</strong>fice was rude or discourteous<br />
• The provider is unable to diagnosis or treat their condition<br />
We immediately supply the provider with a copy <strong>of</strong> the complaint<br />
<strong>and</strong> involve the provider in the solution. We are required by the<br />
Department <strong>of</strong> Health to complete these complaints in 30 days,<br />
therefore; we require your expedited attention to any request we<br />
may have.<br />
6-10 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Referrals<br />
<strong>Blue</strong> Plus<br />
Overview When <strong>Blue</strong> Plus members are referred by their PCC to other<br />
providers, <strong>Blue</strong> Plus needs to be notified by the PCC in order for<br />
claims to process correctly. A referral is not a guarantee <strong>of</strong><br />
payment, but allows the patient to seek medical care outside<br />
the PCC. A referral does not negate the necessity <strong>of</strong> a prior<br />
authorization or preadmission notification, if they are required.<br />
Referrals are in addition to both <strong>of</strong> these procedures for managed<br />
care products.<br />
Once the referral is received from the PCC, <strong>Blue</strong> Plus will generate<br />
a referral letter depending on the type <strong>of</strong> referral (see Referral<br />
Letter).<br />
It is the referred provider’s responsibility to communicate medical<br />
assessments <strong>and</strong> proposed treatment plans to the PCC. To best<br />
coordinate the member’s care, the PCC must have complete<br />
medical information. PCCs may request the information in the<br />
format <strong>of</strong> their choice.<br />
Referral Policy The referral process occurs when a PCC determines that the<br />
patient’s condition requires care outside his or her PCC. A referral<br />
is initiated by the PCC <strong>and</strong> is limited to a specific duration <strong>and</strong><br />
number <strong>of</strong> visits, as determined by the PCC. There are some<br />
situations where a referral is not required (see Referrals Not<br />
Required). A prior authorization may be necessary. See the<br />
section on Prior Authorization, Section 6-16. Policies for<br />
Government Programs may have different requirements. See<br />
Chapter 3 in the <strong>Blue</strong> Plus Provider <strong>Manual</strong>.<br />
The goal <strong>of</strong> the referral process is to ensure continuity <strong>of</strong> care<br />
through coordination with the PCC. When care needs are identified<br />
which cannot be appropriately provided by the PCC, care is<br />
referred.<br />
The objectives <strong>of</strong> referrals are:<br />
• To promote coordination <strong>of</strong> care <strong>and</strong> communication between<br />
patients, PCCs <strong>and</strong> specialty providers.<br />
• To promote appropriate use <strong>of</strong> referral care, thereby reducing<br />
under-utilization or over-utilization <strong>of</strong> services.<br />
• To promote seamless, quality <strong>of</strong> care delivery by facilitating<br />
the use <strong>of</strong> a select, coordinated network <strong>of</strong> primary care <strong>and</strong><br />
specialty providers.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-11
<strong>Blue</strong> Plus<br />
Referral Points Remember these important points about referrals:<br />
• PCCs must have an established referral process.<br />
• PCCs must notify <strong>Blue</strong> Plus <strong>of</strong> authorized referrals via our<br />
provider web self-service product at www.providerhub.com.<br />
• The member may receive services only from the clinic named<br />
in the referral or st<strong>and</strong>ing referral.<br />
• The referral provider or specialist may not refer members to<br />
other providers without written consent from the PCC. If no<br />
referral is given, members will be responsible for any reduced<br />
benefits. Exceptions are made for <strong>Minnesota</strong> Health Care<br />
Program Members.<br />
• In some cases, we will request a second referral if information<br />
from the referred provider’s claim does not match information<br />
received on the initial referral.<br />
• If a member who has a referral or st<strong>and</strong>ing referral changes<br />
PCCs, the referral or st<strong>and</strong>ing referral will no longer be valid<br />
as <strong>of</strong> the date <strong>of</strong> the PCC change. The member’s new PCC<br />
must now coordinate their member’s care.<br />
6-12 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Referral Required If the PCC authorizes the care outside the PCC, referrals are<br />
required to be communicated to <strong>Blue</strong> Plus for:<br />
<strong>Blue</strong> Plus<br />
• Home health care/home IV<br />
• Outpatient surgery<br />
• Psychological testing submitted with a medical diagnosis<br />
• Visits to a specialty provider<br />
• Inpatient skilled nursing facilities (SNF) - a referral is required<br />
along with a prior authorization<br />
• <strong>Minnesota</strong> Health Care Programs <strong>and</strong> Secure<strong>Blue</strong> members do<br />
not require a referral for the SNF charges; but, the provider is<br />
required to send in a Nursing Home Communication Form<br />
• Inpatient admissions – including hospitals<br />
• Inpatient hospital admissions – a referral will be assumed when<br />
the preadmission notification is completed, if the admitting<br />
physician is from the member’s PCC<br />
There are times when a referral is appropriate for behavioral health<br />
services. If this is the case, you can call 1-800-262-0820 or local<br />
(651) 662-5200 to discuss referral needs. This phone number can<br />
also be used to see which providers are in the behavioral health<br />
network. <strong>Minnesota</strong> Health Care Program Members have direct<br />
access to network providers. In rare instances, out-<strong>of</strong>-network<br />
exceptions may be considered. Call the above numbers for further<br />
information.<br />
There also may be exceptions in situations where the patient has<br />
open-access benefits for a particular type <strong>of</strong> service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-13
<strong>Blue</strong> Plus<br />
Referral Not Required We do not require referrals for the services listed below. Claims<br />
will process at the highest level <strong>of</strong> coverage, as if they were<br />
referred, without you authorizing a referral. This process is known<br />
as a referral bypass or referral exception. The referral bypasses<br />
may be in place for ease <strong>of</strong> administration, legislative m<strong>and</strong>ate or<br />
both. They may vary by employer contract or PCC. For complete<br />
information about <strong>Minnesota</strong> Health Care Programs requirements,<br />
see Chapter 3 in the <strong>Blue</strong> Plus Provider <strong>Manual</strong>.<br />
• Abortion <strong>and</strong> sterilization<br />
• Allergy serum when injection is done in the PCC<br />
• Ambulance transportation<br />
• Anesthesia <strong>and</strong> assistant surgeon, if medically necessary (if the<br />
outpatient surgery or inpatient admission is referred)<br />
• Covered services by dentists, endodontists, periodontists,<br />
orthodontists, prosthodontists, <strong>and</strong> oral <strong>and</strong> maxill<strong>of</strong>acial<br />
surgeons.<br />
• Diagnostic X-ray <strong>and</strong> laboratory services only (except MRI)<br />
• Durable medical equipment (DME)<br />
• Emergency services<br />
• Inpatient consultation (if the inpatient admission is referred)<br />
• Inpatient consultation (if the inpatient admission is referred)<br />
• Inpatient delivery/maternity, <strong>and</strong> related services, including<br />
prenatal <strong>and</strong> complications <strong>of</strong> pregnancy<br />
• Inpatient treatment <strong>of</strong> a medical emergency<br />
• Magnetic Resonance Imaging (MRI)<br />
6-14 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Referral Not Required<br />
(continued)<br />
<strong>Blue</strong> Plus<br />
• One postpartum home care visit, if the visit follows an early<br />
discharge. Early discharge for a vaginal delivery would be<br />
within 48 hours <strong>of</strong> delivery <strong>and</strong>, for C-section, within 96 hours<br />
<strong>of</strong> delivery<br />
• Oral <strong>and</strong> maxill<strong>of</strong>acial surgeons<br />
• Orthodontists<br />
• Outpatient emergency room services <strong>and</strong> associated services<br />
• Outpatient observation room<br />
• Prescription drug (pharmacy)<br />
• Services for the diagnosis <strong>of</strong> infertility<br />
• Testing <strong>and</strong> treatment <strong>of</strong> a sexually transmitted disease<br />
• Testing for AIDS or other HIV-related conditions<br />
• Voluntary planning <strong>of</strong> the conception <strong>and</strong> bearing <strong>of</strong> children<br />
PCCs can contact us to implement a PCC-specific referral bypass<br />
for their managed care members. This is beneficial when you<br />
continually refer to a specific provider.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-15
<strong>Blue</strong> Plus<br />
St<strong>and</strong>ing Referral <strong>Minnesota</strong> law provides for a st<strong>and</strong>ing referral. St<strong>and</strong>ing referrals<br />
are for longer-term, ongoing care by a specialty provider. They<br />
may be established at any time at the PCCs discretion. Referrals<br />
must be communicated to <strong>Blue</strong> Plus prior to services being<br />
rendered. PCCs determine the number <strong>of</strong> referral visits <strong>and</strong> the<br />
length, up to 365 days.<br />
M<strong>and</strong>atory st<strong>and</strong>ing referrals to a specialist qualified to treat the<br />
specific condition must be granted, upon request, to a member with<br />
any one <strong>of</strong> the following conditions.<br />
• A chronic health condition<br />
• A life threatening mental or physical condition<br />
• Pregnancy beyond the first trimester if the member’s plan does<br />
not <strong>of</strong>fer open access benefits to<br />
• Ob/gyn network providers<br />
• A degenerative disease or disability<br />
• Any other condition or disease <strong>of</strong> sufficient seriousness <strong>and</strong><br />
complexity to require treatment by a specialist<br />
Routine st<strong>and</strong>ing referrals are still at the discretion <strong>of</strong> the PCC.<br />
PCCs are not required to authorize a referral to accommodate<br />
personal preference, convenience, or other non-medical reason.<br />
While m<strong>and</strong>atory-st<strong>and</strong>ing referrals must be provided, the PCC<br />
can determine the total number <strong>of</strong> visits within the 12-month<br />
period based on the member’s medical condition. If the PCC has<br />
the specialist within its clinic/care system, the PCC may request<br />
that the member receive services there. PCCs must communicate<br />
referrals to <strong>Blue</strong> Plus prior to referred services being rendered.<br />
This law permits specialists, in agreement with the member <strong>and</strong><br />
PCC, to provide primary care services, authorize tests <strong>and</strong> services,<br />
<strong>and</strong> even make secondary referrals. If the PCC does not grant the<br />
member’s st<strong>and</strong>ing referral request, the PCC should inform the<br />
member that he or she can file a complaint with <strong>Blue</strong> Plus by<br />
calling the telephone number on the back <strong>of</strong> the member ID card.<br />
6-16 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
<strong>Blue</strong> Plus<br />
Clarifications <strong>of</strong> Terms Clear communication between <strong>Blue</strong> Plus, the PCC, specialist, <strong>and</strong><br />
the member is very important. At times, definitions <strong>and</strong><br />
underst<strong>and</strong>ing <strong>of</strong> words may differ. To best serve members, a clear<br />
underst<strong>and</strong>ing <strong>of</strong> the meaning <strong>of</strong> the terms referral, prior<br />
authorization, <strong>and</strong> preadmission notification is necessary. Listed<br />
are some clarifications <strong>and</strong> further explanations that are helpful to<br />
fully underst<strong>and</strong>.<br />
Referral:<br />
• A referral is the authorization from the PCC for their members<br />
to seek medical care outside the PCC <strong>and</strong> receive the highest<br />
level <strong>of</strong> the member’s benefits.<br />
• A referral does not mean the service is approved for admission<br />
notification or prior authorization, which is separate from the<br />
referral process.<br />
• A referral does not mean the service is eligible under the<br />
member’s contract. Even if the service is referred, the service<br />
must be eligible under the member’s contract to be eligible for<br />
reimbursement.<br />
• Members may think that a service is referred if you tell them<br />
the service is medically necessary. Be clear when you are<br />
referring services.<br />
• A denied referral does not mean that the service is not<br />
medically necessary. It may simply mean that the PCC may be<br />
able to h<strong>and</strong>le the service within its clinic/care system or at a<br />
different referral provider with which the PCC has developed a<br />
relationship.<br />
• Referrals are not created by <strong>Blue</strong> Plus. Referrals from one<br />
provider to another are established st<strong>and</strong>ard practice. We<br />
simply request that it be communicated to us so we may<br />
process claims correctly. For complete information about<br />
<strong>Minnesota</strong> Health Care Programs, see Chapter 3 <strong>of</strong> the <strong>Blue</strong><br />
Plus Provider <strong>Manual</strong>.<br />
• A verbal referral is not sufficient.. If the PCC authorized a<br />
referral, it needs to be communicated to us (unless a referral<br />
bypass is in place).<br />
• Referrals should be authorized to the entity billing for the<br />
service (contracting provider), not the individual provider who<br />
is performing the service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-17
<strong>Blue</strong> Plus<br />
Clarifications <strong>of</strong> Terms<br />
(continued)<br />
Prior Authorization:<br />
• A prior authorization does not mean that the service is referred.<br />
If a prior authorization is required <strong>and</strong> a provider other than the<br />
PCC is performing the service, a referral is also required.<br />
• An approved prior authorization does not mean the service is<br />
covered under the member’s plan. Members’ benefits may<br />
change.<br />
Admission Notification:<br />
• An admission notification does not mean the service is<br />
referred. If an admission notification is required <strong>and</strong> the PCC<br />
wishes the service to be referred, a referral must be done in<br />
addition to the admission notification. However, when an<br />
admission notification is communicated to us for an inpatient<br />
hospital stay <strong>and</strong> the admitting physician is part <strong>of</strong> the<br />
member’s PCC, we will assume that a referral is authorized.<br />
Referral Letter Referral letters are sent as described below. The reverse side <strong>of</strong> the<br />
referral letter may be used by the specialist to communicate to<br />
your <strong>of</strong>fice the results <strong>of</strong> the services provided.<br />
Referral Letter<br />
(continued)<br />
If the referral is… Then…<br />
To a specialist (not<br />
within the PCC)<br />
For an outpatient<br />
procedure<br />
For an inpatient<br />
procedure<br />
a copy is sent to:<br />
• The referral specialist only if they do not<br />
have access to provider web self-service<br />
• The patient, <strong>and</strong><br />
• Your <strong>of</strong>fice only if you do not have<br />
access to provider web self-service<br />
a copy is sent to:<br />
• The patient, <strong>and</strong><br />
• Your <strong>of</strong>fice, only if you do not have<br />
access to provider web self service<br />
no copies are mailed<br />
Please note that if the PCC or the referred specialist has access to<br />
provider web self-service at providerhub.com referral letters will<br />
not be mailed because they have access to the information<br />
electronically.<br />
6-18 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Sample Patient<br />
Referral Authorization<br />
Letter<br />
If the referral is… Then…<br />
Following is a sample <strong>of</strong> the referral letter that is mailed in the<br />
above situations.<br />
<strong>Blue</strong> Plus<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-19
<strong>Blue</strong> Plus<br />
[Date]<br />
[<strong>Name</strong> <strong>of</strong> patient]<br />
[Address <strong>of</strong> patient]<br />
Copy to:<br />
[<strong>Name</strong> <strong>of</strong> secondary provider]<br />
Dear [name <strong>of</strong> patient]<br />
Patient Referral Notice<br />
Patient:<br />
Identification #:<br />
Member #<br />
Relation to subscriber:<br />
Sex: Date <strong>of</strong> Birth:<br />
Group #<br />
Referral #<br />
This letter is to confirm that your primary care clinic has requested a referral for you to<br />
[insert provider name], for care to be received from ____________ through ________, up to a<br />
maximum <strong>of</strong> _______ visits.<br />
Your <strong>Blue</strong> <strong>Cross</strong>/<strong>Blue</strong> Plus health plan will pay for its share <strong>of</strong> the health services described<br />
above, as defined by the terms <strong>of</strong> your health plan contract, provided that:<br />
1. Your primary care clinic has requested a referral (this letter confirms that this requirement<br />
has been met); <strong>and</strong><br />
2. You are otherwise eligible to receive health plan benefits (for example, you are a currently<br />
enrolled member, you have not reached a lifetime or benefit maximum, <strong>and</strong> your contract<br />
covers the services provided).<br />
Here is a list <strong>of</strong> other conditions that apply. If you have questions, please call the customer<br />
service number on the back <strong>of</strong> your health plan member ID card.<br />
• A new referral request must be submitted by your primary care clinic for any care outside<br />
the dates listed or for more than the maximum number <strong>of</strong> visits noted above.<br />
• This referral is valid only for care provided by [insert provider name].<br />
• If you change your primary care clinic, this referral is no longer valid.<br />
• Any health services related to services excluded in your contract (for example, benefit<br />
exclusions or investigative services) are not covered, even if ordered or provided by your<br />
primary care clinic or the provider to whom you have been referred.<br />
This referral has been made by:<br />
Physician:<br />
Primary Care Clinic:<br />
Clinic Provider #:<br />
Referral care must be provided by:<br />
Provider name:<br />
Provider #:<br />
6-20 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
TO THE REFERRAL SPECIALIST<br />
<strong>Blue</strong> Plus<br />
You or the primary care clinic must approve any hospitalization, tests or special treatments.<br />
Check with the referring physician to determine the participating hospital the clinic uses. Do not<br />
place yourself or the patient at financial risk by performing services not eligible for coverage<br />
under the patient’s health plan, outside the dates specified or for more than the number <strong>of</strong> visits<br />
approved on this referral, or by admitting to a facility not authorized by the referring physician.<br />
Special instructions from the referring physician:<br />
Please use the space below to provide a written report <strong>of</strong> services to the referring physician at:<br />
[address <strong>of</strong> referring physician]<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-21
<strong>Blue</strong> Plus<br />
Special Member Benefits<br />
Overview This section details some <strong>of</strong> the special benefits for <strong>Blue</strong> Plus. It<br />
will assist you in answering some <strong>of</strong> the questions you may have<br />
regarding the benefits. Information in this provider manual is a<br />
general outline. Provider <strong>and</strong> member contracts determine benefits.<br />
Chiropractic Benefits Most members have open-access to a Select network chiropractor.<br />
They may receive eligible chiropractic services without a referral<br />
from their PCC. To receive the highest level <strong>of</strong> the member’s<br />
benefits, the member must use a Select chiropractor.<br />
Continuity <strong>of</strong> Care<br />
After Facility Discharge<br />
Continuity <strong>of</strong> Care<br />
After Facility Discharge<br />
(continued)<br />
Durable Medical<br />
Equipment<br />
Patient care can easily become fragmented <strong>and</strong> compromised as<br />
patients pass from a hospital/facility stay back to the care <strong>of</strong> their<br />
primary care provider. The Joint Commission <strong>of</strong> the Accreditation<br />
<strong>of</strong> Healthcare Organizations (JCAHO) has two Continuum <strong>of</strong> Care<br />
st<strong>and</strong>ards that directly address the follow-up care process <strong>of</strong><br />
patients that are discharged. JCAHO states that the need for<br />
appropriate follow-up plans include:<br />
• Providing continuing care based on the patient’s needs<br />
• Exchanging <strong>of</strong> appropriate information when a patient is<br />
accepted, referred, transferred, or discharged to receive further<br />
care or services<br />
The National Committee for Quality Assurance (NCQA) st<strong>and</strong>ards<br />
require that managed care organizations monitor the continuity <strong>and</strong><br />
coordination <strong>of</strong> care that members receive across practices <strong>and</strong><br />
provider sites. A smooth transition <strong>and</strong> continuity <strong>of</strong> care after<br />
discharge is a need <strong>and</strong> challenge in every episode <strong>of</strong> care. Readmissions<br />
can be caused by gaps in the follow-up process.<br />
• Patient role: Patients need to identify a PCC or follow-up<br />
provider who will coordinate their care after facility discharge.<br />
• Hospital/facility role: Hospitals/facilities are encouraged to<br />
develop systems that capture <strong>and</strong> communicate the patient’s<br />
primary care provider, share information in a timely manner<br />
with the follow-up provider after discharge, provide the patient<br />
with instructions for care after discharge, educate the patient as<br />
needed, <strong>and</strong> obtain permission from the patient to share<br />
information with the follow-up provider.<br />
• PCC or follow-up provider role: PCCs or follow-up<br />
providers need a process in place to receive <strong>and</strong> file medical<br />
information into a patient’s clinic chart in a timely manner.<br />
Members can use any <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Aware participating DME provider.<br />
6-22 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Mental Health <strong>and</strong><br />
Chemical Dependency<br />
Services<br />
<strong>Blue</strong> Plus<br />
<strong>Blue</strong> Plus members may coordinate their evaluation/management<br />
(E/M) or medication management services through their PCC or<br />
their designated behavioral health provider. E/M <strong>and</strong> medication<br />
management services performed outside <strong>of</strong> their PCC or<br />
designated behavioral health provider will require a referral from<br />
the member’s PCC in order to receive the highest level <strong>of</strong> benefits.<br />
Most groups do not require referrals for claims to process at the<br />
highest level. However, member contracts that require the member<br />
to stay in the Select behavioral health network would need<br />
authorization from <strong>Blue</strong> Plus to see a provider outside <strong>of</strong> that<br />
network. PCCs do not need to initiate referrals for patients<br />
requiring mental health/chemical dependency care.<br />
OB/GYN Services State legislation requires open access for specified ob/gyn services<br />
under managed care contracts. When a member obtains eligible<br />
ob/gyn services, she may go to her PCC or elect to seek care from<br />
any ob/gyn network provider without a referral from the PCC <strong>and</strong><br />
receive the highest level <strong>of</strong> her benefits. This benefit is effective<br />
for fully-insured groups. This benefit is optional for self-insured<br />
groups.<br />
OB/GYN Open Access<br />
Additional Services<br />
• Eligible services: The member can go to any ob/gyn network<br />
provider for approved services. The approved services are<br />
considered services billed by a network ob/gyn with a<br />
diagnosis code on our approved list. (See the list later in this<br />
chapter.)<br />
If a member’s needs exp<strong>and</strong> beyond the specified ob/gyn openaccess<br />
benefits, the member needs to be directed back to her<br />
designated PCC or be referred by her PCC in order for the care to<br />
be coordinated by the member’s PCC.<br />
For example, when the ob/gyn provider identifies ovarian cancer<br />
<strong>and</strong> the member needs to see an oncologist, the member should be<br />
directed back to her PCC, because the oncologist is not an ob/gyn<br />
provider. The open access benefit is only for services billed by<br />
ob/gyn providers.<br />
For those members who have an open access benefit, eligible<br />
inpatient <strong>and</strong> outpatient hospital <strong>and</strong> related ob/gyn services are<br />
covered at the member’s highest benefit level. An open access<br />
ob/gyn provider must coordinate the services. We may not be able<br />
to identify these claims during initial processing. Adjustments to<br />
claims may be requested electronically through provider web selfservice,<br />
or by calling Provider Service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-23
<strong>Blue</strong> Plus<br />
OB/GYN Open Access<br />
Diagnosis<br />
Please refer to the following list <strong>of</strong> designated ob/gyn open access<br />
diagnosis codes. Eligible claims submitted with these diagnosis<br />
codes from a specified ob/gyn network provider do not require a<br />
referral, if the patient has the ob/gyn open-access benefit.<br />
Code Description<br />
054.0-054.19 Herpes simplex<br />
078.81-078.89 Other diseases due to viruses <strong>and</strong> Chlamydiae<br />
079.4 Hum an papillomavirus<br />
079.81. 079.89 Other specified viral <strong>and</strong> chlamydial infections<br />
099.0-099.9 Syphilis <strong>and</strong> other venereal disease<br />
112.0-112.9 C<strong>and</strong>idiasis<br />
127.4 Enterobiasis<br />
131.00-131.9 Trichom oniasis<br />
132.2 Phthirus pubis<br />
174.0-184.9 Malignant neoplasm<br />
217-221.9 Benign neoplasm<br />
233.0-233.9 Carcinoma in situ <strong>of</strong> breast <strong>and</strong> genitourinary<br />
system<br />
236.0-236.99 Neoplasm <strong>of</strong> uncertain behavior <strong>of</strong> genitourinary<br />
system<br />
239.3 Neoplasm <strong>of</strong> unspecified nature <strong>of</strong> breast<br />
239.5 Neoplasm <strong>of</strong> unspecified nature <strong>of</strong> other<br />
genitourinary organs<br />
256.0-256.9 Ovarian dysfunction<br />
599.0 Urinary tract infection, site not specified<br />
610.0-611.9 Disorders <strong>of</strong> breast<br />
614.0-616.9 Inflammatory disease <strong>of</strong> female pelvic organs<br />
617.0-627.9 Other disorders <strong>of</strong> female genital tract, infertility<br />
630-677 Complications <strong>of</strong> pregnancy, childbirth <strong>and</strong> the<br />
puerperium<br />
698.1 Pruritus <strong>of</strong> genital organs<br />
752.0-752.9 Congenital anomalies <strong>of</strong> genital organs<br />
6-24 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
OB/GYN Open Access<br />
Diagnosis (continued)<br />
Code Description<br />
780.01-780.99 General symptoms<br />
788.0-788.9 Symptoms involving urinary system<br />
<strong>Blue</strong> Plus<br />
789.1-789.9 Other symptoms involving abdomen <strong>and</strong> pelvis<br />
795.00-795.79 Nonspecific abnormal histological <strong>and</strong><br />
immunological findings<br />
996.32 IUD complications<br />
V01.6 Contact with or exposure to venereal diseases<br />
V07.4 Postmenopausal hormone replacement therapy<br />
V10.3 Personal history <strong>of</strong> malignant neoplasm breast<br />
V10.40-<br />
V10.44<br />
V13.21-<br />
V13.29<br />
Personal history <strong>of</strong> malignant neoplasm female<br />
genital organs<br />
Personal history <strong>of</strong> pre-term labor<br />
Other genital system <strong>and</strong> obstetric disorders<br />
V15.7 Other personal history presenting hazards to<br />
health-contraception<br />
V16.3 Family history <strong>of</strong> malignant neoplasms <strong>of</strong> breast<br />
V16.40-<br />
V16.49<br />
Family history <strong>of</strong> malignant neoplasms <strong>of</strong> genital<br />
organs<br />
V22.0-V28.9 Nor mal pregnancy<br />
Supervision <strong>of</strong> high-risk pregnancy<br />
Postpartum care <strong>and</strong> examination<br />
Contraceptive management<br />
Procreative management<br />
Outcome <strong>of</strong> delivery<br />
Antenatal screening<br />
V45.51-<br />
V45.52<br />
Presence <strong>of</strong> intrauterine contraceptive device<br />
Intrauterine contraceptive device<br />
Presence <strong>of</strong> subdermal contraceptive implant<br />
V61.5-V61.7 Multip arity<br />
Illegitimacy or illegitimate pregnancy<br />
Other unwanted pregnancy<br />
V67.00-V67.9 Follow-up examination<br />
V70.0-V70.9 General medical examination<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10) 6-25
<strong>Blue</strong> Plus<br />
OB/GYN Open Access<br />
Diagnosis (continued)<br />
Code Description<br />
V71.5 Observation following alleged rape or seduction<br />
V72.31-<br />
V72.42<br />
Gynecological examination<br />
Pregnancy examination or test, pregnancy<br />
unconfirmed<br />
V74.5 Special screening examination for venereal<br />
disease<br />
V76.10-<br />
V76.19<br />
Special screening for malignant neoplasms <strong>of</strong><br />
breast<br />
V76.2 Special screening for malignant neoplasms <strong>of</strong><br />
cervix<br />
*Includes all codes (4th or 5th digit) under this category.<br />
Vision Care Fully insured members have direct access to general eye care<br />
services rendered by Aware participating optometrists <strong>and</strong><br />
ophthalmologists. Appropriate ophthalmologist services including<br />
eye examinations <strong>and</strong> Evaluation <strong>and</strong> Management (E/M)<br />
procedure codes as well as CPT codes 65205, 65210, 65220,<br />
65222, <strong>and</strong> 68761 are eligible. Some self-insured groups also<br />
include this benefit. Major surgical procedures <strong>and</strong> follow-up care<br />
will continue to be coordinated through the member’s PCC.<br />
6-26 <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/27/10)
Table <strong>of</strong> Contents<br />
Chapter 7<br />
<strong>Blue</strong>Card ®<br />
<strong>Blue</strong>Card Introduction .............................................................................................................. 7-3<br />
Overview................................................................................................................................7-3<br />
Identifying <strong>Blue</strong>Card ® Members ...........................................................................................7-3<br />
Definitions.............................................................................................................................. 7-7<br />
How the Program Works .......................................................................................................7-7<br />
<strong>Blue</strong>Card Service ....................................................................................................................... 7-8<br />
Claims Questions ...................................................................................................................7-8<br />
Benefits <strong>and</strong> Eligibility ..........................................................................................................7-9<br />
<strong>Blue</strong>Card Preferred Provider Organization (PPO).................................................................7-9<br />
Prior Authorization <strong>and</strong> Preadmission Notification.............................................................7-10<br />
<strong>Blue</strong>Card Claims...................................................................................................................... 7-11<br />
Claims Submission...............................................................................................................7-11<br />
Exclusions............................................................................................................................7-11<br />
Electronic Data Interchange (EDI) Submission...................................................................7-12<br />
Paper Submission.................................................................................................................7-12<br />
Coding.................................................................................................................................. 7-12<br />
Medical Records ..................................................................................................................7-12<br />
Managed Care ......................................................................................................................7-12<br />
Claims Processed by <strong>Blue</strong> <strong>Cross</strong>............................................................................................. 7-13<br />
Claims Notification..............................................................................................................7-13<br />
Policies.................................................................................................................................7-13<br />
Adjustments .........................................................................................................................7-13<br />
Claims Processed by the Member’s Plan............................................................................... 7-14<br />
Claims Notification..............................................................................................................7-14<br />
Policies.................................................................................................................................7-14<br />
Adjustments .........................................................................................................................7-14<br />
Appeals ................................................................................................................................7-14<br />
Medical Records....................................................................................................................... 7-15<br />
Overview..............................................................................................................................7-15<br />
Coordination <strong>of</strong> Benefits (COB) Claims ................................................................................ 7-17<br />
Guidelines ............................................................................................................................7-17<br />
Claim Payment......................................................................................................................... 7-18<br />
Guidelines ............................................................................................................................7-18<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-1
<strong>Blue</strong>Card®<br />
Claim Status Inquiry ............................................................................................................... 7-19<br />
Overview..............................................................................................................................7-19<br />
Calls from Members <strong>and</strong> Others with Claim Questions ...................................................... 7-20<br />
Overview..............................................................................................................................7-20<br />
Traditional Medicare-Related Claims ................................................................................... 7-21<br />
Guidelines ............................................................................................................................7-21<br />
Medicare Advantage Claims through <strong>Blue</strong>Card .................................................................. 7-23<br />
Overview..............................................................................................................................7-23<br />
Types <strong>of</strong> Medicare Advantage Plans ...................................................................................7-24<br />
Eligibility Verification.........................................................................................................7-25<br />
Medicare Advantage Claims Submission ............................................................................7-26<br />
Reimbursement for Medicare Advantage PPO, HMO, POS ...............................................7-26<br />
Reimbursement for Medicare Advantage Private-Fee-for-Service (PFFS).........................7-28<br />
7-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
<strong>Blue</strong>Card Introduction<br />
<strong>Blue</strong>Card®<br />
Overview The <strong>Blue</strong>Card Program links health care providers <strong>and</strong> the<br />
independent <strong>Blue</strong> plans* across the country <strong>and</strong> abroad with a<br />
single electronic network for pr<strong>of</strong>essional, outpatient, inpatient<br />
claims processing <strong>and</strong> reimbursement. The program allows <strong>Blue</strong><br />
<strong>Cross</strong> providers in every state to submit claims for <strong>Blue</strong> <strong>Cross</strong><br />
members to their local <strong>Blue</strong> plan, eliminating the need to track<br />
receivables from multiple <strong>Blue</strong> plans.<br />
Identifying <strong>Blue</strong>Card ®<br />
Members<br />
Through the <strong>Blue</strong>Card program, you can submit claims directly to<br />
<strong>Blue</strong> <strong>Cross</strong> for your patients who have coverage with a <strong>Blue</strong> plan<br />
other than <strong>Blue</strong> <strong>Cross</strong>. <strong>Blue</strong> <strong>Cross</strong> will be your contact for medical<br />
records submission, claims payment, problem resolution <strong>and</strong><br />
adjustments.<br />
<strong>Blue</strong>Card is a national program that enables <strong>Blue</strong> plan members to<br />
obtain healthcare services wherever they are in the United States.<br />
The program links participating healthcare providers with all the<br />
<strong>Blue</strong> <strong>Cross</strong> plans across the nation through a single electronic<br />
network for claims processing <strong>and</strong> reimbursement. Additionally,<br />
the program links providers in more than 200 countries <strong>and</strong><br />
territories worldwide.<br />
* Each <strong>Blue</strong> plan is an independent licensee <strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
<strong>Blue</strong> <strong>Shield</strong> Association.<br />
<strong>Blue</strong>Card members can easily be identified by the three alpha<br />
characters preceding their identification (ID) number <strong>and</strong> the<br />
suitcase logos; either empty, or with letters “PPO” inside, on their<br />
cards. Although the format <strong>of</strong> the identification number may vary<br />
from plan to plan, you can always recognize the trusted <strong>Blue</strong> <strong>Cross</strong><br />
<strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> emblems. Providers are encouraged to make a<br />
copy <strong>of</strong> both the front <strong>and</strong> back <strong>of</strong> the member’s ID card. Please<br />
enter the patient’s ID number on claims submitted exactly as it<br />
appears on the card, including the alpha prefix.<br />
Although all <strong>Blue</strong> plans participate in the <strong>Blue</strong>Card Program, there<br />
are some programs that are exempt such as Medicaid. If the patient<br />
is carrying a current <strong>Blue</strong> <strong>Cross</strong> ID card <strong>and</strong> there is no suitcase<br />
logo on the card, but there is an alpha prefix, claims should still be<br />
filed to <strong>Blue</strong> <strong>Cross</strong> as any other claim. We will facilitate the<br />
processing <strong>of</strong> that claim on your behalf.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-3
<strong>Blue</strong>Card®<br />
Identifying <strong>Blue</strong>Card ®<br />
Members (continued)<br />
Important facts concerning member IDs:<br />
• A correct member ID number includes the alpha prefix (first<br />
three positions) <strong>and</strong> all subsequent characters, up to 17<br />
positions total. This means that you may see cards with ID<br />
numbers between 6 <strong>and</strong> 14 numbers/letters following the alpha<br />
prefix.<br />
• Do not add/delete characters or numbers within the member<br />
ID.<br />
• Do not change the sequence <strong>of</strong> the characters following the<br />
alpha prefix.<br />
• The alpha prefix is critical for the electronic routing <strong>of</strong> specific<br />
HIPAA transactions to the appropriate <strong>Blue</strong> plan.<br />
• Members who are part <strong>of</strong> the Federal Employee Program will<br />
have the letter "R" in front <strong>of</strong> their member ID number.<br />
Examples <strong>of</strong> ID numbers:<br />
ABC1234567<br />
Alpha<br />
Prefix<br />
ABC1234H567<br />
Alpha<br />
Prefix<br />
ABC12345678901234<br />
Alpha<br />
Prefix<br />
As a provider servicing out-<strong>of</strong>-area members, you may find the<br />
following tips helpful:<br />
• Ask the member for the most current ID card at every visit.<br />
Since new ID cards may be issued to members throughout the<br />
year, this will ensure that you have the most up to date<br />
information in your patient’s file.<br />
• Verify with the member that the ID number on the card is not<br />
his/her Social Security number. If it is, call the <strong>Blue</strong>Card<br />
eligibility line 1-800-676-BLUE to verify the ID number.<br />
• Make a copy <strong>of</strong> the front <strong>and</strong> back <strong>of</strong> the member’s ID card<br />
<strong>and</strong> pass this key information on to your billing staff.<br />
NOTE: Member ID numbers must be reported exactly as shown<br />
on the ID card <strong>and</strong> must not be changed or altered. Do not add or<br />
omit any characters from the member ID numbers.<br />
7-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Identifying <strong>Blue</strong>Card ®<br />
Members (continued)<br />
Alpha Prefix<br />
<strong>Blue</strong>Card®<br />
The three-character alpha prefix at the beginning <strong>of</strong> the member’s<br />
identification number is the key element used to identify <strong>and</strong><br />
correctly route claims. The alpha prefix identifies the <strong>Blue</strong> plan or<br />
national account to which the member belongs. It is critical for<br />
confirming a patient’s membership <strong>and</strong> coverage.<br />
To ensure accurate claim processing, it is critical to capture all ID<br />
card data. If the information is not captured correctly, you may<br />
experience a delay with the claim processing. Please make copies<br />
<strong>of</strong> the front <strong>and</strong> back <strong>of</strong> the ID card, <strong>and</strong> pass this key information<br />
to your billing staff.<br />
Do not make up alpha prefixes.<br />
Do not assume that the member’s ID number is the Social Security<br />
number. All <strong>Blue</strong> plans replaced Social Security numbers on<br />
member ID cards with an alternate, unique identifier.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-5
<strong>Blue</strong>Card®<br />
Identifying <strong>Blue</strong>Card ®<br />
Members (continued)<br />
Sample ID Cards<br />
7-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
<strong>Blue</strong>Card®<br />
Definitions Terms that you will hear when dealing with <strong>Blue</strong>Card members:<br />
How the Program<br />
Works<br />
Term Definition<br />
<strong>Blue</strong>Card<br />
Program<br />
A program that enables members to obtain health<br />
care services while traveling or living in another<br />
licensee’s service area <strong>and</strong> receive the benefits <strong>of</strong><br />
their <strong>Blue</strong> <strong>Cross</strong> contract.<br />
The <strong>Blue</strong>Card Program is designed to work as follows:<br />
1. A patient having <strong>Blue</strong> <strong>Cross</strong> coverage receives services at your<br />
<strong>of</strong>fice.<br />
2. You submit the claim to <strong>Blue</strong> <strong>Cross</strong>.<br />
3. <strong>Blue</strong> <strong>Cross</strong> will price the claim according to your contract <strong>and</strong><br />
send the claim electronically to the member’s plan for benefit<br />
determination.<br />
4. The member’s plan applies the member’s benefits <strong>and</strong> sends<br />
the information back to <strong>Blue</strong> <strong>Cross</strong>. They will communicate<br />
the outcome <strong>of</strong> the claim to the member.<br />
5. <strong>Blue</strong> <strong>Cross</strong> will send the electronic remittance advice <strong>and</strong><br />
payment for eligible benefits to you.<br />
6. Deductible <strong>and</strong> coinsurance collection from members can<br />
occur once the claim is adjudicated <strong>and</strong> you receive your<br />
electronic remittance advice (835) or view your remittance<br />
advice on provider web self service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-7
<strong>Blue</strong>Card®<br />
<strong>Blue</strong>Card Service<br />
Claims Questions Provider web self service should be used to check the status <strong>of</strong> a<br />
<strong>Blue</strong>Card claim. Enter only the member’s <strong>Blue</strong> <strong>Cross</strong> ID number<br />
without the alpha prefix <strong>and</strong> the dates <strong>of</strong> service.<br />
Claim status is also available by calling <strong>Blue</strong> <strong>Cross</strong> provider<br />
services. Status is available via a FAX or automated voice<br />
response.<br />
We encourage you to self service so that our provider services staff<br />
is available to assist with any questions or concerns regarding<br />
claims, claims payment <strong>and</strong> problem resolution.<br />
Please pay special attention to the phone prompts to ensure<br />
connection to the correct representative within <strong>Blue</strong> <strong>Cross</strong> provider<br />
services.<br />
<strong>Blue</strong>Card claims cannot be viewed on BLUELINE.<br />
7-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
<strong>Blue</strong>Card®<br />
Benefits <strong>and</strong> Eligibility You may contact the <strong>Blue</strong>Card eligibility number for benefits <strong>and</strong><br />
eligibility 1-800-676-BLUE (2583) for other plans’ members. If<br />
the automated system on the <strong>Blue</strong>Card eligibility line cannot<br />
identify the three digit alpha prefix that is being stated, after the<br />
second failed attempt, you will automatically be transferred to a<br />
<strong>Blue</strong>Card agent. The <strong>Blue</strong>Card agent will need one <strong>of</strong> the<br />
following answers to be accurate in order to validate:<br />
<strong>Blue</strong>Card Preferred<br />
Provider Organization<br />
(PPO)<br />
1. Alpha prefix<br />
2. Plan code<br />
3. <strong>Name</strong> <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> plan<br />
4. Employee name<br />
5. State in which the member’s plan is located (can be found on<br />
the back <strong>of</strong> the member’s ID card)<br />
You will be asked for the alpha prefix on the ID card <strong>and</strong> will then<br />
be transferred to the member’s plan. They will provide the<br />
information requested.<br />
You may also submit a 270 request via provider web self service<br />
for benefits <strong>and</strong> eligibility. In addition, you could send an<br />
electronic request (EDI) via Availity, but you must register to do<br />
that. * Be sure to include:<br />
1. ID number, including alpha prefix<br />
2. Patient first <strong>and</strong> last name<br />
3. Date <strong>of</strong> birth<br />
* Availity registration information: availity.com.<br />
The <strong>Blue</strong>Card PPO program is a national program that <strong>of</strong>fers<br />
members the PPO level <strong>of</strong> benefits when outside their <strong>Blue</strong> plan<br />
area <strong>and</strong> they obtain services from a physician or hospital<br />
designated as a PPO provider.<br />
You will immediately recognize these PPO members by the<br />
special “PPO in a suitcase” logo on their ID card.<br />
<strong>Blue</strong> <strong>Cross</strong> utilizes the Aware® provider network as our <strong>Blue</strong>Card<br />
PPO network. Members can access information about providers in<br />
this network via the toll free number: 1-800-810-BLUE (2583) or<br />
on the <strong>Blue</strong>Card website, bcbs.com.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-9
<strong>Blue</strong>Card®<br />
Prior Authorization <strong>and</strong><br />
Preadmission<br />
Notification<br />
Any required prior authorizations <strong>and</strong>/or preadmission<br />
notifications for members covered by a <strong>Blue</strong> plan besides <strong>Blue</strong><br />
<strong>Cross</strong> must go through the member’s plan. In these cases, the<br />
member is responsible for obtaining prior authorizations <strong>and</strong><br />
preadmission notifications. However, as a courtesy, you may<br />
contact their plan directly for authorizations using the phone<br />
number listed on the back <strong>of</strong> the member’s ID card or by accessing<br />
the Medical Policy/Precertification/Prior Authorization Router via<br />
providers.bluecrossmn.com<br />
When the length <strong>of</strong> an inpatient hospital stay extends past the<br />
previously approved length <strong>of</strong> stay, any additional days must be<br />
approved. Failure to obtain approval for the additional days may<br />
result in claims processing delays <strong>and</strong> potential payment denials. If<br />
prior authorization or preadmission notification is not obtained <strong>and</strong><br />
is required by the patient’s contract, the patient will be liable for<br />
the charges. To avoid delays in the processing <strong>of</strong> your claims,<br />
please assure the necessary approval(s) are obtained in advance <strong>of</strong><br />
services being rendered.<br />
7-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
<strong>Blue</strong>Card Claims<br />
<strong>Blue</strong>Card®<br />
Claims Submission Be sure to include the complete alpha prefix <strong>and</strong> ID number when<br />
submitting claims. The alpha prefix should have at least three<br />
letters, but may have more, as a portion <strong>of</strong> the ID number. You<br />
must submit these claims directly to <strong>Blue</strong> <strong>Cross</strong> (see exclusions<br />
below). Once <strong>Blue</strong> <strong>Cross</strong> processes the claim you will receive<br />
claims information <strong>and</strong> any appropriate payment on your<br />
electronic remittance advice (835).<br />
Some members have been issued identification cards with an alpha<br />
prefix, but for various reasons the claims cannot process through<br />
the <strong>Blue</strong>Card program. You should still submit these claims to<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> we will forward them to the member’s plan for<br />
processing. We will notify you <strong>of</strong> this on your weekly electronic<br />
remittance advice (835). Even though you have been notified that<br />
the member’s plan will be processing the patient’s claim directly,<br />
you should still direct all inquiries regarding that claim to <strong>Blue</strong><br />
<strong>Cross</strong>. We will act as your single point <strong>of</strong> contact for that claim.<br />
See Claims Processed by the Member’s Plan, later in this chapter.<br />
Submit the claim to <strong>Blue</strong> <strong>Cross</strong> when:<br />
• You provide care to a member from <strong>Minnesota</strong>, or<br />
• You provide care to a member who has coverage with a <strong>Blue</strong><br />
plan in another part <strong>of</strong> the country <strong>and</strong> you are located in<br />
<strong>Minnesota</strong>.<br />
Note: Providers who have agreements with both <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
another <strong>Blue</strong> plan should consult with <strong>Blue</strong> <strong>Cross</strong> about the<br />
h<strong>and</strong>ling <strong>of</strong> non-<strong>Minnesota</strong> member claims.<br />
Exclusions The following are exclusions to the <strong>Blue</strong>Card program. Please<br />
submit these claims as instructed on the ID card:<br />
• Dental services covered under a st<strong>and</strong>-alone dental contract.<br />
• Drug claims billed by a pharmacy.<br />
• Federal Employee Program (FEP).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-11
<strong>Blue</strong>Card®<br />
Electronic Data<br />
Interchange (EDI)<br />
Submission<br />
For Electronic Data Interchange submission:<br />
• All <strong>Blue</strong>Card claims must be sent electronically using the<br />
<strong>Minnesota</strong> Uniform Companion Guide. Refer to Chapter 8,<br />
Claims Filing, for more information regarding electronic<br />
submission <strong>of</strong> claims.<br />
• Be sure to include the alpha prefix with no spaces between the<br />
prefix <strong>and</strong> the ID number.<br />
• Be sure to send the subscriber’s ID number as it appears on the<br />
ID card.<br />
• Be sure to include accurate subscriber <strong>and</strong> patient information.<br />
• Be sure to use the correct patient relationship.<br />
Paper Submission • Effective July 15, 2009, all claims from <strong>Minnesota</strong> providers<br />
must be submitted electronically due to <strong>Minnesota</strong> Statute -<br />
62J.536. (Provider Quick Points QP7-09). Refer to Chapter 8,<br />
Claims Filing, for more information regarding claims<br />
submission.<br />
Coding Code claims as you would for local claims. Refer to Chapter 11,<br />
Coding Policies <strong>and</strong> Guidelines, for more coding information.<br />
Medical Records There are times when the member’s plan will require medical<br />
records to review the <strong>Blue</strong>Card claim. These requests should come<br />
to you from us. If the member’s plan contacts you directly, please<br />
forward all requested records to <strong>Blue</strong> <strong>Cross</strong>. We will coordinate<br />
with the member’s plan. Always include the member’s <strong>Blue</strong> <strong>Cross</strong><br />
ID number with the alpha prefix. Participating providers are not<br />
allowed to bill <strong>Blue</strong> <strong>Cross</strong> for medical records. This is part <strong>of</strong> your<br />
provider agreement <strong>and</strong> requests for payment will not be honored.<br />
Managed Care It is generally the responsibility <strong>of</strong> the member’s plan to approve<br />
or deny claims. This is also true for managed care reviews.<br />
Contrary to your st<strong>and</strong>ard provider contract, you will not be<br />
responsible, <strong>and</strong> the patient may be billed as indicated on your<br />
provider remit, for the following denials when applicable to a<br />
member with coverage through a <strong>Blue</strong> plan other than <strong>Blue</strong> <strong>Cross</strong>:<br />
• Investigative services<br />
• Care management charges or penalties<br />
• Medical necessity<br />
7-12 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Claims Processed by <strong>Blue</strong> <strong>Cross</strong><br />
<strong>Blue</strong>Card®<br />
Claims Notification <strong>Blue</strong> <strong>Cross</strong> will issue claims payment <strong>and</strong> notification directly to<br />
you as a participating provider on our st<strong>and</strong>ard electronic<br />
remittance advice (835) or by posting your remittance to provider<br />
web self service. Statements have been sorted to provide a separate<br />
section for <strong>Blue</strong>Card business for providers billing on the CMS-<br />
1500 form or the 837P electronic format. For those providers<br />
billing on the CMS-1450 (UB-92) or the 837I electronic format,<br />
the claims will not be separated.<br />
Your patients’ Explanation <strong>of</strong> Benefits (EOB) will be issued to<br />
them by the home plan. Should there be a discrepancy between the<br />
patient’s EOB <strong>and</strong> your remittance, please send a copy <strong>of</strong> both to<br />
<strong>Blue</strong> <strong>Cross</strong> provider services for review.<br />
Policies When a <strong>Blue</strong>Card claim is received by <strong>Blue</strong> <strong>Cross</strong> the following<br />
procedures must be followed:<br />
• Providers must comply with all st<strong>and</strong>ard contractual<br />
procedures. Patients cannot be billed as follows, except as<br />
otherwise allowed by law:<br />
• prior to the submission <strong>of</strong> the claim<br />
• for any contractual reductions, or<br />
• prior to the finalization <strong>of</strong> their claims<br />
• Providers will not be responsible, <strong>and</strong> patients may be billed,<br />
for the following denials by the member’s plan:<br />
• Investigative services<br />
• Care management charges or penalties<br />
• Medical necessity<br />
• Non-covered services<br />
• <strong>Blue</strong>Card program exempt services (st<strong>and</strong>-alone dental,<br />
drug claims billed by a pharmacy)<br />
Adjustments Contact us if an adjustment is required. We do need to work with<br />
the member’s plan for adjustments; however, your workflow<br />
should not be different. You may continue to contact <strong>Blue</strong> <strong>Cross</strong><br />
provider services for any questions or status on adjustments for<br />
<strong>Blue</strong>Card claims.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-13
<strong>Blue</strong>Card®<br />
Claims Processed by the Member’s Plan<br />
Claims Notification If the member’s plan is processing the claim because it cannot go<br />
through <strong>Blue</strong>Card processing, you will be notified on your weekly<br />
electronic remittance advice (835).<br />
The claim will be documented <strong>and</strong> the remark message will read,<br />
“This claim has been forwarded to the subscriber’s home plan for<br />
processing.” Contact <strong>Blue</strong> <strong>Cross</strong> for any information regarding<br />
this claim, we will contact the member’s plan. You may bill the<br />
member for these services.<br />
Policies Since this is not a <strong>Blue</strong>Card eligible claim, your <strong>Blue</strong> <strong>Cross</strong><br />
provider agreement generally does not apply.<br />
Adjustments Communicate your adjustment request with <strong>Blue</strong> <strong>Cross</strong>. We will<br />
contact the member’s plan on your behalf.<br />
Appeals Please refer to Chapter 10 for information regarding appeals.<br />
7-14 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Medical Records<br />
Overview Medical Records<br />
<strong>Blue</strong>Card®<br />
<strong>Blue</strong> plans around the country have made improvements to the<br />
medical records process to make it more efficient. We now are<br />
able to send <strong>and</strong> receive medical records electronically among<br />
each other. This new method significantly reduces the time it takes<br />
to transmit supporting documentation for our out <strong>of</strong> area claims,<br />
reduces the need to request records multiple times <strong>and</strong> eliminates<br />
lost or misrouted records.<br />
Under what circumstances may the provider get requests for<br />
medical records for out-<strong>of</strong>-area members?<br />
1. As part <strong>of</strong> the pre-authorization process—If you receive<br />
requests for medical records from other <strong>Blue</strong> plans prior to<br />
rendering services, as part <strong>of</strong> the pre-authorization process,<br />
you will be instructed to submit the records directly to the<br />
member’s plan that requested them. This is the only<br />
circumstance where you would not submit them to <strong>Blue</strong> <strong>Cross</strong><br />
<strong>of</strong> <strong>Minnesota</strong>.<br />
2. As part <strong>of</strong> claim review <strong>and</strong> adjudication—These requests will<br />
come from <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> in a form <strong>of</strong> a letter<br />
requesting specific medical records <strong>and</strong> including instructions<br />
for submission.<br />
<strong>Blue</strong>Card medical record process for claim review<br />
1. An initial communication, generally in the form <strong>of</strong> a letter,<br />
should be received by your <strong>of</strong>fice requesting the needed<br />
information.<br />
2. A remittance may be received by your <strong>of</strong>fice indicating the<br />
claim is being denied pending receipt <strong>and</strong> review <strong>of</strong> records.<br />
Occasionally, the medical records you submit might cross in<br />
the mail with the remittance advice for the claim indicating a<br />
need for medical records. A remittance advice is not a<br />
duplicate request for medical records. If you submitted medical<br />
records previously, but received a remittance advice indicating<br />
records were still needed, please contact <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong><br />
<strong>Minnesota</strong> to ensure your original submission has been<br />
received <strong>and</strong> processed. This will prevent duplicate records<br />
being sent unnecessarily.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-15
<strong>Blue</strong>Card®<br />
Overview (continued) 3. If you received only a remittance advice indicating records are<br />
needed, but you did not receive a medical records request<br />
letter, contact <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> to determine if the<br />
records are needed from your <strong>of</strong>fice.<br />
4. Upon receipt <strong>of</strong> the information, the claim will be reviewed to<br />
determine the benefits.<br />
Helpful ways you can assist in timely processing <strong>of</strong> medical<br />
records<br />
1. If the records are requested following submission <strong>of</strong> the claim,<br />
forward all requested medical records to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong><br />
<strong>Minnesota</strong>.<br />
2. Follow the submission instructions given on the request, using<br />
the specified address or FAX number. The address or FAX<br />
number for medical records may be different than the address<br />
you use to submit claims.<br />
3. Include the cover letter you received with the request when<br />
submitting the medical records. This is necessary to make sure<br />
the records are routed properly once received by <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong><br />
<strong>Minnesota</strong>.<br />
4. Please submit the information to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> as<br />
soon as possible to avoid further delay.<br />
5. Only send the information specifically requested. Frequently,<br />
complete medical records are not necessary.<br />
6. Please do not proactively send medical records with the claim.<br />
Unsolicited claim attachments may cause claim payment<br />
delays.<br />
7-16 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Coordination <strong>of</strong> Benefits (COB) Claims<br />
<strong>Blue</strong>Card®<br />
Guidelines Coordination <strong>of</strong> benefits (COB) refers to how we ensure members<br />
receive full benefits <strong>and</strong> prevent double payment for services when<br />
a member has coverage from two or more sources. The member’s<br />
contract language explains the order for which entity has primary<br />
responsibility for payment <strong>and</strong> which entity has secondary<br />
responsibility for payment.<br />
If you discover the member is covered by more that one health<br />
plan, <strong>and</strong>:<br />
• <strong>Blue</strong> <strong>Cross</strong> or any other <strong>Blue</strong> plan is the primary payer, submit<br />
other carrier’s name <strong>and</strong> address with the claim to <strong>Blue</strong> <strong>Cross</strong><br />
<strong>of</strong> <strong>Minnesota</strong>. If you do not include the COB information with<br />
the claim, the member’s <strong>Blue</strong> plan will have to investigate the<br />
claim. This investigation could delay your payment or result in<br />
a post-payment adjustment, which will increase your volume<br />
<strong>of</strong> bookkeeping.<br />
• Other non-<strong>Blue</strong> health plan is primary <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong><br />
<strong>Minnesota</strong> or any other <strong>Blue</strong> plan is secondary, submit the<br />
claim to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> only after receiving payment<br />
from the primary payer, including the explanation <strong>of</strong> payment<br />
from the primary carrier. If you do not include the COB<br />
information with the claim, the member’s <strong>Blue</strong> plan will have<br />
to investigate the claim. This investigation could delay your<br />
payment or result in a post-payment adjustment, which will<br />
increase your volume <strong>of</strong> bookkeeping.<br />
Coordination <strong>of</strong> Benefits Questionnaire<br />
To streamline our claims processing <strong>and</strong> reduce the number <strong>of</strong><br />
denials related to coordination <strong>of</strong> benefits, a COB questionnaire is<br />
now available to you at providers.bluecrossmn.com that will help<br />
you <strong>and</strong> your patients avoid potential claim issues. The COB form<br />
is in the “Other Forms” section in the Forms <strong>and</strong> Publications area.<br />
When you see any <strong>Blue</strong> members <strong>and</strong> you are aware that they<br />
might have other health insurance coverage (that is,. Medicare),<br />
give a copy <strong>of</strong> the questionnaire to them during their visit. Ask<br />
them to complete the form <strong>and</strong> send it to the <strong>Blue</strong> plan through<br />
which they are covered as soon as possible after leaving your<br />
<strong>of</strong>fice. Members will find the address on the back <strong>of</strong> their member<br />
identification card or by calling the customer service numbers<br />
listed on the back <strong>of</strong> the card. Collecting COB information from<br />
members before you file their claim eliminates the need to gather<br />
this information later, thereby reducing processing <strong>and</strong> payment<br />
delays.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-17
<strong>Blue</strong>Card®<br />
Claim Payment<br />
Guidelines • If you have not received payment for a claim, do not resubmit<br />
the claim; it will be denied as a duplicate. This also causes<br />
member confusion because <strong>of</strong> multiple Explanations <strong>of</strong><br />
Benefits (EOBs). <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong>’s st<strong>and</strong>ard time for<br />
claims processing is 17 days. However, claim processing times<br />
at various <strong>Blue</strong> plans vary.<br />
• If you do not receive your payment or a response regarding<br />
your payment, please call <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> provider<br />
services at (651) 662-5200 or 1-800-262-0820 or visit our<br />
website at providerhub.com to check the status <strong>of</strong> your claim.<br />
• In some cases, a member’s <strong>Blue</strong> plan may pend a claim<br />
because medical review or additional information is necessary.<br />
When resolution <strong>of</strong> a pended claim requires additional<br />
information from you, <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> may either ask<br />
you for the information or give the member’s plan permission<br />
to contact you directly.<br />
7-18 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Claim Status Inquiry<br />
Overview <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> is your single point <strong>of</strong> contact for all<br />
claim inquiries.<br />
Claim status inquires can be done by:<br />
<strong>Blue</strong>Card®<br />
• Phone—call provider service at (651) 662-5200 or<br />
1-800-262-0820.<br />
• Electronically—send a HIPAA transaction 276 (claim status<br />
inquiry) to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> via EDI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-19
<strong>Blue</strong>Card®<br />
Calls from Members <strong>and</strong> Others with Claim<br />
Questions<br />
Overview If members contact you, advise them to contact their <strong>Blue</strong> plan <strong>and</strong><br />
refer them to their ID card for a customer service number.<br />
The member’s plan should not contact you directly regarding<br />
claims issues, but if the member’s plan contacts you <strong>and</strong> asks you<br />
to submit the claim to them, refer them to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong><br />
<strong>Minnesota</strong>.<br />
7-20 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Traditional Medicare-Related Claims<br />
Guidelines The following are guidelines for the processing <strong>of</strong> traditional<br />
Medicare-related claims:<br />
<strong>Blue</strong>Card®<br />
• when Medicare is primary payer, submit claims to your local<br />
Medicare intermediary.<br />
• as <strong>of</strong> January 1, 2008, all <strong>Blue</strong> claims are set up to<br />
automatically crossover to the member’s <strong>Blue</strong> plan after being<br />
adjudicated by the Medicare intermediary.<br />
How do I submit Medicare primary / <strong>Blue</strong> plan secondary claims?<br />
• For members with Medicare primary coverage <strong>and</strong> <strong>Blue</strong> plan<br />
secondary coverage, submit claims to your Medicare<br />
intermediary <strong>and</strong>/or Medicare carrier.<br />
• When submitting the claim, it is essential that you enter the<br />
correct <strong>Blue</strong> plan name as the secondary carrier. This may be<br />
different from the local <strong>Blue</strong> plan. Check the member’s ID<br />
card for additional verification.<br />
• Include the alpha prefix as part <strong>of</strong> the member identification<br />
number. The member’s ID will include the alpha prefix in the<br />
first three positions. The alpha prefix is critical for confirming<br />
membership, coverage <strong>and</strong> key to facilitating prompt<br />
payments.<br />
When you receive the remittance advice from the Medicare<br />
intermediary, look to see if the claim has been automatically<br />
forwarded (crossed over) to the <strong>Blue</strong> plan:<br />
• If the remittance advice indicates that the claim was crossed<br />
over, Medicare has forwarded the claim on your behalf to the<br />
appropriate <strong>Blue</strong> plan <strong>and</strong> the claim is in process. There is no<br />
need to resubmit that claim to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong>.<br />
• If the remittance advice indicates that the claim was not<br />
crossed over, submit the claim to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong><br />
with the Medicare remittance advice.<br />
• In some cases, the member identification card may contain a<br />
COBA ID number. If so, be certain to include that number on<br />
your claim.<br />
• For claim status inquiries, contact <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong><br />
through provider web self service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-21
<strong>Blue</strong>Card®<br />
Guidelines (continued) When should I expect to receive payment?<br />
Claims submit to the Medicare intermediary will be crossed over<br />
to the <strong>Blue</strong> plan only after they have been processed. This process<br />
may take up to 14 business days. This means that the Medicare<br />
intermediary will be releasing the claim to the <strong>Blue</strong> plan for<br />
processing about the same time you receive the Medicare<br />
remittance advice. As a result, it may take an additional 14-30<br />
business days for you to receive payment from the <strong>Blue</strong> plan.<br />
What should I do in the meantime?<br />
If you submitted the claim to the Medicare intermediary/carrier,<br />
<strong>and</strong> haven’t received a response to your initial claim submission,<br />
don’t automatically submit another claim. Rather, you should:<br />
• review the automated resubmission cycle on your claim<br />
system.<br />
• wait 30 days.<br />
• check claims status before resubmitting.<br />
Sending another claim, or having your billing agency resubmit<br />
claims automatically, slows down the claim payment process <strong>and</strong><br />
creates confusion for the member.<br />
Who do I contact if I have questions or to check claim status?<br />
If you have questions, please contact <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong><br />
through provider web self service.<br />
7-22 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Medicare Advantage Claims through <strong>Blue</strong>Card<br />
Overview “Medicare Advantage” (MA) is the program alternative to<br />
st<strong>and</strong>ard Medicare Part A <strong>and</strong> Part B fee-for-service coverage;<br />
generally referred to as “traditional Medicare.”<br />
<strong>Blue</strong>Card®<br />
MA <strong>of</strong>fers Medicare beneficiaries several product options (similar<br />
to those available in the commercial market), including health<br />
maintenance organization (HMO), preferred provider organization<br />
(PPO), point-<strong>of</strong>-service (POS) <strong>and</strong> private fee-for-service (PFFS)<br />
plans.<br />
All Medicare Advantage plans must <strong>of</strong>fer beneficiaries at least the<br />
st<strong>and</strong>ard Medicare Part A <strong>and</strong> B benefits, but many <strong>of</strong>fer<br />
additional covered services as well (for example, enhanced vision<br />
<strong>and</strong> dental benefits).<br />
In addition to these products, Medicare Advantage organizations<br />
may also <strong>of</strong>fer a Special Needs Plan (SNP), which can limit<br />
enrollment to subgroups <strong>of</strong> the Medicare population in order to<br />
focus on ensuring that their special needs are met as effectively as<br />
possible.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-23
<strong>Blue</strong>Card®<br />
Types <strong>of</strong> Medicare<br />
Advantage Plans<br />
Medicare Advantage HMO<br />
A Medicare Advantage HMO is a Medicare managed care option<br />
in which members typically receive a set <strong>of</strong> predetermined <strong>and</strong><br />
prepaid services provided by a network <strong>of</strong> physicians <strong>and</strong><br />
hospitals. Generally (except in urgent or emergency care<br />
situations), medical services are only covered when provided by in<br />
network providers. The level <strong>of</strong> benefits <strong>and</strong> the coverage rules<br />
may vary by Medicare Advantage plan.<br />
Medicare Advantage POS<br />
A Medicare Advantage POS program is an option available<br />
through some Medicare HMO programs. It allows members to<br />
determine—at the point <strong>of</strong> service—whether they want to receive<br />
certain designated services within the HMO system, or seek such<br />
services outside the HMO’s provider network (usually at greater<br />
cost to the member). The Medicare Advantage POS plan may<br />
specify which services will be available outside <strong>of</strong> the HMOs<br />
provider network.<br />
Medicare Advantage PPO<br />
A Medicare Advantage PPO is a plan that has a network <strong>of</strong><br />
providers, but unlike traditional HMO products, it allows members<br />
who enroll access to services provided outside the contracted<br />
network <strong>of</strong> providers. Required member cost-sharing may be<br />
greater when covered services are obtained out <strong>of</strong> network.<br />
Medicare Advantage PPO plans may be <strong>of</strong>fered on a local or<br />
regional (frequently multi-state) basis. Special payment <strong>and</strong> other<br />
rules apply to regional PPOs.<br />
Medicare Advantage PFFS<br />
A Medicare Advantage PFFS plan is a plan in which the member<br />
may go to any Medicare approved doctor or hospital that accepts<br />
the plan’s terms <strong>and</strong> conditions <strong>of</strong> participation. Acceptance is<br />
“deemed” to occur where the provider is aware, in advance <strong>of</strong><br />
furnishing services, that the member is enrolled in a PFFS product<br />
<strong>and</strong> where the provider has reasonable access to the terms <strong>and</strong><br />
conditions <strong>of</strong> participation.<br />
The Medicare Advantage organization, rather than the Medicare<br />
program, pays physicians <strong>and</strong> providers on a fee-for-services basis<br />
for services rendered to such members. Members are responsible<br />
for cost-sharing, as specified in the plan.<br />
7-24 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Types <strong>of</strong> Medicare<br />
Advantage Plans<br />
(continued)<br />
Medicare Advantage PFFS varies from the other <strong>Blue</strong> products<br />
you might currently participate in:<br />
<strong>Blue</strong>Card®<br />
• You can see <strong>and</strong> treat any Medicare Advantage PFFS member<br />
without having a contract with <strong>Blue</strong> <strong>Cross</strong>.<br />
• If you do provide services, you will do so under the terms <strong>and</strong><br />
conditions <strong>of</strong> that member’s <strong>Blue</strong> plan.<br />
• Please refer to the back <strong>of</strong> the member’s ID card for<br />
information on accessing the plan’s terms <strong>and</strong> conditions. You<br />
may choose to render services to a MA PFFS member on an<br />
episode <strong>of</strong> care (claim-by-claim) basis.<br />
• MA PFFS terms <strong>and</strong> conditions may vary for each <strong>Blue</strong> <strong>Cross</strong><br />
a plan <strong>and</strong> we advise that you review them before servicing<br />
MA PFFS members.<br />
• Submit your MA PFFS claims to <strong>Blue</strong> <strong>Cross</strong>.<br />
Medicare Advantage Medical Savings Account (MSA)<br />
Medicare Advantage Medical Savings Account (MSA) is a<br />
Medicare health plan option made up <strong>of</strong> two parts. One part is a<br />
Medicare MSA Health Insurance Policy with a high deductible;<br />
The other part is a special savings account where Medicare<br />
deposits money to help members pay their medical bills.<br />
Eligibility Verification • Verify eligibility by contacting 1-800-676-BLUE (2583) <strong>and</strong><br />
providing an alpha prefix or by submitting an electronic<br />
inquiry to www.providerhub.com <strong>and</strong> providing the alpha<br />
prefix.<br />
• If you experience difficulty obtaining eligibility information,<br />
please record the alpha prefix <strong>and</strong> report it to <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong><br />
<strong>Minnesota</strong>.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-25
<strong>Blue</strong>Card®<br />
Medicare Advantage<br />
Claims Submission<br />
Reimbursement for<br />
Medicare Advantage<br />
PPO, HMO, POS<br />
• Submit all Medicare Advantage claims to <strong>Blue</strong> <strong>Cross</strong>.<br />
• Do not bill Medicare directly for any services rendered to a<br />
Medicare Advantage member.<br />
• Payment will be made directly by a <strong>Blue</strong> plan.<br />
Based upon the Centers for Medicare <strong>and</strong> Medicaid Services<br />
(CMS) regulations, if you are a provider who accepts Medicare<br />
assignment <strong>and</strong> you render services to a Medicare Advantage<br />
member for whom you have no obligation to provide services<br />
under your contract with a <strong>Blue</strong> plan, you will generally be<br />
considered a non-contracted provider <strong>and</strong> be reimbursed the<br />
equivalent <strong>of</strong> the current Medicare allowed amount for all covered<br />
services (i.e., the amount you would collect if the beneficiary were<br />
enrolled in traditional Medicare).<br />
Medicare<strong>Blue</strong> PPO <strong>and</strong> Group Medicare<strong>Blue</strong> PPO are regional<br />
Medicare Advantage plans with a Medicare contract.<br />
Medicare<strong>Blue</strong> PPO <strong>and</strong> Group Medicare<strong>Blue</strong> PPO coverage is<br />
separately issued by one <strong>of</strong> the following plans:<br />
• Wellmark <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> Iowa<br />
• <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
• <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> Montana<br />
• <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> Nebraska<br />
• <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> North Dakota<br />
• Wellmark <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> South Dakota<br />
• <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> Wyoming.<br />
Special payment rules apply to hospitals <strong>and</strong> certain other entities<br />
(e.g., skilled nursing facilities) that are non-contracted providers.<br />
Providers should make sure they underst<strong>and</strong> the applicable<br />
Medicare Advantage reimbursement rules.<br />
Other than the applicable member cost-sharing amounts,<br />
reimbursement is made directly by a <strong>Blue</strong> plan or its br<strong>and</strong>ed<br />
member’s affiliate. In general, you may collect only the applicable<br />
cost-sharing (e.g., copayment or coinsurance) amount from the<br />
member at the time <strong>of</strong> service, <strong>and</strong> may not otherwise charge or<br />
balance bill the member.<br />
Note: Enrollee payment responsibilities can include more than<br />
copayments (e.g., deductibles).<br />
Please review the remittance notice concerning Medicare<br />
Advantage plan payment, member’s payment responsibility <strong>and</strong><br />
balance billing limitations.<br />
7-26 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Reimbursement for<br />
Medicare Advantage<br />
PPO, HMO, POS<br />
(continued)<br />
<strong>Blue</strong>Card®<br />
Plan Contract: services for local <strong>and</strong> regional <strong>Blue</strong> Medicare<br />
Advantage members<br />
Situation below is where the provider has a contract with <strong>Blue</strong><br />
<strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> for MA <strong>and</strong> provides service to a <strong>Blue</strong> <strong>Cross</strong><br />
<strong>of</strong> <strong>Minnesota</strong> <strong>Blue</strong> MA member.<br />
If you are a provider who accepts Medicare assignment <strong>and</strong> you<br />
render services to a local or regional Medicare Advantage member<br />
for whom you have an obligation to provide services under your<br />
contract with a <strong>Blue</strong> plan, you will be considered a contracted<br />
provider <strong>and</strong> be reimbursed per the contractual agreement.<br />
Providers should make sure they underst<strong>and</strong> the applicable<br />
Medicare Advantage reimbursement rules <strong>and</strong> their individual<br />
plan contractual arrangements.<br />
Other than the applicable member cost-sharing amounts,<br />
reimbursement is made directly by a <strong>Blue</strong> plan. In general, you<br />
may collect only the applicable cost-sharing (e.g., copayment or<br />
coinsurance) amounts from the member at the time <strong>of</strong> service, <strong>and</strong><br />
may not otherwise charge or balance bill the member.<br />
Please review the remittance notice concerning Medicare<br />
Advantage plan payment, member’s payment responsibility <strong>and</strong><br />
balance billing limitations.<br />
Plan Contract: Services for out-<strong>of</strong>-area Medicare Advantage<br />
<strong>Blue</strong> members<br />
Situation below is where the provider has a contract with <strong>Blue</strong><br />
<strong>Cross</strong> <strong>of</strong> <strong>Minnesota</strong> for local <strong>and</strong> regional MA <strong>and</strong> provides<br />
services for out-<strong>of</strong>-area <strong>Blue</strong> MA members.<br />
If you are a provider who accepts Medicare assignment, has a <strong>Blue</strong><br />
plan contract to provide services for local <strong>and</strong> regional Medicare<br />
Advantage enrollees only, <strong>and</strong> you render services to out-<strong>of</strong>-area<br />
<strong>Blue</strong> Medicare Advantage members, you will be reimbursed at the<br />
Medicare allowed amount (i.e., the amount you would collect if<br />
the beneficiary were enrolled in traditional Medicare). Providers<br />
should make sure they underst<strong>and</strong> the applicable Medicare<br />
Advantage reimbursement rules <strong>and</strong> their individual plan<br />
contractual arrangements.<br />
Other than the applicable member cost-sharing amounts,<br />
reimbursement is made directly by a <strong>Blue</strong> plan. In general, you<br />
may collect only the applicable cost-sharing (e.g., copayment or<br />
coinsurance) amounts from the member at the time <strong>of</strong> service <strong>and</strong><br />
may not otherwise charge or balance bill the member.<br />
Please review the remittance notice concerning Medicare<br />
Advantage plan payment, member’s payment responsibility <strong>and</strong><br />
balance billing limitations.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10) 7-27
<strong>Blue</strong>Card®<br />
Reimbursement for<br />
Medicare Advantage<br />
Private-Fee-for-Service<br />
(PFFS)<br />
Services for out-<strong>of</strong>-area <strong>Blue</strong> Medicare Advantage PFFS<br />
members<br />
Situation below is where the provider renders services for out-<strong>of</strong>area<br />
MA PFFS members.<br />
If you have rendered services for a <strong>Blue</strong> out-<strong>of</strong>-area Medicare<br />
Advantage PFFS member but are not obligated to provide services<br />
to such member under a contract with a <strong>Blue</strong> plan, you will<br />
generally be reimbursed the Medicare allowed amount for all<br />
covered services (i.e., the amount you would collect if the<br />
beneficiary were enrolled in traditional Medicare). Providers<br />
should make sure they underst<strong>and</strong> the applicable Medicare<br />
Advantage reimbursement rules.<br />
Other than the applicable member cost-sharing amounts,<br />
reimbursement is made directly by a <strong>Blue</strong> plan. In general, you<br />
may collect only the applicable cost-sharing (e.g., copayment or<br />
coinsurance) amounts from the member at the time <strong>of</strong> service <strong>and</strong><br />
may not otherwise charge or balance bill the member.<br />
Please review the remittance notice concerning Medicare<br />
Advantage plan payment, member’s payment responsibility <strong>and</strong><br />
balance billing limitations.<br />
7-28 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (12/30/10)
Table <strong>of</strong> Contents<br />
Chapter 8<br />
Claims Filing<br />
Administrative Simplification...................................................................................................8-4<br />
Introduction............................................................................................................................8-4<br />
Web-based Claim Submission, Eligibility, <strong>and</strong> Remittance Tool ......................................... 8-4<br />
Pharmacy <strong>and</strong> Dental Claims................................................................................................. 8-4<br />
Pre-system Edits.....................................................................................................................8-5<br />
Claims with Attachments....................................................................................................... 8-5<br />
Claims with Coordination <strong>of</strong> Benefits ................................................................................... 8-7<br />
Medicare/Uniform Companion Guide Coding Alignment ..................................................8-10<br />
Questions..............................................................................................................................8-11<br />
1500 HICF Form...................................................................................................................... 8-12<br />
Pr<strong>of</strong>essional Claim Submission ...........................................................................................8-12<br />
1500 HICF <strong>Manual</strong> ..............................................................................................................8-12<br />
About the NUCC..................................................................................................................8-12<br />
UB-04 (CMS 1450) Form......................................................................................................... 8-13<br />
Institutional Claim Submission............................................................................................ 8-13<br />
UB-04 <strong>Manual</strong> ..................................................................................................................... 8-13<br />
About the NUBC..................................................................................................................8-13<br />
Ordering Forms <strong>and</strong> <strong>Manual</strong>s ................................................................................................ 8-14<br />
HCPCS, CPT <strong>and</strong> ICD-9-CM <strong>Manual</strong>s ...............................................................................8-14<br />
HIPAA Implementation Guides........................................................................................... 8-14<br />
<strong>Minnesota</strong> Uniform Companion Guides..............................................................................8-14<br />
1500 HICF (CMS-1500) UB-04 (CMS-1450) Forms .........................................................8-14<br />
UB-04 <strong>Manual</strong> ..................................................................................................................... 8-14<br />
1500 HICF <strong>Manual</strong> ..............................................................................................................8-14<br />
Pr<strong>of</strong>essional/837P Billing......................................................................................................... 8-15<br />
Zero Billed Charges .............................................................................................................8-15<br />
Linking <strong>and</strong> Sequencing ...................................................................................................... 8-15<br />
Place <strong>of</strong> Service Codes......................................................................................................... 8-15<br />
Site <strong>of</strong> Service......................................................................................................................8-15<br />
Freest<strong>and</strong>ing Ambulatory Surgery Center Billing ............................................................... 8-16<br />
K3 Segment Usage Instructions for Condition Codes ......................................................... 8-17<br />
Institution (837I) /Facility Billing........................................................................................... 8-18<br />
Claim Format Regulations ...................................................................................................8-18<br />
Procedure Code Regulations................................................................................................ 8-19<br />
Revenue Codes (FL 42) .......................................................................................................8-19<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-1
Claims Filing<br />
HCPCS/ Accommodation Rates/HIPPS Rate Codes (FL 44)..............................................8-19<br />
Duplicate Billing..................................................................................................................8-19<br />
Treatment Room ..................................................................................................................8-20<br />
Observation Room ............................................................................................................... 8-20<br />
Clinic Charges......................................................................................................................8-20<br />
Transfer Case .......................................................................................................................8-20<br />
Single facility claim submission ..........................................................................................8-21<br />
Zero Billed Charges .............................................................................................................8-22<br />
Lactation Education .............................................................................................................8-22<br />
0636 Drugs Requiring Prior Auth........................................................................................ 8-22<br />
Present on Admission (POA)............................................................................................... 8-22<br />
Claims Filing............................................................................................................................. 8-24<br />
Timely Filing .......................................................................................................................8-24<br />
Claims <strong>Cross</strong>over for Medicare <strong>and</strong> Medicare Supplement ................................................ 8-24<br />
Medicare <strong>Cross</strong>over ............................................................................................................. 8-25<br />
837I <strong>Cross</strong>over Information................................................................................................. 8-25<br />
837P <strong>Cross</strong>over Information................................................................................................ 8-25<br />
Duplicate Claims.................................................................................................................. 8-26<br />
Submission <strong>of</strong> Claims .......................................................................................................... 8-26<br />
Cancel/Void <strong>and</strong> Replacement Claims ................................................................................ 8-27<br />
Release <strong>of</strong> Medical Records.................................................................................................8-32<br />
Provider Assistance Requested............................................................................................ 8-32<br />
Medical Records Management Process Improvement.........................................................8-32<br />
Verify Member Identity .......................................................................................................8-32<br />
Verifying Patient Eligibility................................................................................................. 8-33<br />
Basic Character Set Values in the Electronic Transaction................................................... 8-34<br />
Claim Service Dates Restricted to Same Calendar Month .................................................. 8-35<br />
Reporting MNCare <strong>and</strong> Sales Tax ....................................................................................... 8-36<br />
Rural Health Clinics <strong>and</strong> Federally Qualified Health Centers............................................ 8-37<br />
Billing for Medicare Primary............................................................................................... 8-37<br />
Billing Other Than Medicare Primary .................................................................................8-37<br />
Coordination <strong>of</strong> Benefits (COB) ............................................................................................. 8-38<br />
Overview..............................................................................................................................8-38<br />
Primacy Determination ........................................................................................................ 8-38<br />
Coordination <strong>of</strong> Benefits Types .............................................................................................. 8-39<br />
Workers’ Compensation ...................................................................................................... 8-40<br />
No-fault Auto.......................................................................................................................8-40<br />
Subrogation..........................................................................................................................8-40<br />
TEFRA.................................................................................................................................8-41<br />
DEFRA ................................................................................................................................8-41<br />
COBRA................................................................................................................................8-41<br />
OBRA ..................................................................................................................................8-41<br />
Non-Physician Health Care Practitioners ............................................................................. 8-42<br />
Introduction..........................................................................................................................8-42<br />
Eligibility Criteria ................................................................................................................8-42<br />
Definitions............................................................................................................................8-42<br />
8-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims Filing<br />
Employment.........................................................................................................................8-43<br />
Incident To...........................................................................................................................8-43<br />
Direct Supervision ............................................................................................................... 8-44<br />
General Supervision.............................................................................................................8-44<br />
Collaboration/ Independent Practice....................................................................................8-44<br />
Chiropractic Doctors <strong>and</strong> Multidisciplinary Clinics............................................................8-44<br />
Surgical Technicians............................................................................................................8-45<br />
Mid-level Practitioners.........................................................................................................8-45<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-3
Claims Filing<br />
Administrative Simplification<br />
Introduction <strong>Minnesota</strong> Statute 62J.536, requires health care providers <strong>and</strong><br />
group purchasers (payers, health plans) to exchange eligibility<br />
requests, claims <strong>and</strong> remittances electronically using st<strong>and</strong>ard<br />
formats. The intent <strong>of</strong> the law is to reduce costs, simplify <strong>and</strong><br />
speed up health care transactions, <strong>and</strong> to give providers <strong>and</strong> health<br />
plans one set <strong>of</strong> rules to follow for electronic transactions. This<br />
statute applies to all health care providers in <strong>Minnesota</strong>, regardless<br />
<strong>of</strong> participating status.<br />
Web-based Claim<br />
Submission, Eligibility,<br />
<strong>and</strong> Remittance Tool<br />
Pharmacy <strong>and</strong> Dental<br />
Claims<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) <strong>of</strong>fers a nocost,<br />
web-based tool through Availity to comply with the<br />
<strong>Minnesota</strong> Statute 62J.536. Availity, an independent company,<br />
also provides no-cost solutions to obtain eligibility <strong>and</strong> benefits as<br />
well as viewing your remittance information. Availity, an<br />
independent company, is a one stop shop that optimizes<br />
information exchange between multiple heath care stakeholders<br />
through a single secure network. Providers may also take<br />
advantage <strong>of</strong> a range <strong>of</strong> optional, value-added services for a<br />
nominal cost. For more information contact Availity at<br />
availity.com to register for their no-cost web-based tools.<br />
The requirement to submit all claims electronically includes dental<br />
<strong>and</strong> pharmacy formatted claim types. <strong>Blue</strong> <strong>Cross</strong> is completing<br />
system changes to accept <strong>and</strong> properly adjudicate these electronic<br />
claim types. Due to the complexity <strong>of</strong> the changes <strong>and</strong> need for<br />
extensive testing, <strong>Blue</strong> <strong>Cross</strong> can not accept dental formatted or<br />
pharmacy formatted electronic claims at this time. Pharmacy <strong>and</strong><br />
dental providers should continue to submit these claim types on<br />
paper until notified by <strong>Blue</strong> <strong>Cross</strong>.<br />
8-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims Filing<br />
Pre-system Edits <strong>Blue</strong> <strong>Cross</strong> has aligned our pre-system edits with the rules<br />
published in the Uniform Claims Companion Guides found on the<br />
Administrative Uniformity Committee (AUC) website at<br />
health.state.mn.us/auc.<br />
Claims with<br />
Attachments<br />
<strong>Blue</strong> <strong>Cross</strong> accepts claims with attachments electronically. The<br />
claim must adhere to the electronic rules found in the Uniform<br />
Companion Guides <strong>and</strong> include the appropriate populated data as<br />
indicated in section 4.2.3.4 <strong>of</strong> the guides. The related attachment<br />
should be faxed to <strong>Blue</strong> <strong>Cross</strong> at 1-800-793-6928 or mailed to:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
P.O. Box 64338<br />
St. Paul, MN 55164-0338<br />
The attachment cover sheet found on the AUC website must be<br />
used as the first page on each claim attachment. Instructions for<br />
completing the attachment cover sheet are also available on the<br />
AUC website.<br />
<strong>Blue</strong> <strong>Cross</strong> has compiled a list <strong>of</strong> questions <strong>and</strong> answers in<br />
response to provider inquiries regarding sending attachments on<br />
electronic claim transactions.<br />
Questions <strong>and</strong> Answers<br />
1. My clinic has a policy <strong>of</strong> covering all documentation with<br />
an internal cover sheet to protect PHI. Should I be covering<br />
the attachments I am sending with this cover sheet?<br />
No. Per the AUC Guidelines the only acceptable cover sheet<br />
for attachments is the AUC Uniform COVER SHEET For<br />
Health Care Claim Attachments. This form can be modified to<br />
include a PHI message on the bottom <strong>of</strong> the page if you desire,<br />
but is the ONLY acceptable cover sheet when sending<br />
attachments.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-5
Claims Filing<br />
Claims with<br />
Attachments<br />
(continued)<br />
2. Can I send appeals, adjustment requests, status checks <strong>and</strong><br />
general correspondence using the AUC Uniform COVER<br />
SHEET For Health Care Claim Attachments?<br />
No. The AUC Uniform COVER SHEET For Health Care<br />
Claim Attachments is ONLY for use when submitting<br />
attachments for first time claims that have been sent<br />
electronically. It is not to be used for appeals, adjustment<br />
requests, status checks or general correspondence. There are<br />
separate forms <strong>and</strong> FAX numbers for these types <strong>of</strong><br />
correspondence. Please use the appropriate cover sheet for<br />
each type <strong>of</strong> correspondence. Below is a list <strong>of</strong> the forms <strong>and</strong><br />
FAX numbers for each type <strong>of</strong> correspondence:<br />
AUC Uniform COVER SHEET For Health Care Claim<br />
Attachments: 1-800-793-6928 (use for attachment to<br />
original claims only)<br />
AUC Appeal Request Form: (651) 662-2745 (use to submit<br />
claim appeals)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Claim<br />
Adjustment/Status Check Form:<br />
(651) 662-2745 (use to submit adjustments or to request a<br />
status check)<br />
For further reference on the submission <strong>of</strong> attachments,<br />
please visit the AUC website: health.state.mn.us/auc<br />
3. Can I change or remove the AUC Logo on the AUC<br />
Uniform COVER SHEET For Health Care Claim<br />
Attachments?<br />
No. Our automated intake process looks for the AUC Logo<br />
when preparing to scan the attachment. If the LOGO is missing<br />
or has been changed, the automated process cannot take place.<br />
This causes delays in the imaging <strong>of</strong> your document <strong>and</strong><br />
ultimately can lead to delays in the processing <strong>and</strong> payment <strong>of</strong><br />
your claim. This is another reason why you must not use an<br />
internal cover sheet. You must also fax your attachment headup<br />
or top <strong>of</strong> the page first as the recognition s<strong>of</strong>tware only<br />
scans the top third <strong>of</strong> the page for the LOGO.<br />
8-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims with<br />
Attachments<br />
(continued)<br />
Claims with<br />
Coordination <strong>of</strong><br />
Benefits<br />
Claims Filing<br />
4. If I have the Other Insurance Carrier payment information<br />
in the 837 electronic claim transaction, do I also have to<br />
send the EOB in an attachment or notify <strong>Blue</strong> <strong>Cross</strong> that it<br />
is in my <strong>of</strong>fice?<br />
No. Per the AUC Guidelines, you should submit the Other<br />
Insurance Carrier payment information within the 837. HIPAA<br />
regulations forbid populating the claim record with Other<br />
Insurance Carrier information <strong>and</strong> sending the same<br />
information in an attachment. They further forbid sending data<br />
in an attachment that can be codified within the claim record.<br />
5. Can I send the attachment before I send the 837 claim<br />
transaction?<br />
Yes, provided you complete the PWK segment on the 837 with<br />
the appropriate information from the AUC Uniform COVER<br />
SHEET For Health Care Claim Attachments. The PWK<br />
segment must include the Report Type code, Report<br />
Transmission Code <strong>and</strong> the Transaction Control Number (the<br />
Attachment Control Number on the AUC Uniform COVER<br />
SHEET For Health Care Claim Attachments). Failure to<br />
include this information on the 837 will cause delays in<br />
processing <strong>and</strong> payment <strong>and</strong> may result in a denial <strong>of</strong> your<br />
claim.<br />
<strong>Blue</strong> <strong>Cross</strong> accepts electronic claims with previous payer payment<br />
information populated per the requirements in the <strong>Minnesota</strong><br />
Uniform Companion Guides. For proper adjudication claims must<br />
contain all previous payer group codes, ANSI Claim Adjustment<br />
Reason Codes <strong>and</strong> Remittance Advice Remark Codes as you<br />
received them from the previous payer. These claims do not<br />
require an attachment when populated within the claim record.<br />
Refer to the <strong>Minnesota</strong> Uniform Companion Guides, section<br />
4.2.3.5 for more information.<br />
<strong>Blue</strong> <strong>Cross</strong> has compiled a list <strong>of</strong> questions <strong>and</strong> answers in<br />
response to provider inquiries regarding the electronic submission<br />
<strong>of</strong> Coordination <strong>of</strong> Benefits information.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-7
Claims Filing<br />
Claims with<br />
Coordination <strong>of</strong><br />
Benefits (continued)<br />
Questions <strong>and</strong> Answers<br />
1. I underst<strong>and</strong> that there is information on the HIPAA 835<br />
transaction that I have to include on the electronic 837<br />
COB transaction. Can you tell me what I have to include so<br />
I can make sure I get paid accurately?<br />
It is important to use the <strong>Minnesota</strong> Uniform Companion<br />
Guides along with the HIPAA Implementation Guides to<br />
ensure the correct segments <strong>and</strong> elements are completed. The<br />
2320, 2330A, 2330B, <strong>and</strong> the 2430 loops carry a good portion<br />
<strong>of</strong> the COB information a payer needs to process a secondary<br />
claim.<br />
The HIPAA 835 transaction provides most <strong>of</strong> the necessary<br />
information to complete the appropriate segments <strong>and</strong><br />
elements.<br />
The HIPAA 835 transaction from the prior payer(s) should<br />
provide the CAS segments (loops 2100 <strong>and</strong>/or 2110), CLP<br />
segment (loop 2100), <strong>and</strong> the SVC segment (loop 2110), which<br />
are used to complete the 837 COB transaction.<br />
2. I underst<strong>and</strong> the CAS segment is important for the correct<br />
processing <strong>of</strong> my COB 837 transaction. Where do I get the<br />
CAS segment information from?<br />
Again, the CAS segment information on the 837 COB<br />
transactions should come directly from the prior payer(s)<br />
HIPAA 835 or Remittance Advice/Explanation <strong>of</strong> Benefits.<br />
This information must never be altered or combined in any<br />
manner.<br />
3. Do I need to do any combining <strong>of</strong> Claim Adjustment<br />
Reason Codes or change them to specific codes a<br />
Supplemental Insurer might want?<br />
No, when completing the COB information on the 837 use the<br />
information as it was provided on the prior payer(s) HIPAA<br />
835 or Remittance Advice/Explanation <strong>of</strong> Benefits. Never<br />
change or alter any <strong>of</strong> the prior payer(s) payment information<br />
including the Claim Adjustment Reason Codes (CARC), Claim<br />
Adjustment Group Codes, <strong>and</strong> Remittance Advice Remark<br />
Codes. Changing codes is a violation <strong>of</strong> HIPAA <strong>and</strong> could<br />
result in payment errors or processing delays. Per the HIPAA<br />
Implementation Guide, “Codes <strong>and</strong> associated amounts should<br />
come from 835s (Remittance Advice) received on the claim.”<br />
Payers utilize the codes to adjudicate based on the information<br />
sent.<br />
8-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims with<br />
Coordination <strong>of</strong><br />
Benefits (continued)<br />
Claims Filing<br />
4. I know there are Medicare primary claims that should<br />
have crossed over <strong>and</strong> Medicare has had some problems<br />
lately with not being able to cross claims over to<br />
supplemental payers. Should I send all my Medicare<br />
Primary COB claims just in case?<br />
No, “automatic” rebilling <strong>of</strong>ten results in duplicate claims,<br />
increases administrative costs, <strong>and</strong> delays processing. Please<br />
refer to Medicare Primary COB Claim section later in this<br />
chapter.<br />
If your claim is not showing as crossed over on provider web<br />
self-service after 30 days from the date you received your<br />
Medicare payment, then you may submit the claim<br />
electronically populating the claim record with the COB<br />
information exactly as you received it on your Medicare ERA.<br />
5. I have situations where my Medicare primary claims have<br />
been adjusted <strong>and</strong> Medicare is now paying on claims they<br />
have denied. How do I send these COB claims to my<br />
supplemental insurer?<br />
These claims are COB adjustments to the original claim <strong>and</strong><br />
should crossover to us directly from Medicare. Again, please<br />
refer to Medicare Primary COB Claim section later in this<br />
chapter.<br />
If the adjustment did not crossover as it should have within 30<br />
days after you received the updated Medicare ERA, submit an<br />
adjustment/replacement claim.<br />
6. I have a claim where Medicare paid first. They have now<br />
decided to pay one <strong>of</strong> the services on my three line claim.<br />
Should I just send in the COB claim for that one line for<br />
<strong>Blue</strong> <strong>Cross</strong> to pay the coinsurance <strong>and</strong> deductible?<br />
No, never send a partial claim. This would be a violation <strong>of</strong> the<br />
rules in the <strong>Minnesota</strong> Uniform Companion Guides. Again,<br />
this could result in duplicate claims, increased administrative<br />
costs, <strong>and</strong> processing delays. If the prior payer has made a<br />
change to the original or prior claim processing outcome, the<br />
original or prior claim must be adjusted to ensure the<br />
secondary payment is correct. A “partial” claim should never<br />
be sent regardless <strong>of</strong> whether it is an original or adjustment. As<br />
noted in response to question #3 above, if the prior payer has<br />
adjudicated a claim with three services lines, all three service<br />
lines should be sent to the secondary payer. Never alter the<br />
charges <strong>and</strong> critical claim information when sending it to a<br />
secondary / tertiary payer for payment consideration.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-9
Claims Filing<br />
Claims with<br />
Coordination <strong>of</strong><br />
Benefits (continued)<br />
Medicare/Uniform<br />
Companion Guide<br />
Coding Alignment<br />
7. I have talked with other providers <strong>and</strong> they tell me that a<br />
COB claim must balance. What must balance?<br />
The claim paid amounts must be equal to or greater than the<br />
line level paid amounts. The CAS segments must always<br />
reflect exactly what the prior payer has indicated on HIPAA<br />
835 transaction or Remittance Advice/Explanation <strong>of</strong> Benefits.<br />
Do not add or combine the CAS information. Typically, the<br />
pr<strong>of</strong>essional claim allowed <strong>and</strong> paid amounts should not be<br />
greater than the billed amounts. More information regarding<br />
balancing is available in the HIPAA Implementation Guides<br />
available for purchase from Washington Publishing<br />
(wpc-edi.com).<br />
8. When the prior payer is Medicare how do I list them as the<br />
primary payer? Do I list them by the Medicare Office,<br />
CMS, Federal Medicare, the name <strong>of</strong> the Medicare<br />
contractor, etc?<br />
When Medicare is the prior payer, we suggest listing the prior<br />
payer as “Medicare.”<br />
9. I am sending COB in the 837 transaction <strong>and</strong> also sending<br />
the EOB as an attachment with the report type code EB<br />
<strong>and</strong> report transmission code AA. This is to make sure that<br />
you get the COB information.<br />
In these situations, the Report <strong>of</strong> Transmission (PWK02) is AA<br />
indicating the EOB is available upon request at the provider<br />
<strong>of</strong>fice. The HIPAA 837 Implementation Guides, Report <strong>of</strong><br />
Transmission (PWK Segment), states “The PWK segment is<br />
required if there is paper documentation supporting this claim.<br />
The PWK segment should not be used if the information<br />
related to the claim is being sent within the 837 ST-SE<br />
envelope.” Therefore sending the information within the<br />
transaction <strong>and</strong> also sending the PWK would be non-compliant<br />
<strong>and</strong> result in a rejection.<br />
<strong>Blue</strong> <strong>Cross</strong> has made several system modifications to accept<br />
claims coded using the rules indicated by either Medicare or the<br />
<strong>Minnesota</strong> Uniform Companion Guides, Appendix A. Some billed<br />
charges still may not be covered due to member benefits or <strong>Blue</strong><br />
<strong>Cross</strong> payment policy. Code your claims to meet the specifications<br />
set forth in the <strong>Minnesota</strong> Uniform Companion Guides.<br />
8-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims Filing<br />
Questions Questions regarding the content <strong>of</strong> the PA02 electronic reports or<br />
Availity payer reports should be directed to provider services at<br />
(651) 662-5200 or 1-800-262-0820. Questions regarding the payer<br />
electronic reports not being received should be directed to your<br />
clearinghouse. If your clearinghouse is Availity, please refer to<br />
their website at availity.com.<br />
For questions regarding the attachment requirements, attachment<br />
cover sheet <strong>and</strong> related instructions, Coordination <strong>of</strong> Benefits or<br />
coding requirements, refer to the AUC website at<br />
health.state.mn.us/auc.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-11
Claims Filing<br />
1500 HICF Form<br />
Pr<strong>of</strong>essional Claim<br />
Submission<br />
The paper 1500 Health Insurance Claim Form (HICF) (also<br />
referred to as the CMS 1500) is accepted only from out-<strong>of</strong>-state<br />
nonparticipating providers per <strong>Minnesota</strong> Statute 62J.536 <strong>and</strong> the<br />
<strong>Blue</strong> <strong>Cross</strong> provider contracts.<br />
The electronic transaction 837P is the only accepted claim<br />
submission format for pr<strong>of</strong>essional claims.<br />
1500 HICF <strong>Manual</strong> The National Uniform Claim Committee (NUCC) has a reference<br />
instruction manual detailing how to complete the 1500 HICF form.<br />
The purpose <strong>of</strong> this manual is to help st<strong>and</strong>ardize nationally the<br />
manner in which the form is being completed. A copy <strong>of</strong> the<br />
instruction manual is available on the NUCC website -<br />
www.nucc.org.<br />
About the NUCC The National Uniform Claim Committee is a voluntary<br />
organization whose members include representatives from major<br />
provider, payer, health researchers, <strong>and</strong> other organizations<br />
representing billing pr<strong>of</strong>essionals, <strong>and</strong> electronic st<strong>and</strong>ard<br />
developers.<br />
The NUCC maintains the uniform data set known as the National<br />
Uniform Claim Committee Data Set designed for the noninstitutional<br />
claims. The NUCC is also a signatory to a<br />
Memor<strong>and</strong>um <strong>of</strong> Underst<strong>and</strong>ing with five other organizations<br />
designated by the U.S. Department <strong>of</strong> Health <strong>and</strong> Human Services<br />
to collectively serve as the Designated St<strong>and</strong>ard Maintenance<br />
Organizations (DSMO) to the HIPAA Transaction St<strong>and</strong>ard<br />
Implementation Guides.<br />
8-12 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
UB-04 (CMS 1450) Form<br />
Institutional Claim<br />
Submission<br />
Claims Filing<br />
The paper UB-04 (also referred to as the CMS-1450) is accepted<br />
only from out-<strong>of</strong>-state nonparticipating providers per <strong>Minnesota</strong><br />
Statute 62J.536 <strong>and</strong> the <strong>Blue</strong> <strong>Cross</strong> provider contracts.<br />
The electronic transaction 837I is the only accepted claim<br />
submission format for institutional claims.<br />
UB-04 <strong>Manual</strong> The National Uniform Billing Committee (NUBC) publishes a<br />
manual containing the claim data specifications that are submitted<br />
on the 837I or UB-04 claim format <strong>and</strong> guidelines on completion<br />
<strong>of</strong> the UB-04 form.<br />
About the NUBC Established in 1975, the NUBC is the <strong>of</strong>ficial data content body<br />
responsible for maintaining the data set for institutional health care<br />
providers. Representation includes provider, payer, electronic<br />
st<strong>and</strong>ards development organizations, public health data st<strong>and</strong>ards<br />
organizations, <strong>and</strong> others. The NUBC is also one <strong>of</strong> six Designated<br />
St<strong>and</strong>ard Maintenance Organizations (DSMO) responsible for the<br />
maintenance <strong>and</strong> development <strong>of</strong> HIPAA administrative<br />
simplification transaction st<strong>and</strong>ards. (Note: Also see<br />
http://www.nubc.org/INFORMATION_ON_UB-04.pdf)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-13
Claims Filing<br />
Ordering Forms <strong>and</strong> <strong>Manual</strong>s<br />
HCPCS, CPT <strong>and</strong><br />
ICD-9-CM <strong>Manual</strong>s<br />
HIPAA Implementation<br />
Guides<br />
<strong>Minnesota</strong> Uniform<br />
Companion Guides<br />
1500 HICF (CMS-1500)<br />
UB-04 (CMS-1450)<br />
Forms<br />
HCPCS, CPT <strong>and</strong> ICD-9-CM manuals can be purchased from<br />
major bookstores or publishers, such as the American Medical<br />
Association.<br />
To order national Electronic Data Interchange Transaction Set<br />
Implementation guides on paper or electronic versions, contact<br />
Washington Publishing Company.<br />
1-800-972-4334<br />
Or visit their website at:<br />
www.wpc-edi.com<br />
<strong>Minnesota</strong> Uniform Companion Guides containing instructions for<br />
electronic transactions are available free <strong>of</strong> charge on the AUC<br />
website under “Guides” at:<br />
health.state.mn.us/auc/<br />
To order 1500 HICF <strong>and</strong> UB-04 forms contact:<br />
U.S. Government Printing Office<br />
(202) 512-0455 or visit the website at:<br />
cms.hhs.gov/CMSForms/<br />
You may also contact form vendors or publishers, such as the<br />
American Medical Association or the American Hospital<br />
Association.<br />
UB-04 <strong>Manual</strong> To order the UB-04 <strong>Manual</strong> contact:<br />
National Uniform Billing Committee (NUBC) at<br />
nubc.org/become.html for more information <strong>and</strong> an order form,<br />
or call the American Hospital Association at (312) 422-3390 for<br />
questions.<br />
1500 HICF <strong>Manual</strong> The National Uniform Claim Committee 1500 Health Insurance<br />
Claim Form Reference Instruction <strong>Manual</strong> is available at<br />
nucc.org/.<br />
8-14 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Pr<strong>of</strong>essional/837P Billing<br />
Claims Filing<br />
Zero Billed Charges <strong>Blue</strong> <strong>Cross</strong> will allow zero-billing or no charge submission lines<br />
on claims.<br />
Linking <strong>and</strong><br />
Sequencing<br />
It is essential to communicate the primary diagnosis for the service<br />
performed, especially if more than one diagnosis is related to a line<br />
item. Adjudication is based on the first linked diagnosis.<br />
Linking/sequencing rules:<br />
Sequence numbers relate to the ICD-9-CM diagnosis codes as<br />
1, 2, 3 <strong>and</strong> 4.<br />
The primary diagnosis is listed first in the sequence if more<br />
than one diagnosis is related.<br />
Place <strong>of</strong> Service Codes Only nationally assigned place <strong>of</strong> service codes are accepted.<br />
These codes are available at the following web address:<br />
http://www.cms.hhs.gov/Place<strong>of</strong>ServiceCodes/Downloads/place<br />
<strong>of</strong>service.pdf<br />
Site <strong>of</strong> Service <strong>Blue</strong> <strong>Cross</strong> is specifying, for clarity, the difference between a<br />
facility <strong>and</strong> a non-facility with respect to the place <strong>of</strong> service<br />
where a service was rendered. For billing purposes, pr<strong>of</strong>essional<br />
(837P) billers should use an appropriate place <strong>of</strong> service code to<br />
indicate where services were rendered. Examples <strong>of</strong> facilities<br />
include hospitals <strong>and</strong> ambulatory surgery centers. Examples <strong>of</strong><br />
non-facilities include a provider's <strong>of</strong>fice <strong>and</strong> all places not listed<br />
below.<br />
The following is a current comprehensive list <strong>of</strong> facilities, as<br />
defined by <strong>Blue</strong> <strong>Cross</strong>:<br />
Place <strong>of</strong> Service Code Place <strong>of</strong> Service <strong>Name</strong><br />
21 Inpatient hospital<br />
22 Outpatient hospital<br />
23 Emergency room - hospital<br />
24 Ambulatory surgical center<br />
26 Military treatment facility<br />
31 Skilled nursing facility<br />
34 Hospice<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-15
Claims Filing<br />
Site <strong>of</strong> Service<br />
(continued)<br />
Freest<strong>and</strong>ing<br />
Ambulatory Surgery<br />
Center Billing<br />
Place <strong>of</strong> Service Code Place <strong>of</strong> Service <strong>Name</strong><br />
41 Ambulance - l<strong>and</strong><br />
42 Ambulance - air & water<br />
51 Inpatient psychiatric facility<br />
52 Psychiatric facility - partial<br />
53 Community mental health<br />
center<br />
56 Psychiatric residential treatment<br />
center<br />
In order to streamline our administrative processes <strong>and</strong> comply<br />
with regulatory requirements, <strong>Blue</strong> <strong>Cross</strong> contracts with<br />
Freest<strong>and</strong>ing Ambulatory Surgery Centers as pr<strong>of</strong>essional<br />
submitters <strong>and</strong> requires the following guidelines <strong>and</strong> provisions:<br />
Use <strong>of</strong> Pr<strong>of</strong>essional Claims Submission Formats —<br />
Freest<strong>and</strong>ing Ambulatory Surgery Center providers submit<br />
claims utilizing a HIPAA 837P claims transaction, in<br />
compliance with <strong>Minnesota</strong> Statute 62J.52. Use national place<br />
<strong>of</strong> service code 24.<br />
Fee Schedule Based Payment Methodology – APC weights<br />
were used to create fee schedule allowances (Allowance=APC<br />
weight x conversion factor) for each procedure code, as<br />
appropriate.<br />
Recognition <strong>of</strong> Multiple Surgeries <strong>and</strong> Bilateral<br />
Procedures – For multiple surgeries, the procedure with the<br />
highest allowed amount is reimbursed at 100% <strong>of</strong> the allowed<br />
amount. Subsequent services are reimbursed at 50% <strong>of</strong> the<br />
allowed amount. Bilateral surgeries are billed on one line with<br />
the -50 modifier <strong>and</strong> are reimbursed at 150% <strong>of</strong> the allowed<br />
amount.<br />
Adjudication <strong>of</strong> Services at the Claim Line Level – Payment<br />
is calculated at the lesser <strong>of</strong> 100% <strong>of</strong> the provider’s regular<br />
billed charge or the <strong>Blue</strong> <strong>Cross</strong> fee schedule allowance,<br />
implemented at a claim line/service level.<br />
8-16 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Freest<strong>and</strong>ing<br />
Ambulatory Surgery<br />
Center Billing<br />
(continued)<br />
K3 Segment Usage<br />
Instructions for<br />
Condition Codes<br />
Claims Filing<br />
Payment <strong>of</strong> Individual Procedures – APC methodology<br />
determines which services are included/excluded from separate<br />
reimbursement, including implants/devices <strong>and</strong> tissue. Services<br />
excluded from separate reimbursement are listed on the<br />
provider fee schedule with a zero allowance. Pr<strong>of</strong>essional<br />
services, including anesthesia, should not be billed under this<br />
agreement. Individual provider NPI numbers are not required.<br />
Corneal tissue – Claims that contain corneal tissue charges<br />
must be submitted with an attachment containing a copy <strong>of</strong> the<br />
invoice for that corneal tissue.<br />
99199 – The code 99199 (unlisted special service, procedure or<br />
report) will not be considered for separate reimbursement when<br />
submitted by an ASC. 99199 will be denied as provider<br />
liability. No additional reimbursement will be considered on<br />
appeal.<br />
L8699 - Code L8699 (prosthetic implant, not otherwise<br />
specified) will not be considered for separate reimbursement<br />
when submitted by an ASC as it is not part <strong>of</strong> the ASC<br />
contracted fee schedule. L8699 will be denied as provider<br />
liability. No additional reimbursement will be considered on<br />
appeal.<br />
Condition Code<br />
The NUBC has added condition codes to their code set to identify<br />
situations where workers’ compensation requires duplicate or<br />
appeal submissions. The 837P format does not include a<br />
st<strong>and</strong>ardized way <strong>of</strong> reporting condition codes. To report<br />
applicable condition codes on a pr<strong>of</strong>essional claim, the K3<br />
segment should be used.<br />
BG is the qualifier to indicate this value <strong>and</strong> should be followed by<br />
the appropriate condition code (refer to the NUBC Guide <strong>and</strong> Code<br />
Set available from the National Uniform Billing Committee at<br />
nubc.org.<br />
Report at 2300 loop only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-17
Claims Filing<br />
Institution (837I) /Facility Billing<br />
Claim Format<br />
Regulations<br />
HIPAA Administrative Simplification code <strong>and</strong> transaction<br />
regulations dictate the st<strong>and</strong>ard claim format <strong>and</strong> codes for<br />
electronically submitted claims. Institutional claims are billed on<br />
the 837I electronic format. The paper equivalent is the UB-04<br />
claim form.<br />
<strong>Blue</strong> <strong>Cross</strong> considers the following providers as institutional <strong>and</strong><br />
as such, should bill on the institutional claim format (837I).<br />
Category Definition<br />
Home health<br />
agency<br />
HHA is a public agency or private organization<br />
that is primarily engaged in providing skilled<br />
nursing services <strong>and</strong> other therapeutic services,<br />
such as physical therapy, occupational therapy,<br />
medical social services <strong>and</strong> home health aide<br />
services. Home health agencies can be<br />
freest<strong>and</strong>ing or hospital attached. Care is rendered<br />
in the home <strong>and</strong> is in lieu <strong>of</strong> hospital confinement.<br />
Hospice Hospice programs provide health care for<br />
terminally ill patients. Care may be done in the<br />
patient’s home, at special hospice units, or a<br />
separate hospice care facility.<br />
Hospital An institution that provides medical, diagnostic<br />
<strong>and</strong> surgical care. Services can be rendered on an<br />
inpatient or outpatient basis.<br />
Nonresidential<br />
treatment<br />
center<br />
This type <strong>of</strong> institution is the same as a residential<br />
primary treatment center with the exception that<br />
services are rendered on an outpatient basis only.<br />
Nursing home A Skilled Nursing Facility provides skilled<br />
nursing care <strong>and</strong> related services for patients who<br />
require medical or nursing care; or rehabilitation<br />
services for injured, disabled or sick people.<br />
8-18 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claim Format<br />
Regulations<br />
(continued)<br />
Procedure Code<br />
Regulations<br />
Category Definition<br />
Psychiatric<br />
hospital<br />
Residential<br />
primary<br />
treatment<br />
center<br />
(IP chem dep)<br />
Claims Filing<br />
A psychiatric hospital provides care to<br />
emotionally ill patients. These facilities must be<br />
licensed by the state in which they are located.<br />
Residential treatment programs for chemical<br />
dependency are planned <strong>and</strong> purposeful sets <strong>of</strong><br />
conditions <strong>and</strong> events for the care <strong>of</strong> inebriated<br />
<strong>and</strong> drug dependent persons which provides care<br />
<strong>and</strong> treatment for five or more inebriate or drug<br />
dependent persons on a 24 hour basis. Excluded<br />
for this definition are receiving (detoxification)<br />
centers.<br />
The medical procedure code set for inpatient services is ICD-9-<br />
CM procedure codes. Procedure information will be reported on<br />
outpatient claims using HCPCS codes.<br />
Revenue Codes (FL 42) A revenue code identifies a specific accommodation <strong>and</strong>/or<br />
ancillary service or billing calculation. A revenue code is four<br />
characters. The first digit is usually a 0 (zero); however, there are<br />
codes that begin with numbers other than 0 (100X, 210X, 310X). It<br />
is important to report all four digits.<br />
HCPCS/<br />
Accommodation<br />
Rates/HIPPS Rate<br />
Codes (FL 44)<br />
For inpatient bills, the accommodation rate relating to the room<br />
<strong>and</strong> board revenue code is entered.<br />
For outpatient bills, report the HCPCS code, if applicable, to<br />
indicate the specific outpatient service. Some HCPCS codes or<br />
billing situations may require submission <strong>of</strong> modifiers. Modifiers<br />
are reported following the HCPCS code. <strong>Blue</strong> <strong>Cross</strong> accepts all<br />
valid modifiers. Although we currently do not automatically<br />
adjudicate the claim/service based on modifiers, it is still important<br />
to submit all modifiers, if applicable.<br />
Duplicate Billing <strong>Blue</strong> <strong>Cross</strong> will only reimburse the pr<strong>of</strong>essional or clinic services<br />
when a patient is seen in a clinic setting (POS 11). Facilities that<br />
have clinics physically located onsite or next to a hospital<br />
frequently bill an additional claim either electronically or on an<br />
837I with a place <strong>of</strong> service 22 for the same services that the<br />
physician is billing. In some cases, facilities submit revenue code<br />
0361. We consider this practice duplicate billing. Facility overhead<br />
is included in the pr<strong>of</strong>essional reimbursement weighting <strong>and</strong><br />
conversion factor; therefore, complete <strong>and</strong> final reimbursement<br />
will be made on the pr<strong>of</strong>essional claim only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-19
Claims Filing<br />
Treatment Room <strong>Blue</strong> <strong>Cross</strong> considers specialty services <strong>of</strong> a treatment room as an<br />
overhead expense reimbursed as part <strong>of</strong> the physician’s<br />
pr<strong>of</strong>essional fee. Therefore, billing facility fees through the 0760,<br />
0761 or 0769 codes duplicates the physician’s pr<strong>of</strong>essional claim<br />
(837P) <strong>and</strong> will deny as provider liability.<br />
If Medicare if primary, <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong> or <strong>Blue</strong> Plus is secondary,<br />
we will accept the 0760, 0761 or 0769 revenue codes, <strong>and</strong> process<br />
according to Medicare’s guidelines.<br />
Observation Room Observation Care, billed under revenue code 0762, is allowed for<br />
admits <strong>of</strong> fewer than 24 hours. A claim for observation services<br />
over 24 hours will be processed as an inpatient claim.<br />
Clinic Charges Clinic charges, billed under revenue code 051X, are considered an<br />
overhead expense reimbursed as part <strong>of</strong> the physician’s<br />
pr<strong>of</strong>essional fee. Therefore, billing facility fees through the 0510-<br />
0519 revenue codes duplicates the physician’s pr<strong>of</strong>essional claim<br />
<strong>and</strong> will deny as provider liability.<br />
Transfer Case A transfer case is defined as a patient who is being discharged<br />
from one facility to another.<br />
Patient status codes are a required field on the institutional claim<br />
(837I). This code indicates the patient’s status as <strong>of</strong> the “Through”<br />
date <strong>of</strong> the billing period. It is important to note that the patient<br />
status code indicates a destination <strong>and</strong> not a level or type <strong>of</strong> care<br />
received.<br />
When a patient is transferred/discharged to another facility, patient<br />
status may affect reimbursement. All patient status codes are<br />
accepted but not all will result in a transfer case classification. The<br />
following patient status codes are used by <strong>Blue</strong> <strong>Cross</strong> to classify a<br />
transfer case.<br />
Code Definition<br />
02<br />
05<br />
Discharged/Transferred to a Short-Term General Hospital<br />
for Inpatient Care<br />
Discharged/Transferred to a Designated Cancer Center or<br />
Children’s Hospital<br />
Usage Note: Transfers to non-designated cancer hospitals<br />
should use Code 02. A list <strong>of</strong> (National Cancer Institute)<br />
Designated Cancer Centers can be found at<br />
www3.cancer.gov/cancercenters/centerslist.html<br />
8-20 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Transfer Case<br />
(continued)<br />
Code Definition<br />
Claims Filing<br />
43 Discharged/Transferred to a Federal Health Care Facility<br />
65<br />
70<br />
Discharged/Transferred to a Psychiatric Hospital or<br />
Psychiatric Distinct Part Unit <strong>of</strong> a Hospital<br />
Discharged/Transferred to Another Type <strong>of</strong> Health Care<br />
Institution not Defined Elsewhere in this Code List<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-21
Claims Filing<br />
Single facility claim<br />
submission<br />
<strong>Blue</strong> <strong>Cross</strong> generally will not accept additional facility claims for<br />
the same encounter, normally referred to as late charges. To assure<br />
correct adjudication <strong>and</strong> payment <strong>of</strong> services, <strong>Blue</strong> <strong>Cross</strong> requires<br />
all related services to be submitted on the same single facility<br />
claim (837I).<br />
Late charges – A late charge refers to those claims that the<br />
provider is submitting after an admit-through-discharge claim<br />
or for the same encounter. A late charge contains charges<br />
omitted from the original bill <strong>and</strong> the charges are submitted as<br />
an add-on to the original bill. A late charge bill is not allowed<br />
according to the <strong>Minnesota</strong> Uniform Companion Guide for<br />
Institutional Claims. It is also not allowed for paper claim<br />
submission.<br />
Encounter – Encounter means an instance <strong>of</strong> direct<br />
provider/practitioner to patient interaction, in an outpatient<br />
facility setting, for the purpose <strong>of</strong> diagnosing, evaluating or<br />
treating the patient’s condition, <strong>and</strong> during which eligible<br />
health services are rendered to the member.<br />
Exceptions – Exceptions that may justify separate claims may<br />
include:<br />
Separate ER visits – separate emergency room visits on<br />
the same date <strong>of</strong> service<br />
Ambulance services<br />
Late charges – unrelated diagnosis: Outpatient charges<br />
with same date <strong>of</strong> service submitted as separate claims with<br />
unrelated diagnosis will no longer be denied as late<br />
charges. The duplicate review process has been updated<br />
with the following examples <strong>of</strong> exceptions to late charge<br />
(replacement claim) processing. Use these as a guide to<br />
determine if the claim situation meets the criteria as<br />
‘unrelated’.<br />
1. Patient has a mammogram, subsequently, in another<br />
department, the patient received chemotherapy (for<br />
other than breast cancer).<br />
2. Patient receives therapy, subsequently, in another<br />
department, the patient has an electrocardiogram.<br />
3. Patient is seen for a radiation therapy, subsequently,<br />
in another department, the patient is seen for routine<br />
screening.<br />
4. Patient receives therapy <strong>and</strong> subsequently visits the<br />
ER for a unrelated condition (e.g., injury or acute<br />
illness unrelated to the therapy received)<br />
8-22 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims Filing<br />
Zero Billed Charges <strong>Blue</strong> <strong>Cross</strong> will allow zero-billing or no charge submission lines<br />
on claims.<br />
Lactation Education For billing purposes, lactation services are considered to be part <strong>of</strong><br />
the mother’s charges <strong>and</strong> should not be billed on the newborn’s<br />
claim.<br />
0636 Drugs Requiring<br />
Prior Auth<br />
Present on Admission<br />
(POA)<br />
Submit all claims for lactation education on the 837I claim form<br />
using revenue code 0942. These charges must be submitted on the<br />
mother’s original maternity/delivery claim <strong>and</strong> require a narrative<br />
description.<br />
Claims for lactation services submitted under the infant’s name or<br />
number will be rejected.<br />
If lactation education is necessary after discharge, it can be billed<br />
as part <strong>of</strong> the post-partum visit under the mother’s identification<br />
number.<br />
Revenue code 0636, by definition, is for drugs requiring detailed<br />
coding. A HCPCS code must always be submitted with 0636.<br />
However, some drugs that may be submitted under this revenue<br />
code also require prior authorization. The following are examples<br />
that require prior authorization:<br />
IVIG<br />
Aminolevulinic Acid<br />
Factor products<br />
<strong>Blue</strong> <strong>Cross</strong> requires the present on admission (POA) indicator on<br />
all claims (Medicare <strong>and</strong> commercial, including the<br />
Medicare<strong>Blue</strong> SM PPO [Regional PPO] claims, Platinum <strong>Blue</strong> SM<br />
[Cost], Secure<strong>Blue</strong> SM [HMO SNP], Care<strong>Blue</strong> SM [HMO SNP] <strong>and</strong><br />
<strong>Blue</strong> Advantage) for inpatient admissions to general acute care<br />
hospitals.<br />
General Reporting Requirements<br />
The POA indicator is required for all claims involving<br />
Medicare <strong>and</strong> commercial inpatient admissions to general<br />
acute care hospitals.<br />
The POA indicator is assigned to principal <strong>and</strong> secondary<br />
diagnoses.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-23
Claims Filing<br />
Present on Admission<br />
(POA) (continued)<br />
Present on admission is defined as present at the time the order<br />
for inpatient admission occurs. Conditions that develop during<br />
an outpatient encounter while in the emergency room, under<br />
observation or during outpatient surgery are also considered as<br />
present on admission.<br />
If the condition would not be coded <strong>and</strong> reported based on<br />
Uniform Hospital Discharge Data Set definitions <strong>and</strong> current<br />
coding guidelines, then the POA would not be reported.<br />
The POA indicator is not required for the external cause <strong>of</strong><br />
injury code unless it is being reported as an “other diagnosis.”<br />
Critical Access Hospitals, Maryl<strong>and</strong> waiver hospitals, longterm<br />
care hospitals (LTCH), cancer hospitals <strong>and</strong> children’s<br />
inpatient facilities are exempt from this requirement.<br />
Form Completion Instructions<br />
For electronic claims using the 837I, refer to the <strong>Minnesota</strong><br />
Uniform Companion Guide for the Institutional Electronic Health<br />
Care Claim Transaction (ANSI ASC X12 837I). Information on<br />
submission <strong>of</strong> the POA indicator is found in appendix D <strong>of</strong> the<br />
guide. The guide can be accessed at the following link:<br />
health.state.mn.us/auc/mn837i.pdf. POA indicators should only<br />
be submitted along with correlating DX codes.<br />
On UB-04 (CMS-1450) paper claims, the POA indicator is the<br />
eighth digit <strong>of</strong> Form Locator (FL) 67, Principal Diagnosis <strong>and</strong> the<br />
eighth digit <strong>of</strong> each <strong>of</strong> the Other Diagnosis fields FL 67 A-Q. One<br />
POA indicator is submitted per diagnosis. POA indicators should<br />
only be submitted along with correlating diagnosis codes.<br />
Use the POA indicators as you would normally submit to<br />
Medicare. For more information, refer to<br />
cms.hhs.gov/HospitalAcqCond<br />
8-24 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims Filing<br />
Claims Filing<br />
Timely Filing Most member contracts contain a time limit for claims submittal.<br />
The limit is usually six (6) months after the date <strong>of</strong> service, with a<br />
few exceptions. Timely filing for Federal Employee Program<br />
(FEP) members can be found in Chapter 5- ID Cards/Coverage<br />
Options. Participating providers are required to submit original<br />
claims within six (6) months <strong>of</strong> the date <strong>of</strong> service. The provider is<br />
liable for claims not submitted within the timely filing limit.<br />
Claims <strong>Cross</strong>over for<br />
Medicare <strong>and</strong> Medicare<br />
Supplement<br />
For medical care that involves follow-up, such as surgery <strong>and</strong><br />
routine postoperative care, it is most efficient to bill us after all<br />
services have been completed, as long as it is within the time limit.<br />
Replacement Claims<br />
<strong>Blue</strong> <strong>Cross</strong>’ requirements for timely filing <strong>of</strong> replacement claims is<br />
six calendar months from the process date <strong>of</strong> the predecessor claim<br />
There is no timely filing limit on cancel claims (claim frequency<br />
code <strong>of</strong> 8).<br />
Provider-Submitted Appeals<br />
<strong>Blue</strong> <strong>Cross</strong>’ requirements for timely filing <strong>of</strong> provider-submitted<br />
appeals is 90 days from the process date <strong>of</strong> the claim<br />
The claims crossover system reduces your paperwork by using the<br />
Medicare claim form to process both Medicare <strong>and</strong> Medicare<br />
Supplement benefits. Through the crossover, Medicare generates a<br />
second claim automatically for members who have secondary or<br />
supplemental benefits with us. Providers have only one claim form<br />
to submit—the 837P for Medicare Part B or the 837I for Medicare<br />
Part A.<br />
While <strong>Blue</strong> <strong>Cross</strong> can only accept changes from the member, we<br />
encourage providers who are aware <strong>of</strong> Health Insurance Claim<br />
Number (HICN) changes to assist their patients in communicating<br />
this information to us.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-25
Claims Filing<br />
Medicare <strong>Cross</strong>over <strong>Blue</strong> <strong>Cross</strong> provides COBC a weekly eligibility file <strong>of</strong> all <strong>Blue</strong><br />
<strong>Cross</strong> members enrolled for coverage under the Medicare program.<br />
When Medicare processes a claim, the Medicare patient’s HICN<br />
will be compared to the HICNs on the eligibility file sent by us. If<br />
found, the date <strong>of</strong> service on the Medicare claim will be compared<br />
to the <strong>Blue</strong> <strong>Cross</strong> coverage effective <strong>and</strong> cancel dates. If the<br />
claim’s date <strong>of</strong> service falls within those dates, the claim will be<br />
crossed over to us electronically.<br />
837I <strong>Cross</strong>over<br />
Information<br />
837P <strong>Cross</strong>over<br />
Information<br />
The current message indicating the claim was sent to <strong>Blue</strong> <strong>Cross</strong><br />
will continue to be displayed on the patient’s Medicare Summary<br />
Notice (MSN) or on the Explanation <strong>of</strong> Medicare Benefits<br />
(EOMB). Medicare will indicate on the provider’s Remittance<br />
Advice (RA) if the claim was sent to the supplemental insurer. On<br />
the Intermediary RA, claim status codes <strong>of</strong> 19, 20, or 21 indicate<br />
that the claim was crossed over. If the HICN is not found on the<br />
<strong>Blue</strong> <strong>Cross</strong> eligibility file, or if the date <strong>of</strong> service on the claim is<br />
outside the given <strong>Blue</strong> <strong>Cross</strong> coverage effective <strong>and</strong> cancel dates,<br />
the claim will not be forwarded to us electronically.<br />
A note associated with the ANSI remark code indicates which<br />
payer will receive the claim information. Providers will continue to<br />
see MA18 <strong>and</strong> the name <strong>of</strong> the payer on the Medicare RA when<br />
the payment information is forwarded to a single payer. However,<br />
code N89 will be used when the payment information is forwarded<br />
to multiple payers; only one <strong>of</strong> those payers will be named on the<br />
RA even though the payment information is forwarded to multiple<br />
payers.<br />
Paper claims submitted to <strong>Blue</strong> <strong>Cross</strong> with the Medicare RA<br />
attached <strong>and</strong> the N89 remark code stating the payment information<br />
was forwarded to <strong>Blue</strong> <strong>Cross</strong> will be returned to the provider.<br />
Adjusted Medicare B claims will not be crossed over to us.<br />
If the claim is not forwarded, then:<br />
The statement or code indicating the claim was forwarded to us<br />
will not appear on the MSN, EOMB or RA.<br />
The patient or provider must submit the electronic claim to us<br />
populating Medicare’s payment information within the claim<br />
record.<br />
8-26 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims Filing<br />
Duplicate Claims Duplicate billing adds millions <strong>of</strong> dollars each year to health care<br />
administrative costs. Many providers operate under the erroneous<br />
assumption that frequent rebilling leads to faster payment.<br />
Unnecessary rebilling increases your overhead costs as well as<br />
ours. Below are several ways you can help reduce duplicate claims<br />
costs:<br />
When you file the claim, be sure to tell your patients not to bill<br />
on his/her own.<br />
Eliminate ‘‘automatic’’ rebillings. Wait 30 calendar days for us<br />
to process your claim.<br />
Before you rebill use provider web self-service, call<br />
BLUELINE ® , use a 276/277 transaction or call provider<br />
services for claim status information.<br />
Don’t submit previously billed claims with new claims “just to<br />
be safe.” This only delays payment <strong>of</strong> all new claims.<br />
If you receive a Medicare RA showing that the claim has<br />
electronically been ‘‘crossed over’’ to us, do not submit the<br />
paper RA as a claim.<br />
If a claim has been denied, resubmitting the paper RA will only<br />
result in a second denial. Either correct fields on the claim <strong>and</strong><br />
submit a replacement claim or submit an appeal as appropriate.<br />
Submission <strong>of</strong> Claims Our goal is to pay your claims as quickly as possible. By following<br />
the above suggestions, you can help hold down everyone’s<br />
administrative costs.<br />
To ensure the proper administration <strong>of</strong> benefits by <strong>Blue</strong> <strong>Cross</strong>,<br />
providers shall submit claims to <strong>Blue</strong> <strong>Cross</strong> even when their claims<br />
have been paid in full by other third parties such as Medicare.<br />
When submitting claims in these cases, the provider shall populate<br />
the previous payer’s payment information within the claim.<br />
Providers shall submit claims to <strong>Blue</strong> <strong>Cross</strong> for all services<br />
provided, even in cases when the provider suspects a service will<br />
not be covered except charges identified in chapter 9, page 9-5.<br />
This will ensure the proper administration <strong>of</strong> benefits <strong>and</strong> take<br />
advantage <strong>of</strong> changes in coverage that may occur after the provider<br />
checks benefits.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-27
Claims Filing<br />
Cancel/Void <strong>and</strong><br />
Replacement Claims<br />
<strong>Minnesota</strong> statute 62J.536, requires providers to submit all claims<br />
electronically. This requirement includes all cancel <strong>and</strong><br />
replacement claims as well as original submissions. Cancel claims<br />
are claims that should not have been billed or where key claim<br />
information such as the billing provider or patient name were<br />
submitted incorrectly. Replacement claims are sent when data<br />
submitted on the original claim was incorrect or incomplete.<br />
<strong>Minnesota</strong> providers <strong>and</strong> out <strong>of</strong> state providers who participate<br />
with <strong>Blue</strong> <strong>Cross</strong> are no longer allowed to submit adjustment<br />
requests via paper or through provider web self-service at<br />
providerhub.com. Providers are required to adhere to the State <strong>of</strong><br />
<strong>Minnesota</strong> Uniform Companion Guide requirements <strong>and</strong> the AUC<br />
Best Practices for replacement claims. Additionally, provider<br />
services will no longer accept requests to change data elements<br />
within a claim as these should be sent electronically as<br />
replacement claims. Provider services will still accept requests to<br />
adjust claims in situations where the claim processed incorrectly<br />
even though correct information was provided on the original<br />
submission.<br />
Exceptions<br />
Exceptions to this electronic replacement claims enforcement are<br />
as follows:<br />
Dental formatted adjustment requests will still be accepted if<br />
received on paper.<br />
Pharmacy formatted adjustment requests will still be accepted<br />
if received on paper.<br />
Nonparticipating providers that are located in counties that<br />
border <strong>Minnesota</strong> are exempt from the statute, therefore paper<br />
claims will still be accepted from these providers.<br />
Adjustment Requests received from the Veterans<br />
Administration (VA) <strong>and</strong> Indian Health Services.<br />
Additional Information<br />
If you are unable to send electronic replacement <strong>and</strong>/or cancel<br />
claims, <strong>Blue</strong> <strong>Cross</strong> has secured the services <strong>of</strong> Availity to provide<br />
a free web-based tool for provider data entry <strong>of</strong> claims. To learn<br />
more about submitting claims using Availity’s no-cost web-based<br />
tool, go to availity.com.<br />
8-28 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Cancel/Void <strong>and</strong><br />
Replacement Claims<br />
(continued)<br />
Claims Filing<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> its affiliates have completed system changes to<br />
accept <strong>and</strong> properly adjudicate electronic cancel <strong>and</strong> replacement<br />
claims.<br />
Following are some <strong>of</strong> the common questions related to proper<br />
submission requirements. Section A contains general information,<br />
<strong>and</strong> section B is for specific h<strong>and</strong>ling <strong>of</strong> coordination <strong>of</strong> benefits<br />
(COB) related scenarios.<br />
Section A- General Information<br />
1. What is an example <strong>of</strong> a replacement claim? I have read<br />
the AUC description <strong>and</strong> would like some clarity on these<br />
claims.<br />
A replacement claim, to paraphrase the <strong>Minnesota</strong> Uniform<br />
Companion Guides for claims, is used to completely replace a<br />
previously submitted claim when data within the claim record<br />
is added, changed or deleted. An example would be a<br />
pr<strong>of</strong>essional claim sent with all diagnosis pointers set to “1.”<br />
On review by the provider after original payment, it is<br />
determined the second procedure was done in reference to the<br />
third diagnosis on the claim. A replacement claim is sent to<br />
correct the diagnosis pointer on line 2.<br />
See section 4.2.3.2 <strong>of</strong> the <strong>Minnesota</strong> Uniform Companion<br />
Guides <strong>and</strong> the related AUC Replacement/Void Claims Best<br />
Practice available on the AUC website at<br />
health.state.mn.us/auc.<br />
2. Can I send a replacement claim if I have the wrong<br />
subscriber ID on the previous submission?<br />
No. According to the AUC Replacement/Void Claims Best<br />
Practice, “When identifying elements change, a void<br />
submission is required to eliminate the previously submitted<br />
claim.” Changes to identifying information related to the<br />
billing provider, patient, payer, subscriber or statement covers<br />
period dates, require that a cancel claim transaction be<br />
submitted for the original claim <strong>and</strong> that a new claim with the<br />
corrected information be submitted to the payer. These<br />
requirements are similar to the Centers for Medicare &<br />
Medicaid Services (CMS) requirements.<br />
3. Can I send an attachment on a replacement claim?<br />
Yes, if it is relevant to the changes being made on the<br />
replacement claim or needed to support a particular coding<br />
change. For example, the addition <strong>of</strong> a -59 modifier to indicate<br />
that the service being billed is a distinct procedure or service<br />
will require supporting medical documentation to be submitted<br />
with the replacement claim.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-29
Claims Filing<br />
Cancel/Void <strong>and</strong><br />
Replacement Claims<br />
(continued)<br />
4. If <strong>Blue</strong> <strong>Cross</strong> denied my claim because the date <strong>of</strong> injury<br />
was required but not submitted in the claim, can I send an<br />
AUC Appeal Request Form to have the claim reconsidered<br />
<strong>and</strong> list the requested date <strong>of</strong> injury in the Reason for<br />
Appeal section?<br />
No. You must submit a replacement claim with the corrected<br />
data (injury date) in the 837 transaction.<br />
5. What is an appeal?<br />
The <strong>Minnesota</strong> Uniform Companion Guides describe an appeal<br />
as “Provider is requesting a reconsideration <strong>of</strong> a previously<br />
adjudicated claim but there is no additional or corrected data to<br />
be submitted.” For example, you receive a claim denial<br />
because we considered the procedure investigative. Your<br />
request to reconsider must be submitted on the AUC Appeal<br />
Request Form along with supporting documentation following<br />
the instructions in the AUC Submission <strong>of</strong> Appeals Best<br />
Practice. Fax the AUC Appeal Request Form <strong>and</strong> supporting<br />
documentation to <strong>Blue</strong> <strong>Cross</strong> at (651) 662-2745.<br />
6. What are some examples <strong>of</strong> reasons for appeals?<br />
The following is a list <strong>of</strong> reasons to send an appeal, according<br />
to the <strong>Minnesota</strong> Uniform Companion Guide(s) for Claims:<br />
Timely filing denial<br />
Payer allowance<br />
Incorrect benefit applied<br />
Eligibility issues<br />
Benefit accumulation errors<br />
Medical policy/medical necessity<br />
7. All <strong>of</strong> the claim information was submitted correctly;<br />
however, it appears not all claim data I sent was recognized<br />
by the system. Is it acceptable for me to call <strong>Blue</strong> <strong>Cross</strong> to<br />
simply have my claim adjusted using what was previously<br />
submitted or do I need to appeal?<br />
It is acceptable for you to request the claim be adjusted to<br />
recognize the data within the submission through a phone call<br />
to provider services. It would also be acceptable for you to<br />
submit your request using the AUC Appeal Request Form.<br />
8-30 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Cancel/Void <strong>and</strong><br />
Replacement Claims<br />
(continued)<br />
Claims Filing<br />
8. I am sending documentation in response to a request for<br />
additional documentation from <strong>Blue</strong> <strong>Cross</strong>. Do I need to<br />
send a replacement claim with the attached medical<br />
records?<br />
If you are responding to an information request letter sent by<br />
<strong>Blue</strong> <strong>Cross</strong>, regardless <strong>of</strong> whether you have also received a<br />
denial on your remittance, you should submit the requested<br />
information, along with a copy <strong>of</strong> the information request<br />
letter. Do not send an AUC Appeal Request Form. These same<br />
instructions are included on the letter that you receive.<br />
9. I am sending documentation in response to a denial on my<br />
remittance advice from <strong>Blue</strong> <strong>Cross</strong>. Do I need to send a<br />
replacement claim with the supporting information<br />
needed?<br />
If you are sending the additional documentation as a result <strong>of</strong> a<br />
denial on a remittance advice only, <strong>and</strong> not in response to an<br />
information request letter from <strong>Blue</strong> <strong>Cross</strong>, <strong>and</strong> the claim<br />
requires changes to claim data elements (such as date <strong>of</strong> injury,<br />
procedure code changes, diagnosis code changes, etc.), then a<br />
replacement claim must be sent which includes any necessary<br />
attachments.<br />
If you are sending the additional documentation as a result <strong>of</strong> a<br />
denial on a remittance advice only <strong>and</strong> the claim does not<br />
require changes to claim data elements you also may send a<br />
replacement claim.<br />
If you are sending additional documentation because you<br />
believe you did not receive correct payment <strong>and</strong> this<br />
documentation supports your position, you must send the AUC<br />
Appeal Request Form along with the documentation to support<br />
your request.<br />
Section B – COB Related Scenarios<br />
1. How do I send COB information when it was not included<br />
with the previous submission?<br />
Scenario 1<br />
If you have received a HIPAA compliant remittance advice<br />
(835), <strong>and</strong> your system has the capability to populate the<br />
information within a secondary claim, you must submit a<br />
replacement claim with the data appropriately entered<br />
within the claim record.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-31
Claims Filing<br />
Cancel/Void <strong>and</strong><br />
Replacement Claims<br />
(continued)<br />
Scenario 2<br />
If you have not received a HIPAA compliant remittance<br />
advice (835) from the previous payer, you may send a<br />
replacement claim transaction with the addition <strong>of</strong> the<br />
PWK segment <strong>and</strong> send the paper remittance advice from<br />
the previous payer as an attachment.<br />
Note: All <strong>Minnesota</strong> Group Purchasers must provide a<br />
HIPAA <strong>and</strong> State <strong>of</strong> <strong>Minnesota</strong> compliant<br />
remittance advice, <strong>and</strong> providers are required by the<br />
<strong>Minnesota</strong> Uniform Companion Guides (section<br />
4.2.3.5) to submit the previous payment information<br />
electronically using the proper fields within the<br />
claim transactions.<br />
Additional Information<br />
For additional information on these types <strong>of</strong> claims, please refer to<br />
the <strong>Minnesota</strong> Uniform Companion Guides <strong>and</strong> related Best<br />
Practice documentation on the AUC website at<br />
health.state.mn.us/auc/guides.htm.<br />
8-32 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Release <strong>of</strong> Medical<br />
Records<br />
Provider Assistance<br />
Requested<br />
Medical Records<br />
Management Process<br />
Improvement<br />
Claims Filing<br />
The <strong>Minnesota</strong> Statute that states “consent for the release <strong>of</strong><br />
medical records are valid for only one year,” also provides that<br />
consents to release medical records to insurers for purposes <strong>of</strong><br />
claims payment do not expire after one year. Since there are<br />
circumstances where such consents are only valid for one year,<br />
providers may wish to update their records on an annual basis.<br />
Providers are reminded that:<br />
Provider contracts state “The provider shall promptly furnish<br />
any additional information that <strong>Blue</strong> <strong>Cross</strong> or the Plan sponsor<br />
shall reasonably request as necessary to respond to claims.”<br />
HIPAA considers release <strong>of</strong> such records as required for<br />
“business operations.”<br />
ARIs are required under <strong>Minnesota</strong> law.<br />
Providers should gather information from patients on an annual<br />
basis to facilitate timely processing <strong>of</strong> patient claims.<br />
<strong>Blue</strong> <strong>Cross</strong> is improving its medical records management process<br />
to better serve you.<br />
Reduced requests - Changes to the <strong>Blue</strong> Plan internal medical<br />
records procedures will eliminate unnecessary medical record<br />
requests <strong>and</strong> expedite claims processing for members from<br />
other <strong>Blue</strong> Plans.<br />
Clearer instructions - A form will accompany all medical<br />
record requests to facilitate claims processing. The form should<br />
be returned with the requested records.<br />
Verify Member Identity <strong>Blue</strong> <strong>Cross</strong> has received a number <strong>of</strong> calls from our members who<br />
have stated that they did not receive certain services that were<br />
billed under their subscriber identification number.<br />
Upon comparing consent for treatment forms with signatures on<br />
file it appears that such services were provided to an imposter.<br />
In order to prevent this occurrence, providers should take<br />
appropriate steps to verify a member’s identity, such as viewing a<br />
government issued identification card <strong>and</strong> a <strong>Blue</strong> <strong>Cross</strong> member<br />
ID card at each encounter.<br />
If you suspect fraudulent use <strong>of</strong> a member ID card, please call our<br />
fraud hotline at (651) 662-8363. You may remain anonymous.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-33
Claims Filing<br />
Verifying Patient<br />
Eligibility<br />
<strong>Minnesota</strong> Statute 62J.536 requires health care providers <strong>and</strong><br />
group purchasers (payers, plans) to exchange eligibility<br />
information electronically using a st<strong>and</strong>ard format. The intent <strong>of</strong><br />
the law is to reduce costs, simplify <strong>and</strong> speed up health care<br />
transactions, <strong>and</strong> give providers <strong>and</strong> health plans one set <strong>of</strong> rules to<br />
follow for electronic transactions. This statute applies to all health<br />
care providers that request benefit or eligibility information<br />
regardless <strong>of</strong> participating status.<br />
Rules for Checking Eligibility <strong>and</strong> Benefits<br />
According to the <strong>Minnesota</strong> Department <strong>of</strong> Health, the compliant<br />
modes for initial eligibility inquiries <strong>and</strong> responses are either via<br />
provider web self-service (PWSS) or submission <strong>of</strong> the Eligibility<br />
Inquiry <strong>and</strong> Response Electronic Transaction (ANSI ASC X12<br />
270/271). Utilization <strong>of</strong> the Integrated Voice Response system<br />
(IVR) is not considered compliant for this initial exchange. If, after<br />
an initial compliant exchange (via web or EDI), additional<br />
information or review is needed, other modes that are available<br />
may be used, including IVR or a phone call to a service<br />
representative.<br />
The AUC has published a best practice related to checking<br />
eligibility <strong>and</strong> benefits for patients. The best practice covers 4<br />
major areas:<br />
When <strong>and</strong> how to verify<br />
Preferred methods <strong>of</strong> eligibility inquiry<br />
Sharing eligibility information<br />
Data elements that should be used to update information<br />
systems<br />
The recommendation <strong>of</strong> the AUC is that eligibility be checked<br />
for each patient once per calendar month since most eligibility<br />
changes occur at the beginning <strong>of</strong> a month. Please refer to the<br />
best practice at the following link for other helpful tips.<br />
www.health.state.mn.us/auc/bstprac01.pdf<br />
Questions?<br />
If you want to register to receive the electronic eligibility<br />
(270/271) transaction, contact Availity at availity.com.<br />
You can also use the provider web self-service site to check<br />
eligibility <strong>and</strong> benefits. To apply, go to the Welcome page on<br />
www.providerhub.com. Click on the link “Want access to this<br />
online service for your <strong>of</strong>fice?”<br />
8-34 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Basic Character Set<br />
Values in the Electronic<br />
Transaction<br />
Claims Filing<br />
The AUC has published a best practice regarding utilization <strong>of</strong> the<br />
basic character set values within the transaction data.<br />
The basic character set includes some punctuation characters <strong>and</strong><br />
spaces. These values when used unnecessarily can cause issues<br />
with matching to the payers’ enrollment for the provider or the<br />
member; or may cause the data to be incorrectly<br />
extracted/interpreted within the payers’ applications.<br />
If any <strong>of</strong> the punctuation characters within the basic character set<br />
are used as delimiters then they cannot be used in the transmitted<br />
data within a data element.<br />
Punctuation <strong>and</strong> spaces should only be utilized within the elements<br />
when they add value to the data. They should not be used when<br />
their usage is not essential to the interpretation <strong>of</strong> the data content.<br />
Basic character set: uppercase letters (A-Z), numeric digits (0-9),<br />
space ( ), exclamation point (!), double quote (“), single quote (‘),<br />
ampers<strong>and</strong> (&), right parenthesis, left parenthesis, asterisk (*),<br />
period (.), plus sign (+), comma (,), hyphen (-), forward slash (/),<br />
colon (:), semicolon (;), question mark (?), <strong>and</strong> equals sign (=).<br />
Even though the “@” character is in the extended character set it is<br />
allowed for e-mail addresses within the PER segment. This<br />
character must not be used as a delimiter.<br />
Examples to illustrate best practice:<br />
Description Incorrect Examples Correct Example<br />
<strong>Name</strong> Titles (no<br />
period should be<br />
used).<br />
Address – no<br />
periods should be<br />
used as part <strong>of</strong> the<br />
address.<br />
Commas <strong>and</strong><br />
periods should be<br />
used at the end <strong>of</strong> a<br />
sentence in a text<br />
field to separate<br />
from another<br />
sentence within the<br />
text field.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-35<br />
JR.<br />
MR.<br />
PhD.<br />
M.D.<br />
P.O.<br />
AVE.<br />
A PERIOD<br />
WITHIN A<br />
SENTENCE MAY<br />
HAVE VALUE<br />
DESCRIPTION OF<br />
SERVICE IS ABC<br />
JR<br />
MR<br />
PHD<br />
MD<br />
PO<br />
AVE<br />
A PERIOD<br />
WITHIN A<br />
SENTENCE MAY<br />
HAVE VALUE.<br />
DESCRIPTION OF<br />
SERVICE IS ABC.
Claims Filing<br />
Basic Character Set<br />
Values in the Electronic<br />
Transaction<br />
(continued)<br />
Claim Service Dates<br />
Restricted to Same<br />
Calendar Month<br />
Description Incorrect Examples Correct Example<br />
Hyphens <strong>and</strong><br />
apostrophes should<br />
not be used within a<br />
last name field.<br />
Leading <strong>and</strong> trailing<br />
spaces within fields<br />
should not be used.<br />
SMITH-JONES<br />
O’BRIEN<br />
Rendering<br />
practitioner last<br />
name = “_JONES”<br />
or “JONES_”<br />
SMITHJONES<br />
OBRIEN<br />
Rendering<br />
practitioner last<br />
name = “JONES”<br />
The AUC has published a best practice regarding claim service<br />
dates in the same calendar month. The purpose <strong>of</strong> this best practice<br />
is to avoid split claims <strong>and</strong> rejections. Most eligibility changes<br />
occur at the beginning or end <strong>of</strong> a calendar month. Some payer<br />
systems require that claims contain only services that are<br />
associated with a particular eligibility period. Current practice is to<br />
split these claims at the payer site to push through systems or to<br />
reject the claim.<br />
On a pr<strong>of</strong>essional claim, service date spans should only be within<br />
the same calendar month. Multiple claims may be submitted for<br />
different dates within the same calendar month based on the<br />
provider’s billing practices.<br />
On an institutional outpatient claim, statement <strong>and</strong> service date<br />
spans should only be within the same calendar month.<br />
Observation, extended recovery <strong>and</strong> emergency department<br />
services beginning before <strong>and</strong> completing after midnight are<br />
exceptions to this best practice if performed during the same visit.<br />
Procedures beginning on one day <strong>and</strong> ending on another should be<br />
billed together.<br />
This best practice does not apply to an institutional inpatient claim.<br />
Pharmaceuticals should be billed with the administration/dispensed<br />
date rather than a span <strong>of</strong> dates.<br />
Monthly equipment rental should be billed with the start date <strong>of</strong><br />
the rental period only rather than the span <strong>of</strong> days.<br />
Equipment rented on other than monthly basis needs both from <strong>and</strong><br />
through dates. Units <strong>of</strong> service should be reported as one (1) per<br />
rental period. These service date spans should only be within the<br />
same calendar month. Example would be daily rental <strong>of</strong><br />
equipment.<br />
Supplies should be billed with the purchase date rather than the<br />
span <strong>of</strong> days.<br />
8-36 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claim Service Dates<br />
Restricted to Same<br />
Calendar Month<br />
(continued)<br />
Reporting MNCare <strong>and</strong><br />
Sales Tax<br />
Claims Filing<br />
Refer to Appendix A <strong>of</strong> the MN Uniform Companion Guides for<br />
additional guidance on service date coding.<br />
Examples to illustrate best practice:<br />
Example 1 (equipment rental single month):<br />
Equipment is rented for January 17 through February 16. Service<br />
date should be reported as January 17 with no end date.<br />
DTP*472*D8*20080117~<br />
Example 2 (equipment rental multiple months):<br />
Equipment is rented for March 3 through May 15. Should be<br />
submitted as three separate claims, claim one would be reported as<br />
March 3 with no end date; claim two would be reported as April 3<br />
with no end date; claim three would be reported as May 3 with no<br />
end date.<br />
DTP*472*D8*20080303~<br />
DTP*472*D8*20080403~<br />
DTP*472*D8*20080503~<br />
Instructions for MNCare Tax billing only apply if the provider<br />
bills the group purchaser for MNCare Tax. Some providers do not<br />
bill the group purchaser for MNCare Tax. This document DOES<br />
NOT require them to do so but if they do identify the tax it must<br />
be done as follows. Some group purchasers may not reimburse<br />
MNCare Tax unless it is identified in the AMT. Sales tax<br />
instructions for pr<strong>of</strong>essional claims are as follows:<br />
MNCare Tax must be reported as part <strong>of</strong> the line item charge<br />
<strong>and</strong> reported in the corresponding AMT tax segment on the<br />
lines.<br />
Sales tax must be reported using HCPCS code S9999 for the<br />
tax <strong>and</strong> must be billed on the same claim as the related taxable<br />
service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-37
Claims Filing<br />
Rural Health Clinics <strong>and</strong> Federally Qualified Health<br />
Centers<br />
Billing for Medicare<br />
Primary<br />
Billing Other Than<br />
Medicare Primary<br />
Rural Health Clinics (RHC) <strong>and</strong> Federally Qualified Health<br />
Centers (FQHC) are Medicare provider designations. Medicare<br />
requires RHCs <strong>and</strong> FQHCs to bill services in an institutional<br />
format (837I).<br />
Since billing as a RHC or FQHC would be secondary to Medicare,<br />
we will only accept these clinic claims on the 837I.<br />
The claim should be submitted following Medicare billing<br />
requirements (e.g., TOB 071X <strong>and</strong> revenue code 0521 for a clinic<br />
visit to a RHC).<br />
If Medicare is not primary, services must be billed to us as a clinic,<br />
not as a RHC/FQHC, under your <strong>Blue</strong> <strong>Cross</strong> clinic provider<br />
number or NPI <strong>and</strong> submitted as a pr<strong>of</strong>essional claim 837P.<br />
8-38 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Coordination <strong>of</strong> Benefits (COB)<br />
Claims Filing<br />
Overview Third-party payers rely on Coordination <strong>of</strong> Benefits (COB) to<br />
eliminate duplicate payments when a patient has more than one<br />
coverage for health services. Please complete the information<br />
under ‘‘other coverage’’ on claims for your <strong>Blue</strong> <strong>Cross</strong> patients.<br />
List the names <strong>of</strong> any other carriers <strong>and</strong> the member’s ID number,<br />
if possible. We determine which carrier is primary payer <strong>and</strong><br />
ensure that duplicate payments are not made for the same services.<br />
Primacy Determination We follow the National Association <strong>of</strong> Insurance Commissioners<br />
(NAIC) rules to identify the primary insurance carrier.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-39
Claims Filing<br />
Coordination <strong>of</strong> Benefits Types<br />
There are several types <strong>of</strong> coordinating benefits that are outlined below. The only way to<br />
determine what type <strong>of</strong> COB a member has is to contact provider services.<br />
All seven types follow these first three steps:<br />
1. The primary carrier pays appropriate benefits under its contract.<br />
2. The claim is submitted to the secondary plan's carrier.<br />
3. The secondary plan will never pay more than it would pay in the absence <strong>of</strong> coordination.<br />
COB Type 1 <strong>and</strong> 2<br />
(St<strong>and</strong>ard Coordination)<br />
4. The secondary plan pays<br />
the difference between the<br />
higher allowed amount <strong>and</strong><br />
what the primary plan paid.<br />
5. The combined payment <strong>of</strong><br />
the primary <strong>and</strong> secondary<br />
plans will not exceed the total<br />
incurred expenses.<br />
COB Type 3 (Benefits less<br />
Other Insurance Benefits)<br />
4. The secondary plan<br />
processes up to the secondary<br />
plan's allowed amount. The<br />
secondary plan subtracts the<br />
amount the primary plan paid<br />
from the amount it would<br />
have paid without<br />
coordination.<br />
5. If the primary plan paid less<br />
than what the secondary plan<br />
would have paid without<br />
coordination, the secondary<br />
plan pays the difference.<br />
6. If the primary plan paid<br />
more than what the secondary<br />
plan would have paid without<br />
coordination, the secondary<br />
plan pays nothing.<br />
(Integration)<br />
7. The combined payment <strong>of</strong><br />
the primary <strong>and</strong> secondary<br />
plans will not exceed the total<br />
incurred expenses.<br />
COB Type 4 (only with<br />
Medicare)<br />
4. The secondary plan's<br />
allowed amount is determined<br />
by subtracting Medicare's paid<br />
from Medicare's allowed.<br />
5. That amount is reduced by<br />
any applicable deductibles<br />
<strong>and</strong> coinsurance.<br />
6. The combined payment <strong>of</strong><br />
the primary <strong>and</strong> secondary<br />
plans will not exceed the total<br />
incurred expenses.<br />
8-40 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
COB Type 1 <strong>and</strong> 2<br />
(St<strong>and</strong>ard Coordination)<br />
The result:<br />
The patient would not be<br />
responsible for payment <strong>of</strong> a<br />
portion <strong>of</strong> his or her eligible<br />
medical expenses.<br />
COB Type 3 (Benefits less<br />
Other Insurance Benefits)<br />
The result:<br />
The patient is responsible for<br />
any applicable deductible or<br />
coinsurance amounts for<br />
eligible medical expenses<br />
under both plans.<br />
COB Type 4 (only with<br />
Medicare)<br />
The result:<br />
Claims Filing<br />
The patient may be<br />
responsible for a portion <strong>of</strong><br />
his or her eligible medical<br />
expenses.<br />
Note: When coordinating benefits with Medicare all COB Types coordinate up to Medicare's<br />
allowed amount when the provider accepts assignment <strong>and</strong> the provider is located within<br />
the state <strong>of</strong> <strong>Minnesota</strong>. The federal Medicare Secondary Payer (MSP) law dictates when<br />
Medicare pays secondary.<br />
When coordinating benefits with another commercial carrier all COB types coordinate<br />
up to the higher allowed amount between the two plans except when integration is<br />
involved. Integration will coordinate up to <strong>Blue</strong> <strong>Cross</strong>’ allowed amount.<br />
It is important that all charges submitted to the primary payer be submitted to the<br />
secondary payer, even though charges were paid in full.<br />
Workers’<br />
Compensation<br />
In cases where an illness or injury is employment-related, workers’<br />
compensation is primary. If notification is received that the<br />
workers’ compensation carrier has denied the claim, the provider<br />
should submit the claim to <strong>Blue</strong> <strong>Cross</strong> regardless <strong>of</strong> whether the<br />
case is being disputed. It is also helpful to send the other carrier’s<br />
denial statement with the claim.<br />
No-fault Auto The No-fault Automobile Insurance Act calls for automobile<br />
insurance coverage to be primary without regard to cause or fault<br />
for the accident. The health insurance carrier would be the<br />
secondary payer. If notification is received that the no-fault auto<br />
carrier has denied the claim, the provider should submit the claim<br />
to <strong>Blue</strong> <strong>Cross</strong> regardless <strong>of</strong> whether the case is being disputed. It is<br />
also helpful to send the other carrier’s denial statement with the<br />
claim.<br />
Subrogation Subrogation literally means the substitution <strong>of</strong> one person for<br />
another. It is the right to recover payments for a member whose<br />
personal injuries are caused by the negligence or wrongdoing <strong>of</strong><br />
another. <strong>Minnesota</strong> does not have specific statutes or laws that<br />
apply to subrogation. Some group health care coverage plans <strong>and</strong><br />
<strong>Blue</strong> Plus do have subrogation in their certificates or contracts. For<br />
those groups, <strong>Blue</strong> <strong>Cross</strong> will initially pay the claim until the case<br />
is settled.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-41
Claims Filing<br />
TEFRA The 1982 Tax Equity <strong>and</strong> Fiscal Responsibility Act (TEFRA)<br />
applies to employers with 20 or more employees. Under TEFRA,<br />
group health coverage becomes the primary payer <strong>and</strong> Medicare<br />
the secondary payer for active employees between ages 65 <strong>and</strong> 70.<br />
TEFRA applies to active employees from the first day <strong>of</strong> the<br />
month <strong>of</strong> their 65th birthday to the first day <strong>of</strong> the month following<br />
their 70th birthday.<br />
DEFRA Effective January 1, 1985, the Deficit Reduction Act (DEFRA)<br />
exp<strong>and</strong>s the TEFRA aged workers guidelines to include dependent<br />
spouses (ages 65 to 70) <strong>of</strong> actively employed workers under 70.<br />
COBRA On April 7, 1986, the Consolidated Omnibus Budget<br />
Reconciliation Act (COBRA) amended the Working Aged<br />
Provision to eliminate the age 69 limit. Medicare will no longer<br />
become primary payer when an employed person turns age 70 or<br />
the spouse <strong>of</strong> an employed person turns 70. The group remains<br />
primary payer until the employee retires.<br />
OBRA The Omnibus Budget Reconciliation Act (OBRA) <strong>of</strong> 1986<br />
introduces the term ‘‘active individual’’ <strong>and</strong> defines it as the<br />
employee, the employer, or individual associated with the<br />
employer in a business or family relationship. Medicare will now<br />
be the secondary payer for disabled Medicare beneficiaries who<br />
elect to be covered by an employer-based group health plan, either<br />
as current employees or family <strong>of</strong> such employees. The minimum<br />
number <strong>of</strong> employees under this provision is set at 100. The<br />
employer’s insurance pays primary.<br />
8-42 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Non-Physician Health Care Practitioners<br />
Claims Filing<br />
Introduction <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> its affiliates will pay for reasonable <strong>and</strong> necessary<br />
services performed by certain non-physician health care<br />
practitioners. Eligible services are determined by the practitioner’s<br />
scope <strong>of</strong> practice <strong>and</strong> the member’s contract.<br />
Eligibility Criteria Below is the eligibility criteria for non-physician health care<br />
practitioners:<br />
Non-physician health care practitioners must meet applicable<br />
state or federal laws or licensing st<strong>and</strong>ards.<br />
When collaboration is required, non-physician health care<br />
practitioners in independent practice must work in<br />
collaboration with a physician licensed in the state where the<br />
services take place.<br />
A non-physician health care practitioner not eligible as an<br />
independent contractor must be an employee <strong>of</strong> a physician or<br />
limited-license practitioner (such as chiropractor or<br />
optometrist) licensed in the state where the services took place.<br />
The employing provider must be legally <strong>and</strong> medically<br />
responsible for the supervised employee’s services.<br />
Eligible non-physician health care practitioners must apply for<br />
<strong>and</strong> meet <strong>Blue</strong> <strong>Cross</strong> credentialing criteria.<br />
Credentialed or enrolled practitioners must use the <strong>Blue</strong> <strong>Cross</strong><br />
individual provider number or NPI when submitting services.<br />
Services rendered by supervised employees who are not issued<br />
individual provider numbers must be submitted under the<br />
supervising physician’s provider number or NPI. The -U7<br />
modifier should be appended to the HCPCS code to indicate a<br />
non-physician health care practitioner rendered the service.<br />
Services rendered must be eligible under their <strong>Blue</strong> <strong>Cross</strong><br />
provider <strong>and</strong> member contracts <strong>and</strong> the practitioner’s scope <strong>of</strong><br />
practice.<br />
A countersignature <strong>of</strong> notes <strong>and</strong> orders by the employing or<br />
supervising physician is required if the non-physician<br />
practitioner’s licensure <strong>and</strong>/or scope <strong>of</strong> practice requires a<br />
signature.<br />
Definitions Centers for Medicare <strong>and</strong> Medicaid Services (CMS) guidelines are<br />
the basis for the following definitions. For added clarification, we<br />
have further defined supervision as either direct or general.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-43
Claims Filing<br />
Employment As defined by CMS, the non-physician performing an “incidentto”<br />
service may be a part-time, full-time or leased employee <strong>of</strong> the<br />
supervising physician group practice or the legal entity that<br />
employs the supervising physician. A leased employee is a nonphysician<br />
working under a written employee leasing agreement,<br />
which provides that:<br />
The non-physician, although employed by the leasing<br />
company, provides services as the leased employee <strong>of</strong> the<br />
physician or other entity; <strong>and</strong><br />
The physician or other entity has control over all actions taken<br />
by the leased employee with regard to medical services<br />
rendered to the same extent that the physician or other entity<br />
would have such control if the leased employee were directly<br />
employed by the physician or other entity.<br />
To satisfy the employment requirement, the non-physician must be<br />
considered an employee <strong>of</strong> the supervising physician or other<br />
entity under the common law test <strong>of</strong> an employer/employee<br />
relationship.<br />
Services provided by auxiliary personnel not employed by the<br />
physician, physician group practice, or other legal entity are not<br />
covered as incident to a physician’s service.<br />
Incident To “Incident to” physician’s pr<strong>of</strong>essional services means that the<br />
services or supplies are furnished as an integral, although<br />
incidental, part <strong>of</strong> the physician’s personal pr<strong>of</strong>essional services in<br />
the course <strong>of</strong> diagnosis or treatment or an injury or illness.<br />
The practitioner’s service must be furnished as an integral part<br />
<strong>of</strong> the physician’s personal pr<strong>of</strong>essional service in the course <strong>of</strong><br />
diagnosis or treatment <strong>of</strong> an illness or injury.<br />
An employee <strong>of</strong> the physician must render service under the<br />
physician’s direct supervision.<br />
The physician must perform the initial <strong>and</strong> subsequent service<br />
with a frequency that reflects his/her active participation in<br />
managing the course <strong>of</strong> treatment.<br />
Practitioners who are issued individual provider numbers are<br />
considered incident to the physician when performing services<br />
within the same encounter on the same day as the physician.<br />
Incident to services are applicable in the <strong>of</strong>fice place <strong>of</strong> service<br />
only.<br />
8-44 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Claims Filing<br />
Direct Supervision The physician must be present in the <strong>of</strong>fice suite <strong>and</strong> immediately<br />
available to assist <strong>and</strong> direct throughout the performance <strong>of</strong> the<br />
service. Direct personal supervision does not mean that the<br />
physician must be present in the same room with the non-physician<br />
practitioner. A physician cannot provide direct or personal<br />
supervision via telemedicine. Direct supervision is only applicable<br />
in the <strong>of</strong>fice place <strong>of</strong> service.<br />
General Supervision General supervision refers to services furnished under the<br />
physician’s overall direction <strong>and</strong> supervision. The physician does<br />
not have to be physically present in the same <strong>of</strong>fice suite. He or<br />
she may provide general supervision by periodic review <strong>of</strong> the<br />
non-physician’s practice <strong>and</strong> availability either in person or<br />
through electronic communications (telemedicine, telephone, etc.).<br />
Collaboration/<br />
Independent Practice<br />
Chiropractic Doctors<br />
<strong>and</strong> Multidisciplinary<br />
Clinics<br />
Certain practitioners are qualified to set up their own practice.<br />
Although these practitioners work independently <strong>and</strong> do not<br />
require physician supervision, they must work with or collaborate<br />
with a physician. For example, a physical therapist may perform<br />
therapy independently; however, the patient’s physician makes the<br />
initial determination that the patient requires or will benefit from<br />
physical therapy. The physical therapist works in collaboration<br />
with the physician.<br />
Chiropractic doctors must maintain separate provider contracts <strong>and</strong><br />
provider numbers when practicing in a multidisciplinary clinic<br />
setting with medical doctors. <strong>Blue</strong> <strong>Cross</strong> does not allow<br />
chiropractors to bill services as “incident to” a physician’s<br />
services. Services performed by a chiropractor must bill under the<br />
chiropractor’s own provider number.<br />
The assignment <strong>of</strong> a chiropractic provider number is fundamental<br />
to the appropriate processing <strong>of</strong> our member <strong>and</strong> provider<br />
contracts. It allows <strong>Blue</strong> <strong>Cross</strong> to identify the specialty <strong>of</strong> the<br />
individual providing the services. This is especially important to<br />
enable <strong>Blue</strong> <strong>Cross</strong> to correctly administer those contracts that have<br />
visit limitations, exclusions <strong>and</strong> other benefit variances.<br />
A multidisciplinary clinic with medical <strong>and</strong> chiropractic doctors<br />
must adhere to this requirement that independently licensed<br />
chiropractors must maintain separate provider contracts with <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> bill appropriately. There are no exceptions to this policy.<br />
Any deviation from this billing requirement is a violation <strong>of</strong> the<br />
<strong>Blue</strong> <strong>Cross</strong> participating agreement.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12) 8-45
Claims Filing<br />
Surgical Technicians Surgical technicians are considered to be hospital-based<br />
practitioners <strong>and</strong> as such cannot have an independent relationship<br />
with <strong>Blue</strong> <strong>Cross</strong> nor can their services be billed under a<br />
supervising physician’s individual provider number. Surgical<br />
technicians are members <strong>of</strong> the operating team that prepare the<br />
patient <strong>and</strong> the operating room for surgery, transport patients,<br />
observe vital signs <strong>and</strong> check charts during surgery.<br />
Mid-level Practitioners <strong>Blue</strong> <strong>Cross</strong> defines mid-level practitioners based on practitioner<br />
specialties. The practitioner's specialty is established based on their<br />
current state license <strong>and</strong> is appropriately determined during the<br />
credentialing process.<br />
The following is a comprehensive current list <strong>of</strong> mid-level<br />
practitioners:<br />
Adult nurse practitioner<br />
Certified nurse midwife<br />
Clinical nurse specialist<br />
Family nurse practitioner<br />
Gerontological nurse practitioner<br />
Neonatal nurse<br />
OB/GYN nurse practitioner<br />
Optician<br />
Pediatric nurse practitioner<br />
Physician assistant<br />
Public health agency/nurse<br />
Registered nurse first assistant<br />
8-46 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (05/10/12)
Chapter 9<br />
Reimbursement / Reconciliation<br />
Table <strong>of</strong> Contents<br />
Reimbursement .......................................................................................................................... 9-2<br />
Payment Methodology........................................................................................................... 9-2<br />
Direct Payment.......................................................................................................................9-2<br />
Electronic Funds Transfer......................................................................................................9-2<br />
MNCare Tax ..........................................................................................................................9-3<br />
Inpatient Claims Paid at DRG Rates...................................................................................... 9-3<br />
Complication <strong>and</strong> Co-morbidity Defined .............................................................................. 9-4<br />
Serious Preventable Medical Errors....................................................................................... 9-5<br />
Remittance Advice ..................................................................................................................... 9-6<br />
Introduction............................................................................................................................9-6<br />
Sample PDF Remittance Advice............................................................................................9-6<br />
2006 Remittance Advice Change...........................................................................................9-6<br />
ANSI Codes ...........................................................................................................................9-6<br />
Questions <strong>and</strong> Answers.......................................................................................................... 9-7<br />
Remit Balancing Tips ..........................................................................................................9-11<br />
Accounts Receivable Recoupment Report............................................................................. 9-12<br />
Introduction..........................................................................................................................9-12<br />
Accounts Receivable Recoupment Report...........................................................................9-13<br />
Field Descriptions ................................................................................................................ 9-14<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11) 9-1
Reimbursement / Reconciliation<br />
Reimbursement<br />
Payment Methodology Please refer to your provider contract for pr<strong>of</strong>essional provider<br />
payment methodology details.<br />
Direct Payment Because you are a participating provider, we send claims payments<br />
directly to you. Payments are sent weekly.<br />
Effective December 15, 2009, <strong>Minnesota</strong> Statute 62J.536 requires<br />
all health care providers to accept from group purchasers the health<br />
care payment <strong>and</strong> remittance advice transaction (835). The statute<br />
further allows the use <strong>of</strong> web-based technology for complying with<br />
the requirements as long as the data content <strong>and</strong> rules <strong>of</strong> the<br />
<strong>Minnesota</strong> Uniform Companion Guides are followed.<br />
Electronic Funds<br />
Transfer<br />
Beginning second quarter 2011, <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong><br />
<strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus (<strong>Blue</strong> <strong>Cross</strong>) will no longer<br />
print <strong>and</strong> mail any paper remittances. Providers will also not be<br />
able to obtain a printed copy <strong>of</strong> the remittance through provider<br />
services except for remittances produced before February 2010.<br />
Providers must register through Availity to receive the electronic<br />
835 or register for access to our provider portal, provider web selfservice<br />
(PWSS) to view their remittance information. Providers<br />
can register for both options. The full on-line view through the<br />
portal via PWSS was available as <strong>of</strong> September 22, 2010.<br />
A nonparticipating provider generally receives neither direct<br />
reimbursement from <strong>Blue</strong> <strong>Cross</strong> nor a copy <strong>of</strong> the statement for<br />
any member who has <strong>Blue</strong> <strong>Cross</strong> coverage. Members cannot<br />
assign benefits to providers. We pay the member directly for<br />
nonparticipating <strong>Minnesota</strong> or border providers. However, the<br />
provider will be paid directly if the member has<br />
PMAP/<strong>Minnesota</strong>Care coverage.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus <strong>of</strong>fer<br />
Electronic Funds Transfer (EFT). Instead <strong>of</strong> weekly checks with<br />
your remits, you can now receive electronic payments directly into<br />
your facility’s checking or savings account. The funds are securely<br />
transferred via the Automated Clearinghouse (ACH) process.<br />
Electronic payment will streamline your reconciliation process,<br />
eliminate deposit delays due to check h<strong>and</strong>ling, <strong>and</strong> improve cash<br />
flow.<br />
To access a copy <strong>of</strong> the Provider Automatic Payment application,<br />
please visit our website; click on the Provider icon <strong>and</strong> then forms.<br />
9-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11)
Reimbursement / Reconciliation<br />
MNCare Tax Those fee schedules that are impacted by the MNCare tax already<br />
have the 2 percent tax included.<br />
Examples <strong>of</strong> fee schedules that do not include the MNCare tax are<br />
those for Medicaid, Workers’ Compensation, HIAA, Federal<br />
Employee Program, out-<strong>of</strong>-state providers, <strong>and</strong> some specific<br />
provider types.<br />
Inpatient Claims Paid<br />
at DRG Rates<br />
<strong>Blue</strong> <strong>Cross</strong> pays inpatient claims at DRG (Diagnosis-related<br />
group) rates for most hospitals. Some rural hospitals may continue<br />
to be paid at a percentage <strong>of</strong> charge.<br />
About DRGs<br />
The DRG reimbursement methodology has over 500 inpatient<br />
categories <strong>of</strong> care, which are updated annually by the Centers for<br />
Medicare <strong>and</strong> Medicaid Services (CMS). DRGs are a way <strong>of</strong><br />
categorizing inpatient hospital services by diagnosis groups that<br />
have similar patterns <strong>of</strong> hospital resource use <strong>and</strong> similar lengths<br />
<strong>of</strong> stay. DRG assignment is based on the patient’s principal <strong>and</strong><br />
secondary diagnoses, principal <strong>and</strong> secondary procedure codes,<br />
age, sex <strong>and</strong> discharge status. Payments are based on the assigned<br />
DRG case weight, multiplied by a base rate (conversion factor)<br />
that <strong>Blue</strong> <strong>Cross</strong> negotiates with hospitals.<br />
Coding Compliance<br />
Coding compliance relates to the accuracy <strong>and</strong> completeness <strong>of</strong> the<br />
ICD-9-CM diagnosis <strong>and</strong> procedure codes that are used to assign<br />
DRGs <strong>and</strong> determine payment. <strong>Blue</strong> <strong>Cross</strong> requests that hospitals<br />
establish adequate internal procedures to ensure the accuracy <strong>of</strong><br />
claims submissions. <strong>Blue</strong> <strong>Cross</strong> reserves the right to conduct<br />
r<strong>and</strong>om chart audits on a sample <strong>of</strong> records to ensure that<br />
diagnoses submitted justify the DRG <strong>and</strong> adhere to ICD-9-CM<br />
coding rules. Coding errors that are determined to represent a<br />
fraudulent claim may be subject to penalties.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11) 9-3
Reimbursement / Reconciliation<br />
Complication <strong>and</strong> Comorbidity<br />
Defined<br />
According to St. Anthony Publishing, a “complication” is a<br />
condition that arises during a hospital stay <strong>and</strong> prolongs the length<br />
<strong>of</strong> stay by at least one day in approximately 75 percent <strong>of</strong> the<br />
cases. The same source defines “co-morbidity” as a preexisting<br />
condition that, because <strong>of</strong> its presence with a specific diagnosis,<br />
will cause an increase in length <strong>of</strong> stay by at least one day in<br />
approximately 75 percent <strong>of</strong> cases. The condition must affect the<br />
patient’s hospital care by requiring one or more <strong>of</strong> the following:<br />
Clinical evaluation<br />
Therapeutic treatment<br />
Diagnostic studies or procedures<br />
Increased length <strong>of</strong> stay<br />
Increased nursing care <strong>and</strong>/or monitoring<br />
Although there is a st<strong>and</strong>ard list <strong>of</strong> diagnoses that are considered<br />
complications or co-morbidities, if the diagnosis does not require<br />
one or more <strong>of</strong> the above services, it should not be listed as a<br />
diagnosis. The physician must verify <strong>and</strong> document the conditions,<br />
based on clinical findings <strong>and</strong> treatment in the record.<br />
9-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11)
Serious Preventable<br />
Medical Errors<br />
Reimbursement / Reconciliation<br />
When the negligence, omission, or error on the part <strong>of</strong> provider<br />
results in the subscriber incurring additional medical expenses no<br />
payment will be made by <strong>Blue</strong> <strong>Cross</strong> for, nor shall provider bill<br />
either <strong>Blue</strong> <strong>Cross</strong> or the subscriber for said additional medical<br />
expenses. The National Quality Forum has defined certain events<br />
as serious preventable medical errors, <strong>and</strong> these are the situations<br />
for which no payment shall be made by <strong>Blue</strong> <strong>Cross</strong> or the<br />
subscriber.<br />
A listing <strong>of</strong> these events can be found at www.qualityforum.org.<br />
This listing will be updated periodically by the National Quality<br />
Forum.<br />
Examples <strong>of</strong> serious preventable errors include:<br />
Unintended retention <strong>of</strong> a foreign object in a patient after<br />
surgery.<br />
Patient death or serious disability associated with a medication<br />
error (e.g., errors involving the wrong drug, wrong dose, wrong<br />
patient, wrong time, wrong rate, wrong preparation or wrong<br />
route <strong>of</strong> administration).<br />
Surgery performed on the wrong body part.<br />
Surgery performed on the wrong patient.<br />
Wrong surgical procedure performed on a patient.<br />
Infant discharged to the wrong person.<br />
The <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Association's listing <strong>of</strong> recognized<br />
serious preventable errors can be found on the Association's<br />
website at www.bcbs.com.<br />
An implementation guide for appropriate identification <strong>of</strong> serious<br />
preventable errors, including a list <strong>of</strong> ICD-9 CM codes used to<br />
identify serious preventable errors <strong>and</strong>/or Hospital Acquired<br />
Conditions on a claim can also be found at www.bcbs.com.<br />
The <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> Association is an association <strong>of</strong><br />
independent <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> plans.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11) 9-5
Reimbursement / Reconciliation<br />
Remittance Advice<br />
Introduction The provider remittance is made available every week <strong>and</strong> at<br />
month end. The remittance will include claims that are processed<br />
or adjusted before the end <strong>of</strong> the day Friday. You will receive one<br />
remittance for each NPI <strong>and</strong> each type <strong>of</strong> claim (i.e. institutional,<br />
pr<strong>of</strong>essional). You will receive a separate remittance for <strong>Blue</strong><br />
<strong>Cross</strong> members <strong>and</strong> <strong>Blue</strong> Plus members, even if you are not a <strong>Blue</strong><br />
Plus participating provider. The <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus<br />
remittances may vary slightly.<br />
Sample PDF<br />
Remittance Advice<br />
2006 Remittance<br />
Advice Change<br />
Remember to always retain a copy <strong>of</strong> your remittance to meet<br />
HIPAA requirements in a central location for easy retrieval, as<br />
they are an essential resource for your business.<br />
A sample <strong>of</strong> the PDF version <strong>of</strong> the provider remittance with field<br />
descriptions is on our website.<br />
The Health Care Administrative Simplification Act <strong>of</strong> 1996<br />
allowed <strong>Minnesota</strong> health care providers <strong>and</strong> payers the chance to<br />
implement administrative st<strong>and</strong>ards <strong>and</strong> simplified procedures<br />
throughout the industry. A portion <strong>of</strong> the Act required payers to<br />
develop <strong>and</strong> implement a uniform paper Explanation <strong>of</strong> Health<br />
Care Benefits (EOB) <strong>and</strong> Remittance Advice report (remit). The<br />
Act prescribes specific data fields that must appear on the EOB<br />
<strong>and</strong> remit.<br />
ANSI Codes <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus uses all the conventions addressed in the<br />
“<strong>Minnesota</strong> Paper Explanation <strong>of</strong> Benefits <strong>and</strong> Uniform Paper<br />
Remittance Advice Report” manual developed by the<br />
Administrative Uniformity Committee (AUC) in our PDF version<br />
<strong>of</strong> the remittance.<br />
A copy <strong>of</strong> the manual is available on their website at:<br />
www.health.state.mn.us/auc/eobremitmanual2007.pdf or<br />
<strong>Minnesota</strong>’s Bookstore at (651) 297-3000 or 1-800-657-3706.<br />
The guide sets forth the st<strong>and</strong>ard approach to be adopted by payers<br />
<strong>and</strong> providers.<br />
9-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11)
Questions <strong>and</strong> Answers 1. Where will adjusted claims appear?<br />
Reimbursement / Reconciliation<br />
They will appear as claim transactions on the remittance<br />
advice. You will see negative amounts on the cancel <strong>of</strong> the<br />
original claim followed by a new claim to show the final status.<br />
2. How can I identify adjustments in the remittance?<br />
The claim number will be the same as in the original statement,<br />
except the last three digits. For example: If the original claim<br />
ended in 000 the adjusted claim will end in 010. If it needs to<br />
be adjusted again, it will end in 020, etc. If we then make<br />
additional or adjusted payment for that claim, the newly<br />
processed claim will be printed above the original claim.<br />
3. What is a credit balance?<br />
When the amount <strong>of</strong> this payment is not enough to cover the<br />
credits, a credit balance will occur. If the credit balance<br />
occurred on this statement, this amount the will appear in the<br />
PDF version <strong>of</strong> the remit in field #27 along with a code in field<br />
#28. If there were credit balances from previous statements,<br />
that information will be reflected in fields #27 <strong>and</strong> #28. An<br />
Accounts Receivable Recoupment Report is sent separately<br />
<strong>and</strong> prior to the remittance reflecting which claims are being<br />
recouped in this statement period. This report is only sent when<br />
recoupments will be made.<br />
A credit for a <strong>Blue</strong> Plus member will only be recouped from<br />
the <strong>Blue</strong> Plus remittance <strong>and</strong> a credit for a <strong>Blue</strong> <strong>Cross</strong> member<br />
will only be recouped from the <strong>Blue</strong> <strong>Cross</strong> remittance.<br />
4. How do I use the Accounts Receivable Recoupment Report?<br />
This report is sent out under separate cover from the weekly<br />
remittance <strong>and</strong> lists the claims that will be recouped that week.<br />
The amount listed on this report will be reflected in the weekly<br />
remittance. Remember to keep this report in a central location<br />
for easy retrieval.<br />
5. Do I have to credit the member’s account based on the<br />
Accounts Receivable Recoupment Report?<br />
If you already credited the member’s account based on the<br />
remittance that reflected the adjustment, then do not adjust the<br />
member’s account again. This is an internal workflow for your<br />
<strong>of</strong>fice. Adjusting the member’s account using both the weekly<br />
remittance <strong>and</strong> the Accounts Receivable Recoupment Report<br />
may result in duplication.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11) 9-7
Reimbursement / Reconciliation<br />
Questions <strong>and</strong> Answers<br />
(continued)<br />
6. What if there is a claim on my remittance for a patient that<br />
is not ours?<br />
Request an adjustment by contacting provider services. Please<br />
do not send our payment check back to us or send us a refund<br />
check unless we have requested it from you.<br />
7. Why does the check I received not match the amount listed<br />
under Net Payment Activity on the statement?<br />
Less Prior Credit Balances <strong>and</strong> Less Current Credit Balances<br />
will be subtracted from the Net Payment Amount. Your check<br />
should match the amount listed in the Payment Due field on<br />
the statement.<br />
8. What can I bill the patient <strong>and</strong> how can I identify it on the<br />
statement?<br />
The Patient Responsibility field reflects the total patient<br />
liability. This is the amount that the patient is responsible to<br />
pay. However, you may have already billed the member for<br />
copayments up front.<br />
9. What do I have to write-<strong>of</strong>f <strong>and</strong> how can I identify it on the<br />
statement?<br />
The group code 'CO' signifies a provider contractual<br />
obligation. Any amounts associated to the use <strong>of</strong> this code<br />
should be written <strong>of</strong>f.<br />
10. Do members receive their Explanation <strong>of</strong> Health Care<br />
Benefits (EOB) at the same time as providers?<br />
No, the member’s EOB is mailed daily <strong>and</strong> provider’s<br />
remittances are sent or posted weekly. However, we mail<br />
members’ EOBs monthly if there is zero member liability <strong>and</strong><br />
payment was made to the provider. If a member references a<br />
claim that you haven’t received notice on yet, it should be on<br />
your next remittance.<br />
11. How can I identify <strong>Blue</strong>Card ® claims?<br />
The <strong>Blue</strong>Card claims may be identified by the three digit<br />
alpha-prefix on the member’s identification number. <strong>Blue</strong>Card<br />
member's prefix will not be XZA.<br />
9-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11)
Questions <strong>and</strong> Answers<br />
(continued)<br />
12. What does the claim number represent?<br />
Reimbursement / Reconciliation<br />
The claim number is a sequence <strong>of</strong> numbers that identifies each<br />
claim. Knowing what the claim number consists <strong>of</strong> may assist<br />
you in better underst<strong>and</strong>ing the claim. The information below<br />
describes a claim number.<br />
Example: Claim number 5109361034020<br />
5109= Julian date the claim was entered into our claims<br />
processing system. i.e., 109th day <strong>of</strong> 2005<br />
361034= the sequence number for claims entered on that date<br />
020= The first <strong>and</strong> third positions reflects a claim has been<br />
split. If a claim is split, we are unable to process a claim as one<br />
claim so we process it as two. Two main reasons to split a<br />
claim are when benefits have changed in the middle <strong>of</strong> the<br />
claim or there are too many lines for us to process it as one<br />
claim.<br />
The second position reflects if the claim has been adjusted (i.e.,<br />
0= original claim, 1= claim adjusted the first time, 2= claim<br />
adjusted the second time, etc.)<br />
13. How do I request an adjustment or inquiry?<br />
An adjustment should be requested when you notice the<br />
adjudication error. Please remember that if data on the claim<br />
needs to be changed, you must send a complete replacement<br />
claim rather than request an adjustment.<br />
You can request an adjustment by:<br />
Submitting a request through provider web self-service<br />
Fax in the Provider Services Inquiry fax form to:<br />
(651) 662-2745<br />
Mail in a request to:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
P.O. Box 64560<br />
St. Paul, MN 55164-0560<br />
For inquiries:<br />
Provider web self-service is found at:<br />
www.providerhub.com<br />
Call BLUELINE at (651) 662-5200 or 1-800-262-0820<br />
Call provider services at (651) 662-5200 or<br />
1-800-262-0820. Please wait 30 days before checking the<br />
status <strong>of</strong> a claim or adjustment.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11) 9-9
Reimbursement / Reconciliation<br />
Questions <strong>and</strong> Answers<br />
(continued)<br />
14. What do I do with interest payments?<br />
Interest payments that you receive should be posted to a<br />
miscellaneous account. This is money that is yours <strong>and</strong> should<br />
not be posted to the account <strong>of</strong> the member it pertains to. By<br />
posting this money to a member’s account they may end up<br />
with a credit.<br />
15. Are there any limits for making adjustments?<br />
<strong>Blue</strong> <strong>Cross</strong> may make, <strong>and</strong> providers may request, corrective<br />
claim adjustments (recoupments or additional payments) to<br />
previously processed claims for services within 12 months <strong>of</strong><br />
the date a claim is paid or denied unless the adjustment is made<br />
for the following circumstances (<strong>and</strong> thus are not limited to this<br />
12-month period):<br />
One or more insurer is involved, whether primary or<br />
secondary (i.e., Medicare secondary payer, no-fault<br />
automobile coverage, subrogation, coordination <strong>of</strong> benefits,<br />
workers’ compensation, TEFRA, etc.)<br />
The adjustment is required due to provider error (i.e., the<br />
provider should not have billed for services, a claim was a<br />
duplicate <strong>of</strong> a claim previously paid, fraud, incorrect<br />
billing, etc.)<br />
The adjustment is required pursuant to applicable law,<br />
regulation, rule, order or contractual requirement (i.e.,<br />
<strong>Blue</strong>Card claims); or<br />
The adjustment is required as part <strong>of</strong> a contractual<br />
settlement obligation with the provider.<br />
Note that provider errors or data changes require a<br />
replacement claim or cancel claim be submitted within six<br />
months <strong>of</strong> the last adjudication date.<br />
Corrective adjustment requests must be received within 12<br />
months from the date the claim was last paid or denied by<br />
<strong>Blue</strong> <strong>Cross</strong>.<br />
9-10 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11)
Reimbursement / Reconciliation<br />
Remit Balancing Tips Amounts reported in the remittance, if present, must balance at<br />
three levels: service line, claim <strong>and</strong> total remittance.<br />
Service Line Balancing<br />
Although the service payment information is situational, it is<br />
required for all pr<strong>of</strong>essional claims or anytime payment<br />
adjustments are related to specific lines from the original<br />
submitted claim. When used, the submitted service lines minus the<br />
sum <strong>of</strong> all monetary adjustments must equal the amount paid for<br />
the service line.<br />
Charge – Adjustment Amount = Payment Amount<br />
Claim Balancing<br />
Balancing must occur at the claim level so that the submitted<br />
charges minus the sum <strong>of</strong> all monetary adjustments equals the<br />
claim paid amount.<br />
Charge – Adjustment Amount = Claim Payment Amount<br />
Remit Balancing<br />
Within the transaction, the sum <strong>of</strong> all payments minus the sum <strong>of</strong><br />
all adjustments equals the Payment Amount.<br />
Sum <strong>of</strong> all Payments totaled – the Sum <strong>of</strong> all<br />
Adjustments = Total payment amount <strong>of</strong> this remittance<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11) 9-11
Reimbursement / Reconciliation<br />
Accounts Receivable Recoupment Report<br />
Introduction The Accounts Receivable Recoupment Report lists the amount<br />
credited, amount recovered, <strong>and</strong> any balance due on claims for<br />
your patients. It will only be sent if there are funds to be recovered<br />
that week. All the recouped claims for the week (Prior Credit<br />
Balances <strong>and</strong> Current Credit Balances from the remittance) will be<br />
listed on the Accounts Receivable Recoupment Report.<br />
The Report is sent out weekly under separate cover <strong>and</strong> in advance<br />
<strong>of</strong> the remittance. Remember to always keep these reports in a<br />
central location for easy retrieval.<br />
9-12 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11)
Accounts Receivable<br />
Recoupment Report<br />
Reimbursement / Reconciliation<br />
Following is a copy <strong>of</strong> the Accounts Receivable Recoupment<br />
Report. Field descriptions follow the report.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11) 9-13
Reimbursement / Reconciliation<br />
Field Descriptions A brief explanation <strong>of</strong> the fields on the Accounts Receivable<br />
Recoupment Report follows:<br />
<strong>Name</strong> — <strong>Name</strong> <strong>and</strong> address <strong>of</strong> the billing provider.<br />
Page — Page number <strong>of</strong> the report.<br />
Date — This date coincides with the Statement <strong>of</strong> Provider<br />
Claims Paid. The information found on this report reflects the<br />
activity which occurred on the Statement <strong>of</strong> Provider Claims<br />
Paid with this same date.<br />
NPI — National Provider Identifier.<br />
Recovery Date — Credit activity may take place during the<br />
week but actual transactions are not processed until Friday.<br />
This date will reflect the Friday’s date prior to the date <strong>of</strong> your<br />
“Statement <strong>of</strong> Provider/Institutional Claims Paid.”<br />
Sub-ID — Member identification number under which the<br />
credit claim activity occurred. If amounts are being recouped<br />
due to a settlement <strong>of</strong> which you were previously notified.<br />
Patient <strong>Name</strong> — <strong>Name</strong> <strong>of</strong> the patient.<br />
Claim Number — Number <strong>of</strong> the claim which was overpaid<br />
or paid in error by us.<br />
Date Created — Actual date the claim was adjusted by us.<br />
Service Date – Date <strong>of</strong> service on the claim.<br />
Credit Amount — Amount we need to recover from this<br />
claim. If we were unable to recoup the entire amount <strong>of</strong> the<br />
claim from previous statements, this amount will list just the<br />
balance remaining.<br />
Amount Recovered — Amount being recouped on this<br />
statement. This amount is deducted from the Net Payment on<br />
the “Statement <strong>of</strong> Provider/Institutional Claims Paid.”<br />
Balance Due — Amount we still need to recoup from future<br />
statements. If there is a balance, the claim will be listed in<br />
future reports when it is recouped.<br />
Total Credit Activity — Amount <strong>of</strong> overpayment identified<br />
prior to amounts recouped in this statement.<br />
Total Recovered — The total amount <strong>of</strong> overpayments<br />
deducted from your weekly Statement <strong>of</strong><br />
Provider/Institutional Claims Paid for the week.<br />
Balance Due — If the overpayment exceeds what we are<br />
recouping for that statement, the amount still due to us will be<br />
listed here.<br />
9-14 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/02/11)
Table <strong>of</strong> Contents<br />
Chapter 10<br />
Appeals<br />
Provider Appeals...................................................................................................................... 10-2<br />
Introduction..........................................................................................................................10-2<br />
Post Service Claim Appeals.................................................................................................10-2<br />
Appeals <strong>of</strong> Processed Claims............................................................................................... 10-3<br />
Voluntary Second Appeal.................................................................................................... 10-3<br />
Submitting Requests for Post Service Claim Appeals.........................................................10-4<br />
Prior Authorization <strong>and</strong> Preadmission Notification Appeal Process...................................10-4<br />
Prior Authorization <strong>and</strong> Preadmission Notification Appeal ................................................ 10-4<br />
Urgent/Expedited Appeals...................................................................................................10-5<br />
Coding Appeals.................................................................................................................... 10-5<br />
<strong>Blue</strong>Card ® Appeals ..............................................................................................................10-6<br />
<strong>Blue</strong>Card Appeal vs. Adjustments....................................................................................... 10-6<br />
Appealing Claims Processed by the Member’s Plan ........................................................... 10-6<br />
Supporting Documentation .................................................................................................. 10-7<br />
Utilization Review Decision Appeal ...................................................................................10-8<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 10-1
Appeals<br />
Provider Appeals<br />
Introduction Providers are eligible to appeal:<br />
Post Service Claim<br />
Appeals<br />
Post service claim appeals<br />
Prior Authorization <strong>and</strong> Preadmission Notification denials<br />
Coding appeals<br />
For information regarding settlement appeals, refer to your<br />
provider agreement.<br />
For information regarding submission <strong>of</strong> replacement or cancel<br />
claims, refer to Chapter 8 in this manual.<br />
Instructions for the submission <strong>of</strong> appeals are listed in this chapter.<br />
Please read the information carefully to ensure your appeal is<br />
reaching the appropriate area within <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) as that will allow for an efficient <strong>and</strong><br />
timely review <strong>of</strong> your request.<br />
A post service claim appeal is a written request for review.<br />
The <strong>Minnesota</strong> Uniform Companion Guides, version 4.0, dated<br />
March 2009, Section 4.2.3.2, define an appeal as “Provider is<br />
requesting a reconsideration <strong>of</strong> a previously adjudicated claim but<br />
there is no additional or corrected data to be submitted.”<br />
Post service claim appeals require the provider to include with the<br />
request documentation <strong>of</strong> items such as chart notes, medical<br />
records, operative reports <strong>and</strong> letters <strong>of</strong> medical necessity. Appeals<br />
present detailed information in an attempt to change a previous<br />
decision made by <strong>Blue</strong> <strong>Cross</strong>.<br />
All post service claim appeals must be submitted on the AUC<br />
Appeal Request Form available on the AUC web site,<br />
www.health.state.mn.us.auc, along with the supporting<br />
documentation <strong>and</strong> must be mailed or faxed to the Consumer<br />
Service Center.<br />
A post service claim appeal must be requested within 90 days <strong>of</strong><br />
the date claim notification is issued. There is no limit on the dollar<br />
amount for an initial appeal.<br />
A st<strong>and</strong>ard claim appeal submitted with a completed AUC appeal<br />
form <strong>and</strong> attached supporting documentation will be completed<br />
within 60 days <strong>of</strong> receipt. The appeal decision is final unless the<br />
charges in question exceed $500.00. At that time, a voluntary<br />
second level review is available.<br />
10-2 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Appeals <strong>of</strong> Processed<br />
Claims<br />
Voluntary Second<br />
Appeal<br />
Situations brought to appeal include the following categories:<br />
Benefit determinations<br />
Claims processing<br />
Determinations <strong>of</strong> allowed amounts<br />
Provider pr<strong>of</strong>iles<br />
Timely filing denials<br />
Services denied due to lack <strong>of</strong> medical necessity<br />
Appeals<br />
This appeal process does not apply to settlement appeals, medical<br />
necessity <strong>and</strong> prior authorization denials occurring prior to claim<br />
submission.<br />
Voluntary Second Appeals must be filed within 60 days <strong>of</strong> the<br />
notification upholding the decision <strong>of</strong> the initial appeal. To be<br />
eligible for a voluntary second appeal, the amount at issue must be<br />
$500.00 or more. Calculate the amount at issue by subtracting the<br />
deductible, coinsurance, <strong>and</strong> paid amount from the billed charge.<br />
For example:<br />
Billed amount $2,000.00<br />
- (deductible) 500.00<br />
- (coinsurance) 200.00<br />
- (paid amount) 500.00<br />
Amount at issue $ 800.00<br />
If the amount in question is $500.00 or more then this appeal<br />
review may be conducted by the Consumer Service Center as well<br />
as Integrated Health Management.<br />
Claims for the same patient or multiple patients relating to the<br />
same category can be aggregated at this level (you may combine<br />
two or more claims to meet the $500.00 amount-in-controversy<br />
requirement).<br />
Voluntary second appeals must be submitted with additional<br />
information over <strong>and</strong> above what was submitted with the initial<br />
appeal. These requests must also be submitted on an AUC Appeal<br />
form <strong>and</strong> should note “Secondary Appeal” on the form.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 10-3
Appeals<br />
Submitting Requests<br />
for Post Service Claim<br />
Appeals<br />
Prior Authorization <strong>and</strong><br />
Preadmission<br />
Notification Appeal<br />
Process<br />
Prior Authorization <strong>and</strong><br />
Preadmission<br />
Notification Appeal<br />
Post service claim appeals may be mailed or faxed.<br />
Mailing address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Attn: Consumer Service Center<br />
PO Box 64560<br />
St. Paul, MN 55164-0560<br />
Fax: (651) 662-2745<br />
You may appeal a prior authorization request or preadmission<br />
notification request denied as medically unnecessary. Your request<br />
may be initiated by letter or telephone. Written requests should be<br />
addressed to the Consumer Service Center using the address or fax<br />
number provided in the denial letter. An appeal reviewer will<br />
review the case <strong>and</strong> make a final determination.<br />
You may appeal a prior authorization request or a preadmission<br />
notification request denied for benefit administration within 30<br />
days <strong>of</strong> notification. Your request must be in writing <strong>and</strong> should be<br />
addressed to:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Attn: Consumer Service Center<br />
P. O. Box 64560<br />
St. Paul, MN 55164-0560<br />
You may also fax your denied prior authorization appeals to<br />
(651) 662-9517.<br />
When coverage is denied for Prior Authorization or Preadmission<br />
Notification based on medical necessity, <strong>Blue</strong> <strong>Cross</strong> notifies the<br />
provider by telephone <strong>and</strong>/or sends letters to the member, hospital<br />
<strong>and</strong> physician. The physician, member or facility may appeal the<br />
denial. The appeal may be initiated either by letter or by telephone.<br />
<strong>Blue</strong> <strong>Cross</strong>’ review is only a medical necessity review <strong>and</strong> is<br />
subject to all other limitations in the member’s contract. Services<br />
may be denied because <strong>of</strong> exclusions, limitations on preexisting<br />
conditions, <strong>and</strong> medical necessity requirements contained in the<br />
member’s contract. These contract provisions will prevail over a<br />
medical necessity decision. The decision to continue an inpatient<br />
stay or services ultimately rests with the patient <strong>and</strong> the physician.<br />
During the appeal process, all available information is provided to<br />
a physician reviewer who is board certified in the same or similar<br />
general specialty as typically manages the medical condition or<br />
treatment <strong>and</strong> was not involved in the original determination.<br />
10-4 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Urgent/Expedited<br />
Appeals<br />
Appeals<br />
An urgent appeal is done when an initial or continued treatment is<br />
dependent on a quick determination. Urgent is defined as medical<br />
care or treatment with respect to which the application <strong>of</strong> the time<br />
periods for making nonurgent care determinations:<br />
1. Could seriously jeopardize the life or health <strong>of</strong> the claimant or<br />
the ability <strong>of</strong> the claimant to regain maximum function,<br />
although it may not rise to the level <strong>of</strong> being a life-threatening<br />
circumstance, or<br />
2. In the opinion <strong>of</strong> a physician with knowledge <strong>of</strong> the claimant’s<br />
medical condition, would subject the claimant to severe pain<br />
that cannot be adequately managed without the care or<br />
treatment that is the subject <strong>of</strong> the claim.<br />
Urgent appeals are completed within 72 hours <strong>of</strong> receipt <strong>of</strong> the<br />
appeal request, or sooner, based on the medical exigencies <strong>of</strong> the<br />
case. Providers should contact the <strong>Blue</strong> <strong>Cross</strong> clinician who signed<br />
the denial letter to initiate an urgent appeal.<br />
Coding Appeals <strong>Blue</strong> <strong>Cross</strong>’ coding edits are updated at minimum annually to<br />
incorporate new codes, code definition changes <strong>and</strong> edit rule<br />
changes. All claims submitted after the implementation date <strong>of</strong> this<br />
update, regardless <strong>of</strong> service date, will be processed according to<br />
the updated version. Where Medicare’s CCI (Correct Coding<br />
Initiative) edits are identical, we will consider the appeal with<br />
additional documentation; however, the issue is likely to be<br />
upheld. Adjustments, <strong>and</strong>/or request refunds will not be made<br />
when processing changes are a result <strong>of</strong> new code editing rules due<br />
to a s<strong>of</strong>tware version update. Notice <strong>of</strong> this update will be<br />
published in the Provider Press <strong>and</strong>/or a Provider Bulletin.<br />
<strong>Blue</strong> <strong>Cross</strong> has adopted a st<strong>and</strong>ard process to review coding edit<br />
appeals <strong>and</strong> providers have the right to appeal with additional<br />
information. Appeals received without additional information will<br />
not be reviewed. The denial will be upheld.<br />
If you have a question or appeal about our policy regarding a<br />
particular coding combination, provide a written statement <strong>of</strong> the<br />
concern, along with the following <strong>and</strong>/or documentation normally<br />
required for a medical review.<br />
Written explanation supporting the procedures submitted, i.e.,<br />
specific references, specialty specific criteria<br />
Documentation from a recognized authoritative source that<br />
supports your position on the procedure codes submitted<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 10-5
Appeals<br />
Coding Appeals<br />
(continued)<br />
Once received, the inquiry or appeal will be reviewed <strong>and</strong> if<br />
necessary, forwarded to the Integrated Health Management<br />
department for determination. The review may result in approval<br />
or denial <strong>of</strong> the claim, based on review <strong>of</strong> the information<br />
submitted.<br />
Note: Requests to add modifier -24, -25 or -59 to a denied service<br />
must be submitted as replacement claims. All supporting<br />
documentation must also be attached to the replacement<br />
claim.<br />
Appeal requests may be faxed or mailed.<br />
Send your appeal request to the following address:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Attn: Provider Coding Appeals<br />
P.O. Box 64560<br />
St. Paul, MN 55164-0560<br />
Fax appeal requests to: (651) 662-2745<br />
<strong>Blue</strong>Card ® Appeals Appeals for <strong>Blue</strong>Card claims are h<strong>and</strong>led through <strong>Blue</strong> <strong>Cross</strong>.<br />
<strong>Blue</strong>Card Appeal vs.<br />
Adjustments<br />
Appealing Claims<br />
Processed by the<br />
Member’s Plan<br />
Generally, you will not find the appeal process any different. If<br />
coordination is required with the member’s Plan, we will<br />
coordinate it. Appeals for timely filing <strong>of</strong> <strong>Blue</strong>Card claims must be<br />
submitted to the patient’s <strong>Blue</strong> Plan.<br />
<strong>Blue</strong>Card requires that for the following circumstances, new<br />
claims must be submitted. Adjustments /appeals cannot be<br />
reviewed in these instances:<br />
Change an incorrect Individual Provider Number or NPI<br />
Change an incorrect member ID number, including alpha<br />
prefix<br />
Claim was sent in for a patient that is not yours<br />
Claims that are returned to you with either a yellow or green<br />
form attached<br />
Appeals for claims processed by the member’s plan are also<br />
h<strong>and</strong>led by them. However, you should send a completed AUC<br />
Appeal Form <strong>and</strong> the applicable attachments to <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> we<br />
will work with the member’s plan to facilitate your request.<br />
10-6 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Supporting<br />
Documentation<br />
Appeals<br />
The two key elements for submitting documentation with appeal<br />
requests are the patient’s name <strong>and</strong> the date <strong>of</strong> service. Both should<br />
be included on each page <strong>of</strong> the documentation submitted.<br />
Additionally, the documentation should correspond with the dates<br />
<strong>of</strong> service at issue.<br />
When the provider submits the appealed claim, the responsibility<br />
for gathering <strong>and</strong> submitting documentation that supports the<br />
service rests with the provider. We will <strong>of</strong>fer guidance <strong>and</strong><br />
assistance as necessary, but the responsibility for identifying what<br />
is needed <strong>and</strong> where it is located is yours.<br />
The list below includes common types <strong>of</strong> claim denials/reductions<br />
that may be submitted for appeal <strong>and</strong> the sources <strong>of</strong> documentation<br />
suggested for each type. This information is presented as a guide to<br />
assist you <strong>and</strong> is not a complete listing.<br />
Type <strong>of</strong> Denial or<br />
Reduction Documentation<br />
Surgical<br />
Complications<br />
Operative report, chart notes, letter<br />
stating rationale for complication<br />
Medical Necessity Medical records <strong>and</strong> rationale for service<br />
performed<br />
Investigative Medical records <strong>and</strong> rationale for service<br />
performed<br />
Cosmetic Medical records <strong>and</strong> rationale for services<br />
DRG/Category Code Rationale for questioning <strong>of</strong> payment<br />
Private Room Notes, doctor’s order <strong>and</strong> letter <strong>of</strong><br />
medical necessity<br />
Allowed Amount for<br />
unlisted codes<br />
Allowed Amount – for<br />
modified CPT/HCPCS<br />
codes.<br />
Allowed Amount –<br />
excluding unlisted<br />
codes.<br />
Chart notes or invoice, NDC number <strong>and</strong><br />
a letter to review allowance for an<br />
unlisted code. This is independent from<br />
medical necessity review process.<br />
Note: An invoice is required for DME<br />
or supply allowance appeals.<br />
Chart notes, letter <strong>and</strong> operative report<br />
when applicable to review allowance.<br />
Copy <strong>of</strong> fee schedule or provider<br />
agreement.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12) 10-7
Appeals<br />
Supporting<br />
Documentation<br />
(continued)<br />
Utilization Review<br />
Decision Appeal<br />
Type <strong>of</strong> Denial or<br />
Reduction Documentation<br />
Incompatible<br />
Diagnosis<br />
Letter requesting review <strong>of</strong> codes that are<br />
denying as incompatible <strong>and</strong> related notes<br />
Timely Filing Documentation supporting submission <strong>of</strong><br />
a claim after timely filing, such as<br />
secondary coverage, patient expired<br />
during timely filing period, or DME<br />
rental charges that span the timely filing<br />
period. Timely filing is addressed in<br />
Chapter 8.<br />
Coding Edit (Refer to<br />
Chapter 11 for details)<br />
All supporting documentation for<br />
corresponding date <strong>of</strong> service.<br />
Under current external review provisions, Provider or any other<br />
authorized representative may initiate an external review appeal on<br />
behalf <strong>of</strong> a Subscriber, with the express written authorization <strong>of</strong><br />
said Subscriber. Provider <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong> agree that this appeal<br />
process is binding, unless the Subscriber initiates an external<br />
appeal related to Utilization Review decisions. In the event that a<br />
Subscriber, a duly authorized representative <strong>of</strong> the Subscriber, or a<br />
Provider initiates an appeal related to Utilization Review<br />
decisions, <strong>Blue</strong> <strong>Cross</strong> shall abide by all applicable external review<br />
requirements <strong>of</strong> <strong>Minnesota</strong> Statutes, Section 62Q.73.<br />
10-8 <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/19/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Coding)<br />
Table <strong>of</strong> Contents<br />
Coding ....................................................................................................................................... 11-2<br />
Overview..............................................................................................................................11-2<br />
HCPCS Codes...................................................................................................................... 11-2<br />
CPT/Level I..........................................................................................................................11-3<br />
Level II HCPCS ................................................................................................................... 11-5<br />
ICD-9-CM............................................................................................................................11-7<br />
Revenue Codes..................................................................................................................... 11-9<br />
Compatibility .......................................................................................................................11-9<br />
Preventive Care Services ...................................................................................................11-10<br />
Preventive Services Required Under the PPACA .............................................................11-13<br />
General Guides................................................................................................................... 11-22<br />
Zero-billing ........................................................................................................................ 11-22<br />
Coding Edits ........................................................................................................................... 11-23<br />
Overview............................................................................................................................ 11-23<br />
Edit Descriptions................................................................................................................ 11-23<br />
Mutually Exclusive Procedures .........................................................................................11-25<br />
Incidental Procedures.........................................................................................................11-26<br />
Medical Visits on the Same Day as Surgery......................................................................11-27<br />
Global Surgical Package – Pre- <strong>and</strong> Postoperative Services .............................................11-28<br />
Units <strong>of</strong> Service Validation <strong>and</strong> Restriction ......................................................................11-29<br />
General Claims Processing Information ............................................................................ 11-30<br />
Medical <strong>and</strong> Surgical Supplies...........................................................................................11-30<br />
Multiple Surgery Guidelines..............................................................................................11-30<br />
Patient Billing Impact ........................................................................................................11-30<br />
Coding Appeals.................................................................................................................. 11-31<br />
Helpful Coding Tips ..........................................................................................................11-32<br />
Coding Immunizations <strong>and</strong> Injections ...............................................................................11-32<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Coding<br />
Overview <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) requires<br />
submission <strong>of</strong> valid codes to report medical services <strong>and</strong> supplies<br />
on both pr<strong>of</strong>essional <strong>and</strong> institutional claims. This includes<br />
Healthcare Common Procedural Coding System (HCPCS) codes,<br />
International Classification <strong>of</strong> Diseases, 9th Revision, Clinical<br />
Modification (ICD-9-CM) diagnosis <strong>and</strong> procedure codes <strong>and</strong><br />
Revenue codes.<br />
11-2<br />
The Health Insurance Portability <strong>and</strong> Accountability Act (HIPAA)<br />
Transaction <strong>and</strong> Code Set regulation stipulates submission <strong>and</strong><br />
acceptance <strong>of</strong> approved medical code sets. HCPCS <strong>and</strong> ICD-9-CM<br />
codes are among the approved HIPAA medical code sets <strong>and</strong> must<br />
be valid for the actual date <strong>of</strong> the service. If a HCPCS or ICD-9-<br />
CM code is not valid for the date <strong>of</strong> service, the claim will be<br />
returned or denied.<br />
Revenue codes are a data element <strong>of</strong> the institutional claim (837I<br />
or UB-04) <strong>and</strong> must be valid for the date <strong>of</strong> submission. If a<br />
Revenue code is not valid on the date submitted, the claim will be<br />
returned or denied.<br />
HCPCS Codes The HCPCS coding system was developed by CMS (Centers for<br />
Medicare <strong>and</strong> Medicaid Services) to st<strong>and</strong>ardize coding systems<br />
used to process claims for all payers, including Medicare <strong>and</strong><br />
Medicaid. HCPCS is a two level coding system-Level I, a.k.a.,<br />
CPT, <strong>and</strong> Level II, alpha-numeric codes.<br />
All nationally developed codes are accepted; however, coverage is<br />
not guaranteed <strong>and</strong> other restrictions may apply. Services may<br />
deny for various reasons including a subscriber contract exclusion<br />
or service limitation, <strong>Blue</strong> <strong>Cross</strong> corporate or medical policy, or<br />
subject to st<strong>and</strong>ardized coding edits.<br />
HCPCS codes are updated several times throughout the year. The<br />
primary update is January <strong>of</strong> each year. CMS provides updates to<br />
Level II codes on a quarterly basis. In addition to January, code<br />
updates are done in April, July, <strong>and</strong> October. CPT codes are<br />
generally updated only in January; however, the AMA can release<br />
codes early <strong>and</strong> make codes slated for the next year’s publication<br />
available in the prior July.<br />
You will be notified <strong>of</strong> coding updates by Bulletin or the Provider<br />
Press newsletter as to effective date <strong>of</strong> acceptance by <strong>Blue</strong> <strong>Cross</strong>.<br />
Reimbursement <strong>of</strong> new HCPCS/CPT codes billed on pr<strong>of</strong>essional<br />
claims (CMS HICF/837P) will be based on <strong>of</strong> the then current<br />
st<strong>and</strong>ard <strong>Blue</strong> <strong>Cross</strong> fee schedule allowed amount unless explicitly<br />
stated otherwise.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
CPT/Level I Level I or CPT (Current Procedural Terminology) codes are<br />
developed <strong>and</strong> maintained by the American Medical Association.<br />
Each procedure is identified with a five-digit numeric or numericalpha<br />
code. CPT is a set <strong>of</strong> codes, descriptions <strong>and</strong> guidelines<br />
intended to describe procedures <strong>and</strong> services performed by<br />
physicians <strong>and</strong> other health care providers. Inclusion or exclusion<br />
<strong>of</strong> a procedure does not imply any health insurance coverage or<br />
reimbursement policy.<br />
There are eight main sections to the CPT manual, including<br />
subsections with anatomic, procedural, conditions or descriptor<br />
subheadings. All listings are in numeric order except for<br />
Evaluation <strong>and</strong> Management (E/M) codes. E/M codes are the most<br />
frequently used <strong>and</strong> are listed first in the CPT manual<br />
Section Numbers <strong>and</strong> Sequences:<br />
E/M.........................................................99201 to 99499<br />
Anesthesiology.......................................00100 to 01999 <strong>and</strong> 99100<br />
to 99140<br />
Surgery ...................................................10021 to 69990<br />
Radiology ...............................................70010 to 79999<br />
Pathology <strong>and</strong> Laboratory......................80047 to 89398<br />
Medicine (except Anesthesiology).........90281 to 99199 <strong>and</strong> 99500<br />
to 99607<br />
Category II Codes ..................................0001F to 7025F<br />
Category III Codes .................................0019T to 0301T<br />
Modifiers<br />
A modifier is used to indicate that the service or procedure that has<br />
been performed has been altered by some specific circumstance<br />
but has not changed the definition or code. A complete listing <strong>of</strong><br />
modifiers is found in Appendix A <strong>of</strong> CPT. Level I codes are not<br />
limited to CPT modifiers. HCPCS Level II modifiers may also be<br />
used with Level I codes <strong>and</strong>/or in combination with CPT<br />
modifiers.<br />
Genetic Testing Code Modifiers are found in Appendix I <strong>of</strong> CPT.<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
CPT/Level I<br />
(continued)<br />
11-4<br />
CPT Format<br />
CPT codes are five characters in length (either all numeric or<br />
numeric-alpha) <strong>and</strong> designed as st<strong>and</strong>-alone descriptions <strong>of</strong><br />
medical procedures. Some procedures in CPT are not printed in<br />
their entirety but refer back to a common portion <strong>of</strong> the procedure<br />
listed in the preceding entry. These are sometimes referred to as<br />
indented procedures.<br />
For example:<br />
97010......Application <strong>of</strong> a modality to one or more areas; hot or<br />
cold packs<br />
97012......Traction, mechanical<br />
The common part <strong>of</strong> the code 97010 is before the semicolon <strong>and</strong> is<br />
also considered part <strong>of</strong> the code 97012. The full narrative for<br />
97012 is “Application <strong>of</strong> a modality to one or more areas; traction,<br />
mechanical.”<br />
Guidelines<br />
Guidelines are presented at the beginning <strong>of</strong> each <strong>of</strong> the main eight<br />
sections. Some section subheadings may contain instructions or<br />
information specific to those codes.<br />
Code Symbols<br />
Certain symbols may precede a code to indicate additional<br />
information:<br />
New CPT codes will be preceded by a bullet () symbol.<br />
Revised CPT codes will be preceded by a triangle (▲) symbol.<br />
Add-on CPT code will be preceded by a plus () symbol.<br />
Codes that include conscious sedation will be preceded by a<br />
target () symbol.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Level II HCPCS Level II HCPCS are developed <strong>and</strong> maintained by CMS. Level II<br />
consists <strong>of</strong> codes for supplies, materials, injections <strong>and</strong> services.<br />
Each Level II code is identified with a five character<br />
(alphanumeric) code.<br />
Level II codes are generally referred to simply as HCPCS codes to<br />
differentiate them from the Level I (CPT) codes. HCPCS codes are<br />
generally used because CPT has a limited code selection for these<br />
areas. All listings are in alpha category order except for modifiers.<br />
Format<br />
HCPCS codes are five characters in length, consisting <strong>of</strong> one alpha<br />
<strong>and</strong> four numeric characters. Level II codes start with alpha<br />
characters A through V <strong>and</strong> relate to these nationally defined<br />
categories:<br />
A0000-A0999........Transportation Services Including Ambulance<br />
A4000-A8999........Medical <strong>and</strong> Surgical Supplies<br />
A9000-A9999........Administrative, Miscellaneous <strong>and</strong><br />
Investigational<br />
B4000-B9999 ........Enteral <strong>and</strong> Parenteral Therapy<br />
C1000-C9999 ........Outpatient PPS<br />
D0000-D9999........Dental Procedures<br />
E0100-E9999 ........Durable Medical Equipment<br />
G0000-G9999........Procedures/Pr<strong>of</strong>essional Services (Temporary)<br />
(including Injections, Laboratory, Medical<br />
Services, Supplies)<br />
H0001-H2037........Alcohol <strong>and</strong> Drug Abuse Treatment Services<br />
(includes prenatal care codes)<br />
J0000-J9999 ..........Drugs Administered Other than Oral Method<br />
(J0000-J8499 – Other than Chemotherapy,<br />
J8500- J8999 – Oral Chemotherapy Drugs,<br />
J9000-J9999-Chemotherapy Drugs)<br />
K0000-K9999........Temporary Codes (for DMERCS including<br />
Durable Medical Equipment, Orthotics &<br />
Prosthetics, Supplies)<br />
L0000-L4999 ........Orthotics Procedures <strong>and</strong> Devices<br />
L5000-L9999 ........Prosthetic Procedures<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Level II HCPCS<br />
(continued)<br />
11-6<br />
M0000-M0301 ......Medical Services<br />
P0000-P9999.........Pathology <strong>and</strong> Laboratory (including Blood<br />
Products)<br />
Q0000-Q9999........Q Codes (Temporary) (including Injections,<br />
Laboratory, Occupational Therapy, Physical<br />
Therapy)<br />
R0000-R5999 ........Diagnostic Radiology Services (including<br />
Portable X-ray)<br />
S0000-S9999.........Temporary National Codes (Non-Medicare)<br />
T1000-T9999 ........National T Codes Established for State<br />
Medicaid Agencies<br />
V0000- V2799.......Vision Services<br />
V5000- V5399.......Hearing Services<br />
Modifiers<br />
A modifier is used to indicate that the service or supply has been<br />
altered by some specific circumstance but has not changed the<br />
definition or code. A complete listing <strong>of</strong> modifiers is found as an<br />
appendix to the HCPCS manual. Level II codes are not limited to<br />
HCPCS modifiers. CPT modifiers may also be used with Level II<br />
codes <strong>and</strong>/or in combination with HCPCS modifiers.<br />
Code Changes<br />
New HCPCS codes will be preceded by bullet () symbol.<br />
Revised HCPCS codes will be preceded by a triangle ()<br />
symbol.<br />
Reinstated HCPCS codes will be preceded by a circle ()<br />
symbol.<br />
Reinstated codes were previously deleted codes that have been<br />
reactivated.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
ICD-9-CM ICD-9-CM is a statistical classification system that arranges<br />
diseases, injuries <strong>and</strong> procedures into groups. Most ICD-9-CM are<br />
numeric <strong>and</strong> consist <strong>of</strong> three-, four- or five-digit numbers <strong>and</strong> a<br />
description. The coding structure is revised approximately every<br />
10 years by the World Health Organization. Annual updates,<br />
effective October 1, are published by NCVHS <strong>and</strong> CMS.<br />
Code Changes (not all publishers will include this information)<br />
New ICD-9-CM codes will be preceded by a bullet () symbol.<br />
Revised ICD-9-CM codes will be preceded by a triangle ()<br />
symbol.<br />
Format<br />
ICD-9-CM consists <strong>of</strong> three volumes:<br />
Volume I - The Tabular List<br />
Volume I is a numeric listing <strong>of</strong> diagnosis codes <strong>and</strong> descriptions<br />
consisting <strong>of</strong> seventeen chapters that classify diseases <strong>and</strong> injuries.<br />
In addition, two sections <strong>of</strong> supplementary codes (V <strong>and</strong> E codes)<br />
are included.<br />
Most diagnosis codes are four- or five-digit codes. The base ICD-<br />
9-CM diagnosis code consists <strong>of</strong> three digits, which may be further<br />
defined or classified by a fourth or fifth digit following a dot (this<br />
divides <strong>and</strong> identifies the base diagnosis). For example: 738.1 is<br />
the diagnosis “Other acquired deformity <strong>of</strong> head.” “Zygomatic<br />
hyperplasia” is coded as “738.11”. The addition <strong>of</strong> “1” specifically<br />
defines the acquired deformity. Only valid diagnoses, submitted to<br />
their full specificity, are accepted. If a fourth or fifth digit applies<br />
to a specific diagnosis code, it must be submitted.<br />
Volume 2 - The Alphabetical Index<br />
Consists <strong>of</strong> an alphabetic list <strong>of</strong> terms <strong>and</strong> codes.<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
ICD-9-CM (continued) Volume 3 - Procedures: Tabular List <strong>and</strong> Alphabetic Index<br />
11-8<br />
Volume 3 is a numeric listing <strong>of</strong> procedure codes <strong>and</strong> descriptions<br />
consisting <strong>of</strong> 17 chapters containing codes <strong>and</strong> descriptions for<br />
surgical procedures <strong>and</strong> miscellaneous diagnostic <strong>and</strong> therapeutic<br />
procedures. Codes from Volume 3 are intended only for use by<br />
hospitals for inpatient services.<br />
ICD-9-CM procedure codes are two-, three- or four-digit codes.<br />
The base ICD-9-CM procedure code consists <strong>of</strong> two digits that<br />
may be further defined or classified by a third or fourth digit<br />
following a dot (this divides <strong>and</strong> identifies the base procedure). For<br />
example: 50 is the procedure “Operations on liver.” “Closure <strong>of</strong><br />
laceration <strong>of</strong> liver” is coded as “50.61.” The addition <strong>of</strong> “.61”<br />
specifically defines the liver operation. Only valid procedures<br />
submitted to their full specificity, are accepted. If a third or fourth<br />
digit applies to a specific procedures code, it must be submitted.<br />
Linking/Pointing or Sequencing<br />
In the pr<strong>of</strong>essional claim record there are two diagnosis elements -<br />
one is at the header level <strong>of</strong> the claim <strong>and</strong> the other is at the line<br />
level <strong>and</strong> points to the values populated at the claim level. In the<br />
837P electronic transaction record the Diagnosis Code Pointer is<br />
found in the2400 loop - SV107-1, SV107-2, SV107-3, SV107-4.<br />
The primary diagnosis for the service performed must be<br />
appropriately linked to that service, especially if more than one<br />
diagnosis relates to a line item. Up to eight diagnoses can be<br />
submitted per pr<strong>of</strong>essional claim <strong>and</strong> up to four <strong>of</strong> those can be<br />
linked to a detail service line; however, adjudication is based on<br />
the first linked diagnosis.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Revenue Codes Revenue codes are developed by the National Uniform Billing<br />
Committee (NUBC) <strong>and</strong> are used to identify specific<br />
accommodation charges, ancillary service charges, or a type <strong>of</strong><br />
billing calculation. They are only to be submitted on the<br />
institutional electronic claim format (837I).<br />
Format<br />
Revenue codes are four digits in length. The first three digits<br />
define the category <strong>and</strong> the fourth digit defines the subcategory. It<br />
is important for the subcategory to be properly defined for<br />
appropriate payment. For example: 012X is the category for<br />
“Room & Board-Semi-Private (Two Bed)”. While 012X indicates<br />
the type <strong>of</strong> accommodations it does not identify the department or<br />
area in the hospital where the patient is staying. However, the code<br />
0122 (Obstetrics (OB) would properly indicate a semiprivate room<br />
in the OB.<br />
The list <strong>of</strong> revenue code is extensive <strong>and</strong> can be found in the<br />
NUBC UB 04 manual under FORM LOCATOR<br />
SPECIFICATIONS, form locator 42.<br />
HIPAA transaction st<strong>and</strong>ards require submission <strong>of</strong> HCPCS/CPT<br />
codes on outpatient facility claims. Guidelines for submission <strong>of</strong><br />
HCPCS/CPT codes including modifiers can be found in the UB-04<br />
manual under FORM LOCATOR SPECIFICATIONS, form<br />
locator 44.<br />
Compatibility HCPCS <strong>and</strong> ICD-9-CM Codes<br />
<strong>Blue</strong> <strong>Cross</strong> requires that diagnosis codes <strong>and</strong> procedures performed<br />
be compatible. These conditions are identified separately not only<br />
to assure correct coding, but also appropriately apply benefits.<br />
A chart <strong>of</strong> injury, maternity <strong>and</strong> behavioral health conditions <strong>and</strong><br />
the compatible diagnosis codes or ranges is found below. Note that<br />
this is a general guide only <strong>and</strong> is not all inclusive. All diagnoses<br />
must be reported to the fullest specificity.<br />
Condition Compatible Diagnosis Code/Code<br />
Category<br />
Injury 800-977, 980-994, V15.51, V15.59,<br />
V15.6, V66.4, V67.4, V71.3-V71.4,<br />
V71.6<br />
Maternity 630-677, V22-V24, V27, V28<br />
Chemical dependency 303-305. V79.1<br />
Psychiatric care 291-302, 306-319, V11, V40, V70.1-<br />
V70.2, V71.01-V71.09<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Compatibility<br />
(continued)<br />
Preventive Care<br />
Services<br />
11-10<br />
Revenue Codes<br />
Revenue codes must also be compatible with the type <strong>of</strong> facility,<br />
place <strong>of</strong> service <strong>and</strong> type <strong>of</strong> claim. On the 837 institutional claim,<br />
this is the claim facility type code <strong>and</strong> claim frequency code. Some<br />
revenue codes are very specific to the place where the service was<br />
rendered.<br />
For example, the TOB 0111 indicates an original claim for a<br />
hospital inpatient admission through discharge.<br />
Administration <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong>’ preventive care policy includes a<br />
list <strong>of</strong> defined preventive care services according to evidencebased<br />
guidelines. Payment for listed services would be subject to<br />
the subscriber’s coverage options for preventive care <strong>and</strong> cancer<br />
screening. Variations in payment may occur based on self-insured<br />
dollar <strong>and</strong> service limits. Benefits should be verified through use<br />
<strong>of</strong> the electronic eligibility transaction, our provider web self<br />
service site at www.providerhub.com or through BLUELINE.<br />
Services considered preventive<br />
If a patient presents to have these services performed for<br />
preventive purposes, claims will be adjudicated as preventive care<br />
provided the reason for the visit on the claim is listed as<br />
preventive, regardless <strong>of</strong> outcome. <strong>Blue</strong> <strong>Cross</strong>’ administrative<br />
guidelines are as follows:<br />
Service Frequency (does<br />
not apply to <strong>Blue</strong><br />
Plus)<br />
Abdominal Aortic<br />
Aneurysm (AAA)<br />
screening<br />
Vision Screening:<br />
Glaucoma, Acuity,<br />
Refraction<br />
Clinical Practice/<br />
Guidelines<br />
1 per lifetime <strong>Blue</strong> <strong>Cross</strong><br />
1 per year ICSI<br />
Hearing 1 per year ICSI<br />
St<strong>and</strong>ard immunizations Per schedules<br />
determined by<br />
clinical<br />
guidelines<br />
CDC/ACIP<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Preventive Care<br />
Services (continued)<br />
Service Frequency (does<br />
not apply to <strong>Blue</strong><br />
Plus)<br />
Radiology: Osteoporosis<br />
Screening<br />
Laboratory Services:<br />
Cholesterol/Lipid Pr<strong>of</strong>ile,<br />
Urinalysis<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
1 per year ICSI<br />
As recommended<br />
by physician<br />
Diabetes Screening As recommended<br />
by physician<br />
STD Screening: HIV,<br />
Chlamydia, Gonorrhea,<br />
Syphilis<br />
Preventive Medical<br />
Examination for Adults<br />
including Skin Exam,<br />
Testicular Exam, Prostate-<br />
Digital Rectal Exam,<br />
Breast Exam,<br />
Hypertension Screening<br />
As recommended<br />
by physician<br />
As recommended<br />
by physician<br />
Cancer screening paid at the highest level<br />
Clinical Practice/<br />
Guidelines<br />
ICSI<br />
<strong>Blue</strong> <strong>Cross</strong><br />
ICSI/M<strong>and</strong>ate<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
ICSI<br />
Service Frequency Clinical Practice/<br />
Guidelines<br />
Colon Cancer Screening:<br />
Occult Blood<br />
Colon Cancer Screening:<br />
Barium Enema,<br />
Sigmoidoscopy,<br />
Proctosigmoidoscopy<br />
Colon Cancer Screening:<br />
Colonoscopy<br />
Cervical Cancer<br />
Screening: Pap Smear<br />
Breast Cancer Screening:<br />
Conventional Film Screen<br />
Mammography<br />
1 per year ICSI/ACS<br />
As recommended<br />
by physician<br />
As recommended<br />
by physician<br />
ICSI/ACS<br />
ICSI/ACS<br />
1 per year ICSI.ACS<br />
1 per year ICSI.ACS<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Preventive Care<br />
Services (continued)<br />
11-12<br />
Service Frequency (does<br />
not apply to <strong>Blue</strong><br />
Plus)<br />
Prostate Cancer: Prostate<br />
Specific Antigen (PSA)<br />
Ovarian Cancer: CA125,<br />
For those at high risk <strong>and</strong><br />
Trans-vaginal Ultrasound<br />
Clinical Practice/<br />
Guidelines<br />
1 per year <strong>Blue</strong> <strong>Cross</strong>/<br />
M<strong>and</strong>ate<br />
1 per year <strong>Blue</strong> <strong>Cross</strong>/<br />
M<strong>and</strong>ate<br />
Services for consideration under the illness/medical level <strong>of</strong><br />
benefit<br />
Any/all services that have an increased frequency due to an<br />
effort to control or prevent abnormal condition from recurring<br />
Procedures not considered preventive according to evidencebased<br />
guidelines developed as clinical <strong>and</strong> industry st<strong>and</strong>ards;<br />
for example, chest X-rays, urinalysis, complex lab <strong>and</strong><br />
diagnostic imaging procedures<br />
Contraceptive management that is not part <strong>of</strong> Patient Protection<br />
<strong>and</strong> Affordable Care Act (PPACA) women’s preventive<br />
“contraceptive methods <strong>and</strong> counseling”<br />
Eyewear including lenses, frames <strong>and</strong> contract lenses<br />
Using the current version <strong>of</strong> the ICD-9-CM, report the patient’s<br />
condition at the highest level <strong>of</strong> certainty that are related to the<br />
services provided. Both the findings (if any exist) <strong>and</strong> the reason<br />
for the visit should be reported.<br />
Clinical practice guideline abbreviations include:<br />
CDC/ACIP – Centers for Disease Control/Advisory<br />
Committee on Immunization Practices<br />
ICSI – Institute for Clinical Systems Improvement<br />
ACS – American Cancer Society<br />
M<strong>and</strong>ate – M<strong>and</strong>ated by <strong>Minnesota</strong> statute<br />
<strong>Blue</strong> <strong>Cross</strong> – <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong><br />
<strong>Blue</strong> Plus<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Preventive Services<br />
Required Under the<br />
PPACA<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Effective for dates <strong>of</strong> service September 23, 2010 <strong>and</strong> after, the<br />
Patient Protection <strong>and</strong> Affordable Care Act (PPACA) otherwise<br />
known as health care reform (HCR), includes a provision for<br />
preventive services at no cost to eligible subscribers. <strong>Blue</strong> <strong>Cross</strong><br />
has always considered preventive services an essential part <strong>of</strong> a<br />
subscriber’s ongoing care <strong>and</strong> will continue to administer<br />
preventive services in conjunction <strong>and</strong> in accordance with the<br />
administrative <strong>and</strong> recommended guidelines under HCR:<br />
United States Preventive Services Task Force (USPSTF)<br />
ratings <strong>of</strong> A or B<br />
Advisory Committee <strong>of</strong> Immunization Practices (ACIP), under<br />
the Centers for Disease Control <strong>and</strong> Prevention (CDC)<br />
Health Resources <strong>and</strong> Services Administration (HRSA)<br />
Guidelines for Preventive Care <strong>and</strong> Screenings for Women,<br />
Infants, Children <strong>and</strong> Adolescents<br />
<strong>Blue</strong> <strong>Cross</strong>’ Preventive Care Services <strong>and</strong> Administrative<br />
Guidelines already incorporated a majority <strong>of</strong> these<br />
recommendations. As a result <strong>of</strong> PPACA, additional guidelines<br />
have been included under <strong>Blue</strong> <strong>Cross</strong>’ preventive care services to<br />
ensure compliance with the law. Please see the chart below for<br />
more information on the additional services, recommendations <strong>and</strong><br />
suggested coding.<br />
New Preventive<br />
Service<br />
Counseling<br />
related to BRCA<br />
screening<br />
Interventions to<br />
support breastfeeding<br />
Health Care Reform<br />
Recommendation<br />
The USPSTF<br />
recommends that<br />
women whose family<br />
history is associated<br />
with an increased risk<br />
for deleterious<br />
mutations in BRCA1<br />
or BRCA2 genes be<br />
referred for genetic<br />
counseling <strong>and</strong><br />
evaluation for BRCA<br />
testing.<br />
The USPSTF<br />
recommends<br />
interventions during<br />
pregnancy <strong>and</strong> after<br />
birth to promote <strong>and</strong><br />
support breastfeeding.<br />
Suggested Codes<br />
96040, 99401-99404,<br />
<strong>and</strong> S0265 as<br />
preventive with<br />
V16.3, V16.41, V16.8<br />
or V26.33<br />
S9443 as preventive<br />
with V24.1<br />
11-13
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Preventive services<br />
required under the<br />
PPACA (continued)<br />
11-14<br />
New Preventive<br />
Service<br />
Chemoprevention <strong>of</strong><br />
dental caries<br />
Screening for<br />
depression:<br />
adolescents <strong>and</strong> adults<br />
Recommendation for<br />
counseling for a<br />
healthy diet<br />
Health Care Reform<br />
Recommendation<br />
The USPSTF<br />
recommends that<br />
primary care<br />
clinicians administer<br />
oral fluoride<br />
supplementation at<br />
currently<br />
recommended doses<br />
to preschool children<br />
older than 6 months <strong>of</strong><br />
age whose primary<br />
water source is<br />
deficient in fluoride.<br />
The USPSTF<br />
recommends<br />
screening adolescents<br />
<strong>and</strong> adults for<br />
depression when staffassisted<br />
depression<br />
care supports are in<br />
place to assure<br />
accurate diagnosis,<br />
effective treatment<br />
<strong>and</strong> follow-up.<br />
The USPSTF<br />
recommends intensive<br />
behavioral dietary<br />
counseling for adult<br />
patients with<br />
hyperlipidemia <strong>and</strong><br />
other known risk<br />
factors for<br />
cardiovascular <strong>and</strong><br />
diet-related chronic<br />
disease. Intensive<br />
counseling can be<br />
delivered by primary<br />
care clinicians or by<br />
referral to other<br />
specialists, such as<br />
nutritionists or<br />
dietitians.<br />
Suggested Codes<br />
D1206 (age 00-06)<br />
99201-99205, 99211-<br />
99215, 99384-99387<br />
<strong>and</strong> 99394-99397,<br />
G0438,G0439,G0444<br />
as preventive with<br />
V79.0<br />
99401-99404, 99411-<br />
99412, 99078, 97802-<br />
97804, S9452, S9470<br />
as preventive with<br />
V65.3<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Preventive services<br />
required under the<br />
PPACA (continued)<br />
New Preventive<br />
Service<br />
Screening <strong>and</strong><br />
counseling for<br />
obesity: children <strong>and</strong><br />
adults<br />
Recommendation for<br />
counseling for tobacco<br />
use<br />
Recommendation for<br />
counseling for tobacco<br />
use in pregnant<br />
women<br />
Assess for alcohol <strong>and</strong><br />
drug use in<br />
adolescents<br />
Behavioral<br />
assessments for<br />
children<br />
Testing for<br />
tuberculosis in<br />
children<br />
Health Care Reform<br />
Recommendation<br />
The USPSTF<br />
recommends that<br />
clinicians screen all<br />
children <strong>and</strong> adult<br />
patients for obesity<br />
<strong>and</strong> <strong>of</strong>fer intensive<br />
counseling <strong>and</strong><br />
behavioral<br />
interventions to<br />
promote sustained<br />
weight loss for obese<br />
adults.<br />
The USPSTF<br />
recommends that<br />
clinicians ask all<br />
adults about tobacco<br />
use <strong>and</strong> provide<br />
tobacco cessation<br />
interventions for those<br />
who use tobacco<br />
products.<br />
The USPSTF<br />
recommends that<br />
clinicians ask all<br />
pregnant women<br />
about tobacco use <strong>and</strong><br />
provide augmented,<br />
pregnancy-tailored<br />
counseling for those<br />
who smoke.<br />
HRSA recommends<br />
alcohol <strong>and</strong> drug use<br />
assessments for<br />
adolescents<br />
HRSA recommends<br />
behavioral<br />
assessments for<br />
children <strong>of</strong> all ages<br />
HRSA recommends<br />
tuberculin testing for<br />
children at higher risk<br />
<strong>of</strong> tuberculosis<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Suggested Codes<br />
97802-97804, 99078,<br />
99401-99404, 99411-<br />
99412, G0447, G0449<br />
S9470 as preventive<br />
with 278.00 or 278.01<br />
99401-99404, 99406-<br />
99407, 99411-99412,<br />
G0436, G0437, S9453<br />
as preventive with<br />
305.1 or V15.82<br />
99406-99407, G0436,<br />
G0437, S9453 as<br />
preventive with<br />
649.00 or 649.03<br />
G0442, G0443,<br />
H0001, 99408-99409<br />
as preventive with<br />
V65.42 (age 11-20)<br />
99420 as preventive<br />
with V79.0, V79.1,<br />
V79.2, V79.3, V79.8,<br />
V79.9 (age 00-20)<br />
86580 as preventive<br />
with V74.1 (age 00-<br />
20)<br />
11-15
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Preventive services<br />
required under the<br />
PPACA (continued)<br />
11-16<br />
Effective for plan years beginning on or after August 1, 2012,<br />
PPACA requires certain items <strong>and</strong> services covered without cost–<br />
sharing for women as recommended by the:<br />
United States Preventive Services Task Force (USPSTF) ratings<br />
<strong>of</strong> A or B<br />
Advisory Committee <strong>of</strong> Immunization Practices (ACIP), under<br />
the Centers for Disease Control <strong>and</strong> Prevention (CDC)<br />
Health Resources <strong>and</strong> Services Administration (HRSA)<br />
Guidelines for Preventive Care <strong>and</strong> Screenings for Women,<br />
Infants, Children <strong>and</strong> Adolescents<br />
To the extent not described in the USPSTF recommendations,<br />
HRSA was charged with developing comprehensive guidelines for<br />
preventive care <strong>and</strong> screenings for women. As part <strong>of</strong> this process,<br />
HRSA commissioned an Institute <strong>of</strong> Medicine (IOM) report<br />
entitled: “Clinical Preventive Services for Women: Closing the<br />
Gaps”<br />
1. Well–woman visit<br />
2. Screening for gestational diabetes mellitus (GDM)<br />
3. Counseling for sexually transmitted infection (STI)<br />
4. Counseling <strong>and</strong> screening for human hmmunodeficiency virus<br />
(HIV)<br />
5. Counseling <strong>and</strong> screening for interpersonal <strong>and</strong> domestic<br />
violence<br />
6. Breastfeeding support, supplies <strong>and</strong> counseling<br />
7. Human papillomavirus (HPV) testing<br />
8. Contraceptive methods <strong>and</strong> counseling *<br />
* Some employer group plans may be exempt or in temporary safe<br />
harbor status for “contraceptive methods <strong>and</strong> counseling” <strong>and</strong> will<br />
not have to <strong>of</strong>fer women’s preventive “contraceptive methods <strong>and</strong><br />
counseling” until their plan year beginning on or after August 1,<br />
2013. Temporary safe harbor does not apply to individual policies.<br />
Non-preventive care received during a preventive care visit is<br />
subject to normal plan cost sharing.<br />
Please see the chart below for more information on the additional<br />
services, recommendations <strong>and</strong> suggested coding.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
New women’s<br />
preventive service<br />
<strong>Blue</strong> <strong>Cross</strong> coverage<br />
Well-woman visit Well-woman preventive care visit<br />
annually for adult women (ages 12 to<br />
64) to obtain the recommended<br />
preventive services that are age <strong>and</strong><br />
developmentally appropriate, which<br />
may include preconception <strong>and</strong><br />
prenatal care as well as the list <strong>of</strong><br />
services in Table 5 – 6 “Clinical<br />
Preventive Services for Women:<br />
Closing the Gaps” July 2011 report<br />
by the Institute <strong>of</strong> Medicine –<br />
http://iom.edu/Reports/2011/Clinical<br />
-Preventive-Services-for-Women-<br />
Closing-the-Gaps.aspx<br />
Screening for<br />
gestational diabetes<br />
mellitus (GDM)<br />
Counseling for<br />
sexually transmitted<br />
infections (STI)<br />
Based upon ICSI (Institute for<br />
Clinical Systems Improvement)<br />
GDM guideline below:<br />
50 mg oral glucose load<br />
followed one hour later by the<br />
blood draw<br />
If the one-hour (above)<br />
glucose challenge test is<br />
positive, a 100 g load<br />
followed by a 3-hour glucose<br />
tolerance test should be<br />
performed<br />
Note: Confirmation tests in the<br />
2nd bullet (above) will be treated<br />
as preventive ($0 member<br />
liability)<br />
Counseling on STIs, group or<br />
individual sessions, once per year,<br />
30-minute maximum per session for<br />
women regardless <strong>of</strong> sexual activity<br />
Counseling may be similar to the 5Ps<br />
<strong>of</strong> the CDC: partners, prevention <strong>of</strong><br />
pregnancy, protection from STIs,<br />
practices <strong>and</strong> past STIs<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Annual 99384-99386,<br />
99394-99396 as<br />
preventive with<br />
V70.0 or V72.31<br />
Gestational<br />
diabetes screening<br />
for pregnant<br />
women at any<br />
stage (week <strong>of</strong><br />
gestation) in the<br />
pregnancy –<br />
regardless <strong>of</strong><br />
presence <strong>of</strong> highrisk<br />
factors such<br />
as: ethnicity, BMI,<br />
family history,<br />
previous GDM,<br />
patient has DM<br />
82947, 82950,<br />
82951, 83036 as<br />
preventive with<br />
any <strong>of</strong> the<br />
following range:<br />
V22.0-V22.2,<br />
V23.0-V23.3,<br />
V23.41, V23.42,<br />
V23.49, V23.5,<br />
V23.7, V23.81-<br />
V23.87, V23.89 or<br />
V23.9<br />
Annual 99401, 99402,<br />
99411, G0450 as<br />
preventive with<br />
V65.45 or V69.2<br />
11-17
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
New women’s<br />
preventive service<br />
Counseling <strong>and</strong><br />
screening for human<br />
immunodeficiency<br />
virus (HIV)<br />
Counseling <strong>and</strong><br />
screening for<br />
interpersonal <strong>and</strong><br />
domestic violence<br />
11-18<br />
<strong>Blue</strong> <strong>Cross</strong> coverage<br />
Counseling on HIV, group or<br />
individual sessions, once per year,<br />
30-minute maximum per session for<br />
women regardless <strong>of</strong> sexual activity<br />
Counseling up to individual<br />
practitioner but may be similar to the<br />
counseling for STI<br />
Screening for HIV (already paid as<br />
preventive by <strong>Blue</strong> <strong>Cross</strong> prior to<br />
PPACA): lab tests to screen for HIV-<br />
1 or HIV-2 antibodies<br />
Screening up to each individual<br />
practitioner: may be survey or<br />
checklist, usually part <strong>of</strong> st<strong>and</strong>ard<br />
intake/triage for <strong>of</strong>fice visit<br />
Counseling – definition <strong>of</strong><br />
counseling up to each individual<br />
practitioner, group or individual<br />
sessions, no time limit per session,<br />
but only one session per year<br />
covered as preventive (even if<br />
multiple sessions needed)<br />
Counseling:<br />
annual<br />
Screening for STI:<br />
as recommended<br />
by a physician<br />
Counseling:<br />
G0445, G0450,<br />
99401, 99402,<br />
99411 as<br />
preventive with<br />
V65.44, V65.45 or<br />
V69.2<br />
Screening: 86701,<br />
86703, 86689,<br />
G0432, G0433,<br />
G0435, 87390,<br />
87534, 87535, as<br />
preventive<br />
Annual Screening: No<br />
suggested coding.<br />
No coding<br />
available for<br />
screening.<br />
Counseling:<br />
99401-99404, or<br />
99411 or 99412 as<br />
preventive with<br />
V70.0 or V72.31<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
New women’s<br />
preventive service<br />
Breastfeeding support,<br />
supplies <strong>and</strong><br />
counseling<br />
Human papillomavirus<br />
(HPV) testing<br />
<strong>Blue</strong> <strong>Cross</strong> coverage<br />
Support: Per Institute <strong>of</strong> Medicine<br />
(IOM) report: “Clinical Preventive<br />
Services for Women: Closing the<br />
Gaps” employer support <strong>of</strong><br />
breastfeeding such as allowing time<br />
for mother to express milk at the<br />
<strong>of</strong>fice <strong>and</strong> providing quiet <strong>and</strong><br />
private place to express <strong>and</strong>/or store<br />
milk (mother’s room)<br />
Supplies: Purchase, up to 100% <strong>of</strong><br />
allowed charges, <strong>of</strong> manual breast<br />
pump from in-network supplier or<br />
provider<br />
Counseling: Trained provider to<br />
ensure the successful initiation <strong>and</strong><br />
duration <strong>of</strong> breastfeeding. May be<br />
provided as part <strong>of</strong> the hospital or<br />
birthing center delivery stay.<br />
Human papillomavirus DNA testing<br />
in women with normal cytology<br />
results, regardless <strong>of</strong> risk factors or<br />
sexual activity<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Counseling: in<br />
conjunction with<br />
each pregnancy<br />
<strong>Manual</strong> breast<br />
pump: purchase<br />
up to 6 months<br />
post-partum<br />
Screening should<br />
begin at 30 years<br />
<strong>of</strong> age <strong>and</strong> should<br />
occur no more<br />
frequently than<br />
every three years<br />
Support: No<br />
suggested<br />
coding. No<br />
coding available<br />
for support.<br />
Supplies: E0602<br />
Counseling:<br />
S9443 as<br />
preventive with<br />
the following<br />
V24.1,<br />
V22.0-V22.2,<br />
V23.0-V23.3,<br />
V23.41,V23.42,<br />
V23.49, V23.5,<br />
V23.7, V23.81-<br />
V23.87, V23.89<br />
or V23.9<br />
87620, 87621 as<br />
preventive<br />
11-19
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
New women’s<br />
preventive service<br />
Contraceptive methods<br />
<strong>and</strong> counseling *<br />
* Some employer<br />
group plans may be<br />
exempt or in<br />
temporary safe harbor<br />
status for<br />
“contraceptive<br />
methods <strong>and</strong><br />
counseling” <strong>and</strong> will<br />
not have to <strong>of</strong>fer<br />
women’s preventive<br />
“contraceptive<br />
methods <strong>and</strong><br />
counseling” until their<br />
plan year beginning on<br />
or after August 1, 2013<br />
11-20<br />
<strong>Blue</strong> <strong>Cross</strong> coverage<br />
Counseling: Counseling for women<br />
ages 12 to 64 by trained personnel<br />
regarding family planning;<br />
distribution <strong>of</strong> information relating<br />
to family planning, referral to<br />
licensed physicians or local health<br />
agencies for consultation,<br />
examination, medical treatment,<br />
genetic counseling, <strong>and</strong> prescriptions<br />
for the purpose <strong>of</strong> family planning,<br />
<strong>and</strong> the distribution <strong>of</strong> family<br />
planning products, such as: charts,<br />
thermometers, drugs, medical<br />
preparations, <strong>and</strong> contraceptive<br />
devices. Does not include the<br />
performance, or referrals for<br />
encouragement <strong>of</strong> voluntary<br />
termination <strong>of</strong> pregnancy.<br />
Inform any woman requesting<br />
counseling on family planning<br />
methods or procedures <strong>of</strong>:<br />
1. Any methods or procedures<br />
that may be followed (which<br />
may include continuous<br />
abstinence, natural family<br />
planning/rhythm method),<br />
including identification <strong>of</strong><br />
any that are experimental or<br />
may post a health hazard to<br />
the woman,<br />
2. A description <strong>of</strong> any<br />
attendant discomforts or<br />
risks that might reasonably<br />
be expected,<br />
3. A fair explanation <strong>of</strong> likely<br />
results, should a method fail,<br />
4. A description <strong>of</strong> any benefits<br />
that might reasonably be<br />
expected <strong>of</strong> any method,<br />
5. A disclosure <strong>of</strong> appropriate<br />
alternative methods or<br />
procedures,<br />
6. An <strong>of</strong>fer to answer any<br />
inquiries concerning<br />
Counseling:<br />
once/year<br />
Methods: Select<br />
oral<br />
contraceptives,<br />
supplies <strong>and</strong><br />
procedures will be<br />
covered<br />
Counseling:<br />
99384-99386<br />
99394-99396,<br />
S0610, S0612 or<br />
S0613 as<br />
preventive with<br />
V25.01-V25.04,<br />
V25.09, V25.41,<br />
V25.43 or V25.49<br />
Methods: Varies<br />
depending upon<br />
covered drug,<br />
supply or<br />
procedure<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
New women’s<br />
preventive service<br />
Contraceptive methods<br />
<strong>and</strong> counseling *<br />
* Some employer<br />
group plans may be<br />
exempt or in<br />
temporary safe harbor<br />
status for<br />
“contraceptive<br />
methods <strong>and</strong><br />
counseling” <strong>and</strong> will<br />
not have to <strong>of</strong>fer<br />
women’s preventive<br />
“contraceptive<br />
methods <strong>and</strong><br />
counseling” until their<br />
plan year beginning on<br />
or after August 1, 2013<br />
(continued)<br />
Preventive Services<br />
Required Under the<br />
PPACA (continued)<br />
<strong>Blue</strong> <strong>Cross</strong> coverage<br />
An instruction that the person is free<br />
either to decline commencement <strong>of</strong><br />
any method or procedure or to<br />
withdraw consent to a method or<br />
procedure at any reasonable time<br />
Methods:<br />
For women ages 12 to 64; limited to<br />
specific oral contraceptives, supplies<br />
<strong>and</strong> procedures. Coverage may vary<br />
by group <strong>and</strong> pharmacy benefit<br />
manager (PBM) <strong>and</strong> is subject to<br />
change if covered formulary<br />
changes. Members should contact<br />
customer service at the number on<br />
the back <strong>of</strong> their member ID card for<br />
the specific methods covered by their<br />
group or policy.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Not all health plans, policies or employer groups will define or<br />
administer the women’s preventive coverage in the same way.<br />
PPACA requires coverage <strong>of</strong> the women’s preventive items for<br />
non-gr<strong>and</strong>fathered status plans. <strong>Blue</strong> <strong>Cross</strong> made a business<br />
decision to apply the women’s preventive benefits to plans that<br />
accepted the prior PPACA preventive care package (dates <strong>of</strong><br />
service September 23, 2010 <strong>and</strong> after) – some <strong>of</strong> those groups may<br />
be gr<strong>and</strong>fathered status. Also, self–insured groups may <strong>of</strong>fer a<br />
different, or richer, benefit. Groups may have different drugs<br />
covered for “contraceptive methods <strong>and</strong> counseling” depending<br />
upon the pharmacy benefit manager (PBM) they use. Members<br />
should verify their preventive coverage before receiving benefits by<br />
calling the customer service phone number on the back <strong>of</strong> their<br />
member identification (ID) card.<br />
11-21
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
General Guides Submit the code that most accurately identifies the service(s)<br />
performed. Documentation in the patient’s medical record must<br />
support the codes submitted.<br />
11-22<br />
Do not use multiple codes when services can be represented by<br />
a single code, unless otherwise instructed. Fragmented services<br />
(reporting several codes when one adequately defines the<br />
service) will be subject to our coding s<strong>of</strong>tware edits <strong>and</strong> may<br />
be denied.<br />
Unlisted codes should only be used if no code exists to<br />
describe the service or supply. HCPCS codes for unlisted<br />
services require a complete narrative description.<br />
Submit all services for the same date <strong>of</strong> service on the same<br />
claim.<br />
“C” HCPCS codes.<br />
Codes C1000-C9999 are for items classified in newtechnology<br />
ambulatory payment classifications (APCs)<br />
under the outpatient prospective payment systems. These<br />
codes are exclusively for use in billing for institutional<br />
transitional pass-through payments. <strong>Blue</strong> <strong>Cross</strong> does not<br />
use an APC methodology for adjudication or payment <strong>of</strong><br />
claims, thus C codes will not be used in adjudication.<br />
Processing <strong>and</strong> payment will be determined by other<br />
factors on the claim, such as a revenue code.<br />
It is the intention <strong>of</strong> CMS to allow the use <strong>of</strong> the codes by<br />
all payers regardless <strong>of</strong> payment methodology, so C<br />
HCPCS codes will be accepted on institutional (UB-04 or<br />
837I) claims only. However, C codes submitted on a<br />
pr<strong>of</strong>essional claim (CMS HICF/837P), other than<br />
freest<strong>and</strong>ing ambulatory surgical centers (ASC), will deny<br />
as provider liability.<br />
Free-st<strong>and</strong>ing ASC services are submitted on a pr<strong>of</strong>essional<br />
claim format. C-codes may be submitted, as appropriate, on<br />
freest<strong>and</strong>ing ASC claims.<br />
Zero-billing <strong>Blue</strong> <strong>Cross</strong> will allow zero-billing or no-charge claim lines.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Coding Edits<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Overview <strong>Blue</strong> <strong>Cross</strong> uses an automated procedure editing tool. This tool has<br />
been adopted <strong>and</strong> modified by <strong>Blue</strong> <strong>Cross</strong> to assist in a consistent<br />
<strong>and</strong> fair claim review process. The procedure code edits may also<br />
reflect <strong>Blue</strong> <strong>Cross</strong>’ Medical Coverage Guidelines, benefit plans<br />
<strong>and</strong> other <strong>Blue</strong> <strong>Cross</strong> policies. Unbundling, fragmentation,<br />
mutually exclusive procedures, duplicate, obsolete or invalid codes<br />
are all identified through the use <strong>of</strong> this coding edit application.<br />
The procedure code edits are based on CPT guidelines, a review <strong>of</strong><br />
the Center for Medicare <strong>and</strong> Medicaid Services (CMS) Correct<br />
Coding Initiative policies <strong>and</strong> guidelines, specialty society<br />
guidelines, agreed upon industry practices <strong>and</strong> analysis by an<br />
extensive clinical consultant network. This automated review<br />
process is designed to apply the same industry criteria consistently<br />
across all pr<strong>of</strong>essional claims.<br />
Edit Descriptions Procedure Code Unbundling/Replacement<br />
Procedure code unbundling is the submission <strong>of</strong> multiple<br />
procedure codes for a group <strong>of</strong> specific procedures that are<br />
components <strong>of</strong> a single comprehensive code. Procedure<br />
unbundling may occur in one <strong>of</strong> two ways:<br />
A pr<strong>of</strong>essional claim could be submitted that has procedure codes<br />
for both the individual components, <strong>and</strong> the procedure code for the<br />
comprehensive procedure. <strong>Blue</strong> <strong>Cross</strong> would rebundle the<br />
individual component codes into the comprehensive procedure<br />
code for payment.<br />
Procedure unbundling could also occur when a pr<strong>of</strong>essional claim<br />
is submitted with only the individual components <strong>of</strong> the<br />
comprehensive code. In this situation, the s<strong>of</strong>tware will recognize<br />
the relationship between the comprehensive code <strong>and</strong> its individual<br />
components. Then, it will automatically add the comprehensive<br />
code to the claim <strong>and</strong> rebundle the individual components into that<br />
comprehensive code for payment.<br />
11-23
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Edit Descriptions<br />
(continued)<br />
11-24<br />
An example would be billing the following procedure codes<br />
together:<br />
33207......Insertion <strong>of</strong> heart pacemaker, ventricular<br />
33208......Insertion <strong>of</strong> heart pacemaker, atrial <strong>and</strong> ventricular<br />
Procedure 33208 is identified as the primary procedure code. CPT<br />
33207 would be rebundled because it is an integral part <strong>of</strong><br />
procedure 33208. Rather than a line item denial, the procedure <strong>and</strong><br />
related charge will be summed together <strong>and</strong> a new allowance for<br />
the surviving code will be established based on your contracted fee<br />
schedule.<br />
Another example would be billing the following procedure codes<br />
together:<br />
82374......Carbon dioxide<br />
82435......Chloride<br />
84132......Potassium<br />
84295......Sodium<br />
In combination, the four codes above would be rebundled <strong>and</strong><br />
replaced with the more appropriate procedure 80051-electrolyte<br />
panel. Related charges will be summed together <strong>and</strong> the allowance<br />
based on the comprehensive code 80051.<br />
When this edit is applicable, the following message will appear on<br />
your current remittance advice:<br />
This service is a component <strong>of</strong> a procedure that has already<br />
been processed on this or another claim.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Mutually Exclusive<br />
Procedures<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Mutually exclusive procedures exist when a claim is submitted for<br />
two or more procedures that are not usually performed on the same<br />
patient, on the same date <strong>of</strong> service. In mutually exclusive<br />
relationships, the most clinically intense code is recognized for<br />
payment. Clinical intensity is generally based on the total RVU for<br />
the procedures submitted.<br />
An example would be billing the following procedure codes<br />
together:<br />
58260......Vaginal Hysterectomy<br />
58150......Total Abdominal Hysterectomy<br />
Since a hysterectomy would not be performed using two different<br />
approaches, the vaginal hysterectomy would be denied as mutually<br />
exclusive to the abdominal hysterectomy. This edit would result in<br />
the line item denial <strong>of</strong> procedure 58260 <strong>and</strong> would be the<br />
participating network provider’s liability.<br />
Another example would be billing the following procedures<br />
together:<br />
27550......Closed treatment <strong>of</strong> a knee dislocation<br />
27556......Open treatment <strong>of</strong> a knee dislocation<br />
The knee would not be reduced by doing both procedures. The<br />
open procedure would survive as the one that was more clinically<br />
intense. This would result in the line item denial <strong>of</strong> procedure<br />
27550 <strong>and</strong> would be the participating network provider’s liability.<br />
When this edit is applicable, the following message(s) will appear<br />
on your current remittance advice:<br />
Payment is included in the allowance <strong>of</strong> the other procedure.<br />
Service is not payable with other service rendered on the same<br />
date.<br />
These charges are not covered. Less complex procedures with<br />
the same outcome <strong>and</strong> date <strong>of</strong> service as another procedure are<br />
not eligible.<br />
11-25
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Incidental Procedures Incidental is defined as a procedure carried out at the same time as<br />
a primary procedure, but is clinically integral to the performance<br />
<strong>of</strong> the primary procedure, <strong>and</strong> therefore, should not be reimbursed<br />
separately.<br />
11-26<br />
An example would be billing the following procedure codes<br />
together:<br />
59300 .....Episiotomy<br />
59409 .....Vaginal delivery<br />
An episiotomy performed as part <strong>of</strong> the overall management <strong>of</strong> a<br />
delivery does not warrant a separate identification. This would<br />
result in the line item denial <strong>of</strong> procedure 59300 <strong>and</strong> would be the<br />
participating network provider’s responsibility.<br />
Another example would be billing the following procedure codes<br />
together:<br />
44005 .....Enterolysis (lysis <strong>of</strong> adhesions, separate procedure)<br />
44140 .....Partial colectomy with anastomosis<br />
Services that are identified by CPT with the term “separate<br />
procedure” are commonly carried out as an integral component <strong>of</strong><br />
a total service. Separate procedures are not reported in addition to<br />
the total procedure or service <strong>of</strong> which it is considered an integral<br />
component. This would result in the line item denial <strong>of</strong> procedure<br />
44005 <strong>and</strong> would be the participating network provider’s liability.<br />
When this edit is applicable, the following message(s) will appear<br />
on your current remittance advice:<br />
This procedure is incidental to another procedure processed<br />
on this or another claim.<br />
This procedure is incidental to the primary procedure.<br />
Reimbursement is included in the allowance for that primary<br />
procedure.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Medical Visits on the<br />
Same Day as Surgery<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
In keeping with the CPT surgical “package,” related E/M services<br />
are not reimbursed separately when submitted with a procedure<br />
performed on the same day. Modifiers may be used with E/M<br />
services that are not considered part <strong>of</strong> the same day surgical<br />
package. Please refer to the current year’s CPT manual for E/M<br />
services <strong>and</strong> surgery guidelines.<br />
Some <strong>of</strong> the related CPT modifiers would include:<br />
-24 unrelated E/M service by the same physician during a<br />
postoperative period<br />
-25 significant, separately identifiable E/M service by the same<br />
physician on the day <strong>of</strong> a procedure or other service<br />
The provider should add these modifiers when a patient’s<br />
condition requires a significant, separately identifiable service<br />
above <strong>and</strong> beyond the usual care associated with the procedure.<br />
Documentation in your files must support the use <strong>of</strong> modifier –25<br />
with E/M codes as defined in CPT. Use modifier –25 with newpatient<br />
<strong>and</strong> established-patient E/M codes to prevent denial <strong>of</strong><br />
significant, separately identifiable E/M services performed on the<br />
same day as a procedure or other service. Some <strong>of</strong> these other<br />
services are allergy injections, joint injections, chemotherapy<br />
administration, brachytherapy services <strong>and</strong> dialysis. Modifier –25<br />
is not required by <strong>Blue</strong> <strong>Cross</strong> with consultation <strong>and</strong> emergency<br />
room codes.<br />
One <strong>of</strong> the following messages will appear on your current<br />
remittance advice:<br />
Payment is included in the allowance for another<br />
service/procedure<br />
Based on the other services submitted for this service date,<br />
reimbursement is not considered for this medical visit.<br />
Note: Requests to add a modifier -24 or -25 to a denied service<br />
must follow the appeal process. An adjustment request will<br />
not be allowed.<br />
11-27
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Global Surgical<br />
Package – Pre- <strong>and</strong><br />
Postoperative Services<br />
11-28<br />
As defined by CPT, the surgical “package” includes the surgical<br />
operation, local infiltration, metacarpal/digital block or topical<br />
anesthesia when used, <strong>and</strong> the normal, uncomplicated follow-up<br />
care visits. These services, when billed in addition to surgery, are<br />
denied as included in the surgical allowance. The surgical package<br />
includes all normal <strong>and</strong> uncomplicated care including pre- <strong>and</strong><br />
postoperative visits as part <strong>of</strong> the reimbursement for the surgical<br />
procedure. Preoperative visits are defined as visits by the surgeon<br />
or another practitioner in the same practice on the day <strong>of</strong> a surgery<br />
for minor procedures <strong>and</strong> the day before or day <strong>of</strong> major surgical<br />
procedures.<br />
We do not consider new patient codes exceptions to the package.<br />
The fact that the patient is new is not reason alone to exclude the<br />
visits from the global package. <strong>Blue</strong> <strong>Cross</strong> follows the same<br />
postoperative time frames associated with surgical procedures as<br />
Medicare <strong>of</strong> 10 or 90 days. These can be found in the Federal<br />
Register. Routine postoperative medical visits rendered with this<br />
time frame <strong>and</strong> related to the surgery will not be recognized for<br />
separate reimbursement as an unbundled component <strong>of</strong> the total<br />
surgical package.<br />
One <strong>of</strong> the following messages will appear on your current<br />
remittance advice:<br />
This procedure is within the postoperative range for a surgery<br />
found on this or another claim.<br />
This procedure is within the preoperative range for a surgery<br />
found on this or another claim.<br />
Pre- <strong>and</strong> postoperative care is a covered benefit <strong>and</strong> these<br />
services are included in the allowance<br />
Modifiers -55 <strong>and</strong> -56<br />
For <strong>Blue</strong> <strong>Cross</strong>, modifiers –55 <strong>and</strong> –56 for pre- <strong>and</strong> postoperative<br />
care are used with surgery codes.<br />
Modifier –57<br />
Modifier –57 is used to indicate that the E/M service resulted in<br />
the initial decision to perform surgery either the day before a major<br />
surgery (90 day global) or the day <strong>of</strong> a major procedure.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Units <strong>of</strong> Service<br />
Validation <strong>and</strong><br />
Restriction<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
<strong>Blue</strong> <strong>Cross</strong> edits procedure code units on pr<strong>of</strong>essional claims<br />
(837P/1500 HICF).<br />
While each service must be submitted with a unit <strong>of</strong> measurement,<br />
multiple units <strong>of</strong> service per code, per date <strong>of</strong> service are only<br />
applicable if the code definition supports submission <strong>of</strong> more than<br />
one unit. This is usually indicated by words such as each or per.<br />
Additionally, the number <strong>of</strong> units for codes that qualify for<br />
submission <strong>of</strong> multiple units may be subject to limits. Although<br />
<strong>Blue</strong> <strong>Cross</strong> is not following Medicare’s Medically Unlikely Edits<br />
(MUE), the editing logic is similar to MUEs.<br />
This edit will occur in the pre-adjudication phase <strong>of</strong> processing. If<br />
the claim submission does not pass (or fails for greater than one<br />
unit per day) it will stop <strong>and</strong> be rejected back to the provider.<br />
This rejection occurs before the submission is accepted as a claim,<br />
therefore a claim number is not assigned <strong>and</strong> the provider must<br />
correct the data <strong>and</strong> resubmit all charges. There will not be any<br />
duplicate editing or adjustments because a “claim” was not created<br />
in the payer adjudication system.<br />
The error denial message will be:<br />
2045 -- Unit(s) billed is inconsistent with procedure code.<br />
Please correct the claim <strong>and</strong> resubmit.<br />
11-29
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
General Claims<br />
Processing<br />
Information<br />
Medical <strong>and</strong> Surgical<br />
Supplies<br />
Multiple Surgery<br />
Guidelines<br />
11-30<br />
Scope Procedures<br />
Our coding s<strong>of</strong>tware makes the following assumptions when<br />
determining payment for multiple scope procedures billed on the<br />
same date <strong>of</strong> service:<br />
A diagnostic scope is always incidental to a surgical scope.<br />
A diagnostic scope with biopsy is always incidental to a<br />
surgical scope.<br />
A diagnostic scope with or without biopsy is always incidental<br />
to an open surgical procedure in the same area.<br />
A diagnostic scope rebundles to a diagnostic scope with biopsy<br />
unless the code description makes the distinction with biopsy<br />
vs. without biopsy.<br />
CPT descriptions such as: complete vs. partial, with vs.<br />
without, complex vs. simple, etc. means there are two mutually<br />
exclusive codes for the procedures.<br />
Medical <strong>and</strong> surgical supplies during an outpatient or physician<br />
<strong>of</strong>fice visit are included as incidental to the E/M service or<br />
procedure performed, <strong>and</strong> will not be separately reimbursed.<br />
Multiple surgical procedures performed during the same operative<br />
session are processed in accordance with <strong>Blue</strong> <strong>Cross</strong> multiple<br />
surgical guidelines. These guidelines state the primary procedure is<br />
determined as the highest billed charge <strong>and</strong> is reimbursed at 100%<br />
<strong>of</strong> the fee schedule or billed amount, whichever is less. Secondary,<br />
tertiary procedures, etc., again determined in order <strong>of</strong> billed<br />
charge, are reimbursed at 50% <strong>of</strong> the fee schedule or billed<br />
amount, whichever is less, regardless <strong>of</strong> separate site or incision.<br />
In addition, procedures noted in CPT as “modifier –51 exempt” are<br />
not subject to multiple surgery reductions.<br />
Patient Billing Impact The patient is not responsible <strong>and</strong> must not be balance billed for<br />
any procedures for which payment has been denied or reduced by<br />
<strong>Blue</strong> <strong>Cross</strong> as the result <strong>of</strong> a coding edit. Edit denials are designed<br />
to ensure appropriate coding <strong>and</strong> to assist in processing claims<br />
accurately <strong>and</strong> consistently.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>and</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Coding Appeals <strong>Blue</strong> <strong>Cross</strong>’ coding edits are updated at minimum annually, to<br />
incorporate new codes, code definition changes <strong>and</strong> edit rule<br />
changes. All claims submitted after the implementation date <strong>of</strong> this<br />
update, regardless <strong>of</strong> service date, will be processed according to<br />
the updated version. Where Medicare’s CCI (Correct Coding<br />
Initiative) edits are identical, we will consider the appeal with<br />
additional documentation, but the issue may be upheld. No<br />
retrospective payment changes, adjustments, <strong>and</strong>/or request<br />
refunds will be made when processing changes are a result <strong>of</strong> new<br />
code editing rules due to a s<strong>of</strong>tware version update. Notice <strong>of</strong> this<br />
update will be published in the Provider Press or Provider Bulletin,<br />
with a ‘Summary <strong>of</strong> Change’ summarizing new edits.<br />
<strong>Blue</strong> <strong>Cross</strong> has adopted a st<strong>and</strong>ard process to review edit appeals<br />
<strong>and</strong> providers have the right to appeal with additional information.<br />
If you have a question or appeal about our policy regarding a<br />
particular coding combination, provide a written statement <strong>of</strong> the<br />
concern, along with the following information <strong>and</strong>/or<br />
documentation normally required for a medical review.<br />
Written explanation supporting the procedures submitted, e.g.,<br />
specific references, specialty specific criteria<br />
Documentation from a recognized authoritative source that<br />
supports your position on the procedure codes submitted<br />
Once received, the inquiry or appeal will be reviewed <strong>and</strong> if<br />
necessary, forwarded to the medical review department for<br />
determination. The review may result in approval or denial <strong>of</strong> the<br />
claim, based on review <strong>of</strong> the information submitted.<br />
Note: Requests to add modifier -24, -25 or -59 to a denied service<br />
must follow the appeal process. An adjustment request will<br />
not allowed.<br />
Refer to Chapter 10 for additional information regarding<br />
submission <strong>of</strong> appeals.<br />
11-31
Coding Policies <strong>and</strong> Guidelines (Coding)<br />
Helpful Coding Tips We recognize the challenges you have in staying up-to-date with<br />
coding changes. Below are some helpful tips to assist with<br />
accurate <strong>and</strong> effective coding to support correct claim processing<br />
<strong>and</strong> reimbursement.<br />
Coding Immunizations<br />
<strong>and</strong> Injections<br />
11-32<br />
Code using current coding books. Order new CPT <strong>and</strong> HCPCS<br />
manuals every year, as codes are added, deleted <strong>and</strong> revised<br />
annually. Submitting invalid or deleted codes will result in claim<br />
rejection or denials. Web links to review for possible updates:<br />
http://www.ama-assn.org/ama/pub/category/3884.html<br />
http://www.cms.hhs.gov/HCPCSReleaseCodeSets/<br />
http://www.cms.hhs.gov/MLNProducts/<br />
http://www.health.state.mn.us/auc/guides.htm<br />
It is appropriate when administering an immunization or injection<br />
to bill administration codes (90460-90461, 90471-90474, 96372-<br />
96375, G0008-G0010). Reimbursement for vaccines/toxoids <strong>and</strong><br />
immunization administration is currently allowed in addition to<br />
preventive medicine services (99381-99384, 99391-99394, 99401-<br />
99404) <strong>and</strong> newborn care services (99460-99463).<br />
Immunizations<br />
If only an immunization is administered, bill the CPT code for the<br />
vaccine/toxoid administered <strong>and</strong> the applicable CPT administration<br />
code (90460-90474).<br />
Example: A 65-year old patient comes to your <strong>of</strong>fice just for a flu<br />
vaccine. Bill the vaccine code 90658 <strong>and</strong> vaccine administration<br />
code 90471.<br />
Immunizations <strong>and</strong> E/M Visits<br />
E/M codes 99201-99205 <strong>and</strong> 99212-99215 are eligible for separate<br />
reimbursement when billed on the same date <strong>of</strong> service as<br />
vaccine/toxoid codes 90476-90749 <strong>and</strong> the immunization<br />
administration codes 90461-90461.<br />
Example:<br />
A one-year-old established patient has a preventive visit <strong>and</strong> a<br />
polio vaccine. Bill the appropriate preventive visit CPT code<br />
(i.e., 99392), the polio vaccine (i.e., 90712) <strong>and</strong> in this case,<br />
the oral administration code (90473).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Copays)<br />
Table <strong>of</strong> Contents<br />
Office Call Copays...............................................................................................................11-2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/12/10) 11-1
Coding Policies <strong>and</strong> Guidelines (Copays)<br />
Office Call Copays Following is a listing <strong>of</strong> procedure codes to which the <strong>of</strong>fice call<br />
copay may apply when included in the contract benefits. This is not<br />
an all-inclusive list.<br />
11-2<br />
Code Description<br />
90804-90815 Psychotherapy<br />
90847, 90853 Family therapy/ Group therapy<br />
92002-92014 Ophthalm ological services (new or established<br />
patient)<br />
92597 Evaluation for use/fitting <strong>of</strong> voice prosthetic<br />
device<br />
92605,<br />
92607-92608<br />
Evaluation for prescription <strong>of</strong> speech/ non-speech<br />
generating device<br />
97001-97004 Physical <strong>and</strong> occupational evaluations <strong>and</strong><br />
reevaluations<br />
98925-98929 Office or outpatient visit with osteopathic<br />
manipulative therapy<br />
98940-98943 Chiropractic visit with manipulation/adjustment<br />
99201-99215 Office or other outpatient services, new <strong>and</strong><br />
established patient<br />
99218-99220 Initial observation care<br />
99241-99245 Consultations (<strong>of</strong>fice, outpatient) new or<br />
established patient- Based on place <strong>of</strong> service<br />
99354-99357 Prolonged physician services<br />
99381-99387 Preventive medicine, new patient<br />
99391-99397 Preventive medicine, established patient<br />
99401-99404 Preventive medicine individual counseling<br />
99406-99409 Behavior change interventions<br />
99411-99412 Preventive medicine group counseling<br />
99420, 99429 Other preventive medicine services<br />
G0245-G0246 E/M <strong>of</strong> a diabetic patient<br />
H1000, H1001,<br />
H1003<br />
Prenatal risk assessment, high risk antepartum<br />
care, nutrition education<br />
S9401 Anticoagulation clinic, inclusive <strong>of</strong> all services<br />
except laboratory tests, per session<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/12/10)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Modifiers)<br />
Table <strong>of</strong> Contents<br />
Modifiers..............................................................................................................................11-2<br />
Anatomical Modifiers ........................................................................................................11-16<br />
Modifiers Defined by DHS................................................................................................11-17<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11) 11-1
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Modifiers General Guidelines<br />
11-2<br />
Modifiers are two-digit codes that are appended to a service as a<br />
means to indicate that the service/procedure is affected or altered<br />
by a specific circumstance <strong>and</strong> to add specificity, but not changed<br />
in its definition.<br />
Modifiers are found in both CPT <strong>and</strong> HCPCS manuals. CPT<br />
modifiers can be found in Appendix A. Genetic Testing Code<br />
Modifiers are found in Appendix I <strong>of</strong> CPT. A complete list <strong>of</strong><br />
HCPCS modifiers is found as an appendix to the HCPCS manual.<br />
CPT codes are not limited to CPT modifiers. HCPCS codes are not<br />
limited to HCPCS modifiers. HCPCS modifiers may also be used<br />
with CPT codes <strong>and</strong>/or in combination with CPT modifiers. CPT<br />
modifiers may also be used with HCPCS codes <strong>and</strong>/or in<br />
combination with HCPCS modifiers. For example, -TC <strong>and</strong> –76<br />
can be appended to a radiology procedure to indicate the technical<br />
component <strong>of</strong> the services was repeated.<br />
Modifiers may be used to indicate:<br />
A service or procedure has both a pr<strong>of</strong>essional <strong>and</strong> technical<br />
component.<br />
A service or procedure was performed by more than one<br />
physician <strong>and</strong>/or in more than one location.<br />
A service or procedure has been increased or reduced.<br />
Only part <strong>of</strong> a service was performed.<br />
A bilateral procedure was performed.<br />
A service or procedure was provided more than once.<br />
Unusual events occurred.<br />
A DME item is purchased or rented.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Modifiers (continued) It is important to append all appropriate modifiers the first time the<br />
claim is submitted.<br />
Modifiers are also subject to compatibility edits with the procedure<br />
to which they are appended. For example, an Evaluation <strong>and</strong><br />
Management (E/M) service appended with a -59 modifier will be<br />
denied.<br />
Note: If your claim is denied due to lack <strong>of</strong> documentation to<br />
support the use <strong>of</strong> a specific modifier or an invalid<br />
modifier/procedure combination, you may submit a claim<br />
payment appeal or replacement claim. Your appeal must be<br />
in writing <strong>and</strong> accompanied by the necessary<br />
documentation. Replacement claims must include an<br />
attachment with supporting documentation.<br />
The information outlined below is a general guideline regarding<br />
the use <strong>of</strong> modifiers. The list is not all-inclusive. Refer to your<br />
CPT <strong>and</strong> HCPCS for a complete list <strong>of</strong> modifiers. When a specific<br />
service/circumstance requires the use <strong>of</strong> a modifier, the submission<br />
criteria is outlined in the applicable specialty section <strong>of</strong> the Coding<br />
Chapter <strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong>.<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
11-4<br />
**The impact to payment statements below are a general guide<br />
<strong>and</strong> not a guarantee <strong>of</strong> payment**<br />
MOD Description Submission Guidelines Impact to Payment<br />
-22 Increased<br />
Procedural<br />
Services<br />
-24 Unrelated<br />
Evaluation <strong>and</strong><br />
Management<br />
(E/M) Service by<br />
the Same<br />
Physician During<br />
a Post-operative<br />
Period.<br />
Note: <strong>Blue</strong> <strong>Cross</strong><br />
defines the<br />
“same<br />
physician” as the<br />
same physician,<br />
or physicians <strong>of</strong><br />
the same or<br />
similar specialty<br />
within the same<br />
clinical practice.<br />
Requires submission <strong>of</strong> an operative<br />
report, narrative <strong>and</strong>/or other relevant<br />
documentation that adequately describes<br />
what care/service was greater than usually<br />
required.<br />
Do not use modifier –22 when there is an<br />
existing code to describe the service.<br />
By appending the –24 modifier to an<br />
unrelated E/M service you are indicating<br />
that the patient’s condition requires a<br />
significant, separately identifiable E/M<br />
service above <strong>and</strong> beyond the other service<br />
provided, or beyond the usual preoperative<br />
<strong>and</strong> post-operative care<br />
associated with the procedure that was<br />
performed. Services appended with a –24<br />
modifier must be sufficiently documented<br />
in the patient’s medical record that the visit<br />
was unrelated to the post-operative care <strong>of</strong><br />
the procedure. An ICD-9-CM that clearly<br />
indicates that the reason for the encounter<br />
was different <strong>and</strong> unrelated to the postoperative<br />
care may provide sufficient<br />
documentation.<br />
Note: Requests to add a modifier -24 to a<br />
denied service must follow the<br />
replacement claim process. An<br />
adjustment request will not be<br />
allowed.<br />
The availability <strong>of</strong><br />
additional payment<br />
will be determined<br />
based on review <strong>of</strong><br />
supporting<br />
documentation.<br />
Separate payment <strong>of</strong><br />
the E/M may be<br />
allowed.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-25 Significant<br />
Separately<br />
Identifiable<br />
Evaluation <strong>and</strong><br />
Management<br />
(E/M) Service by<br />
the Same<br />
Physician on the<br />
Same Day <strong>of</strong> the<br />
Procedure or<br />
Other Service<br />
-26 Pr<strong>of</strong>essional<br />
Component<br />
-50 Bilateral<br />
Procedure<br />
Use the –25 modifier when an E/M service<br />
is rendered on the same day as a minor<br />
surgical procedure (0 or 10 day global<br />
period).<br />
The use <strong>of</strong> –25 is appropriate only when<br />
the E/M service provided is above <strong>and</strong><br />
beyond the usual pre <strong>and</strong> post-operative<br />
service associated with a procedure.<br />
No documentation needs to be submitted<br />
with the initial claim. However, E/M<br />
services submitted with a –25 modifier are<br />
subject to review. Furthermore, medical<br />
documentation, when requested, needs to<br />
support the significant, separately<br />
identifiable E/M service.<br />
Note: Requests to add a modifier -25 to a<br />
denied service must follow the<br />
replacement claim process. An<br />
adjustment request will not be<br />
allowed.<br />
Certain procedures are a combination <strong>of</strong> a<br />
physician component <strong>and</strong> a technical<br />
component. When the physician<br />
component is reported separately, the<br />
service may be identified by adding the<br />
modifier ‘26’ to the usual procedure<br />
number.<br />
The pr<strong>of</strong>essional component applies to the<br />
physician who interprets the procedure <strong>and</strong><br />
provides a written report.<br />
Surgical procedures performed on bilateral<br />
pieces <strong>of</strong> anatomy should be billed on one<br />
line. The –50 modifier should be appended<br />
to the submitted lines <strong>of</strong> service.<br />
<strong>Blue</strong> <strong>Cross</strong> adheres to CMS’ published list<br />
<strong>of</strong> bilateral procedures<br />
Separate payment <strong>of</strong><br />
the E/M may be<br />
allowed.<br />
Payment is made<br />
based on the<br />
pr<strong>of</strong>essional portion<br />
<strong>of</strong> the RVU<br />
associated with the<br />
service.<br />
Payment is made at<br />
150% <strong>of</strong> the allowed<br />
amount for the<br />
procedure.<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-51 Multiple<br />
Procedures<br />
-52 Reduced<br />
Services<br />
-53 Discontinued<br />
Procedure<br />
11-6<br />
When more than one service is performed<br />
during the same operative session, the –51<br />
modifier may be appended to all secondary<br />
surgical procedures.<br />
It is not necessary to append the –51<br />
modifier to “add on” or to exempt codes.<br />
Applicable code edits will be applied to<br />
services submitted.<br />
Append the –52 modifier to indicate that a<br />
service or procedure is partially reduced or<br />
eliminated at the physician’s discretion.<br />
This provides a means <strong>of</strong> reporting reduced<br />
services without disturbing the<br />
identification <strong>of</strong> the basic service.<br />
Append –53 when the physician elects to<br />
terminate the procedure<br />
The -51 modifier<br />
itself does not affect<br />
payment. Multiple<br />
surgical payment is<br />
based on whether the<br />
surgical procedure<br />
may be subject to a<br />
multiple surgery.<br />
Then the reduction<br />
would be based on the<br />
allowed amount. The<br />
lowest valued<br />
procedure(s) will<br />
have the multiple<br />
surgical reduction<br />
applied. When<br />
covered, payment is<br />
made at 50% <strong>of</strong> the<br />
allowed amount for<br />
all allowable<br />
secondary procedures.<br />
The normal full<br />
charge billed or a<br />
reduced charge for the<br />
procedure may be<br />
submitted. <strong>Blue</strong> <strong>Cross</strong><br />
will pay the lesser <strong>of</strong><br />
either 90% <strong>of</strong> the<br />
physician fee<br />
schedule allowance<br />
for the procedure or<br />
the charge submitted.<br />
The normal full<br />
charge or reduced<br />
charge should be<br />
submitted.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-54 Surgical Care<br />
Only<br />
-55 Post-operative<br />
Management<br />
Only<br />
-56 Pre-operative<br />
Management<br />
Only<br />
Append –54 when one physician performs<br />
intraoperative portion <strong>of</strong> a surgical<br />
procedure while another practitioner(s)<br />
from a different practice provides preoperative<br />
<strong>and</strong>/or post-operative<br />
management.<br />
Surgery should be billed globally (no<br />
modifier) if the pre-, intra-, <strong>and</strong> postoperative<br />
services are rendered by the<br />
same provider or other practitioners who<br />
are employed by the same clinic (same tax<br />
ID number).<br />
Append –55 to the surgical procedure code<br />
only when post-operative is provided by a<br />
different clinic than performed the surgery.<br />
Append the –55 to the surgical procedure<br />
code.<br />
Append –56 to the surgical procedure code<br />
only when pre-operative is provided by a<br />
different clinic than performed the surgery.<br />
Append the –56 to the surgical procedure<br />
code.<br />
Payment is made at<br />
90% <strong>of</strong> the allowed<br />
amount.<br />
Separate payment<br />
may be allowed.<br />
Services will be<br />
denied if the –55<br />
modifier is billed by a<br />
practitioner who is<br />
employed by the same<br />
clinic (same tax<br />
ID number) as the<br />
surgeon.<br />
Separate payment<br />
may be allowed.<br />
Services will be<br />
denied if the –56<br />
modifier is billed by a<br />
practitioner who is<br />
employed by the same<br />
clinic (same tax ID<br />
number) as the<br />
surgeon.<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-57 Decision for<br />
Surgery<br />
11-8<br />
The –57 modifier is appended to indicate<br />
that the E/M service resulted in the initial<br />
decision to perform surgery either the day<br />
before or the day <strong>of</strong> a major surgical<br />
procedure (90-day global period).<br />
Do not append this modifier when a minor<br />
surgical procedure (0-, 10-day global<br />
period) is performed.<br />
The –57 should not be used to report an<br />
E/M service that was pre-planned or prescheduled<br />
the day before or the day <strong>of</strong><br />
surgery, as they would be included as part<br />
<strong>of</strong> the global surgical package. Patients are<br />
normally reevaluated on the date <strong>of</strong> the<br />
actual surgery to assure the service can be<br />
performed. That clearance would be<br />
included in the global period <strong>and</strong> should<br />
not be reported separately.<br />
Note: Requests to add a modifier -57 to a<br />
denied service must follow the<br />
replacement claim process. An<br />
adjustment request will not be<br />
allowed.<br />
Modifer-57 may not<br />
affect edits or<br />
payment. However, if<br />
applicable, the<br />
modifier should be<br />
appended to the E/M.<br />
Services denied may<br />
be considered on<br />
subsequent appeal.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-59 Distinct<br />
Procedural<br />
Service<br />
Modifier –59 may be appended to identify<br />
non-E/M procedures/services that are not<br />
normally reported together, but are<br />
appropriate under the circumstances.<br />
However, when another already<br />
established modifier is appropriate it<br />
should be used rather than modifier –59.<br />
Only if no more descriptive modifier is<br />
available, <strong>and</strong> the use <strong>of</strong> modifier –59 best<br />
explains the circumstances, should<br />
modifier –59 be used. Modifier –59 is<br />
always appended to the component or<br />
lesser procedure code. Documentation<br />
supporting the separate <strong>and</strong> distinct status<br />
must be present in the patient’s medical<br />
record.<br />
A -59 modifier may be appropriate to<br />
indicate a:<br />
Different session<br />
Different procedure<br />
Different anatomical site or organ<br />
system<br />
Separate lesion<br />
Separate incision or excision<br />
Separate injury<br />
Note: Requests to add a modifier -59 to a<br />
denied service must follow the<br />
replacement claim process. An<br />
adjustment request will not be<br />
allowed.<br />
-62 Two Surgeons The use <strong>of</strong> this modifier is appropriate to<br />
identify the use <strong>of</strong> two primary surgeons<br />
when required during a surgical procedure.<br />
Documentation should be submitted to<br />
support the use <strong>of</strong> the –62 modifier.<br />
Modifer-59 may not<br />
affect edits or<br />
payment. However, if<br />
applicable, the<br />
modifier should be<br />
appended to the<br />
service. Generally,<br />
the –59 modifier is<br />
only applicable to<br />
those code<br />
combinations noted in<br />
the Correct Coding<br />
Initiative (CCI) code<br />
list with a modifier<br />
indicator <strong>of</strong> “1” which<br />
specifies the services<br />
are distinct <strong>and</strong><br />
separate <strong>and</strong> thus<br />
allowed. Service<br />
denied may be<br />
considered on<br />
subsequent appeal.<br />
Payment will be<br />
determined based on<br />
the Medicare<br />
Physician Fee<br />
Schedule Database<br />
(MPFSDB) indicators<br />
1 or 2 <strong>and</strong> based on<br />
Medical Review <strong>of</strong><br />
supporting<br />
documentation.<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-66 Surgical Team The use <strong>of</strong> this modifier is appropriate to<br />
identify the services <strong>of</strong> a physician<br />
involved as part <strong>of</strong> a surgical team. Under<br />
some circumstances, highly complex<br />
procedures (requiring the concomitant<br />
services <strong>of</strong> several physicians, <strong>of</strong>ten <strong>of</strong><br />
different specialties) are carried out under<br />
the “surgical team” concept.<br />
-73 Discontinued<br />
out-patient<br />
hospital/<br />
ambulatory<br />
surgery center<br />
(ASC) procedure<br />
prior to the<br />
administration <strong>of</strong><br />
anesthesia<br />
-76 Repeat<br />
Procedure or<br />
Service by Same<br />
Physician<br />
11-10<br />
Due to extenuating circumstances or those<br />
that threaten the well being <strong>of</strong> the patient,<br />
the physician may cancel a surgical or<br />
diagnostic procedure subsequent to the<br />
patient's surgical preparation, but prior to<br />
the administration <strong>of</strong> anesthesia. Under<br />
these circumstances, the intended service<br />
that is prepared for but cancelled can be<br />
reported by its usual procedure number <strong>and</strong><br />
the addition <strong>of</strong> the modifier -73.<br />
The practitioner may need to indicate that a<br />
procedure or service was repeated<br />
subsequent to the original procedure or<br />
service on the same day. This circumstance<br />
may be reported by adding modifier –76 to<br />
the repeated procedure/service.<br />
Note: In situations warranting the use <strong>of</strong><br />
both the –26 <strong>and</strong> –76 modifier (e.g.,<br />
reading multiple chest X-rays <strong>of</strong> a patient<br />
performed on the same day), submit the –<br />
26 modifier in the first position with the<br />
initial procedure <strong>and</strong> the –76 in the first<br />
position for the repeat procedure.<br />
Payment will be<br />
determined based on a<br />
case-by-case basis<br />
<strong>and</strong> review <strong>of</strong><br />
supporting<br />
documentation.<br />
Payment is made at<br />
50% <strong>of</strong> the allowed<br />
amount.<br />
Effective for claims<br />
processed on <strong>and</strong> after<br />
January 1, 2012.<br />
Separate payment <strong>of</strong><br />
the service may be<br />
made.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-77 Repeat<br />
Procedure by<br />
Another<br />
Physician<br />
-79 Unrelated<br />
Procedure or<br />
Service by the<br />
Same Physician<br />
During Postoperative<br />
Period<br />
-80 Assistant<br />
Surgeon<br />
-81 Minimum<br />
Assistant<br />
Surgeon<br />
-82 Assistant<br />
Surgeon (When<br />
Qualified<br />
Resident<br />
Surgeon Not<br />
Available)<br />
The practitioner may need to indicate that a<br />
procedure or service was repeated<br />
subsequent to the original procedure or<br />
service on the same day. This circumstance<br />
may be reported by adding modifier –77 to<br />
the repeated procedure/service.<br />
Note: In situations warranting the use <strong>of</strong><br />
both the –26 <strong>and</strong> –77 modifier (e.g.,<br />
reading multiple chest X-rays <strong>of</strong> a<br />
patient performed on the same day),<br />
submit the –26 modifier in the first<br />
position with the initial procedure<br />
<strong>and</strong> the –77 in the first position for<br />
the repeat procedure.<br />
Append this modifier to<br />
procedures/services performed during the<br />
post-operative period <strong>of</strong> another procedure,<br />
if the procedure/service is unrelated to the<br />
original procedure.<br />
Append this modifier to surgical assists<br />
performed by a physician, nurse<br />
practitioner, physician assistant, or RNFA.<br />
<strong>Blue</strong> <strong>Cross</strong> adheres to CMS’ published list<br />
<strong>of</strong> services eligible for surgical assist.<br />
Append this modifier to surgical assists<br />
performed by a physician, nurse<br />
practitioner, physician assistant, or RNFA.<br />
<strong>Blue</strong> <strong>Cross</strong> adheres to CMS’ published list<br />
<strong>of</strong> services eligible for surgical assist.<br />
Append this modifier to surgical assists<br />
performed by a physician, nurse<br />
practitioner, physician assistant, or RNFA.<br />
<strong>Blue</strong> <strong>Cross</strong> adheres to CMS’ published list<br />
<strong>of</strong> services eligible for surgical assist.<br />
Separate payment <strong>of</strong><br />
the service may be<br />
made.<br />
Separate payment <strong>of</strong><br />
the service may be<br />
made.<br />
Payment is made at<br />
16% <strong>of</strong> the allowed<br />
amount.<br />
Multiple surgery<br />
pricing logic also<br />
applies to assistant at<br />
surgery services.<br />
Payment is made at<br />
16% <strong>of</strong> the allowed<br />
amount.<br />
Multiple surgery<br />
pricing logic also<br />
applies to assistant at<br />
surgery services.<br />
Payment is made at<br />
16% <strong>of</strong> the allowed<br />
amount.<br />
Multiple surgery<br />
pricing logic also<br />
applies to assistant at<br />
surgery services.<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-90 Reference<br />
(outside) Lab<br />
-91 Repeat Clinical<br />
Diagnostic Lab<br />
Test<br />
-99 Multiple<br />
Modifiers<br />
-AA Anesthesia<br />
services<br />
performed<br />
personally by<br />
anesthesiologist<br />
-AD Medical<br />
supervision by a<br />
physician; more<br />
than four<br />
concurrent<br />
anesthesia<br />
procedures<br />
-AS PA, Nurse<br />
Practitioner, or<br />
Clinical Nurse<br />
Specialist<br />
Services for<br />
Assistant at<br />
Surgery<br />
11-12<br />
The use <strong>of</strong> the –90 modifier is appropriate<br />
when a lab provider, not the treating<br />
physician, performs a laboratory<br />
procedure. The –90 modifier should be<br />
appended to the procedure code/test that<br />
was sent to the lab.<br />
Append the modifier to a lab procedure<br />
that was repeated during the day.<br />
Modifier -99 indicates that multiple<br />
modifiers may apply to a particular service.<br />
Because <strong>Blue</strong> <strong>Cross</strong> can accept up to four<br />
modifiers, -99 should be used only if there<br />
are five or more modifiers applicable to a<br />
particular service line. In that<br />
circumstance, if -99 is submitted, the<br />
additional modifiers must be entered on the<br />
narrative record.<br />
Append the modifier when the<br />
anesthesiologist is physically present in the<br />
operating room, personally performs the<br />
induction <strong>and</strong> emergence, <strong>and</strong> directly<br />
monitors the patient throughout the entire<br />
operative procedure.<br />
Append the modifier when the<br />
anesthesiologist supervises more than four<br />
concurrent anesthesia procedures. The<br />
anesthesiologist may perform the induction<br />
<strong>and</strong> emergence but may not be present<br />
during the entire operative session.<br />
Append this modifier to surgical assists<br />
performed by a physician assistant, nurse<br />
practitioner, or clinical nurse specialist.<br />
The modifier does not<br />
impact payment for<br />
the lab test; however,<br />
it may be used in<br />
determining whether<br />
payment will be made<br />
for more than one<br />
type <strong>of</strong> specimen<br />
collection.<br />
Separate payment <strong>of</strong><br />
the service may be<br />
made.<br />
Impact <strong>of</strong> payment or<br />
adjudication may be<br />
based on what the<br />
additional modifier(s)<br />
represents.<br />
Payment is made at<br />
the full-time<br />
anesthesia conversion<br />
rate.<br />
Payment is made at<br />
the part-time<br />
anesthesia conversion<br />
rate.<br />
Payment is made at<br />
16% <strong>of</strong> the allowed<br />
amount.<br />
Multiple surgery<br />
pricing logic also<br />
applies to assistant as<br />
surgery services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-GA Waiver <strong>of</strong><br />
liability<br />
statement on file<br />
The GA modifier (WAIVER OF<br />
LIABILITY STATEMENT ON FILE)<br />
may be submitted when the patient has<br />
signed a waiver specifically for a service<br />
that may not be covered. If the service is<br />
denied, the payment for that service is the<br />
patient’s liability in most cases.<br />
General rules surrounding GA:<br />
1. GA is an acceptable modifier.<br />
Providers may submit this modifier if a<br />
waiver is signed by the patient <strong>and</strong> is<br />
on file with the provider. The waiver<br />
must be for the specific service <strong>and</strong><br />
date only – blanket waivers are not<br />
acceptable.<br />
2. Liability will not be changed under<br />
some circumstances: Denial waiting for<br />
additional information, duplicate<br />
billing, incidental or included in the<br />
basic service rendered denials, <strong>and</strong><br />
denials generated from a coding<br />
s<strong>of</strong>tware decision (such as incidental,<br />
mutually exclusive or visit logic).<br />
These denials will always remain<br />
provider liability regardless if the GA<br />
is submitted.<br />
3. If the service denies provider liability,<br />
the provider may ask for an adjustment<br />
to change to subscriber liability, if<br />
appropriate (incidental <strong>and</strong> coding<br />
s<strong>of</strong>tware denials will remain provider<br />
liability).<br />
For Public Program subscribers, refer to<br />
the <strong>Blue</strong> Plus Provider <strong>Manual</strong>.<br />
If the service is<br />
denied, liability may<br />
be changed to<br />
subscriber liability.<br />
See general rules<br />
under “Submission<br />
Guidelines”.<br />
11-13
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-QJ Services/items<br />
provided to a<br />
prisoner or<br />
patient in state or<br />
local custody,<br />
however the<br />
state or local<br />
government, as<br />
applicable, meets<br />
the requirements<br />
in 42 CFR 411.4<br />
(B)<br />
-QK Medical<br />
direction (by<br />
physician) <strong>of</strong><br />
two, three or<br />
four concurrent<br />
procedures by<br />
qualified<br />
personnel<br />
-QS Monitored<br />
anesthesia care<br />
service<br />
-QX CRNA service<br />
with medical<br />
direction by a<br />
physician<br />
-QY Medical<br />
direction <strong>of</strong> one<br />
Certified<br />
Registered Nurse<br />
Anesthetist<br />
(CRNA) by an<br />
anesthesiologist<br />
11-14<br />
The appropriate use <strong>of</strong> this modifier is<br />
required for our Government Program <strong>and</strong><br />
Public Program subscribers.<br />
The –QJ may be submitted for other<br />
subscribers/products as well, but the<br />
modifier will not affect adjudication.<br />
Append the modifier when the<br />
anesthesiologist supervises more than four<br />
concurrent anesthesia procedures. The<br />
anesthesiologist may perform the induction<br />
<strong>and</strong> emergence but may not be present<br />
during the entire operative session.<br />
Append the modifier when the<br />
anesthesiologist provides specific<br />
anesthesia services to a particular patient<br />
undergoing a planned procedure including<br />
performing a preanesthetic examination, be<br />
physically present in the operating suite,<br />
monitors the patient’s condition, <strong>and</strong> is<br />
prepared to furnish anesthesia services as<br />
necessary.<br />
Append the modifier on the CRNA charges<br />
when the anesthesiologist supervises the<br />
CRNA who performed the anesthesia<br />
procedure. The anesthesiologist may<br />
perform the induction <strong>and</strong> emergence but<br />
may not be present during the entire<br />
operative session.<br />
Append the modifier on the<br />
anesthesiologist charges when the<br />
anesthesiologist supervises the CRNA who<br />
performed the anesthesia procedure. The<br />
anesthesiologist may perform the induction<br />
<strong>and</strong> emergence but may not be present<br />
during the entire operative session.<br />
Services or items will<br />
deny for Government<br />
Program or Public<br />
Program subscribers.<br />
Payment is made at<br />
the part-time<br />
anesthesia conversion<br />
rate.<br />
Payment is made at<br />
the part-time<br />
anesthesia conversion<br />
rate. Only one –QS<br />
service per day will<br />
be allowed.<br />
Payment is made at<br />
the part-time<br />
anesthesia conversion<br />
rate.<br />
Payment is made at<br />
the part-time<br />
anesthesia conversion<br />
rate.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
MOD Description Submission Guidelines Impact to Payment<br />
-QZ CRNA service<br />
without medical<br />
direction by a<br />
physician<br />
-TC Technical<br />
component<br />
Append the modifier when the CRNA is<br />
physically present in the operating room,<br />
personally performs the induction <strong>and</strong><br />
emergence, <strong>and</strong> directly monitors the<br />
patient throughout the entire operative<br />
procedure.<br />
Under certain circumstances, a charge may<br />
be made for the technical component<br />
alone. Under those circumstances the<br />
technical component charge is identified<br />
by adding modifier ‘TC’ to the usual<br />
procedure number.<br />
The technical component applies to the<br />
actual physical performance <strong>of</strong> the service,<br />
which includes the equipment, supplies<br />
<strong>and</strong> personnel.<br />
Payment is made at<br />
the full-time<br />
anesthesia conversion<br />
rate.<br />
Payment is made<br />
based on the technical<br />
portion <strong>of</strong> the RVU<br />
associated with the<br />
service.<br />
11-15
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Anatomical Modifiers The following modifiers indicate a specific anatomic site. Because<br />
these modifiers affect edits <strong>and</strong> payment we suggest they be<br />
submitted in the first modifier position, if applicable. Appropriate<br />
use <strong>of</strong> these modifiers may assure correct claims adjudication.<br />
11-16<br />
E1 Upper left eyelid<br />
E2 Lower left eyelid<br />
E3 Upper right eyelid<br />
E4 Lower right eyelid<br />
F1 Left h<strong>and</strong> second digit<br />
F2 Left h<strong>and</strong> third digit<br />
F3 Left h<strong>and</strong> fourth digit<br />
F4 Left h<strong>and</strong> fifth digit<br />
F5 Right h<strong>and</strong> thumb<br />
F6 Right h<strong>and</strong> second digit<br />
F7 Right h<strong>and</strong> third digit<br />
F8 Right h<strong>and</strong> fourth digit<br />
F9 Right h<strong>and</strong> fifth digit<br />
FA Left h<strong>and</strong> thumb<br />
LC Left circumflex coronary artery<br />
LD Left anterior descending coronary artery<br />
LT Left side (used to identify procedures performed on the left<br />
side <strong>of</strong> the body)<br />
RC Right coronary artery<br />
RT Right side (used to identify procedures performed on the<br />
right side <strong>of</strong> the body)<br />
T1 Left foot second digit<br />
T2 Left foot third digit<br />
T3 Left foot fourth digit<br />
T4 Left foot fifth digit<br />
T5 Right foot great toe<br />
T6 Right foot second digit<br />
T7 Right foot third digit<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
Anatomical Modifiers<br />
(continued)<br />
Modifiers Defined by<br />
DHS<br />
T8 Right foot fourth digit<br />
T9 Right foot fifth digit<br />
TA Left foot great toe<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
The national HCPCS Panel developed several modifiers that could<br />
be defined by the various state Medicaid agencies. The <strong>Minnesota</strong><br />
Department <strong>of</strong> Human Services has defined these as follows.<br />
Each modifier has more than one definition dependent on what<br />
service it is appended to or the program affected. The modifiers are<br />
generally informational only <strong>and</strong>, with the exception <strong>of</strong> –U7,<br />
applicable primarily to services for our PMAP <strong>and</strong> MNCare<br />
subscribers.<br />
U1 Definition 1 = Vulnerable Adult<br />
Case Management<br />
Definition 2 = IEP Physical Therapy<br />
(T1018)<br />
Definition 3 = Access Transportation<br />
Services ATS Coordinator admin fee<br />
(A0080, A0090, A0100, A0110,<br />
A0120, A0140)<br />
Definition 4 = CDCS- Personal<br />
Assistance (T2028)<br />
Definition 5 = Transitional Services-<br />
furniture (T2038)<br />
Definition 6 = Basic complexity<br />
level (Care Coordination/Medical<br />
Home S0280-S0281)<br />
Definition 7 = Added absorbency<br />
(A5421-A4554)<br />
Definition 8 = Dialectical Behavior<br />
Therapy (H2019)<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
11-17
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Modifiers Defined by<br />
DHS (continued)<br />
11-18<br />
U2 Definition 1 = Home Care Case<br />
Management<br />
Definition 2 = IEP Occupational<br />
Therapy (T1018)<br />
Definition 3 = none<br />
Definition 4 = CDCS – Treatment &<br />
Training (T2028)<br />
Definition 5 = Transitional Services-<br />
supplies (T2038)<br />
Definition 6 = Extended complexity<br />
level (Care Coordination/Medical<br />
Home S0280-S0281)<br />
Definition 7 = Maximum absorbency<br />
(A4521-A4554)<br />
U3 Definition 1 = CW-TCM<br />
Definition 2 = IEP Speech Therapy<br />
(T1018)<br />
Definition 3 = NET Broker admin<br />
fee (A0080, A0090, A0100, A0110,<br />
A0120)<br />
Definition 4 = CDCS-<br />
Environmental Modifications <strong>and</strong><br />
Provisions (T2028)<br />
Definition 5 = Approved Assessment<br />
Penalty Reconsideration (T1001)<br />
Definition 6 = Complicating factor,<br />
non-English language (Care<br />
Coordination/Medical Home S0280-<br />
S0281)<br />
Definition 7 = Enhanced service or<br />
item (T1013/Sign or any DMPOS,<br />
etc.) replaces -22 for non-CPT<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
Modifiers Defined by<br />
DHS (continued)<br />
U4 Definition 1 = Service provided via<br />
non face-to-face contact, e.g.,<br />
telephone<br />
Definition 2 = IEP Mental Health<br />
Services T1018)<br />
Definition 3 = NET Taxi or equal,<br />
door to door (A0100)<br />
Definition 4 = CDCS (Consumer<br />
Directed Community Support) - Selfdirection<br />
Support Activities (T2028)<br />
Definition 5 = Overnight study<br />
(E0445)<br />
Definition 6 = Complicating factor;<br />
major active mental health condition<br />
(Care Coordination/Medical Home<br />
S0280-S0281)<br />
Definition 7 = Special population<br />
(Substance abuse treatment H2036,<br />
H0005, H2035, H0020)<br />
U5 Definition 1 = Partial Day (DT&H)<br />
(T2020)<br />
Definition 2 = IEP Nursing Services<br />
(T1018)<br />
Definition 3 = NET Taxi or equal,<br />
wheelchair, curb to curb (A0100)<br />
Definition 4 = End tidal CO 2<br />
monitor, monthly rental (E1399)<br />
Definition 5 = Service Units<br />
available through the notice <strong>of</strong><br />
termination, reduction or denial <strong>of</strong><br />
services (T1019)<br />
Definition 6 = Advanced level<br />
specialist (H0038)<br />
Definition 7 = With medical services<br />
(Substance abuse treatment H2036,<br />
H0005, H2035, H0020)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
11-19
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Modifiers Defined by<br />
DHS (continued)<br />
11-20<br />
U6 Definition 1= Temporary Service<br />
Increase (T1001, T1019)<br />
Definition 2= IEP<br />
PCA/Parapr<strong>of</strong>essional Services<br />
(T1018)<br />
Definition 3 = NET Taxi or equal,<br />
wheelchair, door to door (A0100)<br />
Definition 4 = End tidal CO2 spot<br />
check, weekly rental (E1399)<br />
Definition 5 = none<br />
Definition 6 = none<br />
Definition 7 = Parents with children<br />
(Substance abuse treatment H2036,<br />
H0005, H2035)<br />
U7 Definition 1 = Physician Extender<br />
(medical services)<br />
Definition 2 = IEP Assistive<br />
Technology Devices (T1018)<br />
Definition 3 = NET Bus/train,<br />
monthly pass (A0110)<br />
Definition 4 = Oximeter spot check,<br />
weekly rental (E0445)<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
Append this<br />
modifier to services<br />
by non-credentialed<br />
or non-enrolled<br />
practitioners when<br />
performing incidentto<br />
services under the<br />
direct supervision.<br />
The services would<br />
be reported under<br />
the directing<br />
physician’s provider<br />
number. The<br />
modifier does not<br />
impact payment.<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
Modifiers Defined by<br />
DHS (continued)<br />
U8 Definition 1 = Home Based Mental<br />
Health Service<br />
Definition 2 = IEP Special<br />
Transportation (T1018)<br />
Definition 3 = NET Level <strong>of</strong> need<br />
assessment (LON) (T1023)<br />
Definition 4 = CDCS – Flexible<br />
case management (T2028) separately<br />
recognized component <strong>of</strong> selfdirection<br />
support services<br />
Definition 5 = none<br />
Definition 6 = none<br />
Definition 7 = With MAT<br />
(medication assisted therapy) dosing<br />
(H2036, H0005, H2035)<br />
U9 Definition 1 = Therapeutic Support<br />
Foster Care<br />
Definition 2 = Behavioral<br />
Programming by Aide (S5135)<br />
Definition 3 = NET level <strong>of</strong> need<br />
assessment (LON) II (T1023)<br />
Definition 4 = Corporate settings<br />
(S5140, S5141, T2030 TG, T2032,<br />
T2016, T2017)<br />
Definition 5 = none<br />
Definition 6 = none<br />
Definition 7 = All other MAT drugs<br />
(H0020)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
Append the modifier<br />
if directed in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
11-21
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Modifiers Defined by<br />
DHS (continued)<br />
11-22<br />
UA Definition 1 = Children’s<br />
Therapeutic Services <strong>and</strong> Supports<br />
Definition 2 = Night Supervision<br />
(S5135)<br />
Definition 3 = NET Broker review<br />
(T1023)<br />
Definition 4 = PCA Supervision<br />
(T1019)<br />
Definition 5 = Item, service, or<br />
procedure furnished in conjunction<br />
with a demonstration project (E1399,<br />
T1028, S9441)<br />
Definition 6 = none<br />
Definition 7 = Methadone Plus<br />
(H0020)<br />
UB Definition 1 = Non-reservation<br />
American Indian Chemical Health<br />
only<br />
Definition 2 = 24-Hour Emergency<br />
Service (S5135, S5136)<br />
Definition 3 = NET Taxi or equal,<br />
wheelchair, assisted station to station<br />
(A0100)<br />
Definition 4 = DT & H Pilot Rate C<br />
(T2021)<br />
Definition 5 = Out <strong>of</strong> home Respite<br />
(S5150)<br />
Definition 6 = none<br />
Definition 7 = All other MAT drugs<br />
Plus (H0020)<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)
Modifiers Defined by<br />
DHS (continued)<br />
UC Definition 1 = Specialized<br />
Maintenance Therapy<br />
Definition 2 = Extended Home Care<br />
Services (T1002-03, T1019, S9128-<br />
29, S9131, S5181)<br />
Definition 3 = MNET – Mileage<br />
provided by licensed foster parent<br />
(A0090)<br />
Definition 4= Waiver Case<br />
Management (T1016)<br />
Definition 5 = C&TC Mental Health<br />
Screening (96110)<br />
Definition 6 = none<br />
Definition 7 = Combination cooccurring<br />
mental health with medical<br />
services (Substance abuse treatment<br />
H2036, H0005, H2035, H0020)<br />
UD Definition 1 = Pr<strong>of</strong>essional service<br />
for fitting <strong>and</strong> evaluation <strong>of</strong><br />
customized DME/PO (K0115-<br />
K0116)<br />
Definition 2 = Transitioning to<br />
community living services (90882,<br />
H2017)<br />
Definition 3 = NET Fuel Adjustment<br />
Rate (A0100)<br />
Definition 4 = Family Support Grant<br />
(T2025)<br />
Definition 5 = ER Triage (99201,<br />
99211)<br />
Definition 6 = DRA reporting<br />
exception 340B purchased drug<br />
(HCPCS subset requiring NDC)<br />
Definition 7 = Low intensity<br />
(Substance abuse treatment H2036)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (10/05/11)<br />
Coding Policies <strong>and</strong> Guidelines (Modifiers)<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
Append the modifier<br />
if directed to in<br />
guidelines that may<br />
be found elsewhere<br />
in this manual.<br />
11-23
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Anesthesia)<br />
Table <strong>of</strong> Contents<br />
Overview..............................................................................................................................11-2<br />
Full-time Anesthesia Services.............................................................................................. 11-2<br />
Part-time (Medically Directed) Anesthesia Services...........................................................11-3<br />
Qualifying Circumstances.................................................................................................... 11-3<br />
Physical Status .....................................................................................................................11-4<br />
Qualifying Circumstances <strong>and</strong> Physical Status Submission................................................ 11-4<br />
Electroconvulsive Treatments.............................................................................................. 11-5<br />
Local Anesthesia.................................................................................................................. 11-5<br />
Medical Services <strong>and</strong> Invasive Procedures.......................................................................... 11-5<br />
Epidural Anesthesia for a Surgical Procedure ..................................................................... 11-5<br />
Epidural Anesthesia for Pain Management..........................................................................11-5<br />
Anesthesia for Nerve Blocks ............................................................................................... 11-5<br />
Daily Management <strong>of</strong> Epidural Drug Administration ......................................................... 11-5<br />
Epidural Anesthesia for Labor <strong>and</strong> Delivery ....................................................................... 11-6<br />
Moderate (Conscious) Sedation...........................................................................................11-7<br />
Monitored Anesthesia Care.................................................................................................. 11-7<br />
Patient Controlled Analgesia ...............................................................................................11-7<br />
St<strong>and</strong>by ................................................................................................................................11-7<br />
Documentation..................................................................................................................... 11-8<br />
Time Designation/ Submission............................................................................................ 11-8<br />
Diagnosis Coding................................................................................................................. 11-8<br />
Multiple Surgery .................................................................................................................. 11-8<br />
Cardioversion Restriction ....................................................................................................11-8<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Anesthesia)<br />
Overview <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> accepts the CPT<br />
American Society <strong>of</strong> Anesthesiologists codes (ASA), 00100-<br />
01999, for anesthesia services billed on the 837P claim format. We<br />
do not accept surgical codes submitted with anesthesia modifiers.<br />
All services for the same operative session should be submitted on<br />
the same claim.<br />
Full-time Anesthesia<br />
Services<br />
11-2<br />
We define full-time anesthesia as follows:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Full-time anesthesia services are provided personally by the<br />
anesthesiologist to an individual patient. The anesthesiologist<br />
is physically present in the specific operating room, personally<br />
performs the induction <strong>and</strong> emergence, <strong>and</strong> directly monitors<br />
the patient throughout the entire operative procedure. The<br />
anesthesiologist may leave the specific operating suite to<br />
perform necessary administrative duties. However, the<br />
anesthesiologist does not perform other revenue-generating<br />
procedures when billing full-time anesthesia services. This<br />
definition includes one-on-one supervision <strong>of</strong> a certified<br />
registered nurse anesthetist (CRNA) present in the same<br />
operating suite.<br />
Use modifier AA for full-time physician services.<br />
<strong>Blue</strong> <strong>Cross</strong> also considers anesthesia services provided by<br />
independent CRNA <strong>and</strong> physician-employed CRNA to be fulltime<br />
if the above criteria are met <strong>and</strong> medical direction is not<br />
provided by a physician.<br />
Modifier QZ would be used for full-time CRNA services.<br />
The HCPCS level II modifiers (AA <strong>and</strong> QZ) should be listed<br />
in the first modifier position.<br />
The anesthesia modifiers should only be reported with the CPT<br />
anesthesia codes 00100-01999. Other services (such as nerve<br />
blocks), may be performed by an anesthesiologist or CRNA,<br />
but should not be submitted with an anesthesia modifier.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12)
Part-time (Medically<br />
Directed) Anesthesia<br />
Services<br />
Qualifying<br />
Circumstances<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12)<br />
Coding Policies <strong>and</strong> Guidelines (Anesthesia)<br />
Medically directed anesthesia services are provided by the<br />
anesthesiologist when he or she is supervising two or more<br />
CRNAs. The anesthesiologist may perform the induction <strong>and</strong><br />
emergence but is not necessarily present during the entire<br />
operative session <strong>and</strong> may be supervising two or more procedures<br />
at the same time.<br />
• Use modifier -AD or -QK for the medical direction provided<br />
by a physician (part-time services).<br />
• Use modifier -QY for part-time medical direction <strong>of</strong> one<br />
CRNA by an anesthesiologist.<br />
• Use modifier -QX for medically directed CRNA services (parttime).<br />
• Modifier -QS would be used for part-time monitored<br />
anesthesia care.<br />
The HCPCS level II modifiers (AD, QK, QS, QX <strong>and</strong> QY)<br />
should be listed in the first modifier position.<br />
In accordance with CPT, the following circumstances are<br />
recognized for submission <strong>of</strong> risk. These codes are not st<strong>and</strong>-alone<br />
services. Qualifying circumstance codes billed without an ASA<br />
service on the same claim will be rejected. The corresponding<br />
eligible base units that may be allowed are also listed. Anesthesia<br />
risk factors will be priced independently <strong>of</strong> the anesthesia line for<br />
easier posting <strong>of</strong> payments to accounts <strong>and</strong> greater accuracy <strong>of</strong><br />
payments.<br />
Code Base<br />
Units<br />
Description<br />
99100 1 Anesthesia for patient <strong>of</strong> extreme age; younger<br />
than 1 year <strong>and</strong> older than 70<br />
(List separately in addition to the code for the<br />
primary anesthesia procedure.)<br />
99116 5 Anesthesia complicated by utilization <strong>of</strong> total<br />
body hypothermia<br />
(List separately in addition to the code for the<br />
primary anesthesia procedure.)<br />
99135 5 Anesthesia complicated by utilization <strong>of</strong><br />
controlled hypotension<br />
(List separately in addition to the code for the<br />
primary anesthesia procedure.)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Anesthesia)<br />
11-4<br />
Code Base<br />
Units<br />
Description<br />
99140 2 Anesthesia complicated by emergency<br />
conditions (specify)<br />
(List separately in addition to the code for the<br />
primary anesthesia procedure.) (An emergency is<br />
defined as existing when delay in treatment <strong>of</strong><br />
the patient would lead to a significant increase in<br />
the threat <strong>of</strong> life or body part.)<br />
Physical Status Six levels are currently recognized for patient physical status that<br />
may be used to distinguish various levels <strong>of</strong> complexity <strong>of</strong> the<br />
anesthesia service provided. Submit these physical status modifiers<br />
in the second modifier position, on the same line as the anesthesia<br />
service code. The corresponding eligible base units that may be<br />
allowed are also listed.<br />
Qualifying<br />
Circumstances <strong>and</strong><br />
Physical Status<br />
Submission<br />
Modifier<br />
Base<br />
Units Description<br />
P1 0 Normal, healthy patient<br />
P2 0 Patient with mild systemic disease<br />
P3 1 Patient with severe systemic disease<br />
P4 2 Patient with severe systemic disease that is a<br />
constant threat to life<br />
P5 3 A moribund patient who is not expected to<br />
survive without the operation<br />
P6 0 Declared brain-dead patient whose organs are<br />
being removed for donor purposes<br />
The example below illustrates a claim that is submitted<br />
appropriately. It is for a situation where both qualifying<br />
circumstances <strong>and</strong> physical status may apply.<br />
Procedure<br />
Code Modifier Description<br />
00862 AA P3 Anesthesia for extra- peritoneal<br />
procedures in lower abdomen, including<br />
urinary tract; renal procedures, including<br />
upper one-third <strong>of</strong> ureter, or donor<br />
nephrectomy<br />
Performed by a full-time M.D.<br />
Patient with severe systemic disease<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12)
Electroconvulsive<br />
Treatments<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12)<br />
Coding Policies <strong>and</strong> Guidelines (Anesthesia)<br />
99140 Anesthesia complicated by emergency<br />
conditions<br />
To bill for anesthesia for electroshock treatments (00104), submit<br />
the appropriate anesthesia modifier. Time units <strong>and</strong> risk are<br />
recognized for this service.<br />
Local Anesthesia Local anesthesia, such as a nerve block, is included in the surgical<br />
procedure code. Do not submit a separate charge for this service.<br />
Medical Services <strong>and</strong><br />
Invasive Procedures<br />
Epidural Anesthesia for<br />
a Surgical Procedure<br />
Epidural Anesthesia for<br />
Pain Management<br />
Anesthesia for Nerve<br />
Blocks<br />
Daily Management <strong>of</strong><br />
Epidural Drug<br />
Administration<br />
Anesthesia HCPCS Level II modifiers should be submitted with<br />
ASA codes only. Do not submit anesthesia modifiers with medical<br />
services such as hospital visits, consultations, ventilation<br />
management, CPR, daily epidural management, or with invasive<br />
procedures such as vascular injections or nerve blocks.<br />
The insertion <strong>and</strong> administration <strong>of</strong> an epidural by an anesthesia<br />
provider for anesthesia during a surgical procedure should be<br />
reported with the appropriate anesthesia code. Codes 62311, 62318<br />
or 62319 should not be used.<br />
The insertion <strong>of</strong> an epidural catheter for pain management services<br />
by a qualified provider should be reported with either code 62311,<br />
62318 or 62319, as appropriate. Time units are not appropriate for<br />
codes 62311, 62318 <strong>and</strong> 62319, <strong>and</strong> anesthesia modifiers are not<br />
required.<br />
Anesthesia services for diagnostic or therapeutic nerve blocks <strong>and</strong><br />
injections are submitted under codes 01991 or 01992 only when a<br />
different provider performs the block or injection.<br />
Daily management <strong>of</strong> an epidural catheter performed on the same<br />
date as the insertion <strong>of</strong> the catheter is considered to be included in<br />
the insertion <strong>and</strong> should not be reported separately.<br />
Subsequent daily management <strong>of</strong> epidural drug administration in<br />
the inpatient setting, including daily visits <strong>and</strong> removal <strong>of</strong> the<br />
epidural catheter, may be reported using CPT code 01996 (daily<br />
hospital management <strong>of</strong> epidural or subarachnoid drug<br />
administration).<br />
Do not submit anesthesia modifiers or time for epidural daily<br />
management.<br />
Removal <strong>of</strong> the epidural catheter alone does not constitute daily<br />
management. If the only service performed is removal <strong>of</strong> the<br />
catheter, code 01996 should not be reported. Subsequent daily<br />
management <strong>of</strong> an epidural catheter performed in a setting other<br />
than inpatient hospital should be reported using the appropriate<br />
Evaluation <strong>and</strong> Management code.<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Anesthesia)<br />
Epidural Anesthesia for<br />
Labor <strong>and</strong> Delivery<br />
11-6<br />
Insertion Only<br />
When a provider performs the insertion <strong>of</strong> an epidural catheter for<br />
continuous analgesia, but does not participate in the ongoing<br />
management <strong>and</strong> monitoring <strong>of</strong> the epidural analgesia for labor<br />
<strong>and</strong> delivery, the claim should be for the insertion service only<br />
(code 62319). Time units are not appropriate for code 62319, <strong>and</strong><br />
anesthesia modifiers are not required.<br />
Insertion <strong>and</strong> Management<br />
When a provider inserts the epidural catheter <strong>and</strong> participates in<br />
ongoing management <strong>and</strong> monitoring <strong>of</strong> the patient's epidural<br />
analgesia, the anesthesia code 01967 <strong>and</strong> (if applicable) 01968<br />
should be reported for the complete service using the appropriate<br />
anesthesia modifier, with anesthesia time units for actual face-t<strong>of</strong>ace<br />
time. It would not be appropriate to report 62319 for the<br />
insertion <strong>of</strong> the catheter in addition to the epidural management.<br />
99140<br />
It is also not appropriate to bill the emergency qualifying<br />
circumstance code (99140) with normal deliveries. Emergency<br />
code 99140 applies only to cases where a “delay in treatment<br />
would result in an increased risk to life or body part,” according to<br />
the ASA Relative Value Guide. Do not confuse an inconvenient<br />
case with emergencies, such as a surgery that takes place on the<br />
weekend or after normal business hours.<br />
Management Only<br />
In many cases, a physician will insert the epidural catheter, but a<br />
CRNA is responsible for the ongoing management <strong>and</strong> monitoring<br />
<strong>of</strong> the patient’s epidural analgesia. When this is the case, the<br />
CRNA should submit the anesthesia code 01967 (if applicable)<br />
<strong>and</strong> 01968 using the appropriate anesthesia modifier, with<br />
anesthesia time units for actual face-to-face time.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12)
Moderate (Conscious)<br />
Sedation<br />
Monitored Anesthesia<br />
Care<br />
Patient Controlled<br />
Analgesia<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12)<br />
Coding Policies <strong>and</strong> Guidelines (Anesthesia)<br />
The physician who performs a procedure may bill moderate<br />
sedation, codes 99143-99145, in addition to billing the procedure.<br />
The use <strong>of</strong> these codes requires <strong>and</strong> includes an independent<br />
trained observer. The observer is not eligible to bill for anesthesia.<br />
Do not submit an anesthesia modifier with these codes.<br />
When a second physician, other than the healthcare pr<strong>of</strong>essional<br />
performing the procedure, provides moderate sedation in the<br />
facility setting (e.g., hospital, outpatient hospital/ambulatory<br />
surgery center) the second physician reports 99148-99150. Codes<br />
99148-99150 may not be reported in a non-facility setting (e.g.,<br />
<strong>of</strong>fice).<br />
Do not submit 99143-99150 with procedures that include<br />
conscious sedation as an inherent part <strong>of</strong> providing the procedure.<br />
These procedures are listed in Appendix G <strong>of</strong> the 2012 CPT<br />
manual. The target symbol () will precede applicable codes in<br />
the main body <strong>of</strong> the CPT manual.<br />
Monitored anesthesia care (MAC) refers to instances in which an<br />
anesthesiologist has been called on to provide specific anesthesia<br />
services to a particular patient undergoing a planned procedure. In<br />
this case, the physician performs a preanesthetic examination, is<br />
physically present in the operating suite, monitors the patient’s<br />
condition, makes medical judgments regarding the patient’s<br />
anesthesia needs, <strong>and</strong> is prepared to furnish anesthesia service as<br />
necessary.<br />
For those circumstances under which such care is medically<br />
necessary <strong>and</strong> requested by the performing surgeon, <strong>Blue</strong> <strong>Cross</strong><br />
will allow submission for MAC the same as for any other<br />
anesthesia service.<br />
Use modifier -QS for monitored anesthesia services.<br />
<strong>Blue</strong> <strong>Cross</strong> recognizes that patient-controlled analgesia (PCA) has<br />
demonstrated clear value to the patient. However, we do not<br />
recognize a separate charge for this service because postoperative<br />
pain control has already been included in the reimbursement <strong>of</strong> the<br />
surgical fee, which was paid to the performing surgeon. Patient<br />
controlled analgesia is also given to patients who have not had<br />
surgery (such as cancer patients) for pain control. It will be<br />
covered in such cases.<br />
St<strong>and</strong>by Anesthesia st<strong>and</strong>by occurs when an anesthesiologist or CRNA is<br />
present in case his or her services are required for anesthesia, but<br />
otherwise performs no medical intervention. <strong>Blue</strong> <strong>Cross</strong> does not<br />
cover anesthesia st<strong>and</strong>by. St<strong>and</strong>by services (99360) are considered<br />
ineligible <strong>and</strong> should not be billed to <strong>Blue</strong> <strong>Cross</strong> or the patient.<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Anesthesia)<br />
Documentation The anesthesia record (either at the facility or the provider’s <strong>of</strong>fice)<br />
must clearly identify the pr<strong>of</strong>essional or pr<strong>of</strong>essionals providing<br />
the anesthesia service. For legal reasons, <strong>and</strong> in order to justify<br />
charges, <strong>Blue</strong> <strong>Cross</strong> requests that both the CRNA <strong>and</strong><br />
anesthesiologist signatures be present for medically directed care.<br />
Time Designation/<br />
Submission<br />
11-8<br />
Anesthesia time should be indicated on the 837P claim format in<br />
the unit(s) field <strong>of</strong> the 837P record. Anesthesia time begins when<br />
the anesthesiologist or CRNA begins to prepare the patient for the<br />
induction <strong>of</strong> anesthesia in the operating room, or an equivalent<br />
area, <strong>and</strong> ends when they are no longer in personal attendance.<br />
Code the anesthesia time as minutes in the units <strong>of</strong> service field.<br />
Diagnosis Coding Use ICD-9-CM diagnosis codes. Select the diagnosis code that<br />
best describes the reason for the surgery based on the patient’s<br />
medical record. Diagnosis code V50.1, plastic surgery for<br />
unacceptable cosmetic surgery appearance, may be submitted<br />
when the patient has requested elective surgery <strong>and</strong> that is the only<br />
surgery performed during an operative session.<br />
Multiple Surgery Code anesthesia services associated with multiple or bilateral<br />
surgical procedures performed during the same operative session<br />
with the single anesthesia code that has the highest base unit value.<br />
Cardioversion<br />
Restriction<br />
Cardioversion, CPT code 92960 (cardioversion, elective, electrical<br />
conversion <strong>of</strong> arrhythmia; external) will not be allowed if<br />
submitted by a certified registered nurse anesthetist.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/21/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Behavioral Health)<br />
Table <strong>of</strong> Contents<br />
Behavioral Health for Pr<strong>of</strong>essional Billers (837P) ................................................................ 11-4<br />
Introduction..........................................................................................................................11-4<br />
Practitioners Who Should be Using this Section .................................................................11-4<br />
Units.....................................................................................................................................11-4<br />
Coding Restrictions..............................................................................................................11-4<br />
CTSS Skills Training <strong>and</strong> Development – PMAP/MNCARE Only....................................11-5<br />
Adult Rehabilitation Mental Health Services (ARMHS) – PMAP/MNCARE Only .......... 11-7<br />
Coding for ARMHS – PMAP/MNCARE Only................................................................... 11-7<br />
Eligible Groups for ARMHS ...............................................................................................11-8<br />
Assertive Community Treatment (ACT) ............................................................................. 11-8<br />
Billing for ACT....................................................................................................................11-8<br />
Intensive Residential Treatment Services (IRTS) (Medicaid Government Programs Only)11-9<br />
IRTS/Crisis Provider Eligibility ........................................................................................11-10<br />
IRTS Member Eligibility ...................................................................................................11-11<br />
IRTS Access to Services....................................................................................................11-11<br />
Billing for IRTS or Residential Crisis ...............................................................................11-11<br />
Adult Non-Residential Crisis Services - Public Program Members Only......................... 11-12<br />
MH-TCM Services to <strong>Minnesota</strong> Health Care Programs.................................................. 11-14<br />
Dialectical Behavioral Therapy/DBT - MHCP Members Only ........................................11-16<br />
Autism Spectrum Disorder/EIBI........................................................................................11-18<br />
Psychiatric Consultation to Primary Care Practitioners.....................................................11-22<br />
Psychiatry <strong>and</strong> Chemical Dependency Assessments .........................................................11-25<br />
MHCP Screening Requirements........................................................................................ 11-25<br />
Family Therapy..................................................................................................................11-26<br />
Units for Public Program Members ................................................................................... 11-26<br />
Medication Management ...................................................................................................11-27<br />
Behavioral Health Evaluation & Management (E&M) Office Calls.................................11-28<br />
Nutritional Counseling/Medical Nutrition Therapy Services............................................11-29<br />
Eligibility <strong>of</strong> Dietitians/ Nutritionists ................................................................................11-30<br />
Psychological <strong>and</strong> Neuropsychological Testing ................................................................11-30<br />
Testing Policy ....................................................................................................................11-31<br />
Practitioner Key .................................................................................................................11-37<br />
Policies...............................................................................................................................11-38<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
11-1
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
11-2<br />
Clinical Supervision Under <strong>Minnesota</strong> Rule Part 9505.0371 - MHCP Members Only.... 11-39<br />
DIAMOND Initiative ........................................................................................................ 11-40<br />
Marital Counseling ............................................................................................................ 11-41<br />
Opioid Maintenance Drug Therapy................................................................................... 11-41<br />
Tobacco Cessation............................................................................................................. 11-42<br />
Rule 29 Setting .................................................................................................................. 11-43<br />
Day Treatment................................................................................................................... 11-43<br />
Compatibility..................................................................................................................... 11-43<br />
Health <strong>and</strong> Behavior Assessment <strong>and</strong> Intervention Codes................................................ 11-44<br />
Missed Appointments........................................................................................................ 11-44<br />
Court Ordered Treatment .................................................................................................. 11-45<br />
Guidelines for Court Ordered Evaluations........................................................................ 11-46<br />
Guidelines for Court Ordered Evaluations – Noncovered Services.................................. 11-49<br />
Parity.................................................................................................................................. 11-51<br />
Behavioral Health Quality Improvement Objectives ........................................................ 11-51<br />
Prior Authorization............................................................................................................ 11-53<br />
Referrals ............................................................................................................................ 11-54<br />
Preadmission Notification ................................................................................................. 11-54<br />
Pre-certification <strong>and</strong> Concurrent Review for Inpatient/Residential Mental Health <strong>and</strong><br />
Substance use Disorder Services....................................................................................... 11-55<br />
Groups that Carve Out Behavioral Health Benefits .......................................................... 11-56<br />
Provider Networks............................................................................................................. 11-57<br />
Pr<strong>of</strong>essional Behavioral Health Coding Information..........................................................11-59<br />
Behavioral Health for Institutional (837I) Billers ...............................................................11-85<br />
Introduction ....................................................................................................................... 11-85<br />
Practitioners Who Should be Using this Section............................................................... 11-85<br />
Coding Guidelines............................................................................................................. 11-85<br />
Behavioral Health Evaluation or Testing .......................................................................... 11-85<br />
Units .................................................................................................................................. 11-85<br />
Individual Behavioral Health Therapy .............................................................................. 11-86<br />
Family <strong>and</strong> Group Therapy ............................................................................................... 11-86<br />
Substance Abuse Services ................................................................................................. 11-87<br />
Billing a Behavioral Health Assessment ........................................................................... 11-87<br />
Testing ............................................................................................................................... 11-87<br />
Family Therapy ................................................................................................................. 11-87<br />
Nutritional Counseling/ Dietitians..................................................................................... 11-88<br />
Detox <strong>and</strong> Alcohol/Drug Rehab Services.......................................................................... 11-89<br />
Health <strong>and</strong> Behavior Assessment <strong>and</strong> Intervention Codes................................................ 11-89<br />
Non-Residential Treatment Centers .................................................................................. 11-90<br />
FEP Exclusion <strong>of</strong> Residential Treatment Centers ............................................................. 11-90<br />
Compatibility..................................................................................................................... 11-90<br />
Recreational Therapy......................................................................................................... 11-90<br />
Extended Care <strong>and</strong> Halfway House Room <strong>and</strong> Board (Medicaid Government Programs<br />
Only).................................................................................................................................. 11-91<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Partial Psychiatric Billing ..................................................................................................11-93<br />
Rule 5 - Emotionally H<strong>and</strong>icapped Facilities ....................................................................11-95<br />
Children’s Residential Mental Health (Medicaid Government Programs only) ...............11-95<br />
IRTS (Medicaid Government Programs Only)..................................................................11-96<br />
IRTS/Crisis Provider Eligibility ........................................................................................11-97<br />
IRTS Member Eligibility ...................................................................................................11-98<br />
IRTS Access to Services....................................................................................................11-98<br />
Billing for IRTS or Residential Crisis ...............................................................................11-98<br />
Court Ordered Treatment...................................................................................................11-98<br />
Preadmission Notification.................................................................................................. 11-99<br />
Residential Substance Abuse Admission <strong>and</strong> Concurrent Review Process Change .........11-99<br />
Pre-certification <strong>and</strong> Concurrent Review for Inpatient/Residential Mental Health <strong>and</strong><br />
Substance Use Disorder services .....................................................................................11-100<br />
Referrals...........................................................................................................................11-102<br />
Parity................................................................................................................................11-102<br />
Groups that Carve Out Behavioral Health Benefits.........................................................11-103<br />
Provider Networks ........................................................................................................... 11-103<br />
Institutional Behavioral Health Coding Information....................................................... 11-104<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-3
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Behavioral Health for Pr<strong>of</strong>essional Billers (837P)<br />
Introduction This section <strong>of</strong> the manual is intended for all behavioral health<br />
practitioners who bill on the pr<strong>of</strong>essional claim format (837P).<br />
This section is not intended for practitioners whose services are<br />
billed on the institutional claim format (837I).<br />
Practitioners Who<br />
Should be Using this<br />
Section<br />
11-4<br />
Psychiatrists, Ph.D. level psychologists, master’s level<br />
psychologists, licensed independent clinical social workers,<br />
certified nurse specialists in psychiatry, licensed marriage <strong>and</strong><br />
family therapists, <strong>and</strong> psychiatric mental health nurse practitioners.<br />
Behavioral health practitioners in Rule 29 Clinics <strong>and</strong> Behavioral<br />
Health specialty clinics should bill under the supervising<br />
practitioner's individual provider number <strong>and</strong> with the U7 modifier<br />
attached to the procedure codes submitted on the claim.<br />
Units One or more units should be submitted based on the time<br />
designation within the HCPCS code narrative. If there is no time<br />
designation, the service is considered ‘per session’ <strong>and</strong> only one<br />
unit should be submitted regardless <strong>of</strong> actual time spent.<br />
Coding Restrictions Code Restriction<br />
90845 Psychoanalysis is generally excluded in member<br />
contracts. If it were to be covered, it must be provided<br />
by an MD (psychiatrist).<br />
90846 Family psychotherapy without the patient present may<br />
be excluded in some members’ contracts. It is only<br />
compatible with a behavioral health diagnosis.<br />
90882 Environmental intervention for medical management<br />
purposes is not covered because it is included in the<br />
practitioner's basic service. However, for Public<br />
Program members only, code 90882 is allowed for<br />
transitioning to community living. See the sections on<br />
“Adult Rehabilitation Mental Health Services (ARMHS)<br />
– PMAP/MNCARE Only” <strong>and</strong> “Coding for ARMHS –<br />
PMAP/MNCARE Only.”<br />
90885 Psychiatric evaluation <strong>of</strong> hospital records - not covered<br />
because it is included in the practitioner's basic service<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Restrictions Code Restriction<br />
CTSS Skills Training<br />
<strong>and</strong> Development –<br />
PMAP/MNCARE Only<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
90887 Interpretation or explanation <strong>of</strong> exam results is not<br />
covered because reimbursement is included in the<br />
compensation for the practitioner’s basic service billed<br />
with the testing code. This service may be allowed for<br />
Public Program members within the DHS Policy<br />
guidelines <strong>of</strong> four per year. Services beyond the four<br />
per year will be denied as provider liability.<br />
90889 Preparation <strong>of</strong> report is a contract exclusion <strong>and</strong> is not<br />
covered.<br />
90899 Unlisted psychiatric service or procedure codes must be<br />
submitted with a specific narrative description detailing<br />
exactly what the charge is for along with documentation<br />
<strong>of</strong> time. Unlisted codes may be subject to denial if there<br />
is an existing definitive code describing the service.<br />
Children’s Therapeutic Services <strong>and</strong> Supports (CTSS) providers<br />
should bill HCPCS code H2014, for skills training <strong>and</strong><br />
development services provided to Public Program members. These<br />
services are used exclusively for Public Program members under<br />
the age <strong>of</strong> 21. The appropriate number <strong>of</strong> units must be billed with<br />
this code. Each unit equals 15 minutes <strong>of</strong> service. Providers billing<br />
code H2014 must include the following modifier(s):<br />
UA for individual skills<br />
UA, HR for family skills<br />
UA, HQ for group skills<br />
While the majority <strong>of</strong> CTSS providers specialize in in-home work,<br />
they can also provide services in the <strong>of</strong>fice. H2014 is only one <strong>of</strong><br />
many services under the CTSS umbrella. CTSS providers can bill<br />
all the codes that any other licensed mental health pr<strong>of</strong>essional can<br />
bill. The Skills Training service will <strong>of</strong>ten be done by a nonlicensed<br />
practitioner but should always be billed under the<br />
supervising pr<strong>of</strong>essional’s provider number or NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-5
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
CTSS Skills Training<br />
<strong>and</strong> Development –<br />
PMAP/MNCare Only<br />
(continued)<br />
11-6<br />
Code Restriction<br />
H0046 Mental health services, not otherwise<br />
specified. Use for travel time for in-home<br />
services. Bill 1 unit per 1 minute. A specific<br />
narrative description detailing exactly what<br />
the charge is for must be submitted with this<br />
code.<br />
H2011 Crisis intervention service, per 15 minutes<br />
H2012-UA Behavioral health day treatment, per hour.<br />
Use for therapeutic preschool for Public<br />
Program members.<br />
H2014-UA Skills training <strong>and</strong> development, per 15<br />
minutes. Use for CTSS individual skills<br />
training <strong>and</strong> development services. This code<br />
is covered for Public Program members<br />
under age 21.<br />
H2014-U9 Use for TSFC (Therapeutic Support <strong>of</strong> Foster<br />
Care) service package<br />
H2014-UA,HR Use for CTSS, family skills<br />
H2014-UA,HQ Use for CTSS, group skills<br />
H2015 Comprehensive community support services,<br />
per 15 minutes. Submit with UA modifier for<br />
CTSS Crisis Intervention.<br />
H2019-UA Therapeutic behavioral services, per 15<br />
minutes. Use for CTSS Behavioral Aide level<br />
1 I.<br />
H2019-UA, HM Therapeutic behavioral services, per 15<br />
minutes. Use for CTSS Behavioral Aide<br />
level II.<br />
H2019-UA, HE Therapeutic behavioral services, per 15<br />
minutes. Use for mental health practitioner<br />
direction (supervision) <strong>of</strong> CTSS Behavioral<br />
Aide.<br />
H2020-UA Therapeutic behavioral services, per diem.<br />
Use for CTSS Behavioral Aide level I.<br />
H2020-UA, HM Therapeutic behavioral services, per diem.<br />
Use for CTSS Behavioral Aide level II.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
CTSS Skills Training<br />
<strong>and</strong> Development –<br />
PMAP/MNCare Only<br />
(continued)<br />
Adult Rehabilitation<br />
Mental Health Services<br />
(ARMHS) –<br />
PMAP/MNCARE Only<br />
Coding for ARMHS –<br />
PMAP/MNCARE Only<br />
Code Restriction<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
H2020-UA, HE Therapeutic behavioral services, per diem.<br />
Use for mental health practitioner direction<br />
(supervision) <strong>of</strong> CTSS Behavioral Aide.<br />
H2032 Activity therapy, per 15 minutes. Use for<br />
Therapeutic Camp.<br />
ARMHS is a health plan responsibility for <strong>Blue</strong> Plus ® Public<br />
Program groups. These services are for members with a serious<br />
mental illness.<br />
The following provider specialties are eligible to provide these<br />
services: Multi-specialty clinics, community mental health<br />
clinics, behavioral health clinics, psychiatrists, Ph.D. level<br />
licensed psychologists, master’s level licensed psychologists,<br />
clinical nurse specialists, licensed independent clinical social<br />
workers, licensed marriage/family therapists, <strong>and</strong> psychiatric<br />
mental health nurse practitioners.<br />
Eligible providers must be certified through DHS as Adult<br />
Rehab Mental Health Services providers.<br />
Code Restriction<br />
H2017 Psychosocial Rehab (basic social <strong>and</strong> living<br />
skills) individual by a pr<strong>of</strong>essional<br />
H2017 – HM Psychosocial Rehab individual by a rehab<br />
worker<br />
H2017 – HQ Psychosocial Rehab group by either a<br />
pr<strong>of</strong>essional or rehab worker<br />
H2017 – UD Psychosocial Rehab when transitioning to<br />
Community Living Services<br />
90882 Community Intervention by a pr<strong>of</strong>essional<br />
90882 – HM Community Intervention by a rehab worker<br />
90882 – UD Community Intervention when transitioning to<br />
Community Living Services<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-7
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Eligible Groups for<br />
ARMHS<br />
Assertive Community<br />
Treatment (ACT)<br />
11-8<br />
Code Restriction<br />
H0034 Medication Education individual by a physician,<br />
RN, pharmacist, or PA<br />
H0034 – HQ Medication Education group by a physician, RN,<br />
pharmacist, or PA<br />
Members in the following groups are eligible to receive these<br />
services through <strong>Blue</strong> Plus:<br />
Products Group Numbers<br />
PMAP PP011, PP012, PP014, PP015, PP016, PP017,<br />
PP021, PP022, PP024, PP025, PP026, PP027,<br />
PP031, PP032, PP034, PP035, PP036, PP037<br />
GA/GAMC PP081, PP082, PP084, PP091, PP092, PP094<br />
<strong>Minnesota</strong><br />
Senior Care<br />
Plus<br />
<strong>Minnesota</strong>Care<br />
Exp<strong>and</strong>ed<br />
<strong>Minnesota</strong>Care<br />
Basic Plus,<br />
Basic +1,<br />
Basic +2<br />
Secure<strong>Blue</strong> SM<br />
(HMO SNP)<br />
PP041, PP042, PP044, PP051, PP052, PP054,<br />
PP055, PP056, PP057, PP061, PP062, PP064,<br />
PP071, PP072, PP074, PP075, PP076, PP077<br />
PP111, PP112, PP151, PP152<br />
PP121, PP122, PP131, PP132, PP141, PP142,<br />
PP161, PP162, PP163, PP164<br />
PP200, PP201, PP202, PP210, PP215, PP220,<br />
PP221, PP222, PP230, PP240, PP245, PP250,<br />
PP255, PP260, PP261, PP262, PP270, PP280,<br />
PP281, PP282, PP290<br />
To provide this type <strong>of</strong> treatment, providers must:<br />
Be certified by DHS to provide ARMHS<br />
Be a participating provider with <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>)<br />
Billing for ACT Services must be billed on an 837P electronic claim format<br />
Use HCPCS code H0040 (ACT Program per diem)<br />
For each line item billed, an individual mental health<br />
pr<strong>of</strong>essional or mental health rehab pr<strong>of</strong>essional provider<br />
number must be submitted in loop 2310B <strong>of</strong> the electronic<br />
claim.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Intensive Residential<br />
Treatment Services<br />
(IRTS) (Medicaid<br />
Government Programs<br />
Only)<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
<strong>Blue</strong> <strong>Cross</strong> will reimburse certain categories <strong>of</strong> providers for these<br />
services, which were formerly reimbursed through the <strong>Minnesota</strong><br />
Department <strong>of</strong> Human Services (DHS).<br />
This change was effective for all enrollees in the Prepaid Medical<br />
Assistance Programs (PMAP), <strong>Minnesota</strong> Senior Health Options<br />
(MSHO) <strong>and</strong> <strong>Minnesota</strong> Disabled Health Options (MnDHO).<br />
Crisis response services include:<br />
Crisis assessment<br />
Crisis intervention<br />
Crisis stabilization<br />
Community intervention<br />
The following summarizes provider eligibility, member eligibility<br />
<strong>and</strong> operational requirements for <strong>Blue</strong> Plus providers <strong>of</strong> these<br />
services.<br />
All members <strong>of</strong> the following <strong>Blue</strong> Plus products are eligible to<br />
receive these services:<br />
<strong>Blue</strong> Advantage (<strong>Blue</strong> Plus PMAP, <strong>and</strong> <strong>Minnesota</strong> Senior<br />
CarePlus)<br />
<strong>Minnesota</strong>Care<br />
Care<strong>Blue</strong><br />
Group numbers for these products are listed below.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-9
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Intensive Residential<br />
Treatment Services<br />
(IRTS) (Medicaid<br />
Government Programs<br />
Only) (continued)<br />
IRTS/Crisis Provider<br />
Eligibility<br />
11-10<br />
<strong>Blue</strong> Plus<br />
Products Group Numbers<br />
<strong>Blue</strong> Advantage PP011, PP012, PP014, PP015, PP016,<br />
PP017, PP021, PP022, PP024, PP025,<br />
PP026, PP027, PP031, PP032, PP034,<br />
PP035, PP036, PP037, PP411, PP412,<br />
PP414<br />
<strong>Minnesota</strong> Senior<br />
Care Plus<br />
<strong>Minnesota</strong>Care<br />
Exp<strong>and</strong>ed<br />
<strong>Minnesota</strong>Care<br />
Basic Plus, Basic<br />
+1, Basic +2<br />
PP041, PP042, PP044, PP051, PP052,<br />
PP054, PP055, PP056, PP057, PP061,<br />
PP062, PP064, PP071, PP072, PP074,<br />
PP075, PP076, PP077<br />
PP111, PP112, PP151, PP152<br />
PP121, PP122, PP131, PP132, PP141,<br />
PP142, PP161, PP162, PP163, PP164<br />
Secure<strong>Blue</strong> PP200, PP201, PP202, PP215, PP220,<br />
PP221, PP222, PP240, PP245, PP260,<br />
PP261, PP262, PP280, PP281, PP282<br />
Members with commercial coverage may be eligible to receive<br />
these services. Please verify member eligibility using one <strong>of</strong> the<br />
resources described below under Member eligibility.<br />
To provide this type <strong>of</strong> treatment, providers must:<br />
Be licensed under Rule 36<br />
Have DHS approval<br />
Be a participating provider with <strong>Blue</strong> <strong>Cross</strong><br />
Pr<strong>of</strong>essional treatment services may only be provided by an<br />
eligible IRTS Crisis provider.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
IRTS Member<br />
Eligibility<br />
IRTS Access to<br />
Services<br />
Billing for IRTS or<br />
Residential Crisis<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Providers are expected to check the member’s eligibility before<br />
rendering services. Resources available for verification include:<br />
MN-ITS<br />
www.mn-its.dhs.state.mn.us<br />
EVS<br />
1-800-657-3613<br />
Provider Web Self-Service<br />
www.providerhub.com<br />
Provider Services<br />
1-800-262-0820<br />
Direct access to contracted providers<br />
No prior authorizations required<br />
No referrals required<br />
Non-contracted providers must obtain a referral from provider<br />
services at 1-800-262-0820 prior to delivering treatment.<br />
When reporting room <strong>and</strong> board <strong>and</strong>/or treatment services, report<br />
on the 837I type <strong>of</strong> bill 86X, with the room <strong>and</strong> board <strong>and</strong><br />
treatment services as separate line items. Submit the room <strong>and</strong><br />
board charges under revenue code 1001 <strong>and</strong> the treatment services<br />
under revenue codes 090X or 091X.<br />
When room <strong>and</strong> board <strong>and</strong> treatment are billed to separate entities,<br />
treatment is reported on the 837P, with HCPCS code H0018 or<br />
H0019.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-11
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Adult Non-Residential<br />
Crisis Services - Public<br />
Program Members<br />
Only<br />
11-12<br />
Per the Department <strong>of</strong> Human Services (DHS), adult nonresidential<br />
crisis services for behavioral health diagnoses are a<br />
covered service for some <strong>Minnesota</strong> Health Care Program (Public<br />
Programs) members.<br />
Eligible providers must be enrolled through DHS.<br />
Eligible providers must be enrolled through DHS as Adult<br />
Crisis Response Providers.<br />
<strong>Blue</strong> <strong>Cross</strong> has adopted the same coding changes as outlined below<br />
by the <strong>Minnesota</strong> Department <strong>of</strong> Human Services. This change is<br />
effective for all <strong>Minnesota</strong> Health Care Programs (MHCP)<br />
members.<br />
Adult Mental Health Crisis Services<br />
Use HCPCS code S9484 to bill for adult mental health crisis<br />
services, combining crisis assessment, intervention <strong>and</strong> nonresidential<br />
stabilization. This coding:<br />
complies with HIPAA coding requirements<br />
creates consistency between adult <strong>and</strong> children’s crisis service<br />
billing<br />
eliminates arbitrary distinction between intervention <strong>and</strong><br />
assessment<br />
Do not use HCPCS code H0031 for crisis assessment or H2011 for<br />
crisis intervention.<br />
The following services may be submitted on an 837P claim format.<br />
Enter the actual place <strong>of</strong> service code (POS); POS may not be 23<br />
(emergency department) for mobile team billing.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Adult Non-Residential<br />
Crisis Services - Public<br />
Program Members<br />
Only (continued)<br />
Adult Crisis Service Billing<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Of Service Billing Unit<br />
S9484 adult crisis assessment,<br />
intervention <strong>and</strong> stabilizationindividual,<br />
pr<strong>of</strong>essional<br />
S9484-HM adult crisis stabilization –<br />
individual rehab worker<br />
S9484-HN adult crisis assessment,<br />
intervention <strong>and</strong> stabilization<br />
– individual practitioner<br />
1 unit per 60<br />
minutes<br />
1 unit per 60<br />
minutes<br />
1 unit per 60<br />
minutes<br />
S9484-HQ adult crisis stabilization-group 1 unit per 60<br />
minutes<br />
Additional information<br />
Rehabilitation workers can provide adult crisis stabilization<br />
services only.<br />
The changes listed above do not apply to the coverage, coding or<br />
authorization thresholds for residential crisis stabilization (H0018)<br />
or community intervention (90882).<br />
Pricing <strong>and</strong> Programs Applicability<br />
<strong>Blue</strong> <strong>Cross</strong>’ usual pricing methodology for Public Programs will<br />
apply to these codes. This information applies to the following<br />
programs:<br />
Prepaid Medical Assistance Program (<strong>Blue</strong>Advantage/<br />
PMAP/GAMC) – all groups<br />
<strong>Minnesota</strong> Senior Health Options (MSHO Secure<strong>Blue</strong>)<br />
<strong>Minnesota</strong> Senior Care Plus (<strong>Blue</strong>Advantage MSC+) – all<br />
groups<br />
<strong>Minnesota</strong> Care – all groups<br />
Group Numbers<br />
A complete listing <strong>of</strong> group numbers can be found on the <strong>Blue</strong><br />
<strong>Cross</strong> website at bluecrossmn.com.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-13
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
MH-TCM Services to<br />
<strong>Minnesota</strong> Health Care<br />
Programs<br />
11-14<br />
The <strong>Minnesota</strong> Department <strong>of</strong> Human Services (DHS) has<br />
determined that managed care organizations that contract with<br />
DHS shall be responsible for the provision <strong>of</strong> mental health –<br />
targeted case management (MH-TCM) services for eligible<br />
<strong>Minnesota</strong> Health Care Programs members.<br />
Eligibility<br />
As a contracted provider, your agency must meet Rule 79 criteria<br />
<strong>and</strong> be designated by <strong>Blue</strong> Plus in order to be eligible for<br />
reimbursement for MH-TCM services. Providers are responsible<br />
for checking the member’s eligibility prior to rendering services.<br />
Resources available for verification include:<br />
MN-ITS – www.mn-its.dhs.state.mn.us<br />
Provider web self-service – providerhub.com<br />
Nonparticipating providers must obtain a referral prior to rendering<br />
services for <strong>Blue</strong> Plus members. Contact provider services at<br />
(651) 662-5200 or 1-800-262-0820 for assistance.<br />
Billing<br />
MH-TCM is a pr<strong>of</strong>essional service billed on an 837P claim format.<br />
When billing for MH-TCM, submit the contracting provider NPI<br />
number currently on file with <strong>Blue</strong> Plus. In addition, an individual<br />
rendering NPI number is required.<br />
Eligible <strong>Minnesota</strong> Health Care Programs<br />
Product <strong>Name</strong> Group Numbers<br />
Prepaid Medical Assistance<br />
Program (PMAP) <strong>and</strong><br />
<strong>Minnesota</strong> Senior Care Plus<br />
(MSC+)<br />
All group numbers that begin<br />
with PP0 <strong>and</strong> FPG04<br />
<strong>Minnesota</strong>Care All group numbers that begin<br />
with PP1 <strong>and</strong> FPG10<br />
MSHO – Secure<strong>Blue</strong> All group numbers that begin<br />
with PP2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
MH-TCM Services to<br />
<strong>Minnesota</strong> Health Care<br />
Programs (continued)<br />
Access to Services<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Members have direct access to contracted MH-TCM providers.<br />
<strong>Blue</strong> Plus members:<br />
No prior authorizations required<br />
Members must be determined eligible for MH-TCM<br />
according to Rule 79 criteria<br />
Providers must be contracted <strong>and</strong> designated by <strong>Blue</strong> Plus<br />
Nonparticipating providers must obtain a referral prior to rendering<br />
services for <strong>Blue</strong> Plus members. Contact provider services at<br />
(651) 662-5200 or 1-800-262-0820 for assistance.<br />
Billing<br />
MH-TCM is a pr<strong>of</strong>essional service billed on an 837P claim format.<br />
When billing for MH-TCM, submit the contracting provider NPI<br />
number currently on file with <strong>Blue</strong> Plus. In addition, an individual<br />
rendering NPI number is required.<br />
Procedure<br />
Codes<br />
Modifiers Brief Description Service<br />
Limitations<br />
T2023 HE, HA Face-to-face<br />
contact between<br />
case manager <strong>and</strong><br />
recipient under age<br />
18 years<br />
T2023 HE Face-to-face<br />
contact between<br />
case manager <strong>and</strong><br />
recipient age 18 or<br />
older<br />
T2023 HE, U4 Telephone contact<br />
(recipient 18 years<br />
or older)<br />
1 unit per<br />
month<br />
1 unit per<br />
month<br />
1 unit per<br />
month<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-15
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
MH-TCM Services to<br />
<strong>Minnesota</strong> Health Care<br />
Programs (continued)<br />
Dialectical Behavioral<br />
Therapy/DBT - MHCP<br />
Members Only<br />
11-16<br />
Procedure<br />
Codes<br />
T1017 for<br />
HIS/638 <strong>and</strong><br />
FQHC billing<br />
only<br />
T1017 for<br />
HIS/638 <strong>and</strong><br />
FQHC billing<br />
only<br />
Reimbursement<br />
Modifiers Brief Description Service<br />
Limitations<br />
HE, HA Face-to face<br />
encounter (child<br />
under age 18<br />
years)<br />
HE Face-to face<br />
encounter (age 18<br />
or older)<br />
Per encounter<br />
Per encounter<br />
For MH-TCM, eligible providers should bill 100% <strong>of</strong> the thencurrent<br />
monthly rate established with the county. <strong>Blue</strong> Plus<br />
reimbursement will be 100% <strong>of</strong> charge. Providers shall accept this<br />
reimbursement as payment in full for MH-TCM services.<br />
MHCP adds Dialectical Behavior Therapy (DBT) to covered<br />
mental health outpatient benefits for some MHCP members. The<br />
<strong>Minnesota</strong> Department <strong>of</strong> Human Services (DHS) received federal<br />
approval on October 1, 2010, to add DBT face-to-face services as<br />
an outpatient mental health benefit. This benefit addition is<br />
effective immediately.<br />
Subscriber must meet all <strong>of</strong> the following eligibility<br />
requirements:<br />
Subscriber must be age eighteen (18) or older<br />
Subscriber must be diagnosed with severe symptoms <strong>and</strong><br />
significant dysfunction consistent with the current Diagnostic<br />
<strong>and</strong> Statistical <strong>Manual</strong> <strong>of</strong> Mental Disorders (DSM) criteria for<br />
a Borderline Personality Disorder<br />
Subscriber’s mental health needs cannot be met with available<br />
community-based services or must be provided concurrently<br />
with other community-based services<br />
Subscriber underst<strong>and</strong>s <strong>and</strong> is cognitively capable <strong>of</strong><br />
participating in programming<br />
Subscriber is willing <strong>and</strong> able to follow program policies <strong>and</strong><br />
rules assuring safety <strong>of</strong> self <strong>and</strong> others<br />
Subscriber is at significant risk <strong>of</strong> one or more <strong>of</strong> the<br />
following; a mental health crisis, entering a more restrictive<br />
setting, decompensating functioning or mental health<br />
symptoms, engaging in intentional self-harm<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Dialectical Behavioral<br />
Therapy/DBT - MHCP<br />
Members Only<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
This information applies to the following programs <strong>and</strong> all<br />
subgroups for the group numbers listed:<br />
<strong>Blue</strong>Advantage<br />
PMAP (age 18<br />
<strong>and</strong> older)<br />
<strong>Minnesota</strong>Care<br />
(age 18 <strong>and</strong><br />
older)<br />
<strong>Blue</strong>Advantage<br />
MSC+<br />
Secure<strong>Blue</strong><br />
(HMO SNP)<br />
Provider eligibility requirements:<br />
PP011, PP012, PP014, PP015, PP016, PP017,<br />
PP021, PP022, PP024, PP025, PP026, PP027,<br />
PP031, PP032, PP034, PP035, PP036, PP037,<br />
PP411, PP412, PP414<br />
PP111, PP112, PP121, PP122, PP131, PP132,<br />
PP141, PP142, PP151, PP152, PP161, PP162,<br />
PP163, PP164<br />
PP041, PP042, PP044, PP051, PP052, PP054,<br />
PP055, PP056, PP057, PP061, PP062, PP064,<br />
PP071, PP072, PP074, PP075, PP076, PP077<br />
PP200, PP201, PP202, PP215, PP220, PP221,<br />
PP222, PP240, PP245, PP260, PP261, PP262,<br />
PP280, PP281, PP282<br />
Provider shall be certified by DHS to provide DBT services<br />
Provider shall meet all <strong>Blue</strong> <strong>Cross</strong> credentialing requirements<br />
Provider shall be a participating provider with <strong>Blue</strong> <strong>Cross</strong><br />
Claims submission requirements:<br />
Submit claims on the electronic 837P (pr<strong>of</strong>essional) format<br />
Both a type 1 NPI (rendering provider) <strong>and</strong> type 2 NPI (billing<br />
provider) are required on the claim<br />
Submit individual services using HCPCS code H2019 with the<br />
U1 modifier (services must be face-to-face)<br />
Submit group services using HCPCS code H2019 with the U1<br />
<strong>and</strong> the HQ modifiers (services must be face-to-face)<br />
Payment information<br />
Payment for eligible health services provided to MHCP<br />
subscribers shall be subject to the terms <strong>and</strong> provisions described<br />
in the Provider Service Agreement as renewed annually.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-17
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Autism Spectrum<br />
Disorder/EIBI<br />
11-18<br />
Early Intensive Behavioral Intervention (EIBI) is a term used to<br />
describe an intensive, multidisciplinary approach used to treat the<br />
symptoms <strong>of</strong> a diagnosis <strong>of</strong> autism spectrum disorder (ASD). This<br />
area lacks st<strong>and</strong>ard terminology, but does include intensive early<br />
intervention behavioral therapy (IEIBT), applied behavioral<br />
analysis (ABA), Lovaas <strong>and</strong> discrete trial training (DTT).<br />
To ensure members receive the appropriate quality <strong>and</strong> level <strong>of</strong><br />
care for autism spectrum disorders (ASD) <strong>and</strong> autism early<br />
intensive behavioral interventions (EIBI), providers should refer to<br />
<strong>Blue</strong> <strong>Cross</strong> medical policy (X-44, Autism spectrum disorder:<br />
Early intensive behavioral interventions (EIBI)) relating to<br />
assessment <strong>of</strong> autism spectrum disorder that includes steps to<br />
follow when providing early intensive behavioral interventions.<br />
Autism spectrum disorder: Assessment<br />
Autism spectrum disorder: Early intensive behavioral<br />
interventions (EIBI)<br />
A summary <strong>of</strong> the medical policies are available on<br />
providers.bluecrossmn.com.<br />
Product application<br />
EIBI services are subject to the member’s plan benefits. Some<br />
benefit plans may exclude coverage <strong>of</strong> EIBI services.<br />
Pre-certification/pre-authorization review applies to all EIBI<br />
services for members in fully insured <strong>and</strong> self-insured benefit<br />
plans, <strong>Blue</strong> Advantage (PMAP) programs, <strong>and</strong> <strong>Minnesota</strong>Care<br />
programs when the provider <strong>of</strong> the service is a participating<br />
provider caring for <strong>Blue</strong> <strong>Cross</strong> <strong>Minnesota</strong> members. This does not<br />
include members <strong>of</strong> other <strong>Blue</strong> <strong>Cross</strong> plans.<br />
Pre-certification/pre-authorization review for EIBI services is not<br />
required for members in the following plans:<br />
<strong>Minnesota</strong> Senior Care Plus (MSC+)<br />
Secure<strong>Blue</strong> (HMO SNP)<br />
Platinum <strong>Blue</strong> (Cost)<br />
Medicare<strong>Blue</strong> PPO (Regional PPO)<br />
Medicare supplement<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Autism Spectrum<br />
Disorder/EIBI<br />
(continued)<br />
ASD Assessment Requirements<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
To ensure appropriate care <strong>and</strong> use <strong>of</strong> benefits, <strong>Blue</strong> <strong>Cross</strong> requires<br />
the following to be done prior to the initiation <strong>of</strong> health services<br />
for EIBI:<br />
A comprehensive diagnostic assessment must have been<br />
completed within the past 12 months.<br />
The assessment must be on file in the provider’s <strong>of</strong>fice as part <strong>of</strong><br />
each patient’s medical record.<br />
In addition, providers are expected to follow the diagnostic<br />
assessment st<strong>and</strong>ards as described in the assessment section <strong>of</strong> the<br />
<strong>Blue</strong> <strong>Cross</strong> behavioral health medical policy, autism spectrum<br />
disorder.<br />
Pre-certification/pre-authorization requirements<br />
Pre-certification/pre-authorization will be required for all EIBI<br />
services (procedure codes H2014, H2017 <strong>and</strong> H2019) in<br />
which the level <strong>of</strong> treatment provided consists <strong>of</strong> more than<br />
nine (9) hours per week for intensive therapy. A week is<br />
defined as a period <strong>of</strong> seven consecutive days.<br />
A summary <strong>of</strong> the components <strong>of</strong> the multidisciplinary<br />
Diagnostic Assessment as described in the Autism Spectrum<br />
Disorders: Assessment Medical Policy X-43, must be included<br />
with the authorization request.<br />
A one-visit Diagnostic Assessment (procedure codes 90801 or<br />
90802) may be completed without pre-certification.<br />
Any psychological or neuropsychological testing also requires<br />
pre-certification/pre-authorization before performing services<br />
for a member.<br />
Pre-certification/pre-authorization requirement applies to all<br />
participating providers.<br />
Obtaining pre-certification/pre-authorization<br />
Providers can obtain pre-certification/pre-authorization for EIBI<br />
assessment/services by completing the Early Intensive Behavioral<br />
Intervention Autism Spectrum Disorder Service request form,<br />
which can be found at providers.bluecrossmn.com. Click on<br />
“Forms & publications.” From the drop-down box choose “forms:<br />
preadmission/prior authorization.” The completed form may be<br />
faxed to (651) 662-0854.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-19
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Autism Spectrum<br />
Disorder/EIBI<br />
(continued)<br />
11-20<br />
Claims audits<br />
Routine claim audits have disclosed occurrences where some<br />
providers have been submitting claims for EIBI services that do<br />
not meet medical policy criteria. This is a reminder that providers<br />
must abide by the requirements <strong>of</strong> all medical policies.<br />
This action is being taken to help ensure that members receive the<br />
appropriate level <strong>of</strong> care <strong>and</strong> frequency <strong>of</strong> service for EIBI<br />
services. Failure to provide evidence <strong>of</strong> medical necessity may<br />
result in claim denials.<br />
Coding<br />
Self-insured <strong>and</strong> fully insured plans except for MHCP:<br />
Provider shall submit claims for EIBI services for autism<br />
spectrum disorder using HCPCS codes H2014, H2017 or<br />
H2019. Provider shall only bill for 15 minute face-to-face<br />
sessions, which shall have a value <strong>of</strong> one (1) unit. The codes<br />
listed above replace the use <strong>of</strong> CPT code 90899.<br />
MHCP<br />
For MHCP subscribers eligible for children’s therapeutic<br />
services <strong>and</strong> supports (CTSS) provider shall submit claims for<br />
EIBI services for autism spectrum disorder using HCPCS<br />
codes H2014-UA, H2017 or H2019-UA. Code H2017 is not a<br />
CTSS code; therefore, it should not be billed using the UA<br />
modifier. Provider shall only bill for 15 minute face to-face<br />
sessions, which shall have a value <strong>of</strong> one (1) unit. The codes<br />
listed above replace the use <strong>of</strong> CPT code 90899.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Autism Spectrum<br />
Disorder/EIBI<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
HCPCS codes H2018 <strong>and</strong> H2020:<br />
<strong>Blue</strong> <strong>Cross</strong> will accept HCPCS codes H2018 <strong>and</strong> H2020 but<br />
will not allow reimbursement for these codes. Provider shall<br />
submit the timed codes listed above for reimbursement for<br />
EIBI services.<br />
Other <strong>Blue</strong> <strong>Cross</strong> Plans<br />
If a provider is working with <strong>Blue</strong> Plans outside <strong>of</strong> <strong>Minnesota</strong>, it<br />
may be helpful to identify the code that will be used on the claim<br />
when checking subscriber eligibility <strong>and</strong> benefit information. This<br />
may help to ensure accurate eligibility <strong>and</strong> benefit information<br />
prior to the delivery <strong>of</strong> EIBI services.<br />
Reimbursement<br />
In accordance with a commitment to health care affordability <strong>and</strong><br />
administrative simplification, payment for EIBI services for all<br />
eligible <strong>Blue</strong> <strong>Cross</strong> subscribers shall remain subject to the terms<br />
<strong>and</strong> provisions described under Provider Reimbursement,<br />
<strong>Minnesota</strong> Health Care Programs in the Agreement as renewed<br />
annually by <strong>Blue</strong> <strong>Cross</strong> less subscriber <strong>and</strong> other party liabilities<br />
(e.g., deductibles, coinsurance, non-covered services <strong>and</strong><br />
coordination <strong>of</strong> benefits with other health plans, employer liability<br />
plans, workers’ compensation or automobile plans). Provider<br />
agrees to not request reimbursement for simultaneously provided<br />
individual <strong>and</strong> family services.<br />
Medical Policies <strong>and</strong> Procedures Related to ASD<br />
Providers must comply with all medical policy <strong>and</strong> procedures<br />
including the medical policy <strong>and</strong> procedures for services rendered<br />
for autism spectrum disorder.<br />
Client Related Activity<br />
Any client related activity that is not face-to-face service shall not<br />
be billed separately. Reimbursement for subscriber related activity<br />
that is not a face-to-face service is included in the rate paid for the<br />
codes stated above.<br />
Adherence <strong>and</strong> Enforcement <strong>of</strong> Policy<br />
<strong>Blue</strong> <strong>Cross</strong> retains the right to audit provider’s compliance with the<br />
aforementioned coding <strong>and</strong> reimbursement provisions to ensure<br />
proper administration <strong>of</strong> subscriber benefits <strong>and</strong> payment for<br />
services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-21
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Psychiatric<br />
Consultation to<br />
Primary Care<br />
Practitioners<br />
11-22<br />
The Department <strong>of</strong> Human Services (DHS) has federal approval to<br />
add psychiatric consultation to mental health covered services.<br />
This includes psychiatric consultation by a psychiatrist via<br />
telephone, e-mail, facsimile, or other means <strong>of</strong> communication to<br />
primary care practitioners.<br />
Eligibility is extended to all <strong>Blue</strong> <strong>Cross</strong> fully insured members <strong>and</strong><br />
self-insured members whose groups have elected this coverage.<br />
Psych Consult to PCP Policy<br />
Psychiatric consultation by a psychiatrist via telephone, e-mail,<br />
facsimile, or other means <strong>of</strong> communication to a primary care<br />
practitioners is subject to the following coverage criteria.<br />
Premises Underlying Psychiatric Consultation<br />
Psychiatric consultations must be:<br />
documented in the patient record <strong>and</strong> maintained by the<br />
primary care practitioner<br />
between the physician <strong>and</strong> psychiatrist, compliant with HIPAA<br />
privacy <strong>and</strong> security requirements <strong>and</strong> regulations<br />
provided according to federal requirements <strong>and</strong> data privacy<br />
provisions<br />
With the patient’s consent, psychiatric consultation may be<br />
without the patient present.<br />
Eligible Recipients<br />
To be eligible for psychiatric consultations to primary care<br />
practitioners, recipients:<br />
must be eligible for <strong>Blue</strong> Plus Public Programs through<br />
Medical Assistance (MA), General Assistance Medical Care<br />
(GAMC) or <strong>Minnesota</strong>Care OR must be a fully insured<br />
member, or a self-insured member whose group has elected<br />
this coverage, <strong>and</strong><br />
must be under the care <strong>of</strong> a primary care physician, <strong>and</strong> require<br />
the consultation between a psychiatrist <strong>and</strong> their primary care<br />
practitioner for appropriate medical or mental health treatment,<br />
<strong>and</strong><br />
may be any age<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Psychiatric<br />
Consultation to<br />
Primary Care<br />
Practitioners<br />
(continued)<br />
Eligible Providers<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Providers eligible to request a psychiatric consultation:<br />
Primary care physicians<br />
Nurse practitioners<br />
Clinical nurse specialists<br />
Physician assistants<br />
Only psychiatrists are eligible to provide psychiatric consultation<br />
to primary care practitioners.<br />
Provider Responsibilities<br />
Only the primary care provider may bill for psychiatric<br />
consultations to primary care practitioners.<br />
Primary care clinics <strong>and</strong> the consulting psychiatrists should<br />
have a contract or other formal agreement that defines the<br />
strategy for payment to the consulting psychiatrist <strong>and</strong> ensures<br />
that provider requirements <strong>and</strong> responsibilities are met.<br />
Providers must obtain <strong>and</strong> maintain HIPAA-compliant<br />
technology <strong>and</strong> use HIPAA-compliant privacy <strong>and</strong> security<br />
protections for the recipient. Also, providers must ensure<br />
procedures are in place to prevent a breach in privacy or cause<br />
exposure <strong>of</strong> recipient mental health records to unauthorized<br />
persons.<br />
Covered Service<br />
Communication between a primary care provider <strong>and</strong> a psychiatrist<br />
for consultation or medical management <strong>of</strong> patients is a covered<br />
service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-23
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Psychiatric<br />
Consultation to<br />
Primary Care<br />
Practitioners<br />
(continued)<br />
11-24<br />
Billing<br />
Use the following code <strong>and</strong> modifiers to report this service:<br />
99499 – Unlisted evaluation <strong>and</strong> management service. A<br />
narrative must be submitted as well as the time spent for this<br />
service. This should be reported in the NTE segment <strong>of</strong> the<br />
837P electronic claim format as “(amount <strong>of</strong> time) spent in<br />
telephone consultation with (name <strong>of</strong> psychiatrist).”<br />
Appropriate modifiers as follows:<br />
Basic Consultation: U4, HE<br />
Intermediate Consultation: U4, U5, HE<br />
Complex Consultation: U4, U6, HE<br />
U4 – Case Management via Telephone<br />
The U4 identifies the service as a telephone call.<br />
HE – Mental Health Program<br />
The HE modifier identifies the service as mental health.<br />
Also add modifier -U7 to the appropriate code when the<br />
primary care is provided by a physician extender.<br />
The recipient must be present unless the recipient has granted<br />
permission for the consultation to take place without the recipient<br />
being present.<br />
Authorization requirements, maximum utilization limits <strong>and</strong><br />
thresholds do not currently apply to psychiatric consultation codes.<br />
Note: Telephone service codes 99441-99443 <strong>and</strong> 98966-98968 are<br />
not allowed <strong>and</strong> will deny as provider liability if submitted.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Psychiatry <strong>and</strong><br />
Chemical Dependency<br />
Assessments<br />
MHCP Screening<br />
Requirements<br />
90801 <strong>and</strong> 90802<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
These are “per session” codes. Bill one unit <strong>of</strong> service per<br />
session regardless <strong>of</strong> time.<br />
These codes can be billed with either a chemical dependency<br />
diagnosis or with a psychiatric condition diagnosis.<br />
If the assessment does not reveal a behavioral health condition,<br />
it would be appropriate to bill with the sign or symptom<br />
precipitating the assessment.<br />
Rule 25 – chemical dependency assessors should submit their<br />
assessments with a 90801 or 90802 code on an 837P claim<br />
format.<br />
The 2011 <strong>Minnesota</strong> State Legislature passed <strong>Minnesota</strong> Session<br />
Laws 2011, First Special Session, Chapter 9, Article 8, Section 9.<br />
The legislation directs the Department <strong>of</strong> Human Services<br />
commissioner to require individuals performing chemical<br />
dependency or mental health diagnostic assessments to use the<br />
approved st<strong>and</strong>ardized screening tools to identify whether the<br />
individual being assessed screens positive for a co-occurring<br />
mental health or chemical dependency disorder.<br />
<strong>Blue</strong> <strong>Cross</strong> directs participating providers who provide mental<br />
health diagnostic assessments <strong>and</strong> chemical dependency<br />
assessments for MHCP members to comply with this Legislation.<br />
Follow the instructions related to the screening process <strong>and</strong><br />
screening tools provided by the <strong>Minnesota</strong> Department <strong>of</strong> Human<br />
Services (DHS) in Bulletin 12-53-01 published on January 5,<br />
2012.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-25
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Family Therapy 90846<br />
Units for Public<br />
Program Members<br />
11-26<br />
This code is billed for family therapy when the patient is not<br />
present. There may be specific contract exclusions for some<br />
self-insured groups.<br />
This code should be billed under the specific patient, not under<br />
the member.<br />
Bill one unit per session regardless <strong>of</strong> total time.<br />
This code must be billed with a behavioral health diagnosis.<br />
90847<br />
This code is billed for family therapy when the patient is<br />
present. There may be specific contract exclusions for some<br />
self-insured groups.<br />
This code should be billed under the specific patient, not under<br />
the member.<br />
Bill one unit per session regardless <strong>of</strong> total time.<br />
This code must be billed with a behavioral health diagnosis.<br />
Psychiatric diagnostic interview exams, family psychotherapy<br />
without the patient present, <strong>and</strong> family psychotherapy with the<br />
patient present are all allowed for PMAP <strong>and</strong> MNCare<br />
enrollees, when provided by an MD, LP-PhD., LP-MA,<br />
LICSW, CNS-Psych, PMHNP, LPCC or LMFT.<br />
Note: LPCs <strong>and</strong> LPCCs are ineligible providers for <strong>Minnesota</strong><br />
Health Care Program enrollees.<br />
Codes 90801, 90802, 90846, 90847, 90849, 90853, 90857 <strong>and</strong><br />
90887 must only be reported by session, regardless <strong>of</strong> time.<br />
The unit reported must be “1.” Unit submission for all codes<br />
will be based on the code narrative.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Medication<br />
Management<br />
M0064 <strong>and</strong> 90862<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
It is not appropriate to bill a medication management code on the<br />
same day as an evaluation <strong>and</strong> management code. If both are billed<br />
on the same day, the medication management code will deny as<br />
incidental to the evaluation <strong>and</strong> management code.<br />
Medication management can be billed by a nurse practitioner,<br />
physician assistant, MD, clinical nurse specialist in psychiatry, <strong>and</strong><br />
psychiatric mental health nurse practitioner.<br />
Medication management is compatible with a behavioral health<br />
diagnosis.<br />
This service is eligible when billed in the <strong>of</strong>fice or skilled nursing<br />
facility. It is not an eligible service when billed with an inpatient<br />
place <strong>of</strong> service. A medication management visit billed on the<br />
same day as an inpatient visit will deny as incidental to the<br />
inpatient visit.<br />
Medication management rendered in the outpatient clinic setting<br />
should only be billed on an 837P pr<strong>of</strong>essional claim form. If billed<br />
on a facility claim, it will be denied.<br />
M0064 includes a component for a brief <strong>of</strong>fice visit.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-27
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Behavioral Health<br />
Evaluation &<br />
Management (E&M)<br />
Office Calls<br />
11-28<br />
99201-99215<br />
Only an MD is eligible to bill procedure codes 99201-99205 which<br />
are codes for new patients. Procedure codes 99211-99215 (for<br />
established patients) can be billed by an MD, nurse practitioner,<br />
clinical nurse specialist, clinical nurse specialist in psychiatry,<br />
psychiatric mental health nurse practitioner or a physician<br />
assistant.<br />
These E/M services will not be accumulated towards any dollar or<br />
visit maximums.<br />
For complete information on requirements for <strong>Minnesota</strong> Health<br />
Care Programs, see Chapter 3 <strong>of</strong> the <strong>Blue</strong> Plus <strong>Manual</strong>. <strong>Blue</strong> Plus<br />
members who receive an E/M service billed with a behavioral<br />
health diagnosis by a non-behavioral health practitioner within<br />
their designated primary care clinic will have services reimbursed<br />
according to their behavioral health contract benefit. <strong>Blue</strong> Plus<br />
members who receive a behavioral health E/M service by a nonbehavioral<br />
health practitioner outside their primary care clinic but<br />
not within the Select Behavioral Health Network will need an<br />
approved referral to receive their highest level <strong>of</strong> benefits.<br />
Fee for service (FFS) members who have open access to the<br />
Aware network <strong>and</strong> who receive a behavioral health E/M service<br />
by a non-behavioral health practitioner will have services<br />
reimbursed according to their behavioral health contract benefit.<br />
Behavioral health E/M services provided outside the Aware<br />
network will be subject to the member’s nonparticipating provider<br />
benefit limitations.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Nutritional<br />
Counseling/Medical<br />
Nutrition Therapy<br />
Services<br />
97802-97804, S9470<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Medical nutrition therapy services are usually eligible if billed<br />
with either a behavioral health diagnosis or with a disease related<br />
diagnosis such as obesity or diabetes. Group nutritional therapy<br />
services billed under code 97804 are generally only covered when<br />
submitted with diagnosis codes for anorexia, bulimia, diabetes,<br />
congestive heart failure, <strong>and</strong> some maternity diagnoses. Obesity is<br />
not an eligible diagnosis for code 97804.<br />
There are no limits to the number <strong>of</strong> eligible services a patient<br />
receives if the patient has a fully insured contract. In contrast,<br />
some self-insured contracts may choose to apply contract<br />
variations/exclusions for nutritional counseling/medical nutrition<br />
therapy services.<br />
The contract for Federal Employee Program members (who have<br />
ID numbers beginning with “R”) only allows medical nutrition<br />
therapy services in the following situations: Dietitian assessments<br />
as part <strong>of</strong> a multi-disciplinary eating disorder evaluation; <strong>and</strong><br />
medical nutrition therapy services as part <strong>of</strong> ongoing nutritional<br />
therapy for eating disorders anorexia nervosa (diagnosis code<br />
307.1) <strong>and</strong>/or bulimia nervosa (diagnosis code 307.51.) Coverage<br />
is extended to diabetic educators, dietitians, <strong>and</strong> nutritionists who<br />
bill independently as part <strong>of</strong> a covered diabetic education program<br />
only. Nutritional counseling for up to four visits per year is<br />
covered when billed by a covered provider, although nutritional<br />
counseling for the treatment <strong>of</strong> anorexia <strong>and</strong>/or bulimia billed with<br />
diagnosis codes 307.1 or 307.51 is not subject to the four visit<br />
limitation.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-29
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Eligibility <strong>of</strong> Dietitians/<br />
Nutritionists<br />
Psychological <strong>and</strong><br />
Neuropsychological<br />
Testing<br />
11-30<br />
Registered dietitians <strong>and</strong> licensed nutritionists can bill<br />
independently for procedure codes S9470, 97802, 97803 <strong>and</strong><br />
97804 when billed with eating disorder diagnosis codes 307.1,<br />
307.50 <strong>and</strong> 307.51. No referral is required for the highest benefit<br />
level.<br />
For all other diagnoses, licensed dietitian <strong>and</strong> nutritionist services<br />
must be submitted to <strong>Blue</strong> <strong>Cross</strong> by an eligible medical clinic or<br />
hospital. The individual provider number or NPI <strong>of</strong> the licensed<br />
dietitian or nutritionist must be submitted on the claim. Licensed<br />
dietitians <strong>and</strong> nutritionists can bill for procedure codes S9470,<br />
97802 <strong>and</strong> 97803 for any diagnosis. Procedure code 97804 is not<br />
an eligible service for obesity.<br />
Claims for registered dietitians billing services outside <strong>of</strong><br />
behavioral health diagnoses will deny unless the services are<br />
submitted under the individual provider number or NPI <strong>of</strong> a<br />
supervising physician. The U7 modifier should also be submitted.<br />
96101-96103, 96116, 96118-96125<br />
Each test should be associated with medical necessity <strong>and</strong> not<br />
be a battery <strong>of</strong> tests for screening purposes.<br />
Code 90887 (interpretation or explanation <strong>of</strong> exam results)<br />
should not be billed because reimbursement for these services<br />
is included in the reimbursement for the testing.<br />
The psychological <strong>and</strong> neuropsychological testing codes reflect<br />
who does the testing: a psychologist, a technician or a<br />
computer. <strong>Blue</strong> <strong>Cross</strong> coverage <strong>and</strong> billing policies for these<br />
codes follows the testing policy below.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Testing Policy The <strong>Blue</strong> <strong>Cross</strong> testing policy is found in medical policy X-45,<br />
psychological <strong>and</strong> neuropsychological testing policy. Medical <strong>and</strong><br />
behavioral health policies are available at<br />
providers.bluecrossmn.com under “Medical policy.”<br />
Pre-certification/pre-authorization requirements<br />
Pre-certification/pre-authorization will be required for all<br />
psychological (procedure codes 96101, 96102 <strong>and</strong> 96103) <strong>and</strong><br />
neuropsychological (procedure codes 96116, 96118, 96119,<br />
96120 <strong>and</strong> 96125) testing before performing services for a<br />
member.<br />
A one-visit Diagnostic Assessment (procedure codes 90801 or<br />
90802) may be completed without pre-certification.<br />
All services are subject to the benefit <strong>and</strong> network requirement<br />
provisions as written in the member’s plan.<br />
Pre-certification/pre-authorization requirement applies to<br />
<strong>Minnesota</strong> providers <strong>and</strong> providers outside <strong>of</strong> <strong>Minnesota</strong>.<br />
Obtaining pre-certification/pre-authorization<br />
Providers can obtain pre-certification/pre-authorization for<br />
psychological <strong>and</strong> neuropsychological testing by completing the<br />
Pre-certification/pre-authorization for psychological <strong>and</strong><br />
neuropsychological testing form, which will be available at<br />
providers.bluecrossmn.com. Click on “Forms & publications.”<br />
From the drop-down box choose “forms: pre-admission/prior<br />
authorization.” The completed form may be faxed to<br />
(651) 662-0854.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-31
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Testing Policy<br />
(continued)<br />
11-32<br />
This action is being taken to help ensure that members receive the<br />
appropriate level <strong>of</strong> care <strong>and</strong> frequency <strong>of</strong> service for<br />
psychological <strong>and</strong> neuropsychological testing. Failure to provide<br />
evidence <strong>of</strong> medical necessity may result in claim denials with the<br />
outcome <strong>of</strong> provider liability.<br />
The pre-certification/pre-authorization protocol parallels the<br />
process utilized for other medical/surgical services.<br />
Product Application<br />
Pre-certification/pre-authorization review applies to all<br />
psychological <strong>and</strong> neuropsychological testing for members in fully<br />
insured <strong>and</strong> self-insured benefit plans. Pre-certification/preauthorization<br />
review for psychological <strong>and</strong> neuropsychological<br />
testing is not required for members in the following plans:<br />
<strong>Blue</strong> Advantage (PMAP) programs<br />
<strong>Minnesota</strong>Care programs<br />
<strong>Minnesota</strong> Senior Care Plus (MSC+)<br />
Secure<strong>Blue</strong> (HMO SNP)<br />
Platinum <strong>Blue</strong> (Cost)<br />
Medicare<strong>Blue</strong> PPO (Regional PPO)<br />
Medicare supplement<br />
Code Narrative Units Practitioner General Policies<br />
96101 Psychological testing<br />
(includes psychodiagnostic<br />
assessment <strong>of</strong> emotionality,<br />
intellectual abilities,<br />
personality <strong>and</strong><br />
psychopathology, e.g.,<br />
MMPI, Rorschach, WAIS),<br />
per hour <strong>of</strong> the<br />
psychologist’s or<br />
physician’s time, both faceto-face<br />
time with the patient<br />
<strong>and</strong> time interpreting test<br />
results <strong>and</strong> preparing the<br />
report.<br />
Report one (1)<br />
unit per hour<br />
<strong>of</strong> face-to-face<br />
testing,<br />
interpretation<br />
<strong>and</strong><br />
preparation <strong>of</strong><br />
report.<br />
MD, LP-<br />
PhD, LP-<br />
MA<br />
The psychologist<br />
or psychiatrist<br />
administers <strong>and</strong><br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report.<br />
Billed under the<br />
MD, LP-PhD, LP-<br />
MA individual<br />
provider number or<br />
NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Narrative Units Practitioner General Policies<br />
96102 Psychological testing<br />
(includes psychodiagnostic<br />
assessment <strong>of</strong> emotionality,<br />
intellectual abilities,<br />
personality <strong>and</strong><br />
psychopathology, e.g.,<br />
MMPI <strong>and</strong> WAIS), with<br />
qualified health care<br />
pr<strong>of</strong>essional interpretation<br />
<strong>and</strong> report, administered by<br />
technician, per hour <strong>of</strong><br />
technician time, face-t<strong>of</strong>ace.<br />
96103 Psychological testing<br />
(includes psychodiagnostic<br />
assessment <strong>of</strong> emotionality,<br />
intellectual abilities,<br />
personality <strong>and</strong><br />
psychopathology, e.g.,<br />
MMPI), administered by a<br />
computer, with qualified<br />
health care pr<strong>of</strong>essional<br />
interpretation <strong>and</strong> report.<br />
Report one (1)<br />
unit per hour<br />
<strong>of</strong> face-to-face<br />
testing.<br />
Report one (1)<br />
unit per testing<br />
session<br />
regardless <strong>of</strong><br />
the number <strong>of</strong><br />
tests taken.<br />
MD, LP-<br />
Ph.D., LP-<br />
MA,<br />
LICSW,<br />
CNS-Psych,<br />
LMFT,<br />
LPCC<br />
MD, LP-<br />
Ph.D., LP-<br />
MA,<br />
LICSW,<br />
CNS-Psych,<br />
PMHNP,<br />
LMFT, NP,<br />
PA, LPCC<br />
A technician under<br />
direct supervision,<br />
administers the<br />
test(s).<br />
The supervising<br />
qualified licensed<br />
practitioner<br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report.<br />
Billed under the<br />
supervising<br />
licensed<br />
practitioner<br />
provider number or<br />
NPI.<br />
Patient is alone <strong>and</strong><br />
is taking a<br />
computer-based<br />
test.<br />
A qualified<br />
licensed<br />
practitioner<br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report.<br />
Billed under the<br />
licensed<br />
practitioner<br />
provider number or<br />
NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-33
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Narrative Units Practitioner General Policies<br />
96116 Neurobehavioral status<br />
exam (clinical assessment <strong>of</strong><br />
thinking, reasoning <strong>and</strong><br />
judgment, e.g., acquired<br />
knowledge, attention,<br />
language, memory, planning<br />
<strong>and</strong> problem solving, <strong>and</strong><br />
visual spatial abilities), per<br />
hour <strong>of</strong> the psychologist’s<br />
or physician’s time, both<br />
face-to-face time with the<br />
patient <strong>and</strong> time interpreting<br />
test results <strong>and</strong> preparing<br />
the report.<br />
96118 Neuropsychological testing<br />
(e.g., Halstead-Reitan<br />
neuropsychological battery,<br />
Wechsler memory scales<br />
<strong>and</strong> Wisconsin card sorting<br />
test), per hour <strong>of</strong> the<br />
psychologist’s or<br />
physician’s time, both faceto-face<br />
time with the patient<br />
<strong>and</strong> time interpreting test<br />
results <strong>and</strong> preparing the<br />
report.<br />
11-34<br />
Report one (1)<br />
unit per hour<br />
<strong>of</strong> face-to-face<br />
testing,<br />
interpretation<br />
<strong>and</strong><br />
preparation <strong>of</strong><br />
report.<br />
Report one (1)<br />
unit per hour<br />
<strong>of</strong> face-to-face<br />
testing,<br />
interpretation<br />
<strong>and</strong><br />
preparation <strong>of</strong><br />
report.<br />
MD, LP-<br />
PhD., LP-<br />
MA,<br />
LICSW,<br />
CNS-Psych,<br />
PMHNP,<br />
LMFT, NP,<br />
PA, LPCC<br />
MD, LP-<br />
PhD, LP-<br />
MA<br />
The psychologist<br />
or psychiatrist<br />
administers <strong>and</strong><br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report.<br />
Billed under the<br />
practitioner’s<br />
individual provider<br />
number or NPI.<br />
The psychologist<br />
or psychiatrist<br />
administers <strong>and</strong><br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report.<br />
Billed under the<br />
MD, LP-PhD, LP-<br />
MA individual<br />
provider number or<br />
NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Narrative Units Practitioner General Policies<br />
96119 Neuropsychological testing<br />
(e.g., Halstead-Reitan<br />
neuropsychological battery,<br />
Wechsler memory scales<br />
<strong>and</strong> Wisconsin card sorting<br />
test), with qualified health<br />
care pr<strong>of</strong>essional<br />
interpretation <strong>and</strong> report<br />
administered by technician,<br />
per hour <strong>of</strong> technician time,<br />
face-to-face.<br />
96120 Neuropsychological testing<br />
(e.g., Wisconsin card<br />
sorting test), administered<br />
by a computer, with<br />
qualified health care<br />
pr<strong>of</strong>essional interpretation<br />
<strong>and</strong> report.<br />
Report one (1)<br />
unit per hour<br />
<strong>of</strong> face-to-face<br />
testing.<br />
Report one (1)<br />
unit per testing<br />
session<br />
regardless <strong>of</strong><br />
the number <strong>of</strong><br />
tests taken.<br />
MD, LP-<br />
PhD, LP-<br />
MA<br />
MD, LP-<br />
PhD, LP-<br />
MA<br />
A technician,<br />
under direct<br />
supervision,<br />
administers the<br />
test(s).<br />
The supervising<br />
qualified licensed<br />
practitioner<br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report<br />
Billed under the<br />
supervising<br />
licensed<br />
practitioner<br />
provider number or<br />
NPI.<br />
Patient is alone <strong>and</strong><br />
is taking a<br />
computer-based<br />
test.<br />
A qualified<br />
licensed<br />
practitioner<br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report.<br />
Billed under the<br />
licensed<br />
practitioner<br />
provider number or<br />
NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-35
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Narrative Units Practitioner General Policies<br />
96125 St<strong>and</strong>ardized cognitive<br />
performance testing (e.g.,<br />
Ross information processing<br />
assessment) per hour <strong>of</strong> a<br />
qualified health care<br />
pr<strong>of</strong>essional's time, both<br />
face-to-face time<br />
administering tests to the<br />
patient <strong>and</strong> time interpreting<br />
these test results <strong>and</strong><br />
preparing the report<br />
11-36<br />
Report one (1)<br />
unit per hour<br />
<strong>of</strong> face-to-face<br />
testing,<br />
interpretation<br />
<strong>and</strong><br />
preparation <strong>of</strong><br />
report<br />
MD, LP-<br />
PhD, LP-<br />
MA<br />
The psychologist<br />
or psychiatrist<br />
administers <strong>and</strong><br />
interprets the<br />
test(s) <strong>and</strong> prepares<br />
the report.<br />
Billed under the<br />
MD, LP-PhD, LP-<br />
MA individual<br />
provider number or<br />
NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Practitioner Key MD = Psychiatrist<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
LP-Ph.D. = Licensed Psychologist, Doctorate<br />
LP-MA = Licensed Psychologist, Masters<br />
LICSW = Licensed Clinical Social Worker<br />
CNS-Psych = Clinic Nurse Specialist, Psychiatric Specialty<br />
PMHNP = Psychiatric Mental Health Nurse Practitioner<br />
LMFT = Licensed Marriage <strong>and</strong> Family Therapist<br />
PA = Physician Assistant<br />
NP = Nurse Practitioner<br />
LPC = Licensed Pr<strong>of</strong>essional Counselor (ineligible provider,<br />
unless practicing as part <strong>of</strong> a Rule 29 licensed clinic, a<br />
community health center or a behavioral health clinic per the<br />
<strong>Blue</strong> <strong>Cross</strong> criteria)<br />
LPCC = Licensed Pr<strong>of</strong>essional Clinical Counselor (ineligible<br />
provider, unless practicing as part <strong>of</strong> a Rule 29 licensed clinic,<br />
a community health center or a behavioral health clinic per the<br />
<strong>Blue</strong> <strong>Cross</strong> criteria)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-37
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Policies Policies applicable to the codes on the previous pages:<br />
11-38<br />
Test result interpretation <strong>and</strong> report preparation are an inherent<br />
part <strong>of</strong> the testing service <strong>and</strong> are not separately billable. Only<br />
one testing code may be billed.<br />
Only a licensed psychologist or other licensed health care<br />
pr<strong>of</strong>essional may bill for these psychological <strong>and</strong><br />
neuropsychological tests.<br />
The date <strong>of</strong> service submitted should be the date the testing is<br />
completed, regardless <strong>of</strong> when the report is completed.<br />
Testing, scoring, <strong>and</strong> interpretation done solely by a computer<br />
is not a billable service.<br />
There is no specific definition <strong>of</strong> technician; a technician may<br />
be a psychometrist, student or trainee. Testing administered by<br />
a technician may be billed if the service is rendered under<br />
direct supervision <strong>of</strong> a qualified practitioner <strong>and</strong> if submitted<br />
under the supervising practitioner’s individual provider number<br />
or NPI.<br />
Direct supervision definition: The physician/qualified<br />
practitioner must be present in the same <strong>of</strong>fice (although not<br />
necessarily in the same room as the non-physician/qualified<br />
practitioner) <strong>and</strong> must be immediately available to assist <strong>and</strong><br />
direct throughout the performance <strong>of</strong> the service. A<br />
physician/qualified practitioner cannot provide direct or<br />
personal supervision via telemedicine.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Clinical Supervision<br />
Under <strong>Minnesota</strong> Rule<br />
Part 9505.0371 -<br />
MHCP Members Only<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
<strong>Blue</strong> <strong>Cross</strong> requires clinical supervision to comply with <strong>Minnesota</strong><br />
Rule part 9505.0371 which was adopted <strong>and</strong> implemented on June<br />
28, 2011. Refer to the <strong>Minnesota</strong> Department <strong>of</strong> Human Services<br />
(DHS) Bulletin #11-53-03 for requirements related to clinical<br />
supervision.<br />
The Rule addresses st<strong>and</strong>ards in the following areas:<br />
Eligibility <strong>of</strong> a supervisor<br />
Eligibility <strong>of</strong> a supervisee<br />
Individual <strong>and</strong> group supervision<br />
Clinical supervision plan for each person under supervision<br />
Documentation <strong>of</strong> a supervision session<br />
When clinical supervision documentation is required in a<br />
client’s chart<br />
<strong>Blue</strong> <strong>Cross</strong> will continue to allow clinical supervision that meets<br />
the requirement <strong>of</strong> the new Rule to be done in the following clinic<br />
settings:<br />
Rule 29 Licensed Clinics<br />
Community Mental Health Centers<br />
Behavioral Health Clinics as defined by <strong>Blue</strong> <strong>Cross</strong><br />
Mental Health Designated Essential Community Providers<br />
Multi-specialty Clinics<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-39
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
DIAMOND Initiative <strong>Blue</strong> <strong>Cross</strong> is participating in a collaborative effort along with the<br />
<strong>Minnesota</strong> Department <strong>of</strong> Human Services (DHS) <strong>and</strong> other health<br />
plans in <strong>Minnesota</strong> called the Depression Improvement Across<br />
<strong>Minnesota</strong>, Offering a New Direction (DIAMOND) Initiative. The<br />
DIAMOND Initiative collaborative is organized by the Institute for<br />
Clinical Systems Improvement (ICSI). The goal <strong>of</strong> the DIAMOND<br />
Initiative is to improve care for people who have depression by<br />
providing services through a new care model <strong>of</strong>fered in select<br />
primary care settings.<br />
11-40<br />
Provider Participation<br />
The DIAMOND Initiative will be <strong>of</strong>fered at select primary care<br />
settings that have been approved to participate by ICSI <strong>and</strong> have<br />
been trained in the DIAMOND care model. The DIAMOND care<br />
model includes adding a care manager <strong>and</strong> consulting psychiatrist<br />
to the patient's treatment team. <strong>Blue</strong> <strong>Cross</strong> will be contacting the<br />
select primary care providers who have been approved to<br />
participate by ICSI <strong>and</strong> have been trained in the DIAMOND care<br />
model.<br />
Services <strong>and</strong> Billing<br />
Approved providers should bill using HCPCS code T2022 (case<br />
management, per month), billed as one unit per calendar month, on<br />
a pr<strong>of</strong>essional claim format (837P). This code will include any<br />
services rendered by the care manager, the consultative time the<br />
primary care physician/psychiatrist spends with the care manager,<br />
<strong>and</strong> any non-face-to-face time the physician spends reviewing,<br />
managing or coordinating care on behalf <strong>of</strong> the patient. Services<br />
need to be billed on a monthly basis to the health plan that insured<br />
the patient at the beginning <strong>of</strong> the month in which service<br />
occurred. The provider should bill this code on a monthly basis for<br />
a maximum <strong>of</strong> 12 consecutive months or until the member opts out<br />
<strong>of</strong> the DIAMOND Initiative, whichever comes first.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
DIAMOND Initiative<br />
(continued)<br />
Reimbursement<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Only those primary care providers who have been certified or<br />
approved by ICSI, who have been trained in the DIAMOND care<br />
model, who have been contacted by <strong>Blue</strong> <strong>Cross</strong>, <strong>and</strong> who have<br />
elected to participate in the DIAMOND Initiative will be eligible<br />
for reimbursement. The <strong>Blue</strong> <strong>Cross</strong> allowed amount will be up to<br />
$100 plus applicable <strong>Minnesota</strong>Care tax for eligible members <strong>and</strong><br />
eligible providers up to a maximum <strong>of</strong> 12 consecutive months per<br />
member.<br />
Marital Counseling Diagnosis code V61.10, counseling for marital <strong>and</strong> partner<br />
problems, unspecified.<br />
Generally, marital counseling is a contract exclusion for<br />
members <strong>and</strong> will deny as member responsibility when this<br />
diagnosis code is used as the primary diagnosis. Relationship<br />
improvement/enhancement services or training not related to<br />
the treatment <strong>of</strong> a diagnosable mental health disorder are<br />
generally not covered.<br />
Opioid Maintenance<br />
Drug Therapy<br />
Opioid treatment will be processed at the member’s highest<br />
benefit level if there is coverage for these services in the<br />
member’s contract benefits. No referral is required for <strong>Blue</strong><br />
Plus members. If a member’s contract has no substance abuse<br />
benefits or if a member’s contract has methadone <strong>and</strong>/or<br />
buprenorphine treatment as a contract exclusion, then there is<br />
no coverage for these services.<br />
Only providers that are contracted as a freest<strong>and</strong>ing methadone<br />
clinic can bill methadone treatment services.<br />
The participating freest<strong>and</strong>ing opioid treatment clinics<br />
methadone administration is a pr<strong>of</strong>essional service that should<br />
be billed on an 837P claim format with procedure code H0020<br />
<strong>and</strong> diagnosis code 304.01. This charge will deny if incorrectly<br />
submitted on an 837I. This service is treated as medication<br />
management so will not be counted against any substance<br />
abuse accumulation maximums for the member.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-41
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Opioid Maintenance<br />
Drug Therapy<br />
(continued)<br />
11-42<br />
Buprenorphine administration is a pr<strong>of</strong>essional service that<br />
should be billed on an 837P claim format. This charge will<br />
deny if incorrectly submitted on an 837I. When administered<br />
as part <strong>of</strong> a program, procedure code H0047 (along with a<br />
narrative stating this is for buprenorphine) should be billed<br />
with diagnosis code 304.01. When administered in the <strong>of</strong>fice,<br />
the appropriate <strong>of</strong>fice visit or evaluation management<br />
procedure code should be billed with diagnosis code 304.01.<br />
Buprenorphine administration applies to the member’s<br />
substance abuse benefits for <strong>of</strong>fice visits, <strong>and</strong> these charges<br />
will not be applied to any accumulation maximums for the<br />
member. The injectable form <strong>of</strong> buprenorphine hydrochloride<br />
should be billed as code J0592 with one unit per 0.1 mg<br />
dosage.<br />
Tobacco Cessation Submit diagnosis code 305.1 or V15.82 if the intent is<br />
counseling <strong>and</strong>/or visit to obtain a prescription for smoking<br />
cessation medication/patches.<br />
If linked to an E/M service, a preventative or general illness<br />
benefit will be applied depending on the member’s benefits.<br />
Do not use 305.1 or V15.82 as the primary diagnosis if the<br />
member has a primary behavioral health diagnosis (such as<br />
depression) that is being treated but the member also uses<br />
tobacco. If this is the case, 305.1 or V15.82 should be listed as<br />
a secondary diagnosis.<br />
Hypnotherapy (code 90880), bi<strong>of</strong>eedback (codes 90875-<br />
90876), <strong>and</strong> acupuncture (codes 97810- 97811, 97813-97814)<br />
are considered investigative for treatment <strong>of</strong> tobacco use,<br />
dependence, <strong>and</strong> withdrawal, <strong>and</strong> are ineligible for<br />
reimbursement.<br />
Nicotine replacement therapies <strong>and</strong> bupropion for the treatment<br />
<strong>of</strong> tobacco dependence are subject to the member’s pharmacy<br />
benefits.<br />
Coverage for the treatment <strong>of</strong> tobacco dependence is subject to<br />
the member’s contract benefits.<br />
Any inpatient treatment service for tobacco cessation should be<br />
prior authorized, as they will be reviewed for medical<br />
necessity.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Rule 29 Setting State licensed Rule 29 clinics will have three provider numbers:<br />
Day Treatment H2012<br />
One for services in the clinic<br />
One for MD/Psychiatrists to bill for inpatient services<br />
One for Ph.D. level psychologists to bill for inpatient services<br />
Services should be billed under the appropriate provider number or<br />
NPI.<br />
Rule 29 clinics can only provide outpatient mental health services<br />
under this licensure. Any inpatient services billed under the Rule<br />
29 clinic provider number or NPI will be denied. Some Rule 29<br />
clinics will also be licensed as nonresidential chemical dependency<br />
providers. It is important to keep these two entities separate.<br />
If a patient is being treated for depression secondary to a chemical<br />
dependency, the depression diagnosis should be billed as the<br />
primary diagnosis under the Rule 29 clinic provider number or<br />
NPI.<br />
When non-licensed practitioners treat patients, their services<br />
MUST be billed under the supervising practitioner’s individual<br />
provider number <strong>and</strong> with the U7 modifier or NPI.<br />
Behavioral health day treatment services may be provided at a<br />
licensed Rule 29 facility. Day treatment is a specific<br />
programmatic service where the patient attends a minimum <strong>of</strong><br />
3 hours per day <strong>and</strong> generally 3-5 hours per day, 3-5 days per<br />
week. The services provided within these hours may include<br />
group therapy, living/social skills building groups, educational<br />
groups, <strong>and</strong> some individual time.<br />
Day treatment is billed as a program, rather than under an<br />
individual provider. Bill one line for each day <strong>and</strong> one unit for<br />
each hour the patient attends the program.<br />
Services are reimbursed under the member’s outpatient mental<br />
health benefits.<br />
Compatibility This is a very common <strong>and</strong> frequent cause for claim denials. The<br />
diagnosis code <strong>and</strong> CPT code must be compatible as well as<br />
compatible with the practitioner’s licensure.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-43
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Health <strong>and</strong> Behavior<br />
Assessment <strong>and</strong><br />
Intervention Codes<br />
11-44<br />
96150-96155<br />
Codes 96150-96155 are eligible to be billed by all behavioral<br />
health practitioners. However, per CPT, 96150-96155 describe<br />
services <strong>of</strong>fered to patients who present with established illnesses<br />
or symptoms, are not diagnosed with mental illness, <strong>and</strong> may<br />
benefit from evaluations that focus on biopsychological factors<br />
related to the patients’ physical health status. The primary<br />
diagnosis for the claim line containing these assessment <strong>and</strong><br />
intervention codes should be a non-behavioral health diagnosis<br />
code. (An example would be a newly diagnosed cancer patient or a<br />
patient struggling with infertility.)<br />
Missed Appointments Missed scheduled appointments are not paid for by <strong>Blue</strong> <strong>Cross</strong>.<br />
<strong>Blue</strong> <strong>Cross</strong> recommends that your clinic establish a uniform<br />
cancellation policy requiring 24-hour advance notification. Your<br />
clinic may bill a patient who misses a scheduled behavioral health<br />
appointment, provided that you have notified the member in<br />
writing in advance that this is your policy. A copy <strong>of</strong> this signed<br />
notification should be maintained in your patient’s medical record.<br />
Your patient should be billed no more than your contracted rate.<br />
Government programs such as Prepaid Medical Assistance<br />
(PMAP), <strong>Minnesota</strong>Care <strong>and</strong> Medicare prohibit billing for missed<br />
appointments.<br />
This policy applies to providers, whose scope <strong>of</strong> practice is<br />
behavioral health, including psychiatrists, licensed psychologists<br />
(LP), licensed independent clinical social workers (LICSW),<br />
licensed marriage <strong>and</strong> family therapists (LMFT), registered nurse<br />
clinical specialist (CNS) <strong>and</strong> out-patient chemical dependency<br />
(OPCD) facilities. This policy change is not intended to apply to<br />
medication management provided within the member’s primary<br />
care clinic or internist’s <strong>of</strong>fice.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Missed Appointments<br />
(continued)<br />
Court Ordered<br />
Treatment<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
<strong>Blue</strong> <strong>Cross</strong> expects behavioral health providers to abide by the<br />
following guidelines:<br />
PMAP, <strong>Minnesota</strong>Care <strong>and</strong> Medicare members cannot be<br />
charged for missed appointments.<br />
Providers must establish a reasonable business policy that<br />
allows for patients not to be charged for failed appointments<br />
due to circumstances outside <strong>of</strong> their control.<br />
Providers must abide by guidelines established by the<br />
American Medical Association (AMA) <strong>and</strong> the American<br />
Psychological Association (APA), which state it is ethical for<br />
providers to charge for missed appointments or for<br />
appointments not canceled at least 24 hours in advance, if<br />
patients have been fully advised <strong>of</strong> the possibility <strong>of</strong> such<br />
charges.<br />
When a court order for treatment is based on evaluation <strong>and</strong><br />
recommendation by a physician, licensed Ph.D. level psychologist,<br />
licensed alcohol <strong>and</strong> drug dependency counselor, or a certified<br />
chemical dependency assessor (Rule 25), <strong>Blue</strong> <strong>Cross</strong> will consider<br />
the order medically necessary.<br />
<strong>Blue</strong> <strong>Cross</strong> will provide coverage for these court ordered services<br />
according to the patient’s contract benefits. For example, if the<br />
member does not have inpatient chemical dependency benefits <strong>and</strong><br />
the patient is court ordered into inpatient chemical dependency<br />
treatment, there will be no coverage for the services.<br />
Participating providers should maintain a copy <strong>of</strong> the court order in<br />
the patient’s chart. Nonparticipating providers should fax in the<br />
evaluation <strong>and</strong> court order to Integrated Health Management at<br />
(651) 662-0854 as soon as possible so that the necessary approval<br />
can be entered into the claim system in time to ensure the claim is<br />
paid accurately.<br />
If the court order specifies a certain non-network provider but the<br />
member does not have any benefits for non-network providers,<br />
<strong>Blue</strong> <strong>Cross</strong> will cover the services as they would for any other<br />
network provider. However, fee-for-service members will be<br />
responsible for the difference between the billed amount <strong>and</strong> <strong>Blue</strong><br />
<strong>Cross</strong>’ allowed amount.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-45
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Guidelines for Court<br />
Ordered Evaluations<br />
11-46<br />
An appropriately licensed physician or Ph.D. level psychologist<br />
must perform the mental health assessment. A physician, licensed<br />
alcohol <strong>and</strong> drug dependency counselor, or certified chemical<br />
dependency assessor must perform the chemical dependency<br />
assessment.<br />
The following services are eligible for <strong>Blue</strong> <strong>Cross</strong> coverage<br />
(subject to the terms <strong>of</strong> the member's contract):<br />
Mental health evaluations/diagnostic assessments <strong>and</strong> related<br />
testing<br />
Chemical health evaluations<br />
72 hour holds under the Mental Health Act, Minn. Stat.<br />
253B.05<br />
24-hour mental health observation beds<br />
Mental health evaluations to determine the need for civil<br />
commitment for treatment<br />
Submitting Mental <strong>and</strong>/or Chemical Health Court Ordered<br />
Evaluations<br />
<strong>Blue</strong> <strong>Cross</strong> recognizes that certain court ordered evaluations may<br />
be lengthy <strong>and</strong> wants to ensure equitable reimbursement to<br />
providers for these types <strong>of</strong> evaluations, but the claim submission<br />
must be HIPAA compliant including the restriction <strong>of</strong> units based<br />
on the code narrative. Behavioral health assessments/evaluations<br />
are reported under code 90801. Only one unit <strong>of</strong> service may be<br />
submitted regardless <strong>of</strong> the time spent with the patient. To alert<br />
<strong>Blue</strong> <strong>Cross</strong> that this is a court ordered evaluation, an H9 modifier<br />
must be appended to 90801. Prior authorization is not required;<br />
however, the court order for the evaluation must be on file in the<br />
patient’s medical record.<br />
Court Ordered Evaluation Claim Submission Guideline<br />
HCPCS code: 90801<br />
HCPCS modifier: H9 (court ordered)<br />
Unit: one unit (regardless <strong>of</strong> time spent)<br />
Diagnosis code: appropriate ICD-9-CM mental or chemical<br />
health diagnosis<br />
Coverage <strong>of</strong> follow-up care will depend upon individual member<br />
benefits.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Guidelines for Court<br />
Ordered Evaluations<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
The following are <strong>Blue</strong> <strong>Cross</strong> guidelines regarding Mental<br />
Health Evaluation components: (from <strong>Blue</strong> <strong>Cross</strong> Behavioral<br />
Health Guidelines for Treatment Record Documentation<br />
previously sent to providers by <strong>Blue</strong> <strong>Cross</strong> Quality Improvement.)<br />
The assessment or mental status exam is to identify appropriate<br />
subjective <strong>and</strong> objective information pertinent to the patient's<br />
presenting complaint. The presenting symptoms are to be<br />
clearly identified with the onset, duration <strong>and</strong> intensity<br />
documented.<br />
The assessment contains the patient's presenting problem(s) as<br />
well as relevant psychological or social conditions affecting the<br />
patient's medical or psychiatric status. For children <strong>and</strong><br />
adolescents (18 <strong>and</strong> under), past medical history <strong>and</strong><br />
psychiatric history includes prenatal <strong>and</strong> perinatal events <strong>and</strong> a<br />
complete developmental history (physical, psychological,<br />
social, intellectual, <strong>and</strong> academic).<br />
The mental status exam is to document the patient's affect,<br />
speech, mood, thought content, judgment, insight, attention or<br />
concentration, memory, impulse control, suicidal ideation <strong>and</strong><br />
homicidal ideation.<br />
For patients 10 years <strong>and</strong> older, there is to be an appropriate<br />
notation in the assessment concerning past <strong>and</strong> present use <strong>of</strong><br />
tobacco, alcohol, as well as illicit, prescribed <strong>and</strong> over-thecounter<br />
substances.<br />
Past medical/behavioral history is easily identifiable in the<br />
record <strong>and</strong> includes, if applicable; previous treatment dates,<br />
former provider information, therapeutic interventions <strong>and</strong><br />
responses, source <strong>of</strong> clinical data, relevant family information,<br />
results <strong>of</strong> lab test <strong>and</strong> consultation reports.<br />
To determine if a comprehensive substance abuse evaluation is<br />
needed, a substance abuse screening is to be incorporated into<br />
the assessment <strong>of</strong> all new patients. This can be accomplished<br />
by the use <strong>of</strong> brief questionnaires such as CAGAID or the<br />
AUDIT.<br />
The provider is to have procedures in place for the reassessment<br />
<strong>of</strong> patients who return for treatment after having<br />
been out <strong>of</strong> treatment for an extended period <strong>of</strong> time.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-47
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Guidelines for Court<br />
Ordered Evaluations<br />
(continued)<br />
11-48<br />
The MH evaluation components <strong>of</strong> the following assessments are<br />
eligible for <strong>Blue</strong> <strong>Cross</strong> coverage (subject to the terms <strong>of</strong> the<br />
member's contract):<br />
Civil competency evaluations (evaluation to guide courts in<br />
determining whether a person is mentally competent to manage<br />
his/her own affairs)<br />
Competency <strong>and</strong> diminished capacity evaluations (evaluation<br />
to guide courts in determining whether to award guardianship<br />
<strong>of</strong> an adult)<br />
Domestic violence assessments<br />
Pre-placement assessments (for evaluation prior to county<br />
placement in various settings, which may include foster care,<br />
shelter care, residential treatment, corrections, etc.)<br />
Sex <strong>of</strong>fender evaluations (does not cover the criminal history<br />
review or risk assessment portions as identified in MN Rule<br />
2955.0100, Subp.7. A, B, C, D, G <strong>and</strong> J)<br />
Sex <strong>of</strong>fender evaluations (SOE) performed for forensic<br />
(court ordered) purposes are not reimbursed <strong>and</strong> will be<br />
denied as subscriber liability.<br />
SOE performed as part <strong>of</strong> treatment is eligible for separate<br />
reimbursement. Submit 90899 (unlisted psychiatric service<br />
or procedure) with medical records. Coverage <strong>and</strong>/or<br />
liability will be determined based on review <strong>and</strong> purpose <strong>of</strong><br />
the evaluation.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Guidelines for Court<br />
Ordered Evaluations<br />
(continued)<br />
Guidelines for Court<br />
Ordered Evaluations –<br />
Noncovered Services<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
<strong>Blue</strong> <strong>Cross</strong> does not cover forensic evaluations conducted to<br />
answer specific legal questions.<br />
Forensic Evaluations<br />
In contrast to a mental health evaluation, a forensic evaluation is<br />
conducted primarily to assist the legal system in making decisions<br />
regarding family, civil or criminal matters. In these instances, the<br />
summary <strong>and</strong> conclusions relate directly to the legal issues, <strong>and</strong> the<br />
relationship between psychological factors <strong>and</strong> the legal issues are<br />
described. (For more information go to<br />
www.psychologyinfo.com/forensic/index.html, a link provided<br />
through the American Psychological Association website.)<br />
It is our expectation that a MH pr<strong>of</strong>essional conducting one <strong>of</strong> the<br />
following assessments will use his/her clinical judgment. In the<br />
event that the MH pr<strong>of</strong>essional determines that the member<br />
requires a MH evaluation as a component <strong>of</strong> one <strong>of</strong> these<br />
evaluations for the purpose <strong>of</strong> identifying <strong>and</strong> determining<br />
treatment needs, <strong>Blue</strong> <strong>Cross</strong> will consider the component eligible<br />
for coverage, subject to the terms <strong>of</strong> the member's contract.<br />
The following are examples <strong>of</strong> forensic evaluations that are not<br />
covered by <strong>Blue</strong> <strong>Cross</strong>:<br />
Adoption home studies (evaluation to guide courts in decision<br />
whether to allow adoption <strong>of</strong> children by an individual or<br />
couple)<br />
Adoption readiness evaluations (evaluation to guide courts in<br />
decisions regarding adoption placement planning)<br />
Adult pre-sentencing evaluations (evaluation to guide courts in<br />
determining sentencing <strong>of</strong> adults in criminal matters)<br />
Assessment <strong>of</strong> emotional factors in sexual harassment <strong>and</strong><br />
discrimination (evaluation to guide courts decision regarding<br />
sexual harassment <strong>and</strong>/or discrimination)<br />
Child abuse evaluations, including sexual abuse evaluations<br />
(investigative evaluation to determine presence <strong>and</strong>/or extent<br />
<strong>of</strong> child physical <strong>and</strong>/or sexual abuse)<br />
Child custody evaluations (evaluations to guide the courts<br />
decision in determining who should have custody <strong>of</strong> minor<br />
children)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-49
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Guidelines for Court<br />
Ordered Evaluations –<br />
Noncovered Services<br />
(continued)<br />
11-50<br />
Criminal competency evaluations (evaluation to determine<br />
whether a person is competent to st<strong>and</strong> trial)<br />
Development <strong>of</strong> family reunification plans (service to guide<br />
courts decisions regarding child placement/return to family<br />
setting)<br />
Education classes for DUI <strong>of</strong>fenses (education classes/program<br />
regarding driving under the influence. A CD diagnosis is not<br />
required for attendance.)<br />
Evaluating the credibility <strong>of</strong> child witnesses (evaluation to<br />
guide courts in determining credibility <strong>of</strong> a child witness)<br />
Evaluations <strong>of</strong> juveniles accused <strong>of</strong> criminal acts (evaluation to<br />
guide courts in determining whether a minor should be tried as<br />
an adult)<br />
Evaluations to assess termination <strong>of</strong> parental rights (evaluation<br />
to guide courts decision regarding termination <strong>of</strong> parental<br />
rights)<br />
Juvenile pre-sentencing evaluations (evaluation to guide courts<br />
decision related to sentencing in criminal matters)<br />
Juvenile probation evaluations (evaluation to guide courts<br />
decision related to probation terms in criminal matters)<br />
Mediation <strong>of</strong> parental conflicts about children (service to<br />
provide assistance to parents engaged in a legal dispute over<br />
child custody <strong>and</strong>/or visitation)<br />
Parenting assessments/parental competency evaluation<br />
(evaluation to guide the courts decisions about parental rights,<br />
custody <strong>and</strong> placements)<br />
Personal injury evaluations (evaluation to guide courts decision<br />
in awarding damages related to personal injury)<br />
Visitation risk assessments (evaluations to guide the courts<br />
decision in determining child visitation rights; may include<br />
gr<strong>and</strong>parent visitation.)<br />
Workers’ compensation evaluations (evaluation to determine<br />
extent <strong>of</strong> damage related to a workers’ compensation claim)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Parity Federal laws <strong>and</strong> state m<strong>and</strong>ates dictate mental health parity laws<br />
that are applicable to all fully insured groups. Self-insured groups<br />
are not subject to parity laws <strong>and</strong> legislation unless they choose to<br />
add this benefit.<br />
Behavioral Health<br />
Quality Improvement<br />
Objectives<br />
Parity means that treatment for substance abuse <strong>and</strong>/or mental<br />
health is covered the same as any other inpatient <strong>and</strong>/or outpatient<br />
medical benefit. For example, if a member has coverage for an<br />
illness E/M service from a non-network provider, then that<br />
member will also have coverage for a behavioral health service<br />
from a non-network provider.<br />
Based upon results <strong>of</strong> the 2004 quality improvement activities <strong>and</strong><br />
National Committee for Quality Assurance (NCQA) st<strong>and</strong>ards,<br />
<strong>Blue</strong> <strong>Cross</strong> requires participation from behavioral health providers<br />
in the following activities:<br />
Follow-up After Hospitalization for Mental Illness<br />
Offer appointments to new <strong>and</strong> returning patients within seven<br />
days <strong>of</strong> mental health hospitalization discharge. Appointments<br />
should be provided within the timeframe commensurate with<br />
patient clinical need. <strong>Blue</strong> <strong>Cross</strong> recommends that behavioral<br />
health providers develop an appointment scheduling strategy to<br />
accommodate newly discharged patients, if they have not already<br />
done so.<br />
St<strong>and</strong>ardized Substance Abuse Screenings in Mental Health<br />
Assessments<br />
Routinely utilize st<strong>and</strong>ardized substance abuse screening<br />
questionnaires (e.g., CAGEAID) in mental health assessments<br />
for new patients age 12 <strong>and</strong> older. (Routine substance use<br />
assessment <strong>of</strong> children ages 10 <strong>and</strong> 11 is also recommended.)<br />
Recommend or refer patients for comprehensive substance<br />
abuse assessment based on the screening results <strong>and</strong><br />
corroborating clinical information from the substance use<br />
assessment.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-51
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Behavioral Health<br />
Quality Improvement<br />
Objectives (continued)<br />
11-52<br />
Exchange <strong>of</strong> Information with Primary Care Physicians<br />
Routinely ask all new patients to authorize exchange <strong>of</strong><br />
information with primary care/specialty physicians.<br />
Establish a distinct section in the treatment record, if one does<br />
not exist, dedicated to case management activities. This section<br />
should contain:<br />
Documentation <strong>of</strong> patient authorization/refusal to exchange<br />
information with the physician.<br />
When authorized, documentation <strong>of</strong> communication with<br />
the physician (e.g., report, letter, telephone or e-mail<br />
communication).<br />
When recommending a patient seek psychopharmacologic<br />
treatment from his/her primary care physician or if the<br />
patient’s primary care physician recommended mental<br />
health assessment <strong>and</strong>/or treatment, provide the primary<br />
care physician with the current behavioral health<br />
diagnosis(es), diagnostic criteria (i.e., symptoms with<br />
onset, duration <strong>and</strong> severity) <strong>and</strong> treatment plan, if<br />
applicable.<br />
When authorized, the treating psychiatrist or clinical<br />
nurse specialist should provide the current diagnosis<br />
(es) <strong>and</strong> initial medication management information to<br />
the primary care/specialty physician. This requirement<br />
is important for patient safety.<br />
Appointment Accessibility<br />
Provide routine initial appointments within ten business days<br />
<strong>of</strong> the request.<br />
Provide routine follow-up appointments within ten business<br />
days <strong>of</strong> the initial appointment.<br />
Provide urgent appointments within 24 hours <strong>of</strong> the request.<br />
Provide non-life-threatening-emergency appointments within<br />
six hours <strong>of</strong> the request.<br />
Provide or facilitate life-threatening-emergency care<br />
immediately.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Behavioral Health<br />
Quality Improvement<br />
Objectives (continued)<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Questions, comments or material requests should be directed to:<br />
Attn: Mary Rains R4-18<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus<br />
P.O. Box 64179<br />
St. Paul, MN 55164-0179<br />
Phone: (651) 662-0826 or 1-800-382-2000 x20826<br />
Fax: (651) 662-3625<br />
E-mail: mary_e_rains@bluecrossmn.com<br />
Prior Authorization <strong>Blue</strong> <strong>Cross</strong> does not usually require prior authorization for<br />
outpatient mental health or chemical dependency services provided<br />
within the Select or Aware ® provider networks, depending on<br />
specific contract requirements. Likewise, if the patient has benefits<br />
for behavioral health services from a non-network provider, no<br />
prior authorization is usually required. If the patient does NOT<br />
have benefits for behavioral health services from a non-network<br />
provider, there is no coverage <strong>and</strong> claims will deny as “not<br />
covered.”<br />
A few groups do have specific prior authorization requirements for<br />
behavioral health services. Contact provider services for a specific<br />
group’s requirements:<br />
Phone: 1-800-262-0820 or (651) 662-5200<br />
Fax: (651) 662-2745<br />
Federal Employee Program ® (FEP) (member ID numbers begin<br />
with “R”) members require a prior authorization for all outpatient<br />
mental health <strong>and</strong> substance abuse services before the first visit.<br />
To request a prior authorization, complete the <strong>Minnesota</strong> universal<br />
outpatient mental/chemical health authorization form that is<br />
available on bluecrossmn.com. Select “for health care providers”<br />
then “forms <strong>and</strong> publications” <strong>and</strong> in the drop down box, select<br />
“forms: prior authorization.” If you have questions regarding FEP<br />
members:<br />
Phone: (651) 662-5044 or 1-800-859-2128<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-53
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Prior Authorization<br />
(continued)<br />
11-54<br />
Providers may use the following numbers to submit a prior<br />
authorization request, check on the status <strong>of</strong> a prior authorization<br />
request, or ask questions about prior authorization guidelines for<br />
Behavioral Health Services.<br />
Phone: 1-800-262-0820<br />
Fax: (651) 662-0854 outpatient or inpatient behavioral health<br />
services<br />
Providers should submit a new prior authorization request when<br />
requesting additional services or a change in dates <strong>of</strong> service for a<br />
prior authorization.<br />
Referrals <strong>Blue</strong> <strong>Cross</strong> does not require a referral for patients seeking care<br />
within the Select Behavioral Health Network. For complete<br />
information on requirements for <strong>Minnesota</strong> Health Care Programs,<br />
see Chapter 3 <strong>of</strong> the <strong>Blue</strong> Plus <strong>Manual</strong>.<br />
Preadmission<br />
Notification<br />
Services sought outside the Select Behavioral Health Network but<br />
within the Aware network will be processed according to the<br />
patient’s self-referral benefit, if the patient’s contract has a selfreferral<br />
benefit. If the patient has specialty needs, continuity <strong>of</strong><br />
care issues, transition <strong>of</strong> care issues, or cannot access behavioral<br />
health services within the required provider network within a<br />
reasonable time period, or due to geographical or physical<br />
accessibility reasons, the provider should contact <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
request a referral. A referral will be approved depending on the<br />
patient’s situation.<br />
If services are sought outside both the Select network <strong>and</strong> the<br />
Aware network <strong>and</strong> the member does not have self-referral<br />
benefits, then <strong>Blue</strong> <strong>Cross</strong> should be contacted <strong>and</strong> the situation<br />
reviewed for a possible referral approval.<br />
Call (651) 662-2474 or 1-800-262-0820 or fax form X13459 to<br />
(651) 662-0856 to notify <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> admissions into day<br />
treatment, partial psychiatric or inpatient programs.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Pre-certification <strong>and</strong><br />
Concurrent Review for<br />
Inpatient/Residential<br />
Mental Health <strong>and</strong><br />
Substance use<br />
Disorder Services<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
To help assure that members receive the appropriate level <strong>of</strong> care<br />
for mental health <strong>and</strong> substance use disorder treatment, <strong>Blue</strong><br />
<strong>Cross</strong>, as done with other medical/surgical services, require certain<br />
pre-certification <strong>and</strong> concurrent review protocols for<br />
inpatient/residential services.<br />
This program will continue to exp<strong>and</strong> <strong>and</strong> impacted providers will<br />
receive additional information once these requirements are<br />
exp<strong>and</strong>ed.<br />
Pre-certification <strong>and</strong> concurrent review applies to health services<br />
provided to members in fully insured <strong>and</strong> self-insured benefit<br />
plans, including <strong>Minnesota</strong> Health Care Programs, with the<br />
exception <strong>of</strong> <strong>Minnesota</strong> Senior Care Plus (MSC+), Secure<strong>Blue</strong><br />
(HMO SNP), Platinum <strong>Blue</strong> (Cost) <strong>and</strong> Medicare<strong>Blue</strong> PPO<br />
(Regional PPO) members. Medicare supplement benefit plans are<br />
also excluded from review. This also does not apply to court<br />
ordered admissions to inpatient/residential treatment. Coverage for<br />
court ordered mental health services is detailed in <strong>Minnesota</strong><br />
Statute 62Q.535.<br />
Definitions<br />
"Pre-certification" is defined as an advance review <strong>of</strong> a proposed<br />
facility admission or certain services or procedures in order to<br />
determine whether the proposed admission, services or procedures<br />
meet the medical necessity criteria for payment <strong>and</strong> to ensure that<br />
the subscriber receives the maximum benefits available under the<br />
subscriber’s plan.<br />
"Concurrent review" is defined as ongoing review during the<br />
subscriber’s care to ensure that it meets established medical<br />
criteria in a timely manner <strong>and</strong> certifies the necessity, the<br />
appropriateness <strong>and</strong> quality <strong>of</strong> services during an inpatient<br />
admission.<br />
Pre-certification Requirements<br />
Provider will obtain pre-certification from <strong>Blue</strong> <strong>Cross</strong> before<br />
admitting a member. If admission is emergent or after business<br />
hours, provider will obtain pre-certification within two (2)<br />
business days after the admission.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-55
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Pre-certification <strong>and</strong><br />
Concurrent Review for<br />
Inpatient/Residential<br />
Mental Health <strong>and</strong><br />
Substance use<br />
Disorder Services –<br />
(continued)<br />
Groups that Carve Out<br />
Behavioral Health<br />
Benefits<br />
11-56<br />
Provider shall obtain pre-certification by calling <strong>Blue</strong> <strong>Cross</strong> at<br />
(651) 662 5270 or toll free at 1-800-528-0934. <strong>Blue</strong> <strong>Cross</strong> will use<br />
criteria set forth in the Level <strong>of</strong> Care Utilization System (LOCUS)<br />
<strong>and</strong> Child <strong>and</strong> Adolescent Services Intensity Instrument (CASII)<br />
for mental health or the Dimensions criteria for substance use<br />
disorders in conducting a medical necessity review for the<br />
admission.<br />
Failure to provide evidence <strong>of</strong> medical necessity may result in<br />
claim denials as provider liability.<br />
Concurrent Review Requirements<br />
Providers have a contractual obligation as noted in Chapter 4 <strong>of</strong><br />
the online <strong>Blue</strong> <strong>Cross</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> to<br />
adhere to care management programs. At the time <strong>of</strong> precertification<br />
a date will be established to conduct concurrent<br />
review.<br />
Concurrent review will include verification <strong>of</strong> medical necessity<br />
based on criteria set forth in the LOCUS <strong>and</strong> CASII for mental<br />
health or the Dimensions criteria for substance use disorders.<br />
Failure to provide evidence <strong>of</strong> medical necessity may result in<br />
claim denials as provider liability.<br />
Some self-insured contract with another carrier to manage their<br />
behavioral health benefits. This means that their behavioral health<br />
claims should be filed to the designated third party behavioral<br />
health carrier for processing. This carrier’s information should be<br />
obtained from the patient.<br />
E/M services (codes 99201-99215) <strong>and</strong> medication management<br />
services (codes 90862 or M0064) billed with a behavioral health<br />
diagnosis for carve out group members should be billed to <strong>Blue</strong><br />
<strong>Cross</strong> as long as the practitioner is a non-behavioral health<br />
practitioner or a multi-specialty clinic. If one <strong>of</strong> these services is<br />
denied, <strong>Blue</strong> <strong>Cross</strong> should be contacted for it to be reprocessed.<br />
These services will be paid at the behavioral health benefit but will<br />
not accumulate towards patients’ behavioral health benefit<br />
maximums. Any other behavioral health treatment for carve out<br />
group members that is billed to <strong>Blue</strong> <strong>Cross</strong> will be denied.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Provider Networks There are two behavioral health provider networks: the Select<br />
Behavioral Health Network <strong>and</strong> the Aware network.<br />
Most <strong>Blue</strong> Plus patients are required to utilize a Select provider for<br />
their highest level <strong>of</strong> benefits. Many but not all members have selfreferral<br />
benefits that are applied when services are obtained in the<br />
Aware network. To find a participating Select network provider,<br />
members are encouraged to call <strong>Blue</strong> <strong>Cross</strong> so that a provider best<br />
suited to meet their treatment needs can be found in a convenient<br />
location.<br />
The majority <strong>of</strong> fee-for-service members have direct access to an<br />
Aware network practitioner.<br />
Fully insured groups have the Select Behavioral Health Network.<br />
Some self-insured groups have the Select Behavioral Health<br />
Network while other self-insured groups may choose the Aware<br />
Network. Individual accounts use the Aware Network.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-57
Pr<strong>of</strong>essional Behavioral Health Coding Information<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus<br />
Code Description Units Who May Submit Misc<br />
90801 Psychiatric diagnostic interview exam 1 per session MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90802 Interactive diagnostic interview exam 1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90804 Individual psychotherapy, insight oriented,<br />
<strong>of</strong>fice/outpatient, 20-30 min.<br />
90805 Individual psychotherapy, insight oriented,<br />
<strong>of</strong>fice/outpatient, 20-30 min., w/E/M<br />
90806 Individual psychotherapy, insight oriented,<br />
<strong>of</strong>fice/outpatient, 45-50 min.<br />
90807 Individual psychotherapy, insight oriented,<br />
<strong>of</strong>fice/outpatient, 45-50 min., w/E/M<br />
90808 Individual psychotherapy, insight oriented,<br />
<strong>of</strong>fice/outpatient, 75-80 min.<br />
90809 Individual psychotherapy, insight oriented,<br />
<strong>of</strong>fice/outpatient, 75-80 min., w/E/M<br />
90810 Individual psychotherapy, interactive,<br />
<strong>of</strong>fice/outpatient, 20-30 min.<br />
90811 Individual psychotherapy, interactive,<br />
<strong>of</strong>fice/outpatient, 20-30 min., w/E/M<br />
90812 Individual psychotherapy, interactive,<br />
<strong>of</strong>fice/outpatient, 45-50 min.<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-59
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
90813 Individual psychotherapy, interactive,<br />
<strong>of</strong>fice/outpatient, 45-50 min., w/E/M<br />
90814 Individual psychotherapy, interactive,<br />
<strong>of</strong>fice/outpatient, 75-80 min.<br />
90815 Individual psychotherapy, interactive,<br />
<strong>of</strong>fice/outpatient, 75-80 min., w/E/M<br />
90816 Individual psychotherapy, insight oriented,<br />
inpatient, 20-30 min.<br />
90817 Individual psychotherapy, insight oriented,<br />
inpatient, 20-30 min., w/E/M<br />
90818 Individual psychotherapy, insight oriented,<br />
inpatient, 45-50 min.<br />
90819 Individual psychotherapy, insight oriented,<br />
inpatient, 45-50 min., w/E/M<br />
90821 Individual psychotherapy, insight oriented,<br />
inpatient, 75-80 min.<br />
90822 Individual psychotherapy, insight oriented,<br />
inpatient, 75-80 min., w/E/M<br />
90823 Individual psychotherapy, interactive,<br />
inpatient, 20-30 min.<br />
90824 Individual psychotherapy, interactive,<br />
inpatient, 20-30 min., w/E/M<br />
90826 Individual psychotherapy, interactive,<br />
inpatient, 45-50 min.<br />
11-60<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
90827 Individual psychotherapy, interactive,<br />
inpatient, 45-50 min., w/E/M<br />
90828 Individual psychotherapy, interactive,<br />
inpatient, 75-80 min.<br />
90829 Individual psychotherapy, interactive,<br />
inpatient, 75-80 min., w/E/M<br />
1 per session MD, CNS-Psych, PMHNP<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
90845 Psychoanalysis 1 per session MD only Not covered – may be a<br />
contract exclusion<br />
90846 Family psychotherapy (without patient<br />
present)<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90847 Family psychotherapy (with patient present) 1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90849 Multiple family group psychotherapy 1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90853 Group psychotherapy (other than family) 1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90857 Interactive group psychotherapy 1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90862 Pharmacologic management w/minimal<br />
psychotherapy<br />
90865 Narcosyntheseis for psychiatric diagnostic<br />
<strong>and</strong> therapeutic purposes (e.g., sodium<br />
amobarbital (amytal) interview)<br />
May be a contract<br />
exclusion. Incompatible<br />
with non-BH dx<br />
Incompatible with non-BH<br />
dx<br />
Incompatible with non-BH<br />
dx<br />
Incompatible with non-BH<br />
dx<br />
Incompatible with non-BH<br />
dx<br />
1 per session MD, CNS-Psych, PMHNP, PA, NP Incompatible with non-BH<br />
dx<br />
1 per session MD, CNS-Psych, PMHNP Incompatible with non-BH<br />
dx<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-61
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
90870 Electroconvulsive therapy; (includes<br />
necessary monitoring)<br />
90875 Individual psychophysiological therapy<br />
incorporating bi<strong>of</strong>eedback, 20-30 min.<br />
90876 Individual psychophysiological therapy<br />
incorporating bi<strong>of</strong>eedback, 45-50 min.<br />
11-62<br />
1 per day MD only Incompatible with non-BH<br />
dx<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90880 Hypnotherapy 1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90882 Environmental intervention for medical<br />
management purposes<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, LMFT, LPCC<br />
Incompatible with non-BH<br />
dx<br />
Incompatible with non-BH<br />
dx<br />
Incompatible with non-BH<br />
dx<br />
Not covered - incl. in basic<br />
service (for Public Program<br />
members, allowed for<br />
ARHMS program)<br />
90885 Psychiatric evaluation <strong>of</strong> hospital records 1 per day MD only Not covered - incl. in basic<br />
service<br />
90887 Interpretation or explanation <strong>of</strong> exam results 1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
90889 Preparation <strong>of</strong> report <strong>of</strong> patient’s psychiatric<br />
status<br />
90899 Unlisted psychiatric service or procedure 1 unit- submit<br />
time<br />
Not covered - incl. in basic<br />
service<br />
1 per service MD only Not covered - contract<br />
exclusion<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
Submit narrative <strong>and</strong> time<br />
90901 Bi<strong>of</strong>eedback training by any modality 1 per session MD only Not covered in home POS-<br />
contract exclusion<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
90911 Bi<strong>of</strong>eedback training, perineal muscles,<br />
anorectoal or urethral sphincter, including<br />
EMG <strong>and</strong>/or manometry<br />
96101 Psychological testing, (includes<br />
psychodiagnostic assessment <strong>of</strong> emotionality,<br />
intellectual abilities, personality <strong>and</strong><br />
psychopathology, e.g., MMPI, Rorschach,<br />
WAIS), per hour <strong>of</strong> the psychologist’s or<br />
physician’s time, both face-to-face time<br />
administering tests to the patient <strong>and</strong> time<br />
interpreting test results <strong>and</strong> preparing the<br />
report<br />
96102 Psychological testing (includes<br />
psychodiagnostic assessment <strong>of</strong> emotionality,<br />
intellectual abilities, personality <strong>and</strong><br />
psychopathology, e.g., MMPI <strong>and</strong> WAIS),<br />
with qualified health care pr<strong>of</strong>essional<br />
interpretation <strong>and</strong> report, administered by<br />
technician, per hour <strong>of</strong> technician time, faceto-face<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
1 per session MD only Not covered in home POS-<br />
contract exclusion<br />
1 unit per hour<br />
<strong>of</strong> face-to-face<br />
testing,<br />
interpretation<br />
<strong>and</strong><br />
preparation <strong>of</strong><br />
report<br />
Report 1 unit<br />
per hour <strong>of</strong><br />
face-to-face<br />
testing<br />
MD, LP-Ph.D., LP-MA The psychologist or<br />
psychiatrist administers<br />
<strong>and</strong> interprets the test(s)<br />
<strong>and</strong> prepares the report.<br />
Billed under the MD, LP-<br />
PhD, LP-MA individual<br />
provider number or NPI.<br />
MD, LP-PhD, LP-MA, LICSW, CNS-<br />
Psych, LMFT, LPCC<br />
A technician under direct<br />
supervision, administers<br />
the test(s). The supervising<br />
qualified licensed<br />
practitioner interprets the<br />
test(s) <strong>and</strong> prepares the<br />
report. Billed under the<br />
supervising licensed<br />
practitioner provider<br />
number or NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-63
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
96103 Psychological testing (includes<br />
psychodiagnostic assessment <strong>of</strong> emotionality,<br />
intellectual abilities, personality <strong>and</strong><br />
psychopathology, e.g., MMPI), administered<br />
by a computer, with qualified health care<br />
pr<strong>of</strong>essional interpretation <strong>and</strong> report<br />
96116 Neurobehavioral status exam (clinical<br />
assessment <strong>of</strong> thinking, reasoning <strong>and</strong><br />
judgment, e.g., acquired knowledge, attention,<br />
language, memory, planning <strong>and</strong> problem<br />
solving, <strong>and</strong> visual spatial abilities), per hour<br />
<strong>of</strong> the psychologist’s or physician’s time, both<br />
face-to-face time with the patient <strong>and</strong> time<br />
interpreting test results <strong>and</strong> preparing the<br />
report<br />
96118 Neuropsychological testing (e.g., Halstead-<br />
Reitan neuropsychological battery, Wechsler<br />
memory scales <strong>and</strong> Wisconsin card sorting<br />
test), per hour <strong>of</strong> the psychologist’s or<br />
physician’s time, both face-to-face time<br />
administering tests to the patient <strong>and</strong> time<br />
interpreting test results <strong>and</strong> preparing the<br />
report<br />
11-64<br />
Report 1 unit<br />
per testing<br />
session<br />
regardless <strong>of</strong><br />
number <strong>of</strong> tests<br />
MD, LP-PhD, LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
1 per hour MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
Report 1 unit<br />
per hour <strong>of</strong><br />
face-to-face<br />
testing,<br />
interpretation<br />
<strong>and</strong><br />
preparation <strong>of</strong><br />
report<br />
Patient is alone <strong>and</strong> taking<br />
a computer-based test.<br />
A qualified licensed<br />
practitioner interprets the<br />
test(s) <strong>and</strong> prepares the<br />
report.<br />
Billed under the licensed<br />
practitioner provider<br />
number or NPI.<br />
MD, LP-Ph.D., LP-MA The psychologist or<br />
psychiatrist administers<br />
<strong>and</strong> interprets the test(s)<br />
<strong>and</strong> prepares the report.<br />
Billed under the MD, LP-<br />
PhD, LP-MA individual<br />
provider number or NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
96119 Neuropsychological testing (e.g., Halstead-<br />
Reitan neuropsychological battery, Wechsler<br />
memory scales <strong>and</strong> Wisconsin card sorting<br />
test), with qualified health care pr<strong>of</strong>essional<br />
interpretation <strong>and</strong> report, administered by<br />
technician, per hour <strong>of</strong> technician time, faceto-face<br />
96120 Neuropsychological testing (e.g., Wisconsin<br />
card sorting test), administered by a<br />
computer, with qualified health care<br />
pr<strong>of</strong>essional interpretation <strong>and</strong> report<br />
96125 St<strong>and</strong>ardized cognitive performance testing<br />
(e.g., Ross information processing<br />
assessment) per hour <strong>of</strong> a qualified health care<br />
pr<strong>of</strong>essional's time, both face-to-face time<br />
administering tests to the patient <strong>and</strong> time<br />
interpreting these test results <strong>and</strong> preparing<br />
the report<br />
Report 1 unit<br />
per hour <strong>of</strong><br />
face-to-face<br />
testing<br />
Report 1 unit<br />
per testing<br />
session<br />
regardless <strong>of</strong><br />
number <strong>of</strong> tests<br />
Report 1 unit<br />
per hour <strong>of</strong><br />
face-to-face<br />
testing,<br />
interpretation<br />
<strong>and</strong><br />
preparation <strong>of</strong><br />
report<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
MD, LP-PhD, LP-MA A technician under direct<br />
supervision, administers<br />
the test(s). The supervising<br />
qualified licensed<br />
practitioner interprets the<br />
test(s) <strong>and</strong> prepares the<br />
report. Billed under the<br />
supervising licensed<br />
practitioner provider<br />
number or NPI.<br />
MD, LP-PhD, LP-MA Patient is alone <strong>and</strong> is<br />
taking a computer-based<br />
test. A qualified licensed<br />
practitioner interprets the<br />
test(s) <strong>and</strong> prepares the<br />
report. Billed under the<br />
licensed practitioner<br />
provider number or NPI.<br />
MD, LP-PhD, LP-MA The psychologist or<br />
psychiatrist administers<br />
<strong>and</strong> interprets the test(s)<br />
<strong>and</strong> prepares the report.<br />
Billed under the MD, LP-<br />
PhD, LP-MA individual<br />
provider number or NPI.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-65
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
96150 Health <strong>and</strong> behavior assessment (e.g., healthfocused<br />
clinical interview, behavioral<br />
observations, psychophysiological<br />
monitoring, health-oriented questionnaires),<br />
each 15 minutes face-to-face with the patient;<br />
initial assessment<br />
96151 Health <strong>and</strong> behavior assessment (e.g., healthfocused<br />
clinical interview, behavioral<br />
observations, psychophysiological<br />
monitoring, health-oriented questionnaires),<br />
each 15 minutes face-to-face with the patient;<br />
re-assessment<br />
96152 Health <strong>and</strong> behavior intervention, each 15<br />
minutes, face-to-face; individual<br />
96153 Health <strong>and</strong> behavior intervention, each 15<br />
minutes, face-to-face; group (2 or more<br />
patients)<br />
96154 Health <strong>and</strong> behavior intervention, each 15<br />
minutes, face-to-face; family (with the patient<br />
present)<br />
96155 Health <strong>and</strong> behavior intervention, each 15<br />
minutes, face-to-face; family (without the<br />
patient present)<br />
11-66<br />
1 per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MH/CD diagnosis is NOT<br />
primary diagnosis<br />
MH/CD diagnosis is NOT<br />
primary diagnosis<br />
MH/CD diagnosis is NOT<br />
primary diagnosis<br />
MH/CD diagnosis is NOT<br />
primary diagnosis<br />
MH/CD diagnosis is NOT<br />
primary diagnosis<br />
MH/CD diagnosis is NOT<br />
primary diagnosis<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
98960 Education <strong>and</strong> training for patient selfmanagement<br />
by a qualified, nonphysician<br />
health care pr<strong>of</strong>essional using a st<strong>and</strong>ard<br />
curriculum, face-to-face with the patient<br />
(could include caregiver/family) each 30<br />
minutes; individual patient<br />
98961 Education <strong>and</strong> training for patient selfmanagement<br />
by a qualified, nonphysician<br />
health care pr<strong>of</strong>essional using a st<strong>and</strong>ardized<br />
curriculum, face-to-face with the patient<br />
(could include caregiver/family) each 30<br />
minutes; 2-4 patients<br />
98962 Education <strong>and</strong> training for patient selfmanagement<br />
by a qualified, nonphysician<br />
health care pr<strong>of</strong>essional using a st<strong>and</strong>ardized<br />
curriculum, face-to-face with the patient<br />
(could include caregiver/family) each 30<br />
minutes; 5-8 patients<br />
99201-<br />
99205<br />
99211-<br />
99215<br />
99217-<br />
99220<br />
1 per 30<br />
minutes<br />
1 per 30<br />
minutes<br />
1 per 30<br />
minutes<br />
MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, NP, PA, LPCC<br />
Office or other outpatient E/M – new patient 1 per visit MD, NP, CNS, CNS-psych, PMHNP, PA<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Limited coverage for:<br />
PMAP/MNCare<br />
Diabetes dx<br />
BH dx<br />
Prenatal<br />
Limited coverage for:<br />
PMAP/MNCare<br />
Diabetes dx<br />
BH dx<br />
Prenatal<br />
Limited coverage for:<br />
PMAP/MNCare<br />
Diabetes dx<br />
BH dx<br />
Prenatal<br />
Office or other outpatient E/M – established<br />
patient<br />
1 per visit MD, NP, CNS, CNS-psych, PMHNP, PA<br />
Hospital observation services, initial 1 per visit MD, NP, CNS, CNS-psych, PMHNP, PA Routine dx not allowed<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-67
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
99221-<br />
99223<br />
99224-<br />
99226<br />
99231-<br />
99233<br />
99234-<br />
99236<br />
11-68<br />
Hospital inpatient E/M – initial 1 per visit MD, NP, CNS, CNS-psych, PMHNP, PA,<br />
Approved Mental Health Clinic,<br />
Community Mental Health Center,<br />
Essential Community Provider<br />
Routine dx not allowed<br />
Hospital observation services; subsequent 1 per visit MD, NP, CNS, CNS-psych, PMHNP, PA Routine dx not allowed<br />
Hospital inpatient E/M – subsequent 1 per visit MD, CNS-Psych, NP, PA, CNS, PMHNP,<br />
Approved Mental Health Clinic,<br />
Community Mental Health Center,<br />
Essential Community Provider<br />
Observation or inpatient hospital care 1 per day MD, NP, CNS, CNS-psych, PMHNP, PA,<br />
Approved Mental Health Clinic,<br />
Community Mental Health Center,<br />
Essential Community Provider<br />
99238 Hospital discharge, 30 minutes or less 1 per day MD, Approved Mental Health Clinic,<br />
CNS-Psych, NP, PA, CNS, PMHNP,<br />
Community Mental Health Center,<br />
Essential Community Provider<br />
99239 Hospital discharge, more than 30 minutes 1 per day MD, Approved Mental Health Clinic,<br />
CNS-Psych, NP, PA, CNS, PMHNP,<br />
Community Mental Health Center,<br />
Essential Community Provider<br />
99241-<br />
99245<br />
99251-<br />
99255<br />
Office or other outpatient consultation 1 per session MD only<br />
Inpatient consultation, initial 1 per session MD only<br />
Routine dx not allowed<br />
Routine dx not allowed<br />
Routine dx not allowed<br />
Routine dx not allowed<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
99281-<br />
99285<br />
Emergency department E/M 1 per session MD only<br />
99408 Alcohol <strong>and</strong>/or substance (other than tobacco)<br />
abuse structured screening (e.g., AUDIT,<br />
DAST), <strong>and</strong> brief intervention (SBI) services;<br />
15 to 30 minutes<br />
99409 Alcohol <strong>and</strong>/or substance (other than tobacco)<br />
abuse structured screening (e.g., AUDIT,<br />
DAST), <strong>and</strong> brief intervention (SBI) services;<br />
greater than 30 minutes<br />
G0175 Scheduled interdisciplinary team conference<br />
(minimum <strong>of</strong> three exclusive <strong>of</strong> patient care<br />
nursing staff) with patient present<br />
G0176 Activity therapy, such as music, dance, art or<br />
play therapies not for recreation, related to the<br />
care <strong>and</strong> treatment <strong>of</strong> patient’s disabling<br />
mental health problems, per session (45<br />
minutes or more)<br />
G0177 Training <strong>and</strong> educational services related to<br />
the care <strong>and</strong> treatment <strong>of</strong> patient’s disabling<br />
mental health problems per session (45<br />
minutes or more)<br />
1 per session MD, LP-PhD, LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, LP-PhD, LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
1 per session N/A Denied. If IP or partial<br />
hospital - part <strong>of</strong> hospital<br />
rates. Not payable as OP<br />
therapy code – no medical<br />
necessary care is provided.<br />
1 per session N/A Denied. If IP or partial<br />
hospital - part <strong>of</strong> hospital<br />
rates. Not payable as OP<br />
therapy code – no medical<br />
necessary care is provided.<br />
1 per session N/A Denied. If IP or partial<br />
hospital - part <strong>of</strong> hospital<br />
rates. Not payable as OP<br />
therapy code – no medical<br />
necessary care is provided.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-69
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
G0396 Alcohol <strong>and</strong>/or substance (other than tobacco)<br />
abuse structured assessment (e.g., AUDIT,<br />
DAST), <strong>and</strong> brief intervention 15 to 30<br />
minutes<br />
G0397 Alcohol <strong>and</strong>/or substance (other than tobacco)<br />
abuse structured assessment (e.g., AUDIT,<br />
DAST), <strong>and</strong> intervention, greater than 30<br />
minutes<br />
G0409 Social work <strong>and</strong> psychological services,<br />
directly relating to <strong>and</strong>/or furthering the<br />
patient's rehabilitation goals, each 15 minutes,<br />
face-to-face; individual (services provided by<br />
a CORF-qualified social worker or<br />
11-70<br />
psychologist in a CORF)<br />
G0410 Group psychotherapy other than <strong>of</strong> a<br />
multiple-family group, in a partial<br />
hospitalization setting, approximately 45 to<br />
50 minutes<br />
G0411 Interactive group psychotherapy, in a partial<br />
hospitalization setting, approximately 45 to<br />
50 minutes<br />
G9012 Other specified case management service not<br />
otherwise classified<br />
1 per session MD, LP-PhD, LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, Rule 25, LPCC<br />
1 per session MD, LP-PhD, LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, Rule 25, LPCC<br />
1 per 15<br />
minutes<br />
MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session<br />
MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
H0001 Alcohol <strong>and</strong>/or drug assessment 1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, Rule 25, LPCC<br />
H0002 Behavioral health screening to determine<br />
eligibility for admission to treatment program<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Incompatible with non-BH<br />
dx<br />
Incompatible with non-BH<br />
dx<br />
Incompatible with non-BH<br />
dx<br />
Autism related service only<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
H0003 Alcohol <strong>and</strong>/or drug screening; laboratory<br />
analysis <strong>of</strong> specimens for presence <strong>of</strong> alcohol<br />
<strong>and</strong>/or drugs<br />
H0004 Behavioral health counseling <strong>and</strong> therapy, per<br />
15 minutes<br />
H0005 Alcohol <strong>and</strong>/or drug services; group<br />
counseling by a clinician<br />
H0006 Alcohol <strong>and</strong>/or drug services; case<br />
management<br />
H0007 Alcohol <strong>and</strong>/or drug services; crisis<br />
intervention (outpatient)<br />
H0008 Alcohol <strong>and</strong>/or drug services; sub-acute<br />
detoxification (hospital inpatient)<br />
H0009 Alcohol <strong>and</strong>/or drug services; acute<br />
detoxification (hospital inpatient)<br />
H0010 Alcohol <strong>and</strong>/or drug services; sub-acute<br />
detoxification (residential addiction program<br />
inpatient)<br />
H0011 Alcohol <strong>and</strong>/or drug services; acute<br />
detoxification (residential addiction program<br />
inpatient)<br />
H0012 Alcohol <strong>and</strong>/or drug services; sub-acute<br />
detoxification (residential addiction program<br />
outpatient)<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per 15<br />
minutes<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC, mobile<br />
crisis provider specialty, Rule 29.<br />
1 per session MD, CNS-Psych, PMHNP, NP, PA, CNSmedical<br />
1 per session MD, CNS-Psych, PMHNP, NP, PA, CNSmedical<br />
1 per session MD, CNS-Psych, PMHNP, NP, PA, CNSmedical<br />
1 per session MD, CNS-Psych, PMHNP, NP, PA, CNSmedical<br />
1 per session MD, CNS-Psych, PMHNP, NP, PA, CNSmedical<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Incompatible with non-BH<br />
dx<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Non-covered<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-71
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
H0013 Alcohol <strong>and</strong>/or drug services; acute<br />
detoxification (residential addiction program<br />
outpatient)<br />
H0014 Alcohol <strong>and</strong>/or drug services; ambulatory<br />
detoxification<br />
H0015 Alcohol <strong>and</strong>/or drug services; intensive<br />
outpatient (treatment program that operates at<br />
least 3 hours/day <strong>and</strong> at least 3 days/week <strong>and</strong><br />
is based on an individualized treatment plan),<br />
including assessment, counseling; crisis<br />
intervention, <strong>and</strong> activity therapies or<br />
education<br />
H0016 Alcohol <strong>and</strong>/or drug services;<br />
medical/somatic (medical intervention in<br />
ambulatory setting)<br />
H0017 Behavioral health; residential (hospital<br />
residential treatment program), without room<br />
<strong>and</strong> board, per diem<br />
H0018 Behavioral health; short-term residential<br />
(non-hospital residential treatment program),<br />
without room <strong>and</strong> board, per diem<br />
H0019 Behavioral health; long-term residential (nonmedical,<br />
non-acute care in residential<br />
treatment program where stay is typically<br />
longer than 30 days), without room <strong>and</strong> board,<br />
per diem<br />
11-72<br />
1 per session MD, CNS-Psych, PMHNP, NP, PA, CNSmedical<br />
1 per session MD, CNS-Psych, PMHNP, NP, PA, CNSmedical<br />
1 per session MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per session MD, CNS-Psych, PMHNP, PA, NP, CNS-<br />
Medical<br />
1 per day/diem MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with mental<br />
health dx only.<br />
1 per day/diem IRTS Crisis provider Compatible with mental<br />
health dx only.<br />
1 per day/diem IRTS Crisis provider Compatible with mental<br />
health dx only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
H0020 Alcohol <strong>and</strong>/or drug services; methadone<br />
administration <strong>and</strong>/or service (provision <strong>of</strong> the<br />
drug by a licensed program)<br />
H0021 Alcohol <strong>and</strong>/or drug training service (for staff<br />
<strong>and</strong> personnel not employed by providers)<br />
H0022 Alcohol <strong>and</strong>/or drug intervention service<br />
(planned facilitation)<br />
H0023 Behavioral health outreach service (planned<br />
approach to reach a target population)<br />
H0024 Behavioral health prevention information<br />
dissemination service (one-way direct or nondirect<br />
contact with service audiences to affect<br />
knowledge or attitude)<br />
H0025 Behavioral health prevention education<br />
service (delivery <strong>of</strong> services with target<br />
population to affect knowledge, attitude<br />
<strong>and</strong>/or behavior)<br />
H0026 Alcohol <strong>and</strong>/or drug prevention process<br />
service, community-based (delivery <strong>of</strong><br />
services to develop skills <strong>of</strong> impactors)<br />
1 per session Freest<strong>and</strong>ing Methadone/Opiod clinic,<br />
Substance Abuse Facility<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
Covered when provided<br />
within a methadone clinic<br />
or substance abuse facility.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-73
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
H0027 Alcohol <strong>and</strong>/or drug prevention<br />
environmental service (broad range <strong>of</strong><br />
external activities geared toward modifying<br />
systems in order to mainstream prevention<br />
through policy <strong>and</strong> law)<br />
H0028 Alcohol <strong>and</strong>/or drug prevention problem<br />
identification <strong>and</strong> referral service(e.g. student<br />
assistance <strong>and</strong> employee assistance<br />
programs), does not include assessment<br />
H0029 Alcohol <strong>and</strong>/or drug prevention alternatives<br />
service (services for populations that exclude<br />
alcohol <strong>and</strong> other drug use, e.g. alcohol free<br />
social events)<br />
11-74<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
H0030 Behavioral health hotline service 1 per session N/A Not covered<br />
H0031 Mental health assessment, by non-physician 1 per session LP-Ph.D., LP-MA, LICSW, CNS-Psych,<br />
PMHNP, LMFT, NP, PA, behavioral<br />
health therapist, LPCC<br />
H0032 Mental health service plan development by<br />
non-physician<br />
H0034 Medication training <strong>and</strong> support, per 15<br />
minutes<br />
H0035 Mental health partial hospitalization,<br />
treatment, less than 24 hours<br />
1 per session N/A Not covered<br />
1 per 15<br />
minutes<br />
Behavioral health clinic, MD, LP-Ph.D.,<br />
LP-MA, LICSW, CNS-Psych, LMFT,<br />
LPCC<br />
Generally not covered –<br />
eligible coding for<br />
ARMHS – Public<br />
Program/MNCare only<br />
1 per day Rule 29, approved mental health clinic Compatible with BH dx<br />
only<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
H0036 Community psychiatric supportive treatment,<br />
face-to-face, per 15 minutes<br />
H0037 Community psychiatric supportive treatment<br />
program, per diem<br />
1 per 15<br />
minutes<br />
H0038 Self-help/peer services, per 15 minutes 1 per 15<br />
minutes<br />
H0039 Assertive community treatment, face-to-face,<br />
per 15 minutes<br />
H0040 Assertive community treatment program, per<br />
diem<br />
H0046 Mental health services, not otherwise<br />
specified<br />
H0047 Alcohol <strong>and</strong>/or other drug abuse services, not<br />
otherwise specified<br />
H0048 Alcohol <strong>and</strong>/or other drug testing: collection<br />
<strong>and</strong> h<strong>and</strong>ling only, specimens other than<br />
blood<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
N/A Not covered<br />
1 per day N/A Not covered<br />
1 per 15<br />
minutes<br />
N/A Generally not covered –<br />
may be allowed for PMAP<br />
only<br />
N/A Not covered<br />
1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, behavioral health<br />
clinic, BH Therapist Practitioner, LPCC<br />
1 per day / 1<br />
minute for<br />
travel time<br />
1 unit – submit<br />
time<br />
1 per service<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, behavioral health<br />
clinic, BH Therapist Practitioner, LPCC<br />
PMAP only<br />
PMAP only – use for travel<br />
time for In-Home services.<br />
Requires narrative.<br />
Freest<strong>and</strong>ing methadone/opioid clinic Requires narrative <strong>and</strong><br />
time.<br />
MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT<br />
H0049 Alcohol <strong>and</strong>/or drug screening 1 per service MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
H0050 Alcohol <strong>and</strong>/or drug services, brief<br />
intervention, per 15 minutes<br />
1 per 15<br />
minutes<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
Compatible with alcohol or<br />
substance abuse dx only<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
Compatible with alcohol or<br />
substance abuse dx only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-75
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
H2001 Rehabilitation program, per ½ day 1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
H2010 Comprehensive medication services, per 15<br />
minutes<br />
11-76<br />
1 per 15<br />
minutes<br />
H2011 Crisis intervention service, per 15 minutes 1 per 15<br />
minutes<br />
MD, CNS-Psych, PMHNP, PA, NP<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP,<br />
behavioral health clinic, LPCC<br />
H2012 Behavioral health day treatment, per hour 1 per hour MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
PMAP only<br />
H2013 Psychiatric health facility service, per diem 1 per day N/A Not covered<br />
H2014 Skills training <strong>and</strong> development, per 15<br />
minutes<br />
H2015 Comprehensive community support services,<br />
per 15 minutes<br />
H2016 Comprehensive community support services,<br />
per diem<br />
H2017 Psychosocial rehabilitation services, per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
Incompatible with non-BH<br />
dx<br />
PMAP or autism related<br />
service only<br />
PMAP/MNCare only.<br />
Submit UA modifier for<br />
crisis intervention.<br />
1 per day N/A Not covered<br />
1 per 15<br />
minutes<br />
Behavioral health clinic, MD, LP-Ph.D.,<br />
LP-MA, LICSW, CNS-Psych, LMFT,<br />
LPCC<br />
H2018 Psychosocial rehabilitation services, per diem 1 per day N/A Not covered<br />
Generally not covered –<br />
may be allowed for Public<br />
Program/ MNCare for<br />
ARHMS or autism related<br />
service only<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
H2019 Therapeutic behavioral services, per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
H2020 Therapeutic behavioral services, per diem 1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
H2021 Community based wrap-around services, per<br />
15 minutes<br />
1 per 15<br />
minutes<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
N/A Not covered<br />
PMAP/MNCare or<br />
autism related service<br />
Modifier required:<br />
UA modifier for<br />
MH Behavioral<br />
aide Level 1. HM<br />
modifier for MH<br />
Behavioral aide<br />
Level 2. HE<br />
modifier for MH<br />
Practitioner<br />
direction <strong>of</strong> MH<br />
Behavioral aide.<br />
PMAP/MNCare only<br />
Modifier required:<br />
UA modifier for<br />
MH Behavioral<br />
aide Level 1. HM<br />
modifier for MH<br />
Behavioral aide<br />
Level 2. HE<br />
modifier for MH<br />
Practitioner<br />
direction <strong>of</strong> MH<br />
Behavioral aide.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-77
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
H2022 Community based wrap-around services, per<br />
diem<br />
H2023 Supported employment, per 15 minutes 1 per 15<br />
minutes<br />
11-78<br />
1 per day N/A Not covered<br />
N/A Not covered<br />
H2024 Supported employment, per diem 1 per day N/A Not covered<br />
H2025 Ongoing support to maintain employment, per<br />
15 minutes<br />
H2026 Ongoing support to maintain employment, per<br />
diem<br />
1 per 15<br />
minutes<br />
H2027 Psychoeducational service, per 15 minutes 1 per 15<br />
minutes<br />
H2028 Sexual <strong>of</strong>fender treatment, per 15 minutes 1 per 15<br />
minutes<br />
N/A Not covered<br />
1 per day N/A Not covered<br />
MD, LP-PhD, LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC,<br />
Certified Residential Sex Offender<br />
Treatment Facility<br />
H2029 Sexual <strong>of</strong>fender treatment, per diem 1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC,<br />
Certified Residential Sex Offender<br />
Treatment Facility<br />
H2030 Mental health clubhouse services, per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
H2031 Mental health clubhouse services, per diem 1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
Compatible with bipolar<br />
disorder, schizophrenia,<br />
<strong>and</strong> BPD dx only.<br />
Not allowed with 90801<br />
Not allowed with 90801<br />
Not covered<br />
Not covered<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
H2032 Activity therapy, per 15 minutes 1 per 15<br />
minutes<br />
MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Not covered<br />
H2033 Multisytemic therapy for juveniles 1 per session N/A Generally not covered<br />
H2034 Alcohol <strong>and</strong>/or drug abuse halfway house<br />
services, per diem<br />
H2035 Alcohol <strong>and</strong>/or other drug treatment program,<br />
per hour<br />
H2036 Alcohol <strong>and</strong>/or other drug treatment program,<br />
per diem<br />
H2037 Developmental delay prevention activities,<br />
dependent child <strong>of</strong> client, per 15 minutes<br />
M0064 Brief <strong>of</strong>fice visit for monitoring or changing<br />
drug prescriptions<br />
S3005 Performance measurement, evaluation <strong>of</strong><br />
patient self assessment, depression<br />
1 per day N/A Not covered<br />
1 per hour N/A Not covered<br />
1 per day N/A Not covered<br />
1 per 15<br />
minutes<br />
N/A Not covered<br />
1 per session MD, CNS-Psych, PMHNP, PA, NP Compatible with BH dx<br />
only<br />
1 per session N/A Not covered<br />
S8940 Equestrian/hippotherapy, per session 1 per session N/A Not covered<br />
S9475 Ambulatory setting substance abuse treatment<br />
or detoxification services, per diem<br />
S9480 Intensive outpatient psychiatric services, per<br />
diem<br />
S9482 Family stabilization services, per 15 minutes 1 per 15<br />
minutes<br />
1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, LPCC<br />
1 per day MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
Compatible with CD dx<br />
only<br />
Compatible with BH dx<br />
only<br />
N/A Not covered<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-79
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
S9484 Crisis intervention mental health services, per<br />
hour<br />
S9485 Crisis intervention mental health services, per<br />
diem<br />
T1006 Alcohol <strong>and</strong>/or substance abuse services,<br />
family/couple counseling<br />
T1007 Alcohol <strong>and</strong>/or substance abuse services,<br />
treatment plan development <strong>and</strong>/or<br />
modification<br />
T1009 Child sitting services for children <strong>of</strong> the<br />
individual receiving alcohol <strong>and</strong>/or substance<br />
abuse services<br />
11-80<br />
1 per hour Rule 29, Mobile Crisis, MD, LP-Ph.D.,<br />
LP-MA, LICSW, CNS-Psych, PMHNP,<br />
LMFT, PA, NP, LPCC, approved mental<br />
health clinic, behavioral health clinic<br />
Applicable modifiers:<br />
HM – less than<br />
bachelor’s degree level<br />
HN – bachelor’s degree<br />
level<br />
HQ – group setting<br />
UA – non-MD<br />
pr<strong>of</strong>essional<br />
Child/Adolescent<br />
practitioner<br />
1 per diem Rule 29, Mobile Crisis Applicable modifiers:<br />
1 per session MD, LP-Ph.D., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC<br />
UA – for MH<br />
pr<strong>of</strong>essional<br />
Child/Adolescent<br />
practitioner.<br />
HN – BA level<br />
practitioner.<br />
Compatible with CD dx<br />
only<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
T1010 Meals for individual receiving alcohol <strong>and</strong>/or<br />
substance abuse services (when meals not<br />
included in the program)<br />
T1012 Alcohol <strong>and</strong>/or substance abuse services,<br />
skills development<br />
T1023 Screening to determine the appropriateness <strong>of</strong><br />
consideration <strong>of</strong> an individual for<br />
participation in a specified program, project<br />
or treatment protocol, per encounter<br />
T1024 Evaluation <strong>and</strong> treatment by an integrated,<br />
specialty team contracted to provide<br />
coordinated care to multiple or severely<br />
h<strong>and</strong>icapped children, per encounter<br />
T1025 Intensive, extended multidisciplinary services<br />
provided in a clinic setting to children with<br />
complex medical, physical, mental <strong>and</strong><br />
psychosocial impairments, per diem<br />
T1026 Intensive, extended multidisciplinary services<br />
provided in a clinic setting to children with<br />
complex medical, physical, medical <strong>and</strong><br />
psychosocial impairments per hour<br />
T1027 Family training <strong>and</strong> counseling for child<br />
development, per 15 minutes<br />
T1028 Assessment <strong>of</strong> home, physical <strong>and</strong> family<br />
environment, to determine suitability to meet<br />
patient's medical needs<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
1 per day N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session MD, LP-PhD., LP-MA, LICSW, CNS-<br />
Psych, PMHNP, LMFT, PA, NP, LPCC,<br />
Community Mental Health Center, Rule<br />
29, Essential community provider, BH<br />
clinic<br />
1 per session N/A Not covered<br />
1 per day N/A Not covered<br />
1 per hour N/A Not covered<br />
1 per 15<br />
minutes<br />
N/A Not covered<br />
1 per session N/A Not covered<br />
Autism related service only<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-81
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
T1029 Comprehensive environmental lead<br />
investigation, not including laboratory<br />
analysis, per dwelling<br />
T2010 Preadmission screening <strong>and</strong> resident review<br />
(PASRR) level I identification screening, per<br />
screen<br />
T2011 Preadmission screening <strong>and</strong> resident review<br />
(PASRR) level II evaluation, per evaluation<br />
11-82<br />
1 per session N/A Not covered<br />
1 per screen N/A Not covered<br />
1 per<br />
evaluation<br />
N/A Not covered<br />
T2012 Habilitation, educational; waiver, per diem 1 per day N/A Not covered<br />
T2013 Habilitation, educational, waiver; per hour 1 per hour N/A Not covered<br />
T2014 Habilitation, prevocational, waiver; per diem 1 per day N/A Not covered<br />
T2015 Habilitation, prevocational, waiver; per hour 1 per hour N/A Not covered<br />
T2016 Habilitation, residential, waiver; per diem 1 per day N/A Not covered<br />
T2017 Habilitation, residential, waiver; 15 minutes 1 per 15<br />
minutes<br />
T2018 Habilitation, supported employment, waiver;<br />
per diem<br />
T2019 Habilitation, supported employment, waiver;<br />
per 15 minutes<br />
N/A Not covered<br />
1 per day N/A Not covered<br />
1 per 15<br />
minutes<br />
N/A Not covered<br />
T2020 Day habilitation, waiver; per diem 1 per day N/A Not covered<br />
T2021 Day habilitation, waiver; per 15 minutes 1 per 15<br />
minutes<br />
N/A Not covered<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Code Description Units Who May Submit Misc<br />
T2022 Case management, per month 1 per calendar<br />
month<br />
T2023 Targeted case management; per month 1 per calendar<br />
month<br />
T2024 Service assessment/ plan <strong>of</strong> care<br />
development, waiver<br />
T2025 Waiver services; not otherwise specified<br />
(NOS)<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
N/A Generally not covered<br />
Approved MH Center, BH Clinic,<br />
Community MH Center, CNS – Psych,<br />
LICSW, LP-PhD, LP – MA, LMFT,<br />
PMHNP, LPCC, Social Service Agency<br />
DIAMOND project only<br />
PMAP/MNCare only<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
T2026 Specialized childcare, waiver; per diem 1 per day N/A Not covered<br />
T2027 Specialized childcare, waiver; per 15 minutes 1 per 15<br />
minutes<br />
T2028 Specialized supply, not otherwise specified,<br />
waiver<br />
T2029 Specialized medical equipment, not otherwise<br />
specified, waiver<br />
T2030 Assisted living; waiver, per month 1 per calendar<br />
month<br />
N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
N/A Not covered<br />
T2031 Assisted living; waiver, per diem 1 per day N/A Not covered<br />
T2032 Residential care, not otherwise specified<br />
(NOS), waiver; per month<br />
T2033 Residential care, not otherwise specified<br />
(NOS), waive; per diem<br />
1 per calendar<br />
month<br />
N/A Not covered<br />
1 per day N/A Not covered<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-83
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Who May Submit Misc<br />
T2034 Crisis intervention, waiver; per diem 1 per day N/A Not covered<br />
T2035 Utility services to support medical equipment<br />
<strong>and</strong> assistive technology/ devices, waiver<br />
T2036 Therapeutic camping, overnight, waiver; each<br />
session<br />
T2037 Therapeutic camping day, waiver; each<br />
session<br />
11-84<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
1 per session N/A Not covered<br />
T2038 Community transition, waiver; per service 1 per session N/A Not covered<br />
T2039 Vehicle modifications, waiver; per service 1 per session N/A Not covered<br />
T2040 Financial management, self-directed, waiver;<br />
per 15 minutes<br />
T2041 Supports brokerage, self-directed, waiver; per<br />
15 minutes<br />
T2048 Behavioral health; long-term care residential<br />
(non-acute care in a residential treatment<br />
program where stay is typically longer than<br />
30 days), with room <strong>and</strong> board, per diem<br />
1 per 15<br />
minutes<br />
1 per 15<br />
minutes<br />
N/A Not covered<br />
N/A Not covered<br />
1 per day N/A Not covered<br />
MD = Psychiatrist; LP-Ph.D. = Licensed Psychologist, Doctorate; LP-MA = Licensed Psychologist, Masters; LICSW = Licensed Clinical Social Worker; PA = Physician’s Assistant: NP = Nurse Practitioner, CNS-<br />
Psych = Clinical Nurse Specialist, Psychiatric specialty; PMHNP = Psychiatric Mental Health Nurse Practitioner; LMFT = Licensed Marriage <strong>and</strong> Family Therapist<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Behavioral Health for Institutional (837I) Billers<br />
Introduction This section <strong>of</strong> the manual is intended for all behavioral health<br />
practitioners who bill on the 837I claim format. This section is not<br />
intended for practitioners whose services are billed on the 837P<br />
claim format.<br />
Practitioners Who<br />
Should be Using this<br />
Section<br />
Residential treatment centers, non-residential treatment centers,<br />
Rule 5 facilities, Rule 8 facilities, hospitals, state hospitals <strong>and</strong><br />
treatment centers, freest<strong>and</strong>ing detoxification centers, sex <strong>of</strong>fender<br />
treatment facilities.<br />
Coding Guidelines Use the following codes for submitting behavioral health<br />
evaluation or testing services on the 837I claim format.<br />
Behavioral Health<br />
Evaluation or Testing<br />
Revenue<br />
Code<br />
HCPCS<br />
Code Narrative Time Units<br />
0914 90801 Psychiatric diagnostic<br />
review<br />
0914 90802 Interactive psychiatric<br />
diagnostic interview<br />
0918 96101-<br />
96102<br />
0918 96118-<br />
96119<br />
Psychological testing<br />
per hour<br />
Neuropsychological<br />
testing battery with<br />
interpretation or report<br />
Per<br />
session<br />
Per<br />
session<br />
60<br />
minutes<br />
60<br />
minutes<br />
1 unit<br />
1 unit<br />
1 per<br />
hour<br />
1 per<br />
hour<br />
Units One or more units should be submitted based on the time<br />
designation within the HCPCS code narrative. If there is no time<br />
designation, the service is considered ‘per session’ <strong>and</strong> only one<br />
unit should be submitted regardless <strong>of</strong> the actual time spent.<br />
Unit guidelines are also noted in the appropriate following<br />
sections.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12 11-85
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Individual Behavioral<br />
Health Therapy<br />
Family <strong>and</strong> Group<br />
Therapy<br />
11-86<br />
Revenue<br />
Code<br />
0911 See<br />
HCPCS/<br />
CPT for<br />
approp.<br />
code<br />
HCPCS<br />
Code Narrative Time Units<br />
Psychiatric/<br />
Psychological<br />
service/rehabilitat<br />
ion. Do not use<br />
for CD services.<br />
0912 H2012 Psychiatric/<br />
Psychological<br />
service/partial<br />
hospitalization -<br />
less intensive<br />
0914 See CPT<br />
codes for<br />
individual<br />
therapy<br />
Psychiatric/<br />
psychological<br />
service/individual<br />
therapy<br />
Based on<br />
HCPCS/<br />
CPT<br />
code<br />
used<br />
One line<br />
for each<br />
day the<br />
patient<br />
attends<br />
the<br />
program<br />
Based on<br />
CPT<br />
code<br />
used<br />
Depends<br />
on<br />
HCPCS/<br />
CPT code<br />
used<br />
1 unit for<br />
each hour<br />
the patient<br />
attends<br />
the<br />
program<br />
Depends<br />
CPT code<br />
used<br />
Use these codes when billing behavioral health family <strong>and</strong> group<br />
therapy services on an 837I claim format.<br />
Revenue<br />
Code<br />
0915 See<br />
HCPCS/<br />
CPT<br />
codes for<br />
group<br />
therapy<br />
0916 90846 or<br />
90847<br />
0917 90875 or<br />
90876<br />
0918 96101-<br />
96102,<br />
96118-<br />
96119<br />
HCPCS<br />
Code Narrative Time Units<br />
Psychiatric/<br />
Psychological<br />
service/group<br />
therapy<br />
Psychiatric/<br />
Psychological<br />
service/family<br />
therapy<br />
Psychiatric/<br />
psychological<br />
service/<br />
bi<strong>of</strong>eedback<br />
Psychiatric/<br />
psychological<br />
service/testing<br />
Based on<br />
HCPCS/<br />
CPT<br />
code<br />
used<br />
Per<br />
session<br />
Per<br />
session<br />
60<br />
minute<br />
code<br />
Depends<br />
on<br />
HCPCS/<br />
CPT code<br />
used<br />
One unit<br />
per<br />
session<br />
One unit<br />
per<br />
session<br />
One unit<br />
per 60<br />
minutes<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Substance Abuse<br />
Services<br />
Billing a Behavioral<br />
Health Assessment<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
The <strong>Minnesota</strong> Department <strong>of</strong> Health <strong>Minnesota</strong> Companion<br />
Guide includes a table showing the correct reporting <strong>of</strong> substance<br />
abuse services. See section A.5.3, Table 3, <strong>of</strong> the <strong>Minnesota</strong><br />
Uniform Companion Guide for Institutional Claims at the<br />
following link<br />
http://www.health.state.mn.us/auc/instguide.htm.<br />
The table incorporates both institutional <strong>and</strong> pr<strong>of</strong>essional claim<br />
types for ease <strong>of</strong> reference.<br />
0912, 0944 or 0945 with 90801 or 90802<br />
Bill 0912 <strong>and</strong> 90801/90802 with a mental health, chemical<br />
dependency or alcohol dependency diagnosis code<br />
Bill 0944 <strong>and</strong> 90801/90802 with a chemical dependency<br />
diagnosis code<br />
Bill 0945 <strong>and</strong> 90801/90802 with an alcohol dependency<br />
diagnosis<br />
Testing 0918 with 96101-96103, 96118-96125<br />
Family Therapy 0916 with 90846<br />
Testing is compatible with all behavioral health diagnosis codes.<br />
Revenue code 0916 <strong>and</strong> CPT 90846 is billed for family therapy<br />
when the patient is not present. There may be specific contract<br />
exclusions on for some self-insured groups.<br />
Revenue code 0916 <strong>and</strong> CPT 90846 should be billed under the<br />
specific patient, <strong>and</strong> not under the member.<br />
Bill one unit per session, regardless <strong>of</strong> total time.<br />
0916 with 90847<br />
Revenue code 0916 <strong>and</strong> CPT 90847 is billed for family therapy<br />
when the patient is present. There may be specific contract<br />
exclusions for some self-insured groups.<br />
Revenue code 0916 <strong>and</strong> CPT 90847 should be billed under the<br />
specific patient, <strong>and</strong> not under the member.<br />
Bill one unit per session, regardless <strong>of</strong> total time.<br />
11-87
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Nutritional<br />
Counseling/<br />
Dietitians<br />
11-88<br />
0942 with 97802-97804<br />
Nutritional counseling is usually eligible if billed with either a<br />
behavioral health diagnosis or with a medical diagnosis such as<br />
obesity or diabetes. Group nutritional therapy services billed under<br />
revenue code 0942 with CPT 97804 are generally only covered<br />
when submitted with diagnosis codes for anorexia, bulimia,<br />
diabetes, congestive heart failure, <strong>and</strong> some maternity diagnoses.<br />
Obesity is not an eligible diagnosis for CPT 97804. Outpatient<br />
hospital services billed with revenue code 0942 <strong>and</strong> procedure<br />
codes 97802, 97803 or 97804 are eligible services. There are no<br />
limits to the number <strong>of</strong> eligible services a patient receives if the<br />
patient has a fully insured contract. In contrast, some self-insured<br />
contracts may choose to apply contract variations/exclusions for<br />
nutritional counseling services.<br />
Registered dietitians <strong>and</strong> licensed nutritionists can bill<br />
independently for procedure codes S9470, 97802, 97803 <strong>and</strong><br />
97804 when billed with eating disorder diagnoses 307.1, 307.50<br />
<strong>and</strong> 307.51. No referral is required for the highest benefit level.<br />
For all other diagnoses, licensed dietitian <strong>and</strong> nutritionist services<br />
must be submitted to <strong>Blue</strong> <strong>Cross</strong> by an eligible medical clinic or<br />
hospital. The individual provider number or NPI <strong>of</strong> the licensed<br />
dietitian or nutritionist must be submitted on the claim. Claims for<br />
registered dietitians billing services outside <strong>of</strong> behavioral health<br />
diagnoses will deny unless the services are submitted under the<br />
individual provider number or NPI <strong>of</strong> a supervising physician.<br />
The contract for Federal Employee Program members (who have<br />
ID numbers beginning with “R”) only allows medical nutrition<br />
therapy services in the following situations: Dietitian assessments<br />
as part <strong>of</strong> a multi-disciplinary eating disorder evaluation; <strong>and</strong><br />
medical nutrition therapy services as part <strong>of</strong> ongoing nutritional<br />
therapy for eating disorders anorexia nervosa (diagnosis<br />
code307.1) <strong>and</strong>/or bulimia nervosa (diagnosis code 307.51).<br />
Coverage is extended to diabetic educators, dietitians <strong>and</strong><br />
nutritionists who bill independently as part <strong>of</strong> a covered diabetic<br />
education program only. Nutritional counseling for up to four<br />
visits per year is covered when billed by a covered provider,<br />
although nutritional counseling for the treatment <strong>of</strong> anorexia <strong>and</strong><br />
bulimia billed with diagnosis codes 307.1 or 307.51 is not subject<br />
to the four visit limitation. Outpatient hospital services billed with<br />
revenue code 0942 <strong>and</strong> procedure codes 97802, 97803 <strong>and</strong> 97804<br />
are eligible services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Detox <strong>and</strong><br />
Alcohol/Drug Rehab<br />
Services<br />
Health <strong>and</strong> Behavior<br />
Assessment <strong>and</strong><br />
Intervention Codes<br />
0116, 0126, 0136, 0146, 0156<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Detox is a medically supervised treatment program for alcohol or<br />
drug addiction designed to purge the body <strong>of</strong> intoxicating or<br />
addictive substances. Detox is a medical service that treats<br />
physiological issues. When during this detox process the patient is<br />
not able to participate in a substance abuse treatment program,<br />
detox services are payable out <strong>of</strong> medical benefits, not substance<br />
abuse benefits. It would be appropriate to bill primary diagnosis<br />
code 980.9 when submitting alcohol detox services. It would be<br />
appropriate to bill primary diagnosis code 977.9 when submitting<br />
chemical/drug detox services.<br />
Bill one unit <strong>of</strong> service per night spent in a detox bed.<br />
When billing therapy/treatment services such as revenue code<br />
0944 (drug rehabilitation) or 0945 (alcohol rehabilitation,) a<br />
chemical dependency or alcohol dependency diagnosis code<br />
must be submitted. These services are payable out <strong>of</strong> substance<br />
abuse benefits if the patient’s policy has substance abuse<br />
benefits.<br />
If a patient’s policy does not have a substance abuse benefit,<br />
only room <strong>and</strong> board charges are eligible, typically billed under<br />
revenue code 0126. Detox services will not be paid if billed in<br />
conjunction with a therapy service such as revenue code 0944<br />
or 0945.<br />
If a patient’s policy does have a substance abuse benefit, then<br />
both room <strong>and</strong> board <strong>and</strong> therapy charges are eligible.<br />
Detox does not accumulate towards policy limitations.<br />
Detoxification services are eligible when they are provided in a<br />
state licensed freest<strong>and</strong>ing detoxification center, a hospital or a<br />
residential treatment center.<br />
96150-96155<br />
CPT codes 96150-96155 describe services <strong>of</strong>fered to patients who<br />
present with established illnesses or symptoms <strong>and</strong> who are not<br />
diagnosed with mental illness. The primary diagnosis should be a<br />
non-behavioral health diagnosis code. Codes 96150-96155 should<br />
not be reported with revenue codes 0900-0919 on facility claims.<br />
Codes 96150-96155 may be submitted under revenue code 0940.<br />
11-89
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Non-Residential<br />
Treatment Centers<br />
FEP Exclusion <strong>of</strong><br />
Residential Treatment<br />
Centers<br />
11-90<br />
State licensed non-residential treatment centers generally only bill<br />
outpatient chemical dependency services. A limited number <strong>of</strong><br />
mental health services will be covered in this setting.<br />
Some non-residential treatment centers are dually licensed as both<br />
a Rule 29 clinic <strong>and</strong> a residential treatment center. It is important<br />
to bill appropriate services under each separate entity. Mixing<br />
services <strong>and</strong> provider specialties may cause a claim to deny.<br />
The Federal Employee Program (FEP) benefits specifically<br />
exclude services billed or provided by a residential treatment<br />
center (RTC). To access the 2011 Service Benefit Plan brochure<br />
go to fepblue.org <strong>and</strong> the information is currently available on<br />
pages 70 <strong>and</strong> 86 regarding the RTC exclusion. Affected providers<br />
include all mental health <strong>and</strong> substance abuse RTCs.<br />
All Federal Employee Program members have been notified that<br />
RTCs are not covered providers. <strong>Blue</strong> <strong>Cross</strong> will work with these<br />
members through the case management team to ensure they<br />
continue to receive medically necessary <strong>and</strong> cost-effective<br />
treatment.<br />
Compatibility Compatibility is a frequent <strong>and</strong> common cause <strong>of</strong> claim denials.<br />
Recreational Therapy 0941<br />
Revenue code 0944 should only be billed with a chemical<br />
dependency diagnosis code.<br />
Revenue Code 0945 should only be billed with an alcohol<br />
dependency diagnosis code.<br />
Recreational therapy may be part <strong>of</strong> an approved CD outpatient<br />
program. It is included under the CD program charges <strong>and</strong> should<br />
not be billed separately under revenue code 0941.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Extended Care <strong>and</strong><br />
Halfway House Room<br />
<strong>and</strong> Board (Medicaid<br />
Government Programs<br />
Only)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
<strong>Blue</strong> Plus is responsible for reimbursing providers for extended<br />
care <strong>and</strong> halfway house services for our <strong>Minnesota</strong> Health Care<br />
Program members. This applies only to the government programs<br />
listed below.<br />
To ensure that <strong>Blue</strong> Plus can accurately distinguish, adjudicate the<br />
claim <strong>and</strong> report encounter data to the <strong>Minnesota</strong> Department <strong>of</strong><br />
Human Services (DHS), the room <strong>and</strong> board (R&B) charges for<br />
extended care, halfway house <strong>and</strong> primary residential treatment,<br />
must be submitted in the following manner:<br />
Provider Type Type <strong>of</strong> Bill<br />
Primary<br />
residential<br />
R&B Rev<br />
Code<br />
R&B Rev Code<br />
Description<br />
086X 1002 Behavioral<br />
health<br />
accommodation<br />
– residential<br />
treatment –<br />
chemical<br />
dependency<br />
Extended care 086X 1003 Behavioral<br />
health<br />
accommodation<br />
– supervised<br />
living<br />
Halfway house 086X 1004 Behavioral<br />
health<br />
accommodation<br />
– halfway house<br />
Treatment<br />
Treatment should also be reported in addition to the appropriate<br />
R&B codes noted above. Chemical dependency treatment is<br />
reported using either revenue code 0944 (Drug rehabilitation) or<br />
0945 (Alcohol rehabilitation).<br />
11-91
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Extended Care <strong>and</strong><br />
Halfway House Room<br />
<strong>and</strong> Board (Medicaid<br />
Government Programs<br />
Only) (continued)<br />
11-92<br />
<strong>Blue</strong> Plus<br />
Product <strong>Name</strong> Group Numbers<br />
<strong>Blue</strong> Advantage –<br />
PMAP<br />
<strong>Blue</strong> Advantage –<br />
GA/GAMC<br />
<strong>Blue</strong> Advantage –<br />
MSC+<br />
PP011, PP012, PP014, PP015, PP016,<br />
PP017, PP021, PP022, PP024, PP025,<br />
PP026, PP027, PP031, PP032, PP034,<br />
PP035, PP036, PP037<br />
PP081, PP082, PP084, PP091, PP092, PP094<br />
PP041, PP042, PP044, PP051, PP052,<br />
PP054, PP055, PP056, PP057, PP061,<br />
PP062, PP064, PP071, PP072, PP075,<br />
PP076, PP077<br />
<strong>Minnesota</strong>Care PP161, PP162, PP163, PP164, PP121,<br />
PP122, PP131, PP132, PP141, PP142,<br />
PP111, PP112, PP151, PP152<br />
Secure<strong>Blue</strong> PP200, PP201, PP202, PP210, PP220,<br />
PP221, PP222, PP230, PP240, PP245,<br />
PP250, PP255, PP260, PP261, PP262,<br />
PP270, PP280, PP281, PP282, PP290, PP215<br />
Fax a copy <strong>of</strong> the completed Rule 25 Assessment <strong>and</strong> Placement<br />
Summary, available on line at dhs.state.mn.us admitting<br />
diagnosis code for member, admitting physician/provider (if<br />
applicable) <strong>and</strong> provider’s address.<br />
Fax this information to:<br />
Integrated Health Management-Chemical Dependency<br />
Utilization Management (CD UM) (651) 662-0718.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Extended Care <strong>and</strong><br />
Halfway House Room<br />
<strong>and</strong> Board (Medicaid<br />
Government Programs<br />
Only) (continued)<br />
Partial Psychiatric<br />
Billing<br />
Admission Notification<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
For <strong>Blue</strong> Plus members in the affected groups, please notify <strong>Blue</strong><br />
Plus <strong>of</strong> the member’s extended care or halfway house services by<br />
faxing a copy <strong>of</strong> the following forms to (651) 662-0718:<br />
Chemical Dependency Notification <strong>of</strong> Residential Admission<br />
Form<br />
Rule 25 Assessment <strong>and</strong> Placement Summary<br />
The Chemical Dependency Notification <strong>of</strong> Residential Admission<br />
Form is available at bluecrossmn.com. <strong>Blue</strong> Plus will notify you<br />
that the information has been received.<br />
Discharge Notification<br />
Please notify <strong>Blue</strong> Plus <strong>of</strong> a discharge from extended care or<br />
halfway house services by calling (651) 662-5270 or<br />
1-800-528-0934; prompts will direct you to the correct option to<br />
leave the discharge date. You may also fax discharge information<br />
to (651) 662-0718. When reporting a discharge, please provide the<br />
following information:<br />
Member name <strong>and</strong> ID #<br />
<strong>Blue</strong> Plus case number provided by <strong>Blue</strong> Plus<br />
Provider name, contact name <strong>and</strong> contact phone number<br />
Discharge date<br />
Partial psych services must be billed as an outpatient service under<br />
revenue codes 0912 or 0913. Detailed billing requirements are<br />
listed below.<br />
If your psychiatric unit is Medicare-certified, the following<br />
instructions apply:<br />
Bill using your NPI with the appropriate taxonomy code (partial<br />
psych)<br />
If the patient is not a Medicare member, submit claims using<br />
TOB 013X (Hospital Outpatient) with revenue codes 0912-<br />
0913 <strong>and</strong> HCPCS code H0035. For a child/adolescent program,<br />
use H0035 with the HA modifier.<br />
0912 – Behavioral health treatments/services – partial<br />
hospitalization – less intensive<br />
11-93
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Partial Psychiatric<br />
Billing (continued)<br />
11-94<br />
0913 – Behavioral health treatments/services – partial<br />
hospitalization –intensive<br />
H0035 – Mental health partial hospitalization, treatment,<br />
less than 24 hours<br />
HA – Child/adolescent program<br />
If the patient is a Medicare member, submit claims using TOB<br />
013X, condition code 41 <strong>and</strong> the Medicare-allowed revenue<br />
codes:<br />
0250 – Pharmacy (drugs <strong>and</strong> biologicals) (no HCPCS<br />
required)<br />
043X – Occupational therapy, partial hospitalization<br />
(G0129)<br />
0900 – Behavioral health treatments/services general<br />
(90801, 90802 or 90899)<br />
0904 – Activity therapy, partial hospitalization (G0176)<br />
0914 – Individual psychotherapy (90816, 90817, 90818,<br />
90819, 90821, 90822, 90823, 90824, 90826, 90827, 90828<br />
or 90829)<br />
0915 – Group therapy (90849, 90853 or 90857)<br />
0916 – Family psychotherapy (90846, 90847 or 90849)<br />
0918 – psychiatric testing (96101-96103, 96116, 96118-<br />
96120)<br />
0942 – Education training (G0177)<br />
Partial Program is not Hospital-Based<br />
If your partial program is not hospital-based but is part <strong>of</strong> a<br />
community mental health center in accordance with<br />
MS256B.0625, subd 5 <strong>and</strong> is certified by Medicare to provide<br />
partial hospitalization, bill using your NPI with your partial psych<br />
taxonomy code, using TOB 013X <strong>and</strong> revenue codes 0912-0913.<br />
Hospital outpatient claims generally require submission <strong>of</strong> the<br />
appropriate HCPCS code along with the revenue code. The<br />
behavioral health (0900-0919) <strong>and</strong> the education training (0942)<br />
revenue codes require submission <strong>of</strong> a HCPCS code.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Rule 5 - Emotionally<br />
H<strong>and</strong>icapped Facilities<br />
Children’s Residential<br />
Mental Health<br />
(Medicaid Government<br />
Programs only)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Rule 5 facilities must have state licensure to provide services.<br />
Preadmission notification is recommended.<br />
Services are processed under the patient’s residential benefits<br />
<strong>and</strong> are subject to any day or dollar limitations. Some selfinsured<br />
contracts may deny services as a contract exclusion.<br />
Benefits may end the day the patient turns 18. Each contract<br />
should be checked for clarification on this benefit.<br />
The <strong>Minnesota</strong> Department <strong>of</strong> Human Services (DHS) has<br />
determined that the managed care organizations shall be<br />
responsible for the rehabilitative services <strong>and</strong> other medical costs<br />
for <strong>Minnesota</strong> Health Care Programs members while the child<br />
resides in the children’s residential mental health treatment facility<br />
<strong>and</strong> remains in managed care. In order for <strong>Blue</strong> <strong>Cross</strong> to be in<br />
compliance with this required benefit change, a contract<br />
amendment has been issued to all <strong>Blue</strong> <strong>Cross</strong> participating<br />
children’s residential mental health institutional providers who are<br />
located in <strong>Minnesota</strong> <strong>and</strong> hold host county contracts.<br />
Prior Authorization<br />
Prior authorization from <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> the county will be<br />
required for all children’s residential mental health treatment<br />
facilities. To begin this process, please contact Behavioral Health<br />
Service at 1-800-262-0820.<br />
Coverage<br />
Coverage is subject to the terms <strong>of</strong> the member’s benefit plan.<br />
Provider is responsible to verify eligibility <strong>and</strong> coverage before<br />
services are rendered.<br />
Reimbursement<br />
For the <strong>Minnesota</strong> Health Care Program members affected by this<br />
benefit change, <strong>Blue</strong> Plus will reimburse the provider for the<br />
rehabilitative services at 100 percent (100%) <strong>of</strong> the provider’s<br />
charge. Per diem rates paid to the provider shall be the portion <strong>of</strong><br />
the per-day contract rate that relates to the rehabilitative mental<br />
health services plus two percent (2%) <strong>and</strong> shall not include group<br />
foster care costs or services that are billed to the county <strong>of</strong><br />
financial responsibility.<br />
11-95
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Children’s Residential<br />
Mental Health<br />
(Medicaid Government<br />
Programs only)<br />
(continued)<br />
IRTS (Medicaid<br />
Government Programs<br />
Only)<br />
11-96<br />
Providers may bill <strong>Blue</strong> Plus the then-current county rate at the<br />
percentage determined by DHS to be eligible for reimbursement<br />
by Medical Assistance plus two percent (2%). Further, the<br />
provider should seek reimbursement for the room <strong>and</strong> board<br />
portion <strong>of</strong> facility costs from the local agency (County), not from<br />
<strong>Blue</strong> Plus.<br />
Groups Affected<br />
This change applies to the following <strong>Minnesota</strong> Health Care<br />
Programs:<br />
<strong>Blue</strong> Plus<br />
Product <strong>Name</strong> Group Numbers<br />
<strong>Blue</strong> Advantage (PMAP) PP021, PP022, PP024, PP025,<br />
PP026, PP027<br />
<strong>Minnesota</strong>Care PP111, PP112, PP151, PP152<br />
<strong>Blue</strong> <strong>Cross</strong> will reimburse certain categories <strong>of</strong> providers for these<br />
services, which were formerly reimbursed through the <strong>Minnesota</strong><br />
Department <strong>of</strong> Human Services (DHS).<br />
This change was effective for all enrollees in the Prepaid Medical<br />
Assistance Programs (PMAP), <strong>Minnesota</strong> Senior Health Options<br />
(MSHO) <strong>and</strong> <strong>Minnesota</strong> Disabled Health Options (MnDHO).<br />
Crisis response services include:<br />
Crisis assessment<br />
Crisis intervention<br />
Crisis stabilization<br />
Community intervention<br />
The following summarizes provider eligibility, member eligibility<br />
<strong>and</strong> operational requirements for <strong>Blue</strong> Plus providers <strong>of</strong> these<br />
services.<br />
All members <strong>of</strong> the following <strong>Blue</strong> Plus products are eligible to<br />
receive these services:<br />
<strong>Blue</strong> Advantage (<strong>Blue</strong> Plus PMAP, <strong>and</strong> <strong>Minnesota</strong> Senior<br />
CarePlus)<br />
<strong>Minnesota</strong>Care<br />
Care<strong>Blue</strong><br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
IRTS (Medicaid<br />
Government Programs<br />
Only) (continued)<br />
IRTS/Crisis Provider<br />
Eligibility<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Group numbers for these products are listed below.<br />
<strong>Blue</strong> Plus<br />
Products Group Numbers<br />
<strong>Blue</strong><br />
Advantage<br />
<strong>Minnesota</strong><br />
Senior Care<br />
Plus<br />
<strong>Minnesota</strong>Care<br />
Exp<strong>and</strong>ed<br />
<strong>Minnesota</strong>Care<br />
Basic Plus,<br />
Basic +1,<br />
Basic +2<br />
Secure<strong>Blue</strong><br />
(MSHO)<br />
PP011, PP012, PP014, PP015, PP016, PP017,<br />
PP021, PP022, PP024, PP025, PP026, PP027,<br />
PP031, PP032, PP034, PP035, PP036, PP037,<br />
PP411, PP412, PP414<br />
PP041, PP042, PP044, PP051, PP052, PP054,<br />
PP055, PP056, PP057, PP061, PP062, PP064,<br />
PP071, PP072, PP074, PP075, PP076, PP077<br />
PP111, PP112, PP151, PP152<br />
PP121, PP122, PP131, PP132, PP141, PP142,<br />
PP161, PP162, PP163, PP164<br />
PP200, PP201, PP202, PP215, PP220, PP221,<br />
PP222, PP240, PP245, PP260, PP261, PP262,<br />
PP280, PP281, PP282<br />
Members with commercial coverage may be eligible to receive<br />
these services. Please verify member eligibility using one <strong>of</strong> the<br />
resources described below under Member eligibility.<br />
To provide this type <strong>of</strong> treatment, providers must:<br />
Be licensed under Rule 36<br />
Have DHS approval<br />
Be a participating provider with <strong>Blue</strong> <strong>Cross</strong><br />
Pr<strong>of</strong>essional treatment services may only be provided by an<br />
eligible IRTS Crisis provider.<br />
11-97
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
IRTS Member<br />
Eligibility<br />
IRTS Access to<br />
Services<br />
Billing for IRTS or<br />
Residential Crisis<br />
Court Ordered<br />
Treatment<br />
11-98<br />
Providers are expected to check the member’s eligibility before<br />
rendering services. Resources available for verification include:<br />
MN-ITS<br />
www.mn-its.dhs.state.mn.us<br />
EVS<br />
1-800-657-3613<br />
Provider Web Self-Service<br />
www.providerhub.com<br />
Provider Services<br />
1-800-262-0820<br />
Direct access to contracted providers<br />
No prior authorizations required<br />
No referrals required<br />
Non-contracted providers must obtain a referral from provider<br />
services at 1-800-262-0820 prior to delivering treatment.<br />
When reporting room <strong>and</strong> board <strong>and</strong>/or treatment services, report<br />
on the 837I type <strong>of</strong> bill 86X, with the room <strong>and</strong> board <strong>and</strong><br />
treatment services as separate line items. Submit the room <strong>and</strong><br />
board charges under revenue code 1001 <strong>and</strong> the treatment services<br />
under revenue codes 090X or 091X.<br />
When room <strong>and</strong> board <strong>and</strong> treatment are billed to separate entities,<br />
treatment is reported on the 837P, with HCPCS code H0018 or<br />
H0019.<br />
When a court order for treatment is based on an evaluation <strong>and</strong><br />
recommendation by a physician, licensed Ph.D. level psychologist,<br />
licensed alcohol <strong>and</strong> drug dependency counselor or a certified<br />
chemical dependency assessor (rule 25) we will consider the order<br />
for treatment medically necessary.<br />
<strong>Blue</strong> <strong>Cross</strong> will provide coverage for these court ordered services<br />
according to the patient's contract benefits. For example, if the<br />
member does not have inpatient chemical dependency benefits <strong>and</strong><br />
the patient is court ordered into inpatient chemical dependency<br />
treatment, there will be no coverage for the services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Court Ordered<br />
Treatment<br />
(continued)<br />
Preadmission<br />
Notification<br />
Residential Substance<br />
Abuse Admission <strong>and</strong><br />
Concurrent Review<br />
Process Change<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
If a participating provider is providing services, a copy <strong>of</strong> the court<br />
order should be retained in the patient’s chart in the provider’s<br />
<strong>of</strong>fice. If the patient sees a nonparticipating provider, a copy <strong>of</strong> the<br />
court order <strong>and</strong> MN Universal form should be submitted as soon as<br />
possible so the necessary approval can be entered into the claim<br />
system to ensure accurate payment <strong>of</strong> any claims. This can be<br />
faxed to Integrated Health Management at (651) 662-0854.<br />
If the court order is to a specific non-network provider but the<br />
member does not have any benefits for non-network providers,<br />
<strong>Blue</strong> <strong>Cross</strong> will cover the services as they would for in-network<br />
providers. However, fee-for-service members will be responsible<br />
for the difference between the billed amount <strong>and</strong> <strong>Blue</strong> <strong>Cross</strong>'<br />
allowed amount.<br />
Call (651) 662-2474 or 1-800-262-0820 or fax form X13459 to<br />
(651) 662-0856 to notify <strong>Blue</strong> <strong>Cross</strong> <strong>of</strong> admissions into day<br />
treatment, partial psychiatric or inpatient programs.<br />
PAN Requirements<br />
A PAN is required for all residential substance abuse services,<br />
including services that were previously determined to be halfway<br />
house or extended care. Coverage for services is based on the<br />
specifics <strong>of</strong> each member’s benefits. The PAN requirement is for<br />
all members who are enrolled in a fully insured plan or <strong>Minnesota</strong><br />
Health Care Program.<br />
Concurrent Review<br />
In addition to the PAN requirements, at day 21 <strong>of</strong> an<br />
inpatient/residential stay, a concurrent review is required with a<br />
medical necessity review. <strong>Blue</strong> <strong>Cross</strong> will conduct the medical<br />
necessity review based on an updated completion <strong>of</strong> the<br />
Department <strong>of</strong> Human Services (DHS) Dimensions Criteria <strong>and</strong><br />
the submission <strong>of</strong> a current individualized treatment plan. A copy<br />
<strong>of</strong> the DHS Dimensions Criteria <strong>and</strong> Assessment is located on the<br />
DHS website at<br />
http://edocs.dhs.state.mn.us/lfserver/Legacy/DHS-2794-ENG.<br />
<strong>Blue</strong> <strong>Cross</strong> will not provide courtesy calls to providers notifying<br />
them <strong>of</strong> missing preadmission notification (PAN) or concurrent<br />
review information. If PAN or concurrent review information is<br />
not received, the claim will deny as provider liability.<br />
11-99
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Residential Substance<br />
Abuse Admission <strong>and</strong><br />
Concurrent Review<br />
Process Change<br />
(continued)<br />
Pre-certification <strong>and</strong><br />
Concurrent Review for<br />
Inpatient/Residential<br />
Mental Health <strong>and</strong><br />
Substance Use<br />
Disorder services<br />
11-100<br />
PAN Form<br />
If you have provider web self-service, submit the PAN request<br />
electronically by creating an admission notification on<br />
providerhub.com. A copy <strong>of</strong> the PAN form is also available on<br />
the <strong>Blue</strong> <strong>Cross</strong> website at providers bluecrossmn.com. For<br />
providers that do not have provider web self-service, the PAN<br />
form should be faxed to (651) 662-7006 or called in to<br />
(651) 662-5200 or 1-800-262-0820.<br />
<strong>Blue</strong> <strong>Cross</strong> Policy<br />
Failure to comply with the PAN or concurrent review requirements<br />
within 10 business days from the request will result in claims<br />
being denied as provider liability.<br />
To help assure that members receive the appropriate level <strong>of</strong> care<br />
for mental health <strong>and</strong> substance use disorder treatment, <strong>Blue</strong><br />
<strong>Cross</strong>, as done with other medical/surgical services, implemented<br />
certain pre-certification <strong>and</strong> concurrent review protocols for<br />
inpatient/residential services.<br />
This program will continue to exp<strong>and</strong> throughout 2010, <strong>and</strong><br />
impacted providers will receive additional information once these<br />
requirements are exp<strong>and</strong>ed.<br />
Pre-certification <strong>and</strong> concurrent review applies to health services<br />
provided to members in fully insured <strong>and</strong> self-insured benefit<br />
plans, including <strong>Minnesota</strong> Health Care Programs, with the<br />
exception <strong>of</strong> <strong>Minnesota</strong> Senior Care Plus (MSC+), Secure<strong>Blue</strong><br />
(HMO SNP), (HMO), Platinum <strong>Blue</strong> (Cost) <strong>and</strong> Medicare<strong>Blue</strong><br />
PPO (Regional PPO) members. Medicare supplement benefit plans<br />
are also excluded from review. This also does not apply to court<br />
ordered admissions to inpatient/residential treatment. Coverage for<br />
court ordered mental health services is detailed in <strong>Minnesota</strong><br />
Statute 62Q.535.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Pre-certification <strong>and</strong><br />
Concurrent Review for<br />
Inpatient/Residential<br />
Mental Health <strong>and</strong><br />
Substance Use<br />
Disorder services<br />
(continued)<br />
Definitions<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
"Pre-certification" means an advance review <strong>of</strong> a proposed facility<br />
admission or certain services or procedures in order to determine<br />
whether the proposed admission, services or procedures meet the<br />
medical necessity criteria for payment <strong>and</strong> to ensure that the<br />
subscriber receives the maximum benefits available under the<br />
subscriber’s plan. "Concurrent review" means ongoing review<br />
during the subscriber’s care, to ensure that it meets established<br />
medical criteria in a timely manner <strong>and</strong> certifies the necessity, <strong>and</strong><br />
the appropriateness, <strong>and</strong> quality <strong>of</strong> services during an inpatient<br />
admission.<br />
Pre-certification Requirements<br />
Provider will obtain pre-certification from <strong>Blue</strong> <strong>Cross</strong> before<br />
admitting a member. If admission is emergent or after business<br />
hours, provider will obtain pre-certification within two (2)<br />
business days after the admission.<br />
Provider shall obtain pre-certification by calling <strong>Blue</strong> <strong>Cross</strong> at<br />
(651) 662-5270 or toll free at 1-800-528-0934. <strong>Blue</strong> <strong>Cross</strong> will use<br />
criteria set forth in the Level <strong>of</strong> Care Utilization System (LOCUS)<br />
<strong>and</strong> Child <strong>and</strong> Adolescent Services Intensity Instrument (CASII)<br />
for mental health or the Dimensions criteria for substance use<br />
disorders in conducting a medical necessity review for the<br />
admission.<br />
Failure to provide evidence <strong>of</strong> medical necessity may result in<br />
claim denials as provider liability.<br />
Concurrent Review Requirements<br />
Providers have a contractual obligation as noted in Chapter 4 <strong>of</strong><br />
the online <strong>Blue</strong> <strong>Cross</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> to<br />
adhere to care management programs. At the time <strong>of</strong> precertification<br />
a date will be established to conduct concurrent<br />
review.<br />
Concurrent review will include verification <strong>of</strong> medical necessity<br />
based on criteria set forth in the LOCUS <strong>and</strong> CASII for mental<br />
health or the Dimensions criteria for substance use disorders.<br />
Failure to provide evidence <strong>of</strong> medical necessity may result in<br />
claim denials as provider liability.<br />
11-101
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Referrals <strong>Blue</strong> <strong>Cross</strong> does not require a referral for patients seeking care<br />
within the Select Behavioral Health Network. For complete<br />
information on requirements for <strong>Minnesota</strong> Health Care Programs,<br />
see Chapter 3 <strong>of</strong> the <strong>Blue</strong> Plus <strong>Manual</strong>.<br />
11-102<br />
Services sought outside the Select Behavioral Health Network but<br />
within the Aware network will be processed according to the<br />
patient's self-referral benefit. If the patient has specialty needs,<br />
continuity <strong>of</strong> care issues, transition <strong>of</strong> care issues, or cannot access<br />
behavioral health services within the required provider network<br />
within a reasonable time period or due to geographical or physical<br />
accessibility reasons, the provider should contact <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
request a referral. A referral may be approved depending on the<br />
patient's situation.<br />
If services are sought outside both the Select network <strong>and</strong> the<br />
Aware network <strong>and</strong> the member does not have self-referral<br />
benefits, then <strong>Blue</strong> <strong>Cross</strong> should be contacted <strong>and</strong> the situation<br />
reviewed for a possible referral approval.<br />
Parity Federal <strong>and</strong> state m<strong>and</strong>ates dictate mental health parity laws that<br />
are applicable to all fully insured groups. Self-insured groups are<br />
not subject to parity legislation, but they may elect to follow these<br />
laws.<br />
Parity means that treatment for substance abuse <strong>and</strong>/or mental<br />
health is covered the same as any other inpatient <strong>and</strong>/or outpatient<br />
medical benefit. For example, if a member has coverage for an<br />
illness E/M service from a non-network provider, then that<br />
member will also have coverage for a behavioral health service<br />
from a non-network provider.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Groups that Carve Out<br />
Behavioral Health<br />
Benefits<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Some self-insured groups contract with another carrier to manage<br />
their behavioral health benefits. This means that their behavioral<br />
health claims should be filed to the designated third party<br />
behavioral health carrier for processing. This carrier’s information<br />
should be obtained from the patient.<br />
E/M services (codes 99201-99215) <strong>and</strong> medication management<br />
services (codes 90862 or M0064) billed with a behavioral health<br />
diagnosis for carve out group members should be billed to <strong>Blue</strong><br />
<strong>Cross</strong> as long as the practitioner is a non-behavioral health<br />
practitioner or a multi-specialty clinic. If one <strong>of</strong> these services is<br />
denied, <strong>Blue</strong> <strong>Cross</strong> should be contacted for it to be reprocessed.<br />
These services will be paid at the behavioral health benefit but will<br />
not accumulate towards patients’ behavioral health benefit<br />
maximums. Any other behavioral health treatment for carve out<br />
group members that is billed to <strong>Blue</strong> <strong>Cross</strong> will be denied.<br />
Provider Networks There are two behavioral health provider networks: the Select<br />
Behavioral Health Network <strong>and</strong> the Aware network.<br />
Most <strong>Blue</strong> Plus patients are required to utilize a Select provider for<br />
their highest level <strong>of</strong> benefits. Many but not all members have selfreferral<br />
benefits that are applied when services are obtained in the<br />
Aware network. To find a participating Select network provider,<br />
members are encouraged to call <strong>Blue</strong> <strong>Cross</strong> so that a provider best<br />
suited to meet their treatment needs can be found in a convenient<br />
location.<br />
The majority <strong>of</strong> fee-for-service members have direct access to an<br />
Aware network practitioner.<br />
Fully insured groups have the Select Behavioral Health Network.<br />
Some self-insured groups have the Select Behavioral Health<br />
Network while other self-insured groups may choose the Aware<br />
Network. Individual Accounts use the Aware Network.<br />
11-103
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Institutional Behavioral Health Coding Information<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus<br />
Code Description Units Notes on<br />
Use/Coverage<br />
0900 Behavioral Health Treatments/Services,<br />
General Classification<br />
0901 Behavioral Health Treatments/Services,<br />
Electroshock Treatment<br />
0902 Behavioral Health Treatments/Services,<br />
Milieu Therapy<br />
0903 Behavioral Health Treatments/Services,<br />
Play Therapy<br />
0904 Behavioral Health Treatments/Services,<br />
Activity Therapy<br />
0905 Behavioral Health Treatments/Services,<br />
Intensive Outpatient Services – Psychiatric<br />
0906 Behavioral Health Treatments/Services,<br />
Intensive Outpatient Services – Chemical<br />
Dependency<br />
0907 Behavioral Health Treatments/Services,<br />
Community Behavioral Health Program<br />
(Day Treatment)<br />
0911 Behavioral Health Treatments/Services,<br />
Rehabilitation<br />
0912 Behavioral Health Treatments/Services,<br />
Partial Hospitalization - Less Intensive<br />
11-104<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Not covered<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Not covered<br />
Compatible with<br />
behavioral health<br />
<strong>and</strong> accident dx<br />
only<br />
Only use for<br />
psychiatric<br />
rehabilitation<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12<br />
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Notes on<br />
Use/Coverage<br />
0913 Behavioral Health Treatments/Services,<br />
Partial Hospitalization - Intensive<br />
0914 Behavioral Health Treatments/Services,<br />
Individual Therapy<br />
0915 Behavioral Health Treatments/Services,<br />
Group Therapy<br />
0916 Behavioral Health Treatments/Services,<br />
Family Therapy<br />
0917 Behavioral Health Treatments/Services,<br />
Bio Feedback<br />
0918 Behavioral Health Treatments/Services,<br />
Testing<br />
0919 Behavioral Health Treatments/Services,<br />
Other Behavioral Health<br />
Treatments/Services<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
1 unit based on<br />
CPT/HCPCS<br />
0944 Drug Rehabilitation 1 unit based on<br />
CPT/HCPCS<br />
0945 Alcohol Rehabilitation 1 unit based on<br />
CPT/HCPCS<br />
0949 Other Therapeutic Services 1 unit based on<br />
CPT/HCPCS<br />
1000 Behavioral Health Accommodations,<br />
General Classification<br />
1001 Behavioral Health Accommodations,<br />
Residential Treatment – Psychiatric<br />
1002 Behavioral Health Accommodations,<br />
Residential Treatment – Chemical<br />
Dependency<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Incompatible with<br />
routine, prenatal or<br />
maternity dx<br />
Incompatible with<br />
routine, prenatal or<br />
maternity dx<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Compatible with<br />
behavioral health <strong>and</strong><br />
accident dx only<br />
Requires description <strong>of</strong><br />
service<br />
1 per day Room <strong>and</strong> board<br />
1 per day Room <strong>and</strong> board<br />
1 per day Room <strong>and</strong> board<br />
11-105
Coding Policies <strong>and</strong> Guidelines (Behavioral Health)<br />
Code Description Units Notes on<br />
Use/Coverage<br />
1003 Behavioral Health Accommodations,<br />
Supervised Living<br />
1004 Behavioral Health Accommodations,<br />
Halfway House<br />
1005 Behavioral Health Accommodations,<br />
Group Home<br />
11-106<br />
1 per day Room <strong>and</strong> board<br />
Not covered<br />
1 per day Room <strong>and</strong> board<br />
Not covered<br />
1 per day Room <strong>and</strong> board<br />
Not covered<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 06/19/12
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Chiropractic)<br />
Table <strong>of</strong> Contents<br />
Coding Overview................................................................................................................. 11-2<br />
Examination Codes ..............................................................................................................11-2<br />
Chiropractic Manipulation Treatment.................................................................................. 11-3<br />
Chiropractic Manipulation with Visit .................................................................................. 11-4<br />
<strong>Manual</strong> Therapy................................................................................................................... 11-4<br />
Massage Therapy ................................................................................................................. 11-5<br />
Conjunctive Therapy, Modality: Office, Home or Nursing Home......................................11-6<br />
Maintenance or Palliative Care............................................................................................ 11-6<br />
Source <strong>of</strong> Condition ............................................................................................................. 11-6<br />
Diagnostic Services.............................................................................................................. 11-6<br />
Radiology Coverage Restriction.......................................................................................... 11-7<br />
Practicing in Multidisciplinary Clinics ................................................................................11-7<br />
Documentation Guides......................................................................................................... 11-8<br />
Prior Authorization .............................................................................................................. 11-9<br />
Form Required ..................................................................................................................... 11-9<br />
MHCP Chiropractic Authorization Process....................................................................... 11-10<br />
Compliance Audits............................................................................................................. 11-12<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Coding Overview Chiropractors should use CPT codes when billing for services.<br />
Providers should submit the code that most accurately identifies<br />
the service(s) performed, paying close attention to the attended<br />
versus unattended procedures (for example, 97032 versus 97014).<br />
The fact that a code exists does not guarantee the service is<br />
covered for all <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> members.<br />
The member's health coverage contract defines the services that<br />
are eligible for payment.<br />
Examination Codes An examination includes inspection <strong>of</strong> the patient <strong>and</strong> review <strong>of</strong><br />
diagnostic tests to diagnose disease or evaluate progress. Use <strong>of</strong><br />
the E/M codes must be supported within your medical record.<br />
11-2<br />
Per CPT, "Chiropractic manipulative treatment codes (98940-<br />
98943) include a pre-manipulation patient assessment. Additional<br />
E/M services may be reported separately using the modifier -25, if<br />
the patient's condition requires a significant, separately identifiable<br />
E/M service, above <strong>and</strong> beyond the usual pre-service <strong>and</strong> postservice<br />
work associated with the procedure."<br />
It would be inappropriate to bill 99214, 99215, 99204 or 99205<br />
along with manipulative treatment codes. These will be rejected as<br />
provider liability. Because a level 4 or 5 would require significant<br />
additional work, it would seldom be appropriate to bill both.<br />
Documentation in the patient’s record must support the additional<br />
E/M service.<br />
As noted by the <strong>Minnesota</strong> Chiropractic Association, an E/M<br />
would be appropriate for the following situations:<br />
New Patient<br />
A new patient is one who has not received any pr<strong>of</strong>essional<br />
services from the chiropractor or another chiropractor in the same<br />
group practice within the past three years.<br />
Established Patient – New Injury or Exacerbation<br />
The E/M is needed to obtain history <strong>and</strong> fully evaluate the patient's<br />
condition for an initial treatment plan or, in the event <strong>of</strong> an<br />
exacerbation, modify a previous treatment plan.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
Examination Codes<br />
(continued)<br />
Chiropractic<br />
Manipulation<br />
Treatment<br />
Established Patient – Re-examination<br />
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Periodic examinations are typically performed in order to formally<br />
assess the patient's response to treatment, progress, <strong>and</strong> make<br />
necessary changes to the treatment plan.<br />
For any <strong>of</strong> the above circumstances, a -25 modifier must be<br />
submitted on the E/M service if there was a significant separately<br />
identifiable E/M service.<br />
The chiropractic manipulation treatment codes (CMT) include a<br />
pre-manipulation patient assessment, the adjustment, <strong>and</strong><br />
evaluation <strong>of</strong> the effect <strong>of</strong> treatment. The CMT codes 98940-98942<br />
are used to indicate the number <strong>of</strong> spinal areas manipulated. CMT<br />
code 98943 is used to report chiropractic manipulation <strong>of</strong> one or<br />
more <strong>of</strong> the extra-spinal regions (head region; lower extremities;<br />
upper extremities; rib cage; abdomen).<br />
PRE Service<br />
PRE Service work may include a review <strong>of</strong>:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
the patient’s records<br />
their diagnostic tests<br />
communication with other providers<br />
the actual preparations for care<br />
INTRA Service<br />
INTRA Service work would include:<br />
discussion about the service with the patient<br />
a pertinent evaluation <strong>and</strong> assessment <strong>of</strong> the patient<br />
the procedure<br />
POST Service<br />
POST Service work includes:<br />
an evaluation <strong>and</strong> discussion with the patient about the effect<br />
<strong>of</strong> treatment<br />
arrangement <strong>of</strong> additional services or referral to another<br />
provider<br />
discussion <strong>of</strong> the case with other providers<br />
review <strong>of</strong> literature about the patient’s condition<br />
documenting the service<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Chiropractic<br />
Manipulation with Visit<br />
If an evaluation <strong>and</strong> management service is done with the<br />
manipulation, the E/M will deny unless it is submitted with a -25<br />
modifier, signifying significant, separately identifiable illness or<br />
injury. A level 4 or 5 E/M (99204, 99205, 99214, 99215) will be<br />
denied as provider liability because these levels would require<br />
significant additional work, <strong>and</strong> it is seldom appropriate to bill<br />
both.<br />
<strong>Manual</strong> Therapy 97140, manual therapy techniques (e.g., mobilization/<br />
manipulation, manual lymphatic drainage, manual traction), one or<br />
more regions, each 15 minutes.<br />
11-4<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus will not<br />
reimburse providers for manual therapy services. <strong>Manual</strong> therapy<br />
will deny either as incidental (provider liability) or subscriber<br />
liability.<br />
Provider liable:<br />
<strong>Manual</strong> therapy (97140) will be denied incidental (provider liable)<br />
to chiropractic manipulations billed on the same date <strong>of</strong> service.<br />
The denial will be upheld regardless <strong>of</strong> submission <strong>of</strong> the -59<br />
modifier. Based on chart documentation review, <strong>Blue</strong> <strong>Cross</strong> found<br />
that manual therapy services submitted with the -59 modifier did<br />
not clearly indicate it as a distinct service. Thus we have adopted a<br />
corporate policy to disallow 97140 submitted with the -59<br />
modifier. Additionally, submission <strong>of</strong> the -GA modifier will not<br />
affect or change the denial.<br />
Patient Billing Impact<br />
The patient is not responsible <strong>and</strong> must not be balance billed for<br />
any procedures for which payment has been denied or reduced by<br />
<strong>Blue</strong> <strong>Cross</strong> as the result <strong>of</strong> a coding edit. Edit denials are designed<br />
to ensure appropriate coding <strong>and</strong> to assist in processing claims<br />
accurately <strong>and</strong> consistently.<br />
Subscriber liable:<br />
Coverage for manual therapy (97140) services provided without a<br />
chiropractic manipulation is subject to the members’ contract<br />
benefits.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Massage Therapy 97124 Therapeutic procedure, one or more areas, each 15 minutes;<br />
massage, including effleurage, petrissage <strong>and</strong>/or tapotement<br />
(stroking, compression, percussion).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus will not<br />
reimburse providers for massage therapy services. Massage<br />
therapy will deny either as incidental (provider liability) or<br />
subscriber liability.<br />
Massages that are provided as preparation for a chiropractic<br />
manipulation are considered an integral part <strong>of</strong> the chiropractic<br />
manipulation. As such, we will deny it as provider liability. If a<br />
massage is billed alone, then it will be denied as a subscriber<br />
contract exclusion.<br />
Provider liable:<br />
Massage therapy (97124) will be denied incidental (provider<br />
liable) to chiropractic manipulations billed on the same date <strong>of</strong><br />
service. The denial will be upheld regardless <strong>of</strong> submission <strong>of</strong> the -<br />
59 modifier. Based on chart documentation review, <strong>Blue</strong> <strong>Cross</strong><br />
found that massage therapy services submitted with the -59<br />
modifier did not clearly indicate it as a distinct service. Thus we<br />
have adopted a corporate policy to disallow 97124 submitted with<br />
the -59 modifier. Additionally, submission <strong>of</strong> the -GA modifier<br />
will not affect or change the denial.<br />
Patient Billing Impact<br />
The patient is not responsible <strong>and</strong> must not be balance billed for<br />
any procedures for which payment has been denied or reduced by<br />
<strong>Blue</strong> <strong>Cross</strong> as the result <strong>of</strong> a coding edit. Edit denials are designed<br />
to ensure appropriate coding <strong>and</strong> to assist in processing claims<br />
accurately <strong>and</strong> consistently.<br />
Subscriber liable:<br />
Coverage for massage therapy (97124) services provided without a<br />
chiropractic manipulation is subject to the member’s contract<br />
benefits. Many benefit plans do not cover this service.<br />
An independent massage therapist is an ineligible provider.<br />
When a massage therapist is employed <strong>and</strong> supervised by the<br />
chiropractor, chiropractor should submit procedure code 97124<br />
with a -U7 modifier.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Conjunctive Therapy,<br />
Modality: Office, Home<br />
or Nursing Home<br />
Maintenance or<br />
Palliative Care<br />
Therapies must be used in conjunction with adjustment or<br />
manipulation on the same day for most contracts. If more than one<br />
therapy is done per treatment, submit documentation with the<br />
claim to support the necessity for the additional therapy.<br />
Rehabilitation services that would not result in measurable<br />
progress relative to established goals are non-covered services.<br />
The “AT” modifier distinguishes active/corrective treatment from<br />
maintenance therapy. The AT modifier should be appended to the<br />
chiropractic manipulation (98940-98943). The absence <strong>of</strong> the AT<br />
modifier would indicate maintenance or palliative care.<br />
Source <strong>of</strong> Condition Incorrect coding <strong>of</strong> "source <strong>of</strong> condition" is the major reason for<br />
delay in processing chiropractic claims. Follow the procedures<br />
outlined below to eliminate claim delays.<br />
Illness<br />
Typically an illness diagnosis is found in the 700 range <strong>of</strong><br />
ICD-9-CM codes. If services are not related to a specific injury,<br />
choose a diagnosis code outside <strong>of</strong> the ranges given below.<br />
Injury<br />
Injury is defined as bodily harm caused by an accident. The term<br />
includes all related conditions <strong>and</strong> recurrent symptoms. If services<br />
are related to a specific injury, choose a diagnosis code in the<br />
800-977 <strong>and</strong> 980-994 ranges.<br />
Submit the date <strong>of</strong> injury whenever the services are related to a<br />
specific injury. An exacerbation is not necessarily the result <strong>of</strong> an<br />
injury; therefore the appropriate illness diagnosis should be<br />
submitted.<br />
Diagnostic Services Use CPT codes to submit laboratory <strong>and</strong> X-ray services. The<br />
number <strong>of</strong> services on your claim must be the number <strong>of</strong><br />
procedures performed not the number <strong>of</strong> views taken.<br />
11-6<br />
For example:<br />
Code Units<br />
71020 (Chest X-ray, 2 views) 1<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
Radiology Coverage<br />
Restriction<br />
Practicing in<br />
Multidisciplinary<br />
Clinics<br />
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
<strong>Blue</strong> <strong>Cross</strong> will not reimburse for many imaging services when<br />
billed by a chiropractor. This policy applies to all High Tech<br />
Diagnostic Imaging (HTDI) procedures, including CT Scans <strong>and</strong><br />
MRI services, in addition to the procedures below. This will allow<br />
<strong>Blue</strong> <strong>Cross</strong> to better manage these high-cost radiology services.<br />
These claims will be denied as provider liability.<br />
71260 71550 72192 72193 72194<br />
73221 73721 74150 74160 74170<br />
74183 76140 76496 76536 76800<br />
76856 76870 76977 77057 77080<br />
<strong>Blue</strong> <strong>Cross</strong> will continue to allow chiropractors to order medically<br />
necessary radiology services, as permitted by the provider’s scope<br />
<strong>of</strong> practice. In instances where HTDI is ordered, chiropractors<br />
should direct patients to designated HTDI providers. For additional<br />
information on HTDI requirements, <strong>and</strong> a list <strong>of</strong> HTDI providers<br />
<strong>and</strong> procedures, reference the <strong>Blue</strong> <strong>Cross</strong> website at<br />
providers.bluecrossmn.com <strong>and</strong> select High Tech Diagnostic<br />
Imaging under Tools & Resources.<br />
Services billed for consultation on X-ray exams performed<br />
elsewhere (CPT 76140) will not be payable, as <strong>Blue</strong> <strong>Cross</strong> already<br />
reimburses for both the pr<strong>of</strong>essional <strong>and</strong> technical component <strong>of</strong><br />
most radiology services. Re-interpretation <strong>of</strong> a film is a duplication<br />
<strong>of</strong> these other components.<br />
<strong>Blue</strong> <strong>Cross</strong> will continue to allow chiropractors to perform, bill<br />
<strong>and</strong> be reimbursed for most traditional X-ray films based on the<br />
member’s benefits.<br />
Chiropractors practicing in multidisciplinary clinics shall maintain<br />
a separate contract <strong>and</strong> billing number.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Documentation Guides To avoid denials for medical necessity, the patient’s medical<br />
record must contain certain pertinent information that may be<br />
subject to our review. The Centers for Medicare <strong>and</strong> Medicaid<br />
Services (CMS) in conjunction with the American Medical<br />
Association (AMA) has developed guidelines for the medical<br />
documentation necessary to support a given level <strong>of</strong> evaluation <strong>and</strong><br />
management service. <strong>Blue</strong> <strong>Cross</strong> has adopted these guidelines to<br />
ensure that our members receive quality care <strong>and</strong> that the services<br />
are consistent with the insurance coverage provided. The general<br />
guidelines are listed below:<br />
11-8<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
The medical record should be complete <strong>and</strong> legible.<br />
The documentation <strong>of</strong> each patient encounter should include:<br />
• reason for the encounter <strong>and</strong> relevant history, physical<br />
examination findings <strong>and</strong> prior diagnostic test results<br />
• plan <strong>of</strong> care<br />
Documentation must be signed <strong>and</strong> dated by the practitioner<br />
rendering the service; electronic signature is acceptable but<br />
must be noted on the record.<br />
If not documented, the rationale for ordering diagnostic <strong>and</strong><br />
other ancillary services should be easily inferred.<br />
Past <strong>and</strong> present diagnoses should be accessible to the treating<br />
<strong>and</strong>/or consulting physician.<br />
Appropriate health risk factors should be identified.<br />
The patient’s progress, response <strong>and</strong> changes in treatment, <strong>and</strong><br />
revision <strong>of</strong> diagnosis should be documented.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
Documentation Guides<br />
(continued)<br />
•<br />
•<br />
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
The CPT/HCPCS <strong>and</strong> ICD-9-CM codes reported on the health<br />
insurance claim form or billing statement should be supported<br />
by the documentation in the medical record. Charge slips,<br />
super bills, travel cards, or <strong>of</strong>fice ledgers are not considered<br />
supporting documentation for services provided to a patient.<br />
Use <strong>of</strong> the term IBID <strong>and</strong>/or the use <strong>of</strong> quotation marks to<br />
replace or repeat previously documented information is not<br />
acceptable. All information must be in date-sequence order.<br />
Services not documented as indicated are not covered by <strong>Blue</strong><br />
<strong>Cross</strong>. Patients are not financially liable for services that are<br />
denied for inadequate documentation. In addition, chart<br />
documentation should clearly list the name <strong>of</strong> the practitioner<br />
rendering services to the member, including the names <strong>and</strong><br />
credentials <strong>of</strong> employees providing care under the supervision <strong>of</strong> a<br />
chiropractor.<br />
Prior Authorization Chiropractic services rendered by Aware Chiropractic Providers<br />
are not subject to prior authorization for members <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong><br />
<strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> fully insured groups. For <strong>Blue</strong> <strong>Cross</strong><br />
self-insured groups, it is recommended that prior authorization for<br />
chiropractic services will be done after 20 visits. Benefits are<br />
allowable only for services that are medically necessary. Providers<br />
are encouraged to use provider web self-service or BLUELINE to<br />
obtain member benefits prior to beginning services.<br />
Form Required To obtain prior authorization, providers should complete the<br />
Chiropractic Medical Information Request Form, form number<br />
F4355 R12. This form can be found on the <strong>Blue</strong> <strong>Cross</strong> web site.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
MHCP Chiropractic<br />
Authorization Process<br />
11-10<br />
<strong>Blue</strong> Plus requires prior authorization for chiropractic services<br />
beyond 12 visits per calendar year for <strong>Minnesota</strong> Health Care<br />
Programs members. Commercial lines <strong>of</strong> business are not<br />
impacted by this change.<br />
<strong>Minnesota</strong> Health Care Programs<br />
Group numbers for the affected products are as follows:<br />
Product <strong>Name</strong> Group Numbers<br />
<strong>Blue</strong> Advantage<br />
(PMAP)<br />
PP011, PP012, PP014, PP015, PP016,<br />
PP017, PP021, PP022, PP024, PP025,<br />
PP026, PP027, PP031, PP032, PP034,<br />
PP035, PP036, PP037<br />
<strong>Minnesota</strong>Care PP111, PP112, PP151, PP152, PP121,<br />
PP122, PP131, PP132, PP141, PP142,<br />
PP161, PP162, PP163, PP164<br />
<strong>Minnesota</strong> Senior Care<br />
Plus (MSC+)<br />
Secure<strong>Blue</strong> SM (HMO<br />
SNP)<br />
PP041, PP042, PP044, PP051, PP052,<br />
PP054, PP055, PP056, PP057, PP061,<br />
PP062, PP064, PP071, PP072, PP074,<br />
PP075, PP076, PP077<br />
All group numbers that begin with PP2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
MHCP Chiropractic<br />
Authorization Process<br />
(continued)<br />
Documentation Required<br />
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Prior authorization for visits beyond 12 should be submitted two<br />
weeks in advance <strong>of</strong> reaching the 12th visit. Fax your <strong>Blue</strong> Plus<br />
member requests to: (651) 662-4022 or 1-866-800-1665.<br />
Documentation needs to include all <strong>of</strong> the following information:<br />
•<br />
•<br />
•<br />
•<br />
Evaluation <strong>and</strong> diagnosis: Indicate how the subluxation<br />
diagnosis was determined<br />
Chief complaint: List member’s symptoms<br />
Assessment <strong>and</strong> treatment plan: Provide your physical<br />
assessment <strong>and</strong> treatment plan including when the member will<br />
be discharged, number <strong>of</strong> visits planned <strong>and</strong> frequency planned<br />
Rationale for continued treatment: Provide evidence <strong>of</strong><br />
member’s improvement with chiropractic services<br />
Prior Authorization Process<br />
To initiate prior authorization complete the Chiropractic Medical<br />
Information Request Form found in the forms section <strong>of</strong><br />
providers.bluecrossmn.com. You may also submit supporting<br />
information from your chart records in addition to completing the<br />
form. All documentation needs to be legible.<br />
The timeline for decisions is up to 10 business days. Decisions will<br />
be communicated via telephone or fax, <strong>and</strong> letter. Approvals are<br />
communicated via telephone with a letter as follow up. Denials are<br />
communicated with a fax copy <strong>of</strong> the denial letter <strong>and</strong> a follow-up<br />
letter sent by mail.<br />
MHCP coverage guidelines are followed for <strong>Minnesota</strong> Health<br />
Care Program members. All services must be medically necessary<br />
for continued coverage.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Chiropractic)<br />
Compliance Audits Your provider service agreement includes certain quality assurance<br />
requirements. Pursuant to this agreement, <strong>Blue</strong> <strong>Cross</strong> may conduct<br />
audits to evaluate a provider’s compliance with medical necessity<br />
guidelines <strong>and</strong> st<strong>and</strong>ards <strong>of</strong> practice in the community. Such an<br />
audit could include post-service claims review using provider<br />
utilization thresholds established by <strong>Blue</strong> <strong>Cross</strong> which may result<br />
in provider liability if care is determined to be not medically<br />
necessary or medically inappropriate.<br />
11-12<br />
Medical necessary services are directed toward a diagnosis or<br />
condition that is supported by documented subjective <strong>and</strong> objective<br />
findings. Medically necessary care means health care services are<br />
appropriate, in terms <strong>of</strong> type, frequency level, setting <strong>and</strong> duration,<br />
to the member’s diagnosis or condition, <strong>and</strong> diagnostic testing <strong>and</strong><br />
preventive services (<strong>Minnesota</strong> Rules 4685.0100 Subp.5). The<br />
intensity <strong>of</strong> treatment must be consistent with the severity or acuity<br />
<strong>of</strong> the patient’s current level <strong>of</strong> impairment <strong>and</strong>/or<br />
symptomatology. Additionally, there must be documentation <strong>of</strong><br />
reasonable progress consistent with the intensity <strong>of</strong> treatment <strong>and</strong><br />
the severity/acuity <strong>of</strong> the patient’s condition.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Dental Services)<br />
Table <strong>of</strong> Contents<br />
Medical-Surgical Procedures............................................................................................... 11-2<br />
Prior Authorization .............................................................................................................. 11-3<br />
Claim Form ..........................................................................................................................11-3<br />
Coordination Between Dental <strong>and</strong> Medical Carriers........................................................... 11-4<br />
TMJ Claims Submission......................................................................................................11-4<br />
Diagnostic Studies ............................................................................................................... 11-5<br />
Emergency Room.................................................................................................................11-5<br />
Dental Aware .......................................................................................................................11-5<br />
Dental Procedures <strong>and</strong> Pre-op/Medical Exams.................................................................... 11-5<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Dental Services)<br />
Medical-Surgical<br />
Procedures<br />
11-2<br />
Many <strong>of</strong> our member contracts cover several medical-surgical<br />
procedures that dentists perform. The procedures are:<br />
• Treatment (repair or replacement only) <strong>of</strong> accidental injury to<br />
natural teeth, which is not regular dental repair or maintenance.<br />
• Surgical <strong>and</strong> nonsurgical treatment <strong>of</strong> TMJ <strong>and</strong><br />
craniom<strong>and</strong>ibular disorder.<br />
• Treatment <strong>of</strong> cleft lip <strong>and</strong> palate for a dependent child up to<br />
age 19, if medically necessary.<br />
• Reconstructive surgery to correct a functional physical defect<br />
for dependent children — this would include orthognathic<br />
surgery. Treatment involving dental implants is specifically<br />
excluded.<br />
• Removal <strong>of</strong> cysts/lesion(s)/tumor(s) <strong>and</strong> the accompanying<br />
pathology reports, scans, <strong>and</strong> anesthesia <strong>and</strong> allowable<br />
supplies.<br />
Certain dental services may be reported using either a CPT or<br />
dental HCPCS code. CPT codes are generally five numeric digits.<br />
Dental HCPCS codes, which are developed by the American<br />
Dental Association (ADA), start with the letter D <strong>and</strong> are followed<br />
by four numeric digits.<br />
It is important to note that pricing will vary between a comparable<br />
CPT <strong>and</strong> dental HCPCS code <strong>and</strong> that claims will be reimbursed<br />
based on the pricing associated with the code submitted. Pricing<br />
for CPT codes is based on Resource Based Relative Value System<br />
(RBRVS). Pricing for dental HCPCS codes is based on Delta<br />
Dental pricing.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
Coding Policies <strong>and</strong> Guidelines (Dental Services)<br />
Prior Authorization If a service requires prior authorization, make sure the CPT or<br />
dental HCPCS procedure code on the claim is the same as on the<br />
prior authorization. For example, if a dental HCPCS code is<br />
approved on a prior authorization, use the same code on the claim.<br />
Prior authorization requests<br />
Begin mailing or faxing prior authorization (PA) requests to:<br />
Utilization Management Dept. R4-72<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
P.O. Box 64265<br />
St. Paul, MN 55164-0265<br />
Fax: (651) 662-7816<br />
Prior authorization recommendations<br />
PAs are recommended for the following services:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Surgical TMJ services<br />
Orthognathic/osteotomies<br />
Orthodontics for TMJ <strong>and</strong> cleft lip/palate<br />
Bone grafts<br />
Treatment related to accidental injuries<br />
Claim Form Use an 837P electronic claim format when submitting dentalrelated<br />
claims (the ADA claim form is accepted, but <strong>Blue</strong> <strong>Cross</strong><br />
prefers the 837P). If you are using the ADA form, be sure to<br />
include the diagnosis if the treatment is accident related, for cleft<br />
lip/palate or TMJ diagnosis or include the narrative.<br />
Treatment <strong>of</strong> accidental injury to natural teeth<br />
• Initial treatment must begin within 12 months <strong>of</strong> the accidental<br />
injury <strong>and</strong> completed at 24 months from the date <strong>of</strong> initial<br />
treatment.<br />
• “Injury” does not include bruxism or biting <strong>and</strong> chewing.<br />
• Complete the “date <strong>of</strong> injury” field on the claim. Submit the<br />
appropriate accidental injury diagnosis code on the initial <strong>and</strong><br />
subsequent claims throughout treatment.<br />
• Include documentation in support <strong>of</strong> the accidental injury<br />
diagnosis or narrative description <strong>of</strong> the accident with the<br />
claim.<br />
Note: Prior authorization for anesthesia for children is not<br />
required. Benefits are paid in accordance with the contract.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Dental Services)<br />
Coordination Between<br />
Dental <strong>and</strong> Medical<br />
Carriers<br />
If you perform the types <strong>of</strong> service listed above for your patients,<br />
bill <strong>Blue</strong> <strong>Cross</strong> as usual. If the patient has a dental plan in addition<br />
to a medical-surgical policy, the dental plan is the primary payer.<br />
Note: If you receive payments from both the dental <strong>and</strong> medical<br />
plans for the same services, refund the medical carrier. We<br />
will coordinate up to our U&C allowances or billed charges,<br />
whichever is less.<br />
TMJ Claims Submission The following guidelines should be used when preparing TMJrelated<br />
disorder claims for submission:<br />
11-4<br />
Codes Guidelines<br />
ICM-9-CM The primary diagnosis code should be 524.60-<br />
524.69, temporom<strong>and</strong>ibular joint disorders. All<br />
other primary diagnosis codes submitted for TMJ<br />
<strong>and</strong> craniom<strong>and</strong>ibular disorders will be rejected.<br />
HCPCS<br />
codes<br />
CPT codes<br />
nonsurgical<br />
CPT codes<br />
surgical<br />
The HCPCS code for orthotic therapy should be<br />
D7880. All other orthotic codes submitted for TMJ<br />
<strong>and</strong> craniom<strong>and</strong>ibular disorders will be rejected.<br />
Study casts <strong>and</strong>/or mounted or unmounted study<br />
models are considered an integral part <strong>of</strong> the splint<br />
therapy <strong>and</strong> should not be billed separately.<br />
Orthotic adjustments <strong>and</strong> <strong>of</strong>fice call visits are<br />
considered an integral part <strong>of</strong> the orthotic therapy<br />
<strong>and</strong> should not be billed separately. Only the initial<br />
visit may be billed separately.<br />
The following procedure codes are considered<br />
eligible for reimbursement for surgical services <strong>of</strong><br />
the temporom<strong>and</strong>ibular joint: 21050, 21060, 21070,<br />
21073, 21240, 21242, 21243, 29804 (TMJ<br />
arthroscopy—surgical only).<br />
Note: All postoperative <strong>of</strong>fice visits are considered<br />
an integral part <strong>of</strong> the surgical fee <strong>and</strong> will be<br />
denied if billed separately during the global<br />
surgical period.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)
Coding Policies <strong>and</strong> Guidelines (Dental Services)<br />
Diagnostic Studies The following radiographs are considered eligible for TMJ<br />
disorders when medically necessary.<br />
Procedure Codes<br />
70328 70332 70355 70487<br />
70330 70336 70486 70488<br />
Benefits are not provided for cephalometric radiographs for TMJ<br />
disorders.<br />
Electromyography (EMG), Computerized M<strong>and</strong>ibular Scanner,<br />
Computerized Jaw Tracking/Motion Analysis, Doppler<br />
Auscultation, <strong>and</strong> Sonography/ultrasound are considered<br />
investigative <strong>and</strong> therefore ineligible when used in the diagnosis<br />
<strong>and</strong> treatment <strong>of</strong> temporom<strong>and</strong>ibular <strong>and</strong> craniom<strong>and</strong>ibular<br />
disorders.<br />
Emergency Room Emergency room services submitted with dental diagnosis will be<br />
processed as a medical service.<br />
Dental Aware All dental contracts are being administered by Delta Dental <strong>of</strong><br />
<strong>Minnesota</strong>. Please direct all correspondence to:<br />
Dental Procedures <strong>and</strong><br />
Pre-op/Medical Exams<br />
Delta Dental <strong>of</strong> <strong>Minnesota</strong><br />
P.O. Box 330<br />
Minneapolis, MN 55440<br />
Delta Dental <strong>of</strong> <strong>Minnesota</strong> is independent from <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
<strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong>. Delta Dental is solely responsible for<br />
administration <strong>of</strong> its dental products.<br />
When a member comes to your clinic for a pre-op exam for a<br />
dental related procedure, code the exam as a medical pre-op. The<br />
charges will fall under their medical benefits. Providers should<br />
only code as a pre-op exam if they know the procedure will be<br />
covered.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/12)<br />
11-5
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Durable Medical Equipment)<br />
Table <strong>of</strong> Contents<br />
Durable Medical Equipment (DME) Definition.................................................................. 11-2<br />
Enrollment Requirements when Providing Services to MHCP Subscribers .......................11-2<br />
Prior Authorization Requirements ....................................................................................... 11-3<br />
Ineligible Items ....................................................................................................................11-4<br />
DME Rental Guidelines.......................................................................................................11-5<br />
Medicare Advantage DME Rental Guidelines .................................................................... 11-5<br />
Waivers <strong>and</strong> Upgraded/Deluxe DME ..................................................................................11-7<br />
Waiver Claim Submission ................................................................................................... 11-7<br />
Sample Waiver Form ........................................................................................................... 11-8<br />
DME Coding........................................................................................................................ 11-8<br />
Sales Tax..............................................................................................................................11-9<br />
H<strong>and</strong>ling/ Conveyance......................................................................................................... 11-9<br />
Claims Filing Requirements ................................................................................................ 11-9<br />
Hearing Aids ......................................................................................................................11-10<br />
Oxygen <strong>and</strong> Oxygen Aiding Equipment (includes ventilators).........................................11-12<br />
Portable Oxygen Billing ....................................................................................................11-12<br />
Coding Modifiers............................................................................................................... 11-13<br />
DME Repairs <strong>and</strong> Maintenance (Excluding Oxygen Equipment).....................................11-14<br />
Replacement <strong>of</strong> Purchased Equipment .............................................................................. 11-14<br />
Billing for Supplies............................................................................................................ 11-15<br />
Rental Unit Submission .....................................................................................................11-16<br />
Hospital DME Providers.................................................................................................... 11-16<br />
DME/Supply Internet Purchases........................................................................................ 11-17<br />
E0935 Rental Guides ......................................................................................................... 11-17<br />
Pharmacies Submitting DME Claims ................................................................................11-17<br />
DME <strong>and</strong> Specialty Pharmacy Billed through the <strong>Blue</strong>Card ® Program............................11-18<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> 08/15/2012) 11-1
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Durable Medical<br />
Equipment (DME)<br />
Definition<br />
Enrollment<br />
Requirements when<br />
Providing Services to<br />
MHCP Subscribers<br />
11-2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) defines<br />
DME as equipment <strong>and</strong> related health care supplies <strong>and</strong> services<br />
that are:<br />
able to withst<strong>and</strong> repeated use; <strong>and</strong><br />
used primarily for a medical purpose; <strong>and</strong><br />
generally not useful in the absence <strong>of</strong> illness or injury; <strong>and</strong><br />
determined to be reasonable <strong>and</strong> necessary; <strong>and</strong><br />
prescribed by a physician; <strong>and</strong><br />
represents the most cost-effective alternative.<br />
Effective January 1, 2012, <strong>Minnesota</strong> Statutes Section 256B.0625<br />
requires that DME <strong>and</strong> Orthotic & Prosthetic (O&P) providers be<br />
enrolled as Medicare providers if the provider provides services to<br />
individuals enrolled in <strong>Minnesota</strong> Health Care Programs (MHCP).<br />
This includes subscribers enrolled in <strong>Blue</strong> Advantage (PMAP,<br />
<strong>Minnesota</strong>Care <strong>and</strong> <strong>Minnesota</strong> Senior Care Plus) <strong>and</strong><br />
Secure<strong>Blue</strong> SM (HMO SNP). Enrollment in Medicare requires that<br />
providers accept Medicare’s assignment <strong>of</strong> claims <strong>and</strong> payment for<br />
services. According to the Centers for Medicare & Medicaid<br />
Services (CMS), DME <strong>and</strong> O&P providers are enrolled as<br />
Medicare providers after their Medicare enrollment application has<br />
been completed <strong>and</strong> approved by Medicare.<br />
<strong>Minnesota</strong> Statutes Section 256B.0625, subd. 31 reads, in part, as<br />
follows: “Medical supplies <strong>and</strong> equipment… (b) Vendors <strong>of</strong><br />
durable medical equipment, prosthetics, orthotics, or medical<br />
supplies must enroll as a Medicare provider.”<br />
<strong>Blue</strong> <strong>Cross</strong> participating providers agree to comply with all<br />
applicable state <strong>and</strong> federal laws, rules, regulations, orders <strong>and</strong><br />
requirements. Therefore, all DME <strong>and</strong> O&P participating<br />
providers who provide services/products to MHCP <strong>and</strong> Medicare<br />
subscribers must be enrolled with Medicare per <strong>Minnesota</strong> Statutes<br />
Section 256B.0625.<br />
In addition to the changes noted above, <strong>Blue</strong> <strong>Cross</strong> requires all<br />
DME <strong>and</strong> O&P providers to submit the ordering <strong>and</strong> referring<br />
provider information via loop 2420E in the electronic transaction.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Prior Authorization<br />
Requirements<br />
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Fax all prior authorization requests for <strong>Blue</strong> <strong>Cross</strong> subscribers<br />
using the Prior Authorization Request for DME form (F5893-R02)<br />
to (651) 662-2810. <strong>Blue</strong> <strong>Cross</strong> will approve or deny prior<br />
authorization requests based on a subscriber's contract benefits <strong>and</strong><br />
the criteria defined in applicable medical policies. Prior<br />
authorization requests should be submitted by the DME supplier<br />
who will be providing the equipment <strong>and</strong> should include the<br />
appropriate HCPCS code(s).<br />
For questions about prior authorizations, call (651) 662-5270 or<br />
1-800-528-0934 (choose option 2, then option 4). Providers can<br />
also fax prior authorization questions to (651) 662-2810.<br />
Subscribers should call the number on the back <strong>of</strong> their subscriber<br />
ID card for customer service if they have questions.<br />
To access the most current medical policies including DME prior<br />
authorization (PA) list go to providers.bluecrossmn.com ><br />
“Tools <strong>and</strong> Resources” > Medical Policy.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Ineligible Items The following lists <strong>of</strong> some items that are considered ineligible<br />
DME. There is no need to submit prior authorization requests for<br />
ineligible items.<br />
Abdominal support belts<br />
for pregnant women<br />
Adaptive eating<br />
equipment<br />
Air conditioners<br />
Air filters<br />
Back huggers<br />
Balls for therapy<br />
Bedpans <strong>and</strong> urinals<br />
Bi<strong>of</strong>eedback device,<br />
purchase<br />
Blood pressure cuffs <strong>and</strong><br />
accessories<br />
Car seats<br />
Computer s<strong>of</strong>tware &<br />
hardware<br />
Copes scoliosis brace total<br />
recovery program<br />
Croup tent<br />
Cryocuff (icing device)<br />
Drionic devices (sweating<br />
devices)<br />
11-4<br />
Note: This is not an all-inclusive list. (For Medicaid products, see<br />
DHS website for <strong>Minnesota</strong> Health Care Programs manual.)<br />
Elevators/stairlifts<br />
Exercise equipment (e.g.<br />
bicycles, tricycles,<br />
treadmills <strong>and</strong> ski<br />
machines)<br />
Feeding chairs<br />
Floor sitters<br />
Formula, infant<br />
Grab bars<br />
Heating pads<br />
Home monitors<br />
Incontinence supplies (e.g.<br />
diapers, underpants,<br />
underpads, Attends)<br />
Lifeline medical alert<br />
Maternity belts<br />
Overbed tables<br />
Positioning aids (e.g.<br />
bolsters, wedges)<br />
Reachers<br />
Roman chairs<br />
Scales<br />
StimMaster E4000<br />
Telephone communication<br />
device (TTDY)<br />
Thera cane<br />
Tub stool or bench<br />
Vehicle modifications<br />
(h<strong>and</strong> controls, lifts <strong>and</strong><br />
car seats)<br />
Vitrectomy, seated<br />
support system (special<br />
chair for eye surgery<br />
patients)<br />
Wheelchair vehicle<br />
lift/ramps<br />
Whirlpools/Jacuzzi/hot<br />
tubs<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
DME Rental Guidelines Most DME can only be rented for 10 months. DME is considered<br />
purchased after 10 months <strong>of</strong> rental payments. Ten months rental<br />
for a particular item equals <strong>Blue</strong> <strong>Cross</strong> allowed amount for the<br />
purchase price <strong>of</strong> that item. No additional claims for rental or<br />
purchase <strong>of</strong> the same device should be submitted after the <strong>Blue</strong><br />
<strong>Cross</strong> allowed amount for the purchase price <strong>of</strong> that item has been<br />
met.<br />
Medicare Advantage<br />
DME Rental Guidelines<br />
The following items are rental only:<br />
Ventilators<br />
Negative-pressure ventilators<br />
CPM machines<br />
Oximeters<br />
Airway-pressure monitors oxygen concentrators<br />
Medicare Advantage DME claims are subject to Original Medicare<br />
claims processing supplier guidelines. The total number <strong>of</strong> months<br />
<strong>of</strong> capped rental DME payment is based on the date <strong>of</strong> service <strong>of</strong><br />
the initial capped rental. In all instances, when billing capped<br />
rentals, use the modifiers as outlined in Medicare’s claims<br />
processing manuals.<br />
For capped rentals, <strong>Blue</strong> <strong>Cross</strong> will reimburse monthly rental<br />
claims <strong>of</strong> continuous use for 13 months. The option to purchase<br />
at the 10 th month <strong>of</strong> rental no longer applies. After 13 months<br />
<strong>of</strong> continuous rental, ownership <strong>of</strong> the equipment is transferred<br />
to the subscriber. The first three rental months will be<br />
reimbursed based on the fee schedule amount. For the<br />
remaining rental months, the fee schedule amount will be<br />
reduced by 25 percent.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Medicare Advantage<br />
DME Rental Guidelines<br />
(continued)<br />
11-6<br />
Electric wheelchairs are an exception to this process. A<br />
purchase option must be given to the subscriber at the time the<br />
electric wheelchair is first provided, regardless <strong>of</strong> the initial<br />
date <strong>of</strong> service. <strong>Blue</strong> <strong>Cross</strong> recommends a prior authorization<br />
be completed for all wheelchair purchases. If the subscriber<br />
chooses to rent <strong>and</strong> not purchase the electric wheelchair at the<br />
time the item is provided, the length <strong>of</strong> rental (13 or 15<br />
months) is dependent upon the date <strong>of</strong> the initial rental.<br />
In accordance with Medicare, maintenance <strong>and</strong> service will be<br />
allowed on capped rental <strong>and</strong> where the subscriber chose the<br />
rental option only. Providers should bill for maintenance <strong>and</strong><br />
services using the appropriate HCPCS code <strong>and</strong> the modifier –<br />
MS.<br />
For capped rentals bill for replacement or repair using modifier<br />
RA or RB with the HCPCS code for the item serviced.<br />
RA Replacement <strong>of</strong> a DME, orthotic or prosthetic item.<br />
RB Replacement <strong>of</strong> a part <strong>of</strong> DME, orthotic or prosthetic item<br />
furnished as part <strong>of</strong> a repair.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Waivers <strong>and</strong><br />
Upgraded/Deluxe DME<br />
Waiver Claim<br />
Submission<br />
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
The following is <strong>Blue</strong> <strong>Cross</strong>’ policy for provision <strong>of</strong> upgraded or<br />
deluxe equipment. This policy does not apply to <strong>Minnesota</strong> Health<br />
Care Program subscribers because only medically necessary DME<br />
may be provided <strong>and</strong> billed to these subscribers.<br />
Providers may bill subscribers for an equipment upgrade or deluxe<br />
charge if a waiver is on file <strong>and</strong> the DME charges are billed<br />
correctly to <strong>Blue</strong> <strong>Cross</strong>. <strong>Blue</strong> <strong>Cross</strong> will continue to reimburse<br />
only for medically necessary st<strong>and</strong>ard DME. Providers must ask<br />
for a signed, written waiver that includes the cost for the deluxe<br />
features or upgrade. (A sample waiver form follows.)<br />
The waiver must state ALL <strong>of</strong> the following:<br />
The st<strong>and</strong>ard piece <strong>of</strong> equipment or least costly alternative was<br />
<strong>of</strong>fered to the subscriber; <strong>and</strong><br />
The subscriber is aware <strong>and</strong> agrees that <strong>Blue</strong> <strong>Cross</strong> will only<br />
pay the st<strong>and</strong>ard allowance; <strong>and</strong><br />
The subscriber will be responsible for the deluxe or upgrade<br />
charge in addition to his or her contractual obligation<br />
Providers must keep all signed waivers on file. Do not send waiver<br />
forms to <strong>Blue</strong> <strong>Cross</strong>. <strong>Blue</strong> <strong>Cross</strong> reserves the right to request<br />
waiver forms from a provider's <strong>of</strong>fice when necessary.<br />
Two lines <strong>of</strong> services must be billed. The first line will include the<br />
HCPCS code <strong>and</strong> the charge for the st<strong>and</strong>ard (non-deluxe)<br />
equipment with the GK modifier (in addition to any other<br />
appropriate modifier). This dollar amount will be subject to<br />
contract benefits <strong>and</strong> usual <strong>and</strong> customary reductions.<br />
The second line must include the same HCPCS code with the -GA<br />
modifier (waiver <strong>of</strong> liability statement issued as required by payer<br />
policy, individual case) <strong>and</strong> the amount charged for the upgrade or<br />
deluxe feature.<br />
For example:<br />
E0202 NU GK $550.00 (st<strong>and</strong>ard, charge that will be subject to<br />
st<strong>and</strong>ard allowance <strong>and</strong> subscriber contract benefits)<br />
E0202 GA $150.00 (deluxe/upgrade charge that will be denied<br />
as subscriber liability)<br />
The -GA modifier must be submitted as the first modifier on the<br />
second service line. Other applicable modifiers should be<br />
submitted on the first service line only.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Sample Waiver Form As a participating provider with <strong>Blue</strong> <strong>Cross</strong>, we are obligated to<br />
notify you <strong>of</strong> services that are medically unnecessary. This<br />
notification will allow us to hold you financially responsible for<br />
the upgrade to the DME that you are purchasing.<br />
We have <strong>of</strong>fered you the st<strong>and</strong>ard _______________________<br />
(list type <strong>of</strong> equipment)<br />
at the customary price <strong>of</strong> $________________ .<br />
We have informed you <strong>of</strong> the least costly alternative, which is<br />
the charge for the upgrade or deluxe features is $___________ .<br />
By signing <strong>and</strong> dating this waiver, you are acknowledging that:<br />
You are aware <strong>of</strong> <strong>and</strong> agree that <strong>Blue</strong> <strong>Cross</strong> will allow only<br />
st<strong>and</strong>ard equipment.<br />
Only the allowed amount for the st<strong>and</strong>ard equipment will apply<br />
to deductible <strong>and</strong> coinsurance amounts.<br />
You will be financially responsible for the deluxe or upgrade<br />
charge.<br />
The upgrade charge is in addition to any contractual<br />
obligations you have such as deductible <strong>and</strong> coinsurance<br />
amounts.<br />
Signature ____________________________ Date: _________<br />
DME Coding DME suppliers <strong>and</strong> others who bill supply items should use<br />
HCPCS level II codes. Our research shows that codes E1399 <strong>and</strong><br />
K0108 are used excessively <strong>and</strong> incorrectly. These should be used<br />
ONLY when there is no code listed in the HCPCS manual for the<br />
equipment. Do not use this code for supplies or equipment that can<br />
be coded with a specific code or combination <strong>of</strong> codes.<br />
11-8<br />
Unlisted codes (such as K0108 or E1399) require submission <strong>of</strong> a<br />
narrative describing the equipment along with the Manufacturers<br />
Suggested Retail Price (MSRP).<br />
Additional identification <strong>of</strong> the product or supply can be entered in<br />
the electronic claim in the NTE segment:<br />
837P: Loop 2400, Segment NTE<br />
837I: Loop 2300, Segment NTE<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Sales Tax Sales tax should generally be included in your charge for the item<br />
<strong>and</strong> not reported separately. If submitted, sales tax must be<br />
reported using code S9999 for the tax <strong>and</strong> must be billed on the<br />
same claim as the related taxable service. Code S9999 will be<br />
denied as provider liability.<br />
H<strong>and</strong>ling/<br />
Conveyance<br />
Claims Filing<br />
Requirements<br />
H<strong>and</strong>ling, conveyance, <strong>and</strong>/or any other service in connection with<br />
the implementation <strong>of</strong> an order involving devices (code 99002) is<br />
not separately reimbursable. These charges should be included in<br />
charge for the item.<br />
1. Use the 837P claim form to report your services to <strong>Blue</strong> <strong>Cross</strong>.<br />
To obtain forms, please refer to Chapter 8 – Claims Filing in<br />
this manual.<br />
2. Submit ICD-9-CM codes to report an appropriate diagnosis for<br />
your patient.<br />
3. Use HCPCS level II codes to report your services.<br />
4. Appropriate modifiers are required to indicate rental or<br />
purchase <strong>of</strong> DME, e.g., NU, RR.<br />
5. The place <strong>of</strong> service must be a valid CMS two-digit place <strong>of</strong><br />
service code.<br />
6. Submit units based on narrative description.<br />
DME providers <strong>and</strong> skilled nursing facilities billing for place <strong>of</strong><br />
service 31, 32, or 33, are required to submit an Explanation <strong>of</strong><br />
Medicare Benefits (EOMB) for their services unless the provider<br />
has opted out <strong>of</strong> Medicare. If the provider has opted out then the<br />
provider will need to include the opt-out letter with claims<br />
submitted. Any other place <strong>of</strong> service does require an EOMB. This<br />
applies only to Medicare recipients.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Hearing Aids Hearing aids are generally not covered for most contracts.<br />
11-10<br />
<strong>Minnesota</strong> Health Care Programs hearing aids<br />
<strong>Blue</strong> <strong>Cross</strong> uses the MHCP Hearing Aid Volume Purchase<br />
Contract (which contains the MHCP Hearing Aid Contract) as the<br />
base Medical Assistance Fee Schedule. <strong>Blue</strong> <strong>Cross</strong> will follow the<br />
non-covered code list contained in the MHCP Hearing Aid<br />
Contract <strong>and</strong> the DHS supply limits.<br />
Products affected<br />
The following MHCP products are affected:<br />
<strong>Blue</strong> Advantage (PMAP/GAMC, MSC & MSC+)<br />
<strong>Minnesota</strong>Care<br />
Secure<strong>Blue</strong><br />
MHCP Hearing Aid Volume Purchase Contract<br />
The hearing aid service provider must dispense the hearing aid<br />
according to the hearing aid exam, selection <strong>and</strong> prescription <strong>of</strong> the<br />
otolaryngologist <strong>and</strong> audiologist.<br />
For accurate claims processing, the provider will need to submit an<br />
attachment that includes the manufacturers’ specifications.<br />
Providers should utilize the information contained in the current<br />
MHCP contracts, including manufacturer, model name <strong>and</strong> model<br />
number. This information will need to be included in the<br />
attachment when the claim for reimbursement is submitted. <strong>Blue</strong><br />
<strong>Cross</strong> will verify that the hearing aid billed is a covered benefit for<br />
the subscriber <strong>and</strong> will apply the current MHCP Hearing Aid<br />
Volume Purchase Contract pricing for reimbursement. Items not<br />
included in this pricing will defer to the DHS Medical Assistance<br />
st<strong>and</strong>ard fee schedule or the <strong>Blue</strong> <strong>Cross</strong> st<strong>and</strong>ard fee schedule, as<br />
applicable.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Hearing Aids<br />
(continued)<br />
Website<br />
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
The current MHCP Contract Pricing can be found at:<br />
http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNA<br />
MIC_CONVERSION&RevisionSelectionMethod=LatestReleased<br />
&dDoc<strong>Name</strong>=id_010724<br />
Prior Authorization<br />
If the subscriber requires a hearing aid that is not listed on the<br />
DHS Volume Hearing Aid Purchase Contract, a prior authorization<br />
may be submitted for review <strong>of</strong> coverage to the prior authorization<br />
fax line at (651) 662-2810. Please include the following<br />
information in the request:<br />
Audiologic recommendations, including:<br />
Written recommendations for hearing aid(s), including the<br />
manufacturer specifications<br />
Follow-up plan for determining the effectiveness <strong>of</strong> the hearing<br />
aid<br />
Audiogram or reason why this was not obtained<br />
History <strong>of</strong> previous hearing aid use<br />
Pure tone average<br />
Reason why a st<strong>and</strong>ard hearing aid on the Volume Hearing Aid<br />
Purchase Contract is not appropriate for this subscriber<br />
Binaural Hearing Aid Units<br />
Binaural hearing aid codes should be submitted with 1 unit only.<br />
The set allowance reflects two hearing aids.<br />
When submitting a charge for hearing aid repair, use HCPCS code<br />
V5014. Coverage <strong>of</strong> hearing aids, services <strong>and</strong> supplies is<br />
contractually based.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Oxygen <strong>and</strong> Oxygen<br />
Aiding Equipment<br />
(includes ventilators)<br />
Portable Oxygen<br />
Billing<br />
11-12<br />
Oxygen <strong>and</strong> oxygen aiding equipment are defined as the following<br />
items:<br />
Oxygen<br />
Ventilators<br />
Negative-Pressure Ventilators<br />
Oximeters<br />
Large-Volume Air Compressors<br />
Airway-Pressure Monitors (excluding CPAP)<br />
Oxygen Concentrators <strong>and</strong> Oxygen Conservers<br />
Oxygen equipment is reimbursed on a rental basis only, as long as<br />
the equipment is medically necessary.<br />
Oxygen contents will be reimbursed separately only when the<br />
subscriber owns an oxygen system, or rents or owns only a<br />
portable oxygen system.<br />
The units billed for the following codes should never exceed<br />
one (1) per one-month-date range based on the code narrative:<br />
E0443 - Portable oxygen contents, gaseous (for use only with<br />
portable gaseous systems when no stationary gas or liquid<br />
system is used), one month's supply = 1 unit<br />
E0444 - Portable oxygen contents, liquid (for use only with<br />
portable liquid systems when no stationary gas or liquid system<br />
is used), one month's supply = 1 unit<br />
At this time the Department <strong>of</strong> Human Services (DHS) has<br />
different unit submission guides for billing units for E0443-E0444;<br />
however, those guidelines may be used only for Public Program<br />
claims.<br />
In addition to the oxygen contents only codes, E0443 <strong>and</strong> E0444,<br />
the equipment rental or purchase fees are billed separately as<br />
appropriate, with the corresponding gaseous or liquid system code<br />
as follows:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Portable Oxygen<br />
Billing (continued)<br />
Code Definition<br />
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
E0430 Portable gaseous oxygen system, purchase; includes<br />
regulator, flowmeter, humidifier, cannula or mask,<br />
<strong>and</strong> tubing<br />
E0431 Portable gaseous oxygen system, rental; includes<br />
portable container, regulator, flowmeter, humidifier,<br />
cannula or mask, <strong>and</strong> tubing<br />
E0434 Portable liquid oxygen system, rental; includes<br />
portable container, supply reservoir, humidifier,<br />
flowmeter, refill adaptor, contents gauge, cannula or<br />
mask, <strong>and</strong> tubing<br />
E0435 Portable liquid oxygen system, purchase; includes<br />
portable container, supply reservoir, flowmeter,<br />
humidifier, contents gauge, cannula or mask, tubing<br />
<strong>and</strong> refill adaptor<br />
Coding Modifiers <strong>Blue</strong> <strong>Cross</strong> requires all DME providers to submit procedure code<br />
modifiers to differentiate rental, purchase <strong>and</strong> repair or<br />
replacement <strong>of</strong> DME. Modifiers include the following:<br />
Rental Modifiers:<br />
BR The beneficiary has been informed <strong>of</strong> the purchase <strong>and</strong><br />
rental options <strong>and</strong> has elected to rent the item<br />
LL Lease/rental (Use the LL modifier when DME equipment<br />
rental is to be applied against the purchase price)<br />
RR Rental (Use the RR modifier when DME is to be rented)<br />
Purchase Modifiers:<br />
BP The beneficiary has been informed <strong>of</strong> the purchase <strong>and</strong><br />
rental options <strong>and</strong> has elected to purchase the item<br />
NR New when rented. (Use the NR modifier when DME which<br />
was new at the time <strong>of</strong> rental is subsequently purchased.)<br />
NU New equipment<br />
RA Replacement <strong>of</strong> a DME, orthotic or prosthetic item<br />
RB Replacement <strong>of</strong> a part <strong>of</strong> DME, orthotic or prosthetic item<br />
furnished as part <strong>of</strong> a repair<br />
Note: The modifiers BU or UE are not recognized in processing.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-13
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
DME Repairs <strong>and</strong><br />
Maintenance<br />
(Excluding Oxygen<br />
Equipment)<br />
Replacement <strong>of</strong><br />
Purchased Equipment<br />
11-14<br />
Repair <strong>of</strong> rental DME is not covered.<br />
Exception:<br />
For Medicare Advantage subscribers with a capped rental item<br />
with an initial date on <strong>and</strong> after January 1, 2006, repair may be<br />
billed using modifier -RA or -RB with the HCPCS code for the<br />
item serviced.<br />
RA Replacement <strong>of</strong> a DME orthotic or prosthetic item.<br />
RB Replacement <strong>of</strong> a part <strong>of</strong> DME orthotic or prosthetic item<br />
furnished as part <strong>of</strong> a repair.<br />
Repair may be allowed for purchased DME. To submit repair,<br />
report the HCPCS code for the DME being repaired with the –<br />
RB modifier. Submit K0739 (repair or nonroutine service for<br />
DME other than oxygen equipment requiring the skill <strong>of</strong> a<br />
technician, labor component, per 15 minutes) or K0740 (repair<br />
or nonroutine service for oxygen equipment requiring the skill<br />
<strong>of</strong> a technician, labor component, per 15 minutes) on a separate<br />
line. Include the appropriate number <strong>of</strong> units (one per 15<br />
minutes). The cost <strong>of</strong> the repair (including parts <strong>and</strong> loaner fee)<br />
should not exceed our allowable for the purchase <strong>of</strong> the<br />
equipment.<br />
Charges for maintenance <strong>of</strong> DME are not covered.<br />
Maintenance would be indicated with the –MS modifier.<br />
Exception:<br />
For Medicare Advantage subscribers, maintenance <strong>and</strong> service will<br />
be allowed on capped rental with initial rental dates <strong>of</strong> service<br />
prior to January 1, 2006, <strong>and</strong> where the subscriber chose the rental<br />
option only.<br />
<strong>Blue</strong> <strong>Cross</strong>’ policy is to pay for replacement <strong>of</strong> DME, due to<br />
normal use <strong>and</strong> wear, every five (5) years, unless unusual<br />
circumstances necessitate replacement <strong>of</strong> an item sooner than five<br />
years.<br />
Replacement <strong>of</strong> obsolete or inoperable DME equipment, which has<br />
been purchased, is subject to the same prior authorization<br />
guidelines as the purchase <strong>of</strong> the original equipment.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Billing for Supplies Supply items should be submitted with the HCPCS Level II code<br />
that most appropriately describes the item. Unlisted supply codes<br />
should be used only if there is no other code that describes the<br />
item. A narrative must be submitted with every unlisted code.<br />
Supplies are generally allowed separately only in conjunction with<br />
approved home health care. Reimbursement for supplies used in<br />
the <strong>of</strong>fice is already included in the overhead component <strong>of</strong> the<br />
pr<strong>of</strong>essional service (such as an E/M). Office supplies, such as, but<br />
not limited to, Betadine or alcohol wipes, will be denied.<br />
Payment for supplies is based per narrative description (e.g., each,<br />
per pair, per 100, etc.). It is necessary to identify the total number<br />
<strong>of</strong> each supply in the “units” field <strong>of</strong> the 837P claim format.<br />
It is important to assure the units submitted correctly correspond to<br />
the code chosen to ensure appropriate reimbursement. For<br />
example, disposable gloves can be reported per 100 (a single box)<br />
or per pair. Code A4927 reflects billing per 100. HCPCS code<br />
A4930 reflects billing per pair. The unit descriptions for each code<br />
differ significantly.<br />
Following is the narrative for each glove code along with a coding<br />
example:<br />
Code: A4927 Narrative: Glove, non-sterile, per 100<br />
Example: One 100-count box <strong>of</strong> non-sterile gloves, submit<br />
1 unit in the units field on the 837P claim format.<br />
Code: A4930 Narrative: Gloves, sterile, per pair<br />
Example: One 100-count box <strong>of</strong> sterile gloves, submit 50 units<br />
in the units field on the 837P claim format.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-15
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
Billing for Supplies<br />
(continued)<br />
Gloves are restricted to home use only (for approved home health,<br />
home infusion, or home dialysis services). Eligibility for<br />
reimbursement is subject to subscriber benefits.<br />
The following quantities <strong>of</strong> ostomy <strong>and</strong> urology-related supplies<br />
are considered to be reasonable for a monthly (30-day) period.<br />
When quantities in excess <strong>of</strong> these amounts are supplied to the<br />
same patient for use during the same month, the claim(s) must<br />
contain an explanation <strong>of</strong> the medical necessity for such quantities.<br />
If the documentation is not on the claim, there may be a delay in<br />
processing the claim or the claim may be denied.<br />
Indwelling catheters - two per month<br />
Catheter insertion trays - two per month<br />
Sterile irrigation tray/kit - four per month<br />
Irrigation syringe, bulb or piston - four per month<br />
Bottles <strong>of</strong> irrigation solution - four per month<br />
Bedside drainage bags - four per month<br />
Leg drainage bags - four per month<br />
Bedside drainage bottle, rigid or expendable - one per month<br />
Leg strap, foam or fabric - one per month<br />
Urinary catheters (straight catheter) - 31 per month<br />
Ostomy Pouches - 70 per month<br />
If a subscriber signs a waiver accepting responsibility for supplies<br />
billed in excess <strong>of</strong> recommended guides, bill two lines <strong>of</strong> service.<br />
The first line will include the HCPCS supply code <strong>and</strong> the second<br />
line should be submitted with the same HCPCS code with a –GA<br />
modifier. See “Waivers <strong>and</strong> Upgraded/Deluxe DME” for<br />
additional waiver sample <strong>and</strong> submission information.<br />
Rental Unit Submission Service counts must be submitted on a monthly basis only <strong>and</strong><br />
generally submitted as one (1) service per month, instead <strong>of</strong> 30<br />
units or services. Do not submit claims for more than a thirty-day<br />
supply <strong>of</strong> any related supplies. Rental is on a monthly basis only.<br />
Hospital DME Providers Hospital DME providers are required to bill DME on an 837I<br />
claim form.<br />
11-16<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
DME/Supply Internet<br />
Purchases<br />
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
DME or supplies purchased from Internet auction sites (such as e-<br />
Bay) or private parties are generally not covered. If a DME supply<br />
company is the actual supplier, that provider’s number will be<br />
assigned <strong>and</strong> the claim will be processed per the subscriber’s<br />
benefits. If the provider is not a DME/supply company (e.g.,<br />
private party, estate sale), the claim will be denied.<br />
E0935 Rental Guides Continuous passive motion devices are usually used only for a<br />
short period <strong>of</strong> time during a patient’s recovery period. Therefore,<br />
the HCPCS code E0935 (continuous passive motion exercise<br />
device for use on knee only) is assigned a daily rental allowance<br />
<strong>and</strong> it limited to 21 days <strong>of</strong> rental. Submit one unit for each day <strong>of</strong><br />
rental. For example, if the device is rented for 14 days, indicate 14<br />
in the unit field.<br />
Pharmacies Submitting<br />
DME Claims<br />
Aware agreement<br />
The Aware Agreement states: “Provider shall provide Health<br />
Services to Subscribers for eligible Prescription Drugs which are<br />
authorized by a valid prescription.” This section also includes the<br />
dispensing <strong>of</strong> DME to <strong>Blue</strong> <strong>Cross</strong> subscribers.<br />
Pharmacy responsibilities<br />
It is the responsibility <strong>of</strong> the participating pharmacy to submit the<br />
claims for all such eligible services to <strong>Blue</strong> <strong>Cross</strong> on behalf <strong>of</strong> the<br />
subscriber. The pharmacy may bill subscribers for appropriate<br />
subscriber liability amounts as detailed in the provider service<br />
agreement. This process allows for the proper adjudication <strong>of</strong> the<br />
claim by <strong>Blue</strong> <strong>Cross</strong> in order to correctly determine the applicable<br />
deductible <strong>and</strong>/or coinsurance amounts that may be due from the<br />
subscriber. After the claim is processed by <strong>Blue</strong> <strong>Cross</strong>, you will be<br />
notified <strong>of</strong> the proper amount to bill the subscriber, if any balance<br />
remains due from the subscriber.<br />
It is also the responsibility <strong>of</strong> all participating providers to abide by<br />
all other terms <strong>and</strong> provisions <strong>of</strong> the agreement including, but not<br />
limited to, the administration <strong>of</strong> the coordination <strong>of</strong> benefits<br />
provisions.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)<br />
11-17
Coding Policies <strong>and</strong> Guidelines (Durable Medical Equipment)<br />
DME <strong>and</strong> Specialty<br />
Pharmacy Billed<br />
through the <strong>Blue</strong>Card ®<br />
Program<br />
11-18<br />
<strong>Blue</strong> plans* may contract with providers outside <strong>of</strong> their exclusive<br />
service area for services provided to local <strong>and</strong> <strong>Blue</strong>Card<br />
subscribers within their own service area for DME <strong>and</strong> selfadministered<br />
specialty pharmacy. <strong>Blue</strong> plans may not contract for<br />
such services for their subscribers who receive services outside <strong>of</strong><br />
their service area.<br />
DME<br />
DME providers should file claims to the <strong>Blue</strong> plan in whose<br />
service area the equipment or supplies were shipped or purchased<br />
if the location was a retail store. For example, if a DME device<br />
was delivered to a subscriber in Massachusetts, then the claim<br />
should be filed with <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> Massachusetts.<br />
The claim will be reimbursed based on provider’s participation<br />
status with that <strong>Blue</strong> plan.<br />
Specialty Pharmacy<br />
Self-administered specialty pharmacy providers should file the<br />
claim to the <strong>Blue</strong> plan where the ordering physician is located. The<br />
claim will be reimbursed based on provider’s participation status<br />
with that <strong>Blue</strong> plan.<br />
* Each <strong>Blue</strong> plan is an independent licensee <strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
<strong>Blue</strong> <strong>Shield</strong> Association<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/15/2012)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Home Health, Home Infusion, Hospice)<br />
Table <strong>of</strong> Contents<br />
Definitions............................................................................................................................11-2<br />
Prior Authorization .............................................................................................................. 11-2<br />
Home Health ........................................................................................................................11-3<br />
Elderly Waiver Program ...................................................................................................... 11-4<br />
Referrals <strong>and</strong> Prior Authorization........................................................................................ 11-6<br />
Adult Day Care Bath Services ........................................................................................... 11-11<br />
RAP Claim Submission ..................................................................................................... 11-11<br />
Home Infusion ................................................................................................................... 11-12<br />
Medicare Primary with <strong>Blue</strong> <strong>Cross</strong> Secondary..................................................................11-14<br />
Hospice ..............................................................................................................................11-15<br />
Rules <strong>and</strong> Regulations........................................................................................................11-15<br />
Hospice Billing for Medicare Products..............................................................................11-17<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Definitions Home Health<br />
Home health care is care provided in a patient's home by qualified<br />
personnel.<br />
Home Infusion<br />
Home infusion is the administration <strong>of</strong> medications or nutrition<br />
intravenously or through a feeding tube.<br />
Hospice<br />
Hospice care is a concept <strong>of</strong> care that provides palliative care<br />
(rather than curative care) to a terminally ill patient <strong>and</strong> family.<br />
Prior Authorization All home health services require prior authorization. Hospice<br />
services require prior authorization only for FEP members <strong>and</strong><br />
notification for MHCP members. Prior authorization is required<br />
for the following home infusion services:<br />
11-2<br />
Blood factor products<br />
IVIG<br />
Synagis<br />
Home health, blood factor, IVIG <strong>and</strong> Synagis prior authorization is<br />
performed by:<br />
Utilization Management<br />
Route code: R4-72<br />
(651) 662-5520<br />
1-888-878-0139 ext. 25520<br />
Fax: (651) 662-1004<br />
Address:<br />
P.O. Box 64265<br />
St. Paul, MN 55164-0265<br />
For Government Program members<br />
Utilization Management<br />
Route code: R348<br />
(651) 662-5540<br />
1-800-711-9668<br />
Fax: 651-662-4022 or 1-866-800-1665<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Home Health Examples <strong>of</strong> home health care services requiring review include:<br />
skilled home nursing visits, home health aid services, home social<br />
worker visits, physical therapy, occupational therapy, speech<br />
therapy <strong>and</strong> personal care attendants.<br />
Coverage <strong>of</strong> services is subject to contract benefits <strong>and</strong><br />
limitations.<br />
Services must be skilled versus non-skilled or custodial.<br />
Services must be intermittent <strong>and</strong> <strong>of</strong> a medical nature.<br />
Home health care must be ordered in writing by a physician<br />
<strong>and</strong> performed by a Medicare certified/JCAHO approved home<br />
health agency.<br />
Note: Personal care attendants are not eligible for coverage under<br />
most health plans, with the exception <strong>of</strong> Public Programs.<br />
Services must be submitted on an 837I claim form. The<br />
appropriate revenue code(s) should be submitted for the services<br />
supplied. Associated HCPCS codes must be submitted on each line<br />
or the line may be denied for additional information.<br />
Home Health revenue code categories are:<br />
055X Home Health (HH) - Skilled Nursing<br />
056X Home Health (HH) - Medical Social Services<br />
057X Home Health (HH) - Aide<br />
058X Home Health (HH) - Other Visits<br />
059X Home Health (HH) - Units <strong>of</strong> Service<br />
060X Home Health (HH) – Oxygen<br />
Prior authorization is recommended for all members, regardless <strong>of</strong><br />
plan. For members who are eligible for elderly waiver services, the<br />
home care agency should coordinate with the member’s care<br />
coordinator for home care services. The authorization number<br />
provided by <strong>Blue</strong> <strong>Cross</strong> must be entered in the REF segment on the<br />
electronic 837I.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Elderly Waiver<br />
Program<br />
11-4<br />
The statewide Elderly Waiver Program (EW) is available to<br />
members <strong>of</strong> <strong>Blue</strong> Advantage MSC+ <strong>and</strong> Secure<strong>Blue</strong> SM (HMO<br />
SNP). <strong>Blue</strong> Plus will review all Medicaid <strong>and</strong> Medicare home care<br />
requests <strong>and</strong> determine the number <strong>of</strong> visits based upon medical<br />
necessity, Medicare, <strong>and</strong> state plan guidelines. This is applicable to<br />
all members receiving Medicaid <strong>and</strong> Medicare home care services<br />
including those on Elderly Waiver.<br />
Home care agencies contact the member’s care coordinator for<br />
consultation regarding the member’s plan <strong>of</strong> care. The care<br />
coordinator will need to fax in the 6.04.01 Recommendation for<br />
Authorization <strong>of</strong> MA Home Care Services for members open to a<br />
home <strong>and</strong> community based disability or form 6.04.03 Home Care<br />
Services Recommendation-Non Disability to request <strong>Blue</strong> Plus to<br />
review the services.<br />
<strong>Blue</strong> Plus will obtain medical necessity information from the home<br />
care agency <strong>and</strong> will review the information submitted <strong>and</strong> make a<br />
coverage determination within 10 days <strong>of</strong> receipt <strong>of</strong> the request.<br />
When a determination is made, <strong>Blue</strong> Plus will notify the member<br />
<strong>and</strong> the home care provider via a letter <strong>of</strong> the outcome.<br />
<strong>Blue</strong> Plus will fax the 6.04.01 or 6.04.03 form back to the care<br />
coordinator for their records <strong>and</strong> case mix cap management.<br />
PCA Services<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus contracts with Personal Care Provider<br />
Organizations (PCPO) <strong>and</strong> PCA (Personal Care Assistant) Choice<br />
providers as part <strong>of</strong> our Government Programs Specialty Network.<br />
PCA services are eligible only for reimbursement under certain<br />
Public Program contracts. PCA services may also be furnished<br />
through a contracted home health agency. The following<br />
information describes the programs, eligible services <strong>and</strong> claims<br />
submission requirements.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Elderly Waiver<br />
Program (continued)<br />
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
<strong>Minnesota</strong> Health Care Programs<br />
Group numbers for members who have coverage with <strong>Minnesota</strong><br />
Health Care Programs are as follows:<br />
Product <strong>Name</strong> ID #s / Group Numbers<br />
<strong>Blue</strong> Advantage<br />
(PMAP <strong>and</strong> MSC+)<br />
<strong>Minnesota</strong>Care<br />
Exp<strong>and</strong>ed<br />
ID #s begin with “XZG8” / All group<br />
numbers that begin with PP0<br />
ID #s begin with “XZG8” / All group<br />
numbers that begin with PP1<br />
Secure<strong>Blue</strong> ID #s begin with “XZS8” / All group<br />
numbers that begin with PP2<br />
Program Purpose<br />
<strong>Minnesota</strong>’s PCA program is designed to support people <strong>of</strong> all<br />
ages with disabilities to live independently in the community.<br />
PCAs provide home-based services to people who need help with<br />
activities <strong>of</strong> daily living <strong>and</strong> health-related functions (under<br />
direction <strong>of</strong> an RN or qualified pr<strong>of</strong>essional such as a Social<br />
Worker or Psychologist). PCAs may provide h<strong>and</strong>s-on assistance,<br />
supervision, cueing, redirection <strong>and</strong> intervention for behavior<br />
including observation <strong>and</strong> monitoring. PCA services can be linked<br />
to medical or behavioral health diagnoses <strong>and</strong> are considered a<br />
home care service.<br />
Eligibility for PCA Services<br />
There are three basic requirements for eligibility:<br />
1. The patient must be eligible for, or receiving, Prepaid Medical<br />
Assistance Program (PMAP) or <strong>Minnesota</strong>Care Exp<strong>and</strong>ed<br />
benefits (for pregnant women or children under age 21).<br />
2. The patient must have a physician’s statement <strong>of</strong> need stating<br />
that PCA services are medically necessary.<br />
3. The patient must be able to make decisions about their care or<br />
have a person designated as a Responsible Party (RP) who can<br />
make decisions about the patient’s care. (The RP must<br />
participate in the planning <strong>and</strong> directing <strong>of</strong> PCA services. The<br />
RP cannot be the PCA <strong>and</strong> must be 18 years or older, available<br />
for the patient <strong>and</strong>/or PCA, <strong>and</strong> monitor care a minimum <strong>of</strong><br />
one time per week.)<br />
Note: General Assistance Medical Care (GAMC) members <strong>and</strong><br />
adults enrolled in <strong>Minnesota</strong>Care (except pregnant women)<br />
are not eligible for PCA services. Care<strong>Blue</strong> SM (HMO SNP)<br />
members are eligible for PCA services but their services are<br />
paid by the State <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> not <strong>Blue</strong>Plus.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Referrals <strong>and</strong> Prior<br />
Authorization<br />
11-6<br />
Statement <strong>of</strong> Need for PCA Services<br />
In accordance with <strong>Minnesota</strong> Statute 256B.0655, a physician’s<br />
statement <strong>of</strong> need must be obtained before the start <strong>of</strong> services <strong>and</strong><br />
annually thereafter. The statement <strong>of</strong> need must include the<br />
member’s diagnosis <strong>and</strong> condition for which the PCA services are<br />
needed. The statement <strong>of</strong> need must also be utilized any time there<br />
is a change in the member’s condition that results in a change in<br />
the level <strong>of</strong> PCA services.<br />
The <strong>Minnesota</strong> Council <strong>of</strong> Health Plans has collaborated with all<br />
health plans to develop a universal statement <strong>of</strong> need form for the<br />
PCA program. This statement <strong>of</strong> need form is posted on the MN<br />
Council <strong>of</strong> Health Plans website at www.mnhealthplans.org.<br />
<strong>Blue</strong> <strong>Cross</strong> requires that the form be completed prior to the start <strong>of</strong><br />
any PCA services. Services must be provided by a par provider.<br />
Process for Initiating PCA Services<br />
1. Prior to rendering PCA services to a <strong>Blue</strong> Plus Public<br />
Programs member, providers should contact the member’s case<br />
manager, care coordinator or IHM Utilization review area as<br />
follows:<br />
For <strong>Blue</strong> Advantage PMAP members, contact the<br />
Government Programs Integrated Health Management<br />
Intake at (651) 662-5540 or 1-800-711-9668.<br />
For Secure<strong>Blue</strong> <strong>and</strong> MSC+ members, contact the member’s<br />
county coordinator, if known, to request PCA services. For<br />
assistance in locating the member’s county care<br />
coordinator, contact Government Programs Integrated<br />
Health Management Intake at (651) 662-5540 or at<br />
1-800-711-9868. Secure<strong>Blue</strong> members are those members<br />
with <strong>Minnesota</strong> Senior Health Options (MSHO) coverage<br />
through <strong>Blue</strong> Plus.<br />
2. An assessment <strong>of</strong> the member’s need for PCA services will be<br />
completed by a public health nurse, Elderly Waiver case<br />
manager or county care coordinator that has been trained by<br />
the Department <strong>of</strong> Human Services.<br />
3. Once completed, the PCA assessment should be faxed to<br />
Government Programs Integrated Health Management at<br />
(651) 662-4022 or 1-866-800-1665 for review.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Referrals <strong>and</strong> Prior<br />
Authorization<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
4. A utilization management nurse will review the request using<br />
the state guidelines for PCA services <strong>and</strong> make a coverage<br />
determination. A determination will be made within 10 days<br />
from the date the PCA assessment is received by <strong>Blue</strong>Plus.<br />
5. Once a determination has been made, the member, PCA<br />
agency <strong>and</strong> care coordinator (if applicable) will receive<br />
notification <strong>of</strong> the amount <strong>of</strong> services authorized, date spans<br />
covered <strong>and</strong> an authorization number. If the services have been<br />
denied or reduced, the member’s primary care physician will<br />
also be notified.<br />
Documentation requirements (applies only to providers<br />
employing PCAs)<br />
PCA providers must use a st<strong>and</strong>ardized timesheet for all PCAs.<br />
The timesheet must include the following: the start <strong>and</strong> end time<br />
for each episode <strong>of</strong> PCA service, the services provided, signature<br />
<strong>of</strong> the PCA, signature <strong>of</strong> the member or responsible party, <strong>and</strong> a<br />
statement that false billing is a federal crime.<br />
PCA individual provider number (applies only to providers<br />
employing PCAs)<br />
DHS assigns Medical Assistance provider numbers to each<br />
individual PCA. Only PCAs who have been issued such a number<br />
by DHS <strong>and</strong> have evidence <strong>of</strong> a completed <strong>and</strong> approved<br />
background study (completed by DHS), shall be considered<br />
eligible providers for the purpose <strong>of</strong> rendering care to <strong>Blue</strong> Plus<br />
<strong>Minnesota</strong> Public Program members. Post-service audits will be<br />
conducted to ensure that the criteria are being met.<br />
When billing an 837P claim format, PCA providers must submit<br />
their individual provider ID in the rendering practitioner fields.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Referrals <strong>and</strong> Prior<br />
Authorization<br />
(continued)<br />
11-8<br />
PCA services must be submitted to <strong>Blue</strong> Plus using one date <strong>of</strong><br />
service per claim line. Any claim lines that are submitted with<br />
more than one date <strong>of</strong> service (date span) will be denied for<br />
improper format. All claim lines should have an individual PCA<br />
associated with the service.<br />
All PCA claim lines (T1019), except for those submitted with the<br />
QP supervision modifier, must include at least one <strong>of</strong> the<br />
relationship modifiers on each line (UD or U1). All other HCPCS<br />
code <strong>and</strong> modifier combinations still apply to PCA claims.<br />
Multiple modifiers can be submitted on one line to further identify<br />
services provided. Claims that do not include an appropriate<br />
modifier will be denied. These claims may be reconsidered when<br />
the appropriate modifier is provided.<br />
Participating Home<br />
Health Agencies<br />
Purpose: provide<br />
skilled <strong>and</strong> nonskilled<br />
care <strong>and</strong><br />
supervision<br />
Billing: submit<br />
services on a facility<br />
claim format (837I),<br />
use revenue codes<br />
0570-0579 <strong>and</strong><br />
HCPCS code T1019<br />
PCA Code<br />
or Code &<br />
Modifier Code Narrative<br />
Personal Care<br />
Provider<br />
Organization<br />
Purpose: provide<br />
RN/qualified<br />
pr<strong>of</strong>essional<br />
supervision <strong>and</strong><br />
PCA services only<br />
Billing: submit<br />
services on a<br />
pr<strong>of</strong>essional claim<br />
format (837P) using<br />
the appropriate “T”<br />
HCPCS codes (see<br />
code <strong>and</strong> modifier<br />
list below)<br />
T1001 Nursing assessment/evaluation<br />
PCA Choice<br />
Providers<br />
Purpose: bill PCA<br />
services for the<br />
member.<br />
Member/RP does all<br />
hiring, training <strong>and</strong><br />
supervision <strong>of</strong><br />
PCAs.<br />
Billing: submit<br />
services on a<br />
Pr<strong>of</strong>essional claim<br />
format (837P) using<br />
the appropriate “T”<br />
HCPCS codes (see<br />
code <strong>and</strong> modifier<br />
list below)<br />
Modifier<br />
Instructions<br />
T1001-52 Same as above The –52 modifier is<br />
submitted to<br />
indicate a service<br />
update.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Referrals <strong>and</strong> Prior<br />
Authorization<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
PCA Code<br />
or Code &<br />
Modifier Code Narrative<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
Modifier<br />
Instructions<br />
T1001-U6 Same as above The –U6 modifier is<br />
submitted to<br />
indicate a temporary<br />
service increase.<br />
T1019 Personal care services, per 15<br />
minutes, not for an inpatient or<br />
resident <strong>of</strong> a hospital, nursing<br />
facility, ICF/MR or IMD, part<br />
<strong>of</strong> the individualized plan <strong>of</strong><br />
care treatment (code may not<br />
be used to identify services<br />
provided by home health aide<br />
or certified nursing assistant)<br />
T1019-TT Same as above The –TT modifier is<br />
submitted to<br />
indicate personal<br />
care assistant PCPO<br />
services at a 1:2<br />
ratio (one assistant<br />
to two patients).<br />
T1019-<br />
HQ<br />
T1019-<br />
UA<br />
Same as above The –HQ modifier is<br />
submitted to<br />
indicate personal<br />
care assistant PCPO<br />
services at a 1:3<br />
ratio (one assistant<br />
to three patients).<br />
Same as above The UA modifier is<br />
submitted to<br />
indicate the services<br />
are for supervision<br />
<strong>of</strong> a PCA.<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Referrals <strong>and</strong> Prior<br />
Authorization<br />
(continued)<br />
11-10<br />
PCA Code<br />
or Code &<br />
Modifier Code Narrative<br />
T1019-<br />
UD<br />
Modifier<br />
Instructions<br />
Same as above The UD modifier is<br />
submitted to<br />
indicate personal<br />
care assistant PCPO<br />
services at a 1:1<br />
ratio (one assistant<br />
to one patient). No<br />
relationship to the<br />
member.<br />
T1019-U1 Same as above The UD modifier is<br />
submitted to<br />
indicate personal<br />
care assistant PCPO<br />
services at a 1:1<br />
ratio (one assistant<br />
to one patient).<br />
Parent/Adoptive<br />
Parent, Sibling,<br />
Adult Child,<br />
Gr<strong>and</strong>parent or<br />
Gr<strong>and</strong>child <strong>of</strong> the<br />
member.<br />
T1019-U6 Same as above The U6 modifier is<br />
submitted to<br />
indicate the service<br />
is for a temporary<br />
45-day service<br />
increase.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Adult Day Care Bath<br />
Services<br />
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Bath services provided by Adult Day Care providers are a covered<br />
benefit for Public Program members under the following<br />
programs:<br />
Secure<strong>Blue</strong> – groups beginning with PP2<br />
<strong>Minnesota</strong> Senior Care Plus (MSC+) – groups beginning with<br />
PP0<br />
These members must also be on an Elderly Waiver program.<br />
Services should be coordinated with the member’s care<br />
coordinator <strong>and</strong> part <strong>of</strong> the member’s comprehensive care plan.<br />
The Adult Day Care providers must have record <strong>of</strong> the individual’s<br />
care plan that documents the necessity for the services. Eligible<br />
providers must be listed on the <strong>Minnesota</strong> Department <strong>of</strong> Human<br />
Services website as licensed Adult Day Care providers.<br />
Claim Submission<br />
Submit the claim on the 837P claim format.<br />
Bill code S5100-TF (day care services, adult; per 15 minutes).<br />
Eligible providers may be reimbursed for a maximum <strong>of</strong> two<br />
units <strong>of</strong> service per day.<br />
Enter each date <strong>of</strong> service on a separate line with units <strong>of</strong><br />
service for each date.<br />
Reimbursement will be based on the usual pricing methodology<br />
for Public Programs.<br />
RAP Claim Submission Home health providers submitting Medicare RAP (Request for<br />
Anticipated Payment) claims should submit zero charges ($0.00)<br />
with the HIPPS code on the 0023 revenue code line. Claims<br />
submitted with charge amounts other than $0.00 on the 0023<br />
revenue code line will be denied <strong>and</strong> returned to the provider<br />
without processing.<br />
Products Affected<br />
This change applies to home health RAP claims submitted for the<br />
following Medicare enrollees:<br />
Product <strong>Name</strong> Member ID alpha prefix<br />
Care<strong>Blue</strong> XZS<br />
Secure<strong>Blue</strong> XZS<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Home Infusion Coverage <strong>of</strong> services is subject to contract benefits <strong>and</strong> limitations.<br />
11-12<br />
Home infusion services must be ordered in writing by a physician<br />
<strong>and</strong> performed by a Medicare certified/JCAHO approved home<br />
infusion agency.<br />
Claim Submission<br />
Submit claims using either the electronic ASC ANSI X 12N<br />
837P format using CPT <strong>and</strong> HCPCS codes.<br />
Use the Place <strong>of</strong> Service code 12 (Home) for services provided<br />
in the patient’s home.<br />
Use the Place <strong>of</strong> Service code 11 or 49 for services provided in<br />
a home infusion suite in the provider’s <strong>of</strong>fice.<br />
Pr<strong>of</strong>essional ID numbers are issued with contracts for all<br />
participating home infusion providers. Individual provider<br />
numbers are not required. As always, reimbursement is subject to<br />
the member’s contract benefits.<br />
Per Diem Payment<br />
The HCPCS “S” codes for home infusion services are based on a<br />
“per diem” reimbursement methodology. The per diem includes all<br />
supplies, care coordination <strong>and</strong> pr<strong>of</strong>essional pharmacy services.<br />
The per diem is billed for each day that a patient is on service from<br />
date <strong>of</strong> admission through date <strong>of</strong> discharge. Nursing services <strong>and</strong><br />
drug products are billed separately from the per diem.<br />
Drugs<br />
Code all drugs with a HCPCS or CPT code. If a specific code is<br />
not available you may use J3490, J7799 or J9999. Provide the<br />
narrative, NDC number <strong>and</strong> dosage/units supplied. Related NDC<br />
codes for compounded products are itemized using the LIN <strong>and</strong><br />
CTP segments.<br />
These claims will require manual review.<br />
Use drug units as described in the HCPCS or CPT description <strong>of</strong><br />
the code.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Home Infusion<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Nursing Services<br />
Code home IV nursing visits lasting up to two hours using CPT<br />
code 99601. Report each additional hour beyond the initial two<br />
with 99602 with the appropriate number <strong>of</strong> units.<br />
When provided in the infusion suite <strong>of</strong> a home infusion agency,<br />
code each nursing visit lasting up to two hours using CPT code<br />
99199, with a narrative description. Report each additional hour<br />
beyond the initial two with 99199-52 with the appropriate number<br />
<strong>of</strong> units, in accordance with the NHIA (National Home Infusion<br />
Association) recommendations for billing.<br />
Catheter Care<br />
Bill catheter care per diems (S5498, S5501, S5502) when provided<br />
as a st<strong>and</strong>-alone therapy. Insertion by a nurse <strong>of</strong> a PICC line<br />
(S5522) or midline (S5523) is coded separately from the other<br />
nursing visit code <strong>and</strong> per diem. Supplies required from nonroutine<br />
catheter procedures such as de-clotting supplies (S5517),<br />
repair kits (S5518), PICC insertion supplies (S5520) <strong>and</strong> midline<br />
insertion supplies (S5521) are coded separately.<br />
Prior Authorization<br />
Prior authorization is recommended when supplying IVIG, Factor<br />
products, Aldurazyme, Fabrazyme, Synagis or other drugs not yet<br />
identified. A Prior Authorization can be completed using the<br />
st<strong>and</strong>ard PA form F1676 R9. For the members insured by a <strong>Blue</strong><br />
<strong>Cross</strong> plan <strong>of</strong> another state, check the prior authorization<br />
requirements <strong>of</strong> that state.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-13
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Home Infusion<br />
(continued)<br />
Medicare Primary with<br />
<strong>Blue</strong> <strong>Cross</strong> Secondary<br />
11-14<br />
Multiple Therapies<br />
For multiple therapies in the same category done on the same date<br />
<strong>of</strong> service as primary therapy, append the following modifiers to<br />
the “S” code per diem:<br />
SH- second concurrently administered infusion therapy<br />
SJ- third or more concurrently administered therapy<br />
Notification recommended<br />
Notification to our Case Management department is recommended<br />
for obstetrical patients receiving hydration therapy, tocolytic<br />
therapy (i.e. Terbutaline) or anti-emetic infusion (i.e. Reglan or<br />
Z<strong>of</strong>ran). This serves as notification to <strong>Blue</strong> <strong>Cross</strong> that the patient<br />
may need additional support from our staff by calling<br />
(651) 662-5520.<br />
Medicare Supplement policies will only coordinate with the<br />
services that Medicare allows.<br />
Submit the nursing claims to Medicare Part A. The claim may<br />
crossover to <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> process with your home health<br />
provider number. Agencies who are not certified by Medicare<br />
A should subcontract the nursing portion <strong>of</strong> the service to<br />
Medicare Part A certified home care agency.<br />
Submit the drugs <strong>and</strong> supply charges to Medicare Part B. The<br />
claim may crossover to <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> should process using<br />
your DME provider number.<br />
Verification <strong>of</strong> the crossover may be done on BLUELINE, or<br />
through our secure website. If the claim is not found, attach the<br />
Medicare EOMB <strong>and</strong> cover letter to a paper claim <strong>and</strong> submit<br />
to <strong>Blue</strong> <strong>Cross</strong>.<br />
For services that would be denied by Medicare, but may be<br />
allowed by <strong>Blue</strong> <strong>Cross</strong>:<br />
A Medicare denial is not required. Submit the claim to <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> append the -GY modifier to each line <strong>of</strong> service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Hospice Coverage <strong>of</strong> services is subject to contract benefits <strong>and</strong> limitations.<br />
Hospice care must be ordered in writing by a physician <strong>and</strong><br />
performed by a Medicare certified/JCAHO approved hospice<br />
agency. The member must meet hospice guidelines for admission<br />
into the program.<br />
Services must be submitted on an 837I claim format using a<br />
hospice contracting provider ID number or NPI. The appropriate<br />
revenue code(s) should be submitted for the services supplied.<br />
Hospice revenue codes are 0650-0659.<br />
Prior authorization is required only for FEP members. Effective<br />
April 1, 2012, hospice services require notification for all products<br />
under MHCP to assure proper claims payment.<br />
Rules <strong>and</strong> Regulations The authorization number provided by <strong>Blue</strong> <strong>Cross</strong> must be entered<br />
in the REF segment on the electronic 837I.<br />
The Provider shall have a written eligibility criteria for service<br />
<strong>and</strong> procedures for referral to other sources that include the<br />
following:<br />
1. Policies shall cover all services provided by the provider<br />
directly or under contract.<br />
2. The policies shall define referrals accepted, admissions <strong>of</strong><br />
clients to provider services <strong>and</strong> the discharge <strong>of</strong> clients.<br />
3. Criteria <strong>of</strong> eligibility for the service shall be stated clearly in<br />
reference to such factors as: age groups, geographical area,<br />
hours <strong>of</strong> service (including policy about 8 to 24 hour service<br />
<strong>and</strong> weekend service), social <strong>and</strong> health needs, crises or<br />
emergency services, referral <strong>and</strong> funding sources.<br />
4. Eligibility criteria that apply to the service shall be available to<br />
community pr<strong>of</strong>essionals <strong>and</strong> organizations <strong>and</strong> persons<br />
applying for the service.<br />
5. There shall be a written policy for making referrals for needed<br />
services that are not available through the provider.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-15
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Rules <strong>and</strong> Regulations<br />
(continued)<br />
11-16<br />
The provider shall be required to have policies <strong>and</strong> procedures<br />
which identify:<br />
1. a competent <strong>and</strong> comprehensive assessment <strong>of</strong> client healthrelated<br />
needs;<br />
2. that the home health services provided are appropriate to a<br />
client’s identified needs;<br />
3. that an approved plan <strong>of</strong> care is accurately implemented<br />
through service delivery; <strong>and</strong><br />
4. that the client care <strong>and</strong> treatment, including progress reports<br />
from all disciplines, is correctly documented in an acceptable<br />
clinical record format in a timely manner.<br />
There shall be a written policy explaining procedures for obtaining<br />
referrals from primary care physician’s original signed physician<br />
plan <strong>of</strong> treatment <strong>and</strong> subsequent renewals <strong>of</strong> plan <strong>of</strong> treatment<br />
consistent with provider’s applicable licensure/certification<br />
requirements.<br />
Demonstration <strong>of</strong> Internal Continuity <strong>of</strong> Care/Case<br />
Management shall include the following:<br />
1. The provider shall have policies <strong>and</strong> procedures to assure the<br />
coordination, integration <strong>and</strong> continuity <strong>of</strong> client’s care.<br />
2. There is a written policy statement ensuring the coordination <strong>of</strong><br />
all client services delivered by the provider, according to the<br />
plan <strong>of</strong> care.<br />
3. There is evidence <strong>of</strong> the provider’s ongoing compliance with<br />
policies <strong>and</strong> procedures regarding service coordination,<br />
according to the plan <strong>of</strong> care.<br />
4. The discharge planning process <strong>and</strong> transfer policies are the<br />
same as those under external continuity <strong>of</strong> Care/Case<br />
Management.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Rules <strong>and</strong> Regulations<br />
(continued)<br />
Hospice Billing for<br />
Medicare Products<br />
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
In addition to the other provisions <strong>of</strong> the Agreement <strong>and</strong> these<br />
Rules <strong>and</strong> Regulations, the following special provisions will<br />
apply when providing home health services to members <strong>of</strong><br />
<strong>Blue</strong> <strong>Cross</strong>’ long-term care coverage plans:<br />
1. The provider agrees to request prior authorization <strong>of</strong> home<br />
health services prior to the commencement <strong>of</strong> such services.<br />
2. If the member contract includes coverage for medically<br />
necessary, non-emergency medical transportation, the provider<br />
agrees to arrange for <strong>and</strong> to obtain prior authorization for such<br />
transportation.<br />
Products Affected<br />
Secure<strong>Blue</strong> (except for members who do not have Medicare<br />
coverage)<br />
Care<strong>Blue</strong> (except for members who do not have Medicare<br />
coverage)<br />
Secure<strong>Blue</strong> Medicare Hospice Group Numbers<br />
All claims for members with these group numbers that are<br />
submitted to <strong>Blue</strong> <strong>Cross</strong> with provider specialty B5 (inpatient <strong>and</strong><br />
home hospice) <strong>and</strong> all claims for services related to the terminal<br />
illness will be denied indicating that all claims should be sent to<br />
RHHI.<br />
PP245-ZA PP245-ZC PP245-ZE PP245-ZF PP245-ZM PP245-ZR PP245-ZS PP245-ZV PP245-ZW<br />
PP260-ZA PP260-ZC PP260-ZE PP260-ZF PP260-ZM PP260-ZR PP260-ZS PP260-ZV PP260-ZW<br />
PP261-ZA PP261-ZC PP261-ZE PP261-ZF PP261-ZM PP261-ZR PP261-ZS PP261-ZV PP261-ZW<br />
PP262-ZA PP262-ZC PP262-ZE PP262-ZF PP262-ZM PP262-ZR PP262-ZS PP262-ZV PP262-ZW<br />
PP280-ZA PP280-ZC PP280-ZC PP280-ZF PP280-ZM PP280-ZR PP280-ZS PP280-ZV PP280-ZW<br />
PP281-ZA PP281-ZC PP281-ZE PP281-ZF PP281-ZM PP281-ZR PP281-ZS PP281-ZV PP281-ZW<br />
PP282-ZA PP282-ZC PP282-ZE PP282-ZF PP282-ZM PP282-ZR PP282-ZS PP282-ZV PP282-ZW<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-17
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Hospice Billing for<br />
Medicare Products<br />
(continued)<br />
11-18<br />
Care<strong>Blue</strong> Medicare Hospice Group Numbers<br />
All claims for members with these group numbers that are<br />
submitted to <strong>Blue</strong> <strong>Cross</strong> with provider specialty B5 (inpatient <strong>and</strong><br />
home hospice) <strong>and</strong> all claims for services related to the terminal<br />
illness will be denied indicating that all claims should be sent to<br />
RHHI.<br />
PP301-ZA PP301-ZM PP301-ZP PP301-ZQ<br />
PP303-ZA PP303-ZM PP303-ZP PP303-ZQ<br />
PP305-ZA PP305-ZM PP305-ZP PP305-ZQ<br />
PP313-ZA PP313-ZM PP313-ZP PP313-ZQ<br />
Hospice Billing<br />
Members who have elected Medicare hospice benefits can be<br />
identified by their group number for Secure<strong>Blue</strong> <strong>and</strong> Care<strong>Blue</strong>.<br />
The hospice benefit for all Medicare plans administered by <strong>Blue</strong><br />
<strong>Cross</strong> is maintained through the Regional Home Health <strong>and</strong><br />
Hospice Medicare Intermediary (RHHI).<br />
Secure<strong>Blue</strong>/Care<strong>Blue</strong> Specific Processing<br />
All claims submitted to <strong>Blue</strong> <strong>Cross</strong> with provider specialty B5<br />
(inpatient <strong>and</strong> home hospice) will be denied indicating that all<br />
claims should be sent to RHHI for consideration.<br />
Claims for all other provider specialties for services related to the<br />
terminal illness should be submitted to Medicare for primary<br />
consideration. If submitted to <strong>Blue</strong> <strong>Cross</strong>, these claims will be<br />
denied indicating that all claims related to the terminal illness<br />
should be submitted to Medicare for primary consideration. If the<br />
provider needs to bill for a service never covered by Medicare (for<br />
example, special or common carrier transportation or services with<br />
HCPCS codes that begin with alpha characters H, S or T) these<br />
services can be billed to <strong>Blue</strong> <strong>Cross</strong> directly.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)
Hospice Billing for<br />
Medicare Products<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Home Health, Home Infusion, Hospice)<br />
Claims submitted with a GV modifier indicate services were<br />
provided by a provider not reimbursed through the hospice<br />
provider. These claims need to be submitted to Medicare for<br />
primary consideration. If the claim is submitted to <strong>Blue</strong> <strong>Cross</strong><br />
without Medicare payment information, the claim will be denied<br />
requesting this information. If Medicare payment information is<br />
submitted on the claim, then the Secure<strong>Blue</strong>/Care<strong>Blue</strong> products<br />
will consider payment for the services as the secondary payer.<br />
Institutional room <strong>and</strong> board for Secure<strong>Blue</strong> or Care<strong>Blue</strong> nursing<br />
home members is paid by the <strong>Minnesota</strong> Department <strong>of</strong> Human<br />
Services (DHS). Nursing facility room <strong>and</strong> board claims should be<br />
submitted to DHS for payment. Claims received by <strong>Blue</strong> <strong>Cross</strong> for<br />
these services will be denied indicating that claims for these<br />
services should be sent to DHS for consideration.<br />
Claims Not Related to Terminal Diagnosis<br />
Claims that are not related to a terminal diagnosis may be denied<br />
by RHHI. These claims should then be submitted with a copy <strong>of</strong><br />
the Medicare denial to <strong>Blue</strong> <strong>Cross</strong> for processing. These services<br />
can <strong>of</strong>ten be identified by procedure code modifier GW on<br />
pr<strong>of</strong>essional claims (837-P), or condition code 07 on institutional<br />
claims (837-I).<br />
Notification <strong>of</strong> Hospice Election<br />
<strong>Blue</strong> <strong>Cross</strong> requires hospice providers to notify <strong>Blue</strong> <strong>Cross</strong> when a<br />
member has elected the hospice benefit. For Secure<strong>Blue</strong> <strong>and</strong><br />
Care<strong>Blue</strong> members, the hospice agency should communicate the<br />
hospice election to senior public programs unit at (651) 662-5540<br />
or toll free at 1-800-711-9868.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (07/12/12)<br />
11-19
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Hospital / SNF Care)<br />
Table <strong>of</strong> Contents<br />
Initial Hospital Care............................................................................................................. 11-2<br />
Subsequent Hospital Visits .................................................................................................. 11-2<br />
Critical Care.........................................................................................................................11-2<br />
Hospital Observation Services............................................................................................. 11-3<br />
Observation Care Discharge Day Management...................................................................11-3<br />
Hospital Discharge............................................................................................................... 11-3<br />
Continuing Intensive Care Services..................................................................................... 11-3<br />
Swing Beds ..........................................................................................................................11-3<br />
Skilled Nursing Facility Care ..............................................................................................11-4<br />
SNF Billing for <strong>Blue</strong> Plus Government Program Products .................................................11-4<br />
Medical Necessity Vendor...................................................................................................11-8<br />
Leave <strong>of</strong> Absence (LOA) or Furlough Days........................................................................11-9<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
Initial Hospital Care <strong>Blue</strong> <strong>Cross</strong> patients have coverage for a physician’s daily inpatient<br />
care. Submit a separate charge for medical care on the admission<br />
day, using codes 99221-99223. Always submit this charge as one<br />
unit <strong>of</strong> service.<br />
Subsequent<br />
Hospital Visits<br />
Bill all other inpatient visits as subsequent care, using codes<br />
99231-99233. If the patient is still hospitalized when you bill, use<br />
the last visit as the discharge date on the claim.<br />
Subsequent visits may be combined on one line if all services,<br />
diagnoses, <strong>and</strong> charges are identical, provided by the same<br />
individual provider <strong>and</strong> the dates <strong>of</strong> service are sequential. Each<br />
visit counts as one unit <strong>of</strong> service. The place-<strong>of</strong>-service code is<br />
inpatient hospital (21).<br />
Critical Care Coding <strong>of</strong> Critical Care is based first on the age <strong>of</strong> the patient.<br />
11-2<br />
Neonates - birth through the 28 th postnatal day would utilize<br />
99468 <strong>and</strong> 99469. These are inpatient per day codes.<br />
Pediatrics - 29 days old through 24 months would utilize<br />
99471 <strong>and</strong> 99472. These are inpatient per day codes.<br />
Pediatrics - 2 through 5 years <strong>of</strong> age would utilize 99475 <strong>and</strong><br />
99476. These are inpatient per day codes.<br />
Over 71 months <strong>of</strong> age - anyone older than 71 months would<br />
utilize 99291 <strong>and</strong> 99292. These are time-based codes.<br />
Use code 99291 for up to <strong>and</strong> including 74 minutes <strong>of</strong> critical care.<br />
Submit one unit <strong>of</strong> service for this code. Time duration beyond 74<br />
minutes should be coded as 99292 with the appropriate number <strong>of</strong><br />
units. The narrative for 99292 states “each additional 30 minutes.”<br />
For procedures that include time increments, over 50 percent <strong>of</strong> the<br />
indicated time must be rendered <strong>and</strong> documented in order to bill<br />
for the code <strong>and</strong> any additional unit(s). If code 99292 is reported it<br />
must always be submitted with 99291.<br />
Example:<br />
Critical care for a 26-year-old <strong>of</strong> 2 hours’ duration.<br />
Code Units <strong>of</strong> Service<br />
99291 1<br />
99292 1<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Hospital Observation<br />
Services<br />
Observation Care<br />
Discharge Day<br />
Management<br />
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
<strong>Blue</strong> <strong>Cross</strong> considers hospital stays for 24 hours or more as<br />
inpatient. The hospital observation codes 99218-99220 should not<br />
be submitted if the hospital stay is more than 24 hours.<br />
Subsequent observation is reported under codes 99224-99226.<br />
Evaluation <strong>and</strong> management services on the same date provided in<br />
sites that are related to initiating “observation status” should NOT<br />
be reported separately.<br />
Subsequent visits provided to patients who have been admitted to<br />
the hospital for 24 hours or more should be submitted with codes<br />
99231-99233.<br />
Observation or inpatient care services provided to patients<br />
admitted <strong>and</strong> discharged on the same date <strong>of</strong> service are reported<br />
using codes 99234-99236. The place <strong>of</strong> service can be either<br />
inpatient or outpatient.<br />
The discharge management code 99217 may be submitted for the<br />
day following initial observation care when a physician performs a<br />
final exam, discusses the observation period, provides instructions<br />
for continued care <strong>and</strong> prepares the discharge record.<br />
Hospital Discharge Hospital discharge day management services, 99238 or 99239, are<br />
billable only by the provider who actually discharged the patient<br />
on the actual date <strong>of</strong> discharge. Face-to-face contact is required on<br />
the day <strong>of</strong> discharge.<br />
Continuing Intensive<br />
Care Services<br />
Discharge summaries prepared before the patient is discharged are<br />
not billable.<br />
The codes 99478-99480 are used to report services subsequent to<br />
the day <strong>of</strong> admission provided by a physician directing the<br />
continuing intensive care <strong>of</strong> the low birth weight (LBW), very low<br />
birth weight (VLBW) infant, or normal weight newborn who no<br />
longer meets the definition <strong>of</strong> critically ill but continues to require<br />
intensive observation, frequent interventions <strong>and</strong> other intensive<br />
services. These codes are global 24-hour codes <strong>and</strong> not reported as<br />
hourly services.<br />
Swing Beds If the hospital census reports the patient as inpatient, use inpatient<br />
E/M codes with an inpatient place <strong>of</strong> service. If the patient has<br />
been discharged from inpatient status, use the skilled nursing place<br />
<strong>of</strong> service <strong>and</strong> the corresponding E/M codes 99304-99310.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
Skilled Nursing Facility<br />
Care<br />
SNF Billing for <strong>Blue</strong><br />
Plus Government<br />
Program Products<br />
11-4<br />
Follow the same guidelines for skilled nursing facility care as for<br />
in-hospital medical care above. Use codes 99304-99306 for<br />
medical care on the day <strong>of</strong> admission to a skilled nursing facility.<br />
For follow-up care, use codes 99307-99310. The place-<strong>of</strong>-service<br />
code is 31. Claims for skilled nursing care require admit <strong>and</strong><br />
discharge dates.<br />
Discharge day management codes 99315 or 99316 are used to<br />
report the total duration <strong>of</strong> time spent by a physician for the final<br />
nursing facility discharge <strong>of</strong> a patient.<br />
How to submit the Medicare Assessment line:<br />
Loop <strong>and</strong> Segment<br />
on 837<br />
Description <strong>of</strong> Data Content<br />
Loop 2400, SV201 Revenue Code for SNF PPS, example<br />
“0022.”<br />
Loop 2400, SV202 Three (3) character RUG code with two (2)<br />
character assessment type indicator.<br />
Total <strong>of</strong> five (5) characters; for example<br />
“RVX01.”<br />
Loop 2400, DTP03 The service date <strong>of</strong> the assessment. Service<br />
date must fall within statement covered<br />
period.<br />
Loop 2400, SV205 The number <strong>of</strong> days that apply to the RUG<br />
code in FL 44.<br />
Loop 2400, SV203 Zero-fill this form locator; for example “0 |<br />
00.”<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
SNF Billing for <strong>Blue</strong><br />
Plus Government<br />
Program Products<br />
(continued)<br />
How to bill the room & board line:<br />
Loop <strong>and</strong> Segment<br />
on 837I<br />
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
Description <strong>of</strong> Data Content<br />
Loop 2400, SV201 Revenue Code for room & board; for<br />
example “0120.”<br />
Loop 2400, SV202 The rate charged per day for the room <strong>and</strong><br />
board, for example “174.41.”<br />
Loop 2400, DTP03 Can be left blank.<br />
Loop 2400, SV205 The number <strong>of</strong> days that room <strong>and</strong> board<br />
were provided.<br />
Loop 2400, SV203 The total charge for the room <strong>and</strong> board.<br />
Skilled Nursing Facility Services should be billed with claim<br />
facility type <strong>of</strong> bill code 02XX.<br />
Intensive Service Days (ISD)<br />
Nursing facility providers should bill Intensive Service Days (ISD)<br />
with revenue code 0230.<br />
Providers may request prior authorization <strong>and</strong>, if approved, receive<br />
reimbursement for Intensive Service Days for a resident who is in<br />
skilled or custodial care. ISDs can be considered regardless <strong>of</strong><br />
whether <strong>Blue</strong> Plus or the Department <strong>of</strong> Human Services (DHS) is<br />
responsible for the payment <strong>of</strong> the custodial stay.<br />
If DHS is responsible for the custodial room <strong>and</strong> board, the<br />
nursing facility should prior authorize the ISD <strong>and</strong> then bill to<br />
<strong>Blue</strong> Plus only the revenue code 0230 for the ISD services<br />
provided.<br />
If <strong>Blue</strong> Plus is responsible for the custodial room <strong>and</strong> board, the<br />
nursing facility should prior authorize the ISD <strong>and</strong> then bill the<br />
revenue code 0230 for the ISD services along with normal billing<br />
procedures for the custodial room <strong>and</strong> board.<br />
Medicaid<br />
Custodial days are billed at the Medicaid Case Mix rate as<br />
determined by the MN Department <strong>of</strong> Human Services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
SNF Billing for <strong>Blue</strong><br />
Plus Government<br />
Program Products<br />
(continued)<br />
11-6<br />
How to report the Medicaid Custodial days line<br />
Loop <strong>and</strong> Segment<br />
on 837I<br />
Description <strong>of</strong> Data Content<br />
Loop 2400, SV201 Revenue Code for Medicaid Custodial<br />
days; for example “0100” or “0101.”<br />
Loop 2400, SV202 The rate charged per day for the Medicaid<br />
Custodial days; for example “174.41.”<br />
Loop 2400, DTP03 Can be left blank.<br />
Loop 2400, SV205 The number <strong>of</strong> Medicaid Custodial days<br />
provided.<br />
Loop 2400, SV203 The total charge for the Medicaid Custodial<br />
days.<br />
Bedhold Days for Medicaid subscribers<br />
Loop <strong>and</strong> Segment<br />
on 837I<br />
Description <strong>of</strong> Data Content<br />
Loop 2400, SV201 Revenue Code for Bedhold days; for<br />
example “0185.”<br />
Loop 2400, SV202 The rate charged per day for the Bedhold<br />
day.<br />
Loop 2400, DTP03 Can be left blank.<br />
Loop 2400, SV205 The number <strong>of</strong> Bedhold days provided <strong>and</strong><br />
approved.<br />
Loop 2400, SV203 The total charge for the Bedhold days.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
SNF Billing for <strong>Blue</strong><br />
Plus Government<br />
Program Products<br />
(continued)<br />
Billing for Swing Beds<br />
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
The appropriate type <strong>of</strong> bill for swing bed services is 028X.<br />
Use the correct <strong>Blue</strong> <strong>Cross</strong> provider number or NPI<br />
specifically for billing Swing Beds (xxExx.)<br />
Common send back issues<br />
Loop <strong>and</strong> Segment<br />
on 837I<br />
Description <strong>of</strong> Data Content<br />
Loop 2300, CLM05 Appropriate type <strong>of</strong> bill entered. TOB<br />
should be four digits.<br />
Loop 2010CA,<br />
DMG02<br />
Date <strong>of</strong> birth must be in MMDDCCYY<br />
format.<br />
Loop 2300, DTP03 There must be an admit date.<br />
The admit date cannot be prior to 010102.<br />
(Jan. 1, 2002) (If it is, change to 010102.)<br />
Loop 2400, SV201 Use Revenue Code 0022 to report RUG<br />
Code <strong>and</strong> Assessment Date. Use Revenue<br />
Code 0230 for ISD days.<br />
Loop 2400, SV202 Only use Rates on room <strong>and</strong> board lines.<br />
RUG codes must be five (5) characters.<br />
(Include assessment type indicator.)<br />
Can only be submitted with five (5)<br />
character HCPCS <strong>and</strong> up to four (4)<br />
modifiers.<br />
Loop 2400, DTP03 Service date must fall within statement<br />
covers period.<br />
Loop 2400, SV205 Do not use decimals to report units. (Round<br />
up to the nearest whole number.)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
SNF Billing for <strong>Blue</strong><br />
Plus Government<br />
Program Products<br />
(continued)<br />
Medical Necessity<br />
Vendor<br />
11-8<br />
Tips for Billing<br />
If the stay includes a change in level <strong>of</strong> care, then additional<br />
lines can be added onto the claim as instructed above. Indicate<br />
the number <strong>of</strong> days associated with each level <strong>of</strong> care that is<br />
being billed.<br />
Skilled days <strong>and</strong> nonskilled days should be billed on separate<br />
claims.<br />
Part B eligible services should be billed on a separate form.<br />
Nursing Home Communication Form<br />
A Nursing Home Communication Form is required.<br />
PMAP communication form process remains unchanged<br />
The current requirement for <strong>Blue</strong> Advantage (PMAP) subscribers<br />
<strong>and</strong> SCHA (PMAP) products will remain in place. The PMAP<br />
Communication Form must be faxed to (651) 662-6054 before<br />
claims are submitted.<br />
<strong>Blue</strong> <strong>Cross</strong>, Commercial <strong>Blue</strong> Plus <strong>and</strong> <strong>Blue</strong>Link TPA have an<br />
agreement with McKesson Health Solutions, who provides<br />
medical necessity criteria for the majority <strong>of</strong> hospitals <strong>and</strong> health<br />
care systems in <strong>Minnesota</strong>, for use <strong>of</strong> their InterQual Medical<br />
Necessity Criteria.<br />
Effective March 26, 2012, clinicians, peer reviewers <strong>and</strong> appeals<br />
reviewers will utilize this tool to determine medical necessity <strong>and</strong><br />
level <strong>of</strong> care review for inpatient, long-term acute care, <strong>and</strong> acute<br />
rehabilitation admissions <strong>and</strong> length <strong>of</strong> stay. Criteria are available<br />
for review, on a case-by-case basis, upon request. The <strong>Blue</strong> <strong>Cross</strong><br />
clinician who is communicating the results <strong>of</strong> the case review will<br />
be able to assist you with your questions.<br />
We will extend the use <strong>of</strong> the McKesson InterQual criteria to<br />
behavioral health <strong>and</strong> chemical dependency, along with<br />
chiropractic, physical therapy, occupational therapy, speech<br />
therapy, home health care <strong>and</strong> skilled nursing facility reviews on<br />
April 1, 2012.<br />
Government Programs will also be using McKesson InterQual<br />
Criteria, in addition to Medicare <strong>and</strong> MHCP guidelines, for<br />
inpatient care, long-term acute care, acute rehabilitation care <strong>and</strong><br />
behavioral health services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Leave <strong>of</strong> Absence<br />
(LOA) or Furlough<br />
Days<br />
Coding Policies <strong>and</strong> Guidelines (Hospital / SNF Care)<br />
<strong>Blue</strong> <strong>Cross</strong> does not pay for Leave <strong>of</strong> Absence (LOA) or furlough<br />
days as these are considered a charge or fee to “hold” a bed. Actual<br />
services are not being provided to the patient.<br />
Leave <strong>of</strong> absence (LOA) or furlough days are “time away” dates<br />
during which a patient is discharged from but remains a patient <strong>of</strong><br />
an inpatient hospital, residential treatment program, or Skilled<br />
Nursing Facility. If the member or patient has progressed to the<br />
point <strong>of</strong> being able to be away from the facility, or is expected for<br />
follow-up care or surgery <strong>and</strong> the patient does not require a<br />
hospital level <strong>of</strong> care during the interim period, an LOA or<br />
furlough may be granted.<br />
Leave days may be eligible for MA payment for patients <strong>of</strong> skilled<br />
nursing facility, nursing facility, or boarding care homes. A leave<br />
day must be for hospital leave or therapeutic leave <strong>of</strong> a recipient<br />
who has not been discharged from a nursing facility. A reserved<br />
bed must be held for a recipient on hospital leave or therapeutic<br />
leave. Payment for leave days in an SNF or NF is limited to 60%<br />
<strong>of</strong> the applicable payment rate.<br />
The Leave <strong>of</strong> Absence accommodation revenue codes 018X are<br />
billed to indicate the days that the patient was not in the facility.<br />
These codes indicate routine service charges including zero<br />
charges for holding a room while the patient is temporarily away<br />
from the provider. Use <strong>of</strong> this revenue code also requires that<br />
occurrence span code 74 Noncovered level <strong>of</strong> care/LOA, <strong>and</strong><br />
date(s) <strong>of</strong> the absence.<br />
Leave <strong>of</strong> Absence 018X revenue codes<br />
0180 – Leave <strong>of</strong> Absence—General<br />
0182 – Leave <strong>of</strong> Absence—Patient Convenience<br />
0183 – Leave <strong>of</strong> Absence—Therapeutic Leave<br />
0185 – Leave <strong>of</strong> Absence—Nursing Home (for Hospitalization)<br />
0189 – Leave <strong>of</strong> Absence—Other LOA<br />
Occurrence Span Code 74 – Noncovered Level <strong>of</strong> Care/Leave <strong>of</strong><br />
Absence Dates<br />
This code <strong>and</strong> corresponding dates indicate the from <strong>and</strong> through<br />
dates <strong>of</strong> a period <strong>of</strong> noncovered level <strong>of</strong> care or leave <strong>of</strong> absence in<br />
an otherwise covered stay<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-9
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Laboratory)<br />
Table <strong>of</strong> Contents<br />
Introduction..........................................................................................................................11-2<br />
Organ or Disease-Oriented Panels.......................................................................................11-2<br />
Lyme Disease Titer.............................................................................................................. 11-2<br />
Office Visits.........................................................................................................................11-2<br />
St<strong>and</strong>ing Orders ................................................................................................................... 11-3<br />
Venipunctures <strong>and</strong> Lab H<strong>and</strong>ling ........................................................................................ 11-3<br />
Collection <strong>and</strong> h<strong>and</strong>ling <strong>of</strong> specimens for <strong>Minnesota</strong> Health Care Program Subscribers<br />
only .................................................................................................................................... 11-4<br />
Papanicolaou Smears ........................................................................................................... 11-4<br />
Pregnancy Tests ................................................................................................................... 11-6<br />
Purchased Services/ Outside Lab......................................................................................... 11-6<br />
Stat Lab Charges.................................................................................................................. 11-7<br />
Repeat Lab Services............................................................................................................. 11-7<br />
Genetic Testing Modifiers ...................................................................................................11-7<br />
Lab Billed through the <strong>Blue</strong>Card® Program .......................................................................11-7<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Laboratory)<br />
Introduction <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) does not<br />
allow providers to bill the health plan for laboratory services or<br />
imaging studies that are not ordered by a physician or other<br />
qualified practitioner because in addition to receiving lab or<br />
radiology results, the patient also needs interpretation <strong>of</strong> the tests,<br />
recommendations for future care, <strong>and</strong> a course <strong>of</strong> action that only a<br />
physician or other qualified practitioner can deliver. In addition,<br />
tests must be medically necessary in order to be eligible for<br />
coverage. As a result, we will only issue payment for services that<br />
are coordinated by a physician or other qualified practitioner. A<br />
qualified practitioner is a practitioner recognized as an eligible<br />
provider by <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> practices within the scope <strong>of</strong> his or her<br />
licensure. Specific licensing questions should be directed to your<br />
specialty’s licensing board.<br />
Organ or Disease-<br />
Oriented Panels<br />
Laboratory <strong>and</strong> pathology procedures should be submitted using<br />
the HCPCS level I or II code that best describes the service. CPT<br />
codes 80047-89358 encompass level I codes for the majority <strong>of</strong><br />
laboratory <strong>and</strong> pathology procedures.<br />
The services listed in the pathology <strong>and</strong> laboratory section <strong>of</strong> the<br />
CPT manual may be provided by the pathologist or alternatively<br />
by technologists who are under the supervision <strong>of</strong> the pathologist<br />
or practitioner.<br />
The guidelines outlined below should be adhered to when<br />
submitting laboratory services to <strong>Blue</strong> <strong>Cross</strong>.<br />
The tests listed under each panel (80047-80076) identify the<br />
defined components <strong>of</strong> that panel, <strong>and</strong> all tests listed must be<br />
performed in order to bill for that panel. Tests performed in<br />
addition to those specifically indicated for a particular panel can be<br />
billed separately in addition to the panel code.<br />
Lab panels should be reported as 1 line item with 1 unit per panel.<br />
Lyme Disease Titer Laboratory testing codes for Lyme disease titer are 86617 or<br />
86618.<br />
Office Visits A level-<strong>of</strong>-service <strong>of</strong>fice visit may be submitted in addition to<br />
laboratory tests only when additional separately identifiable<br />
services are provided. Obtaining a specimen for a streptococcus<br />
test, for example, <strong>and</strong> relaying the results to the patient are<br />
included in the reimbursement for the test itself <strong>and</strong> may not be<br />
billed separately. A minimal level <strong>of</strong> service may be submitted if a<br />
brief history <strong>and</strong> examination is performed in addition to the<br />
laboratory test.<br />
11-2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)
Coding Policies <strong>and</strong> Guidelines (Laboratory)<br />
St<strong>and</strong>ing Orders Generally, laboratory tests performed because <strong>of</strong> st<strong>and</strong>ing orders<br />
on file for certain patients are not covered. One example <strong>of</strong> this is a<br />
st<strong>and</strong>ing order for routine screening tests when the patient has no<br />
clinical symptoms or is not taking medications. Laboratory<br />
services based on st<strong>and</strong>ing orders are covered only if you can show<br />
the medical necessity <strong>of</strong> the services through your medical records<br />
or if the patient has routine screening benefits <strong>and</strong> the tests are<br />
coded with an ICD-9-CM as routine services.<br />
Venipunctures <strong>and</strong> Lab<br />
H<strong>and</strong>ling<br />
The following codes apply to venipunctures <strong>and</strong> lab h<strong>and</strong>ling:<br />
Code Description<br />
36415 Collection <strong>of</strong> venous blood by venipuncture<br />
36416 Collection <strong>of</strong> capillary blood specimen (e.g., finger,<br />
heel, ear stick)<br />
99000 H<strong>and</strong>ling <strong>and</strong>/or conveyance <strong>of</strong> specimen for transfer<br />
from the physician’s <strong>of</strong>fice to a laboratory<br />
Code 36415 is submitted when the provider performs a<br />
venipuncture service to collect a blood specimen(s).<br />
As opposed to a venipuncture, a finger/heel/ear stick (36416) is<br />
performed in order to obtain a small amount <strong>of</strong> blood for a<br />
laboratory test.<br />
These codes should be billed only once regardless <strong>of</strong> the number<br />
<strong>of</strong> tests performed from that specimen.<br />
Code 99000 is an adjunct code submitted to indicate h<strong>and</strong>ling<br />
<strong>and</strong>/or conveyance <strong>of</strong> a specimen for transfer from the physician’s<br />
<strong>of</strong>fice to a laboratory. This code is never used for lab services<br />
performed completely within the physician’s <strong>of</strong>fice.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Laboratory)<br />
Venipunctures <strong>and</strong> Lab<br />
H<strong>and</strong>ling (continued)<br />
Collection <strong>and</strong><br />
h<strong>and</strong>ling <strong>of</strong> specimens<br />
for <strong>Minnesota</strong> Health<br />
Care Program<br />
Subscribers only<br />
If the lab is picking up the specimen, there is no h<strong>and</strong>ling cost<br />
incurred <strong>and</strong> the clinic should not bill 99000.<br />
The test that is being done from the specimen must be indicated on<br />
the claim. This can be indicated by submission <strong>of</strong> the lab test code<br />
with the -90 modifier (if you are billing for the test) or narrative<br />
indicating the test code <strong>and</strong>/or name (done if lab will bill for test<br />
instead <strong>of</strong> clinic). If this information is not present on the claim,<br />
the charge will be denied if billed in addition to a venipuncture<br />
code 36415.<br />
For lab tests requiring routine venipuncture <strong>and</strong> subsequently sent<br />
to an outside lab, the physician <strong>of</strong>fice may bill either the<br />
venipuncture service or the h<strong>and</strong>ling charge, but not both<br />
(i.e., 36415 or 99000).<br />
Due to a benefit change dictated by the <strong>Minnesota</strong> Department <strong>of</strong><br />
Human Services effective for dates <strong>of</strong> service February 3, 2012<br />
<strong>and</strong> after <strong>Blue</strong> Plus will no longer reimburse for the collection <strong>of</strong><br />
blood by venipuncture (CPT 36416), capillary (CPT 36415) or<br />
access port (CPT 36591 <strong>and</strong> 36592) in conjunction with another<br />
service for <strong>Minnesota</strong> Health Care Programs Subscribers. These<br />
services (36415, 36416, 36591 <strong>and</strong> 36592) will be denied as<br />
incidental, or included in a primary service when billed in<br />
conjunction with another service.<br />
Papanicolaou Smears The procedure codes, diagnosis codes, specimen collection codes<br />
<strong>and</strong> h<strong>and</strong>ling fee that apply to Papanicolaou smears are detailed<br />
below.<br />
11-4<br />
Procedure Codes<br />
Codes 88142-88154, 88164-88167, 88174-88175, P3000, P3001,<br />
G0123-G0124, <strong>and</strong> G0141, G0143-G0148 are for cytopathology<br />
screening <strong>of</strong> cervical or vaginal smears. Submit the appropriate<br />
code to reflect the service provided.<br />
Procedure code 88141 <strong>and</strong> 88155 are used to report physician<br />
interpretation <strong>of</strong> a cervical or vaginal specimen <strong>and</strong> should be<br />
listed in addition to the screening code chosen when the additional<br />
services are provided.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)
Papanicolaou Smears<br />
(continued)<br />
Diagnosis Codes<br />
Coding Policies <strong>and</strong> Guidelines (Laboratory)<br />
Routine cervical Papanicolaou smears should be reported with<br />
appropriate ICD-9-CM diagnosis codes:<br />
Use this code… In this situation…<br />
V72.32 As part <strong>of</strong> a general gynecological examination<br />
V76.2 Without a general gynecological examination<br />
Pap smears performed due to illness, specific related symptoms,<br />
or relevant personal or family history should be reported with the<br />
most specific ICD-9-CM code available.<br />
Specimen Collection Codes<br />
The specimen collection code for a Pap smear (Q0091) is not<br />
separately reimbursable. Specimen collection is included in the<br />
level <strong>of</strong> service reported for the examination <strong>and</strong> evaluation <strong>and</strong><br />
should not be billed separately. The collection code will be denied<br />
as incidental regardless <strong>of</strong> what, if any, other service is billed with<br />
the code.<br />
H<strong>and</strong>ling Fee<br />
Code 99000 may be submitted for the cost incurred by the clinic<br />
for the h<strong>and</strong>ling <strong>and</strong>/or conveyance <strong>of</strong> the Pap smear for transfer<br />
from the physician’s <strong>of</strong>fice to an outside laboratory. This code is<br />
never submitted for cytopathology screening performed within the<br />
physician’s <strong>of</strong>fice.<br />
Modifier -90 (reference outside laboratory) must also be submitted<br />
when the screening is performed by a party other than the treating<br />
or reporting physician. This modifier would be submitted with the<br />
Pap smear code (e.g., 88150-90). Narrative indicating the test<br />
being done may be submitted in lieu <strong>of</strong> the procedure code <strong>and</strong><br />
modifier if the lab will be billing <strong>Blue</strong> <strong>Cross</strong> for the test instead <strong>of</strong><br />
the clinic.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Laboratory)<br />
Pregnancy Tests Pregnancy tests should be coded as follows:<br />
Purchased Services/<br />
Outside Lab<br />
11-6<br />
Code Description<br />
84702 Quantitative, serum<br />
84703 Qualitative, serum<br />
81025 Urine<br />
Laboratory records must document the method (quantitative or<br />
qualitative) <strong>of</strong> testing done <strong>and</strong> the type <strong>of</strong> specimen used (serum<br />
or urine).<br />
The entity that performs a test should be the one to bill for that<br />
test. However, a provider may, under arrangement with another<br />
provider, bill a service that is purchased from that other provider.<br />
For example, a clinic may bill for a Pap smear that is sent to an<br />
independent lab for analysis, or for an X-ray that is done at a<br />
hospital because the clinic did not have the appropriate equipment.<br />
It is important to remember that only one provider may bill for the<br />
service.<br />
Claims for purchased services should be submitted on the 837P<br />
format as follows:<br />
Loop 2300, CLM05-1 (place <strong>of</strong> service) - enter the place <strong>of</strong><br />
service code where the service was done by the performing<br />
provider.<br />
Loop 2400, SV101-2 (procedure/modifier) - enter the<br />
procedure code <strong>of</strong> the test <strong>and</strong> the modifier 90.<br />
Loop 2400, SV101-1 (ID qual) - enter the two-character<br />
qualifier in the shaded area if there is an ID submitted in 24J<br />
shaded.<br />
Loop 2310B, NM109 or REF02 (rendering provider ID) -<br />
enter the NPI provider number <strong>of</strong> the ordering physician or the<br />
legacy ID if the provider was not NPI eligible.<br />
Loop 2310D (service facility location information) - enter the<br />
name <strong>and</strong> address <strong>of</strong> the performing provider.<br />
Loop 2310D, NM109 (NPI #) or REF02 (service facility<br />
provider) - enter the NPI provider number <strong>of</strong> the service<br />
facility location or the legacy ID if the provider was not NPI<br />
eligible.<br />
Loop 2010AA, NM109 (NPI) or REF02 (billing provider) -<br />
Enter the NPI provider number <strong>of</strong> the billing provider or the<br />
legacy ID if the provider was not NPI eligible.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)<br />
Coding Policies <strong>and</strong> Guidelines (Laboratory)<br />
Stat Lab Charges Charges for stat laboratory requests (S3600 <strong>and</strong> S3601) are not<br />
allowed. If submitted, they will deny as provider liability.<br />
Repeat Lab Services Repeat services require modifier 91 (not 59), unless the narrative<br />
supports submission <strong>of</strong> multiple units.<br />
Genetic Testing<br />
Modifiers<br />
Lab Billed through the<br />
<strong>Blue</strong>Card® Program<br />
Genetic coding modifiers (0A-9Z) are developed <strong>and</strong> maintained<br />
by the AMA. These modifiers are required when reporting a<br />
genetic lab procedure, as appropriate.<br />
<strong>Blue</strong> plans* may contract with providers outside <strong>of</strong> their exclusive<br />
service area for services provided to local <strong>and</strong> <strong>Blue</strong>Card members<br />
within their own service area for independent clinical lab services.<br />
<strong>Blue</strong> plans may not contract for such services for their members<br />
who receive services outside <strong>of</strong> their service area.<br />
Lab<br />
Providers who perform lab services should file the claim to the<br />
<strong>Blue</strong> plan in whose service area the specimen was drawn. The<br />
claim will be reimbursed based on provider’s participation status<br />
with that <strong>Blue</strong> plan.<br />
* Each <strong>Blue</strong> plan is an independent licensee <strong>of</strong> the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong><br />
<strong>Blue</strong> <strong>Shield</strong> Association<br />
11-7
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Maternity)<br />
Table <strong>of</strong> Contents<br />
Global Obstetrical Care........................................................................................................ 11-2<br />
Antepartum Care.................................................................................................................. 11-2<br />
Delivery................................................................................................................................ 11-2<br />
Subsequent VBACs .............................................................................................................11-2<br />
Postpartum Care................................................................................................................... 11-2<br />
Initial Visit <strong>and</strong> Itemized Services.......................................................................................11-2<br />
Submission Options <strong>and</strong> Coding Alternatives .....................................................................11-3<br />
Pre-term Birth Prevention Services ..................................................................................... 11-4<br />
Two Physicians Involved in Care/ Same Tax ID.................................................................11-5<br />
Newborn Care ...................................................................................................................... 11-5<br />
Complications or Unusual Circumstances...........................................................................11-6<br />
Exceptions............................................................................................................................11-6<br />
Lactation Education ............................................................................................................. 11-6<br />
Collection <strong>of</strong> Umbilical Cord Blood.................................................................................... 11-6<br />
Obstetrical Care Coding Alternatives ..................................................................................11-7<br />
Reproduction Treatment ...................................................................................................... 11-8<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
Global Obstetrical Care <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) accepts the<br />
global obstetric care codes 59400, 59510, 59610 <strong>and</strong> 59618, which<br />
include antepartum care, delivery, <strong>and</strong> postpartum care.<br />
Antepartum Care Antepartum care includes the subsequent history <strong>and</strong> physical<br />
examinations, recording <strong>of</strong> weight, height, blood pressures, fetal<br />
heart tones, chemical urinalysis, maternity counseling, <strong>and</strong><br />
monthly visits up to 28 weeks gestation, biweekly visits to 36<br />
weeks gestation, <strong>and</strong> weekly visits until delivery. Any other visits<br />
or services within this time period should be coded separately.<br />
The provider may choose to bill globally, visit-by-visit, or to use<br />
codes 59425 or 59426 for antepartum care. The date <strong>of</strong> service<br />
submitted for antepartum care should be the date <strong>of</strong> delivery.<br />
If antepartum care is not performed for the entire period, code each<br />
E/M service separately.<br />
Delivery Delivery includes admission history <strong>and</strong> physical, management <strong>of</strong><br />
uncomplicated labor, <strong>and</strong> delivery (with or without episiotomy or<br />
forceps). Vaginal delivery only should be submitted with<br />
procedure code 59409 or 59612 (VBAC).<br />
Cesarean (C-section) delivery only should be submitted with code<br />
59514 or 59620 (VBAC).<br />
Only one delivery code should be billed regardless <strong>of</strong> the number<br />
<strong>of</strong> births during that delivery.<br />
Subsequent VBACs Vaginal births after a C-section (VBACs) should be coded using<br />
CPT codes 59618, 59620, 59622 regardless if the vaginal birth is<br />
the first or subsequent following the C-section.<br />
Postpartum Care Postpartum care includes hospital visits <strong>and</strong> one to two <strong>of</strong>fice visits<br />
for usual, uncomplicated postpartum follow-up, urinalysis, <strong>and</strong><br />
hemoglobins. The global codes (59400, 59510, 59610, or 59618)<br />
<strong>and</strong> delivery codes (59410, 59515, 59614, or 59622) include<br />
postpartum care.<br />
Initial Visit <strong>and</strong><br />
Itemized Services<br />
11-2<br />
Submit the postpartum care package (separate procedure) code<br />
59430 only when another provider does the delivery. Submit this<br />
code one time with one unit <strong>of</strong> service. The date <strong>of</strong> service should<br />
be the delivery date.<br />
The initial visit may be billed separately with an appropriate E/M<br />
code. An obstetrical pr<strong>of</strong>ile (80055) <strong>and</strong> any laboratory procedure<br />
codes (other than urinalysis) should also be submitted separately.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Submission Options<br />
<strong>and</strong> Coding<br />
Alternatives<br />
The following submission options are available:<br />
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
The global codes 59400, 59510, 59610, <strong>and</strong> 59618 may be<br />
submitted with one charge. For contracts subject to <strong>Minnesota</strong><br />
legislative m<strong>and</strong>ated benefits <strong>and</strong> others that waive<br />
deductibles, copays, or coinsurance on antepartum care, <strong>Blue</strong><br />
<strong>Cross</strong> will process these services separately from the delivery<br />
<strong>and</strong> postpartum care. The global maternity charge will be split<br />
based on RBRVS (Resource Based Relative Value System)<br />
work values. The provider Remittance Advice will report<br />
procedure code 59426 with a payment at 100 percent <strong>of</strong> the<br />
allowance <strong>and</strong> a delivery code 59410, 59515, 59614, or 59622<br />
with a payment determined according to the contract’s<br />
benefits.<br />
For contracts that are not subject to <strong>Minnesota</strong> legislative<br />
m<strong>and</strong>ated benefits <strong>and</strong>/or where antepartum care is subject to<br />
regular contract benefits, the global codes 59400, 59510,<br />
59610 <strong>and</strong> 59618 will process with the charge <strong>and</strong> code as<br />
submitted.<br />
Providers may submit the appropriate E/M codes for each<br />
antepartum visit individually with the delivery code 59410,<br />
59515, 59614, or 59622 as an alternative to submitting the<br />
global maternity codes 59400, 59510, 59610, or 59618.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
Pre-term Birth<br />
Prevention Services<br />
11-4<br />
<strong>Blue</strong> <strong>Cross</strong> will reimburse for certain pre-term birth prevention<br />
services when the patient’s contract covers these services.<br />
Code Narrative Billing<br />
H1000 Prenatal Care, at-risk assessment<br />
[use the <strong>Minnesota</strong> Pregnancy<br />
Assessment Form, DHS 3294 (1/97)<br />
to complete assessment or the<br />
American College <strong>of</strong> Obstetrics <strong>and</strong><br />
Gynecology (ACOG) pregnancy<br />
assessment form]<br />
H1001 Prenatal care, at-risk enhanced<br />
service; antepartum management<br />
H1003 Prenatal care, at-risk enhanced<br />
services; education<br />
Done twice for<br />
all patients; once<br />
at initial OB visit<br />
<strong>and</strong> once at 24-<br />
28 weeks.<br />
If the patient is<br />
identified via the<br />
assessment as<br />
high risk. This<br />
code may be<br />
billed once.<br />
If the patient is<br />
identified via the<br />
assessment as<br />
high risk. This<br />
code may be<br />
billed once.<br />
The services represented by the prenatal care at-risk codes H1002,<br />
H1004 <strong>and</strong> H1005 are already included in the provider’s normal<br />
prenatal care <strong>and</strong> not separately reimbursed.<br />
Please refer to Chapter 4 Case Management for information on<br />
the <strong>Minnesota</strong> Pregnancy Assessment Form.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Two Physicians<br />
Involved in Care/<br />
Same Tax ID<br />
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
There are situations where the primary physician provides prenatal<br />
<strong>and</strong> postnatal care but does not deliver the baby. The most<br />
common situation noted is when a surgeon from the same medical<br />
group as the primary physician delivers the baby via C-section.<br />
Many times the primary physician is also acting as an assistant-atsurgery.<br />
In the case where both physicians are in the same practice<br />
(same tax ID), <strong>Blue</strong> <strong>Cross</strong> is recommending the following<br />
submission guides:<br />
Same tax-ID – clinic provider number reported for the claim<br />
Surgeon – bills the global C-section (59510); individual<br />
provider number or NPI <strong>of</strong> the surgeon reported on the service<br />
line<br />
Primary physician – bills the C-section assist (59514-80);<br />
individual provider number or NPI <strong>of</strong> the physician reported on<br />
the service line<br />
Provider production <strong>and</strong> disbursement <strong>of</strong> reimbursement is an<br />
internal process. It is the clinic’s responsibility to assure the<br />
providers participating in the patient’s care are appropriately paid.<br />
Newborn Care Submit procedure code 99460 or 99462 <strong>and</strong> diagnosis code V20.1<br />
to bill for routine services in the hospital for well newborns. If the<br />
newborn is ill, submit codes 99221-99223 or 99231--99233 for<br />
hospital visits. Initial hospital care <strong>of</strong> neonates, 28 days <strong>of</strong> age or<br />
less, who require intensive observation, frequent interventions, <strong>and</strong><br />
other intensive care services is reported with code 99477.<br />
Subsequent intensive care for very low birth weight infants is<br />
reported with codes 99478-99480, depending on the weight <strong>of</strong> the<br />
infant. For discharge day management, submit 99238. Pediatric<br />
st<strong>and</strong>by should be submitted with code 99464. St<strong>and</strong>by services<br />
are requested by another physician. The physician may not be<br />
providing care or services to other patients during this period.<br />
St<strong>and</strong>by, 99464, includes the initial stabilization <strong>of</strong> the newborn,<br />
thus services may be denied as incidental to 99464. When billing a<br />
newborn circumcision (54150 or 54160) on the day <strong>of</strong> discharge,<br />
add modifier –25 to code 99238. A diagnosis indicating the<br />
circumcision (V50.2) must be linked as the primary diagnosis to<br />
the circumcision procedure (54150 or 54160).<br />
For neonatal critical care services see codes 99468-99476.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
Complications or<br />
Unusual Circumstances<br />
Submit modifier –22 with specific documentation to justify<br />
additional reimbursement along with the delivery or operative<br />
report for complications during delivery. Unusual circumstances<br />
resulting in extensive antepartum or postpartum care should be<br />
coded separately. A narrative/operative report should be sent with<br />
the claim.<br />
Exceptions These guidelines apply to the majority <strong>of</strong> contracts. Exceptions<br />
include, but are not limited to, the Federal Employee Plan (FEP)<br />
<strong>and</strong> 3M.<br />
The Federal Employee Program contract does not allow<br />
payment for individual visits prior to delivery. Those services<br />
will be rejected. Antepartum care should be submitted as part<br />
<strong>of</strong> the global maternity code after delivery.<br />
For 3M contracts <strong>and</strong> others that require a copayment per visit,<br />
<strong>Blue</strong> <strong>Cross</strong> will request the number <strong>of</strong> antepartum visits if the<br />
global maternity codes 59400, 59510, 59610, or 59618 or the<br />
antepartum codes 59425 or 59426 are submitted.<br />
Lactation Education If done as part <strong>of</strong> the delivery, lactation education should be billed<br />
on the 837I, on the mother’s claim. If this is done after discharge,<br />
it should be incorporated into the E/M for postpartum care.<br />
Collection <strong>of</strong> Umbilical<br />
Cord Blood<br />
11-6<br />
Collection <strong>of</strong> umbilical cord blood may be done at the time <strong>of</strong> a<br />
delivery either for donation to organizations such as the Red <strong>Cross</strong><br />
or per the patient’s request to bank the blood for possible future<br />
need. Regardless <strong>of</strong> intent, cord blood collection is not a<br />
reimbursable service. If billing for the collection per the request <strong>of</strong><br />
the patient, the patient must be notified that this charge will be<br />
their liability. The charge should be submitted using an unlisted<br />
procedure code, such as 59899, with a narrative description <strong>and</strong><br />
will be denied as subscriber liability.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Obstetrical Care<br />
Coding Alternatives<br />
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
Different options are available for billing Obstetrical care. Listed<br />
below are some <strong>of</strong> the variations. Generally, global billing is<br />
preferred.<br />
Global Billing<br />
Global Billing includes the antepartum care, delivery, <strong>and</strong> postpartum<br />
care.<br />
59400 Vaginal delivery<br />
59510 C-section<br />
59610 VBAC<br />
59618 C-section after VBAC<br />
Antepartum Care Only<br />
59425 4 – 6 Visits<br />
59426 7 Visits<br />
E/M Evaluation <strong>and</strong> Management codes billed for each<br />
visit.<br />
Delivery Only<br />
59409 Vaginal delivery<br />
59514 C-section<br />
59612 VBAC<br />
59620 C-section after VBAC<br />
Delivery <strong>and</strong> Post-partum Only<br />
59410 Vaginal delivery<br />
59515 C-section<br />
59614 VBAC<br />
59622 C-section after VBAC<br />
Post-partum Care Only<br />
59430<br />
E/M Evaluation <strong>and</strong> Management codes billed for each<br />
visit<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
Reproduction<br />
Treatment<br />
11-8<br />
All <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus large group fully insured <strong>and</strong> Service<br />
Cooperative plans include a Reproduction Treatment combined<br />
lifetime dollar maximum benefit.<br />
Medical policy<br />
For medical policy information, including medical codes defining<br />
treatment, refer to the reproduction treatment medical policy, II-<br />
02, found on the <strong>Blue</strong> <strong>Cross</strong> website.<br />
Reproduction treatment services<br />
Artificial insemination (AI): The introduction <strong>of</strong> semen from a<br />
donor into a woman’s vagina, cervical canal or uterus by<br />
means other than sexual intercourse.<br />
Intrauterine insemination (IUI): A specific method <strong>of</strong> artificial<br />
insemination in which semen is introduced directly into the<br />
uterus.<br />
Non-investigative assisted reproductive technologies (ART):<br />
Fertility treatments in which both eggs <strong>and</strong> sperm are h<strong>and</strong>led.<br />
ART procedures involve surgically removing eggs from a<br />
woman’s ovaries, combining them with sperm in the laboratory<br />
<strong>and</strong> returning them to the woman’s body or donating them to<br />
another woman.<br />
Non-investigative drugs used to treat anovulation, ovarian<br />
dysfunction or unexplained infertility in women. Reproduction<br />
Treatment drugs include, but are not limited to:<br />
Ovulatory stimulants, including follitropins <strong>and</strong><br />
monotropins<br />
Chorionic gonadotropin (HCG)<br />
Gonadotropin-releasing hormones<br />
Ineligible services include, but are not limited to:<br />
cryopreservation <strong>of</strong> reproductive tissue, embryos, or sperm<br />
thawing <strong>of</strong> cryopreserved reproductive tissue, embryos, or<br />
sperm<br />
management <strong>and</strong>/or storage <strong>of</strong> reproductive tissue, embryos, or<br />
sperm<br />
donor services relating to reproductive tissue, embryos, or<br />
sperm<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Reproduction<br />
Treatment (continued)<br />
Benefit information<br />
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
Services defined by <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus as reproduction<br />
treatment are subject to a combined lifetime dollar maximum per<br />
person for all eligible medical <strong>and</strong> prescription drug services.<br />
Charges related to reproduction treatment will be combined for all<br />
networks. Services related to infertility testing will continue to<br />
process under “physician services” <strong>and</strong> will not be subject to the<br />
lifetime dollar maximum for reproduction treatment.<br />
The dollar maximum is a combination <strong>of</strong> the following services:<br />
Artificial insemination (AI)<br />
Intrauterine insemination (IUI)<br />
Non-investigative assisted reproductive technologies (ART)<br />
Associated lab <strong>and</strong> diagnostic imaging services<br />
Prescription drugs, which include injections either selfadministered<br />
or administered by a health care pr<strong>of</strong>essional <strong>and</strong><br />
oral prescription drugs<br />
Coverage <strong>of</strong> medications is subject to a product-specific<br />
formulary, specialty drug program or other requirements as<br />
outlined within a subscriber’s specific contract benefits.<br />
Prior authorization is only required for benefit plans without dollar<br />
maximum limitations.<br />
Definitions<br />
Infertility testing: Services associated with establishing the<br />
underlying medical condition or cause <strong>of</strong> infertility. This may<br />
include the evaluation <strong>of</strong> female factors (e.g., ovulatory, tubal<br />
or uterine function), male factors (e.g., semen analysis or<br />
urological testing) or a combination <strong>of</strong> both. Infertility testing<br />
involves a physical examination, laboratory studies <strong>and</strong><br />
diagnostic testing performed solely to rule out causes <strong>of</strong><br />
infertility or establish an infertility diagnosis.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Maternity)<br />
Reproduction<br />
Treatment (continued)<br />
11-10<br />
Reproduction treatment: Treatment to enhance the reproductive<br />
ability among subscribers experiencing infertility after a<br />
confirmed diagnosis <strong>of</strong> infertility has been established due to<br />
either female, male factors or unknown causes. Treatment may<br />
involve oral <strong>and</strong>/or injectable medication, surgery, artificial<br />
insemination, intrauterine insemination, assisted reproductive<br />
technologies or a combination <strong>of</strong> these.<br />
Six-cycle: A cycle is defined as one partial or complete<br />
fertilization attempt extending through the implantation phase<br />
only. A treatment cycle can involve both drugs <strong>and</strong><br />
insemination <strong>and</strong> can be timed with the completed menses.<br />
Once a pregnancy is confirmed, the cycles can begin again.<br />
Any cycle billed to the claims administrator using artificial<br />
insemination (AI), intrauterine insemination (IUI) <strong>and</strong>/or<br />
prescription drugs will be applied to the six-cycle maximum. If<br />
the patient ab<strong>and</strong>ons a treatment regimen before the cycle is<br />
complete, the partial cycle may be counted as one <strong>of</strong> the six (6)<br />
eligible cycles or the patient may assume all charges for that<br />
cycle in order to preserve benefits for six (6) complete cycles.<br />
Note: Some self-insured plans may still elect this benefit<br />
instead <strong>of</strong> a dollar maximum.<br />
Disclaimer<br />
The defined reproduction treatment services <strong>and</strong> related coding<br />
applies to all <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> Plus large group fully insured<br />
<strong>and</strong> Service Cooperative plans. <strong>Minnesota</strong> Health Care Programs,<br />
including Prepaid Medical Assistance (PMAP), <strong>Minnesota</strong>Care<br />
(MNCare), <strong>and</strong> General Assistance Medical Care (GAMC),<br />
exclude benefits for reproduction or infertility treatment. Benefits<br />
for self-insured plans may vary. This benefit does not apply to<br />
<strong>Blue</strong> <strong>Cross</strong> Medicare products. Please contact provider services for<br />
additional benefit information. Coverage decisions are subject to<br />
all terms <strong>and</strong> conditions <strong>of</strong> the applicable benefit plan, including<br />
specific exclusions <strong>and</strong> limitations, <strong>and</strong> to applicable state <strong>and</strong>/or<br />
federal law.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Medical Emergency)<br />
Table <strong>of</strong> Contents<br />
Introduction..........................................................................................................................11-2<br />
Criteria for Medical Emergencies........................................................................................ 11-2<br />
Emergency Department Services......................................................................................... 11-3<br />
Extended/After-hours Clinics ..............................................................................................11-4<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Medical Emergency)<br />
Introduction Some subscribers have full coverage for an outpatient medical<br />
emergency, which we generally define as the sudden <strong>and</strong><br />
unexpected onset <strong>of</strong> a condition requiring immediate medical<br />
attention. To receive full benefits, the subscriber must seek care<br />
within specified time limits, usually within 24 to 72 hours <strong>of</strong> the<br />
onset <strong>of</strong> acute symptoms. Accidental injury may not be included in<br />
the medical emergency benefits. Many coverage plans have<br />
separate first-aid or accident benefits.<br />
Criteria for Medical<br />
Emergencies<br />
11-2<br />
Use the guidelines below to determine if you should submit a<br />
claim as a medical emergency. Medical emergency charges<br />
should be submitted with the date <strong>and</strong> time the emergency<br />
occurred. If the emergency is related to pregnancy, also indicate<br />
that the charges were for emergency services.<br />
Were the symptoms sudden, severe <strong>and</strong> life threatening?<br />
Did the condition require immediate medical (not surgical)<br />
attention?<br />
Did the patient see a doctor no later than 72 hours after the<br />
problem began?<br />
Did the time or date <strong>of</strong> the visit indicate it was an emergency?<br />
The following situations generally would not indicate a medical<br />
emergency:<br />
scheduled surgeries or diagnostic procedures such as colon or<br />
IVP X-rays<br />
follow-up visits for further injections, such as antibiotics<br />
suture removal<br />
urgent but non-life-threatening situations seen during regular<br />
<strong>of</strong>fice hours<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)
Emergency<br />
Department Services<br />
Coding Policies <strong>and</strong> Guidelines (Medical Emergency)<br />
Emergency department services (codes 99281-99285) are<br />
submitted by the physician assigned to the emergency room.<br />
Assignment is defined as a formal relationship between the<br />
physician <strong>and</strong> the hospital whereby the physician is solely<br />
responsible for seeing patients in the emergency room during a<br />
specified time period.<br />
Physicians who specialize in emergency medicine <strong>and</strong> use the<br />
emergency department as their place <strong>of</strong> business are generally<br />
considered assigned to the emergency room.<br />
Other physicians who have arrangements with the hospital to be<br />
‘‘on call’’ to see patients in the emergency department during<br />
specific hours may also be considered assigned to the emergency<br />
department while seeing patients there. In this case, the physician’s<br />
primary responsibility is to the emergency department <strong>and</strong> the<br />
arrangement is between the physician <strong>and</strong> the hospital, as opposed<br />
to an agreement between physicians to cover one another’s<br />
patients over the weekend, etc.<br />
Any physician seeing a patient in the emergency department to<br />
which he/she is not assigned must submit level-<strong>of</strong>-service <strong>of</strong>fice<br />
calls according to CPT guidelines.<br />
Emergency department visit evaluation <strong>and</strong> management codes are<br />
restricted to the emergency place <strong>of</strong> service (23), in accordance<br />
with CPT coding rules. Codes 99281-99285 will be denied<br />
provider liable as incompatible if submitted with any place <strong>of</strong><br />
service (POS) other than 23.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Medical Emergency)<br />
Extended/After-hours<br />
Clinics<br />
11-4<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) does not<br />
consider an extended/after-hours clinic to be an emergency<br />
department. An emergency department is defined as an organized<br />
hospital-based facility for the provision <strong>of</strong> unscheduled episodic<br />
services to patients who present for immediate medical attention.<br />
The facility must be available 24 hours a day.<br />
Clinic-based urgent care services may be billed under the place <strong>of</strong><br />
service (POS) 20. The POS code 20 will apply <strong>of</strong>fice benefits to<br />
the services if submitted. DO NOT bill a corresponding facility<br />
claim with the revenue code 0456 if already billing for urgent care<br />
on the pr<strong>of</strong>essional claim (837P). This would be considered<br />
duplicate billing. Hospital-based emergency room urgent care<br />
should be billed on the 837I only with the revenue code 0456.<br />
Codes S9083 (global fee urgent care centers) <strong>and</strong> S9088 (services<br />
provided in an urgent care center) represent where the service was<br />
rendered, not the service itself. Thus, they are not separately<br />
covered <strong>and</strong> will be denied as part <strong>of</strong> the primary service (such as<br />
an E/M).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/23/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Medical Services)<br />
Table <strong>of</strong> Contents<br />
Evaluation <strong>and</strong> Management (E/M)..................................................................................... 11-3<br />
Office or Other Outpatient <strong>and</strong> Initial Inpatient Consultations .........................................11-11<br />
New <strong>and</strong> Established Patients ............................................................................................ 11-12<br />
Preventive Medicine ..........................................................................................................11-12<br />
Hospital Discharge.............................................................................................................11-13<br />
Allergy Testing .................................................................................................................. 11-13<br />
Allergy Immunotherapy.....................................................................................................11-13<br />
Anticoagulation Clinic-S9401 ...........................................................................................11-14<br />
Blood, Occult, Feces Screening......................................................................................... 11-14<br />
Cardiovascular Stress Test................................................................................................ 11-14<br />
Chemotherapy Administration........................................................................................... 11-15<br />
Chemical Dependency Assessment ................................................................................... 11-16<br />
CHF Telemonitoring..........................................................................................................11-16<br />
Day Treatment ................................................................................................................... 11-19<br />
Diabetic Education.............................................................................................................11-19<br />
E-Care Visits......................................................................................................................11-20<br />
Ear Wax Removal..............................................................................................................11-24<br />
G0101.................................................................................................................................11-24<br />
Immunizations.................................................................................................................... 11-25<br />
Billing Options for Medicare Part D Vaccines.................................................................. 11-30<br />
Injections............................................................................................................................11-32<br />
Appealing Unlisted Drug Allowances ............................................................................... 11-33<br />
Infusion Therapy................................................................................................................ 11-34<br />
Injection <strong>and</strong> Infusion Services Restrictions......................................................................11-34<br />
Dispensing Fees ................................................................................................................. 11-34<br />
Interpreter Services ............................................................................................................ 11-34<br />
Transfusion—Blood <strong>and</strong> Blood Products .......................................................................... 11-34<br />
Locum Tenens.................................................................................................................... 11-35<br />
Natural Family Planning.................................................................................................... 11-35<br />
Nicotine Dependence.........................................................................................................11-35<br />
Revenue Codes Used by Facilities 0944 or 0945 ..............................................................11-37<br />
Eligibility to Bill for Specific Procedures/Services...........................................................11-37<br />
Coverage for Tobacco Treatment Medications..................................................................11-38<br />
Noncovered Tobacco Treatments ...................................................................................... 11-38<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
11-2<br />
Medication Therapy Management (MTM) ....................................................................... 11-38<br />
Oral Medication................................................................................................................. 11-40<br />
Non-Physician Health Care Practitioners.......................................................................... 11-40<br />
Practitioners That ARE Credentialed by <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> Issued Individual Provider<br />
Number/NPIs..................................................................................................................... 11-41<br />
Practitioners that are NOT Credentialed by <strong>Blue</strong> <strong>Cross</strong> But Are Issued Individual Provider<br />
Number/NPIs..................................................................................................................... 11-42<br />
Counseling <strong>and</strong>/or Risk Factor Reduction......................................................................... 11-42<br />
Room or Machine Set-Up Charges.................................................................................... 11-42<br />
Supplies in the Office ........................................................................................................ 11-42<br />
Adjunct CPT Codes........................................................................................................... 11-42<br />
Care Plan Oversight Services ............................................................................................ 11-42<br />
Prolonged Physician Services............................................................................................ 11-43<br />
Telephone Calls................................................................................................................. 11-43<br />
Medical Team Conferences............................................................................................... 11-43<br />
Televideo Consultations .................................................................................................... 11-43<br />
Televideo Coverage Exceptions........................................................................................ 11-45<br />
Unusual Travel .................................................................................................................. 11-45<br />
Urgent Care ....................................................................................................................... 11-45<br />
Weight Management Care................................................................................................. 11-46<br />
Assessment Management Program for Fully Insured ....................................................... 11-51<br />
Health Care Home (HCH)................................................................................................. 11-53<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Evaluation <strong>and</strong><br />
Management (E/M)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Evaluation <strong>and</strong> management (E/M) services refer to visits <strong>and</strong><br />
consultations furnished by physicians or other qualified<br />
practitioners.<br />
The E/M section <strong>of</strong> the CPT manual is divided into broad<br />
categories such as <strong>of</strong>fice visits, hospital visits, <strong>and</strong> consultations.<br />
Each section has basic guides or requirements for selection, such<br />
as new versus established patient, or <strong>of</strong>fice versus hospital based<br />
services.<br />
Evaluation <strong>and</strong> Management Basics<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> <strong>and</strong> <strong>Blue</strong> Plus (<strong>Blue</strong><br />
<strong>Cross</strong>) would like to clarify <strong>and</strong> exp<strong>and</strong> on our requirements for<br />
E/M services. The following guides cover how <strong>Blue</strong> <strong>Cross</strong> treats<br />
preventive <strong>and</strong> illness E/M services <strong>and</strong> what <strong>Blue</strong> <strong>Cross</strong> expects<br />
for documentation if the claim is appealed.<br />
Documentation<br />
<strong>Blue</strong> <strong>Cross</strong> requires reasonable documentation that services are<br />
consistent with the health plan coverage provided, that services are<br />
medically necessary, <strong>and</strong> appropriate diagnostic <strong>and</strong>/or therapeutic<br />
services are provided <strong>and</strong>/or the services furnished have been<br />
accurately reported. Documentation does not need to be submitted<br />
with every claim; however, it must be readily available on request<br />
or submitted, as appropriate, with an appeal or replacement claim.<br />
It is important to note that even if all requirements <strong>of</strong> a code are<br />
documented, if medical necessity is not established, the service<br />
may be denied.<br />
The principles <strong>of</strong> documentation listed below are applicable to all<br />
types <strong>of</strong> medical <strong>and</strong> surgical services in all settings. For E/M<br />
services, the nature <strong>and</strong> amount <strong>of</strong> physician work <strong>and</strong><br />
documentation varies by type <strong>of</strong> service, place <strong>of</strong> service <strong>and</strong> the<br />
patient's status. The general principles listed below may be<br />
modified to account for these variable circumstances in providing<br />
E/M services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Evaluation <strong>and</strong><br />
Management (E/M)<br />
(continued)<br />
11-4<br />
1. The medical record should be complete <strong>and</strong> legible. Vitals,<br />
forms, <strong>and</strong> anything pertaining to the visit needs to be<br />
complete <strong>and</strong> contained in the record.<br />
2. The documentation <strong>of</strong> each patient encounter should include:<br />
reason for the encounter <strong>and</strong> relevant history, physical<br />
examination findings <strong>and</strong> prior diagnostic test results;<br />
assessment, clinical impression or diagnosis;<br />
plan for care; <strong>and</strong><br />
date <strong>and</strong> legible identity <strong>of</strong> the observer. On review,<br />
documentation not signed by the physician/practitioner<br />
performing the service will subject the entire visit to denial.<br />
3. If not documented, the rationale for ordering diagnostic <strong>and</strong><br />
other ancillary services should be easily inferred.<br />
4. Past <strong>and</strong> present diagnoses should be accessible to the treating<br />
<strong>and</strong>/or consulting physician.<br />
5. Appropriate health risk factors should be identified.<br />
6. The patient's progress, response to <strong>and</strong> changes in treatment,<br />
<strong>and</strong> revision <strong>of</strong> diagnosis should be documented.<br />
7. The CPT <strong>and</strong> ICD-9-CM codes reported on the health<br />
insurance claim form or billing statement should be supported<br />
by the documentation in the medical record. Include ALL<br />
diagnoses addressed during the encounter. Diagnoses MUST<br />
be coded to the highest degree <strong>of</strong> specificity for accurate risk<br />
adjusted quality review.<br />
Additional reminders:<br />
Use <strong>of</strong> the term IBID (same as above) <strong>and</strong>/or the use <strong>of</strong><br />
quotation marks to replace or repeat previously documented<br />
information is not acceptable. All information must be in datesequence<br />
order.<br />
Use <strong>of</strong> question marks (?) or underline (________) are not<br />
considered to be part <strong>of</strong> a complete medical record. Dictation<br />
transcription should be reviewed by the medical practitioner<br />
<strong>and</strong> updated prior to sign-<strong>of</strong>f to ensure complete medical<br />
records are maintained.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Evaluation <strong>and</strong><br />
Management (E/M)<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Each page in the medical record must contain the patient’s<br />
name <strong>and</strong>/or identification number.<br />
All encounters/entries must be dated.<br />
Services not clearly documented are not covered by <strong>Blue</strong> <strong>Cross</strong><br />
<strong>and</strong> will be denied as participating provider liability. Failing to<br />
submit requested medical records may result in claims being<br />
denied or payment being recouped from a provider. Patients<br />
are not financially liable for services that are denied for<br />
inadequate documentation.<br />
What information would constitute as a plan <strong>of</strong> care?<br />
For a physician’s note to qualify as a plan <strong>of</strong> care, it would need to<br />
contain at least:<br />
the patient’s diagnosis,<br />
long term goals,<br />
<strong>and</strong> the type, amount, duration <strong>and</strong> frequency <strong>of</strong> services.<br />
It must be established before treatment has begun <strong>and</strong> may be<br />
adjusted by the appropriate practitioner.<br />
Time Documentation<br />
The time spent face-to-face with either the patient or family should<br />
be noted for every service. This is particularly important in a<br />
situation where counseling <strong>and</strong>/or coordination <strong>of</strong> care dominates<br />
more than 50 percent <strong>of</strong> the face-to-face physician time. In this<br />
situation, time is considered the key or controlling factor, <strong>and</strong> the<br />
extent <strong>of</strong> counseling <strong>and</strong>/or coordination <strong>of</strong> care must be<br />
documented in the medical record.<br />
Consider that in an eight or nine hour work day; there are a given<br />
number <strong>of</strong> time units which may be allocated to E/M services.<br />
Obviously, the collective time reported, as reflected in the choice<br />
<strong>of</strong> E/M services codes, cannot exceed the amount <strong>of</strong> time available<br />
in the work day.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Evaluation <strong>and</strong><br />
Management (E/M)<br />
(continued)<br />
11-6<br />
1995 <strong>and</strong> 1997 E/M Guidelines<br />
<strong>Blue</strong> <strong>Cross</strong> will accept either the Centers for Medicare <strong>and</strong><br />
Medicaid (CMS) 1995 or 1997 E/M documentation guidelines.<br />
Refer to the following publications for the <strong>of</strong>ficial documentation<br />
guidelines:<br />
1995 Documentation Guidelines for Evaluation <strong>and</strong><br />
Management Services, available at<br />
www.cms.hhs.gov/MLNProducts/Downloads/1995dg.pdf on<br />
the CMS website;<br />
1997 Documentation Guidelines for Evaluation <strong>and</strong><br />
Management Services, available at<br />
www.cms.hhs.gov/MLNProducts/Downloads/MASTER1.p<br />
df on the CMS website.<br />
What are the differences between the 1995 <strong>and</strong> 1997 Medicare<br />
E/M guidelines when it pertains to the different exam levels?<br />
The 1995 Guidelines define the different exam levels as follows:<br />
Problem Focused -- a limited examination <strong>of</strong> the affected<br />
body area or organ system.<br />
Exp<strong>and</strong>ed Problem Focused -- a limited examination <strong>of</strong> the<br />
affected body area or organ system <strong>and</strong> other symptomatic or<br />
related organ system(s).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Evaluation <strong>and</strong><br />
Management (E/M)<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Detailed -- an extended examination <strong>of</strong> the affected body<br />
area(s) <strong>and</strong> other symptomatic or related organ system(s).<br />
Comprehensive -- a general multi-system examination or<br />
complete examination <strong>of</strong> a single organ system.<br />
The 1997 Guidelines contain the following definitions:<br />
Problem Focused Examination -- should include<br />
performance <strong>and</strong> documentation <strong>of</strong> one to five elements<br />
identified by a bullet (o) in one or more organ system(s) or<br />
body area(s).<br />
Exp<strong>and</strong>ed Problem Focused Examination -- should include<br />
performance <strong>and</strong> documentation <strong>of</strong> at least six elements<br />
identified by a bullet (o) in one or more organ system(s) or<br />
body area(s).<br />
Detailed Examination -- should include at least six organ<br />
systems or body areas. For each system/area selected,<br />
performance <strong>and</strong> documentation <strong>of</strong> at least two elements<br />
identified by a bullet (o) is expected. Alternatively, a detailed<br />
examination may include performance <strong>and</strong> documentation <strong>of</strong> at<br />
least twelve elements identified by a bullet (o) in two or more<br />
organ systems or body areas.<br />
Comprehensive Examination -- should include at least nine<br />
organ systems or body areas. For each system/area selected, all<br />
elements <strong>of</strong> the examination identified by a bullet (o) should be<br />
performed, unless specific directions limit the content <strong>of</strong> the<br />
examination. For each area/system, documentation <strong>of</strong> at least<br />
two elements identified by a bullet is expected.<br />
Illness E/M <strong>and</strong> Preventive on Same Date<br />
Preventive E/M services reflect an age <strong>and</strong> gender appropriate<br />
history/exam. The types <strong>of</strong> services will vary <strong>and</strong> include<br />
counseling or anticipatory guidance based on age <strong>and</strong>/or sex.<br />
For example, an E/M preventive service for a 28-year-old adult<br />
female may include a pelvic examination including obtaining a<br />
Pap smear, breast examination, <strong>and</strong> counseling regarding diet <strong>and</strong><br />
exercise, substance abuse, sexual activity, <strong>and</strong> birth control.<br />
What is included in each?<br />
Generally, the following distinguish an evaluation <strong>and</strong><br />
management illness/problem-oriented code (99201-99215) from a<br />
preventive exam code (99381-99397)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Evaluation <strong>and</strong><br />
Management (E/M)<br />
(continued)<br />
11-8<br />
Illness/Problem-oriented Preventive<br />
1. Management 3 Chronic<br />
Conditions, or<br />
2. Chief Complaint<br />
(CC)/Problem oriented<br />
3. History <strong>of</strong> Present Illness<br />
(HPI)/Status <strong>of</strong> conditions<br />
4. Review <strong>of</strong> Systems (ROS)<br />
as applicable<br />
5. Past, Family <strong>and</strong> Social<br />
History (PFSH) as<br />
applicable<br />
6. Appropriate Exam based on<br />
presenting problem<br />
7. Decision<br />
Making/Risk/Treatment<br />
8. Diagnosis-condition, signs<br />
or symptoms<br />
9. Bill Level based on work<br />
performed/risk<br />
1. Patient asymptomatic<br />
2. No CC or PI<br />
3. Comprehensive ROS<br />
4. Comp or interval PFSH<br />
5. Comprehensive Exam<br />
6. Risk Reduction<br />
7. Counseling<br />
8. Diagnosis – V Codes<br />
9. Select Code based on age<br />
<strong>and</strong> new or established<br />
Immunizations <strong>and</strong> ancillary studies involving lab, X-rays or other<br />
procedures/services are not included in either type <strong>of</strong> service <strong>and</strong><br />
should be reported separately using the appropriate diagnosis.<br />
Significant <strong>and</strong> separately identifiable<br />
In the event that a problem or abnormality requires additional work<br />
<strong>and</strong> the performance <strong>of</strong> the key components <strong>of</strong> a problem-oriented<br />
E/M service, modifier -25 should be appended to the<br />
Office/Outpatient code reported. Appending modifier -25 indicates<br />
that a significant, separately identifiable E/M (above <strong>and</strong> beyond<br />
the preventive medicine E/M service) was provided by the same<br />
physician on the same day as the preventive medicine service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Evaluation <strong>and</strong><br />
Management (E/M)<br />
(continued)<br />
What is significant?<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
An issue is considered a “significant issue” when a new or<br />
different abnormality/medical problem or a change or exacerbation<br />
<strong>of</strong> a previous condition is revealed in the process <strong>of</strong> examining the<br />
patient <strong>and</strong> the physician determines it is significant enough to<br />
require additional work to perform the components <strong>of</strong> the<br />
appropriate E/M.<br />
What is identifiable?<br />
Separate documentation or records are not required, but it needs to<br />
be clear to an auditor/someone outside <strong>of</strong> the clinic what<br />
documentation relates to the preventive E/M <strong>and</strong> what to the<br />
illness E/M. The chief complaint for the illness E/M should be<br />
clearly identifiable in the record. The illness complaint or<br />
abnormal finding should not be intermixed within the body <strong>of</strong> the<br />
physical exam documentation. Regardless <strong>of</strong> what guide used, any<br />
part <strong>of</strong> the preventive exam cannot be used again to support the<br />
billing <strong>of</strong> the illness E/M, such as patient history or review <strong>of</strong><br />
systems.<br />
What doesn’t count for extra work for support <strong>of</strong> the illness<br />
E/M?<br />
Prescription refills <strong>and</strong>/or samples for chronic stable conditions<br />
Rule out X-rays<br />
Rule out blood work<br />
Referral to another physician<br />
Decision to “observe” (is not considered treatment)<br />
Chronic or past diagnosis(es) that are not treated (for example,<br />
change in meds)<br />
Results <strong>of</strong> test(s)<br />
If treated at the visit, an uncontrolled diagnosis must be supported<br />
in the documentation in order to be considered.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Evaluation <strong>and</strong><br />
Management (E/M)<br />
(continued)<br />
11-10<br />
Why does <strong>Blue</strong> <strong>Cross</strong> deny level 4 or 5 illness E/Ms with a<br />
preventive E/M?<br />
Codes 99214 <strong>and</strong> 99215 involve a moderate or high complexity<br />
review <strong>and</strong> the focus <strong>of</strong> the visit may no longer be preventive in<br />
nature. Denials may be appealed. All supporting documentation<br />
must be included with the appeal request or will be denied for lack<br />
<strong>of</strong> documentation. For example, if the doctor states “vitals as<br />
noted” or “physical form filled out,” the documentation must state<br />
where it is noted in the chart. This should be included with the<br />
appeal.<br />
Why doesn’t <strong>Blue</strong> <strong>Cross</strong> allow codes 99201-99205 with a<br />
preventive E/M?<br />
New patient illness E/M codes will not be allowed with preventive<br />
E/M codes, including the new patient preventive E/M codes<br />
99381-99387. The additional work for an initial service will be<br />
met in the billing <strong>of</strong> the initial preventive E/M. Any additional<br />
E/M service during the same would be considered established.<br />
Although the CPT manual may not clearly state that a new illnessrelated<br />
E/M should not be billed with a new patient preventive<br />
exam, <strong>Blue</strong> <strong>Cross</strong> will not allow two new patient services at the<br />
same visit based on the rationale stated above. Because the patient<br />
already received pr<strong>of</strong>essional services as part <strong>of</strong> the preventive<br />
E/M, he or she no longer meets the ‘new patient’ criteria. New<br />
patients are those who have not been seen by a member <strong>of</strong> the<br />
group in same specialty during the prior three-year period.<br />
When may it be appropriate to bill an <strong>of</strong>fice visit on the same<br />
day as a procedure?<br />
If the patient comes in only for the procedure – only bill for the<br />
procedure.<br />
If the patient comes in knowing they are going to have the<br />
procedure done, but they also have a new complaint, then the<br />
practitioner may code for the E/M appended with the -25 modifier<br />
<strong>and</strong> the procedure.<br />
If the patient comes in with a new complaint, <strong>and</strong> during that time<br />
the practitioner makes the decision that a particular procedure<br />
needs to be done at that visit, then the practitioner may code for the<br />
procedure <strong>and</strong> the E/M appended with the -25 modifier.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Office or Other<br />
Outpatient <strong>and</strong> Initial<br />
Inpatient<br />
Consultations<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
CMS does not allow submission <strong>of</strong> inpatient <strong>and</strong> outpatient<br />
consultation codes for Medicare claims. This coding <strong>and</strong><br />
submission will be followed only for our Medicare business. There<br />
is no change for all other lines <strong>of</strong> business. <strong>Blue</strong> <strong>Cross</strong> accepts all<br />
valid HIPAA medical codes. The consultation codes 99241-99245<br />
<strong>and</strong> 99251-99255 are still valid CPT codes <strong>and</strong> as such will be<br />
accepted. We expect that the documentation will support any code<br />
submitted.<br />
Consultation codes 99241-99255 include a physician’s services<br />
requested by another physician or other appropriate source, for<br />
further evaluation or management <strong>of</strong> the patient. They are<br />
designated according to place <strong>of</strong> service <strong>and</strong> apply to new or<br />
established patients.<br />
The consultant must document the consult request <strong>and</strong> the reason<br />
for the consult in the patient record <strong>and</strong> must also appear in the<br />
requesting practitioner’s plan <strong>of</strong> care.<br />
The consult request is typically in writing but it may be verbal so<br />
long as both the requestor <strong>and</strong> the consultant document the<br />
conversation in the patient medical record. The consultant must<br />
provide a written report to the requesting practitioner. A reference<br />
to “cc” in the medical record is not sufficient to justify a<br />
consultation.<br />
A consultation may include the diagnostic tests needed to provide<br />
an opinion or advice. If the physician consultant introduces further<br />
therapeutic services, documentation must show that the consultant<br />
recommended a course <strong>of</strong> action at the request <strong>of</strong> the attending<br />
physician. Any subsequent services <strong>and</strong> continuing care rendered<br />
by the consultant cease to be a consultation <strong>and</strong> become<br />
established patient care services. Initial or subsequent services<br />
rendered by a consultant may make an initial consultation invalid<br />
if records show that patient care was immediately assumed as in a<br />
referral.<br />
A referral is the transfer <strong>of</strong> total or specific care <strong>of</strong> a patient from<br />
one physician to another <strong>and</strong> does not constitute a consultation.<br />
Initial evaluation <strong>and</strong> subsequent service for a referral are<br />
designated as level-<strong>of</strong>-service <strong>of</strong>fice visits.<br />
Second or confirmatory consults are coded as the appropriate E/M<br />
for the setting <strong>and</strong> type <strong>of</strong> service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
New <strong>and</strong> Established<br />
Patients<br />
A new patient is one who has not received any pr<strong>of</strong>essional<br />
services from the provider or another provider <strong>of</strong> the same<br />
specialty who belongs to the same group practice within the past<br />
three years.<br />
An established patient is one who has received services from the<br />
provider or another provider <strong>of</strong> the same specialty who belongs to<br />
the same group practice, within the past three years.<br />
Preventive Medicine Routine examinations for adults <strong>and</strong> children should be submitted<br />
with CPT codes 99381-99397, according to the age <strong>of</strong> the patient.<br />
The routine nature <strong>of</strong> the examination should also be indicated by<br />
the ICD-9-CM code submitted (usually a V-code). Illness <strong>and</strong><br />
injury-related visits should be submitted with the <strong>of</strong>fice or<br />
outpatient evaluation <strong>and</strong> management codes 99201-99215 with<br />
the appropriate ICD-9-CM code indicating the illness, injury,<br />
symptom, or complaint.<br />
11-12<br />
The ICD-9-CM code indicates the purpose <strong>of</strong> performing the<br />
examination. Examinations performed in the absence <strong>of</strong><br />
complaints should be billed as preventive medicine to be<br />
compatible with the ICD-9-CM code submitted.<br />
Providers can bill both an E/M code <strong>and</strong> a preventive medicine<br />
code when a patient goes in for a routine exam <strong>and</strong> an<br />
illness/problem that is significant enough to require additional<br />
work is found or addressed. In this case, providers may bill 99381-<br />
99397 with a routine diagnosis code <strong>and</strong> an illness E/M code<br />
99211-99213 with a -25 modifier <strong>and</strong> an illness diagnosis code.<br />
The -25 modifier indicates a significant, separately identifiable<br />
evaluation <strong>and</strong> management service by the same physician on the<br />
day <strong>of</strong> a procedure or service. The appropriate level <strong>of</strong> E/M should<br />
be submitted.<br />
Generally, a level 4 or 5 illness E/M (99214, 99215) is not allowed<br />
in conjunction with a preventive E/M. Because a level 4 or 5<br />
would require significant additional work, it would seldom be<br />
appropriate to bill both. Denials can be appealed, but would<br />
require documentation to support both E/M services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Preventive Medicine<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
The documentation for the E/M must not be combined into or be<br />
part <strong>of</strong> the documentation for the preventive physical. The<br />
problem(s) addressed must be significant enough to require<br />
additional work. All key components for the level E/M reported<br />
must be met <strong>and</strong> supported.<br />
Developmental testing, 96110 or 96111, is considered part <strong>of</strong> an<br />
age appropriate preventive medicine E/M <strong>and</strong> as such, will deny if<br />
billed in addition to the exam. Exceptions are made only for our<br />
Public Program members (PMAP <strong>and</strong> MNCare).<br />
Hospital Discharge Hospital discharge services, 99238 or 99239, can only be billed<br />
when services are performed on the actual date the patient left the<br />
hospital. A discharge is not billable for a patient’s death.<br />
Allergy Testing Allergy testing (95004-95075) refers to the evaluation <strong>of</strong> selective<br />
cutaneous <strong>and</strong> mucous membrane tests to assist in the<br />
determination <strong>of</strong> appropriate immunotherapy.<br />
Allergy<br />
Immunotherapy<br />
Submit the number <strong>of</strong> services in accordance with the CPT<br />
description.<br />
Allergy tests <strong>and</strong> their interpretation are a single entity; do not<br />
submit separately. An <strong>of</strong>fice visit with the modifier –25 may be<br />
submitted in addition to allergy testing only when additional<br />
identifiable services are provided.<br />
Code 95115 should be submitted with one unit <strong>of</strong> service when<br />
one injection is given.<br />
Code 95117 should be submitted with one unit <strong>of</strong> service when<br />
multiple injections are given (regardless <strong>of</strong> the number <strong>of</strong><br />
injections).<br />
Codes 95120-95134 should be submitted with one unit <strong>of</strong><br />
service. 95145-95180 should be submitted with the number <strong>of</strong><br />
services in accordance with the CPT description.<br />
Codes 95115 <strong>and</strong> 95117 include pr<strong>of</strong>essional services<br />
necessary for allergen immunotherapy.<br />
A level-<strong>of</strong>-service <strong>of</strong>fice visit with modifier –25 may be submitted<br />
in addition to an allergy injection only when additional identifiable<br />
services are provided.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-13
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Anticoagulation Clinic-<br />
S9401<br />
Blood, Occult, Feces<br />
Screening<br />
Cardiovascular<br />
Stress Test<br />
11-14<br />
<strong>Blue</strong> <strong>Cross</strong> will accept code S9401 for scheduled visits to an<br />
anticoagulation clinic (S9401 – anticoagulation clinic, inclusive <strong>of</strong><br />
all services except laboratory tests, per session). This service will<br />
be treated <strong>and</strong> reimbursed the same as the evaluation <strong>and</strong><br />
management (E/M) code 99211. Code S9401 will be subject to an<br />
<strong>of</strong>fice call copay.<br />
Code S9401 will not be allowed in addition to an E/M, unless the<br />
E/M represents a significant separately identifiable service. If so,<br />
the E/M should be appended with the –25 modifier <strong>and</strong> the<br />
appropriate diagnosis linked. Additionally, some contracts may not<br />
allow the service <strong>and</strong>/or code. For example, ‘S’ codes are not<br />
accepted for our Medicare products.<br />
Codes 82270 (blood, occult; feces, consecutive collected<br />
specimens with single determination) is to be submitted with one<br />
unit <strong>of</strong> service.<br />
This screening typically tests three specimens, but units <strong>of</strong> service<br />
should reflect the series, not number <strong>of</strong> specimens.<br />
The date <strong>of</strong> service submitted should be the date the test card is<br />
returned to the clinic.<br />
Codes 82271 <strong>and</strong> 82272 are also limited to one unit <strong>of</strong> service.<br />
Code 93015 is the global code for a cardiovascular stress test,<br />
which includes both the pr<strong>of</strong>essional component (interpretation,<br />
report, <strong>and</strong> physician monitoring) <strong>and</strong> the technical component<br />
(tracing). Submit code 93016 for physician supervision only,<br />
without interpretation <strong>and</strong> report. Submit code 93017 for the<br />
technical component only. Submit code 93018 for the pr<strong>of</strong>essional<br />
component only, which includes interpretation report <strong>and</strong><br />
physician monitoring. Submit prolonged services (codes 99354-<br />
99357) only if acute intervention is required beyond routine<br />
physician monitoring during the test.<br />
The monitoring <strong>of</strong> a patient by a physician during a cardiovascular<br />
stress test is considered an integral part <strong>of</strong> the pr<strong>of</strong>essional<br />
component <strong>of</strong> the test <strong>and</strong> not reimbursable as a separate service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Chemotherapy<br />
Administration<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Chemotherapy administration codes are used for services <strong>of</strong> a<br />
physician or qualified assistant employed by <strong>and</strong> under the<br />
supervision <strong>of</strong> a physician. The preparation <strong>of</strong> the chemotherapy<br />
agent(s) <strong>and</strong> related supplies are included in the code for<br />
administration <strong>of</strong> the agent(s). Use the CPT codes below:<br />
Codes 96401-96542 <strong>and</strong> 96549 cover chemotherapy<br />
administration. Specific Level II HCPCS codes should be used<br />
to identify the chemotherapy drug(s) utilized.<br />
When billing a dosage higher than that listed in the HCPCS<br />
<strong>Manual</strong>, use the units field to indicate a higher dosage.<br />
For example: The common dosage for J9070 is 100 mg. but 490<br />
mg. was administered. Submit five units <strong>of</strong> service (round up the<br />
dosage).<br />
Codes J8999 or J9999 should be submitted only if no specific<br />
HCPCS code exist. Specify the drug, dosage <strong>and</strong> NDC code.<br />
When billing an unlisted code, the unit should always be ‘1’.<br />
Chemotherapy codes may be independent <strong>of</strong> the patient’s <strong>of</strong>fice<br />
visit. An <strong>of</strong>fice visit with modifier –25 may be submitted in<br />
addition to or subsequent to chemotherapy administration only<br />
when additional identifiable services are provided.<br />
Pr<strong>of</strong>essional charges <strong>and</strong> codes for chemotherapy administration<br />
should not be submitted when services are administered by<br />
hospital or home health agency personnel.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-15
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Chemical Dependency<br />
Assessment<br />
Often providers perform chemical dependency assessments when a<br />
court <strong>of</strong> law orders an evaluation or a family member requests one.<br />
Under circumstances like these, providers may submit the<br />
following diagnosis code:<br />
V79.1, screening for alcoholism – use when an alcohol or<br />
chemical dependency assessment or evaluation reveals no<br />
illness, abuse, or dependency.<br />
Services billed with a V79.1 code will apply to the member’s<br />
chemical dependency benefit limit.<br />
CHF Telemonitoring <strong>Blue</strong> <strong>Cross</strong> allows coverage for telemonitoring <strong>of</strong> patients with<br />
congestive heart failure (CHF).<br />
11-16<br />
How CHF Telemonitoring Works<br />
CHF telemonitoring utilizes a computerized scale that is placed in<br />
the patient’s home. The scale weighs the patient <strong>and</strong> presents a<br />
series <strong>of</strong> questions to be answered. The data is scored <strong>and</strong><br />
transmitted to the physician’s <strong>of</strong>fice. An exception report<br />
documents <strong>and</strong> stores the patient data. Based on the preset<br />
parameters (weight range/criteria) the clinic may be alerted to<br />
contact the patient for additional evaluation <strong>and</strong>/or intervention.<br />
Reimbursement Requirements<br />
The telemonitoring scale is eligible only as a rental item. The<br />
vendor is responsible for installation, maintenance <strong>and</strong> update <strong>of</strong><br />
the system. Daily monitoring <strong>of</strong> the transmitted data <strong>and</strong><br />
interaction with the patient is the responsibility <strong>of</strong> the clinical<br />
practitioner(s). <strong>Blue</strong> <strong>Cross</strong> assumes that 30 cumulative minutes, or<br />
more, are spent per month performing these activities. To<br />
minimize administrative expenses, we request collection <strong>and</strong><br />
interpretation services to be billed on a monthly basis. However,<br />
each interaction with the patient should be reported as one unit.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
CHF Telemonitoring<br />
(continued)<br />
Billing Guidelines<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Pr<strong>of</strong>essional claim format (837P)<br />
Place <strong>of</strong> service code 11 (clinic)<br />
Submit one claim per month – for scale rental, the date <strong>of</strong><br />
service is first date <strong>of</strong> the month or first date <strong>of</strong> rental<br />
HCPCS Codes:<br />
S9109 – Congestive heart failure telemonitoring,<br />
equipment rental, including telescale, computer system <strong>and</strong><br />
s<strong>of</strong>tware, telephone connections, <strong>and</strong> maintenance, per<br />
month<br />
99091 – Collection <strong>and</strong> interpretation <strong>of</strong> physiologic data<br />
(e.g., ECG, blood pressure, glucose monitoring) digitally<br />
stored <strong>and</strong>/or transmitted by the patient <strong>and</strong>/or caregiver to<br />
the physician or other qualified health care pr<strong>of</strong>essional,<br />
requiring a minimum <strong>of</strong> 30 minutes <strong>of</strong> time<br />
Units:<br />
S9109 - One unit per month for equipment rental<br />
99091 - Total interactions per month (calculated one unit<br />
per patient interaction)<br />
Selected <strong>Blue</strong> Plus members with congestive heart failure (CHF)<br />
<strong>and</strong>/or chronic obstructive pulmonary disease (COPD) can receive<br />
telemonitoring services rendered by a participating homecare<br />
agency through their disease management program.<br />
Homecare agencies, physicians <strong>and</strong> care coordinators may refer a<br />
member with CHF <strong>and</strong>/or COPD to the telemonitoring program.<br />
Members with established homecare services preferably will<br />
remain with the same homecare agency for telemonitoring services<br />
to ensure continuity <strong>of</strong> care. Homecare agencies will be<br />
responsible for coordinating the entire telemonitoring program<br />
with the member <strong>and</strong> physician. Coordination would include:<br />
installation/de-installation, troubleshooting equipment, training,<br />
setting parameters <strong>and</strong> oversight. We expect face-to-face skilled<br />
nurse visits to decrease due to telemonitoring.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-17
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
CHF/COPD<br />
Telemonitoring<br />
Services for<br />
Secure<strong>Blue</strong><br />
(continued)<br />
11-18<br />
Eligibility<br />
This service is currently available only to Secure<strong>Blue</strong> SM (HMO<br />
SNP) members with diagnosis <strong>of</strong> CHF <strong>and</strong>/or COPD who have a<br />
history <strong>of</strong> hospitalization or emergency room visits in the<br />
preceding twelve months. The alpha prefix for these members is<br />
XZS.<br />
Prior Authorization<br />
These services must be prior authorized by a case manager in the<br />
integrated health management government programs department.<br />
The department’s phone number is 1-800-711-9868.<br />
Coding <strong>and</strong> Reimbursement<br />
Participating homecare agencies may bill <strong>Blue</strong> Plus for both<br />
monthly rental <strong>of</strong> telemonitoring equipment <strong>and</strong> collection <strong>and</strong><br />
interpretation <strong>of</strong> telemonitoring data.<br />
The following codes should be utilized on the institutional claim<br />
format (837I) for these services:<br />
Telemonitor Rental<br />
Rental should be billed to <strong>Blue</strong> Plus monthly by either the<br />
homecare agency or the contracted vendor supplying the<br />
monitor. However, only one organization may bill.<br />
Rev.<br />
Code<br />
Description HCPCS Description Reimburs.<br />
0291 Durable<br />
medical<br />
equipment,<br />
rental<br />
S9109 Congestive heart<br />
failure<br />
telemonitoring,<br />
equipment rental,<br />
including telescale,<br />
computer system<br />
<strong>and</strong> s<strong>of</strong>tware,<br />
telephone<br />
connections, <strong>and</strong><br />
maintenance per<br />
month<br />
$88 per<br />
month<br />
(excludes<br />
any<br />
applicable<br />
<strong>Minnesota</strong>C<br />
are tax)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
CHF/COPD<br />
Telemonitoring<br />
Services for<br />
Secure<strong>Blue</strong><br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Data Collection <strong>and</strong> Interpretation<br />
Services should be billed utilizing one unit per month.<br />
Rev.<br />
Code<br />
0780 Telemedicine<br />
– general<br />
classification<br />
Description HCPCS Description Reimburs.<br />
99091 Collection <strong>and</strong><br />
interpretation <strong>of</strong><br />
physiologic data<br />
(e.g.,<br />
ECG, blood<br />
pressure, glucose<br />
monitoring)<br />
digitally stored<br />
<strong>and</strong>/or transmitted<br />
by the patient<br />
<strong>and</strong>/or caregiver<br />
to the physician or<br />
other qualified<br />
health<br />
pr<strong>of</strong>essional,<br />
requiring a<br />
minimum <strong>of</strong> 30<br />
minutes <strong>of</strong> time<br />
$71.48<br />
per month<br />
(excludes<br />
any<br />
applicable<br />
<strong>Minnesota</strong><br />
Care tax)<br />
Day Treatment Submit one unit <strong>of</strong> service per hour for day treatment programs for<br />
behavioral health diagnoses (H2012). Include the actual time <strong>of</strong><br />
therapy on the claim also. Refer to the Behavioral Health section<br />
for additional information.<br />
Diabetic Education <strong>Blue</strong> <strong>Cross</strong> recommends submission <strong>of</strong> HCPCS codes G0108 <strong>and</strong><br />
G0109 for a diabetes education program that meets the National<br />
St<strong>and</strong>ards for Diabetes Self-Management Education <strong>and</strong> obtains<br />
recognition status from the American Diabetes Association (ADA)<br />
or program accreditation from the American Association <strong>of</strong><br />
Diabetes Educators (AADE); however, program recognition or<br />
accreditation does not guarantee reimbursement <strong>of</strong> treatment<br />
which includes Diabetes Self-Management Training, services must<br />
be within the scope <strong>of</strong> an individual practitioner’s registration,<br />
license <strong>and</strong> training.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-19
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
E-Care Visits <strong>Blue</strong> <strong>Cross</strong> allows coverage <strong>of</strong> certain internet E/M visits called E-<br />
Care visits.<br />
11-20<br />
Description<br />
E-Care is a term used to describe limited healthcare services<br />
provided over the Internet. E-Care may also be referred to as<br />
online medical evaluations, online visits, E-visits, E-consultations,<br />
or virtual visit.<br />
E-Care is a member initiated online evaluation <strong>and</strong> management<br />
(E/M) visit provided remotely to patients via the Internet. This<br />
visit is used to address non-urgent medical symptoms including<br />
medication <strong>and</strong> prescription refills or renewals <strong>and</strong> review <strong>of</strong> lab<br />
<strong>and</strong> test results. E-Care visits are not normally ‘real-time’. The<br />
provider responds to the patient’s issue within a prescribed time<br />
limit (usually within 24 hours).<br />
Coverage Criteria<br />
Services obtained from the rendering practitioner by means <strong>of</strong><br />
online email communication via the Internet may be eligible for<br />
coverage for non-urgent care when ALL <strong>of</strong> the following criteria<br />
are met:<br />
The individual initiating the E-Care visit is an established<br />
patient <strong>of</strong> the provider <strong>and</strong> has previously received face-to-face<br />
treatment<br />
In the judgment <strong>of</strong> the practitioner, the E-Care visit is<br />
medically necessary <strong>and</strong> involved sufficient resource use, time<br />
<strong>and</strong> complexity to warrant separate recognition as a unique<br />
event<br />
Written documentation related to the service must be included<br />
in the patient’s medical record <strong>and</strong> should include the<br />
following:<br />
Documentation must support, at minimum, a 99212 level<br />
E/M<br />
Medical information exchange, assessment, <strong>and</strong> plan <strong>of</strong><br />
treatment/care (e.g., symptoms, counseling)<br />
Services must be billed under the rendering practitioner’s<br />
provider number or NPI<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
E-Care Visits<br />
(continued)<br />
Qualifying Criteria<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Qualifying criteria for reimbursement <strong>of</strong> online services are as<br />
follows:<br />
Practitioner responds within on business day AND one or more<br />
<strong>of</strong> the following:<br />
Patient describes new symptoms <strong>and</strong> is requesting intervention<br />
<strong>and</strong>/or advice from practitioner to treat new symptoms<br />
Patient describes ongoing symptoms from a recent acute<br />
problem or chronic health problem <strong>and</strong> is requesting<br />
intervention <strong>and</strong>/or advice from practitioner to treat ongoing<br />
acute problem or chronic health problem<br />
Evidence that practitioner is giving substantive medical advice,<br />
revising treatment plan, prescribing/revising medication,<br />
recommending additional testing, <strong>and</strong>/or providing self care/<br />
patient education information for new <strong>and</strong>/or chronic health<br />
problem<br />
Evidence that practitioner is making a new diagnosis <strong>and</strong> is<br />
prescribing new treatment<br />
Patient requesting interpretation <strong>of</strong> lab <strong>and</strong>/or test results with<br />
evidence that practitioner is providing substantive explanation<br />
<strong>and</strong> recommendations to modify treatment plan, revising<br />
medications, etc.<br />
Evidence that practitioner is providing extended personal<br />
patient counseling that is changing the course <strong>of</strong> treatment <strong>and</strong><br />
impacting the potential health outcome.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-21
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
E-Care Visits<br />
(continued)<br />
11-22<br />
Billing/Coding Information<br />
CODING: 99444 or 98969<br />
99444 – Online evaluation <strong>and</strong> management service<br />
provided by a physician to an established patient, guardian,<br />
or health care provider not originating from a related E/M<br />
service provided within the previous 7 days, using the<br />
internet or similar electronic communications network<br />
98969 – Online assessment <strong>and</strong> management service<br />
provided by a qualified non-physician health care<br />
pr<strong>of</strong>essional to an established patient, guardian, or health<br />
care provider not originating from a related assessment <strong>and</strong><br />
management service provided within the previous 7 days,<br />
using the internet or similar electronic communications<br />
network<br />
COPAY: Code 99444 or 98969 is subject to the member’s<br />
<strong>of</strong>fice call copay.<br />
CLAIM FORMAT: Billed on the pr<strong>of</strong>essional claim format-<br />
837P.<br />
UNITS: One (1). Reimbursement for online medical<br />
evaluations is limited to one per day.<br />
PROVIDER NUMBER: An individual provider number or<br />
NPI is required. Code 99444 is limited to MDs. Code 98969 is<br />
limited to PA, NP, <strong>and</strong> CNS-Medical practitioners.<br />
EDITS: An E-Care visit, 99444 or 98969, will not be allowed<br />
on the same day as another E/M visit. Code 99444 or 98969<br />
will deny as mutually exclusive to these other services. An E-<br />
Care visit will not be allowed as a routine follow-up to surgical<br />
care.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
E-Care Visits<br />
(continued)<br />
Not Covered:<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
E-Care services are not covered when provided for the following:<br />
Provider-initiated e-mail<br />
Appointment scheduling<br />
Refilling or renewing existing prescriptions without substantial<br />
change in clinical situation<br />
Scheduling diagnostic tests<br />
Reporting normal test results<br />
Updating patient information<br />
Providing educational materials<br />
Brief follow-up <strong>of</strong> a medical procedure/service to confirm<br />
stability <strong>of</strong> the patient’s condition without indication <strong>of</strong><br />
complication or new condition including, but not limited to,<br />
routine global surgical follow-up.<br />
Brief discussion to confirm stability <strong>of</strong> the patient’s chronic<br />
condition without change in current treatment.<br />
When information is exchanged <strong>and</strong> the patient is subsequently<br />
asked to come in for an <strong>of</strong>fice visit<br />
A service that would similarly not be charged for in a regular<br />
<strong>of</strong>fice visit<br />
Reminders <strong>of</strong> scheduled <strong>of</strong>fice visits<br />
Requests for a referral<br />
Consultative message exchanges with an individual who is<br />
seen in the provider’s <strong>of</strong>fice immediately afterward<br />
Clarification <strong>of</strong> simple instructions<br />
Note: The following is not an all-inclusive list. E-Care visits may<br />
be denied for reasons other than noted below.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-23
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
E-Care Visits<br />
(continued)<br />
Program Exceptions:<br />
Benefits are determined by the individual member contract<br />
language in effect at the time services were rendered. Check for<br />
patient benefits before services are rendered.<br />
The following groups do not provide for coverage <strong>of</strong> E-Care visits:<br />
Federal Employee Program (FEP)<br />
Medicare Supplements<br />
PMAP/MNCARE<br />
Some self-insured groups<br />
Ear Wax Removal Ear wax removal (removal <strong>of</strong> impacted cerumen) is by CPT<br />
definition a “separate procedure”. Codes designated as separate<br />
procedures should not be reported in addition to the code for the<br />
total procedure or service <strong>of</strong> which it is considered an integral<br />
component. The denial however, may vary depending on what<br />
code(s) is billed with 69210. For example, code 69210 will deny as<br />
incidental to audiometry evaluation <strong>and</strong> speech recognition testing,<br />
but if billed with an <strong>of</strong>fice visit, the E/M will be denied as<br />
incidental to 69210.<br />
G0101 G0101 (cervical or vaginal cancer screening; pelvic <strong>and</strong> clinical<br />
breast examination) is an accepted code. However, G0101 will<br />
deny if billed in conjunction with an E/M service.<br />
11-24<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Immunizations Immunizations are injections separately identified in CPT <strong>and</strong><br />
HCPCS Level II (codes 90476-90749, Q2035-Q2039). Submit the<br />
code which describes the immunization administered. It is<br />
inappropriate to code each component <strong>of</strong> a combination vaccine<br />
separately. The administration code(s) 90460-90461, 90471-<br />
90474, or G0008-G0010 must be reported in addition to the<br />
vaccine <strong>and</strong> toxoid code(s) 90476-90749, Q2035-Q2039.<br />
Type <strong>of</strong><br />
vaccine/toxoid<br />
administration(s)<br />
injection, oral or<br />
intranasal<br />
Immunization Administration Add-ons<br />
The immunization administration codes 90460-90461, 90471-<br />
90474, or G0008-G0010 are reported in addition to the vaccine or<br />
toxoid code(s) 90476-90749, Q2035-Q2039. When giving more<br />
than one vaccine/toxoid, multiple administration codes are<br />
reported. But it is important to choose the correct add-on<br />
administration code. The following are the correct reporting <strong>of</strong><br />
single <strong>and</strong> combinations <strong>of</strong> administration codes.<br />
Although the administration services 90472 <strong>and</strong> 90474 are<br />
considered add-on codes, the modifier 51 does not apply to these<br />
services <strong>and</strong> should not be reported with these codes.<br />
Is there more<br />
than one vaccine/<br />
toxoid?<br />
Is<br />
counseling<br />
included?<br />
No Yes 90460<br />
Correct administration code(s)<br />
injection No No 90471, G0008, G0009, or G0010<br />
injection, oral or<br />
intranasal<br />
Yes Yes 90460 <strong>and</strong> 90461 (X # <strong>of</strong> add’l<br />
vaccines/toxoid components)<br />
injection Yes No 90741, G0008, G0009, or G0010 <strong>and</strong><br />
90472 (X # <strong>of</strong> add’l vaccines/toxoid<br />
components)<br />
oral or intranasal No No 90473<br />
oral or intranasal Yes No 90473 <strong>and</strong> 90474 (X # <strong>of</strong> add’l<br />
vaccines/toxoid components)<br />
injection <strong>and</strong><br />
oral/intranasal<br />
Yes No 90471, G0008, G0009, or G0010 <strong>and</strong><br />
90474 (X # <strong>of</strong> add’l oral/intranasal<br />
vaccines/toxoid components) or<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
90473 <strong>and</strong> 90472 (X # <strong>of</strong> add’l<br />
injected vaccines/toxoid components)<br />
11-25
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Immunizations<br />
(continued)<br />
11-26<br />
Serum from Department <strong>of</strong> Human Services<br />
If receiving serum from the Department <strong>of</strong> Human Services (DHS)<br />
for child immunizations, the provider should bill <strong>Blue</strong> <strong>Cross</strong> for<br />
the administration charge only. Providers should submit the<br />
immunization code with an –SL modifier to indicate the serum was<br />
received from DHS. Providers are required to obtain serum from<br />
DHS for all PMAP enrollees. The administration codes 90460-<br />
90461, 90471-90474, or G0008-G0010 must be reported in<br />
addition to the vaccine. If the vaccine code is submitted it should<br />
be reported with a zero charge. <strong>Blue</strong> <strong>Cross</strong> will allow the line to be<br />
submitted with a $0.01 charge if the provider’s billing systems or<br />
services cannot accommodate a zero charge.<br />
<strong>Minnesota</strong> Health Care Programs (MHCP) payment for<br />
vaccine administration code 90461<br />
<strong>Blue</strong> Plus is following the DHS guidelines for payment <strong>of</strong> vaccine<br />
administration. Based upon these guidelines, only the single or<br />
first vaccine/toxoid component will be reimbursed for <strong>Blue</strong> Plus<br />
MHCP members. <strong>Blue</strong> Plus reminds providers that, effective<br />
January 1, 2011, claim lines submitted for MHCP members with<br />
procedure code 90461 are being denied as part <strong>of</strong> the basic service.<br />
See DHS provider communication below:<br />
MHCP-covered Immunization Administration<br />
(vaccines/toxoids). Use the following codes to report<br />
immunization administration in conjunction with each single or<br />
combination vaccine/toxoid code reported.<br />
Code Use to report<br />
administration <strong>of</strong>:<br />
90471 First vaccine<br />
(single or<br />
combination)<br />
90472 Each additional<br />
vaccine<br />
Administration<br />
route<br />
Percutaneous,<br />
intradermal,<br />
subcutaneous,<br />
intramuscular<br />
Percutaneous,<br />
intradermal,<br />
subcutaneous,<br />
intramuscular<br />
MHCP<br />
limitations<br />
Do not use with<br />
90473<br />
Use with 90471<br />
or 90473; list<br />
separately<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Immunizations<br />
(continued)<br />
Code Use to report<br />
administration <strong>of</strong>:<br />
90473 First vaccine<br />
(single or<br />
combination)<br />
90474 Each additional<br />
vaccine<br />
90460 Single or first<br />
vaccine/toxoid<br />
component <strong>of</strong><br />
combination<br />
vaccine<br />
90461 Each additional<br />
component <strong>of</strong><br />
combination<br />
vaccine<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Administration<br />
route<br />
MHCP<br />
limitations<br />
Oral, intranasal Do not use with<br />
90471<br />
Oral, intranasal Use with 90471<br />
or 90473; list<br />
separately<br />
Any 18 years &<br />
younger<br />
Physician /<br />
health care<br />
pr<strong>of</strong>essional<br />
counseling<br />
required<br />
Any List<br />
separately<br />
Use only<br />
with 90460<br />
(when<br />
performing<br />
physician/<br />
health care<br />
pr<strong>of</strong>essional<br />
counseling)<br />
*There is no<br />
additional<br />
reimbursement<br />
for the<br />
administration <strong>of</strong><br />
the additional<br />
components <strong>of</strong> a<br />
combination<br />
vaccine.<br />
11-27
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Immunizations<br />
(continued)<br />
11-28<br />
*Centers for Disease Control <strong>and</strong> Prevention (CDC) considers the<br />
VFC administration reimbursement amount to be paid on a per<br />
injection basis, not a per component basis.<br />
DHS website reference<br />
To view the DHS specific information go to the following link:<br />
http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DY<br />
NAMIC_CONVERSION&RevisionSelectionMethod=LatestRe<br />
leased&Redirected=true&dDoc<strong>Name</strong>=id_000094<br />
Members impacted<br />
This applies to members enrolled in the following <strong>Blue</strong> Plus plans:<br />
Product name Group numbers<br />
<strong>Blue</strong> Advantage (PMAP) 18<br />
years <strong>and</strong> younger<br />
<strong>Minnesota</strong>Care 18 years <strong>and</strong><br />
younger<br />
PP021, PP022, PP024, PP025,<br />
PP026, PP027, PP031, PP032,<br />
PP034, PP035, PP036, PP037<br />
PP111, PP112, PP151, PP152<br />
Supplies Used in Conjunction with Immunization<br />
Administrations<br />
Syringes, needles or other supplies (A4206-A4209) used in<br />
conjunction with administering any injection, including<br />
immunizations, are considered integral to that administration <strong>and</strong><br />
will be denied as incidental to the administration.<br />
Flu Vaccines<br />
The influenza vaccine codes Q2035-Q2039 were added for<br />
Medicare to identify specific flu vaccine products. Additionally,<br />
Medicare instructed that the existing CPT vaccine code 90658<br />
would no longer be allowed. While our Medicare Advantage plan<br />
will follow Medicare’s requirements, commercial plans will<br />
continue to accept 90658 as well as the new flu vaccine codes.<br />
However, edits will be instituted.<br />
Only one flu vaccine code will be accepted: 90658, Q2035,<br />
Q2036, Q2037, or Q2038. Code Q2039 should not be submitted.<br />
If the vaccine is not specific to the products noted in codes Q2035-<br />
Q2038, <strong>Blue</strong> <strong>Cross</strong> expects the code 90658 to be submitted in lieu<br />
<strong>of</strong> the unlisted code Q2039. As a general policy, claims may be<br />
subject to denial when an unlisted code is submitted when a<br />
definitive code exists. Such would be the case for code Q2039.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Immunizations<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Q2035 Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years <strong>of</strong> age <strong>and</strong> older, for intramuscular use<br />
(Afluria)<br />
Q2036 Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years <strong>of</strong> age <strong>and</strong> older, for intramuscular use<br />
(Flulaval)<br />
Q2037 Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years <strong>of</strong> age <strong>and</strong> older, for intramuscular use<br />
(Fluvirin)<br />
Q2038 Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years <strong>of</strong> age <strong>and</strong> older, for intramuscular use<br />
(Fluzone)<br />
Q2039 Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years <strong>of</strong> age <strong>and</strong> older, for intramuscular use (not<br />
otherwise specified)<br />
90658 Influenza virus vaccine, split virus, when administered to<br />
individuals 3 years <strong>of</strong> age <strong>and</strong> older, for intramuscular use<br />
90718 Restriction for MHCP Members<br />
Due to a change in the DHS fee schedule, <strong>Blue</strong> Plus will not allow<br />
the use <strong>of</strong> code 90718 following the direction set forth by the<br />
Department <strong>of</strong> Human Services (DHS). Following is the DHS<br />
communication:<br />
Immunization <strong>and</strong> Vaccines<br />
MHCP does not cover tetanus <strong>and</strong> diphtheria toxoids vaccine code<br />
(90718). Use the preservative-free tetanus <strong>and</strong> diphtheria toxoids<br />
vaccine code (90714) for both preservative <strong>and</strong> preservative-free<br />
vaccines billing.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-29
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Billing Options for<br />
Medicare Part D<br />
Vaccines<br />
11-30<br />
There is an online option for processing Medicare Part D vaccine<br />
claims electronically. eDispense Part D Vaccine Manager, a<br />
product <strong>of</strong> Dispensing Solutions Inc. (DSI), is a web portal that<br />
provides physicians with real-time claims processing for in-<strong>of</strong>fice<br />
administered vaccines. This system also allows providers to<br />
electronically bill for Part D vaccine administration charges.<br />
eDispense Part D Vaccine Manager allows physicians to bill <strong>Blue</strong><br />
Plus (through its pharmacy benefit manager, Prime Therapeutics)<br />
online for all Part D vaccines like Zostavax, on behalf <strong>of</strong><br />
Secure<strong>Blue</strong>, Medicare<strong>Blue</strong> SM Rx (PDP) <strong>and</strong> Medicare<strong>Blue</strong> PPO<br />
(Regional PPO) members.<br />
Physicians can submit claims for Part D vaccines <strong>and</strong>/or Part D<br />
vaccine administration in two ways: either electronically through<br />
the eDispense website or by using a HICF-1500 <strong>and</strong> following a<br />
paper claims process.<br />
Enrolled with DSI<br />
If you have enrolled with DSI (Part D electronic clearinghouse) to<br />
use their eDispense claims system, you can submit claims for<br />
vaccines <strong>and</strong> vaccine administration through their website. This<br />
website will also allow you to check member eligibility for various<br />
Part D vaccines, as well as to determine the applicable member<br />
copays, if any.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Billing Options for<br />
Medicare Part D<br />
Vaccines (continued)<br />
Additional Information<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
For more information on eDispense <strong>and</strong> how to sign up to use that<br />
system, please visit: https://enroll.edispense.com/ws_enroll or<br />
call DSI at 1-866-522-3386. You can also go to bluecrossmn.com<br />
<strong>and</strong> type “eDispense” in the search option.<br />
Paper Claims<br />
If you decide not to enroll in eDispense, you can use a HICF-1500<br />
form to submit claims for vaccines <strong>and</strong> administration. If you<br />
submit a paper claim, it must include:<br />
NDC number for the vaccine<br />
quantity<br />
a days supply is reported using (1) unit<br />
Paper claims for Secure<strong>Blue</strong> members can be submitted to:<br />
<strong>Blue</strong> Plus<br />
P.O. Box 64813<br />
St. Paul, MN 55164<br />
For the regional products, Medicare<strong>Blue</strong> Rx or Medicare<strong>Blue</strong><br />
PPO, please use the name <strong>of</strong> the product as the addressee when<br />
submitting paper claims:<br />
Medicare<strong>Blue</strong> Rx or Medicare<strong>Blue</strong> PPO (whichever is<br />
appropriate)<br />
P. O. Box 64813<br />
St. Paul, MN 55164<br />
If you have questions regarding claims submitted for the regional<br />
products, please call the member services number on the back <strong>of</strong><br />
the member’s ID card.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-31
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Billing Options for<br />
Medicare Part D<br />
Vaccines (continued)<br />
Questions?<br />
Enrollment <strong>and</strong> claims processing, call Dispensing Solutions’<br />
customer support center at 1-866-522-3386.<br />
<strong>Blue</strong> Plus, contact provider service at (651) 662-5200 or toll free at<br />
1-800-262-0820.<br />
Medicare<strong>Blue</strong> PPO, contact 1-888-457-3009. Links to current<br />
medical policies are available in the provider section <strong>of</strong> our<br />
website, www.YourMedicareSolutions.com.<br />
Injections Therapeutic or diagnostic injections may be subcutaneous,<br />
intramuscular, intra-arterial, or intravenous. These codes do not<br />
include injections for allergen immunotherapy or immunizations.<br />
11-32<br />
Injectable Drug<br />
Submit the HCPCS Level II code that best describes the injection<br />
given in terms <strong>of</strong> the drug <strong>and</strong> dosage. Codes for injections include<br />
the charge for the drug only. When the dosage given is greater than<br />
that listed, use the units field to specify the appropriate number <strong>of</strong><br />
units according to code definition found in the HCPCS manual.<br />
For example:<br />
The patient received 8 mg. <strong>of</strong> haloperiodol. The common<br />
dosage for haloperiodol (J1630) is “up to 5 mg;” 2 UOS<br />
should be submitted. The dosage is rounded up to the next unit.<br />
The administration charge should be submitted separately.<br />
Codes 96379 <strong>and</strong> J3490 are for unlisted therapeutic injections. The<br />
drug name <strong>and</strong> dosage must be included on each claim, as well as<br />
the National Drug Code (NDC) number.<br />
Report the drug name, dosage <strong>and</strong> NDC starting in the loop<br />
2400/NTE segment narrative field for electronic claims.<br />
Administration<br />
Choose the appropriate administration code for the route <strong>of</strong><br />
administration 96365-96379.<br />
It is inappropriate to bill an intravenous injection in addition to an<br />
intravenous infusion on the same date <strong>of</strong> service when an injection<br />
is administered through the same line as the infusion. The provider<br />
may submit the infusion or the injection, but not both.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Injections (continued) Units <strong>of</strong> service reflect the number <strong>of</strong> injections given.<br />
Appealing Unlisted<br />
Drug Allowances<br />
If an <strong>of</strong>fice visit is submitted on the same day <strong>of</strong> the subcutaneous<br />
or intramuscular injection (96372-96376), the administration<br />
would be included in the E/M <strong>and</strong> will deny if submitted<br />
separately.<br />
Supplies used in conjunction with therapeutic administrations<br />
Syringes, needles or other supplies (A4206-A4209) used in<br />
conjunction with administering any injection, including therapeutic<br />
or diagnostic, are considered integral to that administration <strong>and</strong><br />
will be denied as incidental to the administration.<br />
Surgical Injections<br />
Performed as st<strong>and</strong>-alone procedures/services, the injections<br />
should be submitted with the appropriate CPT code for the<br />
administration <strong>of</strong> the injection. In addition, submit the HCPCS<br />
Level II code for the drug. If no specific HCPCS code exists for<br />
the drug, submit J3490 with a narrative indicating the drug name,<br />
dosage <strong>and</strong> NDC.<br />
When surgical injections are performed as part <strong>of</strong> a surgical<br />
procedure, submit the HCPCS Level II code for the drug. The<br />
administration <strong>of</strong> the injection is considered part <strong>of</strong> the surgical<br />
procedure itself <strong>and</strong> should not be submitted separately.<br />
Unlisted drug codes, such as J3490, should only be submitted if<br />
there is no other code that describes the drug given. All unlisted<br />
drugs must be submitted with a narrative, dosage <strong>and</strong> NDC, <strong>and</strong><br />
are manually priced. There may be times when the invoice cost <strong>of</strong><br />
the drug may be significantly higher than our allowance. In this<br />
case, a provider may submit an appeal for additional<br />
reimbursement using the normal appeal process as described in<br />
Chapter 10, “Appeals <strong>of</strong> Processed Claims.” To facilitate the<br />
appeal review, the drug invoice must be submitted with the appeal<br />
for consideration. Additional reimbursement will not be considered<br />
without the invoice.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-33
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Infusion Therapy Infusion therapy as described below excludes chemotherapy. For<br />
prolonged intravenous or subcutaneous infusions performed in the<br />
<strong>of</strong>fice or clinic, submit CPT codes 96365-96371 for the<br />
administration <strong>and</strong> the appropriate HCPCS Level II code for the<br />
drug. When billing a higher dosage than listed in the HCPCS<br />
<strong>Manual</strong>, use the units field to indicate the higher dosage. The CPT<br />
code includes the administration <strong>and</strong> supplies. Submit code J3490<br />
with a narrative indicating the drug name, dosage <strong>and</strong> NDC if a<br />
specific HCPCS code for the drug does not exist. Only a unit <strong>of</strong><br />
one (1) should be reported when submitting an unlisted drug code.<br />
Injection <strong>and</strong> Infusion<br />
Services Restrictions<br />
Codes 96365-96371 typically require direct physician supervision<br />
for any or all purposes <strong>of</strong> patient assessment, provision <strong>of</strong> consent,<br />
safety oversight, <strong>and</strong> intra-service supervision <strong>of</strong> staff.<br />
Pr<strong>of</strong>essional charges for infusion therapy should not be submitted<br />
when the service is administered by the hospital or the home health<br />
agency personnel. Do not use these codes to indicate intradermal,<br />
subcutaneous, intramuscular, or routine IV injections, or<br />
chemotherapy.<br />
<strong>Blue</strong> <strong>Cross</strong> will not allow pr<strong>of</strong>essional 837P charges for<br />
therapeutic, prophylactic, diagnostic injection <strong>and</strong> infusion CPT®<br />
codes (96360-96379) when rendered in certain places <strong>of</strong> service.<br />
Pr<strong>of</strong>essional services (837P) submitted with a facility place <strong>of</strong><br />
service (such as 21, 22 or 23), will deny as provider liability.<br />
Dispensing Fees Drug dispensing fees, Q0510-Q0514, are non-covered <strong>and</strong> will<br />
deny as provider liability. Coverage may be allowed for our<br />
Medicare members.<br />
Interpreter Services Interpreter services are not separately billable or reimbursed for<br />
most members.<br />
Transfusion—Blood<br />
<strong>and</strong> Blood Products<br />
11-34<br />
Refer to the Public Programs section <strong>of</strong> this chapter for interpreter<br />
service guides for Public Program members.<br />
Transfusion <strong>of</strong> blood <strong>and</strong>/or blood products is submitted with code<br />
36430 when administered by a physician or qualified assistant<br />
employed by <strong>and</strong> under the supervision <strong>of</strong> a physician. Preparation<br />
<strong>of</strong> blood <strong>and</strong> blood products is included in the service for<br />
administration <strong>of</strong> the agent.<br />
Pr<strong>of</strong>essional charges/codes for the transfusion <strong>of</strong> blood or blood<br />
products should not be submitted when administered by hospital or<br />
home health agency personnel. Bill the blood separately with the<br />
appropriate HCPCS code.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Locum Tenens A substitute physician who takes over another physician’s practice<br />
when that regular physician is absent for specific reasons (e.g.,<br />
illness, maternity leave, military duty or sabbatical) is generally<br />
referred to as a “locum tenens” physician. The services rendered<br />
by the locum tenens physician may be submitted under the absent<br />
physicians’ provider number or NPI. The modifier Q6 should be<br />
appended to these services. Additional or replacement physicians<br />
not substituting for an absent physician must be credentialed <strong>and</strong><br />
submit claims with their own NPI.<br />
Natural Family<br />
Planning<br />
The natural family planning (NFP) code H1010 (Non-medical<br />
family planning education, per session) is restricted only to those<br />
participating non-clinic providers contracted as a NFP provider.<br />
Clinics/medical practitioners providing NFP would bill their<br />
services using the appropriate evaluation <strong>and</strong> management code.<br />
Nicotine Dependence <strong>Blue</strong> <strong>Cross</strong> covers services for the treatment <strong>of</strong> tobacco<br />
dependence. However, coverage for these services depends on the<br />
type <strong>of</strong> provider submitting the claim, the procedure/service <strong>and</strong><br />
diagnosis codes submitted, <strong>and</strong> the patient’s contract with <strong>Blue</strong><br />
<strong>Cross</strong>. Due to these many variables, exact payment can not be<br />
determined until we receive the claims for processing.<br />
Diagnosis Codes<br />
If the primary reason for the outpatient visit to the clinician is<br />
tobacco use, claims should be submitted with one <strong>of</strong> the following<br />
diagnosis codes:<br />
305.1 tobacco use disorder<br />
V15.82 history <strong>of</strong> tobacco use<br />
Procedure/Service Codes<br />
Clinicians should submit the HCPCS code that reflects the service<br />
furnished. Claims may process differently depending on the code<br />
submitted. The difference reflects the application <strong>of</strong> the member’s<br />
contract benefits.<br />
Evaluation <strong>and</strong> Management (E/M) codes 99201-99215:<br />
Claims submitted using these problem-related visit codes will<br />
process according to the illness portion <strong>of</strong> the patient’s<br />
contract.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-35
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Nicotine Dependence<br />
(continued)<br />
11-36<br />
E/M codes 99241-99245: Claims submitted using these<br />
consultation codes will process according to the illness portion<br />
<strong>of</strong> the patient’s contract when submitted with a tobacco<br />
diagnosis.<br />
E/M codes 99401-99404: Claims submitted using these<br />
preventive counseling codes will process according to the<br />
preventive portion <strong>of</strong> the patient’s contract. These codes may<br />
also be covered under the Patient Protection <strong>and</strong> Affordable<br />
Care Act (PPACA) otherwise known as health care reform<br />
(HCR) <strong>and</strong> as such, will be processed according the preventive<br />
portion <strong>of</strong> the patient’s contract.<br />
Codes 99406 <strong>and</strong> 99407: Claims submitted using these<br />
counseling visit codes will process according to the illness<br />
portion <strong>of</strong> the patient’s contract. These codes may also be<br />
covered under the Patient Protection <strong>and</strong> Affordable Care Act<br />
(PPACA) otherwise known as health care reform (HCR) <strong>and</strong> as<br />
such, will be processed according the preventive portion <strong>of</strong> the<br />
patient’s contract.<br />
Code S9453 for stop-smoking classes is generally not an<br />
eligible service under the patient’s contract; however, may be<br />
covered under the Patient Protection <strong>and</strong> Affordable Care Act<br />
(PPACA) otherwise known as health care reform (HCR) <strong>and</strong> as<br />
such, will be processed according the preventive portion <strong>of</strong> the<br />
patient’s contract.<br />
E/M codes 99384-99387 <strong>and</strong> 99394-99397: These<br />
comprehensive preventive medicine services include<br />
counseling/anticipatory guidance/risk factor reduction<br />
interventions. Tobacco cessation counseling is part <strong>of</strong> a<br />
comprehensive preventative medicine evaluation. Therefore it<br />
is not separately reportable under these codes.<br />
Psychiatric codes 90804-90862: Claims submitted using these<br />
codes will process according to the substance abuse portion <strong>of</strong><br />
the patient’s contract.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Nicotine Dependence<br />
(continued)<br />
Revenue Codes Used<br />
by Facilities 0944 or<br />
0945<br />
Eligibility to Bill for<br />
Specific<br />
Procedures/Services<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Group counseling codes 99411-99412 will process according<br />
to the illness portion <strong>of</strong> the patient’s contract when submitted<br />
with a tobacco diagnosis; however, may be covered under the<br />
Patient Protection <strong>and</strong> Affordable Care Act (PPACA)<br />
otherwise known as health care reform (HCR) <strong>and</strong> as such, will<br />
be processed according the preventive portion <strong>of</strong> the patient’s<br />
contract.<br />
For questions regarding “incident to” services please refer to<br />
Chapter 8 <strong>of</strong> this manual.<br />
Codes for reporting patient documentation or supplemental<br />
tracking for performance measurement (4000F-4001F) may be<br />
submitted. These are zero-billed <strong>and</strong> zero-allowed codes.<br />
Facilities such as hospitals, skilled nursing facilities, <strong>and</strong><br />
residential treatment centers, must bill for tobacco use under<br />
revenue codes 0944 (drug rehabilitation) or 0945 (alcohol<br />
rehabilitation). Claims submitted using these codes will process<br />
according to the substance abuse portion <strong>of</strong> the patient’s contract.<br />
St<strong>and</strong>ard guidelines regarding provider eligibility apply to<br />
procedures/services submitted with a tobacco diagnosis. Provider<br />
eligibility depends on the provider’s scope <strong>of</strong> practice <strong>and</strong> the type<br />
<strong>of</strong> procedure/service being billed. For example, consultation codes<br />
are generally only allowed when performed by a MD; however,<br />
evaluation <strong>and</strong> management codes may be eligible if billed by a<br />
qualified practitioner such as a Nurse Practitioner, or Physician<br />
Assistant. Some procedure/service codes specific to mental health<br />
<strong>and</strong> chemical dependency may have to be performed by a qualified<br />
mental health provider.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-37
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Coverage for Tobacco<br />
Treatment Medications<br />
Noncovered Tobacco<br />
Treatments<br />
Medication Therapy<br />
Management (MTM)<br />
11-38<br />
All fully insured <strong>Blue</strong> <strong>Cross</strong> plans with drug coverage cover stopsmoking<br />
medications. The same copayments <strong>and</strong> deductibles<br />
apply. With a physician’s prescription these patients are eligible<br />
for Zyban <strong>and</strong>/or any FDA-approved nicotine replacement therapy<br />
drug (patch, gum, lozenge, inhaler, <strong>and</strong> nasal spray).<br />
Note #1: In order to trigger this benefit, the patient does need a<br />
physician’s prescription even if the medication is available over<br />
the counter (except as described below in Note #2).<br />
Note #2: <strong>Blue</strong> <strong>Cross</strong> wants to encourage people to use both<br />
counseling <strong>and</strong> medications. Fully insured members who choose to<br />
enroll in the Stop-Smoking Program can trigger their benefit for<br />
either patch, gum, or lozenge without a physician’s prescription if:<br />
they enroll in our free Stop-Smoking Program (phone-based<br />
counseling),<br />
they have pharmacy benefits that cover FDA-approved OTC<br />
NRT <strong>and</strong> these benefits are administered through Prime<br />
Therapeutics, <strong>Blue</strong> <strong>Cross</strong>’ pharmacy benefit manager, <strong>and</strong><br />
the Quit Coach at the Stop-Smoking Program determines that<br />
the member can safely take the medications.<br />
Each self-insured group account chooses whether or not if will<br />
cover prescription <strong>and</strong>/or over-the-counter stop-smoking aids.<br />
Thus coverage varies greatly among self-insured groups. Your<br />
patients who have <strong>Blue</strong> <strong>Cross</strong> coverage through a self-insured<br />
group should call the customer service number on the back <strong>of</strong> their<br />
member ID card to determine if they have coverage for tobacco<br />
treatment medications <strong>and</strong> what restrictions might apply. If you<br />
have questions you may contact <strong>Blue</strong> <strong>Cross</strong> provider services.<br />
Refer to Medical Policy X-21 for information regarding treatments<br />
that are considered INVESTIGATIVE or ineligible for treatment<br />
<strong>of</strong> tobacco use, dependence, <strong>and</strong> withdrawal.<br />
Medication Therapy Management services are a covered benefit<br />
for Prepaid Medical Assistance Program (PMAP) Public Programs<br />
members.<br />
Eligible providers must be enrolled through DHS<br />
Eligible providers must be enrolled through DHS as a certified<br />
MTM pharmacist. Services should be submitted on an 837P claim<br />
format with the following codes:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Medication Therapy<br />
Management (MTM)<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Code Definition Allowed Frequency<br />
99605 Medication Therapy Management<br />
Service(s) provided by a<br />
pharmacist, individual face to face<br />
with patient, with assessment <strong>and</strong><br />
intervention if provided; initial 15<br />
minutes, new patient.<br />
99606 Medication Therapy Management<br />
Service(s) provided by a<br />
pharmacist, individual face to face<br />
with patient, with assessment <strong>and</strong><br />
intervention if provided; initial 15<br />
minutes, established patient.<br />
99607 Medication Therapy Management<br />
Service(s) provided by a<br />
pharmacist, individual face to face<br />
with patient, with assessment <strong>and</strong><br />
intervention if provided; each<br />
additional 15 minutes (list<br />
separately in addition to code for<br />
primary service)<br />
Pricing <strong>and</strong> programs applicability<br />
1 per enrollee per<br />
year<br />
Up to 7 per enrollee<br />
per year<br />
Up to 4 per enrollee<br />
per date <strong>of</strong> service<br />
<strong>Blue</strong> <strong>Cross</strong> has incorporated DHS rates in the usual pricing<br />
methodology for Public Programs for these codes. This<br />
information applies to the following programs <strong>and</strong> group numbers:<br />
Prepaid Medical Assistance Program (PMAP & GAMC) – all<br />
groups beginning with PP0 (Members with Medicare must get<br />
these services through their Medicare Part D plan).<br />
Secure<strong>Blue</strong> – all groups beginning with PP2 (Members with<br />
Medicare must get these services through their Medicare Part<br />
D plan for Medicare-covered services).<br />
<strong>Minnesota</strong> Senior Care – all groups beginning with PP0<br />
(Members with Medicare must get these services through their<br />
Medicare Part D plan).<br />
<strong>Minnesota</strong>Care – Exp<strong>and</strong>ed (PP111, PP112, PP151, PP152),<br />
Basic Plus (PP161, PP162, PP163, PP164), Basic + One<br />
(PP121, PP122), <strong>and</strong> Basic + 2 (PP131, PP132, PP141,<br />
PP142).<br />
This benefit is not covered under the Limited Benefit Set (PP171,<br />
PP172).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-39
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Oral Medication When submitting oral drugs for your <strong>Blue</strong> <strong>Cross</strong> patients, use the<br />
procedure/service codes in your HCPCS manual. HCPCS includes<br />
many codes for oral medications <strong>and</strong> injections that are commonly<br />
dispensed in physicians’ <strong>of</strong>fices.<br />
Non-Physician Health<br />
Care Practitioners<br />
11-40<br />
Use J8499 (prescription drug, oral, nonchemotherapeutic, NOS)<br />
only in limited situations such as after-hours emergency visits,<br />
house calls, or in rural areas where access to a community<br />
pharmacy is limited. Drug name, dosage, <strong>and</strong> NDC must be<br />
included on each claim.<br />
Benefits cannot be extended for drug samples provided by<br />
pharmaceutical companies.<br />
If the service is rendered by a non-physician healthcare<br />
practitioner that we credential, <strong>and</strong>/or verify licensure <strong>and</strong> are<br />
issued individual provider numbers, that practitioner must submit<br />
the services under the individual provider number that <strong>Blue</strong> <strong>Cross</strong><br />
has issued to him or her or NPI.<br />
Some practitioners who are not credentialed or issued individual<br />
provider numbers or NPIs (such as LPN, RN, dietitian), work<br />
under the supervision <strong>of</strong> a physician. The services must be<br />
submitted under the supervising physician’s provider number/NPI.<br />
The -U7 modifier must be submitted with the procedure/service to<br />
indicate these services. This includes those clinics with a<br />
pharmacist on staff. Services would be billed under the supervising<br />
MD with the -U7 modifier.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Practitioners That ARE<br />
Credentialed by <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> Issued<br />
Individual Provider<br />
Number/NPIs<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Acupuncturists (LAc)<br />
Certified Ind. Clinical Social Worker (CICSW)<br />
Certified Marriage <strong>and</strong> Family Therapist (CMFT)<br />
Certified Nurse Midwife (CNM)<br />
Certified Pr<strong>of</strong>essional Counselor (CPC)<br />
Chiropractor (DC)<br />
Dentist (DDS, DMD)<br />
Psychologist (PhD., MA, PsyD., MS, EDD)<br />
Licensed Certified Social Worker (LCSW)<br />
Licensed Ind. Clinical Social Worker (LICSW)<br />
Licensed Ind. Social Worker (LISW)<br />
Licensed Marriage & Family Therapist (LMFT)<br />
Licensed Pr<strong>of</strong>. Clinical Counselor (LPCC)<br />
Optometrist (OD)<br />
Physician Assistant (PA)<br />
Physician (MD, DO)<br />
Podiatrist (DPM)<br />
Psychiatric Mental Health Nurse Practitioner (PMHNP)<br />
Registered Nurse Clinical Specialist (CNS)<br />
Registered Nurse Practitioner (NP)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-41
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Practitioners that<br />
are NOT Credentialed<br />
by <strong>Blue</strong> <strong>Cross</strong> But Are<br />
Issued Individual<br />
Provider Number/NPIs<br />
Counseling <strong>and</strong>/or Risk<br />
Factor Reduction<br />
Room or Machine Set-<br />
Up Charges<br />
Although the following practitioner types do not go through the<br />
credentialing process, they do require an individual provider<br />
number or NPI for claims submission.<br />
Audiologist<br />
Certified Registered Nurse Anesthetist (CRNA)<br />
Licensed Assoc. Counselor (LAC)<br />
Lic. Assoc. Marriage & Family Therapist (LAMFT)<br />
Licensed Psychological Practitioner (LPP)<br />
Occupational Therapist (OT)<br />
Physician Therapist (PT)<br />
Registered Nurse First Assist (RNFA)<br />
Resident<br />
Social Worker (Levels: LISW, LGSW, LSW,<br />
LMSW, CSW, LSW, LMSW, CISW, CASW)<br />
Speech <strong>and</strong> Language Therapist<br />
Individual preventive medicine counseling (codes 99401-99404)<br />
are reimbursed per contract benefits. Group preventive medicine<br />
counseling (codes 99411-99412) may be covered under the Patient<br />
Protection <strong>and</strong> Affordable Care Act (PPACA) otherwise known as<br />
health care reform (HCR).<br />
Room or machine set-up charges are considered to be an integral<br />
part <strong>of</strong> the procedure/service being done. Do not submit separately<br />
for these services.<br />
Supplies in the Office Supplies in the clinic setting are generally included or part <strong>of</strong> the<br />
procedure or service. Codes 99070, A4649 <strong>and</strong> A4550 will be<br />
denied. Other supplies, such as Betadine or alcohol wipes, will<br />
also be denied. Generally, supplies are only allowed separately in<br />
conjunction with approved home health care.<br />
Adjunct CPT Codes Adjunct CPT codes 99024-99060 are designed for the provider to<br />
report special circumstances under which a basic procedure/service<br />
is performed.<br />
Care Plan Oversight<br />
Services<br />
11-42<br />
<strong>Blue</strong> <strong>Cross</strong> does not consider these or provider inconvenience fees<br />
as reimbursable services <strong>and</strong> they are denied as a provider liability.<br />
Care plan oversight services codes 99374-99380 are not<br />
reimbursed by <strong>Blue</strong> <strong>Cross</strong> as a separate service from the evaluation<br />
<strong>and</strong> management codes <strong>and</strong> will deny as provider liability.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Prolonged Physician<br />
Services<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
<strong>Blue</strong> <strong>Cross</strong> reimburses face-to-face prolonged physician services<br />
codes 99354-99357. Codes 99358-99359 are not reimbursed<br />
(prolonged services without face-to-face patient contact) <strong>and</strong> will<br />
deny as provider liability.<br />
Telephone Calls Telephone calls, codes 99441-99443 <strong>and</strong> 98966-98968, are noncovered<br />
services. Calls are considered an integral part <strong>of</strong> other<br />
services the patient receives (usually an evaluation <strong>and</strong><br />
management service) <strong>and</strong> not separately reimbursable.<br />
Medical Team<br />
Conferences<br />
Televideo<br />
Consultations<br />
Medical conferences without face-to-face patient contact, codes<br />
99367-99368, are not reimbursed, <strong>and</strong> will deny as provider<br />
liability.<br />
<strong>Blue</strong> <strong>Cross</strong> provides reimbursement for certain televideo<br />
consultations. These consultations are also sometimes referred to<br />
as telemedicine or telehealth services. Televideo consultations are<br />
interactive audio <strong>and</strong> video communications, permitting real-time<br />
communication between a distant site physician or practitioner <strong>and</strong><br />
the member, who is present <strong>and</strong> participating in the televideo visit<br />
at a remote facility.<br />
Coverage <strong>of</strong> televideo consultations includes consultations, <strong>of</strong>fice<br />
visits, psychotherapy, substance use disorders, as well as the codes<br />
allowed per Medicare policy. Facilities may be reimbursed for the<br />
origination fee. Both the consulting physician <strong>and</strong> the remote clinic<br />
or remote site will submit a claim for their services. The consulting<br />
physician will bill the appropriate CPT evaluation <strong>and</strong><br />
management, psychotherapy code, nutrition therapy or follow-up<br />
telehealth consult code. The remote provider will bill for the<br />
originating site facility fee only. This service is billable on either<br />
the pr<strong>of</strong>essional or institutional claim format.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-43
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Remote Clinic or Remote<br />
Site<br />
CODING Q3014- Telehealth<br />
originating site facility fee<br />
11-44<br />
0780- Telemedicine, General<br />
Classification<br />
Consulting Physician/Practitioner<br />
Note: The –GT modifier must be appended to<br />
all <strong>of</strong> the services below.<br />
–GT– Via interactive audio <strong>and</strong> video<br />
telecommunication systems<br />
99201-99215 – Office or other outpatient<br />
visits<br />
99231-99233 – Subsequent hospital care<br />
services<br />
99307-99310 – Subsequent nursing facility<br />
care services<br />
99241-99255 – Consultations<br />
90801 – Psychiatric diagnostic interview<br />
90804-90809 – Individual psychotherapy<br />
90862-Pharmacologic management<br />
90846 – Family psychotherapy (without the<br />
patient present)<br />
90847 – Family psychotherapy (conjoint<br />
psychotherapy) (with patient present)<br />
90849 – Multiple-family group<br />
psychotherapy<br />
90853 – Group psychotherapy (other than <strong>of</strong><br />
a multiple-family group)<br />
90857 – Interactive group psychotherapy<br />
90951-90952, 90954-90955, 90957-90958,<br />
90960-90961 – ESRD related services<br />
96116 – Neurobehavioral status exam<br />
96150-96154 – Individual <strong>and</strong> group health<br />
<strong>and</strong> behavior assessment <strong>and</strong> intervention<br />
G0108-G0109 – Individual <strong>and</strong> group<br />
kidney disease education services<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
CODING<br />
(continued)<br />
Remote Clinic or Remote<br />
Site<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Consulting Physician/Practitioner<br />
CO-PAY None Co-pays would apply<br />
GLOBAL<br />
PERIOD<br />
Televideo Coverage<br />
Exceptions<br />
Not included in the global<br />
surgical period<br />
G0270, 97802-97803 – Individual medical<br />
nutrition therapy<br />
G0406-G0408 – Follow-up inpatient<br />
telehealth consult<br />
G0420-G0421 – Individual <strong>and</strong> group<br />
kidney disease education services<br />
G0436-G0437, 99406-99407 – Smoking<br />
cessation services<br />
Global surgical package edits apply<br />
Televideo consultations are subject to the terms <strong>of</strong> the member’s<br />
contract <strong>and</strong> may not be covered under the member’s health plan.<br />
The Federal Employee Program (FEP) specifically excludes<br />
televideo consultations. Televideo consultations do not include<br />
telephone calls or Internet consultations. Telephone <strong>and</strong> Internet<br />
consultations are contract exclusions <strong>and</strong> will be denied.<br />
Unusual Travel Unusual travel charges (99082) are non-covered services <strong>and</strong> will<br />
deny as provider liability<br />
Urgent Care Clinic-based urgent care services may be billed under the place <strong>of</strong><br />
service (POS) 20. The POS code 20 will apply <strong>of</strong>fice benefits to<br />
the services if submitted. DO NOT bill a corresponding facility<br />
claim with the revenue code 0456 if already billing for urgent care<br />
on the pr<strong>of</strong>essional claim (837P). This would be considered<br />
duplicate billing.<br />
Hospital based emergency room urgent care should be billed on<br />
the UB-04 only with the revenue code 0456.<br />
Codes S9083 (global fee urgent care centers) <strong>and</strong> S9088 (services<br />
provided in an urgent care center) represent where the service was<br />
rendered, not the service itself. Thus, they are not separately<br />
covered <strong>and</strong> will be denied as part <strong>of</strong> the primary service (such as<br />
E/M).<br />
11-45
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Weight Management<br />
Care<br />
11-46<br />
General Guidelines<br />
In general, <strong>Blue</strong> <strong>Cross</strong> covers services for the treatment <strong>of</strong> obesity,<br />
weight management, nutrition, <strong>and</strong> physical activity counseling.<br />
However, coverage for these services depends on the type <strong>of</strong><br />
provider submitting the claim, the procedure/service <strong>and</strong> diagnosis<br />
codes submitted, <strong>and</strong> the patient’s contract with <strong>Blue</strong> <strong>Cross</strong>. We<br />
encourage you to request that your patients check on their<br />
coverage before extensive services are provided. Due to the many<br />
variables, exact payment can not be determined until we receive<br />
the claim for processing.<br />
Screening <strong>and</strong> counseling for obesity <strong>and</strong> counseling for a healthy<br />
diet are covered under the Patient Protection <strong>and</strong> Affordable Care<br />
Act (PPACA) otherwise known as health care reform (HCR).<br />
The suggested coding for obesity screening <strong>and</strong> counseling<br />
includes 97802-97804, 99078, 99401-99404, 99411-99412,<br />
G0447, G0449 or S9470 as preventive with 278.00 or 278.01.<br />
The suggested coding for counseling for a healthy diet includes<br />
99401-99404, 99411-99412, 99078, 97802-97804, G0447, S9452,<br />
S9470 as preventive with V65.3.<br />
Refer to the information below for screening <strong>and</strong> other services not<br />
subject to PPACA. The outline reviews the following seven<br />
categories as they relate to coverage for services related to obesity,<br />
weight management, nutrition, <strong>and</strong> physical activity counseling.<br />
1. Diagnosis Codes<br />
2. Procedure/Service Codes<br />
3. Eligible Providers<br />
4. Weight Loss Programs<br />
5. Weight Loss Drugs<br />
6. Physical Activity<br />
7. Surgery<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Weight Management<br />
Care (continued)<br />
Diagnosis Codes<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
The physician determines if the patient meets the criteria to be<br />
classified as obese. If the patient meets those criteria, two specific<br />
obesity diagnosis codes may be used:<br />
1. 278.00 Obesity, Unspecified<br />
2. 278.01 Morbid Obesity<br />
In addition to the two specific obesity codes, the provider may also<br />
bill for obesity or weight management counseling with routine<br />
diagnosis codes such as:<br />
1. V65.3 Dietary Surveillance <strong>and</strong> Counseling<br />
2. V70.0 Routine General Medical Examination at a Health Care<br />
Facility.<br />
The obesity diagnosis codes <strong>of</strong> 278.00. 278.01 <strong>and</strong> code V65.3 will<br />
cause claims to pay according to the illness portion <strong>of</strong> the patient’s<br />
contract. All <strong>Blue</strong> <strong>Cross</strong> contracts have benefits for illness-related<br />
services. If the claim is submitted with a routine medical exam<br />
code <strong>of</strong> V70.0, it will pay based on the routine benefits, if any, are<br />
provided by the patient’s contract. Some contracts exclude routine<br />
benefits.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-47
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Weight Management<br />
Care (continued)<br />
11-48<br />
Claims may be submitted for obesity, weight management,<br />
nutrition counseling etc. with the diagnosis <strong>of</strong> the underlying<br />
symptom that brought the patient to the provider. For example, the<br />
claim may be submitted with a diagnosis <strong>of</strong> elevated blood<br />
cholesterol, shortness <strong>of</strong> breath, or diabetes. These claims will<br />
process according to the medical illness benefit.<br />
Procedure/Service Codes<br />
Services for obesity/weight management counseling may be billed<br />
under E/M codes (99201-99215) provided that those services meet<br />
the components <strong>of</strong> an E/M service. These E/M codes are<br />
compatible with all causes, illness or routine related, <strong>and</strong> will pay<br />
according to the diagnosis submitted.<br />
Claims may also be submitted as preventive counseling (99401-<br />
99404). These codes, however, are only compatible with routine<br />
diagnosis codes (e.g., V70.0). Claims submitted with these<br />
procedure/service codes <strong>and</strong> a routine diagnosis code will process<br />
according to the patient’s preventive benefit, provided the patient<br />
has coverage for preventive services. If CPT codes 99401-99404<br />
were submitted with a diagnosis <strong>of</strong> obesity (e.g., 278.00) the claim<br />
would reject because the service was incompatible with the<br />
diagnosis.<br />
Medical nutritional therapy codes (97802, 97803, S9470) may be<br />
billed when counseling patients on obesity or weight management.<br />
These codes are compatible with any diagnosis but are most<br />
appropriate or intended for illness or disease-related diagnoses<br />
such as obesity or diabetes. Note that code 97804 is nutritional<br />
therapy in a group setting. Group therapy services are generally<br />
only covered when submitted with diagnosis codes for anorexia,<br />
bulimia, diabetes, congestive heart failure, <strong>and</strong> some maternity<br />
diagnosis codes.<br />
The FEP contract allows medical nutrition therapy services only<br />
for the following diagnosis codes:<br />
Diagnosis codes 250.XX <strong>and</strong> 648.XX for diabetes <strong>and</strong><br />
gestational diabetes;<br />
Medical nutritional therapy for eating disorders 307.1<br />
(anorexia nervosa) <strong>and</strong> 307.51 (bulimia nervosa); or<br />
Dietitian assessments as part <strong>of</strong> a multi-disciplinary eating<br />
disorder evaluation.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Weight Management<br />
Care (continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Nutritionists, Dietitians <strong>and</strong> other Providers<br />
For many lines <strong>of</strong> business, <strong>Blue</strong> <strong>Cross</strong> pays <strong>Minnesota</strong> licensed<br />
nutritionists, licensed dietitians, <strong>and</strong> registered dietitians directly<br />
for services submitted with an eating disorder code 307.1, 307.50<br />
<strong>and</strong> 307.51. The provider may submit using procedure/service<br />
codes S9470, 97802, 97803, or 97804 based on the service<br />
provided. No referral is necessary for the highest benefit level.<br />
Some self-insured plans, however, may exclude coverage by a<br />
dietitian, so benefits should be verified.<br />
Licensed dietitians <strong>and</strong> licensed nutritionists can bill for<br />
procedure/service codes S9470, 97802, 97803, G0447 <strong>and</strong> G0449<br />
for diagnosis codes other than eating disorders. Services provided<br />
by licensed dietitians <strong>and</strong> nutritionists must be submitted to <strong>Blue</strong><br />
<strong>Cross</strong> using the provider number or NPI <strong>of</strong> an eligible medical<br />
clinic or hospital. The individual provider number or NPI <strong>of</strong> the<br />
licensed dietitian or licensed nutritionist must also be submitted on<br />
the claim.<br />
Registered dietitians billing for services outside <strong>of</strong> behavioral<br />
health diagnosis codes will have those claims denied unless the<br />
services are submitted under the individual provider number <strong>of</strong> a<br />
supervising physician. The –U7 modifier should also be submitted.<br />
Health educators <strong>and</strong> exercise physiologists are not recognized as<br />
eligible providers <strong>and</strong> their services will be rejected if received by<br />
<strong>Blue</strong> <strong>Cross</strong>.<br />
Weight Loss Programs<br />
<strong>Blue</strong> <strong>Cross</strong> does not cover commercial weight loss programs (e.g.,<br />
Nutra-systems, Jenny Craig, LA Weight Loss, Weight Watchers<br />
etc.) with the exception <strong>of</strong> the PMAP contract.<br />
Members <strong>of</strong> <strong>Minnesota</strong>Care, <strong>Blue</strong>Advantage, Secure<strong>Blue</strong> do have<br />
limited weight loss programs benefits, including weight<br />
management <strong>and</strong> nutrition classes.<br />
Weight Loss Drugs<br />
All fully insured groups cover weight loss drugs. Public Program<br />
accounts do not cover weight loss drugs. Each self-insured account<br />
chooses whether or not to cover weight loss drugs. Note that<br />
patients covered by certain State Health Plan products have<br />
specific authorization requirements for weight loss drugs.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-49
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Weight Management<br />
Care (continued)<br />
11-50<br />
Physical Activity<br />
There are no procedure/service codes specifically for physical<br />
activity counseling. Providers typically bill counseling services for<br />
physical activity as an E/M service (99201-99215) provided that<br />
the counseling meets the components <strong>of</strong> an E/M service. There is<br />
no specific diagnosis code for physical activity counseling.<br />
Exercise classes (S9451) are generally non-covered.<br />
The provider may also submit codes for preventive counseling<br />
(99401-99404). These codes however, are only compatible with<br />
routine diagnosis codes (e.g., V70.0). Claims submitted with these<br />
procedure/service codes <strong>and</strong> a routine diagnosis code will process<br />
according to the patient’s preventative benefit, provided the patient<br />
has coverage for preventative services.<br />
Services billed by a personal trainer or an exercise physiologist are<br />
not covered. Claims for their services will be denied as an<br />
ineligible provider, regardless <strong>of</strong> the procedure/service code <strong>and</strong><br />
diagnosis code submitted.<br />
Surgery<br />
<strong>Blue</strong> <strong>Cross</strong> has a detailed medical policy, IV-19, regarding<br />
provider <strong>and</strong> patient eligibility criteria for obesity surgery.<br />
Some groups exclude coverage for obesity surgery in their<br />
contracts. Prior authorization is highly recommended.<br />
Disclaimer: The fine print<br />
This information is designed for reference purposes only <strong>and</strong> does<br />
not guarantee coverage. <strong>Blue</strong> <strong>Cross</strong> will consider each individual<br />
member’s condition <strong>and</strong> unique circumstances in making coverage<br />
determinations. <strong>Blue</strong> <strong>Cross</strong> will also make each determination on a<br />
case-by-case basis <strong>and</strong> according to the terms <strong>and</strong> conditions <strong>of</strong> the<br />
member’s contract, certificate <strong>of</strong> coverage, or summary plan<br />
description, as applicable, including provisions relating to<br />
exclusions <strong>and</strong> limitations. If there is a conflict between the<br />
information above <strong>and</strong> the contract or plan documents, the contract<br />
or plan documents govern.<br />
<strong>Blue</strong> <strong>Cross</strong> reviews its policies <strong>and</strong> coverage periodically <strong>and</strong> may<br />
make changes in the future.<br />
Any providers who have questions about this information are<br />
invited to contact <strong>Blue</strong> <strong>Cross</strong> provider services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Assessment<br />
Management Program<br />
for Fully Insured<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
The Integrated Health Management division <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> utilizes<br />
a management program called Access Management. The program<br />
only applies to fully insured members with commercial Managed<br />
care (<strong>Blue</strong> Plus) <strong>and</strong> preferred provider (Aware ® ) coverage who<br />
are using services at a higher frequency than their known medical<br />
conditions would normally warrant.<br />
Program Details<br />
Members that meet the Access Management program criteria will<br />
be assigned to a specific physician for their primary care needs<br />
who, in turn, will coordinate all their care <strong>and</strong> medication needs.<br />
The member will also be assigned to a single pharmacy <strong>and</strong> a<br />
single hospital. Access to specialty care may be discussed with the<br />
<strong>Blue</strong> <strong>Cross</strong> access manager assigned to the member. Assignment to<br />
the Access Management program is for 24 months.<br />
Member identification<br />
To see if a member is enrolled in the Access Management Program<br />
check the provider web self-service (PWSS) at providerhub.com<br />
or use the 270/271 Eligibility transaction as noted below. For<br />
provider web self-service, follow the link to the HIPAA benefit<br />
view from the Member Benefit Screen. If the member is enrolled<br />
in AMP, it will be indicated in the HIPAA view screen.<br />
Members enrolled in the program will have the letters AMP on<br />
their member ID card. Members currently enrolled will receive<br />
new member ID cards with AMP on them. As individuals are<br />
enrolled in the program a new member ID card will be issued with<br />
AMP on the card. When members exit the program a new member<br />
ID card will be issued without AMP.<br />
Eligibility<br />
If you are not the assigned physician, pharmacy or hospital for a<br />
member in this program, it may affect claims payment should you<br />
provide services to a member enrolled in this program. If we have<br />
received claims from you within 12 months prior to the member<br />
being placed in this program, you will be notified by telephone<br />
<strong>and</strong>/or letter <strong>of</strong> the member’s placement.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-51
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Assessment<br />
Management Program<br />
for Fully Insured<br />
(continued)<br />
11-52<br />
Eligible services provided to a member in the Access Management<br />
program will only be reimbursed when one <strong>of</strong> the following<br />
criteria is met:<br />
The service is provided by the member’s assigned provider<br />
The service is <strong>of</strong> a provider type or type <strong>of</strong> service that is not<br />
listed as needing Access Management. This includes Durable<br />
Medical Equipment (DME), home care, ambulance services,<br />
mental health or chemical health services.<br />
Eligibility Transaction<br />
The following Loops <strong>and</strong> Segments will be populated in the 271<br />
eligibility response when the above Eligibility criteria are met.<br />
HIPAA Version 5010<br />
2110C/D – EB (Subscriber/Dependent Eligibility or<br />
Benefit Information)<br />
EB01 = MC (Managed Care Coordinator)<br />
2110C/D – DTP (Subscriber/Dependent Eligibility/Benefit<br />
Date)<br />
DTP01 = “193” (Period Start)<br />
DTP02 = “D8” ( Date Expressed in Format<br />
CCYYMMDD)<br />
DTP03 = CCYYMMDD (Period Start Date)<br />
2110C/D – MSG (Message Text)<br />
MSG01 = Access Management Program<br />
Additional Information<br />
If one <strong>of</strong> your patients is enrolled in this program, you will be<br />
notified by letter by the access manager. As the primary provider,<br />
you will be coordinating the identified member’s care with the<br />
<strong>Blue</strong> <strong>Cross</strong> access manager.<br />
If you have a patient covered by fully insured commercial<br />
coverage who you believe would benefit from the Access<br />
Management program, contact Cathryn Bashore, manager, at<br />
(651) 662-0733 or Jennifer Jaynes, director, at (651) 662-2346.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Health Care Home<br />
(HCH)<br />
Health Care Home Guidelines<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
<strong>Blue</strong> <strong>Cross</strong> will accept certain claims for payment <strong>of</strong> health care<br />
home (HCH) care coordination services billed via procedure codes<br />
S0280 or S0281.<br />
The development <strong>of</strong> health care homes in <strong>Minnesota</strong> is part <strong>of</strong> the<br />
health care reform legislation passed in <strong>Minnesota</strong> in May 2008.<br />
The legislation includes payment to providers for partnering with<br />
eligible patients <strong>and</strong> families to provide coordination <strong>of</strong> care.<br />
<strong>Blue</strong> Plus' <strong>Minnesota</strong> Department <strong>of</strong> Human Services (DHS) 2010<br />
Contracts require that individuals with complex or chronic<br />
conditions be able to access services through a certified health care<br />
home. These provisions impact individuals enrolled in <strong>Minnesota</strong><br />
Health Care Programs (MHCP), including <strong>Blue</strong> Advantage,<br />
<strong>Minnesota</strong>Care, Secure<strong>Blue</strong>, <strong>Minnesota</strong> Senior Health Options<br />
(MSHO), Special Needs Basic Care (SNBC), <strong>and</strong> <strong>Minnesota</strong><br />
Senior Care Plus (MSC+). These health care home provisions also<br />
impact the <strong>Minnesota</strong> Advantage Health Plan <strong>of</strong>fered by the State<br />
Employee Group.<br />
In addition, <strong>Blue</strong> <strong>Cross</strong> will accept certain claims for payment <strong>of</strong><br />
certified health care home care coordination services for<br />
Subscribers covered under fully insured group contracts, when<br />
billed via procedure codes S0280 or S0281. The benefit will not be<br />
<strong>of</strong>fered to self-insured groups at this time. Individuals enrolled in<br />
our Platinum <strong>Blue</strong> Medicare Cost products or Medicare<br />
Supplement products will also not be affected.<br />
What does this mean for you?<br />
<strong>Blue</strong> <strong>Cross</strong> will not be pursuing separate contracting<br />
arrangements for HCH services at this time. Payment for<br />
services provided to both commercial subscribers <strong>and</strong><br />
<strong>Minnesota</strong> Health Care Programs enrollees will be made at<br />
your then-current contracted rate <strong>of</strong> reimbursement for health<br />
services.<br />
Members will not have copayments or coinsurance for HCH<br />
care coordination, except in the case <strong>of</strong> fully insured<br />
commercial subscribers covered under a health savings account<br />
(HSA), as per Internal Revenue Service requirements (see<br />
below).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-53
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Health Care Home<br />
(HCH) (continued)<br />
11-54<br />
To the extent that <strong>Blue</strong> <strong>Cross</strong> has global payment arrangements<br />
with providers or other alternative reimbursement<br />
arrangements that already include HCH-type care coordination<br />
arrangements <strong>Blue</strong> <strong>Cross</strong> will not give the provider a separate<br />
payment under the HCH requirement.<br />
Enrollment in a health care home is voluntary <strong>and</strong> based on<br />
information collected <strong>and</strong> documented by the provider.<br />
Providers are required to maintain a registry <strong>of</strong> health care<br />
home participants. Health plans have worked with the AUC to<br />
develop st<strong>and</strong>ardized billing codes for health care home<br />
services. Individuals are not prohibited from being enrolled in<br />
more than one HCH, but health plans are only required to pay<br />
for a single HCH for each member.<br />
<strong>Blue</strong> <strong>Cross</strong> will comply with health care home legislation in<br />
the processing <strong>of</strong> care coordination fees incurred by our<br />
impacted State Health Plan members. There will be no cost<br />
sharing for either the <strong>Minnesota</strong> Advantage Health Plan or the<br />
Advantage Consumer Directed Health Plan <strong>of</strong>fered by the State<br />
Employee Group Insurance Plan. Health care home care<br />
coordination will not be a covered service for members <strong>of</strong> the<br />
Public Employee Insurance Plan.<br />
Because <strong>Blue</strong> <strong>Cross</strong> has no administratively feasible way to<br />
identify a member’s “real” HCH, we will pay the first claim<br />
that we receive each month. Additional claims will not be paid.<br />
Certified health care home care coordination services<br />
Certified health care home care coordination services will be<br />
accepted for fully insured commercial business <strong>and</strong> <strong>Minnesota</strong><br />
Health Care Programs for reimbursement under procedure codes<br />
S0280 or S0281, subject to the following limitations:<br />
Subscribers who are not covered under a health savings<br />
account (HSA) plan:<br />
1. For code S0280: Allow once per 12 months for each<br />
patient/provider combination. No patient out <strong>of</strong> pocket<br />
should be applied. The code will be allowed per provider<br />
contract. Code S0280 billed more than once per 12 months<br />
for each patient /provider combination will be denied with<br />
Claim Adjustment Reason Code 119 <strong>and</strong> Remark Code<br />
M90.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Health Care Home<br />
(HCH) (continued)<br />
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
2. For code S0281: Allow once per month for subsequent<br />
months. No patient out <strong>of</strong> pocket should be applied. The<br />
code will be allowed per provider contract. Code S0281<br />
billed more than once per month for each patient will be<br />
denied with Claim Adjustment Reason Code 119 <strong>and</strong><br />
Remark Code M86.<br />
Subscribers who are not covered under an HSA plan members:<br />
1. For code S0280: Allow once per 12 months for each<br />
patient/provider combination. Patient<br />
deductible/coinsurance will apply per Internal Revenue<br />
Service (IRS) regulations. The code will be allowed per<br />
provider contract. Code S0280 billed more than once per<br />
12 months for each patient /provider combination will be<br />
denied with Claim Adjustment Reason Code 119 <strong>and</strong><br />
Remark Code M90.<br />
2. For code S0281: Allow once per month for subsequent<br />
months. Patient deductible/coinsurance will apply per IRS<br />
regulations. The code will be allowed per provider contract.<br />
Code S0281 billed more than once per month for each<br />
patient will be denied with Claim Adjustment Reason Code<br />
119 <strong>and</strong> Remark Code M86.<br />
Coding Submission<br />
The following coding submission guides were developed by the<br />
AUC Medical Code TAG <strong>and</strong> approved by the AUC Operations<br />
Committee. This information is found in the 5010 version <strong>of</strong> the<br />
837P MN Companion Guide, Table A.5.1, Chapter 12.<br />
The Health Care Home Payment Methodology Steering<br />
Committee has determined that five levels <strong>of</strong> patient complexity<br />
should be recognized for health care home payment purposes. In<br />
addition, the complexity level determination must take into<br />
account two supplemental factors (non-English speaking, <strong>and</strong><br />
major active mental health condition). In order to achieve the goals<br />
<strong>of</strong> reporting five levels <strong>of</strong> patient complexity, as well as two<br />
additional supplemental complexity factors, additional qualifiers<br />
(modifiers or condition codes) are needed.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)<br />
11-55
Coding Policies <strong>and</strong> Guidelines (Medical Services)<br />
Health Care Home<br />
(HCH) (continued)<br />
11-56<br />
The Medical Code TAG recommends that interim coding as shown<br />
below be used until new modifiers <strong>and</strong>/or condition codes can be<br />
created at the national level to differentiate health care home<br />
patient complexity levels. The proposed interim solution is to use<br />
U modifiers, in addition to existing TF <strong>and</strong> TG modifiers, with the<br />
following two S codes: S0280 – medical home program,<br />
comprehensive care coordination <strong>and</strong> planning, initial plan; <strong>and</strong><br />
S0281 – medical home program, comprehensive care coordination<br />
<strong>and</strong> planning, maintenance.<br />
Proposed interim solution: Use U modifiers in conjunction with<br />
medical home S codes as shown below:<br />
Patient<br />
Complexity<br />
Level Modifiers<br />
Low (no major<br />
conditions)<br />
Non English<br />
Speaking<br />
No modifier U3 U4<br />
Basic U1 U3 U4<br />
Intermediate TF U3 U4<br />
Extended U2 U3 U4<br />
Complex<br />
(most major<br />
conditions<br />
TG U3 U4<br />
Definitions <strong>of</strong> U codes<br />
Active Mental<br />
Health<br />
Condition<br />
U1 – Care coordination, basic complexity level (used with<br />
S0280 - S0281)<br />
U2 – Care coordination, extended complexity level (used with<br />
S0280 - S0281)<br />
U3 – Care coordination, supplemental factor; non-English<br />
language (used with S0280 – S0281)<br />
U4 – Care coordination, supplemental factor; Major Active<br />
Mental Health Condition (used with S0280 – S0281)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (06/20/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Optometric/Optical Services)<br />
Table <strong>of</strong> Contents<br />
Ophthalmological Services ..................................................................................................11-2<br />
Charges for Lenses <strong>and</strong> Contact Lens Fitting......................................................................11-2<br />
Eyewear billing <strong>and</strong> Reimbursement...................................................................................11-2<br />
Routine Vision Services.......................................................................................................11-2<br />
Vision Therapy Services...................................................................................................... 11-3<br />
Claims Filing Requirements ...............................................................................................11-3<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/15/10) 11-1
Coding Policies <strong>and</strong> Guidelines (Optometric/Optical Services)<br />
Ophthalmological<br />
Services<br />
Charges for Lenses <strong>and</strong><br />
Contact Lens Fitting<br />
Eyewear billing <strong>and</strong><br />
Reimbursement<br />
11-2<br />
<strong>Blue</strong> <strong>Cross</strong> coding policy follows the CPT system <strong>of</strong> descriptive<br />
terms <strong>and</strong> identifying codes for reporting medical services <strong>and</strong><br />
procedures performed by physicians <strong>and</strong> optometrists.<br />
Both E/M codes <strong>and</strong> ophthalmology codes 92002, 92004, 92012,<br />
92014, <strong>and</strong> 92015, may be appropriate to use by optometrists or<br />
ophthalmologists. The level <strong>of</strong> E/M service or the selection <strong>of</strong><br />
ophthalmology codes must appropriately reflect the medical<br />
condition, the medical necessity, the tests performed, <strong>and</strong> be<br />
documented in the patient record. Selection <strong>of</strong> either an E/M code<br />
or an ophthalmology code may be appropriate for routine or<br />
medical diagnoses, <strong>and</strong> should be based on the CPT definitions <strong>of</strong><br />
services provided. Details <strong>of</strong> the patient encounter, as recorded on<br />
the patient record, must meet or exceed the stated CPT<br />
requirements to qualify for the code selected.<br />
<strong>Blue</strong> <strong>Cross</strong> requires that all medical services be performed by the<br />
pr<strong>of</strong>essionals eligible <strong>and</strong> credentialed to perform the service. The<br />
diagnosis <strong>and</strong> CPT coding must appropriately reflect the medical<br />
condition <strong>and</strong> that the medical record reflect the medical necessity<br />
<strong>and</strong> severity <strong>of</strong> the condition.<br />
Submit charges for any type <strong>of</strong> lenses using Level II HCPCS<br />
codes. Any fee for fitting <strong>and</strong> prescription <strong>of</strong> contact lenses may be<br />
reported by submitting a CPT code from the contact lens services<br />
section in addition to the contact lens supply code. The fee for<br />
fitting <strong>and</strong> prescription <strong>of</strong> contact lenses may also be included in<br />
the contact lens charge.<br />
Eyewear claims will be paid to the member, not the provider. This<br />
affects all <strong>of</strong> our members with the exception <strong>of</strong> Prepaid Medical<br />
Assistance Program (PMAP) or <strong>Minnesota</strong> Care (MNCARE)<br />
coverage.<br />
If you bill eyewear for a member, you should bill the eyewear on a<br />
separate claim form from the one used for the eye exam. Use your<br />
optician’s contracting provider number or NPI when billing for the<br />
eyewear. Your optometrist’s contracting provider number or NPI<br />
should be submitted when billing for the eye exam. <strong>Blue</strong> <strong>Cross</strong><br />
requires that eye exams <strong>and</strong> eyewear claims not be billed on the<br />
same claim form.<br />
Routine Vision Services <strong>Blue</strong> Plus contracts allow routine vision exams without a referral.<br />
However, if an illness or problem is discovered, treatment requires<br />
a referral from the patient’s primary care clinic.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/15/10)
Vision Therapy<br />
Services<br />
Claims Filing<br />
Requirements<br />
Coding Policies <strong>and</strong> Guidelines (Optometric/Optical Services)<br />
<strong>Blue</strong> <strong>Cross</strong> will reimburse the initial visit under 92060. Visual<br />
therapy instruction by any method that is provided during the first<br />
visit is included in this description. Separate billing for CPT code<br />
92065 will not be allowed for the initial visit. Vision therapy<br />
services involve non-surgical orthoptics, medical, or sensorymotor<br />
re-education for patients who suffer from conditions such as<br />
strabismus, amblyopia, exotropia, <strong>and</strong>/or esotropia.<br />
All subsequent visits for patient evaluation <strong>and</strong> monitoring <strong>of</strong><br />
treatment will be billed to <strong>Blue</strong> <strong>Cross</strong> under CPT code 92065.<br />
Office calls (99201-99215, 92002-92014) <strong>and</strong> sensorimotor exams<br />
(92060) are not eligible for separate billing from the providers <strong>of</strong><br />
the visual therapy during the course <strong>of</strong> treatment unless a medical<br />
examination is clinically indicated for other reasons.<br />
Use CPT codes or HCPCS level II code to bill your services.<br />
ICD-9-CM codes should be used to submit an appropriate<br />
diagnosis for your patient. Please note the correct code for routine<br />
vision care is V72.0 or 367.0-367.9 completed to the appropriate<br />
fourth <strong>and</strong> fifth digits.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (11/15/10)<br />
11-3
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Pharmacy Services)<br />
Table <strong>of</strong> Contents<br />
Claims Submission................................................................................................................... 11-2<br />
Pharmacy Claims for <strong>Blue</strong> <strong>Cross</strong> Subscribers without a Pharmacy Benefit Manager ........11-2<br />
Claims Filing Requirements ................................................................................................ 11-2<br />
Drug Claims Submission ..................................................................................................... 11-2<br />
Prescribing Physician’s DEA............................................................................................... 11-2<br />
Prior Authorization .............................................................................................................. 11-3<br />
Injectable Drugs...................................................................................................................11-3<br />
Pharmacies Submitting Claims for DME ............................................................................ 11-3<br />
Claim Processing...................................................................................................................... 11-4<br />
NDC Numbers ..................................................................................................................... 11-4<br />
Copays/Coinsurance ............................................................................................................11-4<br />
Vacation Prescription Requests ........................................................................................... 11-4<br />
Prescription Cost Less Than Copay..................................................................................... 11-4<br />
Discounting or Waiving Copays..........................................................................................11-4<br />
Pharmacy Audits.................................................................................................................. 11-4<br />
Drugs ......................................................................................................................................... 11-5<br />
Drug Formulary ................................................................................................................... 11-5<br />
Drugs with a Non-preferred Status ...................................................................................... 11-6<br />
Quantity Limits ....................................................................................................................11-7<br />
Compounded Prescriptions ..................................................................................................11-7<br />
Over-the-Counter Drugs ...................................................................................................... 11-7<br />
Dispense As Written (DAW)...............................................................................................11-8<br />
Investigative Drug Use ........................................................................................................11-8<br />
Drug Programs......................................................................................................................... 11-9<br />
Specialty Drugs....................................................................................................................11-9<br />
Step Therapy Program ....................................................................................................... 11-11<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11) 11-1
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Claims Submission<br />
Pharmacy Claims for<br />
<strong>Blue</strong> <strong>Cross</strong> Subscribers<br />
without a Pharmacy<br />
Benefit Manager<br />
Claims Filing<br />
Requirements<br />
Drug Claims<br />
Submission<br />
Prescribing Physician’s<br />
DEA<br />
11-2<br />
All pharmacies that are contracted with <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong><br />
<strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) are required to submit<br />
prescription charges on behalf <strong>of</strong> any <strong>Blue</strong> <strong>Cross</strong> subscriber, when<br />
a subscriber’s contract does not use a pharmacy benefit manager.<br />
The pharmacy should not request that the subscriber pay for any<br />
services before claim adjudication other than the copayment<br />
amount stated on the subscriber’s member ID card. At this time the<br />
pharmacy claims should be submitted in a paper format. Once the<br />
claim is received at <strong>Blue</strong> <strong>Cross</strong>, the appropriate benefits <strong>and</strong><br />
reimbursement will be applied according to the provider <strong>and</strong><br />
subscriber contracts.<br />
The majority <strong>of</strong> our member contracts contain basic drug coverage.<br />
Drug claims are either processed by <strong>Blue</strong> <strong>Cross</strong> or Prime<br />
Therapeutics. To determine if a drug claim should be submitted to<br />
<strong>Blue</strong> <strong>Cross</strong> or Prime Therapeutics for processing, check the<br />
member’s ID card. If the member has drug processing through<br />
Prime Therapeutics, the medical identification (ID) card will<br />
indicate RxPCN (the carrier code) “PGIGN”. A Prime<br />
Therapeutics provider must be used. You must include the two<br />
digit numeric dependent code, which is indicated before the name<br />
on the member ID card. For an example <strong>of</strong> a member ID card,<br />
refer to bluecrossmn.com. Type in the search field “sample id<br />
card”.<br />
Providers within the Prime Therapeutic network must submit<br />
claims electronically.<br />
If the member has Prime Therapeutics coverage, but the Prime<br />
Therapeutics information is not printed on the member ID card, the<br />
member should pay the prescription in full <strong>and</strong> submit the claim to<br />
Prime Therapeutics for direct reimbursement.<br />
Submit Prime Therapeutics member drug claims to:<br />
Prime Therapeutics<br />
Mail Route BCBSMN<br />
P.O. Box 14501<br />
Lexington, KY 40512-4501<br />
The physician’s NPI (National Provider Identifier) number must be<br />
entered on all electronic or paper claims submitted for payment.<br />
This information is used for drug utilization review aimed at<br />
improving the quality <strong>of</strong> health care delivered to our members.<br />
Leaving this data element out or use <strong>of</strong> a dummy NPI number<br />
constitutes an incomplete pharmacy claim.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Prior Authorization The prescribing physician must obtain prior authorization through<br />
<strong>Blue</strong> <strong>Cross</strong>’s medical review area for certain drugs. Some<br />
examples <strong>of</strong> drugs requiring prior authorization include infertility<br />
drugs <strong>and</strong> growth hormones.<br />
For a complete listing, refer to the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong><br />
<strong>Minnesota</strong> Medical Policy Update. To view medical policies go to<br />
providers.bluecrossmn.com <strong>and</strong> select “Medical policy” under<br />
“Tools & Resources.”<br />
For drugs that require a prior authorization, complete a <strong>Minnesota</strong><br />
Uniform Form for Prescription Drug Prior Authorization (PA)<br />
Requests <strong>and</strong> Formulary Exceptions.<br />
Injectable Drugs Most prescription benefit plans allow injectable processing online.<br />
Be sure to use the appropriate NDC <strong>and</strong> submit your claim<br />
electronically to the processor.<br />
Pharmacies Submitting<br />
Claims for DME<br />
For durable medical equipment, the pharmacy must follow the<br />
normal process for claims submission utilizing the electronic 837P<br />
claim format.<br />
The Aware Agreement, Article III, Section A, "Scope <strong>of</strong> Services"<br />
states: “Provider shall provide Health Services to Subscribers for<br />
eligible Prescription Drugs which are authorized by a valid<br />
prescription.” This section also includes the dispensing <strong>of</strong> durable<br />
medical equipment (DME) to <strong>Blue</strong> <strong>Cross</strong> subscribers.<br />
It is the responsibility <strong>of</strong> the participating pharmacy to submit the<br />
claims for all such eligible services to <strong>Blue</strong> <strong>Cross</strong> on behalf <strong>of</strong> the<br />
subscriber. After the claim is processed by <strong>Blue</strong> <strong>Cross</strong>, you will be<br />
notified <strong>of</strong> the proper amount to bill the subscriber, if any balance<br />
remains due from the subscriber.<br />
It is also the responsibility <strong>of</strong> all participating providers to abide by<br />
all other terms <strong>and</strong> provisions <strong>of</strong> the agreement including, but not<br />
limited to, the administration <strong>of</strong> the coordination <strong>of</strong> benefits<br />
provisions. This process is detailed in Article III, Section M,<br />
Coordination <strong>of</strong> Benefits.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Claim Processing<br />
NDC Numbers The NDC numbers submitted on the pharmacy claim must be<br />
taken from the container from which the drug was dispensed. The<br />
NDC number must match the manufacturer <strong>and</strong> package size.<br />
Copays/Coinsurance The drug copay/coinsurance amount varies for each subscriber.<br />
Rely on “claim response” to correctly identify the amount to<br />
collect from the member. If a member’s contract contains the<br />
formulary amendment, a dual copay may be in effect. Again, rely<br />
on “claim response” to determine the correct amount to collect<br />
from the member.<br />
Vacation Prescription<br />
Requests<br />
Prescription Cost Less<br />
Than Copay<br />
Discounting or Waiving<br />
Copays<br />
Requests for additional drug quantities may be made by the<br />
member, physician, or pharmacist. The member would contact the<br />
customer service number listed on the back <strong>of</strong> their member ID<br />
card. The physician or pharmacist would contact the pharmacy<br />
help desk. Please keep in mind that some drugs are controlled<br />
substances <strong>and</strong> may require a new prescription.<br />
If the cost <strong>of</strong> the prescription is less than a member’s copay, the<br />
member should pay the lesser <strong>of</strong> the allowed amount as shown on<br />
the claims response.<br />
In order to maintain the level <strong>of</strong> subscriber responsibility specified<br />
in <strong>Blue</strong> <strong>Cross</strong> contracts, it is essential that members pay the<br />
agreed-upon copay for preferred <strong>and</strong> non-preferred drugs. Both<br />
member <strong>and</strong> provider agreements specifically state that the copay<br />
must be collected in full. Noncompliance <strong>of</strong> this provision, through<br />
discount or waiver, could result in termination <strong>of</strong> the provider<br />
agreement.<br />
Pharmacy Audits <strong>Blue</strong> <strong>Cross</strong> performs comprehensive pharmacy program integrity<br />
audits to ensure compliance with its programs.<br />
11-4<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)
Drugs<br />
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Drug Formulary <strong>Blue</strong> <strong>Cross</strong> promotes the use <strong>of</strong> the member’s specified drug<br />
formulary. The formularies have been developed to provide a<br />
listing <strong>of</strong> drugs that are safe, effective, high-quality <strong>and</strong><br />
economical.<br />
FlexRx is the st<strong>and</strong>ard <strong>Blue</strong> <strong>Cross</strong> drug list, which provides<br />
our members with broad access to drugs at a reasonable overall<br />
cost.<br />
GenRx is a formulary option designed to maximize costeffectiveness<br />
through the use <strong>of</strong> generic drugs. Br<strong>and</strong> drugs are<br />
on the formulary only when a generic drug is not available to<br />
treat a specific medical condition or when the br<strong>and</strong> drug <strong>of</strong>fers<br />
a significant advantage over generic drugs.<br />
Definitions<br />
Formulary is a list <strong>of</strong> preferred drugs with coverage under the<br />
plan. This list may change during the year.<br />
Preferred drug is a drug that is covered under the plan because<br />
it is included on the formulary drug list.<br />
Non-preferred drug is a drug not on the formulary drug list, but<br />
could be covered under an open pharmacy benefit plan design.<br />
Open pharmacy benefit plan design is a benefit design that<br />
covers most drugs regardless <strong>of</strong> the status (preferred or nonpreferred)<br />
on the formulary drug list. The member’s financial<br />
responsibility will vary based on formulary status <strong>and</strong> benefit<br />
design.<br />
Closed pharmacy benefit plan design is a benefit design that<br />
covers only drugs on the formulary drug list. A member can<br />
get a non-preferred drug, but is responsible for 100% <strong>of</strong> the<br />
cost unless a formulary exception is submitted <strong>and</strong> approved.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Drug Formulary<br />
(continued)<br />
Drugs with a Nonpreferred<br />
Status<br />
11-6<br />
Requesting to add a drug to the formulary<br />
Any participating health care provider may request the addition <strong>of</strong><br />
a non-preferred drug to a preferred status by sending a letter to<br />
<strong>Blue</strong> <strong>Cross</strong>. Include the following:<br />
<strong>Name</strong> <strong>of</strong> prescribing MD<br />
Clinic name<br />
Clinic phone number<br />
Clinic fax number<br />
<strong>Name</strong> <strong>of</strong> drug<br />
<strong>Name</strong> <strong>of</strong> manufacturer<br />
Rationale for adding the drug<br />
A new FDA-approved drug is not considered to be on the drug<br />
formulary until it has been approved by the formulary committee.<br />
To view the formularies go to providers.bluecrossmn.com, click<br />
“More tools & resources” under “Tools & Resources”, <strong>and</strong> then<br />
select “Formularies <strong>and</strong> drug programs”.<br />
Physicians may request coverage <strong>of</strong> a non-preferred drug for a<br />
member by completing the <strong>Minnesota</strong> Uniform Form for<br />
Prescription Drug Prior Authorization (PA) Requests <strong>and</strong><br />
Formulary Exceptions. Member liability for non-preferred drugs is<br />
subject to the member specific benefit design.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Quantity Limits Certain drugs have limits on the quantity that can be given to a<br />
patient during a period <strong>of</strong> time. Quantity limits are set to encourage<br />
appropriate drug usage, enhance drug therapy <strong>and</strong> reduce costs.<br />
Preferred <strong>and</strong> non-preferred drugs may have quantity limits. Check<br />
your plan’s certificate or other materials for benefit details.<br />
Compounded<br />
Prescriptions<br />
Over-the-Counter<br />
Drugs<br />
Drug list <strong>and</strong> request form<br />
FlexRx quantity limit drug list (PDF) – Quantity limits for the<br />
FlexRx formulary. The list is subject to change without notice.<br />
GenRx quantity limit drug list (PDF) – Quantity limits for the<br />
GenRx formulary. The list is subject to change without notice.<br />
Quantity limits override request form (PDF) – The prescriber<br />
must complete <strong>and</strong> submit this form to request a quantity<br />
exception. The prescriber can also get this form by calling<br />
provider services at (651) 662-5200 or 1-800-262-0820.<br />
Compounded prescriptions are considered preferred drugs<br />
provided they contain at least one federal legend drug in the final<br />
product. Use <strong>of</strong> the compound indicator for compounded<br />
prescriptions is reserved for prescriptions requiring the pharmacist<br />
to combine two or more ingredients.<br />
Many drugs a member could once only get with a prescription are<br />
now available over the counter at a local pharmacy. These drugs<br />
are just as safe <strong>and</strong> effective as the prescription versions. Check<br />
the plan’s certificate <strong>of</strong> coverage or other materials for benefit<br />
details.<br />
What it means for the member<br />
If the member has this benefit available, they can get an over-thecounter<br />
drug that’s identical to the prescription version at no cost<br />
to them, or at their plan’s lowest copay amount. The cost depends<br />
on their plan.<br />
How the member gets started<br />
Check the OTC drug list to see if they’re taking a drug that<br />
qualifies – see the OTC drug list (PDF). (The list is subject to<br />
change without notice.)<br />
Write the member’s prescription for the over-the-counter version<br />
<strong>of</strong> the drug.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Dispense As Written<br />
(DAW)<br />
<strong>Blue</strong> <strong>Cross</strong> provides for the payment <strong>of</strong> claims coded ‘‘dispense as<br />
written’’ (DAW). Consistent with state law, DAW must be in the<br />
physician’s h<strong>and</strong>writing or when an oral prescription is given,<br />
specifically stated. Physicians may use DAW to prevent generic<br />
substitution. Only a physician may indicate DAW on a<br />
prescription. Neither member nor pharmacist may change this<br />
status for any reason. A DAW may not always result in a lower<br />
copay. This will be dependent on the patient’s benefit plan.<br />
Investigative Drug Use Drugs used investigatively are not eligible for reimbursement.<br />
11-8<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)
Drug Programs<br />
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Specialty Drugs Specialty drugs are used to treat serious or chronic medical<br />
conditions such as multiple sclerosis, hemophilia, hepatitis <strong>and</strong><br />
rheumatoid arthritis. They are typically injectable <strong>and</strong> can be selfadministered<br />
by a patient or family member.<br />
When a member receives their drugs from a specialty network<br />
supplier, they are assured quality while saving money <strong>and</strong> time.<br />
Contact provider services to verify if the member’s plan has the<br />
specialty drug program as an available benefit.<br />
Quality<br />
The specialty network suppliers are accredited by the Joint<br />
Commission on Accreditation <strong>of</strong> Healthcare Organizations, which<br />
ensures the highest st<strong>and</strong>ard <strong>of</strong> pharmacy care. They’re experts in<br />
supplying drugs <strong>and</strong> services to patients with complex health<br />
conditions.<br />
Convenience<br />
The member can order their specialty drug each month from a<br />
specialty drug supplier, pay their health plan’s applicable innetwork<br />
copay or coinsurance amount <strong>and</strong> eliminate the expense<br />
<strong>of</strong> driving or having to find transportation to a pharmacy to pick up<br />
their drugs.<br />
Specialty Drug List<br />
The Specialty Drug List is available on bluecrossmn.com.<br />
Other prescription drugs<br />
Only select injectable <strong>and</strong> oral drugs are available through the<br />
specialty drug program. Members will need to continue to get their<br />
other prescription drugs through their local pharmacy.<br />
More information<br />
Additional information is available on bluecrossmn.com in<br />
regards to the specialty drug network.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Specialty Drugs<br />
(continued)<br />
11-10<br />
Specialty Network Suppliers<br />
The specialty drug benefit program <strong>of</strong>fers you these choices in<br />
pr<strong>of</strong>essional specialty drug suppliers:<br />
Fairview Specialty Pharmacy, LLC*<br />
1-800-595-7140<br />
(612) 672-5262 (Fax)<br />
www.fairviewspecialtyrx.org<br />
*Fairview can only fill prescriptions for hemophilia, growth<br />
hormone infertility <strong>and</strong> oral chemotherapy drugs.<br />
Triessent<br />
1-888-216-6710<br />
1-866-203-6010 fax<br />
The specialty network suppliers were selected for their outst<strong>and</strong>ing<br />
customer service <strong>and</strong> dedication to patients. These suppliers are<br />
experts in h<strong>and</strong>ling the types <strong>of</strong> drugs you’re taking.<br />
Prime Therapeutics, LLC is an independent company providing<br />
pharmacy benefit management services.<br />
Fairview Specialty Pharmacy, LLC is an independent company<br />
providing pharmacy benefit management services.<br />
Triessent, provided by Prime Therapeutics, a specialty pharmacy<br />
program, is an independent specialty pharmacy program.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)
Coding Policies <strong>and</strong> Guidelines (Pharmacy Services)<br />
Step Therapy Program A step therapy program is an approach to providing drug coverage.<br />
It encourages the use <strong>of</strong> cost-effective prescription drugs, when<br />
appropriate. This means that the member may first need to try an<br />
alternative drug, typically a generic drug, before we will cover<br />
certain drugs prescribed by your doctor. Step therapy programs are<br />
developed using treatment guidelines, clinical evidence <strong>and</strong><br />
research. Check the member’s plan’s certificate <strong>of</strong> coverage or<br />
other materials for benefit details.<br />
What it means for the member or patient<br />
If the member is currently taking a drug that’s included in our step<br />
therapy program, please talk to your patient. Together you can<br />
discuss which drug options are best for the patient. You can decide<br />
whether to write a new prescription or submit a written request for<br />
the member to remain on his/her current drug.<br />
Drug lists <strong>and</strong> authorization form<br />
GenRx Step Therapy program - drug list (PDF) – All users <strong>of</strong><br />
the GenRx formulary have step therapy. The list is subject to<br />
change without notice.<br />
FlexRx Step Therapy program - drug list (PDF) – Step therapy<br />
programs for the FlexRx formulary vary based on employer<br />
group. The list is subject to change without notice.<br />
Step Therapy authorization form (PDF) – Your doctor must<br />
complete <strong>and</strong> submit this form to request an exception to this<br />
program. Your doctor can also get this form by calling<br />
provider services at (651) 662-5200 or 1-800-262-0820.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (08/09/11)<br />
11-11
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Public Programs)<br />
Table <strong>of</strong> Contents<br />
Child <strong>and</strong> Teen Checkups ....................................................................................................11-2<br />
S0302 ................................................................................................................................... 11-4<br />
C&TC Referral Codes..........................................................................................................11-4<br />
Public Health Nursing Services ........................................................................................... 11-5<br />
Interpretive Services ............................................................................................................ 11-6<br />
<strong>Blue</strong> Plus Contracted Interpreter Agencies.......................................................................... 11-9<br />
Community Health Workers.............................................................................................. 11-13<br />
Newborn Circumcision ...................................................................................................... 11-14<br />
Hearing Aid Fee Schedule Update..................................................................................... 11-15<br />
GenRx Formulary ..............................................................................................................11-16<br />
Formulary Exception Process ............................................................................................ 11-17<br />
PCA Billing........................................................................................................................11-19<br />
PCA Billing (continued) ....................................................................................................11-20<br />
Chiropractic, Physical, Occupational, <strong>and</strong> Speech Therapy Authorization.......................11-21<br />
Services to Restricted Recipients....................................................................................... 11-24<br />
MHCP Changes in Prior Authorization .............................................................................11-26<br />
Special Transportation ....................................................................................................... 11-29<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Child <strong>and</strong> Teen<br />
Checkups<br />
Child <strong>and</strong> teen checkups (C&TC) are comprehensive preventive<br />
care services provided to children under the age <strong>of</strong> 21 enrolled in a<br />
public program. These services are usually performed at the<br />
primary care clinic (PCC). They may also be performed by a<br />
public health nurse clinic in the referral network without a referral<br />
from the PCC.<br />
Child <strong>and</strong> teen checkups can be identified by procedure code<br />
S0302 on a claim or on another claim with the same date <strong>of</strong><br />
service. Since these checkups involve additional time spent with<br />
the patient, this code allows the provider to charge a “bump-up”<br />
amount for performing the C&TC.<br />
Covered Services<br />
Anticipatory guidance <strong>and</strong> health education<br />
Assessment <strong>of</strong> physical growth <strong>and</strong> measurements<br />
Health history including mental health, nutrition, <strong>and</strong> chemical<br />
use<br />
Developmental/behavioral assessments<br />
Physical examination including sexual development, oral exam<br />
Immunizations/review<br />
Laboratory tests including blood lead, urinalysis,<br />
hemoglobin/hematocrit <strong>and</strong> other tests as indicated<br />
Vision screening<br />
Hearing screening<br />
Dental checkups - verbal referral for preventive dental care<br />
Diagnosis <strong>and</strong> treatment <strong>of</strong> health conditions listed in the<br />
<strong>Minnesota</strong> Health Care Programs (MHCP) benefit plan <strong>and</strong><br />
others determined to be medically necessary, are also covered<br />
services.<br />
C&TC Component Commonly Billed Code(s) Notes<br />
Anticipatory<br />
Guidance <strong>and</strong> health<br />
education<br />
Measurement –<br />
height, weight, head<br />
circumference, blood<br />
pressure<br />
11-2<br />
99401-99404 This component may be billed separately<br />
only if at least 15 minutes is spent<br />
specifically on this topic.<br />
Not billed separately, part<br />
<strong>of</strong> the E&M<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
C&TC Component Commonly Billed Code(s) Notes<br />
Health History Not billed separately, part<br />
<strong>of</strong> the E&M<br />
Developmental /<br />
Behavioral<br />
Physical – including<br />
sexual development<br />
<strong>and</strong> oral exam<br />
Immunizations /<br />
Vaccines<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
96110 or 96111 This code may be billed if a measurable<br />
tool is used to assess the developmental<br />
<strong>and</strong> behavioral level <strong>of</strong> the child.<br />
99381-99385 or 99391-<br />
99395<br />
90460, 90461, 90470,<br />
90471, 90472, 90473,<br />
90474<br />
Appropriate<br />
vaccine/toxoid code with<br />
an –SL modifier (if the<br />
immunization is available<br />
through the <strong>Minnesota</strong><br />
Vaccines for Children<br />
program).<br />
Laboratory Tests Billed as appropriate<br />
Bill developmental <strong>and</strong> mental health<br />
screenings using:<br />
96110 for an objective, st<strong>and</strong>ardized<br />
developmental screening instrument<br />
96110-UC for a st<strong>and</strong>ardized mental<br />
health screening instrument<br />
This code is billed according to whether<br />
the child is a new or established patient<br />
<strong>and</strong> the age <strong>of</strong> the child.<br />
Administration is billed with the<br />
appropriate administration code(s).<br />
Immunizations are billed with the<br />
appropriate vaccine code appended with<br />
an –SL modifier to indicate the vaccine<br />
was obtained free through the <strong>Minnesota</strong><br />
Vaccines for Children program.<br />
All providers must use the available free<br />
vaccines for MHCP covered children.<br />
Blood Lead 83655 Blood lead screening is a required<br />
component at 12 & 24 months <strong>of</strong> age, but<br />
can occur at other times within these<br />
ranges if necessary. Lead testing is a<br />
federally required component <strong>of</strong> C&TC.<br />
Vision 99173 This code may be billed for children three<br />
years <strong>of</strong> age <strong>and</strong> older to indicate that an<br />
objective screening was performed.<br />
Hearing V5008 or 92551 This code may be billed for children three<br />
years <strong>of</strong> age <strong>and</strong> older to indicate that an<br />
objective screening was performed.<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
C&TC Component Commonly Billed Code(s) Notes<br />
Dental Checkups-<br />
verbal referral<br />
Fluoride Varnish<br />
Application<br />
11-4<br />
Not billed separately, part<br />
<strong>of</strong> the E/M<br />
Dental services processed through Delta<br />
Dental <strong>of</strong> <strong>Minnesota</strong>.<br />
D1206 Billed by PCC or Public Health Nursing<br />
Clinic <strong>and</strong> paid as part <strong>of</strong> the C&TC.<br />
Eligible providers include:<br />
Nurse practitioners<br />
Nurses<br />
Physicians<br />
Physician Assistants<br />
Staff under the supervision <strong>of</strong> the treating<br />
physician<br />
S0302 If HCPCS code S0302 is submitted on a claim for any member<br />
other than an MHCP member, it will be denied as provider<br />
liability. Code S0302, completed early periodic screening<br />
diagnosis <strong>and</strong> treatment service (EPSDT) (list in addition to code<br />
for appropriate evaluation <strong>and</strong> management service), should be<br />
submitted only when a completed well child or child <strong>and</strong> teen<br />
checkup is performed for an MHCP member (i.e., PMAP or<br />
MNCare).<br />
C&TC Referral Codes The C&TC referral codes must be submitted on C&TC claims to<br />
inform state <strong>and</strong> county C&TC staff that a referral was made.<br />
Follow-up assistance is provided by the state <strong>and</strong> county to help<br />
assure follow-up care is received. The C&TC referral codes also<br />
fulfill <strong>Minnesota</strong>’s reporting requirements to the Centers for<br />
Medicare <strong>and</strong> Medicaid Services (CMS) for the number <strong>of</strong><br />
referrals made as a result <strong>of</strong> C&TC screenings.<br />
The C&TC referral code pertains to the entire claim <strong>and</strong> must be<br />
entered as value '01' in loop 2300, CLM12 on the 837P claim. It<br />
documents that a complete C&TC screening was performed for<br />
enhanced/appropriate reimbursement purposes.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Public Health Nursing<br />
Services<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
The following services may be billed by Public Health on a<br />
pr<strong>of</strong>essional claim (837P). These services are eligible under the<br />
Public Nursing Clinic (PHNC) contract without a referral from the<br />
member’s primary care clinic or a prior authorization from <strong>Blue</strong><br />
Plus (these services are found in Chapter 8 <strong>of</strong> the MHCP manual.<br />
If a service requires a physician’s order <strong>and</strong> can be billed to<br />
Medicare or other third party payers, those services are not billable<br />
by Public Health.<br />
In addition, Public Health may bill for Enhanced Services for “At-<br />
Risk” Pregnancies, as well as patient education services found in<br />
Chapter 10 <strong>of</strong> the MHCP manual.<br />
Codes Description<br />
H1002 Care coordination<br />
H1003 Prenatal health education I<br />
Prenatal health education II<br />
Prenatal nutrition education services<br />
H1004 Postpartum follow-up home visit<br />
S9445 Patient education, not otherwise classified, nonphysician<br />
provider, individual, per session<br />
S9446 Patient education, not otherwise classified, nonphysician<br />
provider, group, per session<br />
S9442 Birthing classes, non-physician provider, per session<br />
S9443 Lactation classes, non-physician provider, per session<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Interpretive Services <strong>Blue</strong> Plus contracts with several interpreter agencies to provide<br />
sign <strong>and</strong> spoken interpreter services for members <strong>of</strong> <strong>Blue</strong> Plus<br />
MHCP plans only.<br />
11-6<br />
These members can be identified by their identification numbers,<br />
which begin with “80” (i.e. 80XXXXXXX).<br />
Primary care clinics, physician specialty clinics <strong>and</strong> Select<br />
behavioral health clinics may request a contract in order to provide<br />
<strong>and</strong> bill <strong>Blue</strong> Plus for interpreter services at their sites for MHCP<br />
members. To request a contract, primary care clinics, physician<br />
specialty clinics or Select behavioral health clinics should fax a<br />
request to Theresa Peters-Nelson, Provider Contracting at<br />
(651) 662-6326, or mail your request to:<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong><br />
Attn: Theresa Peters-Nelson, S117<br />
1750 Yankee Doodle Road<br />
Eagan, MN 55121-1600<br />
Effective January 1, 2011, in order to comply with <strong>Minnesota</strong><br />
Department <strong>of</strong> Human Services requirements (in accordance with<br />
<strong>Minnesota</strong> State Statute Sec. 144.058), any interpretation services<br />
provided to <strong>Blue</strong> Plus <strong>Minnesota</strong> Health Care Program members<br />
must be rendered by a registered <strong>and</strong> rostered interpreter with<br />
proper certification.<br />
All providers contracted with <strong>Blue</strong> Plus for provision <strong>of</strong><br />
interpretation services are accountable for ensuring that<br />
interpreters employed by or contracted with their agency meet<br />
these requirements.<br />
Services provided by interpreters who do not meet the<br />
qualifications outlined in the statute are ineligible for payment <strong>and</strong><br />
should not be billed to <strong>Blue</strong> Plus. Interpreters who are not properly<br />
qualified cannot bill either <strong>Blue</strong> Plus or the member.<br />
If the provider does not have a <strong>Blue</strong> Plus interpreter contract <strong>and</strong><br />
schedules interpreter services with an interpretation agency that<br />
does not hold a contract with <strong>Blue</strong> Plus Public Programs customer<br />
service, the interpreter charges are the financial responsibility <strong>of</strong><br />
the provider. Hospitals are responsible for arranging <strong>and</strong><br />
reimbursing for interpreter services for hospital inpatient services.<br />
A <strong>Blue</strong> Plus Public Programs member, clinic, public health agency<br />
or county worker may call <strong>Blue</strong> Plus Public Programs Customer<br />
Service, or the contracted interpreter agency for assistance in<br />
scheduling an interpreter for the member’s covered health services.<br />
The contracted agency will bill <strong>Blue</strong> Plus directly.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Interpretive Services<br />
(continued)<br />
Billing Guides<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
The following guides for reporting interpreter services have been<br />
approved by the MN Administrative Uniform Committee <strong>and</strong> are<br />
listed in the MINNESOTA UNIFORM COMPANION GUIDE<br />
FOR IMPLEMENTATION OF THE ASC X12/005010X222.<br />
HEALTH CARE CLAIM: PROFESSIONAL (837).<br />
Note: Rounding rules apply to all services below. A minimum <strong>of</strong><br />
eight minutes must be spent in order to report one unit.<br />
T1013 -- Face-to-face oral language interpreter services per 15<br />
minutes<br />
T1013-U3 -- Face-to-face sign language interpreter services per 15<br />
minutes<br />
T1013-GT -- Telemedicine interpreter services per 15 minutes<br />
T1013-U4 -- Telephone interpreter services per 15 minutes<br />
T1013-UN, UP, UQ, UR, US Interpreter services provided to<br />
multiple patients in a group setting<br />
T1013-52 -- Interpreter drive time, wait time, no show/cancellation<br />
per 15 minutes<br />
Report one unit per 15 minutes per client<br />
For multiple encounters with the same patient on the same<br />
day, report one line with units reflecting total time with<br />
patient<br />
If more than one type <strong>of</strong> service is provided, report each on<br />
a separate line appended with the -59 modifier; for<br />
example:<br />
T1013-52 x 2 units (30 minutes <strong>of</strong> drive time)<br />
T1013-5259 (12 minutes <strong>of</strong> wait time)<br />
Add narrative(s) in the NTE segment to report the service(s)<br />
rendered. An NTE segment is required for each line.<br />
Reporting drive time versus mileage is based on individual<br />
contract. T1013-52 may not be used for drive time if mileage<br />
(see 99199) is reported<br />
A canceled service may be reported only if the interpreter has<br />
already arrived for the appointment prior to the cancellation<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Interpretive Services<br />
(continued)<br />
11-8<br />
99199 -- Mileage for interpreter service<br />
Reporting mileage versus drive time is based on individual<br />
contract. 99199 may not be used if drive time (T1013-52) is<br />
reported<br />
Report one unit per mile<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
<strong>Blue</strong> Plus Contracted Interpreter Agencies<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Provider Languages Geographic Coverage (By County)<br />
Kim Tong<br />
Phone #:<br />
(612) 724-5962<br />
Midwest Language Banc<br />
Phone #:<br />
(612) 695-6008<br />
Afar, Albanian, American Sign<br />
Language, Amharic, Anuak, Arabic,<br />
Armenian, Belarusian, Berber,<br />
Bosnian, Bulgarian, Burmese,<br />
Cambodian, Cantonese, Creole,<br />
Croatian, Farsi, Filipino, French,<br />
German, Gujarati, Hebrew, Hindi,<br />
Hmong, Indonesian, Italian, Japanese,<br />
Karen, Korean, Krahn, Kurdish,<br />
Laotian, Lithuanian, Macedonian,<br />
M<strong>and</strong>arin, Nepalese, Oromo, Persian,<br />
Polish, Portuguese, Punjabi,<br />
Romanian, Russian, Serbian, Somali,<br />
Spanish, Swahili, Taishanese, Thai,<br />
Tibetan, Tigrinia, Turkish, Ukrainian,<br />
Urdu, Vietnamese, Yiddish<br />
Sign Language—YES<br />
Akkan, Albanian, American Sign<br />
Language (Metro Area Only),<br />
Amharic, Arabic, Armenian, Bashto,<br />
Bassah, Bayer, Belrussian, Bengali,<br />
Burmese, Bhutan, Bosnian, Bulgarian,<br />
Cambodian, Cantonese, Chinese,<br />
Comoren, Creole, Croatian, Cubano,<br />
Dari, Dinka, Ethiopian, Eritrean, Farsi,<br />
Filipino, French, French Krio, Gbanti,<br />
German, Gio, Greek, Gujarati, Hausa,<br />
Hebrew, Hindi, Hmong, Indonesian,<br />
Ibo, Irani, Italian, Japanese, Katchi,<br />
Kissi, Kiswahili, Korean, Kpelleh,<br />
Krahn, Kru, Kurdish, Laotian,<br />
Lingala, Lorma, Lug<strong>and</strong>a, M<strong>and</strong>arin,<br />
M<strong>and</strong>ingo, Mano, Micronesian,<br />
Nepali, Nuer, Oromo, Pashto, Persian,<br />
Pigeon-English, Polish, Portuguese,<br />
Punjabi, Romanian, Russian,<br />
Shanghiese, Sierra Leone, Somali,<br />
Spanish, Swahili, Tagalog ,<br />
Taiwanese, Tamil, Tajik Telugu,<br />
Telegis, Telegu, Temne, Thai,<br />
Thirumalai, Tibetan, Tigrinya, Tomi,<br />
Turkish, Ukrainian, Urdu,<br />
Vietnamese, Wolaff, Yoruba<br />
Sign Language—YES (Metro Area<br />
Only)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
Becker, Brown, Chisago, Clay,<br />
Cottonwood, Dakota, Dodge,<br />
Faribault, Fillmore, Freeborn,<br />
Goodhue, Hennepin, Isanti, Jackson,<br />
K<strong>and</strong>iyohi, Le Sueur, Lyon, Martin,<br />
Meeker, Mower, Murray, Nicollet,<br />
Nobles, Olmsted, Otter Tail,<br />
Pipestone, Ramsey, Redwood,<br />
Renville, Rice, Rock, Scott,<br />
Sherburne, Sioux Falls (South<br />
Dakota), Stearns, Steele, Wabasha,<br />
Waseca, Washington, Watonwan,<br />
Wilkin, Winona, Wright<br />
Aitkin, Anoka, Becker, Beltrami,<br />
Benton, Big Stone, <strong>Blue</strong> Earth,<br />
Brown, Carlton, Carver, Cass,<br />
Chippewa, Chisago, Clay, Clearwater,<br />
Cook, Cottonwood, Crow Wing,<br />
Dakota, Dodge, Douglas, Faribault,<br />
Fillmore, Freeborn, Goodhue, Grant,<br />
Hennepin, Houston, Hubbard, Isanti,<br />
Itasca, Jackson, Kanabec, K<strong>and</strong>iyohi,<br />
Kittson, Koochiching, Lac qui Parle,<br />
Lake, Lake <strong>of</strong> the Woods, Le Sueur,<br />
Lincoln, Lyon, Mahnomen, Marshall,<br />
Martin, McLeod, Meeker, Mille Lacs,<br />
Morrison, Mower, Murray, Nicollet,<br />
Nobles, Norman, Olmsted, Otter Tail,<br />
Pennington, Pine, Pipestone, Polk,<br />
Pope, Ramsey, Red Lake, Redwood,<br />
Renville, Rice, Rock, Roseau, Scott,<br />
Sherburne, Sibley, St Louis, Stearns,<br />
Steele, Stevens, Swift, Todd, Traverse,<br />
Wabasha, Wadena, Waseca,<br />
Washington, Watonwan, Wilkin,<br />
Winona, Wright, Yellow Medicine<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Provider Languages Geographic Coverage (By County)<br />
Project FINE<br />
Phone #:<br />
(507) 452-4100<br />
ARCH Language Network<br />
Phone #:<br />
(651) 789-7897<br />
The Bridge<br />
Phone #:<br />
(320) 259-9239<br />
11-10<br />
Arabic, Bosnian, Bulgarian,<br />
Cambodian, Chinese, Dinka, French,<br />
German, Hmong, Italian, Japanese,<br />
Korean, Laotian, Nepali Portuguese,<br />
Romanian, Russian, Somali, Spanish,<br />
Swahili, Thai, Tibetan, Vietnamese<br />
Sign Language—NO<br />
Afar, Albanian, Amharic, Anuak,<br />
Arabic, Armenian, Belarusian, Berber,<br />
Bhutanese, Burmese, Bosnian,<br />
Cambodian, Cantonese, Creole,<br />
Croatian, Dioula, Eritrean, Farsi,<br />
French, Gujarati, Hindi, Hmong, Igbo,<br />
Italian, Japanese, Karen, Korean,<br />
Laotian, Malinke, M<strong>and</strong>arin, Nepali,<br />
Nuer, Oromo, Pashto, Persian,<br />
Portuguese, Punjabi, Romanian,<br />
Russian, Serbian, Somali, Spanish,<br />
Swahili, Thai, Tigrinya, Turkish,<br />
Ukrainian, Urdu, Vietnamese, Yoruba<br />
Sign Language—NO<br />
American Sign Language, Arabic,<br />
Bangladeshi, Bengali, Bosnian,<br />
Bulgarian, Chinese, French, German,<br />
Gujarati, Hindi, Hmong, Kurdish,<br />
Laotian, Malay, Marathi, Nuer,<br />
Oromo, Portuguese, Punjabi, Pushto,<br />
Romanian, Russian, Serbian, Serbo-<br />
Croatian, Somali, Spanish, Swahili,<br />
Tagalog, Thai, Tigrinya, Ukrainian,<br />
Urdu, Vietnamese<br />
Sign Language--YES<br />
Winona<br />
Anoka, Benton, <strong>Blue</strong> Earth, Carver,<br />
Carver, Chisago, Clay, Dakota,<br />
Faribault, Hennepin, Isanti, Jackson,<br />
K<strong>and</strong>iyohi, Le Sueur, Lincoln, Lyon,<br />
McLeod, Meeker, Mille Lacs,<br />
Mower, Nicollet, Nobles, Norman,<br />
Olmsted, Polk, Ramsey, Red Lake,<br />
Rice, Scott, Sherburne, Sibley, St<br />
Louis, Stearns, Steele, Wabasha,<br />
Waseca, Washington, Winona,<br />
Wright<br />
Anoka, Benton, Carver, Clay, Crow<br />
Wing, Dakota, Hennepin, Isanti, Lyon,<br />
Olmsted (Spanish only), Ramsey,<br />
Redwood, Rice, Scott, Sherburne,<br />
Stearns, Stevens (Spanish only),<br />
Washington, Wright<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Provider Languages Geographic Coverage (By County)<br />
Garden <strong>and</strong> Associates<br />
Phone #:<br />
(952) 920-6160<br />
Afar, Afghan, Akan, Albanian,<br />
Amharic, Anuak, Arabic, Aramaic,<br />
Armenian, Ashante, Asturian, Azeri,<br />
Bahasa, Bana, B<strong>and</strong>i, Bari, Basque,<br />
Bassa, Belarusian, Bengali, Berber,<br />
Bosnian, Breton, Bulgarian, Burmese,<br />
Cambodian, Cantonese, Catalan,<br />
Cherokee, Chinese, Coniagui, Creole,<br />
Croatian, Czech, Dagaare, Dan,<br />
Danish, Dari, Dibo, Dinka, Dutch,<br />
Dzongkha, Egyptian, English,<br />
Esperanto, Estonian, Ethiopian, Ewe,<br />
Fanti, Farsi, Finnish, French, Frisian,<br />
Fulani, Ga, Gaelic, Galego, Gb<strong>and</strong>i,<br />
Georgian, German, Gio, Grebo,<br />
Greek, Gujarati, Guyanese, Haitian<br />
Creole, Hausa, Hawaiian, Hebrew,<br />
Hindi, Hmong, Hungarian, Ibo/Igbo,<br />
Icel<strong>and</strong>ic, Indonesian, Inuit, Irish,<br />
Italian, Japanese, Javanese, Kannada,<br />
Karen, Kazakh, Khmer, Kirghizian,<br />
Kissi, Kona, Korean, Kpelle, Krahn,<br />
Krio, Kru, Kuku, Kurdish, Laotian,<br />
Latin, Latvian, Liberian, Lingala,<br />
Lithuanian, Lorma, Lug<strong>and</strong>a,<br />
Macedonian, Maide, Malagasy,<br />
Malayalam, Malinke, Maltese,<br />
M<strong>and</strong>arin, M<strong>and</strong>ingo, Mano, Marathi,<br />
Marshallese, Mazahua, Mende, Mina,<br />
Moldovian, Mongolian, Navajo,<br />
Nepali, Norwegian, Nuer, Ogoni,<br />
Ojibwa, Oromo, Pashto, Persian,<br />
Polish, Portuguese, Quechua, Quiche,<br />
Romani, Romanian, Romansch,<br />
Rundi, Russian, Samoan, Sarpo,<br />
Senegalese, Serbian, Shanghainese,<br />
Sinhala, Slovak, Slovenian, Somali,<br />
Sotho, Spanish, Sudanese,<br />
Susu/Soussou, Swahili, Tagalog,<br />
Taishanese, Taiwanese, Tamil,<br />
Telugu, Thai, Tibetan, Tigrinya,<br />
Tswana, Turkish, Turkmen, Twi,<br />
Ukrainian, Urdu, Uzbek, Vai,<br />
Vietnamese, Welsh, Wol<strong>of</strong>, Yao,<br />
Yiddish, Yoruba, Zulu<br />
Sign Language—NO<br />
Anoka, Beltrami, Benton, <strong>Blue</strong> Earth,<br />
Carlton, Carver, Chisago, Crow Wing,<br />
Dakota, Dodge, Douglas, Faribault,<br />
Fillmore, Freeborn, Goodhue,<br />
Hennepin, Huston, Isanti, Itasca,<br />
Jackson, K<strong>and</strong>iyohi, Lac qui Parle, Le<br />
Sueur, Marshall, Meeker, McLeod,<br />
Mille Lacs, Morrison, Mower,<br />
Nicollet, Nobles, Olmsted, Pine,<br />
Pipestone, Ramsey, Rice, Scott,<br />
Sherburne, St. Louis, Stearns, Steele,<br />
Todd, Traverse, Wabasha, Waseca,<br />
Washington, Watonwan, Winona,<br />
Wright<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Provider Languages Geographic Coverage (By County)<br />
A-Z Friendly Languages<br />
Phone #:<br />
(763) 566-4312<br />
Intercultural Mutual<br />
Assistance Association<br />
(IMAA)<br />
Phone #:<br />
(507) 289-5960<br />
11-12<br />
Afar, Albanian, Amharic, Arabic,<br />
Armenian, Azerbaijani, Basa,<br />
Belarusian, Bengali, Bosnian (Serbo-<br />
Croatian), Bulgarian, Burmese,<br />
Cebuano, Chinese (Cantonese,<br />
M<strong>and</strong>arin, Toysanese), Czech, Danish,<br />
Dutch, Erithrian, Estonian, Ewe, Farsi,<br />
Finnish, French, Gb<strong>and</strong>i, Geo,<br />
Georgian, German, Grebo, Greek,<br />
Gujarathi, Haitian Creo, Hebrew,<br />
Hindi, Hmong, Hungarian, Idbo,<br />
Indonesian, Italian, Japanese, Kazakh,<br />
Khmer, Kirghiz, Kisi, Korean, Kpelle,<br />
Krahn, Krio, Kru, Kurdish, Latvian,<br />
Laotian, Lebanese, Liberian English,<br />
Lithuanian, Lorma, Lug<strong>and</strong>a,<br />
M<strong>and</strong>ingo, Mano, Moldovan,<br />
Mongolian, Norwegian, Oromo,<br />
Polish, Portuguese, Punjabi, Pushtu,<br />
Romanian, Russian, Sarpo, Slovak,<br />
Slovenian, Somali, Soninke, Spanish,<br />
Susu, Swahili, Swedish, Tadzik,<br />
Tagalog, Tatar, Telugu, Tibetan,<br />
Tigrinya, Turkish, Turkmen, Twi,<br />
Ukranian, Urdu, Uzbek, Vietnamese,<br />
Yoruba<br />
Sign Language—NO<br />
American Sign Language, Amharic,<br />
Anuak, Arabic, ASL, Bari, Bosnian,<br />
Burmese, Cantonese, Creole, Czech,<br />
Dinka, Farsi, Filipino, French,<br />
German, Grebo, Greek, Hindi,<br />
Hmong, Homala, Indonesian, Italian,<br />
Japanese, Kamba, Kiswahili, Khmer,<br />
Korean, Krio, Kurdish, Lango, Lahu,<br />
Lao, Lao-lu, Lao-Tinh, Lokoya,<br />
Lopit, Lotoko, Luo, Mai, M<strong>and</strong>arin,<br />
Mendi, Nuer, Oromo, Pakistani,<br />
Polish, Portuguese, Punjabai,<br />
Quechua, Romanian, Russian,<br />
Somali, Spanish, Swahili, Tagalog,<br />
Temne, Tigrinia, Thai, Turkish, Urdu,<br />
Vietnamese<br />
Sign Language---YES<br />
Anoka, Carver, Chisago, Dakota,<br />
Goodhue, Hennepin, Isanti,<br />
K<strong>and</strong>iyohi, Le Sueur, McLeod,<br />
Mower, Olmsted, Polk, Ramsey, Rice,<br />
Scott, Sherburne, Sibley, Stearns,<br />
Washington, Wright<br />
<strong>Blue</strong> Earth, Dodge, Faribault,<br />
Fillmore, Freeborn, Goodhue,<br />
Houston, Mower, Olmsted, Rice,<br />
Steel, Wabasha, Waseca, Winona<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Community Health<br />
Workers<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
<strong>Blue</strong> Plus may reimburse for certain educational services provided<br />
by Community Health Workers (CHWs).<br />
Practitioner Enrollment Process<br />
A CHW must meet <strong>Minnesota</strong> Department <strong>of</strong> Human Services<br />
(DHS) eligibility requirements, <strong>and</strong> be enrolled through DHS<br />
before requesting enrollment with <strong>Blue</strong> Plus. DHS requirements<br />
are outlined in the MHCP <strong>Manual</strong>, which can be found at<br />
www.dhs.state.mn.us.<br />
Upon receiving a Unique <strong>Minnesota</strong> Provider Identifier (UMPI)<br />
number from DHS, a CHW may then request to be registered with<br />
<strong>Blue</strong> Plus. This process may be initiated by completing the<br />
Individual Practitioner Addition <strong>and</strong> Termination Form, which can<br />
be accessed at bluecrossmn.com. The CHW must be registered<br />
with <strong>Blue</strong> Plus before services can be billed.<br />
Member <strong>and</strong> Service Eligibility<br />
Members enrolled in the following <strong>Blue</strong> Plus plans will have<br />
benefits for services rendered by a CHW:<br />
<strong>Blue</strong> Plus Plan Alpha Prefix<br />
<strong>Blue</strong> Advantage (PMAP/GAMC) XZG<br />
<strong>Minnesota</strong>Care XZG<br />
<strong>Minnesota</strong> Senior Care XZG<br />
<strong>Minnesota</strong> Senior Care + XZG<br />
Secure<strong>Blue</strong> SM (HMO SNP) XZS<br />
Care<strong>Blue</strong> SM (HMO SNP) XZS<br />
In order to be considered eligible for reimbursement, educational<br />
services provided by a CHW must be rendered face to face in a<br />
clinic, outpatient or home setting <strong>and</strong> be related to a medical<br />
diagnosis. In addition, the services must be supervised by a <strong>Blue</strong><br />
<strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> or <strong>Blue</strong> Plus eligible<br />
physician, dentist, public health nurse, mental health pr<strong>of</strong>essional,<br />
or advanced practice registered nurse (APRN).<br />
Reference the MHCP Provider <strong>Manual</strong> for additional information<br />
regarding requirements for physician orders/care plans, medical<br />
record documentation, record keeping <strong>and</strong> curriculum as they<br />
relate to CHWs. This communication can be found at<br />
www.dhs.state.mn.us.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-13
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Community Health<br />
Workers<br />
(continued)<br />
Billing<br />
CHW services should be billed to <strong>Blue</strong> Plus as follows:<br />
Claims format: Pr<strong>of</strong>essional (837P)<br />
Codes: 98960, 98961, 98962 or D1206<br />
Provider Number: Enter the <strong>Blue</strong> Plus individual provider<br />
number or UMPI number <strong>of</strong> the CHW on each service line<br />
Diagnosis: Enter a valid ICD-9-CM diagnosis(es) on the claim<br />
<strong>and</strong> link to the appropriate service line<br />
Reimbursement<br />
<strong>Blue</strong> Plus will utilize our st<strong>and</strong>ard public programs pricing<br />
methodology for reimbursement <strong>of</strong> CHW services.<br />
Newborn Circumcision For members <strong>of</strong> MCHP, claims payment for newborn circumcision<br />
is the responsibility <strong>of</strong> <strong>Blue</strong> Plus. Circumcision coverage is limited<br />
to only those procedures that are medically necessary (a pathologic<br />
condition exists that requires circumcision). This limitation applies<br />
to circumcision for all ages. The newborn circumcision exception<br />
for religious practice was eliminated.<br />
11-14<br />
A prior authorization will be required for all circumcisions for<br />
determination <strong>of</strong> medical necessity.<br />
Member Eligibility<br />
This legislative change in circumcision benefits <strong>and</strong> claims<br />
processing applies to members in all MHCP products:<br />
MHCP Product <strong>Name</strong> Group Number<br />
Begins With<br />
<strong>Blue</strong> Plus: <strong>Blue</strong> Advantage<br />
(PMAP, & MCS+)<br />
PP01, PP02, PP03,<br />
PP04, PP05, PP06,<br />
PP07, PP08, PP09<br />
Members<br />
Alpha Prefix<br />
XZG<br />
<strong>Blue</strong> Plus: <strong>Minnesota</strong>Care PP1 XZG<br />
<strong>Blue</strong> Plus: Secure<strong>Blue</strong> PP3 XZS<br />
<strong>Blue</strong> Plus: Care<strong>Blue</strong> PP3 XZS<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Hearing Aid Fee<br />
Schedule Update<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
<strong>Blue</strong> Plus uses the MHCP Hearing Aid Volume Purchase Contract<br />
(which contains the MHCP Hearing Aid Contract) as the base<br />
Medical Assistance Fee Schedule. <strong>Blue</strong> Plus will follow the noncovered<br />
code list contained in the MHCP Hearing Aid Contract<br />
<strong>and</strong> the DHS supply limits.<br />
Products Affected<br />
The following MHCP products are affected:<br />
<strong>Blue</strong> Advantage (PMAP/GAMC, MSC & MSC+)<br />
<strong>Minnesota</strong>Care<br />
Care<strong>Blue</strong><br />
Secure<strong>Blue</strong><br />
MHCP Hearing Aid Volume Purchase Contract<br />
The hearing aid service provider must dispense the hearing aid<br />
according to the hearing aid exam, selection <strong>and</strong> prescription <strong>of</strong> the<br />
otolaryngologist <strong>and</strong> audiologist.<br />
For accurate claims processing, the provider will need to submit an<br />
attachment that includes the manufacturers’ specifications.<br />
Providers should utilize the information contained in the current<br />
MHCP contracts, including manufacturer, model name <strong>and</strong> model<br />
number. This information will need to be included in the<br />
attachment when the claim for reimbursement is submitted. <strong>Blue</strong><br />
Plus will verify that the hearing aid billed is a covered benefit for<br />
the member <strong>and</strong> will apply the current MHCP Hearing Aid<br />
Volume Purchase Contract pricing for reimbursement. Items not<br />
included in this pricing will defer to the DHS Medical Assistance<br />
st<strong>and</strong>ard fee schedule or the <strong>Blue</strong> Plus st<strong>and</strong>ard fee schedule, as<br />
applicable.<br />
Website<br />
The current MHCP Contract Pricing can be found at:<br />
http://www.dhs.state.mn.us/main/idcplg?IdcService=GET_DY<br />
NAMIC_CONVERSION&RevisionSelectionMethod=LatestRe<br />
leased&dDoc<strong>Name</strong>=id_010724<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-15
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Hearing Aid Fee<br />
Schedule Update<br />
(continued)<br />
Prior Authorization<br />
If the member requires a hearing aid that is not listed on the DHS<br />
Volume Hearing Aid Purchase Contract, a prior authorization may<br />
be submitted for review <strong>of</strong> coverage to the Prior Authorization fax<br />
line at (651) 662-2810. Please include the following information in<br />
the request:<br />
Audiologic recommendations, including:<br />
Written recommendations for hearing aid(s), including the<br />
manufacturer specifications<br />
Follow-up plan for determining the effectiveness <strong>of</strong> the hearing<br />
aid<br />
Audiogram or reason why this was not obtained<br />
History <strong>of</strong> previous hearing aid use<br />
Pure tone average<br />
Reason why a st<strong>and</strong>ard hearing aid on the Volume Hearing Aid<br />
Purchase Contract is not appropriate for this member<br />
GenRx Formulary The drug formulary GenRx will apply for members covered under<br />
<strong>Minnesota</strong> Health Care Programs.<br />
This new formulary <strong>of</strong>fers drugs that have been shown to be safe<br />
<strong>and</strong> effective, while being cost conscious. The GenRx formulary<br />
consists <strong>of</strong> almost all generics, with the exception <strong>of</strong> a few<br />
generics that were not included on the new formulary due to safety<br />
or efficacy concerns. A limited number <strong>of</strong> br<strong>and</strong>-name drugs will<br />
be on formulary to provide appropriate coverage <strong>of</strong> most disease<br />
states.<br />
11-16<br />
What does this mean for you?<br />
You may need to prescribe a different drug that treats the same<br />
symptoms or condition to an MHCP member. Please be aware that<br />
most <strong>of</strong> our Secure<strong>Blue</strong> <strong>and</strong> Care<strong>Blue</strong> members have a Medicare<br />
Part D formulary <strong>and</strong> will not be affected.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
GenRx Formulary<br />
(continued)<br />
Formulary Exception<br />
Process<br />
What steps should you take?<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Determine which <strong>of</strong> your patients' current prescription drugs will<br />
not be on the GenRx drug list. To determine which drugs are on<br />
the new GenRx formulary, visit bluecrossmn.com to view the list<br />
<strong>of</strong> drugs available to MHCP members. Under the orange<br />
“Resources” tab, choose “prescription drugs.” Then click on<br />
“Search the drug lists.” When the pop-up window appears, choose<br />
the GenRx drug list.<br />
What if a member tries to fill a prescription for a drug not<br />
listed in the new formulary?<br />
The prescription will not be filled by the pharmacy. The member<br />
will be referred back to the prescribing physician for a new<br />
prescription.<br />
Dispense as Written (DAW) will not process at point <strong>of</strong> sale until a<br />
formulary exception has been received.<br />
Anti-psychotic drugs<br />
For anti-psychotic drugs prescribed to treat a diagnosed mental<br />
illness or emotional disturbance that are not on the GenRx<br />
formulary, the health care provider prescribing the drug must<br />
certify the following to <strong>Blue</strong> <strong>Cross</strong> in writing:<br />
1. The provider has considered all equivalent drugs on the<br />
formulary <strong>and</strong> has determined that the drug prescribed will best<br />
treat the patient’s condition<br />
2. The drug must be dispensed as written (DAW)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-17
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Formulary Exception<br />
Process<br />
(continued)<br />
11-18<br />
All other Drugs<br />
For all other drugs not on the GenRx formulary, the health care<br />
provider prescribing the drug must follow formulary exception<br />
procedures to request an exception. The health care provider<br />
prescribing the drug must do one <strong>of</strong> the following:<br />
1. attest that the formulary drug causes an adverse reaction in the<br />
patient<br />
2. attest that the formulary drug is contraindicated for the patient<br />
3. attest that the patient has tried <strong>and</strong> failed at least three (or as<br />
many as available, if fewer than three) formulary alternatives<br />
for the diagnosis being treated with the requested medication<br />
4. demonstrate in writing to <strong>Blue</strong> <strong>Cross</strong> that the provider has<br />
considered all equivalent drugs on the formulary <strong>and</strong> has<br />
determined that the drug prescribed will best treat the patient’s<br />
condition<br />
The prescriber may be required to submit medical records that<br />
support the medical necessity for the prescribed non-formulary<br />
drug.<br />
DAW for non-formulary drugs<br />
Prescriptions entered with a DAW for non-formulary drugs will<br />
not process at the point <strong>of</strong> sale until the prescriber has also<br />
completed the second part <strong>of</strong> the process. Members will be<br />
directed to work with their provider to determine if a formulary<br />
drug may work for them. If the provider determines that the nonformulary<br />
drug will best treat the member’s condition, a formulary<br />
exception request must be submitted on the member’s behalf.<br />
What does this mean for you?<br />
Prescriptions written as DAW will not process at point <strong>of</strong> sale until<br />
the certification or demonstration has been received. Members will<br />
be directed to contact their provider to determine if a formulary<br />
drug may work for them. If the provider determines that the nonformulary<br />
drug will best treat the member’s condition, a formulary<br />
exception request must be submitted on the member’s behalf.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Formulary Exception<br />
Process<br />
(continued)<br />
What steps should you take?<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Determine which <strong>of</strong> your patients' current prescription drugs<br />
written as DAW are not on the GenRx drug list. To determine<br />
which drugs are on the GenRx formulary, visit<br />
providers.bluecrossmn.com to view the list <strong>of</strong> drugs available to<br />
<strong>Minnesota</strong> Health Care Programs members. Under the “Tools &<br />
Resources” tab, choose “formulary <strong>and</strong> special program drug<br />
lists.” Then click on “see the lists” under “<strong>Blue</strong> <strong>Cross</strong> formularies”<br />
<strong>and</strong> select “GenRx.<br />
What if a member tries to fill a DAW prescription for a drug<br />
not listed in GenRx?<br />
The prescription will not be filled by the pharmacy until the<br />
certification or demonstration has been received <strong>and</strong> approved.<br />
The member will be referred back to the prescribing physician for<br />
a new prescription <strong>and</strong>/or a formulary exception submission on<br />
their behalf.<br />
Glucose Testing Meters The new GenRx drug formulary for MHCP members will include<br />
only the Bayer CONTOUR <strong>and</strong> BREEZE 2 glucose testing meters<br />
<strong>and</strong> strips. All other meters <strong>and</strong> test strips will be removed from<br />
the drug list.<br />
We are committed to helping you make this change <strong>and</strong> serving<br />
these members' health care needs. If the patient <strong>and</strong> doctor can<br />
show that a glucose meter other than the Bayer CONTOUR or<br />
BREEZE is the best option for a member's treatment, the provider<br />
can ask <strong>Blue</strong> Plus for a formulary exception. For assistance with<br />
this, a member can call the member services number on the back<br />
<strong>of</strong> the member ID card.<br />
PCA Billing Claims for PCA services must be submitted to <strong>Blue</strong> Plus using one<br />
date <strong>of</strong> service per claim line. Any claim lines that are submitted<br />
with more than one date <strong>of</strong> service will be denied for improper<br />
format. All claim lines should have an individual PCA associated<br />
with the service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-19
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
PCA Billing<br />
(continued)<br />
11-20<br />
Individual PCA Enrollment<br />
Individual PCA enrollment forms submitted with incomplete<br />
information will be sent back to the provider unprocessed along<br />
with a letter requesting the missing information. Upon receipt <strong>of</strong> a<br />
complete form, the form will be processed <strong>and</strong>, if appropriate, the<br />
individual will be affiliated with the agency. <strong>Blue</strong> <strong>Cross</strong> will<br />
require individuals to submit their assigned UMPI number on the<br />
enrollment form. <strong>Blue</strong> <strong>Cross</strong> will not enroll an individual PCA that<br />
submits a copy <strong>of</strong> the completed background study in lieu <strong>of</strong> an<br />
UMPI number.<br />
<strong>Minnesota</strong> Health Care Programs<br />
Group numbers for members that have coverage with MHCP are<br />
as follows:<br />
Product <strong>Name</strong> Group Product Group Numbers<br />
<strong>Blue</strong> Advantage (PMAP) PP011, PP012, PP014, PP015, PP016,<br />
PP017, PP021, PP022, PP024, PP025,<br />
PP026, PP027, PP031, PP032,PP034,<br />
PP035, PP036, PP037<br />
<strong>Minnesota</strong>Care Exp<strong>and</strong>ed PP111, PP112, PP151, PP152<br />
<strong>Minnesota</strong> Senior Care<br />
Plus (MSC+)<br />
PP055, PP056, PP057, PP061, PP062,<br />
PP064, PP071, PP072, PP074, PP075,<br />
PP076, PP077<br />
Secure<strong>Blue</strong> All group numbers that begin with<br />
PP2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Chiropractic, Physical,<br />
Occupational, <strong>and</strong><br />
Speech Therapy<br />
Authorization<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Effective January 15, 2011, all <strong>of</strong> the following services provided<br />
to MHCP members will require pre-authorization by <strong>Blue</strong> Plus:<br />
Chiropractic services beyond 12 visits per calendar year<br />
Physical therapy visits beyond 40 visits per calendar year<br />
Occupational therapy visits beyond 40 per calendar year<br />
Speech therapy visits beyond 50 per calendar year<br />
These changes are consistent with changes in <strong>Minnesota</strong> statute<br />
regarding chiropractic <strong>and</strong> therapy services for MHCP members.<br />
Commercial lines <strong>of</strong> business are not impacted by this change.<br />
<strong>Minnesota</strong> Health Care Programs<br />
Group numbers for the affected products are as follows:<br />
Product <strong>Name</strong> Group Product Group Numbers<br />
<strong>Blue</strong> Advantage<br />
(PMAP)<br />
PP011, PP012, PP014, PP015, PP016,<br />
PP017, PP021, PP022, PP024, PP025,<br />
PP026, PP027, PP031, PP032, PP034,<br />
PP035, PP036, PP037<br />
<strong>Minnesota</strong>Care PP111, PP112, PP151, PP152, PP121,<br />
PP122, PP131, PP132, PP141, PP142,<br />
PP161, PP162, PP163, PP164<br />
<strong>Minnesota</strong> Senior Care<br />
Plus (MSC+)<br />
Secure<strong>Blue</strong><br />
PP041, PP042, PP044, PP051, PP052,<br />
PP054, PP055, PP056, PP057, PP061,<br />
PP062, PP064, PP071, PP072, PP074,<br />
PP075, PP076, PP077<br />
All group numbers that begin with PP2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-21
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Chiropractic, Physical,<br />
Occupational, <strong>and</strong><br />
Speech Therapy<br />
Authorization<br />
(continued)<br />
11-22<br />
Outpatient physical, occupational <strong>and</strong> speech therapy services:<br />
Initial evaluation<br />
Any additional evaluations<br />
Plan <strong>of</strong> Care including the following:<br />
Member’s diagnosis<br />
Description <strong>of</strong> member’s functional status / limitations<br />
Treatment plan<br />
Treatment goals (functional, measurable <strong>and</strong> time-specific)<br />
Requested frequency <strong>and</strong> expected duration <strong>of</strong> treatment<br />
Discharge plan<br />
Member’s progress toward goals<br />
Ordering practitioner<br />
Documentation Required<br />
Prior authorization requests should be submitted two weeks in<br />
advance <strong>of</strong> reaching the visit threshold as listed above. Fax your<br />
<strong>Blue</strong> Plus member requests to: (651) 662-4022 or<br />
1-866-800-1665.<br />
Submit the following documentation when requesting an<br />
authorization:<br />
Chiropractic services:<br />
Evaluation <strong>and</strong> diagnosis: Indicate how the subluxation<br />
diagnosis was determined<br />
Chief complaint: List member’s current symptoms<br />
Assessment <strong>and</strong> treatment plan: Provide your physical<br />
assessment <strong>and</strong> treatment plan including when the member will<br />
be discharged, number <strong>of</strong> visits planned <strong>and</strong> frequency <strong>of</strong> visits<br />
planned<br />
Rationale for continued treatment: Provide evidence <strong>of</strong><br />
member’s improvement with chiropractic services <strong>and</strong> goals<br />
for further care<br />
The completed Chiropractic Medical Information Request<br />
form, available in the forms section <strong>of</strong><br />
providers.bluecrossmn.com.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Chiropractic, Physical,<br />
Occupational, <strong>and</strong><br />
Speech Therapy<br />
Authorization<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Outpatient physical, occupational <strong>and</strong> speech therapy services:<br />
Initial evaluation<br />
Any additional evaluations<br />
Plan <strong>of</strong> Care including the following:<br />
Member’s diagnosis<br />
Description <strong>of</strong> member’s functional status / limitations<br />
Treatment plan<br />
Treatment goals (functional, measurable <strong>and</strong> time-specific)<br />
Requested frequency <strong>and</strong> expected duration <strong>of</strong> treatment<br />
Discharge plan<br />
Member’s progress toward goals<br />
Ordering practitioner<br />
Prior Authorization Process<br />
The timeline for decisions is up to ten business days. Decisions<br />
will be communicated via telephone or fax, <strong>and</strong> letter. Approvals<br />
are communicated via telephone with a letter as follow-up. Denials<br />
are communicated with a fax copy <strong>of</strong> the denial letter <strong>and</strong> a followup<br />
letter sent by mail.<br />
MHCP coverage guidelines are followed for MHCP members. All<br />
services must be medically necessary for continued coverage.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-23
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Services to Restricted<br />
Recipients<br />
11-24<br />
Under the <strong>Minnesota</strong> Restricted Recipient Program, either the<br />
Department <strong>of</strong> Human Services (DHS) or <strong>Blue</strong> Plus identifies<br />
members <strong>of</strong> <strong>Blue</strong> Plus MHCP who have used Medicaid services,<br />
most <strong>of</strong>ten prescription drugs or emergency rooms visits for nonemergent<br />
reasons, at a frequency or amount that is not medically<br />
necessary <strong>and</strong>/or who have used health care services that resulted<br />
in unnecessary costs to the program. Once identified, such<br />
recipients will be placed under the care <strong>of</strong> a primary care physician<br />
<strong>and</strong>/or other designated providers who will coordinate their care<br />
for a 24-month or a 36-month period. Although other members <strong>of</strong><br />
<strong>Blue</strong> Plus <strong>Minnesota</strong> Health Care programs require a referral only<br />
to nonparticipating providers, all services to a restricted recipient<br />
from other than the designated primary care physician require a<br />
referral.<br />
Restricted Recipient Program<br />
Placement in the Restricted Recipient Program means that for a<br />
period <strong>of</strong> twenty-four (24) or thirty six (36) months <strong>of</strong> eligibility,<br />
the enrollee must obtain health care services from:<br />
A designated primary care provider located in the enrollee’s or<br />
recipient’s local trade area<br />
A hospital used by the primary care provider<br />
A designated pharmacy<br />
The restriction may include any other type <strong>of</strong> health care service<br />
from a designated provider, including services from a <strong>Blue</strong> Plus<br />
participating Personal Care Provider Organization (PCPO).<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Services to Restricted<br />
Recipients (continued)<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
The DHS <strong>and</strong> health plans have developed a universal restriction,<br />
which is put in place by either the DHS or a health plan, <strong>and</strong> stays<br />
in effect for the entire period <strong>of</strong> restriction, regardless <strong>of</strong> whether<br />
the recipient does any <strong>of</strong> the following:<br />
Changes health plans<br />
Moves from fee-for-service to a health plan<br />
Moves from a health plan to fee-for-service<br />
If you are a designated primary care provider, you can verify this<br />
<strong>and</strong> the restricted recipient status <strong>of</strong> a member through <strong>Blue</strong> Plus<br />
provider service or through MN-ITS, the <strong>Minnesota</strong> Department <strong>of</strong><br />
Human Services (DHS) billing system, at<br />
www.mn-its.dhs.state.mn.us/login.html. Typically, a recipient is<br />
restricted to one primary care physician, pharmacy <strong>and</strong> hospital. A<br />
recipient may also be restricted to other designated providers or be<br />
referred by the primary care physician to other providers, if<br />
appropriate. When a member is restricted only for certain types <strong>of</strong><br />
services, no referral is required to restriction.<br />
Claims Reimbursement<br />
Eligible services provided to a restricted recipient will only be<br />
reimbursed when one <strong>of</strong> the following criteria is met:<br />
The service is provided by the recipient's primary care<br />
physician or his/her designee<br />
The primary care physician has made a referral to another<br />
provider<br />
The service is <strong>of</strong> a provider type or type <strong>of</strong> service that is not<br />
listed as restricted on the recipient's file<br />
Additional Information<br />
Providers may access more information about the <strong>Minnesota</strong><br />
Restricted Recipient Program on the DHS website with the<br />
following link:<br />
www.dhs.state.mn.us/main/idcplg?IdcService=GET_DYNAMI<br />
C_CONVERSION&RevisionSelectionMethod=LatestReleased<br />
&dDoc<strong>Name</strong>=id_008922#mrrp.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-25
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
MHCP Changes in Prior<br />
Authorization<br />
11-26<br />
Unless otherwise noted, prior authorization is required for the<br />
services listed below for <strong>Minnesota</strong> Health Care products.<br />
Commercial lines <strong>of</strong> business are not impacted by this change.<br />
<strong>Minnesota</strong> Health Care Programs<br />
Group numbers for the affected <strong>Blue</strong> Plus products are as follows:<br />
Product <strong>Name</strong> Group Numbers<br />
<strong>Blue</strong> Advantage (PMAP &<br />
GAMC)<br />
PP011, PP012, PP014, PP015,<br />
PP016, PP017, PP021, PP022,<br />
PP024, PP025, PP026, PP027,<br />
PP031, PP032, PP034, PP035,<br />
PP036, PP037, PP081, PP082,<br />
PP084, PP091, PP092, PP094<br />
<strong>Minnesota</strong>Care PP111, PP112, PP121, PP122,<br />
PP131, PP132, PP141, PP142,<br />
PP151, PP152, PP161, PP162,<br />
PP163, PP164<br />
<strong>Minnesota</strong> Senior Care Plus<br />
(MSC+)<br />
PP041, PP042, PP044, PP051,<br />
PP052, PP054, PP055, PP056,<br />
PP057, PP061, PP062, PP064,<br />
PP071, PP072, PP074, PP075,<br />
PP076, PP077<br />
Secure<strong>Blue</strong> All group numbers that begin<br />
with PP2<br />
Care<strong>Blue</strong> All group numbers that begin<br />
with PP3<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Prior authorization changes<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
For <strong>Blue</strong> Advantage, <strong>Minnesota</strong>Care, MSC+, Secure<strong>Blue</strong> <strong>and</strong> Care<strong>Blue</strong> members, prior<br />
authorization is required for the services listed below.<br />
15780 15781 15782 15783 15786<br />
15787 15819 15820 15821 15822<br />
15823 17340 17360 19304 19328<br />
20975 21010 21110 21255 21485<br />
29870 29873 29874 29875 29876<br />
29877 29878 29879 29880 29881<br />
29882 29883 29884 29885 29886<br />
29887 33140 33141 33975 33976<br />
33979 35400 37788 37790 43280<br />
43325 43850 43855 43860<br />
43865 48160 51715 54400 55401<br />
54405 54660 64622 64623 64626<br />
64627 64640 67345 67901 67902<br />
67903 67904 67906 67909 67911<br />
69930 76390 77058 77605<br />
77610 77615 77620 78459 78491<br />
78492 78607 78608 78609 78811<br />
78812 78813 78814 78815 78816<br />
91110 91111 93784 93786 93788<br />
93790<br />
0159T<br />
C8903 C8904 C8905 C8906 C8907<br />
C8908 G0166 G0252 G0289 S2400<br />
S2401 S2402 S2403 S2404 S2405<br />
S2409 S3823 S8035<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-27
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
MHCP Changes in Prior<br />
Authorization<br />
(continued)<br />
11-28<br />
Additional Information<br />
MHCP coverage guidelines are followed for <strong>Minnesota</strong> Health<br />
Care members. All services must be medically necessary for<br />
coverage.<br />
To obtain prior authorization, providers should complete the Pre-<br />
Service Request Form located on the <strong>Blue</strong> <strong>Cross</strong> website at<br />
providers.bluecrossmn.com.<br />
To assure timeliness <strong>of</strong> the review, please submit your request<br />
form at least 14 days in advance <strong>of</strong> the procedure whenever<br />
possible.<br />
Medical Necessity Criteria<br />
To view the medical necessity review criteria for these services go<br />
to providers.bluecrossmn.com <strong>and</strong> select “Medical Policy” under<br />
“Tools & Resources.” The website includes links to:<br />
Prior Authorization Recommendations (Government<br />
Programs)<br />
Coverage Guidelines for DHS Programs<br />
Coding Requirements Reminder<br />
All coding <strong>and</strong> reimbursement is subject to changes, updates, or<br />
other requirements <strong>of</strong> coding rules <strong>and</strong> guidelines. All codes are<br />
subject to federal HIPAA rules, <strong>and</strong> in the case <strong>of</strong> medical code<br />
sets (e.g., HCPCS, CPT, ICD-9-CM), only valid codes for the date<br />
<strong>of</strong> service may be submitted or accepted.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Special Transportation Special Transportation<br />
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Effective January 1, 2012, all Special Transportation rides must be<br />
scheduled through the <strong>Blue</strong>Ride staff. The Special Transportation<br />
Services (STS) providers may not schedule or provide rides<br />
requested directly by members or their representatives. Any such<br />
requests are not eligible for coverage.<br />
<strong>Blue</strong>Ride will schedule the rides <strong>and</strong> fax information to the STS<br />
providers directly with the detailed information regarding the<br />
rides. It will be imperative that STS providers keep all<br />
administrative information up to date at <strong>Blue</strong> Plus.<br />
<strong>Blue</strong>Ride can be reached at (651) 662-8648 or toll-free at<br />
1-866-340-8648. Although <strong>Blue</strong>Ride will occasionally schedule<br />
same-day rides depending on provider availability, we require at<br />
least 24 hours in advance in the metro area <strong>and</strong> two business days<br />
in advance for greater <strong>Minnesota</strong>.<br />
STS providers will be notified <strong>of</strong> scheduled rides via fax from the<br />
<strong>Blue</strong>Ride staff.<br />
Physician Certification <strong>of</strong> Need (CON)<br />
All non-institutionalized eligible MHCP Members must have a<br />
complete, signed CON on file with the STS provider <strong>and</strong> <strong>Blue</strong> Plus<br />
prior to the provision <strong>of</strong> STS transportation. Signed forms will be<br />
valid for one year from date <strong>of</strong> the medical provider’s signature.<br />
Any CONs that are incomplete or unreadable will be considered<br />
invalid, rejected, <strong>and</strong> returned to the STS provider. CONs must be<br />
faxed by the STS provider to <strong>Blue</strong>Ride at (651) 662-2844 before<br />
transportation is provided.<br />
Claims submitted for services provided without a valid CON on<br />
file at <strong>Blue</strong> Plus will not be paid.<br />
Medical providers are NOT obligated to sign a CON. The medical<br />
provider will use their pr<strong>of</strong>essional judgment to determine if the<br />
member requires special transportation <strong>and</strong> indicate that on the<br />
CON.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)<br />
11-29
Coding Policies <strong>and</strong> Guidelines (Public Programs)<br />
Special Transportation<br />
(continued)<br />
11-30<br />
Special Transportation Trip Sheet<br />
STS providers must maintain a special transportation services trip<br />
sheet documenting each ride that is provided to eligible MHCP<br />
Members. The completed trip sheets must be filed in the STS<br />
provider’s <strong>of</strong>fice <strong>and</strong> available for inspection <strong>and</strong> review by <strong>Blue</strong><br />
Plus.<br />
Reimbursement<br />
Reimbursement for services will only be allowed, <strong>and</strong> should only<br />
be billed, when the transportation is to or from a covered medical<br />
or dental service for an eligible MHCP member. Some examples<br />
<strong>of</strong> covered medical services are clinic visits, therapies, eye exams,<br />
etc. Appropriate modifiers must be used when billing for services.<br />
An eligible MHCP member is defined as a member who is<br />
physically or mentally impaired in a manner that keeps him/her<br />
from safely accessing <strong>and</strong> using common carrier transportation. If<br />
an eligible MHCP member does not meet this definition <strong>and</strong> is in<br />
need <strong>of</strong> transportation, please refer them to <strong>Blue</strong>Ride at<br />
1-866-340-8648 so they may talk to a representative.<br />
Point <strong>of</strong> Pick up Zip Code<br />
STS providers must submit the point-<strong>of</strong>-pickup zip code on all<br />
claims. This information should be submitted on an 837P<br />
transaction in the 2310D loop. If this information is not submitted,<br />
the services will be denied.<br />
<strong>Minnesota</strong> rule<br />
Per <strong>Minnesota</strong> Rule 9505.0315 “One-way mileage for special<br />
transportation within the recipient’s local trade area must not<br />
exceed 20 miles for a trip originating in the seven-county<br />
metropolitan area or 40 miles for a trip originating outside <strong>of</strong> the<br />
seven-county metropolitan area if a similar health service is<br />
available within the mileage limitation.” <strong>Blue</strong> Plus requires full<br />
compliance with all applicable state <strong>and</strong> federal laws as stated in<br />
the Provider Service Agreement between <strong>Blue</strong> Plus <strong>and</strong> the<br />
provider.<br />
These provisions, along with all Provider Service Agreement<br />
requirements are subject to audit at any time by <strong>Blue</strong> Plus.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/07/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Radiology Services)<br />
Table <strong>of</strong> Contents<br />
General Guidelines............................................................................................................... 11-2<br />
Diagnosis..............................................................................................................................11-2<br />
Modifiers..............................................................................................................................11-2<br />
Radiation Treatment Management.......................................................................................11-2<br />
Maternity Ultrasound Compatibility....................................................................................11-3<br />
Purchased Services/ Outside Lab......................................................................................... 11-3<br />
Diagnostic <strong>and</strong> Screening Mammogram..............................................................................11-4<br />
76140.................................................................................................................................... 11-4<br />
Comparison X-ray................................................................................................................ 11-4<br />
High-Technology Diagnostic Imaging (HTDI) program..................................................... 11-5<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/2012) 11-1
Coding Policies <strong>and</strong> Guidelines (Radiology Services)<br />
General Guidelines Codes 70010-79999 are used for reporting radiology procedures.<br />
The number <strong>of</strong> services on your claim must be the number <strong>of</strong><br />
procedures performed, not the number <strong>of</strong> views taken.<br />
For example:<br />
Code Number <strong>of</strong> Services<br />
71020 (chest X-ray, two views) 1<br />
Diagnosis A diagnosis code is required for radiology services <strong>and</strong> should<br />
match the services provided. For example, 76805 should have a<br />
maternity diagnosis.<br />
For a preoperative chest X-ray, use ICD-9 code V72.82.<br />
Modifiers Use modifier -26 to indicate a physician’s pr<strong>of</strong>essional component<br />
when only the pr<strong>of</strong>essional component is reported. Likewise, if<br />
only the technical component is being reported, modifier -TC<br />
should be added to the CPT code. We expect the global procedure<br />
to be reported if both components are performed by personnel in<br />
the same clinic.<br />
Radiation Treatment<br />
Management<br />
11-2<br />
Examples:<br />
•<br />
•<br />
•<br />
Global – 71010<br />
Pr<strong>of</strong>essional only – 71010-26<br />
Technical only – 71010-TC<br />
Pr<strong>of</strong>essional bilateral radiology services are reported as two lines<br />
with LT <strong>and</strong> RT modifiers.<br />
The weekly management code is 77427. Radiation treatment<br />
management is reported in units <strong>of</strong> five fractions or treatment<br />
sessions, regardless <strong>of</strong> the actual time period in which the services<br />
are furnished. The services need not be furnished on consecutive<br />
days. Multiple fractions representing two or more treatment<br />
sessions furnished on the same day may be counted separately as<br />
long as there has been a distinct break in therapy sessions, <strong>and</strong> the<br />
fractions are <strong>of</strong> the character usually furnished on different days.<br />
Code 77427 is also reported if there are three <strong>of</strong> four fractions<br />
beyond a multiple <strong>of</strong> five at the end <strong>of</strong> a course <strong>of</strong> treatment; one<br />
or two fractions beyond a multiple <strong>of</strong> five at the end <strong>of</strong> a course <strong>of</strong><br />
treatment are not reported separately.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/2012)
Radiation Treatment<br />
Management Codes<br />
(continued)<br />
Maternity Ultrasound<br />
Compatibility<br />
Purchased Services/<br />
Outside Lab<br />
Coding Policies <strong>and</strong> Guidelines (Radiology Services)<br />
The pr<strong>of</strong>essional services furnished during treatment management<br />
typically consists <strong>of</strong>:<br />
•<br />
•<br />
•<br />
•<br />
Review <strong>of</strong> port films;<br />
Review <strong>of</strong> dosimetry, dose delivery, <strong>and</strong> treatment parameters;<br />
Review <strong>of</strong> patient treatment set-up;<br />
Examination <strong>of</strong> patient for medical evaluation <strong>and</strong><br />
management (e.g., assessment <strong>of</strong> the patient’s response to<br />
treatment, coordination <strong>of</strong> care <strong>and</strong> treatment, review <strong>of</strong><br />
imaging <strong>and</strong>/or lab test results.)<br />
The code 77431 is meant to be utilized for radiation therapy<br />
management that includes the complete course <strong>of</strong> therapy,<br />
consisting <strong>of</strong> one or two fractions only. This code is not meant to<br />
fill in the gaps for the one or two fractions that may be left over at<br />
the end <strong>of</strong> a long course <strong>of</strong> therapy.<br />
The pregnant uterus ultrasound CPT codes 76801-76817 are not<br />
compatible with routine or non-specific diagnoses. This includes<br />
the diagnosis code V72.5 (Radiological examination, not<br />
elsewhere classified). If a definitive diagnosis is not available, a<br />
sign or symptom necessitating the ultrasound should be submitted.<br />
The entity that performs a test should be the one to bill for that<br />
test. However, a provider may, under arrangement with another<br />
provider, bill a service that is purchased from that other provider.<br />
For example, a clinical provider may bill for an X-ray that is done<br />
at a hospital because the clinic did not have the appropriate<br />
equipment. It is important to remember that only one provider may<br />
bill for the service.<br />
Claims for purchased services should be submitted on the<br />
electronic 837 pr<strong>of</strong>essional format as follows:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Place <strong>of</strong> service – enter the place <strong>of</strong> service code where the<br />
service was done by the performing provider.<br />
Procedure/modifier – enter the procedure code <strong>of</strong> the test <strong>and</strong><br />
the modifier 90.<br />
Provider ID – enter the NPI provider number <strong>of</strong> the ordering<br />
physician.<br />
Service facility location – enter the name <strong>and</strong> address <strong>of</strong> the<br />
service facility along with the applicable NPI.<br />
Billing Provider – enter the NPI provider number <strong>of</strong> the billing<br />
provider.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/2012)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Radiology Services)<br />
Diagnostic <strong>and</strong><br />
Screening<br />
Mammogram<br />
Generally, screening <strong>and</strong> diagnostic services done on the same day<br />
are considered mutually exclusive <strong>and</strong> the screening service will<br />
be denied. However, if a diagnostic mammogram is followed by a<br />
screening mammogram on the same day, both may be allowed.<br />
The modifier –GG must be appended to the diagnostic<br />
mammogram code.<br />
76140 Code 76140 (consultation on X-ray examination made elsewhere,<br />
written report) is considered an overread, thus it is not allowed.<br />
Overreads are an additional interpretation <strong>of</strong> a film <strong>and</strong> as such, are<br />
not billable to the plan or the patient as a separate charge.<br />
Comparison X-ray X-rays taken for comparison purposes are generally not covered.<br />
Re-X-rays are allowed if performed at different times <strong>of</strong> day or<br />
before <strong>and</strong> after surgery, such as orthopedic procedures including<br />
casting. Appending a repeat modifier (-76 or -77) will not be<br />
allowed; however, the repeat charge may be considered on appeal.<br />
11-4<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/2012)
High-Technology<br />
Diagnostic Imaging<br />
(HTDI) program<br />
Coding Policies <strong>and</strong> Guidelines (Radiology Services)<br />
<strong>Blue</strong> <strong>Cross</strong> has a relationship with Nuance for the Institute <strong>of</strong><br />
Clinical Systems Improvement (ICSI) sponsored HTDI automated<br />
decision support program.<br />
Key process changes<br />
Ordering providers are required to use a decision support system as<br />
part <strong>of</strong> their process for ordering elective, outpatient HTDI<br />
procedures. This can be performed either by Electronic Medical<br />
Record (EMR) integrated RadPort s<strong>of</strong>tware or the web-based<br />
version. Those providers using other previously approved decision<br />
support systems may continue doing so.<br />
This program applies to the following <strong>Blue</strong> <strong>Cross</strong> products:<br />
• <strong>Blue</strong> <strong>Cross</strong> fully insured members<br />
• A limited number <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> self-insured <strong>Minnesota</strong><br />
members<br />
• <strong>Blue</strong> Plus members enrolled in <strong>Minnesota</strong> Health Care<br />
Programs (MHCP)<br />
All providers must continue to follow Medical <strong>and</strong> Behavioral<br />
Health Policies for selected HTDI procedures as summarized in<br />
the section below.<br />
For more information about the RadPort tool, <strong>and</strong> to schedule<br />
implementation, contact ICSI at (952) 814-7067 or<br />
htdi@icsi.org.<br />
Imaging procedures included in the automated decision<br />
support HTDI program<br />
The new program covers the following elective, outpatient<br />
HTDI procedures:<br />
• Computed tomography <strong>and</strong> angiography (CT/CTA) scans<br />
• Positron emission tomography (PET scans)<br />
• Magnetic resonance imaging <strong>and</strong> magnetic resonance<br />
angiography (MRI/MRA) scans<br />
• Nuclear cardiology scans<br />
• Combinations <strong>of</strong> PET, CT, MRI, etc.<br />
Medical <strong>and</strong> behavioral health policies relating to HTDI<br />
(existing requirements)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/2012)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Radiology Services)<br />
High-Technology<br />
Diagnostic Imaging<br />
(HTDI) program<br />
(continued)<br />
11-6<br />
All providers must follow current pre-certification/pre-authorization<br />
<strong>and</strong> investigative policies in the Medical <strong>and</strong> Behavioral Health<br />
Policy <strong>Manual</strong> for commercial products. The following procedures<br />
have coverage criteria, are subject to medical review <strong>and</strong> continue to<br />
require the st<strong>and</strong>ard pre-certification/pre-authorization process:<br />
•<br />
•<br />
•<br />
• MRI <strong>of</strong> the breast<br />
• CT colonography (virtual colonoscopy) as a screening test for<br />
colorectal cancer<br />
• Computed tomography angiography (CTA) for evaluation <strong>of</strong><br />
coronary arteries, including coronary CT <strong>and</strong> EBCT for calcium<br />
scoring<br />
• PET scans<br />
• SPECT scans case-by-case review<br />
• Capsule endoscopy<br />
Non-covered procedures<br />
•<br />
•<br />
•<br />
Computed tomography angiography (CTA) for evaluation <strong>of</strong><br />
coronary arteries<br />
(retrospective claim review to determine if medical necessity<br />
criteria met)<br />
CT colonography (virtual colonoscopy) as a screening test for<br />
colorectal cancer (pre-certification/pre-authorization required)<br />
MRI <strong>of</strong> the breast<br />
(pre-certification/pre-authorization required EXCEPT in<br />
individuals with biopsy-proven breast cancer)<br />
• Positron emission tomography (PET)<br />
(retrospective claim review to determine if medical necessity<br />
criteria met)<br />
MHCP:<br />
All providers must follow current prior authorization <strong>and</strong><br />
investigative policies in the Medical <strong>and</strong> Behavioral Health Policy<br />
<strong>Manual</strong> for MHCP as defined in your Provider Service Agreement.<br />
The following procedures continue to require the st<strong>and</strong>ard precertification/pre-authorization<br />
process:<br />
These procedures are not covered for either commercial or MHCP<br />
members:<br />
Computed tomography (CT) screening for coronary artery disease<br />
Full-body CT scanning<br />
Spiral CT screening for lung cancer<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/2012)
High-Technology<br />
Diagnostic Imaging<br />
(HTDI) program<br />
(continued)<br />
Members covered by the program<br />
Coding Policies <strong>and</strong> Guidelines (Radiology Services)<br />
This program includes the following <strong>Blue</strong> <strong>Cross</strong> lines <strong>of</strong> business:<br />
• <strong>Blue</strong> <strong>Cross</strong> fully insured members<br />
• A limited number <strong>of</strong> <strong>Blue</strong> <strong>Cross</strong> self-insured <strong>Minnesota</strong> members<br />
• <strong>Blue</strong> Plus members enrolled in <strong>Minnesota</strong> Health Care Programs<br />
(MHCP)<br />
The HTDI program does not apply to any Medicare products or the<br />
Federal Employee Program.<br />
The EMR integrated RadPort s<strong>of</strong>tware or the web-based version will<br />
display the member's name if they are included under the HTDI<br />
program. (<strong>Blue</strong> <strong>Cross</strong> membership feeds to RadPort contain only<br />
members who are part <strong>of</strong> HTDI program, so if the member is not<br />
displayed in RadPort that member is not included.)<br />
Contact information<br />
For more information about pre-certification/pre-authorization <strong>and</strong><br />
medical necessity requirements, etc., please contact provider services at<br />
(651) 662-5200 or 1-800-262-0820.<br />
For more information about the HTDI program, go to<br />
providers.bluecrossmn.com.<br />
For specific questions about Nuance’s RadPort tool, or to schedule<br />
training <strong>and</strong> implementation <strong>of</strong> the tool, contact ICSI at<br />
(952) 814-7067 or htdi@icsi.org.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/06/2012)<br />
11-7
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Rehabilitative Services)<br />
Table <strong>of</strong> Contents<br />
Physical Therapy Modalities................................................................................................11-2<br />
Physical Therapy Procedures...............................................................................................11-2<br />
Physical Therapy Evaluation Codes .................................................................................... 11-3<br />
Occupational Therapy.......................................................................................................... 11-3<br />
Occupational Therapy Evaluation Codes............................................................................. 11-4<br />
Hot <strong>and</strong> Cold Pack Exclusion .............................................................................................. 11-5<br />
TMJ Orthotic Adjustments .................................................................................................. 11-5<br />
Massage <strong>and</strong> <strong>Manual</strong> Therapy Exclusion ............................................................................ 11-5<br />
Speech Therapy <strong>and</strong> Evaluation........................................................................................... 11-7<br />
“Timed” Unit Reporting ...................................................................................................... 11-7<br />
MHCP PT, OT, ST Authorization Process ..........................................................................11-8<br />
Medical Necessity Vendor.................................................................................................11-10<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
Physical Therapy<br />
Modalities<br />
Physical Therapy<br />
Procedures<br />
11-2<br />
The following physical medicine codes require a physician or<br />
therapist to be in constant attendance. Submit the following CPT<br />
codes for physical therapy services:<br />
Code Units <strong>of</strong> Service<br />
97010-97028, 97039 1 unit for each modality<br />
97032-97036 1 unit for each 15 minutes<br />
The following codes should be used for physical therapy<br />
procedures:<br />
Code Units <strong>of</strong> Service<br />
97110- 97124 1 unit for each 15 minutes.<br />
Example:<br />
Coding for therapeutic exercises, 50 minutes:<br />
Code Time Units <strong>of</strong> Service<br />
97110 50 min. 3<br />
For procedures that include time increments, over 50 percent <strong>of</strong> the<br />
indicated time must be rendered <strong>and</strong> documented in order to bill an<br />
additional unit. In the above example, only three units may be<br />
submitted – three units for the first 45 minutes. The remaining five<br />
minutes may not be reported because it is less than 50 percent <strong>of</strong><br />
the 15-minute code increment.<br />
Additional physical therapy codes 97140-97542 <strong>and</strong> 97597-97606<br />
should be used as defined in CPT.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Physical Therapy<br />
Evaluation Codes<br />
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
Physical therapists evaluation <strong>and</strong> re-evaluation services should be<br />
submitted using CPT codes 97001 <strong>and</strong> 97002.<br />
Code Category Units <strong>of</strong> Service<br />
97001-97002 Evaluation <strong>and</strong> re-evaluation 1 unit<br />
These codes may be reported separately if the patient’s condition<br />
requires significant separately identifiable services, above <strong>and</strong><br />
beyond the usual pre-service <strong>and</strong> post-service work associated with<br />
the procedure performed.<br />
The modifier -25 (significant, separately identifiable evaluation<br />
<strong>and</strong> management service by the same physician on the same day as<br />
the procedure or other service) is not valid with the physical<br />
therapy (PT) evaluations <strong>and</strong> re-evaluation codes 97001-97002.<br />
The evaluation or re-evaluation codes will be allowed, as<br />
appropriate, when billed with other physical or occupational<br />
services on the same date. Because the modifier -25 is not valid<br />
with 97001-97002, if submitted, the service will be denied.<br />
Occupational Therapy Listed below are the CPT physical medicine <strong>and</strong> rehabilitation<br />
codes <strong>and</strong> additional codes that occupational therapists may<br />
submit.<br />
Code Category Units <strong>of</strong> Service<br />
97010-97028 Modalities, supervised 1 unit for each modality<br />
97032-97036 Modalities, constant<br />
attendance<br />
97039 Modality, constant<br />
attendance, unlisted<br />
1 unit for each 15<br />
minutes<br />
1 unit<br />
97110-97140 Therapeutic procedures 1 unit for each 15<br />
minutes<br />
97150 Therapeutic<br />
procedure(s), group<br />
1 unit<br />
97530-97542 Therapeutic procedures 1 unit for each 15<br />
minutes<br />
97545 Therapeutic procedures 1 unit<br />
97546 Therapeutic procedures 1 unit for each additional<br />
60 minutes<br />
97597-97606 Active wound<br />
management<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
Unit per session<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
Occupational Therapy<br />
(continued)<br />
Occupational Therapy<br />
Evaluation Codes<br />
11-4<br />
Code Category Units <strong>of</strong> Service<br />
97750-97755 Test <strong>and</strong> measurements 1 unit for each 15<br />
minutes<br />
97760-97762 Orthotic <strong>and</strong> Prosthetic<br />
management<br />
1 unit for each 15<br />
minutes<br />
97799 Other procedures 1 unit (designate time)<br />
29105-29131<br />
<strong>and</strong> 29505-<br />
29515<br />
Splints 1 unit<br />
29240-29280 Strapping 1 unit<br />
92526,<br />
92610-92617<br />
95831-95852<br />
<strong>and</strong> 95999<br />
Special<br />
otorhinolaryngologic<br />
services<br />
Neurology <strong>and</strong><br />
neuromuscular<br />
procedures<br />
1 unit<br />
1 unit<br />
96105 Aphasia assessments 1 unit per hour<br />
96110-96111 Developmental testing 1 unit<br />
Occupational therapists should submit evaluation <strong>and</strong> re-evaluation<br />
services using the CPT codes 97003 <strong>and</strong> 97004.<br />
Code Category Units <strong>of</strong> Service<br />
97003-97004 Evaluation <strong>and</strong> reevaluation<br />
1 unit<br />
These codes may be reported separately if the patient’s condition<br />
requires significant separately identifiable services, above <strong>and</strong><br />
beyond the usual pre-service <strong>and</strong> post-service work associated with<br />
the procedure performed.<br />
The modifier -25 (significant, separately identifiable evaluation<br />
<strong>and</strong> management service by the same physician on the same day as<br />
the procedure or other service) is not valid with the occupational<br />
therapy (OT) evaluations <strong>and</strong> re-evaluation codes 97003-97004.<br />
The evaluation or re-evaluation codes will be allowed, as<br />
appropriate, when billed with other physical or occupational<br />
services on the same date. Because the modifier -25 is not valid<br />
with 97003-97004, if submitted, the service will be denied.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Hot <strong>and</strong> Cold Pack<br />
Exclusion<br />
TMJ Orthotic<br />
Adjustments<br />
Massage <strong>and</strong> <strong>Manual</strong><br />
Therapy Exclusion<br />
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> (<strong>Blue</strong> <strong>Cross</strong>) will not<br />
reimburse providers for the physical medicine hot <strong>and</strong> cold pack<br />
modality, CPT code 97010.<br />
<strong>Blue</strong> <strong>Cross</strong> reviewed the utilization <strong>of</strong> the hot <strong>and</strong> cold pack<br />
therapy code <strong>and</strong> determined that this modality is used in<br />
conjunction with <strong>and</strong>/or to enhance other services performed.<br />
Thus, 97010 will be denied as provider liability, whether billed<br />
alone or with another service.<br />
Adjustments for TMJ orthotics are normally billed under CPT<br />
codes 97760 or 97762. These services are not separately covered<br />
with a TMJ diagnosis. These adjustments are considered an<br />
integral part <strong>of</strong> the splint therapy <strong>and</strong> as such will be denied<br />
regardless if billed alone or with another service.<br />
97760 Orthotic(s) management <strong>and</strong> training (including<br />
assessment <strong>and</strong> fitting when not otherwise reported), upper<br />
extremity(s), lower extremity(s) <strong>and</strong>/or trunk, each 15 minutes<br />
97762 Checkout for orthotic/prosthetic use, established patient,<br />
each 15 minutes<br />
<strong>Blue</strong> <strong>Cross</strong> will not reimburse providers for massage or manual<br />
therapy services. Massage or manual therapy will deny either as<br />
incidental (provider liability) or subscriber liability.<br />
Massages that are provided as preparation for a physical medicine<br />
therapy are considered an integral part <strong>of</strong> the therapy. As such, we<br />
will deny it as provider liability. If a massage is billed alone, then<br />
it may be denied as a subscriber contract exclusion.<br />
Codes<br />
97124 Therapeutic procedure, one or more areas, each 15<br />
minutes; massage, including effleurage, petrissage <strong>and</strong>/or<br />
tapotement (stroking, compression, percussion).<br />
97140 <strong>Manual</strong> therapy techniques (e.g. mobilization /<br />
manipulation, manual lymphatic drainage, manual traction),<br />
one or more regions, each 15 minutes.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
Massage <strong>and</strong> <strong>Manual</strong><br />
Therapy Exclusion<br />
(continued)<br />
11-6<br />
Liability<br />
Provider liable:<br />
Massage <strong>and</strong> manual therapy (97124 <strong>and</strong> 97140) may be denied<br />
incidental or mutually exclusive (provider liable) to physical<br />
medicine procedures billed on the same date <strong>of</strong> service. The code<br />
combinations <strong>and</strong> outcomes are listed below. For information on<br />
incidental <strong>and</strong> mutually exclusive edits refer to Chapter 11, Coding<br />
section. The denial will be upheld regardless <strong>of</strong> submission <strong>of</strong> the -<br />
59 modifier. Additionally, submission <strong>of</strong> the -GA modifier will not<br />
affect or change the denial. Note that the <strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong><br />
<strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong>,<br />
Chapter 11, Coding section prohibits billing a patient where<br />
payment is denied as the result <strong>of</strong> a coding edit:<br />
Massage therapy – 97124 will be denied incidental to the<br />
following codes:<br />
97110, 97112-97113, 97116, 97139-97140, 97150, 97530,<br />
97532-97533, 97535, 97537, 97542, 97545-97546, 98925-<br />
98929, 98940-98943<br />
<strong>Manual</strong> therapy – 97140 will be denied incidental to the<br />
following codes:<br />
97139, 97150, 97545-97546<br />
<strong>Manual</strong> therapy – 97140 will be denied mutually exclusive to the<br />
following codes:<br />
97530, 97532-97533<br />
<strong>Manual</strong> therapy – 97140 currently denies incidental to the<br />
following codes:<br />
98925-98943<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Massage <strong>and</strong> <strong>Manual</strong><br />
Therapy Exclusion<br />
(continued)<br />
Speech Therapy <strong>and</strong><br />
Evaluation<br />
Patient Billing Impact<br />
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
The patient is not responsible <strong>and</strong> must not be balance billed for<br />
any procedures for which payment has been denied or reduced by<br />
<strong>Blue</strong> <strong>Cross</strong> as the result <strong>of</strong> a coding edit. Edit denials are designed<br />
to ensure appropriate coding <strong>and</strong> to assist in processing claims<br />
accurately <strong>and</strong> consistently.<br />
Subscriber liable:<br />
Coverage for massage <strong>and</strong> manual therapy (97124 <strong>and</strong> 97140)<br />
services provided without a physical medicine therapy is subject to<br />
the subscriber’s contract benefits. Some benefit plans may not<br />
cover this service.<br />
Speech therapists, physicians, or M.D. clinics should use CPT<br />
code 92507 for their speech therapy services <strong>and</strong> 92506 for speech<br />
evaluation. Submit one unit <strong>of</strong> service per encounter.<br />
If a speech evaluation is done over a period <strong>of</strong> two days, but only<br />
one report is generated, submit 92506 only once on the day the<br />
evaluation is completed.<br />
“Timed” Unit Reporting When a procedure/service indicates time, more than half <strong>of</strong> the<br />
designated time must be spent performing the service in order for a<br />
unit to be billed. In the case <strong>of</strong> a 15 minute service - at least 8<br />
minutes must be performed, for a 30 minute service - at least 16<br />
minutes, for a 60 minute service - at least 31 minutes, <strong>and</strong> so on.<br />
If more than one modality or therapy is performed, time cannot be<br />
combined to report units. Do not follow Medicare’s rounding rules<br />
for speech, occupational, <strong>and</strong> physical therapy services. Each<br />
modality <strong>and</strong> unit(s) is reported separately by code definition. Do<br />
not combine codes to determine total time units.<br />
For example, if two 15 minute defined modalities are performed<br />
but only 7 minutes or less is spent per modality, neither service<br />
should be reported.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
MHCP PT, OT, ST<br />
Authorization Process<br />
11-8<br />
The following services provided to <strong>Minnesota</strong> Health Care<br />
Program (MHCP) subscribers will require pre-authorization by<br />
<strong>Blue</strong> <strong>Cross</strong>:<br />
Physical therapy visits beyond 40 visits per calendar year<br />
Occupational therapy visits beyond 40 per calendar year<br />
Speech therapy visits beyond 50 per calendar year<br />
Commercial lines <strong>of</strong> business are not impacted by this change.<br />
<strong>Minnesota</strong> Health Care Programs affected:<br />
Product <strong>Name</strong> Group Numbers<br />
<strong>Blue</strong> Advantage (PMAP) PP011, PP012, PP014, PP015,<br />
PP016, PP017, PP021, PP022,<br />
PP024, PP025, PP026, PP027,<br />
PP031, PP032, PP034, PP035,<br />
PP036, PP037, PP4411, PP412,<br />
PP414<br />
<strong>Minnesota</strong>Care PP111, PP112, PP151, PP152,<br />
PP121, PP122, PP131, PP132,<br />
PP141, PP142, PP161, PP162,<br />
PP163, PP164<br />
<strong>Minnesota</strong> Senior Care Plus<br />
(MSC+)<br />
PP041, PP042, PP044, PP051,<br />
PP052, PP054, PP055, PP056,<br />
PP057, PP061, PP062, PP064,<br />
PP071, PP072, PP074, PP075,<br />
PP076, PP077<br />
Secure<strong>Blue</strong> SM (HMO SNP) All group numbers that begin<br />
with PP2<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
MHCP PT, OT, ST<br />
Authorization Process<br />
(continued)<br />
Documentation required<br />
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
Pre-Authorization requests should be submitted 2 weeks in<br />
advance <strong>of</strong> reaching the visit threshold as listed above. Fax your<br />
<strong>Blue</strong> <strong>Cross</strong> subscriber requests to: (651) 662-4022 or<br />
1-866-800-1665.<br />
Submit the following documentation when requesting an<br />
authorization:<br />
Outpatient physical, occupational <strong>and</strong> speech therapy services:<br />
Initial evaluation<br />
Any additional evaluations<br />
Plan <strong>of</strong> Care including the following:<br />
Subscriber’s diagnosis<br />
Description <strong>of</strong> subscriber’s functional status / limitations<br />
Treatment plan<br />
Treatment goals (functional, measurable <strong>and</strong> time-specific)<br />
Requested frequency <strong>and</strong> expected duration <strong>of</strong> treatment<br />
Discharge plan<br />
Subscriber’s progress toward goals<br />
Ordering practitioner<br />
Pre-Authorization process<br />
The timeline for decisions is up to 10 business days. Decisions will<br />
be communicated via telephone or fax, <strong>and</strong> letter. Approvals are<br />
communicated via telephone with a letter as follow-up. Denials are<br />
communicated with a fax copy <strong>of</strong> the denial letter <strong>and</strong> a follow-up<br />
letter sent by mail.<br />
MHCP coverage guidelines are followed for <strong>Minnesota</strong> Health<br />
Care Programs subscribers. All services must be medically<br />
necessary for continued coverage.<br />
Effective February 1, 2012, Specialized Maintenance Therapy is<br />
covered only for children under 21 years <strong>of</strong> age.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Rehabilitative Services)<br />
Medical Necessity<br />
Vendor<br />
11-10<br />
<strong>Blue</strong> <strong>Cross</strong>, Commercial <strong>Blue</strong> Plus, <strong>and</strong> <strong>Blue</strong>Link TPA have an<br />
agreement with McKesson Health Solutions, who provides<br />
medical necessity criteria for the majority <strong>of</strong> hospitals <strong>and</strong> health<br />
care systems in <strong>Minnesota</strong>, for use <strong>of</strong> their InterQual Medical<br />
Necessity Criteria.<br />
Effective March 26, 2012, clinicians, peer reviewers, <strong>and</strong> appeals<br />
reviewers will utilize this tool to determine medical necessity <strong>and</strong><br />
level <strong>of</strong> care review for inpatient, long-term acute care, <strong>and</strong> acute<br />
rehabilitation admissions <strong>and</strong> length <strong>of</strong> stay. Criteria are available<br />
for review, on a case-by-case basis, upon request. The <strong>Blue</strong> <strong>Cross</strong><br />
clinician who is communicating the results <strong>of</strong> the case review will<br />
be able to assist you with your questions.<br />
We will extend the use <strong>of</strong> the McKesson Interqual criteria to<br />
behavioral health <strong>and</strong> chemical dependency, along with<br />
chiropractic, physical therapy, occupational therapy, speech<br />
therapy, home health care, <strong>and</strong> skilled nursing facility reviews on<br />
April 1, 2012.<br />
Government Programs will also be using McKesson InterQual<br />
Criteria, in addition to Medicare <strong>and</strong> MHCP guidelines, for<br />
inpatient care, long-term acute care, acute rehabilitation care <strong>and</strong><br />
behavioral health services.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Chapter 11<br />
Coding Policies <strong>and</strong> Guidelines<br />
(Surgical Services)<br />
Table <strong>of</strong> Contents<br />
General Guidelines............................................................................................................... 11-2<br />
Bilateral Services .................................................................................................................11-2<br />
Unlisted Procedures ............................................................................................................. 11-3<br />
Facility Fees for Office Surgery .......................................................................................... 11-3<br />
Global Surgical Package......................................................................................................11-4<br />
Fractures............................................................................................................................... 11-5<br />
Incidental Surgery................................................................................................................ 11-5<br />
Lesions ................................................................................................................................. 11-5<br />
Surgical Trays <strong>and</strong> Supplies.................................................................................................11-5<br />
Implanted Supplies / Devices...............................................................................................11-6<br />
St<strong>and</strong>by Services.................................................................................................................. 11-6<br />
Treatment <strong>of</strong> Warts .............................................................................................................. 11-6<br />
Acne Treatment/Skin Rejuvenation <strong>and</strong> Rosacea Treatment .............................................. 11-6<br />
Anesthetic Agent Injections.................................................................................................11-7<br />
Intra-articular Hyaluronan Injections for Osteoarthritis ...................................................... 11-8<br />
Liposuction Edit Change...................................................................................................... 11-9<br />
Assistant Surgeons.............................................................................................................11-10<br />
Co-Surgeons.......................................................................................................................11-11<br />
Multiple Surgeries.............................................................................................................. 11-12<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12) 11-1
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
General Guidelines Generally, <strong>Blue</strong> <strong>Cross</strong> covers only surgical procedures performed<br />
by a physician for the treatment <strong>of</strong> illness or injury.<br />
Follow these procedures to bill surgical charges:<br />
Submit each surgical procedure on a separate line.<br />
Surgical units:<br />
Most surgical procedures should be submitted only with one<br />
unit; however, we can accept more than one unit for those<br />
surgical procedure codes whose narrative includes a unit<br />
indicator, such as “each” or “per.” For example, 11201 is an<br />
add-on code to 11200. Code 11201 indicates “each additional<br />
10 lesions.” If 35 skin tags are removed, code 11200 would be<br />
reported with one unit for the first 15 lesions. Code 11201<br />
could be reported with two units for the additional 20 skin tags.<br />
Submit all surgeries performed on the same date on one claim.<br />
List the appropriate procedure code for each one.<br />
Modifier -51 may be used for secondary procedures but is not<br />
required.<br />
Bilateral Services The bilateral modifier –50 is used to indicate cases in which a<br />
procedure normally performed on only one side <strong>of</strong> the body is<br />
performed on both sides. The CPT descriptors for some procedures<br />
specify that the procedure is bilateral. In such cases, the bilateral<br />
modifier should not be used. <strong>Blue</strong> <strong>Cross</strong> requires submission <strong>of</strong><br />
one line for bilateral procedures. Correctly submitted services will<br />
be eligible for 150 percent <strong>of</strong> the procedure allowed amount.<br />
11-2<br />
Certain edits apply to bilateral services:<br />
If a CPT defined bilateral procedure is submitted with a -50<br />
modifier, the service will be denied based on submission <strong>of</strong> an<br />
incorrect procedure/modifier combination.<br />
If more than one line <strong>of</strong> the same procedure code is submitted<br />
– one with the -50 modifier <strong>and</strong> one without – the unmodified<br />
line(s) will be denied as duplicative.<br />
Bilateral services on claims resubmitted will need to be<br />
submitted using the one-line reporting method regardless <strong>of</strong> the<br />
date <strong>of</strong> service.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Bilateral Services<br />
(continued)<br />
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Bilateral billing for freest<strong>and</strong>ing Ambulatory Surgical Centers<br />
Because Medicare differs in bilateral billing instructions for<br />
freest<strong>and</strong>ing ASCs, the <strong>Minnesota</strong> Rule found in Table A.5.1 <strong>of</strong><br />
the <strong>Minnesota</strong> Department <strong>of</strong> Health <strong>Minnesota</strong> Companion Guide<br />
clarifies the bilateral modifier rules for <strong>Minnesota</strong> providers <strong>and</strong><br />
payers.<br />
Modifier 50 should be used on surgical services that can be<br />
performed bilaterally <strong>and</strong> are not already defined as a bilateral<br />
service. When appropriate, report the service appended with the 50<br />
modifier on one line with one unit.<br />
Pr<strong>of</strong>essional bilateral radiology services are reported as two lines<br />
with LT <strong>and</strong> RT modifiers.<br />
Unlisted Procedures If a code cannot be found for a surgical procedure, submit the<br />
unlisted code from the related section <strong>of</strong> CPT <strong>and</strong> attach an<br />
operative report to the claim. If not attached, records will not be<br />
requested <strong>and</strong> the claim will not be processed without the<br />
information.<br />
Facility Fees for Office<br />
Surgery<br />
<strong>Blue</strong> <strong>Cross</strong> does not allow a separate reimbursement for approved<br />
<strong>of</strong>fice surgery suites. No additional reimbursement will be made<br />
for fees associated with procedures performed in <strong>of</strong>fice surgical<br />
suites regardless if the service(s) is modified with the –SU or –SG<br />
modifier. This includes additional units <strong>of</strong> service for the<br />
preoperative preparation, anesthesia <strong>and</strong> surgical trays.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-3
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Global Surgical<br />
Package<br />
11-4<br />
Surgical procedures include the operation itself, local infiltration,<br />
metacarpal/digital block or topical anesthesia, when used, <strong>and</strong><br />
normal, uncomplicated follow-up care. This concept is referred<br />
to as a ‘‘package’’ for surgical procedures, <strong>and</strong> typically begins the<br />
day before surgery. Do not submit separate, itemized services for<br />
uncomplicated surgical follow-up.<br />
Surgeries should be billed globally (one line, one charge,<br />
unmodified) if the surgery itself, pre- <strong>and</strong> post- op services are<br />
performed by either by the same practitioner or by different<br />
practitioners from the same practice/under the same tax ID. If<br />
different practitioners under different tax IDs perform different<br />
portions <strong>of</strong> the surgical package, the pre-, intra-, <strong>and</strong> post-op<br />
services should be split <strong>and</strong> billed appropriately.<br />
Surgical Care Only<br />
The post-operative period includes all visits by the primary<br />
surgeon unless the visit is for a problem unrelated to the diagnosis<br />
for which the surgery was performed or is for an added course <strong>of</strong><br />
treatment other than the follow-up care that is usually associated<br />
with the surgical procedure.<br />
When billing for the surgery only, submit the surgical procedure<br />
code with a -54 modifier <strong>and</strong> an appropriately reduced charge to<br />
reflect that post-operative care was not provided. Reimbursement<br />
for allowable intraoperative services will reflect 90 percent <strong>of</strong> the<br />
physician fee schedule allowance for the procedure.<br />
Pre- or Post-op Management<br />
When billing for pre- <strong>and</strong>/or post-operative services only, submit<br />
the surgical procedure code with the modifier -55 or -56 as<br />
appropriate. Pre- <strong>and</strong>/or post-operative services are billed only one<br />
time <strong>and</strong> include all visits within the designated period. Thus only<br />
one payment will be made for the pre- <strong>and</strong>/or post-op care.<br />
If care during the post-operative period is relinquished to another<br />
practitioner from a different practice, both practitioners should bill<br />
for their portion <strong>of</strong> post-operative care also with the surgical<br />
procedure code <strong>and</strong> the -55 modifier. However, both practitioners<br />
must report the date the care was relinquished. Assumed <strong>and</strong><br />
relinquished care is reported in the 2300 loop/DTP03 <strong>of</strong> the<br />
electronic claim record.<br />
The reimbursement for the post-op care will be divided between<br />
the practitioners based on each practitioner’s portion <strong>of</strong> their postop<br />
care.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Fractures Codes for fracture treatment include the application <strong>and</strong> removal<br />
<strong>of</strong> the first cast. Do not submit separate charges for these casting<br />
services. Submit cast removal codes only if a different physician<br />
does the removal.<br />
Submit codes 29000-29590 for the application <strong>of</strong> casts <strong>and</strong><br />
strapping only when performed as a replacement during the period<br />
<strong>of</strong> follow-up care, per CPT. Additional visits are reportable only if<br />
additional significantly identifiable services are provided at the<br />
time <strong>of</strong> the cast application or strapping. Removal <strong>of</strong> a second or<br />
third cast by the physician who applied it is included in the casting<br />
<strong>and</strong> strapping codes <strong>and</strong> not billable separately.<br />
If cast application or strapping is provided as an initial procedure<br />
in which no surgery is performed (e.g., casting <strong>of</strong> a sprained ankle<br />
or knee, or open or closed treatment), use the appropriate level-<strong>of</strong><strong>of</strong>fice<br />
visit in addition to the appropriate HCPCS code for the<br />
casting supplies. The removal <strong>of</strong> an initial cast (in which no<br />
surgery was performed) should be submitted as an <strong>of</strong>fice visit.<br />
Incidental Surgery <strong>Blue</strong> <strong>Cross</strong> does not cover procedures that are incidental to other<br />
major surgery <strong>and</strong> unrelated to illness, injury, or sterilization.<br />
Incidental surgical procedures do not usually warrant separate<br />
identification.<br />
Lesions Certain CPT codes for the integumentary system indicate a second<br />
or third lesion. Use these codes only with the primary code for the<br />
first lesion. Use an <strong>of</strong>fice call code for treatment <strong>of</strong> wounds,<br />
punctures, abrasions, <strong>and</strong> lacerations that do not require sutures or<br />
debridement.<br />
Surgical Trays <strong>and</strong><br />
Supplies<br />
Codes 11400-11471, for removal <strong>of</strong> benign lesions such as<br />
keratosis, cover a variety <strong>of</strong> techniques. The excision <strong>of</strong> benign<br />
lesions with a laser is considered a variation <strong>of</strong> a surgical excision.<br />
The dimension <strong>and</strong> location <strong>of</strong> the lesion should be recorded in the<br />
operative report. Submit the appropriate code from the range listed<br />
above.<br />
No additional reimbursement will be made for surgical trays,<br />
surgical or other miscellaneous supply codes A4550, A4649, <strong>and</strong><br />
99070. The allowance for these codes is considered bundled into<br />
payment for the other services rendered.<br />
Other supplies used in the <strong>of</strong>fice place <strong>of</strong> service are also generally<br />
considered incidental or bundled into payment for any other<br />
service performed.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-5
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Implanted Supplies /<br />
Devices<br />
Supplies/devices implanted as part <strong>of</strong> the surgical procedure, are<br />
considered integral to the procedure <strong>and</strong> are generally not<br />
separately reimbursable.<br />
St<strong>and</strong>by Services All st<strong>and</strong>by services (code 99360), are not separately reimbursable.<br />
St<strong>and</strong>by is considered incidental regardless <strong>of</strong> what is or is not<br />
billed with that service.<br />
Treatment <strong>of</strong> Warts The treatment <strong>of</strong> warts (verrucae, papillomas) via surgical or laser<br />
excision is considered a variation <strong>of</strong> destruction <strong>of</strong> a benign lesion.<br />
Use the CPT procedure codes 17000-17004.<br />
Acne Treatment/Skin<br />
Rejuvenation <strong>and</strong><br />
Rosacea Treatment<br />
11-6<br />
A cluster <strong>of</strong> warts is considered a single destruction <strong>of</strong> warts <strong>and</strong><br />
should be submitted using one unit <strong>of</strong> service.<br />
Paring or curettement or shaving <strong>of</strong> warts with or without chemical<br />
cauterization should be coded using CPT procedure codes 11055-<br />
11057.<br />
Electrocauterization or ‘‘burning <strong>of</strong>f’’ <strong>of</strong> warts should be coded<br />
using CPT procedure code 17110. This procedure code includes up<br />
to 14 lesions. Fifteen or more lesions are coded as 17111. A cluster<br />
<strong>of</strong> warts is considered a single operative procedure <strong>and</strong> should be<br />
coded as such. Only one unit will be allowed for either code.<br />
<strong>Blue</strong> <strong>Cross</strong> does not recognize the use <strong>of</strong> CPT procedure codes<br />
11420-11446 for the treatment <strong>of</strong> warts. This range <strong>of</strong> codes is<br />
considered for other types <strong>of</strong> skin lesions, such as a keratosis, etc.<br />
The <strong>Blue</strong> <strong>Cross</strong> medical policy II-33, acne treatment/skin<br />
rejuvenation details the policy on these treatments.<br />
<strong>Blue</strong> <strong>Cross</strong> medical policy II-08, rosacea treatment details the<br />
policy on these treatments.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Acne Treatment/ Skin<br />
Rejuvenation <strong>and</strong><br />
Rosacea Treatment<br />
(continued)<br />
Anesthetic Agent<br />
Injections<br />
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
The use <strong>of</strong> laser <strong>and</strong> light therapy, dermabrasion, chemical peels,<br />
surgical debulking <strong>and</strong> electrosurgery to treat rosacea is<br />
considered cosmetic <strong>and</strong> ineligible for reimbursement. The<br />
treatment <strong>of</strong> telangiectasias is considered cosmetic <strong>and</strong> ineligible<br />
for reimbursement.<br />
Claim Audits<br />
Routine claim audits have disclosed that some providers have been<br />
submitting claims for therapies considered investigative, cosmetic<br />
or not medically necessary for acne <strong>and</strong> rosacea treatment.<br />
Adherence <strong>and</strong> Enforcement <strong>of</strong> Policy<br />
Providers must abide by the requirements <strong>of</strong> all Medical Policies.<br />
<strong>Blue</strong> <strong>Cross</strong> is taking action to enforce Medical Policies II-33 <strong>and</strong><br />
II-08 due to the volume <strong>of</strong> inappropriate claims. Claims will be<br />
subject to retrospective review <strong>and</strong> denial, consistent with Medical<br />
Policy. To view medical policies go to<br />
providers.bluecrossmn.com <strong>and</strong> select then “medical policy”<br />
under “tools & resources.”<br />
Codes 64479-64484 indicate anesthetic agent injections in to the<br />
levels <strong>of</strong> the spine. They should be billed per level <strong>and</strong> not per<br />
injection. For example, a patient has an injection <strong>of</strong> the C2 <strong>and</strong> C3<br />
bilaterally. The procedure should be coded as 64479-50 with one<br />
unit. Two injections were given – one on the right <strong>and</strong> one on the<br />
left; however, code 64479 represents cervical or thoracic, single<br />
level.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-7
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Intra-articular<br />
Hyaluronan Injections<br />
for Osteoarthritis<br />
11-8<br />
The <strong>Blue</strong> <strong>Cross</strong> medical policy II-29, intra-articularhyaluronan<br />
injections for osteoarthritis states:<br />
A course <strong>of</strong> three (3) to five (5) weekly injections <strong>of</strong> intra-articular<br />
hyaluronan injections may be considered medically necessary for<br />
the treatment <strong>of</strong> painful osteoarthritis <strong>of</strong> the knee in patients who<br />
have insufficient pain relief from conservative nonpharmacologic<br />
therapy <strong>and</strong> simple analgesics.<br />
Repeated courses <strong>of</strong> intra-articular hyaluronan injections may be<br />
considered medically necessary under both <strong>of</strong> the following<br />
conditions:<br />
Significant pain relief achieved with the prior course <strong>of</strong><br />
injections<br />
At least six (6) months have passed since the prior course<br />
The use <strong>of</strong> intra-articular hyaluronan injections into joints other<br />
than the knee is considered investigative <strong>and</strong> not medically<br />
necessary.<br />
Coverage<br />
Prior authorization is not required. However, services with specific<br />
coverage criteria may be reviewed retrospectively to determine if<br />
criteria are being met. Retrospective denial <strong>of</strong> claims may result if<br />
criteria are not met.<br />
The FDA-approved single dose injection <strong>of</strong> intra-articular<br />
hyaluronan (i.e., Synvisc-One) may be used in lieu <strong>of</strong> the course <strong>of</strong><br />
three (3) to five (5) weekly injections when the medical policy<br />
criteria stated above has been met.<br />
Claim Audits<br />
Routine claim audits have disclosed occurrences where some<br />
providers have been submitting claims for therapies considered<br />
investigative <strong>and</strong> not medically necessary.<br />
Adherence <strong>and</strong> Enforcement <strong>of</strong> Policy<br />
This is a reminder that providers must abide by the requirements <strong>of</strong><br />
all medical policies. <strong>Blue</strong> <strong>Cross</strong> is taking action to enforce Medical<br />
Policy II-29. Claims for the use <strong>of</strong> intra-articular hyaluronan<br />
injections into joints other than the knee will be subject to<br />
retrospective review <strong>and</strong> denial as investigative services are not<br />
eligible for reimbursement.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Liposuction Edit<br />
Change<br />
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Liposuction services, CPT® codes 15876-15879, are subject to<br />
<strong>Blue</strong> <strong>Cross</strong> Medical Policy IV-82, which states that liposuction is<br />
considered incidental when performed in conjunction with another<br />
related primary surgical procedure. Liposuction is considered<br />
investigative as a primary (i.e., st<strong>and</strong>-alone) procedure when the<br />
usual treatment is surgical excision, or cosmetic as a primary<br />
procedure in all other situations. The policy also stipulates that<br />
“consideration for coverage will be given for the following rare<br />
situation: Liposuction for treatment <strong>of</strong> painful lipomas in a person<br />
with adiposis dolorosa that is unresponsive to analgesics.”<br />
Regardless if the liposuction could be allowed per our medical<br />
policy, we consider liposuction clinically integral to the outcome<br />
<strong>of</strong> any related procedure <strong>and</strong> as such, should deny as incidental<br />
when billed with other procedure codes.<br />
Medical Policies<br />
To view medical policies go to providers.bluecrossmn.com <strong>and</strong><br />
select “for health care providers” then “medical policy” under<br />
“tools & resources.”<br />
Incidental Coding Edit<br />
An incidental coding edit was implemented for codes 15876-<br />
15879. These services will deny to any other surgical procedure<br />
code regardless <strong>of</strong> submission <strong>of</strong> the -59 modifier.<br />
Patient Billing Impact<br />
The patient is not responsible <strong>and</strong> must not be balance billed for<br />
any procedures for which payment has been denied or reduced by<br />
<strong>Blue</strong> <strong>Cross</strong> as the result <strong>of</strong> a coding edit. Edit denials are designed<br />
to ensure appropriate coding <strong>and</strong> to assist in processing claims<br />
accurately <strong>and</strong> consistently.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-9
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Assistant Surgeons Almost all <strong>Blue</strong> <strong>Cross</strong> members have coverage for assistant<br />
surgeon’s services when the following criteria are met:<br />
11-10<br />
The surgical assistant is a licensed physician, nurse practitioner<br />
(NP), registered nurse first assistant (RNFA), or physician<br />
assistant (PA).<br />
The surgical assistant’s services are medically necessary. (This<br />
is determined by the complexity <strong>of</strong> the surgery.)<br />
Note: Assist at surgery services rendered by Surgical Techs or<br />
Bachelor <strong>of</strong> Medicine <strong>and</strong> Bachelor <strong>of</strong> Surgery (MBBS)<br />
practitioners are not allowable. Assistant surgery services rendered<br />
by these specialties will be denied as an ineligible provider.<br />
To bill services <strong>of</strong> an assistant surgeon (MD, NP, PA, or RNFA<br />
acting as an assistant at surgery); use the surgical procedure code<br />
with modifier -80.<br />
The modifiers -81, 82 or –AS may also be used for assist services.<br />
Modifier –AS specifically designates the assist as a physician<br />
assistant, nurse practitioner or clinical nurse specialist.<br />
If more than one surgical procedure was done during the same<br />
session, list each procedure separately.<br />
Generally, reimbursement for eligible assistant surgeon services is<br />
16 percent <strong>of</strong> the surgery allowance. When an assistant surgeon is<br />
involved in multiple surgical procedures, the same method used for<br />
determining reimbursement for the primary surgeon shall be used<br />
in determining reimbursement for the assistant surgeon. The<br />
secondary surgeries will be subject to an additional multiple<br />
surgery reduction (50 percent), if appropriate.<br />
We do not publish a list <strong>of</strong> surgeries for which an assistant surgeon<br />
is allowed. Generally, we follow the list that CMS has furnished to<br />
Medicare carriers, for approved codes. However, we may subject<br />
the assist services to additional edits or restrictions. Denied<br />
assist-at surgery claims may be appealed with documentation. The<br />
documentation/operative report should identify the assistant,<br />
credentials, <strong>and</strong> should include the involvement, thus need, for the<br />
assistant.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Assistant Surgeons<br />
(continued)<br />
Assist at surgery using robotics<br />
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
When a robot is used in conjunction with a surgery, an assist-atsurgery<br />
service may be billed for a qualified practitioner (MD,<br />
RNFA, NP, or PA) assisting by operating the machine (robot). The<br />
appropriate surgical code <strong>and</strong> modifier would be billed. However,<br />
separately billed charges for surgical robotics (S2900) will not be<br />
allowed.<br />
Co-Surgeons Co-surgery services are identified by use <strong>of</strong> the CPT modifier–62.<br />
Co-surgery involves a surgical procedure report with a single<br />
procedure code that requires two surgeons <strong>of</strong> different specialties<br />
or a surgical procedure that involves two surgeons performing<br />
parts <strong>of</strong> the procedure simultaneously. The additional surgeon is<br />
not acting as an assistant at surgery (modifier –80 or –AS) or as<br />
part <strong>of</strong> a surgical team (modifier –66).<br />
Documentation must support the use <strong>of</strong> the –62 modifier. An<br />
operative report(s) is required <strong>and</strong> will be requested if not<br />
submitted.<br />
Claims must be coordinated by the surgeons prior to filing their<br />
claims. One operative report may be used, as long as both<br />
surgeons’ responsibilities are identified. The following criteria<br />
must be met:<br />
Co-surgery services should be submitted using the appropriate<br />
CPT surgical procedure code <strong>and</strong> the modifier -62. If more<br />
than one modifier is being reported, list –62 first.<br />
Both providers billing the -62 modifier should normally be<br />
surgeons <strong>of</strong> different specialties. Examples would include<br />
Gynecology/Urology, General Surgery/ENT, etc.<br />
It must be medically necessary <strong>and</strong> an accepted st<strong>and</strong>ard <strong>of</strong><br />
care to have two surgeons <strong>of</strong> different specialties perform the<br />
surgery.<br />
Each surgeon must perform a distinct portion <strong>of</strong> the surgery.<br />
<strong>Blue</strong> <strong>Cross</strong> follows Medicare’s guidelines regarding which<br />
procedures will be reimbursed for co-surgery services. The<br />
MPFSDB indicators are:<br />
0= Co-surgeons not permitted for this procedure.<br />
1= Co-surgeons may be paid if supporting documentation<br />
is supplied to establish medical necessity.<br />
2= Co-surgeons permitted.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)<br />
11-11
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Co-Surgeons<br />
(continued)<br />
11-12<br />
Allowable co-surgery services will be determined on a case-bycase<br />
basis <strong>and</strong> upon review <strong>of</strong> supporting documentation.<br />
Reimbursement will be 62.5 percent <strong>of</strong> the global surgery fee<br />
schedule amount for allowable co-surgery services. Additionally,<br />
global surgery rules will be applied to each <strong>of</strong> the physicians<br />
participating in a co-surgery.<br />
If multiple co-surgeries are submitted <strong>and</strong> allowed, the second or<br />
subsequent surgery would also be subject to a multiple surgery<br />
reduction, if the surgical code itself may be subject to a reduction.<br />
For example, the first co-surgery would be allowed at 62.5 percent.<br />
The second would be allowed at 62.5 percent then further reduced<br />
by 50 percent.<br />
If multiple co-surgeries are submitted <strong>and</strong> allowed, the second or<br />
subsequent surgery would also be subject to a multiple surgery<br />
reduction, if the surgical code itself may be subject to a reduction.<br />
For example, the first co-surgery would be allowed at 62.5 percent.<br />
The second would be allowed at 62.5 percent then further reduced<br />
by 50 percent.<br />
Multiple Surgeries When more than one surgical procedure is performed during the<br />
same operative session, the -51 modifier may be appended to all<br />
secondary surgical procedures; however, it is not necessary to<br />
append this modifier. Applicable code edits will be applied to<br />
services submitted. The -51 modifier itself does not affect<br />
payment.<br />
Payment for multiple surgeries is based on whether the surgical<br />
procedure itself may be subject to a multiple surgery reduction. If<br />
so, this reduction will be based on the highest allowed amount.<br />
Multiple surgery reduction will be applied to the lesser allowed<br />
procedure(s). Payment will be 50 percent <strong>of</strong> the allowed amount<br />
for all covered secondary procedures.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (03/19/12)
Coding Policies <strong>and</strong> Guidelines (Surgical Services)<br />
Co-Surgeons<br />
(continued)<br />
11-14<br />
If multiple co-surgeries are submitted <strong>and</strong> allowed, the second or<br />
subsequent surgery would also be subject to a multiple surgery<br />
reduction, if the surgical code itself may be subject to a reduction.<br />
For example, the first co-surgery would be allowed at 62.5 percent.<br />
The second would be allowed at 62.5 percent then further reduced<br />
by 50 percent.<br />
If multiple co-surgeries are submitted <strong>and</strong> allowed, the second or<br />
subsequent surgery would also be subject to a multiple surgery<br />
reduction, if the surgical code itself may be subject to a reduction.<br />
For example, the first co-surgery would be allowed at 62.5 percent.<br />
The second would be allowed at 62.5 percent then further reduced<br />
by 50 percent.<br />
Multiple Surgeries When more than one surgical procedure is performed during the<br />
same operative session, the -51 modifier may be appended to all<br />
secondary surgical procedures; however, it is not necessary to<br />
append this modifier. Applicable code edits will be applied to<br />
services submitted. The -51 modifier itself does not affect<br />
payment.<br />
Payment for multiple surgeries is based on whether the surgical<br />
procedure itself may be subject to a multiple surgery reduction. If<br />
so, this reduction will be based on the billed amount. Multiple<br />
surgery reduction will be applied to the lesser charge procedure(s).<br />
Payment will be 50 percent <strong>of</strong> the allowed amount for all covered<br />
secondary procedures.<br />
<strong>Blue</strong> <strong>Cross</strong> <strong>and</strong> <strong>Blue</strong> <strong>Shield</strong> <strong>of</strong> <strong>Minnesota</strong> Provider Policy <strong>and</strong> Procedure <strong>Manual</strong> (02/22/11)