2009 Annual Report - Saint Francis Hospital and Medical Center
2009 Annual Report - Saint Francis Hospital and Medical Center
2009 Annual Report - Saint Francis Hospital and Medical Center
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
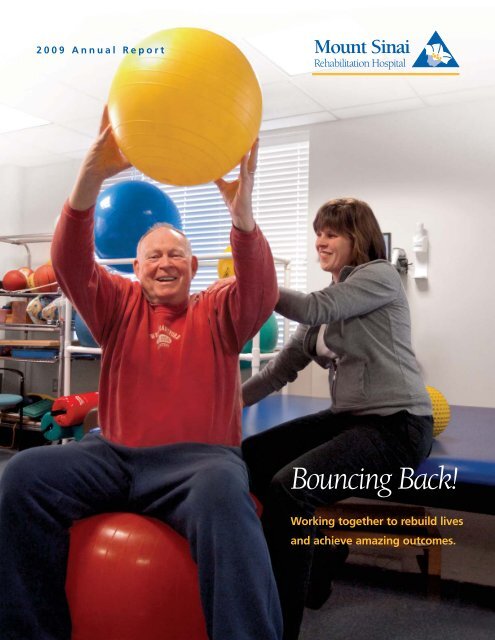
<strong>2009</strong> <strong>Annual</strong> <strong>Report</strong><br />
Bouncing Back!<br />
Working together to rebuild lives<br />
<strong>and</strong> achieve amazing outcomes.
“When I left the hospital after<br />
my accident, I went to Mount<br />
Sinai Rehabilitation <strong>Hospital</strong>.<br />
At Mount Sinai they treated me<br />
like I was their daughter. I don’t<br />
think I would’ve gotten this much<br />
better if it wasn’t for them. I’m<br />
living back on my own <strong>and</strong> I’m<br />
back to work. There are no<br />
words to express how much<br />
gratitude I have.”<br />
~AMY, PUTNAM CT<br />
On the cover: Dr. Tom Halligan, whose<br />
story appears on page 4, works with<br />
Jen Shockley, his physical therapist, to<br />
increase strength <strong>and</strong> coordination.<br />
Mount Sinai Rehabilitation <strong>Hospital</strong><br />
Board of Directors<br />
Officers<br />
Christopher M. Dadlez<br />
President <strong>and</strong> Chief Executive Officer<br />
Howard W. Orr<br />
Chairman<br />
Delores Graham<br />
Vice Chairman<br />
P. Anthony Giorgio, Ph.D.<br />
Secretary<br />
Jeannine Mara<br />
Treasurer<br />
Edward S. Johnson, D.D.S.<br />
Assistant Secretary<br />
CONTENTS<br />
Directors<br />
Michael Cummings<br />
Christopher M. Dadlez<br />
Brad Davis<br />
Wendy E. Elberth<br />
P. Anthony Giorgio, Ph.D.<br />
Delores Graham<br />
Rolf Knoll, M.D.<br />
Jeannine Mara<br />
Howard W. Orr<br />
John Suisman<br />
1 Message from the<br />
President <strong>and</strong> the<br />
Chairman<br />
2 <strong>2009</strong> Highlights<br />
3 Message from the<br />
<strong>Medical</strong> Director<br />
4 A “Christmas Miracle”<br />
6 Acute Rehabilitation Nursing<br />
8 Focus on Physiatry<br />
10 Outpatient Services<br />
12 M<strong>and</strong>ell MS <strong>Center</strong><br />
14 Administration<br />
14 <strong>Medical</strong> Staff<br />
14 Clinical Services<br />
15 Therapy Staff<br />
16 Mount Sinai Foundation
A MESSAGE FROM THE PRESIDENT AND THE CHAIRMAN<br />
The field of medical rehabilitation is in a state of constant<br />
The spectrum of research activities at the M<strong>and</strong>ell <strong>Center</strong><br />
evolution, largely as a result of recent changes in Medicare policy has broadened as well, positioning Mount Sinai as an increasingly<br />
<strong>and</strong> pending national healthcare reform legislation. Although important contributor to the <strong>Saint</strong> <strong>Francis</strong> Care research portfolio.<br />
there is considerable uncertainty surrounding<br />
At a time that is challenging healthcare<br />
these changes, Mount Sinai Rehabilitation<br />
providers everywhere in ways never before<br />
<strong>Hospital</strong> continues to adapt its policies,<br />
At a time that is<br />
experienced, the Mount Sinai team remains<br />
procedures <strong>and</strong> services to remain compliant; challenging healthcare focused on improving outcomes <strong>and</strong> preserving<br />
ensure appropriate reimbursement; <strong>and</strong>,<br />
most importantly, provide exceptional<br />
patient care.<br />
For example, in <strong>2009</strong>, revenues realized<br />
providers everywhere in ways<br />
never before experienced, the<br />
Mount Sinai team remains<br />
access to the valuable care <strong>and</strong> services we<br />
provide.<br />
The success stories incorporated into<br />
this annual report underscore that value <strong>and</strong><br />
through our growth in stroke patient volume focused on improving reflect the true meaning of “Working Together,<br />
continued to compensate, in part, for<br />
outcomes <strong>and</strong> preserving Rebuilding Lives.” Patients <strong>and</strong> families alike<br />
Medicare changes that now exclude most<br />
total joint replacement patients from acute<br />
rehabilitation. This exclusion is unfortunate<br />
because outcome data reflect a more rapid<br />
recovery for joint patients in the acute rehabilitation<br />
setting than any other level of care.<br />
access to the valuable care<br />
<strong>and</strong> services we provide.<br />
benefit from individualized care provided in a<br />
contemporary setting by a dedicated,<br />
multidisciplinary team of skilled professionals.<br />
It is worth explaining that one of the distinguishing factors<br />
of acute rehabilitation is an intensive 3 hours of scheduled therapy<br />
at least 5 out of 7 days per week. As the only freest<strong>and</strong>ing, acute<br />
inpatient rehabilitation facility in Connecticut, Mount Sinai<br />
Rehabilitation <strong>Hospital</strong> is well-prepared to provide this intensity<br />
of care.<br />
In our outpatient setting, growth continues at a brisk pace.<br />
The Mount Sinai sites, in Hartford <strong>and</strong> Bloomfield at the Jewish<br />
Community <strong>Center</strong>, provide a broad array of services; <strong>and</strong> the<br />
Mount Sinai Campus site offers warmwater aqua therapy <strong>and</strong> a<br />
fitness program that many patients continue to use on an<br />
outpatient basis after completing their prescribed treatment.<br />
To date, hospital-based outpatient services are not subject to<br />
therapy caps imposed on other categories of providers.<br />
The M<strong>and</strong>ell <strong>Center</strong> for Multiple Sclerosis at Mount Sinai<br />
has enhanced its services to include a complete functional<br />
evaluation for each new patient. The evaluation encompasses<br />
physical <strong>and</strong> occupational therapy, as well as a speech <strong>and</strong><br />
language assessment. By providing the therapy evaluation at<br />
the <strong>Center</strong>, patients benefit from a comprehensive continuum<br />
of care that is not available elsewhere. The positive<br />
synergy between MS symptom management <strong>and</strong> rehabilitation<br />
services is well understood <strong>and</strong> documented in literature.<br />
Christopher M. Dadlez<br />
President <strong>and</strong> Chief Executive Officer<br />
Howard W. Orr<br />
Chairman
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 2 ]<br />
<strong>2009</strong> Highlights<br />
The Connecticut Adaptive Rowing Program (CARP) enjoyed its most<br />
successful season in <strong>2009</strong> with 22 members rowing on Wednesday<br />
evenings <strong>and</strong> 10 additional members rowing on Monday evenings.<br />
Four teams participated in the Head of the Riverfront Regatta on<br />
October 4, <strong>2009</strong>. This is the 3rd year that events were offered in the<br />
adaptive classification.<br />
The Wii Fit ® system proved to be an<br />
effective rehabilitation tool. Fitness video<br />
games that have the user perform lowerbody<br />
balance <strong>and</strong> weight-shifting activities<br />
help patients with weight-bearing<br />
rehabilitation after an injury or surgery.<br />
The Mount Sinai<br />
Rehabilitation<br />
<strong>Hospital</strong> participates<br />
in a number of<br />
research projects <strong>and</strong><br />
educational training<br />
programs with area<br />
universities <strong>and</strong> high<br />
schools.<br />
Pet Therapy is a popular<br />
program at the Rehab<br />
<strong>Hospital</strong>. The dogs <strong>and</strong><br />
their human partners<br />
provide comfort <strong>and</strong><br />
companionship to patients,<br />
<strong>and</strong> studies show that pets<br />
can lower heart rate <strong>and</strong><br />
blood pressure as well as<br />
being a positive distraction.<br />
The dogs are highly trained<br />
<strong>and</strong> know how to interact<br />
in a special way with each<br />
individual patient.<br />
Volunteers from the Day Treatment Program continue to assist a<br />
steady stream of customers at the Cream <strong>and</strong> Two Sugars coffee shop.<br />
Golfers in Motion — Members of the Connecticut Section of the Professional Golfers<br />
Association volunteered in the “Golfers in Motion” program. The program assists golfers<br />
with physical disabilities to get back on the links. The Connecticut Section PGA Foundation<br />
also awarded the program a grant to purchase adaptive golf equipment to maximize the<br />
independence <strong>and</strong> improve the skills of participants.
A MESSAGE FROM THE MEDICAL DIRECTOR<br />
Mount Sinai Rehabilitation <strong>Hospital</strong>, Connecticut’s only comparisons. So, as Congress continues to wrestle with the<br />
acute rehabilitation hospital, has continued to build on past<br />
complexities of healthcare reform, it is imperative that we advocate<br />
successful initiatives during another busy year.<br />
for continued access to the specialized care <strong>and</strong> services we provide<br />
I invite you to explore this annual report to gain an<br />
to those in need.<br />
underst<strong>and</strong>ing of the importance of outcomes in the field of<br />
I wish to extend my sincere gratitude to our staff for the<br />
rehabilitation. What we like to refer to as a “three-pronged<br />
compassion, commitment, <strong>and</strong> expertise demonstrated on a daily<br />
approach” to patient care allows an<br />
basis; to our Board of Directors <strong>and</strong> generous donors for their<br />
interdisciplinary team to actualize each<br />
vision <strong>and</strong> leadership; <strong>and</strong> finally to our patients<br />
individualized plan of care.<br />
…as Congress continues who inspire us all. It is an honor <strong>and</strong> a privilege<br />
While acute rehabilitation involves<br />
many different medical consultants <strong>and</strong><br />
ancillary services to address complex medical<br />
conditions, it is our outst<strong>and</strong>ing therapists<br />
to wrestle with the<br />
complexities of healthcare<br />
reform, it is imperative<br />
to serve as <strong>Medical</strong> Director of Mount Sinai<br />
Rehabilitation <strong>Hospital</strong>.<br />
(PT, OT <strong>and</strong> Speech), specialized rehabilitation that we advocate for<br />
nursing <strong>and</strong> cutting-edge technology; all<br />
continued access to the<br />
coordinated by physicians board certified in<br />
Physical Medicine <strong>and</strong> Rehabilitation that make<br />
the difference in the outcomes.<br />
Mount Sinai outcomes are consistently<br />
superior to regional <strong>and</strong> national peer<br />
specialized care <strong>and</strong><br />
services we provide to<br />
those in need.<br />
Robert Krug, M.D.<br />
<strong>Medical</strong> Director,<br />
Mount Sinai Rehabilitation <strong>Hospital</strong><br />
Some very healthy numbers<br />
659 discharges<br />
10,007 patient days<br />
228 stroke patients,<br />
continues to be highest<br />
inpatient volume<br />
22,539 outpatient<br />
visits, a 5.5% increase<br />
over 2008<br />
6,192 wellness visits<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 3 ]
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 4 ]<br />
A Christmas<br />
‘Miracle’<br />
PERFORMED WITH THE HELP<br />
OF AN INTENSE PHYSICAL<br />
THERAPY REGIMEN<br />
Dr. Tom Halligan’s stroke was a thief in the night. As he slept, it<br />
stole away with the left side of his body <strong>and</strong> the next morning he<br />
woke to a new <strong>and</strong> frightening reality. When he tried to make his<br />
wife underst<strong>and</strong> that he could not move or get out of bed, she<br />
thought he was pulling one of his jokes on her. After the couple’s<br />
next-door neighbor — an emergency room doctor — confirmed<br />
the seriousness of the situation, an ambulance was called to take<br />
Dr. Halligan to <strong>Saint</strong> <strong>Francis</strong> <strong>Hospital</strong> <strong>and</strong> <strong>Medical</strong> <strong>Center</strong>. Following<br />
a week of acute care, he was moved to Mount Sinai Rehabilitation<br />
<strong>Hospital</strong>.<br />
“When Tom came here, the entire left side of his body was<br />
paralyzed,” says Jen Shockley, M.S.P.T., physical therapist. “He was<br />
still being tube-fed because he couldn’t swallow. He had trouble<br />
speaking, he slept a lot <strong>and</strong> when<br />
he was awake, he couldn’t get out<br />
of bed.”<br />
A retired surgeon with an<br />
active social <strong>and</strong> community life<br />
before the stroke, Dr. Halligan<br />
recalls how helpless he felt. “I<br />
didn’t realize how difficult a thing<br />
just getting out of bed is,” he says. “They had to hoist me with a<br />
sling into the wheelchair. It was scary. I couldn’t assume that I<br />
would ever do anything I had done before. I had no idea what the<br />
future held.”<br />
What the future held was hard work — in the form of<br />
intense therapy sessions with Jen. In the beginning, progress was<br />
painfully slow. “We started with basic exercises in bed,” Jen<br />
explains. “We got him to roll over, then we worked on sitting up.<br />
“<br />
I couldn’t assume that I would ever do<br />
anything I had done before. I had no idea<br />
what the future held.<br />
”<br />
One of Tom’s biggest obstacles was that he had no awareness of<br />
his deficits. He had what we call a ‘field cut,’ <strong>and</strong> he simply didn’t<br />
acknowledge his left side. When he sat up, he would tilt to one<br />
side — <strong>and</strong> not realize what the problem was.”<br />
At one point, Dr. Halligan’s family was told that he was<br />
making insufficient progress <strong>and</strong> might have to be moved to<br />
another facility. Whether it was the knowledge that he could be<br />
leaving or just his sheer determination to succeed, Dr. Halligan <strong>and</strong><br />
his team may never know. But something changed. “You have to<br />
make progress to stay here,” Dr. Halligan points out. “You gotta<br />
st<strong>and</strong> up.” And st<strong>and</strong> up he did. Then he walked, using the parallel<br />
bars in the physical therapy room. Within days he had progressed<br />
to a walker <strong>and</strong> not long after, to a cane.<br />
Ask Dr. Halligan what made<br />
the difference, <strong>and</strong> he’ll tell you<br />
about his team. Besides Jen, his<br />
team included physiatrist Dr.<br />
Thomas Miller; Carrie Burns, M.S.,<br />
O.T.R./L., C.B.I.S., for occupational<br />
therapy; <strong>and</strong> Nicole Scinto, M.S.,<br />
C.C.C.-S.L.P., speech language<br />
pathologist, for speech therapy. “I had seamless care,” he says.<br />
“Everyone on my team knew what I needed. They were on top of<br />
the situation — especially Jen.” Indeed, Jen knew that Dr. Halligan<br />
had the capability to work hard in his therapy sessions, <strong>and</strong> she<br />
saw the time <strong>and</strong> effort pay off. “Tom had the endurance to<br />
tolerate intense therapy. He was motivated <strong>and</strong> he took pride in<br />
what he accomplished. He could tell when he did something better<br />
than the day before.”
“I thought she was gonna kill me,” jokes Dr.<br />
Halligan. “I learned that when she asked me if I<br />
wanted to do something, ‘no’ was not an option.<br />
She was a slavedriver — also ingenious.” To help<br />
Dr. Halligan recognize that he was tilting to one<br />
side, Jen would sit him in front of a full-length<br />
mirror <strong>and</strong> compare his position to hers. She had<br />
him hit a balloon with a badminton racket, an<br />
activity that required not just coordination but<br />
also a light touch. Dr. Halligan also used the Wii<br />
system, which he found challenging. “St<strong>and</strong>ing to<br />
‘bowl’ <strong>and</strong> ‘golf’ tested my stamina, coordination,<br />
timing <strong>and</strong> strength,” he says. During a visit from<br />
his gr<strong>and</strong>sons, Jen set up a game with them that<br />
required Dr. Halligan to move sideways to catch a<br />
soft basketball. He didn’t miss a toss. Dr. Halligan<br />
wells with emotion as he recalls that day. “I knew<br />
I was going to be better after that.”<br />
Dr. Halligan spent both Thanksgiving <strong>and</strong><br />
Christmas at Mount Sinai Rehabilitation <strong>Hospital</strong>. On New Year’s<br />
Eve, he went home, walking out of the hospital on his own. “We<br />
called him our Christmas miracle,” says Jen. “Everyone was<br />
astounded.” Following his discharge, he underwent eight weeks of<br />
outpatient therapy <strong>and</strong> participated in the Adaptive Golf Program,<br />
getting back to the game he loves. He’s also a regular at the Fitness<br />
<strong>Center</strong>. Perhaps most important, he’s giving back. Each week, he<br />
returns to Mount Sinai<br />
Rehabilitation <strong>Hospital</strong> as a<br />
volunteer, talking with patients<br />
<strong>and</strong> their family members,<br />
sharing his experiences <strong>and</strong><br />
offering encouragement.<br />
He also volunteers his medical<br />
services at a walk-in clinic.<br />
“I never dreamed I’d get back<br />
to medicine,” he says, beaming.<br />
Fitness video games helped<br />
Dr. Halligan to improve his<br />
balance <strong>and</strong> coordination<br />
which allowed him to once<br />
again play golf.<br />
Members of Dr. Halligan's treatment team included (from left to right)<br />
Frank Pasini, P.A.-C., Kathy Barone, R.N., Nicole Scinto, M.S., C.C.C.-<br />
S.L.P., Jennifer Shockley, M.S.P.T. <strong>and</strong> Thomas Miller, M.D.<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 5 ]
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 6 ]<br />
On the front lines of<br />
care <strong>and</strong> recovery<br />
ACUTE REHABILITATION NURSING, 24 HOURS A DAY<br />
“<br />
Every aspect of daily life, from<br />
eating <strong>and</strong> dressing to taking<br />
medication <strong>and</strong> transferring from<br />
bed to chair, is an opportunity to put<br />
skills learned in therapy to work.<br />
”<br />
It’s 3 a.m. <strong>and</strong> rehabilitation is in session as a night nurse guides a<br />
patient toward the bathroom. Here, the same instructions <strong>and</strong> the same<br />
encouragement are given as during the day. Twenty-four hours a day,<br />
on all three shifts, rehabilitation is woven into the fabric of life at Mount<br />
Sinai Rehabilitation <strong>Hospital</strong> — <strong>and</strong> the acute rehabilitation nurse is<br />
there. Fully engaged <strong>and</strong> integrated with the rehabilitation process,<br />
the nurse advances <strong>and</strong> reinforces the goals of therapy, all the while<br />
providing ongoing care, education <strong>and</strong> coordination. This complex mix<br />
of roles — <strong>and</strong> the challenges that come with it — sets the acute<br />
rehabilitation nurse apart.
“Rehab nursing is very different from<br />
acute care nursing,” explains Amy Calvo, R.N.,<br />
C.R.R.N. “In the acute care hospital, patients are<br />
evaluated, treated, stabilized <strong>and</strong> discharged.<br />
Here, the focus for most patients is on getting<br />
them home <strong>and</strong> back to their family, work <strong>and</strong><br />
everyday life.” This focus, combined with the<br />
more complex medical needs of today’s patients<br />
(the result of ever-shorter acute hospital stays)<br />
means the rehabilitation nurse must play a<br />
variety of roles. As a caregiver, he or she<br />
performs all the functions normally associated<br />
with nursing. “A patient may not be able to do<br />
much on his or her own at first,” says Amy. “So we’re tending to<br />
basics like feeding, toileting, wound care <strong>and</strong> skin integrity. And<br />
because acute rehab treats the whole person, we’re addressing<br />
psychological <strong>and</strong> social needs as well.” As the patient progresses,<br />
caregiving incorporates rehabilitation strategies. Every aspect of<br />
daily life, from eating <strong>and</strong> dressing to taking medication <strong>and</strong><br />
transferring from bed to chair, is an opportunity to put skills<br />
learned in therapy to work. It’s also an opportunity for education.<br />
“We do a heavy amount of teaching,” Amy says. “Every patient<br />
has a discharge plan when they come here <strong>and</strong> that plan most<br />
often involves the family, because patients will need assistance<br />
when they go home. As educators, we help family members<br />
underst<strong>and</strong> the patient’s medical condition <strong>and</strong> the stages he<br />
or she will go through over time. We also teach them about<br />
medication, wound care <strong>and</strong> quality of life issues. And we make<br />
sure the patient underst<strong>and</strong>s, as much as possible, what he or<br />
she can do in terms of self-care at home.”<br />
As a member of the rehabilitation team, the acute<br />
rehabilitation nurse is part of a coordinated effort to achieve the<br />
best possible outcome for each patient. Nurses attend weekly team<br />
meetings with physiatrists, physician assistants, therapists, case<br />
managers, consultants <strong>and</strong> other adjunct staff. “We talk about<br />
After two years of rehabilitation nursing<br />
experience, a registered nurse may qualify<br />
to sit for the Rehabilitation Registered<br />
Nurse certification examination<br />
administered by the Association of<br />
Rehabilitation Nursing (ARN). C<strong>and</strong>idates<br />
who successfully pass this examination<br />
are awarded the Certified Rehabilitation<br />
Registered Nurse (C.R.R.N.) credential.<br />
where the patient is currently,” Amy explains. “And we go over<br />
therapy <strong>and</strong> nursing goals.” To ensure these goals <strong>and</strong> other vital<br />
information are communicated to everyone who comes in contact<br />
with the patient, they are posted on a white board in the patient’s<br />
room. The board may indicate, for example, the patient’s level of<br />
mobility, speech <strong>and</strong> swallowing abilities, <strong>and</strong> whether he or she<br />
can use a sliding board to transfer from bed to wheelchair. The<br />
therapy schedule is posted as well. While sharing information is<br />
important, patient privacy is safeguarded. “We’re careful with the<br />
type of information we post,” explains Amy. “And what we do<br />
post is all in our own ‘hieroglyphics.’”<br />
Another vital role of acute rehabilitation nursing is the<br />
collaborative relationship with the case manager. Right from<br />
admission, the rehabilitation nurse <strong>and</strong> the case manager focus<br />
on preparing patients for their return home, often to a new <strong>and</strong><br />
different life. Every dimension of this new life is incorporated into<br />
the discharge planning process <strong>and</strong> the rehabilitation nurse is an<br />
integral member of the planning team.<br />
Equipment unique to acute rehabilitation nursing includes the<br />
Arjo Sara Lift (a st<strong>and</strong>ing lift that allows secure transfers); the<br />
Arjo Maxi Move (a mobile passive floor lift); sliding boards for<br />
patients who can bear weight; special reclining chairs for<br />
showering; <strong>and</strong> a rotating disk, which allows patients to change<br />
direction without moving their feet.<br />
[ 7 ]
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 8 ]<br />
Achieving the best quality of life<br />
for each patient<br />
THE PHYSIATRIST TREATS THE WHOLE PERSON,<br />
ADDRESSING PHYSICAL, EMOTIONAL AND SOCIAL NEEDS.<br />
Acute rehabilitation brings together a unique group of<br />
medical professionals who blend <strong>and</strong> coordinate their skills <strong>and</strong><br />
expertise over the full continuum of care. Overseeing <strong>and</strong> directing<br />
that care — <strong>and</strong> the team that provides it — is the physiatrist, a<br />
doctor specializing in physical medicine <strong>and</strong> rehabilitation.<br />
The practice of physiatry took shape during <strong>and</strong> after World<br />
War I as doctors began to use “physiotherapy” in “reconstruction<br />
hospitals” to treat injured soldiers. Today, the scope of physiatry has<br />
broadened to restoring function lost through a variety of injuries,<br />
illnesses <strong>and</strong> disabling conditions. “Physiatry is not<br />
specific to any one disease category,” says<br />
Dr. Thomas Miller, <strong>Medical</strong> Director, Brain Injury<br />
unit <strong>and</strong> Day Treatment Program. “It can address<br />
a wide range of problems, from arthritis <strong>and</strong><br />
sports-related injuries to amputation,<br />
neurological disorders <strong>and</strong> brain injury.” At<br />
Mount Sinai Rehabilitation <strong>Hospital</strong>, the<br />
common denominator for all is an integrated,<br />
team approach to care, personalized for each<br />
patient <strong>and</strong> overseen by the physiatrist.<br />
“All patients admitted to the hospital<br />
are under the care <strong>and</strong> supervision of a<br />
“<br />
It is the physiatrist who develops<br />
the rehabilitation plan of care<br />
<strong>and</strong> assembles the team that will<br />
address the patient’s needs.<br />
”<br />
physiatrist as their primary care physician,” Dr. Miller explains.<br />
“Sometimes there are other consulting physicians — such as<br />
neurologists, cardiologists, orthopedists, urologists, psychologists —<br />
whom we need to bring in or ask questions of.” But it is the<br />
physiatrist who develops the rehabilitation plan of care <strong>and</strong>
The physiatrist reviews consultations <strong>and</strong> reports, incorporating the<br />
input of all team members in overseeing the continuum of care.<br />
assembles the team that will address the patient’s needs. Physician<br />
Assistants (PAs) work closely with the attending physiatrist,<br />
h<strong>and</strong>ling day-to-day management of medical issues. As Dr. Miller<br />
points out, “The PAs are my right h<strong>and</strong>. They interact with the<br />
patient <strong>and</strong> family, work with other team members <strong>and</strong><br />
consultants, write medical orders <strong>and</strong> do discharge paperwork.”<br />
Acute rehabilitation nurses provide patient care 24 hours<br />
a day, complementing <strong>and</strong> supplementing the work of<br />
occupational, physical <strong>and</strong> speech therapists <strong>and</strong> serving<br />
as case managers. Depending on a patient’s particular needs<br />
<strong>and</strong> goals, consultants such as orthotists, prosthetists <strong>and</strong><br />
wheelchair seating specialists may also be part of the<br />
team. “Everybody plays a vital role,” says Dr. Miller. “We like<br />
to say it’s not just a multi-disciplinary team, it’s also an interdisciplinary<br />
team. It’s not only different people doing their<br />
thing; it’s those people doing their thing in a very<br />
coordinated way.”<br />
This kind of coordination enables an intense,<br />
personalized, holistic approach to care — an approach<br />
essential in situations that require a full court press of acute<br />
rehabilitation. A good example is brain injury, where<br />
disability may run the gamut from physical <strong>and</strong> cognitive, to<br />
behavioral <strong>and</strong> emotional. “Brain injury is one of the most<br />
complicated situations in rehab,” Dr. Miller says, “because the<br />
brain controls everything we do. Not just the ability to move, but<br />
thoughts <strong>and</strong> emotions. This has a dramatic impact on the patient<br />
— <strong>and</strong> his or her family.” Once the level of that impact is assessed<br />
(can the patient walk, speak, swallow, eat, dress?) physical<br />
interventions, special equipment, medication, community resources<br />
<strong>and</strong> other services are coordinated <strong>and</strong> implemented to rebuild the<br />
patient’s life, step by step, goal by goal.<br />
In fact, as Dr. Miller says, “Rehabilitation is all about setting<br />
goals — <strong>and</strong> achieving measurable outcomes. There are very<br />
specific outcomes measurements in rehab that consider all the<br />
different activities of daily living a patient needs to do against his<br />
or her current level of function. Based on how much assistance is<br />
needed with these activities, we give the patient a number, on a<br />
0 to 7 scale — from dependent to independent. Then we reassess<br />
that score throughout his or her stay, <strong>and</strong> at discharge. The score<br />
not only indicates how the patient is doing, but how the hospital is<br />
performing as a whole.” For many patients, the focus on goals <strong>and</strong><br />
outcomes doesn’t end with discharge. Rehabilitation — <strong>and</strong> the<br />
physiatrist’s role — continue with outpatient care in the day<br />
treatment program. “It’s still intensive rehab,” says Dr. Miller, “<strong>and</strong><br />
the team still meets on a regular basis to discuss outpatient goals.”<br />
Care also may extend beyond day treatment with visits to the<br />
physiatrist’s office. Throughout, the emphasis is not just on<br />
restoring function, but also a meaningful life — <strong>and</strong> hope for the<br />
future. “It’s not just about therapy”, Dr. Miller explains. “It’s also<br />
about attitude.”<br />
Education is an important component of rehabilitation therapy.<br />
Patients <strong>and</strong> families need to underst<strong>and</strong> the patient’s medical<br />
condition <strong>and</strong> how they can work together to achieve the best<br />
possible outcome.<br />
Following medical school, physiatrists<br />
complete four additional years of residency<br />
training in physical medicine <strong>and</strong><br />
rehabilitation. Specialty board certification<br />
requires written <strong>and</strong> oral examinations<br />
administered by the American Board of<br />
Physical Medicine <strong>and</strong> Rehabilitation<br />
(ABPMR).<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 9 ]
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 10 ]<br />
Serving the community with a full spectrum of<br />
outpatient rehabilitation care<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> also provides comprehensive physical rehabilitation<br />
on an outpatient basis for people who have incurred loss of physical <strong>and</strong>/or cognitive<br />
function through illness, injury, or disease process.<br />
Gym Equipment — The Mountain Laurel Room features modern<br />
therapy <strong>and</strong> exercise equipment to help patients reach their functional<br />
potential. Highly qualified professional staff work with the patient to<br />
identify treatment goals, discharge plans, <strong>and</strong> treatment intensity,<br />
frequency <strong>and</strong> duration in order to maximize results.<br />
Reading Comprehension — Speech <strong>and</strong> language pathologists<br />
assist patients with activities <strong>and</strong> exercises to improve reading<br />
comprehension to better perform routine activities of daily living.<br />
Fine Motor Skills — Exercising workstations <strong>and</strong><br />
boards are used for treatment <strong>and</strong> rehabilitation in<br />
developing fine motor skills <strong>and</strong> exercising forearm,<br />
wrist <strong>and</strong> h<strong>and</strong> muscles.<br />
Swimming Pool — The 92-degree water in the therapeutic pool aids<br />
pain control <strong>and</strong> increases the elasticity of soft tissues. The buoyancy also<br />
aids muscle re-education <strong>and</strong> builds strength. The pool is an integral part<br />
of the hospital’s outpatient community arthritis program.
GAITRite ® Mat — The GAITRite mat,<br />
a portable, instrumented walkway, is<br />
used to analyze details of walking, such<br />
as gait pattern, step length <strong>and</strong> width,<br />
that can guide treatment decisions.<br />
S A T E L L I T E F A C I L I T I E S<br />
FES Stim Bike ® — The FES (functional<br />
electrical stimulation) Stim Bike is used to create<br />
patterned movement of the legs, enabling muscles<br />
to perform cycling work even though the user<br />
may have lost voluntary control of those muscles.<br />
Balance Master ® — The Balance<br />
Master provides assessment <strong>and</strong><br />
retraining of the sensory <strong>and</strong> voluntary<br />
motor control of balance, assisting the<br />
patient in achieving better balance control.<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> also offers a wide variety of outpatient diagnostic <strong>and</strong> treatment services at off-site<br />
locations. Advanced technology <strong>and</strong> treatment, delivered by licensed, registered, <strong>and</strong> certified professional staff, are available<br />
at the Mount Sinai Rehabilitation <strong>Hospital</strong> Physical Therapy <strong>Center</strong> at the M<strong>and</strong>ell Jewish Community <strong>Center</strong> in Bloomfield<br />
<strong>and</strong> at the <strong>Saint</strong> <strong>Francis</strong> <strong>Center</strong> for Rehabilitation <strong>and</strong> Sports Medicine at 95 Woodl<strong>and</strong> Street in Hartford.<br />
M<strong>and</strong>ell Jewish Community <strong>Center</strong> <strong>Saint</strong> <strong>Francis</strong> Care at 95 Woodl<strong>and</strong> Street<br />
Dynavision — Dynavision is used to<br />
evaluate <strong>and</strong> treat patients through forced<br />
cognitive training, honing visual reaction<br />
<strong>and</strong> sensory-motor integration.<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 11 ]
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 12 ]<br />
Caring for MS patients <strong>and</strong> their families<br />
in our community — <strong>and</strong> beyond<br />
At the M<strong>and</strong>ell <strong>Center</strong> for Multiple Sclerosis Care <strong>and</strong> Neuroscience Research, people with MS<br />
are making strides toward a better life with comprehensive care tailored to their individual needs.<br />
A multi-faceted treatment approach is used to address this complex disease, coupling therapeutic<br />
interventions with advanced technology for improved outcomes.<br />
The M<strong>and</strong>ell MS <strong>Center</strong> emphasizes early <strong>and</strong> ongoing treatment.<br />
The neurology team consists of neurologists <strong>and</strong> ancillary care<br />
providers with MS expertise who offer comprehensive treatment to<br />
address the full continuum of care. Services include consultations<br />
<strong>and</strong> evaluations for initial diagnosis <strong>and</strong> second opinion, as well as<br />
ongoing care. In each case, the goal is to control the disease <strong>and</strong><br />
its symptoms.<br />
Rehabilitation services can make an important difference in<br />
helping the MS patient with the challenges of managing everyday<br />
tasks, activities <strong>and</strong> movements.<br />
A physiatrist leads a skilled team of physical <strong>and</strong><br />
occupational therapists <strong>and</strong> speech <strong>and</strong> language<br />
pathologists who help to prevent disability <strong>and</strong><br />
improve function. Spasticity management,<br />
pain control <strong>and</strong> suggested functional<br />
adaptation are also part of the<br />
available services. Infusion<br />
therapy is offered in<br />
a suite dedicated<br />
exclusively to MS<br />
patients. Patients at<br />
the M<strong>and</strong>ell MS <strong>Center</strong><br />
benefit from this<br />
comprehensive approach<br />
to care, taking MS treatment<br />
to exciting new levels.<br />
A patient works with a<br />
member of the research team<br />
using the Anklebot ® , a robotic<br />
device designed to improve a<br />
patient’s ability to walk<br />
through computerized therapy.
Research at the M<strong>and</strong>ell <strong>Center</strong>, led by Neurologist Albert<br />
Lo, M.D., Ph.D., works specifically on underst<strong>and</strong>ing the role of<br />
rehabilitation in multiple sclerosis, from the biological to the<br />
interventional, through a comprehensive research program focused<br />
on improving outcome measures, educating the community <strong>and</strong><br />
studying the effect symptoms of the disease have on the daily life<br />
of a person with MS.<br />
A variety of approaches towards underst<strong>and</strong>ing the patient’s<br />
perspective of living with the disease, how its various forms<br />
progress, treatment of its symptoms, <strong>and</strong> even the effects of a<br />
variety of medications are all of interest. Leading-edge technology<br />
such as the Lokomat ® , Ankle-bot ® <strong>and</strong> GAITRite ® mat, leverage<br />
new discoveries about the adaptability of the human nervous<br />
system.<br />
Working together with the experienced clinical <strong>and</strong><br />
rehabilitation staff, the research team believes that progress in the<br />
area of mobility impairments will be made even more rapidly than<br />
ever before.<br />
“<br />
Leading-edge technology such as the<br />
Lokomat ® , Ankle-bot ® <strong>and</strong> GAITRite ® mat,<br />
leverage new discoveries about the<br />
adaptability of the human nervous system.<br />
”<br />
Members of the Research Team<br />
include from left to right:<br />
Bottom row, Albert Lo, M.D., Ph.D.,<br />
Jennifer Fawcett, Research Coordinator,<br />
Michelle Labas, Research Associate.<br />
Back row, Amy Neal, P.A.-C.,<br />
Wendy McCabe, M.S.P.T.<br />
A patient receives infusion therapy as part of her treatment for MS.<br />
Neurologists are part of the treatment team for patients of<br />
the MS <strong>Center</strong>, providing evaluation <strong>and</strong> treatment<br />
recommendations to help control symptoms <strong>and</strong> disease process.<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 13 ]
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 14 ]<br />
Mount Sinai<br />
Rehabilitation <strong>Hospital</strong><br />
ADMINISTRATION<br />
Christopher M. Dadlez<br />
President <strong>and</strong> Chief Executive<br />
Officer<br />
Edward S. Johnson, D.D.S.<br />
Senior Vice President<br />
Robert Krug, M.D.<br />
<strong>Medical</strong> Director<br />
Maura Murray, CRRN, BSN<br />
Director of Nursing<br />
Joan Page, MA, PT<br />
Director of Clinical Programs<br />
Shirley Fisher<br />
Administrative Associate<br />
MEDICAL STAFF<br />
MEMBERSHIP<br />
ACTIVE STAFF<br />
Raymond Chagnon, M.D.<br />
Robert Krug, M.D.<br />
Thomas Miller, M.D.<br />
ASSOCIATE MEDICAL<br />
STAFF<br />
Michelle Brisman, Ph.D<br />
Cristina Ciocca, Psy.D.<br />
Corinne Harrington, Ph.D.<br />
Beth Karassik, Ph.D.<br />
Howard Oakes, Psy.D.<br />
William Padula, O.D.<br />
Stephen Peters, Ph.D.<br />
Eugene Piasetsky, Psy.D.<br />
Tracey Sondik, Psy.D.<br />
ASSISTANT MEDICAL<br />
STAFF<br />
Denise Abate, APRN<br />
Tara Breslin, PA-C<br />
Sarah Bruns, PA-C<br />
Adrienne M. Clements, APRN<br />
Denise Cologne, PA-C<br />
Concepcion Cortes, APRN<br />
Judith Ebbets, APRN<br />
Eleanor Fritz, APRN<br />
Geriann Gallagher, APRN<br />
Sue Keefe, APRN<br />
Ann Navage, APRN<br />
Amy Neal, PA-C<br />
<strong>Francis</strong> Pasini, PA-C<br />
S<strong>and</strong>ra Rabis, APRN<br />
Nancy Scheetz, APRN<br />
PER DIEM STAFF<br />
Ovanes Borgonos, M.D.<br />
Andrew Ganeles, M.D.<br />
Noam Harel, M.D.<br />
Elizabeth Hill, M.D.<br />
Roger Jou, M.D.<br />
Malik J. Kelly, M.D.<br />
Robert Koorse, M.D.<br />
Haklai Lau, M.D.<br />
David Matuskey, M.D.<br />
Syed Naqvi, M.D.<br />
Maria Quinones, M.D.<br />
Ricardo Ruiz, M.D.<br />
Mark Safalow, M.D.<br />
Christian Sarra, M.D.<br />
Attiya M. Siddiqi, M.D.<br />
David Silver, D.O.<br />
Satyarani Tallapureddy, M.D.<br />
Aliz Tercius, M.D.<br />
Jaykumar R. Thumar, M.D.<br />
David Wolpaw, M.D.<br />
Sergio Yero, M.D.<br />
CONSULTANT STAFF BY<br />
SPECIALTY<br />
DENTISTRY<br />
Paul F. Mitchell, D.M.D.<br />
Mark Schmidt, D.D.S.<br />
J. Robert Stanko, D.M.D.<br />
FAMILY MEDICINE<br />
Patricio Bruno, D.O.<br />
Susan Wiskowski, M.D.<br />
MEDICINE<br />
Ronald Bloom, M.D. (Cardiology)<br />
John Cardone, M.D. (Cardiology)<br />
William Carney, M.D. (Nephrology)<br />
Robert Chamberlain, M.D.<br />
(Cardiology)<br />
Russell Ciafone, M.D. (Cardiology)<br />
Leonard Cohen, M.D. (Allergy)<br />
Ari Geller, D.O. (Nephrology)<br />
Steven Goldenberg, M.D.<br />
(Gastroenterology)<br />
Bruce Gould, M.D.<br />
Carolyn Kosack, M.D. (Cardiology)<br />
Steven Lane, M.D. (Cardiology)<br />
Robert Lyons, M.D. (Infectious<br />
Disease)<br />
Michael Moustakakis, M.D.<br />
(Nephrology)<br />
Visvanathan MuraliDharan, M.D.<br />
(Gastroenterology)<br />
Danilo Pangilinan, M.D.<br />
John Polio, M.D.<br />
(Gastroenterology)<br />
Susan Rabinbowe, M.D.<br />
(Hematology/Oncology)<br />
Mervyn Rimai, M.D.<br />
Frederick Rowl<strong>and</strong>, M.D.<br />
(Geriatrics)<br />
Eytan Rubinstien, M.D. (Infectious<br />
Disease)<br />
Niranjan Sankaranarayanan, M.D.<br />
(Nephrology)<br />
Paul Shapiro, M.D.<br />
(Gastroenterology)<br />
Cheryl Smith, M.D. (Infectious<br />
Disease)<br />
Richard Stone, M.D.<br />
(Gastroenterology)<br />
Paul Stroebel, M.D. (Cardiology)<br />
Michael Teiger, M.D. (Pulmonary)<br />
NEUROLOGY<br />
Gary Belt, M.D.<br />
Phaniraj Iyengar, M.D.<br />
Michael Krinsky, M.D.<br />
Albert C. Lo, M.D.<br />
Zachary Macinski, M.D.<br />
Keshav Rao, M.D.<br />
Peter Wade, M.D.<br />
NEUROSURGERY<br />
Stephen Calderon, M.D.<br />
Bruce Chozick, M.D.<br />
Howard Lantner, M.D.<br />
OBSTETRICS AND GYNECOLOGY<br />
James Egan, M.D.<br />
OPHTHALMOLOGY<br />
Andrew Epstein, M.D.<br />
William Maron, M.D.<br />
ORTHOPEDICS<br />
Michael Aron, M.D.<br />
Steven Bond, M.D.<br />
David Burstein, M.D.<br />
Jesse Eisler, M.D.<br />
Andrew Gabow, M.D.<br />
Robert Green, M.D.<br />
John Mara, M.D.<br />
Paul Murray, M.D.<br />
John O’Brien, M.D.<br />
Steven Selden, M.D.<br />
Anthony Spinella, M.D.<br />
Thomas Stevens, M.D.<br />
Aris Yannopoulos, M.D.<br />
OTOLARYNGOLOGY<br />
Sheldon Nova, M.D.<br />
Ronald Saxon, M.D.<br />
Stephen G. Wolfe, M.D.<br />
PATHOLOGY<br />
George Barrows, M.D.<br />
PEDIATRICS<br />
Ellen Marmer, M.D.<br />
PSYCHIATRY<br />
Luis Gonzalez, M.D.<br />
Ladan Hamdheydari, M.D.<br />
Nina Jacobs, M.D.<br />
Tracey Krasnow, M.D.<br />
John Levine, M.D.<br />
David Matuskey, M.D.<br />
Muhammad I. Munawar, M.D.<br />
Yaser Mushtaq, M.D.<br />
Yann Poncin, M.D.<br />
Eugenia Popescu, M.D.<br />
Osman Qureshi, M.D.<br />
Surita Rao, M.D.<br />
Bruce Rothschild, M.D.<br />
RADIOLOGY<br />
Borden Brown, M.D.<br />
Robert Feld, M.D.<br />
Michael Firestone, M.D.<br />
Clifford Freling, M.D.<br />
Jonathan Getz, M.D.<br />
Pupinder Jaswal, M.D.<br />
Elinor Kron, M.D.<br />
Amy Martin, M.D.<br />
Sean McKeon, M.D.<br />
Peter Morrison, M.D.<br />
Harold Moskowitz, M.D.<br />
Pongsa Pyn Muangman, M.D.<br />
Anthony Posteraro, III, M.D.<br />
Joseph Sala, M.D.<br />
James Slavin, M.D.<br />
George Stohr, M.D.<br />
Michael Twohig, M.D.<br />
George Wislo, M.D.<br />
John Ziewacz, M.D.<br />
Stephen Zink, M.D.<br />
REHABILITATION MEDICINE<br />
Raghubinder Bajwa, M.D.<br />
Michael Saffir, M.D.<br />
SURGERY<br />
Saumitra Banerjee, M.D.<br />
(Colon/Rectal)<br />
David Cherry, M.D. (Colon/Rectal)<br />
Scheuster Christie, M.D.<br />
Scott Fecteau, M.D. (Vascular)<br />
N. Ch<strong>and</strong>ra Narayanan, M.D.<br />
Eugene Sullivan, M.D.(Vascular)<br />
David Walters, M.D. (Colon/Rectal)<br />
SECTION OF PODIATRY<br />
Donna Boccelli, D.P.M.<br />
Rafael Gonzalez-Perez, D.P.M.<br />
Richard Grayson, D.P.M.<br />
Robert Kalman, D.P.M.<br />
Eric Kosofsky, D.P.M.<br />
Elliot Pollack, D.P.M.<br />
Loren Schneider, D.P.M.<br />
Brian Wagner, D.P.M.<br />
Deborah Waterman, D.P.M.<br />
UROLOGY<br />
Peter Bosco, M.D.<br />
James Boyle, M.D.<br />
Carl Gjertson, M.D.<br />
Hugh Kennedy, M.D.<br />
Marlene Murphy-Setzko, M.D.<br />
Adine Regan, M.D.<br />
G. Thomas Trono, M.D.<br />
CLINICAL SERVICES<br />
NURSE MANAGER<br />
Emily Hahn, CRRN, BSN<br />
NURSING STAFF<br />
Gail Abel, RN<br />
Leigh K. Akerlind, RN<br />
Ann Marie Alcide, RN<br />
Nicovia Anderson, CNA<br />
Kathleen Barone, RN<br />
Dianne Bernier, RN<br />
Jajet Brown, CNA<br />
Amy Calvo, RN<br />
Colette L Carroll, RN<br />
S. Shinymol Chemmarappaly, RN<br />
Phyllis Cox-Garvey, RN<br />
Jacqueline Dawkins-Jones, CNA
Maureen Dehaney, LPN<br />
Linda Fader, RN<br />
Renee Fevrier, RN<br />
Hannah Fevrier, LPN<br />
Darnell Glass, RN<br />
Lena Goforth, CNA<br />
Janette Gordon, RN<br />
Gail Gruszczynski, LPN<br />
Claudette Holmes, LPN<br />
Macrina Hopko, RN<br />
Saly Huertas, CNA<br />
Denise Jackson, RN<br />
Beverly Jones, RN<br />
Gosseth Jones, CNA<br />
Juanita Lancaster, LPN<br />
Manuel R. Lopez, RN<br />
Anne MacKenzie, RN<br />
Catherine Mann, LPN<br />
Carmen Martinez, CNA<br />
Laurie Martini, LPN<br />
Simone McDougall, CNA<br />
Reyna McFarl<strong>and</strong>, CNA<br />
Denise Naylor, RN<br />
Darlene Nukis, LPN<br />
Kathy Olson, RN<br />
Nora Osafo, RN<br />
Mayra Oyola, CNA<br />
Patricia Pickett, LPN<br />
Odessa Adren Poplin, RN<br />
Donna Ricketts, RN<br />
Nancy Robinson, RN<br />
Joanne Rose, RN<br />
Sylvia Rubie, CNA<br />
Diane Schank, LPN<br />
Barbara Semple-Cort, RN<br />
Donna Marie Stanford, CNA<br />
Emily Steele, LPN<br />
Otasha Stephens, CNA<br />
Troiano, Lois, LPN<br />
Margaret VanSteenburgh, RN<br />
Monica Walters, RN<br />
Talisha Webb, CNA<br />
Letitia Williams, RN<br />
MANAGER OF CARE<br />
CONTINUUM<br />
Karen M. Prior-Topalis, RN, BSN,<br />
MBA, CCM, A-CCC<br />
QUALITY & OUTCOMES<br />
COORDINATOR<br />
Colin B. Lavoie, RN, BSN<br />
CASE MANAGEMENT<br />
SERVICES<br />
Frances Matkowski, RN<br />
Susan Pearson, MSW<br />
REHABILITATION<br />
ADMISSION NURSES<br />
Denise A. Farrah, RN<br />
Mary Kathryn Harding, RN<br />
Annie L. Parker, RN<br />
Kathy Sylvia, RN<br />
Robin Hinckley Wachs, RN<br />
THERAPY STAFF<br />
REHABILITATION<br />
MANAGERS<br />
Cynthia L. Griffith, MHS, PT, CSCS,<br />
CCRP<br />
Steven M. Kunsman, MSPT, PT, CBIS<br />
Linda Mackay, MA, CCC-SLP,<br />
BRS-S, CBIST<br />
THERAPY STAFF<br />
AUDIOLOGISTS<br />
Claudia Janusko<br />
Margaret R. Pohlman<br />
CERTIFIED OCCUPATIONAL<br />
THERAPY ASSISTANTS<br />
Jennifer U. Allyn<br />
Alyssa Greenberg<br />
Kelly E. Versteeg<br />
Gina Waltos<br />
FITNESS COORDINATOR<br />
Wesley P. Norris<br />
LYMPHEDEMA SPECIALISTS<br />
Nola A. Eddy<br />
Michelle Aafedt<br />
Joanne C. Mitchell<br />
MANDELL CENTER FOR MULTIPLE<br />
SCLEROSIS AND NEUROSCIENCE<br />
RESEARCH<br />
Jennifer Fawcett<br />
Amy C. Neal, PA-C<br />
Michele Labas<br />
Jessica Vegerano<br />
Jacquelyn C. Wright, RN<br />
OCCUPATIONAL THERAPISTS<br />
Janice A. Bane<br />
Nicole Burdick<br />
Deborah Drown<br />
Melissa L. Dusza<br />
Heidi L. Gauthier<br />
Stacy L. Godin<br />
Amy E. Goodwin<br />
Michelle M. Haudeg<strong>and</strong><br />
Melanie Henry<br />
Christina Hillemeir<br />
Fatima Joao<br />
Timothea Kimball<br />
Robin Lindboe<br />
Melanie Morrison Riddle<br />
Bethany Suzanne Pisati<br />
Michelle P. Sacdalan<br />
Robin N. Tripp<br />
Emily H. Vincent<br />
Christopher White<br />
Kimberly Wilson<br />
Kimberley A. Wood<br />
Christy R. Zarlengo<br />
OUTPATIENT COORDINATOR<br />
Pamela Freeman-Brown, RN, Med,<br />
CCM, CRC<br />
OUTREACH COORDINATOR<br />
Matthew D. Durst, MA, PT<br />
PHYSICAL THERAPISTS<br />
Georgia Angelopoulous<br />
Jeffrey Baker<br />
April M. Barthuly<br />
Sarah A. Begina<br />
Sally Campbell<br />
Victor Ch<strong>and</strong>ler<br />
Ruth Clancy<br />
Todd K. Clayton<br />
Stephen T. Davis<br />
Am<strong>and</strong>a L. DeAngelo<br />
Jennifer A. Dearth<br />
Michele Dery<br />
Lisa T. Farr<br />
Eric A. Fay<br />
Laura H. Filipek<br />
Clint R. Galamgam<br />
Thomas Gostyla<br />
Joseph Grabicki<br />
Joan Karpuk<br />
Judith B. Knowlton<br />
Jillian K. Kossbiel<br />
Amy M. Lambert<br />
Deborah A. Ludwig<br />
Wendy McCabe<br />
Paul E. McCloskey<br />
Catherine Milewski<br />
Nancy A. Mullen<br />
Gary E. Naples<br />
Michael G. Perin<br />
Danielle Provost<br />
Barbara A. Robinson<br />
Peggy Romine<br />
Tracey Ruvolo<br />
Deborah H. Ryan<br />
Tamra A. Ryan<br />
Wendy Scutt<br />
Jennifer Shockley<br />
Karen W. Smyth<br />
Kathryn Streb<br />
Bryan R. Tronosky<br />
Patricia Uhl<br />
Kerry Watts<br />
PHYSICAL THERAPIST ASSISTANTS<br />
Christine E. Castler<br />
Denise A. Dieli<br />
Hollie M. Marshall<br />
Michelle C. Russi<br />
REHABILITATION DAY<br />
TREATMENT PROGRAM<br />
COORDINATOR<br />
Tara B. Rothstein, OTR/L, MSW, CBIS<br />
REHABILITATION TECHNICIANS<br />
Mercedes Bello<br />
Kathleen Curtis<br />
Mercedes Garcia<br />
Laura Maldonado<br />
Leonardo Mason<br />
David McNamara<br />
Emilia Neves<br />
Irene Oyola<br />
Grace Simpson<br />
Jason Teles<br />
Joseph Wojtkowiak<br />
SPEECH PATHOLOGISTS<br />
Elizabeth D. Bouchard<br />
Julie Carpenter<br />
Alex<strong>and</strong>ra Carso<br />
Christina Collin<br />
Kelly L. Coyne<br />
Bernadette Fowler<br />
Carley Hauser<br />
Julie Leska<br />
Jessica Levy<br />
Erin Lewis<br />
Julie A. Logan<br />
Gerald R. Nadeau<br />
Lauren A. Quagliaroli<br />
Arlene S. R<strong>and</strong>e<br />
Nicole Scinto<br />
Ashley Zapata<br />
THERAPEUTIC RECREATION<br />
SPECIALIST<br />
Paige McCullough-Casciano<br />
CLINICAL/ADMINISTRATIVE<br />
SUPPORT STAFF<br />
Jenny Almenas<br />
Takisha Archer<br />
Mary Ann Bukowski<br />
Elaine Cloutier<br />
Janet Cormier<br />
Tanya Cruz<br />
Martha Curtis<br />
Nancy Garthwaite<br />
Pauline Howell<br />
Karin Kaczynski<br />
Deborah McGuire<br />
Nelia Oriola<br />
Joanne Plaza<br />
Suzanne Polak<br />
Damaris Rivera<br />
Ana Santillan<br />
Linda Smith<br />
Susan J. Tigno<br />
Herminia Tuell<br />
Theresa E. Turgeon<br />
Andrea Violette<br />
Carleen L. Young<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 15 ]
Mount Sinai Rehabilitation <strong>Hospital</strong> 2 009 <strong>Annual</strong> <strong>Report</strong><br />
[ 16 ]<br />
The Mount Sinai Foundation<br />
continues its long history of support of programs<br />
<strong>and</strong> services to special populations in our community.<br />
Mount Sinai Rehabilitation <strong>Hospital</strong> has been enriched<br />
by the Foundation’s commitment to the <strong>Hospital</strong> <strong>and</strong><br />
the North Campus.<br />
Through the Foundation’s support, patients with<br />
Multiple Sclerosis <strong>and</strong> stroke-related complications<br />
have access to expertise <strong>and</strong> technology not readily<br />
available elsewhere.<br />
The future for the Rehabilitation <strong>Hospital</strong> is bright,<br />
in part because of the members of the Mount Sinai<br />
Foundation who remain committed to our<br />
important work.<br />
Once again we extend our gratitude to the leadership<br />
of the Foundation for continuing to care.<br />
Mount Sinai Foundation, Inc.<br />
Board of Directors<br />
Robert B. Bruner<br />
Robert E. Cohn<br />
Samuel P. Cooley<br />
Christopher M. Dadlez<br />
Robert M. Fechtor<br />
Edward S. Johnson, D.D.S.<br />
E. Merritt McDonough, Sr.<br />
Steven Rosenberg<br />
Roslyne E. Rosenfield<br />
Henry S. Scherer<br />
John R. Suisman<br />
David Title, Ed.D.<br />
Michael Wilde<br />
The <strong>2009</strong> Mount Sinai Rehabilitation <strong>Hospital</strong><br />
Golf Classic was held on Monday, May 18 at<br />
Blue Fox Run Golf Course, in Avon. This year’s<br />
event brought in a record number of participants<br />
<strong>and</strong> proceeds to help Mount Sinai support the<br />
Stroke Rehabilitation Program, specifically the<br />
special technology that will provide invaluable<br />
benefit to our stroke patient population.
PHOTOGRAPHY: JOE DRISCOLL DESIGN: JOHN JOHNSON ART DIRECTION & DESIGN<br />
Working Together, Rebuilding Lives —<br />
is an accurate portrayal of the environment of care at Mount Sinai<br />
Rehabilitation <strong>Hospital</strong> <strong>and</strong> the benefits enjoyed by the patients <strong>and</strong><br />
families who receive our specialized medical rehabilitation care.<br />
The Mount Sinai Team is exceptionally skilled. The technology we<br />
employ is leading-edge, <strong>and</strong> we are constantly upgrading our facilities<br />
<strong>and</strong> exp<strong>and</strong>ing our services. These are the critical elements of the<br />
high-quality care that our communities have come to expect from<br />
Mount Sinai.<br />
As we look beyond the horizon toward the challenges that lie ahead<br />
for healthcare, we know that only through generous philanthropic<br />
support, particularly from those who have benefited from care<br />
provided here, will innovative growth <strong>and</strong> groundbreaking research<br />
be possible. Reimbursement, much of it government-funded, will<br />
simply not meet the need to grow, innovate <strong>and</strong> discover.<br />
Just a few of the wonderful patient stories <strong>and</strong> the important<br />
involvement of our staff are featured in the pages of this report. It is<br />
our hope that they will engage your interest <strong>and</strong> encourage your<br />
support.<br />
Please consider a gift to Mount Sinai Rehabilitation <strong>Hospital</strong> either<br />
now or in your estate planning.<br />
Thank you for your thoughtful consideration.<br />
For more information contact:<br />
Dr. Edward Johnson<br />
Senior Vice President<br />
860-714-2111<br />
Mr. Paul Pendergast<br />
President, <strong>Saint</strong> <strong>Francis</strong> Foundation<br />
860-714-4900
490 Blue Hills Avenue<br />
Hartford, Connecticut 06112<br />
860-714-3500 • 800-789-7709<br />
www.rehabct.com<br />
Our Mission<br />
We are committed to health <strong>and</strong> healing<br />
through excellence,<br />
compassionate care<br />
<strong>and</strong> reverence for the spirituality<br />
of each person.<br />
Our Core Values<br />
RESPECT<br />
We honor the worth <strong>and</strong> dignity of those<br />
we serve <strong>and</strong> with whom we work.<br />
INTEGRITY<br />
We are faithful, trustworthy <strong>and</strong> just.<br />
SERVICE<br />
We reach out to the community,<br />
especially those most in need.<br />
LEADERSHIP<br />
We encourage initiative, creativity,<br />
learning <strong>and</strong> research.<br />
STEWARDSHIP<br />
We care for <strong>and</strong> strengthen<br />
resources entrusted to us.