Chronic Lymphocytic Leukemia - The Leukemia & Lymphoma Society
Chronic Lymphocytic Leukemia - The Leukemia & Lymphoma Society
Chronic Lymphocytic Leukemia - The Leukemia & Lymphoma Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong><br />
JUNE DENNING, CLL Survivor<br />
Revised 2011
A Message From John Walter<br />
President and CEO of <strong>The</strong> <strong>Leukemia</strong> & <strong>Lymphoma</strong> <strong>Society</strong><br />
<strong>The</strong> <strong>Leukemia</strong> & <strong>Lymphoma</strong> <strong>Society</strong> (LLS) is committed to bringing<br />
you the most up-to-date blood cancer information. We know how<br />
important it is for you to have an accurate understanding of your<br />
diagnosis, treatment and support options. With this knowledge, you<br />
can work with members of your oncology team to move forward<br />
with the hope of remission and recovery. Our vision is that one day<br />
the great majority of people who have been diagnosed with <strong>Chronic</strong><br />
<strong>Lymphocytic</strong> <strong>Leukemia</strong> (CLL) will be cured or will be able to manage<br />
their disease with a good quality of life. We hope that the information<br />
in this booklet will help you along your journey.<br />
LLS is the world’s largest voluntary health organization dedicated to<br />
funding blood cancer research, education and patient services. Since<br />
the first funding in 1954, LLS has invested more than $814 million<br />
in research specifically targeting blood cancers. We will continue to<br />
invest in research for cures and in programs and services that improve<br />
the quality of life of people who have CLL and their families.<br />
We wish you well.<br />
John Walter<br />
President and CEO
Table of Contents<br />
2 Introduction<br />
2 Here to Help<br />
5 <strong>Leukemia</strong><br />
6 <strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong><br />
8 Signs and Symptoms<br />
8 Diagnosis<br />
10 Treatment Planning<br />
13 Treatment<br />
18 Complications: CLL or CLL Treatment<br />
20 Clinical Trials<br />
22 Treatment Response and Follow-Up Care<br />
24 Related Diseases<br />
26 Normal Blood and Marrow<br />
28 <strong>The</strong> Lymphatic System<br />
29 Medical Terms<br />
41 More Information<br />
Acknowledgement<br />
<strong>The</strong> <strong>Leukemia</strong> & <strong>Lymphoma</strong> <strong>Society</strong> gratefully acknowledges for his critical<br />
review and important contributions to the material presented in this publication:<br />
John C. Byrd M.D.<br />
D. Warren Brown Chair of <strong>Leukemia</strong> Research<br />
Professor of Medicine, Medicinal Chemistry, and Veterinary Biosciences<br />
Director, Division of Hematology, Department of Internal Medicine<br />
<strong>The</strong> Ohio State University<br />
Columbus, OH<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 1
Introduction<br />
This booklet provides information about chronic lymphocytic leukemia (CLL) for<br />
patients and their families. Brief descriptions of normal blood, bone marrow and<br />
the lymphatic system are provided to help readers better understand the CLLspecific<br />
information in the booklet.<br />
An estimated 105,119 people are living with CLL and 14,570 1 people are expected<br />
to be diagnosed with CLL in the United States in 2011. Doctors have learned a<br />
great deal in the last few decades about CLL. In the last several years, new therapies<br />
have been developed, and outcomes for people living with CLL are steadily<br />
improving. Researchers around the world continue to strive to find a cure for CLL.<br />
1 Howlader N, Noone AM, et al, eds. SEER Cancer Statistics Review, 1975-2008, National Cancer Institute.<br />
Bethesda, MD, www.seer.cancer.gov/csr/1975_2008/, based on November 2010 SEER data submission, posted<br />
to the SEER website, 2011.<br />
This publication is designed to provide accurate and authoritative information about the subject matter<br />
covered. It is distributed as a public service by LLS, with the understanding that LLS is not engaged in<br />
rendering medical or other professional services.<br />
Here to Help<br />
<strong>The</strong> information in this booklet will help you talk to your doctor about the tests<br />
and treatment you need. We encourage you to take the lead in asking questions<br />
and discussing your fears and concerns. <strong>The</strong>se actions will give members of your<br />
healthcare team the opportunity to answer your questions, extend emotional<br />
support and provide any needed referrals.<br />
A diagnosis of CLL is often a shock to the patient, family members and friends.<br />
Denial, depression, hopelessness and fear are some of the reactions people may<br />
have. Keep in mind that<br />
{ { Many people are better able to cope once their treatment plan is established and<br />
they can look forward to recovery.<br />
{ { <strong>The</strong> outlook for people with CLL is continuing to improve. New approaches<br />
to therapy are being studied in clinical trials for patients of all ages and at every<br />
stage of treatment.<br />
LLS Has Ways to Help. Treatment for CLL will affect your daily life, at least for a<br />
time. During and after treatment, you may want to have friends, family members or<br />
caregivers help you get information.<br />
Making treatment choices, paying for medical care, communicating with healthcare<br />
providers, family members and friends—these are some of the stressors that go<br />
page 2 I 800.955.4572 I www.LLS.org
along with a cancer diagnosis. LLS offers free information and patient services for<br />
individuals and families touched by blood cancers.<br />
Speak to an Information Specialist. Information Specialists are master’s level<br />
oncology professionals. <strong>The</strong>y provide accurate up-to-date disease and treatment<br />
information and are available to speak with callers Monday through Friday, 9 a.m.<br />
to 6 p.m. ET at (800) 955-4572. You can email infocenter@LLS.org or chat live<br />
with a Specialist at www.LLS.org.<br />
Language Services. Free language services are available when you speak with an<br />
Information Specialist. Let your doctor know if you want a professional healthcare<br />
interpreter who speaks your native language or uses sign language to be present<br />
during your visit. Many times, this is a free service.<br />
Información en Español. LLS has a number of resources available in Spanish for<br />
patients, caregivers and healthcare professionals. You can read and download these<br />
resources online at www.LLS.org/espanol or order printed copies by mail or phone.<br />
Other Helpful Organizations. Our website, www.LLS.org/resourcedirectory,<br />
offers an extensive list of resources for patients and families about financial<br />
assistance, counseling, transportation, summer camps and other needs.<br />
Chapter Programs and Services. LLS chapter offices around the United States<br />
and Canada offer support and education. Your chapter can arrange for peer-topeer<br />
support through the Patti Robinson Kaufmann First Connection Program. <strong>The</strong><br />
Patient Financial Aid program offers a limited amount of financial aid for qualified<br />
patients. Find your local chapter by calling (800) 955-4572 or by visiting<br />
www.LLS.org/chapterfind.<br />
Co-Pay Assistance Program.This program offers assistance for financially eligible<br />
patients with certain blood cancer diagnoses to help pay for private or public<br />
health insurance premiums and/or co-pay costs for prescription medications.<br />
Check www.LLS.org/copay or call (877) 557-2672 to speak to a Co-Pay Assistance<br />
Program specialist for more eligibility information.<br />
Clinical Trials. Our Information Specialists help patients work with their doctors<br />
to find out about specific clinical trials. Information Specialists conduct clinical-trial<br />
searches for patients, family members and healthcare professionals. You can also<br />
use TrialCheck®, an online clinical-trial search service supported by LLS that offers<br />
patients and caregivers immediate access to listings of blood cancer clinical trials.<br />
Please visit www.LLS.org/clinicaltrials.<br />
Free Materials. LLS publishes many free education and support materials for<br />
patients and healthcare professionals. PDF files can be read online or downloaded.<br />
Free print versions can be ordered. Visit www.LLS.org/resourcecenter.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 3
Telephone/Web Education Programs. LLS provides a number of free,<br />
live telephone and web education programs presented by experts for patients,<br />
caregivers and healthcare professionals. For more information, please visit<br />
www.LLS.org/programs.<br />
Suggestions From Other People Living With Cancer<br />
{ { Get information about choosing a cancer specialist or treatment center.<br />
{ { Find out about financial matters: What does your insurance cover?<br />
What financial assistance is available to you?<br />
{ { Learn about the most current tests and treatments for your type of CLL.<br />
{ { Keep all appointments with the doctor and talk openly about your fears or<br />
concerns or any side effects you experience.<br />
{ { Talk with family and friends about how you feel and how they can help.<br />
{ { Contact your doctor if you have fatigue, fever, pain or sleep problems so<br />
that any issues can be addressed early on.<br />
{ { Get medical advice if you have experienced changes in mood, feelings<br />
of sadness or depression.<br />
Reach Out. You and your loved ones can reach out for support in several ways.<br />
For example:<br />
{ { LLS offers online Blood Cancer Discussion Boards as well as online chats at<br />
www.LLS.org/getinfo.<br />
{ { Local or Internet support groups and blogs can provide forums for support.<br />
{ { Patients with cancer often become acquainted with one another, and these<br />
friendships provide support.<br />
Depression. Treatment for depression has proven benefits for people living<br />
with cancer. Depression is an illness that should be treated even when a person is<br />
undergoing CLL treatment. Seek medical advice if your mood does not improve<br />
over time—for example, if you feel depressed every day for a 2-week period.<br />
Contact LLS or ask your healthcare team for guidance and referrals to other<br />
sources of help, such as counseling services or community programs. For more<br />
information you can contact the National Institute of Mental Health (NIMH)<br />
at www.nimh.nih.gov and enter “depression” in the search box at the top of the<br />
webpage, or call the NIMH toll-free at (866) 615-6464.<br />
Information for Veterans. Veterans with CLL who were exposed to Agent Orange<br />
while serving in Vietnam may be able to get help from the United States Department<br />
of Veterans Affairs. For more information call the Department of Veterans Affairs at<br />
(800) 749-8387 or visit www.publichealth.va.gov/exposures/agentorange.<br />
page 4 I 800.955.4572 I www.LLS.org
We’d Like to Hear From You. We hope this booklet helps you. Please tell us<br />
what you think at www.LLS.org/publicationfeedback. Click on “LLS Disease &<br />
Treatment Publications—Survey for Patients, Family and Friends.”<br />
<strong>Leukemia</strong><br />
<strong>Leukemia</strong> is a cancer of the marrow and blood. <strong>The</strong> four major types of leukemia<br />
are chronic lymphocytic leukemia (CLL), acute lymphoblastic leukemia (ALL),<br />
chronic myeloid leukemia (CML), and acute myeloid leukemia (AML).<br />
<strong>Leukemia</strong> is called “lymphocytic” (or “lymphoblastic”) if the cancerous change<br />
takes place in a type of marrow cell that forms lymphocytes. <strong>Leukemia</strong> is called<br />
“myelogenous” (or “myeloid”) if the cell change takes place in a type of marrow cell<br />
that would normally go on to form red cells, some kinds of white cells and platelets.<br />
<strong>Chronic</strong> leukemia is a slow-growing blood cancer that permits the growth of greater<br />
numbers of more developed cells. In general, these more mature cells can carry out<br />
some of their normal functions. Acute leukemia is a more quickly growing disease<br />
that affects unformed cells or cells that are not yet fully developed. <strong>The</strong>se immature<br />
cells cannot carry out their normal functions.<br />
<strong>The</strong> four main types of leukemia are further classified into subtypes that are based<br />
on specific features of cells. Knowing the subtype of the patient’s disease may help<br />
the doctor to assess how quickly the disease may progress. <strong>The</strong> subtype is important<br />
because the treatment approach may vary according to the disease subtype.<br />
<strong>Lymphocytic</strong> <strong>Leukemia</strong> and <strong>Lymphoma</strong>. <strong>The</strong> World Health Organization<br />
(WHO) includes “lymphocytic leukemias” and “lymphoma” within one<br />
classification. Each of these cancers is the result of a change to a cell that was destined<br />
to be a lymphocyte. However, lymphocytic leukemia and lymphoma originate in<br />
different parts of the body. <strong>Lymphocytic</strong> leukemia develops in the lymphatic tissue<br />
within the marrow. <strong>Lymphoma</strong> begins in a lymph node, or another lymphatic<br />
structure in the skin, the gastrointestinal tract, or some other site in the body.<br />
<strong>Chronic</strong> lymphocytic leukemia (CLL) and small cell lymphocytic lymphoma<br />
(SLL) are often considered to be one disease because they are similar with regard<br />
to incidence, signs and symptoms, genetic features, disease progression and<br />
treatment. <strong>The</strong> leukemic lymphocytes and tissue abnormalities that are observed<br />
in people with SLL are identical to those observed in patients with CLL. However,<br />
in people with SLL, there is more lymph node and lymphoid tissue involvement<br />
and less marrow and blood involvement; in people with CLL, the marrow and<br />
blood are more strikingly affected. Talk to your doctor if you have questions about<br />
your specific diagnosis and treatment.<br />
More information about leukemia and lymphoma can be found in the free LLS<br />
publications Understanding <strong>Leukemia</strong>, <strong>The</strong> <strong>Lymphoma</strong> Guide—Information for<br />
Patients and Caregivers and Non-Hodgkin <strong>Lymphoma</strong>.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 5
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong><br />
<strong>Chronic</strong> lymphocytic leukemia (CLL) results from an acquired (not present at<br />
birth) change (mutation) to the DNA of a single marrow cell that develops into<br />
a lymphocyte.<br />
In 95 percent of people with CLL, the change occurs in a B lymphocyte. In the<br />
other 5 percent of people with CLL, the cell that transforms from normal to<br />
leukemic has the features of a T lymphocyte or a natural killer (NK) cell. Thus, any<br />
of the three major types of lymphocytes (T cells, B cells or NK cells) can undergo a<br />
malignant transformation that causes diseases related to B-cell CLL<br />
(see Related Diseases on page 24).<br />
Scientists do not yet understand what causes this change. Once the marrow cell<br />
undergoes the leukemic change, it multiplies into many cells. CLL cells grow and<br />
survive better than normal cells; over time, they crowd out normal cells.<br />
<strong>The</strong> result is the uncontrolled growth of CLL cells in the marrow, leading to an<br />
increase in the number of CLL cells in the blood. <strong>The</strong> leukemic cells that accumulate<br />
in the marrow in people with CLL do not impede normal blood cell production as<br />
extensively as is the case with acute lymphoblastic leukemia. This is an important<br />
distinction: It is the reason for the generally less severe early course of CLL.<br />
CLL takes different forms. Some people have disease that is slow growing. People<br />
with minimal changes in their blood cell counts (an increase in the number of blood<br />
lymphocytes and little or no decrease in the number of red cells, normal neutrophil<br />
and platelet counts) may have stable disease for years. Other people with CLL have<br />
a faster-growing form of the disease—the CLL cells accumulate in the bone marrow<br />
and blood, and there is a significant decrease in the numbers of red cells and platelets.<br />
People with faster-growing CLL may have<br />
{ { Enlarged lymph nodes that can lead to compression of neighboring organs.<br />
For example, enlarged lymph nodes in the abdomen can interfere with the<br />
functions of the gastrointestinal tract and/or the urinary tract.<br />
{ { A severe immunoglobulin deficiency, sometimes coupled with a low neutrophil<br />
count, which can lead to recurrent infections.<br />
{ { An enlarged spleen which can press on the stomach causing early fullness (satiety)<br />
while eating food and also discomfort in the left upper part of the abdomen.<br />
Causes and Risk Factors. CLL has generally not been associated with any<br />
environmental or external factors. However, the Institute of Medicine of the<br />
National Academy of Sciences issued a report “Veterans and Agent Orange: Update<br />
2002,” which concluded that there was “sufficient evidence of an association”<br />
page 6 I 800.955.4572 I www.LLS.org
etween herbicides used in Vietnam and CLL. For Veterans with Agent Orange<br />
exposure, this may provide additional VA benefits.<br />
First-degree relatives of patients with CLL are three to four times more likely to<br />
develop CLL than people who do not have first-degree relatives with the disease.<br />
However, the risk is still small. For example, the 60-year-old sibling or child of<br />
someone with CLL would have three to four chances in 10,000 of developing the<br />
disease, compared with the one chance in 10,000 for a 60-year-old person without<br />
a family history of the disease.<br />
For information on studies about two or more relatives with a hematologic<br />
malignancy, please visit www.LLS.org/diseaseregistries.<br />
Incidence. CLL is more common in people who are 60 years and older (see<br />
Figure 1). <strong>The</strong> incidence of the disease increases from less than one per 100,000 in<br />
individuals aged 40 to 44 years to more than 30 per 100,000 in individuals aged 80<br />
and older.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong>: Age-Specific Incidence Rates (2004-2008)<br />
Incidence (per 100,000)<br />
36<br />
33<br />
30<br />
27<br />
24<br />
21<br />
18<br />
15<br />
12<br />
9<br />
6<br />
3.3<br />
3<br />
1.8<br />
0 n/a n/a n/a n/a n/a n/a n/a<br />
0.1 0.2 0.6<br />
Signs and Symptoms<br />
CLL symptoms usually develop over time. Early in the course of the disease, CLL<br />
often has little effect on a person’s well-being. Some people with CLL do not have<br />
any symptoms. <strong>The</strong> disease may be suspected because of abnormal results from<br />
blood tests that were ordered either as part of an annual physical or a medical<br />
examination for an unrelated condition. An elevated white cell (lymphocyte) count<br />
is the most common finding that leads a doctor to consider a CLL diagnosis.<br />
People with CLL who do have symptoms may tire more easily, and/or feel short<br />
of breath during day-to-day physical activities—as a result of anemia (low red<br />
cell count). <strong>The</strong>y may lose weight because of decreased appetite and/or increased<br />
use of energy. <strong>The</strong> lymph nodes and spleen may become enlarged as a result of<br />
an accumulation of CLL cells (leukemic lymphocytes). Infections of the skin,<br />
lungs, kidneys or other sites may occur as result of low immunoglobulin levels and<br />
decreased neutrophil counts.<br />
Diagnosis<br />
Blood Cell Count and Examination. <strong>The</strong> diagnosis of CLL is usually evident<br />
from the results of blood cell counts and an examination of blood cells. A person<br />
with CLL will have increased numbers of lymphocytes. Low platelet counts and<br />
low red cell counts may also be present; these counts are usually only slightly<br />
decreased in the early stage of the illness.<br />
Bone Marrow Examination. A bone marrow aspiration and biopsy generally are<br />
not needed to make a diagnosis of CLL. However, these tests are recommended<br />
before treatment begins—the test results provide baseline data that can confirm<br />
other diseases are not present and also be used later on to evaluate the effects<br />
of therapy. Repeat marrow biopsies are helpful in distinguishing disease versus<br />
treatment-related causes of low blood cell counts that do not improve within an<br />
expected period of time after treatment.<br />
In people with CLL, a bone marrow examination will show an increase in the<br />
number of lymphocytes in the marrow and often a decrease in the number of<br />
normal marrow cells. <strong>The</strong> bone marrow biopsy results will also show one of four<br />
patterns characteristic of CLL: nodular, interstitial, mixed or diffuse.<br />
Immunophenotyping. “Immunophenotyping” (or flow cytometry) of<br />
lymphocytes is an important process used to diagnose CLL, and other types of<br />
leukemia and lymphoma, by comparing the cancer cells to normal immune cells.<br />
<strong>The</strong> test results indicate whether or not the person’s lymphocytes are derived<br />
from a single cancer cell (leukemia) or from other conditions in adults that can,<br />
page 8 I 800.955.4572 I www.LLS.org
infrequently, cause an increase in the number of blood lymphocytes from a<br />
noncancerous origin. This test is especially important if the number of lymphocytes<br />
in the blood is only slightly elevated. Immunophenotyping also determines whether<br />
the CLL cells are from a change in either B-cell or T-cell development (see Figure 2).<br />
Most people with CLL have the B-cell type.<br />
Immunophenotyping is done with an instrument called a “flow cytometer.”<br />
A sample of cells from blood or marrow can be tagged with an antibody that is<br />
specific for a site on the cell surface. <strong>The</strong> cells go through the flow cytometer,<br />
passing through a laser beam; if they have the antibody-specific surface feature,<br />
the cells light up and they are counted.<br />
Lymphocyte Development<br />
Other Blood Cells<br />
Stem Cells<br />
Lymphocyte Progenitor<br />
B Cells T Cells NK Cells<br />
Early<br />
Specialized<br />
Lymphocytes<br />
Fully Developed<br />
Specialized<br />
Lymphocytes<br />
Figure 2. I Mutation of DNA can occur when the early specialized lymphocytes are formed or after the<br />
lymphocyte progenitor has differentiated into one of the three specific types of lymphocytes. <strong>The</strong> leukemic<br />
cells may be principally B cells, T cells or natural killer (NK) cells. Most patients have a B-cell type of CLL.<br />
Immunoglobulin Levels. <strong>The</strong> measurement of the concentration of<br />
immunoglobulins (gamma globulins) in the blood is another important test.<br />
Immunoglobulins are proteins called “antibodies” that are made by B cells in<br />
healthy individuals to protect the body from infection. CLL cells do not make<br />
effective antibodies. CLL cells also interfere with the ability of the remaining<br />
normal lymphocytes to make antibodies. As a result, people with CLL often have<br />
low levels of immunoglobulins, which increases their risk of getting infections.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 9
Treatment Planning<br />
Treatment for CLL is always changing due to new treatments and research from<br />
clinical trials. <strong>The</strong>refore, before treatment begins, it is important to consider getting<br />
a second opinion at a center with a CLL-specific expert. Additionally, there are<br />
continuously updated diagnosis and treatment guidelines published by the National<br />
Comprehensive Cancer Network (NCCN) at www.nccn.org, which provide<br />
guidance to doctors.<br />
Staging. Staging for CLL helps doctors to both assess how the disease is expected<br />
to progress over time and also to develop a treatment plan (see Table 1. below).<br />
Staging systems for CLL take into account<br />
{ { <strong>The</strong> elevation of blood and marrow leukemic lymphocyte counts<br />
{ { <strong>The</strong> size and distribution of lymph nodes<br />
{ { <strong>The</strong> spleen size<br />
{ { <strong>The</strong> degree of anemia and the extent of decreased blood platelet counts.<br />
Table 1. Commonly Used CLL Staging Systems<br />
Rai Staging System<br />
Stage and Signs at Diagnosis<br />
Low Risk—0<br />
Abnormal increase in the number of<br />
lymphocytes in the circulating blood and<br />
marrow<br />
Intermediate Risk—I & II<br />
Abnormal increase in the number of<br />
lymphocytes in the circulating blood and<br />
marrow and enlarged lymph nodes<br />
or<br />
Abnormal increase in the number of<br />
lymphocytes in the circulating blood and<br />
marrow and enlarged spleen and/or liver<br />
High Risk—III & IV<br />
Abnormal increase in the number of<br />
lymphocytes in the circulating blood and<br />
marrow and anemia (hemoglobin
Chromosomal Changes. Certain chromosomal changes can help the doctor<br />
to identify those people with CLL who may benefit from closer medical followup<br />
or certain types of therapy. About half of the people with CLL have CLL cells<br />
with chromosomal abnormalities when tested with a method called “G-banding<br />
karyotyping.” About 80 percent of the people with CLL have chromosomal<br />
abnormalities when tested with a method called “fluorescence in situ hybridization<br />
(FISH).” <strong>The</strong> following examples are some of the more common chromosomal<br />
abnormalities:<br />
Del 13q Deletions on the long arm of chromosome 13 (del<br />
13q) are the most common. Del 13q with no other<br />
chromosomal abnormalities is associated with a relatively<br />
more favorable outcome.<br />
Trisomy 12 About 10 to 20 percent of patients have CLL cells with<br />
three copies of chromosome 12 (trisomy 12) instead of<br />
the expected two chromosomes. Trisomy 12 is associated<br />
with intermediate-risk CLL. Trisomy 12 with other<br />
chromosomal abnormalities is associated with a higher risk<br />
than trisomy 12 alone.<br />
Del 11q Up to 20 percent of people with CLL have deletions in<br />
CLL cells in the long arm of chromosome 11 (del 11q).<br />
<strong>The</strong> proportion of CLL patients with del 11q tend to<br />
be younger with large lymph nodes and have high-risk<br />
disease.<br />
Chromosome 14 or Structural abnormalities of chromosome 14 or<br />
Chromosome 6 chromosome 6 in CLL cells also indicate higher-risk<br />
disease.<br />
Del 17p About 5 percent of people with CLL at diagnosis have<br />
deletions in the short arm of chromosome 17 (del 17p).<br />
<strong>The</strong> critical gene in this region that is typically deleted is<br />
TP53. People who have CLL with del 17p tend to have<br />
higher-risk disease and usually do not respond as well to<br />
standard initial therapy. <strong>The</strong>ir CLL treatment needs to be<br />
approached in a different manner.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 11
Other factors may be signs of faster-growing disease (higher-risk CLL) and indicate<br />
the need for closer follow-up with the doctor. For example:<br />
Blood lymphocyte People with CLL whose lymphocyte number doubles in<br />
doubling one year have higher-risk CLL and need closer followup;<br />
a lymphocyte number that remains stable indicates a<br />
relatively lower risk.<br />
CD38 CD is an abbreviation for “cluster designation,” a term<br />
used with a number to identify a specific molecule on the<br />
surface of an immune cell. <strong>The</strong> expression of CD38 on<br />
CLL cells may be an indicator of higher-risk CLL.<br />
B2M A higher level of serum beta 2-microglobulin, (B2M) a<br />
protein that is shed from CLL cells, is associated with a<br />
greater extent of disease. Several studies have found that<br />
B2M and other serum markers, such as CD23, may help<br />
predict survival or progression-free survival. Tests for these<br />
markers need to be standardized, and further study in<br />
clinical trials is needed to evaluate their relative value in<br />
managing the treatments of people with CLL.<br />
Unmutated IgHv <strong>The</strong> unmutated immunoglobulin heavy chain variable<br />
region gene (IgHv) suggests the likelihood of higher-risk<br />
disease. Forty percent of CLL patients at diagnosis will<br />
have this whereas 60 percent will have the more favorable<br />
IgHv mutated disease.<br />
ZAP-70 ZAP-70 (zeta-associated protein 70), when increased, may<br />
be associated with higher-risk disease. It should be noted<br />
that further study in clinical trials is needed to standardize<br />
the assessment of ZAP-70. <strong>The</strong> National Comprehensive<br />
Cancer Network (NCCN) guidelines state that the<br />
evaluation of ZAP-70 expression by flow cytometry can<br />
be challenging and is not recommended outside of a<br />
clinical trial.<br />
page 12 I 800.955.4572 I www.LLS.org
Treatment<br />
Current therapies do not offer patients a cure for CLL, but there are treatments that<br />
help manage the disease. Treatments for CLL include<br />
{ { Watch and wait<br />
{ { Single or combination drug therapy<br />
{ { White cell (neutrophil) growth factors<br />
{ { Radiation therapy (rarely used)<br />
{ { Splenectomy (rarely used)<br />
{ { Treatment in a clinical trial (see page 20).<br />
{ { Drug therapy with new drugs or new drug combinations<br />
{ { High-dose chemotherapy and allogeneic stem cell transplantation.<br />
<strong>The</strong> goals of CLL treatments are to<br />
{ { Slow the growth of the CLL cells<br />
{ { Provide long periods of remission (when there are no signs of CLL and/or<br />
people feel well enough to go about their day-to-day activities)<br />
{ { Improve survival<br />
{ { Help people to feel better if they have infections, fatigue or other symptoms.<br />
Some people with CLL can be managed with a watch and wait approach for years<br />
before the disease progresses. <strong>The</strong> decision to treat a person with CLL is based on a<br />
number of factors (see Table 2).<br />
Table 2. Some Factors That Influence the Decision<br />
to Treat Patients Who Have CLL*<br />
Enlarging lymph nodes<br />
Enlarging spleen<br />
Worsening anemia<br />
Absolute lymphocyte count (>300)**<br />
Falling platelet count<br />
CLL symptoms (such as fatigue, night sweats, weight loss, fever, etc.)<br />
* Several of these factors are often present at the same time.<br />
** Rapidly rising lymphocyte count in asymptomatic patients may not be an independent factor to begin treatment.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 13
A person with CLL is usually treated by a hematologist or an oncologist. People are<br />
advised to consult with a doctor who specializes in treating patients with leukemia<br />
and to discuss their most appropriate treatment options—including whether or not<br />
participation in a clinical trial is recommended.<br />
Watch and Wait. People with CLL who have minimal changes in their blood<br />
counts and no symptoms are usually managed with observation alone. This<br />
approach includes medical examinations and periodic testing to determine whether<br />
the disease is stable or beginning to progress. People with CLL being treated with a<br />
watch and wait approach are counseled by their doctors to seek medical assistance<br />
if they develop fevers or other signs of infection or illness. When, or if, the disease<br />
begins to progress, active treatment is started.<br />
People are often concerned when they receive a diagnosis of CLL and then learn<br />
that they will not begin treatment right away. It is important to know that the<br />
watch and wait approach is the current standard of care for people with CLL who<br />
have minimal changes in their blood counts and no symptoms. Many studies have<br />
compared the watch and wait approach to an early treatment approach for people<br />
with low-risk CLL. To date, no benefits of early treatment for people with low-risk<br />
CLL have been shown. Several studies have confirmed that the use of alkylating<br />
agents in patients with early-stage disease does not prolong survival. <strong>The</strong>re are also<br />
risks of early treatment including potential side effects and treatment complications.<br />
Patients may build up a resistance to the drugs used and would not be able to use<br />
them again when treatment for progressive disease is necessary. Deferred treatment<br />
versus early treatment for people with CLL who are symptom-free is an area of<br />
ongoing study in clinical trials.<br />
Many patients take alternative medicines during this time period. <strong>The</strong> active<br />
ingredient of green tea (EGCG) has been studied preliminarily as a therapy to<br />
prevent CLL progression and has shown very modest results but reasonable safety.<br />
Other agents have not been studied extensively in this area. Patients should discuss<br />
taking such alternative medications with their doctors. For more information<br />
about alternative therapies, see the free LLS publication Integrative Medicine &<br />
Complementary and Alternative <strong>The</strong>rapies as a Part of Blood Cancer Care.<br />
Drug <strong>The</strong>rapies. Patients who have symptomatic, intermediate- and high-risk<br />
disease are usually treated with chemotherapy and/or monoclonal antibody therapy.<br />
<strong>The</strong> choice of recommended treatment generally depends on the patient’s overall<br />
health status, genetic markers in the leukemia cells and the stage of his or her<br />
disease. Age may be a factor for certain types of therapy. Given the importance of<br />
genetics in picking the correct therapy for CLL, it is important that FISH studies<br />
are done to look for del (17p) and del (11q) prior to starting treatment for CLL.<br />
<strong>The</strong> following therapies may be used to treat people with newly diagnosed CLL,<br />
relapsed CLL or refractory CLL (see Relapsed or Refractory CLL on page 17).<br />
page 14 I 800.955.4572 I www.LLS.org
Chemotherapy. Chlorambucil (Leukeran®) is a long-used form of chemotherapy<br />
for CLL. It is a pill (oral) and remains one standard therapy for older patients (65<br />
years or older). Fludarabine (Fludara®) is considered to be one of the most effective<br />
types of chemotherapy for CLL in younger patients. Drug combinations, including<br />
fludarabine and cyclophosphamide (Cytoxan®) were shown to improve response<br />
and remission time of CLL patients. Fludarabine and cyclophosphamide (FC)<br />
combination therapy is most important for treating the genetic group of CLL with<br />
del (11q). Combination of fludarabine with rituximab (Rituxan®) (FR), a CD20<br />
antibody, (see Monoclonal Antibody <strong>The</strong>rapy below) or FC with Rituxan (FCR) is<br />
called “chemoimmunotherapy.” Studies comparing treatment with chemotherapy<br />
(fludarabine or FC) with chemoimmunotherapy (FR or FCR) have shown that FR or<br />
FCR treatment significantly improve the frequency of complete response, remission<br />
duration, and overall survival in previously untreated people with CLL (see Treatment<br />
Response and Follow-Up Care on page 22).<br />
While it is clear that FCR is the best treatment for CLL patients with del (11q), the<br />
benefit of this (versus FR) is not as clear in other genetic groups and is currently being<br />
studied in clinical trials. <strong>The</strong> hesitancy of some doctors to use cyclophosphamide in<br />
FCR, in part, comes from a higher risk that may arise of both short and long-term<br />
complications, such as chronic heart failure. Trials using fludarabine in patients 65<br />
years or older, have not shown as much benefit. Additionally, patients with del (17p)<br />
do not respond as well or for as long to fludarabine-based therapies. <strong>The</strong>refore, if del<br />
(17p) is present on a FISH test, it is important for patients to be evaluated early for<br />
consideration of reduced-intensity allogeneic stem cell transplantation or to strongly<br />
consider participating in a clinical trial.<br />
Bendamustine (Treanda®) is another type of chemotherapy that is approved for<br />
the treatment of CLL. Combination therapy with Treanda and Rituxan in both<br />
untreated and previously treated CLL patients have shown promising results and<br />
are commonly being administered as second-line therapy. A randomized trial is<br />
comparing Treanda and Rituxan to FCR in previously untreated CLL patients.<br />
Patients with del (17p) generally do not respond well or for long to Treanda therapy<br />
as initial therapy.<br />
Monoclonal Antibody <strong>The</strong>rapy. Monoclonal antibodies are proteins that are<br />
bioengineered in the laboratory. Each monoclonal antibody therapy is designed to<br />
recognize a specific molecule on a cell. <strong>The</strong> monoclonal antibody therapy targets<br />
the molecule and attaches to the cell, causing the cell to die.<br />
<strong>The</strong> monoclonal antibody therapies rituximab (Rituxan®), ofatumumab (Arzerra®)and<br />
alemtuzumab (Campath®) are used to treat people with CLL (see Table 3 on page 17).<br />
Rituxan and Arzerra target CD20 on the CLL cell’s surface; Campath targets CD52.<br />
Rituxan is FDA approved for combination with fludarabine and cyclophosphamide<br />
in symptomatic, previously untreated and treated CLL. Arzerra is FDA approved for<br />
the treatment of patients with CLL that is refractory to fludarabine and alemtuzumab.<br />
Campath is FDA approved as a single agent for CLL treatment.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 15
<strong>The</strong>se therapies continue to be studied in clinical trials in combination with<br />
chemotherapy and other biologic therapies such as lenalidomide (Revlimid®).<br />
(see Clinical Trials on page 20).<br />
Whereas most chemotherapy affects normal tissue cells as well as CLL cells,<br />
monoclonal antibody therapy may affect some normal lymphocytes but spare most<br />
other cells. This is particularly true for CD20 antibodies (Rituxan and Arzerra).<br />
Even though the infusion of a monoclonal antibody into a patient’s vein may cause<br />
a short period of fever, chills or low blood pressure, generally people experience less<br />
troubling side effects with monoclonal antibody therapy than with chemotherapy.<br />
<strong>The</strong> drugs most commonly used to treat CLL are shown in Table 3 on page 17.<br />
White Cell (neutrophil) Growth Factors. Treatment for CLL may include<br />
administering blood cell growth factors to improve low white cell counts.<br />
Treatment with white blood cell growth factors may help people with CLL to<br />
tolerate the side effects of higher doses of chemotherapy (see Complications: CLL or<br />
CLL Treatment on page 18).<br />
Radiation <strong>The</strong>rapy. Radiation is sometimes used to shrink large lymph node<br />
masses or masses in locations that interfere with the function of a neighboring body<br />
part, such as the kidney, the gastrointestinal tract or the throat. This treatment is<br />
rarely used in CLL.<br />
Splenectomy. CLL cells can accumulate in the spleen and become problematic in<br />
some people with CLL. Surgical removal (splenectomy) of a very enlarged spleen<br />
may improve blood cell counts. This approach is used selectively because it is only<br />
beneficial if the patient’s spleen is affected by CLL.<br />
page 16 I 800.955.4572 I www.LLS.org
Table 3. Some Drugs Used to Treat <strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong><br />
{ { Bendamustine (Treanda®)<br />
{ { Chlorambucil (Leukeran®)<br />
{ { Cladribine (Leustatin®)<br />
{ { Cyclophosphamide (Cytoxan®)<br />
{ { Doxorubicin (Adriamycin®)<br />
{ { Fludarabine (Fludara®)<br />
{ { Prednisone<br />
{ { Alemtuzumab (Campath®)<br />
{ { Ofatumumab (Arzerra®)<br />
{ { Rituximab (Rituxan®)<br />
{ { GA101*<br />
{ { Xm5574*<br />
{ { TRU-016*<br />
Chemotherapy<br />
Monoclonal Antibody <strong>The</strong>rapy<br />
Other Drugs<br />
{ { PCI-32765 (BTK kinase inhibitor)*<br />
{ { CAL-101 (PI3-kinase inhibitor)*<br />
{ { Flavopiridol (CDK kinase inhibitor)*<br />
{ { Dinaciclib (CDK kinase inhibitor)*<br />
{ { Lenalidomide (Revlimid®)*<br />
[immunomodulator]<br />
* Under study in clinical trials<br />
Relapsed or Refractory CLL. “Relapsed CLL” is the term for disease that<br />
responded to therapy but, after six or more months, stopped responding.<br />
“Refractory disease” is the term for CLL that does not result in a remission (but<br />
may be stable) or disease that gets worse within six months of the last treatment.<br />
People who are treated for relapsed or refractory CLL often have good quality years<br />
of remission after more treatment. Treatment guidelines for people with relapsed<br />
CLL are generally the same as treatment for newly diagnosed people.<br />
People who have refractory CLL with a short time to progression after the first<br />
treatment and/or CLL cells with del 17p often do not respond to standard<br />
chemotherapy. <strong>The</strong>se people are advised to speak to their doctors about whether<br />
or not treatment in a clinical trial is a good option for them. Investigative clinical<br />
protocols for drug therapies or allogeneic stem cell transplantation may offer<br />
appropriate treatment options (see Clinical Trials on page 20).<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 17
Complications: CLL or CLL Treatment<br />
Infection. Infections are a common complication for people with CLL.<br />
Because of this high risk of infections, immediate vaccination for pneumococcal<br />
pneumonia with Prevnar 13® (repeated every 5 years) and a yearly flu vaccine is<br />
recommended. CLL patients do not respond well to vaccines due to their immune<br />
system depression. CLL patients should never receive live vaccines (such as the<br />
shingles vaccine).<br />
A higher risk of infection is caused by<br />
{ { <strong>The</strong> inability of the person’s CLL cells to make antibodies needed to fight infections<br />
{ { <strong>The</strong> effect of chemotherapy, which causes reduced cell counts for certain infectionfighting<br />
white cells in the blood, specifically neutrophils and monocytes.<br />
Antibiotic therapy is usually required to treat bacterial or fungal infections during the<br />
course of the disease. People who get recurrent infections may also receive injections<br />
of immunoglobulin (gamma globulin) on a regular basis to correct the immune<br />
deficiency. While immunoglobulin is expensive, it does have benefit in decreasing<br />
the frequency of infections in CLL patients with low levels of this in the blood.<br />
CLL-related low blood counts are often efficiently corrected by CLL therapy.<br />
However, the use of white cell growth factors may benefit patients who experience<br />
prolonged low white cell counts after treatment. Examples of white cell growth<br />
factors are<br />
{ { Granulocyte-colony stimulating factor (G-CSF) (filgrastim [Neupogen®] or<br />
pegfilgrastim [Neulasta®]) that can increase the number of neutrophils<br />
{ { Granulocyte-macrophage colony-stimulating growth factor (GM-CSF)<br />
(sargramostim [Leukine®]) that can increase the number of neutrophils and<br />
monocytes.<br />
Anemia. Anemia (low numbers of red cells) is a common side effect of<br />
chemotherapy. Some people with CLL may need blood transfusions.<br />
Richter Transformation. In about 3 to 5 percent of people with CLL, the disease<br />
transforms into an aggressive lymphoma because of a change in the characteristics<br />
of the CLL cells. This is much more common in IVgH-unmutated CLL. This<br />
pattern is referred to as a “Richter transformation” or “large cell transformation.”<br />
People with this type of CLL may have significantly enlarged lymph nodes, and<br />
may have fevers and weight loss. Tumors of lymphocytes may also develop in<br />
parts of the body other than the lymph nodes. Richter transformation is treated<br />
with aggressive chemotherapy and reduced-intensity allogeneic transplantation if<br />
feasible. Outcome for patients with Richter transformation is generally poor unless<br />
it is diagnosed prior to receiving a lot of treatment for CLL.<br />
page 18 I 800.955.4572 I www.LLS.org
Prolymphocytes. About 15 percent of people with CLL have leukemia cells that<br />
are a mix of lymphocytes and another type of white cell, called a “prolymphocyte”<br />
(see Figure 3, Panel D). Most people with this type of CLL follow a similar<br />
course to that of other people with CLL. However, for a relatively small subset of<br />
patients with this type of CLL, the blood cells may become mainly composed of<br />
prolymphocytes; the spleen may enlarge further, and the disease may become less<br />
responsive to treatment. In these cases, individuals are encouraged to talk to their<br />
doctors about the potential benefits of treatment in a clinical trial.<br />
Lymphocytes<br />
Panel A Panel B<br />
Panel C<br />
Panel D<br />
Figure 3. I Panel A shows a normal lymphocyte in the blood film of a healthy person. Panel B shows the<br />
increased frequency of lymphocytes in the blood film of a patient with CLL. Panel C shows the appearance<br />
of large granular lymphocytes in a patient with large granular lymphocytic leukemia (the arrows point to the<br />
cluster of granules in the cells), and Panel D shows the cells of prolymphocytic leukemia, which are larger than<br />
those in Panels A and B and have a light area in their nucleus, called a “nucleolus” (see arrow). This structure in<br />
the nucleus is a sign of a more immature or primitive cell.<br />
Autoimmune Hemolytic Anemia. Some people with CLL produce a type of<br />
antibody that works against their own cells. <strong>The</strong>se “autoantibodies” are usually<br />
directed against the patient’s red cells and causes them to be removed rapidly<br />
from the blood. This condition, called “autoimmune hemolytic anemia,” can<br />
worsen the effects of already low red cell counts. <strong>The</strong> “antiglobulin test” or<br />
“Coombs’ test” is used to identify the autoantibodies. Less often, the antibody<br />
works against the platelets. This condition, called “immune thrombocytopenia,”<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 19
esults in significantly decreased platelet counts. <strong>The</strong> drugs prednisone, Rituxan<br />
and cyclosporine are sometimes used to treat autoimmune hemolytic anemia and<br />
immune thrombocytopenia.<br />
Second Cancers. People with CLL have a higher risk than the general population<br />
of developing a second cancer. <strong>The</strong> second cancers that are seen most frequently<br />
are melanoma, soft tissue sarcoma, colorectal cancer, lung cancer, squamous cell<br />
skin cancer and basal cell carcinoma. <strong>The</strong> recurrence rate of basal cell carcinoma<br />
after treatment is also higher for people with CLL compared to that of the general<br />
population. Both treated and untreated people with CLL can develop acute<br />
myeloid leukemia or myelodysplastic syndromes. This complication is more<br />
common after treatment with fludarabine and cyclophosphamide (FC or FCR).<br />
Further evaluation is needed to determine whether treatment with fludarabine<br />
may increase the risk of second solid tumor cancers. It is important to follow up<br />
with your oncologist on a regular basis. More information about long-term and<br />
late effects can be found in the free LLS publication Long-Term and Late Effects of<br />
Treatment in Adults.<br />
Clinical Trials<br />
New approaches to treatment in clinical trials, many of which are being supported<br />
by LLS research programs, hold the promise of increasing the rate of remission and<br />
finding a cure for CLL.<br />
Clinical Trials. Every new drug or treatment regimen goes through a series of<br />
studies called “clinical trials” before it becomes part of standard therapy. Clinical<br />
trials are carefully designed and rigorously reviewed by expert clinicians and<br />
researchers to ensure as much safety and scientific accuracy as possible. Participation<br />
in a carefully conducted clinical trial may be the “best available” therapy. Patient<br />
participation in clinical trials in the past has resulted in the therapies we have today.<br />
LLS Information Specialists, at (800) 955-4572, can offer guidance on how<br />
patients can work with their doctors to determine if a specific clinical trial is an<br />
appropriate treatment option. Information Specialists will conduct individualized<br />
clinical-trial searches for patients, family members and healthcare professionals.<br />
This service is also available at www.LLS.org/clinicaltrials.<br />
Research Approaches. <strong>The</strong>re are clinical trials for newly diagnosed patients and<br />
patients with relapsed or refractory disease. A number of approaches are under<br />
study in clinical trials for the treatment of patients with CLL, as follows:<br />
New Drug Treatments. Specific new drug therapies under study in clinical trials<br />
for people with CLL include<br />
page 20 I 800.955.4572 I www.LLS.org
Kinase Inhibitor <strong>The</strong>rapy. Kinases are enzymes that are found in both normal<br />
cells and cancer cells. Some cancer cells can be targeted by kinase inhibitor drugs<br />
that destroy the cancer cells. Kinase inhibitor drugs may be associated with fewer<br />
side effects than some other chemotherapy agents. <strong>The</strong>re are many different<br />
kinases in CLL cells, including a phosphatidylinositol 3-kinase (PI3-kinase) and<br />
Bruton’s tyrosine kinase (BTK).<br />
Examples of kinase inhibitor therapy include<br />
{ { PCI-32765. PCI-32765 is an orally administered BTK inhibitor that is in<br />
phase II clinical trials for CLL where significant durable remissions have<br />
been observed with single agent activity and it has shown a very favorable<br />
side-effect profile. Efforts to combine PCI-32765 with other agents such as<br />
bendamustine (Treanda®) or ofatumumab (Arzerra®) are ongoing. Phase III<br />
studies are being planned for this agent. This agent does cause temporary<br />
lymphocytosis (high lymphocyte count) when given by itself but this has not<br />
been shown to have any significant clinical consequence.<br />
{ { CAL-101. CAL-101 is an orally administered PI3-kinase inhibitor that is in<br />
phase II clinical trials for CLL where significant durable remissions have been<br />
observed with single agent activity. Efforts to combine CAL-101 with other<br />
agents such as Treanda, rituximab (Rituxan®), or Arzerra are ongoing. Phase<br />
III studies are being planned for this agent. This agent also causes temporary<br />
lymphocytosis (high lymphocyte count) when given by itself but this has not<br />
been shown to have any significant clinical consequence.<br />
{ { Flavopiridol. Flavopiridol is a CDK inhibitor being studied in people with<br />
high-risk genetic features whose CLL has responded to few, if any, standard<br />
treatments. It is being studied to treat CLL or prolymphocytic leukemia<br />
arising from CLL that is refractory to fludarabine.<br />
{ { Dinaciclib. Dinaciclib is a second-generation CDK inhibitor being studied<br />
in patients with relapsed CLL who are not responsive to other therapies. It<br />
has shown activity in this group including patients with high-risk genetic<br />
features.<br />
Monoclonal Antibody. Xm5574 is an antibody that targets CD19 on the<br />
surface of CLL cells. It is being studied in phase I/II clinical trials in CLL.<br />
Immunomodulatory Drug. Lenalidomide (Revlimid®) is an oral drug that<br />
is used to treat patients with myeloma. It stimulates a person’s own immune<br />
system to attack cancer cells. This drug is being evaluated in several CLL trials,<br />
including a phase III study, to determine if Revlimid, given as a maintenance<br />
therapy, is safe and effective in further improving the quality and duration of<br />
the response to treatment. This study will compare the effects of Revlimid with<br />
the effects of a placebo. Revlimid is also being studied as a possible treatment for<br />
people with CLL following second-line therapy. Other studies include Revlimid<br />
with Rituxan or Arzerra; Revlimid, fludarabine and Rituxan combined for<br />
minimally treated and untreated CLL patients; and Revlimid, fludarabine and<br />
cyclophosphamide combined for patients with advanced-relapsed or refractory<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 21
CLL. One problem that has emerged in patients with long-term (maintenance)<br />
use of Revlimid in multiple myeloma has been the occurrence of secondary<br />
cancers. <strong>The</strong> relevance of this finding to CLL is uncertain although the current<br />
trials with Revlimid are being monitored very carefully for this complication.<br />
Improvements in Stem Cell Transplantation. New procedures for allogeneic<br />
stem cell transplantation are being studied in clinical trials. Research teams are now<br />
trying novel ways to reduce the toxicity of transplantation and make it a possible<br />
therapy for more people with CLL.<br />
Allogeneic stem cell transplantation is an investigational treatment option for<br />
people with high-risk CLL that has not responded to other standard therapies. It<br />
may be an appropriate therapy for carefully selected younger people with CLL who<br />
can be matched with a stem cell donor.<br />
A modified form of allogeneic stem cell transplantation called a “reduced-intensity”<br />
or “nonmyeloablative” allogeneic stem cell transplantation may be another<br />
transplant option for CLL patients who do not respond to other treatments.<br />
Patients being prepared for a reduced-intensity transplant receive lower dosages<br />
of chemotherapy drugs and/or radiation in preparation for the transplant,<br />
compared to the dosages given to patients receiving an allogeneic transplant.<br />
Immunosuppressive drugs are used to prevent rejection of the donor stem cells, and<br />
the engraftment of donor immune cells may allow these cells to attack the CLL<br />
cells (called “graft-versus-tumor effect”). <strong>The</strong> theory being tested with a reducedintensity<br />
transplant is that by undergoing less-toxic procedures prior to the stem<br />
cell transplant, the body is better able to withstand the infusion of donor cells.<br />
However, full donor engraftment would still take place, and the desired graftversus-tumor<br />
effect would still occur. This type of transplant is generally done for<br />
high-risk CLL patients with del (17p) early in the course of CLL and also relapsed<br />
patients who have received multiple therapies. Even if transplant is not eventually<br />
pursued, it is important for patients with del (17p) who require therapy and<br />
patients with relapsed CLL to be referred to a transplantation expert relatively early.<br />
We encourage you to contact our Information Specialists and visit www.LLS.org<br />
for more information about specific treatments under study in clinical trials.<br />
Treatment Response<br />
and Follow-Up Care<br />
Treatment Outcomes. Treatment outcomes for people with CLL vary widely,<br />
and expected outcomes are influenced by the stage of the disease, the presence or<br />
lack of various factors associated with higher-risk disease, the overall health of the<br />
patient and other factors. Studies suggest that newer treatment combinations and<br />
approaches may improve the length of survival. People with CLL should consult<br />
with their doctors to discuss individual potential outcomes.<br />
page 22 I 800.955.4572 I www.LLS.org
<strong>The</strong> National Cancer Institute-sponsored Working Group has recommended<br />
criteria to describe responses to CLL therapy. A summary of this information is<br />
presented in Table 4; it may help people with CLL who want to discuss the results<br />
of drug studies with their doctors and to make informed treatment decisions.<br />
Table 4. Responses to CLL <strong>The</strong>rapy<br />
Complete Response (CR)<br />
{ { No evidence of clinical disease for at least two months after the completion<br />
of treatment, including normal blood count (at least 1,500 neutrophils,<br />
100,000 platelets, and 11 g/dL without transfusions<br />
{ { No CLL symptoms or enlarged lymph nodes, enlarged spleen or bone<br />
marrow involvement<br />
Partial Response (PR)<br />
{ { At least a 50 percent reduction in the number of blood lymphocytes and in<br />
lymph node and spleen enlargement<br />
{ { One or more of the following must also be maintained for at least two<br />
months: platelets greater than 100,000/μL; hemoglobin >11 g/dL; or a<br />
50 percent improvement over pretreatment red cell or platelet counts<br />
without transfusions<br />
Nodular Partial Response<br />
{ { Same as CR but with persistent lymphocytic nodules in the marrow<br />
Progressive Disease<br />
At least one of the following:<br />
{ { Increase of at least 50 percent in absolute lymphocyte count or<br />
transformation to higher-risk disease. Lymphocytosis (high lymphocyte<br />
count) can be temporarily seen with the kinase inhibitors PCI-32765 and<br />
CAL-101 and do not indicate progression in absence of other signs<br />
{ { Increase of at least 50 percent in liver or spleen size or new appearance of<br />
enlarged liver or spleen<br />
{ { Increase of at least 50 percent in the sum of the products of at least two<br />
lymph nodes on two consecutive exams performed two weeks apart<br />
{ { New appearance of enlarged lymph nodes<br />
Stable Disease<br />
{ { Absence of CR or PR, without progressive disease<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 23
Follow-Up Care. People with CLL need regular medical follow-up after they have<br />
completed treatment. It is important to assess the full effect of therapy as well as to<br />
identify any return of progressive disease that may require additional therapy.<br />
Minimal Residual Disease. Some people with CLL have such a low level of<br />
remaining CLL cells after treatment that these cells cannot be detected by the<br />
usual clinical tests, such as blood and marrow examinations. <strong>The</strong> term used for<br />
this condition is “minimal residual disease” (MRD). More sensitive tests may be<br />
performed to detect the presence of abnormal cells. <strong>The</strong> methods generally used to<br />
detect MRD in people with CLL are four-color cell flow cytometry and polymerase<br />
chain reaction (PCR). <strong>The</strong> benefit of flow cytometry is its widespread reproducible<br />
use that now is standard as part of clinical trials. <strong>The</strong>se techniques may provide<br />
information that can help the doctor to recognize a disease relapse and to start<br />
treatment again. However, treating asymptomatic patients with MRD remains a<br />
research question and should not be pursued outside of clinical trials.<br />
People who have been treated for CLL and/or other cancers are encouraged to keep<br />
a record of the treatments they have received. It is a good idea to share these records<br />
with the doctors who monitor general health problems, both during treatment and<br />
after treatment ends. Regular screening and monitoring for skin, colorectal, breast<br />
and other types of cancer is advisable.<br />
Related Diseases<br />
<strong>The</strong> diseases mentioned in this section result from the cancerous transformation of<br />
a type of lymphocyte; the accumulation of these cancer cells occurs mainly in the<br />
marrow, the blood and the spleen (see Table 5 on page 25).<br />
<strong>The</strong>re are distinguishing characteristics that enable the hematology oncologist<br />
to identify each disease, including the appearance and the immunophenotype<br />
of the cancer cells; the cells’ varying effects on normal marrow and blood cell<br />
development; and the cells’ varying effects on other parts of the body, such as the<br />
kidneys, bowels and nervous system.<br />
<strong>The</strong> diseases represent a range of clinical severity. At one end of the range, there are<br />
the diseases that may be stable and may not advance in severity for some months or<br />
years, or occasionally indefinitely. At the other end of the range, there are diseases<br />
associated with difficulties that may be present at diagnosis and possibly get worse,<br />
requiring immediate treatment and frequent observation.<br />
page 24 I 800.955.4572 I www.LLS.org
Table 5. CLL and Related Diseases<br />
Less rapidly progressive<br />
<strong>Chronic</strong> lymphocytic leukemia<br />
Hairy cell leukemia*<br />
Large granular lymphocytic leukemia<br />
Small cell lymphocytic lymphoma**<br />
Waldenström macroglobulinemia*<br />
More rapidly progressive<br />
Prolymphocytic leukemia<br />
Mantle cell lymphoma*<br />
Most rapidly progressive<br />
Acute lymphoblastic leukemia*<br />
* For more information, please see the free LLS publication about this disease.<br />
** For more information about small cell lymphocytic lymphoma, please see the free LLS publication<br />
Non-Hodgkin <strong>Lymphoma</strong>.<br />
Large Granular <strong>Lymphocytic</strong> (LGL) <strong>Leukemia</strong>. LGL leukemia is another type<br />
of chronic leukemia of the lymphocytes. It is characterized by larger lymphocytes<br />
containing noticeable granules, which can be seen when the blood is examined<br />
under a microscope (see Figure 3, Panel C, on page 19). <strong>The</strong>se are not features of<br />
cells in other types of CLL. LGL leukemia is either T-cell type or NK-cell type. <strong>The</strong><br />
blood lymphocyte count is always elevated in CLL. However, it is often normal<br />
or low in LGL leukemia. Although the liver and spleen may be enlarged in LGL<br />
leukemia, the lymph nodes are not. This is another feature that distinguishes it<br />
from CLL.<br />
For patients with T-cell LGL leukemia, chemotherapy, if required, with lowdose<br />
methotrexate or cyclophosphamide, or treatment with cyclosporine, an<br />
immunomodulatory drug, may be helpful in improving the neutrophil count and<br />
the red cell count. Granulocyte-colony stimulating factor (G-CSF) may also be<br />
part of therapy to improve neutrophil counts, especially if an infection is present.<br />
Alemtuzumab (Campath®), which destroys large granular lymphocytes, is being<br />
studied in clinical trials as a potential treatment. NK-cell LGL leukemia is very<br />
resistant to therapy.<br />
Prolymphocytic <strong>Leukemia</strong>. This disease can be a B-cell or a T-cell type and<br />
features large numbers of lymphocytes in the blood. <strong>The</strong>se lymphocytes are<br />
a mixture of small lymphocytes akin to CLL cells and large, more immatureappearing<br />
lymphocytes akin to acute lymphoblastic leukemia cells.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 25
In general, prolymphocytic leukemia develops more rapidly than the chronic<br />
form of lymphocytic leukemia, but more slowly than the acute form. It is treated<br />
with the same drugs that are used for other types of lymphocytic leukemia. In<br />
addition, there are a number of clinical trials to study new treatment approaches for<br />
prolymphocytic leukemia.<br />
Normal Blood and Marrow<br />
Blood is composed of plasma and cells suspended in plasma. <strong>The</strong> plasma is largely<br />
made up of water in which many chemicals are dissolved. <strong>The</strong>se chemicals include<br />
{ { Proteins<br />
{ { Albumin, the most common protein in blood<br />
{ { Blood-clotting proteins, made by the liver<br />
{ { Erythropoietin, a protein made by the kidneys that stimulates red<br />
cell production<br />
{ { Immunoglobulins, antibodies made by plasma cells in response to infections<br />
including those we develop from our vaccinations (such as poliovirus<br />
antibodies, which are made by normal plasma cells in the bone marrow)<br />
{ { Hormones (such as thyroid hormone and cortisol)<br />
{ { Minerals (such as iron and magnesium)<br />
{ { Vitamins (such as folate and vitamin B ) 12<br />
{ { Electrolytes (such as calcium, potassium and sodium).<br />
<strong>The</strong> cells suspended in plasma include red cells, platelets and white cells<br />
(neutrophils, monocytes, eosinophils, basophils, and lymphocytes).<br />
{ { <strong>The</strong> red cells make up a little less than half the volume of the blood. <strong>The</strong>y are<br />
filled with hemoglobin, the protein that picks up oxygen in the lungs and<br />
delivers it to the organs all around the body; hemoglobin then picks up carbon<br />
dioxide from the body’s cells and delivers it back to the lungs, where it is<br />
removed when we exhale.<br />
{<br />
{ <strong>The</strong> platelets are small cells (one-tenth the size of red cells) that help stop<br />
bleeding at the site of an injury in the body. For example, when a person has a<br />
cut, the vessels that carry blood are torn open. Platelets stick to the torn surface<br />
of the vessel, clump together and plug up the bleeding site with the help of<br />
blood-clotting proteins such as fibrin and electrolytes such as calcium. Later, a<br />
firm clot forms. <strong>The</strong> vessel wall then heals at the site of the clot and returns to its<br />
normal state.<br />
page 26 I 800.955.4572 I www.LLS.org
{ { <strong>The</strong> neutrophils and monocytes are white cells. <strong>The</strong>y are called “phagocytes”<br />
(eating cells) because they can ingest bacteria or fungi and kill them. Unlike red<br />
cells and platelets, the monocytes can leave the blood and enter the tissue, where<br />
they can attack the invading organisms and help combat infection. Eosinophils<br />
and basophils are types of white cells that respond to allergens or parasites.<br />
{ { Most lymphocytes, another type of white cell, are found in the lymph nodes,<br />
the spleen and the lymphatic channels, but some enter the blood. <strong>The</strong>re are<br />
three major types of lymphocytes: T lymphocytes (T cells), B lymphocytes<br />
(B cells) and natural killer (NK) cells. Each of these cells is a key part of the<br />
immune system.<br />
Marrow is a spongy tissue where blood cell development takes place. It occupies<br />
the central cavity of bones. In newborns, all bones have active marrow. By the time<br />
a person reaches young adulthood, the bones of the hands, feet, arms and legs<br />
no longer contain functioning marrow. In adults, the spine (vertebrae), hip and<br />
shoulder bones, ribs, breastbone and skull contain the marrow that makes blood<br />
cells. <strong>The</strong> process of blood cell formation is called “hematopoiesis.” A small group<br />
of cells, the stem cells, develop into all the blood cells in the marrow by the process<br />
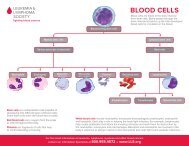
of differentiation (see Figure 4).<br />
Blood Cell & Lymphocyte Development<br />
Multipotential<br />
Hematopoietic Cells<br />
Differentiate & mature into<br />
six types of blood cells<br />
Red Cells<br />
Neutrophils<br />
Eosinophils<br />
Basophils<br />
Monocytes<br />
Platelets<br />
Stem Cells<br />
Multipotential<br />
Lymphoid Cells<br />
Differentiate & mature into<br />
three types of lymphocytes<br />
T Lymphocytes<br />
B Lymphocytes<br />
Natural Killer Cells<br />
Figure 4. I Stem cells develop into blood cells (hematopoiesis) and lymphocytic cells.<br />
In healthy individuals, there are enough stem cells to keep producing new blood cells<br />
continuously. Blood passes through the marrow and picks up the fully developed and<br />
functional red and white cells and platelets for circulation in the blood.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 27
Some stem cells also enter the blood and circulate. <strong>The</strong>y are present in such small<br />
numbers that they cannot be counted or identified by standard blood count tests.<br />
<strong>The</strong>ir presence in the blood is important because they can be collected by a special<br />
technique. <strong>The</strong>re are also methods to induce more stem cells to leave their home in<br />
the marrow and circulate in the blood, allowing a greater number of stem cells to be<br />
collected. If enough stem cells are harvested from a compatible donor, they can be<br />
transplanted into a recipient.<br />
Stem cell circulation, from marrow to blood and back, also occurs in the fetus.<br />
After birth, placental and umbilical cord blood can be collected, stored and used as<br />
a source of stem cells for transplantation.<br />
<strong>The</strong> Lymphatic System<br />
<strong>The</strong> marrow is really two organs in one. <strong>The</strong> first is the blood cell–forming organ.<br />
<strong>The</strong> second is the lymphocyte-forming organ and is a part of the immune system.<br />
<strong>The</strong> marrow produces three main types of lymphocytes:<br />
{ { B lymphocytes (B cells), which make antibodies in response to foreign antigens,<br />
especially microbes<br />
{ { T lymphocytes (T cells), which mature in the thymus. <strong>The</strong> T lymphocytes<br />
have several functions, including assisting B lymphocytes to make antibodies<br />
against invading bacteria, viruses or other microbes. <strong>The</strong> antibody attaches to<br />
the microbe, making it possible for other white cells to recognize the antibody<br />
and pull it into the cell (ingest it) along with its attached microbe. <strong>The</strong> white cell<br />
then kills and digests the microbe<br />
{ { Natural killer (NK) cells, which attack virus-infected cells without requiring an<br />
antibody or other mediation. T cells and NK cells have other functions as well<br />
and are important elements in research efforts to design immunotherapies to<br />
treat lymphoma and other cancers.<br />
<strong>The</strong> lymphocytes circulate through channels called “lymphatics,” which connect the<br />
lymph nodes to each other throughout the body. <strong>The</strong> lymphatic channels collect<br />
into large ducts that empty into blood vessels. Lymphocytes enter the blood via<br />
these ducts. Most lymphocytes are found in the lymph nodes and other parts of<br />
the lymphatic system such as the skin; spleen; tonsils and adenoids (special lymph<br />
nodes); intestinal lining; and, in young people, the thymus.<br />
page 28 I 800.955.4572 I www.LLS.org
Medical Terms<br />
Allogeneic Stem Cell Transplantation. A treatment that uses donor stem cells<br />
to restore a patient’s marrow and blood cells. First, the patient is given conditioning<br />
therapy (high-dose chemotherapy or high-dose chemotherapy with total body<br />
radiation) to treat the leukemia and to “turn off” the patient’s immune system<br />
so that the donor stem cells will not be rejected. A type of transplant called a<br />
“nonmyeloablative” or “reduced-intensity” transplant is under study. It uses lower<br />
doses of conditioning therapy and may be safer, especially for older patients. For more<br />
information, see the free LLS booklet Blood and Marrow Stem Cell Transplantation.<br />
Anemia. A decrease in the number of red cells and, therefore, the hemoglobin<br />
concentration in the blood. This results in a diminished ability of the blood to carry<br />
oxygen. If severe, anemia can cause a pale complexion, weakness, dizziness, fatigue<br />
and shortness of breath on exertion.<br />
Antibodies. Proteins released by plasma cells (derived from B lymphocytes) that<br />
recognize and bind to specific foreign substances called “antigens.” Antibodies<br />
coat, mark for destruction or inactivate foreign particles, such as bacteria, and<br />
viruses or harmful toxins. Antibodies can also be made in the laboratory, in two<br />
ways. Material from species is injected into a different species; the receiving species<br />
recognizes the materials as foreign and make antibodies to it. <strong>The</strong>se antibodies are<br />
usually polyclonal antibodies; that is, they react to multiple targets (antigens). <strong>The</strong><br />
second method involves monoclonal antibodies, which react to only one target<br />
(antigen) and can be used in several important ways. <strong>The</strong>y can be used to identify<br />
and classify types of blood cancers or they can be altered to make them useful in<br />
antibody-mediated immunotherapy.<br />
Apheresis. <strong>The</strong> process of removing certain components of a donor’s blood and<br />
returning the unneeded parts to the donor. <strong>The</strong> process, also called “hemapheresis,”<br />
circulates blood from a donor through a specialized machine, and then back to the<br />
donor. Apheresis makes it possible to remove desired elements from large volumes<br />
of blood. Platelets, red cells, white cells and plasma can be removed separately. This<br />
procedure is also used to remove circulating blood stem cells, which can be frozen,<br />
stored and later used for transplantation instead of marrow stem cells. See Platelet<br />
Transfusion.<br />
Autologous Stem Cell Transplantation. A treatment that uses a patient's<br />
own stem cells to delay the progression of certain blood cancers. <strong>The</strong> autologous<br />
transplantation process takes place after the patient achieves a complete response<br />
(remission), or a good partial response, to induction drug therapy. In this treatment<br />
1) the patient’s stem cells are harvested, usually from the blood; 2) the stem cells<br />
are frozen for later use and the patient receives conditioning drug therapy; and<br />
3) the stem cells are thawed and infused back into the patient through an<br />
indwelling catheter (central line). Patients receive supportive care to help prevent<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 29
and/or manage the side effects. Generally, after 10 to 14 days, blood counts begin<br />
to normalize and the side effects of the conditioning therapy begin to resolve. This<br />
therapy is generally not performed for CLL. For more information about all types<br />
of stem cell transplantation, see the free LLS publication Blood and Marrow Stem<br />
Cell Transplantation.<br />
Banding of Chromosomes. <strong>The</strong> staining of chromosomes with dyes that<br />
highlight transverse bands or regions on the chromosome. <strong>The</strong> bands give the<br />
chromosomes more specific features, allowing individual distinctions to be made<br />
among them. This technique permits more precise identification of chromosomes.<br />
See Fluorescence In Situ Hybridization.<br />
Basophil. A type of white cell that participates in certain allergic reactions.<br />
Beta 2-Microglobulin (B2M). A protein that is shed from CLL cells. <strong>The</strong> degree<br />
of elevation of serum B2M appears to correlate with IgHv mutation status and<br />
ZAP-70. A patient with a high ZAP-70 or an unmutated IgHv gene status is more<br />
likely to have a high B2M level. This test to measure B2M is available in most<br />
laboratories in the United States.<br />
Blast Cells. <strong>The</strong> earliest marrow cells identified by the light microscope. Blasts<br />
represent about 1 to 5 percent of normally developing marrow cells. <strong>The</strong>y are<br />
largely myeloblasts, which are cells that will develop into neutrophils. In normal<br />
lymph nodes, blasts are usually lymphoblasts; that is, cells that are part of<br />
lymphocyte development. In acute leukemias, and in some cases of myelodysplastic<br />
syndromes (MDS), abnormal blast cells (abnormal myeloblasts) accumulate in the<br />
marrow. This accumulation is associated with decreased function of the normal<br />
marrow, leading to decreased numbers of red cells, neutrophils, and platelets in the<br />
blood. <strong>The</strong> reduced number of cells, particularly of red cells, is responsible for the<br />
symptoms of MDS and acute myeloid leukemia (AML).<br />
Bone Marrow. A spongy tissue in the hollow central cavity of the bones that<br />
is the site of blood cell formation. After puberty, the marrow in the spine, ribs,<br />
breastbone, hips, shoulders and skull is most active in blood cell formation. In<br />
adults, the bones of the hands, feet, legs and arms do not contain blood-forming<br />
marrow. In these sites the marrow is filled with fat cells. When marrow cells have<br />
matured into blood cells, they enter the blood that passes through the marrow and<br />
are carried throughout the body.<br />
Bone Marrow Aspiration. A test to examine marrow cells to detect abnormalities.<br />
A marrow sample is usually taken from the patient’s hip bone. After medication<br />
is given to numb the skin, the liquid sample is removed using a special needle<br />
inserted through the bone into the bone marrow. <strong>The</strong> sample is looked at under<br />
a microscope and assessed not only for the presence of leukemia, but also for how<br />
much of it there is. <strong>The</strong> cells obtained can also be used for cytogenetic analysis, flow<br />
cytometry and other tests.<br />
page 30 I 800.955.4572 I www.LLS.org
Bone Marrow Biopsy. A test to examine marrow cells for the presence of<br />
abnormalities. This test differs from a bone marrow aspiration in that a small<br />
amount of bone filled with marrow is removed, usually from the hip (pelvic) bone.<br />
After medication is given to numb the area, a special hollow biopsy needle is used<br />
to remove a core of bone containing marrow. <strong>The</strong> marrow is examined under a<br />
microscope to determine if abnormal cells are present. Bone marrow aspiration and<br />
biopsy may be done in the doctor’s office or in a hospital. <strong>The</strong> two tests are almost<br />
always done together. Both tests are also done after treatment to determine the<br />
proportion of blood cancer cells that have been killed by therapy.<br />
Bone Marrow Transplantation. See Allogeneic Stem Cell Transplantation and<br />
Autologous Stem Cell Transplantation.<br />
CD38. An antigen on CLL cells and other cells. <strong>The</strong> expression of CD38 may be a<br />
marker to assist in predicting CLL progression.<br />
Central Line. A special tube inserted into a large vein in the upper chest. <strong>The</strong><br />
central line, sometimes referred to as an “indwelling catheter,” is tunneled under<br />
the skin of the chest to keep it firmly in place. <strong>The</strong> external end of the catheter can<br />
be used to administer medications, fluids or blood products or to withdraw blood<br />
samples. With meticulous care, central lines can remain in place for long periods<br />
of time (many months) if necessary. <strong>The</strong>y can be capped and remain in place in<br />
patients after they leave the hospital, and be used for outpatient chemotherapy or<br />
blood product administration. Several types of catheters (for example, Groshong®,<br />
Hickman®, and Broviac®) can be used for patients receiving intensive chemotherapy<br />
or nutritional support. <strong>The</strong>re are essentially two types of central lines: the one<br />
described above, in which the tube is outside the skin and requires daily care, and<br />
one called a “port,” which is implanted completely under the skin. A port can be<br />
left in place indefinitely and can be removed when no longer needed. Ports must be<br />
flushed periodically. Patients and/or caregivers are given instructions about caring<br />
for the port. See Port.<br />
Chemotherapy. <strong>The</strong> use of chemicals (drugs or medications) to kill cancer cells.<br />
Numerous chemicals have been developed for this purpose; most act to injure<br />
the DNA of the cancer cells. When the DNA is injured, the cells cannot grow<br />
or survive. Successful chemotherapy depends on the fact that malignant cells<br />
are somewhat more sensitive to the chemicals than normal cells. However, cells<br />
of the marrow are also sensitive to these chemicals, and injury to the cells of the<br />
gastrointestinal tract, skin and hair follicles causes the most common side effects of<br />
chemotherapy, such as mouth sores and hair loss.<br />
Chromosome. Any of the 46 structures (in 23 pairs) in the nucleus of all cells in<br />
the human body (except the red cells) that contain a strand of DNA. This strand is<br />
made up principally of genes, which are specific stretches of the DNA. “Genome”<br />
is the term for an organism’s complete set of DNA. <strong>The</strong> human genome has been<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 31
estimated to contain about 30,000 genes. <strong>The</strong> genes on the X and Y chromosomes<br />
are the determinants of our gender: two X chromosomes produce a female and an<br />
X and a Y chromosome produce a male. Each chromosome has a long arm (called<br />
“q”) and a short arm (called “p”). <strong>The</strong> number or size of chromosomes may be<br />
altered in blood cancer cells as a result of chromosome breakage and rearrangement<br />
(translocation). See Translocation.<br />
Clonal. <strong>The</strong> designation for a population of cells derived from a single transformed<br />
parent cell. Virtually all cancers are derived from a single cell with an injury<br />
(mutation) to its DNA and thus are monoclonal. <strong>Leukemia</strong>, lymphoma, myeloma<br />
and myelodysplastic syndromes are examples of clonal cancers; that is, cancers<br />
derived from a single abnormal cell.<br />
Cluster Designation (CD). A term used with a number to identify a specific<br />
molecule on the surface of an immune cell. It is commonly used in its abbreviated<br />
form, for example, “CD20” (the target of the monoclonal antibody therapy<br />
rituximab [Rituxan®] and “CD52” (the target of the monoclonal antibody therapy<br />
alemtuzumab [Campath®]).<br />
Colony-Stimulating Factor. See Growth Factor.<br />
Cytogenetic Analysis. <strong>The</strong> process of analyzing the number and size of the<br />
chromosomes of cells. Chromosome alterations can be detected, and in some cases<br />
it is possible to identify the actual genes that have been affected. <strong>The</strong>se findings<br />
are very helpful in diagnosing specific types of blood cancers, in determining<br />
treatment approaches and in following the response to treatment. <strong>The</strong> individual<br />
who prepares and examines the chromosomes and interprets the results is called a<br />
“cytogeneticist.”<br />
Differentiation. <strong>The</strong> process by which stem cells give rise to functional cells of<br />
a single blood cell line. Differentiation of stem cells forms red cells, platelets and<br />
white cells (neutrophils, monocytes, eosinophils, basophils and lymphocytes). See<br />
Hematopoiesis.<br />
Eosinophil. A type of white cell that participates in allergic reactions and helps<br />
fight certain parasitic infections.<br />
Erythrocytes. See Red Cells.<br />
Flow Cytometry. A test that permits the identification of specific cell types within<br />
a sample of cells. <strong>The</strong> test may be used to examine blood cells, marrow cells or<br />
cells from a biopsy. A diluted suspension of cells from one of these sources can be<br />
tagged with an antibody specific for a site on the cell surface. <strong>The</strong> antibody has a<br />
chemical attached that will emit light when activated by a laser beam. <strong>The</strong> cells flow<br />
through the instrument called a “flow cytometer”; when the cells pass through its<br />
laser beam, those with the antibody-specific surface feature light up and then can<br />
page 32 I 800.955.4572 I www.LLS.org
e counted. One use of flow cytometry is to determine whether a sample of cells is<br />
composed of T cells or B cells. This permits the doctor to determine if the leukemia<br />
or lymphoma is of the B- or T-cell type. Flow cytometry is also used to select stem<br />
cells from a mixed-cell population so that they can be used later in a stem cell<br />
transplant.<br />
Fluorescence In Situ Hybridization (FISH). A technique for studying<br />
chromosomes in tissue using DNA probes tagged with fluorescent molecules that<br />
emit light of different wavelengths (and different colors). <strong>The</strong> probes match to the<br />
chromosomes within the cells, and the chromosomes fluoresce in color. FISH can<br />
be helpful in assessing risk and treatment needs, and for monitoring treatment<br />
effectiveness, by providing a sensitive test to see abnormal cells, such as cells with<br />
deletions of 17p.<br />
G-Banding Karyotyping. A testing method that makes a certain characteristic<br />
of chromosomes easier to see. A “karyotype” is the systematic arrangement,<br />
using images, of the 46 human chromosomes of a cell. Karyotypes are examined<br />
for deviations from the expected arrangement, number, size, shape or other<br />
characteristics of the chromosomes. Each chromosome pair has a characteristic<br />
banding pattern. To make the banding pattern easier to see, a dye called “Giemsa”<br />
may be used as a stain. This process is also referred to as “G-banding.” Certain<br />
chromosomal abnormalities are associated with specific CLL subtypes. G-banding<br />
karyotyping and other cytogenetic tests provide doctors with information that<br />
contributes to determining the best treatment approach for an individual patient.<br />
This test can take several weeks after samples are obtained from a bone marrow<br />
aspiration, since the cells have to be grown in a laboratory and then stained and<br />
examined individually. Thus, the test takes longer than the FISH test, but has the<br />
advantage of being able to detect any changes that are visible because it does not<br />
rely on specific probes. Usually, both tests are done on samples from the marrow,<br />
especially at the time of diagnosis.<br />
Graft-Versus-Host Disease (GVHD). <strong>The</strong> immune attack by lymphocytes in<br />
a donor’s marrow or blood cell suspension (the graft) against the tissues of the<br />
recipient (the host). <strong>The</strong> immune cells most engaged in this reaction are donor T<br />
lymphocytes, which are present in the donor’s blood or marrow, the source of stem<br />
cells. <strong>The</strong> principal sites of attack are the skin, the liver and the gastrointestinal tract.<br />
<strong>The</strong> reaction does not occur in identical-twin transplants. <strong>The</strong> reaction may be<br />
minimal in closely matched individuals or severe in less well-matched individuals.<br />
<strong>The</strong>se reactions are mediated in part by antigens that are not in the major HLA<br />
system and cannot be matched prior to transplantation. For example, in the case<br />
of a female stem cell donor and a male recipient, factors that are produced by<br />
genes on the male recipient’s Y chromosome may be seen as foreign by the female<br />
donor’s cells, which do not share the genes on the Y chromosome. This fact does<br />
not prohibit female donors and male recipients, but it makes the risk of immune<br />
reaction higher.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 33
Graft-Versus-Tumor Effect (Graft-Versus-<strong>Leukemia</strong> Effect). <strong>The</strong> potential<br />
immune reaction of transplanted (donor) T lymphocytes to recognize and<br />
attack the malignant cells of the recipient. This effect was noted when 1) disease<br />
recurrence after transplant was seen to be more likely if the donor and recipient<br />
were identical twins than if they were nonidentical siblings; 2) disease recurrence<br />
was less likely the more pronounced the graft-versus-host disease was; and<br />
3) the removal of donor T lymphocytes decreased the incidence of graft-versushost<br />
disease (GVHD) but also resulted in a higher frequency of disease relapse.<br />
Each of these observations could be explained best as an immune attack by<br />
donor lymphocytes against recipient tumor cells that, along with the intensive<br />
conditioning treatment, serve to keep the disease in check. This effect seems to be<br />
most active in types of myeloid leukemia, although it may also occur in patients<br />
with other blood cancers.<br />
Granulocyte. A type of white cell that has a large number of granules in the cell<br />
body. Neutrophils, eosinophils and basophils are types of granulocytes.<br />
Growth Factor. A chemical used to stimulate the production of neutrophils and<br />
shorten the period of low neutrophil counts in the blood after chemotherapy.<br />
Granulocyte-colony stimulating factor (G-CSF) and granulocyte-macrophage<br />
colony stimulating factor (GM-CSF) are examples of growth factors that are made<br />
commercially. GM-CSF can also stimulate monocytes.<br />
Hemapheresis. See Apheresis.<br />
Hematologist. A doctor who specializes in the treatment of blood cell diseases.<br />
This person is either an internist who treats adults or a pediatrician who treats<br />
children.<br />
Hematopathologist. See Pathologist.<br />
Hematopoiesis. <strong>The</strong> process of blood cell development in the marrow. <strong>The</strong><br />
most undeveloped cells in the marrow are stem cells. <strong>The</strong>y start the process of<br />
blood cell development. <strong>The</strong> stem cells begin to develop into young or immature<br />
blood cells, such as red cells or various types of white cells. This process is called<br />
“differentiation.” <strong>The</strong> young or immature blood cells then further develop into<br />
fully functional blood cells. This process is called “maturation.” <strong>The</strong> mature<br />
cells leave the marrow, enter the blood and circulate throughout the body.<br />
Hematopoiesis is a continuous process that is active normally throughout life.<br />
<strong>The</strong> reason for this activity is that most blood cells live for short periods and must<br />
be replaced continuously. Red cells live for months, platelets live for a week or two<br />
and white cells live for a few days. About 500 billion blood cells are made each<br />
day. When the marrow is invaded with cancer cells, the constant demand for new<br />
blood cells cannot be met, resulting in a severe deficiency in blood cell counts.<br />
page 34 I 800.955.4572 I www.LLS.org
HLA. <strong>The</strong> abbreviation for “human leukocyte-associated antigen(s).” <strong>The</strong>se antigens<br />
are proteins on the surface of most tissue cells, and they give an individual his or<br />
her unique tissue type. HLA factors are inherited from mother and father, and<br />
the greatest chance of having the same HLA type is between siblings. On average,<br />
one in four siblings is expected to share the same HLA type. <strong>The</strong> testing for HLA<br />
factors is referred to as “tissue typing.” <strong>The</strong>re are six major groups of HLA: A, B,<br />
C, D, Dr, and Dq. <strong>The</strong>se proteins on the cell surface act as antigens when donated<br />
(transplanted) to another individual, the recipient. If the antigens on the donor cells<br />
are identical (as in identical twins) or very similar (as in HLA-matched siblings), the<br />
transplant (donated stem cells) is more likely to survive (engraft) in the recipient.<br />
In addition, the recipient’s body cells are less likely to be attacked by the donated<br />
immune cells (a result called “graft-versus-host disease”).<br />
Immunoglobulin Heavy Chain Variable Region (IgHv) Gene Status. A<br />
marker that can distinguish between CLL subtypes (unmutated IgHv and mutated<br />
IgHv). People with CLL with unmutated IgHv gene status may have a more<br />
progressive form of the disease.<br />
Immunophenotyping. A method that uses the reaction of antibodies with cell<br />
antigens to determine a specific type of cell in a sample of blood cells, marrow cells<br />
or lymph node cells. <strong>The</strong> antibodies react with specific antigens on the cell. A tag is<br />
attached to an antibody so that it can be detected. <strong>The</strong> tag can be identified by the<br />
laboratory equipment used for the test. As cells carrying their array of antigens are<br />
tagged with specific antibodies, they can be identified.<br />
Indwelling Catheter. See Central Line.<br />
Karyotype. <strong>The</strong> systematic arrangement, using images, of the 46 chromosomes in<br />
the human cell in 22 matched pairs (maternal and paternal member of each pair)<br />
by length from longest to shortest and other features, with the sex chromosomes<br />
shown as a separate pair (either XX or XY). <strong>The</strong>se 22 pairs are referred to as<br />
“autosomes.” See Fluorescent In Situ Hybridization.<br />
Leukocytes. See White Cells.<br />
Leukopenia. A decrease below normal in the concentration of blood leukocytes<br />
(white cells).<br />
Lymphadenopathy. Enlargement of lymph nodes.<br />
Lymphatic System. <strong>The</strong> system comprising the lymph nodes, the thymus gland<br />
(in the first several decades of life), the lymphatic channels, the lymphatic tissue of<br />
the marrow, the gastrointestinal tract, the skin and the spleen, along with the T, B<br />
and Natural Killer (NK) lymphocytes contained in those sites.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 35
Lymph Nodes. Small structures, the size of beans that contain large numbers<br />
of lymphocytes and are connected with each other by small channels called<br />
“lymphatics.” <strong>The</strong>se nodes are distributed throughout the body. Enlarged lymph<br />
nodes can be seen, felt or measured by computed tomography (CT) scan or<br />
magnetic resonance imaging (MRI) depending on their location and the degree of<br />
enlargement. In patients with lymphoma and some types of lymphocytic leukemia,<br />
the malignant lymphocytes grow and expand the lymph nodes so that they may<br />
become enlarged.<br />
Lymphocyte. A type of white cell that is the essential cell type in the body’s<br />
immune system. <strong>The</strong>re are three major types of lymphocytes: B lymphocytes,<br />
which produce antibodies to help combat infectious agents such as bacteria, viruses<br />
and fungi; T lymphocytes, which have several functions, including assisting B<br />
lymphocytes in making antibodies; and natural killer (NK) cells, which can attack<br />
virus-infected cells or tumor cells.<br />
Macrophage. See Monocyte/Macrophage.<br />
Minimal Residual Disease (MRD). <strong>The</strong> small amounts of cancer cells that may<br />
remain after treatment, even when blood and marrow may appear to be normal.<br />
<strong>The</strong>se residual cells can only be identified by sensitive molecular techniques.<br />
Monoclonal. See Clonal.<br />
Monocyte/Macrophage. A type of white cell that represents about 5 to 10<br />
percent of the cells in normal human blood. <strong>The</strong> monocyte and the neutrophil<br />
are the two major microbe-eating and microbe-killing cells in the blood. When<br />
monocytes leave the blood and enter the tissue, they are converted to macrophages.<br />
<strong>The</strong> macrophage is the monocyte in action: It can combat infection in the<br />
tissue, ingest dead cells (in this function it is called a “scavenger cell”) and assist<br />
lymphocytes in their immune functions.<br />
Multidrug Resistance (MDR). A characteristic of cells that makes them resistant<br />
to the effects of several different classes of drugs. <strong>The</strong>re are several forms of drug<br />
resistance. <strong>The</strong>y are each determined by genes that govern how the cell will respond<br />
to the chemical agents. One type of multidrug resistance involves the ability to<br />
force several drugs out of cells. <strong>The</strong> outer wall of the cell contains a pump that ejects<br />
chemicals, preventing them from reaching a toxic concentration. <strong>The</strong> resistance<br />
to drugs can be traced to the expression of genes that direct the formation of high<br />
amounts of a protein that prevents the drugs from affecting the malignant cells. If<br />
the gene or genes involved are not expressed or are weakly expressed, the cells are<br />
more sensitive to the drug’s effect. If the genes are highly expressed, the cells are less<br />
sensitive to the drug’s effect.<br />
Mutation. An alteration in a gene that results from a change to a part of the<br />
stretch of DNA that represents the gene. A “germ cell mutation” is present in the<br />
page 36 I 800.955.4572 I www.LLS.org
egg or the sperm and can be transmitted from parent(s) to offspring. A “somatic<br />
cell mutation” occurs in a cell and can result in the growth of that specific tissue<br />
cell into a tumor. Most cancers start after a somatic mutation. In leukemia,<br />
lymphoma or myeloma, a primitive marrow (blood-forming) or lymph node<br />
cell undergoes a somatic mutation (or mutations) that leads to the formation of<br />
a tumor. If a mutation results from a major abnormality of chromosomes, such<br />
as a translocation, it can be detected by cytogenetic examination. Sometimes the<br />
alteration in the gene is more subtle and requires more sensitive tests to identify the<br />
original mutated cell (oncogene).<br />
Myelocyte. A cell of the marrow that is a precursor of the mature granulocytes of<br />
the blood. Myelocytes are not present in the blood of healthy individuals.<br />
Neutropenia. A decrease to a below-normal concentration of neutrophils, a type<br />
of white cell.<br />
Neutrophil. <strong>The</strong> principal phagocyte (microbe-eating cell) in the blood. <strong>The</strong><br />
neutrophil is the main cell that combats infections. Patients with certain blood<br />
cancers or patients who have undergone chemotherapy often do not have sufficient<br />
quantities of neutrophils circulating in their bloodstream. A severe deficiency of<br />
neutrophils increases the patient’s susceptibility to infection. A neutrophil may be<br />
called a “poly” (polymorphonuclear neutrophil) or “seg”(segmented neutrophil)<br />
because its nucleus has several lobes.<br />
Nonmyeloablative Allogeneic Stem Cell Transplantation. See Reduced-<br />
Intensity Stem Cell Transplantation.<br />
Oncologist. A doctor who diagnoses and treats patients with cancer. Oncologists<br />
are usually internists who treat adults or pediatricians who treat children. Radiation<br />
oncologists specialize in the use of radiation to treat cancer. Surgical oncologists<br />
specialize in the use of surgical procedures to diagnose and treat cancer. <strong>The</strong>se<br />
doctors cooperate and collaborate to provide the best treatment plan (surgery,<br />
radiation therapy, chemotherapy or immunotherapy) for the patient.<br />
Pancytopenia. A decrease to a below-normal concentration of all three of the<br />
major blood cell types: red cells, white cells and platelets.<br />
Pathologist. A doctor who identifies disease by studying tissues under a<br />
microscope. A hematopathologist is a type of pathologist who studies diseases<br />
of blood cells by looking at peripheral blood smears, bone marrow aspirates and<br />
biopsies, and lymph nodes and other tissues and uses his or her expertise to identify<br />
diseases such as CLL. In addition to the microscope, a hematopathologist also uses<br />
laboratory values, flow cytometry and molecular diagnostic tests to make the most<br />
accurate diagnosis. <strong>The</strong> hematopathologist works closely with the hematologist or<br />
oncologist who sees the patient and decides on the best treatment based upon the<br />
diagnosis. See Hematopathologist.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 37
Petechiae. Pinhead-sized sites of bleeding in the skin. This type of bleeding results<br />
from a very low platelet count. <strong>The</strong> small hemorrhages are frequently seen on the<br />
legs, feet, trunk and arms. <strong>The</strong>y evolve in color from red to brown, and eventually<br />
disappear. <strong>The</strong>y stop developing when the platelet count increases.<br />
Phagocytes. Cells that readily eat (ingest) microorganisms such as bacteria and<br />
fungi and kill them as a means of protecting against infection. <strong>The</strong> two principal<br />
phagocytes are neutrophils and monocytes. <strong>The</strong>y leave the blood and enter tissue<br />
in which an infection has developed. A severe decrease in the concentrations of<br />
these cells is the principal cause of susceptibility to infection in patients treated with<br />
intensive radiation therapy and/or chemotherapy. Treatment may suppress blood<br />
cell production in the marrow, resulting in deficiencies of these phagocytic cells.<br />
Platelets. Blood cells (about one-tenth the volume of red cells) that stick to the<br />
site of blood vessel injury, aggregate and then seal off the injured blood vessel<br />
to stop bleeding. “Thrombocyte” is another word for platelet and a form of<br />
this word is often used as the prefix in describing disorders of platelets, such as<br />
thrombocytopenia (too few) or thrombocythemia (too many).<br />
Platelet Transfusion. Transfusion of donor platelets, which may be needed to<br />
support some patients treated for blood cancer. <strong>The</strong> platelets can be collected from<br />
several unrelated donors and given as pooled, random-donor platelets. <strong>The</strong> platelets<br />
from about six single-unit blood donors are required to significantly raise the<br />
platelet count in a recipient. Sufficient platelets can be obtained from one donor<br />
by a procedure known as “apheresis.” Platelets are skimmed from large volumes of<br />
blood passing through a specialized machine. <strong>The</strong> red cells and plasma are returned<br />
to the donor. <strong>The</strong> advantage of single-donor platelets is that the patient is not<br />
exposed to the different antigens on platelets from many different people and thus<br />
is less likely to develop antibodies against donor platelets. HLA-matched platelet<br />
transfusion can be given from a related donor who has an identical or very similar<br />
HLA tissue type.<br />
Polymerase Chain Reaction (PCR). A technique to expand trace amounts<br />
of DNA or RNA so that the specific type of the DNA or RNA can be studied<br />
or determined. This technique has become useful in detecting a very low<br />
concentration of residual blood cancer cells, too few to be seen using a microscope.<br />
PCR can detect the presence of one blood cancer cell among 500,000 to one<br />
million blood cancer cells. PCR requires a specific DNA (or RNA) abnormality<br />
or marker, like an oncogene, in cancer cells to be used for identifying residual<br />
abnormal cells.<br />
Port. A small device that is used with a central line that allows access to a vein.<br />
<strong>The</strong> port is placed under the skin of the chest. After the site heals, no dressings are<br />
needed and no special home care is required. To give medicines or nutrition, or to<br />
take blood samples, the doctor or nurse inserts a needle through the skin into the<br />
port. A numbing cream can be put on the skin before the port is used.<br />
page 38 I 800.955.4572 I www.LLS.org
Promyelocyte. A cell that is formed in the transition from an immature cell to a<br />
mature cell during the development cycle for certain types of white cells.<br />
Red Cells. Blood cells (erythrocytes) that carry hemoglobin, which binds oxygen<br />
and carries it to the tissues of the body. Red cells make up about 40 to 45 percent of<br />
the volume of the blood in healthy individuals.<br />
Reduced-Intensity Stem Cell Transplantation. A form of allogeneic<br />
transplantation, now in clinical trials. In reduced intensity transplantation (also<br />
called "nonmyeloablative stem cell transplantation"), patients receive lower<br />
doses of chemotherapy drugs and/or radiation in preparation for the transplant.<br />
Immunosuppressive drugs are used to prevent rejection of the graft (donor<br />
tissue). <strong>The</strong> engraftment of donor immune cells may allow these cells to attack<br />
the disease (graft-versus-leukemia effect). More study is needed to determine the<br />
effectiveness of this treatment for CLL patients. Studies to determine the usefulness<br />
of reduced-intensity stem cell transplantation in older patients are also under way.<br />
For more information about all types of stem cell transplantation, see the free LLS<br />
publication Blood and Marrow Stem Cell Transplantation.<br />
Refractory CLL. <strong>The</strong> term used to describe CLL that does not go into remission or<br />
improve substantially after treatment with standard therapy for the disease. Newly<br />
diagnosed patients or relapsed patients may have refractory disease.<br />
Relapsed CLL. <strong>The</strong> term used to describe CLL that responded to therapy but,<br />
after six or more months, stopped responding.<br />
Remission. <strong>The</strong> disappearance of evidence of a disease, usually as a result of<br />
treatment. <strong>The</strong> words “complete” and “partial” are sometimes used to further define<br />
the term “remission.” Complete remission means that all evidence of the disease is<br />
gone. Partial remission means that the disease is markedly improved by treatment,<br />
but residual evidence of the disease is present.<br />
Resistance to Treatment. <strong>The</strong> ability of cells to grow despite exposure to a<br />
chemical that ordinarily kills cells or inhibits their growth. Refractory disease is the<br />
condition in which a proportion of malignant cells resist the damaging effects of a<br />
drug or drugs. Cells develop drug resistance in several different ways. See Multidrug<br />
Resistance (MDR).<br />
Richter Transformation. In a small number of patients, a progression in their<br />
CLL in which their disease becomes more characteristic of an aggressive lymphoma<br />
such as large cell lymphoma, prolymphocytic transformation, or Hodgkin<br />
lymphoma. This change is not a second cancer, but a transformation of the CLL cells.<br />
Spleen. An organ located in the left upper portion of the abdomen just under<br />
the left side of the diaphragm. It contains clusters of lymphocytes and also filters<br />
old or worn-out cells from the blood. It is often affected in CLL and lymphoma.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 39
Enlargement of the spleen is called “splenomegaly.” Surgical removal of the spleen<br />
is known as “splenectomy.” Certain diseases are treated by removing the spleen.<br />
Most of the functions of the spleen can be performed by other organs, such as the<br />
lymph nodes and liver, but a person whose spleen has been removed is at higher<br />
risk for infection. He or she is given antibiotic therapy immediately at the first sign<br />
of infection, such as a fever.<br />
Stem Cells. Primitive cells in the marrow that are essential to the formation of red<br />
cells, white cells and platelets. Stem cells are largely found in the marrow, but some<br />
leave the marrow and circulate in the blood. Using special techniques, the stem cells<br />
in the blood can be collected, preserved by freezing and later thawed and used for<br />
stem cell therapy. See Hematopoiesis.<br />
Stem Cell Transplantation. See Allogeneic Stem Cell Transplantation;<br />
Autologous Stem Cell Transplantation.<br />
Thrombocytopenia. A decrease to a below-normal concentration of platelets in<br />
the blood.<br />
Translocation. An abnormality of chromosomes in the marrow or lymph node<br />
cells that occurs when a piece of one chromosome breaks off and attaches to<br />
the end of another chromosome. In a balanced translocation, genetic material is<br />
exchanged between two different chromosomes with no gain or loss of genetic<br />
information. When a translocation occurs, the gene at which the break occurs is<br />
altered. This is one form of somatic mutation that may transform the gene into an<br />
oncogene (cancer-causing gene). See Mutation.<br />
White Cells. Any of the five major types of infection-fighting white cells in the<br />
blood: neutrophils, eosinophils, basophils, monocytes and lymphocytes. White cells<br />
are also called “leukocytes.”<br />
ZAP-70. An abbreviation for the cell protein “zeta-associated protein 70.” A high<br />
level of ZAP-70 expression on the cells of patients with B-cell CLL is one of several<br />
factors that may predict more progressive disease. Outside of a research laboratory<br />
this test is generally not very reliable and should not be used.<br />
page 40 I 800.955.4572 I www.LLS.org
More Information<br />
Free LLS publications include<br />
Blood Transfusion<br />
Choosing a Blood Cancer Specialist or Treatment Center<br />
<strong>The</strong> CLL Guide—Information for Patients and Caregivers<br />
Cancer-Related Fatigue Facts<br />
Understanding Clinical Trials for Blood Cancers<br />
Understanding Drug <strong>The</strong>rapy and Managing Side Effects<br />
Understanding Lab and Imaging Tests<br />
Visit “Suggested Reading” at www.LLS.org/resourcecenter to see helpful books on a<br />
wide range of topics.<br />
References<br />
Hallek M, Cheson BD, Catovsky D, et al. Guidelines for the diagnosis and<br />
treatment of chronic lymphocytic leukemia: a report from the International<br />
Workshop on <strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> updating the National Cancer<br />
Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446-5456.<br />
Hallek M, Fischer K, Fingerle-Rowson G, et al. Addition of rituximab to<br />
fludarabine and cyclophosphamide in patients with chronic lymphocytic leukemia:<br />
a randomized, open-label, phase 3 trial. Lancet. 2010;376:1164-1174.<br />
Howlader N, Noone AM, et al, eds. SEER Cancer Statistics Review, 1975-2008,<br />
National Cancer Institute. Bethesda, MD, www.seer.cancer.gov/csr/1975_2008/,<br />
based on November 2010 SEER data submission, posted to the SEER website, 2011.<br />
Accessed November 9, 2011.<br />
Jaglowski SM, Alinari L, Lapalombella R, et al. <strong>The</strong> clinical application<br />
of monoclonal antibodies in chronic lymphocytic leukemia. Blood.<br />
2010;116(19):3705-3714.<br />
Kipps TJ. Chapter 94. <strong>Chronic</strong> lymphocytic leukemia and related diseases. In:<br />
Lichtman MA, Kipps TJ, Seligsohn U, Kaushansky K, Prchal, JT: Williams<br />
Hematology, 8e. Available from: AccessMedicine. Accessed November 9, 2011.<br />
National Comprehensive Cancer Network. Practice Guidelines in<br />
Oncology—v.1.2011. Non-Hodgkin <strong>Lymphoma</strong>. www.nccn.org/professionals/<br />
physician_gls/f_guidelines.asp. Accessed November 9, 2011.<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 41
Woyach JA, Ruppert AS, Heerema NA, et al. Chemoimmunotherapy with<br />
fludarabine and rituximab produces extended overall survival and progression-free<br />
survival in chronic lymphocytic leukemia: long-term follow-up of CALGB study<br />
9712. Journal of Clinical Oncology. 2011;29(10):1349-1355.<br />
Taking Steps to<br />
Cure CancerTM<br />
LIGHTTHENIGHT.ORG 877.LTN.WALK<br />
page 42 I 800.955.4572 I www.LLS.org<br />
<strong>The</strong> <strong>Leukemia</strong> & <strong>Lymphoma</strong> <strong>Society</strong>’s<br />
Light <strong>The</strong> Night Walk
Notes<br />
<strong>Chronic</strong> <strong>Lymphocytic</strong> <strong>Leukemia</strong> I page 43
Notes<br />
page 44 I 800.955.4572 I www.LLS.org
REACH OUT TO OUR<br />
INFORMATION SPECIALISTS<br />
<strong>The</strong> <strong>Leukemia</strong> & <strong>Lymphoma</strong><br />
<strong>Society</strong>’s (LLS) Information<br />
Specialists provide patients,<br />
families and healthcare<br />
professionals with the latest<br />
information on leukemia,<br />
lymphoma and myeloma.<br />
Our team consists of master’s<br />
level oncology professionals who<br />
are available by phone Monday<br />
through Friday, 9 am to 6 pm (ET).<br />
Co-Pay Assistance<br />
LLS’s Co-Pay Assistance Program<br />
helps blood cancer patients cover<br />
the costs of private and public<br />
health insurance premiums,<br />
including Medicare and Medicaid,<br />
and co-pay obligations. Support<br />
for this program is based on the<br />
availability of funds by disease.<br />
For more information,<br />
call 877.557.2672 or<br />
visit www.LLS.org/copay.<br />
For a complete directory of our patient services programs, contact us at<br />
800.955.4572 or www.LLS.org<br />
(Callers may request a language interpreter.)
For more information, please contact:<br />
or:<br />
National Office<br />
1311 Mamaroneck Avenue, Suite 310, White Plains, NY 10605<br />
Contact our Information Specialists 800.955.4572 (Language interpreters available upon request)<br />
www.LLS.org<br />
Our Mission:<br />
Cure leukemia, lymphoma, Hodgkin’s disease and myeloma, and improve the<br />
quality of life of patients and their families.<br />
LLS is a nonprofit organization that relies on the generosity of individual,<br />
foundation and corporate contributions to advance its mission.<br />
PS34 25M 12/11