Neural Tube Defects
Neural Tube Defects
Neural Tube Defects
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Neural</strong> <strong>Tube</strong> <strong>Defects</strong>
When do neural tube defects occur?
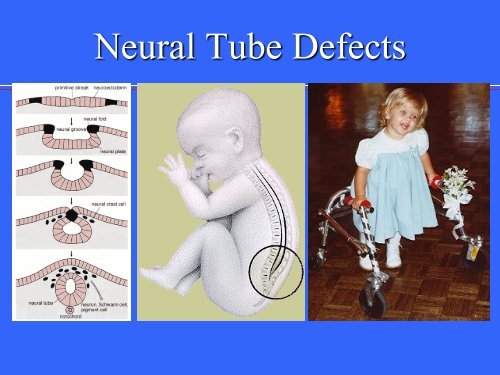
<strong>Neural</strong> <strong>Tube</strong><br />
Development<br />
Normal embryological<br />
development<br />
<strong>Neural</strong> plate<br />
development -18th day<br />
Cranial closure 24th<br />
day (upper spine)<br />
Caudal closure 26th<br />
day (lower spine)
What is Spina Bifida?<br />
A midline defect of the<br />
bone,<br />
skin,<br />
spinal column, &/or<br />
spinal cord.
Does the<br />
mother<br />
generally<br />
know she is<br />
pregnant<br />
when the<br />
neural tube is<br />
developing?<br />
Clinical Considerations<br />
Note this chart illustrates WEEKS of gestation (pregnancy).
Clinical considerations:<br />
At what point could health professionals prevent<br />
the development of neural tube defects?
Preventive Care<br />
• The United States Public Health Service<br />
recommends that: "All women of<br />
childbearing age in the United States who<br />
are capable of becoming pregnant should<br />
consume 0.4 mg of folic acid per day for the<br />
purpose of reducing their risk of having a<br />
pregnancy affected with spina bifida or other<br />
neural tube defects." Folic acid is a "B"<br />
vitamin that can be found in such foods as:<br />
cereals, broccoli, spinach, corn and others,<br />
and also as a vitamin supplement.
Clinical Considerations<br />
What factors contribute to neural tube defects?
Types of Myelodysplasia*<br />
• Spina bifida occulta<br />
• Lipomeningocele<br />
• Meningocele<br />
• Myelomeningocele = Spina Bifida<br />
*defective development of the spinal cord
Spina bifida occulta<br />
(occulta = closed)<br />
A condition<br />
involving<br />
nonfusion of the<br />
halves of the<br />
vertebral arches<br />
without<br />
disturbance of the<br />
underlying neural<br />
tissue<br />
Neurologic pathology
Lipomeningocele<br />
(lipo = fat)<br />
lipoma or fatty tumor<br />
located over the<br />
lumbosacral spine.<br />
Associated with<br />
bowel & bladder<br />
dysfunction<br />
Neurologic pathology<br />
Lipomeningocele
Neurologic pathology<br />
Meningocele (cele = sac)<br />
Fluid-filled sac with meninges involved but neural<br />
tissue unaffected
Types of Myelodysplasia<br />
Myelomeningocele<br />
or spina bifida:<br />
meninges and spinal<br />
tissue protruding<br />
through a dorsal<br />
defect in the<br />
vertebrae
The spinal defect with<br />
myelomeningocele
• Incidence<br />
– 1/1000<br />
• Prevalence<br />
Incidence and Prevalence<br />
– Increased incidence in families of Celtic and<br />
Irish heritage (genetic or environmental?)<br />
– Increased incidence in minorities (genetic or<br />
environmental?)<br />
– Increased incidence in families
Etiology<br />
<strong>Neural</strong> <strong>Tube</strong> defects may result from:<br />
• Combination of environmental and<br />
genetic causes<br />
• Teratogens – Cause developmental<br />
defects<br />
• Nutritional deficiencies - notably, folic<br />
acid deficiency
Diagnosis and Detection<br />
Amniocentesis<br />
AFP - indication of abnormal leakage<br />
Blood test<br />
Maternal blood samples of AFP<br />
Ultrasonography<br />
For locating back lesion vs. cranial signs
Spina bifida is a:<br />
static<br />
Prognosis<br />
non-progressive defect<br />
with worsening from secondary problems.<br />
The prognosis for a normal life span is generally<br />
good for a child with good health habits and a<br />
supportive family/caregiver.
Impairments associated with Spina<br />
Bifida<br />
Physiological changes below the level of the<br />
lesion generally include:<br />
abnormal nerve conduction, resulting in:<br />
somatosensory losses<br />
motor paralysis, including loss of bowel and<br />
bladder control
Impairments associated with Spina<br />
Bifida<br />
Physiological changes below the level of the lesion<br />
generally include:<br />
abnormal nerve conduction, resulting in:<br />
changes in muscle tone*<br />
*Note: Muscle tone can range from flaccid to normal<br />
to spastic; may have UMN signs with/without true<br />
spastic paraparesis; progression of neurologic<br />
dysfunction or change in neurologic status most<br />
concerning
Impairments associated with<br />
Spina Bifida<br />
Anatomical changes below the level of<br />
lesion:<br />
musculoskeletal deformities (scoliosis)<br />
joint and extremity deformities (joint contractures,<br />
club foot, hip subluxations, diminished growth of<br />
non-weight bearing limbs)<br />
osteoporosis<br />
abnormal or damaged nerve tissue
Impairments associated with<br />
Anatomical<br />
changes<br />
associated with a<br />
cervical lesion:<br />
An enlarged head<br />
caused by<br />
hydrocephalus<br />
Spina Bifida<br />
(“water on the<br />
brain” Hydrocephalus
Arnold Chiari Malformation<br />
Arnold Chiari type II<br />
Malformation:<br />
cerebellar hypoplasia<br />
(hypoplasia = reduced<br />
growth)<br />
with caudal displacement<br />
of the hindbrain through<br />
the foramen magnum<br />
usually associated with<br />
hydrocephalus
Health Problems associated with the<br />
Arnold Chiari syndrome<br />
Cranial Nerve Palsies<br />
Visual Deficits<br />
Pressure from the enlarged ventricles<br />
affecting adjacent brain structures<br />
(See Tecklin, page 166, for symptoms<br />
associated with Arnold Chiari syndrome.)
Health Problems associated with the<br />
Arnold Chiari syndrome<br />
Cognitive and perceptual problems:<br />
Potential for lower intellect<br />
Memory deficits<br />
Distractibility<br />
“Cocktail party personality” (chattering<br />
speech - with limited content)<br />
Visual perceptual deficits
Health Problems associated with<br />
Motor dysfunction:<br />
Arnold Chiari syndrome<br />
Upper limb incoordination: halting and<br />
deliberate movement instead of smooth<br />
continuous movement<br />
Spasticity: related to upper motor neuron<br />
lesions
Complications leading to progressive<br />
Tubular cavitation<br />
called a syrinx<br />
neurological dysfunction<br />
• Syringobulbia (syringes occurring in<br />
the brainstem)<br />
• Syringomyelia (syringes anywhere in<br />
the spinal cord)<br />
• Bowel and/or Bladder Dysfunction:<br />
potential for neurogenic bowel and/or<br />
bladder (requires clean, intermittent<br />
catheterization on a regularly timed<br />
schedule)
Hydrocephalus<br />
Hydromyelia<br />
Other Complications<br />
Tethering of the spinal cord: fixation or<br />
tethering of the distal end of the spinal cord<br />
causing intermittent bowstringing of the spinal<br />
cord between the normal cephalic attachment and<br />
the point of tether<br />
Seizures
Related Problems<br />
Skin Breakdown<br />
Decubitus ulcers and other types of<br />
skin breakdown<br />
Obesity<br />
Latex Allergy
• Surgical closure of<br />
back lesion 24-48 hrs<br />
after birth with shunt<br />
insertion within 6<br />
months<br />
Medical Management
Medical Management<br />
• Neurosurgical goals<br />
• Orthopedic goals<br />
• Urologic goals<br />
With the potential of numerous complications in<br />
sight, medical management has a variety of<br />
important goals.<br />
(See Tecklin page 180 for tables listing goals.)
Newborn<br />
Therapeutic positioning pre- and post-surgery for<br />
repair of myelomeningocele.<br />
Keep an eye out for shunt malfunction.
The Young Toddler<br />
Typically seen in a transdisciplinary clinic for<br />
management of multiple and varied medical,<br />
surgical needs, and therapeutic needs.<br />
Transdisciplinary teamwork enhances<br />
communication, prevents delays in care,<br />
coordinates management.<br />
Transdisciplinary team consists of: neurosurgeon,<br />
orthopedist, urologist, PT, OT, nurse, social<br />
worker, and may include others.
Concerns for the Young Toddler<br />
Developmental delay: delayed and<br />
abnormal head and trunk control,<br />
righting, and equilibrium responses<br />
Handling/Positioning: The child needs to<br />
develop upright head control in many<br />
positions
Structural Problems:<br />
• Congenital<br />
deformity with<br />
the following<br />
components:<br />
adductus,<br />
equinus, varus,<br />
and medial<br />
rotation<br />
Club Foot
Structural Problems:<br />
Club Foot<br />
Equinus: due to combination of a plantar-flexed talus,<br />
posterior ankle capsular contracture and shortening of<br />
the gastrocnemius<br />
Varus: frontal plane parallelism of talus and calcaneus,<br />
contracture of the medial subtalar joint capsules and<br />
contracture of the posterior tibialis<br />
Adductus and Medial rotation: metatarsus<br />
adductus, medial deviation of the neck of the talus, and<br />
medial displacement of the talonavicular joint.
Structural Problems<br />
Low Lumbar Paralysis:<br />
“sloppy knees” from<br />
absent lateral<br />
hamstrings (and<br />
active medial<br />
hamstrings and<br />
quads)<br />
Consider the nerves<br />
that innervate these<br />
muscles.
Orthoses and Equipment typical for<br />
• Total contact orthosis<br />
• A-frame (Toronto<br />
standing frame)<br />
• parapodium (Orlau<br />
swivel walker)<br />
• Star Cart<br />
• RGO (new isocentric<br />
RGO)<br />
children with SB<br />
• HKAFO<br />
• rollator walker<br />
• floor reaction AFO<br />
(a.k.a. anti-crouch<br />
orthosis)<br />
• articulating ankle joints<br />
in S1-level lesions<br />
• twister cables
Example of a Parapodium<br />
• Commonly used for<br />
children with high lesions<br />
(T12-L3)<br />
• Offers support to the hips,<br />
knees, and ankles.<br />
• (See Tecklin for additional<br />
descriptions and<br />
illustrations of orthoses<br />
used for various lesion<br />
levels.)
Activities for the Young<br />
Toddler<br />
Stimulate automatic balance responses against<br />
gravity in all positions to activate responses in the<br />
lower extremities.<br />
Encourage brief periods of well-aligned weight-bearing<br />
throughout the day to stimulate acetabular development<br />
(reducing likelihood for hip dysplasia) and prevent<br />
osteoporosis.<br />
Avoid infant walkers, jumper seats, swings, bouncer<br />
chairs, excessive use of infant car seats.
Psychosocial issues:<br />
The Adolescent<br />
• dependency on parents or caretakers<br />
• poor personal hygiene from lack of<br />
independence and motivation,<br />
• need for vocational training<br />
• loss of “cure fantasy” during adolescence
Wheelchair Issues<br />
MY OPINION: I disagree with the statement that<br />
the family should wait until the child is age 5<br />
or 6 to obtain the first wheelchair (p. 181).<br />
Consider the child’s health & quality of life<br />
with and without a wheelchair.<br />
Consult with the family & interdisciplinary team<br />
experts (physicians, Seating Clinic staff, PT<br />
with seating experience,vendors.) before<br />
making wheelchair decisions. Errors are<br />
costly.
The Adult<br />
Need to focus on health promotion and fitness.<br />
Watch for overuse syndrome, especially in<br />
upper extremities. Also, low back pain.<br />
Monitor for safe and properly fitting equipment<br />
(wheelchair, bathroom devices, supportive &<br />
protective shoes<br />
Model advocacy to improve access to<br />
community-based resources.
The Adult<br />
Need to change the status quo:<br />
Despite 21st century medicine and treatment<br />
advances, many children with SB never<br />
achieve independence - many never marry,<br />
never live away from parents. There is not<br />
necessarily a correlation between the level<br />
of independence and level of lesion.
The Challenge<br />
• Look at the case study in your “<strong>Neural</strong> <strong>Tube</strong><br />
<strong>Defects</strong>” handout. Can you answer the<br />
questions posed for the case presented?<br />
• Contact your instructor for answers to<br />
questions posed in the handout.
Sample Documentation<br />
• Look at the sample documentation of a<br />
case featuring a child with spina bifida.<br />
Can you relate the content of the<br />
medical chart to the development of a<br />
PT diagnosis and appropriate plan of<br />
care? (Give it a try.)
Summary<br />
There are several types of neural tube<br />
defects with myelomeningocele (or<br />
spina bifida) being the most commonly<br />
seen by physical therapists.
Summary<br />
A physical therapist examines the<br />
individual with spina bifida for sensory<br />
and motor deficits as well as perceptual<br />
motor deficits that might result from<br />
brain injury secondary to<br />
hydrocephalus or other neurological<br />
complications.
Summary<br />
Common health problems that require<br />
monitoring include:<br />
• musculoskeletal deformities<br />
(scoliosis), joint and extremity<br />
deformities (joint contractures, club<br />
foot, hip subluxations, diminished<br />
growth of non-weight bearing limbs),<br />
osteoporosis
Summary<br />
Neurological/integumentary<br />
complications: abnormal or<br />
damaged nerve tissue (tethering of<br />
spinal cord with growth),skin<br />
breakdown, decubitus ulcers and<br />
other types of skin problems
Summary<br />
Cardiopulmonary problems: risk for<br />
poor cardiovascular fitness<br />
other health concerns: obesity, latex<br />
allergy<br />
psychosocial problems: diminished<br />
self-esteem, poor body image, learned<br />
helplessness, potentially limited social<br />
interaction
Summary<br />
• The role of the PT in the care of an<br />
individual with spina bifida is to<br />
promote functional independence,<br />
prevent complications, and promote<br />
optimal health across the life span.
Slide 1:<br />
Illustrations<br />
http://images.google.com/imgres?imgurl=www.abbottlabs.com.au/images/medcond/spinalcord.gif&imgrefurl<br />
=http://www.abbottlabs.com.au/html/add/medcond/afp.html&hl=en&h=343&w=242&start=16&prev=/i<br />
mages%3Fq%3Dneural%2Btube%2Bdefects%26svnum%3D10%26hl%3Den%26lr%3D%26ie%3DUTF<br />
-8%26oe%3DUTF-8%26sa%3DG<br />
http://www.riken.go.jp/engn/r-world/research/lab/nokagaku/develop/develop/image/01b.gif<br />
http://www.sbagno.org/sb-5.jpg<br />
Slide 4:<br />
http://medicine.ucsd.edu/peds/Pediatric%20Links/Links/Neonatology/<strong>Neural</strong>%20<strong>Tube</strong>%20<strong>Defects</strong>%20N<br />
EJM%20Nov%201999_files/image005.gif<br />
Slide 5:<br />
http://www.med.umich.edu/lrc/coursepages/M1/embryology/embryo/images/neural_crest_and_notocord.gif<br />
Slide 7:<br />
http://www.ohiorepromed.com/images/preg_23.jpg
Slide 10<br />
Illustrations<br />
http://www.stocktonbeachbackpackers.com.au/images/sauna.jpg<br />
Slide 12:<br />
http://www.mercksource.com/ppdocs/us/common/dorlands/dorland/images/fig_s_0040.jpg<br />
.com/displaygraphic.php/411/shutack_fig4-BB.gif<br />
Slide 13:<br />
http://www.kinderchirurgie.ch/atlas/atlasnervensystem/lipomeningocele.JPG<br />
Slide 25:<br />
http://ped1.med.uth.tmc.edu/spinabifida/acmal_files/image002.jpg<br />
Slide 29:<br />
http://images.google.com/imgres?imgurl=www.uottawa.ca/academic/med/hendelman/rscreview/syrinx_mr<br />
i.jpg&imgrefurl=http://www.uottawa.ca/academic/med/hendelman/diagnosis/diagnosissyringomyelia.htm&hl=en&h=235&w=139&start=3&prev=/images%3Fq%3DSyringobulbia%26svnu<br />
m%3D10%26hl%3Den%26lr%3D%26ie%3DUTF-8%26oe%3DUTF-8%26sa%3DG<br />
Slide 40:<br />
http://www.physioroom.com/images/anatomy/hamstring_1.jpg