HIPPA Law - New Jersey City University
HIPPA Law - New Jersey City University
HIPPA Law - New Jersey City University
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
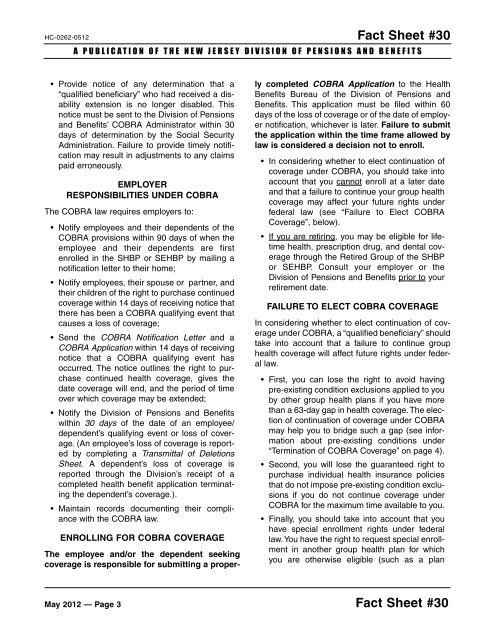
HC-0262-0512 Fact Sheet #30A PUBLICATION OF THE NEW JERSEY DIVISION OF PENSIONS AND BENEFITS• Provide notice of any determination that a“qualified beneficiary” who had received a disabilityextension is no longer disabled. Thisnotice must be sent to the Division of Pensionsand Benefits’ COBRA Administrator within 30days of determination by the Social SecurityAdministration. Failure to provide timely notificationmay result in adjustments to any claimspaid erroneously.EMPLOYERRESPONSIBILITIES UNDER COBRAThe COBRA law requires employers to:• Notify employees and their dependents of theCOBRA provisions within 90 days of when theemployee and their dependents are firstenrolled in the SHBP or SEHBP by mailing anotification letter to their home;• Notify employees, their spouse or partner, andtheir children of the right to purchase continuedcoverage within 14 days of receiving notice thatthere has been a COBRA qualifying event thatcauses a loss of coverage;• Send the COBRA Notification Letter and aCOBRA Application within 14 days of receivingnotice that a COBRA qualifying event hasoccurred. The notice outlines the right to purchasecontinued health coverage, gives thedate coverage will end, and the period of timeover which coverage may be extended;• Notify the Division of Pensions and Benefitswithin 30 days of the date of an employee/dependent’s qualifying event or loss of coverage.(An employee’s loss of coverage is reportedby completing a Transmittal of DeletionsSheet. A dependent’s loss of coverage isreported through the Division’s receipt of acompleted health benefit application terminatingthe dependent’s coverage.).• Maintain records documenting their compliancewith the COBRA law.ENROLLING FOR COBRA COVERAGEThe employee and/or the dependent seekingcoverage is responsible for submitting a properlycompleted COBRA Application to the HealthBenefits Bureau of the Division of Pensions andBenefits. This application must be filed within 60days of the loss of coverage or of the date of employernotification, whichever is later. Failure to submitthe application within the time frame allowed bylaw is considered a decision not to enroll.• In considering whether to elect continuation ofcoverage under COBRA, you should take intoaccount that you cannot enroll at a later dateand that a failure to continue your group healthcoverage may affect your future rights underfederal law (see “Failure to Elect COBRACoverage”, below).• If you are retiring, you may be eligible for lifetimehealth, prescription drug, and dental coveragethrough the Retired Group of the SHBPor SEHBP. Consult your employer or theDivision of Pensions and Benefits prior to yourretirement date.FAILURE TO ELECT COBRA COVERAGEIn considering whether to elect continuation of coverageunder COBRA, a “qualified beneficiary” shouldtake into account that a failure to continue grouphealth coverage will affect future rights under federallaw.• First, you can lose the right to avoid havingpre-existing condition exclusions applied to youby other group health plans if you have morethan a 63-day gap in health coverage. The electionof continuation of coverage under COBRAmay help you to bridge such a gap (see informationabout pre-existing conditions under“Termination of COBRA Coverage” on page 4).• Second, you will lose the guaranteed right topurchase individual health insurance policiesthat do not impose pre-existing condition exclusionsif you do not continue coverage underCOBRA for the maximum time available to you.• Finally, you should take into account that youhave special enrollment rights under federallaw.You have the right to request special enrollmentin another group health plan for whichyou are otherwise eligible (such as a planMay 2012 — Page 3 Fact Sheet #30